User login
Assessing Outcomes Between Risperidone Microspheres and Paliperidone Palmitate Long-Acting Injectable Antipsychotics Among Veterans
Medication nonadherence is common with oral antipsychotic formulations, resulting in relapse, increased morbidity, and more frequent psychiatric hospitalization.1-7 Psychiatric hospitalization and illness decompensation is costly to health care systems and leads to reduced quality of life for veterans and families.6,7 Long-acting injectable antipsychotics (LAIAs) were developed to enhance antipsychotic adherence and improve patient outcomes, including reduced psychiatric hospitalization.8-12
Little outcomes data exist comparing LAIAs, including biweekly risperidone microspheres and monthly paliperidone palmitate.10-13 Risperidone microspheres require a 3-week oral crossover and are administered every 2 weeks, whereas paliperidone palmitate does not require an oral crossover and is administered every 4 weeks. The paliperidone palmitate loading regimen replaces an oral crossover.
The primary objective of this study was to compare the number of psychiatric hospitalizations between veterans administered risperidone microspheres and those on paliperidone palmitate pre- and post-LAIA initiation. Secondary objectives were to assess rehospitalization rates between patients taking risperidone microspheres and paliperidone palmitate, reduction in pre- and posthospitalization rates with LAIAs, and medication adherence.
Methods
This observational study with a retrospective cohort design was conducted at the Veterans Affairs Loma Linda Healthcare System (VALLHS) in California. We examined veterans who were initiated on LAIAs risperidone microspheres or paliperidone palmitate from January 01, 2016 through December 31, 2018. Veterans who were aged ≥ 18 years and received ≥ 2 injections of either risperidone microspheres or paliperidone palmitate during the study period were included. Veterans were excluded if they had received < 2 doses of either LAIA, received the LAIA outside of the review period, were nonadherent to risperidone crossover if they received risperidone microspheres, or transferred their care to another facility. At VALLHS, LAIA injections are administered by a nurse, and veterans must travel to the facility to receive the injections.
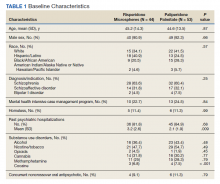
Extracted patient chart elements included participant demographics; diagnoses; comorbid alcohol, nicotine, opioid, or other substance use; duration on LAIA; psychiatric hospitalizations pre- and postinitiation of the LAIA; medication adherence; and medication discontinuation based on clinician documentation and clinic orders (Table 1).
Nonadherence to LAIA was defined as missing an injection by > 3 days for risperidone microspheres and > 7 days for paliperidone palmitate. This time frame was based on pharmacokinetic information listed in the products’ package inserts.14,15 Nonadherence to oral risperidone crossover with risperidone microspheres was defined as ≤ 80% of days covered.
Data Analysis
Patient demographics were analyzed using descriptive statistics and experimental comparisons between the risperidone microspheres and paliperidone palmitate groups to assess baseline differences between groups. Psychiatric hospitalizations pre- and post-LAIA were analyzed with parallel group (between veterans–independent groups) and pre-post (within veterans–dependent groups) designs. Index hospitalizations were examined for a period equivalent to the length of time veterans were on the LAIA. Psychiatric rehospitalization rates were analyzed for patients who had index hospitalizations and were rehospitalized for any period when they were receiving the LAIA. Incidences of pre- and post-LAIA hospitalizations were calculated in 100 person-years.
Parallel-group analysis was analyzed using the χ2 and Mann-Whitney U tests. Pre-post analyses were analyzed using the Wilcoxon rank sum test. P was set at < .05 for statistical significance.
Results
We screened 111 veterans, and 97 were included in this study (risperidone microspheres, 44; paliperidone palmitate, 53). Mean (SD) age was 46 (13.8) years, 92% were male, 38% were White, 94% were diagnosed with schizophrenia or schizoaffective disorder, and 11% were homeless. Substance use was documented as 52% for nicotine products, 40% for alcohol, 31% for cannabis, 27% for methamphetamine, 7% for cocaine, and 3% for opioids. Cannabis, methamphetamine, cocaine, and opioid use were based on clinician documentation and listed as active diagnoses at the time of LAIA initiation. Statistical significance was found in index hospitalizations P = .009) and history of cocaine use disorder (6.8% vs 7.5%, P < .001).
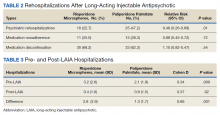
Veterans administered risperidone microspheres had fewer mean (SD) post-LAIA hospitalizations (0.4 [1.0] vs 0.9 [1.5]; P = .02) and were less likely to be rehospitalized (22.7% vs 47.2%, P = .01) compared with paliperidone palmitate. However, veterans taking risperidone microspheres had a shorter mean (SD) treatment duration (41.6 [40.2] vs 58.2 [45.7] weeks, P = .04) compared with paliperidone palmitate, mainly because patients switched to a different LAIA or oral antipsychotic. No differences were detected in nonadherence and discontinuation between risperidone microspheres and paliperidone palmitate. All veterans in the risperidone microspheres group adhered to oral risperidone crossover with an average 87.8% days covered (Table 2).
The average maintenance dose of risperidone microspheres was 42 mg every 2 weeks and 153 mg every 4 weeks for paliperidone palmitate.
Across the sample, 84% of veterans had a previous psychiatric hospitalization, although veterans initiated on risperidone microspheres had significantly higher mean (SD) index hospitalizations than those started on paliperidone palmitate (3.2 [2.6] risperidone microspheres vs 2.1 [1.9] paliperidone palmitate, P = .009). Both groups had significant decreases in mean (SD) hospitalizations (3.2 [2.6] to 0.4 [1.0], risperidone microspheres vs 2.1 [1.9] to 0.9 [1.5] paliperidone palmitate). The risperidone microspheres group had a larger decrease in mean (SD) hospitalizations post-LAIA (2.8 [2.9] risperidone microspheres vs 1.3 [1.7] paliperidone palmitate, P = .001) (Table 3).
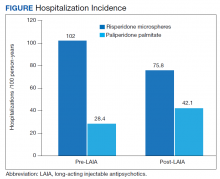
Differences in incidence per 100 person-years between pre- and post-LAIA hospitalizations were larger in risperidone microspheres users than in paliperidone palmitate (73.8 vs 33.7, P = .01) (Figure). No differences between risperidone microspheres and paliperidone palmitate were detected when looking at incidence pre-LAIA (102.2 vs 75.8, P = .22) and post-LAIA (28.4 vs 42.1, P = .38) separately.
Thirty veterans in the risperidone microspheres group discontinued LAIA: 11 were nonadherent, 5 experienced adverse effects (AEs), and 14 discontinued due to inconvenience. Among 33 veterans in the paliperidone palmitate group who discontinued the LAIA, 15 were nonadherent, 11 experienced AEs, 4 stopped due to of inconvenience, and 3 switched to a less frequently administered LAIA. The most common AEs reported were injection site reactions, cholinergic AEs (salivation, lacrimation, urination), orthostasis, and weight gain.
Discussion
The main finding of this study was that initiation of LAIAs significantly reduced hospitalizations. Veterans taking risperidone microspheres had higher index hospitalizations and lower posttreatment hospitalizations compared with paliperidone palmitate. We found that patients initiated on risperidone microspheres had more hospitalizations before use of a LAIA than those initiated on paliperidone palmitate. Risperidone microspheres reduced the number of hospitalization post-LAIA significantly more than paliperidone palmitate. We also found that veterans taking risperidone microspheres were on the medication for less mean (SD) time than those on paliperidone palmitate (41.6 [40.2] vs 58.2 [45.7] weeks; P = .04).
To our knowledge, this is one of the few studies that compared outcomes of psychiatric hospitalizations, medication adherence, and treatment discontinuation between risperidone microspheres and paliperidone palmitate, specifically in a veteran population.16-19 Limosin and colleagues aimed to compare length of stay during the initial hospitalization, rehospitalization risk, and treatment duration between risperidone microspheres and paliperidone palmitate in patients with schizophrenia.16 These researchers detected no differences in initial hospitalization duration and time to rehospitalization between risperidone microspheres and paliperidone palmitate.16 The study revealed a more favorable trend in time to discontinuation for paliperidone palmitate, but switching between LAIAs might have confounded the data.16 The authors note that their study lacked power, and patients on paliperidone palmitate had significantly more nonpsychiatric comorbidities.16 Joshi and colleagues looked at adherence, medication discontinuation, hospitalization rates, emergency department visits, and hospitalization costs between risperidone microspheres and paliperidone palmitate in patients identified in Truven MarketScan Commercial, Medicare Supplemental, and Medicaid Multi-State insurance databases.17 The authors found paliperidone palmitate to be superior in all objectives with better adherence, lower discontinuation rates, less likelihood of hospitalization, fewer emergency department visits, and lower hospitalization costs compared with risperidone microspheres.17 Korell and colleagues aimed to establish reference ranges for plasma concentrations of risperidone and paliperidone among adherent patients.18
The researchers established reference ranges for risperidone and paliperidone plasma concentrations that represented expected variability within a population and were derived from population pharmacokinetic models.18 Gopal and colleagues conducted a post hoc comparison between paliperidone palmitate and oral risperidone during initiation of long-acting injectable risperidone in patients with acute schizophrenia.19 The researchers found that during the first month after initiating long-acting injectable risperidone, paliperidone palmitate without oral supplementation had similar efficacy and safety to oral risperidone among these patients.19
LAIAs can create a steadier drug plasma concentration compared with oral antipsychotics and do not need to be taken daily. These agents improve adherence by reducing the frequency of medication administrations.20-24 Assessing nonadherence is easier with LAIAs by counting missed injections compared with oral antipsychotics that require calculation of percentage of days covered.25
The results in our study are somewhat unexpected in part because of the close relationship between risperidone and paliperidone. Risperidone is converted to paliperidone (9-OH-risperidone) via hepatic cytochrome P450 2D6. Although the molecules do not have identical pharmacologic profiles, it is accepted that they are similar enough that risperidone can establish oral tolerability when transitioning therapy to paliperidone palmitate and vice versa.24 Although the active moiety in risperidone microspheres and paliperidone palmitate is similar, the dosing interval for risperidone microspheres is 2 weeks compared with 4 weeks with paliperidone palmitate. One potential explanation as to why veterans started on risperidone microspheres experienced better outcomes is because they had twice as many office visits with the health care team. Facility procedures dictate veterans receive the LAIA at an on-site clinic. During the visits, a licensed vocational nurse administers the injection and monitors the patient for 15 to 30 minutes afterward.
Despite new LAIAs coming to market, high-quality data examining potential differences in treatment outcomes among agents are limited. This is problematic for clinicians who want to optimize care by understanding how administration schedules or other aspects of LAIA use could modify treatment outcomes. Our results suggest that an advantage might exist in selecting an agent with a more frequent administration schedule, at least initially. This could allow for close monitoring and regular therapeutic contact, which could improve short-term outcomes. This conclusion is supported by meta-analyses, randomized controlled trials, and conceptual articles conducted by Wehring and colleagues, Berwaerts and colleagues, and Parellada and colleagues, respectively, who examined patients on different LAIAs and contact with health care professionals as part of their research.26-28 These researchers concluded that patients who had regular contact with a health care professional had better outcomes when initiated on a LAIA.26-28
Limitations
There are several limitations in this study. Retrospective and observational methods introduce risks of bias and confounding variables. Sample size might have limited statistical power to detect differences. Veterans might have had undocumented pre- or posthospitalizations at other institutions, which was not accounted for and lack of rehospitalization is not conclusive of a positive outcome. Institutions could improve on our study and help to fill gaps in comparative data by conducting larger analyses over longer periods and including more LAIA agents.
Conclusions
Although veterans that were administered risperidone microspheres had a shorter treatment duration, they were less likely to be rehospitalized, had a fewer mean number of post-LAIA hospitalizations, and had a larger difference in incidence in 100 person-years compared with veterans on paliperidone palmitate. Nonadherence and discontinuation rates were comparable between risperidone microspheres and paliperidone palmitate. Future studies could aim to further clarify differences in outcomes among agents or administration schedules.
1. Lehman AF, Lieberman JA, Dixon LB, et al; American Psychiatric Association Steering Committee on Practice Guidelines. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry. 2004;161(suppl 2):1-56.
2. Lieberman JA, Stroup TS, McEvoy JP, et al; Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209-1223. doi:10.1056/NEJMoa051688
3. Swartz MS, Stroup TS, McEvoy JP, et al. What CATIE found: results from the schizophrenia trial. Psychiatr Serv. 2008;59(5):500-506. doi:10.1176/ps.2008.59.5.500
4. Haywood TW, Kravitz HM, Grossman LS, Cavanaugh JL Jr, Davis JM, Lewis DA. Predicting the “revolving door” phenomenon among patients with schizophrenic, schizoaffective, and affective disorders. Am J Psychiatry. 1995;152(6):856-561. doi:10.1176/ajp.152.6.856
5. Morken G, Widen JH, Grawe RW. Non-adherence to antipsychotic medication, relapse and rehospitalisation in recent-onset schizophrenia. BMC Psychiatry. 2008;8:32. doi:10.1186/1471-244X-8-32
6. Weiden PJ, Kozma C, Grogg A, Locklear J. Partial compliance and risk of rehospitalization among California Medicaid patients with schizophrenia. Psychiatr Serv. 2004;55(8):886-891. doi:10.1176/appi.ps.55.8.886
7. Gilmer TP, Dolder CR, Lacro JP, et al. Adherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophrenia. Am J Psychiatry. 2004;161(4):692-699. doi:10.1176/appi.ajp.161.4.692
8. Lafeuille MH, Dean J, Carter V, et al. Systematic review of long-acting injectables versus oral atypical antipsychotics on hospitalization in schizophrenia. Curr Med Res Opin. 2014;30(8):1643-1655. doi:10.1185/03007995.2014.915211
9. Yu W, Wagner TH, Chen S, Barnett PG. Average cost of VA rehabilitation, mental health, and long-term hospital stays. Med Care Res Rev. 2003;60(3 suppl):40S-53S. doi:10.1177/1077558703256724
10. Duncan EJ, Woolson SL, Hamer RM. Treatment compliance in veterans administration schizophrenia spectrum patients treated with risperidone long-acting injectable. Int Clin Psychopharmacol. 2012;27(5):283-290. doi:10.1097/YIC.0b013e328354b534
11. Romstadt N, Wonson E. Outcomes comparison of long-acting injectable antipsychotic initiation in treatment-naïve veterans in the inpatient versus outpatient setting. Ment Health Clin. 2018;8(1):24-27. doi:10.9740/mhc.2018.01.024
12. Dimitropoulos E, Drogemuller L, Wong K. Evaluation of concurrent oral and long-acting injectable antipsychotic prescribing at the Minneapolis Veterans Affairs Health Care System. J Clin Psychopharmacol. 2017;37(5):605-608. doi:10.1097/JCP.0000000000000755
13. Marcus SC, Zummo J, Pettit AR, Stoddard J, Doshi JA. Antipsychotic adherence and rehospitalization in schizophrenia patients receiving oral versus long-acting injectable antipsychotics following hospital discharge. J Manag Care Spec Pharm. 2015;21(9):754-768. doi:10.18553/jmcp.2015.21.9.754
14. Risperdal Consta. Package insert. Janssen Pharmaceutical; 2007.
15. Invega Sustenna. Package insert. Janssen Pharmaceutical; 2009.
16. Limosin F, Belhadi D, Comet D, et al. Comparison of paliperidone palmitate and risperidone long-acting injection in schizophrenic patients: results from a multicenter retrospective cohort study in France. J Clin Psychopharmacol. 2018;38(1):19-26. doi:10.1097/JCP.0000000000000827
17. Joshi K, Pan X, Wang R, Yang E, Benson C. Healthcare resource utilization of second-generation long-acting injectable antipsychotics in schizophrenia: risperidone versus paliperidone palmitate. Curr Med Res Opin. 2016;32(11):1873-1881. doi: 10.1080/03007995.2016.1219706
18. Korell J, Green B, Remmerie B, Vermeulen A. Determination of plasma concentration reference ranges for risperidone and paliperidone. CPT Pharmacometrics Syst Pharmacol. 2017;6(9):589-595. doi:10.1002/psp4.12217
19. Gopal S, Pandina G, Lane R, et al. A post-hoc comparison of paliperidone palmitate to oral risperidone during initiation of long-acting risperidone injection in patients with acute schizophrenia. Innov Clin Neurosci. 2011;8(8):26-33.
20. Marcus SC, Zummo J, Pettit AR, Stoddard J, Doshi JA. Antipsychotic adherence and rehospitalization in schizophrenia patients receiving oral versus long-acting injectable antipsychotics following hospital discharge. J Manag Care Spec Pharm. 2015;21(9):754-768. doi:10.18553/jmcp.2015.21.9.754
21. Romstadt N, Wonson E. Outcomes comparison of long-acting injectable antipsychotic initiation in treatment-naïve veterans in the inpatient versus outpatient setting. Ment Health Clin. 2018;8(1):24-27. doi:10.9740/mhc.2018.01.024
22. Green AI, Brunette MF, Dawson R, et al. Long-acting injectable vs oral risperidone for schizophrenia and co-occurring alcohol use disorder: a randomized trial. J Clin Psychiatry. 2015;76(10):1359-1365. doi:10.4088/JCP.13m08838
23. Rezansoff SN, Moniruzzaman A, Fazel S, Procyshyn R, Somers JM. Adherence to antipsychotic medication among homeless adults in Vancouver, Canada: a 15-year retrospective cohort study. Soc Psychiatry Psychiatr Epidemiol. 2016;51(12):1623-1632. doi:10.1007/s00127-016-1259-7
24. Castillo EG, Stroup TS. Effectiveness of long-acting injectable antipsychotics: a clinical perspective. Evid Based Ment Health. 2015;18(2):36-39. doi:10.1136/eb-2015-102086
25. Marder SR. Overview of partial compliance. J Clin Psychiatry. 2003;64 (suppl 16):3-9.
26. Wehring HJ, Thedford S, Koola M, Kelly DL. Patient and health care provider perspectives on long acting injectable antipsychotics in schizophrenia and the introduction of olanzapine long-acting injection. J Cent Nerv Syst Dis. 2011;2011(3):107-123. doi:10.4137/JCNSD.S4091
27. Berwaerts J, Liu Y, Gopal S, et al. Efficacy and safety of the 3-month formulation of paliperidone palmitate vs placebo for relapse prevention of schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2015;72(8):830-839. doi:10.1001/jamapsychiatry.2015.0241
28. Parellada E, Bioque M. Barriers to the use of long-acting injectable antipsychotics in the management of schizophrenia. CNS Drugs. 2016;30(8):689-701. doi:10.1007/s40263-016-0350-7
Medication nonadherence is common with oral antipsychotic formulations, resulting in relapse, increased morbidity, and more frequent psychiatric hospitalization.1-7 Psychiatric hospitalization and illness decompensation is costly to health care systems and leads to reduced quality of life for veterans and families.6,7 Long-acting injectable antipsychotics (LAIAs) were developed to enhance antipsychotic adherence and improve patient outcomes, including reduced psychiatric hospitalization.8-12
Little outcomes data exist comparing LAIAs, including biweekly risperidone microspheres and monthly paliperidone palmitate.10-13 Risperidone microspheres require a 3-week oral crossover and are administered every 2 weeks, whereas paliperidone palmitate does not require an oral crossover and is administered every 4 weeks. The paliperidone palmitate loading regimen replaces an oral crossover.
The primary objective of this study was to compare the number of psychiatric hospitalizations between veterans administered risperidone microspheres and those on paliperidone palmitate pre- and post-LAIA initiation. Secondary objectives were to assess rehospitalization rates between patients taking risperidone microspheres and paliperidone palmitate, reduction in pre- and posthospitalization rates with LAIAs, and medication adherence.
Methods
This observational study with a retrospective cohort design was conducted at the Veterans Affairs Loma Linda Healthcare System (VALLHS) in California. We examined veterans who were initiated on LAIAs risperidone microspheres or paliperidone palmitate from January 01, 2016 through December 31, 2018. Veterans who were aged ≥ 18 years and received ≥ 2 injections of either risperidone microspheres or paliperidone palmitate during the study period were included. Veterans were excluded if they had received < 2 doses of either LAIA, received the LAIA outside of the review period, were nonadherent to risperidone crossover if they received risperidone microspheres, or transferred their care to another facility. At VALLHS, LAIA injections are administered by a nurse, and veterans must travel to the facility to receive the injections.
Extracted patient chart elements included participant demographics; diagnoses; comorbid alcohol, nicotine, opioid, or other substance use; duration on LAIA; psychiatric hospitalizations pre- and postinitiation of the LAIA; medication adherence; and medication discontinuation based on clinician documentation and clinic orders (Table 1).
Nonadherence to LAIA was defined as missing an injection by > 3 days for risperidone microspheres and > 7 days for paliperidone palmitate. This time frame was based on pharmacokinetic information listed in the products’ package inserts.14,15 Nonadherence to oral risperidone crossover with risperidone microspheres was defined as ≤ 80% of days covered.
Data Analysis
Patient demographics were analyzed using descriptive statistics and experimental comparisons between the risperidone microspheres and paliperidone palmitate groups to assess baseline differences between groups. Psychiatric hospitalizations pre- and post-LAIA were analyzed with parallel group (between veterans–independent groups) and pre-post (within veterans–dependent groups) designs. Index hospitalizations were examined for a period equivalent to the length of time veterans were on the LAIA. Psychiatric rehospitalization rates were analyzed for patients who had index hospitalizations and were rehospitalized for any period when they were receiving the LAIA. Incidences of pre- and post-LAIA hospitalizations were calculated in 100 person-years.
Parallel-group analysis was analyzed using the χ2 and Mann-Whitney U tests. Pre-post analyses were analyzed using the Wilcoxon rank sum test. P was set at < .05 for statistical significance.
Results
We screened 111 veterans, and 97 were included in this study (risperidone microspheres, 44; paliperidone palmitate, 53). Mean (SD) age was 46 (13.8) years, 92% were male, 38% were White, 94% were diagnosed with schizophrenia or schizoaffective disorder, and 11% were homeless. Substance use was documented as 52% for nicotine products, 40% for alcohol, 31% for cannabis, 27% for methamphetamine, 7% for cocaine, and 3% for opioids. Cannabis, methamphetamine, cocaine, and opioid use were based on clinician documentation and listed as active diagnoses at the time of LAIA initiation. Statistical significance was found in index hospitalizations P = .009) and history of cocaine use disorder (6.8% vs 7.5%, P < .001).
Veterans administered risperidone microspheres had fewer mean (SD) post-LAIA hospitalizations (0.4 [1.0] vs 0.9 [1.5]; P = .02) and were less likely to be rehospitalized (22.7% vs 47.2%, P = .01) compared with paliperidone palmitate. However, veterans taking risperidone microspheres had a shorter mean (SD) treatment duration (41.6 [40.2] vs 58.2 [45.7] weeks, P = .04) compared with paliperidone palmitate, mainly because patients switched to a different LAIA or oral antipsychotic. No differences were detected in nonadherence and discontinuation between risperidone microspheres and paliperidone palmitate. All veterans in the risperidone microspheres group adhered to oral risperidone crossover with an average 87.8% days covered (Table 2).
The average maintenance dose of risperidone microspheres was 42 mg every 2 weeks and 153 mg every 4 weeks for paliperidone palmitate.
Across the sample, 84% of veterans had a previous psychiatric hospitalization, although veterans initiated on risperidone microspheres had significantly higher mean (SD) index hospitalizations than those started on paliperidone palmitate (3.2 [2.6] risperidone microspheres vs 2.1 [1.9] paliperidone palmitate, P = .009). Both groups had significant decreases in mean (SD) hospitalizations (3.2 [2.6] to 0.4 [1.0], risperidone microspheres vs 2.1 [1.9] to 0.9 [1.5] paliperidone palmitate). The risperidone microspheres group had a larger decrease in mean (SD) hospitalizations post-LAIA (2.8 [2.9] risperidone microspheres vs 1.3 [1.7] paliperidone palmitate, P = .001) (Table 3).
Differences in incidence per 100 person-years between pre- and post-LAIA hospitalizations were larger in risperidone microspheres users than in paliperidone palmitate (73.8 vs 33.7, P = .01) (Figure). No differences between risperidone microspheres and paliperidone palmitate were detected when looking at incidence pre-LAIA (102.2 vs 75.8, P = .22) and post-LAIA (28.4 vs 42.1, P = .38) separately.
Thirty veterans in the risperidone microspheres group discontinued LAIA: 11 were nonadherent, 5 experienced adverse effects (AEs), and 14 discontinued due to inconvenience. Among 33 veterans in the paliperidone palmitate group who discontinued the LAIA, 15 were nonadherent, 11 experienced AEs, 4 stopped due to of inconvenience, and 3 switched to a less frequently administered LAIA. The most common AEs reported were injection site reactions, cholinergic AEs (salivation, lacrimation, urination), orthostasis, and weight gain.
Discussion
The main finding of this study was that initiation of LAIAs significantly reduced hospitalizations. Veterans taking risperidone microspheres had higher index hospitalizations and lower posttreatment hospitalizations compared with paliperidone palmitate. We found that patients initiated on risperidone microspheres had more hospitalizations before use of a LAIA than those initiated on paliperidone palmitate. Risperidone microspheres reduced the number of hospitalization post-LAIA significantly more than paliperidone palmitate. We also found that veterans taking risperidone microspheres were on the medication for less mean (SD) time than those on paliperidone palmitate (41.6 [40.2] vs 58.2 [45.7] weeks; P = .04).
To our knowledge, this is one of the few studies that compared outcomes of psychiatric hospitalizations, medication adherence, and treatment discontinuation between risperidone microspheres and paliperidone palmitate, specifically in a veteran population.16-19 Limosin and colleagues aimed to compare length of stay during the initial hospitalization, rehospitalization risk, and treatment duration between risperidone microspheres and paliperidone palmitate in patients with schizophrenia.16 These researchers detected no differences in initial hospitalization duration and time to rehospitalization between risperidone microspheres and paliperidone palmitate.16 The study revealed a more favorable trend in time to discontinuation for paliperidone palmitate, but switching between LAIAs might have confounded the data.16 The authors note that their study lacked power, and patients on paliperidone palmitate had significantly more nonpsychiatric comorbidities.16 Joshi and colleagues looked at adherence, medication discontinuation, hospitalization rates, emergency department visits, and hospitalization costs between risperidone microspheres and paliperidone palmitate in patients identified in Truven MarketScan Commercial, Medicare Supplemental, and Medicaid Multi-State insurance databases.17 The authors found paliperidone palmitate to be superior in all objectives with better adherence, lower discontinuation rates, less likelihood of hospitalization, fewer emergency department visits, and lower hospitalization costs compared with risperidone microspheres.17 Korell and colleagues aimed to establish reference ranges for plasma concentrations of risperidone and paliperidone among adherent patients.18
The researchers established reference ranges for risperidone and paliperidone plasma concentrations that represented expected variability within a population and were derived from population pharmacokinetic models.18 Gopal and colleagues conducted a post hoc comparison between paliperidone palmitate and oral risperidone during initiation of long-acting injectable risperidone in patients with acute schizophrenia.19 The researchers found that during the first month after initiating long-acting injectable risperidone, paliperidone palmitate without oral supplementation had similar efficacy and safety to oral risperidone among these patients.19
LAIAs can create a steadier drug plasma concentration compared with oral antipsychotics and do not need to be taken daily. These agents improve adherence by reducing the frequency of medication administrations.20-24 Assessing nonadherence is easier with LAIAs by counting missed injections compared with oral antipsychotics that require calculation of percentage of days covered.25
The results in our study are somewhat unexpected in part because of the close relationship between risperidone and paliperidone. Risperidone is converted to paliperidone (9-OH-risperidone) via hepatic cytochrome P450 2D6. Although the molecules do not have identical pharmacologic profiles, it is accepted that they are similar enough that risperidone can establish oral tolerability when transitioning therapy to paliperidone palmitate and vice versa.24 Although the active moiety in risperidone microspheres and paliperidone palmitate is similar, the dosing interval for risperidone microspheres is 2 weeks compared with 4 weeks with paliperidone palmitate. One potential explanation as to why veterans started on risperidone microspheres experienced better outcomes is because they had twice as many office visits with the health care team. Facility procedures dictate veterans receive the LAIA at an on-site clinic. During the visits, a licensed vocational nurse administers the injection and monitors the patient for 15 to 30 minutes afterward.
Despite new LAIAs coming to market, high-quality data examining potential differences in treatment outcomes among agents are limited. This is problematic for clinicians who want to optimize care by understanding how administration schedules or other aspects of LAIA use could modify treatment outcomes. Our results suggest that an advantage might exist in selecting an agent with a more frequent administration schedule, at least initially. This could allow for close monitoring and regular therapeutic contact, which could improve short-term outcomes. This conclusion is supported by meta-analyses, randomized controlled trials, and conceptual articles conducted by Wehring and colleagues, Berwaerts and colleagues, and Parellada and colleagues, respectively, who examined patients on different LAIAs and contact with health care professionals as part of their research.26-28 These researchers concluded that patients who had regular contact with a health care professional had better outcomes when initiated on a LAIA.26-28
Limitations
There are several limitations in this study. Retrospective and observational methods introduce risks of bias and confounding variables. Sample size might have limited statistical power to detect differences. Veterans might have had undocumented pre- or posthospitalizations at other institutions, which was not accounted for and lack of rehospitalization is not conclusive of a positive outcome. Institutions could improve on our study and help to fill gaps in comparative data by conducting larger analyses over longer periods and including more LAIA agents.
Conclusions
Although veterans that were administered risperidone microspheres had a shorter treatment duration, they were less likely to be rehospitalized, had a fewer mean number of post-LAIA hospitalizations, and had a larger difference in incidence in 100 person-years compared with veterans on paliperidone palmitate. Nonadherence and discontinuation rates were comparable between risperidone microspheres and paliperidone palmitate. Future studies could aim to further clarify differences in outcomes among agents or administration schedules.
Medication nonadherence is common with oral antipsychotic formulations, resulting in relapse, increased morbidity, and more frequent psychiatric hospitalization.1-7 Psychiatric hospitalization and illness decompensation is costly to health care systems and leads to reduced quality of life for veterans and families.6,7 Long-acting injectable antipsychotics (LAIAs) were developed to enhance antipsychotic adherence and improve patient outcomes, including reduced psychiatric hospitalization.8-12
Little outcomes data exist comparing LAIAs, including biweekly risperidone microspheres and monthly paliperidone palmitate.10-13 Risperidone microspheres require a 3-week oral crossover and are administered every 2 weeks, whereas paliperidone palmitate does not require an oral crossover and is administered every 4 weeks. The paliperidone palmitate loading regimen replaces an oral crossover.
The primary objective of this study was to compare the number of psychiatric hospitalizations between veterans administered risperidone microspheres and those on paliperidone palmitate pre- and post-LAIA initiation. Secondary objectives were to assess rehospitalization rates between patients taking risperidone microspheres and paliperidone palmitate, reduction in pre- and posthospitalization rates with LAIAs, and medication adherence.
