User login
Finding a new approach to difficult diagnoses
Reducing – or managing – uncertainty
Beyond its clinical objective, the Socrates Project also seeks to further the discovery of previously unrecognized disease processes.
Many patients do not have a diagnosis that explains their signs and symptoms, despite a thorough evaluation, said Benjamin Singer, MD, assistant professor of pulmonology and critical care at Northwestern Medicine in Chicago. To address that problem, he and his colleagues launched the Socrates Project. The service is intended for difficult diagnoses and is based on Socratic principles, particularly the role of iterative hypothesis testing in the process of diagnosis.
“We began the Socrates Project to assist physicians caring for patients who lack a specific diagnosis. In creating this service, we have found ourselves to be doctors for doctors – formalizing the curbside consultation,” Dr. Singer said.
Northwestern Medicine launched the Socrates Project in 2015. It’s a physician-to-physician consultation service that assists doctors working to diagnose conditions that have so far eluded detection. “Our service’s goal is to improve patient care by providing an opinion to the referring physician on diagnostic possibilities for a particular case and ideas to reduce – or at least manage – diagnostic uncertainty,” they write. “Our service model is similar to a tumor board, which exists as an interdisciplinary group operating in parallel to the clinical services, to provide consensus-based recommendations.”
Hospitalists at other institutions may be interested in starting a similar type of service at their own institution or collaborating with institutions who offer this type of service, Dr. Singer said.
At Northwestern Medicine, they are at work on the project’s next steps. “We are working to generate systematic data about our practice, particularly the types of referrals and outcomes,” he said.
Reference
1. Singer BD, et al. The Socrates Project for Difficult Diagnosis at Northwestern Medicine. J Hosp Med. 2020 February;15(2):116-125. doi:10.12788/jhm.3335.
Reducing – or managing – uncertainty
Reducing – or managing – uncertainty
Beyond its clinical objective, the Socrates Project also seeks to further the discovery of previously unrecognized disease processes.
Many patients do not have a diagnosis that explains their signs and symptoms, despite a thorough evaluation, said Benjamin Singer, MD, assistant professor of pulmonology and critical care at Northwestern Medicine in Chicago. To address that problem, he and his colleagues launched the Socrates Project. The service is intended for difficult diagnoses and is based on Socratic principles, particularly the role of iterative hypothesis testing in the process of diagnosis.
“We began the Socrates Project to assist physicians caring for patients who lack a specific diagnosis. In creating this service, we have found ourselves to be doctors for doctors – formalizing the curbside consultation,” Dr. Singer said.
Northwestern Medicine launched the Socrates Project in 2015. It’s a physician-to-physician consultation service that assists doctors working to diagnose conditions that have so far eluded detection. “Our service’s goal is to improve patient care by providing an opinion to the referring physician on diagnostic possibilities for a particular case and ideas to reduce – or at least manage – diagnostic uncertainty,” they write. “Our service model is similar to a tumor board, which exists as an interdisciplinary group operating in parallel to the clinical services, to provide consensus-based recommendations.”
Hospitalists at other institutions may be interested in starting a similar type of service at their own institution or collaborating with institutions who offer this type of service, Dr. Singer said.
At Northwestern Medicine, they are at work on the project’s next steps. “We are working to generate systematic data about our practice, particularly the types of referrals and outcomes,” he said.
Reference
1. Singer BD, et al. The Socrates Project for Difficult Diagnosis at Northwestern Medicine. J Hosp Med. 2020 February;15(2):116-125. doi:10.12788/jhm.3335.
Beyond its clinical objective, the Socrates Project also seeks to further the discovery of previously unrecognized disease processes.
Many patients do not have a diagnosis that explains their signs and symptoms, despite a thorough evaluation, said Benjamin Singer, MD, assistant professor of pulmonology and critical care at Northwestern Medicine in Chicago. To address that problem, he and his colleagues launched the Socrates Project. The service is intended for difficult diagnoses and is based on Socratic principles, particularly the role of iterative hypothesis testing in the process of diagnosis.
“We began the Socrates Project to assist physicians caring for patients who lack a specific diagnosis. In creating this service, we have found ourselves to be doctors for doctors – formalizing the curbside consultation,” Dr. Singer said.
Northwestern Medicine launched the Socrates Project in 2015. It’s a physician-to-physician consultation service that assists doctors working to diagnose conditions that have so far eluded detection. “Our service’s goal is to improve patient care by providing an opinion to the referring physician on diagnostic possibilities for a particular case and ideas to reduce – or at least manage – diagnostic uncertainty,” they write. “Our service model is similar to a tumor board, which exists as an interdisciplinary group operating in parallel to the clinical services, to provide consensus-based recommendations.”
Hospitalists at other institutions may be interested in starting a similar type of service at their own institution or collaborating with institutions who offer this type of service, Dr. Singer said.
At Northwestern Medicine, they are at work on the project’s next steps. “We are working to generate systematic data about our practice, particularly the types of referrals and outcomes,” he said.
Reference
1. Singer BD, et al. The Socrates Project for Difficult Diagnosis at Northwestern Medicine. J Hosp Med. 2020 February;15(2):116-125. doi:10.12788/jhm.3335.
Is COVID-19 accelerating progress toward high-value care?
As Rachna Rawal, MD, was donning her personal protective equipment (PPE), a process that has become deeply ingrained into her muscle memory, a nurse approached her to ask, “Hey, for Mr. Smith, any chance we can time these labs to be done together with his medication administration? We’ve been in and out of that room a few times already.”
As someone who embraces high-value care, this simple suggestion surprised her. What an easy strategy to minimize room entry with full PPE, lab testing, and patient interruptions. That same day, someone else asked, “Do we need overnight vitals?”
COVID-19 has forced hospitalists to reconsider almost every aspect of care. It feels like every decision we make including things we do routinely – labs, vital signs, imaging – needs to be reassessed to determine the actual benefit to the patient balanced against concerns about staff safety, dwindling PPE supplies, and medication reserves. We are all faced with frequently answering the question, “How will this intervention help the patient?” This question lies at the heart of delivering high-value care.
High-value care is providing the best care possible through efficient use of resources, achieving optimal results for each patient. While high-value care has become a prominent focus over the past decade, COVID-19’s high transmissibility without a cure – and associated scarcity of health care resources – have sparked additional discussions on the front lines about promoting patient outcomes while avoiding waste. Clinicians may not have realized that these were high-value care conversations.
The United States’ health care quality and cost crises, worsened in the face of the current pandemic, have been glaringly apparent for years. Our country is spending more money on health care than anywhere else in the world without desired improvements in patient outcomes. A 2019 JAMA study found that 25% of all health care spending, an estimated $760 to $935 billion, is considered waste, and a significant proportion of this waste is due to repetitive care, overuse and unnecessary care in the U.S.1
Examples of low-value care tests include ordering daily labs in stable medicine inpatients, routine urine electrolytes in acute kidney injury, and folate testing in anemia. The Choosing Wisely® national campaign, Journal of Hospital Medicine’s “Things We Do For No Reason,” and JAMA Internal Medicine’s “Teachable Moment” series have provided guidance on areas where common testing or interventions may not benefit patient outcomes.
The COVID-19 pandemic has raised questions related to other widely-utilized practices: Can medication times be readjusted to allow only one entry into the room? Will these labs or imaging studies actually change management? Are vital checks every 4 hours needed?
Why did it take the COVID-19 threat to our medical system to force many of us to have these discussions? Despite prior efforts to integrate high-value care into hospital practices, long-standing habits and deep-seeded culture are challenging to overcome. Once clinicians develop practice habits, these behaviors tend to persist throughout their careers.2 In many ways, COVID-19 was like hitting a “reset button” as health care professionals were forced to rapidly confront their deeply-ingrained hospital practices and habits. From new protocols for patient rounding to universal masking and social distancing to ground-breaking strategies like awake proning, the response to COVID-19 has represented an unprecedented rapid shift in practice. Previously, consequences of overuse were too downstream or too abstract for clinicians to see in real-time. However, now the ramifications of these choices hit closer to home with obvious potential consequences – like spreading a terrifying virus.
There are three interventions that hospitalists should consider implementing immediately in the COVID-19 era that accelerate us toward high-value care. Routine lab tests, imaging, and overnight vitals represent opportunities to provide patient-centered care while also remaining cognizant of resource utilization.
One area in hospital medicine that has proven challenging to significantly change practice has been routine daily labs. Patients on a general medical inpatient service who are clinically stable generally do not benefit from routine lab work.3 Avoiding these tests does not increase mortality or length of stay in clinically stable patients.3 However, despite this evidence, many patients with COVID-19 and other conditions experience lab draws that are not timed together and are done each morning out of “routine.” Choosing Wisely® recommendations from the Society of Hospital Medicine encourage clinicians to question routine lab work for COVID-19 patients and to consider batching them, if possible.3,4 In COVID-19 patients, the risks of not batching tests are magnified, both in terms of the patient-centered experience and for clinician safety. In essence, COVID-19 has pushed us to consider the elements of safety, PPE conservation and other factors, rather than making decisions based solely on their own comfort, convenience, or historical practice.
Clinicians are also reconsidering the necessity of imaging during the pandemic. The “Things We Do For No Reason” article on “Choosing Wisely® in the COVID-19 era” highlights this well.4 It is more important now than ever to decide whether the timing and type of imaging will change management for your patient. Questions to ask include: Can a portable x-ray be used to avoid patient travel and will that CT scan help your patient? A posterior-anterior/lateral x-ray can potentially provide more information depending on the clinical scenario. However, we now need to assess if that extra information is going to impact patient management. Downstream consequences of these decisions include not only risks to the patient but also infectious exposures for staff and others during patient travel.
Lastly, overnight vital sign checks are another intervention we should analyze through this high-value care lens. The Journal of Hospital Medicine released a “Things We Do For No Reason” article about minimizing overnight vitals to promote uninterrupted sleep at night.5 Deleterious effects of interrupting the sleep of our patients include delirium and patient dissatisfaction.5 Studies have shown the benefits of this approach, yet the shift away from routine overnight vitals has not yet widely occurred.
COVID-19 has pressed us to save PPE and minimize exposure risk; hence, some centers are coordinating the timing of vitals with medication administration times, when feasible. In the stable patient recovering from COVID-19, overnight vitals may not be necessary, particularly if remote monitoring is available. This accomplishes multiple goals: Providing high quality patient care, reducing resource utilization, and minimizing patient nighttime interruptions – all culminating in high-value care.
Even though the COVID-19 pandemic has brought unforeseen emotional, physical, and financial challenges for the health care system and its workers, there may be a silver lining. The pandemic has sparked high-value care discussions, and the urgency of the crisis may be instilling new practices in our daily work. This virus has indeed left a terrible wake of destruction, but may also be a nudge to permanently change our culture of overuse to help us shape the habits of all trainees during this tumultuous time. This experience will hopefully culminate in a culture in which clinicians routinely ask, “How will this intervention help the patient?”
Dr. Rawal is clinical assistant professor of medicine, University of Pittsburgh. Dr. Linker is assistant professor of medicine, Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York. Dr. Moriates is associate professor of internal medicine, Dell Medical School at the University of Texas at Austin.
References
1. Shrank W et al. Waste in The US healthcare system. JAMA. 2019;322(15):1501-9.
2. Chen C et al. Spending patterns in region of residency training and subsequent expenditures for care provided by practicing physicians for Medicare beneficiaries. JAMA. 2014;312(22):2385-93.
3. Eaton KP et al. Evidence-based guidelines to eliminate repetitive laboratory testing. JAMA Intern Med. 2017;177(12):1833-9.
4. Cho H et al. Choosing Wisely in the COVID-19 Era: Preventing harm to healthcare workers. J Hosp Med. 2020;15(6):360-2.
5. Orlov N and Arora V. Things we do for no reason: Routine overnight vital sign checks. J Hosp Med. 2020;15(5):272-27.
As Rachna Rawal, MD, was donning her personal protective equipment (PPE), a process that has become deeply ingrained into her muscle memory, a nurse approached her to ask, “Hey, for Mr. Smith, any chance we can time these labs to be done together with his medication administration? We’ve been in and out of that room a few times already.”
As someone who embraces high-value care, this simple suggestion surprised her. What an easy strategy to minimize room entry with full PPE, lab testing, and patient interruptions. That same day, someone else asked, “Do we need overnight vitals?”
COVID-19 has forced hospitalists to reconsider almost every aspect of care. It feels like every decision we make including things we do routinely – labs, vital signs, imaging – needs to be reassessed to determine the actual benefit to the patient balanced against concerns about staff safety, dwindling PPE supplies, and medication reserves. We are all faced with frequently answering the question, “How will this intervention help the patient?” This question lies at the heart of delivering high-value care.
High-value care is providing the best care possible through efficient use of resources, achieving optimal results for each patient. While high-value care has become a prominent focus over the past decade, COVID-19’s high transmissibility without a cure – and associated scarcity of health care resources – have sparked additional discussions on the front lines about promoting patient outcomes while avoiding waste. Clinicians may not have realized that these were high-value care conversations.
The United States’ health care quality and cost crises, worsened in the face of the current pandemic, have been glaringly apparent for years. Our country is spending more money on health care than anywhere else in the world without desired improvements in patient outcomes. A 2019 JAMA study found that 25% of all health care spending, an estimated $760 to $935 billion, is considered waste, and a significant proportion of this waste is due to repetitive care, overuse and unnecessary care in the U.S.1
Examples of low-value care tests include ordering daily labs in stable medicine inpatients, routine urine electrolytes in acute kidney injury, and folate testing in anemia. The Choosing Wisely® national campaign, Journal of Hospital Medicine’s “Things We Do For No Reason,” and JAMA Internal Medicine’s “Teachable Moment” series have provided guidance on areas where common testing or interventions may not benefit patient outcomes.
The COVID-19 pandemic has raised questions related to other widely-utilized practices: Can medication times be readjusted to allow only one entry into the room? Will these labs or imaging studies actually change management? Are vital checks every 4 hours needed?
Why did it take the COVID-19 threat to our medical system to force many of us to have these discussions? Despite prior efforts to integrate high-value care into hospital practices, long-standing habits and deep-seeded culture are challenging to overcome. Once clinicians develop practice habits, these behaviors tend to persist throughout their careers.2 In many ways, COVID-19 was like hitting a “reset button” as health care professionals were forced to rapidly confront their deeply-ingrained hospital practices and habits. From new protocols for patient rounding to universal masking and social distancing to ground-breaking strategies like awake proning, the response to COVID-19 has represented an unprecedented rapid shift in practice. Previously, consequences of overuse were too downstream or too abstract for clinicians to see in real-time. However, now the ramifications of these choices hit closer to home with obvious potential consequences – like spreading a terrifying virus.
