User login
VA Report Says Endoscope Problems Continue
Grand Rounds: Man, 60, With Abdominal Pain
A 60-year-old white man with a history of hyperlipidemia, hypertension, and anxiety presented with complaints of abdominal pain, localized to an area left of the umbilicus. He described the pain as constant and rated it 6 on a scale of 1 to 10. He said the pain had been present for longer than three weeks.
The man said he had been seen by another health care provider shortly after the pain began, but he did not think the provider took his complaint seriously. At that visit, antacids were prescribed, blood work was ordered, and the man was told to return if there was no improvement. He felt that because he was being treated for anxiety, the provider believed he was just imagining the pain.
At the current visit, the review of systems revealed additional complaints of shakiness and nausea without vomiting, with other findings unremarkable. The persistent pain did not seem related to eating, and the patient had no history of any surgeries that might help explain his current complaints. He had smoked a pack of cigarettes daily for 40 years and had a history of heavy alcohol use, although he denied having consumed any alcohol during the previous five years.
His prescribed medications included gemfibrozil 600 mg per day, hydrochlorothiazide 25 mg each morning, and diazepam 5 mg twice daily, with an OTC antacid.
The patient’s recent laboratory results were normal; they included a complete blood count, comprehensive metabolic panel, liver enzyme levels, and a serum amylase level. The patient weighed 280 lb and his height was 5’10”; his BMI was 40. His temperature was 97.7°F, with a regular heart rate of 88 beats/min; blood pressure, 140/90 mm Hg; and respiratory rate, 18 breaths/min.
The patient did not appear to be in acute distress. A bruit was heard in the indicated area of pain. No mass was palpated, and the width of his aorta could not be determined because of his obesity. His physical exam was otherwise normal.
Abdominal ultrasonography (US) revealed a 5.5-cm abdominal aortic aneurysm (AAA), and the man was referred for immediate surgery. The aneurysm was repaired in an open abdominal procedure with a polyester prosthetic graft. The surgery was successful.
Discussion
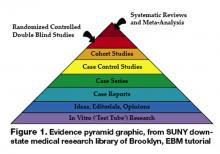
AAA is a permanent bulging area of the aorta that exceeds 3.0 cm in diameter (see Figure 1). It is a potentially life-threatening condition due to the possibility of rupture. Often an aneurysm is asymptomatic until it ruptures, making this a difficult illness to diagnose.1
Each year, an estimated 10,000 deaths result from a ruptured AAA, making this condition the 14th leading cause of death in the United States.2,3 Incidence of AAA appears to have increased over the past two decades. Causes for this may include the aging of the US population, an increase in the number of smokers, and a trend toward diets that are higher in fat.
Prognosis among patients with AAA can be improved with increased awareness of the disease among health care providers, earlier detection of AAAs at risk for rupture, and timely, effective interventions.
Symptomatology
In about one-third of patients with a ruptured AAA, a clinical triad of symptoms is present: abdominal and/or back pain, a pulsatile abdominal mass, and hypotension.4,5 In these cases, according to the American College of Cardiology/American Heart Association (ACC/AHA),4 immediate surgical evaluation is indicated.
Prior to the rupture of an AAA, the patient may feel a pulsing sensation in the abdomen or may experience no symptoms at all. Some patients report vague complaints, such as back, flank, groin, or abdominal pain. Syncope may be the chief complaint as the aneurysm expands, so it is important for primary care providers to be alert to progressive symptoms, including this signal that an aneurysm may exist and may be expanding.6
Pain may also be abrupt and severe in the lower abdomen and back, including tenderness in the area over the aneurysm. Shock can develop rapidly and symptoms such as cyanosis, mottling, altered mental status, tachycardia, and hypotension may be present.1,4
Since symptoms may be vague, the differential diagnosis can be broad (see Table 14,7,8), necessitating a detailed patient history and a careful physical examination. In an elderly patient, low back pain should be evaluated for AAA.9 In addition, acute abdominal pain in a patient older than 50 should be presumed to be a ruptured AAA.8
Risk Factors
A clinician should be familiar with the risk factors for AAA so that diagnosis can be made before a rupture occurs. Male gender and age greater than 65 are important risk factors for AAA, but one of the most important environmental risks is cigarette smoking.9,10 Current smokers are more than seven times more likely than nonsmokers to have an aneurysm.10 Atherosclerosis, which weakens the wall of the aorta, is also believed to contribute to the risk for AAA.11
Other contributing factors include hypertension, chronic obstructive pulmonary disease, hyperlipidemia, and family history. Chronic infection, inflammatory illnesses, and connective tissue disorders (eg, Marfan syndrome) can also increase the risk for aneurysm. Less frequent causes of AAA are trauma and infectious diseases, such as syphilis.1,12
In 85% of patients with femoral aneurysms, AAA has been found to coexist, as it has in 62% of patients with popliteal aneurysms. Patients previously diagnosed with these conditions should be screened for AAA.4,13,14
Diagnosis
An abdominal bruit or a pulsating mass may be found on palpation, but the sensitivity for detection of AAA is related to its size. An aneurysm greater than 5.0 cm has an 82% chance of detection by palpation.15 To assess for the presence of an abdominal aneurysm, the examiner should press the midline between the xiphoid and umbilicus bimanually, firmly but gently.12 There is no evidence to suggest that palpating the abdomen can cause an aneurysm to rupture.
The most useful tests for diagnosis of AAA are US, CT, and MRI.6 US is the simplest and least costly of these diagnostic procedures; it is noninvasive and has a sensitivity of 95% and specificity of nearly 100%. Bedside US can provide a rapid diagnosis in an unstable patient.16
CT is nearly 100% effective in diagnosing AAA and is usually used to help decide on appropriate treatment, as it can determine the size and shape of the aneurysm.17 However, CT should not be used for unstable patients.
MRI is useful in diagnosing AAA, but it is expensive, and inappropriate for unstable patients. Currently, conventional aortography is rarely used for preoperative assessment but may still be used for placement of endovascular devices or in patients with renal complications.1,12
Screening Recommendations
The US Preventive Services Task Force (USPSTF) recommends that all men ages 65 to 74 who have a lifelong history of smoking at least 100 cigarettes should be screened for AAA with abdominal US.3,18 Screening is not recommended for those younger than 65 who have never smoked, but this decision must be individualized to the patient, with other risk factors considered.
The ACC/AHA4 advises that men whose parents or siblings have a history of AAA and who are older than 60 should undergo physical examination and screening US for AAA. In addition, patients with a small AAA should receive US surveillance until the aneurysm reaches 5.5 cm in diameter; survival has not been shown to improve if an AAA is repaired before it reaches this size.1,2,19 In consideration of increased comorbidities and decreased life expectancy, screening is not recommended for men older than 75, but this too should be determined individually.3
Screening for women is not recommended by the USPSTF.3,18 The document states that the prevalence of large AAAs in women is low and that screening may lead to an increased number of unnecessary surgeries with associated morbidity and mortality. Clinical judgment must be used in making this decision, however, as several studies have shown that women have an AAA rupture rate that is three times higher than that in men; they also have an increased in-hospital mortality rate when rupture does occur. Thus, women are less likely to experience AAA but have a worse prognosis when AAA does develop.20-22
Management
The size of an AAA is the most important predictor of rupture. According to the ACC/AHA,4 the associated risk for rupture is about 20% for aneurysms that measure 5.0 cm in diameter, 40% for those measuring at least 6.0 cm, and at least 50% for aneurysms exceeding 7.0 cm.4,23,24 Regarding surveillance of known aneurysms, it is recommended that a patient with an aneurysm smaller than 3.0 cm in diameter requires no further testing. If an AAA measures 3.0 to 4.0 cm, US should be performed yearly; if it is 4.0 to 4.9 cm, US should be performed every six months.4,25
If an identified AAA is larger than 4.5 cm, or if any segment of the aorta is more than 1.5 times the diameter of an adjacent section, referral to a vascular surgeon for further evaluation is indicated. The vascular surgeon should be consulted immediately regarding a symptomatic patient with an AAA, or one with an aneurysm that measures 5.5 cm or larger, as the risk for rupture is high.4,26
Preventing rupture of an AAA is the primary aim in management. Beta-blockers may be used to reduce systolic hypertension in cardiac patients, thus slowing the rate of expansion in those with aortic aneurysms. Patients with a known AAA should undergo frequent monitoring for blood pressure and lipid levels and be advised to stop smoking. Smoking cessation interventions such as behavior modification, nicotine replacement, or bupropion should be offered.27,28
There is evidence that statin use may reduce the size of aneurysms, even in patients without hypercholesterolemia, possibly due to statins’ anti-inflammatory properties.22,29 ACE inhibitors may also be beneficial in reducing AAA growth and in lowering blood pressure. Antiplatelet medications are important in general cardiovascular risk reduction in the patient with AAA. Aspirin is the drug of choice.27,29
Surgical Repair
AAAs are usually repaired by one of two types of surgery: endovascular repair (EVR) or open surgery. Open surgical repair, the more traditional method, involves an incision into the abdomen from the breastbone to below the navel. The weakened area is replaced with a graft made of synthetic material. Open repair of an intact AAA, performed under general anesthesia, takes from three to six hours, and the patient must be hospitalized for five to eight days.30
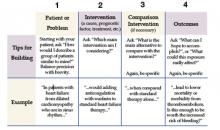
In EVR, the patient is given epidural anesthesia and an incision is made in the right groin, allowing a synthetic stent graft to be threaded by way of a catheter through the femoral artery to repair the lesion (see Figure 2). EVR generally takes two to five hours, followed by a two- to five-day hospital stay. EVR is usually recommended for patients who are at high risk for complications from open operations because of severe cardiopulmonary disease or other risk factors, such as advanced age, morbid obesity, or a history of multiple abdominal operations.1,2,4,19
Prognosis
Patients with a ruptured AAA have a survival rate of less than 50%, with most deaths occurring before surgical repair has been attempted.3,31 In patients with kidney failure resulting from AAA (whether ruptured or unruptured, an AAA can disrupt renal blood flow), the chance for survival is poor. By contrast, the risk for death during surgical graft repair of an AAA is only about 2% to 8%.1,12
In a systematic review, EVR was associated with a lower 30-day mortality rate compared with open surgical repair (1.6% vs 4.7%, respectively), but this reduction did not persist over two years’ follow-up; neither did EVR improve overall survival or quality of life, compared with open surgery.1 Additionally, EVR requires periodic imaging throughout the patient’s life, which is associated with more reinterventions.1,19
Patient Education
Clinicians should encourage all patients to stop smoking, follow a low-cholesterol diet, control hypertension, and exercise regularly to lower the risk for AAAs. Screening recommendations should be explained to patients at risk, as should the signs and symptoms of an aneurysm. These patients should be instructed to call their health care provider immediately if they suspect a problem.
Conclusion
The incidence of AAA is increasing, and primary care providers must be prepared to act promptly in any case of suspected AAA to ensure a safe outcome. For aneurysms measuring greater than 5.5 cm in diameter, open or endovascular surgical repair should be considered. Patients with smaller aneurysms or contraindications for surgery should receive careful medical management and education to reduce the risks of AAA expansion leading to possible rupture.
1. Wilt TJ, Lederle FA, MacDonald R, et al; Agency for Healthcare Research and Quality. Comparison of Endovascular and Open Surgical Repairs for Abdominal Aortic Aneurysm. Rockville, MD: Agency for Healthcare Research and Quality; 2006. AHRQ publication 06-E107. Evidence Report/Technology Assessment 144. www.ahrq.gov/CLINIC/tp/aaareptp.htm. Accessed June 23, 2009.
2. Birkmeyer JD, Upchurch GR Jr. Evidence-based screening and management of abdominal aortic aneurysm. Ann Intern Med. 2007;146(10):749-750.
3. Fleming C, Whitlock EP, Beil TL, Lederle FA. Screening for abdominal aortic aneurysm: a best-evidence systematic review for the US Preventive Services Task Force. Ann Intern Med. 2005;142(3):203-211.
4. Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol. 2006;47(6):1239-1312.
5. Kiell CS, Ernst CB. Advances in management of abdominal aortic aneurysm. Adv Surg. 1993;26:73–98.
6. O’Connor RE. Aneurysm, abdominal. http://emedicine.medscape.com/article/756735-overview. Accessed June 23, 2009.
7. Lederle FA, Parenti CM, Chute EP. Ruptured abdominal aortic aneurysm: the internist as diagnostician. Am J Med. 1994;96:163-167.
8. Cartwright SL, Knudson MP. Evaluation of acute abdominal pain in adults. Am Fam Physician. 2008;77(7): 971-978.
9. Lyon C, Clark DC. Diagnosis of acute abdominal pain in older patients. Am Fam Physician. 2006;74(9):1537-1544.
10. Wilmink TB, Quick CR, Day NE. The association between cigarette smoking and abdominal aortic aneurysms. J Vasc Surg. 1999;30(6):1099-1105.
11. Palazzuoli P, Gallotta M, Guerrieri G, et al. Prevalence of risk factors, coronary and systemic atherosclerosis in abdominal aortic aneurysm: comparison with high cardiovascular risk population. Vasc Health Risk Manag. 2008;4(4):877-883.
12. Sakalihasan N, Limet R, Defawe OD. Abdominal aortic aneurysm. Lancet. 2005;365(9470):1577-1589.
13. Graham LM, Zelenock GB, Whitehouse WM Jr, et al. Clinical significance of arteriosclerotic femoral artery aneurysms. Arch Surg. 1980;115(4):502–507.
14. Whitehouse WM Jr, Wakefield TW, Graham LM, et al. Limb-threatening potential of arteriosclerotic popliteal artery aneurysms. Surgery. 1983;93(5):694–699.
15. Fink HA, Lederle FA, Roth CS, et al. The accuracy of physical examination to detect abdominal aortic aneurysm. Arch Intern Med. 2000;160:833-836.
16. Bentz S, Jones J. Accuracy of emergency department ultrasound scanning in detecting abdominal aortic aneurysm. Emerg Med J. 2006;23(10):803-804.
17. Kvilekval KH, Best IM, Mason RA, et al. The value of computed tomography in the management of symptomatic abdominal aortic aneurysm. J Vasc Surg. 1990;12(1):28-33.
18. US Preventive Services Task Force. Screening for abdominal aortic aneurysm: recommendation statement. Ann Intern Med. 2005;142(3):198-202.
19. Lederle FA, Kane RL, MacDonald R, Wilt TJ. Systematic review: repair of unruptured abdominal aortic aneurysm. Ann Intern Med. 2007;146(10):735-741.
20. McPhee JT, Hill JS, Elami MH. The impact of gender on presentation, therapy, and mortality of abdominal aortic aneurysm in the United States, 2001-2004. J Vasc Surg. 2007;45(5):891-899.
21. Mofidi R, Goldie VJ, Kelman J, et al. Influence of sex on expansion rate of abdominal aortic aneurysms. Br J Surg. 2007;94(3):310-314.
22. Norman PE, Powell JT. Abdominal aortic aneurysm: the prognosis in women is worse than in men. Circulation. 2007;115(22):2865-2869.
23. Englund R, Hudson P, Hanel K, Stanton A. Expansion rates of small abdominal aortic aneurysms. Aust N Z J Surg. 1998;68(1):21–24.
24. Conway KP, Byrne J, Townsend M, Lane IF. Prognosis of patients turned down for conventional abdominal aortic aneurysm repair in the endovascular and sonographic era: Szilagyi revisited? J Vasc Surg. 2001;33(4):752–757.
25. Cook TA, Galland RB. A prospective study to define the optimum rescreening interval for small abdominal aortic aneurysm. Cardiovasc Surg. 1996;4(4):441–444.
26. Kent KC, Zwolak RM, Jaff MR, et al; Society for Vascular Surgery; American Association of Vascular Surgery; Society for Vascular Medicine and Biology. Screening for abdominal aortic aneurysm: a consensus statement. J Vasc Surg. 2004;39(1):267-269.
27. Golledge J, Powell JT. Medical management of abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 2007;4(3):267-273.
28. Sule S, Aronow WS. Management of abdominal aortic aneurysms. Compr Ther. 2009;35(1):3-8.
29. Powell JT. Non-operative or medical management of abdominal aortic aneurysm. Scand J Surg. 2008;97(2): 121-124.
30. Huber TS, Wang JG, Derrow AE, et al. Experience in the United States with intact abdominal aortic aneurysm repair. J Vasc Surg. 2001;33(2):304-310.
31. Adam DJ, Mohan IV, Stuart WP, et al. Community and hospital outcome from ruptured abdominal aortic aneurysm within the catchment area of a regional vascular surgical service. J Vasc Surg. 1999;30(5):922-928.
A 60-year-old white man with a history of hyperlipidemia, hypertension, and anxiety presented with complaints of abdominal pain, localized to an area left of the umbilicus. He described the pain as constant and rated it 6 on a scale of 1 to 10. He said the pain had been present for longer than three weeks.
The man said he had been seen by another health care provider shortly after the pain began, but he did not think the provider took his complaint seriously. At that visit, antacids were prescribed, blood work was ordered, and the man was told to return if there was no improvement. He felt that because he was being treated for anxiety, the provider believed he was just imagining the pain.
At the current visit, the review of systems revealed additional complaints of shakiness and nausea without vomiting, with other findings unremarkable. The persistent pain did not seem related to eating, and the patient had no history of any surgeries that might help explain his current complaints. He had smoked a pack of cigarettes daily for 40 years and had a history of heavy alcohol use, although he denied having consumed any alcohol during the previous five years.
His prescribed medications included gemfibrozil 600 mg per day, hydrochlorothiazide 25 mg each morning, and diazepam 5 mg twice daily, with an OTC antacid.
The patient’s recent laboratory results were normal; they included a complete blood count, comprehensive metabolic panel, liver enzyme levels, and a serum amylase level. The patient weighed 280 lb and his height was 5’10”; his BMI was 40. His temperature was 97.7°F, with a regular heart rate of 88 beats/min; blood pressure, 140/90 mm Hg; and respiratory rate, 18 breaths/min.
The patient did not appear to be in acute distress. A bruit was heard in the indicated area of pain. No mass was palpated, and the width of his aorta could not be determined because of his obesity. His physical exam was otherwise normal.
Abdominal ultrasonography (US) revealed a 5.5-cm abdominal aortic aneurysm (AAA), and the man was referred for immediate surgery. The aneurysm was repaired in an open abdominal procedure with a polyester prosthetic graft. The surgery was successful.
Discussion
AAA is a permanent bulging area of the aorta that exceeds 3.0 cm in diameter (see Figure 1). It is a potentially life-threatening condition due to the possibility of rupture. Often an aneurysm is asymptomatic until it ruptures, making this a difficult illness to diagnose.1
Each year, an estimated 10,000 deaths result from a ruptured AAA, making this condition the 14th leading cause of death in the United States.2,3 Incidence of AAA appears to have increased over the past two decades. Causes for this may include the aging of the US population, an increase in the number of smokers, and a trend toward diets that are higher in fat.
Prognosis among patients with AAA can be improved with increased awareness of the disease among health care providers, earlier detection of AAAs at risk for rupture, and timely, effective interventions.
Symptomatology
In about one-third of patients with a ruptured AAA, a clinical triad of symptoms is present: abdominal and/or back pain, a pulsatile abdominal mass, and hypotension.4,5 In these cases, according to the American College of Cardiology/American Heart Association (ACC/AHA),4 immediate surgical evaluation is indicated.
Prior to the rupture of an AAA, the patient may feel a pulsing sensation in the abdomen or may experience no symptoms at all. Some patients report vague complaints, such as back, flank, groin, or abdominal pain. Syncope may be the chief complaint as the aneurysm expands, so it is important for primary care providers to be alert to progressive symptoms, including this signal that an aneurysm may exist and may be expanding.6
Pain may also be abrupt and severe in the lower abdomen and back, including tenderness in the area over the aneurysm. Shock can develop rapidly and symptoms such as cyanosis, mottling, altered mental status, tachycardia, and hypotension may be present.1,4
Since symptoms may be vague, the differential diagnosis can be broad (see Table 14,7,8), necessitating a detailed patient history and a careful physical examination. In an elderly patient, low back pain should be evaluated for AAA.9 In addition, acute abdominal pain in a patient older than 50 should be presumed to be a ruptured AAA.8
Risk Factors
A clinician should be familiar with the risk factors for AAA so that diagnosis can be made before a rupture occurs. Male gender and age greater than 65 are important risk factors for AAA, but one of the most important environmental risks is cigarette smoking.9,10 Current smokers are more than seven times more likely than nonsmokers to have an aneurysm.10 Atherosclerosis, which weakens the wall of the aorta, is also believed to contribute to the risk for AAA.11
Other contributing factors include hypertension, chronic obstructive pulmonary disease, hyperlipidemia, and family history. Chronic infection, inflammatory illnesses, and connective tissue disorders (eg, Marfan syndrome) can also increase the risk for aneurysm. Less frequent causes of AAA are trauma and infectious diseases, such as syphilis.1,12
In 85% of patients with femoral aneurysms, AAA has been found to coexist, as it has in 62% of patients with popliteal aneurysms. Patients previously diagnosed with these conditions should be screened for AAA.4,13,14
Diagnosis
An abdominal bruit or a pulsating mass may be found on palpation, but the sensitivity for detection of AAA is related to its size. An aneurysm greater than 5.0 cm has an 82% chance of detection by palpation.15 To assess for the presence of an abdominal aneurysm, the examiner should press the midline between the xiphoid and umbilicus bimanually, firmly but gently.12 There is no evidence to suggest that palpating the abdomen can cause an aneurysm to rupture.
The most useful tests for diagnosis of AAA are US, CT, and MRI.6 US is the simplest and least costly of these diagnostic procedures; it is noninvasive and has a sensitivity of 95% and specificity of nearly 100%. Bedside US can provide a rapid diagnosis in an unstable patient.16
CT is nearly 100% effective in diagnosing AAA and is usually used to help decide on appropriate treatment, as it can determine the size and shape of the aneurysm.17 However, CT should not be used for unstable patients.
