User login
Anticoagulation Hub contains news and clinical review articles for physicians seeking the most up-to-date information on the rapidly evolving treatment options for preventing stroke, acute coronary events, deep vein thrombosis, and pulmonary embolism in at-risk patients. The Anticoagulation Hub is powered by Frontline Medical Communications.
Long working hours raised stroke risk
Individuals who worked at least 55 hours a week were about 33% more likely to have a stroke than were those who worked 35-40 hours, according to a large meta-analysis of prospective studies.
The finding is “robust,” wrote Mika Kivimäki, Ph.D., of University College London and his associates. “There was no evidence of between-study heterogeneity, reverse causation bias, or confounding. Furthermore, the association did not vary between men and women or by geographical region, and was independent of the method of stroke ascertainment” (Lancet 2015;386[10005]:1739-46).
“Long working hours were also associated with incident coronary heart disease, but this association was weaker than that for stroke,” they noted.
Past studies have linked long working hours to cardiovascular disease, but prospective data are “scarce, imprecise, and mostly limited to coronary heart disease,” the researchers wrote. To assess relationships between working hours, incident CHD, and stroke, they searched Medline and Embase for studies published through August 2014, and also acquired unpublished data from 20 cohort studies through the Individual-Participant-Data Meta-analysis in Working Populations (IPD-Work) Consortium and open-access databases. These efforts yielded 25 total studies of 24 cohorts in the United States, Europe, and Australia, comprising CHD risk data for almost 604,000 individuals and stroke risk data for almost 529,000, the researchers said.
The studies reported 1,722 strokes and 4,768 new episodes of CHD after an average of 7.2 and 8.5 years of follow-up, respectively, the investigators determined. After accounting for age, sex, and socioeconomic status, individuals who averaged a 55-hour work week were 33% more likely to have a stroke (relative risk, 1.33; 95% confidence interval, 1.11-1.61; P = .002) and a 13% greater risk of CHD (RR, 1.13; 95% CI, 1.02-1.26; P = .02) than were those who worked 35-40 hours per week.
“We recorded a dose-response association for stroke, with RR estimates of 1.10 (95% CI, 0.94 to 1.28; P = .24) for 41 to 48 working hours; 1.27 (1.03 to 1.56; P = .03) for 49 to 54 working hour; and 1.33 (1.11 to 1.61; P = .002) for 55 working hours or more per week, compared with standard working hours (P less than .0001),” the researchers wrote. Based on the findings, “more attention should be paid to the management of vascular risk factors in individuals who work long hours,” they concluded.
The study was funded by the U.K. Medical Research Council, the Economic and Social Research Council, the European Union New and Emerging Risks in Occupational Safety and Health research program, the Finnish Work Environment Fund, the Swedish Research Council for Working Life and Social Research, German Social Accident Insurance, the Danish National Research Centre for the Working Environment, the Academy of Finland, the Ministry of Social Affairs and Employment (Netherlands), the U.S. National Institutes of Health, and the British Heart Foundation. The investigators reported having no conflicts of interest.
Individuals who worked at least 55 hours a week were about 33% more likely to have a stroke than were those who worked 35-40 hours, according to a large meta-analysis of prospective studies.
The finding is “robust,” wrote Mika Kivimäki, Ph.D., of University College London and his associates. “There was no evidence of between-study heterogeneity, reverse causation bias, or confounding. Furthermore, the association did not vary between men and women or by geographical region, and was independent of the method of stroke ascertainment” (Lancet 2015;386[10005]:1739-46).
“Long working hours were also associated with incident coronary heart disease, but this association was weaker than that for stroke,” they noted.
Past studies have linked long working hours to cardiovascular disease, but prospective data are “scarce, imprecise, and mostly limited to coronary heart disease,” the researchers wrote. To assess relationships between working hours, incident CHD, and stroke, they searched Medline and Embase for studies published through August 2014, and also acquired unpublished data from 20 cohort studies through the Individual-Participant-Data Meta-analysis in Working Populations (IPD-Work) Consortium and open-access databases. These efforts yielded 25 total studies of 24 cohorts in the United States, Europe, and Australia, comprising CHD risk data for almost 604,000 individuals and stroke risk data for almost 529,000, the researchers said.
The studies reported 1,722 strokes and 4,768 new episodes of CHD after an average of 7.2 and 8.5 years of follow-up, respectively, the investigators determined. After accounting for age, sex, and socioeconomic status, individuals who averaged a 55-hour work week were 33% more likely to have a stroke (relative risk, 1.33; 95% confidence interval, 1.11-1.61; P = .002) and a 13% greater risk of CHD (RR, 1.13; 95% CI, 1.02-1.26; P = .02) than were those who worked 35-40 hours per week.
“We recorded a dose-response association for stroke, with RR estimates of 1.10 (95% CI, 0.94 to 1.28; P = .24) for 41 to 48 working hours; 1.27 (1.03 to 1.56; P = .03) for 49 to 54 working hour; and 1.33 (1.11 to 1.61; P = .002) for 55 working hours or more per week, compared with standard working hours (P less than .0001),” the researchers wrote. Based on the findings, “more attention should be paid to the management of vascular risk factors in individuals who work long hours,” they concluded.
The study was funded by the U.K. Medical Research Council, the Economic and Social Research Council, the European Union New and Emerging Risks in Occupational Safety and Health research program, the Finnish Work Environment Fund, the Swedish Research Council for Working Life and Social Research, German Social Accident Insurance, the Danish National Research Centre for the Working Environment, the Academy of Finland, the Ministry of Social Affairs and Employment (Netherlands), the U.S. National Institutes of Health, and the British Heart Foundation. The investigators reported having no conflicts of interest.
Individuals who worked at least 55 hours a week were about 33% more likely to have a stroke than were those who worked 35-40 hours, according to a large meta-analysis of prospective studies.
The finding is “robust,” wrote Mika Kivimäki, Ph.D., of University College London and his associates. “There was no evidence of between-study heterogeneity, reverse causation bias, or confounding. Furthermore, the association did not vary between men and women or by geographical region, and was independent of the method of stroke ascertainment” (Lancet 2015;386[10005]:1739-46).
“Long working hours were also associated with incident coronary heart disease, but this association was weaker than that for stroke,” they noted.
Past studies have linked long working hours to cardiovascular disease, but prospective data are “scarce, imprecise, and mostly limited to coronary heart disease,” the researchers wrote. To assess relationships between working hours, incident CHD, and stroke, they searched Medline and Embase for studies published through August 2014, and also acquired unpublished data from 20 cohort studies through the Individual-Participant-Data Meta-analysis in Working Populations (IPD-Work) Consortium and open-access databases. These efforts yielded 25 total studies of 24 cohorts in the United States, Europe, and Australia, comprising CHD risk data for almost 604,000 individuals and stroke risk data for almost 529,000, the researchers said.
The studies reported 1,722 strokes and 4,768 new episodes of CHD after an average of 7.2 and 8.5 years of follow-up, respectively, the investigators determined. After accounting for age, sex, and socioeconomic status, individuals who averaged a 55-hour work week were 33% more likely to have a stroke (relative risk, 1.33; 95% confidence interval, 1.11-1.61; P = .002) and a 13% greater risk of CHD (RR, 1.13; 95% CI, 1.02-1.26; P = .02) than were those who worked 35-40 hours per week.
“We recorded a dose-response association for stroke, with RR estimates of 1.10 (95% CI, 0.94 to 1.28; P = .24) for 41 to 48 working hours; 1.27 (1.03 to 1.56; P = .03) for 49 to 54 working hour; and 1.33 (1.11 to 1.61; P = .002) for 55 working hours or more per week, compared with standard working hours (P less than .0001),” the researchers wrote. Based on the findings, “more attention should be paid to the management of vascular risk factors in individuals who work long hours,” they concluded.
The study was funded by the U.K. Medical Research Council, the Economic and Social Research Council, the European Union New and Emerging Risks in Occupational Safety and Health research program, the Finnish Work Environment Fund, the Swedish Research Council for Working Life and Social Research, German Social Accident Insurance, the Danish National Research Centre for the Working Environment, the Academy of Finland, the Ministry of Social Affairs and Employment (Netherlands), the U.S. National Institutes of Health, and the British Heart Foundation. The investigators reported having no conflicts of interest.
FROM THE LANCET
Key clinical point: Long work weeks were tied to increased stroke risk in a large meta-analysis.
Major finding: Individuals worked an average of at least 55 hours a week were about 33% more likely to have a stroke than were those who worked 35-40 hours (P = .002).
Data source: Meta-analysis of 25 prospective cohort studies from Europe, the United States, and Australia.
Disclosures: The study was funded by a variety of governmental research councils, programs, funds, foundations, ministries, and academies in various countries. The investigators reported having no conflicts of interest.
CDC to celebrate best blood clot prevention strategies
The Centers for Disease Control and Prevention has launched a program to honor hospitals, health systems, and managed care organizations that have implemented effective strategies to prevent health care–associated blood clots.
The HA-VTE Prevention Challenge invites provider organizations around the world to submit evidence of demonstrated successful use of venous thromboembolism (VTE) prevention strategies and interventions. VTE leads to approximately 100,000 premature deaths in the United States every year, according to the CDC, yet as many as 70% of HA-VTEs are preventable, although fewer than half of hospital patients receive appropriate prevention. Indeed, about half of all blood clots happen after a recent hospital stay or surgery.
“Doctors and nurses in hospitals and other health care settings can save lives by implementing the best practices discovered through this challenge,” Dr. Tom Frieden, CDC director, said in a statement. “Tell us about what you are doing and what’s helping prevent blood clots, so we can advance science and save lives together.”
The purpose of the challenge is to highlight the systems, processes, and staffing that contribute to exceptional VTE prevention, according to the CDC. Processes may include the implementation of protocols, risk assessments, and the use of health information technology and clinical decision support tools. Seven of the highest scoring U.S. non-federal hospitals, multihospital systems, hospital networks, and managed care organizations will be recognized as HA-VTE Prevention Champions and will receive a cash award of $10,000 each. Winning submissions from U.S. federal and international entities will be eligible for nonmonetary recognition.
