User login
CMS proposal would allow sharing, selling of claims data
Physicians may soon be able to purchase reports that combine their Medicare and private payer claims data, according to the details of a new government proposal.
The proposed rule, released on Jan. 29, would enable entities approved by the government to share or sell Medicare and private claims information to health providers, suppliers, hospital associations, and medical societies. The new rule, as required by the Medicare Access and CHIP Reauthorization Act (MACRA), seeks to increase transparency about provider performance and generate data uses that improve care delivery, according to a statement from the Centers for Medicare & Medicaid Services.
“Increasing access to analyses and data that include Medicare data will make it easier for stakeholders throughout the healthcare system to make smarter and more informed healthcare decisions,” CMS Acting Administrator Andy Slavitt said in a statement.
Under the rule, qualified entities may provide or sell data or analyses of the data to providers and suppliers. CMS encourages the sharing of data analytics that would assist in quality and patient care improvement activities, including the development of new models of care.
Disclosure or use of data for marketing purposes would be barred.
The rule includes strict privacy and security requirements for all entities receiving Medicare analyses or data.
If finalized, the rule could help practices in their efforts to provide value-based care and perform population management, said Dr. Yul D. Ejnes, chair-emeritus of the American College of Physicians Board of Regents and an internist in private practice in Cranston, R.I.
“A barrier, especially for small groups, is access to all-payer data, since what is available now is often partitioned by payer and not easy to compile into practice-wide data covering all patients,” he said in an interview. “Clearly, there is also a need for analysis of the data that is beyond the reach of most practices and is best done by third parties with the resources and expertise, so making the CMS data available facilitates that.”
However, Dr. Ejnes questioned how much these analyses will cost practices, especially smaller practices.
“Another related issue, beyond CMS’ purview, is how affordable this type of data analysis would be for the small practice that might benefit the most from it, since larger organizations have resources that may make much of this available to its physicians at little or no cost,” he said.
Entities supplying the information to providers must be accepted into the qualified entity program. The program, authorized under the Affordable Care Act, allows organizations that meet certain criteria to access patient-protected Medicare data to produce public reports. Qualified entities must combine the Medicare data with other claims data to produce reports that are “representative of how providers and suppliers are performing across multiple payers.”
Thus far, 13 organizations have been accepted into the program. Of these organizations, 2 have completed public reporting, while the other 11 are preparing for public reporting, according to CMS.
Comments on the new rule are due by March 29.
On Twitter @legal_med
Physicians may soon be able to purchase reports that combine their Medicare and private payer claims data, according to the details of a new government proposal.
The proposed rule, released on Jan. 29, would enable entities approved by the government to share or sell Medicare and private claims information to health providers, suppliers, hospital associations, and medical societies. The new rule, as required by the Medicare Access and CHIP Reauthorization Act (MACRA), seeks to increase transparency about provider performance and generate data uses that improve care delivery, according to a statement from the Centers for Medicare & Medicaid Services.
“Increasing access to analyses and data that include Medicare data will make it easier for stakeholders throughout the healthcare system to make smarter and more informed healthcare decisions,” CMS Acting Administrator Andy Slavitt said in a statement.
Under the rule, qualified entities may provide or sell data or analyses of the data to providers and suppliers. CMS encourages the sharing of data analytics that would assist in quality and patient care improvement activities, including the development of new models of care.
Disclosure or use of data for marketing purposes would be barred.
The rule includes strict privacy and security requirements for all entities receiving Medicare analyses or data.
If finalized, the rule could help practices in their efforts to provide value-based care and perform population management, said Dr. Yul D. Ejnes, chair-emeritus of the American College of Physicians Board of Regents and an internist in private practice in Cranston, R.I.
“A barrier, especially for small groups, is access to all-payer data, since what is available now is often partitioned by payer and not easy to compile into practice-wide data covering all patients,” he said in an interview. “Clearly, there is also a need for analysis of the data that is beyond the reach of most practices and is best done by third parties with the resources and expertise, so making the CMS data available facilitates that.”
However, Dr. Ejnes questioned how much these analyses will cost practices, especially smaller practices.
“Another related issue, beyond CMS’ purview, is how affordable this type of data analysis would be for the small practice that might benefit the most from it, since larger organizations have resources that may make much of this available to its physicians at little or no cost,” he said.
Entities supplying the information to providers must be accepted into the qualified entity program. The program, authorized under the Affordable Care Act, allows organizations that meet certain criteria to access patient-protected Medicare data to produce public reports. Qualified entities must combine the Medicare data with other claims data to produce reports that are “representative of how providers and suppliers are performing across multiple payers.”
Thus far, 13 organizations have been accepted into the program. Of these organizations, 2 have completed public reporting, while the other 11 are preparing for public reporting, according to CMS.
Comments on the new rule are due by March 29.
On Twitter @legal_med
Physicians may soon be able to purchase reports that combine their Medicare and private payer claims data, according to the details of a new government proposal.
The proposed rule, released on Jan. 29, would enable entities approved by the government to share or sell Medicare and private claims information to health providers, suppliers, hospital associations, and medical societies. The new rule, as required by the Medicare Access and CHIP Reauthorization Act (MACRA), seeks to increase transparency about provider performance and generate data uses that improve care delivery, according to a statement from the Centers for Medicare & Medicaid Services.
“Increasing access to analyses and data that include Medicare data will make it easier for stakeholders throughout the healthcare system to make smarter and more informed healthcare decisions,” CMS Acting Administrator Andy Slavitt said in a statement.
Under the rule, qualified entities may provide or sell data or analyses of the data to providers and suppliers. CMS encourages the sharing of data analytics that would assist in quality and patient care improvement activities, including the development of new models of care.
Disclosure or use of data for marketing purposes would be barred.
The rule includes strict privacy and security requirements for all entities receiving Medicare analyses or data.
If finalized, the rule could help practices in their efforts to provide value-based care and perform population management, said Dr. Yul D. Ejnes, chair-emeritus of the American College of Physicians Board of Regents and an internist in private practice in Cranston, R.I.
“A barrier, especially for small groups, is access to all-payer data, since what is available now is often partitioned by payer and not easy to compile into practice-wide data covering all patients,” he said in an interview. “Clearly, there is also a need for analysis of the data that is beyond the reach of most practices and is best done by third parties with the resources and expertise, so making the CMS data available facilitates that.”
However, Dr. Ejnes questioned how much these analyses will cost practices, especially smaller practices.
“Another related issue, beyond CMS’ purview, is how affordable this type of data analysis would be for the small practice that might benefit the most from it, since larger organizations have resources that may make much of this available to its physicians at little or no cost,” he said.
Entities supplying the information to providers must be accepted into the qualified entity program. The program, authorized under the Affordable Care Act, allows organizations that meet certain criteria to access patient-protected Medicare data to produce public reports. Qualified entities must combine the Medicare data with other claims data to produce reports that are “representative of how providers and suppliers are performing across multiple payers.”
Thus far, 13 organizations have been accepted into the program. Of these organizations, 2 have completed public reporting, while the other 11 are preparing for public reporting, according to CMS.
Comments on the new rule are due by March 29.
On Twitter @legal_med
Reaction: Poor methodology mars malpractice study
Physicians and insurers are taking exception to a medical malpractice study published Jan. 28 in the New England Journal of Medicine.
“Once again a study of medical liability claims has based unreliable conclusions on information obtained from the inherently flawed National Practitioner Data Bank,” Dr. Steven J. Stack, president of the American Medical Association, said in an interview.
David M. Studdert, Sc.D., of Stanford (Calif.) University, lead author of the study, said that he stands behind the findings, saying that the methodology used was strong and any significant limitations were noted.
“The data bank is the most authoritative repository of information that we have on medical malpractice claims nationwide,” Dr. Studdert said in an interview. “We don’t have an ability to look across the country at what’s happening with medical malpractice claims in any more comprehensive way than the [data bank]. Is it a perfect source of data? No. It has some limitations.”
The National Practitioner Data Bank (NPDB) is a congressionally mandated repository of medical malpractice payments and certain adverse actions related to health care providers, entities, and suppliers. Dr. Studdert and his colleagues calculated the cumulative distribution of paid claims in two physician populations: U.S. doctors with one or more paid claims and all active U.S. physicians, finding, on summation, that if physicians had one claim paid against them, they were more likely to have a subsequent claim paid against them as well (N Engl J Med. 2016; 374:354-62).
The credibility of the data bank has long been in question. An investigation published by the Government Accountability Office (GAO) in 2000 found that reports collected by the data bank were often untimely, inaccurate, or duplicated, which made it appear that “twice the number of disciplinary actions against a practitioner had been taken.”
In addition, most reports in the NPDB are based on legal settlements that were never adjudicated by a court, proven to involve negligence, or settled with a physician’s consent, according to Dr. Stack of the AMA. “Settlement information offers an incomplete and often misleading indicator of physician quality and competence. The nation’s best physicians who practice cutting-edge medicine and take on the riskiest cases are involved in settlements, yet the [NPDB] information does not acknowledge their high-level of competence.”
The study acknowledged that only 3% of the lawsuits studied were paid through trial verdicts, and that the remaining claims were paid by out-of-court settlements. Dr. Studdert and his colleagues also pointed out that payments do not necessarily indicate that a claim has merit, but that paid claims are “much more likely than unpaid claims to involve substandard care.”
Another study limitation was the unknown extent of underreporting to the NPDB, Dr. Studdert said.
As for the GAO report, the findings analyzed disciplinary actions, while the current study evaluated medical malpractice claims, Dr. Studdert said. Investigators tested for duplicate records during the course of their study and did not find repeated cases.
“That wasn’t an issue with the data we examined,” he said. “The information was very complete. I don’t doubt that the GAO report was correct, but it looks like over the last 15 years there must have been some improvements to the quality of the data bank.”
