User login
Bryn Nelson is a former PhD microbiologist who decided he’d much rather write about microbes than mutate them. After seven years at the science desk of Newsday in New York, Nelson relocated to Seattle as a freelancer, where he has consumed far too much coffee and written features and stories for The Hospitalist, The New York Times, Nature, Scientific American, Science News for Students, Mosaic and many other print and online publications. In addition, he contributed a chapter to The Science Writers’ Handbook and edited two chapters for the six-volume Modernist Cuisine: The Art and Science of Cooking.
ONLINE EXCLUSIVE: Weighing the Costs of Palliative Care
Hospitalist David Mitchell, MD, PhD, was moonlighting in an Ohio hospital when a nurse called him about a gravely ill older patient who was experiencing shortness of breath. Should she administer the diuretic Lasix to help clear his lung congestion?
Dr. Mitchell, now a hospitalist at Sibley Memorial Hospital in Washington, D.C., and a member of SHM’s Performance Standards Committee, decided to see the patient in person and review his charts. He found that the patient had severe dementia, hadn’t walked in months, and was declining despite more than two weeks in the hospital and daily visits by three specialists.
Dr. Mitchell called the patient’s son and explained the situation, then asked whether the son thought his father would want to continue receiving aggressive therapy. “The son said, ‘Oh, no. He would never want to continue like this.’ So we stopped all the treatments, and he died by the next day,” Dr. Mitchell says.
To him, the anecdote highlights how far medicine has to go in providing personalized palliative care that honors the wishes of patients and their families. It also demonstrates how ignoring those wishes and failing to communicate can contribute to the huge costs associated with end-of-life medical care. Every day, the three specialists seeing the patient were recommending the same course of therapy. “But nobody was being the quarterback and saying, ‘Hey, listen. This is not working,’ ” Dr. Mitchell says.
Hospitalists, he says, are in an ideal position to step up and play a pivotal role in providing the kind of patient-centered care that could improve both quality and cost. So far, however, Dr. Mitchell says he’s seen wide variation in how hospitalists communicate with a patient’s family about end-of-life decisions. “For the ones who do have these conversations, the family is almost always glad that somebody finally said, ‘Do we have to do these tests? Do we have to continue to try to save his life?’ ” Dr. Mitchell says.
Time constraints, he says, are the main reason why hospitalists don’t have such conversations more often. “The communication dies when you’re busy.” And the remedy? Dr. Mitchell says the only thing that will help shift the focus from seeing as many patients as possible to making sure every encounter is a high-quality, efficient one is payment reform in the form of bundled payments to hospitals and physicians. In theory, professional standards can encourage more uniformity, he says. “But when it hits the trenches, it’s the payment that speaks.”
Hospitalist David Mitchell, MD, PhD, was moonlighting in an Ohio hospital when a nurse called him about a gravely ill older patient who was experiencing shortness of breath. Should she administer the diuretic Lasix to help clear his lung congestion?
Dr. Mitchell, now a hospitalist at Sibley Memorial Hospital in Washington, D.C., and a member of SHM’s Performance Standards Committee, decided to see the patient in person and review his charts. He found that the patient had severe dementia, hadn’t walked in months, and was declining despite more than two weeks in the hospital and daily visits by three specialists.
Dr. Mitchell called the patient’s son and explained the situation, then asked whether the son thought his father would want to continue receiving aggressive therapy. “The son said, ‘Oh, no. He would never want to continue like this.’ So we stopped all the treatments, and he died by the next day,” Dr. Mitchell says.
To him, the anecdote highlights how far medicine has to go in providing personalized palliative care that honors the wishes of patients and their families. It also demonstrates how ignoring those wishes and failing to communicate can contribute to the huge costs associated with end-of-life medical care. Every day, the three specialists seeing the patient were recommending the same course of therapy. “But nobody was being the quarterback and saying, ‘Hey, listen. This is not working,’ ” Dr. Mitchell says.
Hospitalists, he says, are in an ideal position to step up and play a pivotal role in providing the kind of patient-centered care that could improve both quality and cost. So far, however, Dr. Mitchell says he’s seen wide variation in how hospitalists communicate with a patient’s family about end-of-life decisions. “For the ones who do have these conversations, the family is almost always glad that somebody finally said, ‘Do we have to do these tests? Do we have to continue to try to save his life?’ ” Dr. Mitchell says.
Time constraints, he says, are the main reason why hospitalists don’t have such conversations more often. “The communication dies when you’re busy.” And the remedy? Dr. Mitchell says the only thing that will help shift the focus from seeing as many patients as possible to making sure every encounter is a high-quality, efficient one is payment reform in the form of bundled payments to hospitals and physicians. In theory, professional standards can encourage more uniformity, he says. “But when it hits the trenches, it’s the payment that speaks.”
Hospitalist David Mitchell, MD, PhD, was moonlighting in an Ohio hospital when a nurse called him about a gravely ill older patient who was experiencing shortness of breath. Should she administer the diuretic Lasix to help clear his lung congestion?
Dr. Mitchell, now a hospitalist at Sibley Memorial Hospital in Washington, D.C., and a member of SHM’s Performance Standards Committee, decided to see the patient in person and review his charts. He found that the patient had severe dementia, hadn’t walked in months, and was declining despite more than two weeks in the hospital and daily visits by three specialists.
Dr. Mitchell called the patient’s son and explained the situation, then asked whether the son thought his father would want to continue receiving aggressive therapy. “The son said, ‘Oh, no. He would never want to continue like this.’ So we stopped all the treatments, and he died by the next day,” Dr. Mitchell says.
To him, the anecdote highlights how far medicine has to go in providing personalized palliative care that honors the wishes of patients and their families. It also demonstrates how ignoring those wishes and failing to communicate can contribute to the huge costs associated with end-of-life medical care. Every day, the three specialists seeing the patient were recommending the same course of therapy. “But nobody was being the quarterback and saying, ‘Hey, listen. This is not working,’ ” Dr. Mitchell says.
Hospitalists, he says, are in an ideal position to step up and play a pivotal role in providing the kind of patient-centered care that could improve both quality and cost. So far, however, Dr. Mitchell says he’s seen wide variation in how hospitalists communicate with a patient’s family about end-of-life decisions. “For the ones who do have these conversations, the family is almost always glad that somebody finally said, ‘Do we have to do these tests? Do we have to continue to try to save his life?’ ” Dr. Mitchell says.
Time constraints, he says, are the main reason why hospitalists don’t have such conversations more often. “The communication dies when you’re busy.” And the remedy? Dr. Mitchell says the only thing that will help shift the focus from seeing as many patients as possible to making sure every encounter is a high-quality, efficient one is payment reform in the form of bundled payments to hospitals and physicians. In theory, professional standards can encourage more uniformity, he says. “But when it hits the trenches, it’s the payment that speaks.”
ONLINE EXCLUSIVE: Listen to David Meltzer and Scott Lundberg talk about HM efficiency
ONLINE EXCLUSIVE: The “Weak Link” in Patient Handoffs
Increased handoffs are often viewed as a byproduct of the growth in hospital medicine, with heightened scrutiny on the quality of communication that accompanies these transfers of care. As research suggests, though, finding and fixing the weak links can require persistence.
A study led by Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee, compared a traditional, resident-based model of care to one involving a hospitalist-physician assistant team. Initially, his study found a 6% higher length of stay (LOS) for the hospitalist-physician assistant teams, with no differences in costs or readmission rates.1
But when the researchers pored over their results, they discovered that the increased LOS was limited to patients admitted overnight. Those patients, Dr. Singh says, were admitted by other providers—a night-float resident or faculty hospitalist—and then transferred to the hospitalist-physician assistant teams when they arrived in the morning. These “overflow patients” also were admitted only during busy periods, when limits on the number of admissions by house staff required other arrangements.
To make a direct comparison, Dr. Singh focused on a window from 11 a.m. to 4 p.m., when patients would have an equal probability of being admitted by a resident team or a hospitalist-physician assistant team. From a pool of about 3,000 admitted patients, the study found no significant difference in LOS, cost, readmission rates, or mortality. Instead of highlighting significant differences in models of care, then, Dr. Singh says, his study highlighted a potential weak link in the “treacherous” overnight-to-morning handoffs during busy periods that should be addressed.
“There have been a lot of studies implicating poor communication as a cause of patient-safety issues,” notes Sunil Kripalani, MD, MSc, FHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn. But fewer studies, he says, have shown how to effectively improve communication in a way that improves patient safety.
One focal point is the often incomplete and inadequate nature of discharge summaries. Several models are emerging on how to build a better discharge summary, Dr. Kripalani says, with researchers offering solid recommendations (as multiple presentations at SHM’s annual meeting suggest). The trick is ensuring that those plans can be implemented into practice on a consistent and timely basis.
Dr. Kripalani says at least one straightforward strategy might help improve handoffs, however: building time into the schedule for them, such as 15-minute overlaps between shifts.—BN
Increased handoffs are often viewed as a byproduct of the growth in hospital medicine, with heightened scrutiny on the quality of communication that accompanies these transfers of care. As research suggests, though, finding and fixing the weak links can require persistence.
A study led by Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee, compared a traditional, resident-based model of care to one involving a hospitalist-physician assistant team. Initially, his study found a 6% higher length of stay (LOS) for the hospitalist-physician assistant teams, with no differences in costs or readmission rates.1
But when the researchers pored over their results, they discovered that the increased LOS was limited to patients admitted overnight. Those patients, Dr. Singh says, were admitted by other providers—a night-float resident or faculty hospitalist—and then transferred to the hospitalist-physician assistant teams when they arrived in the morning. These “overflow patients” also were admitted only during busy periods, when limits on the number of admissions by house staff required other arrangements.
To make a direct comparison, Dr. Singh focused on a window from 11 a.m. to 4 p.m., when patients would have an equal probability of being admitted by a resident team or a hospitalist-physician assistant team. From a pool of about 3,000 admitted patients, the study found no significant difference in LOS, cost, readmission rates, or mortality. Instead of highlighting significant differences in models of care, then, Dr. Singh says, his study highlighted a potential weak link in the “treacherous” overnight-to-morning handoffs during busy periods that should be addressed.
“There have been a lot of studies implicating poor communication as a cause of patient-safety issues,” notes Sunil Kripalani, MD, MSc, FHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn. But fewer studies, he says, have shown how to effectively improve communication in a way that improves patient safety.
One focal point is the often incomplete and inadequate nature of discharge summaries. Several models are emerging on how to build a better discharge summary, Dr. Kripalani says, with researchers offering solid recommendations (as multiple presentations at SHM’s annual meeting suggest). The trick is ensuring that those plans can be implemented into practice on a consistent and timely basis.
Dr. Kripalani says at least one straightforward strategy might help improve handoffs, however: building time into the schedule for them, such as 15-minute overlaps between shifts.—BN
Increased handoffs are often viewed as a byproduct of the growth in hospital medicine, with heightened scrutiny on the quality of communication that accompanies these transfers of care. As research suggests, though, finding and fixing the weak links can require persistence.
A study led by Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee, compared a traditional, resident-based model of care to one involving a hospitalist-physician assistant team. Initially, his study found a 6% higher length of stay (LOS) for the hospitalist-physician assistant teams, with no differences in costs or readmission rates.1
But when the researchers pored over their results, they discovered that the increased LOS was limited to patients admitted overnight. Those patients, Dr. Singh says, were admitted by other providers—a night-float resident or faculty hospitalist—and then transferred to the hospitalist-physician assistant teams when they arrived in the morning. These “overflow patients” also were admitted only during busy periods, when limits on the number of admissions by house staff required other arrangements.
To make a direct comparison, Dr. Singh focused on a window from 11 a.m. to 4 p.m., when patients would have an equal probability of being admitted by a resident team or a hospitalist-physician assistant team. From a pool of about 3,000 admitted patients, the study found no significant difference in LOS, cost, readmission rates, or mortality. Instead of highlighting significant differences in models of care, then, Dr. Singh says, his study highlighted a potential weak link in the “treacherous” overnight-to-morning handoffs during busy periods that should be addressed.
“There have been a lot of studies implicating poor communication as a cause of patient-safety issues,” notes Sunil Kripalani, MD, MSc, FHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn. But fewer studies, he says, have shown how to effectively improve communication in a way that improves patient safety.
One focal point is the often incomplete and inadequate nature of discharge summaries. Several models are emerging on how to build a better discharge summary, Dr. Kripalani says, with researchers offering solid recommendations (as multiple presentations at SHM’s annual meeting suggest). The trick is ensuring that those plans can be implemented into practice on a consistent and timely basis.
Dr. Kripalani says at least one straightforward strategy might help improve handoffs, however: building time into the schedule for them, such as 15-minute overlaps between shifts.—BN
A Chilly Reception
The reviews are in, and most healthcare provider groups are finding little to their liking in the proposed rules for the Centers for Medicare & Medicaid Services’ (CMS) voluntary Accountable Care Organization (ACO) program. Organizations like SHM have publically supported the concept of an ACO, but details in the 128 pages of proposed rules released March 31 apparently were not what they had in mind. The problem, as many provider groups detailed in a flurry of letters sent before the June 6 deadline for comments, is too much stick and not enough carrot.
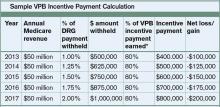
The Patient Protection and Affordable Care Act of 2010, which authorized the program, stipulates that any Medicare savings deriving from ACOs must be divided between CMS and participating organizations. Organizations can choose between two financial models: One track allows participants to retain 60% of overall savings but also requires them to assume financial risk from the start; a second track delays any risk until the third year and offers 50% savings. In exchange, ACOs must achieve an average savings of 2% per patient, as well as meet or beat thresholds for 65 measures of quality.
Organizational Uproar
Critics contend that the recommended rules are so onerous and bureaucratic that the program is likely to attract few takers. In its comment letter, SHM expressed an opinion shared by many: "Although the ACO concept holds much promise, the proposed rule as written presents many barriers to successful ACO development and operations. Establishing an ACO will require an enormous upfront investment from participating providers, but the proposed rule does not allow for enough flexibility to ensure a reasonable return on investment." (Read SHM’s response letter at www.hospital medicine.org/advocacy.)
The American College of Physicians similarly warned that the proposed rules set the bar too high for many would-be participants. "The required administrative, infrastructure, service delivery, and financial resources and the need to accept risk will effectively limit participation to those few large entities already organized under an ACO-like structure; that already have ready access to capital, substantial infrastructure development, and experience operating under an integrative service/payment model (e.g. Medicare Advantage)," the ACP wrote in its response letter (www.acponline.org/run ning_practice/aco/acp_comments.pdf).
The tone was markedly different in letters from consumer and advocacy groups, including one by the Campaign for Better Care, signed by more than 40 organizations (www.nationalpartnership.org). "Overall we believe you are moving in the right direction with the proposed rule, and we applaud your commitment to ensuring ACOs deliver truly patient-centered care," the letter stated. Acknowledging the negative feedback, the letter continued, "While some are concerned about asking too much of ACOs, we cannot expect genuine transformation to be easy, and we know that these new models must be held to standards that ensure they deliver on the promise of better care, better health, and lower cost."
—Michael W. Painter, JD, MD, senior program officer, Robert Wood Johnson Foundation, Princeton, N.J.
Accountability Gap
Michael W. Painter, JD, MD, senior program officer at the Robert Wood Johnson Foundation in Princeton, N.J., helped research and write the foundation’s own comment letter, which he says tried to bridge the divide between provider and patient groups.
"We did get behind the notion of ratcheting up the accountability for quality and cost, including the risk, as soon as it makes sense to do it," he says. "Not dragging our feet, recognizing that we have to do it rapidly, but it has to be balanced by being reasonable to help move from where we are."
Given the mandate for change, Dr. Painter says, the negative tone of many letters from provider organizations shouldn’t be surprising. "What we’re asking the hospital, the health professionals, to do is to change fairly radically and embrace this accountability. So as you just walk through the door of this conversation, it’s not surprising that they would balk," he says. "Nobody wants to take on all of this new responsibility. It’s no fault of theirs; they’ve just been following the rules of the road of the current system and the payment schemes to try to be successful in that environment."
Success, of course, depends on financial stability, and Dr. Painter says the worry that participating ACOs could open themselves up to financial risk too soon is "absolutely a legitimate concern." CMS, he says, should give providers clear guidance and assistance, as well as assurance that the regulations won’t change on them once they’ve enrolled.
So far, at least, CMS has not swayed some of the very institutions that government officials have lauded as examples of how ACOs should be run. In June, the Mayo Clinic in Rochester, Minn., announced that it would not participate. As reported by the Minneapolis Star Tribune, clinic officials said the proposed regulations clashed with Mayo’s existing Medicare operations. One of the clinic’s chief complaints is the proposed requirement that patients be added to oversight boards charged with assessing performance, something that Mayo argues is unnecessary to deliver patient-centered care. Antitrust rules represent another major concern for Mayo and others that argue their dominant position as healthcare providers in rural communities could run afoul of the regulations.
Cleveland Clinic likewise blasted the proposed ACO rules in a letter. "Rather than providing a broad framework that focuses on results as the key criteria of success, the Proposed Rule is replete with (1) prescriptive requirements that have little to do with outcomes, and (2) many detailed governance and reporting requirements that create significant administrative burdens," stated Delos Cosgrove, MD, the clinic’s CEO and president.
Furthermore, Cosgrove’s letter concluded that the shared-savings component "is structured in such a way that creates real uncertainty about whether applicants will be able to achieve success."
The American Medical Group Association went so far as to include in its letter the results of a member survey, which showed 93% would not enroll under the current ACO rules.
No Turning Back
Dr. Painter says the pushback is to be expected. Although the country has no choice but to move toward more accountability, he says, it’s impossible for the first attempt at a proposed rule to be the "magic bullet" that gets it exactly right. "One, this is a radical departure, and two, when you get into the nitty-gritty of the proposed rule and people crunch the numbers, if it’s not going to work for them or it’s simply not enticing enough for them, they [CMS] need to go back to the table and make it that way," he says.
Organizations like the American Medical Association have been particularly vocal about asking CMS to delay issuing its final rule, slated for January. So far, Dr. Painter says, CMS officials have indicated that the timeline will proceed according to schedule, though he notes that providers have raised plenty of valid concerns that should be addressed.
"Would I be surprised if there’s a delay? No. This is a big deal," he says.
Along with some expected rule changes, he says the newly formed Center for Medicare and Medicaid Innovation could play a key role in offering assistance and developing alternative ACO models and pilot programs.
Regardless of whether the voluntary CMS program ultimately pleases both providers and patients, though, one thing seems certain: The accountable-care concept is here to stay.
Bryn Nelson is a freelance medical writer based in Seattle
The reviews are in, and most healthcare provider groups are finding little to their liking in the proposed rules for the Centers for Medicare & Medicaid Services’ (CMS) voluntary Accountable Care Organization (ACO) program. Organizations like SHM have publically supported the concept of an ACO, but details in the 128 pages of proposed rules released March 31 apparently were not what they had in mind. The problem, as many provider groups detailed in a flurry of letters sent before the June 6 deadline for comments, is too much stick and not enough carrot.
The Patient Protection and Affordable Care Act of 2010, which authorized the program, stipulates that any Medicare savings deriving from ACOs must be divided between CMS and participating organizations. Organizations can choose between two financial models: One track allows participants to retain 60% of overall savings but also requires them to assume financial risk from the start; a second track delays any risk until the third year and offers 50% savings. In exchange, ACOs must achieve an average savings of 2% per patient, as well as meet or beat thresholds for 65 measures of quality.