The CDC will accept submissions from Nov. 2, 2015, until Jan. 10, 2016. Winners will be announced in March 2016.
For more information, visit the HA-VTE Prevention Challenge website.
On Twitter: @richpizzi
The Centers for Disease Control and Prevention has launched a program to honor hospitals, health systems, and managed care organizations that have implemented effective strategies to prevent health care–associated blood clots.
The HA-VTE Prevention Challenge invites provider organizations around the world to submit evidence of demonstrated successful use of venous thromboembolism (VTE) prevention strategies and interventions. VTE leads to approximately 100,000 premature deaths in the United States every year, according to the CDC, yet as many as 70% of HA-VTEs are preventable, although fewer than half of hospital patients receive appropriate prevention. Indeed, about half of all blood clots happen after a recent hospital stay or surgery.
“Doctors and nurses in hospitals and other health care settings can save lives by implementing the best practices discovered through this challenge,” Dr. Tom Frieden, CDC director, said in a statement. “Tell us about what you are doing and what’s helping prevent blood clots, so we can advance science and save lives together.”
The purpose of the challenge is to highlight the systems, processes, and staffing that contribute to exceptional VTE prevention, according to the CDC. Processes may include the implementation of protocols, risk assessments, and the use of health information technology and clinical decision support tools. Seven of the highest scoring U.S. non-federal hospitals, multihospital systems, hospital networks, and managed care organizations will be recognized as HA-VTE Prevention Champions and will receive a cash award of $10,000 each. Winning submissions from U.S. federal and international entities will be eligible for nonmonetary recognition.
The CDC will accept submissions from Nov. 2, 2015, until Jan. 10, 2016. Winners will be announced in March 2016.
For more information, visit the HA-VTE Prevention Challenge website.
On Twitter: @richpizzi
The Centers for Disease Control and Prevention has launched a program to honor hospitals, health systems, and managed care organizations that have implemented effective strategies to prevent health care–associated blood clots.
The HA-VTE Prevention Challenge invites provider organizations around the world to submit evidence of demonstrated successful use of venous thromboembolism (VTE) prevention strategies and interventions. VTE leads to approximately 100,000 premature deaths in the United States every year, according to the CDC, yet as many as 70% of HA-VTEs are preventable, although fewer than half of hospital patients receive appropriate prevention. Indeed, about half of all blood clots happen after a recent hospital stay or surgery.
“Doctors and nurses in hospitals and other health care settings can save lives by implementing the best practices discovered through this challenge,” Dr. Tom Frieden, CDC director, said in a statement. “Tell us about what you are doing and what’s helping prevent blood clots, so we can advance science and save lives together.”
The purpose of the challenge is to highlight the systems, processes, and staffing that contribute to exceptional VTE prevention, according to the CDC. Processes may include the implementation of protocols, risk assessments, and the use of health information technology and clinical decision support tools. Seven of the highest scoring U.S. non-federal hospitals, multihospital systems, hospital networks, and managed care organizations will be recognized as HA-VTE Prevention Champions and will receive a cash award of $10,000 each. Winning submissions from U.S. federal and international entities will be eligible for nonmonetary recognition.
The CDC will accept submissions from Nov. 2, 2015, until Jan. 10, 2016. Winners will be announced in March 2016.
For more information, visit the HA-VTE Prevention Challenge website.
On Twitter: @richpizzi
Endovascular thrombectomy vs tPA: better function, same mortality
Endovascular mechanical thrombectomy yielded better function and revascularization rates but similar mortality and intracranial hemorrhage rates as standard medical therapy using tissue plasminogen activator (tPA) in a meta-analysis of eight high-quality randomized clinical trials comparing the two approaches for acute ischemic stroke.
The results were published online Nov. 3 in JAMA.
This meta-analysis included only large multicenter trials published from 2013 to the present. Previous trials and meta-analyses “had several well-recognized limitations” including inconsistent use of vascular imaging to confirm vessel occlusion before randomization, variable use of tPA in patients who eventually were assigned to endovascular therapy, and reliance on less effective and now outdated mechanical devices, said Dr. Jetan H. Badhiwala of the division of neurosurgery, University of Toronto, and his associates.
The eight trials included 2,423 patients (mean age, 67.4 years); 46.7% were women. A total of 1,313 patients underwent endovascular therapy, defined as the intra-arterial use of a microcatheter or other device for mechanical thrombectomy, with or without the local use of a chemical thrombolytic agent. The remaining 1,110 received standard medical therapy (tPA). The interval between stroke onset and endovascular treatment varied from 5 to 12 hours across these studies, with a mean of 3.8 hours.
Patients who had endovascular thrombectomy showed significantly higher rates of functional independence at 90 days (44.6%) than did those who had tPA (31.8%), for an OR of 1.71 and a number needed to treat of 8. The rate of angiographic revascularization at 24 hours also was markedly higher for endovascular thrombectomy (75.8% vs 34.1%), for an OR of 6.49, the investigators said (JAMA 2015;314:1832-43).
However, there were no significant differences between the two study groups in rates of symptomatic intracranial hemorrhage at 90 days (5.7% vs 5.1%) or all-cause mortality at 90 days (15.8% vs 17.8%), and overall morbidity including in-hospital rates of deep venous thrombosis, MI, and pneumonia also were similar.
No sponsor or source of financial support was reported for this study. Dr. Badhiwala and his associates reported having no relevant financial disclosures.
It is important to note some limitations with this well-conducted meta-analysis. First, functional outcomes showed significant heterogeneity, which the authors attributed to variations in patient-, treatment-, and study-related factors.
Second, the confidence intervals for mortality and intracranial hemorrhage were wide, indicating that more data are necessary to fully inform these outcomes.
Third, five of the eight trials were halted early because of the evident superiority of endovascular thrombectomy, which means they fell substantially short (by up to 74%) of their planned sample sizes. This tends to cause overestimation of treatment effects. Fourth, nearly all these strokes involved carotid territory, nearly all the patients were on the young end of the age spectrum, and very few participants had comorbidities such as AF or diabetes. Such favorable characteristics do not reflect real-world experience with ischemic stroke.
Dr. Joanna M. Wardlaw and Dr. Martin S. Dennis are at the Centre for Clinical Brain Sciences at the University of Edinburgh (Scotland). They reported having no relevant financial disclosures. Dr. Wardlaw and Dr. Dennis made these remarks in an editorial accompanying Dr. Badhiwala’s meta-analysis (JAMA 2015;314:1803-4).
It is important to note some limitations with this well-conducted meta-analysis. First, functional outcomes showed significant heterogeneity, which the authors attributed to variations in patient-, treatment-, and study-related factors.
Second, the confidence intervals for mortality and intracranial hemorrhage were wide, indicating that more data are necessary to fully inform these outcomes.
Third, five of the eight trials were halted early because of the evident superiority of endovascular thrombectomy, which means they fell substantially short (by up to 74%) of their planned sample sizes. This tends to cause overestimation of treatment effects. Fourth, nearly all these strokes involved carotid territory, nearly all the patients were on the young end of the age spectrum, and very few participants had comorbidities such as AF or diabetes. Such favorable characteristics do not reflect real-world experience with ischemic stroke.
Dr. Joanna M. Wardlaw and Dr. Martin S. Dennis are at the Centre for Clinical Brain Sciences at the University of Edinburgh (Scotland). They reported having no relevant financial disclosures. Dr. Wardlaw and Dr. Dennis made these remarks in an editorial accompanying Dr. Badhiwala’s meta-analysis (JAMA 2015;314:1803-4).
It is important to note some limitations with this well-conducted meta-analysis. First, functional outcomes showed significant heterogeneity, which the authors attributed to variations in patient-, treatment-, and study-related factors.
Second, the confidence intervals for mortality and intracranial hemorrhage were wide, indicating that more data are necessary to fully inform these outcomes.
Third, five of the eight trials were halted early because of the evident superiority of endovascular thrombectomy, which means they fell substantially short (by up to 74%) of their planned sample sizes. This tends to cause overestimation of treatment effects. Fourth, nearly all these strokes involved carotid territory, nearly all the patients were on the young end of the age spectrum, and very few participants had comorbidities such as AF or diabetes. Such favorable characteristics do not reflect real-world experience with ischemic stroke.
Dr. Joanna M. Wardlaw and Dr. Martin S. Dennis are at the Centre for Clinical Brain Sciences at the University of Edinburgh (Scotland). They reported having no relevant financial disclosures. Dr. Wardlaw and Dr. Dennis made these remarks in an editorial accompanying Dr. Badhiwala’s meta-analysis (JAMA 2015;314:1803-4).
Endovascular mechanical thrombectomy yielded better function and revascularization rates but similar mortality and intracranial hemorrhage rates as standard medical therapy using tissue plasminogen activator (tPA) in a meta-analysis of eight high-quality randomized clinical trials comparing the two approaches for acute ischemic stroke.
The results were published online Nov. 3 in JAMA.
This meta-analysis included only large multicenter trials published from 2013 to the present. Previous trials and meta-analyses “had several well-recognized limitations” including inconsistent use of vascular imaging to confirm vessel occlusion before randomization, variable use of tPA in patients who eventually were assigned to endovascular therapy, and reliance on less effective and now outdated mechanical devices, said Dr. Jetan H. Badhiwala of the division of neurosurgery, University of Toronto, and his associates.
The eight trials included 2,423 patients (mean age, 67.4 years); 46.7% were women. A total of 1,313 patients underwent endovascular therapy, defined as the intra-arterial use of a microcatheter or other device for mechanical thrombectomy, with or without the local use of a chemical thrombolytic agent. The remaining 1,110 received standard medical therapy (tPA). The interval between stroke onset and endovascular treatment varied from 5 to 12 hours across these studies, with a mean of 3.8 hours.
