User login
Richard Franki is the associate editor who writes and creates graphs. He started with the company in 1987, when it was known as the International Medical News Group. In his years as a journalist, Richard has worked for Cap Cities/ABC, Disney, Harcourt, Elsevier, Quadrant, Frontline, and Internet Brands. In the 1990s, he was a contributor to the ill-fated Indications column, predecessor of Livin' on the MDedge.
The human-looking robot therapist will coach your well-being now
Do android therapists dream of electric employees?
Robots. It can be tough to remember that, when they’re not dooming humanity to apocalypse or just telling you that you’re doomed, robots have real-world uses. There are actual robots in the world, and they can do things beyond bend girders, sing about science, or run the navy.
Look, we’ll stop with the pop-culture references when pop culture runs out of robots to reference. It may take a while.
Robots are indelibly rooted in the public consciousness, and that plays into our expectations when we encounter a real-life robot. This leads us into a recent study conducted by researchers at the University of Cambridge, who developed a robot-led mental well-being program that a tech company utilized for 4 weeks. Why choose a robot? Well, why spring for a qualified therapist who requires a salary when you could simply get a robot to do the job for free? Get with the capitalist agenda here. Surely it won’t backfire.
The 26 people enrolled in the study received coaching from one of two robots, both programmed identically to act like mental health coaches, based on interviews with human therapists. Both acted identically and had identical expressions. The only difference between the two was their appearance. QTRobot was nearly a meter tall and looked like a human child; Misty II was much smaller and looked like a toy.
People who received coaching from Misty II were better able to connect and had a better experience than those who received coaching from QTRobot. According to those in the QTRobot group, their expectations didn’t match reality. The robots are good coaches, but they don’t act human. This wasn’t a problem for Misty II, since it doesn’t look human, but for QTRobot, the participants were expecting “to hell with our orders,” but received “Daisy, Daisy, give me your answer do.” When you’ve been programmed to think of robots as metal humans, it can be off-putting to see them act as, well, robots.
That said, all participants found the exercises helpful and were open to receiving more robot-led therapy in the future. And while we’re sure the technology will advance to make robot therapists more empathetic and more human, hopefully scientists won’t go too far. We don’t need depressed robots.
Birthing experience is all in the mindset
Alexa, play Peer Gynt Suite No. 1, Op. 46 - I. Morning Mood.
Birth.
Giving birth is a common experience for many, if not most, female mammals, but wanting it to be a pleasurable one seems distinctly human. There are many methods and practices that may make giving birth an easier and enjoyable experience for the mother, but a new study suggests that the key could be in her mind.
The mindset of the expectant mother during pregnancy, it seems, has some effect on how smooth or intervention-filled delivery is. If the mothers saw their experience as a natural process, they were less likely to need pain medication or a C-section, but mothers who viewed the experience as more of a “medical procedure” were more likely to require more medical supervision and intervention, according to investigators from the University of Bonn (Germany).
Now, the researchers wanted to be super clear in saying that there’s no right or wrong mindset to have. They just focused on the outcomes of those mindsets and whether they actually do have some effect on occurrences.
Apparently, yes.
“Mindsets can be understood as a kind of mental lense that guide our perception of the world around us and can influence our behavior,” Dr. Lisa Hoffmann said in a statement from the university. “The study highlights the importance of psychological factors in childbirth.”
The researchers surveyed 300 women with an online tool before and after delivery and found the effects of the natural process mindset lingered even after giving birth. They had lower rates of depression and posttraumatic stress, which may have a snowballing effect on mother-child bonding after childbirth.
Preparation for the big day, then, should be about more than gathering diapers and shopping for car seats. Women should prepare their minds as well. If it’s going to make giving birth better, why not?
Becoming a parent is going to create a psychological shift, no matter how you slice it.
Giant inflatable colon reported in Utah
Do not be alarmed! Yes, there is a giant inflatable colon currently at large in the Beehive State, but it will not harm you. The giant inflatable colon is in Utah as part of Intermountain Health’s “Let’s get to the bottom of colon cancer tour” and he only wants to help you.
The giant inflatable colon, whose name happens to be Collin, is 12 feet long and weighs 113 pounds. March is Colon Cancer Awareness Month, so Collin is traveling around Utah and Idaho to raise awareness about colon cancer and the various screening options. He is not going to change local weather patterns, eat small children, or take over local governments and raise your taxes.
Instead, Collin is planning to display “portions of a healthy colon, polyps or bumps on the colon, malignant polyps which look more vascular and have more redness, cancerous cells, advanced cancer cells, and Crohn’s disease,” KSL.com said.
Collin the colon is on loan to Intermountain Health from medical device manufacturer Boston Scientific and will be traveling to Spanish Fork, Provo, and Ogden, among other locations in Utah, as well as Burley and Meridian, Idaho, in the coming days.
Collin the colon’s participation in the tour has created some serious buzz in the Colin/Collin community:
- Colin Powell (four-star general and Secretary of State): “Back then, the second-most important topic among the Joint Chiefs of Staff was colon cancer screening. And the Navy guy – I can’t remember his name – was a huge fan of giant inflatable organs.”
- Colin Jost (comedian and Saturday Night Live “Weekend Update” cohost): “He’s funnier than Tucker Carlson and Pete Davidson combined.”
Do android therapists dream of electric employees?
Robots. It can be tough to remember that, when they’re not dooming humanity to apocalypse or just telling you that you’re doomed, robots have real-world uses. There are actual robots in the world, and they can do things beyond bend girders, sing about science, or run the navy.
Look, we’ll stop with the pop-culture references when pop culture runs out of robots to reference. It may take a while.
Robots are indelibly rooted in the public consciousness, and that plays into our expectations when we encounter a real-life robot. This leads us into a recent study conducted by researchers at the University of Cambridge, who developed a robot-led mental well-being program that a tech company utilized for 4 weeks. Why choose a robot? Well, why spring for a qualified therapist who requires a salary when you could simply get a robot to do the job for free? Get with the capitalist agenda here. Surely it won’t backfire.
The 26 people enrolled in the study received coaching from one of two robots, both programmed identically to act like mental health coaches, based on interviews with human therapists. Both acted identically and had identical expressions. The only difference between the two was their appearance. QTRobot was nearly a meter tall and looked like a human child; Misty II was much smaller and looked like a toy.
People who received coaching from Misty II were better able to connect and had a better experience than those who received coaching from QTRobot. According to those in the QTRobot group, their expectations didn’t match reality. The robots are good coaches, but they don’t act human. This wasn’t a problem for Misty II, since it doesn’t look human, but for QTRobot, the participants were expecting “to hell with our orders,” but received “Daisy, Daisy, give me your answer do.” When you’ve been programmed to think of robots as metal humans, it can be off-putting to see them act as, well, robots.
That said, all participants found the exercises helpful and were open to receiving more robot-led therapy in the future. And while we’re sure the technology will advance to make robot therapists more empathetic and more human, hopefully scientists won’t go too far. We don’t need depressed robots.
Birthing experience is all in the mindset
Alexa, play Peer Gynt Suite No. 1, Op. 46 - I. Morning Mood.
Birth.
Giving birth is a common experience for many, if not most, female mammals, but wanting it to be a pleasurable one seems distinctly human. There are many methods and practices that may make giving birth an easier and enjoyable experience for the mother, but a new study suggests that the key could be in her mind.
The mindset of the expectant mother during pregnancy, it seems, has some effect on how smooth or intervention-filled delivery is. If the mothers saw their experience as a natural process, they were less likely to need pain medication or a C-section, but mothers who viewed the experience as more of a “medical procedure” were more likely to require more medical supervision and intervention, according to investigators from the University of Bonn (Germany).
Now, the researchers wanted to be super clear in saying that there’s no right or wrong mindset to have. They just focused on the outcomes of those mindsets and whether they actually do have some effect on occurrences.
Apparently, yes.
“Mindsets can be understood as a kind of mental lense that guide our perception of the world around us and can influence our behavior,” Dr. Lisa Hoffmann said in a statement from the university. “The study highlights the importance of psychological factors in childbirth.”
The researchers surveyed 300 women with an online tool before and after delivery and found the effects of the natural process mindset lingered even after giving birth. They had lower rates of depression and posttraumatic stress, which may have a snowballing effect on mother-child bonding after childbirth.
Preparation for the big day, then, should be about more than gathering diapers and shopping for car seats. Women should prepare their minds as well. If it’s going to make giving birth better, why not?
Becoming a parent is going to create a psychological shift, no matter how you slice it.
Giant inflatable colon reported in Utah
Do not be alarmed! Yes, there is a giant inflatable colon currently at large in the Beehive State, but it will not harm you. The giant inflatable colon is in Utah as part of Intermountain Health’s “Let’s get to the bottom of colon cancer tour” and he only wants to help you.
The giant inflatable colon, whose name happens to be Collin, is 12 feet long and weighs 113 pounds. March is Colon Cancer Awareness Month, so Collin is traveling around Utah and Idaho to raise awareness about colon cancer and the various screening options. He is not going to change local weather patterns, eat small children, or take over local governments and raise your taxes.
Instead, Collin is planning to display “portions of a healthy colon, polyps or bumps on the colon, malignant polyps which look more vascular and have more redness, cancerous cells, advanced cancer cells, and Crohn’s disease,” KSL.com said.
Collin the colon is on loan to Intermountain Health from medical device manufacturer Boston Scientific and will be traveling to Spanish Fork, Provo, and Ogden, among other locations in Utah, as well as Burley and Meridian, Idaho, in the coming days.
Collin the colon’s participation in the tour has created some serious buzz in the Colin/Collin community:
- Colin Powell (four-star general and Secretary of State): “Back then, the second-most important topic among the Joint Chiefs of Staff was colon cancer screening. And the Navy guy – I can’t remember his name – was a huge fan of giant inflatable organs.”
- Colin Jost (comedian and Saturday Night Live “Weekend Update” cohost): “He’s funnier than Tucker Carlson and Pete Davidson combined.”
Do android therapists dream of electric employees?
Robots. It can be tough to remember that, when they’re not dooming humanity to apocalypse or just telling you that you’re doomed, robots have real-world uses. There are actual robots in the world, and they can do things beyond bend girders, sing about science, or run the navy.
Look, we’ll stop with the pop-culture references when pop culture runs out of robots to reference. It may take a while.
Robots are indelibly rooted in the public consciousness, and that plays into our expectations when we encounter a real-life robot. This leads us into a recent study conducted by researchers at the University of Cambridge, who developed a robot-led mental well-being program that a tech company utilized for 4 weeks. Why choose a robot? Well, why spring for a qualified therapist who requires a salary when you could simply get a robot to do the job for free? Get with the capitalist agenda here. Surely it won’t backfire.
The 26 people enrolled in the study received coaching from one of two robots, both programmed identically to act like mental health coaches, based on interviews with human therapists. Both acted identically and had identical expressions. The only difference between the two was their appearance. QTRobot was nearly a meter tall and looked like a human child; Misty II was much smaller and looked like a toy.
People who received coaching from Misty II were better able to connect and had a better experience than those who received coaching from QTRobot. According to those in the QTRobot group, their expectations didn’t match reality. The robots are good coaches, but they don’t act human. This wasn’t a problem for Misty II, since it doesn’t look human, but for QTRobot, the participants were expecting “to hell with our orders,” but received “Daisy, Daisy, give me your answer do.” When you’ve been programmed to think of robots as metal humans, it can be off-putting to see them act as, well, robots.
That said, all participants found the exercises helpful and were open to receiving more robot-led therapy in the future. And while we’re sure the technology will advance to make robot therapists more empathetic and more human, hopefully scientists won’t go too far. We don’t need depressed robots.
Birthing experience is all in the mindset
Alexa, play Peer Gynt Suite No. 1, Op. 46 - I. Morning Mood.
Birth.
Giving birth is a common experience for many, if not most, female mammals, but wanting it to be a pleasurable one seems distinctly human. There are many methods and practices that may make giving birth an easier and enjoyable experience for the mother, but a new study suggests that the key could be in her mind.
The mindset of the expectant mother during pregnancy, it seems, has some effect on how smooth or intervention-filled delivery is. If the mothers saw their experience as a natural process, they were less likely to need pain medication or a C-section, but mothers who viewed the experience as more of a “medical procedure” were more likely to require more medical supervision and intervention, according to investigators from the University of Bonn (Germany).
Now, the researchers wanted to be super clear in saying that there’s no right or wrong mindset to have. They just focused on the outcomes of those mindsets and whether they actually do have some effect on occurrences.
Apparently, yes.
“Mindsets can be understood as a kind of mental lense that guide our perception of the world around us and can influence our behavior,” Dr. Lisa Hoffmann said in a statement from the university. “The study highlights the importance of psychological factors in childbirth.”
The researchers surveyed 300 women with an online tool before and after delivery and found the effects of the natural process mindset lingered even after giving birth. They had lower rates of depression and posttraumatic stress, which may have a snowballing effect on mother-child bonding after childbirth.
Preparation for the big day, then, should be about more than gathering diapers and shopping for car seats. Women should prepare their minds as well. If it’s going to make giving birth better, why not?
Becoming a parent is going to create a psychological shift, no matter how you slice it.
Giant inflatable colon reported in Utah
Do not be alarmed! Yes, there is a giant inflatable colon currently at large in the Beehive State, but it will not harm you. The giant inflatable colon is in Utah as part of Intermountain Health’s “Let’s get to the bottom of colon cancer tour” and he only wants to help you.
The giant inflatable colon, whose name happens to be Collin, is 12 feet long and weighs 113 pounds. March is Colon Cancer Awareness Month, so Collin is traveling around Utah and Idaho to raise awareness about colon cancer and the various screening options. He is not going to change local weather patterns, eat small children, or take over local governments and raise your taxes.
Instead, Collin is planning to display “portions of a healthy colon, polyps or bumps on the colon, malignant polyps which look more vascular and have more redness, cancerous cells, advanced cancer cells, and Crohn’s disease,” KSL.com said.
Collin the colon is on loan to Intermountain Health from medical device manufacturer Boston Scientific and will be traveling to Spanish Fork, Provo, and Ogden, among other locations in Utah, as well as Burley and Meridian, Idaho, in the coming days.
Collin the colon’s participation in the tour has created some serious buzz in the Colin/Collin community:
- Colin Powell (four-star general and Secretary of State): “Back then, the second-most important topic among the Joint Chiefs of Staff was colon cancer screening. And the Navy guy – I can’t remember his name – was a huge fan of giant inflatable organs.”
- Colin Jost (comedian and Saturday Night Live “Weekend Update” cohost): “He’s funnier than Tucker Carlson and Pete Davidson combined.”
