User login
Residual single-site ovarian cancer surpasses multisite outcomes
NEW ORLEANS – When complete resection of advanced-stage, epithelial ovarian cancer is not possible, surgical resection that leaves a small volume of residual tumor at a single site produces significantly better outcomes than leaving minimal residual cancer at multiple sites, according to a review of 510 patients at two U.S. centers.
“In the past, we separated these patients based on whether they had a complete resection, R0 disease, or had 1 cm or less of residual disease” regardless of the number of sites with this small amount of residual tumor. The third category was patients with more than 1 cm of residual tumor at one or more sites, explained Dr. Manning-Geist in an interview. “What we did was break down the patients with 1 cm or less of residual tumor into those with one site or multiple sites. This is the first reported study to use number of sites” as a clinical characteristic for analysis in this context.
The message from the findings is that, while the goal of debulking surgery in patients with advanced epithelial ovarian cancer is complete tumor resection, if that can’t be achieved, the next goal is to leave residual tumor at just a single site, she concluded. A question that remains is whether primary debulking surgery is preferable to neoadjuvant treatment followed by interval debulking surgery. In the results Dr. Manning-Geist presented, patients who underwent primary debulking had better outcomes than those with neoadjuvant therapy followed by interval debulking, but these two subgroups also had different clinical characteristics.
The study used data from 510 patients with stage IIIC or IV epithelial ovarian cancer treated at either Brigham and Women’s or Massachusetts General Hospital during 2010-2015. The study cohort included 240 patients who underwent primary debulking surgery and 270 who first received neoadjuvant chemotherapy and then underwent interval debulking surgery. The patients who received neoadjuvant therapy were, on average, older (65 years vs. 63 years), had a higher prevalence of stage IV disease (44% vs. 16%), and had a higher prevalence of tumors with serous histology (93% vs. 77%), compared with patients who underwent primary debulking.
Complete tumor resections occurred in 39% of the primary debulking patients and in 64% of those who received neoadjuvant therapy; residual disease of 1 cm or less at one site occurred in 17% and 13%, respectively; minimal residual disease at multiple sites remained in 28% and 17% respectively; and the remaining patients had residual disease of more than 1 cm in at least one site, 16% and 6% respectively.
For this analysis, Dr. Manning-Geist and her associates considered residual disease at any of seven possible sites: diaphragm, upper abdomen, bowel mesentary, bowel serosa, abdominal peritoneum, pelvis, and nodal. Even if multiple individual metastases remained within one of these sites after surgery, it was categorized as a single site of residual disease.
Among patients who underwent primary debulking surgery, progression-free survival persisted for a median of 23 months among patients with full resection, 19 months in patients with a single site with minimal residual disease, 13 months among those with multiple sites of residual disease, and 10 months in patients with more than 1 cm of residual tumor. Median overall survival in these four subgroups was not yet reached, 64 months, 50 months, and 49 months, respectively.
Among patients who received neoadjuvant chemotherapy and then underwent interval debulking surgery, median durations of progression-free survival were 14 months, 12 months, 10 months, and 6 months, respectively. Median overall survival rates were 58 months, 37 months, 26 months, and 33 months, respectively. Within each of these four analyses, the differences in both survival and progression-free survival across the four subgroups was statistically significant, with a P less than .001 for each analysis.
In multivariate analyses, among patients who underwent primary debulking surgery, the significant linkages with worsening progression-free and overall survival were age, cancer stage, and amount and site number of residual disease. Among patients who received neoadjuvant chemotherapy followed by interval debulking residual disease diameter and site number of residual tumor was the only significant determinant for both progression-free and overall survival, Dr. Manning-Geist reported.
Dr. Manning-Geist had no disclosures.
SOURCE: Manning-Geist B et al. SGO 2018, Abstract 43.
NEW ORLEANS – When complete resection of advanced-stage, epithelial ovarian cancer is not possible, surgical resection that leaves a small volume of residual tumor at a single site produces significantly better outcomes than leaving minimal residual cancer at multiple sites, according to a review of 510 patients at two U.S. centers.
“In the past, we separated these patients based on whether they had a complete resection, R0 disease, or had 1 cm or less of residual disease” regardless of the number of sites with this small amount of residual tumor. The third category was patients with more than 1 cm of residual tumor at one or more sites, explained Dr. Manning-Geist in an interview. “What we did was break down the patients with 1 cm or less of residual tumor into those with one site or multiple sites. This is the first reported study to use number of sites” as a clinical characteristic for analysis in this context.
The message from the findings is that, while the goal of debulking surgery in patients with advanced epithelial ovarian cancer is complete tumor resection, if that can’t be achieved, the next goal is to leave residual tumor at just a single site, she concluded. A question that remains is whether primary debulking surgery is preferable to neoadjuvant treatment followed by interval debulking surgery. In the results Dr. Manning-Geist presented, patients who underwent primary debulking had better outcomes than those with neoadjuvant therapy followed by interval debulking, but these two subgroups also had different clinical characteristics.
The study used data from 510 patients with stage IIIC or IV epithelial ovarian cancer treated at either Brigham and Women’s or Massachusetts General Hospital during 2010-2015. The study cohort included 240 patients who underwent primary debulking surgery and 270 who first received neoadjuvant chemotherapy and then underwent interval debulking surgery. The patients who received neoadjuvant therapy were, on average, older (65 years vs. 63 years), had a higher prevalence of stage IV disease (44% vs. 16%), and had a higher prevalence of tumors with serous histology (93% vs. 77%), compared with patients who underwent primary debulking.
Complete tumor resections occurred in 39% of the primary debulking patients and in 64% of those who received neoadjuvant therapy; residual disease of 1 cm or less at one site occurred in 17% and 13%, respectively; minimal residual disease at multiple sites remained in 28% and 17% respectively; and the remaining patients had residual disease of more than 1 cm in at least one site, 16% and 6% respectively.
For this analysis, Dr. Manning-Geist and her associates considered residual disease at any of seven possible sites: diaphragm, upper abdomen, bowel mesentary, bowel serosa, abdominal peritoneum, pelvis, and nodal. Even if multiple individual metastases remained within one of these sites after surgery, it was categorized as a single site of residual disease.
Among patients who underwent primary debulking surgery, progression-free survival persisted for a median of 23 months among patients with full resection, 19 months in patients with a single site with minimal residual disease, 13 months among those with multiple sites of residual disease, and 10 months in patients with more than 1 cm of residual tumor. Median overall survival in these four subgroups was not yet reached, 64 months, 50 months, and 49 months, respectively.
Among patients who received neoadjuvant chemotherapy and then underwent interval debulking surgery, median durations of progression-free survival were 14 months, 12 months, 10 months, and 6 months, respectively. Median overall survival rates were 58 months, 37 months, 26 months, and 33 months, respectively. Within each of these four analyses, the differences in both survival and progression-free survival across the four subgroups was statistically significant, with a P less than .001 for each analysis.
In multivariate analyses, among patients who underwent primary debulking surgery, the significant linkages with worsening progression-free and overall survival were age, cancer stage, and amount and site number of residual disease. Among patients who received neoadjuvant chemotherapy followed by interval debulking residual disease diameter and site number of residual tumor was the only significant determinant for both progression-free and overall survival, Dr. Manning-Geist reported.
Dr. Manning-Geist had no disclosures.
SOURCE: Manning-Geist B et al. SGO 2018, Abstract 43.
NEW ORLEANS – When complete resection of advanced-stage, epithelial ovarian cancer is not possible, surgical resection that leaves a small volume of residual tumor at a single site produces significantly better outcomes than leaving minimal residual cancer at multiple sites, according to a review of 510 patients at two U.S. centers.
“In the past, we separated these patients based on whether they had a complete resection, R0 disease, or had 1 cm or less of residual disease” regardless of the number of sites with this small amount of residual tumor. The third category was patients with more than 1 cm of residual tumor at one or more sites, explained Dr. Manning-Geist in an interview. “What we did was break down the patients with 1 cm or less of residual tumor into those with one site or multiple sites. This is the first reported study to use number of sites” as a clinical characteristic for analysis in this context.
The message from the findings is that, while the goal of debulking surgery in patients with advanced epithelial ovarian cancer is complete tumor resection, if that can’t be achieved, the next goal is to leave residual tumor at just a single site, she concluded. A question that remains is whether primary debulking surgery is preferable to neoadjuvant treatment followed by interval debulking surgery. In the results Dr. Manning-Geist presented, patients who underwent primary debulking had better outcomes than those with neoadjuvant therapy followed by interval debulking, but these two subgroups also had different clinical characteristics.
The study used data from 510 patients with stage IIIC or IV epithelial ovarian cancer treated at either Brigham and Women’s or Massachusetts General Hospital during 2010-2015. The study cohort included 240 patients who underwent primary debulking surgery and 270 who first received neoadjuvant chemotherapy and then underwent interval debulking surgery. The patients who received neoadjuvant therapy were, on average, older (65 years vs. 63 years), had a higher prevalence of stage IV disease (44% vs. 16%), and had a higher prevalence of tumors with serous histology (93% vs. 77%), compared with patients who underwent primary debulking.
Complete tumor resections occurred in 39% of the primary debulking patients and in 64% of those who received neoadjuvant therapy; residual disease of 1 cm or less at one site occurred in 17% and 13%, respectively; minimal residual disease at multiple sites remained in 28% and 17% respectively; and the remaining patients had residual disease of more than 1 cm in at least one site, 16% and 6% respectively.
For this analysis, Dr. Manning-Geist and her associates considered residual disease at any of seven possible sites: diaphragm, upper abdomen, bowel mesentary, bowel serosa, abdominal peritoneum, pelvis, and nodal. Even if multiple individual metastases remained within one of these sites after surgery, it was categorized as a single site of residual disease.
Among patients who underwent primary debulking surgery, progression-free survival persisted for a median of 23 months among patients with full resection, 19 months in patients with a single site with minimal residual disease, 13 months among those with multiple sites of residual disease, and 10 months in patients with more than 1 cm of residual tumor. Median overall survival in these four subgroups was not yet reached, 64 months, 50 months, and 49 months, respectively.
Among patients who received neoadjuvant chemotherapy and then underwent interval debulking surgery, median durations of progression-free survival were 14 months, 12 months, 10 months, and 6 months, respectively. Median overall survival rates were 58 months, 37 months, 26 months, and 33 months, respectively. Within each of these four analyses, the differences in both survival and progression-free survival across the four subgroups was statistically significant, with a P less than .001 for each analysis.
In multivariate analyses, among patients who underwent primary debulking surgery, the significant linkages with worsening progression-free and overall survival were age, cancer stage, and amount and site number of residual disease. Among patients who received neoadjuvant chemotherapy followed by interval debulking residual disease diameter and site number of residual tumor was the only significant determinant for both progression-free and overall survival, Dr. Manning-Geist reported.
Dr. Manning-Geist had no disclosures.
SOURCE: Manning-Geist B et al. SGO 2018, Abstract 43.
REPORTING FROM SGO 2018
Key clinical point:
Major finding: Median overall survival after primary debulking was 64 months with single-site residual disease and 50 months with multisite disease.
Study details: Retrospective review of 510 patients from two U.S. centers.
Disclosures: Dr. Manning-Geist had no disclosures.
Source: Manning-Geist BL et al. SGO 2018, Abstract 43.
Surgery after immunotherapy effective in advanced melanoma
CHICAGO – Surgical resection is an effective treatment in selected patients with advanced melanoma treated with checkpoint blockade immunotherapy, according to a study of an institutional database at Memorial Sloan Kettering Cancer Center in New York presented at the Society of Surgical Oncology Annual Cancer Symposium.
“In the era of improved systemic therapy, checkpoint blockade for metastatic melanoma and the ability to surgically resect all disease after treatment is associated with an estimated survival of 75%, better than what’s been previously reported,” said Danielle M. Bello, MD, of Memorial Sloan Kettering.
The study analyzed a cohort of 237 patients who had unresectable stage III and IV melanoma and were treated with checkpoint blockade, including CTLA-4, programmed cell death protein 1 (PD-1), and programmed death-ligand 1 inhibitors, and then had surgical resection during 2003-2017.
Dr. Bello noted two previous studies that had reported encouraging outcomes in advanced melanoma. The first highlighted the role for surgery in stage IV melanoma. In that phase 3 clinical trial, patients had resection of up to five sites of metastatic disease and were then randomized to one of two treatment arms: bacillus Calmette-Guérin and allogeneic whole-cell vaccine (Canvaxin) or bacillus Calmette-Guérin and placebo. While this trial found no difference in overall survival between groups, it did report a 5-year overall survival exceeding 40% in both treatment arms, which highlighted that Stage IV patients who underwent resection of all their disease had survival outcomes superior to outcomes previously reported (Ann Surg Onc. 2017 Dec;24[13]:3991-4000). The second trial, the recent Checkmate 067 trial, emphasized the role of effective systemic checkpoint blockade in advanced stage III and IV melanoma. It reported that patients treated with combined nivolumab/ipilimumab therapy had not reached median overall survival at minimum 36 months of follow-up (N Engl J Med. 2017 Oct 5;377[14]:1345-56).
“We know that checkpoint inhibitor therapy has revolutionized the landscape of unresectable stage III and IV melanoma,” Dr. Bello said. However, despite encouraging trial readouts of overall survival, progression-free survival is a different story. “We know that the median progression-free survival even in our best combination therapy is 11.5 months, meaning that 50% of patients will go on to progress in a year and many will go on to surgical resection of their disease and do quite well,” she said.
Dr. Bello and her coauthors set out to describe outcomes of a “highly selective group” of patients who had surgical resection after checkpoint inhibitor therapy. “The majority of patients in our study had a cutaneous primary melanoma,” she said. Median age was 63 years, and 88% had stage IV disease. Regarding checkpoint blockade regimen, 62% received anti–CTLA-4, and 29% received combination anti–PD-1 and anti–CLTA-4 either sequentially or concomitantly prior to resection.
The median time from the start of immunotherapy to the first operation was 7 months. Forty-six percent had no further postoperative treatment after resection. In those, who did require further treatment, the majority received anti–PD-1 followed by targeted BRAF/MEK therapy, she said.
