User login
Provide appropriate sexual, reproductive health care for transgender patients
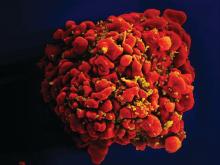
I recently was on a panel of experts discussing how to prevent HIV among transgender youth. Preventing HIV among transgender youth, especially transgender youth of color, remains a challenge for multiple reasons – racism, poverty, stigma, marginalization, and discrimination play a role in the HIV epidemic. A barrier to preventing HIV infections among transgender youth is a lack of knowledge on how to provide them with comprehensive sexual and reproductive health care. Here are some tips and resources that can help you ensure that transgender youth are safe and healthy.
One of the challenges of obtaining a sexual history is asking the right questions For example, if you have a transgender male assigned female at birth, ask whether their partners produce sperm instead of asking about the sex of their partners. A transgender male’s partner may identify as female but is assigned male at birth and uses her penis during sex. Furthermore, a transgender male may be on testosterone, but he still can get pregnant. Asking how they use their organs is just as important. A transgender male who has condomless penile-vaginal sex with multiple partners is at a higher risk for HIV infection than is a transgender male who shares sex toys with his only partner.
Normalizing that you ask a comprehensive sexual history to all your patients regardless of gender identity may put the patient at ease. Many transgender people are reluctant to disclose their gender identity to their provider because they are afraid that the provider may fixate on their sexuality once they do. Stating that you ask sexual health questions to all your patients may prevent the transgender patient from feeling singled out.
Finally, you don’t have to ask a sexual history with every transgender patient, just as you wouldn’t for your cisgender patients. If a patient is complaining of a sprained ankle, a sexual history may not be helpful, compared with obtaining one when a patient comes in with pelvic pain. Many transgender patients avoid care because they are frequently asked about their sexual history or gender identity when these are not relevant to their chief complaint.
Here are some helpful questions to ask when taking a sexual history, according to the University of California, San Francisco, Transgender Care & Treatment Guidelines.1
- Are you having sex? How many sex partners have you had in the past year?
- Who are you having sex with? What types of sex are you having? What parts of your anatomy do you use for sex?
- How do you protect yourself from STIs?
- What STIs have you had in the past, if any? When were you last tested for STIs?
- Has your partner(s) ever been diagnosed with any STIs?
- Do you use alcohol or any drugs when you have sex?
- Do you exchange sex for money, drugs, or a place to stay?
Also, use a trauma-informed approach when working with transgender patients. Many have been victims of sexual trauma. Always have a chaperone accompany you during the exam, explain to the patient what you plan to do and why it is necessary, and allow them to decline (and document their declining the physical exam). Also consider having your patient self-swab for STI screening if appropriate.1
Like obtaining a sexual history, routine screenings for certain types of cancers will be based on the organs the patient has. For example, a transgender woman assigned male at birth will not need a cervical cancer screening, but a transgender man assigned female at birth may need one – if the patient still has a cervix. Cervical cancer screening guidelines are similar for transgender men as it is for nontransgender women, and one should use the same guidelines endorsed by the American Cancer Society, American Society of Colposcopy and Cervical Pathology, American Society of Clinical Pathologists, U.S. Preventive Services Task Force, and the World Health Organization.2-4
Cervical screenings should never be a requirement for testosterone therapy, and no transgender male under the age of 21 years will need cervical screening. The University of California guidelines offers tips on how to make transgender men more comfortable during cervical cancer screening.5
Contraception and menstrual management also are important for transgender patients. Testosterone can induce amenorrhea for transgender men, but it is not good birth control. If a transgender male patient has sex with partners that produce sperm, then the physician should discuss effective birth control options. There is no ideal birth control option for transgender men. One must consider multiple factors including the patient’s desire for pregnancy, desire to cease periods, ease of administration, and risk for thrombosis.
Most transgender men may balk at the idea of taking estrogen-containing contraception, but it is more effective than oral progestin-only pills. Intrauterine devices are highly effective in pregnancy prevention and can achieve amenorrhea in 50% of users within 1 year,but some transmen may become dysphoric with the procedure. 6 The etonogestrel implants also are highly effective birth control, but irregular periods are common, leading to discontinuation. Depot medroxyprogesterone is highly effective in preventing pregnancy and can induce amenorrhea in 70% of users within 1 year and 80% of users in 2 years, but also is associated with weight gain in one-third of users.7 Finally, pubertal blockers can rapidly stop periods for transmen who are severely dysphoric from their menses; however, before achieving amenorrhea, a flare bleed can occur 4-6 weeks after administration.8 Support from a mental health therapist during this time is critical. Pubertal blockers, nevertheless, are not suitable birth control.
When providing affirming sexual and reproductive health care for transgender patients, key principles include focusing on organs and activities over identity. Additionally, screening for certain types of cancers also is dependent on organs. Finally, do not neglect the importance of contraception among transgender men. Taking these principles in consideration will help you provide excellent care for transgender youth.
Dr. Montano is an assistant professor of pediatrics at the University of Pittsburgh and an adolescent medicine physician at the Children’s Hospital of Pittsburgh. He said he had no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. Transgender people and sexually transmitted infections (https://transcare.ucsf.edu/guidelines/stis).
2. CA Cancer J Clin. 2012 May-Jun;62(3):147-72.
3. Ann Intern Med. 2012;156(12):880-91.
4. Cervical cancer screening in developing countries: Report of a WHO consultation. 2002. World Health Organization, Geneva.
5. Screening for cervical cancer for transgender men (https://transcare.ucsf.edu/guidelines/cervical-cancer).
6. Contraception. 2002 Feb;65(2):129-32.
7. Rev Endocr Metab Disord. 2011 Jun;12(2):93-106.
8. Int J Womens Health. 2014 Jun 23;6:631-7.
Resources
Breast cancer screening in transgender men. (https://transcare.ucsf.edu/guidelines/breast-cancer-men).
Screening for breast cancer in transgender women. (https://transcare.ucsf.edu/guidelines/breast-cancer-women).
Transgender health and HIV (https://transcare.ucsf.edu/guidelines/hiv).
Centers for Disease Control and Prevention: HIV and Transgender People (https://www.cdc.gov/hiv/group/gender/transgender/index.html).
I recently was on a panel of experts discussing how to prevent HIV among transgender youth. Preventing HIV among transgender youth, especially transgender youth of color, remains a challenge for multiple reasons – racism, poverty, stigma, marginalization, and discrimination play a role in the HIV epidemic. A barrier to preventing HIV infections among transgender youth is a lack of knowledge on how to provide them with comprehensive sexual and reproductive health care. Here are some tips and resources that can help you ensure that transgender youth are safe and healthy.
One of the challenges of obtaining a sexual history is asking the right questions For example, if you have a transgender male assigned female at birth, ask whether their partners produce sperm instead of asking about the sex of their partners. A transgender male’s partner may identify as female but is assigned male at birth and uses her penis during sex. Furthermore, a transgender male may be on testosterone, but he still can get pregnant. Asking how they use their organs is just as important. A transgender male who has condomless penile-vaginal sex with multiple partners is at a higher risk for HIV infection than is a transgender male who shares sex toys with his only partner.
Normalizing that you ask a comprehensive sexual history to all your patients regardless of gender identity may put the patient at ease. Many transgender people are reluctant to disclose their gender identity to their provider because they are afraid that the provider may fixate on their sexuality once they do. Stating that you ask sexual health questions to all your patients may prevent the transgender patient from feeling singled out.
Finally, you don’t have to ask a sexual history with every transgender patient, just as you wouldn’t for your cisgender patients. If a patient is complaining of a sprained ankle, a sexual history may not be helpful, compared with obtaining one when a patient comes in with pelvic pain. Many transgender patients avoid care because they are frequently asked about their sexual history or gender identity when these are not relevant to their chief complaint.
Here are some helpful questions to ask when taking a sexual history, according to the University of California, San Francisco, Transgender Care & Treatment Guidelines.1
- Are you having sex? How many sex partners have you had in the past year?
- Who are you having sex with? What types of sex are you having? What parts of your anatomy do you use for sex?
- How do you protect yourself from STIs?
- What STIs have you had in the past, if any? When were you last tested for STIs?
- Has your partner(s) ever been diagnosed with any STIs?
- Do you use alcohol or any drugs when you have sex?
- Do you exchange sex for money, drugs, or a place to stay?
Also, use a trauma-informed approach when working with transgender patients. Many have been victims of sexual trauma. Always have a chaperone accompany you during the exam, explain to the patient what you plan to do and why it is necessary, and allow them to decline (and document their declining the physical exam). Also consider having your patient self-swab for STI screening if appropriate.1
Like obtaining a sexual history, routine screenings for certain types of cancers will be based on the organs the patient has. For example, a transgender woman assigned male at birth will not need a cervical cancer screening, but a transgender man assigned female at birth may need one – if the patient still has a cervix. Cervical cancer screening guidelines are similar for transgender men as it is for nontransgender women, and one should use the same guidelines endorsed by the American Cancer Society, American Society of Colposcopy and Cervical Pathology, American Society of Clinical Pathologists, U.S. Preventive Services Task Force, and the World Health Organization.2-4
Cervical screenings should never be a requirement for testosterone therapy, and no transgender male under the age of 21 years will need cervical screening. The University of California guidelines offers tips on how to make transgender men more comfortable during cervical cancer screening.5
Contraception and menstrual management also are important for transgender patients. Testosterone can induce amenorrhea for transgender men, but it is not good birth control. If a transgender male patient has sex with partners that produce sperm, then the physician should discuss effective birth control options. There is no ideal birth control option for transgender men. One must consider multiple factors including the patient’s desire for pregnancy, desire to cease periods, ease of administration, and risk for thrombosis.
Most transgender men may balk at the idea of taking estrogen-containing contraception, but it is more effective than oral progestin-only pills. Intrauterine devices are highly effective in pregnancy prevention and can achieve amenorrhea in 50% of users within 1 year,but some transmen may become dysphoric with the procedure. 6 The etonogestrel implants also are highly effective birth control, but irregular periods are common, leading to discontinuation. Depot medroxyprogesterone is highly effective in preventing pregnancy and can induce amenorrhea in 70% of users within 1 year and 80% of users in 2 years, but also is associated with weight gain in one-third of users.7 Finally, pubertal blockers can rapidly stop periods for transmen who are severely dysphoric from their menses; however, before achieving amenorrhea, a flare bleed can occur 4-6 weeks after administration.8 Support from a mental health therapist during this time is critical. Pubertal blockers, nevertheless, are not suitable birth control.
When providing affirming sexual and reproductive health care for transgender patients, key principles include focusing on organs and activities over identity. Additionally, screening for certain types of cancers also is dependent on organs. Finally, do not neglect the importance of contraception among transgender men. Taking these principles in consideration will help you provide excellent care for transgender youth.
Dr. Montano is an assistant professor of pediatrics at the University of Pittsburgh and an adolescent medicine physician at the Children’s Hospital of Pittsburgh. He said he had no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. Transgender people and sexually transmitted infections (https://transcare.ucsf.edu/guidelines/stis).
2. CA Cancer J Clin. 2012 May-Jun;62(3):147-72.
3. Ann Intern Med. 2012;156(12):880-91.
4. Cervical cancer screening in developing countries: Report of a WHO consultation. 2002. World Health Organization, Geneva.
5. Screening for cervical cancer for transgender men (https://transcare.ucsf.edu/guidelines/cervical-cancer).
6. Contraception. 2002 Feb;65(2):129-32.
7. Rev Endocr Metab Disord. 2011 Jun;12(2):93-106.
8. Int J Womens Health. 2014 Jun 23;6:631-7.
Resources
Breast cancer screening in transgender men. (https://transcare.ucsf.edu/guidelines/breast-cancer-men).
Screening for breast cancer in transgender women. (https://transcare.ucsf.edu/guidelines/breast-cancer-women).
Transgender health and HIV (https://transcare.ucsf.edu/guidelines/hiv).
Centers for Disease Control and Prevention: HIV and Transgender People (https://www.cdc.gov/hiv/group/gender/transgender/index.html).
I recently was on a panel of experts discussing how to prevent HIV among transgender youth. Preventing HIV among transgender youth, especially transgender youth of color, remains a challenge for multiple reasons – racism, poverty, stigma, marginalization, and discrimination play a role in the HIV epidemic. A barrier to preventing HIV infections among transgender youth is a lack of knowledge on how to provide them with comprehensive sexual and reproductive health care. Here are some tips and resources that can help you ensure that transgender youth are safe and healthy.
One of the challenges of obtaining a sexual history is asking the right questions For example, if you have a transgender male assigned female at birth, ask whether their partners produce sperm instead of asking about the sex of their partners. A transgender male’s partner may identify as female but is assigned male at birth and uses her penis during sex. Furthermore, a transgender male may be on testosterone, but he still can get pregnant. Asking how they use their organs is just as important. A transgender male who has condomless penile-vaginal sex with multiple partners is at a higher risk for HIV infection than is a transgender male who shares sex toys with his only partner.
Normalizing that you ask a comprehensive sexual history to all your patients regardless of gender identity may put the patient at ease. Many transgender people are reluctant to disclose their gender identity to their provider because they are afraid that the provider may fixate on their sexuality once they do. Stating that you ask sexual health questions to all your patients may prevent the transgender patient from feeling singled out.
Finally, you don’t have to ask a sexual history with every transgender patient, just as you wouldn’t for your cisgender patients. If a patient is complaining of a sprained ankle, a sexual history may not be helpful, compared with obtaining one when a patient comes in with pelvic pain. Many transgender patients avoid care because they are frequently asked about their sexual history or gender identity when these are not relevant to their chief complaint.
Here are some helpful questions to ask when taking a sexual history, according to the University of California, San Francisco, Transgender Care & Treatment Guidelines.1
- Are you having sex? How many sex partners have you had in the past year?
- Who are you having sex with? What types of sex are you having? What parts of your anatomy do you use for sex?
- How do you protect yourself from STIs?
- What STIs have you had in the past, if any? When were you last tested for STIs?
- Has your partner(s) ever been diagnosed with any STIs?
- Do you use alcohol or any drugs when you have sex?
- Do you exchange sex for money, drugs, or a place to stay?
Also, use a trauma-informed approach when working with transgender patients. Many have been victims of sexual trauma. Always have a chaperone accompany you during the exam, explain to the patient what you plan to do and why it is necessary, and allow them to decline (and document their declining the physical exam). Also consider having your patient self-swab for STI screening if appropriate.1
Like obtaining a sexual history, routine screenings for certain types of cancers will be based on the organs the patient has. For example, a transgender woman assigned male at birth will not need a cervical cancer screening, but a transgender man assigned female at birth may need one – if the patient still has a cervix. Cervical cancer screening guidelines are similar for transgender men as it is for nontransgender women, and one should use the same guidelines endorsed by the American Cancer Society, American Society of Colposcopy and Cervical Pathology, American Society of Clinical Pathologists, U.S. Preventive Services Task Force, and the World Health Organization.2-4
Cervical screenings should never be a requirement for testosterone therapy, and no transgender male under the age of 21 years will need cervical screening. The University of California guidelines offers tips on how to make transgender men more comfortable during cervical cancer screening.5
Contraception and menstrual management also are important for transgender patients. Testosterone can induce amenorrhea for transgender men, but it is not good birth control. If a transgender male patient has sex with partners that produce sperm, then the physician should discuss effective birth control options. There is no ideal birth control option for transgender men. One must consider multiple factors including the patient’s desire for pregnancy, desire to cease periods, ease of administration, and risk for thrombosis.
Most transgender men may balk at the idea of taking estrogen-containing contraception, but it is more effective than oral progestin-only pills. Intrauterine devices are highly effective in pregnancy prevention and can achieve amenorrhea in 50% of users within 1 year,but some transmen may become dysphoric with the procedure. 6 The etonogestrel implants also are highly effective birth control, but irregular periods are common, leading to discontinuation. Depot medroxyprogesterone is highly effective in preventing pregnancy and can induce amenorrhea in 70% of users within 1 year and 80% of users in 2 years, but also is associated with weight gain in one-third of users.7 Finally, pubertal blockers can rapidly stop periods for transmen who are severely dysphoric from their menses; however, before achieving amenorrhea, a flare bleed can occur 4-6 weeks after administration.8 Support from a mental health therapist during this time is critical. Pubertal blockers, nevertheless, are not suitable birth control.
When providing affirming sexual and reproductive health care for transgender patients, key principles include focusing on organs and activities over identity. Additionally, screening for certain types of cancers also is dependent on organs. Finally, do not neglect the importance of contraception among transgender men. Taking these principles in consideration will help you provide excellent care for transgender youth.
Dr. Montano is an assistant professor of pediatrics at the University of Pittsburgh and an adolescent medicine physician at the Children’s Hospital of Pittsburgh. He said he had no relevant financial disclosures. Email him at pdnews@mdedge.com.
References
1. Transgender people and sexually transmitted infections (https://transcare.ucsf.edu/guidelines/stis).
2. CA Cancer J Clin. 2012 May-Jun;62(3):147-72.
3. Ann Intern Med. 2012;156(12):880-91.
4. Cervical cancer screening in developing countries: Report of a WHO consultation. 2002. World Health Organization, Geneva.
5. Screening for cervical cancer for transgender men (https://transcare.ucsf.edu/guidelines/cervical-cancer).
6. Contraception. 2002 Feb;65(2):129-32.
7. Rev Endocr Metab Disord. 2011 Jun;12(2):93-106.
8. Int J Womens Health. 2014 Jun 23;6:631-7.
Resources
Breast cancer screening in transgender men. (https://transcare.ucsf.edu/guidelines/breast-cancer-men).
Screening for breast cancer in transgender women. (https://transcare.ucsf.edu/guidelines/breast-cancer-women).
Transgender health and HIV (https://transcare.ucsf.edu/guidelines/hiv).
Centers for Disease Control and Prevention: HIV and Transgender People (https://www.cdc.gov/hiv/group/gender/transgender/index.html).
Walking the walk
In March 2018, the Human Rights Campaign (HRC), an advocacy organization dedicated to improving the lives of LGBTQ people, released its 11th Annual Healthcare Equality Index. The HEI is an indicator of how inclusive and equitable health care facilities are in providing care for their LGBTQ patients. My own institution, Children’s Hospital of Pittsburgh, scored very high on this index and received the “Leader in LGBTQ Healthcare Equality” designation. The process of receiving this designation is very rigorous, and I am proud of my institution for making great strides in expanding health care access for LGBTQ patients, especially transgender patients. However, this is no time to rest on one’s laurels, as many transgender people still experience challenges and barriers in navigating the health care system.
Insurance access continues to be a problem. I wrote a column in June 2017 about obtaining health care insurance for transgender patients. Preauthorization is common for obtaining cross-sex hormones or pubertal blockers even for insurance companies that are willing to pay for them – a process that can take weeks, even months, to complete. This creates delays in obtaining necessary care for transgender patients. This is just one of the many barriers transgender people face in navigating the health care system.
Increasing access to health care services for transgender patients is more about improving health outcomes than patient satisfaction. Even the smallest policy change may have a meaningful impact on the lives of transgender individuals. A study by Russell et al., in the April 2018 issue of Journal of Adolescent Health found that transgender youth allowed to use their chosen name (instead of the name assigned to them by their parents at birth) were more likely to have fewer depressive symptoms and lower rates of suicidal ideation and suicidal behavior.3 These findings highlight that even a small change can have a huge impact on the health and well-being of this patient population.