Organizational Uproar
Critics contend that the recommended rules are so onerous and bureaucratic that the program is likely to attract few takers. In its comment letter, SHM expressed an opinion shared by many: "Although the ACO concept holds much promise, the proposed rule as written presents many barriers to successful ACO development and operations. Establishing an ACO will require an enormous upfront investment from participating providers, but the proposed rule does not allow for enough flexibility to ensure a reasonable return on investment." (Read SHM’s response letter at www.hospital medicine.org/advocacy.)
The American College of Physicians similarly warned that the proposed rules set the bar too high for many would-be participants. "The required administrative, infrastructure, service delivery, and financial resources and the need to accept risk will effectively limit participation to those few large entities already organized under an ACO-like structure; that already have ready access to capital, substantial infrastructure development, and experience operating under an integrative service/payment model (e.g. Medicare Advantage)," the ACP wrote in its response letter (www.acponline.org/run ning_practice/aco/acp_comments.pdf).
The tone was markedly different in letters from consumer and advocacy groups, including one by the Campaign for Better Care, signed by more than 40 organizations (www.nationalpartnership.org). "Overall we believe you are moving in the right direction with the proposed rule, and we applaud your commitment to ensuring ACOs deliver truly patient-centered care," the letter stated. Acknowledging the negative feedback, the letter continued, "While some are concerned about asking too much of ACOs, we cannot expect genuine transformation to be easy, and we know that these new models must be held to standards that ensure they deliver on the promise of better care, better health, and lower cost."
—Michael W. Painter, JD, MD, senior program officer, Robert Wood Johnson Foundation, Princeton, N.J.
Accountability Gap
Michael W. Painter, JD, MD, senior program officer at the Robert Wood Johnson Foundation in Princeton, N.J., helped research and write the foundation’s own comment letter, which he says tried to bridge the divide between provider and patient groups.
"We did get behind the notion of ratcheting up the accountability for quality and cost, including the risk, as soon as it makes sense to do it," he says. "Not dragging our feet, recognizing that we have to do it rapidly, but it has to be balanced by being reasonable to help move from where we are."
Given the mandate for change, Dr. Painter says, the negative tone of many letters from provider organizations shouldn’t be surprising. "What we’re asking the hospital, the health professionals, to do is to change fairly radically and embrace this accountability. So as you just walk through the door of this conversation, it’s not surprising that they would balk," he says. "Nobody wants to take on all of this new responsibility. It’s no fault of theirs; they’ve just been following the rules of the road of the current system and the payment schemes to try to be successful in that environment."
Success, of course, depends on financial stability, and Dr. Painter says the worry that participating ACOs could open themselves up to financial risk too soon is "absolutely a legitimate concern." CMS, he says, should give providers clear guidance and assistance, as well as assurance that the regulations won’t change on them once they’ve enrolled.
So far, at least, CMS has not swayed some of the very institutions that government officials have lauded as examples of how ACOs should be run. In June, the Mayo Clinic in Rochester, Minn., announced that it would not participate. As reported by the Minneapolis Star Tribune, clinic officials said the proposed regulations clashed with Mayo’s existing Medicare operations. One of the clinic’s chief complaints is the proposed requirement that patients be added to oversight boards charged with assessing performance, something that Mayo argues is unnecessary to deliver patient-centered care. Antitrust rules represent another major concern for Mayo and others that argue their dominant position as healthcare providers in rural communities could run afoul of the regulations.
Cleveland Clinic likewise blasted the proposed ACO rules in a letter. "Rather than providing a broad framework that focuses on results as the key criteria of success, the Proposed Rule is replete with (1) prescriptive requirements that have little to do with outcomes, and (2) many detailed governance and reporting requirements that create significant administrative burdens," stated Delos Cosgrove, MD, the clinic’s CEO and president.
Furthermore, Cosgrove’s letter concluded that the shared-savings component "is structured in such a way that creates real uncertainty about whether applicants will be able to achieve success."
The American Medical Group Association went so far as to include in its letter the results of a member survey, which showed 93% would not enroll under the current ACO rules.
No Turning Back
Dr. Painter says the pushback is to be expected. Although the country has no choice but to move toward more accountability, he says, it’s impossible for the first attempt at a proposed rule to be the "magic bullet" that gets it exactly right. "One, this is a radical departure, and two, when you get into the nitty-gritty of the proposed rule and people crunch the numbers, if it’s not going to work for them or it’s simply not enticing enough for them, they [CMS] need to go back to the table and make it that way," he says.
Organizations like the American Medical Association have been particularly vocal about asking CMS to delay issuing its final rule, slated for January. So far, Dr. Painter says, CMS officials have indicated that the timeline will proceed according to schedule, though he notes that providers have raised plenty of valid concerns that should be addressed.
"Would I be surprised if there’s a delay? No. This is a big deal," he says.
Along with some expected rule changes, he says the newly formed Center for Medicare and Medicaid Innovation could play a key role in offering assistance and developing alternative ACO models and pilot programs.
Regardless of whether the voluntary CMS program ultimately pleases both providers and patients, though, one thing seems certain: The accountable-care concept is here to stay.
Bryn Nelson is a freelance medical writer based in Seattle
The reviews are in, and most healthcare provider groups are finding little to their liking in the proposed rules for the Centers for Medicare & Medicaid Services’ (CMS) voluntary Accountable Care Organization (ACO) program. Organizations like SHM have publically supported the concept of an ACO, but details in the 128 pages of proposed rules released March 31 apparently were not what they had in mind. The problem, as many provider groups detailed in a flurry of letters sent before the June 6 deadline for comments, is too much stick and not enough carrot.
The Patient Protection and Affordable Care Act of 2010, which authorized the program, stipulates that any Medicare savings deriving from ACOs must be divided between CMS and participating organizations. Organizations can choose between two financial models: One track allows participants to retain 60% of overall savings but also requires them to assume financial risk from the start; a second track delays any risk until the third year and offers 50% savings. In exchange, ACOs must achieve an average savings of 2% per patient, as well as meet or beat thresholds for 65 measures of quality.
Organizational Uproar
Critics contend that the recommended rules are so onerous and bureaucratic that the program is likely to attract few takers. In its comment letter, SHM expressed an opinion shared by many: "Although the ACO concept holds much promise, the proposed rule as written presents many barriers to successful ACO development and operations. Establishing an ACO will require an enormous upfront investment from participating providers, but the proposed rule does not allow for enough flexibility to ensure a reasonable return on investment." (Read SHM’s response letter at www.hospital medicine.org/advocacy.)
The American College of Physicians similarly warned that the proposed rules set the bar too high for many would-be participants. "The required administrative, infrastructure, service delivery, and financial resources and the need to accept risk will effectively limit participation to those few large entities already organized under an ACO-like structure; that already have ready access to capital, substantial infrastructure development, and experience operating under an integrative service/payment model (e.g. Medicare Advantage)," the ACP wrote in its response letter (www.acponline.org/run ning_practice/aco/acp_comments.pdf).
The tone was markedly different in letters from consumer and advocacy groups, including one by the Campaign for Better Care, signed by more than 40 organizations (www.nationalpartnership.org). "Overall we believe you are moving in the right direction with the proposed rule, and we applaud your commitment to ensuring ACOs deliver truly patient-centered care," the letter stated. Acknowledging the negative feedback, the letter continued, "While some are concerned about asking too much of ACOs, we cannot expect genuine transformation to be easy, and we know that these new models must be held to standards that ensure they deliver on the promise of better care, better health, and lower cost."
—Michael W. Painter, JD, MD, senior program officer, Robert Wood Johnson Foundation, Princeton, N.J.
Accountability Gap
Michael W. Painter, JD, MD, senior program officer at the Robert Wood Johnson Foundation in Princeton, N.J., helped research and write the foundation’s own comment letter, which he says tried to bridge the divide between provider and patient groups.
"We did get behind the notion of ratcheting up the accountability for quality and cost, including the risk, as soon as it makes sense to do it," he says. "Not dragging our feet, recognizing that we have to do it rapidly, but it has to be balanced by being reasonable to help move from where we are."
Given the mandate for change, Dr. Painter says, the negative tone of many letters from provider organizations shouldn’t be surprising. "What we’re asking the hospital, the health professionals, to do is to change fairly radically and embrace this accountability. So as you just walk through the door of this conversation, it’s not surprising that they would balk," he says. "Nobody wants to take on all of this new responsibility. It’s no fault of theirs; they’ve just been following the rules of the road of the current system and the payment schemes to try to be successful in that environment."
Success, of course, depends on financial stability, and Dr. Painter says the worry that participating ACOs could open themselves up to financial risk too soon is "absolutely a legitimate concern." CMS, he says, should give providers clear guidance and assistance, as well as assurance that the regulations won’t change on them once they’ve enrolled.
So far, at least, CMS has not swayed some of the very institutions that government officials have lauded as examples of how ACOs should be run. In June, the Mayo Clinic in Rochester, Minn., announced that it would not participate. As reported by the Minneapolis Star Tribune, clinic officials said the proposed regulations clashed with Mayo’s existing Medicare operations. One of the clinic’s chief complaints is the proposed requirement that patients be added to oversight boards charged with assessing performance, something that Mayo argues is unnecessary to deliver patient-centered care. Antitrust rules represent another major concern for Mayo and others that argue their dominant position as healthcare providers in rural communities could run afoul of the regulations.
Cleveland Clinic likewise blasted the proposed ACO rules in a letter. "Rather than providing a broad framework that focuses on results as the key criteria of success, the Proposed Rule is replete with (1) prescriptive requirements that have little to do with outcomes, and (2) many detailed governance and reporting requirements that create significant administrative burdens," stated Delos Cosgrove, MD, the clinic’s CEO and president.
Furthermore, Cosgrove’s letter concluded that the shared-savings component "is structured in such a way that creates real uncertainty about whether applicants will be able to achieve success."
The American Medical Group Association went so far as to include in its letter the results of a member survey, which showed 93% would not enroll under the current ACO rules.
No Turning Back
Dr. Painter says the pushback is to be expected. Although the country has no choice but to move toward more accountability, he says, it’s impossible for the first attempt at a proposed rule to be the "magic bullet" that gets it exactly right. "One, this is a radical departure, and two, when you get into the nitty-gritty of the proposed rule and people crunch the numbers, if it’s not going to work for them or it’s simply not enticing enough for them, they [CMS] need to go back to the table and make it that way," he says.
Organizations like the American Medical Association have been particularly vocal about asking CMS to delay issuing its final rule, slated for January. So far, Dr. Painter says, CMS officials have indicated that the timeline will proceed according to schedule, though he notes that providers have raised plenty of valid concerns that should be addressed.
"Would I be surprised if there’s a delay? No. This is a big deal," he says.
Along with some expected rule changes, he says the newly formed Center for Medicare and Medicaid Innovation could play a key role in offering assistance and developing alternative ACO models and pilot programs.
Regardless of whether the voluntary CMS program ultimately pleases both providers and patients, though, one thing seems certain: The accountable-care concept is here to stay.
Bryn Nelson is a freelance medical writer based in Seattle
Are You Delivering on the Promise of Higher Quality?
One hospitalist-led pilot project produced a 61% decrease in heart failure readmission rates. Another resulted in a 33% drop in all-cause readmissions. The numbers might be impressive, but what do they really say about how hospitalists have influenced healthcare quality?
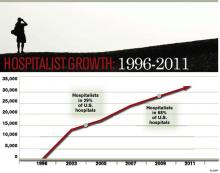
When HM emerged 15 years ago, advocates pitched the fledgling physician specialty as a model of efficient inpatient care, and subsequent findings that the concept led to reductions in length of stay encouraged more hospitals to bolster their staff with the newcomers. With a rising emphasis on quality and patient safety over the past decade, and the new era of pay-for-performance, the hospitalist model of care has expanded to embrace improved quality of care as a chief selling point.
Measuring quality is no easy task, however, and researchers still debate the relative merits of metrics like 30-day readmission rates and inpatient mortality. "Without question, quality measurement is an imperfect science, and all measures will contain some level of imprecision and bias," concluded a recent commentary in Health Affairs.1
Against that backdrop, relatively few studies have looked broadly at the contributions of hospital medicine. Most interventions have been individually tailored to a hospital or instituted at only a few sites, precluding large-scale, head-to-head comparisons.
And so the question remains: Has hospital medicine lived up to its promise on quality?
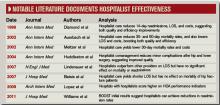
The Evidence
In one of the few national surveys of HM’s impact on patient care, a yearlong comparison of more than 3,600 hospitals found that the roughly 40% that employed hospitalists scored better on multiple Hospital Quality Alliance indicators. The 2009 Archives of Internal Medicine study suggested that hospitals with hospitalists outperformed their counterparts in quality metrics for acute myocardial infarction, pneumonia, overall disease treatment and diagnosis, and counseling and prevention. Congestive heart failure was the only category of the five reviewed that lacked a statistically significant difference.2
A separate editorial, however, argued that the study’s data were not persuasive enough to support the conclusion that hospitalists bring a higher quality of care to the table.3 And even less can be said about the national impact of HM on newly elevated metrics, such as readmission rates. The obligation to gather evidence, in fact, is largely falling upon hospitalists themselves, and the multitude of research abstracts from SHM’s annual meeting in May suggests that plenty of physician scientists are taking the responsibility seriously. Among the presentations, a study led by David Boyte, MD, assistant professor of medicine at Duke University and a hospitalist at Durham Regional Hospital, found that a multidisciplinary approach greatly improved one hospital unit’s 30-day readmission rates for heart failure patients. After a three-month pilot in the cardiac nursing unit, readmission rates fell to 10.7% from 27.6%.4
Although the multidisciplinary effort has included doctors, nurses, nutritionists, pharmacists, unit managers, and other personnel, Dr. Boyte says the involvement of hospitalists has been key to the project’s success. "We feel like we were the main participants who could see the whole picture from a patient-centered perspective," he says. "We were the glue; we were the center node of all the healthcare providers." Based on that dramatic improvement, Dr. Boyte says, the same interventional protocol has been rolled out in three other medical surgical units, and the hospital is using a similar approach to address AMI readmission rates.
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions; www.hospitalmedicine.org/boost )—by far the largest study of how HM is impacting readmission rates—has amassed data from more than 20 hospitals, with more expected from a growing roster of participants. So far, however, the project has only released data from six pilot sites describing the six-month periods before and after the project’s start. Among those sites, initial results suggest that readmission rates fell by an average of more than 20%, to 11.2% from 14.2%.5
Though the early numbers are encouraging, experts say rates from a larger group of participants at the one-year mark will be more telling, as will direct comparisons between BOOST units and nonparticipating counterparts at the same hospitals. Principal investigator Mark Williams, MD, FHM, professor and chief of the division of hospital medicine at the Northwestern University Feinberg School of Medicine in Chicago, says researchers still need to clean up that data before they’re ready to share it publicly.
In the meantime, some individual BOOST case studies are suggesting that hospitalist-led changes could pay big dividends. To help create cohesiveness and a sense of ownership within its HM program, St. Mary’s Health Center in St. Louis started a 20-bed hospitalist unit in 2008. Philip Vaidyan, MD, FACP, head of the hospitalist program and practice group leader for IPC: The Hospitalist Company at St. Mary’s, says one unit, 3 West, has since functioned as a lab for testing new ideas that are then introduced hospitalwide.
One early change was to bring all of the unit’s care providers together, from doctors and nurses to the unit-based case manager and social worker, for 9 a.m. handoff meetings. "We have this collective brain to find unique solutions," Dr. Vaidyan says. After seeing positive trends on length of stay, 30-day readmission rates, and patient satisfaction scores, St. Mary’s upgraded to a 32-bed hospitalist unit in early 2009. That same year, the 525-bed community teaching hospital was accepted into the BOOST program.
The hospitalist unit’s improved quality scores continued under BOOST, leading to a 33% reduction in readmission rates from 2008 to 2010 (to 10.5% from 15.7%). Rates for a nonhospitalist unit, by contrast, hovered around 17%. "For reducing readmissions, people may think that you have to have a higher length of stay," Dr. Vaidyan says. But the unit trended toward a lower length of stay, in addition to its reduced 30-day readmissions and improved patient satisfaction scores.
Flush with success, the 10 physicians and four nurse practitioners in the hospitalist program have since begun spreading their best practices to the rest of the hospital units. "Hospitalists are in the best ‘sweet spot,’ " Dr. Vaidyan says, "partnering with all of the disciplines, bringing them together, and keeping everybody on the same page."
Ironically, pinpointing the contribution of hospitalists is harder when their changes produce an ecological effect throughout an entire institution, says Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee. Even so, he stresses that the impact of the two dozen hospitalists at Medical College Physicians has been felt.
"Coinciding with and following the introduction of our hospitalist program in 2004, we have noticed dramatic decreases in our length of stay throughout medicine services," he says. The same has held true for inpatient mortality. "And that, we feel, is attributable to the standardization of processes introduced by the hospitalist group." Multidisciplinary rounds; whiteboards in patient rooms; and standardized admission orders, prophylactic treatments, and discharge processes—"all of this would’ve been impossible, absolutely impossible, without the hospitalist," he says.
Over the past decade, Dr. Singh’s assessment has been echoed by several studies suggesting that individual hospitalist programs have brought significant improvements in quality measures, such as complication rates and inpatient mortality. In 2002, for example, Andrew Auerbach, MD, MPH, at the University of California San Francisco Medical Center, led a study that compared HM care with that of community physicians in a community-based teaching hospital. Patients cared for by hospitalists, the study found, had a lower risk of death during the hospitalization, as well as at 30 days and 60 days after discharge.6
A separate report by David Meltzer, MD, PhD, and colleagues at the University of Chicago found that an HM program in an academic general medicine service led to a 30% reduction in 30-day mortality rates during its second year of operation.7 And a 2004 study led by Jeanne Huddleston, MD, at the Mayo Clinic College of Medicine in Rochester, Minn., found that a hospitalist-orthopedic co-management model (versus care by orthopedic surgeons with medical consultation) led to more patients being discharged with no complications after elective hip or knee surgery.8 Hospitalist co-management also reduced the rate of minor complications, but had no effect on actual length of stay or cost.
A subsequent study by the same group, however, documented improved efficiency of care through the HM model, but no effect on the mortality of hip fracture patients up to one year after discharge.9 Multiple studies of hospitalist programs, in fact, have seen increased efficiency but little or no impact on inpatient mortality, leading researchers to broadly conclude that such programs can decrease resource use without compromising quality.
In 2007, a retrospective study of nearly 77,000 patients admitted to 45 hospitals with one of seven common diagnoses compared the care delivered by hospitalists, general internists, and family physicians.10 Although the study authors found that hospitalist care yielded a small drop in length of stay, they saw no difference in the inpatient mortality rates or 14-day readmission rates. More recently, mortality has become ensnared in controversy over its reliability as an accurate indicator of quality.

-Shai Gavi, DO, MPH, chief, section of hospital medicine, assistant professor, Stony Brook University School of Medicine, Brookhaven, N.Y.
Half of the Equation
Despite a lack of ideal metrics, another promising sign for HM might be the model’s exportability. Lee Kheng Hock, MMed, senior consultant and head of the Department of Family Medicine and Continuing Care at Singapore General Hospital, says the 1,600-bed hospital began experimenting with the hospitalist model when officials realized the existing care system wasn’t sustainable. Amid an aging population and increasingly complex and fragmented care, Hock views the hospitalist movement as a natural evolution of the healthcare system to meet the needs of a changing environment.