Methods
This observational study with a retrospective cohort design was conducted at the Veterans Affairs Loma Linda Healthcare System (VALLHS) in California. We examined veterans who were initiated on LAIAs risperidone microspheres or paliperidone palmitate from January 01, 2016 through December 31, 2018. Veterans who were aged ≥ 18 years and received ≥ 2 injections of either risperidone microspheres or paliperidone palmitate during the study period were included. Veterans were excluded if they had received < 2 doses of either LAIA, received the LAIA outside of the review period, were nonadherent to risperidone crossover if they received risperidone microspheres, or transferred their care to another facility. At VALLHS, LAIA injections are administered by a nurse, and veterans must travel to the facility to receive the injections.
Extracted patient chart elements included participant demographics; diagnoses; comorbid alcohol, nicotine, opioid, or other substance use; duration on LAIA; psychiatric hospitalizations pre- and postinitiation of the LAIA; medication adherence; and medication discontinuation based on clinician documentation and clinic orders (Table 1).
Nonadherence to LAIA was defined as missing an injection by > 3 days for risperidone microspheres and > 7 days for paliperidone palmitate. This time frame was based on pharmacokinetic information listed in the products’ package inserts.14,15 Nonadherence to oral risperidone crossover with risperidone microspheres was defined as ≤ 80% of days covered.
Data Analysis
Patient demographics were analyzed using descriptive statistics and experimental comparisons between the risperidone microspheres and paliperidone palmitate groups to assess baseline differences between groups. Psychiatric hospitalizations pre- and post-LAIA were analyzed with parallel group (between veterans–independent groups) and pre-post (within veterans–dependent groups) designs. Index hospitalizations were examined for a period equivalent to the length of time veterans were on the LAIA. Psychiatric rehospitalization rates were analyzed for patients who had index hospitalizations and were rehospitalized for any period when they were receiving the LAIA. Incidences of pre- and post-LAIA hospitalizations were calculated in 100 person-years.
Parallel-group analysis was analyzed using the χ2 and Mann-Whitney U tests. Pre-post analyses were analyzed using the Wilcoxon rank sum test. P was set at < .05 for statistical significance.
Results
We screened 111 veterans, and 97 were included in this study (risperidone microspheres, 44; paliperidone palmitate, 53). Mean (SD) age was 46 (13.8) years, 92% were male, 38% were White, 94% were diagnosed with schizophrenia or schizoaffective disorder, and 11% were homeless. Substance use was documented as 52% for nicotine products, 40% for alcohol, 31% for cannabis, 27% for methamphetamine, 7% for cocaine, and 3% for opioids. Cannabis, methamphetamine, cocaine, and opioid use were based on clinician documentation and listed as active diagnoses at the time of LAIA initiation. Statistical significance was found in index hospitalizations P = .009) and history of cocaine use disorder (6.8% vs 7.5%, P < .001).
Veterans administered risperidone microspheres had fewer mean (SD) post-LAIA hospitalizations (0.4 [1.0] vs 0.9 [1.5]; P = .02) and were less likely to be rehospitalized (22.7% vs 47.2%, P = .01) compared with paliperidone palmitate. However, veterans taking risperidone microspheres had a shorter mean (SD) treatment duration (41.6 [40.2] vs 58.2 [45.7] weeks, P = .04) compared with paliperidone palmitate, mainly because patients switched to a different LAIA or oral antipsychotic. No differences were detected in nonadherence and discontinuation between risperidone microspheres and paliperidone palmitate. All veterans in the risperidone microspheres group adhered to oral risperidone crossover with an average 87.8% days covered (Table 2).
The average maintenance dose of risperidone microspheres was 42 mg every 2 weeks and 153 mg every 4 weeks for paliperidone palmitate.
Across the sample, 84% of veterans had a previous psychiatric hospitalization, although veterans initiated on risperidone microspheres had significantly higher mean (SD) index hospitalizations than those started on paliperidone palmitate (3.2 [2.6] risperidone microspheres vs 2.1 [1.9] paliperidone palmitate, P = .009). Both groups had significant decreases in mean (SD) hospitalizations (3.2 [2.6] to 0.4 [1.0], risperidone microspheres vs 2.1 [1.9] to 0.9 [1.5] paliperidone palmitate). The risperidone microspheres group had a larger decrease in mean (SD) hospitalizations post-LAIA (2.8 [2.9] risperidone microspheres vs 1.3 [1.7] paliperidone palmitate, P = .001) (Table 3).
Differences in incidence per 100 person-years between pre- and post-LAIA hospitalizations were larger in risperidone microspheres users than in paliperidone palmitate (73.8 vs 33.7, P = .01) (Figure). No differences between risperidone microspheres and paliperidone palmitate were detected when looking at incidence pre-LAIA (102.2 vs 75.8, P = .22) and post-LAIA (28.4 vs 42.1, P = .38) separately.
Thirty veterans in the risperidone microspheres group discontinued LAIA: 11 were nonadherent, 5 experienced adverse effects (AEs), and 14 discontinued due to inconvenience. Among 33 veterans in the paliperidone palmitate group who discontinued the LAIA, 15 were nonadherent, 11 experienced AEs, 4 stopped due to of inconvenience, and 3 switched to a less frequently administered LAIA. The most common AEs reported were injection site reactions, cholinergic AEs (salivation, lacrimation, urination), orthostasis, and weight gain.
Discussion
The main finding of this study was that initiation of LAIAs significantly reduced hospitalizations. Veterans taking risperidone microspheres had higher index hospitalizations and lower posttreatment hospitalizations compared with paliperidone palmitate. We found that patients initiated on risperidone microspheres had more hospitalizations before use of a LAIA than those initiated on paliperidone palmitate. Risperidone microspheres reduced the number of hospitalization post-LAIA significantly more than paliperidone palmitate. We also found that veterans taking risperidone microspheres were on the medication for less mean (SD) time than those on paliperidone palmitate (41.6 [40.2] vs 58.2 [45.7] weeks; P = .04).
To our knowledge, this is one of the few studies that compared outcomes of psychiatric hospitalizations, medication adherence, and treatment discontinuation between risperidone microspheres and paliperidone palmitate, specifically in a veteran population.16-19 Limosin and colleagues aimed to compare length of stay during the initial hospitalization, rehospitalization risk, and treatment duration between risperidone microspheres and paliperidone palmitate in patients with schizophrenia.16 These researchers detected no differences in initial hospitalization duration and time to rehospitalization between risperidone microspheres and paliperidone palmitate.16 The study revealed a more favorable trend in time to discontinuation for paliperidone palmitate, but switching between LAIAs might have confounded the data.16 The authors note that their study lacked power, and patients on paliperidone palmitate had significantly more nonpsychiatric comorbidities.16 Joshi and colleagues looked at adherence, medication discontinuation, hospitalization rates, emergency department visits, and hospitalization costs between risperidone microspheres and paliperidone palmitate in patients identified in Truven MarketScan Commercial, Medicare Supplemental, and Medicaid Multi-State insurance databases.17 The authors found paliperidone palmitate to be superior in all objectives with better adherence, lower discontinuation rates, less likelihood of hospitalization, fewer emergency department visits, and lower hospitalization costs compared with risperidone microspheres.17 Korell and colleagues aimed to establish reference ranges for plasma concentrations of risperidone and paliperidone among adherent patients.18
The researchers established reference ranges for risperidone and paliperidone plasma concentrations that represented expected variability within a population and were derived from population pharmacokinetic models.18 Gopal and colleagues conducted a post hoc comparison between paliperidone palmitate and oral risperidone during initiation of long-acting injectable risperidone in patients with acute schizophrenia.19 The researchers found that during the first month after initiating long-acting injectable risperidone, paliperidone palmitate without oral supplementation had similar efficacy and safety to oral risperidone among these patients.19
LAIAs can create a steadier drug plasma concentration compared with oral antipsychotics and do not need to be taken daily. These agents improve adherence by reducing the frequency of medication administrations.20-24 Assessing nonadherence is easier with LAIAs by counting missed injections compared with oral antipsychotics that require calculation of percentage of days covered.25
The results in our study are somewhat unexpected in part because of the close relationship between risperidone and paliperidone. Risperidone is converted to paliperidone (9-OH-risperidone) via hepatic cytochrome P450 2D6. Although the molecules do not have identical pharmacologic profiles, it is accepted that they are similar enough that risperidone can establish oral tolerability when transitioning therapy to paliperidone palmitate and vice versa.24 Although the active moiety in risperidone microspheres and paliperidone palmitate is similar, the dosing interval for risperidone microspheres is 2 weeks compared with 4 weeks with paliperidone palmitate. One potential explanation as to why veterans started on risperidone microspheres experienced better outcomes is because they had twice as many office visits with the health care team. Facility procedures dictate veterans receive the LAIA at an on-site clinic. During the visits, a licensed vocational nurse administers the injection and monitors the patient for 15 to 30 minutes afterward.
Despite new LAIAs coming to market, high-quality data examining potential differences in treatment outcomes among agents are limited. This is problematic for clinicians who want to optimize care by understanding how administration schedules or other aspects of LAIA use could modify treatment outcomes. Our results suggest that an advantage might exist in selecting an agent with a more frequent administration schedule, at least initially. This could allow for close monitoring and regular therapeutic contact, which could improve short-term outcomes. This conclusion is supported by meta-analyses, randomized controlled trials, and conceptual articles conducted by Wehring and colleagues, Berwaerts and colleagues, and Parellada and colleagues, respectively, who examined patients on different LAIAs and contact with health care professionals as part of their research.26-28 These researchers concluded that patients who had regular contact with a health care professional had better outcomes when initiated on a LAIA.26-28
Limitations
There are several limitations in this study. Retrospective and observational methods introduce risks of bias and confounding variables. Sample size might have limited statistical power to detect differences. Veterans might have had undocumented pre- or posthospitalizations at other institutions, which was not accounted for and lack of rehospitalization is not conclusive of a positive outcome. Institutions could improve on our study and help to fill gaps in comparative data by conducting larger analyses over longer periods and including more LAIA agents.
Conclusions
Although veterans that were administered risperidone microspheres had a shorter treatment duration, they were less likely to be rehospitalized, had a fewer mean number of post-LAIA hospitalizations, and had a larger difference in incidence in 100 person-years compared with veterans on paliperidone palmitate. Nonadherence and discontinuation rates were comparable between risperidone microspheres and paliperidone palmitate. Future studies could aim to further clarify differences in outcomes among agents or administration schedules.
1. Lehman AF, Lieberman JA, Dixon LB, et al; American Psychiatric Association Steering Committee on Practice Guidelines. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry. 2004;161(suppl 2):1-56.
2. Lieberman JA, Stroup TS, McEvoy JP, et al; Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209-1223. doi:10.1056/NEJMoa051688
3. Swartz MS, Stroup TS, McEvoy JP, et al. What CATIE found: results from the schizophrenia trial. Psychiatr Serv. 2008;59(5):500-506. doi:10.1176/ps.2008.59.5.500
4. Haywood TW, Kravitz HM, Grossman LS, Cavanaugh JL Jr, Davis JM, Lewis DA. Predicting the “revolving door” phenomenon among patients with schizophrenic, schizoaffective, and affective disorders. Am J Psychiatry. 1995;152(6):856-561. doi:10.1176/ajp.152.6.856
5. Morken G, Widen JH, Grawe RW. Non-adherence to antipsychotic medication, relapse and rehospitalisation in recent-onset schizophrenia. BMC Psychiatry. 2008;8:32. doi:10.1186/1471-244X-8-32
6. Weiden PJ, Kozma C, Grogg A, Locklear J. Partial compliance and risk of rehospitalization among California Medicaid patients with schizophrenia. Psychiatr Serv. 2004;55(8):886-891. doi:10.1176/appi.ps.55.8.886
7. Gilmer TP, Dolder CR, Lacro JP, et al. Adherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophrenia. Am J Psychiatry. 2004;161(4):692-699. doi:10.1176/appi.ajp.161.4.692
8. Lafeuille MH, Dean J, Carter V, et al. Systematic review of long-acting injectables versus oral atypical antipsychotics on hospitalization in schizophrenia. Curr Med Res Opin. 2014;30(8):1643-1655. doi:10.1185/03007995.2014.915211
9. Yu W, Wagner TH, Chen S, Barnett PG. Average cost of VA rehabilitation, mental health, and long-term hospital stays. Med Care Res Rev. 2003;60(3 suppl):40S-53S. doi:10.1177/1077558703256724
10. Duncan EJ, Woolson SL, Hamer RM. Treatment compliance in veterans administration schizophrenia spectrum patients treated with risperidone long-acting injectable. Int Clin Psychopharmacol. 2012;27(5):283-290. doi:10.1097/YIC.0b013e328354b534
11. Romstadt N, Wonson E. Outcomes comparison of long-acting injectable antipsychotic initiation in treatment-naïve veterans in the inpatient versus outpatient setting. Ment Health Clin. 2018;8(1):24-27. doi:10.9740/mhc.2018.01.024
12. Dimitropoulos E, Drogemuller L, Wong K. Evaluation of concurrent oral and long-acting injectable antipsychotic prescribing at the Minneapolis Veterans Affairs Health Care System. J Clin Psychopharmacol. 2017;37(5):605-608. doi:10.1097/JCP.0000000000000755
13. Marcus SC, Zummo J, Pettit AR, Stoddard J, Doshi JA. Antipsychotic adherence and rehospitalization in schizophrenia patients receiving oral versus long-acting injectable antipsychotics following hospital discharge. J Manag Care Spec Pharm. 2015;21(9):754-768. doi:10.18553/jmcp.2015.21.9.754
14. Risperdal Consta. Package insert. Janssen Pharmaceutical; 2007.
15. Invega Sustenna. Package insert. Janssen Pharmaceutical; 2009.
16. Limosin F, Belhadi D, Comet D, et al. Comparison of paliperidone palmitate and risperidone long-acting injection in schizophrenic patients: results from a multicenter retrospective cohort study in France. J Clin Psychopharmacol. 2018;38(1):19-26. doi:10.1097/JCP.0000000000000827
17. Joshi K, Pan X, Wang R, Yang E, Benson C. Healthcare resource utilization of second-generation long-acting injectable antipsychotics in schizophrenia: risperidone versus paliperidone palmitate. Curr Med Res Opin. 2016;32(11):1873-1881. doi: 10.1080/03007995.2016.1219706
18. Korell J, Green B, Remmerie B, Vermeulen A. Determination of plasma concentration reference ranges for risperidone and paliperidone. CPT Pharmacometrics Syst Pharmacol. 2017;6(9):589-595. doi:10.1002/psp4.12217
19. Gopal S, Pandina G, Lane R, et al. A post-hoc comparison of paliperidone palmitate to oral risperidone during initiation of long-acting risperidone injection in patients with acute schizophrenia. Innov Clin Neurosci. 2011;8(8):26-33.
20. Marcus SC, Zummo J, Pettit AR, Stoddard J, Doshi JA. Antipsychotic adherence and rehospitalization in schizophrenia patients receiving oral versus long-acting injectable antipsychotics following hospital discharge. J Manag Care Spec Pharm. 2015;21(9):754-768. doi:10.18553/jmcp.2015.21.9.754
21. Romstadt N, Wonson E. Outcomes comparison of long-acting injectable antipsychotic initiation in treatment-naïve veterans in the inpatient versus outpatient setting. Ment Health Clin. 2018;8(1):24-27. doi:10.9740/mhc.2018.01.024
22. Green AI, Brunette MF, Dawson R, et al. Long-acting injectable vs oral risperidone for schizophrenia and co-occurring alcohol use disorder: a randomized trial. J Clin Psychiatry. 2015;76(10):1359-1365. doi:10.4088/JCP.13m08838
23. Rezansoff SN, Moniruzzaman A, Fazel S, Procyshyn R, Somers JM. Adherence to antipsychotic medication among homeless adults in Vancouver, Canada: a 15-year retrospective cohort study. Soc Psychiatry Psychiatr Epidemiol. 2016;51(12):1623-1632. doi:10.1007/s00127-016-1259-7
24. Castillo EG, Stroup TS. Effectiveness of long-acting injectable antipsychotics: a clinical perspective. Evid Based Ment Health. 2015;18(2):36-39. doi:10.1136/eb-2015-102086
25. Marder SR. Overview of partial compliance. J Clin Psychiatry. 2003;64 (suppl 16):3-9.
26. Wehring HJ, Thedford S, Koola M, Kelly DL. Patient and health care provider perspectives on long acting injectable antipsychotics in schizophrenia and the introduction of olanzapine long-acting injection. J Cent Nerv Syst Dis. 2011;2011(3):107-123. doi:10.4137/JCNSD.S4091
27. Berwaerts J, Liu Y, Gopal S, et al. Efficacy and safety of the 3-month formulation of paliperidone palmitate vs placebo for relapse prevention of schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2015;72(8):830-839. doi:10.1001/jamapsychiatry.2015.0241
28. Parellada E, Bioque M. Barriers to the use of long-acting injectable antipsychotics in the management of schizophrenia. CNS Drugs. 2016;30(8):689-701. doi:10.1007/s40263-016-0350-7
1. Lehman AF, Lieberman JA, Dixon LB, et al; American Psychiatric Association Steering Committee on Practice Guidelines. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry. 2004;161(suppl 2):1-56.
2. Lieberman JA, Stroup TS, McEvoy JP, et al; Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209-1223. doi:10.1056/NEJMoa051688
3. Swartz MS, Stroup TS, McEvoy JP, et al. What CATIE found: results from the schizophrenia trial. Psychiatr Serv. 2008;59(5):500-506. doi:10.1176/ps.2008.59.5.500
4. Haywood TW, Kravitz HM, Grossman LS, Cavanaugh JL Jr, Davis JM, Lewis DA. Predicting the “revolving door” phenomenon among patients with schizophrenic, schizoaffective, and affective disorders. Am J Psychiatry. 1995;152(6):856-561. doi:10.1176/ajp.152.6.856
5. Morken G, Widen JH, Grawe RW. Non-adherence to antipsychotic medication, relapse and rehospitalisation in recent-onset schizophrenia. BMC Psychiatry. 2008;8:32. doi:10.1186/1471-244X-8-32
6. Weiden PJ, Kozma C, Grogg A, Locklear J. Partial compliance and risk of rehospitalization among California Medicaid patients with schizophrenia. Psychiatr Serv. 2004;55(8):886-891. doi:10.1176/appi.ps.55.8.886
7. Gilmer TP, Dolder CR, Lacro JP, et al. Adherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophrenia. Am J Psychiatry. 2004;161(4):692-699. doi:10.1176/appi.ajp.161.4.692
8. Lafeuille MH, Dean J, Carter V, et al. Systematic review of long-acting injectables versus oral atypical antipsychotics on hospitalization in schizophrenia. Curr Med Res Opin. 2014;30(8):1643-1655. doi:10.1185/03007995.2014.915211
9. Yu W, Wagner TH, Chen S, Barnett PG. Average cost of VA rehabilitation, mental health, and long-term hospital stays. Med Care Res Rev. 2003;60(3 suppl):40S-53S. doi:10.1177/1077558703256724
10. Duncan EJ, Woolson SL, Hamer RM. Treatment compliance in veterans administration schizophrenia spectrum patients treated with risperidone long-acting injectable. Int Clin Psychopharmacol. 2012;27(5):283-290. doi:10.1097/YIC.0b013e328354b534
11. Romstadt N, Wonson E. Outcomes comparison of long-acting injectable antipsychotic initiation in treatment-naïve veterans in the inpatient versus outpatient setting. Ment Health Clin. 2018;8(1):24-27. doi:10.9740/mhc.2018.01.024
12. Dimitropoulos E, Drogemuller L, Wong K. Evaluation of concurrent oral and long-acting injectable antipsychotic prescribing at the Minneapolis Veterans Affairs Health Care System. J Clin Psychopharmacol. 2017;37(5):605-608. doi:10.1097/JCP.0000000000000755
13. Marcus SC, Zummo J, Pettit AR, Stoddard J, Doshi JA. Antipsychotic adherence and rehospitalization in schizophrenia patients receiving oral versus long-acting injectable antipsychotics following hospital discharge. J Manag Care Spec Pharm. 2015;21(9):754-768. doi:10.18553/jmcp.2015.21.9.754
14. Risperdal Consta. Package insert. Janssen Pharmaceutical; 2007.
15. Invega Sustenna. Package insert. Janssen Pharmaceutical; 2009.
16. Limosin F, Belhadi D, Comet D, et al. Comparison of paliperidone palmitate and risperidone long-acting injection in schizophrenic patients: results from a multicenter retrospective cohort study in France. J Clin Psychopharmacol. 2018;38(1):19-26. doi:10.1097/JCP.0000000000000827
17. Joshi K, Pan X, Wang R, Yang E, Benson C. Healthcare resource utilization of second-generation long-acting injectable antipsychotics in schizophrenia: risperidone versus paliperidone palmitate. Curr Med Res Opin. 2016;32(11):1873-1881. doi: 10.1080/03007995.2016.1219706
18. Korell J, Green B, Remmerie B, Vermeulen A. Determination of plasma concentration reference ranges for risperidone and paliperidone. CPT Pharmacometrics Syst Pharmacol. 2017;6(9):589-595. doi:10.1002/psp4.12217
19. Gopal S, Pandina G, Lane R, et al. A post-hoc comparison of paliperidone palmitate to oral risperidone during initiation of long-acting risperidone injection in patients with acute schizophrenia. Innov Clin Neurosci. 2011;8(8):26-33.
20. Marcus SC, Zummo J, Pettit AR, Stoddard J, Doshi JA. Antipsychotic adherence and rehospitalization in schizophrenia patients receiving oral versus long-acting injectable antipsychotics following hospital discharge. J Manag Care Spec Pharm. 2015;21(9):754-768. doi:10.18553/jmcp.2015.21.9.754
21. Romstadt N, Wonson E. Outcomes comparison of long-acting injectable antipsychotic initiation in treatment-naïve veterans in the inpatient versus outpatient setting. Ment Health Clin. 2018;8(1):24-27. doi:10.9740/mhc.2018.01.024
22. Green AI, Brunette MF, Dawson R, et al. Long-acting injectable vs oral risperidone for schizophrenia and co-occurring alcohol use disorder: a randomized trial. J Clin Psychiatry. 2015;76(10):1359-1365. doi:10.4088/JCP.13m08838
23. Rezansoff SN, Moniruzzaman A, Fazel S, Procyshyn R, Somers JM. Adherence to antipsychotic medication among homeless adults in Vancouver, Canada: a 15-year retrospective cohort study. Soc Psychiatry Psychiatr Epidemiol. 2016;51(12):1623-1632. doi:10.1007/s00127-016-1259-7
24. Castillo EG, Stroup TS. Effectiveness of long-acting injectable antipsychotics: a clinical perspective. Evid Based Ment Health. 2015;18(2):36-39. doi:10.1136/eb-2015-102086
25. Marder SR. Overview of partial compliance. J Clin Psychiatry. 2003;64 (suppl 16):3-9.
26. Wehring HJ, Thedford S, Koola M, Kelly DL. Patient and health care provider perspectives on long acting injectable antipsychotics in schizophrenia and the introduction of olanzapine long-acting injection. J Cent Nerv Syst Dis. 2011;2011(3):107-123. doi:10.4137/JCNSD.S4091
27. Berwaerts J, Liu Y, Gopal S, et al. Efficacy and safety of the 3-month formulation of paliperidone palmitate vs placebo for relapse prevention of schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2015;72(8):830-839. doi:10.1001/jamapsychiatry.2015.0241
28. Parellada E, Bioque M. Barriers to the use of long-acting injectable antipsychotics in the management of schizophrenia. CNS Drugs. 2016;30(8):689-701. doi:10.1007/s40263-016-0350-7
Advocating for children’s health, one page at a time
Everyone can remember a book from their childhood that helped transform them, reinvent them, or turned the world on its head. Characters such as Harry Potter, Franklin the Turtle, Matilda, the Very Hungry Caterpillar, Corduroy, and Nancy Drew, among others, continue to exist in the cultural zeitgeist because they remind us of our childhood and the experience of discovering something innovative and exciting for the first time.
For many young children, introductions to these timeless characters first come from an adult reading to them. Those interactions, starting with watching mouths form words, to exploring pictures, to eventually reading along, leave a lasting impression. “Adults remember being read to,” says pediatrician Perri Klass, MD. “It’s a very powerful thing.”
Dr. Klass serves as national medical director of Reach Out and Read, a nonprofit organization that champions the positive effects of reading and other language-rich activities with young children.
And what better partners to involve in this mission than pediatricians? Before a child reaches the age of 4, the U.S. Department of Health and Human Services recommends that a child visit the pediatrician at least seven times. The Bright Futures/American Academy of Pediatrics suggests as many as 13 pediatrician visits before the child reaches that same milestone. Regardless of the exact number, almost all children are encountering a pediatrician multiple times during the most crucial years of their brain development.
In 1989, physicians Barry Zuckerman, MD, and Robert Needleman, MD, at Boston City Hospital (now Boston Medical Center) realized that they could reach a large population of children and parents, especially those coming from disadvantaged backgrounds, in the pediatrics ward of offices and hospitals all over the country.
The design of Reach Out and Read, the organization they founded, is to work with pediatricians in how they can best support parents in making reading to their children a part of their daily routine, advocating for the importance of books for children, and making sure that a child leaves the office with a book to take home.
Rather than just dumping books onto nervous or busy parents, the organization trains doctors on how to teach parents to read to their children: how to hold the books, how to make it as active as possible, how to point to the pictures and make them come to life, and how to make sure the child is grasping the language.
“You don’t just prop a baby up and read to them,” Dr. Klass told this news organization. “You have to make it interactive.”
Physician-driven success
Now an international organization, Dr. Klass has watched the nonprofit grow tremendously since it began during her fellowship in Boston over three decades ago. The initiative has over 6,100 sites in all 50 states and is able to get books into the hands of 4.2 million children every single year through government aid, individual contributions, and in-kind donations. On average, the organization is able to give parents 6.4 million books annually. Half of the children served every year by the program come from low-income backgrounds.
Dr. Klass ascribed some of the organization’s longevity and success to “practical realism,” its “mission-driven” approach, and its creation by people in primary care who understood the constraints, the upkeep, and the scaling.
“Our organization isn’t looking to pile 10 more things on to the hands of pediatricians who are already very busy,” she said. “We understand that conversation is important with our care providers. We always hear that watching children happily interacting with literature is one of the most rewarding parts of their job. So, we’re saying to them, ‘I want to help you do what you enjoy most.’”
Both Dr. Klass, who is also a presidential appointee to the Advisory Board of the National Institute For Literacy, and Brian Gallagher, MPA, the CEO of Reach Out and Read, said one of the most rewarding parts of their attachment to the organization is working with dedicated physicians all over the country.
“We hear all the time that physicians say working with these tools [from Reach Out and Read] is the most joyful part of their day,” said Mr. Gallagher. “Children are hope for the future and books help them grow.”
Amy Shriver, MD, an Iowa pediatrician and medical director of the Reach Out and Read Iowa Board, admitted that at first she just thought of the organization as a book drive. As Dr. Shriver got closer to the organization, though, she realized how she could utilize the book as a surveillance tool.
“At 6 months through 2 years, I hand the book to the patient, and I can always tell which children are familiar with books by their responses,” she said. After learning about and implementing Reach Out and Read’s ‘model, observe, coach’ methodology, Dr. Shriver said she was wowed by how much it helped families who weren’t reading to their child understand not only how to read with their children but why it’s so important.”
Dr. Shriver said that her clinic has purchased more diverse books to meet the needs of its patient population and has partnered with local libraries and a science center to promote early brain development. The biggest change is that Dr. Shriver finds herself spending more time observing and talking about parent/child relationships since starting with Reach Out and Read.
Mr. Gallagher attributed the organization’s success to the massive amounts of research that back up the practices of the organization. “Our model isn’t just a nice thing to do,” Mr. Gallagher said. “Our practice has been proven to be effective, and that’s why pediatricians continue to work with us. We’ve heard experts say that when they’re advocating for children’s health, they say ‘vaccines, sleep, and Reach Out and Read.’”
Nineteen independent studies have been done profiling the work of Reach Out and Read since its inception. The research has shown that exposure to the organization results in parents reading more often to their children, higher language scores, as well as an improvement in clinic culture and clinician well-being.
In 2014, the American Academy of Pediatrics quoted the research of Reach Out and Read in its policy statement “Literacy Promotion: An Essential Component of Primary Care Pediatric Practice,” which argued that pediatrics should advocate for literacy from birth. The abstract of the study suggests that practicing pediatricians “advise all parents that reading aloud with young children can enhance parent-child relationships and prepare young minds to learn language and early literacy skills ... provide developmentally appropriate books given at health supervision visits for all high-risk, low-income young children ... partnering with other child advocates to influence national messaging and policies that support and promote these key, early shared-reading experiences.”
Adapting to benefit children and parents
Reach Out and Read is not afraid to change with the times. When it began in 1989, there was no guidance for pediatricians on the importance of reading. Mr. Gallagher said that a common question Reach Out and Read received was, “Why not focus on physical health?” The organization was more interested in the shift in pediatric practice overtime.
“We used to advocate starting off kids with books at 6 months old, but we always listen to the research,” Mr. Gallagher said. Now, the organization as well as the American Academy of Pediatrics advocate for beginning at birth. Other publications such as Green Child Magazine and Psychology Today speak of the importance of reading to babies still in the womb. The Proceedings of the National Academy of Sciences published an article in 2013 that suggests that third-trimester babies can not only pick up on language patterns but also can identify words first heard in the womb.
“We aren’t afraid to adjust our practice if it will be more effective and beneficial for children,” Mr. Gallagher said, “We follow the research and share the work that we are doing. It’s important to stay as up to date as possible.”
Although the focus is largely on the health of children, the impact on parents is crucial as well. Mr. Gallagher described the books at the center of the mission as “a vehicle for bonding” between parents and their children. “The relationship-building we see between families is truly quite magical,” he said.
“Parents will say it’s a respite in their day,” Dr. Klass said of the daily practice of reading aloud. She recalled a memory of talking to a mother with two rowdy young boys, who would sit down and read to them, immediately calming them down.
“When parents sit down to read to their children they don’t have to make anything up. It’s a script, it’s a prompt. You have this story, a picture to show. And kids get preferences,” she said. “When they pick a book that they want you to read, they get to exercise some control. It’s a satisfying routine for parents. It helps open up the world to your child. And when kids come over and hand a book to you for you to read together, it’s them saying, ‘I like the way you look, sound, and interact with me when we do this together.’”
A study from Ambulatory Pediatrics demonstrated that families working with Reach Out and Read were more likely to report reading aloud at bedtime, to read aloud three or more days per week, to mention reading aloud as a favorite parenting activity, and to own 10 or more children’s books. The American Journal of Diseases for Children, in a 1991 article co-authored by Needleman and Zuckerman, noted that the effects of Reach Out and Read were greater for those families who were receiving Aid to Families with Dependent Children. In 2015, the Pew Research Center unveiled a report, “Parenting in America” on raising a child in the modern age, the first generation in American history expected, on average, to make less than their parents.
The report stated that “a broad, demographically-based look at the landscape of American families reveals stark parenting divides linked less to philosophies or values and more to economic circumstances and changing family structure.”
As questions of access and privilege loom over the growing world of education, Reach Out and Read is trying to shorten the gap one book at a time. They are hoping, in time, that their model will be able to reach 90% of children in the United States and foster a relationship with reading and protecting children from toxic stress.
