User login
VIDEO: ADA unifies all pediatric HbA1c targets to less than 7.5%
SAN FRANCISCO – The American Diabetes Association has unified the pediatric hemoglobin A1c target values to less than 7.5% for all pediatric age groups, moving away from breaking down glycemic control targets by age. This will also harmonize the HbA1c goals with those of international groups such as the International Society of Pediatric and Adolescent Diabetes (ISPAD).
The change is part of a new position statement released on June 16 during the annual scientific sessions of the American Diabetes Association (Diabetes Care 2014;37:2034-54). The document also for the first time brings together recommendations for care of individuals with type 1 diabetes across all age groups.
In a video interview, Dr. Lori M.B. Laffel, one of the statement’s coauthors and chief of the pediatric, adolescent, and young adult section at Joslin Diabetes Center, Boston, explains the rationale behind this decision. Dr. David Maahs of the University of Colorado, Aurora, discusses the potential concern regarding the risk of hypoglycemia.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
SAN FRANCISCO – The American Diabetes Association has unified the pediatric hemoglobin A1c target values to less than 7.5% for all pediatric age groups, moving away from breaking down glycemic control targets by age. This will also harmonize the HbA1c goals with those of international groups such as the International Society of Pediatric and Adolescent Diabetes (ISPAD).
The change is part of a new position statement released on June 16 during the annual scientific sessions of the American Diabetes Association (Diabetes Care 2014;37:2034-54). The document also for the first time brings together recommendations for care of individuals with type 1 diabetes across all age groups.
In a video interview, Dr. Lori M.B. Laffel, one of the statement’s coauthors and chief of the pediatric, adolescent, and young adult section at Joslin Diabetes Center, Boston, explains the rationale behind this decision. Dr. David Maahs of the University of Colorado, Aurora, discusses the potential concern regarding the risk of hypoglycemia.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
SAN FRANCISCO – The American Diabetes Association has unified the pediatric hemoglobin A1c target values to less than 7.5% for all pediatric age groups, moving away from breaking down glycemic control targets by age. This will also harmonize the HbA1c goals with those of international groups such as the International Society of Pediatric and Adolescent Diabetes (ISPAD).
The change is part of a new position statement released on June 16 during the annual scientific sessions of the American Diabetes Association (Diabetes Care 2014;37:2034-54). The document also for the first time brings together recommendations for care of individuals with type 1 diabetes across all age groups.
In a video interview, Dr. Lori M.B. Laffel, one of the statement’s coauthors and chief of the pediatric, adolescent, and young adult section at Joslin Diabetes Center, Boston, explains the rationale behind this decision. Dr. David Maahs of the University of Colorado, Aurora, discusses the potential concern regarding the risk of hypoglycemia.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
VIDEO: Team approach is best for successful oncofertility clinic
PHILADELPHIA – Whether you want to build an entire oncofertility clinic or just elevate the level of care your current facility offers, an integrated approach to care is key, according to Dr. Leslie A. Appiah, director of oncofertility at the University of Kentucky Medical Center, Lexington.
In a video interview at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology, Dr. Appiah offers suggestions for how oncologists, gynecologists, reproductive endocrinologists, nurse managers, social workers, and others – even when they’re with other institutions – can work together to offer care that adheres to position statements on fertility rights for cancer patients from the American Society of Clinical Oncology and other associations.
Dr. Appiah also discusses how to achieve fluid communication so that fertility can be preserved without delaying cancer treatments, and best practices for oncofertility concerns in the pediatric setting.
On Twitter @whitneymcknight
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHILADELPHIA – Whether you want to build an entire oncofertility clinic or just elevate the level of care your current facility offers, an integrated approach to care is key, according to Dr. Leslie A. Appiah, director of oncofertility at the University of Kentucky Medical Center, Lexington.
In a video interview at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology, Dr. Appiah offers suggestions for how oncologists, gynecologists, reproductive endocrinologists, nurse managers, social workers, and others – even when they’re with other institutions – can work together to offer care that adheres to position statements on fertility rights for cancer patients from the American Society of Clinical Oncology and other associations.
