User login
Karen Appold is a seasoned writer and editor, with more than 20 years of editorial experience and started Write Now Services in 2003. Her scope of work includes writing, editing, and proofreading scholarly peer-reviewed journal content, consumer articles, white papers, and company reports for a variety of medical organizations, businesses, and media. Karen, who holds a BA in English from Penn State University, resides in Lehigh Valley, Pa.
Why Hospitalists Should Embrace Population Health
Population health focuses on the specific health needs of an individual within a defined population.
“In order to truly measure a patient’s health outcomes and identify best practices, providers must evaluate a group of people with similar health needs,” explains Joseph Damore, vice president of population health management for Charlotte-N.C.-based Premier, Inc. “Once we understand a population’s outcomes, we can then target the individual.”
Fundamentally, population health is about individualized care and intervening earlier in order to get a better outcome based on what generally works for the population. It’s also about identifying populations that need specific, targeted care, such as diabetic and oncology patients.
Back in 2003, David A. Kindig MD, PhD, and Greg Stoddart, PhD, defined population health as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group.”1
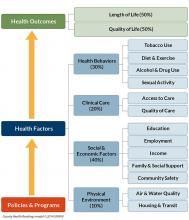
In order to achieve population health, according to Nick Fitterman, MD, SFHM, vice chair of hospital medicine for the Hofstra North Shore-LIJ School of Medicine in Hempstead, N.Y., “it is necessary to reduce health inequities or disparities among different populations due to, among other factors, the social determinants of health, which include social, environmental, cultural, and physical factors.”
Even though the concept of population health emerged more than 25 years ago, Dr. Fitterman points out that, until recently, the U.S. healthcare system has looked at an individual’s episodic illness rather than at population health, which focuses on wellness, prevention, and coordinated care across the continuum.
Marianne McPherson, PhD, MS, senior director of programs, research, and evaluation for the National Institute for Children’s Health Quality in Boston, says it is important for hospitalists to focus on both the patient and the population.
“You need to understand the particular factors facing the patient in front of you and understand that that individual is a product of a variety of different circumstances,” she says. “If you only look at an individual’s health, you can miss important trends across a group of patients within a population or community.
“By looking at both the individual and entire population, you can provide the most effective healthcare and health promotion.”
Government Spearheads Initiatives
With passage of the Patient Protection and Affordable Care Act (ACA) of 2010, the U.S. government helped accelerate the movement toward population health. According to Joshua D. Lenchus, DO, RPh, FACP, SFHM, a veteran hospitalist, president of Jackson Health System Medical Staff, and associate professor of clinical medicine and anesthesiology at the University of Miami Miller School of Medicine, the act’s provisions aim to improve the quality of care and create accountable care organizations (ACOs).
“The idea was to provide patients with insurance coverage, which would improve the access to care of which they were previously deprived,” he says. “With better access, they may receive quality healthcare and the identification and mitigation of disease at an early stage, thereby reducing overall healthcare costs, with the commensurate benefit of a healthy patient population.
“Of course, this is fraught with naïveté, because it explicitly dismisses nonmedical health determinants (i.e., socioeconomic status, education, literacy rate, transportation availability, employment status, individual patient responsibility, and so forth).”
Now, with ACOs, a hospital or healthcare system can manage patient risk with a potential financial gain—if they manage it well. The government shifts the episodic cost of care to an ACO, charges it with achieving health outcome metrics, and allows it to reap the reward of doing so in a cost-effective manner. More risk equals more reward, potentially. But to affect positive change in patient outcomes (e.g. health) in this manner requires acknowledging such external determinants. Hospitals, hospitalists, and physician leaders must seriously consider health determinants and how they impact patients if they are going to adequately address population health.
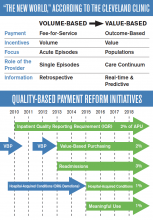
David Nash, MD, MBA, founding dean of the Jefferson College of Population Health at Thomas Jefferson University in Philadelphia, sees the ACA as the major driver of population health, with the payment structure moving from a world of volume to one of value.
“It’s all about demonstrating an improvement in the population’s health,” he says.
In January 2015, U.S. Department of Health and Human Services Secretary Sylvia Mathews Burwell announced that by 2018, 50 cents of every Medicare dollar will be attached to some measure of outcome.2
“So this move, from volume to value, will be the underpinning of the entire population health movement,” Dr. Nash says, “and we will be rewarded based on an improvement in a population’s health, instead of rewards for using resources on a per person basis.”
What’s a Hospitalist to Do?
Hospitalists typically are focused on inpatient care, managing a patient stay and coordinating discharge. Population health is an area, experts say, where hospitalists can extend their expertise in patient care and take a leadership role beyond the hospital.
“Hospitalists need to be aware of population health, embrace it, and help to develop structures within their programs that allow them to more closely partner with social services and case managers,” Dr. Fitterman says. “[You can] coordinate this type of care.”
Listen to more of our interview with Dr. Fitterman.
Dr. Lenchus agrees, noting that hospitalists intersect with population health most at discharge.
“The time point during which we must reconcile our discharge plan with the realities of the patient’s everyday life,” he says. “As we encourage an increasingly active lifestyle, we must pause to ascertain whether or not the patient lives in a neighborhood that is safe for outdoor activity.
As better nutrition is suggested, we must understand that the cost of a meal at a fast food chain is likely cheaper than one at a health food store. And, when arranging for a follow-up appointment, we must account for the bus schedule if a patient depends on that mode of transportation, as well as the potential to be released from work if employed.
“All of these external health determinants play a significant role in patients’ ability to adhere to instructions. Failure to [consider them in the discharge plan] will inevitably result in worsened health outcomes for the patient, and possibly hospital readmission.”
Hospitalists should be aware of the community-based organizations and services that exist, maintaining a working knowledge of who can provide volunteers, aid, food, and clothing to patients in need.
“Hospitalists should help lead or coordinate efforts to catalog these services in a community in which we practice, so we can steer patients toward these facilities,” Dr. Fitterman says. “In the past, we would treat acute medical issues and walk away. Now we need to be involved in patients’ needs, and those of their families.”
Establish a Team
A team-based approach is key to improving patient outcomes upon discharge, Dr. Lenchus says. Hospitalists should interact with social workers and case managers in anticipation of discharge; include the pharmacist in discharge medication counseling sessions. Are there relevant pharmaceutical industry-sponsored programs that can help the patient obtain prescription medications? Does the patient already qualify for some assistance? If the patient is insured, is the medication being prescribed on the formulary, or can it be modified so that it is covered? Could a generic version be prescribed? Does the patient understand the reason for hospitalization, have a follow-up appointment, and know how to take his medications?
Dr. Nash sees physicians as the team captains; physicians know how the system works, because they see it up close every day. The team includes key personnel, such as nurse practitioners, physician assistants, pharmacists, patient navigators, social workers, and patient educators.
“A physician, who might be a hospitalist, ideally will have additional training in both leadership and in population health,” Dr. Nash says.
He also encourages hospitalists to become patient advocates and educators, even though this is not their traditional role.
“They can do a lot to help a hospitalized patient face their challenges,” he says. “Encourage patients to stop smoking, go on a diet, and exercise. When a physician engages in this conversation, it aids in a patient’s ability to tackle challenges.”
For hospitalists who already feel overstretched with demands and overwhelmed with taking on the task of managing population health, Dr. McPherson suggests they learn more about the trend by studying it as part of their continuing education requirements. In addition, many hospitals have a department dedicated to patient safety or quality assurance.
“Ask how they can help the hospital to provide better patient care,” Dr. McPherson says. “Ask patients about their concerns or those of their neighbors. You may start to see trends.”
For example, if you suspect a trend of children who live in a certain housing development having difficulty breathing, try to find out if other hospital units are aware of this. Also try to ascertain whether or not any community groups connected to the hospital are already working to make the housing safer.
Population Health Challenges
The transition to being accountable for the health of a population will most likely be challenging for all providers. It involves significant risk, especially during the transition period, when an organization must live in both worlds (fee-for-service and value-based payment), says Damore, Premier’s vice president of population health management. He says it also requires:
- Enlightened and supportive leadership;
- Information technology to analyze claims and other infrastructure;
- New care management programs to coordinate care across the continuum;
- Agreements that align payment with population health management; and
- Skills and ability to transform a culture to a new value-based model.
To overcome the challenge of incorporating population health, Dr. McPherson suggests hospitals look to their large network of peers and learn from those already doing this, rather than reinventing the wheel. Look for champions to spearhead such initiatives.
“Identify folks who are already oriented in this direction and took steps in this vein,” she says.
Time and money are potential concerns, especially if embarking on a population health initiative will be an additional expense.
“A potential solution would be to look at ways to shift the focus, so that population health becomes integral to proper patient care, from promoting health and well-being to treating illness,” Dr. McPherson says. For example, by minimizing environmentally associated risks, hospitalists might be able to decrease the number of admissions, which will result in a return on your investment and improve population health.
Population health is here to stay, as payment models shift from fee-for-service to the value-based model. Hospitalists should embrace the movement and spearhead initiatives to get others on board. A hospital-wide team approach is advised. And, to save time and money, seek guidance from others who have already been successful. TH
Karen Appold is a medical writer in Pennsylvania.
References
1. Kindig D, Stoddart G. What is population health? Am J Public Health. 2003:93(3):380-383. doi: 10.2105/AJPH.93.3.380
2. Mathews Burwell S. Progress towards achieving better care, smarter spending, healthier people. U.S. Department of Health and Human Services website. January 26, 2015. Available at: http://www.hhs.gov/blog/2015/01/26/progress-towards-better-care-smarter-spending-healthier-people.html. Accessed November 8, 2015.
Population health focuses on the specific health needs of an individual within a defined population.
“In order to truly measure a patient’s health outcomes and identify best practices, providers must evaluate a group of people with similar health needs,” explains Joseph Damore, vice president of population health management for Charlotte-N.C.-based Premier, Inc. “Once we understand a population’s outcomes, we can then target the individual.”
Fundamentally, population health is about individualized care and intervening earlier in order to get a better outcome based on what generally works for the population. It’s also about identifying populations that need specific, targeted care, such as diabetic and oncology patients.
Back in 2003, David A. Kindig MD, PhD, and Greg Stoddart, PhD, defined population health as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group.”1
In order to achieve population health, according to Nick Fitterman, MD, SFHM, vice chair of hospital medicine for the Hofstra North Shore-LIJ School of Medicine in Hempstead, N.Y., “it is necessary to reduce health inequities or disparities among different populations due to, among other factors, the social determinants of health, which include social, environmental, cultural, and physical factors.”
Even though the concept of population health emerged more than 25 years ago, Dr. Fitterman points out that, until recently, the U.S. healthcare system has looked at an individual’s episodic illness rather than at population health, which focuses on wellness, prevention, and coordinated care across the continuum.
Marianne McPherson, PhD, MS, senior director of programs, research, and evaluation for the National Institute for Children’s Health Quality in Boston, says it is important for hospitalists to focus on both the patient and the population.
“You need to understand the particular factors facing the patient in front of you and understand that that individual is a product of a variety of different circumstances,” she says. “If you only look at an individual’s health, you can miss important trends across a group of patients within a population or community.
“By looking at both the individual and entire population, you can provide the most effective healthcare and health promotion.”
Government Spearheads Initiatives
With passage of the Patient Protection and Affordable Care Act (ACA) of 2010, the U.S. government helped accelerate the movement toward population health. According to Joshua D. Lenchus, DO, RPh, FACP, SFHM, a veteran hospitalist, president of Jackson Health System Medical Staff, and associate professor of clinical medicine and anesthesiology at the University of Miami Miller School of Medicine, the act’s provisions aim to improve the quality of care and create accountable care organizations (ACOs).
“The idea was to provide patients with insurance coverage, which would improve the access to care of which they were previously deprived,” he says. “With better access, they may receive quality healthcare and the identification and mitigation of disease at an early stage, thereby reducing overall healthcare costs, with the commensurate benefit of a healthy patient population.
“Of course, this is fraught with naïveté, because it explicitly dismisses nonmedical health determinants (i.e., socioeconomic status, education, literacy rate, transportation availability, employment status, individual patient responsibility, and so forth).”
Now, with ACOs, a hospital or healthcare system can manage patient risk with a potential financial gain—if they manage it well. The government shifts the episodic cost of care to an ACO, charges it with achieving health outcome metrics, and allows it to reap the reward of doing so in a cost-effective manner. More risk equals more reward, potentially. But to affect positive change in patient outcomes (e.g. health) in this manner requires acknowledging such external determinants. Hospitals, hospitalists, and physician leaders must seriously consider health determinants and how they impact patients if they are going to adequately address population health.
David Nash, MD, MBA, founding dean of the Jefferson College of Population Health at Thomas Jefferson University in Philadelphia, sees the ACA as the major driver of population health, with the payment structure moving from a world of volume to one of value.
“It’s all about demonstrating an improvement in the population’s health,” he says.
In January 2015, U.S. Department of Health and Human Services Secretary Sylvia Mathews Burwell announced that by 2018, 50 cents of every Medicare dollar will be attached to some measure of outcome.2
“So this move, from volume to value, will be the underpinning of the entire population health movement,” Dr. Nash says, “and we will be rewarded based on an improvement in a population’s health, instead of rewards for using resources on a per person basis.”
What’s a Hospitalist to Do?
Hospitalists typically are focused on inpatient care, managing a patient stay and coordinating discharge. Population health is an area, experts say, where hospitalists can extend their expertise in patient care and take a leadership role beyond the hospital.
“Hospitalists need to be aware of population health, embrace it, and help to develop structures within their programs that allow them to more closely partner with social services and case managers,” Dr. Fitterman says. “[You can] coordinate this type of care.”
Listen to more of our interview with Dr. Fitterman.
Dr. Lenchus agrees, noting that hospitalists intersect with population health most at discharge.
“The time point during which we must reconcile our discharge plan with the realities of the patient’s everyday life,” he says. “As we encourage an increasingly active lifestyle, we must pause to ascertain whether or not the patient lives in a neighborhood that is safe for outdoor activity.
As better nutrition is suggested, we must understand that the cost of a meal at a fast food chain is likely cheaper than one at a health food store. And, when arranging for a follow-up appointment, we must account for the bus schedule if a patient depends on that mode of transportation, as well as the potential to be released from work if employed.
“All of these external health determinants play a significant role in patients’ ability to adhere to instructions. Failure to [consider them in the discharge plan] will inevitably result in worsened health outcomes for the patient, and possibly hospital readmission.”
Hospitalists should be aware of the community-based organizations and services that exist, maintaining a working knowledge of who can provide volunteers, aid, food, and clothing to patients in need.
“Hospitalists should help lead or coordinate efforts to catalog these services in a community in which we practice, so we can steer patients toward these facilities,” Dr. Fitterman says. “In the past, we would treat acute medical issues and walk away. Now we need to be involved in patients’ needs, and those of their families.”
Establish a Team
A team-based approach is key to improving patient outcomes upon discharge, Dr. Lenchus says. Hospitalists should interact with social workers and case managers in anticipation of discharge; include the pharmacist in discharge medication counseling sessions. Are there relevant pharmaceutical industry-sponsored programs that can help the patient obtain prescription medications? Does the patient already qualify for some assistance? If the patient is insured, is the medication being prescribed on the formulary, or can it be modified so that it is covered? Could a generic version be prescribed? Does the patient understand the reason for hospitalization, have a follow-up appointment, and know how to take his medications?
Dr. Nash sees physicians as the team captains; physicians know how the system works, because they see it up close every day. The team includes key personnel, such as nurse practitioners, physician assistants, pharmacists, patient navigators, social workers, and patient educators.
“A physician, who might be a hospitalist, ideally will have additional training in both leadership and in population health,” Dr. Nash says.
He also encourages hospitalists to become patient advocates and educators, even though this is not their traditional role.
“They can do a lot to help a hospitalized patient face their challenges,” he says. “Encourage patients to stop smoking, go on a diet, and exercise. When a physician engages in this conversation, it aids in a patient’s ability to tackle challenges.”
For hospitalists who already feel overstretched with demands and overwhelmed with taking on the task of managing population health, Dr. McPherson suggests they learn more about the trend by studying it as part of their continuing education requirements. In addition, many hospitals have a department dedicated to patient safety or quality assurance.
“Ask how they can help the hospital to provide better patient care,” Dr. McPherson says. “Ask patients about their concerns or those of their neighbors. You may start to see trends.”
For example, if you suspect a trend of children who live in a certain housing development having difficulty breathing, try to find out if other hospital units are aware of this. Also try to ascertain whether or not any community groups connected to the hospital are already working to make the housing safer.
Population Health Challenges
The transition to being accountable for the health of a population will most likely be challenging for all providers. It involves significant risk, especially during the transition period, when an organization must live in both worlds (fee-for-service and value-based payment), says Damore, Premier’s vice president of population health management. He says it also requires:
- Enlightened and supportive leadership;
- Information technology to analyze claims and other infrastructure;
- New care management programs to coordinate care across the continuum;
- Agreements that align payment with population health management; and
- Skills and ability to transform a culture to a new value-based model.
