User login
Order errors not reduced with limiting number of open records
Background: An estimated 600,000 patients in U.S. hospitals had an order placed in their record that was meant for another patient in 2016. The Office of the National Coordinator for Health Information Technology and the Joint Commission recommend that EHRs limit the number of open records to one at a time based on expert opinion only. There is wide variation in the number of open records allowed among EHRs across the United States currently.
Study design: Randomized clinical trial.
Setting: Large health system in New York.
Synopsis: There were 3,356 clinicians (inpatient, outpatient, ED) randomized in a 1:1 ratio into either a restricted group (one open record at a time) or an unrestricted group (up to four open records at a time). In this study, 12,140,298 orders, in 4,486,631 order sessions, were analyzed with the Wrong-Patient Retract-and-Reorder (RAR) measure to identify wrong-patient orders. The proportion of wrong-patient order sessions were 90.7 vs. 88.0 per 100,000 order sessions for the restricted versus unrestricted groups (odds ratio, 1.03; 95% confidence interval, 0.90-1.20). There were no statistically significant differences in wrong-patient order sessions between the restricted and unrestricted groups in any clinical setting examined (inpatient, outpatient, ED).
Despite the ability to have up to four open records at one time in the unrestricted group, 66% of the order sessions were completed with only one record open in that group. This limited the power of the study to detect a difference in risk of order errors between the restricted and unrestricted groups.
Bottom line: Limiting clinicians to only one open record did not reduce the proportion of wrong-patient orders, compared with allowing up to four open records concurrently.
Citation: Adelman JS et al. Effect of restriction of the number of concurrently open records in an electronic health record on wrong-patient order errors: A randomized clinical trial. JAMA. 2019;32(18):1780-7.
Dr. Field is a hospitalist at Ochsner Health System, New Orleans.
Background: An estimated 600,000 patients in U.S. hospitals had an order placed in their record that was meant for another patient in 2016. The Office of the National Coordinator for Health Information Technology and the Joint Commission recommend that EHRs limit the number of open records to one at a time based on expert opinion only. There is wide variation in the number of open records allowed among EHRs across the United States currently.
Study design: Randomized clinical trial.
Setting: Large health system in New York.
Synopsis: There were 3,356 clinicians (inpatient, outpatient, ED) randomized in a 1:1 ratio into either a restricted group (one open record at a time) or an unrestricted group (up to four open records at a time). In this study, 12,140,298 orders, in 4,486,631 order sessions, were analyzed with the Wrong-Patient Retract-and-Reorder (RAR) measure to identify wrong-patient orders. The proportion of wrong-patient order sessions were 90.7 vs. 88.0 per 100,000 order sessions for the restricted versus unrestricted groups (odds ratio, 1.03; 95% confidence interval, 0.90-1.20). There were no statistically significant differences in wrong-patient order sessions between the restricted and unrestricted groups in any clinical setting examined (inpatient, outpatient, ED).
Despite the ability to have up to four open records at one time in the unrestricted group, 66% of the order sessions were completed with only one record open in that group. This limited the power of the study to detect a difference in risk of order errors between the restricted and unrestricted groups.
Bottom line: Limiting clinicians to only one open record did not reduce the proportion of wrong-patient orders, compared with allowing up to four open records concurrently.
Citation: Adelman JS et al. Effect of restriction of the number of concurrently open records in an electronic health record on wrong-patient order errors: A randomized clinical trial. JAMA. 2019;32(18):1780-7.
Dr. Field is a hospitalist at Ochsner Health System, New Orleans.
Background: An estimated 600,000 patients in U.S. hospitals had an order placed in their record that was meant for another patient in 2016. The Office of the National Coordinator for Health Information Technology and the Joint Commission recommend that EHRs limit the number of open records to one at a time based on expert opinion only. There is wide variation in the number of open records allowed among EHRs across the United States currently.
Study design: Randomized clinical trial.
Setting: Large health system in New York.
Synopsis: There were 3,356 clinicians (inpatient, outpatient, ED) randomized in a 1:1 ratio into either a restricted group (one open record at a time) or an unrestricted group (up to four open records at a time). In this study, 12,140,298 orders, in 4,486,631 order sessions, were analyzed with the Wrong-Patient Retract-and-Reorder (RAR) measure to identify wrong-patient orders. The proportion of wrong-patient order sessions were 90.7 vs. 88.0 per 100,000 order sessions for the restricted versus unrestricted groups (odds ratio, 1.03; 95% confidence interval, 0.90-1.20). There were no statistically significant differences in wrong-patient order sessions between the restricted and unrestricted groups in any clinical setting examined (inpatient, outpatient, ED).
Despite the ability to have up to four open records at one time in the unrestricted group, 66% of the order sessions were completed with only one record open in that group. This limited the power of the study to detect a difference in risk of order errors between the restricted and unrestricted groups.
Bottom line: Limiting clinicians to only one open record did not reduce the proportion of wrong-patient orders, compared with allowing up to four open records concurrently.
Citation: Adelman JS et al. Effect of restriction of the number of concurrently open records in an electronic health record on wrong-patient order errors: A randomized clinical trial. JAMA. 2019;32(18):1780-7.
Dr. Field is a hospitalist at Ochsner Health System, New Orleans.
Hospital vs. outpatient management comparable for elderly syncope patients
Background: In the United States, there are over 1 million visits to EDs for syncope with a greater than 50% hospitalization rate for older adult patients. There remains uncertainty around which patients without an identified cause for the syncope could be discharged from the ED and managed as an outpatient.
Study design: Propensity score analysis.
Setting: EDs from 11 nonprofit academic hospitals.
Synopsis: Prospective data for 2,492 patients aged 60 years and older who did not have an identified cause in the ED for their presenting complaint of syncope were included in the propensity score analysis resulting in a sample size of 1,064 with 532 patients in each of the discharged and hospitalized groups. There was no significant difference in risk of 30-day post-ED serious adverse events between the hospitalized patients (4.89%; 95% confidence interval, 3.06%-6.72%) and discharged patients (2.82%; 95% CI, 1.41%-4.23%; risk difference 2.07%; 95% CI, –0.24% to 4.38%). There was also no statistically significant difference in 30-day mortality post–ED visit.
These results show no clinical benefit in hospitalization for older adults with unexplained syncope after ED evaluation suggesting that it would be reasonable to proceed with outpatient management and evaluation of these patients.
Bottom line: Consider discharging older patients home from the ED who do not have high risk factors and no identified cause of their syncope.
Citation: Probst MA et al. Clinical benefit of hospitalization for older adults with unexplained syncope: A propensity-matched analysis. Ann Emerg Med. 2019 Aug;74(2):260-9.
Dr. Field is a hospitalist at Ochsner Health System, New Orleans.
Background: In the United States, there are over 1 million visits to EDs for syncope with a greater than 50% hospitalization rate for older adult patients. There remains uncertainty around which patients without an identified cause for the syncope could be discharged from the ED and managed as an outpatient.
Study design: Propensity score analysis.
Setting: EDs from 11 nonprofit academic hospitals.
Synopsis: Prospective data for 2,492 patients aged 60 years and older who did not have an identified cause in the ED for their presenting complaint of syncope were included in the propensity score analysis resulting in a sample size of 1,064 with 532 patients in each of the discharged and hospitalized groups. There was no significant difference in risk of 30-day post-ED serious adverse events between the hospitalized patients (4.89%; 95% confidence interval, 3.06%-6.72%) and discharged patients (2.82%; 95% CI, 1.41%-4.23%; risk difference 2.07%; 95% CI, –0.24% to 4.38%). There was also no statistically significant difference in 30-day mortality post–ED visit.
