User login
HM16 Session Analysis: ICD-10 Coding Tips
Presenter: Aziz Ansari, DO, FHM
Summary: With the implementation of ICD-10, correct and specific documentation to ensure proper patient diagnosis categorization has become increasingly important. Hospitalists are urged to understand the impact CDI has on quality and reimbursement.
Quality Impact: Documentation has a direct impact on quality reporting for mortality and complication rates, risk of mortality, as well as severity of illness. Documenting present on admission (POA) also directly impacts the hospital-acquired condition (HAC) classifications.
Reimbursement Impact: Documentation has a direct impact on expected length of stay, case mix index (CMI), cost reporting, and appropriate hospital reimbursement.
HM Takeaways:
- Be clear and specific.
- Document principle diagnosis and secondary diagnoses, and their associated interactions, are critically important.
- Ensure all diagnoses are a part of the discharge summary.
- Avoid saying “History of.”
- It’s OK to document “possible,” “probably,” “likely,” or “suspected.”
- Document “why” the patient has the diagnosis.
- List all differentials, and identify if ruled in or ruled out.
- Indicate acuity, even if obvious.
This presenter also reviewed common CDI opportunities in hospital medicine.
Note: This discussion was specific to the needs of the hospital patient diagnosis and billing, and not related to physician billing and CPT codes.
Presenter: Aziz Ansari, DO, FHM
Summary: With the implementation of ICD-10, correct and specific documentation to ensure proper patient diagnosis categorization has become increasingly important. Hospitalists are urged to understand the impact CDI has on quality and reimbursement.
Quality Impact: Documentation has a direct impact on quality reporting for mortality and complication rates, risk of mortality, as well as severity of illness. Documenting present on admission (POA) also directly impacts the hospital-acquired condition (HAC) classifications.
Reimbursement Impact: Documentation has a direct impact on expected length of stay, case mix index (CMI), cost reporting, and appropriate hospital reimbursement.
HM Takeaways:
- Be clear and specific.
- Document principle diagnosis and secondary diagnoses, and their associated interactions, are critically important.
- Ensure all diagnoses are a part of the discharge summary.
- Avoid saying “History of.”
- It’s OK to document “possible,” “probably,” “likely,” or “suspected.”
- Document “why” the patient has the diagnosis.
- List all differentials, and identify if ruled in or ruled out.
- Indicate acuity, even if obvious.
This presenter also reviewed common CDI opportunities in hospital medicine.
Note: This discussion was specific to the needs of the hospital patient diagnosis and billing, and not related to physician billing and CPT codes.
Presenter: Aziz Ansari, DO, FHM
Summary: With the implementation of ICD-10, correct and specific documentation to ensure proper patient diagnosis categorization has become increasingly important. Hospitalists are urged to understand the impact CDI has on quality and reimbursement.
Quality Impact: Documentation has a direct impact on quality reporting for mortality and complication rates, risk of mortality, as well as severity of illness. Documenting present on admission (POA) also directly impacts the hospital-acquired condition (HAC) classifications.
Reimbursement Impact: Documentation has a direct impact on expected length of stay, case mix index (CMI), cost reporting, and appropriate hospital reimbursement.
HM Takeaways:
- Be clear and specific.
- Document principle diagnosis and secondary diagnoses, and their associated interactions, are critically important.
- Ensure all diagnoses are a part of the discharge summary.
- Avoid saying “History of.”
- It’s OK to document “possible,” “probably,” “likely,” or “suspected.”
- Document “why” the patient has the diagnosis.
- List all differentials, and identify if ruled in or ruled out.
- Indicate acuity, even if obvious.
This presenter also reviewed common CDI opportunities in hospital medicine.
Note: This discussion was specific to the needs of the hospital patient diagnosis and billing, and not related to physician billing and CPT codes.
EHR Report: How Zika virus reveals the fault in our EHRs
It is always noteworthy when the headlines in the medical and mainstream media appear to be the same.
Typically, this means one of two things: 1) Sensationalism has propelled a minor issue into the common lexicon; or 2) a truly serious issue has grown to the point where the whole world is finally taking notice.
With the recent resurgence of Zika virus, something that initially seemed to be the former has unmistakably developed into the latter, and health care providers are again facing an age-old question: How do we adequately fight an evolving and serious illness in the midst of an ever-changing battlefield?
As has been the case countless times before, the answer to this question really lies in early identification. One might think that the advent of modern technology would make this a much easier proposition, but that has not exactly been the case.
In fact, recent Ebola and Zika outbreaks have actually served to demonstrate a big problem in many modern electronic health records: poor clinical decision support.
In this column, we felt it would be helpful to highlight this shortcoming, and make the suggestion that in the world of EHRs …
Change needs to be faster than Zika
Zika virus is not new (it was first identified in the Zika Forest of Uganda in 1947), and neither is the concept of serious mosquito-born illness. While the current Zika hot zones are South America, Central America, Mexico, and the Caribbean, case reports indicate the virus is quickly migrating. At the time of this writing, more than 150 travel-associated cases of Zika have been identified in the continental United States, and it is clear that the consequences of undiagnosed Zika in pregnancy can be devastating.
Furthermore, Zika is just the latest of many viruses to threaten the health and welfare of modern civilization (for example, Ebola, swine flu, SARS, and so on), so screening and prevention is far from a novel idea.
Unfortunately, electronic record vendors don’t seem to have gotten the message that the ability to adapt quickly to public health threats should be a core element of any modern EHR.
On the contrary, EHRs seem to be designed for fixed “best practice” workflows, and updates are often slow in coming (typically requiring a major upgrade or “patch”). This renders them fairly unable to react nimbly to change.
This fact became evident to us as we attempted to implement a reminder for staff members to perform a Zika-focused travel history on all patients. We felt it was critical for this reminder to be prominent, be easy to interact with, and appear at the most appropriate time for screening.
Despite multiple attempts, we discovered that our top-ranked, industry-leading EHR was unable to do this seemingly straightforward task, and eventually we reverted to the age-old practice of hanging signs in all of the exam rooms. These encouraged patients to inform their doctor “of worrisome symptoms or recent travel history to affected areas.”
We refuse to accept the inability of any modern electronic health record to create simple and flexible clinical support rules and improve on the efficacy of the paper sign. This, especially in light of the fact that one of the core requirements of the Meaningful Use (MU) program – for which all EHRs are certified – is clinical decision support!
Unfortunately, the MU guidelines are not specific, so most vendors choose to include a standard set of rules and don’t allow the ability for customization. That just isn’t good enough. If Ebola and Zika have taught the health information technology community one thing, it’s that …
It is time for smarter EHRs!
For many people, the notion of artificial intelligence seems to be science fiction, but they don’t realize they are carrying incredible “AI” devices with them everywhere they go. We are, of course, referring to our cell phones, which seem to be getting more intelligent all the time.
If you own an iPhone, you may have noticed it often seems to know where you are about to drive and how long it will take you to get there. This can be a bit creepy at first, until you realize how helpful – and smart – it actually is.
Essentially, our devices are constantly collecting data, reading the patterns of our lives, and learning ways to enhance them. Smartphones have revolutionized how we communicate, work, and play. Why, then, can’t our electronic health record software do the same?
It will surprise exactly none of our readers that the Meaningful Use program has fallen short of its goal of promoting the true benefits of electronic records. Many critics have suggested that the incentive program has faltered because EHRs have made physicians work harder, without helping them work smarter.
Zika virus proves the critics correct. Beyond creating just simple reminders as mentioned above, EHRs should be able to make intelligent suggestions based on patient data and current practice guidelines.
Some EHRs get it half correct. For example, they are “smart” enough to remind clinicians that women of a certain age should have mammograms, but they fall short in the ability to efficiently update those reminders when the U.S. Preventive Services Task Force updates the screening recommendation (as they did recently).
Other EHRs do allow you to customize preventative health reminders, but do not place them in a position of prominence – so they are easily overlooked by providers as they care for patients.
Few products seem to get it just right, and it’s time for this to change.
Simply put, as questions in the media loom about how to stop this rising threat, we as frontline health care providers should have the tools – and the decision support – required to provide meaningful answers.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
It is always noteworthy when the headlines in the medical and mainstream media appear to be the same.
Typically, this means one of two things: 1) Sensationalism has propelled a minor issue into the common lexicon; or 2) a truly serious issue has grown to the point where the whole world is finally taking notice.
With the recent resurgence of Zika virus, something that initially seemed to be the former has unmistakably developed into the latter, and health care providers are again facing an age-old question: How do we adequately fight an evolving and serious illness in the midst of an ever-changing battlefield?