There are three interventions that hospitalists should consider implementing immediately in the COVID-19 era that accelerate us toward high-value care. Routine lab tests, imaging, and overnight vitals represent opportunities to provide patient-centered care while also remaining cognizant of resource utilization.
One area in hospital medicine that has proven challenging to significantly change practice has been routine daily labs. Patients on a general medical inpatient service who are clinically stable generally do not benefit from routine lab work.3 Avoiding these tests does not increase mortality or length of stay in clinically stable patients.3 However, despite this evidence, many patients with COVID-19 and other conditions experience lab draws that are not timed together and are done each morning out of “routine.” Choosing Wisely® recommendations from the Society of Hospital Medicine encourage clinicians to question routine lab work for COVID-19 patients and to consider batching them, if possible.3,4 In COVID-19 patients, the risks of not batching tests are magnified, both in terms of the patient-centered experience and for clinician safety. In essence, COVID-19 has pushed us to consider the elements of safety, PPE conservation and other factors, rather than making decisions based solely on their own comfort, convenience, or historical practice.
Clinicians are also reconsidering the necessity of imaging during the pandemic. The “Things We Do For No Reason” article on “Choosing Wisely® in the COVID-19 era” highlights this well.4 It is more important now than ever to decide whether the timing and type of imaging will change management for your patient. Questions to ask include: Can a portable x-ray be used to avoid patient travel and will that CT scan help your patient? A posterior-anterior/lateral x-ray can potentially provide more information depending on the clinical scenario. However, we now need to assess if that extra information is going to impact patient management. Downstream consequences of these decisions include not only risks to the patient but also infectious exposures for staff and others during patient travel.
Lastly, overnight vital sign checks are another intervention we should analyze through this high-value care lens. The Journal of Hospital Medicine released a “Things We Do For No Reason” article about minimizing overnight vitals to promote uninterrupted sleep at night.5 Deleterious effects of interrupting the sleep of our patients include delirium and patient dissatisfaction.5 Studies have shown the benefits of this approach, yet the shift away from routine overnight vitals has not yet widely occurred.
COVID-19 has pressed us to save PPE and minimize exposure risk; hence, some centers are coordinating the timing of vitals with medication administration times, when feasible. In the stable patient recovering from COVID-19, overnight vitals may not be necessary, particularly if remote monitoring is available. This accomplishes multiple goals: Providing high quality patient care, reducing resource utilization, and minimizing patient nighttime interruptions – all culminating in high-value care.
Even though the COVID-19 pandemic has brought unforeseen emotional, physical, and financial challenges for the health care system and its workers, there may be a silver lining. The pandemic has sparked high-value care discussions, and the urgency of the crisis may be instilling new practices in our daily work. This virus has indeed left a terrible wake of destruction, but may also be a nudge to permanently change our culture of overuse to help us shape the habits of all trainees during this tumultuous time. This experience will hopefully culminate in a culture in which clinicians routinely ask, “How will this intervention help the patient?”
Dr. Rawal is clinical assistant professor of medicine, University of Pittsburgh. Dr. Linker is assistant professor of medicine, Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York. Dr. Moriates is associate professor of internal medicine, Dell Medical School at the University of Texas at Austin.
References
1. Shrank W et al. Waste in The US healthcare system. JAMA. 2019;322(15):1501-9.
2. Chen C et al. Spending patterns in region of residency training and subsequent expenditures for care provided by practicing physicians for Medicare beneficiaries. JAMA. 2014;312(22):2385-93.
3. Eaton KP et al. Evidence-based guidelines to eliminate repetitive laboratory testing. JAMA Intern Med. 2017;177(12):1833-9.
4. Cho H et al. Choosing Wisely in the COVID-19 Era: Preventing harm to healthcare workers. J Hosp Med. 2020;15(6):360-2.
5. Orlov N and Arora V. Things we do for no reason: Routine overnight vital sign checks. J Hosp Med. 2020;15(5):272-27.
As Rachna Rawal, MD, was donning her personal protective equipment (PPE), a process that has become deeply ingrained into her muscle memory, a nurse approached her to ask, “Hey, for Mr. Smith, any chance we can time these labs to be done together with his medication administration? We’ve been in and out of that room a few times already.”
As someone who embraces high-value care, this simple suggestion surprised her. What an easy strategy to minimize room entry with full PPE, lab testing, and patient interruptions. That same day, someone else asked, “Do we need overnight vitals?”
COVID-19 has forced hospitalists to reconsider almost every aspect of care. It feels like every decision we make including things we do routinely – labs, vital signs, imaging – needs to be reassessed to determine the actual benefit to the patient balanced against concerns about staff safety, dwindling PPE supplies, and medication reserves. We are all faced with frequently answering the question, “How will this intervention help the patient?” This question lies at the heart of delivering high-value care.
High-value care is providing the best care possible through efficient use of resources, achieving optimal results for each patient. While high-value care has become a prominent focus over the past decade, COVID-19’s high transmissibility without a cure – and associated scarcity of health care resources – have sparked additional discussions on the front lines about promoting patient outcomes while avoiding waste. Clinicians may not have realized that these were high-value care conversations.
The United States’ health care quality and cost crises, worsened in the face of the current pandemic, have been glaringly apparent for years. Our country is spending more money on health care than anywhere else in the world without desired improvements in patient outcomes. A 2019 JAMA study found that 25% of all health care spending, an estimated $760 to $935 billion, is considered waste, and a significant proportion of this waste is due to repetitive care, overuse and unnecessary care in the U.S.1
Examples of low-value care tests include ordering daily labs in stable medicine inpatients, routine urine electrolytes in acute kidney injury, and folate testing in anemia. The Choosing Wisely® national campaign, Journal of Hospital Medicine’s “Things We Do For No Reason,” and JAMA Internal Medicine’s “Teachable Moment” series have provided guidance on areas where common testing or interventions may not benefit patient outcomes.
The COVID-19 pandemic has raised questions related to other widely-utilized practices: Can medication times be readjusted to allow only one entry into the room? Will these labs or imaging studies actually change management? Are vital checks every 4 hours needed?
Why did it take the COVID-19 threat to our medical system to force many of us to have these discussions? Despite prior efforts to integrate high-value care into hospital practices, long-standing habits and deep-seeded culture are challenging to overcome. Once clinicians develop practice habits, these behaviors tend to persist throughout their careers.2 In many ways, COVID-19 was like hitting a “reset button” as health care professionals were forced to rapidly confront their deeply-ingrained hospital practices and habits. From new protocols for patient rounding to universal masking and social distancing to ground-breaking strategies like awake proning, the response to COVID-19 has represented an unprecedented rapid shift in practice. Previously, consequences of overuse were too downstream or too abstract for clinicians to see in real-time. However, now the ramifications of these choices hit closer to home with obvious potential consequences – like spreading a terrifying virus.
There are three interventions that hospitalists should consider implementing immediately in the COVID-19 era that accelerate us toward high-value care. Routine lab tests, imaging, and overnight vitals represent opportunities to provide patient-centered care while also remaining cognizant of resource utilization.
One area in hospital medicine that has proven challenging to significantly change practice has been routine daily labs. Patients on a general medical inpatient service who are clinically stable generally do not benefit from routine lab work.3 Avoiding these tests does not increase mortality or length of stay in clinically stable patients.3 However, despite this evidence, many patients with COVID-19 and other conditions experience lab draws that are not timed together and are done each morning out of “routine.” Choosing Wisely® recommendations from the Society of Hospital Medicine encourage clinicians to question routine lab work for COVID-19 patients and to consider batching them, if possible.3,4 In COVID-19 patients, the risks of not batching tests are magnified, both in terms of the patient-centered experience and for clinician safety. In essence, COVID-19 has pushed us to consider the elements of safety, PPE conservation and other factors, rather than making decisions based solely on their own comfort, convenience, or historical practice.
Clinicians are also reconsidering the necessity of imaging during the pandemic. The “Things We Do For No Reason” article on “Choosing Wisely® in the COVID-19 era” highlights this well.4 It is more important now than ever to decide whether the timing and type of imaging will change management for your patient. Questions to ask include: Can a portable x-ray be used to avoid patient travel and will that CT scan help your patient? A posterior-anterior/lateral x-ray can potentially provide more information depending on the clinical scenario. However, we now need to assess if that extra information is going to impact patient management. Downstream consequences of these decisions include not only risks to the patient but also infectious exposures for staff and others during patient travel.
Lastly, overnight vital sign checks are another intervention we should analyze through this high-value care lens. The Journal of Hospital Medicine released a “Things We Do For No Reason” article about minimizing overnight vitals to promote uninterrupted sleep at night.5 Deleterious effects of interrupting the sleep of our patients include delirium and patient dissatisfaction.5 Studies have shown the benefits of this approach, yet the shift away from routine overnight vitals has not yet widely occurred.
COVID-19 has pressed us to save PPE and minimize exposure risk; hence, some centers are coordinating the timing of vitals with medication administration times, when feasible. In the stable patient recovering from COVID-19, overnight vitals may not be necessary, particularly if remote monitoring is available. This accomplishes multiple goals: Providing high quality patient care, reducing resource utilization, and minimizing patient nighttime interruptions – all culminating in high-value care.
Even though the COVID-19 pandemic has brought unforeseen emotional, physical, and financial challenges for the health care system and its workers, there may be a silver lining. The pandemic has sparked high-value care discussions, and the urgency of the crisis may be instilling new practices in our daily work. This virus has indeed left a terrible wake of destruction, but may also be a nudge to permanently change our culture of overuse to help us shape the habits of all trainees during this tumultuous time. This experience will hopefully culminate in a culture in which clinicians routinely ask, “How will this intervention help the patient?”
Dr. Rawal is clinical assistant professor of medicine, University of Pittsburgh. Dr. Linker is assistant professor of medicine, Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York. Dr. Moriates is associate professor of internal medicine, Dell Medical School at the University of Texas at Austin.
References
1. Shrank W et al. Waste in The US healthcare system. JAMA. 2019;322(15):1501-9.
2. Chen C et al. Spending patterns in region of residency training and subsequent expenditures for care provided by practicing physicians for Medicare beneficiaries. JAMA. 2014;312(22):2385-93.
3. Eaton KP et al. Evidence-based guidelines to eliminate repetitive laboratory testing. JAMA Intern Med. 2017;177(12):1833-9.
4. Cho H et al. Choosing Wisely in the COVID-19 Era: Preventing harm to healthcare workers. J Hosp Med. 2020;15(6):360-2.
5. Orlov N and Arora V. Things we do for no reason: Routine overnight vital sign checks. J Hosp Med. 2020;15(5):272-27.
New updates for Choosing Wisely in hospitalized patients with infection
Background: A new update to the Choosing Wisely Campaign was released September 2019.
Study design: Expert consensus recommendations from the American Society for Clinical Pathology.
Synopsis: Eleven of the 30 Choosing Wisely recommendations directly affect hospital medicine. Half of these recommendations are related to infectious diseases. Highlights include:
- Not routinely using broad respiratory viral testing and instead using more targeted approaches to respiratory pathogen tests (e.g., respiratory syncytial virus, influenza A/B, or group A pharyngitis) unless the results will lead to changes to or discontinuations of antimicrobial therapy or isolation.
- Not routinely testing for community gastrointestinal pathogens in patients that develop diarrhea 3 days after hospitalization and to primarily test for Clostridiodes difficile in these patients, unless they are immunocompromised or older adults.
- Not checking procalcitonin unless a specific evidence-based guideline is used for antibiotic stewardship, as it is often used incorrectly without benefit to the patient.
- Not ordering serology for Helicobacter pylori and instead ordering the stool antigen or breath test to test for active infection given higher sensitivity and specificity.
- Not repeating antibody tests for patients with history of hepatitis C and instead ordering a viral load if there is concern for reinfection.
Bottom line: Only order infectious disease tests that will guide changes in clinical management.
Citation: ASCP Effective Test Utilization Steering Committee. Thirty things patients and physicians should question. 2019 Sep 9. Choosingwisely.org.
Dr. Blount is clinical instructor of medicine, hospital medicine, at the Rocky Mountain Veterans Affairs Regional Medical Center, Aurora, Colo.
Background: A new update to the Choosing Wisely Campaign was released September 2019.
Study design: Expert consensus recommendations from the American Society for Clinical Pathology.
Synopsis: Eleven of the 30 Choosing Wisely recommendations directly affect hospital medicine. Half of these recommendations are related to infectious diseases. Highlights include:
- Not routinely using broad respiratory viral testing and instead using more targeted approaches to respiratory pathogen tests (e.g., respiratory syncytial virus, influenza A/B, or group A pharyngitis) unless the results will lead to changes to or discontinuations of antimicrobial therapy or isolation.
- Not routinely testing for community gastrointestinal pathogens in patients that develop diarrhea 3 days after hospitalization and to primarily test for Clostridiodes difficile in these patients, unless they are immunocompromised or older adults.
- Not checking procalcitonin unless a specific evidence-based guideline is used for antibiotic stewardship, as it is often used incorrectly without benefit to the patient.
- Not ordering serology for Helicobacter pylori and instead ordering the stool antigen or breath test to test for active infection given higher sensitivity and specificity.
- Not repeating antibody tests for patients with history of hepatitis C and instead ordering a viral load if there is concern for reinfection.
Bottom line: Only order infectious disease tests that will guide changes in clinical management.
Citation: ASCP Effective Test Utilization Steering Committee. Thirty things patients and physicians should question. 2019 Sep 9. Choosingwisely.org.
Dr. Blount is clinical instructor of medicine, hospital medicine, at the Rocky Mountain Veterans Affairs Regional Medical Center, Aurora, Colo.
Background: A new update to the Choosing Wisely Campaign was released September 2019.
Study design: Expert consensus recommendations from the American Society for Clinical Pathology.
Synopsis: Eleven of the 30 Choosing Wisely recommendations directly affect hospital medicine. Half of these recommendations are related to infectious diseases. Highlights include:
- Not routinely using broad respiratory viral testing and instead using more targeted approaches to respiratory pathogen tests (e.g., respiratory syncytial virus, influenza A/B, or group A pharyngitis) unless the results will lead to changes to or discontinuations of antimicrobial therapy or isolation.
