User login
AAP: Teen access to abortion care is a right
.
“Genuine concern for the best interests of minors argues strongly against mandatory parental consent and notification laws,” the statement authors wrote in the updated policy statement, “The Adolescent’s Right to Confidential Care When Considering Abortion,” published online in Pediatrics.
The AAP Committee on Adolescence, which wrote the policy statement, encourages adolescents to voluntarily involve their parents – or other adults they trust – in decisions surrounding an unintended pregnancy, stating that teens who do will “likely benefit from adult experience, wisdom, emotional support, and financial support.” However, the policy statement also stresses that legally emphasizing parental involvement over a teen’s autonomy can result in barriers to care when timely access is most crucial, especially if a teen is reluctant to tell her parents of the situation (Pediatrics. 2017. doi: 10.1542/peds.2016-3861).
Currently, 37 states require some level of parental involvement in an adolescent’s decision to pursue an abortion. Most of these states will allow a minor to terminate a pregnancy without parental consent in the case of a medical emergency; about half waive the parental involvement requirement when there is evidence of incest, abuse, or neglect. All states with parental involvement laws also have a so-called judicial bypass, allowing a minor to obtain an abortion with a court’s approval; however, because the process can take as long as several weeks, access to medical treatment can be delayed, upping the risk of complications from later-term abortions. Data cited in the statement indicate that following the enactment of parental involvement laws in three states, second-trimester abortion rates increased by as much as 21% (N Engl J Med. 2006;354[10]:1031-8; Fam Plann Perspect. 1995;27[3]:120-2; Women Health. 1995;22[3]:47-58.
Even when a judicial bypass is obtained, a study of 12,000 such petitions obtained in Minnesota and Massachusetts showed that only 21 of them were denied, and half of those were overturned, meaning the outcome was the same, but the potential risks of delaying care were higher (J Adolesc Health. 1991;12[2]:143-7). The AAP statement suggests physicians learn their state requirements for judicial bypass, if any.
The updated statement also refutes the notion that parental involvement laws improve communication within families and lead to better health outcomes for teens facing an unintended pregnancy. Instead, the statement says that on average, minors who discuss pregnancy termination with their parents do so at the same rate as in states with and without such laws, and that a teen is more likely to involve her parents than not, a likelihood that increases the younger a teen is. When she doesn’t choose to discuss it with parents, fear of some sort of danger such as an escalation in any ongoing family tensions, coercion into a decision, or abuse of some kind is often why (Contraception. 2010 Oct;82[4]:310-3; Fam Plann Perspect. 1992 Jul-Aug;24[4]:148-54, 173).
“In a perfect world of butterflies and unicorns, parents and kids have a perfect relationship, but we know that’s not always true. There can be significant discord in families, and parental notification could result in harm to the adolescent, or risk to the family’s tapestry with significant consequences for the family and the adolescent,” Dr. Breuner said.
Dr. Beers argued that while she believed most parents would rather be the one their teen turns to for advice in such a situation, it’s not possible to legislate trust within families, each of which has its own history and unique family culture and style of communication. “This is the type of conversation that doesn’t begin with the acute event. This is the kind of conversation that should begin [at] a very early age between a parent and a child,” she said.
The physician’s role, according to Dr. Beers, is to ensure parents and their children have “a shared understanding of the facts to [rely on] when they talk about what is important to their family and what their family values are.”
The updated statement, originally issued in 1993, roughly coincides with the release of a new Guttmacher Institute report indicating that abortion rates in the United States are at their lowest since passage of Roe v. Wade in 1973. The report credits lower unintended pregnancy rates and better access to contraception, not restrictive abortion legislation, for the drop. The AAP’s updated statement also comes within days of the inauguration of President Donald Trump, whose run-up to election featured rhetoric challenging the status quo of federal abortion laws.
Dr. Breuner said the timing was a coincidence, and that plans to reissue the statement began over 3 years ago as she and her colleagues drew up plans to recommit their membership to protecting the reproductive rights of their patients. “With all of the regulations, restrictions, and decreased access to [abortion] care that are occurring, the academy wanted members to know just how much more difficult it is to obtain an abortion,” she said, noting that access and confidentiality are not the same. “If you can’t get an abortion, what difference does confidentiality make?”
Last year, the Supreme Court reversed a law that would have greatly limited access to abortion in Texas by closing all but nine clinics statewide, burdening them with care for tens of thousands of women annually. Also in 2016, citing a Constitutional violation of a woman’s right to privacy, a federal judge blocked an Indiana law signed by then governor and now vice president Mike Pence, that restricted the reasons a woman could cite to seek an abortion.
Dr. Breuner views this as an erosion of the rights of all women to comprehensive reproductive care, including those of adolescents. “You can’t ‘Google Map’ how to figure this out anymore. The roads are closed and all the ways people say you can get there don’t really lead you there,” she said, noting that the AAP’s statement is in line with several other professional medical societies, including the American College of Obstetricians and Gynecologists and the American Medical Association.
Regardless of timing, the statement should be viewed not through a political – or even partisan – lens, but as a reaffirmation of “core values,” according to Dr. Beers. “We do live in divided times. I think it’s important to circle back to our core values as pediatricians. That’s the agenda – making sure adolescents are healthy, safe, and supported.”
.
“Genuine concern for the best interests of minors argues strongly against mandatory parental consent and notification laws,” the statement authors wrote in the updated policy statement, “The Adolescent’s Right to Confidential Care When Considering Abortion,” published online in Pediatrics.
The AAP Committee on Adolescence, which wrote the policy statement, encourages adolescents to voluntarily involve their parents – or other adults they trust – in decisions surrounding an unintended pregnancy, stating that teens who do will “likely benefit from adult experience, wisdom, emotional support, and financial support.” However, the policy statement also stresses that legally emphasizing parental involvement over a teen’s autonomy can result in barriers to care when timely access is most crucial, especially if a teen is reluctant to tell her parents of the situation (Pediatrics. 2017. doi: 10.1542/peds.2016-3861).
Currently, 37 states require some level of parental involvement in an adolescent’s decision to pursue an abortion. Most of these states will allow a minor to terminate a pregnancy without parental consent in the case of a medical emergency; about half waive the parental involvement requirement when there is evidence of incest, abuse, or neglect. All states with parental involvement laws also have a so-called judicial bypass, allowing a minor to obtain an abortion with a court’s approval; however, because the process can take as long as several weeks, access to medical treatment can be delayed, upping the risk of complications from later-term abortions. Data cited in the statement indicate that following the enactment of parental involvement laws in three states, second-trimester abortion rates increased by as much as 21% (N Engl J Med. 2006;354[10]:1031-8; Fam Plann Perspect. 1995;27[3]:120-2; Women Health. 1995;22[3]:47-58.
Even when a judicial bypass is obtained, a study of 12,000 such petitions obtained in Minnesota and Massachusetts showed that only 21 of them were denied, and half of those were overturned, meaning the outcome was the same, but the potential risks of delaying care were higher (J Adolesc Health. 1991;12[2]:143-7). The AAP statement suggests physicians learn their state requirements for judicial bypass, if any.
The updated statement also refutes the notion that parental involvement laws improve communication within families and lead to better health outcomes for teens facing an unintended pregnancy. Instead, the statement says that on average, minors who discuss pregnancy termination with their parents do so at the same rate as in states with and without such laws, and that a teen is more likely to involve her parents than not, a likelihood that increases the younger a teen is. When she doesn’t choose to discuss it with parents, fear of some sort of danger such as an escalation in any ongoing family tensions, coercion into a decision, or abuse of some kind is often why (Contraception. 2010 Oct;82[4]:310-3; Fam Plann Perspect. 1992 Jul-Aug;24[4]:148-54, 173).
“In a perfect world of butterflies and unicorns, parents and kids have a perfect relationship, but we know that’s not always true. There can be significant discord in families, and parental notification could result in harm to the adolescent, or risk to the family’s tapestry with significant consequences for the family and the adolescent,” Dr. Breuner said.
Dr. Beers argued that while she believed most parents would rather be the one their teen turns to for advice in such a situation, it’s not possible to legislate trust within families, each of which has its own history and unique family culture and style of communication. “This is the type of conversation that doesn’t begin with the acute event. This is the kind of conversation that should begin [at] a very early age between a parent and a child,” she said.
The physician’s role, according to Dr. Beers, is to ensure parents and their children have “a shared understanding of the facts to [rely on] when they talk about what is important to their family and what their family values are.”
The updated statement, originally issued in 1993, roughly coincides with the release of a new Guttmacher Institute report indicating that abortion rates in the United States are at their lowest since passage of Roe v. Wade in 1973. The report credits lower unintended pregnancy rates and better access to contraception, not restrictive abortion legislation, for the drop. The AAP’s updated statement also comes within days of the inauguration of President Donald Trump, whose run-up to election featured rhetoric challenging the status quo of federal abortion laws.
Dr. Breuner said the timing was a coincidence, and that plans to reissue the statement began over 3 years ago as she and her colleagues drew up plans to recommit their membership to protecting the reproductive rights of their patients. “With all of the regulations, restrictions, and decreased access to [abortion] care that are occurring, the academy wanted members to know just how much more difficult it is to obtain an abortion,” she said, noting that access and confidentiality are not the same. “If you can’t get an abortion, what difference does confidentiality make?”
Last year, the Supreme Court reversed a law that would have greatly limited access to abortion in Texas by closing all but nine clinics statewide, burdening them with care for tens of thousands of women annually. Also in 2016, citing a Constitutional violation of a woman’s right to privacy, a federal judge blocked an Indiana law signed by then governor and now vice president Mike Pence, that restricted the reasons a woman could cite to seek an abortion.
Dr. Breuner views this as an erosion of the rights of all women to comprehensive reproductive care, including those of adolescents. “You can’t ‘Google Map’ how to figure this out anymore. The roads are closed and all the ways people say you can get there don’t really lead you there,” she said, noting that the AAP’s statement is in line with several other professional medical societies, including the American College of Obstetricians and Gynecologists and the American Medical Association.
Regardless of timing, the statement should be viewed not through a political – or even partisan – lens, but as a reaffirmation of “core values,” according to Dr. Beers. “We do live in divided times. I think it’s important to circle back to our core values as pediatricians. That’s the agenda – making sure adolescents are healthy, safe, and supported.”
.
“Genuine concern for the best interests of minors argues strongly against mandatory parental consent and notification laws,” the statement authors wrote in the updated policy statement, “The Adolescent’s Right to Confidential Care When Considering Abortion,” published online in Pediatrics.
The AAP Committee on Adolescence, which wrote the policy statement, encourages adolescents to voluntarily involve their parents – or other adults they trust – in decisions surrounding an unintended pregnancy, stating that teens who do will “likely benefit from adult experience, wisdom, emotional support, and financial support.” However, the policy statement also stresses that legally emphasizing parental involvement over a teen’s autonomy can result in barriers to care when timely access is most crucial, especially if a teen is reluctant to tell her parents of the situation (Pediatrics. 2017. doi: 10.1542/peds.2016-3861).
Currently, 37 states require some level of parental involvement in an adolescent’s decision to pursue an abortion. Most of these states will allow a minor to terminate a pregnancy without parental consent in the case of a medical emergency; about half waive the parental involvement requirement when there is evidence of incest, abuse, or neglect. All states with parental involvement laws also have a so-called judicial bypass, allowing a minor to obtain an abortion with a court’s approval; however, because the process can take as long as several weeks, access to medical treatment can be delayed, upping the risk of complications from later-term abortions. Data cited in the statement indicate that following the enactment of parental involvement laws in three states, second-trimester abortion rates increased by as much as 21% (N Engl J Med. 2006;354[10]:1031-8; Fam Plann Perspect. 1995;27[3]:120-2; Women Health. 1995;22[3]:47-58.
Even when a judicial bypass is obtained, a study of 12,000 such petitions obtained in Minnesota and Massachusetts showed that only 21 of them were denied, and half of those were overturned, meaning the outcome was the same, but the potential risks of delaying care were higher (J Adolesc Health. 1991;12[2]:143-7). The AAP statement suggests physicians learn their state requirements for judicial bypass, if any.
The updated statement also refutes the notion that parental involvement laws improve communication within families and lead to better health outcomes for teens facing an unintended pregnancy. Instead, the statement says that on average, minors who discuss pregnancy termination with their parents do so at the same rate as in states with and without such laws, and that a teen is more likely to involve her parents than not, a likelihood that increases the younger a teen is. When she doesn’t choose to discuss it with parents, fear of some sort of danger such as an escalation in any ongoing family tensions, coercion into a decision, or abuse of some kind is often why (Contraception. 2010 Oct;82[4]:310-3; Fam Plann Perspect. 1992 Jul-Aug;24[4]:148-54, 173).
“In a perfect world of butterflies and unicorns, parents and kids have a perfect relationship, but we know that’s not always true. There can be significant discord in families, and parental notification could result in harm to the adolescent, or risk to the family’s tapestry with significant consequences for the family and the adolescent,” Dr. Breuner said.
Dr. Beers argued that while she believed most parents would rather be the one their teen turns to for advice in such a situation, it’s not possible to legislate trust within families, each of which has its own history and unique family culture and style of communication. “This is the type of conversation that doesn’t begin with the acute event. This is the kind of conversation that should begin [at] a very early age between a parent and a child,” she said.
The physician’s role, according to Dr. Beers, is to ensure parents and their children have “a shared understanding of the facts to [rely on] when they talk about what is important to their family and what their family values are.”
