User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Nurses questions answered: Could you face repercussions for your actions?
Nurses are the most trusted profession for one reason. They care.
Nurses are passionate about patient interactions, quality, and giving optimal support, often to the detriment of self-care. Many do not hesitate to voice concerns in an atmosphere that produces anxiety, whether it be regarding supplies, documentation, or staffing. As a result,
In October, three nurses at Ascension Saint Joseph in Joliet, Ill., were escorted off the premises of a hospital emergency room when they began an understaffed shift. They were removed from work by hospital security and then suspended for 1 week. It was a decision that was incomprehensible, because the emergency room faced an overwhelming influx of patients – 46 that evening alone – and only four nurses instead of the more than 10 approved staffing were on duty. Why were they suspended?
Hospital officials have been quiet in responding to their alarmed community as well as in answering the Illinois Nurses Association, who criticized the hospital’s response. It has been suggested that the nurses had been intensely vocal about staffing for several weeks and the hospital might have wanted to silence their voices.
In my opinion, this could be considered a professional repercussion of the post-pandemic work environment. Though the nurses were reinstated after the week expired, nursing organizations believed that the actions of their employer were too harsh.
There was a similar response by employers after a string of large strikes of California nurses earlier this year. For example, a walkout by nurses at Stanford Health Care and Lucile Packard Children’s Hospital resulted in the hospitals withholding wages during the strike period and stating they might withhold health coverage from striking workers.
“Our sincere hope is that an agreement can be reached promptly so that nurses don’t lose additional pay, don’t risk losing the subsidy for employer-paid health benefits, and can return to patient care,” the hospital newsletter StanfordPackardVoice.com reported before the strike began in April. “Nurses who choose to go out on strike will not paid for missed shifts and cannot use PTO, ESL, or Education Hours.”
Nurse: Could a similar repercussion be in my work future?
Nurses may take to picket lines or contact administrators (for example, Human Resources) for multiple reasons, but the most common issues are related to staffing, scheduling, mandatory overtime, or equipment required to do their job: safety or lifting equipment and broken or missing tools for monitoring patients. The lack of hospital security services to assist with violent or threatening patients has also become a concern.
Goodman: The inability to provide safe care is a common fear of all nurses, one that was exacerbated by health care workers leaving during the pandemic, primarily from nursing homes. Although overall safety has improved, that may not be the case in smaller, rural institutions. Staffing for all shifts may also be erratic as the country faces an uphill winter battle with influenza, respiratory syncytial virus, and newer COVID variants.
Report to your supervisor: First, be familiar with your institution’s policy regarding chain of command. Know where to take a complaint when staffing seems unsafe. Contact your immediate supervisor as soon as the situation has been assessed. They might be able to shift resources to your area or find coverage to help. In addition, keep accurate notes related to your actions.
I covered a night shift where I was directly responsible for the care of 13 subacute medical-surgical patients (new admissions and postoperative patients). Patients kept arriving with no regard for the load that was present. One of the patients was completely unhappy with her pain regimen and kept calling for assistance, as is often the case.
While I was doing my best to assess arrivals, another nurse contacted a supervisor. The next thing that happened was an on-site visit by hospital administrators (unusual!) who asked to see my assignment sheet. I had been hesitant to share the list, fearing recrimination from intermediate leadership (this was not my home unit). But it led to an immediate change in staffing. The ordeal ended amicably, but not all do. Thereafter, no nurse was expected to care for more than eight patients on the night shift.
Notify proper authorities: Nurses may believe contacting the Occupational Safety and Health Administration (OSHA) might be helpful; however, OSHA may not have jurisdiction over the hospital, as the Saint Joseph nurses discovered. Working without safety equipment or with reduced supplies (for example, automatic blood pressure cuffs, oxygen saturation monitors, isolation gear) may appear to be a federal complaint, but it depends where the nurse is employed. The hospital in Joliet was covered by the Illinois Department of Public Health.
Federal law entitles you to work in a safe place. Contacting OSHA for direction should not lead to recrimination for nurses. Although OSHA has been overwhelmed with complaints since the onset of the pandemic, their website directs nurses. For example, a whistleblower complaint can be filed up to 30 days after an incident of worker retaliation.
If you are a member of a nursing union, follow union guidelines related to your actions. Thousands of nurses went on strike in the past 2 years. Most remained employed and returned to work with negotiations complete. As far as the nurses in Massachusetts, the state does not have mandatory staffing ratios – most do not – which complicated contract negotiations. At this time, California is the only state that has mandatory nurse-patient ratios written into law.
It is also important to know state law and to be cognizant of nursing organizations within your geographic area. Staying connected means staying informed and having nursing resources.
Respond rationally: An additional reminder for nurses is not to react to a tense situation impulsively. Leaving an assignment unfinished or walking off the job is never a good idea. (A scheduled strike organized by union leaders is different). Leaving work is viewed by institutions as job abandonment and can be grounds for dismissal. Most states are currently “at will” employers, meaning hospitals can terminate nurses without due process.
Above all, know that nurses worry about providing safe practice and avoiding recrimination. Only one of these should be in your future.
Ms. Goodman has no disclosures.
A version of this article first appeared on Medscape.com.
Nurses are the most trusted profession for one reason. They care.
Nurses are passionate about patient interactions, quality, and giving optimal support, often to the detriment of self-care. Many do not hesitate to voice concerns in an atmosphere that produces anxiety, whether it be regarding supplies, documentation, or staffing. As a result,
In October, three nurses at Ascension Saint Joseph in Joliet, Ill., were escorted off the premises of a hospital emergency room when they began an understaffed shift. They were removed from work by hospital security and then suspended for 1 week. It was a decision that was incomprehensible, because the emergency room faced an overwhelming influx of patients – 46 that evening alone – and only four nurses instead of the more than 10 approved staffing were on duty. Why were they suspended?
Hospital officials have been quiet in responding to their alarmed community as well as in answering the Illinois Nurses Association, who criticized the hospital’s response. It has been suggested that the nurses had been intensely vocal about staffing for several weeks and the hospital might have wanted to silence their voices.
In my opinion, this could be considered a professional repercussion of the post-pandemic work environment. Though the nurses were reinstated after the week expired, nursing organizations believed that the actions of their employer were too harsh.
There was a similar response by employers after a string of large strikes of California nurses earlier this year. For example, a walkout by nurses at Stanford Health Care and Lucile Packard Children’s Hospital resulted in the hospitals withholding wages during the strike period and stating they might withhold health coverage from striking workers.
“Our sincere hope is that an agreement can be reached promptly so that nurses don’t lose additional pay, don’t risk losing the subsidy for employer-paid health benefits, and can return to patient care,” the hospital newsletter StanfordPackardVoice.com reported before the strike began in April. “Nurses who choose to go out on strike will not paid for missed shifts and cannot use PTO, ESL, or Education Hours.”
Nurse: Could a similar repercussion be in my work future?
Nurses may take to picket lines or contact administrators (for example, Human Resources) for multiple reasons, but the most common issues are related to staffing, scheduling, mandatory overtime, or equipment required to do their job: safety or lifting equipment and broken or missing tools for monitoring patients. The lack of hospital security services to assist with violent or threatening patients has also become a concern.
Goodman: The inability to provide safe care is a common fear of all nurses, one that was exacerbated by health care workers leaving during the pandemic, primarily from nursing homes. Although overall safety has improved, that may not be the case in smaller, rural institutions. Staffing for all shifts may also be erratic as the country faces an uphill winter battle with influenza, respiratory syncytial virus, and newer COVID variants.
Report to your supervisor: First, be familiar with your institution’s policy regarding chain of command. Know where to take a complaint when staffing seems unsafe. Contact your immediate supervisor as soon as the situation has been assessed. They might be able to shift resources to your area or find coverage to help. In addition, keep accurate notes related to your actions.
I covered a night shift where I was directly responsible for the care of 13 subacute medical-surgical patients (new admissions and postoperative patients). Patients kept arriving with no regard for the load that was present. One of the patients was completely unhappy with her pain regimen and kept calling for assistance, as is often the case.
While I was doing my best to assess arrivals, another nurse contacted a supervisor. The next thing that happened was an on-site visit by hospital administrators (unusual!) who asked to see my assignment sheet. I had been hesitant to share the list, fearing recrimination from intermediate leadership (this was not my home unit). But it led to an immediate change in staffing. The ordeal ended amicably, but not all do. Thereafter, no nurse was expected to care for more than eight patients on the night shift.
Notify proper authorities: Nurses may believe contacting the Occupational Safety and Health Administration (OSHA) might be helpful; however, OSHA may not have jurisdiction over the hospital, as the Saint Joseph nurses discovered. Working without safety equipment or with reduced supplies (for example, automatic blood pressure cuffs, oxygen saturation monitors, isolation gear) may appear to be a federal complaint, but it depends where the nurse is employed. The hospital in Joliet was covered by the Illinois Department of Public Health.
Federal law entitles you to work in a safe place. Contacting OSHA for direction should not lead to recrimination for nurses. Although OSHA has been overwhelmed with complaints since the onset of the pandemic, their website directs nurses. For example, a whistleblower complaint can be filed up to 30 days after an incident of worker retaliation.
If you are a member of a nursing union, follow union guidelines related to your actions. Thousands of nurses went on strike in the past 2 years. Most remained employed and returned to work with negotiations complete. As far as the nurses in Massachusetts, the state does not have mandatory staffing ratios – most do not – which complicated contract negotiations. At this time, California is the only state that has mandatory nurse-patient ratios written into law.
It is also important to know state law and to be cognizant of nursing organizations within your geographic area. Staying connected means staying informed and having nursing resources.
Respond rationally: An additional reminder for nurses is not to react to a tense situation impulsively. Leaving an assignment unfinished or walking off the job is never a good idea. (A scheduled strike organized by union leaders is different). Leaving work is viewed by institutions as job abandonment and can be grounds for dismissal. Most states are currently “at will” employers, meaning hospitals can terminate nurses without due process.
Above all, know that nurses worry about providing safe practice and avoiding recrimination. Only one of these should be in your future.
Ms. Goodman has no disclosures.
A version of this article first appeared on Medscape.com.
Nurses are the most trusted profession for one reason. They care.
Nurses are passionate about patient interactions, quality, and giving optimal support, often to the detriment of self-care. Many do not hesitate to voice concerns in an atmosphere that produces anxiety, whether it be regarding supplies, documentation, or staffing. As a result,
In October, three nurses at Ascension Saint Joseph in Joliet, Ill., were escorted off the premises of a hospital emergency room when they began an understaffed shift. They were removed from work by hospital security and then suspended for 1 week. It was a decision that was incomprehensible, because the emergency room faced an overwhelming influx of patients – 46 that evening alone – and only four nurses instead of the more than 10 approved staffing were on duty. Why were they suspended?
Hospital officials have been quiet in responding to their alarmed community as well as in answering the Illinois Nurses Association, who criticized the hospital’s response. It has been suggested that the nurses had been intensely vocal about staffing for several weeks and the hospital might have wanted to silence their voices.
In my opinion, this could be considered a professional repercussion of the post-pandemic work environment. Though the nurses were reinstated after the week expired, nursing organizations believed that the actions of their employer were too harsh.
There was a similar response by employers after a string of large strikes of California nurses earlier this year. For example, a walkout by nurses at Stanford Health Care and Lucile Packard Children’s Hospital resulted in the hospitals withholding wages during the strike period and stating they might withhold health coverage from striking workers.
“Our sincere hope is that an agreement can be reached promptly so that nurses don’t lose additional pay, don’t risk losing the subsidy for employer-paid health benefits, and can return to patient care,” the hospital newsletter StanfordPackardVoice.com reported before the strike began in April. “Nurses who choose to go out on strike will not paid for missed shifts and cannot use PTO, ESL, or Education Hours.”
Nurse: Could a similar repercussion be in my work future?
Nurses may take to picket lines or contact administrators (for example, Human Resources) for multiple reasons, but the most common issues are related to staffing, scheduling, mandatory overtime, or equipment required to do their job: safety or lifting equipment and broken or missing tools for monitoring patients. The lack of hospital security services to assist with violent or threatening patients has also become a concern.
Goodman: The inability to provide safe care is a common fear of all nurses, one that was exacerbated by health care workers leaving during the pandemic, primarily from nursing homes. Although overall safety has improved, that may not be the case in smaller, rural institutions. Staffing for all shifts may also be erratic as the country faces an uphill winter battle with influenza, respiratory syncytial virus, and newer COVID variants.
Report to your supervisor: First, be familiar with your institution’s policy regarding chain of command. Know where to take a complaint when staffing seems unsafe. Contact your immediate supervisor as soon as the situation has been assessed. They might be able to shift resources to your area or find coverage to help. In addition, keep accurate notes related to your actions.
I covered a night shift where I was directly responsible for the care of 13 subacute medical-surgical patients (new admissions and postoperative patients). Patients kept arriving with no regard for the load that was present. One of the patients was completely unhappy with her pain regimen and kept calling for assistance, as is often the case.
While I was doing my best to assess arrivals, another nurse contacted a supervisor. The next thing that happened was an on-site visit by hospital administrators (unusual!) who asked to see my assignment sheet. I had been hesitant to share the list, fearing recrimination from intermediate leadership (this was not my home unit). But it led to an immediate change in staffing. The ordeal ended amicably, but not all do. Thereafter, no nurse was expected to care for more than eight patients on the night shift.
Notify proper authorities: Nurses may believe contacting the Occupational Safety and Health Administration (OSHA) might be helpful; however, OSHA may not have jurisdiction over the hospital, as the Saint Joseph nurses discovered. Working without safety equipment or with reduced supplies (for example, automatic blood pressure cuffs, oxygen saturation monitors, isolation gear) may appear to be a federal complaint, but it depends where the nurse is employed. The hospital in Joliet was covered by the Illinois Department of Public Health.
Federal law entitles you to work in a safe place. Contacting OSHA for direction should not lead to recrimination for nurses. Although OSHA has been overwhelmed with complaints since the onset of the pandemic, their website directs nurses. For example, a whistleblower complaint can be filed up to 30 days after an incident of worker retaliation.
If you are a member of a nursing union, follow union guidelines related to your actions. Thousands of nurses went on strike in the past 2 years. Most remained employed and returned to work with negotiations complete. As far as the nurses in Massachusetts, the state does not have mandatory staffing ratios – most do not – which complicated contract negotiations. At this time, California is the only state that has mandatory nurse-patient ratios written into law.
It is also important to know state law and to be cognizant of nursing organizations within your geographic area. Staying connected means staying informed and having nursing resources.
Respond rationally: An additional reminder for nurses is not to react to a tense situation impulsively. Leaving an assignment unfinished or walking off the job is never a good idea. (A scheduled strike organized by union leaders is different). Leaving work is viewed by institutions as job abandonment and can be grounds for dismissal. Most states are currently “at will” employers, meaning hospitals can terminate nurses without due process.
Above all, know that nurses worry about providing safe practice and avoiding recrimination. Only one of these should be in your future.
Ms. Goodman has no disclosures.
A version of this article first appeared on Medscape.com.
NRS grants target rosacea’s underlying mechanisms
Two new , according to an announcement by the NRS.
As part of the NRS research grants program, the organization recently awarded $10,000 to Emanual Maverakis, MD, professor of dermatology, University of California, Davis, and research fellow Samantha Herbert, MSPH. Their project will characterize rosacea pathophysiology using single-cell RNA sequencing. This novel analytical technique provides specific information on the signals expressed by different cell types and will help researchers better understand the role each subtype may play in rosacea, along with how these cells interact with each other, according to the NRS press release. New knowledge in the foregoing areas may fuel development of better therapies, the release added.
The NRS awarded its second new-research grant to Arisa Ortiz, MD, director of laser and cosmetic dermatology and associate professor of dermatology, University of California, San Diego. She was awarded $5,000 to examine whether laser therapy affects the skin microbiome, the complex ecosystem of bacteria and other microorganisms that reside on the skin. Studies have detected significant differences – such as higher levels of Demodex folliculorum and Staphylococcus epidermidis and lower levels of Cutibacterium acnes – in the microbiome of skin with rosacea compared with healthy skin. Dr. Ortiz’s research also will probe how blood vessels, which laser therapy often target, contribute to the rosacea disease process.
The NRS also renewed its support of an ongoing study led by Sezen Karakus, MD, assistant professor of ophthalmology at the Johns Hopkins Wilmer Eye Institute, Baltimore. She is studying the role of the ocular-surface microbiome in rosacea pathogenesis. Because ocular rosacea can lead to vision-threatening corneal complications, Dr. Karakus said in the press release, identifying microorganisms present on the ocular surface may spur development of targeted treatment strategies.
A second ongoing study for which the NRS renewed funding is investigating whether certain intracellular signals recently found to be elevated in rosacea lesions may drive skin inflammation, which may be a root cause of rosacea. Emmanuel Contassot, PhD, project leader in the dermatology department at the University Hospital of Basel, Switzerland, is leading the study.
To date, the NRS research grants program has awarded more than $1.6 million to research designed to further elucidate potential causes and other key aspects of rosacea with the goal of advancing treatment, prevention, or potential cure of rosacea.
For interested researchers, the deadline to submit proposals for next year’s grants is June 16, 2023. Forms and instructions are available through the research grants section of the NRS website or by contacting the NRS at 4619 N. Ravenswood Ave., Suite 103, Chicago, IL 60640; 888-662-5874; or info@rosacea.org.
Two new , according to an announcement by the NRS.