- Not routinely testing for community gastrointestinal pathogens in patients that develop diarrhea 3 days after hospitalization and to primarily test for Clostridiodes difficile in these patients, unless they are immunocompromised or older adults.
- Not checking procalcitonin unless a specific evidence-based guideline is used for antibiotic stewardship, as it is often used incorrectly without benefit to the patient.
- Not ordering serology for Helicobacter pylori and instead ordering the stool antigen or breath test to test for active infection given higher sensitivity and specificity.
- Not repeating antibody tests for patients with history of hepatitis C and instead ordering a viral load if there is concern for reinfection.
Bottom line: Only order infectious disease tests that will guide changes in clinical management.
Citation: ASCP Effective Test Utilization Steering Committee. Thirty things patients and physicians should question. 2019 Sep 9. Choosingwisely.org.
Dr. Blount is clinical instructor of medicine, hospital medicine, at the Rocky Mountain Veterans Affairs Regional Medical Center, Aurora, Colo.
Think twice before intensifying BP regimen in older hospitalized patients
Background: It is common practice for providers to intensify antihypertensive regimen during admission for noncardiac conditions even if a patient has a history of well-controlled blood pressure as an outpatient. Many providers have assumed that these changes will benefit patients; however, this outcome had never been studied.
Study design: Retrospective cohort study.
Setting: Veterans Affairs hospitals.
Synopsis: The authors analyzed a well-matched retrospective cohort of 4,056 adults aged 65 years or older with hypertension who were admitted for noncardiac conditions including pneumonia, urinary tract infection, and venous thromboembolism. Half of the cohort was discharged with intensification of their antihypertensives, defined as a new antihypertensive medication or an increase of 20% of a prior medication.
Patients discharged with regimen intensification were more likely to be readmitted (hazard ratio, 1.23; 95% confidence interval, 1.07-1.42; number needed to harm = 27), experience a medication-related serious adverse event (HR, 1.42; 95% CI, 1.06-1.88; NNH = 63), and have a cardiovascular event (HR, 1.65; 95% CI, 1.13-2.4) within 30 days of discharge. At 1 year, no significant difference in mortality, cardiovascular events, or systolic BP were noted between the two groups.
A subgroup analysis of patients with poorly controlled blood pressure as outpatients (defined as systolic blood pressure greater than 140 mm Hg) who had their anti-hypertensive medications intensified did not show significant difference in 30-day readmission, severe adverse events, or cardiovascular events.
Limitations of the study include observational design and majority male sex (97.5%) of the study population.
Bottom line: Intensification of antihypertensive regimen among older adults hospitalized for noncardiac conditions with well-controlled blood pressure as an outpatient can potentially cause harm.
Citation: Anderson TS et al. Clinical outcomes after intensifying antihypertensive medication regimens among older adults at hospital discharge. JAMA Intern Med. 2019 Aug 19. doi: 10.1001/jamainternmed.2019.3007.
Dr. Zarookian is a hospitalist at Maine Medical Center in Portland and Stephens Memorial Hospital in Norway, Maine.
Background: It is common practice for providers to intensify antihypertensive regimen during admission for noncardiac conditions even if a patient has a history of well-controlled blood pressure as an outpatient. Many providers have assumed that these changes will benefit patients; however, this outcome had never been studied.
Study design: Retrospective cohort study.
Setting: Veterans Affairs hospitals.
Synopsis: The authors analyzed a well-matched retrospective cohort of 4,056 adults aged 65 years or older with hypertension who were admitted for noncardiac conditions including pneumonia, urinary tract infection, and venous thromboembolism. Half of the cohort was discharged with intensification of their antihypertensives, defined as a new antihypertensive medication or an increase of 20% of a prior medication.
Patients discharged with regimen intensification were more likely to be readmitted (hazard ratio, 1.23; 95% confidence interval, 1.07-1.42; number needed to harm = 27), experience a medication-related serious adverse event (HR, 1.42; 95% CI, 1.06-1.88; NNH = 63), and have a cardiovascular event (HR, 1.65; 95% CI, 1.13-2.4) within 30 days of discharge. At 1 year, no significant difference in mortality, cardiovascular events, or systolic BP were noted between the two groups.
A subgroup analysis of patients with poorly controlled blood pressure as outpatients (defined as systolic blood pressure greater than 140 mm Hg) who had their anti-hypertensive medications intensified did not show significant difference in 30-day readmission, severe adverse events, or cardiovascular events.
Limitations of the study include observational design and majority male sex (97.5%) of the study population.
Bottom line: Intensification of antihypertensive regimen among older adults hospitalized for noncardiac conditions with well-controlled blood pressure as an outpatient can potentially cause harm.
Citation: Anderson TS et al. Clinical outcomes after intensifying antihypertensive medication regimens among older adults at hospital discharge. JAMA Intern Med. 2019 Aug 19. doi: 10.1001/jamainternmed.2019.3007.
Dr. Zarookian is a hospitalist at Maine Medical Center in Portland and Stephens Memorial Hospital in Norway, Maine.
Background: It is common practice for providers to intensify antihypertensive regimen during admission for noncardiac conditions even if a patient has a history of well-controlled blood pressure as an outpatient. Many providers have assumed that these changes will benefit patients; however, this outcome had never been studied.
Study design: Retrospective cohort study.
Setting: Veterans Affairs hospitals.
Synopsis: The authors analyzed a well-matched retrospective cohort of 4,056 adults aged 65 years or older with hypertension who were admitted for noncardiac conditions including pneumonia, urinary tract infection, and venous thromboembolism. Half of the cohort was discharged with intensification of their antihypertensives, defined as a new antihypertensive medication or an increase of 20% of a prior medication.
Patients discharged with regimen intensification were more likely to be readmitted (hazard ratio, 1.23; 95% confidence interval, 1.07-1.42; number needed to harm = 27), experience a medication-related serious adverse event (HR, 1.42; 95% CI, 1.06-1.88; NNH = 63), and have a cardiovascular event (HR, 1.65; 95% CI, 1.13-2.4) within 30 days of discharge. At 1 year, no significant difference in mortality, cardiovascular events, or systolic BP were noted between the two groups.
A subgroup analysis of patients with poorly controlled blood pressure as outpatients (defined as systolic blood pressure greater than 140 mm Hg) who had their anti-hypertensive medications intensified did not show significant difference in 30-day readmission, severe adverse events, or cardiovascular events.
Limitations of the study include observational design and majority male sex (97.5%) of the study population.
Bottom line: Intensification of antihypertensive regimen among older adults hospitalized for noncardiac conditions with well-controlled blood pressure as an outpatient can potentially cause harm.
Citation: Anderson TS et al. Clinical outcomes after intensifying antihypertensive medication regimens among older adults at hospital discharge. JAMA Intern Med. 2019 Aug 19. doi: 10.1001/jamainternmed.2019.3007.
Dr. Zarookian is a hospitalist at Maine Medical Center in Portland and Stephens Memorial Hospital in Norway, Maine.
Finding meaning in ‘Lean’?
Using systems improvement strategies to support the Quadruple Aim
General background on well-being and burnout
With burnout increasingly recognized as a shared responsibility that requires addressing organizational drivers while supporting individuals to be well,1-4 practical strategies and examples of successful implementation of systems interventions to address burnout will be helpful for service directors to support their staff. The Charter on Physician Well-being, recently developed through collaborative input from multiple organizations, defines guiding principles and key commitments at the societal, organizational, interpersonal, and individual levels and may be a useful framework for organizations that are developing well-being initiatives.5
The charter advocates including physician well-being as a quality improvement metric for health systems, aligned with the concept of the Quadruple Aim of optimizing patient care by enhancing provider experience, promoting high-value care, and improving population health.6 Identifying areas of alignment between the charter’s recommendations and systems improvement strategies that seek to optimize efficiency and reduce waste, such as Lean Management, may help physician leaders to contextualize well-being initiatives more easily within ongoing systems improvement efforts. In this perspective, we provide one division’s experience using the Charter to assess successes and identify additional areas of improvement for well-being initiatives developed using Lean Management methodology.
Past and current state of affairs
In 2011, the division of hospital medicine at Zuckerberg San Francisco General Hospital was established and has seen continual expansion in terms of direct patient care, medical education, and hospital leadership.
In 2015, the division of hospital medicine experienced leadership transitions, faculty attrition, and insufficient recruitment resulting in staffing shortages, service line closure, schedule instability, and ultimately, low morale. A baseline survey conducted using the 2-Item Maslach Burnout Inventory. This survey, which uses one item in the domain of emotional exhaustion and one item in the domain of depersonalization, has shown good correlation with the full Maslach Burnout Inventory.7 At baseline, approximately one-third of the division’s physicians experienced burnout.
In response, a subsequent retreat focused on the three greatest areas of concern identified by the survey: scheduling, faculty development, and well-being.
Like many health systems, the hospital has adopted Lean as its preferred systems-improvement framework. The retreat was structured around the principles of Lean philosophy, and was designed to emulate that of a consolidated Kaizen workshop.
“Kaizen” in Japanese means “change for the better.” A typical Kaizen workshop revolves around rapid problem-solving over the course of 3-5 days, in which a team of people come together to identify and implement significant improvements for a selected process. To this end, the retreat was divided into subgroups for each area of concern. In turn, each subgroup mapped out existing workflows (“value stream”), identified areas of waste and non–value added time, and generated ideas of what an idealized process would be. Next, a root-cause analysis was performed and subsequent interventions (“countermeasures”) developed to address each problem. At the conclusion of the retreat, each subgroup shared a summary of their findings with the larger group.
Moving forward, this information served as a guiding framework for service and division leadership to run small tests of change. We enacted a series of countermeasures over the course of several years, and multiple cycles of improvement work addressed the three areas of concern. We developed an A3 report (a Lean project management tool that incorporates the plan-do-study-act cycle, organizes strategic efforts, and tracks progress on a single page) to summarize and present these initiatives to the Performance Improvement and Patient Safety Committee of the hospital executive leadership team. This structure illustrated alignment with the hospital’s core values (“true north”) of “developing people” and “care experience.”
In 2018, interval surveys demonstrated a gradual reduction of burnout to approximately one-fifth of division physicians as measured by the 2-item Maslach Burnout Inventory.
Initiatives in faculty well-being
The Charter of Physician Well-being outlines a framework to promote well-being among doctors by maximizing a sense of fulfillment and minimizing the harms of burnout. It shares this responsibility among societal, organizational, and interpersonal and individual commitments.5
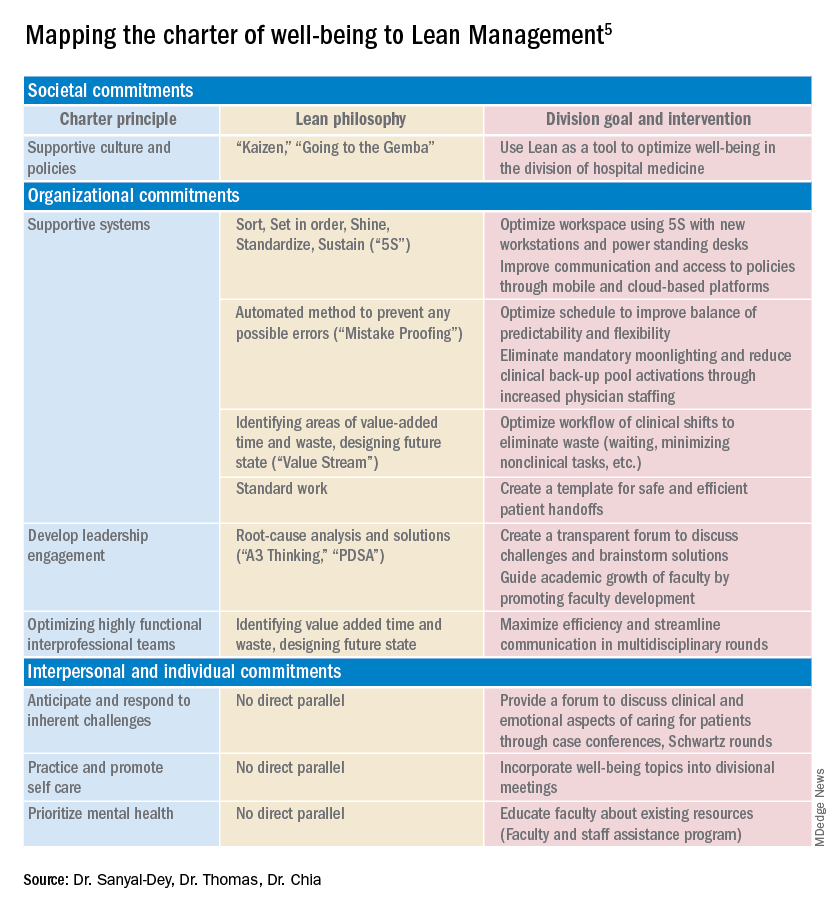
As illustrated above, we used principles of Lean Management to prospectively create initiatives to improve well-being in our division. Lean in health care is designed to optimize primarily the patient experience; its implementation has subsequently demonstrated mixed provider and staff experiences,8,9 and many providers are skeptical of Lean’s potential to improve their own well-being. If, however, Lean is aligned with best practice frameworks for well-being such as those outline in the charter, it may also help to meet the Quadruple Aim of optimizing both provider well-being and patient experience. To further test this hypothesis, we retrospectively categorized our Lean-based interventions into the commitments described by the charter to identify areas of alignment and gaps that were not initially addressed using Lean Management (Table).
Organizational commitments5Supportive systems
We optimized scheduling and enhanced physician staffing by budgeting for a physician staffing buffer each academic year in order to minimize mandatory moonlighting and jeopardy pool activations that result from operating on a thin staffing margin when expected personal leave and reductions in clinical effort occur. Furthermore, we revised scheduling principles to balance patient continuity and individual time off requests while setting limits on the maximum duration of clinical stretches and instituting mandatory minimum time off between them.
Leadership engagement
We initiated monthly operations meetings as a forum to discuss challenges, brainstorm solutions, and message new initiatives with group input. For example, as a result of these meetings, we designed and implemented an additional service line to address the high census, revised the distribution of new patient admissions to level-load clinical shifts, and established a maximum number of weekends worked per month and year. This approach aligns with recommendations to use participatory leadership strategies to enhance physician well-being.10 Engaging both executive level and service level management to focus on burnout and other related well-being metrics is necessary for sustaining such work.
Interprofessional teamwork
We revised multidisciplinary rounds with social work, utilization management, and physical therapy to maximize efficiency and streamline communication by developing standard approaches for each patient presentation.
