User login
Big pharma says it can’t drop drug list prices alone
Top pharmaceutical executives expressed willingness to lower the list prices of their drugs, but only if there were cooperation among all sectors to reform how drugs get from manufacturer to patient.

That theme was common in the testimony of seven pharmaceutical executives before the Senate Finance Committee during a Feb. 26 hearing.
“We are in a system that used to be fit for purpose and really drove enormous savings over the last few years but it is no longer fit for purpose,” Pascal Soriot, executive director and CEO of AstraZeneca, testified before the committee. “It’s one of those situations where nobody in the system can do anything, can fix it by themselves.”
The problem, the executives agreed, is the financial structure of drug delivery that ties list prices and their associated rebates to formulary placement.
“If you went back a few years ago, when we negotiated to get our drugs on formulary, our goal was to have the lowest copay by patients,” Kenneth Frazier, chairman and CEO of Merck, testified before the committee. “Today, the goal is to pay into the supply chain the biggest rebate. That actually puts the patient at a disadvantage since they are the only ones that are paying a portion of the list price. The list price is actually working against the patient.”
When asked why the list prices of prescription drugs are so high, Olivier Brandicourt, MD, CEO of Sanofi, said, “We are trying to get formulary position with those high list price-high rebate. It’s a preferred position. Unfortunately that preferred position doesn’t automatically ensure affordability.”
Mr. Frazier added that if a manufacturer brings a product “with a low list price in this system, you get punished financially and you get no uptake because everyone in the supply chain makes money as a result of a higher list price.”
Executives noted that when accounting for financial incentives such as rebates, discounts, and coupons, net prices for pharmaceuticals have actually come down even as list prices are on the rise to accommodate competition on formulary placement.
But that is obscured at the pharmacy counter, where patients are paying higher and higher out-of-pocket costs because more often than not, payment is tied to the list price of the drug, not the net price after all rebates and other discounts have been taken into consideration.
This is a particular problem in Medicare Part D, said AbbVie Chairman and CEO Richard Gonzalez.
“Due to the structure of the Part D benefit design, patients are charged out-of-pocket costs on a medicine’s list price which does not reflect the market-based rebates that Medicare receives,” he testified.
Despite acknowledging that this is a problem, the executives gathered were hesitant to commit to simply lowering the list prices, or anything for that matter.
The closest the panel came to a commitment to lowering the list prices of their drugs was to do so if all rebates went away in both the public and private sector.
But beyond that, the pharma executives continued to assign responsibility for high out-of-pocket drug costs to other players in the health care system, adding that the only way to change the situation would be to have everyone come to the table simultaneously.
“I understand the dissatisfaction with our industry,” Mr. Frazier said. “I understand why patients are frustrated because they need these medicines and they can’t afford them. I would pledge to do everything that we could, but I would urge you to recognize that the system itself is complex and it is interdependent and no one company can unilaterally lower list prices without running into financial and operating disadvantages that make it impossible to do that. But if we all bring the parties together around the table with the goal of doing what’s best for the patient, I think we can some up with a system that works for all Americans.”
Ultimately, the panel suggested, legislation is going to be required to change the system.
Top pharmaceutical executives expressed willingness to lower the list prices of their drugs, but only if there were cooperation among all sectors to reform how drugs get from manufacturer to patient.

That theme was common in the testimony of seven pharmaceutical executives before the Senate Finance Committee during a Feb. 26 hearing.
“We are in a system that used to be fit for purpose and really drove enormous savings over the last few years but it is no longer fit for purpose,” Pascal Soriot, executive director and CEO of AstraZeneca, testified before the committee. “It’s one of those situations where nobody in the system can do anything, can fix it by themselves.”
The problem, the executives agreed, is the financial structure of drug delivery that ties list prices and their associated rebates to formulary placement.
“If you went back a few years ago, when we negotiated to get our drugs on formulary, our goal was to have the lowest copay by patients,” Kenneth Frazier, chairman and CEO of Merck, testified before the committee. “Today, the goal is to pay into the supply chain the biggest rebate. That actually puts the patient at a disadvantage since they are the only ones that are paying a portion of the list price. The list price is actually working against the patient.”
When asked why the list prices of prescription drugs are so high, Olivier Brandicourt, MD, CEO of Sanofi, said, “We are trying to get formulary position with those high list price-high rebate. It’s a preferred position. Unfortunately that preferred position doesn’t automatically ensure affordability.”
Mr. Frazier added that if a manufacturer brings a product “with a low list price in this system, you get punished financially and you get no uptake because everyone in the supply chain makes money as a result of a higher list price.”
Executives noted that when accounting for financial incentives such as rebates, discounts, and coupons, net prices for pharmaceuticals have actually come down even as list prices are on the rise to accommodate competition on formulary placement.
But that is obscured at the pharmacy counter, where patients are paying higher and higher out-of-pocket costs because more often than not, payment is tied to the list price of the drug, not the net price after all rebates and other discounts have been taken into consideration.
This is a particular problem in Medicare Part D, said AbbVie Chairman and CEO Richard Gonzalez.
“Due to the structure of the Part D benefit design, patients are charged out-of-pocket costs on a medicine’s list price which does not reflect the market-based rebates that Medicare receives,” he testified.
Despite acknowledging that this is a problem, the executives gathered were hesitant to commit to simply lowering the list prices, or anything for that matter.
The closest the panel came to a commitment to lowering the list prices of their drugs was to do so if all rebates went away in both the public and private sector.
But beyond that, the pharma executives continued to assign responsibility for high out-of-pocket drug costs to other players in the health care system, adding that the only way to change the situation would be to have everyone come to the table simultaneously.
“I understand the dissatisfaction with our industry,” Mr. Frazier said. “I understand why patients are frustrated because they need these medicines and they can’t afford them. I would pledge to do everything that we could, but I would urge you to recognize that the system itself is complex and it is interdependent and no one company can unilaterally lower list prices without running into financial and operating disadvantages that make it impossible to do that. But if we all bring the parties together around the table with the goal of doing what’s best for the patient, I think we can some up with a system that works for all Americans.”
Ultimately, the panel suggested, legislation is going to be required to change the system.
Top pharmaceutical executives expressed willingness to lower the list prices of their drugs, but only if there were cooperation among all sectors to reform how drugs get from manufacturer to patient.

That theme was common in the testimony of seven pharmaceutical executives before the Senate Finance Committee during a Feb. 26 hearing.
“We are in a system that used to be fit for purpose and really drove enormous savings over the last few years but it is no longer fit for purpose,” Pascal Soriot, executive director and CEO of AstraZeneca, testified before the committee. “It’s one of those situations where nobody in the system can do anything, can fix it by themselves.”
The problem, the executives agreed, is the financial structure of drug delivery that ties list prices and their associated rebates to formulary placement.
“If you went back a few years ago, when we negotiated to get our drugs on formulary, our goal was to have the lowest copay by patients,” Kenneth Frazier, chairman and CEO of Merck, testified before the committee. “Today, the goal is to pay into the supply chain the biggest rebate. That actually puts the patient at a disadvantage since they are the only ones that are paying a portion of the list price. The list price is actually working against the patient.”
When asked why the list prices of prescription drugs are so high, Olivier Brandicourt, MD, CEO of Sanofi, said, “We are trying to get formulary position with those high list price-high rebate. It’s a preferred position. Unfortunately that preferred position doesn’t automatically ensure affordability.”
Mr. Frazier added that if a manufacturer brings a product “with a low list price in this system, you get punished financially and you get no uptake because everyone in the supply chain makes money as a result of a higher list price.”
Executives noted that when accounting for financial incentives such as rebates, discounts, and coupons, net prices for pharmaceuticals have actually come down even as list prices are on the rise to accommodate competition on formulary placement.
But that is obscured at the pharmacy counter, where patients are paying higher and higher out-of-pocket costs because more often than not, payment is tied to the list price of the drug, not the net price after all rebates and other discounts have been taken into consideration.
This is a particular problem in Medicare Part D, said AbbVie Chairman and CEO Richard Gonzalez.
“Due to the structure of the Part D benefit design, patients are charged out-of-pocket costs on a medicine’s list price which does not reflect the market-based rebates that Medicare receives,” he testified.
Despite acknowledging that this is a problem, the executives gathered were hesitant to commit to simply lowering the list prices, or anything for that matter.
The closest the panel came to a commitment to lowering the list prices of their drugs was to do so if all rebates went away in both the public and private sector.
But beyond that, the pharma executives continued to assign responsibility for high out-of-pocket drug costs to other players in the health care system, adding that the only way to change the situation would be to have everyone come to the table simultaneously.
“I understand the dissatisfaction with our industry,” Mr. Frazier said. “I understand why patients are frustrated because they need these medicines and they can’t afford them. I would pledge to do everything that we could, but I would urge you to recognize that the system itself is complex and it is interdependent and no one company can unilaterally lower list prices without running into financial and operating disadvantages that make it impossible to do that. But if we all bring the parties together around the table with the goal of doing what’s best for the patient, I think we can some up with a system that works for all Americans.”
Ultimately, the panel suggested, legislation is going to be required to change the system.
REPORTING FROM SENATE FINANCE COMMITTEE HEARING
Final ‘Vision’ report addresses MOC woes
Whatever you do, change the name.
That was key among the final recommendations the Vision Initiative Commission submitted to the American Board of Medical Specialties on how to improve the maintenance of certification process.
“A new term that communicates the concept, intent, and expectations of continuing certification programs should be adopted by the ABMS in order to reengage disaffected diplomates and assure the public and other stakeholders that the certificate has enduring meaning and value,” according to the final report. A new term was not suggested.
The commission recommended a continuing certification system with four aims:
- Become a meaningful, contemporary, and relevant professional development activity for diplomates that ensures they remain up-to-date in their specialty.
- Demonstrate a commitment to professional self-regulation to both diplomates and the public.
- Align with international and national standards for certification programs.
- Provide a specialty-based credential that would be of value to diplomates and to multiple stakeholders, including patients, families, the public, and health care institutions.
Testing methods and situations must be simplified and updated, according to the report, which was submitted to ABMS on Feb. 12. Continuing certification “must change to incorporate longitudinal and other innovative formative assessment strategies that support learning, identify knowledge and skills gaps, and help diplomates stay current. The ABMS Boards must offer an alternative to burdensome highly secure, point-in-time examinations of knowledge.” In addition, the boards “must no longer use a single point-in-time examination or a series of single point-in-time assessments as the sole method to determine certification status.”
Instead, the commission recommends that ABMS “move quickly to formative assessment formats that are not characterized by high-stakes summative outcomes (pass/fail), specified time frames for high-stakes assessment, or require burdensome testing formats (such as testing centers or remote proctoring) that are inconsistent with the desired goals for continuing certification – support learning; identify knowledge and skills gaps; and help diplomates stay current.”
The commission also defined how the certification process should be used by other stakeholders.
“ABMS must demonstrate and communicate that continuing certification has value, meaning, and purpose in the health care environment,” the report states. “Hospitals, health systems, payers, and other health care organizations can independently decide what factors are used in credentialing and privileging decisions. ABMS must inform these organizations that continuing certification should not be the only criterion used in these decisions, and these organizations should use a wide portfolio of criteria in these decisions. ABMS must encourage hospitals, health systems, payers, and other health care organizations to not deny credentialing or privileging to a physician solely on the basis of certification status.”
Additionally, the commission report states that “ABMS and the ABMS Boards should collaborate with specialty societies, the [continuing medical education/continuing professional development] community, and other expert stakeholders to develop the infrastructure to support learning activities that produce data-driven advances in clinical practice. The ABMS Boards must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage.”
The report adds that the boards “should readily accept existing activities that diplomates are doing to advance their clinical practice and to provide credit for performing low-resource, high-impact activities as part of their daily practice routine.”
The commission’s final report incorporates a number of changes that physicians offered based on a draft version of the report.