Children and COVID: A look back as the fourth year begins
With 3 years of the COVID-19 experience now past, it’s safe to say that SARS-CoV-2 changed American society in ways that could not have been predicted when the first U.S. cases were reported in January of 2020.
Who would have guessed back then that not one but two vaccines would be developed, approved, and widely distributed before the end of the year? Or that those vaccines would be rejected by large segments of the population on ideological grounds? Could anyone have predicted in early 2020 that schools in 21 states would be forbidden by law to require COVID-19 vaccination in students?
Vaccination is generally considered to be an activity of childhood, but that practice has been turned upside down with COVID-19. Among Americans aged 65 years and older, 95% have received at least one dose of vaccine, versus 27.9% of children younger than 12 years old, according to the Centers for Disease Control and Prevention.
The vaccine situation for children mirrors that of the population as a whole. The oldest children have the highest vaccination rates, and the rates decline along with age: 72.0% of those aged 12-17 years have received at least one dose, compared with 39.8% of 5- to 11-year-olds, 10.5% of 2- to 4-year-olds, and 8.0% of children under age 2, the CDC said on its COVID Data Tracker.
The youngest children were, of course, the last ones to be eligible for the vaccine, but their uptake has been much slower since emergency use was authorized in June of 2022. In the nearly 9 months since then, 9.5% of children aged 4 and under have received at least one dose, versus 66% of children aged 12-15 years in the first 9 months (May 2021 to March 2022).
Altogether, a total of 31.7 million, or 43%, of all children under age 18 had received at least one dose of COVID-19 vaccine as of March 8, 2023, according to the most recent CDC data.
Incidence: Counting COVID
Vaccination and other prevention efforts have tried to stem the tide, but what has COVID actually done to children since the Trump administration declared a nationwide emergency on March 13, 2020?
- 16.6 million cases.
- 186,035 new hospital admissions.
- 2,122 deaths.
Even the proportion of total COVID cases in children, 17.2%, is less than might be expected, given their relatively undervaccinated status.
Seroprevalence estimates seem to support the undercounting of pediatric cases. A survey of commercial laboratories working with the CDC put the seroprevalance of SARS-CoV-2 antibodies in children at 96.3% as of late 2022, based on tests of almost 27,000 specimens performed over an 8-week period from mid-October to mid-December. That would put the number of infected children at 65.7 million children.
Since Omicron
There has not been another major COVID-19 surge since the winter of 2021-2022, when the weekly rate of new cases reached 1,900 per 100,000 population in children aged 16-17 years in early January 2022 – the highest seen among children of any of the CDC’s age groups (0-4, 5-11, 12-15, 16-17) during the entire pandemic. Since the Omicron surge, the highest weekly rate was 221 per 100,000 during the week of May 15-21, again in 16- to 17-year-olds, the CDC reports.
The widely anticipated surge of COVID in the fall and winter of 2022 and 2023 – the so-called “tripledemic” involving influenza and respiratory syncytial virus – did not occur, possibly because so many Americans were vaccinated or previously infected, experts suggested. New-case rates, emergency room visits, and hospitalizations in children have continued to drop as winter comes to a close, CDC data show.
With 3 years of the COVID-19 experience now past, it’s safe to say that SARS-CoV-2 changed American society in ways that could not have been predicted when the first U.S. cases were reported in January of 2020.
Who would have guessed back then that not one but two vaccines would be developed, approved, and widely distributed before the end of the year? Or that those vaccines would be rejected by large segments of the population on ideological grounds? Could anyone have predicted in early 2020 that schools in 21 states would be forbidden by law to require COVID-19 vaccination in students?
Vaccination is generally considered to be an activity of childhood, but that practice has been turned upside down with COVID-19. Among Americans aged 65 years and older, 95% have received at least one dose of vaccine, versus 27.9% of children younger than 12 years old, according to the Centers for Disease Control and Prevention.
The vaccine situation for children mirrors that of the population as a whole. The oldest children have the highest vaccination rates, and the rates decline along with age: 72.0% of those aged 12-17 years have received at least one dose, compared with 39.8% of 5- to 11-year-olds, 10.5% of 2- to 4-year-olds, and 8.0% of children under age 2, the CDC said on its COVID Data Tracker.
The youngest children were, of course, the last ones to be eligible for the vaccine, but their uptake has been much slower since emergency use was authorized in June of 2022. In the nearly 9 months since then, 9.5% of children aged 4 and under have received at least one dose, versus 66% of children aged 12-15 years in the first 9 months (May 2021 to March 2022).
Altogether, a total of 31.7 million, or 43%, of all children under age 18 had received at least one dose of COVID-19 vaccine as of March 8, 2023, according to the most recent CDC data.
Incidence: Counting COVID
Vaccination and other prevention efforts have tried to stem the tide, but what has COVID actually done to children since the Trump administration declared a nationwide emergency on March 13, 2020?
- 16.6 million cases.
- 186,035 new hospital admissions.
- 2,122 deaths.
Even the proportion of total COVID cases in children, 17.2%, is less than might be expected, given their relatively undervaccinated status.
Seroprevalence estimates seem to support the undercounting of pediatric cases. A survey of commercial laboratories working with the CDC put the seroprevalance of SARS-CoV-2 antibodies in children at 96.3% as of late 2022, based on tests of almost 27,000 specimens performed over an 8-week period from mid-October to mid-December. That would put the number of infected children at 65.7 million children.
Since Omicron
There has not been another major COVID-19 surge since the winter of 2021-2022, when the weekly rate of new cases reached 1,900 per 100,000 population in children aged 16-17 years in early January 2022 – the highest seen among children of any of the CDC’s age groups (0-4, 5-11, 12-15, 16-17) during the entire pandemic. Since the Omicron surge, the highest weekly rate was 221 per 100,000 during the week of May 15-21, again in 16- to 17-year-olds, the CDC reports.
The widely anticipated surge of COVID in the fall and winter of 2022 and 2023 – the so-called “tripledemic” involving influenza and respiratory syncytial virus – did not occur, possibly because so many Americans were vaccinated or previously infected, experts suggested. New-case rates, emergency room visits, and hospitalizations in children have continued to drop as winter comes to a close, CDC data show.
With 3 years of the COVID-19 experience now past, it’s safe to say that SARS-CoV-2 changed American society in ways that could not have been predicted when the first U.S. cases were reported in January of 2020.
Who would have guessed back then that not one but two vaccines would be developed, approved, and widely distributed before the end of the year? Or that those vaccines would be rejected by large segments of the population on ideological grounds? Could anyone have predicted in early 2020 that schools in 21 states would be forbidden by law to require COVID-19 vaccination in students?
Vaccination is generally considered to be an activity of childhood, but that practice has been turned upside down with COVID-19. Among Americans aged 65 years and older, 95% have received at least one dose of vaccine, versus 27.9% of children younger than 12 years old, according to the Centers for Disease Control and Prevention.
The vaccine situation for children mirrors that of the population as a whole. The oldest children have the highest vaccination rates, and the rates decline along with age: 72.0% of those aged 12-17 years have received at least one dose, compared with 39.8% of 5- to 11-year-olds, 10.5% of 2- to 4-year-olds, and 8.0% of children under age 2, the CDC said on its COVID Data Tracker.
The youngest children were, of course, the last ones to be eligible for the vaccine, but their uptake has been much slower since emergency use was authorized in June of 2022. In the nearly 9 months since then, 9.5% of children aged 4 and under have received at least one dose, versus 66% of children aged 12-15 years in the first 9 months (May 2021 to March 2022).
Altogether, a total of 31.7 million, or 43%, of all children under age 18 had received at least one dose of COVID-19 vaccine as of March 8, 2023, according to the most recent CDC data.
Incidence: Counting COVID
Vaccination and other prevention efforts have tried to stem the tide, but what has COVID actually done to children since the Trump administration declared a nationwide emergency on March 13, 2020?
- 16.6 million cases.
- 186,035 new hospital admissions.
- 2,122 deaths.
Even the proportion of total COVID cases in children, 17.2%, is less than might be expected, given their relatively undervaccinated status.
Seroprevalence estimates seem to support the undercounting of pediatric cases. A survey of commercial laboratories working with the CDC put the seroprevalance of SARS-CoV-2 antibodies in children at 96.3% as of late 2022, based on tests of almost 27,000 specimens performed over an 8-week period from mid-October to mid-December. That would put the number of infected children at 65.7 million children.
Since Omicron
There has not been another major COVID-19 surge since the winter of 2021-2022, when the weekly rate of new cases reached 1,900 per 100,000 population in children aged 16-17 years in early January 2022 – the highest seen among children of any of the CDC’s age groups (0-4, 5-11, 12-15, 16-17) during the entire pandemic. Since the Omicron surge, the highest weekly rate was 221 per 100,000 during the week of May 15-21, again in 16- to 17-year-olds, the CDC reports.
The widely anticipated surge of COVID in the fall and winter of 2022 and 2023 – the so-called “tripledemic” involving influenza and respiratory syncytial virus – did not occur, possibly because so many Americans were vaccinated or previously infected, experts suggested. New-case rates, emergency room visits, and hospitalizations in children have continued to drop as winter comes to a close, CDC data show.
Ob.gyns. reveal heavier suicide ideation burden than most specialists
Obstetricians and gynecologists are more likely than most specialists to have thoughts of suicide, and almost of quarter of physicians in general reported that they were depressed in a recent survey conducted by Medscape.
“Too much work with too little control is a recipe for depression in anyone,” Andrea Giedinghagen, MD, of Washington University, St. Louis, said in the Medscape Physician Suicide Report: Doctors’ Burden 2023. “Physicians are also still coping with a pandemic – the trauma from COVID-19 didn’t disappear just because the full ICUs did – and with a fractured health care system that virtually guarantees moral distress.”
About 23% of the almost 9,200 survey respondents said that they were depressed in 2022, compared with 21% the previous year. Suicide ideation was down in 2022, however, with 9% of all responding physicians reporting contemplation versus 13% in 2021, based on the results of the latest survey, which was conducted from June 28, 2022, to Oct. 2, 2022.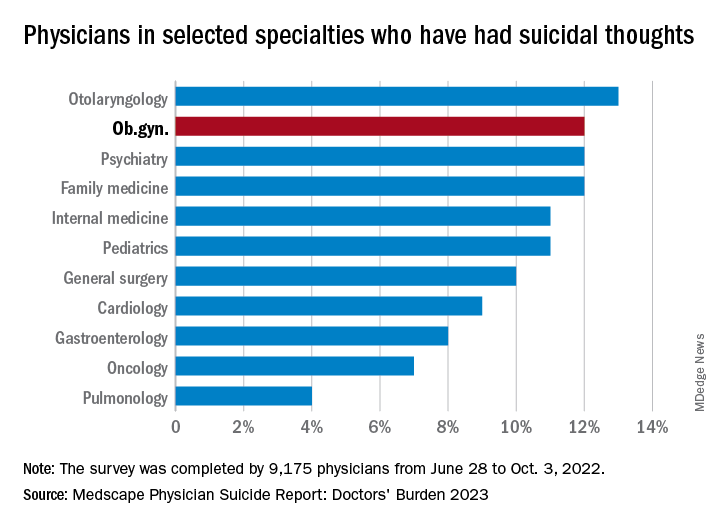
Ob.gyns. were above that average, with 12% reporting suicidal thoughts over the past year, equaling psychiatrists, family physicians, anesthesiologists, and emergency physicians and trailing only the otolaryngologists at 13%. The lowest rate among the 29 specialties included in the report was 4% for pulmonary medicine.
Differences between physicians, general population
Comparisons with the general U.S. population show that physicians are about twice as likely to report thoughts of suicide (9% vs. 4.9%) and to attempt it (1% vs. 0.5%). Among the overall population, however, “females are two to three times more likely to attempt suicide than males are,” noted Perry Lin, MD, national cochair of the American Association of Suicidology’s Physician Suicide Awareness Committee. That was not the case for survey respondents, as men and women both had an attempt rate of 1% and women were slightly ahead in ideation (11% to 9%).
There was a somewhat larger gap when age group was considered. Among physicians aged 57-75 years, 8% had thought about suicide, compared with 10% of those aged 42-56 years and 12% of respondents aged 27-41. This, again, runs counter to the general population, where older men typically deal with higher suicide rates, Michael F. Myers of the State University of New York, Brooklyn, said in the Medscape report.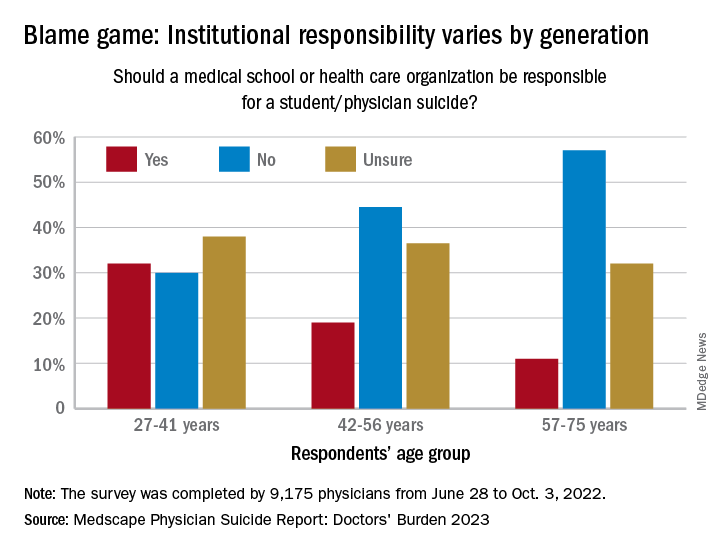
Age also was a factor when responsibility was brought into the equation. Over 30% of the youngest group of respondents (age 27-41) said that medical schools and health care organizations should be held responsible for an individual’s suicide, compared with 19% of those aged 42-56 and 11% of the 57- to 75-year-olds.
That trend was concerning to Dr. Myers: “Most suicides are multifactorial, many stressors coming together all at once in a person’s life, a so-called ‘perfect storm.’ ... But there are suicides each year involving medical students and physicians that have nothing to do with the medical school or place of work.”
Reasons to avoid professional help
Many of the survey respondents also were thinking about third parties when asked why they might not seek professional help for their suicidal thoughts. The most common response, cited by 52%, was that they didn’t need professional help, but 42% didn’t want to risk disclosure to a medical board, 33% were concerned about it being on their insurance record, and 25% were concerned about colleagues finding out.
“Doctors are willing and able to treat suicidal ideation among patients but appear fearful to seek such help themselves. We must do better,” Dr. Lin said in an interview.
