User login
Adverse events occur in LTC residents transitioning from hospital to nursing home
Background: Adverse events in the immediate posthospitalization period are a serious threat to patients 65 years and older who are residents of long-term care facilities. Changes during hospitalization – such as fasting for procedures, immobility, change in surroundings, disruption of sleep, and medication adjustments – can lead to adverse events such as falls, pressure ulcers, adverse drug reactions, and health care–acquired infections. However, the frequency and preventability of these adverse events has not been measured.
Study design: Prospective cohort study.
Setting: Nursing homes in the New England states.
Synopsis: This study sampled 762 hospital discharges for 555 long-term care residents of 32 nursing homes who were discharged from the hospital back to their same long-term care facility and followed for 45 days. A trained nurse reviewed records using a trigger tool developed by the Institute for Healthcare Improvement. Each trigger linked to a possible harm was reviewed by two physicians. Adverse events were categorized into health care–acquired infections and events related to resident care, medications, and procedures. The severity and preventability of each event was assessed.
Of the 555 residents, 65.5% were female and the mean age was 82.2. There were 379 adverse events identified; 52% involved pressure ulcers, skin tears, and falls with injury, which were deemed preventable. Healthcare-acquired infections totaled 28.5% and adverse drug events were 16.5%. Close to half of the events were serious, life threatening, or fatal. The study was limited by subjectivity in classifying the adverse events.
Hospitalists should ensure proper coordination and handoff when transitioning patients back to their nursing home.
Bottom line: Adverse events occur in 4 of 10 discharges from the hospital to long-term care facilities, and most events are preventable.
Citation: Kapoor A et al. Adverse events in long-term care residents transitioning from hospital back to nursing home. JAMA Intern Med. 2019 Jul 22;179(9):1254-61.
Dr. Ali is assistant professor of internal medicine and section chief of hospital medicine at St. Louis University School of Medicine.
Background: Adverse events in the immediate posthospitalization period are a serious threat to patients 65 years and older who are residents of long-term care facilities. Changes during hospitalization – such as fasting for procedures, immobility, change in surroundings, disruption of sleep, and medication adjustments – can lead to adverse events such as falls, pressure ulcers, adverse drug reactions, and health care–acquired infections. However, the frequency and preventability of these adverse events has not been measured.
Study design: Prospective cohort study.
Setting: Nursing homes in the New England states.
Synopsis: This study sampled 762 hospital discharges for 555 long-term care residents of 32 nursing homes who were discharged from the hospital back to their same long-term care facility and followed for 45 days. A trained nurse reviewed records using a trigger tool developed by the Institute for Healthcare Improvement. Each trigger linked to a possible harm was reviewed by two physicians. Adverse events were categorized into health care–acquired infections and events related to resident care, medications, and procedures. The severity and preventability of each event was assessed.
Of the 555 residents, 65.5% were female and the mean age was 82.2. There were 379 adverse events identified; 52% involved pressure ulcers, skin tears, and falls with injury, which were deemed preventable. Healthcare-acquired infections totaled 28.5% and adverse drug events were 16.5%. Close to half of the events were serious, life threatening, or fatal. The study was limited by subjectivity in classifying the adverse events.
Hospitalists should ensure proper coordination and handoff when transitioning patients back to their nursing home.
Bottom line: Adverse events occur in 4 of 10 discharges from the hospital to long-term care facilities, and most events are preventable.
Citation: Kapoor A et al. Adverse events in long-term care residents transitioning from hospital back to nursing home. JAMA Intern Med. 2019 Jul 22;179(9):1254-61.
Dr. Ali is assistant professor of internal medicine and section chief of hospital medicine at St. Louis University School of Medicine.
Background: Adverse events in the immediate posthospitalization period are a serious threat to patients 65 years and older who are residents of long-term care facilities. Changes during hospitalization – such as fasting for procedures, immobility, change in surroundings, disruption of sleep, and medication adjustments – can lead to adverse events such as falls, pressure ulcers, adverse drug reactions, and health care–acquired infections. However, the frequency and preventability of these adverse events has not been measured.
Study design: Prospective cohort study.
Setting: Nursing homes in the New England states.
Synopsis: This study sampled 762 hospital discharges for 555 long-term care residents of 32 nursing homes who were discharged from the hospital back to their same long-term care facility and followed for 45 days. A trained nurse reviewed records using a trigger tool developed by the Institute for Healthcare Improvement. Each trigger linked to a possible harm was reviewed by two physicians. Adverse events were categorized into health care–acquired infections and events related to resident care, medications, and procedures. The severity and preventability of each event was assessed.
Of the 555 residents, 65.5% were female and the mean age was 82.2. There were 379 adverse events identified; 52% involved pressure ulcers, skin tears, and falls with injury, which were deemed preventable. Healthcare-acquired infections totaled 28.5% and adverse drug events were 16.5%. Close to half of the events were serious, life threatening, or fatal. The study was limited by subjectivity in classifying the adverse events.
Hospitalists should ensure proper coordination and handoff when transitioning patients back to their nursing home.
Bottom line: Adverse events occur in 4 of 10 discharges from the hospital to long-term care facilities, and most events are preventable.
Citation: Kapoor A et al. Adverse events in long-term care residents transitioning from hospital back to nursing home. JAMA Intern Med. 2019 Jul 22;179(9):1254-61.
Dr. Ali is assistant professor of internal medicine and section chief of hospital medicine at St. Louis University School of Medicine.
Predicting patient risk of medication-related harm
A new tool is the first of its kind
“An increasing number of older adults are using multiple medicines, and it is important that the benefits are outweighing the risks,” said Nikesh Parekh, MBBS, MPH, lead author of a recent study of a new predictive tool. The study was done in the context of the World Health Organization campaign to halve the incidence of medication-related harm (MRH) by 2022 – reducing MRH following hospital discharge was identified as a priority area.
This works allows clinicians to calculate the risk of a patient suffering MRH post-discharge requiring health care, said Dr. Parekh, a research fellow at Brighton and Sussex Medical School in Great Britain. “This enables practitioners and policy makers to target interventions to reduce MRH at those with highest risk. This should support the delivery of cost-effective care. The knowledge of individual risk can also prompt clinicians to reconsider any high-risk medicines that they intend on prescribing at discharge.”
This is the first prediction tool to calculate individual patient risk of serious MRH post-discharge, he added.The high readmission rate for older adults is often an avoidable pressure for hospitalists, particularly where MRH is the underlying cause. “The prediction tool has the potential to significantly reduce this burden for hospitalists/patients by identifying those individuals at high risk upon discharge and ensuring that monitoring and additional support is provided to them in the community with their medications,” Dr. Parekh said.
This electronic tool could be integrated into the electronic discharge summaries so that the information can be shared with primary care clinicians in a straightforward way. “The risk score should be calculated automatically by a self-population of the tool’s fields from information that exists on the patient within the electronic discharge system.”The tool now needs to be externally validated through testing in new settings to assess its validity and reliability in new populations. “If the tool is found to be usable by hospitalists and demonstrates reasonable predictive accuracy, then it should be implemented widely to reduce the incidence of MRH,” Dr. Parekh said.
Reference
1. Parekh N, et al. Medication-related harm in older adults following hospital discharge: development and validation of a prediction tool. BMJ Qual Saf. Published Online First 2019 Sept 16. doi: 10.1136/bmjqs-2019-009587.
A new tool is the first of its kind
A new tool is the first of its kind
“An increasing number of older adults are using multiple medicines, and it is important that the benefits are outweighing the risks,” said Nikesh Parekh, MBBS, MPH, lead author of a recent study of a new predictive tool. The study was done in the context of the World Health Organization campaign to halve the incidence of medication-related harm (MRH) by 2022 – reducing MRH following hospital discharge was identified as a priority area.
This works allows clinicians to calculate the risk of a patient suffering MRH post-discharge requiring health care, said Dr. Parekh, a research fellow at Brighton and Sussex Medical School in Great Britain. “This enables practitioners and policy makers to target interventions to reduce MRH at those with highest risk. This should support the delivery of cost-effective care. The knowledge of individual risk can also prompt clinicians to reconsider any high-risk medicines that they intend on prescribing at discharge.”
This is the first prediction tool to calculate individual patient risk of serious MRH post-discharge, he added.The high readmission rate for older adults is often an avoidable pressure for hospitalists, particularly where MRH is the underlying cause. “The prediction tool has the potential to significantly reduce this burden for hospitalists/patients by identifying those individuals at high risk upon discharge and ensuring that monitoring and additional support is provided to them in the community with their medications,” Dr. Parekh said.
This electronic tool could be integrated into the electronic discharge summaries so that the information can be shared with primary care clinicians in a straightforward way. “The risk score should be calculated automatically by a self-population of the tool’s fields from information that exists on the patient within the electronic discharge system.”The tool now needs to be externally validated through testing in new settings to assess its validity and reliability in new populations. “If the tool is found to be usable by hospitalists and demonstrates reasonable predictive accuracy, then it should be implemented widely to reduce the incidence of MRH,” Dr. Parekh said.
Reference
1. Parekh N, et al. Medication-related harm in older adults following hospital discharge: development and validation of a prediction tool. BMJ Qual Saf. Published Online First 2019 Sept 16. doi: 10.1136/bmjqs-2019-009587.
“An increasing number of older adults are using multiple medicines, and it is important that the benefits are outweighing the risks,” said Nikesh Parekh, MBBS, MPH, lead author of a recent study of a new predictive tool. The study was done in the context of the World Health Organization campaign to halve the incidence of medication-related harm (MRH) by 2022 – reducing MRH following hospital discharge was identified as a priority area.
This works allows clinicians to calculate the risk of a patient suffering MRH post-discharge requiring health care, said Dr. Parekh, a research fellow at Brighton and Sussex Medical School in Great Britain. “This enables practitioners and policy makers to target interventions to reduce MRH at those with highest risk. This should support the delivery of cost-effective care. The knowledge of individual risk can also prompt clinicians to reconsider any high-risk medicines that they intend on prescribing at discharge.”
This is the first prediction tool to calculate individual patient risk of serious MRH post-discharge, he added.The high readmission rate for older adults is often an avoidable pressure for hospitalists, particularly where MRH is the underlying cause. “The prediction tool has the potential to significantly reduce this burden for hospitalists/patients by identifying those individuals at high risk upon discharge and ensuring that monitoring and additional support is provided to them in the community with their medications,” Dr. Parekh said.
This electronic tool could be integrated into the electronic discharge summaries so that the information can be shared with primary care clinicians in a straightforward way. “The risk score should be calculated automatically by a self-population of the tool’s fields from information that exists on the patient within the electronic discharge system.”The tool now needs to be externally validated through testing in new settings to assess its validity and reliability in new populations. “If the tool is found to be usable by hospitalists and demonstrates reasonable predictive accuracy, then it should be implemented widely to reduce the incidence of MRH,” Dr. Parekh said.
Reference
1. Parekh N, et al. Medication-related harm in older adults following hospital discharge: development and validation of a prediction tool. BMJ Qual Saf. Published Online First 2019 Sept 16. doi: 10.1136/bmjqs-2019-009587.
Monthly needlestick rates suggest a steep learning curve
The rate of injuries with needles and other sharp instruments among hospital staff jumped sharply in July, which suggests the need for safety instruction early in the academic year, researchers say.
“The reason this is important is it gives us an idea of when the best time to intervene might be,” said Jonathan Zampella, MD, an assistant professor of dermatology at New York University.
The findings were published online Nov. 4 in a research letter in JAMA Surgery.
Hundreds of thousands of health care workers incur injuries with needles and other sharp instruments every year, which places them at risk for blood-borne infections.
“Especially amongst dermatologists, it’s not a question of if you get stuck, it’s a question of when,” Dr. Zampella said in an interview. “Most have been stuck at some point in their lives.”
Until now, studies of these injuries have mostly depended on surveys, he said. By contrast, for the current study, Dr. Zampella and colleagues used a dataset of injuries reported to NYU Langone Health’s Occupational Health Services.