The analysis stratified patients into the following three categories based on radiological response to immunotherapy:
- Overall response to checkpoint blockade and the index lesion was either smaller since initiation of therapy or stabilized (12; 5.1%). Half of this group had a pathological complete response.
- Isolated site of progressive disease with residual stable disease elsewhere or as the only site of progressive disease (106; 44.7%).
- Multiple sites of progressive and palliative operations (119; 50.2%).
Median overall survival was 21 months in the entire study cohort with a median follow-up of 23 months, Dr. Bello said. “Those resected to no evidence of disease (NED) – 87 patients – had an estimated 5-year overall survival of 75%.” The NED group did not reach median OS.
The analysis also stratified overall survival by response to immunotherapy. “Patients with responding or stable disease had an estimated 90% 5-year overall survival,” Dr. Bellow said. “Those with one isolated progressive lesion that was resected had a 60% 5-year overall survival.” A more detailed analysis of the latter group found that those who had a resection to NED had an improved overall survival of 75% at 5 years. Resected patients who had residual remaining disease had a 30% 5-year overall survival.
“Further follow-up is needed to assess the durability and contributions of surgery, and further studies are underway to identify biomarkers associated with improved survival after immunotherapy and surgery,” Dr. Bello said.
SOURCE: Bello DM et al. SSO 2018, Abstract 5.
CHICAGO – Surgical resection is an effective treatment in selected patients with advanced melanoma treated with checkpoint blockade immunotherapy, according to a study of an institutional database at Memorial Sloan Kettering Cancer Center in New York presented at the Society of Surgical Oncology Annual Cancer Symposium.
“In the era of improved systemic therapy, checkpoint blockade for metastatic melanoma and the ability to surgically resect all disease after treatment is associated with an estimated survival of 75%, better than what’s been previously reported,” said Danielle M. Bello, MD, of Memorial Sloan Kettering.
The study analyzed a cohort of 237 patients who had unresectable stage III and IV melanoma and were treated with checkpoint blockade, including CTLA-4, programmed cell death protein 1 (PD-1), and programmed death-ligand 1 inhibitors, and then had surgical resection during 2003-2017.
Dr. Bello noted two previous studies that had reported encouraging outcomes in advanced melanoma. The first highlighted the role for surgery in stage IV melanoma. In that phase 3 clinical trial, patients had resection of up to five sites of metastatic disease and were then randomized to one of two treatment arms: bacillus Calmette-Guérin and allogeneic whole-cell vaccine (Canvaxin) or bacillus Calmette-Guérin and placebo. While this trial found no difference in overall survival between groups, it did report a 5-year overall survival exceeding 40% in both treatment arms, which highlighted that Stage IV patients who underwent resection of all their disease had survival outcomes superior to outcomes previously reported (Ann Surg Onc. 2017 Dec;24[13]:3991-4000). The second trial, the recent Checkmate 067 trial, emphasized the role of effective systemic checkpoint blockade in advanced stage III and IV melanoma. It reported that patients treated with combined nivolumab/ipilimumab therapy had not reached median overall survival at minimum 36 months of follow-up (N Engl J Med. 2017 Oct 5;377[14]:1345-56).
“We know that checkpoint inhibitor therapy has revolutionized the landscape of unresectable stage III and IV melanoma,” Dr. Bello said. However, despite encouraging trial readouts of overall survival, progression-free survival is a different story. “We know that the median progression-free survival even in our best combination therapy is 11.5 months, meaning that 50% of patients will go on to progress in a year and many will go on to surgical resection of their disease and do quite well,” she said.
Dr. Bello and her coauthors set out to describe outcomes of a “highly selective group” of patients who had surgical resection after checkpoint inhibitor therapy. “The majority of patients in our study had a cutaneous primary melanoma,” she said. Median age was 63 years, and 88% had stage IV disease. Regarding checkpoint blockade regimen, 62% received anti–CTLA-4, and 29% received combination anti–PD-1 and anti–CLTA-4 either sequentially or concomitantly prior to resection.
The median time from the start of immunotherapy to the first operation was 7 months. Forty-six percent had no further postoperative treatment after resection. In those, who did require further treatment, the majority received anti–PD-1 followed by targeted BRAF/MEK therapy, she said.
The analysis stratified patients into the following three categories based on radiological response to immunotherapy:
- Overall response to checkpoint blockade and the index lesion was either smaller since initiation of therapy or stabilized (12; 5.1%). Half of this group had a pathological complete response.
- Isolated site of progressive disease with residual stable disease elsewhere or as the only site of progressive disease (106; 44.7%).
- Multiple sites of progressive and palliative operations (119; 50.2%).
Median overall survival was 21 months in the entire study cohort with a median follow-up of 23 months, Dr. Bello said. “Those resected to no evidence of disease (NED) – 87 patients – had an estimated 5-year overall survival of 75%.” The NED group did not reach median OS.
The analysis also stratified overall survival by response to immunotherapy. “Patients with responding or stable disease had an estimated 90% 5-year overall survival,” Dr. Bellow said. “Those with one isolated progressive lesion that was resected had a 60% 5-year overall survival.” A more detailed analysis of the latter group found that those who had a resection to NED had an improved overall survival of 75% at 5 years. Resected patients who had residual remaining disease had a 30% 5-year overall survival.
“Further follow-up is needed to assess the durability and contributions of surgery, and further studies are underway to identify biomarkers associated with improved survival after immunotherapy and surgery,” Dr. Bello said.
SOURCE: Bello DM et al. SSO 2018, Abstract 5.
CHICAGO – Surgical resection is an effective treatment in selected patients with advanced melanoma treated with checkpoint blockade immunotherapy, according to a study of an institutional database at Memorial Sloan Kettering Cancer Center in New York presented at the Society of Surgical Oncology Annual Cancer Symposium.
“In the era of improved systemic therapy, checkpoint blockade for metastatic melanoma and the ability to surgically resect all disease after treatment is associated with an estimated survival of 75%, better than what’s been previously reported,” said Danielle M. Bello, MD, of Memorial Sloan Kettering.
The study analyzed a cohort of 237 patients who had unresectable stage III and IV melanoma and were treated with checkpoint blockade, including CTLA-4, programmed cell death protein 1 (PD-1), and programmed death-ligand 1 inhibitors, and then had surgical resection during 2003-2017.
Dr. Bello noted two previous studies that had reported encouraging outcomes in advanced melanoma. The first highlighted the role for surgery in stage IV melanoma. In that phase 3 clinical trial, patients had resection of up to five sites of metastatic disease and were then randomized to one of two treatment arms: bacillus Calmette-Guérin and allogeneic whole-cell vaccine (Canvaxin) or bacillus Calmette-Guérin and placebo. While this trial found no difference in overall survival between groups, it did report a 5-year overall survival exceeding 40% in both treatment arms, which highlighted that Stage IV patients who underwent resection of all their disease had survival outcomes superior to outcomes previously reported (Ann Surg Onc. 2017 Dec;24[13]:3991-4000). The second trial, the recent Checkmate 067 trial, emphasized the role of effective systemic checkpoint blockade in advanced stage III and IV melanoma. It reported that patients treated with combined nivolumab/ipilimumab therapy had not reached median overall survival at minimum 36 months of follow-up (N Engl J Med. 2017 Oct 5;377[14]:1345-56).
“We know that checkpoint inhibitor therapy has revolutionized the landscape of unresectable stage III and IV melanoma,” Dr. Bello said. However, despite encouraging trial readouts of overall survival, progression-free survival is a different story. “We know that the median progression-free survival even in our best combination therapy is 11.5 months, meaning that 50% of patients will go on to progress in a year and many will go on to surgical resection of their disease and do quite well,” she said.
Dr. Bello and her coauthors set out to describe outcomes of a “highly selective group” of patients who had surgical resection after checkpoint inhibitor therapy. “The majority of patients in our study had a cutaneous primary melanoma,” she said. Median age was 63 years, and 88% had stage IV disease. Regarding checkpoint blockade regimen, 62% received anti–CTLA-4, and 29% received combination anti–PD-1 and anti–CLTA-4 either sequentially or concomitantly prior to resection.
The median time from the start of immunotherapy to the first operation was 7 months. Forty-six percent had no further postoperative treatment after resection. In those, who did require further treatment, the majority received anti–PD-1 followed by targeted BRAF/MEK therapy, she said.
The analysis stratified patients into the following three categories based on radiological response to immunotherapy:
- Overall response to checkpoint blockade and the index lesion was either smaller since initiation of therapy or stabilized (12; 5.1%). Half of this group had a pathological complete response.
- Isolated site of progressive disease with residual stable disease elsewhere or as the only site of progressive disease (106; 44.7%).
- Multiple sites of progressive and palliative operations (119; 50.2%).
Median overall survival was 21 months in the entire study cohort with a median follow-up of 23 months, Dr. Bello said. “Those resected to no evidence of disease (NED) – 87 patients – had an estimated 5-year overall survival of 75%.” The NED group did not reach median OS.
The analysis also stratified overall survival by response to immunotherapy. “Patients with responding or stable disease had an estimated 90% 5-year overall survival,” Dr. Bellow said. “Those with one isolated progressive lesion that was resected had a 60% 5-year overall survival.” A more detailed analysis of the latter group found that those who had a resection to NED had an improved overall survival of 75% at 5 years. Resected patients who had residual remaining disease had a 30% 5-year overall survival.
“Further follow-up is needed to assess the durability and contributions of surgery, and further studies are underway to identify biomarkers associated with improved survival after immunotherapy and surgery,” Dr. Bello said.
SOURCE: Bello DM et al. SSO 2018, Abstract 5.
REPORTING FROM SSO 2018
Key clinical point: Surgery after immunotherapy can achieve good outcomes in advanced melanoma.
Major findings: Complete resection achieved an estimated 5-year overall survival of 75%.
Study details: Analysis of a cohort of 237 patients from a prospectively maintained institutional melanoma database who had surgery after immunotherapy for unresectable stage III and IV melanoma during 2003-2017.
Disclosures: Dr. Bello reported having no financial disclosures. Some coauthors reported financial relationships with various pharmaceutical companies.
Source: Bello DM et al. SSO 2018, Abstract 5.
Can cN0 and pCR limit axillary surgery in some breast cancer patients?
CHICAGO – Patients with clinically node-negative HER2-positive or triple-negative breast cancer (TNBC) who achieve a pathological complete response in the breast after neoadjuvant chemotherapy could benefit from clinical trials to evaluate the option of omitting axillary node surgery in this population, according to a retrospective analysis of more than 22,000 cases in the National Cancer Database reported at the Society of Surgical Oncology Annual Cancer Symposium.
Alison U. Barron, MD, breast surgery oncology fellow at Mayo, presented the results. “In patients with HER2+ breast cancer and TNBC who are clinically node negative (cN0) and achieve a breast pathological complete response, this data supports omitting axillary surgery in clinical trials assessing no surgery after neoadjuvant chemotherapy (NAC),” she said. “In patients who present with clinically positive node [cN1] disease with a breast pathological complete response, surgical staging of the axilla is still recommended.”
“Response rates to NAC have increased,” Dr. Barron said. She cited previous reports that showed response rates ranging from 9%-13% for anthracyclines to 19%-26% with the addition of taxanes, and to 60%-70% with the addition of trastuzumab and pertuzumab in HER2+ disease. “Furthermore, we know that tumor biology affects response rates, with TNBC and HER2+ disease having the highest rates of pathologic complete response,” she said.
“In the current era when we frequently operate on patients, we find no residual cancer in the tissue at the time of surgery,” Dr. Barron said. “The question arises as to whether we can limit surgery in patients with a pathological complete response.” While imaging has limited ability to reliably detect pCR with 100% specificity, she noted that recent trials have shown the potential of tumor-bed biopsy to identify pCR in patients after NAC (Ann Surg. Published online Oct. 23, 2017. doi: 10.1097/SLA.0000000000002573; JAMA Surg. 2017;152(7):665-70).
The National Cancer Database data the Mayo researchers analyzed yielded an overall breast pCR of 29%. “When broken down by tumor subtype, we saw significantly higher rates of breast pCR in patients with HER2+ disease (42%, n = 3,107) and TNBC (35%, n = 2,469), compared with patients with hormone-receptor positive (HR+)/HER2-negative disease (12%, n = 1,020),” she said.
When the analysis looked specifically at patients who were clinically node negative at presentation and had a pCR, the rates of positive lymph nodes at the time of surgery were 1.6% in HER2+ patients and 1.7% in TNBC disease, Dr. Barron said. “If there was residual disease in the breast, the nodal positivity rate was significantly higher, at 18% in HER2+ and 12% in TNBC,” she added. In those who were clinical N1, the breast pCR rates were similar – 41% in HER2+ and 35% in TNBC – but nodal positivity rates were significantly higher, at 13% and 14%, respectively.
The HR+/HER2- group had significantly lower rates of pCR: 12% in the cN0 and 13% in the cN1 subgroups. This subgroup also had higher nodal positivity rates – in the cN0 subgroup, 4% in those with a breast pCR and 34% in those with residual disease in the breast, and in the cN1 subgroup, 30% and 83%, respectively.
When the investigators looked at the extent of nodal burden in cN0 patients with breast pCR, they found the rate of N2 and N3 disease was near zero across all biologic subtypes. “In patients who were cN1 at presentation and achieved a breast pCR but had residual axillary disease, the majority had N1 disease with only 1.5%-4% having four or more positive lymph nodes,” Dr. Barron said.
In the discussion, session moderator Carla Fisher, MD, of Indiana University, Indianapolis, said, “While we might not be ready for prime time to not evaluate the lymph nodes of these patients, this study does speak to the importance of establishing N0 and N1 prior to NAC.” In reply to her question about how Mayo routinely evaluates node status prior to NAC, Dr. Barron noted that Mayo performs routine axillary ultrasound. However, the NCDB data does not specify what imaging was done. This is thought to vary across the centers in the NCDB, Dr. Barron said.
