User login
Psilocybin Poison Control Calls Spike in Teens, Young Adults
Calls to US poison centers related to psilocybin more than tripled among teens and more than doubled in young adults between 2019 and 2022, new research suggests. Investigators say the increase may be linked to decriminalization efforts in US cities and states.
METHODOLOGY:
- Investigators used data from the National Poison Data System (NPDS) to identify calls involving psilocybin between January 2013 and December 2022.
- Researchers focused on calls about individuals between the ages of 13 and 25 years.
- Exposures to psilocybin were examined based on demographics, clinical effects, level of care, and medical outcome.
TAKEAWAY:
- During the entire 10-year study period, 4055 psilocybin-involved exposures were reported in the age groups studied, with 66% being single-substance exposures and close to three quarters receiving medical attention.
- Psilocybin’s most common effects were hallucinations or delusions (37% of calls), agitation (28%), tachycardia (20%), and confusion (16%).
- The number of psilocybin-related calls to poison control centers for youth were largely unchanged from 2013 to 2018 but more than tripled among adolescents (aged 13-19 years) from 2019 and 2022 and more than doubled among young adults (aged 20-25 years) between 2018 and 2022 (P < .0001).
IN PRACTICE:
The increase in poison center calls coincides with psilocybin decriminalization efforts in several states in 2019, the authors noted. However, because those efforts only legalized use in adults aged 21 years and older, the rise among younger people is concerning, they added. “As psilocybin may become more widely available, it is important for parents to be aware that psilocybin is also available in edible forms such as chocolate and gummies. And we learned from our experience with edible cannabis that young children can mistake edibles for candy,” lead author Rita Farah, PharmD, MPH, PhD, Blue Ridge Poison Center epidemiologist, said in a news release.
SOURCE:
Christopher Holstege, MD, director of UVA Health’s Blue Ridge Poison Center and chief of the Division of Medical Toxicology at the UVA School of Medicine was the senior and corresponding author of the study. It was published online on February 26 in the Journal of Adolescent Health.
LIMITATIONS:
NPDS data are not designed to assess potential risk factors leading to increases in psilocybin-related cases. Moreover, because reports to poison control centers are voluntary and don’t capture all exposures, NPDS data likely under-represent cases of hallucinogenic mushroom poisonings. Lastly, NPDS data are susceptible to reporting and misclassification biases.
DISCLOSURES:
Funding source was not disclosed. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Calls to US poison centers related to psilocybin more than tripled among teens and more than doubled in young adults between 2019 and 2022, new research suggests. Investigators say the increase may be linked to decriminalization efforts in US cities and states.
METHODOLOGY:
- Investigators used data from the National Poison Data System (NPDS) to identify calls involving psilocybin between January 2013 and December 2022.
- Researchers focused on calls about individuals between the ages of 13 and 25 years.
- Exposures to psilocybin were examined based on demographics, clinical effects, level of care, and medical outcome.
TAKEAWAY:
- During the entire 10-year study period, 4055 psilocybin-involved exposures were reported in the age groups studied, with 66% being single-substance exposures and close to three quarters receiving medical attention.
- Psilocybin’s most common effects were hallucinations or delusions (37% of calls), agitation (28%), tachycardia (20%), and confusion (16%).
- The number of psilocybin-related calls to poison control centers for youth were largely unchanged from 2013 to 2018 but more than tripled among adolescents (aged 13-19 years) from 2019 and 2022 and more than doubled among young adults (aged 20-25 years) between 2018 and 2022 (P < .0001).
IN PRACTICE:
The increase in poison center calls coincides with psilocybin decriminalization efforts in several states in 2019, the authors noted. However, because those efforts only legalized use in adults aged 21 years and older, the rise among younger people is concerning, they added. “As psilocybin may become more widely available, it is important for parents to be aware that psilocybin is also available in edible forms such as chocolate and gummies. And we learned from our experience with edible cannabis that young children can mistake edibles for candy,” lead author Rita Farah, PharmD, MPH, PhD, Blue Ridge Poison Center epidemiologist, said in a news release.
SOURCE:
Christopher Holstege, MD, director of UVA Health’s Blue Ridge Poison Center and chief of the Division of Medical Toxicology at the UVA School of Medicine was the senior and corresponding author of the study. It was published online on February 26 in the Journal of Adolescent Health.
LIMITATIONS:
NPDS data are not designed to assess potential risk factors leading to increases in psilocybin-related cases. Moreover, because reports to poison control centers are voluntary and don’t capture all exposures, NPDS data likely under-represent cases of hallucinogenic mushroom poisonings. Lastly, NPDS data are susceptible to reporting and misclassification biases.
DISCLOSURES:
Funding source was not disclosed. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Calls to US poison centers related to psilocybin more than tripled among teens and more than doubled in young adults between 2019 and 2022, new research suggests. Investigators say the increase may be linked to decriminalization efforts in US cities and states.
METHODOLOGY:
- Investigators used data from the National Poison Data System (NPDS) to identify calls involving psilocybin between January 2013 and December 2022.
- Researchers focused on calls about individuals between the ages of 13 and 25 years.
- Exposures to psilocybin were examined based on demographics, clinical effects, level of care, and medical outcome.
TAKEAWAY:
- During the entire 10-year study period, 4055 psilocybin-involved exposures were reported in the age groups studied, with 66% being single-substance exposures and close to three quarters receiving medical attention.
- Psilocybin’s most common effects were hallucinations or delusions (37% of calls), agitation (28%), tachycardia (20%), and confusion (16%).
- The number of psilocybin-related calls to poison control centers for youth were largely unchanged from 2013 to 2018 but more than tripled among adolescents (aged 13-19 years) from 2019 and 2022 and more than doubled among young adults (aged 20-25 years) between 2018 and 2022 (P < .0001).
IN PRACTICE:
The increase in poison center calls coincides with psilocybin decriminalization efforts in several states in 2019, the authors noted. However, because those efforts only legalized use in adults aged 21 years and older, the rise among younger people is concerning, they added. “As psilocybin may become more widely available, it is important for parents to be aware that psilocybin is also available in edible forms such as chocolate and gummies. And we learned from our experience with edible cannabis that young children can mistake edibles for candy,” lead author Rita Farah, PharmD, MPH, PhD, Blue Ridge Poison Center epidemiologist, said in a news release.
SOURCE:
Christopher Holstege, MD, director of UVA Health’s Blue Ridge Poison Center and chief of the Division of Medical Toxicology at the UVA School of Medicine was the senior and corresponding author of the study. It was published online on February 26 in the Journal of Adolescent Health.
LIMITATIONS:
NPDS data are not designed to assess potential risk factors leading to increases in psilocybin-related cases. Moreover, because reports to poison control centers are voluntary and don’t capture all exposures, NPDS data likely under-represent cases of hallucinogenic mushroom poisonings. Lastly, NPDS data are susceptible to reporting and misclassification biases.
DISCLOSURES:
Funding source was not disclosed. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Prenatal Prescription Opioids Tied to Increased Risk for Preterm Birth
TOPLINE:
Taking a prescription opioid for pain management during pregnancy is associated with an increased risk for spontaneous preterm birth, data from a new case-control study of over 25,000 Medicaid patients showed.
METHODOLOGY:
- Researchers retrospectively reviewed data on pregnant patients enrolled in Tennessee Medicaid who experienced birth of a single baby at ≥ 24 weeks gestation (25,391 with opioid use disorder and 225,696 without).
- Median age of participants was 23 years; 58.1% were non-Hispanic White, 38.7% Black, 2.6% Hispanic, and 0.5% Asian.
- Controls were matched based on pregnancy start date, race, ethnicity, age at delivery (within 2 years), and history of prior preterm birth.
- Sensitivity analysis included the exclusion of opioid prescriptions dispensed within 3 days of the index date to account for potential opioid prescribing associated with labor pain.
TAKEAWAY:
- A total of 18,702 patients (7.4%) filled an opioid prescription during the 60 days prior to the index date.
- Each doubling of opioid morphine milligram equivalents (MMEs) prescribed during the 60 days was associated with a 4% increase in the odds of spontaneous preterm birth compared with no opioid exposure in the matched controls (adjusted odds ratio [aOR], 1.04; 95% CI, 1.01-1.08).
- Overall, 1573 pregnancies filled prescriptions for 900 MMEs or greater, which was associated with at least a 21% increased risk for spontaneous preterm birth compared with no opioid exposure (aOR, 1.21; 95% CI, 1.10-1.33).
- Researchers found no significant difference in odds of spontaneous preterm birth among included opioid types after adjusting for confounders and opioid MMD.
IN PRACTICE:
“This association may appear modest, especially considering that common, one-time prescriptions often fall in the 150-225 MME range, but these findings may provide more caution when prescribing multiple, higher strength opioids,” the authors wrote. “We also caution against the conclusion that lower doses, especially those below 100 MME, are safe; the confidence bands over the low dose range still include odds ratios that are consistent with meaningful harm.”
SOURCE:
Sarah S. Osmundson, MD, MS, of the Department of Obstetrics and Gynecology, Vanderbilt University Medical Center, Nashville, Tennessee, was the senior and corresponding author on the study. The study was published online on February 14 in JAMA Network Open.
LIMITATIONS:
Data are based on opioids prescribed and lack detail on actual use of opioids and nonprescription analgesics. Findings may not be generalizable to other populations or settings outside Medicaid.
DISCLOSURES:
No source of study funding listed. Dr. Osmundson reported receiving grant support from the National Institute on Drug Abuse during the conduct of the study. The other authors’ disclosures are listed on the original paper.
A version of this article appeared on Medscape.com.
TOPLINE:
Taking a prescription opioid for pain management during pregnancy is associated with an increased risk for spontaneous preterm birth, data from a new case-control study of over 25,000 Medicaid patients showed.
METHODOLOGY:
- Researchers retrospectively reviewed data on pregnant patients enrolled in Tennessee Medicaid who experienced birth of a single baby at ≥ 24 weeks gestation (25,391 with opioid use disorder and 225,696 without).
- Median age of participants was 23 years; 58.1% were non-Hispanic White, 38.7% Black, 2.6% Hispanic, and 0.5% Asian.
- Controls were matched based on pregnancy start date, race, ethnicity, age at delivery (within 2 years), and history of prior preterm birth.
- Sensitivity analysis included the exclusion of opioid prescriptions dispensed within 3 days of the index date to account for potential opioid prescribing associated with labor pain.
TAKEAWAY:
- A total of 18,702 patients (7.4%) filled an opioid prescription during the 60 days prior to the index date.
- Each doubling of opioid morphine milligram equivalents (MMEs) prescribed during the 60 days was associated with a 4% increase in the odds of spontaneous preterm birth compared with no opioid exposure in the matched controls (adjusted odds ratio [aOR], 1.04; 95% CI, 1.01-1.08).
- Overall, 1573 pregnancies filled prescriptions for 900 MMEs or greater, which was associated with at least a 21% increased risk for spontaneous preterm birth compared with no opioid exposure (aOR, 1.21; 95% CI, 1.10-1.33).
- Researchers found no significant difference in odds of spontaneous preterm birth among included opioid types after adjusting for confounders and opioid MMD.
IN PRACTICE:
“This association may appear modest, especially considering that common, one-time prescriptions often fall in the 150-225 MME range, but these findings may provide more caution when prescribing multiple, higher strength opioids,” the authors wrote. “We also caution against the conclusion that lower doses, especially those below 100 MME, are safe; the confidence bands over the low dose range still include odds ratios that are consistent with meaningful harm.”
SOURCE:
Sarah S. Osmundson, MD, MS, of the Department of Obstetrics and Gynecology, Vanderbilt University Medical Center, Nashville, Tennessee, was the senior and corresponding author on the study. The study was published online on February 14 in JAMA Network Open.
LIMITATIONS:
Data are based on opioids prescribed and lack detail on actual use of opioids and nonprescription analgesics. Findings may not be generalizable to other populations or settings outside Medicaid.
DISCLOSURES:
No source of study funding listed. Dr. Osmundson reported receiving grant support from the National Institute on Drug Abuse during the conduct of the study. The other authors’ disclosures are listed on the original paper.
A version of this article appeared on Medscape.com.
TOPLINE:
Taking a prescription opioid for pain management during pregnancy is associated with an increased risk for spontaneous preterm birth, data from a new case-control study of over 25,000 Medicaid patients showed.
METHODOLOGY:
- Researchers retrospectively reviewed data on pregnant patients enrolled in Tennessee Medicaid who experienced birth of a single baby at ≥ 24 weeks gestation (25,391 with opioid use disorder and 225,696 without).
- Median age of participants was 23 years; 58.1% were non-Hispanic White, 38.7% Black, 2.6% Hispanic, and 0.5% Asian.
- Controls were matched based on pregnancy start date, race, ethnicity, age at delivery (within 2 years), and history of prior preterm birth.
- Sensitivity analysis included the exclusion of opioid prescriptions dispensed within 3 days of the index date to account for potential opioid prescribing associated with labor pain.
TAKEAWAY:
- A total of 18,702 patients (7.4%) filled an opioid prescription during the 60 days prior to the index date.
- Each doubling of opioid morphine milligram equivalents (MMEs) prescribed during the 60 days was associated with a 4% increase in the odds of spontaneous preterm birth compared with no opioid exposure in the matched controls (adjusted odds ratio [aOR], 1.04; 95% CI, 1.01-1.08).
- Overall, 1573 pregnancies filled prescriptions for 900 MMEs or greater, which was associated with at least a 21% increased risk for spontaneous preterm birth compared with no opioid exposure (aOR, 1.21; 95% CI, 1.10-1.33).
- Researchers found no significant difference in odds of spontaneous preterm birth among included opioid types after adjusting for confounders and opioid MMD.
IN PRACTICE:
“This association may appear modest, especially considering that common, one-time prescriptions often fall in the 150-225 MME range, but these findings may provide more caution when prescribing multiple, higher strength opioids,” the authors wrote. “We also caution against the conclusion that lower doses, especially those below 100 MME, are safe; the confidence bands over the low dose range still include odds ratios that are consistent with meaningful harm.”
SOURCE:
Sarah S. Osmundson, MD, MS, of the Department of Obstetrics and Gynecology, Vanderbilt University Medical Center, Nashville, Tennessee, was the senior and corresponding author on the study. The study was published online on February 14 in JAMA Network Open.
LIMITATIONS:
Data are based on opioids prescribed and lack detail on actual use of opioids and nonprescription analgesics. Findings may not be generalizable to other populations or settings outside Medicaid.
DISCLOSURES:
No source of study funding listed. Dr. Osmundson reported receiving grant support from the National Institute on Drug Abuse during the conduct of the study. The other authors’ disclosures are listed on the original paper.
A version of this article appeared on Medscape.com.
No Link Between Habitual Caffeine Use and Migraine
TOPLINE:
Habitual consumption of caffeine is not associated with frequency, duration, or intensity of episodic migraines, a new study showed.
METHODOLOGY:
- The secondary analysis of a prospective cohort study on sleep in adults with episodic migraine (with or without aura) included a group of 97 people (median age, 31 years; 82% White) with an average of 5.0 ± 3.6 days per month at baseline.
- Participants provided sociodemographic information, medical history, habitual caffeinated beverage consumption, alcohol intake, and lifestyle and psychosocial factors and completed the Center for Epidemiologic Studies- scale, the Perceived Stress Scale, and the Pittsburgh Sleep Quality Index.
- Additionally, they completed twice-daily electronic diaries for the subsequent 6 weeks, reporting headache activity and the use of medications to treat the headache.
TAKEAWAY:
- A total of 67% of participants reported one to two servings of caffeinated beverages per day, 12% reported three to four servings per day, and 21% reported no habitual caffeine consumption.
- After adjusting for age, sex, oral use, and other confounders, mean headache frequency was similar among groups (7.1 days for no caffeine, 7.4 days for one to two servings, and 5.9 days for three to four servings).
- Similarly, adjusted mean headache duration did not differ across levels of caffeinated beverage intake (8.6 hours for no caffeine, 8.5 hours for one to two servings, and 8.8 hours for three to four servings).
- Adjusted mean headache intensity also did not differ among groups.
IN PRACTICE:
“Our findings do not support a recommendation for people with episodic migraine to avoid habitual caffeinated beverage intake,” the authors wrote. However, they noted that habitual caffeine intake may affect systems involved in pain modulation via adenosine signaling. «Therefore, it is possible that habitual caffeine use in those with migraine does not significantly alter adenosine signaling, but significant changes above or below usual consumption may serve as a trigger or contribute to lowering the threshold for an attack to occur along with other triggers,» they added.
SOURCE:
Suzanne M. Bertisch, MD, MPH, assistant professor of medicine, Division of Sleep Medicine, Harvard Medical School, Boston, Massachusetts, was the senior and corresponding author of the study. It was published online in Headache.
