User login
Does laparoscopy have an advantage for emergency VHR?
HOUSTON – The benefits of elective laparoscopic ventral hernia repair over the open approach have been well documented, but, when presented with emergency cases, surgeons still are about 10 times more likely to employ open surgery, possibly exposing patients to greater risk of complications, as well as longer hospital stays, according to an analysis of a national database.
“Despite the benefits of laparoscopic surgery, its utilization in ventral hernia repair (VHR) remains low,” said David Pechman, MD, MBA, of Mount Sinai Beth Israel Medical Center, New York, at the annual meeting of the American Society of Gastrointestinal and Endoscopic Surgeons. “This study suggests that utilization is further decreased in emergency cases. Relative to elective cases, emergency VHR is associated with markedly increased rates of morbidity, giving us more room to improve patient outcomes with the use of laparoscopy in these cases.”
The study analyzed 330 emergency VHR operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database for 2012 and 2013. Thirty-two (9.3%) of those operations were performed laparoscopically, and the remainder were open. Because the sample size of laparoscopic operations was so small, drawing statistically significant conclusions from the findings is difficult without a larger, higher-powered study, Dr. Pechman said. “We do think that further research is warranted and believe that analysis of a larger sample would display that increased utilization of laparoscopy in emergency VHR could significantly improve outcomes.”
The analysis found significant differences in outcomes between the laparoscopic and the open operations for emergency VHR. Average hospital stay after laparoscopic emergency VHR was 2.8 days vs. 5.9 days for open VHR (P = .02). Surgical site infection rates were 0% vs. 7.7% (P = .15). Demographics between both laparoscopic and open groups were similar, Dr. Pechman said.
Session moderator E. Matthew Ritter, MD, of Walter Reed National Military Medical Center, Bethesda, Md., noted that the study conclusion is in line with the goals of SAGES’s minimally invasive surgery initiative to increase utilization of laparoscopy. When referring to the findings Dr. Pechman reported, Dr. Ritter said, “This is a remarkably low complication rate for a procedure that could seemingly have some benefit.”
Dr. Pechman’s response acknowledged the concerns of the surgeons doing the procedures: “A lot of this has to do with surgeon comfort and the preoperative decision-making, especially in an emergency setting.”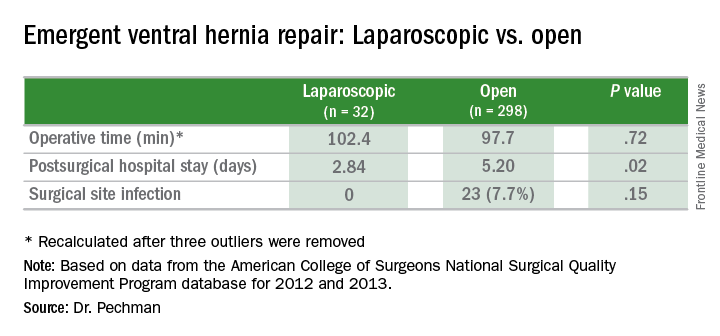
HOUSTON – The benefits of elective laparoscopic ventral hernia repair over the open approach have been well documented, but, when presented with emergency cases, surgeons still are about 10 times more likely to employ open surgery, possibly exposing patients to greater risk of complications, as well as longer hospital stays, according to an analysis of a national database.
“Despite the benefits of laparoscopic surgery, its utilization in ventral hernia repair (VHR) remains low,” said David Pechman, MD, MBA, of Mount Sinai Beth Israel Medical Center, New York, at the annual meeting of the American Society of Gastrointestinal and Endoscopic Surgeons. “This study suggests that utilization is further decreased in emergency cases. Relative to elective cases, emergency VHR is associated with markedly increased rates of morbidity, giving us more room to improve patient outcomes with the use of laparoscopy in these cases.”
The study analyzed 330 emergency VHR operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database for 2012 and 2013. Thirty-two (9.3%) of those operations were performed laparoscopically, and the remainder were open. Because the sample size of laparoscopic operations was so small, drawing statistically significant conclusions from the findings is difficult without a larger, higher-powered study, Dr. Pechman said. “We do think that further research is warranted and believe that analysis of a larger sample would display that increased utilization of laparoscopy in emergency VHR could significantly improve outcomes.”
The analysis found significant differences in outcomes between the laparoscopic and the open operations for emergency VHR. Average hospital stay after laparoscopic emergency VHR was 2.8 days vs. 5.9 days for open VHR (P = .02). Surgical site infection rates were 0% vs. 7.7% (P = .15). Demographics between both laparoscopic and open groups were similar, Dr. Pechman said.
