User login
CMS extends deadline for 2015 EHR attestation
Physicians and hospitals will have an extra 2 weeks to attest to meaningful use of electronic health records in 2015.
The deadline for attesting to 90 days of continuous use during the calendar year for physicians or from Oct. 1, 2014, through the end of 2015 for hospitals is now March 11. Previously, attestations were due Feb. 29 to avoid penalties under the EHR Incentive Program for not meeting meaningful use requirements in 2015.
The deadline was extended to align EHR attestation with the Physician Quality Reporting System, according to CMS officials.
Attestations can be made on the CMS website.
Physicians and hospitals will have an extra 2 weeks to attest to meaningful use of electronic health records in 2015.
The deadline for attesting to 90 days of continuous use during the calendar year for physicians or from Oct. 1, 2014, through the end of 2015 for hospitals is now March 11. Previously, attestations were due Feb. 29 to avoid penalties under the EHR Incentive Program for not meeting meaningful use requirements in 2015.
The deadline was extended to align EHR attestation with the Physician Quality Reporting System, according to CMS officials.
Attestations can be made on the CMS website.
Physicians and hospitals will have an extra 2 weeks to attest to meaningful use of electronic health records in 2015.
The deadline for attesting to 90 days of continuous use during the calendar year for physicians or from Oct. 1, 2014, through the end of 2015 for hospitals is now March 11. Previously, attestations were due Feb. 29 to avoid penalties under the EHR Incentive Program for not meeting meaningful use requirements in 2015.
The deadline was extended to align EHR attestation with the Physician Quality Reporting System, according to CMS officials.
Attestations can be made on the CMS website.
AMA spending tops health-sector lobbying
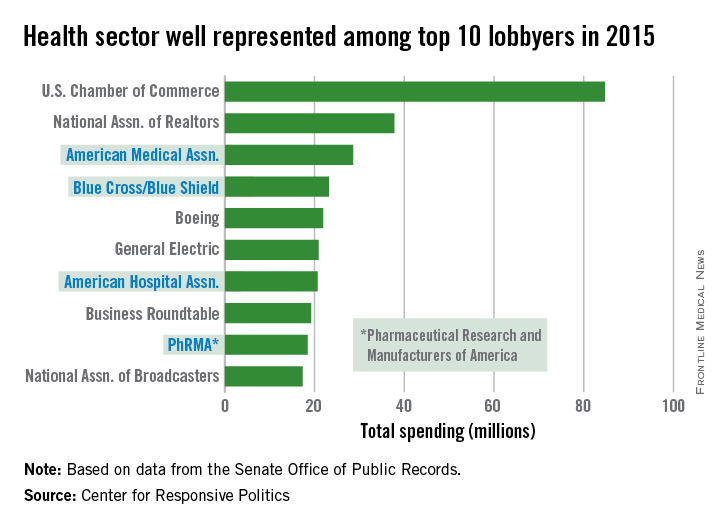
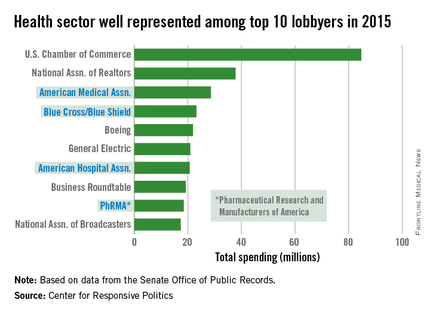
The health sector let itself be heard in Washington in 2015, as the American Medical Association and three other organizations spent their way into the lobbying top 10, according to the Center for Responsive Politics.
The AMA spent $28.6 million on lobbying last year – tops among the health sector and third among all lobbyers. The other health sector entities among the top 10 in spending were Blue Cross/Blue Shield at $23.2 million (fourth overall), the American Hospital Association at $20.7 million (seventh), and the Pharmaceutical Research and Manufacturers of America at $18.4 million (ninth), the center reported.
That’s definitely nothing to sneeze at, but it would have taken the combined spending of all four, about $90.9 million, to surpass the U.S. Chamber of Commerce, which led all lobbyers at $84.7 million.
Total spending on lobbying for the health sector was $507 million in 2015, which was second to “miscellaneous business” (including the Chamber of Commerce) among the center’s 13 ranked sectors. Total spending on lobbying for all sectors was $3.2 billion for the year, according to the center’s calculations, which were based on data from the Senate Office of Public Records.
The health sector let itself be heard in Washington in 2015, as the American Medical Association and three other organizations spent their way into the lobbying top 10, according to the Center for Responsive Politics.
The AMA spent $28.6 million on lobbying last year – tops among the health sector and third among all lobbyers. The other health sector entities among the top 10 in spending were Blue Cross/Blue Shield at $23.2 million (fourth overall), the American Hospital Association at $20.7 million (seventh), and the Pharmaceutical Research and Manufacturers of America at $18.4 million (ninth), the center reported.
That’s definitely nothing to sneeze at, but it would have taken the combined spending of all four, about $90.9 million, to surpass the U.S. Chamber of Commerce, which led all lobbyers at $84.7 million.
Total spending on lobbying for the health sector was $507 million in 2015, which was second to “miscellaneous business” (including the Chamber of Commerce) among the center’s 13 ranked sectors. Total spending on lobbying for all sectors was $3.2 billion for the year, according to the center’s calculations, which were based on data from the Senate Office of Public Records.
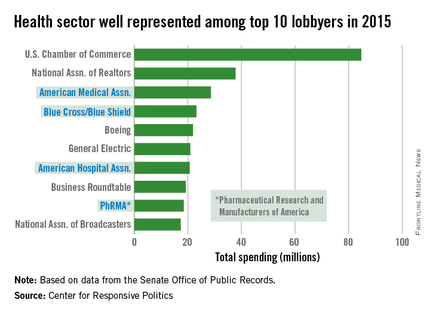
The health sector let itself be heard in Washington in 2015, as the American Medical Association and three other organizations spent their way into the lobbying top 10, according to the Center for Responsive Politics.
The AMA spent $28.6 million on lobbying last year – tops among the health sector and third among all lobbyers. The other health sector entities among the top 10 in spending were Blue Cross/Blue Shield at $23.2 million (fourth overall), the American Hospital Association at $20.7 million (seventh), and the Pharmaceutical Research and Manufacturers of America at $18.4 million (ninth), the center reported.
That’s definitely nothing to sneeze at, but it would have taken the combined spending of all four, about $90.9 million, to surpass the U.S. Chamber of Commerce, which led all lobbyers at $84.7 million.
Total spending on lobbying for the health sector was $507 million in 2015, which was second to “miscellaneous business” (including the Chamber of Commerce) among the center’s 13 ranked sectors. Total spending on lobbying for all sectors was $3.2 billion for the year, according to the center’s calculations, which were based on data from the Senate Office of Public Records.
Law & Medicine: Which doctors get sued?
Question: Doctors are more prone to lawsuits if they:
A. Have been sued before.
B. Spend fewer dollars per hospitalized patient.
C. Show poor communication skills.
D. A and C only.
E. A, B, and C.
Answer: E. Two very recent studies, one by David M. Studdert and the other by Dr. Anupam B. Jena, offer fresh insights into factors linked to the likelihood of a malpractice lawsuit.
The Studdert study concluded that doctors with prior paid claims are at increased risk of incurring yet another lawsuit.1 Instead of simply relying on data from a single insurer or state, the researchers accessed the National Practitioner Data Bank (NPDB) from 2005 through 2014 and identified 66,426 claims paid against 54,099 physicians.
Over that 10-year period, only 1% of physicians accounted for 32% of paid claims. Of all the physicians, 84% incurred only one paid claim during the study period, and 16% had at least two. Four percent of the physicians had at least three. In adjusted analyses, the risk of recurrence increased with the number of previous paid claims.
For example, compared with physicians with a single claim, the 2,160 physicians who had three paid claims had three times the risk of incurring another (hazard ratio, 3.11); this corresponded in absolute terms to a 24% risk within 2 years.
Likelihood of recurrence also varied widely according to specialty. For example, the risk among neurosurgeons was four times greater than that of psychiatrists. As for internists, the risk of recurrence was approximately double that of neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, or obstetrician-gynecologists. The lowest risks of recurrence were seen among psychiatrists (HR, 0.60) and pediatricians (HR, 0.71).
Male physicians had a 38% higher risk of recurrence than did female physicians, and the risk among physicians younger than 35 years was approximately one-third that of their older colleagues (after adjustment for age). Residents had a lower risk of recurrence than did nonresidents, and MDs had a lower risk than did DOs.
Using all 915,564 active physicians in the United States as a denominator, the authors calculated that over the 10-year study period, only 6% of physicians had a paid claim. Note that the 6% figure refers to paid claims reported to the NPDB, which can be expected to be lower than statistics derived from published surveys. These latter studies typically feature self-reported malpractice claims made over a given time period; but it is well known that the majority of such claims are dropped or decided in favor of the doctor, and so will not be reported to the NPDB.
For example, in 2010, the American Medical Association found that 42.2% of 5,825 physicians who responded to its Physician Practice Information survey reported having been sued, with 22.4% sued twice or more.2 The report headlined that by mid career, 61% of doctor have been sued.
Rates varied by specialty, with general surgeons and obstetrician-gynecologists being most likely to be sued (69.2%). Family physicians and general internists had similar rates (38.9% and 34%), and pediatricians and psychiatrists were sued the least.
In that report, male doctors were twice as likely to be sued as were their female counterparts, and physicians in solo and specialty practices were sued more often than those in multispecialty practices. Physicians who had an ownership interest in a practice were also at greater risk, with 47.5% reporting being sued, compared with 33.4% for those with no ownership interest.
The second recent study, reported by Dr. Jena of Harvard Medical School, Boston, and his colleagues, analyzed Florida hospital admissions data covering some 24,000 physicians.3 They found that higher spending by physicians was associated with reduced malpractice claims made the following year.
This pattern held true for physicians in all specialties but one (family practice). For example, among internists, the malpractice risk probability was 1.5% in the bottom spending fifth ($19,725 per admission) and 0.3% in the top fifth ($39,379 per admission). Among obstetricians, the comparable figures were 1.9% and 0.4% respectively.
In addition, a separate subgroup analysis of cesarean-section rates revealed that malpractice claims were approximately halved among obstetricians with rates in the highest fifth, compared with the lowest fifth.
Unfortunately, the Jena study lacked information on illness severity and past malpractice history, and it remains speculative whether increased resource utilization could be attributed entirely to defensive medical practice.4
As interesting as these new reports may be, it is worth remembering that what prompts a lawsuit are poor communication and patient perception that the physician is uncaring and at fault for the bad result.
It is well known that quality of medical care correlates poorly with the filing of malpractice lawsuits, as illustrated in the conclusion of the landmark Harvard study that “medical malpractice litigation infrequently compensates patients injured by medical negligence and rarely identifies, and holds providers accountable for, substandard care.”5 The authors estimated that there was only 1 malpractice claim for every 7.6 adverse events caused by negligence.
In another retrospective chart review study, the quality of treatment as judged by independent peer review was no different in frequently sued versus never-sued obstetricians.6
Communication problems exist in more than 70% of malpractice cases, centering around four themes: 1) deserting the patient; 2) devaluing patient/family views; 3) delivering information poorly; and 4) failing to understand the patient/family perspective.7
Anger, either from the adverse result itself or perceived lack of caring, turns an injured patient into a plaintiff, and lies at the root of all malpractice claims. The patients may not even have a serious injury or a meritorious claim, but they are so frustrated with their physician or the hospital that they contact an attorney to vent their anger.
One experienced attorney volunteered that close to half his malpractice cases could have been avoided through disclosure or apology, noting: “What the patients really wanted was simply an honest explanation of what happened, and, if appropriate, an apology. Unfortunately, when they were not only offered neither, but were rejected as well, they felt doubly wronged and then sought legal counsel.”8
Communicating well begins with active listening. Patients want their doctors to listen to them and to explain their conditions and treatment plans in simple, understandable language. The physician should give them ample opportunity to tell their story and to ask questions.
In one well-publicized study, only 23% of patients were able to complete their opening statement before the doctor interrupted, which occurred, on the average, 18 seconds after the patient began to speak!9
References
1. N Engl J Med. 2016 Jan 28;374(4):354-62.
2. “Medical liability: By late career, 61% of doctors have been sued,” Aug. 16, 2010, American Medical News.
4. “Law & Medicine: Health care costs and defensive medicine,” Jan. 19, 2016, Internal Medicine News.
5. N Engl J Med. 1991 Jul 25;325(4):245-51.
6. JAMA. 1994 Nov 23-30;272(20):1588-91.
7. Arch Intern Med. 1994 Jun 27;154(12):1365-70.
8. Ann Intern Med. 1999 Dec 21;131(12):970-2.
9. Ann Intern Med. 1984 Nov;101(5):692-6.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at siang@hawaii.edu
Question: Doctors are more prone to lawsuits if they:
A. Have been sued before.
B. Spend fewer dollars per hospitalized patient.
C. Show poor communication skills.
D. A and C only.
E. A, B, and C.
Answer: E. Two very recent studies, one by David M. Studdert and the other by Dr. Anupam B. Jena, offer fresh insights into factors linked to the likelihood of a malpractice lawsuit.
The Studdert study concluded that doctors with prior paid claims are at increased risk of incurring yet another lawsuit.1 Instead of simply relying on data from a single insurer or state, the researchers accessed the National Practitioner Data Bank (NPDB) from 2005 through 2014 and identified 66,426 claims paid against 54,099 physicians.
Over that 10-year period, only 1% of physicians accounted for 32% of paid claims. Of all the physicians, 84% incurred only one paid claim during the study period, and 16% had at least two. Four percent of the physicians had at least three. In adjusted analyses, the risk of recurrence increased with the number of previous paid claims.
For example, compared with physicians with a single claim, the 2,160 physicians who had three paid claims had three times the risk of incurring another (hazard ratio, 3.11); this corresponded in absolute terms to a 24% risk within 2 years.
Likelihood of recurrence also varied widely according to specialty. For example, the risk among neurosurgeons was four times greater than that of psychiatrists. As for internists, the risk of recurrence was approximately double that of neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, or obstetrician-gynecologists. The lowest risks of recurrence were seen among psychiatrists (HR, 0.60) and pediatricians (HR, 0.71).
Male physicians had a 38% higher risk of recurrence than did female physicians, and the risk among physicians younger than 35 years was approximately one-third that of their older colleagues (after adjustment for age). Residents had a lower risk of recurrence than did nonresidents, and MDs had a lower risk than did DOs.
Using all 915,564 active physicians in the United States as a denominator, the authors calculated that over the 10-year study period, only 6% of physicians had a paid claim. Note that the 6% figure refers to paid claims reported to the NPDB, which can be expected to be lower than statistics derived from published surveys. These latter studies typically feature self-reported malpractice claims made over a given time period; but it is well known that the majority of such claims are dropped or decided in favor of the doctor, and so will not be reported to the NPDB.
For example, in 2010, the American Medical Association found that 42.2% of 5,825 physicians who responded to its Physician Practice Information survey reported having been sued, with 22.4% sued twice or more.2 The report headlined that by mid career, 61% of doctor have been sued.
Rates varied by specialty, with general surgeons and obstetrician-gynecologists being most likely to be sued (69.2%). Family physicians and general internists had similar rates (38.9% and 34%), and pediatricians and psychiatrists were sued the least.
In that report, male doctors were twice as likely to be sued as were their female counterparts, and physicians in solo and specialty practices were sued more often than those in multispecialty practices. Physicians who had an ownership interest in a practice were also at greater risk, with 47.5% reporting being sued, compared with 33.4% for those with no ownership interest.
The second recent study, reported by Dr. Jena of Harvard Medical School, Boston, and his colleagues, analyzed Florida hospital admissions data covering some 24,000 physicians.3 They found that higher spending by physicians was associated with reduced malpractice claims made the following year.
This pattern held true for physicians in all specialties but one (family practice). For example, among internists, the malpractice risk probability was 1.5% in the bottom spending fifth ($19,725 per admission) and 0.3% in the top fifth ($39,379 per admission). Among obstetricians, the comparable figures were 1.9% and 0.4% respectively.
In addition, a separate subgroup analysis of cesarean-section rates revealed that malpractice claims were approximately halved among obstetricians with rates in the highest fifth, compared with the lowest fifth.
Unfortunately, the Jena study lacked information on illness severity and past malpractice history, and it remains speculative whether increased resource utilization could be attributed entirely to defensive medical practice.4
As interesting as these new reports may be, it is worth remembering that what prompts a lawsuit are poor communication and patient perception that the physician is uncaring and at fault for the bad result.
It is well known that quality of medical care correlates poorly with the filing of malpractice lawsuits, as illustrated in the conclusion of the landmark Harvard study that “medical malpractice litigation infrequently compensates patients injured by medical negligence and rarely identifies, and holds providers accountable for, substandard care.”5 The authors estimated that there was only 1 malpractice claim for every 7.6 adverse events caused by negligence.
In another retrospective chart review study, the quality of treatment as judged by independent peer review was no different in frequently sued versus never-sued obstetricians.6
Communication problems exist in more than 70% of malpractice cases, centering around four themes: 1) deserting the patient; 2) devaluing patient/family views; 3) delivering information poorly; and 4) failing to understand the patient/family perspective.7
Anger, either from the adverse result itself or perceived lack of caring, turns an injured patient into a plaintiff, and lies at the root of all malpractice claims. The patients may not even have a serious injury or a meritorious claim, but they are so frustrated with their physician or the hospital that they contact an attorney to vent their anger.
One experienced attorney volunteered that close to half his malpractice cases could have been avoided through disclosure or apology, noting: “What the patients really wanted was simply an honest explanation of what happened, and, if appropriate, an apology. Unfortunately, when they were not only offered neither, but were rejected as well, they felt doubly wronged and then sought legal counsel.”8
Communicating well begins with active listening. Patients want their doctors to listen to them and to explain their conditions and treatment plans in simple, understandable language. The physician should give them ample opportunity to tell their story and to ask questions.
In one well-publicized study, only 23% of patients were able to complete their opening statement before the doctor interrupted, which occurred, on the average, 18 seconds after the patient began to speak!9
References
1. N Engl J Med. 2016 Jan 28;374(4):354-62.
2. “Medical liability: By late career, 61% of doctors have been sued,” Aug. 16, 2010, American Medical News.
4. “Law & Medicine: Health care costs and defensive medicine,” Jan. 19, 2016, Internal Medicine News.