What can you do to expand access? First, you must educate yourself and teach others. Many providers report never having received education on LGBTQ health during their training,4 and most barriers for transgender patients stem from this lack of training. Second, work with the transgender community – it is very tempting to see your institution’s name on the HEI and think all the work is done, but the lived experiences of transgender patients sometimes are different than what is seen on paper (or online). Team up with local organizations such as PFLAG (formerly known as Parents and Families of Lesbians and Gays) that can create support groups for both transgender youth and their families. Help create a network of referral systems for your transgender patients – the community is often small enough that they know which providers or establishments are safe for transgender individuals. Many transgender patients find this extremely helpful.5 You still wield significant influence in the community, so work with the health care and insurance systems to improve access and coverage for gender-related services. The HRC HEI is becoming coveted by health care institutions. This is a prime opportunity to be involved in committees seeking to improve health care access for transgender individuals. Finally, as there are champions for transgender health in your clinic, there also are champions for transgender health in insurance companies. They often are well known in the community, so find that individual for counseling on how to navigate the insurance system for your transgender patients.
Although an increasing number of health care institutions and clinics are recognizing the health care needs of transgender patients and providing appropriate care, the health care system remains challenging for transgender individuals to navigate. Small policy changes may have a substantial impact on the health and well-being of transgender individuals. Although creating change within an institution may seem like a monumental task, you do have the agency to help create this type change within the system to expand health care access for transgender patients.
Dr. Montano is an assistant professor of pediatrics at the University of Pittsburgh and an adolescent medicine physician at Children’s Hospital of Pittsburgh of UPMC. Email him at pdnews@mdedge.com.
Resources
- HRC HEI: If you’re interested in learning what policies are inclusive and equitable for LGBT patients, check out the HRC HEI scoring criteria. It’s a good place to start if you want to expand health care access for transgender individuals.
- To find out more about the health care legal protections transgender individuals are entitled to, check out the National Center for Transgender Equality.
References
1. Psychol Bull. 2003 Sep;129(5):674-97.
2. “Injustice at every turn: A report of the National Transgender Discrimination Survey.” (Washington: National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011.)
3. J. Adolesc Health. 2018 Apr. doi: 10.1016/j.jadohealth.2018.02.003.
4. Int J Transgenderism. 2008. doi: 10.1300/J485v08n02_08.
5. Transgend Health. 2016 Nov 1;1(1):238-49.
In March 2018, the Human Rights Campaign (HRC), an advocacy organization dedicated to improving the lives of LGBTQ people, released its 11th Annual Healthcare Equality Index. The HEI is an indicator of how inclusive and equitable health care facilities are in providing care for their LGBTQ patients. My own institution, Children’s Hospital of Pittsburgh, scored very high on this index and received the “Leader in LGBTQ Healthcare Equality” designation. The process of receiving this designation is very rigorous, and I am proud of my institution for making great strides in expanding health care access for LGBTQ patients, especially transgender patients. However, this is no time to rest on one’s laurels, as many transgender people still experience challenges and barriers in navigating the health care system.
Insurance access continues to be a problem. I wrote a column in June 2017 about obtaining health care insurance for transgender patients. Preauthorization is common for obtaining cross-sex hormones or pubertal blockers even for insurance companies that are willing to pay for them – a process that can take weeks, even months, to complete. This creates delays in obtaining necessary care for transgender patients. This is just one of the many barriers transgender people face in navigating the health care system.
Increasing access to health care services for transgender patients is more about improving health outcomes than patient satisfaction. Even the smallest policy change may have a meaningful impact on the lives of transgender individuals. A study by Russell et al., in the April 2018 issue of Journal of Adolescent Health found that transgender youth allowed to use their chosen name (instead of the name assigned to them by their parents at birth) were more likely to have fewer depressive symptoms and lower rates of suicidal ideation and suicidal behavior.3 These findings highlight that even a small change can have a huge impact on the health and well-being of this patient population.
What can you do to expand access? First, you must educate yourself and teach others. Many providers report never having received education on LGBTQ health during their training,4 and most barriers for transgender patients stem from this lack of training. Second, work with the transgender community – it is very tempting to see your institution’s name on the HEI and think all the work is done, but the lived experiences of transgender patients sometimes are different than what is seen on paper (or online). Team up with local organizations such as PFLAG (formerly known as Parents and Families of Lesbians and Gays) that can create support groups for both transgender youth and their families. Help create a network of referral systems for your transgender patients – the community is often small enough that they know which providers or establishments are safe for transgender individuals. Many transgender patients find this extremely helpful.5 You still wield significant influence in the community, so work with the health care and insurance systems to improve access and coverage for gender-related services. The HRC HEI is becoming coveted by health care institutions. This is a prime opportunity to be involved in committees seeking to improve health care access for transgender individuals. Finally, as there are champions for transgender health in your clinic, there also are champions for transgender health in insurance companies. They often are well known in the community, so find that individual for counseling on how to navigate the insurance system for your transgender patients.
Although an increasing number of health care institutions and clinics are recognizing the health care needs of transgender patients and providing appropriate care, the health care system remains challenging for transgender individuals to navigate. Small policy changes may have a substantial impact on the health and well-being of transgender individuals. Although creating change within an institution may seem like a monumental task, you do have the agency to help create this type change within the system to expand health care access for transgender patients.
Dr. Montano is an assistant professor of pediatrics at the University of Pittsburgh and an adolescent medicine physician at Children’s Hospital of Pittsburgh of UPMC. Email him at pdnews@mdedge.com.
Resources
- HRC HEI: If you’re interested in learning what policies are inclusive and equitable for LGBT patients, check out the HRC HEI scoring criteria. It’s a good place to start if you want to expand health care access for transgender individuals.
- To find out more about the health care legal protections transgender individuals are entitled to, check out the National Center for Transgender Equality.
References
1. Psychol Bull. 2003 Sep;129(5):674-97.
2. “Injustice at every turn: A report of the National Transgender Discrimination Survey.” (Washington: National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011.)
3. J. Adolesc Health. 2018 Apr. doi: 10.1016/j.jadohealth.2018.02.003.
4. Int J Transgenderism. 2008. doi: 10.1300/J485v08n02_08.
5. Transgend Health. 2016 Nov 1;1(1):238-49.
In March 2018, the Human Rights Campaign (HRC), an advocacy organization dedicated to improving the lives of LGBTQ people, released its 11th Annual Healthcare Equality Index. The HEI is an indicator of how inclusive and equitable health care facilities are in providing care for their LGBTQ patients. My own institution, Children’s Hospital of Pittsburgh, scored very high on this index and received the “Leader in LGBTQ Healthcare Equality” designation. The process of receiving this designation is very rigorous, and I am proud of my institution for making great strides in expanding health care access for LGBTQ patients, especially transgender patients. However, this is no time to rest on one’s laurels, as many transgender people still experience challenges and barriers in navigating the health care system.
Insurance access continues to be a problem. I wrote a column in June 2017 about obtaining health care insurance for transgender patients. Preauthorization is common for obtaining cross-sex hormones or pubertal blockers even for insurance companies that are willing to pay for them – a process that can take weeks, even months, to complete. This creates delays in obtaining necessary care for transgender patients. This is just one of the many barriers transgender people face in navigating the health care system.
Increasing access to health care services for transgender patients is more about improving health outcomes than patient satisfaction. Even the smallest policy change may have a meaningful impact on the lives of transgender individuals. A study by Russell et al., in the April 2018 issue of Journal of Adolescent Health found that transgender youth allowed to use their chosen name (instead of the name assigned to them by their parents at birth) were more likely to have fewer depressive symptoms and lower rates of suicidal ideation and suicidal behavior.3 These findings highlight that even a small change can have a huge impact on the health and well-being of this patient population.
What can you do to expand access? First, you must educate yourself and teach others. Many providers report never having received education on LGBTQ health during their training,4 and most barriers for transgender patients stem from this lack of training. Second, work with the transgender community – it is very tempting to see your institution’s name on the HEI and think all the work is done, but the lived experiences of transgender patients sometimes are different than what is seen on paper (or online). Team up with local organizations such as PFLAG (formerly known as Parents and Families of Lesbians and Gays) that can create support groups for both transgender youth and their families. Help create a network of referral systems for your transgender patients – the community is often small enough that they know which providers or establishments are safe for transgender individuals. Many transgender patients find this extremely helpful.5 You still wield significant influence in the community, so work with the health care and insurance systems to improve access and coverage for gender-related services. The HRC HEI is becoming coveted by health care institutions. This is a prime opportunity to be involved in committees seeking to improve health care access for transgender individuals. Finally, as there are champions for transgender health in your clinic, there also are champions for transgender health in insurance companies. They often are well known in the community, so find that individual for counseling on how to navigate the insurance system for your transgender patients.
Although an increasing number of health care institutions and clinics are recognizing the health care needs of transgender patients and providing appropriate care, the health care system remains challenging for transgender individuals to navigate. Small policy changes may have a substantial impact on the health and well-being of transgender individuals. Although creating change within an institution may seem like a monumental task, you do have the agency to help create this type change within the system to expand health care access for transgender patients.
Dr. Montano is an assistant professor of pediatrics at the University of Pittsburgh and an adolescent medicine physician at Children’s Hospital of Pittsburgh of UPMC. Email him at pdnews@mdedge.com.
Resources
- HRC HEI: If you’re interested in learning what policies are inclusive and equitable for LGBT patients, check out the HRC HEI scoring criteria. It’s a good place to start if you want to expand health care access for transgender individuals.
- To find out more about the health care legal protections transgender individuals are entitled to, check out the National Center for Transgender Equality.
References
1. Psychol Bull. 2003 Sep;129(5):674-97.
2. “Injustice at every turn: A report of the National Transgender Discrimination Survey.” (Washington: National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011.)
3. J. Adolesc Health. 2018 Apr. doi: 10.1016/j.jadohealth.2018.02.003.
4. Int J Transgenderism. 2008. doi: 10.1300/J485v08n02_08.
5. Transgend Health. 2016 Nov 1;1(1):238-49.
Preexposure prophylaxis among LGBT youth
Every prevention effort or treatment has its own risks. Gynecologists must consider the risk for blood clots from using estrogen-containing oral contraceptives versus the risk of blood clots from pregnancy. Endocrinologists must weigh the risk of decreased bone mineral density versus premature closure of growth plates when starting pubertal blockers for children suffering from precocious puberty. Psychologists and primary care providers must consider the risk for increased suicidal thoughts while on selective serotonin reuptake inhibitors versus the risk of completed suicide if the depression remains untreated.
In the United States alone, 22% of HIV infections occur in people aged 13-24 years. Among those with HIV infection, 81% are young men who have sex with men (MSM).1 Among those new infections, young MSM of color are nearly four times as likely to have HIV, compared with white young MSM.2 Moreover, the incidence of HIV infection among transgender individuals is three times higher than the national average.3
What further hampers public health prevention efforts is the stigma and discrimination LGBT youth face in trying to prevent HIV infections: 84% of those aged 15-24 years report recognizing stigma around HIV in the United States.4 In addition, black MSM were more likely than other MSMs to report this kind of stigma.5 And it isn’t enough that LGBT youth have to face stigma and discrimination. In fact, because of it, they often face serious financial challenges. It is estimated that 50% of homeless youth identify as LGBT, and 40% of them were forced out of their homes because of their sexual orientation or gender identity.6 Also, transgender youth have difficulty finding employment because of their gender identity.7 A combination of homelessness or chronic unemployment has driven many LGBT youth to survival sex or sex for money, which puts them at higher risk for HIV infection.7,8 The risk for HIV infection is so high that we should be using all available resources, including PrEP, to address these profound health disparities.
Studies, however, are forthcoming. One study by Hosek et al. that was published in September suggested that PrEP among adolescents can be safe and well tolerated, may not increase the rate of high-risk sexual behaviors, and may not increase the risk of other STDs such as gonorrhea and chlamydia. It must be noted, however, that incidence of HIV was fairly high – the HIV seroconversion rate was 6.4 per 100 person-years. Nevertheless, researchers found the rate of HIV seroconversion was higher among those with lower levels of Truvada in their bodies, compared with the seroconversion rate in those with higher levels of the medication. This suggests that adherence is key in using PrEP to prevent HIV infection.10 Although far from definitive, this small study provides some solid evidence that PrEP is safe and effective in preventing HIV among LGBT youth. More studies that will eventually support its effectiveness and safety are on the way.11
Dr. Montano is an assistant professor of pediatrics at the University of Pittsburgh and an adolescent medicine physician at Children’s Hospital of Pittsburgh of UPMC. Email him at pdnews@frontlinemedcom.com.
Resource
CDC website on PrEP: https://www.cdc.gov/hiv/risk/prep/index.html, with provider guidelines.
References
1. Centers for Disease Control and Prevention. HIV Among Youth fact sheet, April 2017.
2. Centers for Disease Control and Prevention. HIV Surveillance Report, 2015; vol. 27.
3. Centers for Disease Control and Prevention. HIV Among Transgender People.
4. Kaiser Family Foundation. National survey of teens and young adults on HIV/AIDS, Nov. 1, 2012. .
5. J Acquir Immune Defic Syndr. 2016;73(5):547-55.
6. Serving our youth: Findings from a national survey of services providers working with lesbian, gay, bisexual and transgender youth who are homeless or at risk of becoming homeless (The Williams Institute with True Colors and The Palette Fund, 2012).
7. Injustice at every turn: A report of the national transgender discrimination survey (National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011).
8. J Acquir Immune Defic Syndr. 2010 Apr;53(5):661-4.
9. Centers for Disease Control and Prevention. Preexposure prophylaxis for the prevention of HIV infection in the United States: A clinical practice guideline, 2014.
10. JAMA Pediatr. 2017;171(11):1063-71.
11. J Int AIDS Soc. 2016;19. doi: 10.7448/IAS.19.7.21107.
Every prevention effort or treatment has its own risks. Gynecologists must consider the risk for blood clots from using estrogen-containing oral contraceptives versus the risk of blood clots from pregnancy. Endocrinologists must weigh the risk of decreased bone mineral density versus premature closure of growth plates when starting pubertal blockers for children suffering from precocious puberty. Psychologists and primary care providers must consider the risk for increased suicidal thoughts while on selective serotonin reuptake inhibitors versus the risk of completed suicide if the depression remains untreated.
In the United States alone, 22% of HIV infections occur in people aged 13-24 years. Among those with HIV infection, 81% are young men who have sex with men (MSM).1 Among those new infections, young MSM of color are nearly four times as likely to have HIV, compared with white young MSM.2 Moreover, the incidence of HIV infection among transgender individuals is three times higher than the national average.3
What further hampers public health prevention efforts is the stigma and discrimination LGBT youth face in trying to prevent HIV infections: 84% of those aged 15-24 years report recognizing stigma around HIV in the United States.4 In addition, black MSM were more likely than other MSMs to report this kind of stigma.5 And it isn’t enough that LGBT youth have to face stigma and discrimination. In fact, because of it, they often face serious financial challenges. It is estimated that 50% of homeless youth identify as LGBT, and 40% of them were forced out of their homes because of their sexual orientation or gender identity.6 Also, transgender youth have difficulty finding employment because of their gender identity.7 A combination of homelessness or chronic unemployment has driven many LGBT youth to survival sex or sex for money, which puts them at higher risk for HIV infection.7,8 The risk for HIV infection is so high that we should be using all available resources, including PrEP, to address these profound health disparities.
Studies, however, are forthcoming. One study by Hosek et al. that was published in September suggested that PrEP among adolescents can be safe and well tolerated, may not increase the rate of high-risk sexual behaviors, and may not increase the risk of other STDs such as gonorrhea and chlamydia. It must be noted, however, that incidence of HIV was fairly high – the HIV seroconversion rate was 6.4 per 100 person-years. Nevertheless, researchers found the rate of HIV seroconversion was higher among those with lower levels of Truvada in their bodies, compared with the seroconversion rate in those with higher levels of the medication. This suggests that adherence is key in using PrEP to prevent HIV infection.10 Although far from definitive, this small study provides some solid evidence that PrEP is safe and effective in preventing HIV among LGBT youth. More studies that will eventually support its effectiveness and safety are on the way.11
Dr. Montano is an assistant professor of pediatrics at the University of Pittsburgh and an adolescent medicine physician at Children’s Hospital of Pittsburgh of UPMC. Email him at pdnews@frontlinemedcom.com.
Resource
CDC website on PrEP: https://www.cdc.gov/hiv/risk/prep/index.html, with provider guidelines.
References
1. Centers for Disease Control and Prevention. HIV Among Youth fact sheet, April 2017.
2. Centers for Disease Control and Prevention. HIV Surveillance Report, 2015; vol. 27.
3. Centers for Disease Control and Prevention. HIV Among Transgender People.
4. Kaiser Family Foundation. National survey of teens and young adults on HIV/AIDS, Nov. 1, 2012. .
5. J Acquir Immune Defic Syndr. 2016;73(5):547-55.
6. Serving our youth: Findings from a national survey of services providers working with lesbian, gay, bisexual and transgender youth who are homeless or at risk of becoming homeless (The Williams Institute with True Colors and The Palette Fund, 2012).
7. Injustice at every turn: A report of the national transgender discrimination survey (National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011).
8. J Acquir Immune Defic Syndr. 2010 Apr;53(5):661-4.
9. Centers for Disease Control and Prevention. Preexposure prophylaxis for the prevention of HIV infection in the United States: A clinical practice guideline, 2014.
10. JAMA Pediatr. 2017;171(11):1063-71.
11. J Int AIDS Soc. 2016;19. doi: 10.7448/IAS.19.7.21107.
Every prevention effort or treatment has its own risks. Gynecologists must consider the risk for blood clots from using estrogen-containing oral contraceptives versus the risk of blood clots from pregnancy. Endocrinologists must weigh the risk of decreased bone mineral density versus premature closure of growth plates when starting pubertal blockers for children suffering from precocious puberty. Psychologists and primary care providers must consider the risk for increased suicidal thoughts while on selective serotonin reuptake inhibitors versus the risk of completed suicide if the depression remains untreated.
In the United States alone, 22% of HIV infections occur in people aged 13-24 years. Among those with HIV infection, 81% are young men who have sex with men (MSM).1 Among those new infections, young MSM of color are nearly four times as likely to have HIV, compared with white young MSM.2 Moreover, the incidence of HIV infection among transgender individuals is three times higher than the national average.3
What further hampers public health prevention efforts is the stigma and discrimination LGBT youth face in trying to prevent HIV infections: 84% of those aged 15-24 years report recognizing stigma around HIV in the United States.4 In addition, black MSM were more likely than other MSMs to report this kind of stigma.5 And it isn’t enough that LGBT youth have to face stigma and discrimination. In fact, because of it, they often face serious financial challenges. It is estimated that 50% of homeless youth identify as LGBT, and 40% of them were forced out of their homes because of their sexual orientation or gender identity.6 Also, transgender youth have difficulty finding employment because of their gender identity.7 A combination of homelessness or chronic unemployment has driven many LGBT youth to survival sex or sex for money, which puts them at higher risk for HIV infection.7,8 The risk for HIV infection is so high that we should be using all available resources, including PrEP, to address these profound health disparities.
