User login
Opioids overprescribed in elective hernia repair patients
A patient-centered study of postoperative analgesic needs found that surgeons may be overprescribing opioids for pain management after hernia repair operations.
The growing opioid public health crisis – and potential contribution of pain control prescriptions to the crisis – has prompted empirical work on surgeons’ prescribing and actual patient use of opioids (Ann Surg. 2017 Jul 10. doi: 10.1097/SLA.0000000000002365. [Epub ahead of print];J Arthroplasty. 2017;32[8]2395-2398). Excess pain medications are thought to raise the risk of patient dependence and to be potentially diverted to nonpatients’ use. A recent study (Ann Surg. 2017;265:709-16) found that a median of 30 opioid tablets were routinely prescribed by surgeons for pain management after hernia repair.
Konstantinos Mylonas, MD, a research fellow at Massachusetts General Hospital, Boston, and his coinvestigators conducted a prospective, observational study of 185 patients who had an outpatient inguinal hernia repair between October 2015 and September 2016. Participants completed a survey on their pain levels and opioid use during the 2- to 3-week period between their procedure and follow-up appointment (Surgery. 2017 Aug 1. doi: 10.1016/j.surg.2017.06.017).
For postop pain control, the patients were given 10 Vicodin (hydrocodone 5 mg/acetaminophen 325 mg) tablets, although all were advised that they may not require the medication but could instead use acetaminophen or ibuprofen as needed.
Of the 185 patients who were surveyed, 159 (86%) reported taking 4 or less of the 10 opioid tablets prescribed to them, with 110 (60%) reporting taking no tablets at all
While 13 (7%) of the patients did report using nine or more of the prescribed Vicodin tablets, none of the patients surveyed were still taking the pain medication within 7 days of their follow-up appointment.
When asked about how pain affected their returning to daily activities, 123 patients (66.5%) reported not having any pain interference, 42 (22.7%) mentioned slight problems, and 5 (2.7%) were noticeably affected. No patients were unable to return to their daily activities, and those 111 (75%) of the 147 patients who were employed were able to return to work within 3 days of surgery, according to the investigators.
As might be expected, those patients who experienced higher pain levels and persistent pain took more Vicodin tablets, but only one patient required a refill of the original prescription.
Patients were also not blinded to the study, which may have caused them to either take less opioid medication or not report their intake accurately. But the findings suggest that opioid prescribing could be tailored much more narrowly to patients’ needs and to individual procedures than is currently common practice. “Although our study was limited to a single procedure, performed by a single surgeon in a high-volume center, implementing patient-centered, procedure-specific opioid administration strategies may be conceivable across a variety of surgical disciplines,” the investigators concluded.
For the 750,000 inguinal hernia repairs done in the United States each year, prescribing 4 instead of 30 opioid tablets would decrease the number of opioid analgesics dispensed annually for hernia operation from 22.5 million to 3 million,” the investigators wrote. “As a result, 20 million fewer tablets per year would be available for potential diversion and abuse or as a stimulus for the start of opioid dependency.”
The researchers reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
A patient-centered study of postoperative analgesic needs found that surgeons may be overprescribing opioids for pain management after hernia repair operations.
The growing opioid public health crisis – and potential contribution of pain control prescriptions to the crisis – has prompted empirical work on surgeons’ prescribing and actual patient use of opioids (Ann Surg. 2017 Jul 10. doi: 10.1097/SLA.0000000000002365. [Epub ahead of print];J Arthroplasty. 2017;32[8]2395-2398). Excess pain medications are thought to raise the risk of patient dependence and to be potentially diverted to nonpatients’ use. A recent study (Ann Surg. 2017;265:709-16) found that a median of 30 opioid tablets were routinely prescribed by surgeons for pain management after hernia repair.
Konstantinos Mylonas, MD, a research fellow at Massachusetts General Hospital, Boston, and his coinvestigators conducted a prospective, observational study of 185 patients who had an outpatient inguinal hernia repair between October 2015 and September 2016. Participants completed a survey on their pain levels and opioid use during the 2- to 3-week period between their procedure and follow-up appointment (Surgery. 2017 Aug 1. doi: 10.1016/j.surg.2017.06.017).
For postop pain control, the patients were given 10 Vicodin (hydrocodone 5 mg/acetaminophen 325 mg) tablets, although all were advised that they may not require the medication but could instead use acetaminophen or ibuprofen as needed.
Of the 185 patients who were surveyed, 159 (86%) reported taking 4 or less of the 10 opioid tablets prescribed to them, with 110 (60%) reporting taking no tablets at all
While 13 (7%) of the patients did report using nine or more of the prescribed Vicodin tablets, none of the patients surveyed were still taking the pain medication within 7 days of their follow-up appointment.
When asked about how pain affected their returning to daily activities, 123 patients (66.5%) reported not having any pain interference, 42 (22.7%) mentioned slight problems, and 5 (2.7%) were noticeably affected. No patients were unable to return to their daily activities, and those 111 (75%) of the 147 patients who were employed were able to return to work within 3 days of surgery, according to the investigators.
As might be expected, those patients who experienced higher pain levels and persistent pain took more Vicodin tablets, but only one patient required a refill of the original prescription.
Patients were also not blinded to the study, which may have caused them to either take less opioid medication or not report their intake accurately. But the findings suggest that opioid prescribing could be tailored much more narrowly to patients’ needs and to individual procedures than is currently common practice. “Although our study was limited to a single procedure, performed by a single surgeon in a high-volume center, implementing patient-centered, procedure-specific opioid administration strategies may be conceivable across a variety of surgical disciplines,” the investigators concluded.
For the 750,000 inguinal hernia repairs done in the United States each year, prescribing 4 instead of 30 opioid tablets would decrease the number of opioid analgesics dispensed annually for hernia operation from 22.5 million to 3 million,” the investigators wrote. “As a result, 20 million fewer tablets per year would be available for potential diversion and abuse or as a stimulus for the start of opioid dependency.”
The researchers reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
A patient-centered study of postoperative analgesic needs found that surgeons may be overprescribing opioids for pain management after hernia repair operations.
The growing opioid public health crisis – and potential contribution of pain control prescriptions to the crisis – has prompted empirical work on surgeons’ prescribing and actual patient use of opioids (Ann Surg. 2017 Jul 10. doi: 10.1097/SLA.0000000000002365. [Epub ahead of print];J Arthroplasty. 2017;32[8]2395-2398). Excess pain medications are thought to raise the risk of patient dependence and to be potentially diverted to nonpatients’ use. A recent study (Ann Surg. 2017;265:709-16) found that a median of 30 opioid tablets were routinely prescribed by surgeons for pain management after hernia repair.
Konstantinos Mylonas, MD, a research fellow at Massachusetts General Hospital, Boston, and his coinvestigators conducted a prospective, observational study of 185 patients who had an outpatient inguinal hernia repair between October 2015 and September 2016. Participants completed a survey on their pain levels and opioid use during the 2- to 3-week period between their procedure and follow-up appointment (Surgery. 2017 Aug 1. doi: 10.1016/j.surg.2017.06.017).
For postop pain control, the patients were given 10 Vicodin (hydrocodone 5 mg/acetaminophen 325 mg) tablets, although all were advised that they may not require the medication but could instead use acetaminophen or ibuprofen as needed.
Of the 185 patients who were surveyed, 159 (86%) reported taking 4 or less of the 10 opioid tablets prescribed to them, with 110 (60%) reporting taking no tablets at all
While 13 (7%) of the patients did report using nine or more of the prescribed Vicodin tablets, none of the patients surveyed were still taking the pain medication within 7 days of their follow-up appointment.
When asked about how pain affected their returning to daily activities, 123 patients (66.5%) reported not having any pain interference, 42 (22.7%) mentioned slight problems, and 5 (2.7%) were noticeably affected. No patients were unable to return to their daily activities, and those 111 (75%) of the 147 patients who were employed were able to return to work within 3 days of surgery, according to the investigators.
As might be expected, those patients who experienced higher pain levels and persistent pain took more Vicodin tablets, but only one patient required a refill of the original prescription.