Exact numbers of survey respondents were not given by specialty, but about 5% of the 9,175 total responses were completed by ob.gyns. The margin of error for the survey was ±1.02% at the 95% confidence interval.
Obstetricians and gynecologists are more likely than most specialists to have thoughts of suicide, and almost of quarter of physicians in general reported that they were depressed in a recent survey conducted by Medscape.
“Too much work with too little control is a recipe for depression in anyone,” Andrea Giedinghagen, MD, of Washington University, St. Louis, said in the Medscape Physician Suicide Report: Doctors’ Burden 2023. “Physicians are also still coping with a pandemic – the trauma from COVID-19 didn’t disappear just because the full ICUs did – and with a fractured health care system that virtually guarantees moral distress.”
About 23% of the almost 9,200 survey respondents said that they were depressed in 2022, compared with 21% the previous year. Suicide ideation was down in 2022, however, with 9% of all responding physicians reporting contemplation versus 13% in 2021, based on the results of the latest survey, which was conducted from June 28, 2022, to Oct. 2, 2022.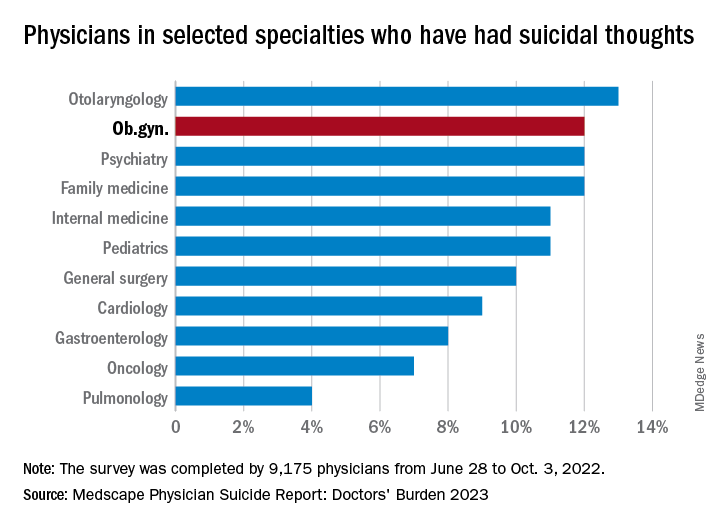
Ob.gyns. were above that average, with 12% reporting suicidal thoughts over the past year, equaling psychiatrists, family physicians, anesthesiologists, and emergency physicians and trailing only the otolaryngologists at 13%. The lowest rate among the 29 specialties included in the report was 4% for pulmonary medicine.
Differences between physicians, general population
Comparisons with the general U.S. population show that physicians are about twice as likely to report thoughts of suicide (9% vs. 4.9%) and to attempt it (1% vs. 0.5%). Among the overall population, however, “females are two to three times more likely to attempt suicide than males are,” noted Perry Lin, MD, national cochair of the American Association of Suicidology’s Physician Suicide Awareness Committee. That was not the case for survey respondents, as men and women both had an attempt rate of 1% and women were slightly ahead in ideation (11% to 9%).
There was a somewhat larger gap when age group was considered. Among physicians aged 57-75 years, 8% had thought about suicide, compared with 10% of those aged 42-56 years and 12% of respondents aged 27-41. This, again, runs counter to the general population, where older men typically deal with higher suicide rates, Michael F. Myers of the State University of New York, Brooklyn, said in the Medscape report.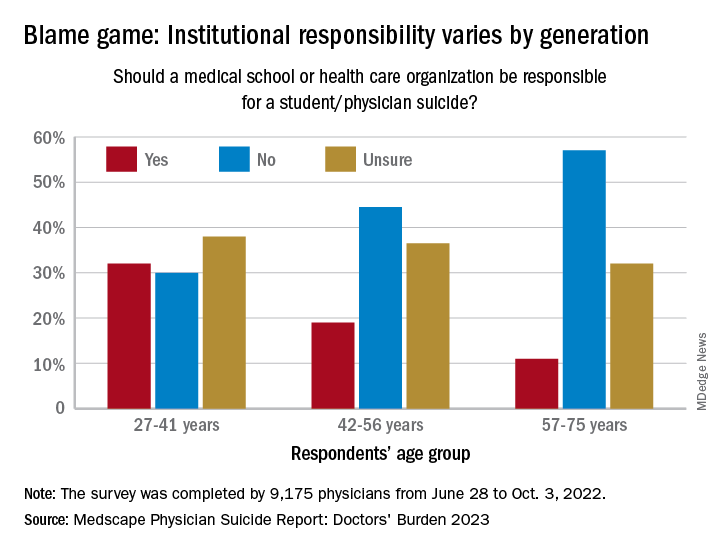
Age also was a factor when responsibility was brought into the equation. Over 30% of the youngest group of respondents (age 27-41) said that medical schools and health care organizations should be held responsible for an individual’s suicide, compared with 19% of those aged 42-56 and 11% of the 57- to 75-year-olds.
That trend was concerning to Dr. Myers: “Most suicides are multifactorial, many stressors coming together all at once in a person’s life, a so-called ‘perfect storm.’ ... But there are suicides each year involving medical students and physicians that have nothing to do with the medical school or place of work.”
Reasons to avoid professional help
Many of the survey respondents also were thinking about third parties when asked why they might not seek professional help for their suicidal thoughts. The most common response, cited by 52%, was that they didn’t need professional help, but 42% didn’t want to risk disclosure to a medical board, 33% were concerned about it being on their insurance record, and 25% were concerned about colleagues finding out.
“Doctors are willing and able to treat suicidal ideation among patients but appear fearful to seek such help themselves. We must do better,” Dr. Lin said in an interview.
Exact numbers of survey respondents were not given by specialty, but about 5% of the 9,175 total responses were completed by ob.gyns. The margin of error for the survey was ±1.02% at the 95% confidence interval.
Obstetricians and gynecologists are more likely than most specialists to have thoughts of suicide, and almost of quarter of physicians in general reported that they were depressed in a recent survey conducted by Medscape.
“Too much work with too little control is a recipe for depression in anyone,” Andrea Giedinghagen, MD, of Washington University, St. Louis, said in the Medscape Physician Suicide Report: Doctors’ Burden 2023. “Physicians are also still coping with a pandemic – the trauma from COVID-19 didn’t disappear just because the full ICUs did – and with a fractured health care system that virtually guarantees moral distress.”
About 23% of the almost 9,200 survey respondents said that they were depressed in 2022, compared with 21% the previous year. Suicide ideation was down in 2022, however, with 9% of all responding physicians reporting contemplation versus 13% in 2021, based on the results of the latest survey, which was conducted from June 28, 2022, to Oct. 2, 2022.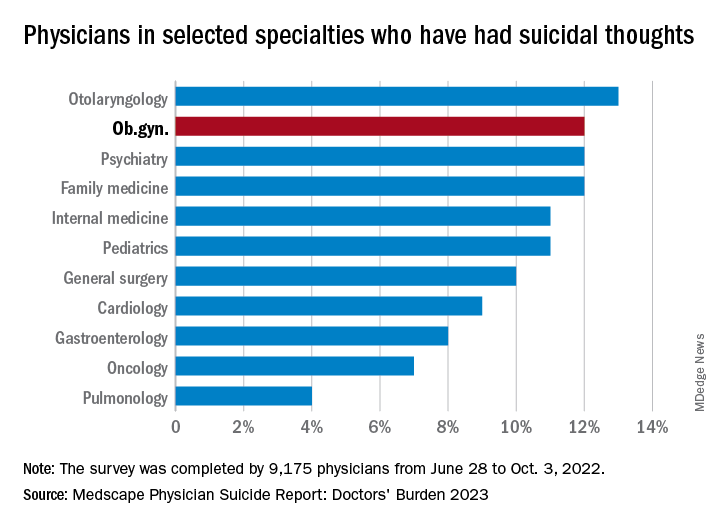
Ob.gyns. were above that average, with 12% reporting suicidal thoughts over the past year, equaling psychiatrists, family physicians, anesthesiologists, and emergency physicians and trailing only the otolaryngologists at 13%. The lowest rate among the 29 specialties included in the report was 4% for pulmonary medicine.
Differences between physicians, general population
Comparisons with the general U.S. population show that physicians are about twice as likely to report thoughts of suicide (9% vs. 4.9%) and to attempt it (1% vs. 0.5%). Among the overall population, however, “females are two to three times more likely to attempt suicide than males are,” noted Perry Lin, MD, national cochair of the American Association of Suicidology’s Physician Suicide Awareness Committee. That was not the case for survey respondents, as men and women both had an attempt rate of 1% and women were slightly ahead in ideation (11% to 9%).
There was a somewhat larger gap when age group was considered. Among physicians aged 57-75 years, 8% had thought about suicide, compared with 10% of those aged 42-56 years and 12% of respondents aged 27-41. This, again, runs counter to the general population, where older men typically deal with higher suicide rates, Michael F. Myers of the State University of New York, Brooklyn, said in the Medscape report.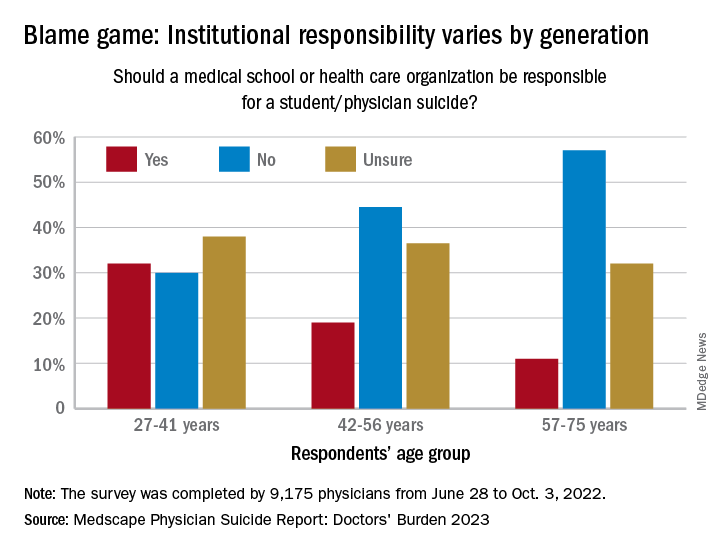
Age also was a factor when responsibility was brought into the equation. Over 30% of the youngest group of respondents (age 27-41) said that medical schools and health care organizations should be held responsible for an individual’s suicide, compared with 19% of those aged 42-56 and 11% of the 57- to 75-year-olds.
That trend was concerning to Dr. Myers: “Most suicides are multifactorial, many stressors coming together all at once in a person’s life, a so-called ‘perfect storm.’ ... But there are suicides each year involving medical students and physicians that have nothing to do with the medical school or place of work.”
Reasons to avoid professional help
Many of the survey respondents also were thinking about third parties when asked why they might not seek professional help for their suicidal thoughts. The most common response, cited by 52%, was that they didn’t need professional help, but 42% didn’t want to risk disclosure to a medical board, 33% were concerned about it being on their insurance record, and 25% were concerned about colleagues finding out.
“Doctors are willing and able to treat suicidal ideation among patients but appear fearful to seek such help themselves. We must do better,” Dr. Lin said in an interview.
Exact numbers of survey respondents were not given by specialty, but about 5% of the 9,175 total responses were completed by ob.gyns. The margin of error for the survey was ±1.02% at the 95% confidence interval.
We have seen the future of healthy muffins, and its name is Roselle
Get ‘em while they’re hot … for your health
Today on the Eating Channel, it’s a very special episode of “Much Ado About Muffin.”
The muffin. For some of us, it’s a good way to pretend we’re not having dessert for breakfast. A bran muffin can be loaded with calcium and fiber, and our beloved blueberry is full of yummy antioxidants and vitamins. Definitely not dessert.
Well, the muffin denial can stop there because there’s a new flavor on the scene, and research suggests it may actually be healthy. (Disclaimer: Muffin may not be considered healthy in Norway.) This new muffin has a name, Roselle, that comes from the calyx extract used in it, which is found in the Hibiscus sabdariffa plant of the same name.
Now, when it comes to new foods, especially ones that are supposed to be healthy, the No. 1 criteria is the same: It has to taste good. Researchers at the Norwegian University of Science and Technology and Amity University in India agreed, but they also set out to make it nutritionally valuable and give it a long shelf life without the addition of preservatives.
Sounds like a tall order, but they figured it out.
Not only is it tasty, but the properties of it could rival your morning multivitamin. Hibiscus extract has huge amounts of antioxidants, like phenolics, which are believed to help prevent cell membrane damage. Foods like vegetables, flax seed, and whole grains also have these antioxidants, but why not just have a Roselle muffin instead? You also get a dose of ascorbic acid without the glass of OJ in the morning.
The ascorbic acid, however, is not there just to help you. It also helps to check the researcher’s third box, shelf life. These naturally rosy-colored pastries will stay mold-free for 6 days without refrigeration at room temperature and without added preservatives.
Our guess, though, is they won’t be on the kitchen counter long enough to find out.
A sobering proposition
If Hollywood is to be believed, there’s no amount of drunkenness that can’t be cured with a cup of coffee or a stern slap in the face. Unfortunately, here in the real world the only thing that can make you less drunk is time. Maybe next time you’ll stop after that seventh Manhattan.
But what if we could beat time? What if there’s an actual sobriety drug out there?
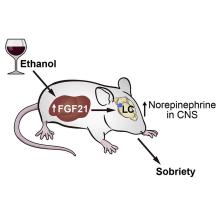
Say hello to fibroblast growth factor 21. Although the liver already does good work filtering out what is essentially poison, it then goes the extra mile and produces fibroblast growth factor 21 (or, as her friends call her, FGF21), a hormone that suppresses the desire to drink, makes you desire water, and protects the liver all at the same time.
Now, FGF21 in its current role is great, but if you’ve ever seen or been a drunk person before, you’ve experienced the lack of interest in listening to reason, especially when it comes from within our own bodies. Who are you to tell us what to do, body? You’re not the boss of us! So a group of scientists decided to push the limits of FGF21. Could it do more than it already does?
First off, they genetically altered a group of mice so that they didn’t produce FGF21 on their own. Then they got them drunk. We’re going to assume they built a scale model of the bar from Cheers and had the mice filter in through the front door as they served their subjects beer out of tiny little glasses.
Once the mice were nice and liquored up, some were given a treatment of FGF21 while others were given a placebo. Lo and behold, the mice given FGF21 recovered about 50% faster than those that received the control treatment. Not exactly instant, but 50% is nothing to sniff at.