As part of the NRS research grants program, the organization recently awarded $10,000 to Emanual Maverakis, MD, professor of dermatology, University of California, Davis, and research fellow Samantha Herbert, MSPH. Their project will characterize rosacea pathophysiology using single-cell RNA sequencing. This novel analytical technique provides specific information on the signals expressed by different cell types and will help researchers better understand the role each subtype may play in rosacea, along with how these cells interact with each other, according to the NRS press release. New knowledge in the foregoing areas may fuel development of better therapies, the release added.
The NRS awarded its second new-research grant to Arisa Ortiz, MD, director of laser and cosmetic dermatology and associate professor of dermatology, University of California, San Diego. She was awarded $5,000 to examine whether laser therapy affects the skin microbiome, the complex ecosystem of bacteria and other microorganisms that reside on the skin. Studies have detected significant differences – such as higher levels of Demodex folliculorum and Staphylococcus epidermidis and lower levels of Cutibacterium acnes – in the microbiome of skin with rosacea compared with healthy skin. Dr. Ortiz’s research also will probe how blood vessels, which laser therapy often target, contribute to the rosacea disease process.
The NRS also renewed its support of an ongoing study led by Sezen Karakus, MD, assistant professor of ophthalmology at the Johns Hopkins Wilmer Eye Institute, Baltimore. She is studying the role of the ocular-surface microbiome in rosacea pathogenesis. Because ocular rosacea can lead to vision-threatening corneal complications, Dr. Karakus said in the press release, identifying microorganisms present on the ocular surface may spur development of targeted treatment strategies.
A second ongoing study for which the NRS renewed funding is investigating whether certain intracellular signals recently found to be elevated in rosacea lesions may drive skin inflammation, which may be a root cause of rosacea. Emmanuel Contassot, PhD, project leader in the dermatology department at the University Hospital of Basel, Switzerland, is leading the study.
To date, the NRS research grants program has awarded more than $1.6 million to research designed to further elucidate potential causes and other key aspects of rosacea with the goal of advancing treatment, prevention, or potential cure of rosacea.
For interested researchers, the deadline to submit proposals for next year’s grants is June 16, 2023. Forms and instructions are available through the research grants section of the NRS website or by contacting the NRS at 4619 N. Ravenswood Ave., Suite 103, Chicago, IL 60640; 888-662-5874; or info@rosacea.org.
Two new , according to an announcement by the NRS.
As part of the NRS research grants program, the organization recently awarded $10,000 to Emanual Maverakis, MD, professor of dermatology, University of California, Davis, and research fellow Samantha Herbert, MSPH. Their project will characterize rosacea pathophysiology using single-cell RNA sequencing. This novel analytical technique provides specific information on the signals expressed by different cell types and will help researchers better understand the role each subtype may play in rosacea, along with how these cells interact with each other, according to the NRS press release. New knowledge in the foregoing areas may fuel development of better therapies, the release added.
The NRS awarded its second new-research grant to Arisa Ortiz, MD, director of laser and cosmetic dermatology and associate professor of dermatology, University of California, San Diego. She was awarded $5,000 to examine whether laser therapy affects the skin microbiome, the complex ecosystem of bacteria and other microorganisms that reside on the skin. Studies have detected significant differences – such as higher levels of Demodex folliculorum and Staphylococcus epidermidis and lower levels of Cutibacterium acnes – in the microbiome of skin with rosacea compared with healthy skin. Dr. Ortiz’s research also will probe how blood vessels, which laser therapy often target, contribute to the rosacea disease process.
The NRS also renewed its support of an ongoing study led by Sezen Karakus, MD, assistant professor of ophthalmology at the Johns Hopkins Wilmer Eye Institute, Baltimore. She is studying the role of the ocular-surface microbiome in rosacea pathogenesis. Because ocular rosacea can lead to vision-threatening corneal complications, Dr. Karakus said in the press release, identifying microorganisms present on the ocular surface may spur development of targeted treatment strategies.
A second ongoing study for which the NRS renewed funding is investigating whether certain intracellular signals recently found to be elevated in rosacea lesions may drive skin inflammation, which may be a root cause of rosacea. Emmanuel Contassot, PhD, project leader in the dermatology department at the University Hospital of Basel, Switzerland, is leading the study.
To date, the NRS research grants program has awarded more than $1.6 million to research designed to further elucidate potential causes and other key aspects of rosacea with the goal of advancing treatment, prevention, or potential cure of rosacea.
For interested researchers, the deadline to submit proposals for next year’s grants is June 16, 2023. Forms and instructions are available through the research grants section of the NRS website or by contacting the NRS at 4619 N. Ravenswood Ave., Suite 103, Chicago, IL 60640; 888-662-5874; or info@rosacea.org.
Rosacea and the gut: Looking into SIBO
, according to speakers at the annual Integrative Dermatology Symposium.
“SIBO is definitely something we test for and treat,” Raja Sivamani, MD, said in an interview after the meeting. Dr. Sivamani practices as an integrative dermatologist at the Pacific Skin Institute in Sacramento and is the director of clinical research at the institute’s research unit, Integrative Skin Science and Research. He led a panel discussion on rosacea and acne at the meeting.
Associations between SIBO and several dermatologic conditions, including systemic sclerosis, have been reported, but the strongest evidence to date involves rosacea. “There’s associative epidemiological evidence showing higher rates of SIBO among those with rosacea, and there are prospective studies” showing clearance of rosacea in patients treated for SIBO, said Dr. Sivamani, also adjunct associate professor of clinical dermatology at the University of California, Davis.
Studies are small, but are “well done and well-designed,” he said in the interview. “Do we need more studies? Absolutely. But what we have now is compelling [enough] for us to take a look at it.”
Findings of rosacea clearance
SIBO’s believed contribution to the pathophysiology of rosacea is part of the increasingly described gut microbiome-skin axis. SIBO has been recognized as a medical phenomenon for many decades and has been defined as an excessive bacterial load in the small bowel that causes gastrointestinal symptoms, according to the 2020 American College of Gastroenterology clinical guideline on SIBO.
Symptoms commonly associated with SIBO overlap with the cardinal symptoms of irritable bowel syndrome (IBS): abdominal pain; diarrhea, constipation, or both; bloating; and flatulence. SIBO can be diagnosed with several validated carbohydrate substrate (glucose or lactulose)–based breath tests that measure hydrogen and/or methane.
Hydrogen-positive breath tests suggest bacterial overgrowth, and methane-positive breath tests suggest small intestinal methanogen overgrowth. Methane is increasingly important and recognized, the AGA guideline says, though it creates a “nomenclature problem in the SIBO framework” because methanogens are not bacteria, the authors note.
In conventional practice, SIBO is typically treated with antibiotics such as rifaximin, and often with short-term dietary modification as well. Integrative medicine typically considers the use of supplements and botanicals in addition to or instead of antibiotics, as well as dietary change and increasingly, a close look at SIBO risk factors to prevent recurrence, Dr. Sivamani said. (His research unit is currently studying the use of herbal protocols as an alternative to antibiotics in patients with SIBO and dermatologic conditions.)
During a presentation on rosacea at the meeting, Neal Bhatia, MD, director of clinical dermatology at Therapeutics Clinical Research, a dermatology treatment and research center in San Diego, said that currently available breath tests for SIBO “are very interesting tools for understanding what may be happening in the gut” and that the “rifaximin data are good.”
He referred to a study reported in the Journal of the American Academy of Dermatology showing that patients with rosacea were significantly more likely to have SIBO (41.7% of 48 patients vs. 5.0% of 40 controls; P < .001), and that 64.5% of rosacea patients who completed treatment with rifaximin had remission of rosacea at a 3-year follow-up.
An earlier crossover study is also notable, he said. This study enrolled 113 consecutive patients with rosacea and 60 age- and sex-matched controls, and randomized those with SIBO (52 of the 113 with rosacea vs. 3 of the 60 controls) to rifaximin or placebo. Rosacea cleared in 20 of the 28 patients in the rifaximin group and greatly improved in 6 of the 28. Of 20 patients in the placebo group, rosacea remained unchanged in 18 and worsened in 2. When patients in the placebo group were switched to rifaximin, SIBO was eradicated in 17 of the 20, and rosacea completely resolved in 15 of those patients, Dr. Bhatia said.
In his view, it will take more time, greater awareness of the rosacea-SIBO link, and a willingness “to take chances” for more dermatologists to consider SIBO during rosacea care. “Breath tests are not something used in the [typical dermatology] clinic right now, but they may make their way in,” he said at the meeting.
In a follow-up interview, Dr. Bhatia emphasized that “it’s really a question of uptake, which always takes a while” and of willingness to “think through the disease from another angle ... especially in patients who are recalcitrant.”
Treatment
Dr. Sivamani said in the interview that a third type of SIBO – hydrogen sulfide–dominant SIBO – is now documented and worth considering when glucose and lactulose breath tests are negative in patients with rosacea who have gastrointestinal symptoms.
The use of breath tests to objectively diagnose SIBO is always best, Dr. Sivamani said, but he will consider empiric therapy in some patients. “I always tell patients [about] the benefits of testing, but if they can’t get the test covered or are unable to pay for the test, and they have symptoms consistent with SIBO, I’m okay doing a trial with therapy,” he said.
Rifaximin, one of the suggested antibiotics listed in the AGA guideline, is a nonabsorbable antibiotic that is FDA-approved for IBS with diarrhea (IBS-D); it has been shown to not negatively affect the growth of beneficial bacteria in the colon.
However, herbals are also an attractive option – alone or in combination with rifaximin or other antibiotics – speakers at the meeting said. In a multicenter retrospective chart review led by investigators at the Johns Hopkins Hospital, herbal therapies were at least as effective as rifaximin for treating SIBO, with similar safety profiles. The response rate for normalizing breath hydrogen testing in patients with SIBO was 46% for herbal therapies and 34% for rifaximin.
Dietary change is also part of treatment, with the reduction of fermentable carbohydrates – often through the Low FODMAP Diet and Specific Carbohydrate Diet – being the dominant theme in dietary intervention for SIBO, according to the AGA guideline.
“There are definitely some food choices you can shift,” said Dr. Sivamani. “I’ll work with patients on FODMAP, though it’s hard to sustain over the long-term and can induce psychological issues. You have to provide other options.”
Dr. Sivamani works with patients on using “a restrictive diet for a short amount of time, with the gradual reintroduction of foods to see [what] foods are and aren’t [causing] flares.” He also works to identify and eliminate risk factors and predisposing factors for SIBO so that recurrence will be less likely.
“SIBO is definitely an entity that is not on the fringes anymore ... it adds to inflammation in the body ... and if you have an inflamed gut, there’s a domino effect that will lead to inflammation elsewhere,” Dr. Sivamani said.
“You want to know, do your patients have SIBO? What subset do they have? Do they have risk factors you can eliminate?” he said. “And then what therapies will you use – pharmaceuticals, supplements and botanicals, or a combination? And finally, what will you do with diet?”
Dr. Bhatia disclosed he has affiliations with Abbvie, Almirall, Arcutis, Arena, Biofrontera, BMS, BI, Brickell, Dermavant, EPI Health, Ferndale, Galderma, Genentech, InCyte, ISDIN, Johnson & Johnson, LaRoche-Posay, Leo, Lilly, Novartis, Ortho, Pfizer, Proctor & Gamble, Regeneron, Sanofi, Stemline, SunPharma, and Verrica. Dr. Sivamani did not provide a disclosure statement.
, according to speakers at the annual Integrative Dermatology Symposium.
“SIBO is definitely something we test for and treat,” Raja Sivamani, MD, said in an interview after the meeting. Dr. Sivamani practices as an integrative dermatologist at the Pacific Skin Institute in Sacramento and is the director of clinical research at the institute’s research unit, Integrative Skin Science and Research. He led a panel discussion on rosacea and acne at the meeting.
Associations between SIBO and several dermatologic conditions, including systemic sclerosis, have been reported, but the strongest evidence to date involves rosacea. “There’s associative epidemiological evidence showing higher rates of SIBO among those with rosacea, and there are prospective studies” showing clearance of rosacea in patients treated for SIBO, said Dr. Sivamani, also adjunct associate professor of clinical dermatology at the University of California, Davis.
Studies are small, but are “well done and well-designed,” he said in the interview. “Do we need more studies? Absolutely. But what we have now is compelling [enough] for us to take a look at it.”
Findings of rosacea clearance
SIBO’s believed contribution to the pathophysiology of rosacea is part of the increasingly described gut microbiome-skin axis. SIBO has been recognized as a medical phenomenon for many decades and has been defined as an excessive bacterial load in the small bowel that causes gastrointestinal symptoms, according to the 2020 American College of Gastroenterology clinical guideline on SIBO.
Symptoms commonly associated with SIBO overlap with the cardinal symptoms of irritable bowel syndrome (IBS): abdominal pain; diarrhea, constipation, or both; bloating; and flatulence. SIBO can be diagnosed with several validated carbohydrate substrate (glucose or lactulose)–based breath tests that measure hydrogen and/or methane.
Hydrogen-positive breath tests suggest bacterial overgrowth, and methane-positive breath tests suggest small intestinal methanogen overgrowth. Methane is increasingly important and recognized, the AGA guideline says, though it creates a “nomenclature problem in the SIBO framework” because methanogens are not bacteria, the authors note.
In conventional practice, SIBO is typically treated with antibiotics such as rifaximin, and often with short-term dietary modification as well. Integrative medicine typically considers the use of supplements and botanicals in addition to or instead of antibiotics, as well as dietary change and increasingly, a close look at SIBO risk factors to prevent recurrence, Dr. Sivamani said. (His research unit is currently studying the use of herbal protocols as an alternative to antibiotics in patients with SIBO and dermatologic conditions.)
During a presentation on rosacea at the meeting, Neal Bhatia, MD, director of clinical dermatology at Therapeutics Clinical Research, a dermatology treatment and research center in San Diego, said that currently available breath tests for SIBO “are very interesting tools for understanding what may be happening in the gut” and that the “rifaximin data are good.”
He referred to a study reported in the Journal of the American Academy of Dermatology showing that patients with rosacea were significantly more likely to have SIBO (41.7% of 48 patients vs. 5.0% of 40 controls; P < .001), and that 64.5% of rosacea patients who completed treatment with rifaximin had remission of rosacea at a 3-year follow-up.
An earlier crossover study is also notable, he said. This study enrolled 113 consecutive patients with rosacea and 60 age- and sex-matched controls, and randomized those with SIBO (52 of the 113 with rosacea vs. 3 of the 60 controls) to rifaximin or placebo. Rosacea cleared in 20 of the 28 patients in the rifaximin group and greatly improved in 6 of the 28. Of 20 patients in the placebo group, rosacea remained unchanged in 18 and worsened in 2. When patients in the placebo group were switched to rifaximin, SIBO was eradicated in 17 of the 20, and rosacea completely resolved in 15 of those patients, Dr. Bhatia said.
In his view, it will take more time, greater awareness of the rosacea-SIBO link, and a willingness “to take chances” for more dermatologists to consider SIBO during rosacea care. “Breath tests are not something used in the [typical dermatology] clinic right now, but they may make their way in,” he said at the meeting.
In a follow-up interview, Dr. Bhatia emphasized that “it’s really a question of uptake, which always takes a while” and of willingness to “think through the disease from another angle ... especially in patients who are recalcitrant.”
Treatment
Dr. Sivamani said in the interview that a third type of SIBO – hydrogen sulfide–dominant SIBO – is now documented and worth considering when glucose and lactulose breath tests are negative in patients with rosacea who have gastrointestinal symptoms.
The use of breath tests to objectively diagnose SIBO is always best, Dr. Sivamani said, but he will consider empiric therapy in some patients. “I always tell patients [about] the benefits of testing, but if they can’t get the test covered or are unable to pay for the test, and they have symptoms consistent with SIBO, I’m okay doing a trial with therapy,” he said.
Rifaximin, one of the suggested antibiotics listed in the AGA guideline, is a nonabsorbable antibiotic that is FDA-approved for IBS with diarrhea (IBS-D); it has been shown to not negatively affect the growth of beneficial bacteria in the colon.
However, herbals are also an attractive option – alone or in combination with rifaximin or other antibiotics – speakers at the meeting said. In a multicenter retrospective chart review led by investigators at the Johns Hopkins Hospital, herbal therapies were at least as effective as rifaximin for treating SIBO, with similar safety profiles. The response rate for normalizing breath hydrogen testing in patients with SIBO was 46% for herbal therapies and 34% for rifaximin.
Dietary change is also part of treatment, with the reduction of fermentable carbohydrates – often through the Low FODMAP Diet and Specific Carbohydrate Diet – being the dominant theme in dietary intervention for SIBO, according to the AGA guideline.
“There are definitely some food choices you can shift,” said Dr. Sivamani. “I’ll work with patients on FODMAP, though it’s hard to sustain over the long-term and can induce psychological issues. You have to provide other options.”
Dr. Sivamani works with patients on using “a restrictive diet for a short amount of time, with the gradual reintroduction of foods to see [what] foods are and aren’t [causing] flares.” He also works to identify and eliminate risk factors and predisposing factors for SIBO so that recurrence will be less likely.
“SIBO is definitely an entity that is not on the fringes anymore ... it adds to inflammation in the body ... and if you have an inflamed gut, there’s a domino effect that will lead to inflammation elsewhere,” Dr. Sivamani said.
“You want to know, do your patients have SIBO? What subset do they have? Do they have risk factors you can eliminate?” he said. “And then what therapies will you use – pharmaceuticals, supplements and botanicals, or a combination? And finally, what will you do with diet?”
