User login
McAneny: Transparency needed for meaningful talk on drug pricing
WASHINGTON – As the rising cost of prescription drugs continues to garner heightened scrutiny from the federal government, one thing is missing from the conversation that would make any solution more effective, according to American Medical Association President Barbara L. McAneny, MD.
“We would like to see transparency from end to end in this pipeline because that is the way we will have the ability to look for savings,” she said in an interview at a national advocacy conference sponsored by the American Medical Association.
“I think we don’t have the information we need to make rational decisions,” she said. “I think the first thing we need to do is to understand the entire pipeline from the basic research that results in a drug’s clinical trials that results in a new drug to the pharmacy benefit managers and all of the ways that they have increased the cost of the drugs all the way to when the patient actually gets it.”
In particular, Dr. McAneny targeted the need for transparency in the role and financial impact pharmacy benefit managers have on the cost of prescription drugs.
“We were told at our state advocacy conference, which we held in January, by an expert who studied pharmacy benefit managers, that 42% of the cost of any drug is attributable to the profits of pharmacy benefit managers,” she said. “To me, that makes me wonder what value do they add that is worth 42% of these exorbitant costs and if they are not adding value, why do we have them in this process?”
She also called on the pharmaceutical manufacturers to be more forthcoming with their financial information regarding marketing and advertising, but she stressed that it needs to be done in a way that does not hinder future development of life-saving therapies.
“We do not want to stifle innovation.” Dr. McAneny said. “As a cancer doctor, I have seen diseases that I used to treat with morphine and sympathy now be diseases that I can treat, where I can restore people to good quality of life and buy them additional years of life because of these drugs. They are amazing and I don’t want to do without them and I want more of them. ... We want to support that research. That is probably worth a lot of the price tag. But how much of that goes to direct-to-consumer advertising? How much of that is the advertising budget? Where can we cut some of this out of the system so that we get the innovation, but we get innovation that all of our patients can afford?”
Another issue that is looming for physicians is a payment rate freeze from 2020-2025 under the Merit-based Incentive Payment System (MIPS) track of the Quality Payment Program, which was created under the Medicare Access and CHIP Reauthorization Act (MACRA).
“A 5-year freeze when my expenses do not freeze is a terrifying thing and could be a practice-ending expense for a lot of practices,” Dr. McAneny warned. “I will point out that independent practices, if they sell to a hospital, the cost of care immediately doubles. The amount that is paid for it, not the cost of delivering it. So that is not a great solution. But we also have this increasing practice expense and a flat rate is not going to help practices survive. So I am very concerned.”
Related to the QPP, Dr. McAneny also wants to see the Centers for Medicare & Medicaid Services do more with physician-developed alternative payment models. The Physician-Focused Payment Model Technical Advisory Committee (PTAC) continues to review and evaluate submissions, but to date, the CMS has yet to implement any of the committee’s recommendations.
“I read all of the PTAC submissions that went to CMS. Some of them I thought were a little on the weak side, but there are a lot of them that I thought were really good ideas. I do not know why CMS did not approve them and fund them and let them be tried,” she said, although she did offer an opinion on why the agency has yet to act on any of them.
“I read their paper saying why they didn’t approve [the recommended physician-developed alternative payment models]. It seemed to me they are waiting for one silver bullet that will fix all of health care. I don’t think a silver bullet is going to fix health care. It’s not an issue. It’s a complicated set of issues. You will not have a quick fix.”
WASHINGTON – As the rising cost of prescription drugs continues to garner heightened scrutiny from the federal government, one thing is missing from the conversation that would make any solution more effective, according to American Medical Association President Barbara L. McAneny, MD.
“We would like to see transparency from end to end in this pipeline because that is the way we will have the ability to look for savings,” she said in an interview at a national advocacy conference sponsored by the American Medical Association.