MRI is useful in diagnosing AAA, but it is expensive, and inappropriate for unstable patients. Currently, conventional aortography is rarely used for preoperative assessment but may still be used for placement of endovascular devices or in patients with renal complications.1,12
Screening Recommendations
The US Preventive Services Task Force (USPSTF) recommends that all men ages 65 to 74 who have a lifelong history of smoking at least 100 cigarettes should be screened for AAA with abdominal US.3,18 Screening is not recommended for those younger than 65 who have never smoked, but this decision must be individualized to the patient, with other risk factors considered.
The ACC/AHA4 advises that men whose parents or siblings have a history of AAA and who are older than 60 should undergo physical examination and screening US for AAA. In addition, patients with a small AAA should receive US surveillance until the aneurysm reaches 5.5 cm in diameter; survival has not been shown to improve if an AAA is repaired before it reaches this size.1,2,19 In consideration of increased comorbidities and decreased life expectancy, screening is not recommended for men older than 75, but this too should be determined individually.3
Screening for women is not recommended by the USPSTF.3,18 The document states that the prevalence of large AAAs in women is low and that screening may lead to an increased number of unnecessary surgeries with associated morbidity and mortality. Clinical judgment must be used in making this decision, however, as several studies have shown that women have an AAA rupture rate that is three times higher than that in men; they also have an increased in-hospital mortality rate when rupture does occur. Thus, women are less likely to experience AAA but have a worse prognosis when AAA does develop.20-22
Management
The size of an AAA is the most important predictor of rupture. According to the ACC/AHA,4 the associated risk for rupture is about 20% for aneurysms that measure 5.0 cm in diameter, 40% for those measuring at least 6.0 cm, and at least 50% for aneurysms exceeding 7.0 cm.4,23,24 Regarding surveillance of known aneurysms, it is recommended that a patient with an aneurysm smaller than 3.0 cm in diameter requires no further testing. If an AAA measures 3.0 to 4.0 cm, US should be performed yearly; if it is 4.0 to 4.9 cm, US should be performed every six months.4,25
If an identified AAA is larger than 4.5 cm, or if any segment of the aorta is more than 1.5 times the diameter of an adjacent section, referral to a vascular surgeon for further evaluation is indicated. The vascular surgeon should be consulted immediately regarding a symptomatic patient with an AAA, or one with an aneurysm that measures 5.5 cm or larger, as the risk for rupture is high.4,26
Preventing rupture of an AAA is the primary aim in management. Beta-blockers may be used to reduce systolic hypertension in cardiac patients, thus slowing the rate of expansion in those with aortic aneurysms. Patients with a known AAA should undergo frequent monitoring for blood pressure and lipid levels and be advised to stop smoking. Smoking cessation interventions such as behavior modification, nicotine replacement, or bupropion should be offered.27,28
There is evidence that statin use may reduce the size of aneurysms, even in patients without hypercholesterolemia, possibly due to statins’ anti-inflammatory properties.22,29 ACE inhibitors may also be beneficial in reducing AAA growth and in lowering blood pressure. Antiplatelet medications are important in general cardiovascular risk reduction in the patient with AAA. Aspirin is the drug of choice.27,29
Surgical Repair
AAAs are usually repaired by one of two types of surgery: endovascular repair (EVR) or open surgery. Open surgical repair, the more traditional method, involves an incision into the abdomen from the breastbone to below the navel. The weakened area is replaced with a graft made of synthetic material. Open repair of an intact AAA, performed under general anesthesia, takes from three to six hours, and the patient must be hospitalized for five to eight days.30
In EVR, the patient is given epidural anesthesia and an incision is made in the right groin, allowing a synthetic stent graft to be threaded by way of a catheter through the femoral artery to repair the lesion (see Figure 2). EVR generally takes two to five hours, followed by a two- to five-day hospital stay. EVR is usually recommended for patients who are at high risk for complications from open operations because of severe cardiopulmonary disease or other risk factors, such as advanced age, morbid obesity, or a history of multiple abdominal operations.1,2,4,19
Prognosis
Patients with a ruptured AAA have a survival rate of less than 50%, with most deaths occurring before surgical repair has been attempted.3,31 In patients with kidney failure resulting from AAA (whether ruptured or unruptured, an AAA can disrupt renal blood flow), the chance for survival is poor. By contrast, the risk for death during surgical graft repair of an AAA is only about 2% to 8%.1,12
In a systematic review, EVR was associated with a lower 30-day mortality rate compared with open surgical repair (1.6% vs 4.7%, respectively), but this reduction did not persist over two years’ follow-up; neither did EVR improve overall survival or quality of life, compared with open surgery.1 Additionally, EVR requires periodic imaging throughout the patient’s life, which is associated with more reinterventions.1,19
Patient Education
Clinicians should encourage all patients to stop smoking, follow a low-cholesterol diet, control hypertension, and exercise regularly to lower the risk for AAAs. Screening recommendations should be explained to patients at risk, as should the signs and symptoms of an aneurysm. These patients should be instructed to call their health care provider immediately if they suspect a problem.
Conclusion
The incidence of AAA is increasing, and primary care providers must be prepared to act promptly in any case of suspected AAA to ensure a safe outcome. For aneurysms measuring greater than 5.5 cm in diameter, open or endovascular surgical repair should be considered. Patients with smaller aneurysms or contraindications for surgery should receive careful medical management and education to reduce the risks of AAA expansion leading to possible rupture.
A 60-year-old white man with a history of hyperlipidemia, hypertension, and anxiety presented with complaints of abdominal pain, localized to an area left of the umbilicus. He described the pain as constant and rated it 6 on a scale of 1 to 10. He said the pain had been present for longer than three weeks.
The man said he had been seen by another health care provider shortly after the pain began, but he did not think the provider took his complaint seriously. At that visit, antacids were prescribed, blood work was ordered, and the man was told to return if there was no improvement. He felt that because he was being treated for anxiety, the provider believed he was just imagining the pain.
At the current visit, the review of systems revealed additional complaints of shakiness and nausea without vomiting, with other findings unremarkable. The persistent pain did not seem related to eating, and the patient had no history of any surgeries that might help explain his current complaints. He had smoked a pack of cigarettes daily for 40 years and had a history of heavy alcohol use, although he denied having consumed any alcohol during the previous five years.
His prescribed medications included gemfibrozil 600 mg per day, hydrochlorothiazide 25 mg each morning, and diazepam 5 mg twice daily, with an OTC antacid.
The patient’s recent laboratory results were normal; they included a complete blood count, comprehensive metabolic panel, liver enzyme levels, and a serum amylase level. The patient weighed 280 lb and his height was 5’10”; his BMI was 40. His temperature was 97.7°F, with a regular heart rate of 88 beats/min; blood pressure, 140/90 mm Hg; and respiratory rate, 18 breaths/min.
The patient did not appear to be in acute distress. A bruit was heard in the indicated area of pain. No mass was palpated, and the width of his aorta could not be determined because of his obesity. His physical exam was otherwise normal.
Abdominal ultrasonography (US) revealed a 5.5-cm abdominal aortic aneurysm (AAA), and the man was referred for immediate surgery. The aneurysm was repaired in an open abdominal procedure with a polyester prosthetic graft. The surgery was successful.
Discussion
AAA is a permanent bulging area of the aorta that exceeds 3.0 cm in diameter (see Figure 1). It is a potentially life-threatening condition due to the possibility of rupture. Often an aneurysm is asymptomatic until it ruptures, making this a difficult illness to diagnose.1
Each year, an estimated 10,000 deaths result from a ruptured AAA, making this condition the 14th leading cause of death in the United States.2,3 Incidence of AAA appears to have increased over the past two decades. Causes for this may include the aging of the US population, an increase in the number of smokers, and a trend toward diets that are higher in fat.
Prognosis among patients with AAA can be improved with increased awareness of the disease among health care providers, earlier detection of AAAs at risk for rupture, and timely, effective interventions.
Symptomatology
In about one-third of patients with a ruptured AAA, a clinical triad of symptoms is present: abdominal and/or back pain, a pulsatile abdominal mass, and hypotension.4,5 In these cases, according to the American College of Cardiology/American Heart Association (ACC/AHA),4 immediate surgical evaluation is indicated.
Prior to the rupture of an AAA, the patient may feel a pulsing sensation in the abdomen or may experience no symptoms at all. Some patients report vague complaints, such as back, flank, groin, or abdominal pain. Syncope may be the chief complaint as the aneurysm expands, so it is important for primary care providers to be alert to progressive symptoms, including this signal that an aneurysm may exist and may be expanding.6
Pain may also be abrupt and severe in the lower abdomen and back, including tenderness in the area over the aneurysm. Shock can develop rapidly and symptoms such as cyanosis, mottling, altered mental status, tachycardia, and hypotension may be present.1,4
Since symptoms may be vague, the differential diagnosis can be broad (see Table 14,7,8), necessitating a detailed patient history and a careful physical examination. In an elderly patient, low back pain should be evaluated for AAA.9 In addition, acute abdominal pain in a patient older than 50 should be presumed to be a ruptured AAA.8
Risk Factors
A clinician should be familiar with the risk factors for AAA so that diagnosis can be made before a rupture occurs. Male gender and age greater than 65 are important risk factors for AAA, but one of the most important environmental risks is cigarette smoking.9,10 Current smokers are more than seven times more likely than nonsmokers to have an aneurysm.10 Atherosclerosis, which weakens the wall of the aorta, is also believed to contribute to the risk for AAA.11
Other contributing factors include hypertension, chronic obstructive pulmonary disease, hyperlipidemia, and family history. Chronic infection, inflammatory illnesses, and connective tissue disorders (eg, Marfan syndrome) can also increase the risk for aneurysm. Less frequent causes of AAA are trauma and infectious diseases, such as syphilis.1,12
In 85% of patients with femoral aneurysms, AAA has been found to coexist, as it has in 62% of patients with popliteal aneurysms. Patients previously diagnosed with these conditions should be screened for AAA.4,13,14
Diagnosis
An abdominal bruit or a pulsating mass may be found on palpation, but the sensitivity for detection of AAA is related to its size. An aneurysm greater than 5.0 cm has an 82% chance of detection by palpation.15 To assess for the presence of an abdominal aneurysm, the examiner should press the midline between the xiphoid and umbilicus bimanually, firmly but gently.12 There is no evidence to suggest that palpating the abdomen can cause an aneurysm to rupture.
The most useful tests for diagnosis of AAA are US, CT, and MRI.6 US is the simplest and least costly of these diagnostic procedures; it is noninvasive and has a sensitivity of 95% and specificity of nearly 100%. Bedside US can provide a rapid diagnosis in an unstable patient.16
CT is nearly 100% effective in diagnosing AAA and is usually used to help decide on appropriate treatment, as it can determine the size and shape of the aneurysm.17 However, CT should not be used for unstable patients.
MRI is useful in diagnosing AAA, but it is expensive, and inappropriate for unstable patients. Currently, conventional aortography is rarely used for preoperative assessment but may still be used for placement of endovascular devices or in patients with renal complications.1,12
Screening Recommendations
The US Preventive Services Task Force (USPSTF) recommends that all men ages 65 to 74 who have a lifelong history of smoking at least 100 cigarettes should be screened for AAA with abdominal US.3,18 Screening is not recommended for those younger than 65 who have never smoked, but this decision must be individualized to the patient, with other risk factors considered.
The ACC/AHA4 advises that men whose parents or siblings have a history of AAA and who are older than 60 should undergo physical examination and screening US for AAA. In addition, patients with a small AAA should receive US surveillance until the aneurysm reaches 5.5 cm in diameter; survival has not been shown to improve if an AAA is repaired before it reaches this size.1,2,19 In consideration of increased comorbidities and decreased life expectancy, screening is not recommended for men older than 75, but this too should be determined individually.3
Screening for women is not recommended by the USPSTF.3,18 The document states that the prevalence of large AAAs in women is low and that screening may lead to an increased number of unnecessary surgeries with associated morbidity and mortality. Clinical judgment must be used in making this decision, however, as several studies have shown that women have an AAA rupture rate that is three times higher than that in men; they also have an increased in-hospital mortality rate when rupture does occur. Thus, women are less likely to experience AAA but have a worse prognosis when AAA does develop.20-22
Management
The size of an AAA is the most important predictor of rupture. According to the ACC/AHA,4 the associated risk for rupture is about 20% for aneurysms that measure 5.0 cm in diameter, 40% for those measuring at least 6.0 cm, and at least 50% for aneurysms exceeding 7.0 cm.4,23,24 Regarding surveillance of known aneurysms, it is recommended that a patient with an aneurysm smaller than 3.0 cm in diameter requires no further testing. If an AAA measures 3.0 to 4.0 cm, US should be performed yearly; if it is 4.0 to 4.9 cm, US should be performed every six months.4,25
If an identified AAA is larger than 4.5 cm, or if any segment of the aorta is more than 1.5 times the diameter of an adjacent section, referral to a vascular surgeon for further evaluation is indicated. The vascular surgeon should be consulted immediately regarding a symptomatic patient with an AAA, or one with an aneurysm that measures 5.5 cm or larger, as the risk for rupture is high.4,26
Preventing rupture of an AAA is the primary aim in management. Beta-blockers may be used to reduce systolic hypertension in cardiac patients, thus slowing the rate of expansion in those with aortic aneurysms. Patients with a known AAA should undergo frequent monitoring for blood pressure and lipid levels and be advised to stop smoking. Smoking cessation interventions such as behavior modification, nicotine replacement, or bupropion should be offered.27,28
There is evidence that statin use may reduce the size of aneurysms, even in patients without hypercholesterolemia, possibly due to statins’ anti-inflammatory properties.22,29 ACE inhibitors may also be beneficial in reducing AAA growth and in lowering blood pressure. Antiplatelet medications are important in general cardiovascular risk reduction in the patient with AAA. Aspirin is the drug of choice.27,29
Surgical Repair
AAAs are usually repaired by one of two types of surgery: endovascular repair (EVR) or open surgery. Open surgical repair, the more traditional method, involves an incision into the abdomen from the breastbone to below the navel. The weakened area is replaced with a graft made of synthetic material. Open repair of an intact AAA, performed under general anesthesia, takes from three to six hours, and the patient must be hospitalized for five to eight days.30
In EVR, the patient is given epidural anesthesia and an incision is made in the right groin, allowing a synthetic stent graft to be threaded by way of a catheter through the femoral artery to repair the lesion (see Figure 2). EVR generally takes two to five hours, followed by a two- to five-day hospital stay. EVR is usually recommended for patients who are at high risk for complications from open operations because of severe cardiopulmonary disease or other risk factors, such as advanced age, morbid obesity, or a history of multiple abdominal operations.1,2,4,19
Prognosis
Patients with a ruptured AAA have a survival rate of less than 50%, with most deaths occurring before surgical repair has been attempted.3,31 In patients with kidney failure resulting from AAA (whether ruptured or unruptured, an AAA can disrupt renal blood flow), the chance for survival is poor. By contrast, the risk for death during surgical graft repair of an AAA is only about 2% to 8%.1,12
In a systematic review, EVR was associated with a lower 30-day mortality rate compared with open surgical repair (1.6% vs 4.7%, respectively), but this reduction did not persist over two years’ follow-up; neither did EVR improve overall survival or quality of life, compared with open surgery.1 Additionally, EVR requires periodic imaging throughout the patient’s life, which is associated with more reinterventions.1,19
Patient Education
Clinicians should encourage all patients to stop smoking, follow a low-cholesterol diet, control hypertension, and exercise regularly to lower the risk for AAAs. Screening recommendations should be explained to patients at risk, as should the signs and symptoms of an aneurysm. These patients should be instructed to call their health care provider immediately if they suspect a problem.
Conclusion
The incidence of AAA is increasing, and primary care providers must be prepared to act promptly in any case of suspected AAA to ensure a safe outcome. For aneurysms measuring greater than 5.5 cm in diameter, open or endovascular surgical repair should be considered. Patients with smaller aneurysms or contraindications for surgery should receive careful medical management and education to reduce the risks of AAA expansion leading to possible rupture.
1. Wilt TJ, Lederle FA, MacDonald R, et al; Agency for Healthcare Research and Quality. Comparison of Endovascular and Open Surgical Repairs for Abdominal Aortic Aneurysm. Rockville, MD: Agency for Healthcare Research and Quality; 2006. AHRQ publication 06-E107. Evidence Report/Technology Assessment 144. www.ahrq.gov/CLINIC/tp/aaareptp.htm. Accessed June 23, 2009.
2. Birkmeyer JD, Upchurch GR Jr. Evidence-based screening and management of abdominal aortic aneurysm. Ann Intern Med. 2007;146(10):749-750.
3. Fleming C, Whitlock EP, Beil TL, Lederle FA. Screening for abdominal aortic aneurysm: a best-evidence systematic review for the US Preventive Services Task Force. Ann Intern Med. 2005;142(3):203-211.
4. Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol. 2006;47(6):1239-1312.
5. Kiell CS, Ernst CB. Advances in management of abdominal aortic aneurysm. Adv Surg. 1993;26:73–98.
6. O’Connor RE. Aneurysm, abdominal. http://emedicine.medscape.com/article/756735-overview. Accessed June 23, 2009.
7. Lederle FA, Parenti CM, Chute EP. Ruptured abdominal aortic aneurysm: the internist as diagnostician. Am J Med. 1994;96:163-167.
8. Cartwright SL, Knudson MP. Evaluation of acute abdominal pain in adults. Am Fam Physician. 2008;77(7): 971-978.
9. Lyon C, Clark DC. Diagnosis of acute abdominal pain in older patients. Am Fam Physician. 2006;74(9):1537-1544.
10. Wilmink TB, Quick CR, Day NE. The association between cigarette smoking and abdominal aortic aneurysms. J Vasc Surg. 1999;30(6):1099-1105.
11. Palazzuoli P, Gallotta M, Guerrieri G, et al. Prevalence of risk factors, coronary and systemic atherosclerosis in abdominal aortic aneurysm: comparison with high cardiovascular risk population. Vasc Health Risk Manag. 2008;4(4):877-883.
12. Sakalihasan N, Limet R, Defawe OD. Abdominal aortic aneurysm. Lancet. 2005;365(9470):1577-1589.
13. Graham LM, Zelenock GB, Whitehouse WM Jr, et al. Clinical significance of arteriosclerotic femoral artery aneurysms. Arch Surg. 1980;115(4):502–507.
14. Whitehouse WM Jr, Wakefield TW, Graham LM, et al. Limb-threatening potential of arteriosclerotic popliteal artery aneurysms. Surgery. 1983;93(5):694–699.
15. Fink HA, Lederle FA, Roth CS, et al. The accuracy of physical examination to detect abdominal aortic aneurysm. Arch Intern Med. 2000;160:833-836.
16. Bentz S, Jones J. Accuracy of emergency department ultrasound scanning in detecting abdominal aortic aneurysm. Emerg Med J. 2006;23(10):803-804.
17. Kvilekval KH, Best IM, Mason RA, et al. The value of computed tomography in the management of symptomatic abdominal aortic aneurysm. J Vasc Surg. 1990;12(1):28-33.
18. US Preventive Services Task Force. Screening for abdominal aortic aneurysm: recommendation statement. Ann Intern Med. 2005;142(3):198-202.
19. Lederle FA, Kane RL, MacDonald R, Wilt TJ. Systematic review: repair of unruptured abdominal aortic aneurysm. Ann Intern Med. 2007;146(10):735-741.
20. McPhee JT, Hill JS, Elami MH. The impact of gender on presentation, therapy, and mortality of abdominal aortic aneurysm in the United States, 2001-2004. J Vasc Surg. 2007;45(5):891-899.
21. Mofidi R, Goldie VJ, Kelman J, et al. Influence of sex on expansion rate of abdominal aortic aneurysms. Br J Surg. 2007;94(3):310-314.
22. Norman PE, Powell JT. Abdominal aortic aneurysm: the prognosis in women is worse than in men. Circulation. 2007;115(22):2865-2869.
23. Englund R, Hudson P, Hanel K, Stanton A. Expansion rates of small abdominal aortic aneurysms. Aust N Z J Surg. 1998;68(1):21–24.
24. Conway KP, Byrne J, Townsend M, Lane IF. Prognosis of patients turned down for conventional abdominal aortic aneurysm repair in the endovascular and sonographic era: Szilagyi revisited? J Vasc Surg. 2001;33(4):752–757.
25. Cook TA, Galland RB. A prospective study to define the optimum rescreening interval for small abdominal aortic aneurysm. Cardiovasc Surg. 1996;4(4):441–444.
26. Kent KC, Zwolak RM, Jaff MR, et al; Society for Vascular Surgery; American Association of Vascular Surgery; Society for Vascular Medicine and Biology. Screening for abdominal aortic aneurysm: a consensus statement. J Vasc Surg. 2004;39(1):267-269.
27. Golledge J, Powell JT. Medical management of abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 2007;4(3):267-273.
28. Sule S, Aronow WS. Management of abdominal aortic aneurysms. Compr Ther. 2009;35(1):3-8.
29. Powell JT. Non-operative or medical management of abdominal aortic aneurysm. Scand J Surg. 2008;97(2): 121-124.
30. Huber TS, Wang JG, Derrow AE, et al. Experience in the United States with intact abdominal aortic aneurysm repair. J Vasc Surg. 2001;33(2):304-310.
31. Adam DJ, Mohan IV, Stuart WP, et al. Community and hospital outcome from ruptured abdominal aortic aneurysm within the catchment area of a regional vascular surgical service. J Vasc Surg. 1999;30(5):922-928.
1. Wilt TJ, Lederle FA, MacDonald R, et al; Agency for Healthcare Research and Quality. Comparison of Endovascular and Open Surgical Repairs for Abdominal Aortic Aneurysm. Rockville, MD: Agency for Healthcare Research and Quality; 2006. AHRQ publication 06-E107. Evidence Report/Technology Assessment 144. www.ahrq.gov/CLINIC/tp/aaareptp.htm. Accessed June 23, 2009.
2. Birkmeyer JD, Upchurch GR Jr. Evidence-based screening and management of abdominal aortic aneurysm. Ann Intern Med. 2007;146(10):749-750.
3. Fleming C, Whitlock EP, Beil TL, Lederle FA. Screening for abdominal aortic aneurysm: a best-evidence systematic review for the US Preventive Services Task Force. Ann Intern Med. 2005;142(3):203-211.
4. Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol. 2006;47(6):1239-1312.
5. Kiell CS, Ernst CB. Advances in management of abdominal aortic aneurysm. Adv Surg. 1993;26:73–98.
6. O’Connor RE. Aneurysm, abdominal. http://emedicine.medscape.com/article/756735-overview. Accessed June 23, 2009.
7. Lederle FA, Parenti CM, Chute EP. Ruptured abdominal aortic aneurysm: the internist as diagnostician. Am J Med. 1994;96:163-167.
8. Cartwright SL, Knudson MP. Evaluation of acute abdominal pain in adults. Am Fam Physician. 2008;77(7): 971-978.
9. Lyon C, Clark DC. Diagnosis of acute abdominal pain in older patients. Am Fam Physician. 2006;74(9):1537-1544.
10. Wilmink TB, Quick CR, Day NE. The association between cigarette smoking and abdominal aortic aneurysms. J Vasc Surg. 1999;30(6):1099-1105.
11. Palazzuoli P, Gallotta M, Guerrieri G, et al. Prevalence of risk factors, coronary and systemic atherosclerosis in abdominal aortic aneurysm: comparison with high cardiovascular risk population. Vasc Health Risk Manag. 2008;4(4):877-883.
12. Sakalihasan N, Limet R, Defawe OD. Abdominal aortic aneurysm. Lancet. 2005;365(9470):1577-1589.
13. Graham LM, Zelenock GB, Whitehouse WM Jr, et al. Clinical significance of arteriosclerotic femoral artery aneurysms. Arch Surg. 1980;115(4):502–507.
14. Whitehouse WM Jr, Wakefield TW, Graham LM, et al. Limb-threatening potential of arteriosclerotic popliteal artery aneurysms. Surgery. 1983;93(5):694–699.
15. Fink HA, Lederle FA, Roth CS, et al. The accuracy of physical examination to detect abdominal aortic aneurysm. Arch Intern Med. 2000;160:833-836.
16. Bentz S, Jones J. Accuracy of emergency department ultrasound scanning in detecting abdominal aortic aneurysm. Emerg Med J. 2006;23(10):803-804.
17. Kvilekval KH, Best IM, Mason RA, et al. The value of computed tomography in the management of symptomatic abdominal aortic aneurysm. J Vasc Surg. 1990;12(1):28-33.
18. US Preventive Services Task Force. Screening for abdominal aortic aneurysm: recommendation statement. Ann Intern Med. 2005;142(3):198-202.
19. Lederle FA, Kane RL, MacDonald R, Wilt TJ. Systematic review: repair of unruptured abdominal aortic aneurysm. Ann Intern Med. 2007;146(10):735-741.
20. McPhee JT, Hill JS, Elami MH. The impact of gender on presentation, therapy, and mortality of abdominal aortic aneurysm in the United States, 2001-2004. J Vasc Surg. 2007;45(5):891-899.
21. Mofidi R, Goldie VJ, Kelman J, et al. Influence of sex on expansion rate of abdominal aortic aneurysms. Br J Surg. 2007;94(3):310-314.
22. Norman PE, Powell JT. Abdominal aortic aneurysm: the prognosis in women is worse than in men. Circulation. 2007;115(22):2865-2869.
23. Englund R, Hudson P, Hanel K, Stanton A. Expansion rates of small abdominal aortic aneurysms. Aust N Z J Surg. 1998;68(1):21–24.
24. Conway KP, Byrne J, Townsend M, Lane IF. Prognosis of patients turned down for conventional abdominal aortic aneurysm repair in the endovascular and sonographic era: Szilagyi revisited? J Vasc Surg. 2001;33(4):752–757.
25. Cook TA, Galland RB. A prospective study to define the optimum rescreening interval for small abdominal aortic aneurysm. Cardiovasc Surg. 1996;4(4):441–444.
26. Kent KC, Zwolak RM, Jaff MR, et al; Society for Vascular Surgery; American Association of Vascular Surgery; Society for Vascular Medicine and Biology. Screening for abdominal aortic aneurysm: a consensus statement. J Vasc Surg. 2004;39(1):267-269.
27. Golledge J, Powell JT. Medical management of abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 2007;4(3):267-273.
28. Sule S, Aronow WS. Management of abdominal aortic aneurysms. Compr Ther. 2009;35(1):3-8.
29. Powell JT. Non-operative or medical management of abdominal aortic aneurysm. Scand J Surg. 2008;97(2): 121-124.
30. Huber TS, Wang JG, Derrow AE, et al. Experience in the United States with intact abdominal aortic aneurysm repair. J Vasc Surg. 2001;33(2):304-310.
31. Adam DJ, Mohan IV, Stuart WP, et al. Community and hospital outcome from ruptured abdominal aortic aneurysm within the catchment area of a regional vascular surgical service. J Vasc Surg. 1999;30(5):922-928.
Botanical Briefs: Common Ivy (Hedera helix)
Multiple Congenital Plaquelike Glomuvenous Malformations With Type 2 Segmental Involvement
Potential caregivers for homebound elderly: More numerous than supposed?
Background This qualitative study examined the experiences and perspectives of caregivers of homebound elderly patients.
Methods We performed in-depth, semistructured interviews with 22 caregivers (average age 59 years) of homebound elderly patients and analyzed them to determine major themes. The homebound patients were part of a house call program of a US academic medical center in Baltimore, Maryland.
Results Caregiver relationships in our study were diverse: 41% were spouses or children, and 41% were unrelated to the homebound patient; 36% were male. We identified 3 themes: (1) caregiving has both positive and negative aspects, (2) caregiver motivation is heterogeneous, and (3) caregivers sometimes undergo transformation as a result of their caregiving experience.
Conclusion Caregiver experience is varied. Interviewees reported a variety of motivations for becoming caregivers and both positive and negative aspects of the experience. Caregivers in this study were diverse with respect to sex and relationship to the patient, suggesting the pool of potential caregivers may be larger than previously thought.
When thinking about long-term home care for the chronically ill elderly, many people automatically imagine a spouse or child as the primary caregiver. In our study, however, 41% of the caregivers interviewed were unrelated to the person receiving the care. In addition to this diversity, we found that motivations for providing care varied among participants; that their different experiences ranged from positive to negative, or a little of both; and that a few caregivers felt their attitudes changed for the better over the course of giving assistance.
We must plan for an aging population
In 2000, 35 million people, or 8% of the US population, were 65 years of age or older. In 2040, there will be 80 million seniors, or 20.4% of the US population.1 The National Long Term Care Survey found that in 1999, 3.9 million Medicare enrollees with a chronic disability were receiving care in their homes. A significant portion of caregiving burden is borne by patients’ relatives and friends; more than 90% of homebound patients were receiving some degree of informal, unpaid assistance.2 As the population ages, more caregivers will be needed to tend chronically ill elders, and most will be informal caregivers.
The reason for our study
Research over the past few decades has found that the burden is significant for those caring for older adults.3-6 Daily challenges and stressors increase the burden caregivers feel in their role.7,8 More recent work has also examined interventions to alleviate caregiver burden.9 Studies of caregivers—published predominately in the social science and nursing literature—have seldom reported on the positive aspects of the role.10-12 Only 1 study in the US medical literature, a national survey, noted positive aspects of the caregiving role.13
Through in-depth interviews, we sought to learn more fully about the experiences of caregivers of chronically ill homebound elderly people.
Methods
Design, setting, study population
This qualitative study of caregivers, a focused ethnography,14 was part of a larger project that interviewed the patients and their doctors. We conducted the study through the Johns Hopkins Geriatrics Center Elder Housecall Program (EHP) from 1997 to 2001. Since 1979, EHP has provided medical and nursing care to generally frail, homebound elderly (mean age 77), predominantly white (82%) and female (69%) patients in a largely blue-collar community in east Baltimore. Annual mortality for patients is 25%.15 We selected a qualitative approach because we wanted to learn more about the experiences and perspectives of the caregivers.
Sampling
The parent study used a purposive and probabilistic sampling strategy to select patients, as described elsewhere.16,17 We found subjects for our caregiver study through the patients, who identified the individuals who assist them. The range of caregiver responsibilities included, but was not limited to, coordinating services, managing medical and financial affairs, and directing such activities as bathing, dressing, and meal preparation. All caregivers we invited to participate did so.
Measurements
We conducted in-depth, semistructured interviews lasting approximately 1 hour. We also collected demographic information. As a starting point for each interview, we used the following brief guide:
- What has your experience as a caregiver for the patient been like?
- Do you recall any particular examples of rewarding aspects of the role?
- Do you recall any particular examples of difficult aspects of the role?
- Are there any particular challenges or important issues in your relationship with the patient that you wish to share?
An investigator trained in qualitative research (JC) asked additional questions, as needed, to further explore caregiver responses. We gave interviewees considerable latitude in commenting on points or topics they considered relevant.
Analysis
Two of this study’s authors (JC, JM) audiotaped, transcribed, and independently coded the interviews, and compared them for agreement. We used an editing style analysis.18 Thematic categories and subcategories became apparent during coding, and we modified them as the interviewing proceeded. We examined and conceptually organized the categories, using the qualitative research software program NUD*IST 4 (Qualitative Solutions and Research Pty Ltd, Victoria, Australia) to facilitate data management and analysis.
A consensus approach
At least 2 investigators participated in each step of the analysis (eg, reading and coding of transcripts; identification, modification, conceptual organization of categories; and selection of themes for presentation). The team made all decisions by consensus.
Human subjects research approval
A Johns Hopkins University School of Medicine Institutional Review Board approved this study, and we obtained written informed consent from all study participants.
Results
We interviewed 22 caregivers (TABLE 1). The number of caregivers per patient ranged from 0 to 3 (20 patients altogether). Most patients had 1 caregiver, but several had 2 or 3. Sixteen interviews involved 1 caregiver, and 3 involved caregiver teams. The average age of the caregivers was 59.3 years, and they had known the patients for an average of 37.4 years. Fourteen of the 22 caregivers (63.6%) were female (a finding similar to results from a Kaiser Family Foundation study in 1998 of 1002 caregivers, in which 64% of the 511 primary caregivers were female).19 Nine of the 22 (40.9%) participants were unrelated to the patient. Caregivers were primarily unpaid relatives or friends (77.3%), but compensated individuals were also included.
Three major themes emerged from analysis of the interview transcripts: (1) positive and negative experiences of caregiving, (2) caregiver motivation, and (3) caregiver transformation. Representative quotes are used to illustrate the themes presented. Specific examples of these themes are shown in TABLE 2.
TABLE 1
Characteristics of the caregivers we interviewed
| Sex | |
| Female | 14/22 (63.6%) |
| Average age | |
| 59.3 years | |
| Ethnicity | |
| Caucasian | 19/22 (86.4%) |
| African American | 3/22 (13.6%) |
| Average length of relationship with patient | |
| 37.4 years | |
| Relationship to patient | |
| Related | 13/22 (59.1%) |
| 1 wife 4 sons 4 daughters 2 grandchildren 1 daughter-in-law 1 grandson-in-law | |
| Unrelated | 9/22 (40.9%) |
| 4 friends (1 paid) 3 paid professional caregivers 1 paid nonprofessional caregiver 1 distant nonblood relative | |
TABLE 2
Common caregiver themes that emerged during interviews
Positive aspects of caregiving
| Negative aspects of caregiving
|
Caregiver motivations
| Caregiver transformation
|
Positive and negative aspects of caregiving
Caregivers described very different experiences of their roles—some only negative, some only positive, and others both positive and negative. Accounts of 6 of the 22 interviewees were essentially value-neutral.
Negative aspects of caregiving. Seven of 22 caregivers reported only negative feelings toward their role, including feeling burdened.
A 62-year-old retired son described how caring for his mother adversely affected his life:
Yeah, I sleep here. I don’t even go to my bed. I haven’t been to bed in over 3 years, because…if I don’t go down as soon as she rings the bell, she can’t hold her water.… I used to go out to Pennsylvania and go up in the battlefield there. I used to go down Skyline Drive, places like that. I can’t do that anymore.
Positive aspects of caregiving. Four caregivers addressed only positive aspects of caregiving.
A 71-year-old retired secretary who was asked if she had encountered any difficulties in caring for her friend said:
I haven’t had any. We’ve become very close friends and her friendship means a lot…I don’t think there’s any problems with going up there…Because I call her before I go to the grocery store to make sure she’s got everything on the list and then I go and just take it up to her and do from there.
Mixed experiences with caregiving. Five of our participants discussed both positive and negative aspects of caregiving; 4 of these 5 lived with the patient.
A 47-year-old machine technician who cared for his grandmother described the benefits his 16-year-old son was receiving from the caregiving arrangement:
It’s been a plus for him to have his great-grandmother living here. I think he enjoys her company, the little stories that go along and plus they always had a good relationship when he was a small child…I would hope he would realize the importance of family and I feel we’re losing that in our society, we’re losing our family. Seems like everybody is moving away and not being associated as close as probably we once were, and you know you realize that sometimes people need a little bit of help and not to be as selfish as you would want to be and maybe learn from that that we all kind of need one another at one time and not to be so independent, like it seems like our society has gone.
He also identified negative aspects of caregiving, including the burdens associated with selling his grandmother’s home and helping her settle into his family’s home:
For the last year it has been kind of hectic with trying to make things easier, doing what needs to be done, taking care of her house. Now that that’s out of the way, that’s a big burden out of the way.
Caregiver motivations
Eight caregivers shared their motivations for deciding to care for a homebound relative or friend. These comments were unsolicited and unexpected. Four caregivers believed they were repaying the patient for help received earlier in life.
A 69-year-old daughter-in-law said the following:
I say to her the same thing I said to my mother: “You took care of me when I was little and I am taking care of you. Now it is my turn.”…I mean we are put on this earth for a purpose and I figure this is our purpose. God put us down here to take care of someone or to help someone.
Potential for caregiver transformation
Another unexpected finding from our study was that 3 interviewees reported that they or their family members were changed by the caregiving experience. Transformations included changing one’s outlook on life, changing one’s views of the caregiving role, and being able to better cope with the death of others.
A 59-year-old homemaker related how her feelings about caregiving changed over time, and she felt she was repaying her mother for help she herself had received:
My major thing in the beginning was I really felt dumped on, like you have to do this whether you want to or not to prevent her from going in a place she didn’t want to go to. But then, after a while, I didn’t feel that way no more because she helped me when I needed help, when my kids were little. She was always there for me.
Discussion
While the medical literature to date has focused on the burdens and difficulties of caregiving, our study shows that caregivers have positive as well as negative experiences in their roles, and that, for some, the experience is a complex mixture of burdens and benefits. Interestingly, 4 of the 5 caregivers who experienced that mixture lived with the patient, suggesting that proximity and increased exposure may result in a more complex experience. In addition to these findings, some caregivers have different motivations for providing care. A small number even describe the experience as transformative.
These findings are consistent with a few studies from the nursing and social science literature that address the positive aspects of caregiving.11,20 For example, 2 studies found that caregivers of patients with dementia experienced both positive and negative aspects of their role.10,12 A recent analysis of a national survey of caregivers noted that two-thirds had feelings of personal reward.13
How can you support caregivers? A deeper understanding of caregivers’ diverse motivations and experiences can help physicians prepare others for this important role, and support and encourage those who are already caring for someone.
You can offer support by discussing with current and prospective caregivers the possibility that the role may bring both positive and negative experiences.
It may also be helpful to describe the potentially transformative nature of caregiving—to point out that some people report that their negative feelings have become more positive in time. In the end, care of dependent elderly patients may improve with such awareness.
Pool of potential caregivers larger than expected. Another finding of our study is the diversity of caregivers. Only 9 of the 22 caregivers interviewed were spouses or children, and only 5 of these 9 were wives or daughters. Among the children, there were just as many sons as daughters. Grandchildren were also represented, and 41% of the caregivers were unrelated to the patient.
Traditionally, many health professionals and the public have looked to female adult children or spouses to care for patients, and the literature on the caregiver experience often represents their views. However, some studies have noted that friends and others are also involved.21 Our finding adds to an evolving understanding that potential caregivers for the homebound elderly can be drawn from a broader pool than first-degree, female relatives.
Limitations of this study. The study sample was small—22 caregivers who live in a particular section of the greater Baltimore metropolitan area. In addition, most of the caregivers were Caucasian and thus do not reflect the ethnic diversity of the United States. As such, we must be cautious in extrapolating these findings to other caregivers in other settings. Nevertheless, we believe that aspects of the caregiver experience reported here will ring true to caregivers who live elsewhere.
Americans are living longer, and many of them have chronic medical problems. An increasing percentage of these elderly will require some level of caregiving to stay in their homes. Future studies might explore in more depth caregiver motivations and caregiver transformation to gain better insight into these important issues.
Acknowledgement
Dr. Carrese received support for this project from the Robert Wood Johnson Generalist Physician Faculty Scholars Program.
Correspondence
Laura A. Hanyok, MD, Johns Hopkins Bayview Medical Center, 5501 Hopkins Bayview Circle, Room 1B.45, Baltimore, MD 21224; lhanyok2@jhmi.edu.
1. Federal Interagency Forum on Aging-Related Statistics: 2006 older Americans update: key indicator of wellness. Available at: http://www.agingstats.gov/agingstatsdotnet/Main_Site/Data/Data_2006.aspx. Accessed June 13, 2008.
2. Wolff JL, Kasper JD. Caregivers of frail elders: updating a national profile. Gerontologist. 2006;46:344-356.
3. Brody EM. The Donald P. Kent Memorial Lecture. Parent care as a normative family stress. Gerontologist. 1986;25:19-29.
4. George LK, Gwyther LP. Caregiver well-being: A multidimensional examination of family caregivers of demented adults. Gerontologist. 1986;26:253-259.
5. Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20:649-655.
6. Zarit SH, Todd PA, Zarit JM. Subjective burden of husbands and wives as caregivers: A longitudinal study. Gerontologist. 1986;26:260-266.
7. Öhman M, Seidenberg S. The experiences of close relatives living with a person with serious chronic illness. Qual Health Res. 2004;14:396-410.
8. Sawatzky JE, Fowler-Kerry S. Impact of caregiving: listening to the voice of informal caregivers. J Psychiatr Ment Health Nurs. 2003;10:277-286.
9. Yin T, Zhou Q, Bashford C. Burden on family members: Caring for frail elderly: a meta-analysis of interventions. Nurs Res. 2002;51:199-208.
10. Andrén S, Elmståhl S. Family caregivers’ subjective experiences of satisfaction in dementia care: aspects of burden, subjective health and sense of coherence. Scand J Caring Sci. 2005;19:157-168.
11. Riedel SE, Fredman L, Langenberg P. Associations among caregiving difficulties, burden, and rewards in caregivers to older post-rehabilitation patients. J Gerontol B Psychol Sci Soc Sci. 1998;53:165-174.
12. Sanders S. Is the glass half empty or half full? Reflections on strain and gain in caregivers of individuals with Alzheimer’s disease. Soc Work Health Care. 2005;40:57-73.
13. Wolff JL, Dy SM, Frick KD, et al. End-of-life care: findings from a national survey of informal caregivers. Arch Intern Med. 2007;167:40-46.
14. Muecke MA. On the evaluation of ethnographies. In: Morse J, ed. Critical Issues in Qualitative Research Methods. Thousand oaks, Calif: Sage Publications; 1994:198-199.
15. Tsuji I, Fox-Whalen S, Finucane TE. Predictors of nursing home placement in community-based long-term care. J Am Geriatr Soc. 1995;43:761-766.
16. Carrese JA, Mullaney JL, Faden RR, et al. Planning for death but not serious future illness: Qualitative study of housebound elderly patients. BMJ. 2002;325:125-127.
17. Russell BH. Research Methods in Anthropology: Qualitative and Quantitative Approaches. 2nd ed. Thousand oaks, Calif: Sage Publications; 1994:95-96.
18. Crabtree BF, Mille WL. Doing Qualitative Research. Newbury Park, Calif: Sage Publications; 1992:18.
19. Donelan K, Hill CA, Hoffman C, et al. Challenged to care: informal caregivers in a changing health system. Health Affairs. 2002. Available at: http://content.healthaffairs.org/cgi/content/full/21/4/222. Accessed June 9, 2009.
20. Jarvis A, Worth A, Porter M. The experience of caring for someone over 75 years of age: results from a Scottish General Practice. J Clin Nurs. 2006;15:1450-1459.
21. Grunfield E, Coyle D, Whelan T, et al. Family caregiver burden; Results of a longitudinal study of breast cancer patient and their principal caregivers. CMAJ. 2004;170:1795-1801.
Background This qualitative study examined the experiences and perspectives of caregivers of homebound elderly patients.
Methods We performed in-depth, semistructured interviews with 22 caregivers (average age 59 years) of homebound elderly patients and analyzed them to determine major themes. The homebound patients were part of a house call program of a US academic medical center in Baltimore, Maryland.
Results Caregiver relationships in our study were diverse: 41% were spouses or children, and 41% were unrelated to the homebound patient; 36% were male. We identified 3 themes: (1) caregiving has both positive and negative aspects, (2) caregiver motivation is heterogeneous, and (3) caregivers sometimes undergo transformation as a result of their caregiving experience.
Conclusion Caregiver experience is varied. Interviewees reported a variety of motivations for becoming caregivers and both positive and negative aspects of the experience. Caregivers in this study were diverse with respect to sex and relationship to the patient, suggesting the pool of potential caregivers may be larger than previously thought.
When thinking about long-term home care for the chronically ill elderly, many people automatically imagine a spouse or child as the primary caregiver. In our study, however, 41% of the caregivers interviewed were unrelated to the person receiving the care. In addition to this diversity, we found that motivations for providing care varied among participants; that their different experiences ranged from positive to negative, or a little of both; and that a few caregivers felt their attitudes changed for the better over the course of giving assistance.