Dr. Bhatia disclosed he has affiliations with Abbvie, Almirall, Arcutis, Arena, Biofrontera, BMS, BI, Brickell, Dermavant, EPI Health, Ferndale, Galderma, Genentech, InCyte, ISDIN, Johnson & Johnson, LaRoche-Posay, Leo, Lilly, Novartis, Ortho, Pfizer, Proctor & Gamble, Regeneron, Sanofi, Stemline, SunPharma, and Verrica. Dr. Sivamani did not provide a disclosure statement.
, according to speakers at the annual Integrative Dermatology Symposium.
“SIBO is definitely something we test for and treat,” Raja Sivamani, MD, said in an interview after the meeting. Dr. Sivamani practices as an integrative dermatologist at the Pacific Skin Institute in Sacramento and is the director of clinical research at the institute’s research unit, Integrative Skin Science and Research. He led a panel discussion on rosacea and acne at the meeting.
Associations between SIBO and several dermatologic conditions, including systemic sclerosis, have been reported, but the strongest evidence to date involves rosacea. “There’s associative epidemiological evidence showing higher rates of SIBO among those with rosacea, and there are prospective studies” showing clearance of rosacea in patients treated for SIBO, said Dr. Sivamani, also adjunct associate professor of clinical dermatology at the University of California, Davis.
Studies are small, but are “well done and well-designed,” he said in the interview. “Do we need more studies? Absolutely. But what we have now is compelling [enough] for us to take a look at it.”
Findings of rosacea clearance
SIBO’s believed contribution to the pathophysiology of rosacea is part of the increasingly described gut microbiome-skin axis. SIBO has been recognized as a medical phenomenon for many decades and has been defined as an excessive bacterial load in the small bowel that causes gastrointestinal symptoms, according to the 2020 American College of Gastroenterology clinical guideline on SIBO.
Symptoms commonly associated with SIBO overlap with the cardinal symptoms of irritable bowel syndrome (IBS): abdominal pain; diarrhea, constipation, or both; bloating; and flatulence. SIBO can be diagnosed with several validated carbohydrate substrate (glucose or lactulose)–based breath tests that measure hydrogen and/or methane.
Hydrogen-positive breath tests suggest bacterial overgrowth, and methane-positive breath tests suggest small intestinal methanogen overgrowth. Methane is increasingly important and recognized, the AGA guideline says, though it creates a “nomenclature problem in the SIBO framework” because methanogens are not bacteria, the authors note.
In conventional practice, SIBO is typically treated with antibiotics such as rifaximin, and often with short-term dietary modification as well. Integrative medicine typically considers the use of supplements and botanicals in addition to or instead of antibiotics, as well as dietary change and increasingly, a close look at SIBO risk factors to prevent recurrence, Dr. Sivamani said. (His research unit is currently studying the use of herbal protocols as an alternative to antibiotics in patients with SIBO and dermatologic conditions.)
During a presentation on rosacea at the meeting, Neal Bhatia, MD, director of clinical dermatology at Therapeutics Clinical Research, a dermatology treatment and research center in San Diego, said that currently available breath tests for SIBO “are very interesting tools for understanding what may be happening in the gut” and that the “rifaximin data are good.”
He referred to a study reported in the Journal of the American Academy of Dermatology showing that patients with rosacea were significantly more likely to have SIBO (41.7% of 48 patients vs. 5.0% of 40 controls; P < .001), and that 64.5% of rosacea patients who completed treatment with rifaximin had remission of rosacea at a 3-year follow-up.
An earlier crossover study is also notable, he said. This study enrolled 113 consecutive patients with rosacea and 60 age- and sex-matched controls, and randomized those with SIBO (52 of the 113 with rosacea vs. 3 of the 60 controls) to rifaximin or placebo. Rosacea cleared in 20 of the 28 patients in the rifaximin group and greatly improved in 6 of the 28. Of 20 patients in the placebo group, rosacea remained unchanged in 18 and worsened in 2. When patients in the placebo group were switched to rifaximin, SIBO was eradicated in 17 of the 20, and rosacea completely resolved in 15 of those patients, Dr. Bhatia said.
In his view, it will take more time, greater awareness of the rosacea-SIBO link, and a willingness “to take chances” for more dermatologists to consider SIBO during rosacea care. “Breath tests are not something used in the [typical dermatology] clinic right now, but they may make their way in,” he said at the meeting.
In a follow-up interview, Dr. Bhatia emphasized that “it’s really a question of uptake, which always takes a while” and of willingness to “think through the disease from another angle ... especially in patients who are recalcitrant.”
Treatment
Dr. Sivamani said in the interview that a third type of SIBO – hydrogen sulfide–dominant SIBO – is now documented and worth considering when glucose and lactulose breath tests are negative in patients with rosacea who have gastrointestinal symptoms.
The use of breath tests to objectively diagnose SIBO is always best, Dr. Sivamani said, but he will consider empiric therapy in some patients. “I always tell patients [about] the benefits of testing, but if they can’t get the test covered or are unable to pay for the test, and they have symptoms consistent with SIBO, I’m okay doing a trial with therapy,” he said.
Rifaximin, one of the suggested antibiotics listed in the AGA guideline, is a nonabsorbable antibiotic that is FDA-approved for IBS with diarrhea (IBS-D); it has been shown to not negatively affect the growth of beneficial bacteria in the colon.
However, herbals are also an attractive option – alone or in combination with rifaximin or other antibiotics – speakers at the meeting said. In a multicenter retrospective chart review led by investigators at the Johns Hopkins Hospital, herbal therapies were at least as effective as rifaximin for treating SIBO, with similar safety profiles. The response rate for normalizing breath hydrogen testing in patients with SIBO was 46% for herbal therapies and 34% for rifaximin.
Dietary change is also part of treatment, with the reduction of fermentable carbohydrates – often through the Low FODMAP Diet and Specific Carbohydrate Diet – being the dominant theme in dietary intervention for SIBO, according to the AGA guideline.
“There are definitely some food choices you can shift,” said Dr. Sivamani. “I’ll work with patients on FODMAP, though it’s hard to sustain over the long-term and can induce psychological issues. You have to provide other options.”
Dr. Sivamani works with patients on using “a restrictive diet for a short amount of time, with the gradual reintroduction of foods to see [what] foods are and aren’t [causing] flares.” He also works to identify and eliminate risk factors and predisposing factors for SIBO so that recurrence will be less likely.
“SIBO is definitely an entity that is not on the fringes anymore ... it adds to inflammation in the body ... and if you have an inflamed gut, there’s a domino effect that will lead to inflammation elsewhere,” Dr. Sivamani said.
“You want to know, do your patients have SIBO? What subset do they have? Do they have risk factors you can eliminate?” he said. “And then what therapies will you use – pharmaceuticals, supplements and botanicals, or a combination? And finally, what will you do with diet?”
Dr. Bhatia disclosed he has affiliations with Abbvie, Almirall, Arcutis, Arena, Biofrontera, BMS, BI, Brickell, Dermavant, EPI Health, Ferndale, Galderma, Genentech, InCyte, ISDIN, Johnson & Johnson, LaRoche-Posay, Leo, Lilly, Novartis, Ortho, Pfizer, Proctor & Gamble, Regeneron, Sanofi, Stemline, SunPharma, and Verrica. Dr. Sivamani did not provide a disclosure statement.
REPORTING FROM IDS 2022
‘Slugging’: A TikTok skin trend that has some merit
They’ve been around for a while and show no signs of going away: videos on TikTok of people, often teens, slathering their face with petroleum jelly and claiming that it’s transformed their skin, cured their acne, or given them an amazing “glow up.”
TikTok videos mentioning petrolatum increased by 46% and Instagram videos by 93% from 2021 to 2022, reported Gabriel Santos Malave, BA, of the Icahn School of Medicine at Mount Sinai, New York, and William D. James, MD, professor of dermatology, University of Pennsylvania, Philadelphia, in a review of petroleum jelly’s uses recently published in Cutis.
The authors said that after application of a moisturizer.
In a typical demonstration, a dermatologist in the United Kingdom showed how she incorporates slugging into her routine in a TikTok video that’s had more than 1 million views.
Unlike many TikTok trends, slugging may not be entirely bad, say dermatologists.
“I think it’s a great way to keep your skin protected and moisturized, especially in those dry, cold winter months,” said dermatologist Mamina Turegano, MD, in a video posted in February 2022. That TikTok video has had more than 6 million views.
Dr. Turegano, who is in private practice in the New Orleans suburb of Metairie, La., told this news organization that she decided to post about slugging after she’d noticed that the topic was trending. Also, she had tried the technique herself when she was a resident in Washington more than a decade ago.
At the time, Dr. Turegano said that she was aware that “putting petroleum jelly on your face was not a normal thing.” But, given its history of being used in dermatology, she gave it a try and found that it worked well for her dry skin, she said.
Dr. Turegano is one among many dermatologists who have joined TikTok to dispel myths, educate, and inform. It’s important for them to be there “to engage and empower the public to become a better consumer of information out there and take ownership of their skin health,” said Jean McGee, MD, PhD, a dermatologist at Beth Israel Deaconess Medical Center, Boston, and assistant professor of dermatology at Harvard Medical School, also in Boston.
Dr. McGee and colleagues studied TikTok content on slugging and found that by far, videos that were created by health care providers were more educational. Dermatologists who posted were more likely to discuss the risks and benefits, whereas so-called “influencers” rarely posted on the risks, according to the study, published in Clinics in Dermatology.
Slugging is generally safe and effective for those who have a compromised skin barrier or “for those who have sensitive skin and can’t tolerate other products but need some form of moisturization,” said Dr. Turegano.
“Its oil-based nature allows it to seal water in the skin by creating a hydrophobic barrier that decreases transepidermal water loss (TEWL),” write Mr. Malave and Dr. James in Cutis. They note that petrolatum reduces TEWL by 98%, compared with only 20% to 30% for other oil-based moisturizers.
Dermatologists have often recommended a “seal and trap” regimen for dry skin or eczema. It involves a short, lukewarm shower, followed by immediately moisturizing with a petrolatum-based ointment, said Dr. McGee.
This could be safe for the face, but “other variables need to be considered,” including use of other topical medications and other skin care practices, she added.
The concept of double-layering a moisturizer and an occlusive agent can be beneficial but more typically for the hands and feet, where the skin can be severely dry and cracked, said Adam Friedman, MD, professor and chair of dermatology, George Washington University, Washington. “I would not recommend that on the face,” Dr. Friedman told this news organization.
He and other dermatologists warned about the potential for slugging – given petroleum jelly’s occlusive nature – to enhance the action of any topical steroid, retinol, or exfoliating agent.
Muneeb Shah, MD, who practices in Mooresville, N.C., is one of the most popular dermatologists on TikTok, with more than 17 million followers. He also warned in a February 2022 video about potential downsides. “Be careful after using retinol or exfoliating acids because it may actually irritate your skin more,” he says in the video.
“Slugging is awesome for some people but not for others, and not for every night,” said Whitney Bowe, MD, on a TikTok video she posted in July. She recommended it for eczema or really dry skin. Dr. Bowe, who practices with Advanced Dermatology in New York, advised those with acne-prone skin to “skip this trend.”
On a web page aimed at the general public, the American Academy of Dermatology similarly cautioned, “Avoid putting petroleum jelly on your face if you are acne-prone, as this may cause breakouts in some people.”
Acne cure or pore clogger?
And yet, plenty of TikTok users claim that it has improved their acne.
One such user posted a before and after video purporting to show that slugging had almost completely eliminated her acne and prior scarring. Not surprisingly, it has been viewed some 9 million times and got 1.5 million “likes.”
Dr. Friedman notes that it’s theoretically possible – but not likely – that acne could improve by slugging, given that acne basically is a disease of barrier disruption. “The idea here is you have disrupted skin barrier throughout the face regardless of whether you have a pimple in that spot or not, so you need to repair it,” he said. “That’s where I think slugging is somewhat on the right track, because by putting an occlusive agent on the skin, you are restoring the barrier element,” he said.
However, applying a thick, greasy ointment on the face could block pores and cause a backup of sebum and dead skin cells, and it could trap bacteria, he said. “Skin barrier protection and repair is central to acne management, but you need to do it in a safe way,” he said. He noted that that means applying an oil-free moisturizer to damp skin.
Dr. Turegano said she has seen slugging improve acne, but it’s hard to say which people with acne-prone skin would be the best candidates. Those who have used harsh products to treat acne and subsequently experienced worsening acne could potentially benefit, she said.
Even so, she said, “I’d be very cautious in anyone with acne.”
Dr. Friedman, Dr. McGee, and Dr. Turegano reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
They’ve been around for a while and show no signs of going away: videos on TikTok of people, often teens, slathering their face with petroleum jelly and claiming that it’s transformed their skin, cured their acne, or given them an amazing “glow up.”
TikTok videos mentioning petrolatum increased by 46% and Instagram videos by 93% from 2021 to 2022, reported Gabriel Santos Malave, BA, of the Icahn School of Medicine at Mount Sinai, New York, and William D. James, MD, professor of dermatology, University of Pennsylvania, Philadelphia, in a review of petroleum jelly’s uses recently published in Cutis.
The authors said that after application of a moisturizer.
In a typical demonstration, a dermatologist in the United Kingdom showed how she incorporates slugging into her routine in a TikTok video that’s had more than 1 million views.
Unlike many TikTok trends, slugging may not be entirely bad, say dermatologists.
“I think it’s a great way to keep your skin protected and moisturized, especially in those dry, cold winter months,” said dermatologist Mamina Turegano, MD, in a video posted in February 2022. That TikTok video has had more than 6 million views.
Dr. Turegano, who is in private practice in the New Orleans suburb of Metairie, La., told this news organization that she decided to post about slugging after she’d noticed that the topic was trending. Also, she had tried the technique herself when she was a resident in Washington more than a decade ago.
At the time, Dr. Turegano said that she was aware that “putting petroleum jelly on your face was not a normal thing.” But, given its history of being used in dermatology, she gave it a try and found that it worked well for her dry skin, she said.
Dr. Turegano is one among many dermatologists who have joined TikTok to dispel myths, educate, and inform. It’s important for them to be there “to engage and empower the public to become a better consumer of information out there and take ownership of their skin health,” said Jean McGee, MD, PhD, a dermatologist at Beth Israel Deaconess Medical Center, Boston, and assistant professor of dermatology at Harvard Medical School, also in Boston.
Dr. McGee and colleagues studied TikTok content on slugging and found that by far, videos that were created by health care providers were more educational. Dermatologists who posted were more likely to discuss the risks and benefits, whereas so-called “influencers” rarely posted on the risks, according to the study, published in Clinics in Dermatology.
Slugging is generally safe and effective for those who have a compromised skin barrier or “for those who have sensitive skin and can’t tolerate other products but need some form of moisturization,” said Dr. Turegano.
“Its oil-based nature allows it to seal water in the skin by creating a hydrophobic barrier that decreases transepidermal water loss (TEWL),” write Mr. Malave and Dr. James in Cutis. They note that petrolatum reduces TEWL by 98%, compared with only 20% to 30% for other oil-based moisturizers.
Dermatologists have often recommended a “seal and trap” regimen for dry skin or eczema. It involves a short, lukewarm shower, followed by immediately moisturizing with a petrolatum-based ointment, said Dr. McGee.
This could be safe for the face, but “other variables need to be considered,” including use of other topical medications and other skin care practices, she added.
The concept of double-layering a moisturizer and an occlusive agent can be beneficial but more typically for the hands and feet, where the skin can be severely dry and cracked, said Adam Friedman, MD, professor and chair of dermatology, George Washington University, Washington. “I would not recommend that on the face,” Dr. Friedman told this news organization.
He and other dermatologists warned about the potential for slugging – given petroleum jelly’s occlusive nature – to enhance the action of any topical steroid, retinol, or exfoliating agent.
Muneeb Shah, MD, who practices in Mooresville, N.C., is one of the most popular dermatologists on TikTok, with more than 17 million followers. He also warned in a February 2022 video about potential downsides. “Be careful after using retinol or exfoliating acids because it may actually irritate your skin more,” he says in the video.
“Slugging is awesome for some people but not for others, and not for every night,” said Whitney Bowe, MD, on a TikTok video she posted in July. She recommended it for eczema or really dry skin. Dr. Bowe, who practices with Advanced Dermatology in New York, advised those with acne-prone skin to “skip this trend.”
On a web page aimed at the general public, the American Academy of Dermatology similarly cautioned, “Avoid putting petroleum jelly on your face if you are acne-prone, as this may cause breakouts in some people.”
Acne cure or pore clogger?
And yet, plenty of TikTok users claim that it has improved their acne.
One such user posted a before and after video purporting to show that slugging had almost completely eliminated her acne and prior scarring. Not surprisingly, it has been viewed some 9 million times and got 1.5 million “likes.”
Dr. Friedman notes that it’s theoretically possible – but not likely – that acne could improve by slugging, given that acne basically is a disease of barrier disruption. “The idea here is you have disrupted skin barrier throughout the face regardless of whether you have a pimple in that spot or not, so you need to repair it,” he said. “That’s where I think slugging is somewhat on the right track, because by putting an occlusive agent on the skin, you are restoring the barrier element,” he said.
However, applying a thick, greasy ointment on the face could block pores and cause a backup of sebum and dead skin cells, and it could trap bacteria, he said. “Skin barrier protection and repair is central to acne management, but you need to do it in a safe way,” he said. He noted that that means applying an oil-free moisturizer to damp skin.