Noted Dr. Boughey, “The findings from this study provide data that can be used moving forward for planning future clinical trials.” She also said that these findings do not alter the current standard of care; that still calls for breast and nodal surgery after NAC. However, the ongoing NRG-BR005 phase II clinical trial is assessing the accuracy of tumor-bed biopsy in these situations (ClinicalTrials.gov Identifier: NCT03188393). “The results from that trial will help inform future trials evaluating eliminating breast surgery in patients with an excellent response to NAC,” Dr. Boughey said. “Those patients could also potentially avoid axillary surgery based on the data we have now.”
Dr. Barron and Dr. Boughey and coauthors reported having no financial disclosures.
SOURCE: Barron AU et al. Society of Surgical Oncology Annual Cancer Symposium, Abstract 48.
CHICAGO – Patients with clinically node-negative HER2-positive or triple-negative breast cancer (TNBC) who achieve a pathological complete response in the breast after neoadjuvant chemotherapy could benefit from clinical trials to evaluate the option of omitting axillary node surgery in this population, according to a retrospective analysis of more than 22,000 cases in the National Cancer Database reported at the Society of Surgical Oncology Annual Cancer Symposium.
Alison U. Barron, MD, breast surgery oncology fellow at Mayo, presented the results. “In patients with HER2+ breast cancer and TNBC who are clinically node negative (cN0) and achieve a breast pathological complete response, this data supports omitting axillary surgery in clinical trials assessing no surgery after neoadjuvant chemotherapy (NAC),” she said. “In patients who present with clinically positive node [cN1] disease with a breast pathological complete response, surgical staging of the axilla is still recommended.”
“Response rates to NAC have increased,” Dr. Barron said. She cited previous reports that showed response rates ranging from 9%-13% for anthracyclines to 19%-26% with the addition of taxanes, and to 60%-70% with the addition of trastuzumab and pertuzumab in HER2+ disease. “Furthermore, we know that tumor biology affects response rates, with TNBC and HER2+ disease having the highest rates of pathologic complete response,” she said.
“In the current era when we frequently operate on patients, we find no residual cancer in the tissue at the time of surgery,” Dr. Barron said. “The question arises as to whether we can limit surgery in patients with a pathological complete response.” While imaging has limited ability to reliably detect pCR with 100% specificity, she noted that recent trials have shown the potential of tumor-bed biopsy to identify pCR in patients after NAC (Ann Surg. Published online Oct. 23, 2017. doi: 10.1097/SLA.0000000000002573; JAMA Surg. 2017;152(7):665-70).
The National Cancer Database data the Mayo researchers analyzed yielded an overall breast pCR of 29%. “When broken down by tumor subtype, we saw significantly higher rates of breast pCR in patients with HER2+ disease (42%, n = 3,107) and TNBC (35%, n = 2,469), compared with patients with hormone-receptor positive (HR+)/HER2-negative disease (12%, n = 1,020),” she said.
When the analysis looked specifically at patients who were clinically node negative at presentation and had a pCR, the rates of positive lymph nodes at the time of surgery were 1.6% in HER2+ patients and 1.7% in TNBC disease, Dr. Barron said. “If there was residual disease in the breast, the nodal positivity rate was significantly higher, at 18% in HER2+ and 12% in TNBC,” she added. In those who were clinical N1, the breast pCR rates were similar – 41% in HER2+ and 35% in TNBC – but nodal positivity rates were significantly higher, at 13% and 14%, respectively.
The HR+/HER2- group had significantly lower rates of pCR: 12% in the cN0 and 13% in the cN1 subgroups. This subgroup also had higher nodal positivity rates – in the cN0 subgroup, 4% in those with a breast pCR and 34% in those with residual disease in the breast, and in the cN1 subgroup, 30% and 83%, respectively.
When the investigators looked at the extent of nodal burden in cN0 patients with breast pCR, they found the rate of N2 and N3 disease was near zero across all biologic subtypes. “In patients who were cN1 at presentation and achieved a breast pCR but had residual axillary disease, the majority had N1 disease with only 1.5%-4% having four or more positive lymph nodes,” Dr. Barron said.
In the discussion, session moderator Carla Fisher, MD, of Indiana University, Indianapolis, said, “While we might not be ready for prime time to not evaluate the lymph nodes of these patients, this study does speak to the importance of establishing N0 and N1 prior to NAC.” In reply to her question about how Mayo routinely evaluates node status prior to NAC, Dr. Barron noted that Mayo performs routine axillary ultrasound. However, the NCDB data does not specify what imaging was done. This is thought to vary across the centers in the NCDB, Dr. Barron said.
Noted Dr. Boughey, “The findings from this study provide data that can be used moving forward for planning future clinical trials.” She also said that these findings do not alter the current standard of care; that still calls for breast and nodal surgery after NAC. However, the ongoing NRG-BR005 phase II clinical trial is assessing the accuracy of tumor-bed biopsy in these situations (ClinicalTrials.gov Identifier: NCT03188393). “The results from that trial will help inform future trials evaluating eliminating breast surgery in patients with an excellent response to NAC,” Dr. Boughey said. “Those patients could also potentially avoid axillary surgery based on the data we have now.”
Dr. Barron and Dr. Boughey and coauthors reported having no financial disclosures.
SOURCE: Barron AU et al. Society of Surgical Oncology Annual Cancer Symposium, Abstract 48.
CHICAGO – Patients with clinically node-negative HER2-positive or triple-negative breast cancer (TNBC) who achieve a pathological complete response in the breast after neoadjuvant chemotherapy could benefit from clinical trials to evaluate the option of omitting axillary node surgery in this population, according to a retrospective analysis of more than 22,000 cases in the National Cancer Database reported at the Society of Surgical Oncology Annual Cancer Symposium.
Alison U. Barron, MD, breast surgery oncology fellow at Mayo, presented the results. “In patients with HER2+ breast cancer and TNBC who are clinically node negative (cN0) and achieve a breast pathological complete response, this data supports omitting axillary surgery in clinical trials assessing no surgery after neoadjuvant chemotherapy (NAC),” she said. “In patients who present with clinically positive node [cN1] disease with a breast pathological complete response, surgical staging of the axilla is still recommended.”
“Response rates to NAC have increased,” Dr. Barron said. She cited previous reports that showed response rates ranging from 9%-13% for anthracyclines to 19%-26% with the addition of taxanes, and to 60%-70% with the addition of trastuzumab and pertuzumab in HER2+ disease. “Furthermore, we know that tumor biology affects response rates, with TNBC and HER2+ disease having the highest rates of pathologic complete response,” she said.
“In the current era when we frequently operate on patients, we find no residual cancer in the tissue at the time of surgery,” Dr. Barron said. “The question arises as to whether we can limit surgery in patients with a pathological complete response.” While imaging has limited ability to reliably detect pCR with 100% specificity, she noted that recent trials have shown the potential of tumor-bed biopsy to identify pCR in patients after NAC (Ann Surg. Published online Oct. 23, 2017. doi: 10.1097/SLA.0000000000002573; JAMA Surg. 2017;152(7):665-70).
The National Cancer Database data the Mayo researchers analyzed yielded an overall breast pCR of 29%. “When broken down by tumor subtype, we saw significantly higher rates of breast pCR in patients with HER2+ disease (42%, n = 3,107) and TNBC (35%, n = 2,469), compared with patients with hormone-receptor positive (HR+)/HER2-negative disease (12%, n = 1,020),” she said.
When the analysis looked specifically at patients who were clinically node negative at presentation and had a pCR, the rates of positive lymph nodes at the time of surgery were 1.6% in HER2+ patients and 1.7% in TNBC disease, Dr. Barron said. “If there was residual disease in the breast, the nodal positivity rate was significantly higher, at 18% in HER2+ and 12% in TNBC,” she added. In those who were clinical N1, the breast pCR rates were similar – 41% in HER2+ and 35% in TNBC – but nodal positivity rates were significantly higher, at 13% and 14%, respectively.
The HR+/HER2- group had significantly lower rates of pCR: 12% in the cN0 and 13% in the cN1 subgroups. This subgroup also had higher nodal positivity rates – in the cN0 subgroup, 4% in those with a breast pCR and 34% in those with residual disease in the breast, and in the cN1 subgroup, 30% and 83%, respectively.
When the investigators looked at the extent of nodal burden in cN0 patients with breast pCR, they found the rate of N2 and N3 disease was near zero across all biologic subtypes. “In patients who were cN1 at presentation and achieved a breast pCR but had residual axillary disease, the majority had N1 disease with only 1.5%-4% having four or more positive lymph nodes,” Dr. Barron said.
In the discussion, session moderator Carla Fisher, MD, of Indiana University, Indianapolis, said, “While we might not be ready for prime time to not evaluate the lymph nodes of these patients, this study does speak to the importance of establishing N0 and N1 prior to NAC.” In reply to her question about how Mayo routinely evaluates node status prior to NAC, Dr. Barron noted that Mayo performs routine axillary ultrasound. However, the NCDB data does not specify what imaging was done. This is thought to vary across the centers in the NCDB, Dr. Barron said.
Noted Dr. Boughey, “The findings from this study provide data that can be used moving forward for planning future clinical trials.” She also said that these findings do not alter the current standard of care; that still calls for breast and nodal surgery after NAC. However, the ongoing NRG-BR005 phase II clinical trial is assessing the accuracy of tumor-bed biopsy in these situations (ClinicalTrials.gov Identifier: NCT03188393). “The results from that trial will help inform future trials evaluating eliminating breast surgery in patients with an excellent response to NAC,” Dr. Boughey said. “Those patients could also potentially avoid axillary surgery based on the data we have now.”
Dr. Barron and Dr. Boughey and coauthors reported having no financial disclosures.
SOURCE: Barron AU et al. Society of Surgical Oncology Annual Cancer Symposium, Abstract 48.
REPORTING FROM SSO 2018
Key clinical point: Neoadjuvant chemotherapy for certain breast cancers achieves low rates of nodal positivity.
Major finding: In clinically node-negative HER2+ and triple-negative disease, nodal positivity after NAC in patients that had breast pathological complete response was less than 2%.
Study details: Review of 22,695 patients in NCDB with clinical T1 or T2 disease from 2010 to 2014.
Disclosure: Dr. Barron and coauthors reported having no financial disclosures.
Source: Barron AU et al. Society of Surgical Oncology Annual Cancer Symposium, Abstract 48.
No increased complication risk with delaying resection for LARC
CHICAGO – Delaying surgery after neoadjuvant therapy for locally advanced rectal cancer for up to 12 weeks does not seem to impact complication rates compared to surgery at 8 weeks or earlier, findings that run counter to results from a major European clinical trial reported in 2016, investigators reported at the Society of Surgical Oncology Annual Cancer Symposium.
“There’s an increasing trend toward delayed surgery beyond eight to 12 weeks after neoadjuvant therapy (NT) for locally advanced rectal cancer (LARC),” said Campbell Roxburgh, FRCS, PhD, of the University of Glasgow in Scotland. “Although we saw an increase in all complications in patients who had surgery beyond 12 weeks, there were no increases in surgical site complications, grade 3-5 complications, or anastomotic leaks. Before 12 weeks we did not observe increases in any type of complication where surgery was performed prior to or after 8 weeks.”
The study involved 798 patients who had received NT for LARC from June 2009 to March 2014 at Memorial Sloan Kettering Cancer Center in New York. The vast majority – 76% (607) – had rectal resection within 16 weeks of completing NT. Among them, 52% (317) had surgery 5-8 weeks after NT, 38% (229) had surgery at 8-12 weeks post-NT, and 10% (61) had surgery 12-16 weeks after completing NT. Those who had surgery beyond 16 weeks mostly had it deferred because they were undergoing nonoperative management in the case of complete clinical response to treatment or had a comorbidity that prevented earlier surgery, Dr. Roxburgh said.
The complication rate was 42.3% among the patients who had surgery up to 16 weeks after NT, Dr. Roxburgh said. The most common complication was surgical site infection (SSI) in 16.6% (101), followed by a grade 3-5 complication in 10.5% (64) and anastomotic leak in 6.4% (39). Overall complication rates among the two groups that had surgery within 12 weeks were not statistically different from the overall complication rate, Dr. Roxburgh said: 42.5% (138) in the 5- to 8-week group; and 36.7% (84) in the 8- to 12-week group. The 12- to16-week group had a complication rate of 56% (34, P = .022).
Dr. Roxburgh noted that the idea of delaying surgery beyond 8 weeks after NT has been a subject of debate, and that these findings run counter to those reported in the GRECCAR-6 trial (J Clin Oncol. 2016;34:3773-80). That study compared groups that had surgery for rectal cancer at 7 and 11 weeks after neoadjuvant radiochemotherapy and found that those in the 11-week group had higher rates of complications.
Dr. Roxburgh also reported on an analysis of the 12- to 16-week subgroup that found the highest complication rates were among those who had low anterior resection (53% vs. 41% in the 5- to 8-week group and 31% in the 8- to 12-week population), and patients who had a poor treatment response (no T-downstaging, 66% vs. 44% and 33%, respectively). Age, pretreatment and posttreatment TNM stages, surgical approach (open or minimally invasive), and year of treatment did not factor in complication rates in the subgroup analysis, Dr. Roxburgh noted.
The univariate regression analysis determined a trend toward increased rates of all complications in the 12- to 16-week group (P = .081). But the multivariate analysis did not find timing of surgery to be an independent risk factor for all complications, Dr. Roxburgh said. “We believe other factors, including tumor location, the type of NT, operative approach, and treatment response, however, were more important on multivariate analysis,” he said. For example, open surgery had an odds ratio of 1.7 (P = .004).
During the discussion, Dr. Roxburgh was asked what would be the optimal timing for resection after NT in LARC. “I would recommend posttreatment assessment with MRI and proctoscopy between 8 to 12 weeks and in the case of residual tumor or incomplete response to treatment, scheduling surgery at that time,” he said.
Dr. Roxburgh and coauthors reported having no financial disclosures.
SOURCE: Roxburgh C, et al. Society of Surgical Oncology Annual Cancer Symposium Abstract No. 3.
CHICAGO – Delaying surgery after neoadjuvant therapy for locally advanced rectal cancer for up to 12 weeks does not seem to impact complication rates compared to surgery at 8 weeks or earlier, findings that run counter to results from a major European clinical trial reported in 2016, investigators reported at the Society of Surgical Oncology Annual Cancer Symposium.