LIMITATIONS:
Serving size was not standardized, and there was no information on the type of caffeinated beverage consumed or about other sources of caffeine. Moreover, the population consisted of relatively healthy participants with episodic migraine and generally low levels of habitual caffeinated beverage intake, which limited the statistical power to detect an association between migraine frequency, duration, and intensity with higher levels of caffeine intake.
DISCLOSURES:
The study was funded by the National Institute of Neurological Disorders and Stroke, the American Sleep Medicine Foundation, and the Harvard Catalyst/Harvard Clinical and Translational Science Center. Dr. Bertisch has done consulting work with Idorsia and ResMed. The other authors’ disclosures are listed in the original paper.
A version of this article appeared on Medscape.com.
TOPLINE:
Habitual consumption of caffeine is not associated with frequency, duration, or intensity of episodic migraines, a new study showed.
METHODOLOGY:
- The secondary analysis of a prospective cohort study on sleep in adults with episodic migraine (with or without aura) included a group of 97 people (median age, 31 years; 82% White) with an average of 5.0 ± 3.6 days per month at baseline.
- Participants provided sociodemographic information, medical history, habitual caffeinated beverage consumption, alcohol intake, and lifestyle and psychosocial factors and completed the Center for Epidemiologic Studies- scale, the Perceived Stress Scale, and the Pittsburgh Sleep Quality Index.
- Additionally, they completed twice-daily electronic diaries for the subsequent 6 weeks, reporting headache activity and the use of medications to treat the headache.
TAKEAWAY:
- A total of 67% of participants reported one to two servings of caffeinated beverages per day, 12% reported three to four servings per day, and 21% reported no habitual caffeine consumption.
- After adjusting for age, sex, oral use, and other confounders, mean headache frequency was similar among groups (7.1 days for no caffeine, 7.4 days for one to two servings, and 5.9 days for three to four servings).
- Similarly, adjusted mean headache duration did not differ across levels of caffeinated beverage intake (8.6 hours for no caffeine, 8.5 hours for one to two servings, and 8.8 hours for three to four servings).
- Adjusted mean headache intensity also did not differ among groups.
IN PRACTICE:
“Our findings do not support a recommendation for people with episodic migraine to avoid habitual caffeinated beverage intake,” the authors wrote. However, they noted that habitual caffeine intake may affect systems involved in pain modulation via adenosine signaling. «Therefore, it is possible that habitual caffeine use in those with migraine does not significantly alter adenosine signaling, but significant changes above or below usual consumption may serve as a trigger or contribute to lowering the threshold for an attack to occur along with other triggers,» they added.
SOURCE:
Suzanne M. Bertisch, MD, MPH, assistant professor of medicine, Division of Sleep Medicine, Harvard Medical School, Boston, Massachusetts, was the senior and corresponding author of the study. It was published online in Headache.
LIMITATIONS:
Serving size was not standardized, and there was no information on the type of caffeinated beverage consumed or about other sources of caffeine. Moreover, the population consisted of relatively healthy participants with episodic migraine and generally low levels of habitual caffeinated beverage intake, which limited the statistical power to detect an association between migraine frequency, duration, and intensity with higher levels of caffeine intake.
DISCLOSURES:
The study was funded by the National Institute of Neurological Disorders and Stroke, the American Sleep Medicine Foundation, and the Harvard Catalyst/Harvard Clinical and Translational Science Center. Dr. Bertisch has done consulting work with Idorsia and ResMed. The other authors’ disclosures are listed in the original paper.
A version of this article appeared on Medscape.com.
TOPLINE:
Habitual consumption of caffeine is not associated with frequency, duration, or intensity of episodic migraines, a new study showed.
METHODOLOGY:
- The secondary analysis of a prospective cohort study on sleep in adults with episodic migraine (with or without aura) included a group of 97 people (median age, 31 years; 82% White) with an average of 5.0 ± 3.6 days per month at baseline.
- Participants provided sociodemographic information, medical history, habitual caffeinated beverage consumption, alcohol intake, and lifestyle and psychosocial factors and completed the Center for Epidemiologic Studies- scale, the Perceived Stress Scale, and the Pittsburgh Sleep Quality Index.
- Additionally, they completed twice-daily electronic diaries for the subsequent 6 weeks, reporting headache activity and the use of medications to treat the headache.
TAKEAWAY:
- A total of 67% of participants reported one to two servings of caffeinated beverages per day, 12% reported three to four servings per day, and 21% reported no habitual caffeine consumption.
- After adjusting for age, sex, oral use, and other confounders, mean headache frequency was similar among groups (7.1 days for no caffeine, 7.4 days for one to two servings, and 5.9 days for three to four servings).
- Similarly, adjusted mean headache duration did not differ across levels of caffeinated beverage intake (8.6 hours for no caffeine, 8.5 hours for one to two servings, and 8.8 hours for three to four servings).
- Adjusted mean headache intensity also did not differ among groups.
IN PRACTICE:
“Our findings do not support a recommendation for people with episodic migraine to avoid habitual caffeinated beverage intake,” the authors wrote. However, they noted that habitual caffeine intake may affect systems involved in pain modulation via adenosine signaling. «Therefore, it is possible that habitual caffeine use in those with migraine does not significantly alter adenosine signaling, but significant changes above or below usual consumption may serve as a trigger or contribute to lowering the threshold for an attack to occur along with other triggers,» they added.
SOURCE:
Suzanne M. Bertisch, MD, MPH, assistant professor of medicine, Division of Sleep Medicine, Harvard Medical School, Boston, Massachusetts, was the senior and corresponding author of the study. It was published online in Headache.
LIMITATIONS:
Serving size was not standardized, and there was no information on the type of caffeinated beverage consumed or about other sources of caffeine. Moreover, the population consisted of relatively healthy participants with episodic migraine and generally low levels of habitual caffeinated beverage intake, which limited the statistical power to detect an association between migraine frequency, duration, and intensity with higher levels of caffeine intake.
DISCLOSURES:
The study was funded by the National Institute of Neurological Disorders and Stroke, the American Sleep Medicine Foundation, and the Harvard Catalyst/Harvard Clinical and Translational Science Center. Dr. Bertisch has done consulting work with Idorsia and ResMed. The other authors’ disclosures are listed in the original paper.
A version of this article appeared on Medscape.com.
Even Moderate Exposure to Radon Tied to Increased Stroke Risk
Exposure to even moderate concentrations of radon is associated with a significant increase in stroke risk, new research suggests.
Even moderate concentrations of radon were associated with a 6% higher stroke risk.
Radon is the second leading cause of lung cancer, but little was known about how exposure to the gas might affect stroke risk in women.
“Our research found an increased risk of stroke among participants exposed to radon above — and as many as 2 picocuries per liter (pCi/L) below — concentrations that usually trigger Environmental Protection Agency recommendations to install a home radon mitigation system,” senior author Eric A. Whitsel, MD, MPH, professor of epidemiology and medicine, University of North Carolina, Chapel Hill, said in a news release.
The study was published online on January 31, 2024, in Neurology.
Women Particularly Affected
Radon is a naturally occurring odorless radioactive gas produced when uranium or radium break down in rocks and soil. Its presence is increasing as a result of climate change, and it is increasingly being found in people’s homes. When inhaled, this air pollutant releases ionizing radiation in the lungs and is seen as second only to smoking as an established cause of lung cancer.
The National Radon Action Plan of the US Environmental Protection Agency (EPA) lays out testing and mitigation guidelines based on the known role of radon in lung carcinogenesis. But radon testing and mitigation are less common than recommended, and the EPA’s action plan doesn’t cover diseases other than lung cancer.
Compared with men, women have a higher rate of stroke and, in the US, typically spend about 11% more hours per day indoors at home, which investigators note highlights a “potential role of the residential environment among other risk factors specific to women.”
Researchers examined longitudinal associations between home radon exposure and incident stroke in 158,910 women at baseline (mean age 63.2 years; 83% White) over a mean follow-up of 13.4 years. During this time, participants experienced a total of 6979 strokes.
Participants’ home addresses were linked to radon concentration data drawn from the US Geological Survey and the EPA, which recommends that average indoor radon concentrations not exceed 4 pCi/L.
The highest radon exposure group resided in areas where average radon concentrations were < 4 pCi/L; the middle exposure group lived in regions with average concentrations of 2-4 pCi/L; and the lowest exposure group lived in areas with average concentrations < 2 pCi/L.
The researchers adjusted for demographic, social, behavioral, and clinical characteristics.
Public Health Implications
The incidence rates of stroke per 100,000 women in the lowest, middle, and highest radon concentration areas were 333, 343, and 349, respectively.
Stroke risk was 6% higher among those in the middle exposure group (adjusted hazard ratio [aHR], 1.06; 95% CI, 0.99-1.13) and 14% higher in the highest exposure group (aHR, 1.14; 95% CI, 1.05-1.22) compared with the lowest exposure group.
Notably, stroke risk was significant even at concentrations ranging from 2 to 4 pCi/L (P = .0004) vs < 2 pCi/L, which is below the EPA›s Radon Action Level for mitigation.
The findings remained robust in sensitivity analyses, although the associations were slightly stronger for ischemic stroke (especially cardioembolic, small-vessel occlusive, and very large artery atherosclerotic) compared with hemorrhagic stroke.
“Radon is an indoor air pollutant that can only be detected through testing that measures concentrations of the gas in homes,” Dr. Whitsel said in the release. “More studies are needed to confirm our findings. Confirmation would present an opportunity to improve public health by addressing an emerging risk factor for stroke.”
The study lacked gender and racial/ethnic diversity, so the findings may not be generalizable to other populations.
“Replication studies of individual-level radon exposures are needed to confirm this positive radon-stroke association,” the authors write. “Confirmation would present a potential opportunity to affect public health by addressing a pervasive environmental risk factor for stroke and thereby merit reconsideration of extant radon policy.”
The study was funded by the National Institute of Environmental Health Sciences and National Heart, Lung, and Blood Institute. Dr. Whitsel and coauthors report no relevant financial relationships.
A version of this article appeared on Medscape.com.
Exposure to even moderate concentrations of radon is associated with a significant increase in stroke risk, new research suggests.
Even moderate concentrations of radon were associated with a 6% higher stroke risk.
Radon is the second leading cause of lung cancer, but little was known about how exposure to the gas might affect stroke risk in women.
“Our research found an increased risk of stroke among participants exposed to radon above — and as many as 2 picocuries per liter (pCi/L) below — concentrations that usually trigger Environmental Protection Agency recommendations to install a home radon mitigation system,” senior author Eric A. Whitsel, MD, MPH, professor of epidemiology and medicine, University of North Carolina, Chapel Hill, said in a news release.
The study was published online on January 31, 2024, in Neurology.
Women Particularly Affected
Radon is a naturally occurring odorless radioactive gas produced when uranium or radium break down in rocks and soil. Its presence is increasing as a result of climate change, and it is increasingly being found in people’s homes. When inhaled, this air pollutant releases ionizing radiation in the lungs and is seen as second only to smoking as an established cause of lung cancer.
The National Radon Action Plan of the US Environmental Protection Agency (EPA) lays out testing and mitigation guidelines based on the known role of radon in lung carcinogenesis. But radon testing and mitigation are less common than recommended, and the EPA’s action plan doesn’t cover diseases other than lung cancer.
Compared with men, women have a higher rate of stroke and, in the US, typically spend about 11% more hours per day indoors at home, which investigators note highlights a “potential role of the residential environment among other risk factors specific to women.”
Researchers examined longitudinal associations between home radon exposure and incident stroke in 158,910 women at baseline (mean age 63.2 years; 83% White) over a mean follow-up of 13.4 years. During this time, participants experienced a total of 6979 strokes.
Participants’ home addresses were linked to radon concentration data drawn from the US Geological Survey and the EPA, which recommends that average indoor radon concentrations not exceed 4 pCi/L.
The highest radon exposure group resided in areas where average radon concentrations were < 4 pCi/L; the middle exposure group lived in regions with average concentrations of 2-4 pCi/L; and the lowest exposure group lived in areas with average concentrations < 2 pCi/L.
The researchers adjusted for demographic, social, behavioral, and clinical characteristics.
Public Health Implications
The incidence rates of stroke per 100,000 women in the lowest, middle, and highest radon concentration areas were 333, 343, and 349, respectively.
Stroke risk was 6% higher among those in the middle exposure group (adjusted hazard ratio [aHR], 1.06; 95% CI, 0.99-1.13) and 14% higher in the highest exposure group (aHR, 1.14; 95% CI, 1.05-1.22) compared with the lowest exposure group.
Notably, stroke risk was significant even at concentrations ranging from 2 to 4 pCi/L (P = .0004) vs < 2 pCi/L, which is below the EPA›s Radon Action Level for mitigation.
The findings remained robust in sensitivity analyses, although the associations were slightly stronger for ischemic stroke (especially cardioembolic, small-vessel occlusive, and very large artery atherosclerotic) compared with hemorrhagic stroke.
“Radon is an indoor air pollutant that can only be detected through testing that measures concentrations of the gas in homes,” Dr. Whitsel said in the release. “More studies are needed to confirm our findings. Confirmation would present an opportunity to improve public health by addressing an emerging risk factor for stroke.”
The study lacked gender and racial/ethnic diversity, so the findings may not be generalizable to other populations.
“Replication studies of individual-level radon exposures are needed to confirm this positive radon-stroke association,” the authors write. “Confirmation would present a potential opportunity to affect public health by addressing a pervasive environmental risk factor for stroke and thereby merit reconsideration of extant radon policy.”
The study was funded by the National Institute of Environmental Health Sciences and National Heart, Lung, and Blood Institute. Dr. Whitsel and coauthors report no relevant financial relationships.
A version of this article appeared on Medscape.com.
Exposure to even moderate concentrations of radon is associated with a significant increase in stroke risk, new research suggests.
Even moderate concentrations of radon were associated with a 6% higher stroke risk.
Radon is the second leading cause of lung cancer, but little was known about how exposure to the gas might affect stroke risk in women.
“Our research found an increased risk of stroke among participants exposed to radon above — and as many as 2 picocuries per liter (pCi/L) below — concentrations that usually trigger Environmental Protection Agency recommendations to install a home radon mitigation system,” senior author Eric A. Whitsel, MD, MPH, professor of epidemiology and medicine, University of North Carolina, Chapel Hill, said in a news release.
The study was published online on January 31, 2024, in Neurology.
Women Particularly Affected
Radon is a naturally occurring odorless radioactive gas produced when uranium or radium break down in rocks and soil. Its presence is increasing as a result of climate change, and it is increasingly being found in people’s homes. When inhaled, this air pollutant releases ionizing radiation in the lungs and is seen as second only to smoking as an established cause of lung cancer.
The National Radon Action Plan of the US Environmental Protection Agency (EPA) lays out testing and mitigation guidelines based on the known role of radon in lung carcinogenesis. But radon testing and mitigation are less common than recommended, and the EPA’s action plan doesn’t cover diseases other than lung cancer.
Compared with men, women have a higher rate of stroke and, in the US, typically spend about 11% more hours per day indoors at home, which investigators note highlights a “potential role of the residential environment among other risk factors specific to women.”
Researchers examined longitudinal associations between home radon exposure and incident stroke in 158,910 women at baseline (mean age 63.2 years; 83% White) over a mean follow-up of 13.4 years. During this time, participants experienced a total of 6979 strokes.
Participants’ home addresses were linked to radon concentration data drawn from the US Geological Survey and the EPA, which recommends that average indoor radon concentrations not exceed 4 pCi/L.
The highest radon exposure group resided in areas where average radon concentrations were < 4 pCi/L; the middle exposure group lived in regions with average concentrations of 2-4 pCi/L; and the lowest exposure group lived in areas with average concentrations < 2 pCi/L.
The researchers adjusted for demographic, social, behavioral, and clinical characteristics.
Public Health Implications
The incidence rates of stroke per 100,000 women in the lowest, middle, and highest radon concentration areas were 333, 343, and 349, respectively.
Stroke risk was 6% higher among those in the middle exposure group (adjusted hazard ratio [aHR], 1.06; 95% CI, 0.99-1.13) and 14% higher in the highest exposure group (aHR, 1.14; 95% CI, 1.05-1.22) compared with the lowest exposure group.
Notably, stroke risk was significant even at concentrations ranging from 2 to 4 pCi/L (P = .0004) vs < 2 pCi/L, which is below the EPA›s Radon Action Level for mitigation.
The findings remained robust in sensitivity analyses, although the associations were slightly stronger for ischemic stroke (especially cardioembolic, small-vessel occlusive, and very large artery atherosclerotic) compared with hemorrhagic stroke.
“Radon is an indoor air pollutant that can only be detected through testing that measures concentrations of the gas in homes,” Dr. Whitsel said in the release. “More studies are needed to confirm our findings. Confirmation would present an opportunity to improve public health by addressing an emerging risk factor for stroke.”