Studies, however, are forthcoming. One study by Hosek et al. that was published in September suggested that PrEP among adolescents can be safe and well tolerated, may not increase the rate of high-risk sexual behaviors, and may not increase the risk of other STDs such as gonorrhea and chlamydia. It must be noted, however, that incidence of HIV was fairly high – the HIV seroconversion rate was 6.4 per 100 person-years. Nevertheless, researchers found the rate of HIV seroconversion was higher among those with lower levels of Truvada in their bodies, compared with the seroconversion rate in those with higher levels of the medication. This suggests that adherence is key in using PrEP to prevent HIV infection.10 Although far from definitive, this small study provides some solid evidence that PrEP is safe and effective in preventing HIV among LGBT youth. More studies that will eventually support its effectiveness and safety are on the way.11
Dr. Montano is an assistant professor of pediatrics at the University of Pittsburgh and an adolescent medicine physician at Children’s Hospital of Pittsburgh of UPMC. Email him at pdnews@frontlinemedcom.com.
Resource
CDC website on PrEP: https://www.cdc.gov/hiv/risk/prep/index.html, with provider guidelines.
References
1. Centers for Disease Control and Prevention. HIV Among Youth fact sheet, April 2017.
2. Centers for Disease Control and Prevention. HIV Surveillance Report, 2015; vol. 27.
3. Centers for Disease Control and Prevention. HIV Among Transgender People.
4. Kaiser Family Foundation. National survey of teens and young adults on HIV/AIDS, Nov. 1, 2012. .
5. J Acquir Immune Defic Syndr. 2016;73(5):547-55.
6. Serving our youth: Findings from a national survey of services providers working with lesbian, gay, bisexual and transgender youth who are homeless or at risk of becoming homeless (The Williams Institute with True Colors and The Palette Fund, 2012).
7. Injustice at every turn: A report of the national transgender discrimination survey (National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011).
8. J Acquir Immune Defic Syndr. 2010 Apr;53(5):661-4.
9. Centers for Disease Control and Prevention. Preexposure prophylaxis for the prevention of HIV infection in the United States: A clinical practice guideline, 2014.
10. JAMA Pediatr. 2017;171(11):1063-71.
11. J Int AIDS Soc. 2016;19. doi: 10.7448/IAS.19.7.21107.
Confronting hate and violence against the LGBT community
It may be unusual for an LGBT health columnist to mention the horrendous events that occurred in Charlottesville, Va., in August 2017. It clearly was a demonstration of hate and violence against racial and ethnic minorities. Unfortunately, the LGBT community – especially LGBT communities of color – are often a target of that kind of hate and violence. This has a detrimental effect on the health of the LGBT community, and I believe that health care providers have a responsibility to address this hate and violence to promote the well-being of this marginalized community.
It cannot be overstated that LGBT individuals frequently experience anti-gay and anti-trans violence. According to the 2015 Federal Bureau of Investigation Hate Crime Statistics, about a fifth of hate crimes reported were based on sexual orientation or gender identity.1 In addition, LGBT youth are eight times as likely to experience bullying at school because of their sexual orientation or gender identity.2 Furthermore, on many surveys on anti-LGBT violence, people of color comprise more than half of the victims.3 There is a strong association between exposure to this violence and the health outcomes of LGBT youth. A study by Russell et al. showed that LGBT youth who were victims of physical violence at school are more likely to be depressed and suicidal and more likely to be diagnosed with an STD,4 and another study showed that LGBT youth who experienced anti-LGBT violence are more likely to engage in substance use.5 The health outcomes from anti-LGBT violence are not limited to the adolescent period – adolescents who experienced this kind of violence are more likely to report higher levels of depression as adults.6 Although researchers still are trying to determine the exact mechanism for these relationships, the most cited (and sensible) explanation is that exposure to anti-LGBT stigma, discrimination, and violence leads to a toxic environment, which in turn increases the risk for mental health problems and maladaptive coping mechanisms (such as substance use) as a response to such an environment.7
What can we do to stand up to the hate and violence against marginalized groups, such as the LGBT community? First, make your office a safe space. With the recent brazen display of hate and violence going around, members the LGBT community are desperate to feel protected. A good place to start is a guide by Advocates for Youth. Second, educate yourself and others. The title physician means “teacher,” and I feel it is your responsibility to teach your peers, colleagues, and the public about how anti-LGBT violence affects the health of LGBT individuals. To be an effective teacher, you need to be up to date on the research on how hatred and intolerance affects the health of the LGBT community. A good place to start is the Human Rights Campaign, which has accurate statistics on anti-LGBT violence and resources to address this problem. Finally, be an advocate. You don’t need to be in the streets with picket signs, nor do you necessarily need to lead the charge against anti-LGBT hate and violence – others will be at the front lines. What you can do is to call for your local, state, and federal government to institute policies that address anti-LGBT violence. Many medical organizations have resources that help health care providers engage with policy makers (check out the American Academy of Pediatrics advocacy page for these resources). Many of our elected officials take our professional opinions seriously.
Anti-gay and anti-trans violence is all too common in the LGBT community, especially violence against LGBT people of color, and this violence can adversely affect their health. Health care providers have a responsibility and the influence to confront these nexuses of hate and intolerance. You don’t need to do something heroic to accomplish this. You are members of a privileged and respected group of professionals, so small actions can coalesce into something that has a large impact on the health and well-being of the communities you serve.
Resources
• Advocates for Youth. Creating Safe Space for GLBTQ Youth: A Toolkit
• Human Rights Campaign. www.hrc.org/resources/
• American Academy of Pediatrics advocacy page: www.aap.org/en-us/advocacy-and-policy/
References
1. U.S. Department of Justice Federal Bureau of Investigation. Uniform Crime Report Hate Crime Statistics, 2015.
2. J Interpers Violence. 2017. doi: 10.1177/0886260517718830.
3. National Coalition of Anti-Violence Programs (NCAVP). Lesbian, Gay, Bisexual, Transgender, Queer and HIV-Affected Hate Violence in 2016.
4. J Sch Health. 2011 May;81(5):223-30.
5. Prev Sci. 2015 Jul;16(5):734-43.
6. Dev Psychol. 2010 Nov;46(6):1580-9.
7. Psychol Bull. 2003 Sep;129(5):674-97.
8. Gallup. Americans Rate Healthcare Providers High on Honesty, Ethics. 2016.
9. The Hippocratic Oath Today. 2001 or Do. No. Harm.
It may be unusual for an LGBT health columnist to mention the horrendous events that occurred in Charlottesville, Va., in August 2017. It clearly was a demonstration of hate and violence against racial and ethnic minorities. Unfortunately, the LGBT community – especially LGBT communities of color – are often a target of that kind of hate and violence. This has a detrimental effect on the health of the LGBT community, and I believe that health care providers have a responsibility to address this hate and violence to promote the well-being of this marginalized community.
It cannot be overstated that LGBT individuals frequently experience anti-gay and anti-trans violence. According to the 2015 Federal Bureau of Investigation Hate Crime Statistics, about a fifth of hate crimes reported were based on sexual orientation or gender identity.1 In addition, LGBT youth are eight times as likely to experience bullying at school because of their sexual orientation or gender identity.2 Furthermore, on many surveys on anti-LGBT violence, people of color comprise more than half of the victims.3 There is a strong association between exposure to this violence and the health outcomes of LGBT youth. A study by Russell et al. showed that LGBT youth who were victims of physical violence at school are more likely to be depressed and suicidal and more likely to be diagnosed with an STD,4 and another study showed that LGBT youth who experienced anti-LGBT violence are more likely to engage in substance use.5 The health outcomes from anti-LGBT violence are not limited to the adolescent period – adolescents who experienced this kind of violence are more likely to report higher levels of depression as adults.6 Although researchers still are trying to determine the exact mechanism for these relationships, the most cited (and sensible) explanation is that exposure to anti-LGBT stigma, discrimination, and violence leads to a toxic environment, which in turn increases the risk for mental health problems and maladaptive coping mechanisms (such as substance use) as a response to such an environment.7
What can we do to stand up to the hate and violence against marginalized groups, such as the LGBT community? First, make your office a safe space. With the recent brazen display of hate and violence going around, members the LGBT community are desperate to feel protected. A good place to start is a guide by Advocates for Youth. Second, educate yourself and others. The title physician means “teacher,” and I feel it is your responsibility to teach your peers, colleagues, and the public about how anti-LGBT violence affects the health of LGBT individuals. To be an effective teacher, you need to be up to date on the research on how hatred and intolerance affects the health of the LGBT community. A good place to start is the Human Rights Campaign, which has accurate statistics on anti-LGBT violence and resources to address this problem. Finally, be an advocate. You don’t need to be in the streets with picket signs, nor do you necessarily need to lead the charge against anti-LGBT hate and violence – others will be at the front lines. What you can do is to call for your local, state, and federal government to institute policies that address anti-LGBT violence. Many medical organizations have resources that help health care providers engage with policy makers (check out the American Academy of Pediatrics advocacy page for these resources). Many of our elected officials take our professional opinions seriously.
Anti-gay and anti-trans violence is all too common in the LGBT community, especially violence against LGBT people of color, and this violence can adversely affect their health. Health care providers have a responsibility and the influence to confront these nexuses of hate and intolerance. You don’t need to do something heroic to accomplish this. You are members of a privileged and respected group of professionals, so small actions can coalesce into something that has a large impact on the health and well-being of the communities you serve.
Resources
• Advocates for Youth. Creating Safe Space for GLBTQ Youth: A Toolkit
• Human Rights Campaign. www.hrc.org/resources/
• American Academy of Pediatrics advocacy page: www.aap.org/en-us/advocacy-and-policy/
References
1. U.S. Department of Justice Federal Bureau of Investigation. Uniform Crime Report Hate Crime Statistics, 2015.
2. J Interpers Violence. 2017. doi: 10.1177/0886260517718830.
3. National Coalition of Anti-Violence Programs (NCAVP). Lesbian, Gay, Bisexual, Transgender, Queer and HIV-Affected Hate Violence in 2016.
4. J Sch Health. 2011 May;81(5):223-30.
5. Prev Sci. 2015 Jul;16(5):734-43.
6. Dev Psychol. 2010 Nov;46(6):1580-9.
7. Psychol Bull. 2003 Sep;129(5):674-97.
8. Gallup. Americans Rate Healthcare Providers High on Honesty, Ethics. 2016.
9. The Hippocratic Oath Today. 2001 or Do. No. Harm.
It may be unusual for an LGBT health columnist to mention the horrendous events that occurred in Charlottesville, Va., in August 2017. It clearly was a demonstration of hate and violence against racial and ethnic minorities. Unfortunately, the LGBT community – especially LGBT communities of color – are often a target of that kind of hate and violence. This has a detrimental effect on the health of the LGBT community, and I believe that health care providers have a responsibility to address this hate and violence to promote the well-being of this marginalized community.
It cannot be overstated that LGBT individuals frequently experience anti-gay and anti-trans violence. According to the 2015 Federal Bureau of Investigation Hate Crime Statistics, about a fifth of hate crimes reported were based on sexual orientation or gender identity.1 In addition, LGBT youth are eight times as likely to experience bullying at school because of their sexual orientation or gender identity.2 Furthermore, on many surveys on anti-LGBT violence, people of color comprise more than half of the victims.3 There is a strong association between exposure to this violence and the health outcomes of LGBT youth. A study by Russell et al. showed that LGBT youth who were victims of physical violence at school are more likely to be depressed and suicidal and more likely to be diagnosed with an STD,4 and another study showed that LGBT youth who experienced anti-LGBT violence are more likely to engage in substance use.5 The health outcomes from anti-LGBT violence are not limited to the adolescent period – adolescents who experienced this kind of violence are more likely to report higher levels of depression as adults.6 Although researchers still are trying to determine the exact mechanism for these relationships, the most cited (and sensible) explanation is that exposure to anti-LGBT stigma, discrimination, and violence leads to a toxic environment, which in turn increases the risk for mental health problems and maladaptive coping mechanisms (such as substance use) as a response to such an environment.7
What can we do to stand up to the hate and violence against marginalized groups, such as the LGBT community? First, make your office a safe space. With the recent brazen display of hate and violence going around, members the LGBT community are desperate to feel protected. A good place to start is a guide by Advocates for Youth. Second, educate yourself and others. The title physician means “teacher,” and I feel it is your responsibility to teach your peers, colleagues, and the public about how anti-LGBT violence affects the health of LGBT individuals. To be an effective teacher, you need to be up to date on the research on how hatred and intolerance affects the health of the LGBT community. A good place to start is the Human Rights Campaign, which has accurate statistics on anti-LGBT violence and resources to address this problem. Finally, be an advocate. You don’t need to be in the streets with picket signs, nor do you necessarily need to lead the charge against anti-LGBT hate and violence – others will be at the front lines. What you can do is to call for your local, state, and federal government to institute policies that address anti-LGBT violence. Many medical organizations have resources that help health care providers engage with policy makers (check out the American Academy of Pediatrics advocacy page for these resources). Many of our elected officials take our professional opinions seriously.
Anti-gay and anti-trans violence is all too common in the LGBT community, especially violence against LGBT people of color, and this violence can adversely affect their health. Health care providers have a responsibility and the influence to confront these nexuses of hate and intolerance. You don’t need to do something heroic to accomplish this. You are members of a privileged and respected group of professionals, so small actions can coalesce into something that has a large impact on the health and well-being of the communities you serve.
Resources
• Advocates for Youth. Creating Safe Space for GLBTQ Youth: A Toolkit
• Human Rights Campaign. www.hrc.org/resources/
• American Academy of Pediatrics advocacy page: www.aap.org/en-us/advocacy-and-policy/
References
1. U.S. Department of Justice Federal Bureau of Investigation. Uniform Crime Report Hate Crime Statistics, 2015.
2. J Interpers Violence. 2017. doi: 10.1177/0886260517718830.
3. National Coalition of Anti-Violence Programs (NCAVP). Lesbian, Gay, Bisexual, Transgender, Queer and HIV-Affected Hate Violence in 2016.
4. J Sch Health. 2011 May;81(5):223-30.
5. Prev Sci. 2015 Jul;16(5):734-43.
6. Dev Psychol. 2010 Nov;46(6):1580-9.
7. Psychol Bull. 2003 Sep;129(5):674-97.
8. Gallup. Americans Rate Healthcare Providers High on Honesty, Ethics. 2016.
9. The Hippocratic Oath Today. 2001 or Do. No. Harm.
Obtaining coverage for transgender and gender-expansive youth
Transgender and gender-expansive youth face many barriers to health care. (Gender-expansive youth are defined as “youth who do not identify with traditional gender roles but are otherwise not confined to one gender narrative or experience.”) Although some of these youth may be fortunate to have a supportive family and access to health care providers proficient in transgender health care, they still face difficulties in having their insurance cover transgender-related services. This is not an impossible task, but it is a constant struggle for many clinicians.
In this column, I will provide some tips and strategies to help clinicians get insurance companies to cover these critical services. However, keep in mind that there is no one-size-fits-all approach to obtaining insurance coverage. In addition, growing uncertainty over the repeal of the Affordable Care Act (ACA) – which was critical in lifting many of the barriers to insurance coverage for transgender individuals – will make this task challenging.
Health insurance is extraordinarily complex. There are multiple private and public plans that vary in the services they cover. This variation is state dependent. And even within states, there is additional variability. Most health insurance plans are purchased by employers, and employers have a choice of what can be covered in their health plans. So even though an insurance company may state that it covers transgender-related services, the patient’s employer may pay for a plan that doesn’t cover such services. The only way to be sure whether a patient’s insurance will cover transgender-related services or not is to contact the insurance provider directly, but with extremely busy schedules and heavy patient loads, this is easier said than done. It would be helpful to have a social worker perform this task, but even having a social worker can be a luxury for some clinics.
The ACA made it easier for transgender individuals to obtain insurance coverage. Three years ago, the U.S. Department of Health and Human Services stated that Medicare’s longstanding exclusion of “transsexual surgical procedures” was no longer valid.1 Although it did not universally ban transgender exclusion policies, it did allow individual states to do so. Thirteen states have explicit policies that ban exclusions of transgender-related services in both private insurance and in Medicaid, and an additional five states have some policies that discourage such practices.2 This allowed some insurance providers and state Medicaid plans to offer coverage of transgender-related services.
Another challenge in obtaining insurance coverage for transgender and gender-expansive youth is claims denial for sex-specific procedures. For example, if a transwoman is designated as “male” in the electronic medical record and requires a breast ultrasound, the insurance company may automatically reject this claim because this procedure is covered for bodies designated as “female.” If the patient’s insurance plan covers transgender-related services, the clinic can notify the insurance company that the patient is transgender; if the patient’s plan does not, then the clinic will need to appeal to the insurance provider. Alternatively, for clinics associated with federally-funded institutions (e.g., most hospitals), the clinician can use Condition Code 45 in the billing to override the sex mismatch, although not all hospitals have implemented this code.3
1. Patient’s identifying information. Usually the patient’s name and date of birth is sufficient. Clinicians should use the patient’s preferred name in the letter, but provide the insurance or legal name of the patient so that the insurance provider can locate the patient’s records.
2. Result of a psychosocial evaluation and diagnosis (if any). Many insurance providers are looking specifically for the gender dysphoria diagnosis.
3. The duration of the referring health professional’s relationship with the patient, which includes the type of evaluation and therapy or counseling (e.g., cognitive behavior therapy or gender coaching).
4. An explanation that the criteria (usually from the World Professional Association for Transgender Health standard of care4 or the Endocrine Society Guidelines titled Endocrine Treatment of Transsexual Persons5) for hormone therapy have been met, and a brief description of the clinical rationale for supporting the client’s request for hormone therapy.
5. A statement that informed consent has been obtained from the patient (or parental permission if the patient is younger than 18 years).
6. A statement that the referring health professional is available for coordination of care.
If the clinician fails to convince the insurance provider of the necessity of covering transgender-related services, the patient still can pay out of pocket. Some hormones can be affordable to certain patients. In the state of Pennsylvania, for example, a 10-mL vial of testosterone can cost anywhere from $60 to $80, and may generally last anywhere from 10 weeks to a year, depending on dosage. Nevertheless, these costs still may be prohibitive for many transgender youth. Many are chronically unemployed or underemployed, or struggle with homelessness.6 Some transgender youth have to the face the excruciatingly difficult choice between having something to eat for the day or living another day with gender dysphoria.
Clinicians should work very hard to make sure that their transgender and gender-expansive patients obtain the care they need. The above strategies may help navigate the complex insurance system. However, insurance policies vary by state, and anti-trans discrimination creates additional barriers to health care. Therefore, clinicians who take care of transgender youth also should advocate for policies that protect these patients from discrimination, and they should advocate for policies that expand medical coverage for this vulnerable population.
Resources
• The Human Rights Campaign keeps a list of insurance plans that cover transgender-related services, but this list is far from comprehensive.
• Healthcare.gov provides some guidance on how to obtain coverage and navigate the insurance system for transgender individuals.
• UCSF Center of Excellence for Transgender Health provides some excellent resources and guidance on obtaining insurance coverage for transgender individuals.
References
1. LGBT Health 2014;1(4):256-8.
2. Map: State Health Insurance Rules: National Center for Transgender Equality, 2016 [Available from: www.transequality.org/issues/resources/map-state-health-insurance-rules].