Interpersonal and individual commitments5Address emotional challenges of physician work
Although these commitments did not have a direct corollary with Lean philosophy, some of these needs were identified by our physician group at our annual retreats. As a result, we initiated a monthly faculty-led noon conference series focused on the clinical challenges of caring for vulnerable populations, a particular source of distress in our practice setting, and revised the division schedule to encourage attendance at the hospital’s Schwartz rounds.
Mental health and self-care
We organized focus groups and faculty development sessions on provider well-being and burnout and dealing with challenging patients and invited the Faculty and Staff Assistance Program, our institution’s mental health service provider, to our weekly division meeting.
Future directions
After using Lean Management as an approach to prospectively improve physician well-being, we were able to use the Charter on Physician Well-being retrospectively as a “checklist” to identify additional gaps for targeted intervention to ensure all commitments are sufficiently addressed.
Overall, we found that, not surprisingly, Lean Management aligned best with the organizational commitments in the charter. Reviewing the organizational commitments, we found our biggest remaining challenges are in building supportive systems, namely ensuring sustainable workloads, offloading and delegating nonphysician tasks, and minimizing the burden of documentation and administration.
Reviewing the societal commitments helped us to identify opportunities for future directions that we may not have otherwise considered. As a safety-net institution, we benefit from a strong sense of mission and shared values within our hospital and division. However, we recognize the need to continue to be vigilant to ensure that our physicians perceive that their own values are aligned with the division’s stated mission. Devoting a Kaizen-style retreat to well-being likely helped, and allocating divisional resources to a well-being committee indirectly helped, to foster a culture of well-being; however, we could more deliberately identify local policies that may benefit from advocacy or revision. Although our faculty identified interventions to improve interpersonal and individual drivers of well-being, these charter commitments did not have direct parallels in Lean philosophy, and organizations may need to deliberately seek to address these commitments outside of a Lean approach. Specifically, by reviewing the charter, we identified opportunities to provide additional resources for peer support and protected time for mental health care and self-care.
Conclusion
Lean Management can be an effective strategy to address many of the organizational commitments outlined in the Charter on Physician Well-being. This approach may be particularly effective for solving local challenges with systems and workflows. Those who use Lean as a primary method to approach systems improvement in support of the Quadruple Aim may need to use additional strategies to address societal and interpersonal and individual commitments outlined in the charter.
Dr. Sanyal-Dey is visiting associate clinical professor of medicine at Zuckerberg San Francisco General Hospital and director of client services, LeanTaaS. Dr. Thomas is associate clinical professor of medicine at Zuckerberg San Francisco General Hospital. Dr. Chia is associate professor of clinical medicine at Zuckerberg San Francisco General Hospital.
References
1. West CP et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016;388(10057):2272-81.
2. Shanafelt TD, Noseworthy JH. Executive leadership and physician: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129-46.
3. Shanafelt T et al. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826-32.
4. Shanafelt T et al. Building a program on well-being: Key design considerations to meet the unique needs of each organization. Acad Med. 2019 Feb;94(2):156-161.
5. Thomas LR et al. Charter on physician well-being. JAMA. 2018;319(15):1541-42.
6. Bodenheimer T, Sinsky C. From triple to quadruple aim: Care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-6.
7. West CP et al. Concurrent Validity of Single-Item Measures of Emotional Exhaustion and Depersonalization in Burnout Assessment. J Gen Intern Med. 2012;27(11):1445-52.
8. Hung DY et al. Experiences of primary care physicians and staff following lean workflow redesign. BMC Health Serv Res. 2018 Apr 10;18(1):274.
9. Zibrowski E et al. Easier and faster is not always better: Grounded theory of the impact of large-scale system transformation on the clinical work of emergency medicine nurses and physicians. JMIR Hum Factors. 2018. doi: 10.2196/11013.
10. Shanafelt TD et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90(4):432-40.
Using systems improvement strategies to support the Quadruple Aim
Using systems improvement strategies to support the Quadruple Aim
General background on well-being and burnout
With burnout increasingly recognized as a shared responsibility that requires addressing organizational drivers while supporting individuals to be well,1-4 practical strategies and examples of successful implementation of systems interventions to address burnout will be helpful for service directors to support their staff. The Charter on Physician Well-being, recently developed through collaborative input from multiple organizations, defines guiding principles and key commitments at the societal, organizational, interpersonal, and individual levels and may be a useful framework for organizations that are developing well-being initiatives.5
The charter advocates including physician well-being as a quality improvement metric for health systems, aligned with the concept of the Quadruple Aim of optimizing patient care by enhancing provider experience, promoting high-value care, and improving population health.6 Identifying areas of alignment between the charter’s recommendations and systems improvement strategies that seek to optimize efficiency and reduce waste, such as Lean Management, may help physician leaders to contextualize well-being initiatives more easily within ongoing systems improvement efforts. In this perspective, we provide one division’s experience using the Charter to assess successes and identify additional areas of improvement for well-being initiatives developed using Lean Management methodology.
Past and current state of affairs
In 2011, the division of hospital medicine at Zuckerberg San Francisco General Hospital was established and has seen continual expansion in terms of direct patient care, medical education, and hospital leadership.
In 2015, the division of hospital medicine experienced leadership transitions, faculty attrition, and insufficient recruitment resulting in staffing shortages, service line closure, schedule instability, and ultimately, low morale. A baseline survey conducted using the 2-Item Maslach Burnout Inventory. This survey, which uses one item in the domain of emotional exhaustion and one item in the domain of depersonalization, has shown good correlation with the full Maslach Burnout Inventory.7 At baseline, approximately one-third of the division’s physicians experienced burnout.
In response, a subsequent retreat focused on the three greatest areas of concern identified by the survey: scheduling, faculty development, and well-being.
Like many health systems, the hospital has adopted Lean as its preferred systems-improvement framework. The retreat was structured around the principles of Lean philosophy, and was designed to emulate that of a consolidated Kaizen workshop.
“Kaizen” in Japanese means “change for the better.” A typical Kaizen workshop revolves around rapid problem-solving over the course of 3-5 days, in which a team of people come together to identify and implement significant improvements for a selected process. To this end, the retreat was divided into subgroups for each area of concern. In turn, each subgroup mapped out existing workflows (“value stream”), identified areas of waste and non–value added time, and generated ideas of what an idealized process would be. Next, a root-cause analysis was performed and subsequent interventions (“countermeasures”) developed to address each problem. At the conclusion of the retreat, each subgroup shared a summary of their findings with the larger group.
Moving forward, this information served as a guiding framework for service and division leadership to run small tests of change. We enacted a series of countermeasures over the course of several years, and multiple cycles of improvement work addressed the three areas of concern. We developed an A3 report (a Lean project management tool that incorporates the plan-do-study-act cycle, organizes strategic efforts, and tracks progress on a single page) to summarize and present these initiatives to the Performance Improvement and Patient Safety Committee of the hospital executive leadership team. This structure illustrated alignment with the hospital’s core values (“true north”) of “developing people” and “care experience.”
In 2018, interval surveys demonstrated a gradual reduction of burnout to approximately one-fifth of division physicians as measured by the 2-item Maslach Burnout Inventory.
Initiatives in faculty well-being
The Charter of Physician Well-being outlines a framework to promote well-being among doctors by maximizing a sense of fulfillment and minimizing the harms of burnout. It shares this responsibility among societal, organizational, and interpersonal and individual commitments.5
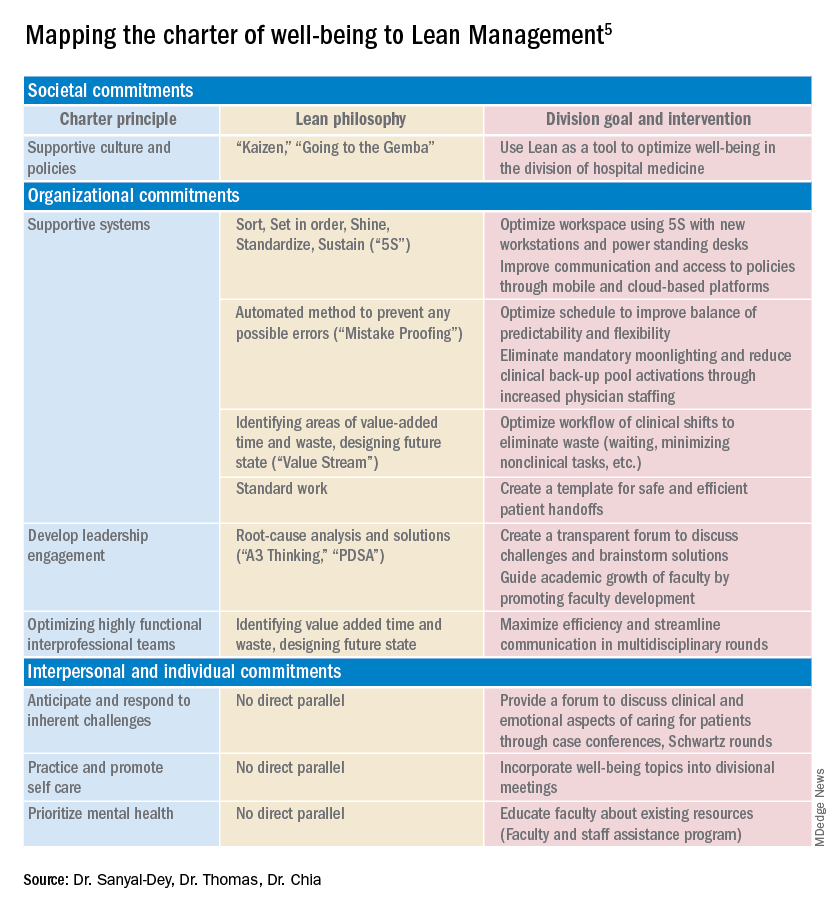
As illustrated above, we used principles of Lean Management to prospectively create initiatives to improve well-being in our division. Lean in health care is designed to optimize primarily the patient experience; its implementation has subsequently demonstrated mixed provider and staff experiences,8,9 and many providers are skeptical of Lean’s potential to improve their own well-being. If, however, Lean is aligned with best practice frameworks for well-being such as those outline in the charter, it may also help to meet the Quadruple Aim of optimizing both provider well-being and patient experience. To further test this hypothesis, we retrospectively categorized our Lean-based interventions into the commitments described by the charter to identify areas of alignment and gaps that were not initially addressed using Lean Management (Table).
Organizational commitments5Supportive systems
We optimized scheduling and enhanced physician staffing by budgeting for a physician staffing buffer each academic year in order to minimize mandatory moonlighting and jeopardy pool activations that result from operating on a thin staffing margin when expected personal leave and reductions in clinical effort occur. Furthermore, we revised scheduling principles to balance patient continuity and individual time off requests while setting limits on the maximum duration of clinical stretches and instituting mandatory minimum time off between them.
Leadership engagement
We initiated monthly operations meetings as a forum to discuss challenges, brainstorm solutions, and message new initiatives with group input. For example, as a result of these meetings, we designed and implemented an additional service line to address the high census, revised the distribution of new patient admissions to level-load clinical shifts, and established a maximum number of weekends worked per month and year. This approach aligns with recommendations to use participatory leadership strategies to enhance physician well-being.10 Engaging both executive level and service level management to focus on burnout and other related well-being metrics is necessary for sustaining such work.
Interprofessional teamwork
We revised multidisciplinary rounds with social work, utilization management, and physical therapy to maximize efficiency and streamline communication by developing standard approaches for each patient presentation.
Interpersonal and individual commitments5Address emotional challenges of physician work
Although these commitments did not have a direct corollary with Lean philosophy, some of these needs were identified by our physician group at our annual retreats. As a result, we initiated a monthly faculty-led noon conference series focused on the clinical challenges of caring for vulnerable populations, a particular source of distress in our practice setting, and revised the division schedule to encourage attendance at the hospital’s Schwartz rounds.
Mental health and self-care
We organized focus groups and faculty development sessions on provider well-being and burnout and dealing with challenging patients and invited the Faculty and Staff Assistance Program, our institution’s mental health service provider, to our weekly division meeting.
Future directions
After using Lean Management as an approach to prospectively improve physician well-being, we were able to use the Charter on Physician Well-being retrospectively as a “checklist” to identify additional gaps for targeted intervention to ensure all commitments are sufficiently addressed.
Overall, we found that, not surprisingly, Lean Management aligned best with the organizational commitments in the charter. Reviewing the organizational commitments, we found our biggest remaining challenges are in building supportive systems, namely ensuring sustainable workloads, offloading and delegating nonphysician tasks, and minimizing the burden of documentation and administration.
Reviewing the societal commitments helped us to identify opportunities for future directions that we may not have otherwise considered. As a safety-net institution, we benefit from a strong sense of mission and shared values within our hospital and division. However, we recognize the need to continue to be vigilant to ensure that our physicians perceive that their own values are aligned with the division’s stated mission. Devoting a Kaizen-style retreat to well-being likely helped, and allocating divisional resources to a well-being committee indirectly helped, to foster a culture of well-being; however, we could more deliberately identify local policies that may benefit from advocacy or revision. Although our faculty identified interventions to improve interpersonal and individual drivers of well-being, these charter commitments did not have direct parallels in Lean philosophy, and organizations may need to deliberately seek to address these commitments outside of a Lean approach. Specifically, by reviewing the charter, we identified opportunities to provide additional resources for peer support and protected time for mental health care and self-care.
Conclusion
Lean Management can be an effective strategy to address many of the organizational commitments outlined in the Charter on Physician Well-being. This approach may be particularly effective for solving local challenges with systems and workflows. Those who use Lean as a primary method to approach systems improvement in support of the Quadruple Aim may need to use additional strategies to address societal and interpersonal and individual commitments outlined in the charter.
Dr. Sanyal-Dey is visiting associate clinical professor of medicine at Zuckerberg San Francisco General Hospital and director of client services, LeanTaaS. Dr. Thomas is associate clinical professor of medicine at Zuckerberg San Francisco General Hospital. Dr. Chia is associate professor of clinical medicine at Zuckerberg San Francisco General Hospital.
References
1. West CP et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016;388(10057):2272-81.
2. Shanafelt TD, Noseworthy JH. Executive leadership and physician: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129-46.
3. Shanafelt T et al. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826-32.
4. Shanafelt T et al. Building a program on well-being: Key design considerations to meet the unique needs of each organization. Acad Med. 2019 Feb;94(2):156-161.