“Every time I look at a newborn, I think about the power of relationships,” said Dr. Shriver, the Iowa-based pediatrician. “I think about how much love passes between infants and their parents, and how shared reading is such a powerful way to show our children we love them. I know from my own experiences how good it feels to snuggle every night and read together. Those moments when the world falls away, and it’s just you, your child, and a book are magical.”
“I want every parent and child to have that experience and create those loving memories. I want all children to feel safe, secure, and loved. I want every child to have the opportunity to use books as a mirror to see themselves and as a window to see the world.”
A version of this article first appeared on Medscape.com.
Everyone can remember a book from their childhood that helped transform them, reinvent them, or turned the world on its head. Characters such as Harry Potter, Franklin the Turtle, Matilda, the Very Hungry Caterpillar, Corduroy, and Nancy Drew, among others, continue to exist in the cultural zeitgeist because they remind us of our childhood and the experience of discovering something innovative and exciting for the first time.
For many young children, introductions to these timeless characters first come from an adult reading to them. Those interactions, starting with watching mouths form words, to exploring pictures, to eventually reading along, leave a lasting impression. “Adults remember being read to,” says pediatrician Perri Klass, MD. “It’s a very powerful thing.”
Dr. Klass serves as national medical director of Reach Out and Read, a nonprofit organization that champions the positive effects of reading and other language-rich activities with young children.
And what better partners to involve in this mission than pediatricians? Before a child reaches the age of 4, the U.S. Department of Health and Human Services recommends that a child visit the pediatrician at least seven times. The Bright Futures/American Academy of Pediatrics suggests as many as 13 pediatrician visits before the child reaches that same milestone. Regardless of the exact number, almost all children are encountering a pediatrician multiple times during the most crucial years of their brain development.
In 1989, physicians Barry Zuckerman, MD, and Robert Needleman, MD, at Boston City Hospital (now Boston Medical Center) realized that they could reach a large population of children and parents, especially those coming from disadvantaged backgrounds, in the pediatrics ward of offices and hospitals all over the country.
The design of Reach Out and Read, the organization they founded, is to work with pediatricians in how they can best support parents in making reading to their children a part of their daily routine, advocating for the importance of books for children, and making sure that a child leaves the office with a book to take home.
Rather than just dumping books onto nervous or busy parents, the organization trains doctors on how to teach parents to read to their children: how to hold the books, how to make it as active as possible, how to point to the pictures and make them come to life, and how to make sure the child is grasping the language.
“You don’t just prop a baby up and read to them,” Dr. Klass told this news organization. “You have to make it interactive.”
Physician-driven success
Now an international organization, Dr. Klass has watched the nonprofit grow tremendously since it began during her fellowship in Boston over three decades ago. The initiative has over 6,100 sites in all 50 states and is able to get books into the hands of 4.2 million children every single year through government aid, individual contributions, and in-kind donations. On average, the organization is able to give parents 6.4 million books annually. Half of the children served every year by the program come from low-income backgrounds.
Dr. Klass ascribed some of the organization’s longevity and success to “practical realism,” its “mission-driven” approach, and its creation by people in primary care who understood the constraints, the upkeep, and the scaling.
“Our organization isn’t looking to pile 10 more things on to the hands of pediatricians who are already very busy,” she said. “We understand that conversation is important with our care providers. We always hear that watching children happily interacting with literature is one of the most rewarding parts of their job. So, we’re saying to them, ‘I want to help you do what you enjoy most.’”
Both Dr. Klass, who is also a presidential appointee to the Advisory Board of the National Institute For Literacy, and Brian Gallagher, MPA, the CEO of Reach Out and Read, said one of the most rewarding parts of their attachment to the organization is working with dedicated physicians all over the country.
“We hear all the time that physicians say working with these tools [from Reach Out and Read] is the most joyful part of their day,” said Mr. Gallagher. “Children are hope for the future and books help them grow.”
Amy Shriver, MD, an Iowa pediatrician and medical director of the Reach Out and Read Iowa Board, admitted that at first she just thought of the organization as a book drive. As Dr. Shriver got closer to the organization, though, she realized how she could utilize the book as a surveillance tool.
“At 6 months through 2 years, I hand the book to the patient, and I can always tell which children are familiar with books by their responses,” she said. After learning about and implementing Reach Out and Read’s ‘model, observe, coach’ methodology, Dr. Shriver said she was wowed by how much it helped families who weren’t reading to their child understand not only how to read with their children but why it’s so important.”
Dr. Shriver said that her clinic has purchased more diverse books to meet the needs of its patient population and has partnered with local libraries and a science center to promote early brain development. The biggest change is that Dr. Shriver finds herself spending more time observing and talking about parent/child relationships since starting with Reach Out and Read.
Mr. Gallagher attributed the organization’s success to the massive amounts of research that back up the practices of the organization. “Our model isn’t just a nice thing to do,” Mr. Gallagher said. “Our practice has been proven to be effective, and that’s why pediatricians continue to work with us. We’ve heard experts say that when they’re advocating for children’s health, they say ‘vaccines, sleep, and Reach Out and Read.’”
Nineteen independent studies have been done profiling the work of Reach Out and Read since its inception. The research has shown that exposure to the organization results in parents reading more often to their children, higher language scores, as well as an improvement in clinic culture and clinician well-being.
In 2014, the American Academy of Pediatrics quoted the research of Reach Out and Read in its policy statement “Literacy Promotion: An Essential Component of Primary Care Pediatric Practice,” which argued that pediatrics should advocate for literacy from birth. The abstract of the study suggests that practicing pediatricians “advise all parents that reading aloud with young children can enhance parent-child relationships and prepare young minds to learn language and early literacy skills ... provide developmentally appropriate books given at health supervision visits for all high-risk, low-income young children ... partnering with other child advocates to influence national messaging and policies that support and promote these key, early shared-reading experiences.”
Adapting to benefit children and parents
Reach Out and Read is not afraid to change with the times. When it began in 1989, there was no guidance for pediatricians on the importance of reading. Mr. Gallagher said that a common question Reach Out and Read received was, “Why not focus on physical health?” The organization was more interested in the shift in pediatric practice overtime.
“We used to advocate starting off kids with books at 6 months old, but we always listen to the research,” Mr. Gallagher said. Now, the organization as well as the American Academy of Pediatrics advocate for beginning at birth. Other publications such as Green Child Magazine and Psychology Today speak of the importance of reading to babies still in the womb. The Proceedings of the National Academy of Sciences published an article in 2013 that suggests that third-trimester babies can not only pick up on language patterns but also can identify words first heard in the womb.
“We aren’t afraid to adjust our practice if it will be more effective and beneficial for children,” Mr. Gallagher said, “We follow the research and share the work that we are doing. It’s important to stay as up to date as possible.”
Although the focus is largely on the health of children, the impact on parents is crucial as well. Mr. Gallagher described the books at the center of the mission as “a vehicle for bonding” between parents and their children. “The relationship-building we see between families is truly quite magical,” he said.
“Parents will say it’s a respite in their day,” Dr. Klass said of the daily practice of reading aloud. She recalled a memory of talking to a mother with two rowdy young boys, who would sit down and read to them, immediately calming them down.
“When parents sit down to read to their children they don’t have to make anything up. It’s a script, it’s a prompt. You have this story, a picture to show. And kids get preferences,” she said. “When they pick a book that they want you to read, they get to exercise some control. It’s a satisfying routine for parents. It helps open up the world to your child. And when kids come over and hand a book to you for you to read together, it’s them saying, ‘I like the way you look, sound, and interact with me when we do this together.’”
A study from Ambulatory Pediatrics demonstrated that families working with Reach Out and Read were more likely to report reading aloud at bedtime, to read aloud three or more days per week, to mention reading aloud as a favorite parenting activity, and to own 10 or more children’s books. The American Journal of Diseases for Children, in a 1991 article co-authored by Needleman and Zuckerman, noted that the effects of Reach Out and Read were greater for those families who were receiving Aid to Families with Dependent Children. In 2015, the Pew Research Center unveiled a report, “Parenting in America” on raising a child in the modern age, the first generation in American history expected, on average, to make less than their parents.
The report stated that “a broad, demographically-based look at the landscape of American families reveals stark parenting divides linked less to philosophies or values and more to economic circumstances and changing family structure.”
As questions of access and privilege loom over the growing world of education, Reach Out and Read is trying to shorten the gap one book at a time. They are hoping, in time, that their model will be able to reach 90% of children in the United States and foster a relationship with reading and protecting children from toxic stress.
“Every time I look at a newborn, I think about the power of relationships,” said Dr. Shriver, the Iowa-based pediatrician. “I think about how much love passes between infants and their parents, and how shared reading is such a powerful way to show our children we love them. I know from my own experiences how good it feels to snuggle every night and read together. Those moments when the world falls away, and it’s just you, your child, and a book are magical.”
“I want every parent and child to have that experience and create those loving memories. I want all children to feel safe, secure, and loved. I want every child to have the opportunity to use books as a mirror to see themselves and as a window to see the world.”
A version of this article first appeared on Medscape.com.
Everyone can remember a book from their childhood that helped transform them, reinvent them, or turned the world on its head. Characters such as Harry Potter, Franklin the Turtle, Matilda, the Very Hungry Caterpillar, Corduroy, and Nancy Drew, among others, continue to exist in the cultural zeitgeist because they remind us of our childhood and the experience of discovering something innovative and exciting for the first time.
For many young children, introductions to these timeless characters first come from an adult reading to them. Those interactions, starting with watching mouths form words, to exploring pictures, to eventually reading along, leave a lasting impression. “Adults remember being read to,” says pediatrician Perri Klass, MD. “It’s a very powerful thing.”
Dr. Klass serves as national medical director of Reach Out and Read, a nonprofit organization that champions the positive effects of reading and other language-rich activities with young children.
And what better partners to involve in this mission than pediatricians? Before a child reaches the age of 4, the U.S. Department of Health and Human Services recommends that a child visit the pediatrician at least seven times. The Bright Futures/American Academy of Pediatrics suggests as many as 13 pediatrician visits before the child reaches that same milestone. Regardless of the exact number, almost all children are encountering a pediatrician multiple times during the most crucial years of their brain development.
In 1989, physicians Barry Zuckerman, MD, and Robert Needleman, MD, at Boston City Hospital (now Boston Medical Center) realized that they could reach a large population of children and parents, especially those coming from disadvantaged backgrounds, in the pediatrics ward of offices and hospitals all over the country.
The design of Reach Out and Read, the organization they founded, is to work with pediatricians in how they can best support parents in making reading to their children a part of their daily routine, advocating for the importance of books for children, and making sure that a child leaves the office with a book to take home.
Rather than just dumping books onto nervous or busy parents, the organization trains doctors on how to teach parents to read to their children: how to hold the books, how to make it as active as possible, how to point to the pictures and make them come to life, and how to make sure the child is grasping the language.
“You don’t just prop a baby up and read to them,” Dr. Klass told this news organization. “You have to make it interactive.”
Physician-driven success
Now an international organization, Dr. Klass has watched the nonprofit grow tremendously since it began during her fellowship in Boston over three decades ago. The initiative has over 6,100 sites in all 50 states and is able to get books into the hands of 4.2 million children every single year through government aid, individual contributions, and in-kind donations. On average, the organization is able to give parents 6.4 million books annually. Half of the children served every year by the program come from low-income backgrounds.
Dr. Klass ascribed some of the organization’s longevity and success to “practical realism,” its “mission-driven” approach, and its creation by people in primary care who understood the constraints, the upkeep, and the scaling.
“Our organization isn’t looking to pile 10 more things on to the hands of pediatricians who are already very busy,” she said. “We understand that conversation is important with our care providers. We always hear that watching children happily interacting with literature is one of the most rewarding parts of their job. So, we’re saying to them, ‘I want to help you do what you enjoy most.’”
Both Dr. Klass, who is also a presidential appointee to the Advisory Board of the National Institute For Literacy, and Brian Gallagher, MPA, the CEO of Reach Out and Read, said one of the most rewarding parts of their attachment to the organization is working with dedicated physicians all over the country.
“We hear all the time that physicians say working with these tools [from Reach Out and Read] is the most joyful part of their day,” said Mr. Gallagher. “Children are hope for the future and books help them grow.”
Amy Shriver, MD, an Iowa pediatrician and medical director of the Reach Out and Read Iowa Board, admitted that at first she just thought of the organization as a book drive. As Dr. Shriver got closer to the organization, though, she realized how she could utilize the book as a surveillance tool.
“At 6 months through 2 years, I hand the book to the patient, and I can always tell which children are familiar with books by their responses,” she said. After learning about and implementing Reach Out and Read’s ‘model, observe, coach’ methodology, Dr. Shriver said she was wowed by how much it helped families who weren’t reading to their child understand not only how to read with their children but why it’s so important.”
Dr. Shriver said that her clinic has purchased more diverse books to meet the needs of its patient population and has partnered with local libraries and a science center to promote early brain development. The biggest change is that Dr. Shriver finds herself spending more time observing and talking about parent/child relationships since starting with Reach Out and Read.
Mr. Gallagher attributed the organization’s success to the massive amounts of research that back up the practices of the organization. “Our model isn’t just a nice thing to do,” Mr. Gallagher said. “Our practice has been proven to be effective, and that’s why pediatricians continue to work with us. We’ve heard experts say that when they’re advocating for children’s health, they say ‘vaccines, sleep, and Reach Out and Read.’”
Nineteen independent studies have been done profiling the work of Reach Out and Read since its inception. The research has shown that exposure to the organization results in parents reading more often to their children, higher language scores, as well as an improvement in clinic culture and clinician well-being.
In 2014, the American Academy of Pediatrics quoted the research of Reach Out and Read in its policy statement “Literacy Promotion: An Essential Component of Primary Care Pediatric Practice,” which argued that pediatrics should advocate for literacy from birth. The abstract of the study suggests that practicing pediatricians “advise all parents that reading aloud with young children can enhance parent-child relationships and prepare young minds to learn language and early literacy skills ... provide developmentally appropriate books given at health supervision visits for all high-risk, low-income young children ... partnering with other child advocates to influence national messaging and policies that support and promote these key, early shared-reading experiences.”
Adapting to benefit children and parents
Reach Out and Read is not afraid to change with the times. When it began in 1989, there was no guidance for pediatricians on the importance of reading. Mr. Gallagher said that a common question Reach Out and Read received was, “Why not focus on physical health?” The organization was more interested in the shift in pediatric practice overtime.
“We used to advocate starting off kids with books at 6 months old, but we always listen to the research,” Mr. Gallagher said. Now, the organization as well as the American Academy of Pediatrics advocate for beginning at birth. Other publications such as Green Child Magazine and Psychology Today speak of the importance of reading to babies still in the womb. The Proceedings of the National Academy of Sciences published an article in 2013 that suggests that third-trimester babies can not only pick up on language patterns but also can identify words first heard in the womb.
“We aren’t afraid to adjust our practice if it will be more effective and beneficial for children,” Mr. Gallagher said, “We follow the research and share the work that we are doing. It’s important to stay as up to date as possible.”
Although the focus is largely on the health of children, the impact on parents is crucial as well. Mr. Gallagher described the books at the center of the mission as “a vehicle for bonding” between parents and their children. “The relationship-building we see between families is truly quite magical,” he said.
“Parents will say it’s a respite in their day,” Dr. Klass said of the daily practice of reading aloud. She recalled a memory of talking to a mother with two rowdy young boys, who would sit down and read to them, immediately calming them down.
“When parents sit down to read to their children they don’t have to make anything up. It’s a script, it’s a prompt. You have this story, a picture to show. And kids get preferences,” she said. “When they pick a book that they want you to read, they get to exercise some control. It’s a satisfying routine for parents. It helps open up the world to your child. And when kids come over and hand a book to you for you to read together, it’s them saying, ‘I like the way you look, sound, and interact with me when we do this together.’”
A study from Ambulatory Pediatrics demonstrated that families working with Reach Out and Read were more likely to report reading aloud at bedtime, to read aloud three or more days per week, to mention reading aloud as a favorite parenting activity, and to own 10 or more children’s books. The American Journal of Diseases for Children, in a 1991 article co-authored by Needleman and Zuckerman, noted that the effects of Reach Out and Read were greater for those families who were receiving Aid to Families with Dependent Children. In 2015, the Pew Research Center unveiled a report, “Parenting in America” on raising a child in the modern age, the first generation in American history expected, on average, to make less than their parents.
The report stated that “a broad, demographically-based look at the landscape of American families reveals stark parenting divides linked less to philosophies or values and more to economic circumstances and changing family structure.”
As questions of access and privilege loom over the growing world of education, Reach Out and Read is trying to shorten the gap one book at a time. They are hoping, in time, that their model will be able to reach 90% of children in the United States and foster a relationship with reading and protecting children from toxic stress.
“Every time I look at a newborn, I think about the power of relationships,” said Dr. Shriver, the Iowa-based pediatrician. “I think about how much love passes between infants and their parents, and how shared reading is such a powerful way to show our children we love them. I know from my own experiences how good it feels to snuggle every night and read together. Those moments when the world falls away, and it’s just you, your child, and a book are magical.”
“I want every parent and child to have that experience and create those loving memories. I want all children to feel safe, secure, and loved. I want every child to have the opportunity to use books as a mirror to see themselves and as a window to see the world.”
A version of this article first appeared on Medscape.com.
The imperfections of being perfect: Recognizing high-functioning anxiety
Motivated, calm, and high-functioning. On the surface, you are the epitome of success. You arrive at work early. You are driven, meet all deadlines and, in fact, excel at tasks. Not only are you successful in your work, but also you appear well put-together – not a single hair out of place. You have a busy social life, always smiling, laughing, or generally in an uplifting mood. On the surface, you have everything together.
Inside, you’re drowning. You’re in constant survival mode – always overthinking, ruminating, and fearful. Your need for self-preservation is in overdrive. You use your anxiety and fear as motivation. You are a people pleaser, need constant reassurance, and are unable to enjoy the present moment. You have an inability to say no regardless of your overloaded schedule. You are mentally and physically fatigued and overworked beyond the brink of exhaustion. You need to take time off but can’t bring yourself to do so. Others wouldn’t see you in this light because you always appear to be doing well.
The portraits I’ve painted here sound like two different people, but in fact are representative of one. High-functioning anxiety, while not a formal health diagnosis, is a term that broadly encapsulates individuals who experience anxiety but also function well in their day-to-day lives. On the surface, They are perceived as overachievers, but this perception fails to recognize and acknowledge the mental health toll required to achieve at such a high level.
I came across this concept when a friend sent me a post on social media. It was a completely new but oddly familiar concept when I first read about high-functioning anxiety. In fact, I related to this concept almost immediately based on interactions with friends and colleagues, and their recollection of stressors over the years in high-stress, high-functioning environments.
In addition to personal interactions, I’ve seen anxiety and mental health at large become more “normalized” on various platforms (e.g., Instagram, TikTok) over the years. Interestingly, normalizing these concepts could be beneficial. For example, they increase awareness, encourage conversations (e.g., creating communities), and minimize the barriers toward understanding and respecting individuals who experience high-functioning anxiety. However, social media also has the potential to be harmful (e.g., “humorizing” the concept or turning it into memes, diminishing the experience).
However, the question that nagged at my mind even further was: What reasons are there, if any, for why high-functioning anxiety is not recognized as a formal diagnosis? Is this concept too new? Difficult to diagnose? Anecdotal evidence seems to suggest that high-functioning anxiety is debilitating and impairs one’s quality of life. There appears to be a need to formally recognize this subtype of anxiety and invest more time and research. Increasing the sphere of knowledge may bring more good than harm, as a way to let others know that it’s okay.
Ms. Lui is an MSc candidate at the University of Toronto and is with the mood disorders psychopharmacology unit, Toronto Western Hospital, University Health Network, also in Toronto. She reported receiving income from Braxia Scientific.
A version of this article first appeared on Medscape.com.
Motivated, calm, and high-functioning. On the surface, you are the epitome of success. You arrive at work early. You are driven, meet all deadlines and, in fact, excel at tasks. Not only are you successful in your work, but also you appear well put-together – not a single hair out of place. You have a busy social life, always smiling, laughing, or generally in an uplifting mood. On the surface, you have everything together.
Inside, you’re drowning. You’re in constant survival mode – always overthinking, ruminating, and fearful. Your need for self-preservation is in overdrive. You use your anxiety and fear as motivation. You are a people pleaser, need constant reassurance, and are unable to enjoy the present moment. You have an inability to say no regardless of your overloaded schedule. You are mentally and physically fatigued and overworked beyond the brink of exhaustion. You need to take time off but can’t bring yourself to do so. Others wouldn’t see you in this light because you always appear to be doing well.
The portraits I’ve painted here sound like two different people, but in fact are representative of one. High-functioning anxiety, while not a formal health diagnosis, is a term that broadly encapsulates individuals who experience anxiety but also function well in their day-to-day lives. On the surface, They are perceived as overachievers, but this perception fails to recognize and acknowledge the mental health toll required to achieve at such a high level.
I came across this concept when a friend sent me a post on social media. It was a completely new but oddly familiar concept when I first read about high-functioning anxiety. In fact, I related to this concept almost immediately based on interactions with friends and colleagues, and their recollection of stressors over the years in high-stress, high-functioning environments.
In addition to personal interactions, I’ve seen anxiety and mental health at large become more “normalized” on various platforms (e.g., Instagram, TikTok) over the years. Interestingly, normalizing these concepts could be beneficial. For example, they increase awareness, encourage conversations (e.g., creating communities), and minimize the barriers toward understanding and respecting individuals who experience high-functioning anxiety. However, social media also has the potential to be harmful (e.g., “humorizing” the concept or turning it into memes, diminishing the experience).
However, the question that nagged at my mind even further was: What reasons are there, if any, for why high-functioning anxiety is not recognized as a formal diagnosis? Is this concept too new? Difficult to diagnose? Anecdotal evidence seems to suggest that high-functioning anxiety is debilitating and impairs one’s quality of life. There appears to be a need to formally recognize this subtype of anxiety and invest more time and research. Increasing the sphere of knowledge may bring more good than harm, as a way to let others know that it’s okay.
Ms. Lui is an MSc candidate at the University of Toronto and is with the mood disorders psychopharmacology unit, Toronto Western Hospital, University Health Network, also in Toronto. She reported receiving income from Braxia Scientific.
A version of this article first appeared on Medscape.com.
Motivated, calm, and high-functioning. On the surface, you are the epitome of success. You arrive at work early. You are driven, meet all deadlines and, in fact, excel at tasks. Not only are you successful in your work, but also you appear well put-together – not a single hair out of place. You have a busy social life, always smiling, laughing, or generally in an uplifting mood. On the surface, you have everything together.
Inside, you’re drowning. You’re in constant survival mode – always overthinking, ruminating, and fearful. Your need for self-preservation is in overdrive. You use your anxiety and fear as motivation. You are a people pleaser, need constant reassurance, and are unable to enjoy the present moment. You have an inability to say no regardless of your overloaded schedule. You are mentally and physically fatigued and overworked beyond the brink of exhaustion. You need to take time off but can’t bring yourself to do so. Others wouldn’t see you in this light because you always appear to be doing well.
The portraits I’ve painted here sound like two different people, but in fact are representative of one. High-functioning anxiety, while not a formal health diagnosis, is a term that broadly encapsulates individuals who experience anxiety but also function well in their day-to-day lives. On the surface, They are perceived as overachievers, but this perception fails to recognize and acknowledge the mental health toll required to achieve at such a high level.
I came across this concept when a friend sent me a post on social media. It was a completely new but oddly familiar concept when I first read about high-functioning anxiety. In fact, I related to this concept almost immediately based on interactions with friends and colleagues, and their recollection of stressors over the years in high-stress, high-functioning environments.
In addition to personal interactions, I’ve seen anxiety and mental health at large become more “normalized” on various platforms (e.g., Instagram, TikTok) over the years. Interestingly, normalizing these concepts could be beneficial. For example, they increase awareness, encourage conversations (e.g., creating communities), and minimize the barriers toward understanding and respecting individuals who experience high-functioning anxiety. However, social media also has the potential to be harmful (e.g., “humorizing” the concept or turning it into memes, diminishing the experience).
However, the question that nagged at my mind even further was: What reasons are there, if any, for why high-functioning anxiety is not recognized as a formal diagnosis? Is this concept too new? Difficult to diagnose? Anecdotal evidence seems to suggest that high-functioning anxiety is debilitating and impairs one’s quality of life. There appears to be a need to formally recognize this subtype of anxiety and invest more time and research. Increasing the sphere of knowledge may bring more good than harm, as a way to let others know that it’s okay.
Ms. Lui is an MSc candidate at the University of Toronto and is with the mood disorders psychopharmacology unit, Toronto Western Hospital, University Health Network, also in Toronto. She reported receiving income from Braxia Scientific.
A version of this article first appeared on Medscape.com.
Is mindfulness key to helping physicians with mental health?
In 2011, the Mayo Clinic began surveying physicians about burnout and found 45% of physicians experienced at least one symptom, such as emotional exhaustion, finding work no longer meaningful, feelings of ineffectiveness, and depersonalizing patients. Associated manifestations can range from headache and insomnia to impaired memory and decreased attention.
Fast forward 10 years to the Medscape National Physician Burnout and Suicide Report, which found that a similar number of physicians (42%) feel burned out. The COVID-19 pandemic only added insult to injury. A Medscape survey that included nearly 5,000 U.S. physicians revealed that about two-thirds (64%) of them reported burnout had intensified during the crisis.
These elevated numbers are being labeled as “a public health crisis” for the impact widespread physician burnout could have on the health of the doctor and patient safety. The relatively consistent levels across the decade seem to suggest that, if health organizations are attempting to improve physician well-being, it doesn’t appear to be working, forcing doctors to find solutions for themselves.
Jill Wener, MD, considers herself part of the 45% burned out 10 years ago. She was working as an internist at Rush University Medical Center in Chicago, but the “existential reality of being a doctor in this world” was wearing on her. “Staying up with the literature, knowing that every day you’re going to go into work without knowing what you’re going to find, threats of lawsuits, the pressure of perfectionism,” Dr. Wener told this news organization. “By the time I hit burnout, everything made me feel like the world was crashing down on me.”
When Dr. Wener encountered someone who meditated twice a day, she was intrigued, even though the self-described “most Type-A, inside-the-box, nonspiritual type, anxious, linear-path doctor” didn’t think people like her could meditate. Dr. Wener is not alone in her hesitation to explore meditation as a means to help prevent burnout because the causes of burnout are primarily linked to external rather than internal factors. Issues including a loss of autonomy, the burden and distraction of electronic health records, and the intense pressure to comply with rules from the government are not things mindfulness can fix.
And because the sources of burnout are primarily environmental and inherent to the current medical system, the suggestion that physicians need to fix themselves with meditation can come as a slap in the face. However, when up against a system slow to change, mindfulness can provide physicians access to the one thing they can control: How they perceive and react to what’s in front of them.
At the recommendation of an acquaintance, Dr. Wener enrolled in a Vedic Meditation (also known as Conscious Health Meditation) course taught by Light Watkins, a well-known traveling instructor, author, and speaker. By the second meeting she was successfully practicing 20 minutes twice a day. This form of mediation traces its roots to the Vedas, ancient Indian texts (also the foundation for yoga), and uses a mantra to settle the mind, transitioning to an awake state of inner contentment.
Three weeks later, Dr. Wener’s daily crying jags ended as did her propensity for road rage. “I felt like I was on the cusp of something life-changing, I just didn’t understand it,” she recalled. “But I knew I was never going to give it up.”
Defining mindfulness
“Mindfulness is being able to be present in the moment that you’re in with acceptance of what it is and without judging it,” said Donna Rockwell, PsyD, a leading mindfulness meditation teacher. The practice of mindfulness is really meditation. Dr. Rockwell explained that the noise of our mind is most often focused on either the past or the future. “We’re either bemoaning something that happened earlier or we’re catastrophizing the future,” she said, which prevents us from being present in the moment.
Meditation allows you to notice when your mind has drifted from the present moment into the past or future. “You gently notice it, label it with a lot of self-compassion, and then bring your mind back by focusing on your breath – going out, going in – and the incoming stimuli through your five senses,” said Dr. Rockwell. “When you’re doing that, you can’t be in the past or future.”
Dr. Rockwell also pointed out that we constantly categorize incoming data of the moment as either “good for me or bad for me,” which gets in the way of simply being present for what you’re facing. “When you’re more fully present, you become more skillful and able to do what this moment is asking of you,” she said. Being mindful allows us to better navigate incoming stimuli, which could be a “code blue” in the ED or a patient who needs another 2 minutes during an office visit.
When Dr. Wener was burned out, she felt unable to adapt whenever something unexpected happened. “When you have no emotional reserves, everything feels like a big deal,” she said. “The meditation gave me what we call adaptation energy; it filled up my tank and kept me from feeling like I was going to lose it at 10 o’clock in the morning.”
Dr. Rockwell explained burnout as an overactive fight or flight response activated by the amygdala. It starts pumping cortisol, our pupils dilate, and our pores open. The prefrontal cortex is offline when we’re experiencing this physiological response because they both can’t be operational at the same time. “When we’re constantly in a ‘fight or flight’ response and don’t have any access to our prefrontal cortex, we are coming from a brain that is pumping cortisol and that leads to burnout,” said Dr. Rockwell.
“Any fight or flight response leaves a mark on your body,” Dr. Wener echoed. “When we go into our state of deep rest in the meditation practice, which is two to five times more restful than sleep, it heals those stress scars.”
Making time for mindfulness
Prescribing mindfulness for physicians is not new. Molecular biologist Jon Kabat-Zinn, PhD, developed Mindfulness-Based Stress Reduction (MBSR) in 1979, a practice that incorporates mindfulness exercises to help people become familiar with their behavior patterns in stressful situations. Thus, instead of reacting, they can respond with a clearer understanding of the circumstance. Dr. Kabat-Zinn initially targeted people with chronic health problems to help them cope with the effects of pain and the condition of their illness, but it has expanded to anyone experiencing challenges in their life, including physicians. A standard MBSR course runs 8 weeks, making it a commitment for most people.
Mindfulness training requires that physicians use what they already have so little of: time.
Dr. Wener was able to take a sabbatical, embarking on a 3-month trip to India to immerse herself in the study of Vedic Meditation. Upon her return, Dr. Wener took a position at Emory University, Atlanta, and has launched a number of CME-accredited meditation courses and retreats. Unlike Dr. Kabat-Zinn, her programs are by physicians and for physicians. She also created an online version of the meditation course to make it more accessible.
For these reasons, Kara Pepper, MD, an internist in outpatient primary care in Atlanta, was drawn to the meditation course. Dr. Pepper was 7 years into practice when she burned out. “The program dovetailed into my burnout recovery,” she said. “It allowed me space to separate myself from the thoughts I was having about work and just recognize them as just that – as thoughts.”
In the course, Dr. Wener teaches the REST Technique, which she says is different than mindfulness in that she encourages the mind to run rampant. “Trying to control the mind can feel very uncomfortable because we always have thoughts,” she says. “We can’t tell the mind to stop thinking just like we can’t tell the heart to stop beating.” Dr. Wener said the REST Technique lets “the mind swim downstream,” allowing the brain to go into a deep state of rest and start to heal from the scars caused by stress.