“I think we don’t have the information we need to make rational decisions,” she said. “I think the first thing we need to do is to understand the entire pipeline from the basic research that results in a drug’s clinical trials that results in a new drug to the pharmacy benefit managers and all of the ways that they have increased the cost of the drugs all the way to when the patient actually gets it.”
In particular, Dr. McAneny targeted the need for transparency in the role and financial impact pharmacy benefit managers have on the cost of prescription drugs.
“We were told at our state advocacy conference, which we held in January, by an expert who studied pharmacy benefit managers, that 42% of the cost of any drug is attributable to the profits of pharmacy benefit managers,” she said. “To me, that makes me wonder what value do they add that is worth 42% of these exorbitant costs and if they are not adding value, why do we have them in this process?”
She also called on the pharmaceutical manufacturers to be more forthcoming with their financial information regarding marketing and advertising, but she stressed that it needs to be done in a way that does not hinder future development of life-saving therapies.
“We do not want to stifle innovation.” Dr. McAneny said. “As a cancer doctor, I have seen diseases that I used to treat with morphine and sympathy now be diseases that I can treat, where I can restore people to good quality of life and buy them additional years of life because of these drugs. They are amazing and I don’t want to do without them and I want more of them. ... We want to support that research. That is probably worth a lot of the price tag. But how much of that goes to direct-to-consumer advertising? How much of that is the advertising budget? Where can we cut some of this out of the system so that we get the innovation, but we get innovation that all of our patients can afford?”
Another issue that is looming for physicians is a payment rate freeze from 2020-2025 under the Merit-based Incentive Payment System (MIPS) track of the Quality Payment Program, which was created under the Medicare Access and CHIP Reauthorization Act (MACRA).
“A 5-year freeze when my expenses do not freeze is a terrifying thing and could be a practice-ending expense for a lot of practices,” Dr. McAneny warned. “I will point out that independent practices, if they sell to a hospital, the cost of care immediately doubles. The amount that is paid for it, not the cost of delivering it. So that is not a great solution. But we also have this increasing practice expense and a flat rate is not going to help practices survive. So I am very concerned.”
Related to the QPP, Dr. McAneny also wants to see the Centers for Medicare & Medicaid Services do more with physician-developed alternative payment models. The Physician-Focused Payment Model Technical Advisory Committee (PTAC) continues to review and evaluate submissions, but to date, the CMS has yet to implement any of the committee’s recommendations.
“I read all of the PTAC submissions that went to CMS. Some of them I thought were a little on the weak side, but there are a lot of them that I thought were really good ideas. I do not know why CMS did not approve them and fund them and let them be tried,” she said, although she did offer an opinion on why the agency has yet to act on any of them.
“I read their paper saying why they didn’t approve [the recommended physician-developed alternative payment models]. It seemed to me they are waiting for one silver bullet that will fix all of health care. I don’t think a silver bullet is going to fix health care. It’s not an issue. It’s a complicated set of issues. You will not have a quick fix.”
WASHINGTON – As the rising cost of prescription drugs continues to garner heightened scrutiny from the federal government, one thing is missing from the conversation that would make any solution more effective, according to American Medical Association President Barbara L. McAneny, MD.
“We would like to see transparency from end to end in this pipeline because that is the way we will have the ability to look for savings,” she said in an interview at a national advocacy conference sponsored by the American Medical Association.
“I think we don’t have the information we need to make rational decisions,” she said. “I think the first thing we need to do is to understand the entire pipeline from the basic research that results in a drug’s clinical trials that results in a new drug to the pharmacy benefit managers and all of the ways that they have increased the cost of the drugs all the way to when the patient actually gets it.”
In particular, Dr. McAneny targeted the need for transparency in the role and financial impact pharmacy benefit managers have on the cost of prescription drugs.
“We were told at our state advocacy conference, which we held in January, by an expert who studied pharmacy benefit managers, that 42% of the cost of any drug is attributable to the profits of pharmacy benefit managers,” she said. “To me, that makes me wonder what value do they add that is worth 42% of these exorbitant costs and if they are not adding value, why do we have them in this process?”
