User login
VIDEO: Routine hysteroscopy found unnecessary after multiple miscarriages
MUNICH – Routinely performed hysteroscopy proved unable to increase the live-birth rate from in vitro fertilization in women who had two to four prior miscarriages after in vitro fertilization, according to results from a multicenter, controlled trial of 656 women.
Based on these findings, hysteroscopy should be limited to women with either a clinical indication or evidence of a uterine abnormality seen on transvaginal ultrasonography. Clinicians should not perform hysteroscopy in all women with a miscarriage history unless they have a reason to suspect that such an abnormality exists, said Dr. Tarek El-Toukhy in a video interview during the annual meeting of the European Society of Human Reproduction and Embryology.
Prior to this trial, some experts had hope that routine hysteroscopy could boost the live-birth rate following in vitro fertilization by 20%, 30%, or more, said Dr. El-Toukhy, a gynecologist at Guy’s and St. Thomas’ Hospital in London. But the finding that routine hysteroscopy failed to provide any benefit suggested that embryonic factors are more important than uterine factors for explaining the serial miscarriages in these women who have no clinical or ultrasound indication of a uterine problem.
Karl Storz supplied the hysteroscopy devices used in the study and training in their use. Dr. El-Toukhy said that he and his associates had no other disclosures.
On Twitter @mitchelzoler
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MUNICH – Routinely performed hysteroscopy proved unable to increase the live-birth rate from in vitro fertilization in women who had two to four prior miscarriages after in vitro fertilization, according to results from a multicenter, controlled trial of 656 women.
Based on these findings, hysteroscopy should be limited to women with either a clinical indication or evidence of a uterine abnormality seen on transvaginal ultrasonography. Clinicians should not perform hysteroscopy in all women with a miscarriage history unless they have a reason to suspect that such an abnormality exists, said Dr. Tarek El-Toukhy in a video interview during the annual meeting of the European Society of Human Reproduction and Embryology.
Prior to this trial, some experts had hope that routine hysteroscopy could boost the live-birth rate following in vitro fertilization by 20%, 30%, or more, said Dr. El-Toukhy, a gynecologist at Guy’s and St. Thomas’ Hospital in London. But the finding that routine hysteroscopy failed to provide any benefit suggested that embryonic factors are more important than uterine factors for explaining the serial miscarriages in these women who have no clinical or ultrasound indication of a uterine problem.
Karl Storz supplied the hysteroscopy devices used in the study and training in their use. Dr. El-Toukhy said that he and his associates had no other disclosures.
On Twitter @mitchelzoler
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MUNICH – Routinely performed hysteroscopy proved unable to increase the live-birth rate from in vitro fertilization in women who had two to four prior miscarriages after in vitro fertilization, according to results from a multicenter, controlled trial of 656 women.
Based on these findings, hysteroscopy should be limited to women with either a clinical indication or evidence of a uterine abnormality seen on transvaginal ultrasonography. Clinicians should not perform hysteroscopy in all women with a miscarriage history unless they have a reason to suspect that such an abnormality exists, said Dr. Tarek El-Toukhy in a video interview during the annual meeting of the European Society of Human Reproduction and Embryology.
Prior to this trial, some experts had hope that routine hysteroscopy could boost the live-birth rate following in vitro fertilization by 20%, 30%, or more, said Dr. El-Toukhy, a gynecologist at Guy’s and St. Thomas’ Hospital in London. But the finding that routine hysteroscopy failed to provide any benefit suggested that embryonic factors are more important than uterine factors for explaining the serial miscarriages in these women who have no clinical or ultrasound indication of a uterine problem.
Karl Storz supplied the hysteroscopy devices used in the study and training in their use. Dr. El-Toukhy said that he and his associates had no other disclosures.
On Twitter @mitchelzoler
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ESHRE 2014
VIDEO: Routine hysteroscopy found unnecessary after multiple miscarriages
MUNICH – Routinely performed hysteroscopy proved unable to increase the live-birth rate from in vitro fertilization in women who had two to four prior miscarriages after in vitro fertilization, according to results from a multicenter, controlled trial of 656 women.