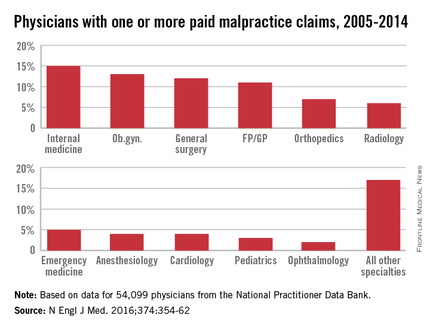
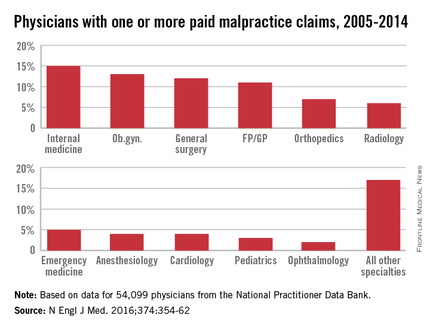
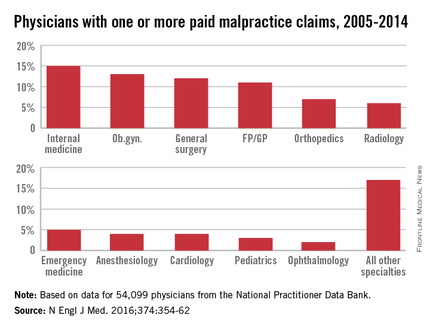
PIAA, a national trade association that represents medical liability insurers, expressed concern over findings that certain specialists face more claims than others.
“We know that certain specialties, such a neurosurgery, obstetrics and gynecology, and others, have been linked with a higher frequency of claims,” PIAA President and CEO Brian K. Atchinson said in a statement. “These doctors experience more claims because of the risk associated with their particular specialty, and not because they are inherently prone to making mistakes more often than their colleagues.”
“Studies have shown that all physicians are likely to be named in at least one medical liability claim during the course of their career with some subject to more based on their specialty,” P. Divya Parikh, PIAA vice president of research, said in a statement. “Thus, this study hasn’t really revealed anything we didn’t already know.”
Dr. Studdert said that he disagrees. “That’s really not an accurate analysis of what our analysis does. Our analysis controls for specialty and then looks at other risk factors for recurrent claims. It’s a regression model.”
On Twitter@legal_med
Physicians and insurers are taking exception to a medical malpractice study published Jan. 28 in the New England Journal of Medicine.
“Once again a study of medical liability claims has based unreliable conclusions on information obtained from the inherently flawed National Practitioner Data Bank,” Dr. Steven J. Stack, president of the American Medical Association, said in an interview.
David M. Studdert, Sc.D., of Stanford (Calif.) University, lead author of the study, said that he stands behind the findings, saying that the methodology used was strong and any significant limitations were noted.
“The data bank is the most authoritative repository of information that we have on medical malpractice claims nationwide,” Dr. Studdert said in an interview. “We don’t have an ability to look across the country at what’s happening with medical malpractice claims in any more comprehensive way than the [data bank]. Is it a perfect source of data? No. It has some limitations.”
The National Practitioner Data Bank (NPDB) is a congressionally mandated repository of medical malpractice payments and certain adverse actions related to health care providers, entities, and suppliers. Dr. Studdert and his colleagues calculated the cumulative distribution of paid claims in two physician populations: U.S. doctors with one or more paid claims and all active U.S. physicians, finding, on summation, that if physicians had one claim paid against them, they were more likely to have a subsequent claim paid against them as well (N Engl J Med. 2016; 374:354-62).
The credibility of the data bank has long been in question. An investigation published by the Government Accountability Office (GAO) in 2000 found that reports collected by the data bank were often untimely, inaccurate, or duplicated, which made it appear that “twice the number of disciplinary actions against a practitioner had been taken.”
In addition, most reports in the NPDB are based on legal settlements that were never adjudicated by a court, proven to involve negligence, or settled with a physician’s consent, according to Dr. Stack of the AMA. “Settlement information offers an incomplete and often misleading indicator of physician quality and competence. The nation’s best physicians who practice cutting-edge medicine and take on the riskiest cases are involved in settlements, yet the [NPDB] information does not acknowledge their high-level of competence.”
The study acknowledged that only 3% of the lawsuits studied were paid through trial verdicts, and that the remaining claims were paid by out-of-court settlements. Dr. Studdert and his colleagues also pointed out that payments do not necessarily indicate that a claim has merit, but that paid claims are “much more likely than unpaid claims to involve substandard care.”
Another study limitation was the unknown extent of underreporting to the NPDB, Dr. Studdert said.
As for the GAO report, the findings analyzed disciplinary actions, while the current study evaluated medical malpractice claims, Dr. Studdert said. Investigators tested for duplicate records during the course of their study and did not find repeated cases.
“That wasn’t an issue with the data we examined,” he said. “The information was very complete. I don’t doubt that the GAO report was correct, but it looks like over the last 15 years there must have been some improvements to the quality of the data bank.”
PIAA, a national trade association that represents medical liability insurers, expressed concern over findings that certain specialists face more claims than others.
“We know that certain specialties, such a neurosurgery, obstetrics and gynecology, and others, have been linked with a higher frequency of claims,” PIAA President and CEO Brian K. Atchinson said in a statement. “These doctors experience more claims because of the risk associated with their particular specialty, and not because they are inherently prone to making mistakes more often than their colleagues.”
“Studies have shown that all physicians are likely to be named in at least one medical liability claim during the course of their career with some subject to more based on their specialty,” P. Divya Parikh, PIAA vice president of research, said in a statement. “Thus, this study hasn’t really revealed anything we didn’t already know.”
Dr. Studdert said that he disagrees. “That’s really not an accurate analysis of what our analysis does. Our analysis controls for specialty and then looks at other risk factors for recurrent claims. It’s a regression model.”
On Twitter@legal_med
Physicians and insurers are taking exception to a medical malpractice study published Jan. 28 in the New England Journal of Medicine.
“Once again a study of medical liability claims has based unreliable conclusions on information obtained from the inherently flawed National Practitioner Data Bank,” Dr. Steven J. Stack, president of the American Medical Association, said in an interview.
David M. Studdert, Sc.D., of Stanford (Calif.) University, lead author of the study, said that he stands behind the findings, saying that the methodology used was strong and any significant limitations were noted.
“The data bank is the most authoritative repository of information that we have on medical malpractice claims nationwide,” Dr. Studdert said in an interview. “We don’t have an ability to look across the country at what’s happening with medical malpractice claims in any more comprehensive way than the [data bank]. Is it a perfect source of data? No. It has some limitations.”
The National Practitioner Data Bank (NPDB) is a congressionally mandated repository of medical malpractice payments and certain adverse actions related to health care providers, entities, and suppliers. Dr. Studdert and his colleagues calculated the cumulative distribution of paid claims in two physician populations: U.S. doctors with one or more paid claims and all active U.S. physicians, finding, on summation, that if physicians had one claim paid against them, they were more likely to have a subsequent claim paid against them as well (N Engl J Med. 2016; 374:354-62).
The credibility of the data bank has long been in question. An investigation published by the Government Accountability Office (GAO) in 2000 found that reports collected by the data bank were often untimely, inaccurate, or duplicated, which made it appear that “twice the number of disciplinary actions against a practitioner had been taken.”
In addition, most reports in the NPDB are based on legal settlements that were never adjudicated by a court, proven to involve negligence, or settled with a physician’s consent, according to Dr. Stack of the AMA. “Settlement information offers an incomplete and often misleading indicator of physician quality and competence. The nation’s best physicians who practice cutting-edge medicine and take on the riskiest cases are involved in settlements, yet the [NPDB] information does not acknowledge their high-level of competence.”
The study acknowledged that only 3% of the lawsuits studied were paid through trial verdicts, and that the remaining claims were paid by out-of-court settlements. Dr. Studdert and his colleagues also pointed out that payments do not necessarily indicate that a claim has merit, but that paid claims are “much more likely than unpaid claims to involve substandard care.”
Another study limitation was the unknown extent of underreporting to the NPDB, Dr. Studdert said.
As for the GAO report, the findings analyzed disciplinary actions, while the current study evaluated medical malpractice claims, Dr. Studdert said. Investigators tested for duplicate records during the course of their study and did not find repeated cases.
“That wasn’t an issue with the data we examined,” he said. “The information was very complete. I don’t doubt that the GAO report was correct, but it looks like over the last 15 years there must have been some improvements to the quality of the data bank.”
PIAA, a national trade association that represents medical liability insurers, expressed concern over findings that certain specialists face more claims than others.
“We know that certain specialties, such a neurosurgery, obstetrics and gynecology, and others, have been linked with a higher frequency of claims,” PIAA President and CEO Brian K. Atchinson said in a statement. “These doctors experience more claims because of the risk associated with their particular specialty, and not because they are inherently prone to making mistakes more often than their colleagues.”
“Studies have shown that all physicians are likely to be named in at least one medical liability claim during the course of their career with some subject to more based on their specialty,” P. Divya Parikh, PIAA vice president of research, said in a statement. “Thus, this study hasn’t really revealed anything we didn’t already know.”
Dr. Studdert said that he disagrees. “That’s really not an accurate analysis of what our analysis does. Our analysis controls for specialty and then looks at other risk factors for recurrent claims. It’s a regression model.”
On Twitter@legal_med
Study: Pay one malpractice claim, expect second
If you pay a medical malpractice claim once, chances are you’ll pay a second claim in the future, according to a study published Jan. 28 in the New England Journal of Medicine (doi: 10.1056/NEJMsa1506137).
David M. Studdert Sc.D., of Stanford (Calif.) University and his colleagues analyzed 66,426 malpractice claims from the National Practitioner Data Bank that were paid against 54,099 physicians between 2005 through 2014. Investigators calculated the cumulative distribution of paid claims in two physician populations: U.S. doctors with one or more paid claims and all active U.S. physicians.
Of all paid claims, 82% involved male physicians. The specialists with the most paid claims were internists (15%), ob.gyns. (13%), general surgeons (12%), and family physicians (11%). Only 3% of the lawsuits were paid through trial verdicts. The remaining claims were paid by out-of-court settlements. The mean payment amount for claims was $371,054, while the median was $204,750.
When using all 915,564 active U.S. physicians as a denominator, only 6% of physicians had a paid claim against them and about 1% had at least two paid claims against them. When looking at physicians with at least one paid claim, 84% had only one paid claim over the study period, accounting for 68% of all paid claims. However, 16% (8,846 physicians) had at least two paid claims, accounting for 32% of all claims. A total of 4% of doctors (2,160 physicians) had at least three paid claims and accounted for 12% of all claims, and 1% (722 physicians) had at least four paid claims and accounted for 5% of all claims.
