User login
Teens report increasingly lax attitude about marijuana use
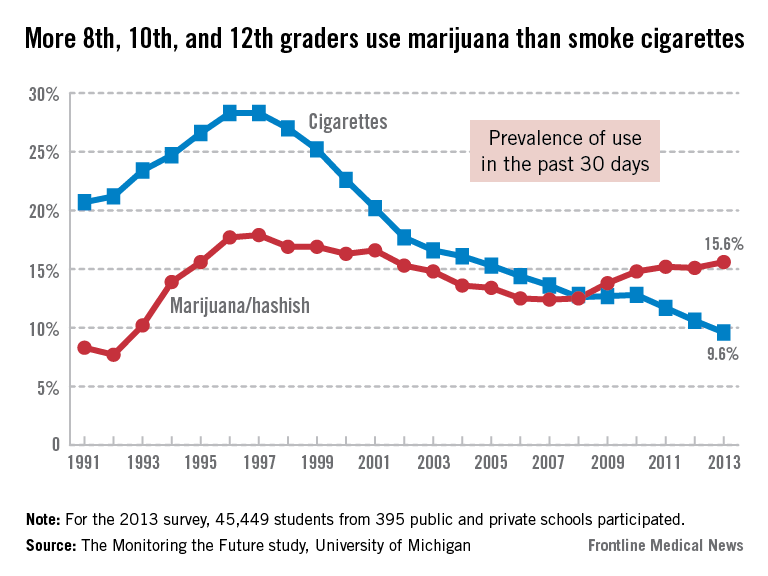
High school students are becoming more accepting of marijuana use, according to findings from the 2013 Monitoring the Future survey. This year’s survey results, released Dec. 18, show that 39.5% of 12th graders view marijuana use as harmful, down from last year’s rate of 44.1%.
The annual survey also reports a rise in marijuana use, compared with past decades, with 6.5% of high school seniors smoking daily, up from 6% in 2003 and 2.4% in 1993. Past-month use of marijuana increased between 2008 to 2013 from 5.8% to 7% among 8th graders, from 13.8% to 18% among 10th graders, and from 19.4% to 22.7% among 12th graders.
Dr. Nora D. Volkow, director of the National Institute on Drug Abuse, said this increase is quite worrying because of the potential effects on developing teenagers’ learning and memory.
"They are more sensitive to the effects in the brain," Dr. Volkow said in a teleconference announcing the results of the survey. "These are very high numbers, because these kids are in school and may be unable to learn properly."
Lloyd D. Johnston, Ph.D., lead investigator of the survey, said the changes in attitude might be related to easier access to pot as a result of medical marijuana legalization in some states, and the recent legalization of recreational marijuana in Colorado and Washington states.
"Medical marijuana and legalization affect perceived risk and prevalence of use," said Dr. Johnston of the University of Michigan’s Institute for Social Research. High school students also might be obtaining the drug through a friend or relative’s medical marijuana prescription, he added.
R. Gil Kerlikowske, director of the Office of National Drug Control Policy, expressed disappointment about the findings about teenagers’ increased use of marijuana. "More teens are now smoking marijuana than smoke cigarettes," he said.
The survey also shows a steady decrease in two areas: cigarette smoking and alcohol abuse. Cigarette use among 8th graders dropped to 14.8%, down from 15.5% in 2012. In 10th and 12th graders, cigarette use decreased from 27.7% to 25.7% and from 39.5% to 38.1%, respectively.
"Needless to say, the decline in cigarette use is very important," Dr. Johnston said. "We’re still seeing progress."
He added that newer drugs, such as bath salts and synthetic marijuana (also known as Spice or K2), were a cause for concern last year, but that recent media coverage has attracted attention to their adverse effects.
"There’s always a concern about new trends," Dr. Johnston said. "It seems the questionnaires get longer every year because there are so many drugs now, and unfortunately, not many leave the scene."
Synthetic marijuana use among high school seniors decreased from 11.3% in 2012 to 7.9% in 2013, and perceived risk of harm of using bath salts increased from 33.2% in 2012 to 59.5% in 2013.
This increased risk awareness is promising, Dr. Johnston said. "I think it’s important that we’ve seen a turnaround."
Abuse of prescription painkillers decreased this year, with Vicodin use among high school seniors dropping from 7.5% in 2012 to 5.3% in 2013. The increased abuse of prescription stimulants such as Adderall, however, continues to be a cause for concern, with 8.7% of 12th graders using amphetamines for nonmedical reasons in 2013, up from 6.8% in 2008.
"These drugs are used not just to get high and have fun, but also to improve performance," Dr. Volkow said. "So they take it prior to exams."
Cocaine and heroin use, though not significantly different from 2012 rates, continue to see a drop in use and currently are at a historic low in all grades. Only 2.6% of high school seniors reported cocaine use in 2013, compared with the peak rate of 6.2% in 1999. Heroin use was even lower, with 0.6% reporting use this year, compared with a peak of 1.5% in 2000.
Inhalants, more likely to be abused by younger students, also saw a decrease, with 5.2% of 8th graders reporting use.
Mr. Kerlikowske of the drug control policy office, said he hopes drug prevention programs in schools and communities will help curb abuse of marijuana in the future. "This should concern every parent, teacher, and employer across the nation," he said. "I continue to call upon all of us to bolster education."
This year’s Monitoring the Future survey featured more than 41,000 participants from 389 public and private schools. Survey participants are asked to report past month, past year, and lifetime use for each drug in the questionnaire. The survey has measured drug use and attitudes in high school seniors since 1975. Eighth and 10th graders were added in 1991.
The survey was sponsored by NIDA and conducted at the University of Michigan.
High school students are becoming more accepting of marijuana use, according to findings from the 2013 Monitoring the Future survey. This year’s survey results, released Dec. 18, show that 39.5% of 12th graders view marijuana use as harmful, down from last year’s rate of 44.1%.
The annual survey also reports a rise in marijuana use, compared with past decades, with 6.5% of high school seniors smoking daily, up from 6% in 2003 and 2.4% in 1993. Past-month use of marijuana increased between 2008 to 2013 from 5.8% to 7% among 8th graders, from 13.8% to 18% among 10th graders, and from 19.4% to 22.7% among 12th graders.
Dr. Nora D. Volkow, director of the National Institute on Drug Abuse, said this increase is quite worrying because of the potential effects on developing teenagers’ learning and memory.
"They are more sensitive to the effects in the brain," Dr. Volkow said in a teleconference announcing the results of the survey. "These are very high numbers, because these kids are in school and may be unable to learn properly."
Lloyd D. Johnston, Ph.D., lead investigator of the survey, said the changes in attitude might be related to easier access to pot as a result of medical marijuana legalization in some states, and the recent legalization of recreational marijuana in Colorado and Washington states.
"Medical marijuana and legalization affect perceived risk and prevalence of use," said Dr. Johnston of the University of Michigan’s Institute for Social Research. High school students also might be obtaining the drug through a friend or relative’s medical marijuana prescription, he added.
R. Gil Kerlikowske, director of the Office of National Drug Control Policy, expressed disappointment about the findings about teenagers’ increased use of marijuana. "More teens are now smoking marijuana than smoke cigarettes," he said.
The survey also shows a steady decrease in two areas: cigarette smoking and alcohol abuse. Cigarette use among 8th graders dropped to 14.8%, down from 15.5% in 2012. In 10th and 12th graders, cigarette use decreased from 27.7% to 25.7% and from 39.5% to 38.1%, respectively.
"Needless to say, the decline in cigarette use is very important," Dr. Johnston said. "We’re still seeing progress."
He added that newer drugs, such as bath salts and synthetic marijuana (also known as Spice or K2), were a cause for concern last year, but that recent media coverage has attracted attention to their adverse effects.
"There’s always a concern about new trends," Dr. Johnston said. "It seems the questionnaires get longer every year because there are so many drugs now, and unfortunately, not many leave the scene."
Synthetic marijuana use among high school seniors decreased from 11.3% in 2012 to 7.9% in 2013, and perceived risk of harm of using bath salts increased from 33.2% in 2012 to 59.5% in 2013.
This increased risk awareness is promising, Dr. Johnston said. "I think it’s important that we’ve seen a turnaround."
Abuse of prescription painkillers decreased this year, with Vicodin use among high school seniors dropping from 7.5% in 2012 to 5.3% in 2013. The increased abuse of prescription stimulants such as Adderall, however, continues to be a cause for concern, with 8.7% of 12th graders using amphetamines for nonmedical reasons in 2013, up from 6.8% in 2008.
"These drugs are used not just to get high and have fun, but also to improve performance," Dr. Volkow said. "So they take it prior to exams."
Cocaine and heroin use, though not significantly different from 2012 rates, continue to see a drop in use and currently are at a historic low in all grades. Only 2.6% of high school seniors reported cocaine use in 2013, compared with the peak rate of 6.2% in 1999. Heroin use was even lower, with 0.6% reporting use this year, compared with a peak of 1.5% in 2000.
Inhalants, more likely to be abused by younger students, also saw a decrease, with 5.2% of 8th graders reporting use.
Mr. Kerlikowske of the drug control policy office, said he hopes drug prevention programs in schools and communities will help curb abuse of marijuana in the future. "This should concern every parent, teacher, and employer across the nation," he said. "I continue to call upon all of us to bolster education."
This year’s Monitoring the Future survey featured more than 41,000 participants from 389 public and private schools. Survey participants are asked to report past month, past year, and lifetime use for each drug in the questionnaire. The survey has measured drug use and attitudes in high school seniors since 1975. Eighth and 10th graders were added in 1991.
The survey was sponsored by NIDA and conducted at the University of Michigan.
High school students are becoming more accepting of marijuana use, according to findings from the 2013 Monitoring the Future survey. This year’s survey results, released Dec. 18, show that 39.5% of 12th graders view marijuana use as harmful, down from last year’s rate of 44.1%.
The annual survey also reports a rise in marijuana use, compared with past decades, with 6.5% of high school seniors smoking daily, up from 6% in 2003 and 2.4% in 1993. Past-month use of marijuana increased between 2008 to 2013 from 5.8% to 7% among 8th graders, from 13.8% to 18% among 10th graders, and from 19.4% to 22.7% among 12th graders.
Dr. Nora D. Volkow, director of the National Institute on Drug Abuse, said this increase is quite worrying because of the potential effects on developing teenagers’ learning and memory.