Based on these findings, hysteroscopy should be limited to women with either a clinical indication or evidence of a uterine abnormality seen on transvaginal ultrasonography. Clinicians should not perform hysteroscopy in all women with a miscarriage history unless they have a reason to suspect that such an abnormality exists, said Dr. Tarek El-Toukhy in a video interview during the annual meeting of the European Society of Human Reproduction and Embryology.
Prior to this trial, some experts had hope that routine hysteroscopy could boost the live-birth rate following in vitro fertilization by 20%, 30%, or more, said Dr. El-Toukhy, a gynecologist at Guy’s and St. Thomas’ Hospital in London. But the finding that routine hysteroscopy failed to provide any benefit suggested that embryonic factors are more important than uterine factors for explaining the serial miscarriages in these women who have no clinical or ultrasound indication of a uterine problem.
Karl Storz supplied the hysteroscopy devices used in the study and training in their use. Dr. El-Toukhy said that he and his associates had no other disclosures.
On Twitter @mitchelzoler
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MUNICH – Routinely performed hysteroscopy proved unable to increase the live-birth rate from in vitro fertilization in women who had two to four prior miscarriages after in vitro fertilization, according to results from a multicenter, controlled trial of 656 women.
Based on these findings, hysteroscopy should be limited to women with either a clinical indication or evidence of a uterine abnormality seen on transvaginal ultrasonography. Clinicians should not perform hysteroscopy in all women with a miscarriage history unless they have a reason to suspect that such an abnormality exists, said Dr. Tarek El-Toukhy in a video interview during the annual meeting of the European Society of Human Reproduction and Embryology.
Prior to this trial, some experts had hope that routine hysteroscopy could boost the live-birth rate following in vitro fertilization by 20%, 30%, or more, said Dr. El-Toukhy, a gynecologist at Guy’s and St. Thomas’ Hospital in London. But the finding that routine hysteroscopy failed to provide any benefit suggested that embryonic factors are more important than uterine factors for explaining the serial miscarriages in these women who have no clinical or ultrasound indication of a uterine problem.
Karl Storz supplied the hysteroscopy devices used in the study and training in their use. Dr. El-Toukhy said that he and his associates had no other disclosures.
On Twitter @mitchelzoler
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MUNICH – Routinely performed hysteroscopy proved unable to increase the live-birth rate from in vitro fertilization in women who had two to four prior miscarriages after in vitro fertilization, according to results from a multicenter, controlled trial of 656 women.
Based on these findings, hysteroscopy should be limited to women with either a clinical indication or evidence of a uterine abnormality seen on transvaginal ultrasonography. Clinicians should not perform hysteroscopy in all women with a miscarriage history unless they have a reason to suspect that such an abnormality exists, said Dr. Tarek El-Toukhy in a video interview during the annual meeting of the European Society of Human Reproduction and Embryology.
Prior to this trial, some experts had hope that routine hysteroscopy could boost the live-birth rate following in vitro fertilization by 20%, 30%, or more, said Dr. El-Toukhy, a gynecologist at Guy’s and St. Thomas’ Hospital in London. But the finding that routine hysteroscopy failed to provide any benefit suggested that embryonic factors are more important than uterine factors for explaining the serial miscarriages in these women who have no clinical or ultrasound indication of a uterine problem.
Karl Storz supplied the hysteroscopy devices used in the study and training in their use. Dr. El-Toukhy said that he and his associates had no other disclosures.
On Twitter @mitchelzoler
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ESHRE 2014
VIDEO: Use late-night salivary cortisol to catch recurrent Cushing’s
CHICAGO – Late-night salivary cortisol exceeded normal limits in 10 women with recurrent Cushing’s disease a mean of 3.5 years after transsphenoidal surgery, but their urinary free cortisol remained in normal limits, according to a retrospective review from the Medical College of Wisconsin, Milwaukee.
That adds strength to the notion that late-night salivary cortisol (LNSC) catches recurrent Cushing’s that’s missed by urinary free cortisol, even though UFC remains a standard screening approach in some places.
The study is tiny and retrospective, but at the joint meeting of the International Congress of Endocrinology and the Endocrine Society, lead investigator Dr. Ty Carroll explained why the findings still matter, and also why two LNSC measurements are better than one.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Late-night salivary cortisol exceeded normal limits in 10 women with recurrent Cushing’s disease a mean of 3.5 years after transsphenoidal surgery, but their urinary free cortisol remained in normal limits, according to a retrospective review from the Medical College of Wisconsin, Milwaukee.