In a recent study, Hock and his colleagues used the hospital’s administrative database to examine the resource use and outcomes of patients cared for in 2008 by family medicine hospitalists or by specialists.11 The comparison, based on several standard metrics, found no significant improvements in quality, with similar inpatient mortality rates and 30-day, all-cause, unscheduled readmission rates regardless of the care delivery method. The study, though, revealed a significantly shorter hospital stay (4.4 days vs. 5.3 days) and lower costs per patient for those cared for by hospitalists ($2,250 vs. $2,500).11
Hock points out that, like his study, most analyses of hospitalist programs have shown an improvement in length of stay and cost of care without any increase in mortality and morbidity. If value equals quality divided by cost, he says, it stands to reason that quality must increase as overall value remains the same but costs decrease.
"The main difference is that the patients received undivided attention from a well-rounded generalist physician who is focused on providing holistic general medical care," Hock says, adding that "it is really a no-brainer that the outcome would be different."
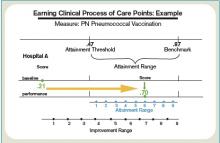
Patients Rule
Other measures like the effectiveness of communication and seamlessness of handoffs often are assessed through their impacts on patient outcomes. But Sunil Kripalani, MD, MSc, SFHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn., says communication is now a primary focal point in Medicare’s new hospital value-based purchasing program (VBP). Within VBP’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) component, worth 30% of a hospital’s sum score, four of the 10 survey-based measures deal directly with communication. Patients’ overall rating and recommendation of hospitals likely will reflect their satisfaction with communication as well. Dr. Kripalani says it’s inevitable that hospitals—and hospitalists—will pay more attention to communication ratings as patients become judges of quality.
The expertise of hospitalists in handling challenging patients also leads to improved quality over time, says Shai Gavi, DO, MPH, chief of the section of hospital medicine and assistant professor of clinical medicine at Stony Brook University School of Medicine in Brookhaven, N.Y. Hospitalists, he says, excel in handling such high-stakes medical issues as gastrointestinal bleeding, pancreatitis, sepsis, and pain management that can quickly impact patient outcomes if not addressed properly and proficiently. "I think there’s significant value to having people who do this on a pretty frequent basis," he says.
And because of their broad day-to-day interactions, Dr. Gavi says, hospitalists are natural choices for committees focused on improving quality. "When we sit on committees, people often look to us for answers and directions because they know we’re on the front lines and we’ve interfaced with all of the services in the hospital," he says. "You have a good view of the whole hospital operation from A to Z, and I think that’s pretty unique to hospitalists."
The Verdict
In a recent issue brief by Lisa Sprague, principal policy analyst at the National Health Policy Forum, she asserts, "Hospitalists have the undeniable advantage of being there when a crisis occurs, when a patient is ready for discharge, and so on."12
So is "being there" the defining concept of hospital medicine, as she subsequently suggests?
Based on both scientific and anecdotal evidence, the contribution of hospitalists to healthcare quality might be better summarized as "being involved." Whether as innovators, navigators, physician champions, the "sweet spot" of interdepartmental partnerships, the "glue" of multidisciplinary teams, or the nuclei of performance committees, hospitalists are increasingly described as being in the middle of efforts to improve quality. On this basis, the discipline appears to be living up to expectations, though experts say more research is needed to better assess the impacts of HM on quality.
Dr. Vaidyan says hospitalists are particularly well positioned to understand what constitutes ideal care from the perspective of patients. "They want to be treated well: That’s patient satisfaction," he says. "They want to have their chief complaint—why they came to the hospital—properly addressed, so you need a coordinated care team. They want to go home early and don’t want come back: That’s low length of stay and a reduction in 30-day readmissions. And they don’t want any hospital-acquired complications."
Treating patients better, then, should be reflected by improved quality, even if the participation of hospitalists cannot be precisely quantified. "Being involved is something that may be difficult to measure," Dr. Gavi says, "but nonetheless, it has an important impact." TH
Bryn Nelson is a medical writer based in Seattle.
References
- Pronovost PJ, Lilford R. Analysis & commentary: A roadmap for improving the performance of performance measures. Health Aff (Millwood). 2011;30(4):569-73.
- López L, Hicks LS, Cohen AP, McKean S, Weissman JS. Hospitalists and the quality of care in hospitals. Arch Intern Med. 2009;169(15):1389-1394.
- Centor RM, Taylor BB. Do hospitalists improve quality? Arch Intern Med. 2009;169(15):1351-1352.
- Boyte D, Verma L, Wightman M. A multidisciplinary approach to reducing heart failure readmissions. J Hosp Med. 2011;6(4)Supp 2:S14.
- Williams MV, Hansen L, Greenwald J, Howell E, et al. BOOST: impact of a quality improvement project to reduce rehospitalizations. J Hosp Med. 2011;6(4) Supp 2:S88. BOOST: impact of a quality improvement project to reduce rehospitalizations.
- Auerbach AD, Wachter RM, Katz P, Showstack J, Baron RB, Goldman L. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859-865.
- Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(1):866-874.
- Huddleston JM, Hall K, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty. Ann Intern Med. 2004;141(1):28-38.
- Batsis JA, Phy MP, Melton LJ, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4): 219–225.
- Lindenauer PK, Rothberg MB, Pekow PS, et al. Outcomes of care by hospitalists, general internists, and family physicians. N Eng J Med. 2007;357:2589-2600.
- Hock Lee K, Yang Y, Soong Yang K, Chi Ong B, Seong Ng H. Bringing generalists into the hospital: outcomes of a family medicine hospitalist model in Singapore. J Hosp Med. 2011;6(3):115-121.
- Sprague L. The hospitalist: better value in inpatient care? National Health Policy Forum website. Available at: www.nhpf.org/library/issue-briefs/IB842_Hospitalist_03-30-11.pdf. Accessed June 28, 2011.
One hospitalist-led pilot project produced a 61% decrease in heart failure readmission rates. Another resulted in a 33% drop in all-cause readmissions. The numbers might be impressive, but what do they really say about how hospitalists have influenced healthcare quality?
When HM emerged 15 years ago, advocates pitched the fledgling physician specialty as a model of efficient inpatient care, and subsequent findings that the concept led to reductions in length of stay encouraged more hospitals to bolster their staff with the newcomers. With a rising emphasis on quality and patient safety over the past decade, and the new era of pay-for-performance, the hospitalist model of care has expanded to embrace improved quality of care as a chief selling point.
Measuring quality is no easy task, however, and researchers still debate the relative merits of metrics like 30-day readmission rates and inpatient mortality. "Without question, quality measurement is an imperfect science, and all measures will contain some level of imprecision and bias," concluded a recent commentary in Health Affairs.1
Against that backdrop, relatively few studies have looked broadly at the contributions of hospital medicine. Most interventions have been individually tailored to a hospital or instituted at only a few sites, precluding large-scale, head-to-head comparisons.
And so the question remains: Has hospital medicine lived up to its promise on quality?
The Evidence
In one of the few national surveys of HM’s impact on patient care, a yearlong comparison of more than 3,600 hospitals found that the roughly 40% that employed hospitalists scored better on multiple Hospital Quality Alliance indicators. The 2009 Archives of Internal Medicine study suggested that hospitals with hospitalists outperformed their counterparts in quality metrics for acute myocardial infarction, pneumonia, overall disease treatment and diagnosis, and counseling and prevention. Congestive heart failure was the only category of the five reviewed that lacked a statistically significant difference.2
A separate editorial, however, argued that the study’s data were not persuasive enough to support the conclusion that hospitalists bring a higher quality of care to the table.3 And even less can be said about the national impact of HM on newly elevated metrics, such as readmission rates. The obligation to gather evidence, in fact, is largely falling upon hospitalists themselves, and the multitude of research abstracts from SHM’s annual meeting in May suggests that plenty of physician scientists are taking the responsibility seriously. Among the presentations, a study led by David Boyte, MD, assistant professor of medicine at Duke University and a hospitalist at Durham Regional Hospital, found that a multidisciplinary approach greatly improved one hospital unit’s 30-day readmission rates for heart failure patients. After a three-month pilot in the cardiac nursing unit, readmission rates fell to 10.7% from 27.6%.4
Although the multidisciplinary effort has included doctors, nurses, nutritionists, pharmacists, unit managers, and other personnel, Dr. Boyte says the involvement of hospitalists has been key to the project’s success. "We feel like we were the main participants who could see the whole picture from a patient-centered perspective," he says. "We were the glue; we were the center node of all the healthcare providers." Based on that dramatic improvement, Dr. Boyte says, the same interventional protocol has been rolled out in three other medical surgical units, and the hospital is using a similar approach to address AMI readmission rates.
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions; www.hospitalmedicine.org/boost )—by far the largest study of how HM is impacting readmission rates—has amassed data from more than 20 hospitals, with more expected from a growing roster of participants. So far, however, the project has only released data from six pilot sites describing the six-month periods before and after the project’s start. Among those sites, initial results suggest that readmission rates fell by an average of more than 20%, to 11.2% from 14.2%.5
Though the early numbers are encouraging, experts say rates from a larger group of participants at the one-year mark will be more telling, as will direct comparisons between BOOST units and nonparticipating counterparts at the same hospitals. Principal investigator Mark Williams, MD, FHM, professor and chief of the division of hospital medicine at the Northwestern University Feinberg School of Medicine in Chicago, says researchers still need to clean up that data before they’re ready to share it publicly.
In the meantime, some individual BOOST case studies are suggesting that hospitalist-led changes could pay big dividends. To help create cohesiveness and a sense of ownership within its HM program, St. Mary’s Health Center in St. Louis started a 20-bed hospitalist unit in 2008. Philip Vaidyan, MD, FACP, head of the hospitalist program and practice group leader for IPC: The Hospitalist Company at St. Mary’s, says one unit, 3 West, has since functioned as a lab for testing new ideas that are then introduced hospitalwide.
One early change was to bring all of the unit’s care providers together, from doctors and nurses to the unit-based case manager and social worker, for 9 a.m. handoff meetings. "We have this collective brain to find unique solutions," Dr. Vaidyan says. After seeing positive trends on length of stay, 30-day readmission rates, and patient satisfaction scores, St. Mary’s upgraded to a 32-bed hospitalist unit in early 2009. That same year, the 525-bed community teaching hospital was accepted into the BOOST program.
The hospitalist unit’s improved quality scores continued under BOOST, leading to a 33% reduction in readmission rates from 2008 to 2010 (to 10.5% from 15.7%). Rates for a nonhospitalist unit, by contrast, hovered around 17%. "For reducing readmissions, people may think that you have to have a higher length of stay," Dr. Vaidyan says. But the unit trended toward a lower length of stay, in addition to its reduced 30-day readmissions and improved patient satisfaction scores.
Flush with success, the 10 physicians and four nurse practitioners in the hospitalist program have since begun spreading their best practices to the rest of the hospital units. "Hospitalists are in the best ‘sweet spot,’ " Dr. Vaidyan says, "partnering with all of the disciplines, bringing them together, and keeping everybody on the same page."
Ironically, pinpointing the contribution of hospitalists is harder when their changes produce an ecological effect throughout an entire institution, says Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee. Even so, he stresses that the impact of the two dozen hospitalists at Medical College Physicians has been felt.
"Coinciding with and following the introduction of our hospitalist program in 2004, we have noticed dramatic decreases in our length of stay throughout medicine services," he says. The same has held true for inpatient mortality. "And that, we feel, is attributable to the standardization of processes introduced by the hospitalist group." Multidisciplinary rounds; whiteboards in patient rooms; and standardized admission orders, prophylactic treatments, and discharge processes—"all of this would’ve been impossible, absolutely impossible, without the hospitalist," he says.
Over the past decade, Dr. Singh’s assessment has been echoed by several studies suggesting that individual hospitalist programs have brought significant improvements in quality measures, such as complication rates and inpatient mortality. In 2002, for example, Andrew Auerbach, MD, MPH, at the University of California San Francisco Medical Center, led a study that compared HM care with that of community physicians in a community-based teaching hospital. Patients cared for by hospitalists, the study found, had a lower risk of death during the hospitalization, as well as at 30 days and 60 days after discharge.6
A separate report by David Meltzer, MD, PhD, and colleagues at the University of Chicago found that an HM program in an academic general medicine service led to a 30% reduction in 30-day mortality rates during its second year of operation.7 And a 2004 study led by Jeanne Huddleston, MD, at the Mayo Clinic College of Medicine in Rochester, Minn., found that a hospitalist-orthopedic co-management model (versus care by orthopedic surgeons with medical consultation) led to more patients being discharged with no complications after elective hip or knee surgery.8 Hospitalist co-management also reduced the rate of minor complications, but had no effect on actual length of stay or cost.
A subsequent study by the same group, however, documented improved efficiency of care through the HM model, but no effect on the mortality of hip fracture patients up to one year after discharge.9 Multiple studies of hospitalist programs, in fact, have seen increased efficiency but little or no impact on inpatient mortality, leading researchers to broadly conclude that such programs can decrease resource use without compromising quality.
In 2007, a retrospective study of nearly 77,000 patients admitted to 45 hospitals with one of seven common diagnoses compared the care delivered by hospitalists, general internists, and family physicians.10 Although the study authors found that hospitalist care yielded a small drop in length of stay, they saw no difference in the inpatient mortality rates or 14-day readmission rates. More recently, mortality has become ensnared in controversy over its reliability as an accurate indicator of quality.

-Shai Gavi, DO, MPH, chief, section of hospital medicine, assistant professor, Stony Brook University School of Medicine, Brookhaven, N.Y.
Half of the Equation
Despite a lack of ideal metrics, another promising sign for HM might be the model’s exportability. Lee Kheng Hock, MMed, senior consultant and head of the Department of Family Medicine and Continuing Care at Singapore General Hospital, says the 1,600-bed hospital began experimenting with the hospitalist model when officials realized the existing care system wasn’t sustainable. Amid an aging population and increasingly complex and fragmented care, Hock views the hospitalist movement as a natural evolution of the healthcare system to meet the needs of a changing environment.
In a recent study, Hock and his colleagues used the hospital’s administrative database to examine the resource use and outcomes of patients cared for in 2008 by family medicine hospitalists or by specialists.11 The comparison, based on several standard metrics, found no significant improvements in quality, with similar inpatient mortality rates and 30-day, all-cause, unscheduled readmission rates regardless of the care delivery method. The study, though, revealed a significantly shorter hospital stay (4.4 days vs. 5.3 days) and lower costs per patient for those cared for by hospitalists ($2,250 vs. $2,500).11
Hock points out that, like his study, most analyses of hospitalist programs have shown an improvement in length of stay and cost of care without any increase in mortality and morbidity. If value equals quality divided by cost, he says, it stands to reason that quality must increase as overall value remains the same but costs decrease.
"The main difference is that the patients received undivided attention from a well-rounded generalist physician who is focused on providing holistic general medical care," Hock says, adding that "it is really a no-brainer that the outcome would be different."
Patients Rule
Other measures like the effectiveness of communication and seamlessness of handoffs often are assessed through their impacts on patient outcomes. But Sunil Kripalani, MD, MSc, SFHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn., says communication is now a primary focal point in Medicare’s new hospital value-based purchasing program (VBP). Within VBP’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) component, worth 30% of a hospital’s sum score, four of the 10 survey-based measures deal directly with communication. Patients’ overall rating and recommendation of hospitals likely will reflect their satisfaction with communication as well. Dr. Kripalani says it’s inevitable that hospitals—and hospitalists—will pay more attention to communication ratings as patients become judges of quality.
The expertise of hospitalists in handling challenging patients also leads to improved quality over time, says Shai Gavi, DO, MPH, chief of the section of hospital medicine and assistant professor of clinical medicine at Stony Brook University School of Medicine in Brookhaven, N.Y. Hospitalists, he says, excel in handling such high-stakes medical issues as gastrointestinal bleeding, pancreatitis, sepsis, and pain management that can quickly impact patient outcomes if not addressed properly and proficiently. "I think there’s significant value to having people who do this on a pretty frequent basis," he says.
And because of their broad day-to-day interactions, Dr. Gavi says, hospitalists are natural choices for committees focused on improving quality. "When we sit on committees, people often look to us for answers and directions because they know we’re on the front lines and we’ve interfaced with all of the services in the hospital," he says. "You have a good view of the whole hospital operation from A to Z, and I think that’s pretty unique to hospitalists."
The Verdict
In a recent issue brief by Lisa Sprague, principal policy analyst at the National Health Policy Forum, she asserts, "Hospitalists have the undeniable advantage of being there when a crisis occurs, when a patient is ready for discharge, and so on."12
So is "being there" the defining concept of hospital medicine, as she subsequently suggests?
Based on both scientific and anecdotal evidence, the contribution of hospitalists to healthcare quality might be better summarized as "being involved." Whether as innovators, navigators, physician champions, the "sweet spot" of interdepartmental partnerships, the "glue" of multidisciplinary teams, or the nuclei of performance committees, hospitalists are increasingly described as being in the middle of efforts to improve quality. On this basis, the discipline appears to be living up to expectations, though experts say more research is needed to better assess the impacts of HM on quality.
Dr. Vaidyan says hospitalists are particularly well positioned to understand what constitutes ideal care from the perspective of patients. "They want to be treated well: That’s patient satisfaction," he says. "They want to have their chief complaint—why they came to the hospital—properly addressed, so you need a coordinated care team. They want to go home early and don’t want come back: That’s low length of stay and a reduction in 30-day readmissions. And they don’t want any hospital-acquired complications."
Treating patients better, then, should be reflected by improved quality, even if the participation of hospitalists cannot be precisely quantified. "Being involved is something that may be difficult to measure," Dr. Gavi says, "but nonetheless, it has an important impact." TH
Bryn Nelson is a medical writer based in Seattle.
References
- Pronovost PJ, Lilford R. Analysis & commentary: A roadmap for improving the performance of performance measures. Health Aff (Millwood). 2011;30(4):569-73.
- López L, Hicks LS, Cohen AP, McKean S, Weissman JS. Hospitalists and the quality of care in hospitals. Arch Intern Med. 2009;169(15):1389-1394.
- Centor RM, Taylor BB. Do hospitalists improve quality? Arch Intern Med. 2009;169(15):1351-1352.
- Boyte D, Verma L, Wightman M. A multidisciplinary approach to reducing heart failure readmissions. J Hosp Med. 2011;6(4)Supp 2:S14.
- Williams MV, Hansen L, Greenwald J, Howell E, et al. BOOST: impact of a quality improvement project to reduce rehospitalizations. J Hosp Med. 2011;6(4) Supp 2:S88. BOOST: impact of a quality improvement project to reduce rehospitalizations.
- Auerbach AD, Wachter RM, Katz P, Showstack J, Baron RB, Goldman L. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859-865.
- Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(1):866-874.
- Huddleston JM, Hall K, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty. Ann Intern Med. 2004;141(1):28-38.
- Batsis JA, Phy MP, Melton LJ, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4): 219–225.
- Lindenauer PK, Rothberg MB, Pekow PS, et al. Outcomes of care by hospitalists, general internists, and family physicians. N Eng J Med. 2007;357:2589-2600.
- Hock Lee K, Yang Y, Soong Yang K, Chi Ong B, Seong Ng H. Bringing generalists into the hospital: outcomes of a family medicine hospitalist model in Singapore. J Hosp Med. 2011;6(3):115-121.