5. N Engl J Med. 1991 Jul 25;325(4):245-51.
6. JAMA. 1994 Nov 23-30;272(20):1588-91.
7. Arch Intern Med. 1994 Jun 27;154(12):1365-70.
8. Ann Intern Med. 1999 Dec 21;131(12):970-2.
9. Ann Intern Med. 1984 Nov;101(5):692-6.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at siang@hawaii.edu
Question: Doctors are more prone to lawsuits if they:
A. Have been sued before.
B. Spend fewer dollars per hospitalized patient.
C. Show poor communication skills.
D. A and C only.
E. A, B, and C.
Answer: E. Two very recent studies, one by David M. Studdert and the other by Dr. Anupam B. Jena, offer fresh insights into factors linked to the likelihood of a malpractice lawsuit.
The Studdert study concluded that doctors with prior paid claims are at increased risk of incurring yet another lawsuit.1 Instead of simply relying on data from a single insurer or state, the researchers accessed the National Practitioner Data Bank (NPDB) from 2005 through 2014 and identified 66,426 claims paid against 54,099 physicians.
Over that 10-year period, only 1% of physicians accounted for 32% of paid claims. Of all the physicians, 84% incurred only one paid claim during the study period, and 16% had at least two. Four percent of the physicians had at least three. In adjusted analyses, the risk of recurrence increased with the number of previous paid claims.
For example, compared with physicians with a single claim, the 2,160 physicians who had three paid claims had three times the risk of incurring another (hazard ratio, 3.11); this corresponded in absolute terms to a 24% risk within 2 years.
Likelihood of recurrence also varied widely according to specialty. For example, the risk among neurosurgeons was four times greater than that of psychiatrists. As for internists, the risk of recurrence was approximately double that of neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, or obstetrician-gynecologists. The lowest risks of recurrence were seen among psychiatrists (HR, 0.60) and pediatricians (HR, 0.71).
Male physicians had a 38% higher risk of recurrence than did female physicians, and the risk among physicians younger than 35 years was approximately one-third that of their older colleagues (after adjustment for age). Residents had a lower risk of recurrence than did nonresidents, and MDs had a lower risk than did DOs.
Using all 915,564 active physicians in the United States as a denominator, the authors calculated that over the 10-year study period, only 6% of physicians had a paid claim. Note that the 6% figure refers to paid claims reported to the NPDB, which can be expected to be lower than statistics derived from published surveys. These latter studies typically feature self-reported malpractice claims made over a given time period; but it is well known that the majority of such claims are dropped or decided in favor of the doctor, and so will not be reported to the NPDB.
For example, in 2010, the American Medical Association found that 42.2% of 5,825 physicians who responded to its Physician Practice Information survey reported having been sued, with 22.4% sued twice or more.2 The report headlined that by mid career, 61% of doctor have been sued.
Rates varied by specialty, with general surgeons and obstetrician-gynecologists being most likely to be sued (69.2%). Family physicians and general internists had similar rates (38.9% and 34%), and pediatricians and psychiatrists were sued the least.
In that report, male doctors were twice as likely to be sued as were their female counterparts, and physicians in solo and specialty practices were sued more often than those in multispecialty practices. Physicians who had an ownership interest in a practice were also at greater risk, with 47.5% reporting being sued, compared with 33.4% for those with no ownership interest.
The second recent study, reported by Dr. Jena of Harvard Medical School, Boston, and his colleagues, analyzed Florida hospital admissions data covering some 24,000 physicians.3 They found that higher spending by physicians was associated with reduced malpractice claims made the following year.
This pattern held true for physicians in all specialties but one (family practice). For example, among internists, the malpractice risk probability was 1.5% in the bottom spending fifth ($19,725 per admission) and 0.3% in the top fifth ($39,379 per admission). Among obstetricians, the comparable figures were 1.9% and 0.4% respectively.
In addition, a separate subgroup analysis of cesarean-section rates revealed that malpractice claims were approximately halved among obstetricians with rates in the highest fifth, compared with the lowest fifth.
Unfortunately, the Jena study lacked information on illness severity and past malpractice history, and it remains speculative whether increased resource utilization could be attributed entirely to defensive medical practice.4
As interesting as these new reports may be, it is worth remembering that what prompts a lawsuit are poor communication and patient perception that the physician is uncaring and at fault for the bad result.
It is well known that quality of medical care correlates poorly with the filing of malpractice lawsuits, as illustrated in the conclusion of the landmark Harvard study that “medical malpractice litigation infrequently compensates patients injured by medical negligence and rarely identifies, and holds providers accountable for, substandard care.”5 The authors estimated that there was only 1 malpractice claim for every 7.6 adverse events caused by negligence.
In another retrospective chart review study, the quality of treatment as judged by independent peer review was no different in frequently sued versus never-sued obstetricians.6
Communication problems exist in more than 70% of malpractice cases, centering around four themes: 1) deserting the patient; 2) devaluing patient/family views; 3) delivering information poorly; and 4) failing to understand the patient/family perspective.7
Anger, either from the adverse result itself or perceived lack of caring, turns an injured patient into a plaintiff, and lies at the root of all malpractice claims. The patients may not even have a serious injury or a meritorious claim, but they are so frustrated with their physician or the hospital that they contact an attorney to vent their anger.
One experienced attorney volunteered that close to half his malpractice cases could have been avoided through disclosure or apology, noting: “What the patients really wanted was simply an honest explanation of what happened, and, if appropriate, an apology. Unfortunately, when they were not only offered neither, but were rejected as well, they felt doubly wronged and then sought legal counsel.”8
Communicating well begins with active listening. Patients want their doctors to listen to them and to explain their conditions and treatment plans in simple, understandable language. The physician should give them ample opportunity to tell their story and to ask questions.
In one well-publicized study, only 23% of patients were able to complete their opening statement before the doctor interrupted, which occurred, on the average, 18 seconds after the patient began to speak!9
References
1. N Engl J Med. 2016 Jan 28;374(4):354-62.
2. “Medical liability: By late career, 61% of doctors have been sued,” Aug. 16, 2010, American Medical News.
4. “Law & Medicine: Health care costs and defensive medicine,” Jan. 19, 2016, Internal Medicine News.
5. N Engl J Med. 1991 Jul 25;325(4):245-51.
6. JAMA. 1994 Nov 23-30;272(20):1588-91.
7. Arch Intern Med. 1994 Jun 27;154(12):1365-70.
8. Ann Intern Med. 1999 Dec 21;131(12):970-2.
9. Ann Intern Med. 1984 Nov;101(5):692-6.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at siang@hawaii.edu
Feds propose update to substance use privacy rules
Proposed federal regulations aim to improve integrated patient care for substance use disorders while preserving patient privacy.
The Health & Human Services department “is proposing to modernize the existing rules because new models are built on a foundation of information sharing to support coordination of patient care; the development of an electronic infrastructure for managing and exchanging patient data; and an increased focus on performance measurement and quality improvement within the health care system,” officials said in a statement Feb. 5.
The last substantive update to the Confidentiality of Alcohol and Drug Abuse Patient Records regulations – officially known as 42 CFR Part 2 – was in 1987, prior to either the push for integrated care or the use of electronic health records, according to HHS.
“Health care delivery has changed dramatically since the Part 2 regulations were originally promulgated and updated in the 1970s and 1980s,” Dianne J. Bourque, a Boston-based health law attorney, said in an interview. “Part 2’s stringent limitations on a provider’s ability to use and disclose patient information for purposes other than treatment creates a risk of drug and alcohol treatment patients being excluded from innovative care models like ACOs, health information exchanges, or population-based initiatives aimed at improving the quality and efficiency of care.”
Under the proposed regulations, health care providers would be allowed to share patient information except any records specifically related to substance abuse treatment; the proposal simultaneously would tighten requirements that any associated, identifying records be sanitized. Upon request, providers would be required to provide patients with a list of all entities with which their information has been shared.
When finalized, the updated regulations should be better aligned with other privacy and data security laws, including HIPAA, Ms. Bourque said.
However, “it will not be a large step and providers will still have to deal with overlapping and inconsistent requirements. For example, a HIPAA business associate is not the same thing as a Part 2 Qualified Service Organization, which creates complexity and potentially confusion for both providers and vendors,” she said. “There will be a learning curve. Providers will have to think carefully about third-party contract and consent form language.”
The proposed changes also would revise the medical emergency exception, giving providers more discretion in determining what constitutes an actual emergency.
Comments will be accepted on the proposed regulation at www.regulations.gov through April 11, 2016.
On Twitter @whitneymcknight
Proposed federal regulations aim to improve integrated patient care for substance use disorders while preserving patient privacy.
The Health & Human Services department “is proposing to modernize the existing rules because new models are built on a foundation of information sharing to support coordination of patient care; the development of an electronic infrastructure for managing and exchanging patient data; and an increased focus on performance measurement and quality improvement within the health care system,” officials said in a statement Feb. 5.
The last substantive update to the Confidentiality of Alcohol and Drug Abuse Patient Records regulations – officially known as 42 CFR Part 2 – was in 1987, prior to either the push for integrated care or the use of electronic health records, according to HHS.
“Health care delivery has changed dramatically since the Part 2 regulations were originally promulgated and updated in the 1970s and 1980s,” Dianne J. Bourque, a Boston-based health law attorney, said in an interview. “Part 2’s stringent limitations on a provider’s ability to use and disclose patient information for purposes other than treatment creates a risk of drug and alcohol treatment patients being excluded from innovative care models like ACOs, health information exchanges, or population-based initiatives aimed at improving the quality and efficiency of care.”
Under the proposed regulations, health care providers would be allowed to share patient information except any records specifically related to substance abuse treatment; the proposal simultaneously would tighten requirements that any associated, identifying records be sanitized. Upon request, providers would be required to provide patients with a list of all entities with which their information has been shared.
When finalized, the updated regulations should be better aligned with other privacy and data security laws, including HIPAA, Ms. Bourque said.
However, “it will not be a large step and providers will still have to deal with overlapping and inconsistent requirements. For example, a HIPAA business associate is not the same thing as a Part 2 Qualified Service Organization, which creates complexity and potentially confusion for both providers and vendors,” she said. “There will be a learning curve. Providers will have to think carefully about third-party contract and consent form language.”
The proposed changes also would revise the medical emergency exception, giving providers more discretion in determining what constitutes an actual emergency.
Comments will be accepted on the proposed regulation at www.regulations.gov through April 11, 2016.
On Twitter @whitneymcknight
Proposed federal regulations aim to improve integrated patient care for substance use disorders while preserving patient privacy.
The Health & Human Services department “is proposing to modernize the existing rules because new models are built on a foundation of information sharing to support coordination of patient care; the development of an electronic infrastructure for managing and exchanging patient data; and an increased focus on performance measurement and quality improvement within the health care system,” officials said in a statement Feb. 5.
The last substantive update to the Confidentiality of Alcohol and Drug Abuse Patient Records regulations – officially known as 42 CFR Part 2 – was in 1987, prior to either the push for integrated care or the use of electronic health records, according to HHS.
“Health care delivery has changed dramatically since the Part 2 regulations were originally promulgated and updated in the 1970s and 1980s,” Dianne J. Bourque, a Boston-based health law attorney, said in an interview. “Part 2’s stringent limitations on a provider’s ability to use and disclose patient information for purposes other than treatment creates a risk of drug and alcohol treatment patients being excluded from innovative care models like ACOs, health information exchanges, or population-based initiatives aimed at improving the quality and efficiency of care.”
Under the proposed regulations, health care providers would be allowed to share patient information except any records specifically related to substance abuse treatment; the proposal simultaneously would tighten requirements that any associated, identifying records be sanitized. Upon request, providers would be required to provide patients with a list of all entities with which their information has been shared.
When finalized, the updated regulations should be better aligned with other privacy and data security laws, including HIPAA, Ms. Bourque said.
However, “it will not be a large step and providers will still have to deal with overlapping and inconsistent requirements. For example, a HIPAA business associate is not the same thing as a Part 2 Qualified Service Organization, which creates complexity and potentially confusion for both providers and vendors,” she said. “There will be a learning curve. Providers will have to think carefully about third-party contract and consent form language.”
The proposed changes also would revise the medical emergency exception, giving providers more discretion in determining what constitutes an actual emergency.
Comments will be accepted on the proposed regulation at www.regulations.gov through April 11, 2016.
On Twitter @whitneymcknight
Data, new partnerships key to prepping for value-based care
AUSTIN, TEX. – Gathering data, seeking new partnerships, and showing leadership are the key ways to prepare for value-based medical practice, according to Houston-based health law attorney Ellie Bane.
“We are entering a whole new world in health care reimbursement,” Ms. Bane said at a conference held by the American Health Lawyers Association. “Physicians who think ahead will be well suited to succeed.”
If you don’t have practice data, start collecting the information today, she advised. Data – such as how long it takes for patients to book appointments, primary reasons for patient visits, and trends on care management – can set doctors apart and create leverage when it comes to new networks.
“You want to have reliable data so that when you go to partner with a health system or a health plan, you can show them what you can offer,” Ms. Bane said in an interview.
If the data do not exist, reach out to payers to see if they can help gather it, Ms. Bane suggested. Some health plans will assign a physician assistant or nurse practitioner to follow up with patients and help collect trend data. Other plans provide nurses or case managers to doctors who participate in certain initiatives such as quality, disease management, or performance improvement programs.
Demonstrating leadership also is key. Be vocal to hospitals and health plans about your interest in alternative payment systems and your desire to lead the transition, she advised. Be proactive by researching clinically-integrated networks, for example, and determining which network may work best for your practice.
“You want to become that value-based champion so that others will want to contract with your group,” she added.
When choosing a health system to partner with, assess whether the system is adequately responsive, can pull data in a timely manner, and can shift as measures change.
“Can your practice do the same thing?” Ms. Bane said. “If quality metrics change, are you able to change your systems to respond?”
Be creative and stay ahead of the curve by searching for novel ways to coordinate services and enlisting guidance, she said.
“A joint venture or Physician-Hospital Organization might have worked 5 years ago, but, it may not be the best model today,” she said. “This is where effective counsel is so helpful. A good health law attorney will be able to think of creative alignment strategies that will benefit the providers, health plans, systems, and – most importantly – patients.”
On Twitter @legal_med
AUSTIN, TEX. – Gathering data, seeking new partnerships, and showing leadership are the key ways to prepare for value-based medical practice, according to Houston-based health law attorney Ellie Bane.
“We are entering a whole new world in health care reimbursement,” Ms. Bane said at a conference held by the American Health Lawyers Association. “Physicians who think ahead will be well suited to succeed.”
If you don’t have practice data, start collecting the information today, she advised. Data – such as how long it takes for patients to book appointments, primary reasons for patient visits, and trends on care management – can set doctors apart and create leverage when it comes to new networks.
“You want to have reliable data so that when you go to partner with a health system or a health plan, you can show them what you can offer,” Ms. Bane said in an interview.
If the data do not exist, reach out to payers to see if they can help gather it, Ms. Bane suggested. Some health plans will assign a physician assistant or nurse practitioner to follow up with patients and help collect trend data. Other plans provide nurses or case managers to doctors who participate in certain initiatives such as quality, disease management, or performance improvement programs.
Demonstrating leadership also is key. Be vocal to hospitals and health plans about your interest in alternative payment systems and your desire to lead the transition, she advised. Be proactive by researching clinically-integrated networks, for example, and determining which network may work best for your practice.
“You want to become that value-based champion so that others will want to contract with your group,” she added.
When choosing a health system to partner with, assess whether the system is adequately responsive, can pull data in a timely manner, and can shift as measures change.
“Can your practice do the same thing?” Ms. Bane said. “If quality metrics change, are you able to change your systems to respond?”
Be creative and stay ahead of the curve by searching for novel ways to coordinate services and enlisting guidance, she said.
“A joint venture or Physician-Hospital Organization might have worked 5 years ago, but, it may not be the best model today,” she said. “This is where effective counsel is so helpful. A good health law attorney will be able to think of creative alignment strategies that will benefit the providers, health plans, systems, and – most importantly – patients.”
On Twitter @legal_med
AUSTIN, TEX. – Gathering data, seeking new partnerships, and showing leadership are the key ways to prepare for value-based medical practice, according to Houston-based health law attorney Ellie Bane.
“We are entering a whole new world in health care reimbursement,” Ms. Bane said at a conference held by the American Health Lawyers Association. “Physicians who think ahead will be well suited to succeed.”
If you don’t have practice data, start collecting the information today, she advised. Data – such as how long it takes for patients to book appointments, primary reasons for patient visits, and trends on care management – can set doctors apart and create leverage when it comes to new networks.
“You want to have reliable data so that when you go to partner with a health system or a health plan, you can show them what you can offer,” Ms. Bane said in an interview.
If the data do not exist, reach out to payers to see if they can help gather it, Ms. Bane suggested. Some health plans will assign a physician assistant or nurse practitioner to follow up with patients and help collect trend data. Other plans provide nurses or case managers to doctors who participate in certain initiatives such as quality, disease management, or performance improvement programs.
Demonstrating leadership also is key. Be vocal to hospitals and health plans about your interest in alternative payment systems and your desire to lead the transition, she advised. Be proactive by researching clinically-integrated networks, for example, and determining which network may work best for your practice.
“You want to become that value-based champion so that others will want to contract with your group,” she added.
When choosing a health system to partner with, assess whether the system is adequately responsive, can pull data in a timely manner, and can shift as measures change.
“Can your practice do the same thing?” Ms. Bane said. “If quality metrics change, are you able to change your systems to respond?”
Be creative and stay ahead of the curve by searching for novel ways to coordinate services and enlisting guidance, she said.
“A joint venture or Physician-Hospital Organization might have worked 5 years ago, but, it may not be the best model today,” she said. “This is where effective counsel is so helpful. A good health law attorney will be able to think of creative alignment strategies that will benefit the providers, health plans, systems, and – most importantly – patients.”
On Twitter @legal_med
EXPERT ANALYSIS FROM THE PHYSICIANS & HOSPITALS LAW INSTITUTE
Six Strategies to Help Hospitalists Improve Communication
As Karen Smith, MD, SFHM, chief of hospital medicine at Children’s National Health System in Washington, D.C., sees it, communication problems often arise at the first possible opportunity, when she’s trying to find out whom to call when she needs to inform a primary care physician or specialist about a hospitalized patient. Sometimes, that information isn’t readily available.
“Which specialist is on and available to talk?” she says.
Then there’s timing.
“By the time we can set up a time to actually talk to people, it’s after normal business hours,” Dr. Smith says. “People aren’t answering their office phones after five. …Your other choice is going through the answering service, but then you get a variety of people and not the person who knows this patient.”
Dr. Smith spearheaded an effort to reach out in a more reliable fashion to community physicians, with a goal of speaking to—or, more commonly, leaving messages with—at least 90% of hospitalized patients’ physicians. They reached the goal, but it was an eye-opening effort.
“The feedback I got from the hospitalists was it’s ‘just so difficult,’” Dr. Smith says. “I’m sitting on the phone waiting to get ahold of someone. Even trying to use administrative people and have them call and contact us, which is kind of complicated to do.”
