User login
Karen Appold is a seasoned writer and editor, with more than 20 years of editorial experience and started Write Now Services in 2003. Her scope of work includes writing, editing, and proofreading scholarly peer-reviewed journal content, consumer articles, white papers, and company reports for a variety of medical organizations, businesses, and media. Karen, who holds a BA in English from Penn State University, resides in Lehigh Valley, Pa.
SHM to induct new Masters in Hospital Medicine
The Society of Hospital Medicine will induct four new Masters in Hospital Medicine (MHM), the society’s highest professional honor, at HM18. Recipients are distinguished by the excellence and significance of their contributions to the field of hospital medicine and health care overall, said Larry Wellikson, MD, MHM, CEO of the Society of Hospital Medicine. They have been selected because of personal character; positions of honor; contributions toward furthering the society’s goals; distinction in practice, education, medical research; and other achievements in science or in the art of hospital medicine.
MHM nominees must be highly accomplished individuals in the hospital medicine specialty. Evidence of their achievements can come from many types of activities, such as excellence in clinical care, health care initiatives, education, research, writing and publication, volunteerism, and administrative positions. Current members of the society’s board are not eligible for nomination or selection.
This is truly the Hall of Fame for hospital medicine. Congratulations to this year’s MHMs.
Andrew Auerbach, MD, MPH, MHM, is professor of medicine in residence at the University of California, San Francisco, where he also serves as director of innovation research for the Center for Digital Health and Innovation. He was one of the first 200 members of the Society of Hospital Medicine when it was first called the National Association of Inpatient Physicians. “I have contributed to the field and society through my research and national role as a hospitalist in high-profile policy and guideline initiatives,” he said. These include formulating guidelines for the Institute of Medicine, American College of Cardiology, and Agency for Healthcare Research and Quality.
Dr. Auerbach has been deeply involved with the society through his role as chair of its Research Committee and Academic Hospitalist Committee for several years. Other accomplishments include being a founding framer of the Academic Hospitalist Academy, contributing to white papers outlining academic hospitalists’ needs, cofounding a national research network for hospitalists, and serving as editor-in-chief of the Journal of Hospital Medicine for 7 years.
“Being named an MHM is wonderful recognition,” he said. “I just hope it does not represent a ‘lifetime achievement’ award – I still have many things I want to accomplish in my career!”
Daniel J. Brotman, MD, MHM, professor of medicine, director of the hospitalist program at Johns Hopkins Hospital, Baltimore, and a member of the Society of Hospital Medicine since 2000, has served in many roles at the organization. These include being a member of the Annual Meeting Planning Committee (2007-2016), course director for the annual meeting (2013, 2014), chair of the Education Committee (2012-2016), and a member of the Research Committee (2008-2015). Dr. Brotman also won the society’s Research Award in 2015. He has been a staple of the editorial team at the Journal of Hospital Medicine since its founding in 2006.
“I am truly honored to be recognized for my participation and leadership in the field of hospital medicine and the society,” he said. “I am humbled to be included among the many luminaries who have won the award in prior years.”
He has been in his current role at Johns Hopkins since 2005, where he has more than tripled the program’s size and grown its academic profile.
“I have had the good fortune to work with a lot of talented faculty members and have helped them advance professionally and academically, while they pushed me to be a better leader,” Dr. Brotman said. “I encourage my team members to participate in the Society of Hospital Medicine; it is a fabulous way to gain leadership opportunities while staying abreast of the most important developments in the field.”
Bob Harrington, MD, MHM, is president and chief medical officer, SurveyVitals, an organization that provides digital patient experience and Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys nationwide to hospitals, health care systems, and physician practices. He believes he is an award recipient because he is a long-time advocate for hospitalists trained in family medicine (HTFMs). “I have always looked for ways to level the playing field for clinical and leadership opportunities for HTFMs,” he said.
Dr. Harrington first became involved with the Society of Hospital Medicine as chair of its Family Medicine Committee in the late 1990s. In that role, his committee looked at unique needs of HTFMs, including hiring practices, providing education to potential employers, and assisting HTFM members in career advancement.
“Our efforts resulted in tremendous growth of the HTFM membership, as these physicians began to view the society as their professional home and not as an internal medicine–dominant organization,” he said. He went on to become the first HTFM to serve on the society’s board and then became the first HTFM to be its president.
“This award is the greatest professional honor that I have received,” Dr. Harrington said. “It is especially important to me, because it is from a group of people whom I hold in the highest professional regard. They always put quality and patients first. I have been privileged to play a small part in that.”
Janet Nagamine, MD, BSN, MHM, is a hospitalist in the department of hospital-based specialty and inpatient palliative care at Kaiser Permanente Hospital in Santa Clara, Calif.
Dr. Nagamine was one of the first 200 people to join the Society of Hospital Medicine. Among her many roles within the society were serving on its board of directors from 2009 to 2014 and chairing the Quality and Safety committee for 5 years.
“I’m honored to be acknowledged in this formal and prestigious way, because my career path hasn’t always followed the traditional course of recipients who receive this type of award,” commented Dr. Nagamine, who has worked in a community hospital for the last 18 years. “This speaks volumes to the type of organization that the Society of Hospital Medicine is, and it makes me proud.”
She started her career as an ICU nurse and spent the last 30 years in various institutional and organizational roles trying to make hospitals a better place.
“At times, I was juggling family responsibilities and had to defer the fancy titles, but I always found a way to contribute meaningfully through my work with the Society of Hospital Medicine.”
The Society of Hospital Medicine will induct four new Masters in Hospital Medicine (MHM), the society’s highest professional honor, at HM18. Recipients are distinguished by the excellence and significance of their contributions to the field of hospital medicine and health care overall, said Larry Wellikson, MD, MHM, CEO of the Society of Hospital Medicine. They have been selected because of personal character; positions of honor; contributions toward furthering the society’s goals; distinction in practice, education, medical research; and other achievements in science or in the art of hospital medicine.
MHM nominees must be highly accomplished individuals in the hospital medicine specialty. Evidence of their achievements can come from many types of activities, such as excellence in clinical care, health care initiatives, education, research, writing and publication, volunteerism, and administrative positions. Current members of the society’s board are not eligible for nomination or selection.
This is truly the Hall of Fame for hospital medicine. Congratulations to this year’s MHMs.
Andrew Auerbach, MD, MPH, MHM, is professor of medicine in residence at the University of California, San Francisco, where he also serves as director of innovation research for the Center for Digital Health and Innovation. He was one of the first 200 members of the Society of Hospital Medicine when it was first called the National Association of Inpatient Physicians. “I have contributed to the field and society through my research and national role as a hospitalist in high-profile policy and guideline initiatives,” he said. These include formulating guidelines for the Institute of Medicine, American College of Cardiology, and Agency for Healthcare Research and Quality.
Dr. Auerbach has been deeply involved with the society through his role as chair of its Research Committee and Academic Hospitalist Committee for several years. Other accomplishments include being a founding framer of the Academic Hospitalist Academy, contributing to white papers outlining academic hospitalists’ needs, cofounding a national research network for hospitalists, and serving as editor-in-chief of the Journal of Hospital Medicine for 7 years.
“Being named an MHM is wonderful recognition,” he said. “I just hope it does not represent a ‘lifetime achievement’ award – I still have many things I want to accomplish in my career!”
Daniel J. Brotman, MD, MHM, professor of medicine, director of the hospitalist program at Johns Hopkins Hospital, Baltimore, and a member of the Society of Hospital Medicine since 2000, has served in many roles at the organization. These include being a member of the Annual Meeting Planning Committee (2007-2016), course director for the annual meeting (2013, 2014), chair of the Education Committee (2012-2016), and a member of the Research Committee (2008-2015). Dr. Brotman also won the society’s Research Award in 2015. He has been a staple of the editorial team at the Journal of Hospital Medicine since its founding in 2006.
“I am truly honored to be recognized for my participation and leadership in the field of hospital medicine and the society,” he said. “I am humbled to be included among the many luminaries who have won the award in prior years.”
He has been in his current role at Johns Hopkins since 2005, where he has more than tripled the program’s size and grown its academic profile.
“I have had the good fortune to work with a lot of talented faculty members and have helped them advance professionally and academically, while they pushed me to be a better leader,” Dr. Brotman said. “I encourage my team members to participate in the Society of Hospital Medicine; it is a fabulous way to gain leadership opportunities while staying abreast of the most important developments in the field.”
Bob Harrington, MD, MHM, is president and chief medical officer, SurveyVitals, an organization that provides digital patient experience and Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys nationwide to hospitals, health care systems, and physician practices. He believes he is an award recipient because he is a long-time advocate for hospitalists trained in family medicine (HTFMs). “I have always looked for ways to level the playing field for clinical and leadership opportunities for HTFMs,” he said.
Dr. Harrington first became involved with the Society of Hospital Medicine as chair of its Family Medicine Committee in the late 1990s. In that role, his committee looked at unique needs of HTFMs, including hiring practices, providing education to potential employers, and assisting HTFM members in career advancement.
“Our efforts resulted in tremendous growth of the HTFM membership, as these physicians began to view the society as their professional home and not as an internal medicine–dominant organization,” he said. He went on to become the first HTFM to serve on the society’s board and then became the first HTFM to be its president.
“This award is the greatest professional honor that I have received,” Dr. Harrington said. “It is especially important to me, because it is from a group of people whom I hold in the highest professional regard. They always put quality and patients first. I have been privileged to play a small part in that.”
Janet Nagamine, MD, BSN, MHM, is a hospitalist in the department of hospital-based specialty and inpatient palliative care at Kaiser Permanente Hospital in Santa Clara, Calif.
Dr. Nagamine was one of the first 200 people to join the Society of Hospital Medicine. Among her many roles within the society were serving on its board of directors from 2009 to 2014 and chairing the Quality and Safety committee for 5 years.
“I’m honored to be acknowledged in this formal and prestigious way, because my career path hasn’t always followed the traditional course of recipients who receive this type of award,” commented Dr. Nagamine, who has worked in a community hospital for the last 18 years. “This speaks volumes to the type of organization that the Society of Hospital Medicine is, and it makes me proud.”
She started her career as an ICU nurse and spent the last 30 years in various institutional and organizational roles trying to make hospitals a better place.
“At times, I was juggling family responsibilities and had to defer the fancy titles, but I always found a way to contribute meaningfully through my work with the Society of Hospital Medicine.”
The Society of Hospital Medicine will induct four new Masters in Hospital Medicine (MHM), the society’s highest professional honor, at HM18. Recipients are distinguished by the excellence and significance of their contributions to the field of hospital medicine and health care overall, said Larry Wellikson, MD, MHM, CEO of the Society of Hospital Medicine. They have been selected because of personal character; positions of honor; contributions toward furthering the society’s goals; distinction in practice, education, medical research; and other achievements in science or in the art of hospital medicine.
MHM nominees must be highly accomplished individuals in the hospital medicine specialty. Evidence of their achievements can come from many types of activities, such as excellence in clinical care, health care initiatives, education, research, writing and publication, volunteerism, and administrative positions. Current members of the society’s board are not eligible for nomination or selection.
This is truly the Hall of Fame for hospital medicine. Congratulations to this year’s MHMs.
Andrew Auerbach, MD, MPH, MHM, is professor of medicine in residence at the University of California, San Francisco, where he also serves as director of innovation research for the Center for Digital Health and Innovation. He was one of the first 200 members of the Society of Hospital Medicine when it was first called the National Association of Inpatient Physicians. “I have contributed to the field and society through my research and national role as a hospitalist in high-profile policy and guideline initiatives,” he said. These include formulating guidelines for the Institute of Medicine, American College of Cardiology, and Agency for Healthcare Research and Quality.
Dr. Auerbach has been deeply involved with the society through his role as chair of its Research Committee and Academic Hospitalist Committee for several years. Other accomplishments include being a founding framer of the Academic Hospitalist Academy, contributing to white papers outlining academic hospitalists’ needs, cofounding a national research network for hospitalists, and serving as editor-in-chief of the Journal of Hospital Medicine for 7 years.
“Being named an MHM is wonderful recognition,” he said. “I just hope it does not represent a ‘lifetime achievement’ award – I still have many things I want to accomplish in my career!”
Daniel J. Brotman, MD, MHM, professor of medicine, director of the hospitalist program at Johns Hopkins Hospital, Baltimore, and a member of the Society of Hospital Medicine since 2000, has served in many roles at the organization. These include being a member of the Annual Meeting Planning Committee (2007-2016), course director for the annual meeting (2013, 2014), chair of the Education Committee (2012-2016), and a member of the Research Committee (2008-2015). Dr. Brotman also won the society’s Research Award in 2015. He has been a staple of the editorial team at the Journal of Hospital Medicine since its founding in 2006.
“I am truly honored to be recognized for my participation and leadership in the field of hospital medicine and the society,” he said. “I am humbled to be included among the many luminaries who have won the award in prior years.”
He has been in his current role at Johns Hopkins since 2005, where he has more than tripled the program’s size and grown its academic profile.
“I have had the good fortune to work with a lot of talented faculty members and have helped them advance professionally and academically, while they pushed me to be a better leader,” Dr. Brotman said. “I encourage my team members to participate in the Society of Hospital Medicine; it is a fabulous way to gain leadership opportunities while staying abreast of the most important developments in the field.”
Bob Harrington, MD, MHM, is president and chief medical officer, SurveyVitals, an organization that provides digital patient experience and Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys nationwide to hospitals, health care systems, and physician practices. He believes he is an award recipient because he is a long-time advocate for hospitalists trained in family medicine (HTFMs). “I have always looked for ways to level the playing field for clinical and leadership opportunities for HTFMs,” he said.
Dr. Harrington first became involved with the Society of Hospital Medicine as chair of its Family Medicine Committee in the late 1990s. In that role, his committee looked at unique needs of HTFMs, including hiring practices, providing education to potential employers, and assisting HTFM members in career advancement.
“Our efforts resulted in tremendous growth of the HTFM membership, as these physicians began to view the society as their professional home and not as an internal medicine–dominant organization,” he said. He went on to become the first HTFM to serve on the society’s board and then became the first HTFM to be its president.
“This award is the greatest professional honor that I have received,” Dr. Harrington said. “It is especially important to me, because it is from a group of people whom I hold in the highest professional regard. They always put quality and patients first. I have been privileged to play a small part in that.”
Janet Nagamine, MD, BSN, MHM, is a hospitalist in the department of hospital-based specialty and inpatient palliative care at Kaiser Permanente Hospital in Santa Clara, Calif.
Dr. Nagamine was one of the first 200 people to join the Society of Hospital Medicine. Among her many roles within the society were serving on its board of directors from 2009 to 2014 and chairing the Quality and Safety committee for 5 years.
“I’m honored to be acknowledged in this formal and prestigious way, because my career path hasn’t always followed the traditional course of recipients who receive this type of award,” commented Dr. Nagamine, who has worked in a community hospital for the last 18 years. “This speaks volumes to the type of organization that the Society of Hospital Medicine is, and it makes me proud.”
She started her career as an ICU nurse and spent the last 30 years in various institutional and organizational roles trying to make hospitals a better place.
“At times, I was juggling family responsibilities and had to defer the fancy titles, but I always found a way to contribute meaningfully through my work with the Society of Hospital Medicine.”
Embracing constant change in a growing practice
Although many physicians resist change, learning how to embrace change and making it work for you are keys to a long, successful practice in hospital medicine, said Thomas McIlraith, MD, SFHM, CLHM, immediate past chairman, department of hospital medicine, and immediate past treasurer of the board of directors of Mercy Medical Group in Sacramento, Calif.
During his Monday, April 9, session, “Scaling Up Your Hospital Medicine Group,” he will share what it was like to work through significant changes as the chair of a department that grew in 12 years from 12 hospitalists – averaging fewer than 100 patients per day – to 84 hospitalists averaging more than 500 patients per day.
“I will be discussing my experiences but relating some universal truths about leadership in hospital medicine that can be applied to all areas of hospital medicine and how to manage change in an environment where change is constant,” said Dr. McIlraith, who will share key lessons that he learned. “I will break it down into the cultural, personal, and structural aspects of thriving in this dynamic environment.”
Dr. McIlraith hopes that attendees will come away with a good understanding of what he dubs the “authority/accountability” equation in physician leadership. “This is a principle that is used to assess what is expected of you in order to be successful as a leader, and if your ‘authority’ is commensurate with your ‘accountability,’ ” he said. “The authority piece of the equation takes many forms: resources, personnel, reporting structure, clerical support, and so forth. The key is to make sure that the authority/accountably equation is balanced not only for you but also for your subordinates.”
One example of an imbalanced authority/accountability equation that he’ll discuss in some detail is becoming a figurehead, in which accountability exists without the necessary authority. “If you end up in that position, get out,” Dr. McIlraith said. He will also discuss an example of where the authority/accountability equation is tipped in the opposite direction, with disastrous consequences.
Dr. McIlraith and Kimberly Bell, MD, who will also present at this session, aim to make it interactive. Dr. Bell currently serves as the divisional director of the CHI Franciscan Inpatient Team located in Tacoma, Wash. “We both have a wealth of experience to offer, but we are not the only ones in attendance who have wisdom to share,” Dr. McIlraith said.
Another goal of this session is to help attendees identify other hospital medicine leaders in comparable situations for the purpose of networking outside of the meeting. The session, although aimed at physician leaders, will be relevant to all hospitalists.
Scaling Up Your Hospital Medicine Group
Monday, 1:35-2:35 p.m.
Grand Ballroom 7B
Although many physicians resist change, learning how to embrace change and making it work for you are keys to a long, successful practice in hospital medicine, said Thomas McIlraith, MD, SFHM, CLHM, immediate past chairman, department of hospital medicine, and immediate past treasurer of the board of directors of Mercy Medical Group in Sacramento, Calif.
During his Monday, April 9, session, “Scaling Up Your Hospital Medicine Group,” he will share what it was like to work through significant changes as the chair of a department that grew in 12 years from 12 hospitalists – averaging fewer than 100 patients per day – to 84 hospitalists averaging more than 500 patients per day.
“I will be discussing my experiences but relating some universal truths about leadership in hospital medicine that can be applied to all areas of hospital medicine and how to manage change in an environment where change is constant,” said Dr. McIlraith, who will share key lessons that he learned. “I will break it down into the cultural, personal, and structural aspects of thriving in this dynamic environment.”
Dr. McIlraith hopes that attendees will come away with a good understanding of what he dubs the “authority/accountability” equation in physician leadership. “This is a principle that is used to assess what is expected of you in order to be successful as a leader, and if your ‘authority’ is commensurate with your ‘accountability,’ ” he said. “The authority piece of the equation takes many forms: resources, personnel, reporting structure, clerical support, and so forth. The key is to make sure that the authority/accountably equation is balanced not only for you but also for your subordinates.”
One example of an imbalanced authority/accountability equation that he’ll discuss in some detail is becoming a figurehead, in which accountability exists without the necessary authority. “If you end up in that position, get out,” Dr. McIlraith said. He will also discuss an example of where the authority/accountability equation is tipped in the opposite direction, with disastrous consequences.
Dr. McIlraith and Kimberly Bell, MD, who will also present at this session, aim to make it interactive. Dr. Bell currently serves as the divisional director of the CHI Franciscan Inpatient Team located in Tacoma, Wash. “We both have a wealth of experience to offer, but we are not the only ones in attendance who have wisdom to share,” Dr. McIlraith said.
Another goal of this session is to help attendees identify other hospital medicine leaders in comparable situations for the purpose of networking outside of the meeting. The session, although aimed at physician leaders, will be relevant to all hospitalists.
Scaling Up Your Hospital Medicine Group
Monday, 1:35-2:35 p.m.
Grand Ballroom 7B
Although many physicians resist change, learning how to embrace change and making it work for you are keys to a long, successful practice in hospital medicine, said Thomas McIlraith, MD, SFHM, CLHM, immediate past chairman, department of hospital medicine, and immediate past treasurer of the board of directors of Mercy Medical Group in Sacramento, Calif.
During his Monday, April 9, session, “Scaling Up Your Hospital Medicine Group,” he will share what it was like to work through significant changes as the chair of a department that grew in 12 years from 12 hospitalists – averaging fewer than 100 patients per day – to 84 hospitalists averaging more than 500 patients per day.
“I will be discussing my experiences but relating some universal truths about leadership in hospital medicine that can be applied to all areas of hospital medicine and how to manage change in an environment where change is constant,” said Dr. McIlraith, who will share key lessons that he learned. “I will break it down into the cultural, personal, and structural aspects of thriving in this dynamic environment.”
Dr. McIlraith hopes that attendees will come away with a good understanding of what he dubs the “authority/accountability” equation in physician leadership. “This is a principle that is used to assess what is expected of you in order to be successful as a leader, and if your ‘authority’ is commensurate with your ‘accountability,’ ” he said. “The authority piece of the equation takes many forms: resources, personnel, reporting structure, clerical support, and so forth. The key is to make sure that the authority/accountably equation is balanced not only for you but also for your subordinates.”
One example of an imbalanced authority/accountability equation that he’ll discuss in some detail is becoming a figurehead, in which accountability exists without the necessary authority. “If you end up in that position, get out,” Dr. McIlraith said. He will also discuss an example of where the authority/accountability equation is tipped in the opposite direction, with disastrous consequences.
Dr. McIlraith and Kimberly Bell, MD, who will also present at this session, aim to make it interactive. Dr. Bell currently serves as the divisional director of the CHI Franciscan Inpatient Team located in Tacoma, Wash. “We both have a wealth of experience to offer, but we are not the only ones in attendance who have wisdom to share,” Dr. McIlraith said.
Another goal of this session is to help attendees identify other hospital medicine leaders in comparable situations for the purpose of networking outside of the meeting. The session, although aimed at physician leaders, will be relevant to all hospitalists.
Scaling Up Your Hospital Medicine Group
Monday, 1:35-2:35 p.m.
Grand Ballroom 7B
How hospitalists can help reduce readmissions
Hospital readmissions are frequent, harmful, and costly. Consider the fact that 18% of Medicare patients can expect to be readmitted within 30 days at a cost of more than $17 billion.1 Recent changes in health care policy aimed at reducing readmission have substantially increased attention to this major health care issue.2
The Affordable Care Act has mandated that the Centers for Medicare & Medicaid Services reduce payment to hospitals with higher-than-expected 30-day readmissions, with its Hospital Readmissions Reduction Program. This has driven rapid growth in the study of patients rehospitalized within 30 days of discharge.3 So what are some strategies that have either been proven to reduce readmissions or show promise in doing so? 
An ounce of prevention
In studying inpatient and outpatient physicians’ perspectives regarding factors contributing to readmission,4 Shoshana Herzig, MD, MPH, assistant professor of medicine, Harvard Medical School, and director of Hospital Medicine Research, Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, and her colleagues identified some potential preventive strategies.
The most commonly endorsed strategy to prevent readmissions by both primary care physicians and hospitalists surveyed involved improving self-management plans at discharge. “This refers to actions such as providing patient-centered discharge instructions (that is, making sure they are written in language that patients can understand) or asking transition coaches to help facilitate a successful transition,” Dr. Herzig said. “This finding is consistent with the fact that the factor most commonly identified as contributing to readmissions was insufficient patient understanding or ability to self-manage. Combined, these findings suggest that strategies to enhance patient understanding of their illness, care plan, and what to expect after hospital discharge, are likely to be important components of successful readmission reduction programs.”
Provisioning of resources to patients to help them manage their care after discharge is also recommended. For example, engaging nurses or pharmacists who can help with issues that arise after discharge may help keep patients out of the hospital.
“Hospitalists should be aware of what resources are available to help patients manage their care,” Dr. Herzig said. For example, if a patient needs periodic blood pressure monitoring, the hospitalist can tell the patient about free blood pressure checkpoints or suggest a home-automated blood pressure monitor.
The study also showed that improved coordination of care between inpatient and outpatient providers, such as sharing medical records, could reduce readmission rates. “This allows for better inpatient care and increased ability for primary care physicians to react appropriately to issues arising after discharge,” Dr. Herzig said. “In the absence of a shared system, hospitalists should complete discharge summaries in a timely fashion and ensure that they’re promptly transmitted to primary care physicians.”
Dr. Herzig said it’s important to note that hospitalists and primary care physicians had different appraisals of reasons for readmission. Therefore, when designing readmission reduction programs or determining specific services to prevent a readmission for a given patient, it is important for hospitalists to obtain input from primary care physicians to ensure that they address all of the potential contributors to readmission for a given patient.
Interviewing patients regarding readmissions
After involved clinicians and independent physician reviewers performed extensive case reviews of more than 700 readmitted patients,6 Ashley Busuttil, MD, FHM, associate section chief, Hospital Medicine, University of California, Los Angeles Department of Medicine; and executive medical director, Medicine Services, UCLA Department of Medicine, and Erin Dowling, MD, assistant clinical professor, General Internal Medicine, Hospitalist Services, UCLA Medical Center, Santa Monica, Calif., and their colleagues were unable to identify which readmissions could have easily been prevented, and found that readmission causality varied extensively.
Through interviews with patients, the researchers determined that patients were more likely to think that their readmission was preventable if they felt unready for discharge during their initial hospitalization. This was despite the fact that patients met what clinicians would consider “ready” by objective, provider-centric criteria: they were medically stable, they had in-home support services, they had follow-up arranged, and so forth. As such, they wanted to put effort into educating and preparing patients for what home will look and feel like posthospitalization to address their feelings of unreadiness.
To that end, the researchers created an enhanced transition initiative that included showing an educational video near the time of admission and a patient-centered discharge checklist to help patients identify questions they might have after discharge. The discharge checklist asks patients to put themselves in the position of being at home and working through scenarios they may face so they will know how to deal with them. For example, if you have pain, who should you call? What should you do if you run out of medication?
Dr. Dowling believes that the hospitalist will, over time, become essential to assessing patient readiness. “As we learn more about how patients approach discharge, hospitalists’ understanding of patient needs beyond straightforward medical care will be crucial to having smoother transitions of care,” she said.
The researchers also explored pain control. As a health system, UCLA Medical Center has formed a multidisciplinary task force to optimize its approach to pain control. “If we can address comfort – for both patients at high risk of readmission and those that aren’t – we hope we can improve symptom control overall,” Dr. Busuttil said. “It’s not uncommon for patients to feel inadequate symptom control at discharge. While this is likely only one component of all the readmission pieces, a patient who feels that their symptoms are not controlled is likely to feel less ready for discharge. Increasing patient readiness, perhaps by increasing symptom control and improving communication regarding symptom management expectations, is a task that the hospitalist is well positioned to address.”