“There’s an increasing trend toward delayed surgery beyond eight to 12 weeks after neoadjuvant therapy (NT) for locally advanced rectal cancer (LARC),” said Campbell Roxburgh, FRCS, PhD, of the University of Glasgow in Scotland. “Although we saw an increase in all complications in patients who had surgery beyond 12 weeks, there were no increases in surgical site complications, grade 3-5 complications, or anastomotic leaks. Before 12 weeks we did not observe increases in any type of complication where surgery was performed prior to or after 8 weeks.”
The study involved 798 patients who had received NT for LARC from June 2009 to March 2014 at Memorial Sloan Kettering Cancer Center in New York. The vast majority – 76% (607) – had rectal resection within 16 weeks of completing NT. Among them, 52% (317) had surgery 5-8 weeks after NT, 38% (229) had surgery at 8-12 weeks post-NT, and 10% (61) had surgery 12-16 weeks after completing NT. Those who had surgery beyond 16 weeks mostly had it deferred because they were undergoing nonoperative management in the case of complete clinical response to treatment or had a comorbidity that prevented earlier surgery, Dr. Roxburgh said.
The complication rate was 42.3% among the patients who had surgery up to 16 weeks after NT, Dr. Roxburgh said. The most common complication was surgical site infection (SSI) in 16.6% (101), followed by a grade 3-5 complication in 10.5% (64) and anastomotic leak in 6.4% (39). Overall complication rates among the two groups that had surgery within 12 weeks were not statistically different from the overall complication rate, Dr. Roxburgh said: 42.5% (138) in the 5- to 8-week group; and 36.7% (84) in the 8- to 12-week group. The 12- to16-week group had a complication rate of 56% (34, P = .022).
Dr. Roxburgh noted that the idea of delaying surgery beyond 8 weeks after NT has been a subject of debate, and that these findings run counter to those reported in the GRECCAR-6 trial (J Clin Oncol. 2016;34:3773-80). That study compared groups that had surgery for rectal cancer at 7 and 11 weeks after neoadjuvant radiochemotherapy and found that those in the 11-week group had higher rates of complications.
Dr. Roxburgh also reported on an analysis of the 12- to 16-week subgroup that found the highest complication rates were among those who had low anterior resection (53% vs. 41% in the 5- to 8-week group and 31% in the 8- to 12-week population), and patients who had a poor treatment response (no T-downstaging, 66% vs. 44% and 33%, respectively). Age, pretreatment and posttreatment TNM stages, surgical approach (open or minimally invasive), and year of treatment did not factor in complication rates in the subgroup analysis, Dr. Roxburgh noted.
The univariate regression analysis determined a trend toward increased rates of all complications in the 12- to 16-week group (P = .081). But the multivariate analysis did not find timing of surgery to be an independent risk factor for all complications, Dr. Roxburgh said. “We believe other factors, including tumor location, the type of NT, operative approach, and treatment response, however, were more important on multivariate analysis,” he said. For example, open surgery had an odds ratio of 1.7 (P = .004).
During the discussion, Dr. Roxburgh was asked what would be the optimal timing for resection after NT in LARC. “I would recommend posttreatment assessment with MRI and proctoscopy between 8 to 12 weeks and in the case of residual tumor or incomplete response to treatment, scheduling surgery at that time,” he said.
Dr. Roxburgh and coauthors reported having no financial disclosures.
SOURCE: Roxburgh C, et al. Society of Surgical Oncology Annual Cancer Symposium Abstract No. 3.
CHICAGO – Delaying surgery after neoadjuvant therapy for locally advanced rectal cancer for up to 12 weeks does not seem to impact complication rates compared to surgery at 8 weeks or earlier, findings that run counter to results from a major European clinical trial reported in 2016, investigators reported at the Society of Surgical Oncology Annual Cancer Symposium.
“There’s an increasing trend toward delayed surgery beyond eight to 12 weeks after neoadjuvant therapy (NT) for locally advanced rectal cancer (LARC),” said Campbell Roxburgh, FRCS, PhD, of the University of Glasgow in Scotland. “Although we saw an increase in all complications in patients who had surgery beyond 12 weeks, there were no increases in surgical site complications, grade 3-5 complications, or anastomotic leaks. Before 12 weeks we did not observe increases in any type of complication where surgery was performed prior to or after 8 weeks.”
The study involved 798 patients who had received NT for LARC from June 2009 to March 2014 at Memorial Sloan Kettering Cancer Center in New York. The vast majority – 76% (607) – had rectal resection within 16 weeks of completing NT. Among them, 52% (317) had surgery 5-8 weeks after NT, 38% (229) had surgery at 8-12 weeks post-NT, and 10% (61) had surgery 12-16 weeks after completing NT. Those who had surgery beyond 16 weeks mostly had it deferred because they were undergoing nonoperative management in the case of complete clinical response to treatment or had a comorbidity that prevented earlier surgery, Dr. Roxburgh said.
The complication rate was 42.3% among the patients who had surgery up to 16 weeks after NT, Dr. Roxburgh said. The most common complication was surgical site infection (SSI) in 16.6% (101), followed by a grade 3-5 complication in 10.5% (64) and anastomotic leak in 6.4% (39). Overall complication rates among the two groups that had surgery within 12 weeks were not statistically different from the overall complication rate, Dr. Roxburgh said: 42.5% (138) in the 5- to 8-week group; and 36.7% (84) in the 8- to 12-week group. The 12- to16-week group had a complication rate of 56% (34, P = .022).
Dr. Roxburgh noted that the idea of delaying surgery beyond 8 weeks after NT has been a subject of debate, and that these findings run counter to those reported in the GRECCAR-6 trial (J Clin Oncol. 2016;34:3773-80). That study compared groups that had surgery for rectal cancer at 7 and 11 weeks after neoadjuvant radiochemotherapy and found that those in the 11-week group had higher rates of complications.
Dr. Roxburgh also reported on an analysis of the 12- to 16-week subgroup that found the highest complication rates were among those who had low anterior resection (53% vs. 41% in the 5- to 8-week group and 31% in the 8- to 12-week population), and patients who had a poor treatment response (no T-downstaging, 66% vs. 44% and 33%, respectively). Age, pretreatment and posttreatment TNM stages, surgical approach (open or minimally invasive), and year of treatment did not factor in complication rates in the subgroup analysis, Dr. Roxburgh noted.
The univariate regression analysis determined a trend toward increased rates of all complications in the 12- to 16-week group (P = .081). But the multivariate analysis did not find timing of surgery to be an independent risk factor for all complications, Dr. Roxburgh said. “We believe other factors, including tumor location, the type of NT, operative approach, and treatment response, however, were more important on multivariate analysis,” he said. For example, open surgery had an odds ratio of 1.7 (P = .004).
During the discussion, Dr. Roxburgh was asked what would be the optimal timing for resection after NT in LARC. “I would recommend posttreatment assessment with MRI and proctoscopy between 8 to 12 weeks and in the case of residual tumor or incomplete response to treatment, scheduling surgery at that time,” he said.
Dr. Roxburgh and coauthors reported having no financial disclosures.
SOURCE: Roxburgh C, et al. Society of Surgical Oncology Annual Cancer Symposium Abstract No. 3.
REPORTING FROM SSO 2018
Key clinical point: Timing of surgery for rectal cancer within 12 weeks of neoadjuvant therapy does not influence complications.
Major finding: Complication rates in early and later surgery groups were 44% and 38%.
Study details: Institutional cohort of 607 patients who had rectal resection within 16 weeks of completing NT between June 2009 and March 2015.
Disclosure: Dr. Roxburgh and coauthors reported having no financial disclosures.
Source: Roxburgh C, et al. Society of Surgical Oncology Annual Cancer Symposium Abstract No. 3.
Accuracy of colon cancer lymph node sampling influenced by location
CHICAGO – Clinical guidelines recommend , but those guidelines may need to be revised to take into account which side the cancer is on to accurately stage a subset of patients with colon cancer, according to results of a prospective, multicenter clinical trial presented at the Society of Surgical Oncology Annual Cancer Symposium.
Ahmed Dehal, MD, of John Wayne Canter Institute in Santa Monica, Calif., presented results of the trial that compared nodal staging in right-sided vs. left-sided colon cancer in two cohorts with T3N0 colon cancer who had at least one lymph node examined: a group of 370 patients from the randomized, multicenter prospective trial; and a sampling of 153,945 patients in the National Cancer Database (NCDB). The latter was used to validate findings in the trial group.
The probability of achieving true nodal negativity when 12 lymph nodes were examined was 64% for left and 68% for right colon cancer in the trial group and 72% and 77% in the NCDB cohort, Dr. Dehal said.
The analysis also examined how many nodes would need to be sampled to achieve probabilities of 85%, 90% and 95% true nodal negativity. This analysis found the numbers were consistently lower for right- vs. left-sided disease, Dr. Dehal said. For example, in the trial cohort, 27 lymph nodes would need be sampled in right-sided disease to achieve 85% probability vs. 31 in left-sided. In the NCDB cohort, those numbers were 21 and 25, respectively.
“The current threshold for adequate nodal sampling does not reliably predict the true nodal negativity in this subgroup of patients,” Dr. Dehal said. “In both cohorts – the trial and NCDB – more lymph nodes are needed to predict the true nodal negativity in patients with left compared to right colon cancer.”
These findings may help to inform revisions to existing clinical guidelines, Dr. Dehal said.
“Current guidelines regarding the minimum number of nodes needed to accurately stage patients with node-negative T3 colon cancer may need to be reevaluated given that the decision to give those patients chemotherapy is largely based on the nodal status,” he said. “More studies are needed to improve our understanding of the impact of sidedness on nodal staging in the colon cancer.”
Dr. Dehal and his coauthors reported having no financial disclosures.
SOURCE: Dehal A et al. Society of Surgical Oncology Annual Cancer Symposium. Abstract #23: Accuracy of nodal staging is influenced by sidedness in colon cancer: Results of a multicenter prospective trial.
*CORRECTION, 4/4/2018; a previous version of this story misidentified the cancer type
CHICAGO – Clinical guidelines recommend , but those guidelines may need to be revised to take into account which side the cancer is on to accurately stage a subset of patients with colon cancer, according to results of a prospective, multicenter clinical trial presented at the Society of Surgical Oncology Annual Cancer Symposium.
Ahmed Dehal, MD, of John Wayne Canter Institute in Santa Monica, Calif., presented results of the trial that compared nodal staging in right-sided vs. left-sided colon cancer in two cohorts with T3N0 colon cancer who had at least one lymph node examined: a group of 370 patients from the randomized, multicenter prospective trial; and a sampling of 153,945 patients in the National Cancer Database (NCDB). The latter was used to validate findings in the trial group.
The probability of achieving true nodal negativity when 12 lymph nodes were examined was 64% for left and 68% for right colon cancer in the trial group and 72% and 77% in the NCDB cohort, Dr. Dehal said.
The analysis also examined how many nodes would need to be sampled to achieve probabilities of 85%, 90% and 95% true nodal negativity. This analysis found the numbers were consistently lower for right- vs. left-sided disease, Dr. Dehal said. For example, in the trial cohort, 27 lymph nodes would need be sampled in right-sided disease to achieve 85% probability vs. 31 in left-sided. In the NCDB cohort, those numbers were 21 and 25, respectively.
“The current threshold for adequate nodal sampling does not reliably predict the true nodal negativity in this subgroup of patients,” Dr. Dehal said. “In both cohorts – the trial and NCDB – more lymph nodes are needed to predict the true nodal negativity in patients with left compared to right colon cancer.”
These findings may help to inform revisions to existing clinical guidelines, Dr. Dehal said.
“Current guidelines regarding the minimum number of nodes needed to accurately stage patients with node-negative T3 colon cancer may need to be reevaluated given that the decision to give those patients chemotherapy is largely based on the nodal status,” he said. “More studies are needed to improve our understanding of the impact of sidedness on nodal staging in the colon cancer.”
Dr. Dehal and his coauthors reported having no financial disclosures.
SOURCE: Dehal A et al. Society of Surgical Oncology Annual Cancer Symposium. Abstract #23: Accuracy of nodal staging is influenced by sidedness in colon cancer: Results of a multicenter prospective trial.
*CORRECTION, 4/4/2018; a previous version of this story misidentified the cancer type
CHICAGO – Clinical guidelines recommend , but those guidelines may need to be revised to take into account which side the cancer is on to accurately stage a subset of patients with colon cancer, according to results of a prospective, multicenter clinical trial presented at the Society of Surgical Oncology Annual Cancer Symposium.
Ahmed Dehal, MD, of John Wayne Canter Institute in Santa Monica, Calif., presented results of the trial that compared nodal staging in right-sided vs. left-sided colon cancer in two cohorts with T3N0 colon cancer who had at least one lymph node examined: a group of 370 patients from the randomized, multicenter prospective trial; and a sampling of 153,945 patients in the National Cancer Database (NCDB). The latter was used to validate findings in the trial group.
The probability of achieving true nodal negativity when 12 lymph nodes were examined was 64% for left and 68% for right colon cancer in the trial group and 72% and 77% in the NCDB cohort, Dr. Dehal said.
The analysis also examined how many nodes would need to be sampled to achieve probabilities of 85%, 90% and 95% true nodal negativity. This analysis found the numbers were consistently lower for right- vs. left-sided disease, Dr. Dehal said. For example, in the trial cohort, 27 lymph nodes would need be sampled in right-sided disease to achieve 85% probability vs. 31 in left-sided. In the NCDB cohort, those numbers were 21 and 25, respectively.
“The current threshold for adequate nodal sampling does not reliably predict the true nodal negativity in this subgroup of patients,” Dr. Dehal said. “In both cohorts – the trial and NCDB – more lymph nodes are needed to predict the true nodal negativity in patients with left compared to right colon cancer.”
These findings may help to inform revisions to existing clinical guidelines, Dr. Dehal said.
“Current guidelines regarding the minimum number of nodes needed to accurately stage patients with node-negative T3 colon cancer may need to be reevaluated given that the decision to give those patients chemotherapy is largely based on the nodal status,” he said. “More studies are needed to improve our understanding of the impact of sidedness on nodal staging in the colon cancer.”
