User login
Your patient bequeathed money to you: Can you accept it?
Michael Victoroff, MD, described the phone call he received from an attorney asking a thorny ethics question involving a patient’s gift to another physician. Dr. Victoroff, a past member of the ethics committee of the American Academy of Family Physicians, had definite thoughts about it.
“The attorney was representing the daughters of an elderly gentleman who had moved from the East Coast to Colorado to be closer to them,” said Dr. Victoroff, who teaches bioethics in the MBA program at the University of Denver and also practices at the University of Colorado School of Medicine.
“The father visited his new primary care physician frequently because he had multiple health issues.”
The patient was happy with the doctor’s medical care and over time that they developed a friendship. Dr. Victoroff emphasized that no sexual or romantic impropriety ever took place between the patient and his physician.
“But the social relationship went beyond the ordinary doctor-patient boundaries. The patient ultimately named the doctor as his health care proxy in the event that he became unable to make decisions regarding his care. He also mentioned he was going to leave her $100,000 in his will,” says Dr. Victoroff.
The physician did accept the role of proxy, “which raises a whole host of ethical issues,” says Dr. Victoroff. As it happened, she was never called upon to exercise that decision-making authority, since the patient died suddenly and was mentally competent at the time.
for her to accept such a substantial bequest from a patient, and they hired an attorney to contest the will.
No law against it
Dennis Hursh, attorney and managing partner of Physician Agreements Health Law, a Pennsylvania-based law firm that represents physicians, noted in an interview that, “the problem isn’t legal per se. Rather, the problem is an ethical one.”
Legally speaking, there’s no prohibition against receiving a bequest or other form of gift from a patient. “People are free to dispose of their estates in whatever way they see fit, and no law technically precludes a physician from accepting a bequest,” says Dr. Victoroff. “But this presupposes there is nothing improper going on, such as extortion, deception, coercion, or exercising undue influence.”
The issue of bequeathing money to their physician gained attention in a recent case that took place in Australia. Peter Alexakis, MD, received a whopping bequest of $24 million from a patient. The elderly patient had changed his will to name Dr. Alexakis as the sole beneficiary – after Dr. Alexakis had visited him at home 92 times during the preceding months. The original heirs filed a lawsuit in Australia’s Supreme Court against Dr. Alexakis, contesting the will.
The lawsuit was unsuccessful in court, but Dr. Alexakis was found guilty of malpractice by Australia’s Health Care Complaints Commission after being reported to the HCCC by the palliative care physicians who were treating the patient. They alleged that Dr. Alexakis had interfered with their care of the patient. The more serious allegation was that the doctor had engaged in a deliberate strategy to exploit the relationship for financial gain.
Dr. Alexakis was chastised by the HCCC for engaging in “obtuse” and “suspicious” behavior and for “blurring the boundaries of the doctor-patient relationship.”
There are three domains – legal, ethical, and practical – when it comes to accepting bequests or any gifts from patients, says Dr. Victoroff.
“[In] the legal domain, for example, if you receive a bequest from anyone, patient or otherwise, you have to know your local laws about estates and taxes and so forth and obey them,” he said.
Attorney Hursh pointed out that the Australian doctor wasn’t found guilty of wrongdoing in a court of law but rather of unethical conduct by the Australian medical licensing entity.
Patients giving gifts is often a part of a physician’s life
When Ian Schorr, MD, first started out in practice, he was surprised that patients began bringing him gifts of food to express gratitude for his care.
“I thought it was unethical to accept their gifts, so I turned them down and wouldn’t accept so much as a cookie,” Dr. Schorr, a now-retired ophthalmologist, told this news organization. “But that changed because my office staff told me that some patients were feeling disappointed and insulted. I realized that some people want to express appreciation in ways that go beyond a monetary payment.”
The next time he received a gift from a patient, he “accepted it gracefully.” And he wrote a thank you note, which he continued to do any time he received a gift from a patient.
Kenneth Prager, MD, professor of clinical medicine, director of clinical ethics and chairman of the Medical Ethics Committee at Columbia University Medical Center, New York, says, “I have literally received hundreds of gifts, the vast majority being tokens of patients’ appreciation,” he said. “I’ll get boxes of chocolate or cakes, or sometimes articles of clothing.”
Occasionally, Dr. Prager receives a “somewhat larger gift” – for example, two tickets to a baseball game. “To reject these gifts would be a slap in the face to the patient,” he says, but “where it gets more ethically cloudy is when a gift is very substantial.”
Dr. Prager has never been offered a “substantial” gift or bequest personally. “But a patient whose brother I cared for has indicated that she has left instructions in her will to endow an associate chair of ethics in my honor, and I didn’t decline that,” he said.
The AMA Code of Ethics confirms that accepting gifts offered “as an expression of gratitude or a reflection of the patient’s cultural tradition” can “enhance the patient-physician relationship.” But sometimes gifts “may signal psychological needs that require the physician’s attention.” Accepting such gifts is “likely to damage the patient-physician relationship.”
Potential damage to the therapeutic relationship applies to all physicians but especially for psychiatrists and mental health professionals. “There are more stringent ethical requirements when it comes to these disciplines, where gift-giving gets into the territory of transference or may have particular psychological meaning, and accepting the gift may muddy the therapeutic waters,” Dr. Victoroff said.
Impact on the patient’s family and on other patients
The AMA statement encourages physicians to be “sensitive to the gift’s value, relative to the patient’s or physician’s means.” Physicians should decline gifts that are “disproportionately or inappropriately large, or when the physician would be uncomfortable to have colleagues know the gift had been accepted.”
They should also decline a bequest from a patient if they have reason to believe that to accept it “would present an emotional or financial hardship to the patient’s family.”
“If Bill Gates were leaving $100,000 to his doctor, I imagine Melinda would be just fine,” Mr. Hursh said. “But under ordinary circumstances, if the patient’s family might feel the impact of the bequest, it would be unethical to accept it and could be grounds for revocation of the doctor’s license.”
The AMA statement also warns physicians that by offering a gift, some patients may be seeking to “secure or influence care or to secure preferential treatment,” which can “undermine physicians’ obligation to provide services fairly to all patients.”
For this reason, bequests are “sticky,” said Laurel Lyckholm, MD, professor of hematology and oncology at West Virginia University School of Medicine. In the case of institutions where patients or community members donate money, “we know whose names are on the plaques that hang on the hospital walls, so it’s a delicate balance. What if there’s only one bed or one ventilator? Will the wife of the donor get preferential treatment?”
Follow institutional policy
A “very small gift, such as a fruitcake, is fine,” says Dr. Lyckholm, author of an essay on accepting gifts from patients. She said there’s a dollar amount ($15) that her institution mandates, above which a gift – even food – is considered too expensive to accept. “I was a nurse before I became a physician, and people always tried to give us gifts because we were so close to the minute-by-minute care of the patients,” she said. “We were not allowed to accept money or anything lavish.”
But in the case of small gifts, “the risk-benefit analysis is that there’s much more risk not to take it and to hurt the patient’s feelings.”
Gifts above $15 are given to charity. “I explain to patients that I’m not allowed to take such a large gift, but I’d love to give it to the hospital’s Rosenbaum Family House that provides patients and their relatives with lodging, or to the homeless shelter in Morgantown.”
Dr. Lyckholm, who serves on the ethics committee at J.W. Ruby Memorial Hospital, once was offered expensive tickets and said to the patient, “This is so incredibly thoughtful and kind, but I can’t accept them. I would like to give the tickets to a charity that can auction them off.”
She advises physicians to find out their institution’s policies. Many institutions have policies about what gifts their staff – whether physicians, nurses, or other health care professionals – can accept.
Passing the ‘smell test’
Accepting a large gift from a patient could potentially make it look like you might have exercised undue influence.
“That concern brings us to the third domain, which is very practical and all about appearances and perceptions,” Dr. Victoroff said.
He noted that there is “an inherent power differential between a physician and a patient. The very nature of the relationship can create a risk of ‘undue influence’ on the doctor’s part, even if it’s not apparent to the doctor.” For this reason, it’s necessary to be utterly transparent about how the bequest came about.
He suggests that if a patient informs you that he or she would like to leave money to you, it might be wise to suggest a meeting with the patient’s family, thus establishing some transparency.
It may not be possible to meet with the patient’s family for logistical reasons or because the patient would prefer not to involve their family in their estate planning. But in any case, it’s advisable to document any conversation in the patient’s chart, Dr. Victoroff advised.
“You should make a contemporaneous note that the patient initiated the suggestion and that you counseled them about the implications, no differently than you would with an interaction of a clinical nature,” he suggests. That way, if money has been left to you and is disputed, there’s a clear record that you didn’t solicit it or use any undue influence to bring it about.
He also recommended getting advice from a trusted colleague or a member of your institution’s ethics committee. “Taking time to get a second opinion about an ethical question is a safeguard, like having a chaperone in the room during an examination.”
Ultimately, “there is no human relationship without potential conflicts of interest. Our job is to manage those as best as we can, and sunlight is the best antidote to bad appearances,” Dr. Victoroff said.
A version of this article appeared on Medscape.com.
Michael Victoroff, MD, described the phone call he received from an attorney asking a thorny ethics question involving a patient’s gift to another physician. Dr. Victoroff, a past member of the ethics committee of the American Academy of Family Physicians, had definite thoughts about it.
“The attorney was representing the daughters of an elderly gentleman who had moved from the East Coast to Colorado to be closer to them,” said Dr. Victoroff, who teaches bioethics in the MBA program at the University of Denver and also practices at the University of Colorado School of Medicine.
“The father visited his new primary care physician frequently because he had multiple health issues.”
The patient was happy with the doctor’s medical care and over time that they developed a friendship. Dr. Victoroff emphasized that no sexual or romantic impropriety ever took place between the patient and his physician.
“But the social relationship went beyond the ordinary doctor-patient boundaries. The patient ultimately named the doctor as his health care proxy in the event that he became unable to make decisions regarding his care. He also mentioned he was going to leave her $100,000 in his will,” says Dr. Victoroff.
The physician did accept the role of proxy, “which raises a whole host of ethical issues,” says Dr. Victoroff. As it happened, she was never called upon to exercise that decision-making authority, since the patient died suddenly and was mentally competent at the time.
for her to accept such a substantial bequest from a patient, and they hired an attorney to contest the will.
No law against it
Dennis Hursh, attorney and managing partner of Physician Agreements Health Law, a Pennsylvania-based law firm that represents physicians, noted in an interview that, “the problem isn’t legal per se. Rather, the problem is an ethical one.”
Legally speaking, there’s no prohibition against receiving a bequest or other form of gift from a patient. “People are free to dispose of their estates in whatever way they see fit, and no law technically precludes a physician from accepting a bequest,” says Dr. Victoroff. “But this presupposes there is nothing improper going on, such as extortion, deception, coercion, or exercising undue influence.”
The issue of bequeathing money to their physician gained attention in a recent case that took place in Australia. Peter Alexakis, MD, received a whopping bequest of $24 million from a patient. The elderly patient had changed his will to name Dr. Alexakis as the sole beneficiary – after Dr. Alexakis had visited him at home 92 times during the preceding months. The original heirs filed a lawsuit in Australia’s Supreme Court against Dr. Alexakis, contesting the will.
The lawsuit was unsuccessful in court, but Dr. Alexakis was found guilty of malpractice by Australia’s Health Care Complaints Commission after being reported to the HCCC by the palliative care physicians who were treating the patient. They alleged that Dr. Alexakis had interfered with their care of the patient. The more serious allegation was that the doctor had engaged in a deliberate strategy to exploit the relationship for financial gain.
Dr. Alexakis was chastised by the HCCC for engaging in “obtuse” and “suspicious” behavior and for “blurring the boundaries of the doctor-patient relationship.”
There are three domains – legal, ethical, and practical – when it comes to accepting bequests or any gifts from patients, says Dr. Victoroff.
“[In] the legal domain, for example, if you receive a bequest from anyone, patient or otherwise, you have to know your local laws about estates and taxes and so forth and obey them,” he said.
Attorney Hursh pointed out that the Australian doctor wasn’t found guilty of wrongdoing in a court of law but rather of unethical conduct by the Australian medical licensing entity.
Patients giving gifts is often a part of a physician’s life
When Ian Schorr, MD, first started out in practice, he was surprised that patients began bringing him gifts of food to express gratitude for his care.
“I thought it was unethical to accept their gifts, so I turned them down and wouldn’t accept so much as a cookie,” Dr. Schorr, a now-retired ophthalmologist, told this news organization. “But that changed because my office staff told me that some patients were feeling disappointed and insulted. I realized that some people want to express appreciation in ways that go beyond a monetary payment.”
The next time he received a gift from a patient, he “accepted it gracefully.” And he wrote a thank you note, which he continued to do any time he received a gift from a patient.
Kenneth Prager, MD, professor of clinical medicine, director of clinical ethics and chairman of the Medical Ethics Committee at Columbia University Medical Center, New York, says, “I have literally received hundreds of gifts, the vast majority being tokens of patients’ appreciation,” he said. “I’ll get boxes of chocolate or cakes, or sometimes articles of clothing.”
Occasionally, Dr. Prager receives a “somewhat larger gift” – for example, two tickets to a baseball game. “To reject these gifts would be a slap in the face to the patient,” he says, but “where it gets more ethically cloudy is when a gift is very substantial.”
Dr. Prager has never been offered a “substantial” gift or bequest personally. “But a patient whose brother I cared for has indicated that she has left instructions in her will to endow an associate chair of ethics in my honor, and I didn’t decline that,” he said.
The AMA Code of Ethics confirms that accepting gifts offered “as an expression of gratitude or a reflection of the patient’s cultural tradition” can “enhance the patient-physician relationship.” But sometimes gifts “may signal psychological needs that require the physician’s attention.” Accepting such gifts is “likely to damage the patient-physician relationship.”
Potential damage to the therapeutic relationship applies to all physicians but especially for psychiatrists and mental health professionals. “There are more stringent ethical requirements when it comes to these disciplines, where gift-giving gets into the territory of transference or may have particular psychological meaning, and accepting the gift may muddy the therapeutic waters,” Dr. Victoroff said.
Impact on the patient’s family and on other patients
The AMA statement encourages physicians to be “sensitive to the gift’s value, relative to the patient’s or physician’s means.” Physicians should decline gifts that are “disproportionately or inappropriately large, or when the physician would be uncomfortable to have colleagues know the gift had been accepted.”
They should also decline a bequest from a patient if they have reason to believe that to accept it “would present an emotional or financial hardship to the patient’s family.”
“If Bill Gates were leaving $100,000 to his doctor, I imagine Melinda would be just fine,” Mr. Hursh said. “But under ordinary circumstances, if the patient’s family might feel the impact of the bequest, it would be unethical to accept it and could be grounds for revocation of the doctor’s license.”
The AMA statement also warns physicians that by offering a gift, some patients may be seeking to “secure or influence care or to secure preferential treatment,” which can “undermine physicians’ obligation to provide services fairly to all patients.”
For this reason, bequests are “sticky,” said Laurel Lyckholm, MD, professor of hematology and oncology at West Virginia University School of Medicine. In the case of institutions where patients or community members donate money, “we know whose names are on the plaques that hang on the hospital walls, so it’s a delicate balance. What if there’s only one bed or one ventilator? Will the wife of the donor get preferential treatment?”
Follow institutional policy
A “very small gift, such as a fruitcake, is fine,” says Dr. Lyckholm, author of an essay on accepting gifts from patients. She said there’s a dollar amount ($15) that her institution mandates, above which a gift – even food – is considered too expensive to accept. “I was a nurse before I became a physician, and people always tried to give us gifts because we were so close to the minute-by-minute care of the patients,” she said. “We were not allowed to accept money or anything lavish.”
But in the case of small gifts, “the risk-benefit analysis is that there’s much more risk not to take it and to hurt the patient’s feelings.”
Gifts above $15 are given to charity. “I explain to patients that I’m not allowed to take such a large gift, but I’d love to give it to the hospital’s Rosenbaum Family House that provides patients and their relatives with lodging, or to the homeless shelter in Morgantown.”
Dr. Lyckholm, who serves on the ethics committee at J.W. Ruby Memorial Hospital, once was offered expensive tickets and said to the patient, “This is so incredibly thoughtful and kind, but I can’t accept them. I would like to give the tickets to a charity that can auction them off.”
She advises physicians to find out their institution’s policies. Many institutions have policies about what gifts their staff – whether physicians, nurses, or other health care professionals – can accept.
Passing the ‘smell test’
Accepting a large gift from a patient could potentially make it look like you might have exercised undue influence.
“That concern brings us to the third domain, which is very practical and all about appearances and perceptions,” Dr. Victoroff said.
He noted that there is “an inherent power differential between a physician and a patient. The very nature of the relationship can create a risk of ‘undue influence’ on the doctor’s part, even if it’s not apparent to the doctor.” For this reason, it’s necessary to be utterly transparent about how the bequest came about.
He suggests that if a patient informs you that he or she would like to leave money to you, it might be wise to suggest a meeting with the patient’s family, thus establishing some transparency.
It may not be possible to meet with the patient’s family for logistical reasons or because the patient would prefer not to involve their family in their estate planning. But in any case, it’s advisable to document any conversation in the patient’s chart, Dr. Victoroff advised.
“You should make a contemporaneous note that the patient initiated the suggestion and that you counseled them about the implications, no differently than you would with an interaction of a clinical nature,” he suggests. That way, if money has been left to you and is disputed, there’s a clear record that you didn’t solicit it or use any undue influence to bring it about.
He also recommended getting advice from a trusted colleague or a member of your institution’s ethics committee. “Taking time to get a second opinion about an ethical question is a safeguard, like having a chaperone in the room during an examination.”
Ultimately, “there is no human relationship without potential conflicts of interest. Our job is to manage those as best as we can, and sunlight is the best antidote to bad appearances,” Dr. Victoroff said.
A version of this article appeared on Medscape.com.
Michael Victoroff, MD, described the phone call he received from an attorney asking a thorny ethics question involving a patient’s gift to another physician. Dr. Victoroff, a past member of the ethics committee of the American Academy of Family Physicians, had definite thoughts about it.
“The attorney was representing the daughters of an elderly gentleman who had moved from the East Coast to Colorado to be closer to them,” said Dr. Victoroff, who teaches bioethics in the MBA program at the University of Denver and also practices at the University of Colorado School of Medicine.
“The father visited his new primary care physician frequently because he had multiple health issues.”
The patient was happy with the doctor’s medical care and over time that they developed a friendship. Dr. Victoroff emphasized that no sexual or romantic impropriety ever took place between the patient and his physician.
“But the social relationship went beyond the ordinary doctor-patient boundaries. The patient ultimately named the doctor as his health care proxy in the event that he became unable to make decisions regarding his care. He also mentioned he was going to leave her $100,000 in his will,” says Dr. Victoroff.
The physician did accept the role of proxy, “which raises a whole host of ethical issues,” says Dr. Victoroff. As it happened, she was never called upon to exercise that decision-making authority, since the patient died suddenly and was mentally competent at the time.
for her to accept such a substantial bequest from a patient, and they hired an attorney to contest the will.
No law against it
Dennis Hursh, attorney and managing partner of Physician Agreements Health Law, a Pennsylvania-based law firm that represents physicians, noted in an interview that, “the problem isn’t legal per se. Rather, the problem is an ethical one.”
Legally speaking, there’s no prohibition against receiving a bequest or other form of gift from a patient. “People are free to dispose of their estates in whatever way they see fit, and no law technically precludes a physician from accepting a bequest,” says Dr. Victoroff. “But this presupposes there is nothing improper going on, such as extortion, deception, coercion, or exercising undue influence.”
The issue of bequeathing money to their physician gained attention in a recent case that took place in Australia. Peter Alexakis, MD, received a whopping bequest of $24 million from a patient. The elderly patient had changed his will to name Dr. Alexakis as the sole beneficiary – after Dr. Alexakis had visited him at home 92 times during the preceding months. The original heirs filed a lawsuit in Australia’s Supreme Court against Dr. Alexakis, contesting the will.
The lawsuit was unsuccessful in court, but Dr. Alexakis was found guilty of malpractice by Australia’s Health Care Complaints Commission after being reported to the HCCC by the palliative care physicians who were treating the patient. They alleged that Dr. Alexakis had interfered with their care of the patient. The more serious allegation was that the doctor had engaged in a deliberate strategy to exploit the relationship for financial gain.
Dr. Alexakis was chastised by the HCCC for engaging in “obtuse” and “suspicious” behavior and for “blurring the boundaries of the doctor-patient relationship.”
There are three domains – legal, ethical, and practical – when it comes to accepting bequests or any gifts from patients, says Dr. Victoroff.
“[In] the legal domain, for example, if you receive a bequest from anyone, patient or otherwise, you have to know your local laws about estates and taxes and so forth and obey them,” he said.
Attorney Hursh pointed out that the Australian doctor wasn’t found guilty of wrongdoing in a court of law but rather of unethical conduct by the Australian medical licensing entity.
Patients giving gifts is often a part of a physician’s life
When Ian Schorr, MD, first started out in practice, he was surprised that patients began bringing him gifts of food to express gratitude for his care.
“I thought it was unethical to accept their gifts, so I turned them down and wouldn’t accept so much as a cookie,” Dr. Schorr, a now-retired ophthalmologist, told this news organization. “But that changed because my office staff told me that some patients were feeling disappointed and insulted. I realized that some people want to express appreciation in ways that go beyond a monetary payment.”
The next time he received a gift from a patient, he “accepted it gracefully.” And he wrote a thank you note, which he continued to do any time he received a gift from a patient.
Kenneth Prager, MD, professor of clinical medicine, director of clinical ethics and chairman of the Medical Ethics Committee at Columbia University Medical Center, New York, says, “I have literally received hundreds of gifts, the vast majority being tokens of patients’ appreciation,” he said. “I’ll get boxes of chocolate or cakes, or sometimes articles of clothing.”
Occasionally, Dr. Prager receives a “somewhat larger gift” – for example, two tickets to a baseball game. “To reject these gifts would be a slap in the face to the patient,” he says, but “where it gets more ethically cloudy is when a gift is very substantial.”
Dr. Prager has never been offered a “substantial” gift or bequest personally. “But a patient whose brother I cared for has indicated that she has left instructions in her will to endow an associate chair of ethics in my honor, and I didn’t decline that,” he said.
The AMA Code of Ethics confirms that accepting gifts offered “as an expression of gratitude or a reflection of the patient’s cultural tradition” can “enhance the patient-physician relationship.” But sometimes gifts “may signal psychological needs that require the physician’s attention.” Accepting such gifts is “likely to damage the patient-physician relationship.”
Potential damage to the therapeutic relationship applies to all physicians but especially for psychiatrists and mental health professionals. “There are more stringent ethical requirements when it comes to these disciplines, where gift-giving gets into the territory of transference or may have particular psychological meaning, and accepting the gift may muddy the therapeutic waters,” Dr. Victoroff said.
Impact on the patient’s family and on other patients
The AMA statement encourages physicians to be “sensitive to the gift’s value, relative to the patient’s or physician’s means.” Physicians should decline gifts that are “disproportionately or inappropriately large, or when the physician would be uncomfortable to have colleagues know the gift had been accepted.”