The researchers also wanted to find out why patients may not use available outpatient resources, and assessed them for decisional conflict – a measure of certainty with decision making – when selecting from multiple options for accessing medical care if they were home postdischarge and began to feel ill again. “Patients with decisional conflict were more likely to state that they would go the emergency room rather than call their primary medical physician or visit an urgent care center,” Dr. Busuttil said.
The health system continues to screen patients for decisional conflict. “When positive, we provide bedside education on when to seek medical care through primary care, urgent care, or the emergency department,” Dr. Busuttil said. “We also provide patients with information on how to access each of these resources.”
While a prior discharge plan may have seemed ideal on paper, time and time again it’s not logistically possible for certain patients. “By having this knowledge gleaned from patient interviews, hospitalists are able to provide feedback to health systems regarding different options of outpatient care that may work for the different patient populations they serve,” Dr. Dowling said.
To understand why one particular patient population is being readmitted requires taking the time to understand that population, Dr. Dowling noted. “While many validated risk stratification tools are available, they may only serve as general guides,” she said. “To impact the population you serve, you must first understand the readmission process as it looks to them.”
Employing the HOSPITAL score
In another effort to reduce hospital readmissions, Jacques Donzé, MD, MSc, associate physician, Bern University Hospital, Switzerland, and research associate, Brigham and Women’s Hospital, Boston, and his colleagues used the HOSPITAL score to identify patients at high risk of 30-day potentially avoidable readmission.
To most efficiently reduce hospital readmissions, hospitals need to target complex and intensive discharge interventions for patients at high risk of potentially avoidable readmission who are more likely to benefit.2 “However, prior research indicates that clinical health care providers are not able to accurately identify which patients are at high risk for readmission,” Dr. Donzé said.
Dr. Donzé believes that several factors may influence the performance of a prediction model, such as the initial selection of the potential predictors, the quality of the derivation method, including readily available predictors commonly available, and including reliable factors that aren’t subject to subjective evaluation. “All of these factors can play a role in the performance and generalizability of the HOSPITAL score,” he said.
When a patient is identified as high risk to be readmitted, hospitalists can take certain actions to prevent readmission. “Interventions are more likely to be effective when they include several components,” Dr. Donzé said. “These include follow-up phone calls and/or home visits, review of the patient’s medication list, patient education, and sending a discharge summary to the patient’s primary care physician in a timely manner. For now, enough evidence for a specific effective multimodal intervention to be generalizable to the majority of patients is lacking.”
Currently, the HOSPITAL score has been validated in approximately 180,000 patients in 14 hospitals across five countries and three continents – always showing good performance and generalizability. The HOSPITAL score includes seven variables readily available before hospital discharge, is easy to use, and is the most widely validated prediction model for readmission, Dr. Donzé said.
Before being implemented into practice, a score should ideally reach the highest level of validation, that is, show its clinical impact. “We expect that the score will not only be able to accurately predict high-risk patients, but using the score will also impact patient care by reducing readmissions when coupled with an appropriate intervention,” Dr. Donzé said.
In summary, research has shown that a variety of methods can be used to reduce hospital readmissions, including studying inpatient and outpatient physicians’ perspectives regarding factors contributing to readmission; interviewing patients regarding readmissions; and identifying patients at high risk of readmission using the HOSPITAL score.
Many researchers are continuing their studies in these areas.
Karen Appold is a medical writer in Pennsylvania.
Using hospitalist reflections as a means to reduce readmissions
Readmission studies and the development of readmission scoring systems and prediction tools rely on data from a large number of patients, typically extracted from administrative databases.
To complement this data, Deanne Kashiwagi, MD, consultant, Hospital Internal Medicine, Mayo Clinic, Rochester, Minn., and her colleagues asked hospitalists to reflect upon the readmissions of patients for whom they cared to add insight into the culture of patient care transitions within the health system.
“We felt there was some value in considering these nuances of the local care environment, which may not be represented in studies drawing from large databases, as potential targets for readmission efforts,” she said.
Dr. Kashiwagi believes that including elements of local practice and culture was the strength of their work. “Groups interested in replicating this reflective process should consider including factors specific to their practices that may contribute to readmission,” she said.
Asking hospitalists to perform reviews has led to implementing changes. Physicians were prompted to schedule earlier follow-up appointments and nurse practitioners and physician assistants have worked to improve the quality of their discharge summaries. The exercise also engaged hospitalists to suggest system changes that might contribute to decreased readmissions, such as a geriatrician-run service (which was recently begun) to provide multidisciplinary acute geriatric care for hospitalized older adults.
“Although large-scale studies are clearly important, readmission review at a more granular level may have merit as well,” Dr. Kashiwagi said, noting that such reviews identify local practice factors that groups may quickly act upon to help decrease readmissions. “Hospitalists readily engaged in this reflective exercise, which yielded actionable information to decrease readmissions.”
In commenting on why a different similar study7 didn’t mimic the results of Mayo Clinic’s study, Dr. Kashiwagi said there were some differences in methodology that may explain the difference in readmission rates. “First, this group excluded patients on dialysis, which in our study was a common comorbidity of our readmitted patients,” she said. “It is also notable that the chart review tool was different. Perhaps there is less representation of local factors, unique to that hospitalist group and their practice culture, than on our review form. These investigators also discussed their readmissions at routine intervals. Additionally, their preintervention readmission rate was lower than Mayo Clinic’s group, and although the readmission rate trended downward postintervention, it did not reach statistical significance.”
References
1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-28.
2. Donzé JD, Williams MV, Robinson EJ, et al. International validity of the HOSPITAL Score to predict 30-day potentially avoidable hospital readmissions. JAMA Intern Med. 2016 Apr;176(4):496-502.
3. Kashiwagi DT, Burton MC, Hakim FA, et al. Reflective practice: a tool for readmission reduction. Am J Med Qual. 2016 May;31(3):265-71.
4. Herzig SJ, Schnipper JL, Doctoroff L, et al. Physician perspectives on factors contributing to readmissions and potential prevention strategies: a multicenter survey. J Gen Intern Med. 2016 Nov;31(11):1287-93. Epub 2016 Jun 9.
5. Allaudeen N, Schnipper JL, Orav EJ, et al. Inability of providers to predict unplanned readmissions. J Gen Intern Med. 2011 Jul;26(7):771-6.
6. Busuttil A, Howard-Anderson J, Dowling EP, et al. Building a comprehensive patient-centered readmission reduction program [abstract]. J Hosp Med. 2016;11(suppl 1).
7. Rana V, Thapa B, Saini SC, et al. Self-reflection as a tool to increase hospitalist participation in readmission quality improvement. Qual Manag Health Care. 2016 Oct/Dec;25(4):219-24.
Hospital readmissions are frequent, harmful, and costly. Consider the fact that 18% of Medicare patients can expect to be readmitted within 30 days at a cost of more than $17 billion.1 Recent changes in health care policy aimed at reducing readmission have substantially increased attention to this major health care issue.2
The Affordable Care Act has mandated that the Centers for Medicare & Medicaid Services reduce payment to hospitals with higher-than-expected 30-day readmissions, with its Hospital Readmissions Reduction Program. This has driven rapid growth in the study of patients rehospitalized within 30 days of discharge.3 So what are some strategies that have either been proven to reduce readmissions or show promise in doing so? 
An ounce of prevention
In studying inpatient and outpatient physicians’ perspectives regarding factors contributing to readmission,4 Shoshana Herzig, MD, MPH, assistant professor of medicine, Harvard Medical School, and director of Hospital Medicine Research, Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, and her colleagues identified some potential preventive strategies.
The most commonly endorsed strategy to prevent readmissions by both primary care physicians and hospitalists surveyed involved improving self-management plans at discharge. “This refers to actions such as providing patient-centered discharge instructions (that is, making sure they are written in language that patients can understand) or asking transition coaches to help facilitate a successful transition,” Dr. Herzig said. “This finding is consistent with the fact that the factor most commonly identified as contributing to readmissions was insufficient patient understanding or ability to self-manage. Combined, these findings suggest that strategies to enhance patient understanding of their illness, care plan, and what to expect after hospital discharge, are likely to be important components of successful readmission reduction programs.”
Provisioning of resources to patients to help them manage their care after discharge is also recommended. For example, engaging nurses or pharmacists who can help with issues that arise after discharge may help keep patients out of the hospital.
“Hospitalists should be aware of what resources are available to help patients manage their care,” Dr. Herzig said. For example, if a patient needs periodic blood pressure monitoring, the hospitalist can tell the patient about free blood pressure checkpoints or suggest a home-automated blood pressure monitor.
The study also showed that improved coordination of care between inpatient and outpatient providers, such as sharing medical records, could reduce readmission rates. “This allows for better inpatient care and increased ability for primary care physicians to react appropriately to issues arising after discharge,” Dr. Herzig said. “In the absence of a shared system, hospitalists should complete discharge summaries in a timely fashion and ensure that they’re promptly transmitted to primary care physicians.”
Dr. Herzig said it’s important to note that hospitalists and primary care physicians had different appraisals of reasons for readmission. Therefore, when designing readmission reduction programs or determining specific services to prevent a readmission for a given patient, it is important for hospitalists to obtain input from primary care physicians to ensure that they address all of the potential contributors to readmission for a given patient.
Interviewing patients regarding readmissions
After involved clinicians and independent physician reviewers performed extensive case reviews of more than 700 readmitted patients,6 Ashley Busuttil, MD, FHM, associate section chief, Hospital Medicine, University of California, Los Angeles Department of Medicine; and executive medical director, Medicine Services, UCLA Department of Medicine, and Erin Dowling, MD, assistant clinical professor, General Internal Medicine, Hospitalist Services, UCLA Medical Center, Santa Monica, Calif., and their colleagues were unable to identify which readmissions could have easily been prevented, and found that readmission causality varied extensively.
Through interviews with patients, the researchers determined that patients were more likely to think that their readmission was preventable if they felt unready for discharge during their initial hospitalization. This was despite the fact that patients met what clinicians would consider “ready” by objective, provider-centric criteria: they were medically stable, they had in-home support services, they had follow-up arranged, and so forth. As such, they wanted to put effort into educating and preparing patients for what home will look and feel like posthospitalization to address their feelings of unreadiness.
To that end, the researchers created an enhanced transition initiative that included showing an educational video near the time of admission and a patient-centered discharge checklist to help patients identify questions they might have after discharge. The discharge checklist asks patients to put themselves in the position of being at home and working through scenarios they may face so they will know how to deal with them. For example, if you have pain, who should you call? What should you do if you run out of medication?
Dr. Dowling believes that the hospitalist will, over time, become essential to assessing patient readiness. “As we learn more about how patients approach discharge, hospitalists’ understanding of patient needs beyond straightforward medical care will be crucial to having smoother transitions of care,” she said.
The researchers also explored pain control. As a health system, UCLA Medical Center has formed a multidisciplinary task force to optimize its approach to pain control. “If we can address comfort – for both patients at high risk of readmission and those that aren’t – we hope we can improve symptom control overall,” Dr. Busuttil said. “It’s not uncommon for patients to feel inadequate symptom control at discharge. While this is likely only one component of all the readmission pieces, a patient who feels that their symptoms are not controlled is likely to feel less ready for discharge. Increasing patient readiness, perhaps by increasing symptom control and improving communication regarding symptom management expectations, is a task that the hospitalist is well positioned to address.”
The researchers also wanted to find out why patients may not use available outpatient resources, and assessed them for decisional conflict – a measure of certainty with decision making – when selecting from multiple options for accessing medical care if they were home postdischarge and began to feel ill again. “Patients with decisional conflict were more likely to state that they would go the emergency room rather than call their primary medical physician or visit an urgent care center,” Dr. Busuttil said.
The health system continues to screen patients for decisional conflict. “When positive, we provide bedside education on when to seek medical care through primary care, urgent care, or the emergency department,” Dr. Busuttil said. “We also provide patients with information on how to access each of these resources.”
While a prior discharge plan may have seemed ideal on paper, time and time again it’s not logistically possible for certain patients. “By having this knowledge gleaned from patient interviews, hospitalists are able to provide feedback to health systems regarding different options of outpatient care that may work for the different patient populations they serve,” Dr. Dowling said.
To understand why one particular patient population is being readmitted requires taking the time to understand that population, Dr. Dowling noted. “While many validated risk stratification tools are available, they may only serve as general guides,” she said. “To impact the population you serve, you must first understand the readmission process as it looks to them.”
Employing the HOSPITAL score
In another effort to reduce hospital readmissions, Jacques Donzé, MD, MSc, associate physician, Bern University Hospital, Switzerland, and research associate, Brigham and Women’s Hospital, Boston, and his colleagues used the HOSPITAL score to identify patients at high risk of 30-day potentially avoidable readmission.
To most efficiently reduce hospital readmissions, hospitals need to target complex and intensive discharge interventions for patients at high risk of potentially avoidable readmission who are more likely to benefit.2 “However, prior research indicates that clinical health care providers are not able to accurately identify which patients are at high risk for readmission,” Dr. Donzé said.
Dr. Donzé believes that several factors may influence the performance of a prediction model, such as the initial selection of the potential predictors, the quality of the derivation method, including readily available predictors commonly available, and including reliable factors that aren’t subject to subjective evaluation. “All of these factors can play a role in the performance and generalizability of the HOSPITAL score,” he said.
When a patient is identified as high risk to be readmitted, hospitalists can take certain actions to prevent readmission. “Interventions are more likely to be effective when they include several components,” Dr. Donzé said. “These include follow-up phone calls and/or home visits, review of the patient’s medication list, patient education, and sending a discharge summary to the patient’s primary care physician in a timely manner. For now, enough evidence for a specific effective multimodal intervention to be generalizable to the majority of patients is lacking.”
Currently, the HOSPITAL score has been validated in approximately 180,000 patients in 14 hospitals across five countries and three continents – always showing good performance and generalizability. The HOSPITAL score includes seven variables readily available before hospital discharge, is easy to use, and is the most widely validated prediction model for readmission, Dr. Donzé said.
Before being implemented into practice, a score should ideally reach the highest level of validation, that is, show its clinical impact. “We expect that the score will not only be able to accurately predict high-risk patients, but using the score will also impact patient care by reducing readmissions when coupled with an appropriate intervention,” Dr. Donzé said.
In summary, research has shown that a variety of methods can be used to reduce hospital readmissions, including studying inpatient and outpatient physicians’ perspectives regarding factors contributing to readmission; interviewing patients regarding readmissions; and identifying patients at high risk of readmission using the HOSPITAL score.
Many researchers are continuing their studies in these areas.
Karen Appold is a medical writer in Pennsylvania.
Using hospitalist reflections as a means to reduce readmissions
Readmission studies and the development of readmission scoring systems and prediction tools rely on data from a large number of patients, typically extracted from administrative databases.
To complement this data, Deanne Kashiwagi, MD, consultant, Hospital Internal Medicine, Mayo Clinic, Rochester, Minn., and her colleagues asked hospitalists to reflect upon the readmissions of patients for whom they cared to add insight into the culture of patient care transitions within the health system.
“We felt there was some value in considering these nuances of the local care environment, which may not be represented in studies drawing from large databases, as potential targets for readmission efforts,” she said.
Dr. Kashiwagi believes that including elements of local practice and culture was the strength of their work. “Groups interested in replicating this reflective process should consider including factors specific to their practices that may contribute to readmission,” she said.
Asking hospitalists to perform reviews has led to implementing changes. Physicians were prompted to schedule earlier follow-up appointments and nurse practitioners and physician assistants have worked to improve the quality of their discharge summaries. The exercise also engaged hospitalists to suggest system changes that might contribute to decreased readmissions, such as a geriatrician-run service (which was recently begun) to provide multidisciplinary acute geriatric care for hospitalized older adults.
“Although large-scale studies are clearly important, readmission review at a more granular level may have merit as well,” Dr. Kashiwagi said, noting that such reviews identify local practice factors that groups may quickly act upon to help decrease readmissions. “Hospitalists readily engaged in this reflective exercise, which yielded actionable information to decrease readmissions.”
In commenting on why a different similar study7 didn’t mimic the results of Mayo Clinic’s study, Dr. Kashiwagi said there were some differences in methodology that may explain the difference in readmission rates. “First, this group excluded patients on dialysis, which in our study was a common comorbidity of our readmitted patients,” she said. “It is also notable that the chart review tool was different. Perhaps there is less representation of local factors, unique to that hospitalist group and their practice culture, than on our review form. These investigators also discussed their readmissions at routine intervals. Additionally, their preintervention readmission rate was lower than Mayo Clinic’s group, and although the readmission rate trended downward postintervention, it did not reach statistical significance.”
References
1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-28.
2. Donzé JD, Williams MV, Robinson EJ, et al. International validity of the HOSPITAL Score to predict 30-day potentially avoidable hospital readmissions. JAMA Intern Med. 2016 Apr;176(4):496-502.
3. Kashiwagi DT, Burton MC, Hakim FA, et al. Reflective practice: a tool for readmission reduction. Am J Med Qual. 2016 May;31(3):265-71.
4. Herzig SJ, Schnipper JL, Doctoroff L, et al. Physician perspectives on factors contributing to readmissions and potential prevention strategies: a multicenter survey. J Gen Intern Med. 2016 Nov;31(11):1287-93. Epub 2016 Jun 9.
5. Allaudeen N, Schnipper JL, Orav EJ, et al. Inability of providers to predict unplanned readmissions. J Gen Intern Med. 2011 Jul;26(7):771-6.
6. Busuttil A, Howard-Anderson J, Dowling EP, et al. Building a comprehensive patient-centered readmission reduction program [abstract]. J Hosp Med. 2016;11(suppl 1).
7. Rana V, Thapa B, Saini SC, et al. Self-reflection as a tool to increase hospitalist participation in readmission quality improvement. Qual Manag Health Care. 2016 Oct/Dec;25(4):219-24.
Hospital readmissions are frequent, harmful, and costly. Consider the fact that 18% of Medicare patients can expect to be readmitted within 30 days at a cost of more than $17 billion.1 Recent changes in health care policy aimed at reducing readmission have substantially increased attention to this major health care issue.2
The Affordable Care Act has mandated that the Centers for Medicare & Medicaid Services reduce payment to hospitals with higher-than-expected 30-day readmissions, with its Hospital Readmissions Reduction Program. This has driven rapid growth in the study of patients rehospitalized within 30 days of discharge.3 So what are some strategies that have either been proven to reduce readmissions or show promise in doing so? 
An ounce of prevention
In studying inpatient and outpatient physicians’ perspectives regarding factors contributing to readmission,4 Shoshana Herzig, MD, MPH, assistant professor of medicine, Harvard Medical School, and director of Hospital Medicine Research, Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, and her colleagues identified some potential preventive strategies.
The most commonly endorsed strategy to prevent readmissions by both primary care physicians and hospitalists surveyed involved improving self-management plans at discharge. “This refers to actions such as providing patient-centered discharge instructions (that is, making sure they are written in language that patients can understand) or asking transition coaches to help facilitate a successful transition,” Dr. Herzig said. “This finding is consistent with the fact that the factor most commonly identified as contributing to readmissions was insufficient patient understanding or ability to self-manage. Combined, these findings suggest that strategies to enhance patient understanding of their illness, care plan, and what to expect after hospital discharge, are likely to be important components of successful readmission reduction programs.”
Provisioning of resources to patients to help them manage their care after discharge is also recommended. For example, engaging nurses or pharmacists who can help with issues that arise after discharge may help keep patients out of the hospital.
“Hospitalists should be aware of what resources are available to help patients manage their care,” Dr. Herzig said. For example, if a patient needs periodic blood pressure monitoring, the hospitalist can tell the patient about free blood pressure checkpoints or suggest a home-automated blood pressure monitor.
The study also showed that improved coordination of care between inpatient and outpatient providers, such as sharing medical records, could reduce readmission rates. “This allows for better inpatient care and increased ability for primary care physicians to react appropriately to issues arising after discharge,” Dr. Herzig said. “In the absence of a shared system, hospitalists should complete discharge summaries in a timely fashion and ensure that they’re promptly transmitted to primary care physicians.”
Dr. Herzig said it’s important to note that hospitalists and primary care physicians had different appraisals of reasons for readmission. Therefore, when designing readmission reduction programs or determining specific services to prevent a readmission for a given patient, it is important for hospitalists to obtain input from primary care physicians to ensure that they address all of the potential contributors to readmission for a given patient.
Interviewing patients regarding readmissions
After involved clinicians and independent physician reviewers performed extensive case reviews of more than 700 readmitted patients,6 Ashley Busuttil, MD, FHM, associate section chief, Hospital Medicine, University of California, Los Angeles Department of Medicine; and executive medical director, Medicine Services, UCLA Department of Medicine, and Erin Dowling, MD, assistant clinical professor, General Internal Medicine, Hospitalist Services, UCLA Medical Center, Santa Monica, Calif., and their colleagues were unable to identify which readmissions could have easily been prevented, and found that readmission causality varied extensively.
Through interviews with patients, the researchers determined that patients were more likely to think that their readmission was preventable if they felt unready for discharge during their initial hospitalization. This was despite the fact that patients met what clinicians would consider “ready” by objective, provider-centric criteria: they were medically stable, they had in-home support services, they had follow-up arranged, and so forth. As such, they wanted to put effort into educating and preparing patients for what home will look and feel like posthospitalization to address their feelings of unreadiness.
To that end, the researchers created an enhanced transition initiative that included showing an educational video near the time of admission and a patient-centered discharge checklist to help patients identify questions they might have after discharge. The discharge checklist asks patients to put themselves in the position of being at home and working through scenarios they may face so they will know how to deal with them. For example, if you have pain, who should you call? What should you do if you run out of medication?
Dr. Dowling believes that the hospitalist will, over time, become essential to assessing patient readiness. “As we learn more about how patients approach discharge, hospitalists’ understanding of patient needs beyond straightforward medical care will be crucial to having smoother transitions of care,” she said.
The researchers also explored pain control. As a health system, UCLA Medical Center has formed a multidisciplinary task force to optimize its approach to pain control. “If we can address comfort – for both patients at high risk of readmission and those that aren’t – we hope we can improve symptom control overall,” Dr. Busuttil said. “It’s not uncommon for patients to feel inadequate symptom control at discharge. While this is likely only one component of all the readmission pieces, a patient who feels that their symptoms are not controlled is likely to feel less ready for discharge. Increasing patient readiness, perhaps by increasing symptom control and improving communication regarding symptom management expectations, is a task that the hospitalist is well positioned to address.”
The researchers also wanted to find out why patients may not use available outpatient resources, and assessed them for decisional conflict – a measure of certainty with decision making – when selecting from multiple options for accessing medical care if they were home postdischarge and began to feel ill again. “Patients with decisional conflict were more likely to state that they would go the emergency room rather than call their primary medical physician or visit an urgent care center,” Dr. Busuttil said.
The health system continues to screen patients for decisional conflict. “When positive, we provide bedside education on when to seek medical care through primary care, urgent care, or the emergency department,” Dr. Busuttil said. “We also provide patients with information on how to access each of these resources.”
While a prior discharge plan may have seemed ideal on paper, time and time again it’s not logistically possible for certain patients. “By having this knowledge gleaned from patient interviews, hospitalists are able to provide feedback to health systems regarding different options of outpatient care that may work for the different patient populations they serve,” Dr. Dowling said.
To understand why one particular patient population is being readmitted requires taking the time to understand that population, Dr. Dowling noted. “While many validated risk stratification tools are available, they may only serve as general guides,” she said. “To impact the population you serve, you must first understand the readmission process as it looks to them.”
Employing the HOSPITAL score
In another effort to reduce hospital readmissions, Jacques Donzé, MD, MSc, associate physician, Bern University Hospital, Switzerland, and research associate, Brigham and Women’s Hospital, Boston, and his colleagues used the HOSPITAL score to identify patients at high risk of 30-day potentially avoidable readmission.
To most efficiently reduce hospital readmissions, hospitals need to target complex and intensive discharge interventions for patients at high risk of potentially avoidable readmission who are more likely to benefit.2 “However, prior research indicates that clinical health care providers are not able to accurately identify which patients are at high risk for readmission,” Dr. Donzé said.
Dr. Donzé believes that several factors may influence the performance of a prediction model, such as the initial selection of the potential predictors, the quality of the derivation method, including readily available predictors commonly available, and including reliable factors that aren’t subject to subjective evaluation. “All of these factors can play a role in the performance and generalizability of the HOSPITAL score,” he said.
When a patient is identified as high risk to be readmitted, hospitalists can take certain actions to prevent readmission. “Interventions are more likely to be effective when they include several components,” Dr. Donzé said. “These include follow-up phone calls and/or home visits, review of the patient’s medication list, patient education, and sending a discharge summary to the patient’s primary care physician in a timely manner. For now, enough evidence for a specific effective multimodal intervention to be generalizable to the majority of patients is lacking.”
Currently, the HOSPITAL score has been validated in approximately 180,000 patients in 14 hospitals across five countries and three continents – always showing good performance and generalizability. The HOSPITAL score includes seven variables readily available before hospital discharge, is easy to use, and is the most widely validated prediction model for readmission, Dr. Donzé said.
Before being implemented into practice, a score should ideally reach the highest level of validation, that is, show its clinical impact. “We expect that the score will not only be able to accurately predict high-risk patients, but using the score will also impact patient care by reducing readmissions when coupled with an appropriate intervention,” Dr. Donzé said.
In summary, research has shown that a variety of methods can be used to reduce hospital readmissions, including studying inpatient and outpatient physicians’ perspectives regarding factors contributing to readmission; interviewing patients regarding readmissions; and identifying patients at high risk of readmission using the HOSPITAL score.
Many researchers are continuing their studies in these areas.
Karen Appold is a medical writer in Pennsylvania.
Using hospitalist reflections as a means to reduce readmissions
Readmission studies and the development of readmission scoring systems and prediction tools rely on data from a large number of patients, typically extracted from administrative databases.
To complement this data, Deanne Kashiwagi, MD, consultant, Hospital Internal Medicine, Mayo Clinic, Rochester, Minn., and her colleagues asked hospitalists to reflect upon the readmissions of patients for whom they cared to add insight into the culture of patient care transitions within the health system.
“We felt there was some value in considering these nuances of the local care environment, which may not be represented in studies drawing from large databases, as potential targets for readmission efforts,” she said.
Dr. Kashiwagi believes that including elements of local practice and culture was the strength of their work. “Groups interested in replicating this reflective process should consider including factors specific to their practices that may contribute to readmission,” she said.
