User login
Anticoagulation Hub contains news and clinical review articles for physicians seeking the most up-to-date information on the rapidly evolving treatment options for preventing stroke, acute coronary events, deep vein thrombosis, and pulmonary embolism in at-risk patients. The Anticoagulation Hub is powered by Frontline Medical Communications.
Idarucizumab approved as first agent to reverse a novel oral anticoagulant
Idarucizumab has been approved by the Food and Drug Administration for reversing the effects of dabigatran, a novel oral anticoagulant.
Specifically, idarucizumab (Praxbind) is intended for use in patients who are taking dabigatran (Pradaxa) during emergency situations when there is a need to reverse its blood-thinning effects, according to an FDA statement. Both drugs are marketed by Boehringer Ingelheim.
“The anticoagulant effects of Pradaxa are important and life-saving for some patients, but there are situations where reversal of the drug’s effects is medically necessary,” said Dr. Richard Pazdur, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Today’s approval offers the medical community an important tool for managing patients taking Pradaxa in emergency or life-threatening situations when bleeding can’t be controlled.”
The decision, released on Oct. 16, was based on efficacy and safety observed in three randomized trials, the largest of which is the ongoing phase III RE-VERSE AD.
Patients were enrolled into two distinct groups in RE-VERSE AD. Group A, with 51 patients, comprised patients on dabigatran experiencing a serious bleeding episode. Group B, with 39 patients, comprised patients on dabigatran who required an urgent surgical procedure. In both, 5 g of idarucizumab solution was administered intravenously. The primary endpoint was maximum percentage reversal of the anticoagulant effect of dabigatran within 4 hours.
In both groups, the median maximum percentage reversal was 100%. Other measures corroborated a rapid and highly effective reversal of anticoagulation. For example, the dilute thrombin time in those who could be evaluated was normalized in 98% of group A and 93% of group B (N Engl J Med. 2015 Aug 6. doi:10.1056/NEJMoa1502000).
Interim results of RE-VERSE AD “show rather convincingly that idarucizumab completely and safely reverses the anticoagulant effects of dabigatran within minutes,” said the lead author, Dr. Charles V. Pollack Jr., chairman of the department of emergency medicine at the University of Pennsylvania, Philadelphia. Dr. Pollack presented the findings at the 2015 International Society of Thrombosis and Haemostatis (ISTH) Congress in June.
Idarucizumab is the first reversal agent for any of the novel oral anticoagulants used as an alternative to warfarin. Unlike warfarin, which can be reversed with vitamin K, the lack of a reversal agent for dabigatran, a direct thrombin inhibitor, and other novel agents, such as rivaroxaban and apixaban, which are direct factor Xa inhibitors, has been a concern for patients who experience unexpected bleeding or face a risk of bleeding because of the need for urgent surgery. The laboratory findings were supported by the clinical findings, according to Dr. Pollack.
“Clinical outcomes were quite good in this multimorbid patient population,” he said. “Restoration of hemostasis as reported by local investigators was achieved in less than 12 hours when assessable, and 92% of the surgical patients were reported to have normal hemostasis at the time of the procedure.”
Idarucizumab was also found safe in this and the two previous randomized studies. In the 237 healthy volunteers evaluated previously, no serious adverse events were reported. In RE-VERSE AD, serious adverse events leading to death included hemorrhagic and thrombotic complications, but there were no off-target side effects, and the deaths occurred in a highly unstable patient population.
“Only one patient experienced a thrombotic complication within 72 hours [of initiating idarucizumab], and that patient had not been restarted on any antithrombotic medications,” Dr. Pollack reported. He noted that no safety concerns arose in patients who were enrolled in the study, but later were found to have normal clotting parameters.
Idarucizumab binds to dabigatran to neutralize its activity. It was given priority review status by the FDA in April 2015. Priority review is now being sought for andexanet, which is a potential reversal agent for the factor Xa inhibitors, according to press releases from the developer, Portola Pharmaceuticals. Idarucizumab and other effective reversal agents – if approved – are expected to increase the utility of novel oral anticoagulants.
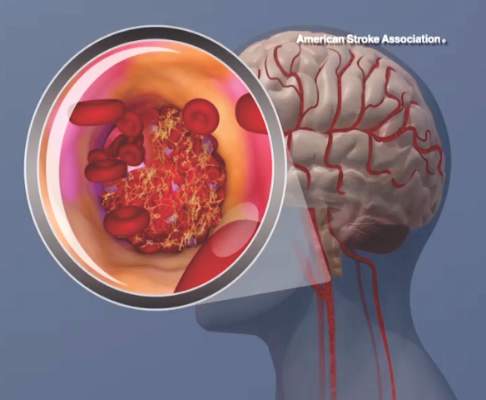
The FDA cautioned in its statement that reversing the effect of dabigatran exposes patients to the risk of blood clots and stroke from their underlying disease, and said that the idarucizumab labeling recommends patients resume their anticoagulant therapy as soon as medically appropriate.
Dr. Pollack disclosed that he has financial relationships with Bristol-Myers Squibb, Daiichi-Sankyo, Janssen, and Pfizer. RE-VERSE AD was supported by Boehringer Ingelheim.
Idarucizumab has been approved by the Food and Drug Administration for reversing the effects of dabigatran, a novel oral anticoagulant.
Specifically, idarucizumab (Praxbind) is intended for use in patients who are taking dabigatran (Pradaxa) during emergency situations when there is a need to reverse its blood-thinning effects, according to an FDA statement. Both drugs are marketed by Boehringer Ingelheim.
“The anticoagulant effects of Pradaxa are important and life-saving for some patients, but there are situations where reversal of the drug’s effects is medically necessary,” said Dr. Richard Pazdur, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Today’s approval offers the medical community an important tool for managing patients taking Pradaxa in emergency or life-threatening situations when bleeding can’t be controlled.”
The decision, released on Oct. 16, was based on efficacy and safety observed in three randomized trials, the largest of which is the ongoing phase III RE-VERSE AD.
Patients were enrolled into two distinct groups in RE-VERSE AD. Group A, with 51 patients, comprised patients on dabigatran experiencing a serious bleeding episode. Group B, with 39 patients, comprised patients on dabigatran who required an urgent surgical procedure. In both, 5 g of idarucizumab solution was administered intravenously. The primary endpoint was maximum percentage reversal of the anticoagulant effect of dabigatran within 4 hours.
In both groups, the median maximum percentage reversal was 100%. Other measures corroborated a rapid and highly effective reversal of anticoagulation. For example, the dilute thrombin time in those who could be evaluated was normalized in 98% of group A and 93% of group B (N Engl J Med. 2015 Aug 6. doi:10.1056/NEJMoa1502000).
Interim results of RE-VERSE AD “show rather convincingly that idarucizumab completely and safely reverses the anticoagulant effects of dabigatran within minutes,” said the lead author, Dr. Charles V. Pollack Jr., chairman of the department of emergency medicine at the University of Pennsylvania, Philadelphia. Dr. Pollack presented the findings at the 2015 International Society of Thrombosis and Haemostatis (ISTH) Congress in June.
Idarucizumab is the first reversal agent for any of the novel oral anticoagulants used as an alternative to warfarin. Unlike warfarin, which can be reversed with vitamin K, the lack of a reversal agent for dabigatran, a direct thrombin inhibitor, and other novel agents, such as rivaroxaban and apixaban, which are direct factor Xa inhibitors, has been a concern for patients who experience unexpected bleeding or face a risk of bleeding because of the need for urgent surgery. The laboratory findings were supported by the clinical findings, according to Dr. Pollack.
“Clinical outcomes were quite good in this multimorbid patient population,” he said. “Restoration of hemostasis as reported by local investigators was achieved in less than 12 hours when assessable, and 92% of the surgical patients were reported to have normal hemostasis at the time of the procedure.”
Idarucizumab was also found safe in this and the two previous randomized studies. In the 237 healthy volunteers evaluated previously, no serious adverse events were reported. In RE-VERSE AD, serious adverse events leading to death included hemorrhagic and thrombotic complications, but there were no off-target side effects, and the deaths occurred in a highly unstable patient population.
“Only one patient experienced a thrombotic complication within 72 hours [of initiating idarucizumab], and that patient had not been restarted on any antithrombotic medications,” Dr. Pollack reported. He noted that no safety concerns arose in patients who were enrolled in the study, but later were found to have normal clotting parameters.