Dr. Pepper said the self-paced online course gave her all the tools she needed, and it was pragmatic and evidence based. “I didn’t feel ‘woo’ or like another gimmick,” she said. Pepper, who continues to practice medicine, became a life coach in 2019 to teach others the skills she uses daily.
An integrated strategy
In a review published in The American Journal of Medicine in 2019, Scott Yates, MD, MBA, from the Center for Executive Medicine in Plano, Tex., found that physicians who had adopted mediation and mindfulness training to decrease anxiety and perceived work stress only experienced modest benefits. In fact, Dr. Yates claims that there’s little data to suggest the long-term benefit of any particular stress management intervention in the prevention of burnout symptoms.
“The often-repeated goals of the Triple Aim [enhancing patient experience, improving population health, and reducing costs] may be unreachable until we recognize and address burnout in health care providers,” Dr. Yates wrote. He recommends adding a fourth goal to specifically address physician wellness, which certainly could include mindfulness training and meditation.
Burnout coach, trainer, and consultant Dike Drummond, MD, also professes that physician wellness must be added as the key fourth ingredient to improving health care. “Burnout is a dilemma, a balancing act,” he said. “It takes an integrated strategy.” The CEO and founder of TheHappyMD.com, Dr. Drummond’s integrated strategy to stop physician burnout has been taught to more than 40,000 physicians in 175 organizations, and one element of that strategy can be mindfulness training.
Dr. Drummond said he doesn’t use the word meditation “because that scares most people”; it takes a commitment and isn’t accessible for a lot of doctors. Instead, he coaches doctors to use a ‘single-breath’ technique to help them reset multiple times throughout the day. “I teach people how to breathe up to the top of their head and then down to the bottom of their feet,” Dr. Drummond said. He calls it the Squeegee Breath Technique because when they exhale, they “wipe away” anything that doesn’t need to be there right now. “If you happen to have a mindfulness practice like meditation, they work synergistically because the calmness you feel in your mediation is available to you at the bottom of these releasing breaths.”
Various studies and surveys provide great detail as to the “why” of physician burnout. And while mindfulness is not the sole answer, it’s something physicians can explore for themselves while health care as an industry looks for a more comprehensive solution.
“It’s not rocket science,” Dr. Drummond insisted. “You want a different result? You’re not satisfied with the way things are now and you want to feel different? You absolutely must do something different.”
A version of this article first appeared on Medscape.com.
In 2011, the Mayo Clinic began surveying physicians about burnout and found 45% of physicians experienced at least one symptom, such as emotional exhaustion, finding work no longer meaningful, feelings of ineffectiveness, and depersonalizing patients. Associated manifestations can range from headache and insomnia to impaired memory and decreased attention.
Fast forward 10 years to the Medscape National Physician Burnout and Suicide Report, which found that a similar number of physicians (42%) feel burned out. The COVID-19 pandemic only added insult to injury. A Medscape survey that included nearly 5,000 U.S. physicians revealed that about two-thirds (64%) of them reported burnout had intensified during the crisis.
These elevated numbers are being labeled as “a public health crisis” for the impact widespread physician burnout could have on the health of the doctor and patient safety. The relatively consistent levels across the decade seem to suggest that, if health organizations are attempting to improve physician well-being, it doesn’t appear to be working, forcing doctors to find solutions for themselves.
Jill Wener, MD, considers herself part of the 45% burned out 10 years ago. She was working as an internist at Rush University Medical Center in Chicago, but the “existential reality of being a doctor in this world” was wearing on her. “Staying up with the literature, knowing that every day you’re going to go into work without knowing what you’re going to find, threats of lawsuits, the pressure of perfectionism,” Dr. Wener told this news organization. “By the time I hit burnout, everything made me feel like the world was crashing down on me.”
When Dr. Wener encountered someone who meditated twice a day, she was intrigued, even though the self-described “most Type-A, inside-the-box, nonspiritual type, anxious, linear-path doctor” didn’t think people like her could meditate. Dr. Wener is not alone in her hesitation to explore meditation as a means to help prevent burnout because the causes of burnout are primarily linked to external rather than internal factors. Issues including a loss of autonomy, the burden and distraction of electronic health records, and the intense pressure to comply with rules from the government are not things mindfulness can fix.
And because the sources of burnout are primarily environmental and inherent to the current medical system, the suggestion that physicians need to fix themselves with meditation can come as a slap in the face. However, when up against a system slow to change, mindfulness can provide physicians access to the one thing they can control: How they perceive and react to what’s in front of them.
At the recommendation of an acquaintance, Dr. Wener enrolled in a Vedic Meditation (also known as Conscious Health Meditation) course taught by Light Watkins, a well-known traveling instructor, author, and speaker. By the second meeting she was successfully practicing 20 minutes twice a day. This form of mediation traces its roots to the Vedas, ancient Indian texts (also the foundation for yoga), and uses a mantra to settle the mind, transitioning to an awake state of inner contentment.
Three weeks later, Dr. Wener’s daily crying jags ended as did her propensity for road rage. “I felt like I was on the cusp of something life-changing, I just didn’t understand it,” she recalled. “But I knew I was never going to give it up.”
Defining mindfulness
“Mindfulness is being able to be present in the moment that you’re in with acceptance of what it is and without judging it,” said Donna Rockwell, PsyD, a leading mindfulness meditation teacher. The practice of mindfulness is really meditation. Dr. Rockwell explained that the noise of our mind is most often focused on either the past or the future. “We’re either bemoaning something that happened earlier or we’re catastrophizing the future,” she said, which prevents us from being present in the moment.
Meditation allows you to notice when your mind has drifted from the present moment into the past or future. “You gently notice it, label it with a lot of self-compassion, and then bring your mind back by focusing on your breath – going out, going in – and the incoming stimuli through your five senses,” said Dr. Rockwell. “When you’re doing that, you can’t be in the past or future.”
Dr. Rockwell also pointed out that we constantly categorize incoming data of the moment as either “good for me or bad for me,” which gets in the way of simply being present for what you’re facing. “When you’re more fully present, you become more skillful and able to do what this moment is asking of you,” she said. Being mindful allows us to better navigate incoming stimuli, which could be a “code blue” in the ED or a patient who needs another 2 minutes during an office visit.
When Dr. Wener was burned out, she felt unable to adapt whenever something unexpected happened. “When you have no emotional reserves, everything feels like a big deal,” she said. “The meditation gave me what we call adaptation energy; it filled up my tank and kept me from feeling like I was going to lose it at 10 o’clock in the morning.”
Dr. Rockwell explained burnout as an overactive fight or flight response activated by the amygdala. It starts pumping cortisol, our pupils dilate, and our pores open. The prefrontal cortex is offline when we’re experiencing this physiological response because they both can’t be operational at the same time. “When we’re constantly in a ‘fight or flight’ response and don’t have any access to our prefrontal cortex, we are coming from a brain that is pumping cortisol and that leads to burnout,” said Dr. Rockwell.
“Any fight or flight response leaves a mark on your body,” Dr. Wener echoed. “When we go into our state of deep rest in the meditation practice, which is two to five times more restful than sleep, it heals those stress scars.”
Making time for mindfulness
Prescribing mindfulness for physicians is not new. Molecular biologist Jon Kabat-Zinn, PhD, developed Mindfulness-Based Stress Reduction (MBSR) in 1979, a practice that incorporates mindfulness exercises to help people become familiar with their behavior patterns in stressful situations. Thus, instead of reacting, they can respond with a clearer understanding of the circumstance. Dr. Kabat-Zinn initially targeted people with chronic health problems to help them cope with the effects of pain and the condition of their illness, but it has expanded to anyone experiencing challenges in their life, including physicians. A standard MBSR course runs 8 weeks, making it a commitment for most people.
Mindfulness training requires that physicians use what they already have so little of: time.
Dr. Wener was able to take a sabbatical, embarking on a 3-month trip to India to immerse herself in the study of Vedic Meditation. Upon her return, Dr. Wener took a position at Emory University, Atlanta, and has launched a number of CME-accredited meditation courses and retreats. Unlike Dr. Kabat-Zinn, her programs are by physicians and for physicians. She also created an online version of the meditation course to make it more accessible.
For these reasons, Kara Pepper, MD, an internist in outpatient primary care in Atlanta, was drawn to the meditation course. Dr. Pepper was 7 years into practice when she burned out. “The program dovetailed into my burnout recovery,” she said. “It allowed me space to separate myself from the thoughts I was having about work and just recognize them as just that – as thoughts.”
In the course, Dr. Wener teaches the REST Technique, which she says is different than mindfulness in that she encourages the mind to run rampant. “Trying to control the mind can feel very uncomfortable because we always have thoughts,” she says. “We can’t tell the mind to stop thinking just like we can’t tell the heart to stop beating.” Dr. Wener said the REST Technique lets “the mind swim downstream,” allowing the brain to go into a deep state of rest and start to heal from the scars caused by stress.
Dr. Pepper said the self-paced online course gave her all the tools she needed, and it was pragmatic and evidence based. “I didn’t feel ‘woo’ or like another gimmick,” she said. Pepper, who continues to practice medicine, became a life coach in 2019 to teach others the skills she uses daily.
An integrated strategy
In a review published in The American Journal of Medicine in 2019, Scott Yates, MD, MBA, from the Center for Executive Medicine in Plano, Tex., found that physicians who had adopted mediation and mindfulness training to decrease anxiety and perceived work stress only experienced modest benefits. In fact, Dr. Yates claims that there’s little data to suggest the long-term benefit of any particular stress management intervention in the prevention of burnout symptoms.
“The often-repeated goals of the Triple Aim [enhancing patient experience, improving population health, and reducing costs] may be unreachable until we recognize and address burnout in health care providers,” Dr. Yates wrote. He recommends adding a fourth goal to specifically address physician wellness, which certainly could include mindfulness training and meditation.
Burnout coach, trainer, and consultant Dike Drummond, MD, also professes that physician wellness must be added as the key fourth ingredient to improving health care. “Burnout is a dilemma, a balancing act,” he said. “It takes an integrated strategy.” The CEO and founder of TheHappyMD.com, Dr. Drummond’s integrated strategy to stop physician burnout has been taught to more than 40,000 physicians in 175 organizations, and one element of that strategy can be mindfulness training.
Dr. Drummond said he doesn’t use the word meditation “because that scares most people”; it takes a commitment and isn’t accessible for a lot of doctors. Instead, he coaches doctors to use a ‘single-breath’ technique to help them reset multiple times throughout the day. “I teach people how to breathe up to the top of their head and then down to the bottom of their feet,” Dr. Drummond said. He calls it the Squeegee Breath Technique because when they exhale, they “wipe away” anything that doesn’t need to be there right now. “If you happen to have a mindfulness practice like meditation, they work synergistically because the calmness you feel in your mediation is available to you at the bottom of these releasing breaths.”
Various studies and surveys provide great detail as to the “why” of physician burnout. And while mindfulness is not the sole answer, it’s something physicians can explore for themselves while health care as an industry looks for a more comprehensive solution.
“It’s not rocket science,” Dr. Drummond insisted. “You want a different result? You’re not satisfied with the way things are now and you want to feel different? You absolutely must do something different.”
A version of this article first appeared on Medscape.com.
In 2011, the Mayo Clinic began surveying physicians about burnout and found 45% of physicians experienced at least one symptom, such as emotional exhaustion, finding work no longer meaningful, feelings of ineffectiveness, and depersonalizing patients. Associated manifestations can range from headache and insomnia to impaired memory and decreased attention.
Fast forward 10 years to the Medscape National Physician Burnout and Suicide Report, which found that a similar number of physicians (42%) feel burned out. The COVID-19 pandemic only added insult to injury. A Medscape survey that included nearly 5,000 U.S. physicians revealed that about two-thirds (64%) of them reported burnout had intensified during the crisis.
These elevated numbers are being labeled as “a public health crisis” for the impact widespread physician burnout could have on the health of the doctor and patient safety. The relatively consistent levels across the decade seem to suggest that, if health organizations are attempting to improve physician well-being, it doesn’t appear to be working, forcing doctors to find solutions for themselves.
Jill Wener, MD, considers herself part of the 45% burned out 10 years ago. She was working as an internist at Rush University Medical Center in Chicago, but the “existential reality of being a doctor in this world” was wearing on her. “Staying up with the literature, knowing that every day you’re going to go into work without knowing what you’re going to find, threats of lawsuits, the pressure of perfectionism,” Dr. Wener told this news organization. “By the time I hit burnout, everything made me feel like the world was crashing down on me.”
When Dr. Wener encountered someone who meditated twice a day, she was intrigued, even though the self-described “most Type-A, inside-the-box, nonspiritual type, anxious, linear-path doctor” didn’t think people like her could meditate. Dr. Wener is not alone in her hesitation to explore meditation as a means to help prevent burnout because the causes of burnout are primarily linked to external rather than internal factors. Issues including a loss of autonomy, the burden and distraction of electronic health records, and the intense pressure to comply with rules from the government are not things mindfulness can fix.
And because the sources of burnout are primarily environmental and inherent to the current medical system, the suggestion that physicians need to fix themselves with meditation can come as a slap in the face. However, when up against a system slow to change, mindfulness can provide physicians access to the one thing they can control: How they perceive and react to what’s in front of them.
At the recommendation of an acquaintance, Dr. Wener enrolled in a Vedic Meditation (also known as Conscious Health Meditation) course taught by Light Watkins, a well-known traveling instructor, author, and speaker. By the second meeting she was successfully practicing 20 minutes twice a day. This form of mediation traces its roots to the Vedas, ancient Indian texts (also the foundation for yoga), and uses a mantra to settle the mind, transitioning to an awake state of inner contentment.
Three weeks later, Dr. Wener’s daily crying jags ended as did her propensity for road rage. “I felt like I was on the cusp of something life-changing, I just didn’t understand it,” she recalled. “But I knew I was never going to give it up.”
Defining mindfulness
“Mindfulness is being able to be present in the moment that you’re in with acceptance of what it is and without judging it,” said Donna Rockwell, PsyD, a leading mindfulness meditation teacher. The practice of mindfulness is really meditation. Dr. Rockwell explained that the noise of our mind is most often focused on either the past or the future. “We’re either bemoaning something that happened earlier or we’re catastrophizing the future,” she said, which prevents us from being present in the moment.
Meditation allows you to notice when your mind has drifted from the present moment into the past or future. “You gently notice it, label it with a lot of self-compassion, and then bring your mind back by focusing on your breath – going out, going in – and the incoming stimuli through your five senses,” said Dr. Rockwell. “When you’re doing that, you can’t be in the past or future.”
Dr. Rockwell also pointed out that we constantly categorize incoming data of the moment as either “good for me or bad for me,” which gets in the way of simply being present for what you’re facing. “When you’re more fully present, you become more skillful and able to do what this moment is asking of you,” she said. Being mindful allows us to better navigate incoming stimuli, which could be a “code blue” in the ED or a patient who needs another 2 minutes during an office visit.
When Dr. Wener was burned out, she felt unable to adapt whenever something unexpected happened. “When you have no emotional reserves, everything feels like a big deal,” she said. “The meditation gave me what we call adaptation energy; it filled up my tank and kept me from feeling like I was going to lose it at 10 o’clock in the morning.”
Dr. Rockwell explained burnout as an overactive fight or flight response activated by the amygdala. It starts pumping cortisol, our pupils dilate, and our pores open. The prefrontal cortex is offline when we’re experiencing this physiological response because they both can’t be operational at the same time. “When we’re constantly in a ‘fight or flight’ response and don’t have any access to our prefrontal cortex, we are coming from a brain that is pumping cortisol and that leads to burnout,” said Dr. Rockwell.
“Any fight or flight response leaves a mark on your body,” Dr. Wener echoed. “When we go into our state of deep rest in the meditation practice, which is two to five times more restful than sleep, it heals those stress scars.”
Making time for mindfulness
Prescribing mindfulness for physicians is not new. Molecular biologist Jon Kabat-Zinn, PhD, developed Mindfulness-Based Stress Reduction (MBSR) in 1979, a practice that incorporates mindfulness exercises to help people become familiar with their behavior patterns in stressful situations. Thus, instead of reacting, they can respond with a clearer understanding of the circumstance. Dr. Kabat-Zinn initially targeted people with chronic health problems to help them cope with the effects of pain and the condition of their illness, but it has expanded to anyone experiencing challenges in their life, including physicians. A standard MBSR course runs 8 weeks, making it a commitment for most people.
Mindfulness training requires that physicians use what they already have so little of: time.
Dr. Wener was able to take a sabbatical, embarking on a 3-month trip to India to immerse herself in the study of Vedic Meditation. Upon her return, Dr. Wener took a position at Emory University, Atlanta, and has launched a number of CME-accredited meditation courses and retreats. Unlike Dr. Kabat-Zinn, her programs are by physicians and for physicians. She also created an online version of the meditation course to make it more accessible.
For these reasons, Kara Pepper, MD, an internist in outpatient primary care in Atlanta, was drawn to the meditation course. Dr. Pepper was 7 years into practice when she burned out. “The program dovetailed into my burnout recovery,” she said. “It allowed me space to separate myself from the thoughts I was having about work and just recognize them as just that – as thoughts.”
In the course, Dr. Wener teaches the REST Technique, which she says is different than mindfulness in that she encourages the mind to run rampant. “Trying to control the mind can feel very uncomfortable because we always have thoughts,” she says. “We can’t tell the mind to stop thinking just like we can’t tell the heart to stop beating.” Dr. Wener said the REST Technique lets “the mind swim downstream,” allowing the brain to go into a deep state of rest and start to heal from the scars caused by stress.
Dr. Pepper said the self-paced online course gave her all the tools she needed, and it was pragmatic and evidence based. “I didn’t feel ‘woo’ or like another gimmick,” she said. Pepper, who continues to practice medicine, became a life coach in 2019 to teach others the skills she uses daily.
An integrated strategy
In a review published in The American Journal of Medicine in 2019, Scott Yates, MD, MBA, from the Center for Executive Medicine in Plano, Tex., found that physicians who had adopted mediation and mindfulness training to decrease anxiety and perceived work stress only experienced modest benefits. In fact, Dr. Yates claims that there’s little data to suggest the long-term benefit of any particular stress management intervention in the prevention of burnout symptoms.
“The often-repeated goals of the Triple Aim [enhancing patient experience, improving population health, and reducing costs] may be unreachable until we recognize and address burnout in health care providers,” Dr. Yates wrote. He recommends adding a fourth goal to specifically address physician wellness, which certainly could include mindfulness training and meditation.
Burnout coach, trainer, and consultant Dike Drummond, MD, also professes that physician wellness must be added as the key fourth ingredient to improving health care. “Burnout is a dilemma, a balancing act,” he said. “It takes an integrated strategy.” The CEO and founder of TheHappyMD.com, Dr. Drummond’s integrated strategy to stop physician burnout has been taught to more than 40,000 physicians in 175 organizations, and one element of that strategy can be mindfulness training.
Dr. Drummond said he doesn’t use the word meditation “because that scares most people”; it takes a commitment and isn’t accessible for a lot of doctors. Instead, he coaches doctors to use a ‘single-breath’ technique to help them reset multiple times throughout the day. “I teach people how to breathe up to the top of their head and then down to the bottom of their feet,” Dr. Drummond said. He calls it the Squeegee Breath Technique because when they exhale, they “wipe away” anything that doesn’t need to be there right now. “If you happen to have a mindfulness practice like meditation, they work synergistically because the calmness you feel in your mediation is available to you at the bottom of these releasing breaths.”
Various studies and surveys provide great detail as to the “why” of physician burnout. And while mindfulness is not the sole answer, it’s something physicians can explore for themselves while health care as an industry looks for a more comprehensive solution.
“It’s not rocket science,” Dr. Drummond insisted. “You want a different result? You’re not satisfied with the way things are now and you want to feel different? You absolutely must do something different.”
A version of this article first appeared on Medscape.com.
Don’t give up on relentless youth depression
As pediatricians, we are acutely aware of the increase in depression in our teen patients. Lifetime prevalence is now approaching 20%, and we are doing our best to help.
The Guidelines for Adolescent Depression in Primary Care (GLAD-PC, 2018) has advice on screening and primary care provider (PCP) management, verifying our role in care. But GLAD-PC also advises “referral to a mental health specialist” in patient scenarios we see multiple times per week. Even when patients are willing and able to go, mental health specialists are in short supply or have months-long waiting lists. What should we do to help the more severely depressed adolescent when immediate referral is not possible? What should we expect of specialist care for what is called treatment-resistant or treatment-refractory depression (TRD)?
To know what to do for a youth with TRD, first you need to know what constitutes an adequate trial of treatment. After diagnosis of major depressive disorder (MDD) from a validated screening tool or an interview based on DSM-5 criteria and an appropriate assessment (as described in GLAD-PC), patients and parents need education on symptoms, course, prognosis including suicide risk, and treatment options. Known TRD risk factors, besides longer or greater depression severity, anhedonia, and poor global functioning, can benefit from being specifically addressed: trauma, bullying, comorbid anxiety or substance use, subsyndromal mania, insomnia, hypothyroidism, nutritional deficiencies from eating disorders, certain genetic variants, LGBTQ identification, family conflict, and parental depression. Screening and assessment for suicidal ideation/attempts is needed initially and in follow-up as MDD increases risk of suicide 30 times.
PCPs can manage mild depression with regular visits every 1-2 weeks for active support for 6-8 weeks. Advise all depressed youth on healthy eating, adequate sleep and exercise, pleasurable activities, and refraining from substance use. With a full response (50%+ reduction in symptom score from baseline), monthly monitoring for symptoms, suicidality, and stressors (phone/televisits suffice) should continue for 6-24 months as half recur. Monitoring with ratings by both youth and parent are recommended and may be required by insurers. Scores below cutoff suggest “remission,” although functioning must be considered. Youth report symptoms best but parents may better report improved functioning and affect that can precede symptom reduction.
If there is no initial response (< 25% decrease in symptom score) or a partial response (25%-49% decrease), PCPs should begin treatment as for moderate depression with either a selective serotonin reuptake inhibitor (SSRI) or psychotherapy. Use of both has the best evidence; cognitive behavior therapy (CBT) and interpersonal psychotherapy for adolescents are equally effective.
Side effects from SSRIs are almost universal with GI upset, headaches, and sexual dysfunction most common, but activation (increased agitation or irritability) may occur. Educate patients about these and encourage tolerating them as they tend to subside in weeks, allowing continuation of these most effective medicines. Activation rarely indicates true mania, which would require stopping and referral.
Moderate depression with only comorbid anxiety may be addressed by PCPs with problem-focused supportive counseling and SSRIs, but mental health consultation or referral also are appropriate. Fluoxetine starting at 5-10 mg/day has best evidence and Food and Drug Administration approval for MDD from age 8. Starting at a higher dose may increase risk of suicidal ideation. Alternatively, escitalopram is FDA approved for MDD at age 12 starting at 10 mg/day, although meta-analyses do not distinguish effectiveness within the SSRI class. Although benefit usually appears within 2 weeks, a trial of at least 4 weeks should be used to assess effect.
If after 4 weeks, the SSRI is tolerated but has little or no response, reassess the diagnosis, try a different SSRI, e.g. sertraline, and add CBT (combined SSRI+CBT has an advantage). To switch SSRIs, reduce the first every 1-2 weeks (by 10-20 mg for fluoxetine; 5-10 for escitalopram) to reduce side effects. If overlapping, the replacement SSRI may start midway in the wean at low dose with patients educated about serotonin syndrome. If instead there was a partial response to the initial SSRI, progressively increase the dose (by 10 mg for fluoxetine or 5 mg for escitalopram monthly) as indicated by symptom change up to the maximum (60-80 mg fluoxetine or 20 mg escitalopram), if needed, and maintain for another 4 weeks. Alternatively, or in addition, start psychotherapy or ask to change current therapy, as therapy focus makes a difference in effect. Initial CBT focus on anxiety acts fastest when anxiety is comorbid.
Once a regimen produces a response, maintain it for 16-20 weeks, the longer for more severe depression. Although three-fourths of mildly to moderately depressed youth are late responders, emerging near 6 weeks, a rapid initial response is associated with better outcome. The recommended 8 weeks on a final tolerated dose constituting an adequate trial before changing may be shortened to 6 weeks in severe unremitting cases. Youth not remitting by 12 weeks should be offered alternative treatment. Referral is recommended for moderately severe depression with comorbidity or severe depression but also for unresponsive moderate depression or by family or clinician preference.
Treatment-resistant depression is defined as “clinically impairing depression symptoms despite an adequate trial of an evidence-based psychotherapy and an antidepressant with grade A evidence (fluoxetine, escitalopram, or sertraline),” sequentially or together; treatment-refractory depression comprises the above with failure on at least two antidepressants, with at least one being grade A. Unfortunately, TRD occurs in 30%-40% of children and remission is only 30%. Low adherence based on pill counts (> 30% missed) or with therapy (fewer than nine visits) should be considered in treatment failures.
With manageable factors addressed, the next step for TRD is treatment augmentation. The best evidence-based augmentation for TRD is CBT; 55% of those receiving CBT responded within 12 weeks. TRD augmentations and interventions with evidence in adults have either no evidence of effect in children (SNRIs, lithium), no randomized controlled trials, or support only from small suggestive studies, e.g., antipsychotics, 16 g/day omega-3 fatty acid supplementation, folic acid supplementation, repetitive transcranial magnetic stimulation, electroconvulsive therapy, or ketamine. Prompt referral to a child psychiatrist is essential for youth classified as TRD as earlier more aggressive treatment may avoid the long-term morbidity of chronic depression.
Fortunately, a meta-analysis of studies showed that PCP medication management visits with monitoring could improve outcomes, even for TRD.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at pdnews@mdedge.com.
Reference
Dwyer J et al. Annual research review: Defining and treating pediatric treatment-resistant depression. J Child Psychol Psychiatry. 2020 March;61(3):312-32.
As pediatricians, we are acutely aware of the increase in depression in our teen patients. Lifetime prevalence is now approaching 20%, and we are doing our best to help.
The Guidelines for Adolescent Depression in Primary Care (GLAD-PC, 2018) has advice on screening and primary care provider (PCP) management, verifying our role in care. But GLAD-PC also advises “referral to a mental health specialist” in patient scenarios we see multiple times per week. Even when patients are willing and able to go, mental health specialists are in short supply or have months-long waiting lists. What should we do to help the more severely depressed adolescent when immediate referral is not possible? What should we expect of specialist care for what is called treatment-resistant or treatment-refractory depression (TRD)?
To know what to do for a youth with TRD, first you need to know what constitutes an adequate trial of treatment. After diagnosis of major depressive disorder (MDD) from a validated screening tool or an interview based on DSM-5 criteria and an appropriate assessment (as described in GLAD-PC), patients and parents need education on symptoms, course, prognosis including suicide risk, and treatment options. Known TRD risk factors, besides longer or greater depression severity, anhedonia, and poor global functioning, can benefit from being specifically addressed: trauma, bullying, comorbid anxiety or substance use, subsyndromal mania, insomnia, hypothyroidism, nutritional deficiencies from eating disorders, certain genetic variants, LGBTQ identification, family conflict, and parental depression. Screening and assessment for suicidal ideation/attempts is needed initially and in follow-up as MDD increases risk of suicide 30 times.
PCPs can manage mild depression with regular visits every 1-2 weeks for active support for 6-8 weeks. Advise all depressed youth on healthy eating, adequate sleep and exercise, pleasurable activities, and refraining from substance use. With a full response (50%+ reduction in symptom score from baseline), monthly monitoring for symptoms, suicidality, and stressors (phone/televisits suffice) should continue for 6-24 months as half recur. Monitoring with ratings by both youth and parent are recommended and may be required by insurers. Scores below cutoff suggest “remission,” although functioning must be considered. Youth report symptoms best but parents may better report improved functioning and affect that can precede symptom reduction.
If there is no initial response (< 25% decrease in symptom score) or a partial response (25%-49% decrease), PCPs should begin treatment as for moderate depression with either a selective serotonin reuptake inhibitor (SSRI) or psychotherapy. Use of both has the best evidence; cognitive behavior therapy (CBT) and interpersonal psychotherapy for adolescents are equally effective.
Side effects from SSRIs are almost universal with GI upset, headaches, and sexual dysfunction most common, but activation (increased agitation or irritability) may occur. Educate patients about these and encourage tolerating them as they tend to subside in weeks, allowing continuation of these most effective medicines. Activation rarely indicates true mania, which would require stopping and referral.
Moderate depression with only comorbid anxiety may be addressed by PCPs with problem-focused supportive counseling and SSRIs, but mental health consultation or referral also are appropriate. Fluoxetine starting at 5-10 mg/day has best evidence and Food and Drug Administration approval for MDD from age 8. Starting at a higher dose may increase risk of suicidal ideation. Alternatively, escitalopram is FDA approved for MDD at age 12 starting at 10 mg/day, although meta-analyses do not distinguish effectiveness within the SSRI class. Although benefit usually appears within 2 weeks, a trial of at least 4 weeks should be used to assess effect.
If after 4 weeks, the SSRI is tolerated but has little or no response, reassess the diagnosis, try a different SSRI, e.g. sertraline, and add CBT (combined SSRI+CBT has an advantage). To switch SSRIs, reduce the first every 1-2 weeks (by 10-20 mg for fluoxetine; 5-10 for escitalopram) to reduce side effects. If overlapping, the replacement SSRI may start midway in the wean at low dose with patients educated about serotonin syndrome. If instead there was a partial response to the initial SSRI, progressively increase the dose (by 10 mg for fluoxetine or 5 mg for escitalopram monthly) as indicated by symptom change up to the maximum (60-80 mg fluoxetine or 20 mg escitalopram), if needed, and maintain for another 4 weeks. Alternatively, or in addition, start psychotherapy or ask to change current therapy, as therapy focus makes a difference in effect. Initial CBT focus on anxiety acts fastest when anxiety is comorbid.
Once a regimen produces a response, maintain it for 16-20 weeks, the longer for more severe depression. Although three-fourths of mildly to moderately depressed youth are late responders, emerging near 6 weeks, a rapid initial response is associated with better outcome. The recommended 8 weeks on a final tolerated dose constituting an adequate trial before changing may be shortened to 6 weeks in severe unremitting cases. Youth not remitting by 12 weeks should be offered alternative treatment. Referral is recommended for moderately severe depression with comorbidity or severe depression but also for unresponsive moderate depression or by family or clinician preference.
Treatment-resistant depression is defined as “clinically impairing depression symptoms despite an adequate trial of an evidence-based psychotherapy and an antidepressant with grade A evidence (fluoxetine, escitalopram, or sertraline),” sequentially or together; treatment-refractory depression comprises the above with failure on at least two antidepressants, with at least one being grade A. Unfortunately, TRD occurs in 30%-40% of children and remission is only 30%. Low adherence based on pill counts (> 30% missed) or with therapy (fewer than nine visits) should be considered in treatment failures.