Before you bring your FGF21 supplement to the bar, though, this research only applies to mice. We don’t know if it works in people. And make sure you stick to booze. If your choice of intoxication is a bit more exotic, FGF21 isn’t going to do anything for you. Yes, the scientists tried. Yes, those mice are living a very interesting life. And yes, we are jealous of drugged-up lab mice.
Supersize your imagination, shrink your snacks
Have you ever heard of the meal-recall effect? Did you know that, in England, a biscuit is really a cookie? Did you also know that the magazine Bon Appétit is not the same as the peer-reviewed journal Appetite? We do … now.
The meal-recall effect is the subsequent reduction in snacking that comes from remembering a recent meal. It was used to great effect in a recent study conducted at the University of Cambridge, which is in England, where they feed their experimental humans cookies but, for some reason, call them biscuits.
For the first part of the study, the participants were invited to dine at Che Laboratory, where they “were given a microwave ready meal of rice and sauce and a cup of water,” according to a statement from the university. As our Uncle Ernie would say, “Gourmet all the way.”
The test subjects were instructed not to eat anything for 3 hours and “then invited back to the lab to perform imagination tasks.” Those who did come back were randomly divided into five different groups, each with a different task:
- Imagine moving their recent lunch at the lab around a plate.
- Recall eating their recent lunch in detail.
- Imagine that the lunch was twice as big and filling as it really was.
- Look at a photograph of spaghetti hoops in tomato sauce and write a description of it before imagining moving the food around a plate.
- Look at a photo of paper clips and rubber bands and imagine moving them around.
Now, at last, we get to the biscuits/cookies, which were the subject of a taste test that “was simply a rouse for covertly assessing snacking,” the investigators explained. As part of that test, participants were told they could eat as many biscuits as they wanted.
When the tables were cleared and the leftovers examined, the group that imagined spaghetti hoops had eaten the most biscuits (75.9 g), followed by the group that imagined paper clips (75.5 g), the moving-their-lunch-around-the-plate group (72.0 g), and the group that relived eating their lunch (70.0 g).
In a victory for the meal-recall effect, the people who imagined their meal being twice as big ate the fewest biscuits (51.1 g). “Your mind can be more powerful than your stomach in dictating how much you eat,” lead author Joanna Szypula, PhD, said in the university statement.
Oh! One more thing. The study appeared in Appetite, which is a peer-reviewed journal, not in Bon Appétit, which is not a peer-reviewed journal. Thanks to the fine folks at both publications for pointing that out to us.
Get ‘em while they’re hot … for your health
Today on the Eating Channel, it’s a very special episode of “Much Ado About Muffin.”
The muffin. For some of us, it’s a good way to pretend we’re not having dessert for breakfast. A bran muffin can be loaded with calcium and fiber, and our beloved blueberry is full of yummy antioxidants and vitamins. Definitely not dessert.
Well, the muffin denial can stop there because there’s a new flavor on the scene, and research suggests it may actually be healthy. (Disclaimer: Muffin may not be considered healthy in Norway.) This new muffin has a name, Roselle, that comes from the calyx extract used in it, which is found in the Hibiscus sabdariffa plant of the same name.
Now, when it comes to new foods, especially ones that are supposed to be healthy, the No. 1 criteria is the same: It has to taste good. Researchers at the Norwegian University of Science and Technology and Amity University in India agreed, but they also set out to make it nutritionally valuable and give it a long shelf life without the addition of preservatives.
Sounds like a tall order, but they figured it out.
Not only is it tasty, but the properties of it could rival your morning multivitamin. Hibiscus extract has huge amounts of antioxidants, like phenolics, which are believed to help prevent cell membrane damage. Foods like vegetables, flax seed, and whole grains also have these antioxidants, but why not just have a Roselle muffin instead? You also get a dose of ascorbic acid without the glass of OJ in the morning.
The ascorbic acid, however, is not there just to help you. It also helps to check the researcher’s third box, shelf life. These naturally rosy-colored pastries will stay mold-free for 6 days without refrigeration at room temperature and without added preservatives.
Our guess, though, is they won’t be on the kitchen counter long enough to find out.
A sobering proposition
If Hollywood is to be believed, there’s no amount of drunkenness that can’t be cured with a cup of coffee or a stern slap in the face. Unfortunately, here in the real world the only thing that can make you less drunk is time. Maybe next time you’ll stop after that seventh Manhattan.
But what if we could beat time? What if there’s an actual sobriety drug out there?
Say hello to fibroblast growth factor 21. Although the liver already does good work filtering out what is essentially poison, it then goes the extra mile and produces fibroblast growth factor 21 (or, as her friends call her, FGF21), a hormone that suppresses the desire to drink, makes you desire water, and protects the liver all at the same time.
Now, FGF21 in its current role is great, but if you’ve ever seen or been a drunk person before, you’ve experienced the lack of interest in listening to reason, especially when it comes from within our own bodies. Who are you to tell us what to do, body? You’re not the boss of us! So a group of scientists decided to push the limits of FGF21. Could it do more than it already does?
First off, they genetically altered a group of mice so that they didn’t produce FGF21 on their own. Then they got them drunk. We’re going to assume they built a scale model of the bar from Cheers and had the mice filter in through the front door as they served their subjects beer out of tiny little glasses.
Once the mice were nice and liquored up, some were given a treatment of FGF21 while others were given a placebo. Lo and behold, the mice given FGF21 recovered about 50% faster than those that received the control treatment. Not exactly instant, but 50% is nothing to sniff at.
Before you bring your FGF21 supplement to the bar, though, this research only applies to mice. We don’t know if it works in people. And make sure you stick to booze. If your choice of intoxication is a bit more exotic, FGF21 isn’t going to do anything for you. Yes, the scientists tried. Yes, those mice are living a very interesting life. And yes, we are jealous of drugged-up lab mice.
Supersize your imagination, shrink your snacks
Have you ever heard of the meal-recall effect? Did you know that, in England, a biscuit is really a cookie? Did you also know that the magazine Bon Appétit is not the same as the peer-reviewed journal Appetite? We do … now.
The meal-recall effect is the subsequent reduction in snacking that comes from remembering a recent meal. It was used to great effect in a recent study conducted at the University of Cambridge, which is in England, where they feed their experimental humans cookies but, for some reason, call them biscuits.
For the first part of the study, the participants were invited to dine at Che Laboratory, where they “were given a microwave ready meal of rice and sauce and a cup of water,” according to a statement from the university. As our Uncle Ernie would say, “Gourmet all the way.”
The test subjects were instructed not to eat anything for 3 hours and “then invited back to the lab to perform imagination tasks.” Those who did come back were randomly divided into five different groups, each with a different task:
- Imagine moving their recent lunch at the lab around a plate.
- Recall eating their recent lunch in detail.
- Imagine that the lunch was twice as big and filling as it really was.
- Look at a photograph of spaghetti hoops in tomato sauce and write a description of it before imagining moving the food around a plate.
- Look at a photo of paper clips and rubber bands and imagine moving them around.
Now, at last, we get to the biscuits/cookies, which were the subject of a taste test that “was simply a rouse for covertly assessing snacking,” the investigators explained. As part of that test, participants were told they could eat as many biscuits as they wanted.
When the tables were cleared and the leftovers examined, the group that imagined spaghetti hoops had eaten the most biscuits (75.9 g), followed by the group that imagined paper clips (75.5 g), the moving-their-lunch-around-the-plate group (72.0 g), and the group that relived eating their lunch (70.0 g).
In a victory for the meal-recall effect, the people who imagined their meal being twice as big ate the fewest biscuits (51.1 g). “Your mind can be more powerful than your stomach in dictating how much you eat,” lead author Joanna Szypula, PhD, said in the university statement.
Oh! One more thing. The study appeared in Appetite, which is a peer-reviewed journal, not in Bon Appétit, which is not a peer-reviewed journal. Thanks to the fine folks at both publications for pointing that out to us.
Get ‘em while they’re hot … for your health
Today on the Eating Channel, it’s a very special episode of “Much Ado About Muffin.”
The muffin. For some of us, it’s a good way to pretend we’re not having dessert for breakfast. A bran muffin can be loaded with calcium and fiber, and our beloved blueberry is full of yummy antioxidants and vitamins. Definitely not dessert.
Well, the muffin denial can stop there because there’s a new flavor on the scene, and research suggests it may actually be healthy. (Disclaimer: Muffin may not be considered healthy in Norway.) This new muffin has a name, Roselle, that comes from the calyx extract used in it, which is found in the Hibiscus sabdariffa plant of the same name.
Now, when it comes to new foods, especially ones that are supposed to be healthy, the No. 1 criteria is the same: It has to taste good. Researchers at the Norwegian University of Science and Technology and Amity University in India agreed, but they also set out to make it nutritionally valuable and give it a long shelf life without the addition of preservatives.
Sounds like a tall order, but they figured it out.
Not only is it tasty, but the properties of it could rival your morning multivitamin. Hibiscus extract has huge amounts of antioxidants, like phenolics, which are believed to help prevent cell membrane damage. Foods like vegetables, flax seed, and whole grains also have these antioxidants, but why not just have a Roselle muffin instead? You also get a dose of ascorbic acid without the glass of OJ in the morning.
The ascorbic acid, however, is not there just to help you. It also helps to check the researcher’s third box, shelf life. These naturally rosy-colored pastries will stay mold-free for 6 days without refrigeration at room temperature and without added preservatives.
Our guess, though, is they won’t be on the kitchen counter long enough to find out.
A sobering proposition
If Hollywood is to be believed, there’s no amount of drunkenness that can’t be cured with a cup of coffee or a stern slap in the face. Unfortunately, here in the real world the only thing that can make you less drunk is time. Maybe next time you’ll stop after that seventh Manhattan.
But what if we could beat time? What if there’s an actual sobriety drug out there?
Say hello to fibroblast growth factor 21. Although the liver already does good work filtering out what is essentially poison, it then goes the extra mile and produces fibroblast growth factor 21 (or, as her friends call her, FGF21), a hormone that suppresses the desire to drink, makes you desire water, and protects the liver all at the same time.
Now, FGF21 in its current role is great, but if you’ve ever seen or been a drunk person before, you’ve experienced the lack of interest in listening to reason, especially when it comes from within our own bodies. Who are you to tell us what to do, body? You’re not the boss of us! So a group of scientists decided to push the limits of FGF21. Could it do more than it already does?
First off, they genetically altered a group of mice so that they didn’t produce FGF21 on their own. Then they got them drunk. We’re going to assume they built a scale model of the bar from Cheers and had the mice filter in through the front door as they served their subjects beer out of tiny little glasses.
Once the mice were nice and liquored up, some were given a treatment of FGF21 while others were given a placebo. Lo and behold, the mice given FGF21 recovered about 50% faster than those that received the control treatment. Not exactly instant, but 50% is nothing to sniff at.
Before you bring your FGF21 supplement to the bar, though, this research only applies to mice. We don’t know if it works in people. And make sure you stick to booze. If your choice of intoxication is a bit more exotic, FGF21 isn’t going to do anything for you. Yes, the scientists tried. Yes, those mice are living a very interesting life. And yes, we are jealous of drugged-up lab mice.
Supersize your imagination, shrink your snacks
Have you ever heard of the meal-recall effect? Did you know that, in England, a biscuit is really a cookie? Did you also know that the magazine Bon Appétit is not the same as the peer-reviewed journal Appetite? We do … now.
The meal-recall effect is the subsequent reduction in snacking that comes from remembering a recent meal. It was used to great effect in a recent study conducted at the University of Cambridge, which is in England, where they feed their experimental humans cookies but, for some reason, call them biscuits.
For the first part of the study, the participants were invited to dine at Che Laboratory, where they “were given a microwave ready meal of rice and sauce and a cup of water,” according to a statement from the university. As our Uncle Ernie would say, “Gourmet all the way.”
The test subjects were instructed not to eat anything for 3 hours and “then invited back to the lab to perform imagination tasks.” Those who did come back were randomly divided into five different groups, each with a different task:
- Imagine moving their recent lunch at the lab around a plate.
- Recall eating their recent lunch in detail.
- Imagine that the lunch was twice as big and filling as it really was.
- Look at a photograph of spaghetti hoops in tomato sauce and write a description of it before imagining moving the food around a plate.
- Look at a photo of paper clips and rubber bands and imagine moving them around.
Now, at last, we get to the biscuits/cookies, which were the subject of a taste test that “was simply a rouse for covertly assessing snacking,” the investigators explained. As part of that test, participants were told they could eat as many biscuits as they wanted.
When the tables were cleared and the leftovers examined, the group that imagined spaghetti hoops had eaten the most biscuits (75.9 g), followed by the group that imagined paper clips (75.5 g), the moving-their-lunch-around-the-plate group (72.0 g), and the group that relived eating their lunch (70.0 g).
In a victory for the meal-recall effect, the people who imagined their meal being twice as big ate the fewest biscuits (51.1 g). “Your mind can be more powerful than your stomach in dictating how much you eat,” lead author Joanna Szypula, PhD, said in the university statement.
Oh! One more thing. The study appeared in Appetite, which is a peer-reviewed journal, not in Bon Appétit, which is not a peer-reviewed journal. Thanks to the fine folks at both publications for pointing that out to us.
Transplant surgeon to 30,000 marathoners: Give me that liver
Surgeon goes the extra half mile for his patient
Sorry medical profession, but it’s Adam Bodzin’s world now. When a donor liver got stuck in the middle of the Philadelphia Half Marathon’s 30,000 participants, Dr. Bodzin, the transplant team’s lead surgeon, took matters into his own hands. And by hands, of course, we mean feet.
Still wearing his hospital scrubs, Dr. Bodzin ran more than half a mile to where the van carrying the liver was stranded, according to the Philadelphia Inquirer. Fortunately, he was able to hitch a ride in a police car for the return trip and didn’t have to run back through the crowd carrying his somewhat unusual package. By package, of course, we mean human liver.
It’s been 3 months since the surgery/marathon and it’s still not clear why the driver had such trouble getting through – he had been trying for more than an hour and half by the time Dr. Bodzin reached him – but the surgery half of the big event was deemed a success and the patient has recovered.
Rick Hasz, president and chief executive officer of the Gift of Life Donor Program, which coordinates organ donation for transplants in the Philadelphia region, told the newspaper that “Dr. Bodzin’s quick action demonstrated his commitment to honoring the selfless generosity of all donors and their families and gives hope to everyone waiting for a second chance at life.”
Should Dr. Bodzin consider a step up from the transplant team to another group that’s fighting for the common good? The recipient of the liver in question seems to think so. “I guess he has a cape on under that white jacket,” 66-year-old Charles Rowe told Fox29. You already know where we’re going with this, right?
Avengers … Assemble.