Dr. Appiah also discusses how to achieve fluid communication so that fertility can be preserved without delaying cancer treatments, and best practices for oncofertility concerns in the pediatric setting.
On Twitter @whitneymcknight
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHILADELPHIA – Whether you want to build an entire oncofertility clinic or just elevate the level of care your current facility offers, an integrated approach to care is key, according to Dr. Leslie A. Appiah, director of oncofertility at the University of Kentucky Medical Center, Lexington.
In a video interview at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology, Dr. Appiah offers suggestions for how oncologists, gynecologists, reproductive endocrinologists, nurse managers, social workers, and others – even when they’re with other institutions – can work together to offer care that adheres to position statements on fertility rights for cancer patients from the American Society of Clinical Oncology and other associations.
Dr. Appiah also discusses how to achieve fluid communication so that fertility can be preserved without delaying cancer treatments, and best practices for oncofertility concerns in the pediatric setting.
On Twitter @whitneymcknight
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE NASPAG ANNUAL MEETING
VIDEO: Teen brain reacts to sugar differently
SAN FRANCISCO — When it comes to glucose ingestion, the adolescent brain reacts differently than the adult brain. That’s according to functional MRI scans comparing the cerebral blood flow of lean adolescents with lean adults, Dr. Ania M. Jastreboff reported June 15 at the annual scientific sessions of the American Diabetes Association.
Researchers found that lean adolescents showed increased cerebral blood flow in several regions, including the reward-motivation region (striatum), the impulse control region (anterior cingulate cortex), and the prefrontal cortex, which is in charge of executive function regulation. All these regions undergo marked developmental changes during adolescence.
In a video interview, Dr. Jastreboff, assistant professor of internal medicine and pediatrics at Yale University, New Haven, Conn., further explains the study’s findings and its implications.
On Twitter @naseemmiller
SAN FRANCISCO — When it comes to glucose ingestion, the adolescent brain reacts differently than the adult brain. That’s according to functional MRI scans comparing the cerebral blood flow of lean adolescents with lean adults, Dr. Ania M. Jastreboff reported June 15 at the annual scientific sessions of the American Diabetes Association.
Researchers found that lean adolescents showed increased cerebral blood flow in several regions, including the reward-motivation region (striatum), the impulse control region (anterior cingulate cortex), and the prefrontal cortex, which is in charge of executive function regulation. All these regions undergo marked developmental changes during adolescence.
In a video interview, Dr. Jastreboff, assistant professor of internal medicine and pediatrics at Yale University, New Haven, Conn., further explains the study’s findings and its implications.
On Twitter @naseemmiller
SAN FRANCISCO — When it comes to glucose ingestion, the adolescent brain reacts differently than the adult brain. That’s according to functional MRI scans comparing the cerebral blood flow of lean adolescents with lean adults, Dr. Ania M. Jastreboff reported June 15 at the annual scientific sessions of the American Diabetes Association.
Researchers found that lean adolescents showed increased cerebral blood flow in several regions, including the reward-motivation region (striatum), the impulse control region (anterior cingulate cortex), and the prefrontal cortex, which is in charge of executive function regulation. All these regions undergo marked developmental changes during adolescence.
In a video interview, Dr. Jastreboff, assistant professor of internal medicine and pediatrics at Yale University, New Haven, Conn., further explains the study’s findings and its implications.
On Twitter @naseemmiller
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
VIDEO: ACC/AHA lipid guidelines and diabetes
SAN FRANCISCO – Those looking for guidance from the American Diabetes Association regarding the guidelines released last fall from the American College of Cardiology and the American Heart Association dropping cholesterol treatment goals will have to wait until next year.
That’s when the ADA’s Clinical Practice Recommendations, released each year in January, will incorporate the Professional Practice Committee’s review of the ACC/AHA guidelines and the evidence behind it. The new recommendations caused some controversy and raised some questions about treatment of certain patient groups, most notably those with diabetes.
The ADA hasn’t recommended any changes to its current guidelines, which still incorporate treatment to target. But it has been reviewing the guidelines to see if it would recommend any changes for its 2015 guidelines.