Asking hospitalists to perform reviews has led to implementing changes. Physicians were prompted to schedule earlier follow-up appointments and nurse practitioners and physician assistants have worked to improve the quality of their discharge summaries. The exercise also engaged hospitalists to suggest system changes that might contribute to decreased readmissions, such as a geriatrician-run service (which was recently begun) to provide multidisciplinary acute geriatric care for hospitalized older adults.
“Although large-scale studies are clearly important, readmission review at a more granular level may have merit as well,” Dr. Kashiwagi said, noting that such reviews identify local practice factors that groups may quickly act upon to help decrease readmissions. “Hospitalists readily engaged in this reflective exercise, which yielded actionable information to decrease readmissions.”
In commenting on why a different similar study7 didn’t mimic the results of Mayo Clinic’s study, Dr. Kashiwagi said there were some differences in methodology that may explain the difference in readmission rates. “First, this group excluded patients on dialysis, which in our study was a common comorbidity of our readmitted patients,” she said. “It is also notable that the chart review tool was different. Perhaps there is less representation of local factors, unique to that hospitalist group and their practice culture, than on our review form. These investigators also discussed their readmissions at routine intervals. Additionally, their preintervention readmission rate was lower than Mayo Clinic’s group, and although the readmission rate trended downward postintervention, it did not reach statistical significance.”
References
1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-28.
2. Donzé JD, Williams MV, Robinson EJ, et al. International validity of the HOSPITAL Score to predict 30-day potentially avoidable hospital readmissions. JAMA Intern Med. 2016 Apr;176(4):496-502.
3. Kashiwagi DT, Burton MC, Hakim FA, et al. Reflective practice: a tool for readmission reduction. Am J Med Qual. 2016 May;31(3):265-71.
4. Herzig SJ, Schnipper JL, Doctoroff L, et al. Physician perspectives on factors contributing to readmissions and potential prevention strategies: a multicenter survey. J Gen Intern Med. 2016 Nov;31(11):1287-93. Epub 2016 Jun 9.
5. Allaudeen N, Schnipper JL, Orav EJ, et al. Inability of providers to predict unplanned readmissions. J Gen Intern Med. 2011 Jul;26(7):771-6.
6. Busuttil A, Howard-Anderson J, Dowling EP, et al. Building a comprehensive patient-centered readmission reduction program [abstract]. J Hosp Med. 2016;11(suppl 1).
7. Rana V, Thapa B, Saini SC, et al. Self-reflection as a tool to increase hospitalist participation in readmission quality improvement. Qual Manag Health Care. 2016 Oct/Dec;25(4):219-24.
Communication tools improve patient experience and satisfaction
How hospitalists and other clinicians communicate with patients impacts a patient’s overall experience and satisfaction. But according to the authors of “Communication the Cleveland Way,”1 a book about how the clinic created and applied communication skills training, “in a culture prioritizing clinical outcomes above all, there can be a tendency to lose sight of one of the most critical aspects of providing effective care: the communication skills that build and foster physician-patient relationships.”
“Studies2,3 have shown that good communication between doctors and patients and among all caregivers who interface with patients directly results in better clinical outcomes, reduced costs, greater patient satisfaction, and lower rates of physician burnout,” the authors wrote.
“It places a special focus on empathy in relationships, and in our case, the provider-patient relationship rather than patient-centered care. The former acknowledges that the thoughts and feelings in both sides of a relationship are important. We know that clinicians, too, can suffer as a result of the care they provide,” Dr. Velez wrote in “Communication the Cleveland Way.”1
“Healthy relationships are based on balance and mutual respect,” Dr Velez said. “Courses made a strong point to practice empathy in order to teach empathy. Clinician participants were gifted with a safe space, an opportunity to share their own skills and expertise, and a chance to be appreciated for what they already do effectively. Most of all, activities were designed to be fun and engaging.” For example, CEHC encouraged and fostered an attitude of exploration, experimentation, and adventure. Various warm-up activities effectively helped the participants enter a more playful space and get into character portrayal.
Dr. Velez credits the CEHC model’s sustainability and success to the early realization that an appreciative approach is effective. In a study3 about the strategy, hospital-employed attending physicians participated in the 8-hour experiential communication skills training course on REDE. The study compared approximately 1,500 “intervention” physicians who attended and 1,900 “nonintervention” physicians who did not attend.
Following the course, scores for physician communication and respect were higher for intervention physicians. Furthermore, physicians showed significant improvement in self-perceptions of empathy and burnout. Some of these gains were sustained for at least 3 months. “This is especially important because in the current health care climate, physicians experience increased burnout,” Dr. Velez notes.
How it works
Because a provider’s connection with a patient occurs when a relationship is established, the REDE course focuses on the beginning of the conversation. “It’s important for clinicians to exhibit value and respect through words and actions when welcoming patients,” Dr. Velez said. “Further, instead of guiding the medical interview with a series of close-ended questions like an interrogator would, we invite the use of open-ended questions and setting an agenda for the visit early on, by asking the patient what they wish to discuss.”
Another key component is empathy, which plays a huge role in patient satisfaction. “Learning how to express empathy is very important,” Dr. Velez said. “A patient may not remember all of the medical details discussed, but human interactions, rapport, expressions of care, support, validation, and acknowledgment of emotions tend to be more indelible.”
Dr. Velez notes that decades of literature regarding effective communication have demonstrated improved outcomes. “If trust in a therapeutic relationship is strong, a patient is more likely to follow instructions and have better engagement with their care plan,” he said. “If a clinician ensures that the patient understands the diagnosis and recommendations, then compliance will increase, especially if the plan is tailored to the patient’s goals and perspective.”
One surprising effect of the REDE course was how it improved relationships among professionals. “Many participants have shared that having a day out of one’s normal schedule, not only to learn, but also to share their own experiences, is quite therapeutic,” Dr. Velez said. “We can extend the same communication strategies to team building, interprofessional interactions, and challenging encounters.”
Study focuses on comportment and communication
In an effort to define optimal care in hospital medicine, a team from Johns Hopkins Health System set out to establish a metric that would comprehensively assess hospitalists’ comportment (which includes behavior as well as general demeanor) and communication to establish norms and expectations when they saw patients at the bedside.
To perform the study,4 chiefs of hospital medicine divisions at five independent hospitals located in Baltimore and Washington identified their most clinically excellent hospitalists. Then, an investigator observed each hospitalist during a routine clinical shift and recorded behaviors believed to be associated with excellent behavior and communication using the hospital medicine comportment and communication observation tool (HMCCOT), said Susrutha Kotwal, MD, assistant professor of medicine at Johns Hopkins University School of Medicine, Baltimore, and lead author. The investigators collected basic demographic information while observing hospitalists for an average of 280 minutes; 26 physicians were observed for 181 separate clinical encounters. Each provider’s mean HMCCOT score was compared with patient satisfaction surveys such as Press Ganey (PG) scores.
Noteworthy is the fact that the distribution of HMCCOT scores were similar when analyzed by age, gender, race, amount of clinical experience, the hospitalist’s clinical workload, hospital, or time spent observing the hospitalist. But the distribution of HMCCOT scores was quite different in new patient encounters, compared with follow-ups (68.1% versus 39.7%). Encounters with patients that generated HMCCOT scores above versus below the mean were longer (13 minutes versus 8.7 minutes). The physicians’ HMCCOT scores were also associated with their PG scores. These findings suggest that improved bedside communication and comportment with patients might also translate into enhanced patient satisfaction.
As a result of the study, a comportment and communication tool was established and validated by following clinically excellent hospitalists at the bedside. “Even among clinically respected hospitalists, the results reveal that there is wide variability in behaviors and communication practices at the bedside,” Dr. Kotwal said.
Employing the tool
Hospitalists can choose whether to perform behaviors in the HMCCOT themselves, while others may wish to watch other hospitalists to give them feedback tied to specific behaviors. “These simple behaviors are intimately linked to excellent communication and comportment, which can serve as the foundation for delivering patient-centered care,” Dr. Kotwal said.
A positive correlation was found between spending more time with patients and higher HMCCOT scores. “Patients’ complaints about doctors often relate to feeling rushed, that their physicians did not listen to them, or that they did not convey information in a clear manner,” Dr. Kotwal said. “When successfully achieved, patient-centered communication has been associated with improved clinical outcomes, including adherence to recommended treatment and better self-management of chronic disease. Many of the components of the HMCCOT described in our study are at the heart of patient-centered care.”
Dr. Kotwal believes HMCCOT is a better strategy to improve patient satisfaction than patient satisfaction surveys because patients can’t always recall which specific provider saw them. In addition, patients’ recall about the provider may be poor because surveys are sent to patients days after they return home. In addition, patients’ recovery and health outcomes are likely to influence their assessment of the doctor. Finally, feedback is known to be most valuable and transformative when it is specific and given in real time. Therefore, a tool that is able to provide feedback at the encounter level should be more helpful than a tool that offers assessment at the level of the admission, particularly when it can be also delivered immediately after the data are collected.5
The study authors conclude that, “Future studies are necessary to determine whether hospitalists of all levels of experience and clinical skill can improve when given data and feedback using the HMCCOT. Larger studies are then needed to assess whether enhancing comportment and communication can truly improve patient satisfaction and clinical outcomes in the hospital. Because hospitalists spend only a small proportion of their clinical time in direct patient care, it is imperative that excellent comportment and communication be established as a goal for every encounter.”
The effectiveness of care team rounds at the bedside
Investigators at the UMass Memorial Medical Center, in Worcester, Mass., studied the effectiveness of assembling the entire care team (i.e., physicians, including residents and attendings, nursing, and clinical pharmacy) to round at the patient’s bedside each morning – in lieu of its traditionally separate rounding strategies – on one unit of its academic hospitalist service for an internal quality program, said Patricia Seymour, MD, FAAFP, assistant professor and family medicine hospitalist education director.
Additionally, academic presentations and discussions were all done in front of patients and their families (with a few exceptions) rather than traditional hallway rounds or sit rounds. Over the course of the project, the hospital also offered residents training around physician behaviors that improve patient satisfaction; provided incentives for nurses and residents to work as a team; and created a welcome visit template for the nursing manager and instruments for patients to enhance engagement. Through all of these cycles, the collaborative rounding strategy continued.
Because Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey scores yielded low response rates for the singular test unit and service, the investigators used a validated patient satisfaction instrument and surveyed patients from the intervention group and patients on the same unit who did not experience this collaborative rounding on their day of discharge. The intervention group had higher satisfaction scores at most of the time points. The unit-based HCAHPS scores (not just study patients) improved during this time period.
“We think the strategy of collaborative rounding yielded positive results for obvious reasons – the entire team was on the same page and the information given to the patient was consistent,” said Dr. Seymour, who notes that the study’s findings weren’t published and the project was completed for an internal quality program. “Doctors had an increased understanding about nursing concerns and the nursing staff expressed improved understanding of patients’ care plans.”
Certainly, face time with the patient was extended because much of the academic discussion occurred at the bedside instead of at another physical location without patient awareness, Dr. Seymour said. She believes the strategy boosted patient satisfaction because it was patient centered. “While this rounding strategy is not the most convenient rounding strategy for nurses or doctors, it consolidates the discussion about the patient’s clinical condition and the plan for the day. The patient experiences a strong sense of being cared for by a unified team and receives consistent messaging,” she said.
Also noteworthy is that job satisfaction for residents and nurses improved on the unit over the study time period because of the expected collaboration that was built into the work flow.
Although the facility is no longer using this communication strategy to the same degree, teaching attendings have seen the value of true bedside rounding and continue to teach this skill to learners. “We have had some challenges with geographic cohorting at our institution, which is essential for this type of team-based strategy,” Dr. Seymour said. “Sustainability requires constant encouragement, oversight, and auditing from team leaders which is also challenging and fluctuates with competing demands.”
The results of this study, and others, show that employing tools to improve communication can also result in improved patient satisfaction and experience.
Karen Appold is a medical writer in Pennsylvania.
References
1. Boissy A, Gilligan T. “Communication the Cleveland Clinic Way: How to drive a relationship-centered strategy for superior patient experience.” New York: McGraw-Hill Education. 2016.
2. Weng HC, Hung CM, Liu YT, et al. Associations between emotional intelligence and doctor burnout, job satisfaction and patient satisfaction. Med Educ. 2011;45:835-42.
3. Boissy A, Windover AK, Bokar D, et al. Communication skills training for physicians improves patient satisfaction. J Gen Intern Med. 2016 Jul;31(7):755-761. doi: 10.1007/s11606-016-3597-2. Epub 2016 Feb 26.
4. Kotwal S, Khaliq W, Landis R, Wright S. Developing a comportment and communication tool for use in hospital medicine. J Hosp Med. 2016 Dec;11(12):853-858. doi: 10.1002/jhm.2647. Epub 2016 Aug 13.
5. Fong Ha J, Longnecker N. Doctor-patient communication: a review. Ochsner J. 2010 Spring; 10(1):38-43.
6. Bodenheimer T, Sinsky C. From Triple to Quadruple Aim: care of the patient requires care of the provider. Ann Fam Med. 2014 Nov;12(6): 573-6. doi: 10.1370/afm.1713.
Bonus Content
Clinicians wary of course's worthiness
Before clinicians took Cleveland Clinic’s Relationship Establishment, Development, and Engagement (REDE) course, only 20% strongly agreed that the course would be valuable, whereas afterward 58% strongly agreed that it was indeed valuable. Less than 1% said it wasn’t valuable.4 “Most likely clinicians had a preconceived notion about how communication courses go, but they were probably surprised at how much these sessions were equally about them as providers as they were about caring for patients,” said Vicente J. Velez, MD, FACP, FHM, a hospitalist who serves as the director of faculty enrichment for the leadership team of CEHC. “This is the power of relationship-centered care, and also why I think the model has been sustainable.”
Physicians also reported that before taking the course, they had moderate levels of burnout and low levels of empathy. After taking it, burnout metrics (i.e., emotional exhaustion, depersonalization, and personal achievement) and empathy improved significantly. “I observed that most are surprised to find out that empathy is a discreet set of skills that can be learned, practiced, observed, measured, and improved upon,” Dr. Velez said. “If taught in a safe and validating environment and if principles of adult learning are followed, improvement can be optimized and sustained.”
Since the REDE course rolled out in 2012, all attending physicians and medical staff members have been trained in it.
Why empathy is preferred over patient-centered care
The Cleveland Clinic intentionally puts a focus on relationship-centered care.
“When there’s an emphasis on patient-centered care, some physicians have a hard time figuring out what to do when the patient wants something that the physician doesn’t feel is appropriate,” said Katie Neuendorf, MD, director for the Center for Excellence in Healthcare Communication. “Patient-centered implies that the patient is always right and that their opinion should win out over the physician’s opinion. In that same scenario, relationship-centered care implies that the relationship should be prioritized, even when there’s disagreement in the plan of care. I can tell my patients that I hear what they are saying, that I empathize with their struggles, that I care about the way the illness is affecting their lives, and that I am here to support them. I can do all of that and still not prescribe a treatment that I feel is inappropriate just because it happens to be what the patient wants.”
The Cleveland Clinic’s Relationship Establishment, Development and Engagement (REDE) course helps clinicians to see the individual that exists beyond a diagnosis. “Having empathy, or putting yourself in the other person’s shoes, is a key step in that process,” Dr. Neuendorf said. “Once a physician understands the patient’s perspective, the treatment for the diagnosis is more meaningful to both the patient and physician. Finding meaning in their work addresses the Quadruple Aim.”
How hospitalists and other clinicians communicate with patients impacts a patient’s overall experience and satisfaction. But according to the authors of “Communication the Cleveland Way,”1 a book about how the clinic created and applied communication skills training, “in a culture prioritizing clinical outcomes above all, there can be a tendency to lose sight of one of the most critical aspects of providing effective care: the communication skills that build and foster physician-patient relationships.”
“Studies2,3 have shown that good communication between doctors and patients and among all caregivers who interface with patients directly results in better clinical outcomes, reduced costs, greater patient satisfaction, and lower rates of physician burnout,” the authors wrote.
“It places a special focus on empathy in relationships, and in our case, the provider-patient relationship rather than patient-centered care. The former acknowledges that the thoughts and feelings in both sides of a relationship are important. We know that clinicians, too, can suffer as a result of the care they provide,” Dr. Velez wrote in “Communication the Cleveland Way.”1
“Healthy relationships are based on balance and mutual respect,” Dr Velez said. “Courses made a strong point to practice empathy in order to teach empathy. Clinician participants were gifted with a safe space, an opportunity to share their own skills and expertise, and a chance to be appreciated for what they already do effectively. Most of all, activities were designed to be fun and engaging.” For example, CEHC encouraged and fostered an attitude of exploration, experimentation, and adventure. Various warm-up activities effectively helped the participants enter a more playful space and get into character portrayal.
Dr. Velez credits the CEHC model’s sustainability and success to the early realization that an appreciative approach is effective. In a study3 about the strategy, hospital-employed attending physicians participated in the 8-hour experiential communication skills training course on REDE. The study compared approximately 1,500 “intervention” physicians who attended and 1,900 “nonintervention” physicians who did not attend.
Following the course, scores for physician communication and respect were higher for intervention physicians. Furthermore, physicians showed significant improvement in self-perceptions of empathy and burnout. Some of these gains were sustained for at least 3 months. “This is especially important because in the current health care climate, physicians experience increased burnout,” Dr. Velez notes.
How it works
Because a provider’s connection with a patient occurs when a relationship is established, the REDE course focuses on the beginning of the conversation. “It’s important for clinicians to exhibit value and respect through words and actions when welcoming patients,” Dr. Velez said. “Further, instead of guiding the medical interview with a series of close-ended questions like an interrogator would, we invite the use of open-ended questions and setting an agenda for the visit early on, by asking the patient what they wish to discuss.”
Another key component is empathy, which plays a huge role in patient satisfaction. “Learning how to express empathy is very important,” Dr. Velez said. “A patient may not remember all of the medical details discussed, but human interactions, rapport, expressions of care, support, validation, and acknowledgment of emotions tend to be more indelible.”
Dr. Velez notes that decades of literature regarding effective communication have demonstrated improved outcomes. “If trust in a therapeutic relationship is strong, a patient is more likely to follow instructions and have better engagement with their care plan,” he said. “If a clinician ensures that the patient understands the diagnosis and recommendations, then compliance will increase, especially if the plan is tailored to the patient’s goals and perspective.”
One surprising effect of the REDE course was how it improved relationships among professionals. “Many participants have shared that having a day out of one’s normal schedule, not only to learn, but also to share their own experiences, is quite therapeutic,” Dr. Velez said. “We can extend the same communication strategies to team building, interprofessional interactions, and challenging encounters.”
Study focuses on comportment and communication
In an effort to define optimal care in hospital medicine, a team from Johns Hopkins Health System set out to establish a metric that would comprehensively assess hospitalists’ comportment (which includes behavior as well as general demeanor) and communication to establish norms and expectations when they saw patients at the bedside.
To perform the study,4 chiefs of hospital medicine divisions at five independent hospitals located in Baltimore and Washington identified their most clinically excellent hospitalists. Then, an investigator observed each hospitalist during a routine clinical shift and recorded behaviors believed to be associated with excellent behavior and communication using the hospital medicine comportment and communication observation tool (HMCCOT), said Susrutha Kotwal, MD, assistant professor of medicine at Johns Hopkins University School of Medicine, Baltimore, and lead author. The investigators collected basic demographic information while observing hospitalists for an average of 280 minutes; 26 physicians were observed for 181 separate clinical encounters. Each provider’s mean HMCCOT score was compared with patient satisfaction surveys such as Press Ganey (PG) scores.
Noteworthy is the fact that the distribution of HMCCOT scores were similar when analyzed by age, gender, race, amount of clinical experience, the hospitalist’s clinical workload, hospital, or time spent observing the hospitalist. But the distribution of HMCCOT scores was quite different in new patient encounters, compared with follow-ups (68.1% versus 39.7%). Encounters with patients that generated HMCCOT scores above versus below the mean were longer (13 minutes versus 8.7 minutes). The physicians’ HMCCOT scores were also associated with their PG scores. These findings suggest that improved bedside communication and comportment with patients might also translate into enhanced patient satisfaction.
As a result of the study, a comportment and communication tool was established and validated by following clinically excellent hospitalists at the bedside. “Even among clinically respected hospitalists, the results reveal that there is wide variability in behaviors and communication practices at the bedside,” Dr. Kotwal said.
Employing the tool
Hospitalists can choose whether to perform behaviors in the HMCCOT themselves, while others may wish to watch other hospitalists to give them feedback tied to specific behaviors. “These simple behaviors are intimately linked to excellent communication and comportment, which can serve as the foundation for delivering patient-centered care,” Dr. Kotwal said.
A positive correlation was found between spending more time with patients and higher HMCCOT scores. “Patients’ complaints about doctors often relate to feeling rushed, that their physicians did not listen to them, or that they did not convey information in a clear manner,” Dr. Kotwal said. “When successfully achieved, patient-centered communication has been associated with improved clinical outcomes, including adherence to recommended treatment and better self-management of chronic disease. Many of the components of the HMCCOT described in our study are at the heart of patient-centered care.”
Dr. Kotwal believes HMCCOT is a better strategy to improve patient satisfaction than patient satisfaction surveys because patients can’t always recall which specific provider saw them. In addition, patients’ recall about the provider may be poor because surveys are sent to patients days after they return home. In addition, patients’ recovery and health outcomes are likely to influence their assessment of the doctor. Finally, feedback is known to be most valuable and transformative when it is specific and given in real time. Therefore, a tool that is able to provide feedback at the encounter level should be more helpful than a tool that offers assessment at the level of the admission, particularly when it can be also delivered immediately after the data are collected.5
The study authors conclude that, “Future studies are necessary to determine whether hospitalists of all levels of experience and clinical skill can improve when given data and feedback using the HMCCOT. Larger studies are then needed to assess whether enhancing comportment and communication can truly improve patient satisfaction and clinical outcomes in the hospital. Because hospitalists spend only a small proportion of their clinical time in direct patient care, it is imperative that excellent comportment and communication be established as a goal for every encounter.”
The effectiveness of care team rounds at the bedside
Investigators at the UMass Memorial Medical Center, in Worcester, Mass., studied the effectiveness of assembling the entire care team (i.e., physicians, including residents and attendings, nursing, and clinical pharmacy) to round at the patient’s bedside each morning – in lieu of its traditionally separate rounding strategies – on one unit of its academic hospitalist service for an internal quality program, said Patricia Seymour, MD, FAAFP, assistant professor and family medicine hospitalist education director.
Additionally, academic presentations and discussions were all done in front of patients and their families (with a few exceptions) rather than traditional hallway rounds or sit rounds. Over the course of the project, the hospital also offered residents training around physician behaviors that improve patient satisfaction; provided incentives for nurses and residents to work as a team; and created a welcome visit template for the nursing manager and instruments for patients to enhance engagement. Through all of these cycles, the collaborative rounding strategy continued.
Because Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey scores yielded low response rates for the singular test unit and service, the investigators used a validated patient satisfaction instrument and surveyed patients from the intervention group and patients on the same unit who did not experience this collaborative rounding on their day of discharge. The intervention group had higher satisfaction scores at most of the time points. The unit-based HCAHPS scores (not just study patients) improved during this time period.
“We think the strategy of collaborative rounding yielded positive results for obvious reasons – the entire team was on the same page and the information given to the patient was consistent,” said Dr. Seymour, who notes that the study’s findings weren’t published and the project was completed for an internal quality program. “Doctors had an increased understanding about nursing concerns and the nursing staff expressed improved understanding of patients’ care plans.”
Certainly, face time with the patient was extended because much of the academic discussion occurred at the bedside instead of at another physical location without patient awareness, Dr. Seymour said. She believes the strategy boosted patient satisfaction because it was patient centered. “While this rounding strategy is not the most convenient rounding strategy for nurses or doctors, it consolidates the discussion about the patient’s clinical condition and the plan for the day. The patient experiences a strong sense of being cared for by a unified team and receives consistent messaging,” she said.
Also noteworthy is that job satisfaction for residents and nurses improved on the unit over the study time period because of the expected collaboration that was built into the work flow.
Although the facility is no longer using this communication strategy to the same degree, teaching attendings have seen the value of true bedside rounding and continue to teach this skill to learners. “We have had some challenges with geographic cohorting at our institution, which is essential for this type of team-based strategy,” Dr. Seymour said. “Sustainability requires constant encouragement, oversight, and auditing from team leaders which is also challenging and fluctuates with competing demands.”
The results of this study, and others, show that employing tools to improve communication can also result in improved patient satisfaction and experience.
Karen Appold is a medical writer in Pennsylvania.
References
1. Boissy A, Gilligan T. “Communication the Cleveland Clinic Way: How to drive a relationship-centered strategy for superior patient experience.” New York: McGraw-Hill Education. 2016.
2. Weng HC, Hung CM, Liu YT, et al. Associations between emotional intelligence and doctor burnout, job satisfaction and patient satisfaction. Med Educ. 2011;45:835-42.
3. Boissy A, Windover AK, Bokar D, et al. Communication skills training for physicians improves patient satisfaction. J Gen Intern Med. 2016 Jul;31(7):755-761. doi: 10.1007/s11606-016-3597-2. Epub 2016 Feb 26.
4. Kotwal S, Khaliq W, Landis R, Wright S. Developing a comportment and communication tool for use in hospital medicine. J Hosp Med. 2016 Dec;11(12):853-858. doi: 10.1002/jhm.2647. Epub 2016 Aug 13.
5. Fong Ha J, Longnecker N. Doctor-patient communication: a review. Ochsner J. 2010 Spring; 10(1):38-43.
6. Bodenheimer T, Sinsky C. From Triple to Quadruple Aim: care of the patient requires care of the provider. Ann Fam Med. 2014 Nov;12(6): 573-6. doi: 10.1370/afm.1713.
Bonus Content
Clinicians wary of course's worthiness
Before clinicians took Cleveland Clinic’s Relationship Establishment, Development, and Engagement (REDE) course, only 20% strongly agreed that the course would be valuable, whereas afterward 58% strongly agreed that it was indeed valuable. Less than 1% said it wasn’t valuable.4 “Most likely clinicians had a preconceived notion about how communication courses go, but they were probably surprised at how much these sessions were equally about them as providers as they were about caring for patients,” said Vicente J. Velez, MD, FACP, FHM, a hospitalist who serves as the director of faculty enrichment for the leadership team of CEHC. “This is the power of relationship-centered care, and also why I think the model has been sustainable.”