Yul Ejnes, MD, MACP, a past chair of the board of regents of the American College of Physicians and an internist at Coastal Medical in R.I., says that if he were grading hospitalist communication with primary care providers on a poor-fair-good-excellent scale, he would give it a “fair.”
“It runs the spectrum from getting nothing—which is rare, I have to say—to getting at least a notification that your patient is in the hospital: ‘Here’s a contact number,’ sometimes with diagnosis,” he says. “And, much less commonly, getting a phone call. That usually occurs when there are questions.”
Dr. Ejnes says consistent communication is not as “robust as I would like it to be.”
“Some institutions do much better than others, in terms of the hospitalist always letting us know patients have come in,” he says. “With others, it doesn’t seem to be part of the institutional culture.”
There has to be a better way.
And, in fact, Dr. Smith and many other hospitalists are developing ways to better use technology to communicate more effectively with primary care, specialists, nurses, and patients. The goal is to make communication more routine, more effective, and more convenient for both parties, all the while—hopefully—improving patient care and strengthening working relationships.
Most of the approaches are not ultra-high tech. Too high tech might, in itself, be a potential barrier to communication for those who might be uncomfortable with new technology. Instead, the initiatives are mostly common sense tweaks to—or new, logical uses of—existing technology.
EHR-Embedded Communication
At Children’s National, Dr. Smith and colleagues use a standardized letter as part of a patient’s electronic health record (EHR). In addition to facts about the patient’s condition, the EHR includes information that makes it easier for physicians to communicate.
“What’s lovely with that is that [the letter] tells the provider the team that they’re on,” she said, adding that teams are divided by letter and color. “It has information on how you can reach the doctor. All of our doctors carry a phone around with them, and so it’s got that number.”
The EHR also includes a note suggesting that physicians avoid calling during rounds and gives them information on how to access the portal, so they can follow along with the patient’s care, should they choose to do so.
The amount of actual contact from primary care physicians? Scarce. Maybe one of 20 pediatricians will actually place a call to the hospitalist, but the response she has received has been positive, Dr. Smith says.
The EHR note also includes a sentence further characterizing the patient’s care, such as: Bobby C. was admitted with bronchiolitis. He’s doing fine; I anticipate he will go home tomorrow.
“Pediatricians have loved that,” she says. “They say, ‘I know exactly what my patient’s there for. I had the ability to call if I want.’”
Smarter Pages
At Vanderbilt University Medical Center in Nashville, Tenn., hospitalists noticed a frequent occurrence with pages: Many times, the hospitalist would only receive a phone number.
“With that, you don’t know which patient it’s about, who called you, how urgent it is, or what they need,” says researcher Sunil Kripalani, MD, MSc, SFHM, associate professor and chief of the section of hospital medicine at Vanderbilt.
It’s a tough spot for a busy hospitalist, who might be on the phone or at a bedside with another patient when three, four, or even five pages come through. The page might just be an FYI requiring no callback. It might be urgent. It might be the same page sent multiple times from different numbers (e.g. nursing moving to various phones). Many times, Dr. Kripalani and his hospitalists have had no way to know.
Now, Vanderbilt has established an online template for text pages, with the following basic information:
- Patient;
- Room number;
- Urgency level;
- Name of the sender;
- Callback number;
- Message; and
- Whether or not a callback is needed.
“That structure is very helpful for allowing physicians to triage which pages to call back and how quickly,” Dr. Kripalani says.
He acknowledges it isn’t “fancy bells and whistles.”
“Sometimes it’s doing the basic things well that makes the difference,” he adds.
The “structured pages” have allowed the nature of pages to be analyzed. Dr. Kripalani and colleagues have found that approximately 5% of pages were about a patient’s dietary status. If the patient was ordered not to receive anything by mouth, pages asked, when did that order expire and what diet should the patient resume?
Now, a prompt for that information is included in the hospital’s order entry system, which has cut the number of pages sent.
Vanderbilt is now looking at other, similar ways to streamline communication.
Patients and iPads
At the University of Colorado Hospital in Denver, researchers had an idea to facilitate communication and patient education: Patients are always inquiring about their discharge status and other facets of their hospitalization; what if they got their own tablet to follow along with everything in real time?1
The only real requirements for the study were that patients had to have Internet access at home and an understanding of how to work a web browser, says Jonathan Pell, MD, SFHM, assistant professor of internal medicine at the University of Colorado in Aurora and a hospitalist at University of Colorado Hospital. Patients were shown how to access their schedule for the day, their medication list and dosing schedule, and test results. Much of the information was delivered in real time, so patients who were told that if a lab result came back at a certain level they could be discharged could perhaps start preparing for that possibility earlier than they might have otherwise.
Researchers found that their patients worried less and reported less confusion. They also found that providing the tablets didn’t cause any increase in workload for doctors or nurses.
Providers and nurses expected that patients would notice medication errors, but that endpoint was not significant. Surprisingly, patients’ understanding of discharge times did not live up to expectations. But the results overall were encouraging enough that the effort will continue.
“We have these mixed results,” Dr. Pell says. “I think it’s good to get something out there in the literature and see what else people may be interested in doing. Our next step is to potentially open up notes to patients and let them see their doctor’s and nurse’s notes during their hospitalization.”
He says that, in some cases, communication with patients is the most crucial channel for hospitalists.
“For the very engaged patient [who has] a busy primary care doctor who’s hard to get in touch with,” he explains, “using the patient, informing them well, and getting them all the information they need is actually the best way to make sure that transition of care is smooth.”
Discharge, Facebook-Style
New England Inpatient Specialists (NEIS), a hospitalist group in North Andover, Mass., has an interesting approach to discharge. Instead of a nurse picking up the phone to make a follow-up appointment for a patient leaving the hospital, a secretary posts a message on “Chatter,” a secure tool similar to Facebook. The technology was developed by Salesforce.com, which offers platforms mainly designed to assist businesses with communication.
The idea behind Chatter is that the primary care office personnel can respond to a post at a time that’s convenient to them.
“All of this is so time-consuming. Why would you want somebody like an RN spending 15 to 20 minutes on the phone setting up an appointment when she could be on the floor?” says Sawad Thotathil, MD, vice president of performance and physician recruitment at NEIS. “Our program secretary will just post a discharge, and then somebody at the practice will look at it when they can and find out what associated information is needed and answer at their own convenience.”
Dr. Thotathil’s group also has been using the Imprivata Cortext secure text messaging system for more than a year, with what he deems “overall positive” results. About 60% of the practices with which NEIS staff need to communicate have signed on to the system.
“That kind of helps in management,” he says. “Sometimes, a patient is in the hospital and you can text the cardiologist, asking if the patient can be taken on for a procedure. That kind of communication, which would have taken longer or would not have happened, is happening now.
“Have we been able to directly link it to better outcomes?” he adds. “No, we haven’t looked at it that way. But what we have seen is that there’s always going to be a variation in how many people in a network actually will use it. ... There are going to be those high users, and there are going to be those providers who are going to be minimally using it.”
Videoconferencing
Pediatric hospitalists at the main hospital at Children’s National have been helping to provide care to children who are seen at five community sites. Dr. Smith says the communication at these sites, mostly from the ED, in which the pediatric hospitalists are helping make medical decisions, has been dramatically enhanced.
“The visual aspect of it changes the whole conversation,” she says. “You could tell them the exact same thing verbally and they are like, ‘OK, that’s fine,’ and there doesn’t seem to be a true understanding of what I’m trying to impart to you. Once people look at the child, all of a sudden there is a true shared mental model of, ‘OK, I understand what you’re doing. What’s going on?’”
Hospitalists also have been spearheading videoconferencing at diabetes clinics, to provide better care at community sites.
“We know what the need is. We know the gap in care,” Dr. Smith says. “We’ve been able to advocate and get those specialists brought out to the community via telemedicine, if it’s too difficult to get out on a regular basis.”
There are no hard data on the effects of the programs, but Dr. Smith says the improvement is noticeable.
“Anecdotally, we’ve seen a decrease in kids coming in with DKA (diabetic ketoacidosis) to the emergency room, so we’ve been able to change some of the trajectory. Many of those kids just didn’t have access to care. [For some], it would be a day’s trip for them to get to one of the academic centers to get follow up. They just wouldn’t go.”
EHR-Facilitated Calls
At Cincinnati Children’s, phone contact with community pediatricians at discharge is established with remarkable consistency: 98% to 99% of the time. The reason? A communication system, “Priority Link,” is connected to the EHR.
When the hospitalist signs a discharge order, the patient’s name is put in a queue. An operator sends out a page to inform the resident that the call is about to be made to the outpatient physician, making sure they’re ready for the call to be made.
“The key innovation was that we were trying to make sure that the inpatient side of it was really ready for the call, so we weren’t placing calls out to doctors and then we weren’t ready,” says Jeffrey Simmons, MD, MSc, associate director of clinical operations and quality in Cincinnati Children’s hospital medicine division.
He says there has been some pushback from pediatricians who feel the calls don’t provide any more value than the discharge summary itself. But the opportunity for questions and for a dialogue makes the calls worthwhile, Dr. Simmons notes. The system could be improved by tailoring communications to the community physicians’ preference—via fax or email, perhaps—and by having the call placed by physicians who are more knowledgeable about the details of the case.
Priority Link also is used to help community physicians with direct admissions for patients who don’t need to go to the ED. The operator coordinates a three-way call among the community physician, the hospitalist, and a nurse familiar with the bed situation.
“That three-way call is really great because we’re big and busy enough that sometimes we need that nurse manager on the phone, too, to No. 1, let us know if there really is a bed and, No. 2, coordinate with the nursing unit,” he says. TH
Tom Collins is a freelance writer in South Florida.
Reference
Pell JM, Mancuso M, Limon S, Oman K, Lin CT. Patient access to electronic health records during hospitalization. JAMA Intern Med. 2015;175(5):856-858. doi: 10.1001/jamainternmed.2015.121.
As Karen Smith, MD, SFHM, chief of hospital medicine at Children’s National Health System in Washington, D.C., sees it, communication problems often arise at the first possible opportunity, when she’s trying to find out whom to call when she needs to inform a primary care physician or specialist about a hospitalized patient. Sometimes, that information isn’t readily available.
“Which specialist is on and available to talk?” she says.
Then there’s timing.
“By the time we can set up a time to actually talk to people, it’s after normal business hours,” Dr. Smith says. “People aren’t answering their office phones after five. …Your other choice is going through the answering service, but then you get a variety of people and not the person who knows this patient.”
Dr. Smith spearheaded an effort to reach out in a more reliable fashion to community physicians, with a goal of speaking to—or, more commonly, leaving messages with—at least 90% of hospitalized patients’ physicians. They reached the goal, but it was an eye-opening effort.
“The feedback I got from the hospitalists was it’s ‘just so difficult,’” Dr. Smith says. “I’m sitting on the phone waiting to get ahold of someone. Even trying to use administrative people and have them call and contact us, which is kind of complicated to do.”
Yul Ejnes, MD, MACP, a past chair of the board of regents of the American College of Physicians and an internist at Coastal Medical in R.I., says that if he were grading hospitalist communication with primary care providers on a poor-fair-good-excellent scale, he would give it a “fair.”
“It runs the spectrum from getting nothing—which is rare, I have to say—to getting at least a notification that your patient is in the hospital: ‘Here’s a contact number,’ sometimes with diagnosis,” he says. “And, much less commonly, getting a phone call. That usually occurs when there are questions.”
Dr. Ejnes says consistent communication is not as “robust as I would like it to be.”
“Some institutions do much better than others, in terms of the hospitalist always letting us know patients have come in,” he says. “With others, it doesn’t seem to be part of the institutional culture.”
There has to be a better way.
And, in fact, Dr. Smith and many other hospitalists are developing ways to better use technology to communicate more effectively with primary care, specialists, nurses, and patients. The goal is to make communication more routine, more effective, and more convenient for both parties, all the while—hopefully—improving patient care and strengthening working relationships.
Most of the approaches are not ultra-high tech. Too high tech might, in itself, be a potential barrier to communication for those who might be uncomfortable with new technology. Instead, the initiatives are mostly common sense tweaks to—or new, logical uses of—existing technology.
EHR-Embedded Communication
At Children’s National, Dr. Smith and colleagues use a standardized letter as part of a patient’s electronic health record (EHR). In addition to facts about the patient’s condition, the EHR includes information that makes it easier for physicians to communicate.
“What’s lovely with that is that [the letter] tells the provider the team that they’re on,” she said, adding that teams are divided by letter and color. “It has information on how you can reach the doctor. All of our doctors carry a phone around with them, and so it’s got that number.”
The EHR also includes a note suggesting that physicians avoid calling during rounds and gives them information on how to access the portal, so they can follow along with the patient’s care, should they choose to do so.
The amount of actual contact from primary care physicians? Scarce. Maybe one of 20 pediatricians will actually place a call to the hospitalist, but the response she has received has been positive, Dr. Smith says.
The EHR note also includes a sentence further characterizing the patient’s care, such as: Bobby C. was admitted with bronchiolitis. He’s doing fine; I anticipate he will go home tomorrow.
“Pediatricians have loved that,” she says. “They say, ‘I know exactly what my patient’s there for. I had the ability to call if I want.’”
Smarter Pages
At Vanderbilt University Medical Center in Nashville, Tenn., hospitalists noticed a frequent occurrence with pages: Many times, the hospitalist would only receive a phone number.
“With that, you don’t know which patient it’s about, who called you, how urgent it is, or what they need,” says researcher Sunil Kripalani, MD, MSc, SFHM, associate professor and chief of the section of hospital medicine at Vanderbilt.
It’s a tough spot for a busy hospitalist, who might be on the phone or at a bedside with another patient when three, four, or even five pages come through. The page might just be an FYI requiring no callback. It might be urgent. It might be the same page sent multiple times from different numbers (e.g. nursing moving to various phones). Many times, Dr. Kripalani and his hospitalists have had no way to know.
Now, Vanderbilt has established an online template for text pages, with the following basic information:
- Patient;
- Room number;
- Urgency level;
- Name of the sender;
- Callback number;
- Message; and
- Whether or not a callback is needed.
“That structure is very helpful for allowing physicians to triage which pages to call back and how quickly,” Dr. Kripalani says.
He acknowledges it isn’t “fancy bells and whistles.”
“Sometimes it’s doing the basic things well that makes the difference,” he adds.
The “structured pages” have allowed the nature of pages to be analyzed. Dr. Kripalani and colleagues have found that approximately 5% of pages were about a patient’s dietary status. If the patient was ordered not to receive anything by mouth, pages asked, when did that order expire and what diet should the patient resume?
Now, a prompt for that information is included in the hospital’s order entry system, which has cut the number of pages sent.
Vanderbilt is now looking at other, similar ways to streamline communication.
Patients and iPads
At the University of Colorado Hospital in Denver, researchers had an idea to facilitate communication and patient education: Patients are always inquiring about their discharge status and other facets of their hospitalization; what if they got their own tablet to follow along with everything in real time?1
The only real requirements for the study were that patients had to have Internet access at home and an understanding of how to work a web browser, says Jonathan Pell, MD, SFHM, assistant professor of internal medicine at the University of Colorado in Aurora and a hospitalist at University of Colorado Hospital. Patients were shown how to access their schedule for the day, their medication list and dosing schedule, and test results. Much of the information was delivered in real time, so patients who were told that if a lab result came back at a certain level they could be discharged could perhaps start preparing for that possibility earlier than they might have otherwise.
Researchers found that their patients worried less and reported less confusion. They also found that providing the tablets didn’t cause any increase in workload for doctors or nurses.
Providers and nurses expected that patients would notice medication errors, but that endpoint was not significant. Surprisingly, patients’ understanding of discharge times did not live up to expectations. But the results overall were encouraging enough that the effort will continue.
“We have these mixed results,” Dr. Pell says. “I think it’s good to get something out there in the literature and see what else people may be interested in doing. Our next step is to potentially open up notes to patients and let them see their doctor’s and nurse’s notes during their hospitalization.”
He says that, in some cases, communication with patients is the most crucial channel for hospitalists.
“For the very engaged patient [who has] a busy primary care doctor who’s hard to get in touch with,” he explains, “using the patient, informing them well, and getting them all the information they need is actually the best way to make sure that transition of care is smooth.”
Discharge, Facebook-Style
New England Inpatient Specialists (NEIS), a hospitalist group in North Andover, Mass., has an interesting approach to discharge. Instead of a nurse picking up the phone to make a follow-up appointment for a patient leaving the hospital, a secretary posts a message on “Chatter,” a secure tool similar to Facebook. The technology was developed by Salesforce.com, which offers platforms mainly designed to assist businesses with communication.
The idea behind Chatter is that the primary care office personnel can respond to a post at a time that’s convenient to them.
“All of this is so time-consuming. Why would you want somebody like an RN spending 15 to 20 minutes on the phone setting up an appointment when she could be on the floor?” says Sawad Thotathil, MD, vice president of performance and physician recruitment at NEIS. “Our program secretary will just post a discharge, and then somebody at the practice will look at it when they can and find out what associated information is needed and answer at their own convenience.”
Dr. Thotathil’s group also has been using the Imprivata Cortext secure text messaging system for more than a year, with what he deems “overall positive” results. About 60% of the practices with which NEIS staff need to communicate have signed on to the system.
“That kind of helps in management,” he says. “Sometimes, a patient is in the hospital and you can text the cardiologist, asking if the patient can be taken on for a procedure. That kind of communication, which would have taken longer or would not have happened, is happening now.
“Have we been able to directly link it to better outcomes?” he adds. “No, we haven’t looked at it that way. But what we have seen is that there’s always going to be a variation in how many people in a network actually will use it. ... There are going to be those high users, and there are going to be those providers who are going to be minimally using it.”
Videoconferencing
Pediatric hospitalists at the main hospital at Children’s National have been helping to provide care to children who are seen at five community sites. Dr. Smith says the communication at these sites, mostly from the ED, in which the pediatric hospitalists are helping make medical decisions, has been dramatically enhanced.
“The visual aspect of it changes the whole conversation,” she says. “You could tell them the exact same thing verbally and they are like, ‘OK, that’s fine,’ and there doesn’t seem to be a true understanding of what I’m trying to impart to you. Once people look at the child, all of a sudden there is a true shared mental model of, ‘OK, I understand what you’re doing. What’s going on?’”
Hospitalists also have been spearheading videoconferencing at diabetes clinics, to provide better care at community sites.
“We know what the need is. We know the gap in care,” Dr. Smith says. “We’ve been able to advocate and get those specialists brought out to the community via telemedicine, if it’s too difficult to get out on a regular basis.”
There are no hard data on the effects of the programs, but Dr. Smith says the improvement is noticeable.
“Anecdotally, we’ve seen a decrease in kids coming in with DKA (diabetic ketoacidosis) to the emergency room, so we’ve been able to change some of the trajectory. Many of those kids just didn’t have access to care. [For some], it would be a day’s trip for them to get to one of the academic centers to get follow up. They just wouldn’t go.”