We must plan for an aging population
In 2000, 35 million people, or 8% of the US population, were 65 years of age or older. In 2040, there will be 80 million seniors, or 20.4% of the US population.1 The National Long Term Care Survey found that in 1999, 3.9 million Medicare enrollees with a chronic disability were receiving care in their homes. A significant portion of caregiving burden is borne by patients’ relatives and friends; more than 90% of homebound patients were receiving some degree of informal, unpaid assistance.2 As the population ages, more caregivers will be needed to tend chronically ill elders, and most will be informal caregivers.
The reason for our study
Research over the past few decades has found that the burden is significant for those caring for older adults.3-6 Daily challenges and stressors increase the burden caregivers feel in their role.7,8 More recent work has also examined interventions to alleviate caregiver burden.9 Studies of caregivers—published predominately in the social science and nursing literature—have seldom reported on the positive aspects of the role.10-12 Only 1 study in the US medical literature, a national survey, noted positive aspects of the caregiving role.13
Through in-depth interviews, we sought to learn more fully about the experiences of caregivers of chronically ill homebound elderly people.
Methods
Design, setting, study population
This qualitative study of caregivers, a focused ethnography,14 was part of a larger project that interviewed the patients and their doctors. We conducted the study through the Johns Hopkins Geriatrics Center Elder Housecall Program (EHP) from 1997 to 2001. Since 1979, EHP has provided medical and nursing care to generally frail, homebound elderly (mean age 77), predominantly white (82%) and female (69%) patients in a largely blue-collar community in east Baltimore. Annual mortality for patients is 25%.15 We selected a qualitative approach because we wanted to learn more about the experiences and perspectives of the caregivers.
Sampling
The parent study used a purposive and probabilistic sampling strategy to select patients, as described elsewhere.16,17 We found subjects for our caregiver study through the patients, who identified the individuals who assist them. The range of caregiver responsibilities included, but was not limited to, coordinating services, managing medical and financial affairs, and directing such activities as bathing, dressing, and meal preparation. All caregivers we invited to participate did so.
Measurements
We conducted in-depth, semistructured interviews lasting approximately 1 hour. We also collected demographic information. As a starting point for each interview, we used the following brief guide:
- What has your experience as a caregiver for the patient been like?
- Do you recall any particular examples of rewarding aspects of the role?
- Do you recall any particular examples of difficult aspects of the role?
- Are there any particular challenges or important issues in your relationship with the patient that you wish to share?
An investigator trained in qualitative research (JC) asked additional questions, as needed, to further explore caregiver responses. We gave interviewees considerable latitude in commenting on points or topics they considered relevant.
Analysis
Two of this study’s authors (JC, JM) audiotaped, transcribed, and independently coded the interviews, and compared them for agreement. We used an editing style analysis.18 Thematic categories and subcategories became apparent during coding, and we modified them as the interviewing proceeded. We examined and conceptually organized the categories, using the qualitative research software program NUD*IST 4 (Qualitative Solutions and Research Pty Ltd, Victoria, Australia) to facilitate data management and analysis.
A consensus approach
At least 2 investigators participated in each step of the analysis (eg, reading and coding of transcripts; identification, modification, conceptual organization of categories; and selection of themes for presentation). The team made all decisions by consensus.
Human subjects research approval
A Johns Hopkins University School of Medicine Institutional Review Board approved this study, and we obtained written informed consent from all study participants.
Results
We interviewed 22 caregivers (TABLE 1). The number of caregivers per patient ranged from 0 to 3 (20 patients altogether). Most patients had 1 caregiver, but several had 2 or 3. Sixteen interviews involved 1 caregiver, and 3 involved caregiver teams. The average age of the caregivers was 59.3 years, and they had known the patients for an average of 37.4 years. Fourteen of the 22 caregivers (63.6%) were female (a finding similar to results from a Kaiser Family Foundation study in 1998 of 1002 caregivers, in which 64% of the 511 primary caregivers were female).19 Nine of the 22 (40.9%) participants were unrelated to the patient. Caregivers were primarily unpaid relatives or friends (77.3%), but compensated individuals were also included.
Three major themes emerged from analysis of the interview transcripts: (1) positive and negative experiences of caregiving, (2) caregiver motivation, and (3) caregiver transformation. Representative quotes are used to illustrate the themes presented. Specific examples of these themes are shown in TABLE 2.
TABLE 1
Characteristics of the caregivers we interviewed
| Sex | |
| Female | 14/22 (63.6%) |
| Average age | |
| 59.3 years | |
| Ethnicity | |
| Caucasian | 19/22 (86.4%) |
| African American | 3/22 (13.6%) |
| Average length of relationship with patient | |
| 37.4 years | |
| Relationship to patient | |
| Related | 13/22 (59.1%) |
| 1 wife 4 sons 4 daughters 2 grandchildren 1 daughter-in-law 1 grandson-in-law | |
| Unrelated | 9/22 (40.9%) |
| 4 friends (1 paid) 3 paid professional caregivers 1 paid nonprofessional caregiver 1 distant nonblood relative | |
TABLE 2
Common caregiver themes that emerged during interviews
Positive aspects of caregiving
| Negative aspects of caregiving
|
Caregiver motivations
| Caregiver transformation
|
Positive and negative aspects of caregiving
Caregivers described very different experiences of their roles—some only negative, some only positive, and others both positive and negative. Accounts of 6 of the 22 interviewees were essentially value-neutral.
Negative aspects of caregiving. Seven of 22 caregivers reported only negative feelings toward their role, including feeling burdened.
A 62-year-old retired son described how caring for his mother adversely affected his life:
Yeah, I sleep here. I don’t even go to my bed. I haven’t been to bed in over 3 years, because…if I don’t go down as soon as she rings the bell, she can’t hold her water.… I used to go out to Pennsylvania and go up in the battlefield there. I used to go down Skyline Drive, places like that. I can’t do that anymore.
Positive aspects of caregiving. Four caregivers addressed only positive aspects of caregiving.
A 71-year-old retired secretary who was asked if she had encountered any difficulties in caring for her friend said:
I haven’t had any. We’ve become very close friends and her friendship means a lot…I don’t think there’s any problems with going up there…Because I call her before I go to the grocery store to make sure she’s got everything on the list and then I go and just take it up to her and do from there.
Mixed experiences with caregiving. Five of our participants discussed both positive and negative aspects of caregiving; 4 of these 5 lived with the patient.
A 47-year-old machine technician who cared for his grandmother described the benefits his 16-year-old son was receiving from the caregiving arrangement:
It’s been a plus for him to have his great-grandmother living here. I think he enjoys her company, the little stories that go along and plus they always had a good relationship when he was a small child…I would hope he would realize the importance of family and I feel we’re losing that in our society, we’re losing our family. Seems like everybody is moving away and not being associated as close as probably we once were, and you know you realize that sometimes people need a little bit of help and not to be as selfish as you would want to be and maybe learn from that that we all kind of need one another at one time and not to be so independent, like it seems like our society has gone.
He also identified negative aspects of caregiving, including the burdens associated with selling his grandmother’s home and helping her settle into his family’s home:
For the last year it has been kind of hectic with trying to make things easier, doing what needs to be done, taking care of her house. Now that that’s out of the way, that’s a big burden out of the way.
Caregiver motivations
Eight caregivers shared their motivations for deciding to care for a homebound relative or friend. These comments were unsolicited and unexpected. Four caregivers believed they were repaying the patient for help received earlier in life.
A 69-year-old daughter-in-law said the following:
I say to her the same thing I said to my mother: “You took care of me when I was little and I am taking care of you. Now it is my turn.”…I mean we are put on this earth for a purpose and I figure this is our purpose. God put us down here to take care of someone or to help someone.
Potential for caregiver transformation
Another unexpected finding from our study was that 3 interviewees reported that they or their family members were changed by the caregiving experience. Transformations included changing one’s outlook on life, changing one’s views of the caregiving role, and being able to better cope with the death of others.
A 59-year-old homemaker related how her feelings about caregiving changed over time, and she felt she was repaying her mother for help she herself had received:
My major thing in the beginning was I really felt dumped on, like you have to do this whether you want to or not to prevent her from going in a place she didn’t want to go to. But then, after a while, I didn’t feel that way no more because she helped me when I needed help, when my kids were little. She was always there for me.
Discussion
While the medical literature to date has focused on the burdens and difficulties of caregiving, our study shows that caregivers have positive as well as negative experiences in their roles, and that, for some, the experience is a complex mixture of burdens and benefits. Interestingly, 4 of the 5 caregivers who experienced that mixture lived with the patient, suggesting that proximity and increased exposure may result in a more complex experience. In addition to these findings, some caregivers have different motivations for providing care. A small number even describe the experience as transformative.
These findings are consistent with a few studies from the nursing and social science literature that address the positive aspects of caregiving.11,20 For example, 2 studies found that caregivers of patients with dementia experienced both positive and negative aspects of their role.10,12 A recent analysis of a national survey of caregivers noted that two-thirds had feelings of personal reward.13
How can you support caregivers? A deeper understanding of caregivers’ diverse motivations and experiences can help physicians prepare others for this important role, and support and encourage those who are already caring for someone.
You can offer support by discussing with current and prospective caregivers the possibility that the role may bring both positive and negative experiences.
It may also be helpful to describe the potentially transformative nature of caregiving—to point out that some people report that their negative feelings have become more positive in time. In the end, care of dependent elderly patients may improve with such awareness.
Pool of potential caregivers larger than expected. Another finding of our study is the diversity of caregivers. Only 9 of the 22 caregivers interviewed were spouses or children, and only 5 of these 9 were wives or daughters. Among the children, there were just as many sons as daughters. Grandchildren were also represented, and 41% of the caregivers were unrelated to the patient.
Traditionally, many health professionals and the public have looked to female adult children or spouses to care for patients, and the literature on the caregiver experience often represents their views. However, some studies have noted that friends and others are also involved.21 Our finding adds to an evolving understanding that potential caregivers for the homebound elderly can be drawn from a broader pool than first-degree, female relatives.
Limitations of this study. The study sample was small—22 caregivers who live in a particular section of the greater Baltimore metropolitan area. In addition, most of the caregivers were Caucasian and thus do not reflect the ethnic diversity of the United States. As such, we must be cautious in extrapolating these findings to other caregivers in other settings. Nevertheless, we believe that aspects of the caregiver experience reported here will ring true to caregivers who live elsewhere.
Americans are living longer, and many of them have chronic medical problems. An increasing percentage of these elderly will require some level of caregiving to stay in their homes. Future studies might explore in more depth caregiver motivations and caregiver transformation to gain better insight into these important issues.
Acknowledgement
Dr. Carrese received support for this project from the Robert Wood Johnson Generalist Physician Faculty Scholars Program.
Correspondence
Laura A. Hanyok, MD, Johns Hopkins Bayview Medical Center, 5501 Hopkins Bayview Circle, Room 1B.45, Baltimore, MD 21224; lhanyok2@jhmi.edu.
Background This qualitative study examined the experiences and perspectives of caregivers of homebound elderly patients.
Methods We performed in-depth, semistructured interviews with 22 caregivers (average age 59 years) of homebound elderly patients and analyzed them to determine major themes. The homebound patients were part of a house call program of a US academic medical center in Baltimore, Maryland.
Results Caregiver relationships in our study were diverse: 41% were spouses or children, and 41% were unrelated to the homebound patient; 36% were male. We identified 3 themes: (1) caregiving has both positive and negative aspects, (2) caregiver motivation is heterogeneous, and (3) caregivers sometimes undergo transformation as a result of their caregiving experience.
Conclusion Caregiver experience is varied. Interviewees reported a variety of motivations for becoming caregivers and both positive and negative aspects of the experience. Caregivers in this study were diverse with respect to sex and relationship to the patient, suggesting the pool of potential caregivers may be larger than previously thought.
When thinking about long-term home care for the chronically ill elderly, many people automatically imagine a spouse or child as the primary caregiver. In our study, however, 41% of the caregivers interviewed were unrelated to the person receiving the care. In addition to this diversity, we found that motivations for providing care varied among participants; that their different experiences ranged from positive to negative, or a little of both; and that a few caregivers felt their attitudes changed for the better over the course of giving assistance.
We must plan for an aging population
In 2000, 35 million people, or 8% of the US population, were 65 years of age or older. In 2040, there will be 80 million seniors, or 20.4% of the US population.1 The National Long Term Care Survey found that in 1999, 3.9 million Medicare enrollees with a chronic disability were receiving care in their homes. A significant portion of caregiving burden is borne by patients’ relatives and friends; more than 90% of homebound patients were receiving some degree of informal, unpaid assistance.2 As the population ages, more caregivers will be needed to tend chronically ill elders, and most will be informal caregivers.
The reason for our study
Research over the past few decades has found that the burden is significant for those caring for older adults.3-6 Daily challenges and stressors increase the burden caregivers feel in their role.7,8 More recent work has also examined interventions to alleviate caregiver burden.9 Studies of caregivers—published predominately in the social science and nursing literature—have seldom reported on the positive aspects of the role.10-12 Only 1 study in the US medical literature, a national survey, noted positive aspects of the caregiving role.13
Through in-depth interviews, we sought to learn more fully about the experiences of caregivers of chronically ill homebound elderly people.
Methods
Design, setting, study population
This qualitative study of caregivers, a focused ethnography,14 was part of a larger project that interviewed the patients and their doctors. We conducted the study through the Johns Hopkins Geriatrics Center Elder Housecall Program (EHP) from 1997 to 2001. Since 1979, EHP has provided medical and nursing care to generally frail, homebound elderly (mean age 77), predominantly white (82%) and female (69%) patients in a largely blue-collar community in east Baltimore. Annual mortality for patients is 25%.15 We selected a qualitative approach because we wanted to learn more about the experiences and perspectives of the caregivers.
Sampling
The parent study used a purposive and probabilistic sampling strategy to select patients, as described elsewhere.16,17 We found subjects for our caregiver study through the patients, who identified the individuals who assist them. The range of caregiver responsibilities included, but was not limited to, coordinating services, managing medical and financial affairs, and directing such activities as bathing, dressing, and meal preparation. All caregivers we invited to participate did so.
Measurements
We conducted in-depth, semistructured interviews lasting approximately 1 hour. We also collected demographic information. As a starting point for each interview, we used the following brief guide:
- What has your experience as a caregiver for the patient been like?
- Do you recall any particular examples of rewarding aspects of the role?
- Do you recall any particular examples of difficult aspects of the role?
- Are there any particular challenges or important issues in your relationship with the patient that you wish to share?
An investigator trained in qualitative research (JC) asked additional questions, as needed, to further explore caregiver responses. We gave interviewees considerable latitude in commenting on points or topics they considered relevant.
Analysis
Two of this study’s authors (JC, JM) audiotaped, transcribed, and independently coded the interviews, and compared them for agreement. We used an editing style analysis.18 Thematic categories and subcategories became apparent during coding, and we modified them as the interviewing proceeded. We examined and conceptually organized the categories, using the qualitative research software program NUD*IST 4 (Qualitative Solutions and Research Pty Ltd, Victoria, Australia) to facilitate data management and analysis.
A consensus approach
At least 2 investigators participated in each step of the analysis (eg, reading and coding of transcripts; identification, modification, conceptual organization of categories; and selection of themes for presentation). The team made all decisions by consensus.
Human subjects research approval
A Johns Hopkins University School of Medicine Institutional Review Board approved this study, and we obtained written informed consent from all study participants.
Results
We interviewed 22 caregivers (TABLE 1). The number of caregivers per patient ranged from 0 to 3 (20 patients altogether). Most patients had 1 caregiver, but several had 2 or 3. Sixteen interviews involved 1 caregiver, and 3 involved caregiver teams. The average age of the caregivers was 59.3 years, and they had known the patients for an average of 37.4 years. Fourteen of the 22 caregivers (63.6%) were female (a finding similar to results from a Kaiser Family Foundation study in 1998 of 1002 caregivers, in which 64% of the 511 primary caregivers were female).19 Nine of the 22 (40.9%) participants were unrelated to the patient. Caregivers were primarily unpaid relatives or friends (77.3%), but compensated individuals were also included.
Three major themes emerged from analysis of the interview transcripts: (1) positive and negative experiences of caregiving, (2) caregiver motivation, and (3) caregiver transformation. Representative quotes are used to illustrate the themes presented. Specific examples of these themes are shown in TABLE 2.
TABLE 1
Characteristics of the caregivers we interviewed
| Sex | |
| Female | 14/22 (63.6%) |
| Average age | |
| 59.3 years | |
| Ethnicity | |
| Caucasian | 19/22 (86.4%) |
| African American | 3/22 (13.6%) |
| Average length of relationship with patient | |
| 37.4 years | |
| Relationship to patient | |
| Related | 13/22 (59.1%) |
| 1 wife 4 sons 4 daughters 2 grandchildren 1 daughter-in-law 1 grandson-in-law | |
| Unrelated | 9/22 (40.9%) |
| 4 friends (1 paid) 3 paid professional caregivers 1 paid nonprofessional caregiver 1 distant nonblood relative | |
TABLE 2
Common caregiver themes that emerged during interviews
Positive aspects of caregiving
| Negative aspects of caregiving
|
Caregiver motivations
| Caregiver transformation
|
Positive and negative aspects of caregiving
Caregivers described very different experiences of their roles—some only negative, some only positive, and others both positive and negative. Accounts of 6 of the 22 interviewees were essentially value-neutral.
Negative aspects of caregiving. Seven of 22 caregivers reported only negative feelings toward their role, including feeling burdened.
A 62-year-old retired son described how caring for his mother adversely affected his life:
Yeah, I sleep here. I don’t even go to my bed. I haven’t been to bed in over 3 years, because…if I don’t go down as soon as she rings the bell, she can’t hold her water.… I used to go out to Pennsylvania and go up in the battlefield there. I used to go down Skyline Drive, places like that. I can’t do that anymore.
Positive aspects of caregiving. Four caregivers addressed only positive aspects of caregiving.
A 71-year-old retired secretary who was asked if she had encountered any difficulties in caring for her friend said:
I haven’t had any. We’ve become very close friends and her friendship means a lot…I don’t think there’s any problems with going up there…Because I call her before I go to the grocery store to make sure she’s got everything on the list and then I go and just take it up to her and do from there.
Mixed experiences with caregiving. Five of our participants discussed both positive and negative aspects of caregiving; 4 of these 5 lived with the patient.
A 47-year-old machine technician who cared for his grandmother described the benefits his 16-year-old son was receiving from the caregiving arrangement:
It’s been a plus for him to have his great-grandmother living here. I think he enjoys her company, the little stories that go along and plus they always had a good relationship when he was a small child…I would hope he would realize the importance of family and I feel we’re losing that in our society, we’re losing our family. Seems like everybody is moving away and not being associated as close as probably we once were, and you know you realize that sometimes people need a little bit of help and not to be as selfish as you would want to be and maybe learn from that that we all kind of need one another at one time and not to be so independent, like it seems like our society has gone.
He also identified negative aspects of caregiving, including the burdens associated with selling his grandmother’s home and helping her settle into his family’s home:
For the last year it has been kind of hectic with trying to make things easier, doing what needs to be done, taking care of her house. Now that that’s out of the way, that’s a big burden out of the way.
Caregiver motivations
Eight caregivers shared their motivations for deciding to care for a homebound relative or friend. These comments were unsolicited and unexpected. Four caregivers believed they were repaying the patient for help received earlier in life.
A 69-year-old daughter-in-law said the following:
I say to her the same thing I said to my mother: “You took care of me when I was little and I am taking care of you. Now it is my turn.”…I mean we are put on this earth for a purpose and I figure this is our purpose. God put us down here to take care of someone or to help someone.
Potential for caregiver transformation
Another unexpected finding from our study was that 3 interviewees reported that they or their family members were changed by the caregiving experience. Transformations included changing one’s outlook on life, changing one’s views of the caregiving role, and being able to better cope with the death of others.
A 59-year-old homemaker related how her feelings about caregiving changed over time, and she felt she was repaying her mother for help she herself had received:
My major thing in the beginning was I really felt dumped on, like you have to do this whether you want to or not to prevent her from going in a place she didn’t want to go to. But then, after a while, I didn’t feel that way no more because she helped me when I needed help, when my kids were little. She was always there for me.
Discussion
While the medical literature to date has focused on the burdens and difficulties of caregiving, our study shows that caregivers have positive as well as negative experiences in their roles, and that, for some, the experience is a complex mixture of burdens and benefits. Interestingly, 4 of the 5 caregivers who experienced that mixture lived with the patient, suggesting that proximity and increased exposure may result in a more complex experience. In addition to these findings, some caregivers have different motivations for providing care. A small number even describe the experience as transformative.
These findings are consistent with a few studies from the nursing and social science literature that address the positive aspects of caregiving.11,20 For example, 2 studies found that caregivers of patients with dementia experienced both positive and negative aspects of their role.10,12 A recent analysis of a national survey of caregivers noted that two-thirds had feelings of personal reward.13
How can you support caregivers? A deeper understanding of caregivers’ diverse motivations and experiences can help physicians prepare others for this important role, and support and encourage those who are already caring for someone.
You can offer support by discussing with current and prospective caregivers the possibility that the role may bring both positive and negative experiences.
It may also be helpful to describe the potentially transformative nature of caregiving—to point out that some people report that their negative feelings have become more positive in time. In the end, care of dependent elderly patients may improve with such awareness.
Pool of potential caregivers larger than expected. Another finding of our study is the diversity of caregivers. Only 9 of the 22 caregivers interviewed were spouses or children, and only 5 of these 9 were wives or daughters. Among the children, there were just as many sons as daughters. Grandchildren were also represented, and 41% of the caregivers were unrelated to the patient.
Traditionally, many health professionals and the public have looked to female adult children or spouses to care for patients, and the literature on the caregiver experience often represents their views. However, some studies have noted that friends and others are also involved.21 Our finding adds to an evolving understanding that potential caregivers for the homebound elderly can be drawn from a broader pool than first-degree, female relatives.
Limitations of this study. The study sample was small—22 caregivers who live in a particular section of the greater Baltimore metropolitan area. In addition, most of the caregivers were Caucasian and thus do not reflect the ethnic diversity of the United States. As such, we must be cautious in extrapolating these findings to other caregivers in other settings. Nevertheless, we believe that aspects of the caregiver experience reported here will ring true to caregivers who live elsewhere.