Physicians also reported that before taking the course, they had moderate levels of burnout and low levels of empathy. After taking it, burnout metrics (i.e., emotional exhaustion, depersonalization, and personal achievement) and empathy improved significantly. “I observed that most are surprised to find out that empathy is a discreet set of skills that can be learned, practiced, observed, measured, and improved upon,” Dr. Velez said. “If taught in a safe and validating environment and if principles of adult learning are followed, improvement can be optimized and sustained.”
Since the REDE course rolled out in 2012, all attending physicians and medical staff members have been trained in it.
Why empathy is preferred over patient-centered care
The Cleveland Clinic intentionally puts a focus on relationship-centered care.
“When there’s an emphasis on patient-centered care, some physicians have a hard time figuring out what to do when the patient wants something that the physician doesn’t feel is appropriate,” said Katie Neuendorf, MD, director for the Center for Excellence in Healthcare Communication. “Patient-centered implies that the patient is always right and that their opinion should win out over the physician’s opinion. In that same scenario, relationship-centered care implies that the relationship should be prioritized, even when there’s disagreement in the plan of care. I can tell my patients that I hear what they are saying, that I empathize with their struggles, that I care about the way the illness is affecting their lives, and that I am here to support them. I can do all of that and still not prescribe a treatment that I feel is inappropriate just because it happens to be what the patient wants.”
The Cleveland Clinic’s Relationship Establishment, Development and Engagement (REDE) course helps clinicians to see the individual that exists beyond a diagnosis. “Having empathy, or putting yourself in the other person’s shoes, is a key step in that process,” Dr. Neuendorf said. “Once a physician understands the patient’s perspective, the treatment for the diagnosis is more meaningful to both the patient and physician. Finding meaning in their work addresses the Quadruple Aim.”
How hospitalists and other clinicians communicate with patients impacts a patient’s overall experience and satisfaction. But according to the authors of “Communication the Cleveland Way,”1 a book about how the clinic created and applied communication skills training, “in a culture prioritizing clinical outcomes above all, there can be a tendency to lose sight of one of the most critical aspects of providing effective care: the communication skills that build and foster physician-patient relationships.”
“Studies2,3 have shown that good communication between doctors and patients and among all caregivers who interface with patients directly results in better clinical outcomes, reduced costs, greater patient satisfaction, and lower rates of physician burnout,” the authors wrote.
“It places a special focus on empathy in relationships, and in our case, the provider-patient relationship rather than patient-centered care. The former acknowledges that the thoughts and feelings in both sides of a relationship are important. We know that clinicians, too, can suffer as a result of the care they provide,” Dr. Velez wrote in “Communication the Cleveland Way.”1
“Healthy relationships are based on balance and mutual respect,” Dr Velez said. “Courses made a strong point to practice empathy in order to teach empathy. Clinician participants were gifted with a safe space, an opportunity to share their own skills and expertise, and a chance to be appreciated for what they already do effectively. Most of all, activities were designed to be fun and engaging.” For example, CEHC encouraged and fostered an attitude of exploration, experimentation, and adventure. Various warm-up activities effectively helped the participants enter a more playful space and get into character portrayal.
Dr. Velez credits the CEHC model’s sustainability and success to the early realization that an appreciative approach is effective. In a study3 about the strategy, hospital-employed attending physicians participated in the 8-hour experiential communication skills training course on REDE. The study compared approximately 1,500 “intervention” physicians who attended and 1,900 “nonintervention” physicians who did not attend.
Following the course, scores for physician communication and respect were higher for intervention physicians. Furthermore, physicians showed significant improvement in self-perceptions of empathy and burnout. Some of these gains were sustained for at least 3 months. “This is especially important because in the current health care climate, physicians experience increased burnout,” Dr. Velez notes.
How it works
Because a provider’s connection with a patient occurs when a relationship is established, the REDE course focuses on the beginning of the conversation. “It’s important for clinicians to exhibit value and respect through words and actions when welcoming patients,” Dr. Velez said. “Further, instead of guiding the medical interview with a series of close-ended questions like an interrogator would, we invite the use of open-ended questions and setting an agenda for the visit early on, by asking the patient what they wish to discuss.”
Another key component is empathy, which plays a huge role in patient satisfaction. “Learning how to express empathy is very important,” Dr. Velez said. “A patient may not remember all of the medical details discussed, but human interactions, rapport, expressions of care, support, validation, and acknowledgment of emotions tend to be more indelible.”
Dr. Velez notes that decades of literature regarding effective communication have demonstrated improved outcomes. “If trust in a therapeutic relationship is strong, a patient is more likely to follow instructions and have better engagement with their care plan,” he said. “If a clinician ensures that the patient understands the diagnosis and recommendations, then compliance will increase, especially if the plan is tailored to the patient’s goals and perspective.”
One surprising effect of the REDE course was how it improved relationships among professionals. “Many participants have shared that having a day out of one’s normal schedule, not only to learn, but also to share their own experiences, is quite therapeutic,” Dr. Velez said. “We can extend the same communication strategies to team building, interprofessional interactions, and challenging encounters.”
Study focuses on comportment and communication
In an effort to define optimal care in hospital medicine, a team from Johns Hopkins Health System set out to establish a metric that would comprehensively assess hospitalists’ comportment (which includes behavior as well as general demeanor) and communication to establish norms and expectations when they saw patients at the bedside.
To perform the study,4 chiefs of hospital medicine divisions at five independent hospitals located in Baltimore and Washington identified their most clinically excellent hospitalists. Then, an investigator observed each hospitalist during a routine clinical shift and recorded behaviors believed to be associated with excellent behavior and communication using the hospital medicine comportment and communication observation tool (HMCCOT), said Susrutha Kotwal, MD, assistant professor of medicine at Johns Hopkins University School of Medicine, Baltimore, and lead author. The investigators collected basic demographic information while observing hospitalists for an average of 280 minutes; 26 physicians were observed for 181 separate clinical encounters. Each provider’s mean HMCCOT score was compared with patient satisfaction surveys such as Press Ganey (PG) scores.
Noteworthy is the fact that the distribution of HMCCOT scores were similar when analyzed by age, gender, race, amount of clinical experience, the hospitalist’s clinical workload, hospital, or time spent observing the hospitalist. But the distribution of HMCCOT scores was quite different in new patient encounters, compared with follow-ups (68.1% versus 39.7%). Encounters with patients that generated HMCCOT scores above versus below the mean were longer (13 minutes versus 8.7 minutes). The physicians’ HMCCOT scores were also associated with their PG scores. These findings suggest that improved bedside communication and comportment with patients might also translate into enhanced patient satisfaction.
As a result of the study, a comportment and communication tool was established and validated by following clinically excellent hospitalists at the bedside. “Even among clinically respected hospitalists, the results reveal that there is wide variability in behaviors and communication practices at the bedside,” Dr. Kotwal said.
Employing the tool
Hospitalists can choose whether to perform behaviors in the HMCCOT themselves, while others may wish to watch other hospitalists to give them feedback tied to specific behaviors. “These simple behaviors are intimately linked to excellent communication and comportment, which can serve as the foundation for delivering patient-centered care,” Dr. Kotwal said.
A positive correlation was found between spending more time with patients and higher HMCCOT scores. “Patients’ complaints about doctors often relate to feeling rushed, that their physicians did not listen to them, or that they did not convey information in a clear manner,” Dr. Kotwal said. “When successfully achieved, patient-centered communication has been associated with improved clinical outcomes, including adherence to recommended treatment and better self-management of chronic disease. Many of the components of the HMCCOT described in our study are at the heart of patient-centered care.”
Dr. Kotwal believes HMCCOT is a better strategy to improve patient satisfaction than patient satisfaction surveys because patients can’t always recall which specific provider saw them. In addition, patients’ recall about the provider may be poor because surveys are sent to patients days after they return home. In addition, patients’ recovery and health outcomes are likely to influence their assessment of the doctor. Finally, feedback is known to be most valuable and transformative when it is specific and given in real time. Therefore, a tool that is able to provide feedback at the encounter level should be more helpful than a tool that offers assessment at the level of the admission, particularly when it can be also delivered immediately after the data are collected.5
The study authors conclude that, “Future studies are necessary to determine whether hospitalists of all levels of experience and clinical skill can improve when given data and feedback using the HMCCOT. Larger studies are then needed to assess whether enhancing comportment and communication can truly improve patient satisfaction and clinical outcomes in the hospital. Because hospitalists spend only a small proportion of their clinical time in direct patient care, it is imperative that excellent comportment and communication be established as a goal for every encounter.”
The effectiveness of care team rounds at the bedside
Investigators at the UMass Memorial Medical Center, in Worcester, Mass., studied the effectiveness of assembling the entire care team (i.e., physicians, including residents and attendings, nursing, and clinical pharmacy) to round at the patient’s bedside each morning – in lieu of its traditionally separate rounding strategies – on one unit of its academic hospitalist service for an internal quality program, said Patricia Seymour, MD, FAAFP, assistant professor and family medicine hospitalist education director.
Additionally, academic presentations and discussions were all done in front of patients and their families (with a few exceptions) rather than traditional hallway rounds or sit rounds. Over the course of the project, the hospital also offered residents training around physician behaviors that improve patient satisfaction; provided incentives for nurses and residents to work as a team; and created a welcome visit template for the nursing manager and instruments for patients to enhance engagement. Through all of these cycles, the collaborative rounding strategy continued.
Because Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey scores yielded low response rates for the singular test unit and service, the investigators used a validated patient satisfaction instrument and surveyed patients from the intervention group and patients on the same unit who did not experience this collaborative rounding on their day of discharge. The intervention group had higher satisfaction scores at most of the time points. The unit-based HCAHPS scores (not just study patients) improved during this time period.
“We think the strategy of collaborative rounding yielded positive results for obvious reasons – the entire team was on the same page and the information given to the patient was consistent,” said Dr. Seymour, who notes that the study’s findings weren’t published and the project was completed for an internal quality program. “Doctors had an increased understanding about nursing concerns and the nursing staff expressed improved understanding of patients’ care plans.”
Certainly, face time with the patient was extended because much of the academic discussion occurred at the bedside instead of at another physical location without patient awareness, Dr. Seymour said. She believes the strategy boosted patient satisfaction because it was patient centered. “While this rounding strategy is not the most convenient rounding strategy for nurses or doctors, it consolidates the discussion about the patient’s clinical condition and the plan for the day. The patient experiences a strong sense of being cared for by a unified team and receives consistent messaging,” she said.
Also noteworthy is that job satisfaction for residents and nurses improved on the unit over the study time period because of the expected collaboration that was built into the work flow.
Although the facility is no longer using this communication strategy to the same degree, teaching attendings have seen the value of true bedside rounding and continue to teach this skill to learners. “We have had some challenges with geographic cohorting at our institution, which is essential for this type of team-based strategy,” Dr. Seymour said. “Sustainability requires constant encouragement, oversight, and auditing from team leaders which is also challenging and fluctuates with competing demands.”
The results of this study, and others, show that employing tools to improve communication can also result in improved patient satisfaction and experience.
Karen Appold is a medical writer in Pennsylvania.
References
1. Boissy A, Gilligan T. “Communication the Cleveland Clinic Way: How to drive a relationship-centered strategy for superior patient experience.” New York: McGraw-Hill Education. 2016.
2. Weng HC, Hung CM, Liu YT, et al. Associations between emotional intelligence and doctor burnout, job satisfaction and patient satisfaction. Med Educ. 2011;45:835-42.
3. Boissy A, Windover AK, Bokar D, et al. Communication skills training for physicians improves patient satisfaction. J Gen Intern Med. 2016 Jul;31(7):755-761. doi: 10.1007/s11606-016-3597-2. Epub 2016 Feb 26.
4. Kotwal S, Khaliq W, Landis R, Wright S. Developing a comportment and communication tool for use in hospital medicine. J Hosp Med. 2016 Dec;11(12):853-858. doi: 10.1002/jhm.2647. Epub 2016 Aug 13.
5. Fong Ha J, Longnecker N. Doctor-patient communication: a review. Ochsner J. 2010 Spring; 10(1):38-43.
6. Bodenheimer T, Sinsky C. From Triple to Quadruple Aim: care of the patient requires care of the provider. Ann Fam Med. 2014 Nov;12(6): 573-6. doi: 10.1370/afm.1713.
Bonus Content
Clinicians wary of course's worthiness
Before clinicians took Cleveland Clinic’s Relationship Establishment, Development, and Engagement (REDE) course, only 20% strongly agreed that the course would be valuable, whereas afterward 58% strongly agreed that it was indeed valuable. Less than 1% said it wasn’t valuable.4 “Most likely clinicians had a preconceived notion about how communication courses go, but they were probably surprised at how much these sessions were equally about them as providers as they were about caring for patients,” said Vicente J. Velez, MD, FACP, FHM, a hospitalist who serves as the director of faculty enrichment for the leadership team of CEHC. “This is the power of relationship-centered care, and also why I think the model has been sustainable.”
Physicians also reported that before taking the course, they had moderate levels of burnout and low levels of empathy. After taking it, burnout metrics (i.e., emotional exhaustion, depersonalization, and personal achievement) and empathy improved significantly. “I observed that most are surprised to find out that empathy is a discreet set of skills that can be learned, practiced, observed, measured, and improved upon,” Dr. Velez said. “If taught in a safe and validating environment and if principles of adult learning are followed, improvement can be optimized and sustained.”
Since the REDE course rolled out in 2012, all attending physicians and medical staff members have been trained in it.
Why empathy is preferred over patient-centered care
The Cleveland Clinic intentionally puts a focus on relationship-centered care.
“When there’s an emphasis on patient-centered care, some physicians have a hard time figuring out what to do when the patient wants something that the physician doesn’t feel is appropriate,” said Katie Neuendorf, MD, director for the Center for Excellence in Healthcare Communication. “Patient-centered implies that the patient is always right and that their opinion should win out over the physician’s opinion. In that same scenario, relationship-centered care implies that the relationship should be prioritized, even when there’s disagreement in the plan of care. I can tell my patients that I hear what they are saying, that I empathize with their struggles, that I care about the way the illness is affecting their lives, and that I am here to support them. I can do all of that and still not prescribe a treatment that I feel is inappropriate just because it happens to be what the patient wants.”
The Cleveland Clinic’s Relationship Establishment, Development and Engagement (REDE) course helps clinicians to see the individual that exists beyond a diagnosis. “Having empathy, or putting yourself in the other person’s shoes, is a key step in that process,” Dr. Neuendorf said. “Once a physician understands the patient’s perspective, the treatment for the diagnosis is more meaningful to both the patient and physician. Finding meaning in their work addresses the Quadruple Aim.”
Set a goal, or two, or three
In today’s health care space, tracking progress and achieving specified metrics are all part of the job. Most fast-paced physician groups incentivize clinicians for efficiency, consistency, quality, and loyalty. Setting and achieving goals, although it might sound somewhat cliche, can play an important role in daily performance, as well as have an impact on long-term satisfaction with an HM career, according to experts in the field.
“Health care insurers and individuals choosing where to obtain health care want evidence that hospitalists are delivering the best care possible,” says Judith S. Treharne, consulting executive at Halley Consulting Group in Westerville, Ohio. “This requires goal setting, measuring performance related to those goals, and continually developing processes that enhance performance in order to achieve goals.”
Hospitalists are at the forefront of healthcare transformations taking place both inside the hospital and when patients are discharged to different settings. The opportunities for setting goals – personal and group-wide – are endless.
For employed hospitalists, goal setting – and achievement – can counter career stagnation, says Sanjay Bhatia, MD, FHM, CDIP.
“They show up, do a job, and go home. Many are not encouraged to develop their careers,” says Dr. Bhatia, chief medical officer, Prime Healthcare–Lower Bucks Hospital, Bristol, Pa.; founding partner, First Docs/Mercer Bucks Medical, Levittown, Pa.; and CEO/president, Prime Clinical Solutions, Freehold, N.J.
Setting goals will help hospitalists establish skill sets and achieve accomplishments that will keep their career growth on track, adds Surinder Yadav, MD, SFHM, vice president of hospital medicine at Emeryville, Calif.–based CEP America, a national organization specializing in acute-care staffing, including hospitalist, intensivist, and emergency medicine programs.
when someone consistently reaches their goals (that is, improving outcomes) and feels accomplished, it enhances engagement of their work, says Treharne, who advises hospitalist groups.
Determine, pursue goals
There are many reasons why goal setting is important. So what guidelines can a hospitalist use to set goals? In order to establish goals for your current role, Treharne advises reviewing your job description – which should be updated as your role evolves.
“Determine what you need to do in order to progress toward meeting these requirements,” she says. “Find out what resources are available to support your efforts.”
Regarding setting career goals, Dr. Jaffer says hospitalists should consider things that really move them.
“For hospitalists in the early stages of their careers, it may take some time to determine them,” he says. “But when a passion develops, hospitalists can identify opportunities which will allow them to create a niche for themselves or an area of expertise.”
Then, hospitalists can work with individuals within their organization and beyond to increase their expertise.
“Find one or more mentors, take educational courses or even pursue an advanced degree, and write about your area of expertise either by publishing articles or abstracts, giving poster presentations, or lecturing,” Dr. Jaffer advises. “That will establish you as an expert and lead to promotions.”
Dr. Bhatia believes it’s natural and important for hospitalists to pursue administrative roles and become experts on how hospitals and post–acute care facilities work, because they transition patients to these institutions and they employ hospitalists. He has also seen hospitalists pursue entrepreneurial goals, such as becoming involved in information technology by developing apps or becoming C-suite executives, and starting other medical-based businesses such as home-based physician visits and telemedicine ventures and even nonmedical-based businesses such as real estate investing. Another avenue is teaching residency programs and developing an academic career.
“The key is to have good teammates, partners, and ancillary staff in each endeavor,” Dr. Bhatia says. “You can learn a lot from them as well. My experiences beyond being a hospitalist make me very valuable as a hospitalist. I’ve found that varied experiences create a synergistic and value-added service to a hospital.”
Stay on target
In order to reach your goals, Dr. Bhatia recommends creating daily task lists as well as setting goals quarterly and annually and evaluating them at those intervals. Determine action steps to reach long-term goals. “I keep these lists on my smartphone, so they’re always in my mind’s eye,” he says. “I look at the big picture on a daily basis and work toward my goals.”
In an effort to help faculty members reach their goals, Dr. Jaffer, when he was a division director at Rush University Medical Center in Chicago, scheduled biannual professional reviews with each team member. It was a formal process adapted from the annual professional review that he learned while at the Cleveland Clinic. Members were asked to complete a faculty self-reflection assessment and answer questions such as:
- Since our last meeting, what committees and educational opportunities have you participated in?
- What types of quality improvement projects and presentations have you done?
- What achievements are you most proud of?
- Regarding the goals you listed at your last review, where have you had the most growth? What would you define as opportunities for growth?
At Rush, Dr. Jaffer asked members of his division to set one or two professional goals each year. “I suggested they set goals that will make them feel fulfilled professionally, so their careers remain gratifying,” he says.
Group goals
Hospitalists should play an integral role in developing a hospital’s strategic and operational plan. “By having hospitalists provide feedback in the planning process, prior to annual finalization of the plan, the hospital’s and hospitalist program’s objectives can be aligned,” Treharne says. “It’s important that their goals align, in order for both to be successful.”
Dr. Jaffer suggests starting at the beginning of each fiscal year. HM groups should, as a team, create quality, operational, and efficiency goals, which align closely with the hospital’s goals. Some examples: clinical productivity work relative value units (wRVUs), doctor-patient communication scores, observed-to-expected length of stay, readmission rates, and percentage of patients discharged by 1 p.m.
“We set goals both as individuals and as a group,” Dr. Jaffer says. “Then, we create a scorecard for each hospitalist on a quarterly basis and share each hospitalist’s data with them, as well as create a group dashboard. As a group, hospitalists can view both individual data and the group’s data. This feedback helps them identify where they need to improve their performance.”
Dr. Bhatia has found that setting group goals on a quarterly basis works well. Goals involve recruitment needs, patient satisfaction, case mix index, Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), utilization, and length of stay.
“Metrics should be recorded and shared monthly by either the hospital’s information technology department or the hospitalist group’s software,” he says.
Data: top of mind
Each provider needs to understand that success for the team also means individual success.
“Focus on helping each other to achieve high performance and high quality care,” Dr. Yadav says. “Engage with each other and with the hospital at large. Aim to be involved in projects and to help find solutions to problems or barriers within the system.”
When you implement a change in a process and expect to see improvement regarding a particular measure, be sure to give the new process adequate time to shift the outcome.
“Many good ideas have been cast aside because they were deemed unsuccessful before there was sufficient time for the process to stabilize and the improvement to be seen,” Treharne says.
When setting targets and measures, set expectations regarding how long the new process will need to be in place prior to evaluating the change.
“Pilot programs are often a good way to try something out before completely changing a process with potential unwanted outcomes,” she says.
If a clinical operational or efficiency goal that involves the whole group and performance is below target, look to best practices to help you achieve success, Dr. Jaffer says. Create a work group and appoint a champion.
Hopefully, reaching your goals will translate into success.
“Success for me is about having a positive impact on people and processes, and being content with my personal life and having time and resources to pursue my passions,” Dr. Jaffer concludes.
Setting Goals for Now and Then
When looking to set goals, Treharne recommends starting with long-term goal setting.
“Set goals for the next year, or five years and beyond, by establishing a vision – dream to be more than you are today,” she says. “Envision a future that gets you excited to participate in change and come to work every day.”
- I could become more valued in my job by doing _____.
- I could make more income by _____.
- I’d like to increase my knowledge of _____.
Then, develop short-term goals that will help you work toward achieving your long-term goals.
“Map out a path from today using the metrics available and applicable to the future state,” Treharne says. “Creating that path allows you to determine the short-term goals. How far can you get in what period of time? Be realistic, but stretch yourself so you’re not complacent.”
Document this path in a quarterly action plan with a complementary monthly tactical plan. Plans should identify accountable parties, resources needed, data requirements, and timelines, Treharne says. Review your progress monthly.
Check in and articulate your goals with those in your inner circle – seek their advice on a regular basis, Uy says. Measure results and be willing to adapt if you’re not progressing as you’ve envisioned.
Karen Appold is a freelance writer in Pennsylvania.
In today’s health care space, tracking progress and achieving specified metrics are all part of the job. Most fast-paced physician groups incentivize clinicians for efficiency, consistency, quality, and loyalty. Setting and achieving goals, although it might sound somewhat cliche, can play an important role in daily performance, as well as have an impact on long-term satisfaction with an HM career, according to experts in the field.
“Health care insurers and individuals choosing where to obtain health care want evidence that hospitalists are delivering the best care possible,” says Judith S. Treharne, consulting executive at Halley Consulting Group in Westerville, Ohio. “This requires goal setting, measuring performance related to those goals, and continually developing processes that enhance performance in order to achieve goals.”
Hospitalists are at the forefront of healthcare transformations taking place both inside the hospital and when patients are discharged to different settings. The opportunities for setting goals – personal and group-wide – are endless.
For employed hospitalists, goal setting – and achievement – can counter career stagnation, says Sanjay Bhatia, MD, FHM, CDIP.
“They show up, do a job, and go home. Many are not encouraged to develop their careers,” says Dr. Bhatia, chief medical officer, Prime Healthcare–Lower Bucks Hospital, Bristol, Pa.; founding partner, First Docs/Mercer Bucks Medical, Levittown, Pa.; and CEO/president, Prime Clinical Solutions, Freehold, N.J.
Setting goals will help hospitalists establish skill sets and achieve accomplishments that will keep their career growth on track, adds Surinder Yadav, MD, SFHM, vice president of hospital medicine at Emeryville, Calif.–based CEP America, a national organization specializing in acute-care staffing, including hospitalist, intensivist, and emergency medicine programs.
when someone consistently reaches their goals (that is, improving outcomes) and feels accomplished, it enhances engagement of their work, says Treharne, who advises hospitalist groups.
Determine, pursue goals
There are many reasons why goal setting is important. So what guidelines can a hospitalist use to set goals? In order to establish goals for your current role, Treharne advises reviewing your job description – which should be updated as your role evolves.
“Determine what you need to do in order to progress toward meeting these requirements,” she says. “Find out what resources are available to support your efforts.”
Regarding setting career goals, Dr. Jaffer says hospitalists should consider things that really move them.
“For hospitalists in the early stages of their careers, it may take some time to determine them,” he says. “But when a passion develops, hospitalists can identify opportunities which will allow them to create a niche for themselves or an area of expertise.”
Then, hospitalists can work with individuals within their organization and beyond to increase their expertise.
“Find one or more mentors, take educational courses or even pursue an advanced degree, and write about your area of expertise either by publishing articles or abstracts, giving poster presentations, or lecturing,” Dr. Jaffer advises. “That will establish you as an expert and lead to promotions.”
Dr. Bhatia believes it’s natural and important for hospitalists to pursue administrative roles and become experts on how hospitals and post–acute care facilities work, because they transition patients to these institutions and they employ hospitalists. He has also seen hospitalists pursue entrepreneurial goals, such as becoming involved in information technology by developing apps or becoming C-suite executives, and starting other medical-based businesses such as home-based physician visits and telemedicine ventures and even nonmedical-based businesses such as real estate investing. Another avenue is teaching residency programs and developing an academic career.
“The key is to have good teammates, partners, and ancillary staff in each endeavor,” Dr. Bhatia says. “You can learn a lot from them as well. My experiences beyond being a hospitalist make me very valuable as a hospitalist. I’ve found that varied experiences create a synergistic and value-added service to a hospital.”
Stay on target
In order to reach your goals, Dr. Bhatia recommends creating daily task lists as well as setting goals quarterly and annually and evaluating them at those intervals. Determine action steps to reach long-term goals. “I keep these lists on my smartphone, so they’re always in my mind’s eye,” he says. “I look at the big picture on a daily basis and work toward my goals.”
In an effort to help faculty members reach their goals, Dr. Jaffer, when he was a division director at Rush University Medical Center in Chicago, scheduled biannual professional reviews with each team member. It was a formal process adapted from the annual professional review that he learned while at the Cleveland Clinic. Members were asked to complete a faculty self-reflection assessment and answer questions such as:
- Since our last meeting, what committees and educational opportunities have you participated in?
- What types of quality improvement projects and presentations have you done?
- What achievements are you most proud of?
- Regarding the goals you listed at your last review, where have you had the most growth? What would you define as opportunities for growth?
At Rush, Dr. Jaffer asked members of his division to set one or two professional goals each year. “I suggested they set goals that will make them feel fulfilled professionally, so their careers remain gratifying,” he says.