The updated statement, originally issued in 1993, roughly coincides with the release of a new Guttmacher Institute report indicating that abortion rates in the United States are at their lowest since passage of Roe v. Wade in 1973. The report credits lower unintended pregnancy rates and better access to contraception, not restrictive abortion legislation, for the drop. The AAP’s updated statement also comes within days of the inauguration of President Donald Trump, whose run-up to election featured rhetoric challenging the status quo of federal abortion laws.
Dr. Breuner said the timing was a coincidence, and that plans to reissue the statement began over 3 years ago as she and her colleagues drew up plans to recommit their membership to protecting the reproductive rights of their patients. “With all of the regulations, restrictions, and decreased access to [abortion] care that are occurring, the academy wanted members to know just how much more difficult it is to obtain an abortion,” she said, noting that access and confidentiality are not the same. “If you can’t get an abortion, what difference does confidentiality make?”
Last year, the Supreme Court reversed a law that would have greatly limited access to abortion in Texas by closing all but nine clinics statewide, burdening them with care for tens of thousands of women annually. Also in 2016, citing a Constitutional violation of a woman’s right to privacy, a federal judge blocked an Indiana law signed by then governor and now vice president Mike Pence, that restricted the reasons a woman could cite to seek an abortion.
Dr. Breuner views this as an erosion of the rights of all women to comprehensive reproductive care, including those of adolescents. “You can’t ‘Google Map’ how to figure this out anymore. The roads are closed and all the ways people say you can get there don’t really lead you there,” she said, noting that the AAP’s statement is in line with several other professional medical societies, including the American College of Obstetricians and Gynecologists and the American Medical Association.
Regardless of timing, the statement should be viewed not through a political – or even partisan – lens, but as a reaffirmation of “core values,” according to Dr. Beers. “We do live in divided times. I think it’s important to circle back to our core values as pediatricians. That’s the agenda – making sure adolescents are healthy, safe, and supported.”
Oral, liquid supplement improves clinical outcomes in lactose-intolerant adults
Adults with self-reported lactose intolerance were shown to have significant improvement in their clinical outcomes, including abdominal pain, after consuming an oral, liquid supplement intended to increase lactose-fermenting gut bacteria, M. Andrea Azcarate-Peril, PhD, assistant professor of medicine at the University of North Carolina, Chapel Hill, and her colleagues have shown in a small phase IIa study (Proc Nat Acad Sci. doi: 10.1073/pnas.1606722113).
In a placebo-controlled, double-blind trial, randomly assigned in a 2:1 ratio and conducted at two U.S. sites, highly purified (more than 95%) short-chain galactooligosaccharide (GOS) was given to 42 adults with a self-reported history of lactose intolerance, confirmed by a hydrogen breath test administered after a 25-g lactose challenge. The 20 controls were given a corn syrup mixture formulated according to the same sweetness and consistency as the test drug. Each study arm was started on its regimen at 1.5 g daily, with incremental increases in dose every 5 days until reaching 15 g. Beginning with their first dose at day 1, through day 35, all participants avoided consumption of dairy foods. Stool samples were collected from both groups at days 0 and 36. After day 36, all participants were asked to resume eating dairy foods. At day 66, stool samples were once again collected. Changes in the microbiome at all endpoints were measured by testing the stools via polymerase chain reaction.
Of the 30 study arm participants for whom complete stool samples were available, 27 were found to have had a bifidobacterial response at day 36, including a significant increase in the lactose-fermenting Bifidobacterium, Faecalibacterium, and Lactobacillus species. The remaining three participants in the study arm were considered nonresponders.
In an interview, Andrew Ritter, whose company, Ritter Pharmaceuticals, sponsored the trial, reported that of the 36 study arm participants who had reported abdominal pain pretreatment, 18 said they no longer had the pain at either endpoint, day 36 or day 66 (P = .019); three of 19 in the placebo group reported they no longer had abdominal pain at either endpoint. The study group was also six times more likely to report lactose tolerance at day 66 compared with their pretreatment levels (P = .0389); 28% of the placebo arm reported lactose tolerance at the endpoints. These results were previously published in Nutrition Journal in 2013. [doi: 10.1186/1475-2891-12-160]
“We’re super excited about these results,” said Mr. Ritter. “This is really one of the first clinical studies in a lactose-intolerant population that shows changes in the microbiome.” As to how long before the treatment will be ready for the Food and Drug Administration approval process, Mr. Ritter said, “We’re probably just a couple of years away.”
Two coauthors are advisers to Ritter Pharmaceuticals, which provided the highly purified GOS used in the study. The North Carolina Agriculture Foundation also provided funding for the study.
Adults with self-reported lactose intolerance were shown to have significant improvement in their clinical outcomes, including abdominal pain, after consuming an oral, liquid supplement intended to increase lactose-fermenting gut bacteria, M. Andrea Azcarate-Peril, PhD, assistant professor of medicine at the University of North Carolina, Chapel Hill, and her colleagues have shown in a small phase IIa study (Proc Nat Acad Sci. doi: 10.1073/pnas.1606722113).
In a placebo-controlled, double-blind trial, randomly assigned in a 2:1 ratio and conducted at two U.S. sites, highly purified (more than 95%) short-chain galactooligosaccharide (GOS) was given to 42 adults with a self-reported history of lactose intolerance, confirmed by a hydrogen breath test administered after a 25-g lactose challenge. The 20 controls were given a corn syrup mixture formulated according to the same sweetness and consistency as the test drug. Each study arm was started on its regimen at 1.5 g daily, with incremental increases in dose every 5 days until reaching 15 g. Beginning with their first dose at day 1, through day 35, all participants avoided consumption of dairy foods. Stool samples were collected from both groups at days 0 and 36. After day 36, all participants were asked to resume eating dairy foods. At day 66, stool samples were once again collected. Changes in the microbiome at all endpoints were measured by testing the stools via polymerase chain reaction.
Of the 30 study arm participants for whom complete stool samples were available, 27 were found to have had a bifidobacterial response at day 36, including a significant increase in the lactose-fermenting Bifidobacterium, Faecalibacterium, and Lactobacillus species. The remaining three participants in the study arm were considered nonresponders.
In an interview, Andrew Ritter, whose company, Ritter Pharmaceuticals, sponsored the trial, reported that of the 36 study arm participants who had reported abdominal pain pretreatment, 18 said they no longer had the pain at either endpoint, day 36 or day 66 (P = .019); three of 19 in the placebo group reported they no longer had abdominal pain at either endpoint. The study group was also six times more likely to report lactose tolerance at day 66 compared with their pretreatment levels (P = .0389); 28% of the placebo arm reported lactose tolerance at the endpoints. These results were previously published in Nutrition Journal in 2013. [doi: 10.1186/1475-2891-12-160]
“We’re super excited about these results,” said Mr. Ritter. “This is really one of the first clinical studies in a lactose-intolerant population that shows changes in the microbiome.” As to how long before the treatment will be ready for the Food and Drug Administration approval process, Mr. Ritter said, “We’re probably just a couple of years away.”
Two coauthors are advisers to Ritter Pharmaceuticals, which provided the highly purified GOS used in the study. The North Carolina Agriculture Foundation also provided funding for the study.
Adults with self-reported lactose intolerance were shown to have significant improvement in their clinical outcomes, including abdominal pain, after consuming an oral, liquid supplement intended to increase lactose-fermenting gut bacteria, M. Andrea Azcarate-Peril, PhD, assistant professor of medicine at the University of North Carolina, Chapel Hill, and her colleagues have shown in a small phase IIa study (Proc Nat Acad Sci. doi: 10.1073/pnas.1606722113).
In a placebo-controlled, double-blind trial, randomly assigned in a 2:1 ratio and conducted at two U.S. sites, highly purified (more than 95%) short-chain galactooligosaccharide (GOS) was given to 42 adults with a self-reported history of lactose intolerance, confirmed by a hydrogen breath test administered after a 25-g lactose challenge. The 20 controls were given a corn syrup mixture formulated according to the same sweetness and consistency as the test drug. Each study arm was started on its regimen at 1.5 g daily, with incremental increases in dose every 5 days until reaching 15 g. Beginning with their first dose at day 1, through day 35, all participants avoided consumption of dairy foods. Stool samples were collected from both groups at days 0 and 36. After day 36, all participants were asked to resume eating dairy foods. At day 66, stool samples were once again collected. Changes in the microbiome at all endpoints were measured by testing the stools via polymerase chain reaction.
Of the 30 study arm participants for whom complete stool samples were available, 27 were found to have had a bifidobacterial response at day 36, including a significant increase in the lactose-fermenting Bifidobacterium, Faecalibacterium, and Lactobacillus species. The remaining three participants in the study arm were considered nonresponders.
In an interview, Andrew Ritter, whose company, Ritter Pharmaceuticals, sponsored the trial, reported that of the 36 study arm participants who had reported abdominal pain pretreatment, 18 said they no longer had the pain at either endpoint, day 36 or day 66 (P = .019); three of 19 in the placebo group reported they no longer had abdominal pain at either endpoint. The study group was also six times more likely to report lactose tolerance at day 66 compared with their pretreatment levels (P = .0389); 28% of the placebo arm reported lactose tolerance at the endpoints. These results were previously published in Nutrition Journal in 2013. [doi: 10.1186/1475-2891-12-160]
“We’re super excited about these results,” said Mr. Ritter. “This is really one of the first clinical studies in a lactose-intolerant population that shows changes in the microbiome.” As to how long before the treatment will be ready for the Food and Drug Administration approval process, Mr. Ritter said, “We’re probably just a couple of years away.”
Two coauthors are advisers to Ritter Pharmaceuticals, which provided the highly purified GOS used in the study. The North Carolina Agriculture Foundation also provided funding for the study.
FROM THE PROCEEDINGS OF THE NATIONAL ACADEMIES OF SCIENCE
Key clinical point:
Major finding: A clinically significant response was seen in patients with lactose intolerance who were given an oral, liquid supplement intended to increase lactose-fermenting bacteria.
Data source: Phase IIa trial of 62 adults with lactose intolerance incrementally dosed with an oral, highly purified (more than 95%) short-chain galactooligosaccharide while dietary dairy was restricted.
Disclosures: Ritter Pharmaceuticals, owned by study coauthor Andrew J. Ritter, funded the study and provided the highly purified GOS used in the study. The North Carolina Agriculture Foundation also provided funding. Two coauthors are advisers to Ritter Pharmaceuticals.
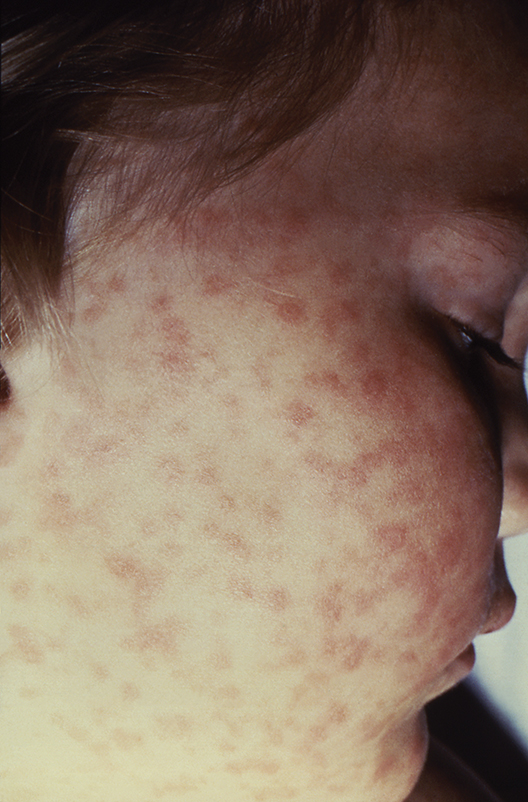
Lab values poor surrogate for detecting pediatric Rocky Mountain spotted fever in children
The three fatalities observed in a retrospective analysis of six cases of Rocky Mountain spotted fever (RMSF) in children were associated with either a delayed diagnosis pending laboratory findings or delayed antirickettsia treatment.
“The fact that all fatal cases died before the convalescent period emphasizes that diagnosis should be based on clinical findings instead of RMSF serologic and histologic testing,” wrote the authors of a study published online in Pediatric Dermatology (2016 Dec 19. doi: 10.1111/pde.13053).
Two of the fatal cases involved delayed antirickettsial therapy after the patients were misdiagnosed with group A streptococcus. None of the six children were initially evaluated for R. rickettsii; they averaged three encounters with their clinician before being admitted for acute inpatient care where they received intravenous doxycycline after nearly a week of symptoms.
“All fatal cases were complicated by neurologic manifestations, including seizures, obtundation, and uncal herniation,” a finding that is consistent with the literature, the authors said.
Although the high fatality rate might be the result of the small study size, Ms. Tull and her coinvestigators concluded that the disease should be considered in all differential diagnoses for children who present with a fever and rash during the summer months in endemic areas, particularly since pediatric cases of the disease are associated with poorer outcomes than in adult cases.
Given that RMSF often remains subclinical in its early stages, and typically presents with nonspecific symptoms of fever, rash, headache, and abdominal pain when it does emerge, physicians might be tempted to defer treatment until after serologic and histologic results are in, as is the standard method. Concerns over doxycycline’s tendency to stain teeth and cause enamel hypoplasia are also common. However, empirical administration could mean the difference between life and death, since treatment within the first 5 days following infection is associated with better outcomes – an algorithm complicated by the fact that symptoms caused by R. rickettsii have been known to take as long as 21 days to appear.
In the study, Ms. Tull and her colleagues found that the average time between exposure to the tick and the onset of symptoms was 6.6 days (range, 1-21 days).