Specialties had a marked impact on the risk of future paid claims. Compared with internists, the risk of recurrence was double among neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, and ob.gyns. Psychiatrists and pediatricians had the lowest risks of recurrence.
Mr. Studdert said that the investigators were surprised to learn the degree to which past paid claims predicted future claims.
“I think if you ask most people who work in the liability insurance industry, they would tell you that’s probably true,” he said in an interview. “But I don’ t think we’ve seen – at least not on this scale – research finding just how sharply claim risk rises with malpractice history. It does suggest for those multiclaim physicians, that there is something going on that is predisposing them to be the subject of malpractice litigation.”
He noted the analysis suggests that it is feasible to predict which physicians are at higher risk for future claims. The information could then be used to develop interventions to address malpractice claims.
“These multiclaim physicians do appear to have some distinctive characteristics, and that gives us some optimism that it might be possible to predict who is going to [become] a multiclaim physician,” Mr. Studdert said. “More work is needed to make sure that’s technically feasible, but if it is, that opens up a lot of possibilities for liability insurers, hospitals ,medical boards, and other regulators to use this information proactively rather than just reacting to events after they happen.”
On Twitter @legal_med
If you pay a medical malpractice claim once, chances are you’ll pay a second claim in the future, according to a study published Jan. 28 in the New England Journal of Medicine (doi: 10.1056/NEJMsa1506137).
David M. Studdert Sc.D., of Stanford (Calif.) University and his colleagues analyzed 66,426 malpractice claims from the National Practitioner Data Bank that were paid against 54,099 physicians between 2005 through 2014. Investigators calculated the cumulative distribution of paid claims in two physician populations: U.S. doctors with one or more paid claims and all active U.S. physicians.
Of all paid claims, 82% involved male physicians. The specialists with the most paid claims were internists (15%), ob.gyns. (13%), general surgeons (12%), and family physicians (11%). Only 3% of the lawsuits were paid through trial verdicts. The remaining claims were paid by out-of-court settlements. The mean payment amount for claims was $371,054, while the median was $204,750.
When using all 915,564 active U.S. physicians as a denominator, only 6% of physicians had a paid claim against them and about 1% had at least two paid claims against them. When looking at physicians with at least one paid claim, 84% had only one paid claim over the study period, accounting for 68% of all paid claims. However, 16% (8,846 physicians) had at least two paid claims, accounting for 32% of all claims. A total of 4% of doctors (2,160 physicians) had at least three paid claims and accounted for 12% of all claims, and 1% (722 physicians) had at least four paid claims and accounted for 5% of all claims.
Specialties had a marked impact on the risk of future paid claims. Compared with internists, the risk of recurrence was double among neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, and ob.gyns. Psychiatrists and pediatricians had the lowest risks of recurrence.
Mr. Studdert said that the investigators were surprised to learn the degree to which past paid claims predicted future claims.
“I think if you ask most people who work in the liability insurance industry, they would tell you that’s probably true,” he said in an interview. “But I don’ t think we’ve seen – at least not on this scale – research finding just how sharply claim risk rises with malpractice history. It does suggest for those multiclaim physicians, that there is something going on that is predisposing them to be the subject of malpractice litigation.”
He noted the analysis suggests that it is feasible to predict which physicians are at higher risk for future claims. The information could then be used to develop interventions to address malpractice claims.
“These multiclaim physicians do appear to have some distinctive characteristics, and that gives us some optimism that it might be possible to predict who is going to [become] a multiclaim physician,” Mr. Studdert said. “More work is needed to make sure that’s technically feasible, but if it is, that opens up a lot of possibilities for liability insurers, hospitals ,medical boards, and other regulators to use this information proactively rather than just reacting to events after they happen.”
On Twitter @legal_med
If you pay a medical malpractice claim once, chances are you’ll pay a second claim in the future, according to a study published Jan. 28 in the New England Journal of Medicine (doi: 10.1056/NEJMsa1506137).
David M. Studdert Sc.D., of Stanford (Calif.) University and his colleagues analyzed 66,426 malpractice claims from the National Practitioner Data Bank that were paid against 54,099 physicians between 2005 through 2014. Investigators calculated the cumulative distribution of paid claims in two physician populations: U.S. doctors with one or more paid claims and all active U.S. physicians.
Of all paid claims, 82% involved male physicians. The specialists with the most paid claims were internists (15%), ob.gyns. (13%), general surgeons (12%), and family physicians (11%). Only 3% of the lawsuits were paid through trial verdicts. The remaining claims were paid by out-of-court settlements. The mean payment amount for claims was $371,054, while the median was $204,750.
When using all 915,564 active U.S. physicians as a denominator, only 6% of physicians had a paid claim against them and about 1% had at least two paid claims against them. When looking at physicians with at least one paid claim, 84% had only one paid claim over the study period, accounting for 68% of all paid claims. However, 16% (8,846 physicians) had at least two paid claims, accounting for 32% of all claims. A total of 4% of doctors (2,160 physicians) had at least three paid claims and accounted for 12% of all claims, and 1% (722 physicians) had at least four paid claims and accounted for 5% of all claims.
Specialties had a marked impact on the risk of future paid claims. Compared with internists, the risk of recurrence was double among neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, and ob.gyns. Psychiatrists and pediatricians had the lowest risks of recurrence.
Mr. Studdert said that the investigators were surprised to learn the degree to which past paid claims predicted future claims.
“I think if you ask most people who work in the liability insurance industry, they would tell you that’s probably true,” he said in an interview. “But I don’ t think we’ve seen – at least not on this scale – research finding just how sharply claim risk rises with malpractice history. It does suggest for those multiclaim physicians, that there is something going on that is predisposing them to be the subject of malpractice litigation.”
He noted the analysis suggests that it is feasible to predict which physicians are at higher risk for future claims. The information could then be used to develop interventions to address malpractice claims.
“These multiclaim physicians do appear to have some distinctive characteristics, and that gives us some optimism that it might be possible to predict who is going to [become] a multiclaim physician,” Mr. Studdert said. “More work is needed to make sure that’s technically feasible, but if it is, that opens up a lot of possibilities for liability insurers, hospitals ,medical boards, and other regulators to use this information proactively rather than just reacting to events after they happen.”
On Twitter @legal_med
Key clinical point: Doctors with one paid medical malpractice claim have a greater chance of future paid claims.
Major finding: Of 54,099 physicians with at least one paid claim,16% had at least two paid claims. Physicians with two paid claims had almost twice the risk of having another paid claim compared with doctors who had only one paid claim against them.
Data source: Analysis of the National Practitioner Data Bank.
Disclosures: David Studdert, Sc.D., and Michelle Mello, Ph.D., reported grant support from the Risk Authority outside of this study.
Defining Patient Experience: 'Everything We Say and Do'
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one ormore of the “key communication” tactics in practice to maintain provider accountability for “Everything we say and do that affects our patients’ thoughts, feelings and well-being.”
As providers, how do we define the patient experience? Over the past year, I have had the pleasure of working with a dedicated group of 15 fellow members on the newly formed SHM Patient Experience Committee. One of our first goals was to define the patient experience in a way that acknowledges our role and its potential impact on patients as emotional beings and not just vessels for their disease.
To this end, we define the patient experience as “everything we say and do that affects our patients’ thoughts, feelings, and well-being.
Although it’s true that patients bring with them their own history and narrative that contribute to their experience, we cannot change that. We can only adjust our own behaviors and actions when we seek to elicit or respond to patients’ concerns and goals.
And although “everything we say and do” is inclusive of providing the most effective and evidence-based medical care at all times, we believe that accurate clinical decision making absolutely must be accompanied by superior communication. By offering clear explanations, listening compassionately, and acknowledging patients’ predicaments with empathy and caring statements, we can restore a degree of humanity to our care that will allow patients to trust that we have their best interests in mind at all times. This is our role in improving the patient experience.
Beginning next month, members of the Patient Experience Committee will be sharing key communication skills and interventions that each of us believes to be important and effective. Each member will share what they do, why they do it, and how it can be done effectively. The items we’ll be focusing on will be taken from the “Core Principles” and “Key Communications,” as compiled by the committee (see Table 1, below). Some have evidence to back them up. Some are common sense. All of them are simply the right thing to do.
We hope you’ll reflect on “everything we say and do” each month as well as share it with your colleagues and teams. And we need look no further for a winning argument to focus on the patient experience than Sir William Osler and one of his most famous quotes: “The good physician treats the disease; the great physician treats the patient who has the disease.”
We’re going for great. Are you with us? TH
Dr. Rudolph is vice president of physician development and patient experience for Tacoma, Wash.–based Sound Physicians. He is chair of SHM’s Patient Experience Committee.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one ormore of the “key communication” tactics in practice to maintain provider accountability for “Everything we say and do that affects our patients’ thoughts, feelings and well-being.”
As providers, how do we define the patient experience? Over the past year, I have had the pleasure of working with a dedicated group of 15 fellow members on the newly formed SHM Patient Experience Committee. One of our first goals was to define the patient experience in a way that acknowledges our role and its potential impact on patients as emotional beings and not just vessels for their disease.
To this end, we define the patient experience as “everything we say and do that affects our patients’ thoughts, feelings, and well-being.
Although it’s true that patients bring with them their own history and narrative that contribute to their experience, we cannot change that. We can only adjust our own behaviors and actions when we seek to elicit or respond to patients’ concerns and goals.
And although “everything we say and do” is inclusive of providing the most effective and evidence-based medical care at all times, we believe that accurate clinical decision making absolutely must be accompanied by superior communication. By offering clear explanations, listening compassionately, and acknowledging patients’ predicaments with empathy and caring statements, we can restore a degree of humanity to our care that will allow patients to trust that we have their best interests in mind at all times. This is our role in improving the patient experience.
Beginning next month, members of the Patient Experience Committee will be sharing key communication skills and interventions that each of us believes to be important and effective. Each member will share what they do, why they do it, and how it can be done effectively. The items we’ll be focusing on will be taken from the “Core Principles” and “Key Communications,” as compiled by the committee (see Table 1, below). Some have evidence to back them up. Some are common sense. All of them are simply the right thing to do.
We hope you’ll reflect on “everything we say and do” each month as well as share it with your colleagues and teams. And we need look no further for a winning argument to focus on the patient experience than Sir William Osler and one of his most famous quotes: “The good physician treats the disease; the great physician treats the patient who has the disease.”