Group goals
Hospitalists should play an integral role in developing a hospital’s strategic and operational plan. “By having hospitalists provide feedback in the planning process, prior to annual finalization of the plan, the hospital’s and hospitalist program’s objectives can be aligned,” Treharne says. “It’s important that their goals align, in order for both to be successful.”
Dr. Jaffer suggests starting at the beginning of each fiscal year. HM groups should, as a team, create quality, operational, and efficiency goals, which align closely with the hospital’s goals. Some examples: clinical productivity work relative value units (wRVUs), doctor-patient communication scores, observed-to-expected length of stay, readmission rates, and percentage of patients discharged by 1 p.m.
“We set goals both as individuals and as a group,” Dr. Jaffer says. “Then, we create a scorecard for each hospitalist on a quarterly basis and share each hospitalist’s data with them, as well as create a group dashboard. As a group, hospitalists can view both individual data and the group’s data. This feedback helps them identify where they need to improve their performance.”
Dr. Bhatia has found that setting group goals on a quarterly basis works well. Goals involve recruitment needs, patient satisfaction, case mix index, Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), utilization, and length of stay.
“Metrics should be recorded and shared monthly by either the hospital’s information technology department or the hospitalist group’s software,” he says.
Data: top of mind
Each provider needs to understand that success for the team also means individual success.
“Focus on helping each other to achieve high performance and high quality care,” Dr. Yadav says. “Engage with each other and with the hospital at large. Aim to be involved in projects and to help find solutions to problems or barriers within the system.”
When you implement a change in a process and expect to see improvement regarding a particular measure, be sure to give the new process adequate time to shift the outcome.
“Many good ideas have been cast aside because they were deemed unsuccessful before there was sufficient time for the process to stabilize and the improvement to be seen,” Treharne says.
When setting targets and measures, set expectations regarding how long the new process will need to be in place prior to evaluating the change.
“Pilot programs are often a good way to try something out before completely changing a process with potential unwanted outcomes,” she says.
If a clinical operational or efficiency goal that involves the whole group and performance is below target, look to best practices to help you achieve success, Dr. Jaffer says. Create a work group and appoint a champion.
Hopefully, reaching your goals will translate into success.
“Success for me is about having a positive impact on people and processes, and being content with my personal life and having time and resources to pursue my passions,” Dr. Jaffer concludes.
Setting Goals for Now and Then
When looking to set goals, Treharne recommends starting with long-term goal setting.
“Set goals for the next year, or five years and beyond, by establishing a vision – dream to be more than you are today,” she says. “Envision a future that gets you excited to participate in change and come to work every day.”
- I could become more valued in my job by doing _____.
- I could make more income by _____.
- I’d like to increase my knowledge of _____.
Then, develop short-term goals that will help you work toward achieving your long-term goals.
“Map out a path from today using the metrics available and applicable to the future state,” Treharne says. “Creating that path allows you to determine the short-term goals. How far can you get in what period of time? Be realistic, but stretch yourself so you’re not complacent.”
Document this path in a quarterly action plan with a complementary monthly tactical plan. Plans should identify accountable parties, resources needed, data requirements, and timelines, Treharne says. Review your progress monthly.
Check in and articulate your goals with those in your inner circle – seek their advice on a regular basis, Uy says. Measure results and be willing to adapt if you’re not progressing as you’ve envisioned.
Karen Appold is a freelance writer in Pennsylvania.
In today’s health care space, tracking progress and achieving specified metrics are all part of the job. Most fast-paced physician groups incentivize clinicians for efficiency, consistency, quality, and loyalty. Setting and achieving goals, although it might sound somewhat cliche, can play an important role in daily performance, as well as have an impact on long-term satisfaction with an HM career, according to experts in the field.
“Health care insurers and individuals choosing where to obtain health care want evidence that hospitalists are delivering the best care possible,” says Judith S. Treharne, consulting executive at Halley Consulting Group in Westerville, Ohio. “This requires goal setting, measuring performance related to those goals, and continually developing processes that enhance performance in order to achieve goals.”
Hospitalists are at the forefront of healthcare transformations taking place both inside the hospital and when patients are discharged to different settings. The opportunities for setting goals – personal and group-wide – are endless.
For employed hospitalists, goal setting – and achievement – can counter career stagnation, says Sanjay Bhatia, MD, FHM, CDIP.
“They show up, do a job, and go home. Many are not encouraged to develop their careers,” says Dr. Bhatia, chief medical officer, Prime Healthcare–Lower Bucks Hospital, Bristol, Pa.; founding partner, First Docs/Mercer Bucks Medical, Levittown, Pa.; and CEO/president, Prime Clinical Solutions, Freehold, N.J.
Setting goals will help hospitalists establish skill sets and achieve accomplishments that will keep their career growth on track, adds Surinder Yadav, MD, SFHM, vice president of hospital medicine at Emeryville, Calif.–based CEP America, a national organization specializing in acute-care staffing, including hospitalist, intensivist, and emergency medicine programs.
when someone consistently reaches their goals (that is, improving outcomes) and feels accomplished, it enhances engagement of their work, says Treharne, who advises hospitalist groups.
Determine, pursue goals
There are many reasons why goal setting is important. So what guidelines can a hospitalist use to set goals? In order to establish goals for your current role, Treharne advises reviewing your job description – which should be updated as your role evolves.
“Determine what you need to do in order to progress toward meeting these requirements,” she says. “Find out what resources are available to support your efforts.”
Regarding setting career goals, Dr. Jaffer says hospitalists should consider things that really move them.
“For hospitalists in the early stages of their careers, it may take some time to determine them,” he says. “But when a passion develops, hospitalists can identify opportunities which will allow them to create a niche for themselves or an area of expertise.”
Then, hospitalists can work with individuals within their organization and beyond to increase their expertise.
“Find one or more mentors, take educational courses or even pursue an advanced degree, and write about your area of expertise either by publishing articles or abstracts, giving poster presentations, or lecturing,” Dr. Jaffer advises. “That will establish you as an expert and lead to promotions.”
Dr. Bhatia believes it’s natural and important for hospitalists to pursue administrative roles and become experts on how hospitals and post–acute care facilities work, because they transition patients to these institutions and they employ hospitalists. He has also seen hospitalists pursue entrepreneurial goals, such as becoming involved in information technology by developing apps or becoming C-suite executives, and starting other medical-based businesses such as home-based physician visits and telemedicine ventures and even nonmedical-based businesses such as real estate investing. Another avenue is teaching residency programs and developing an academic career.
“The key is to have good teammates, partners, and ancillary staff in each endeavor,” Dr. Bhatia says. “You can learn a lot from them as well. My experiences beyond being a hospitalist make me very valuable as a hospitalist. I’ve found that varied experiences create a synergistic and value-added service to a hospital.”
Stay on target
In order to reach your goals, Dr. Bhatia recommends creating daily task lists as well as setting goals quarterly and annually and evaluating them at those intervals. Determine action steps to reach long-term goals. “I keep these lists on my smartphone, so they’re always in my mind’s eye,” he says. “I look at the big picture on a daily basis and work toward my goals.”
In an effort to help faculty members reach their goals, Dr. Jaffer, when he was a division director at Rush University Medical Center in Chicago, scheduled biannual professional reviews with each team member. It was a formal process adapted from the annual professional review that he learned while at the Cleveland Clinic. Members were asked to complete a faculty self-reflection assessment and answer questions such as:
- Since our last meeting, what committees and educational opportunities have you participated in?
- What types of quality improvement projects and presentations have you done?
- What achievements are you most proud of?
- Regarding the goals you listed at your last review, where have you had the most growth? What would you define as opportunities for growth?
At Rush, Dr. Jaffer asked members of his division to set one or two professional goals each year. “I suggested they set goals that will make them feel fulfilled professionally, so their careers remain gratifying,” he says.
Group goals
Hospitalists should play an integral role in developing a hospital’s strategic and operational plan. “By having hospitalists provide feedback in the planning process, prior to annual finalization of the plan, the hospital’s and hospitalist program’s objectives can be aligned,” Treharne says. “It’s important that their goals align, in order for both to be successful.”
Dr. Jaffer suggests starting at the beginning of each fiscal year. HM groups should, as a team, create quality, operational, and efficiency goals, which align closely with the hospital’s goals. Some examples: clinical productivity work relative value units (wRVUs), doctor-patient communication scores, observed-to-expected length of stay, readmission rates, and percentage of patients discharged by 1 p.m.
“We set goals both as individuals and as a group,” Dr. Jaffer says. “Then, we create a scorecard for each hospitalist on a quarterly basis and share each hospitalist’s data with them, as well as create a group dashboard. As a group, hospitalists can view both individual data and the group’s data. This feedback helps them identify where they need to improve their performance.”
Dr. Bhatia has found that setting group goals on a quarterly basis works well. Goals involve recruitment needs, patient satisfaction, case mix index, Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS), utilization, and length of stay.
“Metrics should be recorded and shared monthly by either the hospital’s information technology department or the hospitalist group’s software,” he says.
Data: top of mind
Each provider needs to understand that success for the team also means individual success.
“Focus on helping each other to achieve high performance and high quality care,” Dr. Yadav says. “Engage with each other and with the hospital at large. Aim to be involved in projects and to help find solutions to problems or barriers within the system.”
When you implement a change in a process and expect to see improvement regarding a particular measure, be sure to give the new process adequate time to shift the outcome.
“Many good ideas have been cast aside because they were deemed unsuccessful before there was sufficient time for the process to stabilize and the improvement to be seen,” Treharne says.
When setting targets and measures, set expectations regarding how long the new process will need to be in place prior to evaluating the change.
“Pilot programs are often a good way to try something out before completely changing a process with potential unwanted outcomes,” she says.
If a clinical operational or efficiency goal that involves the whole group and performance is below target, look to best practices to help you achieve success, Dr. Jaffer says. Create a work group and appoint a champion.
Hopefully, reaching your goals will translate into success.
“Success for me is about having a positive impact on people and processes, and being content with my personal life and having time and resources to pursue my passions,” Dr. Jaffer concludes.
Setting Goals for Now and Then
When looking to set goals, Treharne recommends starting with long-term goal setting.
“Set goals for the next year, or five years and beyond, by establishing a vision – dream to be more than you are today,” she says. “Envision a future that gets you excited to participate in change and come to work every day.”
- I could become more valued in my job by doing _____.
- I could make more income by _____.
- I’d like to increase my knowledge of _____.
Then, develop short-term goals that will help you work toward achieving your long-term goals.
“Map out a path from today using the metrics available and applicable to the future state,” Treharne says. “Creating that path allows you to determine the short-term goals. How far can you get in what period of time? Be realistic, but stretch yourself so you’re not complacent.”
Document this path in a quarterly action plan with a complementary monthly tactical plan. Plans should identify accountable parties, resources needed, data requirements, and timelines, Treharne says. Review your progress monthly.
Check in and articulate your goals with those in your inner circle – seek their advice on a regular basis, Uy says. Measure results and be willing to adapt if you’re not progressing as you’ve envisioned.
Karen Appold is a freelance writer in Pennsylvania.
Eight things hospitalists need to know about post-acute care
Whether you’re a hospitalist who works only in a hospital, a hospitalist who works only in a post-acute care (PAC) setting, or a hospitalist who works in both types of facilities, knowing about current trends at PAC facilities and what the future may hold can help you excel in your current capacity and, ultimately, improve patient care.
The Hospitalist tapped experts in the post-acute space to tell us what they thought HM should know about working in PAC – which, in many ways, is quite different from the hospital setting. Here’s a compilation of their top eight must-knows.
1. PAC settings rely more on mid-level medical staff than hospitals do.
PAC facilities employ more mid-level providers, such as nurse practitioners and physician assistants, because they can support the level of medical complexity and decision making 95% of the time, says James D. Tollman, MD, FHM, president of Essex Inpatient Physicians in Boxford, Mass. Further, they are more heavily staffed by licensed practical nurses than are acute-care settings.
Usually, there is no physician or nurse practitioner presence at night. Clinicians rely on nursing staff’s assessment to make decisions regarding changes in patient status during off-hours, says Virginia Cummings, MD, director of long-term care, gerontology division, at Boston-based Beth Israel Deaconess Medical Center.
2. Testing takes longer, and options are limited.
Access to some acute urgent resources such as laboratory testing, imaging tests, and pharmacy products is more challenging at PAC facilities because most of these resources are not on-site. Consequently, there is a time lag between ordering tests and new medications and implementing these orders.
“If a patient needs something performed diagnostically immediately, they usually have to be transported to the emergency room or a facility with the necessary testing equipment,” Dr. Tollman says.
However, Paul T. Liistro, managing partner, Arbors of Hop Brook Limited Partnership in Manchester, Conn., and Vernon Manor Health Care Center in Vernon, Conn., and administrator, Manchester Manor Health Care Center, notes that it’s possible for a laboratory service or mobile diagnostic unit to provide laboratory testing or certain imaging at a PAC facility. More-involved diagnostics, such as an MRI or a PET scan, typically require testing at a remote location.
3. Patient populations mainly include rehab and terminally ill patients.
Patients are typically sent to a PAC facility either to recover from an illness or injury or because they are chronically ill and have exhausted treatment options. Regarding the latter, “They are mostly there for palliation; we don’t perform daily tests or prescribe aggressive medications on these patients,” Dr. Nazir says.
Dr. Cummings explains that PAC clinicians go through “the dying process with the patient.”
“They may or may not have assistance from hospice organizations,” she says, “and when they don’t, [hospitalists] take on the role of palliative-care providers.”
Dr. Cummings has seen an increase in psychiatric patients entering PAC facilities.
“Many patients with chronic psychological problems are aging, and there are fewer inpatient psychiatric beds available to those with concurrent medical and psychiatric problems,” she says. Much of this work is now being done in PAC settings. 
4. You can build a relationship with your patient.
Because the pace of a PAC facility is slower and a patient typically stays in a PAC facility longer than at a hospital, there’s time for a hospitalist to have more in-depth conversations with patients and their families.
“Building a deeper relationship with a patient may give the hospitalist an opportunity to discover the cause of an acute problem,” Dr. Nazir says. “They can go in-depth into the psychosocial aspect of medicine and may be able to find out what led to the initial problem and the real root cause, which can help prevent future recurrences, such as repeat falls or forgetting to take a medication.”
5. Using EHRs can improve transitions.
Care transitions between a hospital and PAC facility can be compromised by a lack of information sharing, and they can affect the quality and safety of patient care, says Dori Cross, a doctoral candidate in health services organization and policy at the University of Michigan School of Public Health in Ann Arbor. Handoffs between providers require information continuity – information that is complete, timely, and in a usable format – to ensure appropriate medical decisions and to provide high-quality care during and after transition.
Electronic health records (EHRs) as well as health information exchanges (HIEs) allow providers to communicate and share patient information. For example, hospitals can send information electronically to PAC facilities (“push” exchange) or make information available online securely for PAC providers to log in and access (“pull” exchange). According to a 2014 survey data by the American Hospital Association, more than 50% of hospitals report sending structured summary-of-care records electronically to long-term care settings; a little less than half of those hospitals (23% of the total sample of hospitals) were also receiving information electronically from long-term care sites.1
“This bidirectional exchange, in particular, can make it easier to share information across provider organizations electronically and, in turn, improve care delivery,” says Ms. Cross, who authored an accepted paper on the subject in the Journal of Post-Acute and Long-Term Medicine.
6. Hospitalists can work with providers in PAC settings to improve transitions.
Despite improvements in the electronic transfer of medical information, gaps still exist and can cause problems. One chasm when discharging patients to a PAC facility, is when a hospital IT system is incapable of communicating with the PAC facility system. In this instance, Dr. Nazir says, the hospitalist “can help bridge the gap.”
“[We] can verbally relay relevant information to physicians at PAC facilities so they understand the patient’s status, needs, and expectations,” he says. “Furthermore, hospitalists and a PAC facility’s administration can brainstorm methods to improve the systems of care so the patient receives more effective and timely care.”
7. Hospitalists switching to the PAC setting should have formal training.
The two main obstacles for hospitalists who change from working in a hospital to a PAC facility are the lack of exposure to PAC work in training and the assumption that it requires the same skills sets of a typical hospitalist, according to Manoj K. Mathew, MD, SFHM, national medical director of Los Angeles–based Agilon Health. The PAC setting has quite a number of differences compared with a hospital setting. For example, some regulations apply specifically to PAC facilities. In addition to formal training, hospitalists can benefit from using SHM’s Post-Acute Care Transitions Toolkit, having a mentor, or using resources from other organizations that function in this space such as The Society for Post-Acute and Long-Term Care Medicine, Dr. Nazir says.
8. A variety of payors and payment models are in play.
Commercial insurers continue to be major payors for PAC, especially for individuals younger than 65 years. Medicare and Medicaid, administered by the Centers for Medicare & Medicaid Services, are the primary payors for patients aged 65 years and older.
“These scorecards are using a variety of criteria to rank providers, such as length of stay, cost, readmissions to hospitals, and quality.”
Because Medicare Part A covers many patients discharged to a PAC setting, any changes in payment incentives or benefit structures by the Medicare program will drive changes in PAC. 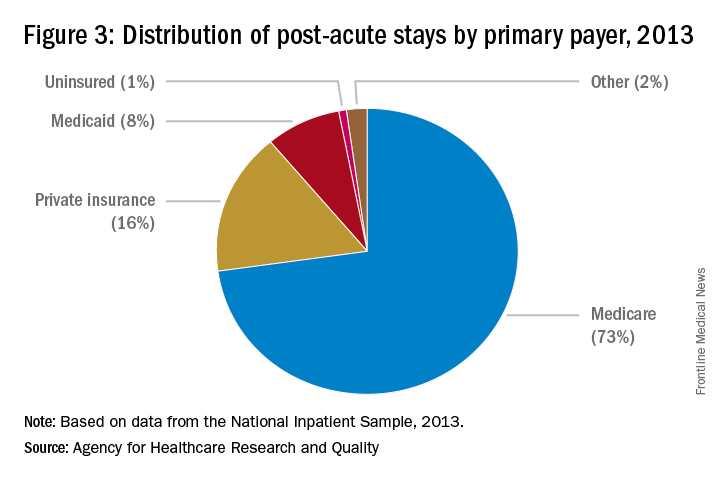
“For example, as Medicare implements payment adjustments for hospitals that have high rates of readmissions, hospitals have a new incentive to work closely with SNFs and other providers of PAC to ensure patients can avoid unnecessary readmissions,” says Tiffany A. Radcliff, PhD, a health economist and associate professor in the department of health policy and management at Texas A&M University School of Public Health in College Station.
Providers must follow the billing rules for each payor. The rules for Medicare payments are outlined on CMS’ website. Bundled payments for PAC under the Medicare Part A program are scheduled to be implemented by 2018.
Reference
Cross DA, Adler-Milstein J. Investing in post-acute care transitions: electronic information exchange between hospitals and long-term care facilities [published online ahead of print Sept. 14, 2016]. JAMDA. doi: http://dx.doi.org/10.1016/j.jamda.2016.07.024.
Whether you’re a hospitalist who works only in a hospital, a hospitalist who works only in a post-acute care (PAC) setting, or a hospitalist who works in both types of facilities, knowing about current trends at PAC facilities and what the future may hold can help you excel in your current capacity and, ultimately, improve patient care.
The Hospitalist tapped experts in the post-acute space to tell us what they thought HM should know about working in PAC – which, in many ways, is quite different from the hospital setting. Here’s a compilation of their top eight must-knows.
1. PAC settings rely more on mid-level medical staff than hospitals do.
PAC facilities employ more mid-level providers, such as nurse practitioners and physician assistants, because they can support the level of medical complexity and decision making 95% of the time, says James D. Tollman, MD, FHM, president of Essex Inpatient Physicians in Boxford, Mass. Further, they are more heavily staffed by licensed practical nurses than are acute-care settings.
Usually, there is no physician or nurse practitioner presence at night. Clinicians rely on nursing staff’s assessment to make decisions regarding changes in patient status during off-hours, says Virginia Cummings, MD, director of long-term care, gerontology division, at Boston-based Beth Israel Deaconess Medical Center.
2. Testing takes longer, and options are limited.
Access to some acute urgent resources such as laboratory testing, imaging tests, and pharmacy products is more challenging at PAC facilities because most of these resources are not on-site. Consequently, there is a time lag between ordering tests and new medications and implementing these orders.
“If a patient needs something performed diagnostically immediately, they usually have to be transported to the emergency room or a facility with the necessary testing equipment,” Dr. Tollman says.
However, Paul T. Liistro, managing partner, Arbors of Hop Brook Limited Partnership in Manchester, Conn., and Vernon Manor Health Care Center in Vernon, Conn., and administrator, Manchester Manor Health Care Center, notes that it’s possible for a laboratory service or mobile diagnostic unit to provide laboratory testing or certain imaging at a PAC facility. More-involved diagnostics, such as an MRI or a PET scan, typically require testing at a remote location.
3. Patient populations mainly include rehab and terminally ill patients.
Patients are typically sent to a PAC facility either to recover from an illness or injury or because they are chronically ill and have exhausted treatment options. Regarding the latter, “They are mostly there for palliation; we don’t perform daily tests or prescribe aggressive medications on these patients,” Dr. Nazir says.
Dr. Cummings explains that PAC clinicians go through “the dying process with the patient.”
“They may or may not have assistance from hospice organizations,” she says, “and when they don’t, [hospitalists] take on the role of palliative-care providers.”
Dr. Cummings has seen an increase in psychiatric patients entering PAC facilities.
“Many patients with chronic psychological problems are aging, and there are fewer inpatient psychiatric beds available to those with concurrent medical and psychiatric problems,” she says. Much of this work is now being done in PAC settings. 
4. You can build a relationship with your patient.
Because the pace of a PAC facility is slower and a patient typically stays in a PAC facility longer than at a hospital, there’s time for a hospitalist to have more in-depth conversations with patients and their families.
“Building a deeper relationship with a patient may give the hospitalist an opportunity to discover the cause of an acute problem,” Dr. Nazir says. “They can go in-depth into the psychosocial aspect of medicine and may be able to find out what led to the initial problem and the real root cause, which can help prevent future recurrences, such as repeat falls or forgetting to take a medication.”
5. Using EHRs can improve transitions.
Care transitions between a hospital and PAC facility can be compromised by a lack of information sharing, and they can affect the quality and safety of patient care, says Dori Cross, a doctoral candidate in health services organization and policy at the University of Michigan School of Public Health in Ann Arbor. Handoffs between providers require information continuity – information that is complete, timely, and in a usable format – to ensure appropriate medical decisions and to provide high-quality care during and after transition.
Electronic health records (EHRs) as well as health information exchanges (HIEs) allow providers to communicate and share patient information. For example, hospitals can send information electronically to PAC facilities (“push” exchange) or make information available online securely for PAC providers to log in and access (“pull” exchange). According to a 2014 survey data by the American Hospital Association, more than 50% of hospitals report sending structured summary-of-care records electronically to long-term care settings; a little less than half of those hospitals (23% of the total sample of hospitals) were also receiving information electronically from long-term care sites.1
“This bidirectional exchange, in particular, can make it easier to share information across provider organizations electronically and, in turn, improve care delivery,” says Ms. Cross, who authored an accepted paper on the subject in the Journal of Post-Acute and Long-Term Medicine.
6. Hospitalists can work with providers in PAC settings to improve transitions.
Despite improvements in the electronic transfer of medical information, gaps still exist and can cause problems. One chasm when discharging patients to a PAC facility, is when a hospital IT system is incapable of communicating with the PAC facility system. In this instance, Dr. Nazir says, the hospitalist “can help bridge the gap.”
“[We] can verbally relay relevant information to physicians at PAC facilities so they understand the patient’s status, needs, and expectations,” he says. “Furthermore, hospitalists and a PAC facility’s administration can brainstorm methods to improve the systems of care so the patient receives more effective and timely care.”
7. Hospitalists switching to the PAC setting should have formal training.
The two main obstacles for hospitalists who change from working in a hospital to a PAC facility are the lack of exposure to PAC work in training and the assumption that it requires the same skills sets of a typical hospitalist, according to Manoj K. Mathew, MD, SFHM, national medical director of Los Angeles–based Agilon Health. The PAC setting has quite a number of differences compared with a hospital setting. For example, some regulations apply specifically to PAC facilities. In addition to formal training, hospitalists can benefit from using SHM’s Post-Acute Care Transitions Toolkit, having a mentor, or using resources from other organizations that function in this space such as The Society for Post-Acute and Long-Term Care Medicine, Dr. Nazir says.
8. A variety of payors and payment models are in play.
Commercial insurers continue to be major payors for PAC, especially for individuals younger than 65 years. Medicare and Medicaid, administered by the Centers for Medicare & Medicaid Services, are the primary payors for patients aged 65 years and older.
“These scorecards are using a variety of criteria to rank providers, such as length of stay, cost, readmissions to hospitals, and quality.”
Because Medicare Part A covers many patients discharged to a PAC setting, any changes in payment incentives or benefit structures by the Medicare program will drive changes in PAC. 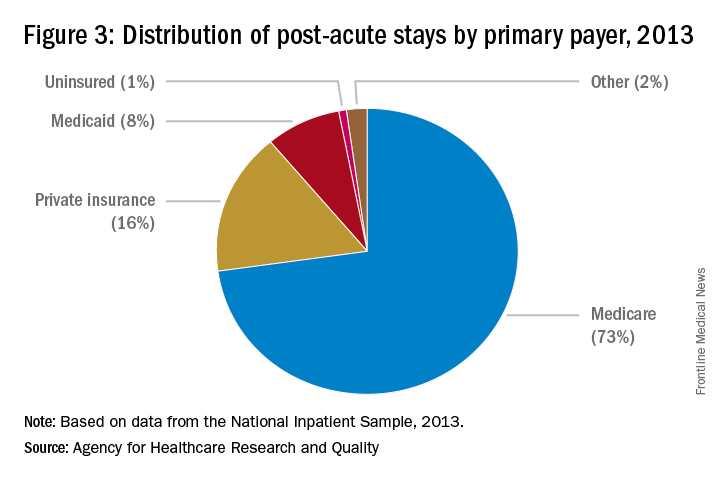
“For example, as Medicare implements payment adjustments for hospitals that have high rates of readmissions, hospitals have a new incentive to work closely with SNFs and other providers of PAC to ensure patients can avoid unnecessary readmissions,” says Tiffany A. Radcliff, PhD, a health economist and associate professor in the department of health policy and management at Texas A&M University School of Public Health in College Station.
Providers must follow the billing rules for each payor. The rules for Medicare payments are outlined on CMS’ website. Bundled payments for PAC under the Medicare Part A program are scheduled to be implemented by 2018.