With manageable factors addressed, the next step for TRD is treatment augmentation. The best evidence-based augmentation for TRD is CBT; 55% of those receiving CBT responded within 12 weeks. TRD augmentations and interventions with evidence in adults have either no evidence of effect in children (SNRIs, lithium), no randomized controlled trials, or support only from small suggestive studies, e.g., antipsychotics, 16 g/day omega-3 fatty acid supplementation, folic acid supplementation, repetitive transcranial magnetic stimulation, electroconvulsive therapy, or ketamine. Prompt referral to a child psychiatrist is essential for youth classified as TRD as earlier more aggressive treatment may avoid the long-term morbidity of chronic depression.
Fortunately, a meta-analysis of studies showed that PCP medication management visits with monitoring could improve outcomes, even for TRD.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at pdnews@mdedge.com.
Reference
Dwyer J et al. Annual research review: Defining and treating pediatric treatment-resistant depression. J Child Psychol Psychiatry. 2020 March;61(3):312-32.
As pediatricians, we are acutely aware of the increase in depression in our teen patients. Lifetime prevalence is now approaching 20%, and we are doing our best to help.
The Guidelines for Adolescent Depression in Primary Care (GLAD-PC, 2018) has advice on screening and primary care provider (PCP) management, verifying our role in care. But GLAD-PC also advises “referral to a mental health specialist” in patient scenarios we see multiple times per week. Even when patients are willing and able to go, mental health specialists are in short supply or have months-long waiting lists. What should we do to help the more severely depressed adolescent when immediate referral is not possible? What should we expect of specialist care for what is called treatment-resistant or treatment-refractory depression (TRD)?
To know what to do for a youth with TRD, first you need to know what constitutes an adequate trial of treatment. After diagnosis of major depressive disorder (MDD) from a validated screening tool or an interview based on DSM-5 criteria and an appropriate assessment (as described in GLAD-PC), patients and parents need education on symptoms, course, prognosis including suicide risk, and treatment options. Known TRD risk factors, besides longer or greater depression severity, anhedonia, and poor global functioning, can benefit from being specifically addressed: trauma, bullying, comorbid anxiety or substance use, subsyndromal mania, insomnia, hypothyroidism, nutritional deficiencies from eating disorders, certain genetic variants, LGBTQ identification, family conflict, and parental depression. Screening and assessment for suicidal ideation/attempts is needed initially and in follow-up as MDD increases risk of suicide 30 times.
PCPs can manage mild depression with regular visits every 1-2 weeks for active support for 6-8 weeks. Advise all depressed youth on healthy eating, adequate sleep and exercise, pleasurable activities, and refraining from substance use. With a full response (50%+ reduction in symptom score from baseline), monthly monitoring for symptoms, suicidality, and stressors (phone/televisits suffice) should continue for 6-24 months as half recur. Monitoring with ratings by both youth and parent are recommended and may be required by insurers. Scores below cutoff suggest “remission,” although functioning must be considered. Youth report symptoms best but parents may better report improved functioning and affect that can precede symptom reduction.
If there is no initial response (< 25% decrease in symptom score) or a partial response (25%-49% decrease), PCPs should begin treatment as for moderate depression with either a selective serotonin reuptake inhibitor (SSRI) or psychotherapy. Use of both has the best evidence; cognitive behavior therapy (CBT) and interpersonal psychotherapy for adolescents are equally effective.
Side effects from SSRIs are almost universal with GI upset, headaches, and sexual dysfunction most common, but activation (increased agitation or irritability) may occur. Educate patients about these and encourage tolerating them as they tend to subside in weeks, allowing continuation of these most effective medicines. Activation rarely indicates true mania, which would require stopping and referral.
Moderate depression with only comorbid anxiety may be addressed by PCPs with problem-focused supportive counseling and SSRIs, but mental health consultation or referral also are appropriate. Fluoxetine starting at 5-10 mg/day has best evidence and Food and Drug Administration approval for MDD from age 8. Starting at a higher dose may increase risk of suicidal ideation. Alternatively, escitalopram is FDA approved for MDD at age 12 starting at 10 mg/day, although meta-analyses do not distinguish effectiveness within the SSRI class. Although benefit usually appears within 2 weeks, a trial of at least 4 weeks should be used to assess effect.
If after 4 weeks, the SSRI is tolerated but has little or no response, reassess the diagnosis, try a different SSRI, e.g. sertraline, and add CBT (combined SSRI+CBT has an advantage). To switch SSRIs, reduce the first every 1-2 weeks (by 10-20 mg for fluoxetine; 5-10 for escitalopram) to reduce side effects. If overlapping, the replacement SSRI may start midway in the wean at low dose with patients educated about serotonin syndrome. If instead there was a partial response to the initial SSRI, progressively increase the dose (by 10 mg for fluoxetine or 5 mg for escitalopram monthly) as indicated by symptom change up to the maximum (60-80 mg fluoxetine or 20 mg escitalopram), if needed, and maintain for another 4 weeks. Alternatively, or in addition, start psychotherapy or ask to change current therapy, as therapy focus makes a difference in effect. Initial CBT focus on anxiety acts fastest when anxiety is comorbid.
Once a regimen produces a response, maintain it for 16-20 weeks, the longer for more severe depression. Although three-fourths of mildly to moderately depressed youth are late responders, emerging near 6 weeks, a rapid initial response is associated with better outcome. The recommended 8 weeks on a final tolerated dose constituting an adequate trial before changing may be shortened to 6 weeks in severe unremitting cases. Youth not remitting by 12 weeks should be offered alternative treatment. Referral is recommended for moderately severe depression with comorbidity or severe depression but also for unresponsive moderate depression or by family or clinician preference.
Treatment-resistant depression is defined as “clinically impairing depression symptoms despite an adequate trial of an evidence-based psychotherapy and an antidepressant with grade A evidence (fluoxetine, escitalopram, or sertraline),” sequentially or together; treatment-refractory depression comprises the above with failure on at least two antidepressants, with at least one being grade A. Unfortunately, TRD occurs in 30%-40% of children and remission is only 30%. Low adherence based on pill counts (> 30% missed) or with therapy (fewer than nine visits) should be considered in treatment failures.
With manageable factors addressed, the next step for TRD is treatment augmentation. The best evidence-based augmentation for TRD is CBT; 55% of those receiving CBT responded within 12 weeks. TRD augmentations and interventions with evidence in adults have either no evidence of effect in children (SNRIs, lithium), no randomized controlled trials, or support only from small suggestive studies, e.g., antipsychotics, 16 g/day omega-3 fatty acid supplementation, folic acid supplementation, repetitive transcranial magnetic stimulation, electroconvulsive therapy, or ketamine. Prompt referral to a child psychiatrist is essential for youth classified as TRD as earlier more aggressive treatment may avoid the long-term morbidity of chronic depression.
Fortunately, a meta-analysis of studies showed that PCP medication management visits with monitoring could improve outcomes, even for TRD.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at pdnews@mdedge.com.
Reference
Dwyer J et al. Annual research review: Defining and treating pediatric treatment-resistant depression. J Child Psychol Psychiatry. 2020 March;61(3):312-32.
The importance of self-compassion for hospitalists
A mindful way relate to ourselves
Physicians, clinicians, providers, healers, and now heroes, are some of the names we have been given throughout history. These titles bring together a universal concept in medicine that all human beings deserve compassion, understanding, and care. However, as health care providers we forget to show ourselves the same compassion we bestow upon others.
Self-compassion is a new way of relating to ourselves. As clinicians, we are trained investigators, delving deeper into what our patient is thinking and feeling. “Tell me more about that. How does that make you feel? That must have been (very painful/scary/frustrating).” These are a few statements we learned in patient interviewing to actively engage with patients, build rapport, solidify trust, validate their concerns, and ultimately obtain the information needed to diagnose and heal.
We know the importance of looking beyond the surface, as more often than not a deeper inspection reveals more to the story. We have uncovered cracks in the foundation, erosion of the roof, worn out siding, and a glimpse into the complexities that make up each individual. We look at our patients, loved ones, and the world with night-vision lenses to uncover what is deeper.
Clinicians are good at directing compassion toward others, but not as good at giving it to themselves.1 Many health care providers may see self-compassion as soft, weak, selfish, or unnecessary. However, mindful self-compassion is a positive practice that opens a pathway for healing, personal growth, and protection against the negative consequences of self-judgment, isolation, anxiety, burnout, and depression.
What is self-compassion?
Kristin Neff, PhD, an associate professor in educational psychology at the University of Texas at Austin, was the first to academically define self-compassion. Self-compassion brings together three core elements – kindness, humanity, and mindfulness.2 Self-compassion involves acting the same way toward yourself when you are having a difficult time as you would toward another person. Instead of mercilessly judging and criticizing yourself for self-perceived inadequacies or shortcomings, self-compassion allows you to ask yourself: “How can I give myself comfort and care in this moment?”
Mindfulness acknowledges a painful experience without resistance or judgment, while being present in the moment with things as they are. Self-compassion provides the emotional safety needed to mindfully open to our pain, disappointments, and defeats. Mindfulness and self-compassion both allow us to live with more acceptance toward ourselves and our lives. Mindfulness asks: “What am I experiencing right now?” Self-compassion asks: “What do I need right now?” When you feel compassion for yourself or another, you recognize that suffering, failure, and imperfection are all part of the shared human experience.
The physiology of self-compassion
When we practice self-compassion, we feel safe and cared for because there is a physiological pathway that explains this response. Self-compassion helps down-regulate the stress response (fight-flight-freeze). When we are triggered by a threat to our self-concept, we are likely to do one, two, or all of three things: we fight ourselves (self-criticism – often our first reaction when things go wrong), we flee from others (isolation), or we freeze (rumination).
Feeling threatened puts stress on the mind and body, and chronic stress leads to anxiety and depression, which hinders emotional and physical well-being. With self-criticism, we are both the attacker and the attacked. When we practice self-compassion, we are deactivating the threat-defense system and activating the care system, releasing oxytocin and endorphins, which reduce stress and increase feelings of safety and security.3
Why is self-compassion important to provider well-being?
Research has shown that individuals who are more self-compassionate tend to have greater happiness, life satisfaction, and motivation; better relationships and physical health; and less anxiety and depression. They also have the resilience needed to cope with stressful life events. The more we practice being kind and compassionate with ourselves, the more we’ll increase the habit of self-compassion, and extend compassion to our patients and loved ones in daily life.4
Why is self-compassion important? When we experience a setback at work or in life, we can become defensive, accuse others, or blame ourselves, especially when we are already under immense stress. These responses are not helpful, productive, or effective to the situation or our personal well-being. Although in the moment it may feel good to be reactive, it is a short-lived feeling that we trade for the longer-lasting effects of learning, resilience, and personal growth. Self-compassion teaches us to connect with our inner imperfections, and what makes us human, as to err is human.
To cultivate a habit of self-compassion itself, it is important to understand that self-compassion is a practice of goodwill, not good feelings. Self-compassion is aimed at the alleviation of suffering, but it does not erase any pain and suffering that does exist. The truth is, we can’t always control external forces – the events of 2020-2021 are a perfect example of this. As a result, we cannot utilize self-compassion as a practice to make our pain disappear or suppress strong emotions.
Instead, self-compassion helps us cultivate the resilience needed to mindfully acknowledge and accept a painful moment or experience, while reminding us to embrace ourselves with kindness and care in response. This builds our internal foundation with support, love, and self-care, while providing the optimal conditions for growth, resilience, and transformation
Self-compassion and the backdraft phenomenon
When you start the practice of self-compassion, you may experience backdraft, a phenomenon in which pain initially increases.5 Backdraft is similar to the stages of grief or when the flames of a burning house become larger when a door is opened and oxygen surges in. Practicing self-compassion may cause a tidal wave of emotions to come to the forefront, but it is likely that if this happens, it needs to happen.
Imagine yourself in a room with two versions of yourself. To the left is your best self that you present to the world, standing tall, organized, well kept, and without any noticeable imperfections. To the right, is the deepest part of your being, laying on the floor, filled with raw emotions – sadness, fear, anger, and love. This version of yourself is vulnerable, open, honest, and imperfect. When looking at each version of yourself, which one is the real you? The right? The left? Maybe it’s both?
Imagine what would happen if you walked over to the version of yourself on the right, sat down, and provided it comfort, and embraced yourself with love and kindness. What would happen if you gave that version of yourself a hug? Seeing your true self, with all the layers peeled away, at the very core of your being, vulnerable, and possibly broken, is a powerful and gut-wrenching experience. It may hurt at first, but once we embrace our own pain and suffering, that is where mindfulness and self-compassion intersect to begin the path to healing. It takes more strength and courage to be the version of ourselves on the right than the version on the left.
What is not self compassion?
Self-compassion is not self-pity, weakness, self-esteem, or selfishness. When individuals feel self-pity, they become immersed in their own problems and feel that they are the only ones in the world who are suffering. Self-compassion makes us more willing to accept, experience, and acknowledge difficult feelings with kindness. This paradoxically helps us process and let go of these feelings without long-term negative consequences, and with a better ability to recognize the suffering of others.
Self-compassion allows us to be our own inner ally and strengthens our ability to cope successfully when life gets hard. Self-compassion will not make you weak and vulnerable. It is a reliable source of inner strength that enhances resilience when faced with difficulties. Research shows self-compassionate people are better able to cope with tough situations like divorce, trauma, and crisis.
Self-compassion and self-esteem are important to well-being; however, they are not the same. Self-esteem refers to a judgment or evaluation of our sense of self-worth, perceived value, or how much we like ourselves. While self-compassion relates to the changing landscape of who we are with kindness and acceptance – especially in times when we feel useless, inadequate, or hopeless – self-esteem allows for greater self-clarity, independent of external circumstances, and acknowledges that all human beings deserve compassion and understanding, not because they possess certain traits or have a certain perceive valued, but because we share the human experience and the human condition of imperfection. Finally, self-compassion is not selfish, as practicing it helps people sustain the act of caring for others and decrease caregiver burnout.6,7
Strategies to practice self-compassion
There are many ways to practice self-compassion. Here are a few experiences created by Dr. Neff, a leader in the field.8
Experience 1: How would you treat a friend?
How do you think things might change if you responded to yourself in the same way you typically respond to a close friend when he or she is suffering? Why not try treating yourself like a good friend and see what happens.
Take out a sheet of paper and write down your answer to the following questions:
- First, think about times when a close friend feels really bad about him or herself or is really struggling in some way. How would you respond to your friend in this situation (especially when you’re at your best)? Write down what you typically do and say and note the tone in which you typically talk to your friends.
- Second, think about times when you feel bad about yourself or are struggling. How do you typically respond to yourself in these situations? Write down what you typically do and say, and note the tone in which you typically talk to your friends.
- Did you notice a difference? If so, ask yourself why. What factors or fears come into play that lead you to treat yourself and others so differently?
- Please write down how you think things might change if you responded to yourself in the same way you typically respond to a close friend when you’re suffering.
Experience 2: Take a self-compassion break
This practice can be used any time of day or night, with others or alone. It will help you remember to evoke the three aspects of self-compassion when you need it most.
Think of a situation in your life that is difficult, that is causing you stress. Call the situation to mind, and if you feel comfortable, allow yourself to experience these feelings and emotions, without judgment and without altering them to what you think they should be.
- Say to yourself one of the following: “This is a difficult moment,” “This is a moment of suffering,” “This is stress,” “This hurts,” or “Ouch.” Doing this step is “mindfulness”: A willingness to observe negative thoughts and emotions with openness and clarity, so that they are held in mindful awareness, without judgment.
- Find your equilibrium of observation with thoughts and feelings. Try not to suppress or deny them and try not to get caught up and swept away by them.
- Remind yourself of the shared human experience. Recognize that suffering and personal difficulty is something that we all go through rather than being something that happens to “me” alone. Remind yourself that “other people feel this way,” “I’m not alone,” and “we all have struggles in life.”
- Be kind to yourself and ask: “What do I need to hear right now to express kindness to myself?” Is there a phrase that speaks to you in your particular situation? For example: “May I give myself the compassion that I need; may I learn to accept myself as I am; may I forgive myself; may I be strong; may I be patient.” There is no wrong answer.
Exercise 3: Explore self-compassion through writing
Everybody has something about themselves that they don’t like; something that causes them to feel shame, to feel insecure, or not “good enough.” This exercise will help you write a letter to yourself about this issue from a place of acceptance and compassion. It can feel uncomfortable at first, but it gets easier with practice.
- Write about an issue you have that makes you feel inadequate or bad about yourself (physical appearance, work, or relationship issue) What emotions do you experience when you think about this aspect of yourself? Try to only feel your emotions exactly as they are – no more, no less – and then write about them.
- Write a letter as if you were talking to a dearly beloved friend who was struggling with the same concerns as you and has the same strengths and weaknesses as you. How would you convey deep compassion, especially for the pain you feel when they judge themselves so harshly? What would you write to your friend to remind them that they are only human, that all people have both strengths and weaknesses? As you write, try to infuse your letter with a strong sense of acceptance, kindness, caring, and desire for their health and happiness.
- After writing the letter, put it aside for a little while. Then come back and read it again, really letting the words sink in. Feel the compassion as it pours into you, soothing and comforting you. Love, connection, and acceptance are a part of your human right. To claim them you need only look within yourself.
Experience 4: Taking care of the caregiver
We work in the very stressful time of the COVID pandemic. As medical providers, we are caregivers to our patients and our families. Yet, we do not give ourselves time to rest, recover, and recharge. Remember, to care for others, you cannot pour from an empty cup.
- Give yourself permission to meet your own needs, recognizing that this will not only enhance your quality of life, it will also enhance your ability to be there for those that rely on you. Our time is limited but self-care can occur both at work and outside of work.
- When you are “off the clock,” be off the clock! Turn off notifications, don’t check email, and be present in your personal lives. If you are constantly answering patient calls or nursing questions until 10 p.m., that means your health care system is in need of an upgrade, as you need the appropriate coverage to give you time to care for yourself, just as well as you care for your patients.
- While at work you can practice self-care. Take 2 minutes to practice relaxation breathing. Take 1 minute to show yourself or another person gratitude. Take 5 minutes before you start writing your notes for the day to listen to relaxing music or a mindful podcast. Take 3 minutes to share three good things that happened in the day with your family or colleagues. Take 5-10 minutes to do chair yoga. Take a self-compassion break.
- Implement a 5-minute wellness break into your group’s daily function with some of the previous mentioned examples. This will allow you to care for and nurture yourself, while also caring for and nurturing others in an environment that cultivates your wellness goals.
As a hospitalist, I can attest that I did not show myself self-compassion nearly as often as I showed compassion to others. I am my own worst critic and my training taught me to suffer in silence, and not seek out others who are experiencing the same thing for fear of being perceived as weak, inadequate, or flawed.
This false notion that we need to always be tough, strong, and without emotion in order to be taken seriously, to advance, or be held in high regard is rubbish and only perpetuated by accepting it. In order to change the culture of medicine, we have to change the way we think and behave. I have practiced self-compassion exercises and it has enhanced my perspective to see that many of us are going through varying degrees of the same thing. It has shown me the positive effects on my inner being and my life. If you are ready to try something new that will benefit your psychological and emotional well-being, and help you through pain, suffering, struggles, and crisis, you have nothing to lose. Be the change, and show yourself self-compassion.
In summary, self-compassion is an attitude of warmth, curiosity, connection, and care. Learning to become more self-compassionate is a process of moving from striving to change our experience and ourselves toward embracing who we are already.9 The practice of self-compassion is giving ourselves what we need in the moment. Even if we are not ready, or it is too painful to fully accept or embrace, we can still plant the seeds that will, with time and patience, grow and bloom.
When we are mindful of our struggles, when we respond to ourselves with compassion, kindness, and give ourselves support in times of difficulty, we learn to embrace ourselves and our lives, our inner and outer imperfections, and provide ourselves with the strength needed to thrive in the most precarious and difficult situations. With self-compassion, we give the world the best of us, instead of what is left of us.
Dr. Williams is vice president of the Hampton Roads chapter of the Society of Hospital Medicine. She is a hospitalist at Sentara Careplex Hospital in Hampton, Va., where she also serves as vice president of the medical executive committee.
References
1. Sanchez-Reilly S et al. Caring for oneself to care for others: Physicians and their self-care. J Community Support Oncol. 2013;11(2):75-81. doi: 10.12788/j.suponc.0003.
2. Neff K. Self-Compassion: An Alternative Conceptualization of a Healthy Attitude Toward Oneself. Self Identity. 2010;2(2):85-101. doi: 10.1080/15298860309032.
3. Neff K et al. The forest and the trees: Examining the association of self-compassion and its positive and negative components with psychological functioning. Self Identity. 2018;17(6):627-45. doi: 10.1080/15298868.2018.1436587.
4. Zessin U et al. The relationship between self-compassion and well-being: A meta-analysis. Appl Psychol Health Well-Being. 2015;7(3):340-64. doi: 10.1111/aphw.12051.
5. Warren R et al. Self-criticism and self-compassion: Risk and resilience. Current Psychiatry. 2016 Dec;15(12):18-21,24-28,32.
6. Neff K. The Five Myths of Self-Compassion. Greater Good Magazine. 2015 Sep 30. https://greatergood.berkeley.edu/article/item/the_five_myths_of_self_compassion.
7. Neff KD and Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. J Clin Psychol. 2013 Jan;69(1):28-44. doi: 10.1002/jclp.21923.
8. Neff K. Self-Compassion Guided Meditations and Exercises. https://self-compassion.org/category/exercises/#exercises.
9. Germer C and Neff KD. Mindful Self-Compassion (MSC), in “The handbook of mindfulness-based programs.” (London: Routledge, 2019, pp. 357-67).
A mindful way relate to ourselves
A mindful way relate to ourselves
Physicians, clinicians, providers, healers, and now heroes, are some of the names we have been given throughout history. These titles bring together a universal concept in medicine that all human beings deserve compassion, understanding, and care. However, as health care providers we forget to show ourselves the same compassion we bestow upon others.
Self-compassion is a new way of relating to ourselves. As clinicians, we are trained investigators, delving deeper into what our patient is thinking and feeling. “Tell me more about that. How does that make you feel? That must have been (very painful/scary/frustrating).” These are a few statements we learned in patient interviewing to actively engage with patients, build rapport, solidify trust, validate their concerns, and ultimately obtain the information needed to diagnose and heal.
We know the importance of looking beyond the surface, as more often than not a deeper inspection reveals more to the story. We have uncovered cracks in the foundation, erosion of the roof, worn out siding, and a glimpse into the complexities that make up each individual. We look at our patients, loved ones, and the world with night-vision lenses to uncover what is deeper.
Clinicians are good at directing compassion toward others, but not as good at giving it to themselves.1 Many health care providers may see self-compassion as soft, weak, selfish, or unnecessary. However, mindful self-compassion is a positive practice that opens a pathway for healing, personal growth, and protection against the negative consequences of self-judgment, isolation, anxiety, burnout, and depression.
What is self-compassion?
Kristin Neff, PhD, an associate professor in educational psychology at the University of Texas at Austin, was the first to academically define self-compassion. Self-compassion brings together three core elements – kindness, humanity, and mindfulness.2 Self-compassion involves acting the same way toward yourself when you are having a difficult time as you would toward another person. Instead of mercilessly judging and criticizing yourself for self-perceived inadequacies or shortcomings, self-compassion allows you to ask yourself: “How can I give myself comfort and care in this moment?”
Mindfulness acknowledges a painful experience without resistance or judgment, while being present in the moment with things as they are. Self-compassion provides the emotional safety needed to mindfully open to our pain, disappointments, and defeats. Mindfulness and self-compassion both allow us to live with more acceptance toward ourselves and our lives. Mindfulness asks: “What am I experiencing right now?” Self-compassion asks: “What do I need right now?” When you feel compassion for yourself or another, you recognize that suffering, failure, and imperfection are all part of the shared human experience.
The physiology of self-compassion
When we practice self-compassion, we feel safe and cared for because there is a physiological pathway that explains this response. Self-compassion helps down-regulate the stress response (fight-flight-freeze). When we are triggered by a threat to our self-concept, we are likely to do one, two, or all of three things: we fight ourselves (self-criticism – often our first reaction when things go wrong), we flee from others (isolation), or we freeze (rumination).
Feeling threatened puts stress on the mind and body, and chronic stress leads to anxiety and depression, which hinders emotional and physical well-being. With self-criticism, we are both the attacker and the attacked. When we practice self-compassion, we are deactivating the threat-defense system and activating the care system, releasing oxytocin and endorphins, which reduce stress and increase feelings of safety and security.3
Why is self-compassion important to provider well-being?
Research has shown that individuals who are more self-compassionate tend to have greater happiness, life satisfaction, and motivation; better relationships and physical health; and less anxiety and depression. They also have the resilience needed to cope with stressful life events. The more we practice being kind and compassionate with ourselves, the more we’ll increase the habit of self-compassion, and extend compassion to our patients and loved ones in daily life.4
Why is self-compassion important? When we experience a setback at work or in life, we can become defensive, accuse others, or blame ourselves, especially when we are already under immense stress. These responses are not helpful, productive, or effective to the situation or our personal well-being. Although in the moment it may feel good to be reactive, it is a short-lived feeling that we trade for the longer-lasting effects of learning, resilience, and personal growth. Self-compassion teaches us to connect with our inner imperfections, and what makes us human, as to err is human.
To cultivate a habit of self-compassion itself, it is important to understand that self-compassion is a practice of goodwill, not good feelings. Self-compassion is aimed at the alleviation of suffering, but it does not erase any pain and suffering that does exist. The truth is, we can’t always control external forces – the events of 2020-2021 are a perfect example of this. As a result, we cannot utilize self-compassion as a practice to make our pain disappear or suppress strong emotions.
Instead, self-compassion helps us cultivate the resilience needed to mindfully acknowledge and accept a painful moment or experience, while reminding us to embrace ourselves with kindness and care in response. This builds our internal foundation with support, love, and self-care, while providing the optimal conditions for growth, resilience, and transformation
Self-compassion and the backdraft phenomenon
When you start the practice of self-compassion, you may experience backdraft, a phenomenon in which pain initially increases.5 Backdraft is similar to the stages of grief or when the flames of a burning house become larger when a door is opened and oxygen surges in. Practicing self-compassion may cause a tidal wave of emotions to come to the forefront, but it is likely that if this happens, it needs to happen.
Imagine yourself in a room with two versions of yourself. To the left is your best self that you present to the world, standing tall, organized, well kept, and without any noticeable imperfections. To the right, is the deepest part of your being, laying on the floor, filled with raw emotions – sadness, fear, anger, and love. This version of yourself is vulnerable, open, honest, and imperfect. When looking at each version of yourself, which one is the real you? The right? The left? Maybe it’s both?
Imagine what would happen if you walked over to the version of yourself on the right, sat down, and provided it comfort, and embraced yourself with love and kindness. What would happen if you gave that version of yourself a hug? Seeing your true self, with all the layers peeled away, at the very core of your being, vulnerable, and possibly broken, is a powerful and gut-wrenching experience. It may hurt at first, but once we embrace our own pain and suffering, that is where mindfulness and self-compassion intersect to begin the path to healing. It takes more strength and courage to be the version of ourselves on the right than the version on the left.
What is not self compassion?
Self-compassion is not self-pity, weakness, self-esteem, or selfishness. When individuals feel self-pity, they become immersed in their own problems and feel that they are the only ones in the world who are suffering. Self-compassion makes us more willing to accept, experience, and acknowledge difficult feelings with kindness. This paradoxically helps us process and let go of these feelings without long-term negative consequences, and with a better ability to recognize the suffering of others.
Self-compassion allows us to be our own inner ally and strengthens our ability to cope successfully when life gets hard. Self-compassion will not make you weak and vulnerable. It is a reliable source of inner strength that enhances resilience when faced with difficulties. Research shows self-compassionate people are better able to cope with tough situations like divorce, trauma, and crisis.
Self-compassion and self-esteem are important to well-being; however, they are not the same. Self-esteem refers to a judgment or evaluation of our sense of self-worth, perceived value, or how much we like ourselves. While self-compassion relates to the changing landscape of who we are with kindness and acceptance – especially in times when we feel useless, inadequate, or hopeless – self-esteem allows for greater self-clarity, independent of external circumstances, and acknowledges that all human beings deserve compassion and understanding, not because they possess certain traits or have a certain perceive valued, but because we share the human experience and the human condition of imperfection. Finally, self-compassion is not selfish, as practicing it helps people sustain the act of caring for others and decrease caregiver burnout.6,7
Strategies to practice self-compassion
There are many ways to practice self-compassion. Here are a few experiences created by Dr. Neff, a leader in the field.8
Experience 1: How would you treat a friend?
How do you think things might change if you responded to yourself in the same way you typically respond to a close friend when he or she is suffering? Why not try treating yourself like a good friend and see what happens.
Take out a sheet of paper and write down your answer to the following questions:
- First, think about times when a close friend feels really bad about him or herself or is really struggling in some way. How would you respond to your friend in this situation (especially when you’re at your best)? Write down what you typically do and say and note the tone in which you typically talk to your friends.
- Second, think about times when you feel bad about yourself or are struggling. How do you typically respond to yourself in these situations? Write down what you typically do and say, and note the tone in which you typically talk to your friends.
- Did you notice a difference? If so, ask yourself why. What factors or fears come into play that lead you to treat yourself and others so differently?
- Please write down how you think things might change if you responded to yourself in the same way you typically respond to a close friend when you’re suffering.
Experience 2: Take a self-compassion break
This practice can be used any time of day or night, with others or alone. It will help you remember to evoke the three aspects of self-compassion when you need it most.
Think of a situation in your life that is difficult, that is causing you stress. Call the situation to mind, and if you feel comfortable, allow yourself to experience these feelings and emotions, without judgment and without altering them to what you think they should be.
- Say to yourself one of the following: “This is a difficult moment,” “This is a moment of suffering,” “This is stress,” “This hurts,” or “Ouch.” Doing this step is “mindfulness”: A willingness to observe negative thoughts and emotions with openness and clarity, so that they are held in mindful awareness, without judgment.
- Find your equilibrium of observation with thoughts and feelings. Try not to suppress or deny them and try not to get caught up and swept away by them.
- Remind yourself of the shared human experience. Recognize that suffering and personal difficulty is something that we all go through rather than being something that happens to “me” alone. Remind yourself that “other people feel this way,” “I’m not alone,” and “we all have struggles in life.”
- Be kind to yourself and ask: “What do I need to hear right now to express kindness to myself?” Is there a phrase that speaks to you in your particular situation? For example: “May I give myself the compassion that I need; may I learn to accept myself as I am; may I forgive myself; may I be strong; may I be patient.” There is no wrong answer.
Exercise 3: Explore self-compassion through writing
Everybody has something about themselves that they don’t like; something that causes them to feel shame, to feel insecure, or not “good enough.” This exercise will help you write a letter to yourself about this issue from a place of acceptance and compassion. It can feel uncomfortable at first, but it gets easier with practice.
- Write about an issue you have that makes you feel inadequate or bad about yourself (physical appearance, work, or relationship issue) What emotions do you experience when you think about this aspect of yourself? Try to only feel your emotions exactly as they are – no more, no less – and then write about them.
- Write a letter as if you were talking to a dearly beloved friend who was struggling with the same concerns as you and has the same strengths and weaknesses as you. How would you convey deep compassion, especially for the pain you feel when they judge themselves so harshly? What would you write to your friend to remind them that they are only human, that all people have both strengths and weaknesses? As you write, try to infuse your letter with a strong sense of acceptance, kindness, caring, and desire for their health and happiness.