That adds strength to the notion that late-night salivary cortisol (LNSC) catches recurrent Cushing’s that’s missed by urinary free cortisol, even though UFC remains a standard screening approach in some places.
The study is tiny and retrospective, but at the joint meeting of the International Congress of Endocrinology and the Endocrine Society, lead investigator Dr. Ty Carroll explained why the findings still matter, and also why two LNSC measurements are better than one.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Late-night salivary cortisol exceeded normal limits in 10 women with recurrent Cushing’s disease a mean of 3.5 years after transsphenoidal surgery, but their urinary free cortisol remained in normal limits, according to a retrospective review from the Medical College of Wisconsin, Milwaukee.
That adds strength to the notion that late-night salivary cortisol (LNSC) catches recurrent Cushing’s that’s missed by urinary free cortisol, even though UFC remains a standard screening approach in some places.
The study is tiny and retrospective, but at the joint meeting of the International Congress of Endocrinology and the Endocrine Society, lead investigator Dr. Ty Carroll explained why the findings still matter, and also why two LNSC measurements are better than one.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ICE/ENDO 2014
VIDEO: Use late-night salivary cortisol to catch recurrent Cushing’s
CHICAGO – Late-night salivary cortisol exceeded normal limits in 10 women with recurrent Cushing’s disease a mean of 3.5 years after transsphenoidal surgery, but their urinary free cortisol remained in normal limits, according to a retrospective review from the Medical College of Wisconsin, Milwaukee.
That adds strength to the notion that late-night salivary cortisol (LNSC) catches recurrent Cushing’s that’s missed by urinary free cortisol, even though UFC remains a standard screening approach in some places.
The study is tiny and retrospective, but at the joint meeting of the International Congress of Endocrinology and the Endocrine Society, lead investigator Dr. Ty Carroll explained why the findings still matter, and also why two LNSC measurements are better than one.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Late-night salivary cortisol exceeded normal limits in 10 women with recurrent Cushing’s disease a mean of 3.5 years after transsphenoidal surgery, but their urinary free cortisol remained in normal limits, according to a retrospective review from the Medical College of Wisconsin, Milwaukee.
That adds strength to the notion that late-night salivary cortisol (LNSC) catches recurrent Cushing’s that’s missed by urinary free cortisol, even though UFC remains a standard screening approach in some places.
The study is tiny and retrospective, but at the joint meeting of the International Congress of Endocrinology and the Endocrine Society, lead investigator Dr. Ty Carroll explained why the findings still matter, and also why two LNSC measurements are better than one.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Late-night salivary cortisol exceeded normal limits in 10 women with recurrent Cushing’s disease a mean of 3.5 years after transsphenoidal surgery, but their urinary free cortisol remained in normal limits, according to a retrospective review from the Medical College of Wisconsin, Milwaukee.
That adds strength to the notion that late-night salivary cortisol (LNSC) catches recurrent Cushing’s that’s missed by urinary free cortisol, even though UFC remains a standard screening approach in some places.
The study is tiny and retrospective, but at the joint meeting of the International Congress of Endocrinology and the Endocrine Society, lead investigator Dr. Ty Carroll explained why the findings still matter, and also why two LNSC measurements are better than one.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ICE/ENDO 2014
VIDEO: Kisspeptin outperforms HCG for early miscarriage prediction
CHICAGO – A one-time measurement of plasma kisspeptin – a family of placental peptides also being studied for fertility treatment – better predicts miscarriage than does serial measurement of human chorionic gonadotropin (HCG), a widely used measure.
British researchers measured both in 993 asymptomatic women at approximately 11 weeks’ gestation, 50 of whom later miscarried. Plasma kisspeptin proved a more accurate predictor of miscarriage than HCG: the area under the receiver operating characteristic (ROC) curve for plasma kisspeptin was 0.899, compared with 0.775 for serum HCG. Plasma kisspeptin above 1,306 pmol/L was associated with a highly significant 87% reduced risk of miscarriage, even after adjusting for age, body mass index, gestational age, smoking, and blood pressure.