Dr. Dehal and his coauthors reported having no financial disclosures.
SOURCE: Dehal A et al. Society of Surgical Oncology Annual Cancer Symposium. Abstract #23: Accuracy of nodal staging is influenced by sidedness in colon cancer: Results of a multicenter prospective trial.
*CORRECTION, 4/4/2018; a previous version of this story misidentified the cancer type
REPORTING FROM SSO 2018
Key clinical point: Sidedness influences the number of lymph nodes needed to predict true nodal negativity in colon cancer.
Major finding: Probability of true nodal negativity when 12 lymph nodes were examined was 64% for left and 68% for right colon cancer.
Study details: Randomized, multicenter trial of ultrastaging in colon cancer in 370 patients and National Cancer Database sampling of 153,945 patients.
Disclosures: Dr. Dehal and his coauthors report having no financial disclosures.
Source: Dehal A et al. Society of Surgical Oncology Annual Cancer Symposium, Abstract 23: Accuracy of nodal staging is influenced by sidedness in colon cancer: Results of a multicenter prospective trial.
Think about breast cancer surveillance for transgender patients
CHICAGO – , said Christel de Blok, MD, sharing results of a Dutch national study.
The study included 3,078 transgender people (2,064 transgender women) who began hormone therapy (HT) at age 18 years or older. The mean age at which transgender women began HT was 33 years; for transgender men, the mean age was 25 years. In all, transgender women in the study had a total of 30,699 person-years of exposure to HT; for transgender men, the figure was 13,155 person-years.
Overall, there were 16 observed cases of breast cancer in transgender women and four in transgender men. After gender-affirming surgery, the transgender women were followed for a median of 146 months, and experienced a median of 193 months of HT. Transgender men who had mastectomies were followed for a median 93 months, and those who had a hysterectomy-oophorectomy were followed for a median 144 months. Transgender men received a median 176 months of HT.
“Breast cancer can still occur after mastectomy in [transgender] men,” Dr. de Blok said at the annual meeting of the Endocrine Society. “What is interesting is that three out of the four cases of breast cancer in [transgender] men happened after mastectomy.”
In the Netherlands, one in eight women and one in 1,000 men will develop cancer at some point during their lives. In patients who have had a subtotal mastectomy and who are BRCA-1/2 carriers, there is still an approximate 5% residual risk of breast cancer, said Dr. de Blok.
A literature review conducted by Dr. de Blok and her colleagues revealed 19 cases of breast cancer in transgender women and 13 in transgender men. However, a more general study of incidence and characteristics of breast cancer in transgender people receiving hormone treatment had not been done, said Dr. de Blok, of the VU University Medical Center, Amsterdam.
The investigators examined data for adult transgender people seen at their center from 1991 to 2017 and started on hormone treatment. This clinic, said Dr. de Blok, sees about 95% of the transgender individuals in the Netherlands.
The study was able to capitalize on comprehensive information from national databases and registries. Investigators drew from a national histopathology and cytopathology registry as well as from a national vital statistics database. A comprehensive cancer database was used to establish both reference incidence values for males and females and the number of expected cases within the study group.
In both transgender men and women, exactly 50% of cases were ductal carcinoma, compared to 85% in the group of reference women.
An additional 31% of the breast cancers in transgender women were lobular, 6% were ductal carcinoma in situ (DCIS), and the remainder were of other types. Of the cancers in transgender women, 82% were estrogen receptor positive, 64% were progesterone receptor positive, and 9% were Her2/neu positive.
For transgender men, there were no lobular carcinomas; 25% were DCIS, and 25% were of other types. Half of the cancers were estrogen receptor positive, and half were progesterone receptor positive; 25% were Her2/neu positive, and there was one case of androgen receptor positive breast cancer.
Dr. de Blok explained that their analysis compared the observed cases in both transgender men and women to the expected number of cases for the same number of males and females, yielding two standardized incidence ratios (SIRs) for each transgender group.
For transgender women, the SIR for breast cancer compared with males was 50.9 (95% confidence interval, 30.1-80.9). The SIR compared to females was 0.3 (95% CI, 0.2-0.4). This reflected the expected case number of 0.3 for males and the 58 expected cases for a matched group of females.
For transgender men, the SIR for breast cancer compared with males was 59.8 (95% CI, 19-144.3), while the SIR compared to females was 0.2 (95% CI, 0.1-0.5). The expected cases for a similar group of males would be 0.1, and for females, 18.
In many cases, whether a transgender person receives standardized screening mammogram reminders will depend on which sex is assigned to that individual in insurance and other administrative databases, Mr. de Blok noted. When electronic health records and other databases have a binary system, at-risk individuals may fall through the cracks.
Dr. de Blok reported no conflicts of interest.
SOURCE: de Blok C, et al. ENDO 2018, abstract OR 25-6.
CHICAGO – , said Christel de Blok, MD, sharing results of a Dutch national study.
The study included 3,078 transgender people (2,064 transgender women) who began hormone therapy (HT) at age 18 years or older. The mean age at which transgender women began HT was 33 years; for transgender men, the mean age was 25 years. In all, transgender women in the study had a total of 30,699 person-years of exposure to HT; for transgender men, the figure was 13,155 person-years.
Overall, there were 16 observed cases of breast cancer in transgender women and four in transgender men. After gender-affirming surgery, the transgender women were followed for a median of 146 months, and experienced a median of 193 months of HT. Transgender men who had mastectomies were followed for a median 93 months, and those who had a hysterectomy-oophorectomy were followed for a median 144 months. Transgender men received a median 176 months of HT.
“Breast cancer can still occur after mastectomy in [transgender] men,” Dr. de Blok said at the annual meeting of the Endocrine Society. “What is interesting is that three out of the four cases of breast cancer in [transgender] men happened after mastectomy.”
In the Netherlands, one in eight women and one in 1,000 men will develop cancer at some point during their lives. In patients who have had a subtotal mastectomy and who are BRCA-1/2 carriers, there is still an approximate 5% residual risk of breast cancer, said Dr. de Blok.
A literature review conducted by Dr. de Blok and her colleagues revealed 19 cases of breast cancer in transgender women and 13 in transgender men. However, a more general study of incidence and characteristics of breast cancer in transgender people receiving hormone treatment had not been done, said Dr. de Blok, of the VU University Medical Center, Amsterdam.
The investigators examined data for adult transgender people seen at their center from 1991 to 2017 and started on hormone treatment. This clinic, said Dr. de Blok, sees about 95% of the transgender individuals in the Netherlands.
The study was able to capitalize on comprehensive information from national databases and registries. Investigators drew from a national histopathology and cytopathology registry as well as from a national vital statistics database. A comprehensive cancer database was used to establish both reference incidence values for males and females and the number of expected cases within the study group.
In both transgender men and women, exactly 50% of cases were ductal carcinoma, compared to 85% in the group of reference women.
An additional 31% of the breast cancers in transgender women were lobular, 6% were ductal carcinoma in situ (DCIS), and the remainder were of other types. Of the cancers in transgender women, 82% were estrogen receptor positive, 64% were progesterone receptor positive, and 9% were Her2/neu positive.
For transgender men, there were no lobular carcinomas; 25% were DCIS, and 25% were of other types. Half of the cancers were estrogen receptor positive, and half were progesterone receptor positive; 25% were Her2/neu positive, and there was one case of androgen receptor positive breast cancer.
Dr. de Blok explained that their analysis compared the observed cases in both transgender men and women to the expected number of cases for the same number of males and females, yielding two standardized incidence ratios (SIRs) for each transgender group.
For transgender women, the SIR for breast cancer compared with males was 50.9 (95% confidence interval, 30.1-80.9). The SIR compared to females was 0.3 (95% CI, 0.2-0.4). This reflected the expected case number of 0.3 for males and the 58 expected cases for a matched group of females.
For transgender men, the SIR for breast cancer compared with males was 59.8 (95% CI, 19-144.3), while the SIR compared to females was 0.2 (95% CI, 0.1-0.5). The expected cases for a similar group of males would be 0.1, and for females, 18.
In many cases, whether a transgender person receives standardized screening mammogram reminders will depend on which sex is assigned to that individual in insurance and other administrative databases, Mr. de Blok noted. When electronic health records and other databases have a binary system, at-risk individuals may fall through the cracks.
Dr. de Blok reported no conflicts of interest.
SOURCE: de Blok C, et al. ENDO 2018, abstract OR 25-6.
CHICAGO – , said Christel de Blok, MD, sharing results of a Dutch national study.
The study included 3,078 transgender people (2,064 transgender women) who began hormone therapy (HT) at age 18 years or older. The mean age at which transgender women began HT was 33 years; for transgender men, the mean age was 25 years. In all, transgender women in the study had a total of 30,699 person-years of exposure to HT; for transgender men, the figure was 13,155 person-years.
Overall, there were 16 observed cases of breast cancer in transgender women and four in transgender men. After gender-affirming surgery, the transgender women were followed for a median of 146 months, and experienced a median of 193 months of HT. Transgender men who had mastectomies were followed for a median 93 months, and those who had a hysterectomy-oophorectomy were followed for a median 144 months. Transgender men received a median 176 months of HT.
“Breast cancer can still occur after mastectomy in [transgender] men,” Dr. de Blok said at the annual meeting of the Endocrine Society. “What is interesting is that three out of the four cases of breast cancer in [transgender] men happened after mastectomy.”
In the Netherlands, one in eight women and one in 1,000 men will develop cancer at some point during their lives. In patients who have had a subtotal mastectomy and who are BRCA-1/2 carriers, there is still an approximate 5% residual risk of breast cancer, said Dr. de Blok.
A literature review conducted by Dr. de Blok and her colleagues revealed 19 cases of breast cancer in transgender women and 13 in transgender men. However, a more general study of incidence and characteristics of breast cancer in transgender people receiving hormone treatment had not been done, said Dr. de Blok, of the VU University Medical Center, Amsterdam.
The investigators examined data for adult transgender people seen at their center from 1991 to 2017 and started on hormone treatment. This clinic, said Dr. de Blok, sees about 95% of the transgender individuals in the Netherlands.
The study was able to capitalize on comprehensive information from national databases and registries. Investigators drew from a national histopathology and cytopathology registry as well as from a national vital statistics database. A comprehensive cancer database was used to establish both reference incidence values for males and females and the number of expected cases within the study group.
In both transgender men and women, exactly 50% of cases were ductal carcinoma, compared to 85% in the group of reference women.
An additional 31% of the breast cancers in transgender women were lobular, 6% were ductal carcinoma in situ (DCIS), and the remainder were of other types. Of the cancers in transgender women, 82% were estrogen receptor positive, 64% were progesterone receptor positive, and 9% were Her2/neu positive.
For transgender men, there were no lobular carcinomas; 25% were DCIS, and 25% were of other types. Half of the cancers were estrogen receptor positive, and half were progesterone receptor positive; 25% were Her2/neu positive, and there was one case of androgen receptor positive breast cancer.
Dr. de Blok explained that their analysis compared the observed cases in both transgender men and women to the expected number of cases for the same number of males and females, yielding two standardized incidence ratios (SIRs) for each transgender group.
For transgender women, the SIR for breast cancer compared with males was 50.9 (95% confidence interval, 30.1-80.9). The SIR compared to females was 0.3 (95% CI, 0.2-0.4). This reflected the expected case number of 0.3 for males and the 58 expected cases for a matched group of females.
For transgender men, the SIR for breast cancer compared with males was 59.8 (95% CI, 19-144.3), while the SIR compared to females was 0.2 (95% CI, 0.1-0.5). The expected cases for a similar group of males would be 0.1, and for females, 18.
In many cases, whether a transgender person receives standardized screening mammogram reminders will depend on which sex is assigned to that individual in insurance and other administrative databases, Mr. de Blok noted. When electronic health records and other databases have a binary system, at-risk individuals may fall through the cracks.
Dr. de Blok reported no conflicts of interest.
SOURCE: de Blok C, et al. ENDO 2018, abstract OR 25-6.
REPORTING FROM ENDO 2018
Key clinical point: Transgender individuals had increased risk of breast cancer similar to a female reference population.
Major finding: Transgender men had a standardized incidence ratio of 59.8 compared to a male reference population.
Study details: Study of 3,078 transgender adults receiving hormone therapy.
Disclosures: Dr. de Blok reported no conflicts of interest.
Source: de Blok C, et al. ENDO 2018, abstract OR 25-6.
Breast cancer care delayed when patients have high deductibles
High-deductible health insurance plans may be bad for women’s health, suggest results of a new study.
An analysis of data on women without evidence of breast cancer who were covered for at least 1 year in a low annual deductible plan and then switched by their employers to high annual deductible plans showed that when women were forced to shell out substantially more money before their insurance kicked in, they were significantly more likely to have delays in diagnostic breast imaging, breast biopsy, and initiation of chemotherapy.
“Such delays might lead to adverse long-term breast cancer outcomes. Policymakers, health insurers, and employers should consider designing or incentivizing health insurance benefits that facilitate transitions through key steps along the cancer care pathway,” wrote J. Frank Wharam, MB, and colleagues at Harvard Medical School and Harvard Pilgrim Health Care Institute in Boston. The report was published in Journal of Clinical Oncology.
The investigators conducted a controlled pre-post study to measure the occurrence of outcomes both before and after women were switched from a low-deductible health plan, defined as a maximum annual deductible of $500 or less, to a high-deductible plan, defined as an annual deductible of $1,000 or more.
The study population comprised 273,499 women aged 25-64 years who had no evidence of breast cancer before they were included in the study. The women had all been enrolled in a low-deductible plan for at least 1 year, and were then switched by employer mandate to a high-deductible plan and followed for up to 4 additional years.
Controls included 2.4 million women matched by time of inclusion whose employers continued to offer only low-deductible health plans.
Although at baseline there were no differences between the study sample and the controls in time to first diagnostic breast imaging, breast biopsy, diagnosis of early stage breast cancer, or initiation of breast cancer chemotherapy, at follow-up the women who had been switched to the high-deductible plans had significant delays in all categories.