Currently, there are no diagnostic tests “that reliably diagnose RMSF during the first 7 days of illness,” and most patients “do not develop detectable antibodies until the second week of illness,” the investigators reported. Even then, sensitivity of indirect fluorescent antibody serum testing after the second week of illness is only between 86% and 94%, they noted. Further, the sensitivity of immunohistochemical (IHC) tissue staining has been reported at 70%, and false-negative IHC results are common in acute disease when antibody response is harder to detect.
Ms. Tull and her colleagues found that five of the six patients in their study had negative IHC testing; two of the six had positive serum antibody titers. For this reason, they concluded that Rocky Mountain spotted fever diagnosis should be based on “clinical history, examination, and laboratory abnormalities” rather than laboratory testing, and urged that “prompt treatment should be instituted empirically.”
The authors did not have any relevant financial disclosures.
The three fatalities observed in a retrospective analysis of six cases of Rocky Mountain spotted fever (RMSF) in children were associated with either a delayed diagnosis pending laboratory findings or delayed antirickettsia treatment.
“The fact that all fatal cases died before the convalescent period emphasizes that diagnosis should be based on clinical findings instead of RMSF serologic and histologic testing,” wrote the authors of a study published online in Pediatric Dermatology (2016 Dec 19. doi: 10.1111/pde.13053).
Two of the fatal cases involved delayed antirickettsial therapy after the patients were misdiagnosed with group A streptococcus. None of the six children were initially evaluated for R. rickettsii; they averaged three encounters with their clinician before being admitted for acute inpatient care where they received intravenous doxycycline after nearly a week of symptoms.
“All fatal cases were complicated by neurologic manifestations, including seizures, obtundation, and uncal herniation,” a finding that is consistent with the literature, the authors said.
Although the high fatality rate might be the result of the small study size, Ms. Tull and her coinvestigators concluded that the disease should be considered in all differential diagnoses for children who present with a fever and rash during the summer months in endemic areas, particularly since pediatric cases of the disease are associated with poorer outcomes than in adult cases.
Given that RMSF often remains subclinical in its early stages, and typically presents with nonspecific symptoms of fever, rash, headache, and abdominal pain when it does emerge, physicians might be tempted to defer treatment until after serologic and histologic results are in, as is the standard method. Concerns over doxycycline’s tendency to stain teeth and cause enamel hypoplasia are also common. However, empirical administration could mean the difference between life and death, since treatment within the first 5 days following infection is associated with better outcomes – an algorithm complicated by the fact that symptoms caused by R. rickettsii have been known to take as long as 21 days to appear.
In the study, Ms. Tull and her colleagues found that the average time between exposure to the tick and the onset of symptoms was 6.6 days (range, 1-21 days).
Currently, there are no diagnostic tests “that reliably diagnose RMSF during the first 7 days of illness,” and most patients “do not develop detectable antibodies until the second week of illness,” the investigators reported. Even then, sensitivity of indirect fluorescent antibody serum testing after the second week of illness is only between 86% and 94%, they noted. Further, the sensitivity of immunohistochemical (IHC) tissue staining has been reported at 70%, and false-negative IHC results are common in acute disease when antibody response is harder to detect.
Ms. Tull and her colleagues found that five of the six patients in their study had negative IHC testing; two of the six had positive serum antibody titers. For this reason, they concluded that Rocky Mountain spotted fever diagnosis should be based on “clinical history, examination, and laboratory abnormalities” rather than laboratory testing, and urged that “prompt treatment should be instituted empirically.”
The authors did not have any relevant financial disclosures.
The three fatalities observed in a retrospective analysis of six cases of Rocky Mountain spotted fever (RMSF) in children were associated with either a delayed diagnosis pending laboratory findings or delayed antirickettsia treatment.
“The fact that all fatal cases died before the convalescent period emphasizes that diagnosis should be based on clinical findings instead of RMSF serologic and histologic testing,” wrote the authors of a study published online in Pediatric Dermatology (2016 Dec 19. doi: 10.1111/pde.13053).
Two of the fatal cases involved delayed antirickettsial therapy after the patients were misdiagnosed with group A streptococcus. None of the six children were initially evaluated for R. rickettsii; they averaged three encounters with their clinician before being admitted for acute inpatient care where they received intravenous doxycycline after nearly a week of symptoms.
“All fatal cases were complicated by neurologic manifestations, including seizures, obtundation, and uncal herniation,” a finding that is consistent with the literature, the authors said.
Although the high fatality rate might be the result of the small study size, Ms. Tull and her coinvestigators concluded that the disease should be considered in all differential diagnoses for children who present with a fever and rash during the summer months in endemic areas, particularly since pediatric cases of the disease are associated with poorer outcomes than in adult cases.
Given that RMSF often remains subclinical in its early stages, and typically presents with nonspecific symptoms of fever, rash, headache, and abdominal pain when it does emerge, physicians might be tempted to defer treatment until after serologic and histologic results are in, as is the standard method. Concerns over doxycycline’s tendency to stain teeth and cause enamel hypoplasia are also common. However, empirical administration could mean the difference between life and death, since treatment within the first 5 days following infection is associated with better outcomes – an algorithm complicated by the fact that symptoms caused by R. rickettsii have been known to take as long as 21 days to appear.
In the study, Ms. Tull and her colleagues found that the average time between exposure to the tick and the onset of symptoms was 6.6 days (range, 1-21 days).
Currently, there are no diagnostic tests “that reliably diagnose RMSF during the first 7 days of illness,” and most patients “do not develop detectable antibodies until the second week of illness,” the investigators reported. Even then, sensitivity of indirect fluorescent antibody serum testing after the second week of illness is only between 86% and 94%, they noted. Further, the sensitivity of immunohistochemical (IHC) tissue staining has been reported at 70%, and false-negative IHC results are common in acute disease when antibody response is harder to detect.
Ms. Tull and her colleagues found that five of the six patients in their study had negative IHC testing; two of the six had positive serum antibody titers. For this reason, they concluded that Rocky Mountain spotted fever diagnosis should be based on “clinical history, examination, and laboratory abnormalities” rather than laboratory testing, and urged that “prompt treatment should be instituted empirically.”
The authors did not have any relevant financial disclosures.
FROM PEDIATRIC DERMATOLOGY
Key clinical point:
Major finding: Half of pediatric patients diagnosed with Rocky Mountain spotted fever died after treatment was delayed.
Data source: A retrospective analysis of 6 pediatric RMSF cases among 3,912 inpatient dermatology consultations over a period of 10 years at a tertiary care center.
Disclosures: The authors did not have any relevant financial disclosures. .
Adolescents, boys, black children most likely to be hospitalized in SJS and TEN
Annual hospitalization rates in the United States for Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) were shown to be higher in adolescents, boys, and black children, in a cross-sectional analysis of discharge records from more than 4,100 hospitals.
Using relevant ICD-9 codes, researchers at Harvard University identified 1,571 patients hospitalized for SJS, TEN, or both in 2009 and 2012, as listed in the Kids Inpatient Database from the Agency for Healthcare Research and Quality. The highest hospitalization rates per 100,000 in each year were for adolescents between 15 and 19 years (P = .01), boys (P = .03), and black children (P = .82). The overall risk of death from these conditions was 1.5% in 2009 and 0.3% in 2012. The data were published online in a brief report (Pediatr Dermatol. 2016 Dec 19. doi: 10.1111/pde.13050).
With the number of SJS- and TEN-related hospitalizations between 0.1 and 1.0 per 100,000, lead author Yusuke Okubo MD, MPH, and his colleagues wrote that their data aligned with previous studies; however, regarding the emphasis on demographic differences, theirs was, to the best of their knowledge, “the first study to reveal these disparities.” Compared with adults, they added, mortality was “remarkably lower” in children.
The authors had no disclosures.
Annual hospitalization rates in the United States for Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) were shown to be higher in adolescents, boys, and black children, in a cross-sectional analysis of discharge records from more than 4,100 hospitals.
Using relevant ICD-9 codes, researchers at Harvard University identified 1,571 patients hospitalized for SJS, TEN, or both in 2009 and 2012, as listed in the Kids Inpatient Database from the Agency for Healthcare Research and Quality. The highest hospitalization rates per 100,000 in each year were for adolescents between 15 and 19 years (P = .01), boys (P = .03), and black children (P = .82). The overall risk of death from these conditions was 1.5% in 2009 and 0.3% in 2012. The data were published online in a brief report (Pediatr Dermatol. 2016 Dec 19. doi: 10.1111/pde.13050).
With the number of SJS- and TEN-related hospitalizations between 0.1 and 1.0 per 100,000, lead author Yusuke Okubo MD, MPH, and his colleagues wrote that their data aligned with previous studies; however, regarding the emphasis on demographic differences, theirs was, to the best of their knowledge, “the first study to reveal these disparities.” Compared with adults, they added, mortality was “remarkably lower” in children.
The authors had no disclosures.
Annual hospitalization rates in the United States for Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) were shown to be higher in adolescents, boys, and black children, in a cross-sectional analysis of discharge records from more than 4,100 hospitals.
Using relevant ICD-9 codes, researchers at Harvard University identified 1,571 patients hospitalized for SJS, TEN, or both in 2009 and 2012, as listed in the Kids Inpatient Database from the Agency for Healthcare Research and Quality. The highest hospitalization rates per 100,000 in each year were for adolescents between 15 and 19 years (P = .01), boys (P = .03), and black children (P = .82). The overall risk of death from these conditions was 1.5% in 2009 and 0.3% in 2012. The data were published online in a brief report (Pediatr Dermatol. 2016 Dec 19. doi: 10.1111/pde.13050).
With the number of SJS- and TEN-related hospitalizations between 0.1 and 1.0 per 100,000, lead author Yusuke Okubo MD, MPH, and his colleagues wrote that their data aligned with previous studies; however, regarding the emphasis on demographic differences, theirs was, to the best of their knowledge, “the first study to reveal these disparities.” Compared with adults, they added, mortality was “remarkably lower” in children.
The authors had no disclosures.
Key clinical point:
Major finding: Hospitalization rates for SJS/TEN were highest among adolescents (aged 15-19) at 1.36 and 1.09 per 100,000 children in 2009 and 2012, respectively.
Data source: An analysis of 1,571 pediatric discharge records for 2009 and 2012 from more than 4,100 hospitals in a national database.
Disclosures: The authors had no disclosures.
BRAIN Initiative could help end mental illness stigma
BETHESDA, MD – Top researchers are optimistic that billions in funding for basic neuroscience research made possible by the 21st Century Cures Act will lead to breakthroughs in the understanding of brain function and dysfunction that could help end the stigma of mental illness.
Under the new law, $6.3 billion are slated for health initiatives over the next decade. The Cancer Moonshot will receive $1.8 billion, precision medicine will receive just under $1.5 billion, and the BRAIN Initiative (Brain Research Through Advancing Innovative Neurotechnologies) will receive just over that amount.
“I know there have been some anxieties about the program’s fragilities given the change in administration,” Dr. Collins told an audience at a meeting of the NIH Brain Institute investigators. “But [passage of the 21st Century Cures Act] should be a source of great reassurance.”
The actual cost of the BRAIN Initiative is expected to top $4.5 billion by the year 2025, funded by a mix of federal and private monies. The National Institute of Mental Health’s typical annual budget is just under $1.5 billion – essentially the same as the amount provided for in the new law. The funds will benefit neuroscience generally, and if successful, understanding of the brain specifically.
The BRAIN Initiative funding is not for clinical studies, however. Instead, it will be spread across what Dr. Collins dubbed, “Team Science,” a multidisciplinary band of investigators, all of whom are expected to help not only identify the brain’s biologic processes but also create the tools needed to reengineer the brain’s circuitry when it malfunctions. Some current BRAIN projects Dr. Collins singled out as worth watching were the use of ultrasound neuromodulation in nonhuman primates, the analysis of individual methylone in cell nuclei, and the development of ultrahigh-resolution 3D brain imaging technology.
“We are moving toward a full bore effort toward technologies that allow us to see what is happening in real time in circuits in the brain,” Dr. Collins said. “Maybe there are certain fundamental operating principles that may have eluded us in the past but which may start to appear.”
In 2016, there were as many neuroscientists as there were engineers of all types – 141 each – named as the principal investigators of projects funded by the initiative, according to NIMH Director Joshua A. Gordon, MD, PhD, who also spoke at the meeting. Among the other disciplines Dr. Gordon said were represented in the 2016 roster of investigators were 61 radiologists, 33 biostatisticians, 47 neurosurgeons, and 69 psychiatrists and psychologists.
The enormous focus on bench science – about 85% of all NIMH funding is for nonclinical research – is not without its critics. In a recent editorial, several prominent academic clinicians urged the NIMH to spend less on futuristic neuroscience and more on the application of therapies for those with mental illness, and on their psychosocial needs (Br J Psychiatry. 2016;208[6]507-9). The last-minute inclusion in the 21st Century Cures Act of several provisions that will have a direct impact in the near future on the plight of those with severe mental illness has the potential to allay some concerns, however.
“My hope is that the [law] will be interpreted from the perspective of making effective treatments available for ... those who are already ill,” Susan M. Essock, PhD, the Edna L. Edison Professor of Medical Psychology (in Psychiatry) at Columbia University, New York, and a cosigner of the editorial, said in an interview.
The law aims to drive evidence-based grant making for programs such as the Recovery After an Initial Schizophrenia Episode (RAISE) integrated care model and expands assisted outpatient treatment for children with serious emotional disturbance, or adults with serious mental illness, among several other provisions.