Dr. Robert E. Ratner, chief scientific and medical officer for the American Diabetes Association, further explained the organization’s position on treatment of lipids in patients with diabetes in a video interview at the annual scientific sessions of the ADA.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The association is also holding a debate at this year’s meeting to discuss the pros and cons of the new lipid guidelines for patients with diabetes.
In a press conference, Dr. Robert Eckel, professor of medicine and Charles A. Boettcher chair in atherosclerosis at University of Colorado, Anschutz Medical Campus, Aurora, said he was in support of the ACC/AHA guidelines, having served on the Task Force on Practice Guidelines, and that he believed that almost all patients with diabetes should be on a statin. He stressed that the new guidelines are evidence based.
But Dr. Henry Ginsberg, Irving Professor of Medicine and Director of the Irving Institute for Clinical and Translational Research at Columbia University, New York, argued that the guidelines’ evidence-based construct was too narrow.
In a video interview, Dr. Ginsberg further discussed his position and his practice tips for physicians.
Both physicians agreed that patients should be treated on an individual basis. For instance, patients who are statin intolerant won’t meet the guidelines’ criteria and "we’ll have to go beyond the guidelines," said Dr. Eckel.
On Twitter @naseemmiller
SAN FRANCISCO – Those looking for guidance from the American Diabetes Association regarding the guidelines released last fall from the American College of Cardiology and the American Heart Association dropping cholesterol treatment goals will have to wait until next year.
That’s when the ADA’s Clinical Practice Recommendations, released each year in January, will incorporate the Professional Practice Committee’s review of the ACC/AHA guidelines and the evidence behind it. The new recommendations caused some controversy and raised some questions about treatment of certain patient groups, most notably those with diabetes.
The ADA hasn’t recommended any changes to its current guidelines, which still incorporate treatment to target. But it has been reviewing the guidelines to see if it would recommend any changes for its 2015 guidelines.
Dr. Robert E. Ratner, chief scientific and medical officer for the American Diabetes Association, further explained the organization’s position on treatment of lipids in patients with diabetes in a video interview at the annual scientific sessions of the ADA.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The association is also holding a debate at this year’s meeting to discuss the pros and cons of the new lipid guidelines for patients with diabetes.
In a press conference, Dr. Robert Eckel, professor of medicine and Charles A. Boettcher chair in atherosclerosis at University of Colorado, Anschutz Medical Campus, Aurora, said he was in support of the ACC/AHA guidelines, having served on the Task Force on Practice Guidelines, and that he believed that almost all patients with diabetes should be on a statin. He stressed that the new guidelines are evidence based.
But Dr. Henry Ginsberg, Irving Professor of Medicine and Director of the Irving Institute for Clinical and Translational Research at Columbia University, New York, argued that the guidelines’ evidence-based construct was too narrow.
In a video interview, Dr. Ginsberg further discussed his position and his practice tips for physicians.
Both physicians agreed that patients should be treated on an individual basis. For instance, patients who are statin intolerant won’t meet the guidelines’ criteria and "we’ll have to go beyond the guidelines," said Dr. Eckel.
On Twitter @naseemmiller
SAN FRANCISCO – Those looking for guidance from the American Diabetes Association regarding the guidelines released last fall from the American College of Cardiology and the American Heart Association dropping cholesterol treatment goals will have to wait until next year.
That’s when the ADA’s Clinical Practice Recommendations, released each year in January, will incorporate the Professional Practice Committee’s review of the ACC/AHA guidelines and the evidence behind it. The new recommendations caused some controversy and raised some questions about treatment of certain patient groups, most notably those with diabetes.
The ADA hasn’t recommended any changes to its current guidelines, which still incorporate treatment to target. But it has been reviewing the guidelines to see if it would recommend any changes for its 2015 guidelines.
Dr. Robert E. Ratner, chief scientific and medical officer for the American Diabetes Association, further explained the organization’s position on treatment of lipids in patients with diabetes in a video interview at the annual scientific sessions of the ADA.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The association is also holding a debate at this year’s meeting to discuss the pros and cons of the new lipid guidelines for patients with diabetes.