5. Thomas LR et al. Charter on physician well-being. JAMA. 2018;319(15):1541-42.
6. Bodenheimer T, Sinsky C. From triple to quadruple aim: Care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-6.
7. West CP et al. Concurrent Validity of Single-Item Measures of Emotional Exhaustion and Depersonalization in Burnout Assessment. J Gen Intern Med. 2012;27(11):1445-52.
8. Hung DY et al. Experiences of primary care physicians and staff following lean workflow redesign. BMC Health Serv Res. 2018 Apr 10;18(1):274.
9. Zibrowski E et al. Easier and faster is not always better: Grounded theory of the impact of large-scale system transformation on the clinical work of emergency medicine nurses and physicians. JMIR Hum Factors. 2018. doi: 10.2196/11013.
10. Shanafelt TD et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90(4):432-40.
General background on well-being and burnout
With burnout increasingly recognized as a shared responsibility that requires addressing organizational drivers while supporting individuals to be well,1-4 practical strategies and examples of successful implementation of systems interventions to address burnout will be helpful for service directors to support their staff. The Charter on Physician Well-being, recently developed through collaborative input from multiple organizations, defines guiding principles and key commitments at the societal, organizational, interpersonal, and individual levels and may be a useful framework for organizations that are developing well-being initiatives.5
The charter advocates including physician well-being as a quality improvement metric for health systems, aligned with the concept of the Quadruple Aim of optimizing patient care by enhancing provider experience, promoting high-value care, and improving population health.6 Identifying areas of alignment between the charter’s recommendations and systems improvement strategies that seek to optimize efficiency and reduce waste, such as Lean Management, may help physician leaders to contextualize well-being initiatives more easily within ongoing systems improvement efforts. In this perspective, we provide one division’s experience using the Charter to assess successes and identify additional areas of improvement for well-being initiatives developed using Lean Management methodology.
Past and current state of affairs
In 2011, the division of hospital medicine at Zuckerberg San Francisco General Hospital was established and has seen continual expansion in terms of direct patient care, medical education, and hospital leadership.
In 2015, the division of hospital medicine experienced leadership transitions, faculty attrition, and insufficient recruitment resulting in staffing shortages, service line closure, schedule instability, and ultimately, low morale. A baseline survey conducted using the 2-Item Maslach Burnout Inventory. This survey, which uses one item in the domain of emotional exhaustion and one item in the domain of depersonalization, has shown good correlation with the full Maslach Burnout Inventory.7 At baseline, approximately one-third of the division’s physicians experienced burnout.
In response, a subsequent retreat focused on the three greatest areas of concern identified by the survey: scheduling, faculty development, and well-being.
Like many health systems, the hospital has adopted Lean as its preferred systems-improvement framework. The retreat was structured around the principles of Lean philosophy, and was designed to emulate that of a consolidated Kaizen workshop.
“Kaizen” in Japanese means “change for the better.” A typical Kaizen workshop revolves around rapid problem-solving over the course of 3-5 days, in which a team of people come together to identify and implement significant improvements for a selected process. To this end, the retreat was divided into subgroups for each area of concern. In turn, each subgroup mapped out existing workflows (“value stream”), identified areas of waste and non–value added time, and generated ideas of what an idealized process would be. Next, a root-cause analysis was performed and subsequent interventions (“countermeasures”) developed to address each problem. At the conclusion of the retreat, each subgroup shared a summary of their findings with the larger group.
Moving forward, this information served as a guiding framework for service and division leadership to run small tests of change. We enacted a series of countermeasures over the course of several years, and multiple cycles of improvement work addressed the three areas of concern. We developed an A3 report (a Lean project management tool that incorporates the plan-do-study-act cycle, organizes strategic efforts, and tracks progress on a single page) to summarize and present these initiatives to the Performance Improvement and Patient Safety Committee of the hospital executive leadership team. This structure illustrated alignment with the hospital’s core values (“true north”) of “developing people” and “care experience.”
In 2018, interval surveys demonstrated a gradual reduction of burnout to approximately one-fifth of division physicians as measured by the 2-item Maslach Burnout Inventory.
Initiatives in faculty well-being
The Charter of Physician Well-being outlines a framework to promote well-being among doctors by maximizing a sense of fulfillment and minimizing the harms of burnout. It shares this responsibility among societal, organizational, and interpersonal and individual commitments.5
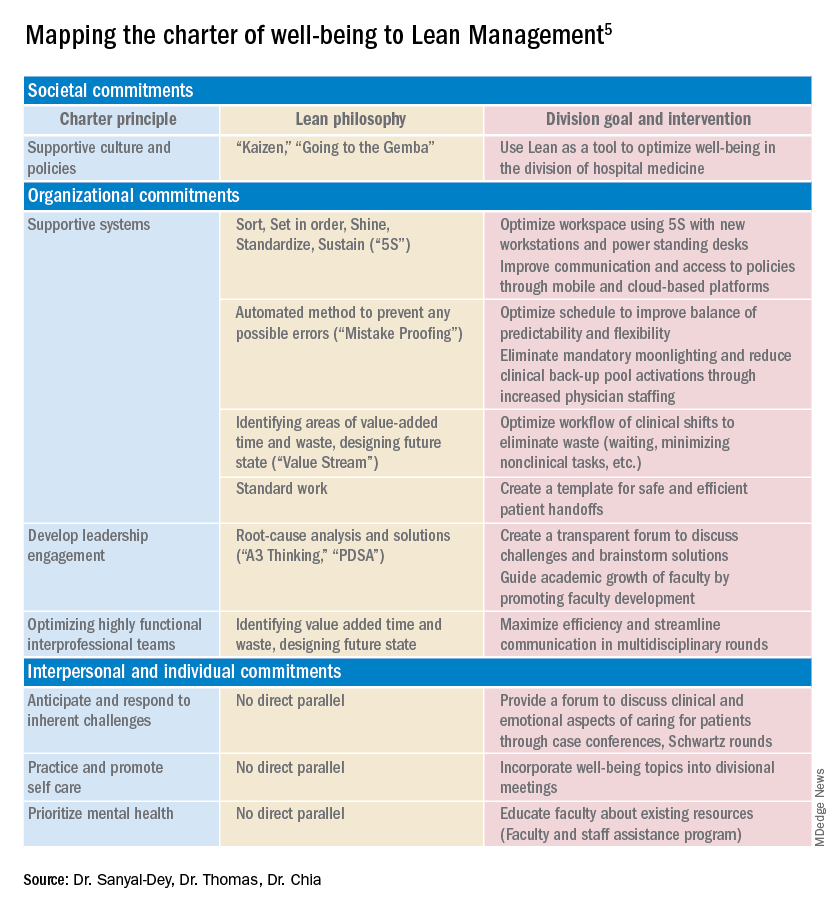
As illustrated above, we used principles of Lean Management to prospectively create initiatives to improve well-being in our division. Lean in health care is designed to optimize primarily the patient experience; its implementation has subsequently demonstrated mixed provider and staff experiences,8,9 and many providers are skeptical of Lean’s potential to improve their own well-being. If, however, Lean is aligned with best practice frameworks for well-being such as those outline in the charter, it may also help to meet the Quadruple Aim of optimizing both provider well-being and patient experience. To further test this hypothesis, we retrospectively categorized our Lean-based interventions into the commitments described by the charter to identify areas of alignment and gaps that were not initially addressed using Lean Management (Table).
Organizational commitments5Supportive systems
We optimized scheduling and enhanced physician staffing by budgeting for a physician staffing buffer each academic year in order to minimize mandatory moonlighting and jeopardy pool activations that result from operating on a thin staffing margin when expected personal leave and reductions in clinical effort occur. Furthermore, we revised scheduling principles to balance patient continuity and individual time off requests while setting limits on the maximum duration of clinical stretches and instituting mandatory minimum time off between them.
Leadership engagement
We initiated monthly operations meetings as a forum to discuss challenges, brainstorm solutions, and message new initiatives with group input. For example, as a result of these meetings, we designed and implemented an additional service line to address the high census, revised the distribution of new patient admissions to level-load clinical shifts, and established a maximum number of weekends worked per month and year. This approach aligns with recommendations to use participatory leadership strategies to enhance physician well-being.10 Engaging both executive level and service level management to focus on burnout and other related well-being metrics is necessary for sustaining such work.
Interprofessional teamwork
We revised multidisciplinary rounds with social work, utilization management, and physical therapy to maximize efficiency and streamline communication by developing standard approaches for each patient presentation.
Interpersonal and individual commitments5Address emotional challenges of physician work
Although these commitments did not have a direct corollary with Lean philosophy, some of these needs were identified by our physician group at our annual retreats. As a result, we initiated a monthly faculty-led noon conference series focused on the clinical challenges of caring for vulnerable populations, a particular source of distress in our practice setting, and revised the division schedule to encourage attendance at the hospital’s Schwartz rounds.
Mental health and self-care
We organized focus groups and faculty development sessions on provider well-being and burnout and dealing with challenging patients and invited the Faculty and Staff Assistance Program, our institution’s mental health service provider, to our weekly division meeting.
Future directions
After using Lean Management as an approach to prospectively improve physician well-being, we were able to use the Charter on Physician Well-being retrospectively as a “checklist” to identify additional gaps for targeted intervention to ensure all commitments are sufficiently addressed.
Overall, we found that, not surprisingly, Lean Management aligned best with the organizational commitments in the charter. Reviewing the organizational commitments, we found our biggest remaining challenges are in building supportive systems, namely ensuring sustainable workloads, offloading and delegating nonphysician tasks, and minimizing the burden of documentation and administration.
Reviewing the societal commitments helped us to identify opportunities for future directions that we may not have otherwise considered. As a safety-net institution, we benefit from a strong sense of mission and shared values within our hospital and division. However, we recognize the need to continue to be vigilant to ensure that our physicians perceive that their own values are aligned with the division’s stated mission. Devoting a Kaizen-style retreat to well-being likely helped, and allocating divisional resources to a well-being committee indirectly helped, to foster a culture of well-being; however, we could more deliberately identify local policies that may benefit from advocacy or revision. Although our faculty identified interventions to improve interpersonal and individual drivers of well-being, these charter commitments did not have direct parallels in Lean philosophy, and organizations may need to deliberately seek to address these commitments outside of a Lean approach. Specifically, by reviewing the charter, we identified opportunities to provide additional resources for peer support and protected time for mental health care and self-care.
Conclusion
Lean Management can be an effective strategy to address many of the organizational commitments outlined in the Charter on Physician Well-being. This approach may be particularly effective for solving local challenges with systems and workflows. Those who use Lean as a primary method to approach systems improvement in support of the Quadruple Aim may need to use additional strategies to address societal and interpersonal and individual commitments outlined in the charter.
Dr. Sanyal-Dey is visiting associate clinical professor of medicine at Zuckerberg San Francisco General Hospital and director of client services, LeanTaaS. Dr. Thomas is associate clinical professor of medicine at Zuckerberg San Francisco General Hospital. Dr. Chia is associate professor of clinical medicine at Zuckerberg San Francisco General Hospital.
References
1. West CP et al. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016;388(10057):2272-81.
2. Shanafelt TD, Noseworthy JH. Executive leadership and physician: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129-46.
3. Shanafelt T et al. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826-32.
4. Shanafelt T et al. Building a program on well-being: Key design considerations to meet the unique needs of each organization. Acad Med. 2019 Feb;94(2):156-161.
5. Thomas LR et al. Charter on physician well-being. JAMA. 2018;319(15):1541-42.
6. Bodenheimer T, Sinsky C. From triple to quadruple aim: Care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-6.
7. West CP et al. Concurrent Validity of Single-Item Measures of Emotional Exhaustion and Depersonalization in Burnout Assessment. J Gen Intern Med. 2012;27(11):1445-52.
8. Hung DY et al. Experiences of primary care physicians and staff following lean workflow redesign. BMC Health Serv Res. 2018 Apr 10;18(1):274.
9. Zibrowski E et al. Easier and faster is not always better: Grounded theory of the impact of large-scale system transformation on the clinical work of emergency medicine nurses and physicians. JMIR Hum Factors. 2018. doi: 10.2196/11013.
10. Shanafelt TD et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc. 2015;90(4):432-40.
Overdiagnosis and overtreatment of COPD appears rampant
Background: COPD is a highly morbid disease, and there is a need for a better understanding of the true prevalence. Little is known regarding overdiagnosis of COPD. According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD), airflow limitation by spirometry is a key criteria for diagnosis.
Study design: Population-based survey.
Setting: Altogether, 23 sites in 20 countries worldwide were included.
Synopsis: The Burden of Obstructive Lung Disease (BOLD) study recruited community-dwelling adults who underwent questionnaires, as well as spirometry. Of the 16,717 participants, 919 self-reported a COPD diagnosis. Of these, more than half were found to not meet obstructive lung disease criteria on spirometry, and therefore were misdiagnosed: 62% when defined as forced expiratory volume in 1 second to forced vital capacity (FEV1/FVC) ratio less than the lower limit of normal and 55% when using the GOLD definition of FEV1/FVC less than 0.7. After patients with reported asthma were excluded, 34% of participants with false-positive COPD were found to be treated with respiratory medications as outpatients.
Overdiagnosis of COPD was noted to be more prevalent in high-income countries than they were in low- to middle-income countries (4.9% versus 1.9% of the participants sampled).
The self-reporting of the diagnosis of COPD is a limitation of the study because it may have artificially inflated the rate of false positives.
Bottom line: Patient-reported diagnoses of COPD should be taken with a degree of caution because of high rates of overdiagnosis and overtreatment.
Citation: Sator L et al. Overdiagnosis of COPD in subjects with unobstructed spirometry. Chest. 2019 Aug;156(2):277-88.
Dr. Gordon is a hospitalist at Maine Medical Center in Portland.
Background: COPD is a highly morbid disease, and there is a need for a better understanding of the true prevalence. Little is known regarding overdiagnosis of COPD. According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD), airflow limitation by spirometry is a key criteria for diagnosis.
Study design: Population-based survey.
Setting: Altogether, 23 sites in 20 countries worldwide were included.
Synopsis: The Burden of Obstructive Lung Disease (BOLD) study recruited community-dwelling adults who underwent questionnaires, as well as spirometry. Of the 16,717 participants, 919 self-reported a COPD diagnosis. Of these, more than half were found to not meet obstructive lung disease criteria on spirometry, and therefore were misdiagnosed: 62% when defined as forced expiratory volume in 1 second to forced vital capacity (FEV1/FVC) ratio less than the lower limit of normal and 55% when using the GOLD definition of FEV1/FVC less than 0.7. After patients with reported asthma were excluded, 34% of participants with false-positive COPD were found to be treated with respiratory medications as outpatients.
