User login
MedPAC eyes scholarships, loan forgiveness to boost primary care ranks
WASHINGTON – according to a proposal presented at a meeting of the Medicare Payment Advisory Commission.
“A Medicare[-based] program would have a specific objective to encourage more physicians to enter primary care and provide primary care to beneficiaries,” MedPAC staffer Ariel Winter said. “By reducing educational debt, a Medicare-specific program would provide a financial incentive for physicians to choose primary care.”
Any program would face some challenges, Mr. Winter noted. Based on evidence, “it’s difficult to predict how physicians would respond if they were offered debt reduction in exchange for a commitment to practice primary care,” as financial considerations are not the only reason why physicians choose a specific career track.
Financing the program would also need to be considered. MedPAC staff recommended using a separate recommendation, one to end the Merit-based Incentive Payment System and use its $500 million put aside as MIPS bonuses to pay for any Medicare-based program.
Staff proposed a pilot program to “test the impact of different design choices on program operations, physician participation, and career choices,” he said. “Policymakers could use the results to improve the program and decide whether to expand it.”
MedPAC Vice Chairman Jon Christianson, PhD, suggested any program be tied to “physicians who practiced in areas where Medicare beneficiaries don’t have adequate access” to primary care doctors.
However, Mr. Winter noted that he is not aware of “any off-the-shelf system that identifies areas where there’s a problem, where there’s a shortage of clinicians for Medicare beneficiaries specifically. I am not sure how you would do that.”
MedPAC member Kathy Buto, former vice president of global health policy at Johnson & Johnson, questioned whether nurse practitioners and physician assistants should be included in the program, as they “are beginning to subspecialize and get out of primary care.” Mr. Winter said it is open for consideration.
MedPAC member Pat Wang, president and CEO of Healthfirst in New York, questioned whether a new program was needed or whether fixing of existing programs, “making them work better” is the way to go given the evidence that the effect of student debt on decision making is mixed.
She suggested that rather than targeting loan forgiveness, maybe the program should be structured more as a bonus payment rather than debt forgiveness as a means of incentivizing people who may not be concerned with debt forgiveness.
Ms. Buto added that questions of autonomy might also need to be addressed. “Physicians often feel like they don’t have control in Medicare, that they’re required to do a lot of things, and that they are subject to the fee schedule. If there were some way to grant more autonomy, control, and convey status that way, whether it has to do with greater flexibility in whatever, payment models and so on, that’s where I think you can begin to shift the status within primary care.”
MedPAC Chairman Francis Crosson, MD, recalled his time at Kaiser Permanente and noted their programs showed success because of the combination of a significant amount of money and time commitment (10 years).
The time commitment became an important part because after that long, physicians became a part of their communities and tended to stay.
“Two or 3 years, from my perspective and my experience, doesn’t work very well,” Dr. Crosson said. “But a significant period of time does, and a significant amount of money does seem to work.”
gtwachtman@mdedge.com
WASHINGTON – according to a proposal presented at a meeting of the Medicare Payment Advisory Commission.
“A Medicare[-based] program would have a specific objective to encourage more physicians to enter primary care and provide primary care to beneficiaries,” MedPAC staffer Ariel Winter said. “By reducing educational debt, a Medicare-specific program would provide a financial incentive for physicians to choose primary care.”
Any program would face some challenges, Mr. Winter noted. Based on evidence, “it’s difficult to predict how physicians would respond if they were offered debt reduction in exchange for a commitment to practice primary care,” as financial considerations are not the only reason why physicians choose a specific career track.
Financing the program would also need to be considered. MedPAC staff recommended using a separate recommendation, one to end the Merit-based Incentive Payment System and use its $500 million put aside as MIPS bonuses to pay for any Medicare-based program.
Staff proposed a pilot program to “test the impact of different design choices on program operations, physician participation, and career choices,” he said. “Policymakers could use the results to improve the program and decide whether to expand it.”
MedPAC Vice Chairman Jon Christianson, PhD, suggested any program be tied to “physicians who practiced in areas where Medicare beneficiaries don’t have adequate access” to primary care doctors.
However, Mr. Winter noted that he is not aware of “any off-the-shelf system that identifies areas where there’s a problem, where there’s a shortage of clinicians for Medicare beneficiaries specifically. I am not sure how you would do that.”
MedPAC member Kathy Buto, former vice president of global health policy at Johnson & Johnson, questioned whether nurse practitioners and physician assistants should be included in the program, as they “are beginning to subspecialize and get out of primary care.” Mr. Winter said it is open for consideration.
MedPAC member Pat Wang, president and CEO of Healthfirst in New York, questioned whether a new program was needed or whether fixing of existing programs, “making them work better” is the way to go given the evidence that the effect of student debt on decision making is mixed.
She suggested that rather than targeting loan forgiveness, maybe the program should be structured more as a bonus payment rather than debt forgiveness as a means of incentivizing people who may not be concerned with debt forgiveness.
Ms. Buto added that questions of autonomy might also need to be addressed. “Physicians often feel like they don’t have control in Medicare, that they’re required to do a lot of things, and that they are subject to the fee schedule. If there were some way to grant more autonomy, control, and convey status that way, whether it has to do with greater flexibility in whatever, payment models and so on, that’s where I think you can begin to shift the status within primary care.”
MedPAC Chairman Francis Crosson, MD, recalled his time at Kaiser Permanente and noted their programs showed success because of the combination of a significant amount of money and time commitment (10 years).
The time commitment became an important part because after that long, physicians became a part of their communities and tended to stay.
“Two or 3 years, from my perspective and my experience, doesn’t work very well,” Dr. Crosson said. “But a significant period of time does, and a significant amount of money does seem to work.”
gtwachtman@mdedge.com
WASHINGTON – according to a proposal presented at a meeting of the Medicare Payment Advisory Commission.
“A Medicare[-based] program would have a specific objective to encourage more physicians to enter primary care and provide primary care to beneficiaries,” MedPAC staffer Ariel Winter said. “By reducing educational debt, a Medicare-specific program would provide a financial incentive for physicians to choose primary care.”
Any program would face some challenges, Mr. Winter noted. Based on evidence, “it’s difficult to predict how physicians would respond if they were offered debt reduction in exchange for a commitment to practice primary care,” as financial considerations are not the only reason why physicians choose a specific career track.
Financing the program would also need to be considered. MedPAC staff recommended using a separate recommendation, one to end the Merit-based Incentive Payment System and use its $500 million put aside as MIPS bonuses to pay for any Medicare-based program.
Staff proposed a pilot program to “test the impact of different design choices on program operations, physician participation, and career choices,” he said. “Policymakers could use the results to improve the program and decide whether to expand it.”
MedPAC Vice Chairman Jon Christianson, PhD, suggested any program be tied to “physicians who practiced in areas where Medicare beneficiaries don’t have adequate access” to primary care doctors.
However, Mr. Winter noted that he is not aware of “any off-the-shelf system that identifies areas where there’s a problem, where there’s a shortage of clinicians for Medicare beneficiaries specifically. I am not sure how you would do that.”
MedPAC member Kathy Buto, former vice president of global health policy at Johnson & Johnson, questioned whether nurse practitioners and physician assistants should be included in the program, as they “are beginning to subspecialize and get out of primary care.” Mr. Winter said it is open for consideration.
MedPAC member Pat Wang, president and CEO of Healthfirst in New York, questioned whether a new program was needed or whether fixing of existing programs, “making them work better” is the way to go given the evidence that the effect of student debt on decision making is mixed.
She suggested that rather than targeting loan forgiveness, maybe the program should be structured more as a bonus payment rather than debt forgiveness as a means of incentivizing people who may not be concerned with debt forgiveness.
Ms. Buto added that questions of autonomy might also need to be addressed. “Physicians often feel like they don’t have control in Medicare, that they’re required to do a lot of things, and that they are subject to the fee schedule. If there were some way to grant more autonomy, control, and convey status that way, whether it has to do with greater flexibility in whatever, payment models and so on, that’s where I think you can begin to shift the status within primary care.”
MedPAC Chairman Francis Crosson, MD, recalled his time at Kaiser Permanente and noted their programs showed success because of the combination of a significant amount of money and time commitment (10 years).
The time commitment became an important part because after that long, physicians became a part of their communities and tended to stay.
“Two or 3 years, from my perspective and my experience, doesn’t work very well,” Dr. Crosson said. “But a significant period of time does, and a significant amount of money does seem to work.”
gtwachtman@mdedge.com
REPORTING FROM A MEDPAC MEETING
Addressing insulin price spikes will require supply chain reform
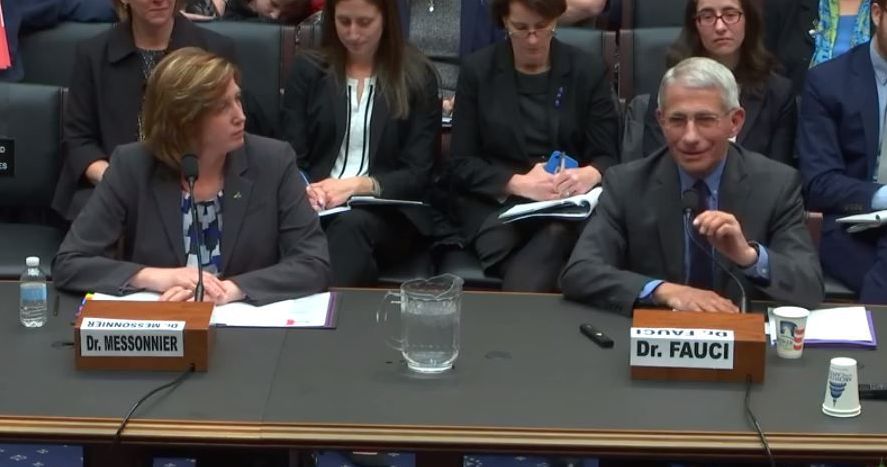
WASHINGTON – panelists said at a House Committee on Energy & Commerce hearing on insulin affordability.
“Each member of the supply chain has a responsibility to help solve this problem,” said Alvin C. Powers, MD, director of the Vanderbilt Diabetes Center at Vanderbilt University, who was speaking on behalf of the Endocrine Society during the April 2 hearing of the committee’s oversight & investigations subcommittee.
Dr. Powers identified all members – manufacturers, payers, pharmacy benefit managers, patients, providers, and Congress – as having a role in developing a solution that will encourage more access to the treatment.
The hearing was the first of two in a series specifically examining the price of insulin. This one focused on the role pricing issues play in terms of access to insulin and patient outcomes.
To highlight the pricing issues, it was noted that a vial of Humalog (insulin lispro) cost $21 when it was launched by Eli Lilly in 1996. It now costs $275 even though it has gone through no changes in formulation or innovation during that time.