These results show no clinical benefit in hospitalization for older adults with unexplained syncope after ED evaluation suggesting that it would be reasonable to proceed with outpatient management and evaluation of these patients.
Bottom line: Consider discharging older patients home from the ED who do not have high risk factors and no identified cause of their syncope.
Citation: Probst MA et al. Clinical benefit of hospitalization for older adults with unexplained syncope: A propensity-matched analysis. Ann Emerg Med. 2019 Aug;74(2):260-9.
Dr. Field is a hospitalist at Ochsner Health System, New Orleans.
Background: In the United States, there are over 1 million visits to EDs for syncope with a greater than 50% hospitalization rate for older adult patients. There remains uncertainty around which patients without an identified cause for the syncope could be discharged from the ED and managed as an outpatient.
Study design: Propensity score analysis.
Setting: EDs from 11 nonprofit academic hospitals.
Synopsis: Prospective data for 2,492 patients aged 60 years and older who did not have an identified cause in the ED for their presenting complaint of syncope were included in the propensity score analysis resulting in a sample size of 1,064 with 532 patients in each of the discharged and hospitalized groups. There was no significant difference in risk of 30-day post-ED serious adverse events between the hospitalized patients (4.89%; 95% confidence interval, 3.06%-6.72%) and discharged patients (2.82%; 95% CI, 1.41%-4.23%; risk difference 2.07%; 95% CI, –0.24% to 4.38%). There was also no statistically significant difference in 30-day mortality post–ED visit.
These results show no clinical benefit in hospitalization for older adults with unexplained syncope after ED evaluation suggesting that it would be reasonable to proceed with outpatient management and evaluation of these patients.
Bottom line: Consider discharging older patients home from the ED who do not have high risk factors and no identified cause of their syncope.
Citation: Probst MA et al. Clinical benefit of hospitalization for older adults with unexplained syncope: A propensity-matched analysis. Ann Emerg Med. 2019 Aug;74(2):260-9.
Dr. Field is a hospitalist at Ochsner Health System, New Orleans.
Goals of care conferences for incapacitated ICU patients
Background: Previous studies suggest that clinicians and surrogates rarely discuss patient values in ICU family conferences about goals of care despite recommendations from international critical care societies.
Study design: Analysis of audiotaped goals of care conferences.
Setting: ICUs in six U.S. academic centers.
Synopsis: The authors analyzed 249 audiotaped family conferences concerning goals of care for severely critically ill, incapacitated patients with acute respiratory distress syndrome and found that information about patient values and preferences was discussed in only 68.4% of the conferences.
Moreover, there was no deliberation about how to apply patient values and preferences to clinical decisions in 55.7% of the conferences. Surrogates were more likely to bring up these elements of shared decision making than were physicians.
Bottom line: Care providers and surrogates of critically ill ICU patients often fail to discuss patient preferences, values, and how they apply to care decisions in goals of care conferences.
Citation: Scheunemann LP et al. Clinician-family communication about patients’ values and preferences in intensive care units. JAMA Intern Med. 2019;179(5):676-84.
Dr. Mastalerz is a hospitalist and medical director of 9A Accountable Care Unit at the Colorado Health Foundation.
Background: Previous studies suggest that clinicians and surrogates rarely discuss patient values in ICU family conferences about goals of care despite recommendations from international critical care societies.
Study design: Analysis of audiotaped goals of care conferences.
Setting: ICUs in six U.S. academic centers.
Synopsis: The authors analyzed 249 audiotaped family conferences concerning goals of care for severely critically ill, incapacitated patients with acute respiratory distress syndrome and found that information about patient values and preferences was discussed in only 68.4% of the conferences.
Moreover, there was no deliberation about how to apply patient values and preferences to clinical decisions in 55.7% of the conferences. Surrogates were more likely to bring up these elements of shared decision making than were physicians.
Bottom line: Care providers and surrogates of critically ill ICU patients often fail to discuss patient preferences, values, and how they apply to care decisions in goals of care conferences.
Citation: Scheunemann LP et al. Clinician-family communication about patients’ values and preferences in intensive care units. JAMA Intern Med. 2019;179(5):676-84.
Dr. Mastalerz is a hospitalist and medical director of 9A Accountable Care Unit at the Colorado Health Foundation.
Background: Previous studies suggest that clinicians and surrogates rarely discuss patient values in ICU family conferences about goals of care despite recommendations from international critical care societies.
Study design: Analysis of audiotaped goals of care conferences.
Setting: ICUs in six U.S. academic centers.
Synopsis: The authors analyzed 249 audiotaped family conferences concerning goals of care for severely critically ill, incapacitated patients with acute respiratory distress syndrome and found that information about patient values and preferences was discussed in only 68.4% of the conferences.
Moreover, there was no deliberation about how to apply patient values and preferences to clinical decisions in 55.7% of the conferences. Surrogates were more likely to bring up these elements of shared decision making than were physicians.
Bottom line: Care providers and surrogates of critically ill ICU patients often fail to discuss patient preferences, values, and how they apply to care decisions in goals of care conferences.
Citation: Scheunemann LP et al. Clinician-family communication about patients’ values and preferences in intensive care units. JAMA Intern Med. 2019;179(5):676-84.
Dr. Mastalerz is a hospitalist and medical director of 9A Accountable Care Unit at the Colorado Health Foundation.
Catheter ablation of AFib improves quality of life more than medications do
Background: Catheter ablation of AFib (primarily pulmonary vein isolation) has been shown to result in better maintenance of sinus rhythm than medications. Small studies of QOL have shown mixed results. Larger trials were needed.
Study design: Open-label randomized multisite clinical trial of catheter ablation (pulmonary vein isolation with additional ablation procedure at the treating physician discretion) versus standard rate and/or rhythm control medications (chosen by clinician discretion). Patients were included for paroxysmal or persistent AFib and either age 65 years or older or age younger than 65 years with one additional stroke risk factor. Quality of life surveys – the Atrial Fibrillation Effect on Quality of Life (AFEQT) questionnaire and the Mayo AF-Specific Symptom Inventory (MAFSI) – were completed at baseline, and at 3, 12, 24, 36, 48, and 60 months.
Setting: 126 centers in 10 countries.
Synopsis: The study included 2,204 patients with median age of 68 years, diagnosed with AFib a median of 1.1 years prior, who were followed for a median of 48 months. The median CHA2DS2-VASc score was 3.0.
Self-reported AFib dropped from 86.0% to 21.1% in the ablation group and from 83.7% to 39.8% in the medication group at 12 months. The AFEQT score (range 0-100, higher score indicating better QOL) increased from 62.9 to 86.4 in the ablation group and increased from 63.1 to 80.9 in the medication group (for a mean difference of 5.3 points [95% confidence interval, 3.7-6.9; P less than .001] favoring ablation). MAFSI symptom frequency score and symptom severity score also showed improvement in symptoms favoring ablation. Post hoc subgroup analysis showed that those with the most severe symptoms had the largest benefit from ablation.
The primary limitation is the lack of patient blinding (may bias self-reported symptoms).