To overcome the challenge of incorporating population health, Dr. McPherson suggests hospitals look to their large network of peers and learn from those already doing this, rather than reinventing the wheel. Look for champions to spearhead such initiatives.
“Identify folks who are already oriented in this direction and took steps in this vein,” she says.
Time and money are potential concerns, especially if embarking on a population health initiative will be an additional expense.
“A potential solution would be to look at ways to shift the focus, so that population health becomes integral to proper patient care, from promoting health and well-being to treating illness,” Dr. McPherson says. For example, by minimizing environmentally associated risks, hospitalists might be able to decrease the number of admissions, which will result in a return on your investment and improve population health.
Population health is here to stay, as payment models shift from fee-for-service to the value-based model. Hospitalists should embrace the movement and spearhead initiatives to get others on board. A hospital-wide team approach is advised. And, to save time and money, seek guidance from others who have already been successful. TH
Karen Appold is a medical writer in Pennsylvania.
References
1. Kindig D, Stoddart G. What is population health? Am J Public Health. 2003:93(3):380-383. doi: 10.2105/AJPH.93.3.380
2. Mathews Burwell S. Progress towards achieving better care, smarter spending, healthier people. U.S. Department of Health and Human Services website. January 26, 2015. Available at: http://www.hhs.gov/blog/2015/01/26/progress-towards-better-care-smarter-spending-healthier-people.html. Accessed November 8, 2015.
Population health focuses on the specific health needs of an individual within a defined population.
“In order to truly measure a patient’s health outcomes and identify best practices, providers must evaluate a group of people with similar health needs,” explains Joseph Damore, vice president of population health management for Charlotte-N.C.-based Premier, Inc. “Once we understand a population’s outcomes, we can then target the individual.”
Fundamentally, population health is about individualized care and intervening earlier in order to get a better outcome based on what generally works for the population. It’s also about identifying populations that need specific, targeted care, such as diabetic and oncology patients.
Back in 2003, David A. Kindig MD, PhD, and Greg Stoddart, PhD, defined population health as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group.”1
In order to achieve population health, according to Nick Fitterman, MD, SFHM, vice chair of hospital medicine for the Hofstra North Shore-LIJ School of Medicine in Hempstead, N.Y., “it is necessary to reduce health inequities or disparities among different populations due to, among other factors, the social determinants of health, which include social, environmental, cultural, and physical factors.”
Even though the concept of population health emerged more than 25 years ago, Dr. Fitterman points out that, until recently, the U.S. healthcare system has looked at an individual’s episodic illness rather than at population health, which focuses on wellness, prevention, and coordinated care across the continuum.
Marianne McPherson, PhD, MS, senior director of programs, research, and evaluation for the National Institute for Children’s Health Quality in Boston, says it is important for hospitalists to focus on both the patient and the population.
“You need to understand the particular factors facing the patient in front of you and understand that that individual is a product of a variety of different circumstances,” she says. “If you only look at an individual’s health, you can miss important trends across a group of patients within a population or community.
“By looking at both the individual and entire population, you can provide the most effective healthcare and health promotion.”
Government Spearheads Initiatives
With passage of the Patient Protection and Affordable Care Act (ACA) of 2010, the U.S. government helped accelerate the movement toward population health. According to Joshua D. Lenchus, DO, RPh, FACP, SFHM, a veteran hospitalist, president of Jackson Health System Medical Staff, and associate professor of clinical medicine and anesthesiology at the University of Miami Miller School of Medicine, the act’s provisions aim to improve the quality of care and create accountable care organizations (ACOs).
“The idea was to provide patients with insurance coverage, which would improve the access to care of which they were previously deprived,” he says. “With better access, they may receive quality healthcare and the identification and mitigation of disease at an early stage, thereby reducing overall healthcare costs, with the commensurate benefit of a healthy patient population.
“Of course, this is fraught with naïveté, because it explicitly dismisses nonmedical health determinants (i.e., socioeconomic status, education, literacy rate, transportation availability, employment status, individual patient responsibility, and so forth).”
Now, with ACOs, a hospital or healthcare system can manage patient risk with a potential financial gain—if they manage it well. The government shifts the episodic cost of care to an ACO, charges it with achieving health outcome metrics, and allows it to reap the reward of doing so in a cost-effective manner. More risk equals more reward, potentially. But to affect positive change in patient outcomes (e.g. health) in this manner requires acknowledging such external determinants. Hospitals, hospitalists, and physician leaders must seriously consider health determinants and how they impact patients if they are going to adequately address population health.
David Nash, MD, MBA, founding dean of the Jefferson College of Population Health at Thomas Jefferson University in Philadelphia, sees the ACA as the major driver of population health, with the payment structure moving from a world of volume to one of value.
“It’s all about demonstrating an improvement in the population’s health,” he says.
In January 2015, U.S. Department of Health and Human Services Secretary Sylvia Mathews Burwell announced that by 2018, 50 cents of every Medicare dollar will be attached to some measure of outcome.2
“So this move, from volume to value, will be the underpinning of the entire population health movement,” Dr. Nash says, “and we will be rewarded based on an improvement in a population’s health, instead of rewards for using resources on a per person basis.”
What’s a Hospitalist to Do?
Hospitalists typically are focused on inpatient care, managing a patient stay and coordinating discharge. Population health is an area, experts say, where hospitalists can extend their expertise in patient care and take a leadership role beyond the hospital.
“Hospitalists need to be aware of population health, embrace it, and help to develop structures within their programs that allow them to more closely partner with social services and case managers,” Dr. Fitterman says. “[You can] coordinate this type of care.”
Listen to more of our interview with Dr. Fitterman.
Dr. Lenchus agrees, noting that hospitalists intersect with population health most at discharge.
“The time point during which we must reconcile our discharge plan with the realities of the patient’s everyday life,” he says. “As we encourage an increasingly active lifestyle, we must pause to ascertain whether or not the patient lives in a neighborhood that is safe for outdoor activity.
As better nutrition is suggested, we must understand that the cost of a meal at a fast food chain is likely cheaper than one at a health food store. And, when arranging for a follow-up appointment, we must account for the bus schedule if a patient depends on that mode of transportation, as well as the potential to be released from work if employed.
“All of these external health determinants play a significant role in patients’ ability to adhere to instructions. Failure to [consider them in the discharge plan] will inevitably result in worsened health outcomes for the patient, and possibly hospital readmission.”
Hospitalists should be aware of the community-based organizations and services that exist, maintaining a working knowledge of who can provide volunteers, aid, food, and clothing to patients in need.
“Hospitalists should help lead or coordinate efforts to catalog these services in a community in which we practice, so we can steer patients toward these facilities,” Dr. Fitterman says. “In the past, we would treat acute medical issues and walk away. Now we need to be involved in patients’ needs, and those of their families.”
Establish a Team
A team-based approach is key to improving patient outcomes upon discharge, Dr. Lenchus says. Hospitalists should interact with social workers and case managers in anticipation of discharge; include the pharmacist in discharge medication counseling sessions. Are there relevant pharmaceutical industry-sponsored programs that can help the patient obtain prescription medications? Does the patient already qualify for some assistance? If the patient is insured, is the medication being prescribed on the formulary, or can it be modified so that it is covered? Could a generic version be prescribed? Does the patient understand the reason for hospitalization, have a follow-up appointment, and know how to take his medications?
Dr. Nash sees physicians as the team captains; physicians know how the system works, because they see it up close every day. The team includes key personnel, such as nurse practitioners, physician assistants, pharmacists, patient navigators, social workers, and patient educators.
“A physician, who might be a hospitalist, ideally will have additional training in both leadership and in population health,” Dr. Nash says.
He also encourages hospitalists to become patient advocates and educators, even though this is not their traditional role.
“They can do a lot to help a hospitalized patient face their challenges,” he says. “Encourage patients to stop smoking, go on a diet, and exercise. When a physician engages in this conversation, it aids in a patient’s ability to tackle challenges.”
For hospitalists who already feel overstretched with demands and overwhelmed with taking on the task of managing population health, Dr. McPherson suggests they learn more about the trend by studying it as part of their continuing education requirements. In addition, many hospitals have a department dedicated to patient safety or quality assurance.
“Ask how they can help the hospital to provide better patient care,” Dr. McPherson says. “Ask patients about their concerns or those of their neighbors. You may start to see trends.”
For example, if you suspect a trend of children who live in a certain housing development having difficulty breathing, try to find out if other hospital units are aware of this. Also try to ascertain whether or not any community groups connected to the hospital are already working to make the housing safer.
Population Health Challenges
The transition to being accountable for the health of a population will most likely be challenging for all providers. It involves significant risk, especially during the transition period, when an organization must live in both worlds (fee-for-service and value-based payment), says Damore, Premier’s vice president of population health management. He says it also requires:
- Enlightened and supportive leadership;
- Information technology to analyze claims and other infrastructure;
- New care management programs to coordinate care across the continuum;
- Agreements that align payment with population health management; and
- Skills and ability to transform a culture to a new value-based model.
To overcome the challenge of incorporating population health, Dr. McPherson suggests hospitals look to their large network of peers and learn from those already doing this, rather than reinventing the wheel. Look for champions to spearhead such initiatives.
“Identify folks who are already oriented in this direction and took steps in this vein,” she says.
Time and money are potential concerns, especially if embarking on a population health initiative will be an additional expense.
“A potential solution would be to look at ways to shift the focus, so that population health becomes integral to proper patient care, from promoting health and well-being to treating illness,” Dr. McPherson says. For example, by minimizing environmentally associated risks, hospitalists might be able to decrease the number of admissions, which will result in a return on your investment and improve population health.
Population health is here to stay, as payment models shift from fee-for-service to the value-based model. Hospitalists should embrace the movement and spearhead initiatives to get others on board. A hospital-wide team approach is advised. And, to save time and money, seek guidance from others who have already been successful. TH
Karen Appold is a medical writer in Pennsylvania.
References
1. Kindig D, Stoddart G. What is population health? Am J Public Health. 2003:93(3):380-383. doi: 10.2105/AJPH.93.3.380
2. Mathews Burwell S. Progress towards achieving better care, smarter spending, healthier people. U.S. Department of Health and Human Services website. January 26, 2015. Available at: http://www.hhs.gov/blog/2015/01/26/progress-towards-better-care-smarter-spending-healthier-people.html. Accessed November 8, 2015.
Population Health Prevails at Two Institutions
Population health—a movement to improve the health of an entire population—is a growing trend driven by the U.S. government. Many health systems are already on board, as healthcare shifts from a fee-for-service system to a value-based system.
One group of Premier Health hospitals and health systems has been collaborating since 2011 to build capabilities to become clinically integrated care networks that are accountable for the health of defined populations within their communities, according to Joseph Damore, vice president of population health management for the Charlotte, N.C-based company.
Damore says Premier has developed a comprehensive framework for the activities and capabilities necessary for successful population health management. Building blocks include:
- Patient-centered foundation (greater patient engagement and involvement in clinical decisions);
- Health home (a primary care medical home);
- High-value network (a set of providers who deliver quality care at an efficient price and whose performance is measured in the areas of cost, quality, and satisfaction);
- Payer partnership (care delivery network providers working with payers to create aligned financial incentives consistent with providing high-value care);
- Population health data management (collecting, analyzing, and reporting data covering all of the care the network’s patient population receives); and
- Network leadership (systematic governance and administration) focused on improving health, managing and coordinating care, and managing per capita cost.
“We’re also working with health systems on initiatives to establish patient-centered foundations and medical homes and create clinically integrated networks, providing our members with a direct roadmap to follow to successfully transition to this new value-based model,” Damore says.
At Jackson Memorial Hospital, one of the nation’s largest safety net hospitals, managing population health is ingrained in staff from day one. Nonetheless, Joshua D. Lenchus, DO, RPh, FACP, SFHM, president of Jackson Health System Medical Staff, says there are opportunities for improvement.
“A more team-based, collaborative approach is being piloted on some floors of our hospital, with specific physician groups,” he says. “Armed with the knowledge of these interventions, we can work on bolstering the pearls and rectifying the pitfalls as we move forward.
“One of our biggest obstacles to success is our patients’ general socioeconomic status.”
A current initiative at Jackson includes piloting a physician-led, multidisciplinary approach to address some of the health determinants. Furthermore, the health system is building additional satellite community clinics and urgent care centers, as it attempts to address disease earlier in the process. Additionally, there is a renewed emphasis on reinforcing the primary care infrastructure to facilitate patient appointment needs, Dr. Lenchus says. TH
Population health—a movement to improve the health of an entire population—is a growing trend driven by the U.S. government. Many health systems are already on board, as healthcare shifts from a fee-for-service system to a value-based system.
One group of Premier Health hospitals and health systems has been collaborating since 2011 to build capabilities to become clinically integrated care networks that are accountable for the health of defined populations within their communities, according to Joseph Damore, vice president of population health management for the Charlotte, N.C-based company.
Damore says Premier has developed a comprehensive framework for the activities and capabilities necessary for successful population health management. Building blocks include:
- Patient-centered foundation (greater patient engagement and involvement in clinical decisions);
- Health home (a primary care medical home);
- High-value network (a set of providers who deliver quality care at an efficient price and whose performance is measured in the areas of cost, quality, and satisfaction);
- Payer partnership (care delivery network providers working with payers to create aligned financial incentives consistent with providing high-value care);
- Population health data management (collecting, analyzing, and reporting data covering all of the care the network’s patient population receives); and
- Network leadership (systematic governance and administration) focused on improving health, managing and coordinating care, and managing per capita cost.
“We’re also working with health systems on initiatives to establish patient-centered foundations and medical homes and create clinically integrated networks, providing our members with a direct roadmap to follow to successfully transition to this new value-based model,” Damore says.
At Jackson Memorial Hospital, one of the nation’s largest safety net hospitals, managing population health is ingrained in staff from day one. Nonetheless, Joshua D. Lenchus, DO, RPh, FACP, SFHM, president of Jackson Health System Medical Staff, says there are opportunities for improvement.
“A more team-based, collaborative approach is being piloted on some floors of our hospital, with specific physician groups,” he says. “Armed with the knowledge of these interventions, we can work on bolstering the pearls and rectifying the pitfalls as we move forward.
“One of our biggest obstacles to success is our patients’ general socioeconomic status.”
A current initiative at Jackson includes piloting a physician-led, multidisciplinary approach to address some of the health determinants. Furthermore, the health system is building additional satellite community clinics and urgent care centers, as it attempts to address disease earlier in the process. Additionally, there is a renewed emphasis on reinforcing the primary care infrastructure to facilitate patient appointment needs, Dr. Lenchus says. TH
Population health—a movement to improve the health of an entire population—is a growing trend driven by the U.S. government. Many health systems are already on board, as healthcare shifts from a fee-for-service system to a value-based system.
One group of Premier Health hospitals and health systems has been collaborating since 2011 to build capabilities to become clinically integrated care networks that are accountable for the health of defined populations within their communities, according to Joseph Damore, vice president of population health management for the Charlotte, N.C-based company.
Damore says Premier has developed a comprehensive framework for the activities and capabilities necessary for successful population health management. Building blocks include:
- Patient-centered foundation (greater patient engagement and involvement in clinical decisions);
- Health home (a primary care medical home);
- High-value network (a set of providers who deliver quality care at an efficient price and whose performance is measured in the areas of cost, quality, and satisfaction);
- Payer partnership (care delivery network providers working with payers to create aligned financial incentives consistent with providing high-value care);
- Population health data management (collecting, analyzing, and reporting data covering all of the care the network’s patient population receives); and
- Network leadership (systematic governance and administration) focused on improving health, managing and coordinating care, and managing per capita cost.
“We’re also working with health systems on initiatives to establish patient-centered foundations and medical homes and create clinically integrated networks, providing our members with a direct roadmap to follow to successfully transition to this new value-based model,” Damore says.
At Jackson Memorial Hospital, one of the nation’s largest safety net hospitals, managing population health is ingrained in staff from day one. Nonetheless, Joshua D. Lenchus, DO, RPh, FACP, SFHM, president of Jackson Health System Medical Staff, says there are opportunities for improvement.
“A more team-based, collaborative approach is being piloted on some floors of our hospital, with specific physician groups,” he says. “Armed with the knowledge of these interventions, we can work on bolstering the pearls and rectifying the pitfalls as we move forward.
“One of our biggest obstacles to success is our patients’ general socioeconomic status.”
A current initiative at Jackson includes piloting a physician-led, multidisciplinary approach to address some of the health determinants. Furthermore, the health system is building additional satellite community clinics and urgent care centers, as it attempts to address disease earlier in the process. Additionally, there is a renewed emphasis on reinforcing the primary care infrastructure to facilitate patient appointment needs, Dr. Lenchus says. TH
Unassigned, Undocumented Patients Take a Toll on Healthcare and Hospitalists
When a patient must remain in the acute care hospital setting—despite being well enough to transition to a lower level of care, costs continue to mount as the patient receives care at the most expensive level.
“But policymakers must understand that reducing support for essential hospitals might save dollars in the short term but ultimately threatens access to care and creates greater costs in the long run,” says Beth Feldpush, DrPH, senior vice president of policy and advocacy for America’s Essential Hospitals in Washington, D.C. The group represents more than 250 essential hospitals, which fill a safety net role and provide communitywide services, such as trauma, neonatal intensive care, and disaster response.