They should also decline a bequest from a patient if they have reason to believe that to accept it “would present an emotional or financial hardship to the patient’s family.”
“If Bill Gates were leaving $100,000 to his doctor, I imagine Melinda would be just fine,” Mr. Hursh said. “But under ordinary circumstances, if the patient’s family might feel the impact of the bequest, it would be unethical to accept it and could be grounds for revocation of the doctor’s license.”
The AMA statement also warns physicians that by offering a gift, some patients may be seeking to “secure or influence care or to secure preferential treatment,” which can “undermine physicians’ obligation to provide services fairly to all patients.”
For this reason, bequests are “sticky,” said Laurel Lyckholm, MD, professor of hematology and oncology at West Virginia University School of Medicine. In the case of institutions where patients or community members donate money, “we know whose names are on the plaques that hang on the hospital walls, so it’s a delicate balance. What if there’s only one bed or one ventilator? Will the wife of the donor get preferential treatment?”
Follow institutional policy
A “very small gift, such as a fruitcake, is fine,” says Dr. Lyckholm, author of an essay on accepting gifts from patients. She said there’s a dollar amount ($15) that her institution mandates, above which a gift – even food – is considered too expensive to accept. “I was a nurse before I became a physician, and people always tried to give us gifts because we were so close to the minute-by-minute care of the patients,” she said. “We were not allowed to accept money or anything lavish.”
But in the case of small gifts, “the risk-benefit analysis is that there’s much more risk not to take it and to hurt the patient’s feelings.”
Gifts above $15 are given to charity. “I explain to patients that I’m not allowed to take such a large gift, but I’d love to give it to the hospital’s Rosenbaum Family House that provides patients and their relatives with lodging, or to the homeless shelter in Morgantown.”
Dr. Lyckholm, who serves on the ethics committee at J.W. Ruby Memorial Hospital, once was offered expensive tickets and said to the patient, “This is so incredibly thoughtful and kind, but I can’t accept them. I would like to give the tickets to a charity that can auction them off.”
She advises physicians to find out their institution’s policies. Many institutions have policies about what gifts their staff – whether physicians, nurses, or other health care professionals – can accept.
Passing the ‘smell test’
Accepting a large gift from a patient could potentially make it look like you might have exercised undue influence.
“That concern brings us to the third domain, which is very practical and all about appearances and perceptions,” Dr. Victoroff said.
He noted that there is “an inherent power differential between a physician and a patient. The very nature of the relationship can create a risk of ‘undue influence’ on the doctor’s part, even if it’s not apparent to the doctor.” For this reason, it’s necessary to be utterly transparent about how the bequest came about.
He suggests that if a patient informs you that he or she would like to leave money to you, it might be wise to suggest a meeting with the patient’s family, thus establishing some transparency.
It may not be possible to meet with the patient’s family for logistical reasons or because the patient would prefer not to involve their family in their estate planning. But in any case, it’s advisable to document any conversation in the patient’s chart, Dr. Victoroff advised.
“You should make a contemporaneous note that the patient initiated the suggestion and that you counseled them about the implications, no differently than you would with an interaction of a clinical nature,” he suggests. That way, if money has been left to you and is disputed, there’s a clear record that you didn’t solicit it or use any undue influence to bring it about.
He also recommended getting advice from a trusted colleague or a member of your institution’s ethics committee. “Taking time to get a second opinion about an ethical question is a safeguard, like having a chaperone in the room during an examination.”
Ultimately, “there is no human relationship without potential conflicts of interest. Our job is to manage those as best as we can, and sunlight is the best antidote to bad appearances,” Dr. Victoroff said.
A version of this article appeared on Medscape.com.
Resident creates AI alternative to U.S. News med school ranking
For decades, pre-med students depended on the annual medical school rankings by U.S. News and World Report to decide where to apply for physician education. But after several prominent med schools pulled out of the rankings, one resident began experimenting with artificial intelligence (AI) to create an alternative.
Brandon Turner MD, MSc, a radiation oncology resident at Massachusetts General Hospital in Boston, developed a free do-it-yourself tool using AI that allows prospective students to rank medical schools based on considerations that are most important to them. His research was published online in JAMA Network Open.
“One of the flaws with conventional ranking systems is that the metrics used in these tools are weighted based on the preferences and views of the people who developed these rankings, but those may not work for everyone,” Dr. Turner told this news organization.
He explained that there are different types of metrics used in the U.S. News ranking: one for research and the other for primary care. “The research rankings carry the most prestige and are the ones that most people know about,” he explained. These metrics take into account factors such as how many grant dollars the medical school receives and the average size of those grants per faculty member, Dr. Turner said.
Admission metrics are also included – for example, the median grade point average or MCAT scores of students who have been accepted. “These don’t tell you anything about the research output of the school, only about how selective the school is,” he said.
Primary care metrics might focus on how many graduates of a given school go into primary care, or how other schools rate the quality of primary care training at a given school – a process called peer assessment, Dr. Turner said.
But even though these might be helpful, students may be more interested in the cost of attendance, average debt, representation of minorities, and how many graduates pass their boards, he said. “U.S. News metrics don’t capture these things, but I included them in my algorithm.”
A U.S. News spokesperson said that the publication continues to help students and their families make decisions about their future education. The spokesperson cited U.S. News’ explanation of how it calculates its rankings. “A school’s overall Best Medical Schools rank should be one consideration and not the lone determinant in where a student applies and accepts,” the article states.
Dr. Turner agreed ranking systems are a good starting point when researching med schools, “but the values reflected in the ranking may not reflect an individual’s goals.”
Tyra-Lee Brett, a premed student at the University of South Florida, Tampa, believes an additional tool for students to evaluate medical schools is needed – and she could potentially see herself using Dr. Turner’s creation.
Still, Ms. Brett, a premed trustee of the American Medical Student Association, doesn’t regard any ranking tool as the “be all and end all.” Rather, she feels that the most effective tool would be based on students’ lived experiences. The AMSA is developing a scorecard in which students grade schools based on their opinions about such issues as housing, family planning, and environmental health, she said.
No prior judgments
To develop his algorithm, Dr. Turner used a branch of AI called “unsupervised learning.” It doesn’t make a prior judgment about what the data should look like, Dr. Turner explained.
“You’re just analyzing natural trends within the data.”
The algorithm tries to find and discover clusters or patterns within the data. “It’s like saying to the algorithm: ‘I want you to tell me what schools you think should be grouped together based on the data I feed you,’ which is the data that the user selects based on his or her personal preferences.”
U.S. News has been transparent about the metrics it uses, Dr. Turner notes. “When I started looking into how rankings are developed, I saw that there was transparency, and the reasoning for choosing the metrics used to develop the ranking was pretty sound,” he said.
“But I didn’t see any justification as to why they chose the particular metrics and weighted them in the way that they did.”
Dr. Turner extracted data from the 2023 U.S. News report, which ranked 109 allopathic medical schools, and applied several scenarios to the results to create his alternative ranking system.
In one scenario, he used the same research metrics used by U.S. News, such as a peer research assessment, median federal research activity per full-time faculty member, median GPA, median MCAT, acceptance rate, and faculty-student ratio.
In another scenario, he included four additional metrics: debt, in-state cost of attendance, USMLE Step 1 passing rate, and percentage of underrepresented students with minority race or ethnicity at the school.
For example, a user can rank the importance of the diversity of the class, amount of debt students expect to incur, and amount of research funding the medical school receives. After selecting those factors, the tool generates tiered results displayed in a circle, a shape chosen to avoid the appearance of the hierarchy associated with traditional rankings, Dr. Turner said.
“A prospective student might not care about acceptance rates and MCAT scores, and instead cares about diversity and debt,” Dr. Turner said. He looks forward to extending this approach to the ranking of colleges as well.
‘Imperfect measures’
“The model and interesting online tool that Dr. Turner created allows a premed [student] to generate custom rankings that are in line with their own priorities,” said Christopher Worsham, MD, MPH, a critical care physician in Mass General’s division of pulmonary and critical care medicine.
But Dr. Worsham, also a teaching associate at Harvard Medical School’s department of health care policy, expressed concern that factors figuring into the rankings by U.S. News and Dr. Turner’s alternative “are imperfect measures of medical school quality.”
For example, a student interested in research might favor federal research funding in their customized rankings with Dr. Turner’s model. “But higher research funding doesn’t necessarily translate into a better education for students, particularly when differentiating between two major research systems,” Dr. Worsham noted.
Dr. Worsham added that neither ranking system accurately predicts the quality of doctors graduating from the schools. Instead, he’d like to see ranking systems based on which schools’ graduates deliver the best patient outcomes, whether that’s through direct patient care, impactful research, or leadership within the health care system.
Michael Sauder, PhD, professor of sociology at the University of Iowa, Iowa City, said the model could offer a valuable alternative to the U.S. News ranking system. It might help users develop their own criteria for determining the ranking of medical schools, which is a big improvement over a “one-size-fits-all” approach, Dr. Sauder said.
And Hanna Stotland, an admission consultant based in Chicago, noted that most students rely on rankings because they “don’t have the luxury of advisers who know the ins and outs of different medical schools.” Given the role that rankings play, Ms. Stotland expects that every new ranking tool will have some influence on students.
This tool in particular “has the potential to be useful for students who have identified values they want their medical school to share.” For example, students who care about racial diversity “could use it to easily identify schools that are successful on that metric,” Ms. Stotland said.
Sujay Ratna, a 2nd-year med student at Icahn School of Medicine at Mount Sinai in New York, said he considered the U.S. News ranking his “go-to tool” when he was applying to med school.
But after reading Dr. Turner’s article, the AMSA membership vice president tried the algorithm. “I definitely would have used it had it existed when I was thinking of what schools to apply to and what [schools] to attend.”
The study had no specific funding. Dr. Turner, Dr. Worsham, Dr. Sauder, Ms. Stotland, Ms. Brett, and Mr. Ratna report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
For decades, pre-med students depended on the annual medical school rankings by U.S. News and World Report to decide where to apply for physician education. But after several prominent med schools pulled out of the rankings, one resident began experimenting with artificial intelligence (AI) to create an alternative.
Brandon Turner MD, MSc, a radiation oncology resident at Massachusetts General Hospital in Boston, developed a free do-it-yourself tool using AI that allows prospective students to rank medical schools based on considerations that are most important to them. His research was published online in JAMA Network Open.
“One of the flaws with conventional ranking systems is that the metrics used in these tools are weighted based on the preferences and views of the people who developed these rankings, but those may not work for everyone,” Dr. Turner told this news organization.
He explained that there are different types of metrics used in the U.S. News ranking: one for research and the other for primary care. “The research rankings carry the most prestige and are the ones that most people know about,” he explained. These metrics take into account factors such as how many grant dollars the medical school receives and the average size of those grants per faculty member, Dr. Turner said.
Admission metrics are also included – for example, the median grade point average or MCAT scores of students who have been accepted. “These don’t tell you anything about the research output of the school, only about how selective the school is,” he said.
Primary care metrics might focus on how many graduates of a given school go into primary care, or how other schools rate the quality of primary care training at a given school – a process called peer assessment, Dr. Turner said.
But even though these might be helpful, students may be more interested in the cost of attendance, average debt, representation of minorities, and how many graduates pass their boards, he said. “U.S. News metrics don’t capture these things, but I included them in my algorithm.”
A U.S. News spokesperson said that the publication continues to help students and their families make decisions about their future education. The spokesperson cited U.S. News’ explanation of how it calculates its rankings. “A school’s overall Best Medical Schools rank should be one consideration and not the lone determinant in where a student applies and accepts,” the article states.
Dr. Turner agreed ranking systems are a good starting point when researching med schools, “but the values reflected in the ranking may not reflect an individual’s goals.”
Tyra-Lee Brett, a premed student at the University of South Florida, Tampa, believes an additional tool for students to evaluate medical schools is needed – and she could potentially see herself using Dr. Turner’s creation.
Still, Ms. Brett, a premed trustee of the American Medical Student Association, doesn’t regard any ranking tool as the “be all and end all.” Rather, she feels that the most effective tool would be based on students’ lived experiences. The AMSA is developing a scorecard in which students grade schools based on their opinions about such issues as housing, family planning, and environmental health, she said.
No prior judgments
To develop his algorithm, Dr. Turner used a branch of AI called “unsupervised learning.” It doesn’t make a prior judgment about what the data should look like, Dr. Turner explained.
“You’re just analyzing natural trends within the data.”
The algorithm tries to find and discover clusters or patterns within the data. “It’s like saying to the algorithm: ‘I want you to tell me what schools you think should be grouped together based on the data I feed you,’ which is the data that the user selects based on his or her personal preferences.”
U.S. News has been transparent about the metrics it uses, Dr. Turner notes. “When I started looking into how rankings are developed, I saw that there was transparency, and the reasoning for choosing the metrics used to develop the ranking was pretty sound,” he said.
“But I didn’t see any justification as to why they chose the particular metrics and weighted them in the way that they did.”
Dr. Turner extracted data from the 2023 U.S. News report, which ranked 109 allopathic medical schools, and applied several scenarios to the results to create his alternative ranking system.
In one scenario, he used the same research metrics used by U.S. News, such as a peer research assessment, median federal research activity per full-time faculty member, median GPA, median MCAT, acceptance rate, and faculty-student ratio.
In another scenario, he included four additional metrics: debt, in-state cost of attendance, USMLE Step 1 passing rate, and percentage of underrepresented students with minority race or ethnicity at the school.
For example, a user can rank the importance of the diversity of the class, amount of debt students expect to incur, and amount of research funding the medical school receives. After selecting those factors, the tool generates tiered results displayed in a circle, a shape chosen to avoid the appearance of the hierarchy associated with traditional rankings, Dr. Turner said.
“A prospective student might not care about acceptance rates and MCAT scores, and instead cares about diversity and debt,” Dr. Turner said. He looks forward to extending this approach to the ranking of colleges as well.
‘Imperfect measures’
“The model and interesting online tool that Dr. Turner created allows a premed [student] to generate custom rankings that are in line with their own priorities,” said Christopher Worsham, MD, MPH, a critical care physician in Mass General’s division of pulmonary and critical care medicine.
But Dr. Worsham, also a teaching associate at Harvard Medical School’s department of health care policy, expressed concern that factors figuring into the rankings by U.S. News and Dr. Turner’s alternative “are imperfect measures of medical school quality.”
For example, a student interested in research might favor federal research funding in their customized rankings with Dr. Turner’s model. “But higher research funding doesn’t necessarily translate into a better education for students, particularly when differentiating between two major research systems,” Dr. Worsham noted.
Dr. Worsham added that neither ranking system accurately predicts the quality of doctors graduating from the schools. Instead, he’d like to see ranking systems based on which schools’ graduates deliver the best patient outcomes, whether that’s through direct patient care, impactful research, or leadership within the health care system.
Michael Sauder, PhD, professor of sociology at the University of Iowa, Iowa City, said the model could offer a valuable alternative to the U.S. News ranking system. It might help users develop their own criteria for determining the ranking of medical schools, which is a big improvement over a “one-size-fits-all” approach, Dr. Sauder said.
And Hanna Stotland, an admission consultant based in Chicago, noted that most students rely on rankings because they “don’t have the luxury of advisers who know the ins and outs of different medical schools.” Given the role that rankings play, Ms. Stotland expects that every new ranking tool will have some influence on students.
This tool in particular “has the potential to be useful for students who have identified values they want their medical school to share.” For example, students who care about racial diversity “could use it to easily identify schools that are successful on that metric,” Ms. Stotland said.
Sujay Ratna, a 2nd-year med student at Icahn School of Medicine at Mount Sinai in New York, said he considered the U.S. News ranking his “go-to tool” when he was applying to med school.
But after reading Dr. Turner’s article, the AMSA membership vice president tried the algorithm. “I definitely would have used it had it existed when I was thinking of what schools to apply to and what [schools] to attend.”
The study had no specific funding. Dr. Turner, Dr. Worsham, Dr. Sauder, Ms. Stotland, Ms. Brett, and Mr. Ratna report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
For decades, pre-med students depended on the annual medical school rankings by U.S. News and World Report to decide where to apply for physician education. But after several prominent med schools pulled out of the rankings, one resident began experimenting with artificial intelligence (AI) to create an alternative.
Brandon Turner MD, MSc, a radiation oncology resident at Massachusetts General Hospital in Boston, developed a free do-it-yourself tool using AI that allows prospective students to rank medical schools based on considerations that are most important to them. His research was published online in JAMA Network Open.
“One of the flaws with conventional ranking systems is that the metrics used in these tools are weighted based on the preferences and views of the people who developed these rankings, but those may not work for everyone,” Dr. Turner told this news organization.
He explained that there are different types of metrics used in the U.S. News ranking: one for research and the other for primary care. “The research rankings carry the most prestige and are the ones that most people know about,” he explained. These metrics take into account factors such as how many grant dollars the medical school receives and the average size of those grants per faculty member, Dr. Turner said.
Admission metrics are also included – for example, the median grade point average or MCAT scores of students who have been accepted. “These don’t tell you anything about the research output of the school, only about how selective the school is,” he said.
Primary care metrics might focus on how many graduates of a given school go into primary care, or how other schools rate the quality of primary care training at a given school – a process called peer assessment, Dr. Turner said.
But even though these might be helpful, students may be more interested in the cost of attendance, average debt, representation of minorities, and how many graduates pass their boards, he said. “U.S. News metrics don’t capture these things, but I included them in my algorithm.”
A U.S. News spokesperson said that the publication continues to help students and their families make decisions about their future education. The spokesperson cited U.S. News’ explanation of how it calculates its rankings. “A school’s overall Best Medical Schools rank should be one consideration and not the lone determinant in where a student applies and accepts,” the article states.
Dr. Turner agreed ranking systems are a good starting point when researching med schools, “but the values reflected in the ranking may not reflect an individual’s goals.”
Tyra-Lee Brett, a premed student at the University of South Florida, Tampa, believes an additional tool for students to evaluate medical schools is needed – and she could potentially see herself using Dr. Turner’s creation.
Still, Ms. Brett, a premed trustee of the American Medical Student Association, doesn’t regard any ranking tool as the “be all and end all.” Rather, she feels that the most effective tool would be based on students’ lived experiences. The AMSA is developing a scorecard in which students grade schools based on their opinions about such issues as housing, family planning, and environmental health, she said.
No prior judgments
To develop his algorithm, Dr. Turner used a branch of AI called “unsupervised learning.” It doesn’t make a prior judgment about what the data should look like, Dr. Turner explained.
“You’re just analyzing natural trends within the data.”
The algorithm tries to find and discover clusters or patterns within the data. “It’s like saying to the algorithm: ‘I want you to tell me what schools you think should be grouped together based on the data I feed you,’ which is the data that the user selects based on his or her personal preferences.”
U.S. News has been transparent about the metrics it uses, Dr. Turner notes. “When I started looking into how rankings are developed, I saw that there was transparency, and the reasoning for choosing the metrics used to develop the ranking was pretty sound,” he said.
“But I didn’t see any justification as to why they chose the particular metrics and weighted them in the way that they did.”
Dr. Turner extracted data from the 2023 U.S. News report, which ranked 109 allopathic medical schools, and applied several scenarios to the results to create his alternative ranking system.
In one scenario, he used the same research metrics used by U.S. News, such as a peer research assessment, median federal research activity per full-time faculty member, median GPA, median MCAT, acceptance rate, and faculty-student ratio.
In another scenario, he included four additional metrics: debt, in-state cost of attendance, USMLE Step 1 passing rate, and percentage of underrepresented students with minority race or ethnicity at the school.
For example, a user can rank the importance of the diversity of the class, amount of debt students expect to incur, and amount of research funding the medical school receives. After selecting those factors, the tool generates tiered results displayed in a circle, a shape chosen to avoid the appearance of the hierarchy associated with traditional rankings, Dr. Turner said.
“A prospective student might not care about acceptance rates and MCAT scores, and instead cares about diversity and debt,” Dr. Turner said. He looks forward to extending this approach to the ranking of colleges as well.
‘Imperfect measures’
“The model and interesting online tool that Dr. Turner created allows a premed [student] to generate custom rankings that are in line with their own priorities,” said Christopher Worsham, MD, MPH, a critical care physician in Mass General’s division of pulmonary and critical care medicine.
But Dr. Worsham, also a teaching associate at Harvard Medical School’s department of health care policy, expressed concern that factors figuring into the rankings by U.S. News and Dr. Turner’s alternative “are imperfect measures of medical school quality.”
For example, a student interested in research might favor federal research funding in their customized rankings with Dr. Turner’s model. “But higher research funding doesn’t necessarily translate into a better education for students, particularly when differentiating between two major research systems,” Dr. Worsham noted.
Dr. Worsham added that neither ranking system accurately predicts the quality of doctors graduating from the schools. Instead, he’d like to see ranking systems based on which schools’ graduates deliver the best patient outcomes, whether that’s through direct patient care, impactful research, or leadership within the health care system.
Michael Sauder, PhD, professor of sociology at the University of Iowa, Iowa City, said the model could offer a valuable alternative to the U.S. News ranking system. It might help users develop their own criteria for determining the ranking of medical schools, which is a big improvement over a “one-size-fits-all” approach, Dr. Sauder said.
And Hanna Stotland, an admission consultant based in Chicago, noted that most students rely on rankings because they “don’t have the luxury of advisers who know the ins and outs of different medical schools.” Given the role that rankings play, Ms. Stotland expects that every new ranking tool will have some influence on students.
This tool in particular “has the potential to be useful for students who have identified values they want their medical school to share.” For example, students who care about racial diversity “could use it to easily identify schools that are successful on that metric,” Ms. Stotland said.
Sujay Ratna, a 2nd-year med student at Icahn School of Medicine at Mount Sinai in New York, said he considered the U.S. News ranking his “go-to tool” when he was applying to med school.
But after reading Dr. Turner’s article, the AMSA membership vice president tried the algorithm. “I definitely would have used it had it existed when I was thinking of what schools to apply to and what [schools] to attend.”
The study had no specific funding. Dr. Turner, Dr. Worsham, Dr. Sauder, Ms. Stotland, Ms. Brett, and Mr. Ratna report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Could colchicine replace aspirin after PCI for ACS?
Dual antiplatelet therapy (DAPT) consisting of aspirin plus a P2Y12 inhibitor has been the standard of care to prevent thrombotic events in patients with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI).
in these patients, while mitigating the increased bleeding risk associated with aspirin.
Investigators conducted a pilot trial in ACS patients treated with drug-eluting stents (DES) who received low-dose colchicine the day after PCI, together with P2Y12 inhibitor (ticagrelor or prasugrel) maintenance therapy. Aspirin use was discontinued.
At 3 months, only 1% of the patients experienced stent thrombosis, and only 1 patient showed high platelet reactivity. Moreover, at 1 month, high-sensitivity C-reactive protein (hs-CRP) and platelet reactivity both decreased, pointing to reduced inflammation.
“In ACS patients undergoing PCI, it is feasible to discontinue aspirin therapy and administer low-dose colchicine on the day after PCI in addition to ticagrelor or prasugrel P2Y12 inhibitors,” write Seung-Yul Lee, MD, CHA Bundang Medical Center, CHA University, Seongnam, South Korea, and colleagues. “This approach is associated with favorable platelet function and inflammatory profiles.”