The study lacked gender and racial/ethnic diversity, so the findings may not be generalizable to other populations.
“Replication studies of individual-level radon exposures are needed to confirm this positive radon-stroke association,” the authors write. “Confirmation would present a potential opportunity to affect public health by addressing a pervasive environmental risk factor for stroke and thereby merit reconsideration of extant radon policy.”
The study was funded by the National Institute of Environmental Health Sciences and National Heart, Lung, and Blood Institute. Dr. Whitsel and coauthors report no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM NEUROLOGY
The Solution to a ‘Common and Hazardous’ Symptom of Bipolar Disorder?
. Notably, investigators said, the drug comes without the typical metabolic side effects, including weight gain, associated with this drug class.
A post hoc analysis of pooled data from two trials comparing two different doses of cariprazine (Vraylar) to placebo showed it was consistently effective not only in alleviating bipolar depression but also in improving symptoms of anxiety.
“Since this was a post hoc analysis, one has to be careful about not overstating the findings,” said study investigator Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, Toronto, Ontario, Canada, and head of the Mood Disorders Psychopharmacology Unit.
“But what we can say is that anxiety has been an under-researched, undertreated symptom dimension in BPD, and these findings about cariprazine are very promising,” said Dr. McIntyre, chair and executive director of the Brain and Cognition Discovery Foundation, also in Toronto.
The analysis was published in International Clinical Psychopharmacology) and was presented as a poster at the 2023 Neuroscience Education Institute, Colorado Springs, Colorado.
Ubiquitous, Common, Hazardous
Anxiety in BPD is “ubiquitous, common, and hazardous,” Dr. McIntyre said. “We talk so much about depression and mania as cardinal presentations, but someone could make a case that in that trifecta, we’re missing anxiety.”
In patients with BPD and anxiety, “the index episode is much more difficult to treat, there’s a longer time to remission, lower rates of recovery, and a shorter time to recurrence,” noted Dr. McIntyre, chair of the board of the Depression and Bipolar Support Alliance.
Anxiety also may “represent a portent of other things that can add more to the trouble, like alcohol, illicit drugs, or cannabis use — especially now that cannabis is no longer illegal,” Dr. McIntyre said.
Unfortunately, he said, “there hasn’t been an organized, systematic approach to developing a therapy for anxiety in BPD.” Rather, patients are prescribed benzodiazepines, gabapentinoids, or selective serotonin reuptake inhibitors, all of which have limitations, he added.
Some atypical antipsychotics such as quetiapine have been shown to be helpful with anxiety but “have a lot of baggage and side effects — especially sedation, somnolence, weight gain, and metabolic problems,” Dr. McIntyre noted.
Cariprazine is a dopamine D3-preferring D3/D2 partial agonist, a serotonin 5-HT1A receptor partial agonist, and 5-HT2B receptor antagonist, which has shown anxiolytic-like activity in rodent models.
It was approved by the US Food and Drug Administration to treat mania, depression, and mixed episodes of BPD in 2015 and BPD in 2019.
Dr. McIntyre and his team believed there was an opportunity in the completed randomized controlled trials of cariprazine in BPD to conduct a post hoc analysis of its impact on anxiety.
‘Cornerstone Mood Stabilizer’
The researchers pooled data from two phase 3, randomized, double-blind, placebo-controlled studies in adults with BPD experiencing a current major depressive episode.
The pooled intention-to-treat population consisted of 952 patients with BPD (mean age, ~43 years; 62% female) randomized to receive either 1.5 mg/d, 3 mg/d of cariprazine, or placebo. Patients were divided into two subsets: Lower or higher anxiety (defined as a Hamilton Anxiety Rating Scale [HAM-A] total score of < 18 and ≥ 18, respectively). Patients also completed the Montgomery-Åsberg Rating Scale (MADRS).
A third of the patients received a placebo, a third received the 1.5 mg/d dose, and a third received the 3 mg/d dose. Demographic and baseline characteristics were similar between the subsets.
Results showed there was a statistically significant change in HAM-A total score for cariprazine 1.5 mg/d (P = .0027). The investigators also found a statistically significant change in MADRS total score change for cariprazine 1.5 mg (P = .0200) in the higher anxiety subset. The rate of remission was significantly greater for cariprazine 1.5 mg/d in the higher and lower anxiety subsets (P = .0172 and P = .0004, respectively).
In addition, the change in HAM-A total score change was statistically significant for cariprazine 1.5 mg/d in the higher anxiety subgroup (P = .0105) and the 3 mg/d dose in the lower anxiety subgroup (P = .0441).
Dr. McIntyre hopes these findings can be replicated in other trials.
“Clinically, I find that many patients who take cariprazine don’t require as many benzodiazepines or other medications for anxiety, and it’s one of the better-tolerated medications without metabolic complications or weight gain, so it’s become a cornerstone mood stabilizer,” he said.
Polypharmacy Avoided
Another recent study retrospectively analyzed medical records of close to 40 adult patients with BPD I who were receiving treatment with aripiprazole for bipolar depression and then switched to cariprazine.
“We wanted to conduct a study in depressed patients who had gained weight on aripiprazole and then directly switched to cariprazine. It improved their mood and helped mitigate weight gain, thereby avoiding polypharmacy of additional antidepressants and weight loss agents,” said study investigator Maxwell Zachary Price, a medical student at Hackensack Meridian School of Medicine, Nutley, New Jersey.
“In our general outpatient psychiatry practice, we’ve treated many adult patients with oral aripiprazole for maintenance of BPD,” the study’s senior investigator, Richard Price, MD, clinical assistant professor of psychiatry at Weill Cornell Medical College, New York City, added.
Aripiprazole is associated with weight gain. Moreover, aripiprazole “hasn’t shown efficacy in managing BPD,” he said.
Most patients in Dr. Price’s practice are insured through Medicaid, which mandates treatment with aripiprazole before covering cariprazine. “We noticed their weight had been creeping up over the years, and they also were experiencing depressive symptoms,” he said.
The requirement to initiate treatment with aripiprazole before switching to cariprazine offered Dr. Price an opportunity to compare the two agents in this real-world setting by retrospectively reviewing the charts of 37 patients with BPD (23 females and 14 males who made the switch). The patients had been taking aripiprazole for a mean duration of 94.9 weeks and had experienced a mean increase in body weight of 16.1% ± 12.3% on aripiprazole before switching.
Patients who were taking 2 mg-10 mg of aripiprazole were switched to 1.5 mg of cariprazine, while those taking ≥ 15 mg of aripiprazole were switched to 3 mg of cariprazine.
“Patients tolerated the switch well and maintained stability during the transition,” and “no patients discontinued cariprazine during the study,” Dr. Price said.
After a mean duration of 36.7 weeks (range, 1-127 weeks), the patients showed a decrease in Clinical Global Impression-Bipolar Severity of Illness Scale score from a mean of 5.0 ± 0.9 to a mean of 2.8 ± 0.7 (t = −12.75, P < .00001).
The patients’ weight dropped from a mean of 90.3± 21.5 kg on aripiprazole to a mean of 83.9 ± 19.2 kg on cariprazine (t = −4.22, P < .001).
Two patients experienced initial nausea that resolved by taking the medication with food, and two experienced initial restlessness that resolved with dosage reduction.
“We found that the patients were lighter in mood, body habitus and weight, and less agitated and their mental alertness and concentration improved as well,” said Dr. Price. He hopes that further research in randomized blinded trials will corroborate the findings.
Hypothesis-Generating Research
Joseph Cerimele, MD, MPH, associate professor of psychiatry and behavioral sciences, University of Washington, Division of Population Health, UW Medicine, Seattle, Washington, said the research findings are “hypothesis-generating.”
Dr. Ciremele, who wasn’t involved with either study, said many clinicians and researchers are trying to tailor treatment options to match patient characteristics, and these studies and other similar research, “help us all ask questions related to concurrent symptoms in bipolar depression.”
However, the post hoc analysis was a secondary analysis of an efficacy trial where individuals with concurrent anxiety disorders were excluded. “So, a next step might be to evaluate this and other treatments in individuals with BPD and concurrent anxiety disorders,” he said.
The study by Jain et al was funded by AbbVie. Dr. McIntyre had received research grant support from CIHR/GACD/National Natural Science Foundation of China and the Milken Institute; speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics Inc., Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome Therapeutics, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular Therapies, NewBridge Pharmaceuticals, Viatris, Abbvie, and Atai Life Sciences. Dr. McIntyre is the CEO of Braxia Scientific Corp. His coauthors’ disclosures are listed in the original paper. Dr. Price had received honoraria from AbbVie, Alkermes, Allergan, Intra-Cellular Therapies, Janssen, Jazz, Lundbeck, Neuronetics, Otsuka, and Supernus. Mr. Price and Dr. Cerimele reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
. Notably, investigators said, the drug comes without the typical metabolic side effects, including weight gain, associated with this drug class.
A post hoc analysis of pooled data from two trials comparing two different doses of cariprazine (Vraylar) to placebo showed it was consistently effective not only in alleviating bipolar depression but also in improving symptoms of anxiety.
“Since this was a post hoc analysis, one has to be careful about not overstating the findings,” said study investigator Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, Toronto, Ontario, Canada, and head of the Mood Disorders Psychopharmacology Unit.
“But what we can say is that anxiety has been an under-researched, undertreated symptom dimension in BPD, and these findings about cariprazine are very promising,” said Dr. McIntyre, chair and executive director of the Brain and Cognition Discovery Foundation, also in Toronto.
The analysis was published in International Clinical Psychopharmacology) and was presented as a poster at the 2023 Neuroscience Education Institute, Colorado Springs, Colorado.
Ubiquitous, Common, Hazardous
Anxiety in BPD is “ubiquitous, common, and hazardous,” Dr. McIntyre said. “We talk so much about depression and mania as cardinal presentations, but someone could make a case that in that trifecta, we’re missing anxiety.”
In patients with BPD and anxiety, “the index episode is much more difficult to treat, there’s a longer time to remission, lower rates of recovery, and a shorter time to recurrence,” noted Dr. McIntyre, chair of the board of the Depression and Bipolar Support Alliance.
Anxiety also may “represent a portent of other things that can add more to the trouble, like alcohol, illicit drugs, or cannabis use — especially now that cannabis is no longer illegal,” Dr. McIntyre said.
Unfortunately, he said, “there hasn’t been an organized, systematic approach to developing a therapy for anxiety in BPD.” Rather, patients are prescribed benzodiazepines, gabapentinoids, or selective serotonin reuptake inhibitors, all of which have limitations, he added.
Some atypical antipsychotics such as quetiapine have been shown to be helpful with anxiety but “have a lot of baggage and side effects — especially sedation, somnolence, weight gain, and metabolic problems,” Dr. McIntyre noted.
Cariprazine is a dopamine D3-preferring D3/D2 partial agonist, a serotonin 5-HT1A receptor partial agonist, and 5-HT2B receptor antagonist, which has shown anxiolytic-like activity in rodent models.
It was approved by the US Food and Drug Administration to treat mania, depression, and mixed episodes of BPD in 2015 and BPD in 2019.
Dr. McIntyre and his team believed there was an opportunity in the completed randomized controlled trials of cariprazine in BPD to conduct a post hoc analysis of its impact on anxiety.
‘Cornerstone Mood Stabilizer’
The researchers pooled data from two phase 3, randomized, double-blind, placebo-controlled studies in adults with BPD experiencing a current major depressive episode.
The pooled intention-to-treat population consisted of 952 patients with BPD (mean age, ~43 years; 62% female) randomized to receive either 1.5 mg/d, 3 mg/d of cariprazine, or placebo. Patients were divided into two subsets: Lower or higher anxiety (defined as a Hamilton Anxiety Rating Scale [HAM-A] total score of < 18 and ≥ 18, respectively). Patients also completed the Montgomery-Åsberg Rating Scale (MADRS).
A third of the patients received a placebo, a third received the 1.5 mg/d dose, and a third received the 3 mg/d dose. Demographic and baseline characteristics were similar between the subsets.
Results showed there was a statistically significant change in HAM-A total score for cariprazine 1.5 mg/d (P = .0027). The investigators also found a statistically significant change in MADRS total score change for cariprazine 1.5 mg (P = .0200) in the higher anxiety subset. The rate of remission was significantly greater for cariprazine 1.5 mg/d in the higher and lower anxiety subsets (P = .0172 and P = .0004, respectively).
In addition, the change in HAM-A total score change was statistically significant for cariprazine 1.5 mg/d in the higher anxiety subgroup (P = .0105) and the 3 mg/d dose in the lower anxiety subgroup (P = .0441).
Dr. McIntyre hopes these findings can be replicated in other trials.
“Clinically, I find that many patients who take cariprazine don’t require as many benzodiazepines or other medications for anxiety, and it’s one of the better-tolerated medications without metabolic complications or weight gain, so it’s become a cornerstone mood stabilizer,” he said.
Polypharmacy Avoided
Another recent study retrospectively analyzed medical records of close to 40 adult patients with BPD I who were receiving treatment with aripiprazole for bipolar depression and then switched to cariprazine.
“We wanted to conduct a study in depressed patients who had gained weight on aripiprazole and then directly switched to cariprazine. It improved their mood and helped mitigate weight gain, thereby avoiding polypharmacy of additional antidepressants and weight loss agents,” said study investigator Maxwell Zachary Price, a medical student at Hackensack Meridian School of Medicine, Nutley, New Jersey.
“In our general outpatient psychiatry practice, we’ve treated many adult patients with oral aripiprazole for maintenance of BPD,” the study’s senior investigator, Richard Price, MD, clinical assistant professor of psychiatry at Weill Cornell Medical College, New York City, added.
Aripiprazole is associated with weight gain. Moreover, aripiprazole “hasn’t shown efficacy in managing BPD,” he said.
Most patients in Dr. Price’s practice are insured through Medicaid, which mandates treatment with aripiprazole before covering cariprazine. “We noticed their weight had been creeping up over the years, and they also were experiencing depressive symptoms,” he said.
The requirement to initiate treatment with aripiprazole before switching to cariprazine offered Dr. Price an opportunity to compare the two agents in this real-world setting by retrospectively reviewing the charts of 37 patients with BPD (23 females and 14 males who made the switch). The patients had been taking aripiprazole for a mean duration of 94.9 weeks and had experienced a mean increase in body weight of 16.1% ± 12.3% on aripiprazole before switching.
Patients who were taking 2 mg-10 mg of aripiprazole were switched to 1.5 mg of cariprazine, while those taking ≥ 15 mg of aripiprazole were switched to 3 mg of cariprazine.
“Patients tolerated the switch well and maintained stability during the transition,” and “no patients discontinued cariprazine during the study,” Dr. Price said.
After a mean duration of 36.7 weeks (range, 1-127 weeks), the patients showed a decrease in Clinical Global Impression-Bipolar Severity of Illness Scale score from a mean of 5.0 ± 0.9 to a mean of 2.8 ± 0.7 (t = −12.75, P < .00001).
The patients’ weight dropped from a mean of 90.3± 21.5 kg on aripiprazole to a mean of 83.9 ± 19.2 kg on cariprazine (t = −4.22, P < .001).
Two patients experienced initial nausea that resolved by taking the medication with food, and two experienced initial restlessness that resolved with dosage reduction.
“We found that the patients were lighter in mood, body habitus and weight, and less agitated and their mental alertness and concentration improved as well,” said Dr. Price. He hopes that further research in randomized blinded trials will corroborate the findings.
Hypothesis-Generating Research
Joseph Cerimele, MD, MPH, associate professor of psychiatry and behavioral sciences, University of Washington, Division of Population Health, UW Medicine, Seattle, Washington, said the research findings are “hypothesis-generating.”
Dr. Ciremele, who wasn’t involved with either study, said many clinicians and researchers are trying to tailor treatment options to match patient characteristics, and these studies and other similar research, “help us all ask questions related to concurrent symptoms in bipolar depression.”
However, the post hoc analysis was a secondary analysis of an efficacy trial where individuals with concurrent anxiety disorders were excluded. “So, a next step might be to evaluate this and other treatments in individuals with BPD and concurrent anxiety disorders,” he said.
The study by Jain et al was funded by AbbVie. Dr. McIntyre had received research grant support from CIHR/GACD/National Natural Science Foundation of China and the Milken Institute; speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics Inc., Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome Therapeutics, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular Therapies, NewBridge Pharmaceuticals, Viatris, Abbvie, and Atai Life Sciences. Dr. McIntyre is the CEO of Braxia Scientific Corp. His coauthors’ disclosures are listed in the original paper. Dr. Price had received honoraria from AbbVie, Alkermes, Allergan, Intra-Cellular Therapies, Janssen, Jazz, Lundbeck, Neuronetics, Otsuka, and Supernus. Mr. Price and Dr. Cerimele reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
. Notably, investigators said, the drug comes without the typical metabolic side effects, including weight gain, associated with this drug class.