We’re going for great. Are you with us? TH
Dr. Rudolph is vice president of physician development and patient experience for Tacoma, Wash.–based Sound Physicians. He is chair of SHM’s Patient Experience Committee.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one ormore of the “key communication” tactics in practice to maintain provider accountability for “Everything we say and do that affects our patients’ thoughts, feelings and well-being.”
As providers, how do we define the patient experience? Over the past year, I have had the pleasure of working with a dedicated group of 15 fellow members on the newly formed SHM Patient Experience Committee. One of our first goals was to define the patient experience in a way that acknowledges our role and its potential impact on patients as emotional beings and not just vessels for their disease.
To this end, we define the patient experience as “everything we say and do that affects our patients’ thoughts, feelings, and well-being.
Although it’s true that patients bring with them their own history and narrative that contribute to their experience, we cannot change that. We can only adjust our own behaviors and actions when we seek to elicit or respond to patients’ concerns and goals.
And although “everything we say and do” is inclusive of providing the most effective and evidence-based medical care at all times, we believe that accurate clinical decision making absolutely must be accompanied by superior communication. By offering clear explanations, listening compassionately, and acknowledging patients’ predicaments with empathy and caring statements, we can restore a degree of humanity to our care that will allow patients to trust that we have their best interests in mind at all times. This is our role in improving the patient experience.
Beginning next month, members of the Patient Experience Committee will be sharing key communication skills and interventions that each of us believes to be important and effective. Each member will share what they do, why they do it, and how it can be done effectively. The items we’ll be focusing on will be taken from the “Core Principles” and “Key Communications,” as compiled by the committee (see Table 1, below). Some have evidence to back them up. Some are common sense. All of them are simply the right thing to do.
We hope you’ll reflect on “everything we say and do” each month as well as share it with your colleagues and teams. And we need look no further for a winning argument to focus on the patient experience than Sir William Osler and one of his most famous quotes: “The good physician treats the disease; the great physician treats the patient who has the disease.”
We’re going for great. Are you with us? TH
Dr. Rudolph is vice president of physician development and patient experience for Tacoma, Wash.–based Sound Physicians. He is chair of SHM’s Patient Experience Committee.
CMS releases applications, instructions for 2015 meaningful use hardship exemptions
The Centers for Medicare & Medicaid Services has released the applications for meaningful use hardship exemptions for 2015.
Physicians who qualify for a hardship exemption must apply by March 15; hospitals must apply by April 1 to avoid being penalized in 2017. Exemptions may be granted for those facing infrastructure-related problems, unforeseen circumstances, lack of face-to-face interactions, or lack of available certified electronic health record systems.
As part of the Patient Access and Medicare Protection Act, passed in December 2015, CMS will be able to process blocks of applications instead of on a case-by-case basis, as it was required to do prior to the new law.
Applications and instructions are available here.
The Centers for Medicare & Medicaid Services has released the applications for meaningful use hardship exemptions for 2015.
Physicians who qualify for a hardship exemption must apply by March 15; hospitals must apply by April 1 to avoid being penalized in 2017. Exemptions may be granted for those facing infrastructure-related problems, unforeseen circumstances, lack of face-to-face interactions, or lack of available certified electronic health record systems.
As part of the Patient Access and Medicare Protection Act, passed in December 2015, CMS will be able to process blocks of applications instead of on a case-by-case basis, as it was required to do prior to the new law.
Applications and instructions are available here.
The Centers for Medicare & Medicaid Services has released the applications for meaningful use hardship exemptions for 2015.
Physicians who qualify for a hardship exemption must apply by March 15; hospitals must apply by April 1 to avoid being penalized in 2017. Exemptions may be granted for those facing infrastructure-related problems, unforeseen circumstances, lack of face-to-face interactions, or lack of available certified electronic health record systems.
As part of the Patient Access and Medicare Protection Act, passed in December 2015, CMS will be able to process blocks of applications instead of on a case-by-case basis, as it was required to do prior to the new law.
Applications and instructions are available here.
Patient records requests: New regs clarify physician responsibilities
The age of the information-empowered patient is upon us. Not only do patients bring the results of their Internet research when they come to the office, they also want to take a record of the clinical encounter with them when they leave.
New HIPAA guidance issued in January by the Health & Human Services Department’s Office of Civil Rights (OCR) aims to help clinicians know how to respond and with what information; it also addresses when patients can be charged for the information.
In the past, physicians and other providers had to “wing it” when it came to unclear rules about patient’s data requests, said Dianne J. Bourque, a Boston health law and HIPAA compliance attorney. “Prior to this, there may not have been readily available guidance that would drill down” to address specific concerns.
When it comes to systems security, physicians and other health providers do not have to put their health IT systems at risk in an effort to meet a request for patient records. For example, Mrs. Smith requests that her protected health information (PHI) be copied onto a thumb drive that she has provided.
In most cases, a covered entity must provide data access in the manner requested by the patient. But the updated guidance states that health providers are not expected to tolerate “unacceptable levels of risk to the security of the PHI on its systems” in responding to requests.
Unlike system security, patient security does not trump patient access. If Mr. Black requests that his records by emailed to him, but a connection cannot be made secure, physicians are still required to send the data.
While OCR requires HIPAA-covered entities to implement reasonable safeguards to protect PHI while in transit, patients have a right to receive a copy of records by unencrypted email if they so wish.
To comply with the new rules, be sure to warn patients of the risks, and confirm that they still want their PHI by unencrypted email. If confirmed, you must comply with the request. This clarification relieves doctors of potential breach notification and liability if the data is intercepted in transit.
The guidance also clarifies how to deliver patients’ data. If PHI is maintained electronically, physicians and other HIPAA-covered entities must be able provide it to patients electronically.
“Because you hold it electronically, you can’t say, ‘Forget it, you have to have paper,’” Ms. Bourque said. “You lose that option when you keep [data] electronically. Maybe you have to go buy a scanner and scan [the document] and email it, but you can’t charge [patients] for the scanner.”
The new guidance also allows patients to get results directly from a clinical laboratory; however, labs are not required to interpret test results. Rather, patients are encouraged to reach out to their physician for such insights.
Overall, the access guidelines appear reasonable and hopefully will relieve hassles for patients in obtaining their health information, said Dr. Sam Slishman, an emergency physician for Sierra Vista Hospital in San Luis Obispo, Calif., and co-founder of Pre-R, a service that provides in-home visits. Dr. Slishman does not foresee the guidance having much impact on his practices.
“It’s crazy to me that patients have to struggle to retrieve their records at all,” he said in an interview. “I routinely send my patients home with at least their lab tests and copies of their radiology reports so they have something to bring to their [primary care physicians]. If they want more, I hand it to them.”
Dr. Rocky D. Bilhartz, an interventional cardiologist in private practice in College Station, Tex., said that he has concerns about the guidelines. Specifically, that doctors may charge a fee to cover the cost of copying records, but that they cannot charge for the cost of searching and retrieving data, said Dr. Bilhartz, who is founder of ECGsource, an online cardiovascular medical education resource.
“Record requests can take significant time for staff to filter through and gather,” he said in an interview. “That time should be reimbursable ... If updated provisions prohibit charging for time spent compiling records, it seems those provisions are a bit out of touch with understanding what those of us on the ground floor must do when a request is received.”
But Dr. Bilhartz acknowledged that he would be unlikely to charge patients for “reasonable” data requests.
“I’m in private practice ... and because of that, I have more market-driven accountability to all my patients,” he said. “Why would I nickel and dime people who I would want to be satisfied patients? For reasonable requests, I would just provide records for free.”
Ms. Bourque notes that while the clarifications are primarily positive for health providers, they present a double-edged sword.
“The good side is that, it has all this detail and it’s really helpful and makes things easier when you have a tricky access request and don’t know what to do,” she said. “The flip side is that once it’s out there, they expect you to read it and pay attention. You start running out of excuses for why you didn’t comply with the access right or why you got it wrong.”
On Twitter @legal_med
The age of the information-empowered patient is upon us. Not only do patients bring the results of their Internet research when they come to the office, they also want to take a record of the clinical encounter with them when they leave.
New HIPAA guidance issued in January by the Health & Human Services Department’s Office of Civil Rights (OCR) aims to help clinicians know how to respond and with what information; it also addresses when patients can be charged for the information.
In the past, physicians and other providers had to “wing it” when it came to unclear rules about patient’s data requests, said Dianne J. Bourque, a Boston health law and HIPAA compliance attorney. “Prior to this, there may not have been readily available guidance that would drill down” to address specific concerns.
When it comes to systems security, physicians and other health providers do not have to put their health IT systems at risk in an effort to meet a request for patient records. For example, Mrs. Smith requests that her protected health information (PHI) be copied onto a thumb drive that she has provided.
In most cases, a covered entity must provide data access in the manner requested by the patient. But the updated guidance states that health providers are not expected to tolerate “unacceptable levels of risk to the security of the PHI on its systems” in responding to requests.
Unlike system security, patient security does not trump patient access. If Mr. Black requests that his records by emailed to him, but a connection cannot be made secure, physicians are still required to send the data.
While OCR requires HIPAA-covered entities to implement reasonable safeguards to protect PHI while in transit, patients have a right to receive a copy of records by unencrypted email if they so wish.
To comply with the new rules, be sure to warn patients of the risks, and confirm that they still want their PHI by unencrypted email. If confirmed, you must comply with the request. This clarification relieves doctors of potential breach notification and liability if the data is intercepted in transit.
The guidance also clarifies how to deliver patients’ data. If PHI is maintained electronically, physicians and other HIPAA-covered entities must be able provide it to patients electronically.
“Because you hold it electronically, you can’t say, ‘Forget it, you have to have paper,’” Ms. Bourque said. “You lose that option when you keep [data] electronically. Maybe you have to go buy a scanner and scan [the document] and email it, but you can’t charge [patients] for the scanner.”
The new guidance also allows patients to get results directly from a clinical laboratory; however, labs are not required to interpret test results. Rather, patients are encouraged to reach out to their physician for such insights.
Overall, the access guidelines appear reasonable and hopefully will relieve hassles for patients in obtaining their health information, said Dr. Sam Slishman, an emergency physician for Sierra Vista Hospital in San Luis Obispo, Calif., and co-founder of Pre-R, a service that provides in-home visits. Dr. Slishman does not foresee the guidance having much impact on his practices.