EHR-Facilitated Calls
At Cincinnati Children’s, phone contact with community pediatricians at discharge is established with remarkable consistency: 98% to 99% of the time. The reason? A communication system, “Priority Link,” is connected to the EHR.
When the hospitalist signs a discharge order, the patient’s name is put in a queue. An operator sends out a page to inform the resident that the call is about to be made to the outpatient physician, making sure they’re ready for the call to be made.
“The key innovation was that we were trying to make sure that the inpatient side of it was really ready for the call, so we weren’t placing calls out to doctors and then we weren’t ready,” says Jeffrey Simmons, MD, MSc, associate director of clinical operations and quality in Cincinnati Children’s hospital medicine division.
He says there has been some pushback from pediatricians who feel the calls don’t provide any more value than the discharge summary itself. But the opportunity for questions and for a dialogue makes the calls worthwhile, Dr. Simmons notes. The system could be improved by tailoring communications to the community physicians’ preference—via fax or email, perhaps—and by having the call placed by physicians who are more knowledgeable about the details of the case.
Priority Link also is used to help community physicians with direct admissions for patients who don’t need to go to the ED. The operator coordinates a three-way call among the community physician, the hospitalist, and a nurse familiar with the bed situation.
“That three-way call is really great because we’re big and busy enough that sometimes we need that nurse manager on the phone, too, to No. 1, let us know if there really is a bed and, No. 2, coordinate with the nursing unit,” he says. TH
Tom Collins is a freelance writer in South Florida.
Reference
Pell JM, Mancuso M, Limon S, Oman K, Lin CT. Patient access to electronic health records during hospitalization. JAMA Intern Med. 2015;175(5):856-858. doi: 10.1001/jamainternmed.2015.121.
As Karen Smith, MD, SFHM, chief of hospital medicine at Children’s National Health System in Washington, D.C., sees it, communication problems often arise at the first possible opportunity, when she’s trying to find out whom to call when she needs to inform a primary care physician or specialist about a hospitalized patient. Sometimes, that information isn’t readily available.
“Which specialist is on and available to talk?” she says.
Then there’s timing.
“By the time we can set up a time to actually talk to people, it’s after normal business hours,” Dr. Smith says. “People aren’t answering their office phones after five. …Your other choice is going through the answering service, but then you get a variety of people and not the person who knows this patient.”
Dr. Smith spearheaded an effort to reach out in a more reliable fashion to community physicians, with a goal of speaking to—or, more commonly, leaving messages with—at least 90% of hospitalized patients’ physicians. They reached the goal, but it was an eye-opening effort.
“The feedback I got from the hospitalists was it’s ‘just so difficult,’” Dr. Smith says. “I’m sitting on the phone waiting to get ahold of someone. Even trying to use administrative people and have them call and contact us, which is kind of complicated to do.”
Yul Ejnes, MD, MACP, a past chair of the board of regents of the American College of Physicians and an internist at Coastal Medical in R.I., says that if he were grading hospitalist communication with primary care providers on a poor-fair-good-excellent scale, he would give it a “fair.”
“It runs the spectrum from getting nothing—which is rare, I have to say—to getting at least a notification that your patient is in the hospital: ‘Here’s a contact number,’ sometimes with diagnosis,” he says. “And, much less commonly, getting a phone call. That usually occurs when there are questions.”
Dr. Ejnes says consistent communication is not as “robust as I would like it to be.”
“Some institutions do much better than others, in terms of the hospitalist always letting us know patients have come in,” he says. “With others, it doesn’t seem to be part of the institutional culture.”
There has to be a better way.
And, in fact, Dr. Smith and many other hospitalists are developing ways to better use technology to communicate more effectively with primary care, specialists, nurses, and patients. The goal is to make communication more routine, more effective, and more convenient for both parties, all the while—hopefully—improving patient care and strengthening working relationships.
Most of the approaches are not ultra-high tech. Too high tech might, in itself, be a potential barrier to communication for those who might be uncomfortable with new technology. Instead, the initiatives are mostly common sense tweaks to—or new, logical uses of—existing technology.
EHR-Embedded Communication
At Children’s National, Dr. Smith and colleagues use a standardized letter as part of a patient’s electronic health record (EHR). In addition to facts about the patient’s condition, the EHR includes information that makes it easier for physicians to communicate.
“What’s lovely with that is that [the letter] tells the provider the team that they’re on,” she said, adding that teams are divided by letter and color. “It has information on how you can reach the doctor. All of our doctors carry a phone around with them, and so it’s got that number.”
The EHR also includes a note suggesting that physicians avoid calling during rounds and gives them information on how to access the portal, so they can follow along with the patient’s care, should they choose to do so.
The amount of actual contact from primary care physicians? Scarce. Maybe one of 20 pediatricians will actually place a call to the hospitalist, but the response she has received has been positive, Dr. Smith says.
The EHR note also includes a sentence further characterizing the patient’s care, such as: Bobby C. was admitted with bronchiolitis. He’s doing fine; I anticipate he will go home tomorrow.
“Pediatricians have loved that,” she says. “They say, ‘I know exactly what my patient’s there for. I had the ability to call if I want.’”
Smarter Pages
At Vanderbilt University Medical Center in Nashville, Tenn., hospitalists noticed a frequent occurrence with pages: Many times, the hospitalist would only receive a phone number.
“With that, you don’t know which patient it’s about, who called you, how urgent it is, or what they need,” says researcher Sunil Kripalani, MD, MSc, SFHM, associate professor and chief of the section of hospital medicine at Vanderbilt.
It’s a tough spot for a busy hospitalist, who might be on the phone or at a bedside with another patient when three, four, or even five pages come through. The page might just be an FYI requiring no callback. It might be urgent. It might be the same page sent multiple times from different numbers (e.g. nursing moving to various phones). Many times, Dr. Kripalani and his hospitalists have had no way to know.
Now, Vanderbilt has established an online template for text pages, with the following basic information:
- Patient;
- Room number;
- Urgency level;
- Name of the sender;
- Callback number;
- Message; and
- Whether or not a callback is needed.
“That structure is very helpful for allowing physicians to triage which pages to call back and how quickly,” Dr. Kripalani says.
He acknowledges it isn’t “fancy bells and whistles.”
“Sometimes it’s doing the basic things well that makes the difference,” he adds.
The “structured pages” have allowed the nature of pages to be analyzed. Dr. Kripalani and colleagues have found that approximately 5% of pages were about a patient’s dietary status. If the patient was ordered not to receive anything by mouth, pages asked, when did that order expire and what diet should the patient resume?
Now, a prompt for that information is included in the hospital’s order entry system, which has cut the number of pages sent.
Vanderbilt is now looking at other, similar ways to streamline communication.
Patients and iPads
At the University of Colorado Hospital in Denver, researchers had an idea to facilitate communication and patient education: Patients are always inquiring about their discharge status and other facets of their hospitalization; what if they got their own tablet to follow along with everything in real time?1
The only real requirements for the study were that patients had to have Internet access at home and an understanding of how to work a web browser, says Jonathan Pell, MD, SFHM, assistant professor of internal medicine at the University of Colorado in Aurora and a hospitalist at University of Colorado Hospital. Patients were shown how to access their schedule for the day, their medication list and dosing schedule, and test results. Much of the information was delivered in real time, so patients who were told that if a lab result came back at a certain level they could be discharged could perhaps start preparing for that possibility earlier than they might have otherwise.
Researchers found that their patients worried less and reported less confusion. They also found that providing the tablets didn’t cause any increase in workload for doctors or nurses.
Providers and nurses expected that patients would notice medication errors, but that endpoint was not significant. Surprisingly, patients’ understanding of discharge times did not live up to expectations. But the results overall were encouraging enough that the effort will continue.
“We have these mixed results,” Dr. Pell says. “I think it’s good to get something out there in the literature and see what else people may be interested in doing. Our next step is to potentially open up notes to patients and let them see their doctor’s and nurse’s notes during their hospitalization.”
He says that, in some cases, communication with patients is the most crucial channel for hospitalists.
“For the very engaged patient [who has] a busy primary care doctor who’s hard to get in touch with,” he explains, “using the patient, informing them well, and getting them all the information they need is actually the best way to make sure that transition of care is smooth.”
Discharge, Facebook-Style
New England Inpatient Specialists (NEIS), a hospitalist group in North Andover, Mass., has an interesting approach to discharge. Instead of a nurse picking up the phone to make a follow-up appointment for a patient leaving the hospital, a secretary posts a message on “Chatter,” a secure tool similar to Facebook. The technology was developed by Salesforce.com, which offers platforms mainly designed to assist businesses with communication.
The idea behind Chatter is that the primary care office personnel can respond to a post at a time that’s convenient to them.
“All of this is so time-consuming. Why would you want somebody like an RN spending 15 to 20 minutes on the phone setting up an appointment when she could be on the floor?” says Sawad Thotathil, MD, vice president of performance and physician recruitment at NEIS. “Our program secretary will just post a discharge, and then somebody at the practice will look at it when they can and find out what associated information is needed and answer at their own convenience.”
Dr. Thotathil’s group also has been using the Imprivata Cortext secure text messaging system for more than a year, with what he deems “overall positive” results. About 60% of the practices with which NEIS staff need to communicate have signed on to the system.
“That kind of helps in management,” he says. “Sometimes, a patient is in the hospital and you can text the cardiologist, asking if the patient can be taken on for a procedure. That kind of communication, which would have taken longer or would not have happened, is happening now.
“Have we been able to directly link it to better outcomes?” he adds. “No, we haven’t looked at it that way. But what we have seen is that there’s always going to be a variation in how many people in a network actually will use it. ... There are going to be those high users, and there are going to be those providers who are going to be minimally using it.”
Videoconferencing
Pediatric hospitalists at the main hospital at Children’s National have been helping to provide care to children who are seen at five community sites. Dr. Smith says the communication at these sites, mostly from the ED, in which the pediatric hospitalists are helping make medical decisions, has been dramatically enhanced.
“The visual aspect of it changes the whole conversation,” she says. “You could tell them the exact same thing verbally and they are like, ‘OK, that’s fine,’ and there doesn’t seem to be a true understanding of what I’m trying to impart to you. Once people look at the child, all of a sudden there is a true shared mental model of, ‘OK, I understand what you’re doing. What’s going on?’”
Hospitalists also have been spearheading videoconferencing at diabetes clinics, to provide better care at community sites.
“We know what the need is. We know the gap in care,” Dr. Smith says. “We’ve been able to advocate and get those specialists brought out to the community via telemedicine, if it’s too difficult to get out on a regular basis.”
There are no hard data on the effects of the programs, but Dr. Smith says the improvement is noticeable.
“Anecdotally, we’ve seen a decrease in kids coming in with DKA (diabetic ketoacidosis) to the emergency room, so we’ve been able to change some of the trajectory. Many of those kids just didn’t have access to care. [For some], it would be a day’s trip for them to get to one of the academic centers to get follow up. They just wouldn’t go.”
EHR-Facilitated Calls
At Cincinnati Children’s, phone contact with community pediatricians at discharge is established with remarkable consistency: 98% to 99% of the time. The reason? A communication system, “Priority Link,” is connected to the EHR.
When the hospitalist signs a discharge order, the patient’s name is put in a queue. An operator sends out a page to inform the resident that the call is about to be made to the outpatient physician, making sure they’re ready for the call to be made.
“The key innovation was that we were trying to make sure that the inpatient side of it was really ready for the call, so we weren’t placing calls out to doctors and then we weren’t ready,” says Jeffrey Simmons, MD, MSc, associate director of clinical operations and quality in Cincinnati Children’s hospital medicine division.
He says there has been some pushback from pediatricians who feel the calls don’t provide any more value than the discharge summary itself. But the opportunity for questions and for a dialogue makes the calls worthwhile, Dr. Simmons notes. The system could be improved by tailoring communications to the community physicians’ preference—via fax or email, perhaps—and by having the call placed by physicians who are more knowledgeable about the details of the case.
Priority Link also is used to help community physicians with direct admissions for patients who don’t need to go to the ED. The operator coordinates a three-way call among the community physician, the hospitalist, and a nurse familiar with the bed situation.
“That three-way call is really great because we’re big and busy enough that sometimes we need that nurse manager on the phone, too, to No. 1, let us know if there really is a bed and, No. 2, coordinate with the nursing unit,” he says. TH
Tom Collins is a freelance writer in South Florida.
Reference
Pell JM, Mancuso M, Limon S, Oman K, Lin CT. Patient access to electronic health records during hospitalization. JAMA Intern Med. 2015;175(5):856-858. doi: 10.1001/jamainternmed.2015.121.
More than 90% of Americans have health insurance, HHS reports
About 12.7 million people have either selected plans or were automatically reenrolled through the federal or state-based individual insurance marketplaces during the open enrollment period for the 2016 plan year, the U.S. Department of Health & Human Services reported.
An additional 400,000 people in Minnesota and New York enrolled through the Basic Health Program, a state-based program that provides health insurance coverage to low-income individuals who would otherwise be eligible to purchase on the exchanges.
“As the Affordable Care Act has taken effect, more than 17.6 million Americans gained coverage through late last summer,” HHS Secretary Sylvia Burwell said during a Feb. 2 teleconference. “More than 90% of Americans are insured. That’s the first time this has ever been true.”
In detailing enrollment through the federal marketplace, HHS reported that of the 9.6 million people who received coverage through the exchange, 42%, or 4 million, were new enrollees.
“While we won’t know how this season’s sign-ups will precisely impact the uninsured rate until later in the year, it’s clear that, with these 4 million people who are new to Medicaid, and the improving economy, we will continue to make progress,” Ms. Burwell said.
The new enrollees are also important to “help refresh” the risk pools, Health Insurance Marketplace CEO Kevin Counihan said during the call. In responding to a question about larger insurers possibly bowing out of the exchanges, he noted that the higher utilizers of health care services were more likely to have joined in the first 2 years, and those new enrollees are likely to be in a different place in terms of their health care needs.
About 12.7 million people have either selected plans or were automatically reenrolled through the federal or state-based individual insurance marketplaces during the open enrollment period for the 2016 plan year, the U.S. Department of Health & Human Services reported.
An additional 400,000 people in Minnesota and New York enrolled through the Basic Health Program, a state-based program that provides health insurance coverage to low-income individuals who would otherwise be eligible to purchase on the exchanges.
“As the Affordable Care Act has taken effect, more than 17.6 million Americans gained coverage through late last summer,” HHS Secretary Sylvia Burwell said during a Feb. 2 teleconference. “More than 90% of Americans are insured. That’s the first time this has ever been true.”
In detailing enrollment through the federal marketplace, HHS reported that of the 9.6 million people who received coverage through the exchange, 42%, or 4 million, were new enrollees.
“While we won’t know how this season’s sign-ups will precisely impact the uninsured rate until later in the year, it’s clear that, with these 4 million people who are new to Medicaid, and the improving economy, we will continue to make progress,” Ms. Burwell said.
The new enrollees are also important to “help refresh” the risk pools, Health Insurance Marketplace CEO Kevin Counihan said during the call. In responding to a question about larger insurers possibly bowing out of the exchanges, he noted that the higher utilizers of health care services were more likely to have joined in the first 2 years, and those new enrollees are likely to be in a different place in terms of their health care needs.
About 12.7 million people have either selected plans or were automatically reenrolled through the federal or state-based individual insurance marketplaces during the open enrollment period for the 2016 plan year, the U.S. Department of Health & Human Services reported.
An additional 400,000 people in Minnesota and New York enrolled through the Basic Health Program, a state-based program that provides health insurance coverage to low-income individuals who would otherwise be eligible to purchase on the exchanges.
“As the Affordable Care Act has taken effect, more than 17.6 million Americans gained coverage through late last summer,” HHS Secretary Sylvia Burwell said during a Feb. 2 teleconference. “More than 90% of Americans are insured. That’s the first time this has ever been true.”
In detailing enrollment through the federal marketplace, HHS reported that of the 9.6 million people who received coverage through the exchange, 42%, or 4 million, were new enrollees.
“While we won’t know how this season’s sign-ups will precisely impact the uninsured rate until later in the year, it’s clear that, with these 4 million people who are new to Medicaid, and the improving economy, we will continue to make progress,” Ms. Burwell said.
The new enrollees are also important to “help refresh” the risk pools, Health Insurance Marketplace CEO Kevin Counihan said during the call. In responding to a question about larger insurers possibly bowing out of the exchanges, he noted that the higher utilizers of health care services were more likely to have joined in the first 2 years, and those new enrollees are likely to be in a different place in terms of their health care needs.
Practice Expanding: The Rising Trend in Hospitalist Co-Management
As the practice of medicine continues to transition to performance-based payment systems, the number of mergers of hospitalists and specialists has surged. Payment models that focus on clinical outcomes and best practices link payment to the ability of physicians to provide efficient, quality healthcare and improve patient outcomes. These payment systems are changing the way healthcare services are delivered by demanding better patient care at a lower cost. The result is increasing pressure on physicians to meet operational and quality goals, or receive less reimbursement for their services.
Studies have shown that the effective use of hospitalists can improve standardized patient care for surgical patients. Hospitalists also provide value to specialists by freeing up time so they can focus on their area of expertise. As a result, co-management arrangements between hospitalists and specialists have become a popular tool to define working relationships and improve the quality of care patients receive.
Hospitalist Evolution
When hospitalists first debuted, they were seen as a threat to primary care physicians and specialists. Over time, they were criticized for performing routine work for specialized physicians. To overcome these negative connotations and prove their worth, hospitalists began co-managing patients for surgical specialists, who soon realized the significant value hospitalist services provided. Not only do they share in the responsibility of care provided to patients, but they also reduce readmissions and costs associated with providing healthcare.
Now there are even specialty hospitalists who specialize in a particular field, such as orthopedics or obstetrics.
Why Co-Management?
Hospitalists add value by helping to alleviate the burden on specialists—providing ED coverage, assisting in the operating room, and rounding on patients. They evaluate surgical patients for medical issues, reconcile medications across the spectrum of a patient’s care, and standardize the patient discharge and communication processes.
Providing these services frees specialists from rounding and allows them to concentrate on their specialty. Hospitalists do not have office-based practices, which allows them to spend their time in the hospital caring for admitted, pre-operative, and post-operative patients.
It is in the pre-operative and post-operative environments where hospitalists have established their extreme value to specialists. Under co-management arrangements, hospitalists are able to ensure that all pre-operative tests are conducted, reports are dictated, and the patient’s medical history is available. Pre-operative evaluations allow the hospitalist to develop a post-operative plan of care and proactively address many medical concerns. Also, the hospitalist is available to see patients immediately after surgery, allowing immediate evaluation and treatment for high blood pressure, diabetic issues, or other medical issues.