She also called on the pharmaceutical manufacturers to be more forthcoming with their financial information regarding marketing and advertising, but she stressed that it needs to be done in a way that does not hinder future development of life-saving therapies.
“We do not want to stifle innovation.” Dr. McAneny said. “As a cancer doctor, I have seen diseases that I used to treat with morphine and sympathy now be diseases that I can treat, where I can restore people to good quality of life and buy them additional years of life because of these drugs. They are amazing and I don’t want to do without them and I want more of them. ... We want to support that research. That is probably worth a lot of the price tag. But how much of that goes to direct-to-consumer advertising? How much of that is the advertising budget? Where can we cut some of this out of the system so that we get the innovation, but we get innovation that all of our patients can afford?”
Another issue that is looming for physicians is a payment rate freeze from 2020-2025 under the Merit-based Incentive Payment System (MIPS) track of the Quality Payment Program, which was created under the Medicare Access and CHIP Reauthorization Act (MACRA).
“A 5-year freeze when my expenses do not freeze is a terrifying thing and could be a practice-ending expense for a lot of practices,” Dr. McAneny warned. “I will point out that independent practices, if they sell to a hospital, the cost of care immediately doubles. The amount that is paid for it, not the cost of delivering it. So that is not a great solution. But we also have this increasing practice expense and a flat rate is not going to help practices survive. So I am very concerned.”
Related to the QPP, Dr. McAneny also wants to see the Centers for Medicare & Medicaid Services do more with physician-developed alternative payment models. The Physician-Focused Payment Model Technical Advisory Committee (PTAC) continues to review and evaluate submissions, but to date, the CMS has yet to implement any of the committee’s recommendations.
“I read all of the PTAC submissions that went to CMS. Some of them I thought were a little on the weak side, but there are a lot of them that I thought were really good ideas. I do not know why CMS did not approve them and fund them and let them be tried,” she said, although she did offer an opinion on why the agency has yet to act on any of them.
“I read their paper saying why they didn’t approve [the recommended physician-developed alternative payment models]. It seemed to me they are waiting for one silver bullet that will fix all of health care. I don’t think a silver bullet is going to fix health care. It’s not an issue. It’s a complicated set of issues. You will not have a quick fix.”
REPORTING FROM THE AMA NATIONAL ADVOCACY CONFERENCE
House committee passes AMA-endorsed firearm bill
WASHINGTON – A bill requiring universal background checks for firearm purchases passed the House Judiciary committee and is expected to pass the full House of Representatives when it comes up for consideration.
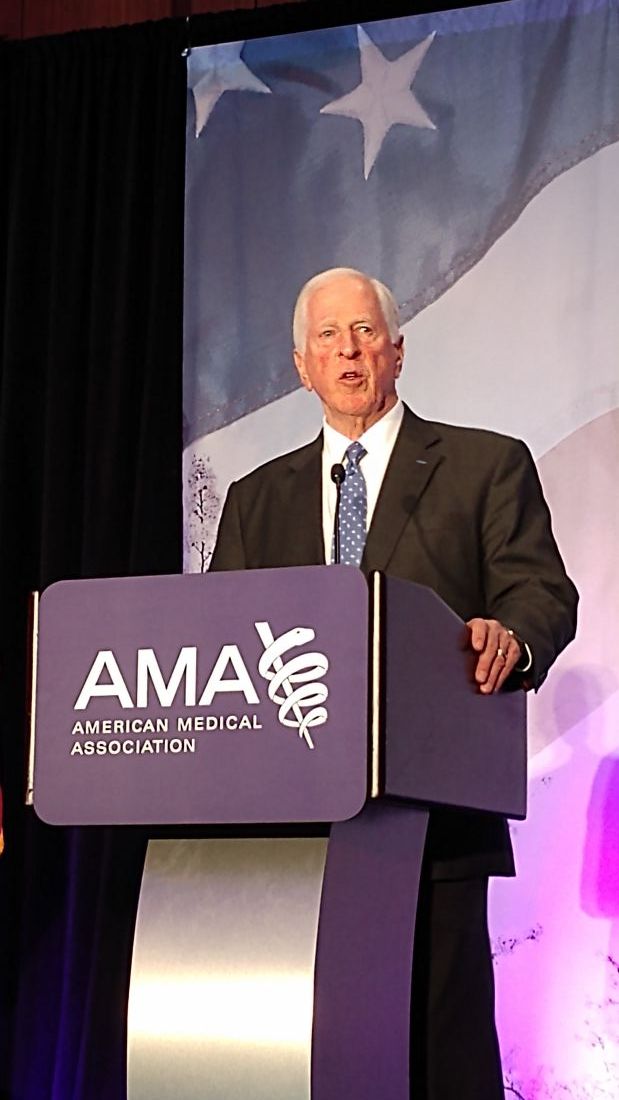