Idarucizumab binds to dabigatran to neutralize its activity. It was given priority review status by the FDA in April 2015. Priority review is now being sought for andexanet, which is a potential reversal agent for the factor Xa inhibitors, according to press releases from the developer, Portola Pharmaceuticals. Idarucizumab and other effective reversal agents – if approved – are expected to increase the utility of novel oral anticoagulants.
The FDA cautioned in its statement that reversing the effect of dabigatran exposes patients to the risk of blood clots and stroke from their underlying disease, and said that the idarucizumab labeling recommends patients resume their anticoagulant therapy as soon as medically appropriate.
Dr. Pollack disclosed that he has financial relationships with Bristol-Myers Squibb, Daiichi-Sankyo, Janssen, and Pfizer. RE-VERSE AD was supported by Boehringer Ingelheim.
Idarucizumab has been approved by the Food and Drug Administration for reversing the effects of dabigatran, a novel oral anticoagulant.
Specifically, idarucizumab (Praxbind) is intended for use in patients who are taking dabigatran (Pradaxa) during emergency situations when there is a need to reverse its blood-thinning effects, according to an FDA statement. Both drugs are marketed by Boehringer Ingelheim.
“The anticoagulant effects of Pradaxa are important and life-saving for some patients, but there are situations where reversal of the drug’s effects is medically necessary,” said Dr. Richard Pazdur, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Today’s approval offers the medical community an important tool for managing patients taking Pradaxa in emergency or life-threatening situations when bleeding can’t be controlled.”
The decision, released on Oct. 16, was based on efficacy and safety observed in three randomized trials, the largest of which is the ongoing phase III RE-VERSE AD.
Patients were enrolled into two distinct groups in RE-VERSE AD. Group A, with 51 patients, comprised patients on dabigatran experiencing a serious bleeding episode. Group B, with 39 patients, comprised patients on dabigatran who required an urgent surgical procedure. In both, 5 g of idarucizumab solution was administered intravenously. The primary endpoint was maximum percentage reversal of the anticoagulant effect of dabigatran within 4 hours.
In both groups, the median maximum percentage reversal was 100%. Other measures corroborated a rapid and highly effective reversal of anticoagulation. For example, the dilute thrombin time in those who could be evaluated was normalized in 98% of group A and 93% of group B (N Engl J Med. 2015 Aug 6. doi:10.1056/NEJMoa1502000).
Interim results of RE-VERSE AD “show rather convincingly that idarucizumab completely and safely reverses the anticoagulant effects of dabigatran within minutes,” said the lead author, Dr. Charles V. Pollack Jr., chairman of the department of emergency medicine at the University of Pennsylvania, Philadelphia. Dr. Pollack presented the findings at the 2015 International Society of Thrombosis and Haemostatis (ISTH) Congress in June.
Idarucizumab is the first reversal agent for any of the novel oral anticoagulants used as an alternative to warfarin. Unlike warfarin, which can be reversed with vitamin K, the lack of a reversal agent for dabigatran, a direct thrombin inhibitor, and other novel agents, such as rivaroxaban and apixaban, which are direct factor Xa inhibitors, has been a concern for patients who experience unexpected bleeding or face a risk of bleeding because of the need for urgent surgery. The laboratory findings were supported by the clinical findings, according to Dr. Pollack.
“Clinical outcomes were quite good in this multimorbid patient population,” he said. “Restoration of hemostasis as reported by local investigators was achieved in less than 12 hours when assessable, and 92% of the surgical patients were reported to have normal hemostasis at the time of the procedure.”
Idarucizumab was also found safe in this and the two previous randomized studies. In the 237 healthy volunteers evaluated previously, no serious adverse events were reported. In RE-VERSE AD, serious adverse events leading to death included hemorrhagic and thrombotic complications, but there were no off-target side effects, and the deaths occurred in a highly unstable patient population.
“Only one patient experienced a thrombotic complication within 72 hours [of initiating idarucizumab], and that patient had not been restarted on any antithrombotic medications,” Dr. Pollack reported. He noted that no safety concerns arose in patients who were enrolled in the study, but later were found to have normal clotting parameters.
Idarucizumab binds to dabigatran to neutralize its activity. It was given priority review status by the FDA in April 2015. Priority review is now being sought for andexanet, which is a potential reversal agent for the factor Xa inhibitors, according to press releases from the developer, Portola Pharmaceuticals. Idarucizumab and other effective reversal agents – if approved – are expected to increase the utility of novel oral anticoagulants.
The FDA cautioned in its statement that reversing the effect of dabigatran exposes patients to the risk of blood clots and stroke from their underlying disease, and said that the idarucizumab labeling recommends patients resume their anticoagulant therapy as soon as medically appropriate.
Dr. Pollack disclosed that he has financial relationships with Bristol-Myers Squibb, Daiichi-Sankyo, Janssen, and Pfizer. RE-VERSE AD was supported by Boehringer Ingelheim.
ESC: Air quality level linked to STEMI risk in men
LONDON – The risk for ST-elevation myocardial infarction (STEMI) increased in men when air quality dipped below acceptable levels as designated by the World Health Organization (WHO), based on the results of an observational study in Belgian.
The relative risk for a STEMI increased by 2.8% (1.026; 95% confidence interval, 1.005-1.048) for every 10 mcg/cm3 rise in fine particulate air pollution and by 5.1% (RR, 1.051; 95% CI, 1.018-1.084) for a comparable rise in nitric oxide air pollution. Ozone level was not associated with the risk for STEMI. Air pollution levels did not affect in-hospital mortality due to STEMI and had no clear effect on patients with coronary artery disease, diabetes or hypertension.
“Of course, it is very interesting that the results are only observed in men. This may be due to a statistical issue, because in our study population, the female group represents less than 25% of the population,” Dr. Jean-François Argacha, a study investigator, said during a press briefing at the annual congress of the European Society of Cardiology.
Subgroup analysis suggested that patients who were aged 75 years and older were more likely to develop STEMI in relation to exposure to particulate matter (RR, 1.046; 95% CI, 1.002-1.092, P = .041). Those aged 54 years and younger seemed more susceptible to nitric oxide levels (RR, 1.071; 95% CI, 1.010-1.136; P = .021).“The detrimental impact of nitric oxide exceeded that of fine particles and may be of particular concern in the younger population,” said Dr. Argacha, a cardiologist at University Hospital Brussels.
Previous research had shown that particulate matter is associated with an increased risk for acute myocardial infarction, but there had been no specific assessments on air pollution’s potential effects on STEMI, according to Dr. Argacha.
The study considered information on 11,428 patients in the Belgian Interdisciplinary Working Group on Acute Cardiology STEMI Registry between 2009 and 2013. Data on national air pollution parameters – particulate matter with an aerodynamic diameter of less than 10 (PM10) or 2.5 (PM2.5) mcm, nitric oxide and ozone – and air temperature were obtained from the Belgian Environment Agency database and adjusted for population density.
A case crossover analysis of STEMI risk was then performed, with risk being adjusted for ambient temperature, day of the week, and the season. The study’s case crossover design ensured that the effects were limited to air pollution and excluded other confounders including respiratory disease and air temperature.
Worldwide, WHO has estimated that poor urban air quality is responsible for around 1.3 million deaths per year, Dr. Argacha observed, noting that air pollution consists of fine (PM2.5) and larger (PM10) particles, nitric oxide, and ozone as well as sulfur dioxide and carbon monoxide.
During the observation period, the mean air pollution levels over the course of 1 year in Belgium were 23.9 mcg/cm3 for PM10, 16.1 mcg/cm3 for PM2.5, and 23.7 mcg/cm3 for nitric oxide. WHO guidelines set a daily limit of 25 mcg/cm3 for PM2.5. Dr. Argacha noted that this limit was exceeded in Belgium on 17.5% of days in the study.
Dr. Oscar Franco, professor of preventative medicine at the Erasmus University Medical Center in Rotterdam, the Netherlands, who cochaired the press conference noted that the European Society of Cardiology recently published a position paper on air pollution on cardiovascular disease (Eur Heart J. 2015;36:83-93) and has launched a major campaign to raise awareness of the detrimental effects that the environment can have on the heart.