- Sprague L. The hospitalist: better value in inpatient care? National Health Policy Forum website. Available at: www.nhpf.org/library/issue-briefs/IB842_Hospitalist_03-30-11.pdf. Accessed June 28, 2011.
One hospitalist-led pilot project produced a 61% decrease in heart failure readmission rates. Another resulted in a 33% drop in all-cause readmissions. The numbers might be impressive, but what do they really say about how hospitalists have influenced healthcare quality?
When HM emerged 15 years ago, advocates pitched the fledgling physician specialty as a model of efficient inpatient care, and subsequent findings that the concept led to reductions in length of stay encouraged more hospitals to bolster their staff with the newcomers. With a rising emphasis on quality and patient safety over the past decade, and the new era of pay-for-performance, the hospitalist model of care has expanded to embrace improved quality of care as a chief selling point.
Measuring quality is no easy task, however, and researchers still debate the relative merits of metrics like 30-day readmission rates and inpatient mortality. "Without question, quality measurement is an imperfect science, and all measures will contain some level of imprecision and bias," concluded a recent commentary in Health Affairs.1
Against that backdrop, relatively few studies have looked broadly at the contributions of hospital medicine. Most interventions have been individually tailored to a hospital or instituted at only a few sites, precluding large-scale, head-to-head comparisons.
And so the question remains: Has hospital medicine lived up to its promise on quality?
The Evidence
In one of the few national surveys of HM’s impact on patient care, a yearlong comparison of more than 3,600 hospitals found that the roughly 40% that employed hospitalists scored better on multiple Hospital Quality Alliance indicators. The 2009 Archives of Internal Medicine study suggested that hospitals with hospitalists outperformed their counterparts in quality metrics for acute myocardial infarction, pneumonia, overall disease treatment and diagnosis, and counseling and prevention. Congestive heart failure was the only category of the five reviewed that lacked a statistically significant difference.2
A separate editorial, however, argued that the study’s data were not persuasive enough to support the conclusion that hospitalists bring a higher quality of care to the table.3 And even less can be said about the national impact of HM on newly elevated metrics, such as readmission rates. The obligation to gather evidence, in fact, is largely falling upon hospitalists themselves, and the multitude of research abstracts from SHM’s annual meeting in May suggests that plenty of physician scientists are taking the responsibility seriously. Among the presentations, a study led by David Boyte, MD, assistant professor of medicine at Duke University and a hospitalist at Durham Regional Hospital, found that a multidisciplinary approach greatly improved one hospital unit’s 30-day readmission rates for heart failure patients. After a three-month pilot in the cardiac nursing unit, readmission rates fell to 10.7% from 27.6%.4
Although the multidisciplinary effort has included doctors, nurses, nutritionists, pharmacists, unit managers, and other personnel, Dr. Boyte says the involvement of hospitalists has been key to the project’s success. "We feel like we were the main participants who could see the whole picture from a patient-centered perspective," he says. "We were the glue; we were the center node of all the healthcare providers." Based on that dramatic improvement, Dr. Boyte says, the same interventional protocol has been rolled out in three other medical surgical units, and the hospital is using a similar approach to address AMI readmission rates.
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions; www.hospitalmedicine.org/boost )—by far the largest study of how HM is impacting readmission rates—has amassed data from more than 20 hospitals, with more expected from a growing roster of participants. So far, however, the project has only released data from six pilot sites describing the six-month periods before and after the project’s start. Among those sites, initial results suggest that readmission rates fell by an average of more than 20%, to 11.2% from 14.2%.5
Though the early numbers are encouraging, experts say rates from a larger group of participants at the one-year mark will be more telling, as will direct comparisons between BOOST units and nonparticipating counterparts at the same hospitals. Principal investigator Mark Williams, MD, FHM, professor and chief of the division of hospital medicine at the Northwestern University Feinberg School of Medicine in Chicago, says researchers still need to clean up that data before they’re ready to share it publicly.
In the meantime, some individual BOOST case studies are suggesting that hospitalist-led changes could pay big dividends. To help create cohesiveness and a sense of ownership within its HM program, St. Mary’s Health Center in St. Louis started a 20-bed hospitalist unit in 2008. Philip Vaidyan, MD, FACP, head of the hospitalist program and practice group leader for IPC: The Hospitalist Company at St. Mary’s, says one unit, 3 West, has since functioned as a lab for testing new ideas that are then introduced hospitalwide.
One early change was to bring all of the unit’s care providers together, from doctors and nurses to the unit-based case manager and social worker, for 9 a.m. handoff meetings. "We have this collective brain to find unique solutions," Dr. Vaidyan says. After seeing positive trends on length of stay, 30-day readmission rates, and patient satisfaction scores, St. Mary’s upgraded to a 32-bed hospitalist unit in early 2009. That same year, the 525-bed community teaching hospital was accepted into the BOOST program.
The hospitalist unit’s improved quality scores continued under BOOST, leading to a 33% reduction in readmission rates from 2008 to 2010 (to 10.5% from 15.7%). Rates for a nonhospitalist unit, by contrast, hovered around 17%. "For reducing readmissions, people may think that you have to have a higher length of stay," Dr. Vaidyan says. But the unit trended toward a lower length of stay, in addition to its reduced 30-day readmissions and improved patient satisfaction scores.
Flush with success, the 10 physicians and four nurse practitioners in the hospitalist program have since begun spreading their best practices to the rest of the hospital units. "Hospitalists are in the best ‘sweet spot,’ " Dr. Vaidyan says, "partnering with all of the disciplines, bringing them together, and keeping everybody on the same page."
Ironically, pinpointing the contribution of hospitalists is harder when their changes produce an ecological effect throughout an entire institution, says Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee. Even so, he stresses that the impact of the two dozen hospitalists at Medical College Physicians has been felt.
"Coinciding with and following the introduction of our hospitalist program in 2004, we have noticed dramatic decreases in our length of stay throughout medicine services," he says. The same has held true for inpatient mortality. "And that, we feel, is attributable to the standardization of processes introduced by the hospitalist group." Multidisciplinary rounds; whiteboards in patient rooms; and standardized admission orders, prophylactic treatments, and discharge processes—"all of this would’ve been impossible, absolutely impossible, without the hospitalist," he says.
Over the past decade, Dr. Singh’s assessment has been echoed by several studies suggesting that individual hospitalist programs have brought significant improvements in quality measures, such as complication rates and inpatient mortality. In 2002, for example, Andrew Auerbach, MD, MPH, at the University of California San Francisco Medical Center, led a study that compared HM care with that of community physicians in a community-based teaching hospital. Patients cared for by hospitalists, the study found, had a lower risk of death during the hospitalization, as well as at 30 days and 60 days after discharge.6
A separate report by David Meltzer, MD, PhD, and colleagues at the University of Chicago found that an HM program in an academic general medicine service led to a 30% reduction in 30-day mortality rates during its second year of operation.7 And a 2004 study led by Jeanne Huddleston, MD, at the Mayo Clinic College of Medicine in Rochester, Minn., found that a hospitalist-orthopedic co-management model (versus care by orthopedic surgeons with medical consultation) led to more patients being discharged with no complications after elective hip or knee surgery.8 Hospitalist co-management also reduced the rate of minor complications, but had no effect on actual length of stay or cost.
A subsequent study by the same group, however, documented improved efficiency of care through the HM model, but no effect on the mortality of hip fracture patients up to one year after discharge.9 Multiple studies of hospitalist programs, in fact, have seen increased efficiency but little or no impact on inpatient mortality, leading researchers to broadly conclude that such programs can decrease resource use without compromising quality.
In 2007, a retrospective study of nearly 77,000 patients admitted to 45 hospitals with one of seven common diagnoses compared the care delivered by hospitalists, general internists, and family physicians.10 Although the study authors found that hospitalist care yielded a small drop in length of stay, they saw no difference in the inpatient mortality rates or 14-day readmission rates. More recently, mortality has become ensnared in controversy over its reliability as an accurate indicator of quality.

-Shai Gavi, DO, MPH, chief, section of hospital medicine, assistant professor, Stony Brook University School of Medicine, Brookhaven, N.Y.
Half of the Equation
Despite a lack of ideal metrics, another promising sign for HM might be the model’s exportability. Lee Kheng Hock, MMed, senior consultant and head of the Department of Family Medicine and Continuing Care at Singapore General Hospital, says the 1,600-bed hospital began experimenting with the hospitalist model when officials realized the existing care system wasn’t sustainable. Amid an aging population and increasingly complex and fragmented care, Hock views the hospitalist movement as a natural evolution of the healthcare system to meet the needs of a changing environment.
In a recent study, Hock and his colleagues used the hospital’s administrative database to examine the resource use and outcomes of patients cared for in 2008 by family medicine hospitalists or by specialists.11 The comparison, based on several standard metrics, found no significant improvements in quality, with similar inpatient mortality rates and 30-day, all-cause, unscheduled readmission rates regardless of the care delivery method. The study, though, revealed a significantly shorter hospital stay (4.4 days vs. 5.3 days) and lower costs per patient for those cared for by hospitalists ($2,250 vs. $2,500).11
Hock points out that, like his study, most analyses of hospitalist programs have shown an improvement in length of stay and cost of care without any increase in mortality and morbidity. If value equals quality divided by cost, he says, it stands to reason that quality must increase as overall value remains the same but costs decrease.
"The main difference is that the patients received undivided attention from a well-rounded generalist physician who is focused on providing holistic general medical care," Hock says, adding that "it is really a no-brainer that the outcome would be different."
Patients Rule
Other measures like the effectiveness of communication and seamlessness of handoffs often are assessed through their impacts on patient outcomes. But Sunil Kripalani, MD, MSc, SFHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn., says communication is now a primary focal point in Medicare’s new hospital value-based purchasing program (VBP). Within VBP’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) component, worth 30% of a hospital’s sum score, four of the 10 survey-based measures deal directly with communication. Patients’ overall rating and recommendation of hospitals likely will reflect their satisfaction with communication as well. Dr. Kripalani says it’s inevitable that hospitals—and hospitalists—will pay more attention to communication ratings as patients become judges of quality.
The expertise of hospitalists in handling challenging patients also leads to improved quality over time, says Shai Gavi, DO, MPH, chief of the section of hospital medicine and assistant professor of clinical medicine at Stony Brook University School of Medicine in Brookhaven, N.Y. Hospitalists, he says, excel in handling such high-stakes medical issues as gastrointestinal bleeding, pancreatitis, sepsis, and pain management that can quickly impact patient outcomes if not addressed properly and proficiently. "I think there’s significant value to having people who do this on a pretty frequent basis," he says.
And because of their broad day-to-day interactions, Dr. Gavi says, hospitalists are natural choices for committees focused on improving quality. "When we sit on committees, people often look to us for answers and directions because they know we’re on the front lines and we’ve interfaced with all of the services in the hospital," he says. "You have a good view of the whole hospital operation from A to Z, and I think that’s pretty unique to hospitalists."
The Verdict
In a recent issue brief by Lisa Sprague, principal policy analyst at the National Health Policy Forum, she asserts, "Hospitalists have the undeniable advantage of being there when a crisis occurs, when a patient is ready for discharge, and so on."12
So is "being there" the defining concept of hospital medicine, as she subsequently suggests?
Based on both scientific and anecdotal evidence, the contribution of hospitalists to healthcare quality might be better summarized as "being involved." Whether as innovators, navigators, physician champions, the "sweet spot" of interdepartmental partnerships, the "glue" of multidisciplinary teams, or the nuclei of performance committees, hospitalists are increasingly described as being in the middle of efforts to improve quality. On this basis, the discipline appears to be living up to expectations, though experts say more research is needed to better assess the impacts of HM on quality.
Dr. Vaidyan says hospitalists are particularly well positioned to understand what constitutes ideal care from the perspective of patients. "They want to be treated well: That’s patient satisfaction," he says. "They want to have their chief complaint—why they came to the hospital—properly addressed, so you need a coordinated care team. They want to go home early and don’t want come back: That’s low length of stay and a reduction in 30-day readmissions. And they don’t want any hospital-acquired complications."
Treating patients better, then, should be reflected by improved quality, even if the participation of hospitalists cannot be precisely quantified. "Being involved is something that may be difficult to measure," Dr. Gavi says, "but nonetheless, it has an important impact." TH
Bryn Nelson is a medical writer based in Seattle.
References
- Pronovost PJ, Lilford R. Analysis & commentary: A roadmap for improving the performance of performance measures. Health Aff (Millwood). 2011;30(4):569-73.
- López L, Hicks LS, Cohen AP, McKean S, Weissman JS. Hospitalists and the quality of care in hospitals. Arch Intern Med. 2009;169(15):1389-1394.
- Centor RM, Taylor BB. Do hospitalists improve quality? Arch Intern Med. 2009;169(15):1351-1352.
- Boyte D, Verma L, Wightman M. A multidisciplinary approach to reducing heart failure readmissions. J Hosp Med. 2011;6(4)Supp 2:S14.
- Williams MV, Hansen L, Greenwald J, Howell E, et al. BOOST: impact of a quality improvement project to reduce rehospitalizations. J Hosp Med. 2011;6(4) Supp 2:S88. BOOST: impact of a quality improvement project to reduce rehospitalizations.
- Auerbach AD, Wachter RM, Katz P, Showstack J, Baron RB, Goldman L. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859-865.
- Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(1):866-874.
- Huddleston JM, Hall K, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty. Ann Intern Med. 2004;141(1):28-38.
- Batsis JA, Phy MP, Melton LJ, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4): 219–225.
- Lindenauer PK, Rothberg MB, Pekow PS, et al. Outcomes of care by hospitalists, general internists, and family physicians. N Eng J Med. 2007;357:2589-2600.
- Hock Lee K, Yang Y, Soong Yang K, Chi Ong B, Seong Ng H. Bringing generalists into the hospital: outcomes of a family medicine hospitalist model in Singapore. J Hosp Med. 2011;6(3):115-121.
- Sprague L. The hospitalist: better value in inpatient care? National Health Policy Forum website. Available at: www.nhpf.org/library/issue-briefs/IB842_Hospitalist_03-30-11.pdf. Accessed June 28, 2011.
Global Perspective
We’ve all heard the stereotypes: Other countries have socialized medicine, rationed care, endless lines, and little incentive for innovation. OK, there might be a grain of truth to the wait times. But healthcare in other developed nations is surprisingly varied in its mix of public and private providers, and it yields high-quality outcomes for a far better price than in the U.S. And yes, international innovation is alive and well.
Head-to-head comparisons can only go so far, with many countries using vastly different metrics to measure quality and efficiency. Nevertheless, the examples of bundling, reference pricing, and patient-reported outcomes offer a glimpse of how large-scale initiatives can help improve outcomes and bottom lines in the hospital and beyond.
Just the Facts
Last November, the nonprofit Commonwealth Fund in New York funded an analysis of healthcare data from the Organisation for Economic Co-operation and Development (OECD), which explains just how expensive healthcare is here.
In 2008, the U.S. spent roughly $7,500 per person on healthcare, an astonishing 50% more than the next closest country: Norway, at about $5,000 per person. And yet we lag behind Norway and almost all of our other peers in mortality rates. Cathy Schoen, senior vice president for policy, research, and evaluation at the Commonwealth Fund, says the OECD statistics also say something about how we use hospitals. Compared with its peers, the U.S. actually spends a smaller fraction of money on hospital care. We’re also on the low end of the number of acute-care hospital beds and hospital discharges per 1,000 people, and below average on the typical length of stay for acute care, at about 5.5 days. “So we’re not using the hospital more, and we’re not staying in it longer,” Schoen says. “Nor do we have way more beds, so it’s not an occupancy issue that’s driving this.”
Instead, the numbers suggest that the tests ordered, the drugs prescribed, the devices implanted, and other medical services offered are driving up costs, at least in part. So what can other countries tell us? As policymakers here debate how to bundle more healthcare payments around episodes of care (see “A Bundle of Nerves,” November 2010, p. 1), European countries including Germany and the Netherlands already are using the payment initiative on a national level to create efficiencies around hospital-based care. And they’ve done it with an American innovation: diagnostic-related groups, or DRGs. Bundling around a hip replacement, for example, includes the cost of the implant, the surgeon, and all of the hospital care. “It gives the hospital overall and all of its physicians an incentive to say, ‘If we could buy supplies cheaper, let’s do it,’ ” Schoen says.
An eye-popping 2007 McKinsey & Company study documents the relative cost of hip and knee replacement surgeries for five countries. In 2004, U.S. doctors performed just over half as many hip replacements per 100,000 people as their German counterparts. Yet the cost of each hip prosthetic averaged more than $4,800 per patient in the U.S.—four times higher than the $1,200 cost in Germany and the $1,400 cost in the United Kingdom.
Part of this difference, Schoen says, is due to supply chain management and involving doctors in the decision-making process. Many countries (and a few integrated health systems in the U.S.) are asking surgeons to help select just one or two prosthetic implants, negotiate for bulk volume pricing, and then track the clinical outcomes of those devices to flag poor performers, she says.
Setting the Bar for New Drugs
Drugs are another big-ticket item, and the U.S. pays almost twice as much per capita as the OECD average. To keep their prices lower, Schoen says, many European countries have information systems that track the relative clinical effectiveness of pharmaceuticals. “And they’re using it to inform the way they cover drugs: not to exclude them from the list of what’s covered, but to do something in Europe that’s called reference pricing,” she adds.
Let’s say a new drug costs 50% more than an older one with roughly equivalent efficacy. Under reference pricing, a doctor can still prescribe the new drug, but the patient must pay all or most of the difference. Such benchmarking has fueled an interesting dynamic. “The brand names that are coming in and want to get some market share will price themselves lower, because if they’re priced really high compared to the reference price, the chances are they just won’t ever get a market share,” Schoen says. As a result, drug prices stay lower.
The concept, although discussed in the U.S., has yet to be widely implemented here. A new study in the April issue of the Journal of Managed Care Pharmacy, however, could cause some cash-strapped governments to take a closer look.1 In the study, the Arkansas State Employee Health Plan used reference pricing for proton-pump inhibitors, using the cost of generic omeprazole as its reference point. Over the 43-month reference-pricing period, net plan costs for the drugs dropped by 49.5% per member per month.
Patient Feedback
A third lesson is that constructive feedback on quality can improve performance, even if no money is attached to outcomes. Like the U.S., Germany is placing a high priority on metrics that evaluate hospital quality. Schoen says the German performance improvement initiative is identifying outliers and providing them with feedback and technical support, but it is not built into the payment system. “They’ve had pretty rapid improvement out of that,” she says, “and I would say we’re learning the same thing in the U.S.”
Initially, Medicare data posted on its Hospital Compare website (www.hospitalcompare.hhs.gov) showed a wide hospital-to-hospital variation in mortality rates for pneumonia, heart attacks, and congestive heart failure. But since then, Schoen says, most outliers on the low end have improved dramatically, even though the only payment incentive was to encourage reporting. In fact, CMS is dropping some core measures from its hospital value-based purchasing program.
Public reporting of quality measures, especially mortality rates, is certainly not without controversy. But Schoen says that if handled properly, disseminating information that suggests a facility’s performance is subpar can tap into the professionalism of its staff and create a strong incentive among them to do better. “That’s something true both internationally and in the U.S.,” she says.
In the U.S., Schoen says, the basic questions asked of patients in the HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) portion of Medicare’s new VBP system represent a good start. But the experiences of other countries, she says, suggest that patient reporting should be directed more at outcomes, similar to a proposal left out of last year’s healthcare reform bill that would have created a feedback system for patients receiving implantable medical devices.