They identified 5,395 such injuries that occurred between January 2000 and February 2020. The total number was similar among surgical and nonsurgical specialists, but the mean incident rate was 4.7 for every 10 people among the nonsurgical staff versus 9.4 for every 10 people in the surgical staff.
Dr. Zampella and colleagues further found that the highest rate of injury, at 16.0 incidents for every 10 people, occurred among urology house staff, followed by orthopedic surgery staff, with 14.1, and general surgery staff, with 14.0. The lowest staff rates were among psychiatrists (0.3), radiation oncologists (1.1), and neurologists (2.4).
But even some nonsurgical specialties had high rates. For example, the rate was 11.5 for pathology house staff and 11.3 for dermatology house staff.
Dr. Zampella said his first reaction to the data was, “What the heck? What are pathologists doing that they are getting needlestick injuries?
“But it makes sense,” he said. “Sometimes they do biopsies, and they do fine-needle aspirations – these kinds of things that we might not be paying as much attention to as we should.”
The finding suggests that nonsurgical specialists should receive more training in injury prevention, he said.
The training should be in person, and it should not just be for first-year residents. “Everybody needs to have refreshers on preventing needlesticks,” he said. “And we have to make sure everyone in the hospital is playing for the same team. Residents are learning, and if they see poor technique by one of their attendings, that’s something they may imitate.”
The study’s primary conclusion regards the importance of seasonality in needlestick and other injuries from sharp instruments.
Among house staff, 9.4% of the injuries occurred in July. The proportion then gradually rose to 10.5% in October before gradually going back down to a low of 6.2% in June.
The difference from one quarter to the next was statistically significant (P = .02).
July is when internships and residencies start, Dr. Zampella pointed out. Among the nonhouse staff, the rate was consistent throughout the year.
This suggests that the beginning of the academic year for trainees was the key factor driving the uptick in injuries, he said.
He said that residents are receiving instruction in injury prevention, but perhaps not at the right time of year. For example, dermatology residents at NYU are given a lecture in needlestick injury prevention in February.
Dr. Zampella has received personal fees from X4 pharmaceuticals. The other authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The rate of injuries with needles and other sharp instruments among hospital staff jumped sharply in July, which suggests the need for safety instruction early in the academic year, researchers say.
“The reason this is important is it gives us an idea of when the best time to intervene might be,” said Jonathan Zampella, MD, an assistant professor of dermatology at New York University.
The findings were published online Nov. 4 in a research letter in JAMA Surgery.
Hundreds of thousands of health care workers incur injuries with needles and other sharp instruments every year, which places them at risk for blood-borne infections.
“Especially amongst dermatologists, it’s not a question of if you get stuck, it’s a question of when,” Dr. Zampella said in an interview. “Most have been stuck at some point in their lives.”
Until now, studies of these injuries have mostly depended on surveys, he said. By contrast, for the current study, Dr. Zampella and colleagues used a dataset of injuries reported to NYU Langone Health’s Occupational Health Services.
They identified 5,395 such injuries that occurred between January 2000 and February 2020. The total number was similar among surgical and nonsurgical specialists, but the mean incident rate was 4.7 for every 10 people among the nonsurgical staff versus 9.4 for every 10 people in the surgical staff.
Dr. Zampella and colleagues further found that the highest rate of injury, at 16.0 incidents for every 10 people, occurred among urology house staff, followed by orthopedic surgery staff, with 14.1, and general surgery staff, with 14.0. The lowest staff rates were among psychiatrists (0.3), radiation oncologists (1.1), and neurologists (2.4).
But even some nonsurgical specialties had high rates. For example, the rate was 11.5 for pathology house staff and 11.3 for dermatology house staff.
Dr. Zampella said his first reaction to the data was, “What the heck? What are pathologists doing that they are getting needlestick injuries?
“But it makes sense,” he said. “Sometimes they do biopsies, and they do fine-needle aspirations – these kinds of things that we might not be paying as much attention to as we should.”
The finding suggests that nonsurgical specialists should receive more training in injury prevention, he said.
The training should be in person, and it should not just be for first-year residents. “Everybody needs to have refreshers on preventing needlesticks,” he said. “And we have to make sure everyone in the hospital is playing for the same team. Residents are learning, and if they see poor technique by one of their attendings, that’s something they may imitate.”
The study’s primary conclusion regards the importance of seasonality in needlestick and other injuries from sharp instruments.
Among house staff, 9.4% of the injuries occurred in July. The proportion then gradually rose to 10.5% in October before gradually going back down to a low of 6.2% in June.
The difference from one quarter to the next was statistically significant (P = .02).
July is when internships and residencies start, Dr. Zampella pointed out. Among the nonhouse staff, the rate was consistent throughout the year.
This suggests that the beginning of the academic year for trainees was the key factor driving the uptick in injuries, he said.
He said that residents are receiving instruction in injury prevention, but perhaps not at the right time of year. For example, dermatology residents at NYU are given a lecture in needlestick injury prevention in February.
Dr. Zampella has received personal fees from X4 pharmaceuticals. The other authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The rate of injuries with needles and other sharp instruments among hospital staff jumped sharply in July, which suggests the need for safety instruction early in the academic year, researchers say.
“The reason this is important is it gives us an idea of when the best time to intervene might be,” said Jonathan Zampella, MD, an assistant professor of dermatology at New York University.
The findings were published online Nov. 4 in a research letter in JAMA Surgery.
Hundreds of thousands of health care workers incur injuries with needles and other sharp instruments every year, which places them at risk for blood-borne infections.
“Especially amongst dermatologists, it’s not a question of if you get stuck, it’s a question of when,” Dr. Zampella said in an interview. “Most have been stuck at some point in their lives.”
Until now, studies of these injuries have mostly depended on surveys, he said. By contrast, for the current study, Dr. Zampella and colleagues used a dataset of injuries reported to NYU Langone Health’s Occupational Health Services.
They identified 5,395 such injuries that occurred between January 2000 and February 2020. The total number was similar among surgical and nonsurgical specialists, but the mean incident rate was 4.7 for every 10 people among the nonsurgical staff versus 9.4 for every 10 people in the surgical staff.
Dr. Zampella and colleagues further found that the highest rate of injury, at 16.0 incidents for every 10 people, occurred among urology house staff, followed by orthopedic surgery staff, with 14.1, and general surgery staff, with 14.0. The lowest staff rates were among psychiatrists (0.3), radiation oncologists (1.1), and neurologists (2.4).
But even some nonsurgical specialties had high rates. For example, the rate was 11.5 for pathology house staff and 11.3 for dermatology house staff.
Dr. Zampella said his first reaction to the data was, “What the heck? What are pathologists doing that they are getting needlestick injuries?
“But it makes sense,” he said. “Sometimes they do biopsies, and they do fine-needle aspirations – these kinds of things that we might not be paying as much attention to as we should.”
The finding suggests that nonsurgical specialists should receive more training in injury prevention, he said.
The training should be in person, and it should not just be for first-year residents. “Everybody needs to have refreshers on preventing needlesticks,” he said. “And we have to make sure everyone in the hospital is playing for the same team. Residents are learning, and if they see poor technique by one of their attendings, that’s something they may imitate.”
The study’s primary conclusion regards the importance of seasonality in needlestick and other injuries from sharp instruments.
Among house staff, 9.4% of the injuries occurred in July. The proportion then gradually rose to 10.5% in October before gradually going back down to a low of 6.2% in June.
The difference from one quarter to the next was statistically significant (P = .02).
July is when internships and residencies start, Dr. Zampella pointed out. Among the nonhouse staff, the rate was consistent throughout the year.
This suggests that the beginning of the academic year for trainees was the key factor driving the uptick in injuries, he said.
He said that residents are receiving instruction in injury prevention, but perhaps not at the right time of year. For example, dermatology residents at NYU are given a lecture in needlestick injury prevention in February.
Dr. Zampella has received personal fees from X4 pharmaceuticals. The other authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
AMA discharge linked to increased readmissions, discontinuity of care
Background: AMA discharges are common (1%-2% of all U.S. discharges) and disproportionately affect vulnerable patient populations, specifically those of lower socioeconomic status and the uninsured. Previous studies have been insufficiently powered to assess the effects of AMA discharge on 30-day readmission rates at a national level.
Study design: Retrospective cohort.
Setting: Community and teaching hospitals in 22 states.
Synopsis: With use of the 2014 Nationwide Readmissions Database of 23,110,641 index hospitalizations of patients 18 years or older, this study found that AMA discharge occurred with 1.3% of admissions. AMA discharge was associated with greater than twice the odds of 30-day readmission, compared with routine discharge. Of patients discharged AMA, 20.2% had an unplanned readmission within 30 days, compared with 10.1% of patients discharged routinely (OR, 2.25; 95% CI, 2.20-2.30; P less than .001).
Patients who were discharged AMA had almost 20 times the odds of undergoing repeat AMA discharge at readmission (OR, 18.41; 95% CI, 17.46-19.41; P less than .001) and twice the odds of presenting to a different hospital (OR, 2.35; 95% CI, 2.22-2.49; P less than .001). The study did not capture readmissions in a different state than that of the index hospital and was limited to the 22 states participating in the 2014 Readmissions Database.
Bottom line: Discharge AMA is associated with significantly higher odds of 30-day readmission, subsequent AMA discharge and presentation to another hospital, compared with routine discharge.
Citation: Kumar N. Burden of 30-day readmissions associated with discharge against medical advice among inpatients in the United States. Am J Med. 2019 Jun;132(6):708-17.
Dr. Webber is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: AMA discharges are common (1%-2% of all U.S. discharges) and disproportionately affect vulnerable patient populations, specifically those of lower socioeconomic status and the uninsured. Previous studies have been insufficiently powered to assess the effects of AMA discharge on 30-day readmission rates at a national level.
Study design: Retrospective cohort.
Setting: Community and teaching hospitals in 22 states.
Synopsis: With use of the 2014 Nationwide Readmissions Database of 23,110,641 index hospitalizations of patients 18 years or older, this study found that AMA discharge occurred with 1.3% of admissions. AMA discharge was associated with greater than twice the odds of 30-day readmission, compared with routine discharge. Of patients discharged AMA, 20.2% had an unplanned readmission within 30 days, compared with 10.1% of patients discharged routinely (OR, 2.25; 95% CI, 2.20-2.30; P less than .001).
Patients who were discharged AMA had almost 20 times the odds of undergoing repeat AMA discharge at readmission (OR, 18.41; 95% CI, 17.46-19.41; P less than .001) and twice the odds of presenting to a different hospital (OR, 2.35; 95% CI, 2.22-2.49; P less than .001). The study did not capture readmissions in a different state than that of the index hospital and was limited to the 22 states participating in the 2014 Readmissions Database.
Bottom line: Discharge AMA is associated with significantly higher odds of 30-day readmission, subsequent AMA discharge and presentation to another hospital, compared with routine discharge.
Citation: Kumar N. Burden of 30-day readmissions associated with discharge against medical advice among inpatients in the United States. Am J Med. 2019 Jun;132(6):708-17.
Dr. Webber is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: AMA discharges are common (1%-2% of all U.S. discharges) and disproportionately affect vulnerable patient populations, specifically those of lower socioeconomic status and the uninsured. Previous studies have been insufficiently powered to assess the effects of AMA discharge on 30-day readmission rates at a national level.
Study design: Retrospective cohort.
Setting: Community and teaching hospitals in 22 states.
Synopsis: With use of the 2014 Nationwide Readmissions Database of 23,110,641 index hospitalizations of patients 18 years or older, this study found that AMA discharge occurred with 1.3% of admissions. AMA discharge was associated with greater than twice the odds of 30-day readmission, compared with routine discharge. Of patients discharged AMA, 20.2% had an unplanned readmission within 30 days, compared with 10.1% of patients discharged routinely (OR, 2.25; 95% CI, 2.20-2.30; P less than .001).
Patients who were discharged AMA had almost 20 times the odds of undergoing repeat AMA discharge at readmission (OR, 18.41; 95% CI, 17.46-19.41; P less than .001) and twice the odds of presenting to a different hospital (OR, 2.35; 95% CI, 2.22-2.49; P less than .001). The study did not capture readmissions in a different state than that of the index hospital and was limited to the 22 states participating in the 2014 Readmissions Database.
