User login
ID Practitioner is an independent news source that provides infectious disease specialists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the infectious disease specialist’s practice. Specialty focus topics include antimicrobial resistance, emerging infections, global ID, hepatitis, HIV, hospital-acquired infections, immunizations and vaccines, influenza, mycoses, pediatric infections, and STIs. Infectious Diseases News is owned by Frontline Medical Communications.
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
section[contains(@class, 'footer-nav-section-wrapper')]
div[contains(@class, 'pane-pub-article-idp')]
div[contains(@class, 'pane-medstat-latest-articles-articles-section')]
div[contains(@class, 'pane-pub-home-idp')]
div[contains(@class, 'pane-pub-topic-idp')]
HIV does not appear to worsen COVID-19 outcomes
People living with HIV who are admitted to the hospital with COVID-19 are no more likely to die than those without HIV, an analysis conducted in New York City shows. This is despite the fact that comorbidities associated with worse COVID-19 outcomes were more common in the HIV group.
“We don’t see any signs that people with HIV should take extra precautions” to protect themselves from COVID-19, said Keith Sigel, MD, associate professor of medicine and infectious diseases at the Icahn School of Medicine at Mount Sinai, New York, and the lead researcher on the study, published online June 28 in Clinical Infectious Diseases.
“We still don’t have a great explanation for why we’re seeing what we’re seeing,” he added. “But we’re glad we’re seeing it.”
The findings have changed how Dr. Sigel talks to his patients with HIV about protecting themselves from COVID-19. Some patients have so curtailed their behavior for fear of acquiring COVID-19 that they aren’t buying groceries or attending needed medical appointments. With these data, Dr. Sigel said he’s comfortable telling his patients, “COVID-19 is bad all by itself, but you don’t need to go crazy. Wear a mask, practice appropriate social distancing and hygiene, but your risk doesn’t appear to be greater.”
The findings conform with those on the lack of association between HIV and COVID-19 severity seen in a cohort study from Spain, a case study from China, and case series from New Jersey, New York City, and Spain.
One of the only regions reporting something different so far is South Africa. There, HIV is the third most common comorbidity associated with death from COVID-19, according to a cohort analysis conducted in the province of Western Cape.
Along with data from HIV prevention and treatment trials, the conference will feature updates on where the world stands in the control of HIV during the COVID-19 pandemic. And for an even more focused look, the IAS COVID-19 Conference will immediately follow that meeting.
The New York City cohort
For their study, Dr. Sigel and colleagues examined the 4402 COVID-19 cases at the Mount Sinai Health System’s five hospitals between March 12 and April 23.
They found 88 people with COVID-19 whose charts showed codes indicating they were living with HIV. All 88 were receiving treatment, and 81% of them had undetectable viral loads documented at COVID admission or in the 12 months prior to admission.
The median age was 61 years, and 40% of the cohort was black and 30% was Hispanic.
Patients in the comparison group – 405 people without HIV from the Veterans Aging Cohort Study who had been admitted to the hospital for COVID-19 – were matched in terms of age, race, and stage of COVID-19.
The study had an 80% power to detect a 15% increase in the absolute risk for death in people with COVID-19, with or without HIV.
Patients with HIV were almost three times as likely to have smoked and were more likely to have chronic obstructive pulmonary disease, cirrhosis, and a history of cancer.
“This was a group of patients that one might suspect would do worse,” Dr. Sigel said. And yet, “we didn’t see any difference in deaths. We didn’t see any difference in respiratory failure.”
In fact, people with HIV required mechanical ventilation less often than those without HIV (18% vs. 23%). And when it came to mortality, one in five people died from COVID-19 during follow-up whether they had HIV or not (21% vs. 20%).
The only factor associated with significantly worse outcomes was a history of organ transplantation, “suggesting that non-HIV causes of immunodeficiency may be more prominent risks for severe outcomes,” Dr. Sigel and colleagues explained.
A surprise association
What’s more, the researchers found a slight association between the use of nucleoside reverse-transcriptase inhibitors (NRTI) by people with HIV and better outcomes in COVID-19. That echoes findings published June 26 in Annals of Internal Medicine, which showed that people with HIV taking the combination of tenofovir disoproxil fumarate plus emtricitabine (Truvada, Gilead Sciences) were less likely to be diagnosed with COVID-19, less likely to be hospitalized, and less likely to die.
This has led some to wonder whether NRTIs have some effect on SARS-CoV-2, the virus that causes COVID-19. Dr. Sigel said he wonders that too, but right now, it’s just musings.
“These studies are not even remotely designed” to show that NRTIs are protective against COVID-19, he explained. “Ours was extremely underpowered to detect that and there was a high potential for confounding.”
“I’d be wary of any study in a subpopulation – which is what we’re dealing with here – that is looking for signals of protection with certain medications,” he added.
A “modest” increase
Using the South African data, released on June 22, public health officials estimate that people with HIV are 2.75 times more likely to die from COVID-19 than those without HIV, making it the third most common comorbidity in people who died from COVID-19, behind diabetes and hypertension. This held true regardless of whether the people with HIV were on treatment.
But when they looked at COVID-19 deaths in the sickest of the sick – those hospitalized with COVID-19 symptoms – HIV was associated with just a 28% increase in the risk for death. The South African researchers called this risk “modest.”
“While these findings may overestimate the effect of HIV on COVID-19 death due to the presence of residual confounding, people living with HIV should be considered a high-risk group for COVID-19 management, with modestly elevated risk of poor outcomes, irrespective of viral suppression,” they wrote.
Epidemiologist Gregorio Millett, MPH, has been tracking the effect of HIV on COVID-19 outcomes since the start of the pandemic in his role as vice president and head of policy at the American Foundation for AIDS Research (amFAR).
Back in April, he and his colleagues looked at rates of COVID-19 deaths and hospitalizations in counties with disproportionate levels of black residents. These areas often overlapped with the communities selected for the Ending the HIV Epidemic plan to control HIV by 2030. What they found was that there was more HIV and COVID-19 in those communities.
What they didn’t find was that people with HIV in those communities had worse outcomes with COVID-19. This remained true even when they reran the analysis after the number of cases of COVID-19 in the United States surpassed 100,000. Those data have yet to be published, Mr. Millett reported.
“HIV does not pop out,” he said. “It’s still social determinants of health. It’s still underlying conditions. It’s still age as a primary factor.”
“People living with HIV are mainly dying of underlying conditions – so all the things associated with COVID-19 – rather than the association being with HIV itself,” he added.
Although he’s not ruling out the possibility that an association like the one in South Africa could emerge, Mr. Millett, who will present a plenary on the context of the HIV epidemic at the IAS conference, said he suspects we won’t see one.
“If we didn’t see an association with the counties that are disproportionately African American, in the black belt where we see high rates of HIV, particularly where we see the social determinants of health that definitely make a difference – if we’re not seeing that association there, where we have a high proportion of African Americans who are at risk both for HIV and COVID-19 – I just don’t think it’s going to emerge,” he said.
This article first appeared on Medscape.com.
People living with HIV who are admitted to the hospital with COVID-19 are no more likely to die than those without HIV, an analysis conducted in New York City shows. This is despite the fact that comorbidities associated with worse COVID-19 outcomes were more common in the HIV group.
“We don’t see any signs that people with HIV should take extra precautions” to protect themselves from COVID-19, said Keith Sigel, MD, associate professor of medicine and infectious diseases at the Icahn School of Medicine at Mount Sinai, New York, and the lead researcher on the study, published online June 28 in Clinical Infectious Diseases.
“We still don’t have a great explanation for why we’re seeing what we’re seeing,” he added. “But we’re glad we’re seeing it.”
The findings have changed how Dr. Sigel talks to his patients with HIV about protecting themselves from COVID-19. Some patients have so curtailed their behavior for fear of acquiring COVID-19 that they aren’t buying groceries or attending needed medical appointments. With these data, Dr. Sigel said he’s comfortable telling his patients, “COVID-19 is bad all by itself, but you don’t need to go crazy. Wear a mask, practice appropriate social distancing and hygiene, but your risk doesn’t appear to be greater.”
The findings conform with those on the lack of association between HIV and COVID-19 severity seen in a cohort study from Spain, a case study from China, and case series from New Jersey, New York City, and Spain.
One of the only regions reporting something different so far is South Africa. There, HIV is the third most common comorbidity associated with death from COVID-19, according to a cohort analysis conducted in the province of Western Cape.
Along with data from HIV prevention and treatment trials, the conference will feature updates on where the world stands in the control of HIV during the COVID-19 pandemic. And for an even more focused look, the IAS COVID-19 Conference will immediately follow that meeting.
The New York City cohort
For their study, Dr. Sigel and colleagues examined the 4402 COVID-19 cases at the Mount Sinai Health System’s five hospitals between March 12 and April 23.
They found 88 people with COVID-19 whose charts showed codes indicating they were living with HIV. All 88 were receiving treatment, and 81% of them had undetectable viral loads documented at COVID admission or in the 12 months prior to admission.
The median age was 61 years, and 40% of the cohort was black and 30% was Hispanic.
Patients in the comparison group – 405 people without HIV from the Veterans Aging Cohort Study who had been admitted to the hospital for COVID-19 – were matched in terms of age, race, and stage of COVID-19.
The study had an 80% power to detect a 15% increase in the absolute risk for death in people with COVID-19, with or without HIV.
Patients with HIV were almost three times as likely to have smoked and were more likely to have chronic obstructive pulmonary disease, cirrhosis, and a history of cancer.
“This was a group of patients that one might suspect would do worse,” Dr. Sigel said. And yet, “we didn’t see any difference in deaths. We didn’t see any difference in respiratory failure.”
In fact, people with HIV required mechanical ventilation less often than those without HIV (18% vs. 23%). And when it came to mortality, one in five people died from COVID-19 during follow-up whether they had HIV or not (21% vs. 20%).
The only factor associated with significantly worse outcomes was a history of organ transplantation, “suggesting that non-HIV causes of immunodeficiency may be more prominent risks for severe outcomes,” Dr. Sigel and colleagues explained.
A surprise association
What’s more, the researchers found a slight association between the use of nucleoside reverse-transcriptase inhibitors (NRTI) by people with HIV and better outcomes in COVID-19. That echoes findings published June 26 in Annals of Internal Medicine, which showed that people with HIV taking the combination of tenofovir disoproxil fumarate plus emtricitabine (Truvada, Gilead Sciences) were less likely to be diagnosed with COVID-19, less likely to be hospitalized, and less likely to die.
This has led some to wonder whether NRTIs have some effect on SARS-CoV-2, the virus that causes COVID-19. Dr. Sigel said he wonders that too, but right now, it’s just musings.
“These studies are not even remotely designed” to show that NRTIs are protective against COVID-19, he explained. “Ours was extremely underpowered to detect that and there was a high potential for confounding.”
“I’d be wary of any study in a subpopulation – which is what we’re dealing with here – that is looking for signals of protection with certain medications,” he added.
A “modest” increase
Using the South African data, released on June 22, public health officials estimate that people with HIV are 2.75 times more likely to die from COVID-19 than those without HIV, making it the third most common comorbidity in people who died from COVID-19, behind diabetes and hypertension. This held true regardless of whether the people with HIV were on treatment.
But when they looked at COVID-19 deaths in the sickest of the sick – those hospitalized with COVID-19 symptoms – HIV was associated with just a 28% increase in the risk for death. The South African researchers called this risk “modest.”
“While these findings may overestimate the effect of HIV on COVID-19 death due to the presence of residual confounding, people living with HIV should be considered a high-risk group for COVID-19 management, with modestly elevated risk of poor outcomes, irrespective of viral suppression,” they wrote.
Epidemiologist Gregorio Millett, MPH, has been tracking the effect of HIV on COVID-19 outcomes since the start of the pandemic in his role as vice president and head of policy at the American Foundation for AIDS Research (amFAR).
Back in April, he and his colleagues looked at rates of COVID-19 deaths and hospitalizations in counties with disproportionate levels of black residents. These areas often overlapped with the communities selected for the Ending the HIV Epidemic plan to control HIV by 2030. What they found was that there was more HIV and COVID-19 in those communities.
What they didn’t find was that people with HIV in those communities had worse outcomes with COVID-19. This remained true even when they reran the analysis after the number of cases of COVID-19 in the United States surpassed 100,000. Those data have yet to be published, Mr. Millett reported.
“HIV does not pop out,” he said. “It’s still social determinants of health. It’s still underlying conditions. It’s still age as a primary factor.”
“People living with HIV are mainly dying of underlying conditions – so all the things associated with COVID-19 – rather than the association being with HIV itself,” he added.
Although he’s not ruling out the possibility that an association like the one in South Africa could emerge, Mr. Millett, who will present a plenary on the context of the HIV epidemic at the IAS conference, said he suspects we won’t see one.
“If we didn’t see an association with the counties that are disproportionately African American, in the black belt where we see high rates of HIV, particularly where we see the social determinants of health that definitely make a difference – if we’re not seeing that association there, where we have a high proportion of African Americans who are at risk both for HIV and COVID-19 – I just don’t think it’s going to emerge,” he said.
This article first appeared on Medscape.com.
People living with HIV who are admitted to the hospital with COVID-19 are no more likely to die than those without HIV, an analysis conducted in New York City shows. This is despite the fact that comorbidities associated with worse COVID-19 outcomes were more common in the HIV group.
“We don’t see any signs that people with HIV should take extra precautions” to protect themselves from COVID-19, said Keith Sigel, MD, associate professor of medicine and infectious diseases at the Icahn School of Medicine at Mount Sinai, New York, and the lead researcher on the study, published online June 28 in Clinical Infectious Diseases.
“We still don’t have a great explanation for why we’re seeing what we’re seeing,” he added. “But we’re glad we’re seeing it.”
The findings have changed how Dr. Sigel talks to his patients with HIV about protecting themselves from COVID-19. Some patients have so curtailed their behavior for fear of acquiring COVID-19 that they aren’t buying groceries or attending needed medical appointments. With these data, Dr. Sigel said he’s comfortable telling his patients, “COVID-19 is bad all by itself, but you don’t need to go crazy. Wear a mask, practice appropriate social distancing and hygiene, but your risk doesn’t appear to be greater.”
The findings conform with those on the lack of association between HIV and COVID-19 severity seen in a cohort study from Spain, a case study from China, and case series from New Jersey, New York City, and Spain.
One of the only regions reporting something different so far is South Africa. There, HIV is the third most common comorbidity associated with death from COVID-19, according to a cohort analysis conducted in the province of Western Cape.
Along with data from HIV prevention and treatment trials, the conference will feature updates on where the world stands in the control of HIV during the COVID-19 pandemic. And for an even more focused look, the IAS COVID-19 Conference will immediately follow that meeting.
The New York City cohort
For their study, Dr. Sigel and colleagues examined the 4402 COVID-19 cases at the Mount Sinai Health System’s five hospitals between March 12 and April 23.
They found 88 people with COVID-19 whose charts showed codes indicating they were living with HIV. All 88 were receiving treatment, and 81% of them had undetectable viral loads documented at COVID admission or in the 12 months prior to admission.
The median age was 61 years, and 40% of the cohort was black and 30% was Hispanic.
Patients in the comparison group – 405 people without HIV from the Veterans Aging Cohort Study who had been admitted to the hospital for COVID-19 – were matched in terms of age, race, and stage of COVID-19.
The study had an 80% power to detect a 15% increase in the absolute risk for death in people with COVID-19, with or without HIV.
Patients with HIV were almost three times as likely to have smoked and were more likely to have chronic obstructive pulmonary disease, cirrhosis, and a history of cancer.
“This was a group of patients that one might suspect would do worse,” Dr. Sigel said. And yet, “we didn’t see any difference in deaths. We didn’t see any difference in respiratory failure.”
In fact, people with HIV required mechanical ventilation less often than those without HIV (18% vs. 23%). And when it came to mortality, one in five people died from COVID-19 during follow-up whether they had HIV or not (21% vs. 20%).
The only factor associated with significantly worse outcomes was a history of organ transplantation, “suggesting that non-HIV causes of immunodeficiency may be more prominent risks for severe outcomes,” Dr. Sigel and colleagues explained.
A surprise association
What’s more, the researchers found a slight association between the use of nucleoside reverse-transcriptase inhibitors (NRTI) by people with HIV and better outcomes in COVID-19. That echoes findings published June 26 in Annals of Internal Medicine, which showed that people with HIV taking the combination of tenofovir disoproxil fumarate plus emtricitabine (Truvada, Gilead Sciences) were less likely to be diagnosed with COVID-19, less likely to be hospitalized, and less likely to die.
This has led some to wonder whether NRTIs have some effect on SARS-CoV-2, the virus that causes COVID-19. Dr. Sigel said he wonders that too, but right now, it’s just musings.
“These studies are not even remotely designed” to show that NRTIs are protective against COVID-19, he explained. “Ours was extremely underpowered to detect that and there was a high potential for confounding.”
“I’d be wary of any study in a subpopulation – which is what we’re dealing with here – that is looking for signals of protection with certain medications,” he added.
A “modest” increase
Using the South African data, released on June 22, public health officials estimate that people with HIV are 2.75 times more likely to die from COVID-19 than those without HIV, making it the third most common comorbidity in people who died from COVID-19, behind diabetes and hypertension. This held true regardless of whether the people with HIV were on treatment.
But when they looked at COVID-19 deaths in the sickest of the sick – those hospitalized with COVID-19 symptoms – HIV was associated with just a 28% increase in the risk for death. The South African researchers called this risk “modest.”
“While these findings may overestimate the effect of HIV on COVID-19 death due to the presence of residual confounding, people living with HIV should be considered a high-risk group for COVID-19 management, with modestly elevated risk of poor outcomes, irrespective of viral suppression,” they wrote.
Epidemiologist Gregorio Millett, MPH, has been tracking the effect of HIV on COVID-19 outcomes since the start of the pandemic in his role as vice president and head of policy at the American Foundation for AIDS Research (amFAR).
Back in April, he and his colleagues looked at rates of COVID-19 deaths and hospitalizations in counties with disproportionate levels of black residents. These areas often overlapped with the communities selected for the Ending the HIV Epidemic plan to control HIV by 2030. What they found was that there was more HIV and COVID-19 in those communities.
What they didn’t find was that people with HIV in those communities had worse outcomes with COVID-19. This remained true even when they reran the analysis after the number of cases of COVID-19 in the United States surpassed 100,000. Those data have yet to be published, Mr. Millett reported.
“HIV does not pop out,” he said. “It’s still social determinants of health. It’s still underlying conditions. It’s still age as a primary factor.”
“People living with HIV are mainly dying of underlying conditions – so all the things associated with COVID-19 – rather than the association being with HIV itself,” he added.