The American College of Physicians commented that it “objects to the use of data regarding quality measures for individual diplomate certification status, because physician-level measures of quality are flawed, and because physician-level data inevitably leads to physician-level documentation burden. Flawed performance measures also often inadequately adjust for patient comorbidities and socioeconomic status, which leads to assessments that do not reflect the actual quality of care.”
Similarly, the American Society of Hematology noted in a statement that it “disagrees with the commission’s recommendation to retain the reporting of practice improvement activities as part of continuous certification due to direct and indirect costs needed to fulfill this requirement on top of requirements for engagement in quality improvement mandated by insurers, institutions, and health systems.”
While the draft report recommended that specialty boards provide aggregated feedback to medical societies, a more individualized dissemination on the gaps in knowledge would be more helpful, according to Doug Henley, MD, CEO of the American Academy of Family Physicians, who said that a more individualized approach would help his organization better provide CME to its members to help fill in the knowledge gaps.
“If we can identify these and use other processes and then target at the individual level to seek improvement, I think that will be a better outcome rather than just x learners don’t do well in diabetic care,” he said in an interview. “That doesn’t really help me in terms of who needs the real education in diabetic care versus who needs it for heart failure.”
The final recommendation notes that ABMS member boards “must collaborate with professional and/or CME/CPD organizations to share data and information to guide and support diplomate engagement in continuing certification.”
The document further clarifies that the boards should examine “the aggregated results from assessments to identify knowledge, skills, and other competency gaps,” and the aggregated data should be shared with specialty societies, CME/CPD providers, quality improvement professionals, and other health care organizations.
One weakness in the draft noted by Dr. Henley was the lack of a more forceful tone within the recommendations. Even though AMBS is not bound by its recommendations, he said that he would like to see stronger language throughout the document.
“We would certainly hope that the ABMS and the member boards will follow the direction of the Vision Commission very directly and succinctly,” he said. “That is why we suggested that some of the recommendations from the Vision Commission should use words like ‘should’ and ‘must’ and not just ‘encourage’ and words like that.”
That recommendation was taken and implemented in the final document.
Societies differed in how often participation in the certification process should occur.
The American College of Rheumatology in its comments challenged a recommendation that certification should be structured to expect participation on an annual basis.
“The ACR supports the importance of ongoing learning,” it stated. “However, no discussion is provided as to how and why the recommendation for annual participation by diplomates was conceived. For some ABMS Boards, an annual requirement will increase physician burden unless continuing certification is modified to a formative pathway. If this recommendation is to be retained, the commission would be encouraged to emphasize that inclusion of annual participation should be part of an overall program structure plan that supports a formative approach to assessment. In addition, the ACR requests that ABMS Boards allow exceptions without penalty to be made to this annual requirement to all for live events.”
The American College of Cardiology took a different point of view with regard to this recommendation.
In its comments, ACC stated that it “concurs with this recommendation. Annual participation is a feature of the ACC’s proposed maintenance of certification solution. The ACC believes that ABMS boards should recognize, and make allowances for, physicians who may, for valid reasons (illness, sabbatical, medical or family issue) may not participate in MOC for a period of a year.” ACC generally concurred with the recommendations in the draft.
The final document presented the commission’s view that the ABMS member boards “need to engage with diplomates on an ongoing basis instead of every 2, 5, or 10 years. The ABMS Boards should develop a diplomate engagement strategy and support the idea that diplomates are committed to learning and continually improving their practice, skills, and competencies. The ABMS Boards should expect that diplomates would engage in some learning, assessment, or advancing practice work annually.”
The American Gastroenterological Association, in its comment letter on the draft, said it was “greatly concerned” about the inclusion of practice improvement data, noting it is “debatable whether it is even within the appropriate domain of the boards to assume responsibility for clinical practice performance and quality assurance.”
The final report states that ABMS “must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage,” and added that “when appropriate, taking advantage of other organizations’ quality improvement and reporting activities should be maximized to avoid additional burdens on diplomates.”
ABMS and its board are not bound to follow any of the recommendations contained within the report, but the commission states that it “expects that the ABMS and the ABMS Boards, in collaboration with professional organizations and other stakeholders, will prioritize these recommendations and develop the necessary strategies and infrastructure to implement them.”
Whatever you do, change the name.
That was key among the final recommendations the Vision Initiative Commission submitted to the American Board of Medical Specialties on how to improve the maintenance of certification process.
“A new term that communicates the concept, intent, and expectations of continuing certification programs should be adopted by the ABMS in order to reengage disaffected diplomates and assure the public and other stakeholders that the certificate has enduring meaning and value,” according to the final report. A new term was not suggested.
The commission recommended a continuing certification system with four aims:
- Become a meaningful, contemporary, and relevant professional development activity for diplomates that ensures they remain up-to-date in their specialty.
- Demonstrate a commitment to professional self-regulation to both diplomates and the public.
- Align with international and national standards for certification programs.
- Provide a specialty-based credential that would be of value to diplomates and to multiple stakeholders, including patients, families, the public, and health care institutions.
Testing methods and situations must be simplified and updated, according to the report, which was submitted to ABMS on Feb. 12. Continuing certification “must change to incorporate longitudinal and other innovative formative assessment strategies that support learning, identify knowledge and skills gaps, and help diplomates stay current. The ABMS Boards must offer an alternative to burdensome highly secure, point-in-time examinations of knowledge.” In addition, the boards “must no longer use a single point-in-time examination or a series of single point-in-time assessments as the sole method to determine certification status.”
Instead, the commission recommends that ABMS “move quickly to formative assessment formats that are not characterized by high-stakes summative outcomes (pass/fail), specified time frames for high-stakes assessment, or require burdensome testing formats (such as testing centers or remote proctoring) that are inconsistent with the desired goals for continuing certification – support learning; identify knowledge and skills gaps; and help diplomates stay current.”
The commission also defined how the certification process should be used by other stakeholders.
“ABMS must demonstrate and communicate that continuing certification has value, meaning, and purpose in the health care environment,” the report states. “Hospitals, health systems, payers, and other health care organizations can independently decide what factors are used in credentialing and privileging decisions. ABMS must inform these organizations that continuing certification should not be the only criterion used in these decisions, and these organizations should use a wide portfolio of criteria in these decisions. ABMS must encourage hospitals, health systems, payers, and other health care organizations to not deny credentialing or privileging to a physician solely on the basis of certification status.”
Additionally, the commission report states that “ABMS and the ABMS Boards should collaborate with specialty societies, the [continuing medical education/continuing professional development] community, and other expert stakeholders to develop the infrastructure to support learning activities that produce data-driven advances in clinical practice. The ABMS Boards must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage.”
The report adds that the boards “should readily accept existing activities that diplomates are doing to advance their clinical practice and to provide credit for performing low-resource, high-impact activities as part of their daily practice routine.”
The commission’s final report incorporates a number of changes that physicians offered based on a draft version of the report.
The American College of Physicians commented that it “objects to the use of data regarding quality measures for individual diplomate certification status, because physician-level measures of quality are flawed, and because physician-level data inevitably leads to physician-level documentation burden. Flawed performance measures also often inadequately adjust for patient comorbidities and socioeconomic status, which leads to assessments that do not reflect the actual quality of care.”
Similarly, the American Society of Hematology noted in a statement that it “disagrees with the commission’s recommendation to retain the reporting of practice improvement activities as part of continuous certification due to direct and indirect costs needed to fulfill this requirement on top of requirements for engagement in quality improvement mandated by insurers, institutions, and health systems.”
While the draft report recommended that specialty boards provide aggregated feedback to medical societies, a more individualized dissemination on the gaps in knowledge would be more helpful, according to Doug Henley, MD, CEO of the American Academy of Family Physicians, who said that a more individualized approach would help his organization better provide CME to its members to help fill in the knowledge gaps.
“If we can identify these and use other processes and then target at the individual level to seek improvement, I think that will be a better outcome rather than just x learners don’t do well in diabetic care,” he said in an interview. “That doesn’t really help me in terms of who needs the real education in diabetic care versus who needs it for heart failure.”
The final recommendation notes that ABMS member boards “must collaborate with professional and/or CME/CPD organizations to share data and information to guide and support diplomate engagement in continuing certification.”
The document further clarifies that the boards should examine “the aggregated results from assessments to identify knowledge, skills, and other competency gaps,” and the aggregated data should be shared with specialty societies, CME/CPD providers, quality improvement professionals, and other health care organizations.
One weakness in the draft noted by Dr. Henley was the lack of a more forceful tone within the recommendations. Even though AMBS is not bound by its recommendations, he said that he would like to see stronger language throughout the document.
“We would certainly hope that the ABMS and the member boards will follow the direction of the Vision Commission very directly and succinctly,” he said. “That is why we suggested that some of the recommendations from the Vision Commission should use words like ‘should’ and ‘must’ and not just ‘encourage’ and words like that.”
That recommendation was taken and implemented in the final document.
Societies differed in how often participation in the certification process should occur.
The American College of Rheumatology in its comments challenged a recommendation that certification should be structured to expect participation on an annual basis.
“The ACR supports the importance of ongoing learning,” it stated. “However, no discussion is provided as to how and why the recommendation for annual participation by diplomates was conceived. For some ABMS Boards, an annual requirement will increase physician burden unless continuing certification is modified to a formative pathway. If this recommendation is to be retained, the commission would be encouraged to emphasize that inclusion of annual participation should be part of an overall program structure plan that supports a formative approach to assessment. In addition, the ACR requests that ABMS Boards allow exceptions without penalty to be made to this annual requirement to all for live events.”
The American College of Cardiology took a different point of view with regard to this recommendation.
In its comments, ACC stated that it “concurs with this recommendation. Annual participation is a feature of the ACC’s proposed maintenance of certification solution. The ACC believes that ABMS boards should recognize, and make allowances for, physicians who may, for valid reasons (illness, sabbatical, medical or family issue) may not participate in MOC for a period of a year.” ACC generally concurred with the recommendations in the draft.
The final document presented the commission’s view that the ABMS member boards “need to engage with diplomates on an ongoing basis instead of every 2, 5, or 10 years. The ABMS Boards should develop a diplomate engagement strategy and support the idea that diplomates are committed to learning and continually improving their practice, skills, and competencies. The ABMS Boards should expect that diplomates would engage in some learning, assessment, or advancing practice work annually.”
The American Gastroenterological Association, in its comment letter on the draft, said it was “greatly concerned” about the inclusion of practice improvement data, noting it is “debatable whether it is even within the appropriate domain of the boards to assume responsibility for clinical practice performance and quality assurance.”
The final report states that ABMS “must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage,” and added that “when appropriate, taking advantage of other organizations’ quality improvement and reporting activities should be maximized to avoid additional burdens on diplomates.”
ABMS and its board are not bound to follow any of the recommendations contained within the report, but the commission states that it “expects that the ABMS and the ABMS Boards, in collaboration with professional organizations and other stakeholders, will prioritize these recommendations and develop the necessary strategies and infrastructure to implement them.”
Whatever you do, change the name.
That was key among the final recommendations the Vision Initiative Commission submitted to the American Board of Medical Specialties on how to improve the maintenance of certification process.
“A new term that communicates the concept, intent, and expectations of continuing certification programs should be adopted by the ABMS in order to reengage disaffected diplomates and assure the public and other stakeholders that the certificate has enduring meaning and value,” according to the final report. A new term was not suggested.
The commission recommended a continuing certification system with four aims:
- Become a meaningful, contemporary, and relevant professional development activity for diplomates that ensures they remain up-to-date in their specialty.
- Demonstrate a commitment to professional self-regulation to both diplomates and the public.
- Align with international and national standards for certification programs.
- Provide a specialty-based credential that would be of value to diplomates and to multiple stakeholders, including patients, families, the public, and health care institutions.