In a press conference, Dr. Robert Eckel, professor of medicine and Charles A. Boettcher chair in atherosclerosis at University of Colorado, Anschutz Medical Campus, Aurora, said he was in support of the ACC/AHA guidelines, having served on the Task Force on Practice Guidelines, and that he believed that almost all patients with diabetes should be on a statin. He stressed that the new guidelines are evidence based.
But Dr. Henry Ginsberg, Irving Professor of Medicine and Director of the Irving Institute for Clinical and Translational Research at Columbia University, New York, argued that the guidelines’ evidence-based construct was too narrow.
In a video interview, Dr. Ginsberg further discussed his position and his practice tips for physicians.
Both physicians agreed that patients should be treated on an individual basis. For instance, patients who are statin intolerant won’t meet the guidelines’ criteria and "we’ll have to go beyond the guidelines," said Dr. Eckel.
On Twitter @naseemmiller
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
VIDEO: Shedding stigma for advocacy, suicide attempt survivors find a voice
LOS ANGELES – Suicide attempt survivors are overcoming the stigma of talking about their attempts and joining together to demand a voice in suicide prevention efforts. Researchers and leaders in the field are hearing that voice and acknowledging them as sources of insight and advocacy that, for too long, have been largely ignored.
Among the signs of that shift – and due largely to their lobbying – the American Association of Suicidology (AAS) recently formed a division for attempt-survivors and launched a blog on the topic.
"It’s a critical voice. There’s no better advocate for mental well-being than someone who has been on the edge of life and death and chosen a path of recovery," said AAS President William Schmitz Jr., Psy.D.
Asked for an example of how this new voice might help, he noted that "there are a lot of clinicians out there who are not trained in the assessment and management of suicidality. I’ve heard stories from some of our attempt survivors that are truly scary – very negative, hostile encounters with the health care system." People who’ve experienced it firsthand offer "a chance for us to open that dialogue," he said at the annual conference of the American Association of Suicidology.
Cara Anna, a journalist and attempt-survivor who helped spearhead the AAS lobbying campaign, stated her case for us at the meeting. She’s a prominent voice in the attempt-survivor community.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LOS ANGELES – Suicide attempt survivors are overcoming the stigma of talking about their attempts and joining together to demand a voice in suicide prevention efforts. Researchers and leaders in the field are hearing that voice and acknowledging them as sources of insight and advocacy that, for too long, have been largely ignored.
Among the signs of that shift – and due largely to their lobbying – the American Association of Suicidology (AAS) recently formed a division for attempt-survivors and launched a blog on the topic.
"It’s a critical voice. There’s no better advocate for mental well-being than someone who has been on the edge of life and death and chosen a path of recovery," said AAS President William Schmitz Jr., Psy.D.
Asked for an example of how this new voice might help, he noted that "there are a lot of clinicians out there who are not trained in the assessment and management of suicidality. I’ve heard stories from some of our attempt survivors that are truly scary – very negative, hostile encounters with the health care system." People who’ve experienced it firsthand offer "a chance for us to open that dialogue," he said at the annual conference of the American Association of Suicidology.
Cara Anna, a journalist and attempt-survivor who helped spearhead the AAS lobbying campaign, stated her case for us at the meeting. She’s a prominent voice in the attempt-survivor community.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LOS ANGELES – Suicide attempt survivors are overcoming the stigma of talking about their attempts and joining together to demand a voice in suicide prevention efforts. Researchers and leaders in the field are hearing that voice and acknowledging them as sources of insight and advocacy that, for too long, have been largely ignored.
Among the signs of that shift – and due largely to their lobbying – the American Association of Suicidology (AAS) recently formed a division for attempt-survivors and launched a blog on the topic.
"It’s a critical voice. There’s no better advocate for mental well-being than someone who has been on the edge of life and death and chosen a path of recovery," said AAS President William Schmitz Jr., Psy.D.
Asked for an example of how this new voice might help, he noted that "there are a lot of clinicians out there who are not trained in the assessment and management of suicidality. I’ve heard stories from some of our attempt survivors that are truly scary – very negative, hostile encounters with the health care system." People who’ve experienced it firsthand offer "a chance for us to open that dialogue," he said at the annual conference of the American Association of Suicidology.