Bottom line: Discharge AMA is associated with significantly higher odds of 30-day readmission, subsequent AMA discharge and presentation to another hospital, compared with routine discharge.
Citation: Kumar N. Burden of 30-day readmissions associated with discharge against medical advice among inpatients in the United States. Am J Med. 2019 Jun;132(6):708-17.
Dr. Webber is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Hospitalists are natural leaders in the COVID-19 battle
Christopher Pribula, MD, a hospitalist at Sanford Broadway Medical Center in Fargo, N.D., didn’t anticipate becoming his hospital’s resident expert on COVID-19. Having just returned from vacation in March, he agreed to cover for a colleague on what would become the special care unit. “When our hospital medicine group decided that it would be the COVID unit, I just ran with it,” he said. Dr. Pribula spent the next 18 days doing 8- to 14-hour shifts and learning as much as he could as the hospital – and the nation – wrestled with the pandemic.
“Because I was the first hospitalist, along with our infectious disease specialist, Dr. Avish Nagpal, to really engage with the virus, people came to me with their questions,” Dr. Pribula said. Working to establish protocols for the care of COVID-19 patients involved a lot of planning, from nursing protocols to discharge planning.
Dr. Pribula was part of the hospital’s incident command structure, thought about how the system could scale up for a potential surge, and worked with the North Dakota Medical Association to reach out to outlying medical centers on safety and infection control. He even drew on his prior work experience as a medical technologist doing negative-pressure containment in a cell-processing facility to help create the hospital’s negative-pressure unit in an old ICU.
“We did a lot of communication from the start. To a certain extent we were making it up as we went along, but we sat down and huddled as a team every day at 9 and 4,” he explained. “We started out with observation and retrospective research, and learned piece by piece. But that’s how science works.”
Hospitalists across the country have played leading roles in their hospitals’ and health systems’ response to the pandemic, and not just because they are on the front lines providing patient care. Their job as doctors who work full-time in the hospital makes them natural leaders in improving clinical quality and hospital administrative protocols as well as studying the latest information and educating their colleagues. Responding to the pandemic has required lots of planning, careful attention to schedules and assignments and staff stress, and working with other departments in the hospital and groups in the community, including public health authorities.
Where is hospital treatment for COVID-19 at today?
As knowledge has grown, Dr. Pribula said, COVID-19 treatment in the hospital has come to incorporate remdesivir, a broad-spectrum antiviral; dexamethasone, a common steroid medication; and convalescent plasma, blood products from people who have recovered from the illness. “We went from no steroids to giving steroids. We went from putting patients on ventilators to avoid acute respiratory distress syndrome (ARDS) initially to now working to avoid intubation at all costs,” he said.
“What we found is that we need to pressure-support these patients. We do proning and CPAP while we let the lungs heal. By the time they arrive at the hospital, more often than not they’re on the backside of the viral load. But now we’re dealing with the body’s inflammatory response.”
Navneet Attri, MD, a hospitalist at Sutter Santa Rosa Regional Hospital in Santa Rosa, Calif., 50 miles north of San Francisco, experienced fears and uncertainties working at a hospital that treated early COVID patients from the Grand Princess cruise ship. Early on, she wrote a post describing her experience for The Hospitalist Leader, the Society of Hospital Medicine’s blog page.
Dr. Attri said she has gone through the gamut of emotions while caring for COVID-19 patients, addressing their fears and trying to support family members who aren’t allowed to enter the hospital to be at their loved one’s side. Sometimes, patient after patient with COVID-19 becomes almost too much. But seeing a lot of them in the intervening 6 months has increased her confidence level.
Understanding of how the disease is spread has continued to evolve, with a recent return to focusing on airborne transmission, she said. Frontline workers need N95 masks and eye shields, even if all of that PPE feels like a burden. Dr. Attri said she hardly notices the PPE anymore. “Putting it on is just a habit.”
She sits on Sonoma County’s COVID-19 surge planning group, which has representatives from the three local hospitals, the public health department, and other community agencies. “I report back to my hospitalist group about the situation in the community. Because our facilities were well prepared, our hospitals have not been overwhelmed,” she said.
The importance of teamwork
Sunil Shah, MD, a hospitalist with Northwell Health’s Southside Hospital in Bay Shore, N.Y., is part of the massive hospital medicine team, including reassigned specialists and volunteers from across the country, deployed at Northwell hospitals in Greater New York City and Long Island during the COVID-19 surge. Northwell probably has cared for more COVID-19 patients than any other health system in the country, and at the height of the surge the intensity of hospital care was like nothing he’s ever seen. But he also expressed gratitude that doctors from other parts of the country were willing to come and help out.
Southside Hospital went almost overnight from a 200-bed acute facility to a full, 350-bed, regional COVID-19–only hospital. “On busy days, our entire hospital was like a floating ICU,” he said. “You’d hear ‘rapid response’ or ‘code blue’ over the intercom every few seconds. Normally we’d have a designated rapid response person for the day, but with COVID, everybody stepped in to help – whoever was closest,” he said.
Majid Sheikh, MD, a hospitalist at Emory University Hospital in Atlanta, also became a go-to COVID-19 expert for his group. “I didn’t specifically volunteer, but my partner and I had the first cases, and the leadership group was happy to have us there,” he explained.
“One interesting thing I learned was the concept of the ‘happy’ hypoxemic patient, who is having a significant drop in oxygen saturation without developing any obvious signs of respiratory distress,” he said. “We’d be checking the accuracy of the reading and trying to figure out if it was real.” Emory was also one of the leaders in studying anticoagulant treatments for COVID-19 patients.
“Six months later I would say we’re definitely getting better outcomes on the floor, and our COVID patients aren’t landing in the ICU as easily,” Dr. Sheikh said. “It was scary at first, and doubly scary when doctors sometimes don’t feel they can say, ‘Hey, I’m scared too,’ or ‘By the way, I really don’t know what I’m doing.’ So, we’d be trying to reassure the patients when the information was coming to us in fragments.”
But he also believes that the pandemic has afforded hospitalists the opportunity to be the clinical detectives they were trained to be, sifting through clues. “I had to think more and really pay attention clinically in a much different way. You could say it was exciting and scary at the same time,” he said.
A human fix in the hospital
Dr. Pribula agreed that the pandemic has been both a difficult experience and a rewarding one. “I think of the people I first admitted. If they had shown up even a month later, would they still be with us?” He believes that his group and his field are going to get to a place where they have solid treatment plans for how to provide optimal care and how to protect providers from exposure.
One of the first COVID-19 patients in Fargo had dementia and was very distressed. “She had no idea why nobody was visiting or why we wouldn’t let her out of her room,” Dr. Pribula said. “Instead of reaching for sedatives, one of our nurses went into the room and talked with her, prayed a rosary, and played two hands of cards with her and didn’t have to sedate her. That’s what people need when they’re alone and scared. It wasn’t a medical fix but a human fix.”
A version of this article originally appeared on Medscape.com.
Christopher Pribula, MD, a hospitalist at Sanford Broadway Medical Center in Fargo, N.D., didn’t anticipate becoming his hospital’s resident expert on COVID-19. Having just returned from vacation in March, he agreed to cover for a colleague on what would become the special care unit. “When our hospital medicine group decided that it would be the COVID unit, I just ran with it,” he said. Dr. Pribula spent the next 18 days doing 8- to 14-hour shifts and learning as much as he could as the hospital – and the nation – wrestled with the pandemic.
“Because I was the first hospitalist, along with our infectious disease specialist, Dr. Avish Nagpal, to really engage with the virus, people came to me with their questions,” Dr. Pribula said. Working to establish protocols for the care of COVID-19 patients involved a lot of planning, from nursing protocols to discharge planning.
Dr. Pribula was part of the hospital’s incident command structure, thought about how the system could scale up for a potential surge, and worked with the North Dakota Medical Association to reach out to outlying medical centers on safety and infection control. He even drew on his prior work experience as a medical technologist doing negative-pressure containment in a cell-processing facility to help create the hospital’s negative-pressure unit in an old ICU.
“We did a lot of communication from the start. To a certain extent we were making it up as we went along, but we sat down and huddled as a team every day at 9 and 4,” he explained. “We started out with observation and retrospective research, and learned piece by piece. But that’s how science works.”
Hospitalists across the country have played leading roles in their hospitals’ and health systems’ response to the pandemic, and not just because they are on the front lines providing patient care. Their job as doctors who work full-time in the hospital makes them natural leaders in improving clinical quality and hospital administrative protocols as well as studying the latest information and educating their colleagues. Responding to the pandemic has required lots of planning, careful attention to schedules and assignments and staff stress, and working with other departments in the hospital and groups in the community, including public health authorities.
Where is hospital treatment for COVID-19 at today?
As knowledge has grown, Dr. Pribula said, COVID-19 treatment in the hospital has come to incorporate remdesivir, a broad-spectrum antiviral; dexamethasone, a common steroid medication; and convalescent plasma, blood products from people who have recovered from the illness. “We went from no steroids to giving steroids. We went from putting patients on ventilators to avoid acute respiratory distress syndrome (ARDS) initially to now working to avoid intubation at all costs,” he said.
“What we found is that we need to pressure-support these patients. We do proning and CPAP while we let the lungs heal. By the time they arrive at the hospital, more often than not they’re on the backside of the viral load. But now we’re dealing with the body’s inflammatory response.”
Navneet Attri, MD, a hospitalist at Sutter Santa Rosa Regional Hospital in Santa Rosa, Calif., 50 miles north of San Francisco, experienced fears and uncertainties working at a hospital that treated early COVID patients from the Grand Princess cruise ship. Early on, she wrote a post describing her experience for The Hospitalist Leader, the Society of Hospital Medicine’s blog page.
Dr. Attri said she has gone through the gamut of emotions while caring for COVID-19 patients, addressing their fears and trying to support family members who aren’t allowed to enter the hospital to be at their loved one’s side. Sometimes, patient after patient with COVID-19 becomes almost too much. But seeing a lot of them in the intervening 6 months has increased her confidence level.
Understanding of how the disease is spread has continued to evolve, with a recent return to focusing on airborne transmission, she said. Frontline workers need N95 masks and eye shields, even if all of that PPE feels like a burden. Dr. Attri said she hardly notices the PPE anymore. “Putting it on is just a habit.”
She sits on Sonoma County’s COVID-19 surge planning group, which has representatives from the three local hospitals, the public health department, and other community agencies. “I report back to my hospitalist group about the situation in the community. Because our facilities were well prepared, our hospitals have not been overwhelmed,” she said.
The importance of teamwork
Sunil Shah, MD, a hospitalist with Northwell Health’s Southside Hospital in Bay Shore, N.Y., is part of the massive hospital medicine team, including reassigned specialists and volunteers from across the country, deployed at Northwell hospitals in Greater New York City and Long Island during the COVID-19 surge. Northwell probably has cared for more COVID-19 patients than any other health system in the country, and at the height of the surge the intensity of hospital care was like nothing he’s ever seen. But he also expressed gratitude that doctors from other parts of the country were willing to come and help out.
Southside Hospital went almost overnight from a 200-bed acute facility to a full, 350-bed, regional COVID-19–only hospital. “On busy days, our entire hospital was like a floating ICU,” he said. “You’d hear ‘rapid response’ or ‘code blue’ over the intercom every few seconds. Normally we’d have a designated rapid response person for the day, but with COVID, everybody stepped in to help – whoever was closest,” he said.
Majid Sheikh, MD, a hospitalist at Emory University Hospital in Atlanta, also became a go-to COVID-19 expert for his group. “I didn’t specifically volunteer, but my partner and I had the first cases, and the leadership group was happy to have us there,” he explained.
“One interesting thing I learned was the concept of the ‘happy’ hypoxemic patient, who is having a significant drop in oxygen saturation without developing any obvious signs of respiratory distress,” he said. “We’d be checking the accuracy of the reading and trying to figure out if it was real.” Emory was also one of the leaders in studying anticoagulant treatments for COVID-19 patients.