3. Health insurance coverage issues for transgender people in the United States: University of California, San Fransisco Center of Excellence for Transgender Health, 2017 [Available from: http://transhealth.ucsf.edu/trans?page=guidelines-insurance].
4. International Journal of Transgenderism 2012;13(4):165-232.
5. J Clin Endocrinol Metab 2009;94(9):3132-54.
6. Injustice at Every Turn: A Report of the National Transgender Discrimination Survey. Washington: National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011.
Transgender and gender-expansive youth face many barriers to health care. (Gender-expansive youth are defined as “youth who do not identify with traditional gender roles but are otherwise not confined to one gender narrative or experience.”) Although some of these youth may be fortunate to have a supportive family and access to health care providers proficient in transgender health care, they still face difficulties in having their insurance cover transgender-related services. This is not an impossible task, but it is a constant struggle for many clinicians.
In this column, I will provide some tips and strategies to help clinicians get insurance companies to cover these critical services. However, keep in mind that there is no one-size-fits-all approach to obtaining insurance coverage. In addition, growing uncertainty over the repeal of the Affordable Care Act (ACA) – which was critical in lifting many of the barriers to insurance coverage for transgender individuals – will make this task challenging.
Health insurance is extraordinarily complex. There are multiple private and public plans that vary in the services they cover. This variation is state dependent. And even within states, there is additional variability. Most health insurance plans are purchased by employers, and employers have a choice of what can be covered in their health plans. So even though an insurance company may state that it covers transgender-related services, the patient’s employer may pay for a plan that doesn’t cover such services. The only way to be sure whether a patient’s insurance will cover transgender-related services or not is to contact the insurance provider directly, but with extremely busy schedules and heavy patient loads, this is easier said than done. It would be helpful to have a social worker perform this task, but even having a social worker can be a luxury for some clinics.
The ACA made it easier for transgender individuals to obtain insurance coverage. Three years ago, the U.S. Department of Health and Human Services stated that Medicare’s longstanding exclusion of “transsexual surgical procedures” was no longer valid.1 Although it did not universally ban transgender exclusion policies, it did allow individual states to do so. Thirteen states have explicit policies that ban exclusions of transgender-related services in both private insurance and in Medicaid, and an additional five states have some policies that discourage such practices.2 This allowed some insurance providers and state Medicaid plans to offer coverage of transgender-related services.
Another challenge in obtaining insurance coverage for transgender and gender-expansive youth is claims denial for sex-specific procedures. For example, if a transwoman is designated as “male” in the electronic medical record and requires a breast ultrasound, the insurance company may automatically reject this claim because this procedure is covered for bodies designated as “female.” If the patient’s insurance plan covers transgender-related services, the clinic can notify the insurance company that the patient is transgender; if the patient’s plan does not, then the clinic will need to appeal to the insurance provider. Alternatively, for clinics associated with federally-funded institutions (e.g., most hospitals), the clinician can use Condition Code 45 in the billing to override the sex mismatch, although not all hospitals have implemented this code.3
1. Patient’s identifying information. Usually the patient’s name and date of birth is sufficient. Clinicians should use the patient’s preferred name in the letter, but provide the insurance or legal name of the patient so that the insurance provider can locate the patient’s records.
2. Result of a psychosocial evaluation and diagnosis (if any). Many insurance providers are looking specifically for the gender dysphoria diagnosis.
3. The duration of the referring health professional’s relationship with the patient, which includes the type of evaluation and therapy or counseling (e.g., cognitive behavior therapy or gender coaching).
4. An explanation that the criteria (usually from the World Professional Association for Transgender Health standard of care4 or the Endocrine Society Guidelines titled Endocrine Treatment of Transsexual Persons5) for hormone therapy have been met, and a brief description of the clinical rationale for supporting the client’s request for hormone therapy.
5. A statement that informed consent has been obtained from the patient (or parental permission if the patient is younger than 18 years).
6. A statement that the referring health professional is available for coordination of care.
If the clinician fails to convince the insurance provider of the necessity of covering transgender-related services, the patient still can pay out of pocket. Some hormones can be affordable to certain patients. In the state of Pennsylvania, for example, a 10-mL vial of testosterone can cost anywhere from $60 to $80, and may generally last anywhere from 10 weeks to a year, depending on dosage. Nevertheless, these costs still may be prohibitive for many transgender youth. Many are chronically unemployed or underemployed, or struggle with homelessness.6 Some transgender youth have to the face the excruciatingly difficult choice between having something to eat for the day or living another day with gender dysphoria.
Clinicians should work very hard to make sure that their transgender and gender-expansive patients obtain the care they need. The above strategies may help navigate the complex insurance system. However, insurance policies vary by state, and anti-trans discrimination creates additional barriers to health care. Therefore, clinicians who take care of transgender youth also should advocate for policies that protect these patients from discrimination, and they should advocate for policies that expand medical coverage for this vulnerable population.
Resources
• The Human Rights Campaign keeps a list of insurance plans that cover transgender-related services, but this list is far from comprehensive.
• Healthcare.gov provides some guidance on how to obtain coverage and navigate the insurance system for transgender individuals.
• UCSF Center of Excellence for Transgender Health provides some excellent resources and guidance on obtaining insurance coverage for transgender individuals.
References
1. LGBT Health 2014;1(4):256-8.
2. Map: State Health Insurance Rules: National Center for Transgender Equality, 2016 [Available from: www.transequality.org/issues/resources/map-state-health-insurance-rules].
3. Health insurance coverage issues for transgender people in the United States: University of California, San Fransisco Center of Excellence for Transgender Health, 2017 [Available from: http://transhealth.ucsf.edu/trans?page=guidelines-insurance].
4. International Journal of Transgenderism 2012;13(4):165-232.
5. J Clin Endocrinol Metab 2009;94(9):3132-54.
6. Injustice at Every Turn: A Report of the National Transgender Discrimination Survey. Washington: National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011.
Transgender and gender-expansive youth face many barriers to health care. (Gender-expansive youth are defined as “youth who do not identify with traditional gender roles but are otherwise not confined to one gender narrative or experience.”) Although some of these youth may be fortunate to have a supportive family and access to health care providers proficient in transgender health care, they still face difficulties in having their insurance cover transgender-related services. This is not an impossible task, but it is a constant struggle for many clinicians.
In this column, I will provide some tips and strategies to help clinicians get insurance companies to cover these critical services. However, keep in mind that there is no one-size-fits-all approach to obtaining insurance coverage. In addition, growing uncertainty over the repeal of the Affordable Care Act (ACA) – which was critical in lifting many of the barriers to insurance coverage for transgender individuals – will make this task challenging.
Health insurance is extraordinarily complex. There are multiple private and public plans that vary in the services they cover. This variation is state dependent. And even within states, there is additional variability. Most health insurance plans are purchased by employers, and employers have a choice of what can be covered in their health plans. So even though an insurance company may state that it covers transgender-related services, the patient’s employer may pay for a plan that doesn’t cover such services. The only way to be sure whether a patient’s insurance will cover transgender-related services or not is to contact the insurance provider directly, but with extremely busy schedules and heavy patient loads, this is easier said than done. It would be helpful to have a social worker perform this task, but even having a social worker can be a luxury for some clinics.
The ACA made it easier for transgender individuals to obtain insurance coverage. Three years ago, the U.S. Department of Health and Human Services stated that Medicare’s longstanding exclusion of “transsexual surgical procedures” was no longer valid.1 Although it did not universally ban transgender exclusion policies, it did allow individual states to do so. Thirteen states have explicit policies that ban exclusions of transgender-related services in both private insurance and in Medicaid, and an additional five states have some policies that discourage such practices.2 This allowed some insurance providers and state Medicaid plans to offer coverage of transgender-related services.
Another challenge in obtaining insurance coverage for transgender and gender-expansive youth is claims denial for sex-specific procedures. For example, if a transwoman is designated as “male” in the electronic medical record and requires a breast ultrasound, the insurance company may automatically reject this claim because this procedure is covered for bodies designated as “female.” If the patient’s insurance plan covers transgender-related services, the clinic can notify the insurance company that the patient is transgender; if the patient’s plan does not, then the clinic will need to appeal to the insurance provider. Alternatively, for clinics associated with federally-funded institutions (e.g., most hospitals), the clinician can use Condition Code 45 in the billing to override the sex mismatch, although not all hospitals have implemented this code.3
1. Patient’s identifying information. Usually the patient’s name and date of birth is sufficient. Clinicians should use the patient’s preferred name in the letter, but provide the insurance or legal name of the patient so that the insurance provider can locate the patient’s records.
2. Result of a psychosocial evaluation and diagnosis (if any). Many insurance providers are looking specifically for the gender dysphoria diagnosis.
3. The duration of the referring health professional’s relationship with the patient, which includes the type of evaluation and therapy or counseling (e.g., cognitive behavior therapy or gender coaching).
4. An explanation that the criteria (usually from the World Professional Association for Transgender Health standard of care4 or the Endocrine Society Guidelines titled Endocrine Treatment of Transsexual Persons5) for hormone therapy have been met, and a brief description of the clinical rationale for supporting the client’s request for hormone therapy.
5. A statement that informed consent has been obtained from the patient (or parental permission if the patient is younger than 18 years).
6. A statement that the referring health professional is available for coordination of care.
If the clinician fails to convince the insurance provider of the necessity of covering transgender-related services, the patient still can pay out of pocket. Some hormones can be affordable to certain patients. In the state of Pennsylvania, for example, a 10-mL vial of testosterone can cost anywhere from $60 to $80, and may generally last anywhere from 10 weeks to a year, depending on dosage. Nevertheless, these costs still may be prohibitive for many transgender youth. Many are chronically unemployed or underemployed, or struggle with homelessness.6 Some transgender youth have to the face the excruciatingly difficult choice between having something to eat for the day or living another day with gender dysphoria.
Clinicians should work very hard to make sure that their transgender and gender-expansive patients obtain the care they need. The above strategies may help navigate the complex insurance system. However, insurance policies vary by state, and anti-trans discrimination creates additional barriers to health care. Therefore, clinicians who take care of transgender youth also should advocate for policies that protect these patients from discrimination, and they should advocate for policies that expand medical coverage for this vulnerable population.
Resources
• The Human Rights Campaign keeps a list of insurance plans that cover transgender-related services, but this list is far from comprehensive.
• Healthcare.gov provides some guidance on how to obtain coverage and navigate the insurance system for transgender individuals.
• UCSF Center of Excellence for Transgender Health provides some excellent resources and guidance on obtaining insurance coverage for transgender individuals.
References
1. LGBT Health 2014;1(4):256-8.
2. Map: State Health Insurance Rules: National Center for Transgender Equality, 2016 [Available from: www.transequality.org/issues/resources/map-state-health-insurance-rules].
3. Health insurance coverage issues for transgender people in the United States: University of California, San Fransisco Center of Excellence for Transgender Health, 2017 [Available from: http://transhealth.ucsf.edu/trans?page=guidelines-insurance].
4. International Journal of Transgenderism 2012;13(4):165-232.
5. J Clin Endocrinol Metab 2009;94(9):3132-54.
6. Injustice at Every Turn: A Report of the National Transgender Discrimination Survey. Washington: National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011.
Why state and school policies matter
Recently North Carolina proposed a bill (House Bill 780) that will ban same-sex marriage in the state, even though the U.S. Supreme Court ruled in 2015 that no states can ban same-sex marriage because doing so violates the 14th Amendment. Although many mainly will argue that H.B. 780 is unconstitutional, this bill also can be detrimental to the health of lesbian, gay, and bisexual (LGB) youth.
In March 2017, JAMA Pediatrics published a study on the association between same-sex marriage laws and the rates of suicide attempts.1 Using data from the Youth Risk Behavior Surveillance System, they analyzed the relationship between state policies that permitted same-sex marriage and self-report of suicide attempts within the last 12 months. Thirty percent of LGB youth (13% of the survey population) reported a suicide attempt in the past year prior to any state policies that permitted same-sex marriage, compared with about 9% of the general population. After states implemented pro–same-sex marriage policies, LGB youth suicide attempts dropped to about 26% – a 14% relative decline. This was not limited to LGB youth. The general youth suicide rates declined from 8.6% to 8% – a 7% relative decline. Although the change in suicide attempts was small, the authors determined that the likelihood it occurred by chance was very slim, and concluded that policies enabling same-sex marriage may be associated with an improvement in population health, especially for LGB youth.
This was not the first study examining the relationship between policies and the health of LGB youth. Mark Hatzenbuehler, PhD, of Columbia University, New York, and his associates have published multiple studies on this topic. Four years earlier, Hatzenbuehler et al. published a study on the relationship between antibullying policies and suicide among LGB youth. Using data from the Oregon Healthy Teen survey (2006-2008), he found that LGB youth who live in counties where there are fewer districts with antibullying policies are more than twice as likely to attempt suicide, compared with LGB youth who live in counties where more districts had antibullying policies. Furthermore, the type of antibullying policy mattered. If a district’s antibullying policy did not prohibit bullying based on sexual orientation, then it had no impact on the suicide attempt rates of LGB youth in that area.2 Similar results were found when the relationship between anti–homophobic bullying policies and LGB suicide attempts was examined in the larger Youth Risk Behavior Surveillance System.3
State and local policies also influence other health outcomes among LGB youth. Hatzenbuehler et al. did another study that examined community-level determinants of tobacco use among LGB youth. Again using the data from the Oregon Healthy Teen Survey, they found that LGB youth living in communities that were more supportive of LGB youth (i.e., communities with a high proportion of same-sex couples living in the area, a high proportion of gay-straight alliances at schools, and LGB-specific antibullying policies) were less likely to smoke cigarettes, compared with LGB youth living in communities that were less supportive.4 A similar study in Canada by Konishi et al. found that schools with gay-straight alliances and anti–homophobic bullying policies were less likely to have LGB youth engaging in risky alcohol or illicit drug use.5
Why do these policies matter? A common theme among these policies is that they can either cause or alleviate stress for LGB youth. States that restrict same-sex marriages or schools that do not have any gay-straight alliances may signal to LGB youth that they are not valued or welcomed, or at the very worse, are despised. This creates a hostile and stressful environment for LGB youth, which raises the risk for mental health problems, such as depression and anxiety, which in turn, raises the risk for substance use and suicide.6 Conversely, the presence of a gay-straight alliance at school or a state that allows same-sex marriage may indicate to LGB youth that they are welcomed, if not just tolerated, and may alleviate this risk. Furthermore, antibullying policies seem to reduce the stress associated with bullying among LGB youth because it may serve as a deterrent to bullying based on sexual orientation. Although passing pro-LGB policies will not solve all the health problems among LGB youth, these policies certainly have an impact.
There might be trepidation among some pediatricians about being vocal on a politically charged policy proposal such as H.B. 780. However, suicide and substance use are major concerns for all physicians – especially pediatricians. Policy makers considering passing laws that can affect their LGB constituents should read these studies to see what kind of influence these proposals can have on the health and well-being of LGB youth. Moreover, health care providers should use their expertise, influence, and standing in their community to support policies that encourage protection for LGB youth and oppose policies that can harm LGB youth. These leaders are responsible for ensuring the health of the people they serve.
Dr. Montano is clinical instructor of pediatrics at the University of Pittsburgh and an adolescent medicine physician at Children’s Hospital of Pittsburgh of UPMC.
References
1. JAMA Pediatr. 2017. doi: 10.1001/jamapediatrics.2016.4529.
2. J Adolesc Health. 2013:S21-6. doi: 10.1016/j.jadohealth.2012.08.010.
3. Am J Public Health. 2014. doi: 10.2105/AJPH.2013.301508.
4. Arch Pediatr Adolesc Med. 2011. doi: 10.1001/archpediatrics.2011.64.
5. Prev Med. 2013. doi: 10.1016/j.ypmed.2013.06.031.
6. Psychol Bull. 2003. doi: 10.1037/0033-2909.129.5.674.
Recently North Carolina proposed a bill (House Bill 780) that will ban same-sex marriage in the state, even though the U.S. Supreme Court ruled in 2015 that no states can ban same-sex marriage because doing so violates the 14th Amendment. Although many mainly will argue that H.B. 780 is unconstitutional, this bill also can be detrimental to the health of lesbian, gay, and bisexual (LGB) youth.
In March 2017, JAMA Pediatrics published a study on the association between same-sex marriage laws and the rates of suicide attempts.1 Using data from the Youth Risk Behavior Surveillance System, they analyzed the relationship between state policies that permitted same-sex marriage and self-report of suicide attempts within the last 12 months. Thirty percent of LGB youth (13% of the survey population) reported a suicide attempt in the past year prior to any state policies that permitted same-sex marriage, compared with about 9% of the general population. After states implemented pro–same-sex marriage policies, LGB youth suicide attempts dropped to about 26% – a 14% relative decline. This was not limited to LGB youth. The general youth suicide rates declined from 8.6% to 8% – a 7% relative decline. Although the change in suicide attempts was small, the authors determined that the likelihood it occurred by chance was very slim, and concluded that policies enabling same-sex marriage may be associated with an improvement in population health, especially for LGB youth.
This was not the first study examining the relationship between policies and the health of LGB youth. Mark Hatzenbuehler, PhD, of Columbia University, New York, and his associates have published multiple studies on this topic. Four years earlier, Hatzenbuehler et al. published a study on the relationship between antibullying policies and suicide among LGB youth. Using data from the Oregon Healthy Teen survey (2006-2008), he found that LGB youth who live in counties where there are fewer districts with antibullying policies are more than twice as likely to attempt suicide, compared with LGB youth who live in counties where more districts had antibullying policies. Furthermore, the type of antibullying policy mattered. If a district’s antibullying policy did not prohibit bullying based on sexual orientation, then it had no impact on the suicide attempt rates of LGB youth in that area.2 Similar results were found when the relationship between anti–homophobic bullying policies and LGB suicide attempts was examined in the larger Youth Risk Behavior Surveillance System.3
State and local policies also influence other health outcomes among LGB youth. Hatzenbuehler et al. did another study that examined community-level determinants of tobacco use among LGB youth. Again using the data from the Oregon Healthy Teen Survey, they found that LGB youth living in communities that were more supportive of LGB youth (i.e., communities with a high proportion of same-sex couples living in the area, a high proportion of gay-straight alliances at schools, and LGB-specific antibullying policies) were less likely to smoke cigarettes, compared with LGB youth living in communities that were less supportive.4 A similar study in Canada by Konishi et al. found that schools with gay-straight alliances and anti–homophobic bullying policies were less likely to have LGB youth engaging in risky alcohol or illicit drug use.5
Why do these policies matter? A common theme among these policies is that they can either cause or alleviate stress for LGB youth. States that restrict same-sex marriages or schools that do not have any gay-straight alliances may signal to LGB youth that they are not valued or welcomed, or at the very worse, are despised. This creates a hostile and stressful environment for LGB youth, which raises the risk for mental health problems, such as depression and anxiety, which in turn, raises the risk for substance use and suicide.6 Conversely, the presence of a gay-straight alliance at school or a state that allows same-sex marriage may indicate to LGB youth that they are welcomed, if not just tolerated, and may alleviate this risk. Furthermore, antibullying policies seem to reduce the stress associated with bullying among LGB youth because it may serve as a deterrent to bullying based on sexual orientation. Although passing pro-LGB policies will not solve all the health problems among LGB youth, these policies certainly have an impact.