- After writing the letter, put it aside for a little while. Then come back and read it again, really letting the words sink in. Feel the compassion as it pours into you, soothing and comforting you. Love, connection, and acceptance are a part of your human right. To claim them you need only look within yourself.
Experience 4: Taking care of the caregiver
We work in the very stressful time of the COVID pandemic. As medical providers, we are caregivers to our patients and our families. Yet, we do not give ourselves time to rest, recover, and recharge. Remember, to care for others, you cannot pour from an empty cup.
- Give yourself permission to meet your own needs, recognizing that this will not only enhance your quality of life, it will also enhance your ability to be there for those that rely on you. Our time is limited but self-care can occur both at work and outside of work.
- When you are “off the clock,” be off the clock! Turn off notifications, don’t check email, and be present in your personal lives. If you are constantly answering patient calls or nursing questions until 10 p.m., that means your health care system is in need of an upgrade, as you need the appropriate coverage to give you time to care for yourself, just as well as you care for your patients.
- While at work you can practice self-care. Take 2 minutes to practice relaxation breathing. Take 1 minute to show yourself or another person gratitude. Take 5 minutes before you start writing your notes for the day to listen to relaxing music or a mindful podcast. Take 3 minutes to share three good things that happened in the day with your family or colleagues. Take 5-10 minutes to do chair yoga. Take a self-compassion break.
- Implement a 5-minute wellness break into your group’s daily function with some of the previous mentioned examples. This will allow you to care for and nurture yourself, while also caring for and nurturing others in an environment that cultivates your wellness goals.
As a hospitalist, I can attest that I did not show myself self-compassion nearly as often as I showed compassion to others. I am my own worst critic and my training taught me to suffer in silence, and not seek out others who are experiencing the same thing for fear of being perceived as weak, inadequate, or flawed.
This false notion that we need to always be tough, strong, and without emotion in order to be taken seriously, to advance, or be held in high regard is rubbish and only perpetuated by accepting it. In order to change the culture of medicine, we have to change the way we think and behave. I have practiced self-compassion exercises and it has enhanced my perspective to see that many of us are going through varying degrees of the same thing. It has shown me the positive effects on my inner being and my life. If you are ready to try something new that will benefit your psychological and emotional well-being, and help you through pain, suffering, struggles, and crisis, you have nothing to lose. Be the change, and show yourself self-compassion.
In summary, self-compassion is an attitude of warmth, curiosity, connection, and care. Learning to become more self-compassionate is a process of moving from striving to change our experience and ourselves toward embracing who we are already.9 The practice of self-compassion is giving ourselves what we need in the moment. Even if we are not ready, or it is too painful to fully accept or embrace, we can still plant the seeds that will, with time and patience, grow and bloom.
When we are mindful of our struggles, when we respond to ourselves with compassion, kindness, and give ourselves support in times of difficulty, we learn to embrace ourselves and our lives, our inner and outer imperfections, and provide ourselves with the strength needed to thrive in the most precarious and difficult situations. With self-compassion, we give the world the best of us, instead of what is left of us.
Dr. Williams is vice president of the Hampton Roads chapter of the Society of Hospital Medicine. She is a hospitalist at Sentara Careplex Hospital in Hampton, Va., where she also serves as vice president of the medical executive committee.
References
1. Sanchez-Reilly S et al. Caring for oneself to care for others: Physicians and their self-care. J Community Support Oncol. 2013;11(2):75-81. doi: 10.12788/j.suponc.0003.
2. Neff K. Self-Compassion: An Alternative Conceptualization of a Healthy Attitude Toward Oneself. Self Identity. 2010;2(2):85-101. doi: 10.1080/15298860309032.
3. Neff K et al. The forest and the trees: Examining the association of self-compassion and its positive and negative components with psychological functioning. Self Identity. 2018;17(6):627-45. doi: 10.1080/15298868.2018.1436587.
4. Zessin U et al. The relationship between self-compassion and well-being: A meta-analysis. Appl Psychol Health Well-Being. 2015;7(3):340-64. doi: 10.1111/aphw.12051.
5. Warren R et al. Self-criticism and self-compassion: Risk and resilience. Current Psychiatry. 2016 Dec;15(12):18-21,24-28,32.
6. Neff K. The Five Myths of Self-Compassion. Greater Good Magazine. 2015 Sep 30. https://greatergood.berkeley.edu/article/item/the_five_myths_of_self_compassion.
7. Neff KD and Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. J Clin Psychol. 2013 Jan;69(1):28-44. doi: 10.1002/jclp.21923.
8. Neff K. Self-Compassion Guided Meditations and Exercises. https://self-compassion.org/category/exercises/#exercises.
9. Germer C and Neff KD. Mindful Self-Compassion (MSC), in “The handbook of mindfulness-based programs.” (London: Routledge, 2019, pp. 357-67).
Physicians, clinicians, providers, healers, and now heroes, are some of the names we have been given throughout history. These titles bring together a universal concept in medicine that all human beings deserve compassion, understanding, and care. However, as health care providers we forget to show ourselves the same compassion we bestow upon others.
Self-compassion is a new way of relating to ourselves. As clinicians, we are trained investigators, delving deeper into what our patient is thinking and feeling. “Tell me more about that. How does that make you feel? That must have been (very painful/scary/frustrating).” These are a few statements we learned in patient interviewing to actively engage with patients, build rapport, solidify trust, validate their concerns, and ultimately obtain the information needed to diagnose and heal.
We know the importance of looking beyond the surface, as more often than not a deeper inspection reveals more to the story. We have uncovered cracks in the foundation, erosion of the roof, worn out siding, and a glimpse into the complexities that make up each individual. We look at our patients, loved ones, and the world with night-vision lenses to uncover what is deeper.
Clinicians are good at directing compassion toward others, but not as good at giving it to themselves.1 Many health care providers may see self-compassion as soft, weak, selfish, or unnecessary. However, mindful self-compassion is a positive practice that opens a pathway for healing, personal growth, and protection against the negative consequences of self-judgment, isolation, anxiety, burnout, and depression.
What is self-compassion?
Kristin Neff, PhD, an associate professor in educational psychology at the University of Texas at Austin, was the first to academically define self-compassion. Self-compassion brings together three core elements – kindness, humanity, and mindfulness.2 Self-compassion involves acting the same way toward yourself when you are having a difficult time as you would toward another person. Instead of mercilessly judging and criticizing yourself for self-perceived inadequacies or shortcomings, self-compassion allows you to ask yourself: “How can I give myself comfort and care in this moment?”
Mindfulness acknowledges a painful experience without resistance or judgment, while being present in the moment with things as they are. Self-compassion provides the emotional safety needed to mindfully open to our pain, disappointments, and defeats. Mindfulness and self-compassion both allow us to live with more acceptance toward ourselves and our lives. Mindfulness asks: “What am I experiencing right now?” Self-compassion asks: “What do I need right now?” When you feel compassion for yourself or another, you recognize that suffering, failure, and imperfection are all part of the shared human experience.
The physiology of self-compassion
When we practice self-compassion, we feel safe and cared for because there is a physiological pathway that explains this response. Self-compassion helps down-regulate the stress response (fight-flight-freeze). When we are triggered by a threat to our self-concept, we are likely to do one, two, or all of three things: we fight ourselves (self-criticism – often our first reaction when things go wrong), we flee from others (isolation), or we freeze (rumination).
Feeling threatened puts stress on the mind and body, and chronic stress leads to anxiety and depression, which hinders emotional and physical well-being. With self-criticism, we are both the attacker and the attacked. When we practice self-compassion, we are deactivating the threat-defense system and activating the care system, releasing oxytocin and endorphins, which reduce stress and increase feelings of safety and security.3
Why is self-compassion important to provider well-being?
Research has shown that individuals who are more self-compassionate tend to have greater happiness, life satisfaction, and motivation; better relationships and physical health; and less anxiety and depression. They also have the resilience needed to cope with stressful life events. The more we practice being kind and compassionate with ourselves, the more we’ll increase the habit of self-compassion, and extend compassion to our patients and loved ones in daily life.4
Why is self-compassion important? When we experience a setback at work or in life, we can become defensive, accuse others, or blame ourselves, especially when we are already under immense stress. These responses are not helpful, productive, or effective to the situation or our personal well-being. Although in the moment it may feel good to be reactive, it is a short-lived feeling that we trade for the longer-lasting effects of learning, resilience, and personal growth. Self-compassion teaches us to connect with our inner imperfections, and what makes us human, as to err is human.
To cultivate a habit of self-compassion itself, it is important to understand that self-compassion is a practice of goodwill, not good feelings. Self-compassion is aimed at the alleviation of suffering, but it does not erase any pain and suffering that does exist. The truth is, we can’t always control external forces – the events of 2020-2021 are a perfect example of this. As a result, we cannot utilize self-compassion as a practice to make our pain disappear or suppress strong emotions.
Instead, self-compassion helps us cultivate the resilience needed to mindfully acknowledge and accept a painful moment or experience, while reminding us to embrace ourselves with kindness and care in response. This builds our internal foundation with support, love, and self-care, while providing the optimal conditions for growth, resilience, and transformation
Self-compassion and the backdraft phenomenon
When you start the practice of self-compassion, you may experience backdraft, a phenomenon in which pain initially increases.5 Backdraft is similar to the stages of grief or when the flames of a burning house become larger when a door is opened and oxygen surges in. Practicing self-compassion may cause a tidal wave of emotions to come to the forefront, but it is likely that if this happens, it needs to happen.
Imagine yourself in a room with two versions of yourself. To the left is your best self that you present to the world, standing tall, organized, well kept, and without any noticeable imperfections. To the right, is the deepest part of your being, laying on the floor, filled with raw emotions – sadness, fear, anger, and love. This version of yourself is vulnerable, open, honest, and imperfect. When looking at each version of yourself, which one is the real you? The right? The left? Maybe it’s both?
Imagine what would happen if you walked over to the version of yourself on the right, sat down, and provided it comfort, and embraced yourself with love and kindness. What would happen if you gave that version of yourself a hug? Seeing your true self, with all the layers peeled away, at the very core of your being, vulnerable, and possibly broken, is a powerful and gut-wrenching experience. It may hurt at first, but once we embrace our own pain and suffering, that is where mindfulness and self-compassion intersect to begin the path to healing. It takes more strength and courage to be the version of ourselves on the right than the version on the left.
What is not self compassion?
Self-compassion is not self-pity, weakness, self-esteem, or selfishness. When individuals feel self-pity, they become immersed in their own problems and feel that they are the only ones in the world who are suffering. Self-compassion makes us more willing to accept, experience, and acknowledge difficult feelings with kindness. This paradoxically helps us process and let go of these feelings without long-term negative consequences, and with a better ability to recognize the suffering of others.
Self-compassion allows us to be our own inner ally and strengthens our ability to cope successfully when life gets hard. Self-compassion will not make you weak and vulnerable. It is a reliable source of inner strength that enhances resilience when faced with difficulties. Research shows self-compassionate people are better able to cope with tough situations like divorce, trauma, and crisis.
Self-compassion and self-esteem are important to well-being; however, they are not the same. Self-esteem refers to a judgment or evaluation of our sense of self-worth, perceived value, or how much we like ourselves. While self-compassion relates to the changing landscape of who we are with kindness and acceptance – especially in times when we feel useless, inadequate, or hopeless – self-esteem allows for greater self-clarity, independent of external circumstances, and acknowledges that all human beings deserve compassion and understanding, not because they possess certain traits or have a certain perceive valued, but because we share the human experience and the human condition of imperfection. Finally, self-compassion is not selfish, as practicing it helps people sustain the act of caring for others and decrease caregiver burnout.6,7
Strategies to practice self-compassion
There are many ways to practice self-compassion. Here are a few experiences created by Dr. Neff, a leader in the field.8
Experience 1: How would you treat a friend?
How do you think things might change if you responded to yourself in the same way you typically respond to a close friend when he or she is suffering? Why not try treating yourself like a good friend and see what happens.
Take out a sheet of paper and write down your answer to the following questions:
- First, think about times when a close friend feels really bad about him or herself or is really struggling in some way. How would you respond to your friend in this situation (especially when you’re at your best)? Write down what you typically do and say and note the tone in which you typically talk to your friends.
- Second, think about times when you feel bad about yourself or are struggling. How do you typically respond to yourself in these situations? Write down what you typically do and say, and note the tone in which you typically talk to your friends.
- Did you notice a difference? If so, ask yourself why. What factors or fears come into play that lead you to treat yourself and others so differently?
- Please write down how you think things might change if you responded to yourself in the same way you typically respond to a close friend when you’re suffering.
Experience 2: Take a self-compassion break
This practice can be used any time of day or night, with others or alone. It will help you remember to evoke the three aspects of self-compassion when you need it most.
Think of a situation in your life that is difficult, that is causing you stress. Call the situation to mind, and if you feel comfortable, allow yourself to experience these feelings and emotions, without judgment and without altering them to what you think they should be.
- Say to yourself one of the following: “This is a difficult moment,” “This is a moment of suffering,” “This is stress,” “This hurts,” or “Ouch.” Doing this step is “mindfulness”: A willingness to observe negative thoughts and emotions with openness and clarity, so that they are held in mindful awareness, without judgment.
- Find your equilibrium of observation with thoughts and feelings. Try not to suppress or deny them and try not to get caught up and swept away by them.
- Remind yourself of the shared human experience. Recognize that suffering and personal difficulty is something that we all go through rather than being something that happens to “me” alone. Remind yourself that “other people feel this way,” “I’m not alone,” and “we all have struggles in life.”
- Be kind to yourself and ask: “What do I need to hear right now to express kindness to myself?” Is there a phrase that speaks to you in your particular situation? For example: “May I give myself the compassion that I need; may I learn to accept myself as I am; may I forgive myself; may I be strong; may I be patient.” There is no wrong answer.
Exercise 3: Explore self-compassion through writing
Everybody has something about themselves that they don’t like; something that causes them to feel shame, to feel insecure, or not “good enough.” This exercise will help you write a letter to yourself about this issue from a place of acceptance and compassion. It can feel uncomfortable at first, but it gets easier with practice.
- Write about an issue you have that makes you feel inadequate or bad about yourself (physical appearance, work, or relationship issue) What emotions do you experience when you think about this aspect of yourself? Try to only feel your emotions exactly as they are – no more, no less – and then write about them.
- Write a letter as if you were talking to a dearly beloved friend who was struggling with the same concerns as you and has the same strengths and weaknesses as you. How would you convey deep compassion, especially for the pain you feel when they judge themselves so harshly? What would you write to your friend to remind them that they are only human, that all people have both strengths and weaknesses? As you write, try to infuse your letter with a strong sense of acceptance, kindness, caring, and desire for their health and happiness.
- After writing the letter, put it aside for a little while. Then come back and read it again, really letting the words sink in. Feel the compassion as it pours into you, soothing and comforting you. Love, connection, and acceptance are a part of your human right. To claim them you need only look within yourself.
Experience 4: Taking care of the caregiver
We work in the very stressful time of the COVID pandemic. As medical providers, we are caregivers to our patients and our families. Yet, we do not give ourselves time to rest, recover, and recharge. Remember, to care for others, you cannot pour from an empty cup.
- Give yourself permission to meet your own needs, recognizing that this will not only enhance your quality of life, it will also enhance your ability to be there for those that rely on you. Our time is limited but self-care can occur both at work and outside of work.
- When you are “off the clock,” be off the clock! Turn off notifications, don’t check email, and be present in your personal lives. If you are constantly answering patient calls or nursing questions until 10 p.m., that means your health care system is in need of an upgrade, as you need the appropriate coverage to give you time to care for yourself, just as well as you care for your patients.
- While at work you can practice self-care. Take 2 minutes to practice relaxation breathing. Take 1 minute to show yourself or another person gratitude. Take 5 minutes before you start writing your notes for the day to listen to relaxing music or a mindful podcast. Take 3 minutes to share three good things that happened in the day with your family or colleagues. Take 5-10 minutes to do chair yoga. Take a self-compassion break.
- Implement a 5-minute wellness break into your group’s daily function with some of the previous mentioned examples. This will allow you to care for and nurture yourself, while also caring for and nurturing others in an environment that cultivates your wellness goals.
As a hospitalist, I can attest that I did not show myself self-compassion nearly as often as I showed compassion to others. I am my own worst critic and my training taught me to suffer in silence, and not seek out others who are experiencing the same thing for fear of being perceived as weak, inadequate, or flawed.
This false notion that we need to always be tough, strong, and without emotion in order to be taken seriously, to advance, or be held in high regard is rubbish and only perpetuated by accepting it. In order to change the culture of medicine, we have to change the way we think and behave. I have practiced self-compassion exercises and it has enhanced my perspective to see that many of us are going through varying degrees of the same thing. It has shown me the positive effects on my inner being and my life. If you are ready to try something new that will benefit your psychological and emotional well-being, and help you through pain, suffering, struggles, and crisis, you have nothing to lose. Be the change, and show yourself self-compassion.
In summary, self-compassion is an attitude of warmth, curiosity, connection, and care. Learning to become more self-compassionate is a process of moving from striving to change our experience and ourselves toward embracing who we are already.9 The practice of self-compassion is giving ourselves what we need in the moment. Even if we are not ready, or it is too painful to fully accept or embrace, we can still plant the seeds that will, with time and patience, grow and bloom.
When we are mindful of our struggles, when we respond to ourselves with compassion, kindness, and give ourselves support in times of difficulty, we learn to embrace ourselves and our lives, our inner and outer imperfections, and provide ourselves with the strength needed to thrive in the most precarious and difficult situations. With self-compassion, we give the world the best of us, instead of what is left of us.
Dr. Williams is vice president of the Hampton Roads chapter of the Society of Hospital Medicine. She is a hospitalist at Sentara Careplex Hospital in Hampton, Va., where she also serves as vice president of the medical executive committee.
References
1. Sanchez-Reilly S et al. Caring for oneself to care for others: Physicians and their self-care. J Community Support Oncol. 2013;11(2):75-81. doi: 10.12788/j.suponc.0003.
2. Neff K. Self-Compassion: An Alternative Conceptualization of a Healthy Attitude Toward Oneself. Self Identity. 2010;2(2):85-101. doi: 10.1080/15298860309032.
3. Neff K et al. The forest and the trees: Examining the association of self-compassion and its positive and negative components with psychological functioning. Self Identity. 2018;17(6):627-45. doi: 10.1080/15298868.2018.1436587.
4. Zessin U et al. The relationship between self-compassion and well-being: A meta-analysis. Appl Psychol Health Well-Being. 2015;7(3):340-64. doi: 10.1111/aphw.12051.
5. Warren R et al. Self-criticism and self-compassion: Risk and resilience. Current Psychiatry. 2016 Dec;15(12):18-21,24-28,32.
6. Neff K. The Five Myths of Self-Compassion. Greater Good Magazine. 2015 Sep 30. https://greatergood.berkeley.edu/article/item/the_five_myths_of_self_compassion.
7. Neff KD and Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. J Clin Psychol. 2013 Jan;69(1):28-44. doi: 10.1002/jclp.21923.
8. Neff K. Self-Compassion Guided Meditations and Exercises. https://self-compassion.org/category/exercises/#exercises.
9. Germer C and Neff KD. Mindful Self-Compassion (MSC), in “The handbook of mindfulness-based programs.” (London: Routledge, 2019, pp. 357-67).
Record-breaking autism rates reported with new CDC criteria
Childhood autism rates are at the highest level since the Centers for Disease Control and Prevention began tracking the disorder in 2000, new data released Dec. 2 show.
The increase likely reflects improvements in diagnosis and identification of autism spectrum disorder (ASD), not an increase in incidence, study authors with the CDC’s Autism and Developmental Disabilities Monitoring (ADDM) Network told this news organization.
Using a new surveillance methodology, researchers found that 2.3% of 8-year-olds in communities in 11 states across the United States had an autism diagnosis in 2018, up from 1.9% in 2016.
A separate report on early identification in 4-year-olds shows that children born in 2014 were 50% more likely to receive an autism diagnosis or ASD special education classification by 48 months of age than those born in 2010, signaling improved early diagnosis.
Taken together, the data suggest efforts to raise awareness about autism are working, though researchers were quick to say much work remains.
“It was not surprising to me and in fact it was reassuring that the number of children diagnosed with autism is higher and is actually approaching prevalence of autism that has been noted in some national surveys of parents,” Stuart Shapira, MD, PhD, associate director for science in CDC’s National Center on Birth Defects and Developmental Disability, told this news organization.
“It means we’re doing a better job of identifying children, which helps to get them into services earlier so they can achieve their best developmental outcome.”
The studies, published online in Morbidity and Mortality Weekly Report, are the first to use a new ASD surveillance protocol that relies on ASD diagnosis or special education classification and billing codes and eliminates comprehensive records analysis by trained clinician reviewers.
Racial disparities
The updated methodology was less labor intensive and reduced the time it took to produce the report, but it is not without its critics, who claim the new protocol will undercount the number of children with ASD.
Created in 2000 and funded by the CDC, the ADDM Network is the only surveillance program in the United States that tracks the number and characteristics of children with ASD in multiple communities in the U.S.
When ADDM released its first report in 2007 from six states and based on data from the year 2000, ASD prevalence was 6.7 per 1,000 children, or 1 in 150 children.
In the latest report, which includes data from 2018, the autism prevalence rate across 11 states was 23.0 per 1,000 children, or 1 in 44 children.
That rate is closer to reported autism prevalence from the National Survey of Children’s Health and the National Health Interview Survey, both of which rely on parent-reported ASD diagnoses.
in Arizona, Arkansas, California, Georgia, Maryland, Minnesota, Missouri, New Jersey, Tennessee, Utah, and Wisconsin.
Children were counted as having autism if their records included an ASD diagnosis, a special education classification of ASD, or an ASD International Classification of Diseases (ICD) code. A total of 5,058 children met those criteria.
Rates of ASD ranged from a low of 1.7% in Missouri to 3.9% in California and were 4.2 times higher in boys than in girls. Just under half of the children with ASD were evaluated by age 36 months.
Although the overall ASD prevalence was similar among White, Black, Hispanic, and Asian/Pacific Islander children, the report highlighted a number of other racial disparities overall and in individual states.
For example, among those with ASD and data on cognitive ability, 35.2% had an intelligence quotient score of 70 or lower. Black children with ASD were far more likely to have an IQ of 70 or less (49.8%) than Hispanic (33.1%) or White (29.7%) children.
“The persistent disparities in co-occurring intellectual disabilities in children with autism is something that we continue to see and suggests that we need to better understand exactly what’s happening,” Matthew Maenner, PhD, an epidemiologist and autism surveillance team lead with the CDC’s National Center on Birth Defects and Developmental Disabilities, told this news organization.
Another long-standing trend observed again in the new report on prevalence among 8-year-olds is low ASD prevalence among Hispanic children. While the overall estimate showed similar autism rates, a closer review of state-level data reveals a different picture.
“In almost half of the sites, Hispanic children were less likely to be identified as having ASD,” he said. “This gets lost if you look only at the overall estimate.”
New methodology
When ADDM released its first report in 2007, autism diagnosis was widely inadequate in the United States. Relying on only confirmed ASD diagnoses would significantly underestimate the number of children with the disorder, so the CDC added “active case finding” to the protocol.
Trained clinician reviewers analyzed individual notes from medical and educational records for every 8-year-old in ADDM Network sites, looking for evidence of characteristics and behaviors associated with autism. The process was labor- and time-intensive and took up to 4 years to complete.
In 2018, the CDC began investigating ways to speed the process and came up with the strategy used in the latest report. The new protocol was faster, easier, and less expensive. Although he says cost was never the deciding factor, Dr. Maenner acknowledges that had they stuck with the original protocol, they would have been forced to reduce the number of ADDM Network sites.
Dr. Maenner argues that a comparison of the two protocols shows the new method doesn’t compromise accuracy and may actually capture children who lacked the medical or educational records the previous protocol required for a count. But not everyone agrees.
“I thought the point was to be as accurate and complete as possible in doing the surveillance,” Walter Zahorodny, PhD, associate professor of pediatrics at Rutgers University, New Brunswick, N.J., and principal investigator of the New Jersey ADDM Network site, told this news organization. “In states where there’s a high detail of information in records, like New Jersey, it’s going to underestimate the count.”
Dr. Zahorodny says the latest data prove his point. In 2016, under the old methodology, ASD prevalence was 3.1% in the state. In 2018, under the new protocol, prevalence was 2.84%, a decrease of about 20% that Dr. Zahorodny pins squarely on the elimination of ADDM clinical reviewers.
But New Jersey is the only state that participated in both the 2016 and 2018 surveillance periods to report a decrease in ASD prevalence. The other eight states all found autism rates in their states went up.
Sydney Pettygrove, PhD, associate professor of public health and pediatrics at the University of Arizona, Tucson, and a principal investigator for the ADDM site in Arizona, told this news organization that when she first learned the CDC was rolling out a new methodology, she and other investigators were concerned.
“People were really upset. I was really upset,” she said. “I had formed an opinion based on the earlier data that this would not be a good idea.”
In 2000, when ASD surveillance began in Arizona, nearly 30% of children identified by ADDM clinical reviewers as having autism had no mention of the disorder in their records. Today, that percentage is closer to 5%.
“In 2000 it would have been catastrophic to try to estimate the prevalence of autism with the new protocol,” said Dr. Pettygrove. As it turns out, under the new protocol, prevalence rates in Arizona increased from 16.0 per 1,000 children in 2016 to 24.9 in 2018.
Built-in bias eliminated?
In addition to speeding up the process, the new methodology might have other benefits as well. Under the old ADDM surveillance protocol, children who lacked certain medical or educational records did not meet the ASD case definition and weren’t counted.
A 2019 study showed that this disproportionately affected Black and Hispanic children, who had significantly less access to health care professionals than White children.
As a result, “the old methodology had a bias built into it,” Maureen Durkin, PhD, DrPH, coauthor of that study and chair of population health sciences at the University of Wisconsin–Madison and principal investigator for the ADDM site in Wisconsin, told this news organization.
“Clinician reviewers ended up putting these children in the ‘suspected ASD’ category because they couldn’t call it a case under the case definition,” Dr. Durkin said. “There was a fairly large percentage of suspected cases and a disproportionate number of those kids were children of color.”
Although she can’t say for sure, Dr. Durkin said it’s possible the new protocol could eliminate some of that bias.
CDC researchers also attribute the new method to an expanded study of early diagnosis among 4-year-olds. In previous years, only a handful of the ADDM Network sites participating in the 8-year-old surveillance project also studied early diagnosis in 4-year-olds.
This year, all 11 sites took part in the early diagnosis analysis, tripling the number of children included in the analysis. That made it possible to include, for the first time, Asian/Pacific Islander children in this analysis.
In the past, ASD prevalence has trended higher in White children, compared with other racial groups. The new data found that ASD prevalence among 4-year-olds was significantly lower in White children (12.9 per 1,000 children) than in Black, Hispanic, or Asian/Pacific Islander children (16.6, 21.1, and 22.7 per 1,000, respectively). Prevalence in American Indian/Alaska Native children was the lowest among all racial groups (11.5 per 1,000).
It’s the first time researchers have seen this pattern in any ADDM report, Kelly Shaw, PhD, lead author of that study and an epidemiologist with the National Center on Birth Defects and Developmental Disability at the CDC, told this news organization.
These data don’t provide clues about the potential cause of that disparity, Dr. Shaw said. It’s likely an indication of better identification of ASD in those communities, she said, and not a sign of increased incidence of autism among Black, Hispanic, or Asian/Pacific Islander children.
“We don’t have any evidence to suggest or expect that autism would be increasing differentially among groups,” Dr. Shaw said.
The data suggest “we are making some progress but there certainly is still room for improvement,” Dr. Shaw said.
Study authors report no conflicts of interest.
A version of this article first appeared on Medscape.com.
Childhood autism rates are at the highest level since the Centers for Disease Control and Prevention began tracking the disorder in 2000, new data released Dec. 2 show.
The increase likely reflects improvements in diagnosis and identification of autism spectrum disorder (ASD), not an increase in incidence, study authors with the CDC’s Autism and Developmental Disabilities Monitoring (ADDM) Network told this news organization.
Using a new surveillance methodology, researchers found that 2.3% of 8-year-olds in communities in 11 states across the United States had an autism diagnosis in 2018, up from 1.9% in 2016.
A separate report on early identification in 4-year-olds shows that children born in 2014 were 50% more likely to receive an autism diagnosis or ASD special education classification by 48 months of age than those born in 2010, signaling improved early diagnosis.
Taken together, the data suggest efforts to raise awareness about autism are working, though researchers were quick to say much work remains.
“It was not surprising to me and in fact it was reassuring that the number of children diagnosed with autism is higher and is actually approaching prevalence of autism that has been noted in some national surveys of parents,” Stuart Shapira, MD, PhD, associate director for science in CDC’s National Center on Birth Defects and Developmental Disability, told this news organization.
“It means we’re doing a better job of identifying children, which helps to get them into services earlier so they can achieve their best developmental outcome.”
The studies, published online in Morbidity and Mortality Weekly Report, are the first to use a new ASD surveillance protocol that relies on ASD diagnosis or special education classification and billing codes and eliminates comprehensive records analysis by trained clinician reviewers.
Racial disparities
The updated methodology was less labor intensive and reduced the time it took to produce the report, but it is not without its critics, who claim the new protocol will undercount the number of children with ASD.
Created in 2000 and funded by the CDC, the ADDM Network is the only surveillance program in the United States that tracks the number and characteristics of children with ASD in multiple communities in the U.S.
When ADDM released its first report in 2007 from six states and based on data from the year 2000, ASD prevalence was 6.7 per 1,000 children, or 1 in 150 children.
In the latest report, which includes data from 2018, the autism prevalence rate across 11 states was 23.0 per 1,000 children, or 1 in 44 children.
That rate is closer to reported autism prevalence from the National Survey of Children’s Health and the National Health Interview Survey, both of which rely on parent-reported ASD diagnoses.
in Arizona, Arkansas, California, Georgia, Maryland, Minnesota, Missouri, New Jersey, Tennessee, Utah, and Wisconsin.
Children were counted as having autism if their records included an ASD diagnosis, a special education classification of ASD, or an ASD International Classification of Diseases (ICD) code. A total of 5,058 children met those criteria.
Rates of ASD ranged from a low of 1.7% in Missouri to 3.9% in California and were 4.2 times higher in boys than in girls. Just under half of the children with ASD were evaluated by age 36 months.
Although the overall ASD prevalence was similar among White, Black, Hispanic, and Asian/Pacific Islander children, the report highlighted a number of other racial disparities overall and in individual states.
For example, among those with ASD and data on cognitive ability, 35.2% had an intelligence quotient score of 70 or lower. Black children with ASD were far more likely to have an IQ of 70 or less (49.8%) than Hispanic (33.1%) or White (29.7%) children.
“The persistent disparities in co-occurring intellectual disabilities in children with autism is something that we continue to see and suggests that we need to better understand exactly what’s happening,” Matthew Maenner, PhD, an epidemiologist and autism surveillance team lead with the CDC’s National Center on Birth Defects and Developmental Disabilities, told this news organization.