As has been the case countless times before, the answer to this question really lies in early identification. One might think that the advent of modern technology would make this a much easier proposition, but that has not exactly been the case.
In fact, recent Ebola and Zika outbreaks have actually served to demonstrate a big problem in many modern electronic health records: poor clinical decision support.
In this column, we felt it would be helpful to highlight this shortcoming, and make the suggestion that in the world of EHRs …
Change needs to be faster than Zika
Zika virus is not new (it was first identified in the Zika Forest of Uganda in 1947), and neither is the concept of serious mosquito-born illness. While the current Zika hot zones are South America, Central America, Mexico, and the Caribbean, case reports indicate the virus is quickly migrating. At the time of this writing, more than 150 travel-associated cases of Zika have been identified in the continental United States, and it is clear that the consequences of undiagnosed Zika in pregnancy can be devastating.
Furthermore, Zika is just the latest of many viruses to threaten the health and welfare of modern civilization (for example, Ebola, swine flu, SARS, and so on), so screening and prevention is far from a novel idea.
Unfortunately, electronic record vendors don’t seem to have gotten the message that the ability to adapt quickly to public health threats should be a core element of any modern EHR.
On the contrary, EHRs seem to be designed for fixed “best practice” workflows, and updates are often slow in coming (typically requiring a major upgrade or “patch”). This renders them fairly unable to react nimbly to change.
This fact became evident to us as we attempted to implement a reminder for staff members to perform a Zika-focused travel history on all patients. We felt it was critical for this reminder to be prominent, be easy to interact with, and appear at the most appropriate time for screening.
Despite multiple attempts, we discovered that our top-ranked, industry-leading EHR was unable to do this seemingly straightforward task, and eventually we reverted to the age-old practice of hanging signs in all of the exam rooms. These encouraged patients to inform their doctor “of worrisome symptoms or recent travel history to affected areas.”
We refuse to accept the inability of any modern electronic health record to create simple and flexible clinical support rules and improve on the efficacy of the paper sign. This, especially in light of the fact that one of the core requirements of the Meaningful Use (MU) program – for which all EHRs are certified – is clinical decision support!
Unfortunately, the MU guidelines are not specific, so most vendors choose to include a standard set of rules and don’t allow the ability for customization. That just isn’t good enough. If Ebola and Zika have taught the health information technology community one thing, it’s that …
It is time for smarter EHRs!
For many people, the notion of artificial intelligence seems to be science fiction, but they don’t realize they are carrying incredible “AI” devices with them everywhere they go. We are, of course, referring to our cell phones, which seem to be getting more intelligent all the time.
If you own an iPhone, you may have noticed it often seems to know where you are about to drive and how long it will take you to get there. This can be a bit creepy at first, until you realize how helpful – and smart – it actually is.
Essentially, our devices are constantly collecting data, reading the patterns of our lives, and learning ways to enhance them. Smartphones have revolutionized how we communicate, work, and play. Why, then, can’t our electronic health record software do the same?
It will surprise exactly none of our readers that the Meaningful Use program has fallen short of its goal of promoting the true benefits of electronic records. Many critics have suggested that the incentive program has faltered because EHRs have made physicians work harder, without helping them work smarter.
Zika virus proves the critics correct. Beyond creating just simple reminders as mentioned above, EHRs should be able to make intelligent suggestions based on patient data and current practice guidelines.
Some EHRs get it half correct. For example, they are “smart” enough to remind clinicians that women of a certain age should have mammograms, but they fall short in the ability to efficiently update those reminders when the U.S. Preventive Services Task Force updates the screening recommendation (as they did recently).
Other EHRs do allow you to customize preventative health reminders, but do not place them in a position of prominence – so they are easily overlooked by providers as they care for patients.
Few products seem to get it just right, and it’s time for this to change.
Simply put, as questions in the media loom about how to stop this rising threat, we as frontline health care providers should have the tools – and the decision support – required to provide meaningful answers.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
It is always noteworthy when the headlines in the medical and mainstream media appear to be the same.
Typically, this means one of two things: 1) Sensationalism has propelled a minor issue into the common lexicon; or 2) a truly serious issue has grown to the point where the whole world is finally taking notice.
With the recent resurgence of Zika virus, something that initially seemed to be the former has unmistakably developed into the latter, and health care providers are again facing an age-old question: How do we adequately fight an evolving and serious illness in the midst of an ever-changing battlefield?
As has been the case countless times before, the answer to this question really lies in early identification. One might think that the advent of modern technology would make this a much easier proposition, but that has not exactly been the case.
In fact, recent Ebola and Zika outbreaks have actually served to demonstrate a big problem in many modern electronic health records: poor clinical decision support.
In this column, we felt it would be helpful to highlight this shortcoming, and make the suggestion that in the world of EHRs …
Change needs to be faster than Zika
Zika virus is not new (it was first identified in the Zika Forest of Uganda in 1947), and neither is the concept of serious mosquito-born illness. While the current Zika hot zones are South America, Central America, Mexico, and the Caribbean, case reports indicate the virus is quickly migrating. At the time of this writing, more than 150 travel-associated cases of Zika have been identified in the continental United States, and it is clear that the consequences of undiagnosed Zika in pregnancy can be devastating.
Furthermore, Zika is just the latest of many viruses to threaten the health and welfare of modern civilization (for example, Ebola, swine flu, SARS, and so on), so screening and prevention is far from a novel idea.
Unfortunately, electronic record vendors don’t seem to have gotten the message that the ability to adapt quickly to public health threats should be a core element of any modern EHR.
On the contrary, EHRs seem to be designed for fixed “best practice” workflows, and updates are often slow in coming (typically requiring a major upgrade or “patch”). This renders them fairly unable to react nimbly to change.
This fact became evident to us as we attempted to implement a reminder for staff members to perform a Zika-focused travel history on all patients. We felt it was critical for this reminder to be prominent, be easy to interact with, and appear at the most appropriate time for screening.
Despite multiple attempts, we discovered that our top-ranked, industry-leading EHR was unable to do this seemingly straightforward task, and eventually we reverted to the age-old practice of hanging signs in all of the exam rooms. These encouraged patients to inform their doctor “of worrisome symptoms or recent travel history to affected areas.”
We refuse to accept the inability of any modern electronic health record to create simple and flexible clinical support rules and improve on the efficacy of the paper sign. This, especially in light of the fact that one of the core requirements of the Meaningful Use (MU) program – for which all EHRs are certified – is clinical decision support!
Unfortunately, the MU guidelines are not specific, so most vendors choose to include a standard set of rules and don’t allow the ability for customization. That just isn’t good enough. If Ebola and Zika have taught the health information technology community one thing, it’s that …
It is time for smarter EHRs!
For many people, the notion of artificial intelligence seems to be science fiction, but they don’t realize they are carrying incredible “AI” devices with them everywhere they go. We are, of course, referring to our cell phones, which seem to be getting more intelligent all the time.
If you own an iPhone, you may have noticed it often seems to know where you are about to drive and how long it will take you to get there. This can be a bit creepy at first, until you realize how helpful – and smart – it actually is.
Essentially, our devices are constantly collecting data, reading the patterns of our lives, and learning ways to enhance them. Smartphones have revolutionized how we communicate, work, and play. Why, then, can’t our electronic health record software do the same?
It will surprise exactly none of our readers that the Meaningful Use program has fallen short of its goal of promoting the true benefits of electronic records. Many critics have suggested that the incentive program has faltered because EHRs have made physicians work harder, without helping them work smarter.
Zika virus proves the critics correct. Beyond creating just simple reminders as mentioned above, EHRs should be able to make intelligent suggestions based on patient data and current practice guidelines.
Some EHRs get it half correct. For example, they are “smart” enough to remind clinicians that women of a certain age should have mammograms, but they fall short in the ability to efficiently update those reminders when the U.S. Preventive Services Task Force updates the screening recommendation (as they did recently).
Other EHRs do allow you to customize preventative health reminders, but do not place them in a position of prominence – so they are easily overlooked by providers as they care for patients.
Few products seem to get it just right, and it’s time for this to change.
Simply put, as questions in the media loom about how to stop this rising threat, we as frontline health care providers should have the tools – and the decision support – required to provide meaningful answers.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
NPs, PAs Vital to Hospital Medicine
Yes, it’s time for another “year ahead” type column where the writer attempts to provide clarity on future events. What does “Hospital Medicine 2016” hold for us? I hope by the time Hospital Medicine 2017 rolls around, everyone will have forgotten the wrong predictions and only remember those that reveal my exceptional clairvoyance and prescient knowledge.