"They are more sensitive to the effects in the brain," Dr. Volkow said in a teleconference announcing the results of the survey. "These are very high numbers, because these kids are in school and may be unable to learn properly."
Lloyd D. Johnston, Ph.D., lead investigator of the survey, said the changes in attitude might be related to easier access to pot as a result of medical marijuana legalization in some states, and the recent legalization of recreational marijuana in Colorado and Washington states.
"Medical marijuana and legalization affect perceived risk and prevalence of use," said Dr. Johnston of the University of Michigan’s Institute for Social Research. High school students also might be obtaining the drug through a friend or relative’s medical marijuana prescription, he added.
R. Gil Kerlikowske, director of the Office of National Drug Control Policy, expressed disappointment about the findings about teenagers’ increased use of marijuana. "More teens are now smoking marijuana than smoke cigarettes," he said.
The survey also shows a steady decrease in two areas: cigarette smoking and alcohol abuse. Cigarette use among 8th graders dropped to 14.8%, down from 15.5% in 2012. In 10th and 12th graders, cigarette use decreased from 27.7% to 25.7% and from 39.5% to 38.1%, respectively.
"Needless to say, the decline in cigarette use is very important," Dr. Johnston said. "We’re still seeing progress."
He added that newer drugs, such as bath salts and synthetic marijuana (also known as Spice or K2), were a cause for concern last year, but that recent media coverage has attracted attention to their adverse effects.
"There’s always a concern about new trends," Dr. Johnston said. "It seems the questionnaires get longer every year because there are so many drugs now, and unfortunately, not many leave the scene."
Synthetic marijuana use among high school seniors decreased from 11.3% in 2012 to 7.9% in 2013, and perceived risk of harm of using bath salts increased from 33.2% in 2012 to 59.5% in 2013.
This increased risk awareness is promising, Dr. Johnston said. "I think it’s important that we’ve seen a turnaround."
Abuse of prescription painkillers decreased this year, with Vicodin use among high school seniors dropping from 7.5% in 2012 to 5.3% in 2013. The increased abuse of prescription stimulants such as Adderall, however, continues to be a cause for concern, with 8.7% of 12th graders using amphetamines for nonmedical reasons in 2013, up from 6.8% in 2008.
"These drugs are used not just to get high and have fun, but also to improve performance," Dr. Volkow said. "So they take it prior to exams."
Cocaine and heroin use, though not significantly different from 2012 rates, continue to see a drop in use and currently are at a historic low in all grades. Only 2.6% of high school seniors reported cocaine use in 2013, compared with the peak rate of 6.2% in 1999. Heroin use was even lower, with 0.6% reporting use this year, compared with a peak of 1.5% in 2000.
Inhalants, more likely to be abused by younger students, also saw a decrease, with 5.2% of 8th graders reporting use.
Mr. Kerlikowske of the drug control policy office, said he hopes drug prevention programs in schools and communities will help curb abuse of marijuana in the future. "This should concern every parent, teacher, and employer across the nation," he said. "I continue to call upon all of us to bolster education."
This year’s Monitoring the Future survey featured more than 41,000 participants from 389 public and private schools. Survey participants are asked to report past month, past year, and lifetime use for each drug in the questionnaire. The survey has measured drug use and attitudes in high school seniors since 1975. Eighth and 10th graders were added in 1991.
The survey was sponsored by NIDA and conducted at the University of Michigan.
FROM A TELECONFERENCE SPONSORED BY THE NIDA
Major finding: Only slightly more than 39% of high school seniors view marijuana use as harmful, compared with 44.1% in 2012.
Data source: A survey of 41, 675 students in grades 8, 10, and 12, from 389 public and private schools in the United States.
Disclosures: The survey was sponsored by the National Institute on Drug Abuse, a division of the National Institutes of Health.
FDA approves Xiaflex for Peyronie’s disease
The Food and Drug Administration has approved the biologic drug Xiaflex (collagenase clostridium histolyticum) for Peyronie’s disease, making it the first FDA-approved medicine for men with the disease.
Xiaflex, originally approved in 2010 to treat the hand deformity Dupuytren’s contracture, is the first available nonsurgical treatment option for Peyronie’s disease, a condition in which scar tissue develops under the skin of the penis to form a lump. This scar tissue causes an abnormal bend during erection that may cause discomfort during intercourse.
"Xiaflex is believed to work for Peyronie’s disease by breaking down the buildup of collagen that causes the curvature deformity," the FDA said in a statement Dec. 6.
A treatment cycle with Xiaflex consists of two injections directly into the collagen-containing part of the penis and one penile modeling procedure. The patient may undergo a maximum of four treatment cycles.
Xiaflex was studied in two trials of a total of 832 men with Peyronie’s disease and a penile curvature deformity of at least 30 degrees. Patients received either placebo or up to four Xiaflex treatment cycles and were followed over 52 weeks.
The FDA reported that Xiaflex "significantly reduced penile curvature deformity and related bothersome effects" compared with placebo, but warned of possible adverse side effects of the drug, such as penile fracture, hematoma, swelling, and pain.
Because of the risk for adverse reactions, Xiaflex for the treatment of Peyronie’s disease is available only through a restricted program under a Risk Evaluation and Mitigation Strategy. The program requires participating doctors to undergo training and certification in the administration of the drug.
Adverse reactions from the use of Xiaflex should be reported to the FDA’s MedWatch Adverse Event Reporting Program online or by calling 800-FDA-1088.
Xiaflex is marketed by Auxilium Pharmaceuticals.
Xiaflex, scar tissue, under the skin of the penis, lump, abnormal bend during erection, discomfort,
The Food and Drug Administration has approved the biologic drug Xiaflex (collagenase clostridium histolyticum) for Peyronie’s disease, making it the first FDA-approved medicine for men with the disease.
Xiaflex, originally approved in 2010 to treat the hand deformity Dupuytren’s contracture, is the first available nonsurgical treatment option for Peyronie’s disease, a condition in which scar tissue develops under the skin of the penis to form a lump. This scar tissue causes an abnormal bend during erection that may cause discomfort during intercourse.
"Xiaflex is believed to work for Peyronie’s disease by breaking down the buildup of collagen that causes the curvature deformity," the FDA said in a statement Dec. 6.
A treatment cycle with Xiaflex consists of two injections directly into the collagen-containing part of the penis and one penile modeling procedure. The patient may undergo a maximum of four treatment cycles.
Xiaflex was studied in two trials of a total of 832 men with Peyronie’s disease and a penile curvature deformity of at least 30 degrees. Patients received either placebo or up to four Xiaflex treatment cycles and were followed over 52 weeks.
The FDA reported that Xiaflex "significantly reduced penile curvature deformity and related bothersome effects" compared with placebo, but warned of possible adverse side effects of the drug, such as penile fracture, hematoma, swelling, and pain.
Because of the risk for adverse reactions, Xiaflex for the treatment of Peyronie’s disease is available only through a restricted program under a Risk Evaluation and Mitigation Strategy. The program requires participating doctors to undergo training and certification in the administration of the drug.
Adverse reactions from the use of Xiaflex should be reported to the FDA’s MedWatch Adverse Event Reporting Program online or by calling 800-FDA-1088.
Xiaflex is marketed by Auxilium Pharmaceuticals.
The Food and Drug Administration has approved the biologic drug Xiaflex (collagenase clostridium histolyticum) for Peyronie’s disease, making it the first FDA-approved medicine for men with the disease.
Xiaflex, originally approved in 2010 to treat the hand deformity Dupuytren’s contracture, is the first available nonsurgical treatment option for Peyronie’s disease, a condition in which scar tissue develops under the skin of the penis to form a lump. This scar tissue causes an abnormal bend during erection that may cause discomfort during intercourse.
"Xiaflex is believed to work for Peyronie’s disease by breaking down the buildup of collagen that causes the curvature deformity," the FDA said in a statement Dec. 6.
A treatment cycle with Xiaflex consists of two injections directly into the collagen-containing part of the penis and one penile modeling procedure. The patient may undergo a maximum of four treatment cycles.
Xiaflex was studied in two trials of a total of 832 men with Peyronie’s disease and a penile curvature deformity of at least 30 degrees. Patients received either placebo or up to four Xiaflex treatment cycles and were followed over 52 weeks.
The FDA reported that Xiaflex "significantly reduced penile curvature deformity and related bothersome effects" compared with placebo, but warned of possible adverse side effects of the drug, such as penile fracture, hematoma, swelling, and pain.
Because of the risk for adverse reactions, Xiaflex for the treatment of Peyronie’s disease is available only through a restricted program under a Risk Evaluation and Mitigation Strategy. The program requires participating doctors to undergo training and certification in the administration of the drug.
Adverse reactions from the use of Xiaflex should be reported to the FDA’s MedWatch Adverse Event Reporting Program online or by calling 800-FDA-1088.
Xiaflex is marketed by Auxilium Pharmaceuticals.
Xiaflex, scar tissue, under the skin of the penis, lump, abnormal bend during erection, discomfort,
Xiaflex, scar tissue, under the skin of the penis, lump, abnormal bend during erection, discomfort,
Headache neuroimaging and medication no-nos highlighted in new list
Patients with stable headaches that meet criteria for migraine should not undergo neuroimaging studies, according to one of five new recommendations developed by the American Headache Society about treatments and tests that may not always be necessary in the treatment of migraines and headaches.
The list of recommendations is part of the American Board of Internal Medicine Foundation’s "Choosing Wisely" campaign, which aims to educate patients and physicians about unnecessary and potentially harmful screening and treatment.
The AHS list was written by a task force approved by the AHS Board of Directors, in consultation with AHS members via an electronic survey.
The other four recommendations are:
• Don’t perform CT imaging for headache when MRI is available, except in emergency settings. "MRI is better for looking at brain tissue, and changes associated with migraines may be more visible on MRI," said Dr. Carolyn Bernstein, a headache medicine specialist and neurologist at Beth Israel Deaconess Medical Center in Brookline, Mass. In addition, "MRI doesn’t expose the patient to radiation, but the CT scan does."
• Don’t recommend surgical deactivation of migraine trigger points outside of a clinical trial.
• Don’t prescribe opioid or butalbital-containing medications as first-line treatment for recurrent headache disorders.