Patients who had endovascular thrombectomy showed significantly higher rates of functional independence at 90 days (44.6%) than did those who had tPA (31.8%), for an OR of 1.71 and a number needed to treat of 8. The rate of angiographic revascularization at 24 hours also was markedly higher for endovascular thrombectomy (75.8% vs 34.1%), for an OR of 6.49, the investigators said (JAMA 2015;314:1832-43).
However, there were no significant differences between the two study groups in rates of symptomatic intracranial hemorrhage at 90 days (5.7% vs 5.1%) or all-cause mortality at 90 days (15.8% vs 17.8%), and overall morbidity including in-hospital rates of deep venous thrombosis, MI, and pneumonia also were similar.
No sponsor or source of financial support was reported for this study. Dr. Badhiwala and his associates reported having no relevant financial disclosures.
Endovascular mechanical thrombectomy yielded better function and revascularization rates but similar mortality and intracranial hemorrhage rates as standard medical therapy using tissue plasminogen activator (tPA) in a meta-analysis of eight high-quality randomized clinical trials comparing the two approaches for acute ischemic stroke.
The results were published online Nov. 3 in JAMA.
This meta-analysis included only large multicenter trials published from 2013 to the present. Previous trials and meta-analyses “had several well-recognized limitations” including inconsistent use of vascular imaging to confirm vessel occlusion before randomization, variable use of tPA in patients who eventually were assigned to endovascular therapy, and reliance on less effective and now outdated mechanical devices, said Dr. Jetan H. Badhiwala of the division of neurosurgery, University of Toronto, and his associates.
The eight trials included 2,423 patients (mean age, 67.4 years); 46.7% were women. A total of 1,313 patients underwent endovascular therapy, defined as the intra-arterial use of a microcatheter or other device for mechanical thrombectomy, with or without the local use of a chemical thrombolytic agent. The remaining 1,110 received standard medical therapy (tPA). The interval between stroke onset and endovascular treatment varied from 5 to 12 hours across these studies, with a mean of 3.8 hours.
Patients who had endovascular thrombectomy showed significantly higher rates of functional independence at 90 days (44.6%) than did those who had tPA (31.8%), for an OR of 1.71 and a number needed to treat of 8. The rate of angiographic revascularization at 24 hours also was markedly higher for endovascular thrombectomy (75.8% vs 34.1%), for an OR of 6.49, the investigators said (JAMA 2015;314:1832-43).
However, there were no significant differences between the two study groups in rates of symptomatic intracranial hemorrhage at 90 days (5.7% vs 5.1%) or all-cause mortality at 90 days (15.8% vs 17.8%), and overall morbidity including in-hospital rates of deep venous thrombosis, MI, and pneumonia also were similar.
No sponsor or source of financial support was reported for this study. Dr. Badhiwala and his associates reported having no relevant financial disclosures.
FROM JAMA
Key clinical point: Endovascular mechanical thrombectomy yielded better function and angiographic revascularization but similar mortality and rate of intracranial hemorrhage compared with standard medical therapy (tPA) for acute ischemic stroke.
Major finding: Patients who had endovascular thrombectomy showed significantly higher rates of functional independence at 90 days (44.6%) than did those who had tPA (31.8%), for an OR of 1.71 and a number needed to treat of 8.
Data source: A meta-analysis of eight high-quality multicenter randomized clinical trials published during 2013-2015 involving 2,423 adults with acute ischemic stroke.
Disclosures: No sponsor or source of financial support was reported for this study. Dr. Badhiwala and his associates reported having no relevant financial disclosures.
Guidelines back multivessel PCI
New recommendations validate the treatment of partially blocked vessels along with the culprit vessel in patients undergoing a primary percutaneous coronary intervention for ST-elevation myocardial infarction (STEMI).
While 2013 guidelines by the American College of Cardiology and the American Heart Association cautioned against multivessel interventions as nonbeneficial in STEMI, evidence from four recent randomized controlled trials now supports the practice as “reasonable,” the updated guidelines say.
Partially blocked vessels may be treated in hemodynamically stable patients at the time of PCI or as a planned staged procedure.
The guidelines, issued Oct 21 by the ACC/AHA and the Society for Cardiovascular Angiography and Interventions, with collaboration from the American College of Emergency Physicians, have been published online in Journal of the American College of Cardiology (2015 Oct 21;10.1016/jacc.2015.10.005), Circulation, and Catheterization and Cardiovascular Interventions.
The guidelines also downgrade a prior recommendation on routine use of manual aspiration thrombectomy before primary PCI to implant a stent, citing evidence from three randomized trials (INFUSE-AMI, TASTE, and TOTAL) in support of the new class III “no benefit” recommendation. Previously, the organizations had considered this treatment strategy reasonable.
For the advice on primary PCI and multivessel treatment, the guideline authors, led by Dr. Glenn N. Levine of Baylor College of Medicine in Houston, identified four trials (PRAMI, CvLPRIT, DANAMI 3-PRIMULTI, PRAGUE-13) in which multivessel PCI, either staged or at the time of primary PCI, was shown to be nonharmful or beneficial in selected patients with STEMI. In three of these trials, multivessel treatment was shown associated with significant reductions in risk of death and other cardiac events compared to culprit-vessel-only treatment.
Previously, “differing inclusion criteria, study protocols, timing of multivessel PCI, statistical heterogeneity, and variable endpoints” made study results on culprit-only vs. multivessel PCI conflicting, Dr. Levine and colleagues wrote.
While the more recent RCTs have helped clarify a benefit or at least lack of harm, “there are insufficient observational data and no randomized data at this time to inform a recommendation with regard to the optimal timing of nonculprit vessel PCI,” the authors wrote, saying further studies were needed. Clinical data, lesion severity and complexity, and the risk of contrast nephropathy should be considered when determining whether to perform primary or staged multivessel PCI.
Earlier recommendations in 2011 and 2013 favoring aspiration thrombectomy before primary PCI had been based largely on the results of one single-center randomized study enrolling about 1,000 patients (Lancet 2008;371:1915-20).
Since then, much larger trials have shown no significant differences in major cardiac events or death in people who received aspiration thrombectomy prior to primary PCI compared with PCI alone, and a meta-analysis of more than 20,000 patients across 17 trials found no significant reduction in death, reinfarction, or stent thrombosis associated with routine aspiration thrombectomy vs. PCI alone (Circ Cardiovasc Interv. 2015;8:e002258).
The guideline authors clarified that the downgraded recommendation of “no benefit” applies only to routine use of aspiration thrombectomy before primary PCI. Current data remain inadequate to determine a benefit for selective or “bailout” aspiration thrombectomy, which is thrombectomy that, though unplanned, had to be used during the procedure because of an unsatisfactory initial result or a complication.
Several of the ACC/AHA/SCAI guideline authors or reviewers, including both vice chairs of the PCI writing committee, disclosed industry relationships.
New recommendations validate the treatment of partially blocked vessels along with the culprit vessel in patients undergoing a primary percutaneous coronary intervention for ST-elevation myocardial infarction (STEMI).
While 2013 guidelines by the American College of Cardiology and the American Heart Association cautioned against multivessel interventions as nonbeneficial in STEMI, evidence from four recent randomized controlled trials now supports the practice as “reasonable,” the updated guidelines say.
Partially blocked vessels may be treated in hemodynamically stable patients at the time of PCI or as a planned staged procedure.
The guidelines, issued Oct 21 by the ACC/AHA and the Society for Cardiovascular Angiography and Interventions, with collaboration from the American College of Emergency Physicians, have been published online in Journal of the American College of Cardiology (2015 Oct 21;10.1016/jacc.2015.10.005), Circulation, and Catheterization and Cardiovascular Interventions.
The guidelines also downgrade a prior recommendation on routine use of manual aspiration thrombectomy before primary PCI to implant a stent, citing evidence from three randomized trials (INFUSE-AMI, TASTE, and TOTAL) in support of the new class III “no benefit” recommendation. Previously, the organizations had considered this treatment strategy reasonable.
For the advice on primary PCI and multivessel treatment, the guideline authors, led by Dr. Glenn N. Levine of Baylor College of Medicine in Houston, identified four trials (PRAMI, CvLPRIT, DANAMI 3-PRIMULTI, PRAGUE-13) in which multivessel PCI, either staged or at the time of primary PCI, was shown to be nonharmful or beneficial in selected patients with STEMI. In three of these trials, multivessel treatment was shown associated with significant reductions in risk of death and other cardiac events compared to culprit-vessel-only treatment.
Previously, “differing inclusion criteria, study protocols, timing of multivessel PCI, statistical heterogeneity, and variable endpoints” made study results on culprit-only vs. multivessel PCI conflicting, Dr. Levine and colleagues wrote.
While the more recent RCTs have helped clarify a benefit or at least lack of harm, “there are insufficient observational data and no randomized data at this time to inform a recommendation with regard to the optimal timing of nonculprit vessel PCI,” the authors wrote, saying further studies were needed. Clinical data, lesion severity and complexity, and the risk of contrast nephropathy should be considered when determining whether to perform primary or staged multivessel PCI.
Earlier recommendations in 2011 and 2013 favoring aspiration thrombectomy before primary PCI had been based largely on the results of one single-center randomized study enrolling about 1,000 patients (Lancet 2008;371:1915-20).
Since then, much larger trials have shown no significant differences in major cardiac events or death in people who received aspiration thrombectomy prior to primary PCI compared with PCI alone, and a meta-analysis of more than 20,000 patients across 17 trials found no significant reduction in death, reinfarction, or stent thrombosis associated with routine aspiration thrombectomy vs. PCI alone (Circ Cardiovasc Interv. 2015;8:e002258).
The guideline authors clarified that the downgraded recommendation of “no benefit” applies only to routine use of aspiration thrombectomy before primary PCI. Current data remain inadequate to determine a benefit for selective or “bailout” aspiration thrombectomy, which is thrombectomy that, though unplanned, had to be used during the procedure because of an unsatisfactory initial result or a complication.