The campaign notes that air and noise pollution are modifiable risk factors for the prevention and control of cardiovascular diseases, and advocated for acceptable limits that reflect WHO levels. Individuals “need to take action,” Dr. Franco urged. The decisions that people make every day – how they get to work for example – could have a potentially huge impact on the environment and health.
Dr. Argacha and Dr. Franco had no disclosures to report.
LONDON – The risk for ST-elevation myocardial infarction (STEMI) increased in men when air quality dipped below acceptable levels as designated by the World Health Organization (WHO), based on the results of an observational study in Belgian.
The relative risk for a STEMI increased by 2.8% (1.026; 95% confidence interval, 1.005-1.048) for every 10 mcg/cm3 rise in fine particulate air pollution and by 5.1% (RR, 1.051; 95% CI, 1.018-1.084) for a comparable rise in nitric oxide air pollution. Ozone level was not associated with the risk for STEMI. Air pollution levels did not affect in-hospital mortality due to STEMI and had no clear effect on patients with coronary artery disease, diabetes or hypertension.
“Of course, it is very interesting that the results are only observed in men. This may be due to a statistical issue, because in our study population, the female group represents less than 25% of the population,” Dr. Jean-François Argacha, a study investigator, said during a press briefing at the annual congress of the European Society of Cardiology.
Subgroup analysis suggested that patients who were aged 75 years and older were more likely to develop STEMI in relation to exposure to particulate matter (RR, 1.046; 95% CI, 1.002-1.092, P = .041). Those aged 54 years and younger seemed more susceptible to nitric oxide levels (RR, 1.071; 95% CI, 1.010-1.136; P = .021).“The detrimental impact of nitric oxide exceeded that of fine particles and may be of particular concern in the younger population,” said Dr. Argacha, a cardiologist at University Hospital Brussels.
Previous research had shown that particulate matter is associated with an increased risk for acute myocardial infarction, but there had been no specific assessments on air pollution’s potential effects on STEMI, according to Dr. Argacha.
The study considered information on 11,428 patients in the Belgian Interdisciplinary Working Group on Acute Cardiology STEMI Registry between 2009 and 2013. Data on national air pollution parameters – particulate matter with an aerodynamic diameter of less than 10 (PM10) or 2.5 (PM2.5) mcm, nitric oxide and ozone – and air temperature were obtained from the Belgian Environment Agency database and adjusted for population density.
A case crossover analysis of STEMI risk was then performed, with risk being adjusted for ambient temperature, day of the week, and the season. The study’s case crossover design ensured that the effects were limited to air pollution and excluded other confounders including respiratory disease and air temperature.
Worldwide, WHO has estimated that poor urban air quality is responsible for around 1.3 million deaths per year, Dr. Argacha observed, noting that air pollution consists of fine (PM2.5) and larger (PM10) particles, nitric oxide, and ozone as well as sulfur dioxide and carbon monoxide.
During the observation period, the mean air pollution levels over the course of 1 year in Belgium were 23.9 mcg/cm3 for PM10, 16.1 mcg/cm3 for PM2.5, and 23.7 mcg/cm3 for nitric oxide. WHO guidelines set a daily limit of 25 mcg/cm3 for PM2.5. Dr. Argacha noted that this limit was exceeded in Belgium on 17.5% of days in the study.
Dr. Oscar Franco, professor of preventative medicine at the Erasmus University Medical Center in Rotterdam, the Netherlands, who cochaired the press conference noted that the European Society of Cardiology recently published a position paper on air pollution on cardiovascular disease (Eur Heart J. 2015;36:83-93) and has launched a major campaign to raise awareness of the detrimental effects that the environment can have on the heart.
The campaign notes that air and noise pollution are modifiable risk factors for the prevention and control of cardiovascular diseases, and advocated for acceptable limits that reflect WHO levels. Individuals “need to take action,” Dr. Franco urged. The decisions that people make every day – how they get to work for example – could have a potentially huge impact on the environment and health.
Dr. Argacha and Dr. Franco had no disclosures to report.
LONDON – The risk for ST-elevation myocardial infarction (STEMI) increased in men when air quality dipped below acceptable levels as designated by the World Health Organization (WHO), based on the results of an observational study in Belgian.
The relative risk for a STEMI increased by 2.8% (1.026; 95% confidence interval, 1.005-1.048) for every 10 mcg/cm3 rise in fine particulate air pollution and by 5.1% (RR, 1.051; 95% CI, 1.018-1.084) for a comparable rise in nitric oxide air pollution. Ozone level was not associated with the risk for STEMI. Air pollution levels did not affect in-hospital mortality due to STEMI and had no clear effect on patients with coronary artery disease, diabetes or hypertension.
“Of course, it is very interesting that the results are only observed in men. This may be due to a statistical issue, because in our study population, the female group represents less than 25% of the population,” Dr. Jean-François Argacha, a study investigator, said during a press briefing at the annual congress of the European Society of Cardiology.
Subgroup analysis suggested that patients who were aged 75 years and older were more likely to develop STEMI in relation to exposure to particulate matter (RR, 1.046; 95% CI, 1.002-1.092, P = .041). Those aged 54 years and younger seemed more susceptible to nitric oxide levels (RR, 1.071; 95% CI, 1.010-1.136; P = .021).“The detrimental impact of nitric oxide exceeded that of fine particles and may be of particular concern in the younger population,” said Dr. Argacha, a cardiologist at University Hospital Brussels.
Previous research had shown that particulate matter is associated with an increased risk for acute myocardial infarction, but there had been no specific assessments on air pollution’s potential effects on STEMI, according to Dr. Argacha.
The study considered information on 11,428 patients in the Belgian Interdisciplinary Working Group on Acute Cardiology STEMI Registry between 2009 and 2013. Data on national air pollution parameters – particulate matter with an aerodynamic diameter of less than 10 (PM10) or 2.5 (PM2.5) mcm, nitric oxide and ozone – and air temperature were obtained from the Belgian Environment Agency database and adjusted for population density.
A case crossover analysis of STEMI risk was then performed, with risk being adjusted for ambient temperature, day of the week, and the season. The study’s case crossover design ensured that the effects were limited to air pollution and excluded other confounders including respiratory disease and air temperature.
Worldwide, WHO has estimated that poor urban air quality is responsible for around 1.3 million deaths per year, Dr. Argacha observed, noting that air pollution consists of fine (PM2.5) and larger (PM10) particles, nitric oxide, and ozone as well as sulfur dioxide and carbon monoxide.
During the observation period, the mean air pollution levels over the course of 1 year in Belgium were 23.9 mcg/cm3 for PM10, 16.1 mcg/cm3 for PM2.5, and 23.7 mcg/cm3 for nitric oxide. WHO guidelines set a daily limit of 25 mcg/cm3 for PM2.5. Dr. Argacha noted that this limit was exceeded in Belgium on 17.5% of days in the study.
Dr. Oscar Franco, professor of preventative medicine at the Erasmus University Medical Center in Rotterdam, the Netherlands, who cochaired the press conference noted that the European Society of Cardiology recently published a position paper on air pollution on cardiovascular disease (Eur Heart J. 2015;36:83-93) and has launched a major campaign to raise awareness of the detrimental effects that the environment can have on the heart.
The campaign notes that air and noise pollution are modifiable risk factors for the prevention and control of cardiovascular diseases, and advocated for acceptable limits that reflect WHO levels. Individuals “need to take action,” Dr. Franco urged. The decisions that people make every day – how they get to work for example – could have a potentially huge impact on the environment and health.
Dr. Argacha and Dr. Franco had no disclosures to report.
AT THE ESC CONGRESS 2015
Key clinical point: Air pollution may be a potentially modifiable risk factor for STEMI in men.
Major finding: The relative risk for a STEMI increased by 2.8% for a 10 mcg/cm3 rise in fine particulate air pollution and by 5.1% for a comparable rise in nitric oxide air pollution.
Data source: 11,428 patients logged in the Belgian Interdisciplinary Working Group on Acute Cardiology STEMI Registry between 2009 and 2013.
Disclosures: Dr. Argacha and Dr. Franco had no disclosures to report.