• Don’t recommend prolonged or frequent use of over-the-counter pain medications for headache. Though "abortive medications" such as Tylenol or Excedrin may be effective in relieving headaches and migraines, patients who take these medications too frequently may develop overuse headache, said Dr. Bernstein, who was not involved in making the recommendations. "People think it’s safe because it’s over the counter," she said. "But the headache can become harder to treat" and become refractory to the medications, leading patients to "ask for something stronger."
Dr. Bernstein recommends that patients track their headaches, either on a calendar or using a free smartphone app such as My Migraine Triggers or iHeadache. "If the frequency picks up and you find yourself reaching for abortive medication more than once a week, see a doctor and explore a preventative plan," she said.
This AHS Choosing Wisely list is being released along with its publication in the November/December issue of the journal Headache.
Patients with stable headaches that meet criteria for migraine should not undergo neuroimaging studies, according to one of five new recommendations developed by the American Headache Society about treatments and tests that may not always be necessary in the treatment of migraines and headaches.
The list of recommendations is part of the American Board of Internal Medicine Foundation’s "Choosing Wisely" campaign, which aims to educate patients and physicians about unnecessary and potentially harmful screening and treatment.
The AHS list was written by a task force approved by the AHS Board of Directors, in consultation with AHS members via an electronic survey.
The other four recommendations are:
• Don’t perform CT imaging for headache when MRI is available, except in emergency settings. "MRI is better for looking at brain tissue, and changes associated with migraines may be more visible on MRI," said Dr. Carolyn Bernstein, a headache medicine specialist and neurologist at Beth Israel Deaconess Medical Center in Brookline, Mass. In addition, "MRI doesn’t expose the patient to radiation, but the CT scan does."
• Don’t recommend surgical deactivation of migraine trigger points outside of a clinical trial.
• Don’t prescribe opioid or butalbital-containing medications as first-line treatment for recurrent headache disorders.
• Don’t recommend prolonged or frequent use of over-the-counter pain medications for headache. Though "abortive medications" such as Tylenol or Excedrin may be effective in relieving headaches and migraines, patients who take these medications too frequently may develop overuse headache, said Dr. Bernstein, who was not involved in making the recommendations. "People think it’s safe because it’s over the counter," she said. "But the headache can become harder to treat" and become refractory to the medications, leading patients to "ask for something stronger."
Dr. Bernstein recommends that patients track their headaches, either on a calendar or using a free smartphone app such as My Migraine Triggers or iHeadache. "If the frequency picks up and you find yourself reaching for abortive medication more than once a week, see a doctor and explore a preventative plan," she said.
This AHS Choosing Wisely list is being released along with its publication in the November/December issue of the journal Headache.
Patients with stable headaches that meet criteria for migraine should not undergo neuroimaging studies, according to one of five new recommendations developed by the American Headache Society about treatments and tests that may not always be necessary in the treatment of migraines and headaches.
The list of recommendations is part of the American Board of Internal Medicine Foundation’s "Choosing Wisely" campaign, which aims to educate patients and physicians about unnecessary and potentially harmful screening and treatment.
The AHS list was written by a task force approved by the AHS Board of Directors, in consultation with AHS members via an electronic survey.
The other four recommendations are:
• Don’t perform CT imaging for headache when MRI is available, except in emergency settings. "MRI is better for looking at brain tissue, and changes associated with migraines may be more visible on MRI," said Dr. Carolyn Bernstein, a headache medicine specialist and neurologist at Beth Israel Deaconess Medical Center in Brookline, Mass. In addition, "MRI doesn’t expose the patient to radiation, but the CT scan does."
• Don’t recommend surgical deactivation of migraine trigger points outside of a clinical trial.
• Don’t prescribe opioid or butalbital-containing medications as first-line treatment for recurrent headache disorders.
• Don’t recommend prolonged or frequent use of over-the-counter pain medications for headache. Though "abortive medications" such as Tylenol or Excedrin may be effective in relieving headaches and migraines, patients who take these medications too frequently may develop overuse headache, said Dr. Bernstein, who was not involved in making the recommendations. "People think it’s safe because it’s over the counter," she said. "But the headache can become harder to treat" and become refractory to the medications, leading patients to "ask for something stronger."
Dr. Bernstein recommends that patients track their headaches, either on a calendar or using a free smartphone app such as My Migraine Triggers or iHeadache. "If the frequency picks up and you find yourself reaching for abortive medication more than once a week, see a doctor and explore a preventative plan," she said.
This AHS Choosing Wisely list is being released along with its publication in the November/December issue of the journal Headache.
The American Academy of Dermatology releases ‘Choosing Wisely’ list of treatments physicians and patients should question
The American Academy of Dermatology has released a list of treatments and screenings that may not always be necessary in dermatologic medicine.
The list of recommendations is part of the American Board of Internal Medicine Foundation’s "Choosing Wisely" campaign, which aims to educate patients and physicians about unnecessary and potentially harmful testing and treatment.
The AAD’s list was created by members of the its Board of Directors; Council on Science and Research, Health Policy and Practice; Council on Government Affairs, Health Policy & Practice; Research Agenda Committee; Clinical Guidelines Committee; Access to Dermatologic Care Committee; Patient Safety and Quality Committee; Resource-Based Relative Value Scale Committee; and the Workgroup on Innovative Payment and Delivery Reform.
The AAD’s Choose Wisely recommendations are as follows:
• Do not prescribe oral antifungal therapy for suspected nail fungus without confirmation of fungal infection. About half of nails with suspected fungus do not actually have a fungal infection. Other nail conditions such as dystrophies may look similar in appearance, so it is important to first confirm the presence of nail disease before starting treatment.
• Do not perform sentinel lymph node biopsy or other diagnostic tests for the evaluation of early, thin melanoma. These tests do not improve survival. Patients with early, thin melanomas have a very low risk of the cancer spreading to the lymph nodes and other parts of the body, and a 97% 5-year survival rate. Also, baseline blood tests and radiographic scans have high false-positive rates and are not the most accurate for detecting cancer that is spreading.
• Do not treat uncomplicated, nonmelanoma skin cancer less than 1 centimeter in size on the trunk and extremities with Mohs micrographic surgery. The use of Mohs micrographic surgery in healthy individuals with low-risk, small, superficial, or nonaggressive squamous cell carcinomas and basal cell carcinomas is not appropriate for skin cancers on the trunk and extremities, as the benefits do not outweigh the risks on these parts of the body. However, Mohs micrographic surgery may be called for in skin cancers on the hands, feet, ankles, shins, nipples, or genitals, as they have a higher risk for recurrence and may require additional surgical considerations.
• Do not use oral antibiotics for treatment of atopic dermatitis unless there is clinical evidence of infection. The presence of Staphylococcus bacteria on the skin of children and adults with atopic dermatitis is common. Though it is widely believed that Staphylococcus bacteria may contribute to skin inflammation, oral antibiotics have not been shown to reduce the symptoms or severity of atopic dermatitis. The use of antibiotics may also lead to antibiotic resistance and cause side effects such as hypersensitivity reactions.
• Do not routinely use topical antibiotics on a surgical wound. This practice has not been shown to reduce the rate of infection, compared with using nonantibiotic ointment or no ointment. Topical antibiotics can aggravate open wounds, thus delaying the healing process. Also, topical antibiotic use carries a significant risk of developing contact dermatitis. Antibiotics should only be used when wounds show symptoms of infection.
For more information about the campaign, visit the AAD website.
The American Academy of Dermatology has released a list of treatments and screenings that may not always be necessary in dermatologic medicine.
The list of recommendations is part of the American Board of Internal Medicine Foundation’s "Choosing Wisely" campaign, which aims to educate patients and physicians about unnecessary and potentially harmful testing and treatment.
The AAD’s list was created by members of the its Board of Directors; Council on Science and Research, Health Policy and Practice; Council on Government Affairs, Health Policy & Practice; Research Agenda Committee; Clinical Guidelines Committee; Access to Dermatologic Care Committee; Patient Safety and Quality Committee; Resource-Based Relative Value Scale Committee; and the Workgroup on Innovative Payment and Delivery Reform.
The AAD’s Choose Wisely recommendations are as follows:
• Do not prescribe oral antifungal therapy for suspected nail fungus without confirmation of fungal infection. About half of nails with suspected fungus do not actually have a fungal infection. Other nail conditions such as dystrophies may look similar in appearance, so it is important to first confirm the presence of nail disease before starting treatment.
• Do not perform sentinel lymph node biopsy or other diagnostic tests for the evaluation of early, thin melanoma. These tests do not improve survival. Patients with early, thin melanomas have a very low risk of the cancer spreading to the lymph nodes and other parts of the body, and a 97% 5-year survival rate. Also, baseline blood tests and radiographic scans have high false-positive rates and are not the most accurate for detecting cancer that is spreading.
• Do not treat uncomplicated, nonmelanoma skin cancer less than 1 centimeter in size on the trunk and extremities with Mohs micrographic surgery. The use of Mohs micrographic surgery in healthy individuals with low-risk, small, superficial, or nonaggressive squamous cell carcinomas and basal cell carcinomas is not appropriate for skin cancers on the trunk and extremities, as the benefits do not outweigh the risks on these parts of the body. However, Mohs micrographic surgery may be called for in skin cancers on the hands, feet, ankles, shins, nipples, or genitals, as they have a higher risk for recurrence and may require additional surgical considerations.
• Do not use oral antibiotics for treatment of atopic dermatitis unless there is clinical evidence of infection. The presence of Staphylococcus bacteria on the skin of children and adults with atopic dermatitis is common. Though it is widely believed that Staphylococcus bacteria may contribute to skin inflammation, oral antibiotics have not been shown to reduce the symptoms or severity of atopic dermatitis. The use of antibiotics may also lead to antibiotic resistance and cause side effects such as hypersensitivity reactions.
• Do not routinely use topical antibiotics on a surgical wound. This practice has not been shown to reduce the rate of infection, compared with using nonantibiotic ointment or no ointment. Topical antibiotics can aggravate open wounds, thus delaying the healing process. Also, topical antibiotic use carries a significant risk of developing contact dermatitis. Antibiotics should only be used when wounds show symptoms of infection.
For more information about the campaign, visit the AAD website.
The American Academy of Dermatology has released a list of treatments and screenings that may not always be necessary in dermatologic medicine.
The list of recommendations is part of the American Board of Internal Medicine Foundation’s "Choosing Wisely" campaign, which aims to educate patients and physicians about unnecessary and potentially harmful testing and treatment.