Testing methods and situations must be simplified and updated, according to the report, which was submitted to ABMS on Feb. 12. Continuing certification “must change to incorporate longitudinal and other innovative formative assessment strategies that support learning, identify knowledge and skills gaps, and help diplomates stay current. The ABMS Boards must offer an alternative to burdensome highly secure, point-in-time examinations of knowledge.” In addition, the boards “must no longer use a single point-in-time examination or a series of single point-in-time assessments as the sole method to determine certification status.”
Instead, the commission recommends that ABMS “move quickly to formative assessment formats that are not characterized by high-stakes summative outcomes (pass/fail), specified time frames for high-stakes assessment, or require burdensome testing formats (such as testing centers or remote proctoring) that are inconsistent with the desired goals for continuing certification – support learning; identify knowledge and skills gaps; and help diplomates stay current.”
The commission also defined how the certification process should be used by other stakeholders.
“ABMS must demonstrate and communicate that continuing certification has value, meaning, and purpose in the health care environment,” the report states. “Hospitals, health systems, payers, and other health care organizations can independently decide what factors are used in credentialing and privileging decisions. ABMS must inform these organizations that continuing certification should not be the only criterion used in these decisions, and these organizations should use a wide portfolio of criteria in these decisions. ABMS must encourage hospitals, health systems, payers, and other health care organizations to not deny credentialing or privileging to a physician solely on the basis of certification status.”
Additionally, the commission report states that “ABMS and the ABMS Boards should collaborate with specialty societies, the [continuing medical education/continuing professional development] community, and other expert stakeholders to develop the infrastructure to support learning activities that produce data-driven advances in clinical practice. The ABMS Boards must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage.”
The report adds that the boards “should readily accept existing activities that diplomates are doing to advance their clinical practice and to provide credit for performing low-resource, high-impact activities as part of their daily practice routine.”
The commission’s final report incorporates a number of changes that physicians offered based on a draft version of the report.
The American College of Physicians commented that it “objects to the use of data regarding quality measures for individual diplomate certification status, because physician-level measures of quality are flawed, and because physician-level data inevitably leads to physician-level documentation burden. Flawed performance measures also often inadequately adjust for patient comorbidities and socioeconomic status, which leads to assessments that do not reflect the actual quality of care.”
Similarly, the American Society of Hematology noted in a statement that it “disagrees with the commission’s recommendation to retain the reporting of practice improvement activities as part of continuous certification due to direct and indirect costs needed to fulfill this requirement on top of requirements for engagement in quality improvement mandated by insurers, institutions, and health systems.”
While the draft report recommended that specialty boards provide aggregated feedback to medical societies, a more individualized dissemination on the gaps in knowledge would be more helpful, according to Doug Henley, MD, CEO of the American Academy of Family Physicians, who said that a more individualized approach would help his organization better provide CME to its members to help fill in the knowledge gaps.
“If we can identify these and use other processes and then target at the individual level to seek improvement, I think that will be a better outcome rather than just x learners don’t do well in diabetic care,” he said in an interview. “That doesn’t really help me in terms of who needs the real education in diabetic care versus who needs it for heart failure.”
The final recommendation notes that ABMS member boards “must collaborate with professional and/or CME/CPD organizations to share data and information to guide and support diplomate engagement in continuing certification.”
The document further clarifies that the boards should examine “the aggregated results from assessments to identify knowledge, skills, and other competency gaps,” and the aggregated data should be shared with specialty societies, CME/CPD providers, quality improvement professionals, and other health care organizations.
One weakness in the draft noted by Dr. Henley was the lack of a more forceful tone within the recommendations. Even though AMBS is not bound by its recommendations, he said that he would like to see stronger language throughout the document.
“We would certainly hope that the ABMS and the member boards will follow the direction of the Vision Commission very directly and succinctly,” he said. “That is why we suggested that some of the recommendations from the Vision Commission should use words like ‘should’ and ‘must’ and not just ‘encourage’ and words like that.”
That recommendation was taken and implemented in the final document.
Societies differed in how often participation in the certification process should occur.
The American College of Rheumatology in its comments challenged a recommendation that certification should be structured to expect participation on an annual basis.
“The ACR supports the importance of ongoing learning,” it stated. “However, no discussion is provided as to how and why the recommendation for annual participation by diplomates was conceived. For some ABMS Boards, an annual requirement will increase physician burden unless continuing certification is modified to a formative pathway. If this recommendation is to be retained, the commission would be encouraged to emphasize that inclusion of annual participation should be part of an overall program structure plan that supports a formative approach to assessment. In addition, the ACR requests that ABMS Boards allow exceptions without penalty to be made to this annual requirement to all for live events.”
The American College of Cardiology took a different point of view with regard to this recommendation.
In its comments, ACC stated that it “concurs with this recommendation. Annual participation is a feature of the ACC’s proposed maintenance of certification solution. The ACC believes that ABMS boards should recognize, and make allowances for, physicians who may, for valid reasons (illness, sabbatical, medical or family issue) may not participate in MOC for a period of a year.” ACC generally concurred with the recommendations in the draft.
The final document presented the commission’s view that the ABMS member boards “need to engage with diplomates on an ongoing basis instead of every 2, 5, or 10 years. The ABMS Boards should develop a diplomate engagement strategy and support the idea that diplomates are committed to learning and continually improving their practice, skills, and competencies. The ABMS Boards should expect that diplomates would engage in some learning, assessment, or advancing practice work annually.”
The American Gastroenterological Association, in its comment letter on the draft, said it was “greatly concerned” about the inclusion of practice improvement data, noting it is “debatable whether it is even within the appropriate domain of the boards to assume responsibility for clinical practice performance and quality assurance.”
The final report states that ABMS “must ensure that their continuing certification programs recognize and document participation in a wide range of quality assessment activities in which diplomates already engage,” and added that “when appropriate, taking advantage of other organizations’ quality improvement and reporting activities should be maximized to avoid additional burdens on diplomates.”
ABMS and its board are not bound to follow any of the recommendations contained within the report, but the commission states that it “expects that the ABMS and the ABMS Boards, in collaboration with professional organizations and other stakeholders, will prioritize these recommendations and develop the necessary strategies and infrastructure to implement them.”
HHS to target step therapy, Stark Law in 2019
WASHINGTON –
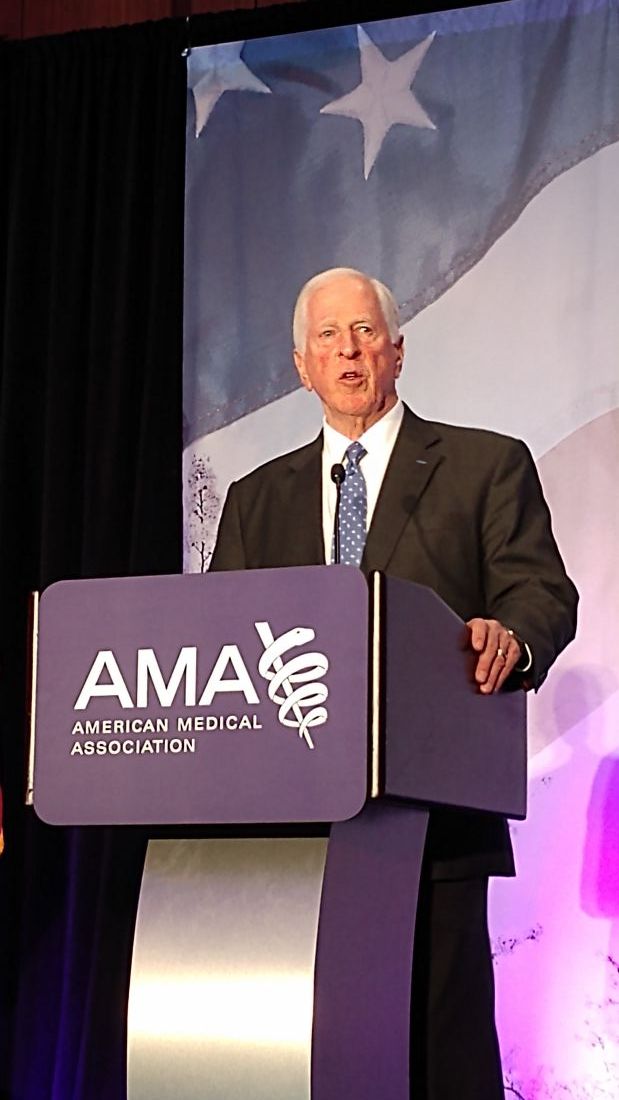
Speaking Feb. 12 at the American Medical Association’s National Advocacy Conference, Secretary Azar said the agency will be looking into ensuring that patients on medical plans who have found a working drug after going through a step-therapy protocol will not have to restart on a drug that has already failed for them if they switch insurance providers.
“I was very disturbed to hear that stable patients switching among insurance plans, like switching among Medicare Advantage plans, can often be required to start over again on a step therapy regimen,” he said.
“This is not just potentially injurious to their health, it’s also penny-wise and pound-foolish,” Secretary Azar continued. “We know that getting a patient on the right drug, at the right time, is one of the best investments we can make in their health, and we do not want to impede physicians from making that happen. We’re looking at how we can address that issue now.”
The other area Secretary Azar highlighted that the agency is working on is making changes to the Stark Law.
“The Stark Law was written with noble purposes in mind, but it was designed for a fee-for-service system, not the kind of system we are moving toward today,” he said. “We’ve heard from many, many stakeholders, including the AMA, about the need to update the enumerated exceptions in the Stark Law to include value-based approaches to care.”
He added that how care coordination interacts with the antikickback statutes and HIPAA are also going to be examined.
He used most of his speech to discuss recent regulatory actions around drug pricing and pushed for support for the Part B drug pricing model that the agency is preparing for a formal proposed rule, despite having received a critical reception from medical societies.
“If you have a small practice that uses infusions, and you don’t want to bear the risk of buy and bill, now you’re off the hook,” he said. “We’ll allow you to work with private vendors who can take the risk for buying the drugs in a way that isn’t possible today. But if you’re part of a much larger practice that’s able to drive a better deal than you could on your own, or want to band together with other practices to do the purchasing, then you can do that, too.”
He continued: “Next is the launch of the actual proposed rule, followed by the rule itself, which, I’ll remind you, is just a model.”
However, despite it being a model under test from the Center for Medicare & Medicaid Innovation, the advanced notice of proposed rule making that was issued in October 2018 suggested that participation in the so-called International Pricing Index model would be mandatory.
AGA is pleased about Secretary Azar’s commitment to ensuring Medicare beneficiaries will continue to have access to and coverage of medications that work for them. Patients should not be forced to switch to a therapy that they have already failed if they change insurance plans. Read more about AGA’s advocacy for similar federal legislation at http://ow.ly/2t3030nLbcB.
AGA, in conjunction with other physician specialty organizations, continues to advocate for changes in the Stark Law to allow physician practices to participate in advanced payment models in the Medicare program that will improve care coordination and patient outcomes.
WASHINGTON –
Speaking Feb. 12 at the American Medical Association’s National Advocacy Conference, Secretary Azar said the agency will be looking into ensuring that patients on medical plans who have found a working drug after going through a step-therapy protocol will not have to restart on a drug that has already failed for them if they switch insurance providers.
“I was very disturbed to hear that stable patients switching among insurance plans, like switching among Medicare Advantage plans, can often be required to start over again on a step therapy regimen,” he said.
“This is not just potentially injurious to their health, it’s also penny-wise and pound-foolish,” Secretary Azar continued. “We know that getting a patient on the right drug, at the right time, is one of the best investments we can make in their health, and we do not want to impede physicians from making that happen. We’re looking at how we can address that issue now.”
The other area Secretary Azar highlighted that the agency is working on is making changes to the Stark Law.
“The Stark Law was written with noble purposes in mind, but it was designed for a fee-for-service system, not the kind of system we are moving toward today,” he said. “We’ve heard from many, many stakeholders, including the AMA, about the need to update the enumerated exceptions in the Stark Law to include value-based approaches to care.”