Lead investigator Dr. Ali Abbara of Imperial College London explained why that matters at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – A one-time measurement of plasma kisspeptin – a family of placental peptides also being studied for fertility treatment – better predicts miscarriage than does serial measurement of human chorionic gonadotropin (HCG), a widely used measure.
British researchers measured both in 993 asymptomatic women at approximately 11 weeks’ gestation, 50 of whom later miscarried. Plasma kisspeptin proved a more accurate predictor of miscarriage than HCG: the area under the receiver operating characteristic (ROC) curve for plasma kisspeptin was 0.899, compared with 0.775 for serum HCG. Plasma kisspeptin above 1,306 pmol/L was associated with a highly significant 87% reduced risk of miscarriage, even after adjusting for age, body mass index, gestational age, smoking, and blood pressure.
Lead investigator Dr. Ali Abbara of Imperial College London explained why that matters at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – A one-time measurement of plasma kisspeptin – a family of placental peptides also being studied for fertility treatment – better predicts miscarriage than does serial measurement of human chorionic gonadotropin (HCG), a widely used measure.
British researchers measured both in 993 asymptomatic women at approximately 11 weeks’ gestation, 50 of whom later miscarried. Plasma kisspeptin proved a more accurate predictor of miscarriage than HCG: the area under the receiver operating characteristic (ROC) curve for plasma kisspeptin was 0.899, compared with 0.775 for serum HCG. Plasma kisspeptin above 1,306 pmol/L was associated with a highly significant 87% reduced risk of miscarriage, even after adjusting for age, body mass index, gestational age, smoking, and blood pressure.
Lead investigator Dr. Ali Abbara of Imperial College London explained why that matters at the joint meeting of the International Congress of Endocrinology and the Endocrine Society.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ICE/ENDO 2014
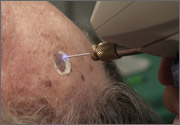
Cryosurgery
VIDEO: Slow tapering worked best for stopping SLE immunosuppression
PARIS – When physicians withdrew immunosuppressant treatment from lupus patients in long-term remission, a gradual tapering down of their immunosuppressant treatment produced a lower rate of subsequent flares than did faster treatment withdrawal, based on experience with 99 patients treated at the University of Toronto.
"This study has answered a very important question," namely, what approach works best when taking patients with systemic lupus erythematosus who are in long-term remission on immunosuppressant therapy off their treatment, said Dr. Zahi Touma, a rheumatologist at the University of Toronto. When patients had their dose tapered down more gradually, they had a reduced rate of flares and needed less immunosuppressant therapy to restart, compared with patients who withdrew from treatment more quickly.
"This is not a validated approach. It is not yet even published," Dr. Touma cautioned during a video interview at the annual European Congress of Rheumatology. But the apparent advantage of more gradual treatment withdrawal "is something we found in this study," he said.
Dr. Touma said that he had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
PARIS – When physicians withdrew immunosuppressant treatment from lupus patients in long-term remission, a gradual tapering down of their immunosuppressant treatment produced a lower rate of subsequent flares than did faster treatment withdrawal, based on experience with 99 patients treated at the University of Toronto.
"This study has answered a very important question," namely, what approach works best when taking patients with systemic lupus erythematosus who are in long-term remission on immunosuppressant therapy off their treatment, said Dr. Zahi Touma, a rheumatologist at the University of Toronto. When patients had their dose tapered down more gradually, they had a reduced rate of flares and needed less immunosuppressant therapy to restart, compared with patients who withdrew from treatment more quickly.
"This is not a validated approach. It is not yet even published," Dr. Touma cautioned during a video interview at the annual European Congress of Rheumatology. But the apparent advantage of more gradual treatment withdrawal "is something we found in this study," he said.
Dr. Touma said that he had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
PARIS – When physicians withdrew immunosuppressant treatment from lupus patients in long-term remission, a gradual tapering down of their immunosuppressant treatment produced a lower rate of subsequent flares than did faster treatment withdrawal, based on experience with 99 patients treated at the University of Toronto.