Overdiagnosis of COPD was noted to be more prevalent in high-income countries than they were in low- to middle-income countries (4.9% versus 1.9% of the participants sampled).
The self-reporting of the diagnosis of COPD is a limitation of the study because it may have artificially inflated the rate of false positives.
Bottom line: Patient-reported diagnoses of COPD should be taken with a degree of caution because of high rates of overdiagnosis and overtreatment.
Citation: Sator L et al. Overdiagnosis of COPD in subjects with unobstructed spirometry. Chest. 2019 Aug;156(2):277-88.
Dr. Gordon is a hospitalist at Maine Medical Center in Portland.
Background: COPD is a highly morbid disease, and there is a need for a better understanding of the true prevalence. Little is known regarding overdiagnosis of COPD. According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD), airflow limitation by spirometry is a key criteria for diagnosis.
Study design: Population-based survey.
Setting: Altogether, 23 sites in 20 countries worldwide were included.
Synopsis: The Burden of Obstructive Lung Disease (BOLD) study recruited community-dwelling adults who underwent questionnaires, as well as spirometry. Of the 16,717 participants, 919 self-reported a COPD diagnosis. Of these, more than half were found to not meet obstructive lung disease criteria on spirometry, and therefore were misdiagnosed: 62% when defined as forced expiratory volume in 1 second to forced vital capacity (FEV1/FVC) ratio less than the lower limit of normal and 55% when using the GOLD definition of FEV1/FVC less than 0.7. After patients with reported asthma were excluded, 34% of participants with false-positive COPD were found to be treated with respiratory medications as outpatients.
Overdiagnosis of COPD was noted to be more prevalent in high-income countries than they were in low- to middle-income countries (4.9% versus 1.9% of the participants sampled).
The self-reporting of the diagnosis of COPD is a limitation of the study because it may have artificially inflated the rate of false positives.
Bottom line: Patient-reported diagnoses of COPD should be taken with a degree of caution because of high rates of overdiagnosis and overtreatment.
Citation: Sator L et al. Overdiagnosis of COPD in subjects with unobstructed spirometry. Chest. 2019 Aug;156(2):277-88.
Dr. Gordon is a hospitalist at Maine Medical Center in Portland.
How can hospitalists change the status quo?
Lean framework for efficiency and empathy of care
“My census is too high.”
“I don’t have enough time to talk to patients.”
“These are outside our scope of practice.”
These are statements that I have heard from colleagues over the last fourteen years as a hospitalist. Back in 1996, when Dr. Bob Wachter coined the term ‘hospitalist,’ we were still in our infancy – the scope of what we could do had yet to be fully realized. Our focus was on providing care for hospitalized patients and improving quality of clinical care and patient safety. As health care organizations began to see the potential for our field, the demands on our services grew. We grew to comanage patients with our surgical colleagues, worked on patient satisfaction, facilitated transitions of care, and attempted to reduce readmissions – all of which improved patient care and the bottom line for our organizations.
Somewhere along the way, we were expected to staff high patient volumes to add more value, but this always seemed to come with compromise in another aspect of care or our own well-being. After all, there are only so many hours in the day and a limit on what one individual can accomplish in that time.
One of the reasons I love hospital medicine is the novelty of what we do – we are creative thinkers. We have the capacity to innovate solutions to hospital problems based on our expertise as frontline providers for our patients. Hospitalists of every discipline staff a large majority of inpatients, which makes our collective experience significant to the management of inpatient health care. We are often the ones tasked with executing improvement projects, but how often are we involved in their design? I know that we collectively have an enormous opportunity to improve our health care practice, both for ourselves, our patients, and the institutions we work for. But more than just being a voice of advocacy, we need to understand how to positively influence the health care structures that allow us to deliver quality patient care.
It is no surprise that the inefficiencies we deal with in our hospitals are many – daily workflow interruptions, delays in results, scheduling issues, communication difficulties. These are not unique to any one institution. The pandemic added more to that plate – PPE deficiencies, patient volume triage, and resource management are examples. Hospitals often contract consultants to help solve these problems, and many utilize a variety of frameworks to improve these system processes. The Lean framework is one of these, and it originated in the manufacturing industry to eliminate waste in systems in the pursuit of efficiency.
In my business training and prior hospital medicine leadership roles, I was educated in Lean thinking and methodologies for improving quality and applied its principles to projects for improving workflow. Last year I attended a virtual conference on ‘Lean Innovation during the pandemic’ for New York region hospitals, and it again highlighted how the Lean management methodology can help improve patient care but importantly, our workflow as clinicians. This got me thinking. Why is Lean well accepted in business and manufacturing circles, but less so in health care?
I think the answer is twofold – knowledge and people.
What is Lean and how can it help us?
The ‘Toyota Production System’-based philosophy has 14 core principles that help eliminate waste in systems in pursuit of efficiency. These principles are the “Toyota Way.” They center around two pillars: continuous improvement and respect for people. The cornerstone of this management methodology is based on efficient processes, developing employees to add value to the organization and continuous improvement through problem-solving and organizational learning.
Lean is often implemented with Six Sigma methodology. Six Sigma has its origins in Motorola. While Lean cuts waste in our systems to provide value, Six Sigma uses DMAIC (Define, Measure, Analyze, Improve, Control) to reduce variation in our processes. When done in its entirety, Lean Six Sigma methodology adds value by increasing efficiency, reducing cost, and improving our everyday work.
Statistical principles suggest that 80% of consequences comes from 20% of causes. Lean methodology and tools allow us to systematically identify root causes for the problems we face and help narrow it down to the ‘vital few.’ In other words, fixing these would give us the most bang for our buck. As hospitalists, we are able to do this better than most because we work in these hospital processes everyday – we truly know the strengths and weaknesses of our systems.
As a hospitalist, I would love for the process of seeing patients in hospitals to be more efficient, less variable, and be more cost-effective for my institution. By eliminating the time wasted performing unnecessary and redundant tasks in my everyday work, I can reallocate that time to patient care – the very reason I chose a career in medicine.
We, the people
There are two common rebuttals I hear for adopting Lean Six Sigma methodology in health care. A frequent misconception is that Lean is all about reducing staff or time with patients. The second is that manufacturing methodologies do not work for a service profession. For instance, an article published on Reuters Events (www.reutersevents.com/supplychain/supply-chain/end-just-time) talks about Lean JIT (Just In Time) inventory as a culprit for creating a supply chain deficit during COVID-19. It is not entirely without merit. However, if done the correct way, Lean is all about involving the frontline worker to create a workflow that would work best for them.
Reducing the waste in our processes and empowering our frontline doctors to be creative in finding solutions naturally leads to cost reduction. The cornerstone of Lean is creating a continuously learning organization and putting your employees at the forefront. I think it is important that Lean principles be utilized within health care – but we cannot push to fix every problem in our systems to perfection at a significant expense to the physician and other health care staff.
Why HM can benefit from Lean
There is no hard and fast rule about the way health care should adopt Lean thinking. It is a way of thinking that aims to balance purpose, people, and process – extremes of inventory management may not be necessary to be successful in health care. Lean tools alone would not create results. John Shook, chairman of Lean Global Network, has said that the social side of Lean needs to be in balance with the technical side. In other words, rigidity and efficiency is good, but so is encouraging creativity and flexibility in thinking within the workforce.
In the crisis created by the novel coronavirus, many hospitals in New York state, including my own, turned to Lean to respond quickly and effectively to the challenges. Lean principles helped them problem-solve and develop strategies to both recover from the pandemic surge and adapt to future problems that could occur. Geographic clustering of patients, PPE supply, OR shut down and ramp up, emergency management offices at the peak of the pandemic, telehealth streamlining, and post-COVID-19 care planning are some areas where the application of Lean resulted in successful responses to the challenges that 2020 brought to our work.
As Warren Bennis said, ‘The manager accepts the status quo; the leader challenges it.’ As hospitalists, we can lead the way our hospitals provide care. Lean is not just a way for hospitals to cut costs (although it helps quite a bit there). Its processes and philosophies could enable hospitalists to maximize potential, efficiency, quality of care, and allow for a balanced work environment. When applied in a manner that focuses on continuous improvement (and is cognizant of its limitations), it has the potential to increase the capability of our service lines and streamline our processes and workday for greater efficiency. As a specialty, we stand to benefit by taking the lead role in choosing how best to improve how we work. We should think outside the box. What better time to do this than now?
Dr. Kanikkannan is a practicing hospitalist and assistant professor of medicine at Albany (N.Y) Medical College. She is a former hospitalist medical director and has served on SHM’s national committees, and is a certified Lean Six Sigma black belt and MBA candidate.
Lean framework for efficiency and empathy of care
Lean framework for efficiency and empathy of care
“My census is too high.”
“I don’t have enough time to talk to patients.”
“These are outside our scope of practice.”
These are statements that I have heard from colleagues over the last fourteen years as a hospitalist. Back in 1996, when Dr. Bob Wachter coined the term ‘hospitalist,’ we were still in our infancy – the scope of what we could do had yet to be fully realized. Our focus was on providing care for hospitalized patients and improving quality of clinical care and patient safety. As health care organizations began to see the potential for our field, the demands on our services grew. We grew to comanage patients with our surgical colleagues, worked on patient satisfaction, facilitated transitions of care, and attempted to reduce readmissions – all of which improved patient care and the bottom line for our organizations.
Somewhere along the way, we were expected to staff high patient volumes to add more value, but this always seemed to come with compromise in another aspect of care or our own well-being. After all, there are only so many hours in the day and a limit on what one individual can accomplish in that time.
One of the reasons I love hospital medicine is the novelty of what we do – we are creative thinkers. We have the capacity to innovate solutions to hospital problems based on our expertise as frontline providers for our patients. Hospitalists of every discipline staff a large majority of inpatients, which makes our collective experience significant to the management of inpatient health care. We are often the ones tasked with executing improvement projects, but how often are we involved in their design? I know that we collectively have an enormous opportunity to improve our health care practice, both for ourselves, our patients, and the institutions we work for. But more than just being a voice of advocacy, we need to understand how to positively influence the health care structures that allow us to deliver quality patient care.
It is no surprise that the inefficiencies we deal with in our hospitals are many – daily workflow interruptions, delays in results, scheduling issues, communication difficulties. These are not unique to any one institution. The pandemic added more to that plate – PPE deficiencies, patient volume triage, and resource management are examples. Hospitals often contract consultants to help solve these problems, and many utilize a variety of frameworks to improve these system processes. The Lean framework is one of these, and it originated in the manufacturing industry to eliminate waste in systems in the pursuit of efficiency.
In my business training and prior hospital medicine leadership roles, I was educated in Lean thinking and methodologies for improving quality and applied its principles to projects for improving workflow. Last year I attended a virtual conference on ‘Lean Innovation during the pandemic’ for New York region hospitals, and it again highlighted how the Lean management methodology can help improve patient care but importantly, our workflow as clinicians. This got me thinking. Why is Lean well accepted in business and manufacturing circles, but less so in health care?
I think the answer is twofold – knowledge and people.
What is Lean and how can it help us?
The ‘Toyota Production System’-based philosophy has 14 core principles that help eliminate waste in systems in pursuit of efficiency. These principles are the “Toyota Way.” They center around two pillars: continuous improvement and respect for people. The cornerstone of this management methodology is based on efficient processes, developing employees to add value to the organization and continuous improvement through problem-solving and organizational learning.
Lean is often implemented with Six Sigma methodology. Six Sigma has its origins in Motorola. While Lean cuts waste in our systems to provide value, Six Sigma uses DMAIC (Define, Measure, Analyze, Improve, Control) to reduce variation in our processes. When done in its entirety, Lean Six Sigma methodology adds value by increasing efficiency, reducing cost, and improving our everyday work.
Statistical principles suggest that 80% of consequences comes from 20% of causes. Lean methodology and tools allow us to systematically identify root causes for the problems we face and help narrow it down to the ‘vital few.’ In other words, fixing these would give us the most bang for our buck. As hospitalists, we are able to do this better than most because we work in these hospital processes everyday – we truly know the strengths and weaknesses of our systems.
As a hospitalist, I would love for the process of seeing patients in hospitals to be more efficient, less variable, and be more cost-effective for my institution. By eliminating the time wasted performing unnecessary and redundant tasks in my everyday work, I can reallocate that time to patient care – the very reason I chose a career in medicine.
We, the people
There are two common rebuttals I hear for adopting Lean Six Sigma methodology in health care. A frequent misconception is that Lean is all about reducing staff or time with patients. The second is that manufacturing methodologies do not work for a service profession. For instance, an article published on Reuters Events (www.reutersevents.com/supplychain/supply-chain/end-just-time) talks about Lean JIT (Just In Time) inventory as a culprit for creating a supply chain deficit during COVID-19. It is not entirely without merit. However, if done the correct way, Lean is all about involving the frontline worker to create a workflow that would work best for them.
Reducing the waste in our processes and empowering our frontline doctors to be creative in finding solutions naturally leads to cost reduction. The cornerstone of Lean is creating a continuously learning organization and putting your employees at the forefront. I think it is important that Lean principles be utilized within health care – but we cannot push to fix every problem in our systems to perfection at a significant expense to the physician and other health care staff.
Why HM can benefit from Lean
There is no hard and fast rule about the way health care should adopt Lean thinking. It is a way of thinking that aims to balance purpose, people, and process – extremes of inventory management may not be necessary to be successful in health care. Lean tools alone would not create results. John Shook, chairman of Lean Global Network, has said that the social side of Lean needs to be in balance with the technical side. In other words, rigidity and efficiency is good, but so is encouraging creativity and flexibility in thinking within the workforce.
In the crisis created by the novel coronavirus, many hospitals in New York state, including my own, turned to Lean to respond quickly and effectively to the challenges. Lean principles helped them problem-solve and develop strategies to both recover from the pandemic surge and adapt to future problems that could occur. Geographic clustering of patients, PPE supply, OR shut down and ramp up, emergency management offices at the peak of the pandemic, telehealth streamlining, and post-COVID-19 care planning are some areas where the application of Lean resulted in successful responses to the challenges that 2020 brought to our work.