Cara Anna, a journalist and attempt-survivor who helped spearhead the AAS lobbying campaign, stated her case for us at the meeting. She’s a prominent voice in the attempt-survivor community.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ANNUAL AAS CONFERENCE
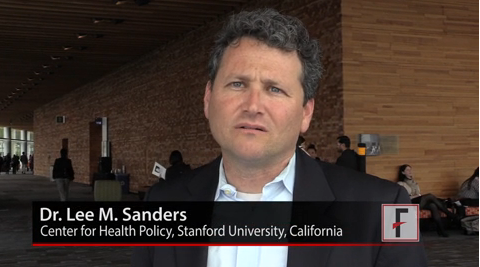
VIDEO: Bottom line on maternal infections and cerebral palsy
VANCOUVER, B.C. – Intra- or extra-amniotic fluid infections during pregnancy elevate the risk of having a child with cerebral palsy, according to analysis of 6 million California birth records – although the findings shows an association, not causality.
Researchers showed that pregnant women who were hospitalized with a diagnosis of chorioamnionitis had a fourfold increase in the risk of having a child with cerebral palsy (CP), while genitourinary and respiratory infections increased that risk twofold.
"I think this is a very important study, and it took us a step further in trying to understand what could cause cerebral palsy," said Dr. Lee M. Sanders, associate professor of pediatrics and codirector of the Center for Policy, Outcomes, and Prevention at Stanford (Calif.) University.
Because the study shows an association only, however, "it’s important not to cause alarm," cautioned Dr. Sanders, who was not involved in the study.
In a video interview, Dr. Sanders explains what’s known so far about this association, the implications of the study’s findings, and the research that’s already underway.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
VANCOUVER, B.C. – Intra- or extra-amniotic fluid infections during pregnancy elevate the risk of having a child with cerebral palsy, according to analysis of 6 million California birth records – although the findings shows an association, not causality.
Researchers showed that pregnant women who were hospitalized with a diagnosis of chorioamnionitis had a fourfold increase in the risk of having a child with cerebral palsy (CP), while genitourinary and respiratory infections increased that risk twofold.
"I think this is a very important study, and it took us a step further in trying to understand what could cause cerebral palsy," said Dr. Lee M. Sanders, associate professor of pediatrics and codirector of the Center for Policy, Outcomes, and Prevention at Stanford (Calif.) University.
Because the study shows an association only, however, "it’s important not to cause alarm," cautioned Dr. Sanders, who was not involved in the study.
In a video interview, Dr. Sanders explains what’s known so far about this association, the implications of the study’s findings, and the research that’s already underway.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
VANCOUVER, B.C. – Intra- or extra-amniotic fluid infections during pregnancy elevate the risk of having a child with cerebral palsy, according to analysis of 6 million California birth records – although the findings shows an association, not causality.
Researchers showed that pregnant women who were hospitalized with a diagnosis of chorioamnionitis had a fourfold increase in the risk of having a child with cerebral palsy (CP), while genitourinary and respiratory infections increased that risk twofold.
"I think this is a very important study, and it took us a step further in trying to understand what could cause cerebral palsy," said Dr. Lee M. Sanders, associate professor of pediatrics and codirector of the Center for Policy, Outcomes, and Prevention at Stanford (Calif.) University.
Because the study shows an association only, however, "it’s important not to cause alarm," cautioned Dr. Sanders, who was not involved in the study.
In a video interview, Dr. Sanders explains what’s known so far about this association, the implications of the study’s findings, and the research that’s already underway.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
AT THE PAS ANNUAL MEETING
Interactive Journal Review on the Treatment of Bipolar Depression
Dr. Henry Nasrallah and Dr. Joseph Calabrese highlight pivotal data from 2 randomized, double-blind, placebo-controlled, short-term clinical studies, published in the February 2014 issue of The American Journal of Psychiatry, that established the efficacy and safety of a treatment option approved for patients with major depressive episodes associated with bipolar I disorder.