Several of the ACC/AHA/SCAI guideline authors or reviewers, including both vice chairs of the PCI writing committee, disclosed industry relationships.
New recommendations validate the treatment of partially blocked vessels along with the culprit vessel in patients undergoing a primary percutaneous coronary intervention for ST-elevation myocardial infarction (STEMI).
While 2013 guidelines by the American College of Cardiology and the American Heart Association cautioned against multivessel interventions as nonbeneficial in STEMI, evidence from four recent randomized controlled trials now supports the practice as “reasonable,” the updated guidelines say.
Partially blocked vessels may be treated in hemodynamically stable patients at the time of PCI or as a planned staged procedure.
The guidelines, issued Oct 21 by the ACC/AHA and the Society for Cardiovascular Angiography and Interventions, with collaboration from the American College of Emergency Physicians, have been published online in Journal of the American College of Cardiology (2015 Oct 21;10.1016/jacc.2015.10.005), Circulation, and Catheterization and Cardiovascular Interventions.
The guidelines also downgrade a prior recommendation on routine use of manual aspiration thrombectomy before primary PCI to implant a stent, citing evidence from three randomized trials (INFUSE-AMI, TASTE, and TOTAL) in support of the new class III “no benefit” recommendation. Previously, the organizations had considered this treatment strategy reasonable.
For the advice on primary PCI and multivessel treatment, the guideline authors, led by Dr. Glenn N. Levine of Baylor College of Medicine in Houston, identified four trials (PRAMI, CvLPRIT, DANAMI 3-PRIMULTI, PRAGUE-13) in which multivessel PCI, either staged or at the time of primary PCI, was shown to be nonharmful or beneficial in selected patients with STEMI. In three of these trials, multivessel treatment was shown associated with significant reductions in risk of death and other cardiac events compared to culprit-vessel-only treatment.
Previously, “differing inclusion criteria, study protocols, timing of multivessel PCI, statistical heterogeneity, and variable endpoints” made study results on culprit-only vs. multivessel PCI conflicting, Dr. Levine and colleagues wrote.
While the more recent RCTs have helped clarify a benefit or at least lack of harm, “there are insufficient observational data and no randomized data at this time to inform a recommendation with regard to the optimal timing of nonculprit vessel PCI,” the authors wrote, saying further studies were needed. Clinical data, lesion severity and complexity, and the risk of contrast nephropathy should be considered when determining whether to perform primary or staged multivessel PCI.
Earlier recommendations in 2011 and 2013 favoring aspiration thrombectomy before primary PCI had been based largely on the results of one single-center randomized study enrolling about 1,000 patients (Lancet 2008;371:1915-20).
Since then, much larger trials have shown no significant differences in major cardiac events or death in people who received aspiration thrombectomy prior to primary PCI compared with PCI alone, and a meta-analysis of more than 20,000 patients across 17 trials found no significant reduction in death, reinfarction, or stent thrombosis associated with routine aspiration thrombectomy vs. PCI alone (Circ Cardiovasc Interv. 2015;8:e002258).
The guideline authors clarified that the downgraded recommendation of “no benefit” applies only to routine use of aspiration thrombectomy before primary PCI. Current data remain inadequate to determine a benefit for selective or “bailout” aspiration thrombectomy, which is thrombectomy that, though unplanned, had to be used during the procedure because of an unsatisfactory initial result or a complication.
Several of the ACC/AHA/SCAI guideline authors or reviewers, including both vice chairs of the PCI writing committee, disclosed industry relationships.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Women usually given dabigatran in lower dose
In real-world practice, women who are prescribed dabigatran for atrial fibrillation (AF) are usually given the lower dose of the drug, even though the higher dose appears to be more protective against stroke, according to Canadian database analysis published online Oct. 27 in Circulation: Cardiovascular Quality and Outcomes.
In RE-LY, the main randomized clinical trial showing that dabigatran is more effective at preventing stroke and provoked fewer bleeding episodes than warfarin, only 37% of the participants were women (N Engl J Med. 2009 Sep 17; 361[12]1139-51).This raises the question of whether the study’s results are truly applicable to women. In addition, the women in that trial showed plasma concentrations of dabigatran that were 30% higher than those in men, suggesting that the drug’s safety profile may differ between women and men. However, there was no mention of sex differences related to outcomes, said Meytal Avgil Tsadok, Ph.D., of the division of clinical epidemiology, McGill University Health Center, Montreal, and her associates.
To examine sex-based differences in prescribing patterns in real-world practice, the investigators performed a population-based cohort study among 631,110 residents of Quebec who were discharged from the hospital with either a primary or a secondary diagnosis of AF during a 14-year period. They identified 15,918 dabigatran users and matched them for comorbidity, age at AF diagnosis, and date of first prescription for anticoagulants with 47,192 warfarin users (control subjects). The 31,786 women and 31,324 men participating in this study were followed for a median of 1.3 years (range, 0-3.2 years) for the development of stroke/TIA, bleeding events, or hospitalization for MI.
The researchers found that dabigatran use differed markedly between women and men. Men were prescribed the lower dose (110 mg) in nearly equal numbers with the higher dose (150 mg) of dabigatran, but women were prescribed the lower dose (64.8%) much more often than the higher dose (35.2%). In a further analysis of the data, women were much more likely than men to fill prescriptions of the lower dose (odds ratio, 1.35). This was true even though women, but not men, showed a trend toward a lower incidence of stroke when prescribed the higher dose of dabigatran, compared with warfarin.
These prescribing practices remained consistent even when the participants were categorized according to age. More women than men used low-dose dabigatran whether they were younger than 75 years of age (22.8% vs. 18.5%) or older than 75 years (83.5% vs. 76.0%). These findings show that, regardless of patient age or comorbidities, “women have 35% higher chances to be prescribed a lower dabigatran dose than men, although women have a higher baseline risk for stroke,” Dr. Tsadok and her associates said (Circ Cardiovasc Qual Outcomes. 2015 Oct 27 [doi: 10.1161/circoutcomes.114.001398]).
The reason for this discrepancy is not yet known. A similar pattern of prescribing was noted in a Danish population-based cohort study. It’s possible that clinicians perceive women as frailer patients than men, “so they tend to be more concerned about safety and, therefore, prescribe women with a lower dose, compromising efficacy,” the investigators said.
Their study was limited in that follow-up was relatively short at approximately 1 year. It is therefore possible that they underestimated the risks of stroke/TIA, bleeding events, or MI hospitalization, Dr. Tsadok and her associates added.
This study was supported by the Canadian Institutes of Health Research. Dr. Tsadok and her associates reported having no relevant financial disclosures.
In real-world practice, women who are prescribed dabigatran for atrial fibrillation (AF) are usually given the lower dose of the drug, even though the higher dose appears to be more protective against stroke, according to Canadian database analysis published online Oct. 27 in Circulation: Cardiovascular Quality and Outcomes.
In RE-LY, the main randomized clinical trial showing that dabigatran is more effective at preventing stroke and provoked fewer bleeding episodes than warfarin, only 37% of the participants were women (N Engl J Med. 2009 Sep 17; 361[12]1139-51).This raises the question of whether the study’s results are truly applicable to women. In addition, the women in that trial showed plasma concentrations of dabigatran that were 30% higher than those in men, suggesting that the drug’s safety profile may differ between women and men. However, there was no mention of sex differences related to outcomes, said Meytal Avgil Tsadok, Ph.D., of the division of clinical epidemiology, McGill University Health Center, Montreal, and her associates.
To examine sex-based differences in prescribing patterns in real-world practice, the investigators performed a population-based cohort study among 631,110 residents of Quebec who were discharged from the hospital with either a primary or a secondary diagnosis of AF during a 14-year period. They identified 15,918 dabigatran users and matched them for comorbidity, age at AF diagnosis, and date of first prescription for anticoagulants with 47,192 warfarin users (control subjects). The 31,786 women and 31,324 men participating in this study were followed for a median of 1.3 years (range, 0-3.2 years) for the development of stroke/TIA, bleeding events, or hospitalization for MI.
The researchers found that dabigatran use differed markedly between women and men. Men were prescribed the lower dose (110 mg) in nearly equal numbers with the higher dose (150 mg) of dabigatran, but women were prescribed the lower dose (64.8%) much more often than the higher dose (35.2%). In a further analysis of the data, women were much more likely than men to fill prescriptions of the lower dose (odds ratio, 1.35). This was true even though women, but not men, showed a trend toward a lower incidence of stroke when prescribed the higher dose of dabigatran, compared with warfarin.
These prescribing practices remained consistent even when the participants were categorized according to age. More women than men used low-dose dabigatran whether they were younger than 75 years of age (22.8% vs. 18.5%) or older than 75 years (83.5% vs. 76.0%). These findings show that, regardless of patient age or comorbidities, “women have 35% higher chances to be prescribed a lower dabigatran dose than men, although women have a higher baseline risk for stroke,” Dr. Tsadok and her associates said (Circ Cardiovasc Qual Outcomes. 2015 Oct 27 [doi: 10.1161/circoutcomes.114.001398]).
The reason for this discrepancy is not yet known. A similar pattern of prescribing was noted in a Danish population-based cohort study. It’s possible that clinicians perceive women as frailer patients than men, “so they tend to be more concerned about safety and, therefore, prescribe women with a lower dose, compromising efficacy,” the investigators said.
Their study was limited in that follow-up was relatively short at approximately 1 year. It is therefore possible that they underestimated the risks of stroke/TIA, bleeding events, or MI hospitalization, Dr. Tsadok and her associates added.
This study was supported by the Canadian Institutes of Health Research. Dr. Tsadok and her associates reported having no relevant financial disclosures.
In real-world practice, women who are prescribed dabigatran for atrial fibrillation (AF) are usually given the lower dose of the drug, even though the higher dose appears to be more protective against stroke, according to Canadian database analysis published online Oct. 27 in Circulation: Cardiovascular Quality and Outcomes.