The AAD’s list was created by members of the its Board of Directors; Council on Science and Research, Health Policy and Practice; Council on Government Affairs, Health Policy & Practice; Research Agenda Committee; Clinical Guidelines Committee; Access to Dermatologic Care Committee; Patient Safety and Quality Committee; Resource-Based Relative Value Scale Committee; and the Workgroup on Innovative Payment and Delivery Reform.
The AAD’s Choose Wisely recommendations are as follows:
• Do not prescribe oral antifungal therapy for suspected nail fungus without confirmation of fungal infection. About half of nails with suspected fungus do not actually have a fungal infection. Other nail conditions such as dystrophies may look similar in appearance, so it is important to first confirm the presence of nail disease before starting treatment.
• Do not perform sentinel lymph node biopsy or other diagnostic tests for the evaluation of early, thin melanoma. These tests do not improve survival. Patients with early, thin melanomas have a very low risk of the cancer spreading to the lymph nodes and other parts of the body, and a 97% 5-year survival rate. Also, baseline blood tests and radiographic scans have high false-positive rates and are not the most accurate for detecting cancer that is spreading.
• Do not treat uncomplicated, nonmelanoma skin cancer less than 1 centimeter in size on the trunk and extremities with Mohs micrographic surgery. The use of Mohs micrographic surgery in healthy individuals with low-risk, small, superficial, or nonaggressive squamous cell carcinomas and basal cell carcinomas is not appropriate for skin cancers on the trunk and extremities, as the benefits do not outweigh the risks on these parts of the body. However, Mohs micrographic surgery may be called for in skin cancers on the hands, feet, ankles, shins, nipples, or genitals, as they have a higher risk for recurrence and may require additional surgical considerations.
• Do not use oral antibiotics for treatment of atopic dermatitis unless there is clinical evidence of infection. The presence of Staphylococcus bacteria on the skin of children and adults with atopic dermatitis is common. Though it is widely believed that Staphylococcus bacteria may contribute to skin inflammation, oral antibiotics have not been shown to reduce the symptoms or severity of atopic dermatitis. The use of antibiotics may also lead to antibiotic resistance and cause side effects such as hypersensitivity reactions.
• Do not routinely use topical antibiotics on a surgical wound. This practice has not been shown to reduce the rate of infection, compared with using nonantibiotic ointment or no ointment. Topical antibiotics can aggravate open wounds, thus delaying the healing process. Also, topical antibiotic use carries a significant risk of developing contact dermatitis. Antibiotics should only be used when wounds show symptoms of infection.
For more information about the campaign, visit the AAD website.
Choosing Wisely in pulmonary medicine means fewer CTs amid low risk
The American College of Chest Physicians has released its list of common but not always necessary tests in pulmonary medicine.
The list was a result of the collaborative efforts of the AACP and the American Thoracic Society, and is part of the ABIM Foundation’s Choosing Wisely campaign, which aims to educate patients and physicians about unnecessary and potentially harmful testing and treatment. The list was released during CHEST 2013, the annual meeting of the ACCP, which is being held in Chicago.
The ACCP’s recommendations are:
• Do not perform CT surveillance for evaluation of indeterminate pulmonary nodules at more frequent intervals or for a longer period of time than recommended by established guidelines. In patients with no cancer history, solid nodules that have not grown over a 2-year period have a very low risk of malignancy. Also, repeating CT scans has not been shown to improve outcomes, and exposes patients to increased radiation over time.
• Do not routinely offer pharmacologic treatment with advanced vasoactive agents approved only for the management of pulmonary arterial hypertension to patients with pulmonary hypertension resulting form left heart disease or hypoxemic lung diseases. There is no established benefit of vasoactive agents for patients with pulmonary hypertension resulting from left heart disease or hypoxemic lung disease.
• For patients recently discharged on supplemental home oxygen following hospitalization for an acute illness, do not renew the prescription without assessing the patient for ongoing hypoxemia. Hypoxemia often resolves after recovery from an acute illness, and continued supplemental oxygen incurs unnecessary costs.
• Do not perform CT angiography to evaluate for possible pulmonary embolism in patients with a low clinical probability and negative results of a highly sensitive d-dimer assay. Clinical practice guidelines indicate that the potential harms of CT angiography outweigh the benefits for patients with a low pretest probability of pulmonary embolism.
• Do not perform CT screening for lung cancer among patients at low risk for lung cancer. Low-dose chest CT screening has the potential to reduce lung cancer death in high-risk patients, but could potentially cause adverse effects such as radiation exposure, high false-positive rates, harms related to downstream evaluation of pulmonary nodules, and overdiagnosis of indolent tumors. Hence, it should be reserved only for patients at high risk of lung cancer (people aged 55-74 with at least a 30 pack-year history of tobacco use, who are either still smoking or quit within the past 15 years).*
The ACCP recommendations and detailed explanations for each will be published in the journal CHEST in 2014. For more information about the Choosing Wisely campaign, click here.
mrajaraman@frontlinemedcom.com
*Correction, 10/29/13: An earlier version of this story misstated the definition of those considered at high risk of lung cancer.
The American College of Chest Physicians has released its list of common but not always necessary tests in pulmonary medicine.
The list was a result of the collaborative efforts of the AACP and the American Thoracic Society, and is part of the ABIM Foundation’s Choosing Wisely campaign, which aims to educate patients and physicians about unnecessary and potentially harmful testing and treatment. The list was released during CHEST 2013, the annual meeting of the ACCP, which is being held in Chicago.
The ACCP’s recommendations are:
• Do not perform CT surveillance for evaluation of indeterminate pulmonary nodules at more frequent intervals or for a longer period of time than recommended by established guidelines. In patients with no cancer history, solid nodules that have not grown over a 2-year period have a very low risk of malignancy. Also, repeating CT scans has not been shown to improve outcomes, and exposes patients to increased radiation over time.
• Do not routinely offer pharmacologic treatment with advanced vasoactive agents approved only for the management of pulmonary arterial hypertension to patients with pulmonary hypertension resulting form left heart disease or hypoxemic lung diseases. There is no established benefit of vasoactive agents for patients with pulmonary hypertension resulting from left heart disease or hypoxemic lung disease.
• For patients recently discharged on supplemental home oxygen following hospitalization for an acute illness, do not renew the prescription without assessing the patient for ongoing hypoxemia. Hypoxemia often resolves after recovery from an acute illness, and continued supplemental oxygen incurs unnecessary costs.
• Do not perform CT angiography to evaluate for possible pulmonary embolism in patients with a low clinical probability and negative results of a highly sensitive d-dimer assay. Clinical practice guidelines indicate that the potential harms of CT angiography outweigh the benefits for patients with a low pretest probability of pulmonary embolism.
• Do not perform CT screening for lung cancer among patients at low risk for lung cancer. Low-dose chest CT screening has the potential to reduce lung cancer death in high-risk patients, but could potentially cause adverse effects such as radiation exposure, high false-positive rates, harms related to downstream evaluation of pulmonary nodules, and overdiagnosis of indolent tumors. Hence, it should be reserved only for patients at high risk of lung cancer (people aged 55-74 with at least a 30 pack-year history of tobacco use, who are either still smoking or quit within the past 15 years).*
The ACCP recommendations and detailed explanations for each will be published in the journal CHEST in 2014. For more information about the Choosing Wisely campaign, click here.
mrajaraman@frontlinemedcom.com
*Correction, 10/29/13: An earlier version of this story misstated the definition of those considered at high risk of lung cancer.
The American College of Chest Physicians has released its list of common but not always necessary tests in pulmonary medicine.
The list was a result of the collaborative efforts of the AACP and the American Thoracic Society, and is part of the ABIM Foundation’s Choosing Wisely campaign, which aims to educate patients and physicians about unnecessary and potentially harmful testing and treatment. The list was released during CHEST 2013, the annual meeting of the ACCP, which is being held in Chicago.
The ACCP’s recommendations are:
• Do not perform CT surveillance for evaluation of indeterminate pulmonary nodules at more frequent intervals or for a longer period of time than recommended by established guidelines. In patients with no cancer history, solid nodules that have not grown over a 2-year period have a very low risk of malignancy. Also, repeating CT scans has not been shown to improve outcomes, and exposes patients to increased radiation over time.
• Do not routinely offer pharmacologic treatment with advanced vasoactive agents approved only for the management of pulmonary arterial hypertension to patients with pulmonary hypertension resulting form left heart disease or hypoxemic lung diseases. There is no established benefit of vasoactive agents for patients with pulmonary hypertension resulting from left heart disease or hypoxemic lung disease.
• For patients recently discharged on supplemental home oxygen following hospitalization for an acute illness, do not renew the prescription without assessing the patient for ongoing hypoxemia. Hypoxemia often resolves after recovery from an acute illness, and continued supplemental oxygen incurs unnecessary costs.
• Do not perform CT angiography to evaluate for possible pulmonary embolism in patients with a low clinical probability and negative results of a highly sensitive d-dimer assay. Clinical practice guidelines indicate that the potential harms of CT angiography outweigh the benefits for patients with a low pretest probability of pulmonary embolism.
• Do not perform CT screening for lung cancer among patients at low risk for lung cancer. Low-dose chest CT screening has the potential to reduce lung cancer death in high-risk patients, but could potentially cause adverse effects such as radiation exposure, high false-positive rates, harms related to downstream evaluation of pulmonary nodules, and overdiagnosis of indolent tumors. Hence, it should be reserved only for patients at high risk of lung cancer (people aged 55-74 with at least a 30 pack-year history of tobacco use, who are either still smoking or quit within the past 15 years).*
The ACCP recommendations and detailed explanations for each will be published in the journal CHEST in 2014. For more information about the Choosing Wisely campaign, click here.
mrajaraman@frontlinemedcom.com
*Correction, 10/29/13: An earlier version of this story misstated the definition of those considered at high risk of lung cancer.
Obstructive sleep apnea is a risk factor for Barrett’s esophagus
Obstructive sleep apnea is a risk factor for Barrett’s esophagus, according to findings published online September 11 in Clinical Gastroenterology and Hepatology.
Researchers from the Mayo Clinic in Rochester, Minn., studied 7,482 patients who had undergone both a diagnostic polysomnogram and esophagogastroduodenoscopy from January 2000 to November 2011.