While the CABANA trial efficacy study (published separately) showed that catheter ablation results in no significant difference in the combined outcome of death, disabling stroke, serious bleeding, or cardiac arrest, the CABANA QOL study, reviewed here, shows that ablation does result in improved QOL and reduced symptoms, compared with medical therapy.
Bottom line: Catheter ablation of AFib can be done safely and successfully at experienced centers. In patients with AFib-related symptoms, ablation reduces symptoms and improves QOL somewhat more than medications do. The most severely symptomatic patients appear to obtain the most benefit.
Citation: Packer DL et al. Effect of catheter ablation vs. antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: The CABANA Randomized Clinical Trial. JAMA. 2019 Mar 15. doi: 10.1001/jama.2019.0693.
Dr. Stafford is a hospitalist at Duke University Health System.
Background: Catheter ablation of AFib (primarily pulmonary vein isolation) has been shown to result in better maintenance of sinus rhythm than medications. Small studies of QOL have shown mixed results. Larger trials were needed.
Study design: Open-label randomized multisite clinical trial of catheter ablation (pulmonary vein isolation with additional ablation procedure at the treating physician discretion) versus standard rate and/or rhythm control medications (chosen by clinician discretion). Patients were included for paroxysmal or persistent AFib and either age 65 years or older or age younger than 65 years with one additional stroke risk factor. Quality of life surveys – the Atrial Fibrillation Effect on Quality of Life (AFEQT) questionnaire and the Mayo AF-Specific Symptom Inventory (MAFSI) – were completed at baseline, and at 3, 12, 24, 36, 48, and 60 months.
Setting: 126 centers in 10 countries.
Synopsis: The study included 2,204 patients with median age of 68 years, diagnosed with AFib a median of 1.1 years prior, who were followed for a median of 48 months. The median CHA2DS2-VASc score was 3.0.
Self-reported AFib dropped from 86.0% to 21.1% in the ablation group and from 83.7% to 39.8% in the medication group at 12 months. The AFEQT score (range 0-100, higher score indicating better QOL) increased from 62.9 to 86.4 in the ablation group and increased from 63.1 to 80.9 in the medication group (for a mean difference of 5.3 points [95% confidence interval, 3.7-6.9; P less than .001] favoring ablation). MAFSI symptom frequency score and symptom severity score also showed improvement in symptoms favoring ablation. Post hoc subgroup analysis showed that those with the most severe symptoms had the largest benefit from ablation.
The primary limitation is the lack of patient blinding (may bias self-reported symptoms).
While the CABANA trial efficacy study (published separately) showed that catheter ablation results in no significant difference in the combined outcome of death, disabling stroke, serious bleeding, or cardiac arrest, the CABANA QOL study, reviewed here, shows that ablation does result in improved QOL and reduced symptoms, compared with medical therapy.
Bottom line: Catheter ablation of AFib can be done safely and successfully at experienced centers. In patients with AFib-related symptoms, ablation reduces symptoms and improves QOL somewhat more than medications do. The most severely symptomatic patients appear to obtain the most benefit.
Citation: Packer DL et al. Effect of catheter ablation vs. antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: The CABANA Randomized Clinical Trial. JAMA. 2019 Mar 15. doi: 10.1001/jama.2019.0693.
Dr. Stafford is a hospitalist at Duke University Health System.
Background: Catheter ablation of AFib (primarily pulmonary vein isolation) has been shown to result in better maintenance of sinus rhythm than medications. Small studies of QOL have shown mixed results. Larger trials were needed.
Study design: Open-label randomized multisite clinical trial of catheter ablation (pulmonary vein isolation with additional ablation procedure at the treating physician discretion) versus standard rate and/or rhythm control medications (chosen by clinician discretion). Patients were included for paroxysmal or persistent AFib and either age 65 years or older or age younger than 65 years with one additional stroke risk factor. Quality of life surveys – the Atrial Fibrillation Effect on Quality of Life (AFEQT) questionnaire and the Mayo AF-Specific Symptom Inventory (MAFSI) – were completed at baseline, and at 3, 12, 24, 36, 48, and 60 months.
Setting: 126 centers in 10 countries.
Synopsis: The study included 2,204 patients with median age of 68 years, diagnosed with AFib a median of 1.1 years prior, who were followed for a median of 48 months. The median CHA2DS2-VASc score was 3.0.
Self-reported AFib dropped from 86.0% to 21.1% in the ablation group and from 83.7% to 39.8% in the medication group at 12 months. The AFEQT score (range 0-100, higher score indicating better QOL) increased from 62.9 to 86.4 in the ablation group and increased from 63.1 to 80.9 in the medication group (for a mean difference of 5.3 points [95% confidence interval, 3.7-6.9; P less than .001] favoring ablation). MAFSI symptom frequency score and symptom severity score also showed improvement in symptoms favoring ablation. Post hoc subgroup analysis showed that those with the most severe symptoms had the largest benefit from ablation.
The primary limitation is the lack of patient blinding (may bias self-reported symptoms).
While the CABANA trial efficacy study (published separately) showed that catheter ablation results in no significant difference in the combined outcome of death, disabling stroke, serious bleeding, or cardiac arrest, the CABANA QOL study, reviewed here, shows that ablation does result in improved QOL and reduced symptoms, compared with medical therapy.
Bottom line: Catheter ablation of AFib can be done safely and successfully at experienced centers. In patients with AFib-related symptoms, ablation reduces symptoms and improves QOL somewhat more than medications do. The most severely symptomatic patients appear to obtain the most benefit.
Citation: Packer DL et al. Effect of catheter ablation vs. antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: The CABANA Randomized Clinical Trial. JAMA. 2019 Mar 15. doi: 10.1001/jama.2019.0693.
Dr. Stafford is a hospitalist at Duke University Health System.
Restriction of Foley catheters in older trauma patients improved outcomes
and led to earlier discharge, findings from a study revealed. The results of the study were reported in an abstract scheduled for release at the annual meeting of the American Academy of Orthopaedic Surgeons. The meeting was canceled because of COVID-19.
“We reduced the use of Foley catheters in our target population by more than 50%, which led to a decrease in the rate of hospital-acquired UTI and positively affected other perioperative outcomes,” reported Sanjit R. Konda, MD, an orthopedic surgeon with New York University Langone Health.
The quality initiative was introduced about 2 years ago specifically to reduce the risk of UTI in older patients admitted for femur or hip fractures. Previously at the level 1 trauma center where this quality initiative was introduced, placement of Foley catheters in these types of patients had been routine.
After the policy change, Foley catheters were only offered to these trauma patients 55 years of age or older when more than three episodes or urinary retention had been documented with a bladder scan. Urinary retention was defined as a volume of at least 600 mL.
When outcomes in 184 patients treated in the 15 months after the policy change were compared with 393 treated in the prior 38 months, Foley catheter use was substantially and significantly reduced (43.5% vs. 95.5%; P < .001), Dr. Konda said in an interview.
Although the lower rate of UTI following the policy change fell short of statistical significance (10.33% vs. 14.5%; P = .167), the policy change was associated with a decreased time to surgery (33.27 vs. 38.54 hours; P = .001), shorter length of stay (6.89 vs. 8.34 days; P < .001), and higher rate of home discharge (22.8% vs. 15.6%; P = .038).
When those who avoided a Foley catheter were compared with those who did not after the policy change, there was a significant reduction in UTI (4.81% vs. 17.4%; P = .014). In addition, patients who avoided a Foley catheter had a decreased time to surgery (P = .014), shorter length of stay (P < .001) and an almost 900% greater likelihood of home discharge (odds ratio, 9.9; P < .001).