He added that how care coordination interacts with the antikickback statutes and HIPAA are also going to be examined.
He used most of his speech to discuss recent regulatory actions around drug pricing and pushed for support for the Part B drug pricing model that the agency is preparing for a formal proposed rule, despite having received a critical reception from medical societies.
“If you have a small practice that uses infusions, and you don’t want to bear the risk of buy and bill, now you’re off the hook,” he said. “We’ll allow you to work with private vendors who can take the risk for buying the drugs in a way that isn’t possible today. But if you’re part of a much larger practice that’s able to drive a better deal than you could on your own, or want to band together with other practices to do the purchasing, then you can do that, too.”
He continued: “Next is the launch of the actual proposed rule, followed by the rule itself, which, I’ll remind you, is just a model.”
However, despite it being a model under test from the Center for Medicare & Medicaid Innovation, the advanced notice of proposed rule making that was issued in October 2018 suggested that participation in the so-called International Pricing Index model would be mandatory.
AGA is pleased about Secretary Azar’s commitment to ensuring Medicare beneficiaries will continue to have access to and coverage of medications that work for them. Patients should not be forced to switch to a therapy that they have already failed if they change insurance plans. Read more about AGA’s advocacy for similar federal legislation at http://ow.ly/2t3030nLbcB.
AGA, in conjunction with other physician specialty organizations, continues to advocate for changes in the Stark Law to allow physician practices to participate in advanced payment models in the Medicare program that will improve care coordination and patient outcomes.
WASHINGTON –
Speaking Feb. 12 at the American Medical Association’s National Advocacy Conference, Secretary Azar said the agency will be looking into ensuring that patients on medical plans who have found a working drug after going through a step-therapy protocol will not have to restart on a drug that has already failed for them if they switch insurance providers.
“I was very disturbed to hear that stable patients switching among insurance plans, like switching among Medicare Advantage plans, can often be required to start over again on a step therapy regimen,” he said.
“This is not just potentially injurious to their health, it’s also penny-wise and pound-foolish,” Secretary Azar continued. “We know that getting a patient on the right drug, at the right time, is one of the best investments we can make in their health, and we do not want to impede physicians from making that happen. We’re looking at how we can address that issue now.”
The other area Secretary Azar highlighted that the agency is working on is making changes to the Stark Law.
“The Stark Law was written with noble purposes in mind, but it was designed for a fee-for-service system, not the kind of system we are moving toward today,” he said. “We’ve heard from many, many stakeholders, including the AMA, about the need to update the enumerated exceptions in the Stark Law to include value-based approaches to care.”
He added that how care coordination interacts with the antikickback statutes and HIPAA are also going to be examined.
He used most of his speech to discuss recent regulatory actions around drug pricing and pushed for support for the Part B drug pricing model that the agency is preparing for a formal proposed rule, despite having received a critical reception from medical societies.
“If you have a small practice that uses infusions, and you don’t want to bear the risk of buy and bill, now you’re off the hook,” he said. “We’ll allow you to work with private vendors who can take the risk for buying the drugs in a way that isn’t possible today. But if you’re part of a much larger practice that’s able to drive a better deal than you could on your own, or want to band together with other practices to do the purchasing, then you can do that, too.”
He continued: “Next is the launch of the actual proposed rule, followed by the rule itself, which, I’ll remind you, is just a model.”
However, despite it being a model under test from the Center for Medicare & Medicaid Innovation, the advanced notice of proposed rule making that was issued in October 2018 suggested that participation in the so-called International Pricing Index model would be mandatory.
AGA is pleased about Secretary Azar’s commitment to ensuring Medicare beneficiaries will continue to have access to and coverage of medications that work for them. Patients should not be forced to switch to a therapy that they have already failed if they change insurance plans. Read more about AGA’s advocacy for similar federal legislation at http://ow.ly/2t3030nLbcB.
AGA, in conjunction with other physician specialty organizations, continues to advocate for changes in the Stark Law to allow physician practices to participate in advanced payment models in the Medicare program that will improve care coordination and patient outcomes.
Health spending: Boomers will spike costs, but growing uninsured will soften their impact
Spending on health care is projected to rise at a faster-than-average rate throughout the next decade, according to the Office of the Actuary at the Centers for Medicare & Medicaid Services.
“Overall, national health spending is projected to grow at 5.5% per year, on average, for 2018-27,” wrote Andrea Sisko, economist in the Office of the Actuary, and colleagues (Health Aff. 2019 Feb 20. doi: 10.1377/hlthaff.2018.05499). “This is faster than the average growth rate experienced following the last recession (3.9% for 2008-2013) and the more recent period inclusive of the Affordable Care Act’s major coverage expansions (5.3% for 2014-16).”
Medicare is projected to see the fastest growth in spending at 7.4% per year “as the shift of the Baby Boom generation into the program continues to result in robust growth in enrollment,” according to the authors.
Private payers should see a corollary slower growth in spending (4.8% per year) over the same period, while Medicaid spending is projected at 5.5% per year.
Faster growth in Medicare spending is expected to come from higher spending on prescription drugs and hospital services, as well as higher fee-for-service payment updates.
Spending increases are projected to be mitigated somewhat by the end of the ACA penalty for not having insurance – which is projected to add 1.3 million people this year to the ranks of the uninsured, according to the report.
Half of the overall growth in health care spending is attributable to rising prices in personal health care prices, on average, Ms. Sisko and colleagues wrote. “Growth in use and intensity is expected to account for just under one-third of the average annual personal health care spending growth, with population growth and the changing age-sex mix of the population accounting for the remainder.”
For those with private insurance, out-of-pocket spending is projected to accelerate to a 3.6% growth rate in 2018 from 2.6% in 2017 “a rate that is consistent with faster income growth as well as with the higher average deductibles for employer-based private health insurance enrollees in 2018 compared to 2017,” the authors note.
“Growth in out-of-pocket spending, which is also primarily influenced by economic factors, is expected to be similar to that of private health insurance spending in 2020-27, at 5%,” they add.
Prescription drug spending also is expected to grow.
“Following growth of just 0.4% in 2017, prescription drug spending is expected to have grown 3.3% in 2018 but still be among the slowest-growing health care sectors,” according to the authors. “Higher utilization growth is anticipated, compared to the relatively low growth in 2016 and 2017, partially driven by an increase in the number of new drug introductions.”
Growth in prescription drug spending is expected to accelerate further to 4.6% in 2019, based on growth in utilization and a “modest increase in drug price growth.”
Starting in 2020, that growth rate is projected to increase, on average, by 6.1% per year, based on the expectation that employers and insurers will lower barriers to maintenance medications for chronic conditions.
In 2019, growth in spending for physician clinical services is projected to accelerate to 5.4% from 4.9% in 2018.
“An acceleration in Medicaid spending growth is the primary factor contributing to the trend, which is in part associated with program’s expansion by additional states,” the authors note.
From 2020 to 2027, growth in spending on physician and clinical services is expected to average 5.4% per year, driven in part by price growth for these services.
“Underlying this acceleration are projected rising costs related to the provision of care,” the report said. “In particular, wages are expected to increase as a result of the supply of physicians not being able to meet expected increases in demand for care connected with the aging population. Furthermore, some of the productivity gains that have been achieved through the use of lower-cost providers as a substitute for physician care within physician practices may be less pronounced in the future, because of limitations such as licensing restrictions on the scope of care that may be provided by nonphysician providers.”
SOURCE: Sisko A et al. Health Aff. 2019 Feb 20. doi: 10.1377/hlthaff.2018.05499.
Spending on health care is projected to rise at a faster-than-average rate throughout the next decade, according to the Office of the Actuary at the Centers for Medicare & Medicaid Services.
“Overall, national health spending is projected to grow at 5.5% per year, on average, for 2018-27,” wrote Andrea Sisko, economist in the Office of the Actuary, and colleagues (Health Aff. 2019 Feb 20. doi: 10.1377/hlthaff.2018.05499). “This is faster than the average growth rate experienced following the last recession (3.9% for 2008-2013) and the more recent period inclusive of the Affordable Care Act’s major coverage expansions (5.3% for 2014-16).”
Medicare is projected to see the fastest growth in spending at 7.4% per year “as the shift of the Baby Boom generation into the program continues to result in robust growth in enrollment,” according to the authors.
Private payers should see a corollary slower growth in spending (4.8% per year) over the same period, while Medicaid spending is projected at 5.5% per year.
Faster growth in Medicare spending is expected to come from higher spending on prescription drugs and hospital services, as well as higher fee-for-service payment updates.
Spending increases are projected to be mitigated somewhat by the end of the ACA penalty for not having insurance – which is projected to add 1.3 million people this year to the ranks of the uninsured, according to the report.
Half of the overall growth in health care spending is attributable to rising prices in personal health care prices, on average, Ms. Sisko and colleagues wrote. “Growth in use and intensity is expected to account for just under one-third of the average annual personal health care spending growth, with population growth and the changing age-sex mix of the population accounting for the remainder.”
For those with private insurance, out-of-pocket spending is projected to accelerate to a 3.6% growth rate in 2018 from 2.6% in 2017 “a rate that is consistent with faster income growth as well as with the higher average deductibles for employer-based private health insurance enrollees in 2018 compared to 2017,” the authors note.
“Growth in out-of-pocket spending, which is also primarily influenced by economic factors, is expected to be similar to that of private health insurance spending in 2020-27, at 5%,” they add.
Prescription drug spending also is expected to grow.
“Following growth of just 0.4% in 2017, prescription drug spending is expected to have grown 3.3% in 2018 but still be among the slowest-growing health care sectors,” according to the authors. “Higher utilization growth is anticipated, compared to the relatively low growth in 2016 and 2017, partially driven by an increase in the number of new drug introductions.”
Growth in prescription drug spending is expected to accelerate further to 4.6% in 2019, based on growth in utilization and a “modest increase in drug price growth.”
Starting in 2020, that growth rate is projected to increase, on average, by 6.1% per year, based on the expectation that employers and insurers will lower barriers to maintenance medications for chronic conditions.
In 2019, growth in spending for physician clinical services is projected to accelerate to 5.4% from 4.9% in 2018.
“An acceleration in Medicaid spending growth is the primary factor contributing to the trend, which is in part associated with program’s expansion by additional states,” the authors note.
From 2020 to 2027, growth in spending on physician and clinical services is expected to average 5.4% per year, driven in part by price growth for these services.
“Underlying this acceleration are projected rising costs related to the provision of care,” the report said. “In particular, wages are expected to increase as a result of the supply of physicians not being able to meet expected increases in demand for care connected with the aging population. Furthermore, some of the productivity gains that have been achieved through the use of lower-cost providers as a substitute for physician care within physician practices may be less pronounced in the future, because of limitations such as licensing restrictions on the scope of care that may be provided by nonphysician providers.”
SOURCE: Sisko A et al. Health Aff. 2019 Feb 20. doi: 10.1377/hlthaff.2018.05499.
Spending on health care is projected to rise at a faster-than-average rate throughout the next decade, according to the Office of the Actuary at the Centers for Medicare & Medicaid Services.
“Overall, national health spending is projected to grow at 5.5% per year, on average, for 2018-27,” wrote Andrea Sisko, economist in the Office of the Actuary, and colleagues (Health Aff. 2019 Feb 20. doi: 10.1377/hlthaff.2018.05499). “This is faster than the average growth rate experienced following the last recession (3.9% for 2008-2013) and the more recent period inclusive of the Affordable Care Act’s major coverage expansions (5.3% for 2014-16).”
Medicare is projected to see the fastest growth in spending at 7.4% per year “as the shift of the Baby Boom generation into the program continues to result in robust growth in enrollment,” according to the authors.