Patients were also not blinded to the study, which may have caused them to either take less opioid medication or not report their intake accurately. But the findings suggest that opioid prescribing could be tailored much more narrowly to patients’ needs and to individual procedures than is currently common practice. “Although our study was limited to a single procedure, performed by a single surgeon in a high-volume center, implementing patient-centered, procedure-specific opioid administration strategies may be conceivable across a variety of surgical disciplines,” the investigators concluded.
For the 750,000 inguinal hernia repairs done in the United States each year, prescribing 4 instead of 30 opioid tablets would decrease the number of opioid analgesics dispensed annually for hernia operation from 22.5 million to 3 million,” the investigators wrote. “As a result, 20 million fewer tablets per year would be available for potential diversion and abuse or as a stimulus for the start of opioid dependency.”
The researchers reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
FROM SURGERY
Key clinical point:
Major finding: Of 185 patients surveyed, 159 (86%) reported taking 4 or less opioid tablets of a 10-tablet prescription.
Data source: Observational study of 185 elective inguinal hernia repair patients between October 2015 and September 2016.
Disclosures: Investigators reported no relevant financial disclosures.
Botox smooths prep for hernia surgery
Injections of onabotulinumtoxinA prior to hernia surgery relaxed the abdominal muscles and increased abdominal wall length by an average of 8 cm, based on data from an observational study of 56 patients. The findings were published online in Surgical Endoscopy.
Although laparoscopic ventral hernia repair has a lower recurrence rate than open repair, expanding the abdominal wall remains a challenge, wrote Omar Rodriguez-Acevedo, MD, of the Hernia Institute Australia, Edgecliff, New South Wales, Australia, and colleagues (Surg Endosc. 2017 Jul 21. doi: 10.1007/s00464-017-5750-3).
Nearly three-fourths of the patients (73%) had at least one previous repair. The patients underwent injections of either 200 units or 300 units of BTA between 7 and 14 days before surgery. The average age of the patients was 60 years, and the average body mass index was 40 kg/m2. A subset of 18 patients with larger defects underwent preoperative progressive pneumoperitoneum (PPP) in addition to receiving BTA injections.
Overall, BTA injections significantly increased lateral abdominal length in all subgroups. On average, the length increase per side was 4.4 cm in the 300-unit group, 3.6 cm in the 200-unit group, 4.2 cm in the BtA-only group, and 3.7 cm in the BTA-plus-PPP group. In a pooled analysis, the average gain in length was 4.0 per side.
No significant difference in abdominal wall lengthening was observed between the 200-unit and 300-unit patients or between the BTA-plus-PPP and BTA-only patients.
Overall, the injections were well tolerated, and no complications required intervention, the researchers said. The most common side effects included superficial bruising at the injection site, bloating sensations, weak coughing, and back pain.
The findings were limited by the small study population and by the short follow-up period, and additional long-term follow-up is needed to identify delayed hernia recurrence, the researchers noted. However, the results suggest that “the flaccid paralysis delivered by BTA resulted in the relaxation, elongation, and thinning of the chronically contracted abdominal lateral wall musculature,” which “consequently facilitates laparoscopic repair and primary closure of large defects under minimal tension,” they said.
The researchers had no financial conflicts to disclose.
Injections of onabotulinumtoxinA prior to hernia surgery relaxed the abdominal muscles and increased abdominal wall length by an average of 8 cm, based on data from an observational study of 56 patients. The findings were published online in Surgical Endoscopy.
Although laparoscopic ventral hernia repair has a lower recurrence rate than open repair, expanding the abdominal wall remains a challenge, wrote Omar Rodriguez-Acevedo, MD, of the Hernia Institute Australia, Edgecliff, New South Wales, Australia, and colleagues (Surg Endosc. 2017 Jul 21. doi: 10.1007/s00464-017-5750-3).
Nearly three-fourths of the patients (73%) had at least one previous repair. The patients underwent injections of either 200 units or 300 units of BTA between 7 and 14 days before surgery. The average age of the patients was 60 years, and the average body mass index was 40 kg/m2. A subset of 18 patients with larger defects underwent preoperative progressive pneumoperitoneum (PPP) in addition to receiving BTA injections.
Overall, BTA injections significantly increased lateral abdominal length in all subgroups. On average, the length increase per side was 4.4 cm in the 300-unit group, 3.6 cm in the 200-unit group, 4.2 cm in the BtA-only group, and 3.7 cm in the BTA-plus-PPP group. In a pooled analysis, the average gain in length was 4.0 per side.
No significant difference in abdominal wall lengthening was observed between the 200-unit and 300-unit patients or between the BTA-plus-PPP and BTA-only patients.
Overall, the injections were well tolerated, and no complications required intervention, the researchers said. The most common side effects included superficial bruising at the injection site, bloating sensations, weak coughing, and back pain.
The findings were limited by the small study population and by the short follow-up period, and additional long-term follow-up is needed to identify delayed hernia recurrence, the researchers noted. However, the results suggest that “the flaccid paralysis delivered by BTA resulted in the relaxation, elongation, and thinning of the chronically contracted abdominal lateral wall musculature,” which “consequently facilitates laparoscopic repair and primary closure of large defects under minimal tension,” they said.
The researchers had no financial conflicts to disclose.
Injections of onabotulinumtoxinA prior to hernia surgery relaxed the abdominal muscles and increased abdominal wall length by an average of 8 cm, based on data from an observational study of 56 patients. The findings were published online in Surgical Endoscopy.
Although laparoscopic ventral hernia repair has a lower recurrence rate than open repair, expanding the abdominal wall remains a challenge, wrote Omar Rodriguez-Acevedo, MD, of the Hernia Institute Australia, Edgecliff, New South Wales, Australia, and colleagues (Surg Endosc. 2017 Jul 21. doi: 10.1007/s00464-017-5750-3).
Nearly three-fourths of the patients (73%) had at least one previous repair. The patients underwent injections of either 200 units or 300 units of BTA between 7 and 14 days before surgery. The average age of the patients was 60 years, and the average body mass index was 40 kg/m2. A subset of 18 patients with larger defects underwent preoperative progressive pneumoperitoneum (PPP) in addition to receiving BTA injections.
Overall, BTA injections significantly increased lateral abdominal length in all subgroups. On average, the length increase per side was 4.4 cm in the 300-unit group, 3.6 cm in the 200-unit group, 4.2 cm in the BtA-only group, and 3.7 cm in the BTA-plus-PPP group. In a pooled analysis, the average gain in length was 4.0 per side.
No significant difference in abdominal wall lengthening was observed between the 200-unit and 300-unit patients or between the BTA-plus-PPP and BTA-only patients.
Overall, the injections were well tolerated, and no complications required intervention, the researchers said. The most common side effects included superficial bruising at the injection site, bloating sensations, weak coughing, and back pain.
The findings were limited by the small study population and by the short follow-up period, and additional long-term follow-up is needed to identify delayed hernia recurrence, the researchers noted. However, the results suggest that “the flaccid paralysis delivered by BTA resulted in the relaxation, elongation, and thinning of the chronically contracted abdominal lateral wall musculature,” which “consequently facilitates laparoscopic repair and primary closure of large defects under minimal tension,” they said.
The researchers had no financial conflicts to disclose.
FROM SURGICAL ENDOSCOPY
Key clinical point: Injection with botulinum toxin A prior to hernia repair serves as an effective surgical preparation by temporarily paralyzing the lateral abdominal wall muscles.
Major finding: A comparison of pre- and post-onabotulinumtoxinA images of the abdominal wall showed an unstretched average increase in length of 8.0 cm.
Data source: A prospective, observational study of 56 adults who underwent elective ventral hernia repairs at a single center.
Disclosures: The researchers had no financial conflicts to disclose.
Umbilical hernia repair during pregnancy safe, but often serious
Umbilical hernia repair during pregnancy is rare and safe, but more than half of surgeries required incarceration or strangulation repair, according to Dr. I.N. Haskins and associates.
A total of 126 pregnant women underwent umbilical hernia repair from 2005 to 2014, according to data collected from the American College of Surgeons National Surgical Quality Improvement Program. All but six women underwent open surgery, and of these 120 patients, 71 had umbilical hernia incarceration or strangulation at the time of surgery.
“Additional studies are needed to determine the long-term recurrence rate of umbilical hernia repairs performed in pregnant patients and the effects of surgical intervention and approach on the fetus,” the investigators concluded.