Dr. Turegano said she has seen slugging improve acne, but it’s hard to say which people with acne-prone skin would be the best candidates. Those who have used harsh products to treat acne and subsequently experienced worsening acne could potentially benefit, she said.
Even so, she said, “I’d be very cautious in anyone with acne.”
Dr. Friedman, Dr. McGee, and Dr. Turegano reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
They’ve been around for a while and show no signs of going away: videos on TikTok of people, often teens, slathering their face with petroleum jelly and claiming that it’s transformed their skin, cured their acne, or given them an amazing “glow up.”
TikTok videos mentioning petrolatum increased by 46% and Instagram videos by 93% from 2021 to 2022, reported Gabriel Santos Malave, BA, of the Icahn School of Medicine at Mount Sinai, New York, and William D. James, MD, professor of dermatology, University of Pennsylvania, Philadelphia, in a review of petroleum jelly’s uses recently published in Cutis.
The authors said that after application of a moisturizer.
In a typical demonstration, a dermatologist in the United Kingdom showed how she incorporates slugging into her routine in a TikTok video that’s had more than 1 million views.
Unlike many TikTok trends, slugging may not be entirely bad, say dermatologists.
“I think it’s a great way to keep your skin protected and moisturized, especially in those dry, cold winter months,” said dermatologist Mamina Turegano, MD, in a video posted in February 2022. That TikTok video has had more than 6 million views.
Dr. Turegano, who is in private practice in the New Orleans suburb of Metairie, La., told this news organization that she decided to post about slugging after she’d noticed that the topic was trending. Also, she had tried the technique herself when she was a resident in Washington more than a decade ago.
At the time, Dr. Turegano said that she was aware that “putting petroleum jelly on your face was not a normal thing.” But, given its history of being used in dermatology, she gave it a try and found that it worked well for her dry skin, she said.
Dr. Turegano is one among many dermatologists who have joined TikTok to dispel myths, educate, and inform. It’s important for them to be there “to engage and empower the public to become a better consumer of information out there and take ownership of their skin health,” said Jean McGee, MD, PhD, a dermatologist at Beth Israel Deaconess Medical Center, Boston, and assistant professor of dermatology at Harvard Medical School, also in Boston.
Dr. McGee and colleagues studied TikTok content on slugging and found that by far, videos that were created by health care providers were more educational. Dermatologists who posted were more likely to discuss the risks and benefits, whereas so-called “influencers” rarely posted on the risks, according to the study, published in Clinics in Dermatology.
Slugging is generally safe and effective for those who have a compromised skin barrier or “for those who have sensitive skin and can’t tolerate other products but need some form of moisturization,” said Dr. Turegano.
“Its oil-based nature allows it to seal water in the skin by creating a hydrophobic barrier that decreases transepidermal water loss (TEWL),” write Mr. Malave and Dr. James in Cutis. They note that petrolatum reduces TEWL by 98%, compared with only 20% to 30% for other oil-based moisturizers.
Dermatologists have often recommended a “seal and trap” regimen for dry skin or eczema. It involves a short, lukewarm shower, followed by immediately moisturizing with a petrolatum-based ointment, said Dr. McGee.
This could be safe for the face, but “other variables need to be considered,” including use of other topical medications and other skin care practices, she added.
The concept of double-layering a moisturizer and an occlusive agent can be beneficial but more typically for the hands and feet, where the skin can be severely dry and cracked, said Adam Friedman, MD, professor and chair of dermatology, George Washington University, Washington. “I would not recommend that on the face,” Dr. Friedman told this news organization.
He and other dermatologists warned about the potential for slugging – given petroleum jelly’s occlusive nature – to enhance the action of any topical steroid, retinol, or exfoliating agent.
Muneeb Shah, MD, who practices in Mooresville, N.C., is one of the most popular dermatologists on TikTok, with more than 17 million followers. He also warned in a February 2022 video about potential downsides. “Be careful after using retinol or exfoliating acids because it may actually irritate your skin more,” he says in the video.
“Slugging is awesome for some people but not for others, and not for every night,” said Whitney Bowe, MD, on a TikTok video she posted in July. She recommended it for eczema or really dry skin. Dr. Bowe, who practices with Advanced Dermatology in New York, advised those with acne-prone skin to “skip this trend.”
On a web page aimed at the general public, the American Academy of Dermatology similarly cautioned, “Avoid putting petroleum jelly on your face if you are acne-prone, as this may cause breakouts in some people.”
Acne cure or pore clogger?
And yet, plenty of TikTok users claim that it has improved their acne.
One such user posted a before and after video purporting to show that slugging had almost completely eliminated her acne and prior scarring. Not surprisingly, it has been viewed some 9 million times and got 1.5 million “likes.”
Dr. Friedman notes that it’s theoretically possible – but not likely – that acne could improve by slugging, given that acne basically is a disease of barrier disruption. “The idea here is you have disrupted skin barrier throughout the face regardless of whether you have a pimple in that spot or not, so you need to repair it,” he said. “That’s where I think slugging is somewhat on the right track, because by putting an occlusive agent on the skin, you are restoring the barrier element,” he said.
However, applying a thick, greasy ointment on the face could block pores and cause a backup of sebum and dead skin cells, and it could trap bacteria, he said. “Skin barrier protection and repair is central to acne management, but you need to do it in a safe way,” he said. He noted that that means applying an oil-free moisturizer to damp skin.
Dr. Turegano said she has seen slugging improve acne, but it’s hard to say which people with acne-prone skin would be the best candidates. Those who have used harsh products to treat acne and subsequently experienced worsening acne could potentially benefit, she said.
Even so, she said, “I’d be very cautious in anyone with acne.”
Dr. Friedman, Dr. McGee, and Dr. Turegano reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Review gives weight to supplements for hair loss
because of small sample sizes, heterogeneity of hair loss types in study subjects, or other limitations.
The review, published online in JAMA Dermatology, notes that “Twelve of the 20 nutritional interventions had high-quality studies suggesting objectively evaluated effectiveness.”
It is “ground breaking,” in part because of its breadth and depth, said Eva Simmons-O’Brien, MD, a dermatologist in Towson, Md., who often recommends supplements for her patients with hair loss. “It basically kind of vindicates what some of us have been doing for a number of years in terms of treating hair loss,” she told this news organization. “It should hopefully make it more commonplace for dermatologists to consider using nutritional supplements as an adjuvant to treating hair loss,” added Dr. Simmons-O’Brien.
The review “is very helpful,” agreed Lynne J. Goldberg, MD, professor of dermatology and pathology and laboratory medicine at Boston University. Dr. Goldberg noted that many patients are already taking supplements and want to know whether they are safe and effective. The review “points out what the problems are; it talks about what the individual ingredients are and what they do, what the problems are; and it concluded that some people may find these helpful. Which is exactly what I tell my patients,” said Dr. Goldberg, who is also director of the Hair Clinic at Boston Medical Center.
“For patients who are highly motivated and eager to try this, we’re hoping that this systematic review serves as a foundation to have a conversation,” study coauthor Arash Mostaghimi, MD, MPA, MPH, of the department of dermatology at Harvard Medical School, told this news organization. “When there’s medical uncertainty and the question is how much risk is one willing to take, the most important thing to do is to present the data and engage in shared decision-making with the patient,” noted Dr. Mostaghimi, who is also director of the inpatient dermatology consult service at Brigham and Women’s Hospital, Boston.
Surprising effectiveness
Going into the study, “we felt it would be likely that majority of nutritional supplements would either not be effective or not studied,” he said.
Dr. Mostaghimi and his coauthors conducted the study because so many patients take nutritional supplements to address hair loss, he said. An initial literature survey yielded more than 6,300 citations, but after screening and reviews, the authors included 30 articles for evaluation.
The review begins with a look at studies of saw palmetto (Serenoa repens), a botanical compound thought to inhibit the enzyme 5-alpha reductase (5AR), which converts testosterone to dihydroxytestosterone (DHT). DHT is a mediator of androgenic alopecia (AGA). The studies suggest that the compound might stabilize hair loss, “although its effect is likely less than that of finasteride,” write the authors. They also note that side effects associated with finasteride, such as sexual dysfunction, were also observed with saw palmetto “but to a lesser extent.”
For AGA, pumpkin seed oil may also be effective and a “potential alternative” to finasteride for AGA, and Forti5, a nutritional supplement that includes botanical 5AR inhibitors and other ingredients, had favorable effects in one study, the authors write. But neither has been compared to finasteride, and the Forti5 study lacked a control group.
The review also examines the micronutrients vitamin D, zinc, B vitamins, and antioxidants. Low levels of vitamin D have been associated with alopecia areata (AA), AGA, and telogen effluvium (TE) in some studies, and zinc deficiencies have been associated with TE, hair breakage, and thinning, according to the review. A single-arm vitamin D study showed improved results at 6 months for women with TE, but there was no control group and TE is self-resolving, the authors add. Studies in patients with normal zinc levels at baseline who had AA or hair loss showed significant hair regrowth and increased hair thickness and density, but the trials were a mishmash of controls and no controls and relied on self-perceived hair-loss data.
Larger more rigorous studies should be done to evaluate zinc’s effectiveness with AA, the authors comment.
Many patients take vitamin B7 (biotin) for hair loss. It has not been studied on its own but was an ingredient in some supplements in the review. Dr. Simmons-O’Brien said that biotin won’t result in new hair growth but that it can help strengthen the new hairs that grow as a result of other therapies. Both she and the study authors note that the Food and Drug Administration has warned against biotin supplementation because it can interfere with troponin and other test results.
The review also finds that immunomodulators –such as Chinese herbal extracts from paeony and glycyrrhizin – were effective in severe AA. Growth hormone modulators targeting deficiencies in insulin growth factor 1 or growth hormone are also promising. Studies of the modulators capsaicin and isoflavones – used topically – spurred hair growth, the authors write.
Products containing marine protein supplements, including Viviscal and Nourkrin, appeared effective in increasing hair counts in men and women, but the studies were funded by the manufacturer and were not well controlled. Side effects with Viviscal included bloating, according to the review.
The multi-ingredient supplements Nutrafol, Omni-Three, Apple Nutraceutical, and Lambdapil were also included in the review. Only Omni-Three showed no effectiveness, but studies of the other supplements had various limitations, including lack of controls and small sample sizes.
Complicated problem, multiple solutions
Given the many reasons for hair loss, multiple solutions are needed, the dermatologists note.
Dr. Mostaghimi said that he’s still a bit skeptical that supplements work as consistently as described or as well as described, given that he and his coauthors were unable to find any negative studies. In talking with patients who are taking supplements, he said that his first aim is to make sure they are safe. At least the supplements in the review have been studied for safety, he added.
He will encourage replacement of vitamin D or zinc or other vitamins or minerals if patients are deficient but said that he does not “actively encourage supplementation.”
Dr. Simmons-O’Brien said that, when evaluating patients with hair loss, she orders lab tests to determine whether the patient has anemia or a thyroid issue or deficiencies in vitamins or minerals or other nutritional deficiencies, asks about diet and styling practices, and takes a scalp biopsy. It is not uncommon to recommend supplementation on the basis of those findings, she added.
“As a hair-loss specialist, my job is to treat the patient at their level, in their framework, in their comfort zone,” said Dr. Goldberg. Some patients don’t want to take medications for hair loss, so she might recommend supplements in those cases but tells patients that they aren’t well studied.
She added that it can be hard to tell whether a supplement is working, particularly if it has multiple ingredients.
Dr. Mostaghimi reported consulting fees from Pfizer, Concert, Lilly, Hims and Hers, Equillium, AbbVie, Digital Diagnostics, and Bioniz and grants from Pfizer, all outside the submitted work. In addition, Dr. Mostaghimi disclosed that he is an associate editor of JAMA Dermatology but was not involved in any of the decisions regarding the review of the manuscript or its acceptance. No other disclosures were reported by the other study authors. Dr. Goldberg reported no disclosures. Dr. Simmons-O›Brien is a medical consultant for Isdin, but not for hair products.
A version of this article first appeared on Medscape.com.
because of small sample sizes, heterogeneity of hair loss types in study subjects, or other limitations.
The review, published online in JAMA Dermatology, notes that “Twelve of the 20 nutritional interventions had high-quality studies suggesting objectively evaluated effectiveness.”
It is “ground breaking,” in part because of its breadth and depth, said Eva Simmons-O’Brien, MD, a dermatologist in Towson, Md., who often recommends supplements for her patients with hair loss. “It basically kind of vindicates what some of us have been doing for a number of years in terms of treating hair loss,” she told this news organization. “It should hopefully make it more commonplace for dermatologists to consider using nutritional supplements as an adjuvant to treating hair loss,” added Dr. Simmons-O’Brien.
The review “is very helpful,” agreed Lynne J. Goldberg, MD, professor of dermatology and pathology and laboratory medicine at Boston University. Dr. Goldberg noted that many patients are already taking supplements and want to know whether they are safe and effective. The review “points out what the problems are; it talks about what the individual ingredients are and what they do, what the problems are; and it concluded that some people may find these helpful. Which is exactly what I tell my patients,” said Dr. Goldberg, who is also director of the Hair Clinic at Boston Medical Center.
“For patients who are highly motivated and eager to try this, we’re hoping that this systematic review serves as a foundation to have a conversation,” study coauthor Arash Mostaghimi, MD, MPA, MPH, of the department of dermatology at Harvard Medical School, told this news organization. “When there’s medical uncertainty and the question is how much risk is one willing to take, the most important thing to do is to present the data and engage in shared decision-making with the patient,” noted Dr. Mostaghimi, who is also director of the inpatient dermatology consult service at Brigham and Women’s Hospital, Boston.
Surprising effectiveness
Going into the study, “we felt it would be likely that majority of nutritional supplements would either not be effective or not studied,” he said.
Dr. Mostaghimi and his coauthors conducted the study because so many patients take nutritional supplements to address hair loss, he said. An initial literature survey yielded more than 6,300 citations, but after screening and reviews, the authors included 30 articles for evaluation.
The review begins with a look at studies of saw palmetto (Serenoa repens), a botanical compound thought to inhibit the enzyme 5-alpha reductase (5AR), which converts testosterone to dihydroxytestosterone (DHT). DHT is a mediator of androgenic alopecia (AGA). The studies suggest that the compound might stabilize hair loss, “although its effect is likely less than that of finasteride,” write the authors. They also note that side effects associated with finasteride, such as sexual dysfunction, were also observed with saw palmetto “but to a lesser extent.”
For AGA, pumpkin seed oil may also be effective and a “potential alternative” to finasteride for AGA, and Forti5, a nutritional supplement that includes botanical 5AR inhibitors and other ingredients, had favorable effects in one study, the authors write. But neither has been compared to finasteride, and the Forti5 study lacked a control group.
The review also examines the micronutrients vitamin D, zinc, B vitamins, and antioxidants. Low levels of vitamin D have been associated with alopecia areata (AA), AGA, and telogen effluvium (TE) in some studies, and zinc deficiencies have been associated with TE, hair breakage, and thinning, according to the review. A single-arm vitamin D study showed improved results at 6 months for women with TE, but there was no control group and TE is self-resolving, the authors add. Studies in patients with normal zinc levels at baseline who had AA or hair loss showed significant hair regrowth and increased hair thickness and density, but the trials were a mishmash of controls and no controls and relied on self-perceived hair-loss data.
Larger more rigorous studies should be done to evaluate zinc’s effectiveness with AA, the authors comment.
Many patients take vitamin B7 (biotin) for hair loss. It has not been studied on its own but was an ingredient in some supplements in the review. Dr. Simmons-O’Brien said that biotin won’t result in new hair growth but that it can help strengthen the new hairs that grow as a result of other therapies. Both she and the study authors note that the Food and Drug Administration has warned against biotin supplementation because it can interfere with troponin and other test results.
The review also finds that immunomodulators –such as Chinese herbal extracts from paeony and glycyrrhizin – were effective in severe AA. Growth hormone modulators targeting deficiencies in insulin growth factor 1 or growth hormone are also promising. Studies of the modulators capsaicin and isoflavones – used topically – spurred hair growth, the authors write.
Products containing marine protein supplements, including Viviscal and Nourkrin, appeared effective in increasing hair counts in men and women, but the studies were funded by the manufacturer and were not well controlled. Side effects with Viviscal included bloating, according to the review.
The multi-ingredient supplements Nutrafol, Omni-Three, Apple Nutraceutical, and Lambdapil were also included in the review. Only Omni-Three showed no effectiveness, but studies of the other supplements had various limitations, including lack of controls and small sample sizes.
Complicated problem, multiple solutions
Given the many reasons for hair loss, multiple solutions are needed, the dermatologists note.
Dr. Mostaghimi said that he’s still a bit skeptical that supplements work as consistently as described or as well as described, given that he and his coauthors were unable to find any negative studies. In talking with patients who are taking supplements, he said that his first aim is to make sure they are safe. At least the supplements in the review have been studied for safety, he added.
He will encourage replacement of vitamin D or zinc or other vitamins or minerals if patients are deficient but said that he does not “actively encourage supplementation.”
Dr. Simmons-O’Brien said that, when evaluating patients with hair loss, she orders lab tests to determine whether the patient has anemia or a thyroid issue or deficiencies in vitamins or minerals or other nutritional deficiencies, asks about diet and styling practices, and takes a scalp biopsy. It is not uncommon to recommend supplementation on the basis of those findings, she added.