The study was published online in JACC: Cardiovascular Interventions.
Safety without compromised efficacy
The U.S. Food and Drug Administration recently approved colchicine 0.5-mg tablets (Lodoco, Agepha Pharma) as the first anti-inflammatory drug shown to reduce the risk for myocardial infarction, stroke, coronary revascularization, and cardiovascular death in adult patients with either established atherosclerotic disease or multiple risk factors for cardiovascular disease. It targets residual inflammation as an underlying cause of cardiovascular events.
Patients after PCI are generally treated using DAPT, but given the risk for increased bleeding associated with aspirin – especially when used long-term – there is a “need to identify strategies associated with a more favorable safety profile without compromising efficacy,” the authors write.
Previous research has yielded mixed results in terms of the discontinuation of aspirin therapy after 1-3 months and maintenance on P2Y12 inhibitor monotherapy. But one trial found colchicine to be effective in reducing recurrent ischemia, and its benefits may be more beneficial with early initiation in the hospital.
In this new study, researchers tested a “strategy that substitutes aspirin with colchicine during the acute phase to maximize the treatment effect of reducing recurrent ischemia and bleeding,” they write. The Mono Antiplatelet and Colchicine Therapy (MACT) single-arm, open-label proof-of-concept study was designed to investigate this approach.
The researchers studied 200 patients with non–ST-segment elevation ACS and ST-segment elevation myocardial infarction (STEMI) who underwent PCI with DES (mean [SD] age, 61.4 [10.7] years; 90% male; 100% of Asian ethnicity), who were receiving either ticagrelor or prasugrel plus a loading dose of aspirin.
On the day after PCI, aspirin was discontinued, and low-dose colchicine (0.6 mg once daily) was administered in addition to the P2Y12 inhibitor. In the case of staged PCI, it was performed under the maintenance of colchicine and ticagrelor or prasugrel.
No other antiplatelet or anticoagulant agents were permitted.
Patients underwent platelet function testing using the VerifyNow P2Y12 assay before discharge. Levels of hs-CRP were measured at admission, at 24 and 48 hours after PCI, and at 1-month follow-up. Clinical follow-up was performed at 1 and at 3 months.
The primary outcome was stent thrombosis within 3 months of follow-up. Secondary outcomes included all-cause mortality, MI, revascularization, major bleeding, a composite of cardiac death, target vessel MI, or target lesion revascularization, P2Y12 reaction units (PRUs), and change in hs-CRP levels between 24 hours post-PCI and 1-month follow-up.
The role of inflammation
Of the original 200 patients, 190 completed the full protocol and were available for follow-up.
The primary outcome occurred in only two patients. It turned out that one of the patients had not been adherent with antiplatelet medications.
“Although bleeding occurred in 36 patients, major bleeding occurred in only 1 patient,” the authors report.
The level of platelet reactivity at discharge was 27 ± 42 PRUs. Most patients (91%) met the criteria for low platelet reactivity, while only 0.5% met the criteria for high platelet reactivity. Platelet reactivity was similar, regardless of which P2Y12 inhibitor (ticagrelor or prasugrel) the patients were taking.
In all patients, the level of inflammation was “reduced considerably” over time: After 1 month, the hs-CRP level decreased from 6.1 mg/L (interquartile range [IQR], 2.6-15.9 mg/L) at 24 hours after PCI to 0.6 mg/L (IQR, 0.4-1.2 mg/L; P < .001).
The prevalence of high-inflammation criteria, defined as hs-CRP ≥ 2 mg/L, decreased significantly, from 81.8% at 24 hours after PCI to 11.8% at 1 month (P < .001).
Major bleeding was rare, they report, with a 3-month incidence of 0.5%.
“Inflammation plays a fundamental role in the development and progression of the atherothrombotic process,” the authors explain. A series of factors also trigger “an intense inflammatory response” in the acute phase of MI, which may lead to adverse myocardial remodeling. In the present study, inflammatory levels were rapidly reduced.
They noted several limitations. For example, all enrolled patients were Asian and were at relatively low bleeding and ischemic risk. “Although ticagrelor or prasugrel is effective regardless of ethnicity, clinical data supporting this de-escalation strategy are limited,” they state. Additionally, there was no control group for comparison.
The findings warrant further investigation, they conclude.
Promising but preliminary
Commenting for this news organization, Francesco Costa, MD, PhD, interventional cardiologist and assistant professor, University of Messina, Sicily, Italy, said he thinks it’s “too early for extensive clinical translation of these findings.”
Rather, larger and more extensive randomized trials are “on their way to give more precise estimates regarding the risks and benefits of early aspirin withdrawal in ACS.”
However, added Dr. Costa, who was not involved with the current research, “in this setting, adding colchicine early looks very promising to mitigate potential thrombotic risk without increasing bleeding risk.”
In the meantime, the study “provides novel insights on early aspirin withdrawal and P2Y12 monotherapy in an unselected population, including [those with] STEMI,” said Dr. Costa, also the coauthor of an accompanying editorial. The findings “could be of particular interest for those patients at extremely high bleeding risk or who are truly intolerant to aspirin, a scenario in which options are limited.”
This study was supported by the Cardiovascular Research Center, Seoul, South Korea. Dr. Lee reports no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. Costa has served on an advisory board for AstraZeneca and has received speaker fees from Chiesi Farmaceutici. His coauthor reports no relevant financial relationships.
A version of this article appeared on Medscape.com.
Dual antiplatelet therapy (DAPT) consisting of aspirin plus a P2Y12 inhibitor has been the standard of care to prevent thrombotic events in patients with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI).
in these patients, while mitigating the increased bleeding risk associated with aspirin.
Investigators conducted a pilot trial in ACS patients treated with drug-eluting stents (DES) who received low-dose colchicine the day after PCI, together with P2Y12 inhibitor (ticagrelor or prasugrel) maintenance therapy. Aspirin use was discontinued.
At 3 months, only 1% of the patients experienced stent thrombosis, and only 1 patient showed high platelet reactivity. Moreover, at 1 month, high-sensitivity C-reactive protein (hs-CRP) and platelet reactivity both decreased, pointing to reduced inflammation.
“In ACS patients undergoing PCI, it is feasible to discontinue aspirin therapy and administer low-dose colchicine on the day after PCI in addition to ticagrelor or prasugrel P2Y12 inhibitors,” write Seung-Yul Lee, MD, CHA Bundang Medical Center, CHA University, Seongnam, South Korea, and colleagues. “This approach is associated with favorable platelet function and inflammatory profiles.”
The study was published online in JACC: Cardiovascular Interventions.
Safety without compromised efficacy
The U.S. Food and Drug Administration recently approved colchicine 0.5-mg tablets (Lodoco, Agepha Pharma) as the first anti-inflammatory drug shown to reduce the risk for myocardial infarction, stroke, coronary revascularization, and cardiovascular death in adult patients with either established atherosclerotic disease or multiple risk factors for cardiovascular disease. It targets residual inflammation as an underlying cause of cardiovascular events.
Patients after PCI are generally treated using DAPT, but given the risk for increased bleeding associated with aspirin – especially when used long-term – there is a “need to identify strategies associated with a more favorable safety profile without compromising efficacy,” the authors write.
Previous research has yielded mixed results in terms of the discontinuation of aspirin therapy after 1-3 months and maintenance on P2Y12 inhibitor monotherapy. But one trial found colchicine to be effective in reducing recurrent ischemia, and its benefits may be more beneficial with early initiation in the hospital.
In this new study, researchers tested a “strategy that substitutes aspirin with colchicine during the acute phase to maximize the treatment effect of reducing recurrent ischemia and bleeding,” they write. The Mono Antiplatelet and Colchicine Therapy (MACT) single-arm, open-label proof-of-concept study was designed to investigate this approach.
The researchers studied 200 patients with non–ST-segment elevation ACS and ST-segment elevation myocardial infarction (STEMI) who underwent PCI with DES (mean [SD] age, 61.4 [10.7] years; 90% male; 100% of Asian ethnicity), who were receiving either ticagrelor or prasugrel plus a loading dose of aspirin.
On the day after PCI, aspirin was discontinued, and low-dose colchicine (0.6 mg once daily) was administered in addition to the P2Y12 inhibitor. In the case of staged PCI, it was performed under the maintenance of colchicine and ticagrelor or prasugrel.
No other antiplatelet or anticoagulant agents were permitted.
Patients underwent platelet function testing using the VerifyNow P2Y12 assay before discharge. Levels of hs-CRP were measured at admission, at 24 and 48 hours after PCI, and at 1-month follow-up. Clinical follow-up was performed at 1 and at 3 months.
The primary outcome was stent thrombosis within 3 months of follow-up. Secondary outcomes included all-cause mortality, MI, revascularization, major bleeding, a composite of cardiac death, target vessel MI, or target lesion revascularization, P2Y12 reaction units (PRUs), and change in hs-CRP levels between 24 hours post-PCI and 1-month follow-up.
The role of inflammation
Of the original 200 patients, 190 completed the full protocol and were available for follow-up.
The primary outcome occurred in only two patients. It turned out that one of the patients had not been adherent with antiplatelet medications.
“Although bleeding occurred in 36 patients, major bleeding occurred in only 1 patient,” the authors report.
The level of platelet reactivity at discharge was 27 ± 42 PRUs. Most patients (91%) met the criteria for low platelet reactivity, while only 0.5% met the criteria for high platelet reactivity. Platelet reactivity was similar, regardless of which P2Y12 inhibitor (ticagrelor or prasugrel) the patients were taking.
In all patients, the level of inflammation was “reduced considerably” over time: After 1 month, the hs-CRP level decreased from 6.1 mg/L (interquartile range [IQR], 2.6-15.9 mg/L) at 24 hours after PCI to 0.6 mg/L (IQR, 0.4-1.2 mg/L; P < .001).
The prevalence of high-inflammation criteria, defined as hs-CRP ≥ 2 mg/L, decreased significantly, from 81.8% at 24 hours after PCI to 11.8% at 1 month (P < .001).
Major bleeding was rare, they report, with a 3-month incidence of 0.5%.
“Inflammation plays a fundamental role in the development and progression of the atherothrombotic process,” the authors explain. A series of factors also trigger “an intense inflammatory response” in the acute phase of MI, which may lead to adverse myocardial remodeling. In the present study, inflammatory levels were rapidly reduced.
They noted several limitations. For example, all enrolled patients were Asian and were at relatively low bleeding and ischemic risk. “Although ticagrelor or prasugrel is effective regardless of ethnicity, clinical data supporting this de-escalation strategy are limited,” they state. Additionally, there was no control group for comparison.
The findings warrant further investigation, they conclude.
Promising but preliminary
Commenting for this news organization, Francesco Costa, MD, PhD, interventional cardiologist and assistant professor, University of Messina, Sicily, Italy, said he thinks it’s “too early for extensive clinical translation of these findings.”
Rather, larger and more extensive randomized trials are “on their way to give more precise estimates regarding the risks and benefits of early aspirin withdrawal in ACS.”
However, added Dr. Costa, who was not involved with the current research, “in this setting, adding colchicine early looks very promising to mitigate potential thrombotic risk without increasing bleeding risk.”
In the meantime, the study “provides novel insights on early aspirin withdrawal and P2Y12 monotherapy in an unselected population, including [those with] STEMI,” said Dr. Costa, also the coauthor of an accompanying editorial. The findings “could be of particular interest for those patients at extremely high bleeding risk or who are truly intolerant to aspirin, a scenario in which options are limited.”
This study was supported by the Cardiovascular Research Center, Seoul, South Korea. Dr. Lee reports no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. Costa has served on an advisory board for AstraZeneca and has received speaker fees from Chiesi Farmaceutici. His coauthor reports no relevant financial relationships.
A version of this article appeared on Medscape.com.
Dual antiplatelet therapy (DAPT) consisting of aspirin plus a P2Y12 inhibitor has been the standard of care to prevent thrombotic events in patients with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI).
in these patients, while mitigating the increased bleeding risk associated with aspirin.
Investigators conducted a pilot trial in ACS patients treated with drug-eluting stents (DES) who received low-dose colchicine the day after PCI, together with P2Y12 inhibitor (ticagrelor or prasugrel) maintenance therapy. Aspirin use was discontinued.
At 3 months, only 1% of the patients experienced stent thrombosis, and only 1 patient showed high platelet reactivity. Moreover, at 1 month, high-sensitivity C-reactive protein (hs-CRP) and platelet reactivity both decreased, pointing to reduced inflammation.
“In ACS patients undergoing PCI, it is feasible to discontinue aspirin therapy and administer low-dose colchicine on the day after PCI in addition to ticagrelor or prasugrel P2Y12 inhibitors,” write Seung-Yul Lee, MD, CHA Bundang Medical Center, CHA University, Seongnam, South Korea, and colleagues. “This approach is associated with favorable platelet function and inflammatory profiles.”
The study was published online in JACC: Cardiovascular Interventions.
Safety without compromised efficacy
The U.S. Food and Drug Administration recently approved colchicine 0.5-mg tablets (Lodoco, Agepha Pharma) as the first anti-inflammatory drug shown to reduce the risk for myocardial infarction, stroke, coronary revascularization, and cardiovascular death in adult patients with either established atherosclerotic disease or multiple risk factors for cardiovascular disease. It targets residual inflammation as an underlying cause of cardiovascular events.
Patients after PCI are generally treated using DAPT, but given the risk for increased bleeding associated with aspirin – especially when used long-term – there is a “need to identify strategies associated with a more favorable safety profile without compromising efficacy,” the authors write.
Previous research has yielded mixed results in terms of the discontinuation of aspirin therapy after 1-3 months and maintenance on P2Y12 inhibitor monotherapy. But one trial found colchicine to be effective in reducing recurrent ischemia, and its benefits may be more beneficial with early initiation in the hospital.
In this new study, researchers tested a “strategy that substitutes aspirin with colchicine during the acute phase to maximize the treatment effect of reducing recurrent ischemia and bleeding,” they write. The Mono Antiplatelet and Colchicine Therapy (MACT) single-arm, open-label proof-of-concept study was designed to investigate this approach.
The researchers studied 200 patients with non–ST-segment elevation ACS and ST-segment elevation myocardial infarction (STEMI) who underwent PCI with DES (mean [SD] age, 61.4 [10.7] years; 90% male; 100% of Asian ethnicity), who were receiving either ticagrelor or prasugrel plus a loading dose of aspirin.
On the day after PCI, aspirin was discontinued, and low-dose colchicine (0.6 mg once daily) was administered in addition to the P2Y12 inhibitor. In the case of staged PCI, it was performed under the maintenance of colchicine and ticagrelor or prasugrel.
No other antiplatelet or anticoagulant agents were permitted.
Patients underwent platelet function testing using the VerifyNow P2Y12 assay before discharge. Levels of hs-CRP were measured at admission, at 24 and 48 hours after PCI, and at 1-month follow-up. Clinical follow-up was performed at 1 and at 3 months.
The primary outcome was stent thrombosis within 3 months of follow-up. Secondary outcomes included all-cause mortality, MI, revascularization, major bleeding, a composite of cardiac death, target vessel MI, or target lesion revascularization, P2Y12 reaction units (PRUs), and change in hs-CRP levels between 24 hours post-PCI and 1-month follow-up.
The role of inflammation
Of the original 200 patients, 190 completed the full protocol and were available for follow-up.
The primary outcome occurred in only two patients. It turned out that one of the patients had not been adherent with antiplatelet medications.
“Although bleeding occurred in 36 patients, major bleeding occurred in only 1 patient,” the authors report.
The level of platelet reactivity at discharge was 27 ± 42 PRUs. Most patients (91%) met the criteria for low platelet reactivity, while only 0.5% met the criteria for high platelet reactivity. Platelet reactivity was similar, regardless of which P2Y12 inhibitor (ticagrelor or prasugrel) the patients were taking.
In all patients, the level of inflammation was “reduced considerably” over time: After 1 month, the hs-CRP level decreased from 6.1 mg/L (interquartile range [IQR], 2.6-15.9 mg/L) at 24 hours after PCI to 0.6 mg/L (IQR, 0.4-1.2 mg/L; P < .001).
The prevalence of high-inflammation criteria, defined as hs-CRP ≥ 2 mg/L, decreased significantly, from 81.8% at 24 hours after PCI to 11.8% at 1 month (P < .001).
Major bleeding was rare, they report, with a 3-month incidence of 0.5%.
“Inflammation plays a fundamental role in the development and progression of the atherothrombotic process,” the authors explain. A series of factors also trigger “an intense inflammatory response” in the acute phase of MI, which may lead to adverse myocardial remodeling. In the present study, inflammatory levels were rapidly reduced.
They noted several limitations. For example, all enrolled patients were Asian and were at relatively low bleeding and ischemic risk. “Although ticagrelor or prasugrel is effective regardless of ethnicity, clinical data supporting this de-escalation strategy are limited,” they state. Additionally, there was no control group for comparison.
The findings warrant further investigation, they conclude.
Promising but preliminary
Commenting for this news organization, Francesco Costa, MD, PhD, interventional cardiologist and assistant professor, University of Messina, Sicily, Italy, said he thinks it’s “too early for extensive clinical translation of these findings.”
Rather, larger and more extensive randomized trials are “on their way to give more precise estimates regarding the risks and benefits of early aspirin withdrawal in ACS.”
However, added Dr. Costa, who was not involved with the current research, “in this setting, adding colchicine early looks very promising to mitigate potential thrombotic risk without increasing bleeding risk.”
In the meantime, the study “provides novel insights on early aspirin withdrawal and P2Y12 monotherapy in an unselected population, including [those with] STEMI,” said Dr. Costa, also the coauthor of an accompanying editorial. The findings “could be of particular interest for those patients at extremely high bleeding risk or who are truly intolerant to aspirin, a scenario in which options are limited.”
This study was supported by the Cardiovascular Research Center, Seoul, South Korea. Dr. Lee reports no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. Costa has served on an advisory board for AstraZeneca and has received speaker fees from Chiesi Farmaceutici. His coauthor reports no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM JACC: CARIOVASCULAR INTERVENTIONS
A better way to measure antidepressant response?
Investigators assessed more than 800 patients with major depressive disorder (MDD) attending a partial hospital program. The patients completed questionnaires about depressive symptoms as well as functioning and broader measures of quality of life (QoL).
Although fewer than 40% were classified as treatment responders on the basis of depressive symptoms, as measured by the Remission from Depression Questionnaire (RDQ), two-thirds met criteria as responders on the Patient Global Rating of Improvement (PGI) scale, which takes into consideration broader domains of life satisfaction.
“The treatments we’re offering patients may be doing a better job than we think in treating depression, because many patients say they feel significantly better, even if their depression symptoms haven’t been diminished by the arbitrary threshold of 50% or greater improvement,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., told this news organization.
“Many of these patients – even if they have ongoing depressive symptoms – nevertheless say treatment has been very or extremely helpful, which is picked by other emphasizes in outcome, such as functioning, quality of life, coping abilities, and positive mental health,” added Dr. Zimmerman, director of the outpatient division at the Partial Hospital Program, Rhode Island Hospital.
The study was published online in the Annals of Clinical Psychiatry.
What’s the best tool?
“Almost all studies of depression treatment rely on measures of symptom severity to evaluate outcome – which is understandable, because a diagnosis of MDD requires a minimum number of symptoms for a sustained period of time,” said Dr. Zimmerman.
However, while important, symptom reduction is only one component of depression treatment. Improving overall function, QoL, and ability to deal with life’s stressors are equally important, he said.
Dr. Zimmerman emphasized he’s an “advocate, supporter, and practitioner of measurement-based care.” This approach, he said, “increases efficiency of the visit and directs me to the areas I should be inquiring about and the areas that need less time for inquiry.”
Measurement tools also enable numerical documentation of how a patient is doing and helps them understand and recognize their improvement.
The question is which tool captures improvements most effectively. Several surveys show that patients value improved functioning and QoL as primary treatment goals, which “is different from the emphasis of symptom improvement found in research,” said Dr. Zimmerman.
A multidimensional questionnaire that assesses functioning, QoL, and coping ability as well as symptoms is more likely to reflect patients’ treatment goals than simply measuring symptoms, he said.
Dr. Zimmerman and his coauthor reported on findings from the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) Project, which “examined the concordance between patients’ global rating of improvement from treatment and responder status, based on a depression symptoms severity scale.”
Doing better than we think
The study was conducted in Rhode Island Hospital’s department of psychiatry partial hospital program, where 844 patients with MDD (65.2% women; mean [SD] age, 36.8 [13.9] years) completed the RDQ – a self-report measure that “assesses constructs that patients consider to be relevant for assessing treatment outcome.” This questionnaire assesses symptom and nonsymptom domains that people consider important when evaluating treatment effectiveness.
To the original 41-item questionnaire, the researchers added 19 items. The final 60-item questionnaire included the following:
- 14 depressive symptoms.
- 11 nondepressive symptoms.
- 5 coping ability/stress tolerance items (for instance, “I had trouble handling pressure”).
- 12 positive mental health items (for instance, “I saw myself as a person of value”).
- 10 functioning items (for instance, “I was socially withdrawn”).
- 8 general well-being/life satisfaction items (for instance, “I was engaging in life rather than hiding from it”).
Patients were divided into three groups:
- Symptom responders (whose scores on the RDQ depressive symptom subscale improved by ≥ 50% from admission to discharge).
- PGI responders, who weren’t symptom responders – that is, who reported global improvement but didn’t improve ≥ 50% on the depression symptom subscale.
- Nonresponders (that is, patients who didn’t respond on the PGI and the depressive symptom subscale).
The researchers compared the three groups on the four symptom domains of the RDQ. Patients also completed the PGI on discharge, and the researchers compared these responses to responses to the RDQ.
Only 38.7% were responders on the depressive symptoms subscale, while 67.4% were PGI responders.
Most patients (91.4%) who were responders on the depressive symptom subscale were also PGI responders, while 32% were PGI responders but not responders on the depressive symptom subscale.
Although 29.2% were nonresponders on both measures, 70.8% were responders on one scale or the other.
As far as the nonsymptom domains, response rates varied between 30% (life satisfaction) to 33.1% (positive mental health).
“If you’re using a measurement tool in practice, I’d recommend one that goes beyond symptom improvement and also captures broader domains,” Dr. Zimmerman said.
‘Better enough’
Commenting on the study, Philip Muskin, MD, professor of psychiatry, Columbia University Medical Center, New York, said the use of symptom-driven rating scales to measure depression response originated in mandates of the U.S. Food and Drug Administration to determine whether a drug being tested in a clinical trial is superior to placebo.
“But there has been, for a long time, the question of whether these people are really better,” said Dr. Muskin, who was not involved with the current study. “Symptomatically, they may show improvement, but do they actually perceive themselves as better?”
Some patients might report, “I’m about 75% myself, but not back to 100%.” Dr. Muskin doesn’t “take these to be hard-and-fast numbers, but patients can tell you how they perceive themselves. This study suggests that if you’re wedded to [symptom measurement] scales, you may not realize that patients are actually getting better. And who decides if a patient is better, or better enough? The patient decides that.”