Even so, hospitals like Dartmouth-Hitchcock Medical Center in Lebanon, N.H., are instituting patient feedback systems on their own, and a National Institutes of Health (NIH) initiative called PROMIS (Patient Reported Outcomes Measurement Information System) is gaining traction. “It’s less blaming, and it’s more informing,” Schoen says. TH
Bryn Nelson is a freelance medical writer based in Seattle.
Reference
- Johnson JT, Neill KK, Davis DA. Five-year examination of utilization and drug cost outcomes associated with benefit design changes including reference pricing for proton pump inhibitors in a state employee health plan. J Manag Care Pharm. 2011;17(3):200-212.
We’ve all heard the stereotypes: Other countries have socialized medicine, rationed care, endless lines, and little incentive for innovation. OK, there might be a grain of truth to the wait times. But healthcare in other developed nations is surprisingly varied in its mix of public and private providers, and it yields high-quality outcomes for a far better price than in the U.S. And yes, international innovation is alive and well.
Head-to-head comparisons can only go so far, with many countries using vastly different metrics to measure quality and efficiency. Nevertheless, the examples of bundling, reference pricing, and patient-reported outcomes offer a glimpse of how large-scale initiatives can help improve outcomes and bottom lines in the hospital and beyond.
Just the Facts
Last November, the nonprofit Commonwealth Fund in New York funded an analysis of healthcare data from the Organisation for Economic Co-operation and Development (OECD), which explains just how expensive healthcare is here.
In 2008, the U.S. spent roughly $7,500 per person on healthcare, an astonishing 50% more than the next closest country: Norway, at about $5,000 per person. And yet we lag behind Norway and almost all of our other peers in mortality rates. Cathy Schoen, senior vice president for policy, research, and evaluation at the Commonwealth Fund, says the OECD statistics also say something about how we use hospitals. Compared with its peers, the U.S. actually spends a smaller fraction of money on hospital care. We’re also on the low end of the number of acute-care hospital beds and hospital discharges per 1,000 people, and below average on the typical length of stay for acute care, at about 5.5 days. “So we’re not using the hospital more, and we’re not staying in it longer,” Schoen says. “Nor do we have way more beds, so it’s not an occupancy issue that’s driving this.”
Instead, the numbers suggest that the tests ordered, the drugs prescribed, the devices implanted, and other medical services offered are driving up costs, at least in part. So what can other countries tell us? As policymakers here debate how to bundle more healthcare payments around episodes of care (see “A Bundle of Nerves,” November 2010, p. 1), European countries including Germany and the Netherlands already are using the payment initiative on a national level to create efficiencies around hospital-based care. And they’ve done it with an American innovation: diagnostic-related groups, or DRGs. Bundling around a hip replacement, for example, includes the cost of the implant, the surgeon, and all of the hospital care. “It gives the hospital overall and all of its physicians an incentive to say, ‘If we could buy supplies cheaper, let’s do it,’ ” Schoen says.
An eye-popping 2007 McKinsey & Company study documents the relative cost of hip and knee replacement surgeries for five countries. In 2004, U.S. doctors performed just over half as many hip replacements per 100,000 people as their German counterparts. Yet the cost of each hip prosthetic averaged more than $4,800 per patient in the U.S.—four times higher than the $1,200 cost in Germany and the $1,400 cost in the United Kingdom.
Part of this difference, Schoen says, is due to supply chain management and involving doctors in the decision-making process. Many countries (and a few integrated health systems in the U.S.) are asking surgeons to help select just one or two prosthetic implants, negotiate for bulk volume pricing, and then track the clinical outcomes of those devices to flag poor performers, she says.
Setting the Bar for New Drugs
Drugs are another big-ticket item, and the U.S. pays almost twice as much per capita as the OECD average. To keep their prices lower, Schoen says, many European countries have information systems that track the relative clinical effectiveness of pharmaceuticals. “And they’re using it to inform the way they cover drugs: not to exclude them from the list of what’s covered, but to do something in Europe that’s called reference pricing,” she adds.
Let’s say a new drug costs 50% more than an older one with roughly equivalent efficacy. Under reference pricing, a doctor can still prescribe the new drug, but the patient must pay all or most of the difference. Such benchmarking has fueled an interesting dynamic. “The brand names that are coming in and want to get some market share will price themselves lower, because if they’re priced really high compared to the reference price, the chances are they just won’t ever get a market share,” Schoen says. As a result, drug prices stay lower.
The concept, although discussed in the U.S., has yet to be widely implemented here. A new study in the April issue of the Journal of Managed Care Pharmacy, however, could cause some cash-strapped governments to take a closer look.1 In the study, the Arkansas State Employee Health Plan used reference pricing for proton-pump inhibitors, using the cost of generic omeprazole as its reference point. Over the 43-month reference-pricing period, net plan costs for the drugs dropped by 49.5% per member per month.
Patient Feedback
A third lesson is that constructive feedback on quality can improve performance, even if no money is attached to outcomes. Like the U.S., Germany is placing a high priority on metrics that evaluate hospital quality. Schoen says the German performance improvement initiative is identifying outliers and providing them with feedback and technical support, but it is not built into the payment system. “They’ve had pretty rapid improvement out of that,” she says, “and I would say we’re learning the same thing in the U.S.”
Initially, Medicare data posted on its Hospital Compare website (www.hospitalcompare.hhs.gov) showed a wide hospital-to-hospital variation in mortality rates for pneumonia, heart attacks, and congestive heart failure. But since then, Schoen says, most outliers on the low end have improved dramatically, even though the only payment incentive was to encourage reporting. In fact, CMS is dropping some core measures from its hospital value-based purchasing program.
Public reporting of quality measures, especially mortality rates, is certainly not without controversy. But Schoen says that if handled properly, disseminating information that suggests a facility’s performance is subpar can tap into the professionalism of its staff and create a strong incentive among them to do better. “That’s something true both internationally and in the U.S.,” she says.
In the U.S., Schoen says, the basic questions asked of patients in the HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) portion of Medicare’s new VBP system represent a good start. But the experiences of other countries, she says, suggest that patient reporting should be directed more at outcomes, similar to a proposal left out of last year’s healthcare reform bill that would have created a feedback system for patients receiving implantable medical devices.
Even so, hospitals like Dartmouth-Hitchcock Medical Center in Lebanon, N.H., are instituting patient feedback systems on their own, and a National Institutes of Health (NIH) initiative called PROMIS (Patient Reported Outcomes Measurement Information System) is gaining traction. “It’s less blaming, and it’s more informing,” Schoen says. TH
Bryn Nelson is a freelance medical writer based in Seattle.
Reference
- Johnson JT, Neill KK, Davis DA. Five-year examination of utilization and drug cost outcomes associated with benefit design changes including reference pricing for proton pump inhibitors in a state employee health plan. J Manag Care Pharm. 2011;17(3):200-212.
We’ve all heard the stereotypes: Other countries have socialized medicine, rationed care, endless lines, and little incentive for innovation. OK, there might be a grain of truth to the wait times. But healthcare in other developed nations is surprisingly varied in its mix of public and private providers, and it yields high-quality outcomes for a far better price than in the U.S. And yes, international innovation is alive and well.
Head-to-head comparisons can only go so far, with many countries using vastly different metrics to measure quality and efficiency. Nevertheless, the examples of bundling, reference pricing, and patient-reported outcomes offer a glimpse of how large-scale initiatives can help improve outcomes and bottom lines in the hospital and beyond.
Just the Facts
Last November, the nonprofit Commonwealth Fund in New York funded an analysis of healthcare data from the Organisation for Economic Co-operation and Development (OECD), which explains just how expensive healthcare is here.
In 2008, the U.S. spent roughly $7,500 per person on healthcare, an astonishing 50% more than the next closest country: Norway, at about $5,000 per person. And yet we lag behind Norway and almost all of our other peers in mortality rates. Cathy Schoen, senior vice president for policy, research, and evaluation at the Commonwealth Fund, says the OECD statistics also say something about how we use hospitals. Compared with its peers, the U.S. actually spends a smaller fraction of money on hospital care. We’re also on the low end of the number of acute-care hospital beds and hospital discharges per 1,000 people, and below average on the typical length of stay for acute care, at about 5.5 days. “So we’re not using the hospital more, and we’re not staying in it longer,” Schoen says. “Nor do we have way more beds, so it’s not an occupancy issue that’s driving this.”
Instead, the numbers suggest that the tests ordered, the drugs prescribed, the devices implanted, and other medical services offered are driving up costs, at least in part. So what can other countries tell us? As policymakers here debate how to bundle more healthcare payments around episodes of care (see “A Bundle of Nerves,” November 2010, p. 1), European countries including Germany and the Netherlands already are using the payment initiative on a national level to create efficiencies around hospital-based care. And they’ve done it with an American innovation: diagnostic-related groups, or DRGs. Bundling around a hip replacement, for example, includes the cost of the implant, the surgeon, and all of the hospital care. “It gives the hospital overall and all of its physicians an incentive to say, ‘If we could buy supplies cheaper, let’s do it,’ ” Schoen says.
An eye-popping 2007 McKinsey & Company study documents the relative cost of hip and knee replacement surgeries for five countries. In 2004, U.S. doctors performed just over half as many hip replacements per 100,000 people as their German counterparts. Yet the cost of each hip prosthetic averaged more than $4,800 per patient in the U.S.—four times higher than the $1,200 cost in Germany and the $1,400 cost in the United Kingdom.
Part of this difference, Schoen says, is due to supply chain management and involving doctors in the decision-making process. Many countries (and a few integrated health systems in the U.S.) are asking surgeons to help select just one or two prosthetic implants, negotiate for bulk volume pricing, and then track the clinical outcomes of those devices to flag poor performers, she says.
Setting the Bar for New Drugs
Drugs are another big-ticket item, and the U.S. pays almost twice as much per capita as the OECD average. To keep their prices lower, Schoen says, many European countries have information systems that track the relative clinical effectiveness of pharmaceuticals. “And they’re using it to inform the way they cover drugs: not to exclude them from the list of what’s covered, but to do something in Europe that’s called reference pricing,” she adds.
Let’s say a new drug costs 50% more than an older one with roughly equivalent efficacy. Under reference pricing, a doctor can still prescribe the new drug, but the patient must pay all or most of the difference. Such benchmarking has fueled an interesting dynamic. “The brand names that are coming in and want to get some market share will price themselves lower, because if they’re priced really high compared to the reference price, the chances are they just won’t ever get a market share,” Schoen says. As a result, drug prices stay lower.
The concept, although discussed in the U.S., has yet to be widely implemented here. A new study in the April issue of the Journal of Managed Care Pharmacy, however, could cause some cash-strapped governments to take a closer look.1 In the study, the Arkansas State Employee Health Plan used reference pricing for proton-pump inhibitors, using the cost of generic omeprazole as its reference point. Over the 43-month reference-pricing period, net plan costs for the drugs dropped by 49.5% per member per month.
Patient Feedback
A third lesson is that constructive feedback on quality can improve performance, even if no money is attached to outcomes. Like the U.S., Germany is placing a high priority on metrics that evaluate hospital quality. Schoen says the German performance improvement initiative is identifying outliers and providing them with feedback and technical support, but it is not built into the payment system. “They’ve had pretty rapid improvement out of that,” she says, “and I would say we’re learning the same thing in the U.S.”
Initially, Medicare data posted on its Hospital Compare website (www.hospitalcompare.hhs.gov) showed a wide hospital-to-hospital variation in mortality rates for pneumonia, heart attacks, and congestive heart failure. But since then, Schoen says, most outliers on the low end have improved dramatically, even though the only payment incentive was to encourage reporting. In fact, CMS is dropping some core measures from its hospital value-based purchasing program.
Public reporting of quality measures, especially mortality rates, is certainly not without controversy. But Schoen says that if handled properly, disseminating information that suggests a facility’s performance is subpar can tap into the professionalism of its staff and create a strong incentive among them to do better. “That’s something true both internationally and in the U.S.,” she says.
In the U.S., Schoen says, the basic questions asked of patients in the HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) portion of Medicare’s new VBP system represent a good start. But the experiences of other countries, she says, suggest that patient reporting should be directed more at outcomes, similar to a proposal left out of last year’s healthcare reform bill that would have created a feedback system for patients receiving implantable medical devices.
Even so, hospitals like Dartmouth-Hitchcock Medical Center in Lebanon, N.H., are instituting patient feedback systems on their own, and a National Institutes of Health (NIH) initiative called PROMIS (Patient Reported Outcomes Measurement Information System) is gaining traction. “It’s less blaming, and it’s more informing,” Schoen says. TH
Bryn Nelson is a freelance medical writer based in Seattle.
Reference
- Johnson JT, Neill KK, Davis DA. Five-year examination of utilization and drug cost outcomes associated with benefit design changes including reference pricing for proton pump inhibitors in a state employee health plan. J Manag Care Pharm. 2011;17(3):200-212.
Marriage of Necessity
Doctors and hospitals need each other. Healthcare reform is requiring hospitals to rely more heavily on physicians to help them meet quality, safety, and efficiency goals. But in return, doctors are demanding more financial security and a larger role in hospital leadership.
Just how far are they willing to take their mutual relationship to meet their individual needs? A new report by professional services company PwC (formerly PricewaterhouseCoopers) examines the mindsets of potential partners, including an online survey of more than 1,000 doctors and in-depth interviews with 28 healthcare executives. The results suggest plenty of opportunities for alignment, though perhaps also the need for serious pre-marriage counseling.
“From Courtship to Marriage Part II” (www.PwC.com/us/PhysicianHospitalAlignment) follows an initial report that emphasizes the element of trust that’s necessary for any doctor-hospital alignment to succeed. This time around, the sequel is focusing on more concrete steps needed to take the budding relationship to the next level and sustain it. In particular, the new report focuses on sharing power (governance), sharing resources (compensation), and sharing outcomes (guidelines).
The PwC report preempts the naysayers by acknowledging at the outset that “hospitals and physicians have been to the altar before, but many of those marriages ended in divorce.” So what’s different from the 1990s, that decade of broken marriages doomed by the irreconcilable differences over capitation?
“Number one is that back in the ’90s, there wasn’t a clear consensus in defining and determining what is quality,” says Warren Skea, a director in the PwC Health Enterprise Growth Practice. In the intervening years, he says, membership societies—SHM among them—and nonprofit organizations, such as the National Quality Forum, have helped address the need to define and measure healthcare quality. The Centers for Medicare & Medicaid Services (CMS) followed up by adopting and implementing some of those measures in programs, including hospital value-based purchasing (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1).
Another missing component in the ’90s, Skea says, was an adequate set of tools for gauging quality. “Even if we did agree what quality was, we couldn’t go back in there and measure it in a valid way,” he explains. “We just didn’t have that capacity.”
A third lesson learned the hard way is that decision-making should involve all physicians, from primary-care doctors to specialists. That power-sharing will be critical, Skea says, as reimbursement models move away from fee-for-service, transaction-based compensation methods and toward paying for outcomes and quality. Silos of care are out, and transitioning patients across a continuum of care is definitely in.
Sound familiar? It should, and the similarity to the hospitalist job description isn’t lost on Skea. “I think hospitalists have served as a very good illustrative example of how physicians can add value to that efficiency equation, improve quality, increase [good] outcomes—all of those things,” he says. In fact, Skea says, the question now is how the quarterback role assumed by hospitalists can be translated or projected to the larger industry and other settings (e.g. outpatient clinics, home care rehabilitation, and continuing care facilities).
Accountable-care organizations (ACOs) are a hot topic in any discussion of better patient transitions and closer doctor-hospital alignments, but they’re hardly the only wedding chapels in town. The new report sketches out the corresponding amenities of a comanagement model and provider-owned plan, and Skea notes that part of the new Center for Medicare & Medicaid Innovation’s mandate will be to investigate other promising methods for encouraging providers to work together.
Leaders, Partners
For most doctors, according to the survey, working together means making joint decisions. More than 90% said they should be involved in “hospital governance activities such as serving on boards, being in management, and taking part in performance.”
“That didn’t surprise me at all; there’s a huge appetite for physicians to be involved in strategic governance and oversight,” Skea says. “That’s where hospitalists have been really good: taking it to that next level of strategy and leadership.”
Next to compensation, he says, governance is the biggest issue for many hospital-affiliated physicians. One wrinkle, however, is what the report’s authors heard from hospital executives. “There’s a recognition by hospital executives that they need those physicians in those governance roles,” Skea says. But the executives felt that more physicians should be trained and educated in business and financial decision-making.
Some of the training strategies, he says, are homegrown. One hospital client, for example, is providing its physicians with courses in statistical analysis, financial modeling, and change management, and referring to the educational package as “MBA in a box.” Other hospitals are steering their physicians toward outside sources of instruction. SHM’s four-day Leadership Academy (www.hospitalmedicine.org/leadership) offers another resource for hospitalists seeking more prominent roles within their institutions.
Along with a desire for more power-sharing, doctors looking to a hospital setting have clearly indicated that they expect to hold their own financially. According to the survey, 83% of doctors considering hospital employment expect to be paid as much as or more than they are currently earning.
And therein lies another potential sticking point. Based on past experience, doctors might expect that hospitals’ financial resources will still allow them to maximize their compensation. But as health reform plays out, Skea cautions, “everybody is going to have to do more with less.”
Compromise Ahead
But other survey results hint at the potential for compromise. According to the report, physicians agreed that half of their compensation should be a fixed salary, while the remaining half could be based on meeting productivity, quality, patient satisfaction, and cost-of-care goals, with the potential for performance rewards. “This shows that physicians realize the health system is changing to track and reward performance and that they can influence the quality and cost of care delivery at the institutional level,” the report states.
And as for the guidelines doctors follow while delivering healthcare, 62% of those surveyed believe nationally accepted guidelines should guide the way they practice medicine; 30% prefer local guidelines.
Skea says he was a bit surprised that nearly 1 in 3 doctors are still resistant to national guidelines, though he believes that number is on the wane. After an initial pushback, he says, doctors seem to be gravitating toward the national standards, due in part to physician societies taking active roles in the discussions.
So what should hospitalists take away from all of this? Skea says they should continue to highlight and demonstrate the value they provide in standardizing care, measuring quality, and improving efficiencies in the four walls of the hospital. “They’ve had a track record, I think they have the mindset, and they’ve had the relationship with hospital executives,” he says.
Hospitalists likely will be called upon to help educate their physician colleagues in other specialties. Because of their background and history of success, Skea says, “they could be one of the real leaders and catalysts for change within an ACO or some of these other more integrated and aligned delivery models, and then move into governance.”
With a little assistance, perhaps this marriage might work after all. TH
Bryn Nelson is a freelance medical writer based in Seattle.
Doctors and hospitals need each other. Healthcare reform is requiring hospitals to rely more heavily on physicians to help them meet quality, safety, and efficiency goals. But in return, doctors are demanding more financial security and a larger role in hospital leadership.
Just how far are they willing to take their mutual relationship to meet their individual needs? A new report by professional services company PwC (formerly PricewaterhouseCoopers) examines the mindsets of potential partners, including an online survey of more than 1,000 doctors and in-depth interviews with 28 healthcare executives. The results suggest plenty of opportunities for alignment, though perhaps also the need for serious pre-marriage counseling.