“As a hair-loss specialist, my job is to treat the patient at their level, in their framework, in their comfort zone,” said Dr. Goldberg. Some patients don’t want to take medications for hair loss, so she might recommend supplements in those cases but tells patients that they aren’t well studied.
She added that it can be hard to tell whether a supplement is working, particularly if it has multiple ingredients.
Dr. Mostaghimi reported consulting fees from Pfizer, Concert, Lilly, Hims and Hers, Equillium, AbbVie, Digital Diagnostics, and Bioniz and grants from Pfizer, all outside the submitted work. In addition, Dr. Mostaghimi disclosed that he is an associate editor of JAMA Dermatology but was not involved in any of the decisions regarding the review of the manuscript or its acceptance. No other disclosures were reported by the other study authors. Dr. Goldberg reported no disclosures. Dr. Simmons-O›Brien is a medical consultant for Isdin, but not for hair products.
A version of this article first appeared on Medscape.com.
because of small sample sizes, heterogeneity of hair loss types in study subjects, or other limitations.
The review, published online in JAMA Dermatology, notes that “Twelve of the 20 nutritional interventions had high-quality studies suggesting objectively evaluated effectiveness.”
It is “ground breaking,” in part because of its breadth and depth, said Eva Simmons-O’Brien, MD, a dermatologist in Towson, Md., who often recommends supplements for her patients with hair loss. “It basically kind of vindicates what some of us have been doing for a number of years in terms of treating hair loss,” she told this news organization. “It should hopefully make it more commonplace for dermatologists to consider using nutritional supplements as an adjuvant to treating hair loss,” added Dr. Simmons-O’Brien.
The review “is very helpful,” agreed Lynne J. Goldberg, MD, professor of dermatology and pathology and laboratory medicine at Boston University. Dr. Goldberg noted that many patients are already taking supplements and want to know whether they are safe and effective. The review “points out what the problems are; it talks about what the individual ingredients are and what they do, what the problems are; and it concluded that some people may find these helpful. Which is exactly what I tell my patients,” said Dr. Goldberg, who is also director of the Hair Clinic at Boston Medical Center.
“For patients who are highly motivated and eager to try this, we’re hoping that this systematic review serves as a foundation to have a conversation,” study coauthor Arash Mostaghimi, MD, MPA, MPH, of the department of dermatology at Harvard Medical School, told this news organization. “When there’s medical uncertainty and the question is how much risk is one willing to take, the most important thing to do is to present the data and engage in shared decision-making with the patient,” noted Dr. Mostaghimi, who is also director of the inpatient dermatology consult service at Brigham and Women’s Hospital, Boston.
Surprising effectiveness
Going into the study, “we felt it would be likely that majority of nutritional supplements would either not be effective or not studied,” he said.
Dr. Mostaghimi and his coauthors conducted the study because so many patients take nutritional supplements to address hair loss, he said. An initial literature survey yielded more than 6,300 citations, but after screening and reviews, the authors included 30 articles for evaluation.
The review begins with a look at studies of saw palmetto (Serenoa repens), a botanical compound thought to inhibit the enzyme 5-alpha reductase (5AR), which converts testosterone to dihydroxytestosterone (DHT). DHT is a mediator of androgenic alopecia (AGA). The studies suggest that the compound might stabilize hair loss, “although its effect is likely less than that of finasteride,” write the authors. They also note that side effects associated with finasteride, such as sexual dysfunction, were also observed with saw palmetto “but to a lesser extent.”
For AGA, pumpkin seed oil may also be effective and a “potential alternative” to finasteride for AGA, and Forti5, a nutritional supplement that includes botanical 5AR inhibitors and other ingredients, had favorable effects in one study, the authors write. But neither has been compared to finasteride, and the Forti5 study lacked a control group.
The review also examines the micronutrients vitamin D, zinc, B vitamins, and antioxidants. Low levels of vitamin D have been associated with alopecia areata (AA), AGA, and telogen effluvium (TE) in some studies, and zinc deficiencies have been associated with TE, hair breakage, and thinning, according to the review. A single-arm vitamin D study showed improved results at 6 months for women with TE, but there was no control group and TE is self-resolving, the authors add. Studies in patients with normal zinc levels at baseline who had AA or hair loss showed significant hair regrowth and increased hair thickness and density, but the trials were a mishmash of controls and no controls and relied on self-perceived hair-loss data.
Larger more rigorous studies should be done to evaluate zinc’s effectiveness with AA, the authors comment.
Many patients take vitamin B7 (biotin) for hair loss. It has not been studied on its own but was an ingredient in some supplements in the review. Dr. Simmons-O’Brien said that biotin won’t result in new hair growth but that it can help strengthen the new hairs that grow as a result of other therapies. Both she and the study authors note that the Food and Drug Administration has warned against biotin supplementation because it can interfere with troponin and other test results.
The review also finds that immunomodulators –such as Chinese herbal extracts from paeony and glycyrrhizin – were effective in severe AA. Growth hormone modulators targeting deficiencies in insulin growth factor 1 or growth hormone are also promising. Studies of the modulators capsaicin and isoflavones – used topically – spurred hair growth, the authors write.
Products containing marine protein supplements, including Viviscal and Nourkrin, appeared effective in increasing hair counts in men and women, but the studies were funded by the manufacturer and were not well controlled. Side effects with Viviscal included bloating, according to the review.
The multi-ingredient supplements Nutrafol, Omni-Three, Apple Nutraceutical, and Lambdapil were also included in the review. Only Omni-Three showed no effectiveness, but studies of the other supplements had various limitations, including lack of controls and small sample sizes.
Complicated problem, multiple solutions
Given the many reasons for hair loss, multiple solutions are needed, the dermatologists note.
Dr. Mostaghimi said that he’s still a bit skeptical that supplements work as consistently as described or as well as described, given that he and his coauthors were unable to find any negative studies. In talking with patients who are taking supplements, he said that his first aim is to make sure they are safe. At least the supplements in the review have been studied for safety, he added.
He will encourage replacement of vitamin D or zinc or other vitamins or minerals if patients are deficient but said that he does not “actively encourage supplementation.”
Dr. Simmons-O’Brien said that, when evaluating patients with hair loss, she orders lab tests to determine whether the patient has anemia or a thyroid issue or deficiencies in vitamins or minerals or other nutritional deficiencies, asks about diet and styling practices, and takes a scalp biopsy. It is not uncommon to recommend supplementation on the basis of those findings, she added.
“As a hair-loss specialist, my job is to treat the patient at their level, in their framework, in their comfort zone,” said Dr. Goldberg. Some patients don’t want to take medications for hair loss, so she might recommend supplements in those cases but tells patients that they aren’t well studied.
She added that it can be hard to tell whether a supplement is working, particularly if it has multiple ingredients.
Dr. Mostaghimi reported consulting fees from Pfizer, Concert, Lilly, Hims and Hers, Equillium, AbbVie, Digital Diagnostics, and Bioniz and grants from Pfizer, all outside the submitted work. In addition, Dr. Mostaghimi disclosed that he is an associate editor of JAMA Dermatology but was not involved in any of the decisions regarding the review of the manuscript or its acceptance. No other disclosures were reported by the other study authors. Dr. Goldberg reported no disclosures. Dr. Simmons-O›Brien is a medical consultant for Isdin, but not for hair products.
A version of this article first appeared on Medscape.com.
Knee lesion that bleeds
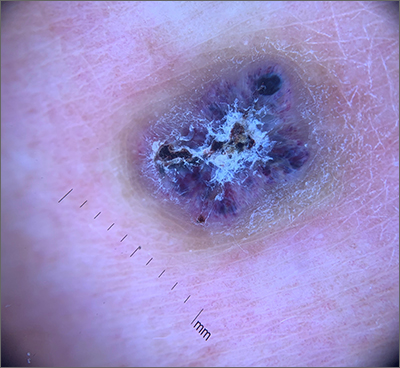
This combination of vascular features with excess keratin fit perfectly with the name of the diagnosis: angiokeratoma. The dark color of the lesion on magnification, or in this case with dermoscopy, showed the lacunar pattern of dilated vessels. The overlying keratin was likely accentuated because it was on an extensor surface; the rim of hyperpigmentation is common for these lesions.
Angiokeratomas result from dilation of the blood vessels underneath the epidermis. There are different inciting events that lead to the 5 different types of angiokeratomas. The overlying epidermal changes are secondary to the underlying process of capillary ectasia.1 This lesion was not part of a cluster, so it was characterized as a solitary angiokeratoma. Smaller lesions are usually less keratinized and are commonly seen on the scrotum and vulva, where there are usually multiple lesions (referred to as angiokeratoma of Fordyce).
Zaballos2 studied the dermoscopic characteristics of 32 solitary angiokeratomas and reported 6 findings in at least half of the solitary lesions. The most common features were dark lacunae in 94% of the lesions, white veil in 91%, and erythema in 69%. Peripheral erythema, red lacunae, and hemorrhagic crusts were all seen at a rate of 53%. The most common location was the lower extremities.
This patient’s previous pathology report from a shave biopsy was found, confirming that the original diagnosis was angiokeratoma. Since the patient’s lesion had not resolved and was symptomatic from minor trauma, he was scheduled to come back in for an elliptical excision to remove the lesion.
Image and text courtesy of Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.
1. Schiller PI, Itin PH. Angiokeratomas: an update. Dermatology. 1996;193:275-282. doi: 10.1159/000246270
2. Zaballos P, Daufí C, Puig S, et al. Dermoscopy of solitary angiokeratomas: a morphological study. Arch Dermatol. 2007;143:318–325. doi:10.1001/archderm.143.3.318
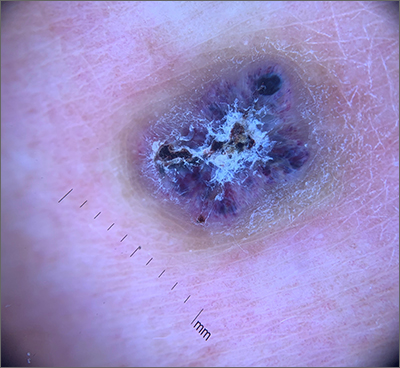
This combination of vascular features with excess keratin fit perfectly with the name of the diagnosis: angiokeratoma. The dark color of the lesion on magnification, or in this case with dermoscopy, showed the lacunar pattern of dilated vessels. The overlying keratin was likely accentuated because it was on an extensor surface; the rim of hyperpigmentation is common for these lesions.
Angiokeratomas result from dilation of the blood vessels underneath the epidermis. There are different inciting events that lead to the 5 different types of angiokeratomas. The overlying epidermal changes are secondary to the underlying process of capillary ectasia.1 This lesion was not part of a cluster, so it was characterized as a solitary angiokeratoma. Smaller lesions are usually less keratinized and are commonly seen on the scrotum and vulva, where there are usually multiple lesions (referred to as angiokeratoma of Fordyce).
Zaballos2 studied the dermoscopic characteristics of 32 solitary angiokeratomas and reported 6 findings in at least half of the solitary lesions. The most common features were dark lacunae in 94% of the lesions, white veil in 91%, and erythema in 69%. Peripheral erythema, red lacunae, and hemorrhagic crusts were all seen at a rate of 53%. The most common location was the lower extremities.
This patient’s previous pathology report from a shave biopsy was found, confirming that the original diagnosis was angiokeratoma. Since the patient’s lesion had not resolved and was symptomatic from minor trauma, he was scheduled to come back in for an elliptical excision to remove the lesion.
Image and text courtesy of Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.
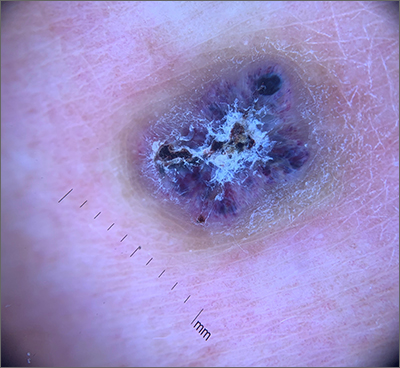
This combination of vascular features with excess keratin fit perfectly with the name of the diagnosis: angiokeratoma. The dark color of the lesion on magnification, or in this case with dermoscopy, showed the lacunar pattern of dilated vessels. The overlying keratin was likely accentuated because it was on an extensor surface; the rim of hyperpigmentation is common for these lesions.
Angiokeratomas result from dilation of the blood vessels underneath the epidermis. There are different inciting events that lead to the 5 different types of angiokeratomas. The overlying epidermal changes are secondary to the underlying process of capillary ectasia.1 This lesion was not part of a cluster, so it was characterized as a solitary angiokeratoma. Smaller lesions are usually less keratinized and are commonly seen on the scrotum and vulva, where there are usually multiple lesions (referred to as angiokeratoma of Fordyce).
Zaballos2 studied the dermoscopic characteristics of 32 solitary angiokeratomas and reported 6 findings in at least half of the solitary lesions. The most common features were dark lacunae in 94% of the lesions, white veil in 91%, and erythema in 69%. Peripheral erythema, red lacunae, and hemorrhagic crusts were all seen at a rate of 53%. The most common location was the lower extremities.
This patient’s previous pathology report from a shave biopsy was found, confirming that the original diagnosis was angiokeratoma. Since the patient’s lesion had not resolved and was symptomatic from minor trauma, he was scheduled to come back in for an elliptical excision to remove the lesion.
Image and text courtesy of Daniel Stulberg, MD, FAAFP, Professor and Chair, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.
1. Schiller PI, Itin PH. Angiokeratomas: an update. Dermatology. 1996;193:275-282. doi: 10.1159/000246270
2. Zaballos P, Daufí C, Puig S, et al. Dermoscopy of solitary angiokeratomas: a morphological study. Arch Dermatol. 2007;143:318–325. doi:10.1001/archderm.143.3.318
1. Schiller PI, Itin PH. Angiokeratomas: an update. Dermatology. 1996;193:275-282. doi: 10.1159/000246270
2. Zaballos P, Daufí C, Puig S, et al. Dermoscopy of solitary angiokeratomas: a morphological study. Arch Dermatol. 2007;143:318–325. doi:10.1001/archderm.143.3.318
‘Meth’ heart failure on the rise, often more severe
a literature review indicates.
MethHF is associated with increased severity for HF, longer inpatient stay, and more readmissions, compared with non-MethHF, the data show.
Clinicians “need to consider methamphetamine as a potential etiology for heart failure and include a substance use history when evaluating patients. Treating methamphetamine use disorder improves heart failure outcomes,” first author Veena Manja, MD, PhD, with Stanford (Calif.) University, said in an interview.
The study was published online in the journal Heart.
Poor outcomes, ‘staggering’ costs
This “thoughtful” review is “important and necessary,” Jonathan Davis, MD, director of the heart failure program, Zuckerberg San Francisco General Hospital, wrote in an editorial in the journal.
Dr. Davis noted that patients with Meth HF are at increased risk for poor outcomes and death and the health care costs related to MethHF are “staggering.”
As an example, inpatient data for California show annual charges related to MethHF rose by 840% from 2008 to 2018, from $41.5 million to $390.2 million, compared with 82% for all HF, which rose from $3.5 billion to $6.8 billion.
Illicit use of methamphetamine – also known as “crystal meth,” “ice,” and “speed” – has been linked to hypertension, MI, stroke, aortic dissection, and sudden death. But until now, there was no comprehensive systematic review of published studies on MethHF.
“Our goal was to compile current knowledge on the topic, increase awareness of this condition and identify areas for future research,” Dr. Manja said.
The researchers reviewed 21 observational studies, mostly from the United States (14 from California), between 1997 and 2020. The mean age of adults with MethHF ranged in age from 35 to 60 and more than half were male (57%).
Illicit methamphetamine was inhaled, injected, swallowed, smoked, and snorted. The reported frequency ranged from daily to every other week, and the total monthly dose ranged from 0.35 g to 24.5 g.
The average duration of meth use before HF diagnosis was 5 years. However, 18% of users developed HF within 1 year of starting to use illicit methamphetamine. In some cases, HF was diagnosed after a single use.
The researchers also note that MethHF with preserved left ventricular ejection fraction, seen in up to 44% of cases, is a distinct entity that may progress to reduced LVEF with continued use.
MethHF is also associated with a greater likelihood of other substance abuse, PTSD, depression, and other heart and kidney disease.
Factors associated with improved MethHF outcomes include female sex, meth abstinence, and adherence to guideline-directed HF therapy.
Improvement in MethHF outcomes is possible even if abstinence is not consistent, a finding that lends support to harm reduction principles of “meeting patients where they are instead of insisting on complete abstinence,” the researchers said.
Large gaps in knowledge
They were unable to combine the results into a meta-analysis because of heterogeneity in study design, population, comparator, and outcome assessment. Also, the overall risk of bias is moderate because of the presence of confounders, selection bias and poor matching, and the overall certainty in the evidence is very low,.
No study evaluated the incidence or prevalence of HF among methamphetamine users and inconsistent history taking and testing in patients with HF impeded accurate MethHF prevalence assessment.
Several studies, however, document an increasing incidence of MethHF, particularly over the past decade.
One study from California reported a 585% increase in MethHF hospital admissions between 2008 and 2018. An analysis of the National Inpatient Survey found a 12-fold increase in annual MethHF hospitalizations between 2002 and 2014.
“The results of this systematic review highlight large gaps in our knowledge” of MethHF, Dr. Manja said in an interview.
“We need to understand the epidemiology, prevalence, factors that confer susceptibility to cardiovascular outcomes, and need research into treatment targeted toward this disease,” Dr. Manja added. “We should consider options to integrate substance use treatment in HF/cardiology/primary care clinics and design a multidisciplinary patient-centered approach.”