A post hoc analysis of pooled data from two trials comparing two different doses of cariprazine (Vraylar) to placebo showed it was consistently effective not only in alleviating bipolar depression but also in improving symptoms of anxiety.
“Since this was a post hoc analysis, one has to be careful about not overstating the findings,” said study investigator Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, Toronto, Ontario, Canada, and head of the Mood Disorders Psychopharmacology Unit.
“But what we can say is that anxiety has been an under-researched, undertreated symptom dimension in BPD, and these findings about cariprazine are very promising,” said Dr. McIntyre, chair and executive director of the Brain and Cognition Discovery Foundation, also in Toronto.
The analysis was published in International Clinical Psychopharmacology) and was presented as a poster at the 2023 Neuroscience Education Institute, Colorado Springs, Colorado.
Ubiquitous, Common, Hazardous
Anxiety in BPD is “ubiquitous, common, and hazardous,” Dr. McIntyre said. “We talk so much about depression and mania as cardinal presentations, but someone could make a case that in that trifecta, we’re missing anxiety.”
In patients with BPD and anxiety, “the index episode is much more difficult to treat, there’s a longer time to remission, lower rates of recovery, and a shorter time to recurrence,” noted Dr. McIntyre, chair of the board of the Depression and Bipolar Support Alliance.
Anxiety also may “represent a portent of other things that can add more to the trouble, like alcohol, illicit drugs, or cannabis use — especially now that cannabis is no longer illegal,” Dr. McIntyre said.
Unfortunately, he said, “there hasn’t been an organized, systematic approach to developing a therapy for anxiety in BPD.” Rather, patients are prescribed benzodiazepines, gabapentinoids, or selective serotonin reuptake inhibitors, all of which have limitations, he added.
Some atypical antipsychotics such as quetiapine have been shown to be helpful with anxiety but “have a lot of baggage and side effects — especially sedation, somnolence, weight gain, and metabolic problems,” Dr. McIntyre noted.
Cariprazine is a dopamine D3-preferring D3/D2 partial agonist, a serotonin 5-HT1A receptor partial agonist, and 5-HT2B receptor antagonist, which has shown anxiolytic-like activity in rodent models.
It was approved by the US Food and Drug Administration to treat mania, depression, and mixed episodes of BPD in 2015 and BPD in 2019.
Dr. McIntyre and his team believed there was an opportunity in the completed randomized controlled trials of cariprazine in BPD to conduct a post hoc analysis of its impact on anxiety.
‘Cornerstone Mood Stabilizer’
The researchers pooled data from two phase 3, randomized, double-blind, placebo-controlled studies in adults with BPD experiencing a current major depressive episode.
The pooled intention-to-treat population consisted of 952 patients with BPD (mean age, ~43 years; 62% female) randomized to receive either 1.5 mg/d, 3 mg/d of cariprazine, or placebo. Patients were divided into two subsets: Lower or higher anxiety (defined as a Hamilton Anxiety Rating Scale [HAM-A] total score of < 18 and ≥ 18, respectively). Patients also completed the Montgomery-Åsberg Rating Scale (MADRS).
A third of the patients received a placebo, a third received the 1.5 mg/d dose, and a third received the 3 mg/d dose. Demographic and baseline characteristics were similar between the subsets.
Results showed there was a statistically significant change in HAM-A total score for cariprazine 1.5 mg/d (P = .0027). The investigators also found a statistically significant change in MADRS total score change for cariprazine 1.5 mg (P = .0200) in the higher anxiety subset. The rate of remission was significantly greater for cariprazine 1.5 mg/d in the higher and lower anxiety subsets (P = .0172 and P = .0004, respectively).
In addition, the change in HAM-A total score change was statistically significant for cariprazine 1.5 mg/d in the higher anxiety subgroup (P = .0105) and the 3 mg/d dose in the lower anxiety subgroup (P = .0441).
Dr. McIntyre hopes these findings can be replicated in other trials.
“Clinically, I find that many patients who take cariprazine don’t require as many benzodiazepines or other medications for anxiety, and it’s one of the better-tolerated medications without metabolic complications or weight gain, so it’s become a cornerstone mood stabilizer,” he said.
Polypharmacy Avoided
Another recent study retrospectively analyzed medical records of close to 40 adult patients with BPD I who were receiving treatment with aripiprazole for bipolar depression and then switched to cariprazine.
“We wanted to conduct a study in depressed patients who had gained weight on aripiprazole and then directly switched to cariprazine. It improved their mood and helped mitigate weight gain, thereby avoiding polypharmacy of additional antidepressants and weight loss agents,” said study investigator Maxwell Zachary Price, a medical student at Hackensack Meridian School of Medicine, Nutley, New Jersey.
“In our general outpatient psychiatry practice, we’ve treated many adult patients with oral aripiprazole for maintenance of BPD,” the study’s senior investigator, Richard Price, MD, clinical assistant professor of psychiatry at Weill Cornell Medical College, New York City, added.
Aripiprazole is associated with weight gain. Moreover, aripiprazole “hasn’t shown efficacy in managing BPD,” he said.
Most patients in Dr. Price’s practice are insured through Medicaid, which mandates treatment with aripiprazole before covering cariprazine. “We noticed their weight had been creeping up over the years, and they also were experiencing depressive symptoms,” he said.
The requirement to initiate treatment with aripiprazole before switching to cariprazine offered Dr. Price an opportunity to compare the two agents in this real-world setting by retrospectively reviewing the charts of 37 patients with BPD (23 females and 14 males who made the switch). The patients had been taking aripiprazole for a mean duration of 94.9 weeks and had experienced a mean increase in body weight of 16.1% ± 12.3% on aripiprazole before switching.
Patients who were taking 2 mg-10 mg of aripiprazole were switched to 1.5 mg of cariprazine, while those taking ≥ 15 mg of aripiprazole were switched to 3 mg of cariprazine.
“Patients tolerated the switch well and maintained stability during the transition,” and “no patients discontinued cariprazine during the study,” Dr. Price said.
After a mean duration of 36.7 weeks (range, 1-127 weeks), the patients showed a decrease in Clinical Global Impression-Bipolar Severity of Illness Scale score from a mean of 5.0 ± 0.9 to a mean of 2.8 ± 0.7 (t = −12.75, P < .00001).
The patients’ weight dropped from a mean of 90.3± 21.5 kg on aripiprazole to a mean of 83.9 ± 19.2 kg on cariprazine (t = −4.22, P < .001).
Two patients experienced initial nausea that resolved by taking the medication with food, and two experienced initial restlessness that resolved with dosage reduction.
“We found that the patients were lighter in mood, body habitus and weight, and less agitated and their mental alertness and concentration improved as well,” said Dr. Price. He hopes that further research in randomized blinded trials will corroborate the findings.
Hypothesis-Generating Research
Joseph Cerimele, MD, MPH, associate professor of psychiatry and behavioral sciences, University of Washington, Division of Population Health, UW Medicine, Seattle, Washington, said the research findings are “hypothesis-generating.”
Dr. Ciremele, who wasn’t involved with either study, said many clinicians and researchers are trying to tailor treatment options to match patient characteristics, and these studies and other similar research, “help us all ask questions related to concurrent symptoms in bipolar depression.”
However, the post hoc analysis was a secondary analysis of an efficacy trial where individuals with concurrent anxiety disorders were excluded. “So, a next step might be to evaluate this and other treatments in individuals with BPD and concurrent anxiety disorders,” he said.
The study by Jain et al was funded by AbbVie. Dr. McIntyre had received research grant support from CIHR/GACD/National Natural Science Foundation of China and the Milken Institute; speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics Inc., Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome Therapeutics, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular Therapies, NewBridge Pharmaceuticals, Viatris, Abbvie, and Atai Life Sciences. Dr. McIntyre is the CEO of Braxia Scientific Corp. His coauthors’ disclosures are listed in the original paper. Dr. Price had received honoraria from AbbVie, Alkermes, Allergan, Intra-Cellular Therapies, Janssen, Jazz, Lundbeck, Neuronetics, Otsuka, and Supernus. Mr. Price and Dr. Cerimele reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
Schizophrenia Med Safe, Effective for Bipolar Mania: Phase 3 Data
Results of the phase 3 randomized double-blind placebo-controlled trial show patients with bipolar mania who received iloperidone had significantly greater change from baseline to 4 weeks on the Young Mania Rating Scale (YMRS) compared with placebo, an improvement detected as early as 14 days from the initial dose.
The incidence of akathisia and extrapyramidal symptoms (EPS) was low in the treatment group, and the medication was well-tolerated.
“This study provides evidence that iloperidone improves the symptoms of bipolar mania in adults and can be a useful treatment option for people with bipolar disorder,” the investigators, led by Rosarelis Torres, PhD, of Vanda Pharmaceuticals, and colleagues wrote.
The study was published online in the Journal of Clinical Psychiatry.
Early Improvement
Iloperidone was first approved by the US Food and Drug Administration in 2009 for treatment of schizophrenia.
The current study included 414 participants (mean age, 43 years; 56% male) across 17 US and international sites. Patients with psychotic features received a fixed daily dose of 24 mg of iloperidone (n = 206) or placebo (n = 208).
Participants completed a screening period of up to 7 days before randomization, followed by a 1-day baseline evaluation period and a 28-day treatment phase.
The primary efficacy endpoint was change from baseline to week 4 on the YMRS (vs placebo), while secondary efficacy endpoints included change from baseline on the Clinical Global Impressions-Severity and Clinical Global Impression of Change scales (CGI-S and CGI-C, respectively).
Compared with placebo, iloperidone was associated with significant improvement of mania symptoms at week 4, with a mean reduction on the YMRS scale of −4.0 (P = .000008), and significant decreases on the CGI-S (mean, −0.4; P = .0005) and CGI-C scales (mean, −0.5; P = .0002).
Statistically significant differences between iloperidone and placebo were observed as early as day 14 and continued through days 21 and 28.
Post hoc analyses found no difference in efficacy even when patients who had received benzodiazepines were excluded, regardless of the presence or absence of psychotic features at baseline.
Favorable Akathisia Profile
As for safety, 68% of patients in the iloperidone group experienced at least one adverse event, compared with 49% of patients in the placebo group.
Patients in the treatment group had a higher rate of withdrawal from the study than those in the placebo group (32.9% vs 27.1%), and more patients in the iloperidone group experienced treatment-emergent adverse events (TEAEs) leading to study drug discontinuation (8.7% vs 5.3%). However, no TEAEs associated with discontinuation occurred in more than two patients in either group, and none of the participants experienced any AE leading to death.
The most common adverse events (AEs) were tachycardia (18%), dizziness (11%), dry mouth (9%), increased alanine aminotransferase (7%), nasal congestion (6%), weight gain (6%), and somnolence (5%).
Five serious AEs were reported in four participants in the treatment group and one in the placebo group. Two were identified as related to the study medication. These included sedation and spontaneous penile erection.
Changes from baseline in clinical laboratory parameters were not largely different between the groups, but there were post-randomization changes in QT interval in three iloperidone patients. The incidence of orthostatic response was also higher for iloperidone vs placebo.
Although “much improved compared to early antipsychotics, SGAs can still cause considerable adverse motor side effects,” the authors wrote. “However, among all SGAs, iloperidone’s akathisia profile is favorable.”
Antipsychotic-induced akathisia has been reported more frequently in patients with bipolar disorder than in those with schizophrenia treated with the same medication, investigators noted.
One study limitation is the fact that long-term efficacy in the prevention of manic or depressive episodes was not assessed.
Potential Second-Line Treatment
Commenting on the study, Richard Louis Price, MD, assistant professor of psychiatry, at Weill Cornell Medical College, New York City, said the findings suggest iloperidone may be “modestly effective” for patients with bipolar 1 mania or mixed episodes.
“It’s helpful to have new treatment options, especially for patients who have difficulty tolerating other agents,” said Dr. Price, who was not involved with the study.
Also commenting on the research, Roger S. McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, Toronto, Ontario, Canada, noted iloperidone’s “interesting antipsychotic pharmacodynamic,” highlighting the drug’s high-binding affinity for serotonin 5HT2A and dopamine D2 and D3 receptors, as well as the noradrenergic α1 receptors.
The drug’s profile “suggests benefit in manic features and agitation, perhaps with a lower propensity to EPS, which is especially important in persons at higher risk, like persons living with bipolar disorder,” Dr. McIntyre said.
Dr. McIntyre, who was not involved with the study, added iloperidone could be a second-line therapy because of its tolerability profile, provided the study results can be replicated.
“When considering alternatives with similar efficacy, absence of titration (or simple titration) minimal to no weight gain, no orthostatic hypotension, and no potential concerns with QT, those alternatives would have to be considered first-line, assuming that the study results are replicated,” he said.
This study was funded by Vanda Pharmaceuticals. The authors’ disclosures are listed in the original paper. Dr. McIntyre had received research grant support from CIHR/GACD/National Natural Science Foundation of China and the Milken Institute; speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine Biosciences, Sunovion, Bausch Health, Axsome Therapeutics, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular Therapies Inc., NewBridge Pharmaceuticals, Viatris, Abbvie, and Atai Life Sciences. McIntyre is the CEO of Braxia Scientific Corp. Dr. Price had received honoraria from AbbVie, Alkermes, Allergan, Intra-Cellular Therapies, Janssen, Jazz, Lundbeck, Neuronetics, Otsuka, and Supernus.
A version of this article appeared on Medscape.com.
Results of the phase 3 randomized double-blind placebo-controlled trial show patients with bipolar mania who received iloperidone had significantly greater change from baseline to 4 weeks on the Young Mania Rating Scale (YMRS) compared with placebo, an improvement detected as early as 14 days from the initial dose.
The incidence of akathisia and extrapyramidal symptoms (EPS) was low in the treatment group, and the medication was well-tolerated.
“This study provides evidence that iloperidone improves the symptoms of bipolar mania in adults and can be a useful treatment option for people with bipolar disorder,” the investigators, led by Rosarelis Torres, PhD, of Vanda Pharmaceuticals, and colleagues wrote.
The study was published online in the Journal of Clinical Psychiatry.
Early Improvement
Iloperidone was first approved by the US Food and Drug Administration in 2009 for treatment of schizophrenia.
The current study included 414 participants (mean age, 43 years; 56% male) across 17 US and international sites. Patients with psychotic features received a fixed daily dose of 24 mg of iloperidone (n = 206) or placebo (n = 208).
Participants completed a screening period of up to 7 days before randomization, followed by a 1-day baseline evaluation period and a 28-day treatment phase.
The primary efficacy endpoint was change from baseline to week 4 on the YMRS (vs placebo), while secondary efficacy endpoints included change from baseline on the Clinical Global Impressions-Severity and Clinical Global Impression of Change scales (CGI-S and CGI-C, respectively).
Compared with placebo, iloperidone was associated with significant improvement of mania symptoms at week 4, with a mean reduction on the YMRS scale of −4.0 (P = .000008), and significant decreases on the CGI-S (mean, −0.4; P = .0005) and CGI-C scales (mean, −0.5; P = .0002).
Statistically significant differences between iloperidone and placebo were observed as early as day 14 and continued through days 21 and 28.
Post hoc analyses found no difference in efficacy even when patients who had received benzodiazepines were excluded, regardless of the presence or absence of psychotic features at baseline.
Favorable Akathisia Profile
As for safety, 68% of patients in the iloperidone group experienced at least one adverse event, compared with 49% of patients in the placebo group.
Patients in the treatment group had a higher rate of withdrawal from the study than those in the placebo group (32.9% vs 27.1%), and more patients in the iloperidone group experienced treatment-emergent adverse events (TEAEs) leading to study drug discontinuation (8.7% vs 5.3%). However, no TEAEs associated with discontinuation occurred in more than two patients in either group, and none of the participants experienced any AE leading to death.
The most common adverse events (AEs) were tachycardia (18%), dizziness (11%), dry mouth (9%), increased alanine aminotransferase (7%), nasal congestion (6%), weight gain (6%), and somnolence (5%).
Five serious AEs were reported in four participants in the treatment group and one in the placebo group. Two were identified as related to the study medication. These included sedation and spontaneous penile erection.
Changes from baseline in clinical laboratory parameters were not largely different between the groups, but there were post-randomization changes in QT interval in three iloperidone patients. The incidence of orthostatic response was also higher for iloperidone vs placebo.
Although “much improved compared to early antipsychotics, SGAs can still cause considerable adverse motor side effects,” the authors wrote. “However, among all SGAs, iloperidone’s akathisia profile is favorable.”
Antipsychotic-induced akathisia has been reported more frequently in patients with bipolar disorder than in those with schizophrenia treated with the same medication, investigators noted.
One study limitation is the fact that long-term efficacy in the prevention of manic or depressive episodes was not assessed.