“From Courtship to Marriage Part II” (www.PwC.com/us/PhysicianHospitalAlignment) follows an initial report that emphasizes the element of trust that’s necessary for any doctor-hospital alignment to succeed. This time around, the sequel is focusing on more concrete steps needed to take the budding relationship to the next level and sustain it. In particular, the new report focuses on sharing power (governance), sharing resources (compensation), and sharing outcomes (guidelines).
The PwC report preempts the naysayers by acknowledging at the outset that “hospitals and physicians have been to the altar before, but many of those marriages ended in divorce.” So what’s different from the 1990s, that decade of broken marriages doomed by the irreconcilable differences over capitation?
“Number one is that back in the ’90s, there wasn’t a clear consensus in defining and determining what is quality,” says Warren Skea, a director in the PwC Health Enterprise Growth Practice. In the intervening years, he says, membership societies—SHM among them—and nonprofit organizations, such as the National Quality Forum, have helped address the need to define and measure healthcare quality. The Centers for Medicare & Medicaid Services (CMS) followed up by adopting and implementing some of those measures in programs, including hospital value-based purchasing (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1).
Another missing component in the ’90s, Skea says, was an adequate set of tools for gauging quality. “Even if we did agree what quality was, we couldn’t go back in there and measure it in a valid way,” he explains. “We just didn’t have that capacity.”
A third lesson learned the hard way is that decision-making should involve all physicians, from primary-care doctors to specialists. That power-sharing will be critical, Skea says, as reimbursement models move away from fee-for-service, transaction-based compensation methods and toward paying for outcomes and quality. Silos of care are out, and transitioning patients across a continuum of care is definitely in.
Sound familiar? It should, and the similarity to the hospitalist job description isn’t lost on Skea. “I think hospitalists have served as a very good illustrative example of how physicians can add value to that efficiency equation, improve quality, increase [good] outcomes—all of those things,” he says. In fact, Skea says, the question now is how the quarterback role assumed by hospitalists can be translated or projected to the larger industry and other settings (e.g. outpatient clinics, home care rehabilitation, and continuing care facilities).
Accountable-care organizations (ACOs) are a hot topic in any discussion of better patient transitions and closer doctor-hospital alignments, but they’re hardly the only wedding chapels in town. The new report sketches out the corresponding amenities of a comanagement model and provider-owned plan, and Skea notes that part of the new Center for Medicare & Medicaid Innovation’s mandate will be to investigate other promising methods for encouraging providers to work together.
Leaders, Partners
For most doctors, according to the survey, working together means making joint decisions. More than 90% said they should be involved in “hospital governance activities such as serving on boards, being in management, and taking part in performance.”
“That didn’t surprise me at all; there’s a huge appetite for physicians to be involved in strategic governance and oversight,” Skea says. “That’s where hospitalists have been really good: taking it to that next level of strategy and leadership.”
Next to compensation, he says, governance is the biggest issue for many hospital-affiliated physicians. One wrinkle, however, is what the report’s authors heard from hospital executives. “There’s a recognition by hospital executives that they need those physicians in those governance roles,” Skea says. But the executives felt that more physicians should be trained and educated in business and financial decision-making.
Some of the training strategies, he says, are homegrown. One hospital client, for example, is providing its physicians with courses in statistical analysis, financial modeling, and change management, and referring to the educational package as “MBA in a box.” Other hospitals are steering their physicians toward outside sources of instruction. SHM’s four-day Leadership Academy (www.hospitalmedicine.org/leadership) offers another resource for hospitalists seeking more prominent roles within their institutions.
Along with a desire for more power-sharing, doctors looking to a hospital setting have clearly indicated that they expect to hold their own financially. According to the survey, 83% of doctors considering hospital employment expect to be paid as much as or more than they are currently earning.
And therein lies another potential sticking point. Based on past experience, doctors might expect that hospitals’ financial resources will still allow them to maximize their compensation. But as health reform plays out, Skea cautions, “everybody is going to have to do more with less.”
Compromise Ahead
But other survey results hint at the potential for compromise. According to the report, physicians agreed that half of their compensation should be a fixed salary, while the remaining half could be based on meeting productivity, quality, patient satisfaction, and cost-of-care goals, with the potential for performance rewards. “This shows that physicians realize the health system is changing to track and reward performance and that they can influence the quality and cost of care delivery at the institutional level,” the report states.
And as for the guidelines doctors follow while delivering healthcare, 62% of those surveyed believe nationally accepted guidelines should guide the way they practice medicine; 30% prefer local guidelines.
Skea says he was a bit surprised that nearly 1 in 3 doctors are still resistant to national guidelines, though he believes that number is on the wane. After an initial pushback, he says, doctors seem to be gravitating toward the national standards, due in part to physician societies taking active roles in the discussions.
So what should hospitalists take away from all of this? Skea says they should continue to highlight and demonstrate the value they provide in standardizing care, measuring quality, and improving efficiencies in the four walls of the hospital. “They’ve had a track record, I think they have the mindset, and they’ve had the relationship with hospital executives,” he says.
Hospitalists likely will be called upon to help educate their physician colleagues in other specialties. Because of their background and history of success, Skea says, “they could be one of the real leaders and catalysts for change within an ACO or some of these other more integrated and aligned delivery models, and then move into governance.”
With a little assistance, perhaps this marriage might work after all. TH
Bryn Nelson is a freelance medical writer based in Seattle.
Doctors and hospitals need each other. Healthcare reform is requiring hospitals to rely more heavily on physicians to help them meet quality, safety, and efficiency goals. But in return, doctors are demanding more financial security and a larger role in hospital leadership.
Just how far are they willing to take their mutual relationship to meet their individual needs? A new report by professional services company PwC (formerly PricewaterhouseCoopers) examines the mindsets of potential partners, including an online survey of more than 1,000 doctors and in-depth interviews with 28 healthcare executives. The results suggest plenty of opportunities for alignment, though perhaps also the need for serious pre-marriage counseling.
“From Courtship to Marriage Part II” (www.PwC.com/us/PhysicianHospitalAlignment) follows an initial report that emphasizes the element of trust that’s necessary for any doctor-hospital alignment to succeed. This time around, the sequel is focusing on more concrete steps needed to take the budding relationship to the next level and sustain it. In particular, the new report focuses on sharing power (governance), sharing resources (compensation), and sharing outcomes (guidelines).
The PwC report preempts the naysayers by acknowledging at the outset that “hospitals and physicians have been to the altar before, but many of those marriages ended in divorce.” So what’s different from the 1990s, that decade of broken marriages doomed by the irreconcilable differences over capitation?
“Number one is that back in the ’90s, there wasn’t a clear consensus in defining and determining what is quality,” says Warren Skea, a director in the PwC Health Enterprise Growth Practice. In the intervening years, he says, membership societies—SHM among them—and nonprofit organizations, such as the National Quality Forum, have helped address the need to define and measure healthcare quality. The Centers for Medicare & Medicaid Services (CMS) followed up by adopting and implementing some of those measures in programs, including hospital value-based purchasing (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1).
Another missing component in the ’90s, Skea says, was an adequate set of tools for gauging quality. “Even if we did agree what quality was, we couldn’t go back in there and measure it in a valid way,” he explains. “We just didn’t have that capacity.”
A third lesson learned the hard way is that decision-making should involve all physicians, from primary-care doctors to specialists. That power-sharing will be critical, Skea says, as reimbursement models move away from fee-for-service, transaction-based compensation methods and toward paying for outcomes and quality. Silos of care are out, and transitioning patients across a continuum of care is definitely in.
Sound familiar? It should, and the similarity to the hospitalist job description isn’t lost on Skea. “I think hospitalists have served as a very good illustrative example of how physicians can add value to that efficiency equation, improve quality, increase [good] outcomes—all of those things,” he says. In fact, Skea says, the question now is how the quarterback role assumed by hospitalists can be translated or projected to the larger industry and other settings (e.g. outpatient clinics, home care rehabilitation, and continuing care facilities).
Accountable-care organizations (ACOs) are a hot topic in any discussion of better patient transitions and closer doctor-hospital alignments, but they’re hardly the only wedding chapels in town. The new report sketches out the corresponding amenities of a comanagement model and provider-owned plan, and Skea notes that part of the new Center for Medicare & Medicaid Innovation’s mandate will be to investigate other promising methods for encouraging providers to work together.
Leaders, Partners
For most doctors, according to the survey, working together means making joint decisions. More than 90% said they should be involved in “hospital governance activities such as serving on boards, being in management, and taking part in performance.”
“That didn’t surprise me at all; there’s a huge appetite for physicians to be involved in strategic governance and oversight,” Skea says. “That’s where hospitalists have been really good: taking it to that next level of strategy and leadership.”
Next to compensation, he says, governance is the biggest issue for many hospital-affiliated physicians. One wrinkle, however, is what the report’s authors heard from hospital executives. “There’s a recognition by hospital executives that they need those physicians in those governance roles,” Skea says. But the executives felt that more physicians should be trained and educated in business and financial decision-making.
Some of the training strategies, he says, are homegrown. One hospital client, for example, is providing its physicians with courses in statistical analysis, financial modeling, and change management, and referring to the educational package as “MBA in a box.” Other hospitals are steering their physicians toward outside sources of instruction. SHM’s four-day Leadership Academy (www.hospitalmedicine.org/leadership) offers another resource for hospitalists seeking more prominent roles within their institutions.
Along with a desire for more power-sharing, doctors looking to a hospital setting have clearly indicated that they expect to hold their own financially. According to the survey, 83% of doctors considering hospital employment expect to be paid as much as or more than they are currently earning.
And therein lies another potential sticking point. Based on past experience, doctors might expect that hospitals’ financial resources will still allow them to maximize their compensation. But as health reform plays out, Skea cautions, “everybody is going to have to do more with less.”
Compromise Ahead
But other survey results hint at the potential for compromise. According to the report, physicians agreed that half of their compensation should be a fixed salary, while the remaining half could be based on meeting productivity, quality, patient satisfaction, and cost-of-care goals, with the potential for performance rewards. “This shows that physicians realize the health system is changing to track and reward performance and that they can influence the quality and cost of care delivery at the institutional level,” the report states.
And as for the guidelines doctors follow while delivering healthcare, 62% of those surveyed believe nationally accepted guidelines should guide the way they practice medicine; 30% prefer local guidelines.
Skea says he was a bit surprised that nearly 1 in 3 doctors are still resistant to national guidelines, though he believes that number is on the wane. After an initial pushback, he says, doctors seem to be gravitating toward the national standards, due in part to physician societies taking active roles in the discussions.
So what should hospitalists take away from all of this? Skea says they should continue to highlight and demonstrate the value they provide in standardizing care, measuring quality, and improving efficiencies in the four walls of the hospital. “They’ve had a track record, I think they have the mindset, and they’ve had the relationship with hospital executives,” he says.
Hospitalists likely will be called upon to help educate their physician colleagues in other specialties. Because of their background and history of success, Skea says, “they could be one of the real leaders and catalysts for change within an ACO or some of these other more integrated and aligned delivery models, and then move into governance.”
With a little assistance, perhaps this marriage might work after all. TH
Bryn Nelson is a freelance medical writer based in Seattle.
Value-Based Purchasing Raises the Stakes
Mock scorecards, interactive blueprints, quality dashboards: Hospitals are frantically seeking out any advantage that might help them excel in a fast-approaching, mandatory competition with millions of dollars on the line. Value-based purchasing (VBP), a program authorized by the Patient Protection and Accountable Care Act of 2010, gives the Centers for Medicare & Medicaid Services (CMS) the power to base a portion of hospital reimbursement payments on how well hospitals perform in 25 core measures.
The move is intended to help CMS flex its muscles and move from being a passive bystander to an active buyer of what its officials have deemed higher-quality healthcare. Analysts and healthcare experts warn that if hospitalists aren’t paying attention, however, they could put themselves at unnecessary risk or lose out on a major opportunity to demonstrate their value in what Patrick Torcson, MD, SFHM, is calling a “team sport.”
Dr. Torcson, chair of SHM’s Performance and Standards Committee, says every hospitalist should be aware of the core-measures concept, which has been around since 2003 in what’s now called the Hospital Inpatient Quality Reporting (IQR) Program. “We’re not reinventing the wheel; we’re just transforming the program from pay-for-reporting to actual pay-for-performance,” he says. Value-based purchasing, though, is raising the stakes considerably. “It’s really significant because it marks the beginning of an era of accountability and true pay-for-performance at the hospital level.”
A major reason for the heightened concern is the structure of the program. In other quality demonstration projects, CMS has established a score to beat: “Anyone above that threshold is in the money. If you didn’t make it, there was no harm, no foul,” says Trent Haywood, MD, JD, chief medical officer of the Irving, Tex.-based for-profit healthcare cooperative VHA Inc.

—Laura Dietzel, PeaceHealth’s program director for High-Tech Meaningful Use
What’s different this time is that value-based purchasing is not a collaboration but a competition in which every hospital is pitted against the entire market, says Dr. Haywood, the former deputy chief medical officer at CMS. It’s also a zero-sum game. That means there will be winners and losers, with the entire cost-neutral program funded by extracting money from the worst performers to financially reward the best. “In this competition-type model, you need to know who you can beat,” he says.
Race to the Top
That new reality has set off a mad scramble among hospitals hoping to gain any edge they can and spawned a cottage industry of consultants, lawyers, and quality specialists advising them on how to maximize their points. The drive to achieve and maintain a high level of performance is also spurring hospitals to seek more individual accountability as they look to minimize their financial risk.
Hospitals’ baseline scores already have been set, and the initial nine-month performance evaluation period begins July 1. Beginning with discharges on Oct. 1, 2012 (fiscal year 2013), the payment phase will kick in. CMS will start by withholding 1% of the base DRG reimbursement paid to hospitals. That money can be earned back based on how well each hospital scores on the performance measures during the evaluation period. The amount initially withheld will rise by 0.25 percentage points per year until it is capped at 2% in 2017 and beyond.
Think of the competition as an annual decathlon with a pool of prize money funded by the participants, except that hospitals will be evaluated on far more measures. So far, the program includes 17 core Clinical Process of Care measures and eight measures based on Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) surveys. Twenty other potential measures are waiting in the wings, including ones related to hospital-acquired conditions, patient safety, inpatient quality, and mortality, some of which likely will be introduced in fiscal year 2014.
CMS intends to monitor and evaluate the program’s impact on access and quality of care, especially for “vulnerable populations,” the percentage of patients who receive appropriate care, the rates of hospital-acquired conditions, and the best practices of high-performing hospitals.
The complicated nature of the rules and scoring, and significant money attached to the competition, have generated deep concern. In October and again in February, healthcare providers bombarded CMS representatives with questions and suggestions during open phone forums, when the regulations were still in flux. Would the rules be fair? Would CMS provide an early warning of impending losses? Was the agency giving too much weight to patient satisfaction scores?
SHM supports the program, stating, “We believe that the Medicare reimbursement system must be changed to promote value, and we strongly support policies that link quality measurement to performance-based payment.”
Other observers, though, have warned of the potential for unintended consequences. If doctors avoid complicated medical cases in order to increase a hospital’s score, for example, are they really improving care? Will poorly performing hospitals get caught in a vicious circle due to declining financial resources?
Some critics have complained that by scoring on a curve rather than on an absolute point system, the value-based purchasing program might not be a quality initiative so much as an opportunity for CMS to reduce hospital payments. “I believe that this is largely a shell game played by the Centers for Medicare & Medicaid Services to give hospitals the idea that they can win at this game, when all but a few will lose,” wrote Richard Rohr, MD, FHM, in his Feb. 1 entry at the Medical Staff Leader blog (http://blogs.hcpro.com/medicalstaff/). Hospitalist subsidies could be a prime target as the cost-reduction pressures rise, wrote Dr. Rohr, who directs HM programs for Guthrie Healthcare System in Sayre, Pa. Enhancing productivity, he stressed, could be the best defense against a rollback in salaries.
Most experts agree that investing in a quality infrastructure will be essential for success, though other hospitalists differ on the potential effects that VBP might have on their profession. “I think a big part of a quality infrastructure is a hospital medicine program,” Dr. Torcson says. In fact, he recommends that hospitalists approach a hospital CFO or CEO and offer their assistance with the program. “I really think that’s the right direction and the right attitude, kind of the way the Samurai used to serve the Japanese emperor,” he explains.
A major reason for taking the initiative, he says, is that value-based purchasing could become the new business case for HM. In the 1990s, hospitalists could put a real number on how much they saved hospitals by reducing length of stay, sparking an investment in HM programs. “I think value-based purchasing is now in the same position,” Dr. Torcson says, “and the savings is actually going to be even more quantifiable for the hospital in terms of their success or failure.”
continued below...
Expectations on the Rise
SHM’s annual meeting this month in Grapevine, Texas (www.hospitalmedicine2011.org), will feature a session on improving HCAHPS scores, and Dr. Torcson has been working on a society task force educating members about how to be successful amid the coming changes. A Web-based toolkit in the works, he says, will highlight best practices for myocardial infarctions, heart failure, surgical care, pneumonia, and patient satisfaction to help hospitalists ensure they have the necessary skill sets. (SHM will offer a full platform of VBP courses by end of 2011.)
“At the individual hospitalist level, once you’ve decided to commit to serving that hospital-level performance agenda, we want SHM to be the place to turn to get the information on best practices and what you need,” Dr. Torcson says.
But first, says Bill Darling, a Washington, D.C., and Austin, Tex.-based partner with Strasburger Attorneys at Law, hospitalists will need a much stronger understanding of hospital expectations. Many hospital officials already are indicating that they’re leaning toward their own pay-for-performance programs to put individual doctors on the hook for negative financial incentives and penalties.
“Ultimately, in these value-based systems,” says Darling, a specialist in healthcare contracts and regulations, “the quality scores for physicians may affect their medical staff privileges or their membership in their group, or their ability to even move to another hospital.”
Moreover, hospital administrators are trying to instill a sense of shared responsibility in maintaining high value-based purchasing scores. “I cannot make a physician prescribe an ACE inhibitor when it’s appropriate to deal with heart failure, but the hospital takes a hit for that,” says Dee Rogers, RN, director of quality and risk management at Magnolia Regional Medical Center in Magnolia, Ark. “Not that I want to see people get their hands slapped—I want to see equal accountability.”
Like other hospitals, Rogers’ 49-bed rural facility is tracking doctors’ performance on quality measures and guidelines as part of its credentialing process. Many facilities are starting to include more comprehensive evaluations as part of their contract renegotiations. Magnolia has one weekend hospitalist and is conducting a feasibility study on whether to launch a full-time hospitalist program on weekdays. If the hospital pursues that program, Rogers says, she’d like to see upfront expectations built into the doctors’ contracts.
PeaceHealth, a faith-based nonprofit healthcare system that operates eight hospitals in Oregon, Washington, and Alaska, is moving in the same direction. “I think we’re getting pretty close—certainly within the next year, probably sooner—of creating a reliable mechanism for physician accountability related to the measures that are included in value-based purchasing,” says Laura Dietzel, PeaceHealth’s program director for High-Tech Meaningful Use. That mechanism will connect specific core measures with specific physicians, not just roles or departments.
“We are really honing in on that kind of a quality dashboard, and [VBP’s arrival] is definitely going to be a big boost toward doing that,” says Dietzel, the health system’s former program manager for core measures. “We are talking about making it part of our credentialing process, part of our privileging process, and part of our physician reimbursement and pay schedule process.”
Dietzel concedes that the health system will need to develop a valid method for ensuring that it correctly records who had the responsibility for key decisions. Apart from the concern over proper credit and blame, Darling warns that doctors who haven’t been paying attention could be left holding the bag.