Your spleen’s due for its 5,000-mile oil change
The human body is an incredible biological machine, capable of performing a countless array of tasks automatically and essentially without flaw, but there’s always room for improvement. After all, there are animals that can regrow entire missing limbs or live for up to 500 years. It would be nice if we could get some of that going.
Rather than any of that cool stuff, a recent survey of 2,000 average Americans revealed that our ambitions for improving the human body are a bit more mundane. The big thing that would make our lives better and easier, according to three-fourths of Americans, would be a built-in “check engine” light in our bodies. Come on guys, starfish can literally be cut in half and not only survive, but become two starfish. Mantis shrimp can punch with a force thousands of times their own weight. If we could punch like they could, we could literally break steel with our fists. Wouldn’t we rather have that?
Apparently not. Fine, we’ll stick with the check engine light.
Maybe it isn’t a huge surprise that we’d like the extra help in figuring out what our body needs. According to the survey, more than 60% of Americans struggle to identify when their body is trying to tell them something important, and only one-third actively checked in with their health every day. Considering about 40% said they feel tired for much of the day and nearly half reported not having a meal with fruits or vegetables in the past 3 days, perhaps a gentle reminder wouldn’t be the worst thing in the world.
So, if we did have a built-in check engine light, what would we use it for? A majority said they’d like to be reminded to drink a glass of water, with 45% saying they wanted to know when to take a nap. Feeling thirsty or tired isn’t quite enough, it seems.
Of course, the technology certainly exists to make the human check engine light a reality. An implanted microchip could absolutely tell us to drink a glass of water, but that would put our health in the hands of tech companies, and you just know Meta and Elon Muskrat wouldn’t pass up the chance for monetization. “Oh, sorry, we could have notified the hospital that you were about to have a heart attack, but you didn’t pay your life subscription this month.”
Sext offenders show more than their, well, you know
As we have become more and more attached to our phones, especially post pandemic, it’s no surprise that sexting – sending sexually explicit images and messages with those phones – has become a fairly common way for people to sexually communicate. And with dating apps just another venture in the dating landscape, regardless of age, sexting is an easy avenue to incite a mood without being physically present.
A recent study, though, has linked sexting with anxiety, sleep issues, depression, and compulsive sexual behaviors. Yikes.
Although the researchers noted that sexting was primarily reciprocal (sending and receiving), “over 50% of adults report sending a sext, while women are up to four times more likely than men to report having received nonconsensual sexts,” said Brenda K. Wiederhold, PhD, editor-in-chief of Cyberpsychology, Behavior, and Social Networking, which published the study, in which Dr. Wiederhold was not involved.
Among the 2,160 U.S. college students who were involved, participants who had only sent sexts reported more anxiety, depression, and sleep problems than other groups (no sexting, received only, reciprocal). There was also a possible connection between sexting, marijuana use, and compulsive sexual behavior, the investigators said in a written statement.
Considering the study population, these data are perhaps not that surprising. For young adults, to receive or send an elusive nude is as common as it once was to give someone flowers. Not that the two things elicit the same reactions. “Many individuals reveal they enjoy consensual sexting and feel it empowers them and builds self-confidence,” Dr. Wiederhold added.
Receiving a nonconsensual sext, though, is definitely going to result in feeling violated and super awkward. Senders beware: Don’t be surprised if you’re ghosted after that.
Surgeon goes the extra half mile for his patient
Sorry medical profession, but it’s Adam Bodzin’s world now. When a donor liver got stuck in the middle of the Philadelphia Half Marathon’s 30,000 participants, Dr. Bodzin, the transplant team’s lead surgeon, took matters into his own hands. And by hands, of course, we mean feet.
Still wearing his hospital scrubs, Dr. Bodzin ran more than half a mile to where the van carrying the liver was stranded, according to the Philadelphia Inquirer. Fortunately, he was able to hitch a ride in a police car for the return trip and didn’t have to run back through the crowd carrying his somewhat unusual package. By package, of course, we mean human liver.
It’s been 3 months since the surgery/marathon and it’s still not clear why the driver had such trouble getting through – he had been trying for more than an hour and half by the time Dr. Bodzin reached him – but the surgery half of the big event was deemed a success and the patient has recovered.
Rick Hasz, president and chief executive officer of the Gift of Life Donor Program, which coordinates organ donation for transplants in the Philadelphia region, told the newspaper that “Dr. Bodzin’s quick action demonstrated his commitment to honoring the selfless generosity of all donors and their families and gives hope to everyone waiting for a second chance at life.”
Should Dr. Bodzin consider a step up from the transplant team to another group that’s fighting for the common good? The recipient of the liver in question seems to think so. “I guess he has a cape on under that white jacket,” 66-year-old Charles Rowe told Fox29. You already know where we’re going with this, right?
Avengers … Assemble.
Your spleen’s due for its 5,000-mile oil change
The human body is an incredible biological machine, capable of performing a countless array of tasks automatically and essentially without flaw, but there’s always room for improvement. After all, there are animals that can regrow entire missing limbs or live for up to 500 years. It would be nice if we could get some of that going.
Rather than any of that cool stuff, a recent survey of 2,000 average Americans revealed that our ambitions for improving the human body are a bit more mundane. The big thing that would make our lives better and easier, according to three-fourths of Americans, would be a built-in “check engine” light in our bodies. Come on guys, starfish can literally be cut in half and not only survive, but become two starfish. Mantis shrimp can punch with a force thousands of times their own weight. If we could punch like they could, we could literally break steel with our fists. Wouldn’t we rather have that?
Apparently not. Fine, we’ll stick with the check engine light.
Maybe it isn’t a huge surprise that we’d like the extra help in figuring out what our body needs. According to the survey, more than 60% of Americans struggle to identify when their body is trying to tell them something important, and only one-third actively checked in with their health every day. Considering about 40% said they feel tired for much of the day and nearly half reported not having a meal with fruits or vegetables in the past 3 days, perhaps a gentle reminder wouldn’t be the worst thing in the world.
So, if we did have a built-in check engine light, what would we use it for? A majority said they’d like to be reminded to drink a glass of water, with 45% saying they wanted to know when to take a nap. Feeling thirsty or tired isn’t quite enough, it seems.
Of course, the technology certainly exists to make the human check engine light a reality. An implanted microchip could absolutely tell us to drink a glass of water, but that would put our health in the hands of tech companies, and you just know Meta and Elon Muskrat wouldn’t pass up the chance for monetization. “Oh, sorry, we could have notified the hospital that you were about to have a heart attack, but you didn’t pay your life subscription this month.”
Sext offenders show more than their, well, you know
As we have become more and more attached to our phones, especially post pandemic, it’s no surprise that sexting – sending sexually explicit images and messages with those phones – has become a fairly common way for people to sexually communicate. And with dating apps just another venture in the dating landscape, regardless of age, sexting is an easy avenue to incite a mood without being physically present.
A recent study, though, has linked sexting with anxiety, sleep issues, depression, and compulsive sexual behaviors. Yikes.
Although the researchers noted that sexting was primarily reciprocal (sending and receiving), “over 50% of adults report sending a sext, while women are up to four times more likely than men to report having received nonconsensual sexts,” said Brenda K. Wiederhold, PhD, editor-in-chief of Cyberpsychology, Behavior, and Social Networking, which published the study, in which Dr. Wiederhold was not involved.
Among the 2,160 U.S. college students who were involved, participants who had only sent sexts reported more anxiety, depression, and sleep problems than other groups (no sexting, received only, reciprocal). There was also a possible connection between sexting, marijuana use, and compulsive sexual behavior, the investigators said in a written statement.
Considering the study population, these data are perhaps not that surprising. For young adults, to receive or send an elusive nude is as common as it once was to give someone flowers. Not that the two things elicit the same reactions. “Many individuals reveal they enjoy consensual sexting and feel it empowers them and builds self-confidence,” Dr. Wiederhold added.
Receiving a nonconsensual sext, though, is definitely going to result in feeling violated and super awkward. Senders beware: Don’t be surprised if you’re ghosted after that.
Surgeon goes the extra half mile for his patient
Sorry medical profession, but it’s Adam Bodzin’s world now. When a donor liver got stuck in the middle of the Philadelphia Half Marathon’s 30,000 participants, Dr. Bodzin, the transplant team’s lead surgeon, took matters into his own hands. And by hands, of course, we mean feet.
Still wearing his hospital scrubs, Dr. Bodzin ran more than half a mile to where the van carrying the liver was stranded, according to the Philadelphia Inquirer. Fortunately, he was able to hitch a ride in a police car for the return trip and didn’t have to run back through the crowd carrying his somewhat unusual package. By package, of course, we mean human liver.
It’s been 3 months since the surgery/marathon and it’s still not clear why the driver had such trouble getting through – he had been trying for more than an hour and half by the time Dr. Bodzin reached him – but the surgery half of the big event was deemed a success and the patient has recovered.
Rick Hasz, president and chief executive officer of the Gift of Life Donor Program, which coordinates organ donation for transplants in the Philadelphia region, told the newspaper that “Dr. Bodzin’s quick action demonstrated his commitment to honoring the selfless generosity of all donors and their families and gives hope to everyone waiting for a second chance at life.”
Should Dr. Bodzin consider a step up from the transplant team to another group that’s fighting for the common good? The recipient of the liver in question seems to think so. “I guess he has a cape on under that white jacket,” 66-year-old Charles Rowe told Fox29. You already know where we’re going with this, right?
Avengers … Assemble.
Your spleen’s due for its 5,000-mile oil change
The human body is an incredible biological machine, capable of performing a countless array of tasks automatically and essentially without flaw, but there’s always room for improvement. After all, there are animals that can regrow entire missing limbs or live for up to 500 years. It would be nice if we could get some of that going.
Rather than any of that cool stuff, a recent survey of 2,000 average Americans revealed that our ambitions for improving the human body are a bit more mundane. The big thing that would make our lives better and easier, according to three-fourths of Americans, would be a built-in “check engine” light in our bodies. Come on guys, starfish can literally be cut in half and not only survive, but become two starfish. Mantis shrimp can punch with a force thousands of times their own weight. If we could punch like they could, we could literally break steel with our fists. Wouldn’t we rather have that?
Apparently not. Fine, we’ll stick with the check engine light.
Maybe it isn’t a huge surprise that we’d like the extra help in figuring out what our body needs. According to the survey, more than 60% of Americans struggle to identify when their body is trying to tell them something important, and only one-third actively checked in with their health every day. Considering about 40% said they feel tired for much of the day and nearly half reported not having a meal with fruits or vegetables in the past 3 days, perhaps a gentle reminder wouldn’t be the worst thing in the world.
So, if we did have a built-in check engine light, what would we use it for? A majority said they’d like to be reminded to drink a glass of water, with 45% saying they wanted to know when to take a nap. Feeling thirsty or tired isn’t quite enough, it seems.
Of course, the technology certainly exists to make the human check engine light a reality. An implanted microchip could absolutely tell us to drink a glass of water, but that would put our health in the hands of tech companies, and you just know Meta and Elon Muskrat wouldn’t pass up the chance for monetization. “Oh, sorry, we could have notified the hospital that you were about to have a heart attack, but you didn’t pay your life subscription this month.”
Sext offenders show more than their, well, you know
As we have become more and more attached to our phones, especially post pandemic, it’s no surprise that sexting – sending sexually explicit images and messages with those phones – has become a fairly common way for people to sexually communicate. And with dating apps just another venture in the dating landscape, regardless of age, sexting is an easy avenue to incite a mood without being physically present.
A recent study, though, has linked sexting with anxiety, sleep issues, depression, and compulsive sexual behaviors. Yikes.
Although the researchers noted that sexting was primarily reciprocal (sending and receiving), “over 50% of adults report sending a sext, while women are up to four times more likely than men to report having received nonconsensual sexts,” said Brenda K. Wiederhold, PhD, editor-in-chief of Cyberpsychology, Behavior, and Social Networking, which published the study, in which Dr. Wiederhold was not involved.
Among the 2,160 U.S. college students who were involved, participants who had only sent sexts reported more anxiety, depression, and sleep problems than other groups (no sexting, received only, reciprocal). There was also a possible connection between sexting, marijuana use, and compulsive sexual behavior, the investigators said in a written statement.
Considering the study population, these data are perhaps not that surprising. For young adults, to receive or send an elusive nude is as common as it once was to give someone flowers. Not that the two things elicit the same reactions. “Many individuals reveal they enjoy consensual sexting and feel it empowers them and builds self-confidence,” Dr. Wiederhold added.
Receiving a nonconsensual sext, though, is definitely going to result in feeling violated and super awkward. Senders beware: Don’t be surprised if you’re ghosted after that.
Isolated nail psoriasis may bring arthritis into play
for dermatologists to improve their diagnostic accuracy,” investigators said in a research letter.
Diagnosis of isolated NP was delayed by almost 3 years among the 87 cases recorded and “arthritis was most often diagnosed concurrently with NP,” at a major nail referral center between Jan. 1, 2001, and Dec. 21, 2022, Michelle J. Chang of Drexel University, Philadelphia, and associates reported.
In what the authors say is, “the largest study documenting clinical and histologic features in patients with isolated NP,” the two most common clinical features were onycholysis and nail plate pitting, seen in 79% and 70% of cases, respectively. No other single feature had a prevalence higher than 28%.
The most frequent clinical dyad was onycholysis and pitting in 66% of patients, followed by onycholysis/nail thickening in 33% and onycholysis/splinter hemorrhage in 32%. The most common histologic features were parakeratosis in 79% and neutrophil infiltration in 48%, the investigators said.
Psoriatic arthritis (PsA), a focus of the study, occurred in 10 (11%) of the 87 individuals with isolated NP. Considering this finding, and “the close proximity between the nail apparatus and joint, we hypothesize a reciprocal relationship, with nail unit inflammation precipitating PsA,” Ms. Chang and associates wrote.
Senior author, Shari Lipner, MD, PhD, of the department of dermatology, Weill Cornell Medicine, New York, is a consultant for Ortho-Dermatologics, Hoth Therapeutics, and BelleTorus. Ms. Chang and the two other investigators had no conflicts of interest to declare.
for dermatologists to improve their diagnostic accuracy,” investigators said in a research letter.
Diagnosis of isolated NP was delayed by almost 3 years among the 87 cases recorded and “arthritis was most often diagnosed concurrently with NP,” at a major nail referral center between Jan. 1, 2001, and Dec. 21, 2022, Michelle J. Chang of Drexel University, Philadelphia, and associates reported.
In what the authors say is, “the largest study documenting clinical and histologic features in patients with isolated NP,” the two most common clinical features were onycholysis and nail plate pitting, seen in 79% and 70% of cases, respectively. No other single feature had a prevalence higher than 28%.