In sum, the hospitalist is responsible for the medical care of the specialist’s patients, and the specialist is able to focus on the specialty services he or she provides. Providing these services gives hospitalists the opportunity to anticipate problems and overcome issues, which results in more efficient care, shorter lengths of stay in the hospital, and improved patient satisfaction. Such results make hospitalists critical to success in performance-based payment systems.
Successful Co-Management Arrangements
A key to success in establishing a co-management arrangement between a hospitalist and a specialist is setting forth the parameters of the relationship in a written agreement. It is particularly important that the relationship foster equality among the parties, regardless of who is the attending physician of record. The parties should be jointly responsible for patient care, with the hospitalist treating the patient’s general medical concerns and the specialist focusing on techniques within his specialty to improve the patient’s issues.
The agreement should clearly state the responsibilities of each party, including delineating the party responsible for decisions such as admission and discharge. It should address resources and set forth the standardized processes and protocols to be used when treating patients.
Specialists can vary in their treatment of patients, so it is best to document their expectations at the onset of the relationship. Also, successful co-management is contingent upon regular communication between the hospitalist and the specialist. It is important to establish those boundaries in advance to prevent miscommunication down the road.
In particular, the agreement should explicitly describe the lines of authority and how conflicts will be addressed.
Final Thoughts
Co-management is a growing trend that can provide an opportunity for hospitalists to expand their practice and reinforce their value to both specialists and the hospital. The improved quality of care and patient satisfaction that is associated with hospitalist services can be crucial to maximizing reimbursement under a value-based reimbursement system. TH
As the practice of medicine continues to transition to performance-based payment systems, the number of mergers of hospitalists and specialists has surged. Payment models that focus on clinical outcomes and best practices link payment to the ability of physicians to provide efficient, quality healthcare and improve patient outcomes. These payment systems are changing the way healthcare services are delivered by demanding better patient care at a lower cost. The result is increasing pressure on physicians to meet operational and quality goals, or receive less reimbursement for their services.
Studies have shown that the effective use of hospitalists can improve standardized patient care for surgical patients. Hospitalists also provide value to specialists by freeing up time so they can focus on their area of expertise. As a result, co-management arrangements between hospitalists and specialists have become a popular tool to define working relationships and improve the quality of care patients receive.
Hospitalist Evolution
When hospitalists first debuted, they were seen as a threat to primary care physicians and specialists. Over time, they were criticized for performing routine work for specialized physicians. To overcome these negative connotations and prove their worth, hospitalists began co-managing patients for surgical specialists, who soon realized the significant value hospitalist services provided. Not only do they share in the responsibility of care provided to patients, but they also reduce readmissions and costs associated with providing healthcare.
Now there are even specialty hospitalists who specialize in a particular field, such as orthopedics or obstetrics.
Why Co-Management?
Hospitalists add value by helping to alleviate the burden on specialists—providing ED coverage, assisting in the operating room, and rounding on patients. They evaluate surgical patients for medical issues, reconcile medications across the spectrum of a patient’s care, and standardize the patient discharge and communication processes.
Providing these services frees specialists from rounding and allows them to concentrate on their specialty. Hospitalists do not have office-based practices, which allows them to spend their time in the hospital caring for admitted, pre-operative, and post-operative patients.
It is in the pre-operative and post-operative environments where hospitalists have established their extreme value to specialists. Under co-management arrangements, hospitalists are able to ensure that all pre-operative tests are conducted, reports are dictated, and the patient’s medical history is available. Pre-operative evaluations allow the hospitalist to develop a post-operative plan of care and proactively address many medical concerns. Also, the hospitalist is available to see patients immediately after surgery, allowing immediate evaluation and treatment for high blood pressure, diabetic issues, or other medical issues.
In sum, the hospitalist is responsible for the medical care of the specialist’s patients, and the specialist is able to focus on the specialty services he or she provides. Providing these services gives hospitalists the opportunity to anticipate problems and overcome issues, which results in more efficient care, shorter lengths of stay in the hospital, and improved patient satisfaction. Such results make hospitalists critical to success in performance-based payment systems.
Successful Co-Management Arrangements
A key to success in establishing a co-management arrangement between a hospitalist and a specialist is setting forth the parameters of the relationship in a written agreement. It is particularly important that the relationship foster equality among the parties, regardless of who is the attending physician of record. The parties should be jointly responsible for patient care, with the hospitalist treating the patient’s general medical concerns and the specialist focusing on techniques within his specialty to improve the patient’s issues.
The agreement should clearly state the responsibilities of each party, including delineating the party responsible for decisions such as admission and discharge. It should address resources and set forth the standardized processes and protocols to be used when treating patients.
Specialists can vary in their treatment of patients, so it is best to document their expectations at the onset of the relationship. Also, successful co-management is contingent upon regular communication between the hospitalist and the specialist. It is important to establish those boundaries in advance to prevent miscommunication down the road.
In particular, the agreement should explicitly describe the lines of authority and how conflicts will be addressed.
Final Thoughts
Co-management is a growing trend that can provide an opportunity for hospitalists to expand their practice and reinforce their value to both specialists and the hospital. The improved quality of care and patient satisfaction that is associated with hospitalist services can be crucial to maximizing reimbursement under a value-based reimbursement system. TH
As the practice of medicine continues to transition to performance-based payment systems, the number of mergers of hospitalists and specialists has surged. Payment models that focus on clinical outcomes and best practices link payment to the ability of physicians to provide efficient, quality healthcare and improve patient outcomes. These payment systems are changing the way healthcare services are delivered by demanding better patient care at a lower cost. The result is increasing pressure on physicians to meet operational and quality goals, or receive less reimbursement for their services.
Studies have shown that the effective use of hospitalists can improve standardized patient care for surgical patients. Hospitalists also provide value to specialists by freeing up time so they can focus on their area of expertise. As a result, co-management arrangements between hospitalists and specialists have become a popular tool to define working relationships and improve the quality of care patients receive.
Hospitalist Evolution
When hospitalists first debuted, they were seen as a threat to primary care physicians and specialists. Over time, they were criticized for performing routine work for specialized physicians. To overcome these negative connotations and prove their worth, hospitalists began co-managing patients for surgical specialists, who soon realized the significant value hospitalist services provided. Not only do they share in the responsibility of care provided to patients, but they also reduce readmissions and costs associated with providing healthcare.
Now there are even specialty hospitalists who specialize in a particular field, such as orthopedics or obstetrics.
Why Co-Management?
Hospitalists add value by helping to alleviate the burden on specialists—providing ED coverage, assisting in the operating room, and rounding on patients. They evaluate surgical patients for medical issues, reconcile medications across the spectrum of a patient’s care, and standardize the patient discharge and communication processes.
Providing these services frees specialists from rounding and allows them to concentrate on their specialty. Hospitalists do not have office-based practices, which allows them to spend their time in the hospital caring for admitted, pre-operative, and post-operative patients.
It is in the pre-operative and post-operative environments where hospitalists have established their extreme value to specialists. Under co-management arrangements, hospitalists are able to ensure that all pre-operative tests are conducted, reports are dictated, and the patient’s medical history is available. Pre-operative evaluations allow the hospitalist to develop a post-operative plan of care and proactively address many medical concerns. Also, the hospitalist is available to see patients immediately after surgery, allowing immediate evaluation and treatment for high blood pressure, diabetic issues, or other medical issues.
In sum, the hospitalist is responsible for the medical care of the specialist’s patients, and the specialist is able to focus on the specialty services he or she provides. Providing these services gives hospitalists the opportunity to anticipate problems and overcome issues, which results in more efficient care, shorter lengths of stay in the hospital, and improved patient satisfaction. Such results make hospitalists critical to success in performance-based payment systems.
Successful Co-Management Arrangements
A key to success in establishing a co-management arrangement between a hospitalist and a specialist is setting forth the parameters of the relationship in a written agreement. It is particularly important that the relationship foster equality among the parties, regardless of who is the attending physician of record. The parties should be jointly responsible for patient care, with the hospitalist treating the patient’s general medical concerns and the specialist focusing on techniques within his specialty to improve the patient’s issues.
The agreement should clearly state the responsibilities of each party, including delineating the party responsible for decisions such as admission and discharge. It should address resources and set forth the standardized processes and protocols to be used when treating patients.
Specialists can vary in their treatment of patients, so it is best to document their expectations at the onset of the relationship. Also, successful co-management is contingent upon regular communication between the hospitalist and the specialist. It is important to establish those boundaries in advance to prevent miscommunication down the road.
In particular, the agreement should explicitly describe the lines of authority and how conflicts will be addressed.
Final Thoughts
Co-management is a growing trend that can provide an opportunity for hospitalists to expand their practice and reinforce their value to both specialists and the hospital. The improved quality of care and patient satisfaction that is associated with hospitalist services can be crucial to maximizing reimbursement under a value-based reimbursement system. TH
Doctors to APM committee: Remember specialists
Physicians are calling on a new federal advisory committee to be sure to include specialists in the coming value-based alternative payment models.
Created by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), the Physician-Focused Payment Model Technical Advisory Committee (PTAC) is charged with providing comments and recommendations on physician payment models to the Health & Human Services department. At the committee’s first meeting on Feb. 1, members heard from a number of physician associations that expressed disappointment about the role of specialists in current value-based payment models and requested more attention as new models move forward.
“We believe [the Centers for Medicare & Medicaid Services] needs to allow for the widest range of innovative ideas to ensure the greatest number of physicians are not only able to participate, but succeed in future payment models,” said Jenna Kappel, health policy director for the American Academy of Otolaryngology–Head and Neck Surgery. “We are hopeful there will be opportunities for specialists to participate and thrive in [alternative payment models] in the future. However, the current CMS definition of an alternative payment entity provides very limited opportunities for models that include the participation of specialists.”
The American College of Emergency Physicians concurred.
“There have been a significant number of [Center for Medicare & Medicaid Innovation] grants and state Medicaid proposals that include an emergency department [ED] visit as a failure metric,” said Barbara Tomar, federal affairs director for ACEP. “We understand that to a certain point ... but there are always going to be a proportion of patients [who] have serious diseases or conditions that will have exacerbations, and they’re going to land in the ED. This really should be acknowledged in a lot of the alternative payment models.”
Committee members acknowledged concerns about APMs and outlined goals for developing an effective proposal review process.
“We need to involve everybody in developing innovative payment models that do away with all frustration that physicians are currently experiencing and get to better results and higher value,” said committee member Robert A. Berenson, an internist and former vice chair of the Medicare Payment Advisory Commission. “At the same time, these payment models not only have to be elegant in their conception, but they have to be operationally and administratively feasible. ... They need to be such that most payers can adopt them, not simply CMS or Medicare or a state Medicaid agency,” Dr. Berenson said.
Transparency, inclusion, and education are primary aims of the committee, said committee member Dr. Kavita Patel, an internist and senior fellow at the Brookings Institution, Washington.
“Part of my responsibility, having looked at other payment models as well as the trials and tribulations of not just the practicing clinician, but the practicing team is [considering] how the team is going to adapt and learn and strive in this environment,” Dr. Patel said. “So much of what we try to do is think about the financial incentives. We also need to think about what are we asking clinicians to measure? What are we asking patients and families to report on and how do we have the two align?”
Officials at the CMS Innovation Center have said that proposed APMs will be submitted first to PTAC for recommendations and then will go to HHS. The Secretary will make comments about the proposals on the CMS website, followed by testing consideration. Potential evaluation factors include the strength of the evidence base, the potential for cost savings, the probability of model success, feasibility, scalability, and demographic, clinical, and geographic diversity.
“Obviously, we’re not looking for slam dunk data that say it always will be effective because if it were, we wouldn’t need to do the test, but we need some evidence that this is potentially a worthwhile investment,” said Dr. Hoangmai H. Pham, director of accountable care programs at the CMS Innovation Center.
CMS officials stressed that models should be designed as broadly as possible. A proposal can include multiple interventions, but should include a similar theme, procedure, or condition to address.
“It gives us the opportunity to find efficiencies,” Dr. Pham said. “It’s much easier to have one model with multiple tracks that you can ask one application contractor to handle as opposed to six. Much easier to ask for all the payment shared system changes in 1 change request rather than 32. That’s another reason we would urge you to favor comprehensive models.”
CMS officials plan to issue a proposed rule on APMs in April and a final rule Nov. 1.
On Twitter @legal_med
Physicians are calling on a new federal advisory committee to be sure to include specialists in the coming value-based alternative payment models.
Created by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), the Physician-Focused Payment Model Technical Advisory Committee (PTAC) is charged with providing comments and recommendations on physician payment models to the Health & Human Services department. At the committee’s first meeting on Feb. 1, members heard from a number of physician associations that expressed disappointment about the role of specialists in current value-based payment models and requested more attention as new models move forward.
“We believe [the Centers for Medicare & Medicaid Services] needs to allow for the widest range of innovative ideas to ensure the greatest number of physicians are not only able to participate, but succeed in future payment models,” said Jenna Kappel, health policy director for the American Academy of Otolaryngology–Head and Neck Surgery. “We are hopeful there will be opportunities for specialists to participate and thrive in [alternative payment models] in the future. However, the current CMS definition of an alternative payment entity provides very limited opportunities for models that include the participation of specialists.”
The American College of Emergency Physicians concurred.
“There have been a significant number of [Center for Medicare & Medicaid Innovation] grants and state Medicaid proposals that include an emergency department [ED] visit as a failure metric,” said Barbara Tomar, federal affairs director for ACEP. “We understand that to a certain point ... but there are always going to be a proportion of patients [who] have serious diseases or conditions that will have exacerbations, and they’re going to land in the ED. This really should be acknowledged in a lot of the alternative payment models.”
Committee members acknowledged concerns about APMs and outlined goals for developing an effective proposal review process.
“We need to involve everybody in developing innovative payment models that do away with all frustration that physicians are currently experiencing and get to better results and higher value,” said committee member Robert A. Berenson, an internist and former vice chair of the Medicare Payment Advisory Commission. “At the same time, these payment models not only have to be elegant in their conception, but they have to be operationally and administratively feasible. ... They need to be such that most payers can adopt them, not simply CMS or Medicare or a state Medicaid agency,” Dr. Berenson said.
Transparency, inclusion, and education are primary aims of the committee, said committee member Dr. Kavita Patel, an internist and senior fellow at the Brookings Institution, Washington.
“Part of my responsibility, having looked at other payment models as well as the trials and tribulations of not just the practicing clinician, but the practicing team is [considering] how the team is going to adapt and learn and strive in this environment,” Dr. Patel said. “So much of what we try to do is think about the financial incentives. We also need to think about what are we asking clinicians to measure? What are we asking patients and families to report on and how do we have the two align?”
Officials at the CMS Innovation Center have said that proposed APMs will be submitted first to PTAC for recommendations and then will go to HHS. The Secretary will make comments about the proposals on the CMS website, followed by testing consideration. Potential evaluation factors include the strength of the evidence base, the potential for cost savings, the probability of model success, feasibility, scalability, and demographic, clinical, and geographic diversity.
“Obviously, we’re not looking for slam dunk data that say it always will be effective because if it were, we wouldn’t need to do the test, but we need some evidence that this is potentially a worthwhile investment,” said Dr. Hoangmai H. Pham, director of accountable care programs at the CMS Innovation Center.
CMS officials stressed that models should be designed as broadly as possible. A proposal can include multiple interventions, but should include a similar theme, procedure, or condition to address.
“It gives us the opportunity to find efficiencies,” Dr. Pham said. “It’s much easier to have one model with multiple tracks that you can ask one application contractor to handle as opposed to six. Much easier to ask for all the payment shared system changes in 1 change request rather than 32. That’s another reason we would urge you to favor comprehensive models.”
CMS officials plan to issue a proposed rule on APMs in April and a final rule Nov. 1.
On Twitter @legal_med
Physicians are calling on a new federal advisory committee to be sure to include specialists in the coming value-based alternative payment models.
Created by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), the Physician-Focused Payment Model Technical Advisory Committee (PTAC) is charged with providing comments and recommendations on physician payment models to the Health & Human Services department. At the committee’s first meeting on Feb. 1, members heard from a number of physician associations that expressed disappointment about the role of specialists in current value-based payment models and requested more attention as new models move forward.
“We believe [the Centers for Medicare & Medicaid Services] needs to allow for the widest range of innovative ideas to ensure the greatest number of physicians are not only able to participate, but succeed in future payment models,” said Jenna Kappel, health policy director for the American Academy of Otolaryngology–Head and Neck Surgery. “We are hopeful there will be opportunities for specialists to participate and thrive in [alternative payment models] in the future. However, the current CMS definition of an alternative payment entity provides very limited opportunities for models that include the participation of specialists.”
The American College of Emergency Physicians concurred.
“There have been a significant number of [Center for Medicare & Medicaid Innovation] grants and state Medicaid proposals that include an emergency department [ED] visit as a failure metric,” said Barbara Tomar, federal affairs director for ACEP. “We understand that to a certain point ... but there are always going to be a proportion of patients [who] have serious diseases or conditions that will have exacerbations, and they’re going to land in the ED. This really should be acknowledged in a lot of the alternative payment models.”
Committee members acknowledged concerns about APMs and outlined goals for developing an effective proposal review process.
“We need to involve everybody in developing innovative payment models that do away with all frustration that physicians are currently experiencing and get to better results and higher value,” said committee member Robert A. Berenson, an internist and former vice chair of the Medicare Payment Advisory Commission. “At the same time, these payment models not only have to be elegant in their conception, but they have to be operationally and administratively feasible. ... They need to be such that most payers can adopt them, not simply CMS or Medicare or a state Medicaid agency,” Dr. Berenson said.
Transparency, inclusion, and education are primary aims of the committee, said committee member Dr. Kavita Patel, an internist and senior fellow at the Brookings Institution, Washington.
“Part of my responsibility, having looked at other payment models as well as the trials and tribulations of not just the practicing clinician, but the practicing team is [considering] how the team is going to adapt and learn and strive in this environment,” Dr. Patel said. “So much of what we try to do is think about the financial incentives. We also need to think about what are we asking clinicians to measure? What are we asking patients and families to report on and how do we have the two align?”
Officials at the CMS Innovation Center have said that proposed APMs will be submitted first to PTAC for recommendations and then will go to HHS. The Secretary will make comments about the proposals on the CMS website, followed by testing consideration. Potential evaluation factors include the strength of the evidence base, the potential for cost savings, the probability of model success, feasibility, scalability, and demographic, clinical, and geographic diversity.
“Obviously, we’re not looking for slam dunk data that say it always will be effective because if it were, we wouldn’t need to do the test, but we need some evidence that this is potentially a worthwhile investment,” said Dr. Hoangmai H. Pham, director of accountable care programs at the CMS Innovation Center.
CMS officials stressed that models should be designed as broadly as possible. A proposal can include multiple interventions, but should include a similar theme, procedure, or condition to address.