For some, the initiative’s cross-specialty structure and hefty price tag are worthwhile if it means filling the void of basic science necessary to explain the mechanics of mental illness, a void often filled with attitudes leading to the stigmatization of people who are ill.
Dr. Mayberg said she believes that a “systems approach” to behavior will emerge over time as interdisciplinary BRAIN Initiative researchers are given the freedom to make necessary discoveries, often when least expected, and are urged to share what they find. “Real fundamental changes happen by accident, in my experience. They are rarely planned. It happens when there are a lot of clues. A diversified portfolio has to be the answer, because nobody is smart enough to do it all [alone]. The goal is diversified, evidence-based approaches. ... Science has to make fundamental progress on how the brain works, because we’re obviously missing something clinically,” she said.
The ultimate goals of the initiative are to understand human beings and to improve the human condition by alleviating suffering, according to Brian Litt, MD, professor of neurology and bioengineering at the University of Pennsylvania, Philadelphia, and a moderator of a panel focused on the clinical implications of BRAIN research.
“If you think about the fundamental problems that affect our society and many around the world, they’re not just diseases like Parkinson’s or epilepsy, they are the disorders of mood, addiction, violence, anger, and a number of other conditions that affect behavior that are part of the neurological spectrum that affects the way our society functions,” Dr. Litt, a clinician specializing in treating people with epilepsy, told the audience.
Rather than create a neuroengineered super race, he said, fundamental neuroscience is about helping humans reach their fullest potential. For his support of this, Dr. Litt said he makes “no apologies. As a clinician, I am not sorry to be involved in fundamental neuroscience where ... incremental discoveries can create cures.”
As science favors cures, policy inevitably will evolve, perhaps even making current interventions relics of ignorance. “Psychosocial intervention is what you do when you have an absence of knowing how to cure,” said Dr. Mayberg. “It might be that [currently] what we treat is maladaptation to the primary problem.”
The key for clinicians, she said, will be to keep up with the latest literature. “Clinicians have to be aware of what’s exciting, of what should be in their armamentarium.”
Dr. Collins, Dr. Gordon, Dr. Essock, and Dr. Mayberg had no disclosures. Dr. Litt has cofounded several companies, including Blackfynn and Neuropace, and has served as a consultant and licensed technology to several companies.
BETHESDA, MD – Top researchers are optimistic that billions in funding for basic neuroscience research made possible by the 21st Century Cures Act will lead to breakthroughs in the understanding of brain function and dysfunction that could help end the stigma of mental illness.
Under the new law, $6.3 billion are slated for health initiatives over the next decade. The Cancer Moonshot will receive $1.8 billion, precision medicine will receive just under $1.5 billion, and the BRAIN Initiative (Brain Research Through Advancing Innovative Neurotechnologies) will receive just over that amount.
“I know there have been some anxieties about the program’s fragilities given the change in administration,” Dr. Collins told an audience at a meeting of the NIH Brain Institute investigators. “But [passage of the 21st Century Cures Act] should be a source of great reassurance.”
The actual cost of the BRAIN Initiative is expected to top $4.5 billion by the year 2025, funded by a mix of federal and private monies. The National Institute of Mental Health’s typical annual budget is just under $1.5 billion – essentially the same as the amount provided for in the new law. The funds will benefit neuroscience generally, and if successful, understanding of the brain specifically.
The BRAIN Initiative funding is not for clinical studies, however. Instead, it will be spread across what Dr. Collins dubbed, “Team Science,” a multidisciplinary band of investigators, all of whom are expected to help not only identify the brain’s biologic processes but also create the tools needed to reengineer the brain’s circuitry when it malfunctions. Some current BRAIN projects Dr. Collins singled out as worth watching were the use of ultrasound neuromodulation in nonhuman primates, the analysis of individual methylone in cell nuclei, and the development of ultrahigh-resolution 3D brain imaging technology.
“We are moving toward a full bore effort toward technologies that allow us to see what is happening in real time in circuits in the brain,” Dr. Collins said. “Maybe there are certain fundamental operating principles that may have eluded us in the past but which may start to appear.”
In 2016, there were as many neuroscientists as there were engineers of all types – 141 each – named as the principal investigators of projects funded by the initiative, according to NIMH Director Joshua A. Gordon, MD, PhD, who also spoke at the meeting. Among the other disciplines Dr. Gordon said were represented in the 2016 roster of investigators were 61 radiologists, 33 biostatisticians, 47 neurosurgeons, and 69 psychiatrists and psychologists.
The enormous focus on bench science – about 85% of all NIMH funding is for nonclinical research – is not without its critics. In a recent editorial, several prominent academic clinicians urged the NIMH to spend less on futuristic neuroscience and more on the application of therapies for those with mental illness, and on their psychosocial needs (Br J Psychiatry. 2016;208[6]507-9). The last-minute inclusion in the 21st Century Cures Act of several provisions that will have a direct impact in the near future on the plight of those with severe mental illness has the potential to allay some concerns, however.
“My hope is that the [law] will be interpreted from the perspective of making effective treatments available for ... those who are already ill,” Susan M. Essock, PhD, the Edna L. Edison Professor of Medical Psychology (in Psychiatry) at Columbia University, New York, and a cosigner of the editorial, said in an interview.
The law aims to drive evidence-based grant making for programs such as the Recovery After an Initial Schizophrenia Episode (RAISE) integrated care model and expands assisted outpatient treatment for children with serious emotional disturbance, or adults with serious mental illness, among several other provisions.
For some, the initiative’s cross-specialty structure and hefty price tag are worthwhile if it means filling the void of basic science necessary to explain the mechanics of mental illness, a void often filled with attitudes leading to the stigmatization of people who are ill.
Dr. Mayberg said she believes that a “systems approach” to behavior will emerge over time as interdisciplinary BRAIN Initiative researchers are given the freedom to make necessary discoveries, often when least expected, and are urged to share what they find. “Real fundamental changes happen by accident, in my experience. They are rarely planned. It happens when there are a lot of clues. A diversified portfolio has to be the answer, because nobody is smart enough to do it all [alone]. The goal is diversified, evidence-based approaches. ... Science has to make fundamental progress on how the brain works, because we’re obviously missing something clinically,” she said.
The ultimate goals of the initiative are to understand human beings and to improve the human condition by alleviating suffering, according to Brian Litt, MD, professor of neurology and bioengineering at the University of Pennsylvania, Philadelphia, and a moderator of a panel focused on the clinical implications of BRAIN research.
“If you think about the fundamental problems that affect our society and many around the world, they’re not just diseases like Parkinson’s or epilepsy, they are the disorders of mood, addiction, violence, anger, and a number of other conditions that affect behavior that are part of the neurological spectrum that affects the way our society functions,” Dr. Litt, a clinician specializing in treating people with epilepsy, told the audience.
Rather than create a neuroengineered super race, he said, fundamental neuroscience is about helping humans reach their fullest potential. For his support of this, Dr. Litt said he makes “no apologies. As a clinician, I am not sorry to be involved in fundamental neuroscience where ... incremental discoveries can create cures.”
As science favors cures, policy inevitably will evolve, perhaps even making current interventions relics of ignorance. “Psychosocial intervention is what you do when you have an absence of knowing how to cure,” said Dr. Mayberg. “It might be that [currently] what we treat is maladaptation to the primary problem.”
The key for clinicians, she said, will be to keep up with the latest literature. “Clinicians have to be aware of what’s exciting, of what should be in their armamentarium.”
Dr. Collins, Dr. Gordon, Dr. Essock, and Dr. Mayberg had no disclosures. Dr. Litt has cofounded several companies, including Blackfynn and Neuropace, and has served as a consultant and licensed technology to several companies.
BETHESDA, MD – Top researchers are optimistic that billions in funding for basic neuroscience research made possible by the 21st Century Cures Act will lead to breakthroughs in the understanding of brain function and dysfunction that could help end the stigma of mental illness.
Under the new law, $6.3 billion are slated for health initiatives over the next decade. The Cancer Moonshot will receive $1.8 billion, precision medicine will receive just under $1.5 billion, and the BRAIN Initiative (Brain Research Through Advancing Innovative Neurotechnologies) will receive just over that amount.
“I know there have been some anxieties about the program’s fragilities given the change in administration,” Dr. Collins told an audience at a meeting of the NIH Brain Institute investigators. “But [passage of the 21st Century Cures Act] should be a source of great reassurance.”
The actual cost of the BRAIN Initiative is expected to top $4.5 billion by the year 2025, funded by a mix of federal and private monies. The National Institute of Mental Health’s typical annual budget is just under $1.5 billion – essentially the same as the amount provided for in the new law. The funds will benefit neuroscience generally, and if successful, understanding of the brain specifically.
The BRAIN Initiative funding is not for clinical studies, however. Instead, it will be spread across what Dr. Collins dubbed, “Team Science,” a multidisciplinary band of investigators, all of whom are expected to help not only identify the brain’s biologic processes but also create the tools needed to reengineer the brain’s circuitry when it malfunctions. Some current BRAIN projects Dr. Collins singled out as worth watching were the use of ultrasound neuromodulation in nonhuman primates, the analysis of individual methylone in cell nuclei, and the development of ultrahigh-resolution 3D brain imaging technology.
“We are moving toward a full bore effort toward technologies that allow us to see what is happening in real time in circuits in the brain,” Dr. Collins said. “Maybe there are certain fundamental operating principles that may have eluded us in the past but which may start to appear.”
In 2016, there were as many neuroscientists as there were engineers of all types – 141 each – named as the principal investigators of projects funded by the initiative, according to NIMH Director Joshua A. Gordon, MD, PhD, who also spoke at the meeting. Among the other disciplines Dr. Gordon said were represented in the 2016 roster of investigators were 61 radiologists, 33 biostatisticians, 47 neurosurgeons, and 69 psychiatrists and psychologists.
The enormous focus on bench science – about 85% of all NIMH funding is for nonclinical research – is not without its critics. In a recent editorial, several prominent academic clinicians urged the NIMH to spend less on futuristic neuroscience and more on the application of therapies for those with mental illness, and on their psychosocial needs (Br J Psychiatry. 2016;208[6]507-9). The last-minute inclusion in the 21st Century Cures Act of several provisions that will have a direct impact in the near future on the plight of those with severe mental illness has the potential to allay some concerns, however.
“My hope is that the [law] will be interpreted from the perspective of making effective treatments available for ... those who are already ill,” Susan M. Essock, PhD, the Edna L. Edison Professor of Medical Psychology (in Psychiatry) at Columbia University, New York, and a cosigner of the editorial, said in an interview.
The law aims to drive evidence-based grant making for programs such as the Recovery After an Initial Schizophrenia Episode (RAISE) integrated care model and expands assisted outpatient treatment for children with serious emotional disturbance, or adults with serious mental illness, among several other provisions.
For some, the initiative’s cross-specialty structure and hefty price tag are worthwhile if it means filling the void of basic science necessary to explain the mechanics of mental illness, a void often filled with attitudes leading to the stigmatization of people who are ill.
Dr. Mayberg said she believes that a “systems approach” to behavior will emerge over time as interdisciplinary BRAIN Initiative researchers are given the freedom to make necessary discoveries, often when least expected, and are urged to share what they find. “Real fundamental changes happen by accident, in my experience. They are rarely planned. It happens when there are a lot of clues. A diversified portfolio has to be the answer, because nobody is smart enough to do it all [alone]. The goal is diversified, evidence-based approaches. ... Science has to make fundamental progress on how the brain works, because we’re obviously missing something clinically,” she said.
The ultimate goals of the initiative are to understand human beings and to improve the human condition by alleviating suffering, according to Brian Litt, MD, professor of neurology and bioengineering at the University of Pennsylvania, Philadelphia, and a moderator of a panel focused on the clinical implications of BRAIN research.
“If you think about the fundamental problems that affect our society and many around the world, they’re not just diseases like Parkinson’s or epilepsy, they are the disorders of mood, addiction, violence, anger, and a number of other conditions that affect behavior that are part of the neurological spectrum that affects the way our society functions,” Dr. Litt, a clinician specializing in treating people with epilepsy, told the audience.
Rather than create a neuroengineered super race, he said, fundamental neuroscience is about helping humans reach their fullest potential. For his support of this, Dr. Litt said he makes “no apologies. As a clinician, I am not sorry to be involved in fundamental neuroscience where ... incremental discoveries can create cures.”
As science favors cures, policy inevitably will evolve, perhaps even making current interventions relics of ignorance. “Psychosocial intervention is what you do when you have an absence of knowing how to cure,” said Dr. Mayberg. “It might be that [currently] what we treat is maladaptation to the primary problem.”
The key for clinicians, she said, will be to keep up with the latest literature. “Clinicians have to be aware of what’s exciting, of what should be in their armamentarium.”
Dr. Collins, Dr. Gordon, Dr. Essock, and Dr. Mayberg had no disclosures. Dr. Litt has cofounded several companies, including Blackfynn and Neuropace, and has served as a consultant and licensed technology to several companies.
EXPERT ANALYSIS AT AN NIH ADVISORY COUNCIL MEETING
FDA eases mental health warnings in smoking cessation drugs’ labels
Labels on two smoking cessation treatments will offer less severe warnings for mental health risk potentials in people with no history of psychiatric disorders, the Food and Drug Administration has announced.
Varenicline (Chantix) will no longer include a boxed warning for serious mental health side effects. The label for bupropion (Zyban) will still include a boxed warning, but language describing the potential for serious psychiatric adverse events will no longer appear within it. Updates will also be made to both labels to describe side effects on mood, behavior, or thinking.
