User login
American Heart Association (AHA): Scientific Sessions 2015
Medicare fumbles penalties for excess heart failure readmissions
ORLANDO – When the Centers for Medicare & Medicaid Services imposes financial penalties on hospitals because of excess readmissions for heart failure, the agency gets it wrong nearly 30% of the time, Hung-Mo Lin, Sc.D. asserted at the American Heart Association scientific sessions.
The problem, she said, is that the agency’s 2012 Inpatient Prospective Payment System Final Rule relies on a formula for estimating the risk-standardized excess readmission ratio that doesn’t take into account the uncertainties surrounding the measurements.
This has serious consequences in terms of the resultant substantial probability of hospital misclassification errors, according to Dr. Lin of the Icahn School of Medicine at Mount Sinai, New York.
How substantial is this error rate? To find out, Dr. Lin and her coworkers retroactively applied the CMS formula to roughly 1.5 million heart failure admissions at nearly 5,000 U.S. hospitals during 2005-2008, then developed confidence intervals for the individual hospitals’ excess readmission ratios and ran the numbers again, this time using the updated formula. They determined that the false-penalty rate was 27.5% for the 2,381 hospitals with an elevated excess admission ratio as defined by the current CMS formula.
Conversely, among the 2,549 hospitals that would have been labeled as good performers using the CMS formula and hence not subject to a punitive payment adjustment, 28.8% actually turned out to be poor performers with excessive heart failure readmissions. Those hospitals would have wrongly escaped penalties, she explained.
Hospital volume mattered. When the investigators stratified their results by hospital volume, they found that the probability of hospital misclassification was twice as great for small hospitals – that is, those in the two bottom quintiles for patient volume – compared to hospitals in the top quintile.
Dr. Lin reported having no financial conflicts regarding this health policy study.
ORLANDO – When the Centers for Medicare & Medicaid Services imposes financial penalties on hospitals because of excess readmissions for heart failure, the agency gets it wrong nearly 30% of the time, Hung-Mo Lin, Sc.D. asserted at the American Heart Association scientific sessions.
The problem, she said, is that the agency’s 2012 Inpatient Prospective Payment System Final Rule relies on a formula for estimating the risk-standardized excess readmission ratio that doesn’t take into account the uncertainties surrounding the measurements.
This has serious consequences in terms of the resultant substantial probability of hospital misclassification errors, according to Dr. Lin of the Icahn School of Medicine at Mount Sinai, New York.
How substantial is this error rate? To find out, Dr. Lin and her coworkers retroactively applied the CMS formula to roughly 1.5 million heart failure admissions at nearly 5,000 U.S. hospitals during 2005-2008, then developed confidence intervals for the individual hospitals’ excess readmission ratios and ran the numbers again, this time using the updated formula. They determined that the false-penalty rate was 27.5% for the 2,381 hospitals with an elevated excess admission ratio as defined by the current CMS formula.
Conversely, among the 2,549 hospitals that would have been labeled as good performers using the CMS formula and hence not subject to a punitive payment adjustment, 28.8% actually turned out to be poor performers with excessive heart failure readmissions. Those hospitals would have wrongly escaped penalties, she explained.
Hospital volume mattered. When the investigators stratified their results by hospital volume, they found that the probability of hospital misclassification was twice as great for small hospitals – that is, those in the two bottom quintiles for patient volume – compared to hospitals in the top quintile.
Dr. Lin reported having no financial conflicts regarding this health policy study.
ORLANDO – When the Centers for Medicare & Medicaid Services imposes financial penalties on hospitals because of excess readmissions for heart failure, the agency gets it wrong nearly 30% of the time, Hung-Mo Lin, Sc.D. asserted at the American Heart Association scientific sessions.
The problem, she said, is that the agency’s 2012 Inpatient Prospective Payment System Final Rule relies on a formula for estimating the risk-standardized excess readmission ratio that doesn’t take into account the uncertainties surrounding the measurements.
This has serious consequences in terms of the resultant substantial probability of hospital misclassification errors, according to Dr. Lin of the Icahn School of Medicine at Mount Sinai, New York.
How substantial is this error rate? To find out, Dr. Lin and her coworkers retroactively applied the CMS formula to roughly 1.5 million heart failure admissions at nearly 5,000 U.S. hospitals during 2005-2008, then developed confidence intervals for the individual hospitals’ excess readmission ratios and ran the numbers again, this time using the updated formula. They determined that the false-penalty rate was 27.5% for the 2,381 hospitals with an elevated excess admission ratio as defined by the current CMS formula.
Conversely, among the 2,549 hospitals that would have been labeled as good performers using the CMS formula and hence not subject to a punitive payment adjustment, 28.8% actually turned out to be poor performers with excessive heart failure readmissions. Those hospitals would have wrongly escaped penalties, she explained.
Hospital volume mattered. When the investigators stratified their results by hospital volume, they found that the probability of hospital misclassification was twice as great for small hospitals – that is, those in the two bottom quintiles for patient volume – compared to hospitals in the top quintile.
Dr. Lin reported having no financial conflicts regarding this health policy study.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Nearly 30% of hospitals penalized by Medicare for excess heart failure readmissions are misclassified as such, and a roughly equal percentage of hospitals are wrongly categorized as good performers.
Major finding: The formula Medicare uses to calculate risk-standardized excess heart failure readmission ratios is flawed in that it ignores the uncertainty of the measurements, leading to erroneous imposition of financial penalties.
Data source: This study entailed calculating the level of uncertainty in the Medicare formula, then retroactively applying the formula to nearly 1.5 million heart failure admissions at almost 5,000 U.S. hospitals.
Disclosures: The presenter reported having no financial conflicts regarding this health policy study.
Vegetarianism may protect against heart failure
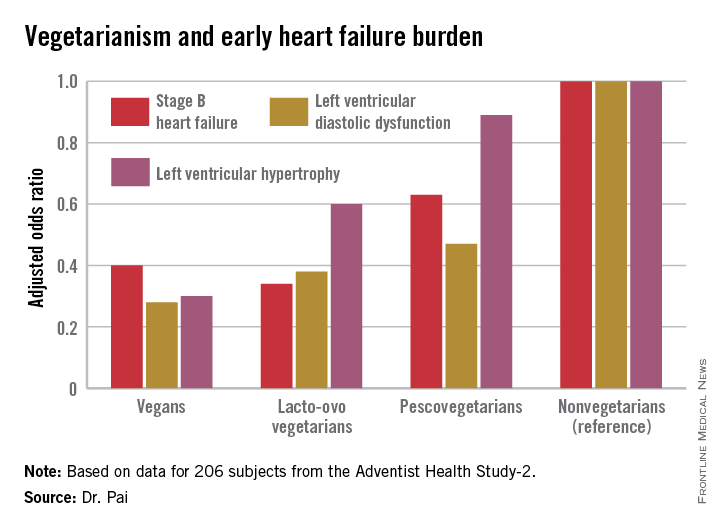
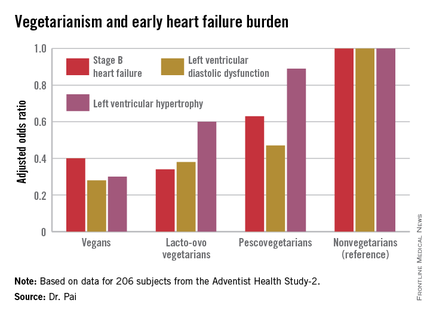
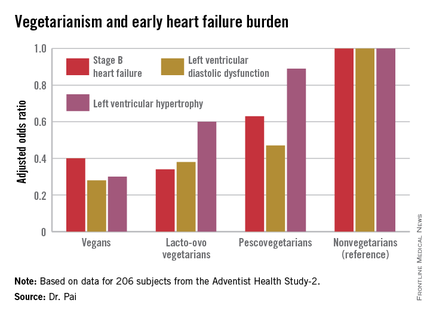
ORLANDO – Elderly individuals who consumed a vegan diet – no meat, fish, dairy, or eggs – were at an adjusted 72% lower risk of prevalent left ventricular diastolic dysfunction as well as 70% lower risk of left ventricular hypertrophy than were nonvegetarians in the Adventist Health Study-2.
The landmark Adventist Health Study-2 (AHS-2) is an ongoing observational epidemiologic study that includes 96,000 subjects. In previously reported findings from AHS-2, a vegetarian diet was associated with reduced risks of diabetes, hypertension, metabolic syndrome, overweight/obesity, all-cause mortality, and some cancers, compared with a nonvegetarian diet of similar caloric intake (Am J Clin Nutr. 2014 Jul;100[suppl 1]:353s-8s).
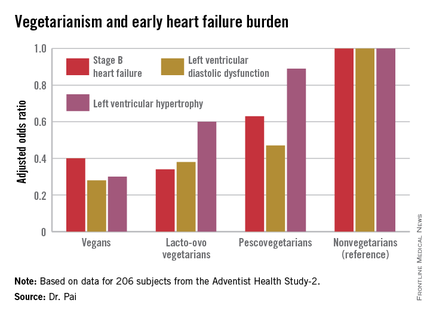
Because heart failure is a massive and growing problem, affecting 6 million Americans at a direct health care cost of $40 billion annually, AHS-2 investigators decided to look at the relationship between diet and heart failure, Dr. Ramdas G. Pai explained at the American Heart Association scientific sessions.
He and his coinvestigators at Loma Linda (Calif.) University brought in a random sample of 206 AHS-2 participants for a clinic visit which included a full echocardiographic assessment. The cohort had a mean age of 74 years. Echocardiography revealed that left ventricular diastolic dysfunction was present in 60% of subjects, left ventricular hypertrophy in 10%, and an increased left atrial volume index in 45%.
The study population consisted of roughly equal numbers of vegans, lacto-ovo vegetarians as defined by consumption of meat or fish less than once per month and dairy and/or eggs more than once weekly, pescovegetarians who eat fish more than once per month, and meat-eating nonvegetarians.
In a multivariate analysis adjusted for age, race, gender, body surface area, diabetes, hypertension, and history of coronary heart disease, a stepwise increase was seen in the prevalence of early stage B heart failure and its echocardiographic risk factors with increasing nonvegetarianism.