“Our hospitals, which already operate at a loss on average, cannot continue to sustain federal and state funding cuts,” Dr. Feldpush says. “Access to care for vulnerable patients and entire communities will suffer if we continue to chip away at crucial sources of support, such as Medicaid and Medicare disproportionate share hospital funding and payment for outpatient services.”
The Affordable Care Act (ACA) makes many changes to the healthcare system that are designed to improve the quality, value of, and access to healthcare services.
“While many are good in theory, they have faced challenges in practice,” Dr. Feldpush says.
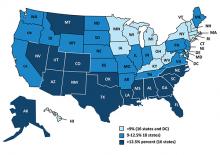
For example, the law’s authors included deep cuts to Medicaid and Medicare disproportionate share hospital (DSH) payments, which support hospitals that provide a large volume of uncompensated care. They made these cuts with the assumption that Medicare expansion and the ACA health insurance marketplace would significantly increase coverage, lessening the need for DSH payments. The U.S. Supreme Court’s decision to give states the option of expanding Medicaid has resulted in expansion in only about half of the states, however.
“But the DSH cuts remain, meaning our hospitals are getting significantly less support for the same or more uncompensated care,” Dr. Feldpush says.
Likewise, the ACA put into place many quality incentive programs for Medicare, including those designed to reduce preventable readmissions and hospital-acquired conditions and to encourage more value-based purchasing.
“The goals are obviously good ones, but the quality measures used to calculate incentive payments or penalties fail to account for the sociodemographic challenges our patients face—and that our hospitals can’t control,” she says. “So, these programs disproportionately penalize our hospitals, which, in turn, creates a vicious circle that reduces the funding they need to make improvements.”
Access to equitable healthcare for low-income, uninsured, and other vulnerable patients is a national problem, Dr. Feldpush continues. But the severity of the problem can vary by community and region—in states that have chosen not to expand their Medicaid programs, for example, or in economically depressed areas. TH
When a patient must remain in the acute care hospital setting—despite being well enough to transition to a lower level of care, costs continue to mount as the patient receives care at the most expensive level.
“But policymakers must understand that reducing support for essential hospitals might save dollars in the short term but ultimately threatens access to care and creates greater costs in the long run,” says Beth Feldpush, DrPH, senior vice president of policy and advocacy for America’s Essential Hospitals in Washington, D.C. The group represents more than 250 essential hospitals, which fill a safety net role and provide communitywide services, such as trauma, neonatal intensive care, and disaster response.
“Our hospitals, which already operate at a loss on average, cannot continue to sustain federal and state funding cuts,” Dr. Feldpush says. “Access to care for vulnerable patients and entire communities will suffer if we continue to chip away at crucial sources of support, such as Medicaid and Medicare disproportionate share hospital funding and payment for outpatient services.”
The Affordable Care Act (ACA) makes many changes to the healthcare system that are designed to improve the quality, value of, and access to healthcare services.
“While many are good in theory, they have faced challenges in practice,” Dr. Feldpush says.
For example, the law’s authors included deep cuts to Medicaid and Medicare disproportionate share hospital (DSH) payments, which support hospitals that provide a large volume of uncompensated care. They made these cuts with the assumption that Medicare expansion and the ACA health insurance marketplace would significantly increase coverage, lessening the need for DSH payments. The U.S. Supreme Court’s decision to give states the option of expanding Medicaid has resulted in expansion in only about half of the states, however.
“But the DSH cuts remain, meaning our hospitals are getting significantly less support for the same or more uncompensated care,” Dr. Feldpush says.
Likewise, the ACA put into place many quality incentive programs for Medicare, including those designed to reduce preventable readmissions and hospital-acquired conditions and to encourage more value-based purchasing.
“The goals are obviously good ones, but the quality measures used to calculate incentive payments or penalties fail to account for the sociodemographic challenges our patients face—and that our hospitals can’t control,” she says. “So, these programs disproportionately penalize our hospitals, which, in turn, creates a vicious circle that reduces the funding they need to make improvements.”
Access to equitable healthcare for low-income, uninsured, and other vulnerable patients is a national problem, Dr. Feldpush continues. But the severity of the problem can vary by community and region—in states that have chosen not to expand their Medicaid programs, for example, or in economically depressed areas. TH
When a patient must remain in the acute care hospital setting—despite being well enough to transition to a lower level of care, costs continue to mount as the patient receives care at the most expensive level.
“But policymakers must understand that reducing support for essential hospitals might save dollars in the short term but ultimately threatens access to care and creates greater costs in the long run,” says Beth Feldpush, DrPH, senior vice president of policy and advocacy for America’s Essential Hospitals in Washington, D.C. The group represents more than 250 essential hospitals, which fill a safety net role and provide communitywide services, such as trauma, neonatal intensive care, and disaster response.
“Our hospitals, which already operate at a loss on average, cannot continue to sustain federal and state funding cuts,” Dr. Feldpush says. “Access to care for vulnerable patients and entire communities will suffer if we continue to chip away at crucial sources of support, such as Medicaid and Medicare disproportionate share hospital funding and payment for outpatient services.”
The Affordable Care Act (ACA) makes many changes to the healthcare system that are designed to improve the quality, value of, and access to healthcare services.
“While many are good in theory, they have faced challenges in practice,” Dr. Feldpush says.
For example, the law’s authors included deep cuts to Medicaid and Medicare disproportionate share hospital (DSH) payments, which support hospitals that provide a large volume of uncompensated care. They made these cuts with the assumption that Medicare expansion and the ACA health insurance marketplace would significantly increase coverage, lessening the need for DSH payments. The U.S. Supreme Court’s decision to give states the option of expanding Medicaid has resulted in expansion in only about half of the states, however.
“But the DSH cuts remain, meaning our hospitals are getting significantly less support for the same or more uncompensated care,” Dr. Feldpush says.
Likewise, the ACA put into place many quality incentive programs for Medicare, including those designed to reduce preventable readmissions and hospital-acquired conditions and to encourage more value-based purchasing.
“The goals are obviously good ones, but the quality measures used to calculate incentive payments or penalties fail to account for the sociodemographic challenges our patients face—and that our hospitals can’t control,” she says. “So, these programs disproportionately penalize our hospitals, which, in turn, creates a vicious circle that reduces the funding they need to make improvements.”
Access to equitable healthcare for low-income, uninsured, and other vulnerable patients is a national problem, Dr. Feldpush continues. But the severity of the problem can vary by community and region—in states that have chosen not to expand their Medicaid programs, for example, or in economically depressed areas. TH
Unassigned, Undocumented Inpatients Present Challenges; Some Hospitalists Have Solutions
Hospitalists are charged with giving the best of care and treatment, regardless of whether or not a patient is insured or has a PCP to transition to after discharge. But patients who do not have insurance or a PCP pose many challenges to hospitalists, as well as the healthcare systems they work in. Although some hospitals and health systems have found ways to address these challenges, issues persist, with high costs to care for these patients topping the list. In 2013, the cost of community hospitals’ uncompensated care climbed to $46.4 billion.1
Typically, undocumented and unassigned patients face many social and economic challenges. Many of these patients are unemployed or work as independent contractors without employer-offered health insurance. Some have multiple jobs, can’t take time off from work for doctor appointments, or are undocumented workers.
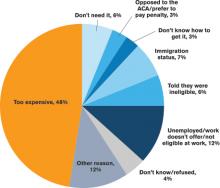
More patients have acquired health insurance in recent years as a result of the Affordable Care Act (ACA) and Medicaid expansion; however, some eligible people never complete the necessary forms.
With or without insurance, some patients don’t establish primary care because they have been healthy, have difficulty navigating the healthcare system, lack transportation, or desire more culturally tailored care. Some Medicare and Medicaid patients don’t have a PCP in their community who accepts these programs.
Treatment Challenges
Uninsured patients often are sicker and have more complex conditions than those with insurance, according to Beth Feldpush, DrPH, senior vice president of policy and advocacy at the nonprofit trade group America’s Essential Hospitals, which is based in Washington, D.C., and represents 250 safety net hospitals throughout the U.S.
“Because they can’t afford regular preventive and primary care, they forgo needed healthcare services until their conditions worsen and they require costly hospital care,” says Dr. Feldpush. Uninsured patients often lack the resources for follow-up care to help them recover and stay well. She says more than half of all inpatient discharges and outpatient visits at her groups’ hospitals are for uninsured or Medicaid patients.
When an uninsured patient is discharged from the hospital, finding follow-up care can be difficult.
“Their ability to get an appointment to see a PCP is extremely limited, because many providers don’t see patients without health insurance,” says Scott Sears, MD, MBA, chief clinical officer of Tacoma, Wash.-based Sound Physicians. Dr. Sears notes that in some hospitalist programs, as many as 40% of hospitalized patients lack insurance. “But without secured follow-up care, hospitalists are hesitant to send patients home, because they could relapse.”
Typically, these patients are not completely well and should be transferred to a skilled nursing or hospice facility; however, many facilities won’t accept them without insurance. Often, these patients need a PCP to monitor them with laboratory tests and other follow-up tests, to prescribe and monitor medications, and to ensure that they are following their plan of care.
At some medical facilities, subspecialists who consult on patients may screen them and refuse to see anyone without health insurance.
“So even though some patients may need subspecialty support, they may not have access to it,” Dr. Sears says. “While some patients without insurance qualify for Medicaid or other programs, due to the amount of paperwork and time to enroll, they end up staying in the hospital even though they are ready for discharge.”
Transitional Challenges
Most patients admitted to the hospital either have exacerbations of chronic conditions or a new diagnosis. “It’s rare to hospitalize a patient with a discrete illness that wouldn’t need care after discharge, so having a robust PCP partner is critical to a patient’s health,” says Honora Englander, MD, medical director of the Care Transitions Innovation (C-TRAIN) program at Oregon Health and Science University (OHSU) in Portland. For many patients, psychosocial complexity complicates their transition out of the hospital. An effective system needs to address a patient’s mental health, housing, and other social needs.
It may take four to six weeks for a patient without an established PCP to get a new patient appointment. “This is a huge impediment, as the patient won’t have anyone to ensure that he or she continues along the proper care path,” Dr. Sears says.
“Studies estimate that more than half of medication errors that patients experience occur during transitions and after discharge,” Dr. Sears says.2 “Intervention with a healthcare provider who can review proper use after discharge can dramatically reduce errors and [improve] patient outcomes.”
Rates of patients without a PCP vary by region for Sound Physicians. In the northwest region, about 25% of admitted patients lack a PCP; in the gulf region, the figure can be as high as 60%.
“In Texas, there is a large number of patients and not as many PCPs,” he adds. “There is also a larger percentage of patients without health insurance. Sometimes patients have coverage but have never established care with a PCP.”
As a result of not having a PCP to transition to, some patients return to the hospital soon after discharge, Dr. Feldpush notes.
Tips for Treating Uninsured Patients
Some facilities have found successful ways to help hospitalized patients without health insurance. Dr. Sears says that hospitalists can investigate which clinics accept uninsured patients or which local physician groups are willing to see them after discharge, in exchange for hospitalists taking care of them in the hospital. They also can investigate the community-based insurance programs that are available.
Teresa Coker, MSN, ARNP, FNP-BC, a Sound Physicians program manager at Mercy Medical Center in Cedar Rapids, Iowa, says that when patients lack insurance at her hospital, an organization will review the patient’s case, determine insurance eligibility, and assist the patient in completing the appropriate paperwork. When patients are not eligible, they are instructed to inquire about the hospital’s charity care program if they receive a bill they are unable to pay.
In addition, the community has a free health clinic that serves those without insurance. “Patients are given the address and hours prior to discharge, because it is walk-in only,” Coker says. “All patients are recommended to follow up within one week, or sooner if medications are needed.”
Dr. Englander advocates that physicians take into account medication costs, transportation, and other social considerations when planning care after hospitalization. The team at OHSU developed a low-cost formulary (based in part on widely available $4 plans from national pharmacy chains), and OHSU provides medications for uninsured patients in the program for up to 30 days following discharge.
For patients who can’t afford the $4 drug plan, case managers offer coupons for $4 prescriptions, says Malik Merchant, MD, area medical officer for the Schumachergroup in Harker Heights, Texas. He says that as many as 30% of the patients in his area are undocumented or unassigned. For more expensive medications, a social worker offers pharmaceutical company coupons when they are available. The institution also has a small budget to pay for drugs.
Dr. Merchant has found the biggest challenge to be the transition of care from inpatient to outpatient.
“Case managers and social workers prepare a financial worksheet that provides the possibility of overall cost savings for the institution, if patients are willing to participate in some upfront cost,” he says. “When our parent institution came on board, we developed contracts with local pharmacies, [a] skilled nursing facility, and PCPs to take these patients until they recovered from an acute illness. Our institution paid for these services at a reduced rate but saved money by reducing the length of their hospital stay.”
Dr. Feldpush says her group’s hospitals work hard to reach the uninsured. South Florida’s Memorial Healthcare System (MHS) created the Health Intervention with Targeted Services (HITS) Program, an outreach initiative that links patients with insurance programs or medical homes.3 The HITS team used a geographic information system map to target 15 neighborhoods with the highest rates of hospitalized, uninsured patients. Over a six-month period, the team approached these neighborhoods using various outreach strategies, such as health fairs, educational workshops, and door-to-door visits.3
Approximately 6,910 HITS participants have been enrolled in Medicaid, Florida’s children’s health insurance program, or an MHS community health center. Over a three-year study period, MHS saved $284,856 in the ED, about $2.8 million in inpatient costs, and roughly $4 million overall.3
Barriers to Follow-Up Care
Whether you are looking to help uninsured patients, those without a PCP, or both, the key is to try to fill in the gaps.
“As hospitalists, we need to work with pharmacists, case managers and social workers, and others to identify affordable and effective ways to provide care,” Dr. Englander says. “Interprofessional team members, community partners, and family members can help hospitalists understand patient and population health needs and available resources.”
In an effort to close transitional care gaps, OHSU developed the C-TRAIN program, a multi-component transitional care intervention that includes four main elements:
- Transitional care nurse who sees patients in the hospital, makes home visits, and helps coordinate care 30 days post-discharge;
- Inpatient pharmacy consultation and prescription medications at discharge from a low-cost, value-based formulary;
- Medical home linkages, whereby OHSU partners with and provides payment to three community clinics to provide primary care for uninsured patients; and
- Monthly implementation team meetings that convene diverse healthcare stakeholders to integrate elements of the healthcare system and engage in ongoing quality improvement.
The Schumachergroup has also found an effective solution.
“The department head of our case managers and social workers made an agreement with a local multispecialty group,” Dr. Merchant says. “The group agreed to take all discharged patients and be their PCP for 30 days, even if the patient couldn’t pay, in exchange for receiving all patients who had good insurance but did not have an established PCP.
“This has worked well. Every patient discharged from our facility has a PCP listed at discharge, and the unit clerk makes an appointment and documents it in the electronic medical record.”
Sound Physicians has set up a service line, called transitional care services, to smooth transitions of care after discharge for up to 90 days, depending on their clinical needs. It hires providers who work in post-acute facilities and who can also visit patients at home. After discharge, a nurse practitioner will visit the patient, connect him or her with a PCP, and get the patient access to care.
“Smaller hospitalist groups could set up post-discharge clinics,” Dr. Sears suggests, “so when they discharge a patient without a PCP, [the patient] could return to see one of the hospitalists there.”
Mount Carmel East Hospital, a Sound Physicians’ hospital in Columbus, Ohio, has a financial assistance program.
“The case management department provides community health resources to patients who are insured but have no PCP,” says Shelli Morris, RN. “We also have a hotline that patients can call for a list of PCPs that are accepting new patients.”
When a patient lacks insurance or a PCP, Morris is contacted by the physician or case management to provide a referral to a neighborhood health clinic. “Then, as a courtesy, we set up a post-hospital follow-up appointment,” she says.
By working with other care team members at facilities such as outpatient clinics and pharmacies, hospitalists and other staff have been able to improve care for patients without insurance or a PCP after discharge. Knowing the funding that is available, as well as programs to help these patients, is also integral.
Karen Appold is a medical writer in Pennsylvania.
References
- American Hospital Association. American Hospital Association Uncompensated Hospital Care Cost Fact Sheet. Accessed October 8, 2015.
- The Office of the National Coordinator for Health Information Technology. Health IT in long-term and post acute care: issue brief. March 15, 2013. Accessed October 8, 2015.
- Addison E. Gage award winner HITS the streets to connect with the uninsured. America’s Essential Hospitals. July 22, 2014. Accessed October 8, 2015.
- DeNavas C, Proctor BD, Smith JC. Income, poverty, and health insurance coverage in the United States: 2010. United States Census Bureau. September 2011. Accessed October 8, 2015.
- United States Census Bureau. People without health insurance coverage by selected characteristics: 2010 and 2011. Accessed October 8, 2015.
- Coughlin TA, Holahan J, Caswell K, McGrath M. Uncompensated care for the uninsured in 2013: a detailed examination. The Henry J. Kaiser Family Foundation. May 30, 2014. Accessed October 8, 2015.