Potential Second-Line Treatment
Commenting on the study, Richard Louis Price, MD, assistant professor of psychiatry, at Weill Cornell Medical College, New York City, said the findings suggest iloperidone may be “modestly effective” for patients with bipolar 1 mania or mixed episodes.
“It’s helpful to have new treatment options, especially for patients who have difficulty tolerating other agents,” said Dr. Price, who was not involved with the study.
Also commenting on the research, Roger S. McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, Toronto, Ontario, Canada, noted iloperidone’s “interesting antipsychotic pharmacodynamic,” highlighting the drug’s high-binding affinity for serotonin 5HT2A and dopamine D2 and D3 receptors, as well as the noradrenergic α1 receptors.
The drug’s profile “suggests benefit in manic features and agitation, perhaps with a lower propensity to EPS, which is especially important in persons at higher risk, like persons living with bipolar disorder,” Dr. McIntyre said.
Dr. McIntyre, who was not involved with the study, added iloperidone could be a second-line therapy because of its tolerability profile, provided the study results can be replicated.
“When considering alternatives with similar efficacy, absence of titration (or simple titration) minimal to no weight gain, no orthostatic hypotension, and no potential concerns with QT, those alternatives would have to be considered first-line, assuming that the study results are replicated,” he said.
This study was funded by Vanda Pharmaceuticals. The authors’ disclosures are listed in the original paper. Dr. McIntyre had received research grant support from CIHR/GACD/National Natural Science Foundation of China and the Milken Institute; speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine Biosciences, Sunovion, Bausch Health, Axsome Therapeutics, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular Therapies Inc., NewBridge Pharmaceuticals, Viatris, Abbvie, and Atai Life Sciences. McIntyre is the CEO of Braxia Scientific Corp. Dr. Price had received honoraria from AbbVie, Alkermes, Allergan, Intra-Cellular Therapies, Janssen, Jazz, Lundbeck, Neuronetics, Otsuka, and Supernus.
A version of this article appeared on Medscape.com.
Results of the phase 3 randomized double-blind placebo-controlled trial show patients with bipolar mania who received iloperidone had significantly greater change from baseline to 4 weeks on the Young Mania Rating Scale (YMRS) compared with placebo, an improvement detected as early as 14 days from the initial dose.
The incidence of akathisia and extrapyramidal symptoms (EPS) was low in the treatment group, and the medication was well-tolerated.
“This study provides evidence that iloperidone improves the symptoms of bipolar mania in adults and can be a useful treatment option for people with bipolar disorder,” the investigators, led by Rosarelis Torres, PhD, of Vanda Pharmaceuticals, and colleagues wrote.
The study was published online in the Journal of Clinical Psychiatry.
Early Improvement
Iloperidone was first approved by the US Food and Drug Administration in 2009 for treatment of schizophrenia.
The current study included 414 participants (mean age, 43 years; 56% male) across 17 US and international sites. Patients with psychotic features received a fixed daily dose of 24 mg of iloperidone (n = 206) or placebo (n = 208).
Participants completed a screening period of up to 7 days before randomization, followed by a 1-day baseline evaluation period and a 28-day treatment phase.
The primary efficacy endpoint was change from baseline to week 4 on the YMRS (vs placebo), while secondary efficacy endpoints included change from baseline on the Clinical Global Impressions-Severity and Clinical Global Impression of Change scales (CGI-S and CGI-C, respectively).
Compared with placebo, iloperidone was associated with significant improvement of mania symptoms at week 4, with a mean reduction on the YMRS scale of −4.0 (P = .000008), and significant decreases on the CGI-S (mean, −0.4; P = .0005) and CGI-C scales (mean, −0.5; P = .0002).
Statistically significant differences between iloperidone and placebo were observed as early as day 14 and continued through days 21 and 28.
Post hoc analyses found no difference in efficacy even when patients who had received benzodiazepines were excluded, regardless of the presence or absence of psychotic features at baseline.
Favorable Akathisia Profile
As for safety, 68% of patients in the iloperidone group experienced at least one adverse event, compared with 49% of patients in the placebo group.
Patients in the treatment group had a higher rate of withdrawal from the study than those in the placebo group (32.9% vs 27.1%), and more patients in the iloperidone group experienced treatment-emergent adverse events (TEAEs) leading to study drug discontinuation (8.7% vs 5.3%). However, no TEAEs associated with discontinuation occurred in more than two patients in either group, and none of the participants experienced any AE leading to death.
The most common adverse events (AEs) were tachycardia (18%), dizziness (11%), dry mouth (9%), increased alanine aminotransferase (7%), nasal congestion (6%), weight gain (6%), and somnolence (5%).
Five serious AEs were reported in four participants in the treatment group and one in the placebo group. Two were identified as related to the study medication. These included sedation and spontaneous penile erection.
Changes from baseline in clinical laboratory parameters were not largely different between the groups, but there were post-randomization changes in QT interval in three iloperidone patients. The incidence of orthostatic response was also higher for iloperidone vs placebo.
Although “much improved compared to early antipsychotics, SGAs can still cause considerable adverse motor side effects,” the authors wrote. “However, among all SGAs, iloperidone’s akathisia profile is favorable.”
Antipsychotic-induced akathisia has been reported more frequently in patients with bipolar disorder than in those with schizophrenia treated with the same medication, investigators noted.
One study limitation is the fact that long-term efficacy in the prevention of manic or depressive episodes was not assessed.
Potential Second-Line Treatment
Commenting on the study, Richard Louis Price, MD, assistant professor of psychiatry, at Weill Cornell Medical College, New York City, said the findings suggest iloperidone may be “modestly effective” for patients with bipolar 1 mania or mixed episodes.
“It’s helpful to have new treatment options, especially for patients who have difficulty tolerating other agents,” said Dr. Price, who was not involved with the study.
Also commenting on the research, Roger S. McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, Toronto, Ontario, Canada, noted iloperidone’s “interesting antipsychotic pharmacodynamic,” highlighting the drug’s high-binding affinity for serotonin 5HT2A and dopamine D2 and D3 receptors, as well as the noradrenergic α1 receptors.
The drug’s profile “suggests benefit in manic features and agitation, perhaps with a lower propensity to EPS, which is especially important in persons at higher risk, like persons living with bipolar disorder,” Dr. McIntyre said.
Dr. McIntyre, who was not involved with the study, added iloperidone could be a second-line therapy because of its tolerability profile, provided the study results can be replicated.
“When considering alternatives with similar efficacy, absence of titration (or simple titration) minimal to no weight gain, no orthostatic hypotension, and no potential concerns with QT, those alternatives would have to be considered first-line, assuming that the study results are replicated,” he said.
This study was funded by Vanda Pharmaceuticals. The authors’ disclosures are listed in the original paper. Dr. McIntyre had received research grant support from CIHR/GACD/National Natural Science Foundation of China and the Milken Institute; speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine Biosciences, Sunovion, Bausch Health, Axsome Therapeutics, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular Therapies Inc., NewBridge Pharmaceuticals, Viatris, Abbvie, and Atai Life Sciences. McIntyre is the CEO of Braxia Scientific Corp. Dr. Price had received honoraria from AbbVie, Alkermes, Allergan, Intra-Cellular Therapies, Janssen, Jazz, Lundbeck, Neuronetics, Otsuka, and Supernus.
A version of this article appeared on Medscape.com.
No Impact of Legalized Cannabis on Opioid Prescriptions, Mortality
TOPLINE:
Legalization of recreational and medical cannabis is not associated with a reduction in opioid prescriptions or overall opioid overdose mortality, a new study suggested. However, investigators did find that recreational cannabis laws may be tied to a potential reduction in synthetic opioid deaths.
METHODOLOGY:
- Investigators analyzed state-level data from the US Centers for Disease Control and Prevention and other databases (2006-2020) on the number of opioid prescriptions (per 100,000 persons).
- Prescription opioids included buprenorphine (except products to treat opioid use disorder), codeine, fentanyl, hydrocodone, hydromorphone, methadone, morphine, oxycodone, oxymorphone, propoxyphene, tapentadol, and tramadol.
- Researchers used regression analyses to account for poverty rates and real gross domestic product and a generalized difference-in-differences method that accounted for staggered implementation of cannabis laws.
TAKEAWAY:
- During the full study period, 13 states legalized recreational cannabis and 23 legalized medical cannabis.
- No statistically significant association was found between recreational cannabis laws and opioid prescriptions (3.08 fewer prescriptions per 100 persons; P = .17) or overall opioid overdose mortality (3.05 fewer deaths per 100,000; P = .24).
- The changes in outcomes associated with medical cannabis laws were larger in magnitude than those for recreational cannabis laws but also not statistically significant (3.54 additional prescriptions per 100 persons; P = .17 and 3.09 additional deaths per 100,000; P = .07).
- A potential reduction was found in synthetic opioid deaths associated specifically with states that had recreational cannabis laws (4.9 fewer deaths per 100,000; P = .04), but there were no differences in overdose deaths with other opioids.
IN PRACTICE:
“These results contrast with recent studies that suggested that recreational and medical cannabis legalization are associated with reductions in opioid prescriptions and medical cannabis legalization is associated with an increase in opioid mortality,” the authors wrote.
SOURCE:
Hai V. Nguyen, PhD, of the School of Pharmacy, Memorial University of Newfoundland, St. John’s, Canada, was the lead and corresponding author of the study. It was published online on January 19, 2024, in JAMA Health Forum.
A version of this article appeared on Medscape.com.
TOPLINE:
Legalization of recreational and medical cannabis is not associated with a reduction in opioid prescriptions or overall opioid overdose mortality, a new study suggested. However, investigators did find that recreational cannabis laws may be tied to a potential reduction in synthetic opioid deaths.
METHODOLOGY:
- Investigators analyzed state-level data from the US Centers for Disease Control and Prevention and other databases (2006-2020) on the number of opioid prescriptions (per 100,000 persons).
- Prescription opioids included buprenorphine (except products to treat opioid use disorder), codeine, fentanyl, hydrocodone, hydromorphone, methadone, morphine, oxycodone, oxymorphone, propoxyphene, tapentadol, and tramadol.
- Researchers used regression analyses to account for poverty rates and real gross domestic product and a generalized difference-in-differences method that accounted for staggered implementation of cannabis laws.
TAKEAWAY:
- During the full study period, 13 states legalized recreational cannabis and 23 legalized medical cannabis.
- No statistically significant association was found between recreational cannabis laws and opioid prescriptions (3.08 fewer prescriptions per 100 persons; P = .17) or overall opioid overdose mortality (3.05 fewer deaths per 100,000; P = .24).
- The changes in outcomes associated with medical cannabis laws were larger in magnitude than those for recreational cannabis laws but also not statistically significant (3.54 additional prescriptions per 100 persons; P = .17 and 3.09 additional deaths per 100,000; P = .07).
- A potential reduction was found in synthetic opioid deaths associated specifically with states that had recreational cannabis laws (4.9 fewer deaths per 100,000; P = .04), but there were no differences in overdose deaths with other opioids.
IN PRACTICE:
“These results contrast with recent studies that suggested that recreational and medical cannabis legalization are associated with reductions in opioid prescriptions and medical cannabis legalization is associated with an increase in opioid mortality,” the authors wrote.
SOURCE:
Hai V. Nguyen, PhD, of the School of Pharmacy, Memorial University of Newfoundland, St. John’s, Canada, was the lead and corresponding author of the study. It was published online on January 19, 2024, in JAMA Health Forum.
A version of this article appeared on Medscape.com.
TOPLINE:
Legalization of recreational and medical cannabis is not associated with a reduction in opioid prescriptions or overall opioid overdose mortality, a new study suggested. However, investigators did find that recreational cannabis laws may be tied to a potential reduction in synthetic opioid deaths.
METHODOLOGY:
- Investigators analyzed state-level data from the US Centers for Disease Control and Prevention and other databases (2006-2020) on the number of opioid prescriptions (per 100,000 persons).
- Prescription opioids included buprenorphine (except products to treat opioid use disorder), codeine, fentanyl, hydrocodone, hydromorphone, methadone, morphine, oxycodone, oxymorphone, propoxyphene, tapentadol, and tramadol.
- Researchers used regression analyses to account for poverty rates and real gross domestic product and a generalized difference-in-differences method that accounted for staggered implementation of cannabis laws.
TAKEAWAY:
- During the full study period, 13 states legalized recreational cannabis and 23 legalized medical cannabis.
- No statistically significant association was found between recreational cannabis laws and opioid prescriptions (3.08 fewer prescriptions per 100 persons; P = .17) or overall opioid overdose mortality (3.05 fewer deaths per 100,000; P = .24).
- The changes in outcomes associated with medical cannabis laws were larger in magnitude than those for recreational cannabis laws but also not statistically significant (3.54 additional prescriptions per 100 persons; P = .17 and 3.09 additional deaths per 100,000; P = .07).
- A potential reduction was found in synthetic opioid deaths associated specifically with states that had recreational cannabis laws (4.9 fewer deaths per 100,000; P = .04), but there were no differences in overdose deaths with other opioids.
IN PRACTICE:
“These results contrast with recent studies that suggested that recreational and medical cannabis legalization are associated with reductions in opioid prescriptions and medical cannabis legalization is associated with an increase in opioid mortality,” the authors wrote.
SOURCE:
Hai V. Nguyen, PhD, of the School of Pharmacy, Memorial University of Newfoundland, St. John’s, Canada, was the lead and corresponding author of the study. It was published online on January 19, 2024, in JAMA Health Forum.
A version of this article appeared on Medscape.com.
OCD Tied to a Twofold Increased Risk for All-Cause Mortality
TOPLINE:
Obsessive-compulsive disorder (OCD) is linked to a twofold increased risk for all-cause mortality and a heightened risk for death from both natural and unnatural causes, a new study showed.
METHODOLOGY:
- Investigators studied a population-based cohort (58% female) of 61,378 people with OCD and 613,780 unaffected individuals from several Swedish population registers and a sibling cohort of 34,085 people with OCD (58% female) and 47,874 unaffected full siblings (48% female).
- The median 8.1-year follow-up and median age at first diagnosis of OCD were 27 years.
- The researchers used Cox proportional hazard models, adjusting for birth year, sex, county, country of birth (Sweden vs abroad), and sociodemographic variables.
TAKEAWAY:
- (adjusted hazard ratio [aHR], 1.82; 95% CI, 1.76-1.89), an almost threefold higher risk for mortality due to unnatural causes (aHR, 3.30; 95% CI, 3.05-3.57), and a higher risk for mortality due to natural causes (aHR, 1.31; 95% CI, 1.24-1.37).
- Of all the unnatural causes of death, suicide was most common (hazard ratio [HR], 4.90; 95% CI, 4.40-5.46), followed by accidents (HR, 1.92; 95% CI, 1.68-2.19).
- Similar results were found in the sibling comparison, where the HR of all-cause mortality was 1.85 (95% CI, 1.67-2.03), death from natural causes was 1.51 (95% CI, 1.35-1.68), and death from unnatural causes was 3.10 (95% CI, 2.52-3.80).
- Natural causes of death that were higher in the OCD vs non-OCD cohort included endocrine, nutritional, and metabolic diseases; mental and behavioral disorders; and diseases of the nervous, circulatory, respiratory, digestive, and genitourinary systems.
IN PRACTICE:
“Better surveillance, prevention, and early intervention strategies should be implemented to reduce the risk of fatal outcomes in people with OCD,” the authors wrote.
SOURCE:
Lorena Fernández de la Cruz, PhD, of Karolinska Institutet, Solna, Sweden, led the study, which was published online on January 17 in the British Medical Journal.
LIMITATIONS:
The study does not establish causality. Registry data used by the investigators only included diagnoses made in specialist care and may not have included diagnoses made in other settings. It is also unclear whether the findings, derived from a Swedish population, can be generalized to other populations, health systems, and medical practices.
DISCLOSURES:
The study was funded by the Swedish Council for Health, Working Life and Welfare, Region Stockholm, the Swedish Society of Medicine, and Karolinska Institutet. Dr. de la Cruz received royalties for contributing articles to UpToDate and Wolters Kluwer Health and for editorial work from Elsevier outside the submitted work. See the paper for disclosures of the other authors.
A version of this article appeared on Medscape.com.
TOPLINE:
Obsessive-compulsive disorder (OCD) is linked to a twofold increased risk for all-cause mortality and a heightened risk for death from both natural and unnatural causes, a new study showed.
METHODOLOGY:
- Investigators studied a population-based cohort (58% female) of 61,378 people with OCD and 613,780 unaffected individuals from several Swedish population registers and a sibling cohort of 34,085 people with OCD (58% female) and 47,874 unaffected full siblings (48% female).
- The median 8.1-year follow-up and median age at first diagnosis of OCD were 27 years.