In RE-LY, the main randomized clinical trial showing that dabigatran is more effective at preventing stroke and provoked fewer bleeding episodes than warfarin, only 37% of the participants were women (N Engl J Med. 2009 Sep 17; 361[12]1139-51).This raises the question of whether the study’s results are truly applicable to women. In addition, the women in that trial showed plasma concentrations of dabigatran that were 30% higher than those in men, suggesting that the drug’s safety profile may differ between women and men. However, there was no mention of sex differences related to outcomes, said Meytal Avgil Tsadok, Ph.D., of the division of clinical epidemiology, McGill University Health Center, Montreal, and her associates.
To examine sex-based differences in prescribing patterns in real-world practice, the investigators performed a population-based cohort study among 631,110 residents of Quebec who were discharged from the hospital with either a primary or a secondary diagnosis of AF during a 14-year period. They identified 15,918 dabigatran users and matched them for comorbidity, age at AF diagnosis, and date of first prescription for anticoagulants with 47,192 warfarin users (control subjects). The 31,786 women and 31,324 men participating in this study were followed for a median of 1.3 years (range, 0-3.2 years) for the development of stroke/TIA, bleeding events, or hospitalization for MI.
The researchers found that dabigatran use differed markedly between women and men. Men were prescribed the lower dose (110 mg) in nearly equal numbers with the higher dose (150 mg) of dabigatran, but women were prescribed the lower dose (64.8%) much more often than the higher dose (35.2%). In a further analysis of the data, women were much more likely than men to fill prescriptions of the lower dose (odds ratio, 1.35). This was true even though women, but not men, showed a trend toward a lower incidence of stroke when prescribed the higher dose of dabigatran, compared with warfarin.
These prescribing practices remained consistent even when the participants were categorized according to age. More women than men used low-dose dabigatran whether they were younger than 75 years of age (22.8% vs. 18.5%) or older than 75 years (83.5% vs. 76.0%). These findings show that, regardless of patient age or comorbidities, “women have 35% higher chances to be prescribed a lower dabigatran dose than men, although women have a higher baseline risk for stroke,” Dr. Tsadok and her associates said (Circ Cardiovasc Qual Outcomes. 2015 Oct 27 [doi: 10.1161/circoutcomes.114.001398]).
The reason for this discrepancy is not yet known. A similar pattern of prescribing was noted in a Danish population-based cohort study. It’s possible that clinicians perceive women as frailer patients than men, “so they tend to be more concerned about safety and, therefore, prescribe women with a lower dose, compromising efficacy,” the investigators said.
Their study was limited in that follow-up was relatively short at approximately 1 year. It is therefore possible that they underestimated the risks of stroke/TIA, bleeding events, or MI hospitalization, Dr. Tsadok and her associates added.
This study was supported by the Canadian Institutes of Health Research. Dr. Tsadok and her associates reported having no relevant financial disclosures.
FROM CIRCULATION: CARDIOVASCULAR QUALITY AND OUTCOMES
Key clinical point: Women prescribed dabigatran for AF are usually given the lower dose of the drug, for unknown reasons.
Major finding: Men were prescribed the lower dose (110 mg) in nearly equal numbers with the higher dose (150 mg) of dabigatran, but women were prescribed the lower dose (64.8%) much more often than the higher dose (35.2%).
Data source: An analysis of prescribing patterns in a population-based cohort of 31,786 women and 31,324 men who had AF living in Quebec.
Disclosures: This study was supported by the Canadian Institutes of Health Research. Dr. Tsadok and her associates reported having no relevant financial disclosures.
VIDEO: ASAP 2 trial will test Watchman in warfarin-contraindicated patients
Now that the Watchman device for left atrial appendage closure is on the U.S. market, target patients are those with atrial fibrillation who can tolerate at least a brief, 6-week course of treatment with warfarin – which is what the device’s labeling demands – but are poor candidates for long-term treatment with oral anticoagulation because they have had a serious bleeding episode while on anticoagulant treatment, Dr. Vivek Y. Reddy said in an interview.
Another type of atrial fibrillation patient who is potentially a prime target for Watchman placement are those with a complete contraindication to warfarin treatment, but as of now this makes then ineligible to receive the device. This category of patient will be the target of the ASAP 2 trial, a large, multicenter trial planned to start by the end of 2015 that will randomize atrial fibrillation patients ineligible to receive any oral anticoagulation to receive Watchman followed by a 6-month period of dual antiplatelet therapy or to current standard therapy for such patients with aspirin alone, said Dr. Reddy, professor of medicine and director of the cardiac arrhythmia service at Mount Sinai Hospital in New York.
The ASAP 2 trial follows the pilot study ASAP (ASA Plavix Feasibility Study With WATCHMAN Left Atrial Appendage Closure Technology) that Dr. Reddy led and ran at four centers in Europe placing Watchman in patients ineligible to receive any oral anticoagulant treatment followed by 6 months of dual antiplatelet therapy. The ASAP results showed that this approach could be safe and effective (J Am Coll Cardiol. 2013 Jun 25;61[25]:2551-6.).
Patients with a total contraindication against treatment with warfarin or another oral anticoagulant “have the greatest need,” said Dr. Reddy. “The problem is we don’t have much safety data” for these patients, and while the results from the ASAP trial showed the device can be safely placed just using dual antiplatelet therapy the numbers were small and the device is not approved for use in this setting, he said.
Dr. Reddy has been an advisor to and received research grants from Atritech/Boston Scientific, the companies that developed and now market Watchman.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
Now that the Watchman device for left atrial appendage closure is on the U.S. market, target patients are those with atrial fibrillation who can tolerate at least a brief, 6-week course of treatment with warfarin – which is what the device’s labeling demands – but are poor candidates for long-term treatment with oral anticoagulation because they have had a serious bleeding episode while on anticoagulant treatment, Dr. Vivek Y. Reddy said in an interview.
Another type of atrial fibrillation patient who is potentially a prime target for Watchman placement are those with a complete contraindication to warfarin treatment, but as of now this makes then ineligible to receive the device. This category of patient will be the target of the ASAP 2 trial, a large, multicenter trial planned to start by the end of 2015 that will randomize atrial fibrillation patients ineligible to receive any oral anticoagulation to receive Watchman followed by a 6-month period of dual antiplatelet therapy or to current standard therapy for such patients with aspirin alone, said Dr. Reddy, professor of medicine and director of the cardiac arrhythmia service at Mount Sinai Hospital in New York.
The ASAP 2 trial follows the pilot study ASAP (ASA Plavix Feasibility Study With WATCHMAN Left Atrial Appendage Closure Technology) that Dr. Reddy led and ran at four centers in Europe placing Watchman in patients ineligible to receive any oral anticoagulant treatment followed by 6 months of dual antiplatelet therapy. The ASAP results showed that this approach could be safe and effective (J Am Coll Cardiol. 2013 Jun 25;61[25]:2551-6.).
Patients with a total contraindication against treatment with warfarin or another oral anticoagulant “have the greatest need,” said Dr. Reddy. “The problem is we don’t have much safety data” for these patients, and while the results from the ASAP trial showed the device can be safely placed just using dual antiplatelet therapy the numbers were small and the device is not approved for use in this setting, he said.
Dr. Reddy has been an advisor to and received research grants from Atritech/Boston Scientific, the companies that developed and now market Watchman.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
Now that the Watchman device for left atrial appendage closure is on the U.S. market, target patients are those with atrial fibrillation who can tolerate at least a brief, 6-week course of treatment with warfarin – which is what the device’s labeling demands – but are poor candidates for long-term treatment with oral anticoagulation because they have had a serious bleeding episode while on anticoagulant treatment, Dr. Vivek Y. Reddy said in an interview.
Another type of atrial fibrillation patient who is potentially a prime target for Watchman placement are those with a complete contraindication to warfarin treatment, but as of now this makes then ineligible to receive the device. This category of patient will be the target of the ASAP 2 trial, a large, multicenter trial planned to start by the end of 2015 that will randomize atrial fibrillation patients ineligible to receive any oral anticoagulation to receive Watchman followed by a 6-month period of dual antiplatelet therapy or to current standard therapy for such patients with aspirin alone, said Dr. Reddy, professor of medicine and director of the cardiac arrhythmia service at Mount Sinai Hospital in New York.
The ASAP 2 trial follows the pilot study ASAP (ASA Plavix Feasibility Study With WATCHMAN Left Atrial Appendage Closure Technology) that Dr. Reddy led and ran at four centers in Europe placing Watchman in patients ineligible to receive any oral anticoagulant treatment followed by 6 months of dual antiplatelet therapy. The ASAP results showed that this approach could be safe and effective (J Am Coll Cardiol. 2013 Jun 25;61[25]:2551-6.).
Patients with a total contraindication against treatment with warfarin or another oral anticoagulant “have the greatest need,” said Dr. Reddy. “The problem is we don’t have much safety data” for these patients, and while the results from the ASAP trial showed the device can be safely placed just using dual antiplatelet therapy the numbers were small and the device is not approved for use in this setting, he said.
Dr. Reddy has been an advisor to and received research grants from Atritech/Boston Scientific, the companies that developed and now market Watchman.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
Every 10° C temperature drop increases STEMI risk by 7%
LONDON – For every 10° C drop in the highest daily air temperature, the risk for ST-elevation myocardial infraction was found to increase by 7% in a Canadian study.
Researchers at the University of Manitoba in Winnipeg performed a retrospective study of all STEMI cases that had occurred in the city during 2009-2014 and linked them to daily air temperatures collected from Environment Canada.
“There is a clear correlation between cold weather and heart attacks,” said Dr. Shuangbo Liu, who presented the findings at the annual congress of the European Society of Cardiology. Previous studies have shown that the incidence of, hospitalization for, and death as a result of, MI are all increased as the weather gets colder. But until now, it wasn’t known what the specific relationship between temperature drops and the rate of STEMI was, she explained.