The implication is that a population shift toward a more vegetarian-oriented diet might reduce the overall burden of heart failure in the community, according to Dr. Pai.
He reported having no financial conflicts of interest regarding the AHS-2 analysis.
ORLANDO – Elderly individuals who consumed a vegan diet – no meat, fish, dairy, or eggs – were at an adjusted 72% lower risk of prevalent left ventricular diastolic dysfunction as well as 70% lower risk of left ventricular hypertrophy than were nonvegetarians in the Adventist Health Study-2.
The landmark Adventist Health Study-2 (AHS-2) is an ongoing observational epidemiologic study that includes 96,000 subjects. In previously reported findings from AHS-2, a vegetarian diet was associated with reduced risks of diabetes, hypertension, metabolic syndrome, overweight/obesity, all-cause mortality, and some cancers, compared with a nonvegetarian diet of similar caloric intake (Am J Clin Nutr. 2014 Jul;100[suppl 1]:353s-8s).
Because heart failure is a massive and growing problem, affecting 6 million Americans at a direct health care cost of $40 billion annually, AHS-2 investigators decided to look at the relationship between diet and heart failure, Dr. Ramdas G. Pai explained at the American Heart Association scientific sessions.
He and his coinvestigators at Loma Linda (Calif.) University brought in a random sample of 206 AHS-2 participants for a clinic visit which included a full echocardiographic assessment. The cohort had a mean age of 74 years. Echocardiography revealed that left ventricular diastolic dysfunction was present in 60% of subjects, left ventricular hypertrophy in 10%, and an increased left atrial volume index in 45%.
The study population consisted of roughly equal numbers of vegans, lacto-ovo vegetarians as defined by consumption of meat or fish less than once per month and dairy and/or eggs more than once weekly, pescovegetarians who eat fish more than once per month, and meat-eating nonvegetarians.
In a multivariate analysis adjusted for age, race, gender, body surface area, diabetes, hypertension, and history of coronary heart disease, a stepwise increase was seen in the prevalence of early stage B heart failure and its echocardiographic risk factors with increasing nonvegetarianism.
The implication is that a population shift toward a more vegetarian-oriented diet might reduce the overall burden of heart failure in the community, according to Dr. Pai.
He reported having no financial conflicts of interest regarding the AHS-2 analysis.
ORLANDO – Elderly individuals who consumed a vegan diet – no meat, fish, dairy, or eggs – were at an adjusted 72% lower risk of prevalent left ventricular diastolic dysfunction as well as 70% lower risk of left ventricular hypertrophy than were nonvegetarians in the Adventist Health Study-2.
The landmark Adventist Health Study-2 (AHS-2) is an ongoing observational epidemiologic study that includes 96,000 subjects. In previously reported findings from AHS-2, a vegetarian diet was associated with reduced risks of diabetes, hypertension, metabolic syndrome, overweight/obesity, all-cause mortality, and some cancers, compared with a nonvegetarian diet of similar caloric intake (Am J Clin Nutr. 2014 Jul;100[suppl 1]:353s-8s).
Because heart failure is a massive and growing problem, affecting 6 million Americans at a direct health care cost of $40 billion annually, AHS-2 investigators decided to look at the relationship between diet and heart failure, Dr. Ramdas G. Pai explained at the American Heart Association scientific sessions.
He and his coinvestigators at Loma Linda (Calif.) University brought in a random sample of 206 AHS-2 participants for a clinic visit which included a full echocardiographic assessment. The cohort had a mean age of 74 years. Echocardiography revealed that left ventricular diastolic dysfunction was present in 60% of subjects, left ventricular hypertrophy in 10%, and an increased left atrial volume index in 45%.
The study population consisted of roughly equal numbers of vegans, lacto-ovo vegetarians as defined by consumption of meat or fish less than once per month and dairy and/or eggs more than once weekly, pescovegetarians who eat fish more than once per month, and meat-eating nonvegetarians.
In a multivariate analysis adjusted for age, race, gender, body surface area, diabetes, hypertension, and history of coronary heart disease, a stepwise increase was seen in the prevalence of early stage B heart failure and its echocardiographic risk factors with increasing nonvegetarianism.
The implication is that a population shift toward a more vegetarian-oriented diet might reduce the overall burden of heart failure in the community, according to Dr. Pai.
He reported having no financial conflicts of interest regarding the AHS-2 analysis.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: The closer one gets to a vegan diet, the less likely are echocardiographic risk factors for early heart failure.
Major finding: Vegans were 60% less likely to have stage B heart failure than were nonvegetarians.
Data source: This study examined echocardiographic findings associated with early heart failure in 206 participants in the observational Adventist Health Study-2.
Disclosures: The presenter reported having no financial conflicts of interest regarding this study.
Cold Weather Linked to Increase in Strokes, MI
ORLANDO – Cold temperature days were associated with a 28% increase in the risk of MI and a 15% increase in stroke over an 18-year period in Ontario, Hong Chen, Ph.D., reported at the American Heart Association scientific sessions.
The relationship between air temperature and cardiovascular events mapped out as a U-shaped pattern, with the lowest-risk trough occurring on days when the temperature averaged 54º F. However, the U-shape was skewed such that the increased risk achieved significance on the cold but not hot days, according to Dr. Chen of Public Health Ontario and the University of Toronto.
He and his coinvestigators looked at the relationship between daily temperature and cardiovascular risk because the epidemiologic data in this area was sparse even though there are intriguing animal studies suggesting that extreme cold weather can induce a prothrombotic inflammatory reaction and hypercoagulable state.
The investigators matched daily temperature and cardiovascular hospital admission data for all 14 health districts in the sprawling province of Ontario for the period 1996-2013. During the study period, there were 443,447 hospitalizations for acute MI, 355,837 for stroke, 237,979 for ischemic stroke, and 1.4 million admissions coded as ischemic heart disease.
In a multivariate analysis controlling for influenza activity, air pollution levels, relative humidity, and day of the week, the adjusted rate of admissions for MI was 28% greater on the coldest 1% of days than on days where the temperature averaged the optimal 54º F. The coldest days were also associated with a 12% increase in the risk of admission for ischemic heart disease, a 15% increase in stroke, and a 19% increase in ischemic stroke.
Dr. Chen and his coworkers also examined their mountain of data to see how selected comorbid conditions might affect temperature-related risk. They found that the risk of admission for ischemic heart disease on cold days was greatest among individuals with a history of conduction disorders, while the risk of cold-related stroke was highest in Ontarians with preexisting arrhythmias.
Dr. Chen reported having no financial conflicts of interest regarding this public health study.
ORLANDO – Cold temperature days were associated with a 28% increase in the risk of MI and a 15% increase in stroke over an 18-year period in Ontario, Hong Chen, Ph.D., reported at the American Heart Association scientific sessions.
The relationship between air temperature and cardiovascular events mapped out as a U-shaped pattern, with the lowest-risk trough occurring on days when the temperature averaged 54º F. However, the U-shape was skewed such that the increased risk achieved significance on the cold but not hot days, according to Dr. Chen of Public Health Ontario and the University of Toronto.
He and his coinvestigators looked at the relationship between daily temperature and cardiovascular risk because the epidemiologic data in this area was sparse even though there are intriguing animal studies suggesting that extreme cold weather can induce a prothrombotic inflammatory reaction and hypercoagulable state.
The investigators matched daily temperature and cardiovascular hospital admission data for all 14 health districts in the sprawling province of Ontario for the period 1996-2013. During the study period, there were 443,447 hospitalizations for acute MI, 355,837 for stroke, 237,979 for ischemic stroke, and 1.4 million admissions coded as ischemic heart disease.
In a multivariate analysis controlling for influenza activity, air pollution levels, relative humidity, and day of the week, the adjusted rate of admissions for MI was 28% greater on the coldest 1% of days than on days where the temperature averaged the optimal 54º F. The coldest days were also associated with a 12% increase in the risk of admission for ischemic heart disease, a 15% increase in stroke, and a 19% increase in ischemic stroke.
Dr. Chen and his coworkers also examined their mountain of data to see how selected comorbid conditions might affect temperature-related risk. They found that the risk of admission for ischemic heart disease on cold days was greatest among individuals with a history of conduction disorders, while the risk of cold-related stroke was highest in Ontarians with preexisting arrhythmias.
Dr. Chen reported having no financial conflicts of interest regarding this public health study.
ORLANDO – Cold temperature days were associated with a 28% increase in the risk of MI and a 15% increase in stroke over an 18-year period in Ontario, Hong Chen, Ph.D., reported at the American Heart Association scientific sessions.
The relationship between air temperature and cardiovascular events mapped out as a U-shaped pattern, with the lowest-risk trough occurring on days when the temperature averaged 54º F. However, the U-shape was skewed such that the increased risk achieved significance on the cold but not hot days, according to Dr. Chen of Public Health Ontario and the University of Toronto.
He and his coinvestigators looked at the relationship between daily temperature and cardiovascular risk because the epidemiologic data in this area was sparse even though there are intriguing animal studies suggesting that extreme cold weather can induce a prothrombotic inflammatory reaction and hypercoagulable state.
The investigators matched daily temperature and cardiovascular hospital admission data for all 14 health districts in the sprawling province of Ontario for the period 1996-2013. During the study period, there were 443,447 hospitalizations for acute MI, 355,837 for stroke, 237,979 for ischemic stroke, and 1.4 million admissions coded as ischemic heart disease.
In a multivariate analysis controlling for influenza activity, air pollution levels, relative humidity, and day of the week, the adjusted rate of admissions for MI was 28% greater on the coldest 1% of days than on days where the temperature averaged the optimal 54º F. The coldest days were also associated with a 12% increase in the risk of admission for ischemic heart disease, a 15% increase in stroke, and a 19% increase in ischemic stroke.
Dr. Chen and his coworkers also examined their mountain of data to see how selected comorbid conditions might affect temperature-related risk. They found that the risk of admission for ischemic heart disease on cold days was greatest among individuals with a history of conduction disorders, while the risk of cold-related stroke was highest in Ontarians with preexisting arrhythmias.
Dr. Chen reported having no financial conflicts of interest regarding this public health study.