Rep. Mike Thompson (R-Calif.), chairman of the House Gun Violence Prevention Task Force, thanked the American Medical Association for its endorsement and support of the bill a day before its Feb. 13 committee passage during a speech at a national advocacy conference sponsored by the AMA.
“The new legislation, H.R. 8, which you have endorsed, would put in place universal background checks,” Rep. Thompson said. “This means anybody who buys a gun would have to go through a background check to make sure they are not a criminal, to make sure they are not dangerously mentally ill and a danger to themselves or others.”
The committee passed the Bipartisan Background Checks Act of 2019 by a 23-15 vote. It would require a background check on all firearms transfers, including private sales, with limited exemptions for firearms given as gifts between family members and those transferred for hunting, target shooting, and self-defense.
A second bill, the Enhanced Background Checks Act (H.R. 1112), passed 21-14 during the same session. That bill would close a loophole that currently allows a licensed dealer to transfer a firearm after 3 days if the background check system has not yet reported back.
Rep. Thompson credited the newest members of Congress with pushing these bills to the forefront.
“During the last midterm election, there was a sea change in attitude around gun violence prevention,” Rep. Thompson noted. “All 40 members of the Democratic-elected class who took a seat ran on gun violence prevention. So they came to Washington with more of a willingness to deal with this issue.”
H.R. 8 has 231 cosponsors – 226 Democrats and 5 Republicans – meaning it has more than enough support to pass in the full House, should all cosponsors remain on board.
Getting the bill passed in the Republican-controlled Senate will be a challenge and Rep. Thompson encouraged doctors to continue their advocacy on this legislation.
“You guys have been fabulous,” he said. “Without your help, we would not be where we are today. I can tell you that this bill will pass the House within the first 100 days and will go to the Senate. That is when you will have to start working again. ... Once it goes to the Senate, there is going to be a reluctance to take it up. We need to make sure that every U.S. senator hears from every doc and every doc’s family and every doc’s friend and every doc’s assistant and everybody else and their brother that this important so we can turn up the heat and make sure they take up the issue of background checks. It works. It saves lives.”
WASHINGTON – A bill requiring universal background checks for firearm purchases passed the House Judiciary committee and is expected to pass the full House of Representatives when it comes up for consideration.
Rep. Mike Thompson (R-Calif.), chairman of the House Gun Violence Prevention Task Force, thanked the American Medical Association for its endorsement and support of the bill a day before its Feb. 13 committee passage during a speech at a national advocacy conference sponsored by the AMA.
“The new legislation, H.R. 8, which you have endorsed, would put in place universal background checks,” Rep. Thompson said. “This means anybody who buys a gun would have to go through a background check to make sure they are not a criminal, to make sure they are not dangerously mentally ill and a danger to themselves or others.”