He added that some patients won’t achieve complete remission. “Even if I can’t get the person to be 100% better, I’m glad if I can help them become ‘better enough’ to function in life, do things, go to work, and improve in quality-of-life domains.”
The study received no outside funding. Dr. Zimmerman and his coauthor and Dr. Muskin report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators assessed more than 800 patients with major depressive disorder (MDD) attending a partial hospital program. The patients completed questionnaires about depressive symptoms as well as functioning and broader measures of quality of life (QoL).
Although fewer than 40% were classified as treatment responders on the basis of depressive symptoms, as measured by the Remission from Depression Questionnaire (RDQ), two-thirds met criteria as responders on the Patient Global Rating of Improvement (PGI) scale, which takes into consideration broader domains of life satisfaction.
“The treatments we’re offering patients may be doing a better job than we think in treating depression, because many patients say they feel significantly better, even if their depression symptoms haven’t been diminished by the arbitrary threshold of 50% or greater improvement,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., told this news organization.
“Many of these patients – even if they have ongoing depressive symptoms – nevertheless say treatment has been very or extremely helpful, which is picked by other emphasizes in outcome, such as functioning, quality of life, coping abilities, and positive mental health,” added Dr. Zimmerman, director of the outpatient division at the Partial Hospital Program, Rhode Island Hospital.
The study was published online in the Annals of Clinical Psychiatry.
What’s the best tool?
“Almost all studies of depression treatment rely on measures of symptom severity to evaluate outcome – which is understandable, because a diagnosis of MDD requires a minimum number of symptoms for a sustained period of time,” said Dr. Zimmerman.
However, while important, symptom reduction is only one component of depression treatment. Improving overall function, QoL, and ability to deal with life’s stressors are equally important, he said.
Dr. Zimmerman emphasized he’s an “advocate, supporter, and practitioner of measurement-based care.” This approach, he said, “increases efficiency of the visit and directs me to the areas I should be inquiring about and the areas that need less time for inquiry.”
Measurement tools also enable numerical documentation of how a patient is doing and helps them understand and recognize their improvement.
The question is which tool captures improvements most effectively. Several surveys show that patients value improved functioning and QoL as primary treatment goals, which “is different from the emphasis of symptom improvement found in research,” said Dr. Zimmerman.
A multidimensional questionnaire that assesses functioning, QoL, and coping ability as well as symptoms is more likely to reflect patients’ treatment goals than simply measuring symptoms, he said.
Dr. Zimmerman and his coauthor reported on findings from the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) Project, which “examined the concordance between patients’ global rating of improvement from treatment and responder status, based on a depression symptoms severity scale.”
Doing better than we think
The study was conducted in Rhode Island Hospital’s department of psychiatry partial hospital program, where 844 patients with MDD (65.2% women; mean [SD] age, 36.8 [13.9] years) completed the RDQ – a self-report measure that “assesses constructs that patients consider to be relevant for assessing treatment outcome.” This questionnaire assesses symptom and nonsymptom domains that people consider important when evaluating treatment effectiveness.
To the original 41-item questionnaire, the researchers added 19 items. The final 60-item questionnaire included the following:
- 14 depressive symptoms.
- 11 nondepressive symptoms.
- 5 coping ability/stress tolerance items (for instance, “I had trouble handling pressure”).
- 12 positive mental health items (for instance, “I saw myself as a person of value”).
- 10 functioning items (for instance, “I was socially withdrawn”).
- 8 general well-being/life satisfaction items (for instance, “I was engaging in life rather than hiding from it”).
Patients were divided into three groups:
- Symptom responders (whose scores on the RDQ depressive symptom subscale improved by ≥ 50% from admission to discharge).
- PGI responders, who weren’t symptom responders – that is, who reported global improvement but didn’t improve ≥ 50% on the depression symptom subscale.
- Nonresponders (that is, patients who didn’t respond on the PGI and the depressive symptom subscale).
The researchers compared the three groups on the four symptom domains of the RDQ. Patients also completed the PGI on discharge, and the researchers compared these responses to responses to the RDQ.
Only 38.7% were responders on the depressive symptoms subscale, while 67.4% were PGI responders.
Most patients (91.4%) who were responders on the depressive symptom subscale were also PGI responders, while 32% were PGI responders but not responders on the depressive symptom subscale.
Although 29.2% were nonresponders on both measures, 70.8% were responders on one scale or the other.
As far as the nonsymptom domains, response rates varied between 30% (life satisfaction) to 33.1% (positive mental health).
“If you’re using a measurement tool in practice, I’d recommend one that goes beyond symptom improvement and also captures broader domains,” Dr. Zimmerman said.
‘Better enough’
Commenting on the study, Philip Muskin, MD, professor of psychiatry, Columbia University Medical Center, New York, said the use of symptom-driven rating scales to measure depression response originated in mandates of the U.S. Food and Drug Administration to determine whether a drug being tested in a clinical trial is superior to placebo.
“But there has been, for a long time, the question of whether these people are really better,” said Dr. Muskin, who was not involved with the current study. “Symptomatically, they may show improvement, but do they actually perceive themselves as better?”
Some patients might report, “I’m about 75% myself, but not back to 100%.” Dr. Muskin doesn’t “take these to be hard-and-fast numbers, but patients can tell you how they perceive themselves. This study suggests that if you’re wedded to [symptom measurement] scales, you may not realize that patients are actually getting better. And who decides if a patient is better, or better enough? The patient decides that.”
He added that some patients won’t achieve complete remission. “Even if I can’t get the person to be 100% better, I’m glad if I can help them become ‘better enough’ to function in life, do things, go to work, and improve in quality-of-life domains.”
The study received no outside funding. Dr. Zimmerman and his coauthor and Dr. Muskin report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators assessed more than 800 patients with major depressive disorder (MDD) attending a partial hospital program. The patients completed questionnaires about depressive symptoms as well as functioning and broader measures of quality of life (QoL).
Although fewer than 40% were classified as treatment responders on the basis of depressive symptoms, as measured by the Remission from Depression Questionnaire (RDQ), two-thirds met criteria as responders on the Patient Global Rating of Improvement (PGI) scale, which takes into consideration broader domains of life satisfaction.
“The treatments we’re offering patients may be doing a better job than we think in treating depression, because many patients say they feel significantly better, even if their depression symptoms haven’t been diminished by the arbitrary threshold of 50% or greater improvement,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., told this news organization.
“Many of these patients – even if they have ongoing depressive symptoms – nevertheless say treatment has been very or extremely helpful, which is picked by other emphasizes in outcome, such as functioning, quality of life, coping abilities, and positive mental health,” added Dr. Zimmerman, director of the outpatient division at the Partial Hospital Program, Rhode Island Hospital.
The study was published online in the Annals of Clinical Psychiatry.
What’s the best tool?
“Almost all studies of depression treatment rely on measures of symptom severity to evaluate outcome – which is understandable, because a diagnosis of MDD requires a minimum number of symptoms for a sustained period of time,” said Dr. Zimmerman.
However, while important, symptom reduction is only one component of depression treatment. Improving overall function, QoL, and ability to deal with life’s stressors are equally important, he said.
Dr. Zimmerman emphasized he’s an “advocate, supporter, and practitioner of measurement-based care.” This approach, he said, “increases efficiency of the visit and directs me to the areas I should be inquiring about and the areas that need less time for inquiry.”
Measurement tools also enable numerical documentation of how a patient is doing and helps them understand and recognize their improvement.
The question is which tool captures improvements most effectively. Several surveys show that patients value improved functioning and QoL as primary treatment goals, which “is different from the emphasis of symptom improvement found in research,” said Dr. Zimmerman.
A multidimensional questionnaire that assesses functioning, QoL, and coping ability as well as symptoms is more likely to reflect patients’ treatment goals than simply measuring symptoms, he said.
Dr. Zimmerman and his coauthor reported on findings from the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) Project, which “examined the concordance between patients’ global rating of improvement from treatment and responder status, based on a depression symptoms severity scale.”
Doing better than we think
The study was conducted in Rhode Island Hospital’s department of psychiatry partial hospital program, where 844 patients with MDD (65.2% women; mean [SD] age, 36.8 [13.9] years) completed the RDQ – a self-report measure that “assesses constructs that patients consider to be relevant for assessing treatment outcome.” This questionnaire assesses symptom and nonsymptom domains that people consider important when evaluating treatment effectiveness.
To the original 41-item questionnaire, the researchers added 19 items. The final 60-item questionnaire included the following:
- 14 depressive symptoms.
- 11 nondepressive symptoms.
- 5 coping ability/stress tolerance items (for instance, “I had trouble handling pressure”).
- 12 positive mental health items (for instance, “I saw myself as a person of value”).
- 10 functioning items (for instance, “I was socially withdrawn”).
- 8 general well-being/life satisfaction items (for instance, “I was engaging in life rather than hiding from it”).
Patients were divided into three groups:
- Symptom responders (whose scores on the RDQ depressive symptom subscale improved by ≥ 50% from admission to discharge).
- PGI responders, who weren’t symptom responders – that is, who reported global improvement but didn’t improve ≥ 50% on the depression symptom subscale.
- Nonresponders (that is, patients who didn’t respond on the PGI and the depressive symptom subscale).
The researchers compared the three groups on the four symptom domains of the RDQ. Patients also completed the PGI on discharge, and the researchers compared these responses to responses to the RDQ.
Only 38.7% were responders on the depressive symptoms subscale, while 67.4% were PGI responders.
Most patients (91.4%) who were responders on the depressive symptom subscale were also PGI responders, while 32% were PGI responders but not responders on the depressive symptom subscale.
Although 29.2% were nonresponders on both measures, 70.8% were responders on one scale or the other.
As far as the nonsymptom domains, response rates varied between 30% (life satisfaction) to 33.1% (positive mental health).
“If you’re using a measurement tool in practice, I’d recommend one that goes beyond symptom improvement and also captures broader domains,” Dr. Zimmerman said.
‘Better enough’
Commenting on the study, Philip Muskin, MD, professor of psychiatry, Columbia University Medical Center, New York, said the use of symptom-driven rating scales to measure depression response originated in mandates of the U.S. Food and Drug Administration to determine whether a drug being tested in a clinical trial is superior to placebo.
“But there has been, for a long time, the question of whether these people are really better,” said Dr. Muskin, who was not involved with the current study. “Symptomatically, they may show improvement, but do they actually perceive themselves as better?”
Some patients might report, “I’m about 75% myself, but not back to 100%.” Dr. Muskin doesn’t “take these to be hard-and-fast numbers, but patients can tell you how they perceive themselves. This study suggests that if you’re wedded to [symptom measurement] scales, you may not realize that patients are actually getting better. And who decides if a patient is better, or better enough? The patient decides that.”
He added that some patients won’t achieve complete remission. “Even if I can’t get the person to be 100% better, I’m glad if I can help them become ‘better enough’ to function in life, do things, go to work, and improve in quality-of-life domains.”
The study received no outside funding. Dr. Zimmerman and his coauthor and Dr. Muskin report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF CLINICAL PSYCHIATRY
Physician-assisted suicide for mental illness – right or wrong?
Until recently, this contentious issue applied only to patients with physical illnesses who want to end their suffering and who seek out a physician willing to assist with that objective. In the United States and other countries, this is the patient population who may be able to avail themselves of this option.
However, newly proposed legislation in Canada – which has the largest number of physician-assisted deaths worldwide – would expand the indication for MAID to include serious mental illness. Originally set to be passed in March 2023, the law has been deferred for final decision until March 2024.
A recent commentary by psychiatrist Dinah Miller, MD, explored the ethics of this proposed legislation for mental health professionals. “To offer the option of death facilitated by the very person who is trying to get [patients with serious mental illness] better seems so counter to everything I have learned and contradicts our role as psychiatrists who work so hard to prevent suicide,” Dr. Miller wrote. “As psychiatrists, do we offer hope to our most vulnerable patients, or do we offer death? Do we rail against suicide, or do we facilitate it?”
Dr. Miller’s piece garnered a huge amount of reader response that included many laudatory comments: a “nuanced and open-ended inquiry here,” “timely and honest,” and “beautifully written.” One reader thanked the author for “this thoughtful, questioning, and open reflection on what it means to be a psychiatrist facing a thorny and deeply personal practice and philosophical question.”
Cognitive distortion or objective reality?
Many readers were opposed to any type of physician involvement in hastening a patient’s death, regardless of whether the condition is medical or psychiatric. “Let others who wish to die make their own arrangement without the aid of the medical profession,” one reader wrote.
But others felt that for those with terminal physical illnesses or intractable pain, it is justified for medical professionals to either facilitate death or, at the very least, withhold life-prolonging treatments.
A critical-care physician described responding to families’ accusations that withdrawal of life-sustaining measures means “playing God.” On the contrary, the physician wrote, “there is a limit to our abilities; and withdrawing those life-prolonging interventions allows nature or God or whatever to play a role and take its course.”
Another U.S. reader pointed out that “multiple polls in this country have shown that the majority of the general public, physicians in general and psychiatrists in particular, support the option of MAID for the terminally ill. They do not find it at variance with their calling as physicians.”
“I and many of my elderly friends don’t fear death but fear prolonged dementia with its dependency and lack of quality of life,” one reader wrote. “We would be much more at peace if we could put in our advanced directive that we request MAID once some point of dependency has been reached.”
Another wrote that in the event of entering a state of “degrading dependency and hardship on the family, please let me go peacefully, without burdening others, into that good night [of death].”
Many felt that not only physical illness but also the prospect of cognitive degeneration – specifically dementia – also justifies assisting patient death.
“Enormous suffering”
One Canadian reader noted that provisions for advance consent are now in place in Canada for those facing the prospect of neurodegenerative disease and who are still mentally competent to make such decisions.
But therein lies the rub – the concept of an advanced directive goes to the question of decisional capacity. Dr. Miller noted that “depression distorts cognition and leads many patients to believe that they would be better off dead and that their loves ones would be better off without them.”
The concept of “cognitive distortion” implies that the illness itself may impede the decisional capacity required for an advanced directive or a decision made in the moment, in the absence of such a directive. Dr. Miller asked, “How do we determine whether patients with serious mental illness are competent to make such a decision or whether it is mental illness that is driving their perception of a future without hope?”
One reader attested to this from personal experience. “As both a physician and a sufferer of severe, often profound depression for 50 years, I can confidently say that ... the pursuit of death is the result of an impaired mental state, which simultaneously prevents a rational decision.”
Another agreed. “As a psychiatrist, I treated suicidal patients almost every day of my 27-year career. I believe in making every effort to prevent the suicide of a healthy depressed person and I do not support MAID for psychiatric conditions. But I do support MAID for the terminally ill.”
Other readers disagreed. In the words of one commentator, “I think that if we are going to help mentally ill people, we have to consider their choices. The stress imposed by a severe/intractable mental illness is as bad as any other devastating medical illness. If no one is going to hold their hand in life (as support services are limited and psychiatric treatments often fail), allow a medical professional to hold their hand through their final moments.”
A psychiatrist described very ill patients with treatment-resistant bipolar disorder who had not only received medications, including ketamine, but had also received electroconvulsive therapy and still did not respond.
“Their suffering is enormous and the truth is that there is no improvement for more than a few days or weeks and later they return to their hell. Appreciating that they would be better off dead for themselves and their families is not always a cognitive distortion but an objective evaluation of their reality.”
However, as another reader pointed out, an issue with the argument presented here is that it presupposes that MAID requires “clinical justification.” But in Canada, “MAID ... is understood as an expression of personal autonomy. Rooted in liberal political philosophy of individualism ... approval for death need not be based on a clinical assessment.” Instead, “death is seen as a ‘right’ that the state must therefore provide.”
Another form of eugenics?
Dr. Miller raised the ethical implications of racial and socioeconomic factors playing a role in the consideration of MAID for those with psychiatric illness.
“Might those who are poor, who have less access to expensive treatment options and social support, be more likely to request facilitated death?” she asks. “Do we risk facilitating a patient’s demise when other options are unavailable because of a lack of access to treatment or when social and financial struggles exacerbate a person’s hopelessness? Should we worry that psychiatric euthanasia will turn into a form of eugenics where those who can’t contribute are made to feel that they should bow out?”
Several readers agreed. “Looking at the disproportionate burden of illness, rates of imprisonment, and application of the death penalty indicates to me that race and socioeconomic status will be an immediate factor in how, where, and with whom MAID for mental illness would be practice in much, if not all, of the U.S.,” wrote one physician.
A Canadian reader expressed similar concerns. “I’ve seen a handful of people, including someone I considered a good friend, opt for MAID because it was easier than living as a disabled person in poverty without adequate mental health care.”
Another Canadian clinician noted that offering people good care can make all the difference. “As a Canadian mental health clinician who served youth with severe mental illness for over 20 years through our socialized medical network, I can attest to the difference good care usually makes in shifting clients from despair and a commitment to death to embracing life once again. Let’s not, as clinicians, embrace easing a government/state-sanctioned pathway to death.”
Some readers believe that these types of issues can’t be solved with a blanket approach, noting that each case is different. “Real life is always more complicated than academic discussions. Having served on a hospital ethics committee, I know that each case is unique,” one reader noted.
Another reader added, “I think all we can do as physicians is to let people decide for themselves and participate only if our conscience allows.”
A version of this article first appeared on Medscape.com.
Until recently, this contentious issue applied only to patients with physical illnesses who want to end their suffering and who seek out a physician willing to assist with that objective. In the United States and other countries, this is the patient population who may be able to avail themselves of this option.
However, newly proposed legislation in Canada – which has the largest number of physician-assisted deaths worldwide – would expand the indication for MAID to include serious mental illness. Originally set to be passed in March 2023, the law has been deferred for final decision until March 2024.
A recent commentary by psychiatrist Dinah Miller, MD, explored the ethics of this proposed legislation for mental health professionals. “To offer the option of death facilitated by the very person who is trying to get [patients with serious mental illness] better seems so counter to everything I have learned and contradicts our role as psychiatrists who work so hard to prevent suicide,” Dr. Miller wrote. “As psychiatrists, do we offer hope to our most vulnerable patients, or do we offer death? Do we rail against suicide, or do we facilitate it?”
Dr. Miller’s piece garnered a huge amount of reader response that included many laudatory comments: a “nuanced and open-ended inquiry here,” “timely and honest,” and “beautifully written.” One reader thanked the author for “this thoughtful, questioning, and open reflection on what it means to be a psychiatrist facing a thorny and deeply personal practice and philosophical question.”
Cognitive distortion or objective reality?
Many readers were opposed to any type of physician involvement in hastening a patient’s death, regardless of whether the condition is medical or psychiatric. “Let others who wish to die make their own arrangement without the aid of the medical profession,” one reader wrote.
But others felt that for those with terminal physical illnesses or intractable pain, it is justified for medical professionals to either facilitate death or, at the very least, withhold life-prolonging treatments.
A critical-care physician described responding to families’ accusations that withdrawal of life-sustaining measures means “playing God.” On the contrary, the physician wrote, “there is a limit to our abilities; and withdrawing those life-prolonging interventions allows nature or God or whatever to play a role and take its course.”
Another U.S. reader pointed out that “multiple polls in this country have shown that the majority of the general public, physicians in general and psychiatrists in particular, support the option of MAID for the terminally ill. They do not find it at variance with their calling as physicians.”
“I and many of my elderly friends don’t fear death but fear prolonged dementia with its dependency and lack of quality of life,” one reader wrote. “We would be much more at peace if we could put in our advanced directive that we request MAID once some point of dependency has been reached.”
Another wrote that in the event of entering a state of “degrading dependency and hardship on the family, please let me go peacefully, without burdening others, into that good night [of death].”
Many felt that not only physical illness but also the prospect of cognitive degeneration – specifically dementia – also justifies assisting patient death.
“Enormous suffering”
One Canadian reader noted that provisions for advance consent are now in place in Canada for those facing the prospect of neurodegenerative disease and who are still mentally competent to make such decisions.
But therein lies the rub – the concept of an advanced directive goes to the question of decisional capacity. Dr. Miller noted that “depression distorts cognition and leads many patients to believe that they would be better off dead and that their loves ones would be better off without them.”
The concept of “cognitive distortion” implies that the illness itself may impede the decisional capacity required for an advanced directive or a decision made in the moment, in the absence of such a directive. Dr. Miller asked, “How do we determine whether patients with serious mental illness are competent to make such a decision or whether it is mental illness that is driving their perception of a future without hope?”
One reader attested to this from personal experience. “As both a physician and a sufferer of severe, often profound depression for 50 years, I can confidently say that ... the pursuit of death is the result of an impaired mental state, which simultaneously prevents a rational decision.”
Another agreed. “As a psychiatrist, I treated suicidal patients almost every day of my 27-year career. I believe in making every effort to prevent the suicide of a healthy depressed person and I do not support MAID for psychiatric conditions. But I do support MAID for the terminally ill.”
Other readers disagreed. In the words of one commentator, “I think that if we are going to help mentally ill people, we have to consider their choices. The stress imposed by a severe/intractable mental illness is as bad as any other devastating medical illness. If no one is going to hold their hand in life (as support services are limited and psychiatric treatments often fail), allow a medical professional to hold their hand through their final moments.”
A psychiatrist described very ill patients with treatment-resistant bipolar disorder who had not only received medications, including ketamine, but had also received electroconvulsive therapy and still did not respond.
“Their suffering is enormous and the truth is that there is no improvement for more than a few days or weeks and later they return to their hell. Appreciating that they would be better off dead for themselves and their families is not always a cognitive distortion but an objective evaluation of their reality.”
However, as another reader pointed out, an issue with the argument presented here is that it presupposes that MAID requires “clinical justification.” But in Canada, “MAID ... is understood as an expression of personal autonomy. Rooted in liberal political philosophy of individualism ... approval for death need not be based on a clinical assessment.” Instead, “death is seen as a ‘right’ that the state must therefore provide.”
Another form of eugenics?
Dr. Miller raised the ethical implications of racial and socioeconomic factors playing a role in the consideration of MAID for those with psychiatric illness.
“Might those who are poor, who have less access to expensive treatment options and social support, be more likely to request facilitated death?” she asks. “Do we risk facilitating a patient’s demise when other options are unavailable because of a lack of access to treatment or when social and financial struggles exacerbate a person’s hopelessness? Should we worry that psychiatric euthanasia will turn into a form of eugenics where those who can’t contribute are made to feel that they should bow out?”
Several readers agreed. “Looking at the disproportionate burden of illness, rates of imprisonment, and application of the death penalty indicates to me that race and socioeconomic status will be an immediate factor in how, where, and with whom MAID for mental illness would be practice in much, if not all, of the U.S.,” wrote one physician.
A Canadian reader expressed similar concerns. “I’ve seen a handful of people, including someone I considered a good friend, opt for MAID because it was easier than living as a disabled person in poverty without adequate mental health care.”
Another Canadian clinician noted that offering people good care can make all the difference. “As a Canadian mental health clinician who served youth with severe mental illness for over 20 years through our socialized medical network, I can attest to the difference good care usually makes in shifting clients from despair and a commitment to death to embracing life once again. Let’s not, as clinicians, embrace easing a government/state-sanctioned pathway to death.”
Some readers believe that these types of issues can’t be solved with a blanket approach, noting that each case is different. “Real life is always more complicated than academic discussions. Having served on a hospital ethics committee, I know that each case is unique,” one reader noted.