AT THE AHA SCIENTIFIC SESSIONS
Cold weather linked to increase in strokes, MI
ORLANDO – Cold temperature days were associated with a 28% increase in the risk of MI and a 15% increase in stroke over an 18-year period in Ontario, Hong Chen, Ph.D., reported at the American Heart Association scientific sessions.
The relationship between air temperature and cardiovascular events mapped out as a U-shaped pattern, with the lowest-risk trough occurring on days when the temperature averaged 54º F. However, the U-shape was skewed such that the increased risk achieved significance on the cold but not hot days, according to Dr. Chen of Public Health Ontario and the University of Toronto.
He and his coinvestigators looked at the relationship between daily temperature and cardiovascular risk because the epidemiologic data in this area was sparse even though there are intriguing animal studies suggesting that extreme cold weather can induce a prothrombotic inflammatory reaction and hypercoagulable state.
The investigators matched daily temperature and cardiovascular hospital admission data for all 14 health districts in the sprawling province of Ontario for the period 1996-2013. During the study period, there were 443,447 hospitalizations for acute MI, 355,837 for stroke, 237,979 for ischemic stroke, and 1.4 million admissions coded as ischemic heart disease.
In a multivariate analysis controlling for influenza activity, air pollution levels, relative humidity, and day of the week, the adjusted rate of admissions for MI was 28% greater on the coldest 1% of days than on days where the temperature averaged the optimal 54º F. The coldest days were also associated with a 12% increase in the risk of admission for ischemic heart disease, a 15% increase in stroke, and a 19% increase in ischemic stroke.
Dr. Chen and his coworkers also examined their mountain of data to see how selected comorbid conditions might affect temperature-related risk. They found that the risk of admission for ischemic heart disease on cold days was greatest among individuals with a history of conduction disorders, while the risk of cold-related stroke was highest in Ontarians with preexisting arrhythmias.
Dr. Chen reported having no financial conflicts of interest regarding this public health study.
ORLANDO – Cold temperature days were associated with a 28% increase in the risk of MI and a 15% increase in stroke over an 18-year period in Ontario, Hong Chen, Ph.D., reported at the American Heart Association scientific sessions.
The relationship between air temperature and cardiovascular events mapped out as a U-shaped pattern, with the lowest-risk trough occurring on days when the temperature averaged 54º F. However, the U-shape was skewed such that the increased risk achieved significance on the cold but not hot days, according to Dr. Chen of Public Health Ontario and the University of Toronto.
He and his coinvestigators looked at the relationship between daily temperature and cardiovascular risk because the epidemiologic data in this area was sparse even though there are intriguing animal studies suggesting that extreme cold weather can induce a prothrombotic inflammatory reaction and hypercoagulable state.
The investigators matched daily temperature and cardiovascular hospital admission data for all 14 health districts in the sprawling province of Ontario for the period 1996-2013. During the study period, there were 443,447 hospitalizations for acute MI, 355,837 for stroke, 237,979 for ischemic stroke, and 1.4 million admissions coded as ischemic heart disease.
In a multivariate analysis controlling for influenza activity, air pollution levels, relative humidity, and day of the week, the adjusted rate of admissions for MI was 28% greater on the coldest 1% of days than on days where the temperature averaged the optimal 54º F. The coldest days were also associated with a 12% increase in the risk of admission for ischemic heart disease, a 15% increase in stroke, and a 19% increase in ischemic stroke.
Dr. Chen and his coworkers also examined their mountain of data to see how selected comorbid conditions might affect temperature-related risk. They found that the risk of admission for ischemic heart disease on cold days was greatest among individuals with a history of conduction disorders, while the risk of cold-related stroke was highest in Ontarians with preexisting arrhythmias.
Dr. Chen reported having no financial conflicts of interest regarding this public health study.
ORLANDO – Cold temperature days were associated with a 28% increase in the risk of MI and a 15% increase in stroke over an 18-year period in Ontario, Hong Chen, Ph.D., reported at the American Heart Association scientific sessions.
The relationship between air temperature and cardiovascular events mapped out as a U-shaped pattern, with the lowest-risk trough occurring on days when the temperature averaged 54º F. However, the U-shape was skewed such that the increased risk achieved significance on the cold but not hot days, according to Dr. Chen of Public Health Ontario and the University of Toronto.
He and his coinvestigators looked at the relationship between daily temperature and cardiovascular risk because the epidemiologic data in this area was sparse even though there are intriguing animal studies suggesting that extreme cold weather can induce a prothrombotic inflammatory reaction and hypercoagulable state.
The investigators matched daily temperature and cardiovascular hospital admission data for all 14 health districts in the sprawling province of Ontario for the period 1996-2013. During the study period, there were 443,447 hospitalizations for acute MI, 355,837 for stroke, 237,979 for ischemic stroke, and 1.4 million admissions coded as ischemic heart disease.
In a multivariate analysis controlling for influenza activity, air pollution levels, relative humidity, and day of the week, the adjusted rate of admissions for MI was 28% greater on the coldest 1% of days than on days where the temperature averaged the optimal 54º F. The coldest days were also associated with a 12% increase in the risk of admission for ischemic heart disease, a 15% increase in stroke, and a 19% increase in ischemic stroke.
Dr. Chen and his coworkers also examined their mountain of data to see how selected comorbid conditions might affect temperature-related risk. They found that the risk of admission for ischemic heart disease on cold days was greatest among individuals with a history of conduction disorders, while the risk of cold-related stroke was highest in Ontarians with preexisting arrhythmias.
Dr. Chen reported having no financial conflicts of interest regarding this public health study.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Expect noticeably more hospital admissions for stroke and ischemic heart disease on cold weather days.
Major finding: Cold weather brought a 15% increase in the risk of hospital admission for stroke and a 28% rise in admissions for acute MI in Ontario, compared with days when the average temperature was 54º F.
Data source: This retrospective study looked at the association between daily temperature and the risk of hospital admission for acute MI, stroke, and other cardiovascular events over an 18-year period across Ontario.
Disclosures: The presenter reported having no financial conflicts of interest regarding this public health study.
67% of teens have substantial cardiometabolic risk burden, blood donor survey shows
ORLANDO – Fully two-thirds of nearly 25,000 Dallas-area volunteer blood donors ages 16-19 had elevated or borderline total cholesterol, blood pressure, and/or hemoglobin A1c, Dr. Merlyn H. Sayers reported at the American Heart Association scientific sessions.
“It is startling that such a significant percentage of these young, ostensibly healthy volunteers have abnormal cardiometabolic health metrics,” observed Dr. Sayers, president and chief executive officer of Carter BloodCare of Bedford, Tex., a nonprofit organization that is the largest blood bank in the state.
After all, he noted, longitudinal studies have clearly shown that cardiometabolic risk factors present in adolescence will persist into adulthood and are associated with increased risks of cardiovascular disease and diabetes. Moreover, it’s troubling, albeit not really surprising, that for the most part these adolescents don’t seem to care about their cardiometabolic risk, the hematologist-oncologist added.
“We give all these youngsters an opportunity to go to the Carter BloodCare website and confidentially retrieve their values. But despite all manner of urging on our part that these results are important, at best only about 20% of the individuals actually do so, and that rate varies substantially by race and ethnicity,” according to Dr. Sayers. “Where appropriate, we need to find ways to impose behavior modification on a group that is relatively resistant to guidance and intervention. Even the best kids, as teenagers, really don’t take this sort of advice about their health risk very seriously. They regard themselves as immortal during their teenage years.”
Noting that behavioral change is not a core strength among transfusion medicine specialists, Dr. Sayers appealed to his audience of cardiologists for suggestions as to how to encourage lifestyle modification in this youthful group without browbeating them to the point that they’re driven off from becoming serial blood donors.
It’s not widely appreciated that across the U.S. during the school year, 20% of all unpaid blood donors are high school students. These high school blood drives provide an as-yet untapped opportunity to screen adolescents for cardiometabolic risk at low cost and minimal inconvenience to participants, said Dr. Sayers of the University of Texas, Dallas.
“We need allies to help us to ensure we get the kids’ attention better,” he explained. “I want to leave you with the sense that perhaps you will see these blood drives as an opportunity to find interventions that might address primordial prevention of cardiometabolic risk.”
He presented a study of 24,925 youths aged 16-19 who donated blood to Carter BloodCare during 2011-2012. Since blood is drawn for obligatory infectious diseases screening at each donation, Dr. Sayers and coinvestigators were able to measure nonfasting total cholesterol and HbA1c in every teen donor. Blood pressure is also measured at every donation.
The investigators used widely accepted definitions of elevated blood pressure, cholesterol, and HbA1c: namely, at least 140/80 mm Hg, 200 mg/dL, and 6.5%, respectively.
While the percentage of teen blood donors with borderline or elevated levels of all three cardiometabolic risk factors was in the low single figures, 21% of boys and 15% of girls were positive for two out of the three.
The prevalence of cardiometabolic risk factors varied by ethnicity. Sixteen percent of white adolescents had elevated or borderline levels of two risk factors. So did 24% of African Americans, 22% of Asian Americans, and 18% of Hispanics.
“These are really staggering results,” commented session chair Dr. Seth S. Martin of Johns Hopkins University, Baltimore. “This is a call to action now that you’ve identified all these kids who are on a trajectory that doesn’t look good.”
As to how physicians can help to favorably alter that trajectory, however, audience members admitted to being stumped, especially since many young people stop going to a primary care physician for preventive care during their teenage years.
“The big problem here is how to use this information to initiate lifestyle change,” observed Dr. Lewis H. Kuller, professor and past chair of epidemiology at the University of Pittsburgh.
Dr. Sayers reported having no financial conflicts regarding his study.
ORLANDO – Fully two-thirds of nearly 25,000 Dallas-area volunteer blood donors ages 16-19 had elevated or borderline total cholesterol, blood pressure, and/or hemoglobin A1c, Dr. Merlyn H. Sayers reported at the American Heart Association scientific sessions.
“It is startling that such a significant percentage of these young, ostensibly healthy volunteers have abnormal cardiometabolic health metrics,” observed Dr. Sayers, president and chief executive officer of Carter BloodCare of Bedford, Tex., a nonprofit organization that is the largest blood bank in the state.