The most frequent clinical dyad was onycholysis and pitting in 66% of patients, followed by onycholysis/nail thickening in 33% and onycholysis/splinter hemorrhage in 32%. The most common histologic features were parakeratosis in 79% and neutrophil infiltration in 48%, the investigators said.
Psoriatic arthritis (PsA), a focus of the study, occurred in 10 (11%) of the 87 individuals with isolated NP. Considering this finding, and “the close proximity between the nail apparatus and joint, we hypothesize a reciprocal relationship, with nail unit inflammation precipitating PsA,” Ms. Chang and associates wrote.
Senior author, Shari Lipner, MD, PhD, of the department of dermatology, Weill Cornell Medicine, New York, is a consultant for Ortho-Dermatologics, Hoth Therapeutics, and BelleTorus. Ms. Chang and the two other investigators had no conflicts of interest to declare.
for dermatologists to improve their diagnostic accuracy,” investigators said in a research letter.
Diagnosis of isolated NP was delayed by almost 3 years among the 87 cases recorded and “arthritis was most often diagnosed concurrently with NP,” at a major nail referral center between Jan. 1, 2001, and Dec. 21, 2022, Michelle J. Chang of Drexel University, Philadelphia, and associates reported.
In what the authors say is, “the largest study documenting clinical and histologic features in patients with isolated NP,” the two most common clinical features were onycholysis and nail plate pitting, seen in 79% and 70% of cases, respectively. No other single feature had a prevalence higher than 28%.
The most frequent clinical dyad was onycholysis and pitting in 66% of patients, followed by onycholysis/nail thickening in 33% and onycholysis/splinter hemorrhage in 32%. The most common histologic features were parakeratosis in 79% and neutrophil infiltration in 48%, the investigators said.
Psoriatic arthritis (PsA), a focus of the study, occurred in 10 (11%) of the 87 individuals with isolated NP. Considering this finding, and “the close proximity between the nail apparatus and joint, we hypothesize a reciprocal relationship, with nail unit inflammation precipitating PsA,” Ms. Chang and associates wrote.
Senior author, Shari Lipner, MD, PhD, of the department of dermatology, Weill Cornell Medicine, New York, is a consultant for Ortho-Dermatologics, Hoth Therapeutics, and BelleTorus. Ms. Chang and the two other investigators had no conflicts of interest to declare.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
A purple warrior rises in the battle against diabetes
One-eyed, one-horned, flying purple veggie eater
Big Fruits and Vegetables is at it again. You notice how they’re always like “Oh, vegetables are good for your health,” and “Eating fruits every day makes you live longer,” but come on. It’s a marketing ploy, leading us astray from our personal savior, McDonald’s.
Just look at this latest bit of research: According to researchers from Finland, eating purple vegetables can protect against diabetes. Considering nearly 40 million Americans have diabetes (and nearly 100 million have prediabetes), anything to reduce the incidence of diabetes (people with diabetes account for one-fourth of every dollar spent in U.S. health care) would be beneficial. So, let’s humor the fruits and veggies people this time and hear them out.
It all comes down to a chemical called anthocyanin, which is a pigment that gives fruits and vegetables such as blueberries, radishes, and red cabbages their purplish color. Anthocyanin also has probiotic and anti-inflammatory effects, meaning it can help improve intestinal lining health and regulate glucose and lipid metabolic pathways. Obviously, good things if you want to avoid diabetes.
The investigators also found that, while standard anthocyanin was beneficial, acylated anthocyanin (which has an acyl group added to the sugar molecules of anthocyanin) is really what you want to go for. The acylated version, found in abundance in purple potatoes, purple carrots, radishes, and red cabbages, is tougher to digest, but the positive effects it has in the body are enhanced over the standard version.
Now, this all a compelling bit of research, but at the end of the day, you’re still eating fruits and vegetables, and we are red-blooded Americans here. We don’t do healthy foods. Although, if you were to dye our burgers with anthocyanin and make them purple, you’d have our attention. Purple is our favorite color.
Manuka honey better as building material than antibiotic
Milk, according to the old saying, builds strong bones, but when it comes to patients with bone loss caused by various medical reasons, researchers found that manuka honey, produced only in New Zealand and some parts of Australia, may also do the job. They soaked collagen scaffolds used for bone implants in various concentrations of the honey and found that 5% led to higher mineral formation and osteoprotegerin production, which suggests increased bone production.
But, and this is a pretty big one, the other half of the study – testing manuka honey’s ability to ward off bacteria – wasn’t so successful. Bone implants, apparently, count for almost half of all hospital-acquired infections, which obviously can put a damper on the healing process. The hope was that a biomaterial would be more effective than something like metal in lessening bacteria formation. Nope.
When the researchers soaked paper disks in honey and added them to cultures of Pseudomonas aeruginosa and Staphylococcus aureus, none of the various concentrations stopped bacterial growth in the scaffolding, even when they added antibiotics.
The sticky conclusion, you could say, is more bitter than sweet.
It may sound like Korn, but can it play ‘Freak on a Leash’?
Like all right-thinking Americans, we love corn, corn-based products, and almost corn. Corn on the cob grilled in the husk? Mmm. Plus, we’re big fans of the band Korn. Also, we once had a reporter here named Tim Kirn. And don’t even get us started with Karn. Best Family Feud host ever.
But what about Quorn? Oh sure, the fungi-based meat alternative is full of yummy mycoprotein, but can it prevent colorectal cancer? Can we add Quorn to our favorites list? Let’s see what Science has to say.
Researchers at Northumbria University in Newcastle upon Tyne, England, fed a group of 20 men some meat (240 g/day) for 2 weeks – hopefully, they were allowed to eat some other food as well – and then gave them the same amount of Quorn, excuse us, fungi-derived mycoprotein equivalents, for 2 more weeks, with a 4-week washout period in between.
Levels of cancer-causing chemicals known as genotoxins fell significantly in the mycoprotein phase but rose during the meat phase. The mycoprotein diet also improved gut health “by increasing the abundance of protective bacteria such as Lactobacilli, Roseburia, and Akkermansia, which are associated with offering protection against chemically induced tumours, inflammation and bowel cancer,” they said in a statement from the university.
The meat phase, on the other hand, resulted in an increase in “gut bacteria linked with issues such as cancer, cardiovascular diseases, weight gain and other negative health outcomes,” they noted.
Science, then, seems to approve of Quorn, and that’s good enough for us. We’re adding Quorn to our diet, starting with a fungi-derived mycoproteinburger tonight while we’re watching the Cornell Big Red take the court against their archrivals, the Big Green of Dartmouth College. GO RED!
One-eyed, one-horned, flying purple veggie eater
Big Fruits and Vegetables is at it again. You notice how they’re always like “Oh, vegetables are good for your health,” and “Eating fruits every day makes you live longer,” but come on. It’s a marketing ploy, leading us astray from our personal savior, McDonald’s.
Just look at this latest bit of research: According to researchers from Finland, eating purple vegetables can protect against diabetes. Considering nearly 40 million Americans have diabetes (and nearly 100 million have prediabetes), anything to reduce the incidence of diabetes (people with diabetes account for one-fourth of every dollar spent in U.S. health care) would be beneficial. So, let’s humor the fruits and veggies people this time and hear them out.
It all comes down to a chemical called anthocyanin, which is a pigment that gives fruits and vegetables such as blueberries, radishes, and red cabbages their purplish color. Anthocyanin also has probiotic and anti-inflammatory effects, meaning it can help improve intestinal lining health and regulate glucose and lipid metabolic pathways. Obviously, good things if you want to avoid diabetes.
The investigators also found that, while standard anthocyanin was beneficial, acylated anthocyanin (which has an acyl group added to the sugar molecules of anthocyanin) is really what you want to go for. The acylated version, found in abundance in purple potatoes, purple carrots, radishes, and red cabbages, is tougher to digest, but the positive effects it has in the body are enhanced over the standard version.
Now, this all a compelling bit of research, but at the end of the day, you’re still eating fruits and vegetables, and we are red-blooded Americans here. We don’t do healthy foods. Although, if you were to dye our burgers with anthocyanin and make them purple, you’d have our attention. Purple is our favorite color.
Manuka honey better as building material than antibiotic
Milk, according to the old saying, builds strong bones, but when it comes to patients with bone loss caused by various medical reasons, researchers found that manuka honey, produced only in New Zealand and some parts of Australia, may also do the job. They soaked collagen scaffolds used for bone implants in various concentrations of the honey and found that 5% led to higher mineral formation and osteoprotegerin production, which suggests increased bone production.
But, and this is a pretty big one, the other half of the study – testing manuka honey’s ability to ward off bacteria – wasn’t so successful. Bone implants, apparently, count for almost half of all hospital-acquired infections, which obviously can put a damper on the healing process. The hope was that a biomaterial would be more effective than something like metal in lessening bacteria formation. Nope.
When the researchers soaked paper disks in honey and added them to cultures of Pseudomonas aeruginosa and Staphylococcus aureus, none of the various concentrations stopped bacterial growth in the scaffolding, even when they added antibiotics.
The sticky conclusion, you could say, is more bitter than sweet.
It may sound like Korn, but can it play ‘Freak on a Leash’?
Like all right-thinking Americans, we love corn, corn-based products, and almost corn. Corn on the cob grilled in the husk? Mmm. Plus, we’re big fans of the band Korn. Also, we once had a reporter here named Tim Kirn. And don’t even get us started with Karn. Best Family Feud host ever.
But what about Quorn? Oh sure, the fungi-based meat alternative is full of yummy mycoprotein, but can it prevent colorectal cancer? Can we add Quorn to our favorites list? Let’s see what Science has to say.
Researchers at Northumbria University in Newcastle upon Tyne, England, fed a group of 20 men some meat (240 g/day) for 2 weeks – hopefully, they were allowed to eat some other food as well – and then gave them the same amount of Quorn, excuse us, fungi-derived mycoprotein equivalents, for 2 more weeks, with a 4-week washout period in between.
Levels of cancer-causing chemicals known as genotoxins fell significantly in the mycoprotein phase but rose during the meat phase. The mycoprotein diet also improved gut health “by increasing the abundance of protective bacteria such as Lactobacilli, Roseburia, and Akkermansia, which are associated with offering protection against chemically induced tumours, inflammation and bowel cancer,” they said in a statement from the university.
The meat phase, on the other hand, resulted in an increase in “gut bacteria linked with issues such as cancer, cardiovascular diseases, weight gain and other negative health outcomes,” they noted.
Science, then, seems to approve of Quorn, and that’s good enough for us. We’re adding Quorn to our diet, starting with a fungi-derived mycoproteinburger tonight while we’re watching the Cornell Big Red take the court against their archrivals, the Big Green of Dartmouth College. GO RED!
One-eyed, one-horned, flying purple veggie eater
Big Fruits and Vegetables is at it again. You notice how they’re always like “Oh, vegetables are good for your health,” and “Eating fruits every day makes you live longer,” but come on. It’s a marketing ploy, leading us astray from our personal savior, McDonald’s.
Just look at this latest bit of research: According to researchers from Finland, eating purple vegetables can protect against diabetes. Considering nearly 40 million Americans have diabetes (and nearly 100 million have prediabetes), anything to reduce the incidence of diabetes (people with diabetes account for one-fourth of every dollar spent in U.S. health care) would be beneficial. So, let’s humor the fruits and veggies people this time and hear them out.
It all comes down to a chemical called anthocyanin, which is a pigment that gives fruits and vegetables such as blueberries, radishes, and red cabbages their purplish color. Anthocyanin also has probiotic and anti-inflammatory effects, meaning it can help improve intestinal lining health and regulate glucose and lipid metabolic pathways. Obviously, good things if you want to avoid diabetes.
The investigators also found that, while standard anthocyanin was beneficial, acylated anthocyanin (which has an acyl group added to the sugar molecules of anthocyanin) is really what you want to go for. The acylated version, found in abundance in purple potatoes, purple carrots, radishes, and red cabbages, is tougher to digest, but the positive effects it has in the body are enhanced over the standard version.
Now, this all a compelling bit of research, but at the end of the day, you’re still eating fruits and vegetables, and we are red-blooded Americans here. We don’t do healthy foods. Although, if you were to dye our burgers with anthocyanin and make them purple, you’d have our attention. Purple is our favorite color.
Manuka honey better as building material than antibiotic
Milk, according to the old saying, builds strong bones, but when it comes to patients with bone loss caused by various medical reasons, researchers found that manuka honey, produced only in New Zealand and some parts of Australia, may also do the job. They soaked collagen scaffolds used for bone implants in various concentrations of the honey and found that 5% led to higher mineral formation and osteoprotegerin production, which suggests increased bone production.
But, and this is a pretty big one, the other half of the study – testing manuka honey’s ability to ward off bacteria – wasn’t so successful. Bone implants, apparently, count for almost half of all hospital-acquired infections, which obviously can put a damper on the healing process. The hope was that a biomaterial would be more effective than something like metal in lessening bacteria formation. Nope.
When the researchers soaked paper disks in honey and added them to cultures of Pseudomonas aeruginosa and Staphylococcus aureus, none of the various concentrations stopped bacterial growth in the scaffolding, even when they added antibiotics.
The sticky conclusion, you could say, is more bitter than sweet.
It may sound like Korn, but can it play ‘Freak on a Leash’?
Like all right-thinking Americans, we love corn, corn-based products, and almost corn. Corn on the cob grilled in the husk? Mmm. Plus, we’re big fans of the band Korn. Also, we once had a reporter here named Tim Kirn. And don’t even get us started with Karn. Best Family Feud host ever.
But what about Quorn? Oh sure, the fungi-based meat alternative is full of yummy mycoprotein, but can it prevent colorectal cancer? Can we add Quorn to our favorites list? Let’s see what Science has to say.
Researchers at Northumbria University in Newcastle upon Tyne, England, fed a group of 20 men some meat (240 g/day) for 2 weeks – hopefully, they were allowed to eat some other food as well – and then gave them the same amount of Quorn, excuse us, fungi-derived mycoprotein equivalents, for 2 more weeks, with a 4-week washout period in between.
Levels of cancer-causing chemicals known as genotoxins fell significantly in the mycoprotein phase but rose during the meat phase. The mycoprotein diet also improved gut health “by increasing the abundance of protective bacteria such as Lactobacilli, Roseburia, and Akkermansia, which are associated with offering protection against chemically induced tumours, inflammation and bowel cancer,” they said in a statement from the university.
The meat phase, on the other hand, resulted in an increase in “gut bacteria linked with issues such as cancer, cardiovascular diseases, weight gain and other negative health outcomes,” they noted.