NP and PA Practice in Hospital Medicine Will Continue to Grow
Well, it doesn’t take a crystal ball or tarot cards to predict this. One only has to look at the data. The 2012 State of Hospital Medicine report revealed that 51.7% of hospital medicine groups (HMGs) employed nurse practitioners (NPs) and/or physician assistants (PAs) in their practice. Two short years later, the survey showed 83% of HMGs reported having NPs and/or PAs in their groups. That is an astounding amount of growth in a short period of time, which brings me to my next prediction.
HMGs Will Have to Continue to Figure Out How to Hire and Deploy NPs and PAs in Sensible Ways
I know that statement is very controversial. Not. But the true work of utilizing NP and PA providers in hospitalist practice is not in the hiring; it’s how to use these providers in thoughtful, sensible, and cost-effective ways.
A group leader really needs to know and understand the drivers behind the need for these hires as well as understand the financial landscape in the hiring. Are you hiring an NP/PA because you want to reduce your provider workforce cost? Are you hiring to target quality outcomes in a specific patient population? Are you hiring to staff your observation unit, freeing up your physicians for higher-acuity work? Are you hiring to treat and improve physician burnout? Or is this the only carbon-based life form you can attract to the outer boroughs of your northern clime in the deepest, darkest days of January?
All these may or may not be good reasons, but understanding those variables will help you get the right person for the right reason and will help you evaluate the return on investment and the impact on practice.
Diversity Prevents Disease
Much like the potato monoculture of McDonald’s french fries increasing the risk of potato diseases, monoculture in your hospitalist group may breed burnout and bad attitudes. Diversity of experience, perspective, and skill set may inoculate your group, keeping the dreaded crispy coated from complaining about schedule, workload, or acuity or, worse yet, simply leaving.
I don’t have data to support this, but I have heard anecdotally from more than one HMG leader that the addition of NP/PA providers to physician teams has improved physician satisfaction. SHM obviously agrees with this philosophy, as they value and support the value of a “big tent” philosophy. This big tent includes all types of people who contribute to the culture of this organization, making it stronger, more nimble and innovative, and definitely more fun.
Diversity in providers can only have a positive impact on your organization’s culture.
Whatever the Reason You Hire Them, Get Ready for Change
Be prepared for evolution. You may have initially hired an NP or PA simply to do admissions or to see all of your orthopedic co-management patients. But over time, your practice is going to morph and evolve, hopefully, in positive ways. Bring your NP/PA colleagues along for the ride; pull up a chair to the table. They may be able to provide new direction, support, or service lines to your practice in ways you hadn’t considered.
NP/PA providers’ abilities and ambitions will change over time as well. Make sure that change goes both ways. You may find that their influence and impact on your organization’s productivity and growth go beyond their industry. Consider utilizing NP/PA providers in novel ways; maybe they have great onboarding skills, are fabulous at scheduling, or can look at a spreadsheet without going cross-eyed or bald.
Change is growth. And growth is good. Unless you would rather die.
HM Needs to Develop Innovative Care Models; NPs/PAs Provide a Platform for Innovation
Inpatient medicine is changing in a rapid and unpredictable way. Some of the necessity of that work is driven by financial incentives and quality indicators, but necessity is the biggest driver of all. People, patients, and providers are getting old (thank God it’s not just me). There simply are not enough physicians to care for our rapidly aging population, or if there are, they are all employed in sunny Southern California. How we respond to this threat or opportunity is one of our most important charges. We own the inpatient kingdom. We need to lead with benevolence and thoughtfulness. We need to really look ahead and identify new ways to manage the complexity of a system whose complexity continues to mutate like some avian virus. I can’t see a future without a crucial role played by my NP/PA brethren. Can we begin this conversation with the long view in mind and really begin to own this in a true and responsible way?
Thanks for your attention, and remember, in 2017 you will have forgotten all the ways, if any, that I was wrong. TH
Ms. Cardin is a nurse practitioner in the Section of Hospital Medicine at the University of Chicago and is chair of SHM’s NP/PA Committee. She is a newly elected SHM board member.
Yes, it’s time for another “year ahead” type column where the writer attempts to provide clarity on future events. What does “Hospital Medicine 2016” hold for us? I hope by the time Hospital Medicine 2017 rolls around, everyone will have forgotten the wrong predictions and only remember those that reveal my exceptional clairvoyance and prescient knowledge.
NP and PA Practice in Hospital Medicine Will Continue to Grow
Well, it doesn’t take a crystal ball or tarot cards to predict this. One only has to look at the data. The 2012 State of Hospital Medicine report revealed that 51.7% of hospital medicine groups (HMGs) employed nurse practitioners (NPs) and/or physician assistants (PAs) in their practice. Two short years later, the survey showed 83% of HMGs reported having NPs and/or PAs in their groups. That is an astounding amount of growth in a short period of time, which brings me to my next prediction.
HMGs Will Have to Continue to Figure Out How to Hire and Deploy NPs and PAs in Sensible Ways
I know that statement is very controversial. Not. But the true work of utilizing NP and PA providers in hospitalist practice is not in the hiring; it’s how to use these providers in thoughtful, sensible, and cost-effective ways.
A group leader really needs to know and understand the drivers behind the need for these hires as well as understand the financial landscape in the hiring. Are you hiring an NP/PA because you want to reduce your provider workforce cost? Are you hiring to target quality outcomes in a specific patient population? Are you hiring to staff your observation unit, freeing up your physicians for higher-acuity work? Are you hiring to treat and improve physician burnout? Or is this the only carbon-based life form you can attract to the outer boroughs of your northern clime in the deepest, darkest days of January?
All these may or may not be good reasons, but understanding those variables will help you get the right person for the right reason and will help you evaluate the return on investment and the impact on practice.
Diversity Prevents Disease
Much like the potato monoculture of McDonald’s french fries increasing the risk of potato diseases, monoculture in your hospitalist group may breed burnout and bad attitudes. Diversity of experience, perspective, and skill set may inoculate your group, keeping the dreaded crispy coated from complaining about schedule, workload, or acuity or, worse yet, simply leaving.
I don’t have data to support this, but I have heard anecdotally from more than one HMG leader that the addition of NP/PA providers to physician teams has improved physician satisfaction. SHM obviously agrees with this philosophy, as they value and support the value of a “big tent” philosophy. This big tent includes all types of people who contribute to the culture of this organization, making it stronger, more nimble and innovative, and definitely more fun.
Diversity in providers can only have a positive impact on your organization’s culture.
Whatever the Reason You Hire Them, Get Ready for Change
Be prepared for evolution. You may have initially hired an NP or PA simply to do admissions or to see all of your orthopedic co-management patients. But over time, your practice is going to morph and evolve, hopefully, in positive ways. Bring your NP/PA colleagues along for the ride; pull up a chair to the table. They may be able to provide new direction, support, or service lines to your practice in ways you hadn’t considered.
NP/PA providers’ abilities and ambitions will change over time as well. Make sure that change goes both ways. You may find that their influence and impact on your organization’s productivity and growth go beyond their industry. Consider utilizing NP/PA providers in novel ways; maybe they have great onboarding skills, are fabulous at scheduling, or can look at a spreadsheet without going cross-eyed or bald.
Change is growth. And growth is good. Unless you would rather die.
HM Needs to Develop Innovative Care Models; NPs/PAs Provide a Platform for Innovation
Inpatient medicine is changing in a rapid and unpredictable way. Some of the necessity of that work is driven by financial incentives and quality indicators, but necessity is the biggest driver of all. People, patients, and providers are getting old (thank God it’s not just me). There simply are not enough physicians to care for our rapidly aging population, or if there are, they are all employed in sunny Southern California. How we respond to this threat or opportunity is one of our most important charges. We own the inpatient kingdom. We need to lead with benevolence and thoughtfulness. We need to really look ahead and identify new ways to manage the complexity of a system whose complexity continues to mutate like some avian virus. I can’t see a future without a crucial role played by my NP/PA brethren. Can we begin this conversation with the long view in mind and really begin to own this in a true and responsible way?
Thanks for your attention, and remember, in 2017 you will have forgotten all the ways, if any, that I was wrong. TH
Ms. Cardin is a nurse practitioner in the Section of Hospital Medicine at the University of Chicago and is chair of SHM’s NP/PA Committee. She is a newly elected SHM board member.