“It’s crazy to me that patients have to struggle to retrieve their records at all,” he said in an interview. “I routinely send my patients home with at least their lab tests and copies of their radiology reports so they have something to bring to their [primary care physicians]. If they want more, I hand it to them.”
Dr. Rocky D. Bilhartz, an interventional cardiologist in private practice in College Station, Tex., said that he has concerns about the guidelines. Specifically, that doctors may charge a fee to cover the cost of copying records, but that they cannot charge for the cost of searching and retrieving data, said Dr. Bilhartz, who is founder of ECGsource, an online cardiovascular medical education resource.
“Record requests can take significant time for staff to filter through and gather,” he said in an interview. “That time should be reimbursable ... If updated provisions prohibit charging for time spent compiling records, it seems those provisions are a bit out of touch with understanding what those of us on the ground floor must do when a request is received.”
But Dr. Bilhartz acknowledged that he would be unlikely to charge patients for “reasonable” data requests.
“I’m in private practice ... and because of that, I have more market-driven accountability to all my patients,” he said. “Why would I nickel and dime people who I would want to be satisfied patients? For reasonable requests, I would just provide records for free.”
Ms. Bourque notes that while the clarifications are primarily positive for health providers, they present a double-edged sword.
“The good side is that, it has all this detail and it’s really helpful and makes things easier when you have a tricky access request and don’t know what to do,” she said. “The flip side is that once it’s out there, they expect you to read it and pay attention. You start running out of excuses for why you didn’t comply with the access right or why you got it wrong.”
On Twitter @legal_med
The age of the information-empowered patient is upon us. Not only do patients bring the results of their Internet research when they come to the office, they also want to take a record of the clinical encounter with them when they leave.
New HIPAA guidance issued in January by the Health & Human Services Department’s Office of Civil Rights (OCR) aims to help clinicians know how to respond and with what information; it also addresses when patients can be charged for the information.
In the past, physicians and other providers had to “wing it” when it came to unclear rules about patient’s data requests, said Dianne J. Bourque, a Boston health law and HIPAA compliance attorney. “Prior to this, there may not have been readily available guidance that would drill down” to address specific concerns.
When it comes to systems security, physicians and other health providers do not have to put their health IT systems at risk in an effort to meet a request for patient records. For example, Mrs. Smith requests that her protected health information (PHI) be copied onto a thumb drive that she has provided.
In most cases, a covered entity must provide data access in the manner requested by the patient. But the updated guidance states that health providers are not expected to tolerate “unacceptable levels of risk to the security of the PHI on its systems” in responding to requests.
Unlike system security, patient security does not trump patient access. If Mr. Black requests that his records by emailed to him, but a connection cannot be made secure, physicians are still required to send the data.
While OCR requires HIPAA-covered entities to implement reasonable safeguards to protect PHI while in transit, patients have a right to receive a copy of records by unencrypted email if they so wish.
To comply with the new rules, be sure to warn patients of the risks, and confirm that they still want their PHI by unencrypted email. If confirmed, you must comply with the request. This clarification relieves doctors of potential breach notification and liability if the data is intercepted in transit.
The guidance also clarifies how to deliver patients’ data. If PHI is maintained electronically, physicians and other HIPAA-covered entities must be able provide it to patients electronically.
“Because you hold it electronically, you can’t say, ‘Forget it, you have to have paper,’” Ms. Bourque said. “You lose that option when you keep [data] electronically. Maybe you have to go buy a scanner and scan [the document] and email it, but you can’t charge [patients] for the scanner.”
The new guidance also allows patients to get results directly from a clinical laboratory; however, labs are not required to interpret test results. Rather, patients are encouraged to reach out to their physician for such insights.
Overall, the access guidelines appear reasonable and hopefully will relieve hassles for patients in obtaining their health information, said Dr. Sam Slishman, an emergency physician for Sierra Vista Hospital in San Luis Obispo, Calif., and co-founder of Pre-R, a service that provides in-home visits. Dr. Slishman does not foresee the guidance having much impact on his practices.
“It’s crazy to me that patients have to struggle to retrieve their records at all,” he said in an interview. “I routinely send my patients home with at least their lab tests and copies of their radiology reports so they have something to bring to their [primary care physicians]. If they want more, I hand it to them.”
Dr. Rocky D. Bilhartz, an interventional cardiologist in private practice in College Station, Tex., said that he has concerns about the guidelines. Specifically, that doctors may charge a fee to cover the cost of copying records, but that they cannot charge for the cost of searching and retrieving data, said Dr. Bilhartz, who is founder of ECGsource, an online cardiovascular medical education resource.
“Record requests can take significant time for staff to filter through and gather,” he said in an interview. “That time should be reimbursable ... If updated provisions prohibit charging for time spent compiling records, it seems those provisions are a bit out of touch with understanding what those of us on the ground floor must do when a request is received.”
But Dr. Bilhartz acknowledged that he would be unlikely to charge patients for “reasonable” data requests.
“I’m in private practice ... and because of that, I have more market-driven accountability to all my patients,” he said. “Why would I nickel and dime people who I would want to be satisfied patients? For reasonable requests, I would just provide records for free.”
Ms. Bourque notes that while the clarifications are primarily positive for health providers, they present a double-edged sword.
“The good side is that, it has all this detail and it’s really helpful and makes things easier when you have a tricky access request and don’t know what to do,” she said. “The flip side is that once it’s out there, they expect you to read it and pay attention. You start running out of excuses for why you didn’t comply with the access right or why you got it wrong.”
On Twitter @legal_med
CMS: IT changes are coming, but not here yet
Don’t walk away from meaningful use quite yet. That’s the message from CMS leaders Andy Slavitt and Dr. Karen DeSalvo.
Mr. Slavitt, acting administrator of the Centers for Medicare & Medicaid Services, announced on Jan. 11 that change would be coming to health care IT. “The meaningful use program as it has existed will now be effectively over and replaced with something better,” he said at the annual J.P. Morgan Healthcare Conference.
In a blog post intended to elaborate on those statements, Mr. Slavitt and Dr. DeSalvo, National Coordinator for Health IT, wrote that “the approach to meaningful use under the [Medicare Access & CHIP Reauthorization Act of 2015 (MACRA)] won’t happen overnight. Our goal in communicating our principles now is to give everyone time to plan for what’s next and to continue to give us input. We encourage you to look for the MACRA regulations this year; in the meantime, our existing regulations – including meaningful use stage 3 – are still in effect.”
Although CMS had been hinting since late in 2015 that it was considering dropping or modifying the meaningful use program, Mr. Slavitt made it official during the J.P. Morgan conference. The latest announcement asks providers to have patience with this process. “We will continue to listen and learn and make improvements based on what happens on the front line,” Mr. Slavitt and Dr. DeSalvo wrote. “The process will be ongoing, not an instant fix and we must all commit to learning and improving and collaborating on the best solutions.”
Since health IT changes under MACRA apply only to Medicare, the CMS leaders pointed out that electronic health record incentives for Medicaid and Medicare hospitals are unchanged; however, they noted that the agency would seek ways to help health care institutions streamline their IT needs as well.
The blog post also pointed out that late last year, CMS was given the authority to allow groups of providers – rather than individuals – to receive hardship exemptions under meaningful use. “This should make the process much simpler for physicians and their practice managers in the future. We will be releasing guidance on this new process soon,” Mr. Slavitt and Dr. DeSalvo noted.
The American Medical Association lauded the coming changes to health IT. This is “a win for patients, physicians and common sense,” Dr. Steven J. Sack said in a statement.
But as CMS forges ahead with new tech mandates, others advised the agency not to throw away the good with the bad.
“We are heartened that CMS has its ears to the ground and is trying to shape the program in a way that will be genuinely beneficial for providers and patients,” Ed Park, chief operating officer at AthenaHealth, a Boston-based health IT solutions firm, said in an interview. “With that said, just because providers found meaningful use stage 2 hard doesn’t by itself make it a bad program.”
This latest information out of CMS would seem to reinforce Mr. Slavitt’s promise to the investors at the J.P. Morgan conference that the move away from meaningful use would be to “start small and leave a lot of tool-building opportunities for the private sector.” He told attendees that CMS would level the playing field for start-ups and new entrants into the health IT space who can help providers securely transfer patient data and close the loops on referrals and other essentials of continuous care.
Some are not so optimistic about the private sector’s ability to help make MACRA a sustained reality, however. “As to whether the systems will be ready for the new payment regime, I am not holding my breath,” Johnathan Graham, a health economist and senior fellow at the National Center for Policy Analysis, Washington, D.C., said in an interview.
Even with updated technologies, physician satisfaction will not rise overall, he predicted, because of what he referred to as a too-slow rate of growth in Medicare’s Part B budget.
He also called out MACRA payment adjustments as onerous to physicians: The implementation of MACRA’s range of positive or negative payment adjustments in the MIPS program of minus 3.5% to plus 4.5% in 2019, plus or minus 5% in 2020, plus or minus 7% in 2021, and plus or minus 9% after that, meaning that the more providers who score above the threshold for the positive payment update, the narrower the update will be to each practice.
“I think MACRA will fall apart within 2 or 3 years as practicing physicians learn they are in a dog-eat-dog environment, or zero-sum game. The can will get kicked down the road just like meaningful use was,” Mr. Graham said.
But forcing doctors to face off is the point, according to Mr. Park: “Our health care system is on a transformational journey and we should all expect it to be hard. We want to encourage CMS to continue to keep the bar high on the right things and we hope that CMS doesn’t water down merit-based incentive pay so that the definition of success is that everyone succeeds.”
On Twitter @whitneymcknight
Don’t walk away from meaningful use quite yet. That’s the message from CMS leaders Andy Slavitt and Dr. Karen DeSalvo.
Mr. Slavitt, acting administrator of the Centers for Medicare & Medicaid Services, announced on Jan. 11 that change would be coming to health care IT. “The meaningful use program as it has existed will now be effectively over and replaced with something better,” he said at the annual J.P. Morgan Healthcare Conference.
In a blog post intended to elaborate on those statements, Mr. Slavitt and Dr. DeSalvo, National Coordinator for Health IT, wrote that “the approach to meaningful use under the [Medicare Access & CHIP Reauthorization Act of 2015 (MACRA)] won’t happen overnight. Our goal in communicating our principles now is to give everyone time to plan for what’s next and to continue to give us input. We encourage you to look for the MACRA regulations this year; in the meantime, our existing regulations – including meaningful use stage 3 – are still in effect.”