Although he’s not ruling out the possibility that an association like the one in South Africa could emerge, Mr. Millett, who will present a plenary on the context of the HIV epidemic at the IAS conference, said he suspects we won’t see one.
“If we didn’t see an association with the counties that are disproportionately African American, in the black belt where we see high rates of HIV, particularly where we see the social determinants of health that definitely make a difference – if we’re not seeing that association there, where we have a high proportion of African Americans who are at risk both for HIV and COVID-19 – I just don’t think it’s going to emerge,” he said.
This article first appeared on Medscape.com.
FROM AIDS 2020
Daily Recap: Lifestyle vs. genes in breast cancer showdown; Big pharma sues over insulin affordability law
Here are the stories our MDedge editors across specialties think you need to know about today:
Lifestyle choices may reduce breast cancer risk regardless of genetics
A “favorable” lifestyle was associated with a reduced risk of breast cancer even among women at high genetic risk for the disease in a study of more than 90,000 women, researchers reported.
The findings suggest that, regardless of genetic risk, women may be able to reduce their risk of developing breast cancer by getting adequate levels of exercise; maintaining a healthy weight; and limiting or eliminating use of alcohol, oral contraceptives, and hormone replacement therapy.
“These data should empower patients that they can impact on their overall health and reduce the risk of developing breast cancer,” said William Gradishar, MD, who was not invovled with the study. Read more.
Primary care practices may lose $68K per physician this year
Primary care practices stand to lose almost $68,000 per full-time physician this year as COVID-19 causes care delays and cancellations, researchers estimate. And while some outpatient care has started to rebound to near baseline appointment levels, other ambulatory specialties remain dramatically down from prepandemic rates.
Dermatology and rheumatology visits have recovered, but some specialties have cumulative deficits that are particularly concerning. For example, pediatric visits were down by 47% in the 3 months since March 15, and pulmonology visits were down 45% in that time.
This primary care estimate is without a potential second wave of COVID-19, noted Sanjay Basu, MD, director of research and population health at Collective Health in San Francisco, and colleagues.
“We expect ongoing turbulent times, so having a prospective payment could unleash the capacity for primary care practices to be creative in the way they care for their patients,” Daniel Horn, MD, director of population health and quality at Massachusetts General Hospital in Boston, said in an interview. Read more.
Big pharma sues to block Minnesota insulin affordability law
The Pharmaceutical Research and Manufacturers Association (PhRMA) is suing the state of Minnesota in an attempt to overturn a law that requires insulin makers to provide an emergency supply to individuals free of charge.
In the July 1 filing, PhRMA’s attorneys said the law is unconstitutional. It “order[s] pharmaceutical manufacturers to give insulin to state residents, on the state’s prescribed terms, at no charge to the recipients and without compensating the manufacturers in any way.”
The state has estimated that as many as 30,000 Minnesotans would be eligible for free insulin in the first year of the program. The drugmakers strenuously objected, noting that would mean they would “be compelled to provide 173,800 monthly supplies of free insulin” just in the first year.
“There is nothing in the U.S. Constitution that prevents states from saving the lives of its citizens who are in imminent danger,” said Mayo Clinic hematologist S. Vincent Rajkumar, MD. “The only motives for this lawsuit in my opinion are greed and the worry that other states may also choose to put lives of patients ahead of pharma profits.” Read more.
Despite guidelines, kids get opioids & steroids for pneumonia, sinusitis
A significant percentage of children receive opioids and systemic corticosteroids for pneumonia and sinusitis despite guidelines, according to an analysis of 2016 Medicaid data from South Carolina.
Prescriptions for these drugs were more likely after visits to EDs than after ambulatory visits, researchers reported in Pediatrics.
“Each of the 828 opioid and 2,737 systemic steroid prescriptions in the data set represent a potentially inappropriate prescription,” wrote Karina G. Phang, MD, MPH, of Geisinger Medical Center in Danville, Pa., and colleagues. “These rates appear excessive given that the use of these medications is not supported by available research or recommended in national guidelines.” Read more.
Study supports changing classification of RCC
The definition of stage IV renal cell carcinoma (RCC) should be expanded to include lymph node–positive stage III disease, according to a population-level cohort study published in Cancer.
While patients with lymph node–negative stage III disease had superior overall survival at 5 years, survival rates were similar between patients with node–positive stage III disease and stage IV disease. This supports reclassifying stage III node-positive RCC to stage IV, according to researchers.
“Prior institutional studies have indicated that, among patients with stage III disease, those with lymph node disease have worse oncologic outcomes and experience survival that is similar to that of patients with American Joint Committee on Cancer (AJCC) stage IV disease,” wrote Arnav Srivastava, MD, of Rutgers Cancer Institute of New Jersey, New Brunswick, and colleagues. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Lifestyle choices may reduce breast cancer risk regardless of genetics
A “favorable” lifestyle was associated with a reduced risk of breast cancer even among women at high genetic risk for the disease in a study of more than 90,000 women, researchers reported.
The findings suggest that, regardless of genetic risk, women may be able to reduce their risk of developing breast cancer by getting adequate levels of exercise; maintaining a healthy weight; and limiting or eliminating use of alcohol, oral contraceptives, and hormone replacement therapy.
“These data should empower patients that they can impact on their overall health and reduce the risk of developing breast cancer,” said William Gradishar, MD, who was not invovled with the study. Read more.
Primary care practices may lose $68K per physician this year
Primary care practices stand to lose almost $68,000 per full-time physician this year as COVID-19 causes care delays and cancellations, researchers estimate. And while some outpatient care has started to rebound to near baseline appointment levels, other ambulatory specialties remain dramatically down from prepandemic rates.
Dermatology and rheumatology visits have recovered, but some specialties have cumulative deficits that are particularly concerning. For example, pediatric visits were down by 47% in the 3 months since March 15, and pulmonology visits were down 45% in that time.
This primary care estimate is without a potential second wave of COVID-19, noted Sanjay Basu, MD, director of research and population health at Collective Health in San Francisco, and colleagues.
“We expect ongoing turbulent times, so having a prospective payment could unleash the capacity for primary care practices to be creative in the way they care for their patients,” Daniel Horn, MD, director of population health and quality at Massachusetts General Hospital in Boston, said in an interview. Read more.
Big pharma sues to block Minnesota insulin affordability law
The Pharmaceutical Research and Manufacturers Association (PhRMA) is suing the state of Minnesota in an attempt to overturn a law that requires insulin makers to provide an emergency supply to individuals free of charge.
In the July 1 filing, PhRMA’s attorneys said the law is unconstitutional. It “order[s] pharmaceutical manufacturers to give insulin to state residents, on the state’s prescribed terms, at no charge to the recipients and without compensating the manufacturers in any way.”
The state has estimated that as many as 30,000 Minnesotans would be eligible for free insulin in the first year of the program. The drugmakers strenuously objected, noting that would mean they would “be compelled to provide 173,800 monthly supplies of free insulin” just in the first year.
“There is nothing in the U.S. Constitution that prevents states from saving the lives of its citizens who are in imminent danger,” said Mayo Clinic hematologist S. Vincent Rajkumar, MD. “The only motives for this lawsuit in my opinion are greed and the worry that other states may also choose to put lives of patients ahead of pharma profits.” Read more.
Despite guidelines, kids get opioids & steroids for pneumonia, sinusitis
A significant percentage of children receive opioids and systemic corticosteroids for pneumonia and sinusitis despite guidelines, according to an analysis of 2016 Medicaid data from South Carolina.
Prescriptions for these drugs were more likely after visits to EDs than after ambulatory visits, researchers reported in Pediatrics.
“Each of the 828 opioid and 2,737 systemic steroid prescriptions in the data set represent a potentially inappropriate prescription,” wrote Karina G. Phang, MD, MPH, of Geisinger Medical Center in Danville, Pa., and colleagues. “These rates appear excessive given that the use of these medications is not supported by available research or recommended in national guidelines.” Read more.
Study supports changing classification of RCC
The definition of stage IV renal cell carcinoma (RCC) should be expanded to include lymph node–positive stage III disease, according to a population-level cohort study published in Cancer.
While patients with lymph node–negative stage III disease had superior overall survival at 5 years, survival rates were similar between patients with node–positive stage III disease and stage IV disease. This supports reclassifying stage III node-positive RCC to stage IV, according to researchers.
“Prior institutional studies have indicated that, among patients with stage III disease, those with lymph node disease have worse oncologic outcomes and experience survival that is similar to that of patients with American Joint Committee on Cancer (AJCC) stage IV disease,” wrote Arnav Srivastava, MD, of Rutgers Cancer Institute of New Jersey, New Brunswick, and colleagues. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Lifestyle choices may reduce breast cancer risk regardless of genetics
A “favorable” lifestyle was associated with a reduced risk of breast cancer even among women at high genetic risk for the disease in a study of more than 90,000 women, researchers reported.
The findings suggest that, regardless of genetic risk, women may be able to reduce their risk of developing breast cancer by getting adequate levels of exercise; maintaining a healthy weight; and limiting or eliminating use of alcohol, oral contraceptives, and hormone replacement therapy.
“These data should empower patients that they can impact on their overall health and reduce the risk of developing breast cancer,” said William Gradishar, MD, who was not invovled with the study. Read more.
Primary care practices may lose $68K per physician this year
Primary care practices stand to lose almost $68,000 per full-time physician this year as COVID-19 causes care delays and cancellations, researchers estimate. And while some outpatient care has started to rebound to near baseline appointment levels, other ambulatory specialties remain dramatically down from prepandemic rates.
Dermatology and rheumatology visits have recovered, but some specialties have cumulative deficits that are particularly concerning. For example, pediatric visits were down by 47% in the 3 months since March 15, and pulmonology visits were down 45% in that time.
This primary care estimate is without a potential second wave of COVID-19, noted Sanjay Basu, MD, director of research and population health at Collective Health in San Francisco, and colleagues.
“We expect ongoing turbulent times, so having a prospective payment could unleash the capacity for primary care practices to be creative in the way they care for their patients,” Daniel Horn, MD, director of population health and quality at Massachusetts General Hospital in Boston, said in an interview. Read more.
Big pharma sues to block Minnesota insulin affordability law
The Pharmaceutical Research and Manufacturers Association (PhRMA) is suing the state of Minnesota in an attempt to overturn a law that requires insulin makers to provide an emergency supply to individuals free of charge.
In the July 1 filing, PhRMA’s attorneys said the law is unconstitutional. It “order[s] pharmaceutical manufacturers to give insulin to state residents, on the state’s prescribed terms, at no charge to the recipients and without compensating the manufacturers in any way.”
The state has estimated that as many as 30,000 Minnesotans would be eligible for free insulin in the first year of the program. The drugmakers strenuously objected, noting that would mean they would “be compelled to provide 173,800 monthly supplies of free insulin” just in the first year.
“There is nothing in the U.S. Constitution that prevents states from saving the lives of its citizens who are in imminent danger,” said Mayo Clinic hematologist S. Vincent Rajkumar, MD. “The only motives for this lawsuit in my opinion are greed and the worry that other states may also choose to put lives of patients ahead of pharma profits.” Read more.
Despite guidelines, kids get opioids & steroids for pneumonia, sinusitis
A significant percentage of children receive opioids and systemic corticosteroids for pneumonia and sinusitis despite guidelines, according to an analysis of 2016 Medicaid data from South Carolina.
Prescriptions for these drugs were more likely after visits to EDs than after ambulatory visits, researchers reported in Pediatrics.
“Each of the 828 opioid and 2,737 systemic steroid prescriptions in the data set represent a potentially inappropriate prescription,” wrote Karina G. Phang, MD, MPH, of Geisinger Medical Center in Danville, Pa., and colleagues. “These rates appear excessive given that the use of these medications is not supported by available research or recommended in national guidelines.” Read more.
Study supports changing classification of RCC
The definition of stage IV renal cell carcinoma (RCC) should be expanded to include lymph node–positive stage III disease, according to a population-level cohort study published in Cancer.
While patients with lymph node–negative stage III disease had superior overall survival at 5 years, survival rates were similar between patients with node–positive stage III disease and stage IV disease. This supports reclassifying stage III node-positive RCC to stage IV, according to researchers.
“Prior institutional studies have indicated that, among patients with stage III disease, those with lymph node disease have worse oncologic outcomes and experience survival that is similar to that of patients with American Joint Committee on Cancer (AJCC) stage IV disease,” wrote Arnav Srivastava, MD, of Rutgers Cancer Institute of New Jersey, New Brunswick, and colleagues. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Higher stroke rates seen among patients with COVID-19 compared with influenza
, according to a retrospective cohort study conducted at New York–Presbyterian Hospital and Weill Cornell Medicine, New York. “These findings suggest that clinicians should be vigilant for symptoms and signs of acute ischemic stroke in patients with COVID-19 so that time-sensitive interventions, such as thrombolysis and thrombectomy, can be instituted if possible to reduce the burden of long-term disability,” wrote Alexander E. Merkler and colleagues. Their report is in JAMA Neurology.
While several recent publications have “raised the possibility” of this link, none have had an appropriate control group, noted Dr. Merkler of the department of neurology, Weill Cornell Medicine. “Further elucidation of thrombotic mechanisms in patients with COVID-19 may yield better strategies to prevent disabling thrombotic complications like ischemic stroke,” he added.
An increased risk of stroke
The study included 1,916 adults with confirmed COVID-19 (median age 64 years) who were either hospitalized or visited an emergency department between March 4 and May 2, 2020. These cases were compared with a historical cohort of 1,486 patients (median age 62 years) who were hospitalized with laboratory-confirmed influenza A or B between January 1, 2016, and May 31, 2018.
Among the patients with COVID-19, a diagnosis of cerebrovascular disease during hospitalization, a brain computed tomography (CT), or brain magnetic resonance imaging (MRI) was an indication of possible ischemic stroke. These records were then independently reviewed by two board-certified attending neurologists (with a third resolving any disagreement) to adjudicate a final stroke diagnosis. In the influenza cohort, the Cornell Acute Stroke Academic Registry (CAESAR) was used to ascertain ischemic strokes.
The study identified 31 patients with stroke among the COVID-19 cohort (1.6%; 95% confidence interval, 1.1%-2.3%) and 3 in the influenza cohort (0.2%; 95% CI, 0.0%-0.6%). After adjustment for age, sex, and race, stroke risk was almost 8 times higher in the COVID-19 cohort (OR, 7.6; 95% CI, 2.3-25.2).
This association “persisted across multiple sensitivity analyses, with the magnitude of relative associations ranging from 4.0 to 9,” wrote the authors. “This included a sensitivity analysis that adjusted for the number of vascular risk factors and ICU admissions (OR, 4.6; 95% CI, 1.4-15.7).”
The median age of patients with COVID-19 and stroke was 69 years, and the median duration of COVID-19 symptom onset to stroke diagnosis was 16 days. Stroke symptoms were the presenting complaint in only 26% of the patients, while the remainder developing stroke while hospitalized, and more than a third (35%) of all strokes occurred in patients who were mechanically ventilated with severe COVID-19. Inpatient mortality was considerably higher among patients with COVID-19 with stroke versus without (32% vs. 14%; P = .003).
In patients with COVID-19 “most ischemic strokes occurred in older age groups, those with traditional stroke risk factors, and people of color,” wrote the authors. “We also noted that initial plasma D-dimer levels were nearly 3-fold higher in those who received a diagnosis of ischemic stroke than in those who did not” (1.930 mcg/mL vs. 0.682 mcg/mL).
The authors suggested several possible explanations for the elevated risk of stroke in COVID-19. Acute viral illnesses are known to trigger inflammation, and COVID-19 in particular is associated with “a vigorous inflammatory response accompanied by coagulopathy, with elevated D-dimer levels and the frequent presence of antiphospholipid antibodies,” they wrote. The infection is also associated with more severe respiratory syndrome compared with influenza, as well as a heightened risk for complications such as atrial arrhythmias, myocardial infarction, heart failure, myocarditis, and venous thromboses, all of which likely contribute to the risk of ischemic stroke.”
COVID or conventional risk factors?
Asked to comment on the study, Benedict Michael, MBChB (Hons), MRCP (Neurol), PhD, from the United Kingdom’s Coronerve Studies Group, a collaborative initiative to study the neurological features of COVID-19, said in an interview that “this study suggests many cases of stroke are occurring in older patients with multiple existing conventional and well recognized risks for stroke, and may simply represent decompensation during sepsis.”
Dr. Michael, a senior clinician scientist fellow at the University of Liverpool and an honorary consultant neurologist at the Walton Centre, was the senior author on a recently published UK-wide surveillance study on the neurological and neuropsychiatric complications of COVID-19 (Lancet Psychiatry. 2020 Jun 25. doi: 10.1016/S2215-0366[20]30287-X).
He said among patients in the New York study, “those with COVID and a stroke appeared to have many conventional risk factors for stroke (and often at higher percentages than COVID patients without a stroke), e.g. hypertension, overweight, diabetes, hyperlipidemia, existing vascular disease affecting the coronary arteries and atrial fibrillation. To establish evidence-based treatment pathways, clearly further studies are needed to determine the biological mechanisms underlying the seemingly higher rate of stroke with COVID-19 than influenza; but this must especially focus on those younger patients without conventional risk factors for stroke (which are largely not included in this study).”
SOURCE: Merkler AE et al. JAMA Neurol. doi: 10.1001/jamaneurol.2020.2730.
, according to a retrospective cohort study conducted at New York–Presbyterian Hospital and Weill Cornell Medicine, New York. “These findings suggest that clinicians should be vigilant for symptoms and signs of acute ischemic stroke in patients with COVID-19 so that time-sensitive interventions, such as thrombolysis and thrombectomy, can be instituted if possible to reduce the burden of long-term disability,” wrote Alexander E. Merkler and colleagues. Their report is in JAMA Neurology.
While several recent publications have “raised the possibility” of this link, none have had an appropriate control group, noted Dr. Merkler of the department of neurology, Weill Cornell Medicine. “Further elucidation of thrombotic mechanisms in patients with COVID-19 may yield better strategies to prevent disabling thrombotic complications like ischemic stroke,” he added.
An increased risk of stroke
The study included 1,916 adults with confirmed COVID-19 (median age 64 years) who were either hospitalized or visited an emergency department between March 4 and May 2, 2020. These cases were compared with a historical cohort of 1,486 patients (median age 62 years) who were hospitalized with laboratory-confirmed influenza A or B between January 1, 2016, and May 31, 2018.
Among the patients with COVID-19, a diagnosis of cerebrovascular disease during hospitalization, a brain computed tomography (CT), or brain magnetic resonance imaging (MRI) was an indication of possible ischemic stroke. These records were then independently reviewed by two board-certified attending neurologists (with a third resolving any disagreement) to adjudicate a final stroke diagnosis. In the influenza cohort, the Cornell Acute Stroke Academic Registry (CAESAR) was used to ascertain ischemic strokes.