"This study has answered a very important question," namely, what approach works best when taking patients with systemic lupus erythematosus who are in long-term remission on immunosuppressant therapy off their treatment, said Dr. Zahi Touma, a rheumatologist at the University of Toronto. When patients had their dose tapered down more gradually, they had a reduced rate of flares and needed less immunosuppressant therapy to restart, compared with patients who withdrew from treatment more quickly.
"This is not a validated approach. It is not yet even published," Dr. Touma cautioned during a video interview at the annual European Congress of Rheumatology. But the apparent advantage of more gradual treatment withdrawal "is something we found in this study," he said.
Dr. Touma said that he had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
AT THE EULAR CONGRESS 2014
VIDEO: Sarilumab shows RA safety, efficacy in phase III trial
PARIS – Treatment with the interleukin-6–blocking drug sarilumab led to statistically significant and clinically meaningful improvements in patients with rheumatoid arthritis in a multicenter, placebo controlled, phase III trial with 1,197 patients.
The safety and efficacy results from the SARIL-RA-MOBILITY trial are the first outcomes from a panel of phase III studies of sarilumab in patients with rheumatoid arthritis, said Dr. Mark Genovese at the annual European Congress of Rheumatology. The results showed that treatment with sarilumab plus methotrexate led to less joint damage over time, compared with methotrexate plus placebo, a benefit that should result in patients feeling better, said Dr. Genovese, professor of medicine and co-chief of the division of immunology and rheumatology at Stanford (Calif.) University.
Sarilumab is the first agent to progress this far in testing from a novel class of immunosuppressive drugs that work by blocking interleukin-6. Having safe drugs from a new class available to treat patients with rheumatoid arthritis holds promise for better controlling this disease in patients who inadequately respond to existing drug options, Dr. Genovese said in a video interview.
The SARIL-RA-MOBILITY trial was sponsored by Sanofi and Regeneron, the companies developing the drug. Dr. Genovese said that he has been a consultant to and received research support from Sanofi. Several of the coauthors are employees of Sanofi or Regeneron.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
PARIS – Treatment with the interleukin-6–blocking drug sarilumab led to statistically significant and clinically meaningful improvements in patients with rheumatoid arthritis in a multicenter, placebo controlled, phase III trial with 1,197 patients.
The safety and efficacy results from the SARIL-RA-MOBILITY trial are the first outcomes from a panel of phase III studies of sarilumab in patients with rheumatoid arthritis, said Dr. Mark Genovese at the annual European Congress of Rheumatology. The results showed that treatment with sarilumab plus methotrexate led to less joint damage over time, compared with methotrexate plus placebo, a benefit that should result in patients feeling better, said Dr. Genovese, professor of medicine and co-chief of the division of immunology and rheumatology at Stanford (Calif.) University.
Sarilumab is the first agent to progress this far in testing from a novel class of immunosuppressive drugs that work by blocking interleukin-6. Having safe drugs from a new class available to treat patients with rheumatoid arthritis holds promise for better controlling this disease in patients who inadequately respond to existing drug options, Dr. Genovese said in a video interview.
The SARIL-RA-MOBILITY trial was sponsored by Sanofi and Regeneron, the companies developing the drug. Dr. Genovese said that he has been a consultant to and received research support from Sanofi. Several of the coauthors are employees of Sanofi or Regeneron.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
PARIS – Treatment with the interleukin-6–blocking drug sarilumab led to statistically significant and clinically meaningful improvements in patients with rheumatoid arthritis in a multicenter, placebo controlled, phase III trial with 1,197 patients.
The safety and efficacy results from the SARIL-RA-MOBILITY trial are the first outcomes from a panel of phase III studies of sarilumab in patients with rheumatoid arthritis, said Dr. Mark Genovese at the annual European Congress of Rheumatology. The results showed that treatment with sarilumab plus methotrexate led to less joint damage over time, compared with methotrexate plus placebo, a benefit that should result in patients feeling better, said Dr. Genovese, professor of medicine and co-chief of the division of immunology and rheumatology at Stanford (Calif.) University.
Sarilumab is the first agent to progress this far in testing from a novel class of immunosuppressive drugs that work by blocking interleukin-6. Having safe drugs from a new class available to treat patients with rheumatoid arthritis holds promise for better controlling this disease in patients who inadequately respond to existing drug options, Dr. Genovese said in a video interview.