“Six months later I would say we’re definitely getting better outcomes on the floor, and our COVID patients aren’t landing in the ICU as easily,” Dr. Sheikh said. “It was scary at first, and doubly scary when doctors sometimes don’t feel they can say, ‘Hey, I’m scared too,’ or ‘By the way, I really don’t know what I’m doing.’ So, we’d be trying to reassure the patients when the information was coming to us in fragments.”
But he also believes that the pandemic has afforded hospitalists the opportunity to be the clinical detectives they were trained to be, sifting through clues. “I had to think more and really pay attention clinically in a much different way. You could say it was exciting and scary at the same time,” he said.
A human fix in the hospital
Dr. Pribula agreed that the pandemic has been both a difficult experience and a rewarding one. “I think of the people I first admitted. If they had shown up even a month later, would they still be with us?” He believes that his group and his field are going to get to a place where they have solid treatment plans for how to provide optimal care and how to protect providers from exposure.
One of the first COVID-19 patients in Fargo had dementia and was very distressed. “She had no idea why nobody was visiting or why we wouldn’t let her out of her room,” Dr. Pribula said. “Instead of reaching for sedatives, one of our nurses went into the room and talked with her, prayed a rosary, and played two hands of cards with her and didn’t have to sedate her. That’s what people need when they’re alone and scared. It wasn’t a medical fix but a human fix.”
A version of this article originally appeared on Medscape.com.
Christopher Pribula, MD, a hospitalist at Sanford Broadway Medical Center in Fargo, N.D., didn’t anticipate becoming his hospital’s resident expert on COVID-19. Having just returned from vacation in March, he agreed to cover for a colleague on what would become the special care unit. “When our hospital medicine group decided that it would be the COVID unit, I just ran with it,” he said. Dr. Pribula spent the next 18 days doing 8- to 14-hour shifts and learning as much as he could as the hospital – and the nation – wrestled with the pandemic.
“Because I was the first hospitalist, along with our infectious disease specialist, Dr. Avish Nagpal, to really engage with the virus, people came to me with their questions,” Dr. Pribula said. Working to establish protocols for the care of COVID-19 patients involved a lot of planning, from nursing protocols to discharge planning.
Dr. Pribula was part of the hospital’s incident command structure, thought about how the system could scale up for a potential surge, and worked with the North Dakota Medical Association to reach out to outlying medical centers on safety and infection control. He even drew on his prior work experience as a medical technologist doing negative-pressure containment in a cell-processing facility to help create the hospital’s negative-pressure unit in an old ICU.
“We did a lot of communication from the start. To a certain extent we were making it up as we went along, but we sat down and huddled as a team every day at 9 and 4,” he explained. “We started out with observation and retrospective research, and learned piece by piece. But that’s how science works.”
Hospitalists across the country have played leading roles in their hospitals’ and health systems’ response to the pandemic, and not just because they are on the front lines providing patient care. Their job as doctors who work full-time in the hospital makes them natural leaders in improving clinical quality and hospital administrative protocols as well as studying the latest information and educating their colleagues. Responding to the pandemic has required lots of planning, careful attention to schedules and assignments and staff stress, and working with other departments in the hospital and groups in the community, including public health authorities.
Where is hospital treatment for COVID-19 at today?
As knowledge has grown, Dr. Pribula said, COVID-19 treatment in the hospital has come to incorporate remdesivir, a broad-spectrum antiviral; dexamethasone, a common steroid medication; and convalescent plasma, blood products from people who have recovered from the illness. “We went from no steroids to giving steroids. We went from putting patients on ventilators to avoid acute respiratory distress syndrome (ARDS) initially to now working to avoid intubation at all costs,” he said.
“What we found is that we need to pressure-support these patients. We do proning and CPAP while we let the lungs heal. By the time they arrive at the hospital, more often than not they’re on the backside of the viral load. But now we’re dealing with the body’s inflammatory response.”
Navneet Attri, MD, a hospitalist at Sutter Santa Rosa Regional Hospital in Santa Rosa, Calif., 50 miles north of San Francisco, experienced fears and uncertainties working at a hospital that treated early COVID patients from the Grand Princess cruise ship. Early on, she wrote a post describing her experience for The Hospitalist Leader, the Society of Hospital Medicine’s blog page.
Dr. Attri said she has gone through the gamut of emotions while caring for COVID-19 patients, addressing their fears and trying to support family members who aren’t allowed to enter the hospital to be at their loved one’s side. Sometimes, patient after patient with COVID-19 becomes almost too much. But seeing a lot of them in the intervening 6 months has increased her confidence level.
Understanding of how the disease is spread has continued to evolve, with a recent return to focusing on airborne transmission, she said. Frontline workers need N95 masks and eye shields, even if all of that PPE feels like a burden. Dr. Attri said she hardly notices the PPE anymore. “Putting it on is just a habit.”
She sits on Sonoma County’s COVID-19 surge planning group, which has representatives from the three local hospitals, the public health department, and other community agencies. “I report back to my hospitalist group about the situation in the community. Because our facilities were well prepared, our hospitals have not been overwhelmed,” she said.
The importance of teamwork
Sunil Shah, MD, a hospitalist with Northwell Health’s Southside Hospital in Bay Shore, N.Y., is part of the massive hospital medicine team, including reassigned specialists and volunteers from across the country, deployed at Northwell hospitals in Greater New York City and Long Island during the COVID-19 surge. Northwell probably has cared for more COVID-19 patients than any other health system in the country, and at the height of the surge the intensity of hospital care was like nothing he’s ever seen. But he also expressed gratitude that doctors from other parts of the country were willing to come and help out.
Southside Hospital went almost overnight from a 200-bed acute facility to a full, 350-bed, regional COVID-19–only hospital. “On busy days, our entire hospital was like a floating ICU,” he said. “You’d hear ‘rapid response’ or ‘code blue’ over the intercom every few seconds. Normally we’d have a designated rapid response person for the day, but with COVID, everybody stepped in to help – whoever was closest,” he said.
Majid Sheikh, MD, a hospitalist at Emory University Hospital in Atlanta, also became a go-to COVID-19 expert for his group. “I didn’t specifically volunteer, but my partner and I had the first cases, and the leadership group was happy to have us there,” he explained.
“One interesting thing I learned was the concept of the ‘happy’ hypoxemic patient, who is having a significant drop in oxygen saturation without developing any obvious signs of respiratory distress,” he said. “We’d be checking the accuracy of the reading and trying to figure out if it was real.” Emory was also one of the leaders in studying anticoagulant treatments for COVID-19 patients.
“Six months later I would say we’re definitely getting better outcomes on the floor, and our COVID patients aren’t landing in the ICU as easily,” Dr. Sheikh said. “It was scary at first, and doubly scary when doctors sometimes don’t feel they can say, ‘Hey, I’m scared too,’ or ‘By the way, I really don’t know what I’m doing.’ So, we’d be trying to reassure the patients when the information was coming to us in fragments.”
But he also believes that the pandemic has afforded hospitalists the opportunity to be the clinical detectives they were trained to be, sifting through clues. “I had to think more and really pay attention clinically in a much different way. You could say it was exciting and scary at the same time,” he said.
A human fix in the hospital
Dr. Pribula agreed that the pandemic has been both a difficult experience and a rewarding one. “I think of the people I first admitted. If they had shown up even a month later, would they still be with us?” He believes that his group and his field are going to get to a place where they have solid treatment plans for how to provide optimal care and how to protect providers from exposure.
One of the first COVID-19 patients in Fargo had dementia and was very distressed. “She had no idea why nobody was visiting or why we wouldn’t let her out of her room,” Dr. Pribula said. “Instead of reaching for sedatives, one of our nurses went into the room and talked with her, prayed a rosary, and played two hands of cards with her and didn’t have to sedate her. That’s what people need when they’re alone and scared. It wasn’t a medical fix but a human fix.”
A version of this article originally appeared on Medscape.com.
PICC lines often used inappropriately in advanced CKD patients
Background: PICC insertion is associated with risk for venous thrombosis and stenosis. National guidelines recommend avoiding PICC lines in patients with CKD stage 3b (glomerular filtration rate less than 45 mL/min per 1.73 m2) in order to preserve venous integrity for future creation of arteriovenous fistula, which is the ideal vascular access for hemodialysis.
Study design: Prospective cohort.
Setting: 52 hospitals in Michigan.
Synopsis: Data obtained from inpatients within the Michigan Hospital Medicine Safety Consortium between 2013 and 2016 showed that, of 20,545 total PICCs placed, 23% were placed in patients with a glomerular filtration rate less than 45 mL/min per 1.73 m2, and 3.2% were placed in those receiving dialysis. PICC placement in advanced CKD was more common in the ICU than in the ward setting, and placement more frequently utilized multilumen instead of single-lumen catheters. PICC-related complications were not more common in advanced CKD but were more often seen in the ICU and with multilumen PICCs. About one-quarter of PICCs were used for durations of less than 5 days.
The study is limited by lack of data in a subset of patients who had no documented GFR (2.7%) or missing covariate data (2.7%). The inability to ascertain other clinical information, such as nephrology approval of PICC, functional AV fistula or other hemodialysis access, or PICC complications after discharge further limit the findings.
Hospitalists should first decide if a PICC line is truly indicated, and if so, carefully weigh the risks and benefits of PICC placement in patients with advanced CKD.
Bottom line: PICC placement is common and often inappropriate in hospitalized patients with advanced CKD.
Citation: Paje D et al. Use of peripherally inserted central catheters in patients with advanced chronic kidney disease A prospective cohort study. Ann Intern Med. 2019 Jun 4;171:10-8.
Dr. Hageman is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: PICC insertion is associated with risk for venous thrombosis and stenosis. National guidelines recommend avoiding PICC lines in patients with CKD stage 3b (glomerular filtration rate less than 45 mL/min per 1.73 m2) in order to preserve venous integrity for future creation of arteriovenous fistula, which is the ideal vascular access for hemodialysis.
Study design: Prospective cohort.
Setting: 52 hospitals in Michigan.
Synopsis: Data obtained from inpatients within the Michigan Hospital Medicine Safety Consortium between 2013 and 2016 showed that, of 20,545 total PICCs placed, 23% were placed in patients with a glomerular filtration rate less than 45 mL/min per 1.73 m2, and 3.2% were placed in those receiving dialysis. PICC placement in advanced CKD was more common in the ICU than in the ward setting, and placement more frequently utilized multilumen instead of single-lumen catheters. PICC-related complications were not more common in advanced CKD but were more often seen in the ICU and with multilumen PICCs. About one-quarter of PICCs were used for durations of less than 5 days.
The study is limited by lack of data in a subset of patients who had no documented GFR (2.7%) or missing covariate data (2.7%). The inability to ascertain other clinical information, such as nephrology approval of PICC, functional AV fistula or other hemodialysis access, or PICC complications after discharge further limit the findings.
Hospitalists should first decide if a PICC line is truly indicated, and if so, carefully weigh the risks and benefits of PICC placement in patients with advanced CKD.
Bottom line: PICC placement is common and often inappropriate in hospitalized patients with advanced CKD.
Citation: Paje D et al. Use of peripherally inserted central catheters in patients with advanced chronic kidney disease A prospective cohort study. Ann Intern Med. 2019 Jun 4;171:10-8.
Dr. Hageman is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: PICC insertion is associated with risk for venous thrombosis and stenosis. National guidelines recommend avoiding PICC lines in patients with CKD stage 3b (glomerular filtration rate less than 45 mL/min per 1.73 m2) in order to preserve venous integrity for future creation of arteriovenous fistula, which is the ideal vascular access for hemodialysis.
Study design: Prospective cohort.
Setting: 52 hospitals in Michigan.