"In this subset of patients, the presence of OSA [obstructive sleep apnea] was associated with an 80% increased risk of [Barrett’s esophagus], compared to subjects without OSA and [Barrett’s esophagus]," wrote study author Dr. Prasad G. Iyer and his colleagues (Clin. Gastroenterol. Hepatol. 2013 September;11:1108-14.e5).
Several overlapping risk factors exist for obstructive sleep apnea and Barrett’s esophagus (BE), including obesity, gastroesophageal reflux disease (GERD), male gender, and older age. This study was designed to explore whether there is a relationship between obstructive sleep apnea and Barrett’s esophagus independent of these factors.
Subjects were categorized into four groups: diagnosis of BE but not OSA; OSA but not BE; both; or neither. Of the 7,482 patients, 2,480 did not have a diagnosis of OSA or BE; 83 had BE but not OSA; 4,641 had OSA but not BE; and 278 had a diagnosis of both.
The study authors used univariable models assessing age, sex, body mass index, GERD, and smoking history to determine the association between OSA and BE. GERD and OSA were associated with Barrett’s esophagus. A multiple-variable analysis was performed to observe the association of OSA with BE, adjusting for other factors. Patients with OSA were about 80% more at risk for having Barrett’s esophagus than were subjects without OSA or Barrett’s esophagus.
"This association was dose dependent, with an increase in severity of OSA being associated with an increased risk of Barrett’s esophagus," wrote the authors.
Additionally, since "the association of [Barrett’s esophagus] and OSA could be confounded by gastroesophageal reflux," the researchers also performed analyses to determine whether this relationship was independent of a GERD diagnosis. In a univariate analysis, both OSA and GERD were associated with BE, and in a multiple-variable analysis demonstrated that "both OSA and GERD were "independently associated with an increased risk of Barrett’s esophagus."
Dr. Iyer and his colleagues cited a few limitations to this study. First, the study’s design did not allow for exploration of a specific mechanism for how OSA predisposes individuals to Barrett’s esophagus. Second, the ability to accurately assess the association of OSA with GERD was limited by a lack of an established clinical definition of GERD. Finally, the use of ICD-9 codes to diagnose conditions may have resulted in overestimates in the sample.
The authors concluded that further research is needed to confirm that these findings can be applied to the general population and to explore whether treatment for OSA may help reverse this risk.
They also added that given the "asymptomatic nature" of Barrett’s esophagus and the higher risk of esophageal adenocarcinoma, patients with OSA may benefit from BE screening.
Dr. Iyer and his colleagues disclosed that this study was supported in part by the American College of Gastroenterology, the National Institute of Diabetes, Digestive and Kidney Disease; and the Edward C. Rosenow Endowed Professorship Internal Medicine Residency Award at the Mayo Clinic.
Obstructive sleep apnea is a risk factor for Barrett’s esophagus, according to findings published online September 11 in Clinical Gastroenterology and Hepatology.
Researchers from the Mayo Clinic in Rochester, Minn., studied 7,482 patients who had undergone both a diagnostic polysomnogram and esophagogastroduodenoscopy from January 2000 to November 2011.
"In this subset of patients, the presence of OSA [obstructive sleep apnea] was associated with an 80% increased risk of [Barrett’s esophagus], compared to subjects without OSA and [Barrett’s esophagus]," wrote study author Dr. Prasad G. Iyer and his colleagues (Clin. Gastroenterol. Hepatol. 2013 September;11:1108-14.e5).
Several overlapping risk factors exist for obstructive sleep apnea and Barrett’s esophagus (BE), including obesity, gastroesophageal reflux disease (GERD), male gender, and older age. This study was designed to explore whether there is a relationship between obstructive sleep apnea and Barrett’s esophagus independent of these factors.
Subjects were categorized into four groups: diagnosis of BE but not OSA; OSA but not BE; both; or neither. Of the 7,482 patients, 2,480 did not have a diagnosis of OSA or BE; 83 had BE but not OSA; 4,641 had OSA but not BE; and 278 had a diagnosis of both.
The study authors used univariable models assessing age, sex, body mass index, GERD, and smoking history to determine the association between OSA and BE. GERD and OSA were associated with Barrett’s esophagus. A multiple-variable analysis was performed to observe the association of OSA with BE, adjusting for other factors. Patients with OSA were about 80% more at risk for having Barrett’s esophagus than were subjects without OSA or Barrett’s esophagus.
"This association was dose dependent, with an increase in severity of OSA being associated with an increased risk of Barrett’s esophagus," wrote the authors.
Additionally, since "the association of [Barrett’s esophagus] and OSA could be confounded by gastroesophageal reflux," the researchers also performed analyses to determine whether this relationship was independent of a GERD diagnosis. In a univariate analysis, both OSA and GERD were associated with BE, and in a multiple-variable analysis demonstrated that "both OSA and GERD were "independently associated with an increased risk of Barrett’s esophagus."
Dr. Iyer and his colleagues cited a few limitations to this study. First, the study’s design did not allow for exploration of a specific mechanism for how OSA predisposes individuals to Barrett’s esophagus. Second, the ability to accurately assess the association of OSA with GERD was limited by a lack of an established clinical definition of GERD. Finally, the use of ICD-9 codes to diagnose conditions may have resulted in overestimates in the sample.
The authors concluded that further research is needed to confirm that these findings can be applied to the general population and to explore whether treatment for OSA may help reverse this risk.
They also added that given the "asymptomatic nature" of Barrett’s esophagus and the higher risk of esophageal adenocarcinoma, patients with OSA may benefit from BE screening.
Dr. Iyer and his colleagues disclosed that this study was supported in part by the American College of Gastroenterology, the National Institute of Diabetes, Digestive and Kidney Disease; and the Edward C. Rosenow Endowed Professorship Internal Medicine Residency Award at the Mayo Clinic.
Obstructive sleep apnea is a risk factor for Barrett’s esophagus, according to findings published online September 11 in Clinical Gastroenterology and Hepatology.
Researchers from the Mayo Clinic in Rochester, Minn., studied 7,482 patients who had undergone both a diagnostic polysomnogram and esophagogastroduodenoscopy from January 2000 to November 2011.
"In this subset of patients, the presence of OSA [obstructive sleep apnea] was associated with an 80% increased risk of [Barrett’s esophagus], compared to subjects without OSA and [Barrett’s esophagus]," wrote study author Dr. Prasad G. Iyer and his colleagues (Clin. Gastroenterol. Hepatol. 2013 September;11:1108-14.e5).
Several overlapping risk factors exist for obstructive sleep apnea and Barrett’s esophagus (BE), including obesity, gastroesophageal reflux disease (GERD), male gender, and older age. This study was designed to explore whether there is a relationship between obstructive sleep apnea and Barrett’s esophagus independent of these factors.
Subjects were categorized into four groups: diagnosis of BE but not OSA; OSA but not BE; both; or neither. Of the 7,482 patients, 2,480 did not have a diagnosis of OSA or BE; 83 had BE but not OSA; 4,641 had OSA but not BE; and 278 had a diagnosis of both.
The study authors used univariable models assessing age, sex, body mass index, GERD, and smoking history to determine the association between OSA and BE. GERD and OSA were associated with Barrett’s esophagus. A multiple-variable analysis was performed to observe the association of OSA with BE, adjusting for other factors. Patients with OSA were about 80% more at risk for having Barrett’s esophagus than were subjects without OSA or Barrett’s esophagus.
"This association was dose dependent, with an increase in severity of OSA being associated with an increased risk of Barrett’s esophagus," wrote the authors.
Additionally, since "the association of [Barrett’s esophagus] and OSA could be confounded by gastroesophageal reflux," the researchers also performed analyses to determine whether this relationship was independent of a GERD diagnosis. In a univariate analysis, both OSA and GERD were associated with BE, and in a multiple-variable analysis demonstrated that "both OSA and GERD were "independently associated with an increased risk of Barrett’s esophagus."
Dr. Iyer and his colleagues cited a few limitations to this study. First, the study’s design did not allow for exploration of a specific mechanism for how OSA predisposes individuals to Barrett’s esophagus. Second, the ability to accurately assess the association of OSA with GERD was limited by a lack of an established clinical definition of GERD. Finally, the use of ICD-9 codes to diagnose conditions may have resulted in overestimates in the sample.
The authors concluded that further research is needed to confirm that these findings can be applied to the general population and to explore whether treatment for OSA may help reverse this risk.
They also added that given the "asymptomatic nature" of Barrett’s esophagus and the higher risk of esophageal adenocarcinoma, patients with OSA may benefit from BE screening.
Dr. Iyer and his colleagues disclosed that this study was supported in part by the American College of Gastroenterology, the National Institute of Diabetes, Digestive and Kidney Disease; and the Edward C. Rosenow Endowed Professorship Internal Medicine Residency Award at the Mayo Clinic.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Major finding: The presence of OSA was associated with an 80% increased risk of Barrett’s esophagus, compared with subjects without OSA.
Data source: A case-control study of 7,482 patients who underwent both a polysomnogram and esophagogastroduodenoscopy and were screened for OSA and BE using ICD-9 codes.
Disclosures: The study was supported in part by the American College of Gastroenterology, the National Institute of Diabetes, Digestive and Kidney Disease; and the Edward C. Rosenow Endowed Professorship Internal Medicine Residency Award at the Mayo Clinic.
SGIM releases new Choosing Wisely recommendations
The Society of General Internal Medicine has released a new list of recommendations, "Five Things Physicians and Patients Should Question."
The list is part of the ABIM Foundation’s Choosing Wisely campaign to educate patients and physicians about unnecessary and potentially harmful testing and treatment.
SGIM’s recommendations are:
• Don’t recommend daily home finger glucose testing in patients with type 2 diabetes who are not using insulin. Although the self-monitoring of blood glucose is important for maintaining glucose control in patients with type 1 diabetes, there is no benefit in patients with type 2 diabetes who are not on insulin or hypoglycemia medications.
• Don’t perform routine general health checks for asymptomatic adults. As opposed to office visits for acute illness or chronic care management, regularly scheduled general health checks without a specific cause have not been shown to be effective in reducing morbidity, mortality, or hospitalization.
• Don’t perform routine preoperative testing before low-risk surgical procedures. Preoperative assessment is expected before surgical procedures, but results in unnecessary delays and avoidable costs for low-risk surgical procedures.