Hospitalists are charged with giving the best of care and treatment, regardless of whether or not a patient is insured or has a PCP to transition to after discharge. But patients who do not have insurance or a PCP pose many challenges to hospitalists, as well as the healthcare systems they work in. Although some hospitals and health systems have found ways to address these challenges, issues persist, with high costs to care for these patients topping the list. In 2013, the cost of community hospitals’ uncompensated care climbed to $46.4 billion.1
Typically, undocumented and unassigned patients face many social and economic challenges. Many of these patients are unemployed or work as independent contractors without employer-offered health insurance. Some have multiple jobs, can’t take time off from work for doctor appointments, or are undocumented workers.
More patients have acquired health insurance in recent years as a result of the Affordable Care Act (ACA) and Medicaid expansion; however, some eligible people never complete the necessary forms.
With or without insurance, some patients don’t establish primary care because they have been healthy, have difficulty navigating the healthcare system, lack transportation, or desire more culturally tailored care. Some Medicare and Medicaid patients don’t have a PCP in their community who accepts these programs.
Treatment Challenges
Uninsured patients often are sicker and have more complex conditions than those with insurance, according to Beth Feldpush, DrPH, senior vice president of policy and advocacy at the nonprofit trade group America’s Essential Hospitals, which is based in Washington, D.C., and represents 250 safety net hospitals throughout the U.S.
“Because they can’t afford regular preventive and primary care, they forgo needed healthcare services until their conditions worsen and they require costly hospital care,” says Dr. Feldpush. Uninsured patients often lack the resources for follow-up care to help them recover and stay well. She says more than half of all inpatient discharges and outpatient visits at her groups’ hospitals are for uninsured or Medicaid patients.
When an uninsured patient is discharged from the hospital, finding follow-up care can be difficult.
“Their ability to get an appointment to see a PCP is extremely limited, because many providers don’t see patients without health insurance,” says Scott Sears, MD, MBA, chief clinical officer of Tacoma, Wash.-based Sound Physicians. Dr. Sears notes that in some hospitalist programs, as many as 40% of hospitalized patients lack insurance. “But without secured follow-up care, hospitalists are hesitant to send patients home, because they could relapse.”
Typically, these patients are not completely well and should be transferred to a skilled nursing or hospice facility; however, many facilities won’t accept them without insurance. Often, these patients need a PCP to monitor them with laboratory tests and other follow-up tests, to prescribe and monitor medications, and to ensure that they are following their plan of care.
At some medical facilities, subspecialists who consult on patients may screen them and refuse to see anyone without health insurance.
“So even though some patients may need subspecialty support, they may not have access to it,” Dr. Sears says. “While some patients without insurance qualify for Medicaid or other programs, due to the amount of paperwork and time to enroll, they end up staying in the hospital even though they are ready for discharge.”
Transitional Challenges
Most patients admitted to the hospital either have exacerbations of chronic conditions or a new diagnosis. “It’s rare to hospitalize a patient with a discrete illness that wouldn’t need care after discharge, so having a robust PCP partner is critical to a patient’s health,” says Honora Englander, MD, medical director of the Care Transitions Innovation (C-TRAIN) program at Oregon Health and Science University (OHSU) in Portland. For many patients, psychosocial complexity complicates their transition out of the hospital. An effective system needs to address a patient’s mental health, housing, and other social needs.
It may take four to six weeks for a patient without an established PCP to get a new patient appointment. “This is a huge impediment, as the patient won’t have anyone to ensure that he or she continues along the proper care path,” Dr. Sears says.
“Studies estimate that more than half of medication errors that patients experience occur during transitions and after discharge,” Dr. Sears says.2 “Intervention with a healthcare provider who can review proper use after discharge can dramatically reduce errors and [improve] patient outcomes.”
Rates of patients without a PCP vary by region for Sound Physicians. In the northwest region, about 25% of admitted patients lack a PCP; in the gulf region, the figure can be as high as 60%.
“In Texas, there is a large number of patients and not as many PCPs,” he adds. “There is also a larger percentage of patients without health insurance. Sometimes patients have coverage but have never established care with a PCP.”
As a result of not having a PCP to transition to, some patients return to the hospital soon after discharge, Dr. Feldpush notes.
Tips for Treating Uninsured Patients
Some facilities have found successful ways to help hospitalized patients without health insurance. Dr. Sears says that hospitalists can investigate which clinics accept uninsured patients or which local physician groups are willing to see them after discharge, in exchange for hospitalists taking care of them in the hospital. They also can investigate the community-based insurance programs that are available.
Teresa Coker, MSN, ARNP, FNP-BC, a Sound Physicians program manager at Mercy Medical Center in Cedar Rapids, Iowa, says that when patients lack insurance at her hospital, an organization will review the patient’s case, determine insurance eligibility, and assist the patient in completing the appropriate paperwork. When patients are not eligible, they are instructed to inquire about the hospital’s charity care program if they receive a bill they are unable to pay.
In addition, the community has a free health clinic that serves those without insurance. “Patients are given the address and hours prior to discharge, because it is walk-in only,” Coker says. “All patients are recommended to follow up within one week, or sooner if medications are needed.”
Dr. Englander advocates that physicians take into account medication costs, transportation, and other social considerations when planning care after hospitalization. The team at OHSU developed a low-cost formulary (based in part on widely available $4 plans from national pharmacy chains), and OHSU provides medications for uninsured patients in the program for up to 30 days following discharge.
For patients who can’t afford the $4 drug plan, case managers offer coupons for $4 prescriptions, says Malik Merchant, MD, area medical officer for the Schumachergroup in Harker Heights, Texas. He says that as many as 30% of the patients in his area are undocumented or unassigned. For more expensive medications, a social worker offers pharmaceutical company coupons when they are available. The institution also has a small budget to pay for drugs.
Dr. Merchant has found the biggest challenge to be the transition of care from inpatient to outpatient.
“Case managers and social workers prepare a financial worksheet that provides the possibility of overall cost savings for the institution, if patients are willing to participate in some upfront cost,” he says. “When our parent institution came on board, we developed contracts with local pharmacies, [a] skilled nursing facility, and PCPs to take these patients until they recovered from an acute illness. Our institution paid for these services at a reduced rate but saved money by reducing the length of their hospital stay.”
Dr. Feldpush says her group’s hospitals work hard to reach the uninsured. South Florida’s Memorial Healthcare System (MHS) created the Health Intervention with Targeted Services (HITS) Program, an outreach initiative that links patients with insurance programs or medical homes.3 The HITS team used a geographic information system map to target 15 neighborhoods with the highest rates of hospitalized, uninsured patients. Over a six-month period, the team approached these neighborhoods using various outreach strategies, such as health fairs, educational workshops, and door-to-door visits.3
Approximately 6,910 HITS participants have been enrolled in Medicaid, Florida’s children’s health insurance program, or an MHS community health center. Over a three-year study period, MHS saved $284,856 in the ED, about $2.8 million in inpatient costs, and roughly $4 million overall.3
Barriers to Follow-Up Care
Whether you are looking to help uninsured patients, those without a PCP, or both, the key is to try to fill in the gaps.
“As hospitalists, we need to work with pharmacists, case managers and social workers, and others to identify affordable and effective ways to provide care,” Dr. Englander says. “Interprofessional team members, community partners, and family members can help hospitalists understand patient and population health needs and available resources.”
In an effort to close transitional care gaps, OHSU developed the C-TRAIN program, a multi-component transitional care intervention that includes four main elements:
- Transitional care nurse who sees patients in the hospital, makes home visits, and helps coordinate care 30 days post-discharge;
- Inpatient pharmacy consultation and prescription medications at discharge from a low-cost, value-based formulary;
- Medical home linkages, whereby OHSU partners with and provides payment to three community clinics to provide primary care for uninsured patients; and
- Monthly implementation team meetings that convene diverse healthcare stakeholders to integrate elements of the healthcare system and engage in ongoing quality improvement.
The Schumachergroup has also found an effective solution.
“The department head of our case managers and social workers made an agreement with a local multispecialty group,” Dr. Merchant says. “The group agreed to take all discharged patients and be their PCP for 30 days, even if the patient couldn’t pay, in exchange for receiving all patients who had good insurance but did not have an established PCP.
“This has worked well. Every patient discharged from our facility has a PCP listed at discharge, and the unit clerk makes an appointment and documents it in the electronic medical record.”
Sound Physicians has set up a service line, called transitional care services, to smooth transitions of care after discharge for up to 90 days, depending on their clinical needs. It hires providers who work in post-acute facilities and who can also visit patients at home. After discharge, a nurse practitioner will visit the patient, connect him or her with a PCP, and get the patient access to care.
“Smaller hospitalist groups could set up post-discharge clinics,” Dr. Sears suggests, “so when they discharge a patient without a PCP, [the patient] could return to see one of the hospitalists there.”
Mount Carmel East Hospital, a Sound Physicians’ hospital in Columbus, Ohio, has a financial assistance program.
“The case management department provides community health resources to patients who are insured but have no PCP,” says Shelli Morris, RN. “We also have a hotline that patients can call for a list of PCPs that are accepting new patients.”
When a patient lacks insurance or a PCP, Morris is contacted by the physician or case management to provide a referral to a neighborhood health clinic. “Then, as a courtesy, we set up a post-hospital follow-up appointment,” she says.
By working with other care team members at facilities such as outpatient clinics and pharmacies, hospitalists and other staff have been able to improve care for patients without insurance or a PCP after discharge. Knowing the funding that is available, as well as programs to help these patients, is also integral.
Karen Appold is a medical writer in Pennsylvania.
References
- American Hospital Association. American Hospital Association Uncompensated Hospital Care Cost Fact Sheet. Accessed October 8, 2015.
- The Office of the National Coordinator for Health Information Technology. Health IT in long-term and post acute care: issue brief. March 15, 2013. Accessed October 8, 2015.
- Addison E. Gage award winner HITS the streets to connect with the uninsured. America’s Essential Hospitals. July 22, 2014. Accessed October 8, 2015.
- DeNavas C, Proctor BD, Smith JC. Income, poverty, and health insurance coverage in the United States: 2010. United States Census Bureau. September 2011. Accessed October 8, 2015.
- United States Census Bureau. People without health insurance coverage by selected characteristics: 2010 and 2011. Accessed October 8, 2015.
- Coughlin TA, Holahan J, Caswell K, McGrath M. Uncompensated care for the uninsured in 2013: a detailed examination. The Henry J. Kaiser Family Foundation. May 30, 2014. Accessed October 8, 2015.
Hospitalists are charged with giving the best of care and treatment, regardless of whether or not a patient is insured or has a PCP to transition to after discharge. But patients who do not have insurance or a PCP pose many challenges to hospitalists, as well as the healthcare systems they work in. Although some hospitals and health systems have found ways to address these challenges, issues persist, with high costs to care for these patients topping the list. In 2013, the cost of community hospitals’ uncompensated care climbed to $46.4 billion.1
Typically, undocumented and unassigned patients face many social and economic challenges. Many of these patients are unemployed or work as independent contractors without employer-offered health insurance. Some have multiple jobs, can’t take time off from work for doctor appointments, or are undocumented workers.
More patients have acquired health insurance in recent years as a result of the Affordable Care Act (ACA) and Medicaid expansion; however, some eligible people never complete the necessary forms.
With or without insurance, some patients don’t establish primary care because they have been healthy, have difficulty navigating the healthcare system, lack transportation, or desire more culturally tailored care. Some Medicare and Medicaid patients don’t have a PCP in their community who accepts these programs.
Treatment Challenges
Uninsured patients often are sicker and have more complex conditions than those with insurance, according to Beth Feldpush, DrPH, senior vice president of policy and advocacy at the nonprofit trade group America’s Essential Hospitals, which is based in Washington, D.C., and represents 250 safety net hospitals throughout the U.S.
“Because they can’t afford regular preventive and primary care, they forgo needed healthcare services until their conditions worsen and they require costly hospital care,” says Dr. Feldpush. Uninsured patients often lack the resources for follow-up care to help them recover and stay well. She says more than half of all inpatient discharges and outpatient visits at her groups’ hospitals are for uninsured or Medicaid patients.
When an uninsured patient is discharged from the hospital, finding follow-up care can be difficult.
“Their ability to get an appointment to see a PCP is extremely limited, because many providers don’t see patients without health insurance,” says Scott Sears, MD, MBA, chief clinical officer of Tacoma, Wash.-based Sound Physicians. Dr. Sears notes that in some hospitalist programs, as many as 40% of hospitalized patients lack insurance. “But without secured follow-up care, hospitalists are hesitant to send patients home, because they could relapse.”
Typically, these patients are not completely well and should be transferred to a skilled nursing or hospice facility; however, many facilities won’t accept them without insurance. Often, these patients need a PCP to monitor them with laboratory tests and other follow-up tests, to prescribe and monitor medications, and to ensure that they are following their plan of care.
At some medical facilities, subspecialists who consult on patients may screen them and refuse to see anyone without health insurance.
“So even though some patients may need subspecialty support, they may not have access to it,” Dr. Sears says. “While some patients without insurance qualify for Medicaid or other programs, due to the amount of paperwork and time to enroll, they end up staying in the hospital even though they are ready for discharge.”
Transitional Challenges
Most patients admitted to the hospital either have exacerbations of chronic conditions or a new diagnosis. “It’s rare to hospitalize a patient with a discrete illness that wouldn’t need care after discharge, so having a robust PCP partner is critical to a patient’s health,” says Honora Englander, MD, medical director of the Care Transitions Innovation (C-TRAIN) program at Oregon Health and Science University (OHSU) in Portland. For many patients, psychosocial complexity complicates their transition out of the hospital. An effective system needs to address a patient’s mental health, housing, and other social needs.
It may take four to six weeks for a patient without an established PCP to get a new patient appointment. “This is a huge impediment, as the patient won’t have anyone to ensure that he or she continues along the proper care path,” Dr. Sears says.
“Studies estimate that more than half of medication errors that patients experience occur during transitions and after discharge,” Dr. Sears says.2 “Intervention with a healthcare provider who can review proper use after discharge can dramatically reduce errors and [improve] patient outcomes.”
Rates of patients without a PCP vary by region for Sound Physicians. In the northwest region, about 25% of admitted patients lack a PCP; in the gulf region, the figure can be as high as 60%.
“In Texas, there is a large number of patients and not as many PCPs,” he adds. “There is also a larger percentage of patients without health insurance. Sometimes patients have coverage but have never established care with a PCP.”
As a result of not having a PCP to transition to, some patients return to the hospital soon after discharge, Dr. Feldpush notes.
Tips for Treating Uninsured Patients
Some facilities have found successful ways to help hospitalized patients without health insurance. Dr. Sears says that hospitalists can investigate which clinics accept uninsured patients or which local physician groups are willing to see them after discharge, in exchange for hospitalists taking care of them in the hospital. They also can investigate the community-based insurance programs that are available.
Teresa Coker, MSN, ARNP, FNP-BC, a Sound Physicians program manager at Mercy Medical Center in Cedar Rapids, Iowa, says that when patients lack insurance at her hospital, an organization will review the patient’s case, determine insurance eligibility, and assist the patient in completing the appropriate paperwork. When patients are not eligible, they are instructed to inquire about the hospital’s charity care program if they receive a bill they are unable to pay.
In addition, the community has a free health clinic that serves those without insurance. “Patients are given the address and hours prior to discharge, because it is walk-in only,” Coker says. “All patients are recommended to follow up within one week, or sooner if medications are needed.”
Dr. Englander advocates that physicians take into account medication costs, transportation, and other social considerations when planning care after hospitalization. The team at OHSU developed a low-cost formulary (based in part on widely available $4 plans from national pharmacy chains), and OHSU provides medications for uninsured patients in the program for up to 30 days following discharge.
For patients who can’t afford the $4 drug plan, case managers offer coupons for $4 prescriptions, says Malik Merchant, MD, area medical officer for the Schumachergroup in Harker Heights, Texas. He says that as many as 30% of the patients in his area are undocumented or unassigned. For more expensive medications, a social worker offers pharmaceutical company coupons when they are available. The institution also has a small budget to pay for drugs.
Dr. Merchant has found the biggest challenge to be the transition of care from inpatient to outpatient.
“Case managers and social workers prepare a financial worksheet that provides the possibility of overall cost savings for the institution, if patients are willing to participate in some upfront cost,” he says. “When our parent institution came on board, we developed contracts with local pharmacies, [a] skilled nursing facility, and PCPs to take these patients until they recovered from an acute illness. Our institution paid for these services at a reduced rate but saved money by reducing the length of their hospital stay.”
Dr. Feldpush says her group’s hospitals work hard to reach the uninsured. South Florida’s Memorial Healthcare System (MHS) created the Health Intervention with Targeted Services (HITS) Program, an outreach initiative that links patients with insurance programs or medical homes.3 The HITS team used a geographic information system map to target 15 neighborhoods with the highest rates of hospitalized, uninsured patients. Over a six-month period, the team approached these neighborhoods using various outreach strategies, such as health fairs, educational workshops, and door-to-door visits.3
Approximately 6,910 HITS participants have been enrolled in Medicaid, Florida’s children’s health insurance program, or an MHS community health center. Over a three-year study period, MHS saved $284,856 in the ED, about $2.8 million in inpatient costs, and roughly $4 million overall.3
Barriers to Follow-Up Care
Whether you are looking to help uninsured patients, those without a PCP, or both, the key is to try to fill in the gaps.