In addition, varenicline’s label will reflect trial data showing its superior efficacy, compared with oral bupropion or nicotine patch. Although a patient medication guide will still be included with each prescription, the risk evaluation and mitigation strategy that prompted the guide will no longer be in place.
Earlier this year, two FDA advisory committees voted in favor of updating varenicline’s label, based on data from a randomized, controlled trial of more than 8,000 smokers, half of whom had a history of psychiatric disorders.
The trial showed no clinically significant difference in risk of adverse events across the smoking cessation treatments varenicline, bupropion, nicotine patch, or placebo study arms, although the risk was higher in the psychiatric cohorts in each.
Overall, 2% of those without a history of mental illness experienced neuropsychiatric adverse events, compared with between 5% and 7% of those with such a history.
The trial was cosponsored by Pfizer, maker of Chantix, and GlaxoSmithKline, maker of Zyban.
The FDA approved varenicline for smoking cessation in 2006 and approved bupropion, which also is indicated to treat depression and seasonal affective disorder, in 1997. After numerous postmarketing reports of increased incidents of psychiatric disorders occurring in smokers who used either drug, the agency added the boxed warning to each in 2009.
FDA officials advised clinicians to guard against changes in mental health status in smokers using these therapies. However, “the results of the trial confirm that the benefits of stopping smoking outweigh the risks of these medicines,” they noted.
On Twitter @whitneymcknight
Labels on two smoking cessation treatments will offer less severe warnings for mental health risk potentials in people with no history of psychiatric disorders, the Food and Drug Administration has announced.
Varenicline (Chantix) will no longer include a boxed warning for serious mental health side effects. The label for bupropion (Zyban) will still include a boxed warning, but language describing the potential for serious psychiatric adverse events will no longer appear within it. Updates will also be made to both labels to describe side effects on mood, behavior, or thinking.
In addition, varenicline’s label will reflect trial data showing its superior efficacy, compared with oral bupropion or nicotine patch. Although a patient medication guide will still be included with each prescription, the risk evaluation and mitigation strategy that prompted the guide will no longer be in place.
Earlier this year, two FDA advisory committees voted in favor of updating varenicline’s label, based on data from a randomized, controlled trial of more than 8,000 smokers, half of whom had a history of psychiatric disorders.
The trial showed no clinically significant difference in risk of adverse events across the smoking cessation treatments varenicline, bupropion, nicotine patch, or placebo study arms, although the risk was higher in the psychiatric cohorts in each.
Overall, 2% of those without a history of mental illness experienced neuropsychiatric adverse events, compared with between 5% and 7% of those with such a history.
The trial was cosponsored by Pfizer, maker of Chantix, and GlaxoSmithKline, maker of Zyban.
The FDA approved varenicline for smoking cessation in 2006 and approved bupropion, which also is indicated to treat depression and seasonal affective disorder, in 1997. After numerous postmarketing reports of increased incidents of psychiatric disorders occurring in smokers who used either drug, the agency added the boxed warning to each in 2009.
FDA officials advised clinicians to guard against changes in mental health status in smokers using these therapies. However, “the results of the trial confirm that the benefits of stopping smoking outweigh the risks of these medicines,” they noted.
On Twitter @whitneymcknight
Labels on two smoking cessation treatments will offer less severe warnings for mental health risk potentials in people with no history of psychiatric disorders, the Food and Drug Administration has announced.
Varenicline (Chantix) will no longer include a boxed warning for serious mental health side effects. The label for bupropion (Zyban) will still include a boxed warning, but language describing the potential for serious psychiatric adverse events will no longer appear within it. Updates will also be made to both labels to describe side effects on mood, behavior, or thinking.
In addition, varenicline’s label will reflect trial data showing its superior efficacy, compared with oral bupropion or nicotine patch. Although a patient medication guide will still be included with each prescription, the risk evaluation and mitigation strategy that prompted the guide will no longer be in place.
Earlier this year, two FDA advisory committees voted in favor of updating varenicline’s label, based on data from a randomized, controlled trial of more than 8,000 smokers, half of whom had a history of psychiatric disorders.
The trial showed no clinically significant difference in risk of adverse events across the smoking cessation treatments varenicline, bupropion, nicotine patch, or placebo study arms, although the risk was higher in the psychiatric cohorts in each.
Overall, 2% of those without a history of mental illness experienced neuropsychiatric adverse events, compared with between 5% and 7% of those with such a history.
The trial was cosponsored by Pfizer, maker of Chantix, and GlaxoSmithKline, maker of Zyban.
The FDA approved varenicline for smoking cessation in 2006 and approved bupropion, which also is indicated to treat depression and seasonal affective disorder, in 1997. After numerous postmarketing reports of increased incidents of psychiatric disorders occurring in smokers who used either drug, the agency added the boxed warning to each in 2009.
FDA officials advised clinicians to guard against changes in mental health status in smokers using these therapies. However, “the results of the trial confirm that the benefits of stopping smoking outweigh the risks of these medicines,” they noted.
On Twitter @whitneymcknight
Is better reporting to blame for the rise maternal mortality rates?
Better surveillance could be responsible for increased rates of U.S. maternal mortality, a sign that previous estimates were too low, according to a new study.
For more than 2 decades, rates of maternal deaths have increased significantly, climbing from 7.55 per 100,000 live births in 1993 to 9.88 in 1999, and rising again to 21.5 in 2014. This means the relative risk of maternal death between 2014 and 1993 was 2.84, while it was 2.17 between 2014 and 1999.
Although rising rates of obesity and other chronic conditions are often theorized as possible factors in the spiking maternal death rates K.S. Joseph, MD, PhD, of the University of British Columbia, Vancouver, and his colleagues suggest the more likely causes are improved maternal death surveillance and changes in how these deaths are coded.
This conclusion is based on a retrospective cohort analysis of maternal deaths and live births from 1993-2014 as recorded in the National Center for Health Statistics and the Wide-Ranging Online Data for Epidemiologic Research files of the Centers for Disease Control and Prevention (Obstet Gynecol 2017;129:91-100).
Surveillance and reporting changes have been implemented across the country over the last few decades. During the 1990s, some states began including a separate question regarding pregnancy on death certificates. Starting in 2003, pregnancy was added to the standardized checklist of causes of death on certificates used nationwide, although state-by-state implementation has varied. In addition, in 1999, ICD-10 codes for underlying causes of death were introduced, including O96 and O97 for late maternal deaths, O26.8 for specified pregnancy-related conditions, and O99 for other maternal diseases classifiable elsewhere.
When Dr. Joseph and his colleagues excluded from their analysis maternal deaths coded according to the new ICD-10 codes primarily related to renal disease and other maternal diseases classifiable elsewhere, the increase between 1999 and 2014 was erased, dropping the relative risk to 1.09 (95% CI, 0.94-1.27).
Adjustment for improvements in surveillance also wiped out the temporal increase in maternal mortality rates for a relative risk of 1.06 for 2013 compared to 1993 (95% CI, 0.90-1.25).
“Reports of temporal increases in maternal mortality rates in the United States have led to shock and soul-searching by clinicians,” the investigators wrote. “In fact, maternal deaths from conditions historically associated with high case fatality rates including preeclampsia, eclampsia, complications of labor and delivery, antepartum and postpartum hemorrhage, and abortion either declined substantially or remained stable between 1999 and 2014.”
The investigators did not report having any potential conflicts of interest.
Better surveillance could be responsible for increased rates of U.S. maternal mortality, a sign that previous estimates were too low, according to a new study.
For more than 2 decades, rates of maternal deaths have increased significantly, climbing from 7.55 per 100,000 live births in 1993 to 9.88 in 1999, and rising again to 21.5 in 2014. This means the relative risk of maternal death between 2014 and 1993 was 2.84, while it was 2.17 between 2014 and 1999.
Although rising rates of obesity and other chronic conditions are often theorized as possible factors in the spiking maternal death rates K.S. Joseph, MD, PhD, of the University of British Columbia, Vancouver, and his colleagues suggest the more likely causes are improved maternal death surveillance and changes in how these deaths are coded.
This conclusion is based on a retrospective cohort analysis of maternal deaths and live births from 1993-2014 as recorded in the National Center for Health Statistics and the Wide-Ranging Online Data for Epidemiologic Research files of the Centers for Disease Control and Prevention (Obstet Gynecol 2017;129:91-100).
Surveillance and reporting changes have been implemented across the country over the last few decades. During the 1990s, some states began including a separate question regarding pregnancy on death certificates. Starting in 2003, pregnancy was added to the standardized checklist of causes of death on certificates used nationwide, although state-by-state implementation has varied. In addition, in 1999, ICD-10 codes for underlying causes of death were introduced, including O96 and O97 for late maternal deaths, O26.8 for specified pregnancy-related conditions, and O99 for other maternal diseases classifiable elsewhere.
When Dr. Joseph and his colleagues excluded from their analysis maternal deaths coded according to the new ICD-10 codes primarily related to renal disease and other maternal diseases classifiable elsewhere, the increase between 1999 and 2014 was erased, dropping the relative risk to 1.09 (95% CI, 0.94-1.27).
Adjustment for improvements in surveillance also wiped out the temporal increase in maternal mortality rates for a relative risk of 1.06 for 2013 compared to 1993 (95% CI, 0.90-1.25).
“Reports of temporal increases in maternal mortality rates in the United States have led to shock and soul-searching by clinicians,” the investigators wrote. “In fact, maternal deaths from conditions historically associated with high case fatality rates including preeclampsia, eclampsia, complications of labor and delivery, antepartum and postpartum hemorrhage, and abortion either declined substantially or remained stable between 1999 and 2014.”
The investigators did not report having any potential conflicts of interest.
Better surveillance could be responsible for increased rates of U.S. maternal mortality, a sign that previous estimates were too low, according to a new study.
For more than 2 decades, rates of maternal deaths have increased significantly, climbing from 7.55 per 100,000 live births in 1993 to 9.88 in 1999, and rising again to 21.5 in 2014. This means the relative risk of maternal death between 2014 and 1993 was 2.84, while it was 2.17 between 2014 and 1999.
Although rising rates of obesity and other chronic conditions are often theorized as possible factors in the spiking maternal death rates K.S. Joseph, MD, PhD, of the University of British Columbia, Vancouver, and his colleagues suggest the more likely causes are improved maternal death surveillance and changes in how these deaths are coded.
This conclusion is based on a retrospective cohort analysis of maternal deaths and live births from 1993-2014 as recorded in the National Center for Health Statistics and the Wide-Ranging Online Data for Epidemiologic Research files of the Centers for Disease Control and Prevention (Obstet Gynecol 2017;129:91-100).
Surveillance and reporting changes have been implemented across the country over the last few decades. During the 1990s, some states began including a separate question regarding pregnancy on death certificates. Starting in 2003, pregnancy was added to the standardized checklist of causes of death on certificates used nationwide, although state-by-state implementation has varied. In addition, in 1999, ICD-10 codes for underlying causes of death were introduced, including O96 and O97 for late maternal deaths, O26.8 for specified pregnancy-related conditions, and O99 for other maternal diseases classifiable elsewhere.
When Dr. Joseph and his colleagues excluded from their analysis maternal deaths coded according to the new ICD-10 codes primarily related to renal disease and other maternal diseases classifiable elsewhere, the increase between 1999 and 2014 was erased, dropping the relative risk to 1.09 (95% CI, 0.94-1.27).
Adjustment for improvements in surveillance also wiped out the temporal increase in maternal mortality rates for a relative risk of 1.06 for 2013 compared to 1993 (95% CI, 0.90-1.25).
“Reports of temporal increases in maternal mortality rates in the United States have led to shock and soul-searching by clinicians,” the investigators wrote. “In fact, maternal deaths from conditions historically associated with high case fatality rates including preeclampsia, eclampsia, complications of labor and delivery, antepartum and postpartum hemorrhage, and abortion either declined substantially or remained stable between 1999 and 2014.”
The investigators did not report having any potential conflicts of interest.
Key clinical point:
Major finding: The relative risk for maternal death was 2.17 between 1999 and 2014, but dropped to 1.09 when certain new ICD-10 codes were excluded.
Data source: Retrospective cohort study of maternal deaths recorded in federal health data from 1993-2004.
Disclosures: The investigators did not report any potential conflicts of interest.
Spike in Colombian microcephaly cases linked to Zika infection early in pregnancy
Colombia experienced a fourfold increase in cases of microcephaly following the Zika virus outbreak in 2016, with temporal evidence suggesting that infection in the first months of pregnancy poses the greatest risk to the fetus of microcephaly.
From January 31 through mid-November 2016, there were 476 cases of microcephaly reported in Colombia, four times the rate of cases reported during the same period in 2015. In July 2016, there was a ninefold increase in Colombian microcephaly cases reported, compared with July 2015, according to data published in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report.
Based on an average full-term gestation – because the 24-week period from the peak of Colombia’s Zika virus outbreak occurred simultaneously with the peak in reported microcephaly cases – there is a temporal suggestion that the greatest risk for microcephaly is associated with Zika virus infection during the first half of pregnancy, according to the authors of the report. Of the reported cases of microcephaly in 2016, 432 were live-born infants and 44 were pregnancy losses (MMWR. 2016 Dec 9. doi: 10.15585/mmwr.mm6549e1).
Of Colombia’s reported 105,000 cases of Zika virus occurring between August 9, 2015, and November 12, 2016, nearly 20,000 cases were in pregnant women, according to the Instituto Nacional de Salud.
The findings reinforce previous data indicating the correlation between early Zika virus-infection and microcephaly (N Engl J Med. 2016;374:1981-7. doi: 10.1056/NEJMsr1604338), although the report’s authors cautioned there are several confounders to these data, including that the surveillance was passive, not all reported cases of Zika virus infection were confirmed by a laboratory, and not all cases might have been reported.