Compared with controls, the hazard ratios (HR) for each parameter were as follows:
Time to first diagnostic breast imaging: HR = 0.96 (95% confidence interval 0.94-0.96)
Time to first breast biopsy: HR = 0.92 (0.89-0.95)
Time to early stage breast cancer diagnosis: HR = 0.83 (0.78-0.90)
Time to breast cancer chemotherapy: HR = 0.79 (0.72-0.86)
“The findings imply that the high out-of-pocket obligations under HDHPs [high-deductible health plans] might be a barrier to timely receipt of essential breast cancer services. Women in HDHPs might either delay presenting for concerning symptoms or, if proceeding along the pathway from breast cancer screening to diagnostic testing to treatment, be hesitant to undergo subsequent (and generally more expensive) care,” the authors wrote.
They noted that initially modest delays in diagnostic imaging appeared to snowball into longer delays as women proceeded through stages of care.
They recommend a strategy whereby insurers carve out exemptions to high deductibles for services such as diagnostic imaging and breast biopsy.
SOURCE: Wharam et al. J Clin Oncol. 2018 Feb 28. doi: 10.1200/JCO.2017.75.2501.
High-deductible health insurance plans may be bad for women’s health, suggest results of a new study.
An analysis of data on women without evidence of breast cancer who were covered for at least 1 year in a low annual deductible plan and then switched by their employers to high annual deductible plans showed that when women were forced to shell out substantially more money before their insurance kicked in, they were significantly more likely to have delays in diagnostic breast imaging, breast biopsy, and initiation of chemotherapy.
“Such delays might lead to adverse long-term breast cancer outcomes. Policymakers, health insurers, and employers should consider designing or incentivizing health insurance benefits that facilitate transitions through key steps along the cancer care pathway,” wrote J. Frank Wharam, MB, and colleagues at Harvard Medical School and Harvard Pilgrim Health Care Institute in Boston. The report was published in Journal of Clinical Oncology.
The investigators conducted a controlled pre-post study to measure the occurrence of outcomes both before and after women were switched from a low-deductible health plan, defined as a maximum annual deductible of $500 or less, to a high-deductible plan, defined as an annual deductible of $1,000 or more.
The study population comprised 273,499 women aged 25-64 years who had no evidence of breast cancer before they were included in the study. The women had all been enrolled in a low-deductible plan for at least 1 year, and were then switched by employer mandate to a high-deductible plan and followed for up to 4 additional years.
Controls included 2.4 million women matched by time of inclusion whose employers continued to offer only low-deductible health plans.
Although at baseline there were no differences between the study sample and the controls in time to first diagnostic breast imaging, breast biopsy, diagnosis of early stage breast cancer, or initiation of breast cancer chemotherapy, at follow-up the women who had been switched to the high-deductible plans had significant delays in all categories.
Compared with controls, the hazard ratios (HR) for each parameter were as follows:
Time to first diagnostic breast imaging: HR = 0.96 (95% confidence interval 0.94-0.96)
Time to first breast biopsy: HR = 0.92 (0.89-0.95)
Time to early stage breast cancer diagnosis: HR = 0.83 (0.78-0.90)
Time to breast cancer chemotherapy: HR = 0.79 (0.72-0.86)
“The findings imply that the high out-of-pocket obligations under HDHPs [high-deductible health plans] might be a barrier to timely receipt of essential breast cancer services. Women in HDHPs might either delay presenting for concerning symptoms or, if proceeding along the pathway from breast cancer screening to diagnostic testing to treatment, be hesitant to undergo subsequent (and generally more expensive) care,” the authors wrote.
They noted that initially modest delays in diagnostic imaging appeared to snowball into longer delays as women proceeded through stages of care.
They recommend a strategy whereby insurers carve out exemptions to high deductibles for services such as diagnostic imaging and breast biopsy.
SOURCE: Wharam et al. J Clin Oncol. 2018 Feb 28. doi: 10.1200/JCO.2017.75.2501.
High-deductible health insurance plans may be bad for women’s health, suggest results of a new study.
An analysis of data on women without evidence of breast cancer who were covered for at least 1 year in a low annual deductible plan and then switched by their employers to high annual deductible plans showed that when women were forced to shell out substantially more money before their insurance kicked in, they were significantly more likely to have delays in diagnostic breast imaging, breast biopsy, and initiation of chemotherapy.
“Such delays might lead to adverse long-term breast cancer outcomes. Policymakers, health insurers, and employers should consider designing or incentivizing health insurance benefits that facilitate transitions through key steps along the cancer care pathway,” wrote J. Frank Wharam, MB, and colleagues at Harvard Medical School and Harvard Pilgrim Health Care Institute in Boston. The report was published in Journal of Clinical Oncology.
The investigators conducted a controlled pre-post study to measure the occurrence of outcomes both before and after women were switched from a low-deductible health plan, defined as a maximum annual deductible of $500 or less, to a high-deductible plan, defined as an annual deductible of $1,000 or more.
The study population comprised 273,499 women aged 25-64 years who had no evidence of breast cancer before they were included in the study. The women had all been enrolled in a low-deductible plan for at least 1 year, and were then switched by employer mandate to a high-deductible plan and followed for up to 4 additional years.
Controls included 2.4 million women matched by time of inclusion whose employers continued to offer only low-deductible health plans.
Although at baseline there were no differences between the study sample and the controls in time to first diagnostic breast imaging, breast biopsy, diagnosis of early stage breast cancer, or initiation of breast cancer chemotherapy, at follow-up the women who had been switched to the high-deductible plans had significant delays in all categories.
Compared with controls, the hazard ratios (HR) for each parameter were as follows:
Time to first diagnostic breast imaging: HR = 0.96 (95% confidence interval 0.94-0.96)
Time to first breast biopsy: HR = 0.92 (0.89-0.95)
Time to early stage breast cancer diagnosis: HR = 0.83 (0.78-0.90)
Time to breast cancer chemotherapy: HR = 0.79 (0.72-0.86)
“The findings imply that the high out-of-pocket obligations under HDHPs [high-deductible health plans] might be a barrier to timely receipt of essential breast cancer services. Women in HDHPs might either delay presenting for concerning symptoms or, if proceeding along the pathway from breast cancer screening to diagnostic testing to treatment, be hesitant to undergo subsequent (and generally more expensive) care,” the authors wrote.
They noted that initially modest delays in diagnostic imaging appeared to snowball into longer delays as women proceeded through stages of care.
They recommend a strategy whereby insurers carve out exemptions to high deductibles for services such as diagnostic imaging and breast biopsy.
SOURCE: Wharam et al. J Clin Oncol. 2018 Feb 28. doi: 10.1200/JCO.2017.75.2501.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Many women have high-deductible health plans that may discourage them from seeking essential care when needed.
Major finding: Women with an employer-mandated switch from a low- to high-deductible health plan had significant delays in diagnostic imaging, biopsy, diagnosis, and cancer care.
Study details: Controlled pre-post study of data on 273,499 women and 2.4 million controls.
Disclosures: The study was supported by National Cancer Institute and National Institute of Health grants. Dr. Wharam and three coauthors reported no conflicts of interest. Three coauthors reported honoraria and/or consulting/advisory roles with various companies.
Source: Wharam et al. J Clin Oncol. 2018 Feb 28. doi: 10.1200/JCO.2017.75.2501.
VIDEO: Model supports endoscopic resection for some T1b esophageal adenocarcinomas
Endoscopic treatment of T1a esophageal adenocarcinoma outperformed esophagectomy across a range of ages and comorbidity levels in a Markov model.
Esophagectomy produced 0.16 more unadjusted life-years, but led to 0.27 fewer quality-adjusted life-years (QALYs), in the hypothetical case of a 75-year-old man with T1aN0M0 esophageal adenocarcinoma (EAC) and a Charlson comorbidity index score of 0, reported Jacqueline N. Chu, MD, of Massachusetts General Hospital, Boston, and her associates. “[We] believe QALYs are a more important endpoint because of the significant morbidity associated with esophagectomy,” they wrote in the March issue of Clinical Gastroenterology and Hepatology.
Source: American Gastroenterological Association
In contrast, the model portrayed the management of T1b EAC as “an individualized decision” – esophagectomy was preferable in 60- to 70-year-old patients with T1b EAC, but serial endoscopic treatment was better when patients were older, with more comorbidities, the researchers said. “For the sickest patients, those aged 80 and older with comorbidity index of 2, endoscopic treatment not only provided more QALYs but more unadjusted life years as well.”
Treatment of T1a EAC is transitioning from esophagectomy to serial endoscopic resection, which physicians still tend to regard as too risky in T1b EAC. The Markov model evaluated the efficacy and cost efficacy of the two approaches in hypothetical T1a and T1b patients of various ages and comorbidities, using cancer death data from the Surveillance, Epidemiology, and End Results (SEER) Medicare database and published cost data converted to 2017 U.S. dollars based on the U.S. Bureau of Labor Statistics’ Consumer Price Index.
Like the T1a case, the T1b base case consisted of a 75-year-old man with a Charlson comorbidity index of 0. Esophagectomy produced 0.72 more unadjusted life years than did endoscopic treatment (5.73 vs. 5.01) while yielding 0.22 more QALYs (4.07 vs. 3.85, respectively). Esophagectomy cost $156,981 more, but the model did not account for costs of chemotherapy and radiation or palliative care, all of which are more likely with endoscopic resection than esophagectomy, the researchers noted.
In sensitivity analyses, endoscopic treatment optimized quality of life in T1b EAC patients who were older than 80 years and had a comorbidity index of 1 or 2. Beyond that, treatment choice depended on posttreatment variables. “[If] a patient considered his or her quality of life postesophagectomy nearly equal to, or preferable to, [that] postendoscopic treatment, esophagectomy would be the optimal treatment strategy,” the investigators wrote. “An example would be the patient who would rather have an esophagectomy than worry about recurrence with endoscopic treatment.”
Pathologic analysis of T1a EACs can be inconsistent, and the model did not test whether high versus low pathologic risk affected treatment preference, the researchers said. They added data on T1NOS (T1 not otherwise specified) EACs to the model because the SEER-Medicare database included so few T1b endoscopic cases, but T1NOS patients had the worst outcomes and were in fact probably higher stage than T1. Fully 31% of endoscopy patients were T1NOS, compared with only 11% of esophagectomy patients, which would have biased the model against endoscopic treatment, according to the investigators.
The National Institutes of Health provided funding. Dr. Chu reported having no conflicts of interest. Three coinvestigators disclosed ties to CSA Medical, Ninepoint, C2 Therapeutics, Medtronic, and Trio Medicines. The remaining coinvestigators had no conflicts.
SOURCE: Chu JN et al. Clin Gastroenterol Hepatol. 2017 Nov 24. doi: 10.1016/j.cgh.2017.10.024.
Endoscopic treatment of T1a esophageal adenocarcinoma outperformed esophagectomy across a range of ages and comorbidity levels in a Markov model.
Esophagectomy produced 0.16 more unadjusted life-years, but led to 0.27 fewer quality-adjusted life-years (QALYs), in the hypothetical case of a 75-year-old man with T1aN0M0 esophageal adenocarcinoma (EAC) and a Charlson comorbidity index score of 0, reported Jacqueline N. Chu, MD, of Massachusetts General Hospital, Boston, and her associates. “[We] believe QALYs are a more important endpoint because of the significant morbidity associated with esophagectomy,” they wrote in the March issue of Clinical Gastroenterology and Hepatology.
Source: American Gastroenterological Association
In contrast, the model portrayed the management of T1b EAC as “an individualized decision” – esophagectomy was preferable in 60- to 70-year-old patients with T1b EAC, but serial endoscopic treatment was better when patients were older, with more comorbidities, the researchers said. “For the sickest patients, those aged 80 and older with comorbidity index of 2, endoscopic treatment not only provided more QALYs but more unadjusted life years as well.”
Treatment of T1a EAC is transitioning from esophagectomy to serial endoscopic resection, which physicians still tend to regard as too risky in T1b EAC. The Markov model evaluated the efficacy and cost efficacy of the two approaches in hypothetical T1a and T1b patients of various ages and comorbidities, using cancer death data from the Surveillance, Epidemiology, and End Results (SEER) Medicare database and published cost data converted to 2017 U.S. dollars based on the U.S. Bureau of Labor Statistics’ Consumer Price Index.
Like the T1a case, the T1b base case consisted of a 75-year-old man with a Charlson comorbidity index of 0. Esophagectomy produced 0.72 more unadjusted life years than did endoscopic treatment (5.73 vs. 5.01) while yielding 0.22 more QALYs (4.07 vs. 3.85, respectively). Esophagectomy cost $156,981 more, but the model did not account for costs of chemotherapy and radiation or palliative care, all of which are more likely with endoscopic resection than esophagectomy, the researchers noted.
In sensitivity analyses, endoscopic treatment optimized quality of life in T1b EAC patients who were older than 80 years and had a comorbidity index of 1 or 2. Beyond that, treatment choice depended on posttreatment variables. “[If] a patient considered his or her quality of life postesophagectomy nearly equal to, or preferable to, [that] postendoscopic treatment, esophagectomy would be the optimal treatment strategy,” the investigators wrote. “An example would be the patient who would rather have an esophagectomy than worry about recurrence with endoscopic treatment.”
Pathologic analysis of T1a EACs can be inconsistent, and the model did not test whether high versus low pathologic risk affected treatment preference, the researchers said. They added data on T1NOS (T1 not otherwise specified) EACs to the model because the SEER-Medicare database included so few T1b endoscopic cases, but T1NOS patients had the worst outcomes and were in fact probably higher stage than T1. Fully 31% of endoscopy patients were T1NOS, compared with only 11% of esophagectomy patients, which would have biased the model against endoscopic treatment, according to the investigators.
The National Institutes of Health provided funding. Dr. Chu reported having no conflicts of interest. Three coinvestigators disclosed ties to CSA Medical, Ninepoint, C2 Therapeutics, Medtronic, and Trio Medicines. The remaining coinvestigators had no conflicts.
SOURCE: Chu JN et al. Clin Gastroenterol Hepatol. 2017 Nov 24. doi: 10.1016/j.cgh.2017.10.024.