For subacute STEMI, thrombectomy adds no benefit to PCI
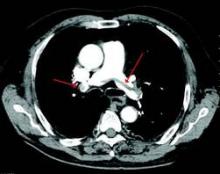
The addition of thrombectomy to percutaneous coronary intervention didn’t improve cardiac flow or clinical endpoints any more than PCI alone in patients with a subacute ST-elevation myocardial infarction.
Thrombosis aspiration decreased microvascular obstruction less than 1% more than did PCI alone – 2.5% vs. 3% of the left ventricular mass, Dr. Steffan Desch said at the Transcatheter Cardiovascular Therapeutics annual meeting. There were also no significant differences in infarct size, myocardial salvage, or left ventricular ejection fraction, he said at the meeting sponsored by the Cardiovascular Research Foundation.
“Routine manual thrombectomy and aspiration didn’t show any significant reduction in microvascular obstruction on imaging,” said Dr. Desch of University Heart Center, Lübeck, Germany. “This finding was supported by a variety of secondary endpoints, none of them significantly beneficial.”
The study, which was simultaneously published online (JACC Cardiovasc Interv. 2015. doi: 10.1016/j.jcin.2015.09.010), gives the first firm evidence that clot removal is not particularly helpful to patients who present late after symptom onset. With a mean development time of 28 hours, thrombi in this cohort were more mature, with higher fibrin content than the typically soft material seen in patients with acute ST-elevation myocardial infarction (STEMI). When the clot becomes denser and more organized, it is likely less suitable for aspiration, he said.
The cohort comprised 152 patients who presented in a 12- to 48-hour window after onset of symptoms. They were randomized to either standard PCI or to clot aspiration followed by PCI. The primary outcome was the extent of major vessel occlusion on magnetic resonance imaging conducted 1-4 days after the intervention. Secondary outcomes included infarct size, myocardial salvage, and left ventricular volume and ejection fraction.
Patients were a mean of 66 years old, with typical baseline characteristics. Most were men; hypertension was common (about 70%). About half had signs of ongoing ischemia at admission. The door-to-balloon time was 78 minutes in the combination therapy group and 62 minutes in the PCI-only group. Most (62.5%) had a complete occlusion of the culprit vessel.
In addition to providing no benefit in microvascular occlusion, aspiration did not significantly improve TIMI flow grade above that achieved with PCI only. After the intervention, 78% of those in the thrombectomy group and 69% of those in the PCI group achieved a TIMI flow grade 3. Nor was there a significant difference in myocardial blush grade (70% vs. 65%). When troponin T values were used to assess enzymatic infarct size, they were similar in both groups at 24 and 48 hours.
Clinical outcomes were similar as well. All-cause mortality was 3% in the aspiration group and 5% in the PCI-only group; cardiovascular death occurred in 3% and 4%, respectively. There were no reinfarctions and no stent thromboses. One stroke occurred in a patient who underwent PCI alone.
Dr. Desch noted in the published article that the study took all comers, rather than selecting for specific patient characteristics. Therefore, he said “it is possible that thrombus aspiration might only be advantageous in specific subsets of patients such as those with large thrombus burden, total occlusion or reduced flow.”
The study was funded by a research grant from Medtronic. Dr. Desch reported grant/research support from Medtronic.
The addition of thrombectomy to percutaneous coronary intervention didn’t improve cardiac flow or clinical endpoints any more than PCI alone in patients with a subacute ST-elevation myocardial infarction.
Thrombosis aspiration decreased microvascular obstruction less than 1% more than did PCI alone – 2.5% vs. 3% of the left ventricular mass, Dr. Steffan Desch said at the Transcatheter Cardiovascular Therapeutics annual meeting. There were also no significant differences in infarct size, myocardial salvage, or left ventricular ejection fraction, he said at the meeting sponsored by the Cardiovascular Research Foundation.
“Routine manual thrombectomy and aspiration didn’t show any significant reduction in microvascular obstruction on imaging,” said Dr. Desch of University Heart Center, Lübeck, Germany. “This finding was supported by a variety of secondary endpoints, none of them significantly beneficial.”
The study, which was simultaneously published online (JACC Cardiovasc Interv. 2015. doi: 10.1016/j.jcin.2015.09.010), gives the first firm evidence that clot removal is not particularly helpful to patients who present late after symptom onset. With a mean development time of 28 hours, thrombi in this cohort were more mature, with higher fibrin content than the typically soft material seen in patients with acute ST-elevation myocardial infarction (STEMI). When the clot becomes denser and more organized, it is likely less suitable for aspiration, he said.
The cohort comprised 152 patients who presented in a 12- to 48-hour window after onset of symptoms. They were randomized to either standard PCI or to clot aspiration followed by PCI. The primary outcome was the extent of major vessel occlusion on magnetic resonance imaging conducted 1-4 days after the intervention. Secondary outcomes included infarct size, myocardial salvage, and left ventricular volume and ejection fraction.
Patients were a mean of 66 years old, with typical baseline characteristics. Most were men; hypertension was common (about 70%). About half had signs of ongoing ischemia at admission. The door-to-balloon time was 78 minutes in the combination therapy group and 62 minutes in the PCI-only group. Most (62.5%) had a complete occlusion of the culprit vessel.
In addition to providing no benefit in microvascular occlusion, aspiration did not significantly improve TIMI flow grade above that achieved with PCI only. After the intervention, 78% of those in the thrombectomy group and 69% of those in the PCI group achieved a TIMI flow grade 3. Nor was there a significant difference in myocardial blush grade (70% vs. 65%). When troponin T values were used to assess enzymatic infarct size, they were similar in both groups at 24 and 48 hours.
Clinical outcomes were similar as well. All-cause mortality was 3% in the aspiration group and 5% in the PCI-only group; cardiovascular death occurred in 3% and 4%, respectively. There were no reinfarctions and no stent thromboses. One stroke occurred in a patient who underwent PCI alone.
Dr. Desch noted in the published article that the study took all comers, rather than selecting for specific patient characteristics. Therefore, he said “it is possible that thrombus aspiration might only be advantageous in specific subsets of patients such as those with large thrombus burden, total occlusion or reduced flow.”
The study was funded by a research grant from Medtronic. Dr. Desch reported grant/research support from Medtronic.
The addition of thrombectomy to percutaneous coronary intervention didn’t improve cardiac flow or clinical endpoints any more than PCI alone in patients with a subacute ST-elevation myocardial infarction.
Thrombosis aspiration decreased microvascular obstruction less than 1% more than did PCI alone – 2.5% vs. 3% of the left ventricular mass, Dr. Steffan Desch said at the Transcatheter Cardiovascular Therapeutics annual meeting. There were also no significant differences in infarct size, myocardial salvage, or left ventricular ejection fraction, he said at the meeting sponsored by the Cardiovascular Research Foundation.
“Routine manual thrombectomy and aspiration didn’t show any significant reduction in microvascular obstruction on imaging,” said Dr. Desch of University Heart Center, Lübeck, Germany. “This finding was supported by a variety of secondary endpoints, none of them significantly beneficial.”
The study, which was simultaneously published online (JACC Cardiovasc Interv. 2015. doi: 10.1016/j.jcin.2015.09.010), gives the first firm evidence that clot removal is not particularly helpful to patients who present late after symptom onset. With a mean development time of 28 hours, thrombi in this cohort were more mature, with higher fibrin content than the typically soft material seen in patients with acute ST-elevation myocardial infarction (STEMI). When the clot becomes denser and more organized, it is likely less suitable for aspiration, he said.
The cohort comprised 152 patients who presented in a 12- to 48-hour window after onset of symptoms. They were randomized to either standard PCI or to clot aspiration followed by PCI. The primary outcome was the extent of major vessel occlusion on magnetic resonance imaging conducted 1-4 days after the intervention. Secondary outcomes included infarct size, myocardial salvage, and left ventricular volume and ejection fraction.
Patients were a mean of 66 years old, with typical baseline characteristics. Most were men; hypertension was common (about 70%). About half had signs of ongoing ischemia at admission. The door-to-balloon time was 78 minutes in the combination therapy group and 62 minutes in the PCI-only group. Most (62.5%) had a complete occlusion of the culprit vessel.