After all, he noted, longitudinal studies have clearly shown that cardiometabolic risk factors present in adolescence will persist into adulthood and are associated with increased risks of cardiovascular disease and diabetes. Moreover, it’s troubling, albeit not really surprising, that for the most part these adolescents don’t seem to care about their cardiometabolic risk, the hematologist-oncologist added.
“We give all these youngsters an opportunity to go to the Carter BloodCare website and confidentially retrieve their values. But despite all manner of urging on our part that these results are important, at best only about 20% of the individuals actually do so, and that rate varies substantially by race and ethnicity,” according to Dr. Sayers. “Where appropriate, we need to find ways to impose behavior modification on a group that is relatively resistant to guidance and intervention. Even the best kids, as teenagers, really don’t take this sort of advice about their health risk very seriously. They regard themselves as immortal during their teenage years.”
Noting that behavioral change is not a core strength among transfusion medicine specialists, Dr. Sayers appealed to his audience of cardiologists for suggestions as to how to encourage lifestyle modification in this youthful group without browbeating them to the point that they’re driven off from becoming serial blood donors.
It’s not widely appreciated that across the U.S. during the school year, 20% of all unpaid blood donors are high school students. These high school blood drives provide an as-yet untapped opportunity to screen adolescents for cardiometabolic risk at low cost and minimal inconvenience to participants, said Dr. Sayers of the University of Texas, Dallas.
“We need allies to help us to ensure we get the kids’ attention better,” he explained. “I want to leave you with the sense that perhaps you will see these blood drives as an opportunity to find interventions that might address primordial prevention of cardiometabolic risk.”
He presented a study of 24,925 youths aged 16-19 who donated blood to Carter BloodCare during 2011-2012. Since blood is drawn for obligatory infectious diseases screening at each donation, Dr. Sayers and coinvestigators were able to measure nonfasting total cholesterol and HbA1c in every teen donor. Blood pressure is also measured at every donation.
The investigators used widely accepted definitions of elevated blood pressure, cholesterol, and HbA1c: namely, at least 140/80 mm Hg, 200 mg/dL, and 6.5%, respectively.
While the percentage of teen blood donors with borderline or elevated levels of all three cardiometabolic risk factors was in the low single figures, 21% of boys and 15% of girls were positive for two out of the three.
The prevalence of cardiometabolic risk factors varied by ethnicity. Sixteen percent of white adolescents had elevated or borderline levels of two risk factors. So did 24% of African Americans, 22% of Asian Americans, and 18% of Hispanics.
“These are really staggering results,” commented session chair Dr. Seth S. Martin of Johns Hopkins University, Baltimore. “This is a call to action now that you’ve identified all these kids who are on a trajectory that doesn’t look good.”
As to how physicians can help to favorably alter that trajectory, however, audience members admitted to being stumped, especially since many young people stop going to a primary care physician for preventive care during their teenage years.
“The big problem here is how to use this information to initiate lifestyle change,” observed Dr. Lewis H. Kuller, professor and past chair of epidemiology at the University of Pittsburgh.
Dr. Sayers reported having no financial conflicts regarding his study.
ORLANDO – Fully two-thirds of nearly 25,000 Dallas-area volunteer blood donors ages 16-19 had elevated or borderline total cholesterol, blood pressure, and/or hemoglobin A1c, Dr. Merlyn H. Sayers reported at the American Heart Association scientific sessions.
“It is startling that such a significant percentage of these young, ostensibly healthy volunteers have abnormal cardiometabolic health metrics,” observed Dr. Sayers, president and chief executive officer of Carter BloodCare of Bedford, Tex., a nonprofit organization that is the largest blood bank in the state.
After all, he noted, longitudinal studies have clearly shown that cardiometabolic risk factors present in adolescence will persist into adulthood and are associated with increased risks of cardiovascular disease and diabetes. Moreover, it’s troubling, albeit not really surprising, that for the most part these adolescents don’t seem to care about their cardiometabolic risk, the hematologist-oncologist added.
“We give all these youngsters an opportunity to go to the Carter BloodCare website and confidentially retrieve their values. But despite all manner of urging on our part that these results are important, at best only about 20% of the individuals actually do so, and that rate varies substantially by race and ethnicity,” according to Dr. Sayers. “Where appropriate, we need to find ways to impose behavior modification on a group that is relatively resistant to guidance and intervention. Even the best kids, as teenagers, really don’t take this sort of advice about their health risk very seriously. They regard themselves as immortal during their teenage years.”
Noting that behavioral change is not a core strength among transfusion medicine specialists, Dr. Sayers appealed to his audience of cardiologists for suggestions as to how to encourage lifestyle modification in this youthful group without browbeating them to the point that they’re driven off from becoming serial blood donors.
It’s not widely appreciated that across the U.S. during the school year, 20% of all unpaid blood donors are high school students. These high school blood drives provide an as-yet untapped opportunity to screen adolescents for cardiometabolic risk at low cost and minimal inconvenience to participants, said Dr. Sayers of the University of Texas, Dallas.
“We need allies to help us to ensure we get the kids’ attention better,” he explained. “I want to leave you with the sense that perhaps you will see these blood drives as an opportunity to find interventions that might address primordial prevention of cardiometabolic risk.”
He presented a study of 24,925 youths aged 16-19 who donated blood to Carter BloodCare during 2011-2012. Since blood is drawn for obligatory infectious diseases screening at each donation, Dr. Sayers and coinvestigators were able to measure nonfasting total cholesterol and HbA1c in every teen donor. Blood pressure is also measured at every donation.
The investigators used widely accepted definitions of elevated blood pressure, cholesterol, and HbA1c: namely, at least 140/80 mm Hg, 200 mg/dL, and 6.5%, respectively.
While the percentage of teen blood donors with borderline or elevated levels of all three cardiometabolic risk factors was in the low single figures, 21% of boys and 15% of girls were positive for two out of the three.
The prevalence of cardiometabolic risk factors varied by ethnicity. Sixteen percent of white adolescents had elevated or borderline levels of two risk factors. So did 24% of African Americans, 22% of Asian Americans, and 18% of Hispanics.
“These are really staggering results,” commented session chair Dr. Seth S. Martin of Johns Hopkins University, Baltimore. “This is a call to action now that you’ve identified all these kids who are on a trajectory that doesn’t look good.”
As to how physicians can help to favorably alter that trajectory, however, audience members admitted to being stumped, especially since many young people stop going to a primary care physician for preventive care during their teenage years.
“The big problem here is how to use this information to initiate lifestyle change,” observed Dr. Lewis H. Kuller, professor and past chair of epidemiology at the University of Pittsburgh.
Dr. Sayers reported having no financial conflicts regarding his study.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Two-thirds of 16- to 19-year-olds have borderline or frank hypertension, hypercholesterolemia, and/or high blood glucose.
Major finding: Of a very large group of 16- to 19-year-old blood donors, 67% had borderline or elevated total cholesterol, blood pressure, and/or hemoglobin A1c levels.
Data source: A retrospective analysis of total cholesterol, blood pressure, and HbA1c levels in 24,925 Dallas-area blood donors aged 16-19.
Disclosures: The presenter reported having no financial conflicts of interest regarding this study.
Bystander CPR rising in children with cardiac arrest
ORLANDO – Bystander CPR was provided in 49% of U.S. cases of pediatric out-of-hospital cardiac arrest during 2013-2014, a major improvement over the 35% rate in a prior study 15 years ago, Dr. Maryam Y. Naim reported at the American Heart Association scientific sessions.
She presented an analysis of 2,176 out-of-hospital cardiac arrests (OHCA) in patients up to age 18 years who were included in the Cardiac Arrest Registry to Enhance Survival (CARES), the nation’s largest OHCA registry. Patients with traumatic OHCA and those whose bystander CPR (BCPR) was provided by a health care professional weren’t included.
Overall, the rate of neurologically favorable survival in pediatric recipients of BCPR was 11%, compared with 7% when BCPR wasn’t provided. But the results were far more impressive in the 14% of cardiac arrests that occurred outside the home, where the rate of neurologically favorable survival in BCPR recipients was 34%, more than twice the 15% figure for nonrecipients, according to Dr. Naim, a pediatrician and cardiac intensivist at Children’s Hospital of Philadelphia and the University of Pennsylvania.
Infants accounted for 47% of all pediatric OHCA, and in these youngest patients BCPR was of no benefit.
“The most common etiology of cardiac arrest in infants is sudden infant death syndrome. These are children who are found unresponsive in their cribs, and sometimes they’ve been dead a long time. We need to find something different for this population: perhaps developing a monitor to signal when an infant stops breathing or the heart rate goes down,” she said.
The fact that the BCPR rate in pediatric OHCA has climbed to 49% speaks well for public health efforts to improve education and awareness. Of those who received BCPR during 2013 and 2014, half got compression-only CPR, suggesting increasing adherence to the 2010 AHA guidelines for CPR and emergency cardiovascular care, which emphasized compression-only CPR as a viable alternative to conventional CPR, Dr. Naim added.
Her study highlighted a racial disparity in the application of BCPR in children and adolescents: Sixty percent of white youths with OHCA received BCPR, compared with 42% of blacks and 48% of Hispanics.
“About 70% of all bystander CPR was provided by a family member at home. So there’s really an opportunity there, especially in minority communities, to further increase education and awareness about bystander CPR, teaching family members to do it and also how to call 911 to start the chain of response,” she said.
Dr. Naim reported having no financial conflicts regarding her study.
ORLANDO – Bystander CPR was provided in 49% of U.S. cases of pediatric out-of-hospital cardiac arrest during 2013-2014, a major improvement over the 35% rate in a prior study 15 years ago, Dr. Maryam Y. Naim reported at the American Heart Association scientific sessions.
She presented an analysis of 2,176 out-of-hospital cardiac arrests (OHCA) in patients up to age 18 years who were included in the Cardiac Arrest Registry to Enhance Survival (CARES), the nation’s largest OHCA registry. Patients with traumatic OHCA and those whose bystander CPR (BCPR) was provided by a health care professional weren’t included.