Although CMS had been hinting since late in 2015 that it was considering dropping or modifying the meaningful use program, Mr. Slavitt made it official during the J.P. Morgan conference. The latest announcement asks providers to have patience with this process. “We will continue to listen and learn and make improvements based on what happens on the front line,” Mr. Slavitt and Dr. DeSalvo wrote. “The process will be ongoing, not an instant fix and we must all commit to learning and improving and collaborating on the best solutions.”
Since health IT changes under MACRA apply only to Medicare, the CMS leaders pointed out that electronic health record incentives for Medicaid and Medicare hospitals are unchanged; however, they noted that the agency would seek ways to help health care institutions streamline their IT needs as well.
The blog post also pointed out that late last year, CMS was given the authority to allow groups of providers – rather than individuals – to receive hardship exemptions under meaningful use. “This should make the process much simpler for physicians and their practice managers in the future. We will be releasing guidance on this new process soon,” Mr. Slavitt and Dr. DeSalvo noted.
The American Medical Association lauded the coming changes to health IT. This is “a win for patients, physicians and common sense,” Dr. Steven J. Sack said in a statement.
But as CMS forges ahead with new tech mandates, others advised the agency not to throw away the good with the bad.
“We are heartened that CMS has its ears to the ground and is trying to shape the program in a way that will be genuinely beneficial for providers and patients,” Ed Park, chief operating officer at AthenaHealth, a Boston-based health IT solutions firm, said in an interview. “With that said, just because providers found meaningful use stage 2 hard doesn’t by itself make it a bad program.”
This latest information out of CMS would seem to reinforce Mr. Slavitt’s promise to the investors at the J.P. Morgan conference that the move away from meaningful use would be to “start small and leave a lot of tool-building opportunities for the private sector.” He told attendees that CMS would level the playing field for start-ups and new entrants into the health IT space who can help providers securely transfer patient data and close the loops on referrals and other essentials of continuous care.
Some are not so optimistic about the private sector’s ability to help make MACRA a sustained reality, however. “As to whether the systems will be ready for the new payment regime, I am not holding my breath,” Johnathan Graham, a health economist and senior fellow at the National Center for Policy Analysis, Washington, D.C., said in an interview.
Even with updated technologies, physician satisfaction will not rise overall, he predicted, because of what he referred to as a too-slow rate of growth in Medicare’s Part B budget.
He also called out MACRA payment adjustments as onerous to physicians: The implementation of MACRA’s range of positive or negative payment adjustments in the MIPS program of minus 3.5% to plus 4.5% in 2019, plus or minus 5% in 2020, plus or minus 7% in 2021, and plus or minus 9% after that, meaning that the more providers who score above the threshold for the positive payment update, the narrower the update will be to each practice.
“I think MACRA will fall apart within 2 or 3 years as practicing physicians learn they are in a dog-eat-dog environment, or zero-sum game. The can will get kicked down the road just like meaningful use was,” Mr. Graham said.
But forcing doctors to face off is the point, according to Mr. Park: “Our health care system is on a transformational journey and we should all expect it to be hard. We want to encourage CMS to continue to keep the bar high on the right things and we hope that CMS doesn’t water down merit-based incentive pay so that the definition of success is that everyone succeeds.”
On Twitter @whitneymcknight
Don’t walk away from meaningful use quite yet. That’s the message from CMS leaders Andy Slavitt and Dr. Karen DeSalvo.
Mr. Slavitt, acting administrator of the Centers for Medicare & Medicaid Services, announced on Jan. 11 that change would be coming to health care IT. “The meaningful use program as it has existed will now be effectively over and replaced with something better,” he said at the annual J.P. Morgan Healthcare Conference.
In a blog post intended to elaborate on those statements, Mr. Slavitt and Dr. DeSalvo, National Coordinator for Health IT, wrote that “the approach to meaningful use under the [Medicare Access & CHIP Reauthorization Act of 2015 (MACRA)] won’t happen overnight. Our goal in communicating our principles now is to give everyone time to plan for what’s next and to continue to give us input. We encourage you to look for the MACRA regulations this year; in the meantime, our existing regulations – including meaningful use stage 3 – are still in effect.”
Although CMS had been hinting since late in 2015 that it was considering dropping or modifying the meaningful use program, Mr. Slavitt made it official during the J.P. Morgan conference. The latest announcement asks providers to have patience with this process. “We will continue to listen and learn and make improvements based on what happens on the front line,” Mr. Slavitt and Dr. DeSalvo wrote. “The process will be ongoing, not an instant fix and we must all commit to learning and improving and collaborating on the best solutions.”
Since health IT changes under MACRA apply only to Medicare, the CMS leaders pointed out that electronic health record incentives for Medicaid and Medicare hospitals are unchanged; however, they noted that the agency would seek ways to help health care institutions streamline their IT needs as well.
The blog post also pointed out that late last year, CMS was given the authority to allow groups of providers – rather than individuals – to receive hardship exemptions under meaningful use. “This should make the process much simpler for physicians and their practice managers in the future. We will be releasing guidance on this new process soon,” Mr. Slavitt and Dr. DeSalvo noted.
The American Medical Association lauded the coming changes to health IT. This is “a win for patients, physicians and common sense,” Dr. Steven J. Sack said in a statement.
But as CMS forges ahead with new tech mandates, others advised the agency not to throw away the good with the bad.
“We are heartened that CMS has its ears to the ground and is trying to shape the program in a way that will be genuinely beneficial for providers and patients,” Ed Park, chief operating officer at AthenaHealth, a Boston-based health IT solutions firm, said in an interview. “With that said, just because providers found meaningful use stage 2 hard doesn’t by itself make it a bad program.”
This latest information out of CMS would seem to reinforce Mr. Slavitt’s promise to the investors at the J.P. Morgan conference that the move away from meaningful use would be to “start small and leave a lot of tool-building opportunities for the private sector.” He told attendees that CMS would level the playing field for start-ups and new entrants into the health IT space who can help providers securely transfer patient data and close the loops on referrals and other essentials of continuous care.
Some are not so optimistic about the private sector’s ability to help make MACRA a sustained reality, however. “As to whether the systems will be ready for the new payment regime, I am not holding my breath,” Johnathan Graham, a health economist and senior fellow at the National Center for Policy Analysis, Washington, D.C., said in an interview.
Even with updated technologies, physician satisfaction will not rise overall, he predicted, because of what he referred to as a too-slow rate of growth in Medicare’s Part B budget.
He also called out MACRA payment adjustments as onerous to physicians: The implementation of MACRA’s range of positive or negative payment adjustments in the MIPS program of minus 3.5% to plus 4.5% in 2019, plus or minus 5% in 2020, plus or minus 7% in 2021, and plus or minus 9% after that, meaning that the more providers who score above the threshold for the positive payment update, the narrower the update will be to each practice.
“I think MACRA will fall apart within 2 or 3 years as practicing physicians learn they are in a dog-eat-dog environment, or zero-sum game. The can will get kicked down the road just like meaningful use was,” Mr. Graham said.
But forcing doctors to face off is the point, according to Mr. Park: “Our health care system is on a transformational journey and we should all expect it to be hard. We want to encourage CMS to continue to keep the bar high on the right things and we hope that CMS doesn’t water down merit-based incentive pay so that the definition of success is that everyone succeeds.”
On Twitter @whitneymcknight
Alternative payment models: MedPAC says keep it simple
WASHINGTON – A federal advisory panel has straightforward advice for the government as it shifts towards value-based health care: Keep it simple.
At the Jan. 15 meeting of the Medicare Payment Advisory Commission (MedPAC), Commissioner Warner Thomas said, “I think one of our first principles should be to try to simplify this because it’s very complicated for a provider to try to understand what path to take and how to play in these situations. We want providers to engage in this and I think there is a lot of aversion because folks don’t understand it, and they’re not sure where to play or where not to play.”
Officials at the Centers for Medicare & Medicaid Services are drafting the regulations needed to implement the Medicare Access & CHIP Reauthorization Act (MACRA); the proposed regulations are expected in the Spring.
MedPAC staff offered a number of principles they hope to see incorporated into the final design for alternative payment models (APMs) under the law, including:
• Incentive payments to providers should be distributed only if the entities they are a part of are able to successfully control cost, improve quality, or both.
• Entities should have enough beneficiaries to detect changes in spending and quality.
• Entities should be at risk for total Part A and Part B spending; in the future, Part D also might be measured.
• Entities should be allowed to share savings with beneficiaries.
• Regulatory relief should be possible.
Several MedPAC commissioners focused on how physicians are viewing the risk they will be asked to assume in an APM.
APMs are “an attempt to sort of jump start a movement in the direction of risk taking from a group that I don’t think is very thrilled about taking financial risk and has shown it by their actual practice in the face of efforts at least to nudge them in this direction,” said Commissioner Bill Gradison Jr., a former congressman from Ohio who served on the House Committee on Ways and Means. “Having said that, I wish I had a better understanding of the motivation of physicians in terms of what might move them in this direction. The assumption here is that the money will move them, and maybe it’s that simple, but I am not too sure about that.”
Commissioner Jack Hoadley, Ph.D., of the Health Policy Institute at Georgetown University, Washington, noted that the if there is too little risk involved, there tends to be little movement in changing the behavior.
Dr. Hoadley suggested that CMS could consider “looking at some of the models by which risk can be structured so it puts plenty of money on the line but it doesn’t do it in a way that’s going to get complicated in terms of physicians owing money back.”
Commissioners also recommended a tight threshold, at least early on, to show that cost containment and/or quality improvement are well established before an entity can move into an APM and receive a financial incentive.
“Let’s keep the initial round and definition tight and actually demand a track record before we qualify something as an alternative payment mechanism,” said Commissioner Kathy Buto, a U.S. and international health policy consultant and former deputy executive secretary in the U.S. Health & Human Services Department. “Once you open this up, you can’t close it down. You cannot walk it back. We are talking about paying a lot more money, 5% more and if the definition is too loose and too many entities get into it, you can never walk it back and you will be just adding to the expenditures.”
WASHINGTON – A federal advisory panel has straightforward advice for the government as it shifts towards value-based health care: Keep it simple.