Yes, it’s time for another “year ahead” type column where the writer attempts to provide clarity on future events. What does “Hospital Medicine 2016” hold for us? I hope by the time Hospital Medicine 2017 rolls around, everyone will have forgotten the wrong predictions and only remember those that reveal my exceptional clairvoyance and prescient knowledge.
NP and PA Practice in Hospital Medicine Will Continue to Grow
Well, it doesn’t take a crystal ball or tarot cards to predict this. One only has to look at the data. The 2012 State of Hospital Medicine report revealed that 51.7% of hospital medicine groups (HMGs) employed nurse practitioners (NPs) and/or physician assistants (PAs) in their practice. Two short years later, the survey showed 83% of HMGs reported having NPs and/or PAs in their groups. That is an astounding amount of growth in a short period of time, which brings me to my next prediction.
HMGs Will Have to Continue to Figure Out How to Hire and Deploy NPs and PAs in Sensible Ways
I know that statement is very controversial. Not. But the true work of utilizing NP and PA providers in hospitalist practice is not in the hiring; it’s how to use these providers in thoughtful, sensible, and cost-effective ways.
A group leader really needs to know and understand the drivers behind the need for these hires as well as understand the financial landscape in the hiring. Are you hiring an NP/PA because you want to reduce your provider workforce cost? Are you hiring to target quality outcomes in a specific patient population? Are you hiring to staff your observation unit, freeing up your physicians for higher-acuity work? Are you hiring to treat and improve physician burnout? Or is this the only carbon-based life form you can attract to the outer boroughs of your northern clime in the deepest, darkest days of January?
All these may or may not be good reasons, but understanding those variables will help you get the right person for the right reason and will help you evaluate the return on investment and the impact on practice.
Diversity Prevents Disease
Much like the potato monoculture of McDonald’s french fries increasing the risk of potato diseases, monoculture in your hospitalist group may breed burnout and bad attitudes. Diversity of experience, perspective, and skill set may inoculate your group, keeping the dreaded crispy coated from complaining about schedule, workload, or acuity or, worse yet, simply leaving.
I don’t have data to support this, but I have heard anecdotally from more than one HMG leader that the addition of NP/PA providers to physician teams has improved physician satisfaction. SHM obviously agrees with this philosophy, as they value and support the value of a “big tent” philosophy. This big tent includes all types of people who contribute to the culture of this organization, making it stronger, more nimble and innovative, and definitely more fun.
Diversity in providers can only have a positive impact on your organization’s culture.
Whatever the Reason You Hire Them, Get Ready for Change
Be prepared for evolution. You may have initially hired an NP or PA simply to do admissions or to see all of your orthopedic co-management patients. But over time, your practice is going to morph and evolve, hopefully, in positive ways. Bring your NP/PA colleagues along for the ride; pull up a chair to the table. They may be able to provide new direction, support, or service lines to your practice in ways you hadn’t considered.
NP/PA providers’ abilities and ambitions will change over time as well. Make sure that change goes both ways. You may find that their influence and impact on your organization’s productivity and growth go beyond their industry. Consider utilizing NP/PA providers in novel ways; maybe they have great onboarding skills, are fabulous at scheduling, or can look at a spreadsheet without going cross-eyed or bald.
Change is growth. And growth is good. Unless you would rather die.
HM Needs to Develop Innovative Care Models; NPs/PAs Provide a Platform for Innovation
Inpatient medicine is changing in a rapid and unpredictable way. Some of the necessity of that work is driven by financial incentives and quality indicators, but necessity is the biggest driver of all. People, patients, and providers are getting old (thank God it’s not just me). There simply are not enough physicians to care for our rapidly aging population, or if there are, they are all employed in sunny Southern California. How we respond to this threat or opportunity is one of our most important charges. We own the inpatient kingdom. We need to lead with benevolence and thoughtfulness. We need to really look ahead and identify new ways to manage the complexity of a system whose complexity continues to mutate like some avian virus. I can’t see a future without a crucial role played by my NP/PA brethren. Can we begin this conversation with the long view in mind and really begin to own this in a true and responsible way?
Thanks for your attention, and remember, in 2017 you will have forgotten all the ways, if any, that I was wrong. TH
Ms. Cardin is a nurse practitioner in the Section of Hospital Medicine at the University of Chicago and is chair of SHM’s NP/PA Committee. She is a newly elected SHM board member.
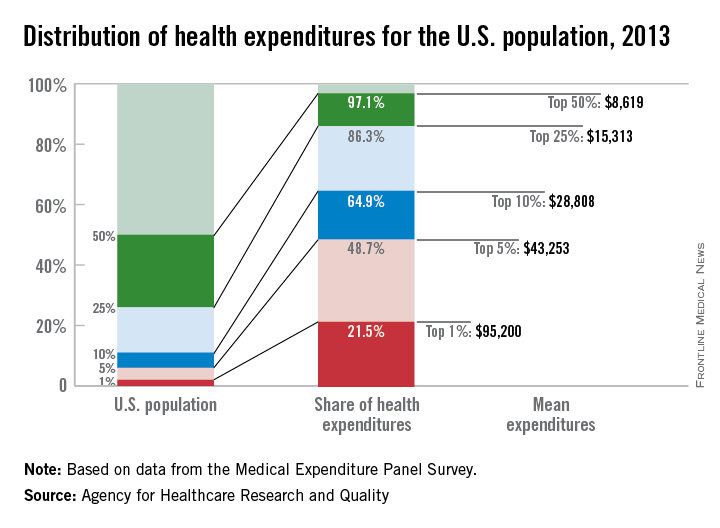
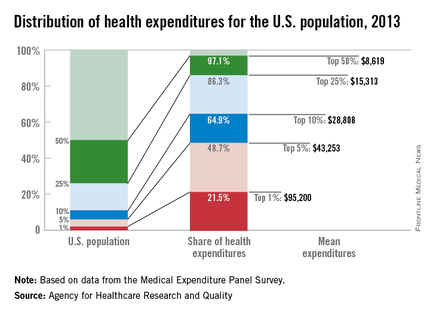
Health spending less concentrated among highest-cost population
Good news for the Occupy movement: The 99% have gained some ground.
The 1% of the U.S. population with the highest health care expenses accounted for 21.5% of all health care expenditures in 2013. That may be a lot, but it’s down from 28% in 1996, according to the Agency for Healthcare Research and Quality.
What’s more, the top 5% of the population ranked by their health care expenses dropped to 48.7% of total spending in 2013, after accounting for more than half in 1996, the AHRQ reported.
Health care expenditures for the U.S. civilian noninstitutionalized population totaled $1.4 trillion in 2013, with mean spending of $4,436 per person. The top 1%, by comparison, had mean spending of $95,200 each, and for the top 5% the figure was $43,253 per person. The top 50% of the population had mean per-person spending of $8,619 and accounted for 97.1% of all health care expenditures, leaving just 2.9% of the total to the lower-cost 50% of the population, the AHRQ said.
Looking at the distribution by race and ethnicity, the top 5% of whites accounted for 45.3% of all spending incurred by whites, compared with 50.8% of all Asian spending for the top 5% of Asians, with corresponding numbers of 56.3% for blacks and 57.3% for Hispanics. Mean spending per person was somewhat reversed, however, at $26,491 for Asian five-percenters, $28,868 for Hispanics, $45,574 for blacks, and $46,809 for whites, according to data from the Medical Expenditure Panel Survey.
Good news for the Occupy movement: The 99% have gained some ground.
The 1% of the U.S. population with the highest health care expenses accounted for 21.5% of all health care expenditures in 2013. That may be a lot, but it’s down from 28% in 1996, according to the Agency for Healthcare Research and Quality.
What’s more, the top 5% of the population ranked by their health care expenses dropped to 48.7% of total spending in 2013, after accounting for more than half in 1996, the AHRQ reported.
Health care expenditures for the U.S. civilian noninstitutionalized population totaled $1.4 trillion in 2013, with mean spending of $4,436 per person. The top 1%, by comparison, had mean spending of $95,200 each, and for the top 5% the figure was $43,253 per person. The top 50% of the population had mean per-person spending of $8,619 and accounted for 97.1% of all health care expenditures, leaving just 2.9% of the total to the lower-cost 50% of the population, the AHRQ said.
Looking at the distribution by race and ethnicity, the top 5% of whites accounted for 45.3% of all spending incurred by whites, compared with 50.8% of all Asian spending for the top 5% of Asians, with corresponding numbers of 56.3% for blacks and 57.3% for Hispanics. Mean spending per person was somewhat reversed, however, at $26,491 for Asian five-percenters, $28,868 for Hispanics, $45,574 for blacks, and $46,809 for whites, according to data from the Medical Expenditure Panel Survey.