Overall, the rate of neurologically favorable survival in pediatric recipients of BCPR was 11%, compared with 7% when BCPR wasn’t provided. But the results were far more impressive in the 14% of cardiac arrests that occurred outside the home, where the rate of neurologically favorable survival in BCPR recipients was 34%, more than twice the 15% figure for nonrecipients, according to Dr. Naim, a pediatrician and cardiac intensivist at Children’s Hospital of Philadelphia and the University of Pennsylvania.
Infants accounted for 47% of all pediatric OHCA, and in these youngest patients BCPR was of no benefit.
“The most common etiology of cardiac arrest in infants is sudden infant death syndrome. These are children who are found unresponsive in their cribs, and sometimes they’ve been dead a long time. We need to find something different for this population: perhaps developing a monitor to signal when an infant stops breathing or the heart rate goes down,” she said.
The fact that the BCPR rate in pediatric OHCA has climbed to 49% speaks well for public health efforts to improve education and awareness. Of those who received BCPR during 2013 and 2014, half got compression-only CPR, suggesting increasing adherence to the 2010 AHA guidelines for CPR and emergency cardiovascular care, which emphasized compression-only CPR as a viable alternative to conventional CPR, Dr. Naim added.
Her study highlighted a racial disparity in the application of BCPR in children and adolescents: Sixty percent of white youths with OHCA received BCPR, compared with 42% of blacks and 48% of Hispanics.
“About 70% of all bystander CPR was provided by a family member at home. So there’s really an opportunity there, especially in minority communities, to further increase education and awareness about bystander CPR, teaching family members to do it and also how to call 911 to start the chain of response,” she said.
Dr. Naim reported having no financial conflicts regarding her study.
ORLANDO – Bystander CPR was provided in 49% of U.S. cases of pediatric out-of-hospital cardiac arrest during 2013-2014, a major improvement over the 35% rate in a prior study 15 years ago, Dr. Maryam Y. Naim reported at the American Heart Association scientific sessions.
She presented an analysis of 2,176 out-of-hospital cardiac arrests (OHCA) in patients up to age 18 years who were included in the Cardiac Arrest Registry to Enhance Survival (CARES), the nation’s largest OHCA registry. Patients with traumatic OHCA and those whose bystander CPR (BCPR) was provided by a health care professional weren’t included.
Overall, the rate of neurologically favorable survival in pediatric recipients of BCPR was 11%, compared with 7% when BCPR wasn’t provided. But the results were far more impressive in the 14% of cardiac arrests that occurred outside the home, where the rate of neurologically favorable survival in BCPR recipients was 34%, more than twice the 15% figure for nonrecipients, according to Dr. Naim, a pediatrician and cardiac intensivist at Children’s Hospital of Philadelphia and the University of Pennsylvania.
Infants accounted for 47% of all pediatric OHCA, and in these youngest patients BCPR was of no benefit.
“The most common etiology of cardiac arrest in infants is sudden infant death syndrome. These are children who are found unresponsive in their cribs, and sometimes they’ve been dead a long time. We need to find something different for this population: perhaps developing a monitor to signal when an infant stops breathing or the heart rate goes down,” she said.
The fact that the BCPR rate in pediatric OHCA has climbed to 49% speaks well for public health efforts to improve education and awareness. Of those who received BCPR during 2013 and 2014, half got compression-only CPR, suggesting increasing adherence to the 2010 AHA guidelines for CPR and emergency cardiovascular care, which emphasized compression-only CPR as a viable alternative to conventional CPR, Dr. Naim added.
Her study highlighted a racial disparity in the application of BCPR in children and adolescents: Sixty percent of white youths with OHCA received BCPR, compared with 42% of blacks and 48% of Hispanics.
“About 70% of all bystander CPR was provided by a family member at home. So there’s really an opportunity there, especially in minority communities, to further increase education and awareness about bystander CPR, teaching family members to do it and also how to call 911 to start the chain of response,” she said.
Dr. Naim reported having no financial conflicts regarding her study.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Nearly half of all children and adolescents with out-of-hospital cardiac arrest in 2013-2014 got bystander CPR.
Major finding: The rate of neurologically favorable survival in pediatric patients with out-of-hospital cardiac arrest who receive bystander CPR is 34%, compared with 15% in those who don’t get the intervention.
Data source: An analysis of 2,176 out-of-hospital cardiac arrests in the Cardiac Arrest Registry to Enhance Survival during 2013 and 2014.
Disclosures: The presenter reported having no financial conflicts regarding her study.
ACC/AHA risk estimator underpredicts in HIV+ individuals
ORLANDO – The 2013 ACC/AHA atherosclerotic cardiovascular disease risk calculator isn’t reliably applicable to HIV-positive adults in its present form because it consistently underpredicts their MI risk, Dr. Michael J. Feinstein reported at the American Heart Association scientific sessions.
That’s the bad news. The good news is that “a simple, data-derived refit of the pooled cohort equations may improve the model’s performance in HIV-positive individuals,” said Dr. Feinstein of Northwestern University, Chicago.
Tweaking the risk calculator to enhance its accuracy in the HIV-positive population is particularly important because this population is growing in size and aging. And as Dr. Feinstein and coinvestigators showed in another study presented at the AHA meeting, the proportion of deaths due to cardiovascular disease in HIV-positive adults is shooting upward as they live longer because of treatment advances.
The investigators’ analysis of data from the Centers for Disease Control and Prevention national Wonder database showed that the proportion of deaths due to cardiovascular disease more than doubled between 1999 and 2013. Meanwhile, proportionate cardiovascular disease mortality declined by 22% in the general population and by 28% among individuals with inflammatory polyarthropathies.
That the ACC/AHA risk calculator in its present form doesn’t perform adequately in HIV-positive individuals hadn’t previously been shown, but it doesn’t really come as a surprise, according to Dr. Feinstein. After all, it’s known that this population is at 1.5- to 2-fold increased risk for MI and roughly 5-fold increased risk for sudden cardiac death, compared to the general population, where the risk calculator works best.
“Most data suggest that even in the setting of optimally treated HIV and undetectable viral load there’s still an underlying viral reservoir that appears to be driving inflammation and atherothrombotic and even nonatherothrombotic events in this population,” he said.
Dr. Feinstein and coworkers evaluated the 2013 ACC/AHA risk calculator in 11,901 HIV-positive black or white adults enrolled in the Centers for AIDS Research Network of Integrated Clinical Systems (CNICS) database for whom 5-year follow-up was available; 52% of the subjects were aged 40 or older at baseline.
Running each of these nearly 12,000 subjects through the risk calculator, the predicted result was that 103 of them would have an acute MI during the 5-year follow-up period. In reality, 132 MIs were observed. The discrepancy between the risk calculator predictions and observed MI rates was greatest in the 63% of HIV-positive subjects deemed at low risk, with an estimated 10-year risk of atherosclerotic cardiovascular disease of less than 5%.
Among white men, the risk calculator was remarkably consistent in underpredicting MIs. Regardless of whether the risk calculator put their estimated 10-year risk at less than 5%, 5% to less than 7.5%, 7.5% to less than 10%, or at least 10%, the actual observed MI rates were 67%-68% greater across the board than predicted.
Dr. Feinstein and coworkers refit the ACC/AHA risk calculator on a trial basis by incorporating variables related to HIV-positivity into the risk equations. Then they reanalyzed the tool’s performance in the same nearly 12,000 HIV-infected subjects. They found the discrimination and calibration of the revised risk equations improved substantially and met the standard of “acceptable” by statisticians’ standards.
The next step in this ongoing CNICS project will be to validate the provisionally refit risk calculator’s performance in a separate database of HIV-infected adults with adjudicated MIs. If the results are again positive, it will be a relatively straightforward matter to introduce the revisions into the ACC/AHA risk calculator, particularly since the senior coinvestigator in this project is Dr. Donald M. Lloyd-Jones, also of Northwestern University, who played a central role in developing the 2013 risk calculator.
Dr. Feinstein reported having no financial conflicts regarding this study.
ORLANDO – The 2013 ACC/AHA atherosclerotic cardiovascular disease risk calculator isn’t reliably applicable to HIV-positive adults in its present form because it consistently underpredicts their MI risk, Dr. Michael J. Feinstein reported at the American Heart Association scientific sessions.
That’s the bad news. The good news is that “a simple, data-derived refit of the pooled cohort equations may improve the model’s performance in HIV-positive individuals,” said Dr. Feinstein of Northwestern University, Chicago.
Tweaking the risk calculator to enhance its accuracy in the HIV-positive population is particularly important because this population is growing in size and aging. And as Dr. Feinstein and coinvestigators showed in another study presented at the AHA meeting, the proportion of deaths due to cardiovascular disease in HIV-positive adults is shooting upward as they live longer because of treatment advances.
The investigators’ analysis of data from the Centers for Disease Control and Prevention national Wonder database showed that the proportion of deaths due to cardiovascular disease more than doubled between 1999 and 2013. Meanwhile, proportionate cardiovascular disease mortality declined by 22% in the general population and by 28% among individuals with inflammatory polyarthropathies.
That the ACC/AHA risk calculator in its present form doesn’t perform adequately in HIV-positive individuals hadn’t previously been shown, but it doesn’t really come as a surprise, according to Dr. Feinstein. After all, it’s known that this population is at 1.5- to 2-fold increased risk for MI and roughly 5-fold increased risk for sudden cardiac death, compared to the general population, where the risk calculator works best.
“Most data suggest that even in the setting of optimally treated HIV and undetectable viral load there’s still an underlying viral reservoir that appears to be driving inflammation and atherothrombotic and even nonatherothrombotic events in this population,” he said.
Dr. Feinstein and coworkers evaluated the 2013 ACC/AHA risk calculator in 11,901 HIV-positive black or white adults enrolled in the Centers for AIDS Research Network of Integrated Clinical Systems (CNICS) database for whom 5-year follow-up was available; 52% of the subjects were aged 40 or older at baseline.
Running each of these nearly 12,000 subjects through the risk calculator, the predicted result was that 103 of them would have an acute MI during the 5-year follow-up period. In reality, 132 MIs were observed. The discrepancy between the risk calculator predictions and observed MI rates was greatest in the 63% of HIV-positive subjects deemed at low risk, with an estimated 10-year risk of atherosclerotic cardiovascular disease of less than 5%.