The SARIL-RA-MOBILITY trial was sponsored by Sanofi and Regeneron, the companies developing the drug. Dr. Genovese said that he has been a consultant to and received research support from Sanofi. Several of the coauthors are employees of Sanofi or Regeneron.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
AT THE EULAR CONGRESS 2014
Some SSRIs are better than others for pregnant women
VIDEO: Gene profiling could signal start of personalized medicine in RA
PARIS – A set of genetic polymorphisms is beginning to allow researchers to predict which patients with rheumatoid arthritis will have a severe disease course, as well as determine their response to treatment and risk of death.
Changes in amino acids at positions 71 and 74 of the HLA-DRB1 gene, which are a part of the "shared epitope" that is already known to increase genetic susceptibility for rheumatoid arthritis, as well as a new polymorphism at position 11 of the HLA-DRB1 gene that is outside the shared epitope, are key to this effort. These polymorphisms predicted the radiologic outcome of rheumatoid arthritis patients, response to anti-tumor necrosis factor therapy, and mortality in an analysis of blood samples from three independent multicenter, prospective cohort studies. The three polymorphisms defined 16 haplotypes whose effects on RA susceptibility range from protective to increasing risk and were perfectly correlated with the observed levels of disease susceptibility.
Further studies will be necessary to validate the associations observed with the sets of polymorphisms, said Dr. Sebastien Viatte, first author of the study and a research fellow at the Centre for Musculoskeletal Research at the University of Manchester (England). Nonetheless, the results are an important step in showing that "genetics can be used to predict disease outcomes and is ... likely to enter the clinic within 5-10 years," he said in a video interview at the annual European Congress of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PARIS – A set of genetic polymorphisms is beginning to allow researchers to predict which patients with rheumatoid arthritis will have a severe disease course, as well as determine their response to treatment and risk of death.
Changes in amino acids at positions 71 and 74 of the HLA-DRB1 gene, which are a part of the "shared epitope" that is already known to increase genetic susceptibility for rheumatoid arthritis, as well as a new polymorphism at position 11 of the HLA-DRB1 gene that is outside the shared epitope, are key to this effort. These polymorphisms predicted the radiologic outcome of rheumatoid arthritis patients, response to anti-tumor necrosis factor therapy, and mortality in an analysis of blood samples from three independent multicenter, prospective cohort studies. The three polymorphisms defined 16 haplotypes whose effects on RA susceptibility range from protective to increasing risk and were perfectly correlated with the observed levels of disease susceptibility.
Further studies will be necessary to validate the associations observed with the sets of polymorphisms, said Dr. Sebastien Viatte, first author of the study and a research fellow at the Centre for Musculoskeletal Research at the University of Manchester (England). Nonetheless, the results are an important step in showing that "genetics can be used to predict disease outcomes and is ... likely to enter the clinic within 5-10 years," he said in a video interview at the annual European Congress of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PARIS – A set of genetic polymorphisms is beginning to allow researchers to predict which patients with rheumatoid arthritis will have a severe disease course, as well as determine their response to treatment and risk of death.
Changes in amino acids at positions 71 and 74 of the HLA-DRB1 gene, which are a part of the "shared epitope" that is already known to increase genetic susceptibility for rheumatoid arthritis, as well as a new polymorphism at position 11 of the HLA-DRB1 gene that is outside the shared epitope, are key to this effort. These polymorphisms predicted the radiologic outcome of rheumatoid arthritis patients, response to anti-tumor necrosis factor therapy, and mortality in an analysis of blood samples from three independent multicenter, prospective cohort studies. The three polymorphisms defined 16 haplotypes whose effects on RA susceptibility range from protective to increasing risk and were perfectly correlated with the observed levels of disease susceptibility.
Further studies will be necessary to validate the associations observed with the sets of polymorphisms, said Dr. Sebastien Viatte, first author of the study and a research fellow at the Centre for Musculoskeletal Research at the University of Manchester (England). Nonetheless, the results are an important step in showing that "genetics can be used to predict disease outcomes and is ... likely to enter the clinic within 5-10 years," he said in a video interview at the annual European Congress of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE EULAR CONGRESS 2014