Kasia Lipska, MD, of Yale University School of Medicine noted that a summer 2017 survey conducted by the Yale Diabetes Center found that one in four patients took less than the prescribed dose of insulin specifically because of the cost of insulin.
William Cefalu, MD, chief scientific, medical, and mission officer at the American Diabetes Association, echoed comments from Dr. Powers about pricing and suggested that simply going after list price is not a complete solution.
“There is also no guarantee that if the list price drops there [will] be substantive changes throughout the supply chain,” Dr. Cefalu said, adding that there needs to be a move away from a system based on high list prices and rebates and toward a system that ensures that any negotiated rebate or discount will find its way to the patient at the pharmacy counter.
“That’s what is not happening now,” Dr. Cefalu added. “Unless you can control what happens downstream in the intermediaries and what happens to the patient, there is no guarantee that just dropping list prices ... is going to get the job done.”
Aaron Kowalski, PhD, chief mission officer of JDRF, an organization that funds research into type 1 diabetes, also called out insurers as a part of the problem.
“What we are seeing in the community is people being switched [from their prescribed insulin for nonmedical reasons] by their insurance companies, not by the choice of their physician or the patient, which is just not the right way to practice medicine.”
He relayed an anecdote about a woman who went from having her blood sugar well controlled to dealing with severe cases of hyperglycemia because of changes in the medical coverage of her insulin. It took 8 hours on the phone with the insurance company, not to mention countless hours spent by the physician, to get the situation corrected and to get the proper insulin covered.
“This is a broken part of the system,” Dr. Kowalski said.
Dr. Cefalu noted that data are needed on the medical impact of switching for nonmedical reasons, such as changes to insurance coverage.
Christel Marchand Aprigliano, chief executive officer of the Diabetes Patient Advocacy Coalition, also relayed an anecdote of a friend who had suffered medical consequences of nonmedical switching of his insulin and then having to deal with his insurer’s fail-first policy before they would cover his original, medically effective insulin.
“Insurance has been denied twice because they believe that insulins are interchangeable, which they aren’t,” she said.
Michael Burgess, MD, (R-Texas) asked rhetorically during the hearing whether it would make sense for payers to simply provide insulin at no cost to patients, given the cost of medical complications resulting from lack of proper use as a result of pricing likely is much higher than covering insulin completely.
While specific legislative proposals were not discussed during the hearing, one thing that the panelists agreed would help to clarify all the factors that are contributing to the pricing increases is clear, transparent information about the finances surrounding the insulin as the product moves through the supply chain.
The Food and Drug Administration is also doing its part. Although the agency was not a participant in the hearing, the agency’s commissioner, Scott Gottlieb, MD, released a statement on the same day as the hearing in which he touted efforts in the biosimilar space that could spur competition.
“Once an interchangeable insulin product is approved and available on the market, it can be substituted for the reference product at the pharmacy, potentially leading to increased access [to insulin] and lower costs for patients,” he said in the statement. “The FDA anticipates that biosimilar and interchangeable insulin products will bring the competition that’s needed to help [deliver] affordable treatment options to patients.”
Dr Gottlieb did not say when a biosimilar insulin might be available on the market.
The second hearing in this series has not been scheduled, but is expected to take place the week of April 8 and will feature representatives from three insulin manufacturers and other participants in the supply chain.
WASHINGTON – panelists said at a House Committee on Energy & Commerce hearing on insulin affordability.
“Each member of the supply chain has a responsibility to help solve this problem,” said Alvin C. Powers, MD, director of the Vanderbilt Diabetes Center at Vanderbilt University, who was speaking on behalf of the Endocrine Society during the April 2 hearing of the committee’s oversight & investigations subcommittee.
Dr. Powers identified all members – manufacturers, payers, pharmacy benefit managers, patients, providers, and Congress – as having a role in developing a solution that will encourage more access to the treatment.
The hearing was the first of two in a series specifically examining the price of insulin. This one focused on the role pricing issues play in terms of access to insulin and patient outcomes.
To highlight the pricing issues, it was noted that a vial of Humalog (insulin lispro) cost $21 when it was launched by Eli Lilly in 1996. It now costs $275 even though it has gone through no changes in formulation or innovation during that time.
Kasia Lipska, MD, of Yale University School of Medicine noted that a summer 2017 survey conducted by the Yale Diabetes Center found that one in four patients took less than the prescribed dose of insulin specifically because of the cost of insulin.
William Cefalu, MD, chief scientific, medical, and mission officer at the American Diabetes Association, echoed comments from Dr. Powers about pricing and suggested that simply going after list price is not a complete solution.
“There is also no guarantee that if the list price drops there [will] be substantive changes throughout the supply chain,” Dr. Cefalu said, adding that there needs to be a move away from a system based on high list prices and rebates and toward a system that ensures that any negotiated rebate or discount will find its way to the patient at the pharmacy counter.
“That’s what is not happening now,” Dr. Cefalu added. “Unless you can control what happens downstream in the intermediaries and what happens to the patient, there is no guarantee that just dropping list prices ... is going to get the job done.”
Aaron Kowalski, PhD, chief mission officer of JDRF, an organization that funds research into type 1 diabetes, also called out insurers as a part of the problem.
“What we are seeing in the community is people being switched [from their prescribed insulin for nonmedical reasons] by their insurance companies, not by the choice of their physician or the patient, which is just not the right way to practice medicine.”
He relayed an anecdote about a woman who went from having her blood sugar well controlled to dealing with severe cases of hyperglycemia because of changes in the medical coverage of her insulin. It took 8 hours on the phone with the insurance company, not to mention countless hours spent by the physician, to get the situation corrected and to get the proper insulin covered.
“This is a broken part of the system,” Dr. Kowalski said.
Dr. Cefalu noted that data are needed on the medical impact of switching for nonmedical reasons, such as changes to insurance coverage.
Christel Marchand Aprigliano, chief executive officer of the Diabetes Patient Advocacy Coalition, also relayed an anecdote of a friend who had suffered medical consequences of nonmedical switching of his insulin and then having to deal with his insurer’s fail-first policy before they would cover his original, medically effective insulin.
“Insurance has been denied twice because they believe that insulins are interchangeable, which they aren’t,” she said.
Michael Burgess, MD, (R-Texas) asked rhetorically during the hearing whether it would make sense for payers to simply provide insulin at no cost to patients, given the cost of medical complications resulting from lack of proper use as a result of pricing likely is much higher than covering insulin completely.
While specific legislative proposals were not discussed during the hearing, one thing that the panelists agreed would help to clarify all the factors that are contributing to the pricing increases is clear, transparent information about the finances surrounding the insulin as the product moves through the supply chain.
The Food and Drug Administration is also doing its part. Although the agency was not a participant in the hearing, the agency’s commissioner, Scott Gottlieb, MD, released a statement on the same day as the hearing in which he touted efforts in the biosimilar space that could spur competition.
“Once an interchangeable insulin product is approved and available on the market, it can be substituted for the reference product at the pharmacy, potentially leading to increased access [to insulin] and lower costs for patients,” he said in the statement. “The FDA anticipates that biosimilar and interchangeable insulin products will bring the competition that’s needed to help [deliver] affordable treatment options to patients.”
Dr Gottlieb did not say when a biosimilar insulin might be available on the market.
The second hearing in this series has not been scheduled, but is expected to take place the week of April 8 and will feature representatives from three insulin manufacturers and other participants in the supply chain.
WASHINGTON – panelists said at a House Committee on Energy & Commerce hearing on insulin affordability.
“Each member of the supply chain has a responsibility to help solve this problem,” said Alvin C. Powers, MD, director of the Vanderbilt Diabetes Center at Vanderbilt University, who was speaking on behalf of the Endocrine Society during the April 2 hearing of the committee’s oversight & investigations subcommittee.
Dr. Powers identified all members – manufacturers, payers, pharmacy benefit managers, patients, providers, and Congress – as having a role in developing a solution that will encourage more access to the treatment.
The hearing was the first of two in a series specifically examining the price of insulin. This one focused on the role pricing issues play in terms of access to insulin and patient outcomes.
To highlight the pricing issues, it was noted that a vial of Humalog (insulin lispro) cost $21 when it was launched by Eli Lilly in 1996. It now costs $275 even though it has gone through no changes in formulation or innovation during that time.
Kasia Lipska, MD, of Yale University School of Medicine noted that a summer 2017 survey conducted by the Yale Diabetes Center found that one in four patients took less than the prescribed dose of insulin specifically because of the cost of insulin.
William Cefalu, MD, chief scientific, medical, and mission officer at the American Diabetes Association, echoed comments from Dr. Powers about pricing and suggested that simply going after list price is not a complete solution.
“There is also no guarantee that if the list price drops there [will] be substantive changes throughout the supply chain,” Dr. Cefalu said, adding that there needs to be a move away from a system based on high list prices and rebates and toward a system that ensures that any negotiated rebate or discount will find its way to the patient at the pharmacy counter.
“That’s what is not happening now,” Dr. Cefalu added. “Unless you can control what happens downstream in the intermediaries and what happens to the patient, there is no guarantee that just dropping list prices ... is going to get the job done.”
Aaron Kowalski, PhD, chief mission officer of JDRF, an organization that funds research into type 1 diabetes, also called out insurers as a part of the problem.
“What we are seeing in the community is people being switched [from their prescribed insulin for nonmedical reasons] by their insurance companies, not by the choice of their physician or the patient, which is just not the right way to practice medicine.”
He relayed an anecdote about a woman who went from having her blood sugar well controlled to dealing with severe cases of hyperglycemia because of changes in the medical coverage of her insulin. It took 8 hours on the phone with the insurance company, not to mention countless hours spent by the physician, to get the situation corrected and to get the proper insulin covered.
“This is a broken part of the system,” Dr. Kowalski said.
Dr. Cefalu noted that data are needed on the medical impact of switching for nonmedical reasons, such as changes to insurance coverage.
Christel Marchand Aprigliano, chief executive officer of the Diabetes Patient Advocacy Coalition, also relayed an anecdote of a friend who had suffered medical consequences of nonmedical switching of his insulin and then having to deal with his insurer’s fail-first policy before they would cover his original, medically effective insulin.
“Insurance has been denied twice because they believe that insulins are interchangeable, which they aren’t,” she said.
Michael Burgess, MD, (R-Texas) asked rhetorically during the hearing whether it would make sense for payers to simply provide insulin at no cost to patients, given the cost of medical complications resulting from lack of proper use as a result of pricing likely is much higher than covering insulin completely.
While specific legislative proposals were not discussed during the hearing, one thing that the panelists agreed would help to clarify all the factors that are contributing to the pricing increases is clear, transparent information about the finances surrounding the insulin as the product moves through the supply chain.