Another reader added, “I think all we can do as physicians is to let people decide for themselves and participate only if our conscience allows.”
A version of this article first appeared on Medscape.com.
Until recently, this contentious issue applied only to patients with physical illnesses who want to end their suffering and who seek out a physician willing to assist with that objective. In the United States and other countries, this is the patient population who may be able to avail themselves of this option.
However, newly proposed legislation in Canada – which has the largest number of physician-assisted deaths worldwide – would expand the indication for MAID to include serious mental illness. Originally set to be passed in March 2023, the law has been deferred for final decision until March 2024.
A recent commentary by psychiatrist Dinah Miller, MD, explored the ethics of this proposed legislation for mental health professionals. “To offer the option of death facilitated by the very person who is trying to get [patients with serious mental illness] better seems so counter to everything I have learned and contradicts our role as psychiatrists who work so hard to prevent suicide,” Dr. Miller wrote. “As psychiatrists, do we offer hope to our most vulnerable patients, or do we offer death? Do we rail against suicide, or do we facilitate it?”
Dr. Miller’s piece garnered a huge amount of reader response that included many laudatory comments: a “nuanced and open-ended inquiry here,” “timely and honest,” and “beautifully written.” One reader thanked the author for “this thoughtful, questioning, and open reflection on what it means to be a psychiatrist facing a thorny and deeply personal practice and philosophical question.”
Cognitive distortion or objective reality?
Many readers were opposed to any type of physician involvement in hastening a patient’s death, regardless of whether the condition is medical or psychiatric. “Let others who wish to die make their own arrangement without the aid of the medical profession,” one reader wrote.
But others felt that for those with terminal physical illnesses or intractable pain, it is justified for medical professionals to either facilitate death or, at the very least, withhold life-prolonging treatments.
A critical-care physician described responding to families’ accusations that withdrawal of life-sustaining measures means “playing God.” On the contrary, the physician wrote, “there is a limit to our abilities; and withdrawing those life-prolonging interventions allows nature or God or whatever to play a role and take its course.”
Another U.S. reader pointed out that “multiple polls in this country have shown that the majority of the general public, physicians in general and psychiatrists in particular, support the option of MAID for the terminally ill. They do not find it at variance with their calling as physicians.”
“I and many of my elderly friends don’t fear death but fear prolonged dementia with its dependency and lack of quality of life,” one reader wrote. “We would be much more at peace if we could put in our advanced directive that we request MAID once some point of dependency has been reached.”
Another wrote that in the event of entering a state of “degrading dependency and hardship on the family, please let me go peacefully, without burdening others, into that good night [of death].”
Many felt that not only physical illness but also the prospect of cognitive degeneration – specifically dementia – also justifies assisting patient death.
“Enormous suffering”
One Canadian reader noted that provisions for advance consent are now in place in Canada for those facing the prospect of neurodegenerative disease and who are still mentally competent to make such decisions.
But therein lies the rub – the concept of an advanced directive goes to the question of decisional capacity. Dr. Miller noted that “depression distorts cognition and leads many patients to believe that they would be better off dead and that their loves ones would be better off without them.”
The concept of “cognitive distortion” implies that the illness itself may impede the decisional capacity required for an advanced directive or a decision made in the moment, in the absence of such a directive. Dr. Miller asked, “How do we determine whether patients with serious mental illness are competent to make such a decision or whether it is mental illness that is driving their perception of a future without hope?”
One reader attested to this from personal experience. “As both a physician and a sufferer of severe, often profound depression for 50 years, I can confidently say that ... the pursuit of death is the result of an impaired mental state, which simultaneously prevents a rational decision.”
Another agreed. “As a psychiatrist, I treated suicidal patients almost every day of my 27-year career. I believe in making every effort to prevent the suicide of a healthy depressed person and I do not support MAID for psychiatric conditions. But I do support MAID for the terminally ill.”
Other readers disagreed. In the words of one commentator, “I think that if we are going to help mentally ill people, we have to consider their choices. The stress imposed by a severe/intractable mental illness is as bad as any other devastating medical illness. If no one is going to hold their hand in life (as support services are limited and psychiatric treatments often fail), allow a medical professional to hold their hand through their final moments.”
A psychiatrist described very ill patients with treatment-resistant bipolar disorder who had not only received medications, including ketamine, but had also received electroconvulsive therapy and still did not respond.
“Their suffering is enormous and the truth is that there is no improvement for more than a few days or weeks and later they return to their hell. Appreciating that they would be better off dead for themselves and their families is not always a cognitive distortion but an objective evaluation of their reality.”
However, as another reader pointed out, an issue with the argument presented here is that it presupposes that MAID requires “clinical justification.” But in Canada, “MAID ... is understood as an expression of personal autonomy. Rooted in liberal political philosophy of individualism ... approval for death need not be based on a clinical assessment.” Instead, “death is seen as a ‘right’ that the state must therefore provide.”
Another form of eugenics?
Dr. Miller raised the ethical implications of racial and socioeconomic factors playing a role in the consideration of MAID for those with psychiatric illness.
“Might those who are poor, who have less access to expensive treatment options and social support, be more likely to request facilitated death?” she asks. “Do we risk facilitating a patient’s demise when other options are unavailable because of a lack of access to treatment or when social and financial struggles exacerbate a person’s hopelessness? Should we worry that psychiatric euthanasia will turn into a form of eugenics where those who can’t contribute are made to feel that they should bow out?”
Several readers agreed. “Looking at the disproportionate burden of illness, rates of imprisonment, and application of the death penalty indicates to me that race and socioeconomic status will be an immediate factor in how, where, and with whom MAID for mental illness would be practice in much, if not all, of the U.S.,” wrote one physician.
A Canadian reader expressed similar concerns. “I’ve seen a handful of people, including someone I considered a good friend, opt for MAID because it was easier than living as a disabled person in poverty without adequate mental health care.”
Another Canadian clinician noted that offering people good care can make all the difference. “As a Canadian mental health clinician who served youth with severe mental illness for over 20 years through our socialized medical network, I can attest to the difference good care usually makes in shifting clients from despair and a commitment to death to embracing life once again. Let’s not, as clinicians, embrace easing a government/state-sanctioned pathway to death.”
Some readers believe that these types of issues can’t be solved with a blanket approach, noting that each case is different. “Real life is always more complicated than academic discussions. Having served on a hospital ethics committee, I know that each case is unique,” one reader noted.
Another reader added, “I think all we can do as physicians is to let people decide for themselves and participate only if our conscience allows.”
A version of this article first appeared on Medscape.com.
Inhaling pleasant scents during sleep tied to a dramatic boost in cognition
In a small, randomized controlled trial researchers found that when cognitively normal individuals were exposed to the scent of an essential oil for 2 hours every night over 6 months, they experienced a 226% improvement in memory compared with a control group who received only a trace amount of the diffused scent.
In addition, functional magnetic resonance imaging (fMRI) showed that those in the enriched group had improved functioning of the left uncinate fasciculus, an area of the brain linked to memory and cognition, which typically declines with age.
“To my knowledge, that level of [memory] improvement is far greater than anything that has been reported for healthy older adults and we also found a critical memory pathway in their brains improved to a similar extent relative to unenriched older adults,” senior investigator Michael Leon, PhD, professor emeritus, University of California, Irvine, said in an interview.
The study was published online in Frontiers of Neuroscience.
The brain’s “superhighway”
Olfactory enrichment “involves the daily exposure of individuals to multiple odorants” and has been shown in mouse models to improve memory and neurogenesis, the investigators noted.
A previous study showed that exposure to individual essential oils for 30 minutes a day over 3 months induced neurogenesis in the olfactory bulb and the hippocampus.
“The olfactory system is the only sense that has a direct ‘superhighway’ input to the memory centers areas of the brain; all the other senses have to reach those brain areas through what you might call the ‘side streets’ of the brain, and so consequently, they have much less impact on maintaining the health of those memory centers.”
When olfaction is compromised, “the memory centers of the brain start to deteriorate and, conversely, when people are given olfactory enrichment, their memory areas become larger and more functional,” he added.
Olfactory dysfunction is the first symptom of Alzheimer’s disease (AD) and is also found in virtually all neurological and psychiatric disorders.
“I’ve counted 68 of them – including anorexia, anxiety, [attention-deficit/hyperactivity disorder], depression, epilepsy, and stroke. In fact, by mid-life, your all-cause mortality can be predicted by your ability to smell things,” Dr. Leon said.
Dr. Leon and colleagues previously developed an effective treatment for autism using environmental enrichment that focused on odor stimulation, along with stimulating other senses. “We then considered the possibility that olfactory enrichment alone might improve brain function.”
Rose, orange, eucalyptus …
For the study, the researchers randomly assigned 43 older adults, aged 60-85 years, to receive either nightly exposure to essential oil scents delivered via a diffuser (n = 20; mean [SD] age, 70.1 [6.6] years) or to a sham control with only trace amounts of odorants (n = 23; mean age, 69.2 [7.1] years) for a period of 6 months.
The intervention group was exposed to a single odorant, delivered through a diffuser, for 2 hours nightly, rotating through seven pleasant aromas each week. They included rose, orange, eucalyptus, lemon, peppermint, rosemary, and lavender scents.
All participants completed a battery of tests at baseline, including the Mini-Mental State Examination (MMSE), which confirmed normal cognitive functioning. At baseline and after a 6-month follow-up, participants completed the Rey Auditory Verbal Learning Test (RAVLT) as well as three subsets of the Wechsler Adult Intelligence Scale–Third Edition (WAIS-III).
Olfactory system function was assessed using “Sniffin Sticks,” allowing the researchers to determine if olfactory enrichment enhanced olfactory performance.
Participants underwent fMRI at baseline and again at 6 months.
Brain imaging results showed a “clear, statistically significant 226% difference between enriched and control older adults in performance on the RAVLT, which evaluates learning and memory (timepoint × group interaction; F = 6.63; P = .02; Cohen’s d = 1.08; a “large effect size”).
They also found a significant change in the mean diffusivity of the left uncinate fasciculus in the enriched group compared with the controls (timepoint × group interaction; F = 4.39; P = .043; h 2 p = .101; a “medium-size effect”).
The uncinate fasciculus is a “major pathway” connecting the basolateral amygdala and the entorhinal cortex to the prefrontal cortex. This pathway deteriorates in aging and in AD and “has been suggested to play a role in mediating episodic memory, language, socio-emotional processing, and selecting among competing memories during retrieval.”
No significant differences were found between the groups in olfactory ability.
Limitations of the study include its small sample size. The investigators hope the findings will “stimulate larger scale clinical trials systematically testing the therapeutic efficacy of olfactory enrichment in treating memory loss in older adults.”
Exciting but preliminary
Commenting for this article, Donald Wilson, PhD, professor of child and adolescent psychiatry and of neuroscience and physiology, the Child Study Center, NYU Langone Medical Center, New York, said that multiple studies have “demonstrated that problems with sense of smell are associated with and sometimes can precede other symptoms for many disorders, including AD, Parkinson’s disease, and depression.”
Recent work has suggested that this relationship can be “bidirectional” – for example, losing one’s sense of smell might promote depression, while depressive disorder might lead to impaired smell, according to Dr. Wilson, also director and senior research scientist, the Emotional Brain Institute, Nathan Kline Institute for Psychiatric Research. He was not involved with the study.
This “two-way interaction” may raise the possibility that “improving olfaction could impact nonolfactory disorders.”
This paper “brings together” previous research findings to show that odors during bedtime can improve some aspects of cognitive function and circuits that are known to be important for memory and cognition – which Dr. Wilson called “a very exciting, though relatively preliminary, finding.”
A caveat is that several measures of cognitive function were assessed and only one (verbal memory) showed clear improvement.
Nevertheless, there’s “very strong interest now in the olfactory and nonolfactory aspects of odor training and this training expands the training possibilities to sleep. This could be a powerful tool for cognitive improvement and/or rescue if follow-up studies support these findings,” Dr. Wilson said.
A version of this article appeared on Medscape.com.
In a small, randomized controlled trial researchers found that when cognitively normal individuals were exposed to the scent of an essential oil for 2 hours every night over 6 months, they experienced a 226% improvement in memory compared with a control group who received only a trace amount of the diffused scent.
In addition, functional magnetic resonance imaging (fMRI) showed that those in the enriched group had improved functioning of the left uncinate fasciculus, an area of the brain linked to memory and cognition, which typically declines with age.
“To my knowledge, that level of [memory] improvement is far greater than anything that has been reported for healthy older adults and we also found a critical memory pathway in their brains improved to a similar extent relative to unenriched older adults,” senior investigator Michael Leon, PhD, professor emeritus, University of California, Irvine, said in an interview.
The study was published online in Frontiers of Neuroscience.
The brain’s “superhighway”
Olfactory enrichment “involves the daily exposure of individuals to multiple odorants” and has been shown in mouse models to improve memory and neurogenesis, the investigators noted.
A previous study showed that exposure to individual essential oils for 30 minutes a day over 3 months induced neurogenesis in the olfactory bulb and the hippocampus.
“The olfactory system is the only sense that has a direct ‘superhighway’ input to the memory centers areas of the brain; all the other senses have to reach those brain areas through what you might call the ‘side streets’ of the brain, and so consequently, they have much less impact on maintaining the health of those memory centers.”
When olfaction is compromised, “the memory centers of the brain start to deteriorate and, conversely, when people are given olfactory enrichment, their memory areas become larger and more functional,” he added.
Olfactory dysfunction is the first symptom of Alzheimer’s disease (AD) and is also found in virtually all neurological and psychiatric disorders.
“I’ve counted 68 of them – including anorexia, anxiety, [attention-deficit/hyperactivity disorder], depression, epilepsy, and stroke. In fact, by mid-life, your all-cause mortality can be predicted by your ability to smell things,” Dr. Leon said.
Dr. Leon and colleagues previously developed an effective treatment for autism using environmental enrichment that focused on odor stimulation, along with stimulating other senses. “We then considered the possibility that olfactory enrichment alone might improve brain function.”
Rose, orange, eucalyptus …
For the study, the researchers randomly assigned 43 older adults, aged 60-85 years, to receive either nightly exposure to essential oil scents delivered via a diffuser (n = 20; mean [SD] age, 70.1 [6.6] years) or to a sham control with only trace amounts of odorants (n = 23; mean age, 69.2 [7.1] years) for a period of 6 months.
The intervention group was exposed to a single odorant, delivered through a diffuser, for 2 hours nightly, rotating through seven pleasant aromas each week. They included rose, orange, eucalyptus, lemon, peppermint, rosemary, and lavender scents.
All participants completed a battery of tests at baseline, including the Mini-Mental State Examination (MMSE), which confirmed normal cognitive functioning. At baseline and after a 6-month follow-up, participants completed the Rey Auditory Verbal Learning Test (RAVLT) as well as three subsets of the Wechsler Adult Intelligence Scale–Third Edition (WAIS-III).
Olfactory system function was assessed using “Sniffin Sticks,” allowing the researchers to determine if olfactory enrichment enhanced olfactory performance.
Participants underwent fMRI at baseline and again at 6 months.
Brain imaging results showed a “clear, statistically significant 226% difference between enriched and control older adults in performance on the RAVLT, which evaluates learning and memory (timepoint × group interaction; F = 6.63; P = .02; Cohen’s d = 1.08; a “large effect size”).
They also found a significant change in the mean diffusivity of the left uncinate fasciculus in the enriched group compared with the controls (timepoint × group interaction; F = 4.39; P = .043; h 2 p = .101; a “medium-size effect”).
The uncinate fasciculus is a “major pathway” connecting the basolateral amygdala and the entorhinal cortex to the prefrontal cortex. This pathway deteriorates in aging and in AD and “has been suggested to play a role in mediating episodic memory, language, socio-emotional processing, and selecting among competing memories during retrieval.”
No significant differences were found between the groups in olfactory ability.
Limitations of the study include its small sample size. The investigators hope the findings will “stimulate larger scale clinical trials systematically testing the therapeutic efficacy of olfactory enrichment in treating memory loss in older adults.”
Exciting but preliminary
Commenting for this article, Donald Wilson, PhD, professor of child and adolescent psychiatry and of neuroscience and physiology, the Child Study Center, NYU Langone Medical Center, New York, said that multiple studies have “demonstrated that problems with sense of smell are associated with and sometimes can precede other symptoms for many disorders, including AD, Parkinson’s disease, and depression.”
Recent work has suggested that this relationship can be “bidirectional” – for example, losing one’s sense of smell might promote depression, while depressive disorder might lead to impaired smell, according to Dr. Wilson, also director and senior research scientist, the Emotional Brain Institute, Nathan Kline Institute for Psychiatric Research. He was not involved with the study.
This “two-way interaction” may raise the possibility that “improving olfaction could impact nonolfactory disorders.”
This paper “brings together” previous research findings to show that odors during bedtime can improve some aspects of cognitive function and circuits that are known to be important for memory and cognition – which Dr. Wilson called “a very exciting, though relatively preliminary, finding.”
A caveat is that several measures of cognitive function were assessed and only one (verbal memory) showed clear improvement.
Nevertheless, there’s “very strong interest now in the olfactory and nonolfactory aspects of odor training and this training expands the training possibilities to sleep. This could be a powerful tool for cognitive improvement and/or rescue if follow-up studies support these findings,” Dr. Wilson said.
A version of this article appeared on Medscape.com.
In a small, randomized controlled trial researchers found that when cognitively normal individuals were exposed to the scent of an essential oil for 2 hours every night over 6 months, they experienced a 226% improvement in memory compared with a control group who received only a trace amount of the diffused scent.
In addition, functional magnetic resonance imaging (fMRI) showed that those in the enriched group had improved functioning of the left uncinate fasciculus, an area of the brain linked to memory and cognition, which typically declines with age.
“To my knowledge, that level of [memory] improvement is far greater than anything that has been reported for healthy older adults and we also found a critical memory pathway in their brains improved to a similar extent relative to unenriched older adults,” senior investigator Michael Leon, PhD, professor emeritus, University of California, Irvine, said in an interview.
The study was published online in Frontiers of Neuroscience.
The brain’s “superhighway”
Olfactory enrichment “involves the daily exposure of individuals to multiple odorants” and has been shown in mouse models to improve memory and neurogenesis, the investigators noted.
A previous study showed that exposure to individual essential oils for 30 minutes a day over 3 months induced neurogenesis in the olfactory bulb and the hippocampus.
“The olfactory system is the only sense that has a direct ‘superhighway’ input to the memory centers areas of the brain; all the other senses have to reach those brain areas through what you might call the ‘side streets’ of the brain, and so consequently, they have much less impact on maintaining the health of those memory centers.”
When olfaction is compromised, “the memory centers of the brain start to deteriorate and, conversely, when people are given olfactory enrichment, their memory areas become larger and more functional,” he added.
Olfactory dysfunction is the first symptom of Alzheimer’s disease (AD) and is also found in virtually all neurological and psychiatric disorders.
“I’ve counted 68 of them – including anorexia, anxiety, [attention-deficit/hyperactivity disorder], depression, epilepsy, and stroke. In fact, by mid-life, your all-cause mortality can be predicted by your ability to smell things,” Dr. Leon said.
Dr. Leon and colleagues previously developed an effective treatment for autism using environmental enrichment that focused on odor stimulation, along with stimulating other senses. “We then considered the possibility that olfactory enrichment alone might improve brain function.”
Rose, orange, eucalyptus …
For the study, the researchers randomly assigned 43 older adults, aged 60-85 years, to receive either nightly exposure to essential oil scents delivered via a diffuser (n = 20; mean [SD] age, 70.1 [6.6] years) or to a sham control with only trace amounts of odorants (n = 23; mean age, 69.2 [7.1] years) for a period of 6 months.
The intervention group was exposed to a single odorant, delivered through a diffuser, for 2 hours nightly, rotating through seven pleasant aromas each week. They included rose, orange, eucalyptus, lemon, peppermint, rosemary, and lavender scents.
All participants completed a battery of tests at baseline, including the Mini-Mental State Examination (MMSE), which confirmed normal cognitive functioning. At baseline and after a 6-month follow-up, participants completed the Rey Auditory Verbal Learning Test (RAVLT) as well as three subsets of the Wechsler Adult Intelligence Scale–Third Edition (WAIS-III).
Olfactory system function was assessed using “Sniffin Sticks,” allowing the researchers to determine if olfactory enrichment enhanced olfactory performance.
Participants underwent fMRI at baseline and again at 6 months.
Brain imaging results showed a “clear, statistically significant 226% difference between enriched and control older adults in performance on the RAVLT, which evaluates learning and memory (timepoint × group interaction; F = 6.63; P = .02; Cohen’s d = 1.08; a “large effect size”).
They also found a significant change in the mean diffusivity of the left uncinate fasciculus in the enriched group compared with the controls (timepoint × group interaction; F = 4.39; P = .043; h 2 p = .101; a “medium-size effect”).
The uncinate fasciculus is a “major pathway” connecting the basolateral amygdala and the entorhinal cortex to the prefrontal cortex. This pathway deteriorates in aging and in AD and “has been suggested to play a role in mediating episodic memory, language, socio-emotional processing, and selecting among competing memories during retrieval.”
No significant differences were found between the groups in olfactory ability.
Limitations of the study include its small sample size. The investigators hope the findings will “stimulate larger scale clinical trials systematically testing the therapeutic efficacy of olfactory enrichment in treating memory loss in older adults.”
Exciting but preliminary
Commenting for this article, Donald Wilson, PhD, professor of child and adolescent psychiatry and of neuroscience and physiology, the Child Study Center, NYU Langone Medical Center, New York, said that multiple studies have “demonstrated that problems with sense of smell are associated with and sometimes can precede other symptoms for many disorders, including AD, Parkinson’s disease, and depression.”
Recent work has suggested that this relationship can be “bidirectional” – for example, losing one’s sense of smell might promote depression, while depressive disorder might lead to impaired smell, according to Dr. Wilson, also director and senior research scientist, the Emotional Brain Institute, Nathan Kline Institute for Psychiatric Research. He was not involved with the study.
This “two-way interaction” may raise the possibility that “improving olfaction could impact nonolfactory disorders.”
This paper “brings together” previous research findings to show that odors during bedtime can improve some aspects of cognitive function and circuits that are known to be important for memory and cognition – which Dr. Wilson called “a very exciting, though relatively preliminary, finding.”
A caveat is that several measures of cognitive function were assessed and only one (verbal memory) showed clear improvement.
Nevertheless, there’s “very strong interest now in the olfactory and nonolfactory aspects of odor training and this training expands the training possibilities to sleep. This could be a powerful tool for cognitive improvement and/or rescue if follow-up studies support these findings,” Dr. Wilson said.
A version of this article appeared on Medscape.com.
FROM FRONTIERS IN NEUROSCIENCE
LAAO tied to fewer post-fall bleeds than DOACs in AF
Left atrial appendage occlusion (LAAO) is associated with fewer injuries and less bleeding from falls than anticoagulant medications in patients with atrial fibrillation (AF) and a previous stroke, a new cohort study suggests.
Investigators prospectively followed more than 1,250 patients with AF and a previous ischemic stroke. Approximately half underwent LAAO, while the other half were treated with direct oral anticoagulants (DOACs). Patients were followed for close to 2 years.