The study identified 31 patients with stroke among the COVID-19 cohort (1.6%; 95% confidence interval, 1.1%-2.3%) and 3 in the influenza cohort (0.2%; 95% CI, 0.0%-0.6%). After adjustment for age, sex, and race, stroke risk was almost 8 times higher in the COVID-19 cohort (OR, 7.6; 95% CI, 2.3-25.2).
This association “persisted across multiple sensitivity analyses, with the magnitude of relative associations ranging from 4.0 to 9,” wrote the authors. “This included a sensitivity analysis that adjusted for the number of vascular risk factors and ICU admissions (OR, 4.6; 95% CI, 1.4-15.7).”
The median age of patients with COVID-19 and stroke was 69 years, and the median duration of COVID-19 symptom onset to stroke diagnosis was 16 days. Stroke symptoms were the presenting complaint in only 26% of the patients, while the remainder developing stroke while hospitalized, and more than a third (35%) of all strokes occurred in patients who were mechanically ventilated with severe COVID-19. Inpatient mortality was considerably higher among patients with COVID-19 with stroke versus without (32% vs. 14%; P = .003).
In patients with COVID-19 “most ischemic strokes occurred in older age groups, those with traditional stroke risk factors, and people of color,” wrote the authors. “We also noted that initial plasma D-dimer levels were nearly 3-fold higher in those who received a diagnosis of ischemic stroke than in those who did not” (1.930 mcg/mL vs. 0.682 mcg/mL).
The authors suggested several possible explanations for the elevated risk of stroke in COVID-19. Acute viral illnesses are known to trigger inflammation, and COVID-19 in particular is associated with “a vigorous inflammatory response accompanied by coagulopathy, with elevated D-dimer levels and the frequent presence of antiphospholipid antibodies,” they wrote. The infection is also associated with more severe respiratory syndrome compared with influenza, as well as a heightened risk for complications such as atrial arrhythmias, myocardial infarction, heart failure, myocarditis, and venous thromboses, all of which likely contribute to the risk of ischemic stroke.”
COVID or conventional risk factors?
Asked to comment on the study, Benedict Michael, MBChB (Hons), MRCP (Neurol), PhD, from the United Kingdom’s Coronerve Studies Group, a collaborative initiative to study the neurological features of COVID-19, said in an interview that “this study suggests many cases of stroke are occurring in older patients with multiple existing conventional and well recognized risks for stroke, and may simply represent decompensation during sepsis.”
Dr. Michael, a senior clinician scientist fellow at the University of Liverpool and an honorary consultant neurologist at the Walton Centre, was the senior author on a recently published UK-wide surveillance study on the neurological and neuropsychiatric complications of COVID-19 (Lancet Psychiatry. 2020 Jun 25. doi: 10.1016/S2215-0366[20]30287-X).
He said among patients in the New York study, “those with COVID and a stroke appeared to have many conventional risk factors for stroke (and often at higher percentages than COVID patients without a stroke), e.g. hypertension, overweight, diabetes, hyperlipidemia, existing vascular disease affecting the coronary arteries and atrial fibrillation. To establish evidence-based treatment pathways, clearly further studies are needed to determine the biological mechanisms underlying the seemingly higher rate of stroke with COVID-19 than influenza; but this must especially focus on those younger patients without conventional risk factors for stroke (which are largely not included in this study).”
SOURCE: Merkler AE et al. JAMA Neurol. doi: 10.1001/jamaneurol.2020.2730.
, according to a retrospective cohort study conducted at New York–Presbyterian Hospital and Weill Cornell Medicine, New York. “These findings suggest that clinicians should be vigilant for symptoms and signs of acute ischemic stroke in patients with COVID-19 so that time-sensitive interventions, such as thrombolysis and thrombectomy, can be instituted if possible to reduce the burden of long-term disability,” wrote Alexander E. Merkler and colleagues. Their report is in JAMA Neurology.
While several recent publications have “raised the possibility” of this link, none have had an appropriate control group, noted Dr. Merkler of the department of neurology, Weill Cornell Medicine. “Further elucidation of thrombotic mechanisms in patients with COVID-19 may yield better strategies to prevent disabling thrombotic complications like ischemic stroke,” he added.
An increased risk of stroke
The study included 1,916 adults with confirmed COVID-19 (median age 64 years) who were either hospitalized or visited an emergency department between March 4 and May 2, 2020. These cases were compared with a historical cohort of 1,486 patients (median age 62 years) who were hospitalized with laboratory-confirmed influenza A or B between January 1, 2016, and May 31, 2018.
Among the patients with COVID-19, a diagnosis of cerebrovascular disease during hospitalization, a brain computed tomography (CT), or brain magnetic resonance imaging (MRI) was an indication of possible ischemic stroke. These records were then independently reviewed by two board-certified attending neurologists (with a third resolving any disagreement) to adjudicate a final stroke diagnosis. In the influenza cohort, the Cornell Acute Stroke Academic Registry (CAESAR) was used to ascertain ischemic strokes.
The study identified 31 patients with stroke among the COVID-19 cohort (1.6%; 95% confidence interval, 1.1%-2.3%) and 3 in the influenza cohort (0.2%; 95% CI, 0.0%-0.6%). After adjustment for age, sex, and race, stroke risk was almost 8 times higher in the COVID-19 cohort (OR, 7.6; 95% CI, 2.3-25.2).
This association “persisted across multiple sensitivity analyses, with the magnitude of relative associations ranging from 4.0 to 9,” wrote the authors. “This included a sensitivity analysis that adjusted for the number of vascular risk factors and ICU admissions (OR, 4.6; 95% CI, 1.4-15.7).”
The median age of patients with COVID-19 and stroke was 69 years, and the median duration of COVID-19 symptom onset to stroke diagnosis was 16 days. Stroke symptoms were the presenting complaint in only 26% of the patients, while the remainder developing stroke while hospitalized, and more than a third (35%) of all strokes occurred in patients who were mechanically ventilated with severe COVID-19. Inpatient mortality was considerably higher among patients with COVID-19 with stroke versus without (32% vs. 14%; P = .003).
In patients with COVID-19 “most ischemic strokes occurred in older age groups, those with traditional stroke risk factors, and people of color,” wrote the authors. “We also noted that initial plasma D-dimer levels were nearly 3-fold higher in those who received a diagnosis of ischemic stroke than in those who did not” (1.930 mcg/mL vs. 0.682 mcg/mL).
The authors suggested several possible explanations for the elevated risk of stroke in COVID-19. Acute viral illnesses are known to trigger inflammation, and COVID-19 in particular is associated with “a vigorous inflammatory response accompanied by coagulopathy, with elevated D-dimer levels and the frequent presence of antiphospholipid antibodies,” they wrote. The infection is also associated with more severe respiratory syndrome compared with influenza, as well as a heightened risk for complications such as atrial arrhythmias, myocardial infarction, heart failure, myocarditis, and venous thromboses, all of which likely contribute to the risk of ischemic stroke.”
COVID or conventional risk factors?
Asked to comment on the study, Benedict Michael, MBChB (Hons), MRCP (Neurol), PhD, from the United Kingdom’s Coronerve Studies Group, a collaborative initiative to study the neurological features of COVID-19, said in an interview that “this study suggests many cases of stroke are occurring in older patients with multiple existing conventional and well recognized risks for stroke, and may simply represent decompensation during sepsis.”
Dr. Michael, a senior clinician scientist fellow at the University of Liverpool and an honorary consultant neurologist at the Walton Centre, was the senior author on a recently published UK-wide surveillance study on the neurological and neuropsychiatric complications of COVID-19 (Lancet Psychiatry. 2020 Jun 25. doi: 10.1016/S2215-0366[20]30287-X).
He said among patients in the New York study, “those with COVID and a stroke appeared to have many conventional risk factors for stroke (and often at higher percentages than COVID patients without a stroke), e.g. hypertension, overweight, diabetes, hyperlipidemia, existing vascular disease affecting the coronary arteries and atrial fibrillation. To establish evidence-based treatment pathways, clearly further studies are needed to determine the biological mechanisms underlying the seemingly higher rate of stroke with COVID-19 than influenza; but this must especially focus on those younger patients without conventional risk factors for stroke (which are largely not included in this study).”
SOURCE: Merkler AE et al. JAMA Neurol. doi: 10.1001/jamaneurol.2020.2730.
FROM JAMA NEUROLOGY
Physician shortage grows in latest projections
Fifteen-year projections for the shortage of primary care and specialty physicians in the United States grew to between 54,000 and 139,000 in the latest annual report by the Association of American Medical Colleges.
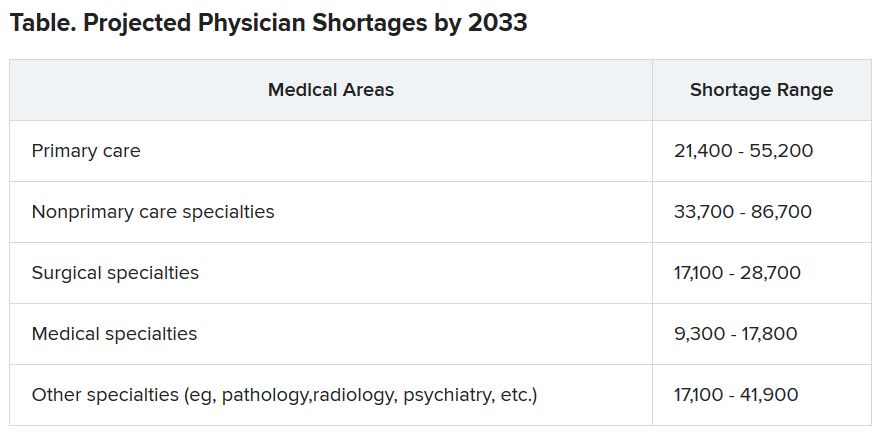
Those estimates are up from last year’s projections of a shortfall of 46,900-121,900 by 2032.
The Complexities of Physician Supply and Demand: Projections from 2018 to 2033, was the sixth annual study conducted for the AAMC by the Life Science division of global analytics firm IHS Markit.
This analysis, conducted in 2019, includes supply and demand scenarios but predates the COVID-19 pandemic.
In a telephone press briefing this morning, David J. Skorton, MD, AAMC’s president and CEO, told reporters that the pandemic has highlighted the acute effects of physician shortages.
“We’ve seen in stark detail how fragile and quickly overwhelmed America’s health care system truly is, and we’re nowhere near out of the woods with this public health emergency yet,” he said.
The persistent shortages mean people “will have ongoing difficulty accessing the care that they need, especially as we all age.”
Some of the biggest shortages will be seen in non–primary care specialists. Dr. Skorton notes that, during the pandemic, shortages of specialists in hospital settings, including critical care, emergency medicine, pulmonology, and infectious disease, are an urgent concern.
Population trends continue to be the biggest drivers of the shortage. Report authors found that by 2033, the U.S. population is expected to grow by 10.4% from 327 million to 361 million, with wide differences by age.
The under-18 population is expected to grow by 3.9%, whereas the numbers of those aged 65 and older is expected to balloon by 45.1% in that time, thus stoking demand for specialties focused on care for older Americans.
Physician age is also a large factor in the projections. More than two in five currently active physicians will be 65 or older in the next 10 years, according to the report. A wave of retirements will have a large impact on the supply of physicians.
The report explains that the projected shortages remain under predictable scenarios: an increase in the use of advanced practice nurses (APRNs) and physician assistants (PAs), more care in alternate settings such as retail clinics, and changes in payment and delivery.
According to the report, the supply of APRNs and PAs is on track to double over the next 15 years (with growth rates varying by APRN and PA specialty).
“At current rates of production, by 2033 APRN supply will grow by 276,000 [full-time equivalents (FTEs)] and PA supply by nearly 138,000 FTEs,” the report states.
However, authors acknowledge there is scant evidence on what effect these numbers will have on demand for physicians.
The report points out that if underserved communities were able to access health care in numbers similar to those without barriers imposed by where they live or what insurance they have, demand could rise beyond the projections in this report by an additional 74,000 to 145,000 physicians.
Stemming the shortages
The first step in addressing the shortage, Dr. Skorton said, is assuring a healthy physician pipeline to meet the demand for generations.
“One essential step that we believe Congress must take is to end the freeze that has been in place since 1997 that limits federal support for residency training of new physicians,” Skorton said.
He noted that AAMC supports the bipartisan Resident Physician Shortage Reduction Act, introduced to Congress in 2019, which calls for an increase in Medicare support for 3000 new residency positions each year over the next 5 years.
However, additional steps are needed, including enabling advanced practice providers to play a greater role in increasing the health care workforce, Dr. Skorton said.
Pointing out some of the effects of physician shortages, Janis M. Orlowski, MD, chief health care officer for the AAMC, noted that high rates of maternal morbidity are partially linked to lack of adequate numbers of physicians in the United States, and a lack of behavioral health specialists has exacerbated effects of the opioid epidemic.
Shortages are already evident in the current pandemic, she added, saying, “Today we see governors calling for retired physicians or physicians from other states to come and help battle the pandemic within their states.”
The report explains that long-term effects on physician numbers from the pandemic likely will include workforce exits because of COVID-19 deaths, early retirements from burnout, or a shift in interest in certain specialties.
Karen Fisher, JD, chief public policy officer for AAMC, said telehealth will also play an important role in bridging gaps in access to care, and its importance has already been seen in this first wave of the pandemic.
She noted that temporary federal waivers have made it easier for those enrolled in Medicare, Medicaid, and the Children’s Health Insurance Program to receive telehealth services during the pandemic.
Expanding the access to telehealth permanently will be important in helping to fill gaps, Ms. Fisher said.
Dr. Skorton, Dr. Orlowski, and Ms. Fisher have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Fifteen-year projections for the shortage of primary care and specialty physicians in the United States grew to between 54,000 and 139,000 in the latest annual report by the Association of American Medical Colleges.
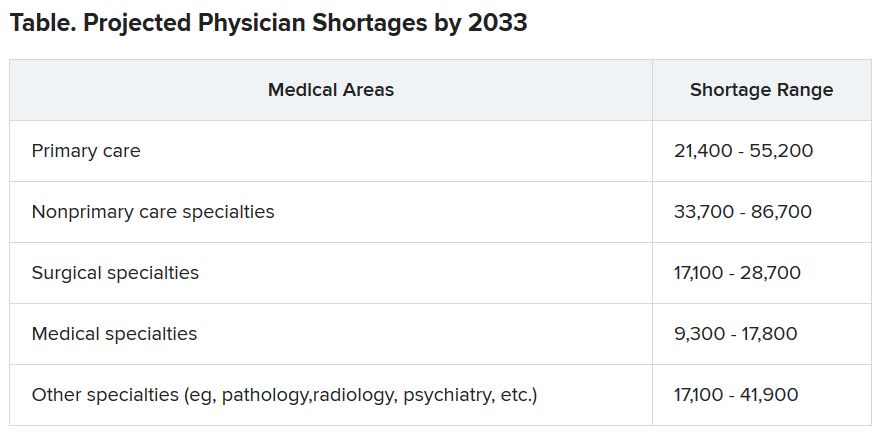
Those estimates are up from last year’s projections of a shortfall of 46,900-121,900 by 2032.
The Complexities of Physician Supply and Demand: Projections from 2018 to 2033, was the sixth annual study conducted for the AAMC by the Life Science division of global analytics firm IHS Markit.
This analysis, conducted in 2019, includes supply and demand scenarios but predates the COVID-19 pandemic.
In a telephone press briefing this morning, David J. Skorton, MD, AAMC’s president and CEO, told reporters that the pandemic has highlighted the acute effects of physician shortages.
“We’ve seen in stark detail how fragile and quickly overwhelmed America’s health care system truly is, and we’re nowhere near out of the woods with this public health emergency yet,” he said.
The persistent shortages mean people “will have ongoing difficulty accessing the care that they need, especially as we all age.”
Some of the biggest shortages will be seen in non–primary care specialists. Dr. Skorton notes that, during the pandemic, shortages of specialists in hospital settings, including critical care, emergency medicine, pulmonology, and infectious disease, are an urgent concern.
Population trends continue to be the biggest drivers of the shortage. Report authors found that by 2033, the U.S. population is expected to grow by 10.4% from 327 million to 361 million, with wide differences by age.
The under-18 population is expected to grow by 3.9%, whereas the numbers of those aged 65 and older is expected to balloon by 45.1% in that time, thus stoking demand for specialties focused on care for older Americans.
Physician age is also a large factor in the projections. More than two in five currently active physicians will be 65 or older in the next 10 years, according to the report. A wave of retirements will have a large impact on the supply of physicians.
The report explains that the projected shortages remain under predictable scenarios: an increase in the use of advanced practice nurses (APRNs) and physician assistants (PAs), more care in alternate settings such as retail clinics, and changes in payment and delivery.
According to the report, the supply of APRNs and PAs is on track to double over the next 15 years (with growth rates varying by APRN and PA specialty).
“At current rates of production, by 2033 APRN supply will grow by 276,000 [full-time equivalents (FTEs)] and PA supply by nearly 138,000 FTEs,” the report states.
However, authors acknowledge there is scant evidence on what effect these numbers will have on demand for physicians.
The report points out that if underserved communities were able to access health care in numbers similar to those without barriers imposed by where they live or what insurance they have, demand could rise beyond the projections in this report by an additional 74,000 to 145,000 physicians.
Stemming the shortages
The first step in addressing the shortage, Dr. Skorton said, is assuring a healthy physician pipeline to meet the demand for generations.
“One essential step that we believe Congress must take is to end the freeze that has been in place since 1997 that limits federal support for residency training of new physicians,” Skorton said.
He noted that AAMC supports the bipartisan Resident Physician Shortage Reduction Act, introduced to Congress in 2019, which calls for an increase in Medicare support for 3000 new residency positions each year over the next 5 years.
However, additional steps are needed, including enabling advanced practice providers to play a greater role in increasing the health care workforce, Dr. Skorton said.
Pointing out some of the effects of physician shortages, Janis M. Orlowski, MD, chief health care officer for the AAMC, noted that high rates of maternal morbidity are partially linked to lack of adequate numbers of physicians in the United States, and a lack of behavioral health specialists has exacerbated effects of the opioid epidemic.
Shortages are already evident in the current pandemic, she added, saying, “Today we see governors calling for retired physicians or physicians from other states to come and help battle the pandemic within their states.”
The report explains that long-term effects on physician numbers from the pandemic likely will include workforce exits because of COVID-19 deaths, early retirements from burnout, or a shift in interest in certain specialties.
Karen Fisher, JD, chief public policy officer for AAMC, said telehealth will also play an important role in bridging gaps in access to care, and its importance has already been seen in this first wave of the pandemic.