“It gives us the opportunity to find efficiencies,” Dr. Pham said. “It’s much easier to have one model with multiple tracks that you can ask one application contractor to handle as opposed to six. Much easier to ask for all the payment shared system changes in 1 change request rather than 32. That’s another reason we would urge you to favor comprehensive models.”
CMS officials plan to issue a proposed rule on APMs in April and a final rule Nov. 1.
On Twitter @legal_med
First EDition: News for and about the practice of emergency medicine
WHO Declares ‘Public Health Emergency’ for Microcephaly Linked to Zika Virus
BY MARY ELLEN SCHNEIDER
Frontline Medical News
The World Health Organization (WHO) has declared a “public health emergency of international concern” related to the clusters of microcephaly and other neurological complications reported in Brazil and earlier in French Polynesia. Though there is a strong association between these cases and the Zika virus, a causal link still has not been scientifically proven, according to the WHO.
The WHO’s emergency declaration clears the way for the international health community to move forward with a coordinated response. Dr Margaret Chan, WHO Director-General, said her organization plans to take a number of precautionary measures, including improving surveillance and detection of infections, congenital malformations, and neurological complications. They will also work with countries to intensify control of mosquito populations and help expedite the development of diagnostic tests and vaccines to protect at-risk populations.
The recommendations came after a February 1 meeting of the International Health Regulations Emergency Committee, which Dr Chan convened in response to the Zika virus outbreak and the observed increase in neurological disorders and neonatal malformations.
The group of 18 experts advised that the clusters of microcephaly and other complications constitute an “extraordinary event and a public health threat to other parts of the world.” The group did not recommend any restrictions on travel or trade with areas where the Zika virus transmission is ongoing, however.
“At present, the most important protective measures are the control of mosquito populations and the prevention of mosquito bites in at-risk individuals, especially pregnant women,” Dr Chan said during a press briefing.
Dr Chan said it’s unclear how long it will take to determine if Zika virus is causing the uptick in microcephaly and other congenital malformations and neurological abnormalities, but health officials are working to set up case-control studies.
Preparing for Zika Virus Outbreaks
BY DEEPAK CHITNIS
Frontline Medical News
The recent spike in Zika virus cases in Central and South America brings with it the alarming risk— and even the expectation—of outbreaks occuring in the United States. How should US-based clinicians prepare for the inevitable?
“The current outbreaks of Zika virus are the first of their kind in the Americas, so there isn’t a previous history of Zika virus spreading into the [United States],” explained Dr Joy St. John, director of surveillance, disease prevention, and control at the Caribbean Public Health Agency in Trinidad.
But now that the virus has hit the United States, with a confirmed case in Texas and more emerging since then, Dr St. John said the most important thing is for US health care providers to recognize the signs and symptoms of Zika virus infection. Carried and transmitted by the Aedes aegypti species of mosquito, Zika virus symptoms are relatively mild, consisting predominantly of maculopapular rash, fever, arthralgia, myalgia, and conjunctivitis. Only one in five individuals with a Zika virus infection develop symptoms, but patients who present as such and who have traveled to Central or South America in the week prior to the onset of symptoms should be considered likely infected.
“At present, there is no rapid test available for diagnosis of Zika,” said Dr St. John. “Diagnosis is primarily based on detection of viral RNA from clinical serum specimens in acutely ill patients.”
To that end, polymerase chain reaction (PCR) testing can be conducted on serum samples collected within 3 to 5 days of symptom onset. Beyond that, elevated levels of immunoglobulin M antibodies can be confirmed by serology, based on the neutralization, seroconversion or four-fold increase of Zika-specific antibodies in paired samples. However, Dr St. John warned that “Due to the possibility of cross reactivity with other viruses, for example, dengue, it is strongly recommended samples be collected early enough for PCR testing.”
Zika and Pregnancy
Zika virus has now been identified in 14 countries and territories worldwide, and while most infected patients experience relatively mild symptoms, Zika becomes very concerning when it infects a pregnant woman, as there have been cases of microcephaly in children whose mothers were infected with Zika virus during pregnancy. Although the association of microcephaly with Zika virus infection during pregnancy has not been definitively confirmed, the Centers for Disease Control and Prevention (CDC) have already issued a warning to Americans—particularly pregnant women—about traveling to high-risk areas.
“Scientifically, we’re not 100% sure if Zika virus is causing microcephaly, [but] what we’re seeing is in certain Brazilian districts, there’s been a 20-fold increase in rates of microcephaly at the same time that there’s been a lot more Zika virus in pregnant women,” explained Dr Sanjaya Senanayake of Australian National University in Canberra.
According to data from the CDC, 1,248 suspected cases of microcephaly had been reported in Brazil as of November 28, 2015, compared to the annual rate of just 150 to 200 such cases during 2010 through 2014. “Examination of the fetus [and] amniotic fluid, in some cases, has shown Zika virus, so there seems to be an association,” Dr Senanayake clarified, adding that “the [ANVISA – Brazilian Health Surveillance Agency] has told women in certain districts where there’s been a lot of microcephaly not to get pregnant.”
Brazil is set to host millions of guests from around the world as the 2016 Olympics get underway in only a few months’ time. Women who are pregnant or anticipate becoming pregnant should consider the risks if they are planning to travel to Rio de Janeiro. The risk of microcephaly does not apply to infected women who are not pregnant, however, as the CDC states that “Zika virus usually remains in the blood of an infected person for only a few days to a week,” and therefore “does not pose a risk of birth defects for future pregnancies.”
Dr St. Joy also stated that “public health personnel are still cautioning pregnant women to take special care to avoid mosquito bites during their pregnancies,” adding that the “[Pan-American Health Organization] is working on its guidelines for surveillance of congenital abnormalities.”
Clinical Insights
With treatment options so sparse—there is no vaccine or drug available specifically meant to combat a Zika virus infection—what can healthcare providers do for their patients? The CDC advises health care providers to “treat the symptoms,” which means telling patients to stay in bed, stay hydrated, and, most importantly, stay away from aspirins and NSAIDs “until dengue can be ruled out to reduce the risk of hemorrhage.” Acetaminophen or paracetamol are safe to use, in order to mitigate fever symptoms.
Those who are infected are also advised to stay indoors and remain as isolated as possible for at least a week after symptoms first present. While the risk of a domestic outbreak is probably low, Dr St. John said, the more exposure a Zika virus-infected individual has to the outside world, the more likely they are to be bitten by another mosquito, which can then carry and transmit the virus to another person.
“Chikungunya and dengue virus, which are transmitted by the same vectors [as Zika virus], have not managed to establish ongoing transmission in the United States despite repeated importations, [so] it is likely that Zika virus’ spread would follow a similar pattern,” Dr St. John noted.
Though rare, sexual transmission of Zika virus has also been found in at least one case, although it had been previously suspected for some time. In December 2013, a 44-year-old Tahitian man sought treatment for hematospermia. Analysis of his sperm, however, found Zika virus, indicating possible sexual transmission of the virus.
“The observation that [Zika virus] RNA was detectable in urine after viremia clearance in blood suggests that, as found for [dengue] and [West Nile virus] infections, urine samples can yield evidence of [Zika virus] for late diagnosis, but more investigation is needed,” the study concluded.
“The best way to control all this is to control the mosquito,” said Dr Senanayake. “You get a four-for-one deal; not only do you get rid of Zika virus, but also chikungunya, dengue, and yellow fever.” Dr Senanayake added that advanced research is currently underway in mosquito control efforts, including the idea of releasing mosquitoes into the wild that have been genetically modified so they cannot breed.
Now that the Illinois Department of Health has confirmed two new cases of Zika virus infection in that state, with other new cases cropping up in Saint Martin, Guadeloupe, and El Salvador, providers should remain vigilant, taking note of patients who have traveled to afflicted regions and show mosquito bites. Person-to-person transmission is “rare as hen’s teeth,” said Dr Senanayake, which is to say, it is highly unlikely to occur. Nonetheless, he said information and communication is the best way to ensure that Zika virus does not spread widely in the United States.
Study Characterizes Intracerebral Hemorrhage With New Oral Anticoagulants
BY MARY ANN MOON
FROM JAMA NEUROLOGY
Vitals Key clinical point: Intracerebral hemorrhage (ICH) related to new oral anticoagulants frequently involves hematoma expansion and does not appear to respond to prothrombin complex concentrate. Major finding: Mortality was 28%; 65% of survivors had unfavorable outcomes; and substantial hematoma expansion occurred in 38% of patients. Data source: A prospective, multicenter, observational study involving 61 patients treated during a 3-year period in Germany. Disclosures: The RASUNOA registry was supported by the University Hospital Heidelberg. Dr Purrucker reported receiving support from Pfizer unrelated to this study, and his associates reported ties to numerous industry sources. |
Intracerebral hemorrhage related to non–vitamin-K antagonist oral anticoagulants carries a high mortality and frequently involves hematoma expansion, according to a report published online December 14 in JAMA Neurology.1
The characteristics and natural history of acute-phase non–vitamin-K antagonist oral anticoagulant (NOAC)-associated intracerebral hemorrhage “are largely unknown,” and there are no prospective data concerning hematoma expansion or the effectiveness of prothrombin complex concentrate in limiting that expansion by reversing anticoagulation. Nevertheless, current recommendations suggest that clinicians consider administering prothrombin complex concentrate in this patient population, said Dr Jan C. Purrucker of the department of neurology at Heidelberg (Germany) University and his associates.1
Dr Purrucker and his associates performed the ICH substudy of the Registry of Acute Stroke Under New Oral Anticoagulants (RASUNOA), a prospective registry with certified stroke units in Germany. For their substudy, the investigators focused on 61 adults with a mean age of 76 years (range, 46-97 years) who were taking novel anticoagulants (NOACs; [apixaban, dabigatran etexilate, or rivaroxaban]) and had moderate to severe neurologic deficits and a median hematoma volume of 10.8 mL at presentation. Prothrombin complex concentrate was given to 35 (57%).
Mortality was high; 10 (16%) patients died during the acute inpatient stay and 17 (28%) at 3 months. Of the survivors, 65% had an unfavorable outcome. Substantial hematoma expansion—defined as a 33% or greater relative increase or 6 mL or greater absolute increase in intracerebral hemorrhage volume—affected 38% of patients. “This proportion was within the range reported for vitamin-K antagonist–associated intracerebral hemorrhage (36%-56%) and is higher, compared with that related to intracerebral hemorrhage in patients not receiving anticoagulation (12%-26%),” the researchers wrote.
Both larger hematoma volume at baseline (odds ratio [OR], 2.37) and intraventricular extension at baseline (OR, 8.13) strongly correlated with adverse outcomes. In contrast, prothrombin-complex concentrate failed to limit lesion expansion or avert adverse outcomes. This might be because patients given the treatment tended to have more severe initial neurologic deficits and more unfavorable hematoma location than did those who were not given prothrombin complex concentrate. In any case, “our study design, the limited sample size, and the potential for confounding by indication do not allow any [firm] conclusions regarding a potential association between prothrombin-complex concentrate treatment and outcome,” they noted.
It is important to note that in the study by Dr Purrucker and his colleagues, the median time from symptom onset to the first brain imaging was 14 hours and that fully 25% of patients presented for treatment more than 22 hours after noticing their initial symptoms. In contrast, patients with spontaneous hypertensive intracerebral hemorrhage present much earlier, usually within 6 hours. This indicates that the bleeding in NOAC-associated hemorrhagic stroke often is gradual and prolonged, an “oozing” process rather than the explosive type of process seen in spontaneous hemorrhagic stroke.
It is almost certain that if this cohort had undergone imaging at 3 hours rather than at 14 hours after symptom onset, the frequency of hematoma expansion would have approached 100% rather than 38%.
Dr Stephan A. Mayer is at Mount Sinai University, New York. He reported having no relevant financial disclosures. Dr Mayer made these remarks in an editorial accompanying Dr Purrucker’s report (Mayer, SA. Emergency Reversal of Novel Oral Anticoagulants. Help Is on the Way. JAMA Neurol. doi:10.1001/jamaneurol.2015.3884).
FDA Approves Treatment for Chemotherapy, Overdoses, Life-threatening Toxicities
BY ELIZABETH MECHCATIE
Frontline Medical News
Uridine triacetate, a pyrimidine analogue, has been approved for the emergency treatment of fluorouracil or capecitabine overdoses in adults and children, and for patients who develop “certain severe or life-threatening toxicities within 4 days of receiving” these treatments, the Food and Drug Administration (FDA) announced on December 11, 2015.
“Today’s approval is a first-of-its-kind therapy that can potentially save lives following overdose or life-threatening toxicity from these chemotherapy agents,” Dr Richard Pazdur, director of the office of hematology and oncology products in the FDA’s Center for Drug Evaluation and Research, said in the FDA statement.1 It will be marketed as Vistogard by Wellstat Therapeutics.
Uridine comes in an oral granule formulation that can be mixed into soft foods or, when necessary, administered via a nasogastric or gastrostomy tube, the prescribing information states. The indication is for use after an overdose “regardless of the presence of symptoms,” and for treating “early-onset, severe, or life-threatening toxicity affecting the cardiac or central nervous system, and/or early-onset, unusually severe adverse reactions (eg, gastrointestinal toxicity and/or neutropenia) within 96 hours following the end of fluorouracil or capecitabine administration,” according to the prescribing information.
Uridine blocks cell damage and cell death caused by fluorouracil chemotherapy, according to the statement.
Uridine was evaluated in two studies of 135 adults and children with cancer treated for a fluorouracil or capecitabine overdose or for early-onset severe or life-threatening toxicities within 96 hours after receiving fluorouracil. Among those treated for an overdose, 97% were alive 30 days after treatment, and among those treated for early-onset severe or life-threatening toxicity, 89% were alive 30 days after treatment. In addition, 33% of the patients resumed chemotherapy within 30 days, according to the FDA statement. Diarrhea, vomiting, and nausea were the most common adverse events associated with treatment.
FDA Advisory Committees Support Changing Codeine Contraindications for Children
BY DEEPAK CHITNIS
AT AN FDA ADVISORY COMMITTEE MEETING
SILVER SPRING, MD—Food and Drug Administration advisory committees have voted overwhelmingly to support expanding the current contraindication for codeine to preclude its use for any pain management in all children under age 18 years.
Twenty members of the FDA’s Pulmonary-Allergy Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee voted on December 10 for the contraindication. Six members elected to contraindicate for any pain management in children younger than 12 years old, and another two members voted only to contraindicate for children younger than age 6 years. One committee member voted not to make any changes to the current contraindications for codeine.
The joint advisory panel also voted to contraindicate the use of codeine for the treatment of cough in all children younger than age 18 years by a similarly robust margin: 20 members voted for contraindicating in all pediatric patients, five voted to contraindicate only in patients younger than age 12 years, one voted to contraindicate in children younger than age 6 years, and three members voted not to make any changes at all.
The final voting question, asking whether to remove codeine from the FDA monograph for over-the-counter use in treating cough in children, was almost unanimously supported by the voting members of both committees. One member supported removing codeine from the monograph only for children under age 2 years.
The decision to vote on approving amendments to the contraindications for codeine use—which would affect not just the monogram, but labeling as well—comes on the heels of the FDA announcing last summer that they would be investigating the safety of codeine-containing drugs in children.
The joint advisory panel cited reports of respiratory depression and death in pediatric patients, variability of codeine metabolism based upon CYP2D6 activity, and the fact that “some regulatory agencies have restricted use of codeine for both cough and analgesia in pediatric patients” as their key reasons for considering the changes to current contraindications, according to Dr Sally Seymour, the FDA’s Deputy Director for Safety.
The FDA is not required to follow the advice of its advisory panels. No members of the panel reported any relevant financial conflicts of interest.
80% of Emergency Physicians Say Mental Health Crisis Response Needs Overhaul
BY WHITNEY MCKNIGHT
Frontline Medical News
Vitals Key clinical point: A new model of psychiatric ED care is being developed by the Coalition on Psychiatric Emergencies (COPE), to improve care, outcomes, and net costs. Major finding: 8 in 10 emergency physicians (EPs) believe a lack of training and resources keep them from meeting a growing demand for emergency mental health services. Data source: American College of Emergency Physicians (ACEP) survey of 1,500 EPs nationwide. Disclosures: COPE is underwritten in part by Teva Pharmaceuticals. |
Emergency medicine professionals have teamed up with mental health workers and patient advocates to call for a new model of care for ED patients in mental health crisis.
The Coalition on Psychiatric Emergencies,” is focused on improving the delivery of emergency psychiatric care, and is supported by more than 30 national emergency medicine, mental health, and patient advocate groups, including the ACEP, the American Psychiatric Association, and the National Alliance on Mental Illness (NAMI). The action comes on the heels of a survey that found 80% of 1,500 US EPs think the system for treating people in acute mental health crisis is broken.
“It’s time we think about doing things differently,” Dr Michael Gerardi, COPE Steering Committee Chair and immediate past president of ACEP, said in a statement. “Through this unique collaboration, the Coalition on Psychiatric Emergencies will focus on developing a more unified treatment model and improving the treatment experience for both patients and health care providers. We want to provide the best care for all our patients and reduce health care costs.”
Among its several goals, the coalition seeks to shorten the time between when a person in mental health crisis presents to the ED and is admitted to an inpatient psychiatric bed. In a recent NAMI survey of 1,400 families, 38% waited more than 7 hours in the ED before seeing a mental health professional. For 21% of those families, the wait was more than 10 hours.
The Coalition on Psychiatric Emergencies also seeks adequate education and training for all emergency personnel who care for patients experiencing psychiatric emergencies.
“Emergency department staff need proper training not only on how to handle behavioral health emergencies, but also on how to initiate care for patients who may remain in the ED setting for long periods of time,” Dr Lorenzo Norris, director of inpatient psychiatric services at George Washington University Hospital in Washington, DC, said in an interview. “Establishing these new systems will likely require robust funding efforts.”
‘‘There is a growing need for change. At our hospital, we have definitely seen an uptick in the number of patients seeking emergency psychiatric care,” Dr Norris said. “Our approach has been to hire a clinician whose sole duty is to work collaboratively with patients and ED staff. It’s the first step in our ultimate goal of creating an ED behavioral health team that includes a psychiatrist, an emergency physician, nursing staff, social worker, and others who can provide the patient with comprehensive care at the initial point of contact.”
Currently in the United States, there are no standard protocols for a psychiatric emergency, according to the National Institute of Mental Health. The online survey was conducted within the ACEP membership between July 1 through 31, 2015. The response rate was 6% and the margin of error of 2.5%.
- Study Characterizes Intracerebral Hemorrhage With New Oral Anticoagulants
- Parrucker JC, Haas K, Rizos T, et al. Early Clinical and Radiological Course, Management, and Outcome of Intracerebral Hemorrhage Related to New Oral Anticoagulants. JAMA Neurol. doi:10.1001/jamaneurol.2015.3682.