Science, then, seems to approve of Quorn, and that’s good enough for us. We’re adding Quorn to our diet, starting with a fungi-derived mycoproteinburger tonight while we’re watching the Cornell Big Red take the court against their archrivals, the Big Green of Dartmouth College. GO RED!
Antibiotics and SJS/TEN: Study provides global prevalence
of SJS/TEN in connection with antibiotics.
“SJS/TEN is considered the most severe form of drug hypersensitivity reaction, and antibiotics are an important risk,” Erika Yue Lee, MD, and associates wrote in JAMA Dermatology.
Their analysis, which involved 38 studies published since 1987 with 2,917 patients from more than 20 countries, showed that 86% of all SJS/TEN cases were associated with a single drug, with the rest involving multiple drug triggers, infections, or other causes. More than a quarter (28%) of those patients had used an antibiotic, and the sulfonamides were the class most often triggering SJS/TEN, said Dr. Lee of the University of Toronto and associates.
Sulfonamides were responsible for 32% of the antibiotic-associated cases, which works out to 11% of all SJS/TEN cases included in the analysis. Penicillins were next with 22% of all antibiotic-associated cases, followed by the cephalosporins (11%), fluoroquinolones (4%), and macrolides (2%), the investigators reported.
A subgroup analysis conducted by age indicated that “there was no difference in the proportion of antibiotics associated with SJS/TEN between adult and pediatric groups,” they noted.
There were differences, however, among the various antibiotic classes. Sulfonamides represented 54% of antibiotic-triggered reactions in children, compared with 25% in adults, but adults were significantly more likely to have cephalosporin (23%) and fluoroquinolone (5%) involvement than were children (2% and 0, respectively). Macrolide-induced SJS/TEN was more common in children (18% vs. 1%), while the penicillin rate was 18% for both age groups, Dr. Lee and associates said.
A second subgroup analysis establishing the proportion of antibiotic-induced SJS/TEN by continent ranked Australia highest with 43%, but that was based on only one study of 42 patients. North America was slightly lower at 37%, but the analysis included 14 studies and 932 patients. Asia’s 16 studies and 1,298 patients were divided into three regions, with the lowest being the southeast at 16%, according to the researchers.
“Global sulfonamide antibiotic use has been decreasing since 2000 despite an ongoing upward trend of use in other antibiotic classes,” they wrote, but “antibiotics remain one of the most common culprit drugs for SJS/TEN in both adults and children worldwide.”
One of Dr. Lee’s associates has received personal fees from Janssen, AstraZeneca, UpToDate, Verve, BioCryst, Regeneron Pharmaceuticals, and Novavax and has served as codirector of IIID Pty Ltd, which holds a patent for HLA-B*57:01 testing and has a patent pending for detection of HLA-A*32:01 in connection with diagnosing drug reaction without any financial remuneration outside this study.
of SJS/TEN in connection with antibiotics.
“SJS/TEN is considered the most severe form of drug hypersensitivity reaction, and antibiotics are an important risk,” Erika Yue Lee, MD, and associates wrote in JAMA Dermatology.
Their analysis, which involved 38 studies published since 1987 with 2,917 patients from more than 20 countries, showed that 86% of all SJS/TEN cases were associated with a single drug, with the rest involving multiple drug triggers, infections, or other causes. More than a quarter (28%) of those patients had used an antibiotic, and the sulfonamides were the class most often triggering SJS/TEN, said Dr. Lee of the University of Toronto and associates.
Sulfonamides were responsible for 32% of the antibiotic-associated cases, which works out to 11% of all SJS/TEN cases included in the analysis. Penicillins were next with 22% of all antibiotic-associated cases, followed by the cephalosporins (11%), fluoroquinolones (4%), and macrolides (2%), the investigators reported.
A subgroup analysis conducted by age indicated that “there was no difference in the proportion of antibiotics associated with SJS/TEN between adult and pediatric groups,” they noted.
There were differences, however, among the various antibiotic classes. Sulfonamides represented 54% of antibiotic-triggered reactions in children, compared with 25% in adults, but adults were significantly more likely to have cephalosporin (23%) and fluoroquinolone (5%) involvement than were children (2% and 0, respectively). Macrolide-induced SJS/TEN was more common in children (18% vs. 1%), while the penicillin rate was 18% for both age groups, Dr. Lee and associates said.
A second subgroup analysis establishing the proportion of antibiotic-induced SJS/TEN by continent ranked Australia highest with 43%, but that was based on only one study of 42 patients. North America was slightly lower at 37%, but the analysis included 14 studies and 932 patients. Asia’s 16 studies and 1,298 patients were divided into three regions, with the lowest being the southeast at 16%, according to the researchers.
“Global sulfonamide antibiotic use has been decreasing since 2000 despite an ongoing upward trend of use in other antibiotic classes,” they wrote, but “antibiotics remain one of the most common culprit drugs for SJS/TEN in both adults and children worldwide.”
One of Dr. Lee’s associates has received personal fees from Janssen, AstraZeneca, UpToDate, Verve, BioCryst, Regeneron Pharmaceuticals, and Novavax and has served as codirector of IIID Pty Ltd, which holds a patent for HLA-B*57:01 testing and has a patent pending for detection of HLA-A*32:01 in connection with diagnosing drug reaction without any financial remuneration outside this study.
of SJS/TEN in connection with antibiotics.
“SJS/TEN is considered the most severe form of drug hypersensitivity reaction, and antibiotics are an important risk,” Erika Yue Lee, MD, and associates wrote in JAMA Dermatology.
Their analysis, which involved 38 studies published since 1987 with 2,917 patients from more than 20 countries, showed that 86% of all SJS/TEN cases were associated with a single drug, with the rest involving multiple drug triggers, infections, or other causes. More than a quarter (28%) of those patients had used an antibiotic, and the sulfonamides were the class most often triggering SJS/TEN, said Dr. Lee of the University of Toronto and associates.
Sulfonamides were responsible for 32% of the antibiotic-associated cases, which works out to 11% of all SJS/TEN cases included in the analysis. Penicillins were next with 22% of all antibiotic-associated cases, followed by the cephalosporins (11%), fluoroquinolones (4%), and macrolides (2%), the investigators reported.
A subgroup analysis conducted by age indicated that “there was no difference in the proportion of antibiotics associated with SJS/TEN between adult and pediatric groups,” they noted.
There were differences, however, among the various antibiotic classes. Sulfonamides represented 54% of antibiotic-triggered reactions in children, compared with 25% in adults, but adults were significantly more likely to have cephalosporin (23%) and fluoroquinolone (5%) involvement than were children (2% and 0, respectively). Macrolide-induced SJS/TEN was more common in children (18% vs. 1%), while the penicillin rate was 18% for both age groups, Dr. Lee and associates said.
A second subgroup analysis establishing the proportion of antibiotic-induced SJS/TEN by continent ranked Australia highest with 43%, but that was based on only one study of 42 patients. North America was slightly lower at 37%, but the analysis included 14 studies and 932 patients. Asia’s 16 studies and 1,298 patients were divided into three regions, with the lowest being the southeast at 16%, according to the researchers.
“Global sulfonamide antibiotic use has been decreasing since 2000 despite an ongoing upward trend of use in other antibiotic classes,” they wrote, but “antibiotics remain one of the most common culprit drugs for SJS/TEN in both adults and children worldwide.”
One of Dr. Lee’s associates has received personal fees from Janssen, AstraZeneca, UpToDate, Verve, BioCryst, Regeneron Pharmaceuticals, and Novavax and has served as codirector of IIID Pty Ltd, which holds a patent for HLA-B*57:01 testing and has a patent pending for detection of HLA-A*32:01 in connection with diagnosing drug reaction without any financial remuneration outside this study.
FROM JAMA DERMATOLOGY
Medicare ‘offers’ cancer patient a choice: Less life or more debt
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
We’re gonna need a bigger meth lab
In case you’ve been living under a rock for the past 15 years, the TV show “Breaking Bad” details the spiraling rise and downfall of a high school chemistry teacher who, after developing a case of terminal lung cancer, starts producing methamphetamine to provide for his family in response to the steep cost of treatment for his cancer.
Meanwhile, here in 2023 in the real world, we have Paul Davis, a retired physician in Ohio, who’s being forced to choose between an expensive cancer treatment and bankrupting his family, since Medicare’s decided it doesn’t want to cover the cost. Hey, we’ve seen this one before!
A bit of backstory: In November 2019, Dr. Davis was diagnosed with uveal melanoma, a very rare type of cancer that affects eye tissue. The news got worse in 2022 when the cancer spread to his liver, a move which typically proves fatal within a year. However, in a stroke of great news, the Food and Drug Administration approved the drug Kimmtrak earlier that year, which could be used to treat his cancer. Not cure, of course, but it would give him more time.
His initial treatments with the drug went fine and were covered, but when he transferred his care from a hospital in Columbus to one closer to home, big problem. Medicare decided it didn’t like that hospital and abruptly cut off coverage, denying the local hospital’s claims. That leaves Dr. Davis on the hook for his cancer treatment, and it’s what you might call expensive. Expensive to the tune of $50,000.
A week.
Apparently the coding the local hospital submitted was wrong, indicating that Dr. Davis was receiving Kimmtrak for a type of cancer that the FDA hadn’t approved the drug for. So until the government bureaucracy works itself out, his treatment is on hold, leaving all his faith in Medicare working quickly to rectify its mistake. If it can rectify its mistake. We’re not hopeful.
And in case you were wondering, if Dr. Davis wanted to go full Walter White, the average street price of meth is about $20-$60 per gram, so to pay for his treatment, he’d need to make at least a kilogram of meth every week. That’s, uh, quite a lot of illegal drug, or what we here at the LOTME office would call a fun Saturday night.
When you give a mouse a movie
Researchers have been successfully testing Alzheimer drugs on mice for years, but none of the drugs has proved successful in humans. Recent work, however, might have found the missing link, and it’s a combination no one ever thought of before: mice and movies.
Turns out that Orson Welles’ 1958 film noir classic “Touch of Evil” tapped a part of the mouse brain that has been overlooked: the hippocampus, which is crucial for learning and memory. Previous researchers thought it was just used as a kind of GPS system, but that’s only partially true.
Not only did the mice choose to pay attention to the movie clip, but the hippocampus responded to the visual stimuli only when the rodents saw the scenes from the clip later in the order that they were presented and not in a scrambled order. These findings represent a “major paradigm shift” in studying mouse recall, Mayank Mehta, PhD, of the University of California, Los Angeles, said in a statement from the school.
This breakthrough could run parallel to Alzheimer’s patients struggling with similar defects. “Selective and episodic activation of the mouse hippocampus using a human movie opens up the possibility of directly testing human episodic memory disorders and therapies using mouse neurons, a major step forward,” said coauthor Chinmay Purandare, PhD, who is now at the University of California, San Francisco.
Who would have thought that a classic film would help advance Alzheimer research?
A less human way to study mosquitoes
We here at LOTME have a history with mosquitoes. We know they don’t like us, and they know that we don’t like them. Trust us, they know. So when humans gain a little ground in the war against the buzzy little bloodsuckers, we want to share the joy.
To know the enemy, scientists have to study the enemy, but there is a problem. “Many mosquito experiments still rely on human volunteers and animal subjects,” bioengineering graduate student Kevin Janson, said in a statement from Rice University. Most people don’t like being bitten by mosquitoes, so that kind of testing can be expensive.
Is there a way to automate the collection and processing of mosquito behavior data using inexpensive cameras and machine-learning software? We’re glad you asked, because Mr. Janson and the research team, which includes bioengineers from Rice and tropical medicine experts from Tulane University, have managed to eliminate the need for live volunteers by using patches of synthetic skin made with a 3D printer.
“Each patch of gelatin-like hydrogel comes complete with tiny passageways that can be filled with flowing blood” from a chicken, sheep, or cow, they explained, and proof-of-concept testing showed that mosquitoes would feed on hydrogels without any repellent and stay away from those treated with a repellent.
To conduct the feeding tests, the blood-infused hydrogels are placed in a clear plastic box that is surrounded by cameras.
A bunch of mosquitoes are then tossed in the box and the cameras record all their insect activities: how often they land at each location, how long they stay, whether or not they bite, how long they feed, etc. Humans don’t have to watch and don’t have to be food sources.
Humans don’t have to be food sources, and we just pictured the future of mosquito control. Imagine a dozen Arnold Schwarzenegger–style Terminators, covered in 3D-printed skin, walking through your neighborhood in the summer while wearing sweat-soaked, brightly colored clothing. The mosquitoes wouldn’t be able to stay away, but guess what? They’re feeding off robots with nonhuman skin and nonhuman blood, so we win. It’s good to have a cerebral cortex.
Getting medieval on brain surgery
Let’s get one thing clear: The so-called “Dark Ages” were not nearly as dark as they’re made out to be. For one thing, there’s a world beyond Western Europe. The Roman Empire didn’t collapse everywhere. But even in Western Europe, the centuries between the fall of Rome and the Renaissance were hardly lacking in cultural development.
That said, we wouldn’t want to be in the position of the seventh-century noblewoman whose remains were recently uncovered in a Byzantine fortress in central Italy with multiple cross-shaped incisions in her skull. Yes, this unfortunate woman underwent at least two brain surgeries.
Then again, maybe not. Nothing like it had been discovered at the site, and while the markings – signs of a procedure called trepanation – can be surgical in nature, there are other explanations. For example, the Avar people practiced ritual trepanation during the same time period, but they were hundreds of miles away in the Carpathian mountains, and there was no evidence to support that a different form of ritualistic trepanation ever took place in Byzantine-era Italy.
The investigators then moved on to a form of judicial punishment called decalvatio, which involves mutilation by scalping. Look, the Dark Ages weren’t dark, but no one said they were fun. Anyway, this was discarded, since decalvatio was only meted out to soldiers who deserted the battlefield.
That brings us back to surgery. While one of the trepanations was fully engraved into her skull, indicating that the woman died soon after the surgery, she also bore indications of a healed trepanation. A 50% success rate isn’t terrible for our medieval surgeon. Sure, the Incas managed 80%, but even during the Civil War brain surgery only had a 50% success rate. And that’s the end of the story, nothing more to say about our medieval Italian woman.
Nope. Nothing at all.
Fine. While a surgical procedure was deemed most likely, the study investigators found no direct evidence of a medical condition. No trauma, no tumor, nothing. Just a couple of suggestions of “a systemic pathological condition,” they said. Okay, we swear, it really wasn’t that bad in the Middle [Editor’s note: Approximately 5,000 more words on medieval culture not included. This is a medical column, thank you very much.]