She noted that temporary federal waivers have made it easier for those enrolled in Medicare, Medicaid, and the Children’s Health Insurance Program to receive telehealth services during the pandemic.
Expanding the access to telehealth permanently will be important in helping to fill gaps, Ms. Fisher said.
Dr. Skorton, Dr. Orlowski, and Ms. Fisher have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Fifteen-year projections for the shortage of primary care and specialty physicians in the United States grew to between 54,000 and 139,000 in the latest annual report by the Association of American Medical Colleges.
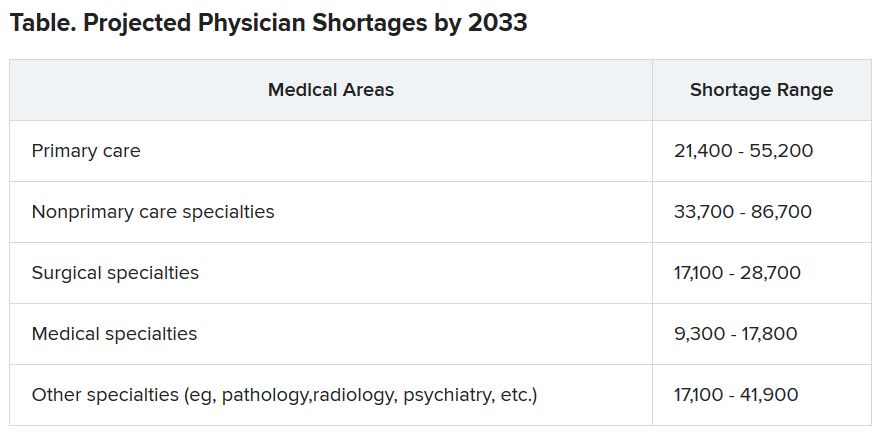
Those estimates are up from last year’s projections of a shortfall of 46,900-121,900 by 2032.
The Complexities of Physician Supply and Demand: Projections from 2018 to 2033, was the sixth annual study conducted for the AAMC by the Life Science division of global analytics firm IHS Markit.
This analysis, conducted in 2019, includes supply and demand scenarios but predates the COVID-19 pandemic.
In a telephone press briefing this morning, David J. Skorton, MD, AAMC’s president and CEO, told reporters that the pandemic has highlighted the acute effects of physician shortages.
“We’ve seen in stark detail how fragile and quickly overwhelmed America’s health care system truly is, and we’re nowhere near out of the woods with this public health emergency yet,” he said.
The persistent shortages mean people “will have ongoing difficulty accessing the care that they need, especially as we all age.”
Some of the biggest shortages will be seen in non–primary care specialists. Dr. Skorton notes that, during the pandemic, shortages of specialists in hospital settings, including critical care, emergency medicine, pulmonology, and infectious disease, are an urgent concern.
Population trends continue to be the biggest drivers of the shortage. Report authors found that by 2033, the U.S. population is expected to grow by 10.4% from 327 million to 361 million, with wide differences by age.
The under-18 population is expected to grow by 3.9%, whereas the numbers of those aged 65 and older is expected to balloon by 45.1% in that time, thus stoking demand for specialties focused on care for older Americans.
Physician age is also a large factor in the projections. More than two in five currently active physicians will be 65 or older in the next 10 years, according to the report. A wave of retirements will have a large impact on the supply of physicians.
The report explains that the projected shortages remain under predictable scenarios: an increase in the use of advanced practice nurses (APRNs) and physician assistants (PAs), more care in alternate settings such as retail clinics, and changes in payment and delivery.
According to the report, the supply of APRNs and PAs is on track to double over the next 15 years (with growth rates varying by APRN and PA specialty).
“At current rates of production, by 2033 APRN supply will grow by 276,000 [full-time equivalents (FTEs)] and PA supply by nearly 138,000 FTEs,” the report states.
However, authors acknowledge there is scant evidence on what effect these numbers will have on demand for physicians.
The report points out that if underserved communities were able to access health care in numbers similar to those without barriers imposed by where they live or what insurance they have, demand could rise beyond the projections in this report by an additional 74,000 to 145,000 physicians.
Stemming the shortages
The first step in addressing the shortage, Dr. Skorton said, is assuring a healthy physician pipeline to meet the demand for generations.
“One essential step that we believe Congress must take is to end the freeze that has been in place since 1997 that limits federal support for residency training of new physicians,” Skorton said.
He noted that AAMC supports the bipartisan Resident Physician Shortage Reduction Act, introduced to Congress in 2019, which calls for an increase in Medicare support for 3000 new residency positions each year over the next 5 years.
However, additional steps are needed, including enabling advanced practice providers to play a greater role in increasing the health care workforce, Dr. Skorton said.
Pointing out some of the effects of physician shortages, Janis M. Orlowski, MD, chief health care officer for the AAMC, noted that high rates of maternal morbidity are partially linked to lack of adequate numbers of physicians in the United States, and a lack of behavioral health specialists has exacerbated effects of the opioid epidemic.
Shortages are already evident in the current pandemic, she added, saying, “Today we see governors calling for retired physicians or physicians from other states to come and help battle the pandemic within their states.”
The report explains that long-term effects on physician numbers from the pandemic likely will include workforce exits because of COVID-19 deaths, early retirements from burnout, or a shift in interest in certain specialties.
Karen Fisher, JD, chief public policy officer for AAMC, said telehealth will also play an important role in bridging gaps in access to care, and its importance has already been seen in this first wave of the pandemic.
She noted that temporary federal waivers have made it easier for those enrolled in Medicare, Medicaid, and the Children’s Health Insurance Program to receive telehealth services during the pandemic.
Expanding the access to telehealth permanently will be important in helping to fill gaps, Ms. Fisher said.
Dr. Skorton, Dr. Orlowski, and Ms. Fisher have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Diagnostic criteria may miss some MIS-C cases, experts say
New data from active surveillance of the severe inflammatory condition associated with COVID-19 in previously healthy children provide further insight into the prevalence and course of the rare syndrome, but experts are concerned that current diagnostic criteria may not capture the true scope of the problem.
In separate reports published online June 29 in the New England Journal of Medicine, researchers from the New York State Department of Health and the Centers for Disease Control and Prevention (CDC) describe the epidemiology and clinical features of multisystem inflammatory syndrome in children (MIS-C) on the basis of information derived from targeted surveillance programs in New York State and across the country.
For the New York study, Elizabeth M. Dufort, MD, from the New York Department of Health in Albany and colleagues analyzed MIS-C surveillance data from 106 hospitals across the state. Of 191 suspected MIS-C cases reported to the Department of Health from March 1 through May 10, 99 met the state’s interim case definition of the condition and were included in the analysis.
The incidence rate for MIS-C was two cases per 100,000 individuals younger than 21 years, whereas the incidence rate of confirmed COVID-19 cases in this age group was 322 per 100,000. Most cases occurred approximately 1 month after the state’s COVID-19 peak.
“Among our patients, predominantly from the New York Metropolitan Region, 40% were black and 36% were Hispanic. This may be a reflection of the well-documented elevated incidence of SARS-CoV-2 infection among black and Hispanic communities,” the authors report.
All children presented with fever or chills, and most had tachycardia (97%) and gastrointestinal symptoms (80%). Rash (60%), conjunctival infection (56%), hypotension (32%), and mucosal changes (27%) were reported. Among all of the children, levels of inflammatory markers were elevated, including levels of C-reactive protein (100%), D-dimer (91%), and troponin (71%). More than one third of the patients (36%) were diagnosed with myocarditis, and an additional 16% had clinical myocarditis.
Of the full cohort, 80% of the children required intensive care, 62% received vasopressor support, and two children died.
The high prevalence of cardiac dysfunction or depression, coagulopathy, gastrointestinal symptoms, mild respiratory symptoms, and indications for supplemental oxygen in patients with MIS-C stands in contrast to the clinical picture observed in most acute cases of COVID-19 in hospitalized children, the authors write.
“Although most children have mild or no illness from SARS-CoV-2 infection, MIS-C may follow Covid-19 or asymptomatic SARS-CoV-2 infection. Recognition of the syndrome and early identification of children with MIS-C, including early monitoring of blood pressure and electrocardiographic and echocardiographic evaluation, could inform appropriate supportive care and other potential therapeutic options,” they continue.
The incidence of MIS-C among children infected with SARS-CoV-2 is unclear because children with COVID-19 often have mild or no symptoms and because children are not tested as frequently, the authors state. For this reason, “[i]t is crucial to establish surveillance for MIS-C cases, particularly in communities with higher levels of SARS-CoV-2 transmission.”
Important Differences From Kawasaki Disease
In a separate study, Leora R. Feldstein, MD, of the CDC, and colleagues report 186 cases of MIS-C collected through targeted surveillance of pediatric health centers in 26 US states from March 15 to May 20, 2020. As with the New York cohort, a disproportionate number of children in this cohort were black (25%) and Hispanic or Latino (31%).
Similar to the New York cohort, 80% of the children in this group required intensive care, 48% received vasoactive support, 20% required invasive mechanical ventilation, and four children died. Skin rashes, gastrointestinal symptoms, cardiovascular and hematologic effects, mucous changes, and elevations of inflammatory biomarkers were also similarly observed.
The researchers note that, although many of the features of MIS-C overlap with Kawasaki disease, there are some important differences, particularly with respect to the nature of cardiovascular involvement. “Approximately 5% of children with Kawasaki’s disease in the United States present with cardiovascular shock leading to vasopressor or inotropic support, as compared with 50% of the patients in our series,” the authors write.
In addition, coronary-artery aneurysms affect approximately one quarter of Kawasaki disease patients within 21 days of disease onset. “In our series, a maximum z score of 2.5 or higher in the left anterior descending or right coronary artery was reported in 8% of the patients overall and in 9% of patients with echocardiograms,” they report.
Additional differentiating features include patient age and race/ethnicity. Kawasaki disease occurs most commonly in children younger than 5 years. The median age in the multistate study was 8.3 years, and nearly half of the children in the New York cohort were in the 6- to 12-year age group. Further, Kawasaki disease is disproportionately prevalent in children of Asian descent.
Despite the differences, “until more is known about long-term cardiac sequelae of MIS-C, providers could consider following Kawasaki’s disease guidelines for follow-up, which recommend repeat echocardiographic imaging at 1 to 2 weeks.”
As was the case in the New York series, treatment in the multistate cohort most commonly included intravenous immunoglobulin and systemic glucocorticoids. Optimal management, however, will require a better understanding of the pathogenesis of MIS-C, Feldstein and colleagues write.
Questions Remain
With the accumulating data on this syndrome, the MIS-C picture seems to be getting incrementally clearer, but there is still much uncertainty, according to Michael Levin, FMedSci, PhD, from the Department of Infectious Disease, Imperial College London, United Kingdom.
“The recognition and description of new diseases often resemble the parable of the blind men and the elephant, with each declaring that the part of the beast they have touched fully defines it,” he writes in an accompanying editorial.
“As the coronavirus disease 2019 (Covid-19) pandemic has evolved, case reports have appeared describing children with unusual febrile illnesses that have features of Kawasaki’s disease, toxic shock syndrome, acute abdominal conditions, and encephalopathy, along with other reports of children with fever, elevated inflammatory markers, and multisystem involvement. It is now apparent that these reports were describing different clinical presentations of a new childhood inflammatory disorder.”
Although a consistent clinical picture is emerging, “[t]he published reports have used a variety of hastily developed case definitions based on the most severe cases, possibly missing less serious cases,” Levin writes. In particular, both the CDC and World Health Organization definitions require evidence of SARS-CoV-2 infection or exposure, which might contribute to underrecognition and underreporting because asymptomatic infections are common and antibody testing is not universally available.
“There is concern that children meeting current diagnostic criteria for MIS-C are the ‘tip of the iceberg,’ and a bigger problem may be lurking below the waterline,” Levin states. With approximately 1000 cases of the syndrome reported worldwide, “do we now have a clear picture of the new disorder, or as in the story of the blind men and the elephant, has only part of the beast been described?”
Adrienne Randolph, MD, of Boston Children’s Hospital, who is a coauthor of the multistate report, agrees that there is still much to learn about MIS-C before the whole beast can be understood. In an interview with Medscape Medical News, she listed the following key questions that have yet to be answered:
- Why do some children get MIS-C and not others?
- What is the long-term outcome of children with MIS-C?
- How can we differentiate MIS-C from acute COVID-19 infection in children with respiratory failure?
- Does MIS-C occur in young adults?
Randolph said her team is taking the best path forward toward answering these questions, including conducting a second study to identify risk factors for MIS-C and longer-term follow-up studies with the National Institutes of Health. “We are also getting consent to collect blood samples and look at other tests to help distinguish MIS-C from acute COVID-19 infection,” she said. She encouraged heightened awareness among physicians who care for young adults to consider MIS-C in patients aged 21 years and older who present with similar signs and symptoms.
On the basis of the answers to these and additional questions, the case definitions for MIS-C may need refinement to capture the wider spectrum of illness, Levin writes in his editorial. “The challenges of this new condition will now be to understand its pathophysiological mechanisms, to develop diagnostics, and to define the best treatment.”
Kleinman has received grants from the Health Services Resources Administration outside the submitted work. Maddux has received grants from the NIH/NICHD and the Francis Family Foundation outside the submitted work. Randolph has received grants from Genentech and personal fees from La Jolla Pharma outside the submitted work and others from the CDC during the conduct of the study.
This article first appeared on Medscape.com.
New data from active surveillance of the severe inflammatory condition associated with COVID-19 in previously healthy children provide further insight into the prevalence and course of the rare syndrome, but experts are concerned that current diagnostic criteria may not capture the true scope of the problem.
In separate reports published online June 29 in the New England Journal of Medicine, researchers from the New York State Department of Health and the Centers for Disease Control and Prevention (CDC) describe the epidemiology and clinical features of multisystem inflammatory syndrome in children (MIS-C) on the basis of information derived from targeted surveillance programs in New York State and across the country.
For the New York study, Elizabeth M. Dufort, MD, from the New York Department of Health in Albany and colleagues analyzed MIS-C surveillance data from 106 hospitals across the state. Of 191 suspected MIS-C cases reported to the Department of Health from March 1 through May 10, 99 met the state’s interim case definition of the condition and were included in the analysis.
The incidence rate for MIS-C was two cases per 100,000 individuals younger than 21 years, whereas the incidence rate of confirmed COVID-19 cases in this age group was 322 per 100,000. Most cases occurred approximately 1 month after the state’s COVID-19 peak.
“Among our patients, predominantly from the New York Metropolitan Region, 40% were black and 36% were Hispanic. This may be a reflection of the well-documented elevated incidence of SARS-CoV-2 infection among black and Hispanic communities,” the authors report.
All children presented with fever or chills, and most had tachycardia (97%) and gastrointestinal symptoms (80%). Rash (60%), conjunctival infection (56%), hypotension (32%), and mucosal changes (27%) were reported. Among all of the children, levels of inflammatory markers were elevated, including levels of C-reactive protein (100%), D-dimer (91%), and troponin (71%). More than one third of the patients (36%) were diagnosed with myocarditis, and an additional 16% had clinical myocarditis.
Of the full cohort, 80% of the children required intensive care, 62% received vasopressor support, and two children died.
The high prevalence of cardiac dysfunction or depression, coagulopathy, gastrointestinal symptoms, mild respiratory symptoms, and indications for supplemental oxygen in patients with MIS-C stands in contrast to the clinical picture observed in most acute cases of COVID-19 in hospitalized children, the authors write.
“Although most children have mild or no illness from SARS-CoV-2 infection, MIS-C may follow Covid-19 or asymptomatic SARS-CoV-2 infection. Recognition of the syndrome and early identification of children with MIS-C, including early monitoring of blood pressure and electrocardiographic and echocardiographic evaluation, could inform appropriate supportive care and other potential therapeutic options,” they continue.
The incidence of MIS-C among children infected with SARS-CoV-2 is unclear because children with COVID-19 often have mild or no symptoms and because children are not tested as frequently, the authors state. For this reason, “[i]t is crucial to establish surveillance for MIS-C cases, particularly in communities with higher levels of SARS-CoV-2 transmission.”
Important Differences From Kawasaki Disease
In a separate study, Leora R. Feldstein, MD, of the CDC, and colleagues report 186 cases of MIS-C collected through targeted surveillance of pediatric health centers in 26 US states from March 15 to May 20, 2020. As with the New York cohort, a disproportionate number of children in this cohort were black (25%) and Hispanic or Latino (31%).
Similar to the New York cohort, 80% of the children in this group required intensive care, 48% received vasoactive support, 20% required invasive mechanical ventilation, and four children died. Skin rashes, gastrointestinal symptoms, cardiovascular and hematologic effects, mucous changes, and elevations of inflammatory biomarkers were also similarly observed.
The researchers note that, although many of the features of MIS-C overlap with Kawasaki disease, there are some important differences, particularly with respect to the nature of cardiovascular involvement. “Approximately 5% of children with Kawasaki’s disease in the United States present with cardiovascular shock leading to vasopressor or inotropic support, as compared with 50% of the patients in our series,” the authors write.
In addition, coronary-artery aneurysms affect approximately one quarter of Kawasaki disease patients within 21 days of disease onset. “In our series, a maximum z score of 2.5 or higher in the left anterior descending or right coronary artery was reported in 8% of the patients overall and in 9% of patients with echocardiograms,” they report.
Additional differentiating features include patient age and race/ethnicity. Kawasaki disease occurs most commonly in children younger than 5 years. The median age in the multistate study was 8.3 years, and nearly half of the children in the New York cohort were in the 6- to 12-year age group. Further, Kawasaki disease is disproportionately prevalent in children of Asian descent.
Despite the differences, “until more is known about long-term cardiac sequelae of MIS-C, providers could consider following Kawasaki’s disease guidelines for follow-up, which recommend repeat echocardiographic imaging at 1 to 2 weeks.”
As was the case in the New York series, treatment in the multistate cohort most commonly included intravenous immunoglobulin and systemic glucocorticoids. Optimal management, however, will require a better understanding of the pathogenesis of MIS-C, Feldstein and colleagues write.
Questions Remain
With the accumulating data on this syndrome, the MIS-C picture seems to be getting incrementally clearer, but there is still much uncertainty, according to Michael Levin, FMedSci, PhD, from the Department of Infectious Disease, Imperial College London, United Kingdom.
“The recognition and description of new diseases often resemble the parable of the blind men and the elephant, with each declaring that the part of the beast they have touched fully defines it,” he writes in an accompanying editorial.