Slightly more than 20% of patients fell during that period in each group, and , who were not taking anticoagulants. The risk for a major bleed, including an intracranial bleed, was 70% lower in the LAAO group.
LAAO has previously been considered for people at risk of bleeding events – for example, those with gastrointestinal (GI) bleeds, bruising, or intracranial bleeding – but had not yet been studied in those at risk for falls, coauthor Moussa Mansour, MD, professor of medicine, Harvard Medical School, and director of the Atrial Fibrillation Program at Massachusetts General Hospital, Boston, said in an interview.
This is the first study to focus on LAAO specifically for those at risk for falling and demonstrated that the LAAO has utility in this population as well, which is important because the U.S. population is an aging population, and at advanced ages, “people’s balance becomes unsteady and they are at high risk of falling,” he said.
The findings were published online as a research letter in the Journal of the American College of Cardiology.
Multidisciplinary collaboration
“More than one in five of our neurology patients with AF fall – many with devastating consequences – making stroke prevention extremely challenging,” senior author MingMing Ning, MD, MMsc, associate professor of neurology, Harvard Medical School, and director of the Cardio-Neurology and the Clinical Proteomics Research Center at Massachusetts General Hospital, Boston, said in an interview.
“There is a dire need to tailor treatment to keep our patients safe while preventing future strokes,” she said.
Anticoagulants are effective in stroke prevention in these patients but are associated with a higher risk for major bleeding, especially after a fall.
The current prospective observational study recruited 1,266 stroke patients who were treated either with LAAO or DOACs (n = 570 and 696, respectively). Patients were followed for a median of 1.8 years (IQR: 0.9-3.0).
During the follow-up period, 22.6% of LAAO-treated patients and 22.7% of DOAC-treated patients sustained a fall (mean age 78.9 years, 57.4% male and 79.1 years, 52.5% male respectively).
Fall severity, evaluated via the Injury Severity Score, was less in the LAAO vs. the DOAC group, with ISS scores of 1 (IQR 1-4) vs. 4 (IQR 1.75-9).
LAAO was associated with significantly reduced severity of fall-related injuries (OR, –1.09, 95% confidence interval [CI], –1.52 to –0.66; P < .001) – a finding that remained statistically significant after adjustment for confounders such as age, sex, and comorbidities contributing to fall risk, such as hypertension, hyperlipidemia, and diabetes.
The incidence of major trauma (defined as ISS >15) was lower in the LAAO group, compared to the DOAC group (0.8% vs. 6.3%, respectively, P = .026), and LAAO-treated patients had a shorter length of hospital stay, with fewer LAAO patients compared with DOAC patients staying in the hospital for more than 3 days (17% vs. 29.1%, respectively, P = .018).
The risk for major post-fall bleeding was lower in the LAAO vs. the DOAC group (4.7% vs. 15.2%, AOR, 0.29; 95% CI, 0.11-0.73; P = .009) – a finding that included intracranial bleeding (3.1% vs. 9.5%; AOR, 0.29; 95% CI, 0.09-0.90; P = .033).
“Many people are living to advanced ages, where their balance becomes unsteady, and in addition, we have an increase in the prevalence of AF because people are living longer and it’s a disease of the elderly, because we have more hypertension, and we also have more tools to diagnose AF. It’s almost a ‘perfect storm’ situation, and we need effective interventions in this population,” said Dr. Mansour.
Before the study, people at risk for falling were not being considered for LAAO; but now, “we believe they should be considered,” he added. “And although people in the current study had all experienced an ischemic stroke, any patient at risk of a fall will potentially benefit.”
Beyond demonstrating the role of LAAO in reducing the risk of post-fall bleeding injuries, the study – which was conducted by specialists in neurology and cardiology among other fields – highlights the importance of multidisciplinary collaboration, which is “key” for effective stroke prevention, Dr. Ning said.
She emphasized that “we need to learn from our patients and tailor treatment to their needs. A patient’s risk of falling, lifestyle, and medication adherence are all important for individualizing care and improving quality of life.”
Better option
Commenting for this article, Andrea Natale, MD, executive medical director, Texas Cardiac Arrhythmia Institute at St. David’s Medical Center, Austin, said the authors “should be commended for this prospective study on real-world patients that has yielded highly meaningful data from a clinical standpoint.”
Dr. Natale, who was not involved with the study, said it has “several strong points,” such as a fairly large sample size, exclusive population with a history of AF-related stroke, long follow-up duration, evaluation of fall incidents by blinded experts, and severity of fall assessed by a validated questionnaire.
“This is the first study that directly compared the outcomes of traumatic fall in patients receiving LAAO vs. DOAC,” he said. “Given that history of fall is an independent predictor of bleeding and death, the study findings by Deng et al. offer the hope for a safer life with the LAAO option in the aging, fall-prone AF population.”
The take-home message is that, in patients with history of stroke, LAAO “is a better option, in terms of significantly reduced injury severity and shortened hospital length of stay after traumatic falls,” Dr. Natale said.
This study was supported in part by research grants from Boston Scientific, the Leducq Foundation, and the National Institutes of Health. The authors reported no relevant financial relationships. Dr. Natale is a consultant for Abbott, Baylis, Biosense Webster, Biotronik, Boston Scientific, and Medtronic.
A version of this article appeared on Medscape.com.
Left atrial appendage occlusion (LAAO) is associated with fewer injuries and less bleeding from falls than anticoagulant medications in patients with atrial fibrillation (AF) and a previous stroke, a new cohort study suggests.
Investigators prospectively followed more than 1,250 patients with AF and a previous ischemic stroke. Approximately half underwent LAAO, while the other half were treated with direct oral anticoagulants (DOACs). Patients were followed for close to 2 years.
Slightly more than 20% of patients fell during that period in each group, and , who were not taking anticoagulants. The risk for a major bleed, including an intracranial bleed, was 70% lower in the LAAO group.
LAAO has previously been considered for people at risk of bleeding events – for example, those with gastrointestinal (GI) bleeds, bruising, or intracranial bleeding – but had not yet been studied in those at risk for falls, coauthor Moussa Mansour, MD, professor of medicine, Harvard Medical School, and director of the Atrial Fibrillation Program at Massachusetts General Hospital, Boston, said in an interview.
This is the first study to focus on LAAO specifically for those at risk for falling and demonstrated that the LAAO has utility in this population as well, which is important because the U.S. population is an aging population, and at advanced ages, “people’s balance becomes unsteady and they are at high risk of falling,” he said.
The findings were published online as a research letter in the Journal of the American College of Cardiology.
Multidisciplinary collaboration
“More than one in five of our neurology patients with AF fall – many with devastating consequences – making stroke prevention extremely challenging,” senior author MingMing Ning, MD, MMsc, associate professor of neurology, Harvard Medical School, and director of the Cardio-Neurology and the Clinical Proteomics Research Center at Massachusetts General Hospital, Boston, said in an interview.
“There is a dire need to tailor treatment to keep our patients safe while preventing future strokes,” she said.
Anticoagulants are effective in stroke prevention in these patients but are associated with a higher risk for major bleeding, especially after a fall.
The current prospective observational study recruited 1,266 stroke patients who were treated either with LAAO or DOACs (n = 570 and 696, respectively). Patients were followed for a median of 1.8 years (IQR: 0.9-3.0).
During the follow-up period, 22.6% of LAAO-treated patients and 22.7% of DOAC-treated patients sustained a fall (mean age 78.9 years, 57.4% male and 79.1 years, 52.5% male respectively).
Fall severity, evaluated via the Injury Severity Score, was less in the LAAO vs. the DOAC group, with ISS scores of 1 (IQR 1-4) vs. 4 (IQR 1.75-9).
LAAO was associated with significantly reduced severity of fall-related injuries (OR, –1.09, 95% confidence interval [CI], –1.52 to –0.66; P < .001) – a finding that remained statistically significant after adjustment for confounders such as age, sex, and comorbidities contributing to fall risk, such as hypertension, hyperlipidemia, and diabetes.
The incidence of major trauma (defined as ISS >15) was lower in the LAAO group, compared to the DOAC group (0.8% vs. 6.3%, respectively, P = .026), and LAAO-treated patients had a shorter length of hospital stay, with fewer LAAO patients compared with DOAC patients staying in the hospital for more than 3 days (17% vs. 29.1%, respectively, P = .018).
The risk for major post-fall bleeding was lower in the LAAO vs. the DOAC group (4.7% vs. 15.2%, AOR, 0.29; 95% CI, 0.11-0.73; P = .009) – a finding that included intracranial bleeding (3.1% vs. 9.5%; AOR, 0.29; 95% CI, 0.09-0.90; P = .033).
“Many people are living to advanced ages, where their balance becomes unsteady, and in addition, we have an increase in the prevalence of AF because people are living longer and it’s a disease of the elderly, because we have more hypertension, and we also have more tools to diagnose AF. It’s almost a ‘perfect storm’ situation, and we need effective interventions in this population,” said Dr. Mansour.
Before the study, people at risk for falling were not being considered for LAAO; but now, “we believe they should be considered,” he added. “And although people in the current study had all experienced an ischemic stroke, any patient at risk of a fall will potentially benefit.”
Beyond demonstrating the role of LAAO in reducing the risk of post-fall bleeding injuries, the study – which was conducted by specialists in neurology and cardiology among other fields – highlights the importance of multidisciplinary collaboration, which is “key” for effective stroke prevention, Dr. Ning said.
She emphasized that “we need to learn from our patients and tailor treatment to their needs. A patient’s risk of falling, lifestyle, and medication adherence are all important for individualizing care and improving quality of life.”
Better option
Commenting for this article, Andrea Natale, MD, executive medical director, Texas Cardiac Arrhythmia Institute at St. David’s Medical Center, Austin, said the authors “should be commended for this prospective study on real-world patients that has yielded highly meaningful data from a clinical standpoint.”
Dr. Natale, who was not involved with the study, said it has “several strong points,” such as a fairly large sample size, exclusive population with a history of AF-related stroke, long follow-up duration, evaluation of fall incidents by blinded experts, and severity of fall assessed by a validated questionnaire.
“This is the first study that directly compared the outcomes of traumatic fall in patients receiving LAAO vs. DOAC,” he said. “Given that history of fall is an independent predictor of bleeding and death, the study findings by Deng et al. offer the hope for a safer life with the LAAO option in the aging, fall-prone AF population.”
The take-home message is that, in patients with history of stroke, LAAO “is a better option, in terms of significantly reduced injury severity and shortened hospital length of stay after traumatic falls,” Dr. Natale said.
This study was supported in part by research grants from Boston Scientific, the Leducq Foundation, and the National Institutes of Health. The authors reported no relevant financial relationships. Dr. Natale is a consultant for Abbott, Baylis, Biosense Webster, Biotronik, Boston Scientific, and Medtronic.
A version of this article appeared on Medscape.com.
Left atrial appendage occlusion (LAAO) is associated with fewer injuries and less bleeding from falls than anticoagulant medications in patients with atrial fibrillation (AF) and a previous stroke, a new cohort study suggests.
Investigators prospectively followed more than 1,250 patients with AF and a previous ischemic stroke. Approximately half underwent LAAO, while the other half were treated with direct oral anticoagulants (DOACs). Patients were followed for close to 2 years.
Slightly more than 20% of patients fell during that period in each group, and , who were not taking anticoagulants. The risk for a major bleed, including an intracranial bleed, was 70% lower in the LAAO group.
LAAO has previously been considered for people at risk of bleeding events – for example, those with gastrointestinal (GI) bleeds, bruising, or intracranial bleeding – but had not yet been studied in those at risk for falls, coauthor Moussa Mansour, MD, professor of medicine, Harvard Medical School, and director of the Atrial Fibrillation Program at Massachusetts General Hospital, Boston, said in an interview.
This is the first study to focus on LAAO specifically for those at risk for falling and demonstrated that the LAAO has utility in this population as well, which is important because the U.S. population is an aging population, and at advanced ages, “people’s balance becomes unsteady and they are at high risk of falling,” he said.
The findings were published online as a research letter in the Journal of the American College of Cardiology.
Multidisciplinary collaboration
“More than one in five of our neurology patients with AF fall – many with devastating consequences – making stroke prevention extremely challenging,” senior author MingMing Ning, MD, MMsc, associate professor of neurology, Harvard Medical School, and director of the Cardio-Neurology and the Clinical Proteomics Research Center at Massachusetts General Hospital, Boston, said in an interview.
“There is a dire need to tailor treatment to keep our patients safe while preventing future strokes,” she said.
Anticoagulants are effective in stroke prevention in these patients but are associated with a higher risk for major bleeding, especially after a fall.
The current prospective observational study recruited 1,266 stroke patients who were treated either with LAAO or DOACs (n = 570 and 696, respectively). Patients were followed for a median of 1.8 years (IQR: 0.9-3.0).
During the follow-up period, 22.6% of LAAO-treated patients and 22.7% of DOAC-treated patients sustained a fall (mean age 78.9 years, 57.4% male and 79.1 years, 52.5% male respectively).
Fall severity, evaluated via the Injury Severity Score, was less in the LAAO vs. the DOAC group, with ISS scores of 1 (IQR 1-4) vs. 4 (IQR 1.75-9).
LAAO was associated with significantly reduced severity of fall-related injuries (OR, –1.09, 95% confidence interval [CI], –1.52 to –0.66; P < .001) – a finding that remained statistically significant after adjustment for confounders such as age, sex, and comorbidities contributing to fall risk, such as hypertension, hyperlipidemia, and diabetes.
The incidence of major trauma (defined as ISS >15) was lower in the LAAO group, compared to the DOAC group (0.8% vs. 6.3%, respectively, P = .026), and LAAO-treated patients had a shorter length of hospital stay, with fewer LAAO patients compared with DOAC patients staying in the hospital for more than 3 days (17% vs. 29.1%, respectively, P = .018).
The risk for major post-fall bleeding was lower in the LAAO vs. the DOAC group (4.7% vs. 15.2%, AOR, 0.29; 95% CI, 0.11-0.73; P = .009) – a finding that included intracranial bleeding (3.1% vs. 9.5%; AOR, 0.29; 95% CI, 0.09-0.90; P = .033).
“Many people are living to advanced ages, where their balance becomes unsteady, and in addition, we have an increase in the prevalence of AF because people are living longer and it’s a disease of the elderly, because we have more hypertension, and we also have more tools to diagnose AF. It’s almost a ‘perfect storm’ situation, and we need effective interventions in this population,” said Dr. Mansour.
Before the study, people at risk for falling were not being considered for LAAO; but now, “we believe they should be considered,” he added. “And although people in the current study had all experienced an ischemic stroke, any patient at risk of a fall will potentially benefit.”
Beyond demonstrating the role of LAAO in reducing the risk of post-fall bleeding injuries, the study – which was conducted by specialists in neurology and cardiology among other fields – highlights the importance of multidisciplinary collaboration, which is “key” for effective stroke prevention, Dr. Ning said.
She emphasized that “we need to learn from our patients and tailor treatment to their needs. A patient’s risk of falling, lifestyle, and medication adherence are all important for individualizing care and improving quality of life.”
Better option
Commenting for this article, Andrea Natale, MD, executive medical director, Texas Cardiac Arrhythmia Institute at St. David’s Medical Center, Austin, said the authors “should be commended for this prospective study on real-world patients that has yielded highly meaningful data from a clinical standpoint.”
Dr. Natale, who was not involved with the study, said it has “several strong points,” such as a fairly large sample size, exclusive population with a history of AF-related stroke, long follow-up duration, evaluation of fall incidents by blinded experts, and severity of fall assessed by a validated questionnaire.
“This is the first study that directly compared the outcomes of traumatic fall in patients receiving LAAO vs. DOAC,” he said. “Given that history of fall is an independent predictor of bleeding and death, the study findings by Deng et al. offer the hope for a safer life with the LAAO option in the aging, fall-prone AF population.”
The take-home message is that, in patients with history of stroke, LAAO “is a better option, in terms of significantly reduced injury severity and shortened hospital length of stay after traumatic falls,” Dr. Natale said.
This study was supported in part by research grants from Boston Scientific, the Leducq Foundation, and the National Institutes of Health. The authors reported no relevant financial relationships. Dr. Natale is a consultant for Abbott, Baylis, Biosense Webster, Biotronik, Boston Scientific, and Medtronic.
A version of this article appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Cognitive problems transient after AFib ablation
Investigators randomly assigned 100 patients with symptomatic AFib who had failed at least one anti-arrhythmic drug (AAD) to ongoing therapy or to AFib catheter ablation. Patients were followed for 1 year, and changes in cognitive performance were assessed at baseline and at 3, 6, and 12 months.
Although patients in the ablation arm initially showed more cognitive dysfunction than those in the medical arm, at 6 months, the gap was smaller, and at 12 months, no patients in the ablation arm showed signs of cognitive dysfunction. In fact, more than 1 in 10 showed signs of cognitive improvement, compared with no patients in the medical arm.
The study was published online in the July issue of JACC: Clinical Electrophysiology.
Important pillar
Previous research has shown that AFib is associated with cognitive dysfunction independently of stroke, “suggesting that AFib is an additional risk factor for cognitive impairment,” the authors write.
Catheter ablation is an “important pillar” in the management of patients with AFib that is refractory to medical therapy, but postoperative cognitive dysfunction (POCD) may occur in the immediate aftermath of the procedure, they note. Little is known about whether these cognitive changes persist long term, and no randomized studies have investigated this issue.
The researchers randomly assigned 100 patients with symptomatic paroxysmal or persistent AFib who had failed greater than or equal to 1 AAD to receive either medical management or catheter ablation. The mean age of the patients was 59 plus or minus 12 years, 32% were women, and 46% had persistent AFib.
Medical management consisted of optimization of AADs to maintain sinus rhythm. For those who underwent ablation, AADs were discontinued five half-lives prior to the procedure (with the exception of amiodarone).
Participants were followed for 12 months after enrollment. Clinical reviews and cognitive testing were performed at 3, 6, and 12 months during that time.
AADs and oral anticoagulation were weaned and were discontinued 3 months after the procedure, depending on each patient’s individual risk profile.
Cognitive testing included the Consortium to Establish a Registry for Alzheimer’s Disease (CERAD) Auditory Verbal Learning Test and Semantic Fluency test; the Controlled Oral Word Association test; and the Trail Making Task (parts A and B).
Participants also completed the University of Toronto AFib Symptom Severity Scale at baseline and at all follow-up visits.
The primary endpoint was prevalence of new-onset cognitive dysfunction. Main secondary endpoints included improvement in cognitive function during follow-up; AFib recurrence and AFib function during follow-up; AAD use during follow-up; and changes to AFib symptom severity assessment scores during follow-up.
More research needed
Of the 100 participants, 96 completed the study protocol (52 in the ablation group and 48 in the medical management group). There were no significant differences between the groups regarding baseline demographics, clinical AFib risk factors, and echocardiographic parameters.
At 3 months, new-onset cognitive dysfunction was detected across a wide range of the neuropsychological tests in 14% of participants in the ablation arm, versus 2% of participants in the medical arm (P = .03)
But at 6 months, only 4% of patients in the ablation arm displayed cognitive dysfunction, compared again with 2% in the medical arm (P = .60). And by 12 months, there were no patients with detectable cognitive dysfunction in the ablation arm, compared with the same patient who showed cognitive impairment in the medical arm (P = .30).
Longer ablation time was an independent predictor of new-onset cognitive dysfunction (odds ratio, 1.30; 95% CI, 1.01-1.60; P = .003).
When patients with and those without new-onset cognitive dysfunction were compared, no differences were found in arrhythmia recurrence or AFib burden post ablation.
At 12 months, 14% of those in the ablation arm showed improvement in cognitive performance, compared with no participants in the medical arm (P = .007).
Compared with participants who had no change in cognitive performance, those who had a significant improvement had a trend toward lower AFib recurrence rates (29% vs. 48%; P = .30). However, both groups were found to have a low AFib burden over the 12 months. And the use of AADs at the 12-month mark was significantly lower among those with versus those without cognitive improvement (0% vs. 38%; P = .04).
As early as 3 months post procedure and then at 12 months, participants in the ablation group had significant improvement in AFib-related symptoms, compared with those in the medical arm (for both, P < .001).
“Among a contemporary cohort of symptomatic paroxysmal and persistent AFib patients, catheter ablation was associated with a transient decline in cognitive function in the short-term, followed by recovery at 12 months,” the authors conclude.
They note that further large studies “are required to determine with AFib ablation may prevent the longer-term neurocognitive decline and dementia development associated with AFib.”
‘Reassuring’ findings
In a comment, Andrea Natale, MD, executive medical director, Texas Cardiac Arrhythmia Institute at St. David’s Medical Center, Austin, said POCD is “very likely due to the vulnerable state of mind and the stress that the patients encounter while undergoing the cardiac procedure,” as well as postsurgical inflammation, which “can cause brief functional alterations in the brain, leading to temporary cognitive impairment.” Inadequate preprocedural anticoagulation may also play a role.
Dr. Natale, co-author of an accompanying editorial, said it’s “prudent” when evaluating cognitive function to use questionnaires that are “sensitive to mild cognitive impairment,” such as the Montreal Cognitive Assessment or the Mini-Mental State Examination.
Additionally, “post-ablation cognitive function should be assessed way after the blanking period to avoid any plausible impact of inflammation, medications, the feeling of being overwhelmed, and the stress of undergoing a cardiac procedure,” advised Dr. Natale, who was not involved with the study.
Also commenting, Matthew Hyman, MD, PhD, an electrophysiologist and assistant professor of medicine at the Hospital of the University of Pennsylvania, called it a “well-done and very reassuring study.”
Dr. Hyman, who was also not part of the research team, added that previous work has shown an association between AFib and dementia, “and it remains to be seen if patients with rhythm control over longer durations than the current studies have the best outcomes.”
The authors of the study are supported by the National Health and Medical Research Council research scholarship. One author of the study is supported by a practitioner fellowship from the National Health and Medical Research Council; has received research support from Biosense Webster, Boston Scientific, Abbott, and Medtronic; and has served on the advisory board of Boston Scientific and Biosense Webster. Dr. Natale is a consultant for Abbott, Baylis, Biosense Webster, Biotronik, Boston Scientific, and Medtronic. Dr. Hyman is a consultant/speaker for Abbott, Biosense Webster and Boston Scientific.
A version of this article first appeared on Medscape.com.
Investigators randomly assigned 100 patients with symptomatic AFib who had failed at least one anti-arrhythmic drug (AAD) to ongoing therapy or to AFib catheter ablation. Patients were followed for 1 year, and changes in cognitive performance were assessed at baseline and at 3, 6, and 12 months.
Although patients in the ablation arm initially showed more cognitive dysfunction than those in the medical arm, at 6 months, the gap was smaller, and at 12 months, no patients in the ablation arm showed signs of cognitive dysfunction. In fact, more than 1 in 10 showed signs of cognitive improvement, compared with no patients in the medical arm.
The study was published online in the July issue of JACC: Clinical Electrophysiology.
Important pillar
Previous research has shown that AFib is associated with cognitive dysfunction independently of stroke, “suggesting that AFib is an additional risk factor for cognitive impairment,” the authors write.