In addition to providing no benefit in microvascular occlusion, aspiration did not significantly improve TIMI flow grade above that achieved with PCI only. After the intervention, 78% of those in the thrombectomy group and 69% of those in the PCI group achieved a TIMI flow grade 3. Nor was there a significant difference in myocardial blush grade (70% vs. 65%). When troponin T values were used to assess enzymatic infarct size, they were similar in both groups at 24 and 48 hours.
Clinical outcomes were similar as well. All-cause mortality was 3% in the aspiration group and 5% in the PCI-only group; cardiovascular death occurred in 3% and 4%, respectively. There were no reinfarctions and no stent thromboses. One stroke occurred in a patient who underwent PCI alone.
Dr. Desch noted in the published article that the study took all comers, rather than selecting for specific patient characteristics. Therefore, he said “it is possible that thrombus aspiration might only be advantageous in specific subsets of patients such as those with large thrombus burden, total occlusion or reduced flow.”
The study was funded by a research grant from Medtronic. Dr. Desch reported grant/research support from Medtronic.
AT TCT 2015
Key clinical point: Thrombus aspiration doesn’t reduce microvascular obstruction in subacute STEMI patients undergoing PCI late after symptom onset.
Major finding: Thrombosis aspiration improved microvascular obstruction less than 1% more than did PCI alone – 2.5% vs. 3% of the left ventricular mass – and conferred no other indications of clinical benefit.
Data source: The study randomized 152 patients with late-presentation STEMI to PCI alone or to thrombectomy plus PCI.
Disclosures: The study was funded by a research grant from Medtronic. Dr. Desch reported grant/research support from Medtronic.
New CPR guide sets compression limits, scratches vasopressin
New guidelines on cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) set upper limits on chest compression rate and depth, add naloxone to the care of suspected opioid abusers, and remove vasopressin from the advanced cardiac life support (ACLS) algorithm.
The American Heart Association published its revised guidelines Oct. 15 in Circulation. The AHA released its previous guidelines in 2010.
“Everyone has a role to play in the chain of survival – from bystanders to dispatchers, emergency responders to health care providers,” Dr. Mark Creager said in a statement. “When everyone knows their role, knows CPR, and works together, we can dramatically improve cardiac arrest victims’ chances of survival,” said Dr. Creager, AHA president and director of the Heart and Vascular Center at Dartmouth-Hitchcock Medical Center, Lebanon, N.H.
The 2015 guidelines’ new recommendations include the following:
• Resuscitation pathways. The guidelines note that the resuscitation pathways are very different for patients who experience cardiac arrest present in either a hospital setting (IHCA) or out-of-hospital setting (OHCA). In OHCA, the patient depends on lay rescuers to not only recognize the situation but also call for help, initiate CPR, and, if available, administer defibrillation until emergency medical personnel arrive. However, IHCA involves prevention of cardiac arrest and smooth delivery of care in a multidisciplinary setting.
• Layperson CPR. Untrained lay rescuers should provide compression-only CPR for OHCA. Trained lay rescuers who are able to provide rescue breaths should begin CPR with compressions followed by breaths at a ratio of 30 compressions to two breaths. Compression-only CPR is easier to perform for untrained lay rescuers, the guidelines note, and survival rates are similar using CPR with or without rescue breaths in adult cardiac arrest with a cardiac etiology.
• Compression rate and depth. The new guidelines set upper limits on chest compression depth and heart rate, recommending a compression rate of 100-120 compressions per minute with a depth of at least 2 inches, not to exceed 2.4 inches in adults.
• Social media dispatching. Despite limited evidence, the guideline authors said that it may be reasonable for communities to use social media technologies to alert lay rescuers with mobile phones about nearby OHCA cases.
• Naloxone and opioid addiction. Also new to the guidelines is the recommended use of naloxone for patients with suspected or known opioid addiction by appropriately trained lay rescuers or basic life support (BLS) providers.
• CPR training. The guidelines highlight several changes to simplify health care provider training in CPR. For example, trained rescuers can simultaneously perform some tasks to reduce the time to initiate chest compressions. Likewise, in a team of trained rescuers, multiple steps such as activating the emergency response system, chest compression, ventilation, and defibrillator retrieval can be accomplished simultaneously.
• High-quality CPR. Finally, the guidelines focus on emphasizing high-quality CPR with adequate compression rate and depth, complete chest recoil, few interruptions to compressions, and appropriate ventilation.
The guidelines offer several changes to advanced cardiac life support (ACLS). The algorithm was simplified by removing vasopressin, because the authors note that “the combined use of vasopressin and epinephrine offers no advantage to using standard-dose epinephrine in cardiac arrest.”
Likewise, the guidelines note conflicting studies to support the use of lidocaine after return of spontaneous circulation (ROSC). “However, the initiation or continuation of lidocaine may be considered immediately after ROSC from VF/pulseless ventricular tachycardia cardiac arrest,” the guideline authors wrote. Finally, the guidelines highlight updates in post–cardiac arrest care, including a wider range of target temperatures, between 32° C and 36° C, to be maintained for at least 24 hours in comatose adults with ROSC after cardiac arrest. In comparison, the 2010 guidelines called for a target temperature range of 32° C to 34° C for 12-24 hours. The guidelines also detail new updates for acute coronary syndrome, pediatric BLS, pediatric ACLS, and neonatal resuscitation.
As the AHA updates its CPR guidelines, it’s also important for lay rescuers and health providers to update their own training, noted Dr. Clifton Callaway, chair of the AHA’s Emergency Cardiovascular Care (ECC) committee.
“Research shows resuscitation skills can decline within a few months after training – far before the 2-year period in which basic and advanced life support skills are currently evaluated,” cautioned Dr. Callaway, professor of emergency medicine at the University of Pittsburgh. “Frequent training with shorter intervals of basic and advanced cardiovascular life support skills may be helpful for providers who are likely to encounter a cardiac arrest to ensure the patient receives high-quality CPR,” he added.
New guidelines on cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) set upper limits on chest compression rate and depth, add naloxone to the care of suspected opioid abusers, and remove vasopressin from the advanced cardiac life support (ACLS) algorithm.
The American Heart Association published its revised guidelines Oct. 15 in Circulation. The AHA released its previous guidelines in 2010.
“Everyone has a role to play in the chain of survival – from bystanders to dispatchers, emergency responders to health care providers,” Dr. Mark Creager said in a statement. “When everyone knows their role, knows CPR, and works together, we can dramatically improve cardiac arrest victims’ chances of survival,” said Dr. Creager, AHA president and director of the Heart and Vascular Center at Dartmouth-Hitchcock Medical Center, Lebanon, N.H.
The 2015 guidelines’ new recommendations include the following:
• Resuscitation pathways. The guidelines note that the resuscitation pathways are very different for patients who experience cardiac arrest present in either a hospital setting (IHCA) or out-of-hospital setting (OHCA). In OHCA, the patient depends on lay rescuers to not only recognize the situation but also call for help, initiate CPR, and, if available, administer defibrillation until emergency medical personnel arrive. However, IHCA involves prevention of cardiac arrest and smooth delivery of care in a multidisciplinary setting.
• Layperson CPR. Untrained lay rescuers should provide compression-only CPR for OHCA. Trained lay rescuers who are able to provide rescue breaths should begin CPR with compressions followed by breaths at a ratio of 30 compressions to two breaths. Compression-only CPR is easier to perform for untrained lay rescuers, the guidelines note, and survival rates are similar using CPR with or without rescue breaths in adult cardiac arrest with a cardiac etiology.
• Compression rate and depth. The new guidelines set upper limits on chest compression depth and heart rate, recommending a compression rate of 100-120 compressions per minute with a depth of at least 2 inches, not to exceed 2.4 inches in adults.
• Social media dispatching. Despite limited evidence, the guideline authors said that it may be reasonable for communities to use social media technologies to alert lay rescuers with mobile phones about nearby OHCA cases.
• Naloxone and opioid addiction. Also new to the guidelines is the recommended use of naloxone for patients with suspected or known opioid addiction by appropriately trained lay rescuers or basic life support (BLS) providers.
• CPR training. The guidelines highlight several changes to simplify health care provider training in CPR. For example, trained rescuers can simultaneously perform some tasks to reduce the time to initiate chest compressions. Likewise, in a team of trained rescuers, multiple steps such as activating the emergency response system, chest compression, ventilation, and defibrillator retrieval can be accomplished simultaneously.