If a hospitalist contract doesn’t discuss how payments will be handled with bundling, value-based purchasing, accountable care, and other models coming down the pike, Darling says, “it may be that you’ve bought a pig in a poke and that you’re just hoping for the kindness of strangers.” Likewise, if a hospital underperforms on its VBP scores due to a lack of investment or training, he asks, will its physicians also look bad on paper? The perceived guilt by association might hurt their chances at finding employment elsewhere if other hospital administrators fear that doctors from poorly performing facilities will hurt their scores as well.
To avoid the most dire “What if?” scenarios, hospitals are enlisting their staff and trying out new tools to help them identify and address trouble spots. At Dr. Torcson’s own hospital, 237-bed St. Tammany Parish Hospital in Covington, La., hospitalists and other staff members are scrutinizing the core measures and tweaking guidelines and best practices to make sure the facility is in top form. Based on initial modeling, the hospital expects to earn back all of its withheld reimbursements, though Dr. Torcson says the push is still on to increase the cushion.
A few QI organizations that contract with CMS, including Seattle-based Qualis Health, have developed interactive calculators or mock scorecards to help hospitals determine where they stand in the value-based purchasing scrum. Patricia Richardson, MA, RCP, director of quality and risk for 50-bed Samaritan Hospital in Moses Lake, Wash., says the hospital has worked with Qualis (www.qualishealth.org) on a scorecard to help staff understand which measures need attention and what the financial repercussions would be if the hospital doesn’t improve.
After earlier pushback from doctors on some core measures, quality-review specialist Rebecca Johnson says Samaritan began posting how individual doctors were performing. “And, over time, that motivated them,” she says. “Nobody wants to be the guy in the red.” Johnson says the hospital’s four hospitalists, though, have been fully engaged. “Our hospitalists are very interested in how we’re doing,” she says. “When I’m on the floor doing my reviews, they consistently ask—all of them—‘How are we doing on the core measures?’ ”
Although Richardson concedes that Samaritan still has work to do to increase its patient-satisfaction scores, she’s hopeful that more education and engagement of both patients and staff will begin to pay off. Initiatives that have recruited patients as active participants in helping the hospital improve might help boost patient satisfaction scores, and internal competitions could help motivate the medical staff.
Setting upfront expectations about the hospital stay during the admissions process also can help. Richardson says patients naturally compare a hospital’s noise level to that of their own homes unless a doctor or other staff member provides the proper context. Letting patients know what to expect and reminding them that they’ll likely have to be awakened a few times during the night can make a big difference in whether they rate the hospital as being sufficiently quiet, she says.
Competition Breeds Cooperation
Hospitals likely will be able to differentiate themselves the most through the national competition’s patient perception of care scores, VHA Inc.’s Dr. Haywood says, largely because the contenders have had less time to prepare for them than for the clinical process-of-care measures. Among the eight HCAHPS measures, Dr. Haywood says, focusing on doctor communication, nurse communication, hospital staff responsiveness, and a quiet room might provide the biggest return on investment.
“If physicians don’t communicate effectively with the nurses, then the nurse communication score goes down because the patients assume that the nurses know the care plan,” he says. “A typical question that we see all the time is that the nurse will ask the patient, ‘Did the doctor come and see you today?’ And if the patient says yes, then the nurse will ask, ‘Well, what did the doctor say?’ because the nurse doesn’t know.”
With VBP in mind, Dr. Haywood’s health system repurposed part of its catalogue of Web-based blueprints designed to help hospitals improve their clinical practices (see Figure 2, below). The cooperative is now making its collection of more than 100 blueprints available to its members to help them prop up sagging core measure scores. All depict best-practice solutions in an easy-to-remember visual format, based on weeklong site visits to exemplary hospitals from a clinical team that includes a cultural anthropologist and graphic artist.
Arkansas’ Magnolia already exceeds the national average for every HCAHPS score except the overall rating, a score that will likely increase because most patient evaluations were conducted before a new facility replaced the previous, aging hospital in February 2010. Rogers says Magnolia’s weekend hospitalist has helped with continuity of care—an important factor for maintaining high satisfaction in a small, rural community where doctors tend to see the same elderly patients on a frequent basis. The patients know the hospitalist by name, she says, “so they almost have as much of a relationship to him as they do with their primary-care physician.”
Rogers says the weekend hospitalist also has helped improve some of the hospital’s lagging pneumonia-related scores by educating and communicating with other members of the medical staff about their respective responsibilities. Because he has gained the trust of his peers, Rogers says, he’s helped the hospital get more buy-in from them as well.
Embracing the role of VBP champion, Dr. Torcson says, could help further define the worth of hospitalists to their employers. And with a trend toward more individual physician accountability, rising to the occasion now could help hospitalists stay on top of their own game. TH
Bryn Nelson is a freelance medical writer in Seattle.
Mock scorecards, interactive blueprints, quality dashboards: Hospitals are frantically seeking out any advantage that might help them excel in a fast-approaching, mandatory competition with millions of dollars on the line. Value-based purchasing (VBP), a program authorized by the Patient Protection and Accountable Care Act of 2010, gives the Centers for Medicare & Medicaid Services (CMS) the power to base a portion of hospital reimbursement payments on how well hospitals perform in 25 core measures.
The move is intended to help CMS flex its muscles and move from being a passive bystander to an active buyer of what its officials have deemed higher-quality healthcare. Analysts and healthcare experts warn that if hospitalists aren’t paying attention, however, they could put themselves at unnecessary risk or lose out on a major opportunity to demonstrate their value in what Patrick Torcson, MD, SFHM, is calling a “team sport.”
Dr. Torcson, chair of SHM’s Performance and Standards Committee, says every hospitalist should be aware of the core-measures concept, which has been around since 2003 in what’s now called the Hospital Inpatient Quality Reporting (IQR) Program. “We’re not reinventing the wheel; we’re just transforming the program from pay-for-reporting to actual pay-for-performance,” he says. Value-based purchasing, though, is raising the stakes considerably. “It’s really significant because it marks the beginning of an era of accountability and true pay-for-performance at the hospital level.”
A major reason for the heightened concern is the structure of the program. In other quality demonstration projects, CMS has established a score to beat: “Anyone above that threshold is in the money. If you didn’t make it, there was no harm, no foul,” says Trent Haywood, MD, JD, chief medical officer of the Irving, Tex.-based for-profit healthcare cooperative VHA Inc.

—Laura Dietzel, PeaceHealth’s program director for High-Tech Meaningful Use
What’s different this time is that value-based purchasing is not a collaboration but a competition in which every hospital is pitted against the entire market, says Dr. Haywood, the former deputy chief medical officer at CMS. It’s also a zero-sum game. That means there will be winners and losers, with the entire cost-neutral program funded by extracting money from the worst performers to financially reward the best. “In this competition-type model, you need to know who you can beat,” he says.
Race to the Top
That new reality has set off a mad scramble among hospitals hoping to gain any edge they can and spawned a cottage industry of consultants, lawyers, and quality specialists advising them on how to maximize their points. The drive to achieve and maintain a high level of performance is also spurring hospitals to seek more individual accountability as they look to minimize their financial risk.
Hospitals’ baseline scores already have been set, and the initial nine-month performance evaluation period begins July 1. Beginning with discharges on Oct. 1, 2012 (fiscal year 2013), the payment phase will kick in. CMS will start by withholding 1% of the base DRG reimbursement paid to hospitals. That money can be earned back based on how well each hospital scores on the performance measures during the evaluation period. The amount initially withheld will rise by 0.25 percentage points per year until it is capped at 2% in 2017 and beyond.
Think of the competition as an annual decathlon with a pool of prize money funded by the participants, except that hospitals will be evaluated on far more measures. So far, the program includes 17 core Clinical Process of Care measures and eight measures based on Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) surveys. Twenty other potential measures are waiting in the wings, including ones related to hospital-acquired conditions, patient safety, inpatient quality, and mortality, some of which likely will be introduced in fiscal year 2014.
CMS intends to monitor and evaluate the program’s impact on access and quality of care, especially for “vulnerable populations,” the percentage of patients who receive appropriate care, the rates of hospital-acquired conditions, and the best practices of high-performing hospitals.
The complicated nature of the rules and scoring, and significant money attached to the competition, have generated deep concern. In October and again in February, healthcare providers bombarded CMS representatives with questions and suggestions during open phone forums, when the regulations were still in flux. Would the rules be fair? Would CMS provide an early warning of impending losses? Was the agency giving too much weight to patient satisfaction scores?
SHM supports the program, stating, “We believe that the Medicare reimbursement system must be changed to promote value, and we strongly support policies that link quality measurement to performance-based payment.”
Other observers, though, have warned of the potential for unintended consequences. If doctors avoid complicated medical cases in order to increase a hospital’s score, for example, are they really improving care? Will poorly performing hospitals get caught in a vicious circle due to declining financial resources?
Some critics have complained that by scoring on a curve rather than on an absolute point system, the value-based purchasing program might not be a quality initiative so much as an opportunity for CMS to reduce hospital payments. “I believe that this is largely a shell game played by the Centers for Medicare & Medicaid Services to give hospitals the idea that they can win at this game, when all but a few will lose,” wrote Richard Rohr, MD, FHM, in his Feb. 1 entry at the Medical Staff Leader blog (http://blogs.hcpro.com/medicalstaff/). Hospitalist subsidies could be a prime target as the cost-reduction pressures rise, wrote Dr. Rohr, who directs HM programs for Guthrie Healthcare System in Sayre, Pa. Enhancing productivity, he stressed, could be the best defense against a rollback in salaries.
Most experts agree that investing in a quality infrastructure will be essential for success, though other hospitalists differ on the potential effects that VBP might have on their profession. “I think a big part of a quality infrastructure is a hospital medicine program,” Dr. Torcson says. In fact, he recommends that hospitalists approach a hospital CFO or CEO and offer their assistance with the program. “I really think that’s the right direction and the right attitude, kind of the way the Samurai used to serve the Japanese emperor,” he explains.
A major reason for taking the initiative, he says, is that value-based purchasing could become the new business case for HM. In the 1990s, hospitalists could put a real number on how much they saved hospitals by reducing length of stay, sparking an investment in HM programs. “I think value-based purchasing is now in the same position,” Dr. Torcson says, “and the savings is actually going to be even more quantifiable for the hospital in terms of their success or failure.”
continued below...
Expectations on the Rise
SHM’s annual meeting this month in Grapevine, Texas (www.hospitalmedicine2011.org), will feature a session on improving HCAHPS scores, and Dr. Torcson has been working on a society task force educating members about how to be successful amid the coming changes. A Web-based toolkit in the works, he says, will highlight best practices for myocardial infarctions, heart failure, surgical care, pneumonia, and patient satisfaction to help hospitalists ensure they have the necessary skill sets. (SHM will offer a full platform of VBP courses by end of 2011.)
“At the individual hospitalist level, once you’ve decided to commit to serving that hospital-level performance agenda, we want SHM to be the place to turn to get the information on best practices and what you need,” Dr. Torcson says.
But first, says Bill Darling, a Washington, D.C., and Austin, Tex.-based partner with Strasburger Attorneys at Law, hospitalists will need a much stronger understanding of hospital expectations. Many hospital officials already are indicating that they’re leaning toward their own pay-for-performance programs to put individual doctors on the hook for negative financial incentives and penalties.
“Ultimately, in these value-based systems,” says Darling, a specialist in healthcare contracts and regulations, “the quality scores for physicians may affect their medical staff privileges or their membership in their group, or their ability to even move to another hospital.”
Moreover, hospital administrators are trying to instill a sense of shared responsibility in maintaining high value-based purchasing scores. “I cannot make a physician prescribe an ACE inhibitor when it’s appropriate to deal with heart failure, but the hospital takes a hit for that,” says Dee Rogers, RN, director of quality and risk management at Magnolia Regional Medical Center in Magnolia, Ark. “Not that I want to see people get their hands slapped—I want to see equal accountability.”
Like other hospitals, Rogers’ 49-bed rural facility is tracking doctors’ performance on quality measures and guidelines as part of its credentialing process. Many facilities are starting to include more comprehensive evaluations as part of their contract renegotiations. Magnolia has one weekend hospitalist and is conducting a feasibility study on whether to launch a full-time hospitalist program on weekdays. If the hospital pursues that program, Rogers says, she’d like to see upfront expectations built into the doctors’ contracts.
PeaceHealth, a faith-based nonprofit healthcare system that operates eight hospitals in Oregon, Washington, and Alaska, is moving in the same direction. “I think we’re getting pretty close—certainly within the next year, probably sooner—of creating a reliable mechanism for physician accountability related to the measures that are included in value-based purchasing,” says Laura Dietzel, PeaceHealth’s program director for High-Tech Meaningful Use. That mechanism will connect specific core measures with specific physicians, not just roles or departments.
“We are really honing in on that kind of a quality dashboard, and [VBP’s arrival] is definitely going to be a big boost toward doing that,” says Dietzel, the health system’s former program manager for core measures. “We are talking about making it part of our credentialing process, part of our privileging process, and part of our physician reimbursement and pay schedule process.”
Dietzel concedes that the health system will need to develop a valid method for ensuring that it correctly records who had the responsibility for key decisions. Apart from the concern over proper credit and blame, Darling warns that doctors who haven’t been paying attention could be left holding the bag.
If a hospitalist contract doesn’t discuss how payments will be handled with bundling, value-based purchasing, accountable care, and other models coming down the pike, Darling says, “it may be that you’ve bought a pig in a poke and that you’re just hoping for the kindness of strangers.” Likewise, if a hospital underperforms on its VBP scores due to a lack of investment or training, he asks, will its physicians also look bad on paper? The perceived guilt by association might hurt their chances at finding employment elsewhere if other hospital administrators fear that doctors from poorly performing facilities will hurt their scores as well.
To avoid the most dire “What if?” scenarios, hospitals are enlisting their staff and trying out new tools to help them identify and address trouble spots. At Dr. Torcson’s own hospital, 237-bed St. Tammany Parish Hospital in Covington, La., hospitalists and other staff members are scrutinizing the core measures and tweaking guidelines and best practices to make sure the facility is in top form. Based on initial modeling, the hospital expects to earn back all of its withheld reimbursements, though Dr. Torcson says the push is still on to increase the cushion.
A few QI organizations that contract with CMS, including Seattle-based Qualis Health, have developed interactive calculators or mock scorecards to help hospitals determine where they stand in the value-based purchasing scrum. Patricia Richardson, MA, RCP, director of quality and risk for 50-bed Samaritan Hospital in Moses Lake, Wash., says the hospital has worked with Qualis (www.qualishealth.org) on a scorecard to help staff understand which measures need attention and what the financial repercussions would be if the hospital doesn’t improve.
After earlier pushback from doctors on some core measures, quality-review specialist Rebecca Johnson says Samaritan began posting how individual doctors were performing. “And, over time, that motivated them,” she says. “Nobody wants to be the guy in the red.” Johnson says the hospital’s four hospitalists, though, have been fully engaged. “Our hospitalists are very interested in how we’re doing,” she says. “When I’m on the floor doing my reviews, they consistently ask—all of them—‘How are we doing on the core measures?’ ”
Although Richardson concedes that Samaritan still has work to do to increase its patient-satisfaction scores, she’s hopeful that more education and engagement of both patients and staff will begin to pay off. Initiatives that have recruited patients as active participants in helping the hospital improve might help boost patient satisfaction scores, and internal competitions could help motivate the medical staff.
Setting upfront expectations about the hospital stay during the admissions process also can help. Richardson says patients naturally compare a hospital’s noise level to that of their own homes unless a doctor or other staff member provides the proper context. Letting patients know what to expect and reminding them that they’ll likely have to be awakened a few times during the night can make a big difference in whether they rate the hospital as being sufficiently quiet, she says.
Competition Breeds Cooperation
Hospitals likely will be able to differentiate themselves the most through the national competition’s patient perception of care scores, VHA Inc.’s Dr. Haywood says, largely because the contenders have had less time to prepare for them than for the clinical process-of-care measures. Among the eight HCAHPS measures, Dr. Haywood says, focusing on doctor communication, nurse communication, hospital staff responsiveness, and a quiet room might provide the biggest return on investment.
“If physicians don’t communicate effectively with the nurses, then the nurse communication score goes down because the patients assume that the nurses know the care plan,” he says. “A typical question that we see all the time is that the nurse will ask the patient, ‘Did the doctor come and see you today?’ And if the patient says yes, then the nurse will ask, ‘Well, what did the doctor say?’ because the nurse doesn’t know.”
With VBP in mind, Dr. Haywood’s health system repurposed part of its catalogue of Web-based blueprints designed to help hospitals improve their clinical practices (see Figure 2, below). The cooperative is now making its collection of more than 100 blueprints available to its members to help them prop up sagging core measure scores. All depict best-practice solutions in an easy-to-remember visual format, based on weeklong site visits to exemplary hospitals from a clinical team that includes a cultural anthropologist and graphic artist.
Arkansas’ Magnolia already exceeds the national average for every HCAHPS score except the overall rating, a score that will likely increase because most patient evaluations were conducted before a new facility replaced the previous, aging hospital in February 2010. Rogers says Magnolia’s weekend hospitalist has helped with continuity of care—an important factor for maintaining high satisfaction in a small, rural community where doctors tend to see the same elderly patients on a frequent basis. The patients know the hospitalist by name, she says, “so they almost have as much of a relationship to him as they do with their primary-care physician.”
Rogers says the weekend hospitalist also has helped improve some of the hospital’s lagging pneumonia-related scores by educating and communicating with other members of the medical staff about their respective responsibilities. Because he has gained the trust of his peers, Rogers says, he’s helped the hospital get more buy-in from them as well.
Embracing the role of VBP champion, Dr. Torcson says, could help further define the worth of hospitalists to their employers. And with a trend toward more individual physician accountability, rising to the occasion now could help hospitalists stay on top of their own game. TH
Bryn Nelson is a freelance medical writer in Seattle.
Mock scorecards, interactive blueprints, quality dashboards: Hospitals are frantically seeking out any advantage that might help them excel in a fast-approaching, mandatory competition with millions of dollars on the line. Value-based purchasing (VBP), a program authorized by the Patient Protection and Accountable Care Act of 2010, gives the Centers for Medicare & Medicaid Services (CMS) the power to base a portion of hospital reimbursement payments on how well hospitals perform in 25 core measures.
The move is intended to help CMS flex its muscles and move from being a passive bystander to an active buyer of what its officials have deemed higher-quality healthcare. Analysts and healthcare experts warn that if hospitalists aren’t paying attention, however, they could put themselves at unnecessary risk or lose out on a major opportunity to demonstrate their value in what Patrick Torcson, MD, SFHM, is calling a “team sport.”
Dr. Torcson, chair of SHM’s Performance and Standards Committee, says every hospitalist should be aware of the core-measures concept, which has been around since 2003 in what’s now called the Hospital Inpatient Quality Reporting (IQR) Program. “We’re not reinventing the wheel; we’re just transforming the program from pay-for-reporting to actual pay-for-performance,” he says. Value-based purchasing, though, is raising the stakes considerably. “It’s really significant because it marks the beginning of an era of accountability and true pay-for-performance at the hospital level.”
A major reason for the heightened concern is the structure of the program. In other quality demonstration projects, CMS has established a score to beat: “Anyone above that threshold is in the money. If you didn’t make it, there was no harm, no foul,” says Trent Haywood, MD, JD, chief medical officer of the Irving, Tex.-based for-profit healthcare cooperative VHA Inc.