Synopsis: Data obtained from inpatients within the Michigan Hospital Medicine Safety Consortium between 2013 and 2016 showed that, of 20,545 total PICCs placed, 23% were placed in patients with a glomerular filtration rate less than 45 mL/min per 1.73 m2, and 3.2% were placed in those receiving dialysis. PICC placement in advanced CKD was more common in the ICU than in the ward setting, and placement more frequently utilized multilumen instead of single-lumen catheters. PICC-related complications were not more common in advanced CKD but were more often seen in the ICU and with multilumen PICCs. About one-quarter of PICCs were used for durations of less than 5 days.
The study is limited by lack of data in a subset of patients who had no documented GFR (2.7%) or missing covariate data (2.7%). The inability to ascertain other clinical information, such as nephrology approval of PICC, functional AV fistula or other hemodialysis access, or PICC complications after discharge further limit the findings.
Hospitalists should first decide if a PICC line is truly indicated, and if so, carefully weigh the risks and benefits of PICC placement in patients with advanced CKD.
Bottom line: PICC placement is common and often inappropriate in hospitalized patients with advanced CKD.
Citation: Paje D et al. Use of peripherally inserted central catheters in patients with advanced chronic kidney disease A prospective cohort study. Ann Intern Med. 2019 Jun 4;171:10-8.
Dr. Hageman is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Hospitalists and unit-based assignments
What seems like a usual day to a seasoned hospitalist can be a daunting task for a new hospitalist. A routine day as a hospitalist begins with prerounding, organizing, familiarizing, and gathering data on the list of patients, and most importantly prioritizing the tasks for the day. I have experienced both traditional and unit-based rounding models, and the geographic (unit-based) rounding model stands out for me.
The push for geographic rounding comes from the need to achieve excellence in patient care, coordination with nursing staff, higher HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores, better provider satisfaction, and efficiency in work flow and in documentation. The goal is typically to use this well-established tool to provide quality care to acutely ill patients admitted to the hospital, creating an environment of improved communication with the staff. It’s a “patient-centered care” model – if the patient wants to see a physician, it’s quicker to get to the patient and provides more visibility for the physician. These encounters result in improved patient-provider relationships, which in turn influences HCAHPS scores. Proximity encourages empathy, better work flow, and productivity.
The American health care system is intense and complex, and effective hospital medicine groups (HMGs) strive to provide quality care. Performance of an effective HMG is often scored on a “balanced score card.” The “balanced score” evaluates performance on domains such as clinical quality and safety, financial stability, HCAHPS, and operational effectiveness (length of stay and readmission rates). In my experience, effective unit-based rounding positively influences all the measures of the balanced score card.
Multidisciplinary roundings (MDRs) provide a platform where “the team” meets every morning to discuss the daily plan of care, everyone gets on the same page, and unit-based assignments facilitate hospitalist participation in MDRs. MDRs typically are a collaborative effort between care team members, such as a case manager, nurse, and hospitalist, physical therapist, and pharmacist. Each team member provides a precise input. Team members feel accountable and are better prepared for the day. It’s easier to develop a rapport with your patient when the same organized, comprehensive plan of care gets communicated to the patient.

It is important that each team member is prepared prior to the rounds. The total time for the rounds is often tightly controlled, as a fundamental concern is that MDRs can take up too much time. Use of a checklist or whiteboard during the unit-based rounds can improve efficiency. Midday MDRs are another gem in patient care, where the team proactively addresses early barriers in patient care and discharge plans for the next day.
The 2020 State of Hospital Medicine report highlights utilization of unit-based rounding, including breakdowns based on employment model. In groups serving adults patients only, 43% of university/medical school practices utilized unit-based assignments versus 48% for hospital-employed HMGs and only 32% for HMGs employed by multistate management companies. In HMGs that served pediatric patients only, 27% utilized unit-based assignments.
Undoubtedly geographic rounding has its own challenges. The pros and cons and the feasibility needs to be determined by each HMG. It’s often best to conduct the unit-based rounds on a few units and then roll it out to all the floors.
An important prerequisite to establishing a unit-based model for rounding is a detailed data analysis of total number of patients in various units to ensure there is adequate staffing. It must be practical to localize providers to different units, and complexity of various units can differ. At Lahey Hospital and Medical Center in Burlington, Mass., an efficient unit-based model has been achieved with complex units typically assigned two providers. Units including oncology and the progressive care unit can be a challenge, because of higher intensity and patient turnover.

Each unit is tagged to another unit in the same geographical area; these units are designated “sister pods.” The intention of these units is to strike a balance and level off patient load when needed. This process helps with standardization of the work between the providers. A big challenge of the unit-based model is to understand that it’s not always feasible to maintain consistency in patient assignments. Some patients can get transferred to a different unit due to limited telemetry and specialty units. At Lahey the provider manages their own patient as “patient drift” happens, in an attempt to maintain continuity of care.
The ultimate goal of unit-based assignments is to improve quality, financial, and operational metrics for the organization and take a deeper dive into provider and staff satisfaction. The simplest benefit for a hospitalist is to reduce travel time while rounding.
Education and teaching opportunities during the daily MDRs are still debatable. Another big step in this area may be a “resident-centered MDR” with the dual goals of improving both quality of care and resident education by focusing on evidence-based medicine.
Dr. Puri is a hospitalist at Lahey Hospital and Medical Center in Burlington, Mass.
What seems like a usual day to a seasoned hospitalist can be a daunting task for a new hospitalist. A routine day as a hospitalist begins with prerounding, organizing, familiarizing, and gathering data on the list of patients, and most importantly prioritizing the tasks for the day. I have experienced both traditional and unit-based rounding models, and the geographic (unit-based) rounding model stands out for me.
The push for geographic rounding comes from the need to achieve excellence in patient care, coordination with nursing staff, higher HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores, better provider satisfaction, and efficiency in work flow and in documentation. The goal is typically to use this well-established tool to provide quality care to acutely ill patients admitted to the hospital, creating an environment of improved communication with the staff. It’s a “patient-centered care” model – if the patient wants to see a physician, it’s quicker to get to the patient and provides more visibility for the physician. These encounters result in improved patient-provider relationships, which in turn influences HCAHPS scores. Proximity encourages empathy, better work flow, and productivity.
The American health care system is intense and complex, and effective hospital medicine groups (HMGs) strive to provide quality care. Performance of an effective HMG is often scored on a “balanced score card.” The “balanced score” evaluates performance on domains such as clinical quality and safety, financial stability, HCAHPS, and operational effectiveness (length of stay and readmission rates). In my experience, effective unit-based rounding positively influences all the measures of the balanced score card.
Multidisciplinary roundings (MDRs) provide a platform where “the team” meets every morning to discuss the daily plan of care, everyone gets on the same page, and unit-based assignments facilitate hospitalist participation in MDRs. MDRs typically are a collaborative effort between care team members, such as a case manager, nurse, and hospitalist, physical therapist, and pharmacist. Each team member provides a precise input. Team members feel accountable and are better prepared for the day. It’s easier to develop a rapport with your patient when the same organized, comprehensive plan of care gets communicated to the patient.

It is important that each team member is prepared prior to the rounds. The total time for the rounds is often tightly controlled, as a fundamental concern is that MDRs can take up too much time. Use of a checklist or whiteboard during the unit-based rounds can improve efficiency. Midday MDRs are another gem in patient care, where the team proactively addresses early barriers in patient care and discharge plans for the next day.
The 2020 State of Hospital Medicine report highlights utilization of unit-based rounding, including breakdowns based on employment model. In groups serving adults patients only, 43% of university/medical school practices utilized unit-based assignments versus 48% for hospital-employed HMGs and only 32% for HMGs employed by multistate management companies. In HMGs that served pediatric patients only, 27% utilized unit-based assignments.
Undoubtedly geographic rounding has its own challenges. The pros and cons and the feasibility needs to be determined by each HMG. It’s often best to conduct the unit-based rounds on a few units and then roll it out to all the floors.
An important prerequisite to establishing a unit-based model for rounding is a detailed data analysis of total number of patients in various units to ensure there is adequate staffing. It must be practical to localize providers to different units, and complexity of various units can differ. At Lahey Hospital and Medical Center in Burlington, Mass., an efficient unit-based model has been achieved with complex units typically assigned two providers. Units including oncology and the progressive care unit can be a challenge, because of higher intensity and patient turnover.

Each unit is tagged to another unit in the same geographical area; these units are designated “sister pods.” The intention of these units is to strike a balance and level off patient load when needed. This process helps with standardization of the work between the providers. A big challenge of the unit-based model is to understand that it’s not always feasible to maintain consistency in patient assignments. Some patients can get transferred to a different unit due to limited telemetry and specialty units. At Lahey the provider manages their own patient as “patient drift” happens, in an attempt to maintain continuity of care.
The ultimate goal of unit-based assignments is to improve quality, financial, and operational metrics for the organization and take a deeper dive into provider and staff satisfaction. The simplest benefit for a hospitalist is to reduce travel time while rounding.
Education and teaching opportunities during the daily MDRs are still debatable. Another big step in this area may be a “resident-centered MDR” with the dual goals of improving both quality of care and resident education by focusing on evidence-based medicine.
Dr. Puri is a hospitalist at Lahey Hospital and Medical Center in Burlington, Mass.
What seems like a usual day to a seasoned hospitalist can be a daunting task for a new hospitalist. A routine day as a hospitalist begins with prerounding, organizing, familiarizing, and gathering data on the list of patients, and most importantly prioritizing the tasks for the day. I have experienced both traditional and unit-based rounding models, and the geographic (unit-based) rounding model stands out for me.
The push for geographic rounding comes from the need to achieve excellence in patient care, coordination with nursing staff, higher HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores, better provider satisfaction, and efficiency in work flow and in documentation. The goal is typically to use this well-established tool to provide quality care to acutely ill patients admitted to the hospital, creating an environment of improved communication with the staff. It’s a “patient-centered care” model – if the patient wants to see a physician, it’s quicker to get to the patient and provides more visibility for the physician. These encounters result in improved patient-provider relationships, which in turn influences HCAHPS scores. Proximity encourages empathy, better work flow, and productivity.
The American health care system is intense and complex, and effective hospital medicine groups (HMGs) strive to provide quality care. Performance of an effective HMG is often scored on a “balanced score card.” The “balanced score” evaluates performance on domains such as clinical quality and safety, financial stability, HCAHPS, and operational effectiveness (length of stay and readmission rates). In my experience, effective unit-based rounding positively influences all the measures of the balanced score card.
Multidisciplinary roundings (MDRs) provide a platform where “the team” meets every morning to discuss the daily plan of care, everyone gets on the same page, and unit-based assignments facilitate hospitalist participation in MDRs. MDRs typically are a collaborative effort between care team members, such as a case manager, nurse, and hospitalist, physical therapist, and pharmacist. Each team member provides a precise input. Team members feel accountable and are better prepared for the day. It’s easier to develop a rapport with your patient when the same organized, comprehensive plan of care gets communicated to the patient.

It is important that each team member is prepared prior to the rounds. The total time for the rounds is often tightly controlled, as a fundamental concern is that MDRs can take up too much time. Use of a checklist or whiteboard during the unit-based rounds can improve efficiency. Midday MDRs are another gem in patient care, where the team proactively addresses early barriers in patient care and discharge plans for the next day.
The 2020 State of Hospital Medicine report highlights utilization of unit-based rounding, including breakdowns based on employment model. In groups serving adults patients only, 43% of university/medical school practices utilized unit-based assignments versus 48% for hospital-employed HMGs and only 32% for HMGs employed by multistate management companies. In HMGs that served pediatric patients only, 27% utilized unit-based assignments.
Undoubtedly geographic rounding has its own challenges. The pros and cons and the feasibility needs to be determined by each HMG. It’s often best to conduct the unit-based rounds on a few units and then roll it out to all the floors.
An important prerequisite to establishing a unit-based model for rounding is a detailed data analysis of total number of patients in various units to ensure there is adequate staffing. It must be practical to localize providers to different units, and complexity of various units can differ. At Lahey Hospital and Medical Center in Burlington, Mass., an efficient unit-based model has been achieved with complex units typically assigned two providers. Units including oncology and the progressive care unit can be a challenge, because of higher intensity and patient turnover.