Watch the video here:
Dr. Henry Nasrallah and Dr. Joseph Calabrese highlight pivotal data from 2 randomized, double-blind, placebo-controlled, short-term clinical studies, published in the February 2014 issue of The American Journal of Psychiatry, that established the efficacy and safety of a treatment option approved for patients with major depressive episodes associated with bipolar I disorder.
Watch the video here:
Dr. Henry Nasrallah and Dr. Joseph Calabrese highlight pivotal data from 2 randomized, double-blind, placebo-controlled, short-term clinical studies, published in the February 2014 issue of The American Journal of Psychiatry, that established the efficacy and safety of a treatment option approved for patients with major depressive episodes associated with bipolar I disorder.
Watch the video here:
Thomas Roth, PhD
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Sonia Ancoli-Israel, PhD
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO: Cranial ultrasound better than temporal artery biopsy for GCA
PARIS – Cranial ultrasound was more sensitive and just as specific as was temporal artery biopsy for the diagnosis of giant cell arteritis, based on the results of a retrospective cohort study reported by Dr. Adam Croft at a press conference held during the annual European Congress of Rheumatology.
Given that ultrasound is noninvasive, associated with fewer risks, and more sensitive than biopsy, "temporal artery biopsy may now be unnecessary (when) clinical suspicion of GCA [giant cell arteritis] is high or quite low," said Dr. Croft of the University of Birmingham, England. "Cranial ultrasound may soon replace temporal artery biopsy in the assessment of patients with a suspected diagnosis of GCA in routine clinical practice."
Giant cell arteritis typically is associated with severe headaches and scalp tenderness on the sides of the forehead that must be distinguished from more benign causes of headache. In GCA, these symptoms result from ocular arterial inflammation and narrowing that respond to high-dose steroid therapy.
The findings were seen in a study of 87 patients who underwent cranial duplex ultrasound for suspected GCA. At 3-month follow-up, 36 patients (41%) had a confirmed clinical diagnosis of giant cell arteritis. Of the 30 patients with a positive cranial ultrasound result, 29 went on to have a confirmed diagnosis. Of the 36 patients with more than three American College of Rheumatology criteria, 21 (58%) had a diagnosis of GCA.
When compared with clinical diagnosis, ultrasound had 81% sensitivity and 98% specificity with a positive likelihood ratio of 41 and a negative likelihood ratio 0.2. The positive predictive value was 97% and the negative predictive value was 88%, he said. In other words, with a positive ultrasound finding, the probability of giant cell arteritis was 41 times higher.
In contrast, when compared with clinical diagnosis, temporal artery biopsy had a sensitivity of 53% and a specificity of 100%. The positive likelihood ratio was 2.3 and the negative likelihood ratio 0.2. The positive predictive value was 100% and the negative predictive value was 47%.
Relying on temporal arterial biopsy results alone leaves "patients at risk of missing out on potentially sight-saving steroid treatment, or of being treated with high-dose steroids unnecessarily," he said. Further, temporal artery biopsy is not without risks. The biopsy can miss the artery and can result is permanent facial nerve damage. A negative biopsy rarely informs practice.
The availability of cranial ultrasound depends on whether one’s practice is located near facilities with the infrastructure and the availability of well-trained rheumatologists and radiologists who can do the scan rapidly, Dr. Croft said in a video interview.
Dr. Croft had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @maryjodales
PARIS – Cranial ultrasound was more sensitive and just as specific as was temporal artery biopsy for the diagnosis of giant cell arteritis, based on the results of a retrospective cohort study reported by Dr. Adam Croft at a press conference held during the annual European Congress of Rheumatology.
Given that ultrasound is noninvasive, associated with fewer risks, and more sensitive than biopsy, "temporal artery biopsy may now be unnecessary (when) clinical suspicion of GCA [giant cell arteritis] is high or quite low," said Dr. Croft of the University of Birmingham, England. "Cranial ultrasound may soon replace temporal artery biopsy in the assessment of patients with a suspected diagnosis of GCA in routine clinical practice."
Giant cell arteritis typically is associated with severe headaches and scalp tenderness on the sides of the forehead that must be distinguished from more benign causes of headache. In GCA, these symptoms result from ocular arterial inflammation and narrowing that respond to high-dose steroid therapy.