Among white men, the risk calculator was remarkably consistent in underpredicting MIs. Regardless of whether the risk calculator put their estimated 10-year risk at less than 5%, 5% to less than 7.5%, 7.5% to less than 10%, or at least 10%, the actual observed MI rates were 67%-68% greater across the board than predicted.
Dr. Feinstein and coworkers refit the ACC/AHA risk calculator on a trial basis by incorporating variables related to HIV-positivity into the risk equations. Then they reanalyzed the tool’s performance in the same nearly 12,000 HIV-infected subjects. They found the discrimination and calibration of the revised risk equations improved substantially and met the standard of “acceptable” by statisticians’ standards.
The next step in this ongoing CNICS project will be to validate the provisionally refit risk calculator’s performance in a separate database of HIV-infected adults with adjudicated MIs. If the results are again positive, it will be a relatively straightforward matter to introduce the revisions into the ACC/AHA risk calculator, particularly since the senior coinvestigator in this project is Dr. Donald M. Lloyd-Jones, also of Northwestern University, who played a central role in developing the 2013 risk calculator.
Dr. Feinstein reported having no financial conflicts regarding this study.
ORLANDO – The 2013 ACC/AHA atherosclerotic cardiovascular disease risk calculator isn’t reliably applicable to HIV-positive adults in its present form because it consistently underpredicts their MI risk, Dr. Michael J. Feinstein reported at the American Heart Association scientific sessions.
That’s the bad news. The good news is that “a simple, data-derived refit of the pooled cohort equations may improve the model’s performance in HIV-positive individuals,” said Dr. Feinstein of Northwestern University, Chicago.
Tweaking the risk calculator to enhance its accuracy in the HIV-positive population is particularly important because this population is growing in size and aging. And as Dr. Feinstein and coinvestigators showed in another study presented at the AHA meeting, the proportion of deaths due to cardiovascular disease in HIV-positive adults is shooting upward as they live longer because of treatment advances.
The investigators’ analysis of data from the Centers for Disease Control and Prevention national Wonder database showed that the proportion of deaths due to cardiovascular disease more than doubled between 1999 and 2013. Meanwhile, proportionate cardiovascular disease mortality declined by 22% in the general population and by 28% among individuals with inflammatory polyarthropathies.
That the ACC/AHA risk calculator in its present form doesn’t perform adequately in HIV-positive individuals hadn’t previously been shown, but it doesn’t really come as a surprise, according to Dr. Feinstein. After all, it’s known that this population is at 1.5- to 2-fold increased risk for MI and roughly 5-fold increased risk for sudden cardiac death, compared to the general population, where the risk calculator works best.
“Most data suggest that even in the setting of optimally treated HIV and undetectable viral load there’s still an underlying viral reservoir that appears to be driving inflammation and atherothrombotic and even nonatherothrombotic events in this population,” he said.
Dr. Feinstein and coworkers evaluated the 2013 ACC/AHA risk calculator in 11,901 HIV-positive black or white adults enrolled in the Centers for AIDS Research Network of Integrated Clinical Systems (CNICS) database for whom 5-year follow-up was available; 52% of the subjects were aged 40 or older at baseline.
Running each of these nearly 12,000 subjects through the risk calculator, the predicted result was that 103 of them would have an acute MI during the 5-year follow-up period. In reality, 132 MIs were observed. The discrepancy between the risk calculator predictions and observed MI rates was greatest in the 63% of HIV-positive subjects deemed at low risk, with an estimated 10-year risk of atherosclerotic cardiovascular disease of less than 5%.
Among white men, the risk calculator was remarkably consistent in underpredicting MIs. Regardless of whether the risk calculator put their estimated 10-year risk at less than 5%, 5% to less than 7.5%, 7.5% to less than 10%, or at least 10%, the actual observed MI rates were 67%-68% greater across the board than predicted.
Dr. Feinstein and coworkers refit the ACC/AHA risk calculator on a trial basis by incorporating variables related to HIV-positivity into the risk equations. Then they reanalyzed the tool’s performance in the same nearly 12,000 HIV-infected subjects. They found the discrimination and calibration of the revised risk equations improved substantially and met the standard of “acceptable” by statisticians’ standards.
The next step in this ongoing CNICS project will be to validate the provisionally refit risk calculator’s performance in a separate database of HIV-infected adults with adjudicated MIs. If the results are again positive, it will be a relatively straightforward matter to introduce the revisions into the ACC/AHA risk calculator, particularly since the senior coinvestigator in this project is Dr. Donald M. Lloyd-Jones, also of Northwestern University, who played a central role in developing the 2013 risk calculator.
Dr. Feinstein reported having no financial conflicts regarding this study.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: The 2013 ACC/AHA risk estimator needs a tune-up before it can be reliably applied to HIV-infected adults.
Major finding: Observed rates of acute MI over time in HIV-positive white men were 67%-68% higher than predicted by the 2013 ACC/AHA atherosclerotic cardiovascular disease risk calculator regardless of whether the men were deemed at low, intermediate, or high baseline risk.
Data source: A study comparing the predicted number of acute MIs in a population of nearly 12,000 HIV-positive adults over a 5-year period as determined via the 2013 ACC/AHA atherosclerotic cardiovascular disease risk calculator with the actual observed number of adjudicated MIs.
Disclosures: The study was conducted free of commercial support. The presenter reported having no financial conflicts of interest.
AHA: Ezetimibe reduces ischemic stroke risk
ORLANDO – The combination of ezetimibe/simvastatin significantly reduced the risk of nonhemorrhagic stroke compared with simvastatin alone, with a particularly striking benefit seen in patients with prior history of stroke, in a new analysis from the landmark IMPROVE-IT trial.
“We believe these data support the use of intensive lipid lowering therapy, which includes ezetimibe to prevent ischemic stroke,” Dr. Stephen D. Wiviott said in reporting the findings at the American Heart Association scientific sessions.
He presented a prespecified secondary analysis from IMPROVE-IT, a double-blind study in which 18,144 patients on background optimal medical management were randomized post–acute coronary syndrome to simvastatin/ezetimibe at 40/10 mg/day (Vytorin) or simvastatin (Zocor) at 40 mg/day. At a median of 6 years of follow-up, the primary composite cardiovascular outcome was significantly reduced by 6% in the dual-therapy group compared with statin monotherapy, with a number-needed-to-treat (NNT) of 50, as previously reported (N Engl J Med. 2015 Jun 18;372[25]:2387-97).
The impetus for the prespecified stroke analysis was that up until IMPROVE-IT, no LDL cholesterol–lowering therapy other than statins had ever been shown to protect against stroke. The Cholesterol Trialists’ Collaboration meta-analysis, involving roughly 173,000 subjects, previously showed that statin therapy reduces ischemic stroke risk by 20% per 1 mmol/L of LDL lowering (Lancet. 2012 Aug 11;380[9841]:581-90). The question was, could add-on ezetimibe decrease stroke risk even further?
Stroke occurred in 641 patients during follow-up. As adjudicated by independent neurologists, 82% of the strokes were nonhemorrhagic, 16% were hemorrhagic, and 2% were unknown. The 14% relative risk reduction in overall stroke with simvastatin/ezetimibe compared with simvastatin, with rates of 4.2% versus 4.8%, just missed achieving statistical significance (P = .052). A significant 21% reduction in nonhemorrhagic strokes was seen with dual therapy, where the incidence during follow-up was 3.4%, compared with 4.1% with simvastatin alone, but this effect was dampened by a numeric albeit statistically nonsignificant absolute 0.2% increase in hemorrhagic strokes in the simvastatin/ezetimibe group.
Far more impressive was the stroke-prevention benefit of simvastatin/ezetimibe among the 1,071 subjects with prior stroke or TIA at baseline. Their nonhemorrhagic stroke rate during follow-up was 10.2% with simvastatin/ezetimibe versus 18.8% with simvastatin alone, for a 40% relative risk reduction favoring dual lipid-lowering therapy and an NNT of about 20. Again, there was no significant difference in hemorrhagic stroke between the two treatment arms, noted Dr. Wiviott of Brigham and Womens Hospital, Boston.
The stroke-prevention benefit achieved by adding ezetimibe to simvastatin was seen regardless of patient age, gender, renal function, baseline LDL cholesterol level, or other prespecified subcategories.
IMPROVE-IT was sponsored by Merck. Dr. Wiviott reported receiving research grants from Merck, AstraZeneca, and Eisai and serving as a consultant to nine pharmaceutical companies.
ORLANDO – The combination of ezetimibe/simvastatin significantly reduced the risk of nonhemorrhagic stroke compared with simvastatin alone, with a particularly striking benefit seen in patients with prior history of stroke, in a new analysis from the landmark IMPROVE-IT trial.
“We believe these data support the use of intensive lipid lowering therapy, which includes ezetimibe to prevent ischemic stroke,” Dr. Stephen D. Wiviott said in reporting the findings at the American Heart Association scientific sessions.
He presented a prespecified secondary analysis from IMPROVE-IT, a double-blind study in which 18,144 patients on background optimal medical management were randomized post–acute coronary syndrome to simvastatin/ezetimibe at 40/10 mg/day (Vytorin) or simvastatin (Zocor) at 40 mg/day. At a median of 6 years of follow-up, the primary composite cardiovascular outcome was significantly reduced by 6% in the dual-therapy group compared with statin monotherapy, with a number-needed-to-treat (NNT) of 50, as previously reported (N Engl J Med. 2015 Jun 18;372[25]:2387-97).
The impetus for the prespecified stroke analysis was that up until IMPROVE-IT, no LDL cholesterol–lowering therapy other than statins had ever been shown to protect against stroke. The Cholesterol Trialists’ Collaboration meta-analysis, involving roughly 173,000 subjects, previously showed that statin therapy reduces ischemic stroke risk by 20% per 1 mmol/L of LDL lowering (Lancet. 2012 Aug 11;380[9841]:581-90). The question was, could add-on ezetimibe decrease stroke risk even further?