The Food and Drug Administration is also doing its part. Although the agency was not a participant in the hearing, the agency’s commissioner, Scott Gottlieb, MD, released a statement on the same day as the hearing in which he touted efforts in the biosimilar space that could spur competition.
“Once an interchangeable insulin product is approved and available on the market, it can be substituted for the reference product at the pharmacy, potentially leading to increased access [to insulin] and lower costs for patients,” he said in the statement. “The FDA anticipates that biosimilar and interchangeable insulin products will bring the competition that’s needed to help [deliver] affordable treatment options to patients.”
Dr Gottlieb did not say when a biosimilar insulin might be available on the market.
The second hearing in this series has not been scheduled, but is expected to take place the week of April 8 and will feature representatives from three insulin manufacturers and other participants in the supply chain.
REPORTING FROM A HOUSE ENERGY & COMMERCE SUBCOMMITTEE HEARING
FDA proposes updates to mammography regulations
Proposed changes to federal mammography regulations aim to provide more information for doctors and patients, as well as standardize patient information on breast density’s impact on screening.
The Food and Drug Administration posted a new proposed rule online March 27 that would “expand the information mammography facilities must provide to patients and health care professionals, allowing for more informed medical decision making,” the agency said in a statement. “It would also modernize mammography quality standards and better position the FDA to enforce regulations that apply to the safety and quality of mammography services.”
Key among the proposed changes is the addition of breast density information to the summary letter provided to patients and to the medical report provided to referring health care professionals.
“The FDA is proposing specific language that would explain how breast density can influence the accuracy of mammography and would recommend patients with dense breasts talk to their health care provider about high breast density and how it relates to breast cancer risk and their individual situation,” the agency said in a statement.
Laurie Margolies, MD, section chief of breast imaging at Mount Sinai Health System in New York, said the regulations would bring some uniformity to the communication process.
“It builds on the experience of the 37 states and the District of Columbia, all of whom have passed dense breast notification laws, and can serve to unify those disparate regulations into one that would be uniform throughout the country to give one clear message to women and health care providers,” Dr. Margolies said in an interview.
She noted that dense breasts are very common and communicating issues that are related to them, including the potential need for supplemental screening, are important.
“Almost half of American women have dense breasts and why that is significant is because the dense breast issue not only increases one’s risk of getting breast cancer, but it also can hide small breast cancers on the mammogram,” she said.
If you take 1,000 women with dense breasts and then do a breast ultrasound as a supplemental screening measure, “you will find three more small node-negative breast cancers that would not have come to light if you didn’t do the extra supplemental screening,” underscoring the importance of communicating dense breast information, she continued.
FDA also is seeking to enhance information provided to health care professionals by codifying three additional categories for mammogram assessments, including the addition of the “known biopsy proven malignancy” category, which the agency says would help identify which scans were being used to evaluate treatment of already diagnosed cancers.
Both patients and health care professionals would receive more detailed information about the mammography facility under the proposed rule.
FDA is proposing modernization of quality standards to help the agency enforce regulations, including giving the agency the authority to notify patients and health care professionals directly if a mammography facility does not meet quality standards and that a reevaluation or repeat of the exam at a different facility may be needed. The proposed amendments also include requiring that only digital accessory components specifically FDA approved or cleared for mammography be used or that facilities use components that otherwise meet the requirements, and stronger record-keeping requirements.
Dr. Margolies did note one potential deficiency in the proposed rule – the lack of any information on health insurance coverage of supplemental screening for women with dense breasts, though she noted this may not fall under the FDA’s authority.
“It would do the most good if everybody could get the supplemental screening without regards to their ability to pay for it out of pocket,” she said.
The proposal amends regulations issued under the Mammography Quality Standards Act of 1992, which gives FDA oversight authority over mammography facilities, including accreditation, certification, annual inspection, and enforcement of standards.
Comments on the proposal are due 90 days after the proposed rule is published in the Federal Register, which is scheduled for March 28.
Proposed changes to federal mammography regulations aim to provide more information for doctors and patients, as well as standardize patient information on breast density’s impact on screening.
The Food and Drug Administration posted a new proposed rule online March 27 that would “expand the information mammography facilities must provide to patients and health care professionals, allowing for more informed medical decision making,” the agency said in a statement. “It would also modernize mammography quality standards and better position the FDA to enforce regulations that apply to the safety and quality of mammography services.”
Key among the proposed changes is the addition of breast density information to the summary letter provided to patients and to the medical report provided to referring health care professionals.
“The FDA is proposing specific language that would explain how breast density can influence the accuracy of mammography and would recommend patients with dense breasts talk to their health care provider about high breast density and how it relates to breast cancer risk and their individual situation,” the agency said in a statement.
Laurie Margolies, MD, section chief of breast imaging at Mount Sinai Health System in New York, said the regulations would bring some uniformity to the communication process.
“It builds on the experience of the 37 states and the District of Columbia, all of whom have passed dense breast notification laws, and can serve to unify those disparate regulations into one that would be uniform throughout the country to give one clear message to women and health care providers,” Dr. Margolies said in an interview.
She noted that dense breasts are very common and communicating issues that are related to them, including the potential need for supplemental screening, are important.
“Almost half of American women have dense breasts and why that is significant is because the dense breast issue not only increases one’s risk of getting breast cancer, but it also can hide small breast cancers on the mammogram,” she said.
If you take 1,000 women with dense breasts and then do a breast ultrasound as a supplemental screening measure, “you will find three more small node-negative breast cancers that would not have come to light if you didn’t do the extra supplemental screening,” underscoring the importance of communicating dense breast information, she continued.
FDA also is seeking to enhance information provided to health care professionals by codifying three additional categories for mammogram assessments, including the addition of the “known biopsy proven malignancy” category, which the agency says would help identify which scans were being used to evaluate treatment of already diagnosed cancers.
Both patients and health care professionals would receive more detailed information about the mammography facility under the proposed rule.
FDA is proposing modernization of quality standards to help the agency enforce regulations, including giving the agency the authority to notify patients and health care professionals directly if a mammography facility does not meet quality standards and that a reevaluation or repeat of the exam at a different facility may be needed. The proposed amendments also include requiring that only digital accessory components specifically FDA approved or cleared for mammography be used or that facilities use components that otherwise meet the requirements, and stronger record-keeping requirements.
Dr. Margolies did note one potential deficiency in the proposed rule – the lack of any information on health insurance coverage of supplemental screening for women with dense breasts, though she noted this may not fall under the FDA’s authority.
“It would do the most good if everybody could get the supplemental screening without regards to their ability to pay for it out of pocket,” she said.
The proposal amends regulations issued under the Mammography Quality Standards Act of 1992, which gives FDA oversight authority over mammography facilities, including accreditation, certification, annual inspection, and enforcement of standards.
Comments on the proposal are due 90 days after the proposed rule is published in the Federal Register, which is scheduled for March 28.
Proposed changes to federal mammography regulations aim to provide more information for doctors and patients, as well as standardize patient information on breast density’s impact on screening.
The Food and Drug Administration posted a new proposed rule online March 27 that would “expand the information mammography facilities must provide to patients and health care professionals, allowing for more informed medical decision making,” the agency said in a statement. “It would also modernize mammography quality standards and better position the FDA to enforce regulations that apply to the safety and quality of mammography services.”
Key among the proposed changes is the addition of breast density information to the summary letter provided to patients and to the medical report provided to referring health care professionals.
“The FDA is proposing specific language that would explain how breast density can influence the accuracy of mammography and would recommend patients with dense breasts talk to their health care provider about high breast density and how it relates to breast cancer risk and their individual situation,” the agency said in a statement.
Laurie Margolies, MD, section chief of breast imaging at Mount Sinai Health System in New York, said the regulations would bring some uniformity to the communication process.
“It builds on the experience of the 37 states and the District of Columbia, all of whom have passed dense breast notification laws, and can serve to unify those disparate regulations into one that would be uniform throughout the country to give one clear message to women and health care providers,” Dr. Margolies said in an interview.
She noted that dense breasts are very common and communicating issues that are related to them, including the potential need for supplemental screening, are important.
“Almost half of American women have dense breasts and why that is significant is because the dense breast issue not only increases one’s risk of getting breast cancer, but it also can hide small breast cancers on the mammogram,” she said.
If you take 1,000 women with dense breasts and then do a breast ultrasound as a supplemental screening measure, “you will find three more small node-negative breast cancers that would not have come to light if you didn’t do the extra supplemental screening,” underscoring the importance of communicating dense breast information, she continued.
FDA also is seeking to enhance information provided to health care professionals by codifying three additional categories for mammogram assessments, including the addition of the “known biopsy proven malignancy” category, which the agency says would help identify which scans were being used to evaluate treatment of already diagnosed cancers.
Both patients and health care professionals would receive more detailed information about the mammography facility under the proposed rule.
FDA is proposing modernization of quality standards to help the agency enforce regulations, including giving the agency the authority to notify patients and health care professionals directly if a mammography facility does not meet quality standards and that a reevaluation or repeat of the exam at a different facility may be needed. The proposed amendments also include requiring that only digital accessory components specifically FDA approved or cleared for mammography be used or that facilities use components that otherwise meet the requirements, and stronger record-keeping requirements.
Dr. Margolies did note one potential deficiency in the proposed rule – the lack of any information on health insurance coverage of supplemental screening for women with dense breasts, though she noted this may not fall under the FDA’s authority.
“It would do the most good if everybody could get the supplemental screening without regards to their ability to pay for it out of pocket,” she said.
The proposal amends regulations issued under the Mammography Quality Standards Act of 1992, which gives FDA oversight authority over mammography facilities, including accreditation, certification, annual inspection, and enforcement of standards.
Comments on the proposal are due 90 days after the proposed rule is published in the Federal Register, which is scheduled for March 28.
DoJ refuses to challenge Texas ACA ruling
The U.S. Department of Justice has signaled it will not oppose any aspect of the recent court ruling to invalidate the Affordable Care Act.
“The Department of Justice has determined that the district court’s judgment should be affirmed, according to a March 25 letter to the U.S. Court of Appeal for the Fifth Circuit in New Orleans. “Because the United States is not urging that any portion of the district court’s judgment be reversed, the government intends to file a brief on the appellees’ schedule.”
At the onset of the trial in the U.S. District Court for the Northern District of Texas, the DOJ had initially challenged portions of the ACA, including declaring guaranteed issue unconstitutional by arguing that it could not be enacted with no penalty for failure to obtain coverage.
However, the judge ruled in the Texas v. United States case that the tax bill passed by Congress in December 2017 effectively rendered the entire health law unconstitutional.