The findings were seen in a study of 87 patients who underwent cranial duplex ultrasound for suspected GCA. At 3-month follow-up, 36 patients (41%) had a confirmed clinical diagnosis of giant cell arteritis. Of the 30 patients with a positive cranial ultrasound result, 29 went on to have a confirmed diagnosis. Of the 36 patients with more than three American College of Rheumatology criteria, 21 (58%) had a diagnosis of GCA.
When compared with clinical diagnosis, ultrasound had 81% sensitivity and 98% specificity with a positive likelihood ratio of 41 and a negative likelihood ratio 0.2. The positive predictive value was 97% and the negative predictive value was 88%, he said. In other words, with a positive ultrasound finding, the probability of giant cell arteritis was 41 times higher.
In contrast, when compared with clinical diagnosis, temporal artery biopsy had a sensitivity of 53% and a specificity of 100%. The positive likelihood ratio was 2.3 and the negative likelihood ratio 0.2. The positive predictive value was 100% and the negative predictive value was 47%.
Relying on temporal arterial biopsy results alone leaves "patients at risk of missing out on potentially sight-saving steroid treatment, or of being treated with high-dose steroids unnecessarily," he said. Further, temporal artery biopsy is not without risks. The biopsy can miss the artery and can result is permanent facial nerve damage. A negative biopsy rarely informs practice.
The availability of cranial ultrasound depends on whether one’s practice is located near facilities with the infrastructure and the availability of well-trained rheumatologists and radiologists who can do the scan rapidly, Dr. Croft said in a video interview.
Dr. Croft had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @maryjodales
PARIS – Cranial ultrasound was more sensitive and just as specific as was temporal artery biopsy for the diagnosis of giant cell arteritis, based on the results of a retrospective cohort study reported by Dr. Adam Croft at a press conference held during the annual European Congress of Rheumatology.
Given that ultrasound is noninvasive, associated with fewer risks, and more sensitive than biopsy, "temporal artery biopsy may now be unnecessary (when) clinical suspicion of GCA [giant cell arteritis] is high or quite low," said Dr. Croft of the University of Birmingham, England. "Cranial ultrasound may soon replace temporal artery biopsy in the assessment of patients with a suspected diagnosis of GCA in routine clinical practice."
Giant cell arteritis typically is associated with severe headaches and scalp tenderness on the sides of the forehead that must be distinguished from more benign causes of headache. In GCA, these symptoms result from ocular arterial inflammation and narrowing that respond to high-dose steroid therapy.
The findings were seen in a study of 87 patients who underwent cranial duplex ultrasound for suspected GCA. At 3-month follow-up, 36 patients (41%) had a confirmed clinical diagnosis of giant cell arteritis. Of the 30 patients with a positive cranial ultrasound result, 29 went on to have a confirmed diagnosis. Of the 36 patients with more than three American College of Rheumatology criteria, 21 (58%) had a diagnosis of GCA.
When compared with clinical diagnosis, ultrasound had 81% sensitivity and 98% specificity with a positive likelihood ratio of 41 and a negative likelihood ratio 0.2. The positive predictive value was 97% and the negative predictive value was 88%, he said. In other words, with a positive ultrasound finding, the probability of giant cell arteritis was 41 times higher.
In contrast, when compared with clinical diagnosis, temporal artery biopsy had a sensitivity of 53% and a specificity of 100%. The positive likelihood ratio was 2.3 and the negative likelihood ratio 0.2. The positive predictive value was 100% and the negative predictive value was 47%.
Relying on temporal arterial biopsy results alone leaves "patients at risk of missing out on potentially sight-saving steroid treatment, or of being treated with high-dose steroids unnecessarily," he said. Further, temporal artery biopsy is not without risks. The biopsy can miss the artery and can result is permanent facial nerve damage. A negative biopsy rarely informs practice.
The availability of cranial ultrasound depends on whether one’s practice is located near facilities with the infrastructure and the availability of well-trained rheumatologists and radiologists who can do the scan rapidly, Dr. Croft said in a video interview.
Dr. Croft had no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @maryjodales
AT THE EULAR CONGRESS 2014