At the Jan. 15 meeting of the Medicare Payment Advisory Commission (MedPAC), Commissioner Warner Thomas said, “I think one of our first principles should be to try to simplify this because it’s very complicated for a provider to try to understand what path to take and how to play in these situations. We want providers to engage in this and I think there is a lot of aversion because folks don’t understand it, and they’re not sure where to play or where not to play.”
Officials at the Centers for Medicare & Medicaid Services are drafting the regulations needed to implement the Medicare Access & CHIP Reauthorization Act (MACRA); the proposed regulations are expected in the Spring.
MedPAC staff offered a number of principles they hope to see incorporated into the final design for alternative payment models (APMs) under the law, including:
• Incentive payments to providers should be distributed only if the entities they are a part of are able to successfully control cost, improve quality, or both.
• Entities should have enough beneficiaries to detect changes in spending and quality.
• Entities should be at risk for total Part A and Part B spending; in the future, Part D also might be measured.
• Entities should be allowed to share savings with beneficiaries.
• Regulatory relief should be possible.
Several MedPAC commissioners focused on how physicians are viewing the risk they will be asked to assume in an APM.
APMs are “an attempt to sort of jump start a movement in the direction of risk taking from a group that I don’t think is very thrilled about taking financial risk and has shown it by their actual practice in the face of efforts at least to nudge them in this direction,” said Commissioner Bill Gradison Jr., a former congressman from Ohio who served on the House Committee on Ways and Means. “Having said that, I wish I had a better understanding of the motivation of physicians in terms of what might move them in this direction. The assumption here is that the money will move them, and maybe it’s that simple, but I am not too sure about that.”
Commissioner Jack Hoadley, Ph.D., of the Health Policy Institute at Georgetown University, Washington, noted that the if there is too little risk involved, there tends to be little movement in changing the behavior.
Dr. Hoadley suggested that CMS could consider “looking at some of the models by which risk can be structured so it puts plenty of money on the line but it doesn’t do it in a way that’s going to get complicated in terms of physicians owing money back.”
Commissioners also recommended a tight threshold, at least early on, to show that cost containment and/or quality improvement are well established before an entity can move into an APM and receive a financial incentive.
“Let’s keep the initial round and definition tight and actually demand a track record before we qualify something as an alternative payment mechanism,” said Commissioner Kathy Buto, a U.S. and international health policy consultant and former deputy executive secretary in the U.S. Health & Human Services Department. “Once you open this up, you can’t close it down. You cannot walk it back. We are talking about paying a lot more money, 5% more and if the definition is too loose and too many entities get into it, you can never walk it back and you will be just adding to the expenditures.”
WASHINGTON – A federal advisory panel has straightforward advice for the government as it shifts towards value-based health care: Keep it simple.
At the Jan. 15 meeting of the Medicare Payment Advisory Commission (MedPAC), Commissioner Warner Thomas said, “I think one of our first principles should be to try to simplify this because it’s very complicated for a provider to try to understand what path to take and how to play in these situations. We want providers to engage in this and I think there is a lot of aversion because folks don’t understand it, and they’re not sure where to play or where not to play.”
Officials at the Centers for Medicare & Medicaid Services are drafting the regulations needed to implement the Medicare Access & CHIP Reauthorization Act (MACRA); the proposed regulations are expected in the Spring.
MedPAC staff offered a number of principles they hope to see incorporated into the final design for alternative payment models (APMs) under the law, including:
• Incentive payments to providers should be distributed only if the entities they are a part of are able to successfully control cost, improve quality, or both.
• Entities should have enough beneficiaries to detect changes in spending and quality.
• Entities should be at risk for total Part A and Part B spending; in the future, Part D also might be measured.
• Entities should be allowed to share savings with beneficiaries.
• Regulatory relief should be possible.
Several MedPAC commissioners focused on how physicians are viewing the risk they will be asked to assume in an APM.
APMs are “an attempt to sort of jump start a movement in the direction of risk taking from a group that I don’t think is very thrilled about taking financial risk and has shown it by their actual practice in the face of efforts at least to nudge them in this direction,” said Commissioner Bill Gradison Jr., a former congressman from Ohio who served on the House Committee on Ways and Means. “Having said that, I wish I had a better understanding of the motivation of physicians in terms of what might move them in this direction. The assumption here is that the money will move them, and maybe it’s that simple, but I am not too sure about that.”
Commissioner Jack Hoadley, Ph.D., of the Health Policy Institute at Georgetown University, Washington, noted that the if there is too little risk involved, there tends to be little movement in changing the behavior.
Dr. Hoadley suggested that CMS could consider “looking at some of the models by which risk can be structured so it puts plenty of money on the line but it doesn’t do it in a way that’s going to get complicated in terms of physicians owing money back.”
Commissioners also recommended a tight threshold, at least early on, to show that cost containment and/or quality improvement are well established before an entity can move into an APM and receive a financial incentive.
“Let’s keep the initial round and definition tight and actually demand a track record before we qualify something as an alternative payment mechanism,” said Commissioner Kathy Buto, a U.S. and international health policy consultant and former deputy executive secretary in the U.S. Health & Human Services Department. “Once you open this up, you can’t close it down. You cannot walk it back. We are talking about paying a lot more money, 5% more and if the definition is too loose and too many entities get into it, you can never walk it back and you will be just adding to the expenditures.”
AT A MEDPAC MEETING
Study eyes sleep-wake cycles in EMS clinicians
SAN DIEGO – Among emergency medical services clinicians, shift length alone was not associated with sleep duration, sleep quality, or self-reported fatigue at the start or end of shift work, preliminary results from a pilot study showed.
“There is a compelling need to address the sleep health and fatigue of EMS clinicians,” lead study author P. Daniel Patterson, Ph.D., said in an interview. “Reports of EMS clinicians falling asleep while driving ambulances have increased in recent history. There is a palpable concern for the safety of patients and clinicians. Prior studies show half of EMS clinicians report excessive mental and physical fatigue while at work; half get less than 6 hours of sleep daily, half rate their sleep quality as poor, and more than one-third report excessive daytime sleepiness.”
In an effort to characterize the sleep-wake and shift patterns of EMS clinicians working diverse shift schedules, Dr. Patterson, research director for MedCenter Air in the department of emergency medicine at Carolinas HealthCare System Medical Center, Charlotte, N.C., and his associates randomly selected 20 EMS clinicians participating in a randomized pilot trial that used text messaging to determine how real-time assessments of perceived sleepiness and fatigue impacts alertness and other behavior during shift work. These individuals provided detailed sleep diaries for 14 straight days in addition to reports of their fatigue in real time during shift work. The researchers used descriptive statistics to characterize sleep patterns in relation to shift work and self-reported fatigue during shifts.
Of the 20 study participants, 14 recorded at least one shift during the 14-day observation period. The mean number of shifts among these 14 participants was five, the most common shift duration worked was 24 hours (49%), and they had a mean of 34 hours off between scheduled shifts. Dr. Patterson, who is a practicing, nationally registered paramedic, reported at the annual meeting of the National Association of EMS Physicians that the shift length for eight of the study participants did not vary, while six worked shifts that ranged from 5 to 48 hours. The researchers found that when participants worked an extended shift of 24 hours, they slept significantly less before the shift than when working a shift of shorter duration (P = .0001). Participants who worked 24-hour shifts averaged 4.9 hours of sleep/rest during scheduled shifts, compared with 0.5 hours of total sleep/rest during shifts of shorter duration (P less than .0001). Dr. Patterson also reported that there appeared to be no differences based on shift duration (24 hours vs. other duration) in total sleep during the 24 hours after a scheduled shift.
He underscored the preliminary nature of the findings and acknowledged the potential for selection bias. “Much of our data are based on clinician self-report. Where possible, we used reliable and valid instruments and tools tested in the EMS setting to improve the internal validity.”
In a separate study presented during a poster session at the meeting, Dr. Patterson and his associates reported they are analyzing detailed sleep diaries and other sleep health information to evaluate psychomotor vigilance in more than 100 air-medical clinicians located in the South, Midwest, and Northeast United States.
Dr. Patterson also made a plea for EMS clinicians to participate in studies focused on their sleep health and fatigue. “We need these data to guide the development of fatigue risk management programs.”
Dr. Patterson disclosed that the study involving 14 EMS clinicians was funded by the Pittsburgh Emergency Medicine Foundation, the MedEvac Foundation, and by a career development award from the National Center for Resources and the National Institutes of Health. He reported that funding for the second study of air-medical clinicians is funded by the MedEvac Foundation.
SAN DIEGO – Among emergency medical services clinicians, shift length alone was not associated with sleep duration, sleep quality, or self-reported fatigue at the start or end of shift work, preliminary results from a pilot study showed.
“There is a compelling need to address the sleep health and fatigue of EMS clinicians,” lead study author P. Daniel Patterson, Ph.D., said in an interview. “Reports of EMS clinicians falling asleep while driving ambulances have increased in recent history. There is a palpable concern for the safety of patients and clinicians. Prior studies show half of EMS clinicians report excessive mental and physical fatigue while at work; half get less than 6 hours of sleep daily, half rate their sleep quality as poor, and more than one-third report excessive daytime sleepiness.”
In an effort to characterize the sleep-wake and shift patterns of EMS clinicians working diverse shift schedules, Dr. Patterson, research director for MedCenter Air in the department of emergency medicine at Carolinas HealthCare System Medical Center, Charlotte, N.C., and his associates randomly selected 20 EMS clinicians participating in a randomized pilot trial that used text messaging to determine how real-time assessments of perceived sleepiness and fatigue impacts alertness and other behavior during shift work. These individuals provided detailed sleep diaries for 14 straight days in addition to reports of their fatigue in real time during shift work. The researchers used descriptive statistics to characterize sleep patterns in relation to shift work and self-reported fatigue during shifts.
Of the 20 study participants, 14 recorded at least one shift during the 14-day observation period. The mean number of shifts among these 14 participants was five, the most common shift duration worked was 24 hours (49%), and they had a mean of 34 hours off between scheduled shifts. Dr. Patterson, who is a practicing, nationally registered paramedic, reported at the annual meeting of the National Association of EMS Physicians that the shift length for eight of the study participants did not vary, while six worked shifts that ranged from 5 to 48 hours. The researchers found that when participants worked an extended shift of 24 hours, they slept significantly less before the shift than when working a shift of shorter duration (P = .0001). Participants who worked 24-hour shifts averaged 4.9 hours of sleep/rest during scheduled shifts, compared with 0.5 hours of total sleep/rest during shifts of shorter duration (P less than .0001). Dr. Patterson also reported that there appeared to be no differences based on shift duration (24 hours vs. other duration) in total sleep during the 24 hours after a scheduled shift.