Another long-standing trend observed again in the new report on prevalence among 8-year-olds is low ASD prevalence among Hispanic children. While the overall estimate showed similar autism rates, a closer review of state-level data reveals a different picture.
“In almost half of the sites, Hispanic children were less likely to be identified as having ASD,” he said. “This gets lost if you look only at the overall estimate.”
New methodology
When ADDM released its first report in 2007, autism diagnosis was widely inadequate in the United States. Relying on only confirmed ASD diagnoses would significantly underestimate the number of children with the disorder, so the CDC added “active case finding” to the protocol.
Trained clinician reviewers analyzed individual notes from medical and educational records for every 8-year-old in ADDM Network sites, looking for evidence of characteristics and behaviors associated with autism. The process was labor- and time-intensive and took up to 4 years to complete.
In 2018, the CDC began investigating ways to speed the process and came up with the strategy used in the latest report. The new protocol was faster, easier, and less expensive. Although he says cost was never the deciding factor, Dr. Maenner acknowledges that had they stuck with the original protocol, they would have been forced to reduce the number of ADDM Network sites.
Dr. Maenner argues that a comparison of the two protocols shows the new method doesn’t compromise accuracy and may actually capture children who lacked the medical or educational records the previous protocol required for a count. But not everyone agrees.
“I thought the point was to be as accurate and complete as possible in doing the surveillance,” Walter Zahorodny, PhD, associate professor of pediatrics at Rutgers University, New Brunswick, N.J., and principal investigator of the New Jersey ADDM Network site, told this news organization. “In states where there’s a high detail of information in records, like New Jersey, it’s going to underestimate the count.”
Dr. Zahorodny says the latest data prove his point. In 2016, under the old methodology, ASD prevalence was 3.1% in the state. In 2018, under the new protocol, prevalence was 2.84%, a decrease of about 20% that Dr. Zahorodny pins squarely on the elimination of ADDM clinical reviewers.
But New Jersey is the only state that participated in both the 2016 and 2018 surveillance periods to report a decrease in ASD prevalence. The other eight states all found autism rates in their states went up.
Sydney Pettygrove, PhD, associate professor of public health and pediatrics at the University of Arizona, Tucson, and a principal investigator for the ADDM site in Arizona, told this news organization that when she first learned the CDC was rolling out a new methodology, she and other investigators were concerned.
“People were really upset. I was really upset,” she said. “I had formed an opinion based on the earlier data that this would not be a good idea.”
In 2000, when ASD surveillance began in Arizona, nearly 30% of children identified by ADDM clinical reviewers as having autism had no mention of the disorder in their records. Today, that percentage is closer to 5%.
“In 2000 it would have been catastrophic to try to estimate the prevalence of autism with the new protocol,” said Dr. Pettygrove. As it turns out, under the new protocol, prevalence rates in Arizona increased from 16.0 per 1,000 children in 2016 to 24.9 in 2018.
Built-in bias eliminated?
In addition to speeding up the process, the new methodology might have other benefits as well. Under the old ADDM surveillance protocol, children who lacked certain medical or educational records did not meet the ASD case definition and weren’t counted.
A 2019 study showed that this disproportionately affected Black and Hispanic children, who had significantly less access to health care professionals than White children.
As a result, “the old methodology had a bias built into it,” Maureen Durkin, PhD, DrPH, coauthor of that study and chair of population health sciences at the University of Wisconsin–Madison and principal investigator for the ADDM site in Wisconsin, told this news organization.
“Clinician reviewers ended up putting these children in the ‘suspected ASD’ category because they couldn’t call it a case under the case definition,” Dr. Durkin said. “There was a fairly large percentage of suspected cases and a disproportionate number of those kids were children of color.”
Although she can’t say for sure, Dr. Durkin said it’s possible the new protocol could eliminate some of that bias.
CDC researchers also attribute the new method to an expanded study of early diagnosis among 4-year-olds. In previous years, only a handful of the ADDM Network sites participating in the 8-year-old surveillance project also studied early diagnosis in 4-year-olds.
This year, all 11 sites took part in the early diagnosis analysis, tripling the number of children included in the analysis. That made it possible to include, for the first time, Asian/Pacific Islander children in this analysis.
In the past, ASD prevalence has trended higher in White children, compared with other racial groups. The new data found that ASD prevalence among 4-year-olds was significantly lower in White children (12.9 per 1,000 children) than in Black, Hispanic, or Asian/Pacific Islander children (16.6, 21.1, and 22.7 per 1,000, respectively). Prevalence in American Indian/Alaska Native children was the lowest among all racial groups (11.5 per 1,000).
It’s the first time researchers have seen this pattern in any ADDM report, Kelly Shaw, PhD, lead author of that study and an epidemiologist with the National Center on Birth Defects and Developmental Disability at the CDC, told this news organization.
These data don’t provide clues about the potential cause of that disparity, Dr. Shaw said. It’s likely an indication of better identification of ASD in those communities, she said, and not a sign of increased incidence of autism among Black, Hispanic, or Asian/Pacific Islander children.
“We don’t have any evidence to suggest or expect that autism would be increasing differentially among groups,” Dr. Shaw said.
The data suggest “we are making some progress but there certainly is still room for improvement,” Dr. Shaw said.
Study authors report no conflicts of interest.
A version of this article first appeared on Medscape.com.
Childhood autism rates are at the highest level since the Centers for Disease Control and Prevention began tracking the disorder in 2000, new data released Dec. 2 show.
The increase likely reflects improvements in diagnosis and identification of autism spectrum disorder (ASD), not an increase in incidence, study authors with the CDC’s Autism and Developmental Disabilities Monitoring (ADDM) Network told this news organization.
Using a new surveillance methodology, researchers found that 2.3% of 8-year-olds in communities in 11 states across the United States had an autism diagnosis in 2018, up from 1.9% in 2016.
A separate report on early identification in 4-year-olds shows that children born in 2014 were 50% more likely to receive an autism diagnosis or ASD special education classification by 48 months of age than those born in 2010, signaling improved early diagnosis.
Taken together, the data suggest efforts to raise awareness about autism are working, though researchers were quick to say much work remains.
“It was not surprising to me and in fact it was reassuring that the number of children diagnosed with autism is higher and is actually approaching prevalence of autism that has been noted in some national surveys of parents,” Stuart Shapira, MD, PhD, associate director for science in CDC’s National Center on Birth Defects and Developmental Disability, told this news organization.
“It means we’re doing a better job of identifying children, which helps to get them into services earlier so they can achieve their best developmental outcome.”
The studies, published online in Morbidity and Mortality Weekly Report, are the first to use a new ASD surveillance protocol that relies on ASD diagnosis or special education classification and billing codes and eliminates comprehensive records analysis by trained clinician reviewers.
Racial disparities
The updated methodology was less labor intensive and reduced the time it took to produce the report, but it is not without its critics, who claim the new protocol will undercount the number of children with ASD.
Created in 2000 and funded by the CDC, the ADDM Network is the only surveillance program in the United States that tracks the number and characteristics of children with ASD in multiple communities in the U.S.
When ADDM released its first report in 2007 from six states and based on data from the year 2000, ASD prevalence was 6.7 per 1,000 children, or 1 in 150 children.
In the latest report, which includes data from 2018, the autism prevalence rate across 11 states was 23.0 per 1,000 children, or 1 in 44 children.
That rate is closer to reported autism prevalence from the National Survey of Children’s Health and the National Health Interview Survey, both of which rely on parent-reported ASD diagnoses.
in Arizona, Arkansas, California, Georgia, Maryland, Minnesota, Missouri, New Jersey, Tennessee, Utah, and Wisconsin.
Children were counted as having autism if their records included an ASD diagnosis, a special education classification of ASD, or an ASD International Classification of Diseases (ICD) code. A total of 5,058 children met those criteria.
Rates of ASD ranged from a low of 1.7% in Missouri to 3.9% in California and were 4.2 times higher in boys than in girls. Just under half of the children with ASD were evaluated by age 36 months.
Although the overall ASD prevalence was similar among White, Black, Hispanic, and Asian/Pacific Islander children, the report highlighted a number of other racial disparities overall and in individual states.
For example, among those with ASD and data on cognitive ability, 35.2% had an intelligence quotient score of 70 or lower. Black children with ASD were far more likely to have an IQ of 70 or less (49.8%) than Hispanic (33.1%) or White (29.7%) children.
“The persistent disparities in co-occurring intellectual disabilities in children with autism is something that we continue to see and suggests that we need to better understand exactly what’s happening,” Matthew Maenner, PhD, an epidemiologist and autism surveillance team lead with the CDC’s National Center on Birth Defects and Developmental Disabilities, told this news organization.
Another long-standing trend observed again in the new report on prevalence among 8-year-olds is low ASD prevalence among Hispanic children. While the overall estimate showed similar autism rates, a closer review of state-level data reveals a different picture.
“In almost half of the sites, Hispanic children were less likely to be identified as having ASD,” he said. “This gets lost if you look only at the overall estimate.”
New methodology
When ADDM released its first report in 2007, autism diagnosis was widely inadequate in the United States. Relying on only confirmed ASD diagnoses would significantly underestimate the number of children with the disorder, so the CDC added “active case finding” to the protocol.
Trained clinician reviewers analyzed individual notes from medical and educational records for every 8-year-old in ADDM Network sites, looking for evidence of characteristics and behaviors associated with autism. The process was labor- and time-intensive and took up to 4 years to complete.
In 2018, the CDC began investigating ways to speed the process and came up with the strategy used in the latest report. The new protocol was faster, easier, and less expensive. Although he says cost was never the deciding factor, Dr. Maenner acknowledges that had they stuck with the original protocol, they would have been forced to reduce the number of ADDM Network sites.
Dr. Maenner argues that a comparison of the two protocols shows the new method doesn’t compromise accuracy and may actually capture children who lacked the medical or educational records the previous protocol required for a count. But not everyone agrees.
“I thought the point was to be as accurate and complete as possible in doing the surveillance,” Walter Zahorodny, PhD, associate professor of pediatrics at Rutgers University, New Brunswick, N.J., and principal investigator of the New Jersey ADDM Network site, told this news organization. “In states where there’s a high detail of information in records, like New Jersey, it’s going to underestimate the count.”
Dr. Zahorodny says the latest data prove his point. In 2016, under the old methodology, ASD prevalence was 3.1% in the state. In 2018, under the new protocol, prevalence was 2.84%, a decrease of about 20% that Dr. Zahorodny pins squarely on the elimination of ADDM clinical reviewers.
But New Jersey is the only state that participated in both the 2016 and 2018 surveillance periods to report a decrease in ASD prevalence. The other eight states all found autism rates in their states went up.
Sydney Pettygrove, PhD, associate professor of public health and pediatrics at the University of Arizona, Tucson, and a principal investigator for the ADDM site in Arizona, told this news organization that when she first learned the CDC was rolling out a new methodology, she and other investigators were concerned.
“People were really upset. I was really upset,” she said. “I had formed an opinion based on the earlier data that this would not be a good idea.”
In 2000, when ASD surveillance began in Arizona, nearly 30% of children identified by ADDM clinical reviewers as having autism had no mention of the disorder in their records. Today, that percentage is closer to 5%.
“In 2000 it would have been catastrophic to try to estimate the prevalence of autism with the new protocol,” said Dr. Pettygrove. As it turns out, under the new protocol, prevalence rates in Arizona increased from 16.0 per 1,000 children in 2016 to 24.9 in 2018.
Built-in bias eliminated?
In addition to speeding up the process, the new methodology might have other benefits as well. Under the old ADDM surveillance protocol, children who lacked certain medical or educational records did not meet the ASD case definition and weren’t counted.
A 2019 study showed that this disproportionately affected Black and Hispanic children, who had significantly less access to health care professionals than White children.
As a result, “the old methodology had a bias built into it,” Maureen Durkin, PhD, DrPH, coauthor of that study and chair of population health sciences at the University of Wisconsin–Madison and principal investigator for the ADDM site in Wisconsin, told this news organization.
“Clinician reviewers ended up putting these children in the ‘suspected ASD’ category because they couldn’t call it a case under the case definition,” Dr. Durkin said. “There was a fairly large percentage of suspected cases and a disproportionate number of those kids were children of color.”
Although she can’t say for sure, Dr. Durkin said it’s possible the new protocol could eliminate some of that bias.
CDC researchers also attribute the new method to an expanded study of early diagnosis among 4-year-olds. In previous years, only a handful of the ADDM Network sites participating in the 8-year-old surveillance project also studied early diagnosis in 4-year-olds.
This year, all 11 sites took part in the early diagnosis analysis, tripling the number of children included in the analysis. That made it possible to include, for the first time, Asian/Pacific Islander children in this analysis.
In the past, ASD prevalence has trended higher in White children, compared with other racial groups. The new data found that ASD prevalence among 4-year-olds was significantly lower in White children (12.9 per 1,000 children) than in Black, Hispanic, or Asian/Pacific Islander children (16.6, 21.1, and 22.7 per 1,000, respectively). Prevalence in American Indian/Alaska Native children was the lowest among all racial groups (11.5 per 1,000).
It’s the first time researchers have seen this pattern in any ADDM report, Kelly Shaw, PhD, lead author of that study and an epidemiologist with the National Center on Birth Defects and Developmental Disability at the CDC, told this news organization.
These data don’t provide clues about the potential cause of that disparity, Dr. Shaw said. It’s likely an indication of better identification of ASD in those communities, she said, and not a sign of increased incidence of autism among Black, Hispanic, or Asian/Pacific Islander children.
“We don’t have any evidence to suggest or expect that autism would be increasing differentially among groups,” Dr. Shaw said.
The data suggest “we are making some progress but there certainly is still room for improvement,” Dr. Shaw said.
Study authors report no conflicts of interest.
A version of this article first appeared on Medscape.com.
The gender pay gap, care economy, and mental health
According to an analysis by the Pew Research Center and a report by the National Women’s Law Center, women were earning approximately $0.83-$0.84 for every $1.00 earned by their male counterparts in 2020. Accordingly, women would need to work an additional 42 days to receive compensation for earnings by men during that year. Moreover, these gaps exist with respect to race inequalities. For example, Black and Latinx women who are working full-time were reported to earn approximately $0.64 and $0.57, respectively, for every $1.00 compared with their white, non-Hispanic male counterparts. Striking, isn’t it?
The gender pay gap also affects physicians. A 2021 Medscape survey found that male physicians earn 35% more than female physicians. The biggest gap seems to be between male and female specialists, with men earning $376,000 and women $283,000.
Gender inequality and COVID-19
In addition to workplace responsibilities, women are more likely to take on unpaid positions in the informal care economy – examples of these tasks include cleaning, grocery shopping, and child care. In fact, the COVID-19 pandemic has increased the burden of unpaid care work among women, which often incurs a significant impact on their participation in the paid economy.
A study in the United States evaluating the impact of gender inequality during COVID-19 suggested that the rise in unemployment among women during this time may be related to decreased occupational flexibility. Accordingly, the closure of schools and caregiving facilities has translated into increased responsibilities as the informal caregiver, and a decreased ability to fulfill work obligations. Consequently, women may be overwhelmed and unable to maintain their employment status, are limited in their work opportunities, and/or are furloughed or passed over for promotions.
Gendered pay gaps affect mental health
A study by Platt and colleagues investigated the relationship between gendered wage gaps and gendered disparities in depression and anxiety disorders. Researchers found that females with a lower income compared with their matched male counterparts were more likely to experience depression and generalized anxiety disorders (i.e., they were 2.4 times more likely to experience depression and 4 times more likely to experience anxiety), while women who earned more than men did not report a significant difference in depression there were reduced gaps in the prevalence of anxiety disorders. As such, it has been suggested that wage gap inequalities are a contributing factor to gendered mental health disparities.
Reduced pay is not only a signifier of reduced returns on human capital. It may also have implications for one’s role in the care economy (e.g., greater time allocation as a result of reduced return), and may result in a higher likelihood for relocation as it relates to a partner’s work, overqualification for a position, inflexible work schedules, and reduced work autonomy.
Wage inequalities may act as a proxy for workplace inequalities such as promotions, prestigious projects, limited upward mobility, and internalized negative workplace experiences, all of which may contribute to increased sleep loss, stress, and related mental health stressors.
One might say, “A few cents, so what?” We should encourage conversations around the gender pay gap and develop strategies to combat this economic and social disparity.
Ms. Lui completed an HBSc global health specialist degree at the University of Toronto, where she is now an MSc candidate. She has received income from Braxia Scientific Corp. A version of this article first appeared on Medscape.com.
According to an analysis by the Pew Research Center and a report by the National Women’s Law Center, women were earning approximately $0.83-$0.84 for every $1.00 earned by their male counterparts in 2020. Accordingly, women would need to work an additional 42 days to receive compensation for earnings by men during that year. Moreover, these gaps exist with respect to race inequalities. For example, Black and Latinx women who are working full-time were reported to earn approximately $0.64 and $0.57, respectively, for every $1.00 compared with their white, non-Hispanic male counterparts. Striking, isn’t it?
The gender pay gap also affects physicians. A 2021 Medscape survey found that male physicians earn 35% more than female physicians. The biggest gap seems to be between male and female specialists, with men earning $376,000 and women $283,000.
Gender inequality and COVID-19
In addition to workplace responsibilities, women are more likely to take on unpaid positions in the informal care economy – examples of these tasks include cleaning, grocery shopping, and child care. In fact, the COVID-19 pandemic has increased the burden of unpaid care work among women, which often incurs a significant impact on their participation in the paid economy.
A study in the United States evaluating the impact of gender inequality during COVID-19 suggested that the rise in unemployment among women during this time may be related to decreased occupational flexibility. Accordingly, the closure of schools and caregiving facilities has translated into increased responsibilities as the informal caregiver, and a decreased ability to fulfill work obligations. Consequently, women may be overwhelmed and unable to maintain their employment status, are limited in their work opportunities, and/or are furloughed or passed over for promotions.
Gendered pay gaps affect mental health
A study by Platt and colleagues investigated the relationship between gendered wage gaps and gendered disparities in depression and anxiety disorders. Researchers found that females with a lower income compared with their matched male counterparts were more likely to experience depression and generalized anxiety disorders (i.e., they were 2.4 times more likely to experience depression and 4 times more likely to experience anxiety), while women who earned more than men did not report a significant difference in depression there were reduced gaps in the prevalence of anxiety disorders. As such, it has been suggested that wage gap inequalities are a contributing factor to gendered mental health disparities.
Reduced pay is not only a signifier of reduced returns on human capital. It may also have implications for one’s role in the care economy (e.g., greater time allocation as a result of reduced return), and may result in a higher likelihood for relocation as it relates to a partner’s work, overqualification for a position, inflexible work schedules, and reduced work autonomy.
Wage inequalities may act as a proxy for workplace inequalities such as promotions, prestigious projects, limited upward mobility, and internalized negative workplace experiences, all of which may contribute to increased sleep loss, stress, and related mental health stressors.
One might say, “A few cents, so what?” We should encourage conversations around the gender pay gap and develop strategies to combat this economic and social disparity.
Ms. Lui completed an HBSc global health specialist degree at the University of Toronto, where she is now an MSc candidate. She has received income from Braxia Scientific Corp. A version of this article first appeared on Medscape.com.
According to an analysis by the Pew Research Center and a report by the National Women’s Law Center, women were earning approximately $0.83-$0.84 for every $1.00 earned by their male counterparts in 2020. Accordingly, women would need to work an additional 42 days to receive compensation for earnings by men during that year. Moreover, these gaps exist with respect to race inequalities. For example, Black and Latinx women who are working full-time were reported to earn approximately $0.64 and $0.57, respectively, for every $1.00 compared with their white, non-Hispanic male counterparts. Striking, isn’t it?
The gender pay gap also affects physicians. A 2021 Medscape survey found that male physicians earn 35% more than female physicians. The biggest gap seems to be between male and female specialists, with men earning $376,000 and women $283,000.
Gender inequality and COVID-19
In addition to workplace responsibilities, women are more likely to take on unpaid positions in the informal care economy – examples of these tasks include cleaning, grocery shopping, and child care. In fact, the COVID-19 pandemic has increased the burden of unpaid care work among women, which often incurs a significant impact on their participation in the paid economy.
A study in the United States evaluating the impact of gender inequality during COVID-19 suggested that the rise in unemployment among women during this time may be related to decreased occupational flexibility. Accordingly, the closure of schools and caregiving facilities has translated into increased responsibilities as the informal caregiver, and a decreased ability to fulfill work obligations. Consequently, women may be overwhelmed and unable to maintain their employment status, are limited in their work opportunities, and/or are furloughed or passed over for promotions.
Gendered pay gaps affect mental health
A study by Platt and colleagues investigated the relationship between gendered wage gaps and gendered disparities in depression and anxiety disorders. Researchers found that females with a lower income compared with their matched male counterparts were more likely to experience depression and generalized anxiety disorders (i.e., they were 2.4 times more likely to experience depression and 4 times more likely to experience anxiety), while women who earned more than men did not report a significant difference in depression there were reduced gaps in the prevalence of anxiety disorders. As such, it has been suggested that wage gap inequalities are a contributing factor to gendered mental health disparities.
Reduced pay is not only a signifier of reduced returns on human capital. It may also have implications for one’s role in the care economy (e.g., greater time allocation as a result of reduced return), and may result in a higher likelihood for relocation as it relates to a partner’s work, overqualification for a position, inflexible work schedules, and reduced work autonomy.
Wage inequalities may act as a proxy for workplace inequalities such as promotions, prestigious projects, limited upward mobility, and internalized negative workplace experiences, all of which may contribute to increased sleep loss, stress, and related mental health stressors.
One might say, “A few cents, so what?” We should encourage conversations around the gender pay gap and develop strategies to combat this economic and social disparity.
Ms. Lui completed an HBSc global health specialist degree at the University of Toronto, where she is now an MSc candidate. She has received income from Braxia Scientific Corp. A version of this article first appeared on Medscape.com.
COVID-19 and the immunocompromised physician
Working feverishly to complete the myriad patient notes accumulated throughout a hectic day, my phone vibrated – alerting me to a number that, over the past several years, has wrought uncertainty, grief, and overwhelming relief. Answering hesitantly, I listened to my physician’s pharmacist inform me of unexpected and alarming news.
Since COVID-19 was first identified more than 1 year ago, more than 770,000 people have died in the United States. In the wake of those losses, countless grieve while attempting to navigate a future without their loved ones. Meanwhile, scientists worked feverishly to combat a pandemic relentless in contagion. As health care professionals, we work tirelessly against the sharpened scythe of death, toiling day after day without an identifiable end. All the while, advocacy has prevailed as the need for personal protective equipment, improved ventilation systems, sanitization measures, and other mitigation measures, such as mask wearing and social distancing, echoed swiftly across the nation and around the world.
But, as the months have progressed, and life has seemingly transitioned toward a parallel version of reality, subsections of communities have grown restless. Several nontherapeutic, ineffective, and falsely touted regimens have been promoted. Amid the chaos of misinformation, most medical professionals have sought support from respected journals and infectious disease experts to filter out jargon and piece together scientifically sound protocols. Although many lives have prevailed by way of those advancements, mixed messages about interventions have emerged – and in many quarters across the country, anger, resistance, and outright refusal have prevailed.
Yet, we – the medical community – have forged ever onward as the cases continued and the death toll steadily climbed. In many cases, physicians who are years removed from critical care training have been thrust into COVID units, while residents have shifted toward working outside of their chosen specialty. Outpatient offices have closed, salaries have been cut, and furloughs have loomed as days fade into months. Beset with exhaustion and uncertainty, sacrifice has become a common thread that intrinsically united us against an unrelenting foe.
Most people continued navigating the many changes and made concerted efforts to mimic our prepandemic lives. Working from home in makeshift offices, dusting off math skills to assist children through the doldrums of distance learning, and mastering various audiovisual platforms, we reinforced social bonds and forged new connections echoing the hallmark resilience reminiscent of our shared distant ancestry.
As of this writing, thanks to our work – and that of scientists and policy makers – about 69% of Americans have received at least one dose of vaccine, and vaccines are widely available to children 5 and older. But it has been disheartening to watch misinformation about vaccine research and development propagated by political figures, social media, and lay people.
Processing the phone call
While listening to my physician’s pharmacist, I slowed my breaths in an effort to find calm. Years of navigating the American health care industry had left me both equipped and ill-prepared for the unexpected. I listened intently to the pharmacist’s words while staring blankly at a computer screen – uncertain of what had felt so assured not 10 minutes earlier.
That’s when I got the news. The intravenous medication that aided in my stabilization had suffered a critical shortage because of its successful use in the treatment of patients with COVID-19 pneumonia – patients who, in a majority of cases, had likely refused the vaccines. As result, the medication that had enabled my return to work, active engagement in nonwork pursuits, and most importantly, equipped my body to thrive despite the damage it had suffered, suddenly vanished.
Gently placing my phone on the desk, my heart beat rapidly as tears steadily streamed down my face. Staring blankly ahead, my hands gradually balled into fists as I let out a sound of fear, agony, and uncertainty. Screaming at everything and nothing, nausea swelled as panic flooded my body. In that moment, I ruminated on the conversation with the pharmacist. There had been no discussion, no option for me to maintain accessibility to this valuable medicine. Consequently, I felt helpless. Although the same medication, albeit a different mechanism of delivery, was promptly chosen as an adequate substitute, there was no guarantee of it bestowing the same degree of efficacy. So I was terrified, envisioning the progress made over several years as plummeting into an abyss of pain and despair. What are those of us who have chosen medicine as our profession but are immunocompromised expected to make of this?
Over the next several weeks, I diligently adhered to the new regimen and focused on positive mentation. Nevertheless, day by day, the symptoms worsened; eventually, I became bed ridden. I tried to gather what little composure remained to reschedule patients and justify the resounding guilt of perceived failure. I remember the sweet and gentle look of my child as I once again could not summon the strength to play pretend. This felt overwhelming. Would I ever go back to work? Would I see my child grow? No amount of pleading or screaming would change the fact that a medical system chose to roll the dice on my health. In a haze of discomfort and betrayal, I wondered how a physician or medical facility could justify removing medication from someone reliant upon it. How do we choose the appropriate allocation of resources when the consequences are potentially catastrophic?
Searching for context
When a country is founded on the mission of rising as a leading world power built upon the concepts of freedom, basic human rights, and individuality while supporting an infrastructure of capitalism, power, and control, crises – particularly those related to public health – can fan deep divisions. Here in the United States, we have seen misinterpretation, misunderstanding, and bitter indignation fuel the flames of provocation as protests of mask mandates, distance learning, and social distancing were touted as violating the very core upon which the country was established. Frustration, palpable among health care professionals, grew ever greater as the importance of vaccination in quelling virus mutations and decreasing morbidity and mortality were openly disparaged and ignored.
Not only have we watched people refuse the vaccines, but some are ignoring other mitigation measures. So the question becomes: How are we, as health care professionals trying to maintain a therapeutic alliance with those who reject lifesaving practices, expected to process this? Sitting in appointments and attempting interventions without judgment feels impractical and nearly impossible – particularly when the behaviors of these patients have the potential of violating our own health and well-being. How do we remain altruistic in our endeavors when those who seek our care seem callously indifferent to our lives – and to those of our families?
Measuring the value of life
Within the fevered haze of this past year, many stories highlighting grim realities have captured the media spotlight. From individuals unable to have emergency evaluations because of facilities being inundated by COVID-19 patients to individuals prematurely discharged, hospital bed shortages, and financial pressures from insurance companies. In reciting the phrase “Primum non noncere,” we physicians are committing to providing fair and competent medical treatment. At times, urgent decisions are necessary but are always made in the best interest of the patient(s). Ultimately, I am left debating how these agonizing weeks served any meaningful purpose. Moreover, when choosing the many over the few, what are the determinant factors? I am left asking: What is the value of a life?
Philosophically, this ethical dilemma is captured succinctly via the “trolley problem,” formulated in 1967 by Philippa Foot, MD. This is how Dr. Foot’s formulation unfolds: Close your eyes, and imagine you are inside a trolley careening unhindered down the rumbling tracks. Straight ahead you see five people bound to the tracks in imminent danger of being struck, and on the other side, one person is tied to the tracks. Do you continue the same course – thereby condemning five innocent people to death – or do you make the active decision to switch tracks, therefore consigning the one to their fate? Envision the people what do they look like? How old are they? If the one were a small child or a close friend, would that alter your decision? How does one make such a harrowing choice knowing the irreversible consequences? Depending on your action, this quandary falls within two primary schools of thought: Utilitarianism, which posits that the best action is the greatest good for the greatest number of people, and deontologicalism, which suggests that action is inherently right or wrong regardless of the consequences. Therefore, the decision to save the five is not favored.
However simplistic those scenarios may read, such principles when viewed through different lenses, they form the basis of medical ethics. In effect, every acute decision, every aspect of treatment is predicated upon the principles of nonmaleficence, beneficence, utility, distributive justice, and autonomy. Yet, the manner in which they are applied is highly contingent upon myriad variables. For example, sociopolitical factors, including population size (rural versus urban), economics (impoverished versus wealthy), as well as demographic factors (age, ethnicity, gender, sexuality) can highly influence and sometimes unknowingly influence interpretation and allocation of health care resources. This dilemma does not yield easily applicable and universal solutions. Nevertheless, it is paramount to evaluate policies effectively and tediously, particularly those with detrimental ramifications. Likewise, remaining flexible in our willingness to explore alternative solutions and encourage open discord among those with opposing viewpoints is key to instituting individual or institutional change that values the one as it values the many.
After several weeks of acute illness and a variety of short-acting interventions, I received approval to resume intravenous therapy. While the saga has ultimately reached a satisfactory conclusion, I am left with stupefied disbelief toward the people who took a gamble on my health. I am facing a battle between understanding the obligation of medicine to provide ethical and reasonable care without hesitation or judgment versus embittered resentment when faced with those who openly campaign against lifesaving interventions, such as the COVID-19 vaccine. For me, each day and the one that follows is riddled with complicated emotion. Every time I prematurely cease activity out of discomfort and weariness, I worry about my increasingly foreboding workload. In those moments, in that place of questions without answers, I remember that someone somewhere ultimately decided to switch the trolley’s track.
Dr. Thomas is a board-certified adult psychiatrist with interests in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. Dr. Thomas has no conflicts of interest.
Working feverishly to complete the myriad patient notes accumulated throughout a hectic day, my phone vibrated – alerting me to a number that, over the past several years, has wrought uncertainty, grief, and overwhelming relief. Answering hesitantly, I listened to my physician’s pharmacist inform me of unexpected and alarming news.
Since COVID-19 was first identified more than 1 year ago, more than 770,000 people have died in the United States. In the wake of those losses, countless grieve while attempting to navigate a future without their loved ones. Meanwhile, scientists worked feverishly to combat a pandemic relentless in contagion. As health care professionals, we work tirelessly against the sharpened scythe of death, toiling day after day without an identifiable end. All the while, advocacy has prevailed as the need for personal protective equipment, improved ventilation systems, sanitization measures, and other mitigation measures, such as mask wearing and social distancing, echoed swiftly across the nation and around the world.