Endoscopic treatment of T1a esophageal adenocarcinoma outperformed esophagectomy across a range of ages and comorbidity levels in a Markov model.
Esophagectomy produced 0.16 more unadjusted life-years, but led to 0.27 fewer quality-adjusted life-years (QALYs), in the hypothetical case of a 75-year-old man with T1aN0M0 esophageal adenocarcinoma (EAC) and a Charlson comorbidity index score of 0, reported Jacqueline N. Chu, MD, of Massachusetts General Hospital, Boston, and her associates. “[We] believe QALYs are a more important endpoint because of the significant morbidity associated with esophagectomy,” they wrote in the March issue of Clinical Gastroenterology and Hepatology.
Source: American Gastroenterological Association
In contrast, the model portrayed the management of T1b EAC as “an individualized decision” – esophagectomy was preferable in 60- to 70-year-old patients with T1b EAC, but serial endoscopic treatment was better when patients were older, with more comorbidities, the researchers said. “For the sickest patients, those aged 80 and older with comorbidity index of 2, endoscopic treatment not only provided more QALYs but more unadjusted life years as well.”
Treatment of T1a EAC is transitioning from esophagectomy to serial endoscopic resection, which physicians still tend to regard as too risky in T1b EAC. The Markov model evaluated the efficacy and cost efficacy of the two approaches in hypothetical T1a and T1b patients of various ages and comorbidities, using cancer death data from the Surveillance, Epidemiology, and End Results (SEER) Medicare database and published cost data converted to 2017 U.S. dollars based on the U.S. Bureau of Labor Statistics’ Consumer Price Index.
Like the T1a case, the T1b base case consisted of a 75-year-old man with a Charlson comorbidity index of 0. Esophagectomy produced 0.72 more unadjusted life years than did endoscopic treatment (5.73 vs. 5.01) while yielding 0.22 more QALYs (4.07 vs. 3.85, respectively). Esophagectomy cost $156,981 more, but the model did not account for costs of chemotherapy and radiation or palliative care, all of which are more likely with endoscopic resection than esophagectomy, the researchers noted.
In sensitivity analyses, endoscopic treatment optimized quality of life in T1b EAC patients who were older than 80 years and had a comorbidity index of 1 or 2. Beyond that, treatment choice depended on posttreatment variables. “[If] a patient considered his or her quality of life postesophagectomy nearly equal to, or preferable to, [that] postendoscopic treatment, esophagectomy would be the optimal treatment strategy,” the investigators wrote. “An example would be the patient who would rather have an esophagectomy than worry about recurrence with endoscopic treatment.”
Pathologic analysis of T1a EACs can be inconsistent, and the model did not test whether high versus low pathologic risk affected treatment preference, the researchers said. They added data on T1NOS (T1 not otherwise specified) EACs to the model because the SEER-Medicare database included so few T1b endoscopic cases, but T1NOS patients had the worst outcomes and were in fact probably higher stage than T1. Fully 31% of endoscopy patients were T1NOS, compared with only 11% of esophagectomy patients, which would have biased the model against endoscopic treatment, according to the investigators.
The National Institutes of Health provided funding. Dr. Chu reported having no conflicts of interest. Three coinvestigators disclosed ties to CSA Medical, Ninepoint, C2 Therapeutics, Medtronic, and Trio Medicines. The remaining coinvestigators had no conflicts.
SOURCE: Chu JN et al. Clin Gastroenterol Hepatol. 2017 Nov 24. doi: 10.1016/j.cgh.2017.10.024.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: A Markov model supports endoscopic resection for some T1b esophageal adenocarcinomas.
Major finding: Endoscopic resection was preferred in T1b patients who were more than 80 years old or had a Charlson comorbidity index of 1or 2.
Data source: A Markov model with Surveillance, Epidemiology, and End Results (SEER) Medicare mortality data and published cost data converted to 2017 U.S. dollars based on the national Consumer Price Index.
Disclosures: The National Institutes of Health provided funding. Dr. Chu reported having no conflicts of interest. Three coinvestigators disclosed ties to CSA Medical, Ninepoint, C2 Therapeutics, Medtronic, and Trio Medicines. The remaining coinvestigators had no conflicts.
Source: Chu JN et al. Clin Gastroenterol Hepatol .2017 Nov 24. doi: 10.1016/j.cgh.2017.10.024.
Liver cancer deaths expected to increase again in 2018
Liver cancer mortality for 2018 is expected to be lowest in Utah and highest in Hawaii.
A total of 30,200 deaths from liver and intrahepatic bile duct cancer are predicted for the year in the United States by the American Cancer Society (ACS) in its Cancer Facts & Figures 2018, based on analysis of 2001-2015 data from the National Center for Health Statistics. That’s up from the 28,920 predicted by the ACS for 2017.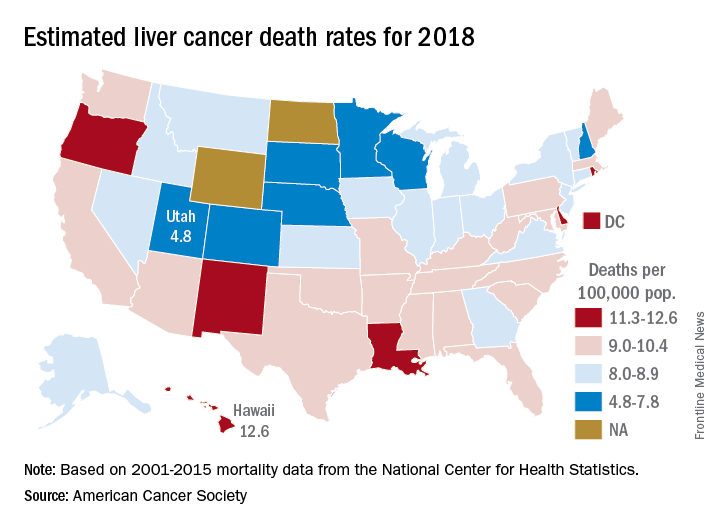
Mortality from liver cancer has been rising since the early 1980s, and in the last 10 years for which data are available (2006-2015), it increased by 2.5% per year. Over almost the same period (2005-2014), incidence rose by approximately 3% a year, and 42,220 new cases are expected in 2018, the ACS noted.
Over the most recent 5 years with available data (2011-2015), racial and ethnic disparities put American Indian/Alaska Natives at the highest mortality risk – 14.8 per 100,000 for men and 7.0 for women – followed by Asian/Pacific Islanders at 14.0 and 6.0, respectively. Non-Hispanic whites had the lowest rates: 8.2 for men and 3.4 for women, according to the ACS report.
Read more about the ACS’s research and estimates here.
Liver cancer mortality for 2018 is expected to be lowest in Utah and highest in Hawaii.
A total of 30,200 deaths from liver and intrahepatic bile duct cancer are predicted for the year in the United States by the American Cancer Society (ACS) in its Cancer Facts & Figures 2018, based on analysis of 2001-2015 data from the National Center for Health Statistics. That’s up from the 28,920 predicted by the ACS for 2017.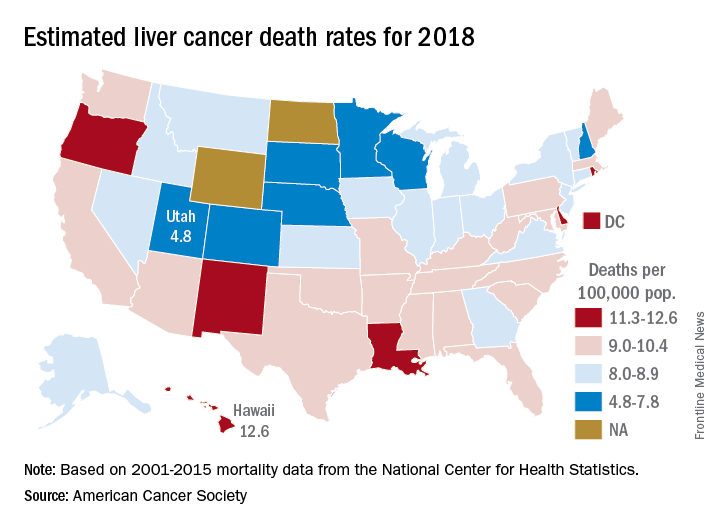
Mortality from liver cancer has been rising since the early 1980s, and in the last 10 years for which data are available (2006-2015), it increased by 2.5% per year. Over almost the same period (2005-2014), incidence rose by approximately 3% a year, and 42,220 new cases are expected in 2018, the ACS noted.
Over the most recent 5 years with available data (2011-2015), racial and ethnic disparities put American Indian/Alaska Natives at the highest mortality risk – 14.8 per 100,000 for men and 7.0 for women – followed by Asian/Pacific Islanders at 14.0 and 6.0, respectively. Non-Hispanic whites had the lowest rates: 8.2 for men and 3.4 for women, according to the ACS report.
Read more about the ACS’s research and estimates here.
Liver cancer mortality for 2018 is expected to be lowest in Utah and highest in Hawaii.
A total of 30,200 deaths from liver and intrahepatic bile duct cancer are predicted for the year in the United States by the American Cancer Society (ACS) in its Cancer Facts & Figures 2018, based on analysis of 2001-2015 data from the National Center for Health Statistics. That’s up from the 28,920 predicted by the ACS for 2017.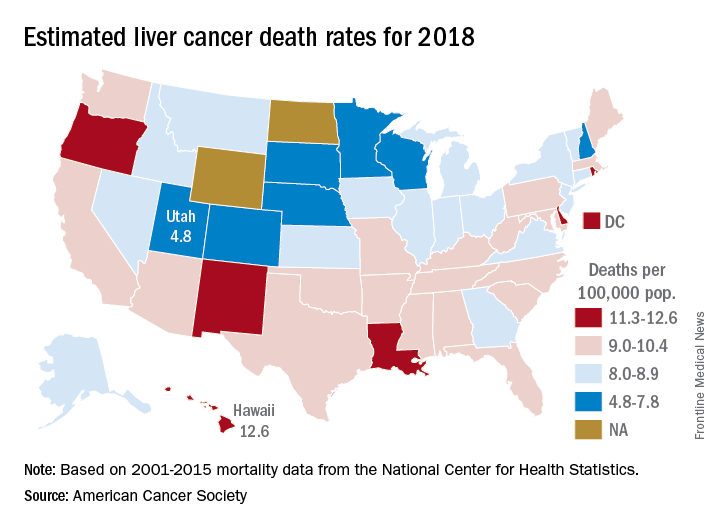
Mortality from liver cancer has been rising since the early 1980s, and in the last 10 years for which data are available (2006-2015), it increased by 2.5% per year. Over almost the same period (2005-2014), incidence rose by approximately 3% a year, and 42,220 new cases are expected in 2018, the ACS noted.
Over the most recent 5 years with available data (2011-2015), racial and ethnic disparities put American Indian/Alaska Natives at the highest mortality risk – 14.8 per 100,000 for men and 7.0 for women – followed by Asian/Pacific Islanders at 14.0 and 6.0, respectively. Non-Hispanic whites had the lowest rates: 8.2 for men and 3.4 for women, according to the ACS report.
Read more about the ACS’s research and estimates here.
ROBOT trial compares surgical approaches to esophagectomy
SAN FRANCISCO – Patients undergoing had less morbidity and pain and similarly good oncologic outcomes, when the surgery was performed by robot-assisted laparoscopy instead of by the open technique, a phase 3 clinical trial has found.
Investigators of the ROBOT (Robot-assisted Thoracolaparoscopic Esophagectomy vs. Open Transthoracic Esophagectomy) trial, led by Pieter C. van der Sluis, MD, a surgeon at the University Medical Center Utrecht, the Netherlands, randomized 112 patients with resectable esophageal cancer to open transthoracic esophagectomy – considered to be the gold standard – or robot-assisted minimally invasive thoracolaparoscopic esophagectomy.
“Robot-assisted minimally invasive thoracolaparoscopic esophagectomy versus open transthoracic esophagectomy improves postoperative outcome. There were no differences in oncologic outcomes, and our oncologic outcomes were in concordance with the highest standards nowadays,” Dr. van der Sluis summarized. “This trial provides evidence for the minimally invasive approach over the open approach, and especially the robot-assisted minimally invasive esophagectomy.”
The investigators will report a full cost comparison separately. “We see that costs are lower, though not significantly lower, with the robot,” he said, giving a preview. “We are going to show that the real costs of the operation are in the complications. When you have complications that involve the ICU and reoperations, some patients are in the hospital for months after the surgery. So by investing a little extra money in the surgical procedure, you might actually get it back by reducing the complications.”
When asked by an attendee why the trial did not compare robotic esophagectomy with thoracoscopic esophagectomy, Dr. van der Sluis noted that such comparison is complicated by many factors; for example, the challenge of finding surgeons skilled in both techniques, and the likelihood of small differences in outcomes, potentially requiring enrollment of thousands of patients to have adequate study power. “We concluded that such a trial might not be feasible,” he said.
Parsing the findings
“The complication rates [in this trial] are very high in the robotic and open groups, much higher than reported in some well-controlled prospective and retrospective studies,” commented session attendee Kenneth Meredith, MD, FACS, professor at Florida State University, Sarasota, and director of gastrointestinal oncology, Sarasota Memorial Institute for Cancer Care.
He wondered how extensive the investigators’ experience with robotics was and how many cases they had done on their learning curve. Data from his group suggest that surgeons must perform 29 cases of robotic esophagectomy before the complication rate drops (Dis Esophagus. 2017;30:1-7).
“That’s more then half of the patients in the robotic arm of their study,” he noted in an interview. “I find this needs to be explained. If the authors are past their learning curve, why were the complication rates so high?” Additionally, the 80% rate in the open group “is among the highest I’ve seen in many years.”
The lack of significant differences in complete resection rate and in lymph node harvest was also surprising, as he and other robotics users have found that this technique can improve these outcomes, Dr. Meredith added. This could likewise be a learning curve phenomenon.
Although ROBOT’s comparison of robotic with open esophagectomy is relevant, “it would have been more relevant to compare robotic to minimally invasive esophagectomy [MIE],” he maintained, as MIE has been shown to improve outcomes relative to open surgery (Lancet. 2012;379:1887-92).