Americans are living longer, and many of them have chronic medical problems. An increasing percentage of these elderly will require some level of caregiving to stay in their homes. Future studies might explore in more depth caregiver motivations and caregiver transformation to gain better insight into these important issues.
Acknowledgement
Dr. Carrese received support for this project from the Robert Wood Johnson Generalist Physician Faculty Scholars Program.
Correspondence
Laura A. Hanyok, MD, Johns Hopkins Bayview Medical Center, 5501 Hopkins Bayview Circle, Room 1B.45, Baltimore, MD 21224; lhanyok2@jhmi.edu.
1. Federal Interagency Forum on Aging-Related Statistics: 2006 older Americans update: key indicator of wellness. Available at: http://www.agingstats.gov/agingstatsdotnet/Main_Site/Data/Data_2006.aspx. Accessed June 13, 2008.
2. Wolff JL, Kasper JD. Caregivers of frail elders: updating a national profile. Gerontologist. 2006;46:344-356.
3. Brody EM. The Donald P. Kent Memorial Lecture. Parent care as a normative family stress. Gerontologist. 1986;25:19-29.
4. George LK, Gwyther LP. Caregiver well-being: A multidimensional examination of family caregivers of demented adults. Gerontologist. 1986;26:253-259.
5. Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20:649-655.
6. Zarit SH, Todd PA, Zarit JM. Subjective burden of husbands and wives as caregivers: A longitudinal study. Gerontologist. 1986;26:260-266.
7. Öhman M, Seidenberg S. The experiences of close relatives living with a person with serious chronic illness. Qual Health Res. 2004;14:396-410.
8. Sawatzky JE, Fowler-Kerry S. Impact of caregiving: listening to the voice of informal caregivers. J Psychiatr Ment Health Nurs. 2003;10:277-286.
9. Yin T, Zhou Q, Bashford C. Burden on family members: Caring for frail elderly: a meta-analysis of interventions. Nurs Res. 2002;51:199-208.
10. Andrén S, Elmståhl S. Family caregivers’ subjective experiences of satisfaction in dementia care: aspects of burden, subjective health and sense of coherence. Scand J Caring Sci. 2005;19:157-168.
11. Riedel SE, Fredman L, Langenberg P. Associations among caregiving difficulties, burden, and rewards in caregivers to older post-rehabilitation patients. J Gerontol B Psychol Sci Soc Sci. 1998;53:165-174.
12. Sanders S. Is the glass half empty or half full? Reflections on strain and gain in caregivers of individuals with Alzheimer’s disease. Soc Work Health Care. 2005;40:57-73.
13. Wolff JL, Dy SM, Frick KD, et al. End-of-life care: findings from a national survey of informal caregivers. Arch Intern Med. 2007;167:40-46.
14. Muecke MA. On the evaluation of ethnographies. In: Morse J, ed. Critical Issues in Qualitative Research Methods. Thousand oaks, Calif: Sage Publications; 1994:198-199.
15. Tsuji I, Fox-Whalen S, Finucane TE. Predictors of nursing home placement in community-based long-term care. J Am Geriatr Soc. 1995;43:761-766.
16. Carrese JA, Mullaney JL, Faden RR, et al. Planning for death but not serious future illness: Qualitative study of housebound elderly patients. BMJ. 2002;325:125-127.
17. Russell BH. Research Methods in Anthropology: Qualitative and Quantitative Approaches. 2nd ed. Thousand oaks, Calif: Sage Publications; 1994:95-96.
18. Crabtree BF, Mille WL. Doing Qualitative Research. Newbury Park, Calif: Sage Publications; 1992:18.
19. Donelan K, Hill CA, Hoffman C, et al. Challenged to care: informal caregivers in a changing health system. Health Affairs. 2002. Available at: http://content.healthaffairs.org/cgi/content/full/21/4/222. Accessed June 9, 2009.
20. Jarvis A, Worth A, Porter M. The experience of caring for someone over 75 years of age: results from a Scottish General Practice. J Clin Nurs. 2006;15:1450-1459.
21. Grunfield E, Coyle D, Whelan T, et al. Family caregiver burden; Results of a longitudinal study of breast cancer patient and their principal caregivers. CMAJ. 2004;170:1795-1801.
1. Federal Interagency Forum on Aging-Related Statistics: 2006 older Americans update: key indicator of wellness. Available at: http://www.agingstats.gov/agingstatsdotnet/Main_Site/Data/Data_2006.aspx. Accessed June 13, 2008.
2. Wolff JL, Kasper JD. Caregivers of frail elders: updating a national profile. Gerontologist. 2006;46:344-356.
3. Brody EM. The Donald P. Kent Memorial Lecture. Parent care as a normative family stress. Gerontologist. 1986;25:19-29.
4. George LK, Gwyther LP. Caregiver well-being: A multidimensional examination of family caregivers of demented adults. Gerontologist. 1986;26:253-259.
5. Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20:649-655.
6. Zarit SH, Todd PA, Zarit JM. Subjective burden of husbands and wives as caregivers: A longitudinal study. Gerontologist. 1986;26:260-266.
7. Öhman M, Seidenberg S. The experiences of close relatives living with a person with serious chronic illness. Qual Health Res. 2004;14:396-410.
8. Sawatzky JE, Fowler-Kerry S. Impact of caregiving: listening to the voice of informal caregivers. J Psychiatr Ment Health Nurs. 2003;10:277-286.
9. Yin T, Zhou Q, Bashford C. Burden on family members: Caring for frail elderly: a meta-analysis of interventions. Nurs Res. 2002;51:199-208.
10. Andrén S, Elmståhl S. Family caregivers’ subjective experiences of satisfaction in dementia care: aspects of burden, subjective health and sense of coherence. Scand J Caring Sci. 2005;19:157-168.
11. Riedel SE, Fredman L, Langenberg P. Associations among caregiving difficulties, burden, and rewards in caregivers to older post-rehabilitation patients. J Gerontol B Psychol Sci Soc Sci. 1998;53:165-174.
12. Sanders S. Is the glass half empty or half full? Reflections on strain and gain in caregivers of individuals with Alzheimer’s disease. Soc Work Health Care. 2005;40:57-73.
13. Wolff JL, Dy SM, Frick KD, et al. End-of-life care: findings from a national survey of informal caregivers. Arch Intern Med. 2007;167:40-46.
14. Muecke MA. On the evaluation of ethnographies. In: Morse J, ed. Critical Issues in Qualitative Research Methods. Thousand oaks, Calif: Sage Publications; 1994:198-199.
15. Tsuji I, Fox-Whalen S, Finucane TE. Predictors of nursing home placement in community-based long-term care. J Am Geriatr Soc. 1995;43:761-766.
16. Carrese JA, Mullaney JL, Faden RR, et al. Planning for death but not serious future illness: Qualitative study of housebound elderly patients. BMJ. 2002;325:125-127.
17. Russell BH. Research Methods in Anthropology: Qualitative and Quantitative Approaches. 2nd ed. Thousand oaks, Calif: Sage Publications; 1994:95-96.
18. Crabtree BF, Mille WL. Doing Qualitative Research. Newbury Park, Calif: Sage Publications; 1992:18.
19. Donelan K, Hill CA, Hoffman C, et al. Challenged to care: informal caregivers in a changing health system. Health Affairs. 2002. Available at: http://content.healthaffairs.org/cgi/content/full/21/4/222. Accessed June 9, 2009.
20. Jarvis A, Worth A, Porter M. The experience of caring for someone over 75 years of age: results from a Scottish General Practice. J Clin Nurs. 2006;15:1450-1459.
21. Grunfield E, Coyle D, Whelan T, et al. Family caregiver burden; Results of a longitudinal study of breast cancer patient and their principal caregivers. CMAJ. 2004;170:1795-1801.
Preventive services: The good, the bad, and the unproven
The past 12 months have been busy ones for the United States Preventive Services Task Force (USPSTF), which issued 34 new recommendations since our last Practice Alert on the group’s activity a year ago. Some recommendations address controversial topics, such as cholesterol screening, and several others—on topics such as prostate cancer screening and acceptable tests for detecting colorectal cancer—differ from those of such prominent groups as the American Cancer Society (ACS).
TABLE 1 provides a breakdown of the 5 categories of USPSTF recommendations (A, B, C, D, I). We’ll start with recent D recommendations (TABLE 2), services the Task Force recommends against, to emphasize that some preventive measures—even if they are widely touted—either provide no benefit or cause more harms than benefits.
TABLE 1
USPSTF recommendation categories
| A Recommendation: The Task Force recommends the service. There is high certainty that the net benefit is substantial. |
| B Recommendation: The Task Force recommends this service. There is high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate to substantial. |
| C Recommendation: The Task Force recommends against routinely providing the service. There may be considerations that support providing the service in an individual patient. There is at least moderate certainty that the net benefit is small. |
| D Recommendation: The Task Force recommends against the service. There is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits. |
| I Statement: The Task Force concludes that the current evidence is insufficient to assess the balance of benefits and harms of the service. Evidence is lacking, of poor quality, or conflicting, and the balance of benefits and harms cannot be determined. |
TABLE 2
The USPSTF recommends AGAINST
|
What not to do
The most notable new D recommendations advise against screening men ≥75 years of age for prostate cancer and against screening for colorectal cancer after age 85. The Task Force also recommends against routine screening for colorectal cancer after age 75, although individual patient considerations may influence your decision about this screen for patients between ages 76 and 85. Bear in mind that the benefits of early detection of colon cancer decline after age 75 because of the time lag between early intervention and benefit and because of competing causes of morbidity and mortality.1
Cancer screening controversies. The recommendations for an age cutoff for prostate and colon cancer screening differ from those of the ACS, which lists no age cutoff for screening for either condition.2 In fact, the Task Force does not recommend screening for prostate cancer at all. Its rationale is that before age 75, the evidence is insufficient to evaluate benefits and harms, and after 75 there is good evidence that screening does more harm than good. The ACS no longer recommends routine prostate cancer screening, but does say that when a patient leaves the decision to the physician, screening should be performed.
Thumbs down on these, too. The Task Force now recommends against using spirometry to screen for chronic obstructive pulmonary disease and against using aspirin for preventing stroke in women <55 years and myocardial infarction (MI) in men <45 years. (See below for a fuller discussion of aspirin as a preventive measure.) The Task Force also recommends against screening for asymptomatic bacteriuria in men and nonpregnant women.
Recommended interventions
Now for the preventive interventions the USPSTF advises you to perform. They include:
Prescribing low-dose aspirin. The most complicated positive recommendations are those for low-dose aspirin to prevent MI in men and stroke in women. Aspirin is effective in preventing these conditions, but carries the risk of major gastrointestinal (GI) bleeding and cerebral hemorrhage. For younger patients, as we’ve seen in the previous section, the Task Force finds the risks of prophylactic low-dose aspirin therapy outweigh the benefits. But for older patients (men between the ages of 45 and 79 years and women ages 55-79), aspirin is recommended when the potential benefit of reducing the incidence of MI in men and stroke in women outweigh the harms. To assist clinicians in weighing the potential benefits and harms, the USPSTF provides a link to a coronary heart disease risk calculator, as well as several tables comparing numbers of prevented heart attacks for men and strokes for women by age and risk category, as well as risks of bleeding complications.3
Screening for hypercholesterolemia. The Task Force’s recommendations for dyslipidemia screening differ markedly from those of the American Heart Association and the Final Report of the National Cholesterol Education Program (NCEP) Expert Panel, which recommend routine screening for all adults starting at age 20 with no age cutoff.4 The USPSTF recommends deferring screening until patients are older, except for those at increased risk of coronary heart disease. This controversy was described in a 2008 Practice Alert.5
Screening for diabetes. The only asymptomatic patients the Task Force recommends screening for diabetes are those with a sustained blood pressure of more than 135/80 mm Hg, treated or untreated. The American Diabetes Association (ADA) would cast a wider net, recommending that you consider screening for prediabetes or diabetes in those ≥45 years of age, particularly in those with a body mass index of ≥25 kg/m2, and in overweight patients <45 years of age who have another risk factor for diabetes.6
Screening for colorectal cancer. The Task Force recommends screening adults starting at age 50 until age 75, using fecal occult blood testing, sigmoidoscopy, or colonoscopy. The ACS also recommends these screening modalities, but adds CT colonography and fecal DNA testing to the list of acceptable methods. The USPSTF found insufficient evidence to evaluate the benefits and harms of these newer tests and expressed concern over the high rate of incidental findings and the unknown long-term effects of radiation from CT colonography.
Screening adolescents. The Task Force is in favor of screening teenagers for major depressive disorder (MDD), as long as systems are in place to provide accurate diagnosis, therapy, and follow-up. High-intensity behavioral counseling for sexually active teens and adults at risk is also endorsed for the prevention of sexually transmitted infections. In both areas, however, the Task Force recognizes that adequately addressing these issues will require more than brief office- or clinic-based interventions.
Caring for pregnant women and newborns. According to the USPSTF, pregnant women should be screened for asymptomatic bacteriuria, advised to take a daily folic acid supplement, counseled about tobacco use, and encouraged to breastfeed. Newborns should be screened for congenital hypothyroidism, phenylketonuria, and hearing loss. These most recent A and B recommendations from the USPSTF are summarized in TABLE 3.
TABLE 3
The USPSTF recommends FOR
| CARDIOVASCULAR DISEASE PREVENTION |
|
| CANCER SCREENING |
|
| PREGNANCY |
|
| NEWBORNS |
|
| ADOLESCENTS |
|
Not proven
When evidence is not available, some organizations are willing to issue guidelines based on expert opinion or consensus. Not so the USPSTF. When the Task Force members find current evidence is not sufficient to make a judgment, they put the intervention into Category I, for Insufficient. The new I recommendations range from aspirin to prevent MI and stroke in those ≥80 years to screening children for MDD and performing whole body skin examinations to detect early manifestations of skin cancer. The new I recommendations are listed in TABLE 4.
TABLE 4
Evidence is INSUFFICIENT to recommend for or against
|
What’s the take-home message?
All of these recent Task Force decisions add substantially to the full set of Task Force recommendations, which can be found at www.ahrq.gov/CLINIC/uspstfix.htm. Given the large number of level A and B recommendations from the Task Force, clinicians are faced with the dilemma of limited time to accomplish all the recommendations. It is reasonable to concentrate on the positive recommendations and avoid performing the interventions recommended against. The interventions in the “I” category are not as clear-cut and clinicians will continue to struggle with them, particularly when other professional organizations recommend them.
CORRESPONDENCE
Doug Campos-Outcalt, MD, MPA, 550 E. Van Buren, Phoenix, AZ 85004; dougco@u.arizona.edu.
1. US Preventive Services Task Force. Screening for colorectal cancer. October 2008. Available at: www.ahrq.gov/clinic/uspstf/uspscolo.htm. Accessed June 3, 2009.
2. American Cancer Society guidelines for early detection of cancer. Last revised May 21, 2009. Available at: http://www.cancer.org/docroot/PED/content/PED_2_3X_ACS_Cancer_Detection_Guidelines_36.asp?sitearea=PED. Accessed June 3, 2009.
3. US Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: recommendation statement. March 2009. Available at: http://www.ahrq.gov/clinic/uspstf09/aspirincvd/aspcvdrs.htm. Accessed June 3, 2009.
4. National Cholesterol Education Program. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation. 2002;106:3143-3421.Available at: http://circ.ahajournals.org/cgi/content/full/106/25/3143. Accessed June 3, 2009.
5. Campos-Outcalt D. USPSTF scales back approach to lipid screening for women. J Fam Pract. 2008;57:740-742.
6. American Diabetes Association. Standards of medical care in diabetes—2008. Diabetes Care. 2008;31(suppl 1):S12-S54.
The past 12 months have been busy ones for the United States Preventive Services Task Force (USPSTF), which issued 34 new recommendations since our last Practice Alert on the group’s activity a year ago. Some recommendations address controversial topics, such as cholesterol screening, and several others—on topics such as prostate cancer screening and acceptable tests for detecting colorectal cancer—differ from those of such prominent groups as the American Cancer Society (ACS).
TABLE 1 provides a breakdown of the 5 categories of USPSTF recommendations (A, B, C, D, I). We’ll start with recent D recommendations (TABLE 2), services the Task Force recommends against, to emphasize that some preventive measures—even if they are widely touted—either provide no benefit or cause more harms than benefits.
TABLE 1
USPSTF recommendation categories
| A Recommendation: The Task Force recommends the service. There is high certainty that the net benefit is substantial. |
| B Recommendation: The Task Force recommends this service. There is high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate to substantial. |
| C Recommendation: The Task Force recommends against routinely providing the service. There may be considerations that support providing the service in an individual patient. There is at least moderate certainty that the net benefit is small. |
| D Recommendation: The Task Force recommends against the service. There is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits. |
| I Statement: The Task Force concludes that the current evidence is insufficient to assess the balance of benefits and harms of the service. Evidence is lacking, of poor quality, or conflicting, and the balance of benefits and harms cannot be determined. |
TABLE 2
The USPSTF recommends AGAINST
|
What not to do
The most notable new D recommendations advise against screening men ≥75 years of age for prostate cancer and against screening for colorectal cancer after age 85. The Task Force also recommends against routine screening for colorectal cancer after age 75, although individual patient considerations may influence your decision about this screen for patients between ages 76 and 85. Bear in mind that the benefits of early detection of colon cancer decline after age 75 because of the time lag between early intervention and benefit and because of competing causes of morbidity and mortality.1
Cancer screening controversies. The recommendations for an age cutoff for prostate and colon cancer screening differ from those of the ACS, which lists no age cutoff for screening for either condition.2 In fact, the Task Force does not recommend screening for prostate cancer at all. Its rationale is that before age 75, the evidence is insufficient to evaluate benefits and harms, and after 75 there is good evidence that screening does more harm than good. The ACS no longer recommends routine prostate cancer screening, but does say that when a patient leaves the decision to the physician, screening should be performed.
Thumbs down on these, too. The Task Force now recommends against using spirometry to screen for chronic obstructive pulmonary disease and against using aspirin for preventing stroke in women <55 years and myocardial infarction (MI) in men <45 years. (See below for a fuller discussion of aspirin as a preventive measure.) The Task Force also recommends against screening for asymptomatic bacteriuria in men and nonpregnant women.
Recommended interventions
Now for the preventive interventions the USPSTF advises you to perform. They include:
Prescribing low-dose aspirin. The most complicated positive recommendations are those for low-dose aspirin to prevent MI in men and stroke in women. Aspirin is effective in preventing these conditions, but carries the risk of major gastrointestinal (GI) bleeding and cerebral hemorrhage. For younger patients, as we’ve seen in the previous section, the Task Force finds the risks of prophylactic low-dose aspirin therapy outweigh the benefits. But for older patients (men between the ages of 45 and 79 years and women ages 55-79), aspirin is recommended when the potential benefit of reducing the incidence of MI in men and stroke in women outweigh the harms. To assist clinicians in weighing the potential benefits and harms, the USPSTF provides a link to a coronary heart disease risk calculator, as well as several tables comparing numbers of prevented heart attacks for men and strokes for women by age and risk category, as well as risks of bleeding complications.3
Screening for hypercholesterolemia. The Task Force’s recommendations for dyslipidemia screening differ markedly from those of the American Heart Association and the Final Report of the National Cholesterol Education Program (NCEP) Expert Panel, which recommend routine screening for all adults starting at age 20 with no age cutoff.4 The USPSTF recommends deferring screening until patients are older, except for those at increased risk of coronary heart disease. This controversy was described in a 2008 Practice Alert.5
Screening for diabetes. The only asymptomatic patients the Task Force recommends screening for diabetes are those with a sustained blood pressure of more than 135/80 mm Hg, treated or untreated. The American Diabetes Association (ADA) would cast a wider net, recommending that you consider screening for prediabetes or diabetes in those ≥45 years of age, particularly in those with a body mass index of ≥25 kg/m2, and in overweight patients <45 years of age who have another risk factor for diabetes.6
Screening for colorectal cancer. The Task Force recommends screening adults starting at age 50 until age 75, using fecal occult blood testing, sigmoidoscopy, or colonoscopy. The ACS also recommends these screening modalities, but adds CT colonography and fecal DNA testing to the list of acceptable methods. The USPSTF found insufficient evidence to evaluate the benefits and harms of these newer tests and expressed concern over the high rate of incidental findings and the unknown long-term effects of radiation from CT colonography.
Screening adolescents. The Task Force is in favor of screening teenagers for major depressive disorder (MDD), as long as systems are in place to provide accurate diagnosis, therapy, and follow-up. High-intensity behavioral counseling for sexually active teens and adults at risk is also endorsed for the prevention of sexually transmitted infections. In both areas, however, the Task Force recognizes that adequately addressing these issues will require more than brief office- or clinic-based interventions.
Caring for pregnant women and newborns. According to the USPSTF, pregnant women should be screened for asymptomatic bacteriuria, advised to take a daily folic acid supplement, counseled about tobacco use, and encouraged to breastfeed. Newborns should be screened for congenital hypothyroidism, phenylketonuria, and hearing loss. These most recent A and B recommendations from the USPSTF are summarized in TABLE 3.
TABLE 3
The USPSTF recommends FOR
| CARDIOVASCULAR DISEASE PREVENTION |
|
| CANCER SCREENING |
|
| PREGNANCY |
|
| NEWBORNS |
|
| ADOLESCENTS |
|
Not proven
When evidence is not available, some organizations are willing to issue guidelines based on expert opinion or consensus. Not so the USPSTF. When the Task Force members find current evidence is not sufficient to make a judgment, they put the intervention into Category I, for Insufficient. The new I recommendations range from aspirin to prevent MI and stroke in those ≥80 years to screening children for MDD and performing whole body skin examinations to detect early manifestations of skin cancer. The new I recommendations are listed in TABLE 4.
TABLE 4
Evidence is INSUFFICIENT to recommend for or against
|
What’s the take-home message?
All of these recent Task Force decisions add substantially to the full set of Task Force recommendations, which can be found at www.ahrq.gov/CLINIC/uspstfix.htm. Given the large number of level A and B recommendations from the Task Force, clinicians are faced with the dilemma of limited time to accomplish all the recommendations. It is reasonable to concentrate on the positive recommendations and avoid performing the interventions recommended against. The interventions in the “I” category are not as clear-cut and clinicians will continue to struggle with them, particularly when other professional organizations recommend them.