Dr. Davis agreed. This work “highlights that the standard of care academically and clinically must be a broad team across the care spectrum to simultaneously address methamphetamine use, heart failure, and social determinants of health.”
This research had no specific funding. Dr. Manja and Dr. Davis reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
a literature review indicates.
MethHF is associated with increased severity for HF, longer inpatient stay, and more readmissions, compared with non-MethHF, the data show.
Clinicians “need to consider methamphetamine as a potential etiology for heart failure and include a substance use history when evaluating patients. Treating methamphetamine use disorder improves heart failure outcomes,” first author Veena Manja, MD, PhD, with Stanford (Calif.) University, said in an interview.
The study was published online in the journal Heart.
Poor outcomes, ‘staggering’ costs
This “thoughtful” review is “important and necessary,” Jonathan Davis, MD, director of the heart failure program, Zuckerberg San Francisco General Hospital, wrote in an editorial in the journal.
Dr. Davis noted that patients with Meth HF are at increased risk for poor outcomes and death and the health care costs related to MethHF are “staggering.”
As an example, inpatient data for California show annual charges related to MethHF rose by 840% from 2008 to 2018, from $41.5 million to $390.2 million, compared with 82% for all HF, which rose from $3.5 billion to $6.8 billion.
Illicit use of methamphetamine – also known as “crystal meth,” “ice,” and “speed” – has been linked to hypertension, MI, stroke, aortic dissection, and sudden death. But until now, there was no comprehensive systematic review of published studies on MethHF.
“Our goal was to compile current knowledge on the topic, increase awareness of this condition and identify areas for future research,” Dr. Manja said.
The researchers reviewed 21 observational studies, mostly from the United States (14 from California), between 1997 and 2020. The mean age of adults with MethHF ranged in age from 35 to 60 and more than half were male (57%).
Illicit methamphetamine was inhaled, injected, swallowed, smoked, and snorted. The reported frequency ranged from daily to every other week, and the total monthly dose ranged from 0.35 g to 24.5 g.
The average duration of meth use before HF diagnosis was 5 years. However, 18% of users developed HF within 1 year of starting to use illicit methamphetamine. In some cases, HF was diagnosed after a single use.
The researchers also note that MethHF with preserved left ventricular ejection fraction, seen in up to 44% of cases, is a distinct entity that may progress to reduced LVEF with continued use.
MethHF is also associated with a greater likelihood of other substance abuse, PTSD, depression, and other heart and kidney disease.
Factors associated with improved MethHF outcomes include female sex, meth abstinence, and adherence to guideline-directed HF therapy.
Improvement in MethHF outcomes is possible even if abstinence is not consistent, a finding that lends support to harm reduction principles of “meeting patients where they are instead of insisting on complete abstinence,” the researchers said.
Large gaps in knowledge
They were unable to combine the results into a meta-analysis because of heterogeneity in study design, population, comparator, and outcome assessment. Also, the overall risk of bias is moderate because of the presence of confounders, selection bias and poor matching, and the overall certainty in the evidence is very low,.
No study evaluated the incidence or prevalence of HF among methamphetamine users and inconsistent history taking and testing in patients with HF impeded accurate MethHF prevalence assessment.
Several studies, however, document an increasing incidence of MethHF, particularly over the past decade.
One study from California reported a 585% increase in MethHF hospital admissions between 2008 and 2018. An analysis of the National Inpatient Survey found a 12-fold increase in annual MethHF hospitalizations between 2002 and 2014.
“The results of this systematic review highlight large gaps in our knowledge” of MethHF, Dr. Manja said in an interview.
“We need to understand the epidemiology, prevalence, factors that confer susceptibility to cardiovascular outcomes, and need research into treatment targeted toward this disease,” Dr. Manja added. “We should consider options to integrate substance use treatment in HF/cardiology/primary care clinics and design a multidisciplinary patient-centered approach.”
Dr. Davis agreed. This work “highlights that the standard of care academically and clinically must be a broad team across the care spectrum to simultaneously address methamphetamine use, heart failure, and social determinants of health.”
This research had no specific funding. Dr. Manja and Dr. Davis reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
a literature review indicates.
MethHF is associated with increased severity for HF, longer inpatient stay, and more readmissions, compared with non-MethHF, the data show.
Clinicians “need to consider methamphetamine as a potential etiology for heart failure and include a substance use history when evaluating patients. Treating methamphetamine use disorder improves heart failure outcomes,” first author Veena Manja, MD, PhD, with Stanford (Calif.) University, said in an interview.
The study was published online in the journal Heart.
Poor outcomes, ‘staggering’ costs
This “thoughtful” review is “important and necessary,” Jonathan Davis, MD, director of the heart failure program, Zuckerberg San Francisco General Hospital, wrote in an editorial in the journal.
Dr. Davis noted that patients with Meth HF are at increased risk for poor outcomes and death and the health care costs related to MethHF are “staggering.”
As an example, inpatient data for California show annual charges related to MethHF rose by 840% from 2008 to 2018, from $41.5 million to $390.2 million, compared with 82% for all HF, which rose from $3.5 billion to $6.8 billion.
Illicit use of methamphetamine – also known as “crystal meth,” “ice,” and “speed” – has been linked to hypertension, MI, stroke, aortic dissection, and sudden death. But until now, there was no comprehensive systematic review of published studies on MethHF.
“Our goal was to compile current knowledge on the topic, increase awareness of this condition and identify areas for future research,” Dr. Manja said.
The researchers reviewed 21 observational studies, mostly from the United States (14 from California), between 1997 and 2020. The mean age of adults with MethHF ranged in age from 35 to 60 and more than half were male (57%).
Illicit methamphetamine was inhaled, injected, swallowed, smoked, and snorted. The reported frequency ranged from daily to every other week, and the total monthly dose ranged from 0.35 g to 24.5 g.
The average duration of meth use before HF diagnosis was 5 years. However, 18% of users developed HF within 1 year of starting to use illicit methamphetamine. In some cases, HF was diagnosed after a single use.
The researchers also note that MethHF with preserved left ventricular ejection fraction, seen in up to 44% of cases, is a distinct entity that may progress to reduced LVEF with continued use.
MethHF is also associated with a greater likelihood of other substance abuse, PTSD, depression, and other heart and kidney disease.
Factors associated with improved MethHF outcomes include female sex, meth abstinence, and adherence to guideline-directed HF therapy.
Improvement in MethHF outcomes is possible even if abstinence is not consistent, a finding that lends support to harm reduction principles of “meeting patients where they are instead of insisting on complete abstinence,” the researchers said.
Large gaps in knowledge
They were unable to combine the results into a meta-analysis because of heterogeneity in study design, population, comparator, and outcome assessment. Also, the overall risk of bias is moderate because of the presence of confounders, selection bias and poor matching, and the overall certainty in the evidence is very low,.
No study evaluated the incidence or prevalence of HF among methamphetamine users and inconsistent history taking and testing in patients with HF impeded accurate MethHF prevalence assessment.
Several studies, however, document an increasing incidence of MethHF, particularly over the past decade.
One study from California reported a 585% increase in MethHF hospital admissions between 2008 and 2018. An analysis of the National Inpatient Survey found a 12-fold increase in annual MethHF hospitalizations between 2002 and 2014.
“The results of this systematic review highlight large gaps in our knowledge” of MethHF, Dr. Manja said in an interview.
“We need to understand the epidemiology, prevalence, factors that confer susceptibility to cardiovascular outcomes, and need research into treatment targeted toward this disease,” Dr. Manja added. “We should consider options to integrate substance use treatment in HF/cardiology/primary care clinics and design a multidisciplinary patient-centered approach.”
Dr. Davis agreed. This work “highlights that the standard of care academically and clinically must be a broad team across the care spectrum to simultaneously address methamphetamine use, heart failure, and social determinants of health.”
This research had no specific funding. Dr. Manja and Dr. Davis reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM HEART
Vaccination cuts long COVID risk for rheumatic disease patients
Patients with rheumatic disease are at least half as likely to develop long COVID after a SARS-CoV-2 infection if they have been fully vaccinated against COVID-19, according to research published in Annals of the Rheumatic Diseases (2022 Nov 28. doi: 10.1136/ard-2022-223439).
“Moreover, those who were vaccinated prior to getting COVID-19 had less pain and fatigue after their infection,” Zachary S. Wallace, MD, MSc, an assistant professor of medicine at Harvard Medical School, Boston, and a study author, said in an interview. “These findings reinforce the importance of vaccination in this population.”
Messaging around the value of COVID vaccination has been confusing for some with rheumatic disease “because our concern regarding a blunted response to vaccination has led many patients to think that they do not provide much benefit if they are on immunosuppression,” Dr. Wallace said. “In our cohort, which included many patients on immunosuppression of varying degrees, being vaccinated was quite beneficial.”
Leonard H. Calabrese, DO, director of the R.J. Fasenmyer Center for Clinical Immunology and a professor of medicine at the Cleveland Clinic, said in an interview that the study is an “extremely important contribution to our understanding of COVID-19 and its pattern of recovery in patients with immune-mediated inflammatory diseases [IMIDs].” Remaining unanswered questions are “whether patients with IMIDs develop more frequent PASC [post–acute sequelae of COVID-19] from COVID-19 and, if so, is it milder or more severe, and does it differ in its clinical phenotype?”
Long COVID risk assessed at 4 weeks and 3 months after infection
The researchers prospectively tracked 280 adult patients in the Mass General Brigham health care system in the greater Boston area who had systemic autoimmune rheumatic diseases and had an acute COVID-19 infection between March 2020 and July 2022. Patients were an average 53 years old, and most were White (82%) and female (80%). More than half (59%) had inflammatory arthritis, a quarter (24%) had connective tissue disease, and most others had a vasculitis condition or multiple conditions.
A total of 11% of patients were unvaccinated, 28% were partially vaccinated with one mRNA COVID-19 vaccine dose, and 41% were fully vaccinated with two mRNA vaccine doses or one Johnson & Johnson dose. The 116 fully vaccinated patients were considered to have a breakthrough infection while the other 164 were considered to have a nonbreakthrough infection. The breakthrough and nonbreakthrough groups were similar in terms of age, sex, race, ethnicity, smoking status, and type of rheumatic disease. Comorbidities were also similar, except obesity, which was more common in the non–breakthrough infection group (25%) than the breakthrough infection group (10%).
The researchers queried patients on their COVID-19 symptoms, how long symptoms lasted, treatments they received, and hospitalization details. COVID-19 symptoms assessed included fever, sore throat, new cough, nasal congestion/rhinorrhea, dyspnea, chest pain, rash, myalgia, fatigue/malaise, headache, nausea/vomiting, diarrhea, anosmia, dysgeusia, and joint pain.
Patients completed surveys about symptoms at 4 weeks and 3 months after infection. Long COVID, or PASC, was defined as any persistent symptom at the times assessed.
Vaccinated patients fared better across outcomes
At 4 weeks after infection, 41% of fully vaccinated patients had at least one persistent symptom, compared with 54% of unvaccinated or partially vaccinated patients (P = .04). At 3 months after infection, 21% of fully vaccinated patients had at least one persistent symptom, compared with 41% of unvaccinated or partially vaccinated patients (P < .0001).
Vaccinated patients were half as likely to have long COVID at 4 weeks after infection (adjusted odds ratio, 0.49) and 90% less likely to have long COVID 3 months after infection (aOR, 0.1), after adjustment for age, sex, race, comorbidities, and use of any of four immune-suppressing medications (anti-CD20 monoclonal antibodies, methotrexate, mycophenolate, or glucocorticoids).
Fully vaccinated patients with breakthrough infections had an average 21 additional days without symptoms during follow-up, compared with unvaccinated and partially vaccinated patients (P = .04).
Reduced risk of long COVID did not change for vaccinated patients after sensitivity analyses for those who did not receive nirmatrelvir/ritonavir (Paxlovid) or monoclonal antibodies, those who didn’t receive any COVID-19-related treatment, those who completed their questionnaires within 6 months after infection, and those who were not hospitalized.
“One important message is that among those who did get PASC, the severity appears similar among those with and without a breakthrough infection,” Dr. Wallace said. “This highlights the need for ongoing research to improve recognition, diagnosis, and treatment of PASC.”
Many more breakthrough infections (72%) than nonbreakthrough infections (2%) occurred during Omicron. The authors acknowledged that different variants might play a role in different long COVID risks but said such potential confounding is unlikely to fully explain the results.
“Even with data suggesting that the Omicron variants may be intrinsically less severe, vaccination still has an impact on severity of infection, rates of hospitalization, and other outcomes and thus may play a role in the risk of PASC,” lead author Naomi Patel, MD, an instructor at Harvard Medical School and a rheumatologist at Massachusetts General Hospital, said in an interview. “A study evaluating the proportions with PASC by vaccination status during the time in which a single variant is predominant, such as the early Omicron era, could help to better assess the more isolated impact of vaccination on PASC.”
Dr. Calabrese said he is convinced that Omicron infections are less likely to result in more severe forms of acute COVID than pre-Omicron infections, and he suspects Omicron infections are also less likely to result in long COVID, although less evidence currently supports this hypothesis.
Hospitalization was more common in unvaccinated/partly vaccinated patients than in vaccinated patients (27% vs. 5%; P = .001). Although pain and fatigue were lower in those with breakthrough infections, functional scores and health-related quality of life were similar in both groups.
Some symptoms significantly differed between vaccinated and unvaccinated/partly vaccinated groups, possibly caused partly by different variants. Nasal congestion was more common (73%) in those with breakthrough infections than in those with nonbreakthrough infections (46%; P < .0001). Those who were unvaccinated/partly vaccinated were significantly more likely to have loss of smell (46% vs. 22%) or taste (45% vs. 28%) or to have joint pain (11% vs. 4%).
Treatment with nirmatrelvir/ritonavir was also more common in vaccinated patients (12%) than in unvaccinated/partly vaccinated patients (1%; P < .0001), as was treatment with monoclonal antibodies (34% vs. 8%; P < .0001).
The study was limited by its low diversity and being at a single health care system, the authors said. Study coauthor Jeffrey A. Sparks, MD, MMSc, an assistant professor of medicine at Brigham and Women’s Hospital and Harvard Medical School, said in an interview that the group is planning additional studies as their cohort grows, including “investigating the relationships between COVID-19 and specific rheumatic diseases and immunomodulating medications, expansion of autoimmunity and systemic inflammation, and lung damage among specific patient populations.”
Dr. Calabrese said it will be important for follow-up study of the symptomatic patients to “determine how many of these patients will fit the clinical picture of long COVID or long-haul phenotypes over the months and years ahead, including documenting exertional malaise and quality of life.
This study only assessed patients who received zero, one, or two doses of a vaccine, but many patients with rheumatic disease today will likely have received booster doses. However, Dr. Calabrese said it would be difficult to quantify whether a third, fourth, or fifth dose offers additional protection from long-term COVID complications after full vaccination or hybrid vaccination.
The research was funded by the Rheumatology Research Foundation, the National Institutes of Health, the R. Bruce and Joan M. Mickey Research Scholar Fund, and the Llura Gund Award for Rheumatoid Arthritis Research and Care. Dr. Wallace has received research support from Bristol-Myers Squibb and Principia/Sanofi and consulting fees from Zenas BioPharma, Horizon, Sanofi, Shionogi, Viela Bio, and Medpace. Dr. Sparks has received research support from Bristol-Myers Squibb and consulting fees from AbbVie, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Gilead, Inova Diagnostics, Janssen, Optum, and Pfizer. Dr. Patel has received consulting fees from FVC Health. Calabrese has consulted for Genentech, Sanofi-Regeneron, AstraZeneca, and GlaxoSmithKline.
A version of this article first appeared on Medscape.com.
Patients with rheumatic disease are at least half as likely to develop long COVID after a SARS-CoV-2 infection if they have been fully vaccinated against COVID-19, according to research published in Annals of the Rheumatic Diseases (2022 Nov 28. doi: 10.1136/ard-2022-223439).
“Moreover, those who were vaccinated prior to getting COVID-19 had less pain and fatigue after their infection,” Zachary S. Wallace, MD, MSc, an assistant professor of medicine at Harvard Medical School, Boston, and a study author, said in an interview. “These findings reinforce the importance of vaccination in this population.”
Messaging around the value of COVID vaccination has been confusing for some with rheumatic disease “because our concern regarding a blunted response to vaccination has led many patients to think that they do not provide much benefit if they are on immunosuppression,” Dr. Wallace said. “In our cohort, which included many patients on immunosuppression of varying degrees, being vaccinated was quite beneficial.”
Leonard H. Calabrese, DO, director of the R.J. Fasenmyer Center for Clinical Immunology and a professor of medicine at the Cleveland Clinic, said in an interview that the study is an “extremely important contribution to our understanding of COVID-19 and its pattern of recovery in patients with immune-mediated inflammatory diseases [IMIDs].” Remaining unanswered questions are “whether patients with IMIDs develop more frequent PASC [post–acute sequelae of COVID-19] from COVID-19 and, if so, is it milder or more severe, and does it differ in its clinical phenotype?”
Long COVID risk assessed at 4 weeks and 3 months after infection
The researchers prospectively tracked 280 adult patients in the Mass General Brigham health care system in the greater Boston area who had systemic autoimmune rheumatic diseases and had an acute COVID-19 infection between March 2020 and July 2022. Patients were an average 53 years old, and most were White (82%) and female (80%). More than half (59%) had inflammatory arthritis, a quarter (24%) had connective tissue disease, and most others had a vasculitis condition or multiple conditions.