Private payers should see a corollary slower growth in spending (4.8% per year) over the same period, while Medicaid spending is projected at 5.5% per year.
Faster growth in Medicare spending is expected to come from higher spending on prescription drugs and hospital services, as well as higher fee-for-service payment updates.
Spending increases are projected to be mitigated somewhat by the end of the ACA penalty for not having insurance – which is projected to add 1.3 million people this year to the ranks of the uninsured, according to the report.
Half of the overall growth in health care spending is attributable to rising prices in personal health care prices, on average, Ms. Sisko and colleagues wrote. “Growth in use and intensity is expected to account for just under one-third of the average annual personal health care spending growth, with population growth and the changing age-sex mix of the population accounting for the remainder.”
For those with private insurance, out-of-pocket spending is projected to accelerate to a 3.6% growth rate in 2018 from 2.6% in 2017 “a rate that is consistent with faster income growth as well as with the higher average deductibles for employer-based private health insurance enrollees in 2018 compared to 2017,” the authors note.
“Growth in out-of-pocket spending, which is also primarily influenced by economic factors, is expected to be similar to that of private health insurance spending in 2020-27, at 5%,” they add.
Prescription drug spending also is expected to grow.
“Following growth of just 0.4% in 2017, prescription drug spending is expected to have grown 3.3% in 2018 but still be among the slowest-growing health care sectors,” according to the authors. “Higher utilization growth is anticipated, compared to the relatively low growth in 2016 and 2017, partially driven by an increase in the number of new drug introductions.”
Growth in prescription drug spending is expected to accelerate further to 4.6% in 2019, based on growth in utilization and a “modest increase in drug price growth.”
Starting in 2020, that growth rate is projected to increase, on average, by 6.1% per year, based on the expectation that employers and insurers will lower barriers to maintenance medications for chronic conditions.
In 2019, growth in spending for physician clinical services is projected to accelerate to 5.4% from 4.9% in 2018.
“An acceleration in Medicaid spending growth is the primary factor contributing to the trend, which is in part associated with program’s expansion by additional states,” the authors note.
From 2020 to 2027, growth in spending on physician and clinical services is expected to average 5.4% per year, driven in part by price growth for these services.
“Underlying this acceleration are projected rising costs related to the provision of care,” the report said. “In particular, wages are expected to increase as a result of the supply of physicians not being able to meet expected increases in demand for care connected with the aging population. Furthermore, some of the productivity gains that have been achieved through the use of lower-cost providers as a substitute for physician care within physician practices may be less pronounced in the future, because of limitations such as licensing restrictions on the scope of care that may be provided by nonphysician providers.”
SOURCE: Sisko A et al. Health Aff. 2019 Feb 20. doi: 10.1377/hlthaff.2018.05499.
FROM HEALTH AFFAIRS
Matching clinical, claims data essential for value-based care
Finding success in alternative payment models is going to require infusing clinical data into administrative claims data.
This was the key takeaway of an analysis of data from a participant in the Oncology Care Model (OCM), a value-based episodic payment model being tested by the Centers for Medicare & Medicaid Service’s Center for Medicare and Medicaid Innovation.
Researchers looked at administrative claims data and infused into it clinical data from 377 6-month-long episode payments pertaining to 210 prostate cancer patients participating at a single OCM site to see if the combination could be used to develop more useful information that OCM participants could use to help improve care and control costs.
“In order to introduce these clinical factors, what we did was divide the patients that were included in our analysis into different disease-state treatment dyads,” Anish Parikh, MD, of Icahn School of Medicine at Mount Sinai, New York, said in an interview. Dr. Parikh is a coauthor of a report detailing the results of the analysis that was published in the Journal of Oncology Practice.
“Then we did a comparative cost analysis using the OCM’s data in this framework,” he continued. “We introduced these clinical factors this administrative claims data and then ran a comparative cost analysis to see what were the contributions to cost of care for each of these dyads.”
The analysis found that the most excessive expenses in prostate cancer treatment were seen in metastatic, castration-resistant dyads containing second-line hormone therapy (ratio of observed to expected expenses [O/E], 2.66), chemotherapy (O/E, 2.09) and radium-223/sipuleucel-T (O/E, 3.01).
During the observation period, the CMS updated the payment model, and a singular change correcting for castration-resistant prostate cancer resulted in up to a 38% increase in O/E for hormone-sensitive dyads and up to a 58% decrease in O/E for castration-resistant dyads. The update improved the overall O/E for all episodes by 22%, from 1.48 to 1.15.
The analysis “really is a demonstration of how sensitive this model is to clinical factors and how necessary and important it is to include clinical data into the administrative claims data whenever possible in order to make the model more accurate and usable,” Dr. Parikh said.
The investigators reported no conflicts of interest.
SOURCE: Parikh A et al. J Oncol Pract. 2019 Feb 11. doi: 10.1200/JOP.18.00336.
Finding success in alternative payment models is going to require infusing clinical data into administrative claims data.
This was the key takeaway of an analysis of data from a participant in the Oncology Care Model (OCM), a value-based episodic payment model being tested by the Centers for Medicare & Medicaid Service’s Center for Medicare and Medicaid Innovation.
Researchers looked at administrative claims data and infused into it clinical data from 377 6-month-long episode payments pertaining to 210 prostate cancer patients participating at a single OCM site to see if the combination could be used to develop more useful information that OCM participants could use to help improve care and control costs.
“In order to introduce these clinical factors, what we did was divide the patients that were included in our analysis into different disease-state treatment dyads,” Anish Parikh, MD, of Icahn School of Medicine at Mount Sinai, New York, said in an interview. Dr. Parikh is a coauthor of a report detailing the results of the analysis that was published in the Journal of Oncology Practice.
“Then we did a comparative cost analysis using the OCM’s data in this framework,” he continued. “We introduced these clinical factors this administrative claims data and then ran a comparative cost analysis to see what were the contributions to cost of care for each of these dyads.”
The analysis found that the most excessive expenses in prostate cancer treatment were seen in metastatic, castration-resistant dyads containing second-line hormone therapy (ratio of observed to expected expenses [O/E], 2.66), chemotherapy (O/E, 2.09) and radium-223/sipuleucel-T (O/E, 3.01).
During the observation period, the CMS updated the payment model, and a singular change correcting for castration-resistant prostate cancer resulted in up to a 38% increase in O/E for hormone-sensitive dyads and up to a 58% decrease in O/E for castration-resistant dyads. The update improved the overall O/E for all episodes by 22%, from 1.48 to 1.15.
The analysis “really is a demonstration of how sensitive this model is to clinical factors and how necessary and important it is to include clinical data into the administrative claims data whenever possible in order to make the model more accurate and usable,” Dr. Parikh said.
The investigators reported no conflicts of interest.
SOURCE: Parikh A et al. J Oncol Pract. 2019 Feb 11. doi: 10.1200/JOP.18.00336.
Finding success in alternative payment models is going to require infusing clinical data into administrative claims data.
This was the key takeaway of an analysis of data from a participant in the Oncology Care Model (OCM), a value-based episodic payment model being tested by the Centers for Medicare & Medicaid Service’s Center for Medicare and Medicaid Innovation.
Researchers looked at administrative claims data and infused into it clinical data from 377 6-month-long episode payments pertaining to 210 prostate cancer patients participating at a single OCM site to see if the combination could be used to develop more useful information that OCM participants could use to help improve care and control costs.
“In order to introduce these clinical factors, what we did was divide the patients that were included in our analysis into different disease-state treatment dyads,” Anish Parikh, MD, of Icahn School of Medicine at Mount Sinai, New York, said in an interview. Dr. Parikh is a coauthor of a report detailing the results of the analysis that was published in the Journal of Oncology Practice.
“Then we did a comparative cost analysis using the OCM’s data in this framework,” he continued. “We introduced these clinical factors this administrative claims data and then ran a comparative cost analysis to see what were the contributions to cost of care for each of these dyads.”
The analysis found that the most excessive expenses in prostate cancer treatment were seen in metastatic, castration-resistant dyads containing second-line hormone therapy (ratio of observed to expected expenses [O/E], 2.66), chemotherapy (O/E, 2.09) and radium-223/sipuleucel-T (O/E, 3.01).
During the observation period, the CMS updated the payment model, and a singular change correcting for castration-resistant prostate cancer resulted in up to a 38% increase in O/E for hormone-sensitive dyads and up to a 58% decrease in O/E for castration-resistant dyads. The update improved the overall O/E for all episodes by 22%, from 1.48 to 1.15.
The analysis “really is a demonstration of how sensitive this model is to clinical factors and how necessary and important it is to include clinical data into the administrative claims data whenever possible in order to make the model more accurate and usable,” Dr. Parikh said.
The investigators reported no conflicts of interest.
SOURCE: Parikh A et al. J Oncol Pract. 2019 Feb 11. doi: 10.1200/JOP.18.00336.
FROM THE JOURNAL OF ONCOLOGY PRACTICE
McAneny: Transparency needed for meaningful talk on drug pricing
WASHINGTON – As the rising cost of prescription drugs continues to garner heightened scrutiny from the federal government, one thing is missing from the conversation that would make any solution more effective, according to American Medical Association President Barbara L. McAneny, MD.
“We would like to see transparency from end to end in this pipeline because that is the way we will have the ability to look for savings,” she said in an interview at a national advocacy conference sponsored by the American Medical Association.
“I think we don’t have the information we need to make rational decisions,” she said. “I think the first thing we need to do is to understand the entire pipeline from the basic research that results in a drug’s clinical trials that results in a new drug to the pharmacy benefit managers and all of the ways that they have increased the cost of the drugs all the way to when the patient actually gets it.”
In particular, Dr. McAneny targeted the need for transparency in the role and financial impact pharmacy benefit managers have on the cost of prescription drugs.
“We were told at our state advocacy conference, which we held in January, by an expert who studied pharmacy benefit managers, that 42% of the cost of any drug is attributable to the profits of pharmacy benefit managers,” she said. “To me, that makes me wonder what value do they add that is worth 42% of these exorbitant costs and if they are not adding value, why do we have them in this process?”
She also called on the pharmaceutical manufacturers to be more forthcoming with their financial information regarding marketing and advertising, but she stressed that it needs to be done in a way that does not hinder future development of life-saving therapies.
“We do not want to stifle innovation.” Dr. McAneny said. “As a cancer doctor, I have seen diseases that I used to treat with morphine and sympathy now be diseases that I can treat, where I can restore people to good quality of life and buy them additional years of life because of these drugs. They are amazing and I don’t want to do without them and I want more of them. ... We want to support that research. That is probably worth a lot of the price tag. But how much of that goes to direct-to-consumer advertising? How much of that is the advertising budget? Where can we cut some of this out of the system so that we get the innovation, but we get innovation that all of our patients can afford?”
Another issue that is looming for physicians is a payment rate freeze from 2020-2025 under the Merit-based Incentive Payment System (MIPS) track of the Quality Payment Program, which was created under the Medicare Access and CHIP Reauthorization Act (MACRA).
“A 5-year freeze when my expenses do not freeze is a terrifying thing and could be a practice-ending expense for a lot of practices,” Dr. McAneny warned. “I will point out that independent practices, if they sell to a hospital, the cost of care immediately doubles. The amount that is paid for it, not the cost of delivering it. So that is not a great solution. But we also have this increasing practice expense and a flat rate is not going to help practices survive. So I am very concerned.”
Related to the QPP, Dr. McAneny also wants to see the Centers for Medicare & Medicaid Services do more with physician-developed alternative payment models. The Physician-Focused Payment Model Technical Advisory Committee (PTAC) continues to review and evaluate submissions, but to date, the CMS has yet to implement any of the committee’s recommendations.
“I read all of the PTAC submissions that went to CMS. Some of them I thought were a little on the weak side, but there are a lot of them that I thought were really good ideas. I do not know why CMS did not approve them and fund them and let them be tried,” she said, although she did offer an opinion on why the agency has yet to act on any of them.