“We said before that the district court’s decision was misguided and wrong. So, too, is the government’s reversal to now support it,” Matt Eyles, president and CEO of America’s Health Insurance Plans said in a statement. “This harmful position puts coverage at risk for more than 100 million Americans that rely on it. We will continue to engage on this issue as it continues through the appeals process so we can support and strengthen affordable coverage for every American.”
The U.S. Department of Justice has signaled it will not oppose any aspect of the recent court ruling to invalidate the Affordable Care Act.
“The Department of Justice has determined that the district court’s judgment should be affirmed, according to a March 25 letter to the U.S. Court of Appeal for the Fifth Circuit in New Orleans. “Because the United States is not urging that any portion of the district court’s judgment be reversed, the government intends to file a brief on the appellees’ schedule.”
At the onset of the trial in the U.S. District Court for the Northern District of Texas, the DOJ had initially challenged portions of the ACA, including declaring guaranteed issue unconstitutional by arguing that it could not be enacted with no penalty for failure to obtain coverage.
However, the judge ruled in the Texas v. United States case that the tax bill passed by Congress in December 2017 effectively rendered the entire health law unconstitutional.
“We said before that the district court’s decision was misguided and wrong. So, too, is the government’s reversal to now support it,” Matt Eyles, president and CEO of America’s Health Insurance Plans said in a statement. “This harmful position puts coverage at risk for more than 100 million Americans that rely on it. We will continue to engage on this issue as it continues through the appeals process so we can support and strengthen affordable coverage for every American.”
The U.S. Department of Justice has signaled it will not oppose any aspect of the recent court ruling to invalidate the Affordable Care Act.
“The Department of Justice has determined that the district court’s judgment should be affirmed, according to a March 25 letter to the U.S. Court of Appeal for the Fifth Circuit in New Orleans. “Because the United States is not urging that any portion of the district court’s judgment be reversed, the government intends to file a brief on the appellees’ schedule.”
At the onset of the trial in the U.S. District Court for the Northern District of Texas, the DOJ had initially challenged portions of the ACA, including declaring guaranteed issue unconstitutional by arguing that it could not be enacted with no penalty for failure to obtain coverage.
However, the judge ruled in the Texas v. United States case that the tax bill passed by Congress in December 2017 effectively rendered the entire health law unconstitutional.
“We said before that the district court’s decision was misguided and wrong. So, too, is the government’s reversal to now support it,” Matt Eyles, president and CEO of America’s Health Insurance Plans said in a statement. “This harmful position puts coverage at risk for more than 100 million Americans that rely on it. We will continue to engage on this issue as it continues through the appeals process so we can support and strengthen affordable coverage for every American.”
MIPS: Nearly 20% of small/solo practices took a pay cut in first year
Most clinicians participating in the Quality Payment Program’s Merit-Based Incentive Payment System (MIPS) received some kind of positive payment adjustment, with small and solo practices fairing not so well.
Overall, 93% of the 1.1 million clinicians who participated in 2017 received a pay bump, according to data released by the Centers for Medicare & Medicaid Services. Of those, about 755,000 (71%) received an exceptional performance payment adjustment of 1.88% and about 230,000 (22%) received a smaller adjustment of 0.2%. About 21,000 (2%) received no adjustment and nearly 52,000 (5%) saw their Medicare reimbursements cut by 4%.
The majority of those receiving pay cuts – about 43,000 (83%) – were in small or solo practices. About one in five participating clinicians in small or solo practices took a pay cut, according to CMS data.
“We weren’t surprised there at all,” Brian Outland, director of regulatory affairs at the American College of Physicians, said in an interview. “We felt that this was the way things were going to go, that small practices would be the ones in the negative.”
Less than half of participants in small or solo practices (44%, or about 101,000) received the exceptional performance bonus of 1.88%, while another approximately 68,000 (30%) received the 0.2% positive adjustment. About 18,000 (8%) received no adjustment.
The imbalance between large and small practices reveals a fundamental design flaw in the MIPS program, Mr. Outland noted.
“This program as presently designed does not certainly create an even playing field for large and small practices,” he said. “We think they need to simplify the MIPS program and make it easier for these smaller practices to be able to comply with the requirements and lessen the performance gap between large and small practices.”
Unless changes are made to help smaller practices perform better, “we feel this is going to continue in the future,” he added.
Outcomes for rural participants closely mirrored the national figures, with 65% (about 106,000) receiving the exceptional performance bonus of 1.88%, 28% (about 46,000) receiving 0.2% adjustment, 6% (about 9,300) receiving the 4% cut, and 1% (about 2,500) receiving no adjustment at all.
Clinicians in small and solo practices “still face challenges to full participation, which is why we will continue to provide direct technical assistance to these clinicians through the Small, Underserved, and Rural Support initiative to help alleviate barriers and create pathways for improvement and success,” CMS officials noted in the report.
SOURCE: Centers for Medicare & Medicaid Services. 2017 QPP Experience Report.
Most clinicians participating in the Quality Payment Program’s Merit-Based Incentive Payment System (MIPS) received some kind of positive payment adjustment, with small and solo practices fairing not so well.
Overall, 93% of the 1.1 million clinicians who participated in 2017 received a pay bump, according to data released by the Centers for Medicare & Medicaid Services. Of those, about 755,000 (71%) received an exceptional performance payment adjustment of 1.88% and about 230,000 (22%) received a smaller adjustment of 0.2%. About 21,000 (2%) received no adjustment and nearly 52,000 (5%) saw their Medicare reimbursements cut by 4%.
The majority of those receiving pay cuts – about 43,000 (83%) – were in small or solo practices. About one in five participating clinicians in small or solo practices took a pay cut, according to CMS data.
“We weren’t surprised there at all,” Brian Outland, director of regulatory affairs at the American College of Physicians, said in an interview. “We felt that this was the way things were going to go, that small practices would be the ones in the negative.”
Less than half of participants in small or solo practices (44%, or about 101,000) received the exceptional performance bonus of 1.88%, while another approximately 68,000 (30%) received the 0.2% positive adjustment. About 18,000 (8%) received no adjustment.
The imbalance between large and small practices reveals a fundamental design flaw in the MIPS program, Mr. Outland noted.
“This program as presently designed does not certainly create an even playing field for large and small practices,” he said. “We think they need to simplify the MIPS program and make it easier for these smaller practices to be able to comply with the requirements and lessen the performance gap between large and small practices.”
Unless changes are made to help smaller practices perform better, “we feel this is going to continue in the future,” he added.
Outcomes for rural participants closely mirrored the national figures, with 65% (about 106,000) receiving the exceptional performance bonus of 1.88%, 28% (about 46,000) receiving 0.2% adjustment, 6% (about 9,300) receiving the 4% cut, and 1% (about 2,500) receiving no adjustment at all.
Clinicians in small and solo practices “still face challenges to full participation, which is why we will continue to provide direct technical assistance to these clinicians through the Small, Underserved, and Rural Support initiative to help alleviate barriers and create pathways for improvement and success,” CMS officials noted in the report.
SOURCE: Centers for Medicare & Medicaid Services. 2017 QPP Experience Report.
Most clinicians participating in the Quality Payment Program’s Merit-Based Incentive Payment System (MIPS) received some kind of positive payment adjustment, with small and solo practices fairing not so well.
Overall, 93% of the 1.1 million clinicians who participated in 2017 received a pay bump, according to data released by the Centers for Medicare & Medicaid Services. Of those, about 755,000 (71%) received an exceptional performance payment adjustment of 1.88% and about 230,000 (22%) received a smaller adjustment of 0.2%. About 21,000 (2%) received no adjustment and nearly 52,000 (5%) saw their Medicare reimbursements cut by 4%.
The majority of those receiving pay cuts – about 43,000 (83%) – were in small or solo practices. About one in five participating clinicians in small or solo practices took a pay cut, according to CMS data.
“We weren’t surprised there at all,” Brian Outland, director of regulatory affairs at the American College of Physicians, said in an interview. “We felt that this was the way things were going to go, that small practices would be the ones in the negative.”
Less than half of participants in small or solo practices (44%, or about 101,000) received the exceptional performance bonus of 1.88%, while another approximately 68,000 (30%) received the 0.2% positive adjustment. About 18,000 (8%) received no adjustment.
The imbalance between large and small practices reveals a fundamental design flaw in the MIPS program, Mr. Outland noted.
“This program as presently designed does not certainly create an even playing field for large and small practices,” he said. “We think they need to simplify the MIPS program and make it easier for these smaller practices to be able to comply with the requirements and lessen the performance gap between large and small practices.”
Unless changes are made to help smaller practices perform better, “we feel this is going to continue in the future,” he added.
Outcomes for rural participants closely mirrored the national figures, with 65% (about 106,000) receiving the exceptional performance bonus of 1.88%, 28% (about 46,000) receiving 0.2% adjustment, 6% (about 9,300) receiving the 4% cut, and 1% (about 2,500) receiving no adjustment at all.
Clinicians in small and solo practices “still face challenges to full participation, which is why we will continue to provide direct technical assistance to these clinicians through the Small, Underserved, and Rural Support initiative to help alleviate barriers and create pathways for improvement and success,” CMS officials noted in the report.
SOURCE: Centers for Medicare & Medicaid Services. 2017 QPP Experience Report.
Female radiation oncologists taking in smaller Medicare payments
Female radiation oncologists are receiving less reimbursement from Medicare, compared with their male counterparts, according to a new study.
An examination of Medicare claims submitted by 4,393 radiation oncologists in 2016 (1,133 women) revealed that female physicians in the non–facility-based setting submitted a mean of 1,051 fewer charges, collected a mean of $143,610 less in revenue, and used a mean of 1.32 fewer billing codes. In the facility-based setting, female radiation oncologists submitted a mean of 423 fewer charges, collected a mean of $26,735 less in revenue, and submitted a mean of 1.28 fewer billing codes.
Additionally, the study noted that women accounted for 46 of the 397 most highly productive radiation oncologists in the facility-based setting and collected a mean of $33,206 less than men who were similarly productive. In the non–facility-based setting, women represented 54 of the 326 most highly productive radiation oncologists and collected $345,944 less than similarly productive men.
“Our study illustrates a gap between the sexes in Medicare charges and collection for radiation oncologists, the latter of which is possibly attributable to female physicians consistently submitting fewer charges and charging for services that are less well reimbursed,” Luca Valle, MD, of the University of California, Los Angeles, and colleagues wrote in JAMA Network Open.
The authors identified a number of factors that could be contributing to the discrepancy, the first of which could be traditional gender roles, particularly related to domestic responsibilities.
“A flexible work schedule and opportunities for part-time employment have been shown to be attractive options for female radiation oncologists; thus less clinical activity may be a natural consequence of the value-based labor choices that female practitioners make, particularly within a sex-structured society within which women continue to be expected to shoulder a greater share of domestic responsibilities,” Dr. Valle and colleagues wrote.