Each unit is tagged to another unit in the same geographical area; these units are designated “sister pods.” The intention of these units is to strike a balance and level off patient load when needed. This process helps with standardization of the work between the providers. A big challenge of the unit-based model is to understand that it’s not always feasible to maintain consistency in patient assignments. Some patients can get transferred to a different unit due to limited telemetry and specialty units. At Lahey the provider manages their own patient as “patient drift” happens, in an attempt to maintain continuity of care.
The ultimate goal of unit-based assignments is to improve quality, financial, and operational metrics for the organization and take a deeper dive into provider and staff satisfaction. The simplest benefit for a hospitalist is to reduce travel time while rounding.
Education and teaching opportunities during the daily MDRs are still debatable. Another big step in this area may be a “resident-centered MDR” with the dual goals of improving both quality of care and resident education by focusing on evidence-based medicine.
Dr. Puri is a hospitalist at Lahey Hospital and Medical Center in Burlington, Mass.
The ally in the waiting room
Improving communication with patients’ loved ones
We think of a patient’s recovery happening in multiple locations – in a hospital room or a rehabilitation facility, for example. But many clinicians may not consider the opportunity to aid healing that lies in the waiting room.
The waiting room is where a patient’s loved ones often are and they, sometimes more than anyone, can unlock the path to a patient’s quicker recovery. Friends and family can offer encouragement, as they have an existing bond of trust that can help if a patient needs reinforcement to take their medications or follow other health care advice. But if loved ones are going to help patients, they need help from clinicians. Beyond being potential allies, they are also hurting, experiencing worry or confusion in a world of medical jargon.
The coronavirus changes the relationship of patients and their loved ones, as patients are often isolated or limited in the number of visitors they are allowed to see. A smartphone replaces the smiling faces of friends and relatives at their bedside, and a text is a poor substitute for a hug.
The Hospitalist asked some experienced hospitalists for insight on how best to communicate with patients’ loved ones to improve outcomes for all, medically and emotionally.
Team approach
“Patients feel isolated, terrified, and vulnerable but still need an advocate in the hospital, so daily communication with a patient’s loved one is important to give a sense that the patient is looked after,” said Kari Esbensen, MD, PhD, a hospitalist and palliative care expert at Emory University Hospital Midtown, Atlanta.
Glenn Rosenbluth, MD, a pediatric hospitalist and director, quality and safety programs, at the University of California, San Francisco, Benioff Children’s Hospital, agreed. He said that the most important thing is to communicate, period.
“We fall into this pattern of ‘out of sight, out of mind,’ ” he said. “We need to take the extra step to find out who a patient’s loved ones are. If it is a clinical visit, ask the patient, or maybe get the information from a caseworker, or just pay attention to who is dropping in to see the patient. Having a second person available to jot down notes, or having a handy list of questions – it all helps the patient. We forget that sometimes it can seem like a whirlwind for the patient when they are hurting. We have to remember that a loved one is important to a patient’s care team and we need to include them, empower them, and show that we want to hear their voices.”
Dr. Esbensen said it is critical to start off on the right foot when communicating with a patient’s loved one, especially during the current pandemic.
“With COVID-19, the most important thing is to speak honestly, to say hope for the best but prepare for the worst-case scenario,” Dr. Esbensen said. “We’ve seen that conditions can shift dramatically in short periods of time. The loved one needs to have a sense of the positive and negative possibilities. Families tend to lack understanding of the changes in the patient that are caused by COVID-19. The patient can come out of the hospital debilitated, very different than when they entered the hospital, and we need to warn people close to them about this. Unrealistic expectations need to be guarded against if a patient’s loved ones are going to help.”
Perhaps the best form of communication with a patient’s loved ones is an often-forgotten skill: listening.
“Get an idea from the patient’s loved ones of what the issues are, as well as their idea of what they think of the disease and how it spreads,” Dr. Esbensen said. “Sometimes they are right on target but sometimes there are misinterpretations and we need to help them understand it better. It’s not a ‘one-size-fits-all’ speech that we should give, but try to say, ‘tell me what you think is going on, what you think you’ve heard, and what you’re worried about,’ and learn what is most important to the patient. Start on those terms and adapt; this way you can correct and address what makes them most fearful, which can be different for each loved one. For some, the concern could be that they have children or other vulnerable people in the house. Finding out these other issues is important.”
Venkatrao Medarametla, MD, SFHM, medical director for hospital medicine at Baystate Medical Center, Springfield, Mass., emphasized that, in a time when hospitalists are being pulled in every direction, it is easy to lose your attention.
“It’s very important that family members know you’re present with them,” he said. “This can be an emotional time and they need empathy. It’s very easy for our list of tasks to get in the way of communicating, including with our body language.”
Dr. Medarametla said one of the reasons to communicate with patients’ loved ones is to calm them – a patient’s relatives or their friends may not be under your medical care, but they are still human beings.
“A lot of people just want information and want to be helpful, but we also need to realize that, while we are caring for many patients, this one person is the patient they are focused on,” said Laura Nell Hodo, MD, a pediatric hospitalist at Kravis Children’s Hospital at Mount Sinai in New York. “Don’t rush, and if you know that a patient’s loved one needs more time, make sure it can be found – if not then, at least later on the phone. Fifteen to 20 minutes may be what’s needed, and you can’t shortchange them.”
Dr. Hodo said that a patient’s loved ones often do not realize it is possible to receive phone calls from hospitalists. “We need to remind them that they can get in touch with us. We have to remember how helpless they can feel and how they want to understand what is happening in the hospital.”
For medical adherence issues, sometimes it is best to communicate with the patient and loved one at the same time, Dr. Hodo advised. “Whether it’s for medication or postdischarge exercises, if they both receive the information together it can reinforce adherence. But you also need to remember that the patient may only want a loved one told about certain things, or possibly nothing at all. We need to make sure we understand the patient’s wishes, regardless of whether we think a person close to them can be an ally or not.”
Dr. Esbensen also noted that a loved one can give hospitalists important clues to the emotional components of a patient’s care.
“I remember a patient whose wife told me how he worked in a garage, how he was strong and did not want people to think he was a weak guy just because of what was happening to him,” Dr. Esbensen said. “I didn’t know that he felt he might be perceived in this way. I mentioned to him how I learned he was a good mechanic and he perked up and felt seen in a different light. These things make a difference.”
But when is the best time to speak with a patient’s loved ones? Since much communication is done via phone during the pandemic, there are different philosophies.
“We had a debate among colleagues to see how each of us did it,” Dr. Esbensen said. “Some try to call after each patient encounter, while they are outside the room and it’s fresh in their mind, but others find it better to make the call after their rounds, to give the person their full attention. Most of the time I try to do it that way.”
She noted that, in the current environment, a phone call may be better than a face-to-face conversation with patients’ loved ones.
“We’re covered in so much gear to protect us from the coronavirus that it can feel like a great distance exists between us and the person with whom we’re speaking,” she said. “It’s strange, but the phone can make the conversation seem more relaxed and may get people to open up more.”
Even when they leave
All the hospitalists affirmed that loved ones can make a big difference for the patient through all aspects of care. Long after a patient returns home, the support of loved ones can have a profound impact in speeding healing and improving long-term outcomes.
Dr. Esbensen said COVID-19 and other serious illnesses can leave a patient needing support, and maybe a “push” when feeling low keeps them from adhering to medical advice.
“It’s not just in the hospital but after discharge,” she said. “A person offering support can really help patients throughout their journey, and much success in recovering from illness occurs after the transition home. Having the support of that one person a patient trusts can be critical.”
Dr. Hodo believes that the coronavirus pandemic could forever change the way hospitalists communicate with patients and their loved ones.
“I work in pediatrics and we know serious medical decisions can’t be made without guardians or parents,” she said. “But in adult medicine doctors may not automatically ask the patient about calling someone for input on decision-making. With COVID, you cannot assume a patient is on their own, because there are protocols keeping people from physically being present in the patient’s room. My experience from working in adult coronavirus units is that the thinking about the loved ones’ role in patient care – and communication with them – might just change. … At least, I hope so.”
Quick takeaways for hospitalists
- Get beyond personal protective equipment. A conversation with a patient’s loved one might be easier to achieve via phone, without all the protective gear in the way.
- Encourage adherence. Speaking with patients and loved ones together may be more effective. They may reach agreement quicker on how best to adhere to medical advice.
- Loved ones offer clues. They might give you a better sense of a patient’s worries, or help you to connect better with those in your care.
- Be present. You have a long to-do list but do not let empathy fall off it, even if you feel overwhelmed.
Improving communication with patients’ loved ones
Improving communication with patients’ loved ones
We think of a patient’s recovery happening in multiple locations – in a hospital room or a rehabilitation facility, for example. But many clinicians may not consider the opportunity to aid healing that lies in the waiting room.
The waiting room is where a patient’s loved ones often are and they, sometimes more than anyone, can unlock the path to a patient’s quicker recovery. Friends and family can offer encouragement, as they have an existing bond of trust that can help if a patient needs reinforcement to take their medications or follow other health care advice. But if loved ones are going to help patients, they need help from clinicians. Beyond being potential allies, they are also hurting, experiencing worry or confusion in a world of medical jargon.
The coronavirus changes the relationship of patients and their loved ones, as patients are often isolated or limited in the number of visitors they are allowed to see. A smartphone replaces the smiling faces of friends and relatives at their bedside, and a text is a poor substitute for a hug.
The Hospitalist asked some experienced hospitalists for insight on how best to communicate with patients’ loved ones to improve outcomes for all, medically and emotionally.
Team approach
“Patients feel isolated, terrified, and vulnerable but still need an advocate in the hospital, so daily communication with a patient’s loved one is important to give a sense that the patient is looked after,” said Kari Esbensen, MD, PhD, a hospitalist and palliative care expert at Emory University Hospital Midtown, Atlanta.
Glenn Rosenbluth, MD, a pediatric hospitalist and director, quality and safety programs, at the University of California, San Francisco, Benioff Children’s Hospital, agreed. He said that the most important thing is to communicate, period.
“We fall into this pattern of ‘out of sight, out of mind,’ ” he said. “We need to take the extra step to find out who a patient’s loved ones are. If it is a clinical visit, ask the patient, or maybe get the information from a caseworker, or just pay attention to who is dropping in to see the patient. Having a second person available to jot down notes, or having a handy list of questions – it all helps the patient. We forget that sometimes it can seem like a whirlwind for the patient when they are hurting. We have to remember that a loved one is important to a patient’s care team and we need to include them, empower them, and show that we want to hear their voices.”
Dr. Esbensen said it is critical to start off on the right foot when communicating with a patient’s loved one, especially during the current pandemic.
“With COVID-19, the most important thing is to speak honestly, to say hope for the best but prepare for the worst-case scenario,” Dr. Esbensen said. “We’ve seen that conditions can shift dramatically in short periods of time. The loved one needs to have a sense of the positive and negative possibilities. Families tend to lack understanding of the changes in the patient that are caused by COVID-19. The patient can come out of the hospital debilitated, very different than when they entered the hospital, and we need to warn people close to them about this. Unrealistic expectations need to be guarded against if a patient’s loved ones are going to help.”
Perhaps the best form of communication with a patient’s loved ones is an often-forgotten skill: listening.
“Get an idea from the patient’s loved ones of what the issues are, as well as their idea of what they think of the disease and how it spreads,” Dr. Esbensen said. “Sometimes they are right on target but sometimes there are misinterpretations and we need to help them understand it better. It’s not a ‘one-size-fits-all’ speech that we should give, but try to say, ‘tell me what you think is going on, what you think you’ve heard, and what you’re worried about,’ and learn what is most important to the patient. Start on those terms and adapt; this way you can correct and address what makes them most fearful, which can be different for each loved one. For some, the concern could be that they have children or other vulnerable people in the house. Finding out these other issues is important.”
Venkatrao Medarametla, MD, SFHM, medical director for hospital medicine at Baystate Medical Center, Springfield, Mass., emphasized that, in a time when hospitalists are being pulled in every direction, it is easy to lose your attention.