The committee passed the Bipartisan Background Checks Act of 2019 by a 23-15 vote. It would require a background check on all firearms transfers, including private sales, with limited exemptions for firearms given as gifts between family members and those transferred for hunting, target shooting, and self-defense.
A second bill, the Enhanced Background Checks Act (H.R. 1112), passed 21-14 during the same session. That bill would close a loophole that currently allows a licensed dealer to transfer a firearm after 3 days if the background check system has not yet reported back.
Rep. Thompson credited the newest members of Congress with pushing these bills to the forefront.
“During the last midterm election, there was a sea change in attitude around gun violence prevention,” Rep. Thompson noted. “All 40 members of the Democratic-elected class who took a seat ran on gun violence prevention. So they came to Washington with more of a willingness to deal with this issue.”
H.R. 8 has 231 cosponsors – 226 Democrats and 5 Republicans – meaning it has more than enough support to pass in the full House, should all cosponsors remain on board.
Getting the bill passed in the Republican-controlled Senate will be a challenge and Rep. Thompson encouraged doctors to continue their advocacy on this legislation.
“You guys have been fabulous,” he said. “Without your help, we would not be where we are today. I can tell you that this bill will pass the House within the first 100 days and will go to the Senate. That is when you will have to start working again. ... Once it goes to the Senate, there is going to be a reluctance to take it up. We need to make sure that every U.S. senator hears from every doc and every doc’s family and every doc’s friend and every doc’s assistant and everybody else and their brother that this important so we can turn up the heat and make sure they take up the issue of background checks. It works. It saves lives.”
WASHINGTON – A bill requiring universal background checks for firearm purchases passed the House Judiciary committee and is expected to pass the full House of Representatives when it comes up for consideration.
Rep. Mike Thompson (R-Calif.), chairman of the House Gun Violence Prevention Task Force, thanked the American Medical Association for its endorsement and support of the bill a day before its Feb. 13 committee passage during a speech at a national advocacy conference sponsored by the AMA.
“The new legislation, H.R. 8, which you have endorsed, would put in place universal background checks,” Rep. Thompson said. “This means anybody who buys a gun would have to go through a background check to make sure they are not a criminal, to make sure they are not dangerously mentally ill and a danger to themselves or others.”
The committee passed the Bipartisan Background Checks Act of 2019 by a 23-15 vote. It would require a background check on all firearms transfers, including private sales, with limited exemptions for firearms given as gifts between family members and those transferred for hunting, target shooting, and self-defense.
A second bill, the Enhanced Background Checks Act (H.R. 1112), passed 21-14 during the same session. That bill would close a loophole that currently allows a licensed dealer to transfer a firearm after 3 days if the background check system has not yet reported back.
Rep. Thompson credited the newest members of Congress with pushing these bills to the forefront.
“During the last midterm election, there was a sea change in attitude around gun violence prevention,” Rep. Thompson noted. “All 40 members of the Democratic-elected class who took a seat ran on gun violence prevention. So they came to Washington with more of a willingness to deal with this issue.”
H.R. 8 has 231 cosponsors – 226 Democrats and 5 Republicans – meaning it has more than enough support to pass in the full House, should all cosponsors remain on board.
Getting the bill passed in the Republican-controlled Senate will be a challenge and Rep. Thompson encouraged doctors to continue their advocacy on this legislation.
“You guys have been fabulous,” he said. “Without your help, we would not be where we are today. I can tell you that this bill will pass the House within the first 100 days and will go to the Senate. That is when you will have to start working again. ... Once it goes to the Senate, there is going to be a reluctance to take it up. We need to make sure that every U.S. senator hears from every doc and every doc’s family and every doc’s friend and every doc’s assistant and everybody else and their brother that this important so we can turn up the heat and make sure they take up the issue of background checks. It works. It saves lives.”
REPORTING FROM AMA NATIONAL ADVOCACY CONFERENCE