“As the coronavirus disease 2019 (Covid-19) pandemic has evolved, case reports have appeared describing children with unusual febrile illnesses that have features of Kawasaki’s disease, toxic shock syndrome, acute abdominal conditions, and encephalopathy, along with other reports of children with fever, elevated inflammatory markers, and multisystem involvement. It is now apparent that these reports were describing different clinical presentations of a new childhood inflammatory disorder.”
Although a consistent clinical picture is emerging, “[t]he published reports have used a variety of hastily developed case definitions based on the most severe cases, possibly missing less serious cases,” Levin writes. In particular, both the CDC and World Health Organization definitions require evidence of SARS-CoV-2 infection or exposure, which might contribute to underrecognition and underreporting because asymptomatic infections are common and antibody testing is not universally available.
“There is concern that children meeting current diagnostic criteria for MIS-C are the ‘tip of the iceberg,’ and a bigger problem may be lurking below the waterline,” Levin states. With approximately 1000 cases of the syndrome reported worldwide, “do we now have a clear picture of the new disorder, or as in the story of the blind men and the elephant, has only part of the beast been described?”
Adrienne Randolph, MD, of Boston Children’s Hospital, who is a coauthor of the multistate report, agrees that there is still much to learn about MIS-C before the whole beast can be understood. In an interview with Medscape Medical News, she listed the following key questions that have yet to be answered:
- Why do some children get MIS-C and not others?
- What is the long-term outcome of children with MIS-C?
- How can we differentiate MIS-C from acute COVID-19 infection in children with respiratory failure?
- Does MIS-C occur in young adults?
Randolph said her team is taking the best path forward toward answering these questions, including conducting a second study to identify risk factors for MIS-C and longer-term follow-up studies with the National Institutes of Health. “We are also getting consent to collect blood samples and look at other tests to help distinguish MIS-C from acute COVID-19 infection,” she said. She encouraged heightened awareness among physicians who care for young adults to consider MIS-C in patients aged 21 years and older who present with similar signs and symptoms.
On the basis of the answers to these and additional questions, the case definitions for MIS-C may need refinement to capture the wider spectrum of illness, Levin writes in his editorial. “The challenges of this new condition will now be to understand its pathophysiological mechanisms, to develop diagnostics, and to define the best treatment.”
Kleinman has received grants from the Health Services Resources Administration outside the submitted work. Maddux has received grants from the NIH/NICHD and the Francis Family Foundation outside the submitted work. Randolph has received grants from Genentech and personal fees from La Jolla Pharma outside the submitted work and others from the CDC during the conduct of the study.
This article first appeared on Medscape.com.
New data from active surveillance of the severe inflammatory condition associated with COVID-19 in previously healthy children provide further insight into the prevalence and course of the rare syndrome, but experts are concerned that current diagnostic criteria may not capture the true scope of the problem.
In separate reports published online June 29 in the New England Journal of Medicine, researchers from the New York State Department of Health and the Centers for Disease Control and Prevention (CDC) describe the epidemiology and clinical features of multisystem inflammatory syndrome in children (MIS-C) on the basis of information derived from targeted surveillance programs in New York State and across the country.
For the New York study, Elizabeth M. Dufort, MD, from the New York Department of Health in Albany and colleagues analyzed MIS-C surveillance data from 106 hospitals across the state. Of 191 suspected MIS-C cases reported to the Department of Health from March 1 through May 10, 99 met the state’s interim case definition of the condition and were included in the analysis.
The incidence rate for MIS-C was two cases per 100,000 individuals younger than 21 years, whereas the incidence rate of confirmed COVID-19 cases in this age group was 322 per 100,000. Most cases occurred approximately 1 month after the state’s COVID-19 peak.
“Among our patients, predominantly from the New York Metropolitan Region, 40% were black and 36% were Hispanic. This may be a reflection of the well-documented elevated incidence of SARS-CoV-2 infection among black and Hispanic communities,” the authors report.
All children presented with fever or chills, and most had tachycardia (97%) and gastrointestinal symptoms (80%). Rash (60%), conjunctival infection (56%), hypotension (32%), and mucosal changes (27%) were reported. Among all of the children, levels of inflammatory markers were elevated, including levels of C-reactive protein (100%), D-dimer (91%), and troponin (71%). More than one third of the patients (36%) were diagnosed with myocarditis, and an additional 16% had clinical myocarditis.
Of the full cohort, 80% of the children required intensive care, 62% received vasopressor support, and two children died.
The high prevalence of cardiac dysfunction or depression, coagulopathy, gastrointestinal symptoms, mild respiratory symptoms, and indications for supplemental oxygen in patients with MIS-C stands in contrast to the clinical picture observed in most acute cases of COVID-19 in hospitalized children, the authors write.
“Although most children have mild or no illness from SARS-CoV-2 infection, MIS-C may follow Covid-19 or asymptomatic SARS-CoV-2 infection. Recognition of the syndrome and early identification of children with MIS-C, including early monitoring of blood pressure and electrocardiographic and echocardiographic evaluation, could inform appropriate supportive care and other potential therapeutic options,” they continue.
The incidence of MIS-C among children infected with SARS-CoV-2 is unclear because children with COVID-19 often have mild or no symptoms and because children are not tested as frequently, the authors state. For this reason, “[i]t is crucial to establish surveillance for MIS-C cases, particularly in communities with higher levels of SARS-CoV-2 transmission.”
Important Differences From Kawasaki Disease
In a separate study, Leora R. Feldstein, MD, of the CDC, and colleagues report 186 cases of MIS-C collected through targeted surveillance of pediatric health centers in 26 US states from March 15 to May 20, 2020. As with the New York cohort, a disproportionate number of children in this cohort were black (25%) and Hispanic or Latino (31%).
Similar to the New York cohort, 80% of the children in this group required intensive care, 48% received vasoactive support, 20% required invasive mechanical ventilation, and four children died. Skin rashes, gastrointestinal symptoms, cardiovascular and hematologic effects, mucous changes, and elevations of inflammatory biomarkers were also similarly observed.
The researchers note that, although many of the features of MIS-C overlap with Kawasaki disease, there are some important differences, particularly with respect to the nature of cardiovascular involvement. “Approximately 5% of children with Kawasaki’s disease in the United States present with cardiovascular shock leading to vasopressor or inotropic support, as compared with 50% of the patients in our series,” the authors write.
In addition, coronary-artery aneurysms affect approximately one quarter of Kawasaki disease patients within 21 days of disease onset. “In our series, a maximum z score of 2.5 or higher in the left anterior descending or right coronary artery was reported in 8% of the patients overall and in 9% of patients with echocardiograms,” they report.
Additional differentiating features include patient age and race/ethnicity. Kawasaki disease occurs most commonly in children younger than 5 years. The median age in the multistate study was 8.3 years, and nearly half of the children in the New York cohort were in the 6- to 12-year age group. Further, Kawasaki disease is disproportionately prevalent in children of Asian descent.
Despite the differences, “until more is known about long-term cardiac sequelae of MIS-C, providers could consider following Kawasaki’s disease guidelines for follow-up, which recommend repeat echocardiographic imaging at 1 to 2 weeks.”
As was the case in the New York series, treatment in the multistate cohort most commonly included intravenous immunoglobulin and systemic glucocorticoids. Optimal management, however, will require a better understanding of the pathogenesis of MIS-C, Feldstein and colleagues write.
Questions Remain
With the accumulating data on this syndrome, the MIS-C picture seems to be getting incrementally clearer, but there is still much uncertainty, according to Michael Levin, FMedSci, PhD, from the Department of Infectious Disease, Imperial College London, United Kingdom.
“The recognition and description of new diseases often resemble the parable of the blind men and the elephant, with each declaring that the part of the beast they have touched fully defines it,” he writes in an accompanying editorial.
“As the coronavirus disease 2019 (Covid-19) pandemic has evolved, case reports have appeared describing children with unusual febrile illnesses that have features of Kawasaki’s disease, toxic shock syndrome, acute abdominal conditions, and encephalopathy, along with other reports of children with fever, elevated inflammatory markers, and multisystem involvement. It is now apparent that these reports were describing different clinical presentations of a new childhood inflammatory disorder.”
Although a consistent clinical picture is emerging, “[t]he published reports have used a variety of hastily developed case definitions based on the most severe cases, possibly missing less serious cases,” Levin writes. In particular, both the CDC and World Health Organization definitions require evidence of SARS-CoV-2 infection or exposure, which might contribute to underrecognition and underreporting because asymptomatic infections are common and antibody testing is not universally available.
“There is concern that children meeting current diagnostic criteria for MIS-C are the ‘tip of the iceberg,’ and a bigger problem may be lurking below the waterline,” Levin states. With approximately 1000 cases of the syndrome reported worldwide, “do we now have a clear picture of the new disorder, or as in the story of the blind men and the elephant, has only part of the beast been described?”
Adrienne Randolph, MD, of Boston Children’s Hospital, who is a coauthor of the multistate report, agrees that there is still much to learn about MIS-C before the whole beast can be understood. In an interview with Medscape Medical News, she listed the following key questions that have yet to be answered:
- Why do some children get MIS-C and not others?
- What is the long-term outcome of children with MIS-C?
- How can we differentiate MIS-C from acute COVID-19 infection in children with respiratory failure?
- Does MIS-C occur in young adults?
Randolph said her team is taking the best path forward toward answering these questions, including conducting a second study to identify risk factors for MIS-C and longer-term follow-up studies with the National Institutes of Health. “We are also getting consent to collect blood samples and look at other tests to help distinguish MIS-C from acute COVID-19 infection,” she said. She encouraged heightened awareness among physicians who care for young adults to consider MIS-C in patients aged 21 years and older who present with similar signs and symptoms.
On the basis of the answers to these and additional questions, the case definitions for MIS-C may need refinement to capture the wider spectrum of illness, Levin writes in his editorial. “The challenges of this new condition will now be to understand its pathophysiological mechanisms, to develop diagnostics, and to define the best treatment.”
Kleinman has received grants from the Health Services Resources Administration outside the submitted work. Maddux has received grants from the NIH/NICHD and the Francis Family Foundation outside the submitted work. Randolph has received grants from Genentech and personal fees from La Jolla Pharma outside the submitted work and others from the CDC during the conduct of the study.
This article first appeared on Medscape.com.
Captopril questioned for diabetes patients in COVID-19 setting
Captopril appears to be associated with a higher rate of pulmonary adverse reactions in patients with diabetes than that of other ACE inhibitors or angiotensin receptor blockers (ARBs) and therefore may not be the best choice for patients with diabetes and COVID-19, a new study suggests.
The study was published online in the Journal of the American Pharmacists Association.
The authors, led by Emma G. Stafford, PharmD, University of Missouri-Kansas City School of Pharmacy, note that diabetes seems to confer a higher risk of adverse outcomes in COVID-19 infection and there is conflicting data on the contribution of ACE inhibitors and ARBs, commonly used medications in diabetes, on the mortality and morbidity of COVID-19.
“In light of the recent COVID-19 outbreak, more research is needed to understand the effects that diabetes (and its medications) may have on the respiratory system and how that could affect the management of diseases such as COVID-19,” they say.
“Although ACE inhibitors and ARBs are generally considered to have similar adverse event profiles, evaluation of postmarketing adverse events may shed light on minute differences that could have important clinical impacts,” they add.
For the current study, the researchers analyzed data from multiple publicly available data sources on adverse drug reactions in patients with diabetes taking ACE inhibitors or ARBs. The data included all adverse drug events (ADEs) reported nationally to the US Food and Drug Administration and internationally to the Medical Dictionary for Regulatory Activities (MedDRA).
Results showed that captopril, the first ACE inhibitor approved back in 1981, has a higher incidence of pulmonary ADEs in patients with diabetes as compared with other ACE-inhibitor drugs (P = .005) as well as a statistically significant difference in pulmonary events compared with ARBs (P = .012).
“These analyses suggest that pharmacists and clinicians will need to consider the specific medication’s adverse event profile, particularly captopril, on how it may affect infections and other acute disease states that alter pulmonary function, such as COVID-19,” the authors conclude.
They say that the high incidence of pulmonary adverse drug effects with captopril “highlights the fact that the drugs belonging in one class are not identical and that its pharmacokinetics and pharmacodynamics can affect the patients’ health especially during acute processes like COVID-19.”
“This is especially important as current observational studies of COVID-19 patients tend to group drugs within a class and are not analyzing the potential differences within each class,” they add.
They note that ACE inhibitors can be broadly classified into 3 structural classes: sulfhydryl-, dicarboxyl-, and phosphorous- containing molecules. Notably, captopril is the only currently available ACE inhibitor belonging to the sulfhydryl-containing class and may explain the higher incidence of adverse drug effects observed, they comment.
“Health care providers have been left with many questions when treating patients with COVID-19, including how ACE inhibitors or ARBs may affect their clinical course. Results from this study may be helpful when prescribing or continuing ACE inhibitors or ARBs for patients with diabetes and infections or illnesses that may affect pulmonary function, such as COVID-19,” they conclude.
Questioning safety in COVID-19 an “overreach”
Commenting for Medscape Medical News, Michael A. Weber, MD, professor of medicine at State University of New York, said he thought the current article appears to overreach in questioning captopril’s safety in the COVID-19 setting.
“Captopril was the first ACE inhibitor available for clinical use. In early prescribing its dosage was not well understood and it might have been administered in excessive amounts,” Weber notes.
“There were some renal and other adverse effects reported that at first were attributed to the fact that captopril, unlike any other popular ACE inhibitors, contained a sulfhydryl (SH) group in its molecule,” he said. “It is not clear whether this feature could be responsible for the increased pulmonary side effects and potential danger to COVID-19 patients now reported with captopril in this new pharmacy article.”
But he adds: “The article contains no evidence that the effect of captopril or any other ACE inhibitor on the pulmonary ACE-2 enzyme has a deleterious effect on outcomes of COVID-19 disease. In any case, captopril — which should be prescribed in a twice-daily dose — is not frequently prescribed these days since newer ACE inhibitors are effective with just once-daily dosing.”
This article first appeared on Medscape.com.
Captopril appears to be associated with a higher rate of pulmonary adverse reactions in patients with diabetes than that of other ACE inhibitors or angiotensin receptor blockers (ARBs) and therefore may not be the best choice for patients with diabetes and COVID-19, a new study suggests.
The study was published online in the Journal of the American Pharmacists Association.
The authors, led by Emma G. Stafford, PharmD, University of Missouri-Kansas City School of Pharmacy, note that diabetes seems to confer a higher risk of adverse outcomes in COVID-19 infection and there is conflicting data on the contribution of ACE inhibitors and ARBs, commonly used medications in diabetes, on the mortality and morbidity of COVID-19.
“In light of the recent COVID-19 outbreak, more research is needed to understand the effects that diabetes (and its medications) may have on the respiratory system and how that could affect the management of diseases such as COVID-19,” they say.
“Although ACE inhibitors and ARBs are generally considered to have similar adverse event profiles, evaluation of postmarketing adverse events may shed light on minute differences that could have important clinical impacts,” they add.
For the current study, the researchers analyzed data from multiple publicly available data sources on adverse drug reactions in patients with diabetes taking ACE inhibitors or ARBs. The data included all adverse drug events (ADEs) reported nationally to the US Food and Drug Administration and internationally to the Medical Dictionary for Regulatory Activities (MedDRA).
Results showed that captopril, the first ACE inhibitor approved back in 1981, has a higher incidence of pulmonary ADEs in patients with diabetes as compared with other ACE-inhibitor drugs (P = .005) as well as a statistically significant difference in pulmonary events compared with ARBs (P = .012).
“These analyses suggest that pharmacists and clinicians will need to consider the specific medication’s adverse event profile, particularly captopril, on how it may affect infections and other acute disease states that alter pulmonary function, such as COVID-19,” the authors conclude.
They say that the high incidence of pulmonary adverse drug effects with captopril “highlights the fact that the drugs belonging in one class are not identical and that its pharmacokinetics and pharmacodynamics can affect the patients’ health especially during acute processes like COVID-19.”
“This is especially important as current observational studies of COVID-19 patients tend to group drugs within a class and are not analyzing the potential differences within each class,” they add.
They note that ACE inhibitors can be broadly classified into 3 structural classes: sulfhydryl-, dicarboxyl-, and phosphorous- containing molecules. Notably, captopril is the only currently available ACE inhibitor belonging to the sulfhydryl-containing class and may explain the higher incidence of adverse drug effects observed, they comment.
“Health care providers have been left with many questions when treating patients with COVID-19, including how ACE inhibitors or ARBs may affect their clinical course. Results from this study may be helpful when prescribing or continuing ACE inhibitors or ARBs for patients with diabetes and infections or illnesses that may affect pulmonary function, such as COVID-19,” they conclude.
Questioning safety in COVID-19 an “overreach”
Commenting for Medscape Medical News, Michael A. Weber, MD, professor of medicine at State University of New York, said he thought the current article appears to overreach in questioning captopril’s safety in the COVID-19 setting.
“Captopril was the first ACE inhibitor available for clinical use. In early prescribing its dosage was not well understood and it might have been administered in excessive amounts,” Weber notes.
“There were some renal and other adverse effects reported that at first were attributed to the fact that captopril, unlike any other popular ACE inhibitors, contained a sulfhydryl (SH) group in its molecule,” he said. “It is not clear whether this feature could be responsible for the increased pulmonary side effects and potential danger to COVID-19 patients now reported with captopril in this new pharmacy article.”
But he adds: “The article contains no evidence that the effect of captopril or any other ACE inhibitor on the pulmonary ACE-2 enzyme has a deleterious effect on outcomes of COVID-19 disease. In any case, captopril — which should be prescribed in a twice-daily dose — is not frequently prescribed these days since newer ACE inhibitors are effective with just once-daily dosing.”
This article first appeared on Medscape.com.
Captopril appears to be associated with a higher rate of pulmonary adverse reactions in patients with diabetes than that of other ACE inhibitors or angiotensin receptor blockers (ARBs) and therefore may not be the best choice for patients with diabetes and COVID-19, a new study suggests.
The study was published online in the Journal of the American Pharmacists Association.
The authors, led by Emma G. Stafford, PharmD, University of Missouri-Kansas City School of Pharmacy, note that diabetes seems to confer a higher risk of adverse outcomes in COVID-19 infection and there is conflicting data on the contribution of ACE inhibitors and ARBs, commonly used medications in diabetes, on the mortality and morbidity of COVID-19.
“In light of the recent COVID-19 outbreak, more research is needed to understand the effects that diabetes (and its medications) may have on the respiratory system and how that could affect the management of diseases such as COVID-19,” they say.
“Although ACE inhibitors and ARBs are generally considered to have similar adverse event profiles, evaluation of postmarketing adverse events may shed light on minute differences that could have important clinical impacts,” they add.