Find the study in Hernia (doi: 10.1007/s10029-017-1633-8).
Umbilical hernia repair during pregnancy is rare and safe, but more than half of surgeries required incarceration or strangulation repair, according to Dr. I.N. Haskins and associates.
A total of 126 pregnant women underwent umbilical hernia repair from 2005 to 2014, according to data collected from the American College of Surgeons National Surgical Quality Improvement Program. All but six women underwent open surgery, and of these 120 patients, 71 had umbilical hernia incarceration or strangulation at the time of surgery.
“Additional studies are needed to determine the long-term recurrence rate of umbilical hernia repairs performed in pregnant patients and the effects of surgical intervention and approach on the fetus,” the investigators concluded.
Find the study in Hernia (doi: 10.1007/s10029-017-1633-8).
Umbilical hernia repair during pregnancy is rare and safe, but more than half of surgeries required incarceration or strangulation repair, according to Dr. I.N. Haskins and associates.
A total of 126 pregnant women underwent umbilical hernia repair from 2005 to 2014, according to data collected from the American College of Surgeons National Surgical Quality Improvement Program. All but six women underwent open surgery, and of these 120 patients, 71 had umbilical hernia incarceration or strangulation at the time of surgery.
“Additional studies are needed to determine the long-term recurrence rate of umbilical hernia repairs performed in pregnant patients and the effects of surgical intervention and approach on the fetus,” the investigators concluded.
Find the study in Hernia (doi: 10.1007/s10029-017-1633-8).
FROM HERNIA
Clinical trial: Mesh Type in Ventral Hernia Repair
The Mesh Type in Ventral Hernia Repair trial is an interventional study currently recruiting patients scheduled for open ventral hernia repair.
Half of ventral hernia repairs utilize synthetic mesh, while the other half use biologic mesh. There is currently little solid evidence that one mesh type is better than the other, although the study investigators hypothesize that biologic mesh is superior to synthetic.
Patients will be included in the trial if they are scheduled for open ventral hernia repair at LBJ General Hospital in Houston and are at least 18 years old. Patients will be excluded if they have an active infection, are unlikely to survive the next 2 years, are individuals in whom a prosthetic would not normally be placed, or are unlikely to follow up.
The primary endpoint goal is zero complications 1 year after the operation. Secondary endpoint goals include patient-centered outcomes, cost, Dindo-Clavien complications (grades I-IV), and to be complication free 3 years after the operation.
Recruitment began on March 27, 2017, and the study is expected to include 50 people. The primary study endpoint will be completed March 31, 2019, with the full study being completed March 31, 2022.
Find more information at the study page on Clinicaltrials.gov.
The Mesh Type in Ventral Hernia Repair trial is an interventional study currently recruiting patients scheduled for open ventral hernia repair.
Half of ventral hernia repairs utilize synthetic mesh, while the other half use biologic mesh. There is currently little solid evidence that one mesh type is better than the other, although the study investigators hypothesize that biologic mesh is superior to synthetic.
Patients will be included in the trial if they are scheduled for open ventral hernia repair at LBJ General Hospital in Houston and are at least 18 years old. Patients will be excluded if they have an active infection, are unlikely to survive the next 2 years, are individuals in whom a prosthetic would not normally be placed, or are unlikely to follow up.
The primary endpoint goal is zero complications 1 year after the operation. Secondary endpoint goals include patient-centered outcomes, cost, Dindo-Clavien complications (grades I-IV), and to be complication free 3 years after the operation.
Recruitment began on March 27, 2017, and the study is expected to include 50 people. The primary study endpoint will be completed March 31, 2019, with the full study being completed March 31, 2022.
Find more information at the study page on Clinicaltrials.gov.
The Mesh Type in Ventral Hernia Repair trial is an interventional study currently recruiting patients scheduled for open ventral hernia repair.
Half of ventral hernia repairs utilize synthetic mesh, while the other half use biologic mesh. There is currently little solid evidence that one mesh type is better than the other, although the study investigators hypothesize that biologic mesh is superior to synthetic.
Patients will be included in the trial if they are scheduled for open ventral hernia repair at LBJ General Hospital in Houston and are at least 18 years old. Patients will be excluded if they have an active infection, are unlikely to survive the next 2 years, are individuals in whom a prosthetic would not normally be placed, or are unlikely to follow up.
The primary endpoint goal is zero complications 1 year after the operation. Secondary endpoint goals include patient-centered outcomes, cost, Dindo-Clavien complications (grades I-IV), and to be complication free 3 years after the operation.
Recruitment began on March 27, 2017, and the study is expected to include 50 people. The primary study endpoint will be completed March 31, 2019, with the full study being completed March 31, 2022.
Find more information at the study page on Clinicaltrials.gov.
SUMMARY FROM CLINICALTRIALS.GOV
Robotic-assisted IHR causes fewer complications in obese patients
Obese people undergoing inguinal hernia repair experienced fewer complications when the surgery was robotic assisted, compared to open repairs, according to Ramachandra Kolachalam, MD, and his associates.
A total of 148 robotic-assisted repairs (RHRs) and 113 open repairs were included in the study. Of open repair (OHR) patients, 11.5% experienced postoperative complications post discharge, compared with only 2.7% of RHR patients. OHR patients also had lower rates of concomitant procedures (16.8% vs. 29.7%) and bilateral repairs (11.5% vs. 35.1%). Morbidity rates did not differ significantly between the groups.
“Robotic-assisted inguinal hernia repair could lead to increased acceptance of minimally invasive hernia repair with the associated clinical benefits to patients, including those who are obese with higher comorbidities and higher American Surgery Association scores. A prospective study of obesity in RHR is warranted to confirm our findings,” the investigators concluded.
Find the full study in Surgical Endoscopy (2017. doi: 10.1007/s00464-017-5665-z).
Obese people undergoing inguinal hernia repair experienced fewer complications when the surgery was robotic assisted, compared to open repairs, according to Ramachandra Kolachalam, MD, and his associates.
A total of 148 robotic-assisted repairs (RHRs) and 113 open repairs were included in the study. Of open repair (OHR) patients, 11.5% experienced postoperative complications post discharge, compared with only 2.7% of RHR patients. OHR patients also had lower rates of concomitant procedures (16.8% vs. 29.7%) and bilateral repairs (11.5% vs. 35.1%). Morbidity rates did not differ significantly between the groups.
“Robotic-assisted inguinal hernia repair could lead to increased acceptance of minimally invasive hernia repair with the associated clinical benefits to patients, including those who are obese with higher comorbidities and higher American Surgery Association scores. A prospective study of obesity in RHR is warranted to confirm our findings,” the investigators concluded.
Find the full study in Surgical Endoscopy (2017. doi: 10.1007/s00464-017-5665-z).
Obese people undergoing inguinal hernia repair experienced fewer complications when the surgery was robotic assisted, compared to open repairs, according to Ramachandra Kolachalam, MD, and his associates.
A total of 148 robotic-assisted repairs (RHRs) and 113 open repairs were included in the study. Of open repair (OHR) patients, 11.5% experienced postoperative complications post discharge, compared with only 2.7% of RHR patients. OHR patients also had lower rates of concomitant procedures (16.8% vs. 29.7%) and bilateral repairs (11.5% vs. 35.1%). Morbidity rates did not differ significantly between the groups.
“Robotic-assisted inguinal hernia repair could lead to increased acceptance of minimally invasive hernia repair with the associated clinical benefits to patients, including those who are obese with higher comorbidities and higher American Surgery Association scores. A prospective study of obesity in RHR is warranted to confirm our findings,” the investigators concluded.
Find the full study in Surgical Endoscopy (2017. doi: 10.1007/s00464-017-5665-z).
FROM SURGICAL ENDOSCOPY
No easy answers for parastomal hernia repair
SEATTLE – At present, laparoscopic Sugarbaker repair is probably the best surgical option for parastomal hernias when stomas can’t be reversed, according to Mark Gudgeon, MS, FRCS, a consultant general surgeon at the Frimley Park Hospital in England.
Parastomal hernias are common in colorectal surgery; more than a quarter of ileostomy stomas and well over half of colostomy stomas herniate within 10 years of placement, leading to pain, leakage, appliance problems, and embarrassment for patients. There’s also the risk of bowel obstruction and strangulation. “It’s something that’s a challenge to all of us. It’s a very difficult problem,” Dr. Gudgeon said at the American Society of Colon and Rectal Surgeons annual meeting.