The authors reported no relevant disclosures.
Colombia experienced a fourfold increase in cases of microcephaly following the Zika virus outbreak in 2016, with temporal evidence suggesting that infection in the first months of pregnancy poses the greatest risk to the fetus of microcephaly.
From January 31 through mid-November 2016, there were 476 cases of microcephaly reported in Colombia, four times the rate of cases reported during the same period in 2015. In July 2016, there was a ninefold increase in Colombian microcephaly cases reported, compared with July 2015, according to data published in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report.
Based on an average full-term gestation – because the 24-week period from the peak of Colombia’s Zika virus outbreak occurred simultaneously with the peak in reported microcephaly cases – there is a temporal suggestion that the greatest risk for microcephaly is associated with Zika virus infection during the first half of pregnancy, according to the authors of the report. Of the reported cases of microcephaly in 2016, 432 were live-born infants and 44 were pregnancy losses (MMWR. 2016 Dec 9. doi: 10.15585/mmwr.mm6549e1).
Of Colombia’s reported 105,000 cases of Zika virus occurring between August 9, 2015, and November 12, 2016, nearly 20,000 cases were in pregnant women, according to the Instituto Nacional de Salud.
The findings reinforce previous data indicating the correlation between early Zika virus-infection and microcephaly (N Engl J Med. 2016;374:1981-7. doi: 10.1056/NEJMsr1604338), although the report’s authors cautioned there are several confounders to these data, including that the surveillance was passive, not all reported cases of Zika virus infection were confirmed by a laboratory, and not all cases might have been reported.
The authors reported no relevant disclosures.
Colombia experienced a fourfold increase in cases of microcephaly following the Zika virus outbreak in 2016, with temporal evidence suggesting that infection in the first months of pregnancy poses the greatest risk to the fetus of microcephaly.
From January 31 through mid-November 2016, there were 476 cases of microcephaly reported in Colombia, four times the rate of cases reported during the same period in 2015. In July 2016, there was a ninefold increase in Colombian microcephaly cases reported, compared with July 2015, according to data published in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report.
Based on an average full-term gestation – because the 24-week period from the peak of Colombia’s Zika virus outbreak occurred simultaneously with the peak in reported microcephaly cases – there is a temporal suggestion that the greatest risk for microcephaly is associated with Zika virus infection during the first half of pregnancy, according to the authors of the report. Of the reported cases of microcephaly in 2016, 432 were live-born infants and 44 were pregnancy losses (MMWR. 2016 Dec 9. doi: 10.15585/mmwr.mm6549e1).
Of Colombia’s reported 105,000 cases of Zika virus occurring between August 9, 2015, and November 12, 2016, nearly 20,000 cases were in pregnant women, according to the Instituto Nacional de Salud.
The findings reinforce previous data indicating the correlation between early Zika virus-infection and microcephaly (N Engl J Med. 2016;374:1981-7. doi: 10.1056/NEJMsr1604338), although the report’s authors cautioned there are several confounders to these data, including that the surveillance was passive, not all reported cases of Zika virus infection were confirmed by a laboratory, and not all cases might have been reported.
The authors reported no relevant disclosures.
FROM MMWR
Key clinical point:
Major finding: In 2016, a fourfold increase in microcephaly cases occurred in Colombia compared with 2015. Most cases coincided with women who were in their first trimester at the Zika outbreak’s inception.
Data source: National passive surveillance data of reported birth defects from Colombia’s Instituto Nacional de Salud.
Disclosures: The authors reported no relevant disclosures.
Landmark psychosocial guidelines for diabetes spark debate over the ideal vs. the practical
, but some question whether endocrinologists and others are up to the task of providing the extensive mental health services called for in the document.
Although the American Diabetes Association has often addressed the specific psychosocial concerns of persons with diabetes, the ADA’s first-ever position statement on the subject reflects a state-of-the-art approach to delivering integrated mental health and specialty services to this patient population. That alone makes the document a milestone in diabetes care, according to Yehuda Handelsman, MD, , medical director of the Metabolic Institute of America in Tarzana, Calif., and chair of the American College of Endocrinology 2011 Comprehensive Diabetes Guidelines. “It raises the importance of the psychological being in diabetes. This has been mentioned before in guidelines, but it has never been the focus. In that respect, this [document] is very important,” Dr. Handelsman said in an interview.
The guidelines detail the most common psychological factors facing persons with diabetes throughout the life span, including diabetes distress, depression, anxiety, eating disorders, and diabetes-related cognitive dysfunction later in life. There is also a section addressing considerations such as mental and emotional preparation before and after bariatric surgery. Clinicians are urged to practice preventive care by assessing patients’ mental states regularly. A list of age-appropriate resources for screens and other measurement tools is included in the guidelines.
Despite the guidelines’ thoroughness, Dr. Handelsman said he is not optimistic they will change much in the way of practice. “The people who wrote this are psychologists and other mental health professionals. This is what they do. When we endocrinologists see patients, we don’t have these [skills]. It’s not so easy to incorporate these suggestions into daily practice,” Dr. Handelsman, said.
“The paper addresses all service providers who help care for people with diabetes. That presumes a starting point of primary care physicians, but includes specialists and team members such as certified diabetes educators, registered nurses, nutritionists, behavioral practitioners, and so on.”
Plenty of integrated care models for diabetes care [are] already in existence, said Dr. Young-Hyman, who is also a certified diabetes educator.
One such clinic is operated by Richard Hellman, MD, , a past president of the American Association of Clinical Endocrinologists. His North Kansas City diabetes specialty clinic has offered psychosocial services to patients for much of its 30 years. The clinic’s focus is not on primary care, but many of his patients’ health needs are met by approaching their chronic illness care in a comprehensive way, according to Dr. Hellman. The clinic’s multidisciplinary team includes certified diabetes educators, nurse practitioners, physician assistants, dietitians, a clinical psychologist, and registered nurses.
Since passage of the Affordable Care Act, the zeitgeist has been a move away from fee for service care provided by a single clinician, to collaborative models. While talk of the incoming U.S. president and Congress dismantling the law has caused some uncertainty over how physician reimbursements will be structured in the future, pressure from health insurers to keep in place value-based care models – particularly for chronic illness management – may remain regardless of the ACA’s ultimate fate.
“The evidence is that when people with diabetes who also have stress or mood disorders get the care they need, they are more productive and healthier, and both insurers and employers save money,” Dr. Hellman said.
It is what might happen should primary care physicians find themselves facing either having to meet standards of care for a number of chronic illnesses or forfeit reimbursements. Such a scenario should concern policymakers dealing with the delivery of chronic illness care, according to Dr. Hellman, who has experience relevant to these issues as a member of the Physician Consortium for Performance Improvement since 2000 and the National Quality Forum Diabetes/Metabolism Technical Advisory Panel from 2009 to 2012.
“Payment strategies to force change are a blunt tool that often don’t work well. There is so much complexity. People often have kidney or heart disease. It’s hard to write policy with so much variation going on,” he said.
Adding mental health screening and referrals likely works well for all models of chronic illness care, according to Victor L. Roberts, MD, MBA, a clinical endocrinologist in Winter Park, Fla.
However, “I don’t see how a primary care doctor will have the time to [follow all the guidelines] and determine what is going on with the patient’s mental health,” observed Dr. Roberts, who works with many central Florida primary care clinics.
“But they can tell if someone is mildly or moderately depressed, and they can refer the patient for evaluation just like you would refer them for an EKG, a blood test, or a consultation to an endocrinologist,” he added. “Look at depression as a comorbidity.”
Not treating depression and anxiety as medical conditions means patient outcomes are almost guaranteed to be poor, he said.
“If someone is depressed, they are not listening. They’re worried, they’re not paying attention, their ability to incorporate new information is impaired,” Dr. Roberts added. That leads to less facility for self care and can contribute to a bidirectional conundrum of depression and worsening health, particularly in diabetes.
An embrace of value-based care as envisioned by the guidelines’ authors is irrelevant, however, if qualified mental health specialists – particularly those trained specifically in the psychosocial needs of people with diabetes – are nowhere to be found. “I [practice] in the middle of Los Angeles, and I can tell you that in a 30-mile radius, there is not a psychologist anywhere that I can refer a diabetes patient to,” Dr. Handelsman said.
To that end, the ADA has developed a partnership with the American Psychological Association to educate psychologists about the kinds of mental health challenges specific to patients with diabetes. The curriculum will be introduced later this year during the ADA’s scientific sessions meeting. At present, none of the classes are accredited, but Dr. Young-Hyman said her “pie-in-the-sky dream” would be to expand the program and continuing medical education units.
“We see the capacity issues and want to address them,” Dr. Young-Hyman said. That alone may not be enough to change practice in the specialty setting where integrated care, as provided by Dr. Hellman’s clinic, currently is the exception, according to Dr. Handelsman.
Although he said it was likely that guidelines issued by ACE will be expanded to incorporate the ADA’s recommendations, he challenged the ADA to advocate directly to endocrinology societies to educate them on the practical application of their recommendations.
“Take the guidelines and make us use them,” he said in the interview. Otherwise, because most clinical endocrinologists are not trained to address psychosocial concerns, unless a specialist already has an interest in mental health, Dr. Handelsman said that specialist largely will ignore this document. “Some in the field will read it ... but we will not take it to the streets.”
Despite his “guarded optimism,” neither does Dr. Roberts see how practice for primary care physicians will change much – at least, not in the near future, given what he called the already “bone crushing” constraints on their time.
Yet, he warned that not dealing with mental health issues means not delivering complete care.
“Depression is a complication of diabetes, in my expert opinion,” Dr. Roberts cautioned.
“Primary care physicians need to not sidestep this. They need to make it clear to their patients that dealing with depression is part and parcel of dealing with their chronic disease. The position statement can at least be a clarion call to consider mental health a medical condition that we can address in a matter-of-fact way.”
The American Diabetes Association’s recommendations for psychosocial care in diabetes are as follows:
• Integrate psychosocial care with collaborative, patient-centered medical care, and provide psychosocial care to all people with diabetes, with the goals of optimizing health outcomes and health-related quality of life. (Evidence level A.)
• Consider assessing symptoms of diabetes distress, depression, anxiety, and disordered eating and of cognitive capacities using patient-appropriate standardized/validated tools at the initial visit, at periodic intervals, and when there is a change in disease, treatment, or life circumstance. Include caregivers and family members in this assessment. (Evidence level B.)
• Consider monitoring patient performance of self-management behaviors as well as psychosocial factors impacting the person’s self-management. (Evidence level E.)
• Consider assessing life circumstances that can affect physical and psychological health outcomes and their incorporation into intervention strategies. (Evidence level E.)
• Address psychosocial problems upon identification. If an intervention cannot be initiated during the visit when the problem is identified, a follow-up visit or referral to a qualified behavioral health care provider may be scheduled during that visit. (Evidence level E.)
Dr. Handelsman chaired the American College of Endocrinology 2011 Comprehensive Diabetes Guidelines committee and is the immediate past president of ACE. Dr. Hellman is an editorial board member of Diabetes Care. Dr. Young-Hyman had no relevant disclosures.
, but some question whether endocrinologists and others are up to the task of providing the extensive mental health services called for in the document.
Although the American Diabetes Association has often addressed the specific psychosocial concerns of persons with diabetes, the ADA’s first-ever position statement on the subject reflects a state-of-the-art approach to delivering integrated mental health and specialty services to this patient population. That alone makes the document a milestone in diabetes care, according to Yehuda Handelsman, MD, , medical director of the Metabolic Institute of America in Tarzana, Calif., and chair of the American College of Endocrinology 2011 Comprehensive Diabetes Guidelines. “It raises the importance of the psychological being in diabetes. This has been mentioned before in guidelines, but it has never been the focus. In that respect, this [document] is very important,” Dr. Handelsman said in an interview.
The guidelines detail the most common psychological factors facing persons with diabetes throughout the life span, including diabetes distress, depression, anxiety, eating disorders, and diabetes-related cognitive dysfunction later in life. There is also a section addressing considerations such as mental and emotional preparation before and after bariatric surgery. Clinicians are urged to practice preventive care by assessing patients’ mental states regularly. A list of age-appropriate resources for screens and other measurement tools is included in the guidelines.
Despite the guidelines’ thoroughness, Dr. Handelsman said he is not optimistic they will change much in the way of practice. “The people who wrote this are psychologists and other mental health professionals. This is what they do. When we endocrinologists see patients, we don’t have these [skills]. It’s not so easy to incorporate these suggestions into daily practice,” Dr. Handelsman, said.
“The paper addresses all service providers who help care for people with diabetes. That presumes a starting point of primary care physicians, but includes specialists and team members such as certified diabetes educators, registered nurses, nutritionists, behavioral practitioners, and so on.”
Plenty of integrated care models for diabetes care [are] already in existence, said Dr. Young-Hyman, who is also a certified diabetes educator.
One such clinic is operated by Richard Hellman, MD, , a past president of the American Association of Clinical Endocrinologists. His North Kansas City diabetes specialty clinic has offered psychosocial services to patients for much of its 30 years. The clinic’s focus is not on primary care, but many of his patients’ health needs are met by approaching their chronic illness care in a comprehensive way, according to Dr. Hellman. The clinic’s multidisciplinary team includes certified diabetes educators, nurse practitioners, physician assistants, dietitians, a clinical psychologist, and registered nurses.