“There are many high-volume centers in MIE but not necessarily robotics. The two are often mutually exclusive, and a multicenter trial in which each center performs high volumes of their respective technique, rather then mandating each center perform an operation they may not be facile in,” would be practical, Dr. Meredith concluded.
Study details
“The main objective in our trial was to reduce surgical trauma and reduce the percentage of complications,” Dr. van der Sluis told attendees of the symposium, sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Results showed that compared with peers in the open surgery group, patients in the robotic-assisted surgery group specifically had a lower rate of pulmonary complications (32% vs. 58%, P = .005), largely due to a reduction in rate of pneumonia (28% vs. 55%, P = .005), and a lower rate of cardiac complications (22% vs. 47%, P = .006), almost entirely due to a reduction in rate of atrial fibrillation (22% vs. 46%, P = .01).
There was a trend toward fewer wound infections with robotics (4% vs. 14%, P = .09), with a large difference in thoracic wound infections (0% vs. 9%, P = .06).
The two groups were statistically indistinguishable on rates of anastomotic leakage (24% and 20%) and recurrent laryngeal nerve injury (9% and 11%). The fairly high rate of anastomotic leakage was likely due to the center’s use of cervical anastomosis at the time of the trial, according to Dr. van der Sluis; they have since started using thoracic anastomosis, and will report results with that technique soon.
There was also no significant difference between groups in the rate of in-hospital mortality (4% with robotic surgery and 2% with open surgery), median hospital length of stay (14 and 16 days), and ICU length of stay (1 day in each group).
Patients in the robotics group more commonly had functional recovery within 2 weeks (70% vs. 51%, P = .04). And on the Quality of Life Questionnaire Core 30, they had better scores for health-related quality of life at discharge (57.9 vs 44.6, P = .02) and at 6 weeks (68.7 vs. 57.6, P = .03), and for physical functioning at discharge (54.5 vs. 41.0, P = .03) and 6 weeks (69.3 vs. 58.6, P = .049).
The two groups were similar on rates of R0 resection (93% and 96%) and median number of lymph nodes retrieved (27 and 25), reported Dr. van der Sluis. Pain during the first 14 days after surgery was lower for the robotics group (P = .003).
With a median follow-up of 40 months, the robotics and open groups did not differ significantly on disease-free survival (median, 26 and 28 months) and overall survival (not reached in either group).
Dr. van der Sluis disclosed no relevant conflicts of interest.
SOURCE: van der Sluis PC et al. 2018 GI Cancer Symposium, Abstract 156148
SAN FRANCISCO – Patients undergoing had less morbidity and pain and similarly good oncologic outcomes, when the surgery was performed by robot-assisted laparoscopy instead of by the open technique, a phase 3 clinical trial has found.
Investigators of the ROBOT (Robot-assisted Thoracolaparoscopic Esophagectomy vs. Open Transthoracic Esophagectomy) trial, led by Pieter C. van der Sluis, MD, a surgeon at the University Medical Center Utrecht, the Netherlands, randomized 112 patients with resectable esophageal cancer to open transthoracic esophagectomy – considered to be the gold standard – or robot-assisted minimally invasive thoracolaparoscopic esophagectomy.
“Robot-assisted minimally invasive thoracolaparoscopic esophagectomy versus open transthoracic esophagectomy improves postoperative outcome. There were no differences in oncologic outcomes, and our oncologic outcomes were in concordance with the highest standards nowadays,” Dr. van der Sluis summarized. “This trial provides evidence for the minimally invasive approach over the open approach, and especially the robot-assisted minimally invasive esophagectomy.”
The investigators will report a full cost comparison separately. “We see that costs are lower, though not significantly lower, with the robot,” he said, giving a preview. “We are going to show that the real costs of the operation are in the complications. When you have complications that involve the ICU and reoperations, some patients are in the hospital for months after the surgery. So by investing a little extra money in the surgical procedure, you might actually get it back by reducing the complications.”
When asked by an attendee why the trial did not compare robotic esophagectomy with thoracoscopic esophagectomy, Dr. van der Sluis noted that such comparison is complicated by many factors; for example, the challenge of finding surgeons skilled in both techniques, and the likelihood of small differences in outcomes, potentially requiring enrollment of thousands of patients to have adequate study power. “We concluded that such a trial might not be feasible,” he said.
Parsing the findings
“The complication rates [in this trial] are very high in the robotic and open groups, much higher than reported in some well-controlled prospective and retrospective studies,” commented session attendee Kenneth Meredith, MD, FACS, professor at Florida State University, Sarasota, and director of gastrointestinal oncology, Sarasota Memorial Institute for Cancer Care.
He wondered how extensive the investigators’ experience with robotics was and how many cases they had done on their learning curve. Data from his group suggest that surgeons must perform 29 cases of robotic esophagectomy before the complication rate drops (Dis Esophagus. 2017;30:1-7).
“That’s more then half of the patients in the robotic arm of their study,” he noted in an interview. “I find this needs to be explained. If the authors are past their learning curve, why were the complication rates so high?” Additionally, the 80% rate in the open group “is among the highest I’ve seen in many years.”
The lack of significant differences in complete resection rate and in lymph node harvest was also surprising, as he and other robotics users have found that this technique can improve these outcomes, Dr. Meredith added. This could likewise be a learning curve phenomenon.
Although ROBOT’s comparison of robotic with open esophagectomy is relevant, “it would have been more relevant to compare robotic to minimally invasive esophagectomy [MIE],” he maintained, as MIE has been shown to improve outcomes relative to open surgery (Lancet. 2012;379:1887-92).
“There are many high-volume centers in MIE but not necessarily robotics. The two are often mutually exclusive, and a multicenter trial in which each center performs high volumes of their respective technique, rather then mandating each center perform an operation they may not be facile in,” would be practical, Dr. Meredith concluded.
Study details
“The main objective in our trial was to reduce surgical trauma and reduce the percentage of complications,” Dr. van der Sluis told attendees of the symposium, sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Results showed that compared with peers in the open surgery group, patients in the robotic-assisted surgery group specifically had a lower rate of pulmonary complications (32% vs. 58%, P = .005), largely due to a reduction in rate of pneumonia (28% vs. 55%, P = .005), and a lower rate of cardiac complications (22% vs. 47%, P = .006), almost entirely due to a reduction in rate of atrial fibrillation (22% vs. 46%, P = .01).
There was a trend toward fewer wound infections with robotics (4% vs. 14%, P = .09), with a large difference in thoracic wound infections (0% vs. 9%, P = .06).
The two groups were statistically indistinguishable on rates of anastomotic leakage (24% and 20%) and recurrent laryngeal nerve injury (9% and 11%). The fairly high rate of anastomotic leakage was likely due to the center’s use of cervical anastomosis at the time of the trial, according to Dr. van der Sluis; they have since started using thoracic anastomosis, and will report results with that technique soon.
There was also no significant difference between groups in the rate of in-hospital mortality (4% with robotic surgery and 2% with open surgery), median hospital length of stay (14 and 16 days), and ICU length of stay (1 day in each group).
Patients in the robotics group more commonly had functional recovery within 2 weeks (70% vs. 51%, P = .04). And on the Quality of Life Questionnaire Core 30, they had better scores for health-related quality of life at discharge (57.9 vs 44.6, P = .02) and at 6 weeks (68.7 vs. 57.6, P = .03), and for physical functioning at discharge (54.5 vs. 41.0, P = .03) and 6 weeks (69.3 vs. 58.6, P = .049).
The two groups were similar on rates of R0 resection (93% and 96%) and median number of lymph nodes retrieved (27 and 25), reported Dr. van der Sluis. Pain during the first 14 days after surgery was lower for the robotics group (P = .003).
With a median follow-up of 40 months, the robotics and open groups did not differ significantly on disease-free survival (median, 26 and 28 months) and overall survival (not reached in either group).
Dr. van der Sluis disclosed no relevant conflicts of interest.
SOURCE: van der Sluis PC et al. 2018 GI Cancer Symposium, Abstract 156148
SAN FRANCISCO – Patients undergoing had less morbidity and pain and similarly good oncologic outcomes, when the surgery was performed by robot-assisted laparoscopy instead of by the open technique, a phase 3 clinical trial has found.
Investigators of the ROBOT (Robot-assisted Thoracolaparoscopic Esophagectomy vs. Open Transthoracic Esophagectomy) trial, led by Pieter C. van der Sluis, MD, a surgeon at the University Medical Center Utrecht, the Netherlands, randomized 112 patients with resectable esophageal cancer to open transthoracic esophagectomy – considered to be the gold standard – or robot-assisted minimally invasive thoracolaparoscopic esophagectomy.
“Robot-assisted minimally invasive thoracolaparoscopic esophagectomy versus open transthoracic esophagectomy improves postoperative outcome. There were no differences in oncologic outcomes, and our oncologic outcomes were in concordance with the highest standards nowadays,” Dr. van der Sluis summarized. “This trial provides evidence for the minimally invasive approach over the open approach, and especially the robot-assisted minimally invasive esophagectomy.”
The investigators will report a full cost comparison separately. “We see that costs are lower, though not significantly lower, with the robot,” he said, giving a preview. “We are going to show that the real costs of the operation are in the complications. When you have complications that involve the ICU and reoperations, some patients are in the hospital for months after the surgery. So by investing a little extra money in the surgical procedure, you might actually get it back by reducing the complications.”
When asked by an attendee why the trial did not compare robotic esophagectomy with thoracoscopic esophagectomy, Dr. van der Sluis noted that such comparison is complicated by many factors; for example, the challenge of finding surgeons skilled in both techniques, and the likelihood of small differences in outcomes, potentially requiring enrollment of thousands of patients to have adequate study power. “We concluded that such a trial might not be feasible,” he said.
Parsing the findings
“The complication rates [in this trial] are very high in the robotic and open groups, much higher than reported in some well-controlled prospective and retrospective studies,” commented session attendee Kenneth Meredith, MD, FACS, professor at Florida State University, Sarasota, and director of gastrointestinal oncology, Sarasota Memorial Institute for Cancer Care.
He wondered how extensive the investigators’ experience with robotics was and how many cases they had done on their learning curve. Data from his group suggest that surgeons must perform 29 cases of robotic esophagectomy before the complication rate drops (Dis Esophagus. 2017;30:1-7).
“That’s more then half of the patients in the robotic arm of their study,” he noted in an interview. “I find this needs to be explained. If the authors are past their learning curve, why were the complication rates so high?” Additionally, the 80% rate in the open group “is among the highest I’ve seen in many years.”
The lack of significant differences in complete resection rate and in lymph node harvest was also surprising, as he and other robotics users have found that this technique can improve these outcomes, Dr. Meredith added. This could likewise be a learning curve phenomenon.
Although ROBOT’s comparison of robotic with open esophagectomy is relevant, “it would have been more relevant to compare robotic to minimally invasive esophagectomy [MIE],” he maintained, as MIE has been shown to improve outcomes relative to open surgery (Lancet. 2012;379:1887-92).
“There are many high-volume centers in MIE but not necessarily robotics. The two are often mutually exclusive, and a multicenter trial in which each center performs high volumes of their respective technique, rather then mandating each center perform an operation they may not be facile in,” would be practical, Dr. Meredith concluded.
Study details
“The main objective in our trial was to reduce surgical trauma and reduce the percentage of complications,” Dr. van der Sluis told attendees of the symposium, sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Results showed that compared with peers in the open surgery group, patients in the robotic-assisted surgery group specifically had a lower rate of pulmonary complications (32% vs. 58%, P = .005), largely due to a reduction in rate of pneumonia (28% vs. 55%, P = .005), and a lower rate of cardiac complications (22% vs. 47%, P = .006), almost entirely due to a reduction in rate of atrial fibrillation (22% vs. 46%, P = .01).
There was a trend toward fewer wound infections with robotics (4% vs. 14%, P = .09), with a large difference in thoracic wound infections (0% vs. 9%, P = .06).
The two groups were statistically indistinguishable on rates of anastomotic leakage (24% and 20%) and recurrent laryngeal nerve injury (9% and 11%). The fairly high rate of anastomotic leakage was likely due to the center’s use of cervical anastomosis at the time of the trial, according to Dr. van der Sluis; they have since started using thoracic anastomosis, and will report results with that technique soon.
There was also no significant difference between groups in the rate of in-hospital mortality (4% with robotic surgery and 2% with open surgery), median hospital length of stay (14 and 16 days), and ICU length of stay (1 day in each group).
Patients in the robotics group more commonly had functional recovery within 2 weeks (70% vs. 51%, P = .04). And on the Quality of Life Questionnaire Core 30, they had better scores for health-related quality of life at discharge (57.9 vs 44.6, P = .02) and at 6 weeks (68.7 vs. 57.6, P = .03), and for physical functioning at discharge (54.5 vs. 41.0, P = .03) and 6 weeks (69.3 vs. 58.6, P = .049).
The two groups were similar on rates of R0 resection (93% and 96%) and median number of lymph nodes retrieved (27 and 25), reported Dr. van der Sluis. Pain during the first 14 days after surgery was lower for the robotics group (P = .003).
With a median follow-up of 40 months, the robotics and open groups did not differ significantly on disease-free survival (median, 26 and 28 months) and overall survival (not reached in either group).
Dr. van der Sluis disclosed no relevant conflicts of interest.
SOURCE: van der Sluis PC et al. 2018 GI Cancer Symposium, Abstract 156148
REPORTING FROM THE 2018 GI CANCERS SYMPOSIUM
Key clinical point: Patients with esophageal cancer undergoing esophagectomy are less likely to experience complications when the surgery is performed robotically.
Major finding: Compared with open transthoracic esophagectomy, robot-assisted minimally invasive thoracolaparoscopic esophagectomy had a lower rate of MCDC grade 2 or higher surgery-related postoperative complications (59% vs. 80%).
Data source: A single-center phase 3 randomized controlled trial among 112 patients with resectable esophageal cancer.
Disclosures: Dr. van der Sluis disclosed no relevant conflicts of interest.
Source: van der Sluis PC et al. 2018 GI Cancer Symposium, Abstract 156148