“As hospitalists, we need to work with pharmacists, case managers and social workers, and others to identify affordable and effective ways to provide care,” Dr. Englander says. “Interprofessional team members, community partners, and family members can help hospitalists understand patient and population health needs and available resources.”
In an effort to close transitional care gaps, OHSU developed the C-TRAIN program, a multi-component transitional care intervention that includes four main elements:
- Transitional care nurse who sees patients in the hospital, makes home visits, and helps coordinate care 30 days post-discharge;
- Inpatient pharmacy consultation and prescription medications at discharge from a low-cost, value-based formulary;
- Medical home linkages, whereby OHSU partners with and provides payment to three community clinics to provide primary care for uninsured patients; and
- Monthly implementation team meetings that convene diverse healthcare stakeholders to integrate elements of the healthcare system and engage in ongoing quality improvement.
The Schumachergroup has also found an effective solution.
“The department head of our case managers and social workers made an agreement with a local multispecialty group,” Dr. Merchant says. “The group agreed to take all discharged patients and be their PCP for 30 days, even if the patient couldn’t pay, in exchange for receiving all patients who had good insurance but did not have an established PCP.
“This has worked well. Every patient discharged from our facility has a PCP listed at discharge, and the unit clerk makes an appointment and documents it in the electronic medical record.”
Sound Physicians has set up a service line, called transitional care services, to smooth transitions of care after discharge for up to 90 days, depending on their clinical needs. It hires providers who work in post-acute facilities and who can also visit patients at home. After discharge, a nurse practitioner will visit the patient, connect him or her with a PCP, and get the patient access to care.
“Smaller hospitalist groups could set up post-discharge clinics,” Dr. Sears suggests, “so when they discharge a patient without a PCP, [the patient] could return to see one of the hospitalists there.”
Mount Carmel East Hospital, a Sound Physicians’ hospital in Columbus, Ohio, has a financial assistance program.
“The case management department provides community health resources to patients who are insured but have no PCP,” says Shelli Morris, RN. “We also have a hotline that patients can call for a list of PCPs that are accepting new patients.”
When a patient lacks insurance or a PCP, Morris is contacted by the physician or case management to provide a referral to a neighborhood health clinic. “Then, as a courtesy, we set up a post-hospital follow-up appointment,” she says.
By working with other care team members at facilities such as outpatient clinics and pharmacies, hospitalists and other staff have been able to improve care for patients without insurance or a PCP after discharge. Knowing the funding that is available, as well as programs to help these patients, is also integral.
Karen Appold is a medical writer in Pennsylvania.
References
- American Hospital Association. American Hospital Association Uncompensated Hospital Care Cost Fact Sheet. Accessed October 8, 2015.
- The Office of the National Coordinator for Health Information Technology. Health IT in long-term and post acute care: issue brief. March 15, 2013. Accessed October 8, 2015.
- Addison E. Gage award winner HITS the streets to connect with the uninsured. America’s Essential Hospitals. July 22, 2014. Accessed October 8, 2015.
- DeNavas C, Proctor BD, Smith JC. Income, poverty, and health insurance coverage in the United States: 2010. United States Census Bureau. September 2011. Accessed October 8, 2015.
- United States Census Bureau. People without health insurance coverage by selected characteristics: 2010 and 2011. Accessed October 8, 2015.
- Coughlin TA, Holahan J, Caswell K, McGrath M. Uncompensated care for the uninsured in 2013: a detailed examination. The Henry J. Kaiser Family Foundation. May 30, 2014. Accessed October 8, 2015.
LISTEN NOW: Scott Sears, MD, Discusses Hospitalist Challenges with Unassigned, Uninsured Patients
Hospitalists Play Vital Role in Patients’ View of Hospital Stay
Special Reports
Hospitalists are often perceived as the face of the hospital, whether that is their official responsibility or not. They are on the front lines of hearing, seeing, and understanding where gaps exist in a patient’s experience.
“Whenever I hear a patient complain, I can almost piece together what happened without having to interview other staff,” says Jairy C. Hunter III, MD, MBA, SFHM, associate CMO for care transitions at the Medical University of South Carolina in Charleston.
“Up to this point, there hasn’t been as much accountability regarding customer satisfaction in our industry compared to other industries,” Dr. Hunter says.
The paradigm shift has occurred because payers are demanding it. They want value and satisfaction in what they are paying for. In fact, there is a movement to try to standardize procedures whenever possible, such as the amount of time it takes someone to answer a call bell or the volume of noise in a hallway.
“Patients are being asked questions about such topics in surveys,” Dr. Hunter says. “Although these types of questions don’t involve medical decision-making or a course of treatment, they do include personal interactions that influence how patients feel about their hospital experience.”
Another reason for the shift is the significant increase in the use of electronic communication devices and the explosion of online ratings of consumer products and services. Naturally, consumers want access to accurate and easy-to-use information about the quality of healthcare services.
Patient experience surveys focus on how patients’ experienced or perceived key aspects of their care, not how satisfied they were with their care.1 One way a hospital can measure patient experience is with the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey, which was developed by the Centers for Medicare and Medicaid Services (CMS) and the Agency for Healthcare Research and Quality (AHRQ).2 Although other patient satisfaction/experience vendors offer surveys, the Deficit Reduction Act of 2005 states that all Inpatient Prospective Payment Systems (IPPS) hospitals who wish to receive their full annual payment update must collect and submit HCAHPS data to CMS.
The HCAHPS survey, which employs standardized survey instrument and data collection methodology to measure patients’ perspectives on hospital care, is administered to a random sample of patients throughout the year. CMS cleans, adjusts, and analyzes the data and then publicly reports the results. All CAHPS products are available at no cost at www.cahps.ahrq.gov.2
Christine Crofton, PhD, director of CAHPS in Rockville, Md., notes that the HCAHPS survey focuses on patient experience measures because they are considered more understandable, unambiguous, actionable, and objective compared to general satisfaction ratings. Although CAHPS surveys do ask respondents to provide overall ratings (e.g. rate the physician on a scale of one to 10), their primary focus is to ask patients to report on their experiences with specific aspects of care in order to provide information that is not biased by different expectations.
For example, if a patient doesn’t understand what symptoms or problems to report to his or her provider after leaving the hospital, the lack of understanding could lead to a complication, a worsening condition, or readmission.
“A specific survey question about written discharge instructions will give hospital administrators more actionable information concerning an increase in readmission rates than a response to a 10-point satisfaction scale,” Dr. Crofton explains.
Efforts to Improve
At medical institutions across the nation, hospitalists and their team members are making conscious efforts to improve the patient experience in light of the growing importance of surveys. Baylor Scott and White Health in Round Rock, Texas, offers a lecture series and provider coaching as part of its continuing education program. The training, says Trina E. Dorrah, MD, MPH, a BSWH hospitalist and physician director for quality improvement, encompasses such topics as:
- Dealing with difficult patient scenarios;
- Patient experience improvement tips;
- Tips to improve providers’ explanations; and
- Tips to improve patients’ understanding.
Dr. Dorrah uses one-on-one shadowing to help providers improve the patient experience.
“I accompany the provider when visiting the patient and observe his or her interactions,” she says. “This enables me to help providers to see what skills they can incorporate to positively impact patient experience.”
Interdisciplinary rounds have also helped to improve the patient experience.
“Patients want to know that their entire healthcare team is focused on them and that they are working together to improve their experience,” Dr. Dorrah says. On weekdays, hospitalists lead interdisciplinary rounds with the rest of the care team, including case management, nursing, and therapy. “We discuss our patients and ensure that we are all on the same page regarding the plan.”
In addition, hospitalists round with nurses each morning. “Everyone benefits,” Dr. Dorrah says. “The patient gets more coordinated care and the nurse is better educated about the plan of care for the day. The number of pages from the nurse to the physician is also reduced because the nurse better understands the care plan.”
BSWH, which uses Press Ganey Associates to administer HCAHPS surveys, considers the scores for the doctor communication domain when establishing a hospitalist team goal for the year.
“If our team reaches the goal, the leadership/administrative team rewards the hospitalist team with a financial bonus,” Dr. Dorrah says.
Lawrence General Hospital, in Lawrence, Mass., which also uses Press Ganey Associates to administer and manage its HCAHPS satisfaction surveys, is working to increase the ability of hospitalists and other caregivers to proactively meet and exceed patients’ needs with its Five-to-Thrive program. The program consists of these five strategies:
- Care-Out-Loud: an initiative that charges every clinical and nonclinical staff member to be present, sensitive, and compassionate to the patient and explain each step of the clinical interaction;
- Manager rounding on staff and patients;
- Hourly staff rounding on patients;
- Interdisciplinary bedside rounding; and
- Senior leader rounding.
“It is based on best practice tactics that aim to improve the overall patient and family experience,” says Damaris Valera, MS, CMPE, director of the hospital’s Service Excellence Program.
Cogent Healthcare at University of Florida Health in Jacksonville, Fla., places a large emphasis on AIDET principles—acknowledge, introduce, duration, explanation, and thank you—during each patient encounter, says Larry Sharp, MD, SFHM, system medical director. AIDET principles entail offering a pleasant greeting and introducing yourself to patients, keeping patients abreast of wait times, explaining procedures, and thanking patients for the opportunity to participate in their care.
The medical director makes shadow rounds with providers and then ghost rounds by surveying the patients after rounds to get the patients’ direct feedback about encounters.
“We provide information to our providers from these rounds as a method to improve care,” Dr. Sharp says.
Northwestern University Feinberg School of Medicine in Chicago trains hospitalists on communication skills and consequently saw a trend toward improved satisfaction scores and used physician face cards to improve patients’ knowledge of the names and roles of physicians, which did not impact patient satisfaction, reports Kevin J. O’Leary, MD, MS, SFHM, associate professor of medicine, chief of the division of hospital medicine, and associate chair for quality in the department of medicine at Northwestern.3,4 Findings were published in the Journal of Hospital Medicine.
“These efforts have reinforced the need for multifaceted interventions,” Dr. O’Leary says. “Alone, each one has had little effect, but combined they may have a greater effect. The data is intended to be formative and to identify opportunities to learn.”
Additional improvements have been made due to a better understanding of drivers of low satisfaction.
“Unit medical directors [hospitalists] have started to visit patients to get a qualitative sense of what things affect patient experience,” Dr. O’Leary says. As a result, two previously unidentified issues—ED personnel making promises that can’t be kept to patients and patients receiving conflicting information from specialist consultants and hospitalists—surfaced which could now be addressed.”
Challenges and Limitations
Despite their best efforts to improve the patient experience, hospitalists face myriad obstacles. First, the HCAHPS survey asks about the collective care delivered by doctors during the hospitalization, as opposed to the care given by one particular hospitalist.
“One challenge hospitalists face by not having individual data is not knowing which hospitalists excel at the patient experience and which ones do not,” Dr. Dorrah says. “When no one feels that he or she is the problem, it is difficult to hold individual hospitalists accountable.”

Another problem, Dr. Dorrah reports, stems from the fact that patients may see more than one physician—perhaps several hospitalists or specialists—during their hospitalization. When the HCAHPS survey asks patients to assess the care given by all physicians, patients consider the care given by multiple different physicians.
“Therefore, it is difficult to hold a particular hospitalist accountable for the physician communication domain when he or she is not the only provider influencing patients’ perceptions.”
Some hospital systems still have chosen to attribute HCAHPS doctor communication scores to individual hospitalists. These health systems address the issue by attributing the survey results to the admitting physician, the discharging physician, or all hospitalists who participated in the patient’s care.
“None of these methods are perfect, but health systems are increasingly wanting to ensure their inpatient providers are as invested in the patient experience as their outpatient physicians,” Dr. Dorrah says.
Another obstacle hospitalist groups face is the fact that more attention is given to raising HCAHPS survey scores than to improving the overall patient experience.
“In an effort to raise survey scores, hospitals often lose sight of what truly matters to patients,” Dr. Dorrah says. “Many things contribute to a positive or negative patient experience that are not necessarily measured by the survey. If you only pay attention to the survey, your hospital may overlook things that truly matter to your patients.”
Finally, with the increasing focus on the patient experience, the focus on maintaining a good provider experience can fall short.
“While it’s tempting to ask hospitalists to do more—see more patients, take on more responsibility, and participate in more committees—if hospitals fail to provide a positive environment for their hospitalists, they will have a difficult time fully engaging their hospitalists with the patient experience,” Dr. Dorrah says.
Some situations are out of the hospitalists’ hands. A patient may get upset or angry, and the cause is outside of anyone’s control.
“They may have to spend a night in the emergency department or have an unfavorable outcome,” Dr. Hunter says. “In those instances, employ the art of personal interaction—try to empathize with patients and let them know that you care about them.”
Another limitation, Dr. Sharp says, is that you can’t specifically script encounters to “teach to the test,” by using verbiage with the patient that is verbatim from the satisfaction survey questions.
“Nor can we directly control the temperature in patients’ rooms or the quality of their food,” he says. “We also do not have direct control over a negative experience in the emergency department before patients are referred to us, and many surveys show that it is very difficult to overcome a bad experience.”
Tools at Your Fingertips
As a result of the growing emphasis on patient-centered care, SHM created a Patient Experience Committee this year. SHM defines patient experience as “everything we say and do that affects our patients’ thoughts, feelings, and well-being.” The committee is looking at the issues at hand and defining the patient experience and what makes it good.
“We are looking at success stories, as well as not so successful stories, from some of our members to identify what seems to work and what doesn’t work,” says Dr. Sharp, a member of the committee. “By identifying best practices, we can then share this knowledge with the rest of the society, along with methods to implement these practices. We can centralize the gathered knowledge and data and then analyze and make it available to SHM members for their implementation and use.”
The hospitalist plays a key role in the patient experience. Now, more than ever, it’s important to do what you can to make it positive. Consider initiatives you might want to participate in—and perhaps even start your own.
Karen Appold is a medical writer in Pennsylvania.
References
- Consumer Assessment of Healthcare Providers & Systems (CAHPS). CMS.gov. Accessed August 2, 2015.
- Survey of patients’ experiences (HCAHPS). Medicare.gov/Hospital Compare. Accessed August 2, 2015.
- O’Leary KJ, Darling TA, Rauworth J, Williams MV. Impact of hospitalist communication-skills training on patient-satisfaction scores. J Hosp Med. 2013;8(6):315-320.
- Simons Y, Caprio T, Furiasse N, Kriss M, Williams MV, O’Leary KJ. The impact of facecards on patients’ knowledge, satisfaction, trust, and agreement with hospital physicians: a pilot study. J Hosp Med. 2014;9(3):137-141.
Special Reports
Hospitalists are often perceived as the face of the hospital, whether that is their official responsibility or not. They are on the front lines of hearing, seeing, and understanding where gaps exist in a patient’s experience.
“Whenever I hear a patient complain, I can almost piece together what happened without having to interview other staff,” says Jairy C. Hunter III, MD, MBA, SFHM, associate CMO for care transitions at the Medical University of South Carolina in Charleston.
“Up to this point, there hasn’t been as much accountability regarding customer satisfaction in our industry compared to other industries,” Dr. Hunter says.
The paradigm shift has occurred because payers are demanding it. They want value and satisfaction in what they are paying for. In fact, there is a movement to try to standardize procedures whenever possible, such as the amount of time it takes someone to answer a call bell or the volume of noise in a hallway.
“Patients are being asked questions about such topics in surveys,” Dr. Hunter says. “Although these types of questions don’t involve medical decision-making or a course of treatment, they do include personal interactions that influence how patients feel about their hospital experience.”
Another reason for the shift is the significant increase in the use of electronic communication devices and the explosion of online ratings of consumer products and services. Naturally, consumers want access to accurate and easy-to-use information about the quality of healthcare services.
Patient experience surveys focus on how patients’ experienced or perceived key aspects of their care, not how satisfied they were with their care.1 One way a hospital can measure patient experience is with the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey, which was developed by the Centers for Medicare and Medicaid Services (CMS) and the Agency for Healthcare Research and Quality (AHRQ).2 Although other patient satisfaction/experience vendors offer surveys, the Deficit Reduction Act of 2005 states that all Inpatient Prospective Payment Systems (IPPS) hospitals who wish to receive their full annual payment update must collect and submit HCAHPS data to CMS.
The HCAHPS survey, which employs standardized survey instrument and data collection methodology to measure patients’ perspectives on hospital care, is administered to a random sample of patients throughout the year. CMS cleans, adjusts, and analyzes the data and then publicly reports the results. All CAHPS products are available at no cost at www.cahps.ahrq.gov.2
Christine Crofton, PhD, director of CAHPS in Rockville, Md., notes that the HCAHPS survey focuses on patient experience measures because they are considered more understandable, unambiguous, actionable, and objective compared to general satisfaction ratings. Although CAHPS surveys do ask respondents to provide overall ratings (e.g. rate the physician on a scale of one to 10), their primary focus is to ask patients to report on their experiences with specific aspects of care in order to provide information that is not biased by different expectations.