“It’s very important that family members know you’re present with them,” he said. “This can be an emotional time and they need empathy. It’s very easy for our list of tasks to get in the way of communicating, including with our body language.”
Dr. Medarametla said one of the reasons to communicate with patients’ loved ones is to calm them – a patient’s relatives or their friends may not be under your medical care, but they are still human beings.
“A lot of people just want information and want to be helpful, but we also need to realize that, while we are caring for many patients, this one person is the patient they are focused on,” said Laura Nell Hodo, MD, a pediatric hospitalist at Kravis Children’s Hospital at Mount Sinai in New York. “Don’t rush, and if you know that a patient’s loved one needs more time, make sure it can be found – if not then, at least later on the phone. Fifteen to 20 minutes may be what’s needed, and you can’t shortchange them.”
Dr. Hodo said that a patient’s loved ones often do not realize it is possible to receive phone calls from hospitalists. “We need to remind them that they can get in touch with us. We have to remember how helpless they can feel and how they want to understand what is happening in the hospital.”
For medical adherence issues, sometimes it is best to communicate with the patient and loved one at the same time, Dr. Hodo advised. “Whether it’s for medication or postdischarge exercises, if they both receive the information together it can reinforce adherence. But you also need to remember that the patient may only want a loved one told about certain things, or possibly nothing at all. We need to make sure we understand the patient’s wishes, regardless of whether we think a person close to them can be an ally or not.”
Dr. Esbensen also noted that a loved one can give hospitalists important clues to the emotional components of a patient’s care.
“I remember a patient whose wife told me how he worked in a garage, how he was strong and did not want people to think he was a weak guy just because of what was happening to him,” Dr. Esbensen said. “I didn’t know that he felt he might be perceived in this way. I mentioned to him how I learned he was a good mechanic and he perked up and felt seen in a different light. These things make a difference.”
But when is the best time to speak with a patient’s loved ones? Since much communication is done via phone during the pandemic, there are different philosophies.
“We had a debate among colleagues to see how each of us did it,” Dr. Esbensen said. “Some try to call after each patient encounter, while they are outside the room and it’s fresh in their mind, but others find it better to make the call after their rounds, to give the person their full attention. Most of the time I try to do it that way.”
She noted that, in the current environment, a phone call may be better than a face-to-face conversation with patients’ loved ones.
“We’re covered in so much gear to protect us from the coronavirus that it can feel like a great distance exists between us and the person with whom we’re speaking,” she said. “It’s strange, but the phone can make the conversation seem more relaxed and may get people to open up more.”
Even when they leave
All the hospitalists affirmed that loved ones can make a big difference for the patient through all aspects of care. Long after a patient returns home, the support of loved ones can have a profound impact in speeding healing and improving long-term outcomes.
Dr. Esbensen said COVID-19 and other serious illnesses can leave a patient needing support, and maybe a “push” when feeling low keeps them from adhering to medical advice.
“It’s not just in the hospital but after discharge,” she said. “A person offering support can really help patients throughout their journey, and much success in recovering from illness occurs after the transition home. Having the support of that one person a patient trusts can be critical.”
Dr. Hodo believes that the coronavirus pandemic could forever change the way hospitalists communicate with patients and their loved ones.
“I work in pediatrics and we know serious medical decisions can’t be made without guardians or parents,” she said. “But in adult medicine doctors may not automatically ask the patient about calling someone for input on decision-making. With COVID, you cannot assume a patient is on their own, because there are protocols keeping people from physically being present in the patient’s room. My experience from working in adult coronavirus units is that the thinking about the loved ones’ role in patient care – and communication with them – might just change. … At least, I hope so.”
Quick takeaways for hospitalists
- Get beyond personal protective equipment. A conversation with a patient’s loved one might be easier to achieve via phone, without all the protective gear in the way.
- Encourage adherence. Speaking with patients and loved ones together may be more effective. They may reach agreement quicker on how best to adhere to medical advice.
- Loved ones offer clues. They might give you a better sense of a patient’s worries, or help you to connect better with those in your care.
- Be present. You have a long to-do list but do not let empathy fall off it, even if you feel overwhelmed.
We think of a patient’s recovery happening in multiple locations – in a hospital room or a rehabilitation facility, for example. But many clinicians may not consider the opportunity to aid healing that lies in the waiting room.
The waiting room is where a patient’s loved ones often are and they, sometimes more than anyone, can unlock the path to a patient’s quicker recovery. Friends and family can offer encouragement, as they have an existing bond of trust that can help if a patient needs reinforcement to take their medications or follow other health care advice. But if loved ones are going to help patients, they need help from clinicians. Beyond being potential allies, they are also hurting, experiencing worry or confusion in a world of medical jargon.
The coronavirus changes the relationship of patients and their loved ones, as patients are often isolated or limited in the number of visitors they are allowed to see. A smartphone replaces the smiling faces of friends and relatives at their bedside, and a text is a poor substitute for a hug.
The Hospitalist asked some experienced hospitalists for insight on how best to communicate with patients’ loved ones to improve outcomes for all, medically and emotionally.
Team approach
“Patients feel isolated, terrified, and vulnerable but still need an advocate in the hospital, so daily communication with a patient’s loved one is important to give a sense that the patient is looked after,” said Kari Esbensen, MD, PhD, a hospitalist and palliative care expert at Emory University Hospital Midtown, Atlanta.
Glenn Rosenbluth, MD, a pediatric hospitalist and director, quality and safety programs, at the University of California, San Francisco, Benioff Children’s Hospital, agreed. He said that the most important thing is to communicate, period.
“We fall into this pattern of ‘out of sight, out of mind,’ ” he said. “We need to take the extra step to find out who a patient’s loved ones are. If it is a clinical visit, ask the patient, or maybe get the information from a caseworker, or just pay attention to who is dropping in to see the patient. Having a second person available to jot down notes, or having a handy list of questions – it all helps the patient. We forget that sometimes it can seem like a whirlwind for the patient when they are hurting. We have to remember that a loved one is important to a patient’s care team and we need to include them, empower them, and show that we want to hear their voices.”
Dr. Esbensen said it is critical to start off on the right foot when communicating with a patient’s loved one, especially during the current pandemic.
“With COVID-19, the most important thing is to speak honestly, to say hope for the best but prepare for the worst-case scenario,” Dr. Esbensen said. “We’ve seen that conditions can shift dramatically in short periods of time. The loved one needs to have a sense of the positive and negative possibilities. Families tend to lack understanding of the changes in the patient that are caused by COVID-19. The patient can come out of the hospital debilitated, very different than when they entered the hospital, and we need to warn people close to them about this. Unrealistic expectations need to be guarded against if a patient’s loved ones are going to help.”
Perhaps the best form of communication with a patient’s loved ones is an often-forgotten skill: listening.
“Get an idea from the patient’s loved ones of what the issues are, as well as their idea of what they think of the disease and how it spreads,” Dr. Esbensen said. “Sometimes they are right on target but sometimes there are misinterpretations and we need to help them understand it better. It’s not a ‘one-size-fits-all’ speech that we should give, but try to say, ‘tell me what you think is going on, what you think you’ve heard, and what you’re worried about,’ and learn what is most important to the patient. Start on those terms and adapt; this way you can correct and address what makes them most fearful, which can be different for each loved one. For some, the concern could be that they have children or other vulnerable people in the house. Finding out these other issues is important.”
Venkatrao Medarametla, MD, SFHM, medical director for hospital medicine at Baystate Medical Center, Springfield, Mass., emphasized that, in a time when hospitalists are being pulled in every direction, it is easy to lose your attention.
“It’s very important that family members know you’re present with them,” he said. “This can be an emotional time and they need empathy. It’s very easy for our list of tasks to get in the way of communicating, including with our body language.”
Dr. Medarametla said one of the reasons to communicate with patients’ loved ones is to calm them – a patient’s relatives or their friends may not be under your medical care, but they are still human beings.
“A lot of people just want information and want to be helpful, but we also need to realize that, while we are caring for many patients, this one person is the patient they are focused on,” said Laura Nell Hodo, MD, a pediatric hospitalist at Kravis Children’s Hospital at Mount Sinai in New York. “Don’t rush, and if you know that a patient’s loved one needs more time, make sure it can be found – if not then, at least later on the phone. Fifteen to 20 minutes may be what’s needed, and you can’t shortchange them.”
Dr. Hodo said that a patient’s loved ones often do not realize it is possible to receive phone calls from hospitalists. “We need to remind them that they can get in touch with us. We have to remember how helpless they can feel and how they want to understand what is happening in the hospital.”
For medical adherence issues, sometimes it is best to communicate with the patient and loved one at the same time, Dr. Hodo advised. “Whether it’s for medication or postdischarge exercises, if they both receive the information together it can reinforce adherence. But you also need to remember that the patient may only want a loved one told about certain things, or possibly nothing at all. We need to make sure we understand the patient’s wishes, regardless of whether we think a person close to them can be an ally or not.”
Dr. Esbensen also noted that a loved one can give hospitalists important clues to the emotional components of a patient’s care.
“I remember a patient whose wife told me how he worked in a garage, how he was strong and did not want people to think he was a weak guy just because of what was happening to him,” Dr. Esbensen said. “I didn’t know that he felt he might be perceived in this way. I mentioned to him how I learned he was a good mechanic and he perked up and felt seen in a different light. These things make a difference.”
But when is the best time to speak with a patient’s loved ones? Since much communication is done via phone during the pandemic, there are different philosophies.
“We had a debate among colleagues to see how each of us did it,” Dr. Esbensen said. “Some try to call after each patient encounter, while they are outside the room and it’s fresh in their mind, but others find it better to make the call after their rounds, to give the person their full attention. Most of the time I try to do it that way.”
She noted that, in the current environment, a phone call may be better than a face-to-face conversation with patients’ loved ones.
“We’re covered in so much gear to protect us from the coronavirus that it can feel like a great distance exists between us and the person with whom we’re speaking,” she said. “It’s strange, but the phone can make the conversation seem more relaxed and may get people to open up more.”
Even when they leave
All the hospitalists affirmed that loved ones can make a big difference for the patient through all aspects of care. Long after a patient returns home, the support of loved ones can have a profound impact in speeding healing and improving long-term outcomes.
Dr. Esbensen said COVID-19 and other serious illnesses can leave a patient needing support, and maybe a “push” when feeling low keeps them from adhering to medical advice.
“It’s not just in the hospital but after discharge,” she said. “A person offering support can really help patients throughout their journey, and much success in recovering from illness occurs after the transition home. Having the support of that one person a patient trusts can be critical.”
Dr. Hodo believes that the coronavirus pandemic could forever change the way hospitalists communicate with patients and their loved ones.
“I work in pediatrics and we know serious medical decisions can’t be made without guardians or parents,” she said. “But in adult medicine doctors may not automatically ask the patient about calling someone for input on decision-making. With COVID, you cannot assume a patient is on their own, because there are protocols keeping people from physically being present in the patient’s room. My experience from working in adult coronavirus units is that the thinking about the loved ones’ role in patient care – and communication with them – might just change. … At least, I hope so.”
Quick takeaways for hospitalists
- Get beyond personal protective equipment. A conversation with a patient’s loved one might be easier to achieve via phone, without all the protective gear in the way.
- Encourage adherence. Speaking with patients and loved ones together may be more effective. They may reach agreement quicker on how best to adhere to medical advice.
- Loved ones offer clues. They might give you a better sense of a patient’s worries, or help you to connect better with those in your care.
- Be present. You have a long to-do list but do not let empathy fall off it, even if you feel overwhelmed.
A dedicated mobility technician improves inpatient mobility
Background: Studies have shown improved hospital outcomes in patients who ambulate regularly. Many assisted mobility protocols aimed at ambulating patients multiple times daily are nurse centered. However, implementation is difficult because of the large number of nursing duties and difficulty finding time away from other competing responsibilities.
Study design: Single-blind randomized controlled trial.
Setting: Single-center 1,440-bed tertiary care hospital.