- FDA Approves Treatment for Chemotherapy, Overdoses, Life-threatening Toxicities
- US Food and Drug Administration. FDA approves first emergency treatment for overdose of certain types of chemotherapy [FDA News Release]. December 11, 2015. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm476919.htm.
WHO Declares ‘Public Health Emergency’ for Microcephaly Linked to Zika Virus
BY MARY ELLEN SCHNEIDER
Frontline Medical News
The World Health Organization (WHO) has declared a “public health emergency of international concern” related to the clusters of microcephaly and other neurological complications reported in Brazil and earlier in French Polynesia. Though there is a strong association between these cases and the Zika virus, a causal link still has not been scientifically proven, according to the WHO.
The WHO’s emergency declaration clears the way for the international health community to move forward with a coordinated response. Dr Margaret Chan, WHO Director-General, said her organization plans to take a number of precautionary measures, including improving surveillance and detection of infections, congenital malformations, and neurological complications. They will also work with countries to intensify control of mosquito populations and help expedite the development of diagnostic tests and vaccines to protect at-risk populations.
The recommendations came after a February 1 meeting of the International Health Regulations Emergency Committee, which Dr Chan convened in response to the Zika virus outbreak and the observed increase in neurological disorders and neonatal malformations.
The group of 18 experts advised that the clusters of microcephaly and other complications constitute an “extraordinary event and a public health threat to other parts of the world.” The group did not recommend any restrictions on travel or trade with areas where the Zika virus transmission is ongoing, however.
“At present, the most important protective measures are the control of mosquito populations and the prevention of mosquito bites in at-risk individuals, especially pregnant women,” Dr Chan said during a press briefing.
Dr Chan said it’s unclear how long it will take to determine if Zika virus is causing the uptick in microcephaly and other congenital malformations and neurological abnormalities, but health officials are working to set up case-control studies.
Preparing for Zika Virus Outbreaks
BY DEEPAK CHITNIS
Frontline Medical News
The recent spike in Zika virus cases in Central and South America brings with it the alarming risk— and even the expectation—of outbreaks occuring in the United States. How should US-based clinicians prepare for the inevitable?
“The current outbreaks of Zika virus are the first of their kind in the Americas, so there isn’t a previous history of Zika virus spreading into the [United States],” explained Dr Joy St. John, director of surveillance, disease prevention, and control at the Caribbean Public Health Agency in Trinidad.
But now that the virus has hit the United States, with a confirmed case in Texas and more emerging since then, Dr St. John said the most important thing is for US health care providers to recognize the signs and symptoms of Zika virus infection. Carried and transmitted by the Aedes aegypti species of mosquito, Zika virus symptoms are relatively mild, consisting predominantly of maculopapular rash, fever, arthralgia, myalgia, and conjunctivitis. Only one in five individuals with a Zika virus infection develop symptoms, but patients who present as such and who have traveled to Central or South America in the week prior to the onset of symptoms should be considered likely infected.
“At present, there is no rapid test available for diagnosis of Zika,” said Dr St. John. “Diagnosis is primarily based on detection of viral RNA from clinical serum specimens in acutely ill patients.”
To that end, polymerase chain reaction (PCR) testing can be conducted on serum samples collected within 3 to 5 days of symptom onset. Beyond that, elevated levels of immunoglobulin M antibodies can be confirmed by serology, based on the neutralization, seroconversion or four-fold increase of Zika-specific antibodies in paired samples. However, Dr St. John warned that “Due to the possibility of cross reactivity with other viruses, for example, dengue, it is strongly recommended samples be collected early enough for PCR testing.”
Zika and Pregnancy
Zika virus has now been identified in 14 countries and territories worldwide, and while most infected patients experience relatively mild symptoms, Zika becomes very concerning when it infects a pregnant woman, as there have been cases of microcephaly in children whose mothers were infected with Zika virus during pregnancy. Although the association of microcephaly with Zika virus infection during pregnancy has not been definitively confirmed, the Centers for Disease Control and Prevention (CDC) have already issued a warning to Americans—particularly pregnant women—about traveling to high-risk areas.
“Scientifically, we’re not 100% sure if Zika virus is causing microcephaly, [but] what we’re seeing is in certain Brazilian districts, there’s been a 20-fold increase in rates of microcephaly at the same time that there’s been a lot more Zika virus in pregnant women,” explained Dr Sanjaya Senanayake of Australian National University in Canberra.
According to data from the CDC, 1,248 suspected cases of microcephaly had been reported in Brazil as of November 28, 2015, compared to the annual rate of just 150 to 200 such cases during 2010 through 2014. “Examination of the fetus [and] amniotic fluid, in some cases, has shown Zika virus, so there seems to be an association,” Dr Senanayake clarified, adding that “the [ANVISA – Brazilian Health Surveillance Agency] has told women in certain districts where there’s been a lot of microcephaly not to get pregnant.”
Brazil is set to host millions of guests from around the world as the 2016 Olympics get underway in only a few months’ time. Women who are pregnant or anticipate becoming pregnant should consider the risks if they are planning to travel to Rio de Janeiro. The risk of microcephaly does not apply to infected women who are not pregnant, however, as the CDC states that “Zika virus usually remains in the blood of an infected person for only a few days to a week,” and therefore “does not pose a risk of birth defects for future pregnancies.”
Dr St. Joy also stated that “public health personnel are still cautioning pregnant women to take special care to avoid mosquito bites during their pregnancies,” adding that the “[Pan-American Health Organization] is working on its guidelines for surveillance of congenital abnormalities.”
Clinical Insights
With treatment options so sparse—there is no vaccine or drug available specifically meant to combat a Zika virus infection—what can healthcare providers do for their patients? The CDC advises health care providers to “treat the symptoms,” which means telling patients to stay in bed, stay hydrated, and, most importantly, stay away from aspirins and NSAIDs “until dengue can be ruled out to reduce the risk of hemorrhage.” Acetaminophen or paracetamol are safe to use, in order to mitigate fever symptoms.
Those who are infected are also advised to stay indoors and remain as isolated as possible for at least a week after symptoms first present. While the risk of a domestic outbreak is probably low, Dr St. John said, the more exposure a Zika virus-infected individual has to the outside world, the more likely they are to be bitten by another mosquito, which can then carry and transmit the virus to another person.
“Chikungunya and dengue virus, which are transmitted by the same vectors [as Zika virus], have not managed to establish ongoing transmission in the United States despite repeated importations, [so] it is likely that Zika virus’ spread would follow a similar pattern,” Dr St. John noted.
Though rare, sexual transmission of Zika virus has also been found in at least one case, although it had been previously suspected for some time. In December 2013, a 44-year-old Tahitian man sought treatment for hematospermia. Analysis of his sperm, however, found Zika virus, indicating possible sexual transmission of the virus.
“The observation that [Zika virus] RNA was detectable in urine after viremia clearance in blood suggests that, as found for [dengue] and [West Nile virus] infections, urine samples can yield evidence of [Zika virus] for late diagnosis, but more investigation is needed,” the study concluded.
“The best way to control all this is to control the mosquito,” said Dr Senanayake. “You get a four-for-one deal; not only do you get rid of Zika virus, but also chikungunya, dengue, and yellow fever.” Dr Senanayake added that advanced research is currently underway in mosquito control efforts, including the idea of releasing mosquitoes into the wild that have been genetically modified so they cannot breed.
Now that the Illinois Department of Health has confirmed two new cases of Zika virus infection in that state, with other new cases cropping up in Saint Martin, Guadeloupe, and El Salvador, providers should remain vigilant, taking note of patients who have traveled to afflicted regions and show mosquito bites. Person-to-person transmission is “rare as hen’s teeth,” said Dr Senanayake, which is to say, it is highly unlikely to occur. Nonetheless, he said information and communication is the best way to ensure that Zika virus does not spread widely in the United States.
Study Characterizes Intracerebral Hemorrhage With New Oral Anticoagulants
BY MARY ANN MOON
FROM JAMA NEUROLOGY
Vitals Key clinical point: Intracerebral hemorrhage (ICH) related to new oral anticoagulants frequently involves hematoma expansion and does not appear to respond to prothrombin complex concentrate. Major finding: Mortality was 28%; 65% of survivors had unfavorable outcomes; and substantial hematoma expansion occurred in 38% of patients. Data source: A prospective, multicenter, observational study involving 61 patients treated during a 3-year period in Germany. Disclosures: The RASUNOA registry was supported by the University Hospital Heidelberg. Dr Purrucker reported receiving support from Pfizer unrelated to this study, and his associates reported ties to numerous industry sources. |
Intracerebral hemorrhage related to non–vitamin-K antagonist oral anticoagulants carries a high mortality and frequently involves hematoma expansion, according to a report published online December 14 in JAMA Neurology.1
The characteristics and natural history of acute-phase non–vitamin-K antagonist oral anticoagulant (NOAC)-associated intracerebral hemorrhage “are largely unknown,” and there are no prospective data concerning hematoma expansion or the effectiveness of prothrombin complex concentrate in limiting that expansion by reversing anticoagulation. Nevertheless, current recommendations suggest that clinicians consider administering prothrombin complex concentrate in this patient population, said Dr Jan C. Purrucker of the department of neurology at Heidelberg (Germany) University and his associates.1
Dr Purrucker and his associates performed the ICH substudy of the Registry of Acute Stroke Under New Oral Anticoagulants (RASUNOA), a prospective registry with certified stroke units in Germany. For their substudy, the investigators focused on 61 adults with a mean age of 76 years (range, 46-97 years) who were taking novel anticoagulants (NOACs; [apixaban, dabigatran etexilate, or rivaroxaban]) and had moderate to severe neurologic deficits and a median hematoma volume of 10.8 mL at presentation. Prothrombin complex concentrate was given to 35 (57%).
Mortality was high; 10 (16%) patients died during the acute inpatient stay and 17 (28%) at 3 months. Of the survivors, 65% had an unfavorable outcome. Substantial hematoma expansion—defined as a 33% or greater relative increase or 6 mL or greater absolute increase in intracerebral hemorrhage volume—affected 38% of patients. “This proportion was within the range reported for vitamin-K antagonist–associated intracerebral hemorrhage (36%-56%) and is higher, compared with that related to intracerebral hemorrhage in patients not receiving anticoagulation (12%-26%),” the researchers wrote.
Both larger hematoma volume at baseline (odds ratio [OR], 2.37) and intraventricular extension at baseline (OR, 8.13) strongly correlated with adverse outcomes. In contrast, prothrombin-complex concentrate failed to limit lesion expansion or avert adverse outcomes. This might be because patients given the treatment tended to have more severe initial neurologic deficits and more unfavorable hematoma location than did those who were not given prothrombin complex concentrate. In any case, “our study design, the limited sample size, and the potential for confounding by indication do not allow any [firm] conclusions regarding a potential association between prothrombin-complex concentrate treatment and outcome,” they noted.
It is important to note that in the study by Dr Purrucker and his colleagues, the median time from symptom onset to the first brain imaging was 14 hours and that fully 25% of patients presented for treatment more than 22 hours after noticing their initial symptoms. In contrast, patients with spontaneous hypertensive intracerebral hemorrhage present much earlier, usually within 6 hours. This indicates that the bleeding in NOAC-associated hemorrhagic stroke often is gradual and prolonged, an “oozing” process rather than the explosive type of process seen in spontaneous hemorrhagic stroke.
It is almost certain that if this cohort had undergone imaging at 3 hours rather than at 14 hours after symptom onset, the frequency of hematoma expansion would have approached 100% rather than 38%.
Dr Stephan A. Mayer is at Mount Sinai University, New York. He reported having no relevant financial disclosures. Dr Mayer made these remarks in an editorial accompanying Dr Purrucker’s report (Mayer, SA. Emergency Reversal of Novel Oral Anticoagulants. Help Is on the Way. JAMA Neurol. doi:10.1001/jamaneurol.2015.3884).
FDA Approves Treatment for Chemotherapy, Overdoses, Life-threatening Toxicities
BY ELIZABETH MECHCATIE
Frontline Medical News
Uridine triacetate, a pyrimidine analogue, has been approved for the emergency treatment of fluorouracil or capecitabine overdoses in adults and children, and for patients who develop “certain severe or life-threatening toxicities within 4 days of receiving” these treatments, the Food and Drug Administration (FDA) announced on December 11, 2015.
“Today’s approval is a first-of-its-kind therapy that can potentially save lives following overdose or life-threatening toxicity from these chemotherapy agents,” Dr Richard Pazdur, director of the office of hematology and oncology products in the FDA’s Center for Drug Evaluation and Research, said in the FDA statement.1 It will be marketed as Vistogard by Wellstat Therapeutics.
Uridine comes in an oral granule formulation that can be mixed into soft foods or, when necessary, administered via a nasogastric or gastrostomy tube, the prescribing information states. The indication is for use after an overdose “regardless of the presence of symptoms,” and for treating “early-onset, severe, or life-threatening toxicity affecting the cardiac or central nervous system, and/or early-onset, unusually severe adverse reactions (eg, gastrointestinal toxicity and/or neutropenia) within 96 hours following the end of fluorouracil or capecitabine administration,” according to the prescribing information.
Uridine blocks cell damage and cell death caused by fluorouracil chemotherapy, according to the statement.
Uridine was evaluated in two studies of 135 adults and children with cancer treated for a fluorouracil or capecitabine overdose or for early-onset severe or life-threatening toxicities within 96 hours after receiving fluorouracil. Among those treated for an overdose, 97% were alive 30 days after treatment, and among those treated for early-onset severe or life-threatening toxicity, 89% were alive 30 days after treatment. In addition, 33% of the patients resumed chemotherapy within 30 days, according to the FDA statement. Diarrhea, vomiting, and nausea were the most common adverse events associated with treatment.
FDA Advisory Committees Support Changing Codeine Contraindications for Children
BY DEEPAK CHITNIS
AT AN FDA ADVISORY COMMITTEE MEETING
SILVER SPRING, MD—Food and Drug Administration advisory committees have voted overwhelmingly to support expanding the current contraindication for codeine to preclude its use for any pain management in all children under age 18 years.
Twenty members of the FDA’s Pulmonary-Allergy Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee voted on December 10 for the contraindication. Six members elected to contraindicate for any pain management in children younger than 12 years old, and another two members voted only to contraindicate for children younger than age 6 years. One committee member voted not to make any changes to the current contraindications for codeine.
The joint advisory panel also voted to contraindicate the use of codeine for the treatment of cough in all children younger than age 18 years by a similarly robust margin: 20 members voted for contraindicating in all pediatric patients, five voted to contraindicate only in patients younger than age 12 years, one voted to contraindicate in children younger than age 6 years, and three members voted not to make any changes at all.
The final voting question, asking whether to remove codeine from the FDA monograph for over-the-counter use in treating cough in children, was almost unanimously supported by the voting members of both committees. One member supported removing codeine from the monograph only for children under age 2 years.
The decision to vote on approving amendments to the contraindications for codeine use—which would affect not just the monogram, but labeling as well—comes on the heels of the FDA announcing last summer that they would be investigating the safety of codeine-containing drugs in children.
The joint advisory panel cited reports of respiratory depression and death in pediatric patients, variability of codeine metabolism based upon CYP2D6 activity, and the fact that “some regulatory agencies have restricted use of codeine for both cough and analgesia in pediatric patients” as their key reasons for considering the changes to current contraindications, according to Dr Sally Seymour, the FDA’s Deputy Director for Safety.
The FDA is not required to follow the advice of its advisory panels. No members of the panel reported any relevant financial conflicts of interest.
80% of Emergency Physicians Say Mental Health Crisis Response Needs Overhaul
BY WHITNEY MCKNIGHT
Frontline Medical News
Vitals Key clinical point: A new model of psychiatric ED care is being developed by the Coalition on Psychiatric Emergencies (COPE), to improve care, outcomes, and net costs. Major finding: 8 in 10 emergency physicians (EPs) believe a lack of training and resources keep them from meeting a growing demand for emergency mental health services. Data source: American College of Emergency Physicians (ACEP) survey of 1,500 EPs nationwide. Disclosures: COPE is underwritten in part by Teva Pharmaceuticals. |
Emergency medicine professionals have teamed up with mental health workers and patient advocates to call for a new model of care for ED patients in mental health crisis.
The Coalition on Psychiatric Emergencies,” is focused on improving the delivery of emergency psychiatric care, and is supported by more than 30 national emergency medicine, mental health, and patient advocate groups, including the ACEP, the American Psychiatric Association, and the National Alliance on Mental Illness (NAMI). The action comes on the heels of a survey that found 80% of 1,500 US EPs think the system for treating people in acute mental health crisis is broken.
“It’s time we think about doing things differently,” Dr Michael Gerardi, COPE Steering Committee Chair and immediate past president of ACEP, said in a statement. “Through this unique collaboration, the Coalition on Psychiatric Emergencies will focus on developing a more unified treatment model and improving the treatment experience for both patients and health care providers. We want to provide the best care for all our patients and reduce health care costs.”
Among its several goals, the coalition seeks to shorten the time between when a person in mental health crisis presents to the ED and is admitted to an inpatient psychiatric bed. In a recent NAMI survey of 1,400 families, 38% waited more than 7 hours in the ED before seeing a mental health professional. For 21% of those families, the wait was more than 10 hours.
The Coalition on Psychiatric Emergencies also seeks adequate education and training for all emergency personnel who care for patients experiencing psychiatric emergencies.
“Emergency department staff need proper training not only on how to handle behavioral health emergencies, but also on how to initiate care for patients who may remain in the ED setting for long periods of time,” Dr Lorenzo Norris, director of inpatient psychiatric services at George Washington University Hospital in Washington, DC, said in an interview. “Establishing these new systems will likely require robust funding efforts.”
‘‘There is a growing need for change. At our hospital, we have definitely seen an uptick in the number of patients seeking emergency psychiatric care,” Dr Norris said. “Our approach has been to hire a clinician whose sole duty is to work collaboratively with patients and ED staff. It’s the first step in our ultimate goal of creating an ED behavioral health team that includes a psychiatrist, an emergency physician, nursing staff, social worker, and others who can provide the patient with comprehensive care at the initial point of contact.”
Currently in the United States, there are no standard protocols for a psychiatric emergency, according to the National Institute of Mental Health. The online survey was conducted within the ACEP membership between July 1 through 31, 2015. The response rate was 6% and the margin of error of 2.5%.
WHO Declares ‘Public Health Emergency’ for Microcephaly Linked to Zika Virus
BY MARY ELLEN SCHNEIDER
Frontline Medical News
The World Health Organization (WHO) has declared a “public health emergency of international concern” related to the clusters of microcephaly and other neurological complications reported in Brazil and earlier in French Polynesia. Though there is a strong association between these cases and the Zika virus, a causal link still has not been scientifically proven, according to the WHO.