For example, if a patient doesn’t understand what symptoms or problems to report to his or her provider after leaving the hospital, the lack of understanding could lead to a complication, a worsening condition, or readmission.
“A specific survey question about written discharge instructions will give hospital administrators more actionable information concerning an increase in readmission rates than a response to a 10-point satisfaction scale,” Dr. Crofton explains.
Efforts to Improve
At medical institutions across the nation, hospitalists and their team members are making conscious efforts to improve the patient experience in light of the growing importance of surveys. Baylor Scott and White Health in Round Rock, Texas, offers a lecture series and provider coaching as part of its continuing education program. The training, says Trina E. Dorrah, MD, MPH, a BSWH hospitalist and physician director for quality improvement, encompasses such topics as:
- Dealing with difficult patient scenarios;
- Patient experience improvement tips;
- Tips to improve providers’ explanations; and
- Tips to improve patients’ understanding.
Dr. Dorrah uses one-on-one shadowing to help providers improve the patient experience.
“I accompany the provider when visiting the patient and observe his or her interactions,” she says. “This enables me to help providers to see what skills they can incorporate to positively impact patient experience.”
Interdisciplinary rounds have also helped to improve the patient experience.
“Patients want to know that their entire healthcare team is focused on them and that they are working together to improve their experience,” Dr. Dorrah says. On weekdays, hospitalists lead interdisciplinary rounds with the rest of the care team, including case management, nursing, and therapy. “We discuss our patients and ensure that we are all on the same page regarding the plan.”
In addition, hospitalists round with nurses each morning. “Everyone benefits,” Dr. Dorrah says. “The patient gets more coordinated care and the nurse is better educated about the plan of care for the day. The number of pages from the nurse to the physician is also reduced because the nurse better understands the care plan.”
BSWH, which uses Press Ganey Associates to administer HCAHPS surveys, considers the scores for the doctor communication domain when establishing a hospitalist team goal for the year.
“If our team reaches the goal, the leadership/administrative team rewards the hospitalist team with a financial bonus,” Dr. Dorrah says.
Lawrence General Hospital, in Lawrence, Mass., which also uses Press Ganey Associates to administer and manage its HCAHPS satisfaction surveys, is working to increase the ability of hospitalists and other caregivers to proactively meet and exceed patients’ needs with its Five-to-Thrive program. The program consists of these five strategies:
- Care-Out-Loud: an initiative that charges every clinical and nonclinical staff member to be present, sensitive, and compassionate to the patient and explain each step of the clinical interaction;
- Manager rounding on staff and patients;
- Hourly staff rounding on patients;
- Interdisciplinary bedside rounding; and
- Senior leader rounding.
“It is based on best practice tactics that aim to improve the overall patient and family experience,” says Damaris Valera, MS, CMPE, director of the hospital’s Service Excellence Program.
Cogent Healthcare at University of Florida Health in Jacksonville, Fla., places a large emphasis on AIDET principles—acknowledge, introduce, duration, explanation, and thank you—during each patient encounter, says Larry Sharp, MD, SFHM, system medical director. AIDET principles entail offering a pleasant greeting and introducing yourself to patients, keeping patients abreast of wait times, explaining procedures, and thanking patients for the opportunity to participate in their care.
The medical director makes shadow rounds with providers and then ghost rounds by surveying the patients after rounds to get the patients’ direct feedback about encounters.
“We provide information to our providers from these rounds as a method to improve care,” Dr. Sharp says.
Northwestern University Feinberg School of Medicine in Chicago trains hospitalists on communication skills and consequently saw a trend toward improved satisfaction scores and used physician face cards to improve patients’ knowledge of the names and roles of physicians, which did not impact patient satisfaction, reports Kevin J. O’Leary, MD, MS, SFHM, associate professor of medicine, chief of the division of hospital medicine, and associate chair for quality in the department of medicine at Northwestern.3,4 Findings were published in the Journal of Hospital Medicine.
“These efforts have reinforced the need for multifaceted interventions,” Dr. O’Leary says. “Alone, each one has had little effect, but combined they may have a greater effect. The data is intended to be formative and to identify opportunities to learn.”
Additional improvements have been made due to a better understanding of drivers of low satisfaction.
“Unit medical directors [hospitalists] have started to visit patients to get a qualitative sense of what things affect patient experience,” Dr. O’Leary says. As a result, two previously unidentified issues—ED personnel making promises that can’t be kept to patients and patients receiving conflicting information from specialist consultants and hospitalists—surfaced which could now be addressed.”
Challenges and Limitations
Despite their best efforts to improve the patient experience, hospitalists face myriad obstacles. First, the HCAHPS survey asks about the collective care delivered by doctors during the hospitalization, as opposed to the care given by one particular hospitalist.
“One challenge hospitalists face by not having individual data is not knowing which hospitalists excel at the patient experience and which ones do not,” Dr. Dorrah says. “When no one feels that he or she is the problem, it is difficult to hold individual hospitalists accountable.”

Another problem, Dr. Dorrah reports, stems from the fact that patients may see more than one physician—perhaps several hospitalists or specialists—during their hospitalization. When the HCAHPS survey asks patients to assess the care given by all physicians, patients consider the care given by multiple different physicians.
“Therefore, it is difficult to hold a particular hospitalist accountable for the physician communication domain when he or she is not the only provider influencing patients’ perceptions.”
Some hospital systems still have chosen to attribute HCAHPS doctor communication scores to individual hospitalists. These health systems address the issue by attributing the survey results to the admitting physician, the discharging physician, or all hospitalists who participated in the patient’s care.
“None of these methods are perfect, but health systems are increasingly wanting to ensure their inpatient providers are as invested in the patient experience as their outpatient physicians,” Dr. Dorrah says.
Another obstacle hospitalist groups face is the fact that more attention is given to raising HCAHPS survey scores than to improving the overall patient experience.
“In an effort to raise survey scores, hospitals often lose sight of what truly matters to patients,” Dr. Dorrah says. “Many things contribute to a positive or negative patient experience that are not necessarily measured by the survey. If you only pay attention to the survey, your hospital may overlook things that truly matter to your patients.”
Finally, with the increasing focus on the patient experience, the focus on maintaining a good provider experience can fall short.
“While it’s tempting to ask hospitalists to do more—see more patients, take on more responsibility, and participate in more committees—if hospitals fail to provide a positive environment for their hospitalists, they will have a difficult time fully engaging their hospitalists with the patient experience,” Dr. Dorrah says.
Some situations are out of the hospitalists’ hands. A patient may get upset or angry, and the cause is outside of anyone’s control.
“They may have to spend a night in the emergency department or have an unfavorable outcome,” Dr. Hunter says. “In those instances, employ the art of personal interaction—try to empathize with patients and let them know that you care about them.”
Another limitation, Dr. Sharp says, is that you can’t specifically script encounters to “teach to the test,” by using verbiage with the patient that is verbatim from the satisfaction survey questions.
“Nor can we directly control the temperature in patients’ rooms or the quality of their food,” he says. “We also do not have direct control over a negative experience in the emergency department before patients are referred to us, and many surveys show that it is very difficult to overcome a bad experience.”
Tools at Your Fingertips
As a result of the growing emphasis on patient-centered care, SHM created a Patient Experience Committee this year. SHM defines patient experience as “everything we say and do that affects our patients’ thoughts, feelings, and well-being.” The committee is looking at the issues at hand and defining the patient experience and what makes it good.
“We are looking at success stories, as well as not so successful stories, from some of our members to identify what seems to work and what doesn’t work,” says Dr. Sharp, a member of the committee. “By identifying best practices, we can then share this knowledge with the rest of the society, along with methods to implement these practices. We can centralize the gathered knowledge and data and then analyze and make it available to SHM members for their implementation and use.”
The hospitalist plays a key role in the patient experience. Now, more than ever, it’s important to do what you can to make it positive. Consider initiatives you might want to participate in—and perhaps even start your own.
Karen Appold is a medical writer in Pennsylvania.
References
- Consumer Assessment of Healthcare Providers & Systems (CAHPS). CMS.gov. Accessed August 2, 2015.
- Survey of patients’ experiences (HCAHPS). Medicare.gov/Hospital Compare. Accessed August 2, 2015.
- O’Leary KJ, Darling TA, Rauworth J, Williams MV. Impact of hospitalist communication-skills training on patient-satisfaction scores. J Hosp Med. 2013;8(6):315-320.
- Simons Y, Caprio T, Furiasse N, Kriss M, Williams MV, O’Leary KJ. The impact of facecards on patients’ knowledge, satisfaction, trust, and agreement with hospital physicians: a pilot study. J Hosp Med. 2014;9(3):137-141.
Special Reports
Hospitalists are often perceived as the face of the hospital, whether that is their official responsibility or not. They are on the front lines of hearing, seeing, and understanding where gaps exist in a patient’s experience.
“Whenever I hear a patient complain, I can almost piece together what happened without having to interview other staff,” says Jairy C. Hunter III, MD, MBA, SFHM, associate CMO for care transitions at the Medical University of South Carolina in Charleston.
“Up to this point, there hasn’t been as much accountability regarding customer satisfaction in our industry compared to other industries,” Dr. Hunter says.
The paradigm shift has occurred because payers are demanding it. They want value and satisfaction in what they are paying for. In fact, there is a movement to try to standardize procedures whenever possible, such as the amount of time it takes someone to answer a call bell or the volume of noise in a hallway.
“Patients are being asked questions about such topics in surveys,” Dr. Hunter says. “Although these types of questions don’t involve medical decision-making or a course of treatment, they do include personal interactions that influence how patients feel about their hospital experience.”
Another reason for the shift is the significant increase in the use of electronic communication devices and the explosion of online ratings of consumer products and services. Naturally, consumers want access to accurate and easy-to-use information about the quality of healthcare services.
Patient experience surveys focus on how patients’ experienced or perceived key aspects of their care, not how satisfied they were with their care.1 One way a hospital can measure patient experience is with the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey, which was developed by the Centers for Medicare and Medicaid Services (CMS) and the Agency for Healthcare Research and Quality (AHRQ).2 Although other patient satisfaction/experience vendors offer surveys, the Deficit Reduction Act of 2005 states that all Inpatient Prospective Payment Systems (IPPS) hospitals who wish to receive their full annual payment update must collect and submit HCAHPS data to CMS.
The HCAHPS survey, which employs standardized survey instrument and data collection methodology to measure patients’ perspectives on hospital care, is administered to a random sample of patients throughout the year. CMS cleans, adjusts, and analyzes the data and then publicly reports the results. All CAHPS products are available at no cost at www.cahps.ahrq.gov.2
Christine Crofton, PhD, director of CAHPS in Rockville, Md., notes that the HCAHPS survey focuses on patient experience measures because they are considered more understandable, unambiguous, actionable, and objective compared to general satisfaction ratings. Although CAHPS surveys do ask respondents to provide overall ratings (e.g. rate the physician on a scale of one to 10), their primary focus is to ask patients to report on their experiences with specific aspects of care in order to provide information that is not biased by different expectations.
For example, if a patient doesn’t understand what symptoms or problems to report to his or her provider after leaving the hospital, the lack of understanding could lead to a complication, a worsening condition, or readmission.
“A specific survey question about written discharge instructions will give hospital administrators more actionable information concerning an increase in readmission rates than a response to a 10-point satisfaction scale,” Dr. Crofton explains.
Efforts to Improve
At medical institutions across the nation, hospitalists and their team members are making conscious efforts to improve the patient experience in light of the growing importance of surveys. Baylor Scott and White Health in Round Rock, Texas, offers a lecture series and provider coaching as part of its continuing education program. The training, says Trina E. Dorrah, MD, MPH, a BSWH hospitalist and physician director for quality improvement, encompasses such topics as:
- Dealing with difficult patient scenarios;
- Patient experience improvement tips;
- Tips to improve providers’ explanations; and
- Tips to improve patients’ understanding.
Dr. Dorrah uses one-on-one shadowing to help providers improve the patient experience.
“I accompany the provider when visiting the patient and observe his or her interactions,” she says. “This enables me to help providers to see what skills they can incorporate to positively impact patient experience.”
Interdisciplinary rounds have also helped to improve the patient experience.
“Patients want to know that their entire healthcare team is focused on them and that they are working together to improve their experience,” Dr. Dorrah says. On weekdays, hospitalists lead interdisciplinary rounds with the rest of the care team, including case management, nursing, and therapy. “We discuss our patients and ensure that we are all on the same page regarding the plan.”
In addition, hospitalists round with nurses each morning. “Everyone benefits,” Dr. Dorrah says. “The patient gets more coordinated care and the nurse is better educated about the plan of care for the day. The number of pages from the nurse to the physician is also reduced because the nurse better understands the care plan.”
BSWH, which uses Press Ganey Associates to administer HCAHPS surveys, considers the scores for the doctor communication domain when establishing a hospitalist team goal for the year.
“If our team reaches the goal, the leadership/administrative team rewards the hospitalist team with a financial bonus,” Dr. Dorrah says.
Lawrence General Hospital, in Lawrence, Mass., which also uses Press Ganey Associates to administer and manage its HCAHPS satisfaction surveys, is working to increase the ability of hospitalists and other caregivers to proactively meet and exceed patients’ needs with its Five-to-Thrive program. The program consists of these five strategies:
- Care-Out-Loud: an initiative that charges every clinical and nonclinical staff member to be present, sensitive, and compassionate to the patient and explain each step of the clinical interaction;
- Manager rounding on staff and patients;
- Hourly staff rounding on patients;
- Interdisciplinary bedside rounding; and
- Senior leader rounding.
“It is based on best practice tactics that aim to improve the overall patient and family experience,” says Damaris Valera, MS, CMPE, director of the hospital’s Service Excellence Program.
Cogent Healthcare at University of Florida Health in Jacksonville, Fla., places a large emphasis on AIDET principles—acknowledge, introduce, duration, explanation, and thank you—during each patient encounter, says Larry Sharp, MD, SFHM, system medical director. AIDET principles entail offering a pleasant greeting and introducing yourself to patients, keeping patients abreast of wait times, explaining procedures, and thanking patients for the opportunity to participate in their care.
The medical director makes shadow rounds with providers and then ghost rounds by surveying the patients after rounds to get the patients’ direct feedback about encounters.
“We provide information to our providers from these rounds as a method to improve care,” Dr. Sharp says.
Northwestern University Feinberg School of Medicine in Chicago trains hospitalists on communication skills and consequently saw a trend toward improved satisfaction scores and used physician face cards to improve patients’ knowledge of the names and roles of physicians, which did not impact patient satisfaction, reports Kevin J. O’Leary, MD, MS, SFHM, associate professor of medicine, chief of the division of hospital medicine, and associate chair for quality in the department of medicine at Northwestern.3,4 Findings were published in the Journal of Hospital Medicine.
“These efforts have reinforced the need for multifaceted interventions,” Dr. O’Leary says. “Alone, each one has had little effect, but combined they may have a greater effect. The data is intended to be formative and to identify opportunities to learn.”
Additional improvements have been made due to a better understanding of drivers of low satisfaction.
“Unit medical directors [hospitalists] have started to visit patients to get a qualitative sense of what things affect patient experience,” Dr. O’Leary says. As a result, two previously unidentified issues—ED personnel making promises that can’t be kept to patients and patients receiving conflicting information from specialist consultants and hospitalists—surfaced which could now be addressed.”
Challenges and Limitations
Despite their best efforts to improve the patient experience, hospitalists face myriad obstacles. First, the HCAHPS survey asks about the collective care delivered by doctors during the hospitalization, as opposed to the care given by one particular hospitalist.
“One challenge hospitalists face by not having individual data is not knowing which hospitalists excel at the patient experience and which ones do not,” Dr. Dorrah says. “When no one feels that he or she is the problem, it is difficult to hold individual hospitalists accountable.”

Another problem, Dr. Dorrah reports, stems from the fact that patients may see more than one physician—perhaps several hospitalists or specialists—during their hospitalization. When the HCAHPS survey asks patients to assess the care given by all physicians, patients consider the care given by multiple different physicians.
“Therefore, it is difficult to hold a particular hospitalist accountable for the physician communication domain when he or she is not the only provider influencing patients’ perceptions.”
Some hospital systems still have chosen to attribute HCAHPS doctor communication scores to individual hospitalists. These health systems address the issue by attributing the survey results to the admitting physician, the discharging physician, or all hospitalists who participated in the patient’s care.
“None of these methods are perfect, but health systems are increasingly wanting to ensure their inpatient providers are as invested in the patient experience as their outpatient physicians,” Dr. Dorrah says.
Another obstacle hospitalist groups face is the fact that more attention is given to raising HCAHPS survey scores than to improving the overall patient experience.
“In an effort to raise survey scores, hospitals often lose sight of what truly matters to patients,” Dr. Dorrah says. “Many things contribute to a positive or negative patient experience that are not necessarily measured by the survey. If you only pay attention to the survey, your hospital may overlook things that truly matter to your patients.”
Finally, with the increasing focus on the patient experience, the focus on maintaining a good provider experience can fall short.
“While it’s tempting to ask hospitalists to do more—see more patients, take on more responsibility, and participate in more committees—if hospitals fail to provide a positive environment for their hospitalists, they will have a difficult time fully engaging their hospitalists with the patient experience,” Dr. Dorrah says.