Since passage of the Affordable Care Act, the zeitgeist has been a move away from fee for service care provided by a single clinician, to collaborative models. While talk of the incoming U.S. president and Congress dismantling the law has caused some uncertainty over how physician reimbursements will be structured in the future, pressure from health insurers to keep in place value-based care models – particularly for chronic illness management – may remain regardless of the ACA’s ultimate fate.
“The evidence is that when people with diabetes who also have stress or mood disorders get the care they need, they are more productive and healthier, and both insurers and employers save money,” Dr. Hellman said.
It is what might happen should primary care physicians find themselves facing either having to meet standards of care for a number of chronic illnesses or forfeit reimbursements. Such a scenario should concern policymakers dealing with the delivery of chronic illness care, according to Dr. Hellman, who has experience relevant to these issues as a member of the Physician Consortium for Performance Improvement since 2000 and the National Quality Forum Diabetes/Metabolism Technical Advisory Panel from 2009 to 2012.
“Payment strategies to force change are a blunt tool that often don’t work well. There is so much complexity. People often have kidney or heart disease. It’s hard to write policy with so much variation going on,” he said.
Adding mental health screening and referrals likely works well for all models of chronic illness care, according to Victor L. Roberts, MD, MBA, a clinical endocrinologist in Winter Park, Fla.
However, “I don’t see how a primary care doctor will have the time to [follow all the guidelines] and determine what is going on with the patient’s mental health,” observed Dr. Roberts, who works with many central Florida primary care clinics.
“But they can tell if someone is mildly or moderately depressed, and they can refer the patient for evaluation just like you would refer them for an EKG, a blood test, or a consultation to an endocrinologist,” he added. “Look at depression as a comorbidity.”
Not treating depression and anxiety as medical conditions means patient outcomes are almost guaranteed to be poor, he said.
“If someone is depressed, they are not listening. They’re worried, they’re not paying attention, their ability to incorporate new information is impaired,” Dr. Roberts added. That leads to less facility for self care and can contribute to a bidirectional conundrum of depression and worsening health, particularly in diabetes.
An embrace of value-based care as envisioned by the guidelines’ authors is irrelevant, however, if qualified mental health specialists – particularly those trained specifically in the psychosocial needs of people with diabetes – are nowhere to be found. “I [practice] in the middle of Los Angeles, and I can tell you that in a 30-mile radius, there is not a psychologist anywhere that I can refer a diabetes patient to,” Dr. Handelsman said.
To that end, the ADA has developed a partnership with the American Psychological Association to educate psychologists about the kinds of mental health challenges specific to patients with diabetes. The curriculum will be introduced later this year during the ADA’s scientific sessions meeting. At present, none of the classes are accredited, but Dr. Young-Hyman said her “pie-in-the-sky dream” would be to expand the program and continuing medical education units.
“We see the capacity issues and want to address them,” Dr. Young-Hyman said. That alone may not be enough to change practice in the specialty setting where integrated care, as provided by Dr. Hellman’s clinic, currently is the exception, according to Dr. Handelsman.
Although he said it was likely that guidelines issued by ACE will be expanded to incorporate the ADA’s recommendations, he challenged the ADA to advocate directly to endocrinology societies to educate them on the practical application of their recommendations.
“Take the guidelines and make us use them,” he said in the interview. Otherwise, because most clinical endocrinologists are not trained to address psychosocial concerns, unless a specialist already has an interest in mental health, Dr. Handelsman said that specialist largely will ignore this document. “Some in the field will read it ... but we will not take it to the streets.”
Despite his “guarded optimism,” neither does Dr. Roberts see how practice for primary care physicians will change much – at least, not in the near future, given what he called the already “bone crushing” constraints on their time.
Yet, he warned that not dealing with mental health issues means not delivering complete care.
“Depression is a complication of diabetes, in my expert opinion,” Dr. Roberts cautioned.
“Primary care physicians need to not sidestep this. They need to make it clear to their patients that dealing with depression is part and parcel of dealing with their chronic disease. The position statement can at least be a clarion call to consider mental health a medical condition that we can address in a matter-of-fact way.”
The American Diabetes Association’s recommendations for psychosocial care in diabetes are as follows:
• Integrate psychosocial care with collaborative, patient-centered medical care, and provide psychosocial care to all people with diabetes, with the goals of optimizing health outcomes and health-related quality of life. (Evidence level A.)
• Consider assessing symptoms of diabetes distress, depression, anxiety, and disordered eating and of cognitive capacities using patient-appropriate standardized/validated tools at the initial visit, at periodic intervals, and when there is a change in disease, treatment, or life circumstance. Include caregivers and family members in this assessment. (Evidence level B.)
• Consider monitoring patient performance of self-management behaviors as well as psychosocial factors impacting the person’s self-management. (Evidence level E.)
• Consider assessing life circumstances that can affect physical and psychological health outcomes and their incorporation into intervention strategies. (Evidence level E.)
• Address psychosocial problems upon identification. If an intervention cannot be initiated during the visit when the problem is identified, a follow-up visit or referral to a qualified behavioral health care provider may be scheduled during that visit. (Evidence level E.)
Dr. Handelsman chaired the American College of Endocrinology 2011 Comprehensive Diabetes Guidelines committee and is the immediate past president of ACE. Dr. Hellman is an editorial board member of Diabetes Care. Dr. Young-Hyman had no relevant disclosures.
, but some question whether endocrinologists and others are up to the task of providing the extensive mental health services called for in the document.
Although the American Diabetes Association has often addressed the specific psychosocial concerns of persons with diabetes, the ADA’s first-ever position statement on the subject reflects a state-of-the-art approach to delivering integrated mental health and specialty services to this patient population. That alone makes the document a milestone in diabetes care, according to Yehuda Handelsman, MD, , medical director of the Metabolic Institute of America in Tarzana, Calif., and chair of the American College of Endocrinology 2011 Comprehensive Diabetes Guidelines. “It raises the importance of the psychological being in diabetes. This has been mentioned before in guidelines, but it has never been the focus. In that respect, this [document] is very important,” Dr. Handelsman said in an interview.
The guidelines detail the most common psychological factors facing persons with diabetes throughout the life span, including diabetes distress, depression, anxiety, eating disorders, and diabetes-related cognitive dysfunction later in life. There is also a section addressing considerations such as mental and emotional preparation before and after bariatric surgery. Clinicians are urged to practice preventive care by assessing patients’ mental states regularly. A list of age-appropriate resources for screens and other measurement tools is included in the guidelines.
Despite the guidelines’ thoroughness, Dr. Handelsman said he is not optimistic they will change much in the way of practice. “The people who wrote this are psychologists and other mental health professionals. This is what they do. When we endocrinologists see patients, we don’t have these [skills]. It’s not so easy to incorporate these suggestions into daily practice,” Dr. Handelsman, said.
“The paper addresses all service providers who help care for people with diabetes. That presumes a starting point of primary care physicians, but includes specialists and team members such as certified diabetes educators, registered nurses, nutritionists, behavioral practitioners, and so on.”
Plenty of integrated care models for diabetes care [are] already in existence, said Dr. Young-Hyman, who is also a certified diabetes educator.
One such clinic is operated by Richard Hellman, MD, , a past president of the American Association of Clinical Endocrinologists. His North Kansas City diabetes specialty clinic has offered psychosocial services to patients for much of its 30 years. The clinic’s focus is not on primary care, but many of his patients’ health needs are met by approaching their chronic illness care in a comprehensive way, according to Dr. Hellman. The clinic’s multidisciplinary team includes certified diabetes educators, nurse practitioners, physician assistants, dietitians, a clinical psychologist, and registered nurses.
Since passage of the Affordable Care Act, the zeitgeist has been a move away from fee for service care provided by a single clinician, to collaborative models. While talk of the incoming U.S. president and Congress dismantling the law has caused some uncertainty over how physician reimbursements will be structured in the future, pressure from health insurers to keep in place value-based care models – particularly for chronic illness management – may remain regardless of the ACA’s ultimate fate.
“The evidence is that when people with diabetes who also have stress or mood disorders get the care they need, they are more productive and healthier, and both insurers and employers save money,” Dr. Hellman said.
It is what might happen should primary care physicians find themselves facing either having to meet standards of care for a number of chronic illnesses or forfeit reimbursements. Such a scenario should concern policymakers dealing with the delivery of chronic illness care, according to Dr. Hellman, who has experience relevant to these issues as a member of the Physician Consortium for Performance Improvement since 2000 and the National Quality Forum Diabetes/Metabolism Technical Advisory Panel from 2009 to 2012.
“Payment strategies to force change are a blunt tool that often don’t work well. There is so much complexity. People often have kidney or heart disease. It’s hard to write policy with so much variation going on,” he said.
Adding mental health screening and referrals likely works well for all models of chronic illness care, according to Victor L. Roberts, MD, MBA, a clinical endocrinologist in Winter Park, Fla.
However, “I don’t see how a primary care doctor will have the time to [follow all the guidelines] and determine what is going on with the patient’s mental health,” observed Dr. Roberts, who works with many central Florida primary care clinics.
“But they can tell if someone is mildly or moderately depressed, and they can refer the patient for evaluation just like you would refer them for an EKG, a blood test, or a consultation to an endocrinologist,” he added. “Look at depression as a comorbidity.”
Not treating depression and anxiety as medical conditions means patient outcomes are almost guaranteed to be poor, he said.
“If someone is depressed, they are not listening. They’re worried, they’re not paying attention, their ability to incorporate new information is impaired,” Dr. Roberts added. That leads to less facility for self care and can contribute to a bidirectional conundrum of depression and worsening health, particularly in diabetes.
An embrace of value-based care as envisioned by the guidelines’ authors is irrelevant, however, if qualified mental health specialists – particularly those trained specifically in the psychosocial needs of people with diabetes – are nowhere to be found. “I [practice] in the middle of Los Angeles, and I can tell you that in a 30-mile radius, there is not a psychologist anywhere that I can refer a diabetes patient to,” Dr. Handelsman said.
To that end, the ADA has developed a partnership with the American Psychological Association to educate psychologists about the kinds of mental health challenges specific to patients with diabetes. The curriculum will be introduced later this year during the ADA’s scientific sessions meeting. At present, none of the classes are accredited, but Dr. Young-Hyman said her “pie-in-the-sky dream” would be to expand the program and continuing medical education units.
“We see the capacity issues and want to address them,” Dr. Young-Hyman said. That alone may not be enough to change practice in the specialty setting where integrated care, as provided by Dr. Hellman’s clinic, currently is the exception, according to Dr. Handelsman.
Although he said it was likely that guidelines issued by ACE will be expanded to incorporate the ADA’s recommendations, he challenged the ADA to advocate directly to endocrinology societies to educate them on the practical application of their recommendations.
“Take the guidelines and make us use them,” he said in the interview. Otherwise, because most clinical endocrinologists are not trained to address psychosocial concerns, unless a specialist already has an interest in mental health, Dr. Handelsman said that specialist largely will ignore this document. “Some in the field will read it ... but we will not take it to the streets.”
Despite his “guarded optimism,” neither does Dr. Roberts see how practice for primary care physicians will change much – at least, not in the near future, given what he called the already “bone crushing” constraints on their time.
Yet, he warned that not dealing with mental health issues means not delivering complete care.
“Depression is a complication of diabetes, in my expert opinion,” Dr. Roberts cautioned.
“Primary care physicians need to not sidestep this. They need to make it clear to their patients that dealing with depression is part and parcel of dealing with their chronic disease. The position statement can at least be a clarion call to consider mental health a medical condition that we can address in a matter-of-fact way.”
The American Diabetes Association’s recommendations for psychosocial care in diabetes are as follows:
• Integrate psychosocial care with collaborative, patient-centered medical care, and provide psychosocial care to all people with diabetes, with the goals of optimizing health outcomes and health-related quality of life. (Evidence level A.)
• Consider assessing symptoms of diabetes distress, depression, anxiety, and disordered eating and of cognitive capacities using patient-appropriate standardized/validated tools at the initial visit, at periodic intervals, and when there is a change in disease, treatment, or life circumstance. Include caregivers and family members in this assessment. (Evidence level B.)
• Consider monitoring patient performance of self-management behaviors as well as psychosocial factors impacting the person’s self-management. (Evidence level E.)
• Consider assessing life circumstances that can affect physical and psychological health outcomes and their incorporation into intervention strategies. (Evidence level E.)
• Address psychosocial problems upon identification. If an intervention cannot be initiated during the visit when the problem is identified, a follow-up visit or referral to a qualified behavioral health care provider may be scheduled during that visit. (Evidence level E.)
Dr. Handelsman chaired the American College of Endocrinology 2011 Comprehensive Diabetes Guidelines committee and is the immediate past president of ACE. Dr. Hellman is an editorial board member of Diabetes Care. Dr. Young-Hyman had no relevant disclosures.
FROM DIABETES CARE
Serious mental illness gets serious attention in 21st Century Cures Act
WASHINGTON – Bipartisan legislation to improve care of patients with serious mental illness is just a pen stroke from passage, now that the 21st Century Cures Act is headed for the President’s desk.
While the mental health care reform provisions in the legislation (H.R. 34) will impact mental health services broadly, the bulk of the reform language comes from H.R. 2646, a bill sponsored by Rep. Tim Murphy (R-Penn.), which was intended to reverse decades of fragmented – and at times nonexistent – care for persons with serious mental illness.
The legislation calls for the expanded use of assisted outpatient treatment, federal guidance on how states can be reimbursed for offering inpatient psychiatric services, better data collection on mental health services paid for with state and federal dollars, new oversight of the federal agency in charge of mental health, and clarification of HIPAA laws, among other provisions.