Catheter ablation is an “important pillar” in the management of patients with AFib that is refractory to medical therapy, but postoperative cognitive dysfunction (POCD) may occur in the immediate aftermath of the procedure, they note. Little is known about whether these cognitive changes persist long term, and no randomized studies have investigated this issue.
The researchers randomly assigned 100 patients with symptomatic paroxysmal or persistent AFib who had failed greater than or equal to 1 AAD to receive either medical management or catheter ablation. The mean age of the patients was 59 plus or minus 12 years, 32% were women, and 46% had persistent AFib.
Medical management consisted of optimization of AADs to maintain sinus rhythm. For those who underwent ablation, AADs were discontinued five half-lives prior to the procedure (with the exception of amiodarone).
Participants were followed for 12 months after enrollment. Clinical reviews and cognitive testing were performed at 3, 6, and 12 months during that time.
AADs and oral anticoagulation were weaned and were discontinued 3 months after the procedure, depending on each patient’s individual risk profile.
Cognitive testing included the Consortium to Establish a Registry for Alzheimer’s Disease (CERAD) Auditory Verbal Learning Test and Semantic Fluency test; the Controlled Oral Word Association test; and the Trail Making Task (parts A and B).
Participants also completed the University of Toronto AFib Symptom Severity Scale at baseline and at all follow-up visits.
The primary endpoint was prevalence of new-onset cognitive dysfunction. Main secondary endpoints included improvement in cognitive function during follow-up; AFib recurrence and AFib function during follow-up; AAD use during follow-up; and changes to AFib symptom severity assessment scores during follow-up.
More research needed
Of the 100 participants, 96 completed the study protocol (52 in the ablation group and 48 in the medical management group). There were no significant differences between the groups regarding baseline demographics, clinical AFib risk factors, and echocardiographic parameters.
At 3 months, new-onset cognitive dysfunction was detected across a wide range of the neuropsychological tests in 14% of participants in the ablation arm, versus 2% of participants in the medical arm (P = .03)
But at 6 months, only 4% of patients in the ablation arm displayed cognitive dysfunction, compared again with 2% in the medical arm (P = .60). And by 12 months, there were no patients with detectable cognitive dysfunction in the ablation arm, compared with the same patient who showed cognitive impairment in the medical arm (P = .30).
Longer ablation time was an independent predictor of new-onset cognitive dysfunction (odds ratio, 1.30; 95% CI, 1.01-1.60; P = .003).
When patients with and those without new-onset cognitive dysfunction were compared, no differences were found in arrhythmia recurrence or AFib burden post ablation.
At 12 months, 14% of those in the ablation arm showed improvement in cognitive performance, compared with no participants in the medical arm (P = .007).
Compared with participants who had no change in cognitive performance, those who had a significant improvement had a trend toward lower AFib recurrence rates (29% vs. 48%; P = .30). However, both groups were found to have a low AFib burden over the 12 months. And the use of AADs at the 12-month mark was significantly lower among those with versus those without cognitive improvement (0% vs. 38%; P = .04).
As early as 3 months post procedure and then at 12 months, participants in the ablation group had significant improvement in AFib-related symptoms, compared with those in the medical arm (for both, P < .001).
“Among a contemporary cohort of symptomatic paroxysmal and persistent AFib patients, catheter ablation was associated with a transient decline in cognitive function in the short-term, followed by recovery at 12 months,” the authors conclude.
They note that further large studies “are required to determine with AFib ablation may prevent the longer-term neurocognitive decline and dementia development associated with AFib.”
‘Reassuring’ findings
In a comment, Andrea Natale, MD, executive medical director, Texas Cardiac Arrhythmia Institute at St. David’s Medical Center, Austin, said POCD is “very likely due to the vulnerable state of mind and the stress that the patients encounter while undergoing the cardiac procedure,” as well as postsurgical inflammation, which “can cause brief functional alterations in the brain, leading to temporary cognitive impairment.” Inadequate preprocedural anticoagulation may also play a role.
Dr. Natale, co-author of an accompanying editorial, said it’s “prudent” when evaluating cognitive function to use questionnaires that are “sensitive to mild cognitive impairment,” such as the Montreal Cognitive Assessment or the Mini-Mental State Examination.
Additionally, “post-ablation cognitive function should be assessed way after the blanking period to avoid any plausible impact of inflammation, medications, the feeling of being overwhelmed, and the stress of undergoing a cardiac procedure,” advised Dr. Natale, who was not involved with the study.
Also commenting, Matthew Hyman, MD, PhD, an electrophysiologist and assistant professor of medicine at the Hospital of the University of Pennsylvania, called it a “well-done and very reassuring study.”
Dr. Hyman, who was also not part of the research team, added that previous work has shown an association between AFib and dementia, “and it remains to be seen if patients with rhythm control over longer durations than the current studies have the best outcomes.”
The authors of the study are supported by the National Health and Medical Research Council research scholarship. One author of the study is supported by a practitioner fellowship from the National Health and Medical Research Council; has received research support from Biosense Webster, Boston Scientific, Abbott, and Medtronic; and has served on the advisory board of Boston Scientific and Biosense Webster. Dr. Natale is a consultant for Abbott, Baylis, Biosense Webster, Biotronik, Boston Scientific, and Medtronic. Dr. Hyman is a consultant/speaker for Abbott, Biosense Webster and Boston Scientific.
A version of this article first appeared on Medscape.com.
Investigators randomly assigned 100 patients with symptomatic AFib who had failed at least one anti-arrhythmic drug (AAD) to ongoing therapy or to AFib catheter ablation. Patients were followed for 1 year, and changes in cognitive performance were assessed at baseline and at 3, 6, and 12 months.
Although patients in the ablation arm initially showed more cognitive dysfunction than those in the medical arm, at 6 months, the gap was smaller, and at 12 months, no patients in the ablation arm showed signs of cognitive dysfunction. In fact, more than 1 in 10 showed signs of cognitive improvement, compared with no patients in the medical arm.
The study was published online in the July issue of JACC: Clinical Electrophysiology.
Important pillar
Previous research has shown that AFib is associated with cognitive dysfunction independently of stroke, “suggesting that AFib is an additional risk factor for cognitive impairment,” the authors write.
Catheter ablation is an “important pillar” in the management of patients with AFib that is refractory to medical therapy, but postoperative cognitive dysfunction (POCD) may occur in the immediate aftermath of the procedure, they note. Little is known about whether these cognitive changes persist long term, and no randomized studies have investigated this issue.
The researchers randomly assigned 100 patients with symptomatic paroxysmal or persistent AFib who had failed greater than or equal to 1 AAD to receive either medical management or catheter ablation. The mean age of the patients was 59 plus or minus 12 years, 32% were women, and 46% had persistent AFib.
Medical management consisted of optimization of AADs to maintain sinus rhythm. For those who underwent ablation, AADs were discontinued five half-lives prior to the procedure (with the exception of amiodarone).
Participants were followed for 12 months after enrollment. Clinical reviews and cognitive testing were performed at 3, 6, and 12 months during that time.
AADs and oral anticoagulation were weaned and were discontinued 3 months after the procedure, depending on each patient’s individual risk profile.
Cognitive testing included the Consortium to Establish a Registry for Alzheimer’s Disease (CERAD) Auditory Verbal Learning Test and Semantic Fluency test; the Controlled Oral Word Association test; and the Trail Making Task (parts A and B).
Participants also completed the University of Toronto AFib Symptom Severity Scale at baseline and at all follow-up visits.
The primary endpoint was prevalence of new-onset cognitive dysfunction. Main secondary endpoints included improvement in cognitive function during follow-up; AFib recurrence and AFib function during follow-up; AAD use during follow-up; and changes to AFib symptom severity assessment scores during follow-up.
More research needed
Of the 100 participants, 96 completed the study protocol (52 in the ablation group and 48 in the medical management group). There were no significant differences between the groups regarding baseline demographics, clinical AFib risk factors, and echocardiographic parameters.
At 3 months, new-onset cognitive dysfunction was detected across a wide range of the neuropsychological tests in 14% of participants in the ablation arm, versus 2% of participants in the medical arm (P = .03)
But at 6 months, only 4% of patients in the ablation arm displayed cognitive dysfunction, compared again with 2% in the medical arm (P = .60). And by 12 months, there were no patients with detectable cognitive dysfunction in the ablation arm, compared with the same patient who showed cognitive impairment in the medical arm (P = .30).
Longer ablation time was an independent predictor of new-onset cognitive dysfunction (odds ratio, 1.30; 95% CI, 1.01-1.60; P = .003).
When patients with and those without new-onset cognitive dysfunction were compared, no differences were found in arrhythmia recurrence or AFib burden post ablation.
At 12 months, 14% of those in the ablation arm showed improvement in cognitive performance, compared with no participants in the medical arm (P = .007).
Compared with participants who had no change in cognitive performance, those who had a significant improvement had a trend toward lower AFib recurrence rates (29% vs. 48%; P = .30). However, both groups were found to have a low AFib burden over the 12 months. And the use of AADs at the 12-month mark was significantly lower among those with versus those without cognitive improvement (0% vs. 38%; P = .04).
As early as 3 months post procedure and then at 12 months, participants in the ablation group had significant improvement in AFib-related symptoms, compared with those in the medical arm (for both, P < .001).
“Among a contemporary cohort of symptomatic paroxysmal and persistent AFib patients, catheter ablation was associated with a transient decline in cognitive function in the short-term, followed by recovery at 12 months,” the authors conclude.
They note that further large studies “are required to determine with AFib ablation may prevent the longer-term neurocognitive decline and dementia development associated with AFib.”
‘Reassuring’ findings
In a comment, Andrea Natale, MD, executive medical director, Texas Cardiac Arrhythmia Institute at St. David’s Medical Center, Austin, said POCD is “very likely due to the vulnerable state of mind and the stress that the patients encounter while undergoing the cardiac procedure,” as well as postsurgical inflammation, which “can cause brief functional alterations in the brain, leading to temporary cognitive impairment.” Inadequate preprocedural anticoagulation may also play a role.
Dr. Natale, co-author of an accompanying editorial, said it’s “prudent” when evaluating cognitive function to use questionnaires that are “sensitive to mild cognitive impairment,” such as the Montreal Cognitive Assessment or the Mini-Mental State Examination.
Additionally, “post-ablation cognitive function should be assessed way after the blanking period to avoid any plausible impact of inflammation, medications, the feeling of being overwhelmed, and the stress of undergoing a cardiac procedure,” advised Dr. Natale, who was not involved with the study.
Also commenting, Matthew Hyman, MD, PhD, an electrophysiologist and assistant professor of medicine at the Hospital of the University of Pennsylvania, called it a “well-done and very reassuring study.”
Dr. Hyman, who was also not part of the research team, added that previous work has shown an association between AFib and dementia, “and it remains to be seen if patients with rhythm control over longer durations than the current studies have the best outcomes.”
The authors of the study are supported by the National Health and Medical Research Council research scholarship. One author of the study is supported by a practitioner fellowship from the National Health and Medical Research Council; has received research support from Biosense Webster, Boston Scientific, Abbott, and Medtronic; and has served on the advisory board of Boston Scientific and Biosense Webster. Dr. Natale is a consultant for Abbott, Baylis, Biosense Webster, Biotronik, Boston Scientific, and Medtronic. Dr. Hyman is a consultant/speaker for Abbott, Biosense Webster and Boston Scientific.
A version of this article first appeared on Medscape.com.
FROM JACC: CLINICAL ELECTROPHYSIOLOGY
Nonstimulants: A better option for ADHD?
.
Investigators studied patients who started out taking atomoxetine and, after a washout period, initiated treatment with viloxazine. Participants’ ADHD symptoms were assessed prior to initiation of each treatment and after 4 weeks.
Children and adults showed significantly larger improvement in inattentiveness and hyperactivity/impulsivity when taking viloxazine vs. atomoxetine, with almost all patients preferring the former to the latter, according to results of the study.
In addition, close to one half of the study participants were taking a prior stimulant, and 85% were able to taper off stimulant treatment. Viloxazine’s effects were more rapid than were those of atomoxetine.
“It is timely to have a rapidly acting, and highly effective nonstimulant option across the full spectrum of ADHD symptoms, for both children and adults, in light of recent stimulant shortages and the new [Food and Drug Administration] boxed warnings regarding increased mortality associated with overuse of stimulants” study investigator Maxwell Z. Price, a medical student at Hackensack Meridian School of Medicine, Nutley, N.J., said in an interview.
Nonstimulant treatment options
Study coauthor Richard L. Price, MD, noted that the study was conducted to find a more acceptable alternative to psychostimulant treatments for ADHD, which are currently considered the “gold standard.”
Although they are effective, said Dr. Price, they are fraught with adverse effects, including appetite suppression, insomnia, exacerbation of mood disorders, anxiety, tics, or misuse.
Atomoxetine, a nonstimulant option, has been around for a few decades and is often used in combination with a stimulant medication. However, he said, the drug has a mild effect, requires frequent dosage adjustment, takes a long time to work, and people have “soured” on its utility, Dr. Price added.
Like atomoxetine, viloxazine is a selective norepinephrine inhibitor that has been used an antidepressant in Europe for 30 years. It was recently reformulated as an extended-release medication and approved by the FDA for pediatric and adult ADHD.
However, unlike atomoxetine, viloxazine is associated with increased prefrontal cortex 5-hydroxytrytamine, norepinephrine, and dopamine levels in vivo.
There have been no head-to-head trials comparing the two agents. However, even in head-to-head ADHD medication trials, the agents that are under investigation are typically compared in matched patients. The current investigators wanted to compare the two agents in the same patients whose insurers mandate a trial of generic atomoxetine prior to covering branded viloxazine.
“We wanted to find out whether patients taking atomoxetine for ADHD combined type would experience improvement in ADHD symptoms following voluntary, open-label switch to viloxazine,” said Dr. Price.
The researchers studied 50 patients who presented with ADHD combined type and had no other psychiatric, medical, or substance-related comorbidities or prior exposure to atomoxetine or viloxazine.
The study included 35 children (mean age, 11.9 ± 2.9 years; 94.3% male) and 15 adults (mean age, 29.3 ± 9.0 years; 73.3% male). Of these, 42.9% and 73.3%, respectively, were taking concurrent stimulants.
Patients received mean doses of atomoxetine once daily followed by viloxazine once daily after a 5-day washout period between the two drugs. Participants were seen weekly for titration and monitoring.
At baseline, the pediatric ADHD–Rating Scale 5 (ADHD-RS-5) and the Adult Investigator Symptoms Rating Scale (AISRS) were completed, then again after 4 weeks of treatment with atomoxetine (or upon earlier response or discontinuation due to side effects, whichever came first), and 5 days after discontinuing atomoxetine, which “reestablished the baseline score.” The same protocol was then repeated with viloxazine.
‘Paradigm shift’
At baseline, the total ADHD-RS-5 mean score was 40.3 ± 10.3. Improvements at 4 weeks were greater in viloxazine vs atomoxetine, with scores of 13.9 ± 10.2 vs 33.1 ± 12.1, respectively (t = -10.12, P < .00001). In inattention and hyperactivity/impulsivity, the t values were –8.57 and –9.87, respectively (both P values < .0001).
Similarly, from the baseline total, AISRS mean score of 37.3 ± 11.8, improvements were greater on viloxazine vs. atomoxetine, with scores of 11.9 ± 9.4 vs. 28.8 ± 14.9, respectively (t = −4.18, P = .0009 overall; for inattention, t = −3.50, P > .004 and for hyperactivity/impulsivity, t = 3.90, P > .002).
By 2 weeks, 86% of patients taking viloxazine reported a positive response vs. 14% when taking atomoxetine.
Side effects were lower in viloxazine vs. atomoxetine, with 36% of patients discontinuing treatment with atomoxetine because of side effects that included gastrointestinal upset, irritability, fatigue, and insomnia vs. 4% who discontinued viloxazine because of fatigue.
Almost all participants (96%) preferred viloxazine over atomoxetine and 85% were able to taper off stimulant treatment following stabilization on viloxazine.
“These were not small differences,” said Dr. Richard L. Price. “These were clinically and statistically meaningful differences.”
The findings could represent “a paradigm shift for the field” because “we always think of starting ADHD treatment with stimulants, but perhaps treatment with viloxazine could help patients to avoid stimulants entirely,” he suggested.
Real-world study
Commenting for this article, Greg Mattingly, MD, associate clinical professor, Washington University, St. Louis, called it “a timely addition to the clinical literature where for the first time ever we have two nonstimulant options approved for adults with ADHD.”
This real-world clinic study “yields many answers,” said Dr. Mattingly, president-elect of the American Professional Society of ADHD and Related Disorders (APSARD), who was not involved with the study.
“Simply put, this real-world study of 50 clinic patients found that viloxazine ER had faster onset, was significantly more effective, and was preferred by 96% of patients as compared to atomoxetine,” he said.
“Another intriguing part of the study that will be of high interest to both patients and providers was that, of those initially treated concurrently with stimulant and viloxazine ER, 85% were able to discontinue their stimulant medication,” Dr. Mattingly added.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The open access fee was funded by the investigators. Dr. Maxwell Z. Price certifies that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript. Dr. Richard L. Price has received honoraria from AbbVie, Alkermes, Idorsia, Intra-Cellular Therapies, Janssen, Jazz, Lundbeck, Neuronetics, Otsuka, and Supernus. Dr. Mattingly reports financial disclosures with various pharmaceutical companies, which are listed in full in the paper.
A version of this article first appeared on Medscape.com.
.
Investigators studied patients who started out taking atomoxetine and, after a washout period, initiated treatment with viloxazine. Participants’ ADHD symptoms were assessed prior to initiation of each treatment and after 4 weeks.
Children and adults showed significantly larger improvement in inattentiveness and hyperactivity/impulsivity when taking viloxazine vs. atomoxetine, with almost all patients preferring the former to the latter, according to results of the study.
In addition, close to one half of the study participants were taking a prior stimulant, and 85% were able to taper off stimulant treatment. Viloxazine’s effects were more rapid than were those of atomoxetine.
“It is timely to have a rapidly acting, and highly effective nonstimulant option across the full spectrum of ADHD symptoms, for both children and adults, in light of recent stimulant shortages and the new [Food and Drug Administration] boxed warnings regarding increased mortality associated with overuse of stimulants” study investigator Maxwell Z. Price, a medical student at Hackensack Meridian School of Medicine, Nutley, N.J., said in an interview.
Nonstimulant treatment options
Study coauthor Richard L. Price, MD, noted that the study was conducted to find a more acceptable alternative to psychostimulant treatments for ADHD, which are currently considered the “gold standard.”
Although they are effective, said Dr. Price, they are fraught with adverse effects, including appetite suppression, insomnia, exacerbation of mood disorders, anxiety, tics, or misuse.
Atomoxetine, a nonstimulant option, has been around for a few decades and is often used in combination with a stimulant medication. However, he said, the drug has a mild effect, requires frequent dosage adjustment, takes a long time to work, and people have “soured” on its utility, Dr. Price added.
Like atomoxetine, viloxazine is a selective norepinephrine inhibitor that has been used an antidepressant in Europe for 30 years. It was recently reformulated as an extended-release medication and approved by the FDA for pediatric and adult ADHD.
However, unlike atomoxetine, viloxazine is associated with increased prefrontal cortex 5-hydroxytrytamine, norepinephrine, and dopamine levels in vivo.
There have been no head-to-head trials comparing the two agents. However, even in head-to-head ADHD medication trials, the agents that are under investigation are typically compared in matched patients. The current investigators wanted to compare the two agents in the same patients whose insurers mandate a trial of generic atomoxetine prior to covering branded viloxazine.
“We wanted to find out whether patients taking atomoxetine for ADHD combined type would experience improvement in ADHD symptoms following voluntary, open-label switch to viloxazine,” said Dr. Price.
The researchers studied 50 patients who presented with ADHD combined type and had no other psychiatric, medical, or substance-related comorbidities or prior exposure to atomoxetine or viloxazine.
The study included 35 children (mean age, 11.9 ± 2.9 years; 94.3% male) and 15 adults (mean age, 29.3 ± 9.0 years; 73.3% male). Of these, 42.9% and 73.3%, respectively, were taking concurrent stimulants.
Patients received mean doses of atomoxetine once daily followed by viloxazine once daily after a 5-day washout period between the two drugs. Participants were seen weekly for titration and monitoring.
At baseline, the pediatric ADHD–Rating Scale 5 (ADHD-RS-5) and the Adult Investigator Symptoms Rating Scale (AISRS) were completed, then again after 4 weeks of treatment with atomoxetine (or upon earlier response or discontinuation due to side effects, whichever came first), and 5 days after discontinuing atomoxetine, which “reestablished the baseline score.” The same protocol was then repeated with viloxazine.
‘Paradigm shift’
At baseline, the total ADHD-RS-5 mean score was 40.3 ± 10.3. Improvements at 4 weeks were greater in viloxazine vs atomoxetine, with scores of 13.9 ± 10.2 vs 33.1 ± 12.1, respectively (t = -10.12, P < .00001). In inattention and hyperactivity/impulsivity, the t values were –8.57 and –9.87, respectively (both P values < .0001).
Similarly, from the baseline total, AISRS mean score of 37.3 ± 11.8, improvements were greater on viloxazine vs. atomoxetine, with scores of 11.9 ± 9.4 vs. 28.8 ± 14.9, respectively (t = −4.18, P = .0009 overall; for inattention, t = −3.50, P > .004 and for hyperactivity/impulsivity, t = 3.90, P > .002).
By 2 weeks, 86% of patients taking viloxazine reported a positive response vs. 14% when taking atomoxetine.
Side effects were lower in viloxazine vs. atomoxetine, with 36% of patients discontinuing treatment with atomoxetine because of side effects that included gastrointestinal upset, irritability, fatigue, and insomnia vs. 4% who discontinued viloxazine because of fatigue.
Almost all participants (96%) preferred viloxazine over atomoxetine and 85% were able to taper off stimulant treatment following stabilization on viloxazine.
“These were not small differences,” said Dr. Richard L. Price. “These were clinically and statistically meaningful differences.”
The findings could represent “a paradigm shift for the field” because “we always think of starting ADHD treatment with stimulants, but perhaps treatment with viloxazine could help patients to avoid stimulants entirely,” he suggested.
Real-world study
Commenting for this article, Greg Mattingly, MD, associate clinical professor, Washington University, St. Louis, called it “a timely addition to the clinical literature where for the first time ever we have two nonstimulant options approved for adults with ADHD.”
This real-world clinic study “yields many answers,” said Dr. Mattingly, president-elect of the American Professional Society of ADHD and Related Disorders (APSARD), who was not involved with the study.
“Simply put, this real-world study of 50 clinic patients found that viloxazine ER had faster onset, was significantly more effective, and was preferred by 96% of patients as compared to atomoxetine,” he said.
“Another intriguing part of the study that will be of high interest to both patients and providers was that, of those initially treated concurrently with stimulant and viloxazine ER, 85% were able to discontinue their stimulant medication,” Dr. Mattingly added.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The open access fee was funded by the investigators. Dr. Maxwell Z. Price certifies that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript. Dr. Richard L. Price has received honoraria from AbbVie, Alkermes, Idorsia, Intra-Cellular Therapies, Janssen, Jazz, Lundbeck, Neuronetics, Otsuka, and Supernus. Dr. Mattingly reports financial disclosures with various pharmaceutical companies, which are listed in full in the paper.