“This quality initiative does increase the number of bladder scans required, meaning more work for nurses, but the program was developed in collaboration with our nursing staff, who were supportive of the goals,” Dr. Konda reported.
Reducing the incidence of UTI is an important initiative because the Centers for Medicare & Medicaid Services and other third-party payers employ this as a quality metric, according to Dr. Konda. This explains why hospital administrators generally embrace effective strategies to reduce UTI rates.
The improvement in outcomes, including the reduction in UTIs and length of stay, has cost implications, which will be evaluated in a future analysis, according to Dr. Konda.
Although this quality initiative was undertaken in a level 1 trauma center, Dr. Konda believes the same principles can be applied to other settings.
Jennifer A. Meddings, MD, an associate professor of medicine at the University of Michigan, Ann Arbor, agreed. Active in the evaluation of strategies to reduce hospital-acquired complications, Dr. Meddings published a study of procedural appropriateness ratings to guide strategies for improving the likelihood that catheters are employed only when needed (BMJ Qual Saf. 2019;28:56-66).
“In addition to avoiding UTI, reducing unnecessary placement of Foley catheters also eliminates the risk of trauma to the urinary tract,” Dr. Meddings said. This is a complication that is not well appreciated because the trauma is not always documented, according to Dr. Meddings, who believes increased risk of both UTI and urinary tract trauma should discourage use of Foley catheters when there is not a specific indication.
Although there are criteria other than excess bladder volume to determine when to consider a Foley catheter, Dr. Meddings encourages any systematic approach that increases the likelihood that catheters are not placed unnecessarily. She emphasized that a hip fracture by itself “is not a criterion for catheterization.”
Dr. Konda reported a financial relationship with Stryker.
and led to earlier discharge, findings from a study revealed. The results of the study were reported in an abstract scheduled for release at the annual meeting of the American Academy of Orthopaedic Surgeons. The meeting was canceled because of COVID-19.
“We reduced the use of Foley catheters in our target population by more than 50%, which led to a decrease in the rate of hospital-acquired UTI and positively affected other perioperative outcomes,” reported Sanjit R. Konda, MD, an orthopedic surgeon with New York University Langone Health.
The quality initiative was introduced about 2 years ago specifically to reduce the risk of UTI in older patients admitted for femur or hip fractures. Previously at the level 1 trauma center where this quality initiative was introduced, placement of Foley catheters in these types of patients had been routine.
After the policy change, Foley catheters were only offered to these trauma patients 55 years of age or older when more than three episodes or urinary retention had been documented with a bladder scan. Urinary retention was defined as a volume of at least 600 mL.
When outcomes in 184 patients treated in the 15 months after the policy change were compared with 393 treated in the prior 38 months, Foley catheter use was substantially and significantly reduced (43.5% vs. 95.5%; P < .001), Dr. Konda said in an interview.
Although the lower rate of UTI following the policy change fell short of statistical significance (10.33% vs. 14.5%; P = .167), the policy change was associated with a decreased time to surgery (33.27 vs. 38.54 hours; P = .001), shorter length of stay (6.89 vs. 8.34 days; P < .001), and higher rate of home discharge (22.8% vs. 15.6%; P = .038).
When those who avoided a Foley catheter were compared with those who did not after the policy change, there was a significant reduction in UTI (4.81% vs. 17.4%; P = .014). In addition, patients who avoided a Foley catheter had a decreased time to surgery (P = .014), shorter length of stay (P < .001) and an almost 900% greater likelihood of home discharge (odds ratio, 9.9; P < .001).
“This quality initiative does increase the number of bladder scans required, meaning more work for nurses, but the program was developed in collaboration with our nursing staff, who were supportive of the goals,” Dr. Konda reported.
Reducing the incidence of UTI is an important initiative because the Centers for Medicare & Medicaid Services and other third-party payers employ this as a quality metric, according to Dr. Konda. This explains why hospital administrators generally embrace effective strategies to reduce UTI rates.
The improvement in outcomes, including the reduction in UTIs and length of stay, has cost implications, which will be evaluated in a future analysis, according to Dr. Konda.
Although this quality initiative was undertaken in a level 1 trauma center, Dr. Konda believes the same principles can be applied to other settings.
Jennifer A. Meddings, MD, an associate professor of medicine at the University of Michigan, Ann Arbor, agreed. Active in the evaluation of strategies to reduce hospital-acquired complications, Dr. Meddings published a study of procedural appropriateness ratings to guide strategies for improving the likelihood that catheters are employed only when needed (BMJ Qual Saf. 2019;28:56-66).
“In addition to avoiding UTI, reducing unnecessary placement of Foley catheters also eliminates the risk of trauma to the urinary tract,” Dr. Meddings said. This is a complication that is not well appreciated because the trauma is not always documented, according to Dr. Meddings, who believes increased risk of both UTI and urinary tract trauma should discourage use of Foley catheters when there is not a specific indication.
Although there are criteria other than excess bladder volume to determine when to consider a Foley catheter, Dr. Meddings encourages any systematic approach that increases the likelihood that catheters are not placed unnecessarily. She emphasized that a hip fracture by itself “is not a criterion for catheterization.”
Dr. Konda reported a financial relationship with Stryker.
and led to earlier discharge, findings from a study revealed. The results of the study were reported in an abstract scheduled for release at the annual meeting of the American Academy of Orthopaedic Surgeons. The meeting was canceled because of COVID-19.
“We reduced the use of Foley catheters in our target population by more than 50%, which led to a decrease in the rate of hospital-acquired UTI and positively affected other perioperative outcomes,” reported Sanjit R. Konda, MD, an orthopedic surgeon with New York University Langone Health.
The quality initiative was introduced about 2 years ago specifically to reduce the risk of UTI in older patients admitted for femur or hip fractures. Previously at the level 1 trauma center where this quality initiative was introduced, placement of Foley catheters in these types of patients had been routine.
After the policy change, Foley catheters were only offered to these trauma patients 55 years of age or older when more than three episodes or urinary retention had been documented with a bladder scan. Urinary retention was defined as a volume of at least 600 mL.
When outcomes in 184 patients treated in the 15 months after the policy change were compared with 393 treated in the prior 38 months, Foley catheter use was substantially and significantly reduced (43.5% vs. 95.5%; P < .001), Dr. Konda said in an interview.
Although the lower rate of UTI following the policy change fell short of statistical significance (10.33% vs. 14.5%; P = .167), the policy change was associated with a decreased time to surgery (33.27 vs. 38.54 hours; P = .001), shorter length of stay (6.89 vs. 8.34 days; P < .001), and higher rate of home discharge (22.8% vs. 15.6%; P = .038).
When those who avoided a Foley catheter were compared with those who did not after the policy change, there was a significant reduction in UTI (4.81% vs. 17.4%; P = .014). In addition, patients who avoided a Foley catheter had a decreased time to surgery (P = .014), shorter length of stay (P < .001) and an almost 900% greater likelihood of home discharge (odds ratio, 9.9; P < .001).
“This quality initiative does increase the number of bladder scans required, meaning more work for nurses, but the program was developed in collaboration with our nursing staff, who were supportive of the goals,” Dr. Konda reported.
Reducing the incidence of UTI is an important initiative because the Centers for Medicare & Medicaid Services and other third-party payers employ this as a quality metric, according to Dr. Konda. This explains why hospital administrators generally embrace effective strategies to reduce UTI rates.