- The researchers used Cox proportional hazard models, adjusting for birth year, sex, county, country of birth (Sweden vs abroad), and sociodemographic variables.
TAKEAWAY:
- (adjusted hazard ratio [aHR], 1.82; 95% CI, 1.76-1.89), an almost threefold higher risk for mortality due to unnatural causes (aHR, 3.30; 95% CI, 3.05-3.57), and a higher risk for mortality due to natural causes (aHR, 1.31; 95% CI, 1.24-1.37).
- Of all the unnatural causes of death, suicide was most common (hazard ratio [HR], 4.90; 95% CI, 4.40-5.46), followed by accidents (HR, 1.92; 95% CI, 1.68-2.19).
- Similar results were found in the sibling comparison, where the HR of all-cause mortality was 1.85 (95% CI, 1.67-2.03), death from natural causes was 1.51 (95% CI, 1.35-1.68), and death from unnatural causes was 3.10 (95% CI, 2.52-3.80).
- Natural causes of death that were higher in the OCD vs non-OCD cohort included endocrine, nutritional, and metabolic diseases; mental and behavioral disorders; and diseases of the nervous, circulatory, respiratory, digestive, and genitourinary systems.
IN PRACTICE:
“Better surveillance, prevention, and early intervention strategies should be implemented to reduce the risk of fatal outcomes in people with OCD,” the authors wrote.
SOURCE:
Lorena Fernández de la Cruz, PhD, of Karolinska Institutet, Solna, Sweden, led the study, which was published online on January 17 in the British Medical Journal.
LIMITATIONS:
The study does not establish causality. Registry data used by the investigators only included diagnoses made in specialist care and may not have included diagnoses made in other settings. It is also unclear whether the findings, derived from a Swedish population, can be generalized to other populations, health systems, and medical practices.
DISCLOSURES:
The study was funded by the Swedish Council for Health, Working Life and Welfare, Region Stockholm, the Swedish Society of Medicine, and Karolinska Institutet. Dr. de la Cruz received royalties for contributing articles to UpToDate and Wolters Kluwer Health and for editorial work from Elsevier outside the submitted work. See the paper for disclosures of the other authors.
A version of this article appeared on Medscape.com.
TOPLINE:
Obsessive-compulsive disorder (OCD) is linked to a twofold increased risk for all-cause mortality and a heightened risk for death from both natural and unnatural causes, a new study showed.
METHODOLOGY:
- Investigators studied a population-based cohort (58% female) of 61,378 people with OCD and 613,780 unaffected individuals from several Swedish population registers and a sibling cohort of 34,085 people with OCD (58% female) and 47,874 unaffected full siblings (48% female).
- The median 8.1-year follow-up and median age at first diagnosis of OCD were 27 years.
- The researchers used Cox proportional hazard models, adjusting for birth year, sex, county, country of birth (Sweden vs abroad), and sociodemographic variables.
TAKEAWAY:
- (adjusted hazard ratio [aHR], 1.82; 95% CI, 1.76-1.89), an almost threefold higher risk for mortality due to unnatural causes (aHR, 3.30; 95% CI, 3.05-3.57), and a higher risk for mortality due to natural causes (aHR, 1.31; 95% CI, 1.24-1.37).
- Of all the unnatural causes of death, suicide was most common (hazard ratio [HR], 4.90; 95% CI, 4.40-5.46), followed by accidents (HR, 1.92; 95% CI, 1.68-2.19).
- Similar results were found in the sibling comparison, where the HR of all-cause mortality was 1.85 (95% CI, 1.67-2.03), death from natural causes was 1.51 (95% CI, 1.35-1.68), and death from unnatural causes was 3.10 (95% CI, 2.52-3.80).
- Natural causes of death that were higher in the OCD vs non-OCD cohort included endocrine, nutritional, and metabolic diseases; mental and behavioral disorders; and diseases of the nervous, circulatory, respiratory, digestive, and genitourinary systems.
IN PRACTICE:
“Better surveillance, prevention, and early intervention strategies should be implemented to reduce the risk of fatal outcomes in people with OCD,” the authors wrote.
SOURCE:
Lorena Fernández de la Cruz, PhD, of Karolinska Institutet, Solna, Sweden, led the study, which was published online on January 17 in the British Medical Journal.
LIMITATIONS:
The study does not establish causality. Registry data used by the investigators only included diagnoses made in specialist care and may not have included diagnoses made in other settings. It is also unclear whether the findings, derived from a Swedish population, can be generalized to other populations, health systems, and medical practices.
DISCLOSURES:
The study was funded by the Swedish Council for Health, Working Life and Welfare, Region Stockholm, the Swedish Society of Medicine, and Karolinska Institutet. Dr. de la Cruz received royalties for contributing articles to UpToDate and Wolters Kluwer Health and for editorial work from Elsevier outside the submitted work. See the paper for disclosures of the other authors.
A version of this article appeared on Medscape.com.
PCPs Increasingly Chained to EHRs
If you feel like the day doesn’t hold enough hours for you to get your work done, you’re right: (EHRs).
Investigators followed 141 academic PCPs between May 2019 and March 2023 and found they spent considerably more time engaging in EHR tasks during the final year of the study than in the prepandemic period. EHR time increased by over 8% on days with scheduled appointments and almost 20% on days without scheduled appointments.
“Physicians spend an unsustainable amount of time on EHR-based work, and that amount has increased steadily from 2019 to 2023,” Christine Sinsky, MD, vice president of professional satisfaction at the American Medical Association (AMA) and the senior author of the study, told this news organization. “It is imperative for healthcare systems to develop strategies to change the overall EHR workload trajectory to minimize PCPs’ occupational stress, including improved workflows, where the work is more appropriately distributed amongst the team.”
The study was published online on January 22, 2024, in the Annals of Family Medicine.
‘Pajama Time’
Dr. Sinsky said the motivation for conducting the current study was that PCPs have reported an increase in their workload, especially EHR tasks outside of work (“pajama time”) since the onset of the pandemic.
The research followed up on a 2017 analysis from the same group and other findings showing an increase in the time physicians spend in EHR tasks and the number of Inbox messages they receive from patients seeking medical advice increased during the months following the start of the pandemic.
“As a busy practicing PCP with a large panel of patients, my sense was that the workload was increasing even more, which is what our study confirmed,” said Brian G. Arndt, MD, of the Department of Family Medicine and Community Heath at the University of Wisconsin School of Medicine and Public Health, in Madison, Wisconsin, who led the new study.
The researchers analyzed EHR usage of 141 academic PCPs practicing family medicine, internal medicine, and general pediatrics, two thirds (66.7%) of whom were female. They compared the amount of time spent on EHR tasks during four timespans:
- May 2019 to February 2020
- June 2020 to March 2021
- May 2021 to March 2022
- April 2022 to March 2023
Each PCP’s time and Inbox message volume were calculated and then normalized over 8 hours of scheduled clinic appointments.
Increased Time, Increased Burnout
The study found evidence PCPs have reduced their clinical hours in response to their growing digital workload.
“We have a serious shortage of primary care physicians,” Dr. Sinsky said. “When PCPs cut back their clinical [work] as a coping mechanism for an unmanageable workload, this further exacerbates the primary care shortage, reducing access to care for patients.”
The researchers found increases from the first prepandemic period to the final period of their study in average time that PCPs spent at the EHR per 8 hours of scheduled clinic appointments (Table).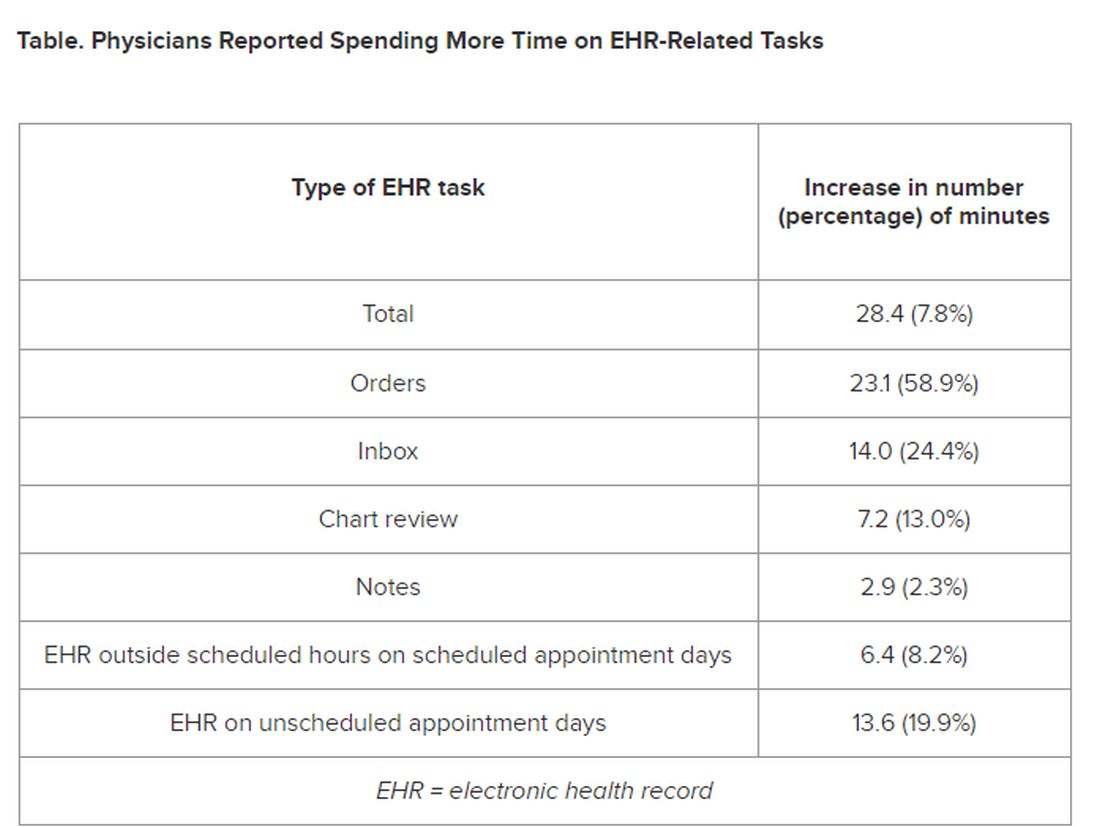
PCPs were inundated with several types of EHR-related responsibilities, including more medical advice requests (+55.5%) and more prescription messages (+19.5%) per 8 hours of scheduled clinic appointments. On the other hand, they had slightly fewer patient calls (−10.5%) and messages concerning test results (−2.7%).
A recent study of 307 PCPs across 31 primary care practices paralleled these findings. It found that physicians spent 36.2 minutes on the EHR per visit (interquartile range, 28.9-45.7 minutes). Included were 6.2 minutes of “pajama time” per visit and 7.8 minutes on the EHR per visit.
The amount of EHR time exceeded the amount of time allotted to a primary care visit (30 minutes). The authors commented that the EHR time burden “and the burnout associated with this burden represent a serious threat to the primary care physician workforce.”
“As more health systems across the country transition from fee-for-service to value-based payment arrangements, they need to balance the time PCPs and their care teams need for face-to-face care — in-person or video visits — with the increasing asynchronous care patients are seeking from us through the portal, for example, MyChart,” Dr. Arndt said.
Sinsky noted that when patients receive care from a PCP, quality is higher and costs are lower. “When access to primary care is further limited by virtue of physicians being overwhelmed by administrative work implemented via the EHR, so that they are reducing their hours, then we can expect negative consequences for patient care and costs of care.”
Tips for Reducing EHR Time
Arndt noted that some “brief investments” of time with patients “lead to high rates of return on decreased MyChart messaging.” For example, he has said to patients: “In the future, there’s no need to respond in MyChart with a ‘Thank you.’” Or “In the future, if you have questions from preappointment labs, no need to send me a separate message in MyChart prior to your visit since they’re typically just a few days out. I look closely at your labs and would always pick up the phone and call you if there was anything more urgent or pressing that needs more immediate action.”
Sinsky recommended two “high-yield opportunities” to reduce EHR-associated workload. The AMA offers a brief Inbox reduction checklist as well as a detailed toolkit to guide physicians and operational leaders in reducing the volume of unnecessary Inbox messages, she said.
Distribution of work among the team also can reduce the time physicians spent on order entry. “It doesn’t take a medical school education to enter orders for flu shots, lipid profiles, mammograms, and other tests, and yet we have primary care physicians around the country spending an hour or more per 8 hours of patient visits on this task,” she said.
‘Growing Mountain’
Sally Baxter, MD, assistant professor of ophthalmology and division chief for Ophthalmology Informatics and Data Sciences at University of California San Diego, said, “Studies like this ... are important for continuing to quantify the burden of EHR work and to evaluate potential interventions to reduce this burden and subsequent burnout.”
Baxter’s health system allows physicians to bill for asynchronous messaging when certain eligibility criteria are met. “This can deter frivolous messaging and also provide some compensation for the work involved,” she said.
“In addition, we’ve recently piloted using AI tools to help draft replies to patient messages in the EHR as another approach to tackling this important issue,” said Baxter, who wasn’t involved with the current study.
Eve Rittenberg, MD, an assistant professor at Harvard Medical School and a PCP at Brigham and Women’s Hospital Fish Center for Women’s Health, in Boston, recommended that healthcare systems “monitor EHR workload across gender, specialty, and other variables to develop equitable support and compensation models.”
Dr. Rittenberg, who wasn’t involved with the current study, said healthcare systems should consider supporting physicians by blocking out time during clinic sessions to manage their EHR work. “Cross-coverage systems are vital so that on their days off, physicians can unplug from the computer and know that their patients’ needs are being met,” she added.
This work was supported in part by the AMA Practice Transformation Initiative: EHR-Use Metrics Research which provided grant funding to several of the authors. Sinsky is employed by the AMA. Dr. Arndt and coauthors disclosed no relevant financial information. Dr. Baxter received nonfinancial support from Optonmed and Topcon for research studies and collaborated with some of the study authors on other research but not this particular study. Dr. Rittenberg received internal funding from the Brigham Care Redesign Incubator and Startup Program, Brigham and Women’s Hospital, for a previous pilot project of inbasket cross-coverage. She had no relevant current disclosures.
A version of this article appeared on Medscape.com.
If you feel like the day doesn’t hold enough hours for you to get your work done, you’re right: (EHRs).
Investigators followed 141 academic PCPs between May 2019 and March 2023 and found they spent considerably more time engaging in EHR tasks during the final year of the study than in the prepandemic period. EHR time increased by over 8% on days with scheduled appointments and almost 20% on days without scheduled appointments.
“Physicians spend an unsustainable amount of time on EHR-based work, and that amount has increased steadily from 2019 to 2023,” Christine Sinsky, MD, vice president of professional satisfaction at the American Medical Association (AMA) and the senior author of the study, told this news organization. “It is imperative for healthcare systems to develop strategies to change the overall EHR workload trajectory to minimize PCPs’ occupational stress, including improved workflows, where the work is more appropriately distributed amongst the team.”
The study was published online on January 22, 2024, in the Annals of Family Medicine.
‘Pajama Time’
Dr. Sinsky said the motivation for conducting the current study was that PCPs have reported an increase in their workload, especially EHR tasks outside of work (“pajama time”) since the onset of the pandemic.
The research followed up on a 2017 analysis from the same group and other findings showing an increase in the time physicians spend in EHR tasks and the number of Inbox messages they receive from patients seeking medical advice increased during the months following the start of the pandemic.
“As a busy practicing PCP with a large panel of patients, my sense was that the workload was increasing even more, which is what our study confirmed,” said Brian G. Arndt, MD, of the Department of Family Medicine and Community Heath at the University of Wisconsin School of Medicine and Public Health, in Madison, Wisconsin, who led the new study.
The researchers analyzed EHR usage of 141 academic PCPs practicing family medicine, internal medicine, and general pediatrics, two thirds (66.7%) of whom were female. They compared the amount of time spent on EHR tasks during four timespans:
- May 2019 to February 2020
- June 2020 to March 2021
- May 2021 to March 2022
- April 2022 to March 2023
Each PCP’s time and Inbox message volume were calculated and then normalized over 8 hours of scheduled clinic appointments.
Increased Time, Increased Burnout
The study found evidence PCPs have reduced their clinical hours in response to their growing digital workload.
“We have a serious shortage of primary care physicians,” Dr. Sinsky said. “When PCPs cut back their clinical [work] as a coping mechanism for an unmanageable workload, this further exacerbates the primary care shortage, reducing access to care for patients.”