For the current study, the researchers analyzed data from multiple publicly available data sources on adverse drug reactions in patients with diabetes taking ACE inhibitors or ARBs. The data included all adverse drug events (ADEs) reported nationally to the US Food and Drug Administration and internationally to the Medical Dictionary for Regulatory Activities (MedDRA).
Results showed that captopril, the first ACE inhibitor approved back in 1981, has a higher incidence of pulmonary ADEs in patients with diabetes as compared with other ACE-inhibitor drugs (P = .005) as well as a statistically significant difference in pulmonary events compared with ARBs (P = .012).
“These analyses suggest that pharmacists and clinicians will need to consider the specific medication’s adverse event profile, particularly captopril, on how it may affect infections and other acute disease states that alter pulmonary function, such as COVID-19,” the authors conclude.
They say that the high incidence of pulmonary adverse drug effects with captopril “highlights the fact that the drugs belonging in one class are not identical and that its pharmacokinetics and pharmacodynamics can affect the patients’ health especially during acute processes like COVID-19.”
“This is especially important as current observational studies of COVID-19 patients tend to group drugs within a class and are not analyzing the potential differences within each class,” they add.
They note that ACE inhibitors can be broadly classified into 3 structural classes: sulfhydryl-, dicarboxyl-, and phosphorous- containing molecules. Notably, captopril is the only currently available ACE inhibitor belonging to the sulfhydryl-containing class and may explain the higher incidence of adverse drug effects observed, they comment.
“Health care providers have been left with many questions when treating patients with COVID-19, including how ACE inhibitors or ARBs may affect their clinical course. Results from this study may be helpful when prescribing or continuing ACE inhibitors or ARBs for patients with diabetes and infections or illnesses that may affect pulmonary function, such as COVID-19,” they conclude.
Questioning safety in COVID-19 an “overreach”
Commenting for Medscape Medical News, Michael A. Weber, MD, professor of medicine at State University of New York, said he thought the current article appears to overreach in questioning captopril’s safety in the COVID-19 setting.
“Captopril was the first ACE inhibitor available for clinical use. In early prescribing its dosage was not well understood and it might have been administered in excessive amounts,” Weber notes.
“There were some renal and other adverse effects reported that at first were attributed to the fact that captopril, unlike any other popular ACE inhibitors, contained a sulfhydryl (SH) group in its molecule,” he said. “It is not clear whether this feature could be responsible for the increased pulmonary side effects and potential danger to COVID-19 patients now reported with captopril in this new pharmacy article.”
But he adds: “The article contains no evidence that the effect of captopril or any other ACE inhibitor on the pulmonary ACE-2 enzyme has a deleterious effect on outcomes of COVID-19 disease. In any case, captopril — which should be prescribed in a twice-daily dose — is not frequently prescribed these days since newer ACE inhibitors are effective with just once-daily dosing.”
This article first appeared on Medscape.com.
Daily Recap: Migraine affects pregnancy planning; FDA okays urothelial carcinoma therapy
Here are the stories our MDedge editors across specialties think you need to know about today:
Migraine is often a deciding factor in pregnancy planning
Migraine can significantly influence a woman’s decision to have children, new research shows.
Results from a multicenter study of more than 600 women showed that, among participants with migraine, those who were younger, had menstrual migraine, or had chronic migraine were more likely to decide to not become pregnant.
“Women who avoided pregnancy due to migraine were most concerned that migraine would make raising a child difficult, that the migraine medications they take would have a negative impact on their child’s development, and that their migraine pattern would worsen during or just after pregnancy,” said study investigator Ryotaro Ishii, MD, PhD, a visiting scientist at Mayo Clinic in Phoenix.
The findings were presented at the virtual annual meeting of the American Headache Society. Read more.
FDA approves avelumab as maintenance for urothelial carcinoma
The Food and Drug Administration has approved avelumab (Bavencio) as a maintenance treatment for patients with locally advanced or metastatic urothelial carcinoma (UC) that has not progressed after first-line platinum-containing chemotherapy.
The new maintenance therapy indication for avelumab is based on efficacy demonstrated in the JAVELIN Bladder 100 trial. Results from this trial were presented as part of the American Society of Clinical Oncology virtual scientific program.
The new indication adds to avelumab use in other patient populations, including people with locally advanced or metastatic UC who experience disease progression during or following platinum-containing chemotherapy. The FDA also previously approved avelumab for patients who experienced UC progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy. The FDA first approved marketing of avelumab in 2017. Other uses include treatment of metastatic Merkel cell carcinoma and first-line treatment of advanced renal cell carcinoma in combination with axitinib. Read more.
Lifestyle changes may explain skin lesions in pandemic-era patients
Two European prospective case series found no direct association between skin lesions on the hands and feet and SARS-CoV-2 in young people, which raises questions about other contributing factors, such as lockdown conditions, which may be clarified with additional research. The study appeared in JAMA Dermatology.
Meanwhile, data from the American Academy of Dermatology and a recent paper from the British Journal of Dermatology suggest a real association exists, at in least some patients.
“It’s going to be true that most patients with toe lesions are PCR [polymerase chain reaction]-negative because it tends to be a late phenomenon when patients are no longer shedding virus,” explained Lindy P. Fox, MD, professor of dermatology at the University of California, San Francisco, who was not an author of either study. Read more.
Take-home test strips allow drug users to detect fentanyl
Illicit drug users seem to overwhelmingly appreciate being able to use take-home test strips to detect the presence of dangerous fentanyl in opioids and other drugs, a new study finds.
More than 95% said they’d use the inexpensive strips again.
“These tests accurately detect fentanyl in the drug supply, and they can be a valuable addition to other drug prevention strategies,” the study’s lead author and addiction medicine specialist Sukhpreet Klaire, MD, of the British Columbia Center on Substance Use in Vancouver, said in an interview.
Dr. Klaire presented the study findings at the virtual annual meeting of the College on Problems of Drug Dependence. Read more.
New data back use of medical cannabis for epilepsy, pain, anxiety
Two new studies offer positive news about medical cannabis, suggesting that marijuana products improve physical and cognitive symptoms, boost quality of life, and rarely produce signs of problematic use.
In one study, patients with epilepsy who used medical cannabis were nearly half as likely to have needed an emergency department visit within the last 30 days as was a control group. In the other study, just 3 of 54 subjects who used medical cannabis showed signs of possible cannabis use disorder (CUD) over 12 months.
The findings show that “there is improvement in a range of outcome variables, and the adverse effects seem to be minimal, compared to what we might have hypothesized based on the bulk of the literature on the negative effects of cannabis on health outcomes,” cannabis researcher Ziva Cooper, PhD, of the University of California at Los Angeles, said in an interview. Dr. Cooper moderated a session about the studies at the virtual annual meeting of the College on Problems of Drug Dependence. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Migraine is often a deciding factor in pregnancy planning
Migraine can significantly influence a woman’s decision to have children, new research shows.
Results from a multicenter study of more than 600 women showed that, among participants with migraine, those who were younger, had menstrual migraine, or had chronic migraine were more likely to decide to not become pregnant.
“Women who avoided pregnancy due to migraine were most concerned that migraine would make raising a child difficult, that the migraine medications they take would have a negative impact on their child’s development, and that their migraine pattern would worsen during or just after pregnancy,” said study investigator Ryotaro Ishii, MD, PhD, a visiting scientist at Mayo Clinic in Phoenix.
The findings were presented at the virtual annual meeting of the American Headache Society. Read more.
FDA approves avelumab as maintenance for urothelial carcinoma
The Food and Drug Administration has approved avelumab (Bavencio) as a maintenance treatment for patients with locally advanced or metastatic urothelial carcinoma (UC) that has not progressed after first-line platinum-containing chemotherapy.
The new maintenance therapy indication for avelumab is based on efficacy demonstrated in the JAVELIN Bladder 100 trial. Results from this trial were presented as part of the American Society of Clinical Oncology virtual scientific program.
The new indication adds to avelumab use in other patient populations, including people with locally advanced or metastatic UC who experience disease progression during or following platinum-containing chemotherapy. The FDA also previously approved avelumab for patients who experienced UC progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy. The FDA first approved marketing of avelumab in 2017. Other uses include treatment of metastatic Merkel cell carcinoma and first-line treatment of advanced renal cell carcinoma in combination with axitinib. Read more.
Lifestyle changes may explain skin lesions in pandemic-era patients
Two European prospective case series found no direct association between skin lesions on the hands and feet and SARS-CoV-2 in young people, which raises questions about other contributing factors, such as lockdown conditions, which may be clarified with additional research. The study appeared in JAMA Dermatology.
Meanwhile, data from the American Academy of Dermatology and a recent paper from the British Journal of Dermatology suggest a real association exists, at in least some patients.
“It’s going to be true that most patients with toe lesions are PCR [polymerase chain reaction]-negative because it tends to be a late phenomenon when patients are no longer shedding virus,” explained Lindy P. Fox, MD, professor of dermatology at the University of California, San Francisco, who was not an author of either study. Read more.
Take-home test strips allow drug users to detect fentanyl
Illicit drug users seem to overwhelmingly appreciate being able to use take-home test strips to detect the presence of dangerous fentanyl in opioids and other drugs, a new study finds.
More than 95% said they’d use the inexpensive strips again.
“These tests accurately detect fentanyl in the drug supply, and they can be a valuable addition to other drug prevention strategies,” the study’s lead author and addiction medicine specialist Sukhpreet Klaire, MD, of the British Columbia Center on Substance Use in Vancouver, said in an interview.
Dr. Klaire presented the study findings at the virtual annual meeting of the College on Problems of Drug Dependence. Read more.
New data back use of medical cannabis for epilepsy, pain, anxiety
Two new studies offer positive news about medical cannabis, suggesting that marijuana products improve physical and cognitive symptoms, boost quality of life, and rarely produce signs of problematic use.
In one study, patients with epilepsy who used medical cannabis were nearly half as likely to have needed an emergency department visit within the last 30 days as was a control group. In the other study, just 3 of 54 subjects who used medical cannabis showed signs of possible cannabis use disorder (CUD) over 12 months.
The findings show that “there is improvement in a range of outcome variables, and the adverse effects seem to be minimal, compared to what we might have hypothesized based on the bulk of the literature on the negative effects of cannabis on health outcomes,” cannabis researcher Ziva Cooper, PhD, of the University of California at Los Angeles, said in an interview. Dr. Cooper moderated a session about the studies at the virtual annual meeting of the College on Problems of Drug Dependence. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Migraine is often a deciding factor in pregnancy planning
Migraine can significantly influence a woman’s decision to have children, new research shows.
Results from a multicenter study of more than 600 women showed that, among participants with migraine, those who were younger, had menstrual migraine, or had chronic migraine were more likely to decide to not become pregnant.
“Women who avoided pregnancy due to migraine were most concerned that migraine would make raising a child difficult, that the migraine medications they take would have a negative impact on their child’s development, and that their migraine pattern would worsen during or just after pregnancy,” said study investigator Ryotaro Ishii, MD, PhD, a visiting scientist at Mayo Clinic in Phoenix.
The findings were presented at the virtual annual meeting of the American Headache Society. Read more.
FDA approves avelumab as maintenance for urothelial carcinoma
The Food and Drug Administration has approved avelumab (Bavencio) as a maintenance treatment for patients with locally advanced or metastatic urothelial carcinoma (UC) that has not progressed after first-line platinum-containing chemotherapy.
The new maintenance therapy indication for avelumab is based on efficacy demonstrated in the JAVELIN Bladder 100 trial. Results from this trial were presented as part of the American Society of Clinical Oncology virtual scientific program.
The new indication adds to avelumab use in other patient populations, including people with locally advanced or metastatic UC who experience disease progression during or following platinum-containing chemotherapy. The FDA also previously approved avelumab for patients who experienced UC progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy. The FDA first approved marketing of avelumab in 2017. Other uses include treatment of metastatic Merkel cell carcinoma and first-line treatment of advanced renal cell carcinoma in combination with axitinib. Read more.
Lifestyle changes may explain skin lesions in pandemic-era patients
Two European prospective case series found no direct association between skin lesions on the hands and feet and SARS-CoV-2 in young people, which raises questions about other contributing factors, such as lockdown conditions, which may be clarified with additional research. The study appeared in JAMA Dermatology.
Meanwhile, data from the American Academy of Dermatology and a recent paper from the British Journal of Dermatology suggest a real association exists, at in least some patients.
“It’s going to be true that most patients with toe lesions are PCR [polymerase chain reaction]-negative because it tends to be a late phenomenon when patients are no longer shedding virus,” explained Lindy P. Fox, MD, professor of dermatology at the University of California, San Francisco, who was not an author of either study. Read more.
Take-home test strips allow drug users to detect fentanyl
Illicit drug users seem to overwhelmingly appreciate being able to use take-home test strips to detect the presence of dangerous fentanyl in opioids and other drugs, a new study finds.
More than 95% said they’d use the inexpensive strips again.
“These tests accurately detect fentanyl in the drug supply, and they can be a valuable addition to other drug prevention strategies,” the study’s lead author and addiction medicine specialist Sukhpreet Klaire, MD, of the British Columbia Center on Substance Use in Vancouver, said in an interview.
Dr. Klaire presented the study findings at the virtual annual meeting of the College on Problems of Drug Dependence. Read more.
New data back use of medical cannabis for epilepsy, pain, anxiety
Two new studies offer positive news about medical cannabis, suggesting that marijuana products improve physical and cognitive symptoms, boost quality of life, and rarely produce signs of problematic use.
In one study, patients with epilepsy who used medical cannabis were nearly half as likely to have needed an emergency department visit within the last 30 days as was a control group. In the other study, just 3 of 54 subjects who used medical cannabis showed signs of possible cannabis use disorder (CUD) over 12 months.
The findings show that “there is improvement in a range of outcome variables, and the adverse effects seem to be minimal, compared to what we might have hypothesized based on the bulk of the literature on the negative effects of cannabis on health outcomes,” cannabis researcher Ziva Cooper, PhD, of the University of California at Los Angeles, said in an interview. Dr. Cooper moderated a session about the studies at the virtual annual meeting of the College on Problems of Drug Dependence. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Lawmakers question mental health disclosure rules
State medical licensing queries criticized
Several federal lawmakers on June 30 questioned state policies that require disclosure of mental health treatment as part of medical licensing applications and renewals, citing concerns about creating barriers to psychiatric care for clinicians.
Mental health–related questions on state medical boards’ licensing applications are especially worrisome with many clinicians, including ED staff, immersed in the physical and emotional challenges involved in treating waves of people with COVID-19, lawmakers said during a hearing of the House Energy and Commerce Committee’s health panel.
“We must consider the mental health of the providers on the front lines of the pandemic,” said Rep. Morgan Griffith, a Virginia Republican.
The issue of state medical boards’ disclosure rules was not on the official agenda for the House Energy and Commerce health subcommittee’s hearing. And there was no discussion of any specific state medical board’s regulations. The Energy and Commerce health subcommittee is working on more than 20 bills related to mental health, including measures intended to aid first responders, such as firemen and emergency medical personnel, and students.
This hearing marked an early stage in the process for a planned package of mental health legislation, said Rep. Michael C. Burgess, MD, of Texas, who is the top Republican on the Energy and Commerce health subcommittee. There may be opportunities as this legislation advances to add provisions intended to aid physicians, said Dr. Burgess, who practiced for many years as an ob.gyn. before being elected to Congress.
“We knew that suicide was a problem among our colleagues prior to the onset of this coronavirus epidemic and I know it is more pronounced now,” he said.
Dr. Burgess then solicited specific recommendations from the hearing’s witnesses on steps needed to help clinicians’ mental health.
The first suggestion offered in reply by Jeffrey L. Geller, MD, MPH, appearing in his role as president of the American Psychiatric Association, was that Congress should look for ways to encourage states to alter their licensing procedures.
The hearing comes on the heels of the APA, the American Academy of Family Physicians, and more than 40 other groups having jointly signed a statement calling for changes to disclosure rules about mental health.
“Licensing and credentialing applications by covered entities should only employ narrowly focused questions that address current functional impairment,” the statement said. “Additionally, we strongly support The Joint Commission (TJC) statement on Removing Barriers to Mental Health Care for Clinicians and Health Care Staff. TJC ‘supports the removal of any barriers that inhibit clinicians and health care staff from accessing mental health care services.’ ”
Physicians and other clinicians must be able to safely secure treatment for mental or other health issues, just as any other individual,” the groups wrote. “A provider’s history of mental illness or substance use disorder should not be used as any indication of their current or future ability to practice competently and without impairment.”
Also among the signers to this statement was the Federation of State Medical Boards, which has been leading an effort for years to change licensing.
In 2018, the FSMB recommended state medical boards reconsider whether it is necessary to include probing questions about a physician applicant’s mental health, addiction, or substance use on applications for medical licensure or their renewal. While the intent of these questions may be to protect patients, these queries can discourage physicians from getting needed help, the FSMB said.
Several states have since revised or considered revising their license applications and renewals. In May 2020, The Joint Commission urged broader adoption of recommendations from the FSMB and the American Medical Association to limit queries about clinicians’ mental health to “conditions that currently impair the clinicians’ ability to perform their job.”
“We strongly encourage organizations to not ask about past history of mental health conditions or treatment,” said The Joint Commission, which accredits hospitals, in a statement. “It is critical that we ensure health care workers can feel free to access mental health resources.”
Rep. Susan Brooks, an Indiana Republican who is an attorney, suggested there may need to be a broader look at how state officials pose questions about past mental health treatment to people in many professions, including her own.
“It does build on the stigma on accessing services” to know a state or licensing authority may question a professional about receiving treatment for mental health, she said.
Also at the hearing, Rep. Nanette Diaz Barragán, a California Democrat, spoke of her own reaction to seeing a question about mental health treatment while applying for a White House internship. During her college years, Rep. Barragán had to cope with her father’s terminal illness.
“I remember thinking to myself: ‘Jeez, if I end up seeing a mental health expert maybe one day I couldn’t work in government,’ ” she said.
State medical licensing queries criticized
State medical licensing queries criticized
Several federal lawmakers on June 30 questioned state policies that require disclosure of mental health treatment as part of medical licensing applications and renewals, citing concerns about creating barriers to psychiatric care for clinicians.
Mental health–related questions on state medical boards’ licensing applications are especially worrisome with many clinicians, including ED staff, immersed in the physical and emotional challenges involved in treating waves of people with COVID-19, lawmakers said during a hearing of the House Energy and Commerce Committee’s health panel.
“We must consider the mental health of the providers on the front lines of the pandemic,” said Rep. Morgan Griffith, a Virginia Republican.
The issue of state medical boards’ disclosure rules was not on the official agenda for the House Energy and Commerce health subcommittee’s hearing. And there was no discussion of any specific state medical board’s regulations. The Energy and Commerce health subcommittee is working on more than 20 bills related to mental health, including measures intended to aid first responders, such as firemen and emergency medical personnel, and students.