As Warren Bennis said, ‘The manager accepts the status quo; the leader challenges it.’ As hospitalists, we can lead the way our hospitals provide care. Lean is not just a way for hospitals to cut costs (although it helps quite a bit there). Its processes and philosophies could enable hospitalists to maximize potential, efficiency, quality of care, and allow for a balanced work environment. When applied in a manner that focuses on continuous improvement (and is cognizant of its limitations), it has the potential to increase the capability of our service lines and streamline our processes and workday for greater efficiency. As a specialty, we stand to benefit by taking the lead role in choosing how best to improve how we work. We should think outside the box. What better time to do this than now?
Dr. Kanikkannan is a practicing hospitalist and assistant professor of medicine at Albany (N.Y) Medical College. She is a former hospitalist medical director and has served on SHM’s national committees, and is a certified Lean Six Sigma black belt and MBA candidate.
“My census is too high.”
“I don’t have enough time to talk to patients.”
“These are outside our scope of practice.”
These are statements that I have heard from colleagues over the last fourteen years as a hospitalist. Back in 1996, when Dr. Bob Wachter coined the term ‘hospitalist,’ we were still in our infancy – the scope of what we could do had yet to be fully realized. Our focus was on providing care for hospitalized patients and improving quality of clinical care and patient safety. As health care organizations began to see the potential for our field, the demands on our services grew. We grew to comanage patients with our surgical colleagues, worked on patient satisfaction, facilitated transitions of care, and attempted to reduce readmissions – all of which improved patient care and the bottom line for our organizations.
Somewhere along the way, we were expected to staff high patient volumes to add more value, but this always seemed to come with compromise in another aspect of care or our own well-being. After all, there are only so many hours in the day and a limit on what one individual can accomplish in that time.
One of the reasons I love hospital medicine is the novelty of what we do – we are creative thinkers. We have the capacity to innovate solutions to hospital problems based on our expertise as frontline providers for our patients. Hospitalists of every discipline staff a large majority of inpatients, which makes our collective experience significant to the management of inpatient health care. We are often the ones tasked with executing improvement projects, but how often are we involved in their design? I know that we collectively have an enormous opportunity to improve our health care practice, both for ourselves, our patients, and the institutions we work for. But more than just being a voice of advocacy, we need to understand how to positively influence the health care structures that allow us to deliver quality patient care.
It is no surprise that the inefficiencies we deal with in our hospitals are many – daily workflow interruptions, delays in results, scheduling issues, communication difficulties. These are not unique to any one institution. The pandemic added more to that plate – PPE deficiencies, patient volume triage, and resource management are examples. Hospitals often contract consultants to help solve these problems, and many utilize a variety of frameworks to improve these system processes. The Lean framework is one of these, and it originated in the manufacturing industry to eliminate waste in systems in the pursuit of efficiency.
In my business training and prior hospital medicine leadership roles, I was educated in Lean thinking and methodologies for improving quality and applied its principles to projects for improving workflow. Last year I attended a virtual conference on ‘Lean Innovation during the pandemic’ for New York region hospitals, and it again highlighted how the Lean management methodology can help improve patient care but importantly, our workflow as clinicians. This got me thinking. Why is Lean well accepted in business and manufacturing circles, but less so in health care?
I think the answer is twofold – knowledge and people.
What is Lean and how can it help us?
The ‘Toyota Production System’-based philosophy has 14 core principles that help eliminate waste in systems in pursuit of efficiency. These principles are the “Toyota Way.” They center around two pillars: continuous improvement and respect for people. The cornerstone of this management methodology is based on efficient processes, developing employees to add value to the organization and continuous improvement through problem-solving and organizational learning.
Lean is often implemented with Six Sigma methodology. Six Sigma has its origins in Motorola. While Lean cuts waste in our systems to provide value, Six Sigma uses DMAIC (Define, Measure, Analyze, Improve, Control) to reduce variation in our processes. When done in its entirety, Lean Six Sigma methodology adds value by increasing efficiency, reducing cost, and improving our everyday work.
Statistical principles suggest that 80% of consequences comes from 20% of causes. Lean methodology and tools allow us to systematically identify root causes for the problems we face and help narrow it down to the ‘vital few.’ In other words, fixing these would give us the most bang for our buck. As hospitalists, we are able to do this better than most because we work in these hospital processes everyday – we truly know the strengths and weaknesses of our systems.
As a hospitalist, I would love for the process of seeing patients in hospitals to be more efficient, less variable, and be more cost-effective for my institution. By eliminating the time wasted performing unnecessary and redundant tasks in my everyday work, I can reallocate that time to patient care – the very reason I chose a career in medicine.
We, the people
There are two common rebuttals I hear for adopting Lean Six Sigma methodology in health care. A frequent misconception is that Lean is all about reducing staff or time with patients. The second is that manufacturing methodologies do not work for a service profession. For instance, an article published on Reuters Events (www.reutersevents.com/supplychain/supply-chain/end-just-time) talks about Lean JIT (Just In Time) inventory as a culprit for creating a supply chain deficit during COVID-19. It is not entirely without merit. However, if done the correct way, Lean is all about involving the frontline worker to create a workflow that would work best for them.
Reducing the waste in our processes and empowering our frontline doctors to be creative in finding solutions naturally leads to cost reduction. The cornerstone of Lean is creating a continuously learning organization and putting your employees at the forefront. I think it is important that Lean principles be utilized within health care – but we cannot push to fix every problem in our systems to perfection at a significant expense to the physician and other health care staff.
Why HM can benefit from Lean
There is no hard and fast rule about the way health care should adopt Lean thinking. It is a way of thinking that aims to balance purpose, people, and process – extremes of inventory management may not be necessary to be successful in health care. Lean tools alone would not create results. John Shook, chairman of Lean Global Network, has said that the social side of Lean needs to be in balance with the technical side. In other words, rigidity and efficiency is good, but so is encouraging creativity and flexibility in thinking within the workforce.
In the crisis created by the novel coronavirus, many hospitals in New York state, including my own, turned to Lean to respond quickly and effectively to the challenges. Lean principles helped them problem-solve and develop strategies to both recover from the pandemic surge and adapt to future problems that could occur. Geographic clustering of patients, PPE supply, OR shut down and ramp up, emergency management offices at the peak of the pandemic, telehealth streamlining, and post-COVID-19 care planning are some areas where the application of Lean resulted in successful responses to the challenges that 2020 brought to our work.
As Warren Bennis said, ‘The manager accepts the status quo; the leader challenges it.’ As hospitalists, we can lead the way our hospitals provide care. Lean is not just a way for hospitals to cut costs (although it helps quite a bit there). Its processes and philosophies could enable hospitalists to maximize potential, efficiency, quality of care, and allow for a balanced work environment. When applied in a manner that focuses on continuous improvement (and is cognizant of its limitations), it has the potential to increase the capability of our service lines and streamline our processes and workday for greater efficiency. As a specialty, we stand to benefit by taking the lead role in choosing how best to improve how we work. We should think outside the box. What better time to do this than now?
Dr. Kanikkannan is a practicing hospitalist and assistant professor of medicine at Albany (N.Y) Medical College. She is a former hospitalist medical director and has served on SHM’s national committees, and is a certified Lean Six Sigma black belt and MBA candidate.
Reducing admissions for alcohol withdrawal syndrome
Hospitalists can drive major changes with a QI project
Hospitalists in the VA system see patients with symptoms of alcohol withdrawal frequently – there are about 33,000 hospital admissions each year for alcohol withdrawal syndrome (AWS), says Robert Patrick, MD, of the Louis Stokes Cleveland VA Medical Center.
“By contrast, the number of admissions for the largest ambulatory care sensitive condition (heart failure) is only about 28,000,” he said. “If alcohol detox were an ambulatory care sensitive condition, it would be the largest in the VA by a substantial margin.”The purpose of the project he and his co-author, Laura Brown, MD, created to address the problem was to increase the number of patients treated for AWS as outpatients and decrease hospital admissions – without increasing readmissions or clinical deterioration.
They introduced four core operational changes for their study:
1. Standardized risk stratification in the Emergency Department (ED) to identify low risk patients for outpatient treatment.
2. Benzodiazepine sparing symptom triggered medication regimen.
3. Daily clinical dashboard surveillance and risk stratification for continued hospital stay.
4. Telephone follow-up for patients discharged from the ED or hospital.
With these changes in place, eight months of data showed a 50% reduction in AWS admissions and a 40% reduction in length of stays.
Their conclusion? “A well designed and executed QI project can dramatically reduce hospitalist workload, while at the same time improving patient safety,” Dr. Patrick said. “Hospitalists just have to be willing to think outside the box, work with nursing and coordinate care outside of the hospital to make it happen.”
He added a caveat for hospital medicine groups still in a fee-for-service environment. “This saves money for the payer, not the hospital,” he said. “In our case they are one and the same, so the ROI is huge. If you are part of an ACO this is probably true for you, but I would check with your ACO first.”
Reference
1. Patrick RM, Brown LZ. Decreasing Admissions, Readmissions and Length of Stay While Improving Patent Safety for Alcohol Withdrawal Syndrome. Abstract published at Hospital Medicine 2019, March 24-27, National Harbor, Md. Abstract Plenary. https://www.shmabstracts.com/abstract/decreasing-admissions-readmissions-and-length-of-stay-while-improving-patient-safety-for-alcohol-withdrawal-syndrome/.
Hospitalists can drive major changes with a QI project
Hospitalists can drive major changes with a QI project
Hospitalists in the VA system see patients with symptoms of alcohol withdrawal frequently – there are about 33,000 hospital admissions each year for alcohol withdrawal syndrome (AWS), says Robert Patrick, MD, of the Louis Stokes Cleveland VA Medical Center.
“By contrast, the number of admissions for the largest ambulatory care sensitive condition (heart failure) is only about 28,000,” he said. “If alcohol detox were an ambulatory care sensitive condition, it would be the largest in the VA by a substantial margin.”The purpose of the project he and his co-author, Laura Brown, MD, created to address the problem was to increase the number of patients treated for AWS as outpatients and decrease hospital admissions – without increasing readmissions or clinical deterioration.
They introduced four core operational changes for their study:
1. Standardized risk stratification in the Emergency Department (ED) to identify low risk patients for outpatient treatment.
2. Benzodiazepine sparing symptom triggered medication regimen.
3. Daily clinical dashboard surveillance and risk stratification for continued hospital stay.
4. Telephone follow-up for patients discharged from the ED or hospital.
With these changes in place, eight months of data showed a 50% reduction in AWS admissions and a 40% reduction in length of stays.
Their conclusion? “A well designed and executed QI project can dramatically reduce hospitalist workload, while at the same time improving patient safety,” Dr. Patrick said. “Hospitalists just have to be willing to think outside the box, work with nursing and coordinate care outside of the hospital to make it happen.”
He added a caveat for hospital medicine groups still in a fee-for-service environment. “This saves money for the payer, not the hospital,” he said. “In our case they are one and the same, so the ROI is huge. If you are part of an ACO this is probably true for you, but I would check with your ACO first.”
Reference
1. Patrick RM, Brown LZ. Decreasing Admissions, Readmissions and Length of Stay While Improving Patent Safety for Alcohol Withdrawal Syndrome. Abstract published at Hospital Medicine 2019, March 24-27, National Harbor, Md. Abstract Plenary. https://www.shmabstracts.com/abstract/decreasing-admissions-readmissions-and-length-of-stay-while-improving-patient-safety-for-alcohol-withdrawal-syndrome/.
Hospitalists in the VA system see patients with symptoms of alcohol withdrawal frequently – there are about 33,000 hospital admissions each year for alcohol withdrawal syndrome (AWS), says Robert Patrick, MD, of the Louis Stokes Cleveland VA Medical Center.
“By contrast, the number of admissions for the largest ambulatory care sensitive condition (heart failure) is only about 28,000,” he said. “If alcohol detox were an ambulatory care sensitive condition, it would be the largest in the VA by a substantial margin.”The purpose of the project he and his co-author, Laura Brown, MD, created to address the problem was to increase the number of patients treated for AWS as outpatients and decrease hospital admissions – without increasing readmissions or clinical deterioration.
They introduced four core operational changes for their study:
1. Standardized risk stratification in the Emergency Department (ED) to identify low risk patients for outpatient treatment.
2. Benzodiazepine sparing symptom triggered medication regimen.
3. Daily clinical dashboard surveillance and risk stratification for continued hospital stay.
4. Telephone follow-up for patients discharged from the ED or hospital.
With these changes in place, eight months of data showed a 50% reduction in AWS admissions and a 40% reduction in length of stays.
Their conclusion? “A well designed and executed QI project can dramatically reduce hospitalist workload, while at the same time improving patient safety,” Dr. Patrick said. “Hospitalists just have to be willing to think outside the box, work with nursing and coordinate care outside of the hospital to make it happen.”
He added a caveat for hospital medicine groups still in a fee-for-service environment. “This saves money for the payer, not the hospital,” he said. “In our case they are one and the same, so the ROI is huge. If you are part of an ACO this is probably true for you, but I would check with your ACO first.”
Reference
1. Patrick RM, Brown LZ. Decreasing Admissions, Readmissions and Length of Stay While Improving Patent Safety for Alcohol Withdrawal Syndrome. Abstract published at Hospital Medicine 2019, March 24-27, National Harbor, Md. Abstract Plenary. https://www.shmabstracts.com/abstract/decreasing-admissions-readmissions-and-length-of-stay-while-improving-patient-safety-for-alcohol-withdrawal-syndrome/.
Rounding to make the hospital go ‘round
Hospitalists and performance incentive measures
No matter how you spin it, hospitalists are key to making the world of the hospital go ‘round, making their daily work of paramount interest to both hospitals and health systems.
Hospitalists are the primary attending physicians for patients in the hospital while also bridging the patient and their needs to the services of other subspecialists, allied health professionals, and when needed, postacute services. In this way, patients are efficiently moved along the acute care experience with multiple process and outcome measures being recorded along the way.
Some of these common performance incentive measures are determined by the Centers for Medicare and Medicaid Services while others may be of interest to third party payers. Often surrogate markers of process metrics (i.e. order set usage for certain diagnoses) are measured and incentivized as a way of directionally measuring small steps that each hospitalist can reliably control toward a presumably associated improvement in mortality or readmissions, for instance. Still other measures such as length of stay or timely completion of documentation have more to do with hospital operations, regulatory governance, and finance.
There are a variety of performance incentive metrics reported in the 2020 SoHM Report. Survey respondents could choose all measures that applied as compensation measures for their group in the past year. The most common metrics reported include patient satisfaction (48.7%), citizenship (45.8%), accuracy or timeliness of documentation (32.8%), and clinical process measures (30.7%).