The improvement in outcomes, including the reduction in UTIs and length of stay, has cost implications, which will be evaluated in a future analysis, according to Dr. Konda.
Although this quality initiative was undertaken in a level 1 trauma center, Dr. Konda believes the same principles can be applied to other settings.
Jennifer A. Meddings, MD, an associate professor of medicine at the University of Michigan, Ann Arbor, agreed. Active in the evaluation of strategies to reduce hospital-acquired complications, Dr. Meddings published a study of procedural appropriateness ratings to guide strategies for improving the likelihood that catheters are employed only when needed (BMJ Qual Saf. 2019;28:56-66).
“In addition to avoiding UTI, reducing unnecessary placement of Foley catheters also eliminates the risk of trauma to the urinary tract,” Dr. Meddings said. This is a complication that is not well appreciated because the trauma is not always documented, according to Dr. Meddings, who believes increased risk of both UTI and urinary tract trauma should discourage use of Foley catheters when there is not a specific indication.
Although there are criteria other than excess bladder volume to determine when to consider a Foley catheter, Dr. Meddings encourages any systematic approach that increases the likelihood that catheters are not placed unnecessarily. She emphasized that a hip fracture by itself “is not a criterion for catheterization.”
Dr. Konda reported a financial relationship with Stryker.
FROM AAOS 2020
QI initiative can decrease unnecessary IV treatment of asymptomatic hypertension
Background: Limited research suggests IV treatment of asymptomatic hypertension may be widespread and unhelpful. There is potential for unnecessary treatment to have adverse outcomes, such as hypotension.
Study design: Retrospective cohort study.
Setting: A single academic hospital.
Synopsis: Of 2,306 inpatients with asymptomatic hypertension, 11% were treated with IV medications to lower their blood pressure. Patients with indications for stricter blood pressure control (such as stroke, intracranial hemorrhage, aortic dissection) were excluded from the study. Following the baseline period, an education intervention was employed that included presentations, handouts, and posters. A second phase of quality improvement intervention included adjustment of the electronic medical record blood pressure alert parameters from more than 160/90 to more than 180/90. After these interventions, a lower percentage of patients received IV blood pressure medications for asymptomatic hypertension without a significant change in the number of rapid response calls, ICU transfers, or code blues. Limitations include that this is a single-center study and it is unclear if the performance improvement seen will be maintained over time.
Bottom line: IV antihypertensive use for asymptomatic hypertension is common despite lack of data to support its use, and reduced use is possible using quality improvement interventions.
Citation: Jacobs Z et al. Reducing unnecessary treatment of asymptomatic elevated blood pressure with intravenous medications on the general internal medicine wards: a quality improvement initiative. J Hosp Med. 2019 Mar;14(3):144-50.
Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and an assistant professor of medicine at Duke University.
Background: Limited research suggests IV treatment of asymptomatic hypertension may be widespread and unhelpful. There is potential for unnecessary treatment to have adverse outcomes, such as hypotension.
Study design: Retrospective cohort study.
Setting: A single academic hospital.
Synopsis: Of 2,306 inpatients with asymptomatic hypertension, 11% were treated with IV medications to lower their blood pressure. Patients with indications for stricter blood pressure control (such as stroke, intracranial hemorrhage, aortic dissection) were excluded from the study. Following the baseline period, an education intervention was employed that included presentations, handouts, and posters. A second phase of quality improvement intervention included adjustment of the electronic medical record blood pressure alert parameters from more than 160/90 to more than 180/90. After these interventions, a lower percentage of patients received IV blood pressure medications for asymptomatic hypertension without a significant change in the number of rapid response calls, ICU transfers, or code blues. Limitations include that this is a single-center study and it is unclear if the performance improvement seen will be maintained over time.
Bottom line: IV antihypertensive use for asymptomatic hypertension is common despite lack of data to support its use, and reduced use is possible using quality improvement interventions.
Citation: Jacobs Z et al. Reducing unnecessary treatment of asymptomatic elevated blood pressure with intravenous medications on the general internal medicine wards: a quality improvement initiative. J Hosp Med. 2019 Mar;14(3):144-50.
Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and an assistant professor of medicine at Duke University.
Background: Limited research suggests IV treatment of asymptomatic hypertension may be widespread and unhelpful. There is potential for unnecessary treatment to have adverse outcomes, such as hypotension.
Study design: Retrospective cohort study.
Setting: A single academic hospital.
Synopsis: Of 2,306 inpatients with asymptomatic hypertension, 11% were treated with IV medications to lower their blood pressure. Patients with indications for stricter blood pressure control (such as stroke, intracranial hemorrhage, aortic dissection) were excluded from the study. Following the baseline period, an education intervention was employed that included presentations, handouts, and posters. A second phase of quality improvement intervention included adjustment of the electronic medical record blood pressure alert parameters from more than 160/90 to more than 180/90. After these interventions, a lower percentage of patients received IV blood pressure medications for asymptomatic hypertension without a significant change in the number of rapid response calls, ICU transfers, or code blues. Limitations include that this is a single-center study and it is unclear if the performance improvement seen will be maintained over time.
Bottom line: IV antihypertensive use for asymptomatic hypertension is common despite lack of data to support its use, and reduced use is possible using quality improvement interventions.
Citation: Jacobs Z et al. Reducing unnecessary treatment of asymptomatic elevated blood pressure with intravenous medications on the general internal medicine wards: a quality improvement initiative. J Hosp Med. 2019 Mar;14(3):144-50.
Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and an assistant professor of medicine at Duke University.
Patients’ perceptions and high hospital use
Background: A small proportion of patients accounts for a large proportion of hospital use and readmissions. As hospitals and hospitalists focus efforts to improve transitions of care, there is a paucity of data that incorporates patients’ perspectives into the design of these programs.
Study design: Qualitative research study.
Setting: Northwestern Memorial Hospital, a single urban academic medical center in Chicago.
Synopsis: Eligible patients had two unplanned 30-day readmissions within the prior 12 months in addition to one or more of the following: at least one readmission in the last 6 months; a referral from a patient’s medical provider; or at least three observation visits.
A research coordinator conducted one-on-one semistructured interviews. Each interview was recorded, transcribed, and then coded using a team-based approach; 26 patients completed the interview process. From the analysis, four major themes emerged: Major medical problems were universal but high hospital use onset varied; participants noted that fluctuations in their course were often related to social, economic, and psychological stressors; onset and progression of episodes seemed uncontrollable and unpredictable; participants preferred to avoid hospitalization and sought care when attempts at self-management failed. The major limitation of this study was the small sample size located at one medical center, creating a data pool that is potentially not generalizable to other medical centers. These findings, however, are an important reminder to focus our interventions with patients’ needs and perceptions in mind.
Bottom line: Frequently hospitalized patients have insights into factors contributing to their high hospital use. Engaging patients in this discussion can enable us to create sustainable patient-centered programs that avoid rehospitalization.
Citation: O’Leary KJ et al. Frequently hospitalized patients’ perceptions of factors contributing to high hospital use. J Hosp Med. 2019 Mar 20;14:e1-6.
Dr. Richardson is a hospitalist at Duke University Health System.
Background: A small proportion of patients accounts for a large proportion of hospital use and readmissions. As hospitals and hospitalists focus efforts to improve transitions of care, there is a paucity of data that incorporates patients’ perspectives into the design of these programs.
Study design: Qualitative research study.