• Don’t recommend cancer screening in adults with a life expectancy of less than 10 years. Though cancer screening can be lifesaving in healthy at-risk patients, patients with life expectancies of less than 10 years are unlikely to reap the long-term benefits from screening, and are more susceptible to the harmful complications of testing.
• Don’t place, or leave in place, peripherally inserted central catheters (PICC) for patient or provider convenience. PICCs are common devices that are associated with complications such as central line–associated bloodstream infection and venous thromboembolism. Placement of PICCs should be limited, and the catheters should be removed without delay when they no longer serve a purpose.
The Society of General Internal Medicine has released a new list of recommendations, "Five Things Physicians and Patients Should Question."
The list is part of the ABIM Foundation’s Choosing Wisely campaign to educate patients and physicians about unnecessary and potentially harmful testing and treatment.
SGIM’s recommendations are:
• Don’t recommend daily home finger glucose testing in patients with type 2 diabetes who are not using insulin. Although the self-monitoring of blood glucose is important for maintaining glucose control in patients with type 1 diabetes, there is no benefit in patients with type 2 diabetes who are not on insulin or hypoglycemia medications.
• Don’t perform routine general health checks for asymptomatic adults. As opposed to office visits for acute illness or chronic care management, regularly scheduled general health checks without a specific cause have not been shown to be effective in reducing morbidity, mortality, or hospitalization.
• Don’t perform routine preoperative testing before low-risk surgical procedures. Preoperative assessment is expected before surgical procedures, but results in unnecessary delays and avoidable costs for low-risk surgical procedures.
• Don’t recommend cancer screening in adults with a life expectancy of less than 10 years. Though cancer screening can be lifesaving in healthy at-risk patients, patients with life expectancies of less than 10 years are unlikely to reap the long-term benefits from screening, and are more susceptible to the harmful complications of testing.
• Don’t place, or leave in place, peripherally inserted central catheters (PICC) for patient or provider convenience. PICCs are common devices that are associated with complications such as central line–associated bloodstream infection and venous thromboembolism. Placement of PICCs should be limited, and the catheters should be removed without delay when they no longer serve a purpose.
The Society of General Internal Medicine has released a new list of recommendations, "Five Things Physicians and Patients Should Question."
The list is part of the ABIM Foundation’s Choosing Wisely campaign to educate patients and physicians about unnecessary and potentially harmful testing and treatment.
SGIM’s recommendations are:
• Don’t recommend daily home finger glucose testing in patients with type 2 diabetes who are not using insulin. Although the self-monitoring of blood glucose is important for maintaining glucose control in patients with type 1 diabetes, there is no benefit in patients with type 2 diabetes who are not on insulin or hypoglycemia medications.
• Don’t perform routine general health checks for asymptomatic adults. As opposed to office visits for acute illness or chronic care management, regularly scheduled general health checks without a specific cause have not been shown to be effective in reducing morbidity, mortality, or hospitalization.
• Don’t perform routine preoperative testing before low-risk surgical procedures. Preoperative assessment is expected before surgical procedures, but results in unnecessary delays and avoidable costs for low-risk surgical procedures.
• Don’t recommend cancer screening in adults with a life expectancy of less than 10 years. Though cancer screening can be lifesaving in healthy at-risk patients, patients with life expectancies of less than 10 years are unlikely to reap the long-term benefits from screening, and are more susceptible to the harmful complications of testing.
• Don’t place, or leave in place, peripherally inserted central catheters (PICC) for patient or provider convenience. PICCs are common devices that are associated with complications such as central line–associated bloodstream infection and venous thromboembolism. Placement of PICCs should be limited, and the catheters should be removed without delay when they no longer serve a purpose.
U.S. breastfeeding rates on the rise
Breastfeeding rates in the United States are on the rise, according to a new report from the Centers for Disease Control and Prevention.
The 2013 CDC Breastfeeding Report Card shows an increase in breastfeeding among U.S. children over the past 10 years, from 71% in 2000 to 77% in 2010.
Among babies born in 2010, 49% were breastfeeding at 6 months, up from 35% in 2000. The percentage of babies being breastfed at 12 months also increased, from 16% in 2000 to 27% in 2010. The findings come from a state-by-state analysis of provisional birth data taken from the 2010 births segment of the National Immunization Survey.
"While there is concern that infants are not breastfed for as long as recommended, the National Immunization Survey data show continued progress has been made over the last 10 years," the report authors wrote.
The CDC also reported a rise in the percent of facilities implementing practices that keep mothers and newborns together after birth. Data from the Maternity Practices in Infant Nutrition and Care survey show that the percentage of hospitals with 90% or more of infants having skin-to-skin contact with their mother following birth increased from 41% in 2007 to 54% in 2011. The percent of facilities with at least 90% of newborns and mothers staying in the same room increased from 30% to 37%.
The agency’s "Healthy People 2020" initiative has established a target breastfeeding rate of about 82% for the year 2020 and aims to increase the rate at 6 months and 12 months to about 61% and 34%, respectively.
CDC will continue interviews with caregivers of children born in 2010 through December 2013. Final estimates are expected in August 2014.
Breastfeeding rates in the United States are on the rise, according to a new report from the Centers for Disease Control and Prevention.
The 2013 CDC Breastfeeding Report Card shows an increase in breastfeeding among U.S. children over the past 10 years, from 71% in 2000 to 77% in 2010.
Among babies born in 2010, 49% were breastfeeding at 6 months, up from 35% in 2000. The percentage of babies being breastfed at 12 months also increased, from 16% in 2000 to 27% in 2010. The findings come from a state-by-state analysis of provisional birth data taken from the 2010 births segment of the National Immunization Survey.
"While there is concern that infants are not breastfed for as long as recommended, the National Immunization Survey data show continued progress has been made over the last 10 years," the report authors wrote.
The CDC also reported a rise in the percent of facilities implementing practices that keep mothers and newborns together after birth. Data from the Maternity Practices in Infant Nutrition and Care survey show that the percentage of hospitals with 90% or more of infants having skin-to-skin contact with their mother following birth increased from 41% in 2007 to 54% in 2011. The percent of facilities with at least 90% of newborns and mothers staying in the same room increased from 30% to 37%.
The agency’s "Healthy People 2020" initiative has established a target breastfeeding rate of about 82% for the year 2020 and aims to increase the rate at 6 months and 12 months to about 61% and 34%, respectively.
CDC will continue interviews with caregivers of children born in 2010 through December 2013. Final estimates are expected in August 2014.
Breastfeeding rates in the United States are on the rise, according to a new report from the Centers for Disease Control and Prevention.
The 2013 CDC Breastfeeding Report Card shows an increase in breastfeeding among U.S. children over the past 10 years, from 71% in 2000 to 77% in 2010.
Among babies born in 2010, 49% were breastfeeding at 6 months, up from 35% in 2000. The percentage of babies being breastfed at 12 months also increased, from 16% in 2000 to 27% in 2010. The findings come from a state-by-state analysis of provisional birth data taken from the 2010 births segment of the National Immunization Survey.
"While there is concern that infants are not breastfed for as long as recommended, the National Immunization Survey data show continued progress has been made over the last 10 years," the report authors wrote.
The CDC also reported a rise in the percent of facilities implementing practices that keep mothers and newborns together after birth. Data from the Maternity Practices in Infant Nutrition and Care survey show that the percentage of hospitals with 90% or more of infants having skin-to-skin contact with their mother following birth increased from 41% in 2007 to 54% in 2011. The percent of facilities with at least 90% of newborns and mothers staying in the same room increased from 30% to 37%.
The agency’s "Healthy People 2020" initiative has established a target breastfeeding rate of about 82% for the year 2020 and aims to increase the rate at 6 months and 12 months to about 61% and 34%, respectively.
CDC will continue interviews with caregivers of children born in 2010 through December 2013. Final estimates are expected in August 2014.
FROM THE 2013 CDC BREASTFEEDING REPORT CARD
Major finding: The percentage of babies in the United States who breastfeed has increased from 71% in 2000 to 77% in 2010.
Data source: A state-by-state analysis of provisional birth data from the National Immunization Survey.
Mixed state bipolar episodes reconceptualized
A new study has proposed a more nuanced approach for the diagnosis and treatment of mixed episodes in bipolar I patients.
The study, conducted by Dr. Isabella Pacchiarotti and her colleagues implemented a "factor structure" approach toward acute mood episodes, with the goal of deconstructing mixed episodes in particular.
Researchers studied 187 bipolar I patients hospitalized for an acute episode – manic, depressive, or mixed – and diagnosed using DSM-IV-TR criteria. Patients were evaluated for manic, mixed, and depressive symptoms using the Brief Psychiatric Rating Scale (BPRS 4.0), the Hamilton Depression Rating Scale (HDRS-21), and the Young Mania Rating Scale (YMRS). Patients also completed a self-reported temperament evaluation after discharge, reported Dr. Pacchiarotti of the Bipolar Disorders Program at the Institute of Clinical Neuroscience, University of Barcelona.
A principal component factor analysis performed on the BPRS found five clinically relevant factors: psychosis (factor 1), euphoric mania (factor 2), "mixity" (factor 3), dysphoria (factor 4), and inhibited depression (factor 5).
Psychosis was characterized by positive loading for bizarre behavior, unusual thought content, hallucinations, disorientation, conceptual disorganization, mannerisms and posturing, distractibility, and self-neglect. Euphoric mania was characterized by elevated mood and grandiosity, with negative loading for depression, guilt, suicidality, somatic concern, tension, and anxiety. "Mixity" was defined by suicidality, excitement, motor hyperactivity, tension, and anxiety, with negative loading for motor retardation. Dysphoria had positive loading for hostility, uncooperativeness, and suspiciousness. Lastly, inhibited depression was defined by depression, guilt, motor retardation, emotional withdrawal, and blunted affect.
The investigators also performed an analysis to determine which factors were associated with depressive, manic, and mixed mood. No association was found between depressive episodes and any of the five factors. However, manic episodes were a predictor of psychosis and euphoric mania (factors 1 and 2), and mixed episodes were associated with mixity (factor 3). None of the episode types were predictors of dysphoria or inhibited depression (factors 3 and 4).
An important result of this study is the discovery of the mixity factor, which provides a more comprehensive profile of mixed episodes than does the conventional combination of manic and depressive symptoms. "Most mixed state scholars feel DSM-IV criteria for mixed states to be too restrictive," the authors wrote in their report. This study endorses the existence of two subtypes of mixed episodes: one defined by factor 3 and characterized by an anxious-agitated dimension, and the other defined by factor 4, characterized by irritability and dysphoria.