A total of 11% of patients were unvaccinated, 28% were partially vaccinated with one mRNA COVID-19 vaccine dose, and 41% were fully vaccinated with two mRNA vaccine doses or one Johnson & Johnson dose. The 116 fully vaccinated patients were considered to have a breakthrough infection while the other 164 were considered to have a nonbreakthrough infection. The breakthrough and nonbreakthrough groups were similar in terms of age, sex, race, ethnicity, smoking status, and type of rheumatic disease. Comorbidities were also similar, except obesity, which was more common in the non–breakthrough infection group (25%) than the breakthrough infection group (10%).
The researchers queried patients on their COVID-19 symptoms, how long symptoms lasted, treatments they received, and hospitalization details. COVID-19 symptoms assessed included fever, sore throat, new cough, nasal congestion/rhinorrhea, dyspnea, chest pain, rash, myalgia, fatigue/malaise, headache, nausea/vomiting, diarrhea, anosmia, dysgeusia, and joint pain.
Patients completed surveys about symptoms at 4 weeks and 3 months after infection. Long COVID, or PASC, was defined as any persistent symptom at the times assessed.
Vaccinated patients fared better across outcomes
At 4 weeks after infection, 41% of fully vaccinated patients had at least one persistent symptom, compared with 54% of unvaccinated or partially vaccinated patients (P = .04). At 3 months after infection, 21% of fully vaccinated patients had at least one persistent symptom, compared with 41% of unvaccinated or partially vaccinated patients (P < .0001).
Vaccinated patients were half as likely to have long COVID at 4 weeks after infection (adjusted odds ratio, 0.49) and 90% less likely to have long COVID 3 months after infection (aOR, 0.1), after adjustment for age, sex, race, comorbidities, and use of any of four immune-suppressing medications (anti-CD20 monoclonal antibodies, methotrexate, mycophenolate, or glucocorticoids).
Fully vaccinated patients with breakthrough infections had an average 21 additional days without symptoms during follow-up, compared with unvaccinated and partially vaccinated patients (P = .04).
Reduced risk of long COVID did not change for vaccinated patients after sensitivity analyses for those who did not receive nirmatrelvir/ritonavir (Paxlovid) or monoclonal antibodies, those who didn’t receive any COVID-19-related treatment, those who completed their questionnaires within 6 months after infection, and those who were not hospitalized.
“One important message is that among those who did get PASC, the severity appears similar among those with and without a breakthrough infection,” Dr. Wallace said. “This highlights the need for ongoing research to improve recognition, diagnosis, and treatment of PASC.”
Many more breakthrough infections (72%) than nonbreakthrough infections (2%) occurred during Omicron. The authors acknowledged that different variants might play a role in different long COVID risks but said such potential confounding is unlikely to fully explain the results.
“Even with data suggesting that the Omicron variants may be intrinsically less severe, vaccination still has an impact on severity of infection, rates of hospitalization, and other outcomes and thus may play a role in the risk of PASC,” lead author Naomi Patel, MD, an instructor at Harvard Medical School and a rheumatologist at Massachusetts General Hospital, said in an interview. “A study evaluating the proportions with PASC by vaccination status during the time in which a single variant is predominant, such as the early Omicron era, could help to better assess the more isolated impact of vaccination on PASC.”
Dr. Calabrese said he is convinced that Omicron infections are less likely to result in more severe forms of acute COVID than pre-Omicron infections, and he suspects Omicron infections are also less likely to result in long COVID, although less evidence currently supports this hypothesis.
Hospitalization was more common in unvaccinated/partly vaccinated patients than in vaccinated patients (27% vs. 5%; P = .001). Although pain and fatigue were lower in those with breakthrough infections, functional scores and health-related quality of life were similar in both groups.
Some symptoms significantly differed between vaccinated and unvaccinated/partly vaccinated groups, possibly caused partly by different variants. Nasal congestion was more common (73%) in those with breakthrough infections than in those with nonbreakthrough infections (46%; P < .0001). Those who were unvaccinated/partly vaccinated were significantly more likely to have loss of smell (46% vs. 22%) or taste (45% vs. 28%) or to have joint pain (11% vs. 4%).
Treatment with nirmatrelvir/ritonavir was also more common in vaccinated patients (12%) than in unvaccinated/partly vaccinated patients (1%; P < .0001), as was treatment with monoclonal antibodies (34% vs. 8%; P < .0001).
The study was limited by its low diversity and being at a single health care system, the authors said. Study coauthor Jeffrey A. Sparks, MD, MMSc, an assistant professor of medicine at Brigham and Women’s Hospital and Harvard Medical School, said in an interview that the group is planning additional studies as their cohort grows, including “investigating the relationships between COVID-19 and specific rheumatic diseases and immunomodulating medications, expansion of autoimmunity and systemic inflammation, and lung damage among specific patient populations.”
Dr. Calabrese said it will be important for follow-up study of the symptomatic patients to “determine how many of these patients will fit the clinical picture of long COVID or long-haul phenotypes over the months and years ahead, including documenting exertional malaise and quality of life.
This study only assessed patients who received zero, one, or two doses of a vaccine, but many patients with rheumatic disease today will likely have received booster doses. However, Dr. Calabrese said it would be difficult to quantify whether a third, fourth, or fifth dose offers additional protection from long-term COVID complications after full vaccination or hybrid vaccination.
The research was funded by the Rheumatology Research Foundation, the National Institutes of Health, the R. Bruce and Joan M. Mickey Research Scholar Fund, and the Llura Gund Award for Rheumatoid Arthritis Research and Care. Dr. Wallace has received research support from Bristol-Myers Squibb and Principia/Sanofi and consulting fees from Zenas BioPharma, Horizon, Sanofi, Shionogi, Viela Bio, and Medpace. Dr. Sparks has received research support from Bristol-Myers Squibb and consulting fees from AbbVie, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Gilead, Inova Diagnostics, Janssen, Optum, and Pfizer. Dr. Patel has received consulting fees from FVC Health. Calabrese has consulted for Genentech, Sanofi-Regeneron, AstraZeneca, and GlaxoSmithKline.
A version of this article first appeared on Medscape.com.
Patients with rheumatic disease are at least half as likely to develop long COVID after a SARS-CoV-2 infection if they have been fully vaccinated against COVID-19, according to research published in Annals of the Rheumatic Diseases (2022 Nov 28. doi: 10.1136/ard-2022-223439).
“Moreover, those who were vaccinated prior to getting COVID-19 had less pain and fatigue after their infection,” Zachary S. Wallace, MD, MSc, an assistant professor of medicine at Harvard Medical School, Boston, and a study author, said in an interview. “These findings reinforce the importance of vaccination in this population.”
Messaging around the value of COVID vaccination has been confusing for some with rheumatic disease “because our concern regarding a blunted response to vaccination has led many patients to think that they do not provide much benefit if they are on immunosuppression,” Dr. Wallace said. “In our cohort, which included many patients on immunosuppression of varying degrees, being vaccinated was quite beneficial.”
Leonard H. Calabrese, DO, director of the R.J. Fasenmyer Center for Clinical Immunology and a professor of medicine at the Cleveland Clinic, said in an interview that the study is an “extremely important contribution to our understanding of COVID-19 and its pattern of recovery in patients with immune-mediated inflammatory diseases [IMIDs].” Remaining unanswered questions are “whether patients with IMIDs develop more frequent PASC [post–acute sequelae of COVID-19] from COVID-19 and, if so, is it milder or more severe, and does it differ in its clinical phenotype?”
Long COVID risk assessed at 4 weeks and 3 months after infection
The researchers prospectively tracked 280 adult patients in the Mass General Brigham health care system in the greater Boston area who had systemic autoimmune rheumatic diseases and had an acute COVID-19 infection between March 2020 and July 2022. Patients were an average 53 years old, and most were White (82%) and female (80%). More than half (59%) had inflammatory arthritis, a quarter (24%) had connective tissue disease, and most others had a vasculitis condition or multiple conditions.
A total of 11% of patients were unvaccinated, 28% were partially vaccinated with one mRNA COVID-19 vaccine dose, and 41% were fully vaccinated with two mRNA vaccine doses or one Johnson & Johnson dose. The 116 fully vaccinated patients were considered to have a breakthrough infection while the other 164 were considered to have a nonbreakthrough infection. The breakthrough and nonbreakthrough groups were similar in terms of age, sex, race, ethnicity, smoking status, and type of rheumatic disease. Comorbidities were also similar, except obesity, which was more common in the non–breakthrough infection group (25%) than the breakthrough infection group (10%).
The researchers queried patients on their COVID-19 symptoms, how long symptoms lasted, treatments they received, and hospitalization details. COVID-19 symptoms assessed included fever, sore throat, new cough, nasal congestion/rhinorrhea, dyspnea, chest pain, rash, myalgia, fatigue/malaise, headache, nausea/vomiting, diarrhea, anosmia, dysgeusia, and joint pain.
Patients completed surveys about symptoms at 4 weeks and 3 months after infection. Long COVID, or PASC, was defined as any persistent symptom at the times assessed.
Vaccinated patients fared better across outcomes
At 4 weeks after infection, 41% of fully vaccinated patients had at least one persistent symptom, compared with 54% of unvaccinated or partially vaccinated patients (P = .04). At 3 months after infection, 21% of fully vaccinated patients had at least one persistent symptom, compared with 41% of unvaccinated or partially vaccinated patients (P < .0001).
Vaccinated patients were half as likely to have long COVID at 4 weeks after infection (adjusted odds ratio, 0.49) and 90% less likely to have long COVID 3 months after infection (aOR, 0.1), after adjustment for age, sex, race, comorbidities, and use of any of four immune-suppressing medications (anti-CD20 monoclonal antibodies, methotrexate, mycophenolate, or glucocorticoids).
Fully vaccinated patients with breakthrough infections had an average 21 additional days without symptoms during follow-up, compared with unvaccinated and partially vaccinated patients (P = .04).
Reduced risk of long COVID did not change for vaccinated patients after sensitivity analyses for those who did not receive nirmatrelvir/ritonavir (Paxlovid) or monoclonal antibodies, those who didn’t receive any COVID-19-related treatment, those who completed their questionnaires within 6 months after infection, and those who were not hospitalized.
“One important message is that among those who did get PASC, the severity appears similar among those with and without a breakthrough infection,” Dr. Wallace said. “This highlights the need for ongoing research to improve recognition, diagnosis, and treatment of PASC.”
Many more breakthrough infections (72%) than nonbreakthrough infections (2%) occurred during Omicron. The authors acknowledged that different variants might play a role in different long COVID risks but said such potential confounding is unlikely to fully explain the results.
“Even with data suggesting that the Omicron variants may be intrinsically less severe, vaccination still has an impact on severity of infection, rates of hospitalization, and other outcomes and thus may play a role in the risk of PASC,” lead author Naomi Patel, MD, an instructor at Harvard Medical School and a rheumatologist at Massachusetts General Hospital, said in an interview. “A study evaluating the proportions with PASC by vaccination status during the time in which a single variant is predominant, such as the early Omicron era, could help to better assess the more isolated impact of vaccination on PASC.”
Dr. Calabrese said he is convinced that Omicron infections are less likely to result in more severe forms of acute COVID than pre-Omicron infections, and he suspects Omicron infections are also less likely to result in long COVID, although less evidence currently supports this hypothesis.
Hospitalization was more common in unvaccinated/partly vaccinated patients than in vaccinated patients (27% vs. 5%; P = .001). Although pain and fatigue were lower in those with breakthrough infections, functional scores and health-related quality of life were similar in both groups.
Some symptoms significantly differed between vaccinated and unvaccinated/partly vaccinated groups, possibly caused partly by different variants. Nasal congestion was more common (73%) in those with breakthrough infections than in those with nonbreakthrough infections (46%; P < .0001). Those who were unvaccinated/partly vaccinated were significantly more likely to have loss of smell (46% vs. 22%) or taste (45% vs. 28%) or to have joint pain (11% vs. 4%).
Treatment with nirmatrelvir/ritonavir was also more common in vaccinated patients (12%) than in unvaccinated/partly vaccinated patients (1%; P < .0001), as was treatment with monoclonal antibodies (34% vs. 8%; P < .0001).
The study was limited by its low diversity and being at a single health care system, the authors said. Study coauthor Jeffrey A. Sparks, MD, MMSc, an assistant professor of medicine at Brigham and Women’s Hospital and Harvard Medical School, said in an interview that the group is planning additional studies as their cohort grows, including “investigating the relationships between COVID-19 and specific rheumatic diseases and immunomodulating medications, expansion of autoimmunity and systemic inflammation, and lung damage among specific patient populations.”
Dr. Calabrese said it will be important for follow-up study of the symptomatic patients to “determine how many of these patients will fit the clinical picture of long COVID or long-haul phenotypes over the months and years ahead, including documenting exertional malaise and quality of life.
This study only assessed patients who received zero, one, or two doses of a vaccine, but many patients with rheumatic disease today will likely have received booster doses. However, Dr. Calabrese said it would be difficult to quantify whether a third, fourth, or fifth dose offers additional protection from long-term COVID complications after full vaccination or hybrid vaccination.
The research was funded by the Rheumatology Research Foundation, the National Institutes of Health, the R. Bruce and Joan M. Mickey Research Scholar Fund, and the Llura Gund Award for Rheumatoid Arthritis Research and Care. Dr. Wallace has received research support from Bristol-Myers Squibb and Principia/Sanofi and consulting fees from Zenas BioPharma, Horizon, Sanofi, Shionogi, Viela Bio, and Medpace. Dr. Sparks has received research support from Bristol-Myers Squibb and consulting fees from AbbVie, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Gilead, Inova Diagnostics, Janssen, Optum, and Pfizer. Dr. Patel has received consulting fees from FVC Health. Calabrese has consulted for Genentech, Sanofi-Regeneron, AstraZeneca, and GlaxoSmithKline.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF THE RHEUMATIC DISEASES
Children and COVID: Hospitalizations provide a tale of two sources
New cases of COVID-19 in children largely held steady over the Thanksgiving holiday, but hospital admissions are telling a somewhat different story.
New pediatric COVID cases for the week ending on Thanksgiving (11/18-11/24) were up by 5.3% over the previous week, but in the most recent week (11/25-12/1) new cases dropped by 2.6%, according to state data collected by the American Academy of Pediatrics and the Children’s Hospital Association.
In both weeks, though, the total case count stayed below 30,000 – a streak that has now lasted 8 weeks – so the actual number of weekly cases remained fairly low, the AAP/CHA weekly report indicates.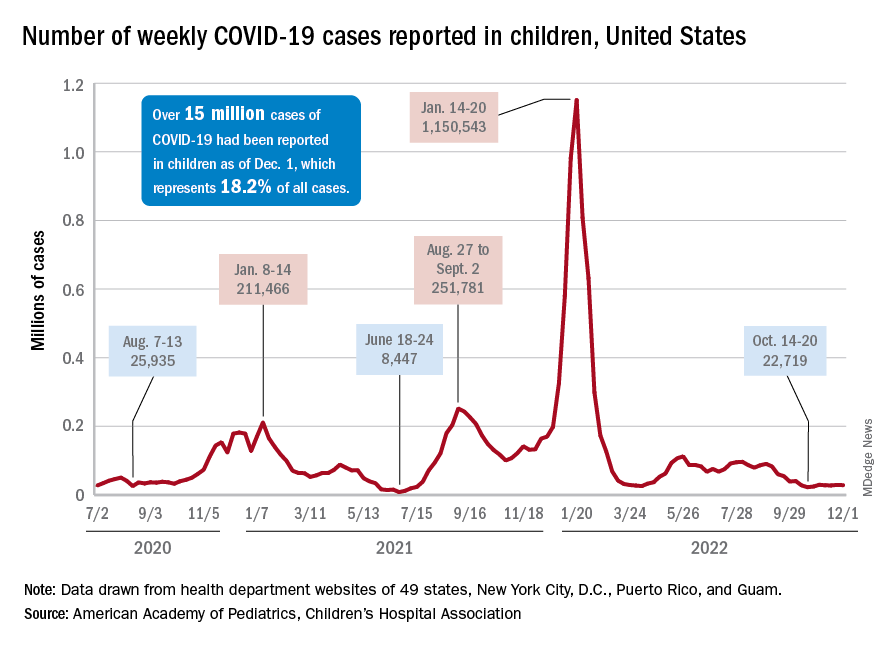
The nation’s emergency departments also experienced a small Thanksgiving bump, as the proportion of visits with diagnosed COVID went from 1.0% of all ED visits for children aged 0-11 years on Nov. 14 to 2.0% on Nov. 27, just 3 days after the official holiday, based on data from the Centers for Disease Control and Prevention. The rate was down to 1.5% on Dec. 1, and similar patterns can be seen for children aged 12-15 and 16-17 years.
New hospital admissions, on the other hand, seem to be following a different path, at least according to the CDC. The hospitalization rate for children aged 0-17 years bottomed out at 0.16 new admissions per 100,000 population back on Oct. 21 and has climbed fairly steadily since then. It was up to 0.20 per 100,000 by Nov. 14, had reached 0.22 per 100,000 on Thanksgiving day (11/24), and then continued to 0.26 per 100,000 by Dec. 2, the latest date for which CDC data are available.