But, as the months have progressed, and life has seemingly transitioned toward a parallel version of reality, subsections of communities have grown restless. Several nontherapeutic, ineffective, and falsely touted regimens have been promoted. Amid the chaos of misinformation, most medical professionals have sought support from respected journals and infectious disease experts to filter out jargon and piece together scientifically sound protocols. Although many lives have prevailed by way of those advancements, mixed messages about interventions have emerged – and in many quarters across the country, anger, resistance, and outright refusal have prevailed.
Yet, we – the medical community – have forged ever onward as the cases continued and the death toll steadily climbed. In many cases, physicians who are years removed from critical care training have been thrust into COVID units, while residents have shifted toward working outside of their chosen specialty. Outpatient offices have closed, salaries have been cut, and furloughs have loomed as days fade into months. Beset with exhaustion and uncertainty, sacrifice has become a common thread that intrinsically united us against an unrelenting foe.
Most people continued navigating the many changes and made concerted efforts to mimic our prepandemic lives. Working from home in makeshift offices, dusting off math skills to assist children through the doldrums of distance learning, and mastering various audiovisual platforms, we reinforced social bonds and forged new connections echoing the hallmark resilience reminiscent of our shared distant ancestry.
As of this writing, thanks to our work – and that of scientists and policy makers – about 69% of Americans have received at least one dose of vaccine, and vaccines are widely available to children 5 and older. But it has been disheartening to watch misinformation about vaccine research and development propagated by political figures, social media, and lay people.
Processing the phone call
While listening to my physician’s pharmacist, I slowed my breaths in an effort to find calm. Years of navigating the American health care industry had left me both equipped and ill-prepared for the unexpected. I listened intently to the pharmacist’s words while staring blankly at a computer screen – uncertain of what had felt so assured not 10 minutes earlier.
That’s when I got the news. The intravenous medication that aided in my stabilization had suffered a critical shortage because of its successful use in the treatment of patients with COVID-19 pneumonia – patients who, in a majority of cases, had likely refused the vaccines. As result, the medication that had enabled my return to work, active engagement in nonwork pursuits, and most importantly, equipped my body to thrive despite the damage it had suffered, suddenly vanished.
Gently placing my phone on the desk, my heart beat rapidly as tears steadily streamed down my face. Staring blankly ahead, my hands gradually balled into fists as I let out a sound of fear, agony, and uncertainty. Screaming at everything and nothing, nausea swelled as panic flooded my body. In that moment, I ruminated on the conversation with the pharmacist. There had been no discussion, no option for me to maintain accessibility to this valuable medicine. Consequently, I felt helpless. Although the same medication, albeit a different mechanism of delivery, was promptly chosen as an adequate substitute, there was no guarantee of it bestowing the same degree of efficacy. So I was terrified, envisioning the progress made over several years as plummeting into an abyss of pain and despair. What are those of us who have chosen medicine as our profession but are immunocompromised expected to make of this?
Over the next several weeks, I diligently adhered to the new regimen and focused on positive mentation. Nevertheless, day by day, the symptoms worsened; eventually, I became bed ridden. I tried to gather what little composure remained to reschedule patients and justify the resounding guilt of perceived failure. I remember the sweet and gentle look of my child as I once again could not summon the strength to play pretend. This felt overwhelming. Would I ever go back to work? Would I see my child grow? No amount of pleading or screaming would change the fact that a medical system chose to roll the dice on my health. In a haze of discomfort and betrayal, I wondered how a physician or medical facility could justify removing medication from someone reliant upon it. How do we choose the appropriate allocation of resources when the consequences are potentially catastrophic?
Searching for context
When a country is founded on the mission of rising as a leading world power built upon the concepts of freedom, basic human rights, and individuality while supporting an infrastructure of capitalism, power, and control, crises – particularly those related to public health – can fan deep divisions. Here in the United States, we have seen misinterpretation, misunderstanding, and bitter indignation fuel the flames of provocation as protests of mask mandates, distance learning, and social distancing were touted as violating the very core upon which the country was established. Frustration, palpable among health care professionals, grew ever greater as the importance of vaccination in quelling virus mutations and decreasing morbidity and mortality were openly disparaged and ignored.
Not only have we watched people refuse the vaccines, but some are ignoring other mitigation measures. So the question becomes: How are we, as health care professionals trying to maintain a therapeutic alliance with those who reject lifesaving practices, expected to process this? Sitting in appointments and attempting interventions without judgment feels impractical and nearly impossible – particularly when the behaviors of these patients have the potential of violating our own health and well-being. How do we remain altruistic in our endeavors when those who seek our care seem callously indifferent to our lives – and to those of our families?
Measuring the value of life
Within the fevered haze of this past year, many stories highlighting grim realities have captured the media spotlight. From individuals unable to have emergency evaluations because of facilities being inundated by COVID-19 patients to individuals prematurely discharged, hospital bed shortages, and financial pressures from insurance companies. In reciting the phrase “Primum non noncere,” we physicians are committing to providing fair and competent medical treatment. At times, urgent decisions are necessary but are always made in the best interest of the patient(s). Ultimately, I am left debating how these agonizing weeks served any meaningful purpose. Moreover, when choosing the many over the few, what are the determinant factors? I am left asking: What is the value of a life?
Philosophically, this ethical dilemma is captured succinctly via the “trolley problem,” formulated in 1967 by Philippa Foot, MD. This is how Dr. Foot’s formulation unfolds: Close your eyes, and imagine you are inside a trolley careening unhindered down the rumbling tracks. Straight ahead you see five people bound to the tracks in imminent danger of being struck, and on the other side, one person is tied to the tracks. Do you continue the same course – thereby condemning five innocent people to death – or do you make the active decision to switch tracks, therefore consigning the one to their fate? Envision the people what do they look like? How old are they? If the one were a small child or a close friend, would that alter your decision? How does one make such a harrowing choice knowing the irreversible consequences? Depending on your action, this quandary falls within two primary schools of thought: Utilitarianism, which posits that the best action is the greatest good for the greatest number of people, and deontologicalism, which suggests that action is inherently right or wrong regardless of the consequences. Therefore, the decision to save the five is not favored.
However simplistic those scenarios may read, such principles when viewed through different lenses, they form the basis of medical ethics. In effect, every acute decision, every aspect of treatment is predicated upon the principles of nonmaleficence, beneficence, utility, distributive justice, and autonomy. Yet, the manner in which they are applied is highly contingent upon myriad variables. For example, sociopolitical factors, including population size (rural versus urban), economics (impoverished versus wealthy), as well as demographic factors (age, ethnicity, gender, sexuality) can highly influence and sometimes unknowingly influence interpretation and allocation of health care resources. This dilemma does not yield easily applicable and universal solutions. Nevertheless, it is paramount to evaluate policies effectively and tediously, particularly those with detrimental ramifications. Likewise, remaining flexible in our willingness to explore alternative solutions and encourage open discord among those with opposing viewpoints is key to instituting individual or institutional change that values the one as it values the many.
After several weeks of acute illness and a variety of short-acting interventions, I received approval to resume intravenous therapy. While the saga has ultimately reached a satisfactory conclusion, I am left with stupefied disbelief toward the people who took a gamble on my health. I am facing a battle between understanding the obligation of medicine to provide ethical and reasonable care without hesitation or judgment versus embittered resentment when faced with those who openly campaign against lifesaving interventions, such as the COVID-19 vaccine. For me, each day and the one that follows is riddled with complicated emotion. Every time I prematurely cease activity out of discomfort and weariness, I worry about my increasingly foreboding workload. In those moments, in that place of questions without answers, I remember that someone somewhere ultimately decided to switch the trolley’s track.
Dr. Thomas is a board-certified adult psychiatrist with interests in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. Dr. Thomas has no conflicts of interest.
Working feverishly to complete the myriad patient notes accumulated throughout a hectic day, my phone vibrated – alerting me to a number that, over the past several years, has wrought uncertainty, grief, and overwhelming relief. Answering hesitantly, I listened to my physician’s pharmacist inform me of unexpected and alarming news.
Since COVID-19 was first identified more than 1 year ago, more than 770,000 people have died in the United States. In the wake of those losses, countless grieve while attempting to navigate a future without their loved ones. Meanwhile, scientists worked feverishly to combat a pandemic relentless in contagion. As health care professionals, we work tirelessly against the sharpened scythe of death, toiling day after day without an identifiable end. All the while, advocacy has prevailed as the need for personal protective equipment, improved ventilation systems, sanitization measures, and other mitigation measures, such as mask wearing and social distancing, echoed swiftly across the nation and around the world.
But, as the months have progressed, and life has seemingly transitioned toward a parallel version of reality, subsections of communities have grown restless. Several nontherapeutic, ineffective, and falsely touted regimens have been promoted. Amid the chaos of misinformation, most medical professionals have sought support from respected journals and infectious disease experts to filter out jargon and piece together scientifically sound protocols. Although many lives have prevailed by way of those advancements, mixed messages about interventions have emerged – and in many quarters across the country, anger, resistance, and outright refusal have prevailed.
Yet, we – the medical community – have forged ever onward as the cases continued and the death toll steadily climbed. In many cases, physicians who are years removed from critical care training have been thrust into COVID units, while residents have shifted toward working outside of their chosen specialty. Outpatient offices have closed, salaries have been cut, and furloughs have loomed as days fade into months. Beset with exhaustion and uncertainty, sacrifice has become a common thread that intrinsically united us against an unrelenting foe.
Most people continued navigating the many changes and made concerted efforts to mimic our prepandemic lives. Working from home in makeshift offices, dusting off math skills to assist children through the doldrums of distance learning, and mastering various audiovisual platforms, we reinforced social bonds and forged new connections echoing the hallmark resilience reminiscent of our shared distant ancestry.
As of this writing, thanks to our work – and that of scientists and policy makers – about 69% of Americans have received at least one dose of vaccine, and vaccines are widely available to children 5 and older. But it has been disheartening to watch misinformation about vaccine research and development propagated by political figures, social media, and lay people.
Processing the phone call
While listening to my physician’s pharmacist, I slowed my breaths in an effort to find calm. Years of navigating the American health care industry had left me both equipped and ill-prepared for the unexpected. I listened intently to the pharmacist’s words while staring blankly at a computer screen – uncertain of what had felt so assured not 10 minutes earlier.
That’s when I got the news. The intravenous medication that aided in my stabilization had suffered a critical shortage because of its successful use in the treatment of patients with COVID-19 pneumonia – patients who, in a majority of cases, had likely refused the vaccines. As result, the medication that had enabled my return to work, active engagement in nonwork pursuits, and most importantly, equipped my body to thrive despite the damage it had suffered, suddenly vanished.
Gently placing my phone on the desk, my heart beat rapidly as tears steadily streamed down my face. Staring blankly ahead, my hands gradually balled into fists as I let out a sound of fear, agony, and uncertainty. Screaming at everything and nothing, nausea swelled as panic flooded my body. In that moment, I ruminated on the conversation with the pharmacist. There had been no discussion, no option for me to maintain accessibility to this valuable medicine. Consequently, I felt helpless. Although the same medication, albeit a different mechanism of delivery, was promptly chosen as an adequate substitute, there was no guarantee of it bestowing the same degree of efficacy. So I was terrified, envisioning the progress made over several years as plummeting into an abyss of pain and despair. What are those of us who have chosen medicine as our profession but are immunocompromised expected to make of this?
Over the next several weeks, I diligently adhered to the new regimen and focused on positive mentation. Nevertheless, day by day, the symptoms worsened; eventually, I became bed ridden. I tried to gather what little composure remained to reschedule patients and justify the resounding guilt of perceived failure. I remember the sweet and gentle look of my child as I once again could not summon the strength to play pretend. This felt overwhelming. Would I ever go back to work? Would I see my child grow? No amount of pleading or screaming would change the fact that a medical system chose to roll the dice on my health. In a haze of discomfort and betrayal, I wondered how a physician or medical facility could justify removing medication from someone reliant upon it. How do we choose the appropriate allocation of resources when the consequences are potentially catastrophic?
Searching for context
When a country is founded on the mission of rising as a leading world power built upon the concepts of freedom, basic human rights, and individuality while supporting an infrastructure of capitalism, power, and control, crises – particularly those related to public health – can fan deep divisions. Here in the United States, we have seen misinterpretation, misunderstanding, and bitter indignation fuel the flames of provocation as protests of mask mandates, distance learning, and social distancing were touted as violating the very core upon which the country was established. Frustration, palpable among health care professionals, grew ever greater as the importance of vaccination in quelling virus mutations and decreasing morbidity and mortality were openly disparaged and ignored.
Not only have we watched people refuse the vaccines, but some are ignoring other mitigation measures. So the question becomes: How are we, as health care professionals trying to maintain a therapeutic alliance with those who reject lifesaving practices, expected to process this? Sitting in appointments and attempting interventions without judgment feels impractical and nearly impossible – particularly when the behaviors of these patients have the potential of violating our own health and well-being. How do we remain altruistic in our endeavors when those who seek our care seem callously indifferent to our lives – and to those of our families?
Measuring the value of life
Within the fevered haze of this past year, many stories highlighting grim realities have captured the media spotlight. From individuals unable to have emergency evaluations because of facilities being inundated by COVID-19 patients to individuals prematurely discharged, hospital bed shortages, and financial pressures from insurance companies. In reciting the phrase “Primum non noncere,” we physicians are committing to providing fair and competent medical treatment. At times, urgent decisions are necessary but are always made in the best interest of the patient(s). Ultimately, I am left debating how these agonizing weeks served any meaningful purpose. Moreover, when choosing the many over the few, what are the determinant factors? I am left asking: What is the value of a life?
Philosophically, this ethical dilemma is captured succinctly via the “trolley problem,” formulated in 1967 by Philippa Foot, MD. This is how Dr. Foot’s formulation unfolds: Close your eyes, and imagine you are inside a trolley careening unhindered down the rumbling tracks. Straight ahead you see five people bound to the tracks in imminent danger of being struck, and on the other side, one person is tied to the tracks. Do you continue the same course – thereby condemning five innocent people to death – or do you make the active decision to switch tracks, therefore consigning the one to their fate? Envision the people what do they look like? How old are they? If the one were a small child or a close friend, would that alter your decision? How does one make such a harrowing choice knowing the irreversible consequences? Depending on your action, this quandary falls within two primary schools of thought: Utilitarianism, which posits that the best action is the greatest good for the greatest number of people, and deontologicalism, which suggests that action is inherently right or wrong regardless of the consequences. Therefore, the decision to save the five is not favored.
However simplistic those scenarios may read, such principles when viewed through different lenses, they form the basis of medical ethics. In effect, every acute decision, every aspect of treatment is predicated upon the principles of nonmaleficence, beneficence, utility, distributive justice, and autonomy. Yet, the manner in which they are applied is highly contingent upon myriad variables. For example, sociopolitical factors, including population size (rural versus urban), economics (impoverished versus wealthy), as well as demographic factors (age, ethnicity, gender, sexuality) can highly influence and sometimes unknowingly influence interpretation and allocation of health care resources. This dilemma does not yield easily applicable and universal solutions. Nevertheless, it is paramount to evaluate policies effectively and tediously, particularly those with detrimental ramifications. Likewise, remaining flexible in our willingness to explore alternative solutions and encourage open discord among those with opposing viewpoints is key to instituting individual or institutional change that values the one as it values the many.
After several weeks of acute illness and a variety of short-acting interventions, I received approval to resume intravenous therapy. While the saga has ultimately reached a satisfactory conclusion, I am left with stupefied disbelief toward the people who took a gamble on my health. I am facing a battle between understanding the obligation of medicine to provide ethical and reasonable care without hesitation or judgment versus embittered resentment when faced with those who openly campaign against lifesaving interventions, such as the COVID-19 vaccine. For me, each day and the one that follows is riddled with complicated emotion. Every time I prematurely cease activity out of discomfort and weariness, I worry about my increasingly foreboding workload. In those moments, in that place of questions without answers, I remember that someone somewhere ultimately decided to switch the trolley’s track.
Dr. Thomas is a board-certified adult psychiatrist with interests in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. Dr. Thomas has no conflicts of interest.
Children with uncontrolled asthma at higher risk of being bullied
The risk of bullying and teasing is higher in children and young people with poorer asthma control, an international study reported. Published online in the Archives of Disease in Childhood, the Room to Breathe survey of 943 children in six countries found 9.9% had experienced asthma-related bullying or teasing (n = 93).
Children with well-controlled disease, however, were less likely to report being victimized by asthma-related bullying/teasing: odds ratio, 0.51; 95% confidence interval, 0.23-0.84; P = .006).
“It’s important for pediatricians to recognize that children and young people with asthma commonly report bullying or teasing as a result of their condition,” Will Carroll, MD, of the Paediatric Respiratory Service at Staffordshire Children’s Hospital at Royal Stoke, Stoke-on-Trent, England, told this news organization. “Pediatricians should talk to children themselves with asthma about this and not just their parents, and efforts should be made to improve asthma control whenever possible.”
Though common and potentially long-lasting in its effects, bullying is rarely addressed by health care professionals, the U.K. authors said.
But things may differ in the United States. According to Mark Welles, MD, a pediatrician at Cohen Children’s Medical Center at Northwell Health in Queen’s, N.Y., and regional cochair of the American Academy of Pediatrics antibullying committee, young doctors here are trained to ask about bullying when seeing a child, no matter what the reason for the visit. “It’s important to build a rapport with the child, and you need to ask about the disease they may have but also generally ask, ‘How are things at school? Is everyone nice to you?’ It is becoming more common practice to ask this,” said Dr. Welles, who was not involved with the U.K. research.
The U.K. study drew on unpublished data from the Room to Breathe survey conducted by Dr. Carroll’s group during 2008-2009 in Canada, the United Kingdom, Greece, Hungary, South Africa, and the Netherlands. Only 358 of 930 (38.5%) children were found to be well controlled according to current Global Initiative for Asthma symptom-control criteria.
The analysis also found a highly significant association (P < .0001) between Childhood Asthma Control Test (C-ACT) score and reported bullying/teasing, with bullied children having lower scores. C-ACT–defined controlled asthma scores of 20 or higher were significantly associated with a lower risk of bullying (OR, 0.46; 95% CI, 0.28-0.76; P = .001).
In other study findings, harassment was more common in children whose asthma was serious enough to entail activity restriction (OR, 1.74; 95% CI, 1.11-2.75; P = .010) and who described their asthma as “bad” (OR, 3.02; 95% CI, 1.86-4.85; P < .001), as well as those whose parents reported ongoing asthma-related health worries (OR, 1.64; 95% CI, 1.04-2.58; P = .024).
“When a child is clearly different from others, such as having bad asthma or being limited in activities due to asthma, they stand out more and are more frequently bullied,” said Tracy Evian Waasdorp, PhD, MSEd, director of research for school-based bullying and social-emotional learning at Children’s Hospital of Philadelphia, and also not a participant in the U.K. study.
In contrast to the 10% bullying rate in Dr. Carroll’s study, Dr. Waasdorp referred to a CHOP analysis of more than 64,000 youth from a Northeastern state in which those with asthma were 40% more likely to be victims of in-person bullying and 70% were more likely to be cyberbullied than youth without asthma. “Having a medical condition can therefore put you at risk of being bullied regardless of what country you live in,” she said.
CHOP policy encourages practitioners to routinely ask about bullying and to provide handouts and resources for parents, she added.
Interestingly, the U.K. investigators found that open public use of spacers was not associated with asthma-related bullying, nor was parental worry at diagnosis or parental concern about steroid use.
But according to Dr. Welles, “Kids may be using the inhaler in front of other kids, and they may be embarrassed and not want to be seen as different. So they may not use the inhaler when needed for gym class or sports, forcing them to sit out and then potentially be bullied again. It’s a vicious cycle.”
Previous research has identified the bullying and teasing of children with food allergies.
Behaviors have included allergy-specific harassment such as smearing peanut butter on a youngster’s forehead or putting peanut butter cookie crumbs in a child’s lunch box.
“In our survey we asked the question ‘Have you been teased or bullied because of your asthma?’ but we didn’t ask what form this took,” Dr. Carroll said. “But we were surprised at just how many children said yes. It’s time for more research, I think.”
“There are never enough studies around this,” added Dr. Welles. “Bullying, whether because of asthma or otherwise, has the potential for long-term effects well into adulthood.”
In the meantime, asthma consultations should incorporate specific questions about bullying. They should also be child focused in order to gain a representative appreciation of asthma control and its effect on the child’s life.
“As pediatricians, we need to be continuously supporting parents and find the help they need to address any mental health issues,” Dr. Welles said. “Every pediatrician and parent needs to be aware and recognize when something is different in their child’s life. Please don’t ignore it.”
Dr. Waasdorp stressed that school and other communities should be aware that children with asthma may be at increased risk for aggression and harmful interactions related to their asthma. “Programming to reduce bullying should focus broadly on shifting the climate so that bullying is not perceived to be normative and on improving ‘upstander,’ or positive bystander, responses.” she said.
The original survey was funded by Nycomed (Zurich). No additional funding was requested for the current analysis. Dr. Carroll reported personal fees from GlaxoSmithKline, Novartis, and Trudell Medical International outside the submitted work. Dr. Welles and Dr. Waasdorp disclosed no competing interests relevant to their comments.
The risk of bullying and teasing is higher in children and young people with poorer asthma control, an international study reported. Published online in the Archives of Disease in Childhood, the Room to Breathe survey of 943 children in six countries found 9.9% had experienced asthma-related bullying or teasing (n = 93).
Children with well-controlled disease, however, were less likely to report being victimized by asthma-related bullying/teasing: odds ratio, 0.51; 95% confidence interval, 0.23-0.84; P = .006).
“It’s important for pediatricians to recognize that children and young people with asthma commonly report bullying or teasing as a result of their condition,” Will Carroll, MD, of the Paediatric Respiratory Service at Staffordshire Children’s Hospital at Royal Stoke, Stoke-on-Trent, England, told this news organization. “Pediatricians should talk to children themselves with asthma about this and not just their parents, and efforts should be made to improve asthma control whenever possible.”
Though common and potentially long-lasting in its effects, bullying is rarely addressed by health care professionals, the U.K. authors said.
But things may differ in the United States. According to Mark Welles, MD, a pediatrician at Cohen Children’s Medical Center at Northwell Health in Queen’s, N.Y., and regional cochair of the American Academy of Pediatrics antibullying committee, young doctors here are trained to ask about bullying when seeing a child, no matter what the reason for the visit. “It’s important to build a rapport with the child, and you need to ask about the disease they may have but also generally ask, ‘How are things at school? Is everyone nice to you?’ It is becoming more common practice to ask this,” said Dr. Welles, who was not involved with the U.K. research.
The U.K. study drew on unpublished data from the Room to Breathe survey conducted by Dr. Carroll’s group during 2008-2009 in Canada, the United Kingdom, Greece, Hungary, South Africa, and the Netherlands. Only 358 of 930 (38.5%) children were found to be well controlled according to current Global Initiative for Asthma symptom-control criteria.
The analysis also found a highly significant association (P < .0001) between Childhood Asthma Control Test (C-ACT) score and reported bullying/teasing, with bullied children having lower scores. C-ACT–defined controlled asthma scores of 20 or higher were significantly associated with a lower risk of bullying (OR, 0.46; 95% CI, 0.28-0.76; P = .001).
In other study findings, harassment was more common in children whose asthma was serious enough to entail activity restriction (OR, 1.74; 95% CI, 1.11-2.75; P = .010) and who described their asthma as “bad” (OR, 3.02; 95% CI, 1.86-4.85; P < .001), as well as those whose parents reported ongoing asthma-related health worries (OR, 1.64; 95% CI, 1.04-2.58; P = .024).
“When a child is clearly different from others, such as having bad asthma or being limited in activities due to asthma, they stand out more and are more frequently bullied,” said Tracy Evian Waasdorp, PhD, MSEd, director of research for school-based bullying and social-emotional learning at Children’s Hospital of Philadelphia, and also not a participant in the U.K. study.
In contrast to the 10% bullying rate in Dr. Carroll’s study, Dr. Waasdorp referred to a CHOP analysis of more than 64,000 youth from a Northeastern state in which those with asthma were 40% more likely to be victims of in-person bullying and 70% were more likely to be cyberbullied than youth without asthma. “Having a medical condition can therefore put you at risk of being bullied regardless of what country you live in,” she said.
CHOP policy encourages practitioners to routinely ask about bullying and to provide handouts and resources for parents, she added.
Interestingly, the U.K. investigators found that open public use of spacers was not associated with asthma-related bullying, nor was parental worry at diagnosis or parental concern about steroid use.
But according to Dr. Welles, “Kids may be using the inhaler in front of other kids, and they may be embarrassed and not want to be seen as different. So they may not use the inhaler when needed for gym class or sports, forcing them to sit out and then potentially be bullied again. It’s a vicious cycle.”
Previous research has identified the bullying and teasing of children with food allergies.
Behaviors have included allergy-specific harassment such as smearing peanut butter on a youngster’s forehead or putting peanut butter cookie crumbs in a child’s lunch box.
“In our survey we asked the question ‘Have you been teased or bullied because of your asthma?’ but we didn’t ask what form this took,” Dr. Carroll said. “But we were surprised at just how many children said yes. It’s time for more research, I think.”
“There are never enough studies around this,” added Dr. Welles. “Bullying, whether because of asthma or otherwise, has the potential for long-term effects well into adulthood.”
In the meantime, asthma consultations should incorporate specific questions about bullying. They should also be child focused in order to gain a representative appreciation of asthma control and its effect on the child’s life.
“As pediatricians, we need to be continuously supporting parents and find the help they need to address any mental health issues,” Dr. Welles said. “Every pediatrician and parent needs to be aware and recognize when something is different in their child’s life. Please don’t ignore it.”
Dr. Waasdorp stressed that school and other communities should be aware that children with asthma may be at increased risk for aggression and harmful interactions related to their asthma. “Programming to reduce bullying should focus broadly on shifting the climate so that bullying is not perceived to be normative and on improving ‘upstander,’ or positive bystander, responses.” she said.
The original survey was funded by Nycomed (Zurich). No additional funding was requested for the current analysis. Dr. Carroll reported personal fees from GlaxoSmithKline, Novartis, and Trudell Medical International outside the submitted work. Dr. Welles and Dr. Waasdorp disclosed no competing interests relevant to their comments.
The risk of bullying and teasing is higher in children and young people with poorer asthma control, an international study reported. Published online in the Archives of Disease in Childhood, the Room to Breathe survey of 943 children in six countries found 9.9% had experienced asthma-related bullying or teasing (n = 93).
Children with well-controlled disease, however, were less likely to report being victimized by asthma-related bullying/teasing: odds ratio, 0.51; 95% confidence interval, 0.23-0.84; P = .006).
“It’s important for pediatricians to recognize that children and young people with asthma commonly report bullying or teasing as a result of their condition,” Will Carroll, MD, of the Paediatric Respiratory Service at Staffordshire Children’s Hospital at Royal Stoke, Stoke-on-Trent, England, told this news organization. “Pediatricians should talk to children themselves with asthma about this and not just their parents, and efforts should be made to improve asthma control whenever possible.”
Though common and potentially long-lasting in its effects, bullying is rarely addressed by health care professionals, the U.K. authors said.
But things may differ in the United States. According to Mark Welles, MD, a pediatrician at Cohen Children’s Medical Center at Northwell Health in Queen’s, N.Y., and regional cochair of the American Academy of Pediatrics antibullying committee, young doctors here are trained to ask about bullying when seeing a child, no matter what the reason for the visit. “It’s important to build a rapport with the child, and you need to ask about the disease they may have but also generally ask, ‘How are things at school? Is everyone nice to you?’ It is becoming more common practice to ask this,” said Dr. Welles, who was not involved with the U.K. research.
The U.K. study drew on unpublished data from the Room to Breathe survey conducted by Dr. Carroll’s group during 2008-2009 in Canada, the United Kingdom, Greece, Hungary, South Africa, and the Netherlands. Only 358 of 930 (38.5%) children were found to be well controlled according to current Global Initiative for Asthma symptom-control criteria.
The analysis also found a highly significant association (P < .0001) between Childhood Asthma Control Test (C-ACT) score and reported bullying/teasing, with bullied children having lower scores. C-ACT–defined controlled asthma scores of 20 or higher were significantly associated with a lower risk of bullying (OR, 0.46; 95% CI, 0.28-0.76; P = .001).
In other study findings, harassment was more common in children whose asthma was serious enough to entail activity restriction (OR, 1.74; 95% CI, 1.11-2.75; P = .010) and who described their asthma as “bad” (OR, 3.02; 95% CI, 1.86-4.85; P < .001), as well as those whose parents reported ongoing asthma-related health worries (OR, 1.64; 95% CI, 1.04-2.58; P = .024).
“When a child is clearly different from others, such as having bad asthma or being limited in activities due to asthma, they stand out more and are more frequently bullied,” said Tracy Evian Waasdorp, PhD, MSEd, director of research for school-based bullying and social-emotional learning at Children’s Hospital of Philadelphia, and also not a participant in the U.K. study.
In contrast to the 10% bullying rate in Dr. Carroll’s study, Dr. Waasdorp referred to a CHOP analysis of more than 64,000 youth from a Northeastern state in which those with asthma were 40% more likely to be victims of in-person bullying and 70% were more likely to be cyberbullied than youth without asthma. “Having a medical condition can therefore put you at risk of being bullied regardless of what country you live in,” she said.
CHOP policy encourages practitioners to routinely ask about bullying and to provide handouts and resources for parents, she added.
Interestingly, the U.K. investigators found that open public use of spacers was not associated with asthma-related bullying, nor was parental worry at diagnosis or parental concern about steroid use.
But according to Dr. Welles, “Kids may be using the inhaler in front of other kids, and they may be embarrassed and not want to be seen as different. So they may not use the inhaler when needed for gym class or sports, forcing them to sit out and then potentially be bullied again. It’s a vicious cycle.”
Previous research has identified the bullying and teasing of children with food allergies.
Behaviors have included allergy-specific harassment such as smearing peanut butter on a youngster’s forehead or putting peanut butter cookie crumbs in a child’s lunch box.
“In our survey we asked the question ‘Have you been teased or bullied because of your asthma?’ but we didn’t ask what form this took,” Dr. Carroll said. “But we were surprised at just how many children said yes. It’s time for more research, I think.”
“There are never enough studies around this,” added Dr. Welles. “Bullying, whether because of asthma or otherwise, has the potential for long-term effects well into adulthood.”
In the meantime, asthma consultations should incorporate specific questions about bullying. They should also be child focused in order to gain a representative appreciation of asthma control and its effect on the child’s life.
“As pediatricians, we need to be continuously supporting parents and find the help they need to address any mental health issues,” Dr. Welles said. “Every pediatrician and parent needs to be aware and recognize when something is different in their child’s life. Please don’t ignore it.”
Dr. Waasdorp stressed that school and other communities should be aware that children with asthma may be at increased risk for aggression and harmful interactions related to their asthma. “Programming to reduce bullying should focus broadly on shifting the climate so that bullying is not perceived to be normative and on improving ‘upstander,’ or positive bystander, responses.” she said.
The original survey was funded by Nycomed (Zurich). No additional funding was requested for the current analysis. Dr. Carroll reported personal fees from GlaxoSmithKline, Novartis, and Trudell Medical International outside the submitted work. Dr. Welles and Dr. Waasdorp disclosed no competing interests relevant to their comments.
FROM ARCHIVES OF DISEASE IN CHILDHOOD