Reference
Cross DA, Adler-Milstein J. Investing in post-acute care transitions: electronic information exchange between hospitals and long-term care facilities [published online ahead of print Sept. 14, 2016]. JAMDA. doi: http://dx.doi.org/10.1016/j.jamda.2016.07.024.
Whether you’re a hospitalist who works only in a hospital, a hospitalist who works only in a post-acute care (PAC) setting, or a hospitalist who works in both types of facilities, knowing about current trends at PAC facilities and what the future may hold can help you excel in your current capacity and, ultimately, improve patient care.
The Hospitalist tapped experts in the post-acute space to tell us what they thought HM should know about working in PAC – which, in many ways, is quite different from the hospital setting. Here’s a compilation of their top eight must-knows.
1. PAC settings rely more on mid-level medical staff than hospitals do.
PAC facilities employ more mid-level providers, such as nurse practitioners and physician assistants, because they can support the level of medical complexity and decision making 95% of the time, says James D. Tollman, MD, FHM, president of Essex Inpatient Physicians in Boxford, Mass. Further, they are more heavily staffed by licensed practical nurses than are acute-care settings.
Usually, there is no physician or nurse practitioner presence at night. Clinicians rely on nursing staff’s assessment to make decisions regarding changes in patient status during off-hours, says Virginia Cummings, MD, director of long-term care, gerontology division, at Boston-based Beth Israel Deaconess Medical Center.
2. Testing takes longer, and options are limited.
Access to some acute urgent resources such as laboratory testing, imaging tests, and pharmacy products is more challenging at PAC facilities because most of these resources are not on-site. Consequently, there is a time lag between ordering tests and new medications and implementing these orders.
“If a patient needs something performed diagnostically immediately, they usually have to be transported to the emergency room or a facility with the necessary testing equipment,” Dr. Tollman says.
However, Paul T. Liistro, managing partner, Arbors of Hop Brook Limited Partnership in Manchester, Conn., and Vernon Manor Health Care Center in Vernon, Conn., and administrator, Manchester Manor Health Care Center, notes that it’s possible for a laboratory service or mobile diagnostic unit to provide laboratory testing or certain imaging at a PAC facility. More-involved diagnostics, such as an MRI or a PET scan, typically require testing at a remote location.
3. Patient populations mainly include rehab and terminally ill patients.
Patients are typically sent to a PAC facility either to recover from an illness or injury or because they are chronically ill and have exhausted treatment options. Regarding the latter, “They are mostly there for palliation; we don’t perform daily tests or prescribe aggressive medications on these patients,” Dr. Nazir says.
Dr. Cummings explains that PAC clinicians go through “the dying process with the patient.”
“They may or may not have assistance from hospice organizations,” she says, “and when they don’t, [hospitalists] take on the role of palliative-care providers.”
Dr. Cummings has seen an increase in psychiatric patients entering PAC facilities.
“Many patients with chronic psychological problems are aging, and there are fewer inpatient psychiatric beds available to those with concurrent medical and psychiatric problems,” she says. Much of this work is now being done in PAC settings. 
4. You can build a relationship with your patient.
Because the pace of a PAC facility is slower and a patient typically stays in a PAC facility longer than at a hospital, there’s time for a hospitalist to have more in-depth conversations with patients and their families.
“Building a deeper relationship with a patient may give the hospitalist an opportunity to discover the cause of an acute problem,” Dr. Nazir says. “They can go in-depth into the psychosocial aspect of medicine and may be able to find out what led to the initial problem and the real root cause, which can help prevent future recurrences, such as repeat falls or forgetting to take a medication.”
5. Using EHRs can improve transitions.
Care transitions between a hospital and PAC facility can be compromised by a lack of information sharing, and they can affect the quality and safety of patient care, says Dori Cross, a doctoral candidate in health services organization and policy at the University of Michigan School of Public Health in Ann Arbor. Handoffs between providers require information continuity – information that is complete, timely, and in a usable format – to ensure appropriate medical decisions and to provide high-quality care during and after transition.
Electronic health records (EHRs) as well as health information exchanges (HIEs) allow providers to communicate and share patient information. For example, hospitals can send information electronically to PAC facilities (“push” exchange) or make information available online securely for PAC providers to log in and access (“pull” exchange). According to a 2014 survey data by the American Hospital Association, more than 50% of hospitals report sending structured summary-of-care records electronically to long-term care settings; a little less than half of those hospitals (23% of the total sample of hospitals) were also receiving information electronically from long-term care sites.1
“This bidirectional exchange, in particular, can make it easier to share information across provider organizations electronically and, in turn, improve care delivery,” says Ms. Cross, who authored an accepted paper on the subject in the Journal of Post-Acute and Long-Term Medicine.
6. Hospitalists can work with providers in PAC settings to improve transitions.
Despite improvements in the electronic transfer of medical information, gaps still exist and can cause problems. One chasm when discharging patients to a PAC facility, is when a hospital IT system is incapable of communicating with the PAC facility system. In this instance, Dr. Nazir says, the hospitalist “can help bridge the gap.”
“[We] can verbally relay relevant information to physicians at PAC facilities so they understand the patient’s status, needs, and expectations,” he says. “Furthermore, hospitalists and a PAC facility’s administration can brainstorm methods to improve the systems of care so the patient receives more effective and timely care.”
7. Hospitalists switching to the PAC setting should have formal training.
The two main obstacles for hospitalists who change from working in a hospital to a PAC facility are the lack of exposure to PAC work in training and the assumption that it requires the same skills sets of a typical hospitalist, according to Manoj K. Mathew, MD, SFHM, national medical director of Los Angeles–based Agilon Health. The PAC setting has quite a number of differences compared with a hospital setting. For example, some regulations apply specifically to PAC facilities. In addition to formal training, hospitalists can benefit from using SHM’s Post-Acute Care Transitions Toolkit, having a mentor, or using resources from other organizations that function in this space such as The Society for Post-Acute and Long-Term Care Medicine, Dr. Nazir says.
8. A variety of payors and payment models are in play.
Commercial insurers continue to be major payors for PAC, especially for individuals younger than 65 years. Medicare and Medicaid, administered by the Centers for Medicare & Medicaid Services, are the primary payors for patients aged 65 years and older.
“These scorecards are using a variety of criteria to rank providers, such as length of stay, cost, readmissions to hospitals, and quality.”
Because Medicare Part A covers many patients discharged to a PAC setting, any changes in payment incentives or benefit structures by the Medicare program will drive changes in PAC. 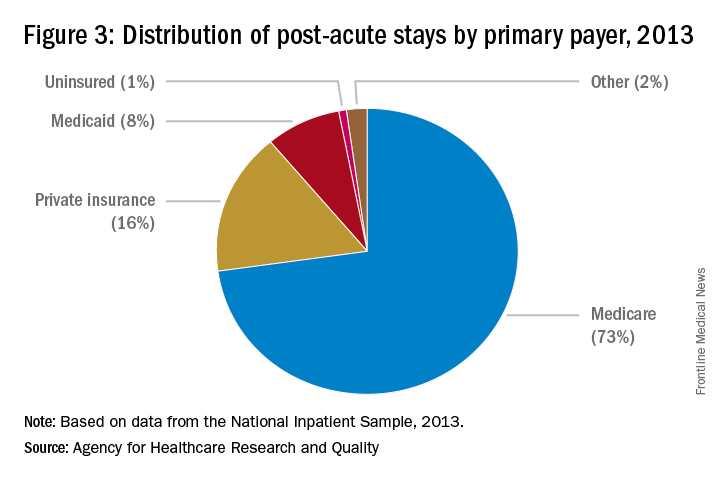
“For example, as Medicare implements payment adjustments for hospitals that have high rates of readmissions, hospitals have a new incentive to work closely with SNFs and other providers of PAC to ensure patients can avoid unnecessary readmissions,” says Tiffany A. Radcliff, PhD, a health economist and associate professor in the department of health policy and management at Texas A&M University School of Public Health in College Station.
Providers must follow the billing rules for each payor. The rules for Medicare payments are outlined on CMS’ website. Bundled payments for PAC under the Medicare Part A program are scheduled to be implemented by 2018.
Reference
Cross DA, Adler-Milstein J. Investing in post-acute care transitions: electronic information exchange between hospitals and long-term care facilities [published online ahead of print Sept. 14, 2016]. JAMDA. doi: http://dx.doi.org/10.1016/j.jamda.2016.07.024.
Tips for Working with Difficult Doctors
As a hospitalist, caring for critically ill or injured patients can be stressful and demanding. Working with difficult doctors, those who exhibit intimidating and disruptive behaviors such as verbal outbursts and physical threats as well as passive activities such as refusing to perform assigned tasks, can make the work environment even more challenging.1 Some docs are routinely reluctant—or refuse—to answer questions or return phone calls or pages. Some communicate in condescending language or voice intonation; some are brutally impatient.1
The most difficult doctors to work with are those who are not aligned with the hospital’s or treatment team’s goals and those who aren’t open to feedback and coaching, says Rob Zipper, MD, MMM, SFHM, regional chief medical officer of Sound Physicians, based in Tacoma, Wash.
“If physicians are aware of a practice’s guidelines and goals but simply won’t comply with them, it makes it harder on everyone else who is pulling the ship in the same direction,” he says.
Unruly physicians don’t just annoy their coworkers. According to a sentinel event alert from The Joint Commission, they can:
- foster medical errors;
- contribute to poor patient satisfaction;
- contribute to preventable adverse outcomes;
- increase the cost of care;
- undermine team effectiveness; and
- cause qualified clinicians, administrators, and managers to seek new positions in more professional environments.1
“These issues are all connected,” says Stephen R. Nichols, MD, chief of clinical operations performance at the Schumacher Group in Brownwood, Texas. “Disruptive behaviors create mitigated communications and dissatisfaction among staff, which bleeds over into other aspects that are involved secondarily.”
Stephen M. Paskoff, Esq., president and CEO of ELI in Atlanta, can attest to the most severe consequences of bad behavior on patient care.
At one institution, a surgeon’s disruptive behavior lead to a coworker forgetting to perform a procedure and a patient dying.2 In another incident, the emergency department stopped calling on a medical subspecialist who was predictably abusive. The subspecialist knew how to treat a specific patient with an unusual intervention. Since the specialist was not consulted initially, the patient ended up in the intensive care unit.2
One bad hospitalist can bring down the reputation of an entire team.
“Many programs are incentivized based on medical staff and primary-care physicians’ perceptions of their care, so there are direct and indirect consequences,” Dr. Zipper says.
The bottom line, says Felix Aguirre, MD, SFHM, vice president of medical affairs at IPC Healthcare in North Hollywood, Calif., is that it only takes one bad experience to tarnish a group, but it takes many positive experiences to erase the damage.
The Roots of Evil
Intimidating and disruptive behavior stems from both individual and systemic factors. Care providers who exhibit characteristics such as self-centeredness, immaturity, or defensiveness can be more prone to unprofessional behavior. They can lack interpersonal, coping, or conflict-management skills.1
Systemic factors are marked by pressures related to increased productivity demands, cost-containment requirements, embedded hierarchies, and fear of litigation in the healthcare environment. These pressures can be further exacerbated by changes to or differences in the authority, autonomy, empowerment, and roles or values of professionals on the healthcare team as well as by the continual daily changes in shifts, rotations, and interdepartmental support staff. This dynamic creates challenges for interprofessional communication and development of trust among team members.1
According to The Joint Commission, intimidating and disruptive behaviors are often manifested by healthcare professionals in positions of power.1 But other members of the care team can be problematic as well.
“In my experience, conflicts usually revolve around different perspectives and objectives, even if both parties are acting respectfully,” Dr. Zipper says. “Sometimes, however, providers or other care team members are tired or stressed and don’t behave professionally.”
Paskoff, who has more than 40 years of experience in healthcare-related workplace issues, including serving as an investigator for the U.S. Equal Employment Opportunity Commission, says some doctors learn bad behaviors from their mentors and that behaviors can be passed down through generations because they are tolerated.
“When I asked one physician who had outstanding training and an outstanding technical reputation how he became abusive, he said, ‘I learned from the best.’” Paskoff was actually able to track the doctor’s training to the late 1800s and physicians who were known for similar behaviors.
Confronting Those Who Misbehave
Dr. Zipper says physicians should confront behavioral issues directly.
“I will typically discuss a complaint with a doctor privately, and ask him or her what happened without being accusatory,” he says. “I try to provide as much concrete and objective information as I can. The doctor needs to know that you are trying to help him or her succeed. That said, if something is clearly bad behavior, feedback should be direct and include a statement such as, ‘This is not how we behave in this practice.’”
At times, it may not be possible to discuss an emergent matter, such as during a code blue.
“However, I will often ask if anyone on the code team has any ideas or concerns before ending the code,” Dr. Nichols says. “Then after the critical time has passed, it is important to debrief and reconnect with the team, especially the less-experienced members who may have lingering concerns.”
For many employees, however, it is difficult to report disruptive behaviors. This is due to a fear of retaliation and the stigma associated with “blowing the whistle” on a colleague as well as a general reluctance to confront an intimidator.1
If an employee cannot muster the courage to confront a disruptive coworker or if the issue isn’t resolved by talking with the difficult individual, an employee should be a good citizen and report bad behavior to the appropriate hospital authority in a timely manner, says A. Kevin Troutman, Esq., a partner at Fisher Phillips in Houston and a former healthcare human resources executive.
Hospitals accredited by The Joint Commission are required to create a code of conduct that defines disruptive and inappropriate behaviors. In addition, leaders must create and implement a process for managing these behaviors.1
Helping Difficult Doctors
After a physician or another employee has been called out for bad behavior, steps need to be taken to correct the problem. Robert Fuller, Esq., an attorney with Nelson Hardiman, LLP, in Los Angeles, has found a positive-oriented intervention called “the 3-Ds”—which stands for diagnose, design, and do—that has been a successful tool for achieving positive change. The strategy involves a supervisor and employee mutually developing a worksheet to diagnose the problem. Next, they design a remediation and improvement plan. Finally, they implement the plan and specify dates to achieve certain milestones. Coworkers should be informed of the plan and be urged to support it.
“Make it clear that the positive aspect of this plan turns to progressive discipline, including termination, if the employee doesn’t improve or abandons the plan of action,” Fuller says. In most cases, troublemakers will make a sincere effort to control disruptive tendencies.
Troutman suggests enlisting the assistance of a respected peer.
“Have a senior-level doctor help the noncompliant physician understand why his or her behavior creates problems for everyone, including the doctor himself,” he says. “Also, consider connecting compensation and other rewards to job performance, which encompasses good behavior and good citizenship within the organization. Make expectations and consequences clear.”
If an employee has a recent change in behavior, ask if there is a reason.
“It is my experience that sudden changes in behaviors are often the result of a personal or clinical issue, so it is important and humane to make certain that there is not some other cause for the change before assuming someone is simply being disruptive or difficult,” Dr. Nichols says.
Many healthcare institutions are now setting up centers of professionalism. Paskoff reports that The Center for Professionalism and Peer Support (CPPS) was created in 2008 at Brigham and Women’s Hospital in Boston to educate the hospital community regarding professionalism and manage unprofessional behavior.3 CPPS has established standards of behavior and a framework to deal with difficult behaviors.
“An employee is told what he or she is doing wrong, receives counseling, and is given resources to improve,” he explains. “If an employee doesn’t improve, he or she is told that the behavior won’t be tolerated.”
Dismissing Bad Employees
After addressing the specifics of unacceptable behavior and explaining the consequences of repeating it, leadership should monitor subsequent conduct and provide feedback.
“If the employee commits other violations or behaves badly, promptly address the misconduct again and make it clear that further such actions will not be tolerated,” Troutman says. “Expect immediate and sustained improvement and compliance. Be consistent, and if bad conduct continues after an opportunity to improve, do not prolong anyone’s suffering. Instead, terminate the disruptive employee. When you do, make the reasons clear.”
Karen Appold is a medical writer in Pennsylvania.
References
- Behaviors that undermine a culture of safety. The Joint Commission website. Accessed April 17, 2015.
- Whittemore AD, New England Society for Vascular Surgery. The impact of professionalism on safe surgical care. J Vasc Surg. 2007;45(2):415-419.
- Shapiro J, Whittemore A, Tsen LC. Instituting a culture of professionalism: the establishment of a center for professionalism and peer support. Jt Comm J Qual Patient Saf. 2014;40(4):168-177.
As a hospitalist, caring for critically ill or injured patients can be stressful and demanding. Working with difficult doctors, those who exhibit intimidating and disruptive behaviors such as verbal outbursts and physical threats as well as passive activities such as refusing to perform assigned tasks, can make the work environment even more challenging.1 Some docs are routinely reluctant—or refuse—to answer questions or return phone calls or pages. Some communicate in condescending language or voice intonation; some are brutally impatient.1
The most difficult doctors to work with are those who are not aligned with the hospital’s or treatment team’s goals and those who aren’t open to feedback and coaching, says Rob Zipper, MD, MMM, SFHM, regional chief medical officer of Sound Physicians, based in Tacoma, Wash.
“If physicians are aware of a practice’s guidelines and goals but simply won’t comply with them, it makes it harder on everyone else who is pulling the ship in the same direction,” he says.
Unruly physicians don’t just annoy their coworkers. According to a sentinel event alert from The Joint Commission, they can:
- foster medical errors;
- contribute to poor patient satisfaction;
- contribute to preventable adverse outcomes;
- increase the cost of care;
- undermine team effectiveness; and
- cause qualified clinicians, administrators, and managers to seek new positions in more professional environments.1
“These issues are all connected,” says Stephen R. Nichols, MD, chief of clinical operations performance at the Schumacher Group in Brownwood, Texas. “Disruptive behaviors create mitigated communications and dissatisfaction among staff, which bleeds over into other aspects that are involved secondarily.”
Stephen M. Paskoff, Esq., president and CEO of ELI in Atlanta, can attest to the most severe consequences of bad behavior on patient care.
At one institution, a surgeon’s disruptive behavior lead to a coworker forgetting to perform a procedure and a patient dying.2 In another incident, the emergency department stopped calling on a medical subspecialist who was predictably abusive. The subspecialist knew how to treat a specific patient with an unusual intervention. Since the specialist was not consulted initially, the patient ended up in the intensive care unit.2
One bad hospitalist can bring down the reputation of an entire team.
“Many programs are incentivized based on medical staff and primary-care physicians’ perceptions of their care, so there are direct and indirect consequences,” Dr. Zipper says.
The bottom line, says Felix Aguirre, MD, SFHM, vice president of medical affairs at IPC Healthcare in North Hollywood, Calif., is that it only takes one bad experience to tarnish a group, but it takes many positive experiences to erase the damage.
The Roots of Evil
Intimidating and disruptive behavior stems from both individual and systemic factors. Care providers who exhibit characteristics such as self-centeredness, immaturity, or defensiveness can be more prone to unprofessional behavior. They can lack interpersonal, coping, or conflict-management skills.1
Systemic factors are marked by pressures related to increased productivity demands, cost-containment requirements, embedded hierarchies, and fear of litigation in the healthcare environment. These pressures can be further exacerbated by changes to or differences in the authority, autonomy, empowerment, and roles or values of professionals on the healthcare team as well as by the continual daily changes in shifts, rotations, and interdepartmental support staff. This dynamic creates challenges for interprofessional communication and development of trust among team members.1
According to The Joint Commission, intimidating and disruptive behaviors are often manifested by healthcare professionals in positions of power.1 But other members of the care team can be problematic as well.
“In my experience, conflicts usually revolve around different perspectives and objectives, even if both parties are acting respectfully,” Dr. Zipper says. “Sometimes, however, providers or other care team members are tired or stressed and don’t behave professionally.”
Paskoff, who has more than 40 years of experience in healthcare-related workplace issues, including serving as an investigator for the U.S. Equal Employment Opportunity Commission, says some doctors learn bad behaviors from their mentors and that behaviors can be passed down through generations because they are tolerated.
“When I asked one physician who had outstanding training and an outstanding technical reputation how he became abusive, he said, ‘I learned from the best.’” Paskoff was actually able to track the doctor’s training to the late 1800s and physicians who were known for similar behaviors.
Confronting Those Who Misbehave
Dr. Zipper says physicians should confront behavioral issues directly.
“I will typically discuss a complaint with a doctor privately, and ask him or her what happened without being accusatory,” he says. “I try to provide as much concrete and objective information as I can. The doctor needs to know that you are trying to help him or her succeed. That said, if something is clearly bad behavior, feedback should be direct and include a statement such as, ‘This is not how we behave in this practice.’”
At times, it may not be possible to discuss an emergent matter, such as during a code blue.
“However, I will often ask if anyone on the code team has any ideas or concerns before ending the code,” Dr. Nichols says. “Then after the critical time has passed, it is important to debrief and reconnect with the team, especially the less-experienced members who may have lingering concerns.”
For many employees, however, it is difficult to report disruptive behaviors. This is due to a fear of retaliation and the stigma associated with “blowing the whistle” on a colleague as well as a general reluctance to confront an intimidator.1
If an employee cannot muster the courage to confront a disruptive coworker or if the issue isn’t resolved by talking with the difficult individual, an employee should be a good citizen and report bad behavior to the appropriate hospital authority in a timely manner, says A. Kevin Troutman, Esq., a partner at Fisher Phillips in Houston and a former healthcare human resources executive.
Hospitals accredited by The Joint Commission are required to create a code of conduct that defines disruptive and inappropriate behaviors. In addition, leaders must create and implement a process for managing these behaviors.1
Helping Difficult Doctors
After a physician or another employee has been called out for bad behavior, steps need to be taken to correct the problem. Robert Fuller, Esq., an attorney with Nelson Hardiman, LLP, in Los Angeles, has found a positive-oriented intervention called “the 3-Ds”—which stands for diagnose, design, and do—that has been a successful tool for achieving positive change. The strategy involves a supervisor and employee mutually developing a worksheet to diagnose the problem. Next, they design a remediation and improvement plan. Finally, they implement the plan and specify dates to achieve certain milestones. Coworkers should be informed of the plan and be urged to support it.
“Make it clear that the positive aspect of this plan turns to progressive discipline, including termination, if the employee doesn’t improve or abandons the plan of action,” Fuller says. In most cases, troublemakers will make a sincere effort to control disruptive tendencies.
Troutman suggests enlisting the assistance of a respected peer.
“Have a senior-level doctor help the noncompliant physician understand why his or her behavior creates problems for everyone, including the doctor himself,” he says. “Also, consider connecting compensation and other rewards to job performance, which encompasses good behavior and good citizenship within the organization. Make expectations and consequences clear.”
If an employee has a recent change in behavior, ask if there is a reason.
“It is my experience that sudden changes in behaviors are often the result of a personal or clinical issue, so it is important and humane to make certain that there is not some other cause for the change before assuming someone is simply being disruptive or difficult,” Dr. Nichols says.
Many healthcare institutions are now setting up centers of professionalism. Paskoff reports that The Center for Professionalism and Peer Support (CPPS) was created in 2008 at Brigham and Women’s Hospital in Boston to educate the hospital community regarding professionalism and manage unprofessional behavior.3 CPPS has established standards of behavior and a framework to deal with difficult behaviors.
“An employee is told what he or she is doing wrong, receives counseling, and is given resources to improve,” he explains. “If an employee doesn’t improve, he or she is told that the behavior won’t be tolerated.”
Dismissing Bad Employees
After addressing the specifics of unacceptable behavior and explaining the consequences of repeating it, leadership should monitor subsequent conduct and provide feedback.
“If the employee commits other violations or behaves badly, promptly address the misconduct again and make it clear that further such actions will not be tolerated,” Troutman says. “Expect immediate and sustained improvement and compliance. Be consistent, and if bad conduct continues after an opportunity to improve, do not prolong anyone’s suffering. Instead, terminate the disruptive employee. When you do, make the reasons clear.”
Karen Appold is a medical writer in Pennsylvania.
References
- Behaviors that undermine a culture of safety. The Joint Commission website. Accessed April 17, 2015.
- Whittemore AD, New England Society for Vascular Surgery. The impact of professionalism on safe surgical care. J Vasc Surg. 2007;45(2):415-419.
- Shapiro J, Whittemore A, Tsen LC. Instituting a culture of professionalism: the establishment of a center for professionalism and peer support. Jt Comm J Qual Patient Saf. 2014;40(4):168-177.
As a hospitalist, caring for critically ill or injured patients can be stressful and demanding. Working with difficult doctors, those who exhibit intimidating and disruptive behaviors such as verbal outbursts and physical threats as well as passive activities such as refusing to perform assigned tasks, can make the work environment even more challenging.1 Some docs are routinely reluctant—or refuse—to answer questions or return phone calls or pages. Some communicate in condescending language or voice intonation; some are brutally impatient.1
The most difficult doctors to work with are those who are not aligned with the hospital’s or treatment team’s goals and those who aren’t open to feedback and coaching, says Rob Zipper, MD, MMM, SFHM, regional chief medical officer of Sound Physicians, based in Tacoma, Wash.
“If physicians are aware of a practice’s guidelines and goals but simply won’t comply with them, it makes it harder on everyone else who is pulling the ship in the same direction,” he says.
Unruly physicians don’t just annoy their coworkers. According to a sentinel event alert from The Joint Commission, they can:
- foster medical errors;
- contribute to poor patient satisfaction;
- contribute to preventable adverse outcomes;
- increase the cost of care;
- undermine team effectiveness; and
- cause qualified clinicians, administrators, and managers to seek new positions in more professional environments.1
“These issues are all connected,” says Stephen R. Nichols, MD, chief of clinical operations performance at the Schumacher Group in Brownwood, Texas. “Disruptive behaviors create mitigated communications and dissatisfaction among staff, which bleeds over into other aspects that are involved secondarily.”
Stephen M. Paskoff, Esq., president and CEO of ELI in Atlanta, can attest to the most severe consequences of bad behavior on patient care.
At one institution, a surgeon’s disruptive behavior lead to a coworker forgetting to perform a procedure and a patient dying.2 In another incident, the emergency department stopped calling on a medical subspecialist who was predictably abusive. The subspecialist knew how to treat a specific patient with an unusual intervention. Since the specialist was not consulted initially, the patient ended up in the intensive care unit.2
One bad hospitalist can bring down the reputation of an entire team.
“Many programs are incentivized based on medical staff and primary-care physicians’ perceptions of their care, so there are direct and indirect consequences,” Dr. Zipper says.