In addition, the authors provided recommendations for diagnostic improvements based on the findings of this paper. First, the DSM-IV excludes anxiety and includes psychomotor retardation in the diagnosis of mixed states, though the current research has found at least one group of bipolar I patients who presented with anxiety and did not have psychomotor retardation. The researchers suggested expanding the current diagnostic criteria to include this subset of bipolar patients.
The authors listed a few limitations to this study. First, the sample size was rather small. Second, this study analyzed only bipolar I patients, and did not assess individuals who were bipolar hypomanic or depressed with subsyndromal symptoms of opposite polarity. Third, this study did not evaluate patients over all phases of illness, only when they were admitted to the hospital. Fourth, most patients in this study were on medication when they were hospitalized, which might have affected results, particularly in factor 3. Lastly, further research is needed to generate more psychometric measures of mixed states, as few are currently available.
The authors of this study expressed hope that these new insights into the factor structure of bipolar episodes will result in improved diagnostic and treatment options in the future.
The study was funded by the several entities, including the Spanish Ministry of Economy and Competitiveness, and the Instituto de Salud Carlos III, Madrid.
A new study has proposed a more nuanced approach for the diagnosis and treatment of mixed episodes in bipolar I patients.
The study, conducted by Dr. Isabella Pacchiarotti and her colleagues implemented a "factor structure" approach toward acute mood episodes, with the goal of deconstructing mixed episodes in particular.
Researchers studied 187 bipolar I patients hospitalized for an acute episode – manic, depressive, or mixed – and diagnosed using DSM-IV-TR criteria. Patients were evaluated for manic, mixed, and depressive symptoms using the Brief Psychiatric Rating Scale (BPRS 4.0), the Hamilton Depression Rating Scale (HDRS-21), and the Young Mania Rating Scale (YMRS). Patients also completed a self-reported temperament evaluation after discharge, reported Dr. Pacchiarotti of the Bipolar Disorders Program at the Institute of Clinical Neuroscience, University of Barcelona.
A principal component factor analysis performed on the BPRS found five clinically relevant factors: psychosis (factor 1), euphoric mania (factor 2), "mixity" (factor 3), dysphoria (factor 4), and inhibited depression (factor 5).
Psychosis was characterized by positive loading for bizarre behavior, unusual thought content, hallucinations, disorientation, conceptual disorganization, mannerisms and posturing, distractibility, and self-neglect. Euphoric mania was characterized by elevated mood and grandiosity, with negative loading for depression, guilt, suicidality, somatic concern, tension, and anxiety. "Mixity" was defined by suicidality, excitement, motor hyperactivity, tension, and anxiety, with negative loading for motor retardation. Dysphoria had positive loading for hostility, uncooperativeness, and suspiciousness. Lastly, inhibited depression was defined by depression, guilt, motor retardation, emotional withdrawal, and blunted affect.
The investigators also performed an analysis to determine which factors were associated with depressive, manic, and mixed mood. No association was found between depressive episodes and any of the five factors. However, manic episodes were a predictor of psychosis and euphoric mania (factors 1 and 2), and mixed episodes were associated with mixity (factor 3). None of the episode types were predictors of dysphoria or inhibited depression (factors 3 and 4).
An important result of this study is the discovery of the mixity factor, which provides a more comprehensive profile of mixed episodes than does the conventional combination of manic and depressive symptoms. "Most mixed state scholars feel DSM-IV criteria for mixed states to be too restrictive," the authors wrote in their report. This study endorses the existence of two subtypes of mixed episodes: one defined by factor 3 and characterized by an anxious-agitated dimension, and the other defined by factor 4, characterized by irritability and dysphoria.
In addition, the authors provided recommendations for diagnostic improvements based on the findings of this paper. First, the DSM-IV excludes anxiety and includes psychomotor retardation in the diagnosis of mixed states, though the current research has found at least one group of bipolar I patients who presented with anxiety and did not have psychomotor retardation. The researchers suggested expanding the current diagnostic criteria to include this subset of bipolar patients.
The authors listed a few limitations to this study. First, the sample size was rather small. Second, this study analyzed only bipolar I patients, and did not assess individuals who were bipolar hypomanic or depressed with subsyndromal symptoms of opposite polarity. Third, this study did not evaluate patients over all phases of illness, only when they were admitted to the hospital. Fourth, most patients in this study were on medication when they were hospitalized, which might have affected results, particularly in factor 3. Lastly, further research is needed to generate more psychometric measures of mixed states, as few are currently available.
The authors of this study expressed hope that these new insights into the factor structure of bipolar episodes will result in improved diagnostic and treatment options in the future.
The study was funded by the several entities, including the Spanish Ministry of Economy and Competitiveness, and the Instituto de Salud Carlos III, Madrid.
A new study has proposed a more nuanced approach for the diagnosis and treatment of mixed episodes in bipolar I patients.
The study, conducted by Dr. Isabella Pacchiarotti and her colleagues implemented a "factor structure" approach toward acute mood episodes, with the goal of deconstructing mixed episodes in particular.
Researchers studied 187 bipolar I patients hospitalized for an acute episode – manic, depressive, or mixed – and diagnosed using DSM-IV-TR criteria. Patients were evaluated for manic, mixed, and depressive symptoms using the Brief Psychiatric Rating Scale (BPRS 4.0), the Hamilton Depression Rating Scale (HDRS-21), and the Young Mania Rating Scale (YMRS). Patients also completed a self-reported temperament evaluation after discharge, reported Dr. Pacchiarotti of the Bipolar Disorders Program at the Institute of Clinical Neuroscience, University of Barcelona.
A principal component factor analysis performed on the BPRS found five clinically relevant factors: psychosis (factor 1), euphoric mania (factor 2), "mixity" (factor 3), dysphoria (factor 4), and inhibited depression (factor 5).
Psychosis was characterized by positive loading for bizarre behavior, unusual thought content, hallucinations, disorientation, conceptual disorganization, mannerisms and posturing, distractibility, and self-neglect. Euphoric mania was characterized by elevated mood and grandiosity, with negative loading for depression, guilt, suicidality, somatic concern, tension, and anxiety. "Mixity" was defined by suicidality, excitement, motor hyperactivity, tension, and anxiety, with negative loading for motor retardation. Dysphoria had positive loading for hostility, uncooperativeness, and suspiciousness. Lastly, inhibited depression was defined by depression, guilt, motor retardation, emotional withdrawal, and blunted affect.
The investigators also performed an analysis to determine which factors were associated with depressive, manic, and mixed mood. No association was found between depressive episodes and any of the five factors. However, manic episodes were a predictor of psychosis and euphoric mania (factors 1 and 2), and mixed episodes were associated with mixity (factor 3). None of the episode types were predictors of dysphoria or inhibited depression (factors 3 and 4).
An important result of this study is the discovery of the mixity factor, which provides a more comprehensive profile of mixed episodes than does the conventional combination of manic and depressive symptoms. "Most mixed state scholars feel DSM-IV criteria for mixed states to be too restrictive," the authors wrote in their report. This study endorses the existence of two subtypes of mixed episodes: one defined by factor 3 and characterized by an anxious-agitated dimension, and the other defined by factor 4, characterized by irritability and dysphoria.
In addition, the authors provided recommendations for diagnostic improvements based on the findings of this paper. First, the DSM-IV excludes anxiety and includes psychomotor retardation in the diagnosis of mixed states, though the current research has found at least one group of bipolar I patients who presented with anxiety and did not have psychomotor retardation. The researchers suggested expanding the current diagnostic criteria to include this subset of bipolar patients.
The authors listed a few limitations to this study. First, the sample size was rather small. Second, this study analyzed only bipolar I patients, and did not assess individuals who were bipolar hypomanic or depressed with subsyndromal symptoms of opposite polarity. Third, this study did not evaluate patients over all phases of illness, only when they were admitted to the hospital. Fourth, most patients in this study were on medication when they were hospitalized, which might have affected results, particularly in factor 3. Lastly, further research is needed to generate more psychometric measures of mixed states, as few are currently available.
The authors of this study expressed hope that these new insights into the factor structure of bipolar episodes will result in improved diagnostic and treatment options in the future.
The study was funded by the several entities, including the Spanish Ministry of Economy and Competitiveness, and the Instituto de Salud Carlos III, Madrid.
FROM THE JOURNAL OF AFFECTIVE DISORDERS
Major finding: This study uncovered five factors of bipolar episodes: psychosis, euphoric mania, mixity, dysphoria, and inhibited depression.
Data source: An assessment of 187 DSM-IV-TR-diagnosed bipolar I patients using the Brief Psychiatric Rating Scale (BPRS 4.0)
Disclosures: The study was funded by several entities, including the Spanish Ministry of Economy and Competitiveness, and the Instituto de Salud Carlos III, Madrid.
Exercise frequency matters for reducing stroke risk, at least for men
Exercising to the point of inducing a sweat at least four times per week may have a protective effect against stroke, according to the results of a large, population-based, longitudinal study of people in the "Stroke Belt" of the Southern United States.
The study, conducted by Michelle N. McDonnell, Ph.D., of the University of South Australia, Adelaide, and her colleagues, confirms previous reports about the effect of exercise on stroke risk, but it is the first to find a dose-response effect of exercise on stroke risk only in men and not in women. Men who exercised to the point of sweating at least four times per week had a significantly lower risk of stroke than did men who exercised one to three times per week. However, women who exercised at either level of frequency did not have a significantly lower risk of stroke, compared with women who did not exercise (Stroke 2013 July 18 [doi:10.1161/STROKEAHA.113.001538]).
The Reasons for Geographic and Racial Differences in Stroke (REGARDS) study assessed 27,348 participants aged 45 years or older who self-reported their frequency of moderate to vigorous physical activity within three categories: none, one to three times per week, and four or more times per week. Intensity of physical activity was determined by whether the exercise induced sweat in participants.
The researchers obtained demographic information and medical history via telephone, and conducted in-person follow-up interviews to take participants’ physical measurements. They conducted follow-up interviews with participants every 6 months to assess for potential stroke risk for a mean of 5.7 years, collecting data on demographics, socioeconomic factors, stroke risk factors (including mass index, smoking status, alcohol use, diabetes, and hypertension), and physical health limitations.