The researchers found increases from the first prepandemic period to the final period of their study in average time that PCPs spent at the EHR per 8 hours of scheduled clinic appointments (Table).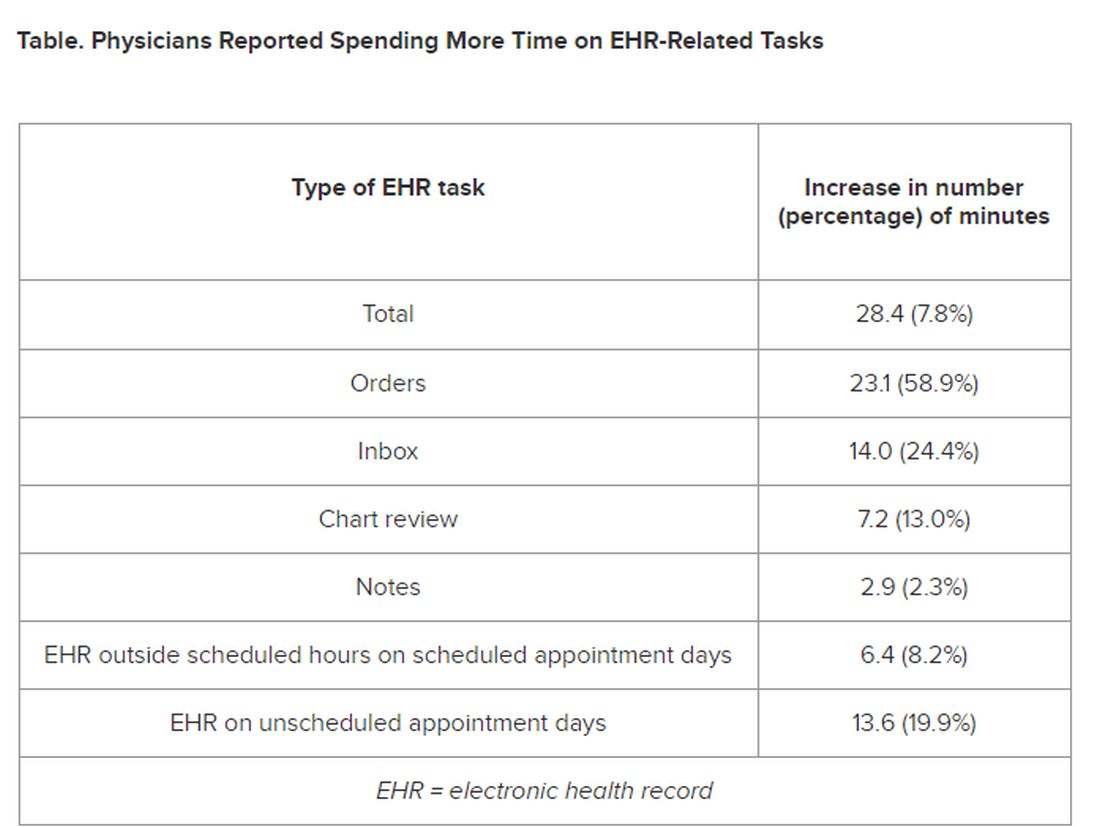
PCPs were inundated with several types of EHR-related responsibilities, including more medical advice requests (+55.5%) and more prescription messages (+19.5%) per 8 hours of scheduled clinic appointments. On the other hand, they had slightly fewer patient calls (−10.5%) and messages concerning test results (−2.7%).
A recent study of 307 PCPs across 31 primary care practices paralleled these findings. It found that physicians spent 36.2 minutes on the EHR per visit (interquartile range, 28.9-45.7 minutes). Included were 6.2 minutes of “pajama time” per visit and 7.8 minutes on the EHR per visit.
The amount of EHR time exceeded the amount of time allotted to a primary care visit (30 minutes). The authors commented that the EHR time burden “and the burnout associated with this burden represent a serious threat to the primary care physician workforce.”
“As more health systems across the country transition from fee-for-service to value-based payment arrangements, they need to balance the time PCPs and their care teams need for face-to-face care — in-person or video visits — with the increasing asynchronous care patients are seeking from us through the portal, for example, MyChart,” Dr. Arndt said.
Sinsky noted that when patients receive care from a PCP, quality is higher and costs are lower. “When access to primary care is further limited by virtue of physicians being overwhelmed by administrative work implemented via the EHR, so that they are reducing their hours, then we can expect negative consequences for patient care and costs of care.”
Tips for Reducing EHR Time
Arndt noted that some “brief investments” of time with patients “lead to high rates of return on decreased MyChart messaging.” For example, he has said to patients: “In the future, there’s no need to respond in MyChart with a ‘Thank you.’” Or “In the future, if you have questions from preappointment labs, no need to send me a separate message in MyChart prior to your visit since they’re typically just a few days out. I look closely at your labs and would always pick up the phone and call you if there was anything more urgent or pressing that needs more immediate action.”
Sinsky recommended two “high-yield opportunities” to reduce EHR-associated workload. The AMA offers a brief Inbox reduction checklist as well as a detailed toolkit to guide physicians and operational leaders in reducing the volume of unnecessary Inbox messages, she said.
Distribution of work among the team also can reduce the time physicians spent on order entry. “It doesn’t take a medical school education to enter orders for flu shots, lipid profiles, mammograms, and other tests, and yet we have primary care physicians around the country spending an hour or more per 8 hours of patient visits on this task,” she said.
‘Growing Mountain’
Sally Baxter, MD, assistant professor of ophthalmology and division chief for Ophthalmology Informatics and Data Sciences at University of California San Diego, said, “Studies like this ... are important for continuing to quantify the burden of EHR work and to evaluate potential interventions to reduce this burden and subsequent burnout.”
Baxter’s health system allows physicians to bill for asynchronous messaging when certain eligibility criteria are met. “This can deter frivolous messaging and also provide some compensation for the work involved,” she said.
“In addition, we’ve recently piloted using AI tools to help draft replies to patient messages in the EHR as another approach to tackling this important issue,” said Baxter, who wasn’t involved with the current study.
Eve Rittenberg, MD, an assistant professor at Harvard Medical School and a PCP at Brigham and Women’s Hospital Fish Center for Women’s Health, in Boston, recommended that healthcare systems “monitor EHR workload across gender, specialty, and other variables to develop equitable support and compensation models.”
Dr. Rittenberg, who wasn’t involved with the current study, said healthcare systems should consider supporting physicians by blocking out time during clinic sessions to manage their EHR work. “Cross-coverage systems are vital so that on their days off, physicians can unplug from the computer and know that their patients’ needs are being met,” she added.
This work was supported in part by the AMA Practice Transformation Initiative: EHR-Use Metrics Research which provided grant funding to several of the authors. Sinsky is employed by the AMA. Dr. Arndt and coauthors disclosed no relevant financial information. Dr. Baxter received nonfinancial support from Optonmed and Topcon for research studies and collaborated with some of the study authors on other research but not this particular study. Dr. Rittenberg received internal funding from the Brigham Care Redesign Incubator and Startup Program, Brigham and Women’s Hospital, for a previous pilot project of inbasket cross-coverage. She had no relevant current disclosures.
A version of this article appeared on Medscape.com.
If you feel like the day doesn’t hold enough hours for you to get your work done, you’re right: (EHRs).
Investigators followed 141 academic PCPs between May 2019 and March 2023 and found they spent considerably more time engaging in EHR tasks during the final year of the study than in the prepandemic period. EHR time increased by over 8% on days with scheduled appointments and almost 20% on days without scheduled appointments.
“Physicians spend an unsustainable amount of time on EHR-based work, and that amount has increased steadily from 2019 to 2023,” Christine Sinsky, MD, vice president of professional satisfaction at the American Medical Association (AMA) and the senior author of the study, told this news organization. “It is imperative for healthcare systems to develop strategies to change the overall EHR workload trajectory to minimize PCPs’ occupational stress, including improved workflows, where the work is more appropriately distributed amongst the team.”
The study was published online on January 22, 2024, in the Annals of Family Medicine.
‘Pajama Time’
Dr. Sinsky said the motivation for conducting the current study was that PCPs have reported an increase in their workload, especially EHR tasks outside of work (“pajama time”) since the onset of the pandemic.
The research followed up on a 2017 analysis from the same group and other findings showing an increase in the time physicians spend in EHR tasks and the number of Inbox messages they receive from patients seeking medical advice increased during the months following the start of the pandemic.
“As a busy practicing PCP with a large panel of patients, my sense was that the workload was increasing even more, which is what our study confirmed,” said Brian G. Arndt, MD, of the Department of Family Medicine and Community Heath at the University of Wisconsin School of Medicine and Public Health, in Madison, Wisconsin, who led the new study.
The researchers analyzed EHR usage of 141 academic PCPs practicing family medicine, internal medicine, and general pediatrics, two thirds (66.7%) of whom were female. They compared the amount of time spent on EHR tasks during four timespans:
- May 2019 to February 2020
- June 2020 to March 2021
- May 2021 to March 2022
- April 2022 to March 2023
Each PCP’s time and Inbox message volume were calculated and then normalized over 8 hours of scheduled clinic appointments.
Increased Time, Increased Burnout
The study found evidence PCPs have reduced their clinical hours in response to their growing digital workload.
“We have a serious shortage of primary care physicians,” Dr. Sinsky said. “When PCPs cut back their clinical [work] as a coping mechanism for an unmanageable workload, this further exacerbates the primary care shortage, reducing access to care for patients.”
The researchers found increases from the first prepandemic period to the final period of their study in average time that PCPs spent at the EHR per 8 hours of scheduled clinic appointments (Table).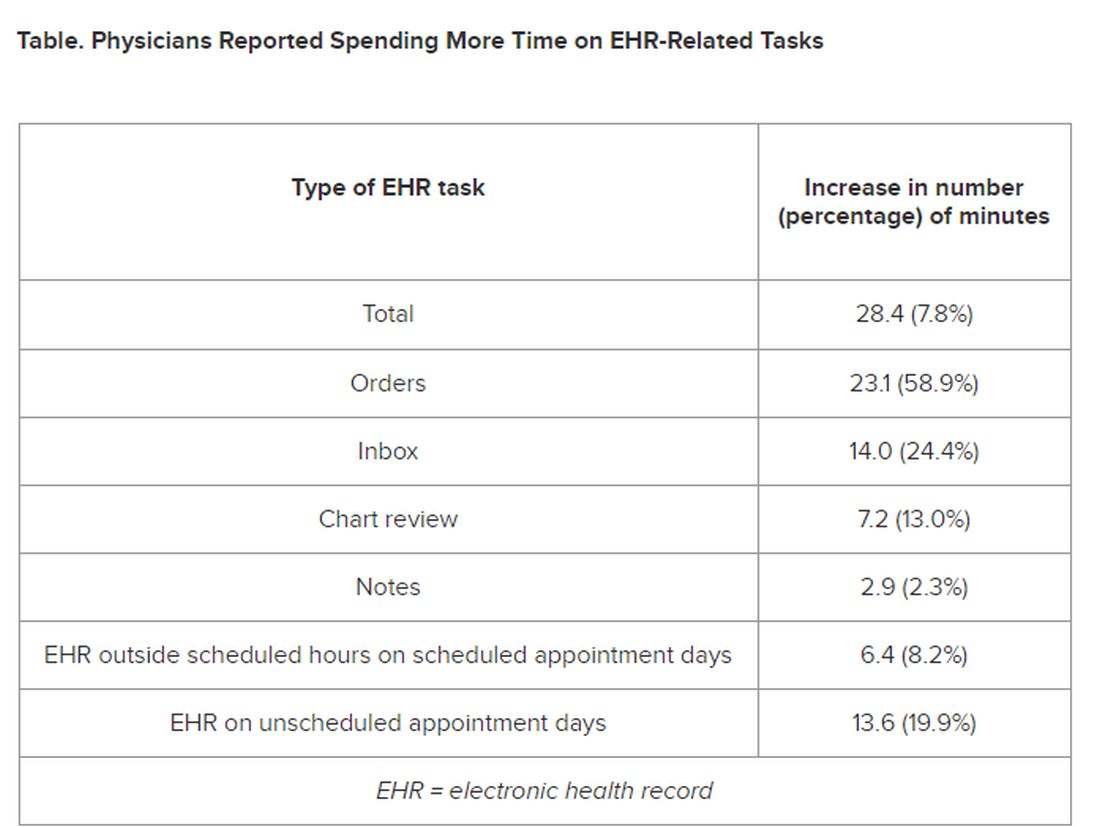
PCPs were inundated with several types of EHR-related responsibilities, including more medical advice requests (+55.5%) and more prescription messages (+19.5%) per 8 hours of scheduled clinic appointments. On the other hand, they had slightly fewer patient calls (−10.5%) and messages concerning test results (−2.7%).
A recent study of 307 PCPs across 31 primary care practices paralleled these findings. It found that physicians spent 36.2 minutes on the EHR per visit (interquartile range, 28.9-45.7 minutes). Included were 6.2 minutes of “pajama time” per visit and 7.8 minutes on the EHR per visit.
The amount of EHR time exceeded the amount of time allotted to a primary care visit (30 minutes). The authors commented that the EHR time burden “and the burnout associated with this burden represent a serious threat to the primary care physician workforce.”
“As more health systems across the country transition from fee-for-service to value-based payment arrangements, they need to balance the time PCPs and their care teams need for face-to-face care — in-person or video visits — with the increasing asynchronous care patients are seeking from us through the portal, for example, MyChart,” Dr. Arndt said.
Sinsky noted that when patients receive care from a PCP, quality is higher and costs are lower. “When access to primary care is further limited by virtue of physicians being overwhelmed by administrative work implemented via the EHR, so that they are reducing their hours, then we can expect negative consequences for patient care and costs of care.”
Tips for Reducing EHR Time
Arndt noted that some “brief investments” of time with patients “lead to high rates of return on decreased MyChart messaging.” For example, he has said to patients: “In the future, there’s no need to respond in MyChart with a ‘Thank you.’” Or “In the future, if you have questions from preappointment labs, no need to send me a separate message in MyChart prior to your visit since they’re typically just a few days out. I look closely at your labs and would always pick up the phone and call you if there was anything more urgent or pressing that needs more immediate action.”
Sinsky recommended two “high-yield opportunities” to reduce EHR-associated workload. The AMA offers a brief Inbox reduction checklist as well as a detailed toolkit to guide physicians and operational leaders in reducing the volume of unnecessary Inbox messages, she said.
Distribution of work among the team also can reduce the time physicians spent on order entry. “It doesn’t take a medical school education to enter orders for flu shots, lipid profiles, mammograms, and other tests, and yet we have primary care physicians around the country spending an hour or more per 8 hours of patient visits on this task,” she said.
‘Growing Mountain’
Sally Baxter, MD, assistant professor of ophthalmology and division chief for Ophthalmology Informatics and Data Sciences at University of California San Diego, said, “Studies like this ... are important for continuing to quantify the burden of EHR work and to evaluate potential interventions to reduce this burden and subsequent burnout.”
Baxter’s health system allows physicians to bill for asynchronous messaging when certain eligibility criteria are met. “This can deter frivolous messaging and also provide some compensation for the work involved,” she said.
“In addition, we’ve recently piloted using AI tools to help draft replies to patient messages in the EHR as another approach to tackling this important issue,” said Baxter, who wasn’t involved with the current study.
Eve Rittenberg, MD, an assistant professor at Harvard Medical School and a PCP at Brigham and Women’s Hospital Fish Center for Women’s Health, in Boston, recommended that healthcare systems “monitor EHR workload across gender, specialty, and other variables to develop equitable support and compensation models.”
Dr. Rittenberg, who wasn’t involved with the current study, said healthcare systems should consider supporting physicians by blocking out time during clinic sessions to manage their EHR work. “Cross-coverage systems are vital so that on their days off, physicians can unplug from the computer and know that their patients’ needs are being met,” she added.
This work was supported in part by the AMA Practice Transformation Initiative: EHR-Use Metrics Research which provided grant funding to several of the authors. Sinsky is employed by the AMA. Dr. Arndt and coauthors disclosed no relevant financial information. Dr. Baxter received nonfinancial support from Optonmed and Topcon for research studies and collaborated with some of the study authors on other research but not this particular study. Dr. Rittenberg received internal funding from the Brigham Care Redesign Incubator and Startup Program, Brigham and Women’s Hospital, for a previous pilot project of inbasket cross-coverage. She had no relevant current disclosures.
A version of this article appeared on Medscape.com.
Robotic Garment Improves Stride in Patient With Parkinson’s Disease
A wearable, soft, robotic device could help patients with Parkinson’s disease (PD) walk without experiencing freezing of gait (FoG), early research suggested.
The robotic apparel, worn around the hips and thighs, gently pushes the hips as the leg swings, facilitating a longer stride and preventing FoG, a common disorder in PD that affects nearly all patients over the disease course.
The small, proof-of-concept study included one person with PD. But investigators noted the reduction in freezing and falls and improvement in walking distance and speed was dramatic. Incidence of FoG decreased from 63% to just 6% when the patient wore the robotic garment outdoors. Wearing the device indoors eliminated freezing altogether.