• High-quality CPR. Finally, the guidelines focus on emphasizing high-quality CPR with adequate compression rate and depth, complete chest recoil, few interruptions to compressions, and appropriate ventilation.
The guidelines offer several changes to advanced cardiac life support (ACLS). The algorithm was simplified by removing vasopressin, because the authors note that “the combined use of vasopressin and epinephrine offers no advantage to using standard-dose epinephrine in cardiac arrest.”
Likewise, the guidelines note conflicting studies to support the use of lidocaine after return of spontaneous circulation (ROSC). “However, the initiation or continuation of lidocaine may be considered immediately after ROSC from VF/pulseless ventricular tachycardia cardiac arrest,” the guideline authors wrote. Finally, the guidelines highlight updates in post–cardiac arrest care, including a wider range of target temperatures, between 32° C and 36° C, to be maintained for at least 24 hours in comatose adults with ROSC after cardiac arrest. In comparison, the 2010 guidelines called for a target temperature range of 32° C to 34° C for 12-24 hours. The guidelines also detail new updates for acute coronary syndrome, pediatric BLS, pediatric ACLS, and neonatal resuscitation.
As the AHA updates its CPR guidelines, it’s also important for lay rescuers and health providers to update their own training, noted Dr. Clifton Callaway, chair of the AHA’s Emergency Cardiovascular Care (ECC) committee.
“Research shows resuscitation skills can decline within a few months after training – far before the 2-year period in which basic and advanced life support skills are currently evaluated,” cautioned Dr. Callaway, professor of emergency medicine at the University of Pittsburgh. “Frequent training with shorter intervals of basic and advanced cardiovascular life support skills may be helpful for providers who are likely to encounter a cardiac arrest to ensure the patient receives high-quality CPR,” he added.
New guidelines on cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) set upper limits on chest compression rate and depth, add naloxone to the care of suspected opioid abusers, and remove vasopressin from the advanced cardiac life support (ACLS) algorithm.
The American Heart Association published its revised guidelines Oct. 15 in Circulation. The AHA released its previous guidelines in 2010.
“Everyone has a role to play in the chain of survival – from bystanders to dispatchers, emergency responders to health care providers,” Dr. Mark Creager said in a statement. “When everyone knows their role, knows CPR, and works together, we can dramatically improve cardiac arrest victims’ chances of survival,” said Dr. Creager, AHA president and director of the Heart and Vascular Center at Dartmouth-Hitchcock Medical Center, Lebanon, N.H.
The 2015 guidelines’ new recommendations include the following:
• Resuscitation pathways. The guidelines note that the resuscitation pathways are very different for patients who experience cardiac arrest present in either a hospital setting (IHCA) or out-of-hospital setting (OHCA). In OHCA, the patient depends on lay rescuers to not only recognize the situation but also call for help, initiate CPR, and, if available, administer defibrillation until emergency medical personnel arrive. However, IHCA involves prevention of cardiac arrest and smooth delivery of care in a multidisciplinary setting.
• Layperson CPR. Untrained lay rescuers should provide compression-only CPR for OHCA. Trained lay rescuers who are able to provide rescue breaths should begin CPR with compressions followed by breaths at a ratio of 30 compressions to two breaths. Compression-only CPR is easier to perform for untrained lay rescuers, the guidelines note, and survival rates are similar using CPR with or without rescue breaths in adult cardiac arrest with a cardiac etiology.
• Compression rate and depth. The new guidelines set upper limits on chest compression depth and heart rate, recommending a compression rate of 100-120 compressions per minute with a depth of at least 2 inches, not to exceed 2.4 inches in adults.
• Social media dispatching. Despite limited evidence, the guideline authors said that it may be reasonable for communities to use social media technologies to alert lay rescuers with mobile phones about nearby OHCA cases.
• Naloxone and opioid addiction. Also new to the guidelines is the recommended use of naloxone for patients with suspected or known opioid addiction by appropriately trained lay rescuers or basic life support (BLS) providers.
• CPR training. The guidelines highlight several changes to simplify health care provider training in CPR. For example, trained rescuers can simultaneously perform some tasks to reduce the time to initiate chest compressions. Likewise, in a team of trained rescuers, multiple steps such as activating the emergency response system, chest compression, ventilation, and defibrillator retrieval can be accomplished simultaneously.
• High-quality CPR. Finally, the guidelines focus on emphasizing high-quality CPR with adequate compression rate and depth, complete chest recoil, few interruptions to compressions, and appropriate ventilation.
The guidelines offer several changes to advanced cardiac life support (ACLS). The algorithm was simplified by removing vasopressin, because the authors note that “the combined use of vasopressin and epinephrine offers no advantage to using standard-dose epinephrine in cardiac arrest.”
Likewise, the guidelines note conflicting studies to support the use of lidocaine after return of spontaneous circulation (ROSC). “However, the initiation or continuation of lidocaine may be considered immediately after ROSC from VF/pulseless ventricular tachycardia cardiac arrest,” the guideline authors wrote. Finally, the guidelines highlight updates in post–cardiac arrest care, including a wider range of target temperatures, between 32° C and 36° C, to be maintained for at least 24 hours in comatose adults with ROSC after cardiac arrest. In comparison, the 2010 guidelines called for a target temperature range of 32° C to 34° C for 12-24 hours. The guidelines also detail new updates for acute coronary syndrome, pediatric BLS, pediatric ACLS, and neonatal resuscitation.
As the AHA updates its CPR guidelines, it’s also important for lay rescuers and health providers to update their own training, noted Dr. Clifton Callaway, chair of the AHA’s Emergency Cardiovascular Care (ECC) committee.
“Research shows resuscitation skills can decline within a few months after training – far before the 2-year period in which basic and advanced life support skills are currently evaluated,” cautioned Dr. Callaway, professor of emergency medicine at the University of Pittsburgh. “Frequent training with shorter intervals of basic and advanced cardiovascular life support skills may be helpful for providers who are likely to encounter a cardiac arrest to ensure the patient receives high-quality CPR,” he added.
FROM CIRCULATION
TCT: Novel drug-coated stent bests bare-metal in patients at high bleeding risk
A novel drug-coated stent halved the need for repeat revascularization and had a superior safety profile, compared with a bare-metal stent, in patients with a high risk of bleeding in the LEADERS FREE trial.
The results could mean that these typically older, sicker patients in whom dual antiplatelet therapy is contraindicated because of hemorrhage risk now have a wider range of revascularization options, said lead investigator Dr. Philip Urban.
“Patients who have a high risk of bleeding during percutaneous coronary intervention (PCI) are often excluded from stent and drug trials but constitute a rapidly growing proportion of PCI candidates, and they suffer high event rates,” said Dr. Urban, director of interventional cardiology at La Tour Hospital in Geneva. As the life expectancy increases, the implications are profound because roughly one-fifth of all PCI patients globally could be candidates for this type of treatment.
The data were presented at the Transcatheter Cardiovascular Therapeutics annual meeting, which was sponsored by the Cardiovascular Research Foundation. The results also were published online (N Engl J Med. 2015 Oct 14. doi: 10.1056/NEJMoa1503943).
“I hope these results will change practice as early as next week in Europe and elsewhere,” he said. The device is currently CE marked in Europe and is available in some parts of Asia. A clinical trial for the device is currently in the preliminary stages in the United States.
The current standard for PCI in patients at high risk for hemorrhage is to use bare-metal, instead of drug-eluting, stents. Although this protocol lowers the potential risk for bleeding and other complications often caused by extended dual antiplatelet therapy (DAPT), it exposes these patients to a higher risk of restenosis.
Rather than use a drug delivery polymer, the Biolimus A9-coated BioFreedom (Biosensors International) is polymer free and uses a stainless steel stent microstructured to hold a proprietary lipophilic drug on its outer surface. The drug is absorbed by the body within a month of placement.
The first of its kind, the double-blinded LEADERS FREE trial randomly assigned 2,466 PCI patients at high risk for bleeding to receive either the test stent or the standard platform Gazelle bare-metal stent. The procedures were performed at nearly 70 participating sites around the world, excluding the United States. More than half of all patients were accessed transradially, which was preferable to transfemoral access, according to Dr. Urban, because of the lower associated bleeding rates.