There might be trepidation among some pediatricians about being vocal on a politically charged policy proposal such as H.B. 780. However, suicide and substance use are major concerns for all physicians – especially pediatricians. Policy makers considering passing laws that can affect their LGB constituents should read these studies to see what kind of influence these proposals can have on the health and well-being of LGB youth. Moreover, health care providers should use their expertise, influence, and standing in their community to support policies that encourage protection for LGB youth and oppose policies that can harm LGB youth. These leaders are responsible for ensuring the health of the people they serve.
Dr. Montano is clinical instructor of pediatrics at the University of Pittsburgh and an adolescent medicine physician at Children’s Hospital of Pittsburgh of UPMC.
References
1. JAMA Pediatr. 2017. doi: 10.1001/jamapediatrics.2016.4529.
2. J Adolesc Health. 2013:S21-6. doi: 10.1016/j.jadohealth.2012.08.010.
3. Am J Public Health. 2014. doi: 10.2105/AJPH.2013.301508.
4. Arch Pediatr Adolesc Med. 2011. doi: 10.1001/archpediatrics.2011.64.
5. Prev Med. 2013. doi: 10.1016/j.ypmed.2013.06.031.
6. Psychol Bull. 2003. doi: 10.1037/0033-2909.129.5.674.
Recently North Carolina proposed a bill (House Bill 780) that will ban same-sex marriage in the state, even though the U.S. Supreme Court ruled in 2015 that no states can ban same-sex marriage because doing so violates the 14th Amendment. Although many mainly will argue that H.B. 780 is unconstitutional, this bill also can be detrimental to the health of lesbian, gay, and bisexual (LGB) youth.
In March 2017, JAMA Pediatrics published a study on the association between same-sex marriage laws and the rates of suicide attempts.1 Using data from the Youth Risk Behavior Surveillance System, they analyzed the relationship between state policies that permitted same-sex marriage and self-report of suicide attempts within the last 12 months. Thirty percent of LGB youth (13% of the survey population) reported a suicide attempt in the past year prior to any state policies that permitted same-sex marriage, compared with about 9% of the general population. After states implemented pro–same-sex marriage policies, LGB youth suicide attempts dropped to about 26% – a 14% relative decline. This was not limited to LGB youth. The general youth suicide rates declined from 8.6% to 8% – a 7% relative decline. Although the change in suicide attempts was small, the authors determined that the likelihood it occurred by chance was very slim, and concluded that policies enabling same-sex marriage may be associated with an improvement in population health, especially for LGB youth.
This was not the first study examining the relationship between policies and the health of LGB youth. Mark Hatzenbuehler, PhD, of Columbia University, New York, and his associates have published multiple studies on this topic. Four years earlier, Hatzenbuehler et al. published a study on the relationship between antibullying policies and suicide among LGB youth. Using data from the Oregon Healthy Teen survey (2006-2008), he found that LGB youth who live in counties where there are fewer districts with antibullying policies are more than twice as likely to attempt suicide, compared with LGB youth who live in counties where more districts had antibullying policies. Furthermore, the type of antibullying policy mattered. If a district’s antibullying policy did not prohibit bullying based on sexual orientation, then it had no impact on the suicide attempt rates of LGB youth in that area.2 Similar results were found when the relationship between anti–homophobic bullying policies and LGB suicide attempts was examined in the larger Youth Risk Behavior Surveillance System.3
State and local policies also influence other health outcomes among LGB youth. Hatzenbuehler et al. did another study that examined community-level determinants of tobacco use among LGB youth. Again using the data from the Oregon Healthy Teen Survey, they found that LGB youth living in communities that were more supportive of LGB youth (i.e., communities with a high proportion of same-sex couples living in the area, a high proportion of gay-straight alliances at schools, and LGB-specific antibullying policies) were less likely to smoke cigarettes, compared with LGB youth living in communities that were less supportive.4 A similar study in Canada by Konishi et al. found that schools with gay-straight alliances and anti–homophobic bullying policies were less likely to have LGB youth engaging in risky alcohol or illicit drug use.5
Why do these policies matter? A common theme among these policies is that they can either cause or alleviate stress for LGB youth. States that restrict same-sex marriages or schools that do not have any gay-straight alliances may signal to LGB youth that they are not valued or welcomed, or at the very worse, are despised. This creates a hostile and stressful environment for LGB youth, which raises the risk for mental health problems, such as depression and anxiety, which in turn, raises the risk for substance use and suicide.6 Conversely, the presence of a gay-straight alliance at school or a state that allows same-sex marriage may indicate to LGB youth that they are welcomed, if not just tolerated, and may alleviate this risk. Furthermore, antibullying policies seem to reduce the stress associated with bullying among LGB youth because it may serve as a deterrent to bullying based on sexual orientation. Although passing pro-LGB policies will not solve all the health problems among LGB youth, these policies certainly have an impact.
There might be trepidation among some pediatricians about being vocal on a politically charged policy proposal such as H.B. 780. However, suicide and substance use are major concerns for all physicians – especially pediatricians. Policy makers considering passing laws that can affect their LGB constituents should read these studies to see what kind of influence these proposals can have on the health and well-being of LGB youth. Moreover, health care providers should use their expertise, influence, and standing in their community to support policies that encourage protection for LGB youth and oppose policies that can harm LGB youth. These leaders are responsible for ensuring the health of the people they serve.
Dr. Montano is clinical instructor of pediatrics at the University of Pittsburgh and an adolescent medicine physician at Children’s Hospital of Pittsburgh of UPMC.
References
1. JAMA Pediatr. 2017. doi: 10.1001/jamapediatrics.2016.4529.
2. J Adolesc Health. 2013:S21-6. doi: 10.1016/j.jadohealth.2012.08.010.
3. Am J Public Health. 2014. doi: 10.2105/AJPH.2013.301508.
4. Arch Pediatr Adolesc Med. 2011. doi: 10.1001/archpediatrics.2011.64.
5. Prev Med. 2013. doi: 10.1016/j.ypmed.2013.06.031.
6. Psychol Bull. 2003. doi: 10.1037/0033-2909.129.5.674.
Eating disorders in transgender youth
The field of transgender health is growing. What began as a lone German physician in 1918 defying the norms of treating gender identity as a disease now has burgeoned into a field that includes 1,079 PubMed articles,two medical guidelines1,2, and a multitude of books. As we learn more about the complexity of gender and gender identity, we also are discovering potential problems that occur when providing care to our transgender patients. One is eating disorders.
A systematic review by Jones et al. showed only a handful of studies on eating disorders in transgender individuals, most of them restricted to case studies.3 In some situations, the issue of gender identity arises during treatment for an eating disorder, as the individual realizes that body dissatisfaction is due to the gender identity instead of a fear of gaining weight. In other cases, a transgender person in the process of transitioning to the affirmed gender develops an eating disorder.
There are two larger quantitative studies on eating disorders among transgender individuals. One study of 289,024 college students reveals that transgender students, compared to cisgender students, are almost five times as likely to report an eating disorder and two times as likely to use unhealthy compensatory methods (e.g., vomiting) for weight control.4 Another study of almost 2,500 teenagers shows that transgender individuals are almost three times as likely to restrict their eating, almost nine times as likely to take diet pills, and seven times as likely to take laxatives.5
The most commonly suggested reason for the possible elevated risk for eating disorders among transgender individuals is that many of them are trying to achieve the unrealistic standards of the ideal masculine or feminine body type. Another explanation is that eating disorders among transgender individuals are maladaptive coping mechanisms to stress from antitrans stigma and discrimination.4 However, these explanations are not mutually exclusive and could simultaneously drive disordered eating among transgender individuals.
To further appreciate the relationship between these two conditions, one must understand their similarities and differences. The Diagnostic Statistical Manual of Mental Disorders V characterizes eating disorders as “a persistent disturbance of eating or eating-related behavior that results in the altered consumption or absorption of food and ... significantly impairs physical health or psychosocial functioning.”6 Anorexia nervosa and bulimia nervosa are driven by fear of gaining weight or by a self-esteem unduly influenced by weight or appearance.6
Gender dysphoria, in comparison, is the distress caused by the incongruence between one’s gender identity and one’s anatomy, along with the desire to have the characteristics of one’s affirmed gender identity. This condition also could severely alter physical and psychosocial functioning,7 partly because of the distress from the incongruence, and partly because of the stress from antitrans stigma and discrimination, as an individual attempts to match the body with the gender identity8 (e.g., wearing clothing to match the gender identity).
The higher risk of developing an eating disorder among transgender individuals makes sense. Dissatisfaction with one’s body characterizes both conditions. The high standards on what is masculine or feminine affects everyone, especially transgender individuals who may feel that they’re “far behind” when they begin to transition to their affirmed gender. In addition, both involve identity. Those who have anorexia nervosa also incorporate this into their own identity.9 This is why treating an eating disorder can be very difficult.
Finally, individuals afflicted by an eating disorder or gender dysphoria engage in certain behaviors to achieve their desired appearance. However, this is where the similarities end. One major distinction between an eating disorder and gender dysphoria is the treatment approach. The goal in treating an eating disorder is to discourage the disordered behavior and encourage healthier eating habits and a more positive body image. Affirming the identity of someone with an eating disorder can be deadly, as it will encourage more disordered eating.10 In contrast, affirming the identity of someone with gender dysphoria through social transition, cross-sex hormones, and/or surgical reassignment is life-saving and therapeutic.11
There is little guidance on how to treat the these disorders simultaneously. What complicates treating both conditions at the same time is that when an eating disorder is accompanied by another mental health disorder (e.g., substance use), one condition over the other is prioritized.12 There is no guidance on whether the eating disorder or gender dysphoria should take priority over the other, or if it is possible to treat both conditions at the same time.
Strandjord et al. suggest a hierarchal approach, in which life-threatening issues (such as suicide or electrolyte disturbances) take priority.13 In addition, if the patient is malnourished, weight restoration should be the initial focus. A patient who is severely malnourished may not have the cognitive capacity nor the physiological ability to manage comorbidities such as anxiety or depression,12 much less have the capacity to process something as complex as gender and gender identity, nor understand the steps necessary for a successful transition to the affirmed gender. However, this does not mean providers should wait to successfully manage an eating disorder before addressing gender dysphoria. Studies have suggested that gender-affirming medical therapies (e.g., cross sex hormones) can be therapeutic for both gender dysphoria and eating disorder symptoms.14 Finally, because of the two ways a transgender patient with an eating disorder can present, I recommend screening for eating disorders in transgender individuals and inquiring about gender identity among those with an eating disorder. Doing so may save a life.
References
1. J Clin Endocrinol Metab. 2009 Sep;94(9):3132-54.
2. Adv Urol. 2012;2012:581712.
3. Int Rev Psychiatry. 2016;28(1):81-94.
4. J Adolesc Health. 2015 Aug;57(2):144-9.
5. J Adolesc Health. 2016. doi: 10.1016/j.jadohealth.2016.08.027.
6. Feeding and Eating Disorders. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. (Washington: American Psychiatric Association, 2013).
7. Gender Dysphoria. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. (Washington: American Psychiatric Association, 2013).
8. Psychol Bull. 2003 Sep;129(5):674-97.
9. Int J Law Psychiatry. 2003 Sep-Oct;26(5):533-48.
10. Arch Gen Psychiatry. 2011 Jul;68(7):724-31.
11. Clin Endocrinol (Oxf). 2010 Feb;72(2):214-31.
12. CNS drugs. 2006;20(8):655-63.
13. Int J Eat Disord. 2015 Nov;48(7):942-5.
14. Eat Disord. 2012;20(4):300-11.
The field of transgender health is growing. What began as a lone German physician in 1918 defying the norms of treating gender identity as a disease now has burgeoned into a field that includes 1,079 PubMed articles,two medical guidelines1,2, and a multitude of books. As we learn more about the complexity of gender and gender identity, we also are discovering potential problems that occur when providing care to our transgender patients. One is eating disorders.
A systematic review by Jones et al. showed only a handful of studies on eating disorders in transgender individuals, most of them restricted to case studies.3 In some situations, the issue of gender identity arises during treatment for an eating disorder, as the individual realizes that body dissatisfaction is due to the gender identity instead of a fear of gaining weight. In other cases, a transgender person in the process of transitioning to the affirmed gender develops an eating disorder.
There are two larger quantitative studies on eating disorders among transgender individuals. One study of 289,024 college students reveals that transgender students, compared to cisgender students, are almost five times as likely to report an eating disorder and two times as likely to use unhealthy compensatory methods (e.g., vomiting) for weight control.4 Another study of almost 2,500 teenagers shows that transgender individuals are almost three times as likely to restrict their eating, almost nine times as likely to take diet pills, and seven times as likely to take laxatives.5
The most commonly suggested reason for the possible elevated risk for eating disorders among transgender individuals is that many of them are trying to achieve the unrealistic standards of the ideal masculine or feminine body type. Another explanation is that eating disorders among transgender individuals are maladaptive coping mechanisms to stress from antitrans stigma and discrimination.4 However, these explanations are not mutually exclusive and could simultaneously drive disordered eating among transgender individuals.
To further appreciate the relationship between these two conditions, one must understand their similarities and differences. The Diagnostic Statistical Manual of Mental Disorders V characterizes eating disorders as “a persistent disturbance of eating or eating-related behavior that results in the altered consumption or absorption of food and ... significantly impairs physical health or psychosocial functioning.”6 Anorexia nervosa and bulimia nervosa are driven by fear of gaining weight or by a self-esteem unduly influenced by weight or appearance.6
Gender dysphoria, in comparison, is the distress caused by the incongruence between one’s gender identity and one’s anatomy, along with the desire to have the characteristics of one’s affirmed gender identity. This condition also could severely alter physical and psychosocial functioning,7 partly because of the distress from the incongruence, and partly because of the stress from antitrans stigma and discrimination, as an individual attempts to match the body with the gender identity8 (e.g., wearing clothing to match the gender identity).
The higher risk of developing an eating disorder among transgender individuals makes sense. Dissatisfaction with one’s body characterizes both conditions. The high standards on what is masculine or feminine affects everyone, especially transgender individuals who may feel that they’re “far behind” when they begin to transition to their affirmed gender. In addition, both involve identity. Those who have anorexia nervosa also incorporate this into their own identity.9 This is why treating an eating disorder can be very difficult.
Finally, individuals afflicted by an eating disorder or gender dysphoria engage in certain behaviors to achieve their desired appearance. However, this is where the similarities end. One major distinction between an eating disorder and gender dysphoria is the treatment approach. The goal in treating an eating disorder is to discourage the disordered behavior and encourage healthier eating habits and a more positive body image. Affirming the identity of someone with an eating disorder can be deadly, as it will encourage more disordered eating.10 In contrast, affirming the identity of someone with gender dysphoria through social transition, cross-sex hormones, and/or surgical reassignment is life-saving and therapeutic.11
There is little guidance on how to treat the these disorders simultaneously. What complicates treating both conditions at the same time is that when an eating disorder is accompanied by another mental health disorder (e.g., substance use), one condition over the other is prioritized.12 There is no guidance on whether the eating disorder or gender dysphoria should take priority over the other, or if it is possible to treat both conditions at the same time.
Strandjord et al. suggest a hierarchal approach, in which life-threatening issues (such as suicide or electrolyte disturbances) take priority.13 In addition, if the patient is malnourished, weight restoration should be the initial focus. A patient who is severely malnourished may not have the cognitive capacity nor the physiological ability to manage comorbidities such as anxiety or depression,12 much less have the capacity to process something as complex as gender and gender identity, nor understand the steps necessary for a successful transition to the affirmed gender. However, this does not mean providers should wait to successfully manage an eating disorder before addressing gender dysphoria. Studies have suggested that gender-affirming medical therapies (e.g., cross sex hormones) can be therapeutic for both gender dysphoria and eating disorder symptoms.14 Finally, because of the two ways a transgender patient with an eating disorder can present, I recommend screening for eating disorders in transgender individuals and inquiring about gender identity among those with an eating disorder. Doing so may save a life.
References
1. J Clin Endocrinol Metab. 2009 Sep;94(9):3132-54.
2. Adv Urol. 2012;2012:581712.
3. Int Rev Psychiatry. 2016;28(1):81-94.
4. J Adolesc Health. 2015 Aug;57(2):144-9.
5. J Adolesc Health. 2016. doi: 10.1016/j.jadohealth.2016.08.027.
6. Feeding and Eating Disorders. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. (Washington: American Psychiatric Association, 2013).
7. Gender Dysphoria. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. (Washington: American Psychiatric Association, 2013).
8. Psychol Bull. 2003 Sep;129(5):674-97.
9. Int J Law Psychiatry. 2003 Sep-Oct;26(5):533-48.
10. Arch Gen Psychiatry. 2011 Jul;68(7):724-31.
11. Clin Endocrinol (Oxf). 2010 Feb;72(2):214-31.
12. CNS drugs. 2006;20(8):655-63.
13. Int J Eat Disord. 2015 Nov;48(7):942-5.
14. Eat Disord. 2012;20(4):300-11.
The field of transgender health is growing. What began as a lone German physician in 1918 defying the norms of treating gender identity as a disease now has burgeoned into a field that includes 1,079 PubMed articles,two medical guidelines1,2, and a multitude of books. As we learn more about the complexity of gender and gender identity, we also are discovering potential problems that occur when providing care to our transgender patients. One is eating disorders.
A systematic review by Jones et al. showed only a handful of studies on eating disorders in transgender individuals, most of them restricted to case studies.3 In some situations, the issue of gender identity arises during treatment for an eating disorder, as the individual realizes that body dissatisfaction is due to the gender identity instead of a fear of gaining weight. In other cases, a transgender person in the process of transitioning to the affirmed gender develops an eating disorder.
There are two larger quantitative studies on eating disorders among transgender individuals. One study of 289,024 college students reveals that transgender students, compared to cisgender students, are almost five times as likely to report an eating disorder and two times as likely to use unhealthy compensatory methods (e.g., vomiting) for weight control.4 Another study of almost 2,500 teenagers shows that transgender individuals are almost three times as likely to restrict their eating, almost nine times as likely to take diet pills, and seven times as likely to take laxatives.5
The most commonly suggested reason for the possible elevated risk for eating disorders among transgender individuals is that many of them are trying to achieve the unrealistic standards of the ideal masculine or feminine body type. Another explanation is that eating disorders among transgender individuals are maladaptive coping mechanisms to stress from antitrans stigma and discrimination.4 However, these explanations are not mutually exclusive and could simultaneously drive disordered eating among transgender individuals.
To further appreciate the relationship between these two conditions, one must understand their similarities and differences. The Diagnostic Statistical Manual of Mental Disorders V characterizes eating disorders as “a persistent disturbance of eating or eating-related behavior that results in the altered consumption or absorption of food and ... significantly impairs physical health or psychosocial functioning.”6 Anorexia nervosa and bulimia nervosa are driven by fear of gaining weight or by a self-esteem unduly influenced by weight or appearance.6
Gender dysphoria, in comparison, is the distress caused by the incongruence between one’s gender identity and one’s anatomy, along with the desire to have the characteristics of one’s affirmed gender identity. This condition also could severely alter physical and psychosocial functioning,7 partly because of the distress from the incongruence, and partly because of the stress from antitrans stigma and discrimination, as an individual attempts to match the body with the gender identity8 (e.g., wearing clothing to match the gender identity).