Good news for the Occupy movement: The 99% have gained some ground.
The 1% of the U.S. population with the highest health care expenses accounted for 21.5% of all health care expenditures in 2013. That may be a lot, but it’s down from 28% in 1996, according to the Agency for Healthcare Research and Quality.
What’s more, the top 5% of the population ranked by their health care expenses dropped to 48.7% of total spending in 2013, after accounting for more than half in 1996, the AHRQ reported.
Health care expenditures for the U.S. civilian noninstitutionalized population totaled $1.4 trillion in 2013, with mean spending of $4,436 per person. The top 1%, by comparison, had mean spending of $95,200 each, and for the top 5% the figure was $43,253 per person. The top 50% of the population had mean per-person spending of $8,619 and accounted for 97.1% of all health care expenditures, leaving just 2.9% of the total to the lower-cost 50% of the population, the AHRQ said.
Looking at the distribution by race and ethnicity, the top 5% of whites accounted for 45.3% of all spending incurred by whites, compared with 50.8% of all Asian spending for the top 5% of Asians, with corresponding numbers of 56.3% for blacks and 57.3% for Hispanics. Mean spending per person was somewhat reversed, however, at $26,491 for Asian five-percenters, $28,868 for Hispanics, $45,574 for blacks, and $46,809 for whites, according to data from the Medical Expenditure Panel Survey.
VIDEO: What are physicians’ top legal risks in 2016?
AUSTIN, TEX. – With ongoing changes in health delivery and ever-increasing government scrutiny over care, physicians face a number of pressing legal risks this year.
At an American Health Lawyers Association meeting, Birmingham, Ala., health law attorney William W. Horton shared the top legal dangers for doctors in 2016.
From False Claims Act investigations and whistle-blower claims to liability connected to value-based care, clinicians have a lot to consider, said Mr. Horton, who is chair of the American Bar Association Health Law Section.
In a video interview, Mr. Horton also discussed how to reduce liability and limit government inquiries.
On Twitter @legal_med
AUSTIN, TEX. – With ongoing changes in health delivery and ever-increasing government scrutiny over care, physicians face a number of pressing legal risks this year.
At an American Health Lawyers Association meeting, Birmingham, Ala., health law attorney William W. Horton shared the top legal dangers for doctors in 2016.
From False Claims Act investigations and whistle-blower claims to liability connected to value-based care, clinicians have a lot to consider, said Mr. Horton, who is chair of the American Bar Association Health Law Section.
In a video interview, Mr. Horton also discussed how to reduce liability and limit government inquiries.
On Twitter @legal_med
AUSTIN, TEX. – With ongoing changes in health delivery and ever-increasing government scrutiny over care, physicians face a number of pressing legal risks this year.
At an American Health Lawyers Association meeting, Birmingham, Ala., health law attorney William W. Horton shared the top legal dangers for doctors in 2016.
From False Claims Act investigations and whistle-blower claims to liability connected to value-based care, clinicians have a lot to consider, said Mr. Horton, who is chair of the American Bar Association Health Law Section.
In a video interview, Mr. Horton also discussed how to reduce liability and limit government inquiries.
On Twitter @legal_med
EXPERT ANALYSIS FROM THE PHYSICIANS AND HOSPITALS LAW INSTITUTE
Medicare reaches first quality-based goal early
At least 30% of Medicare payments are now tied to quality, the Centers for Medicare & Medicaid Services announced March 3. Federal officials originally had aimed to achieve this milestone by the end of 2016.
“Thanks to tools provided by the Affordable Care Act, an estimated 30% of Medicare payments are now tied to alternative payment models such as accountable care organizations and bundled payments,” Dr. Patrick Conway, chief medical officer at CMS, said during a press conference.
Approximately $117 billion in Medicare payments in 2016 will be tied to these alternative payment models out of a projected $380 billion in total fee-for-service payments, Dr. Conway said.
Additionally, hospital readmissions were reduced by an estimated 565,000 between 2010 and 2015 and hospital-acquired conditions were reduced by 17% between 2010 and 2014.
Dr. Conway cited three factors for these improvements in health care quality.
First, he noted that there is broad buy-in to the notion that payment systems need to evolve to paying for quality over quantity.
“We see providers, states, communities, payers across this country moving to alternative payment models,” he said, adding that many in the public and private side are participating in the Health Care Payment Learning and Action Network, further demonstrating the drive toward value-based payments.
Second, “We’ve made adjustments to a number of our models and improved them,” he continued. “So with accountable care organizations, we continue to see increase in participation. We think this is because we continue to improve the model over time.” The same is true, he added, with bundled payment models.
And finally, he said “I think at the end of the day, people know this is the right thing to do. It’s the right thing to do for our patients. It’s the right thing to do for our health system.”
In response to a question as to whether the bar was set too low, considering that 20% of payments were tied to quality already when the goal was announced in January 2015, Dr. Conway said that even within the agency, some thought the 30% goal was too ambitious. No new goal for 2016 has been set.
CMS is now focused on part two of the goal: 50% of payments tied to quality by the end of 2018.
Two programs in the near term that will help achieve that are programs related to knee and hip replacement and oncology care.
At least 30% of Medicare payments are now tied to quality, the Centers for Medicare & Medicaid Services announced March 3. Federal officials originally had aimed to achieve this milestone by the end of 2016.
“Thanks to tools provided by the Affordable Care Act, an estimated 30% of Medicare payments are now tied to alternative payment models such as accountable care organizations and bundled payments,” Dr. Patrick Conway, chief medical officer at CMS, said during a press conference.
Approximately $117 billion in Medicare payments in 2016 will be tied to these alternative payment models out of a projected $380 billion in total fee-for-service payments, Dr. Conway said.
Additionally, hospital readmissions were reduced by an estimated 565,000 between 2010 and 2015 and hospital-acquired conditions were reduced by 17% between 2010 and 2014.
Dr. Conway cited three factors for these improvements in health care quality.
First, he noted that there is broad buy-in to the notion that payment systems need to evolve to paying for quality over quantity.
“We see providers, states, communities, payers across this country moving to alternative payment models,” he said, adding that many in the public and private side are participating in the Health Care Payment Learning and Action Network, further demonstrating the drive toward value-based payments.
Second, “We’ve made adjustments to a number of our models and improved them,” he continued. “So with accountable care organizations, we continue to see increase in participation. We think this is because we continue to improve the model over time.” The same is true, he added, with bundled payment models.
And finally, he said “I think at the end of the day, people know this is the right thing to do. It’s the right thing to do for our patients. It’s the right thing to do for our health system.”
In response to a question as to whether the bar was set too low, considering that 20% of payments were tied to quality already when the goal was announced in January 2015, Dr. Conway said that even within the agency, some thought the 30% goal was too ambitious. No new goal for 2016 has been set.
CMS is now focused on part two of the goal: 50% of payments tied to quality by the end of 2018.
Two programs in the near term that will help achieve that are programs related to knee and hip replacement and oncology care.
At least 30% of Medicare payments are now tied to quality, the Centers for Medicare & Medicaid Services announced March 3. Federal officials originally had aimed to achieve this milestone by the end of 2016.
“Thanks to tools provided by the Affordable Care Act, an estimated 30% of Medicare payments are now tied to alternative payment models such as accountable care organizations and bundled payments,” Dr. Patrick Conway, chief medical officer at CMS, said during a press conference.
Approximately $117 billion in Medicare payments in 2016 will be tied to these alternative payment models out of a projected $380 billion in total fee-for-service payments, Dr. Conway said.
Additionally, hospital readmissions were reduced by an estimated 565,000 between 2010 and 2015 and hospital-acquired conditions were reduced by 17% between 2010 and 2014.
Dr. Conway cited three factors for these improvements in health care quality.
First, he noted that there is broad buy-in to the notion that payment systems need to evolve to paying for quality over quantity.
“We see providers, states, communities, payers across this country moving to alternative payment models,” he said, adding that many in the public and private side are participating in the Health Care Payment Learning and Action Network, further demonstrating the drive toward value-based payments.
Second, “We’ve made adjustments to a number of our models and improved them,” he continued. “So with accountable care organizations, we continue to see increase in participation. We think this is because we continue to improve the model over time.” The same is true, he added, with bundled payment models.
And finally, he said “I think at the end of the day, people know this is the right thing to do. It’s the right thing to do for our patients. It’s the right thing to do for our health system.”