“This is big,” Rep. Murphy said at a press conference Dec. 5. “After all the tears and suffering … know that those times when you felt no one was willing to listen, and you were ready to give up, now there is hope.”
Treatment vs. incarceration
Currently, states and communities can draw from $80 million dollars in federal grants for assisted outpatient treatment for patients with serious mental illness. The new legislation adds another $20 million and extends availability of the funding until 2022. It also allows state criminal justice systems to use assisted outpatient treatment grants to treat convicted criminals with serious mental illness instead of incarcerating them.
“[In prison], their illness gets worse, not better, creating a turnstile through which they will return time and again through our criminal justice system,” Senate Majority Whip John Cornyn (R.-Tex.) said during the press conference.
Paying for inpatient psychiatric care
The Cures Act also strengthens momentum for overhauling the Medicaid Institutions of Mental Diseases (IMD) exclusion, long a focus of mental health care advocates who view it as a governor on the number of psychiatric beds available nationally.
The exclusion prohibits any medical facility with more than 16 beds from using federal funds to pay for inpatient mental health care for adults under age 65 years. The Cures Act requires the Centers for Medicare & Medicaid Services to offer guidance on how states can use Medicaid demonstration projects to provide innovative inpatient psychiatric services using these waivers.
This follows an April 2016 CMS final rule that matches state funding dollar-per-dollar for up to 15 days of inpatient psychiatric treatment given to Medicaid managed care patients.
Although Rep. Murphy’s original bill called for abolishing the exclusion, he and other advocates are not disappointed in the progress made so far. “We didn’t get everything we wanted, but we needed everything we got,” he said.
“That 15 days was a massive win,” Frankie Berger, advocacy director of the Treatment Advocacy Center in Arlington, Va., said in an interview. “Now we have this legislation that requires CMS to tell state Medicaid directors what their wiggle room is when solving the problem on how to get care to these patients. If you read between the lines, this is care that is going to be provided by an IMD.”
The legislation also calls for more data collection and evaluation of IMDs, something that until now has been missing, Ms. Berger said. “A lot of us who work on this issue have found there is absolutely no data on where IMDs are, or who the folks are that are getting treatment in them. We need that information to make good choices,” she said.
“I think we will find savings as we expand the number of psychiatric beds … [and persons with serious mental illness] do not end up in jail cells, homeless, or in the morgue,” Sen. Bill Cassidy (R-La.) said at the press conference. He predicted that for each additional psychiatric bed introduced, savings would amount to between $30,000 and $50,000.
Restructuring, clarifying
The Cures Act reforms also restructure the Substance Abuse and Mental Health Services Administration, putting it under the authority of a new assistant secretary of Health and Human Services and giving it a chief medical officer. The law calls for the new CMO to have “real-world” experience treating patients with serious mental illness. The reformed SAMHSA will have responsibility for centralizing data collection to be used in creating best practices in mental health care. These reforms are particular victories for Rep. Murphy who has railed against the agency for years, citing its lack of medically trained leadership and lack of evidence-based approaches to care.
HIPAA requirements in serious mental illness are also clarified.
“Existing HIPAA laws are badly misunderstood,” said Sen. Chris Murphy (D-Conn.) at the briefing. “Many physicians think there is an outright ban on sharing [patient health] information.”
The legislation calls for the U.S. Department of Health and Human Services secretary to clarify when providers can disclose protected health information related to the treatment of an adult with a mental illness or substance use disorder.
“I would argue that [HIPAA] may be an area we will have to work on down the line, if the education campaign doesn’t work, but we will give this a try,” said Sen. Murphy, who has cosponsored legislation to do so.
As passed, the mental health provisions of the 21st Century Cures Act are an amalgamation of several bills introduced during the 114th Congress and are unique in that they largely were written by health care professionals with direct, relevant experience. Rep. Murphy is a clinical psychologist, while Rep. Cassidy is a physician with experience treating uninsured and incarcerated patients. Rep. Eddie Bernice Johnson (D-Tex.), who cosponsored Rep. Murphy’s bill, previously served as chief psychiatric nurse at the Dallas Veterans Affairs Medical Center.
WASHINGTON – Bipartisan legislation to improve care of patients with serious mental illness is just a pen stroke from passage, now that the 21st Century Cures Act is headed for the President’s desk.
While the mental health care reform provisions in the legislation (H.R. 34) will impact mental health services broadly, the bulk of the reform language comes from H.R. 2646, a bill sponsored by Rep. Tim Murphy (R-Penn.), which was intended to reverse decades of fragmented – and at times nonexistent – care for persons with serious mental illness.
The legislation calls for the expanded use of assisted outpatient treatment, federal guidance on how states can be reimbursed for offering inpatient psychiatric services, better data collection on mental health services paid for with state and federal dollars, new oversight of the federal agency in charge of mental health, and clarification of HIPAA laws, among other provisions.
“This is big,” Rep. Murphy said at a press conference Dec. 5. “After all the tears and suffering … know that those times when you felt no one was willing to listen, and you were ready to give up, now there is hope.”
Treatment vs. incarceration
Currently, states and communities can draw from $80 million dollars in federal grants for assisted outpatient treatment for patients with serious mental illness. The new legislation adds another $20 million and extends availability of the funding until 2022. It also allows state criminal justice systems to use assisted outpatient treatment grants to treat convicted criminals with serious mental illness instead of incarcerating them.
“[In prison], their illness gets worse, not better, creating a turnstile through which they will return time and again through our criminal justice system,” Senate Majority Whip John Cornyn (R.-Tex.) said during the press conference.
Paying for inpatient psychiatric care
The Cures Act also strengthens momentum for overhauling the Medicaid Institutions of Mental Diseases (IMD) exclusion, long a focus of mental health care advocates who view it as a governor on the number of psychiatric beds available nationally.
The exclusion prohibits any medical facility with more than 16 beds from using federal funds to pay for inpatient mental health care for adults under age 65 years. The Cures Act requires the Centers for Medicare & Medicaid Services to offer guidance on how states can use Medicaid demonstration projects to provide innovative inpatient psychiatric services using these waivers.
This follows an April 2016 CMS final rule that matches state funding dollar-per-dollar for up to 15 days of inpatient psychiatric treatment given to Medicaid managed care patients.
Although Rep. Murphy’s original bill called for abolishing the exclusion, he and other advocates are not disappointed in the progress made so far. “We didn’t get everything we wanted, but we needed everything we got,” he said.
“That 15 days was a massive win,” Frankie Berger, advocacy director of the Treatment Advocacy Center in Arlington, Va., said in an interview. “Now we have this legislation that requires CMS to tell state Medicaid directors what their wiggle room is when solving the problem on how to get care to these patients. If you read between the lines, this is care that is going to be provided by an IMD.”
The legislation also calls for more data collection and evaluation of IMDs, something that until now has been missing, Ms. Berger said. “A lot of us who work on this issue have found there is absolutely no data on where IMDs are, or who the folks are that are getting treatment in them. We need that information to make good choices,” she said.
“I think we will find savings as we expand the number of psychiatric beds … [and persons with serious mental illness] do not end up in jail cells, homeless, or in the morgue,” Sen. Bill Cassidy (R-La.) said at the press conference. He predicted that for each additional psychiatric bed introduced, savings would amount to between $30,000 and $50,000.
Restructuring, clarifying
The Cures Act reforms also restructure the Substance Abuse and Mental Health Services Administration, putting it under the authority of a new assistant secretary of Health and Human Services and giving it a chief medical officer. The law calls for the new CMO to have “real-world” experience treating patients with serious mental illness. The reformed SAMHSA will have responsibility for centralizing data collection to be used in creating best practices in mental health care. These reforms are particular victories for Rep. Murphy who has railed against the agency for years, citing its lack of medically trained leadership and lack of evidence-based approaches to care.
HIPAA requirements in serious mental illness are also clarified.
“Existing HIPAA laws are badly misunderstood,” said Sen. Chris Murphy (D-Conn.) at the briefing. “Many physicians think there is an outright ban on sharing [patient health] information.”
The legislation calls for the U.S. Department of Health and Human Services secretary to clarify when providers can disclose protected health information related to the treatment of an adult with a mental illness or substance use disorder.
“I would argue that [HIPAA] may be an area we will have to work on down the line, if the education campaign doesn’t work, but we will give this a try,” said Sen. Murphy, who has cosponsored legislation to do so.
As passed, the mental health provisions of the 21st Century Cures Act are an amalgamation of several bills introduced during the 114th Congress and are unique in that they largely were written by health care professionals with direct, relevant experience. Rep. Murphy is a clinical psychologist, while Rep. Cassidy is a physician with experience treating uninsured and incarcerated patients. Rep. Eddie Bernice Johnson (D-Tex.), who cosponsored Rep. Murphy’s bill, previously served as chief psychiatric nurse at the Dallas Veterans Affairs Medical Center.
WASHINGTON – Bipartisan legislation to improve care of patients with serious mental illness is just a pen stroke from passage, now that the 21st Century Cures Act is headed for the President’s desk.
While the mental health care reform provisions in the legislation (H.R. 34) will impact mental health services broadly, the bulk of the reform language comes from H.R. 2646, a bill sponsored by Rep. Tim Murphy (R-Penn.), which was intended to reverse decades of fragmented – and at times nonexistent – care for persons with serious mental illness.
The legislation calls for the expanded use of assisted outpatient treatment, federal guidance on how states can be reimbursed for offering inpatient psychiatric services, better data collection on mental health services paid for with state and federal dollars, new oversight of the federal agency in charge of mental health, and clarification of HIPAA laws, among other provisions.
“This is big,” Rep. Murphy said at a press conference Dec. 5. “After all the tears and suffering … know that those times when you felt no one was willing to listen, and you were ready to give up, now there is hope.”
Treatment vs. incarceration
Currently, states and communities can draw from $80 million dollars in federal grants for assisted outpatient treatment for patients with serious mental illness. The new legislation adds another $20 million and extends availability of the funding until 2022. It also allows state criminal justice systems to use assisted outpatient treatment grants to treat convicted criminals with serious mental illness instead of incarcerating them.
“[In prison], their illness gets worse, not better, creating a turnstile through which they will return time and again through our criminal justice system,” Senate Majority Whip John Cornyn (R.-Tex.) said during the press conference.
Paying for inpatient psychiatric care
The Cures Act also strengthens momentum for overhauling the Medicaid Institutions of Mental Diseases (IMD) exclusion, long a focus of mental health care advocates who view it as a governor on the number of psychiatric beds available nationally.
The exclusion prohibits any medical facility with more than 16 beds from using federal funds to pay for inpatient mental health care for adults under age 65 years. The Cures Act requires the Centers for Medicare & Medicaid Services to offer guidance on how states can use Medicaid demonstration projects to provide innovative inpatient psychiatric services using these waivers.
This follows an April 2016 CMS final rule that matches state funding dollar-per-dollar for up to 15 days of inpatient psychiatric treatment given to Medicaid managed care patients.
Although Rep. Murphy’s original bill called for abolishing the exclusion, he and other advocates are not disappointed in the progress made so far. “We didn’t get everything we wanted, but we needed everything we got,” he said.
“That 15 days was a massive win,” Frankie Berger, advocacy director of the Treatment Advocacy Center in Arlington, Va., said in an interview. “Now we have this legislation that requires CMS to tell state Medicaid directors what their wiggle room is when solving the problem on how to get care to these patients. If you read between the lines, this is care that is going to be provided by an IMD.”
The legislation also calls for more data collection and evaluation of IMDs, something that until now has been missing, Ms. Berger said. “A lot of us who work on this issue have found there is absolutely no data on where IMDs are, or who the folks are that are getting treatment in them. We need that information to make good choices,” she said.
“I think we will find savings as we expand the number of psychiatric beds … [and persons with serious mental illness] do not end up in jail cells, homeless, or in the morgue,” Sen. Bill Cassidy (R-La.) said at the press conference. He predicted that for each additional psychiatric bed introduced, savings would amount to between $30,000 and $50,000.
Restructuring, clarifying
The Cures Act reforms also restructure the Substance Abuse and Mental Health Services Administration, putting it under the authority of a new assistant secretary of Health and Human Services and giving it a chief medical officer. The law calls for the new CMO to have “real-world” experience treating patients with serious mental illness. The reformed SAMHSA will have responsibility for centralizing data collection to be used in creating best practices in mental health care. These reforms are particular victories for Rep. Murphy who has railed against the agency for years, citing its lack of medically trained leadership and lack of evidence-based approaches to care.
HIPAA requirements in serious mental illness are also clarified.
“Existing HIPAA laws are badly misunderstood,” said Sen. Chris Murphy (D-Conn.) at the briefing. “Many physicians think there is an outright ban on sharing [patient health] information.”
The legislation calls for the U.S. Department of Health and Human Services secretary to clarify when providers can disclose protected health information related to the treatment of an adult with a mental illness or substance use disorder.
“I would argue that [HIPAA] may be an area we will have to work on down the line, if the education campaign doesn’t work, but we will give this a try,” said Sen. Murphy, who has cosponsored legislation to do so.
As passed, the mental health provisions of the 21st Century Cures Act are an amalgamation of several bills introduced during the 114th Congress and are unique in that they largely were written by health care professionals with direct, relevant experience. Rep. Murphy is a clinical psychologist, while Rep. Cassidy is a physician with experience treating uninsured and incarcerated patients. Rep. Eddie Bernice Johnson (D-Tex.), who cosponsored Rep. Murphy’s bill, previously served as chief psychiatric nurse at the Dallas Veterans Affairs Medical Center.