STEMIs typically occur as a result of acute rupture of an atherosclerotic plaque, but although the risk factors for the development for the plaques have been widely studied, the risk factors for rupture are not so well defined. There is some suggestion that colder weather is linked to factors that might predispose to plaque rupture, such as an increased cardiac workload, higher blood pressure, and an increased procoagulant state.
Winnipeg is one of the coldest large cities in the world in winter, but has more temperate fall and spring seasons with hot and dry summers, and so provided the ideal place to study the effect of environmental temperature on the risk of STEMI, Dr. Liu said.
Over the 6-year retrospective audit period, 1,817 STEMIs were recorded. Only STEMIs that were reported within 12 hours of admission were included in the analyses, with almost all (95%) patients undergoing primary percutaneous coronary intervention.
The highest daily temperature reached was 20° C on 31% of the study days, 0°-20° on 38% of the study days, and less than 0° on 32% of the study days.
The cold – but not warm – weather was associated with the risk of STEMI, with the daily high temperature being the strongest predictor of having a heart attack. On the study days where the highest temperature reached was less than 0°, the STEMI event rate was 0.94 per day. This rate was significantly higher than that when the daily high temperature was above 0°, at a rate of 0.79 per day overall (P less than .001)
STEMI rates on days that were 0°-10°, 10°-20°, 20°-30°, and 30° and above were 0.89, 0.81, 0.74, and 0.61 per day, respectively.
Although any snowfall in the last 2 days was predictive of STEMI on univariate analysis, upping the risk by 20%, it did not remain so after adjustment for temperature.
The daily high temperatures on the 1-2 days preceding STEMI were found to be predictive in univariate analyses, increasing the relative risk by 19%-20% (P less than .001).
Dr. Liu acknowledged the limitations of using retrospective administrative data and that further prospective validation of the results would be needed. However, these data are “thought provoking,” she said, and suggest that increasing public awareness is needed and perhaps health care resources need to be reallocated to help prevent the seasonal surge in STEMI observed in the study.
Dr. Liu reported having no relevant financial disclosures.
LONDON – For every 10° C drop in the highest daily air temperature, the risk for ST-elevation myocardial infraction was found to increase by 7% in a Canadian study.
Researchers at the University of Manitoba in Winnipeg performed a retrospective study of all STEMI cases that had occurred in the city during 2009-2014 and linked them to daily air temperatures collected from Environment Canada.
“There is a clear correlation between cold weather and heart attacks,” said Dr. Shuangbo Liu, who presented the findings at the annual congress of the European Society of Cardiology. Previous studies have shown that the incidence of, hospitalization for, and death as a result of, MI are all increased as the weather gets colder. But until now, it wasn’t known what the specific relationship between temperature drops and the rate of STEMI was, she explained.
STEMIs typically occur as a result of acute rupture of an atherosclerotic plaque, but although the risk factors for the development for the plaques have been widely studied, the risk factors for rupture are not so well defined. There is some suggestion that colder weather is linked to factors that might predispose to plaque rupture, such as an increased cardiac workload, higher blood pressure, and an increased procoagulant state.
Winnipeg is one of the coldest large cities in the world in winter, but has more temperate fall and spring seasons with hot and dry summers, and so provided the ideal place to study the effect of environmental temperature on the risk of STEMI, Dr. Liu said.
Over the 6-year retrospective audit period, 1,817 STEMIs were recorded. Only STEMIs that were reported within 12 hours of admission were included in the analyses, with almost all (95%) patients undergoing primary percutaneous coronary intervention.
The highest daily temperature reached was 20° C on 31% of the study days, 0°-20° on 38% of the study days, and less than 0° on 32% of the study days.
The cold – but not warm – weather was associated with the risk of STEMI, with the daily high temperature being the strongest predictor of having a heart attack. On the study days where the highest temperature reached was less than 0°, the STEMI event rate was 0.94 per day. This rate was significantly higher than that when the daily high temperature was above 0°, at a rate of 0.79 per day overall (P less than .001)
STEMI rates on days that were 0°-10°, 10°-20°, 20°-30°, and 30° and above were 0.89, 0.81, 0.74, and 0.61 per day, respectively.
Although any snowfall in the last 2 days was predictive of STEMI on univariate analysis, upping the risk by 20%, it did not remain so after adjustment for temperature.
The daily high temperatures on the 1-2 days preceding STEMI were found to be predictive in univariate analyses, increasing the relative risk by 19%-20% (P less than .001).
Dr. Liu acknowledged the limitations of using retrospective administrative data and that further prospective validation of the results would be needed. However, these data are “thought provoking,” she said, and suggest that increasing public awareness is needed and perhaps health care resources need to be reallocated to help prevent the seasonal surge in STEMI observed in the study.
Dr. Liu reported having no relevant financial disclosures.
LONDON – For every 10° C drop in the highest daily air temperature, the risk for ST-elevation myocardial infraction was found to increase by 7% in a Canadian study.
Researchers at the University of Manitoba in Winnipeg performed a retrospective study of all STEMI cases that had occurred in the city during 2009-2014 and linked them to daily air temperatures collected from Environment Canada.
“There is a clear correlation between cold weather and heart attacks,” said Dr. Shuangbo Liu, who presented the findings at the annual congress of the European Society of Cardiology. Previous studies have shown that the incidence of, hospitalization for, and death as a result of, MI are all increased as the weather gets colder. But until now, it wasn’t known what the specific relationship between temperature drops and the rate of STEMI was, she explained.
STEMIs typically occur as a result of acute rupture of an atherosclerotic plaque, but although the risk factors for the development for the plaques have been widely studied, the risk factors for rupture are not so well defined. There is some suggestion that colder weather is linked to factors that might predispose to plaque rupture, such as an increased cardiac workload, higher blood pressure, and an increased procoagulant state.
Winnipeg is one of the coldest large cities in the world in winter, but has more temperate fall and spring seasons with hot and dry summers, and so provided the ideal place to study the effect of environmental temperature on the risk of STEMI, Dr. Liu said.
Over the 6-year retrospective audit period, 1,817 STEMIs were recorded. Only STEMIs that were reported within 12 hours of admission were included in the analyses, with almost all (95%) patients undergoing primary percutaneous coronary intervention.
The highest daily temperature reached was 20° C on 31% of the study days, 0°-20° on 38% of the study days, and less than 0° on 32% of the study days.
The cold – but not warm – weather was associated with the risk of STEMI, with the daily high temperature being the strongest predictor of having a heart attack. On the study days where the highest temperature reached was less than 0°, the STEMI event rate was 0.94 per day. This rate was significantly higher than that when the daily high temperature was above 0°, at a rate of 0.79 per day overall (P less than .001)
STEMI rates on days that were 0°-10°, 10°-20°, 20°-30°, and 30° and above were 0.89, 0.81, 0.74, and 0.61 per day, respectively.
Although any snowfall in the last 2 days was predictive of STEMI on univariate analysis, upping the risk by 20%, it did not remain so after adjustment for temperature.
The daily high temperatures on the 1-2 days preceding STEMI were found to be predictive in univariate analyses, increasing the relative risk by 19%-20% (P less than .001).
Dr. Liu acknowledged the limitations of using retrospective administrative data and that further prospective validation of the results would be needed. However, these data are “thought provoking,” she said, and suggest that increasing public awareness is needed and perhaps health care resources need to be reallocated to help prevent the seasonal surge in STEMI observed in the study.
Dr. Liu reported having no relevant financial disclosures.
Key clinical point: As the air temperature gets progressively lower, the STEMI risk increases.
Major finding: The STEMI event rate was 0.94 per day when the daily high temperature was below 0° C vs. 0.79 per day when it was above 0° C (P less than .001).
Data source: A retrospective audit of all 1,817 cases of STEMI occurring in Winnipeg between 2009 and 2014.
Disclosures: Dr. Liu reported having no relevant financial disclosures.
Low incidence of DVT reported after percutaneous EVAR
Completely percutaneous endovascular aortic aneurysm repair (PEVAR) has become more common, using the suture-mediated “preclose” technique. The rate of periprocedural, iatrogenic, acute deep vein thrombosis (DVT), hitherto unknown, was found to be low for this approach, according to a study reported by Dr. Courtney E. Morgan and her colleagues at the Northwestern University, Chicago.
The researchers assessed 52 consecutive patients (44 men) with a mean age of 73 years, who underwent PEVAR at their center. Only 6% had a prior history of DVT (J Vasc Surg. 2015 Aug; 62:351-4).
Acute DVT was seen in four patients on postoperative day 1. These four DVTs comprised one femoropopliteal, and three calf DVTs. Three of these patients had associated risk factors: history of DVT (two patients); active smokers (one patient); and obesity (body mass index greater than 30 kg/m2 in all three patients).
At 2 weeks postoperatively, 75% of the DVTs had resolved.
“We found an overall rate of proximal DVT of 4% after PEVAR, which increased to 13% when calf-vein DVTs were included. Most patients with postoperative DVT had preexisting risk factors, which suggests that routine duplex ultrasound screening after PEVAR is not necessary unless there exist preclinical risk factors or postprocedural clinical indications suggestive of DVT,” the authors concluded.
Two of the researchers have received funding and/or served as speakers/consultants for device companies involved in EVAR.
Read the full study online in the Journal of Vascular Surgery.
Completely percutaneous endovascular aortic aneurysm repair (PEVAR) has become more common, using the suture-mediated “preclose” technique. The rate of periprocedural, iatrogenic, acute deep vein thrombosis (DVT), hitherto unknown, was found to be low for this approach, according to a study reported by Dr. Courtney E. Morgan and her colleagues at the Northwestern University, Chicago.
The researchers assessed 52 consecutive patients (44 men) with a mean age of 73 years, who underwent PEVAR at their center. Only 6% had a prior history of DVT (J Vasc Surg. 2015 Aug; 62:351-4).
Acute DVT was seen in four patients on postoperative day 1. These four DVTs comprised one femoropopliteal, and three calf DVTs. Three of these patients had associated risk factors: history of DVT (two patients); active smokers (one patient); and obesity (body mass index greater than 30 kg/m2 in all three patients).