In response to a question as to whether the bar was set too low, considering that 20% of payments were tied to quality already when the goal was announced in January 2015, Dr. Conway said that even within the agency, some thought the 30% goal was too ambitious. No new goal for 2016 has been set.
CMS is now focused on part two of the goal: 50% of payments tied to quality by the end of 2018.
Two programs in the near term that will help achieve that are programs related to knee and hip replacement and oncology care.
AARP: Retail drug prices rising faster than inflation
Retail prices for medications used most commonly by Medicare patients rose almost 10% in 2013 – more than six times faster than the rate of inflation, according to an analysis by the AARP Public Policy Institute.
In 2013, “the average annual cost of drug therapy for prescription drugs, based on the AARP combined market basket used in this study, was over $11,000 per year,” according to the report In comparison, the average Social Security benefit was $15,526, the median income for Medicare beneficiaries was $23,500 and the median U.S. household income was $52,250.
Price increases for traditional and specialty brand prescription drugs rose faster than generics, eliminating any offset the declines in generic prices might have had.
The report examined drug prices from 2006 to 2013 for a combined market basket of 622 brand name and generic versions of traditional and specialty prescription drugs.
Of the 397 drugs that were on the market for all years, the average retail price increased 81%.
Retail prices for medications used most commonly by Medicare patients rose almost 10% in 2013 – more than six times faster than the rate of inflation, according to an analysis by the AARP Public Policy Institute.
In 2013, “the average annual cost of drug therapy for prescription drugs, based on the AARP combined market basket used in this study, was over $11,000 per year,” according to the report In comparison, the average Social Security benefit was $15,526, the median income for Medicare beneficiaries was $23,500 and the median U.S. household income was $52,250.
Price increases for traditional and specialty brand prescription drugs rose faster than generics, eliminating any offset the declines in generic prices might have had.
The report examined drug prices from 2006 to 2013 for a combined market basket of 622 brand name and generic versions of traditional and specialty prescription drugs.
Of the 397 drugs that were on the market for all years, the average retail price increased 81%.
Retail prices for medications used most commonly by Medicare patients rose almost 10% in 2013 – more than six times faster than the rate of inflation, according to an analysis by the AARP Public Policy Institute.
In 2013, “the average annual cost of drug therapy for prescription drugs, based on the AARP combined market basket used in this study, was over $11,000 per year,” according to the report In comparison, the average Social Security benefit was $15,526, the median income for Medicare beneficiaries was $23,500 and the median U.S. household income was $52,250.
Price increases for traditional and specialty brand prescription drugs rose faster than generics, eliminating any offset the declines in generic prices might have had.
The report examined drug prices from 2006 to 2013 for a combined market basket of 622 brand name and generic versions of traditional and specialty prescription drugs.
Of the 397 drugs that were on the market for all years, the average retail price increased 81%.
CMS extends EHR hardship exemption deadline to July 1
Physicians and hospitals seeking a hardship exemption for not being able to meet meaningful use requirements in 2015 will have more time to file their application.
Applications for both groups are now due July 1. Previously, the deadline was March 15 for physicians and other eligible professionals and April 1 for hospitals.
The Centers for Medicare & Medicaid Services said in a statement that it is “extending the deadline so providers have sufficient time to submit their applications to avoid adjustments to their Medicare payments in 2017.”
An agency spokesman did not have any details on how many exemption requests have been made to date, nor did he say how many the agency was expecting.
Last year, Congress approved a process to allow the CMS to batch process hardship exemption requests. Before that, law required that the agency consider requests on a case by case basis.
Filing instructions for a hardship exemption can be found here.
Physicians and hospitals seeking a hardship exemption for not being able to meet meaningful use requirements in 2015 will have more time to file their application.
Applications for both groups are now due July 1. Previously, the deadline was March 15 for physicians and other eligible professionals and April 1 for hospitals.
The Centers for Medicare & Medicaid Services said in a statement that it is “extending the deadline so providers have sufficient time to submit their applications to avoid adjustments to their Medicare payments in 2017.”
An agency spokesman did not have any details on how many exemption requests have been made to date, nor did he say how many the agency was expecting.
Last year, Congress approved a process to allow the CMS to batch process hardship exemption requests. Before that, law required that the agency consider requests on a case by case basis.
Filing instructions for a hardship exemption can be found here.
Physicians and hospitals seeking a hardship exemption for not being able to meet meaningful use requirements in 2015 will have more time to file their application.
Applications for both groups are now due July 1. Previously, the deadline was March 15 for physicians and other eligible professionals and April 1 for hospitals.
The Centers for Medicare & Medicaid Services said in a statement that it is “extending the deadline so providers have sufficient time to submit their applications to avoid adjustments to their Medicare payments in 2017.”
An agency spokesman did not have any details on how many exemption requests have been made to date, nor did he say how many the agency was expecting.
Last year, Congress approved a process to allow the CMS to batch process hardship exemption requests. Before that, law required that the agency consider requests on a case by case basis.
Filing instructions for a hardship exemption can be found here.
Expert counsel: Selling a practice during a government investigation
AUSTIN,TEX. – There a lot of tough questions to answer when selling a medical practice during a government investigation, according to Morristown, N.J.–based health law attorney Glenn P. Prives.
How much information should potential buyers know about the case? Should the investigation be resolved before the sale? A wrong move in any direction may reduce sale profits or harm the investigation’s defense,
Mr. Prives said at an American Health Lawyers Association meeting.
Selling a practice in the midst of state or federal inquires has become more common in this era of increased government scrutiny, he said. Probes may include inquiries related to the False Claims Act, Stark Law, or Anti-Kickback Statute.
“Because of how hard the government is coming down on health care issues, more and more practices are finding themselves dealing with the government in an unfavorable light,” he said in an interview. “At the same time, you’ve got mass consolidation in the health care industry overall. Put those together, and it’s becoming more and more common” to sell a practice during an investigation.
“Just because the seller’s practice is under investigation does not mean it can’t be sold,” Mr. Prives said. “It requires extra effort and caution, but a deal is still possible.”
Be cautious about how much information about the investigation is disclosed to buyers, Mr. Prives warned. During the due diligence process, purchasers typically want to review the practice’s finances, leases, disciplinary complaints, malpractice history, and other pertinent information.
Be careful not to inadvertently waive the attorney-client privilege when divulging information to a potential buyer, Mr. Prives said. “Oftentimes, you’re dealing with health care laws that are vague and gray and broad. Physicians, like other health care providers, will engage health care attorneys to give them confidential advice on different structures. If [sellers] share that information with the buyer, and they have arguably lost the privilege, that advice may find its way into the government’s hands, which could be very damaging to the seller.”
Consider entering into a joint defense agreement, a contract that allows two parties conducting a transaction to freely share information about an investigation without waiving the attorney-client privilege. However, there is mixed case law about how effective joint defense agreements are in preserving the privilege, Mr. Prives said.
A better idea may be to limit disclosures to buyers to a “need to know” basis and provide more information only as the deal gets further along. Share enough information to keep the buyer engaged, but carefully frame issues to best position the practice in transaction negotiations, Mr. Prives advised.
There are pros and cons as to whether to resolve the investigation before closing the transaction, he said.
The selling physician may want to have the inquiry wrapped up before the sale is final to avoid the buyer’s involvement in the case. If the inquiry is ongoing, the buyer will likely want a large escrow or hold back in the purchase price, Mr. Prives said in an interview. In addition, the buyer may want to be part of discussions with the government about the case resolution.
“That can be a double-edged sword for the physician-seller,” he said. “Their objections are not necessarily aligned. The sellers are going to want to resolve the immediate issues and be done with it because they’re selling their business. The buyer cares less about the monetary payment to the government and is more concerned about what’s it’s going to have to do going forward to satisfy the government.”
On the other hand, the buyer may lose interest if kept waiting until the case is resolved.
“Many times when these investigations start, the sellers don’t know if they’ve done anything wrong or their exact role,” Mr. Prives said. “If a seller waits until the investigation is done, they may be waiting years, and a buyer is unlikely to be around for years. That’s the advantage for not waiting and doing the deal anyway.”
A wise move is to negotiate into the purchase agreement that the seller will take the lead in all government negotiations if the transaction closes before the investigation is complete, he added. Remember, however, that the deal will not likely close unless the buyer can approve or veto the final settlement. Ensure through buyer negotiations that such final confirmation is the only influence buyers can have on resolutions, he said.
“Basically, [conduct] everything until it’s about to be tied up with a nice bow, and then send that document over to the buyer for approval or disapproval,” he said. “That way the seller-physician will control the process, but satisfy that the buyer has final approval before everything is done.”