A version of this article first appeared on Medscape.com.
.
Investigators studied patients who started out taking atomoxetine and, after a washout period, initiated treatment with viloxazine. Participants’ ADHD symptoms were assessed prior to initiation of each treatment and after 4 weeks.
Children and adults showed significantly larger improvement in inattentiveness and hyperactivity/impulsivity when taking viloxazine vs. atomoxetine, with almost all patients preferring the former to the latter, according to results of the study.
In addition, close to one half of the study participants were taking a prior stimulant, and 85% were able to taper off stimulant treatment. Viloxazine’s effects were more rapid than were those of atomoxetine.
“It is timely to have a rapidly acting, and highly effective nonstimulant option across the full spectrum of ADHD symptoms, for both children and adults, in light of recent stimulant shortages and the new [Food and Drug Administration] boxed warnings regarding increased mortality associated with overuse of stimulants” study investigator Maxwell Z. Price, a medical student at Hackensack Meridian School of Medicine, Nutley, N.J., said in an interview.
Nonstimulant treatment options
Study coauthor Richard L. Price, MD, noted that the study was conducted to find a more acceptable alternative to psychostimulant treatments for ADHD, which are currently considered the “gold standard.”
Although they are effective, said Dr. Price, they are fraught with adverse effects, including appetite suppression, insomnia, exacerbation of mood disorders, anxiety, tics, or misuse.
Atomoxetine, a nonstimulant option, has been around for a few decades and is often used in combination with a stimulant medication. However, he said, the drug has a mild effect, requires frequent dosage adjustment, takes a long time to work, and people have “soured” on its utility, Dr. Price added.
Like atomoxetine, viloxazine is a selective norepinephrine inhibitor that has been used an antidepressant in Europe for 30 years. It was recently reformulated as an extended-release medication and approved by the FDA for pediatric and adult ADHD.
However, unlike atomoxetine, viloxazine is associated with increased prefrontal cortex 5-hydroxytrytamine, norepinephrine, and dopamine levels in vivo.
There have been no head-to-head trials comparing the two agents. However, even in head-to-head ADHD medication trials, the agents that are under investigation are typically compared in matched patients. The current investigators wanted to compare the two agents in the same patients whose insurers mandate a trial of generic atomoxetine prior to covering branded viloxazine.
“We wanted to find out whether patients taking atomoxetine for ADHD combined type would experience improvement in ADHD symptoms following voluntary, open-label switch to viloxazine,” said Dr. Price.
The researchers studied 50 patients who presented with ADHD combined type and had no other psychiatric, medical, or substance-related comorbidities or prior exposure to atomoxetine or viloxazine.
The study included 35 children (mean age, 11.9 ± 2.9 years; 94.3% male) and 15 adults (mean age, 29.3 ± 9.0 years; 73.3% male). Of these, 42.9% and 73.3%, respectively, were taking concurrent stimulants.
Patients received mean doses of atomoxetine once daily followed by viloxazine once daily after a 5-day washout period between the two drugs. Participants were seen weekly for titration and monitoring.
At baseline, the pediatric ADHD–Rating Scale 5 (ADHD-RS-5) and the Adult Investigator Symptoms Rating Scale (AISRS) were completed, then again after 4 weeks of treatment with atomoxetine (or upon earlier response or discontinuation due to side effects, whichever came first), and 5 days after discontinuing atomoxetine, which “reestablished the baseline score.” The same protocol was then repeated with viloxazine.
‘Paradigm shift’
At baseline, the total ADHD-RS-5 mean score was 40.3 ± 10.3. Improvements at 4 weeks were greater in viloxazine vs atomoxetine, with scores of 13.9 ± 10.2 vs 33.1 ± 12.1, respectively (t = -10.12, P < .00001). In inattention and hyperactivity/impulsivity, the t values were –8.57 and –9.87, respectively (both P values < .0001).
Similarly, from the baseline total, AISRS mean score of 37.3 ± 11.8, improvements were greater on viloxazine vs. atomoxetine, with scores of 11.9 ± 9.4 vs. 28.8 ± 14.9, respectively (t = −4.18, P = .0009 overall; for inattention, t = −3.50, P > .004 and for hyperactivity/impulsivity, t = 3.90, P > .002).
By 2 weeks, 86% of patients taking viloxazine reported a positive response vs. 14% when taking atomoxetine.
Side effects were lower in viloxazine vs. atomoxetine, with 36% of patients discontinuing treatment with atomoxetine because of side effects that included gastrointestinal upset, irritability, fatigue, and insomnia vs. 4% who discontinued viloxazine because of fatigue.
Almost all participants (96%) preferred viloxazine over atomoxetine and 85% were able to taper off stimulant treatment following stabilization on viloxazine.
“These were not small differences,” said Dr. Richard L. Price. “These were clinically and statistically meaningful differences.”
The findings could represent “a paradigm shift for the field” because “we always think of starting ADHD treatment with stimulants, but perhaps treatment with viloxazine could help patients to avoid stimulants entirely,” he suggested.
Real-world study
Commenting for this article, Greg Mattingly, MD, associate clinical professor, Washington University, St. Louis, called it “a timely addition to the clinical literature where for the first time ever we have two nonstimulant options approved for adults with ADHD.”
This real-world clinic study “yields many answers,” said Dr. Mattingly, president-elect of the American Professional Society of ADHD and Related Disorders (APSARD), who was not involved with the study.
“Simply put, this real-world study of 50 clinic patients found that viloxazine ER had faster onset, was significantly more effective, and was preferred by 96% of patients as compared to atomoxetine,” he said.
“Another intriguing part of the study that will be of high interest to both patients and providers was that, of those initially treated concurrently with stimulant and viloxazine ER, 85% were able to discontinue their stimulant medication,” Dr. Mattingly added.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The open access fee was funded by the investigators. Dr. Maxwell Z. Price certifies that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript. Dr. Richard L. Price has received honoraria from AbbVie, Alkermes, Idorsia, Intra-Cellular Therapies, Janssen, Jazz, Lundbeck, Neuronetics, Otsuka, and Supernus. Dr. Mattingly reports financial disclosures with various pharmaceutical companies, which are listed in full in the paper.
A version of this article first appeared on Medscape.com.
FROM CNS DRUGS
Even exercise by ‘weekend warriors’ can cut CV risk
Moderate to vigorous physical activity (MVPA) is a familiar and established approach to reducing cardiovascular (CV) risk, but it’s often believed that the exercise should be spread out across the week rather than concentrated within a couple of days.
A challenge to that view comes from an observational study of accelerometer-confirmed exercise in almost 90,000 people in their 60s. It suggests,
Researchers compared three patterns of MVPA in their subjects who wore accelerometers on their wrists for 1 week. Active WW subjects obtained at least 2.5 hours of exercise weekly, with at least half the amount completed over 1-2 days; “active regular” subjects achieved that exercise level but not mostly during 1 or 2 days; and those who were “inactive” fell short of 2.5 hours of exercise during the week. The group used a median exercise threshold of 3 hours, 50 minutes in a separate analysis.
The “active” groups, compared with inactive subjects, achieved similar and significant reductions in risk for incident atrial fibrillation (AF), myocardial infarction (MI), stroke, and heart failure (HF) over a median follow-up of 6.3 years at both weekly exercise thresholds, the group reported.
“The take-home [message] is that efforts to optimize activity, even if concentrated within just a day or 2 each week, should be expected to result in improved cardiovascular risk profiles,” lead author Shaan Khurshid, MD, MPH, Massachusetts General Hospital, Boston, said in an interview.
The study was published online in JAMA.
The research “provides novel data on patterns of physical activity accumulation and the risk of developing cardiovascular diseases,” observed Peter Katzmarzyk, PhD, Pennington Biomedical Research Center, Baton Rouge, La., in an interview. He was not involved with the research. Its “marked strengths,” he noted, include a large sample population and “use of accelerometers to measure physical activity levels and patterns.”
Moreover, Dr. Katzmarzyk said, its findings are “important” for showing that physical activity “can be accumulated throughout the week in different ways, which opens up more options for busy people to get their physical activity in.”
Current guidelines from the World Health Organization and the American Heart Association recommend at least 150 minutes of MVPA weekly to lower risk for cardiovascular disease and death, but do not specify an optimal exercise time frame. The U.K. National Health Service recommends MVPA daily or spread evenly over perhaps 4-5 days.
“The weekend warrior pattern has been studied previously, but typically relying on self-reported data, which may be biased, or [in studies] too small to look at specific cardiovascular outcomes,” Dr. Khurshid explained.
In the UK Biobank database, he said, “We saw the opportunity to leverage the largest sample of measured activity to date” to address the question of whether exercise time pattern “affects specific major cardiovascular diseases differently,” Dr. Khurshid said
The primary analysis assessed exercise amount in a week based on the guideline-recommended threshold of at least 2.5 hours; a 3-hour, 50-minutes threshold was used in a secondary analysis. The group assessed multiple thresholds because optimal MVPS levels derived from wrist-based accelerometers are “unclear,” he said.
The sample consisted of 89,573 participants with a mean age 62; slightly more than half (56%) were women. Based on the weekly MVPA threshold of 2.5 hours , the WW, active regular, and inactive groups made up 42.2%, 24%, and 33.7% of the population, respectively.
Compared with the inactive group, the two active groups both showed significant risk reductions for the four clinical outcomes, to similar degrees, in multivariate analysis. The results were similar at the 230-minute weekly exercise threshold for incident AF, MI, and HF but not for stroke.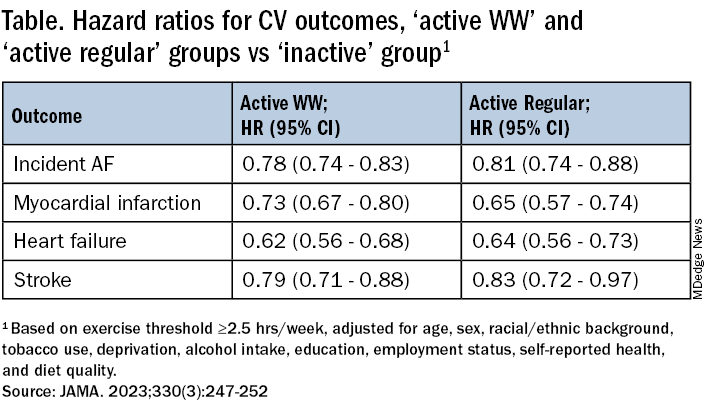
The findings were similarly consistent at the 3-hour, 50-minutes median threshold, although stroke differences were no longer significant.
Patients should be encouraged to exercise at recommended levels, “and should not be discouraged if, for whatever reasons, they are able to focus exercise within only 1 or a few days of the week,” said Dr. Khurshid. “Our findings suggest that it is the volume of activity, rather than the pattern, that matters most.”
The report notes several limitations of the study, including the exercise observation period limited to 1 week and that participants could have modified their behavior during the observation period. Also, the participants were almost all White, so the results may not be generalizable to other populations.
Clinicians should familiarize themselves with the “full range of recommendations” presented in the “Physical Activity Guidelines for Americans, 2nd Edition” “and personalize prescriptions by setting achievable physical activity goals” based on age, physical abilities, and activity levels, states an accompanying editorial from Dr. Katzmarzyk and John M. Jakicic, PhD, University of Kansas Medical Center, Kansas City.
Although MVPA at the recommended level of at least 2.5 hours per week will certainly be beneficial, they write, “the public health message should also clearly convey that every minute counts, especially among the three-quarters of U.S. adults who do not achieve that goal.”
Dr. Khurshid reported no relevant financial relationships; disclosures for the other authors are in the original article. Dr. Katzmarzyk reports no relevant financial relationships. Dr. Jakicic discloses receiving personal fees from Wondr Health, WW International (formerly Weight Watchers), and Educational Initiatives and grants from Epitomee Medical.
A version of this article appeared on Medscape.com.
Moderate to vigorous physical activity (MVPA) is a familiar and established approach to reducing cardiovascular (CV) risk, but it’s often believed that the exercise should be spread out across the week rather than concentrated within a couple of days.
A challenge to that view comes from an observational study of accelerometer-confirmed exercise in almost 90,000 people in their 60s. It suggests,
Researchers compared three patterns of MVPA in their subjects who wore accelerometers on their wrists for 1 week. Active WW subjects obtained at least 2.5 hours of exercise weekly, with at least half the amount completed over 1-2 days; “active regular” subjects achieved that exercise level but not mostly during 1 or 2 days; and those who were “inactive” fell short of 2.5 hours of exercise during the week. The group used a median exercise threshold of 3 hours, 50 minutes in a separate analysis.
The “active” groups, compared with inactive subjects, achieved similar and significant reductions in risk for incident atrial fibrillation (AF), myocardial infarction (MI), stroke, and heart failure (HF) over a median follow-up of 6.3 years at both weekly exercise thresholds, the group reported.
“The take-home [message] is that efforts to optimize activity, even if concentrated within just a day or 2 each week, should be expected to result in improved cardiovascular risk profiles,” lead author Shaan Khurshid, MD, MPH, Massachusetts General Hospital, Boston, said in an interview.
The study was published online in JAMA.
The research “provides novel data on patterns of physical activity accumulation and the risk of developing cardiovascular diseases,” observed Peter Katzmarzyk, PhD, Pennington Biomedical Research Center, Baton Rouge, La., in an interview. He was not involved with the research. Its “marked strengths,” he noted, include a large sample population and “use of accelerometers to measure physical activity levels and patterns.”
Moreover, Dr. Katzmarzyk said, its findings are “important” for showing that physical activity “can be accumulated throughout the week in different ways, which opens up more options for busy people to get their physical activity in.”
Current guidelines from the World Health Organization and the American Heart Association recommend at least 150 minutes of MVPA weekly to lower risk for cardiovascular disease and death, but do not specify an optimal exercise time frame. The U.K. National Health Service recommends MVPA daily or spread evenly over perhaps 4-5 days.
“The weekend warrior pattern has been studied previously, but typically relying on self-reported data, which may be biased, or [in studies] too small to look at specific cardiovascular outcomes,” Dr. Khurshid explained.
In the UK Biobank database, he said, “We saw the opportunity to leverage the largest sample of measured activity to date” to address the question of whether exercise time pattern “affects specific major cardiovascular diseases differently,” Dr. Khurshid said
The primary analysis assessed exercise amount in a week based on the guideline-recommended threshold of at least 2.5 hours; a 3-hour, 50-minutes threshold was used in a secondary analysis. The group assessed multiple thresholds because optimal MVPS levels derived from wrist-based accelerometers are “unclear,” he said.
The sample consisted of 89,573 participants with a mean age 62; slightly more than half (56%) were women. Based on the weekly MVPA threshold of 2.5 hours , the WW, active regular, and inactive groups made up 42.2%, 24%, and 33.7% of the population, respectively.
Compared with the inactive group, the two active groups both showed significant risk reductions for the four clinical outcomes, to similar degrees, in multivariate analysis. The results were similar at the 230-minute weekly exercise threshold for incident AF, MI, and HF but not for stroke.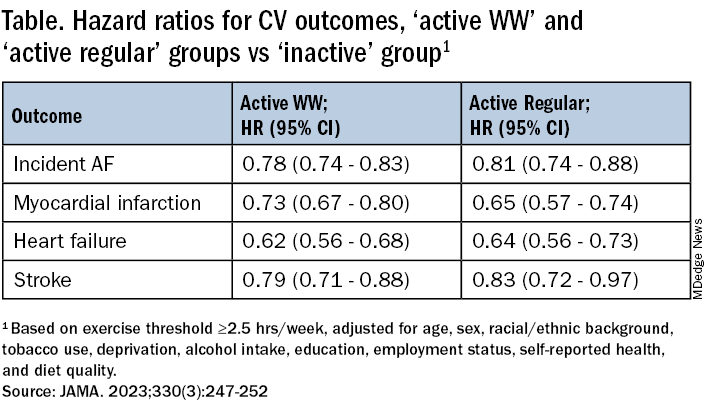
The findings were similarly consistent at the 3-hour, 50-minutes median threshold, although stroke differences were no longer significant.
Patients should be encouraged to exercise at recommended levels, “and should not be discouraged if, for whatever reasons, they are able to focus exercise within only 1 or a few days of the week,” said Dr. Khurshid. “Our findings suggest that it is the volume of activity, rather than the pattern, that matters most.”
The report notes several limitations of the study, including the exercise observation period limited to 1 week and that participants could have modified their behavior during the observation period. Also, the participants were almost all White, so the results may not be generalizable to other populations.
Clinicians should familiarize themselves with the “full range of recommendations” presented in the “Physical Activity Guidelines for Americans, 2nd Edition” “and personalize prescriptions by setting achievable physical activity goals” based on age, physical abilities, and activity levels, states an accompanying editorial from Dr. Katzmarzyk and John M. Jakicic, PhD, University of Kansas Medical Center, Kansas City.
Although MVPA at the recommended level of at least 2.5 hours per week will certainly be beneficial, they write, “the public health message should also clearly convey that every minute counts, especially among the three-quarters of U.S. adults who do not achieve that goal.”
Dr. Khurshid reported no relevant financial relationships; disclosures for the other authors are in the original article. Dr. Katzmarzyk reports no relevant financial relationships. Dr. Jakicic discloses receiving personal fees from Wondr Health, WW International (formerly Weight Watchers), and Educational Initiatives and grants from Epitomee Medical.
A version of this article appeared on Medscape.com.
Moderate to vigorous physical activity (MVPA) is a familiar and established approach to reducing cardiovascular (CV) risk, but it’s often believed that the exercise should be spread out across the week rather than concentrated within a couple of days.
A challenge to that view comes from an observational study of accelerometer-confirmed exercise in almost 90,000 people in their 60s. It suggests,
Researchers compared three patterns of MVPA in their subjects who wore accelerometers on their wrists for 1 week. Active WW subjects obtained at least 2.5 hours of exercise weekly, with at least half the amount completed over 1-2 days; “active regular” subjects achieved that exercise level but not mostly during 1 or 2 days; and those who were “inactive” fell short of 2.5 hours of exercise during the week. The group used a median exercise threshold of 3 hours, 50 minutes in a separate analysis.
The “active” groups, compared with inactive subjects, achieved similar and significant reductions in risk for incident atrial fibrillation (AF), myocardial infarction (MI), stroke, and heart failure (HF) over a median follow-up of 6.3 years at both weekly exercise thresholds, the group reported.
“The take-home [message] is that efforts to optimize activity, even if concentrated within just a day or 2 each week, should be expected to result in improved cardiovascular risk profiles,” lead author Shaan Khurshid, MD, MPH, Massachusetts General Hospital, Boston, said in an interview.
The study was published online in JAMA.
The research “provides novel data on patterns of physical activity accumulation and the risk of developing cardiovascular diseases,” observed Peter Katzmarzyk, PhD, Pennington Biomedical Research Center, Baton Rouge, La., in an interview. He was not involved with the research. Its “marked strengths,” he noted, include a large sample population and “use of accelerometers to measure physical activity levels and patterns.”
Moreover, Dr. Katzmarzyk said, its findings are “important” for showing that physical activity “can be accumulated throughout the week in different ways, which opens up more options for busy people to get their physical activity in.”
Current guidelines from the World Health Organization and the American Heart Association recommend at least 150 minutes of MVPA weekly to lower risk for cardiovascular disease and death, but do not specify an optimal exercise time frame. The U.K. National Health Service recommends MVPA daily or spread evenly over perhaps 4-5 days.
“The weekend warrior pattern has been studied previously, but typically relying on self-reported data, which may be biased, or [in studies] too small to look at specific cardiovascular outcomes,” Dr. Khurshid explained.
In the UK Biobank database, he said, “We saw the opportunity to leverage the largest sample of measured activity to date” to address the question of whether exercise time pattern “affects specific major cardiovascular diseases differently,” Dr. Khurshid said
The primary analysis assessed exercise amount in a week based on the guideline-recommended threshold of at least 2.5 hours; a 3-hour, 50-minutes threshold was used in a secondary analysis. The group assessed multiple thresholds because optimal MVPS levels derived from wrist-based accelerometers are “unclear,” he said.
The sample consisted of 89,573 participants with a mean age 62; slightly more than half (56%) were women. Based on the weekly MVPA threshold of 2.5 hours , the WW, active regular, and inactive groups made up 42.2%, 24%, and 33.7% of the population, respectively.
Compared with the inactive group, the two active groups both showed significant risk reductions for the four clinical outcomes, to similar degrees, in multivariate analysis. The results were similar at the 230-minute weekly exercise threshold for incident AF, MI, and HF but not for stroke.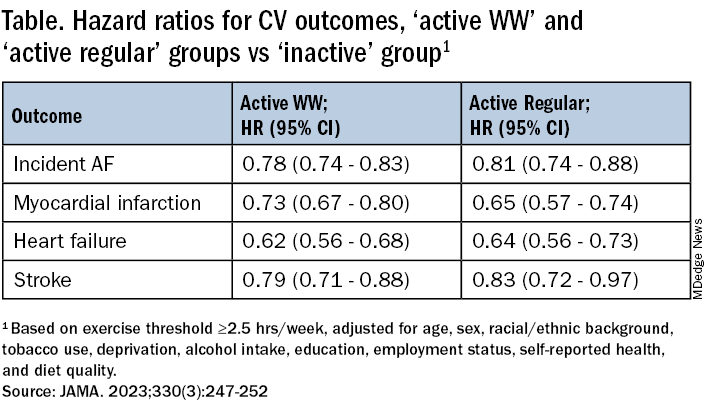
The findings were similarly consistent at the 3-hour, 50-minutes median threshold, although stroke differences were no longer significant.
Patients should be encouraged to exercise at recommended levels, “and should not be discouraged if, for whatever reasons, they are able to focus exercise within only 1 or a few days of the week,” said Dr. Khurshid. “Our findings suggest that it is the volume of activity, rather than the pattern, that matters most.”
The report notes several limitations of the study, including the exercise observation period limited to 1 week and that participants could have modified their behavior during the observation period. Also, the participants were almost all White, so the results may not be generalizable to other populations.
Clinicians should familiarize themselves with the “full range of recommendations” presented in the “Physical Activity Guidelines for Americans, 2nd Edition” “and personalize prescriptions by setting achievable physical activity goals” based on age, physical abilities, and activity levels, states an accompanying editorial from Dr. Katzmarzyk and John M. Jakicic, PhD, University of Kansas Medical Center, Kansas City.
Although MVPA at the recommended level of at least 2.5 hours per week will certainly be beneficial, they write, “the public health message should also clearly convey that every minute counts, especially among the three-quarters of U.S. adults who do not achieve that goal.”
Dr. Khurshid reported no relevant financial relationships; disclosures for the other authors are in the original article. Dr. Katzmarzyk reports no relevant financial relationships. Dr. Jakicic discloses receiving personal fees from Wondr Health, WW International (formerly Weight Watchers), and Educational Initiatives and grants from Epitomee Medical.
A version of this article appeared on Medscape.com.
FROM JAMA