The authors also suggested that women “prioritize time spent with a given patient versus number of patients seen, and that extra time spent counseling patients is not reflected in HCPCS [Healthcare Common Procedure Coding System] code volume.”
Another possibility is the ongoing issues of gender discrimination, leaving female physicians to receive less referrals and fewer opportunities to care for patients, despite the authors noting that there is “no evidence to suggest that women are less competent and have more limited aspirations for their medical careers than men.”
Also contributing to the discrepancy is that women may have a greater portion of less well-reimbursed technologies (that is, three-dimensional conformal therapies used for treating breast cancer) rather than more favorably reimbursed technologies, such as intensity modulation radiation therapy, which is typically used for treating genitourinary malignant neoplasms.
“The sex-based distinctions in subspecialization may develop because men are more attuned to the possibility of differences in revenue generation, or because radiation oncology subspecialties that women choose [or are encouraged to choose] involve less revenue-generating ‘communal’ attributes rather than more favorably reimbursed ‘agentic’ attributes,” Dr. Valle and colleagues wrote.
The authors also suggest that it is possible that, when presented with multiple treatment options, female radiation oncologists are more likely to choose the more cost-effective option, “as women in other specialties have shown to adhere more closely to clinical guidelines, practice value-based care, forgo costly interventions, and engage in shared decision making with patients more frequently.”
The authors noted that the study was limited by using only Medicare payment data and it is not clear whether the same pattern occurs in different payer environments, such as Medicare Advantage or commercial insurance. It is also limited by the snapshot of a single year.
One coauthor reported receiving stock options from Equity Quotient; personal fees from Amgen and Vizient; and grants from the National Institutes of Health, the Doris Duke Foundation, the Greenwall Foundation, the Komen Foundation, and Blue Cross Blue Shield of Michigan; another reported receiving personal fees from ViewRay.
SOURCE: Valle L et al. JAMA Netw Open. 2019 Mar 22. doi: 10.1001/jamanetworkopen.2019.0932.
Female radiation oncologists are receiving less reimbursement from Medicare, compared with their male counterparts, according to a new study.
An examination of Medicare claims submitted by 4,393 radiation oncologists in 2016 (1,133 women) revealed that female physicians in the non–facility-based setting submitted a mean of 1,051 fewer charges, collected a mean of $143,610 less in revenue, and used a mean of 1.32 fewer billing codes. In the facility-based setting, female radiation oncologists submitted a mean of 423 fewer charges, collected a mean of $26,735 less in revenue, and submitted a mean of 1.28 fewer billing codes.
Additionally, the study noted that women accounted for 46 of the 397 most highly productive radiation oncologists in the facility-based setting and collected a mean of $33,206 less than men who were similarly productive. In the non–facility-based setting, women represented 54 of the 326 most highly productive radiation oncologists and collected $345,944 less than similarly productive men.
“Our study illustrates a gap between the sexes in Medicare charges and collection for radiation oncologists, the latter of which is possibly attributable to female physicians consistently submitting fewer charges and charging for services that are less well reimbursed,” Luca Valle, MD, of the University of California, Los Angeles, and colleagues wrote in JAMA Network Open.
The authors identified a number of factors that could be contributing to the discrepancy, the first of which could be traditional gender roles, particularly related to domestic responsibilities.
“A flexible work schedule and opportunities for part-time employment have been shown to be attractive options for female radiation oncologists; thus less clinical activity may be a natural consequence of the value-based labor choices that female practitioners make, particularly within a sex-structured society within which women continue to be expected to shoulder a greater share of domestic responsibilities,” Dr. Valle and colleagues wrote.
The authors also suggested that women “prioritize time spent with a given patient versus number of patients seen, and that extra time spent counseling patients is not reflected in HCPCS [Healthcare Common Procedure Coding System] code volume.”
Another possibility is the ongoing issues of gender discrimination, leaving female physicians to receive less referrals and fewer opportunities to care for patients, despite the authors noting that there is “no evidence to suggest that women are less competent and have more limited aspirations for their medical careers than men.”
Also contributing to the discrepancy is that women may have a greater portion of less well-reimbursed technologies (that is, three-dimensional conformal therapies used for treating breast cancer) rather than more favorably reimbursed technologies, such as intensity modulation radiation therapy, which is typically used for treating genitourinary malignant neoplasms.
“The sex-based distinctions in subspecialization may develop because men are more attuned to the possibility of differences in revenue generation, or because radiation oncology subspecialties that women choose [or are encouraged to choose] involve less revenue-generating ‘communal’ attributes rather than more favorably reimbursed ‘agentic’ attributes,” Dr. Valle and colleagues wrote.
The authors also suggest that it is possible that, when presented with multiple treatment options, female radiation oncologists are more likely to choose the more cost-effective option, “as women in other specialties have shown to adhere more closely to clinical guidelines, practice value-based care, forgo costly interventions, and engage in shared decision making with patients more frequently.”
The authors noted that the study was limited by using only Medicare payment data and it is not clear whether the same pattern occurs in different payer environments, such as Medicare Advantage or commercial insurance. It is also limited by the snapshot of a single year.
One coauthor reported receiving stock options from Equity Quotient; personal fees from Amgen and Vizient; and grants from the National Institutes of Health, the Doris Duke Foundation, the Greenwall Foundation, the Komen Foundation, and Blue Cross Blue Shield of Michigan; another reported receiving personal fees from ViewRay.
SOURCE: Valle L et al. JAMA Netw Open. 2019 Mar 22. doi: 10.1001/jamanetworkopen.2019.0932.
Female radiation oncologists are receiving less reimbursement from Medicare, compared with their male counterparts, according to a new study.
An examination of Medicare claims submitted by 4,393 radiation oncologists in 2016 (1,133 women) revealed that female physicians in the non–facility-based setting submitted a mean of 1,051 fewer charges, collected a mean of $143,610 less in revenue, and used a mean of 1.32 fewer billing codes. In the facility-based setting, female radiation oncologists submitted a mean of 423 fewer charges, collected a mean of $26,735 less in revenue, and submitted a mean of 1.28 fewer billing codes.
Additionally, the study noted that women accounted for 46 of the 397 most highly productive radiation oncologists in the facility-based setting and collected a mean of $33,206 less than men who were similarly productive. In the non–facility-based setting, women represented 54 of the 326 most highly productive radiation oncologists and collected $345,944 less than similarly productive men.
“Our study illustrates a gap between the sexes in Medicare charges and collection for radiation oncologists, the latter of which is possibly attributable to female physicians consistently submitting fewer charges and charging for services that are less well reimbursed,” Luca Valle, MD, of the University of California, Los Angeles, and colleagues wrote in JAMA Network Open.
The authors identified a number of factors that could be contributing to the discrepancy, the first of which could be traditional gender roles, particularly related to domestic responsibilities.
“A flexible work schedule and opportunities for part-time employment have been shown to be attractive options for female radiation oncologists; thus less clinical activity may be a natural consequence of the value-based labor choices that female practitioners make, particularly within a sex-structured society within which women continue to be expected to shoulder a greater share of domestic responsibilities,” Dr. Valle and colleagues wrote.
The authors also suggested that women “prioritize time spent with a given patient versus number of patients seen, and that extra time spent counseling patients is not reflected in HCPCS [Healthcare Common Procedure Coding System] code volume.”
Another possibility is the ongoing issues of gender discrimination, leaving female physicians to receive less referrals and fewer opportunities to care for patients, despite the authors noting that there is “no evidence to suggest that women are less competent and have more limited aspirations for their medical careers than men.”
Also contributing to the discrepancy is that women may have a greater portion of less well-reimbursed technologies (that is, three-dimensional conformal therapies used for treating breast cancer) rather than more favorably reimbursed technologies, such as intensity modulation radiation therapy, which is typically used for treating genitourinary malignant neoplasms.
“The sex-based distinctions in subspecialization may develop because men are more attuned to the possibility of differences in revenue generation, or because radiation oncology subspecialties that women choose [or are encouraged to choose] involve less revenue-generating ‘communal’ attributes rather than more favorably reimbursed ‘agentic’ attributes,” Dr. Valle and colleagues wrote.
The authors also suggest that it is possible that, when presented with multiple treatment options, female radiation oncologists are more likely to choose the more cost-effective option, “as women in other specialties have shown to adhere more closely to clinical guidelines, practice value-based care, forgo costly interventions, and engage in shared decision making with patients more frequently.”
The authors noted that the study was limited by using only Medicare payment data and it is not clear whether the same pattern occurs in different payer environments, such as Medicare Advantage or commercial insurance. It is also limited by the snapshot of a single year.
One coauthor reported receiving stock options from Equity Quotient; personal fees from Amgen and Vizient; and grants from the National Institutes of Health, the Doris Duke Foundation, the Greenwall Foundation, the Komen Foundation, and Blue Cross Blue Shield of Michigan; another reported receiving personal fees from ViewRay.
SOURCE: Valle L et al. JAMA Netw Open. 2019 Mar 22. doi: 10.1001/jamanetworkopen.2019.0932.
FROM JAMA NETWORK OPEN
MedPAC puts Part B reference pricing, binding arbitration on the table
Much of the presentation, offered during the commission’s March meeting, was general ideas with more work to come in terms of fleshing out the details. An ambitious goal of having something ready for the commission’s June 2019 report to Congress was set.
The policy recommendations for reference pricing, to be used when multiple similar drugs are available, and binding arbitration, to be used on new entrants to the market with limited or no competition, are being designed to work with the previously recommended drug value program, but could be implemented on their own.
In general, the reference pricing policy would set a maximum payment rate for a group of drugs with similar health effects based on the minimum, median, or other point along the range of prices for all drugs in that group. Providers would be incentivized to choose a lower-cost alternative when clinically appropriate.
Beneficiaries who still want access to a higher-cost drug would be on the hook for the difference through cost-sharing mechanisms.
MedPAC staff presented two options for setting the reference price. One would be to establish the price based on internal Medicare data. The other would take international pricing into consideration.
Binding arbitration, which is already a component of the drug value program, would be expanded. In the program described by staff, Medicare and the manufacturer would each come to the table with a price and the arbitrator (either an individual or a panel) would set one price.
Potential cost savings from one or both programs was not addressed
“It seems like an important thing for us to understand in order to know the potential impact ... through these two levers that work on different parts of the spend problem,” said Commissioner Dana Safran, head of measurement for the health care venture formed by Amazon, Berkshire Hathaway, and JPMorgan Chase.
Staff said it would work on making that determination.
Commissioners raised additional questions on operational details.
Marjorie Ginsburg, founding executive director of the Center for Healthcare Decisions Inc. in Sacramento, Calif., questioned what would happen if a manufacturer declined to participate in the arbitration process and whether that would mean Medicare would not cover a drug in that circumstance.