The higher risk of developing an eating disorder among transgender individuals makes sense. Dissatisfaction with one’s body characterizes both conditions. The high standards on what is masculine or feminine affects everyone, especially transgender individuals who may feel that they’re “far behind” when they begin to transition to their affirmed gender. In addition, both involve identity. Those who have anorexia nervosa also incorporate this into their own identity.9 This is why treating an eating disorder can be very difficult.
Finally, individuals afflicted by an eating disorder or gender dysphoria engage in certain behaviors to achieve their desired appearance. However, this is where the similarities end. One major distinction between an eating disorder and gender dysphoria is the treatment approach. The goal in treating an eating disorder is to discourage the disordered behavior and encourage healthier eating habits and a more positive body image. Affirming the identity of someone with an eating disorder can be deadly, as it will encourage more disordered eating.10 In contrast, affirming the identity of someone with gender dysphoria through social transition, cross-sex hormones, and/or surgical reassignment is life-saving and therapeutic.11
There is little guidance on how to treat the these disorders simultaneously. What complicates treating both conditions at the same time is that when an eating disorder is accompanied by another mental health disorder (e.g., substance use), one condition over the other is prioritized.12 There is no guidance on whether the eating disorder or gender dysphoria should take priority over the other, or if it is possible to treat both conditions at the same time.
Strandjord et al. suggest a hierarchal approach, in which life-threatening issues (such as suicide or electrolyte disturbances) take priority.13 In addition, if the patient is malnourished, weight restoration should be the initial focus. A patient who is severely malnourished may not have the cognitive capacity nor the physiological ability to manage comorbidities such as anxiety or depression,12 much less have the capacity to process something as complex as gender and gender identity, nor understand the steps necessary for a successful transition to the affirmed gender. However, this does not mean providers should wait to successfully manage an eating disorder before addressing gender dysphoria. Studies have suggested that gender-affirming medical therapies (e.g., cross sex hormones) can be therapeutic for both gender dysphoria and eating disorder symptoms.14 Finally, because of the two ways a transgender patient with an eating disorder can present, I recommend screening for eating disorders in transgender individuals and inquiring about gender identity among those with an eating disorder. Doing so may save a life.
References
1. J Clin Endocrinol Metab. 2009 Sep;94(9):3132-54.
2. Adv Urol. 2012;2012:581712.
3. Int Rev Psychiatry. 2016;28(1):81-94.
4. J Adolesc Health. 2015 Aug;57(2):144-9.
5. J Adolesc Health. 2016. doi: 10.1016/j.jadohealth.2016.08.027.
6. Feeding and Eating Disorders. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. (Washington: American Psychiatric Association, 2013).
7. Gender Dysphoria. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. (Washington: American Psychiatric Association, 2013).
8. Psychol Bull. 2003 Sep;129(5):674-97.
9. Int J Law Psychiatry. 2003 Sep-Oct;26(5):533-48.
10. Arch Gen Psychiatry. 2011 Jul;68(7):724-31.
11. Clin Endocrinol (Oxf). 2010 Feb;72(2):214-31.
12. CNS drugs. 2006;20(8):655-63.
13. Int J Eat Disord. 2015 Nov;48(7):942-5.
14. Eat Disord. 2012;20(4):300-11.
Addressing sexuality, gender identity issues is key to positive outcomes
A while ago, I gave a talk on LGBT health to a group of primary care pediatricians. Although I was glad that they invited me to speak, I also sensed some discomfort in the audience. At the end of the lecture, many pediatricians told me that they were uncomfortable with bringing up the topic of sexuality and gender identity with their patients, and others wanted guidance on how to ask questions on sexuality and gender identity.
There are many barriers for primary pediatricians in addressing sexuality and gender identity concerns in their patients. First, pediatricians often will have up to 15 minutes for a visit, so they will have little time to address a complex issue. Second, primary care pediatricians may have known many of their patients since birth, and asking questions on sexuality and gender can feel awkward. Finally, many pediatricians may be working in more conservative areas in the country where asking questions on sexuality and gender identity may be controversial.
Although a very important topic, there is not much empirical evidence on how to ask questions on sexuality and gender appropriately, and most of these recommendations are based on my own experience working with LGBT youth. Regardless, I hope these pointers will help the primary care pediatrician address the needs of LGBT youth efficiently and with sensitivity.
Tip No. 1: The environment counts
I cannot overstate how important it is to make your clinic a welcoming place for LGBT youth. Having various signs and stickers – like rainbow flags or the Human Rights Campaign sticker – will signal to LGBT youth that they are safe in your clinic. Creating a safe and welcoming environment is important because many people in the LGBT community have experienced rejection and discrimination from their primary care doctors.1 Making your clinic a safe space will make it easier and efficient for patients to ask questions about sexuality and gender identity (see Dr. Gaya Chelvakumar’s column “Creating safe spaces for LGBTQ youth, families in health care settings” at pediatricnews.com).
Tip No. 2: Consider the context
Most likely, many presenting complaints – such as colds or sports injuries – of your adolescent patients will not involve sexual orientation or gender identity. There are exceptions. If you suspect an STD, then the risk for certain infections, such as HIV2 or gonorrhea of the anus or of the pharynx3 are higher in gay young men. For the latter, your screening method would be different (that is, obtaining a pharyngeal swab or an anal swab instead of a urine sample). Also, because many LGBT youth have higher rates of mental health problems compared with heterosexual youth,4 you may want to ask questions about sexuality or gender identity to patients complaining of depressive or anxiety symptoms. This is especially important for transgender youth, because the implementation of pubertal blockers or cross-sex hormones can be therapeutic.5 To prevent or reduce many of these health problems, asking about sexuality and gender identity is a good idea during the well visit, when you may have more time.
Tip No. 3: Not all developmental stages are considered equal
Adolescence is a period of rapid and phasic growth. Formation of an identity is one of the major psychosocial tasks for adolescence,6 and sexuality and gender are important identities. In general, in early adolescence identity becomes an issue as the teenager gains autonomy from parents. I typically start asking questions about sexuality and gender when the patient is 11 or 12, because many children may not understand sexuality and gender identity at a younger age. At these ages, I ask these questions with the parents in the room, then I ask them confidentially on subsequent well visits. This approach serves two purposes: it will prepare the adolescent for these complex and thought-provoking questions in future encounters, and it gives the parents an idea of the type of questions you will ask the children when they are old enough for the confidential visit, helping parents feel more comfortable in stepping out of the room during this time.
Tip No. 4: Keep it confidential
Many adolescents are reluctant to see a doctor, even if they are sick. The primary reason adolescents do not seek care is the fear that the provider will tell their parents about their illness.7 Although this should be applicable to all of your adolescent patients, you should make an extra effort to explicitly state to LGBT patients that the clinic visit is confidential (with the exception of risk of suicide, homicide, or child abuse). This is important for LGBT youth who are not out to their parents and may be in danger if they do come out.8
Tip No. 5: Normalize, normalize, normalize
Because of the stigma and discrimination surrounding sexual orientation and gender identity, many LGBT youth will be reluctant to disclose their sexual orientation or gender identity to their health care providers. At the same time, heterosexual youth may think that you’re asking them questions about sexuality or gender identity because you suspect them to be a member of the LGBT community. To avoid this awkward situation, many pediatricians do not ask these questions at all. A good remedy for this is to preface your questions about sexual orientation or gender identity by saying that you ask these questions to all your patients – that way no one feels singled out.
Tip No. 6: Ask for permission
As previously mentioned, members of the LGBT community may experience discrimination from their health care providers after disclosing to them their sexual orientation or gender identity.1 This rejection can be traumatizing for LGBT youth, making them reluctant to discuss any issues related to sexual orientation or gender identity with any medical provider. As part of the trauma-informed approach, asking for permission before delving into issues related to sexual orientation and gender identity will give LGBT patients a sense of control, especially in an environment where there is a significant power differential.
Tip No. 7: Treat this as a skill
Despite the pressures for primary care pediatricians to maintain an efficient and effective clinical practice, many strive to learn new skills to provide the best care for their patients. Asking questions about sexuality and gender identity should be one of those skills. As with any skill, it will feel unnatural at first, and it will require practice. Mastering this skill, however, will help you address the health needs of this vulnerable population.
Asking questions about sexuality and gender identity is difficult for the primary care pediatrician. Hopefully, these tips can help you develop this important skill. It will also help you reach out to a population that is wary of the health care system.
References
1. J Am Board Fam Med. 2016;29(1):156-60.
2. https://www.cdc.gov/hiv/group/msm/index.html.
3. https://www.cdc.gov/std/tg2015/default.htm.
4. J Adolesc Health. 2011;49(2):115-23.
5. Nat Rev Endocrinol. 2011;7(8):466-72.
6. Neinstein LS. Adolescent health care: a practical guide. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2008.
7. J Adolesc Health. 2007;40(3):218-26.
8. Am J Orthopsychiatry. 1998;68(3):361-71.
Dr. Montano is an adolescent medicine fellow at Children’s Hospital of Pittsburgh of the University of Pittsburgh Medical Center and a postdoctoral fellow in the department of pediatrics at the University of Pittsburgh. Email him at pdnews@frontlinemedcom.com.
A while ago, I gave a talk on LGBT health to a group of primary care pediatricians. Although I was glad that they invited me to speak, I also sensed some discomfort in the audience. At the end of the lecture, many pediatricians told me that they were uncomfortable with bringing up the topic of sexuality and gender identity with their patients, and others wanted guidance on how to ask questions on sexuality and gender identity.
There are many barriers for primary pediatricians in addressing sexuality and gender identity concerns in their patients. First, pediatricians often will have up to 15 minutes for a visit, so they will have little time to address a complex issue. Second, primary care pediatricians may have known many of their patients since birth, and asking questions on sexuality and gender can feel awkward. Finally, many pediatricians may be working in more conservative areas in the country where asking questions on sexuality and gender identity may be controversial.
Although a very important topic, there is not much empirical evidence on how to ask questions on sexuality and gender appropriately, and most of these recommendations are based on my own experience working with LGBT youth. Regardless, I hope these pointers will help the primary care pediatrician address the needs of LGBT youth efficiently and with sensitivity.
Tip No. 1: The environment counts
I cannot overstate how important it is to make your clinic a welcoming place for LGBT youth. Having various signs and stickers – like rainbow flags or the Human Rights Campaign sticker – will signal to LGBT youth that they are safe in your clinic. Creating a safe and welcoming environment is important because many people in the LGBT community have experienced rejection and discrimination from their primary care doctors.1 Making your clinic a safe space will make it easier and efficient for patients to ask questions about sexuality and gender identity (see Dr. Gaya Chelvakumar’s column “Creating safe spaces for LGBTQ youth, families in health care settings” at pediatricnews.com).
Tip No. 2: Consider the context
Most likely, many presenting complaints – such as colds or sports injuries – of your adolescent patients will not involve sexual orientation or gender identity. There are exceptions. If you suspect an STD, then the risk for certain infections, such as HIV2 or gonorrhea of the anus or of the pharynx3 are higher in gay young men. For the latter, your screening method would be different (that is, obtaining a pharyngeal swab or an anal swab instead of a urine sample). Also, because many LGBT youth have higher rates of mental health problems compared with heterosexual youth,4 you may want to ask questions about sexuality or gender identity to patients complaining of depressive or anxiety symptoms. This is especially important for transgender youth, because the implementation of pubertal blockers or cross-sex hormones can be therapeutic.5 To prevent or reduce many of these health problems, asking about sexuality and gender identity is a good idea during the well visit, when you may have more time.
Tip No. 3: Not all developmental stages are considered equal
Adolescence is a period of rapid and phasic growth. Formation of an identity is one of the major psychosocial tasks for adolescence,6 and sexuality and gender are important identities. In general, in early adolescence identity becomes an issue as the teenager gains autonomy from parents. I typically start asking questions about sexuality and gender when the patient is 11 or 12, because many children may not understand sexuality and gender identity at a younger age. At these ages, I ask these questions with the parents in the room, then I ask them confidentially on subsequent well visits. This approach serves two purposes: it will prepare the adolescent for these complex and thought-provoking questions in future encounters, and it gives the parents an idea of the type of questions you will ask the children when they are old enough for the confidential visit, helping parents feel more comfortable in stepping out of the room during this time.
Tip No. 4: Keep it confidential
Many adolescents are reluctant to see a doctor, even if they are sick. The primary reason adolescents do not seek care is the fear that the provider will tell their parents about their illness.7 Although this should be applicable to all of your adolescent patients, you should make an extra effort to explicitly state to LGBT patients that the clinic visit is confidential (with the exception of risk of suicide, homicide, or child abuse). This is important for LGBT youth who are not out to their parents and may be in danger if they do come out.8
Tip No. 5: Normalize, normalize, normalize
Because of the stigma and discrimination surrounding sexual orientation and gender identity, many LGBT youth will be reluctant to disclose their sexual orientation or gender identity to their health care providers. At the same time, heterosexual youth may think that you’re asking them questions about sexuality or gender identity because you suspect them to be a member of the LGBT community. To avoid this awkward situation, many pediatricians do not ask these questions at all. A good remedy for this is to preface your questions about sexual orientation or gender identity by saying that you ask these questions to all your patients – that way no one feels singled out.
Tip No. 6: Ask for permission
As previously mentioned, members of the LGBT community may experience discrimination from their health care providers after disclosing to them their sexual orientation or gender identity.1 This rejection can be traumatizing for LGBT youth, making them reluctant to discuss any issues related to sexual orientation or gender identity with any medical provider. As part of the trauma-informed approach, asking for permission before delving into issues related to sexual orientation and gender identity will give LGBT patients a sense of control, especially in an environment where there is a significant power differential.
Tip No. 7: Treat this as a skill
Despite the pressures for primary care pediatricians to maintain an efficient and effective clinical practice, many strive to learn new skills to provide the best care for their patients. Asking questions about sexuality and gender identity should be one of those skills. As with any skill, it will feel unnatural at first, and it will require practice. Mastering this skill, however, will help you address the health needs of this vulnerable population.
Asking questions about sexuality and gender identity is difficult for the primary care pediatrician. Hopefully, these tips can help you develop this important skill. It will also help you reach out to a population that is wary of the health care system.
References
1. J Am Board Fam Med. 2016;29(1):156-60.
2. https://www.cdc.gov/hiv/group/msm/index.html.
3. https://www.cdc.gov/std/tg2015/default.htm.
4. J Adolesc Health. 2011;49(2):115-23.
5. Nat Rev Endocrinol. 2011;7(8):466-72.
6. Neinstein LS. Adolescent health care: a practical guide. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2008.
7. J Adolesc Health. 2007;40(3):218-26.
8. Am J Orthopsychiatry. 1998;68(3):361-71.
Dr. Montano is an adolescent medicine fellow at Children’s Hospital of Pittsburgh of the University of Pittsburgh Medical Center and a postdoctoral fellow in the department of pediatrics at the University of Pittsburgh. Email him at pdnews@frontlinemedcom.com.
A while ago, I gave a talk on LGBT health to a group of primary care pediatricians. Although I was glad that they invited me to speak, I also sensed some discomfort in the audience. At the end of the lecture, many pediatricians told me that they were uncomfortable with bringing up the topic of sexuality and gender identity with their patients, and others wanted guidance on how to ask questions on sexuality and gender identity.
There are many barriers for primary pediatricians in addressing sexuality and gender identity concerns in their patients. First, pediatricians often will have up to 15 minutes for a visit, so they will have little time to address a complex issue. Second, primary care pediatricians may have known many of their patients since birth, and asking questions on sexuality and gender can feel awkward. Finally, many pediatricians may be working in more conservative areas in the country where asking questions on sexuality and gender identity may be controversial.
Although a very important topic, there is not much empirical evidence on how to ask questions on sexuality and gender appropriately, and most of these recommendations are based on my own experience working with LGBT youth. Regardless, I hope these pointers will help the primary care pediatrician address the needs of LGBT youth efficiently and with sensitivity.
Tip No. 1: The environment counts
I cannot overstate how important it is to make your clinic a welcoming place for LGBT youth. Having various signs and stickers – like rainbow flags or the Human Rights Campaign sticker – will signal to LGBT youth that they are safe in your clinic. Creating a safe and welcoming environment is important because many people in the LGBT community have experienced rejection and discrimination from their primary care doctors.1 Making your clinic a safe space will make it easier and efficient for patients to ask questions about sexuality and gender identity (see Dr. Gaya Chelvakumar’s column “Creating safe spaces for LGBTQ youth, families in health care settings” at pediatricnews.com).
Tip No. 2: Consider the context
Most likely, many presenting complaints – such as colds or sports injuries – of your adolescent patients will not involve sexual orientation or gender identity. There are exceptions. If you suspect an STD, then the risk for certain infections, such as HIV2 or gonorrhea of the anus or of the pharynx3 are higher in gay young men. For the latter, your screening method would be different (that is, obtaining a pharyngeal swab or an anal swab instead of a urine sample). Also, because many LGBT youth have higher rates of mental health problems compared with heterosexual youth,4 you may want to ask questions about sexuality or gender identity to patients complaining of depressive or anxiety symptoms. This is especially important for transgender youth, because the implementation of pubertal blockers or cross-sex hormones can be therapeutic.5 To prevent or reduce many of these health problems, asking about sexuality and gender identity is a good idea during the well visit, when you may have more time.
Tip No. 3: Not all developmental stages are considered equal
Adolescence is a period of rapid and phasic growth. Formation of an identity is one of the major psychosocial tasks for adolescence,6 and sexuality and gender are important identities. In general, in early adolescence identity becomes an issue as the teenager gains autonomy from parents. I typically start asking questions about sexuality and gender when the patient is 11 or 12, because many children may not understand sexuality and gender identity at a younger age. At these ages, I ask these questions with the parents in the room, then I ask them confidentially on subsequent well visits. This approach serves two purposes: it will prepare the adolescent for these complex and thought-provoking questions in future encounters, and it gives the parents an idea of the type of questions you will ask the children when they are old enough for the confidential visit, helping parents feel more comfortable in stepping out of the room during this time.
Tip No. 4: Keep it confidential
Many adolescents are reluctant to see a doctor, even if they are sick. The primary reason adolescents do not seek care is the fear that the provider will tell their parents about their illness.7 Although this should be applicable to all of your adolescent patients, you should make an extra effort to explicitly state to LGBT patients that the clinic visit is confidential (with the exception of risk of suicide, homicide, or child abuse). This is important for LGBT youth who are not out to their parents and may be in danger if they do come out.8
Tip No. 5: Normalize, normalize, normalize
Because of the stigma and discrimination surrounding sexual orientation and gender identity, many LGBT youth will be reluctant to disclose their sexual orientation or gender identity to their health care providers. At the same time, heterosexual youth may think that you’re asking them questions about sexuality or gender identity because you suspect them to be a member of the LGBT community. To avoid this awkward situation, many pediatricians do not ask these questions at all. A good remedy for this is to preface your questions about sexual orientation or gender identity by saying that you ask these questions to all your patients – that way no one feels singled out.
Tip No. 6: Ask for permission
As previously mentioned, members of the LGBT community may experience discrimination from their health care providers after disclosing to them their sexual orientation or gender identity.1 This rejection can be traumatizing for LGBT youth, making them reluctant to discuss any issues related to sexual orientation or gender identity with any medical provider. As part of the trauma-informed approach, asking for permission before delving into issues related to sexual orientation and gender identity will give LGBT patients a sense of control, especially in an environment where there is a significant power differential.