All patients were given 1 month of antiplatelet therapy after their intervention: about two-thirds of each group received DAPT and one-third received triple antiplatelet therapy. All were then switched to aspirin alone for 1 year.
At 390 days, there was nearly a 50% reduction in the need for repeat revascularization in the 1,221 patients receiving the drug-coated stent (5.1%), compared with 1,221 receiving the bare-metal stent (9.8%), with the difference reaching statistical significance for superiority for this primary efficacy endpoint (P < .001 for superiority).
Patients in the study arm also had a 29% reduction in risk of cardiac death, myocardial infarction, or stent thrombosis, the primary safety endpoint. At 390 days, these events occurred in 9.4% of the drug coated–stent patients, compared with 12.9% of the controls, a statistically significant difference for both noninferiority (P < .0001) and superiority (P = .005).
The study was done in patients typically excluded from such a trial, although, according to Dr. Urban, the PCI procedures performed were no more complex than usual. More than half the patients, three-quarters of whom were men in their mid- to late-70s, also had a range of comorbidities such as diabetes, kidney disease, and atrial fibrillation. Patients taking anticoagulants, those who had experienced a stroke within the past year, those expected to have major surgery within the year, and those who had undergone cancer treatment within the past 3 years also were included.
Bleeding events in the year following did not differ significantly between groups: 18.1% in the study group and 19.1% of controls had BARC 1-5 bleeding; 13.9% in the test arm and 14.7% of controls had BARC 2-5 events; and 7.2% in the study group and 7.3% of controls experienced BARC 3-5 events.
In the past, Dr. Urban had theorized that the trial would help to quantify not only risk for hemorrhage, but also the thrombotic risk in this patient population. In an interview, Dr. Urban said that, while the stent thrombosis rate was nearly identical in both groups in the trial, “the safety advantage of the drug-coated stent was especially apparent in the more thrombotic milieu.”
LEADERS FREE was underwritten by Biosensors International, maker of the BioFreedom stent. Dr. Urban and several of his coinvestigators disclosed relationships with device makers, including Edward Lifesciences, Terumo, Abbott Vascular, and Quest Medical.
On Twitter @whitneymcknight
A novel drug-coated stent halved the need for repeat revascularization and had a superior safety profile, compared with a bare-metal stent, in patients with a high risk of bleeding in the LEADERS FREE trial.
The results could mean that these typically older, sicker patients in whom dual antiplatelet therapy is contraindicated because of hemorrhage risk now have a wider range of revascularization options, said lead investigator Dr. Philip Urban.
“Patients who have a high risk of bleeding during percutaneous coronary intervention (PCI) are often excluded from stent and drug trials but constitute a rapidly growing proportion of PCI candidates, and they suffer high event rates,” said Dr. Urban, director of interventional cardiology at La Tour Hospital in Geneva. As the life expectancy increases, the implications are profound because roughly one-fifth of all PCI patients globally could be candidates for this type of treatment.
The data were presented at the Transcatheter Cardiovascular Therapeutics annual meeting, which was sponsored by the Cardiovascular Research Foundation. The results also were published online (N Engl J Med. 2015 Oct 14. doi: 10.1056/NEJMoa1503943).
“I hope these results will change practice as early as next week in Europe and elsewhere,” he said. The device is currently CE marked in Europe and is available in some parts of Asia. A clinical trial for the device is currently in the preliminary stages in the United States.
The current standard for PCI in patients at high risk for hemorrhage is to use bare-metal, instead of drug-eluting, stents. Although this protocol lowers the potential risk for bleeding and other complications often caused by extended dual antiplatelet therapy (DAPT), it exposes these patients to a higher risk of restenosis.
Rather than use a drug delivery polymer, the Biolimus A9-coated BioFreedom (Biosensors International) is polymer free and uses a stainless steel stent microstructured to hold a proprietary lipophilic drug on its outer surface. The drug is absorbed by the body within a month of placement.
The first of its kind, the double-blinded LEADERS FREE trial randomly assigned 2,466 PCI patients at high risk for bleeding to receive either the test stent or the standard platform Gazelle bare-metal stent. The procedures were performed at nearly 70 participating sites around the world, excluding the United States. More than half of all patients were accessed transradially, which was preferable to transfemoral access, according to Dr. Urban, because of the lower associated bleeding rates.
All patients were given 1 month of antiplatelet therapy after their intervention: about two-thirds of each group received DAPT and one-third received triple antiplatelet therapy. All were then switched to aspirin alone for 1 year.
At 390 days, there was nearly a 50% reduction in the need for repeat revascularization in the 1,221 patients receiving the drug-coated stent (5.1%), compared with 1,221 receiving the bare-metal stent (9.8%), with the difference reaching statistical significance for superiority for this primary efficacy endpoint (P < .001 for superiority).
Patients in the study arm also had a 29% reduction in risk of cardiac death, myocardial infarction, or stent thrombosis, the primary safety endpoint. At 390 days, these events occurred in 9.4% of the drug coated–stent patients, compared with 12.9% of the controls, a statistically significant difference for both noninferiority (P < .0001) and superiority (P = .005).
The study was done in patients typically excluded from such a trial, although, according to Dr. Urban, the PCI procedures performed were no more complex than usual. More than half the patients, three-quarters of whom were men in their mid- to late-70s, also had a range of comorbidities such as diabetes, kidney disease, and atrial fibrillation. Patients taking anticoagulants, those who had experienced a stroke within the past year, those expected to have major surgery within the year, and those who had undergone cancer treatment within the past 3 years also were included.
Bleeding events in the year following did not differ significantly between groups: 18.1% in the study group and 19.1% of controls had BARC 1-5 bleeding; 13.9% in the test arm and 14.7% of controls had BARC 2-5 events; and 7.2% in the study group and 7.3% of controls experienced BARC 3-5 events.
In the past, Dr. Urban had theorized that the trial would help to quantify not only risk for hemorrhage, but also the thrombotic risk in this patient population. In an interview, Dr. Urban said that, while the stent thrombosis rate was nearly identical in both groups in the trial, “the safety advantage of the drug-coated stent was especially apparent in the more thrombotic milieu.”
LEADERS FREE was underwritten by Biosensors International, maker of the BioFreedom stent. Dr. Urban and several of his coinvestigators disclosed relationships with device makers, including Edward Lifesciences, Terumo, Abbott Vascular, and Quest Medical.
On Twitter @whitneymcknight
A novel drug-coated stent halved the need for repeat revascularization and had a superior safety profile, compared with a bare-metal stent, in patients with a high risk of bleeding in the LEADERS FREE trial.
The results could mean that these typically older, sicker patients in whom dual antiplatelet therapy is contraindicated because of hemorrhage risk now have a wider range of revascularization options, said lead investigator Dr. Philip Urban.
“Patients who have a high risk of bleeding during percutaneous coronary intervention (PCI) are often excluded from stent and drug trials but constitute a rapidly growing proportion of PCI candidates, and they suffer high event rates,” said Dr. Urban, director of interventional cardiology at La Tour Hospital in Geneva. As the life expectancy increases, the implications are profound because roughly one-fifth of all PCI patients globally could be candidates for this type of treatment.
The data were presented at the Transcatheter Cardiovascular Therapeutics annual meeting, which was sponsored by the Cardiovascular Research Foundation. The results also were published online (N Engl J Med. 2015 Oct 14. doi: 10.1056/NEJMoa1503943).
“I hope these results will change practice as early as next week in Europe and elsewhere,” he said. The device is currently CE marked in Europe and is available in some parts of Asia. A clinical trial for the device is currently in the preliminary stages in the United States.
The current standard for PCI in patients at high risk for hemorrhage is to use bare-metal, instead of drug-eluting, stents. Although this protocol lowers the potential risk for bleeding and other complications often caused by extended dual antiplatelet therapy (DAPT), it exposes these patients to a higher risk of restenosis.
Rather than use a drug delivery polymer, the Biolimus A9-coated BioFreedom (Biosensors International) is polymer free and uses a stainless steel stent microstructured to hold a proprietary lipophilic drug on its outer surface. The drug is absorbed by the body within a month of placement.