Setting: Northwestern Memorial Hospital, a single urban academic medical center in Chicago.
Synopsis: Eligible patients had two unplanned 30-day readmissions within the prior 12 months in addition to one or more of the following: at least one readmission in the last 6 months; a referral from a patient’s medical provider; or at least three observation visits.
A research coordinator conducted one-on-one semistructured interviews. Each interview was recorded, transcribed, and then coded using a team-based approach; 26 patients completed the interview process. From the analysis, four major themes emerged: Major medical problems were universal but high hospital use onset varied; participants noted that fluctuations in their course were often related to social, economic, and psychological stressors; onset and progression of episodes seemed uncontrollable and unpredictable; participants preferred to avoid hospitalization and sought care when attempts at self-management failed. The major limitation of this study was the small sample size located at one medical center, creating a data pool that is potentially not generalizable to other medical centers. These findings, however, are an important reminder to focus our interventions with patients’ needs and perceptions in mind.
Bottom line: Frequently hospitalized patients have insights into factors contributing to their high hospital use. Engaging patients in this discussion can enable us to create sustainable patient-centered programs that avoid rehospitalization.
Citation: O’Leary KJ et al. Frequently hospitalized patients’ perceptions of factors contributing to high hospital use. J Hosp Med. 2019 Mar 20;14:e1-6.
Dr. Richardson is a hospitalist at Duke University Health System.
Background: A small proportion of patients accounts for a large proportion of hospital use and readmissions. As hospitals and hospitalists focus efforts to improve transitions of care, there is a paucity of data that incorporates patients’ perspectives into the design of these programs.
Study design: Qualitative research study.
Setting: Northwestern Memorial Hospital, a single urban academic medical center in Chicago.
Synopsis: Eligible patients had two unplanned 30-day readmissions within the prior 12 months in addition to one or more of the following: at least one readmission in the last 6 months; a referral from a patient’s medical provider; or at least three observation visits.
A research coordinator conducted one-on-one semistructured interviews. Each interview was recorded, transcribed, and then coded using a team-based approach; 26 patients completed the interview process. From the analysis, four major themes emerged: Major medical problems were universal but high hospital use onset varied; participants noted that fluctuations in their course were often related to social, economic, and psychological stressors; onset and progression of episodes seemed uncontrollable and unpredictable; participants preferred to avoid hospitalization and sought care when attempts at self-management failed. The major limitation of this study was the small sample size located at one medical center, creating a data pool that is potentially not generalizable to other medical centers. These findings, however, are an important reminder to focus our interventions with patients’ needs and perceptions in mind.
Bottom line: Frequently hospitalized patients have insights into factors contributing to their high hospital use. Engaging patients in this discussion can enable us to create sustainable patient-centered programs that avoid rehospitalization.
Citation: O’Leary KJ et al. Frequently hospitalized patients’ perceptions of factors contributing to high hospital use. J Hosp Med. 2019 Mar 20;14:e1-6.
Dr. Richardson is a hospitalist at Duke University Health System.
Reducing low-value preop care for cataract surgery patients
Background: Although multiple randomized, controlled trials have shown that routine preoperative testing prior to cataract surgery has low yield, most Medicare beneficiaries continue to undergo this testing. The American Board of Internal Medicine started the Choosing Wisely campaign to help educate patients and providers about a crisis of unnecessary testing and procedures. This prompted multiple centers to create quality improvement (QI) projects to decrease low-value care.
_
Study design: Observational study of a health system quality improvement initiative.
Setting: Two academic, safety-net hospitals in Los Angeles.
Synopsis: The intervention hospital’s QI nurse underwent an extensive formal QI training program, followed by educating all health care team members involved in preoperative care for cataract patients. New guidelines were created and circulated, with a stated goal of eliminating routine preoperative visits and testing. The control hospital continued their usual preoperative care.
Preoperative visits decreased from 93% to 24% in the intervention group and increased from 89% to 91% in the control group (between-group difference, −71%; 95% confidence interval, –80% to –62%). Chest x-rays, laboratory tests, and electrocardiograms also had a similar decrease in the intervention group.
The intervention hospital lost $42,241 the first year because of training costs but 3-year projections estimated $67,241 in savings. The authors estimated $217,322 savings in 3 years from a societal perspective. Interestingly, the decrease in utilization would lead to financial loss in fee-for-service payment ($88,151 loss in 3 years).
No causal relationship can be established since this was an observational study. Several assumptions were made for the cost analysis. Results are less generalizable since the study was at hospitals in a single city and health system. It is unclear which component of the QI initiative was most effective.
Bottom line: A multidisciplinary, multicomponent initiative can be successful in decreasing low-value preoperative testing of patients undergoing cataract surgery. Although this results in cost savings overall and for capitated payment systems, it would actually cause revenue loss in fee-for-service systems. This emphasizes a potential barrier to eradicate low-value care.
Citation: Mafi JN et al. Evaluation of an intervention to reduce low-value preoperative care for patients undergoing cataract surgery at a safety-net health system. JAMA Intern Med. Published online 2019 Mar 25. doi: 10.1001/jamainternmed.2018.8358.
Dr. Menon is a hospitalist at Duke University Health System.
Background: Although multiple randomized, controlled trials have shown that routine preoperative testing prior to cataract surgery has low yield, most Medicare beneficiaries continue to undergo this testing. The American Board of Internal Medicine started the Choosing Wisely campaign to help educate patients and providers about a crisis of unnecessary testing and procedures. This prompted multiple centers to create quality improvement (QI) projects to decrease low-value care.
_
Study design: Observational study of a health system quality improvement initiative.
Setting: Two academic, safety-net hospitals in Los Angeles.
Synopsis: The intervention hospital’s QI nurse underwent an extensive formal QI training program, followed by educating all health care team members involved in preoperative care for cataract patients. New guidelines were created and circulated, with a stated goal of eliminating routine preoperative visits and testing. The control hospital continued their usual preoperative care.
Preoperative visits decreased from 93% to 24% in the intervention group and increased from 89% to 91% in the control group (between-group difference, −71%; 95% confidence interval, –80% to –62%). Chest x-rays, laboratory tests, and electrocardiograms also had a similar decrease in the intervention group.
The intervention hospital lost $42,241 the first year because of training costs but 3-year projections estimated $67,241 in savings. The authors estimated $217,322 savings in 3 years from a societal perspective. Interestingly, the decrease in utilization would lead to financial loss in fee-for-service payment ($88,151 loss in 3 years).
No causal relationship can be established since this was an observational study. Several assumptions were made for the cost analysis. Results are less generalizable since the study was at hospitals in a single city and health system. It is unclear which component of the QI initiative was most effective.
Bottom line: A multidisciplinary, multicomponent initiative can be successful in decreasing low-value preoperative testing of patients undergoing cataract surgery. Although this results in cost savings overall and for capitated payment systems, it would actually cause revenue loss in fee-for-service systems. This emphasizes a potential barrier to eradicate low-value care.
Citation: Mafi JN et al. Evaluation of an intervention to reduce low-value preoperative care for patients undergoing cataract surgery at a safety-net health system. JAMA Intern Med. Published online 2019 Mar 25. doi: 10.1001/jamainternmed.2018.8358.
Dr. Menon is a hospitalist at Duke University Health System.