This hearing marked an early stage in the process for a planned package of mental health legislation, said Rep. Michael C. Burgess, MD, of Texas, who is the top Republican on the Energy and Commerce health subcommittee. There may be opportunities as this legislation advances to add provisions intended to aid physicians, said Dr. Burgess, who practiced for many years as an ob.gyn. before being elected to Congress.
“We knew that suicide was a problem among our colleagues prior to the onset of this coronavirus epidemic and I know it is more pronounced now,” he said.
Dr. Burgess then solicited specific recommendations from the hearing’s witnesses on steps needed to help clinicians’ mental health.
The first suggestion offered in reply by Jeffrey L. Geller, MD, MPH, appearing in his role as president of the American Psychiatric Association, was that Congress should look for ways to encourage states to alter their licensing procedures.
The hearing comes on the heels of the APA, the American Academy of Family Physicians, and more than 40 other groups having jointly signed a statement calling for changes to disclosure rules about mental health.
“Licensing and credentialing applications by covered entities should only employ narrowly focused questions that address current functional impairment,” the statement said. “Additionally, we strongly support The Joint Commission (TJC) statement on Removing Barriers to Mental Health Care for Clinicians and Health Care Staff. TJC ‘supports the removal of any barriers that inhibit clinicians and health care staff from accessing mental health care services.’ ”
Physicians and other clinicians must be able to safely secure treatment for mental or other health issues, just as any other individual,” the groups wrote. “A provider’s history of mental illness or substance use disorder should not be used as any indication of their current or future ability to practice competently and without impairment.”
Also among the signers to this statement was the Federation of State Medical Boards, which has been leading an effort for years to change licensing.
In 2018, the FSMB recommended state medical boards reconsider whether it is necessary to include probing questions about a physician applicant’s mental health, addiction, or substance use on applications for medical licensure or their renewal. While the intent of these questions may be to protect patients, these queries can discourage physicians from getting needed help, the FSMB said.
Several states have since revised or considered revising their license applications and renewals. In May 2020, The Joint Commission urged broader adoption of recommendations from the FSMB and the American Medical Association to limit queries about clinicians’ mental health to “conditions that currently impair the clinicians’ ability to perform their job.”
“We strongly encourage organizations to not ask about past history of mental health conditions or treatment,” said The Joint Commission, which accredits hospitals, in a statement. “It is critical that we ensure health care workers can feel free to access mental health resources.”
Rep. Susan Brooks, an Indiana Republican who is an attorney, suggested there may need to be a broader look at how state officials pose questions about past mental health treatment to people in many professions, including her own.
“It does build on the stigma on accessing services” to know a state or licensing authority may question a professional about receiving treatment for mental health, she said.
Also at the hearing, Rep. Nanette Diaz Barragán, a California Democrat, spoke of her own reaction to seeing a question about mental health treatment while applying for a White House internship. During her college years, Rep. Barragán had to cope with her father’s terminal illness.
“I remember thinking to myself: ‘Jeez, if I end up seeing a mental health expert maybe one day I couldn’t work in government,’ ” she said.
Several federal lawmakers on June 30 questioned state policies that require disclosure of mental health treatment as part of medical licensing applications and renewals, citing concerns about creating barriers to psychiatric care for clinicians.
Mental health–related questions on state medical boards’ licensing applications are especially worrisome with many clinicians, including ED staff, immersed in the physical and emotional challenges involved in treating waves of people with COVID-19, lawmakers said during a hearing of the House Energy and Commerce Committee’s health panel.
“We must consider the mental health of the providers on the front lines of the pandemic,” said Rep. Morgan Griffith, a Virginia Republican.
The issue of state medical boards’ disclosure rules was not on the official agenda for the House Energy and Commerce health subcommittee’s hearing. And there was no discussion of any specific state medical board’s regulations. The Energy and Commerce health subcommittee is working on more than 20 bills related to mental health, including measures intended to aid first responders, such as firemen and emergency medical personnel, and students.
This hearing marked an early stage in the process for a planned package of mental health legislation, said Rep. Michael C. Burgess, MD, of Texas, who is the top Republican on the Energy and Commerce health subcommittee. There may be opportunities as this legislation advances to add provisions intended to aid physicians, said Dr. Burgess, who practiced for many years as an ob.gyn. before being elected to Congress.
“We knew that suicide was a problem among our colleagues prior to the onset of this coronavirus epidemic and I know it is more pronounced now,” he said.
Dr. Burgess then solicited specific recommendations from the hearing’s witnesses on steps needed to help clinicians’ mental health.
The first suggestion offered in reply by Jeffrey L. Geller, MD, MPH, appearing in his role as president of the American Psychiatric Association, was that Congress should look for ways to encourage states to alter their licensing procedures.
The hearing comes on the heels of the APA, the American Academy of Family Physicians, and more than 40 other groups having jointly signed a statement calling for changes to disclosure rules about mental health.
“Licensing and credentialing applications by covered entities should only employ narrowly focused questions that address current functional impairment,” the statement said. “Additionally, we strongly support The Joint Commission (TJC) statement on Removing Barriers to Mental Health Care for Clinicians and Health Care Staff. TJC ‘supports the removal of any barriers that inhibit clinicians and health care staff from accessing mental health care services.’ ”
Physicians and other clinicians must be able to safely secure treatment for mental or other health issues, just as any other individual,” the groups wrote. “A provider’s history of mental illness or substance use disorder should not be used as any indication of their current or future ability to practice competently and without impairment.”
Also among the signers to this statement was the Federation of State Medical Boards, which has been leading an effort for years to change licensing.
In 2018, the FSMB recommended state medical boards reconsider whether it is necessary to include probing questions about a physician applicant’s mental health, addiction, or substance use on applications for medical licensure or their renewal. While the intent of these questions may be to protect patients, these queries can discourage physicians from getting needed help, the FSMB said.
Several states have since revised or considered revising their license applications and renewals. In May 2020, The Joint Commission urged broader adoption of recommendations from the FSMB and the American Medical Association to limit queries about clinicians’ mental health to “conditions that currently impair the clinicians’ ability to perform their job.”
“We strongly encourage organizations to not ask about past history of mental health conditions or treatment,” said The Joint Commission, which accredits hospitals, in a statement. “It is critical that we ensure health care workers can feel free to access mental health resources.”
Rep. Susan Brooks, an Indiana Republican who is an attorney, suggested there may need to be a broader look at how state officials pose questions about past mental health treatment to people in many professions, including her own.
“It does build on the stigma on accessing services” to know a state or licensing authority may question a professional about receiving treatment for mental health, she said.
Also at the hearing, Rep. Nanette Diaz Barragán, a California Democrat, spoke of her own reaction to seeing a question about mental health treatment while applying for a White House internship. During her college years, Rep. Barragán had to cope with her father’s terminal illness.
“I remember thinking to myself: ‘Jeez, if I end up seeing a mental health expert maybe one day I couldn’t work in government,’ ” she said.
FROM A HOUSE ENERGY AND COMMERCE’S HEALTH SUBCOMMITTEE HEARING
Cushing’s and COVID-19: Nontraditional symptoms keys to assessment, treatments
Do not rely on more traditional signs and symptoms of COVID-19 like fever and dyspnea when assessing patients with Cushing’s syndrome for the novel coronavirus, Rosario Pivonello, MD, PhD, and colleagues urged.
Physicians evaluating patients with Cushing’s syndrome for COVID-19 “should be suspicious of any change in health status of their patients with Cushing’s syndrome, rather than relying on fever and [dyspnea] as typical features,” Dr. Pivonello, an endocrinologist with the University of Naples (Italy) Federico II, and colleagues wrote in a commentary published in The Lancet Diabetes & Endocrinology.
COVID-19 symptoms are a unique concern among patients with Cushing’s syndrome because many of the cardiometabolic and immune impairments that place someone at higher risk of more severe disease or mortality for the novel coronavirus – such as obesity, hypertension, diabetes, and immunodeficiency syndromes – are also shared with Cushing’s syndrome.
Increased cardiovascular risk factors and susceptibility to severe infection are “two leading causes of death” for patients with Cushing’s syndrome, Dr. Pivonello and colleagues noted.
The immunocompromised state of patients with Cushing’s syndrome may make detection of COVID-19 infection difficult, the authors say. For example, fever is a common symptom of patients with COVID-19, but in patients with active Cushing’s syndrome, “low-grade chronic inflammation and the poor immune response might limit febrile response in the early phase of infection,” Dr. Pivonello and colleagues wrote.
In other cases, because Cushing’s syndrome and COVID-19 have overlapping symptoms, it may be difficult to attribute a particular symptom to either disease. Dyspnea is a common symptom of COVID-19, but may present in Cushing’s syndrome because of “cardiac insufficiency or weakness of respiratory muscles,” the authors wrote. Instead, physicians should look to other COVID-19 symptoms, such as cough, dysgeusia, anosmia, and diarrhea, for signs of the disease.
Patients with Cushing’s syndrome may also be predisposed to a more severe course of COVID-19 because of the prevalence of obesity, hypertension, or diabetes in these patients, which have been identified as comorbidities that increase the likelihood of severe COVID-19 and progression to acute respiratory distress syndrome (ARDS). “However, a key element in the development of ARDS during COVID-19 is the exaggerated cellular response induced by the cytokine increase, leading to massive alveolar–capillary wall damage and a decline in gas exchange,” Dr. Pivonello and colleagues wrote. “Because patients with Cushing’s syndrome might not mount a normal cytokine response, these patients might [paradoxically] be less prone to develop severe ARDS with COVID-19.”
As both Cushing’s syndrome and COVID-19 are associated with hypercoagulability, the authors “strongly advise” using low-molecular-weight heparin in hospitalized patients with active Cushing’s syndrome who develop COVID-19. In both diseases, there is also a risk of longer duration of viral infections and opportunistic infections such as atypical bacterial and invasive fungal infections. For this reason, the authors also recommended patients with Cushing’s syndrome who have COVID-19 be placed on prolonged antiviral and broad-spectrum antibiotic treatment as a prophylactic measure.
During the pandemic, avoiding surgery for Cushing’s syndrome should be considered to reduce the likelihood of acquiring COVID-19 in a hospital setting, the authors wrote. Medical therapy can be temporarily used where appropriate, such as using ketoconazole, metyrapone, osilodrostat, and etomidate to lower cortisol levels. They acknowledge that some cases of malignant Cushing’s syndrome may require “expeditious definitive diagnosis and proper surgical resolution.”
After remission, while infection risk should be significantly lowered, other comorbidities like obesity, hypertension, diabetes, and thromboembolic diathesis may remain. “Because these are features associated with an increased death risk in patients with COVID-19, patients with Cushing’s syndrome in remission should be considered a high-risk population and consequently adopt adequate self-protection strategies to [minimize] contagion risk,” the authors wrote.
Dr. Pivonello reported relationships with Novartis, Strongbridge Biopharma, HRA Pharma, Ipsen, Shire, and Pfizer, Corcept Therapeutics, IBSA Farmaceutici, Ferring, and Italfarmaco in the form of receiving grants and/or personal fees. One coauthor reported receiving grants and/or nonfinancial support from Takeda, Ipsen, Shire, Pfizer, and Corcept Therapeutics. One coauthor reported receiving grants and personal fees from Novartis and Strongbridge, and grants from Millendo Therapeutics. Another coauthor reported receiving grants and/or personal fees from Novartis, Ipsen, Shire, Pfizer, Italfarmaco, Lilly, Merck, and Novo Nordisk. The other authors reported no relevant conflicts of interest.
SOURCE: Pivonello R et al. Lancet Diabetes Endocrinol. 2020 Jun 9. doi: 10.1016/S2213-8587(20)30215-1.
Do not rely on more traditional signs and symptoms of COVID-19 like fever and dyspnea when assessing patients with Cushing’s syndrome for the novel coronavirus, Rosario Pivonello, MD, PhD, and colleagues urged.
Physicians evaluating patients with Cushing’s syndrome for COVID-19 “should be suspicious of any change in health status of their patients with Cushing’s syndrome, rather than relying on fever and [dyspnea] as typical features,” Dr. Pivonello, an endocrinologist with the University of Naples (Italy) Federico II, and colleagues wrote in a commentary published in The Lancet Diabetes & Endocrinology.
COVID-19 symptoms are a unique concern among patients with Cushing’s syndrome because many of the cardiometabolic and immune impairments that place someone at higher risk of more severe disease or mortality for the novel coronavirus – such as obesity, hypertension, diabetes, and immunodeficiency syndromes – are also shared with Cushing’s syndrome.
Increased cardiovascular risk factors and susceptibility to severe infection are “two leading causes of death” for patients with Cushing’s syndrome, Dr. Pivonello and colleagues noted.
The immunocompromised state of patients with Cushing’s syndrome may make detection of COVID-19 infection difficult, the authors say. For example, fever is a common symptom of patients with COVID-19, but in patients with active Cushing’s syndrome, “low-grade chronic inflammation and the poor immune response might limit febrile response in the early phase of infection,” Dr. Pivonello and colleagues wrote.
In other cases, because Cushing’s syndrome and COVID-19 have overlapping symptoms, it may be difficult to attribute a particular symptom to either disease. Dyspnea is a common symptom of COVID-19, but may present in Cushing’s syndrome because of “cardiac insufficiency or weakness of respiratory muscles,” the authors wrote. Instead, physicians should look to other COVID-19 symptoms, such as cough, dysgeusia, anosmia, and diarrhea, for signs of the disease.
Patients with Cushing’s syndrome may also be predisposed to a more severe course of COVID-19 because of the prevalence of obesity, hypertension, or diabetes in these patients, which have been identified as comorbidities that increase the likelihood of severe COVID-19 and progression to acute respiratory distress syndrome (ARDS). “However, a key element in the development of ARDS during COVID-19 is the exaggerated cellular response induced by the cytokine increase, leading to massive alveolar–capillary wall damage and a decline in gas exchange,” Dr. Pivonello and colleagues wrote. “Because patients with Cushing’s syndrome might not mount a normal cytokine response, these patients might [paradoxically] be less prone to develop severe ARDS with COVID-19.”
As both Cushing’s syndrome and COVID-19 are associated with hypercoagulability, the authors “strongly advise” using low-molecular-weight heparin in hospitalized patients with active Cushing’s syndrome who develop COVID-19. In both diseases, there is also a risk of longer duration of viral infections and opportunistic infections such as atypical bacterial and invasive fungal infections. For this reason, the authors also recommended patients with Cushing’s syndrome who have COVID-19 be placed on prolonged antiviral and broad-spectrum antibiotic treatment as a prophylactic measure.
During the pandemic, avoiding surgery for Cushing’s syndrome should be considered to reduce the likelihood of acquiring COVID-19 in a hospital setting, the authors wrote. Medical therapy can be temporarily used where appropriate, such as using ketoconazole, metyrapone, osilodrostat, and etomidate to lower cortisol levels. They acknowledge that some cases of malignant Cushing’s syndrome may require “expeditious definitive diagnosis and proper surgical resolution.”
After remission, while infection risk should be significantly lowered, other comorbidities like obesity, hypertension, diabetes, and thromboembolic diathesis may remain. “Because these are features associated with an increased death risk in patients with COVID-19, patients with Cushing’s syndrome in remission should be considered a high-risk population and consequently adopt adequate self-protection strategies to [minimize] contagion risk,” the authors wrote.
Dr. Pivonello reported relationships with Novartis, Strongbridge Biopharma, HRA Pharma, Ipsen, Shire, and Pfizer, Corcept Therapeutics, IBSA Farmaceutici, Ferring, and Italfarmaco in the form of receiving grants and/or personal fees. One coauthor reported receiving grants and/or nonfinancial support from Takeda, Ipsen, Shire, Pfizer, and Corcept Therapeutics. One coauthor reported receiving grants and personal fees from Novartis and Strongbridge, and grants from Millendo Therapeutics. Another coauthor reported receiving grants and/or personal fees from Novartis, Ipsen, Shire, Pfizer, Italfarmaco, Lilly, Merck, and Novo Nordisk. The other authors reported no relevant conflicts of interest.
SOURCE: Pivonello R et al. Lancet Diabetes Endocrinol. 2020 Jun 9. doi: 10.1016/S2213-8587(20)30215-1.
Do not rely on more traditional signs and symptoms of COVID-19 like fever and dyspnea when assessing patients with Cushing’s syndrome for the novel coronavirus, Rosario Pivonello, MD, PhD, and colleagues urged.
Physicians evaluating patients with Cushing’s syndrome for COVID-19 “should be suspicious of any change in health status of their patients with Cushing’s syndrome, rather than relying on fever and [dyspnea] as typical features,” Dr. Pivonello, an endocrinologist with the University of Naples (Italy) Federico II, and colleagues wrote in a commentary published in The Lancet Diabetes & Endocrinology.
COVID-19 symptoms are a unique concern among patients with Cushing’s syndrome because many of the cardiometabolic and immune impairments that place someone at higher risk of more severe disease or mortality for the novel coronavirus – such as obesity, hypertension, diabetes, and immunodeficiency syndromes – are also shared with Cushing’s syndrome.
Increased cardiovascular risk factors and susceptibility to severe infection are “two leading causes of death” for patients with Cushing’s syndrome, Dr. Pivonello and colleagues noted.
The immunocompromised state of patients with Cushing’s syndrome may make detection of COVID-19 infection difficult, the authors say. For example, fever is a common symptom of patients with COVID-19, but in patients with active Cushing’s syndrome, “low-grade chronic inflammation and the poor immune response might limit febrile response in the early phase of infection,” Dr. Pivonello and colleagues wrote.
In other cases, because Cushing’s syndrome and COVID-19 have overlapping symptoms, it may be difficult to attribute a particular symptom to either disease. Dyspnea is a common symptom of COVID-19, but may present in Cushing’s syndrome because of “cardiac insufficiency or weakness of respiratory muscles,” the authors wrote. Instead, physicians should look to other COVID-19 symptoms, such as cough, dysgeusia, anosmia, and diarrhea, for signs of the disease.
Patients with Cushing’s syndrome may also be predisposed to a more severe course of COVID-19 because of the prevalence of obesity, hypertension, or diabetes in these patients, which have been identified as comorbidities that increase the likelihood of severe COVID-19 and progression to acute respiratory distress syndrome (ARDS). “However, a key element in the development of ARDS during COVID-19 is the exaggerated cellular response induced by the cytokine increase, leading to massive alveolar–capillary wall damage and a decline in gas exchange,” Dr. Pivonello and colleagues wrote. “Because patients with Cushing’s syndrome might not mount a normal cytokine response, these patients might [paradoxically] be less prone to develop severe ARDS with COVID-19.”