It can be difficult to decide whether or not to even offer patients a surgical fix because they often fail, and sometimes lead to fistulas and well-known mesh complications. Obese patients are “a no-go because they do not do well, and neither do smokers. Both are things patients have an opportunity to correct before we go ahead with surgery,” Dr. Gudgeon said.
On top of that, about 6% of repair patients die from complications. Patients “don’t believe that at first, but when you rub it in, a lot of them will change their minds” about surgery. “These patients don’t do well,” so avoid surgery when possible, he said. “Pain can be dealt with; leakage can be dealt with; cosmesis can be accepted,” especially with the help of stoma specialists who are experts in the art of appliance fit and support garments, Dr. Gudgeon said.
If the decision to operate is made, forget about suture repair, Dr. Gudgeon recommended. It should be “abandoned. I know it still goes on, but the evidence speaks for itself: [hernias] just come back again.”
Dr. Gudgeon suggested that it may be best to reverse the stoma, if possible, and repair the defect. Relocating the stoma “is always an attractive alternative,” and laparoscopic mesh keyhole repairs are straightforward. But the risk of recurrence is high, he said.
The Food and Drug Administration recently found that there’s not much difference between synthetic and biologic mesh, so Dr. Gudgeon said he usually opts for synthetics because they are less expensive.
He reported speakers’ fees from Intuitive, Medtronic, and Cook Medical.
SEATTLE – At present, laparoscopic Sugarbaker repair is probably the best surgical option for parastomal hernias when stomas can’t be reversed, according to Mark Gudgeon, MS, FRCS, a consultant general surgeon at the Frimley Park Hospital in England.
Parastomal hernias are common in colorectal surgery; more than a quarter of ileostomy stomas and well over half of colostomy stomas herniate within 10 years of placement, leading to pain, leakage, appliance problems, and embarrassment for patients. There’s also the risk of bowel obstruction and strangulation. “It’s something that’s a challenge to all of us. It’s a very difficult problem,” Dr. Gudgeon said at the American Society of Colon and Rectal Surgeons annual meeting.
It can be difficult to decide whether or not to even offer patients a surgical fix because they often fail, and sometimes lead to fistulas and well-known mesh complications. Obese patients are “a no-go because they do not do well, and neither do smokers. Both are things patients have an opportunity to correct before we go ahead with surgery,” Dr. Gudgeon said.
On top of that, about 6% of repair patients die from complications. Patients “don’t believe that at first, but when you rub it in, a lot of them will change their minds” about surgery. “These patients don’t do well,” so avoid surgery when possible, he said. “Pain can be dealt with; leakage can be dealt with; cosmesis can be accepted,” especially with the help of stoma specialists who are experts in the art of appliance fit and support garments, Dr. Gudgeon said.
If the decision to operate is made, forget about suture repair, Dr. Gudgeon recommended. It should be “abandoned. I know it still goes on, but the evidence speaks for itself: [hernias] just come back again.”
Dr. Gudgeon suggested that it may be best to reverse the stoma, if possible, and repair the defect. Relocating the stoma “is always an attractive alternative,” and laparoscopic mesh keyhole repairs are straightforward. But the risk of recurrence is high, he said.
The Food and Drug Administration recently found that there’s not much difference between synthetic and biologic mesh, so Dr. Gudgeon said he usually opts for synthetics because they are less expensive.
He reported speakers’ fees from Intuitive, Medtronic, and Cook Medical.
SEATTLE – At present, laparoscopic Sugarbaker repair is probably the best surgical option for parastomal hernias when stomas can’t be reversed, according to Mark Gudgeon, MS, FRCS, a consultant general surgeon at the Frimley Park Hospital in England.
Parastomal hernias are common in colorectal surgery; more than a quarter of ileostomy stomas and well over half of colostomy stomas herniate within 10 years of placement, leading to pain, leakage, appliance problems, and embarrassment for patients. There’s also the risk of bowel obstruction and strangulation. “It’s something that’s a challenge to all of us. It’s a very difficult problem,” Dr. Gudgeon said at the American Society of Colon and Rectal Surgeons annual meeting.
It can be difficult to decide whether or not to even offer patients a surgical fix because they often fail, and sometimes lead to fistulas and well-known mesh complications. Obese patients are “a no-go because they do not do well, and neither do smokers. Both are things patients have an opportunity to correct before we go ahead with surgery,” Dr. Gudgeon said.
On top of that, about 6% of repair patients die from complications. Patients “don’t believe that at first, but when you rub it in, a lot of them will change their minds” about surgery. “These patients don’t do well,” so avoid surgery when possible, he said. “Pain can be dealt with; leakage can be dealt with; cosmesis can be accepted,” especially with the help of stoma specialists who are experts in the art of appliance fit and support garments, Dr. Gudgeon said.
If the decision to operate is made, forget about suture repair, Dr. Gudgeon recommended. It should be “abandoned. I know it still goes on, but the evidence speaks for itself: [hernias] just come back again.”
Dr. Gudgeon suggested that it may be best to reverse the stoma, if possible, and repair the defect. Relocating the stoma “is always an attractive alternative,” and laparoscopic mesh keyhole repairs are straightforward. But the risk of recurrence is high, he said.
The Food and Drug Administration recently found that there’s not much difference between synthetic and biologic mesh, so Dr. Gudgeon said he usually opts for synthetics because they are less expensive.
He reported speakers’ fees from Intuitive, Medtronic, and Cook Medical.
EXPERT ANALYSIS AT THE ASCRS ANNUAL MEETING
Pregnancy boosts risk of ventral hernia recurrence
Pregnancy is associated with a significant increase in the risk of ventral hernia recurrence after repair, according to a population-based cohort study published online in the American Journal of Surgery.
Analysis of registry data from 3,578 Danish women of reproductive age who had previously undergone ventral hernia repair showed that subsequent pregnancy was associated with a 56% higher risk of recurrence (95% confidence interval, 1.09-2.25; P = .016), compared with women who did not get pregnant (Am J Surg. 2017 April 5. doi: 10.1016/j.amjsurg.2017.03.044).
They noted that few studies have directly reported on the rate of ventral hernia recurrence after pregnancy, and the results that do exist are conflicting.
The overall rate of ventral hernia recurrence in the cohort was 12.5%, 67.9% of whom subsequently underwent reoperation to repair. The median time from hernia repair to pregnancy was 1.1 years, and median follow-up was 3.1 years.
Umbilical and incisional hernia repair were independently associated with a higher risk of recurrence (hazard ratio, 1.55 and 3.30, respectively) than epigastric repair, while larger hernia defects also increased the risk of recurrence.
“According to Laplace’s law, both the abdominal wall stretch and the raised intra-abdominal pressure theoretically strain the repaired ventral hernia site and are likely involved in the associated increased risk of recurrence,” the authors wrote. “Furthermore, prolonged duration of the second stage of labor and the use of manual fundal pressure might increase the risk of ventral hernia recurrence.”
The authors pointed out that inadequate fixation and lateral detachment of the mesh material were the most commonly reported mechanisms involved in ventral hernia recurrence after mesh repair. The fact that most mesh materials are far less elastic than the abdominal wall could account for the association between pregnancy and recurrence.
Based on the findings, they suggested that elective surgery for incisional or umbilical hernia repair be postponed until after the last planned pregnancy and that female patients of reproductive age be counseled on the increased risk of recurrence with pregnancy should they choose to undergo ventral hernia repair. They also noted that the natural course of an untreated ventral hernia, how it responds to pregnancy, and the risk of emergency repair during pregnancy need further investigation.
The study was supported by grants from Edgar Schnohr, MD, Dr MSc & Wife Gilberte Schnohr’s Foundation, and Bispebjerg Hospital. No conflicts of interest were declared.
Pregnancy is associated with a significant increase in the risk of ventral hernia recurrence after repair, according to a population-based cohort study published online in the American Journal of Surgery.
Analysis of registry data from 3,578 Danish women of reproductive age who had previously undergone ventral hernia repair showed that subsequent pregnancy was associated with a 56% higher risk of recurrence (95% confidence interval, 1.09-2.25; P = .016), compared with women who did not get pregnant (Am J Surg. 2017 April 5. doi: 10.1016/j.amjsurg.2017.03.044).