The bottom line, says Felix Aguirre, MD, SFHM, vice president of medical affairs at IPC Healthcare in North Hollywood, Calif., is that it only takes one bad experience to tarnish a group, but it takes many positive experiences to erase the damage.
The Roots of Evil
Intimidating and disruptive behavior stems from both individual and systemic factors. Care providers who exhibit characteristics such as self-centeredness, immaturity, or defensiveness can be more prone to unprofessional behavior. They can lack interpersonal, coping, or conflict-management skills.1
Systemic factors are marked by pressures related to increased productivity demands, cost-containment requirements, embedded hierarchies, and fear of litigation in the healthcare environment. These pressures can be further exacerbated by changes to or differences in the authority, autonomy, empowerment, and roles or values of professionals on the healthcare team as well as by the continual daily changes in shifts, rotations, and interdepartmental support staff. This dynamic creates challenges for interprofessional communication and development of trust among team members.1
According to The Joint Commission, intimidating and disruptive behaviors are often manifested by healthcare professionals in positions of power.1 But other members of the care team can be problematic as well.
“In my experience, conflicts usually revolve around different perspectives and objectives, even if both parties are acting respectfully,” Dr. Zipper says. “Sometimes, however, providers or other care team members are tired or stressed and don’t behave professionally.”
Paskoff, who has more than 40 years of experience in healthcare-related workplace issues, including serving as an investigator for the U.S. Equal Employment Opportunity Commission, says some doctors learn bad behaviors from their mentors and that behaviors can be passed down through generations because they are tolerated.
“When I asked one physician who had outstanding training and an outstanding technical reputation how he became abusive, he said, ‘I learned from the best.’” Paskoff was actually able to track the doctor’s training to the late 1800s and physicians who were known for similar behaviors.
Confronting Those Who Misbehave
Dr. Zipper says physicians should confront behavioral issues directly.
“I will typically discuss a complaint with a doctor privately, and ask him or her what happened without being accusatory,” he says. “I try to provide as much concrete and objective information as I can. The doctor needs to know that you are trying to help him or her succeed. That said, if something is clearly bad behavior, feedback should be direct and include a statement such as, ‘This is not how we behave in this practice.’”
At times, it may not be possible to discuss an emergent matter, such as during a code blue.
“However, I will often ask if anyone on the code team has any ideas or concerns before ending the code,” Dr. Nichols says. “Then after the critical time has passed, it is important to debrief and reconnect with the team, especially the less-experienced members who may have lingering concerns.”
For many employees, however, it is difficult to report disruptive behaviors. This is due to a fear of retaliation and the stigma associated with “blowing the whistle” on a colleague as well as a general reluctance to confront an intimidator.1
If an employee cannot muster the courage to confront a disruptive coworker or if the issue isn’t resolved by talking with the difficult individual, an employee should be a good citizen and report bad behavior to the appropriate hospital authority in a timely manner, says A. Kevin Troutman, Esq., a partner at Fisher Phillips in Houston and a former healthcare human resources executive.
Hospitals accredited by The Joint Commission are required to create a code of conduct that defines disruptive and inappropriate behaviors. In addition, leaders must create and implement a process for managing these behaviors.1
Helping Difficult Doctors
After a physician or another employee has been called out for bad behavior, steps need to be taken to correct the problem. Robert Fuller, Esq., an attorney with Nelson Hardiman, LLP, in Los Angeles, has found a positive-oriented intervention called “the 3-Ds”—which stands for diagnose, design, and do—that has been a successful tool for achieving positive change. The strategy involves a supervisor and employee mutually developing a worksheet to diagnose the problem. Next, they design a remediation and improvement plan. Finally, they implement the plan and specify dates to achieve certain milestones. Coworkers should be informed of the plan and be urged to support it.
“Make it clear that the positive aspect of this plan turns to progressive discipline, including termination, if the employee doesn’t improve or abandons the plan of action,” Fuller says. In most cases, troublemakers will make a sincere effort to control disruptive tendencies.
Troutman suggests enlisting the assistance of a respected peer.
“Have a senior-level doctor help the noncompliant physician understand why his or her behavior creates problems for everyone, including the doctor himself,” he says. “Also, consider connecting compensation and other rewards to job performance, which encompasses good behavior and good citizenship within the organization. Make expectations and consequences clear.”
If an employee has a recent change in behavior, ask if there is a reason.
“It is my experience that sudden changes in behaviors are often the result of a personal or clinical issue, so it is important and humane to make certain that there is not some other cause for the change before assuming someone is simply being disruptive or difficult,” Dr. Nichols says.
Many healthcare institutions are now setting up centers of professionalism. Paskoff reports that The Center for Professionalism and Peer Support (CPPS) was created in 2008 at Brigham and Women’s Hospital in Boston to educate the hospital community regarding professionalism and manage unprofessional behavior.3 CPPS has established standards of behavior and a framework to deal with difficult behaviors.
“An employee is told what he or she is doing wrong, receives counseling, and is given resources to improve,” he explains. “If an employee doesn’t improve, he or she is told that the behavior won’t be tolerated.”
Dismissing Bad Employees
After addressing the specifics of unacceptable behavior and explaining the consequences of repeating it, leadership should monitor subsequent conduct and provide feedback.
“If the employee commits other violations or behaves badly, promptly address the misconduct again and make it clear that further such actions will not be tolerated,” Troutman says. “Expect immediate and sustained improvement and compliance. Be consistent, and if bad conduct continues after an opportunity to improve, do not prolong anyone’s suffering. Instead, terminate the disruptive employee. When you do, make the reasons clear.”
Karen Appold is a medical writer in Pennsylvania.
References
- Behaviors that undermine a culture of safety. The Joint Commission website. Accessed April 17, 2015.
- Whittemore AD, New England Society for Vascular Surgery. The impact of professionalism on safe surgical care. J Vasc Surg. 2007;45(2):415-419.
- Shapiro J, Whittemore A, Tsen LC. Instituting a culture of professionalism: the establishment of a center for professionalism and peer support. Jt Comm J Qual Patient Saf. 2014;40(4):168-177.
Experts Suggest Ways to Deal with Challenges Surrounding Care of Psychiatric Patients
In 1955, there was one psychiatric bed for every 300 Americans. By 2005, following the widespread shuttering or downsizing of psychiatric hospitals in the 1990s, that number had shrunk to one bed for every 3,000 Americans.1
In 2008, an estimated 39.8 million Americans age 18 or older had mental illness, which represents 17.7% of U.S. adults.2 In 2013, this number rose to an estimated 43.8 million, or 18.5% of U.S. adults (see Figure 1).3
“It’s like we have returned to the early 19th century, when mentally ill persons were held in prisons or temporarily kept in hospital settings,” says Ricardo Bianco, PsyD, program director of the Master of Arts in counseling and health psychology at William James College in Newton, Mass. “The problem is that the healthcare system did not catch up to absorb the mentally ill population.
“As a result, hospital staffs are inadequately trained, there is insufficient funding for these patients, and there are not enough human resource personnel to manage them. Consequently, hospitalists are overwhelmed with cases that should be primarily treated by psychologists, psychiatrists, and social workers.”
According to David M. Grace, MD, SFHM, hospitalist and senior medical officer at the Schumacher Group in Lafayette, La., two groups of psychiatric patients present to the acute-care hospital environment: those who are there for a primary psychiatric problem and those who have a medical problem and a psychiatric comorbidity. The first group of patients presents distinct challenges. U.S. hospitals lack two-thirds of the minimum number of beds needed to care for this population. The second group is problematic because psychiatric issues often cloud the medical issues of a patient, increasing both diagnostic uncertainty and resource utilization.
Challenges Abound
Psychiatric patients present a number of problems for hospitalists. First, it is difficult to decipher what comprises a psychiatric issue and what does not because “many psychiatric conditions manifest as physical symptoms and they often require significant resource consumption to diagnose,” Dr. Grace says. Secondly, some patients present with a severe primary psychiatric problem in which they are homicidal, suicidal, or gravely disabled.
In addition, psychiatric patients tend to have a greater incidence of noncompliance with imaging, laboratory work, medication, and general medical care, says Daniel Sussman, MD, a hospitalist at IPC Healthcare, Inc., based in North Hollywood, Calif. He also serves as interim chairman in the department of psychiatry at St. John’s Episcopal Hospital in Far Rockaway, N.Y.
Clinically, potential interactions between psychiatric medications and medically related prescription drugs are always a concern, notes Dr. Sussman, who says more than 70% of patients admitted to St. John’s Episcopal Hospital have a major psychiatric illness in addition to their medical problem. Psychiatric medications, which patients may have tolerated well when they were stable, may be too sedating when patients are ill. Side effects and adverse reactions of psychotropic medications must also be considered when diagnosing and treating medical illnesses. Metabolic syndrome is more commonly seen and is a factor in the development and subsequent treatment of other illnesses.
Another challenge stems from the fact that patients with substantial psychiatric comorbidities can have significant and rapid mood and behavioral changes as well as sudden, volatile, and aggressive outbursts—both verbal and physical.
“Staff members who interact with the patient are at risk if an outburst occurs,” says Emily Fingado, MD, FAAP, a pediatric hospitalist and clinical assistant professor of pediatrics at Nemours/Alfred I. duPont Hospital for Children (Nemours/AIDHC) of the Sidney Kimmel Medical College at Thomas Jefferson University in Wilmington, Del.
Such situations can become scary, particularly if someone with psychiatric expertise is not available to intervene. This can be very frustrating for hospitalists who want to provide high-level care but may lack the training needed to be successful with such patients. This can ultimately lead to burnout, says Sarah Rivelli, MD, medical director of psychiatry clinical services at Duke University Hospital and Duke University Medical Center in Durham, N.C.
Another challenge is that although there are protocols in place designed to follow specific steps for patients with physical illnesses or disorders, that’s not the case for psychiatric illness. “Many hospital facilities are not designed, or have yet to implement, protocols to attend to mentally ill individuals,” Dr. Bianco says.
Because of the unpredictability of patients and lack of practice protocols, mental illness can introduce a wild card into the standard treatment process. A more individualized approach with these patients is needed, but with increasing focus on length of stay and operational efficiency, medical and nursing staffs are pressured to do things quickly and to do more with less. It can be very time-consuming for a nurse to have to explain to paranoid patients why they should take their medication or for a phlebotomist to try to calm patients in order to obtain blood. When patients refuse needed tests, or only provide a limited history, the hospitalist ends up working with incomplete information, which makes choosing and monitoring the treatment approach problematic.
A Look at Best Practices
In light of challenges, some best practices have been identified for handling psychiatric patients. As previously mentioned, most hospital staffs have limited formal training in interacting with psychiatric patients. In fact, the American Board of Internal Medicine only devotes 4% of the certification exam to psychiatry.4
Ideally, staff members who care for psychiatric patients will have specialized or additional training in managing patients with psychiatric conditions or comorbidities. Nemours/AIDHC has a committee assigned to evaluate psychiatric patients’ care and help manage them when a behavioral emergency occurs, Dr. Fingado says. This team, which has been trained on de-escalation, restraint techniques and policies, as well as medications to use in these situations, intervenes when patients have an aggressive event that places patients, visitors, or staff at risk. The team includes nursing staff, the hospitalist on-call, and security personnel and involves the social work, psychology, and psychiatry departments.
Training focused on treating patients with psychiatric conditions should include how to recognize substance abuse and treat substance withdrawal because mental illness and substance abuse often track together, Dr. Sussman notes. At St. John’s Episcopal Hospital, patients with chronic mental illness are not the ones who typically become aggressive or violent. Rather, this is more often the case among patients with substance abuse either in states of acute intoxication or withdrawal.
Recently, Dr. Sussman has seen a significant increase in patients who abuse K2, or spice, a synthetic form of cannabis. Side effects of using K2 include rapid heart rate, anxiety, hallucinations, and paranoia to the point of delusional thinking. These side effects can frequently wax and wane for days after the drug is used, and they can be associated with significant psychomotor agitation and assaultive behavior.
When patients abuse flake, another synthetic drug that has been reported in the Southeast, they tend to become very paranoid and violent. “These patients can be extremely unpredictable and aggressive,” he says. “Patients with dementia can be impulsive and aggressive during care, and caution is needed, but it’s not a directed violence like that seen in patients who are agitated secondary to substance abuse.”
Dr. Bianco advises having a predetermined triage system or a scale that can assess and measure patients’ level of psychological distress, which can ensure timely and appropriate evaluation and treatment of psychiatric patients, as well as toxicology screens and mental health protocols, which can aid in diagnosis.
“Technology is an important tool in facilitating integration, including identifying and screening patients, tracking patient progress, encouraging adherence to clinical protocols, facilitating communication between providers, and evaluating the impact of integrated programs,” Dr. Bianco says. Academic hospitals struggle less with this problem, he adds, because they tend to be more adequately funded in all areas of operations, including the field of mental health.
IPC Healthcare hospitalist James N. Horst, DO, a psychiatrist who manages mental health patients in a long-term care and nursing home facility, says he has found standardized general screening tools to be useful. The Hamilton Depression Scale, Beck Anxiety Inventory, and CAGE exam for chemical dependency can be easily administered and scored in any facility setting, he says. These tests include self-administered questions to which the patient answers yes or no. Laboratory work is a secondary tool in psychiatry since few mental illness disorders are based on medical comorbidities.
Dr. Sussman looks to the past, when psychiatrists were part of medical teams rounding in hospitals, for a solution. “An integrated model provides an approach where patient care is less compartmentalized,” he says. “In this model, clinicians are responsible for making sure their patient is treated, not simply focusing on their individual area of expertise. This involves working more closely with an integrated care management team.”
Ideally, this will occur at every level of care: outpatient, inpatient, and emergency department (ED). New York State is attempting to redesign the Medicaid system in this fashion, with the goal of improving overall care and reducing reliance on inpatient treatment to provide that care. This is an enormous initiative, costing more than $8 billion. If successful, it will result in a more patient-centered care system that treats the whole individual, not just the illness, and will positively impact patients’ overall health.
For now, St. John’s Episcopal Hospital has an active psychiatric consultation liaison service that is staffed by both in-house residents and attending physicians who are there 24-7 to help with psychiatric patients.
A ‘Utopia Management’ Perspective
In a dream world, patients with significant psychiatric problems or comorbidities would have coordinated, multidisciplinary care from admission to discharge, Dr. Fingado adds. Ideally, hospitals would have dedicated rooms or areas in the ED that are safe for patients and staff. Psychiatric patients who require observation or admission to a non-psychiatric hospital would be placed in rooms or units dedicated for psychiatric patients, again providing safety for patients and staff, Dr. Fingado surmises.
In addition, all staff members would have training in behavioral health management, including instruction on de-escalation, restraint techniques, and medication use for patients. Ideally, units would be staffed by specially trained aides, nurses, and healthcare providers (i.e., physician assistants, nurse practitioners, physicians), as well as psychologists and psychiatrists, Dr. Fingado says. This type of management would require buy-in from a multitude of groups, including healthcare administrators, nursing and provider staff, as well as health insurance companies. A reallocation or increase in funds would be needed to help build and staff these types of management models and locations, she adds.
In a perfect world, all hospitalized patients would be adequately screened for mental health issues and have their issues appropriately addressed by well-qualified professionals in real time, Dr. Grace says. Telemedicine services have great potential in helping to meet that goal, he says, and more relaxed regulatory guidelines around telemedicine could help make such physician-patient interactions less difficult. Many, if not most, hospitals currently have limited or no access to qualified mental health professionals, a conundrum based on supply, reimbursement, and need.
“Telemedicine, which is already having great success in neurology and intensive care unit medicine, is a great fit for this space,” Dr. Grace says. “Widespread access to a tele-psychiatrist would bring significant tangible benefits to patients, hospitals, hospital staff, and the population at large, who ultimately pay for healthcare in the nation.”
Dr. Horst says he believes everyone who treats psychiatric patients should have education in psychiatric medicine education. One way to achieve this would be to mandate continuing medical education coursework in mental health disorders.
The Reality of a Utopia
Traditionally, our healthcare system has been designed to react to illness, meaning that physicians treat illnesses when individuals become sick.
“But as science and technology now better understand the etiology of most illnesses, we are more equipped to design more preventative interventions rather than wait for individuals to become sick,” Dr. Bianco says. “Prevention interventions require an initial investment that the healthcare system is not necessarily willing to invest in at this time and a shift in the way it charges for services. If the healthcare system is unwilling to go that route, and we know we can prevent many illnesses by shifting the focus of treatment, consequently, human suffering is augmented and quality of life jeopardized.”
More recently, the general population and providers have acknowledged that healing takes place more effectively when it is applied in more integrated approaches (i.e., the utilization of the bio-psycho-social-spiritual model), Dr. Bianco adds. This greater appreciation is demonstrated by different research studies applied to different populations (both the general public and different providers). Despite this, the system (i.e., training) does not support a full integration of interventions.
“The system continues to operate under the traditional medical model that is fragmented and hyper-specialized,” Dr. Bianco says. “Science has demonstrated that the mind and the body work in more complex ways, requiring a more holistic approach to treatment. Although all segments among providers now understand and accept that, the system they dwell in does not support the daily challenges of treatment.
“Treatment continues to be fragmented as it is the medical model. At this point, at a minimum, a hospital should have a psychiatric department composed of individuals who are adequately trained (e.g., health psychology, behavioral medicine) to absorb a portion of individuals who primarily present with mental health issues.” TH
Karen Appold is a freelance medical writer in Pennsylvania.
References
- Torrey EF, Kennard AD, Eslinger D, Lamb R, Pavle J. More mentally ill persons are in jails and prisons than hospitals: a survey of the states. Treatment Advocacy Center website. Available at: http://www.treatmentadvocacycenter.org/storage/documents/final_jails_v_hospitals_study.pdf. May 2010. Accessed August 18, 2015.
- Results from the 2013 national survey on drug use and health: mental health detailed tables. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, U.S. Department of Health & Human Services website. Available at: http://www.samhsa.gov/data/sites/default/files/2013MHDetTabs/NSDUH-MHDetTabs2013.pdf. Accessed August 19, 2015.
- Any mental illness among adults. National Institute of Mental Health website. Available at: http://www.nimh.nih.gov/health/statistics/prevalence/any-mental-illness-ami-among-adults.shtml. Accessed August 19, 2015.
- Internal medicine certification examination blueprint. American Board of Internal Medicine website. Available at: https://www.abim.org/pdf/blueprint/im_cert.pdf. January 2015. Accessed August 19, 2015.
In 1955, there was one psychiatric bed for every 300 Americans. By 2005, following the widespread shuttering or downsizing of psychiatric hospitals in the 1990s, that number had shrunk to one bed for every 3,000 Americans.1
In 2008, an estimated 39.8 million Americans age 18 or older had mental illness, which represents 17.7% of U.S. adults.2 In 2013, this number rose to an estimated 43.8 million, or 18.5% of U.S. adults (see Figure 1).3
“It’s like we have returned to the early 19th century, when mentally ill persons were held in prisons or temporarily kept in hospital settings,” says Ricardo Bianco, PsyD, program director of the Master of Arts in counseling and health psychology at William James College in Newton, Mass. “The problem is that the healthcare system did not catch up to absorb the mentally ill population.
“As a result, hospital staffs are inadequately trained, there is insufficient funding for these patients, and there are not enough human resource personnel to manage them. Consequently, hospitalists are overwhelmed with cases that should be primarily treated by psychologists, psychiatrists, and social workers.”
According to David M. Grace, MD, SFHM, hospitalist and senior medical officer at the Schumacher Group in Lafayette, La., two groups of psychiatric patients present to the acute-care hospital environment: those who are there for a primary psychiatric problem and those who have a medical problem and a psychiatric comorbidity. The first group of patients presents distinct challenges. U.S. hospitals lack two-thirds of the minimum number of beds needed to care for this population. The second group is problematic because psychiatric issues often cloud the medical issues of a patient, increasing both diagnostic uncertainty and resource utilization.
Challenges Abound
Psychiatric patients present a number of problems for hospitalists. First, it is difficult to decipher what comprises a psychiatric issue and what does not because “many psychiatric conditions manifest as physical symptoms and they often require significant resource consumption to diagnose,” Dr. Grace says. Secondly, some patients present with a severe primary psychiatric problem in which they are homicidal, suicidal, or gravely disabled.
In addition, psychiatric patients tend to have a greater incidence of noncompliance with imaging, laboratory work, medication, and general medical care, says Daniel Sussman, MD, a hospitalist at IPC Healthcare, Inc., based in North Hollywood, Calif. He also serves as interim chairman in the department of psychiatry at St. John’s Episcopal Hospital in Far Rockaway, N.Y.
Clinically, potential interactions between psychiatric medications and medically related prescription drugs are always a concern, notes Dr. Sussman, who says more than 70% of patients admitted to St. John’s Episcopal Hospital have a major psychiatric illness in addition to their medical problem. Psychiatric medications, which patients may have tolerated well when they were stable, may be too sedating when patients are ill. Side effects and adverse reactions of psychotropic medications must also be considered when diagnosing and treating medical illnesses. Metabolic syndrome is more commonly seen and is a factor in the development and subsequent treatment of other illnesses.
Another challenge stems from the fact that patients with substantial psychiatric comorbidities can have significant and rapid mood and behavioral changes as well as sudden, volatile, and aggressive outbursts—both verbal and physical.
“Staff members who interact with the patient are at risk if an outburst occurs,” says Emily Fingado, MD, FAAP, a pediatric hospitalist and clinical assistant professor of pediatrics at Nemours/Alfred I. duPont Hospital for Children (Nemours/AIDHC) of the Sidney Kimmel Medical College at Thomas Jefferson University in Wilmington, Del.
Such situations can become scary, particularly if someone with psychiatric expertise is not available to intervene. This can be very frustrating for hospitalists who want to provide high-level care but may lack the training needed to be successful with such patients. This can ultimately lead to burnout, says Sarah Rivelli, MD, medical director of psychiatry clinical services at Duke University Hospital and Duke University Medical Center in Durham, N.C.
Another challenge is that although there are protocols in place designed to follow specific steps for patients with physical illnesses or disorders, that’s not the case for psychiatric illness. “Many hospital facilities are not designed, or have yet to implement, protocols to attend to mentally ill individuals,” Dr. Bianco says.
Because of the unpredictability of patients and lack of practice protocols, mental illness can introduce a wild card into the standard treatment process. A more individualized approach with these patients is needed, but with increasing focus on length of stay and operational efficiency, medical and nursing staffs are pressured to do things quickly and to do more with less. It can be very time-consuming for a nurse to have to explain to paranoid patients why they should take their medication or for a phlebotomist to try to calm patients in order to obtain blood. When patients refuse needed tests, or only provide a limited history, the hospitalist ends up working with incomplete information, which makes choosing and monitoring the treatment approach problematic.
A Look at Best Practices
In light of challenges, some best practices have been identified for handling psychiatric patients. As previously mentioned, most hospital staffs have limited formal training in interacting with psychiatric patients. In fact, the American Board of Internal Medicine only devotes 4% of the certification exam to psychiatry.4
Ideally, staff members who care for psychiatric patients will have specialized or additional training in managing patients with psychiatric conditions or comorbidities. Nemours/AIDHC has a committee assigned to evaluate psychiatric patients’ care and help manage them when a behavioral emergency occurs, Dr. Fingado says. This team, which has been trained on de-escalation, restraint techniques and policies, as well as medications to use in these situations, intervenes when patients have an aggressive event that places patients, visitors, or staff at risk. The team includes nursing staff, the hospitalist on-call, and security personnel and involves the social work, psychology, and psychiatry departments.
Training focused on treating patients with psychiatric conditions should include how to recognize substance abuse and treat substance withdrawal because mental illness and substance abuse often track together, Dr. Sussman notes. At St. John’s Episcopal Hospital, patients with chronic mental illness are not the ones who typically become aggressive or violent. Rather, this is more often the case among patients with substance abuse either in states of acute intoxication or withdrawal.
Recently, Dr. Sussman has seen a significant increase in patients who abuse K2, or spice, a synthetic form of cannabis. Side effects of using K2 include rapid heart rate, anxiety, hallucinations, and paranoia to the point of delusional thinking. These side effects can frequently wax and wane for days after the drug is used, and they can be associated with significant psychomotor agitation and assaultive behavior.
When patients abuse flake, another synthetic drug that has been reported in the Southeast, they tend to become very paranoid and violent. “These patients can be extremely unpredictable and aggressive,” he says. “Patients with dementia can be impulsive and aggressive during care, and caution is needed, but it’s not a directed violence like that seen in patients who are agitated secondary to substance abuse.”
Dr. Bianco advises having a predetermined triage system or a scale that can assess and measure patients’ level of psychological distress, which can ensure timely and appropriate evaluation and treatment of psychiatric patients, as well as toxicology screens and mental health protocols, which can aid in diagnosis.
“Technology is an important tool in facilitating integration, including identifying and screening patients, tracking patient progress, encouraging adherence to clinical protocols, facilitating communication between providers, and evaluating the impact of integrated programs,” Dr. Bianco says. Academic hospitals struggle less with this problem, he adds, because they tend to be more adequately funded in all areas of operations, including the field of mental health.
IPC Healthcare hospitalist James N. Horst, DO, a psychiatrist who manages mental health patients in a long-term care and nursing home facility, says he has found standardized general screening tools to be useful. The Hamilton Depression Scale, Beck Anxiety Inventory, and CAGE exam for chemical dependency can be easily administered and scored in any facility setting, he says. These tests include self-administered questions to which the patient answers yes or no. Laboratory work is a secondary tool in psychiatry since few mental illness disorders are based on medical comorbidities.
Dr. Sussman looks to the past, when psychiatrists were part of medical teams rounding in hospitals, for a solution. “An integrated model provides an approach where patient care is less compartmentalized,” he says. “In this model, clinicians are responsible for making sure their patient is treated, not simply focusing on their individual area of expertise. This involves working more closely with an integrated care management team.”
Ideally, this will occur at every level of care: outpatient, inpatient, and emergency department (ED). New York State is attempting to redesign the Medicaid system in this fashion, with the goal of improving overall care and reducing reliance on inpatient treatment to provide that care. This is an enormous initiative, costing more than $8 billion. If successful, it will result in a more patient-centered care system that treats the whole individual, not just the illness, and will positively impact patients’ overall health.
For now, St. John’s Episcopal Hospital has an active psychiatric consultation liaison service that is staffed by both in-house residents and attending physicians who are there 24-7 to help with psychiatric patients.