Jay Crosson, MD, noted that “Congress would have to … figure out how to deal with that circumstance. ... We would not want to end up with a system that would deny coverage” of effective medications for Medicare beneficiaries.
Another area affecting both issues was the potential for cross subsidization of drugs.
Jonathan Perlin, MD, president of clinical services and chief medical officer of HCA Healthcare of Nashville, Tenn., questioned whether this could open a door for a provider buying at a cheaper government price and using the drugs across patients not from Medicare or whether it could lead to higher prices being charged to commercial payers.
MedPAC staff member Kim Neuman said that “there would need to be some back end reconciliations that would happen to ensure that the stock that was then administered to Medicare patients was provided at a price that was no higher than that ceiling. ... We haven’t scoped out implications for other payers.”
Commissioner Kathy Buto, independent consultant and former vice president of global health policy at Johnson & Johnson, inquired about whether a drug would be made available upon launch while reference pricing or arbitration processes were in progress.
Commissioners also inquired as to how the reference pricing aspects will be operationalized into conversations between the doctor and the patient.
Ms. Buto also cautioned that using a reference pricing scheme could alter the dynamic of pricing competition that has companies competing against a reference price rather than doing what they can to lower prices beyond that.
Much of the presentation, offered during the commission’s March meeting, was general ideas with more work to come in terms of fleshing out the details. An ambitious goal of having something ready for the commission’s June 2019 report to Congress was set.
The policy recommendations for reference pricing, to be used when multiple similar drugs are available, and binding arbitration, to be used on new entrants to the market with limited or no competition, are being designed to work with the previously recommended drug value program, but could be implemented on their own.
In general, the reference pricing policy would set a maximum payment rate for a group of drugs with similar health effects based on the minimum, median, or other point along the range of prices for all drugs in that group. Providers would be incentivized to choose a lower-cost alternative when clinically appropriate.
Beneficiaries who still want access to a higher-cost drug would be on the hook for the difference through cost-sharing mechanisms.
MedPAC staff presented two options for setting the reference price. One would be to establish the price based on internal Medicare data. The other would take international pricing into consideration.
Binding arbitration, which is already a component of the drug value program, would be expanded. In the program described by staff, Medicare and the manufacturer would each come to the table with a price and the arbitrator (either an individual or a panel) would set one price.
Potential cost savings from one or both programs was not addressed
“It seems like an important thing for us to understand in order to know the potential impact ... through these two levers that work on different parts of the spend problem,” said Commissioner Dana Safran, head of measurement for the health care venture formed by Amazon, Berkshire Hathaway, and JPMorgan Chase.
Staff said it would work on making that determination.
Commissioners raised additional questions on operational details.
Marjorie Ginsburg, founding executive director of the Center for Healthcare Decisions Inc. in Sacramento, Calif., questioned what would happen if a manufacturer declined to participate in the arbitration process and whether that would mean Medicare would not cover a drug in that circumstance.
Jay Crosson, MD, noted that “Congress would have to … figure out how to deal with that circumstance. ... We would not want to end up with a system that would deny coverage” of effective medications for Medicare beneficiaries.
Another area affecting both issues was the potential for cross subsidization of drugs.
Jonathan Perlin, MD, president of clinical services and chief medical officer of HCA Healthcare of Nashville, Tenn., questioned whether this could open a door for a provider buying at a cheaper government price and using the drugs across patients not from Medicare or whether it could lead to higher prices being charged to commercial payers.
MedPAC staff member Kim Neuman said that “there would need to be some back end reconciliations that would happen to ensure that the stock that was then administered to Medicare patients was provided at a price that was no higher than that ceiling. ... We haven’t scoped out implications for other payers.”
Commissioner Kathy Buto, independent consultant and former vice president of global health policy at Johnson & Johnson, inquired about whether a drug would be made available upon launch while reference pricing or arbitration processes were in progress.
Commissioners also inquired as to how the reference pricing aspects will be operationalized into conversations between the doctor and the patient.
Ms. Buto also cautioned that using a reference pricing scheme could alter the dynamic of pricing competition that has companies competing against a reference price rather than doing what they can to lower prices beyond that.
Much of the presentation, offered during the commission’s March meeting, was general ideas with more work to come in terms of fleshing out the details. An ambitious goal of having something ready for the commission’s June 2019 report to Congress was set.
The policy recommendations for reference pricing, to be used when multiple similar drugs are available, and binding arbitration, to be used on new entrants to the market with limited or no competition, are being designed to work with the previously recommended drug value program, but could be implemented on their own.
In general, the reference pricing policy would set a maximum payment rate for a group of drugs with similar health effects based on the minimum, median, or other point along the range of prices for all drugs in that group. Providers would be incentivized to choose a lower-cost alternative when clinically appropriate.
Beneficiaries who still want access to a higher-cost drug would be on the hook for the difference through cost-sharing mechanisms.
MedPAC staff presented two options for setting the reference price. One would be to establish the price based on internal Medicare data. The other would take international pricing into consideration.
Binding arbitration, which is already a component of the drug value program, would be expanded. In the program described by staff, Medicare and the manufacturer would each come to the table with a price and the arbitrator (either an individual or a panel) would set one price.
Potential cost savings from one or both programs was not addressed
“It seems like an important thing for us to understand in order to know the potential impact ... through these two levers that work on different parts of the spend problem,” said Commissioner Dana Safran, head of measurement for the health care venture formed by Amazon, Berkshire Hathaway, and JPMorgan Chase.
Staff said it would work on making that determination.
Commissioners raised additional questions on operational details.
Marjorie Ginsburg, founding executive director of the Center for Healthcare Decisions Inc. in Sacramento, Calif., questioned what would happen if a manufacturer declined to participate in the arbitration process and whether that would mean Medicare would not cover a drug in that circumstance.
Jay Crosson, MD, noted that “Congress would have to … figure out how to deal with that circumstance. ... We would not want to end up with a system that would deny coverage” of effective medications for Medicare beneficiaries.
Another area affecting both issues was the potential for cross subsidization of drugs.
Jonathan Perlin, MD, president of clinical services and chief medical officer of HCA Healthcare of Nashville, Tenn., questioned whether this could open a door for a provider buying at a cheaper government price and using the drugs across patients not from Medicare or whether it could lead to higher prices being charged to commercial payers.
MedPAC staff member Kim Neuman said that “there would need to be some back end reconciliations that would happen to ensure that the stock that was then administered to Medicare patients was provided at a price that was no higher than that ceiling. ... We haven’t scoped out implications for other payers.”
Commissioner Kathy Buto, independent consultant and former vice president of global health policy at Johnson & Johnson, inquired about whether a drug would be made available upon launch while reference pricing or arbitration processes were in progress.
Commissioners also inquired as to how the reference pricing aspects will be operationalized into conversations between the doctor and the patient.
Ms. Buto also cautioned that using a reference pricing scheme could alter the dynamic of pricing competition that has companies competing against a reference price rather than doing what they can to lower prices beyond that.
REPORTING FROM A MEDPAC MEETING
Will patient rewards for lower-cost choices impact physicians?
“In the first 12 months of the rewards program, we observed a 2.1% relative reduction in prices across all services eligible for the program,” according to Christopher Whaley, PhD, an associate policy researcher at the RAND Corporation, and his colleagues. “This effect was most evident for MRIs, for which there was a 4.7% reduction in prices.”
The rewards program offered $25-$500 for making lower-cost choices among 131 elective services. Rewards value was based on the provider’s price and service, yielding savings of $2.3 million, or roughly $8 per person across the 269,875 employees and dependents eligible for the rewards program.
Patients who were willing to price-shop chose to save money on imaging tests including ultrasounds, mammograms, and MRIs, Dr. Whaley and his colleagues wrote.
However, initial results showed very little impact in pricing for surgical procedures, including minor (such as breast biopsy), moderate (such as arthroscopy), and major (such as hip and knee replacements), covered by the rewards program.
“There are several potential explanations for this variation across types of services,” the authors wrote. “To receive a reward, patients may need to receive care from a provider different from the one their physician initially recommended. Compared to circumstances where they need an invasive procedure, patients may feel more comfortable asking the provider for a new referral for imaging services.”
An established doctor/patient relationship could have dimmed patient interest in seeking lower cost surgical procedures.
“There is also the complexity of switching their care,” the authors wrote. “For a surgical procedure, switching providers is particularly complex, as it requires identifying a lower-price provider and potentially getting another preoperative visit.”
Quality, while also playing a role in patient choice, is not a factor in the how the rewards program is structured.
“Patients may view imaging services more as commodity services and therefore may be more likely to switch, while patients may be more worried about the quality of lower-price surgeons.”
Building further on that, Dr. Whaley said in an interview that if the program becomes more widely used and successful, it could start to instill more price-shopping for procedures and create levers for pricing wars among local physicians.
“We don’t know if there will be an impact for procedural services in later years,” he said. “On one hand, patients simply may not be willing to price shop for these services. On the other hand, patients may learn about price-shopping for these services or the insurance company might continue to develop the model and try to get patients to shop.”
This, in turn, could potentially affect the dynamic of negotiations between providers and insurance companies for network placement, Dr. Whaley noted.
“It could be a ‘stick’ for insurers to use for negotiations with higher-priced providers. Insurers could say, ‘unless you lower your prices, we’ll pay patients to go to your competitor,’” something he said could ultimately be beneficial to lower-cost providers.
Dr. Whaley also noted that there was a small reduction (0.3 percentage points) in overall health care use among patients using reward-eligible services.
“The intervention population still had to pay their usual out-of-pocket payments, and a patient’s out-of-pocket expense was much higher than the reward amount, on average,” he said. “Therefore, this reduction in utilization may be due to patients’ using the price-shopping tool, becoming more aware of these out-of-pocket liabilities, and deciding to not get care from any provider.”
SOURCE: Whaley C et al. Health Aff (Millwood). 2019 Mar;38(3):440-7.
“In the first 12 months of the rewards program, we observed a 2.1% relative reduction in prices across all services eligible for the program,” according to Christopher Whaley, PhD, an associate policy researcher at the RAND Corporation, and his colleagues. “This effect was most evident for MRIs, for which there was a 4.7% reduction in prices.”
The rewards program offered $25-$500 for making lower-cost choices among 131 elective services. Rewards value was based on the provider’s price and service, yielding savings of $2.3 million, or roughly $8 per person across the 269,875 employees and dependents eligible for the rewards program.
Patients who were willing to price-shop chose to save money on imaging tests including ultrasounds, mammograms, and MRIs, Dr. Whaley and his colleagues wrote.
However, initial results showed very little impact in pricing for surgical procedures, including minor (such as breast biopsy), moderate (such as arthroscopy), and major (such as hip and knee replacements), covered by the rewards program.