Background: Although multiple randomized, controlled trials have shown that routine preoperative testing prior to cataract surgery has low yield, most Medicare beneficiaries continue to undergo this testing. The American Board of Internal Medicine started the Choosing Wisely campaign to help educate patients and providers about a crisis of unnecessary testing and procedures. This prompted multiple centers to create quality improvement (QI) projects to decrease low-value care.
_
Study design: Observational study of a health system quality improvement initiative.
Setting: Two academic, safety-net hospitals in Los Angeles.
Synopsis: The intervention hospital’s QI nurse underwent an extensive formal QI training program, followed by educating all health care team members involved in preoperative care for cataract patients. New guidelines were created and circulated, with a stated goal of eliminating routine preoperative visits and testing. The control hospital continued their usual preoperative care.
Preoperative visits decreased from 93% to 24% in the intervention group and increased from 89% to 91% in the control group (between-group difference, −71%; 95% confidence interval, –80% to –62%). Chest x-rays, laboratory tests, and electrocardiograms also had a similar decrease in the intervention group.
The intervention hospital lost $42,241 the first year because of training costs but 3-year projections estimated $67,241 in savings. The authors estimated $217,322 savings in 3 years from a societal perspective. Interestingly, the decrease in utilization would lead to financial loss in fee-for-service payment ($88,151 loss in 3 years).
No causal relationship can be established since this was an observational study. Several assumptions were made for the cost analysis. Results are less generalizable since the study was at hospitals in a single city and health system. It is unclear which component of the QI initiative was most effective.
Bottom line: A multidisciplinary, multicomponent initiative can be successful in decreasing low-value preoperative testing of patients undergoing cataract surgery. Although this results in cost savings overall and for capitated payment systems, it would actually cause revenue loss in fee-for-service systems. This emphasizes a potential barrier to eradicate low-value care.
Citation: Mafi JN et al. Evaluation of an intervention to reduce low-value preoperative care for patients undergoing cataract surgery at a safety-net health system. JAMA Intern Med. Published online 2019 Mar 25. doi: 10.1001/jamainternmed.2018.8358.
Dr. Menon is a hospitalist at Duke University Health System.
Evaluating complications of midline catheters
Background: Midline catheters have gained popularity in inpatient medical settings as a convenient alternative to PICC lines. This is primarily because of the ability to avoid central line–associated bloodstream infections (CLABSI) since these catheters terminate in the peripheral veins and cannot be reported as such. Additionally, they are potentially able to dwell longer than are traditional peripheral intravenous catheters. However, insufficient data exist to accurately describe the rate of complications in these catheters, as prior studies are based on single-center experiences.
Study design: Multicenter prospective cohort study.
Setting: Hospital medicine ward or medical ICU.
Synopsis: With use of a large database of adult patients from a quality initiative supported by Blue Cross Blue Shield of Michigan and Blue Care Network, this study identified 1,161 patients who had midline catheters placed and showed a 10.3% complication rate, of which 66.7% were minor (dislodgment, leaking, infiltration, or superficial thrombophlebitis) rather than major complications (occlusion, symptomatic upper-extremity deep venous thrombosis, or bloodstream infection). However, a similar rate of removal of the catheters was reported for major and minor complications (53.8% vs. 52.5%; P = .90). Across sites, there was substantial variation in utilization rates (0.97%-12.92%; P less than .001), dwell time and indication for use, and complication rates (3.4%-16.7%; P = .07).
The article does not provide guidance on when and how midline catheters should be used in order to minimize risk; nor does it include a comparison with traditional peripheral intravenous catheters or with PICC lines. Further studies are needed to guide indications and practices for catheter placement in order to minimize risk. Providers should continue to carefully consider the risks and benefits of midline catheter placement in individual cases.
Bottom line: Midline catheter placement more commonly leads to minor rather than major complications, though patterns of use and outcomes vary substantially across sites.
Citation: Chopra V et al. Variation in use and outcomes related to midline catheters: results from a multicentre pilot study. BMJ Qual Saf. 2019 Mar 18. doi: 10.1136/bmjqs-2018-008554.
Dr. Marcantonio is a Med-Peds hospitalist at Duke University Health System.
Background: Midline catheters have gained popularity in inpatient medical settings as a convenient alternative to PICC lines. This is primarily because of the ability to avoid central line–associated bloodstream infections (CLABSI) since these catheters terminate in the peripheral veins and cannot be reported as such. Additionally, they are potentially able to dwell longer than are traditional peripheral intravenous catheters. However, insufficient data exist to accurately describe the rate of complications in these catheters, as prior studies are based on single-center experiences.
Study design: Multicenter prospective cohort study.
Setting: Hospital medicine ward or medical ICU.
Synopsis: With use of a large database of adult patients from a quality initiative supported by Blue Cross Blue Shield of Michigan and Blue Care Network, this study identified 1,161 patients who had midline catheters placed and showed a 10.3% complication rate, of which 66.7% were minor (dislodgment, leaking, infiltration, or superficial thrombophlebitis) rather than major complications (occlusion, symptomatic upper-extremity deep venous thrombosis, or bloodstream infection). However, a similar rate of removal of the catheters was reported for major and minor complications (53.8% vs. 52.5%; P = .90). Across sites, there was substantial variation in utilization rates (0.97%-12.92%; P less than .001), dwell time and indication for use, and complication rates (3.4%-16.7%; P = .07).
The article does not provide guidance on when and how midline catheters should be used in order to minimize risk; nor does it include a comparison with traditional peripheral intravenous catheters or with PICC lines. Further studies are needed to guide indications and practices for catheter placement in order to minimize risk. Providers should continue to carefully consider the risks and benefits of midline catheter placement in individual cases.
Bottom line: Midline catheter placement more commonly leads to minor rather than major complications, though patterns of use and outcomes vary substantially across sites.
Citation: Chopra V et al. Variation in use and outcomes related to midline catheters: results from a multicentre pilot study. BMJ Qual Saf. 2019 Mar 18. doi: 10.1136/bmjqs-2018-008554.
Dr. Marcantonio is a Med-Peds hospitalist at Duke University Health System.
Background: Midline catheters have gained popularity in inpatient medical settings as a convenient alternative to PICC lines. This is primarily because of the ability to avoid central line–associated bloodstream infections (CLABSI) since these catheters terminate in the peripheral veins and cannot be reported as such. Additionally, they are potentially able to dwell longer than are traditional peripheral intravenous catheters. However, insufficient data exist to accurately describe the rate of complications in these catheters, as prior studies are based on single-center experiences.
Study design: Multicenter prospective cohort study.
Setting: Hospital medicine ward or medical ICU.
Synopsis: With use of a large database of adult patients from a quality initiative supported by Blue Cross Blue Shield of Michigan and Blue Care Network, this study identified 1,161 patients who had midline catheters placed and showed a 10.3% complication rate, of which 66.7% were minor (dislodgment, leaking, infiltration, or superficial thrombophlebitis) rather than major complications (occlusion, symptomatic upper-extremity deep venous thrombosis, or bloodstream infection). However, a similar rate of removal of the catheters was reported for major and minor complications (53.8% vs. 52.5%; P = .90). Across sites, there was substantial variation in utilization rates (0.97%-12.92%; P less than .001), dwell time and indication for use, and complication rates (3.4%-16.7%; P = .07).
The article does not provide guidance on when and how midline catheters should be used in order to minimize risk; nor does it include a comparison with traditional peripheral intravenous catheters or with PICC lines. Further studies are needed to guide indications and practices for catheter placement in order to minimize risk. Providers should continue to carefully consider the risks and benefits of midline catheter placement in individual cases.