Stroke occurred in 641 patients during follow-up. As adjudicated by independent neurologists, 82% of the strokes were nonhemorrhagic, 16% were hemorrhagic, and 2% were unknown. The 14% relative risk reduction in overall stroke with simvastatin/ezetimibe compared with simvastatin, with rates of 4.2% versus 4.8%, just missed achieving statistical significance (P = .052). A significant 21% reduction in nonhemorrhagic strokes was seen with dual therapy, where the incidence during follow-up was 3.4%, compared with 4.1% with simvastatin alone, but this effect was dampened by a numeric albeit statistically nonsignificant absolute 0.2% increase in hemorrhagic strokes in the simvastatin/ezetimibe group.
Far more impressive was the stroke-prevention benefit of simvastatin/ezetimibe among the 1,071 subjects with prior stroke or TIA at baseline. Their nonhemorrhagic stroke rate during follow-up was 10.2% with simvastatin/ezetimibe versus 18.8% with simvastatin alone, for a 40% relative risk reduction favoring dual lipid-lowering therapy and an NNT of about 20. Again, there was no significant difference in hemorrhagic stroke between the two treatment arms, noted Dr. Wiviott of Brigham and Womens Hospital, Boston.
The stroke-prevention benefit achieved by adding ezetimibe to simvastatin was seen regardless of patient age, gender, renal function, baseline LDL cholesterol level, or other prespecified subcategories.
IMPROVE-IT was sponsored by Merck. Dr. Wiviott reported receiving research grants from Merck, AstraZeneca, and Eisai and serving as a consultant to nine pharmaceutical companies.
ORLANDO – The combination of ezetimibe/simvastatin significantly reduced the risk of nonhemorrhagic stroke compared with simvastatin alone, with a particularly striking benefit seen in patients with prior history of stroke, in a new analysis from the landmark IMPROVE-IT trial.
“We believe these data support the use of intensive lipid lowering therapy, which includes ezetimibe to prevent ischemic stroke,” Dr. Stephen D. Wiviott said in reporting the findings at the American Heart Association scientific sessions.
He presented a prespecified secondary analysis from IMPROVE-IT, a double-blind study in which 18,144 patients on background optimal medical management were randomized post–acute coronary syndrome to simvastatin/ezetimibe at 40/10 mg/day (Vytorin) or simvastatin (Zocor) at 40 mg/day. At a median of 6 years of follow-up, the primary composite cardiovascular outcome was significantly reduced by 6% in the dual-therapy group compared with statin monotherapy, with a number-needed-to-treat (NNT) of 50, as previously reported (N Engl J Med. 2015 Jun 18;372[25]:2387-97).
The impetus for the prespecified stroke analysis was that up until IMPROVE-IT, no LDL cholesterol–lowering therapy other than statins had ever been shown to protect against stroke. The Cholesterol Trialists’ Collaboration meta-analysis, involving roughly 173,000 subjects, previously showed that statin therapy reduces ischemic stroke risk by 20% per 1 mmol/L of LDL lowering (Lancet. 2012 Aug 11;380[9841]:581-90). The question was, could add-on ezetimibe decrease stroke risk even further?
Stroke occurred in 641 patients during follow-up. As adjudicated by independent neurologists, 82% of the strokes were nonhemorrhagic, 16% were hemorrhagic, and 2% were unknown. The 14% relative risk reduction in overall stroke with simvastatin/ezetimibe compared with simvastatin, with rates of 4.2% versus 4.8%, just missed achieving statistical significance (P = .052). A significant 21% reduction in nonhemorrhagic strokes was seen with dual therapy, where the incidence during follow-up was 3.4%, compared with 4.1% with simvastatin alone, but this effect was dampened by a numeric albeit statistically nonsignificant absolute 0.2% increase in hemorrhagic strokes in the simvastatin/ezetimibe group.
Far more impressive was the stroke-prevention benefit of simvastatin/ezetimibe among the 1,071 subjects with prior stroke or TIA at baseline. Their nonhemorrhagic stroke rate during follow-up was 10.2% with simvastatin/ezetimibe versus 18.8% with simvastatin alone, for a 40% relative risk reduction favoring dual lipid-lowering therapy and an NNT of about 20. Again, there was no significant difference in hemorrhagic stroke between the two treatment arms, noted Dr. Wiviott of Brigham and Womens Hospital, Boston.
The stroke-prevention benefit achieved by adding ezetimibe to simvastatin was seen regardless of patient age, gender, renal function, baseline LDL cholesterol level, or other prespecified subcategories.
IMPROVE-IT was sponsored by Merck. Dr. Wiviott reported receiving research grants from Merck, AstraZeneca, and Eisai and serving as a consultant to nine pharmaceutical companies.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Intensive lipid-lowering therapy that incorporates ezetimibe provides enhanced protection against ischemic stroke.
Major finding: In patients with a baseline history of stroke who were on simvastatin/ezetimibe after an acute coronary syndrome, the risk of nonhemorrhagic stroke during 6 years of follow-up was reduced by 40%, compared with lipid-lowering via simvastatin alone.
Data source: A prespecified secondary analysis of stroke incidence during a median 6 years of follow-up in the double-blind, randomized, 18,144-patient IMPROVE-IT trial.
Disclosures: Merck sponsored the study. The presenter reported receiving a research grant from Merck and serving as a consultant to numerous pharmaceutical companies.
AHA: COPD Doubles Sudden Cardiac Death Risk in Hypertensives
ORLANDO – A second, confirmatory major study has shown that chronic obstructive pulmonary disease independently increases the risk of sudden cardiac death severalfold.
COPD was associated with a roughly twofold increased risk of sudden cardiac death (SCD) in hypertensive patients with COPD, compared with those without the pulmonary disease, in the Scandinavian Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) trial, Dr. Peter M. Okin reported at the American Heart Association scientific sessions.
Moreover, aggressive blood pressure lowering in the hypertensive COPD patients didn’t negate this risk, added Dr. Okin of Cornell University in New York.
The impetus for his secondary analysis of LIFE data was an earlier report from the landmark, population-based Rotterdam Heart Study. Among 1,615 participants with COPD, the age- and sex-adjusted risk of SCD was 1.34-fold greater than in nearly 12,000 controls. This increased SCD risk climbed to 2.12-fold during the first 2,000 days following diagnosis of COPD and reached 3.58-fold among those with frequent COPD exacerbations during this period (Eur Heart J. 2015 Jul 14;36[27]:1754-61).
Dr. Okin’s secondary analysis of LIFE data included 9,193 hypertensive subjects with ECG evidence of left ventricular hypertrophy who were randomized to lisinopril- or atenolol-based blood pressure lowering to a target of 140/90 mm Hg or less. A history of COPD was present in 385 patients (4.2%) at enrollment.
During a mean 4.8 years of prospective follow-up, 178 patients experienced SCD, a prespecified secondary endpoint in the LIFE trial. The incidence rate was 9 cases per 1,000 patient-years in those with COPD and 3.8 per 1,000 person-years in those without the pulmonary disease.
In a univariate analysis, a history of COPD was associated with a 2.36-fold increased risk of SCD during follow-up. In a multivariate analysis extensively adjusted for potential confounders – treatment arm, age, race, gender, history of atrial fibrillation, baseline serum creatinine and serum glucose, stroke or TIA, as well as on-treatment blood pressure, heart rate, QRS duration, HDL cholesterol level, use of a statin or hydrochlorothiazide, and incident MI or heart failure – COPD remained associated with a 1.82-fold increased risk of SCD, the cardiologist reported.
“These results suggest the need for additional studies to assess whether there are targeted therapies that can reduce the risk of SCD in patients with COPD,” he concluded.
As previously reported, the main finding in LIFE was that losartan conferred benefits beyond blood pressure control (Lancet. 2002 Mar 23;359[9311]:995-1003).
Dr. Okin reported serving as a consultant to Novartis.
ORLANDO – A second, confirmatory major study has shown that chronic obstructive pulmonary disease independently increases the risk of sudden cardiac death severalfold.
COPD was associated with a roughly twofold increased risk of sudden cardiac death (SCD) in hypertensive patients with COPD, compared with those without the pulmonary disease, in the Scandinavian Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) trial, Dr. Peter M. Okin reported at the American Heart Association scientific sessions.
Moreover, aggressive blood pressure lowering in the hypertensive COPD patients didn’t negate this risk, added Dr. Okin of Cornell University in New York.
The impetus for his secondary analysis of LIFE data was an earlier report from the landmark, population-based Rotterdam Heart Study. Among 1,615 participants with COPD, the age- and sex-adjusted risk of SCD was 1.34-fold greater than in nearly 12,000 controls. This increased SCD risk climbed to 2.12-fold during the first 2,000 days following diagnosis of COPD and reached 3.58-fold among those with frequent COPD exacerbations during this period (Eur Heart J. 2015 Jul 14;36[27]:1754-61).
Dr. Okin’s secondary analysis of LIFE data included 9,193 hypertensive subjects with ECG evidence of left ventricular hypertrophy who were randomized to lisinopril- or atenolol-based blood pressure lowering to a target of 140/90 mm Hg or less. A history of COPD was present in 385 patients (4.2%) at enrollment.
During a mean 4.8 years of prospective follow-up, 178 patients experienced SCD, a prespecified secondary endpoint in the LIFE trial. The incidence rate was 9 cases per 1,000 patient-years in those with COPD and 3.8 per 1,000 person-years in those without the pulmonary disease.
In a univariate analysis, a history of COPD was associated with a 2.36-fold increased risk of SCD during follow-up. In a multivariate analysis extensively adjusted for potential confounders – treatment arm, age, race, gender, history of atrial fibrillation, baseline serum creatinine and serum glucose, stroke or TIA, as well as on-treatment blood pressure, heart rate, QRS duration, HDL cholesterol level, use of a statin or hydrochlorothiazide, and incident MI or heart failure – COPD remained associated with a 1.82-fold increased risk of SCD, the cardiologist reported.
“These results suggest the need for additional studies to assess whether there are targeted therapies that can reduce the risk of SCD in patients with COPD,” he concluded.
As previously reported, the main finding in LIFE was that losartan conferred benefits beyond blood pressure control (Lancet. 2002 Mar 23;359[9311]:995-1003).
Dr. Okin reported serving as a consultant to Novartis.
ORLANDO – A second, confirmatory major study has shown that chronic obstructive pulmonary disease independently increases the risk of sudden cardiac death severalfold.