They noted that few studies have directly reported on the rate of ventral hernia recurrence after pregnancy, and the results that do exist are conflicting.
The overall rate of ventral hernia recurrence in the cohort was 12.5%, 67.9% of whom subsequently underwent reoperation to repair. The median time from hernia repair to pregnancy was 1.1 years, and median follow-up was 3.1 years.
Umbilical and incisional hernia repair were independently associated with a higher risk of recurrence (hazard ratio, 1.55 and 3.30, respectively) than epigastric repair, while larger hernia defects also increased the risk of recurrence.
“According to Laplace’s law, both the abdominal wall stretch and the raised intra-abdominal pressure theoretically strain the repaired ventral hernia site and are likely involved in the associated increased risk of recurrence,” the authors wrote. “Furthermore, prolonged duration of the second stage of labor and the use of manual fundal pressure might increase the risk of ventral hernia recurrence.”
The authors pointed out that inadequate fixation and lateral detachment of the mesh material were the most commonly reported mechanisms involved in ventral hernia recurrence after mesh repair. The fact that most mesh materials are far less elastic than the abdominal wall could account for the association between pregnancy and recurrence.
Based on the findings, they suggested that elective surgery for incisional or umbilical hernia repair be postponed until after the last planned pregnancy and that female patients of reproductive age be counseled on the increased risk of recurrence with pregnancy should they choose to undergo ventral hernia repair. They also noted that the natural course of an untreated ventral hernia, how it responds to pregnancy, and the risk of emergency repair during pregnancy need further investigation.
The study was supported by grants from Edgar Schnohr, MD, Dr MSc & Wife Gilberte Schnohr’s Foundation, and Bispebjerg Hospital. No conflicts of interest were declared.
Pregnancy is associated with a significant increase in the risk of ventral hernia recurrence after repair, according to a population-based cohort study published online in the American Journal of Surgery.
Analysis of registry data from 3,578 Danish women of reproductive age who had previously undergone ventral hernia repair showed that subsequent pregnancy was associated with a 56% higher risk of recurrence (95% confidence interval, 1.09-2.25; P = .016), compared with women who did not get pregnant (Am J Surg. 2017 April 5. doi: 10.1016/j.amjsurg.2017.03.044).
They noted that few studies have directly reported on the rate of ventral hernia recurrence after pregnancy, and the results that do exist are conflicting.
The overall rate of ventral hernia recurrence in the cohort was 12.5%, 67.9% of whom subsequently underwent reoperation to repair. The median time from hernia repair to pregnancy was 1.1 years, and median follow-up was 3.1 years.
Umbilical and incisional hernia repair were independently associated with a higher risk of recurrence (hazard ratio, 1.55 and 3.30, respectively) than epigastric repair, while larger hernia defects also increased the risk of recurrence.
“According to Laplace’s law, both the abdominal wall stretch and the raised intra-abdominal pressure theoretically strain the repaired ventral hernia site and are likely involved in the associated increased risk of recurrence,” the authors wrote. “Furthermore, prolonged duration of the second stage of labor and the use of manual fundal pressure might increase the risk of ventral hernia recurrence.”
The authors pointed out that inadequate fixation and lateral detachment of the mesh material were the most commonly reported mechanisms involved in ventral hernia recurrence after mesh repair. The fact that most mesh materials are far less elastic than the abdominal wall could account for the association between pregnancy and recurrence.
Based on the findings, they suggested that elective surgery for incisional or umbilical hernia repair be postponed until after the last planned pregnancy and that female patients of reproductive age be counseled on the increased risk of recurrence with pregnancy should they choose to undergo ventral hernia repair. They also noted that the natural course of an untreated ventral hernia, how it responds to pregnancy, and the risk of emergency repair during pregnancy need further investigation.
The study was supported by grants from Edgar Schnohr, MD, Dr MSc & Wife Gilberte Schnohr’s Foundation, and Bispebjerg Hospital. No conflicts of interest were declared.
FROM THE AMERICAN JOURNAL OF SURGERY
Key clinical point: Pregnancy after ventral hernia repair can significantly increase the risk of recurrence.
Major finding: Pregnancy is associated with a 56% increase in the risk of recurrence of ventral hernia after repair.
Data source: A population-based cohort study of 3,578 women of reproductive age who underwent ventral hernia repair.
Disclosures: The study was supported by grants from Edgar Schnohr MD, Dr MSc & Wife Gilberte Schnohr’s Foundation, and Bispebjerg Hospital. No conflicts of interest were declared.
Same-day discharge for lap hiatal procedures found feasible, safe
HOUSTON – Selected patients who need operations, such as paraesophageal hernia repair and Heller myotomy, for benign hiatal diseases can have laparoscopic outpatient procedures with outcomes comparable with those of inpatients, a Canadian retrospective cohort study found.
“When comparing planned day-case patients with those who had planned admissions, we found that postoperative complication was the only statistically significant different outcome. Our data show same-day discharge resulted in no postoperative mortality, and no difference in postoperative morbidity, emergency room visits, and readmissions compared to traditional inpatient care,” said Juan Carlos Molina, MD, of McGill University Health Centre in Montreal, reporting the study results at the annual meeting of the American Society of Gastrointestinal and Endoscopic Surgeons.
The McGill researchers analyzed outcomes for 261 patients who had laparoscopic hiatal procedures from April 2011 to August 2016 – 163 as inpatients, 98 as outpatients, whom the study called planned day-case patients. The outpatient cohort consisted of younger patients (aged 60 vs. 66 years), but otherwise demographics between the two cohorts were similar. Discharge requirements after same-day hiatal procedures were the same as those for other outpatient procedures, Dr. Molina said.
The procedures included primary or revisional paraesophageal hernia repair (PEHR) in 123 (47.1%) patients; Heller myotomy in 94 (36%), 9 of which also underwent resection of an epiphrenic diverticulum; and Nissen fundoplication for gastroesophageal reflux disease in 44 (16.9%), of which 20 (45.5%) had a concomitant type I hiatal hernia. Among PEHR patients, 90% were at least type III.
“We include complex cases, such as revisional surgery, massive paraesophageal hernias, patients who had previous treatments for achalasia before surgery, or concurrent epiphrenic diverticulum resection,” Dr. Molina said. “To our knowledge, this report is the first to describe successful outpatient surgery in these complex patients, with comparable outcomes to admitted patients and to those described for more well-established outpatient procedures.”
The overall success rate of planned day surgery was 81.6%. Of the 18 unplanned admissions, patient preference to stay in the hospital and pain were the most common factors. Dr. Molina-Franjola said, “We identified factors that might be predictors of unplanned admission, and we found that female [sex], intraoperative complication, postoperative complications, and procedure performed in the afternoon were significant risk factors.”
Women accounted for 94.4% of the unplanned admissions after outpatient surgery, and PEHR/fundoplication represented 72.2% of unplanned admissions. No day-case patients with unplanned admission group required a reoperation within 30 days, although one who did not have an unplanned admission did.
With time, the share of outpatient procedures increased, Dr. Molina said. “In 2011, around 10% of procedures were day-case and that increased progressively to 67% in 2016,” he said.
Dr. Molina said that patients were sent home with antinauseates and instructions to call immediately if nausea or vomiting ensued. About 5% of outpatients returned for reflux, nausea, or vomiting, he said.
Dr. Molina reported having no financial disclosures.
HOUSTON – Selected patients who need operations, such as paraesophageal hernia repair and Heller myotomy, for benign hiatal diseases can have laparoscopic outpatient procedures with outcomes comparable with those of inpatients, a Canadian retrospective cohort study found.
“When comparing planned day-case patients with those who had planned admissions, we found that postoperative complication was the only statistically significant different outcome. Our data show same-day discharge resulted in no postoperative mortality, and no difference in postoperative morbidity, emergency room visits, and readmissions compared to traditional inpatient care,” said Juan Carlos Molina, MD, of McGill University Health Centre in Montreal, reporting the study results at the annual meeting of the American Society of Gastrointestinal and Endoscopic Surgeons.