Bottom line: Midline catheter placement more commonly leads to minor rather than major complications, though patterns of use and outcomes vary substantially across sites.
Citation: Chopra V et al. Variation in use and outcomes related to midline catheters: results from a multicentre pilot study. BMJ Qual Saf. 2019 Mar 18. doi: 10.1136/bmjqs-2018-008554.
Dr. Marcantonio is a Med-Peds hospitalist at Duke University Health System.
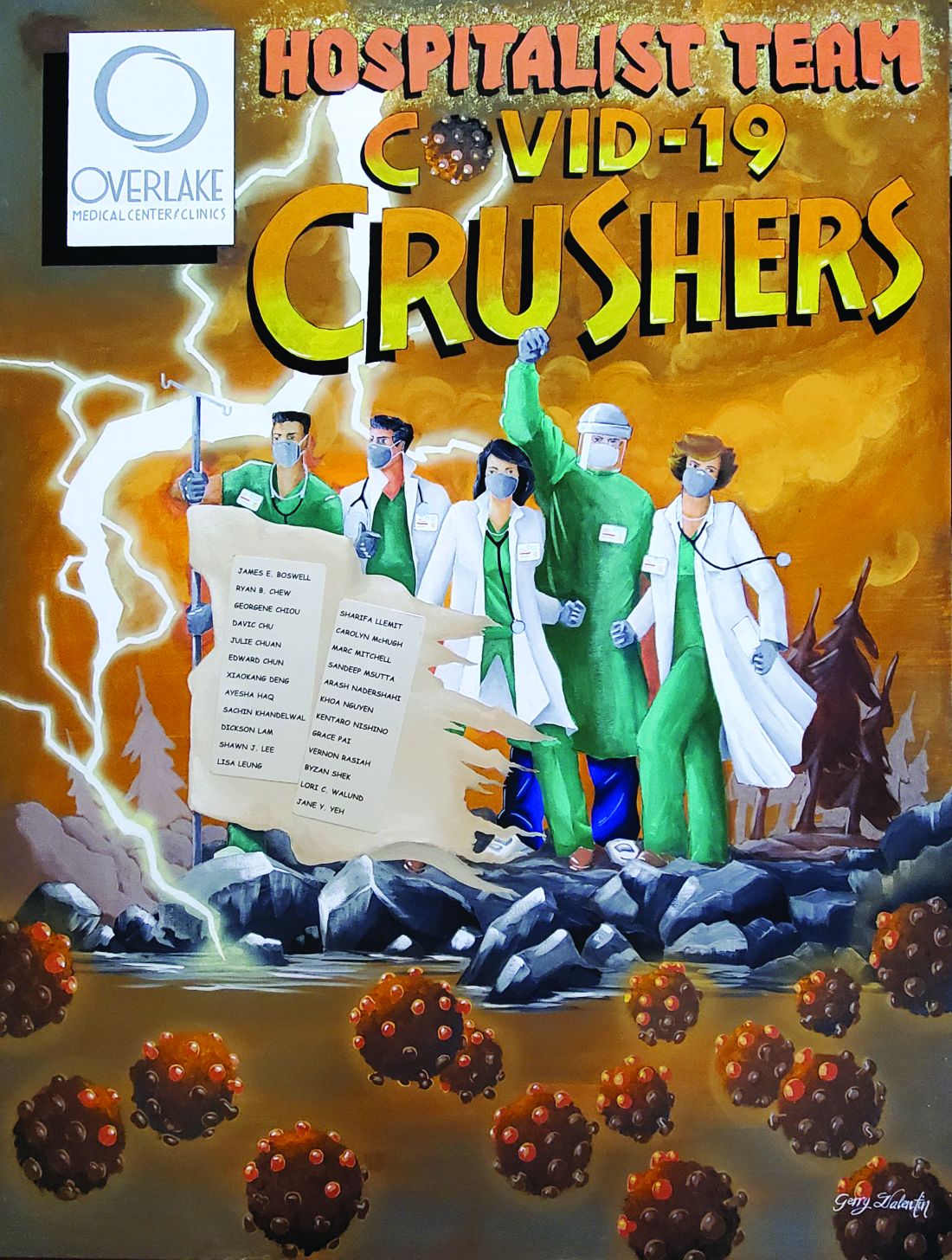
COVID-19 crushers: An appreciation of hospitalists
The hospitalist team at Overlake Medical Center and Clinics in Bellevue, Wash., has been a major partner of our Clinical Documentation Integrity Department in achieving its goal of accurately capturing the quality care patients receive on their records.
For many years, we have been witnesses of our hospitalists’ hard work, and the unique challenges of this pandemic further showed their tenacity and resilience. I thought that the best way to tell this story is through the poster accompanying this article.
To the viewer, this demonstrates the fierce battle raging between our hospitalists and the invisible foe, COVID-19. To my hospitalist colleagues, this is a constant reminder, albeit visually, that you are appreciated, admired and valued – not only by the CDI Department but by the whole organization as well.
Beyond my local colleagues, I would like to also thank the hospitalists working around the globe for their dedication and resolve in fighting this pandemic.
Mr. Valentin is a nurse and Certified Clinical Documentation Integrity Specialist at Overlake Medical Center and Clinics, Bellevue, Wash. His clinical specialties within nursing practice are in the OR, acute inpatient psychiatry, and the AIDS Unit.
The hospitalist team at Overlake Medical Center and Clinics in Bellevue, Wash., has been a major partner of our Clinical Documentation Integrity Department in achieving its goal of accurately capturing the quality care patients receive on their records.
For many years, we have been witnesses of our hospitalists’ hard work, and the unique challenges of this pandemic further showed their tenacity and resilience. I thought that the best way to tell this story is through the poster accompanying this article.
To the viewer, this demonstrates the fierce battle raging between our hospitalists and the invisible foe, COVID-19. To my hospitalist colleagues, this is a constant reminder, albeit visually, that you are appreciated, admired and valued – not only by the CDI Department but by the whole organization as well.
Beyond my local colleagues, I would like to also thank the hospitalists working around the globe for their dedication and resolve in fighting this pandemic.
Mr. Valentin is a nurse and Certified Clinical Documentation Integrity Specialist at Overlake Medical Center and Clinics, Bellevue, Wash. His clinical specialties within nursing practice are in the OR, acute inpatient psychiatry, and the AIDS Unit.
The hospitalist team at Overlake Medical Center and Clinics in Bellevue, Wash., has been a major partner of our Clinical Documentation Integrity Department in achieving its goal of accurately capturing the quality care patients receive on their records.
For many years, we have been witnesses of our hospitalists’ hard work, and the unique challenges of this pandemic further showed their tenacity and resilience. I thought that the best way to tell this story is through the poster accompanying this article.
To the viewer, this demonstrates the fierce battle raging between our hospitalists and the invisible foe, COVID-19. To my hospitalist colleagues, this is a constant reminder, albeit visually, that you are appreciated, admired and valued – not only by the CDI Department but by the whole organization as well.
Beyond my local colleagues, I would like to also thank the hospitalists working around the globe for their dedication and resolve in fighting this pandemic.
Mr. Valentin is a nurse and Certified Clinical Documentation Integrity Specialist at Overlake Medical Center and Clinics, Bellevue, Wash. His clinical specialties within nursing practice are in the OR, acute inpatient psychiatry, and the AIDS Unit.