On Twitter@legal_med
AUSTIN,TEX. – There a lot of tough questions to answer when selling a medical practice during a government investigation, according to Morristown, N.J.–based health law attorney Glenn P. Prives.
How much information should potential buyers know about the case? Should the investigation be resolved before the sale? A wrong move in any direction may reduce sale profits or harm the investigation’s defense,
Mr. Prives said at an American Health Lawyers Association meeting.
Selling a practice in the midst of state or federal inquires has become more common in this era of increased government scrutiny, he said. Probes may include inquiries related to the False Claims Act, Stark Law, or Anti-Kickback Statute.
“Because of how hard the government is coming down on health care issues, more and more practices are finding themselves dealing with the government in an unfavorable light,” he said in an interview. “At the same time, you’ve got mass consolidation in the health care industry overall. Put those together, and it’s becoming more and more common” to sell a practice during an investigation.
“Just because the seller’s practice is under investigation does not mean it can’t be sold,” Mr. Prives said. “It requires extra effort and caution, but a deal is still possible.”
Be cautious about how much information about the investigation is disclosed to buyers, Mr. Prives warned. During the due diligence process, purchasers typically want to review the practice’s finances, leases, disciplinary complaints, malpractice history, and other pertinent information.
Be careful not to inadvertently waive the attorney-client privilege when divulging information to a potential buyer, Mr. Prives said. “Oftentimes, you’re dealing with health care laws that are vague and gray and broad. Physicians, like other health care providers, will engage health care attorneys to give them confidential advice on different structures. If [sellers] share that information with the buyer, and they have arguably lost the privilege, that advice may find its way into the government’s hands, which could be very damaging to the seller.”
Consider entering into a joint defense agreement, a contract that allows two parties conducting a transaction to freely share information about an investigation without waiving the attorney-client privilege. However, there is mixed case law about how effective joint defense agreements are in preserving the privilege, Mr. Prives said.
A better idea may be to limit disclosures to buyers to a “need to know” basis and provide more information only as the deal gets further along. Share enough information to keep the buyer engaged, but carefully frame issues to best position the practice in transaction negotiations, Mr. Prives advised.
There are pros and cons as to whether to resolve the investigation before closing the transaction, he said.
The selling physician may want to have the inquiry wrapped up before the sale is final to avoid the buyer’s involvement in the case. If the inquiry is ongoing, the buyer will likely want a large escrow or hold back in the purchase price, Mr. Prives said in an interview. In addition, the buyer may want to be part of discussions with the government about the case resolution.
“That can be a double-edged sword for the physician-seller,” he said. “Their objections are not necessarily aligned. The sellers are going to want to resolve the immediate issues and be done with it because they’re selling their business. The buyer cares less about the monetary payment to the government and is more concerned about what’s it’s going to have to do going forward to satisfy the government.”
On the other hand, the buyer may lose interest if kept waiting until the case is resolved.
“Many times when these investigations start, the sellers don’t know if they’ve done anything wrong or their exact role,” Mr. Prives said. “If a seller waits until the investigation is done, they may be waiting years, and a buyer is unlikely to be around for years. That’s the advantage for not waiting and doing the deal anyway.”
A wise move is to negotiate into the purchase agreement that the seller will take the lead in all government negotiations if the transaction closes before the investigation is complete, he added. Remember, however, that the deal will not likely close unless the buyer can approve or veto the final settlement. Ensure through buyer negotiations that such final confirmation is the only influence buyers can have on resolutions, he said.
“Basically, [conduct] everything until it’s about to be tied up with a nice bow, and then send that document over to the buyer for approval or disapproval,” he said. “That way the seller-physician will control the process, but satisfy that the buyer has final approval before everything is done.”
On Twitter@legal_med
AUSTIN,TEX. – There a lot of tough questions to answer when selling a medical practice during a government investigation, according to Morristown, N.J.–based health law attorney Glenn P. Prives.
How much information should potential buyers know about the case? Should the investigation be resolved before the sale? A wrong move in any direction may reduce sale profits or harm the investigation’s defense,
Mr. Prives said at an American Health Lawyers Association meeting.
Selling a practice in the midst of state or federal inquires has become more common in this era of increased government scrutiny, he said. Probes may include inquiries related to the False Claims Act, Stark Law, or Anti-Kickback Statute.
“Because of how hard the government is coming down on health care issues, more and more practices are finding themselves dealing with the government in an unfavorable light,” he said in an interview. “At the same time, you’ve got mass consolidation in the health care industry overall. Put those together, and it’s becoming more and more common” to sell a practice during an investigation.
“Just because the seller’s practice is under investigation does not mean it can’t be sold,” Mr. Prives said. “It requires extra effort and caution, but a deal is still possible.”
Be cautious about how much information about the investigation is disclosed to buyers, Mr. Prives warned. During the due diligence process, purchasers typically want to review the practice’s finances, leases, disciplinary complaints, malpractice history, and other pertinent information.
Be careful not to inadvertently waive the attorney-client privilege when divulging information to a potential buyer, Mr. Prives said. “Oftentimes, you’re dealing with health care laws that are vague and gray and broad. Physicians, like other health care providers, will engage health care attorneys to give them confidential advice on different structures. If [sellers] share that information with the buyer, and they have arguably lost the privilege, that advice may find its way into the government’s hands, which could be very damaging to the seller.”
Consider entering into a joint defense agreement, a contract that allows two parties conducting a transaction to freely share information about an investigation without waiving the attorney-client privilege. However, there is mixed case law about how effective joint defense agreements are in preserving the privilege, Mr. Prives said.
A better idea may be to limit disclosures to buyers to a “need to know” basis and provide more information only as the deal gets further along. Share enough information to keep the buyer engaged, but carefully frame issues to best position the practice in transaction negotiations, Mr. Prives advised.
There are pros and cons as to whether to resolve the investigation before closing the transaction, he said.
The selling physician may want to have the inquiry wrapped up before the sale is final to avoid the buyer’s involvement in the case. If the inquiry is ongoing, the buyer will likely want a large escrow or hold back in the purchase price, Mr. Prives said in an interview. In addition, the buyer may want to be part of discussions with the government about the case resolution.
“That can be a double-edged sword for the physician-seller,” he said. “Their objections are not necessarily aligned. The sellers are going to want to resolve the immediate issues and be done with it because they’re selling their business. The buyer cares less about the monetary payment to the government and is more concerned about what’s it’s going to have to do going forward to satisfy the government.”
On the other hand, the buyer may lose interest if kept waiting until the case is resolved.
“Many times when these investigations start, the sellers don’t know if they’ve done anything wrong or their exact role,” Mr. Prives said. “If a seller waits until the investigation is done, they may be waiting years, and a buyer is unlikely to be around for years. That’s the advantage for not waiting and doing the deal anyway.”
A wise move is to negotiate into the purchase agreement that the seller will take the lead in all government negotiations if the transaction closes before the investigation is complete, he added. Remember, however, that the deal will not likely close unless the buyer can approve or veto the final settlement. Ensure through buyer negotiations that such final confirmation is the only influence buyers can have on resolutions, he said.
“Basically, [conduct] everything until it’s about to be tied up with a nice bow, and then send that document over to the buyer for approval or disapproval,” he said. “That way the seller-physician will control the process, but satisfy that the buyer has final approval before everything is done.”
On Twitter@legal_med
AT THE PHYSICIANS AND HOSPITALS LAW INSTITUTE
HHS to doctors: We hear your health IT woes
LAS VEGAS – Federal officials have spent months listening to doctors’ complaints about their frustrating EHRs and are responding with a core group of changes to simplify and standardize health IT.
“We’ve made a great start, but we’re still at a stage where technology often hurts rather than helps physicians to provide better care,” Andy Slavitt, acting administrator of the Centers for Medicare & Medicaid Services, said March 1 at the annual meeting of the Health Information and Management Systems Society.
He provided some examples of complaints he hears from doctors: “Ordering aspirin takes eight clicks on the computer; to order full-strength aspirin, 16,” he said as the audience laughed.
And, “the systems don’t talk to each other. It’s actually the opposite. I can’t even access the hospital because of a firewall, and I can’t even get into the EMR at the hospital to look at patient records.”
And, “I can’t track my patients’ referrals,” or “I sent them to the hospital and I don’t know what happened.”
Mr. Slavitt said that he has 700 complaints from doctors just like those. “But the good news is that they’re not describing problems that we don’t know how to solve.”