CORRESPONDENCE
Doug Campos-Outcalt, MD, MPA, 550 E. Van Buren, Phoenix, AZ 85004; dougco@u.arizona.edu.
The past 12 months have been busy ones for the United States Preventive Services Task Force (USPSTF), which issued 34 new recommendations since our last Practice Alert on the group’s activity a year ago. Some recommendations address controversial topics, such as cholesterol screening, and several others—on topics such as prostate cancer screening and acceptable tests for detecting colorectal cancer—differ from those of such prominent groups as the American Cancer Society (ACS).
TABLE 1 provides a breakdown of the 5 categories of USPSTF recommendations (A, B, C, D, I). We’ll start with recent D recommendations (TABLE 2), services the Task Force recommends against, to emphasize that some preventive measures—even if they are widely touted—either provide no benefit or cause more harms than benefits.
TABLE 1
USPSTF recommendation categories
| A Recommendation: The Task Force recommends the service. There is high certainty that the net benefit is substantial. |
| B Recommendation: The Task Force recommends this service. There is high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate to substantial. |
| C Recommendation: The Task Force recommends against routinely providing the service. There may be considerations that support providing the service in an individual patient. There is at least moderate certainty that the net benefit is small. |
| D Recommendation: The Task Force recommends against the service. There is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits. |
| I Statement: The Task Force concludes that the current evidence is insufficient to assess the balance of benefits and harms of the service. Evidence is lacking, of poor quality, or conflicting, and the balance of benefits and harms cannot be determined. |
TABLE 2
The USPSTF recommends AGAINST
|
What not to do
The most notable new D recommendations advise against screening men ≥75 years of age for prostate cancer and against screening for colorectal cancer after age 85. The Task Force also recommends against routine screening for colorectal cancer after age 75, although individual patient considerations may influence your decision about this screen for patients between ages 76 and 85. Bear in mind that the benefits of early detection of colon cancer decline after age 75 because of the time lag between early intervention and benefit and because of competing causes of morbidity and mortality.1
Cancer screening controversies. The recommendations for an age cutoff for prostate and colon cancer screening differ from those of the ACS, which lists no age cutoff for screening for either condition.2 In fact, the Task Force does not recommend screening for prostate cancer at all. Its rationale is that before age 75, the evidence is insufficient to evaluate benefits and harms, and after 75 there is good evidence that screening does more harm than good. The ACS no longer recommends routine prostate cancer screening, but does say that when a patient leaves the decision to the physician, screening should be performed.
Thumbs down on these, too. The Task Force now recommends against using spirometry to screen for chronic obstructive pulmonary disease and against using aspirin for preventing stroke in women <55 years and myocardial infarction (MI) in men <45 years. (See below for a fuller discussion of aspirin as a preventive measure.) The Task Force also recommends against screening for asymptomatic bacteriuria in men and nonpregnant women.
Recommended interventions
Now for the preventive interventions the USPSTF advises you to perform. They include:
Prescribing low-dose aspirin. The most complicated positive recommendations are those for low-dose aspirin to prevent MI in men and stroke in women. Aspirin is effective in preventing these conditions, but carries the risk of major gastrointestinal (GI) bleeding and cerebral hemorrhage. For younger patients, as we’ve seen in the previous section, the Task Force finds the risks of prophylactic low-dose aspirin therapy outweigh the benefits. But for older patients (men between the ages of 45 and 79 years and women ages 55-79), aspirin is recommended when the potential benefit of reducing the incidence of MI in men and stroke in women outweigh the harms. To assist clinicians in weighing the potential benefits and harms, the USPSTF provides a link to a coronary heart disease risk calculator, as well as several tables comparing numbers of prevented heart attacks for men and strokes for women by age and risk category, as well as risks of bleeding complications.3
Screening for hypercholesterolemia. The Task Force’s recommendations for dyslipidemia screening differ markedly from those of the American Heart Association and the Final Report of the National Cholesterol Education Program (NCEP) Expert Panel, which recommend routine screening for all adults starting at age 20 with no age cutoff.4 The USPSTF recommends deferring screening until patients are older, except for those at increased risk of coronary heart disease. This controversy was described in a 2008 Practice Alert.5
Screening for diabetes. The only asymptomatic patients the Task Force recommends screening for diabetes are those with a sustained blood pressure of more than 135/80 mm Hg, treated or untreated. The American Diabetes Association (ADA) would cast a wider net, recommending that you consider screening for prediabetes or diabetes in those ≥45 years of age, particularly in those with a body mass index of ≥25 kg/m2, and in overweight patients <45 years of age who have another risk factor for diabetes.6
Screening for colorectal cancer. The Task Force recommends screening adults starting at age 50 until age 75, using fecal occult blood testing, sigmoidoscopy, or colonoscopy. The ACS also recommends these screening modalities, but adds CT colonography and fecal DNA testing to the list of acceptable methods. The USPSTF found insufficient evidence to evaluate the benefits and harms of these newer tests and expressed concern over the high rate of incidental findings and the unknown long-term effects of radiation from CT colonography.
Screening adolescents. The Task Force is in favor of screening teenagers for major depressive disorder (MDD), as long as systems are in place to provide accurate diagnosis, therapy, and follow-up. High-intensity behavioral counseling for sexually active teens and adults at risk is also endorsed for the prevention of sexually transmitted infections. In both areas, however, the Task Force recognizes that adequately addressing these issues will require more than brief office- or clinic-based interventions.
Caring for pregnant women and newborns. According to the USPSTF, pregnant women should be screened for asymptomatic bacteriuria, advised to take a daily folic acid supplement, counseled about tobacco use, and encouraged to breastfeed. Newborns should be screened for congenital hypothyroidism, phenylketonuria, and hearing loss. These most recent A and B recommendations from the USPSTF are summarized in TABLE 3.
TABLE 3
The USPSTF recommends FOR
| CARDIOVASCULAR DISEASE PREVENTION |
|
| CANCER SCREENING |
|
| PREGNANCY |
|
| NEWBORNS |
|
| ADOLESCENTS |
|
Not proven
When evidence is not available, some organizations are willing to issue guidelines based on expert opinion or consensus. Not so the USPSTF. When the Task Force members find current evidence is not sufficient to make a judgment, they put the intervention into Category I, for Insufficient. The new I recommendations range from aspirin to prevent MI and stroke in those ≥80 years to screening children for MDD and performing whole body skin examinations to detect early manifestations of skin cancer. The new I recommendations are listed in TABLE 4.
TABLE 4
Evidence is INSUFFICIENT to recommend for or against
|
What’s the take-home message?
All of these recent Task Force decisions add substantially to the full set of Task Force recommendations, which can be found at www.ahrq.gov/CLINIC/uspstfix.htm. Given the large number of level A and B recommendations from the Task Force, clinicians are faced with the dilemma of limited time to accomplish all the recommendations. It is reasonable to concentrate on the positive recommendations and avoid performing the interventions recommended against. The interventions in the “I” category are not as clear-cut and clinicians will continue to struggle with them, particularly when other professional organizations recommend them.
CORRESPONDENCE
Doug Campos-Outcalt, MD, MPA, 550 E. Van Buren, Phoenix, AZ 85004; dougco@u.arizona.edu.
1. US Preventive Services Task Force. Screening for colorectal cancer. October 2008. Available at: www.ahrq.gov/clinic/uspstf/uspscolo.htm. Accessed June 3, 2009.
2. American Cancer Society guidelines for early detection of cancer. Last revised May 21, 2009. Available at: http://www.cancer.org/docroot/PED/content/PED_2_3X_ACS_Cancer_Detection_Guidelines_36.asp?sitearea=PED. Accessed June 3, 2009.
3. US Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: recommendation statement. March 2009. Available at: http://www.ahrq.gov/clinic/uspstf09/aspirincvd/aspcvdrs.htm. Accessed June 3, 2009.
4. National Cholesterol Education Program. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation. 2002;106:3143-3421.Available at: http://circ.ahajournals.org/cgi/content/full/106/25/3143. Accessed June 3, 2009.
5. Campos-Outcalt D. USPSTF scales back approach to lipid screening for women. J Fam Pract. 2008;57:740-742.
6. American Diabetes Association. Standards of medical care in diabetes—2008. Diabetes Care. 2008;31(suppl 1):S12-S54.
1. US Preventive Services Task Force. Screening for colorectal cancer. October 2008. Available at: www.ahrq.gov/clinic/uspstf/uspscolo.htm. Accessed June 3, 2009.
2. American Cancer Society guidelines for early detection of cancer. Last revised May 21, 2009. Available at: http://www.cancer.org/docroot/PED/content/PED_2_3X_ACS_Cancer_Detection_Guidelines_36.asp?sitearea=PED. Accessed June 3, 2009.
3. US Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: recommendation statement. March 2009. Available at: http://www.ahrq.gov/clinic/uspstf09/aspirincvd/aspcvdrs.htm. Accessed June 3, 2009.
4. National Cholesterol Education Program. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation. 2002;106:3143-3421.Available at: http://circ.ahajournals.org/cgi/content/full/106/25/3143. Accessed June 3, 2009.
5. Campos-Outcalt D. USPSTF scales back approach to lipid screening for women. J Fam Pract. 2008;57:740-742.
6. American Diabetes Association. Standards of medical care in diabetes—2008. Diabetes Care. 2008;31(suppl 1):S12-S54.
ACOG guidelines for HIV screening don’t always acknowledge coding reality
Routine screening for the human immunodeficiency virus (HIV) is recommended for all women 19 to 64 years old, according to guidelines issued in August 2008 by the American College of Obstetricians and Gynecologists (ACOG). In addition, ACOG recommends that women outside that age range who have a risk factor for HIV infection undergo targeted screening.
To accomplish these goals, ACOG suggests “opt-out” HIV screening, in which the patient is notified that HIV testing will be performed as a routine part of gynecologic and obstetric care unless she declines it.
Opt-out testing may not always be feasible, however, because many payers still require that you counsel the patient about the HIV test before it is performed, as well as have her sign a consent form.
Information about individual states’ requirements for testing, counseling, and informed consent can be found at the Compendium of State HIV Testing Laws, Quick Reference Guide for Clinicians (March 17, 2009), prepared by the National HIV/AIDS Clinicians’ Consultation Center at www.nccc.ucsf.edu/StateLaws/About%20Compendium/Quick%20Reference%20Guide.pdf.
The patient may be offered the test during any of the following:
- her preventive health checkup
- an office visit for a presenting problem
- a scheduled obstetric visit.
When you provide counseling, bill for it!
Counseling for HIV in the absence of the condition is considered a preventive service, which is reported using 99401–99404 (Preventive medicine counseling and/or risk factor reduction intervention(s) provided to an individual), based on total counseling time between 15 and 60 minutes (reported in 15-minute increments). Such preventive counseling can be reported in addition to a problem E/M service by adding the modifier -25 (Significant, separately identifiable evaluation and management service by the same physician on the same day of the procedure or other service) to the problem E/M code. It can also be reported separately at the time of an obstetric visit. However, such counseling is not covered when it is conducted during a preventive exam.
Include the proper diagnostic code
Diagnostic coding, following these ICD-9 rules, lets the payer know why the service is being rendered:
- Report V73.89 (Screening for other specified viral disease) if the patient is being seen to determine her HIV status.
- Report V69.8 (Other problems related to lifestyle) as a secondary diagnosis if the patient is in a group known to be at high risk of HIV infection.
- Report V65.44 (HIV counseling) for counseling provided during the encounter for the test, or use this code to report the visit at which the patient returns to discuss her result.
Just what constitutes “routine” testing?
The ACOG guidelines are unclear as to what, exactly, “routine” testing means. Is an ObGyn expected to test a patient once in her lifetime, annually, or any time her life partner changes?
These specifics are not addressed in the ACOG recommendations. Based on similar recommendations from the Centers for Disease Control and Prevention (CDC) and the US Preventive Services Task Force (USPSTF), however, you might surmise the following:
- Test all patients 19 to 64 years old for HIV at least once.
- Test all patients at high risk of contracting HIV annually. (High-risk groups include women who receive a blood transfusion, practice unsafe sex, or have a new sexual partner who has not been tested.)
- Test all women each time they become pregnant.
- HIV screening be carried out after the patient is notified that testing will be performed, unless she declines (opt-out screening)
- any person who is at high risk of contracting HIV be screened at least annually
- separate written consent for HIV testing not be required (general consent for medical care should be sufficient to encompass consent for HIV testing)
- prevention counseling not be required with HIV diagnostic testing or as part of HIV screening programs in health-care settings
- among pregnant women, HIV screening be included in the routine panel of prenatal screening tests
- every pregnant woman be screened for HIV after she is notified that testing will be performed, unless she declines (opt-out screening)
- separate written consent for HIV testing not be required for pregnant women (general consent for medical care should be sufficient to encompass consent for HIV testing)
- repeat screening in the third trimester be carried out in certain jurisdictions that have an elevated rate of HIV infection among pregnant women.
Obviously, the CDC’s call for opt-out screening and its recommendation against informed consent for HIV testing contradict the requirements of some states, so it is important to know the regulations where you practice.
Routine screening for the human immunodeficiency virus (HIV) is recommended for all women 19 to 64 years old, according to guidelines issued in August 2008 by the American College of Obstetricians and Gynecologists (ACOG). In addition, ACOG recommends that women outside that age range who have a risk factor for HIV infection undergo targeted screening.
To accomplish these goals, ACOG suggests “opt-out” HIV screening, in which the patient is notified that HIV testing will be performed as a routine part of gynecologic and obstetric care unless she declines it.
Opt-out testing may not always be feasible, however, because many payers still require that you counsel the patient about the HIV test before it is performed, as well as have her sign a consent form.
Information about individual states’ requirements for testing, counseling, and informed consent can be found at the Compendium of State HIV Testing Laws, Quick Reference Guide for Clinicians (March 17, 2009), prepared by the National HIV/AIDS Clinicians’ Consultation Center at www.nccc.ucsf.edu/StateLaws/About%20Compendium/Quick%20Reference%20Guide.pdf.
The patient may be offered the test during any of the following:
- her preventive health checkup
- an office visit for a presenting problem
- a scheduled obstetric visit.
When you provide counseling, bill for it!
Counseling for HIV in the absence of the condition is considered a preventive service, which is reported using 99401–99404 (Preventive medicine counseling and/or risk factor reduction intervention(s) provided to an individual), based on total counseling time between 15 and 60 minutes (reported in 15-minute increments). Such preventive counseling can be reported in addition to a problem E/M service by adding the modifier -25 (Significant, separately identifiable evaluation and management service by the same physician on the same day of the procedure or other service) to the problem E/M code. It can also be reported separately at the time of an obstetric visit. However, such counseling is not covered when it is conducted during a preventive exam.
Include the proper diagnostic code
Diagnostic coding, following these ICD-9 rules, lets the payer know why the service is being rendered:
- Report V73.89 (Screening for other specified viral disease) if the patient is being seen to determine her HIV status.
- Report V69.8 (Other problems related to lifestyle) as a secondary diagnosis if the patient is in a group known to be at high risk of HIV infection.
- Report V65.44 (HIV counseling) for counseling provided during the encounter for the test, or use this code to report the visit at which the patient returns to discuss her result.
Just what constitutes “routine” testing?
The ACOG guidelines are unclear as to what, exactly, “routine” testing means. Is an ObGyn expected to test a patient once in her lifetime, annually, or any time her life partner changes?
These specifics are not addressed in the ACOG recommendations. Based on similar recommendations from the Centers for Disease Control and Prevention (CDC) and the US Preventive Services Task Force (USPSTF), however, you might surmise the following:
- Test all patients 19 to 64 years old for HIV at least once.
- Test all patients at high risk of contracting HIV annually. (High-risk groups include women who receive a blood transfusion, practice unsafe sex, or have a new sexual partner who has not been tested.)
- Test all women each time they become pregnant.
- HIV screening be carried out after the patient is notified that testing will be performed, unless she declines (opt-out screening)
- any person who is at high risk of contracting HIV be screened at least annually
- separate written consent for HIV testing not be required (general consent for medical care should be sufficient to encompass consent for HIV testing)
- prevention counseling not be required with HIV diagnostic testing or as part of HIV screening programs in health-care settings
- among pregnant women, HIV screening be included in the routine panel of prenatal screening tests
- every pregnant woman be screened for HIV after she is notified that testing will be performed, unless she declines (opt-out screening)
- separate written consent for HIV testing not be required for pregnant women (general consent for medical care should be sufficient to encompass consent for HIV testing)
- repeat screening in the third trimester be carried out in certain jurisdictions that have an elevated rate of HIV infection among pregnant women.
Obviously, the CDC’s call for opt-out screening and its recommendation against informed consent for HIV testing contradict the requirements of some states, so it is important to know the regulations where you practice.
Routine screening for the human immunodeficiency virus (HIV) is recommended for all women 19 to 64 years old, according to guidelines issued in August 2008 by the American College of Obstetricians and Gynecologists (ACOG). In addition, ACOG recommends that women outside that age range who have a risk factor for HIV infection undergo targeted screening.
To accomplish these goals, ACOG suggests “opt-out” HIV screening, in which the patient is notified that HIV testing will be performed as a routine part of gynecologic and obstetric care unless she declines it.
Opt-out testing may not always be feasible, however, because many payers still require that you counsel the patient about the HIV test before it is performed, as well as have her sign a consent form.
Information about individual states’ requirements for testing, counseling, and informed consent can be found at the Compendium of State HIV Testing Laws, Quick Reference Guide for Clinicians (March 17, 2009), prepared by the National HIV/AIDS Clinicians’ Consultation Center at www.nccc.ucsf.edu/StateLaws/About%20Compendium/Quick%20Reference%20Guide.pdf.
The patient may be offered the test during any of the following:
- her preventive health checkup
- an office visit for a presenting problem
- a scheduled obstetric visit.
When you provide counseling, bill for it!
Counseling for HIV in the absence of the condition is considered a preventive service, which is reported using 99401–99404 (Preventive medicine counseling and/or risk factor reduction intervention(s) provided to an individual), based on total counseling time between 15 and 60 minutes (reported in 15-minute increments). Such preventive counseling can be reported in addition to a problem E/M service by adding the modifier -25 (Significant, separately identifiable evaluation and management service by the same physician on the same day of the procedure or other service) to the problem E/M code. It can also be reported separately at the time of an obstetric visit. However, such counseling is not covered when it is conducted during a preventive exam.
Include the proper diagnostic code
Diagnostic coding, following these ICD-9 rules, lets the payer know why the service is being rendered:
- Report V73.89 (Screening for other specified viral disease) if the patient is being seen to determine her HIV status.
- Report V69.8 (Other problems related to lifestyle) as a secondary diagnosis if the patient is in a group known to be at high risk of HIV infection.
- Report V65.44 (HIV counseling) for counseling provided during the encounter for the test, or use this code to report the visit at which the patient returns to discuss her result.
Just what constitutes “routine” testing?
The ACOG guidelines are unclear as to what, exactly, “routine” testing means. Is an ObGyn expected to test a patient once in her lifetime, annually, or any time her life partner changes?
These specifics are not addressed in the ACOG recommendations. Based on similar recommendations from the Centers for Disease Control and Prevention (CDC) and the US Preventive Services Task Force (USPSTF), however, you might surmise the following:
- Test all patients 19 to 64 years old for HIV at least once.
- Test all patients at high risk of contracting HIV annually. (High-risk groups include women who receive a blood transfusion, practice unsafe sex, or have a new sexual partner who has not been tested.)
- Test all women each time they become pregnant.
- HIV screening be carried out after the patient is notified that testing will be performed, unless she declines (opt-out screening)
- any person who is at high risk of contracting HIV be screened at least annually
- separate written consent for HIV testing not be required (general consent for medical care should be sufficient to encompass consent for HIV testing)
- prevention counseling not be required with HIV diagnostic testing or as part of HIV screening programs in health-care settings
- among pregnant women, HIV screening be included in the routine panel of prenatal screening tests
- every pregnant woman be screened for HIV after she is notified that testing will be performed, unless she declines (opt-out screening)
- separate written consent for HIV testing not be required for pregnant women (general consent for medical care should be sufficient to encompass consent for HIV testing)
- repeat screening in the third trimester be carried out in certain jurisdictions that have an elevated rate of HIV infection among pregnant women.
Obviously, the CDC’s call for opt-out screening and its recommendation against informed consent for HIV testing contradict the requirements of some states, so it is important to know the regulations where you practice.
The Child With Migraine
More often than not the child who presents with recurrent or chronic headaches will be experiencing migraines. Pediatric migraine is very common; in fact, it is one of the top five health problems for children. General pediatricians treat the majority of these children, up to 90%. There are not enough pediatric neurologists in the United States to take care of all of these children. For example, given the prevalence rate of 10%, an estimated 60,000 children and adolescents experience migraine out of the 2.4 million people in the Cincinnati draw area for my institution. Obviously, they cannot all be referred to a specialist.
The most important thing for you to do is to rule out secondary headaches. Differentiate primary headaches (such as migraine and tension headaches) from secondary ones, being skeptical of the secondary presentations. If a secondary etiology is suspected and the headaches do not resolve, then reassess, but the headaches may be primary ones.
Ask patients and parents about headache symptoms because often the symptoms are initially missed. Standardized criteria such as the American Academy of Neurology practice parameters on the treatment of migraine headache in children and adolescents can guide your diagnosis and management (Neurology 2004;63:2215–24). If the clinical picture does not fit these criteria, consider further evaluation of the child.
After your differential diagnosis, perform a complete neurologic examination. If findings are abnormal on the neurologic exam, consider an MRI. Such imaging also may be warranted for children with exclusively occipital headaches, if they experience a crescendo or abrupt change in headaches, or if they lack a relevant family history.
Almost all other tests are less useful and do not help prior to referral to a pediatric neurologist. We do not need EEGs, sinus x-rays, or CT exams, which have lots of unnecessary radiation. We routinely check riboflavin and coenzyme Q10 levels, but this may be beyond the level of general pediatricians.