The hospitalization story, however, offers yet another twist. The New York Times, using data from the U.S. Department of Health & Human Services, reports that new COVID-related admissions have held steady at 1.0 per 100,000 since Nov. 18. The rate is much higher than has been reported by the CDC, but no increase can be seen in recent weeks among children, which is not the case for Americans overall, Medscape recently reported.
New cases of COVID-19 in children largely held steady over the Thanksgiving holiday, but hospital admissions are telling a somewhat different story.
New pediatric COVID cases for the week ending on Thanksgiving (11/18-11/24) were up by 5.3% over the previous week, but in the most recent week (11/25-12/1) new cases dropped by 2.6%, according to state data collected by the American Academy of Pediatrics and the Children’s Hospital Association.
In both weeks, though, the total case count stayed below 30,000 – a streak that has now lasted 8 weeks – so the actual number of weekly cases remained fairly low, the AAP/CHA weekly report indicates.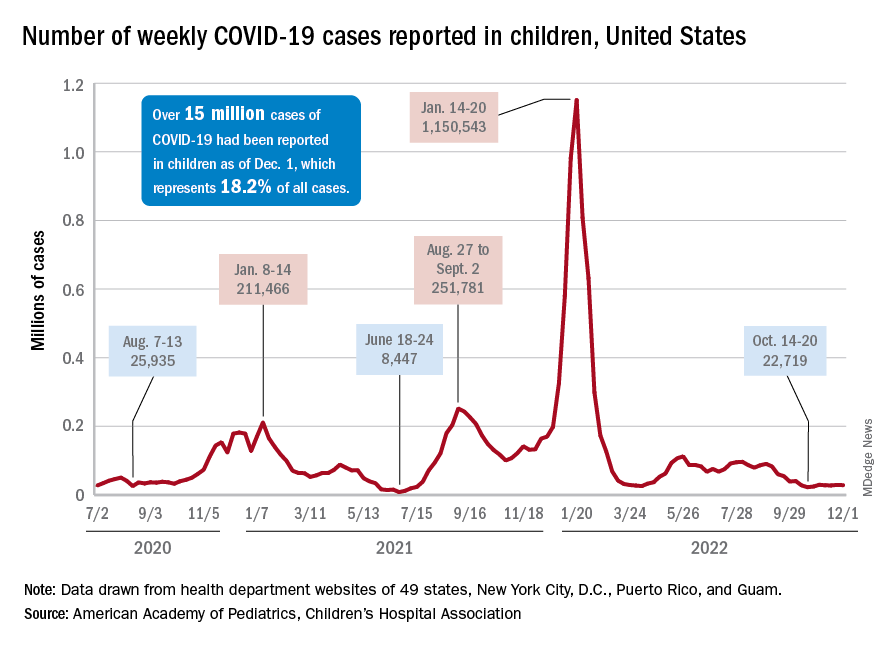
The nation’s emergency departments also experienced a small Thanksgiving bump, as the proportion of visits with diagnosed COVID went from 1.0% of all ED visits for children aged 0-11 years on Nov. 14 to 2.0% on Nov. 27, just 3 days after the official holiday, based on data from the Centers for Disease Control and Prevention. The rate was down to 1.5% on Dec. 1, and similar patterns can be seen for children aged 12-15 and 16-17 years.
New hospital admissions, on the other hand, seem to be following a different path, at least according to the CDC. The hospitalization rate for children aged 0-17 years bottomed out at 0.16 new admissions per 100,000 population back on Oct. 21 and has climbed fairly steadily since then. It was up to 0.20 per 100,000 by Nov. 14, had reached 0.22 per 100,000 on Thanksgiving day (11/24), and then continued to 0.26 per 100,000 by Dec. 2, the latest date for which CDC data are available.
The hospitalization story, however, offers yet another twist. The New York Times, using data from the U.S. Department of Health & Human Services, reports that new COVID-related admissions have held steady at 1.0 per 100,000 since Nov. 18. The rate is much higher than has been reported by the CDC, but no increase can be seen in recent weeks among children, which is not the case for Americans overall, Medscape recently reported.
New cases of COVID-19 in children largely held steady over the Thanksgiving holiday, but hospital admissions are telling a somewhat different story.
New pediatric COVID cases for the week ending on Thanksgiving (11/18-11/24) were up by 5.3% over the previous week, but in the most recent week (11/25-12/1) new cases dropped by 2.6%, according to state data collected by the American Academy of Pediatrics and the Children’s Hospital Association.
In both weeks, though, the total case count stayed below 30,000 – a streak that has now lasted 8 weeks – so the actual number of weekly cases remained fairly low, the AAP/CHA weekly report indicates.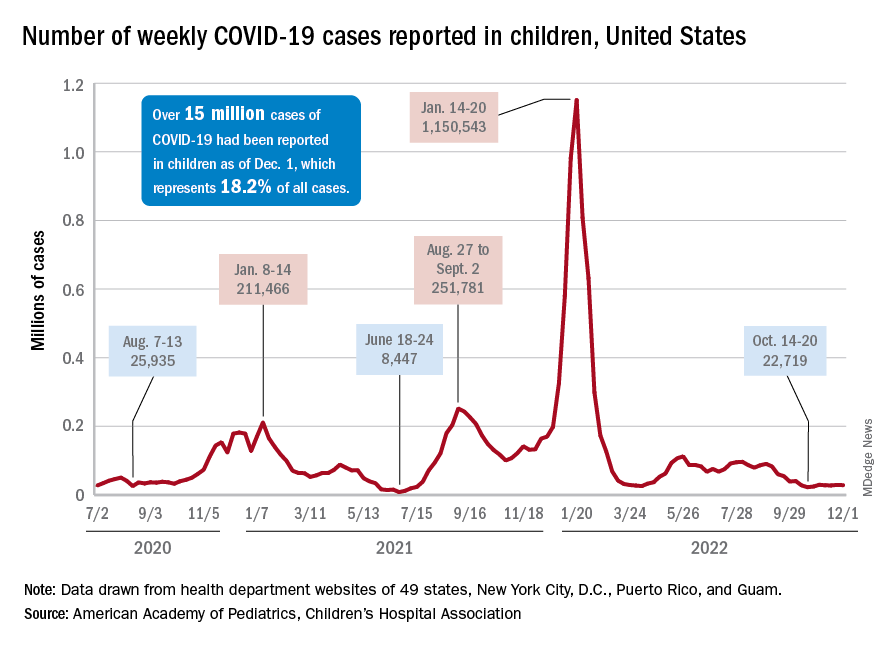
The nation’s emergency departments also experienced a small Thanksgiving bump, as the proportion of visits with diagnosed COVID went from 1.0% of all ED visits for children aged 0-11 years on Nov. 14 to 2.0% on Nov. 27, just 3 days after the official holiday, based on data from the Centers for Disease Control and Prevention. The rate was down to 1.5% on Dec. 1, and similar patterns can be seen for children aged 12-15 and 16-17 years.
New hospital admissions, on the other hand, seem to be following a different path, at least according to the CDC. The hospitalization rate for children aged 0-17 years bottomed out at 0.16 new admissions per 100,000 population back on Oct. 21 and has climbed fairly steadily since then. It was up to 0.20 per 100,000 by Nov. 14, had reached 0.22 per 100,000 on Thanksgiving day (11/24), and then continued to 0.26 per 100,000 by Dec. 2, the latest date for which CDC data are available.
The hospitalization story, however, offers yet another twist. The New York Times, using data from the U.S. Department of Health & Human Services, reports that new COVID-related admissions have held steady at 1.0 per 100,000 since Nov. 18. The rate is much higher than has been reported by the CDC, but no increase can be seen in recent weeks among children, which is not the case for Americans overall, Medscape recently reported.
Youths have strong opinions on language about body weight
With youth obesity on the rise – an estimated 1 in 5 youths are impacted by obesity, according to the Centers for Disease Control and Prevention – conversations about healthy weight are becoming more commonplace, not only in the pediatrician’s office, but at home, too. But the language we use around this sensitive topic is important, as youths are acutely aware that words have a direct impact on their mental health.
Sixteen-year-old Avery DiCocco of Northbrook, Ill., knows how vulnerable teenagers feel.
“I think it definitely matters the way that parents and doctors address weight,” she said. “You never know who may be insecure, and using negative words could go a lot further than they think with impacting self-esteem.”
A new study published in Pediatrics brings light to the words that parents (and providers) use when speaking to youths (ages 10-17) about their weight.
Researchers from the University of Connecticut Rudd Center for Food Policy & Health, Hartford, led an online survey of youths and their parents. Those who took part were asked about 27 terms related to body weight. Parents were asked to comment on their use of these words, while youths commented on the emotional response. The researchers said 1,936 parents and 2,032 adolescents were surveyed between September and December 2021.
Although results skewed toward the use of more positive words, such as “healthy weight,” over terms like “obese,” “fat” or “large,” there was variation across ethnicity, sexual orientation, and weight status. For example, it was noted in the study, funded by WW International, that preference for the word “curvy” was higher among Hispanic/Latino youths, sexual minority youths, and those with a body mass index in the 95th percentile, compared with their White, heterosexual, and lower-weight peers.
Words matter
In 2017, the American Academy of Pediatrics came out with a policy statement on weight stigma and the need for doctors to use more neutral language and less stigmatizing terms in practice when discussing weight among youths.
But one of the reasons this new study is important, said Gregory Germain, MD, associate chief of pediatrics at Yale New Haven (Conn.) Children’s Hospital, is that this study focuses on parents who interact with their kids much more often than a pediatrician who sees them a few times a year.
“Parental motivation, discussion, interaction on a consistent basis – that dialogue is so critical in kids with obesity,” said Germain, who stresses that all adults, coaches, and educators should consider this study as well.
“When we think about those detrimental impacts on mental health when more stigmatizing language is used, just us being more mindful in how we are talking to youth can make such a profound impact,” said Rebecca Kamody, PhD, a clinical psychologist at Yale University, with a research and clinical focus on eating and weight disorders.
“In essence, this is a low-hanging fruit intervention,” she said.
Dr. Kamody recommends we take a lesson from “cultural humility” in psychology to understand how to approach this with kids, calling for “the humbleness as parents or providers in asking someone what they want used to make it the safest place for a discussion with our youth.”
One piece of the puzzle
Dr. Germain and Dr. Kamody agreed that language in discussing this topic is important but that we need to recognize that this topic in general is extremely tricky.
For one, “there are these very real metabolic complications of having high weight at a young age,” said Kamody, who stresses the need for balance to make real change.
Dr. Germain agreed. “Finding a fine line between discussing obesity and not kicking your kid into disordered eating is important.”
The researchers also recognize the limits of an online study, where self-reporting parents may not want to admit using negative weight terminology, but certainly believe it’s a start in identifying some of the undesirable patterns that may be occurring when it comes to weight.
“The overarching message is a positive one, that with our preteens and teenage kids, we need to watch our language, to create a nonjudgmental and safe environment to discuss weight and any issue involved with taking care of themselves,” said Dr. Germain.
A version of this article first appeared on Medscape.com.
With youth obesity on the rise – an estimated 1 in 5 youths are impacted by obesity, according to the Centers for Disease Control and Prevention – conversations about healthy weight are becoming more commonplace, not only in the pediatrician’s office, but at home, too. But the language we use around this sensitive topic is important, as youths are acutely aware that words have a direct impact on their mental health.
Sixteen-year-old Avery DiCocco of Northbrook, Ill., knows how vulnerable teenagers feel.
“I think it definitely matters the way that parents and doctors address weight,” she said. “You never know who may be insecure, and using negative words could go a lot further than they think with impacting self-esteem.”
A new study published in Pediatrics brings light to the words that parents (and providers) use when speaking to youths (ages 10-17) about their weight.
Researchers from the University of Connecticut Rudd Center for Food Policy & Health, Hartford, led an online survey of youths and their parents. Those who took part were asked about 27 terms related to body weight. Parents were asked to comment on their use of these words, while youths commented on the emotional response. The researchers said 1,936 parents and 2,032 adolescents were surveyed between September and December 2021.
Although results skewed toward the use of more positive words, such as “healthy weight,” over terms like “obese,” “fat” or “large,” there was variation across ethnicity, sexual orientation, and weight status. For example, it was noted in the study, funded by WW International, that preference for the word “curvy” was higher among Hispanic/Latino youths, sexual minority youths, and those with a body mass index in the 95th percentile, compared with their White, heterosexual, and lower-weight peers.
Words matter
In 2017, the American Academy of Pediatrics came out with a policy statement on weight stigma and the need for doctors to use more neutral language and less stigmatizing terms in practice when discussing weight among youths.
But one of the reasons this new study is important, said Gregory Germain, MD, associate chief of pediatrics at Yale New Haven (Conn.) Children’s Hospital, is that this study focuses on parents who interact with their kids much more often than a pediatrician who sees them a few times a year.
“Parental motivation, discussion, interaction on a consistent basis – that dialogue is so critical in kids with obesity,” said Germain, who stresses that all adults, coaches, and educators should consider this study as well.
“When we think about those detrimental impacts on mental health when more stigmatizing language is used, just us being more mindful in how we are talking to youth can make such a profound impact,” said Rebecca Kamody, PhD, a clinical psychologist at Yale University, with a research and clinical focus on eating and weight disorders.
“In essence, this is a low-hanging fruit intervention,” she said.
Dr. Kamody recommends we take a lesson from “cultural humility” in psychology to understand how to approach this with kids, calling for “the humbleness as parents or providers in asking someone what they want used to make it the safest place for a discussion with our youth.”
One piece of the puzzle
Dr. Germain and Dr. Kamody agreed that language in discussing this topic is important but that we need to recognize that this topic in general is extremely tricky.
For one, “there are these very real metabolic complications of having high weight at a young age,” said Kamody, who stresses the need for balance to make real change.
Dr. Germain agreed. “Finding a fine line between discussing obesity and not kicking your kid into disordered eating is important.”
The researchers also recognize the limits of an online study, where self-reporting parents may not want to admit using negative weight terminology, but certainly believe it’s a start in identifying some of the undesirable patterns that may be occurring when it comes to weight.
“The overarching message is a positive one, that with our preteens and teenage kids, we need to watch our language, to create a nonjudgmental and safe environment to discuss weight and any issue involved with taking care of themselves,” said Dr. Germain.
A version of this article first appeared on Medscape.com.
With youth obesity on the rise – an estimated 1 in 5 youths are impacted by obesity, according to the Centers for Disease Control and Prevention – conversations about healthy weight are becoming more commonplace, not only in the pediatrician’s office, but at home, too. But the language we use around this sensitive topic is important, as youths are acutely aware that words have a direct impact on their mental health.
Sixteen-year-old Avery DiCocco of Northbrook, Ill., knows how vulnerable teenagers feel.
“I think it definitely matters the way that parents and doctors address weight,” she said. “You never know who may be insecure, and using negative words could go a lot further than they think with impacting self-esteem.”
A new study published in Pediatrics brings light to the words that parents (and providers) use when speaking to youths (ages 10-17) about their weight.
Researchers from the University of Connecticut Rudd Center for Food Policy & Health, Hartford, led an online survey of youths and their parents. Those who took part were asked about 27 terms related to body weight. Parents were asked to comment on their use of these words, while youths commented on the emotional response. The researchers said 1,936 parents and 2,032 adolescents were surveyed between September and December 2021.
Although results skewed toward the use of more positive words, such as “healthy weight,” over terms like “obese,” “fat” or “large,” there was variation across ethnicity, sexual orientation, and weight status. For example, it was noted in the study, funded by WW International, that preference for the word “curvy” was higher among Hispanic/Latino youths, sexual minority youths, and those with a body mass index in the 95th percentile, compared with their White, heterosexual, and lower-weight peers.
Words matter
In 2017, the American Academy of Pediatrics came out with a policy statement on weight stigma and the need for doctors to use more neutral language and less stigmatizing terms in practice when discussing weight among youths.
But one of the reasons this new study is important, said Gregory Germain, MD, associate chief of pediatrics at Yale New Haven (Conn.) Children’s Hospital, is that this study focuses on parents who interact with their kids much more often than a pediatrician who sees them a few times a year.
“Parental motivation, discussion, interaction on a consistent basis – that dialogue is so critical in kids with obesity,” said Germain, who stresses that all adults, coaches, and educators should consider this study as well.
“When we think about those detrimental impacts on mental health when more stigmatizing language is used, just us being more mindful in how we are talking to youth can make such a profound impact,” said Rebecca Kamody, PhD, a clinical psychologist at Yale University, with a research and clinical focus on eating and weight disorders.
“In essence, this is a low-hanging fruit intervention,” she said.
Dr. Kamody recommends we take a lesson from “cultural humility” in psychology to understand how to approach this with kids, calling for “the humbleness as parents or providers in asking someone what they want used to make it the safest place for a discussion with our youth.”
One piece of the puzzle
Dr. Germain and Dr. Kamody agreed that language in discussing this topic is important but that we need to recognize that this topic in general is extremely tricky.
For one, “there are these very real metabolic complications of having high weight at a young age,” said Kamody, who stresses the need for balance to make real change.
Dr. Germain agreed. “Finding a fine line between discussing obesity and not kicking your kid into disordered eating is important.”
The researchers also recognize the limits of an online study, where self-reporting parents may not want to admit using negative weight terminology, but certainly believe it’s a start in identifying some of the undesirable patterns that may be occurring when it comes to weight.
“The overarching message is a positive one, that with our preteens and teenage kids, we need to watch our language, to create a nonjudgmental and safe environment to discuss weight and any issue involved with taking care of themselves,” said Dr. Germain.
A version of this article first appeared on Medscape.com.
FROM PEDIATRICS