The WHO’s emergency declaration clears the way for the international health community to move forward with a coordinated response. Dr Margaret Chan, WHO Director-General, said her organization plans to take a number of precautionary measures, including improving surveillance and detection of infections, congenital malformations, and neurological complications. They will also work with countries to intensify control of mosquito populations and help expedite the development of diagnostic tests and vaccines to protect at-risk populations.
The recommendations came after a February 1 meeting of the International Health Regulations Emergency Committee, which Dr Chan convened in response to the Zika virus outbreak and the observed increase in neurological disorders and neonatal malformations.
The group of 18 experts advised that the clusters of microcephaly and other complications constitute an “extraordinary event and a public health threat to other parts of the world.” The group did not recommend any restrictions on travel or trade with areas where the Zika virus transmission is ongoing, however.
“At present, the most important protective measures are the control of mosquito populations and the prevention of mosquito bites in at-risk individuals, especially pregnant women,” Dr Chan said during a press briefing.
Dr Chan said it’s unclear how long it will take to determine if Zika virus is causing the uptick in microcephaly and other congenital malformations and neurological abnormalities, but health officials are working to set up case-control studies.
Preparing for Zika Virus Outbreaks
BY DEEPAK CHITNIS
Frontline Medical News
The recent spike in Zika virus cases in Central and South America brings with it the alarming risk— and even the expectation—of outbreaks occuring in the United States. How should US-based clinicians prepare for the inevitable?
“The current outbreaks of Zika virus are the first of their kind in the Americas, so there isn’t a previous history of Zika virus spreading into the [United States],” explained Dr Joy St. John, director of surveillance, disease prevention, and control at the Caribbean Public Health Agency in Trinidad.
But now that the virus has hit the United States, with a confirmed case in Texas and more emerging since then, Dr St. John said the most important thing is for US health care providers to recognize the signs and symptoms of Zika virus infection. Carried and transmitted by the Aedes aegypti species of mosquito, Zika virus symptoms are relatively mild, consisting predominantly of maculopapular rash, fever, arthralgia, myalgia, and conjunctivitis. Only one in five individuals with a Zika virus infection develop symptoms, but patients who present as such and who have traveled to Central or South America in the week prior to the onset of symptoms should be considered likely infected.
“At present, there is no rapid test available for diagnosis of Zika,” said Dr St. John. “Diagnosis is primarily based on detection of viral RNA from clinical serum specimens in acutely ill patients.”
To that end, polymerase chain reaction (PCR) testing can be conducted on serum samples collected within 3 to 5 days of symptom onset. Beyond that, elevated levels of immunoglobulin M antibodies can be confirmed by serology, based on the neutralization, seroconversion or four-fold increase of Zika-specific antibodies in paired samples. However, Dr St. John warned that “Due to the possibility of cross reactivity with other viruses, for example, dengue, it is strongly recommended samples be collected early enough for PCR testing.”
Zika and Pregnancy
Zika virus has now been identified in 14 countries and territories worldwide, and while most infected patients experience relatively mild symptoms, Zika becomes very concerning when it infects a pregnant woman, as there have been cases of microcephaly in children whose mothers were infected with Zika virus during pregnancy. Although the association of microcephaly with Zika virus infection during pregnancy has not been definitively confirmed, the Centers for Disease Control and Prevention (CDC) have already issued a warning to Americans—particularly pregnant women—about traveling to high-risk areas.
“Scientifically, we’re not 100% sure if Zika virus is causing microcephaly, [but] what we’re seeing is in certain Brazilian districts, there’s been a 20-fold increase in rates of microcephaly at the same time that there’s been a lot more Zika virus in pregnant women,” explained Dr Sanjaya Senanayake of Australian National University in Canberra.
According to data from the CDC, 1,248 suspected cases of microcephaly had been reported in Brazil as of November 28, 2015, compared to the annual rate of just 150 to 200 such cases during 2010 through 2014. “Examination of the fetus [and] amniotic fluid, in some cases, has shown Zika virus, so there seems to be an association,” Dr Senanayake clarified, adding that “the [ANVISA – Brazilian Health Surveillance Agency] has told women in certain districts where there’s been a lot of microcephaly not to get pregnant.”
Brazil is set to host millions of guests from around the world as the 2016 Olympics get underway in only a few months’ time. Women who are pregnant or anticipate becoming pregnant should consider the risks if they are planning to travel to Rio de Janeiro. The risk of microcephaly does not apply to infected women who are not pregnant, however, as the CDC states that “Zika virus usually remains in the blood of an infected person for only a few days to a week,” and therefore “does not pose a risk of birth defects for future pregnancies.”
Dr St. Joy also stated that “public health personnel are still cautioning pregnant women to take special care to avoid mosquito bites during their pregnancies,” adding that the “[Pan-American Health Organization] is working on its guidelines for surveillance of congenital abnormalities.”
Clinical Insights
With treatment options so sparse—there is no vaccine or drug available specifically meant to combat a Zika virus infection—what can healthcare providers do for their patients? The CDC advises health care providers to “treat the symptoms,” which means telling patients to stay in bed, stay hydrated, and, most importantly, stay away from aspirins and NSAIDs “until dengue can be ruled out to reduce the risk of hemorrhage.” Acetaminophen or paracetamol are safe to use, in order to mitigate fever symptoms.
Those who are infected are also advised to stay indoors and remain as isolated as possible for at least a week after symptoms first present. While the risk of a domestic outbreak is probably low, Dr St. John said, the more exposure a Zika virus-infected individual has to the outside world, the more likely they are to be bitten by another mosquito, which can then carry and transmit the virus to another person.
“Chikungunya and dengue virus, which are transmitted by the same vectors [as Zika virus], have not managed to establish ongoing transmission in the United States despite repeated importations, [so] it is likely that Zika virus’ spread would follow a similar pattern,” Dr St. John noted.
Though rare, sexual transmission of Zika virus has also been found in at least one case, although it had been previously suspected for some time. In December 2013, a 44-year-old Tahitian man sought treatment for hematospermia. Analysis of his sperm, however, found Zika virus, indicating possible sexual transmission of the virus.
“The observation that [Zika virus] RNA was detectable in urine after viremia clearance in blood suggests that, as found for [dengue] and [West Nile virus] infections, urine samples can yield evidence of [Zika virus] for late diagnosis, but more investigation is needed,” the study concluded.
“The best way to control all this is to control the mosquito,” said Dr Senanayake. “You get a four-for-one deal; not only do you get rid of Zika virus, but also chikungunya, dengue, and yellow fever.” Dr Senanayake added that advanced research is currently underway in mosquito control efforts, including the idea of releasing mosquitoes into the wild that have been genetically modified so they cannot breed.
Now that the Illinois Department of Health has confirmed two new cases of Zika virus infection in that state, with other new cases cropping up in Saint Martin, Guadeloupe, and El Salvador, providers should remain vigilant, taking note of patients who have traveled to afflicted regions and show mosquito bites. Person-to-person transmission is “rare as hen’s teeth,” said Dr Senanayake, which is to say, it is highly unlikely to occur. Nonetheless, he said information and communication is the best way to ensure that Zika virus does not spread widely in the United States.
Study Characterizes Intracerebral Hemorrhage With New Oral Anticoagulants
BY MARY ANN MOON
FROM JAMA NEUROLOGY
Vitals Key clinical point: Intracerebral hemorrhage (ICH) related to new oral anticoagulants frequently involves hematoma expansion and does not appear to respond to prothrombin complex concentrate. Major finding: Mortality was 28%; 65% of survivors had unfavorable outcomes; and substantial hematoma expansion occurred in 38% of patients. Data source: A prospective, multicenter, observational study involving 61 patients treated during a 3-year period in Germany. Disclosures: The RASUNOA registry was supported by the University Hospital Heidelberg. Dr Purrucker reported receiving support from Pfizer unrelated to this study, and his associates reported ties to numerous industry sources. |
Intracerebral hemorrhage related to non–vitamin-K antagonist oral anticoagulants carries a high mortality and frequently involves hematoma expansion, according to a report published online December 14 in JAMA Neurology.1
The characteristics and natural history of acute-phase non–vitamin-K antagonist oral anticoagulant (NOAC)-associated intracerebral hemorrhage “are largely unknown,” and there are no prospective data concerning hematoma expansion or the effectiveness of prothrombin complex concentrate in limiting that expansion by reversing anticoagulation. Nevertheless, current recommendations suggest that clinicians consider administering prothrombin complex concentrate in this patient population, said Dr Jan C. Purrucker of the department of neurology at Heidelberg (Germany) University and his associates.1
Dr Purrucker and his associates performed the ICH substudy of the Registry of Acute Stroke Under New Oral Anticoagulants (RASUNOA), a prospective registry with certified stroke units in Germany. For their substudy, the investigators focused on 61 adults with a mean age of 76 years (range, 46-97 years) who were taking novel anticoagulants (NOACs; [apixaban, dabigatran etexilate, or rivaroxaban]) and had moderate to severe neurologic deficits and a median hematoma volume of 10.8 mL at presentation. Prothrombin complex concentrate was given to 35 (57%).
Mortality was high; 10 (16%) patients died during the acute inpatient stay and 17 (28%) at 3 months. Of the survivors, 65% had an unfavorable outcome. Substantial hematoma expansion—defined as a 33% or greater relative increase or 6 mL or greater absolute increase in intracerebral hemorrhage volume—affected 38% of patients. “This proportion was within the range reported for vitamin-K antagonist–associated intracerebral hemorrhage (36%-56%) and is higher, compared with that related to intracerebral hemorrhage in patients not receiving anticoagulation (12%-26%),” the researchers wrote.
Both larger hematoma volume at baseline (odds ratio [OR], 2.37) and intraventricular extension at baseline (OR, 8.13) strongly correlated with adverse outcomes. In contrast, prothrombin-complex concentrate failed to limit lesion expansion or avert adverse outcomes. This might be because patients given the treatment tended to have more severe initial neurologic deficits and more unfavorable hematoma location than did those who were not given prothrombin complex concentrate. In any case, “our study design, the limited sample size, and the potential for confounding by indication do not allow any [firm] conclusions regarding a potential association between prothrombin-complex concentrate treatment and outcome,” they noted.
It is important to note that in the study by Dr Purrucker and his colleagues, the median time from symptom onset to the first brain imaging was 14 hours and that fully 25% of patients presented for treatment more than 22 hours after noticing their initial symptoms. In contrast, patients with spontaneous hypertensive intracerebral hemorrhage present much earlier, usually within 6 hours. This indicates that the bleeding in NOAC-associated hemorrhagic stroke often is gradual and prolonged, an “oozing” process rather than the explosive type of process seen in spontaneous hemorrhagic stroke.
It is almost certain that if this cohort had undergone imaging at 3 hours rather than at 14 hours after symptom onset, the frequency of hematoma expansion would have approached 100% rather than 38%.
Dr Stephan A. Mayer is at Mount Sinai University, New York. He reported having no relevant financial disclosures. Dr Mayer made these remarks in an editorial accompanying Dr Purrucker’s report (Mayer, SA. Emergency Reversal of Novel Oral Anticoagulants. Help Is on the Way. JAMA Neurol. doi:10.1001/jamaneurol.2015.3884).
FDA Approves Treatment for Chemotherapy, Overdoses, Life-threatening Toxicities
BY ELIZABETH MECHCATIE
Frontline Medical News
Uridine triacetate, a pyrimidine analogue, has been approved for the emergency treatment of fluorouracil or capecitabine overdoses in adults and children, and for patients who develop “certain severe or life-threatening toxicities within 4 days of receiving” these treatments, the Food and Drug Administration (FDA) announced on December 11, 2015.
“Today’s approval is a first-of-its-kind therapy that can potentially save lives following overdose or life-threatening toxicity from these chemotherapy agents,” Dr Richard Pazdur, director of the office of hematology and oncology products in the FDA’s Center for Drug Evaluation and Research, said in the FDA statement.1 It will be marketed as Vistogard by Wellstat Therapeutics.
Uridine comes in an oral granule formulation that can be mixed into soft foods or, when necessary, administered via a nasogastric or gastrostomy tube, the prescribing information states. The indication is for use after an overdose “regardless of the presence of symptoms,” and for treating “early-onset, severe, or life-threatening toxicity affecting the cardiac or central nervous system, and/or early-onset, unusually severe adverse reactions (eg, gastrointestinal toxicity and/or neutropenia) within 96 hours following the end of fluorouracil or capecitabine administration,” according to the prescribing information.
Uridine blocks cell damage and cell death caused by fluorouracil chemotherapy, according to the statement.
Uridine was evaluated in two studies of 135 adults and children with cancer treated for a fluorouracil or capecitabine overdose or for early-onset severe or life-threatening toxicities within 96 hours after receiving fluorouracil. Among those treated for an overdose, 97% were alive 30 days after treatment, and among those treated for early-onset severe or life-threatening toxicity, 89% were alive 30 days after treatment. In addition, 33% of the patients resumed chemotherapy within 30 days, according to the FDA statement. Diarrhea, vomiting, and nausea were the most common adverse events associated with treatment.
FDA Advisory Committees Support Changing Codeine Contraindications for Children
BY DEEPAK CHITNIS
AT AN FDA ADVISORY COMMITTEE MEETING
SILVER SPRING, MD—Food and Drug Administration advisory committees have voted overwhelmingly to support expanding the current contraindication for codeine to preclude its use for any pain management in all children under age 18 years.
Twenty members of the FDA’s Pulmonary-Allergy Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee voted on December 10 for the contraindication. Six members elected to contraindicate for any pain management in children younger than 12 years old, and another two members voted only to contraindicate for children younger than age 6 years. One committee member voted not to make any changes to the current contraindications for codeine.
The joint advisory panel also voted to contraindicate the use of codeine for the treatment of cough in all children younger than age 18 years by a similarly robust margin: 20 members voted for contraindicating in all pediatric patients, five voted to contraindicate only in patients younger than age 12 years, one voted to contraindicate in children younger than age 6 years, and three members voted not to make any changes at all.
The final voting question, asking whether to remove codeine from the FDA monograph for over-the-counter use in treating cough in children, was almost unanimously supported by the voting members of both committees. One member supported removing codeine from the monograph only for children under age 2 years.
The decision to vote on approving amendments to the contraindications for codeine use—which would affect not just the monogram, but labeling as well—comes on the heels of the FDA announcing last summer that they would be investigating the safety of codeine-containing drugs in children.
The joint advisory panel cited reports of respiratory depression and death in pediatric patients, variability of codeine metabolism based upon CYP2D6 activity, and the fact that “some regulatory agencies have restricted use of codeine for both cough and analgesia in pediatric patients” as their key reasons for considering the changes to current contraindications, according to Dr Sally Seymour, the FDA’s Deputy Director for Safety.
The FDA is not required to follow the advice of its advisory panels. No members of the panel reported any relevant financial conflicts of interest.
80% of Emergency Physicians Say Mental Health Crisis Response Needs Overhaul
BY WHITNEY MCKNIGHT
Frontline Medical News
Vitals Key clinical point: A new model of psychiatric ED care is being developed by the Coalition on Psychiatric Emergencies (COPE), to improve care, outcomes, and net costs. Major finding: 8 in 10 emergency physicians (EPs) believe a lack of training and resources keep them from meeting a growing demand for emergency mental health services. Data source: American College of Emergency Physicians (ACEP) survey of 1,500 EPs nationwide. Disclosures: COPE is underwritten in part by Teva Pharmaceuticals. |
Emergency medicine professionals have teamed up with mental health workers and patient advocates to call for a new model of care for ED patients in mental health crisis.
The Coalition on Psychiatric Emergencies,” is focused on improving the delivery of emergency psychiatric care, and is supported by more than 30 national emergency medicine, mental health, and patient advocate groups, including the ACEP, the American Psychiatric Association, and the National Alliance on Mental Illness (NAMI). The action comes on the heels of a survey that found 80% of 1,500 US EPs think the system for treating people in acute mental health crisis is broken.
“It’s time we think about doing things differently,” Dr Michael Gerardi, COPE Steering Committee Chair and immediate past president of ACEP, said in a statement. “Through this unique collaboration, the Coalition on Psychiatric Emergencies will focus on developing a more unified treatment model and improving the treatment experience for both patients and health care providers. We want to provide the best care for all our patients and reduce health care costs.”
Among its several goals, the coalition seeks to shorten the time between when a person in mental health crisis presents to the ED and is admitted to an inpatient psychiatric bed. In a recent NAMI survey of 1,400 families, 38% waited more than 7 hours in the ED before seeing a mental health professional. For 21% of those families, the wait was more than 10 hours.
The Coalition on Psychiatric Emergencies also seeks adequate education and training for all emergency personnel who care for patients experiencing psychiatric emergencies.
“Emergency department staff need proper training not only on how to handle behavioral health emergencies, but also on how to initiate care for patients who may remain in the ED setting for long periods of time,” Dr Lorenzo Norris, director of inpatient psychiatric services at George Washington University Hospital in Washington, DC, said in an interview. “Establishing these new systems will likely require robust funding efforts.”
‘‘There is a growing need for change. At our hospital, we have definitely seen an uptick in the number of patients seeking emergency psychiatric care,” Dr Norris said. “Our approach has been to hire a clinician whose sole duty is to work collaboratively with patients and ED staff. It’s the first step in our ultimate goal of creating an ED behavioral health team that includes a psychiatrist, an emergency physician, nursing staff, social worker, and others who can provide the patient with comprehensive care at the initial point of contact.”
Currently in the United States, there are no standard protocols for a psychiatric emergency, according to the National Institute of Mental Health. The online survey was conducted within the ACEP membership between July 1 through 31, 2015. The response rate was 6% and the margin of error of 2.5%.
- Study Characterizes Intracerebral Hemorrhage With New Oral Anticoagulants
- Parrucker JC, Haas K, Rizos T, et al. Early Clinical and Radiological Course, Management, and Outcome of Intracerebral Hemorrhage Related to New Oral Anticoagulants. JAMA Neurol. doi:10.1001/jamaneurol.2015.3682.
- FDA Approves Treatment for Chemotherapy, Overdoses, Life-threatening Toxicities
- US Food and Drug Administration. FDA approves first emergency treatment for overdose of certain types of chemotherapy [FDA News Release]. December 11, 2015. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm476919.htm.
- Study Characterizes Intracerebral Hemorrhage With New Oral Anticoagulants
- Parrucker JC, Haas K, Rizos T, et al. Early Clinical and Radiological Course, Management, and Outcome of Intracerebral Hemorrhage Related to New Oral Anticoagulants. JAMA Neurol. doi:10.1001/jamaneurol.2015.3682.
- FDA Approves Treatment for Chemotherapy, Overdoses, Life-threatening Toxicities
- US Food and Drug Administration. FDA approves first emergency treatment for overdose of certain types of chemotherapy [FDA News Release]. December 11, 2015. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm476919.htm.