Referral to a specialist is appropriate when the above strategies are not working and if the headaches do not improve. Also refer if a child has chronic daily headaches (defined as 15 or more days per month), if a child is missing a lot of school or other activities of daily living, and/or if the history and diagnosis do not seem to fit the presentation.
Optimal treatment is a standardized strategy that incorporates acute and preventive pharmacologic strategies, as well as biobehavioral treatments.
Appropriate NSAID use, for example, can aid a child with an acute presentation. For example, prescribe 10 mg/kg of ibuprofen at onset, and do not exceed three dosages per week. In addition, be familiar with at least one triptan at appropriate dosing (an adult dose for teenagers).
Also be comfortable with at least one age-appropriate, preventive agent. Amitriptyline is the easiest to use. The recommended dosage regimen is 1 mg/kg titrated up slowly (over a period of 8–10 weeks) for about 2–3 months at full dose to allow sufficient time for clinical effect. I also advise against the use of cyproheptadine for teenagers with migraines because of the appetite effect.
Adequate fluid intake without caffeine, exercise at least three to four times per week, and sufficient regular sleep (8–9 hours, for example) are important components of biobehavioral treatment. In addition, educate patients and parents about the importance of a healthy, balanced diet. Instruct patients not to skip meals. We do not recommend avoidance of particular foods, and the evidence supports this stance. It is more important to make healthy food choices.
More often than not the child who presents with recurrent or chronic headaches will be experiencing migraines. Pediatric migraine is very common; in fact, it is one of the top five health problems for children. General pediatricians treat the majority of these children, up to 90%. There are not enough pediatric neurologists in the United States to take care of all of these children. For example, given the prevalence rate of 10%, an estimated 60,000 children and adolescents experience migraine out of the 2.4 million people in the Cincinnati draw area for my institution. Obviously, they cannot all be referred to a specialist.
The most important thing for you to do is to rule out secondary headaches. Differentiate primary headaches (such as migraine and tension headaches) from secondary ones, being skeptical of the secondary presentations. If a secondary etiology is suspected and the headaches do not resolve, then reassess, but the headaches may be primary ones.
Ask patients and parents about headache symptoms because often the symptoms are initially missed. Standardized criteria such as the American Academy of Neurology practice parameters on the treatment of migraine headache in children and adolescents can guide your diagnosis and management (Neurology 2004;63:2215–24). If the clinical picture does not fit these criteria, consider further evaluation of the child.
After your differential diagnosis, perform a complete neurologic examination. If findings are abnormal on the neurologic exam, consider an MRI. Such imaging also may be warranted for children with exclusively occipital headaches, if they experience a crescendo or abrupt change in headaches, or if they lack a relevant family history.
Almost all other tests are less useful and do not help prior to referral to a pediatric neurologist. We do not need EEGs, sinus x-rays, or CT exams, which have lots of unnecessary radiation. We routinely check riboflavin and coenzyme Q10 levels, but this may be beyond the level of general pediatricians.
Referral to a specialist is appropriate when the above strategies are not working and if the headaches do not improve. Also refer if a child has chronic daily headaches (defined as 15 or more days per month), if a child is missing a lot of school or other activities of daily living, and/or if the history and diagnosis do not seem to fit the presentation.
Optimal treatment is a standardized strategy that incorporates acute and preventive pharmacologic strategies, as well as biobehavioral treatments.
Appropriate NSAID use, for example, can aid a child with an acute presentation. For example, prescribe 10 mg/kg of ibuprofen at onset, and do not exceed three dosages per week. In addition, be familiar with at least one triptan at appropriate dosing (an adult dose for teenagers).
Also be comfortable with at least one age-appropriate, preventive agent. Amitriptyline is the easiest to use. The recommended dosage regimen is 1 mg/kg titrated up slowly (over a period of 8–10 weeks) for about 2–3 months at full dose to allow sufficient time for clinical effect. I also advise against the use of cyproheptadine for teenagers with migraines because of the appetite effect.
Adequate fluid intake without caffeine, exercise at least three to four times per week, and sufficient regular sleep (8–9 hours, for example) are important components of biobehavioral treatment. In addition, educate patients and parents about the importance of a healthy, balanced diet. Instruct patients not to skip meals. We do not recommend avoidance of particular foods, and the evidence supports this stance. It is more important to make healthy food choices.
More often than not the child who presents with recurrent or chronic headaches will be experiencing migraines. Pediatric migraine is very common; in fact, it is one of the top five health problems for children. General pediatricians treat the majority of these children, up to 90%. There are not enough pediatric neurologists in the United States to take care of all of these children. For example, given the prevalence rate of 10%, an estimated 60,000 children and adolescents experience migraine out of the 2.4 million people in the Cincinnati draw area for my institution. Obviously, they cannot all be referred to a specialist.
The most important thing for you to do is to rule out secondary headaches. Differentiate primary headaches (such as migraine and tension headaches) from secondary ones, being skeptical of the secondary presentations. If a secondary etiology is suspected and the headaches do not resolve, then reassess, but the headaches may be primary ones.
Ask patients and parents about headache symptoms because often the symptoms are initially missed. Standardized criteria such as the American Academy of Neurology practice parameters on the treatment of migraine headache in children and adolescents can guide your diagnosis and management (Neurology 2004;63:2215–24). If the clinical picture does not fit these criteria, consider further evaluation of the child.
After your differential diagnosis, perform a complete neurologic examination. If findings are abnormal on the neurologic exam, consider an MRI. Such imaging also may be warranted for children with exclusively occipital headaches, if they experience a crescendo or abrupt change in headaches, or if they lack a relevant family history.
Almost all other tests are less useful and do not help prior to referral to a pediatric neurologist. We do not need EEGs, sinus x-rays, or CT exams, which have lots of unnecessary radiation. We routinely check riboflavin and coenzyme Q10 levels, but this may be beyond the level of general pediatricians.
Referral to a specialist is appropriate when the above strategies are not working and if the headaches do not improve. Also refer if a child has chronic daily headaches (defined as 15 or more days per month), if a child is missing a lot of school or other activities of daily living, and/or if the history and diagnosis do not seem to fit the presentation.
Optimal treatment is a standardized strategy that incorporates acute and preventive pharmacologic strategies, as well as biobehavioral treatments.
Appropriate NSAID use, for example, can aid a child with an acute presentation. For example, prescribe 10 mg/kg of ibuprofen at onset, and do not exceed three dosages per week. In addition, be familiar with at least one triptan at appropriate dosing (an adult dose for teenagers).
Also be comfortable with at least one age-appropriate, preventive agent. Amitriptyline is the easiest to use. The recommended dosage regimen is 1 mg/kg titrated up slowly (over a period of 8–10 weeks) for about 2–3 months at full dose to allow sufficient time for clinical effect. I also advise against the use of cyproheptadine for teenagers with migraines because of the appetite effect.
Adequate fluid intake without caffeine, exercise at least three to four times per week, and sufficient regular sleep (8–9 hours, for example) are important components of biobehavioral treatment. In addition, educate patients and parents about the importance of a healthy, balanced diet. Instruct patients not to skip meals. We do not recommend avoidance of particular foods, and the evidence supports this stance. It is more important to make healthy food choices.
Evidence-Based Medicine and the Hospitalist
The terms “hospital medicine” and “evidence-based medicine” (EBM) are both recent arrivals in the history of medicine. Both have spread through medicine at a rapid pace, highlighting the attraction and fundamental soundness of their core ideas. Much has been written about the benefits of the hospitalist movement regarding quality, patient throughput and financial indicators. The next phase in the revolution of patient care is the confluence of technology, EBM, and hospital medicine. One of the pillars for the continued success of the hospital medicine movement will be EBM. EBM must become an integral part of the skill set for all hospitalists.
EBM is an analytical approach with a fundamental knowledge base and a set of tools. The exponential growth of clinical information requires that physicians use an analytical approach for answering clinical questions and keeping up-to-date. This may be easier if you work at an academic center rather than a non-teaching hospital, although this is not guaranteed. Regardless of the working environment, an analytical approach will be needed if we are to build on initial success and unrealized potential to improve quality and patient safety.
The term “EBM” was introduced by a group of clinician researchers and educators at McMaster University during the early 1990s. It was initially defined as “a systemic approach to analyzed published research as the basis of clinical decision making.” Subsequently, as the EBM movement matured as a discipline, the early proponents and developers provided a more complete definition: “Evidence based medicine is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence-based medicine means integrating individual clinical expertise with the best available external clinical evidence from systematic research (1).”
Of course, the concept of practicing medicine based on the scientific method has been around for years. The days of bloodletting with leeches are behind us, but rigorous scientific evaluation of medicine reached critical mass only in the last century. The first double-blind randomized controlled trial (RCT) was conducted in 1931; the study tested the use of sanocrysin for treatment of tuberculosis (2). Since then, there has been an exponential growth in clinical trials. This information explosion requires new approaches to integrating the ever-increasing knowledge with patient care; the concurrent revolution in information technology provides opportunities limited only by our own imaginations.
EBM is not without its critics: “It is cookbook medicine,” “It focuses on cost efficiency,” “I can’t find an RCT that fits my patient,” and “It doesn’t take into account the clinician’s experience” are often argued points. If EBM is not used effectively, all the criticisms are appropriate. Sacket, one of the earliest proponents and likely EBM’s most eloquent champion, refuted the claim that EBM is “cookbook medicine.” He argued that EBM requires a bottom-up approach that integrates the best external evidence with individual clinical expertise and patients’ choice. External clinical evidence informs, but does not replace, individual clinical expertise. The physician must decide whether the external evidence applies to the individual patient at all and, if so, how it should be integrated into a clinical decision (1).
Neither is EBM strictly about RCTs and meta-analysis. It’s about tracking down the best available evidence for your question and, thus, your patient. Sometimes a cohort study is best when you want to find the prognosis of a certain illness. Similarly, a cross-sectional study may be most appropriate when you’re trying to determine the sensitivity and specificity of a test. If a disease once thought universally fatal is proven otherwise in a case report, then a randomized control trial is hardly necessary. Finally, an RCT or meta-analysis is not always going to be available for the disease process you are dealing with, but EBM gives us the skill set to look down the evidence pyramid and find the next best thing (Figure 1).
It is also clear that EBM is not about cost cutting, although many hospital medicine programs were started with this as the primary goal, given the current healthcare environment. Certainly fears exist that EBM is being used by healthcare managers, organizations, and administrators as a cost-efficiency tool. It may be that good evidence is cost-efficient in certain situations, while in others it may require the healthcare system to invest more in itself if available evidence supports doing so. Thus it is imperative that hospitalists accept the challenge of incorporating EBM into their daily practice and become leaders in its application, with patient safety and quality of care as primary goals. If we don’t, others will define the role of EBM for us, with a potential for poor outcomes for the patient and the profession.
The EBM skill set and its tools are being continuously refined, with the evidence pyramid as one of the most basic principles (3). This evidence pyramid is a model for grading the evidence. It puts in perspective the different grades of evidence or study designs. For example, a systematic review of randomized controlled trials that show consistent results provides the highest quality evidence and is ranked accordingly in the pyramid. In contrast, a case report or case series of a treatment would be ranked much lower.
The first step in incorporating EBM into one’s daily practice requires an understanding of its analytical approach and access to the necessary tools. The process begins with asking a question that is answerable. A well-built clinical question is one that benefits the patient and clinician. Such questions are directly relevant to patient problems and phrased in ways that direct your search to relevant and precise answers.
In forming the question the following process, referred to as the PICO method, is helpful (4).
With the question formed, consider what type of question you have. This is often referred to as the typology of the question.
- Clinical Findings: Gathering and interpreting findings from the history, clinical examination, and test results.
- Etiology: Identifying causes for disease.
- Differential Diagnosis: Ranking by likelihood, seriousness, and treatability of the patients problem.
- Prognosis: Figuring out how to estimate the likely clinical course and complications over time of the disease
- Therapy: Selecting treatments to offer that do more good than harm and that are worth the effort and cost of using them.
- Prevention: Reducing the chance of disease by identifying and modifying risk factors and how to diagnose disease early by screening.
- Self-improvement: Keeping up-to-date, improve your clinical skills, and run a better, more efficient clinical practice.
The types of questions can next be matched to the type of research that may provide the answer:
- Diagnosis: prospective cohort study with good quality validation against “gold standard.”
- Prognosis: prospective cohort study.
- Therapy or prevention: prospective, randomized controlled clinical trial (RCT).
- Harm/Etiology: RCT, cohort or case-control study (probably retrospective).
- Economic: analysis of sensible costs against evidence-based outcome.
Once the question has been formed, the following steps lie ahead: finding the evidence, critically appraising the evidence, acting on the evidence, and, finally, evaluating one’s performance. Very much like the formation of the question, each of the subsequent steps involves an analytical approach that can be mastered. Technology—particularly personal computers, the Internet and PDAs—has made the task of mastering EBM easier in many ways. The additional steps in using EBM effectively will be addressed in future articles. A list of useful links is provided below.
http://library.downstate.edu/EBM2/contents.htm
http://healthsystem.virginia.edu/internet/library/collections/ebm/index.cfm
Dr. Kathuria may be reached at Navneet.kathuria@mssm.edu.
Endnotes
- Guyatt GH, Haynes RB, Jaeschke RZ, et al. Users’ guides to the medical literature: XXV. Evidence-based medicine: principles for applying the users’ guides to patient care. Evidence-Based Medicine Working Group. JAMA. 2000;284:1290-6.
- Claridge, J, Fabian, T. History and Development of Evidence Based Medicine. World Journal of Surgery 2005
- Guyatt GH, Haynes RB, et. al. Users’ guides to the medical literature: XXV. Evidence-Based Medicine: Principles for Applying the Users’ Guides to Patient Care. 2000;284:1290-1296
- Sackett DL, Richardson WS, Rosenberg W, Haynes RB (1997). Evidence-based medicine: How to practice and teach EBM. New York: Churchill Livingston
The terms “hospital medicine” and “evidence-based medicine” (EBM) are both recent arrivals in the history of medicine. Both have spread through medicine at a rapid pace, highlighting the attraction and fundamental soundness of their core ideas. Much has been written about the benefits of the hospitalist movement regarding quality, patient throughput and financial indicators. The next phase in the revolution of patient care is the confluence of technology, EBM, and hospital medicine. One of the pillars for the continued success of the hospital medicine movement will be EBM. EBM must become an integral part of the skill set for all hospitalists.
EBM is an analytical approach with a fundamental knowledge base and a set of tools. The exponential growth of clinical information requires that physicians use an analytical approach for answering clinical questions and keeping up-to-date. This may be easier if you work at an academic center rather than a non-teaching hospital, although this is not guaranteed. Regardless of the working environment, an analytical approach will be needed if we are to build on initial success and unrealized potential to improve quality and patient safety.
The term “EBM” was introduced by a group of clinician researchers and educators at McMaster University during the early 1990s. It was initially defined as “a systemic approach to analyzed published research as the basis of clinical decision making.” Subsequently, as the EBM movement matured as a discipline, the early proponents and developers provided a more complete definition: “Evidence based medicine is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence-based medicine means integrating individual clinical expertise with the best available external clinical evidence from systematic research (1).”
Of course, the concept of practicing medicine based on the scientific method has been around for years. The days of bloodletting with leeches are behind us, but rigorous scientific evaluation of medicine reached critical mass only in the last century. The first double-blind randomized controlled trial (RCT) was conducted in 1931; the study tested the use of sanocrysin for treatment of tuberculosis (2). Since then, there has been an exponential growth in clinical trials. This information explosion requires new approaches to integrating the ever-increasing knowledge with patient care; the concurrent revolution in information technology provides opportunities limited only by our own imaginations.
EBM is not without its critics: “It is cookbook medicine,” “It focuses on cost efficiency,” “I can’t find an RCT that fits my patient,” and “It doesn’t take into account the clinician’s experience” are often argued points. If EBM is not used effectively, all the criticisms are appropriate. Sacket, one of the earliest proponents and likely EBM’s most eloquent champion, refuted the claim that EBM is “cookbook medicine.” He argued that EBM requires a bottom-up approach that integrates the best external evidence with individual clinical expertise and patients’ choice. External clinical evidence informs, but does not replace, individual clinical expertise. The physician must decide whether the external evidence applies to the individual patient at all and, if so, how it should be integrated into a clinical decision (1).
Neither is EBM strictly about RCTs and meta-analysis. It’s about tracking down the best available evidence for your question and, thus, your patient. Sometimes a cohort study is best when you want to find the prognosis of a certain illness. Similarly, a cross-sectional study may be most appropriate when you’re trying to determine the sensitivity and specificity of a test. If a disease once thought universally fatal is proven otherwise in a case report, then a randomized control trial is hardly necessary. Finally, an RCT or meta-analysis is not always going to be available for the disease process you are dealing with, but EBM gives us the skill set to look down the evidence pyramid and find the next best thing (Figure 1).
It is also clear that EBM is not about cost cutting, although many hospital medicine programs were started with this as the primary goal, given the current healthcare environment. Certainly fears exist that EBM is being used by healthcare managers, organizations, and administrators as a cost-efficiency tool. It may be that good evidence is cost-efficient in certain situations, while in others it may require the healthcare system to invest more in itself if available evidence supports doing so. Thus it is imperative that hospitalists accept the challenge of incorporating EBM into their daily practice and become leaders in its application, with patient safety and quality of care as primary goals. If we don’t, others will define the role of EBM for us, with a potential for poor outcomes for the patient and the profession.
The EBM skill set and its tools are being continuously refined, with the evidence pyramid as one of the most basic principles (3). This evidence pyramid is a model for grading the evidence. It puts in perspective the different grades of evidence or study designs. For example, a systematic review of randomized controlled trials that show consistent results provides the highest quality evidence and is ranked accordingly in the pyramid. In contrast, a case report or case series of a treatment would be ranked much lower.
The first step in incorporating EBM into one’s daily practice requires an understanding of its analytical approach and access to the necessary tools. The process begins with asking a question that is answerable. A well-built clinical question is one that benefits the patient and clinician. Such questions are directly relevant to patient problems and phrased in ways that direct your search to relevant and precise answers.
In forming the question the following process, referred to as the PICO method, is helpful (4).
With the question formed, consider what type of question you have. This is often referred to as the typology of the question.
- Clinical Findings: Gathering and interpreting findings from the history, clinical examination, and test results.
- Etiology: Identifying causes for disease.
- Differential Diagnosis: Ranking by likelihood, seriousness, and treatability of the patients problem.
- Prognosis: Figuring out how to estimate the likely clinical course and complications over time of the disease
- Therapy: Selecting treatments to offer that do more good than harm and that are worth the effort and cost of using them.
- Prevention: Reducing the chance of disease by identifying and modifying risk factors and how to diagnose disease early by screening.
- Self-improvement: Keeping up-to-date, improve your clinical skills, and run a better, more efficient clinical practice.
The types of questions can next be matched to the type of research that may provide the answer:
- Diagnosis: prospective cohort study with good quality validation against “gold standard.”
- Prognosis: prospective cohort study.
- Therapy or prevention: prospective, randomized controlled clinical trial (RCT).
- Harm/Etiology: RCT, cohort or case-control study (probably retrospective).
- Economic: analysis of sensible costs against evidence-based outcome.
Once the question has been formed, the following steps lie ahead: finding the evidence, critically appraising the evidence, acting on the evidence, and, finally, evaluating one’s performance. Very much like the formation of the question, each of the subsequent steps involves an analytical approach that can be mastered. Technology—particularly personal computers, the Internet and PDAs—has made the task of mastering EBM easier in many ways. The additional steps in using EBM effectively will be addressed in future articles. A list of useful links is provided below.
http://library.downstate.edu/EBM2/contents.htm
http://healthsystem.virginia.edu/internet/library/collections/ebm/index.cfm
Dr. Kathuria may be reached at Navneet.kathuria@mssm.edu.
Endnotes
- Guyatt GH, Haynes RB, Jaeschke RZ, et al. Users’ guides to the medical literature: XXV. Evidence-based medicine: principles for applying the users’ guides to patient care. Evidence-Based Medicine Working Group. JAMA. 2000;284:1290-6.
- Claridge, J, Fabian, T. History and Development of Evidence Based Medicine. World Journal of Surgery 2005
- Guyatt GH, Haynes RB, et. al. Users’ guides to the medical literature: XXV. Evidence-Based Medicine: Principles for Applying the Users’ Guides to Patient Care. 2000;284:1290-1296
- Sackett DL, Richardson WS, Rosenberg W, Haynes RB (1997). Evidence-based medicine: How to practice and teach EBM. New York: Churchill Livingston
The terms “hospital medicine” and “evidence-based medicine” (EBM) are both recent arrivals in the history of medicine. Both have spread through medicine at a rapid pace, highlighting the attraction and fundamental soundness of their core ideas. Much has been written about the benefits of the hospitalist movement regarding quality, patient throughput and financial indicators. The next phase in the revolution of patient care is the confluence of technology, EBM, and hospital medicine. One of the pillars for the continued success of the hospital medicine movement will be EBM. EBM must become an integral part of the skill set for all hospitalists.
EBM is an analytical approach with a fundamental knowledge base and a set of tools. The exponential growth of clinical information requires that physicians use an analytical approach for answering clinical questions and keeping up-to-date. This may be easier if you work at an academic center rather than a non-teaching hospital, although this is not guaranteed. Regardless of the working environment, an analytical approach will be needed if we are to build on initial success and unrealized potential to improve quality and patient safety.
The term “EBM” was introduced by a group of clinician researchers and educators at McMaster University during the early 1990s. It was initially defined as “a systemic approach to analyzed published research as the basis of clinical decision making.” Subsequently, as the EBM movement matured as a discipline, the early proponents and developers provided a more complete definition: “Evidence based medicine is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence-based medicine means integrating individual clinical expertise with the best available external clinical evidence from systematic research (1).”
Of course, the concept of practicing medicine based on the scientific method has been around for years. The days of bloodletting with leeches are behind us, but rigorous scientific evaluation of medicine reached critical mass only in the last century. The first double-blind randomized controlled trial (RCT) was conducted in 1931; the study tested the use of sanocrysin for treatment of tuberculosis (2). Since then, there has been an exponential growth in clinical trials. This information explosion requires new approaches to integrating the ever-increasing knowledge with patient care; the concurrent revolution in information technology provides opportunities limited only by our own imaginations.