And, he said, solving them is exactly what the CMS and a host of other agencies within the Health and Human Services department are trying to do with a raft of new proposed rules and announcements designed to more easily connect patients and providers with health care information necessary to provide better care.
Mr. Slavitt’s view of the EHR situation was echoed by Dr. Karen DeSalvo, national coordinator for Health Information Technology, who said that her husband is a practicing physician with real time frustrations.
“That’s my dinner conversation,” she said. “He’s a very clinically busy emergency medicine doc, and he wants the system to enable his workflow, and just like many physicians, it’s the same common refrain.”
Part of the solution is a proposed rule announced March 1 that would allow the Office of the National Coordinator for Heath Information Technology (ONC) to directly review certified health IT systems “and take action necessary including requiring the correction of nonconformities found in health IT … and suspending and terminating certifications.”
The proposed rule would:
• Enable ONC to directly review certified health IT products, including certified EHRs, and address circumstances such as potential risks to public health and safety. This would complement the existing responsibilities of ONC-Authorized Certification Bodies.
• Give ONC direct oversight of health IT testing bodies.
• Publish information on the performance of certified EHRs and other certified health IT products so that users can easily understand both the positive and negative aspects of each product.
Also on March 1, ONC announced $625,000 worth of challenge awards to encourage the development of mobile apps that patients and physicians can use to manage health information. The challenge will encourage the use of open, standardized application programming interfaces and one federal programming language standard (the Health Level 7 – Fast Healthcare Interoperability Resources or FHIR).
More expected rule making will come in several months to roll out expectations under MACRA, the Medicare Access & CHIP Reauthorization Act of 2015, including the Merit-Based Incentive Payment System (MIPS) and more alternative payment models such as accountable care organizations and bundled payment plans.
Under MIPS, Mr. Slavitt said, Congress is asking to measure quality, resource use, use of technology and practice improvement.
In addition, Mr. Slavitt said the CMS intends to roll out EHR requirements for long-term care facilities and behavioral health care providers. And, he said, “significant, significant effort and rules are underway” to improve quality and access for patients under the Medicaid program.
“I need physicians who are committed and who feel that part of their role is to take care of people who need care the most, who have lower socioeconomic status and who are more difficult to treat.”
LAS VEGAS – Federal officials have spent months listening to doctors’ complaints about their frustrating EHRs and are responding with a core group of changes to simplify and standardize health IT.
“We’ve made a great start, but we’re still at a stage where technology often hurts rather than helps physicians to provide better care,” Andy Slavitt, acting administrator of the Centers for Medicare & Medicaid Services, said March 1 at the annual meeting of the Health Information and Management Systems Society.
He provided some examples of complaints he hears from doctors: “Ordering aspirin takes eight clicks on the computer; to order full-strength aspirin, 16,” he said as the audience laughed.
And, “the systems don’t talk to each other. It’s actually the opposite. I can’t even access the hospital because of a firewall, and I can’t even get into the EMR at the hospital to look at patient records.”
And, “I can’t track my patients’ referrals,” or “I sent them to the hospital and I don’t know what happened.”
Mr. Slavitt said that he has 700 complaints from doctors just like those. “But the good news is that they’re not describing problems that we don’t know how to solve.”
And, he said, solving them is exactly what the CMS and a host of other agencies within the Health and Human Services department are trying to do with a raft of new proposed rules and announcements designed to more easily connect patients and providers with health care information necessary to provide better care.
Mr. Slavitt’s view of the EHR situation was echoed by Dr. Karen DeSalvo, national coordinator for Health Information Technology, who said that her husband is a practicing physician with real time frustrations.
“That’s my dinner conversation,” she said. “He’s a very clinically busy emergency medicine doc, and he wants the system to enable his workflow, and just like many physicians, it’s the same common refrain.”
Part of the solution is a proposed rule announced March 1 that would allow the Office of the National Coordinator for Heath Information Technology (ONC) to directly review certified health IT systems “and take action necessary including requiring the correction of nonconformities found in health IT … and suspending and terminating certifications.”
The proposed rule would:
• Enable ONC to directly review certified health IT products, including certified EHRs, and address circumstances such as potential risks to public health and safety. This would complement the existing responsibilities of ONC-Authorized Certification Bodies.
• Give ONC direct oversight of health IT testing bodies.
• Publish information on the performance of certified EHRs and other certified health IT products so that users can easily understand both the positive and negative aspects of each product.
Also on March 1, ONC announced $625,000 worth of challenge awards to encourage the development of mobile apps that patients and physicians can use to manage health information. The challenge will encourage the use of open, standardized application programming interfaces and one federal programming language standard (the Health Level 7 – Fast Healthcare Interoperability Resources or FHIR).
More expected rule making will come in several months to roll out expectations under MACRA, the Medicare Access & CHIP Reauthorization Act of 2015, including the Merit-Based Incentive Payment System (MIPS) and more alternative payment models such as accountable care organizations and bundled payment plans.
Under MIPS, Mr. Slavitt said, Congress is asking to measure quality, resource use, use of technology and practice improvement.
In addition, Mr. Slavitt said the CMS intends to roll out EHR requirements for long-term care facilities and behavioral health care providers. And, he said, “significant, significant effort and rules are underway” to improve quality and access for patients under the Medicaid program.
“I need physicians who are committed and who feel that part of their role is to take care of people who need care the most, who have lower socioeconomic status and who are more difficult to treat.”
LAS VEGAS – Federal officials have spent months listening to doctors’ complaints about their frustrating EHRs and are responding with a core group of changes to simplify and standardize health IT.
“We’ve made a great start, but we’re still at a stage where technology often hurts rather than helps physicians to provide better care,” Andy Slavitt, acting administrator of the Centers for Medicare & Medicaid Services, said March 1 at the annual meeting of the Health Information and Management Systems Society.
He provided some examples of complaints he hears from doctors: “Ordering aspirin takes eight clicks on the computer; to order full-strength aspirin, 16,” he said as the audience laughed.
And, “the systems don’t talk to each other. It’s actually the opposite. I can’t even access the hospital because of a firewall, and I can’t even get into the EMR at the hospital to look at patient records.”
And, “I can’t track my patients’ referrals,” or “I sent them to the hospital and I don’t know what happened.”
Mr. Slavitt said that he has 700 complaints from doctors just like those. “But the good news is that they’re not describing problems that we don’t know how to solve.”
And, he said, solving them is exactly what the CMS and a host of other agencies within the Health and Human Services department are trying to do with a raft of new proposed rules and announcements designed to more easily connect patients and providers with health care information necessary to provide better care.
Mr. Slavitt’s view of the EHR situation was echoed by Dr. Karen DeSalvo, national coordinator for Health Information Technology, who said that her husband is a practicing physician with real time frustrations.
“That’s my dinner conversation,” she said. “He’s a very clinically busy emergency medicine doc, and he wants the system to enable his workflow, and just like many physicians, it’s the same common refrain.”
Part of the solution is a proposed rule announced March 1 that would allow the Office of the National Coordinator for Heath Information Technology (ONC) to directly review certified health IT systems “and take action necessary including requiring the correction of nonconformities found in health IT … and suspending and terminating certifications.”
The proposed rule would:
• Enable ONC to directly review certified health IT products, including certified EHRs, and address circumstances such as potential risks to public health and safety. This would complement the existing responsibilities of ONC-Authorized Certification Bodies.
• Give ONC direct oversight of health IT testing bodies.
• Publish information on the performance of certified EHRs and other certified health IT products so that users can easily understand both the positive and negative aspects of each product.
Also on March 1, ONC announced $625,000 worth of challenge awards to encourage the development of mobile apps that patients and physicians can use to manage health information. The challenge will encourage the use of open, standardized application programming interfaces and one federal programming language standard (the Health Level 7 – Fast Healthcare Interoperability Resources or FHIR).
More expected rule making will come in several months to roll out expectations under MACRA, the Medicare Access & CHIP Reauthorization Act of 2015, including the Merit-Based Incentive Payment System (MIPS) and more alternative payment models such as accountable care organizations and bundled payment plans.
Under MIPS, Mr. Slavitt said, Congress is asking to measure quality, resource use, use of technology and practice improvement.
In addition, Mr. Slavitt said the CMS intends to roll out EHR requirements for long-term care facilities and behavioral health care providers. And, he said, “significant, significant effort and rules are underway” to improve quality and access for patients under the Medicaid program.
“I need physicians who are committed and who feel that part of their role is to take care of people who need care the most, who have lower socioeconomic status and who are more difficult to treat.”
AT HIMSS16