“There are several potential explanations for this variation across types of services,” the authors wrote. “To receive a reward, patients may need to receive care from a provider different from the one their physician initially recommended. Compared to circumstances where they need an invasive procedure, patients may feel more comfortable asking the provider for a new referral for imaging services.”
An established doctor/patient relationship could have dimmed patient interest in seeking lower cost surgical procedures.
“There is also the complexity of switching their care,” the authors wrote. “For a surgical procedure, switching providers is particularly complex, as it requires identifying a lower-price provider and potentially getting another preoperative visit.”
Quality, while also playing a role in patient choice, is not a factor in the how the rewards program is structured.
“Patients may view imaging services more as commodity services and therefore may be more likely to switch, while patients may be more worried about the quality of lower-price surgeons.”
Building further on that, Dr. Whaley said in an interview that if the program becomes more widely used and successful, it could start to instill more price-shopping for procedures and create levers for pricing wars among local physicians.
“We don’t know if there will be an impact for procedural services in later years,” he said. “On one hand, patients simply may not be willing to price shop for these services. On the other hand, patients may learn about price-shopping for these services or the insurance company might continue to develop the model and try to get patients to shop.”
This, in turn, could potentially affect the dynamic of negotiations between providers and insurance companies for network placement, Dr. Whaley noted.
“It could be a ‘stick’ for insurers to use for negotiations with higher-priced providers. Insurers could say, ‘unless you lower your prices, we’ll pay patients to go to your competitor,’” something he said could ultimately be beneficial to lower-cost providers.
Dr. Whaley also noted that there was a small reduction (0.3 percentage points) in overall health care use among patients using reward-eligible services.
“The intervention population still had to pay their usual out-of-pocket payments, and a patient’s out-of-pocket expense was much higher than the reward amount, on average,” he said. “Therefore, this reduction in utilization may be due to patients’ using the price-shopping tool, becoming more aware of these out-of-pocket liabilities, and deciding to not get care from any provider.”
SOURCE: Whaley C et al. Health Aff (Millwood). 2019 Mar;38(3):440-7.
“In the first 12 months of the rewards program, we observed a 2.1% relative reduction in prices across all services eligible for the program,” according to Christopher Whaley, PhD, an associate policy researcher at the RAND Corporation, and his colleagues. “This effect was most evident for MRIs, for which there was a 4.7% reduction in prices.”
The rewards program offered $25-$500 for making lower-cost choices among 131 elective services. Rewards value was based on the provider’s price and service, yielding savings of $2.3 million, or roughly $8 per person across the 269,875 employees and dependents eligible for the rewards program.
Patients who were willing to price-shop chose to save money on imaging tests including ultrasounds, mammograms, and MRIs, Dr. Whaley and his colleagues wrote.
However, initial results showed very little impact in pricing for surgical procedures, including minor (such as breast biopsy), moderate (such as arthroscopy), and major (such as hip and knee replacements), covered by the rewards program.
“There are several potential explanations for this variation across types of services,” the authors wrote. “To receive a reward, patients may need to receive care from a provider different from the one their physician initially recommended. Compared to circumstances where they need an invasive procedure, patients may feel more comfortable asking the provider for a new referral for imaging services.”
An established doctor/patient relationship could have dimmed patient interest in seeking lower cost surgical procedures.
“There is also the complexity of switching their care,” the authors wrote. “For a surgical procedure, switching providers is particularly complex, as it requires identifying a lower-price provider and potentially getting another preoperative visit.”
Quality, while also playing a role in patient choice, is not a factor in the how the rewards program is structured.
“Patients may view imaging services more as commodity services and therefore may be more likely to switch, while patients may be more worried about the quality of lower-price surgeons.”
Building further on that, Dr. Whaley said in an interview that if the program becomes more widely used and successful, it could start to instill more price-shopping for procedures and create levers for pricing wars among local physicians.
“We don’t know if there will be an impact for procedural services in later years,” he said. “On one hand, patients simply may not be willing to price shop for these services. On the other hand, patients may learn about price-shopping for these services or the insurance company might continue to develop the model and try to get patients to shop.”
This, in turn, could potentially affect the dynamic of negotiations between providers and insurance companies for network placement, Dr. Whaley noted.
“It could be a ‘stick’ for insurers to use for negotiations with higher-priced providers. Insurers could say, ‘unless you lower your prices, we’ll pay patients to go to your competitor,’” something he said could ultimately be beneficial to lower-cost providers.
Dr. Whaley also noted that there was a small reduction (0.3 percentage points) in overall health care use among patients using reward-eligible services.
“The intervention population still had to pay their usual out-of-pocket payments, and a patient’s out-of-pocket expense was much higher than the reward amount, on average,” he said. “Therefore, this reduction in utilization may be due to patients’ using the price-shopping tool, becoming more aware of these out-of-pocket liabilities, and deciding to not get care from any provider.”
SOURCE: Whaley C et al. Health Aff (Millwood). 2019 Mar;38(3):440-7.
FROM HEALTH AFFAIRS
Scott Gottlieb to step down as FDA commissioner
According to reports, he is stepping down to spend more time with his family, who live in Westport, Conn. He splits time between there and Washington. He was confirmed by the Senate in May 2017 with five Democrats and one independent joining Republicans in voting him in.
President Trump confirmed Dr. Gottlieb’s resignation, praising him in a tweet for the “terrific job” he has done in this role and commending his efforts to help “us to lower drug prices, get a record number of generic drugs approved and onto the market, and so many other things. ”
Dr. Gottlieb’s legacy may be his work on regulating e-cigarettes, although that work is unfinished. His passion for this subject can be found in a statement made in Nov. 2018, announcing an advanced notice of proposed rule making to regulate e-cigarettes.
“Today, I’m pursuing actions aimed at addressing the disturbing trend of youth nicotine use and continuing to advance the historic declines we’ve achieved in recent years in the rates of combustible cigarette use among kids,” Dr. Gottlieb said in the statement.
More recently, the agency announced March 4 enforcement actions aimed at both retailers and manufacturers, including requesting a meeting with Walgreens to discuss the nearly 1,800 violations the chain has amassed across the country for selling tobacco products to minors.
“Because tobacco use is almost always initiated and established during adolescence, early intervention ‒ including making sure tobacco products aren’t being marketed to, sold to, or used by kids ‒ is critical,” he said in announcing the enforcement actions. He added that the FDA will “continue vigorous enforcement activities, with a sustained campaign to monitor, penalize, and help prevent e-cigarette sales to minors in retail locations, including manufacturers’ Internet storefronts, as well as take additional steps to tackle other concerns related to the youth access and appeal of these products. The FDA is also exploring additional enforcement avenues to target violative sales and marketing practices by manufacturers and retailers.”
The American Heart Association praised Dr. Gottlieb’s work.
“Commissioner Gottlieb departs the FDA having established himself as a tireless champion of tobacco control,” the organization said in a statement. “He elevated the war on tobacco use – and particularly the epidemic of electronic cigarette use among youth – to unprecedented levels. Because of his efforts, millions more people nationwide are aware of the grave threats posed by e-cigarettes and other tobacco products that are addicting a new generation of youth. We urge the FDA in the strongest possible terms to move forward with effective regulation of an industry that continues to prioritize profits over the lives of consumers.”
Department of Health & Human Services Secretary Alex Azar acknowledged Dr. Gottlieb’s work in combating youth e-cigarette use among a number of areas that the outgoing official has had a positive impact on.
“Scott’s leadership inspired historic results from the FDA team, which delivered record approvals of both innovative treatments and affordable generic drugs, while advancing important policies to confront opioid addiction, tobacco and youth e-cigarette use, chronic disease, and more,” Secretary Azar said in a statement. “The public health of our country is better off for the work Scott and the entire FDA team have done over the last two years.”
Under his leadership, FDA has approved a record number of generic drugs, although many still are not on the market yet.
In the area of opioids, his tenure could be a mixed bag as the FDA on the one hand removed an opioid product from the market, but on the other, controversially approved a new, powerful one.
According to reports, he is stepping down to spend more time with his family, who live in Westport, Conn. He splits time between there and Washington. He was confirmed by the Senate in May 2017 with five Democrats and one independent joining Republicans in voting him in.
President Trump confirmed Dr. Gottlieb’s resignation, praising him in a tweet for the “terrific job” he has done in this role and commending his efforts to help “us to lower drug prices, get a record number of generic drugs approved and onto the market, and so many other things. ”
Dr. Gottlieb’s legacy may be his work on regulating e-cigarettes, although that work is unfinished. His passion for this subject can be found in a statement made in Nov. 2018, announcing an advanced notice of proposed rule making to regulate e-cigarettes.
“Today, I’m pursuing actions aimed at addressing the disturbing trend of youth nicotine use and continuing to advance the historic declines we’ve achieved in recent years in the rates of combustible cigarette use among kids,” Dr. Gottlieb said in the statement.
More recently, the agency announced March 4 enforcement actions aimed at both retailers and manufacturers, including requesting a meeting with Walgreens to discuss the nearly 1,800 violations the chain has amassed across the country for selling tobacco products to minors.
“Because tobacco use is almost always initiated and established during adolescence, early intervention ‒ including making sure tobacco products aren’t being marketed to, sold to, or used by kids ‒ is critical,” he said in announcing the enforcement actions. He added that the FDA will “continue vigorous enforcement activities, with a sustained campaign to monitor, penalize, and help prevent e-cigarette sales to minors in retail locations, including manufacturers’ Internet storefronts, as well as take additional steps to tackle other concerns related to the youth access and appeal of these products. The FDA is also exploring additional enforcement avenues to target violative sales and marketing practices by manufacturers and retailers.”
The American Heart Association praised Dr. Gottlieb’s work.
“Commissioner Gottlieb departs the FDA having established himself as a tireless champion of tobacco control,” the organization said in a statement. “He elevated the war on tobacco use – and particularly the epidemic of electronic cigarette use among youth – to unprecedented levels. Because of his efforts, millions more people nationwide are aware of the grave threats posed by e-cigarettes and other tobacco products that are addicting a new generation of youth. We urge the FDA in the strongest possible terms to move forward with effective regulation of an industry that continues to prioritize profits over the lives of consumers.”
Department of Health & Human Services Secretary Alex Azar acknowledged Dr. Gottlieb’s work in combating youth e-cigarette use among a number of areas that the outgoing official has had a positive impact on.
“Scott’s leadership inspired historic results from the FDA team, which delivered record approvals of both innovative treatments and affordable generic drugs, while advancing important policies to confront opioid addiction, tobacco and youth e-cigarette use, chronic disease, and more,” Secretary Azar said in a statement. “The public health of our country is better off for the work Scott and the entire FDA team have done over the last two years.”