Session moderator E. Matthew Ritter, MD, of Walter Reed National Military Medical Center, Bethesda, Md., noted that the study conclusion is in line with the goals of SAGES’s minimally invasive surgery initiative to increase utilization of laparoscopy. When referring to the findings Dr. Pechman reported, Dr. Ritter said, “This is a remarkably low complication rate for a procedure that could seemingly have some benefit.”
Dr. Pechman’s response acknowledged the concerns of the surgeons doing the procedures: “A lot of this has to do with surgeon comfort and the preoperative decision-making, especially in an emergency setting.”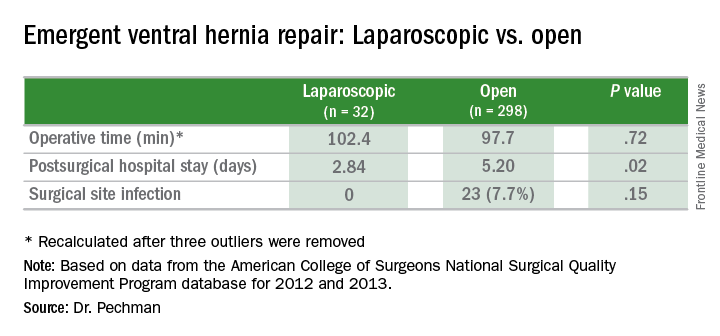
HOUSTON – The benefits of elective laparoscopic ventral hernia repair over the open approach have been well documented, but, when presented with emergency cases, surgeons still are about 10 times more likely to employ open surgery, possibly exposing patients to greater risk of complications, as well as longer hospital stays, according to an analysis of a national database.
“Despite the benefits of laparoscopic surgery, its utilization in ventral hernia repair (VHR) remains low,” said David Pechman, MD, MBA, of Mount Sinai Beth Israel Medical Center, New York, at the annual meeting of the American Society of Gastrointestinal and Endoscopic Surgeons. “This study suggests that utilization is further decreased in emergency cases. Relative to elective cases, emergency VHR is associated with markedly increased rates of morbidity, giving us more room to improve patient outcomes with the use of laparoscopy in these cases.”
The study analyzed 330 emergency VHR operations in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database for 2012 and 2013. Thirty-two (9.3%) of those operations were performed laparoscopically, and the remainder were open. Because the sample size of laparoscopic operations was so small, drawing statistically significant conclusions from the findings is difficult without a larger, higher-powered study, Dr. Pechman said. “We do think that further research is warranted and believe that analysis of a larger sample would display that increased utilization of laparoscopy in emergency VHR could significantly improve outcomes.”
The analysis found significant differences in outcomes between the laparoscopic and the open operations for emergency VHR. Average hospital stay after laparoscopic emergency VHR was 2.8 days vs. 5.9 days for open VHR (P = .02). Surgical site infection rates were 0% vs. 7.7% (P = .15). Demographics between both laparoscopic and open groups were similar, Dr. Pechman said.
Session moderator E. Matthew Ritter, MD, of Walter Reed National Military Medical Center, Bethesda, Md., noted that the study conclusion is in line with the goals of SAGES’s minimally invasive surgery initiative to increase utilization of laparoscopy. When referring to the findings Dr. Pechman reported, Dr. Ritter said, “This is a remarkably low complication rate for a procedure that could seemingly have some benefit.”
Dr. Pechman’s response acknowledged the concerns of the surgeons doing the procedures: “A lot of this has to do with surgeon comfort and the preoperative decision-making, especially in an emergency setting.”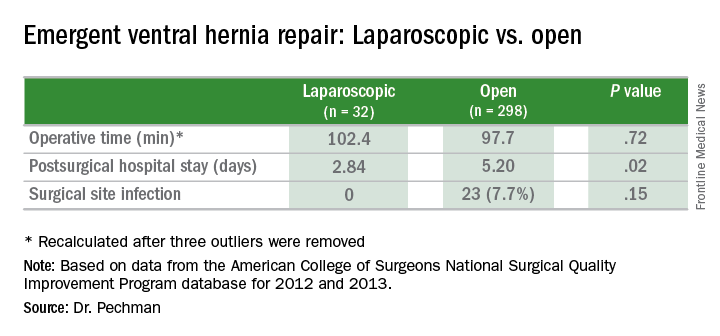
Key clinical point: Outcomes of laparoscopic ventral hernia repair (VHR) may be superior to those for open surgery in the emergency setting.
Major finding: Average hospital stay after laparoscopic emergency VHR was 2.8 days vs. 5.9 days for open surgery, and surgical site infection rates were 0% vs. 7.7%.
Data source: Analysis of 329 cases of emergency VHR enrolled in the American College of Surgeons National Surgical Quality Improvement Program in 2012 and 2013.
Disclosures: Dr. Pechman reported no financial disclosures.