“I read their paper saying why they didn’t approve [the recommended physician-developed alternative payment models]. It seemed to me they are waiting for one silver bullet that will fix all of health care. I don’t think a silver bullet is going to fix health care. It’s not an issue. It’s a complicated set of issues. You will not have a quick fix.”
WASHINGTON – As the rising cost of prescription drugs continues to garner heightened scrutiny from the federal government, one thing is missing from the conversation that would make any solution more effective, according to American Medical Association President Barbara L. McAneny, MD.
“We would like to see transparency from end to end in this pipeline because that is the way we will have the ability to look for savings,” she said in an interview at a national advocacy conference sponsored by the American Medical Association.
“I think we don’t have the information we need to make rational decisions,” she said. “I think the first thing we need to do is to understand the entire pipeline from the basic research that results in a drug’s clinical trials that results in a new drug to the pharmacy benefit managers and all of the ways that they have increased the cost of the drugs all the way to when the patient actually gets it.”
In particular, Dr. McAneny targeted the need for transparency in the role and financial impact pharmacy benefit managers have on the cost of prescription drugs.
“We were told at our state advocacy conference, which we held in January, by an expert who studied pharmacy benefit managers, that 42% of the cost of any drug is attributable to the profits of pharmacy benefit managers,” she said. “To me, that makes me wonder what value do they add that is worth 42% of these exorbitant costs and if they are not adding value, why do we have them in this process?”
She also called on the pharmaceutical manufacturers to be more forthcoming with their financial information regarding marketing and advertising, but she stressed that it needs to be done in a way that does not hinder future development of life-saving therapies.
“We do not want to stifle innovation.” Dr. McAneny said. “As a cancer doctor, I have seen diseases that I used to treat with morphine and sympathy now be diseases that I can treat, where I can restore people to good quality of life and buy them additional years of life because of these drugs. They are amazing and I don’t want to do without them and I want more of them. ... We want to support that research. That is probably worth a lot of the price tag. But how much of that goes to direct-to-consumer advertising? How much of that is the advertising budget? Where can we cut some of this out of the system so that we get the innovation, but we get innovation that all of our patients can afford?”
Another issue that is looming for physicians is a payment rate freeze from 2020-2025 under the Merit-based Incentive Payment System (MIPS) track of the Quality Payment Program, which was created under the Medicare Access and CHIP Reauthorization Act (MACRA).
“A 5-year freeze when my expenses do not freeze is a terrifying thing and could be a practice-ending expense for a lot of practices,” Dr. McAneny warned. “I will point out that independent practices, if they sell to a hospital, the cost of care immediately doubles. The amount that is paid for it, not the cost of delivering it. So that is not a great solution. But we also have this increasing practice expense and a flat rate is not going to help practices survive. So I am very concerned.”
Related to the QPP, Dr. McAneny also wants to see the Centers for Medicare & Medicaid Services do more with physician-developed alternative payment models. The Physician-Focused Payment Model Technical Advisory Committee (PTAC) continues to review and evaluate submissions, but to date, the CMS has yet to implement any of the committee’s recommendations.
“I read all of the PTAC submissions that went to CMS. Some of them I thought were a little on the weak side, but there are a lot of them that I thought were really good ideas. I do not know why CMS did not approve them and fund them and let them be tried,” she said, although she did offer an opinion on why the agency has yet to act on any of them.
“I read their paper saying why they didn’t approve [the recommended physician-developed alternative payment models]. It seemed to me they are waiting for one silver bullet that will fix all of health care. I don’t think a silver bullet is going to fix health care. It’s not an issue. It’s a complicated set of issues. You will not have a quick fix.”
WASHINGTON – As the rising cost of prescription drugs continues to garner heightened scrutiny from the federal government, one thing is missing from the conversation that would make any solution more effective, according to American Medical Association President Barbara L. McAneny, MD.
“We would like to see transparency from end to end in this pipeline because that is the way we will have the ability to look for savings,” she said in an interview at a national advocacy conference sponsored by the American Medical Association.
“I think we don’t have the information we need to make rational decisions,” she said. “I think the first thing we need to do is to understand the entire pipeline from the basic research that results in a drug’s clinical trials that results in a new drug to the pharmacy benefit managers and all of the ways that they have increased the cost of the drugs all the way to when the patient actually gets it.”
In particular, Dr. McAneny targeted the need for transparency in the role and financial impact pharmacy benefit managers have on the cost of prescription drugs.
“We were told at our state advocacy conference, which we held in January, by an expert who studied pharmacy benefit managers, that 42% of the cost of any drug is attributable to the profits of pharmacy benefit managers,” she said. “To me, that makes me wonder what value do they add that is worth 42% of these exorbitant costs and if they are not adding value, why do we have them in this process?”
She also called on the pharmaceutical manufacturers to be more forthcoming with their financial information regarding marketing and advertising, but she stressed that it needs to be done in a way that does not hinder future development of life-saving therapies.
“We do not want to stifle innovation.” Dr. McAneny said. “As a cancer doctor, I have seen diseases that I used to treat with morphine and sympathy now be diseases that I can treat, where I can restore people to good quality of life and buy them additional years of life because of these drugs. They are amazing and I don’t want to do without them and I want more of them. ... We want to support that research. That is probably worth a lot of the price tag. But how much of that goes to direct-to-consumer advertising? How much of that is the advertising budget? Where can we cut some of this out of the system so that we get the innovation, but we get innovation that all of our patients can afford?”
Another issue that is looming for physicians is a payment rate freeze from 2020-2025 under the Merit-based Incentive Payment System (MIPS) track of the Quality Payment Program, which was created under the Medicare Access and CHIP Reauthorization Act (MACRA).
“A 5-year freeze when my expenses do not freeze is a terrifying thing and could be a practice-ending expense for a lot of practices,” Dr. McAneny warned. “I will point out that independent practices, if they sell to a hospital, the cost of care immediately doubles. The amount that is paid for it, not the cost of delivering it. So that is not a great solution. But we also have this increasing practice expense and a flat rate is not going to help practices survive. So I am very concerned.”
Related to the QPP, Dr. McAneny also wants to see the Centers for Medicare & Medicaid Services do more with physician-developed alternative payment models. The Physician-Focused Payment Model Technical Advisory Committee (PTAC) continues to review and evaluate submissions, but to date, the CMS has yet to implement any of the committee’s recommendations.
“I read all of the PTAC submissions that went to CMS. Some of them I thought were a little on the weak side, but there are a lot of them that I thought were really good ideas. I do not know why CMS did not approve them and fund them and let them be tried,” she said, although she did offer an opinion on why the agency has yet to act on any of them.
“I read their paper saying why they didn’t approve [the recommended physician-developed alternative payment models]. It seemed to me they are waiting for one silver bullet that will fix all of health care. I don’t think a silver bullet is going to fix health care. It’s not an issue. It’s a complicated set of issues. You will not have a quick fix.”
REPORTING FROM THE AMA NATIONAL ADVOCACY CONFERENCE
House committee passes AMA-endorsed firearm bill
WASHINGTON – A bill requiring universal background checks for firearm purchases passed the House Judiciary committee and is expected to pass the full House of Representatives when it comes up for consideration.
Rep. Mike Thompson (R-Calif.), chairman of the House Gun Violence Prevention Task Force, thanked the American Medical Association for its endorsement and support of the bill a day before its Feb. 13 committee passage during a speech at a national advocacy conference sponsored by the AMA.
“The new legislation, H.R. 8, which you have endorsed, would put in place universal background checks,” Rep. Thompson said. “This means anybody who buys a gun would have to go through a background check to make sure they are not a criminal, to make sure they are not dangerously mentally ill and a danger to themselves or others.”
The committee passed the Bipartisan Background Checks Act of 2019 by a 23-15 vote. It would require a background check on all firearms transfers, including private sales, with limited exemptions for firearms given as gifts between family members and those transferred for hunting, target shooting, and self-defense.
A second bill, the Enhanced Background Checks Act (H.R. 1112), passed 21-14 during the same session. That bill would close a loophole that currently allows a licensed dealer to transfer a firearm after 3 days if the background check system has not yet reported back.
Rep. Thompson credited the newest members of Congress with pushing these bills to the forefront.
“During the last midterm election, there was a sea change in attitude around gun violence prevention,” Rep. Thompson noted. “All 40 members of the Democratic-elected class who took a seat ran on gun violence prevention. So they came to Washington with more of a willingness to deal with this issue.”
H.R. 8 has 231 cosponsors – 226 Democrats and 5 Republicans – meaning it has more than enough support to pass in the full House, should all cosponsors remain on board.
Getting the bill passed in the Republican-controlled Senate will be a challenge and Rep. Thompson encouraged doctors to continue their advocacy on this legislation.
“You guys have been fabulous,” he said. “Without your help, we would not be where we are today. I can tell you that this bill will pass the House within the first 100 days and will go to the Senate. That is when you will have to start working again. ... Once it goes to the Senate, there is going to be a reluctance to take it up. We need to make sure that every U.S. senator hears from every doc and every doc’s family and every doc’s friend and every doc’s assistant and everybody else and their brother that this important so we can turn up the heat and make sure they take up the issue of background checks. It works. It saves lives.”
WASHINGTON – A bill requiring universal background checks for firearm purchases passed the House Judiciary committee and is expected to pass the full House of Representatives when it comes up for consideration.
Rep. Mike Thompson (R-Calif.), chairman of the House Gun Violence Prevention Task Force, thanked the American Medical Association for its endorsement and support of the bill a day before its Feb. 13 committee passage during a speech at a national advocacy conference sponsored by the AMA.
“The new legislation, H.R. 8, which you have endorsed, would put in place universal background checks,” Rep. Thompson said. “This means anybody who buys a gun would have to go through a background check to make sure they are not a criminal, to make sure they are not dangerously mentally ill and a danger to themselves or others.”
The committee passed the Bipartisan Background Checks Act of 2019 by a 23-15 vote. It would require a background check on all firearms transfers, including private sales, with limited exemptions for firearms given as gifts between family members and those transferred for hunting, target shooting, and self-defense.
A second bill, the Enhanced Background Checks Act (H.R. 1112), passed 21-14 during the same session. That bill would close a loophole that currently allows a licensed dealer to transfer a firearm after 3 days if the background check system has not yet reported back.
Rep. Thompson credited the newest members of Congress with pushing these bills to the forefront.
“During the last midterm election, there was a sea change in attitude around gun violence prevention,” Rep. Thompson noted. “All 40 members of the Democratic-elected class who took a seat ran on gun violence prevention. So they came to Washington with more of a willingness to deal with this issue.”
H.R. 8 has 231 cosponsors – 226 Democrats and 5 Republicans – meaning it has more than enough support to pass in the full House, should all cosponsors remain on board.
Getting the bill passed in the Republican-controlled Senate will be a challenge and Rep. Thompson encouraged doctors to continue their advocacy on this legislation.
“You guys have been fabulous,” he said. “Without your help, we would not be where we are today. I can tell you that this bill will pass the House within the first 100 days and will go to the Senate. That is when you will have to start working again. ... Once it goes to the Senate, there is going to be a reluctance to take it up. We need to make sure that every U.S. senator hears from every doc and every doc’s family and every doc’s friend and every doc’s assistant and everybody else and their brother that this important so we can turn up the heat and make sure they take up the issue of background checks. It works. It saves lives.”
WASHINGTON – A bill requiring universal background checks for firearm purchases passed the House Judiciary committee and is expected to pass the full House of Representatives when it comes up for consideration.
Rep. Mike Thompson (R-Calif.), chairman of the House Gun Violence Prevention Task Force, thanked the American Medical Association for its endorsement and support of the bill a day before its Feb. 13 committee passage during a speech at a national advocacy conference sponsored by the AMA.