Under his leadership, FDA has approved a record number of generic drugs, although many still are not on the market yet.
In the area of opioids, his tenure could be a mixed bag as the FDA on the one hand removed an opioid product from the market, but on the other, controversially approved a new, powerful one.
According to reports, he is stepping down to spend more time with his family, who live in Westport, Conn. He splits time between there and Washington. He was confirmed by the Senate in May 2017 with five Democrats and one independent joining Republicans in voting him in.
President Trump confirmed Dr. Gottlieb’s resignation, praising him in a tweet for the “terrific job” he has done in this role and commending his efforts to help “us to lower drug prices, get a record number of generic drugs approved and onto the market, and so many other things. ”
Dr. Gottlieb’s legacy may be his work on regulating e-cigarettes, although that work is unfinished. His passion for this subject can be found in a statement made in Nov. 2018, announcing an advanced notice of proposed rule making to regulate e-cigarettes.
“Today, I’m pursuing actions aimed at addressing the disturbing trend of youth nicotine use and continuing to advance the historic declines we’ve achieved in recent years in the rates of combustible cigarette use among kids,” Dr. Gottlieb said in the statement.
More recently, the agency announced March 4 enforcement actions aimed at both retailers and manufacturers, including requesting a meeting with Walgreens to discuss the nearly 1,800 violations the chain has amassed across the country for selling tobacco products to minors.
“Because tobacco use is almost always initiated and established during adolescence, early intervention ‒ including making sure tobacco products aren’t being marketed to, sold to, or used by kids ‒ is critical,” he said in announcing the enforcement actions. He added that the FDA will “continue vigorous enforcement activities, with a sustained campaign to monitor, penalize, and help prevent e-cigarette sales to minors in retail locations, including manufacturers’ Internet storefronts, as well as take additional steps to tackle other concerns related to the youth access and appeal of these products. The FDA is also exploring additional enforcement avenues to target violative sales and marketing practices by manufacturers and retailers.”
The American Heart Association praised Dr. Gottlieb’s work.
“Commissioner Gottlieb departs the FDA having established himself as a tireless champion of tobacco control,” the organization said in a statement. “He elevated the war on tobacco use – and particularly the epidemic of electronic cigarette use among youth – to unprecedented levels. Because of his efforts, millions more people nationwide are aware of the grave threats posed by e-cigarettes and other tobacco products that are addicting a new generation of youth. We urge the FDA in the strongest possible terms to move forward with effective regulation of an industry that continues to prioritize profits over the lives of consumers.”
Department of Health & Human Services Secretary Alex Azar acknowledged Dr. Gottlieb’s work in combating youth e-cigarette use among a number of areas that the outgoing official has had a positive impact on.
“Scott’s leadership inspired historic results from the FDA team, which delivered record approvals of both innovative treatments and affordable generic drugs, while advancing important policies to confront opioid addiction, tobacco and youth e-cigarette use, chronic disease, and more,” Secretary Azar said in a statement. “The public health of our country is better off for the work Scott and the entire FDA team have done over the last two years.”
Under his leadership, FDA has approved a record number of generic drugs, although many still are not on the market yet.
In the area of opioids, his tenure could be a mixed bag as the FDA on the one hand removed an opioid product from the market, but on the other, controversially approved a new, powerful one.
Fauci, Messonnier testify on measles outbreaks
Officials from the Centers for Disease Control and Prevention and the National Institute for Allergy and Infectious Diseases stressed the safety of measles vaccines and warned that misinformation is among the factors keeping more children from being vaccinated.
With nearly 160 cases of measles in 10 states during Jan. 1–Feb. 21, a disease once eradicated from the United States is resurfacing, with most cases affecting those who have not been vaccinated.
“Measles outbreaks have been and continue to be a constant threat to the health of the American people,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the CDC, testified at a Feb. 27 hearing of the Oversight and Investigations Subcommittee of the House Energy and Commerce Committee.
She noted that unvaccinated Americans traveling abroad are at risk for contracting the infection, and thus are at risk of spreading it when they return home. Foreigners coming to the country also carry the potential to spread the infection.
“Nationally, we enjoy high measles vaccination coverage,” Dr. Messonnier said.”There are pockets of people who are vaccine hesitant, who delay or even refuse to vaccinate themselves and their children. Outbreaks of measles occur when measles gets into these communities of unvaccinated people.”
She noted that those who eschew vaccination tend to live near one another and share common religious beliefs or racial or ethnic backgrounds.
She continued that vaccine hesitancy “is the result of the misunderstanding of the risk and seriousness of disease, combined with misinformation of the safety and effectiveness of vaccines. However, the specific issues fueling hesitancy varies by community.”
Strategies to increase vaccination need to be localized with national support from the CDC, Dr. Messonnier said, adding that rapid response is critical to control outbreaks.
Anthony Fauci, MD, director of the National Institute for Allergy and Infectious Diseases at NIH, agreed.
“I consider it really an irony that you have one of the most contagious viruses known to man juxtaposed against one of the most effective vaccines that we have and yet we don’t do and have not done what could be done, namely completely eliminate and eradicate this virus,” Dr. Fauci said.
Dr. Messonnier stressed that the only way to protect against measles is to get vaccinated.
“If they have questions, they should talk to their doctor,” she added. “Their doctor can provide them with more information about measles, answer their questions and reassure them so they go ahead and get vaccinated.”
Dr. Fauci concurred and added that “we should look upon it in two approaches. One, it’s for the safety of your own child. The other is a responsibility to the community. ... We all have a responsibility to be part of that umbrella of herd immunity and once it goes down below a certain percentage, then you have danger to the entire society.”
He stressed that the CDC is a good website to combat much of the misinformation that is floating around on the Internet.
The committee panel, while taking an interest in the recent outbreaks, did not hint at any specific legislative actions were being considered.
Officials from the Centers for Disease Control and Prevention and the National Institute for Allergy and Infectious Diseases stressed the safety of measles vaccines and warned that misinformation is among the factors keeping more children from being vaccinated.
With nearly 160 cases of measles in 10 states during Jan. 1–Feb. 21, a disease once eradicated from the United States is resurfacing, with most cases affecting those who have not been vaccinated.
“Measles outbreaks have been and continue to be a constant threat to the health of the American people,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the CDC, testified at a Feb. 27 hearing of the Oversight and Investigations Subcommittee of the House Energy and Commerce Committee.
She noted that unvaccinated Americans traveling abroad are at risk for contracting the infection, and thus are at risk of spreading it when they return home. Foreigners coming to the country also carry the potential to spread the infection.
“Nationally, we enjoy high measles vaccination coverage,” Dr. Messonnier said.”There are pockets of people who are vaccine hesitant, who delay or even refuse to vaccinate themselves and their children. Outbreaks of measles occur when measles gets into these communities of unvaccinated people.”
She noted that those who eschew vaccination tend to live near one another and share common religious beliefs or racial or ethnic backgrounds.
She continued that vaccine hesitancy “is the result of the misunderstanding of the risk and seriousness of disease, combined with misinformation of the safety and effectiveness of vaccines. However, the specific issues fueling hesitancy varies by community.”
Strategies to increase vaccination need to be localized with national support from the CDC, Dr. Messonnier said, adding that rapid response is critical to control outbreaks.
Anthony Fauci, MD, director of the National Institute for Allergy and Infectious Diseases at NIH, agreed.
“I consider it really an irony that you have one of the most contagious viruses known to man juxtaposed against one of the most effective vaccines that we have and yet we don’t do and have not done what could be done, namely completely eliminate and eradicate this virus,” Dr. Fauci said.
Dr. Messonnier stressed that the only way to protect against measles is to get vaccinated.
“If they have questions, they should talk to their doctor,” she added. “Their doctor can provide them with more information about measles, answer their questions and reassure them so they go ahead and get vaccinated.”
Dr. Fauci concurred and added that “we should look upon it in two approaches. One, it’s for the safety of your own child. The other is a responsibility to the community. ... We all have a responsibility to be part of that umbrella of herd immunity and once it goes down below a certain percentage, then you have danger to the entire society.”
He stressed that the CDC is a good website to combat much of the misinformation that is floating around on the Internet.
The committee panel, while taking an interest in the recent outbreaks, did not hint at any specific legislative actions were being considered.
Officials from the Centers for Disease Control and Prevention and the National Institute for Allergy and Infectious Diseases stressed the safety of measles vaccines and warned that misinformation is among the factors keeping more children from being vaccinated.
With nearly 160 cases of measles in 10 states during Jan. 1–Feb. 21, a disease once eradicated from the United States is resurfacing, with most cases affecting those who have not been vaccinated.
“Measles outbreaks have been and continue to be a constant threat to the health of the American people,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the CDC, testified at a Feb. 27 hearing of the Oversight and Investigations Subcommittee of the House Energy and Commerce Committee.
She noted that unvaccinated Americans traveling abroad are at risk for contracting the infection, and thus are at risk of spreading it when they return home. Foreigners coming to the country also carry the potential to spread the infection.
“Nationally, we enjoy high measles vaccination coverage,” Dr. Messonnier said.”There are pockets of people who are vaccine hesitant, who delay or even refuse to vaccinate themselves and their children. Outbreaks of measles occur when measles gets into these communities of unvaccinated people.”
She noted that those who eschew vaccination tend to live near one another and share common religious beliefs or racial or ethnic backgrounds.
She continued that vaccine hesitancy “is the result of the misunderstanding of the risk and seriousness of disease, combined with misinformation of the safety and effectiveness of vaccines. However, the specific issues fueling hesitancy varies by community.”
Strategies to increase vaccination need to be localized with national support from the CDC, Dr. Messonnier said, adding that rapid response is critical to control outbreaks.
Anthony Fauci, MD, director of the National Institute for Allergy and Infectious Diseases at NIH, agreed.
“I consider it really an irony that you have one of the most contagious viruses known to man juxtaposed against one of the most effective vaccines that we have and yet we don’t do and have not done what could be done, namely completely eliminate and eradicate this virus,” Dr. Fauci said.
Dr. Messonnier stressed that the only way to protect against measles is to get vaccinated.
“If they have questions, they should talk to their doctor,” she added. “Their doctor can provide them with more information about measles, answer their questions and reassure them so they go ahead and get vaccinated.”
Dr. Fauci concurred and added that “we should look upon it in two approaches. One, it’s for the safety of your own child. The other is a responsibility to the community. ... We all have a responsibility to be part of that umbrella of herd immunity and once it goes down below a certain percentage, then you have danger to the entire society.”
He stressed that the CDC is a good website to combat much of the misinformation that is floating around on the Internet.
The committee panel, while taking an interest in the recent outbreaks, did not hint at any specific legislative actions were being considered.
REPORTING FROM HOUSE COMMITTEE HEARING