COPD was associated with a roughly twofold increased risk of sudden cardiac death (SCD) in hypertensive patients with COPD, compared with those without the pulmonary disease, in the Scandinavian Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) trial, Dr. Peter M. Okin reported at the American Heart Association scientific sessions.
Moreover, aggressive blood pressure lowering in the hypertensive COPD patients didn’t negate this risk, added Dr. Okin of Cornell University in New York.
The impetus for his secondary analysis of LIFE data was an earlier report from the landmark, population-based Rotterdam Heart Study. Among 1,615 participants with COPD, the age- and sex-adjusted risk of SCD was 1.34-fold greater than in nearly 12,000 controls. This increased SCD risk climbed to 2.12-fold during the first 2,000 days following diagnosis of COPD and reached 3.58-fold among those with frequent COPD exacerbations during this period (Eur Heart J. 2015 Jul 14;36[27]:1754-61).
Dr. Okin’s secondary analysis of LIFE data included 9,193 hypertensive subjects with ECG evidence of left ventricular hypertrophy who were randomized to lisinopril- or atenolol-based blood pressure lowering to a target of 140/90 mm Hg or less. A history of COPD was present in 385 patients (4.2%) at enrollment.
During a mean 4.8 years of prospective follow-up, 178 patients experienced SCD, a prespecified secondary endpoint in the LIFE trial. The incidence rate was 9 cases per 1,000 patient-years in those with COPD and 3.8 per 1,000 person-years in those without the pulmonary disease.
In a univariate analysis, a history of COPD was associated with a 2.36-fold increased risk of SCD during follow-up. In a multivariate analysis extensively adjusted for potential confounders – treatment arm, age, race, gender, history of atrial fibrillation, baseline serum creatinine and serum glucose, stroke or TIA, as well as on-treatment blood pressure, heart rate, QRS duration, HDL cholesterol level, use of a statin or hydrochlorothiazide, and incident MI or heart failure – COPD remained associated with a 1.82-fold increased risk of SCD, the cardiologist reported.
“These results suggest the need for additional studies to assess whether there are targeted therapies that can reduce the risk of SCD in patients with COPD,” he concluded.
As previously reported, the main finding in LIFE was that losartan conferred benefits beyond blood pressure control (Lancet. 2002 Mar 23;359[9311]:995-1003).
Dr. Okin reported serving as a consultant to Novartis.
AT THE AHA SCIENTIFIC SESSIONS
AHA: COPD doubles sudden cardiac death risk in hypertensives
ORLANDO – A second, confirmatory major study has shown that chronic obstructive pulmonary disease independently increases the risk of sudden cardiac death severalfold.
COPD was associated with a roughly twofold increased risk of sudden cardiac death (SCD) in hypertensive patients with COPD, compared with those without the pulmonary disease, in the Scandinavian Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) trial, Dr. Peter M. Okin reported at the American Heart Association scientific sessions.
Moreover, aggressive blood pressure lowering in the hypertensive COPD patients didn’t negate this risk, added Dr. Okin of Cornell University in New York.
The impetus for his secondary analysis of LIFE data was an earlier report from the landmark, population-based Rotterdam Heart Study. Among 1,615 participants with COPD, the age- and sex-adjusted risk of SCD was 1.34-fold greater than in nearly 12,000 controls. This increased SCD risk climbed to 2.12-fold during the first 2,000 days following diagnosis of COPD and reached 3.58-fold among those with frequent COPD exacerbations during this period (Eur Heart J. 2015 Jul 14;36[27]:1754-61).
Dr. Okin’s secondary analysis of LIFE data included 9,193 hypertensive subjects with ECG evidence of left ventricular hypertrophy who were randomized to lisinopril- or atenolol-based blood pressure lowering to a target of 140/90 mm Hg or less. A history of COPD was present in 385 patients (4.2%) at enrollment.
During a mean 4.8 years of prospective follow-up, 178 patients experienced SCD, a prespecified secondary endpoint in the LIFE trial. The incidence rate was 9 cases per 1,000 patient-years in those with COPD and 3.8 per 1,000 person-years in those without the pulmonary disease.
In a univariate analysis, a history of COPD was associated with a 2.36-fold increased risk of SCD during follow-up. In a multivariate analysis extensively adjusted for potential confounders – treatment arm, age, race, gender, history of atrial fibrillation, baseline serum creatinine and serum glucose, stroke or TIA, as well as on-treatment blood pressure, heart rate, QRS duration, HDL cholesterol level, use of a statin or hydrochlorothiazide, and incident MI or heart failure – COPD remained associated with a 1.82-fold increased risk of SCD, the cardiologist reported.
“These results suggest the need for additional studies to assess whether there are targeted therapies that can reduce the risk of SCD in patients with COPD,” he concluded.
As previously reported, the main finding in LIFE was that losartan conferred benefits beyond blood pressure control (Lancet. 2002 Mar 23;359[9311]:995-1003).
Dr. Okin reported serving as a consultant to Novartis.
ORLANDO – A second, confirmatory major study has shown that chronic obstructive pulmonary disease independently increases the risk of sudden cardiac death severalfold.
COPD was associated with a roughly twofold increased risk of sudden cardiac death (SCD) in hypertensive patients with COPD, compared with those without the pulmonary disease, in the Scandinavian Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) trial, Dr. Peter M. Okin reported at the American Heart Association scientific sessions.
Moreover, aggressive blood pressure lowering in the hypertensive COPD patients didn’t negate this risk, added Dr. Okin of Cornell University in New York.
The impetus for his secondary analysis of LIFE data was an earlier report from the landmark, population-based Rotterdam Heart Study. Among 1,615 participants with COPD, the age- and sex-adjusted risk of SCD was 1.34-fold greater than in nearly 12,000 controls. This increased SCD risk climbed to 2.12-fold during the first 2,000 days following diagnosis of COPD and reached 3.58-fold among those with frequent COPD exacerbations during this period (Eur Heart J. 2015 Jul 14;36[27]:1754-61).
Dr. Okin’s secondary analysis of LIFE data included 9,193 hypertensive subjects with ECG evidence of left ventricular hypertrophy who were randomized to lisinopril- or atenolol-based blood pressure lowering to a target of 140/90 mm Hg or less. A history of COPD was present in 385 patients (4.2%) at enrollment.
During a mean 4.8 years of prospective follow-up, 178 patients experienced SCD, a prespecified secondary endpoint in the LIFE trial. The incidence rate was 9 cases per 1,000 patient-years in those with COPD and 3.8 per 1,000 person-years in those without the pulmonary disease.
In a univariate analysis, a history of COPD was associated with a 2.36-fold increased risk of SCD during follow-up. In a multivariate analysis extensively adjusted for potential confounders – treatment arm, age, race, gender, history of atrial fibrillation, baseline serum creatinine and serum glucose, stroke or TIA, as well as on-treatment blood pressure, heart rate, QRS duration, HDL cholesterol level, use of a statin or hydrochlorothiazide, and incident MI or heart failure – COPD remained associated with a 1.82-fold increased risk of SCD, the cardiologist reported.
“These results suggest the need for additional studies to assess whether there are targeted therapies that can reduce the risk of SCD in patients with COPD,” he concluded.
As previously reported, the main finding in LIFE was that losartan conferred benefits beyond blood pressure control (Lancet. 2002 Mar 23;359[9311]:995-1003).
Dr. Okin reported serving as a consultant to Novartis.
ORLANDO – A second, confirmatory major study has shown that chronic obstructive pulmonary disease independently increases the risk of sudden cardiac death severalfold.
COPD was associated with a roughly twofold increased risk of sudden cardiac death (SCD) in hypertensive patients with COPD, compared with those without the pulmonary disease, in the Scandinavian Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) trial, Dr. Peter M. Okin reported at the American Heart Association scientific sessions.
Moreover, aggressive blood pressure lowering in the hypertensive COPD patients didn’t negate this risk, added Dr. Okin of Cornell University in New York.
The impetus for his secondary analysis of LIFE data was an earlier report from the landmark, population-based Rotterdam Heart Study. Among 1,615 participants with COPD, the age- and sex-adjusted risk of SCD was 1.34-fold greater than in nearly 12,000 controls. This increased SCD risk climbed to 2.12-fold during the first 2,000 days following diagnosis of COPD and reached 3.58-fold among those with frequent COPD exacerbations during this period (Eur Heart J. 2015 Jul 14;36[27]:1754-61).
Dr. Okin’s secondary analysis of LIFE data included 9,193 hypertensive subjects with ECG evidence of left ventricular hypertrophy who were randomized to lisinopril- or atenolol-based blood pressure lowering to a target of 140/90 mm Hg or less. A history of COPD was present in 385 patients (4.2%) at enrollment.
During a mean 4.8 years of prospective follow-up, 178 patients experienced SCD, a prespecified secondary endpoint in the LIFE trial. The incidence rate was 9 cases per 1,000 patient-years in those with COPD and 3.8 per 1,000 person-years in those without the pulmonary disease.
In a univariate analysis, a history of COPD was associated with a 2.36-fold increased risk of SCD during follow-up. In a multivariate analysis extensively adjusted for potential confounders – treatment arm, age, race, gender, history of atrial fibrillation, baseline serum creatinine and serum glucose, stroke or TIA, as well as on-treatment blood pressure, heart rate, QRS duration, HDL cholesterol level, use of a statin or hydrochlorothiazide, and incident MI or heart failure – COPD remained associated with a 1.82-fold increased risk of SCD, the cardiologist reported.
“These results suggest the need for additional studies to assess whether there are targeted therapies that can reduce the risk of SCD in patients with COPD,” he concluded.
As previously reported, the main finding in LIFE was that losartan conferred benefits beyond blood pressure control (Lancet. 2002 Mar 23;359[9311]:995-1003).
Dr. Okin reported serving as a consultant to Novartis.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Two large studies link chronic obstructive pulmonary disease with increased risk of sudden cardiac death.
Major finding: Patients with COPD and hypertension had nearly a twofold increased risk of sudden cardiac death, compared with hypertensives without the pulmonary disease.
Data source: This was a secondary analysis comparing sudden cardiac death rates in 385 hypertensive patients with and nearly 12,000 without COPD, all participants in the LIFE trial.
Disclosures: The presenter reported serving as a consultant to Novartis.