—Laura Dietzel, PeaceHealth’s program director for High-Tech Meaningful Use
What’s different this time is that value-based purchasing is not a collaboration but a competition in which every hospital is pitted against the entire market, says Dr. Haywood, the former deputy chief medical officer at CMS. It’s also a zero-sum game. That means there will be winners and losers, with the entire cost-neutral program funded by extracting money from the worst performers to financially reward the best. “In this competition-type model, you need to know who you can beat,” he says.
Race to the Top
That new reality has set off a mad scramble among hospitals hoping to gain any edge they can and spawned a cottage industry of consultants, lawyers, and quality specialists advising them on how to maximize their points. The drive to achieve and maintain a high level of performance is also spurring hospitals to seek more individual accountability as they look to minimize their financial risk.
Hospitals’ baseline scores already have been set, and the initial nine-month performance evaluation period begins July 1. Beginning with discharges on Oct. 1, 2012 (fiscal year 2013), the payment phase will kick in. CMS will start by withholding 1% of the base DRG reimbursement paid to hospitals. That money can be earned back based on how well each hospital scores on the performance measures during the evaluation period. The amount initially withheld will rise by 0.25 percentage points per year until it is capped at 2% in 2017 and beyond.
Think of the competition as an annual decathlon with a pool of prize money funded by the participants, except that hospitals will be evaluated on far more measures. So far, the program includes 17 core Clinical Process of Care measures and eight measures based on Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) surveys. Twenty other potential measures are waiting in the wings, including ones related to hospital-acquired conditions, patient safety, inpatient quality, and mortality, some of which likely will be introduced in fiscal year 2014.
CMS intends to monitor and evaluate the program’s impact on access and quality of care, especially for “vulnerable populations,” the percentage of patients who receive appropriate care, the rates of hospital-acquired conditions, and the best practices of high-performing hospitals.
The complicated nature of the rules and scoring, and significant money attached to the competition, have generated deep concern. In October and again in February, healthcare providers bombarded CMS representatives with questions and suggestions during open phone forums, when the regulations were still in flux. Would the rules be fair? Would CMS provide an early warning of impending losses? Was the agency giving too much weight to patient satisfaction scores?
SHM supports the program, stating, “We believe that the Medicare reimbursement system must be changed to promote value, and we strongly support policies that link quality measurement to performance-based payment.”
Other observers, though, have warned of the potential for unintended consequences. If doctors avoid complicated medical cases in order to increase a hospital’s score, for example, are they really improving care? Will poorly performing hospitals get caught in a vicious circle due to declining financial resources?
Some critics have complained that by scoring on a curve rather than on an absolute point system, the value-based purchasing program might not be a quality initiative so much as an opportunity for CMS to reduce hospital payments. “I believe that this is largely a shell game played by the Centers for Medicare & Medicaid Services to give hospitals the idea that they can win at this game, when all but a few will lose,” wrote Richard Rohr, MD, FHM, in his Feb. 1 entry at the Medical Staff Leader blog (http://blogs.hcpro.com/medicalstaff/). Hospitalist subsidies could be a prime target as the cost-reduction pressures rise, wrote Dr. Rohr, who directs HM programs for Guthrie Healthcare System in Sayre, Pa. Enhancing productivity, he stressed, could be the best defense against a rollback in salaries.
Most experts agree that investing in a quality infrastructure will be essential for success, though other hospitalists differ on the potential effects that VBP might have on their profession. “I think a big part of a quality infrastructure is a hospital medicine program,” Dr. Torcson says. In fact, he recommends that hospitalists approach a hospital CFO or CEO and offer their assistance with the program. “I really think that’s the right direction and the right attitude, kind of the way the Samurai used to serve the Japanese emperor,” he explains.
A major reason for taking the initiative, he says, is that value-based purchasing could become the new business case for HM. In the 1990s, hospitalists could put a real number on how much they saved hospitals by reducing length of stay, sparking an investment in HM programs. “I think value-based purchasing is now in the same position,” Dr. Torcson says, “and the savings is actually going to be even more quantifiable for the hospital in terms of their success or failure.”
continued below...
Expectations on the Rise
SHM’s annual meeting this month in Grapevine, Texas (www.hospitalmedicine2011.org), will feature a session on improving HCAHPS scores, and Dr. Torcson has been working on a society task force educating members about how to be successful amid the coming changes. A Web-based toolkit in the works, he says, will highlight best practices for myocardial infarctions, heart failure, surgical care, pneumonia, and patient satisfaction to help hospitalists ensure they have the necessary skill sets. (SHM will offer a full platform of VBP courses by end of 2011.)
“At the individual hospitalist level, once you’ve decided to commit to serving that hospital-level performance agenda, we want SHM to be the place to turn to get the information on best practices and what you need,” Dr. Torcson says.
But first, says Bill Darling, a Washington, D.C., and Austin, Tex.-based partner with Strasburger Attorneys at Law, hospitalists will need a much stronger understanding of hospital expectations. Many hospital officials already are indicating that they’re leaning toward their own pay-for-performance programs to put individual doctors on the hook for negative financial incentives and penalties.
“Ultimately, in these value-based systems,” says Darling, a specialist in healthcare contracts and regulations, “the quality scores for physicians may affect their medical staff privileges or their membership in their group, or their ability to even move to another hospital.”
Moreover, hospital administrators are trying to instill a sense of shared responsibility in maintaining high value-based purchasing scores. “I cannot make a physician prescribe an ACE inhibitor when it’s appropriate to deal with heart failure, but the hospital takes a hit for that,” says Dee Rogers, RN, director of quality and risk management at Magnolia Regional Medical Center in Magnolia, Ark. “Not that I want to see people get their hands slapped—I want to see equal accountability.”
Like other hospitals, Rogers’ 49-bed rural facility is tracking doctors’ performance on quality measures and guidelines as part of its credentialing process. Many facilities are starting to include more comprehensive evaluations as part of their contract renegotiations. Magnolia has one weekend hospitalist and is conducting a feasibility study on whether to launch a full-time hospitalist program on weekdays. If the hospital pursues that program, Rogers says, she’d like to see upfront expectations built into the doctors’ contracts.
PeaceHealth, a faith-based nonprofit healthcare system that operates eight hospitals in Oregon, Washington, and Alaska, is moving in the same direction. “I think we’re getting pretty close—certainly within the next year, probably sooner—of creating a reliable mechanism for physician accountability related to the measures that are included in value-based purchasing,” says Laura Dietzel, PeaceHealth’s program director for High-Tech Meaningful Use. That mechanism will connect specific core measures with specific physicians, not just roles or departments.
“We are really honing in on that kind of a quality dashboard, and [VBP’s arrival] is definitely going to be a big boost toward doing that,” says Dietzel, the health system’s former program manager for core measures. “We are talking about making it part of our credentialing process, part of our privileging process, and part of our physician reimbursement and pay schedule process.”
Dietzel concedes that the health system will need to develop a valid method for ensuring that it correctly records who had the responsibility for key decisions. Apart from the concern over proper credit and blame, Darling warns that doctors who haven’t been paying attention could be left holding the bag.
If a hospitalist contract doesn’t discuss how payments will be handled with bundling, value-based purchasing, accountable care, and other models coming down the pike, Darling says, “it may be that you’ve bought a pig in a poke and that you’re just hoping for the kindness of strangers.” Likewise, if a hospital underperforms on its VBP scores due to a lack of investment or training, he asks, will its physicians also look bad on paper? The perceived guilt by association might hurt their chances at finding employment elsewhere if other hospital administrators fear that doctors from poorly performing facilities will hurt their scores as well.
To avoid the most dire “What if?” scenarios, hospitals are enlisting their staff and trying out new tools to help them identify and address trouble spots. At Dr. Torcson’s own hospital, 237-bed St. Tammany Parish Hospital in Covington, La., hospitalists and other staff members are scrutinizing the core measures and tweaking guidelines and best practices to make sure the facility is in top form. Based on initial modeling, the hospital expects to earn back all of its withheld reimbursements, though Dr. Torcson says the push is still on to increase the cushion.
A few QI organizations that contract with CMS, including Seattle-based Qualis Health, have developed interactive calculators or mock scorecards to help hospitals determine where they stand in the value-based purchasing scrum. Patricia Richardson, MA, RCP, director of quality and risk for 50-bed Samaritan Hospital in Moses Lake, Wash., says the hospital has worked with Qualis (www.qualishealth.org) on a scorecard to help staff understand which measures need attention and what the financial repercussions would be if the hospital doesn’t improve.
After earlier pushback from doctors on some core measures, quality-review specialist Rebecca Johnson says Samaritan began posting how individual doctors were performing. “And, over time, that motivated them,” she says. “Nobody wants to be the guy in the red.” Johnson says the hospital’s four hospitalists, though, have been fully engaged. “Our hospitalists are very interested in how we’re doing,” she says. “When I’m on the floor doing my reviews, they consistently ask—all of them—‘How are we doing on the core measures?’ ”
Although Richardson concedes that Samaritan still has work to do to increase its patient-satisfaction scores, she’s hopeful that more education and engagement of both patients and staff will begin to pay off. Initiatives that have recruited patients as active participants in helping the hospital improve might help boost patient satisfaction scores, and internal competitions could help motivate the medical staff.
Setting upfront expectations about the hospital stay during the admissions process also can help. Richardson says patients naturally compare a hospital’s noise level to that of their own homes unless a doctor or other staff member provides the proper context. Letting patients know what to expect and reminding them that they’ll likely have to be awakened a few times during the night can make a big difference in whether they rate the hospital as being sufficiently quiet, she says.
Competition Breeds Cooperation
Hospitals likely will be able to differentiate themselves the most through the national competition’s patient perception of care scores, VHA Inc.’s Dr. Haywood says, largely because the contenders have had less time to prepare for them than for the clinical process-of-care measures. Among the eight HCAHPS measures, Dr. Haywood says, focusing on doctor communication, nurse communication, hospital staff responsiveness, and a quiet room might provide the biggest return on investment.
“If physicians don’t communicate effectively with the nurses, then the nurse communication score goes down because the patients assume that the nurses know the care plan,” he says. “A typical question that we see all the time is that the nurse will ask the patient, ‘Did the doctor come and see you today?’ And if the patient says yes, then the nurse will ask, ‘Well, what did the doctor say?’ because the nurse doesn’t know.”
With VBP in mind, Dr. Haywood’s health system repurposed part of its catalogue of Web-based blueprints designed to help hospitals improve their clinical practices (see Figure 2, below). The cooperative is now making its collection of more than 100 blueprints available to its members to help them prop up sagging core measure scores. All depict best-practice solutions in an easy-to-remember visual format, based on weeklong site visits to exemplary hospitals from a clinical team that includes a cultural anthropologist and graphic artist.
Arkansas’ Magnolia already exceeds the national average for every HCAHPS score except the overall rating, a score that will likely increase because most patient evaluations were conducted before a new facility replaced the previous, aging hospital in February 2010. Rogers says Magnolia’s weekend hospitalist has helped with continuity of care—an important factor for maintaining high satisfaction in a small, rural community where doctors tend to see the same elderly patients on a frequent basis. The patients know the hospitalist by name, she says, “so they almost have as much of a relationship to him as they do with their primary-care physician.”
Rogers says the weekend hospitalist also has helped improve some of the hospital’s lagging pneumonia-related scores by educating and communicating with other members of the medical staff about their respective responsibilities. Because he has gained the trust of his peers, Rogers says, he’s helped the hospital get more buy-in from them as well.
Embracing the role of VBP champion, Dr. Torcson says, could help further define the worth of hospitalists to their employers. And with a trend toward more individual physician accountability, rising to the occasion now could help hospitalists stay on top of their own game. TH
Bryn Nelson is a freelance medical writer in Seattle.
ONLINE EXCLUSIVE: Hospitals Forced to Adapt Amid Shifting Slate of Quality Measures
With the arrival of value-based purchasing (VBP), many hospitals have faced hard decisions about where to allocate scarce resources to maximize their performance potential. In some cases, those decisions have been made even more difficult by a set of core measures still very much in flux. For hospitalists, that means the ability to quickly adapt and reprioritize will be in high demand as measures are added or subtracted from the value-based purchasing program.
In the proposed program rules released in mid-January, CMS initially selected 17 core clinical measures from a list of 28 eligible candidates included in the Hospital Inpatient Quality Reporting (IQR) Program (https://www.cms.gov/HospitalQualityInits/08_HospitalRHQDAPU.asp) and also listed on the public Hospital Compare website (www.hospitalcompare.hhs.gov/) for at least one year. CMS explained its decision to withhold some of the remaining core measures from the program by noting that they were “topped out” and thus provided a poor basis of comparison among hospitals. Others, according to the agency, were of little value or were encouraging bad behavior.
CMS used the latter reason in its explanation for why it was not including an eligible core measure on administering antibiotics to pneumonia patients within six hours of their arrival at a hospital. “We do not believe that this measure is appropriate for inclusion because it could lead to inappropriate antibiotic use,” the rules stated. For that measure and others not recommended for inclusion in the hospital VBP program, CMS added that it would propose retiring them “in the near future.”

—Laura M. Dietzel, program director for High-Tech Meaningful Use, PeaceHealth
Laura M. Dietzel, program director for High-Tech Meaningful Use at PeaceHealth, a faith-based healthcare system that operates eight hospitals in three Western states, says CMS’ short statement caught her health system off-guard and forced a rapid shift in its priorities. “We were really focusing on moving some numbers and making some technology changes for some core measures that now, based on what CMS has in the proposed value-based purchasing, will not be around even as of next year,” she says.
Dietzel says the move to high-tech tools like electronic medical records (EMRs) has further complicated how hospitals and healthcare systems like PeaceHealth are preparing for the VBP program. For two other measures that relate to pneumonia immunization, she says, some of PeaceHealth’s hospitals have “less than ideal” scores that could potentially create some financial risk.
An EMR system on tap for next year, she says, likely will help the hospitals significantly improve their scores. But what should they do between now and then: Reinvent the wheel to prop up their numbers, only to do it again in a year? Or should they take a temporary hit until the more comprehensive system is in place?
Similar questions are likely to confront more healthcare providers as the program expands and evolves. Even as it will likely retire some measures in fiscal year 2014, CMS will add more from a list of 20 related to hospital-acquired conditions and complications, patient safety indicators, inpatient quality indicators, and mortality rates.
With the arrival of value-based purchasing (VBP), many hospitals have faced hard decisions about where to allocate scarce resources to maximize their performance potential. In some cases, those decisions have been made even more difficult by a set of core measures still very much in flux. For hospitalists, that means the ability to quickly adapt and reprioritize will be in high demand as measures are added or subtracted from the value-based purchasing program.
In the proposed program rules released in mid-January, CMS initially selected 17 core clinical measures from a list of 28 eligible candidates included in the Hospital Inpatient Quality Reporting (IQR) Program (https://www.cms.gov/HospitalQualityInits/08_HospitalRHQDAPU.asp) and also listed on the public Hospital Compare website (www.hospitalcompare.hhs.gov/) for at least one year. CMS explained its decision to withhold some of the remaining core measures from the program by noting that they were “topped out” and thus provided a poor basis of comparison among hospitals. Others, according to the agency, were of little value or were encouraging bad behavior.
CMS used the latter reason in its explanation for why it was not including an eligible core measure on administering antibiotics to pneumonia patients within six hours of their arrival at a hospital. “We do not believe that this measure is appropriate for inclusion because it could lead to inappropriate antibiotic use,” the rules stated. For that measure and others not recommended for inclusion in the hospital VBP program, CMS added that it would propose retiring them “in the near future.”

—Laura M. Dietzel, program director for High-Tech Meaningful Use, PeaceHealth
Laura M. Dietzel, program director for High-Tech Meaningful Use at PeaceHealth, a faith-based healthcare system that operates eight hospitals in three Western states, says CMS’ short statement caught her health system off-guard and forced a rapid shift in its priorities. “We were really focusing on moving some numbers and making some technology changes for some core measures that now, based on what CMS has in the proposed value-based purchasing, will not be around even as of next year,” she says.
Dietzel says the move to high-tech tools like electronic medical records (EMRs) has further complicated how hospitals and healthcare systems like PeaceHealth are preparing for the VBP program. For two other measures that relate to pneumonia immunization, she says, some of PeaceHealth’s hospitals have “less than ideal” scores that could potentially create some financial risk.
An EMR system on tap for next year, she says, likely will help the hospitals significantly improve their scores. But what should they do between now and then: Reinvent the wheel to prop up their numbers, only to do it again in a year? Or should they take a temporary hit until the more comprehensive system is in place?
Similar questions are likely to confront more healthcare providers as the program expands and evolves. Even as it will likely retire some measures in fiscal year 2014, CMS will add more from a list of 20 related to hospital-acquired conditions and complications, patient safety indicators, inpatient quality indicators, and mortality rates.
With the arrival of value-based purchasing (VBP), many hospitals have faced hard decisions about where to allocate scarce resources to maximize their performance potential. In some cases, those decisions have been made even more difficult by a set of core measures still very much in flux. For hospitalists, that means the ability to quickly adapt and reprioritize will be in high demand as measures are added or subtracted from the value-based purchasing program.
In the proposed program rules released in mid-January, CMS initially selected 17 core clinical measures from a list of 28 eligible candidates included in the Hospital Inpatient Quality Reporting (IQR) Program (https://www.cms.gov/HospitalQualityInits/08_HospitalRHQDAPU.asp) and also listed on the public Hospital Compare website (www.hospitalcompare.hhs.gov/) for at least one year. CMS explained its decision to withhold some of the remaining core measures from the program by noting that they were “topped out” and thus provided a poor basis of comparison among hospitals. Others, according to the agency, were of little value or were encouraging bad behavior.
CMS used the latter reason in its explanation for why it was not including an eligible core measure on administering antibiotics to pneumonia patients within six hours of their arrival at a hospital. “We do not believe that this measure is appropriate for inclusion because it could lead to inappropriate antibiotic use,” the rules stated. For that measure and others not recommended for inclusion in the hospital VBP program, CMS added that it would propose retiring them “in the near future.”

—Laura M. Dietzel, program director for High-Tech Meaningful Use, PeaceHealth
Laura M. Dietzel, program director for High-Tech Meaningful Use at PeaceHealth, a faith-based healthcare system that operates eight hospitals in three Western states, says CMS’ short statement caught her health system off-guard and forced a rapid shift in its priorities. “We were really focusing on moving some numbers and making some technology changes for some core measures that now, based on what CMS has in the proposed value-based purchasing, will not be around even as of next year,” she says.
Dietzel says the move to high-tech tools like electronic medical records (EMRs) has further complicated how hospitals and healthcare systems like PeaceHealth are preparing for the VBP program. For two other measures that relate to pneumonia immunization, she says, some of PeaceHealth’s hospitals have “less than ideal” scores that could potentially create some financial risk.
An EMR system on tap for next year, she says, likely will help the hospitals significantly improve their scores. But what should they do between now and then: Reinvent the wheel to prop up their numbers, only to do it again in a year? Or should they take a temporary hit until the more comprehensive system is in place?
Similar questions are likely to confront more healthcare providers as the program expands and evolves. Even as it will likely retire some measures in fiscal year 2014, CMS will add more from a list of 20 related to hospital-acquired conditions and complications, patient safety indicators, inpatient quality indicators, and mortality rates.