It is important to acknowledge that most of these metrics are objective measurements and can be measured down to the individual physician. However, some of the objective measures, such as patient satisfaction data, must rely on agreed upon methods of attribution – which can include anything from attributing based on admitting physician, discharging attending, or the attending with the greatest number of days (i.e. daily charges) seeing the patient. Because of challenges with attribution, groups may opt for group measurement of metrics for some of the compensation metrics where attribution is most muddy.
For performance incentive metrics that may be more subjective, such as citizenship, it is important for hospitalist leaders to consider having a method of determining a person’s contribution with a rubric as well as some shared decision making among a committee of leaders or team members to promote fairness in compensation.
Hospital leaders must also recognize that what is measured will lead to “performance” in that area. The perfect example here is the “early morning discharge time/orders” which is a compensation metric in 27.6% of hospitalist groups. Most agree that having some early discharges, up to maybe 25%-30% of the total number of discharges before noon, can be helpful with hospital throughput. The trick here is that if a patient can be discharged that early, it is likely that some of those patients could have gone home the evening prior. It is important for hospitalist physician leaders and administrators to think about the behaviors that are incentivized in compensation metrics to ensure that the result is indeed helpful.
Other hospitalist compensation metrics such as readmissions are most effectively addressed if there are multiple physician teams working toward the same metric. Hospitalist work does effect readmissions within the first 7 days of discharge based on available evidence.1 Preventing readmissions from days 8-30 following discharge are more amenable to outpatient and home-based interventions. Also, effective readmission work involves collaboration among the emergency physician team, surgeons, primary care, and subspecialty physicians. So while having this as a compensation metric will gain the attention of hospitalist physicians, the work will be most effective when it is shared with other teams.
Overall, performance incentive metrics for hospitalists can be effective in allowing hospitals and hospitalist groups to partner toward achieving important outcomes for patients. Easy and frequent sharing of data on meaningful metrics with hospitalists is important to effect change. Also, hospital leadership can facilitate collaboration among nursing and multiple physician groups to promote a team culture with hospitalists in achieving goals related to performance incentive metrics.
Dr. McNeal is the division director of inpatient medicine at Baylor Scott & White Medical Center in Temple, Tex.
Reference
1. Graham, et al. Preventability of Early Versus Late Hospital Readmissions in a National Cohort of General Medicine Patients. Ann Intern Med. 2018 Jun 5;168(11):766-74.
Hospitalists and performance incentive measures
Hospitalists and performance incentive measures
No matter how you spin it, hospitalists are key to making the world of the hospital go ‘round, making their daily work of paramount interest to both hospitals and health systems.
Hospitalists are the primary attending physicians for patients in the hospital while also bridging the patient and their needs to the services of other subspecialists, allied health professionals, and when needed, postacute services. In this way, patients are efficiently moved along the acute care experience with multiple process and outcome measures being recorded along the way.
Some of these common performance incentive measures are determined by the Centers for Medicare and Medicaid Services while others may be of interest to third party payers. Often surrogate markers of process metrics (i.e. order set usage for certain diagnoses) are measured and incentivized as a way of directionally measuring small steps that each hospitalist can reliably control toward a presumably associated improvement in mortality or readmissions, for instance. Still other measures such as length of stay or timely completion of documentation have more to do with hospital operations, regulatory governance, and finance.
There are a variety of performance incentive metrics reported in the 2020 SoHM Report. Survey respondents could choose all measures that applied as compensation measures for their group in the past year. The most common metrics reported include patient satisfaction (48.7%), citizenship (45.8%), accuracy or timeliness of documentation (32.8%), and clinical process measures (30.7%).
It is important to acknowledge that most of these metrics are objective measurements and can be measured down to the individual physician. However, some of the objective measures, such as patient satisfaction data, must rely on agreed upon methods of attribution – which can include anything from attributing based on admitting physician, discharging attending, or the attending with the greatest number of days (i.e. daily charges) seeing the patient. Because of challenges with attribution, groups may opt for group measurement of metrics for some of the compensation metrics where attribution is most muddy.
For performance incentive metrics that may be more subjective, such as citizenship, it is important for hospitalist leaders to consider having a method of determining a person’s contribution with a rubric as well as some shared decision making among a committee of leaders or team members to promote fairness in compensation.
Hospital leaders must also recognize that what is measured will lead to “performance” in that area. The perfect example here is the “early morning discharge time/orders” which is a compensation metric in 27.6% of hospitalist groups. Most agree that having some early discharges, up to maybe 25%-30% of the total number of discharges before noon, can be helpful with hospital throughput. The trick here is that if a patient can be discharged that early, it is likely that some of those patients could have gone home the evening prior. It is important for hospitalist physician leaders and administrators to think about the behaviors that are incentivized in compensation metrics to ensure that the result is indeed helpful.
Other hospitalist compensation metrics such as readmissions are most effectively addressed if there are multiple physician teams working toward the same metric. Hospitalist work does effect readmissions within the first 7 days of discharge based on available evidence.1 Preventing readmissions from days 8-30 following discharge are more amenable to outpatient and home-based interventions. Also, effective readmission work involves collaboration among the emergency physician team, surgeons, primary care, and subspecialty physicians. So while having this as a compensation metric will gain the attention of hospitalist physicians, the work will be most effective when it is shared with other teams.
Overall, performance incentive metrics for hospitalists can be effective in allowing hospitals and hospitalist groups to partner toward achieving important outcomes for patients. Easy and frequent sharing of data on meaningful metrics with hospitalists is important to effect change. Also, hospital leadership can facilitate collaboration among nursing and multiple physician groups to promote a team culture with hospitalists in achieving goals related to performance incentive metrics.
Dr. McNeal is the division director of inpatient medicine at Baylor Scott & White Medical Center in Temple, Tex.
Reference
1. Graham, et al. Preventability of Early Versus Late Hospital Readmissions in a National Cohort of General Medicine Patients. Ann Intern Med. 2018 Jun 5;168(11):766-74.
No matter how you spin it, hospitalists are key to making the world of the hospital go ‘round, making their daily work of paramount interest to both hospitals and health systems.
Hospitalists are the primary attending physicians for patients in the hospital while also bridging the patient and their needs to the services of other subspecialists, allied health professionals, and when needed, postacute services. In this way, patients are efficiently moved along the acute care experience with multiple process and outcome measures being recorded along the way.
Some of these common performance incentive measures are determined by the Centers for Medicare and Medicaid Services while others may be of interest to third party payers. Often surrogate markers of process metrics (i.e. order set usage for certain diagnoses) are measured and incentivized as a way of directionally measuring small steps that each hospitalist can reliably control toward a presumably associated improvement in mortality or readmissions, for instance. Still other measures such as length of stay or timely completion of documentation have more to do with hospital operations, regulatory governance, and finance.
There are a variety of performance incentive metrics reported in the 2020 SoHM Report. Survey respondents could choose all measures that applied as compensation measures for their group in the past year. The most common metrics reported include patient satisfaction (48.7%), citizenship (45.8%), accuracy or timeliness of documentation (32.8%), and clinical process measures (30.7%).
It is important to acknowledge that most of these metrics are objective measurements and can be measured down to the individual physician. However, some of the objective measures, such as patient satisfaction data, must rely on agreed upon methods of attribution – which can include anything from attributing based on admitting physician, discharging attending, or the attending with the greatest number of days (i.e. daily charges) seeing the patient. Because of challenges with attribution, groups may opt for group measurement of metrics for some of the compensation metrics where attribution is most muddy.
For performance incentive metrics that may be more subjective, such as citizenship, it is important for hospitalist leaders to consider having a method of determining a person’s contribution with a rubric as well as some shared decision making among a committee of leaders or team members to promote fairness in compensation.
Hospital leaders must also recognize that what is measured will lead to “performance” in that area. The perfect example here is the “early morning discharge time/orders” which is a compensation metric in 27.6% of hospitalist groups. Most agree that having some early discharges, up to maybe 25%-30% of the total number of discharges before noon, can be helpful with hospital throughput. The trick here is that if a patient can be discharged that early, it is likely that some of those patients could have gone home the evening prior. It is important for hospitalist physician leaders and administrators to think about the behaviors that are incentivized in compensation metrics to ensure that the result is indeed helpful.
Other hospitalist compensation metrics such as readmissions are most effectively addressed if there are multiple physician teams working toward the same metric. Hospitalist work does effect readmissions within the first 7 days of discharge based on available evidence.1 Preventing readmissions from days 8-30 following discharge are more amenable to outpatient and home-based interventions. Also, effective readmission work involves collaboration among the emergency physician team, surgeons, primary care, and subspecialty physicians. So while having this as a compensation metric will gain the attention of hospitalist physicians, the work will be most effective when it is shared with other teams.
Overall, performance incentive metrics for hospitalists can be effective in allowing hospitals and hospitalist groups to partner toward achieving important outcomes for patients. Easy and frequent sharing of data on meaningful metrics with hospitalists is important to effect change. Also, hospital leadership can facilitate collaboration among nursing and multiple physician groups to promote a team culture with hospitalists in achieving goals related to performance incentive metrics.
Dr. McNeal is the division director of inpatient medicine at Baylor Scott & White Medical Center in Temple, Tex.
Reference
1. Graham, et al. Preventability of Early Versus Late Hospital Readmissions in a National Cohort of General Medicine Patients. Ann Intern Med. 2018 Jun 5;168(11):766-74.
Higher 10-day mortality of lower-acuity patients during times of increased ED crowding
Background: Studies have assessed mortality effect from ED crowding on high-acuity patients, but limited evidence exists for how this affects lower-acuity patients who are discharged home.
Study design: Retrospective cohort study.
Setting: Emergency department, Karolinska University Hospital, Solna, Sweden.
Synopsis: During 2009-2016, 705,813 encounters seen in the ED, triaged to lower-acuity levels 3-5 and discharged without further hospitalization needs were identified. A total of 623 patients died within 10 days of the initial ED visit (0.09%). The study evaluated the association of 10-day mortality with mean ED length of stay and ED-occupancy ratio.
The study demonstrated an increased 10-day mortality for mean ED length of stay of 8 hours or more vs. less than 2 hours (adjusted odds ratio, 5.86; 95% CI, 2.15-15.94). It also found an increased mortality rate for occupancy ratio quartiles with an aOR for quartiles 2, 3, and 4 vs. quartile 1 of 1.48 (95% CI, 1.14-1.92), 1.63 (95% CI, 1.24-2.14), and 1.53 (95% CI, 1.15-2.03), respectively.
While this suggests increased 10-day mortality in this patient population, additional studies should be conducted to determine if this risk is caused by ED crowding and length of stay or by current limitations in triage scoring.
Bottom line: There is an increased 10-day mortality rate for lower-acuity triaged patients who were discharged from the ED without hospitalization experiencing increased ED length of stay and during times of ED crowding.
Citation: Berg L et al. Associations between crowding and 10-day mortality among patients allocated lower triage acuity levels without need of acute hospital care on departure from the emergency department. Ann Emerg Med. 2019 Sep;74(3):345-56.
Dr. Merando is a hospitalist and assistant professor of internal medicine at St. Louis University School of Medicine.
Background: Studies have assessed mortality effect from ED crowding on high-acuity patients, but limited evidence exists for how this affects lower-acuity patients who are discharged home.
Study design: Retrospective cohort study.
Setting: Emergency department, Karolinska University Hospital, Solna, Sweden.
Synopsis: During 2009-2016, 705,813 encounters seen in the ED, triaged to lower-acuity levels 3-5 and discharged without further hospitalization needs were identified. A total of 623 patients died within 10 days of the initial ED visit (0.09%). The study evaluated the association of 10-day mortality with mean ED length of stay and ED-occupancy ratio.
The study demonstrated an increased 10-day mortality for mean ED length of stay of 8 hours or more vs. less than 2 hours (adjusted odds ratio, 5.86; 95% CI, 2.15-15.94). It also found an increased mortality rate for occupancy ratio quartiles with an aOR for quartiles 2, 3, and 4 vs. quartile 1 of 1.48 (95% CI, 1.14-1.92), 1.63 (95% CI, 1.24-2.14), and 1.53 (95% CI, 1.15-2.03), respectively.
While this suggests increased 10-day mortality in this patient population, additional studies should be conducted to determine if this risk is caused by ED crowding and length of stay or by current limitations in triage scoring.
Bottom line: There is an increased 10-day mortality rate for lower-acuity triaged patients who were discharged from the ED without hospitalization experiencing increased ED length of stay and during times of ED crowding.
Citation: Berg L et al. Associations between crowding and 10-day mortality among patients allocated lower triage acuity levels without need of acute hospital care on departure from the emergency department. Ann Emerg Med. 2019 Sep;74(3):345-56.
Dr. Merando is a hospitalist and assistant professor of internal medicine at St. Louis University School of Medicine.
Background: Studies have assessed mortality effect from ED crowding on high-acuity patients, but limited evidence exists for how this affects lower-acuity patients who are discharged home.
Study design: Retrospective cohort study.
Setting: Emergency department, Karolinska University Hospital, Solna, Sweden.
Synopsis: During 2009-2016, 705,813 encounters seen in the ED, triaged to lower-acuity levels 3-5 and discharged without further hospitalization needs were identified. A total of 623 patients died within 10 days of the initial ED visit (0.09%). The study evaluated the association of 10-day mortality with mean ED length of stay and ED-occupancy ratio.
The study demonstrated an increased 10-day mortality for mean ED length of stay of 8 hours or more vs. less than 2 hours (adjusted odds ratio, 5.86; 95% CI, 2.15-15.94). It also found an increased mortality rate for occupancy ratio quartiles with an aOR for quartiles 2, 3, and 4 vs. quartile 1 of 1.48 (95% CI, 1.14-1.92), 1.63 (95% CI, 1.24-2.14), and 1.53 (95% CI, 1.15-2.03), respectively.
While this suggests increased 10-day mortality in this patient population, additional studies should be conducted to determine if this risk is caused by ED crowding and length of stay or by current limitations in triage scoring.
Bottom line: There is an increased 10-day mortality rate for lower-acuity triaged patients who were discharged from the ED without hospitalization experiencing increased ED length of stay and during times of ED crowding.
Citation: Berg L et al. Associations between crowding and 10-day mortality among patients allocated lower triage acuity levels without need of acute hospital care on departure from the emergency department. Ann Emerg Med. 2019 Sep;74(3):345-56.
Dr. Merando is a hospitalist and assistant professor of internal medicine at St. Louis University School of Medicine.