“The new legislation, H.R. 8, which you have endorsed, would put in place universal background checks,” Rep. Thompson said. “This means anybody who buys a gun would have to go through a background check to make sure they are not a criminal, to make sure they are not dangerously mentally ill and a danger to themselves or others.”
The committee passed the Bipartisan Background Checks Act of 2019 by a 23-15 vote. It would require a background check on all firearms transfers, including private sales, with limited exemptions for firearms given as gifts between family members and those transferred for hunting, target shooting, and self-defense.
A second bill, the Enhanced Background Checks Act (H.R. 1112), passed 21-14 during the same session. That bill would close a loophole that currently allows a licensed dealer to transfer a firearm after 3 days if the background check system has not yet reported back.
Rep. Thompson credited the newest members of Congress with pushing these bills to the forefront.
“During the last midterm election, there was a sea change in attitude around gun violence prevention,” Rep. Thompson noted. “All 40 members of the Democratic-elected class who took a seat ran on gun violence prevention. So they came to Washington with more of a willingness to deal with this issue.”
H.R. 8 has 231 cosponsors – 226 Democrats and 5 Republicans – meaning it has more than enough support to pass in the full House, should all cosponsors remain on board.
Getting the bill passed in the Republican-controlled Senate will be a challenge and Rep. Thompson encouraged doctors to continue their advocacy on this legislation.
“You guys have been fabulous,” he said. “Without your help, we would not be where we are today. I can tell you that this bill will pass the House within the first 100 days and will go to the Senate. That is when you will have to start working again. ... Once it goes to the Senate, there is going to be a reluctance to take it up. We need to make sure that every U.S. senator hears from every doc and every doc’s family and every doc’s friend and every doc’s assistant and everybody else and their brother that this important so we can turn up the heat and make sure they take up the issue of background checks. It works. It saves lives.”
REPORTING FROM AMA NATIONAL ADVOCACY CONFERENCE
ONC aims to help docs, patients with information sharing in proposed rule
The Office of the National Coordinator of Health Information Technology is looking to adopt standardized application programming interfaces (APIs) in an effort to boost interoperability of health data.
The Department of Health & Human Services office posted a proposed rule Feb. 11, 2019, that would, according to an agency press release, “help allow individuals to securely and easily access structured and unstructured EHI [electronic health information] formats using smartphones and other mobile devices.”
“We think our rule is going to help reduce burden and improve care,” Michael Lipinski, director of the Regulatory Affairs Division in the ONC Office of Policy, said in an interview. “It is going to do that through technology. With the APIs, you should be able to get to your information easier and have it readily available. Whether that is from another health care provider or using other health care products through the API to improve care, you will have that ability between the certified API and the information blocking policies to use third party developers and their products.”
The proposed rule also included a requirement that EHRs certified by ONC be able to easily export information contained within the EHR and make the format used to extract and export the data contained within the EHR publicly available.
“Another third party developer can build to that and offer competing services to pull that information out,” Mr. Lipinski said. “That would obviously help if you were choosing to switch [EHRs] if you didn’t like the features you were getting from your EHR. ... That functionality should help if you want to do that.”
The standardizing of APIs to help the delivery of data will go hand in hand with information blocking aspects of the proposed rule, which defines the few exceptions where an activity would not be considered information blocking, such as when engaging in practices will prevent patient harm; engaging in consistent, nondiscriminatory practices to protect patient privacy; and implementing practices to promote the security of health information.
Mr. Lipinski said these changes will help prevent providers from hiding behind HIPAA rules as the excuse to not share patient information, which will help with care coordination. “From a provider’s perspective, this should help them get more access to information, more access in a structured way and then easily get and share that information.”
Ultimately, Mr. Lipinski said, the goal is “to increase competition and lower cost while still improving the quality of care for patients.”
The Office of the National Coordinator of Health Information Technology is looking to adopt standardized application programming interfaces (APIs) in an effort to boost interoperability of health data.
The Department of Health & Human Services office posted a proposed rule Feb. 11, 2019, that would, according to an agency press release, “help allow individuals to securely and easily access structured and unstructured EHI [electronic health information] formats using smartphones and other mobile devices.”
“We think our rule is going to help reduce burden and improve care,” Michael Lipinski, director of the Regulatory Affairs Division in the ONC Office of Policy, said in an interview. “It is going to do that through technology. With the APIs, you should be able to get to your information easier and have it readily available. Whether that is from another health care provider or using other health care products through the API to improve care, you will have that ability between the certified API and the information blocking policies to use third party developers and their products.”
The proposed rule also included a requirement that EHRs certified by ONC be able to easily export information contained within the EHR and make the format used to extract and export the data contained within the EHR publicly available.
“Another third party developer can build to that and offer competing services to pull that information out,” Mr. Lipinski said. “That would obviously help if you were choosing to switch [EHRs] if you didn’t like the features you were getting from your EHR. ... That functionality should help if you want to do that.”
The standardizing of APIs to help the delivery of data will go hand in hand with information blocking aspects of the proposed rule, which defines the few exceptions where an activity would not be considered information blocking, such as when engaging in practices will prevent patient harm; engaging in consistent, nondiscriminatory practices to protect patient privacy; and implementing practices to promote the security of health information.
Mr. Lipinski said these changes will help prevent providers from hiding behind HIPAA rules as the excuse to not share patient information, which will help with care coordination. “From a provider’s perspective, this should help them get more access to information, more access in a structured way and then easily get and share that information.”
Ultimately, Mr. Lipinski said, the goal is “to increase competition and lower cost while still improving the quality of care for patients.”
The Office of the National Coordinator of Health Information Technology is looking to adopt standardized application programming interfaces (APIs) in an effort to boost interoperability of health data.
The Department of Health & Human Services office posted a proposed rule Feb. 11, 2019, that would, according to an agency press release, “help allow individuals to securely and easily access structured and unstructured EHI [electronic health information] formats using smartphones and other mobile devices.”
“We think our rule is going to help reduce burden and improve care,” Michael Lipinski, director of the Regulatory Affairs Division in the ONC Office of Policy, said in an interview. “It is going to do that through technology. With the APIs, you should be able to get to your information easier and have it readily available. Whether that is from another health care provider or using other health care products through the API to improve care, you will have that ability between the certified API and the information blocking policies to use third party developers and their products.”
The proposed rule also included a requirement that EHRs certified by ONC be able to easily export information contained within the EHR and make the format used to extract and export the data contained within the EHR publicly available.
“Another third party developer can build to that and offer competing services to pull that information out,” Mr. Lipinski said. “That would obviously help if you were choosing to switch [EHRs] if you didn’t like the features you were getting from your EHR. ... That functionality should help if you want to do that.”
The standardizing of APIs to help the delivery of data will go hand in hand with information blocking aspects of the proposed rule, which defines the few exceptions where an activity would not be considered information blocking, such as when engaging in practices will prevent patient harm; engaging in consistent, nondiscriminatory practices to protect patient privacy; and implementing practices to promote the security of health information.
Mr. Lipinski said these changes will help prevent providers from hiding behind HIPAA rules as the excuse to not share patient information, which will help with care coordination. “From a provider’s perspective, this should help them get more access to information, more access in a structured way and then easily get and share that information.”
Ultimately, Mr. Lipinski said, the goal is “to increase competition and lower cost while still improving the quality of care for patients.”
HHS to target step therapy, Stark Law in 2019
WASHINGTON –
Speaking Feb. 12 at the American Medical Association’s National Advocacy Conference, Secretary Azar said the agency will be looking into ensuring that patients on medical plans who have found a working drug after going through a step-therapy protocol will not have to restart on a drug that has already failed for them if they switch insurance providers.
“I was very disturbed to hear that stable patients switching among insurance plans, like switching among Medicare Advantage plans, can often be required to start over again on a step therapy regimen,” he said.
“This is not just potentially injurious to their health, it’s also penny-wise and pound-foolish,” Secretary Azar continued. “We know that getting a patient on the right drug, at the right time, is one of the best investments we can make in their health, and we do not want to impede physicians from making that happen. We’re looking at how we can address that issue now.”
The other area Secretary Azar highlighted that the agency is working on is making changes to the Stark Law.
“The Stark Law was written with noble purposes in mind, but it was designed for a fee-for-service system, not the kind of system we are moving toward today,” he said. “We’ve heard from many, many stakeholders, including the AMA, about the need to update the enumerated exceptions in the Stark Law to include value-based approaches to care.”
He added that how care coordination interacts with the antikickback statutes and HIPAA are also going to be examined.
Secretary Azar did not offer any timelines or other more specific details about how the agency plans to tackle these issues.
He used most of his speech to discuss recent regulatory actions around drug pricing and pushed for support for the Part B drug pricing model that the agency is preparing for a formal proposed rule, despite having received a critical reception from medical societies.
“If you have a small practice that uses infusions, and you don’t want to bear the risk of buy and bill, now you’re off the hook,” he said. “We’ll allow you to work with private vendors who can take the risk for buying the drugs in a way that isn’t possible today. But if you’re part of a much larger practice that’s able to drive a better deal than you could on your own, or want to band together with other practices to do the purchasing, then you can do that, too.”
He continued: “Next is the launch of the actual proposed rule, followed by the rule itself, which, I’ll remind you, is just a model.”
However, despite it being a model under test from the Center for Medicare & Medicaid Innovation, the advanced notice of proposed rule making that was issued in October 2018 suggested that participation in the so-called International Pricing Index model would be mandatory.
Secretary Azar did not acknowledge any mandatory participation in his pitch for support, noting that CMMI models “are carefully assessed. We will closely monitor how the model will affect clinical outcomes, including patients’ adherence to their drugs. We believe that the lower costs will, of course, mean better patient access to drugs, better adherence, and better outcomes for the care you provide. That is the goal.”
WASHINGTON –
Speaking Feb. 12 at the American Medical Association’s National Advocacy Conference, Secretary Azar said the agency will be looking into ensuring that patients on medical plans who have found a working drug after going through a step-therapy protocol will not have to restart on a drug that has already failed for them if they switch insurance providers.
“I was very disturbed to hear that stable patients switching among insurance plans, like switching among Medicare Advantage plans, can often be required to start over again on a step therapy regimen,” he said.
“This is not just potentially injurious to their health, it’s also penny-wise and pound-foolish,” Secretary Azar continued. “We know that getting a patient on the right drug, at the right time, is one of the best investments we can make in their health, and we do not want to impede physicians from making that happen. We’re looking at how we can address that issue now.”
The other area Secretary Azar highlighted that the agency is working on is making changes to the Stark Law.
“The Stark Law was written with noble purposes in mind, but it was designed for a fee-for-service system, not the kind of system we are moving toward today,” he said. “We’ve heard from many, many stakeholders, including the AMA, about the need to update the enumerated exceptions in the Stark Law to include value-based approaches to care.”
He added that how care coordination interacts with the antikickback statutes and HIPAA are also going to be examined.
Secretary Azar did not offer any timelines or other more specific details about how the agency plans to tackle these issues.
He used most of his speech to discuss recent regulatory actions around drug pricing and pushed for support for the Part B drug pricing model that the agency is preparing for a formal proposed rule, despite having received a critical reception from medical societies.
“If you have a small practice that uses infusions, and you don’t want to bear the risk of buy and bill, now you’re off the hook,” he said. “We’ll allow you to work with private vendors who can take the risk for buying the drugs in a way that isn’t possible today. But if you’re part of a much larger practice that’s able to drive a better deal than you could on your own, or want to band together with other practices to do the purchasing, then you can do that, too.”
He continued: “Next is the launch of the actual proposed rule, followed by the rule itself, which, I’ll remind you, is just a model.”
However, despite it being a model under test from the Center for Medicare & Medicaid Innovation, the advanced notice of proposed rule making that was issued in October 2018 suggested that participation in the so-called International Pricing Index model would be mandatory.