A total of 918 confirmed stroke/transient ischemic attack cases occurred over the follow-up period, with a significant association between activity and stroke. The most physically active participants had a lower body mass index and prevalence of diabetes and were male, white, and highly educated with high incomes. Participants who reported no physical activity had a 20% greater risk for stroke than did participants who exercised at least four times per week (hazard ratio = 1.20; 95% confidence interval, 1.01-1.42), after adjustment for age, sex, race, and age-race interaction. This remained the same after further adjustments were made for region, urban/rural residence, and socioeconomic status.
The hazard ratio was 1.16 for individuals who did not exercise, compared with those who did so one to three times per week, but it was not statistically significant and was further reduced when additional adjustments were made for region, urban/rural residence, and socioeconomic status.
Exercising at least four times per week was similarly protective against both ischemic and hemorrhagic stroke.
A statistical model in the study that added stroke risk factors attenuated the effects of exercising at least four times per week to the point where it was no longer significant. Individuals who regularly participated in physical activity were more likely to be moderate or heavy consumers of alcohol, leading the investigators to suggest that exercise’s benefit on reducing stroke risk "is likely to be explained for the most part by the positive effect that physical activity has on body mass index, hypertension, and diabetes mellitus, although physical activity also has the potential to reduce stroke risk because of other biological actions (e.g., improving endothelial function and reducing platelet activity)," the investigators wrote.
When Dr. McDonnell and her associates stratified the participants according to sex, they found that men who exercised one to three times per week had a significantly higher risk of stroke than did men who exercised at least four times per week, with hazard ratios ranging from 1.26 to 1.30. Surprisingly, men who did not exercise had no significantly increased risk of stroke. For exercise frequencies of one to three times per week and four or more times per week, women had no change in the risk of stroke, compared with women who did not exercise.
The authors identified a few limitations to this study. First, the "sweat question," though considered a valid assessment of activity, may not account for light to moderate intensity activities such as walking or cycling. Second, the researchers’ measure of physical activity does not measure duration or type of activity. Third, physical activities were categorized at the beginning of the study, with stroke events occurring years later. Lastly, some stroke cases could have been missed if the participants did not seek medical care.
Dr. McDonnell reported receiving support from a National Health and Medical Research Council of Australia fellowship. The other authors reported having no relevant financial disclosures. The REGARDS study was funded by the National Institute of Neurological Disorders and Stroke.
Exercising to the point of inducing a sweat at least four times per week may have a protective effect against stroke, according to the results of a large, population-based, longitudinal study of people in the "Stroke Belt" of the Southern United States.
The study, conducted by Michelle N. McDonnell, Ph.D., of the University of South Australia, Adelaide, and her colleagues, confirms previous reports about the effect of exercise on stroke risk, but it is the first to find a dose-response effect of exercise on stroke risk only in men and not in women. Men who exercised to the point of sweating at least four times per week had a significantly lower risk of stroke than did men who exercised one to three times per week. However, women who exercised at either level of frequency did not have a significantly lower risk of stroke, compared with women who did not exercise (Stroke 2013 July 18 [doi:10.1161/STROKEAHA.113.001538]).
The Reasons for Geographic and Racial Differences in Stroke (REGARDS) study assessed 27,348 participants aged 45 years or older who self-reported their frequency of moderate to vigorous physical activity within three categories: none, one to three times per week, and four or more times per week. Intensity of physical activity was determined by whether the exercise induced sweat in participants.
The researchers obtained demographic information and medical history via telephone, and conducted in-person follow-up interviews to take participants’ physical measurements. They conducted follow-up interviews with participants every 6 months to assess for potential stroke risk for a mean of 5.7 years, collecting data on demographics, socioeconomic factors, stroke risk factors (including mass index, smoking status, alcohol use, diabetes, and hypertension), and physical health limitations.
A total of 918 confirmed stroke/transient ischemic attack cases occurred over the follow-up period, with a significant association between activity and stroke. The most physically active participants had a lower body mass index and prevalence of diabetes and were male, white, and highly educated with high incomes. Participants who reported no physical activity had a 20% greater risk for stroke than did participants who exercised at least four times per week (hazard ratio = 1.20; 95% confidence interval, 1.01-1.42), after adjustment for age, sex, race, and age-race interaction. This remained the same after further adjustments were made for region, urban/rural residence, and socioeconomic status.
The hazard ratio was 1.16 for individuals who did not exercise, compared with those who did so one to three times per week, but it was not statistically significant and was further reduced when additional adjustments were made for region, urban/rural residence, and socioeconomic status.
Exercising at least four times per week was similarly protective against both ischemic and hemorrhagic stroke.
A statistical model in the study that added stroke risk factors attenuated the effects of exercising at least four times per week to the point where it was no longer significant. Individuals who regularly participated in physical activity were more likely to be moderate or heavy consumers of alcohol, leading the investigators to suggest that exercise’s benefit on reducing stroke risk "is likely to be explained for the most part by the positive effect that physical activity has on body mass index, hypertension, and diabetes mellitus, although physical activity also has the potential to reduce stroke risk because of other biological actions (e.g., improving endothelial function and reducing platelet activity)," the investigators wrote.
When Dr. McDonnell and her associates stratified the participants according to sex, they found that men who exercised one to three times per week had a significantly higher risk of stroke than did men who exercised at least four times per week, with hazard ratios ranging from 1.26 to 1.30. Surprisingly, men who did not exercise had no significantly increased risk of stroke. For exercise frequencies of one to three times per week and four or more times per week, women had no change in the risk of stroke, compared with women who did not exercise.
The authors identified a few limitations to this study. First, the "sweat question," though considered a valid assessment of activity, may not account for light to moderate intensity activities such as walking or cycling. Second, the researchers’ measure of physical activity does not measure duration or type of activity. Third, physical activities were categorized at the beginning of the study, with stroke events occurring years later. Lastly, some stroke cases could have been missed if the participants did not seek medical care.
Dr. McDonnell reported receiving support from a National Health and Medical Research Council of Australia fellowship. The other authors reported having no relevant financial disclosures. The REGARDS study was funded by the National Institute of Neurological Disorders and Stroke.
Exercising to the point of inducing a sweat at least four times per week may have a protective effect against stroke, according to the results of a large, population-based, longitudinal study of people in the "Stroke Belt" of the Southern United States.
The study, conducted by Michelle N. McDonnell, Ph.D., of the University of South Australia, Adelaide, and her colleagues, confirms previous reports about the effect of exercise on stroke risk, but it is the first to find a dose-response effect of exercise on stroke risk only in men and not in women. Men who exercised to the point of sweating at least four times per week had a significantly lower risk of stroke than did men who exercised one to three times per week. However, women who exercised at either level of frequency did not have a significantly lower risk of stroke, compared with women who did not exercise (Stroke 2013 July 18 [doi:10.1161/STROKEAHA.113.001538]).
The Reasons for Geographic and Racial Differences in Stroke (REGARDS) study assessed 27,348 participants aged 45 years or older who self-reported their frequency of moderate to vigorous physical activity within three categories: none, one to three times per week, and four or more times per week. Intensity of physical activity was determined by whether the exercise induced sweat in participants.
The researchers obtained demographic information and medical history via telephone, and conducted in-person follow-up interviews to take participants’ physical measurements. They conducted follow-up interviews with participants every 6 months to assess for potential stroke risk for a mean of 5.7 years, collecting data on demographics, socioeconomic factors, stroke risk factors (including mass index, smoking status, alcohol use, diabetes, and hypertension), and physical health limitations.
A total of 918 confirmed stroke/transient ischemic attack cases occurred over the follow-up period, with a significant association between activity and stroke. The most physically active participants had a lower body mass index and prevalence of diabetes and were male, white, and highly educated with high incomes. Participants who reported no physical activity had a 20% greater risk for stroke than did participants who exercised at least four times per week (hazard ratio = 1.20; 95% confidence interval, 1.01-1.42), after adjustment for age, sex, race, and age-race interaction. This remained the same after further adjustments were made for region, urban/rural residence, and socioeconomic status.
The hazard ratio was 1.16 for individuals who did not exercise, compared with those who did so one to three times per week, but it was not statistically significant and was further reduced when additional adjustments were made for region, urban/rural residence, and socioeconomic status.
Exercising at least four times per week was similarly protective against both ischemic and hemorrhagic stroke.
A statistical model in the study that added stroke risk factors attenuated the effects of exercising at least four times per week to the point where it was no longer significant. Individuals who regularly participated in physical activity were more likely to be moderate or heavy consumers of alcohol, leading the investigators to suggest that exercise’s benefit on reducing stroke risk "is likely to be explained for the most part by the positive effect that physical activity has on body mass index, hypertension, and diabetes mellitus, although physical activity also has the potential to reduce stroke risk because of other biological actions (e.g., improving endothelial function and reducing platelet activity)," the investigators wrote.
When Dr. McDonnell and her associates stratified the participants according to sex, they found that men who exercised one to three times per week had a significantly higher risk of stroke than did men who exercised at least four times per week, with hazard ratios ranging from 1.26 to 1.30. Surprisingly, men who did not exercise had no significantly increased risk of stroke. For exercise frequencies of one to three times per week and four or more times per week, women had no change in the risk of stroke, compared with women who did not exercise.
The authors identified a few limitations to this study. First, the "sweat question," though considered a valid assessment of activity, may not account for light to moderate intensity activities such as walking or cycling. Second, the researchers’ measure of physical activity does not measure duration or type of activity. Third, physical activities were categorized at the beginning of the study, with stroke events occurring years later. Lastly, some stroke cases could have been missed if the participants did not seek medical care.
Dr. McDonnell reported receiving support from a National Health and Medical Research Council of Australia fellowship. The other authors reported having no relevant financial disclosures. The REGARDS study was funded by the National Institute of Neurological Disorders and Stroke.
FROM STROKE
Major finding: Moderate to vigorous physical activity four or more times per week in men was associated with a lower stroke risk, compared with exercise one to three times per week.
Data source: A population-based longitudinal study of 27,348 participants aged 45 years or older, residing in the "Stroke Belt" region of the United States.
Disclosures: Michelle N. McDonnell, Ph.D., reported receiving support from a National Health and Medical Research Council of Australia fellowship. The other authors reported having no relevant financial disclosures. The REGARDS study was funded by the National Institute of Neurological Disorders and Stroke.