EBM is not without its critics: “It is cookbook medicine,” “It focuses on cost efficiency,” “I can’t find an RCT that fits my patient,” and “It doesn’t take into account the clinician’s experience” are often argued points. If EBM is not used effectively, all the criticisms are appropriate. Sacket, one of the earliest proponents and likely EBM’s most eloquent champion, refuted the claim that EBM is “cookbook medicine.” He argued that EBM requires a bottom-up approach that integrates the best external evidence with individual clinical expertise and patients’ choice. External clinical evidence informs, but does not replace, individual clinical expertise. The physician must decide whether the external evidence applies to the individual patient at all and, if so, how it should be integrated into a clinical decision (1).
Neither is EBM strictly about RCTs and meta-analysis. It’s about tracking down the best available evidence for your question and, thus, your patient. Sometimes a cohort study is best when you want to find the prognosis of a certain illness. Similarly, a cross-sectional study may be most appropriate when you’re trying to determine the sensitivity and specificity of a test. If a disease once thought universally fatal is proven otherwise in a case report, then a randomized control trial is hardly necessary. Finally, an RCT or meta-analysis is not always going to be available for the disease process you are dealing with, but EBM gives us the skill set to look down the evidence pyramid and find the next best thing (Figure 1).
It is also clear that EBM is not about cost cutting, although many hospital medicine programs were started with this as the primary goal, given the current healthcare environment. Certainly fears exist that EBM is being used by healthcare managers, organizations, and administrators as a cost-efficiency tool. It may be that good evidence is cost-efficient in certain situations, while in others it may require the healthcare system to invest more in itself if available evidence supports doing so. Thus it is imperative that hospitalists accept the challenge of incorporating EBM into their daily practice and become leaders in its application, with patient safety and quality of care as primary goals. If we don’t, others will define the role of EBM for us, with a potential for poor outcomes for the patient and the profession.
The EBM skill set and its tools are being continuously refined, with the evidence pyramid as one of the most basic principles (3). This evidence pyramid is a model for grading the evidence. It puts in perspective the different grades of evidence or study designs. For example, a systematic review of randomized controlled trials that show consistent results provides the highest quality evidence and is ranked accordingly in the pyramid. In contrast, a case report or case series of a treatment would be ranked much lower.
The first step in incorporating EBM into one’s daily practice requires an understanding of its analytical approach and access to the necessary tools. The process begins with asking a question that is answerable. A well-built clinical question is one that benefits the patient and clinician. Such questions are directly relevant to patient problems and phrased in ways that direct your search to relevant and precise answers.
In forming the question the following process, referred to as the PICO method, is helpful (4).
With the question formed, consider what type of question you have. This is often referred to as the typology of the question.
- Clinical Findings: Gathering and interpreting findings from the history, clinical examination, and test results.
- Etiology: Identifying causes for disease.
- Differential Diagnosis: Ranking by likelihood, seriousness, and treatability of the patients problem.
- Prognosis: Figuring out how to estimate the likely clinical course and complications over time of the disease
- Therapy: Selecting treatments to offer that do more good than harm and that are worth the effort and cost of using them.
- Prevention: Reducing the chance of disease by identifying and modifying risk factors and how to diagnose disease early by screening.
- Self-improvement: Keeping up-to-date, improve your clinical skills, and run a better, more efficient clinical practice.
The types of questions can next be matched to the type of research that may provide the answer:
- Diagnosis: prospective cohort study with good quality validation against “gold standard.”
- Prognosis: prospective cohort study.
- Therapy or prevention: prospective, randomized controlled clinical trial (RCT).
- Harm/Etiology: RCT, cohort or case-control study (probably retrospective).
- Economic: analysis of sensible costs against evidence-based outcome.
Once the question has been formed, the following steps lie ahead: finding the evidence, critically appraising the evidence, acting on the evidence, and, finally, evaluating one’s performance. Very much like the formation of the question, each of the subsequent steps involves an analytical approach that can be mastered. Technology—particularly personal computers, the Internet and PDAs—has made the task of mastering EBM easier in many ways. The additional steps in using EBM effectively will be addressed in future articles. A list of useful links is provided below.
http://library.downstate.edu/EBM2/contents.htm
http://healthsystem.virginia.edu/internet/library/collections/ebm/index.cfm
Dr. Kathuria may be reached at Navneet.kathuria@mssm.edu.
Endnotes
- Guyatt GH, Haynes RB, Jaeschke RZ, et al. Users’ guides to the medical literature: XXV. Evidence-based medicine: principles for applying the users’ guides to patient care. Evidence-Based Medicine Working Group. JAMA. 2000;284:1290-6.
- Claridge, J, Fabian, T. History and Development of Evidence Based Medicine. World Journal of Surgery 2005
- Guyatt GH, Haynes RB, et. al. Users’ guides to the medical literature: XXV. Evidence-Based Medicine: Principles for Applying the Users’ Guides to Patient Care. 2000;284:1290-1296
- Sackett DL, Richardson WS, Rosenberg W, Haynes RB (1997). Evidence-based medicine: How to practice and teach EBM. New York: Churchill Livingston
What Is a Laborist?
One of the interesting things about hospital medicine is our diversity. It is an evolutionary construct and can be both a strength and a concern as we all try to create and define our new specialty.
Most hospitalists are trained as general internists. This wasn’t always so. As recently as 1997 almost 50% of hospitalists were internal medical subspecialists. The thinking at that time was that because infectious disease docs, pulmonologists, intensivists, and others were already in the hospital seeing ill patients, why couldn’t they just also be hospitalists?
Well, it turned out they wanted to be infectious disease specialists and pulmonologists and they soon found out that being a hospitalist is somewhat different than these other specialties.
Now hospital medicine is a popular career path for those finishing a general internal medicine residency, as well as for those who are finding a career as a hospitalist preferable to their original choice as in traditional internal medicine. (See “Trendwatch: The Specialization of Hospital Medicine,” p. 27.)
PEDIATRICIANS AND FAMILY PRACTICE
At the same time, even though only 3% of hospitalists are family practitioners, more than 90% of hospitalists in Canada come out of family practice training. Increasingly, young graduates of family practice residency programs are choosing to become hospitalists.
And let’s not forget the pediatricians. Pediatricians comprise about 9% of all hospitalists, and more than 200 pediatric hospitalists got together for the largest pediatric hospital medicine meeting ever in Denver at the end of July. (See the “Pediatric Special Section,” p. 33.) It was an impressive community of pediatric hospitalists. Most children’s hospitals and many community hospitals now have pediatric hospital medicine groups. Most of the pediatric inpatient care in this country is now provided by hospitalists and pediatric subspecialists.
In fact, those who have taken training in med-peds are finding that a career as a hospitalist is a nice fit, and they are welcomed by those who care for children and adults in the hospital.
But hospital medicine is not only about physician caregivers. More than 5% of hospitalists in this country are nonphysician providers, either nurse practitioners or physician assistants. As the demand for hospitalists rapidly increases many hospital medicine groups find that adding nurse practitioners or physician assistants helps them to complete the workforce they need to have in place to meet their clinical and administrative demands.
And hospital medicine includes pharmacists, case managers, and administrators to round out the inpatient team. Each of these professions is developing “hospital medicine specialists” looking for skills and experiences to allow them to help facilitate the work of the hospitalists and to use a team approach to achieve the rapidly expanded expectations of hospital medicine groups.
EDUCATION AND CERTIFICATION ISSUES
This growing conglomeration of healthcare professionals in one specialty presents unique issues. Some of these come in the form of diverse and expanding educational needs. The patient wants to be assured that no matter where the individual hospitalist started his or her training, the hospitalist will bring to the bedside the appropriate skills for their acute medical problems. This leads to having SHM develop courses in critical care skills, perioperative medicine, leadership, and the like.
Yet even though the endpoint may need to be similar for all hospitalists, it takes a fine touch and significant customization to craft educational materials when many hospitalists may start from a different base point.
When it comes to potential credentialing in hospital medicine, there is not a clear path to create a certification in hospital medicine. The solution for the 80% of hospitalists trained in internal medicine may very well be through the American Board of Internal Medicine (ABIM), but the pediatric and family practice solution will need to involve the American Board of Pediatrics (ABP) and the American Board of Family Medicine (ABFP), respectively. And this doesn’t even begin to address the credentialing needs of the nonphysicians.
Further, as SHM looks to represent all of the diverse elements that form the fabric of hospital medicine, we need to be in touch with the American College of Physicians, the American Academy of Pediatrics, the American Academy of Family Physicians, the Society of General Internal Medicine, the Ambulatory Pediatric Association, the American Association of Critical Care Nurses, the American Society of Health System Pharmacists, the American
Academy of Physicians Assistants, the American Academy of Nurse Practitioners, and many other important substantial medical professional societies; members of each believe that their organization relates to a segment of hospital medicine.
DIVERSITY CREATES NEW SOLUTIONS
The good part of this diversity is that as SHM helps to build this new specialty we are able to include so many unique vantage points. This strategy of inclusion allows for new ideas to percolate to the surface and leads to innovation and creativity. In fashioning the hospital of the future, “old think” must not rule the day. One way to change the outcome is to change those who are at the table.
If hospital medicine is to be part of the process of creating a hospital that is patient-centered, relies on measurable quality improvement, and delivers care by teams of healthcare professionals, then we need to open the tent and let in different perspectives. In SHM’s ongoing quality improvement efforts in heart failure and glycemic control, this is our approach—with meaningful input from hospitalists, subspecialists, nurses, pharmacists, and many other stakeholders in hospital medicine. This will lead to a different and—let’s hope—better outcome.
LABORISTS AND SURGICALISTS
And there are more wrinkles in the hospitalist world all the time. Recently USA Today wrote a story about “laborists” as hospitals try to solve access to obstetrical services by having contracted laborists on site 24/7. Some hospitals have to be creative when their community surgeons aren’t available for trauma care and some hospitals have contracted with orthopedists and general surgeons as “surgicalists.”
Are these the latest additions to the roll call of hospital medicine or just a footnote or an asterisk? Time and the marketplace will tell.
Besides the basic training for hospitalists there are many variations determined by site of practice and employment model. Whether we are talking about the differences between academic
hospital medicine or that practiced in community hospitals, or the uniqueness of a small group of hospitalists at only one hospital or a large multistate group of hospitalists in 10 states with 400 hospitalists, we are all part of hospital medicine.
In the end, hospital medicine is defined more by its common goals and its common values regardless of initial training or mode of practice. At this time in healthcare, many are looking for healthcare professionals to have the skills and the energy to create the hospital
of the future that will be a better place to work and to get the best care. SHM is committed to harnessing the diversity of our specialty to do our part to create a better future. With your help, we can get there. TH
Dr. Wellikson has been the CEO of SHM since 2000.
One of the interesting things about hospital medicine is our diversity. It is an evolutionary construct and can be both a strength and a concern as we all try to create and define our new specialty.
Most hospitalists are trained as general internists. This wasn’t always so. As recently as 1997 almost 50% of hospitalists were internal medical subspecialists. The thinking at that time was that because infectious disease docs, pulmonologists, intensivists, and others were already in the hospital seeing ill patients, why couldn’t they just also be hospitalists?
Well, it turned out they wanted to be infectious disease specialists and pulmonologists and they soon found out that being a hospitalist is somewhat different than these other specialties.
Now hospital medicine is a popular career path for those finishing a general internal medicine residency, as well as for those who are finding a career as a hospitalist preferable to their original choice as in traditional internal medicine. (See “Trendwatch: The Specialization of Hospital Medicine,” p. 27.)
PEDIATRICIANS AND FAMILY PRACTICE
At the same time, even though only 3% of hospitalists are family practitioners, more than 90% of hospitalists in Canada come out of family practice training. Increasingly, young graduates of family practice residency programs are choosing to become hospitalists.
And let’s not forget the pediatricians. Pediatricians comprise about 9% of all hospitalists, and more than 200 pediatric hospitalists got together for the largest pediatric hospital medicine meeting ever in Denver at the end of July. (See the “Pediatric Special Section,” p. 33.) It was an impressive community of pediatric hospitalists. Most children’s hospitals and many community hospitals now have pediatric hospital medicine groups. Most of the pediatric inpatient care in this country is now provided by hospitalists and pediatric subspecialists.
In fact, those who have taken training in med-peds are finding that a career as a hospitalist is a nice fit, and they are welcomed by those who care for children and adults in the hospital.
But hospital medicine is not only about physician caregivers. More than 5% of hospitalists in this country are nonphysician providers, either nurse practitioners or physician assistants. As the demand for hospitalists rapidly increases many hospital medicine groups find that adding nurse practitioners or physician assistants helps them to complete the workforce they need to have in place to meet their clinical and administrative demands.
And hospital medicine includes pharmacists, case managers, and administrators to round out the inpatient team. Each of these professions is developing “hospital medicine specialists” looking for skills and experiences to allow them to help facilitate the work of the hospitalists and to use a team approach to achieve the rapidly expanded expectations of hospital medicine groups.
EDUCATION AND CERTIFICATION ISSUES
This growing conglomeration of healthcare professionals in one specialty presents unique issues. Some of these come in the form of diverse and expanding educational needs. The patient wants to be assured that no matter where the individual hospitalist started his or her training, the hospitalist will bring to the bedside the appropriate skills for their acute medical problems. This leads to having SHM develop courses in critical care skills, perioperative medicine, leadership, and the like.
Yet even though the endpoint may need to be similar for all hospitalists, it takes a fine touch and significant customization to craft educational materials when many hospitalists may start from a different base point.
When it comes to potential credentialing in hospital medicine, there is not a clear path to create a certification in hospital medicine. The solution for the 80% of hospitalists trained in internal medicine may very well be through the American Board of Internal Medicine (ABIM), but the pediatric and family practice solution will need to involve the American Board of Pediatrics (ABP) and the American Board of Family Medicine (ABFP), respectively. And this doesn’t even begin to address the credentialing needs of the nonphysicians.
Further, as SHM looks to represent all of the diverse elements that form the fabric of hospital medicine, we need to be in touch with the American College of Physicians, the American Academy of Pediatrics, the American Academy of Family Physicians, the Society of General Internal Medicine, the Ambulatory Pediatric Association, the American Association of Critical Care Nurses, the American Society of Health System Pharmacists, the American
Academy of Physicians Assistants, the American Academy of Nurse Practitioners, and many other important substantial medical professional societies; members of each believe that their organization relates to a segment of hospital medicine.
DIVERSITY CREATES NEW SOLUTIONS
The good part of this diversity is that as SHM helps to build this new specialty we are able to include so many unique vantage points. This strategy of inclusion allows for new ideas to percolate to the surface and leads to innovation and creativity. In fashioning the hospital of the future, “old think” must not rule the day. One way to change the outcome is to change those who are at the table.
If hospital medicine is to be part of the process of creating a hospital that is patient-centered, relies on measurable quality improvement, and delivers care by teams of healthcare professionals, then we need to open the tent and let in different perspectives. In SHM’s ongoing quality improvement efforts in heart failure and glycemic control, this is our approach—with meaningful input from hospitalists, subspecialists, nurses, pharmacists, and many other stakeholders in hospital medicine. This will lead to a different and—let’s hope—better outcome.
LABORISTS AND SURGICALISTS
And there are more wrinkles in the hospitalist world all the time. Recently USA Today wrote a story about “laborists” as hospitals try to solve access to obstetrical services by having contracted laborists on site 24/7. Some hospitals have to be creative when their community surgeons aren’t available for trauma care and some hospitals have contracted with orthopedists and general surgeons as “surgicalists.”
Are these the latest additions to the roll call of hospital medicine or just a footnote or an asterisk? Time and the marketplace will tell.
Besides the basic training for hospitalists there are many variations determined by site of practice and employment model. Whether we are talking about the differences between academic
hospital medicine or that practiced in community hospitals, or the uniqueness of a small group of hospitalists at only one hospital or a large multistate group of hospitalists in 10 states with 400 hospitalists, we are all part of hospital medicine.
In the end, hospital medicine is defined more by its common goals and its common values regardless of initial training or mode of practice. At this time in healthcare, many are looking for healthcare professionals to have the skills and the energy to create the hospital
of the future that will be a better place to work and to get the best care. SHM is committed to harnessing the diversity of our specialty to do our part to create a better future. With your help, we can get there. TH
Dr. Wellikson has been the CEO of SHM since 2000.
One of the interesting things about hospital medicine is our diversity. It is an evolutionary construct and can be both a strength and a concern as we all try to create and define our new specialty.
Most hospitalists are trained as general internists. This wasn’t always so. As recently as 1997 almost 50% of hospitalists were internal medical subspecialists. The thinking at that time was that because infectious disease docs, pulmonologists, intensivists, and others were already in the hospital seeing ill patients, why couldn’t they just also be hospitalists?
Well, it turned out they wanted to be infectious disease specialists and pulmonologists and they soon found out that being a hospitalist is somewhat different than these other specialties.
Now hospital medicine is a popular career path for those finishing a general internal medicine residency, as well as for those who are finding a career as a hospitalist preferable to their original choice as in traditional internal medicine. (See “Trendwatch: The Specialization of Hospital Medicine,” p. 27.)
PEDIATRICIANS AND FAMILY PRACTICE
At the same time, even though only 3% of hospitalists are family practitioners, more than 90% of hospitalists in Canada come out of family practice training. Increasingly, young graduates of family practice residency programs are choosing to become hospitalists.
And let’s not forget the pediatricians. Pediatricians comprise about 9% of all hospitalists, and more than 200 pediatric hospitalists got together for the largest pediatric hospital medicine meeting ever in Denver at the end of July. (See the “Pediatric Special Section,” p. 33.) It was an impressive community of pediatric hospitalists. Most children’s hospitals and many community hospitals now have pediatric hospital medicine groups. Most of the pediatric inpatient care in this country is now provided by hospitalists and pediatric subspecialists.
In fact, those who have taken training in med-peds are finding that a career as a hospitalist is a nice fit, and they are welcomed by those who care for children and adults in the hospital.
But hospital medicine is not only about physician caregivers. More than 5% of hospitalists in this country are nonphysician providers, either nurse practitioners or physician assistants. As the demand for hospitalists rapidly increases many hospital medicine groups find that adding nurse practitioners or physician assistants helps them to complete the workforce they need to have in place to meet their clinical and administrative demands.
And hospital medicine includes pharmacists, case managers, and administrators to round out the inpatient team. Each of these professions is developing “hospital medicine specialists” looking for skills and experiences to allow them to help facilitate the work of the hospitalists and to use a team approach to achieve the rapidly expanded expectations of hospital medicine groups.
EDUCATION AND CERTIFICATION ISSUES
This growing conglomeration of healthcare professionals in one specialty presents unique issues. Some of these come in the form of diverse and expanding educational needs. The patient wants to be assured that no matter where the individual hospitalist started his or her training, the hospitalist will bring to the bedside the appropriate skills for their acute medical problems. This leads to having SHM develop courses in critical care skills, perioperative medicine, leadership, and the like.
Yet even though the endpoint may need to be similar for all hospitalists, it takes a fine touch and significant customization to craft educational materials when many hospitalists may start from a different base point.
When it comes to potential credentialing in hospital medicine, there is not a clear path to create a certification in hospital medicine. The solution for the 80% of hospitalists trained in internal medicine may very well be through the American Board of Internal Medicine (ABIM), but the pediatric and family practice solution will need to involve the American Board of Pediatrics (ABP) and the American Board of Family Medicine (ABFP), respectively. And this doesn’t even begin to address the credentialing needs of the nonphysicians.
Further, as SHM looks to represent all of the diverse elements that form the fabric of hospital medicine, we need to be in touch with the American College of Physicians, the American Academy of Pediatrics, the American Academy of Family Physicians, the Society of General Internal Medicine, the Ambulatory Pediatric Association, the American Association of Critical Care Nurses, the American Society of Health System Pharmacists, the American
Academy of Physicians Assistants, the American Academy of Nurse Practitioners, and many other important substantial medical professional societies; members of each believe that their organization relates to a segment of hospital medicine.
DIVERSITY CREATES NEW SOLUTIONS
The good part of this diversity is that as SHM helps to build this new specialty we are able to include so many unique vantage points. This strategy of inclusion allows for new ideas to percolate to the surface and leads to innovation and creativity. In fashioning the hospital of the future, “old think” must not rule the day. One way to change the outcome is to change those who are at the table.
If hospital medicine is to be part of the process of creating a hospital that is patient-centered, relies on measurable quality improvement, and delivers care by teams of healthcare professionals, then we need to open the tent and let in different perspectives. In SHM’s ongoing quality improvement efforts in heart failure and glycemic control, this is our approach—with meaningful input from hospitalists, subspecialists, nurses, pharmacists, and many other stakeholders in hospital medicine. This will lead to a different and—let’s hope—better outcome.
LABORISTS AND SURGICALISTS
And there are more wrinkles in the hospitalist world all the time. Recently USA Today wrote a story about “laborists” as hospitals try to solve access to obstetrical services by having contracted laborists on site 24/7. Some hospitals have to be creative when their community surgeons aren’t available for trauma care and some hospitals have contracted with orthopedists and general surgeons as “surgicalists.”
Are these the latest additions to the roll call of hospital medicine or just a footnote or an asterisk? Time and the marketplace will tell.
Besides the basic training for hospitalists there are many variations determined by site of practice and employment model. Whether we are talking about the differences between academic
hospital medicine or that practiced in community hospitals, or the uniqueness of a small group of hospitalists at only one hospital or a large multistate group of hospitalists in 10 states with 400 hospitalists, we are all part of hospital medicine.
In the end, hospital medicine is defined more by its common goals and its common values regardless of initial training or mode of practice. At this time in healthcare, many are looking for healthcare professionals to have the skills and the energy to create the hospital
of the future that will be a better place to work and to get the best care. SHM is committed to harnessing the diversity of our specialty to do our part to create a better future. With your help, we can get there. TH
Dr. Wellikson has been the CEO of SHM since 2000.