Some situations are out of the hospitalists’ hands. A patient may get upset or angry, and the cause is outside of anyone’s control.
“They may have to spend a night in the emergency department or have an unfavorable outcome,” Dr. Hunter says. “In those instances, employ the art of personal interaction—try to empathize with patients and let them know that you care about them.”
Another limitation, Dr. Sharp says, is that you can’t specifically script encounters to “teach to the test,” by using verbiage with the patient that is verbatim from the satisfaction survey questions.
“Nor can we directly control the temperature in patients’ rooms or the quality of their food,” he says. “We also do not have direct control over a negative experience in the emergency department before patients are referred to us, and many surveys show that it is very difficult to overcome a bad experience.”
Tools at Your Fingertips
As a result of the growing emphasis on patient-centered care, SHM created a Patient Experience Committee this year. SHM defines patient experience as “everything we say and do that affects our patients’ thoughts, feelings, and well-being.” The committee is looking at the issues at hand and defining the patient experience and what makes it good.
“We are looking at success stories, as well as not so successful stories, from some of our members to identify what seems to work and what doesn’t work,” says Dr. Sharp, a member of the committee. “By identifying best practices, we can then share this knowledge with the rest of the society, along with methods to implement these practices. We can centralize the gathered knowledge and data and then analyze and make it available to SHM members for their implementation and use.”
The hospitalist plays a key role in the patient experience. Now, more than ever, it’s important to do what you can to make it positive. Consider initiatives you might want to participate in—and perhaps even start your own.
Karen Appold is a medical writer in Pennsylvania.
References
- Consumer Assessment of Healthcare Providers & Systems (CAHPS). CMS.gov. Accessed August 2, 2015.
- Survey of patients’ experiences (HCAHPS). Medicare.gov/Hospital Compare. Accessed August 2, 2015.
- O’Leary KJ, Darling TA, Rauworth J, Williams MV. Impact of hospitalist communication-skills training on patient-satisfaction scores. J Hosp Med. 2013;8(6):315-320.
- Simons Y, Caprio T, Furiasse N, Kriss M, Williams MV, O’Leary KJ. The impact of facecards on patients’ knowledge, satisfaction, trust, and agreement with hospital physicians: a pilot study. J Hosp Med. 2014;9(3):137-141.
Rise of the Chief Patient Experience Officer
The Cleveland Clinic was the first major academic medical center to make improving patient experience a strategic goal. In 2007, the medical institution hired its first chief patient experience officer (CXO) and established the Office of Patient Experience. These were also firsts.
“When we took a step back to evaluate why we come to work every day, we realized it’s for one reason—the patients,” says Adrienne Boissy, MD, MA, the clinic’s CXO. “Toby [Cosgrove, MD, president and CEO of Cleveland Clinic] had some key early experiences, which prompted us to think about patient experience as an organizational priority. These experiences led him to recognize the importance of caring for the soul of the patient, not just the body.
“The CXO was embedded into our executive team, which effectively wove it into our fabric.”
Since then, more than 60 other medical institutions across the country have followed suit.
But improving patient experience isn’t just “nice to do,” Dr. Boissy says. “The great part of these shifts in healthcare is that the government has created the burning platform for us. Organizations won’t survive in the current market if they don’t make it a strategic priority.”
So what are the key drivers of a positive patient experience?
“You cannot deliver an exceptional patient experience without safe care, high quality, or high value,” says Dr. Boissy, who adds that hospitalists shouldn’t underestimate their role in the patient’s experience.
“Hospitalists are leaders whether they have an official title or not,” she adds. “People watch how they behave and interact with patients and colleagues. Raising your own awareness about your ability to influence is key. Model the skills you hope to embed.”
The Cleveland Clinic was the first major academic medical center to make improving patient experience a strategic goal. In 2007, the medical institution hired its first chief patient experience officer (CXO) and established the Office of Patient Experience. These were also firsts.
“When we took a step back to evaluate why we come to work every day, we realized it’s for one reason—the patients,” says Adrienne Boissy, MD, MA, the clinic’s CXO. “Toby [Cosgrove, MD, president and CEO of Cleveland Clinic] had some key early experiences, which prompted us to think about patient experience as an organizational priority. These experiences led him to recognize the importance of caring for the soul of the patient, not just the body.
“The CXO was embedded into our executive team, which effectively wove it into our fabric.”
Since then, more than 60 other medical institutions across the country have followed suit.
But improving patient experience isn’t just “nice to do,” Dr. Boissy says. “The great part of these shifts in healthcare is that the government has created the burning platform for us. Organizations won’t survive in the current market if they don’t make it a strategic priority.”
So what are the key drivers of a positive patient experience?
“You cannot deliver an exceptional patient experience without safe care, high quality, or high value,” says Dr. Boissy, who adds that hospitalists shouldn’t underestimate their role in the patient’s experience.
“Hospitalists are leaders whether they have an official title or not,” she adds. “People watch how they behave and interact with patients and colleagues. Raising your own awareness about your ability to influence is key. Model the skills you hope to embed.”
The Cleveland Clinic was the first major academic medical center to make improving patient experience a strategic goal. In 2007, the medical institution hired its first chief patient experience officer (CXO) and established the Office of Patient Experience. These were also firsts.
“When we took a step back to evaluate why we come to work every day, we realized it’s for one reason—the patients,” says Adrienne Boissy, MD, MA, the clinic’s CXO. “Toby [Cosgrove, MD, president and CEO of Cleveland Clinic] had some key early experiences, which prompted us to think about patient experience as an organizational priority. These experiences led him to recognize the importance of caring for the soul of the patient, not just the body.
“The CXO was embedded into our executive team, which effectively wove it into our fabric.”
Since then, more than 60 other medical institutions across the country have followed suit.
But improving patient experience isn’t just “nice to do,” Dr. Boissy says. “The great part of these shifts in healthcare is that the government has created the burning platform for us. Organizations won’t survive in the current market if they don’t make it a strategic priority.”
So what are the key drivers of a positive patient experience?
“You cannot deliver an exceptional patient experience without safe care, high quality, or high value,” says Dr. Boissy, who adds that hospitalists shouldn’t underestimate their role in the patient’s experience.
“Hospitalists are leaders whether they have an official title or not,” she adds. “People watch how they behave and interact with patients and colleagues. Raising your own awareness about your ability to influence is key. Model the skills you hope to embed.”
LISTEN NOW: Vladimir Cadet, MPH, discusses alarm fatigue challenges and solutions
VLADIMIR N. CADET, MPH, associate with the Applied Solutions Group at ECRI Institute in Plymouth Meeting, Pa., discusses why it can be challenging for hospitals to reduce alarm fatigue and provides strategies to address this growing problem.
VLADIMIR N. CADET, MPH, associate with the Applied Solutions Group at ECRI Institute in Plymouth Meeting, Pa., discusses why it can be challenging for hospitals to reduce alarm fatigue and provides strategies to address this growing problem.
VLADIMIR N. CADET, MPH, associate with the Applied Solutions Group at ECRI Institute in Plymouth Meeting, Pa., discusses why it can be challenging for hospitals to reduce alarm fatigue and provides strategies to address this growing problem.
Hospitalists Key to Addressing Medical Device Alarm Fatigue
Everyday, throughout the day, hospitalists and other healthcare workers are inundated with alerts and warnings and notifications from medical and communication devices. The sheer number of alarms can be extremely overwhelming.
“In any given unit, there may be hundreds of alarms per patient, per day,” says Ronald Wyatt, MD, MHA, medical director of the division of healthcare improvement at The Joint Commission in Oakbrook Terrace, Ill. “That amounts to tens of thousands of alarms each day.”
And, although the intent of these alarms may be good, studies show that 80% to 99% of alarms generated by such medical devices as ventilators, blood pressure monitors, and electrocardiograms are false and/or don’t actually require any clinical intervention.1-4 What’s even more alarming is that clinicians become desensitized—even immune—to the sounds, experiencing what has been called “alarm fatigue.” In response to the constant barrage of noise, clinicians may turn alarms down or off, or adjust alarm settings outside limits that are safe and appropriate for the patient.5
The extent to which alarm fatigue has affected patients is unknown. From 2009 to 2012, The Joint Commission reported 98 alarm-related events. Of these, 80 resulted in death, 13 in permanent loss of function, and five in unexpected additional care or extended stay. Because sentinel event reporting to The Joint Commission is voluntary, Dr. Wyatt estimates that the organization is notified of less than 10% of such events.
Maria Cvach, DNP, RN, MSN, CCRN, DNP, assistant director of nursing for clinical standards at The Johns Hopkins Hospital in Baltimore, Md., says that from 2005 to 2008, there were 566 alarm-related deaths reported to the U.S. Food and Drug Administration’s Manufacturer and User Facility Device Experience (MAUDE) database. “Most experts agree that this is grossly underreported,” says Cvach, who has led alarm system improvement efforts at Hopkins since 2006.
In addition to being a patient safety issue, alarm fatigue has other consequences, Cvach says. Patients and families lose trust in staff when alarms go unanswered. Excessive noise can result in patient and staff harm. Research demonstrates that noise can negatively affect patients’ cardiovascular and immune systems and can increase length of hospital stays. Staff may develop stress symptoms and headaches. In addition, hospitals could face litigation from missed alarms and patient events.
From Bad to Worse
Experts agree that alarm fatigue is getting worse system-wide. ECRI Institute, a nonprofit organization that uses applied scientific research in healthcare to establish best practices for improving patient care, has listed alarm hazards as the number one health technology device hazard for the past three years. This persistent danger has made the top 10 since the list’s inception.6
Cvach says alarm fatigue is fairly easy to recognize.
“If you’re on a unit and hear alarms but do not see anyone addressing them, you are probably witnessing alarm fatigue,” she says. “If you ask staff what is alarming and they indicate that they didn’t notice an alarm ringing, it is likely alarm fatigue. Staff have indicated that sometimes alarms are like ‘white noise.’ [Alarms] go unnoticed because they are considered part of the environment and [staff] are accustomed to them.”
Jairy C. Hunter III, MD, MBA, SFHM, hospitalist and associate CMO for care transitions at Medical University of South Carolina (MUSC) in Charleston, believes alarm fatigue is a problem at every hospital, including his own. In addition to being bombarded with medical device alarms, he is constantly receiving notifications via cell phone, pager, and computers.
“Personally, I feel that I suffer from it [alarm fatigue],” says Dr. Hunter, a member of Team Hospitalist. “When I’m not at work and check my phones, I may realize that I missed answering a few notifications.”
He says that sometimes too much information “may be a bad thing, because we aren’t able to discern what is important and what isn’t. Studies have shown that, in general, people are not good at multi-tasking.”7

Reduction Efforts
Dr. Wyatt believes the corrective actions organizations have implemented to reduce alarm fatigue are not optimal, because the problem is worsening. In addition, the number of patients who are connected to alarm-based devices will continue to increase.
He maintains that hospitalists are uniquely positioned to “team up” with housestaff and tackle this issue.
“Unlike other physicians, [hospitalists] are in the hospital around the clock,” he says.
Dr. Wyatt suggests a good starting point is determining the baseline number of device alarms per day. Then answer these questions:
- How many required clinical intervention?
- How many resulted in harm or death?
- What are the organization’s current monitor alarm default parameters?
- How can we adjust alarms to indicate actionable alarms?
Another tip: Work with engineers and equipment manufacturers to customize alarms and notifications, so staff can readily recognize those that need immediate attention.
Cvach says that unnecessary patient monitoring results in excessive nuisance alarms. Patients should only be monitored when clinically necessary. To determine necessity, refer to the American Heart Association’s Practice Standards for Electrocardiographic Monitoring in Hospital Settings.8
“Alarms should be individualized for patients to make them most useful,” she explains. “Defaults should be customized based on the patient population.”
Cvach also recommends momentarily pausing alarms when assisting patients with turning, suctioning, bathing, and so forth, and changing electrodes regularly.
From a personal perspective, Dr. Hunter suggests that hospitalists turn off as many nonessential notifications as possible and have separate devices for work and personal usage. Reset the tolerance for only certain important types of messages.
“I indicate specific parameters for a nurse or another provider to call me in certain circumstances,” Dr. Hunter says. “That grabs my attention more than a text or e-mail.”
Telling Patients
Vladimir N. Cadet, MPH, an associate with ECRI Institute’s Applied Solutions Group in Plymouth Meeting, Pa., says hospitalists should communicate to patients and their family members, many of whom also suffer from alarm fatigue, the importance of allowing health practitioners to address alarms to minimize the potential for delayed responses or missed alarms.
Patients should be told to notify staff if a medical device alarm goes unanswered, Cvach adds. To facilitate adequate sleep, patients can request earplugs or put on restful music.
Karen Appold is freelance writer in Pennsylvania.
References
- Lawless ST. Crying wolf: false alarms in a pediatric intensive care unit. Crit Care Med. 1994;22(6):981-985.
- Tsien CL, Fackler JC. Poor prognosis of existing monitors in the intensive care unit. Crit Care Med. 1997;25(4):614-619.
- Chambrin MC, Ravaux P, Calvelo-Aros D, Jaborska A, Chopin C, Boniface B. Multicentric study of monitoring alarms in the adult intensive care unit (ICU): a descriptive analysis. Intensive Care Med. 1999;25(12):1360-1366.
- Atzema C, Schull MJ, Borgundvaag B, Slaughter GRD, Lee CK. Alarmed: adverse events in low-risk patients with chest pain receiving electrocardiographic monitoring in the emergency department: a pilot study. Am J Emerg Med. 2006;24(1):62-67.
- Keller JP, Diefes R, Graham K, Meyers M, Pelczarski K. Association for the Advancement of Medical Instrumentation. Why clinical alarms are a “top ten” hazard: how you can help reduce the risk. Horizons. Spring 2011. Available at: http://www.aami.org/htsi/alarms/pdfs/Alarms%20Horizons_Secure_Watermarked.pdf. Accessed March 8, 2015.
- ECRI Institute. Top 10 health technology hazards for 2015. Available at: https://www.ecri.org/press/Pages/ECRI-Institute-Announces-Top-10-Health-Technology-Hazards-for-2015.aspx. Accessed March 8, 2015
- Weigl M1, Müller A, Sevdalis N, Angerer P. Relationships of multitasking, physicians’ strain, and performance: an observational study in ward physicians. J Patient Saf. 2013 Mar;9(1):18-23. doi: 10.1097/PTS.0b013e31826b7b87.
- Drew B, Califf RM, Funk M, et al. Practice standards for electrocardiographic monitoring in hospital settings. Circulation. 2004;110:2721-2746.
Everyday, throughout the day, hospitalists and other healthcare workers are inundated with alerts and warnings and notifications from medical and communication devices. The sheer number of alarms can be extremely overwhelming.
“In any given unit, there may be hundreds of alarms per patient, per day,” says Ronald Wyatt, MD, MHA, medical director of the division of healthcare improvement at The Joint Commission in Oakbrook Terrace, Ill. “That amounts to tens of thousands of alarms each day.”
And, although the intent of these alarms may be good, studies show that 80% to 99% of alarms generated by such medical devices as ventilators, blood pressure monitors, and electrocardiograms are false and/or don’t actually require any clinical intervention.1-4 What’s even more alarming is that clinicians become desensitized—even immune—to the sounds, experiencing what has been called “alarm fatigue.” In response to the constant barrage of noise, clinicians may turn alarms down or off, or adjust alarm settings outside limits that are safe and appropriate for the patient.5
The extent to which alarm fatigue has affected patients is unknown. From 2009 to 2012, The Joint Commission reported 98 alarm-related events. Of these, 80 resulted in death, 13 in permanent loss of function, and five in unexpected additional care or extended stay. Because sentinel event reporting to The Joint Commission is voluntary, Dr. Wyatt estimates that the organization is notified of less than 10% of such events.
Maria Cvach, DNP, RN, MSN, CCRN, DNP, assistant director of nursing for clinical standards at The Johns Hopkins Hospital in Baltimore, Md., says that from 2005 to 2008, there were 566 alarm-related deaths reported to the U.S. Food and Drug Administration’s Manufacturer and User Facility Device Experience (MAUDE) database. “Most experts agree that this is grossly underreported,” says Cvach, who has led alarm system improvement efforts at Hopkins since 2006.
In addition to being a patient safety issue, alarm fatigue has other consequences, Cvach says. Patients and families lose trust in staff when alarms go unanswered. Excessive noise can result in patient and staff harm. Research demonstrates that noise can negatively affect patients’ cardiovascular and immune systems and can increase length of hospital stays. Staff may develop stress symptoms and headaches. In addition, hospitals could face litigation from missed alarms and patient events.
From Bad to Worse
Experts agree that alarm fatigue is getting worse system-wide. ECRI Institute, a nonprofit organization that uses applied scientific research in healthcare to establish best practices for improving patient care, has listed alarm hazards as the number one health technology device hazard for the past three years. This persistent danger has made the top 10 since the list’s inception.6
Cvach says alarm fatigue is fairly easy to recognize.
“If you’re on a unit and hear alarms but do not see anyone addressing them, you are probably witnessing alarm fatigue,” she says. “If you ask staff what is alarming and they indicate that they didn’t notice an alarm ringing, it is likely alarm fatigue. Staff have indicated that sometimes alarms are like ‘white noise.’ [Alarms] go unnoticed because they are considered part of the environment and [staff] are accustomed to them.”