The McGill researchers analyzed outcomes for 261 patients who had laparoscopic hiatal procedures from April 2011 to August 2016 – 163 as inpatients, 98 as outpatients, whom the study called planned day-case patients. The outpatient cohort consisted of younger patients (aged 60 vs. 66 years), but otherwise demographics between the two cohorts were similar. Discharge requirements after same-day hiatal procedures were the same as those for other outpatient procedures, Dr. Molina said.
The procedures included primary or revisional paraesophageal hernia repair (PEHR) in 123 (47.1%) patients; Heller myotomy in 94 (36%), 9 of which also underwent resection of an epiphrenic diverticulum; and Nissen fundoplication for gastroesophageal reflux disease in 44 (16.9%), of which 20 (45.5%) had a concomitant type I hiatal hernia. Among PEHR patients, 90% were at least type III.
“We include complex cases, such as revisional surgery, massive paraesophageal hernias, patients who had previous treatments for achalasia before surgery, or concurrent epiphrenic diverticulum resection,” Dr. Molina said. “To our knowledge, this report is the first to describe successful outpatient surgery in these complex patients, with comparable outcomes to admitted patients and to those described for more well-established outpatient procedures.”
The overall success rate of planned day surgery was 81.6%. Of the 18 unplanned admissions, patient preference to stay in the hospital and pain were the most common factors. Dr. Molina-Franjola said, “We identified factors that might be predictors of unplanned admission, and we found that female [sex], intraoperative complication, postoperative complications, and procedure performed in the afternoon were significant risk factors.”
Women accounted for 94.4% of the unplanned admissions after outpatient surgery, and PEHR/fundoplication represented 72.2% of unplanned admissions. No day-case patients with unplanned admission group required a reoperation within 30 days, although one who did not have an unplanned admission did.
With time, the share of outpatient procedures increased, Dr. Molina said. “In 2011, around 10% of procedures were day-case and that increased progressively to 67% in 2016,” he said.
Dr. Molina said that patients were sent home with antinauseates and instructions to call immediately if nausea or vomiting ensued. About 5% of outpatients returned for reflux, nausea, or vomiting, he said.
Dr. Molina reported having no financial disclosures.
HOUSTON – Selected patients who need operations, such as paraesophageal hernia repair and Heller myotomy, for benign hiatal diseases can have laparoscopic outpatient procedures with outcomes comparable with those of inpatients, a Canadian retrospective cohort study found.
“When comparing planned day-case patients with those who had planned admissions, we found that postoperative complication was the only statistically significant different outcome. Our data show same-day discharge resulted in no postoperative mortality, and no difference in postoperative morbidity, emergency room visits, and readmissions compared to traditional inpatient care,” said Juan Carlos Molina, MD, of McGill University Health Centre in Montreal, reporting the study results at the annual meeting of the American Society of Gastrointestinal and Endoscopic Surgeons.
The McGill researchers analyzed outcomes for 261 patients who had laparoscopic hiatal procedures from April 2011 to August 2016 – 163 as inpatients, 98 as outpatients, whom the study called planned day-case patients. The outpatient cohort consisted of younger patients (aged 60 vs. 66 years), but otherwise demographics between the two cohorts were similar. Discharge requirements after same-day hiatal procedures were the same as those for other outpatient procedures, Dr. Molina said.
The procedures included primary or revisional paraesophageal hernia repair (PEHR) in 123 (47.1%) patients; Heller myotomy in 94 (36%), 9 of which also underwent resection of an epiphrenic diverticulum; and Nissen fundoplication for gastroesophageal reflux disease in 44 (16.9%), of which 20 (45.5%) had a concomitant type I hiatal hernia. Among PEHR patients, 90% were at least type III.
“We include complex cases, such as revisional surgery, massive paraesophageal hernias, patients who had previous treatments for achalasia before surgery, or concurrent epiphrenic diverticulum resection,” Dr. Molina said. “To our knowledge, this report is the first to describe successful outpatient surgery in these complex patients, with comparable outcomes to admitted patients and to those described for more well-established outpatient procedures.”
The overall success rate of planned day surgery was 81.6%. Of the 18 unplanned admissions, patient preference to stay in the hospital and pain were the most common factors. Dr. Molina-Franjola said, “We identified factors that might be predictors of unplanned admission, and we found that female [sex], intraoperative complication, postoperative complications, and procedure performed in the afternoon were significant risk factors.”
Women accounted for 94.4% of the unplanned admissions after outpatient surgery, and PEHR/fundoplication represented 72.2% of unplanned admissions. No day-case patients with unplanned admission group required a reoperation within 30 days, although one who did not have an unplanned admission did.
With time, the share of outpatient procedures increased, Dr. Molina said. “In 2011, around 10% of procedures were day-case and that increased progressively to 67% in 2016,” he said.
Dr. Molina said that patients were sent home with antinauseates and instructions to call immediately if nausea or vomiting ensued. About 5% of outpatients returned for reflux, nausea, or vomiting, he said.
Dr. Molina reported having no financial disclosures.
AT SAGES 2017
Key clinical point: Same-day surgery for benign laparoscopic hiatal procedures have outcomes comparable with those of inpatient procedures.
Major finding: Postoperative complications were 9.2% for outpatient operations vs. 19% for inpatient, and 81.7% of patients who had same-day surgery did not have an unplanned admission.
Data source: Retrospective single-center study of 261 patients who had inpatient and outpatient laparoscopic hiatal procedures from April 2011 to August 2016.
Disclosures: Dr. Molina-Franjola reported having no financial disclosures.
Does laparoscopy have an advantage for emergency VHR?
HOUSTON – The benefits of elective laparoscopic ventral hernia repair over the open approach have been well documented, but, when presented with emergency cases, surgeons still are about 10 times more likely to employ open surgery, possibly exposing patients to greater risk of complications, as well as longer hospital stays, according to an analysis of a national database.
“Despite the benefits of laparoscopic surgery, its utilization in ventral hernia repair (VHR) remains low,” said David Pechman, MD, MBA, of Mount Sinai Beth Israel Medical Center, New York, at the annual meeting of the American Society of Gastrointestinal and Endoscopic Surgeons. “This study suggests that utilization is further decreased in emergency cases. Relative to elective cases, emergency VHR is associated with markedly increased rates of morbidity, giving us more room to improve patient outcomes with the use of laparoscopy in these cases.”
The study analyzed 330 emergency VHR operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database for 2012 and 2013. Thirty-two (9.3%) of those operations were performed laparoscopically, and the remainder were open. Because the sample size of laparoscopic operations was so small, drawing statistically significant conclusions from the findings is difficult without a larger, higher-powered study, Dr. Pechman said. “We do think that further research is warranted and believe that analysis of a larger sample would display that increased utilization of laparoscopy in emergency VHR could significantly improve outcomes.”
The analysis found significant differences in outcomes between the laparoscopic and the open operations for emergency VHR. Average hospital stay after laparoscopic emergency VHR was 2.8 days vs. 5.9 days for open VHR (P = .02). Surgical site infection rates were 0% vs. 7.7% (P = .15). Demographics between both laparoscopic and open groups were similar, Dr. Pechman said.
Session moderator E. Matthew Ritter, MD, of Walter Reed National Military Medical Center, Bethesda, Md., noted that the study conclusion is in line with the goals of SAGES’s minimally invasive surgery initiative to increase utilization of laparoscopy. When referring to the findings Dr. Pechman reported, Dr. Ritter said, “This is a remarkably low complication rate for a procedure that could seemingly have some benefit.”
Dr. Pechman’s response acknowledged the concerns of the surgeons doing the procedures: “A lot of this has to do with surgeon comfort and the preoperative decision-making, especially in an emergency setting.”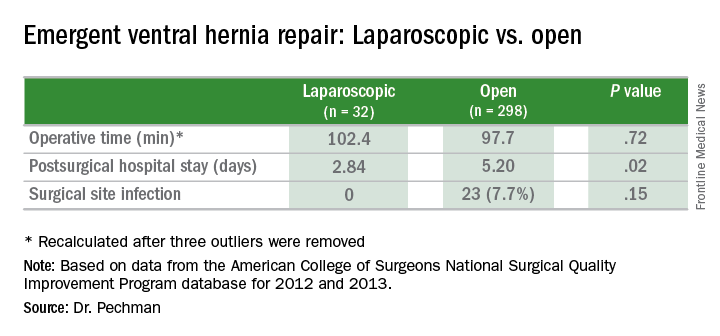
HOUSTON – The benefits of elective laparoscopic ventral hernia repair over the open approach have been well documented, but, when presented with emergency cases, surgeons still are about 10 times more likely to employ open surgery, possibly exposing patients to greater risk of complications, as well as longer hospital stays, according to an analysis of a national database.