A ‘Utopia Management’ Perspective
In a dream world, patients with significant psychiatric problems or comorbidities would have coordinated, multidisciplinary care from admission to discharge, Dr. Fingado adds. Ideally, hospitals would have dedicated rooms or areas in the ED that are safe for patients and staff. Psychiatric patients who require observation or admission to a non-psychiatric hospital would be placed in rooms or units dedicated for psychiatric patients, again providing safety for patients and staff, Dr. Fingado surmises.
In addition, all staff members would have training in behavioral health management, including instruction on de-escalation, restraint techniques, and medication use for patients. Ideally, units would be staffed by specially trained aides, nurses, and healthcare providers (i.e., physician assistants, nurse practitioners, physicians), as well as psychologists and psychiatrists, Dr. Fingado says. This type of management would require buy-in from a multitude of groups, including healthcare administrators, nursing and provider staff, as well as health insurance companies. A reallocation or increase in funds would be needed to help build and staff these types of management models and locations, she adds.
In a perfect world, all hospitalized patients would be adequately screened for mental health issues and have their issues appropriately addressed by well-qualified professionals in real time, Dr. Grace says. Telemedicine services have great potential in helping to meet that goal, he says, and more relaxed regulatory guidelines around telemedicine could help make such physician-patient interactions less difficult. Many, if not most, hospitals currently have limited or no access to qualified mental health professionals, a conundrum based on supply, reimbursement, and need.
“Telemedicine, which is already having great success in neurology and intensive care unit medicine, is a great fit for this space,” Dr. Grace says. “Widespread access to a tele-psychiatrist would bring significant tangible benefits to patients, hospitals, hospital staff, and the population at large, who ultimately pay for healthcare in the nation.”
Dr. Horst says he believes everyone who treats psychiatric patients should have education in psychiatric medicine education. One way to achieve this would be to mandate continuing medical education coursework in mental health disorders.
The Reality of a Utopia
Traditionally, our healthcare system has been designed to react to illness, meaning that physicians treat illnesses when individuals become sick.
“But as science and technology now better understand the etiology of most illnesses, we are more equipped to design more preventative interventions rather than wait for individuals to become sick,” Dr. Bianco says. “Prevention interventions require an initial investment that the healthcare system is not necessarily willing to invest in at this time and a shift in the way it charges for services. If the healthcare system is unwilling to go that route, and we know we can prevent many illnesses by shifting the focus of treatment, consequently, human suffering is augmented and quality of life jeopardized.”
More recently, the general population and providers have acknowledged that healing takes place more effectively when it is applied in more integrated approaches (i.e., the utilization of the bio-psycho-social-spiritual model), Dr. Bianco adds. This greater appreciation is demonstrated by different research studies applied to different populations (both the general public and different providers). Despite this, the system (i.e., training) does not support a full integration of interventions.
“The system continues to operate under the traditional medical model that is fragmented and hyper-specialized,” Dr. Bianco says. “Science has demonstrated that the mind and the body work in more complex ways, requiring a more holistic approach to treatment. Although all segments among providers now understand and accept that, the system they dwell in does not support the daily challenges of treatment.
“Treatment continues to be fragmented as it is the medical model. At this point, at a minimum, a hospital should have a psychiatric department composed of individuals who are adequately trained (e.g., health psychology, behavioral medicine) to absorb a portion of individuals who primarily present with mental health issues.” TH
Karen Appold is a freelance medical writer in Pennsylvania.
References
- Torrey EF, Kennard AD, Eslinger D, Lamb R, Pavle J. More mentally ill persons are in jails and prisons than hospitals: a survey of the states. Treatment Advocacy Center website. Available at: http://www.treatmentadvocacycenter.org/storage/documents/final_jails_v_hospitals_study.pdf. May 2010. Accessed August 18, 2015.
- Results from the 2013 national survey on drug use and health: mental health detailed tables. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, U.S. Department of Health & Human Services website. Available at: http://www.samhsa.gov/data/sites/default/files/2013MHDetTabs/NSDUH-MHDetTabs2013.pdf. Accessed August 19, 2015.
- Any mental illness among adults. National Institute of Mental Health website. Available at: http://www.nimh.nih.gov/health/statistics/prevalence/any-mental-illness-ami-among-adults.shtml. Accessed August 19, 2015.
- Internal medicine certification examination blueprint. American Board of Internal Medicine website. Available at: https://www.abim.org/pdf/blueprint/im_cert.pdf. January 2015. Accessed August 19, 2015.
In 1955, there was one psychiatric bed for every 300 Americans. By 2005, following the widespread shuttering or downsizing of psychiatric hospitals in the 1990s, that number had shrunk to one bed for every 3,000 Americans.1
In 2008, an estimated 39.8 million Americans age 18 or older had mental illness, which represents 17.7% of U.S. adults.2 In 2013, this number rose to an estimated 43.8 million, or 18.5% of U.S. adults (see Figure 1).3
“It’s like we have returned to the early 19th century, when mentally ill persons were held in prisons or temporarily kept in hospital settings,” says Ricardo Bianco, PsyD, program director of the Master of Arts in counseling and health psychology at William James College in Newton, Mass. “The problem is that the healthcare system did not catch up to absorb the mentally ill population.
“As a result, hospital staffs are inadequately trained, there is insufficient funding for these patients, and there are not enough human resource personnel to manage them. Consequently, hospitalists are overwhelmed with cases that should be primarily treated by psychologists, psychiatrists, and social workers.”
According to David M. Grace, MD, SFHM, hospitalist and senior medical officer at the Schumacher Group in Lafayette, La., two groups of psychiatric patients present to the acute-care hospital environment: those who are there for a primary psychiatric problem and those who have a medical problem and a psychiatric comorbidity. The first group of patients presents distinct challenges. U.S. hospitals lack two-thirds of the minimum number of beds needed to care for this population. The second group is problematic because psychiatric issues often cloud the medical issues of a patient, increasing both diagnostic uncertainty and resource utilization.
Challenges Abound
Psychiatric patients present a number of problems for hospitalists. First, it is difficult to decipher what comprises a psychiatric issue and what does not because “many psychiatric conditions manifest as physical symptoms and they often require significant resource consumption to diagnose,” Dr. Grace says. Secondly, some patients present with a severe primary psychiatric problem in which they are homicidal, suicidal, or gravely disabled.
In addition, psychiatric patients tend to have a greater incidence of noncompliance with imaging, laboratory work, medication, and general medical care, says Daniel Sussman, MD, a hospitalist at IPC Healthcare, Inc., based in North Hollywood, Calif. He also serves as interim chairman in the department of psychiatry at St. John’s Episcopal Hospital in Far Rockaway, N.Y.
Clinically, potential interactions between psychiatric medications and medically related prescription drugs are always a concern, notes Dr. Sussman, who says more than 70% of patients admitted to St. John’s Episcopal Hospital have a major psychiatric illness in addition to their medical problem. Psychiatric medications, which patients may have tolerated well when they were stable, may be too sedating when patients are ill. Side effects and adverse reactions of psychotropic medications must also be considered when diagnosing and treating medical illnesses. Metabolic syndrome is more commonly seen and is a factor in the development and subsequent treatment of other illnesses.
Another challenge stems from the fact that patients with substantial psychiatric comorbidities can have significant and rapid mood and behavioral changes as well as sudden, volatile, and aggressive outbursts—both verbal and physical.
“Staff members who interact with the patient are at risk if an outburst occurs,” says Emily Fingado, MD, FAAP, a pediatric hospitalist and clinical assistant professor of pediatrics at Nemours/Alfred I. duPont Hospital for Children (Nemours/AIDHC) of the Sidney Kimmel Medical College at Thomas Jefferson University in Wilmington, Del.
Such situations can become scary, particularly if someone with psychiatric expertise is not available to intervene. This can be very frustrating for hospitalists who want to provide high-level care but may lack the training needed to be successful with such patients. This can ultimately lead to burnout, says Sarah Rivelli, MD, medical director of psychiatry clinical services at Duke University Hospital and Duke University Medical Center in Durham, N.C.
Another challenge is that although there are protocols in place designed to follow specific steps for patients with physical illnesses or disorders, that’s not the case for psychiatric illness. “Many hospital facilities are not designed, or have yet to implement, protocols to attend to mentally ill individuals,” Dr. Bianco says.
Because of the unpredictability of patients and lack of practice protocols, mental illness can introduce a wild card into the standard treatment process. A more individualized approach with these patients is needed, but with increasing focus on length of stay and operational efficiency, medical and nursing staffs are pressured to do things quickly and to do more with less. It can be very time-consuming for a nurse to have to explain to paranoid patients why they should take their medication or for a phlebotomist to try to calm patients in order to obtain blood. When patients refuse needed tests, or only provide a limited history, the hospitalist ends up working with incomplete information, which makes choosing and monitoring the treatment approach problematic.
A Look at Best Practices
In light of challenges, some best practices have been identified for handling psychiatric patients. As previously mentioned, most hospital staffs have limited formal training in interacting with psychiatric patients. In fact, the American Board of Internal Medicine only devotes 4% of the certification exam to psychiatry.4
Ideally, staff members who care for psychiatric patients will have specialized or additional training in managing patients with psychiatric conditions or comorbidities. Nemours/AIDHC has a committee assigned to evaluate psychiatric patients’ care and help manage them when a behavioral emergency occurs, Dr. Fingado says. This team, which has been trained on de-escalation, restraint techniques and policies, as well as medications to use in these situations, intervenes when patients have an aggressive event that places patients, visitors, or staff at risk. The team includes nursing staff, the hospitalist on-call, and security personnel and involves the social work, psychology, and psychiatry departments.
Training focused on treating patients with psychiatric conditions should include how to recognize substance abuse and treat substance withdrawal because mental illness and substance abuse often track together, Dr. Sussman notes. At St. John’s Episcopal Hospital, patients with chronic mental illness are not the ones who typically become aggressive or violent. Rather, this is more often the case among patients with substance abuse either in states of acute intoxication or withdrawal.
Recently, Dr. Sussman has seen a significant increase in patients who abuse K2, or spice, a synthetic form of cannabis. Side effects of using K2 include rapid heart rate, anxiety, hallucinations, and paranoia to the point of delusional thinking. These side effects can frequently wax and wane for days after the drug is used, and they can be associated with significant psychomotor agitation and assaultive behavior.
When patients abuse flake, another synthetic drug that has been reported in the Southeast, they tend to become very paranoid and violent. “These patients can be extremely unpredictable and aggressive,” he says. “Patients with dementia can be impulsive and aggressive during care, and caution is needed, but it’s not a directed violence like that seen in patients who are agitated secondary to substance abuse.”
Dr. Bianco advises having a predetermined triage system or a scale that can assess and measure patients’ level of psychological distress, which can ensure timely and appropriate evaluation and treatment of psychiatric patients, as well as toxicology screens and mental health protocols, which can aid in diagnosis.
“Technology is an important tool in facilitating integration, including identifying and screening patients, tracking patient progress, encouraging adherence to clinical protocols, facilitating communication between providers, and evaluating the impact of integrated programs,” Dr. Bianco says. Academic hospitals struggle less with this problem, he adds, because they tend to be more adequately funded in all areas of operations, including the field of mental health.
IPC Healthcare hospitalist James N. Horst, DO, a psychiatrist who manages mental health patients in a long-term care and nursing home facility, says he has found standardized general screening tools to be useful. The Hamilton Depression Scale, Beck Anxiety Inventory, and CAGE exam for chemical dependency can be easily administered and scored in any facility setting, he says. These tests include self-administered questions to which the patient answers yes or no. Laboratory work is a secondary tool in psychiatry since few mental illness disorders are based on medical comorbidities.
Dr. Sussman looks to the past, when psychiatrists were part of medical teams rounding in hospitals, for a solution. “An integrated model provides an approach where patient care is less compartmentalized,” he says. “In this model, clinicians are responsible for making sure their patient is treated, not simply focusing on their individual area of expertise. This involves working more closely with an integrated care management team.”
Ideally, this will occur at every level of care: outpatient, inpatient, and emergency department (ED). New York State is attempting to redesign the Medicaid system in this fashion, with the goal of improving overall care and reducing reliance on inpatient treatment to provide that care. This is an enormous initiative, costing more than $8 billion. If successful, it will result in a more patient-centered care system that treats the whole individual, not just the illness, and will positively impact patients’ overall health.
For now, St. John’s Episcopal Hospital has an active psychiatric consultation liaison service that is staffed by both in-house residents and attending physicians who are there 24-7 to help with psychiatric patients.
A ‘Utopia Management’ Perspective
In a dream world, patients with significant psychiatric problems or comorbidities would have coordinated, multidisciplinary care from admission to discharge, Dr. Fingado adds. Ideally, hospitals would have dedicated rooms or areas in the ED that are safe for patients and staff. Psychiatric patients who require observation or admission to a non-psychiatric hospital would be placed in rooms or units dedicated for psychiatric patients, again providing safety for patients and staff, Dr. Fingado surmises.
In addition, all staff members would have training in behavioral health management, including instruction on de-escalation, restraint techniques, and medication use for patients. Ideally, units would be staffed by specially trained aides, nurses, and healthcare providers (i.e., physician assistants, nurse practitioners, physicians), as well as psychologists and psychiatrists, Dr. Fingado says. This type of management would require buy-in from a multitude of groups, including healthcare administrators, nursing and provider staff, as well as health insurance companies. A reallocation or increase in funds would be needed to help build and staff these types of management models and locations, she adds.
In a perfect world, all hospitalized patients would be adequately screened for mental health issues and have their issues appropriately addressed by well-qualified professionals in real time, Dr. Grace says. Telemedicine services have great potential in helping to meet that goal, he says, and more relaxed regulatory guidelines around telemedicine could help make such physician-patient interactions less difficult. Many, if not most, hospitals currently have limited or no access to qualified mental health professionals, a conundrum based on supply, reimbursement, and need.
“Telemedicine, which is already having great success in neurology and intensive care unit medicine, is a great fit for this space,” Dr. Grace says. “Widespread access to a tele-psychiatrist would bring significant tangible benefits to patients, hospitals, hospital staff, and the population at large, who ultimately pay for healthcare in the nation.”
Dr. Horst says he believes everyone who treats psychiatric patients should have education in psychiatric medicine education. One way to achieve this would be to mandate continuing medical education coursework in mental health disorders.
The Reality of a Utopia
Traditionally, our healthcare system has been designed to react to illness, meaning that physicians treat illnesses when individuals become sick.
“But as science and technology now better understand the etiology of most illnesses, we are more equipped to design more preventative interventions rather than wait for individuals to become sick,” Dr. Bianco says. “Prevention interventions require an initial investment that the healthcare system is not necessarily willing to invest in at this time and a shift in the way it charges for services. If the healthcare system is unwilling to go that route, and we know we can prevent many illnesses by shifting the focus of treatment, consequently, human suffering is augmented and quality of life jeopardized.”
More recently, the general population and providers have acknowledged that healing takes place more effectively when it is applied in more integrated approaches (i.e., the utilization of the bio-psycho-social-spiritual model), Dr. Bianco adds. This greater appreciation is demonstrated by different research studies applied to different populations (both the general public and different providers). Despite this, the system (i.e., training) does not support a full integration of interventions.
“The system continues to operate under the traditional medical model that is fragmented and hyper-specialized,” Dr. Bianco says. “Science has demonstrated that the mind and the body work in more complex ways, requiring a more holistic approach to treatment. Although all segments among providers now understand and accept that, the system they dwell in does not support the daily challenges of treatment.
“Treatment continues to be fragmented as it is the medical model. At this point, at a minimum, a hospital should have a psychiatric department composed of individuals who are adequately trained (e.g., health psychology, behavioral medicine) to absorb a portion of individuals who primarily present with mental health issues.” TH
Karen Appold is a freelance medical writer in Pennsylvania.
References
- Torrey EF, Kennard AD, Eslinger D, Lamb R, Pavle J. More mentally ill persons are in jails and prisons than hospitals: a survey of the states. Treatment Advocacy Center website. Available at: http://www.treatmentadvocacycenter.org/storage/documents/final_jails_v_hospitals_study.pdf. May 2010. Accessed August 18, 2015.
- Results from the 2013 national survey on drug use and health: mental health detailed tables. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, U.S. Department of Health & Human Services website. Available at: http://www.samhsa.gov/data/sites/default/files/2013MHDetTabs/NSDUH-MHDetTabs2013.pdf. Accessed August 19, 2015.
- Any mental illness among adults. National Institute of Mental Health website. Available at: http://www.nimh.nih.gov/health/statistics/prevalence/any-mental-illness-ami-among-adults.shtml. Accessed August 19, 2015.
- Internal medicine certification examination blueprint. American Board of Internal Medicine website. Available at: https://www.abim.org/pdf/blueprint/im_cert.pdf. January 2015. Accessed August 19, 2015.
Utah Health Sciences Center Realizes Significant Savings from Cost-Analysis Tool
Most healthcare systems don’t know or understand their cost of care at the unit that matters, i.e., the actual cost of care for an individual patient. Knowing this, University of Utah Health Sciences Center (UHSC) sought to develop methodologies using clinical data that would enable it to determine cost of care. Ultimately, a team led by systems, data, and analytics personnel, and including hospitalists, created an analytics framework known as value driven outcomes (VDO) using an agile methodology. Evaluation consisted of measurement against project objectives, including implementation timeliness, system performance, completeness, accuracy, extensibility, adoption, satisfaction, and the ability to support value improvement.1
“The initial results of employing the cost-savings tool have been exciting. For example, a 30% reduction in the cost of an orthopedic joint replacement—an inpatient hospital procedure—was realized,” says Robert C. Pendleton, MD, chief medical quality officer and professor of medicine at the University of Utah in Salt Lake City.
In another instance, hospitalists at UHSC led an initiative to reduce the use of unnecessary laboratory tests. That resulted in $400,000 in cost savings in the first year.
Another UHSC hospitalist used data to reduce unnecessary telemetry utilization by 60% on the hospitalist service.
“The accumulative impact of these initiatives, among others, will be a savings of millions of dollars annually by making process changes,” says Dr. Pendleton, a hospitalist who served on the executive steering committee that designed the web-based tool. “Our early experience shows that there is a lot of waste in the healthcare system.”
Along with the costing tool, quality and outcome measures were integrated so that the actual value of care (best outcomes at the lowest cost) could be assessed and incrementally improved.
Widespread Use?
Dr. Pendleton believes the tool could become popular among hospitalists, explaining that the field is known as the “leading system thinkers in healthcare.”
“By their nature, if you give them meaningful data and they can compare themselves to their peers, they are highly engaged to determine where waste in their hospitals exists and to lead improvement efforts,” he says.
UHSC is currently in the process of rolling out the VDO tool systemwide to its 1,200 faculty members. The rollout will take six to 12 months. In the next year, it’s also working to define and integrate outcome measures for the top 50 medical conditions it treats, which will allow it to robustly assess the value of care delivery.
“Success will equally be to increase quality without an increase in cost,” he says.
What’s more, Dr. Pendleton says efforts are in the works to make the self-intuitive system available to institutions nationwide. For example, the center is working to address technical complexities resulting from the use of multiple electronic health record vendors.
“The goal is to make it usable in every environment so we can support other organizations in the most effective ways,” he says.
Although the tool is very easy to use, stakeholders are providing feedback that allows for continuous improvements in how data are presented.
“Anyone with basic computer skills and the ability to interpret bar charts and basic graphs can use it,” Dr. Pendleton says. The center also offers a 15-minute, confidential, training module and a one-hour, one-on-one training session with an analyst. TH
Karen Appold is a freelance author in Pennsylvania.
Reference
- Kawamoto K, Martin CJ, Williams K, et al. Value driven outcomes (VDO): a pragmatic, modular, and extensible software framework for understanding and improving health care costs and outcomes. J Am Med Inform Assoc. 2015;22(1):223-235.
Most healthcare systems don’t know or understand their cost of care at the unit that matters, i.e., the actual cost of care for an individual patient. Knowing this, University of Utah Health Sciences Center (UHSC) sought to develop methodologies using clinical data that would enable it to determine cost of care. Ultimately, a team led by systems, data, and analytics personnel, and including hospitalists, created an analytics framework known as value driven outcomes (VDO) using an agile methodology. Evaluation consisted of measurement against project objectives, including implementation timeliness, system performance, completeness, accuracy, extensibility, adoption, satisfaction, and the ability to support value improvement.1
“The initial results of employing the cost-savings tool have been exciting. For example, a 30% reduction in the cost of an orthopedic joint replacement—an inpatient hospital procedure—was realized,” says Robert C. Pendleton, MD, chief medical quality officer and professor of medicine at the University of Utah in Salt Lake City.
In another instance, hospitalists at UHSC led an initiative to reduce the use of unnecessary laboratory tests. That resulted in $400,000 in cost savings in the first year.
Another UHSC hospitalist used data to reduce unnecessary telemetry utilization by 60% on the hospitalist service.
“The accumulative impact of these initiatives, among others, will be a savings of millions of dollars annually by making process changes,” says Dr. Pendleton, a hospitalist who served on the executive steering committee that designed the web-based tool. “Our early experience shows that there is a lot of waste in the healthcare system.”
Along with the costing tool, quality and outcome measures were integrated so that the actual value of care (best outcomes at the lowest cost) could be assessed and incrementally improved.
Widespread Use?
Dr. Pendleton believes the tool could become popular among hospitalists, explaining that the field is known as the “leading system thinkers in healthcare.”
“By their nature, if you give them meaningful data and they can compare themselves to their peers, they are highly engaged to determine where waste in their hospitals exists and to lead improvement efforts,” he says.
UHSC is currently in the process of rolling out the VDO tool systemwide to its 1,200 faculty members. The rollout will take six to 12 months. In the next year, it’s also working to define and integrate outcome measures for the top 50 medical conditions it treats, which will allow it to robustly assess the value of care delivery.
“Success will equally be to increase quality without an increase in cost,” he says.
What’s more, Dr. Pendleton says efforts are in the works to make the self-intuitive system available to institutions nationwide. For example, the center is working to address technical complexities resulting from the use of multiple electronic health record vendors.
“The goal is to make it usable in every environment so we can support other organizations in the most effective ways,” he says.
Although the tool is very easy to use, stakeholders are providing feedback that allows for continuous improvements in how data are presented.
“Anyone with basic computer skills and the ability to interpret bar charts and basic graphs can use it,” Dr. Pendleton says. The center also offers a 15-minute, confidential, training module and a one-hour, one-on-one training session with an analyst. TH
Karen Appold is a freelance author in Pennsylvania.
Reference
- Kawamoto K, Martin CJ, Williams K, et al. Value driven outcomes (VDO): a pragmatic, modular, and extensible software framework for understanding and improving health care costs and outcomes. J Am Med Inform Assoc. 2015;22(1):223-235.
Most healthcare systems don’t know or understand their cost of care at the unit that matters, i.e., the actual cost of care for an individual patient. Knowing this, University of Utah Health Sciences Center (UHSC) sought to develop methodologies using clinical data that would enable it to determine cost of care. Ultimately, a team led by systems, data, and analytics personnel, and including hospitalists, created an analytics framework known as value driven outcomes (VDO) using an agile methodology. Evaluation consisted of measurement against project objectives, including implementation timeliness, system performance, completeness, accuracy, extensibility, adoption, satisfaction, and the ability to support value improvement.1
“The initial results of employing the cost-savings tool have been exciting. For example, a 30% reduction in the cost of an orthopedic joint replacement—an inpatient hospital procedure—was realized,” says Robert C. Pendleton, MD, chief medical quality officer and professor of medicine at the University of Utah in Salt Lake City.
In another instance, hospitalists at UHSC led an initiative to reduce the use of unnecessary laboratory tests. That resulted in $400,000 in cost savings in the first year.
Another UHSC hospitalist used data to reduce unnecessary telemetry utilization by 60% on the hospitalist service.
“The accumulative impact of these initiatives, among others, will be a savings of millions of dollars annually by making process changes,” says Dr. Pendleton, a hospitalist who served on the executive steering committee that designed the web-based tool. “Our early experience shows that there is a lot of waste in the healthcare system.”
Along with the costing tool, quality and outcome measures were integrated so that the actual value of care (best outcomes at the lowest cost) could be assessed and incrementally improved.
Widespread Use?
Dr. Pendleton believes the tool could become popular among hospitalists, explaining that the field is known as the “leading system thinkers in healthcare.”
“By their nature, if you give them meaningful data and they can compare themselves to their peers, they are highly engaged to determine where waste in their hospitals exists and to lead improvement efforts,” he says.
UHSC is currently in the process of rolling out the VDO tool systemwide to its 1,200 faculty members. The rollout will take six to 12 months. In the next year, it’s also working to define and integrate outcome measures for the top 50 medical conditions it treats, which will allow it to robustly assess the value of care delivery.
“Success will equally be to increase quality without an increase in cost,” he says.
What’s more, Dr. Pendleton says efforts are in the works to make the self-intuitive system available to institutions nationwide. For example, the center is working to address technical complexities resulting from the use of multiple electronic health record vendors.
“The goal is to make it usable in every environment so we can support other organizations in the most effective ways,” he says.
Although the tool is very easy to use, stakeholders are providing feedback that allows for continuous improvements in how data are presented.
“Anyone with basic computer skills and the ability to interpret bar charts and basic graphs can use it,” Dr. Pendleton says. The center also offers a 15-minute, confidential, training module and a one-hour, one-on-one training session with an analyst. TH
Karen Appold is a freelance author in Pennsylvania.
Reference
- Kawamoto K, Martin CJ, Williams K, et al. Value driven outcomes (VDO): a pragmatic, modular, and extensible software framework for understanding and improving health care costs and outcomes. J Am Med Inform Assoc. 2015;22(1):223-235.
Nick Fitterman, MD, SFHM, Discusses Population Health and Hospital Medicine's Role
Nick Fitterman, MD, SFHM, vice chair of hospital medicine for the Hofstra North Shore-LIJ School of Medicine in Hempstead, N.Y., and North Shore-Long Island Jewish Health System in New Hyde Park, N.Y., discusses how hospital medicine factors into population health—where is the intersection and what is the hospitalist’s role?
Nick Fitterman, MD, SFHM, vice chair of hospital medicine for the Hofstra North Shore-LIJ School of Medicine in Hempstead, N.Y., and North Shore-Long Island Jewish Health System in New Hyde Park, N.Y., discusses how hospital medicine factors into population health—where is the intersection and what is the hospitalist’s role?
Nick Fitterman, MD, SFHM, vice chair of hospital medicine for the Hofstra North Shore-LIJ School of Medicine in Hempstead, N.Y., and North Shore-Long Island Jewish Health System in New Hyde Park, N.Y., discusses how hospital medicine factors into population health—where is the intersection and what is the hospitalist’s role?