Tip No. 7: Treat this as a skill
Despite the pressures for primary care pediatricians to maintain an efficient and effective clinical practice, many strive to learn new skills to provide the best care for their patients. Asking questions about sexuality and gender identity should be one of those skills. As with any skill, it will feel unnatural at first, and it will require practice. Mastering this skill, however, will help you address the health needs of this vulnerable population.
Asking questions about sexuality and gender identity is difficult for the primary care pediatrician. Hopefully, these tips can help you develop this important skill. It will also help you reach out to a population that is wary of the health care system.
References
1. J Am Board Fam Med. 2016;29(1):156-60.
2. https://www.cdc.gov/hiv/group/msm/index.html.
3. https://www.cdc.gov/std/tg2015/default.htm.
4. J Adolesc Health. 2011;49(2):115-23.
5. Nat Rev Endocrinol. 2011;7(8):466-72.
6. Neinstein LS. Adolescent health care: a practical guide. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2008.
7. J Adolesc Health. 2007;40(3):218-26.
8. Am J Orthopsychiatry. 1998;68(3):361-71.
Dr. Montano is an adolescent medicine fellow at Children’s Hospital of Pittsburgh of the University of Pittsburgh Medical Center and a postdoctoral fellow in the department of pediatrics at the University of Pittsburgh. Email him at pdnews@frontlinemedcom.com.
Fear and hope: Helping LGBT youth cope with the 2016 election results
The day after the election, Time magazine reported an increased call volume to the Trevor Project, an organization that provides suicide counseling for LGBT youth.1 A colleague of mine who works closely with the Trevor Project told me that this was the second-highest call volume the organization has received since its inception.
Regardless of your political affiliation, we all can agree that this year’s election was divisive. Many minority groups, including the LGBT community, felt singled out. Although many of us have seen contentious elections in our lifetimes, teenagers, especially LGBT youth, are sensitive to this divisiveness.
Many LGBT youth who called the Trevor Project had expressed fear about the future. Whenever someone becomes suicidal, they have an overwhelming sense of hopelessness.2 Many perceive that the upcoming administration may be hostile to the LGBT community, and because many fear that this new administration may undo all the progress made in LGBT rights in the last 8 years, they have little hope for the future. Numerous reports of increased hate-crime incidents since the start of the election season last year may have exacerbated this feeling of hopelessness.3 This hopelessness may cause many to feel that the best way out is through suicide. Others feel that their sexual orientation or gender identity may be an additional burden to their family during this new era, and so to relieve them of this burden, they consider ending their own lives.4
For adults who have seen many administrations come and go, this may seem like hyperbole. But we have the advantage of living through various elections and administrations, knowing that they were not as catastrophic as others claimed. However, for many LGBT teens or young adults, this is probably their first election after reaching adolescence since Obama was elected in 2008. The Obama administration has been friendly to the LGBT community,5 and for LGBT youth, the upcoming Trump administration may be a substantial departure from this friendliness. In addition, people across the political spectrum have stoked fears among LGBT youth that the new administration will be devastating for the LGBT community. Adolescents, compared with adults, respond more strongly to the limbic system of the brain – the part of the brain involved in emotional processing, which includes fear.6 This fear will override any attempt by the prefrontal cortex – the part of the brain involved in cognitive processing6 – to put the results of this election within context and within perspective. In other words, it is easier for the adolescent brain to become much more despondent over a disappointing outcome.
What can providers do for LGBT youth who feel distressed over the outcome of the election? The approach is twofold. First, address the emotions emanating from the limbic system. Once this influence is dampened, engage the prefrontal cortex to process the emotions and address these fears in a more constructive way.
For LGBT youth who are actively suicidal, providers should first determine the risk for suicide (for example, determine the level of family support, access to lethal means of suicide, etc.) Then, depending on the risk, create a suicide safety plan that will help the teen or young adult cope with the distress. For more information on how to address suicidality among LGBT youth, please see my previous column (“It does get better... with your help: Preventing suicide,” October 2016, page 30).
Recognize and validate the fears of LGBT youth. Do not dismiss their fears as an overreaction. Because of the adolescent brain’s responsiveness to the limbic system, their fears and emotions are much more intense than are those of adults. Allow them to express how worried they are about the future. Remind them that you are their advocate and that your goal is to keep them safe. Remind your LGBT patients that people who have advocated for them did not disappear overnight because of the election. Some parents of my LGBT patients have pointed out that many LGBT youth feel safer when a nonfamily member advocates for them; therefore, it is essential to remind your LGBT patients about your role as their physician and their advocate.
Another way to support your LGBT patients during this stressful time is to help create a safe environment for them, especially at school. There are some concerns about an increase in antigay and antitrans harassment and bullying since the election.7 Schools are doing their best to respond appropriately to these incidents.8 Fortunately, many schools are responsive to physicians’ recommendations for preventing and addressing school bullying.9 For more information on how providers can address bullying of LGBT youth in school, please refer to my column on bullying (“Bullying,” May 2016, p.1).
Once you reduce the responsiveness of the adolescent brain to the limbic system, you then can focus on the prefrontal cortex to help adolescents engage and cope with their distress. Have them recall from their civics classes that the United States government has checks and balances and that one person does not have unilateral power. Remind the adolescent that administrations and governments do not last forever and that there is an opportunity to change administrations every 4 years.
One of the most powerful ways to engage the prefrontal cortex of the distressed adolescent is to provide the individual with opportunities to be an active member of the community. They can volunteer in many organizations that share their values and beliefs. These organizations do not need to be political, but they should provide some service to the community. This will remind the adolescents that they can have an impact on their own lives and in the lives of others. Volunteering in these organizations will give them a sense of purpose and create a stronger connection to their communities10 – both are antidotes to the intense feeling of despair and hopelessness.
The fear and concerns that LGBT youth have over the election results are intense and deserve attention. Their neurobiology and lack of experience make these fears much more powerful. Providers, parents, and advocates have the responsibility to address these fears, remind LGBT youth that they are their advocates, and remind LGBT youth of the ability to influence the outcomes of their own lives. Providing skills to cope with disappointing outcomes also will prepare LGBT youth for the challenges of adulthood and for the many elections to come.
Resources
AAP: Talking to your children about the election
HealthyChildren.org: How to support your child’s resilience in a time of crisis
Suicide Prevention Lifeline: Patient safety plan template
References
1. “Donald Trump Win Causes Spike in Crisis Support Line Calls,” Time magazine, Nov. 9, 2016.
2. Int Rev Psychiatry. 1992;4(2):177-84.
3. “U.S. Hate Crimes Surge 6%, Fueled by Attacks on Muslims,” the New York Times, Nov. 14, 2016.
4. Arch Suicide Res. 2015;19(3):385-400.
5. “The president of the United States shifted the mainstream in one interview,” Newsweek, May 13, 2012.
6. Neuropsychiatric Disease and Treatment. 2013;9:449-61.
7. “This is Trump’s America: LGBT community fears surge in hate crimes following reports of homophobic attacks,” Salon magazine, Nov. 13, 2016.
8. “School officials grapple with bullying, harassment after election,” Lansing State Journal, Nov. 13, 2016.
9. “Roles for pediatricians in bullying prevention and intervention,” StopBullying.gov, 2016.
10. Adv Psych Treatment. 2014;20(3):217-24.
Dr. Montano is an adolescent medicine fellow at Children’s Hospital of Pittsburgh of the University of Pittsburgh Medical Center and a postdoctoral fellow in the department of pediatrics the University of Pittsburgh. Email him at pdnews@frontlinemedcom.com.
The day after the election, Time magazine reported an increased call volume to the Trevor Project, an organization that provides suicide counseling for LGBT youth.1 A colleague of mine who works closely with the Trevor Project told me that this was the second-highest call volume the organization has received since its inception.
Regardless of your political affiliation, we all can agree that this year’s election was divisive. Many minority groups, including the LGBT community, felt singled out. Although many of us have seen contentious elections in our lifetimes, teenagers, especially LGBT youth, are sensitive to this divisiveness.
Many LGBT youth who called the Trevor Project had expressed fear about the future. Whenever someone becomes suicidal, they have an overwhelming sense of hopelessness.2 Many perceive that the upcoming administration may be hostile to the LGBT community, and because many fear that this new administration may undo all the progress made in LGBT rights in the last 8 years, they have little hope for the future. Numerous reports of increased hate-crime incidents since the start of the election season last year may have exacerbated this feeling of hopelessness.3 This hopelessness may cause many to feel that the best way out is through suicide. Others feel that their sexual orientation or gender identity may be an additional burden to their family during this new era, and so to relieve them of this burden, they consider ending their own lives.4
For adults who have seen many administrations come and go, this may seem like hyperbole. But we have the advantage of living through various elections and administrations, knowing that they were not as catastrophic as others claimed. However, for many LGBT teens or young adults, this is probably their first election after reaching adolescence since Obama was elected in 2008. The Obama administration has been friendly to the LGBT community,5 and for LGBT youth, the upcoming Trump administration may be a substantial departure from this friendliness. In addition, people across the political spectrum have stoked fears among LGBT youth that the new administration will be devastating for the LGBT community. Adolescents, compared with adults, respond more strongly to the limbic system of the brain – the part of the brain involved in emotional processing, which includes fear.6 This fear will override any attempt by the prefrontal cortex – the part of the brain involved in cognitive processing6 – to put the results of this election within context and within perspective. In other words, it is easier for the adolescent brain to become much more despondent over a disappointing outcome.
What can providers do for LGBT youth who feel distressed over the outcome of the election? The approach is twofold. First, address the emotions emanating from the limbic system. Once this influence is dampened, engage the prefrontal cortex to process the emotions and address these fears in a more constructive way.
For LGBT youth who are actively suicidal, providers should first determine the risk for suicide (for example, determine the level of family support, access to lethal means of suicide, etc.) Then, depending on the risk, create a suicide safety plan that will help the teen or young adult cope with the distress. For more information on how to address suicidality among LGBT youth, please see my previous column (“It does get better... with your help: Preventing suicide,” October 2016, page 30).
Recognize and validate the fears of LGBT youth. Do not dismiss their fears as an overreaction. Because of the adolescent brain’s responsiveness to the limbic system, their fears and emotions are much more intense than are those of adults. Allow them to express how worried they are about the future. Remind them that you are their advocate and that your goal is to keep them safe. Remind your LGBT patients that people who have advocated for them did not disappear overnight because of the election. Some parents of my LGBT patients have pointed out that many LGBT youth feel safer when a nonfamily member advocates for them; therefore, it is essential to remind your LGBT patients about your role as their physician and their advocate.
Another way to support your LGBT patients during this stressful time is to help create a safe environment for them, especially at school. There are some concerns about an increase in antigay and antitrans harassment and bullying since the election.7 Schools are doing their best to respond appropriately to these incidents.8 Fortunately, many schools are responsive to physicians’ recommendations for preventing and addressing school bullying.9 For more information on how providers can address bullying of LGBT youth in school, please refer to my column on bullying (“Bullying,” May 2016, p.1).
Once you reduce the responsiveness of the adolescent brain to the limbic system, you then can focus on the prefrontal cortex to help adolescents engage and cope with their distress. Have them recall from their civics classes that the United States government has checks and balances and that one person does not have unilateral power. Remind the adolescent that administrations and governments do not last forever and that there is an opportunity to change administrations every 4 years.
One of the most powerful ways to engage the prefrontal cortex of the distressed adolescent is to provide the individual with opportunities to be an active member of the community. They can volunteer in many organizations that share their values and beliefs. These organizations do not need to be political, but they should provide some service to the community. This will remind the adolescents that they can have an impact on their own lives and in the lives of others. Volunteering in these organizations will give them a sense of purpose and create a stronger connection to their communities10 – both are antidotes to the intense feeling of despair and hopelessness.
The fear and concerns that LGBT youth have over the election results are intense and deserve attention. Their neurobiology and lack of experience make these fears much more powerful. Providers, parents, and advocates have the responsibility to address these fears, remind LGBT youth that they are their advocates, and remind LGBT youth of the ability to influence the outcomes of their own lives. Providing skills to cope with disappointing outcomes also will prepare LGBT youth for the challenges of adulthood and for the many elections to come.
Resources
AAP: Talking to your children about the election
HealthyChildren.org: How to support your child’s resilience in a time of crisis
Suicide Prevention Lifeline: Patient safety plan template
References
1. “Donald Trump Win Causes Spike in Crisis Support Line Calls,” Time magazine, Nov. 9, 2016.
2. Int Rev Psychiatry. 1992;4(2):177-84.
3. “U.S. Hate Crimes Surge 6%, Fueled by Attacks on Muslims,” the New York Times, Nov. 14, 2016.
4. Arch Suicide Res. 2015;19(3):385-400.
5. “The president of the United States shifted the mainstream in one interview,” Newsweek, May 13, 2012.
6. Neuropsychiatric Disease and Treatment. 2013;9:449-61.
7. “This is Trump’s America: LGBT community fears surge in hate crimes following reports of homophobic attacks,” Salon magazine, Nov. 13, 2016.
8. “School officials grapple with bullying, harassment after election,” Lansing State Journal, Nov. 13, 2016.
9. “Roles for pediatricians in bullying prevention and intervention,” StopBullying.gov, 2016.
10. Adv Psych Treatment. 2014;20(3):217-24.
Dr. Montano is an adolescent medicine fellow at Children’s Hospital of Pittsburgh of the University of Pittsburgh Medical Center and a postdoctoral fellow in the department of pediatrics the University of Pittsburgh. Email him at pdnews@frontlinemedcom.com.
The day after the election, Time magazine reported an increased call volume to the Trevor Project, an organization that provides suicide counseling for LGBT youth.1 A colleague of mine who works closely with the Trevor Project told me that this was the second-highest call volume the organization has received since its inception.
Regardless of your political affiliation, we all can agree that this year’s election was divisive. Many minority groups, including the LGBT community, felt singled out. Although many of us have seen contentious elections in our lifetimes, teenagers, especially LGBT youth, are sensitive to this divisiveness.
Many LGBT youth who called the Trevor Project had expressed fear about the future. Whenever someone becomes suicidal, they have an overwhelming sense of hopelessness.2 Many perceive that the upcoming administration may be hostile to the LGBT community, and because many fear that this new administration may undo all the progress made in LGBT rights in the last 8 years, they have little hope for the future. Numerous reports of increased hate-crime incidents since the start of the election season last year may have exacerbated this feeling of hopelessness.3 This hopelessness may cause many to feel that the best way out is through suicide. Others feel that their sexual orientation or gender identity may be an additional burden to their family during this new era, and so to relieve them of this burden, they consider ending their own lives.4
For adults who have seen many administrations come and go, this may seem like hyperbole. But we have the advantage of living through various elections and administrations, knowing that they were not as catastrophic as others claimed. However, for many LGBT teens or young adults, this is probably their first election after reaching adolescence since Obama was elected in 2008. The Obama administration has been friendly to the LGBT community,5 and for LGBT youth, the upcoming Trump administration may be a substantial departure from this friendliness. In addition, people across the political spectrum have stoked fears among LGBT youth that the new administration will be devastating for the LGBT community. Adolescents, compared with adults, respond more strongly to the limbic system of the brain – the part of the brain involved in emotional processing, which includes fear.6 This fear will override any attempt by the prefrontal cortex – the part of the brain involved in cognitive processing6 – to put the results of this election within context and within perspective. In other words, it is easier for the adolescent brain to become much more despondent over a disappointing outcome.
What can providers do for LGBT youth who feel distressed over the outcome of the election? The approach is twofold. First, address the emotions emanating from the limbic system. Once this influence is dampened, engage the prefrontal cortex to process the emotions and address these fears in a more constructive way.
For LGBT youth who are actively suicidal, providers should first determine the risk for suicide (for example, determine the level of family support, access to lethal means of suicide, etc.) Then, depending on the risk, create a suicide safety plan that will help the teen or young adult cope with the distress. For more information on how to address suicidality among LGBT youth, please see my previous column (“It does get better... with your help: Preventing suicide,” October 2016, page 30).
Recognize and validate the fears of LGBT youth. Do not dismiss their fears as an overreaction. Because of the adolescent brain’s responsiveness to the limbic system, their fears and emotions are much more intense than are those of adults. Allow them to express how worried they are about the future. Remind them that you are their advocate and that your goal is to keep them safe. Remind your LGBT patients that people who have advocated for them did not disappear overnight because of the election. Some parents of my LGBT patients have pointed out that many LGBT youth feel safer when a nonfamily member advocates for them; therefore, it is essential to remind your LGBT patients about your role as their physician and their advocate.
Another way to support your LGBT patients during this stressful time is to help create a safe environment for them, especially at school. There are some concerns about an increase in antigay and antitrans harassment and bullying since the election.7 Schools are doing their best to respond appropriately to these incidents.8 Fortunately, many schools are responsive to physicians’ recommendations for preventing and addressing school bullying.9 For more information on how providers can address bullying of LGBT youth in school, please refer to my column on bullying (“Bullying,” May 2016, p.1).
Once you reduce the responsiveness of the adolescent brain to the limbic system, you then can focus on the prefrontal cortex to help adolescents engage and cope with their distress. Have them recall from their civics classes that the United States government has checks and balances and that one person does not have unilateral power. Remind the adolescent that administrations and governments do not last forever and that there is an opportunity to change administrations every 4 years.
One of the most powerful ways to engage the prefrontal cortex of the distressed adolescent is to provide the individual with opportunities to be an active member of the community. They can volunteer in many organizations that share their values and beliefs. These organizations do not need to be political, but they should provide some service to the community. This will remind the adolescents that they can have an impact on their own lives and in the lives of others. Volunteering in these organizations will give them a sense of purpose and create a stronger connection to their communities10 – both are antidotes to the intense feeling of despair and hopelessness.
The fear and concerns that LGBT youth have over the election results are intense and deserve attention. Their neurobiology and lack of experience make these fears much more powerful. Providers, parents, and advocates have the responsibility to address these fears, remind LGBT youth that they are their advocates, and remind LGBT youth of the ability to influence the outcomes of their own lives. Providing skills to cope with disappointing outcomes also will prepare LGBT youth for the challenges of adulthood and for the many elections to come.
Resources
AAP: Talking to your children about the election
HealthyChildren.org: How to support your child’s resilience in a time of crisis
Suicide Prevention Lifeline: Patient safety plan template
References
1. “Donald Trump Win Causes Spike in Crisis Support Line Calls,” Time magazine, Nov. 9, 2016.
2. Int Rev Psychiatry. 1992;4(2):177-84.
3. “U.S. Hate Crimes Surge 6%, Fueled by Attacks on Muslims,” the New York Times, Nov. 14, 2016.
4. Arch Suicide Res. 2015;19(3):385-400.
5. “The president of the United States shifted the mainstream in one interview,” Newsweek, May 13, 2012.
6. Neuropsychiatric Disease and Treatment. 2013;9:449-61.
7. “This is Trump’s America: LGBT community fears surge in hate crimes following reports of homophobic attacks,” Salon magazine, Nov. 13, 2016.
8. “School officials grapple with bullying, harassment after election,” Lansing State Journal, Nov. 13, 2016.