At 2 weeks postoperatively, 75% of the DVTs had resolved.
“We found an overall rate of proximal DVT of 4% after PEVAR, which increased to 13% when calf-vein DVTs were included. Most patients with postoperative DVT had preexisting risk factors, which suggests that routine duplex ultrasound screening after PEVAR is not necessary unless there exist preclinical risk factors or postprocedural clinical indications suggestive of DVT,” the authors concluded.
Two of the researchers have received funding and/or served as speakers/consultants for device companies involved in EVAR.
Read the full study online in the Journal of Vascular Surgery.
Completely percutaneous endovascular aortic aneurysm repair (PEVAR) has become more common, using the suture-mediated “preclose” technique. The rate of periprocedural, iatrogenic, acute deep vein thrombosis (DVT), hitherto unknown, was found to be low for this approach, according to a study reported by Dr. Courtney E. Morgan and her colleagues at the Northwestern University, Chicago.
The researchers assessed 52 consecutive patients (44 men) with a mean age of 73 years, who underwent PEVAR at their center. Only 6% had a prior history of DVT (J Vasc Surg. 2015 Aug; 62:351-4).
Acute DVT was seen in four patients on postoperative day 1. These four DVTs comprised one femoropopliteal, and three calf DVTs. Three of these patients had associated risk factors: history of DVT (two patients); active smokers (one patient); and obesity (body mass index greater than 30 kg/m2 in all three patients).
At 2 weeks postoperatively, 75% of the DVTs had resolved.
“We found an overall rate of proximal DVT of 4% after PEVAR, which increased to 13% when calf-vein DVTs were included. Most patients with postoperative DVT had preexisting risk factors, which suggests that routine duplex ultrasound screening after PEVAR is not necessary unless there exist preclinical risk factors or postprocedural clinical indications suggestive of DVT,” the authors concluded.
Two of the researchers have received funding and/or served as speakers/consultants for device companies involved in EVAR.
Read the full study online in the Journal of Vascular Surgery.
FROM THE JOURNAL OF VASCULAR SURGERY
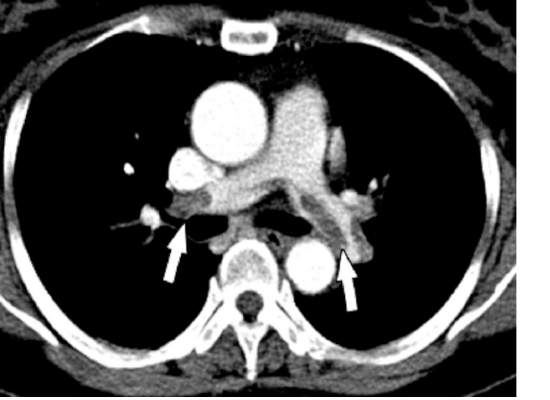
Mean platelet volume higher in DVT patients with PE than without
Mean platelet volume (MPV) has been associated with deep vein thrombosis (DVT), but it also appears to be a potential predictor of the presence of pulmonary embolism (PE), according to a retrospective analysis of patients reported by Dr. Atilla Icli of Ahi Evran University, Kirsehir, Turkey, and his colleagues.
The researchers assessed three groups of patients among those admitted to the emergency department or outpatient clinic of two university hospitals during 2005-2014. The patient study groups consisted of 98 patients with DVT and PE (48 men; mean age, 56.8 years); 97 patients with DVT without PE (48 men; mean age, 54.2 years); and 98 patients admitted with suspicion of DVT, but confirmed to be free of DVT and PE (45 men; mean age, 55.0 years) (Heart Lung Circulation. 2015 Nov;24[11]:1081-6).
There were no statistically significant differences between the groups with regard to sex, age, body mass index, or comorbidities such as hypertension or diabetes. Blood samples were drawn from all patients and assessed for MPV.
MPV was significantly higher in all DVT patients than controls (9.3 femtoliter vs. 7.9 fL; P less than .001) and in DVT patients with PE as compared to DVT patients without PE (9.9 fL vs. 8.7 fL, respectively; P less than .001). A cut-off point was seen where the rate of PE was significantly higher in patients with MPV greater than 9.15 fL, as compared with those with MPV equal to or below 9.15 fL. In addition, the presence of PE in patients with DVT was independently associated with MPV (odds ratio, 22.2; P less than .001).
“Our findings suggest that MPVs are elevated in patients with DVT, and higher MPVs may be associated with this group of patients,” Dr. Icli and his colleagues concluded.
The authors indicated that they had no relevant conflicts.
Read the full study online in Heart, Lung and Circulation.
Mean platelet volume (MPV) has been associated with deep vein thrombosis (DVT), but it also appears to be a potential predictor of the presence of pulmonary embolism (PE), according to a retrospective analysis of patients reported by Dr. Atilla Icli of Ahi Evran University, Kirsehir, Turkey, and his colleagues.
The researchers assessed three groups of patients among those admitted to the emergency department or outpatient clinic of two university hospitals during 2005-2014. The patient study groups consisted of 98 patients with DVT and PE (48 men; mean age, 56.8 years); 97 patients with DVT without PE (48 men; mean age, 54.2 years); and 98 patients admitted with suspicion of DVT, but confirmed to be free of DVT and PE (45 men; mean age, 55.0 years) (Heart Lung Circulation. 2015 Nov;24[11]:1081-6).
There were no statistically significant differences between the groups with regard to sex, age, body mass index, or comorbidities such as hypertension or diabetes. Blood samples were drawn from all patients and assessed for MPV.
MPV was significantly higher in all DVT patients than controls (9.3 femtoliter vs. 7.9 fL; P less than .001) and in DVT patients with PE as compared to DVT patients without PE (9.9 fL vs. 8.7 fL, respectively; P less than .001). A cut-off point was seen where the rate of PE was significantly higher in patients with MPV greater than 9.15 fL, as compared with those with MPV equal to or below 9.15 fL. In addition, the presence of PE in patients with DVT was independently associated with MPV (odds ratio, 22.2; P less than .001).
“Our findings suggest that MPVs are elevated in patients with DVT, and higher MPVs may be associated with this group of patients,” Dr. Icli and his colleagues concluded.
The authors indicated that they had no relevant conflicts.
Read the full study online in Heart, Lung and Circulation.
Mean platelet volume (MPV) has been associated with deep vein thrombosis (DVT), but it also appears to be a potential predictor of the presence of pulmonary embolism (PE), according to a retrospective analysis of patients reported by Dr. Atilla Icli of Ahi Evran University, Kirsehir, Turkey, and his colleagues.
The researchers assessed three groups of patients among those admitted to the emergency department or outpatient clinic of two university hospitals during 2005-2014. The patient study groups consisted of 98 patients with DVT and PE (48 men; mean age, 56.8 years); 97 patients with DVT without PE (48 men; mean age, 54.2 years); and 98 patients admitted with suspicion of DVT, but confirmed to be free of DVT and PE (45 men; mean age, 55.0 years) (Heart Lung Circulation. 2015 Nov;24[11]:1081-6).
There were no statistically significant differences between the groups with regard to sex, age, body mass index, or comorbidities such as hypertension or diabetes. Blood samples were drawn from all patients and assessed for MPV.
MPV was significantly higher in all DVT patients than controls (9.3 femtoliter vs. 7.9 fL; P less than .001) and in DVT patients with PE as compared to DVT patients without PE (9.9 fL vs. 8.7 fL, respectively; P less than .001). A cut-off point was seen where the rate of PE was significantly higher in patients with MPV greater than 9.15 fL, as compared with those with MPV equal to or below 9.15 fL. In addition, the presence of PE in patients with DVT was independently associated with MPV (odds ratio, 22.2; P less than .001).
“Our findings suggest that MPVs are elevated in patients with DVT, and higher MPVs may be associated with this group of patients,” Dr. Icli and his colleagues concluded.
The authors indicated that they had no relevant conflicts.
Read the full study online in Heart, Lung and Circulation.
FROM HEART, LUNG AND CIRCULATION
Depression, hypertension combo compounds cardiovascular risk
LONDON – The combination of depression and very high systolic blood pressure increased the risk for a major cardiovascular event by 83%, compared with normal blood pressure and no depression, in patients with existing heart disease, diabetes, or stroke.
In a large family practice–based study, the hazard ratio for first hospital admission due to myocardial infarction, stroke or heart failure, or cardiovascular death in patients with high (at least 160 mm Hg) systolic blood pressure who were also depressed was 1.83, a highly significant difference compared with individuals with normal BP and no depression.
The presence of depression also significantly increased the risk for these cardiovascular events by 36% in patients with lower systolic BPs, compared with those with normal BP and no depression.
“Patients with existing heart disease, diabetes, or stroke are more likely to have another heart attack or another stroke or die from heart problems than the general population,” Dr. Bhautesh Jani of the Institute of Health and Wellbeing, University of Glasgow (Scotland), said at the annual congress of the European Society of Cardiology.
“In particular, those who have extremes of blood pressure or those who have depressive symptoms are at higher risk, which has been shown by previous evidence. What is relatively unknown is the combined effect of having extremes of blood pressure and depressive symptoms together, and our study tried to address that problem,” Dr. Jani explained.
The study involved more than 35,500 individuals with existing heart disease, diabetes, or stroke living in Scotland, of whom 3,939 (11%) had at least one major cardiovascular event that needed hospital admission during a 4-year period. Patients had been divided into groups based on their systolic BP, and depressive symptoms were assessed using the Hospital Anxiety and Depression Scale (HADS) during 2008-2009. A HADS score of more than 7 was considered indicative of depression.
Dr. Jani noted that all the results were adjusted for multiple confounding factors, including age, gender, socioeconomic status, number of comorbid conditions, total cholesterol values, body mass index, and the initiation of antidepressant medication.
“The key implications I would suggest are for secondary prevention and to perhaps focus our resources on monitoring blood pressure and providing treatment in patients with associated depressive symptoms,” Dr. Jani proposed.