Jairy C. Hunter III, MD, MBA, SFHM, hospitalist and associate CMO for care transitions at Medical University of South Carolina (MUSC) in Charleston, believes alarm fatigue is a problem at every hospital, including his own. In addition to being bombarded with medical device alarms, he is constantly receiving notifications via cell phone, pager, and computers.
“Personally, I feel that I suffer from it [alarm fatigue],” says Dr. Hunter, a member of Team Hospitalist. “When I’m not at work and check my phones, I may realize that I missed answering a few notifications.”
He says that sometimes too much information “may be a bad thing, because we aren’t able to discern what is important and what isn’t. Studies have shown that, in general, people are not good at multi-tasking.”7

Reduction Efforts
Dr. Wyatt believes the corrective actions organizations have implemented to reduce alarm fatigue are not optimal, because the problem is worsening. In addition, the number of patients who are connected to alarm-based devices will continue to increase.
He maintains that hospitalists are uniquely positioned to “team up” with housestaff and tackle this issue.
“Unlike other physicians, [hospitalists] are in the hospital around the clock,” he says.
Dr. Wyatt suggests a good starting point is determining the baseline number of device alarms per day. Then answer these questions:
- How many required clinical intervention?
- How many resulted in harm or death?
- What are the organization’s current monitor alarm default parameters?
- How can we adjust alarms to indicate actionable alarms?
Another tip: Work with engineers and equipment manufacturers to customize alarms and notifications, so staff can readily recognize those that need immediate attention.
Cvach says that unnecessary patient monitoring results in excessive nuisance alarms. Patients should only be monitored when clinically necessary. To determine necessity, refer to the American Heart Association’s Practice Standards for Electrocardiographic Monitoring in Hospital Settings.8
“Alarms should be individualized for patients to make them most useful,” she explains. “Defaults should be customized based on the patient population.”
Cvach also recommends momentarily pausing alarms when assisting patients with turning, suctioning, bathing, and so forth, and changing electrodes regularly.
From a personal perspective, Dr. Hunter suggests that hospitalists turn off as many nonessential notifications as possible and have separate devices for work and personal usage. Reset the tolerance for only certain important types of messages.
“I indicate specific parameters for a nurse or another provider to call me in certain circumstances,” Dr. Hunter says. “That grabs my attention more than a text or e-mail.”
Telling Patients
Vladimir N. Cadet, MPH, an associate with ECRI Institute’s Applied Solutions Group in Plymouth Meeting, Pa., says hospitalists should communicate to patients and their family members, many of whom also suffer from alarm fatigue, the importance of allowing health practitioners to address alarms to minimize the potential for delayed responses or missed alarms.
Patients should be told to notify staff if a medical device alarm goes unanswered, Cvach adds. To facilitate adequate sleep, patients can request earplugs or put on restful music.
Karen Appold is freelance writer in Pennsylvania.
References
- Lawless ST. Crying wolf: false alarms in a pediatric intensive care unit. Crit Care Med. 1994;22(6):981-985.
- Tsien CL, Fackler JC. Poor prognosis of existing monitors in the intensive care unit. Crit Care Med. 1997;25(4):614-619.
- Chambrin MC, Ravaux P, Calvelo-Aros D, Jaborska A, Chopin C, Boniface B. Multicentric study of monitoring alarms in the adult intensive care unit (ICU): a descriptive analysis. Intensive Care Med. 1999;25(12):1360-1366.
- Atzema C, Schull MJ, Borgundvaag B, Slaughter GRD, Lee CK. Alarmed: adverse events in low-risk patients with chest pain receiving electrocardiographic monitoring in the emergency department: a pilot study. Am J Emerg Med. 2006;24(1):62-67.
- Keller JP, Diefes R, Graham K, Meyers M, Pelczarski K. Association for the Advancement of Medical Instrumentation. Why clinical alarms are a “top ten” hazard: how you can help reduce the risk. Horizons. Spring 2011. Available at: http://www.aami.org/htsi/alarms/pdfs/Alarms%20Horizons_Secure_Watermarked.pdf. Accessed March 8, 2015.
- ECRI Institute. Top 10 health technology hazards for 2015. Available at: https://www.ecri.org/press/Pages/ECRI-Institute-Announces-Top-10-Health-Technology-Hazards-for-2015.aspx. Accessed March 8, 2015
- Weigl M1, Müller A, Sevdalis N, Angerer P. Relationships of multitasking, physicians’ strain, and performance: an observational study in ward physicians. J Patient Saf. 2013 Mar;9(1):18-23. doi: 10.1097/PTS.0b013e31826b7b87.
- Drew B, Califf RM, Funk M, et al. Practice standards for electrocardiographic monitoring in hospital settings. Circulation. 2004;110:2721-2746.
Everyday, throughout the day, hospitalists and other healthcare workers are inundated with alerts and warnings and notifications from medical and communication devices. The sheer number of alarms can be extremely overwhelming.
“In any given unit, there may be hundreds of alarms per patient, per day,” says Ronald Wyatt, MD, MHA, medical director of the division of healthcare improvement at The Joint Commission in Oakbrook Terrace, Ill. “That amounts to tens of thousands of alarms each day.”
And, although the intent of these alarms may be good, studies show that 80% to 99% of alarms generated by such medical devices as ventilators, blood pressure monitors, and electrocardiograms are false and/or don’t actually require any clinical intervention.1-4 What’s even more alarming is that clinicians become desensitized—even immune—to the sounds, experiencing what has been called “alarm fatigue.” In response to the constant barrage of noise, clinicians may turn alarms down or off, or adjust alarm settings outside limits that are safe and appropriate for the patient.5
The extent to which alarm fatigue has affected patients is unknown. From 2009 to 2012, The Joint Commission reported 98 alarm-related events. Of these, 80 resulted in death, 13 in permanent loss of function, and five in unexpected additional care or extended stay. Because sentinel event reporting to The Joint Commission is voluntary, Dr. Wyatt estimates that the organization is notified of less than 10% of such events.
Maria Cvach, DNP, RN, MSN, CCRN, DNP, assistant director of nursing for clinical standards at The Johns Hopkins Hospital in Baltimore, Md., says that from 2005 to 2008, there were 566 alarm-related deaths reported to the U.S. Food and Drug Administration’s Manufacturer and User Facility Device Experience (MAUDE) database. “Most experts agree that this is grossly underreported,” says Cvach, who has led alarm system improvement efforts at Hopkins since 2006.
In addition to being a patient safety issue, alarm fatigue has other consequences, Cvach says. Patients and families lose trust in staff when alarms go unanswered. Excessive noise can result in patient and staff harm. Research demonstrates that noise can negatively affect patients’ cardiovascular and immune systems and can increase length of hospital stays. Staff may develop stress symptoms and headaches. In addition, hospitals could face litigation from missed alarms and patient events.
From Bad to Worse
Experts agree that alarm fatigue is getting worse system-wide. ECRI Institute, a nonprofit organization that uses applied scientific research in healthcare to establish best practices for improving patient care, has listed alarm hazards as the number one health technology device hazard for the past three years. This persistent danger has made the top 10 since the list’s inception.6
Cvach says alarm fatigue is fairly easy to recognize.
“If you’re on a unit and hear alarms but do not see anyone addressing them, you are probably witnessing alarm fatigue,” she says. “If you ask staff what is alarming and they indicate that they didn’t notice an alarm ringing, it is likely alarm fatigue. Staff have indicated that sometimes alarms are like ‘white noise.’ [Alarms] go unnoticed because they are considered part of the environment and [staff] are accustomed to them.”
Jairy C. Hunter III, MD, MBA, SFHM, hospitalist and associate CMO for care transitions at Medical University of South Carolina (MUSC) in Charleston, believes alarm fatigue is a problem at every hospital, including his own. In addition to being bombarded with medical device alarms, he is constantly receiving notifications via cell phone, pager, and computers.
“Personally, I feel that I suffer from it [alarm fatigue],” says Dr. Hunter, a member of Team Hospitalist. “When I’m not at work and check my phones, I may realize that I missed answering a few notifications.”
He says that sometimes too much information “may be a bad thing, because we aren’t able to discern what is important and what isn’t. Studies have shown that, in general, people are not good at multi-tasking.”7

Reduction Efforts
Dr. Wyatt believes the corrective actions organizations have implemented to reduce alarm fatigue are not optimal, because the problem is worsening. In addition, the number of patients who are connected to alarm-based devices will continue to increase.
He maintains that hospitalists are uniquely positioned to “team up” with housestaff and tackle this issue.
“Unlike other physicians, [hospitalists] are in the hospital around the clock,” he says.
Dr. Wyatt suggests a good starting point is determining the baseline number of device alarms per day. Then answer these questions:
- How many required clinical intervention?
- How many resulted in harm or death?
- What are the organization’s current monitor alarm default parameters?
- How can we adjust alarms to indicate actionable alarms?
Another tip: Work with engineers and equipment manufacturers to customize alarms and notifications, so staff can readily recognize those that need immediate attention.
Cvach says that unnecessary patient monitoring results in excessive nuisance alarms. Patients should only be monitored when clinically necessary. To determine necessity, refer to the American Heart Association’s Practice Standards for Electrocardiographic Monitoring in Hospital Settings.8
“Alarms should be individualized for patients to make them most useful,” she explains. “Defaults should be customized based on the patient population.”
Cvach also recommends momentarily pausing alarms when assisting patients with turning, suctioning, bathing, and so forth, and changing electrodes regularly.
From a personal perspective, Dr. Hunter suggests that hospitalists turn off as many nonessential notifications as possible and have separate devices for work and personal usage. Reset the tolerance for only certain important types of messages.
“I indicate specific parameters for a nurse or another provider to call me in certain circumstances,” Dr. Hunter says. “That grabs my attention more than a text or e-mail.”
Telling Patients
Vladimir N. Cadet, MPH, an associate with ECRI Institute’s Applied Solutions Group in Plymouth Meeting, Pa., says hospitalists should communicate to patients and their family members, many of whom also suffer from alarm fatigue, the importance of allowing health practitioners to address alarms to minimize the potential for delayed responses or missed alarms.
Patients should be told to notify staff if a medical device alarm goes unanswered, Cvach adds. To facilitate adequate sleep, patients can request earplugs or put on restful music.
Karen Appold is freelance writer in Pennsylvania.
References
- Lawless ST. Crying wolf: false alarms in a pediatric intensive care unit. Crit Care Med. 1994;22(6):981-985.
- Tsien CL, Fackler JC. Poor prognosis of existing monitors in the intensive care unit. Crit Care Med. 1997;25(4):614-619.
- Chambrin MC, Ravaux P, Calvelo-Aros D, Jaborska A, Chopin C, Boniface B. Multicentric study of monitoring alarms in the adult intensive care unit (ICU): a descriptive analysis. Intensive Care Med. 1999;25(12):1360-1366.
- Atzema C, Schull MJ, Borgundvaag B, Slaughter GRD, Lee CK. Alarmed: adverse events in low-risk patients with chest pain receiving electrocardiographic monitoring in the emergency department: a pilot study. Am J Emerg Med. 2006;24(1):62-67.
- Keller JP, Diefes R, Graham K, Meyers M, Pelczarski K. Association for the Advancement of Medical Instrumentation. Why clinical alarms are a “top ten” hazard: how you can help reduce the risk. Horizons. Spring 2011. Available at: http://www.aami.org/htsi/alarms/pdfs/Alarms%20Horizons_Secure_Watermarked.pdf. Accessed March 8, 2015.
- ECRI Institute. Top 10 health technology hazards for 2015. Available at: https://www.ecri.org/press/Pages/ECRI-Institute-Announces-Top-10-Health-Technology-Hazards-for-2015.aspx. Accessed March 8, 2015
- Weigl M1, Müller A, Sevdalis N, Angerer P. Relationships of multitasking, physicians’ strain, and performance: an observational study in ward physicians. J Patient Saf. 2013 Mar;9(1):18-23. doi: 10.1097/PTS.0b013e31826b7b87.
- Drew B, Califf RM, Funk M, et al. Practice standards for electrocardiographic monitoring in hospital settings. Circulation. 2004;110:2721-2746.
Tips for Reducing Medical Device Alarm Fatigue
In April 2013, The Joint Commission issued a Sentinel Event Alert that provided hospitals with recommendations for assessing their individual circumstances and developing a systematic, coordinated approach regarding medical device alarms.
The recommendations correspond with those of the Association for the Advancement of Medical Instrumentation (AAMI) and ECRI Institute. Most of the information and guidance provided in these alerts is drawn from The Joint Commission’s Sentinel Event Database, a voluntary reporting system for serious adverse events in healthcare.
The recommendations include the following:
- Create a process for safe alarm management and response in high-risk areas;
- Inventory alarm-equipped medical devices used for high-risk areas and conditions, and identify default alarm settings;
- Have guidelines for tailoring alarm settings and limits for individual patients; and
- Inspect, check, and maintain alarm-equipped devices.
The Joint Commission alert also recommended training and education for all clinical care team members on safe alarm management and response in high-risk areas. Organizations should also consider ways to reduce nuisance alarm signals.
“Patient harm and death that is caused by factors related to alarm management has persisted as the top patient safety issue,” says Ronald Wyatt, MD, MHA, medical director of the division of healthcare improvement at The Joint Commission in Oakbrook Terrace, Ill.
In addition to the alert and existing accreditation standards regarding alarm safety, The Joint Commission issued 2014 National Patient Safety Goals to help healthcare organizations address this issue.
Beginning in January 2014, hospitals were required to identify the most important alarms to manage based on their own internal situations. In phase 2, beginning in January 2016, hospitals will be expected to develop and implement specific components of alarm policies and procedures that address such items as clinically appropriate settings, when settings can be changed, and who is allowed to make such changes. Requirements only apply to organizations accredited by The Joint Commission.
In April 2013, The Joint Commission issued a Sentinel Event Alert that provided hospitals with recommendations for assessing their individual circumstances and developing a systematic, coordinated approach regarding medical device alarms.
The recommendations correspond with those of the Association for the Advancement of Medical Instrumentation (AAMI) and ECRI Institute. Most of the information and guidance provided in these alerts is drawn from The Joint Commission’s Sentinel Event Database, a voluntary reporting system for serious adverse events in healthcare.
The recommendations include the following:
- Create a process for safe alarm management and response in high-risk areas;
- Inventory alarm-equipped medical devices used for high-risk areas and conditions, and identify default alarm settings;
- Have guidelines for tailoring alarm settings and limits for individual patients; and
- Inspect, check, and maintain alarm-equipped devices.
The Joint Commission alert also recommended training and education for all clinical care team members on safe alarm management and response in high-risk areas. Organizations should also consider ways to reduce nuisance alarm signals.
“Patient harm and death that is caused by factors related to alarm management has persisted as the top patient safety issue,” says Ronald Wyatt, MD, MHA, medical director of the division of healthcare improvement at The Joint Commission in Oakbrook Terrace, Ill.
In addition to the alert and existing accreditation standards regarding alarm safety, The Joint Commission issued 2014 National Patient Safety Goals to help healthcare organizations address this issue.
Beginning in January 2014, hospitals were required to identify the most important alarms to manage based on their own internal situations. In phase 2, beginning in January 2016, hospitals will be expected to develop and implement specific components of alarm policies and procedures that address such items as clinically appropriate settings, when settings can be changed, and who is allowed to make such changes. Requirements only apply to organizations accredited by The Joint Commission.
In April 2013, The Joint Commission issued a Sentinel Event Alert that provided hospitals with recommendations for assessing their individual circumstances and developing a systematic, coordinated approach regarding medical device alarms.
The recommendations correspond with those of the Association for the Advancement of Medical Instrumentation (AAMI) and ECRI Institute. Most of the information and guidance provided in these alerts is drawn from The Joint Commission’s Sentinel Event Database, a voluntary reporting system for serious adverse events in healthcare.
The recommendations include the following:
- Create a process for safe alarm management and response in high-risk areas;
- Inventory alarm-equipped medical devices used for high-risk areas and conditions, and identify default alarm settings;
- Have guidelines for tailoring alarm settings and limits for individual patients; and
- Inspect, check, and maintain alarm-equipped devices.
The Joint Commission alert also recommended training and education for all clinical care team members on safe alarm management and response in high-risk areas. Organizations should also consider ways to reduce nuisance alarm signals.
“Patient harm and death that is caused by factors related to alarm management has persisted as the top patient safety issue,” says Ronald Wyatt, MD, MHA, medical director of the division of healthcare improvement at The Joint Commission in Oakbrook Terrace, Ill.
In addition to the alert and existing accreditation standards regarding alarm safety, The Joint Commission issued 2014 National Patient Safety Goals to help healthcare organizations address this issue.
Beginning in January 2014, hospitals were required to identify the most important alarms to manage based on their own internal situations. In phase 2, beginning in January 2016, hospitals will be expected to develop and implement specific components of alarm policies and procedures that address such items as clinically appropriate settings, when settings can be changed, and who is allowed to make such changes. Requirements only apply to organizations accredited by The Joint Commission.