Synopsis: This study randomized 102 moderately impaired adult inpatients aged 60 years and older with Activity Measures for Post-Acute Care mobility scores of 16-20 to either dedicated regular ambulation sessions with mobility technicians or usual care with hospital nurse–driven protocol. Patients who achieved greater than 400 steps were more likely to discharge to home rather than post–acute care (71% vs. 46%; P = .01). Assisted ambulation did not decrease length of stay or affect the discharge disposition, but it did increase the total daily number of steps taken by patients (1,182 vs. 726; P = .02, per-protocol analysis) and the patients’ mobility scores (18.90 vs. 18.27, P = .04).
Bottom line: A dedicated mobility technician to provide assisted ambulation for older inpatients can improve patient mobility.
Citation: Hamilton AC et al. Increasing mobility via in-hospital ambulation protocol delivered by mobility technicians: A pilot randomized controlled trial. J Hosp Med. 2019;14:272-7.
Dr. Nelson is a hospitalist at Ochsner Health System, New Orleans.
Background: Studies have shown improved hospital outcomes in patients who ambulate regularly. Many assisted mobility protocols aimed at ambulating patients multiple times daily are nurse centered. However, implementation is difficult because of the large number of nursing duties and difficulty finding time away from other competing responsibilities.
Study design: Single-blind randomized controlled trial.
Setting: Single-center 1,440-bed tertiary care hospital.
Synopsis: This study randomized 102 moderately impaired adult inpatients aged 60 years and older with Activity Measures for Post-Acute Care mobility scores of 16-20 to either dedicated regular ambulation sessions with mobility technicians or usual care with hospital nurse–driven protocol. Patients who achieved greater than 400 steps were more likely to discharge to home rather than post–acute care (71% vs. 46%; P = .01). Assisted ambulation did not decrease length of stay or affect the discharge disposition, but it did increase the total daily number of steps taken by patients (1,182 vs. 726; P = .02, per-protocol analysis) and the patients’ mobility scores (18.90 vs. 18.27, P = .04).
Bottom line: A dedicated mobility technician to provide assisted ambulation for older inpatients can improve patient mobility.
Citation: Hamilton AC et al. Increasing mobility via in-hospital ambulation protocol delivered by mobility technicians: A pilot randomized controlled trial. J Hosp Med. 2019;14:272-7.
Dr. Nelson is a hospitalist at Ochsner Health System, New Orleans.
Background: Studies have shown improved hospital outcomes in patients who ambulate regularly. Many assisted mobility protocols aimed at ambulating patients multiple times daily are nurse centered. However, implementation is difficult because of the large number of nursing duties and difficulty finding time away from other competing responsibilities.
Study design: Single-blind randomized controlled trial.
Setting: Single-center 1,440-bed tertiary care hospital.
Synopsis: This study randomized 102 moderately impaired adult inpatients aged 60 years and older with Activity Measures for Post-Acute Care mobility scores of 16-20 to either dedicated regular ambulation sessions with mobility technicians or usual care with hospital nurse–driven protocol. Patients who achieved greater than 400 steps were more likely to discharge to home rather than post–acute care (71% vs. 46%; P = .01). Assisted ambulation did not decrease length of stay or affect the discharge disposition, but it did increase the total daily number of steps taken by patients (1,182 vs. 726; P = .02, per-protocol analysis) and the patients’ mobility scores (18.90 vs. 18.27, P = .04).
Bottom line: A dedicated mobility technician to provide assisted ambulation for older inpatients can improve patient mobility.
Citation: Hamilton AC et al. Increasing mobility via in-hospital ambulation protocol delivered by mobility technicians: A pilot randomized controlled trial. J Hosp Med. 2019;14:272-7.
Dr. Nelson is a hospitalist at Ochsner Health System, New Orleans.
Septicemia first among hospital inpatient costs
according to a recent analysis from the Agency for Healthcare Research and Quality.
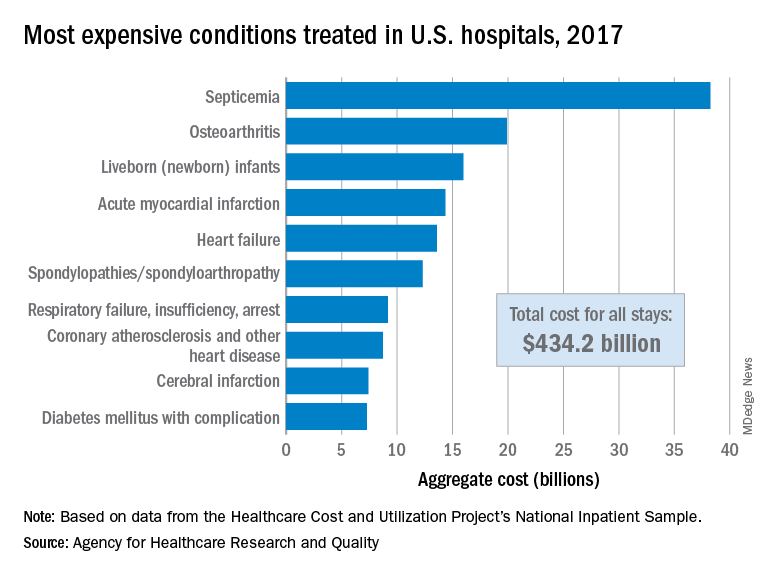
The single most expensive inpatient condition that year, representing about 8.8% of all hospital costs, was septicemia at $38.2 billion, nearly double the $19.9 billion spent on the next most expensive condition, osteoarthritis, Lan Liang, PhD, of the AHRQ, and associates said in a statistical brief.
These figures “represent the hospital’s costs to produce the services – not the amount paid for services by payers – and they do not include separately billed physician fees associated with the hospitalization,” they noted.
Third in overall cost for 2017 but first in total number of stays were live-born infants, with 3.7 million admissions costing just under $16 billion. Hospital costs for acute myocardial infarction ($14.3 billion) made it the fourth most expensive condition, with heart failure fifth at $13.6 billion, based on data from the Healthcare Cost and Utilization Project’s National Inpatient Sample.
The 20 most expensive conditions, which also included coronary atherosclerosis, pneumonia, renal failure, and lower-limb fracture, accounted for close to 47% of all hospital costs and over 43% of all stays in 2017. The total amount spent by hospitals that year, $1.1 trillion, constituted nearly a third of all health care expenditures and was 4.7% higher than in 2016, Dr. Liang and associates reported.
“Although this growth represented deceleration, compared with the 5.8% increase between 2014 and 2015, the consistent year-to-year rise in hospital-related expenses remains a central concern among policymakers,” they wrote.
according to a recent analysis from the Agency for Healthcare Research and Quality.
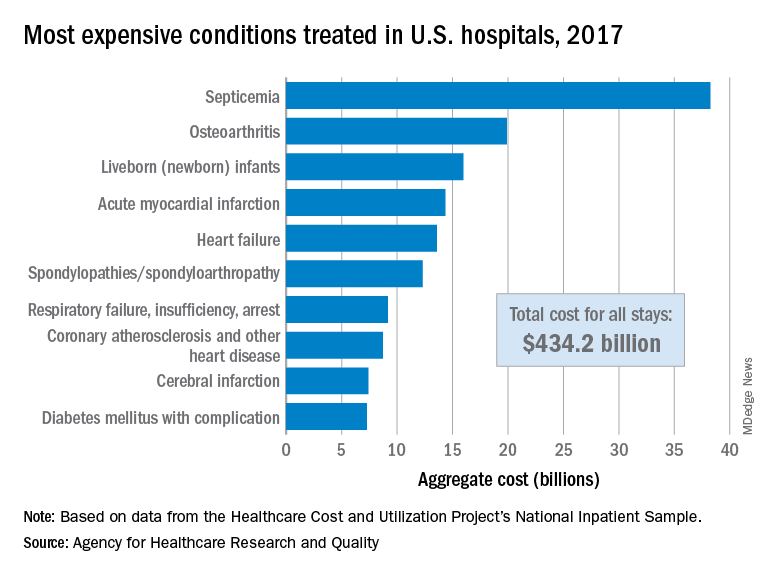
The single most expensive inpatient condition that year, representing about 8.8% of all hospital costs, was septicemia at $38.2 billion, nearly double the $19.9 billion spent on the next most expensive condition, osteoarthritis, Lan Liang, PhD, of the AHRQ, and associates said in a statistical brief.
These figures “represent the hospital’s costs to produce the services – not the amount paid for services by payers – and they do not include separately billed physician fees associated with the hospitalization,” they noted.
Third in overall cost for 2017 but first in total number of stays were live-born infants, with 3.7 million admissions costing just under $16 billion. Hospital costs for acute myocardial infarction ($14.3 billion) made it the fourth most expensive condition, with heart failure fifth at $13.6 billion, based on data from the Healthcare Cost and Utilization Project’s National Inpatient Sample.
The 20 most expensive conditions, which also included coronary atherosclerosis, pneumonia, renal failure, and lower-limb fracture, accounted for close to 47% of all hospital costs and over 43% of all stays in 2017. The total amount spent by hospitals that year, $1.1 trillion, constituted nearly a third of all health care expenditures and was 4.7% higher than in 2016, Dr. Liang and associates reported.
“Although this growth represented deceleration, compared with the 5.8% increase between 2014 and 2015, the consistent year-to-year rise in hospital-related expenses remains a central concern among policymakers,” they wrote.
according to a recent analysis from the Agency for Healthcare Research and Quality.
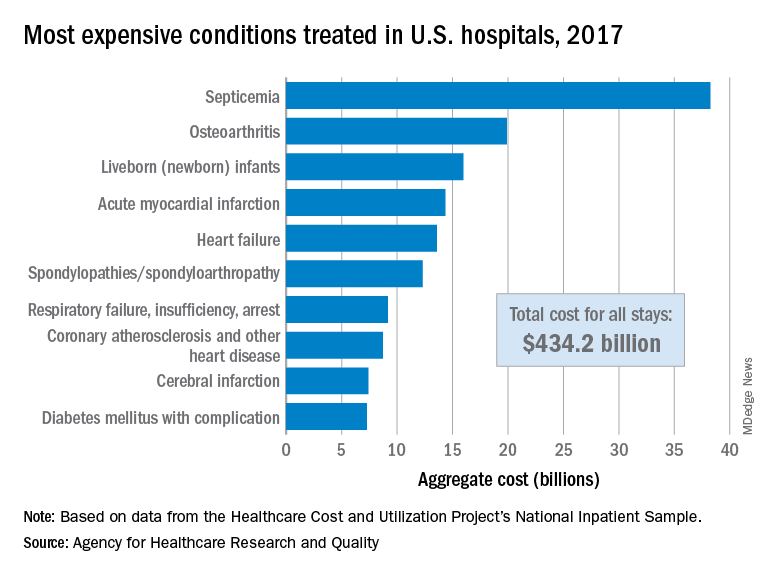
The single most expensive inpatient condition that year, representing about 8.8% of all hospital costs, was septicemia at $38.2 billion, nearly double the $19.9 billion spent on the next most expensive condition, osteoarthritis, Lan Liang, PhD, of the AHRQ, and associates said in a statistical brief.
These figures “represent the hospital’s costs to produce the services – not the amount paid for services by payers – and they do not include separately billed physician fees associated with the hospitalization,” they noted.
Third in overall cost for 2017 but first in total number of stays were live-born infants, with 3.7 million admissions costing just under $16 billion. Hospital costs for acute myocardial infarction ($14.3 billion) made it the fourth most expensive condition, with heart failure fifth at $13.6 billion, based on data from the Healthcare Cost and Utilization Project’s National Inpatient Sample.
The 20 most expensive conditions, which also included coronary atherosclerosis, pneumonia, renal failure, and lower-limb fracture, accounted for close to 47% of all hospital costs and over 43% of all stays in 2017. The total amount spent by hospitals that year, $1.1 trillion, constituted nearly a third of all health care expenditures and was 4.7% higher than in 2016, Dr. Liang and associates reported.
“Although this growth represented deceleration, compared with the 5.8% increase between 2014 and 2015, the consistent year-to-year rise in hospital-related expenses remains a central concern among policymakers,” they wrote.