Dr. Christi Deaton, professor of clinical nursing research at the University of Cambridge (England), who commented on the study findings, noted that it highlighted the importance of raising awareness among both clinicians and patients of the potential risk associated with a combination of hypertension and depression, particularly among patients with a high level of other risk factors for further cardiovascular events.
“Screening patients for depression is very simple to do and you can start with a couple of questions asking about whether or not the patient felt sad or had low mood, and then go on to use other screening tools,” she observed. “All providers should be screening patients and thinking about the synergy of these two risk factors,” she said.
Other research presented at the ESC Congress by cardiologist Dr. Salim Hayek of Emory University in Atlanta also highlighted the importance of screening for depression, this time in patients with angina. In a study of 5,202 adults enrolled in the university’s biobank between 2004 and 2013 and who underwent left heart catheterization, patients with frequent chest pain were found to have more depressive symptoms than those without angina. Depressive symptoms in this study were assessed using the Patient Health Questionnaire (PHQ-9).
“Chest pain was more frequent in patients with mild depression with and without coronary artery disease, regardless of sex or history of myocardial infarction,” Dr. Hayek said. After multivariate analysis, depression was the most important predictor of frequent chest pain, he added. Other factors independently associated with chest pain frequency were female sex, coronary artery disease severity, history of MI, body mass index, and high blood lipid levels.
“At follow-up, a decrease in depressive symptoms was associated with improvement in chest pain,” Dr. Hayek said, but patients with depression who were revascularized did not show an improvement in chest pain.
The findings suggest that the association between chest pain and depression was independent of the underlying arterial disease and further studies are needed to look at the effect of revascularization and angina relief on depressive symptoms, and conversely if antidepressant medications could help alleviate chest pain.
The study Dr. Jani presented was funded by the Scottish Government. Dr. Jani and Dr. Hayek both reported having no disclosures.
This article was updated February 3, 2016.
LONDON – The combination of depression and very high systolic blood pressure increased the risk for a major cardiovascular event by 83%, compared with normal blood pressure and no depression, in patients with existing heart disease, diabetes, or stroke.
In a large family practice–based study, the hazard ratio for first hospital admission due to myocardial infarction, stroke or heart failure, or cardiovascular death in patients with high (at least 160 mm Hg) systolic blood pressure who were also depressed was 1.83, a highly significant difference compared with individuals with normal BP and no depression.
The presence of depression also significantly increased the risk for these cardiovascular events by 36% in patients with lower systolic BPs, compared with those with normal BP and no depression.
“Patients with existing heart disease, diabetes, or stroke are more likely to have another heart attack or another stroke or die from heart problems than the general population,” Dr. Bhautesh Jani of the Institute of Health and Wellbeing, University of Glasgow (Scotland), said at the annual congress of the European Society of Cardiology.
“In particular, those who have extremes of blood pressure or those who have depressive symptoms are at higher risk, which has been shown by previous evidence. What is relatively unknown is the combined effect of having extremes of blood pressure and depressive symptoms together, and our study tried to address that problem,” Dr. Jani explained.
The study involved more than 35,500 individuals with existing heart disease, diabetes, or stroke living in Scotland, of whom 3,939 (11%) had at least one major cardiovascular event that needed hospital admission during a 4-year period. Patients had been divided into groups based on their systolic BP, and depressive symptoms were assessed using the Hospital Anxiety and Depression Scale (HADS) during 2008-2009. A HADS score of more than 7 was considered indicative of depression.
Dr. Jani noted that all the results were adjusted for multiple confounding factors, including age, gender, socioeconomic status, number of comorbid conditions, total cholesterol values, body mass index, and the initiation of antidepressant medication.
“The key implications I would suggest are for secondary prevention and to perhaps focus our resources on monitoring blood pressure and providing treatment in patients with associated depressive symptoms,” Dr. Jani proposed.
Dr. Christi Deaton, professor of clinical nursing research at the University of Cambridge (England), who commented on the study findings, noted that it highlighted the importance of raising awareness among both clinicians and patients of the potential risk associated with a combination of hypertension and depression, particularly among patients with a high level of other risk factors for further cardiovascular events.
“Screening patients for depression is very simple to do and you can start with a couple of questions asking about whether or not the patient felt sad or had low mood, and then go on to use other screening tools,” she observed. “All providers should be screening patients and thinking about the synergy of these two risk factors,” she said.
Other research presented at the ESC Congress by cardiologist Dr. Salim Hayek of Emory University in Atlanta also highlighted the importance of screening for depression, this time in patients with angina. In a study of 5,202 adults enrolled in the university’s biobank between 2004 and 2013 and who underwent left heart catheterization, patients with frequent chest pain were found to have more depressive symptoms than those without angina. Depressive symptoms in this study were assessed using the Patient Health Questionnaire (PHQ-9).
“Chest pain was more frequent in patients with mild depression with and without coronary artery disease, regardless of sex or history of myocardial infarction,” Dr. Hayek said. After multivariate analysis, depression was the most important predictor of frequent chest pain, he added. Other factors independently associated with chest pain frequency were female sex, coronary artery disease severity, history of MI, body mass index, and high blood lipid levels.
“At follow-up, a decrease in depressive symptoms was associated with improvement in chest pain,” Dr. Hayek said, but patients with depression who were revascularized did not show an improvement in chest pain.
The findings suggest that the association between chest pain and depression was independent of the underlying arterial disease and further studies are needed to look at the effect of revascularization and angina relief on depressive symptoms, and conversely if antidepressant medications could help alleviate chest pain.
The study Dr. Jani presented was funded by the Scottish Government. Dr. Jani and Dr. Hayek both reported having no disclosures.
This article was updated February 3, 2016.
LONDON – The combination of depression and very high systolic blood pressure increased the risk for a major cardiovascular event by 83%, compared with normal blood pressure and no depression, in patients with existing heart disease, diabetes, or stroke.
In a large family practice–based study, the hazard ratio for first hospital admission due to myocardial infarction, stroke or heart failure, or cardiovascular death in patients with high (at least 160 mm Hg) systolic blood pressure who were also depressed was 1.83, a highly significant difference compared with individuals with normal BP and no depression.
The presence of depression also significantly increased the risk for these cardiovascular events by 36% in patients with lower systolic BPs, compared with those with normal BP and no depression.
“Patients with existing heart disease, diabetes, or stroke are more likely to have another heart attack or another stroke or die from heart problems than the general population,” Dr. Bhautesh Jani of the Institute of Health and Wellbeing, University of Glasgow (Scotland), said at the annual congress of the European Society of Cardiology.
“In particular, those who have extremes of blood pressure or those who have depressive symptoms are at higher risk, which has been shown by previous evidence. What is relatively unknown is the combined effect of having extremes of blood pressure and depressive symptoms together, and our study tried to address that problem,” Dr. Jani explained.
The study involved more than 35,500 individuals with existing heart disease, diabetes, or stroke living in Scotland, of whom 3,939 (11%) had at least one major cardiovascular event that needed hospital admission during a 4-year period. Patients had been divided into groups based on their systolic BP, and depressive symptoms were assessed using the Hospital Anxiety and Depression Scale (HADS) during 2008-2009. A HADS score of more than 7 was considered indicative of depression.
Dr. Jani noted that all the results were adjusted for multiple confounding factors, including age, gender, socioeconomic status, number of comorbid conditions, total cholesterol values, body mass index, and the initiation of antidepressant medication.
“The key implications I would suggest are for secondary prevention and to perhaps focus our resources on monitoring blood pressure and providing treatment in patients with associated depressive symptoms,” Dr. Jani proposed.
Dr. Christi Deaton, professor of clinical nursing research at the University of Cambridge (England), who commented on the study findings, noted that it highlighted the importance of raising awareness among both clinicians and patients of the potential risk associated with a combination of hypertension and depression, particularly among patients with a high level of other risk factors for further cardiovascular events.
“Screening patients for depression is very simple to do and you can start with a couple of questions asking about whether or not the patient felt sad or had low mood, and then go on to use other screening tools,” she observed. “All providers should be screening patients and thinking about the synergy of these two risk factors,” she said.
Other research presented at the ESC Congress by cardiologist Dr. Salim Hayek of Emory University in Atlanta also highlighted the importance of screening for depression, this time in patients with angina. In a study of 5,202 adults enrolled in the university’s biobank between 2004 and 2013 and who underwent left heart catheterization, patients with frequent chest pain were found to have more depressive symptoms than those without angina. Depressive symptoms in this study were assessed using the Patient Health Questionnaire (PHQ-9).
“Chest pain was more frequent in patients with mild depression with and without coronary artery disease, regardless of sex or history of myocardial infarction,” Dr. Hayek said. After multivariate analysis, depression was the most important predictor of frequent chest pain, he added. Other factors independently associated with chest pain frequency were female sex, coronary artery disease severity, history of MI, body mass index, and high blood lipid levels.
“At follow-up, a decrease in depressive symptoms was associated with improvement in chest pain,” Dr. Hayek said, but patients with depression who were revascularized did not show an improvement in chest pain.
The findings suggest that the association between chest pain and depression was independent of the underlying arterial disease and further studies are needed to look at the effect of revascularization and angina relief on depressive symptoms, and conversely if antidepressant medications could help alleviate chest pain.
The study Dr. Jani presented was funded by the Scottish Government. Dr. Jani and Dr. Hayek both reported having no disclosures.
This article was updated February 3, 2016.
AT THE ESC CONGRESS 2015
Key clinical point: Better monitoring and management of both hypertension and depression could help reduce further cardiovascular morbidity and mortality.
Major finding: The rate of major cardiovascular events was 83% higher in depressed patients with very high (at least 160 mm Hg) systolic BP, compared with individuals with normal pressure and no depression.
Data source: Large family practice study of 35,537 patients with existing coronary heart disease, diabetes, or stroke followed up for 4 years.
Disclosures: The study Dr. Jani presented was funded by the Scottish Government. Dr. Jani had no disclosures.