“Despite the benefits of laparoscopic surgery, its utilization in ventral hernia repair (VHR) remains low,” said David Pechman, MD, MBA, of Mount Sinai Beth Israel Medical Center, New York, at the annual meeting of the American Society of Gastrointestinal and Endoscopic Surgeons. “This study suggests that utilization is further decreased in emergency cases. Relative to elective cases, emergency VHR is associated with markedly increased rates of morbidity, giving us more room to improve patient outcomes with the use of laparoscopy in these cases.”
The study analyzed 330 emergency VHR operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database for 2012 and 2013. Thirty-two (9.3%) of those operations were performed laparoscopically, and the remainder were open. Because the sample size of laparoscopic operations was so small, drawing statistically significant conclusions from the findings is difficult without a larger, higher-powered study, Dr. Pechman said. “We do think that further research is warranted and believe that analysis of a larger sample would display that increased utilization of laparoscopy in emergency VHR could significantly improve outcomes.”
The analysis found significant differences in outcomes between the laparoscopic and the open operations for emergency VHR. Average hospital stay after laparoscopic emergency VHR was 2.8 days vs. 5.9 days for open VHR (P = .02). Surgical site infection rates were 0% vs. 7.7% (P = .15). Demographics between both laparoscopic and open groups were similar, Dr. Pechman said.
Session moderator E. Matthew Ritter, MD, of Walter Reed National Military Medical Center, Bethesda, Md., noted that the study conclusion is in line with the goals of SAGES’s minimally invasive surgery initiative to increase utilization of laparoscopy. When referring to the findings Dr. Pechman reported, Dr. Ritter said, “This is a remarkably low complication rate for a procedure that could seemingly have some benefit.”
Dr. Pechman’s response acknowledged the concerns of the surgeons doing the procedures: “A lot of this has to do with surgeon comfort and the preoperative decision-making, especially in an emergency setting.”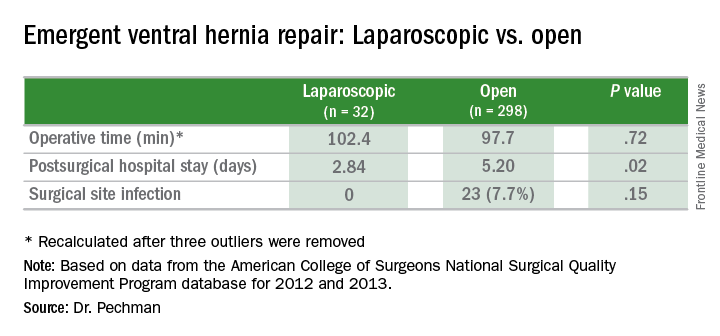
HOUSTON – The benefits of elective laparoscopic ventral hernia repair over the open approach have been well documented, but, when presented with emergency cases, surgeons still are about 10 times more likely to employ open surgery, possibly exposing patients to greater risk of complications, as well as longer hospital stays, according to an analysis of a national database.
“Despite the benefits of laparoscopic surgery, its utilization in ventral hernia repair (VHR) remains low,” said David Pechman, MD, MBA, of Mount Sinai Beth Israel Medical Center, New York, at the annual meeting of the American Society of Gastrointestinal and Endoscopic Surgeons. “This study suggests that utilization is further decreased in emergency cases. Relative to elective cases, emergency VHR is associated with markedly increased rates of morbidity, giving us more room to improve patient outcomes with the use of laparoscopy in these cases.”
The study analyzed 330 emergency VHR operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database for 2012 and 2013. Thirty-two (9.3%) of those operations were performed laparoscopically, and the remainder were open. Because the sample size of laparoscopic operations was so small, drawing statistically significant conclusions from the findings is difficult without a larger, higher-powered study, Dr. Pechman said. “We do think that further research is warranted and believe that analysis of a larger sample would display that increased utilization of laparoscopy in emergency VHR could significantly improve outcomes.”
The analysis found significant differences in outcomes between the laparoscopic and the open operations for emergency VHR. Average hospital stay after laparoscopic emergency VHR was 2.8 days vs. 5.9 days for open VHR (P = .02). Surgical site infection rates were 0% vs. 7.7% (P = .15). Demographics between both laparoscopic and open groups were similar, Dr. Pechman said.
Session moderator E. Matthew Ritter, MD, of Walter Reed National Military Medical Center, Bethesda, Md., noted that the study conclusion is in line with the goals of SAGES’s minimally invasive surgery initiative to increase utilization of laparoscopy. When referring to the findings Dr. Pechman reported, Dr. Ritter said, “This is a remarkably low complication rate for a procedure that could seemingly have some benefit.”
Dr. Pechman’s response acknowledged the concerns of the surgeons doing the procedures: “A lot of this has to do with surgeon comfort and the preoperative decision-making, especially in an emergency setting.”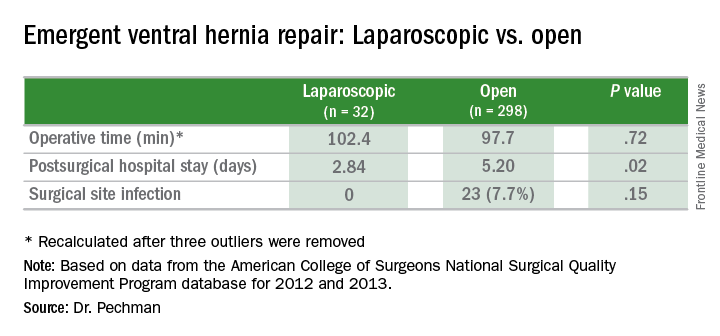
Key clinical point: Outcomes of laparoscopic ventral hernia repair (VHR) may be superior to those for open surgery in the emergency setting.
Major finding: Average hospital stay after laparoscopic emergency VHR was 2.8 days vs. 5.9 days for open surgery, and surgical site infection rates were 0% vs. 7.7%.
Data source: Analysis of 329 cases of emergency VHR enrolled in the American College of Surgeons National Surgical Quality Improvement Program in 2012 and 2013.
Disclosures: Dr. Pechman reported no financial disclosures.
Robot-assisted surgery: Twice the price
HOUSTON – Robot-assisted operations for inguinal hernia repair (IHR) and cholecystectomy have grown steadily in recent years, but these procedures can be done equally well by traditional operations at a fraction of the cost, according to a study from Geisinger Medical Center in Pennsylvania.
Ellen Vogels, DO, of Geisinger, reported results of a study of 1,248 cholecystectomies and 723 initial IHRs from 2007 to 2016. The cholecystectomies were done via robot-assisted surgery or laparoscopy in the hospital or via laparoscopy in an ambulatory surgery center (ASC). The IHRs were done robotically, open, or laparoscopically in the hospital, or open or laparoscopically in an ASC.
Dr. Vogels quoted statistics from the ECRI Institute that showed robotic surgery procedures have increased 178% between 2009 and 2014, and the two procedures the group studied are the most frequently performed robotic procedures.
Within the Geisinger system, the study found a 3:1 cost disparity for IHR: $6,292 total cost for hospital-based robotic surgery vs. $3,421 for ASC-based laparoscopy IHR and $1,853 for ASC-based open repair. For cholecystectomy, the disparity isn’t as wide – it’s 2:1 – but is still significant: Total costs for hospital-based robotic surgery are $6,057 vs. $3,443 for ASC-based cholecystectomy and $3,270 for hospital-based laparoscopic cholecystectomy (the study did not include any open cholecystectomies).
Total costs not only include costs for the procedure but also all related pre- and postoperative care. The cost analysis did not account for the cost of the robot, including maintenance contracts, or costs for laparoscopic instruments. Variable costs also ranged from about $3,000 for robotic IHR to $942 for ASC open repair – which means the lowest per-procedure cost for the latter was around $900.