Pound of flesh buys less prison time
Pound of flesh buys less prison time
We should all have more Shakespeare in our lives. Yeah, yeah, Shakespeare is meant to be played, not read, and it can be a struggle to herd teenagers through the Bard’s interesting and bloody tragedies, but even a perfunctory reading of “The Merchant of Venice” would hopefully have prevented the dystopian nightmare Massachusetts has presented us with today.
The United States has a massive shortage of donor organs. This is an unfortunate truth. So, to combat this issue, a pair of Massachusetts congresspeople have proposed HD 3822, which would allow prisoners to donate organs and/or bone marrow (a pound of flesh, so to speak) in exchange for up to a year in reduced prison time. Yes, that’s right. Give up pieces of yourself and the state of Massachusetts will deign to reduce your long prison sentence.
Oh, and before you dismiss this as typical Republican antics, the bill was sponsored by two Democrats, and in a statement one of them hoped to address racial disparities in organ donation, as people of color are much less likely to receive organs. Never mind that Black people are imprisoned at a much higher rate than Whites.
Yeah, this whole thing is what people in the business like to call an ethical disaster.
Fortunately, the bill will likely never be passed and it’s probably illegal anyway. A federal law from 1984 (how’s that for a coincidence) prevents people from donating organs for use in human transplantation in exchange for “valuable consideration.” In other words, you can’t sell your organs for profit, and in this case, reducing prison time would probably count as valuable consideration in the eyes of the courts.
Oh, and in case you’ve never read Merchant of Venice, Shylock, the character looking for the pound of flesh as payment for a debt? He’s the villain. In fact, it’s pretty safe to say that anyone looking to extract payment from human dismemberment is probably the bad guy of the story. Apparently that wasn’t clear.
How do you stop a fungi? With a deadly guy
Thanks to the new HBO series “The Last of Us,” there’s been a lot of talk about the upcoming fungi-pocalypse, as the show depicts the real-life “zombie fungus” Cordyceps turning humans into, you know, zombies.
No need to worry, ladies and gentleman, because science has discovered a way to turn back the fungal horde. A heroic, and environmentally friendly, alternative to chemical pesticides “in the fight against resistant fungi [that] are now resistant to antimycotics – partly because they are used in large quantities in agricultural fields,” investigators at the Leibniz Institute for Natural Product Research and Infection Biology in Jena, Germany, said in a written statement.
We are, of course, talking about Keanu Reeves. Wait a second. He’s not even in “The Last of Us.” Sorry folks, we are being told that it really is Keanu Reeves. Our champion in the inevitable fungal pandemic is movie star Keanu Reeves. Sort of. It’s actually keanumycin, a substance produced by bacteria of the genus Pseudomonas.
Really? Keanumycin? “The lipopeptides kill so efficiently that we named them after Keanu Reeves because he, too, is extremely deadly in his roles,” lead author Sebastian Götze, PhD, explained.
Dr. Götze and his associates had been working with pseudomonads for quite a while before they were able to isolate the toxins responsible for their ability to kill amoebae, which resemble fungi in some characteristics. When then finally tried the keanumycin against gray mold rot on hydrangea leaves, the intensely contemplative star of “The Matrix” and “John Wick” – sorry, wrong Keanu – the bacterial derivative significantly inhibited growth of the fungus, they said.
Additional testing has shown that keanumycin is not highly toxic to human cells and is effective against fungi such as Candida albicans in very low concentrations, which makes it a good candidate for future pharmaceutical development.
To that news there can be only one response from the substance’s namesake.
High fat, bye parasites
Fat. Fat. Fat. Seems like everyone is trying to avoid it these days, but fat may be good thing when it comes to weaseling out a parasite.
The parasite in this case is the whipworm, aka Trichuris trichiura. You can find this guy in the intestines of millions of people, where it causes long-lasting infections. Yikes … Researchers have found that the plan of attack to get rid of this invasive species is to boost the immune system, but instead of vitamin C and zinc it’s fat they’re pumping in. Yes, fat.
The developing countries with poor sewage that are at the highest risk for contracting parasites such as this also are among those where people ingest cheaper diets that are generally higher in fat. The investigators were interested to see how a high-fat diet would affect immune responses to the whipworms.
And, as with almost everything else, the researchers turned to mice, which were introduced to a closely related species, Trichuris muris.
A high-fat diet, rather than obesity itself, increases a molecule on T-helper cells called ST2, and this allows an increased T-helper 2 response, effectively giving eviction notices to the parasites in the intestinal lining.
To say the least, the researchers were surprised since “high-fat diets are mostly associated with increased pathology during disease,” said senior author Richard Grencis, PhD, of the University of Manchester (England), who noted that ST2 is not normally triggered with a standard diet in mice but the high-fat diet gave it a boost and an “alternate pathway” out.
Now before you start ordering extra-large fries at the drive-through to keep the whipworms away, the researchers added that they “have previously published that weight loss can aid the expulsion of a different gut parasite worm.” Figures.
Once again, though, signs are pointing to the gut for improved health.
Pound of flesh buys less prison time
We should all have more Shakespeare in our lives. Yeah, yeah, Shakespeare is meant to be played, not read, and it can be a struggle to herd teenagers through the Bard’s interesting and bloody tragedies, but even a perfunctory reading of “The Merchant of Venice” would hopefully have prevented the dystopian nightmare Massachusetts has presented us with today.
The United States has a massive shortage of donor organs. This is an unfortunate truth. So, to combat this issue, a pair of Massachusetts congresspeople have proposed HD 3822, which would allow prisoners to donate organs and/or bone marrow (a pound of flesh, so to speak) in exchange for up to a year in reduced prison time. Yes, that’s right. Give up pieces of yourself and the state of Massachusetts will deign to reduce your long prison sentence.
Oh, and before you dismiss this as typical Republican antics, the bill was sponsored by two Democrats, and in a statement one of them hoped to address racial disparities in organ donation, as people of color are much less likely to receive organs. Never mind that Black people are imprisoned at a much higher rate than Whites.
Yeah, this whole thing is what people in the business like to call an ethical disaster.
Fortunately, the bill will likely never be passed and it’s probably illegal anyway. A federal law from 1984 (how’s that for a coincidence) prevents people from donating organs for use in human transplantation in exchange for “valuable consideration.” In other words, you can’t sell your organs for profit, and in this case, reducing prison time would probably count as valuable consideration in the eyes of the courts.
Oh, and in case you’ve never read Merchant of Venice, Shylock, the character looking for the pound of flesh as payment for a debt? He’s the villain. In fact, it’s pretty safe to say that anyone looking to extract payment from human dismemberment is probably the bad guy of the story. Apparently that wasn’t clear.
How do you stop a fungi? With a deadly guy
Thanks to the new HBO series “The Last of Us,” there’s been a lot of talk about the upcoming fungi-pocalypse, as the show depicts the real-life “zombie fungus” Cordyceps turning humans into, you know, zombies.
No need to worry, ladies and gentleman, because science has discovered a way to turn back the fungal horde. A heroic, and environmentally friendly, alternative to chemical pesticides “in the fight against resistant fungi [that] are now resistant to antimycotics – partly because they are used in large quantities in agricultural fields,” investigators at the Leibniz Institute for Natural Product Research and Infection Biology in Jena, Germany, said in a written statement.
We are, of course, talking about Keanu Reeves. Wait a second. He’s not even in “The Last of Us.” Sorry folks, we are being told that it really is Keanu Reeves. Our champion in the inevitable fungal pandemic is movie star Keanu Reeves. Sort of. It’s actually keanumycin, a substance produced by bacteria of the genus Pseudomonas.
Really? Keanumycin? “The lipopeptides kill so efficiently that we named them after Keanu Reeves because he, too, is extremely deadly in his roles,” lead author Sebastian Götze, PhD, explained.
Dr. Götze and his associates had been working with pseudomonads for quite a while before they were able to isolate the toxins responsible for their ability to kill amoebae, which resemble fungi in some characteristics. When then finally tried the keanumycin against gray mold rot on hydrangea leaves, the intensely contemplative star of “The Matrix” and “John Wick” – sorry, wrong Keanu – the bacterial derivative significantly inhibited growth of the fungus, they said.
Additional testing has shown that keanumycin is not highly toxic to human cells and is effective against fungi such as Candida albicans in very low concentrations, which makes it a good candidate for future pharmaceutical development.
To that news there can be only one response from the substance’s namesake.
High fat, bye parasites
Fat. Fat. Fat. Seems like everyone is trying to avoid it these days, but fat may be good thing when it comes to weaseling out a parasite.
The parasite in this case is the whipworm, aka Trichuris trichiura. You can find this guy in the intestines of millions of people, where it causes long-lasting infections. Yikes … Researchers have found that the plan of attack to get rid of this invasive species is to boost the immune system, but instead of vitamin C and zinc it’s fat they’re pumping in. Yes, fat.
The developing countries with poor sewage that are at the highest risk for contracting parasites such as this also are among those where people ingest cheaper diets that are generally higher in fat. The investigators were interested to see how a high-fat diet would affect immune responses to the whipworms.
And, as with almost everything else, the researchers turned to mice, which were introduced to a closely related species, Trichuris muris.
A high-fat diet, rather than obesity itself, increases a molecule on T-helper cells called ST2, and this allows an increased T-helper 2 response, effectively giving eviction notices to the parasites in the intestinal lining.
To say the least, the researchers were surprised since “high-fat diets are mostly associated with increased pathology during disease,” said senior author Richard Grencis, PhD, of the University of Manchester (England), who noted that ST2 is not normally triggered with a standard diet in mice but the high-fat diet gave it a boost and an “alternate pathway” out.
Now before you start ordering extra-large fries at the drive-through to keep the whipworms away, the researchers added that they “have previously published that weight loss can aid the expulsion of a different gut parasite worm.” Figures.
Once again, though, signs are pointing to the gut for improved health.
Pound of flesh buys less prison time
We should all have more Shakespeare in our lives. Yeah, yeah, Shakespeare is meant to be played, not read, and it can be a struggle to herd teenagers through the Bard’s interesting and bloody tragedies, but even a perfunctory reading of “The Merchant of Venice” would hopefully have prevented the dystopian nightmare Massachusetts has presented us with today.
The United States has a massive shortage of donor organs. This is an unfortunate truth. So, to combat this issue, a pair of Massachusetts congresspeople have proposed HD 3822, which would allow prisoners to donate organs and/or bone marrow (a pound of flesh, so to speak) in exchange for up to a year in reduced prison time. Yes, that’s right. Give up pieces of yourself and the state of Massachusetts will deign to reduce your long prison sentence.
Oh, and before you dismiss this as typical Republican antics, the bill was sponsored by two Democrats, and in a statement one of them hoped to address racial disparities in organ donation, as people of color are much less likely to receive organs. Never mind that Black people are imprisoned at a much higher rate than Whites.
Yeah, this whole thing is what people in the business like to call an ethical disaster.
Fortunately, the bill will likely never be passed and it’s probably illegal anyway. A federal law from 1984 (how’s that for a coincidence) prevents people from donating organs for use in human transplantation in exchange for “valuable consideration.” In other words, you can’t sell your organs for profit, and in this case, reducing prison time would probably count as valuable consideration in the eyes of the courts.
Oh, and in case you’ve never read Merchant of Venice, Shylock, the character looking for the pound of flesh as payment for a debt? He’s the villain. In fact, it’s pretty safe to say that anyone looking to extract payment from human dismemberment is probably the bad guy of the story. Apparently that wasn’t clear.
How do you stop a fungi? With a deadly guy
Thanks to the new HBO series “The Last of Us,” there’s been a lot of talk about the upcoming fungi-pocalypse, as the show depicts the real-life “zombie fungus” Cordyceps turning humans into, you know, zombies.
No need to worry, ladies and gentleman, because science has discovered a way to turn back the fungal horde. A heroic, and environmentally friendly, alternative to chemical pesticides “in the fight against resistant fungi [that] are now resistant to antimycotics – partly because they are used in large quantities in agricultural fields,” investigators at the Leibniz Institute for Natural Product Research and Infection Biology in Jena, Germany, said in a written statement.
We are, of course, talking about Keanu Reeves. Wait a second. He’s not even in “The Last of Us.” Sorry folks, we are being told that it really is Keanu Reeves. Our champion in the inevitable fungal pandemic is movie star Keanu Reeves. Sort of. It’s actually keanumycin, a substance produced by bacteria of the genus Pseudomonas.
Really? Keanumycin? “The lipopeptides kill so efficiently that we named them after Keanu Reeves because he, too, is extremely deadly in his roles,” lead author Sebastian Götze, PhD, explained.
Dr. Götze and his associates had been working with pseudomonads for quite a while before they were able to isolate the toxins responsible for their ability to kill amoebae, which resemble fungi in some characteristics. When then finally tried the keanumycin against gray mold rot on hydrangea leaves, the intensely contemplative star of “The Matrix” and “John Wick” – sorry, wrong Keanu – the bacterial derivative significantly inhibited growth of the fungus, they said.
Additional testing has shown that keanumycin is not highly toxic to human cells and is effective against fungi such as Candida albicans in very low concentrations, which makes it a good candidate for future pharmaceutical development.
To that news there can be only one response from the substance’s namesake.
High fat, bye parasites
Fat. Fat. Fat. Seems like everyone is trying to avoid it these days, but fat may be good thing when it comes to weaseling out a parasite.
The parasite in this case is the whipworm, aka Trichuris trichiura. You can find this guy in the intestines of millions of people, where it causes long-lasting infections. Yikes … Researchers have found that the plan of attack to get rid of this invasive species is to boost the immune system, but instead of vitamin C and zinc it’s fat they’re pumping in. Yes, fat.
The developing countries with poor sewage that are at the highest risk for contracting parasites such as this also are among those where people ingest cheaper diets that are generally higher in fat. The investigators were interested to see how a high-fat diet would affect immune responses to the whipworms.
And, as with almost everything else, the researchers turned to mice, which were introduced to a closely related species, Trichuris muris.
A high-fat diet, rather than obesity itself, increases a molecule on T-helper cells called ST2, and this allows an increased T-helper 2 response, effectively giving eviction notices to the parasites in the intestinal lining.
To say the least, the researchers were surprised since “high-fat diets are mostly associated with increased pathology during disease,” said senior author Richard Grencis, PhD, of the University of Manchester (England), who noted that ST2 is not normally triggered with a standard diet in mice but the high-fat diet gave it a boost and an “alternate pathway” out.
Now before you start ordering extra-large fries at the drive-through to keep the whipworms away, the researchers added that they “have previously published that weight loss can aid the expulsion of a different gut parasite worm.” Figures.
Once again, though, signs are pointing to the gut for improved health.