As both Cushing’s syndrome and COVID-19 are associated with hypercoagulability, the authors “strongly advise” using low-molecular-weight heparin in hospitalized patients with active Cushing’s syndrome who develop COVID-19. In both diseases, there is also a risk of longer duration of viral infections and opportunistic infections such as atypical bacterial and invasive fungal infections. For this reason, the authors also recommended patients with Cushing’s syndrome who have COVID-19 be placed on prolonged antiviral and broad-spectrum antibiotic treatment as a prophylactic measure.
During the pandemic, avoiding surgery for Cushing’s syndrome should be considered to reduce the likelihood of acquiring COVID-19 in a hospital setting, the authors wrote. Medical therapy can be temporarily used where appropriate, such as using ketoconazole, metyrapone, osilodrostat, and etomidate to lower cortisol levels. They acknowledge that some cases of malignant Cushing’s syndrome may require “expeditious definitive diagnosis and proper surgical resolution.”
After remission, while infection risk should be significantly lowered, other comorbidities like obesity, hypertension, diabetes, and thromboembolic diathesis may remain. “Because these are features associated with an increased death risk in patients with COVID-19, patients with Cushing’s syndrome in remission should be considered a high-risk population and consequently adopt adequate self-protection strategies to [minimize] contagion risk,” the authors wrote.
Dr. Pivonello reported relationships with Novartis, Strongbridge Biopharma, HRA Pharma, Ipsen, Shire, and Pfizer, Corcept Therapeutics, IBSA Farmaceutici, Ferring, and Italfarmaco in the form of receiving grants and/or personal fees. One coauthor reported receiving grants and/or nonfinancial support from Takeda, Ipsen, Shire, Pfizer, and Corcept Therapeutics. One coauthor reported receiving grants and personal fees from Novartis and Strongbridge, and grants from Millendo Therapeutics. Another coauthor reported receiving grants and/or personal fees from Novartis, Ipsen, Shire, Pfizer, Italfarmaco, Lilly, Merck, and Novo Nordisk. The other authors reported no relevant conflicts of interest.
SOURCE: Pivonello R et al. Lancet Diabetes Endocrinol. 2020 Jun 9. doi: 10.1016/S2213-8587(20)30215-1.
FROM THE LANCET DIABETES & ENDOCRINOLOGY
Lifestyle changes may explain skin lesions in pandemic-era patients
such as lockdown conditions, which may be clarified with additional research.
Lindy P. Fox, MD, professor of dermatology at the University of California, San Francisco, who was not an author of either study, urged caution in interpreting these results. Data from the American Academy of Dermatology and a recent paper from the British Journal of Dermatology suggest a real association exists, at in least some patients. “It’s going to be true that most patients with toe lesions are PCR [polymerase chain reaction]-negative because it tends to be a late phenomenon when patients are no longer shedding virus,” Dr. Fox said in an interview.
Reports about chickenpox-like vesicles, urticaria, and other skin lesions in SARS-CoV-2 patients have circulated in the clinical literature and the media. Acute acro-ischemia has been cited as a potential sign of infection in adolescents and children.
One of the European studies, which was published in JAMA Dermatology, explored this association in 20 patients aged 1-18 years (mean age, 12.3 years), who presented with new-onset acral inflammatory lesions in their hands and feet at La Fe University Hospital, in Valencia, during the country’s peak quarantine period in April. Investigators conducted blood tests and reverse transcriptase–PCR (RT-PCR) for SARS-CoV-2, and six patients had skin biopsies.
Juncal Roca-Ginés, MD, of the department of dermatology, at the Hospital Universitario y Politécnico in La Fe, and coauthors, identified acral erythema in 6 (30%) of the cases, dactylitis in 4 (20%), purpuric maculopapules in 7 (35%), and a mixed pattern in 3 (15%). Serologic and viral testing yielded no positive results for SARS-CoV-2 or other viruses, and none of the patients exhibited COVID-19 symptoms such as fever, dry cough, sore throat, myalgia, or taste or smell disorders. In other findings, 45% of the patients had a history of vascular reactive disease of the hands, and 75% reported walking barefoot in their homes while staying at home. Only two patients reported taking medications.
In the six patients who had a biopsy, the findings were characteristic of chillblains, “confirming the clinical impression,” the authors wrote. Concluding that they could not show a relationship between acute acral skin changes and COVID-19, they noted that “other studies with improved microbiologic tests or molecular techniques aimed at demonstrating the presence of SARS-CoV-2 in the skin may help to clarify this problem.”
The other case series, which was also published in JAMA Dermatology and included 31 adults at a hospital in Brussels, who had recently developed chillblains, also looked for a connection between SARS-CoV-2 and chilblains, in April. Most of the participants were in their teens or 20s. Lesions had appeared on hands, feet, or on both extremities within 1-30 days of consultation, presenting as erythematous or purplish erythematous macules, occasionally with central vesicular or bullous lesions or necrotic areas. Patients reported pain, burning, and itching.
Skin biopsies were obtained in 22 patients and confirmed the diagnosis of chilblains; of the 15 with immunofluorescence analyses, 7 patients were found to have vasculitis of small-diameter vessels.
Of the 31 patients, 20 (64%) reported mild symptoms consistent with SARS-CoV-2, yet none of the RT-PCR or serologic test results showed signs of the virus in all 31 patients. “Because some patients had experienced chilblains for more than 15 days [under 30 days or less] at the time of inclusion, we can reasonably exclude the possibility that serologic testing was done too soon,” observed the authors. They also didn’t find eosinopenia, lymphopenia, and hyperferritinemia, which have been associated with COVID-19, they added.
Changes in lifestyle conditions during the pandemic may explain the appearance of these lesions, according to the authors of both studies, who mentioned that walking around in socks or bare feet and reduced physical activity could have indirectly led to the development of skin lesions.
It’s also possible that young people have less severe disease and a delayed reaction to the virus, Ignacio Torres-Navarro, MD, a dermatologist with La Fe University and the Spanish study’s corresponding author, said in an interview. Their feet may lack maturity in neurovascular regulation and/or the eccrine glands, which can happen in other diseases such as neutrophilic idiopathic eccrine hidradenitis. “In this context, perhaps there was an observational bias of the parents to the children when this manifestation was reported in the media. However, nothing has been demonstrated,” he said.
In an accompanying editor’s note, Claudia Hernandez, MD, of the departments of dermatology and pediatrics, Rush University Medical Center, Chicago, and Anna L. Bruckner, MD, of the departments of dermatology and pediatrics at the University of Colorado, Aurora, wrote that “it is still unclear whether a viral cytopathic process vs a viral reaction pattern or other mechanism is responsible for ‘COVID toes.’ ” Lack of confirmatory testing and reliance on indirect evidence of infection complicates this further, they noted, adding that “dermatologists must be aware of the protean cutaneous findings that are possibly associated with COVID-19, even if our understanding of their origins remains incomplete.”
In an interview, Dr. Fox, a member of the AAD’s’s COVID-19 Registry task force, offered other possible reasons for the negative antibody tests in the studies. The assay might not have been testing the correct antigen, or the timing of the test might not have been optimal. “More studies will help this become less controversial,” she said.
The authors of the two case series acknowledged potential limitations of their studies. Neither was large in scope: Both took place over a week’s time and included small cohorts. The Belgian study had no control group or long-term follow-up. Little is still known about the clinical manifestations and detection methods for SARS-CoV-2, noted the authors of the Spanish study.
The Spanish study received funding La Fe University Hospital’s department of dermatology, and the authors had no disclosures. The Belgian study received support from the Fondation Saint-Luc, which provided academic funding for its lead author, Marie Baeck, MD, PhD. Another author of this study received personal fees from the Fondation Saint-Luc and personal fees and nonfinancial support from Bioderma. The authors of the editor’s note had no disclosures.
SOURCES: Roca-Ginés J et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2340; Herman A et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2368.
such as lockdown conditions, which may be clarified with additional research.
Lindy P. Fox, MD, professor of dermatology at the University of California, San Francisco, who was not an author of either study, urged caution in interpreting these results. Data from the American Academy of Dermatology and a recent paper from the British Journal of Dermatology suggest a real association exists, at in least some patients. “It’s going to be true that most patients with toe lesions are PCR [polymerase chain reaction]-negative because it tends to be a late phenomenon when patients are no longer shedding virus,” Dr. Fox said in an interview.
Reports about chickenpox-like vesicles, urticaria, and other skin lesions in SARS-CoV-2 patients have circulated in the clinical literature and the media. Acute acro-ischemia has been cited as a potential sign of infection in adolescents and children.
One of the European studies, which was published in JAMA Dermatology, explored this association in 20 patients aged 1-18 years (mean age, 12.3 years), who presented with new-onset acral inflammatory lesions in their hands and feet at La Fe University Hospital, in Valencia, during the country’s peak quarantine period in April. Investigators conducted blood tests and reverse transcriptase–PCR (RT-PCR) for SARS-CoV-2, and six patients had skin biopsies.
Juncal Roca-Ginés, MD, of the department of dermatology, at the Hospital Universitario y Politécnico in La Fe, and coauthors, identified acral erythema in 6 (30%) of the cases, dactylitis in 4 (20%), purpuric maculopapules in 7 (35%), and a mixed pattern in 3 (15%). Serologic and viral testing yielded no positive results for SARS-CoV-2 or other viruses, and none of the patients exhibited COVID-19 symptoms such as fever, dry cough, sore throat, myalgia, or taste or smell disorders. In other findings, 45% of the patients had a history of vascular reactive disease of the hands, and 75% reported walking barefoot in their homes while staying at home. Only two patients reported taking medications.
In the six patients who had a biopsy, the findings were characteristic of chillblains, “confirming the clinical impression,” the authors wrote. Concluding that they could not show a relationship between acute acral skin changes and COVID-19, they noted that “other studies with improved microbiologic tests or molecular techniques aimed at demonstrating the presence of SARS-CoV-2 in the skin may help to clarify this problem.”
The other case series, which was also published in JAMA Dermatology and included 31 adults at a hospital in Brussels, who had recently developed chillblains, also looked for a connection between SARS-CoV-2 and chilblains, in April. Most of the participants were in their teens or 20s. Lesions had appeared on hands, feet, or on both extremities within 1-30 days of consultation, presenting as erythematous or purplish erythematous macules, occasionally with central vesicular or bullous lesions or necrotic areas. Patients reported pain, burning, and itching.
Skin biopsies were obtained in 22 patients and confirmed the diagnosis of chilblains; of the 15 with immunofluorescence analyses, 7 patients were found to have vasculitis of small-diameter vessels.
Of the 31 patients, 20 (64%) reported mild symptoms consistent with SARS-CoV-2, yet none of the RT-PCR or serologic test results showed signs of the virus in all 31 patients. “Because some patients had experienced chilblains for more than 15 days [under 30 days or less] at the time of inclusion, we can reasonably exclude the possibility that serologic testing was done too soon,” observed the authors. They also didn’t find eosinopenia, lymphopenia, and hyperferritinemia, which have been associated with COVID-19, they added.
Changes in lifestyle conditions during the pandemic may explain the appearance of these lesions, according to the authors of both studies, who mentioned that walking around in socks or bare feet and reduced physical activity could have indirectly led to the development of skin lesions.
It’s also possible that young people have less severe disease and a delayed reaction to the virus, Ignacio Torres-Navarro, MD, a dermatologist with La Fe University and the Spanish study’s corresponding author, said in an interview. Their feet may lack maturity in neurovascular regulation and/or the eccrine glands, which can happen in other diseases such as neutrophilic idiopathic eccrine hidradenitis. “In this context, perhaps there was an observational bias of the parents to the children when this manifestation was reported in the media. However, nothing has been demonstrated,” he said.
In an accompanying editor’s note, Claudia Hernandez, MD, of the departments of dermatology and pediatrics, Rush University Medical Center, Chicago, and Anna L. Bruckner, MD, of the departments of dermatology and pediatrics at the University of Colorado, Aurora, wrote that “it is still unclear whether a viral cytopathic process vs a viral reaction pattern or other mechanism is responsible for ‘COVID toes.’ ” Lack of confirmatory testing and reliance on indirect evidence of infection complicates this further, they noted, adding that “dermatologists must be aware of the protean cutaneous findings that are possibly associated with COVID-19, even if our understanding of their origins remains incomplete.”
In an interview, Dr. Fox, a member of the AAD’s’s COVID-19 Registry task force, offered other possible reasons for the negative antibody tests in the studies. The assay might not have been testing the correct antigen, or the timing of the test might not have been optimal. “More studies will help this become less controversial,” she said.
The authors of the two case series acknowledged potential limitations of their studies. Neither was large in scope: Both took place over a week’s time and included small cohorts. The Belgian study had no control group or long-term follow-up. Little is still known about the clinical manifestations and detection methods for SARS-CoV-2, noted the authors of the Spanish study.
The Spanish study received funding La Fe University Hospital’s department of dermatology, and the authors had no disclosures. The Belgian study received support from the Fondation Saint-Luc, which provided academic funding for its lead author, Marie Baeck, MD, PhD. Another author of this study received personal fees from the Fondation Saint-Luc and personal fees and nonfinancial support from Bioderma. The authors of the editor’s note had no disclosures.
SOURCES: Roca-Ginés J et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2340; Herman A et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2368.
such as lockdown conditions, which may be clarified with additional research.
Lindy P. Fox, MD, professor of dermatology at the University of California, San Francisco, who was not an author of either study, urged caution in interpreting these results. Data from the American Academy of Dermatology and a recent paper from the British Journal of Dermatology suggest a real association exists, at in least some patients. “It’s going to be true that most patients with toe lesions are PCR [polymerase chain reaction]-negative because it tends to be a late phenomenon when patients are no longer shedding virus,” Dr. Fox said in an interview.
Reports about chickenpox-like vesicles, urticaria, and other skin lesions in SARS-CoV-2 patients have circulated in the clinical literature and the media. Acute acro-ischemia has been cited as a potential sign of infection in adolescents and children.
One of the European studies, which was published in JAMA Dermatology, explored this association in 20 patients aged 1-18 years (mean age, 12.3 years), who presented with new-onset acral inflammatory lesions in their hands and feet at La Fe University Hospital, in Valencia, during the country’s peak quarantine period in April. Investigators conducted blood tests and reverse transcriptase–PCR (RT-PCR) for SARS-CoV-2, and six patients had skin biopsies.
Juncal Roca-Ginés, MD, of the department of dermatology, at the Hospital Universitario y Politécnico in La Fe, and coauthors, identified acral erythema in 6 (30%) of the cases, dactylitis in 4 (20%), purpuric maculopapules in 7 (35%), and a mixed pattern in 3 (15%). Serologic and viral testing yielded no positive results for SARS-CoV-2 or other viruses, and none of the patients exhibited COVID-19 symptoms such as fever, dry cough, sore throat, myalgia, or taste or smell disorders. In other findings, 45% of the patients had a history of vascular reactive disease of the hands, and 75% reported walking barefoot in their homes while staying at home. Only two patients reported taking medications.
In the six patients who had a biopsy, the findings were characteristic of chillblains, “confirming the clinical impression,” the authors wrote. Concluding that they could not show a relationship between acute acral skin changes and COVID-19, they noted that “other studies with improved microbiologic tests or molecular techniques aimed at demonstrating the presence of SARS-CoV-2 in the skin may help to clarify this problem.”
The other case series, which was also published in JAMA Dermatology and included 31 adults at a hospital in Brussels, who had recently developed chillblains, also looked for a connection between SARS-CoV-2 and chilblains, in April. Most of the participants were in their teens or 20s. Lesions had appeared on hands, feet, or on both extremities within 1-30 days of consultation, presenting as erythematous or purplish erythematous macules, occasionally with central vesicular or bullous lesions or necrotic areas. Patients reported pain, burning, and itching.
Skin biopsies were obtained in 22 patients and confirmed the diagnosis of chilblains; of the 15 with immunofluorescence analyses, 7 patients were found to have vasculitis of small-diameter vessels.
Of the 31 patients, 20 (64%) reported mild symptoms consistent with SARS-CoV-2, yet none of the RT-PCR or serologic test results showed signs of the virus in all 31 patients. “Because some patients had experienced chilblains for more than 15 days [under 30 days or less] at the time of inclusion, we can reasonably exclude the possibility that serologic testing was done too soon,” observed the authors. They also didn’t find eosinopenia, lymphopenia, and hyperferritinemia, which have been associated with COVID-19, they added.
Changes in lifestyle conditions during the pandemic may explain the appearance of these lesions, according to the authors of both studies, who mentioned that walking around in socks or bare feet and reduced physical activity could have indirectly led to the development of skin lesions.
It’s also possible that young people have less severe disease and a delayed reaction to the virus, Ignacio Torres-Navarro, MD, a dermatologist with La Fe University and the Spanish study’s corresponding author, said in an interview. Their feet may lack maturity in neurovascular regulation and/or the eccrine glands, which can happen in other diseases such as neutrophilic idiopathic eccrine hidradenitis. “In this context, perhaps there was an observational bias of the parents to the children when this manifestation was reported in the media. However, nothing has been demonstrated,” he said.
In an accompanying editor’s note, Claudia Hernandez, MD, of the departments of dermatology and pediatrics, Rush University Medical Center, Chicago, and Anna L. Bruckner, MD, of the departments of dermatology and pediatrics at the University of Colorado, Aurora, wrote that “it is still unclear whether a viral cytopathic process vs a viral reaction pattern or other mechanism is responsible for ‘COVID toes.’ ” Lack of confirmatory testing and reliance on indirect evidence of infection complicates this further, they noted, adding that “dermatologists must be aware of the protean cutaneous findings that are possibly associated with COVID-19, even if our understanding of their origins remains incomplete.”
In an interview, Dr. Fox, a member of the AAD’s’s COVID-19 Registry task force, offered other possible reasons for the negative antibody tests in the studies. The assay might not have been testing the correct antigen, or the timing of the test might not have been optimal. “More studies will help this become less controversial,” she said.
The authors of the two case series acknowledged potential limitations of their studies. Neither was large in scope: Both took place over a week’s time and included small cohorts. The Belgian study had no control group or long-term follow-up. Little is still known about the clinical manifestations and detection methods for SARS-CoV-2, noted the authors of the Spanish study.
The Spanish study received funding La Fe University Hospital’s department of dermatology, and the authors had no disclosures. The Belgian study received support from the Fondation Saint-Luc, which provided academic funding for its lead author, Marie Baeck, MD, PhD. Another author of this study received personal fees from the Fondation Saint-Luc and personal fees and nonfinancial support from Bioderma. The authors of the editor’s note had no disclosures.
SOURCES: Roca-Ginés J et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2340; Herman A et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2368.