He underscored the preliminary nature of the findings and acknowledged the potential for selection bias. “Much of our data are based on clinician self-report. Where possible, we used reliable and valid instruments and tools tested in the EMS setting to improve the internal validity.”
In a separate study presented during a poster session at the meeting, Dr. Patterson and his associates reported they are analyzing detailed sleep diaries and other sleep health information to evaluate psychomotor vigilance in more than 100 air-medical clinicians located in the South, Midwest, and Northeast United States.
Dr. Patterson also made a plea for EMS clinicians to participate in studies focused on their sleep health and fatigue. “We need these data to guide the development of fatigue risk management programs.”
Dr. Patterson disclosed that the study involving 14 EMS clinicians was funded by the Pittsburgh Emergency Medicine Foundation, the MedEvac Foundation, and by a career development award from the National Center for Resources and the National Institutes of Health. He reported that funding for the second study of air-medical clinicians is funded by the MedEvac Foundation.
SAN DIEGO – Among emergency medical services clinicians, shift length alone was not associated with sleep duration, sleep quality, or self-reported fatigue at the start or end of shift work, preliminary results from a pilot study showed.
“There is a compelling need to address the sleep health and fatigue of EMS clinicians,” lead study author P. Daniel Patterson, Ph.D., said in an interview. “Reports of EMS clinicians falling asleep while driving ambulances have increased in recent history. There is a palpable concern for the safety of patients and clinicians. Prior studies show half of EMS clinicians report excessive mental and physical fatigue while at work; half get less than 6 hours of sleep daily, half rate their sleep quality as poor, and more than one-third report excessive daytime sleepiness.”
In an effort to characterize the sleep-wake and shift patterns of EMS clinicians working diverse shift schedules, Dr. Patterson, research director for MedCenter Air in the department of emergency medicine at Carolinas HealthCare System Medical Center, Charlotte, N.C., and his associates randomly selected 20 EMS clinicians participating in a randomized pilot trial that used text messaging to determine how real-time assessments of perceived sleepiness and fatigue impacts alertness and other behavior during shift work. These individuals provided detailed sleep diaries for 14 straight days in addition to reports of their fatigue in real time during shift work. The researchers used descriptive statistics to characterize sleep patterns in relation to shift work and self-reported fatigue during shifts.
Of the 20 study participants, 14 recorded at least one shift during the 14-day observation period. The mean number of shifts among these 14 participants was five, the most common shift duration worked was 24 hours (49%), and they had a mean of 34 hours off between scheduled shifts. Dr. Patterson, who is a practicing, nationally registered paramedic, reported at the annual meeting of the National Association of EMS Physicians that the shift length for eight of the study participants did not vary, while six worked shifts that ranged from 5 to 48 hours. The researchers found that when participants worked an extended shift of 24 hours, they slept significantly less before the shift than when working a shift of shorter duration (P = .0001). Participants who worked 24-hour shifts averaged 4.9 hours of sleep/rest during scheduled shifts, compared with 0.5 hours of total sleep/rest during shifts of shorter duration (P less than .0001). Dr. Patterson also reported that there appeared to be no differences based on shift duration (24 hours vs. other duration) in total sleep during the 24 hours after a scheduled shift.
He underscored the preliminary nature of the findings and acknowledged the potential for selection bias. “Much of our data are based on clinician self-report. Where possible, we used reliable and valid instruments and tools tested in the EMS setting to improve the internal validity.”
In a separate study presented during a poster session at the meeting, Dr. Patterson and his associates reported they are analyzing detailed sleep diaries and other sleep health information to evaluate psychomotor vigilance in more than 100 air-medical clinicians located in the South, Midwest, and Northeast United States.
Dr. Patterson also made a plea for EMS clinicians to participate in studies focused on their sleep health and fatigue. “We need these data to guide the development of fatigue risk management programs.”
Dr. Patterson disclosed that the study involving 14 EMS clinicians was funded by the Pittsburgh Emergency Medicine Foundation, the MedEvac Foundation, and by a career development award from the National Center for Resources and the National Institutes of Health. He reported that funding for the second study of air-medical clinicians is funded by the MedEvac Foundation.
AT NAEMSP 2016
Hawaii healthiest U.S. state in 2015, North Carolina most improved
For the fourth year in a row, Hawaii was named the healthiest state in America by the United Health Foundation in the 2015 edition of “America’s Health Rankings.”
A low obesity prevalence, low rate of preventable hospitalizations, few poor mental health days, and an 11% increase in immunization among children aged 19-35 months in 2015 helped make Hawaii the healthiest state over second-ranked Vermont. Massachusetts ranked third, with Minnesota and New Hampshire rounding out the top five.
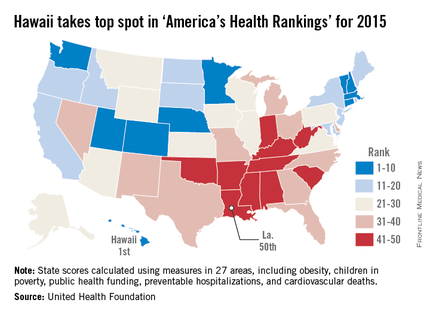
At the other end of the list, Louisiana replaced Mississippi as the least healthy state in 2015. Mississippi rose by one spot to 49th, however, followed by Arkansas at 48th, West Virginia at 47th, and Alabama at 46th.
The most improved state for 2015 was North Carolina, moving six spots up from 37th to 31st. Other states that saw significant moves upward were Maine, Washington, Delaware, and Kentucky. The largest decline was by Oregon, which dropped eight spots to 20th from 12th. New Mexico, Alabama, North Dakota, Texas, and West Virginia also made considerable downward movements.
Overall, the United States saw a significant decrease in preventable hospitalizations, physical inactivity, smoking, cardiovascular deaths, and infant mortality, and an increase in recommended vaccination coverage. Obesity rates increased, however, as did diabetes rates, drug deaths, and children living in poverty, and no progress was made in reducing premature deaths.
“America’s Health Rankings” is a joint effort by the United Health Foundation and the American Public Health Association. It is funded entirely by the private, not-for-profit United Health Foundation, founded by UnitedHealth Group, which operates UnitedHealthcare.
For the fourth year in a row, Hawaii was named the healthiest state in America by the United Health Foundation in the 2015 edition of “America’s Health Rankings.”
A low obesity prevalence, low rate of preventable hospitalizations, few poor mental health days, and an 11% increase in immunization among children aged 19-35 months in 2015 helped make Hawaii the healthiest state over second-ranked Vermont. Massachusetts ranked third, with Minnesota and New Hampshire rounding out the top five.
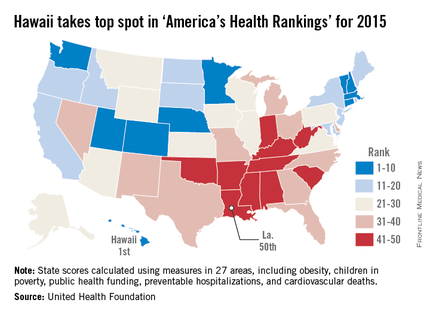
At the other end of the list, Louisiana replaced Mississippi as the least healthy state in 2015. Mississippi rose by one spot to 49th, however, followed by Arkansas at 48th, West Virginia at 47th, and Alabama at 46th.
The most improved state for 2015 was North Carolina, moving six spots up from 37th to 31st. Other states that saw significant moves upward were Maine, Washington, Delaware, and Kentucky. The largest decline was by Oregon, which dropped eight spots to 20th from 12th. New Mexico, Alabama, North Dakota, Texas, and West Virginia also made considerable downward movements.
Overall, the United States saw a significant decrease in preventable hospitalizations, physical inactivity, smoking, cardiovascular deaths, and infant mortality, and an increase in recommended vaccination coverage. Obesity rates increased, however, as did diabetes rates, drug deaths, and children living in poverty, and no progress was made in reducing premature deaths.
“America’s Health Rankings” is a joint effort by the United Health Foundation and the American Public Health Association. It is funded entirely by the private, not-for-profit United Health Foundation, founded by UnitedHealth Group, which operates UnitedHealthcare.
For the fourth year in a row, Hawaii was named the healthiest state in America by the United Health Foundation in the 2015 edition of “America’s Health Rankings.”
A low obesity prevalence, low rate of preventable hospitalizations, few poor mental health days, and an 11% increase in immunization among children aged 19-35 months in 2015 helped make Hawaii the healthiest state over second-ranked Vermont. Massachusetts ranked third, with Minnesota and New Hampshire rounding out the top five.
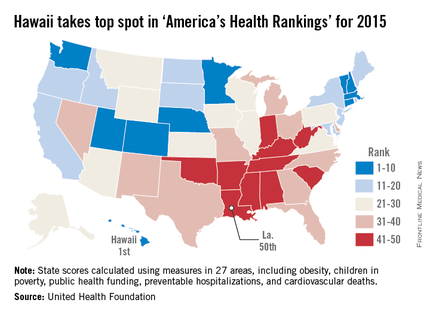
At the other end of the list, Louisiana replaced Mississippi as the least healthy state in 2015. Mississippi rose by one spot to 49th, however, followed by Arkansas at 48th, West Virginia at 47th, and Alabama at 46th.
The most improved state for 2015 was North Carolina, moving six spots up from 37th to 31st. Other states that saw significant moves upward were Maine, Washington, Delaware, and Kentucky. The largest decline was by Oregon, which dropped eight spots to 20th from 12th. New Mexico, Alabama, North Dakota, Texas, and West Virginia also made considerable downward movements.
Overall, the United States saw a significant decrease in preventable hospitalizations, physical inactivity, smoking, cardiovascular deaths, and infant mortality, and an increase in recommended vaccination coverage. Obesity rates increased, however, as did diabetes rates, drug deaths, and children living in poverty, and no progress was made in reducing premature deaths.
“America’s Health Rankings” is a joint effort by the United Health Foundation and the American Public Health Association. It is funded entirely by the private, not-for-profit United Health Foundation, founded by UnitedHealth Group, which operates UnitedHealthcare.