“Translating this into the fact that cholecystectomies and inguinal hernia repairs are the most often performed general surgery procedures, ambulatory surgery centers can save over $60 billion over the next 10 years in just overhead costs as well as increased efficiency,” Dr. Vogels said.
The study also found access issues depending on where patients had their operations. “As far as service and access in our institution alone, we found that patients going to the main hospital spent as much as two times longer getting these procedures done as compared to the ambulatory surgery centers,” Dr. Vogels said.
Robotic procedures also required longer operative times, the study found – an average of 109 minutes for IHR vs. about an hour for ASC procedures and hospital-based open surgery (but averaging 78 minutes for in-hospital laparoscopy); and 73 minutes for robotic cholecystectomy, 60 minutes for hospital laparoscopy, and 45 minutes for ASC laparoscopy.
Robotic session moderator Dmitry Oleynikov, MD, FACS, of the University of Nebraska Medical Center, Omaha, asked Dr. Vogels if putting a robotic platform in an ambulatory surgery setting would make it more cost effective.
That’s not practical from a cost or efficiency perspective, she said.
“When you look at the cost of the ASCs, specifically in the hernia group, the lowest-cost hernia repair is about $800; with the robot it’s going to be significantly higher than that, up to three times higher than that,” Dr. Vogels replied. “Then you’re also changing all those simple ambulatory surgery procedures to more involved robotic procedures, so it’s hard to justify doing that in the ASC.”
Dr. Vogels and her coauthors had no relevant financial disclosures.
HOUSTON – Robot-assisted operations for inguinal hernia repair (IHR) and cholecystectomy have grown steadily in recent years, but these procedures can be done equally well by traditional operations at a fraction of the cost, according to a study from Geisinger Medical Center in Pennsylvania.
Ellen Vogels, DO, of Geisinger, reported results of a study of 1,248 cholecystectomies and 723 initial IHRs from 2007 to 2016. The cholecystectomies were done via robot-assisted surgery or laparoscopy in the hospital or via laparoscopy in an ambulatory surgery center (ASC). The IHRs were done robotically, open, or laparoscopically in the hospital, or open or laparoscopically in an ASC.
Dr. Vogels quoted statistics from the ECRI Institute that showed robotic surgery procedures have increased 178% between 2009 and 2014, and the two procedures the group studied are the most frequently performed robotic procedures.
Within the Geisinger system, the study found a 3:1 cost disparity for IHR: $6,292 total cost for hospital-based robotic surgery vs. $3,421 for ASC-based laparoscopy IHR and $1,853 for ASC-based open repair. For cholecystectomy, the disparity isn’t as wide – it’s 2:1 – but is still significant: Total costs for hospital-based robotic surgery are $6,057 vs. $3,443 for ASC-based cholecystectomy and $3,270 for hospital-based laparoscopic cholecystectomy (the study did not include any open cholecystectomies).
Total costs not only include costs for the procedure but also all related pre- and postoperative care. The cost analysis did not account for the cost of the robot, including maintenance contracts, or costs for laparoscopic instruments. Variable costs also ranged from about $3,000 for robotic IHR to $942 for ASC open repair – which means the lowest per-procedure cost for the latter was around $900.
“Translating this into the fact that cholecystectomies and inguinal hernia repairs are the most often performed general surgery procedures, ambulatory surgery centers can save over $60 billion over the next 10 years in just overhead costs as well as increased efficiency,” Dr. Vogels said.
The study also found access issues depending on where patients had their operations. “As far as service and access in our institution alone, we found that patients going to the main hospital spent as much as two times longer getting these procedures done as compared to the ambulatory surgery centers,” Dr. Vogels said.
Robotic procedures also required longer operative times, the study found – an average of 109 minutes for IHR vs. about an hour for ASC procedures and hospital-based open surgery (but averaging 78 minutes for in-hospital laparoscopy); and 73 minutes for robotic cholecystectomy, 60 minutes for hospital laparoscopy, and 45 minutes for ASC laparoscopy.
Robotic session moderator Dmitry Oleynikov, MD, FACS, of the University of Nebraska Medical Center, Omaha, asked Dr. Vogels if putting a robotic platform in an ambulatory surgery setting would make it more cost effective.
That’s not practical from a cost or efficiency perspective, she said.
“When you look at the cost of the ASCs, specifically in the hernia group, the lowest-cost hernia repair is about $800; with the robot it’s going to be significantly higher than that, up to three times higher than that,” Dr. Vogels replied. “Then you’re also changing all those simple ambulatory surgery procedures to more involved robotic procedures, so it’s hard to justify doing that in the ASC.”
Dr. Vogels and her coauthors had no relevant financial disclosures.
HOUSTON – Robot-assisted operations for inguinal hernia repair (IHR) and cholecystectomy have grown steadily in recent years, but these procedures can be done equally well by traditional operations at a fraction of the cost, according to a study from Geisinger Medical Center in Pennsylvania.
Ellen Vogels, DO, of Geisinger, reported results of a study of 1,248 cholecystectomies and 723 initial IHRs from 2007 to 2016. The cholecystectomies were done via robot-assisted surgery or laparoscopy in the hospital or via laparoscopy in an ambulatory surgery center (ASC). The IHRs were done robotically, open, or laparoscopically in the hospital, or open or laparoscopically in an ASC.
Dr. Vogels quoted statistics from the ECRI Institute that showed robotic surgery procedures have increased 178% between 2009 and 2014, and the two procedures the group studied are the most frequently performed robotic procedures.
Within the Geisinger system, the study found a 3:1 cost disparity for IHR: $6,292 total cost for hospital-based robotic surgery vs. $3,421 for ASC-based laparoscopy IHR and $1,853 for ASC-based open repair. For cholecystectomy, the disparity isn’t as wide – it’s 2:1 – but is still significant: Total costs for hospital-based robotic surgery are $6,057 vs. $3,443 for ASC-based cholecystectomy and $3,270 for hospital-based laparoscopic cholecystectomy (the study did not include any open cholecystectomies).
Total costs not only include costs for the procedure but also all related pre- and postoperative care. The cost analysis did not account for the cost of the robot, including maintenance contracts, or costs for laparoscopic instruments. Variable costs also ranged from about $3,000 for robotic IHR to $942 for ASC open repair – which means the lowest per-procedure cost for the latter was around $900.
“Translating this into the fact that cholecystectomies and inguinal hernia repairs are the most often performed general surgery procedures, ambulatory surgery centers can save over $60 billion over the next 10 years in just overhead costs as well as increased efficiency,” Dr. Vogels said.
The study also found access issues depending on where patients had their operations. “As far as service and access in our institution alone, we found that patients going to the main hospital spent as much as two times longer getting these procedures done as compared to the ambulatory surgery centers,” Dr. Vogels said.
Robotic procedures also required longer operative times, the study found – an average of 109 minutes for IHR vs. about an hour for ASC procedures and hospital-based open surgery (but averaging 78 minutes for in-hospital laparoscopy); and 73 minutes for robotic cholecystectomy, 60 minutes for hospital laparoscopy, and 45 minutes for ASC laparoscopy.
Robotic session moderator Dmitry Oleynikov, MD, FACS, of the University of Nebraska Medical Center, Omaha, asked Dr. Vogels if putting a robotic platform in an ambulatory surgery setting would make it more cost effective.
That’s not practical from a cost or efficiency perspective, she said.
“When you look at the cost of the ASCs, specifically in the hernia group, the lowest-cost hernia repair is about $800; with the robot it’s going to be significantly higher than that, up to three times higher than that,” Dr. Vogels replied. “Then you’re also changing all those simple ambulatory surgery procedures to more involved robotic procedures, so it’s hard to justify doing that in the ASC.”
Dr. Vogels and her coauthors had no relevant financial disclosures.
AT SAGES 2017
Key clinical point: Outcomes for robot-assisted inguinal hernia repair and cholecystectomy are similar to those for outpatient open and laparoscopic procedures.
Major finding: Robotic IHR costs up to three times more than open outpatient surgery, and robotic cholecystectomy costs twice as much as outpatient surgery.
Data source: Study of 1,971 in-hospital robotic, laparoscopic, and open procedures, and outpatient laparoscopic and open operations done from 2007 to 2016 at Geisinger Medical Center.
Disclosures: Dr. Vogels and coauthors reported having no financial disclosures.