Secretary Azar did not acknowledge any mandatory participation in his pitch for support, noting that CMMI models “are carefully assessed. We will closely monitor how the model will affect clinical outcomes, including patients’ adherence to their drugs. We believe that the lower costs will, of course, mean better patient access to drugs, better adherence, and better outcomes for the care you provide. That is the goal.”
WASHINGTON –
Speaking Feb. 12 at the American Medical Association’s National Advocacy Conference, Secretary Azar said the agency will be looking into ensuring that patients on medical plans who have found a working drug after going through a step-therapy protocol will not have to restart on a drug that has already failed for them if they switch insurance providers.
“I was very disturbed to hear that stable patients switching among insurance plans, like switching among Medicare Advantage plans, can often be required to start over again on a step therapy regimen,” he said.
“This is not just potentially injurious to their health, it’s also penny-wise and pound-foolish,” Secretary Azar continued. “We know that getting a patient on the right drug, at the right time, is one of the best investments we can make in their health, and we do not want to impede physicians from making that happen. We’re looking at how we can address that issue now.”
The other area Secretary Azar highlighted that the agency is working on is making changes to the Stark Law.
“The Stark Law was written with noble purposes in mind, but it was designed for a fee-for-service system, not the kind of system we are moving toward today,” he said. “We’ve heard from many, many stakeholders, including the AMA, about the need to update the enumerated exceptions in the Stark Law to include value-based approaches to care.”
He added that how care coordination interacts with the antikickback statutes and HIPAA are also going to be examined.
Secretary Azar did not offer any timelines or other more specific details about how the agency plans to tackle these issues.
He used most of his speech to discuss recent regulatory actions around drug pricing and pushed for support for the Part B drug pricing model that the agency is preparing for a formal proposed rule, despite having received a critical reception from medical societies.
“If you have a small practice that uses infusions, and you don’t want to bear the risk of buy and bill, now you’re off the hook,” he said. “We’ll allow you to work with private vendors who can take the risk for buying the drugs in a way that isn’t possible today. But if you’re part of a much larger practice that’s able to drive a better deal than you could on your own, or want to band together with other practices to do the purchasing, then you can do that, too.”
He continued: “Next is the launch of the actual proposed rule, followed by the rule itself, which, I’ll remind you, is just a model.”
However, despite it being a model under test from the Center for Medicare & Medicaid Innovation, the advanced notice of proposed rule making that was issued in October 2018 suggested that participation in the so-called International Pricing Index model would be mandatory.
Secretary Azar did not acknowledge any mandatory participation in his pitch for support, noting that CMMI models “are carefully assessed. We will closely monitor how the model will affect clinical outcomes, including patients’ adherence to their drugs. We believe that the lower costs will, of course, mean better patient access to drugs, better adherence, and better outcomes for the care you provide. That is the goal.”
REPORTING FROM AMA NATIONAL ADVOCACY CONFERENCE
President Trump calls for end to HIV/AIDS, pediatric cancer
HIV/AIDS, pediatric cancer research, abortion, prescription drug prices, and preexisting conditions were among the health care highlights of President Donald Trump’s second State of the Union address Feb. 5.

Mr. Trump promised to push for funds to end HIV/AIDS and childhood cancer within in 10 years. “In recent years, we have made remarkable progress in the fight against HIV and AIDS. Scientific breakthroughs have brought a once-distant dream within reach,” he said to assembled members of Congress and leaders of the executive and judicial branches of government. “My budget will ask Democrats and Republicans to make the needed commitment to eliminate the HIV epidemic in the United States within 10 years.”
Following the speech, Alex Azar, secretary of the Department of Health and Human Services, offered more details in a blog post on the agency’s website.
Funding for the initiative, dubbed “Ending the HIV Epidemic: A Plan for America,” will have three components.
The first involves increasing investments in “geographic hotspots” though existing programs like the Ryan White HIV/AIDS Program and a new community health center–based program to provide antiretroviral therapy (ART) and preexposure prophylaxis (PrEP) to those at the highest risk of contracting the disease.
Second is the use of data to track where the disease is spreading most rapidly to help target prevention, care, and treatment at the local level. The third will provide funds for the creation of a local HIV HealthForce in these targeted areas to expand HIV prevention and treatment efforts.
A fact sheet on this initiative called for a 75% reduction in new cases of HIV infection in 5 years and at least a 90% reduction within 10 years.
President Trump called for similar efforts to address pediatric cancer.
“Tonight I am also asking you to join me in another fight that all American can get behind – the fight against childhood cancer,” he said, adding that his budget request will come with a line item of $500 million over 10 years to fund research. “Many childhood cancers have not seen new therapies in decades.”
President Trump also asked Congress to legislate a prohibition of late-term abortion.
“There could be no greater contrast to the beautiful image of a mother holding her infant child than the chilling displays our nation saw in recent days,” he said. “Lawmakers in New York cheered with delight upon the passage of legislation that would allow a baby to be ripped from the mother’s womb moments from birth. These are living, feeling beautiful babies who will never get the chance to share their love and their dreams with the world. ... Let us work together to build a culture that cherishes innocent life.”
He also touched on the recurring themes regarding lowering the cost of health care and prescription drugs, as well as protecting those with preexisting conditions, something he called a major priority.
“It’s unacceptable that Americans pay vastly more than people in other countries for the exact same drugs, often made in the exact same place. This is wrong. This is unfair and together we will stop it, and we will stop it fast,” he said.
He did not offer any specific policy recommendation on how to address prescription drug costs, other than a comment on the need for greater price transparency.
“I am asking Congress to pass legislation that finally takes on the problem of global freeloading and delivers fairness and price transparency for American patients,” he said.
“We should also require drug companies, insurance companies, and hospitals to disclose real prices to foster competition and bring costs way down.”
SOURCE: Trump D. State of the Union Address, Feb. 5, 2019.
HIV/AIDS, pediatric cancer research, abortion, prescription drug prices, and preexisting conditions were among the health care highlights of President Donald Trump’s second State of the Union address Feb. 5.

Mr. Trump promised to push for funds to end HIV/AIDS and childhood cancer within in 10 years. “In recent years, we have made remarkable progress in the fight against HIV and AIDS. Scientific breakthroughs have brought a once-distant dream within reach,” he said to assembled members of Congress and leaders of the executive and judicial branches of government. “My budget will ask Democrats and Republicans to make the needed commitment to eliminate the HIV epidemic in the United States within 10 years.”
Following the speech, Alex Azar, secretary of the Department of Health and Human Services, offered more details in a blog post on the agency’s website.
Funding for the initiative, dubbed “Ending the HIV Epidemic: A Plan for America,” will have three components.
The first involves increasing investments in “geographic hotspots” though existing programs like the Ryan White HIV/AIDS Program and a new community health center–based program to provide antiretroviral therapy (ART) and preexposure prophylaxis (PrEP) to those at the highest risk of contracting the disease.
Second is the use of data to track where the disease is spreading most rapidly to help target prevention, care, and treatment at the local level. The third will provide funds for the creation of a local HIV HealthForce in these targeted areas to expand HIV prevention and treatment efforts.
A fact sheet on this initiative called for a 75% reduction in new cases of HIV infection in 5 years and at least a 90% reduction within 10 years.
President Trump called for similar efforts to address pediatric cancer.
“Tonight I am also asking you to join me in another fight that all American can get behind – the fight against childhood cancer,” he said, adding that his budget request will come with a line item of $500 million over 10 years to fund research. “Many childhood cancers have not seen new therapies in decades.”
President Trump also asked Congress to legislate a prohibition of late-term abortion.
“There could be no greater contrast to the beautiful image of a mother holding her infant child than the chilling displays our nation saw in recent days,” he said. “Lawmakers in New York cheered with delight upon the passage of legislation that would allow a baby to be ripped from the mother’s womb moments from birth. These are living, feeling beautiful babies who will never get the chance to share their love and their dreams with the world. ... Let us work together to build a culture that cherishes innocent life.”
He also touched on the recurring themes regarding lowering the cost of health care and prescription drugs, as well as protecting those with preexisting conditions, something he called a major priority.
“It’s unacceptable that Americans pay vastly more than people in other countries for the exact same drugs, often made in the exact same place. This is wrong. This is unfair and together we will stop it, and we will stop it fast,” he said.
He did not offer any specific policy recommendation on how to address prescription drug costs, other than a comment on the need for greater price transparency.
“I am asking Congress to pass legislation that finally takes on the problem of global freeloading and delivers fairness and price transparency for American patients,” he said.
“We should also require drug companies, insurance companies, and hospitals to disclose real prices to foster competition and bring costs way down.”
SOURCE: Trump D. State of the Union Address, Feb. 5, 2019.
HIV/AIDS, pediatric cancer research, abortion, prescription drug prices, and preexisting conditions were among the health care highlights of President Donald Trump’s second State of the Union address Feb. 5.

Mr. Trump promised to push for funds to end HIV/AIDS and childhood cancer within in 10 years. “In recent years, we have made remarkable progress in the fight against HIV and AIDS. Scientific breakthroughs have brought a once-distant dream within reach,” he said to assembled members of Congress and leaders of the executive and judicial branches of government. “My budget will ask Democrats and Republicans to make the needed commitment to eliminate the HIV epidemic in the United States within 10 years.”
Following the speech, Alex Azar, secretary of the Department of Health and Human Services, offered more details in a blog post on the agency’s website.
Funding for the initiative, dubbed “Ending the HIV Epidemic: A Plan for America,” will have three components.
The first involves increasing investments in “geographic hotspots” though existing programs like the Ryan White HIV/AIDS Program and a new community health center–based program to provide antiretroviral therapy (ART) and preexposure prophylaxis (PrEP) to those at the highest risk of contracting the disease.
Second is the use of data to track where the disease is spreading most rapidly to help target prevention, care, and treatment at the local level. The third will provide funds for the creation of a local HIV HealthForce in these targeted areas to expand HIV prevention and treatment efforts.
A fact sheet on this initiative called for a 75% reduction in new cases of HIV infection in 5 years and at least a 90% reduction within 10 years.
President Trump called for similar efforts to address pediatric cancer.
“Tonight I am also asking you to join me in another fight that all American can get behind – the fight against childhood cancer,” he said, adding that his budget request will come with a line item of $500 million over 10 years to fund research. “Many childhood cancers have not seen new therapies in decades.”
President Trump also asked Congress to legislate a prohibition of late-term abortion.
“There could be no greater contrast to the beautiful image of a mother holding her infant child than the chilling displays our nation saw in recent days,” he said. “Lawmakers in New York cheered with delight upon the passage of legislation that would allow a baby to be ripped from the mother’s womb moments from birth. These are living, feeling beautiful babies who will never get the chance to share their love and their dreams with the world. ... Let us work together to build a culture that cherishes innocent life.”
He also touched on the recurring themes regarding lowering the cost of health care and prescription drugs, as well as protecting those with preexisting conditions, something he called a major priority.
“It’s unacceptable that Americans pay vastly more than people in other countries for the exact same drugs, often made in the exact same place. This is wrong. This is unfair and together we will stop it, and we will stop it fast,” he said.
He did not offer any specific policy recommendation on how to address prescription drug costs, other than a comment on the need for greater price transparency.
“I am asking Congress to pass legislation that finally takes on the problem of global freeloading and delivers fairness and price transparency for American patients,” he said.
“We should also require drug companies, insurance companies, and hospitals to disclose real prices to foster competition and bring costs way down.”
SOURCE: Trump D. State of the Union Address, Feb. 5, 2019.
Key clinical point: President Trump calls for an end to HIV/AIDS and pediatric cancer in 10 years.
Major finding: His budget will request $500 million for cancer research and as yet undisclosed amount for HIV/AIDS research.
Study details: More specific details on the proposals will likely come when the president makes his budget submission to Congress in the coming weeks.
Disclosures: There are no disclosures.
Source: Trump D. State of the Union Address, Feb. 5, 2019.