9. “Roles for pediatricians in bullying prevention and intervention,” StopBullying.gov, 2016.
10. Adv Psych Treatment. 2014;20(3):217-24.
Dr. Montano is an adolescent medicine fellow at Children’s Hospital of Pittsburgh of the University of Pittsburgh Medical Center and a postdoctoral fellow in the department of pediatrics the University of Pittsburgh. Email him at pdnews@frontlinemedcom.com.
It does get better ... with your help: Preventing suicide
Suicide continues to be a major public health problem in the United States. It is the second leading cause of death in young people aged 10-24 years, according to 2010 injury data from the Centers from Disease Control and Prevention.1 This problem disproportionately affects lesbian, gay, bisexual, and transgender (LGBT) youth. Compared to their heterosexual peers, LGBT youth are four times as likely to attempt suicide.2 In addition, almost 50% of transgender youth have attempted suicide.3
Why are LGBT youth at high risk for suicide? Antigay and antitrans stigma and discrimination against LGBT youth create a very stressful environment. For example, LGBT youth are two times more likely than are heterosexual youth to experience bullying4 because of their sexual orientation, and half of transgender youth have reported bullying because of their gender identity.3 LGBT youth tend to perceive lower levels of parental support than do heterosexual youth.5-8 A combination of harassment from peers and decreased perceived support from families increases the risk for suicide in LGBT youth.
However, there are factors that can reduce this risk. LGBT youth whose parents reject their sexual orientation or gender identity are eight times as likely to be suicidal,3,9 while in contrast, LGBT youth whose parents are more accepting are less likely to be suicidal.10 These studies underscore the importance of social support in reducing the stress from antigay and antitrans discrimination, and therefore, play a role in preventing suicide.
Health care providers are another source of support for LGBT youth. They can play a role in providing education and preventing suicide in this population because many victims of suicide have visited a health care provider before attempting to kill themselves.11 It is important for providers to screen for suicide in their patients. Although there is no lab test for suicidal ideation, suicidal adolescents tend to have certain risk factors. In addition to being LGBT, being bullied, and having a lack of social support, other risk factors are psychiatric illness, a history of being impulsive, alcohol and substance abuse, and most important of all, a previous suicide attempt.12
When screening for suicide risk, always remember that at the beginning of any visit with an adolescent, remind them about confidentiality and its limits (e.g., breaking confidentiality if the patient is suicidal). Although this appears counterintuitive, it actually builds rapport between you and the patient. If you don’t discuss the limits of confidentiality beforehand and have to break it because the patient is suicidal, the patient is less likely to tell you again in the future. Once you suspect suicidal ideation based on the above risk factors, you can ask:
• Have you thought about ending your own life or would you rather be dead?
• Have you done something to harm yourself or to end your life?
• Have you considered ways to end your own life?12
Some clinicians have expressed concern over asking about suicide in their adolescent patients, but doing so does not induce suicidal thoughts.13 If a patient does express any of the above, the clinician must then inquire about other risk factors that increase the individual’s chances of completing suicide. The American Association of Suicidology has listed several warning signs of imminent suicide, which can be remembered with the acronym IS PATH WARM. This stands for Ideation, Substance use, Purposelessness, heightened Anxiety, feeling Trapped, feeling Hopeless, Withdrawal from friends and family, uncontrollable Anger, engaging in Reckless behavior, and dramatic Mood changes.14
If a patient threatens to kill him/herself, has a specific plan to do so, or speaks about death and suicide, then the clinician must act immediately. Although sending a patient to the emergency department is the safest option, it is not the only option. If a good support system is present, and the patient lives in an environment where he or she does not have the means to carry out a suicide (e.g., there are no guns in the home), then the clinician can create a safety plan for the patient. A safety plan is different from a “no suicide contract.” A no suicide contract is a written commitment that the patient does not engage in suicidal behavior. Many experts caution against a no suicide contract because it can create a false sense of security for the clinician and does not address the strategies needed to combat feelings of suicidality.15,16
Usually with a safety plan, the clinician and the patient identify several people the patient can contact if the patient feels suicidal. In addition, the clinician and the patient can discuss ways the patient can cope with his/her feelings or distract himself/herself from suicidal thoughts (e.g., going out for a walk, watching a movie, etc.). Finally, if these methods fail, patients are provided with emergency hotlines or directed to the emergency department. The Suicide Prevention Resource Center has a template of a patient safety plan.
Finally, clinicians should be proactive in preventing suicide, especially for LGBT youth. Because bullying is a risk factor for suicide, and because LGBT youth are disproportionately affected by bullying, clinicians should advocate for antibullying school policies and advocate for schools to be more LGBT friendly. Clinicians also should speak to the community about suicide, its warning signs, and how to address it. Just like with any disease, prevention is the most effective form of treatment.
As clinicians, we should always be on the lookout for suicide in our young patients, especially LGBT youth. For many LGBT youth, we may be the only source of support. If patients are suicidal, we should work with them to determine how to keep the them safe. We have a powerful voice in the community. We can advocate for making schools safe for LGBT youth and educate the community in suicide prevention. Such a powerful voice proclaiming that it gets better can save a life.
Resources
• The Trevor Project: A non-profit organization dedicated to prevent suicide in LGBT Youth (www.thetrevorproject.org)
• It Gets Better Project: Another website dedicated to preventing suicide in LGBT youth by promoting the message that life will improve for LGBT teens (www.itgetsbetter.org)
• Patient Safety Plan Template from the Suicide Prevention Resource Center (www.sprc.org)
References
1. CDC. NCIPC. Web-based Injury Statistics Query and Reporting System (WISQARS). 2010.
2. MMWR Surveill Summ. 2011 Jun 10;60(7):1-133.
3. Injustice at Every Turn: A Report of the National Transgender Discrimination Survey. (Washington: National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011).
4. J Adolesc Health. 2014 Sep;55(3):432-8.
5. J Youth Adolesc. 2013 Mar;42(3):376-93.
6. J Youth Adolesc. 2010 Oct;39(10):1189-98.
7. School Psychology Review. 2008;37(2):202-16.
8. J Homosex. 2010;57(2):287-309.
9. Pediatrics. 2009 Jan;123(1):346-52.
10. J Child Adolesc Psychiatr Nurs. 2010 Nov;23(4):205-13.
11. Mayo Clin Proc. 2011 Aug;86(8):792-800.
12. Ital J Pediatr. 2015 Jul 7;41:49.
13. Ment Health Fam Med. 2008 Dec;5(4):229-35.
14. Know the Warning Signs of Suicide. American Association of Suicidology.
15. J Psychiatr Ment Health Nurs. 2008 Aug;15(6):512-22.
16. J Amer Acad Psych Law. 1999;27(3):445-50.
Dr. Montano is a physician at Children’s Hospital of Pittsburgh of UPMC and a clinical instructor of pediatrics at the University of Pittsburgh School of Medicine.
Suicide continues to be a major public health problem in the United States. It is the second leading cause of death in young people aged 10-24 years, according to 2010 injury data from the Centers from Disease Control and Prevention.1 This problem disproportionately affects lesbian, gay, bisexual, and transgender (LGBT) youth. Compared to their heterosexual peers, LGBT youth are four times as likely to attempt suicide.2 In addition, almost 50% of transgender youth have attempted suicide.3
Why are LGBT youth at high risk for suicide? Antigay and antitrans stigma and discrimination against LGBT youth create a very stressful environment. For example, LGBT youth are two times more likely than are heterosexual youth to experience bullying4 because of their sexual orientation, and half of transgender youth have reported bullying because of their gender identity.3 LGBT youth tend to perceive lower levels of parental support than do heterosexual youth.5-8 A combination of harassment from peers and decreased perceived support from families increases the risk for suicide in LGBT youth.
However, there are factors that can reduce this risk. LGBT youth whose parents reject their sexual orientation or gender identity are eight times as likely to be suicidal,3,9 while in contrast, LGBT youth whose parents are more accepting are less likely to be suicidal.10 These studies underscore the importance of social support in reducing the stress from antigay and antitrans discrimination, and therefore, play a role in preventing suicide.
Health care providers are another source of support for LGBT youth. They can play a role in providing education and preventing suicide in this population because many victims of suicide have visited a health care provider before attempting to kill themselves.11 It is important for providers to screen for suicide in their patients. Although there is no lab test for suicidal ideation, suicidal adolescents tend to have certain risk factors. In addition to being LGBT, being bullied, and having a lack of social support, other risk factors are psychiatric illness, a history of being impulsive, alcohol and substance abuse, and most important of all, a previous suicide attempt.12
When screening for suicide risk, always remember that at the beginning of any visit with an adolescent, remind them about confidentiality and its limits (e.g., breaking confidentiality if the patient is suicidal). Although this appears counterintuitive, it actually builds rapport between you and the patient. If you don’t discuss the limits of confidentiality beforehand and have to break it because the patient is suicidal, the patient is less likely to tell you again in the future. Once you suspect suicidal ideation based on the above risk factors, you can ask:
• Have you thought about ending your own life or would you rather be dead?
• Have you done something to harm yourself or to end your life?
• Have you considered ways to end your own life?12
Some clinicians have expressed concern over asking about suicide in their adolescent patients, but doing so does not induce suicidal thoughts.13 If a patient does express any of the above, the clinician must then inquire about other risk factors that increase the individual’s chances of completing suicide. The American Association of Suicidology has listed several warning signs of imminent suicide, which can be remembered with the acronym IS PATH WARM. This stands for Ideation, Substance use, Purposelessness, heightened Anxiety, feeling Trapped, feeling Hopeless, Withdrawal from friends and family, uncontrollable Anger, engaging in Reckless behavior, and dramatic Mood changes.14
If a patient threatens to kill him/herself, has a specific plan to do so, or speaks about death and suicide, then the clinician must act immediately. Although sending a patient to the emergency department is the safest option, it is not the only option. If a good support system is present, and the patient lives in an environment where he or she does not have the means to carry out a suicide (e.g., there are no guns in the home), then the clinician can create a safety plan for the patient. A safety plan is different from a “no suicide contract.” A no suicide contract is a written commitment that the patient does not engage in suicidal behavior. Many experts caution against a no suicide contract because it can create a false sense of security for the clinician and does not address the strategies needed to combat feelings of suicidality.15,16
Usually with a safety plan, the clinician and the patient identify several people the patient can contact if the patient feels suicidal. In addition, the clinician and the patient can discuss ways the patient can cope with his/her feelings or distract himself/herself from suicidal thoughts (e.g., going out for a walk, watching a movie, etc.). Finally, if these methods fail, patients are provided with emergency hotlines or directed to the emergency department. The Suicide Prevention Resource Center has a template of a patient safety plan.
Finally, clinicians should be proactive in preventing suicide, especially for LGBT youth. Because bullying is a risk factor for suicide, and because LGBT youth are disproportionately affected by bullying, clinicians should advocate for antibullying school policies and advocate for schools to be more LGBT friendly. Clinicians also should speak to the community about suicide, its warning signs, and how to address it. Just like with any disease, prevention is the most effective form of treatment.
As clinicians, we should always be on the lookout for suicide in our young patients, especially LGBT youth. For many LGBT youth, we may be the only source of support. If patients are suicidal, we should work with them to determine how to keep the them safe. We have a powerful voice in the community. We can advocate for making schools safe for LGBT youth and educate the community in suicide prevention. Such a powerful voice proclaiming that it gets better can save a life.
Resources
• The Trevor Project: A non-profit organization dedicated to prevent suicide in LGBT Youth (www.thetrevorproject.org)
• It Gets Better Project: Another website dedicated to preventing suicide in LGBT youth by promoting the message that life will improve for LGBT teens (www.itgetsbetter.org)
• Patient Safety Plan Template from the Suicide Prevention Resource Center (www.sprc.org)
References
1. CDC. NCIPC. Web-based Injury Statistics Query and Reporting System (WISQARS). 2010.
2. MMWR Surveill Summ. 2011 Jun 10;60(7):1-133.
3. Injustice at Every Turn: A Report of the National Transgender Discrimination Survey. (Washington: National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011).
4. J Adolesc Health. 2014 Sep;55(3):432-8.
5. J Youth Adolesc. 2013 Mar;42(3):376-93.
6. J Youth Adolesc. 2010 Oct;39(10):1189-98.
7. School Psychology Review. 2008;37(2):202-16.
8. J Homosex. 2010;57(2):287-309.
9. Pediatrics. 2009 Jan;123(1):346-52.
10. J Child Adolesc Psychiatr Nurs. 2010 Nov;23(4):205-13.
11. Mayo Clin Proc. 2011 Aug;86(8):792-800.
12. Ital J Pediatr. 2015 Jul 7;41:49.
13. Ment Health Fam Med. 2008 Dec;5(4):229-35.
14. Know the Warning Signs of Suicide. American Association of Suicidology.
15. J Psychiatr Ment Health Nurs. 2008 Aug;15(6):512-22.
16. J Amer Acad Psych Law. 1999;27(3):445-50.
Dr. Montano is a physician at Children’s Hospital of Pittsburgh of UPMC and a clinical instructor of pediatrics at the University of Pittsburgh School of Medicine.
Suicide continues to be a major public health problem in the United States. It is the second leading cause of death in young people aged 10-24 years, according to 2010 injury data from the Centers from Disease Control and Prevention.1 This problem disproportionately affects lesbian, gay, bisexual, and transgender (LGBT) youth. Compared to their heterosexual peers, LGBT youth are four times as likely to attempt suicide.2 In addition, almost 50% of transgender youth have attempted suicide.3
Why are LGBT youth at high risk for suicide? Antigay and antitrans stigma and discrimination against LGBT youth create a very stressful environment. For example, LGBT youth are two times more likely than are heterosexual youth to experience bullying4 because of their sexual orientation, and half of transgender youth have reported bullying because of their gender identity.3 LGBT youth tend to perceive lower levels of parental support than do heterosexual youth.5-8 A combination of harassment from peers and decreased perceived support from families increases the risk for suicide in LGBT youth.
However, there are factors that can reduce this risk. LGBT youth whose parents reject their sexual orientation or gender identity are eight times as likely to be suicidal,3,9 while in contrast, LGBT youth whose parents are more accepting are less likely to be suicidal.10 These studies underscore the importance of social support in reducing the stress from antigay and antitrans discrimination, and therefore, play a role in preventing suicide.
Health care providers are another source of support for LGBT youth. They can play a role in providing education and preventing suicide in this population because many victims of suicide have visited a health care provider before attempting to kill themselves.11 It is important for providers to screen for suicide in their patients. Although there is no lab test for suicidal ideation, suicidal adolescents tend to have certain risk factors. In addition to being LGBT, being bullied, and having a lack of social support, other risk factors are psychiatric illness, a history of being impulsive, alcohol and substance abuse, and most important of all, a previous suicide attempt.12
When screening for suicide risk, always remember that at the beginning of any visit with an adolescent, remind them about confidentiality and its limits (e.g., breaking confidentiality if the patient is suicidal). Although this appears counterintuitive, it actually builds rapport between you and the patient. If you don’t discuss the limits of confidentiality beforehand and have to break it because the patient is suicidal, the patient is less likely to tell you again in the future. Once you suspect suicidal ideation based on the above risk factors, you can ask:
• Have you thought about ending your own life or would you rather be dead?
• Have you done something to harm yourself or to end your life?
• Have you considered ways to end your own life?12
Some clinicians have expressed concern over asking about suicide in their adolescent patients, but doing so does not induce suicidal thoughts.13 If a patient does express any of the above, the clinician must then inquire about other risk factors that increase the individual’s chances of completing suicide. The American Association of Suicidology has listed several warning signs of imminent suicide, which can be remembered with the acronym IS PATH WARM. This stands for Ideation, Substance use, Purposelessness, heightened Anxiety, feeling Trapped, feeling Hopeless, Withdrawal from friends and family, uncontrollable Anger, engaging in Reckless behavior, and dramatic Mood changes.14
If a patient threatens to kill him/herself, has a specific plan to do so, or speaks about death and suicide, then the clinician must act immediately. Although sending a patient to the emergency department is the safest option, it is not the only option. If a good support system is present, and the patient lives in an environment where he or she does not have the means to carry out a suicide (e.g., there are no guns in the home), then the clinician can create a safety plan for the patient. A safety plan is different from a “no suicide contract.” A no suicide contract is a written commitment that the patient does not engage in suicidal behavior. Many experts caution against a no suicide contract because it can create a false sense of security for the clinician and does not address the strategies needed to combat feelings of suicidality.15,16
Usually with a safety plan, the clinician and the patient identify several people the patient can contact if the patient feels suicidal. In addition, the clinician and the patient can discuss ways the patient can cope with his/her feelings or distract himself/herself from suicidal thoughts (e.g., going out for a walk, watching a movie, etc.). Finally, if these methods fail, patients are provided with emergency hotlines or directed to the emergency department. The Suicide Prevention Resource Center has a template of a patient safety plan.
Finally, clinicians should be proactive in preventing suicide, especially for LGBT youth. Because bullying is a risk factor for suicide, and because LGBT youth are disproportionately affected by bullying, clinicians should advocate for antibullying school policies and advocate for schools to be more LGBT friendly. Clinicians also should speak to the community about suicide, its warning signs, and how to address it. Just like with any disease, prevention is the most effective form of treatment.
As clinicians, we should always be on the lookout for suicide in our young patients, especially LGBT youth. For many LGBT youth, we may be the only source of support. If patients are suicidal, we should work with them to determine how to keep the them safe. We have a powerful voice in the community. We can advocate for making schools safe for LGBT youth and educate the community in suicide prevention. Such a powerful voice proclaiming that it gets better can save a life.
Resources
• The Trevor Project: A non-profit organization dedicated to prevent suicide in LGBT Youth (www.thetrevorproject.org)
• It Gets Better Project: Another website dedicated to preventing suicide in LGBT youth by promoting the message that life will improve for LGBT teens (www.itgetsbetter.org)
• Patient Safety Plan Template from the Suicide Prevention Resource Center (www.sprc.org)
References
1. CDC. NCIPC. Web-based Injury Statistics Query and Reporting System (WISQARS). 2010.
2. MMWR Surveill Summ. 2011 Jun 10;60(7):1-133.
3. Injustice at Every Turn: A Report of the National Transgender Discrimination Survey. (Washington: National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011).
4. J Adolesc Health. 2014 Sep;55(3):432-8.
5. J Youth Adolesc. 2013 Mar;42(3):376-93.
6. J Youth Adolesc. 2010 Oct;39(10):1189-98.
7. School Psychology Review. 2008;37(2):202-16.
8. J Homosex. 2010;57(2):287-309.
9. Pediatrics. 2009 Jan;123(1):346-52.
10. J Child Adolesc Psychiatr Nurs. 2010 Nov;23(4):205-13.
11. Mayo Clin Proc. 2011 Aug;86(8):792-800.
12. Ital J Pediatr. 2015 Jul 7;41:49.
13. Ment Health Fam Med. 2008 Dec;5(4):229-35.
14. Know the Warning Signs of Suicide. American Association of Suicidology.
15. J Psychiatr Ment Health Nurs. 2008 Aug;15(6):512-22.
16. J Amer Acad Psych Law. 1999;27(3):445-50.
Dr. Montano is a physician at Children’s Hospital of Pittsburgh of UPMC and a clinical instructor of pediatrics at the University of Pittsburgh School of Medicine.