“We demonstrate proof-of-concept that FoG can be averted using a soft robotic device — a machine that aims to apply physical assistance to movement with minimal restriction, a fundamentally different approach to rigid exoskeletons,” lead investigators Conor Walsh, PhD, and Terry Ellis, PhD, PT, told this news organization.
Walsh is a professor at Harvard John A. Paulson School of Engineering and Applied Sciences in Boston, and Ellis is a professor and chair of the physical therapy department and director of the Center for Neurorehabilitation, Boston University, Boston, Massachusetts.
The study was published online on January 5, 2024, in Nature Medicine.
Disabling Disturbance
From a biomechanical perspective, FoG is manifested by an overt breakdown in spatial and temporal mechanics of walking. The impaired limb coordination occurs during the “swing phase” of the gait cycle.
There are currently no interventions that prevent FoG. Available treatment interventions include pharmacotherapy, such as dopamine replacement; deep brain stimulation (DBS) of the subthalamic nucleus; and behavioral interventions, such as cueing strategies. All have shown only modest effects in reducing FoG and, in some cases, might even worsen it, the investigators noted.
“This challenge led us to become interested in leveraging soft wearable robots to deliver mechanical cues to disrupt aberrant gait mechanics and prevent FOG in people with PD,” Dr. Walsh and Dr. Ellis said.
“Wearable robots” have been used to augment kinematics in neurologic conditions, such as stroke, cerebral palsy, and spinal cord injury. Harnessing this technology to address FoG required “a collaboration between engineers, rehabilitation scientists, physical therapists, biomechanists, and apparel designers,” the researchers said.
The wearable robotic device uses cable-driven actuators, which enable physical movement by converting electrical energy into mechanical force, and sensors worn around the waist and thighs. Using motion data collected by the sensors, algorithms estimate the phase of the walking cycle and generate assistive forces in concert with biological muscles.
Real-World Testing
The researchers tested the robotic garment on a 73-year-old man with idiopathic PD of 10-year duration. The man’s ongoing pharmacologic treatment included 1.5 tablets of 25- to 100-mg carbidopa/levodopa taken four times per day, one tablet of 100-mg amantadine twice per day, and one tablet of 200-mg entacapone taken four times per day.
He had also undergone DBS to the globus pallidus internus and utilized behavioral strategies. Despite these interventions, he continued to endure more than 10 episodes of FoG per day and numerous falls.
The patient tended to use walls to stabilize himself when walking. Freezing episodes were observed mostly when he walked in open hallways, turned, walked outdoors, and when he tried to walk and talk simultaneously.
The research was conducted over a 6-month period, with a total of five study sessions that consisted of walking trials. Four were administered in the laboratory. The fifth was conducted in a real-world outdoor community setting.
During the first visit, a biomechanical analysis of walking was performed under single-task conditions during the medication-on phase.
Testing was usually conducted during medication-on phase and under single-task conditions. But testing conditions also included attention-demanding dual tasks and single-task walking during the medication-off phase.
The researchers compared the effects of the assistance of the robotic apparel to no apparel and with the apparel turned off. They measured the percentage of time spent freezing and the total distance walked.
Robust Response
The participant demonstrated a “robust response” to the robotic apparel. With the garment’s assistance, FoG was eliminated when worn indoors, and walking distance increased by 55%. The participant walked faster and had a 25% reduction in gait variability.
These beneficial effects were repeated across multiple days as well as different types of provoking conditions and environmental contexts. When the device was tried outdoors, FoG decreased from 63% to 6% of the time. The patient was also able to simultaneously walk and talk without freezing.
“When the device assisted with hip flexion during the terminal stance phase of walking (when lifting the toe), FoG was instantaneously eliminated during inner walking, accompanied by clinically significant improvement in walking speeds and distance,” Dr. Walsh and Dr. Ellis reported.
The approach “suggests the potential benefits of a ‘bottom-up’ rather than a ‘top-down’ solution to treating gait freezing,” they commented. “We see that restoring almost-normal biomechanics alters the peripheral dynamics of gait and may influence the central processing of gait control.”
Bringing Hope
Rebecca Gilbert MD, PhD, chief mission officer, American Parkinson Disease Association, said this new approach is “exciting.”
Whether the benefits will be as robust in other people with PD “remains to be seen,” said Dr. Gilbert, who was not involved with the study.
“The paper states that multiple experimental variables utilizing the device could potentially be adjusted to serve different people with PD, and these will need to be tested in clinical trials as well,” Dr. Gilbert said.
Additionally, “the device itself is complex and may be challenging to get on and off without help, which may limit its usability in the community,” Dr. Gilbert noted.
Although more work is needed, the study “represents a remarkable proof of concept that brings hope to those with FoG,” she added.
These “promising findings prompt further investigation to validate the effects of the robotic apparel on a broader range of individuals with PD experiencing FoG and across various FoG phenotypes and environments and task contexts, complemented with FoG metrics that include quantification of the severity of the freezing episodes,” Walsh and Ellis added.
This study was based on work supported by the National Science Foundation, the National Institutes of Health, and the Massachusetts Technology Collaborative, Collaborative Research and Development Matching Grant. This work was also partially funded by the John A. Paulson School of Engineering and Applied Sciences at Harvard University as well as received financial support from the Samsung Scholarship.
A version of this article appeared on Medscape.com.
A wearable, soft, robotic device could help patients with Parkinson’s disease (PD) walk without experiencing freezing of gait (FoG), early research suggested.
The robotic apparel, worn around the hips and thighs, gently pushes the hips as the leg swings, facilitating a longer stride and preventing FoG, a common disorder in PD that affects nearly all patients over the disease course.
The small, proof-of-concept study included one person with PD. But investigators noted the reduction in freezing and falls and improvement in walking distance and speed was dramatic. Incidence of FoG decreased from 63% to just 6% when the patient wore the robotic garment outdoors. Wearing the device indoors eliminated freezing altogether.
“We demonstrate proof-of-concept that FoG can be averted using a soft robotic device — a machine that aims to apply physical assistance to movement with minimal restriction, a fundamentally different approach to rigid exoskeletons,” lead investigators Conor Walsh, PhD, and Terry Ellis, PhD, PT, told this news organization.
Walsh is a professor at Harvard John A. Paulson School of Engineering and Applied Sciences in Boston, and Ellis is a professor and chair of the physical therapy department and director of the Center for Neurorehabilitation, Boston University, Boston, Massachusetts.
The study was published online on January 5, 2024, in Nature Medicine.
Disabling Disturbance
From a biomechanical perspective, FoG is manifested by an overt breakdown in spatial and temporal mechanics of walking. The impaired limb coordination occurs during the “swing phase” of the gait cycle.
There are currently no interventions that prevent FoG. Available treatment interventions include pharmacotherapy, such as dopamine replacement; deep brain stimulation (DBS) of the subthalamic nucleus; and behavioral interventions, such as cueing strategies. All have shown only modest effects in reducing FoG and, in some cases, might even worsen it, the investigators noted.
“This challenge led us to become interested in leveraging soft wearable robots to deliver mechanical cues to disrupt aberrant gait mechanics and prevent FOG in people with PD,” Dr. Walsh and Dr. Ellis said.
“Wearable robots” have been used to augment kinematics in neurologic conditions, such as stroke, cerebral palsy, and spinal cord injury. Harnessing this technology to address FoG required “a collaboration between engineers, rehabilitation scientists, physical therapists, biomechanists, and apparel designers,” the researchers said.
The wearable robotic device uses cable-driven actuators, which enable physical movement by converting electrical energy into mechanical force, and sensors worn around the waist and thighs. Using motion data collected by the sensors, algorithms estimate the phase of the walking cycle and generate assistive forces in concert with biological muscles.
Real-World Testing
The researchers tested the robotic garment on a 73-year-old man with idiopathic PD of 10-year duration. The man’s ongoing pharmacologic treatment included 1.5 tablets of 25- to 100-mg carbidopa/levodopa taken four times per day, one tablet of 100-mg amantadine twice per day, and one tablet of 200-mg entacapone taken four times per day.
He had also undergone DBS to the globus pallidus internus and utilized behavioral strategies. Despite these interventions, he continued to endure more than 10 episodes of FoG per day and numerous falls.
The patient tended to use walls to stabilize himself when walking. Freezing episodes were observed mostly when he walked in open hallways, turned, walked outdoors, and when he tried to walk and talk simultaneously.
The research was conducted over a 6-month period, with a total of five study sessions that consisted of walking trials. Four were administered in the laboratory. The fifth was conducted in a real-world outdoor community setting.
During the first visit, a biomechanical analysis of walking was performed under single-task conditions during the medication-on phase.
Testing was usually conducted during medication-on phase and under single-task conditions. But testing conditions also included attention-demanding dual tasks and single-task walking during the medication-off phase.
The researchers compared the effects of the assistance of the robotic apparel to no apparel and with the apparel turned off. They measured the percentage of time spent freezing and the total distance walked.
Robust Response
The participant demonstrated a “robust response” to the robotic apparel. With the garment’s assistance, FoG was eliminated when worn indoors, and walking distance increased by 55%. The participant walked faster and had a 25% reduction in gait variability.
These beneficial effects were repeated across multiple days as well as different types of provoking conditions and environmental contexts. When the device was tried outdoors, FoG decreased from 63% to 6% of the time. The patient was also able to simultaneously walk and talk without freezing.
“When the device assisted with hip flexion during the terminal stance phase of walking (when lifting the toe), FoG was instantaneously eliminated during inner walking, accompanied by clinically significant improvement in walking speeds and distance,” Dr. Walsh and Dr. Ellis reported.
The approach “suggests the potential benefits of a ‘bottom-up’ rather than a ‘top-down’ solution to treating gait freezing,” they commented. “We see that restoring almost-normal biomechanics alters the peripheral dynamics of gait and may influence the central processing of gait control.”
Bringing Hope
Rebecca Gilbert MD, PhD, chief mission officer, American Parkinson Disease Association, said this new approach is “exciting.”
Whether the benefits will be as robust in other people with PD “remains to be seen,” said Dr. Gilbert, who was not involved with the study.
“The paper states that multiple experimental variables utilizing the device could potentially be adjusted to serve different people with PD, and these will need to be tested in clinical trials as well,” Dr. Gilbert said.
Additionally, “the device itself is complex and may be challenging to get on and off without help, which may limit its usability in the community,” Dr. Gilbert noted.
Although more work is needed, the study “represents a remarkable proof of concept that brings hope to those with FoG,” she added.
These “promising findings prompt further investigation to validate the effects of the robotic apparel on a broader range of individuals with PD experiencing FoG and across various FoG phenotypes and environments and task contexts, complemented with FoG metrics that include quantification of the severity of the freezing episodes,” Walsh and Ellis added.
This study was based on work supported by the National Science Foundation, the National Institutes of Health, and the Massachusetts Technology Collaborative, Collaborative Research and Development Matching Grant. This work was also partially funded by the John A. Paulson School of Engineering and Applied Sciences at Harvard University as well as received financial support from the Samsung Scholarship.
A version of this article appeared on Medscape.com.
A wearable, soft, robotic device could help patients with Parkinson’s disease (PD) walk without experiencing freezing of gait (FoG), early research suggested.
The robotic apparel, worn around the hips and thighs, gently pushes the hips as the leg swings, facilitating a longer stride and preventing FoG, a common disorder in PD that affects nearly all patients over the disease course.
The small, proof-of-concept study included one person with PD. But investigators noted the reduction in freezing and falls and improvement in walking distance and speed was dramatic. Incidence of FoG decreased from 63% to just 6% when the patient wore the robotic garment outdoors. Wearing the device indoors eliminated freezing altogether.
“We demonstrate proof-of-concept that FoG can be averted using a soft robotic device — a machine that aims to apply physical assistance to movement with minimal restriction, a fundamentally different approach to rigid exoskeletons,” lead investigators Conor Walsh, PhD, and Terry Ellis, PhD, PT, told this news organization.
Walsh is a professor at Harvard John A. Paulson School of Engineering and Applied Sciences in Boston, and Ellis is a professor and chair of the physical therapy department and director of the Center for Neurorehabilitation, Boston University, Boston, Massachusetts.
The study was published online on January 5, 2024, in Nature Medicine.
Disabling Disturbance
From a biomechanical perspective, FoG is manifested by an overt breakdown in spatial and temporal mechanics of walking. The impaired limb coordination occurs during the “swing phase” of the gait cycle.
There are currently no interventions that prevent FoG. Available treatment interventions include pharmacotherapy, such as dopamine replacement; deep brain stimulation (DBS) of the subthalamic nucleus; and behavioral interventions, such as cueing strategies. All have shown only modest effects in reducing FoG and, in some cases, might even worsen it, the investigators noted.
“This challenge led us to become interested in leveraging soft wearable robots to deliver mechanical cues to disrupt aberrant gait mechanics and prevent FOG in people with PD,” Dr. Walsh and Dr. Ellis said.
“Wearable robots” have been used to augment kinematics in neurologic conditions, such as stroke, cerebral palsy, and spinal cord injury. Harnessing this technology to address FoG required “a collaboration between engineers, rehabilitation scientists, physical therapists, biomechanists, and apparel designers,” the researchers said.
The wearable robotic device uses cable-driven actuators, which enable physical movement by converting electrical energy into mechanical force, and sensors worn around the waist and thighs. Using motion data collected by the sensors, algorithms estimate the phase of the walking cycle and generate assistive forces in concert with biological muscles.
Real-World Testing
The researchers tested the robotic garment on a 73-year-old man with idiopathic PD of 10-year duration. The man’s ongoing pharmacologic treatment included 1.5 tablets of 25- to 100-mg carbidopa/levodopa taken four times per day, one tablet of 100-mg amantadine twice per day, and one tablet of 200-mg entacapone taken four times per day.
He had also undergone DBS to the globus pallidus internus and utilized behavioral strategies. Despite these interventions, he continued to endure more than 10 episodes of FoG per day and numerous falls.
The patient tended to use walls to stabilize himself when walking. Freezing episodes were observed mostly when he walked in open hallways, turned, walked outdoors, and when he tried to walk and talk simultaneously.
The research was conducted over a 6-month period, with a total of five study sessions that consisted of walking trials. Four were administered in the laboratory. The fifth was conducted in a real-world outdoor community setting.
During the first visit, a biomechanical analysis of walking was performed under single-task conditions during the medication-on phase.
Testing was usually conducted during medication-on phase and under single-task conditions. But testing conditions also included attention-demanding dual tasks and single-task walking during the medication-off phase.
The researchers compared the effects of the assistance of the robotic apparel to no apparel and with the apparel turned off. They measured the percentage of time spent freezing and the total distance walked.
Robust Response
The participant demonstrated a “robust response” to the robotic apparel. With the garment’s assistance, FoG was eliminated when worn indoors, and walking distance increased by 55%. The participant walked faster and had a 25% reduction in gait variability.
These beneficial effects were repeated across multiple days as well as different types of provoking conditions and environmental contexts. When the device was tried outdoors, FoG decreased from 63% to 6% of the time. The patient was also able to simultaneously walk and talk without freezing.
“When the device assisted with hip flexion during the terminal stance phase of walking (when lifting the toe), FoG was instantaneously eliminated during inner walking, accompanied by clinically significant improvement in walking speeds and distance,” Dr. Walsh and Dr. Ellis reported.
The approach “suggests the potential benefits of a ‘bottom-up’ rather than a ‘top-down’ solution to treating gait freezing,” they commented. “We see that restoring almost-normal biomechanics alters the peripheral dynamics of gait and may influence the central processing of gait control.”
Bringing Hope
Rebecca Gilbert MD, PhD, chief mission officer, American Parkinson Disease Association, said this new approach is “exciting.”
Whether the benefits will be as robust in other people with PD “remains to be seen,” said Dr. Gilbert, who was not involved with the study.
“The paper states that multiple experimental variables utilizing the device could potentially be adjusted to serve different people with PD, and these will need to be tested in clinical trials as well,” Dr. Gilbert said.
Additionally, “the device itself is complex and may be challenging to get on and off without help, which may limit its usability in the community,” Dr. Gilbert noted.
Although more work is needed, the study “represents a remarkable proof of concept that brings hope to those with FoG,” she added.
These “promising findings prompt further investigation to validate the effects of the robotic apparel on a broader range of individuals with PD experiencing FoG and across various FoG phenotypes and environments and task contexts, complemented with FoG metrics that include quantification of the severity of the freezing episodes,” Walsh and Ellis added.
This study was based on work supported by the National Science Foundation, the National Institutes of Health, and the Massachusetts Technology Collaborative, Collaborative Research and Development Matching Grant. This work was also partially funded by the John A. Paulson School of Engineering and Applied Sciences at Harvard University as well as received financial support from the Samsung Scholarship.
A version of this article appeared on Medscape.com.