The first of its kind, the double-blinded LEADERS FREE trial randomly assigned 2,466 PCI patients at high risk for bleeding to receive either the test stent or the standard platform Gazelle bare-metal stent. The procedures were performed at nearly 70 participating sites around the world, excluding the United States. More than half of all patients were accessed transradially, which was preferable to transfemoral access, according to Dr. Urban, because of the lower associated bleeding rates.
All patients were given 1 month of antiplatelet therapy after their intervention: about two-thirds of each group received DAPT and one-third received triple antiplatelet therapy. All were then switched to aspirin alone for 1 year.
At 390 days, there was nearly a 50% reduction in the need for repeat revascularization in the 1,221 patients receiving the drug-coated stent (5.1%), compared with 1,221 receiving the bare-metal stent (9.8%), with the difference reaching statistical significance for superiority for this primary efficacy endpoint (P < .001 for superiority).
Patients in the study arm also had a 29% reduction in risk of cardiac death, myocardial infarction, or stent thrombosis, the primary safety endpoint. At 390 days, these events occurred in 9.4% of the drug coated–stent patients, compared with 12.9% of the controls, a statistically significant difference for both noninferiority (P < .0001) and superiority (P = .005).
The study was done in patients typically excluded from such a trial, although, according to Dr. Urban, the PCI procedures performed were no more complex than usual. More than half the patients, three-quarters of whom were men in their mid- to late-70s, also had a range of comorbidities such as diabetes, kidney disease, and atrial fibrillation. Patients taking anticoagulants, those who had experienced a stroke within the past year, those expected to have major surgery within the year, and those who had undergone cancer treatment within the past 3 years also were included.
Bleeding events in the year following did not differ significantly between groups: 18.1% in the study group and 19.1% of controls had BARC 1-5 bleeding; 13.9% in the test arm and 14.7% of controls had BARC 2-5 events; and 7.2% in the study group and 7.3% of controls experienced BARC 3-5 events.
In the past, Dr. Urban had theorized that the trial would help to quantify not only risk for hemorrhage, but also the thrombotic risk in this patient population. In an interview, Dr. Urban said that, while the stent thrombosis rate was nearly identical in both groups in the trial, “the safety advantage of the drug-coated stent was especially apparent in the more thrombotic milieu.”
LEADERS FREE was underwritten by Biosensors International, maker of the BioFreedom stent. Dr. Urban and several of his coinvestigators disclosed relationships with device makers, including Edward Lifesciences, Terumo, Abbott Vascular, and Quest Medical.
On Twitter @whitneymcknight
AT TCT 2015
Key clinical point: Older, sicker acute coronary syndrome patients at higher risk for hemorrhage may now have more PCI options.
Major finding: At 390 days, 5.1% of PCI patients given a drug-coated stent plus 1 month of DAPT required revascularization, compared with 9.8% of the bare metal–stented control group given 1 month of DAPT; 9.4% of those given a drug-coated stent plus 1 month DAPT had adverse events vs. 12.9% of controls.
Data source: LEADERS FREE is a prospective, double-blinded, randomized controlled trial of 2,466 PCI patients at high risk for bleeding.
Disclosures: The study was underwritten by Biosensors International, maker of the BioFreedom stent.
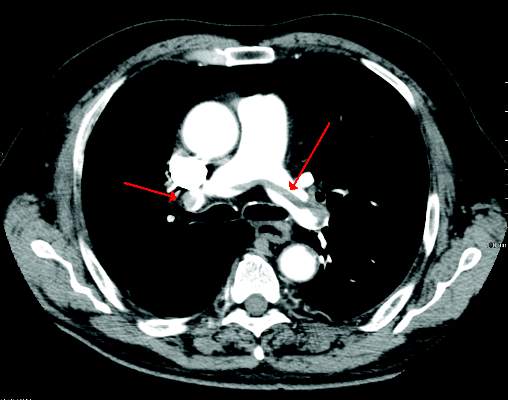
TCT: Routine thrombectomy with PCI raises stroke risk 66% in STEMI patients
Routine manual thrombectomy during percutaneous coronary intervention offers no significant long-term benefit over PCI alone for patients with acute ST-segment–elevation myocardial infarction.
In fact, thrombectomy was associated with a 66% increase in stroke risk in the year following a heart attack, Dr. Sanjit Jolly reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
A 1-year analysis of the TOTAL trial confirmed the study’s recently published 1-month findings: Routine thrombectomy isn’t any better than PCI alone in the clinical outcomes of cardiovascular death, myocardial infarction, cardiogenic shock, or heart failure.
As it was at 1 month, however, stroke at 1 year was significantly more common; it occurred in 60 patients (1.2%) in the thrombectomy group and 36 (0.7%) in the PCI-alone group, for an increase in risk of 66% (P = .015).
The findings were simultaneously published online (Lancet 2015 Oct 13 doi: 10.1016/ S0140-6736[15]00448-1).
“Based on these endpoints, manual thrombectomy can no longer be recommended as a primary strategy in these patients,” Dr. Jolly said at the meeting, which was sponsored by the Cardiovascular Research Foundation.
Despite the unequivocal findings, it’s unclear when clinicians will completely embrace TOTAL’s results, noted Dr. Jolly of McMaster University, Hamilton, Ont.
“Unfortunately, practice has not changed with these findings. It often takes time for new evidence to get translated into the clinic, although some of my colleagues have told me that the results are giving them pause, causing them to use less thrombus aspiration. But interventional cardiologists are very visually driven. If we see something, we want to take it out. So it may take some time for these to be adopted,” he said.
The Thromwbectomy With PCI Versus PCI Alone in Patients With STEMI (TOTAL) trial randomized 10,723 patients to percutaneous coronary intervention with or without routine manual thrombectomy. The primary outcome was a composite of death from cardiovascular causes, recurrent myocardial infarction, cardiogenic shock, or New York Heart Association class IV heart failure within 180 days. The key safety outcome was stroke within 30 days.
The TOTAL results showed no difference in the primary outcome between thrombectomy and PCI patients (6.9% vs. 7%) (N Engl J Med. 2015 Apr 9;372[15]:1389-98).
Rates of cardiovascular death were similar (3% in each group) as were those for a combination of the primary outcome plus stent thrombosis or revascularization (10% in each group). Patients who had a thrombectomy were twice as likely to have a stroke within 30 days, although the absolute numbers were small (0.7% vs. 0.3%; HR, 2.06).
The 1-year follow-up study provided important perspective about the long-term risks and benefits of the two strategies.
There was no difference in the rate of the composite endpoint, which occurred in 7.8% of each group. Cardiovascular death occurred in 3.6% of the thrombectomy group and 3.8% of the PCI-alone group. There were similar rates of recurrent heart attack (2.5% vs. 2.3%), cardiogenic shock (1.9% vs. 2.1%), and class IV heart failure (2.1% vs. 1.9%).
The finding of significantly elevated stroke risk at 30 days was also present at 1 year, occurring in 1.2% of the thrombectomy patients and 0.7% of the PCI-alone patients (HR, 1.66; P = .015). The risk of a combination of stroke or transient ischemic attack was also increased significantly, by 65%, occurring in 1.4% and 0.9%, respectively (HR, 1.65; P = .008).
To further confirm the findings, Dr. Jolly also presented a meta-analysis of all-cause mortality in 20,352 patients involved in 16 studies comparing PCI plus thrombectomy with PCI alone. The meta-analysis also found that routine thrombectomy conferred no mortality benefit over PCI.
It did, however, confirm a 43% increased risk of stroke in PCI plus thrombectomy vs. PCI alone, at 0.9% and 0.6% (P = .03).
TOTAL was funded by the Canadian Institutes of Health Research, the Canadian Network and Centre for Trials Internationally, and Medtronic. Dr. Jolly received grants from Medtronic during the study.
On Twitter @Alz_Gal
Routine manual thrombectomy during percutaneous coronary intervention offers no significant long-term benefit over PCI alone for patients with acute ST-segment–elevation myocardial infarction.
In fact, thrombectomy was associated with a 66% increase in stroke risk in the year following a heart attack, Dr. Sanjit Jolly reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
A 1-year analysis of the TOTAL trial confirmed the study’s recently published 1-month findings: Routine thrombectomy isn’t any better than PCI alone in the clinical outcomes of cardiovascular death, myocardial infarction, cardiogenic shock, or heart failure.
As it was at 1 month, however, stroke at 1 year was significantly more common; it occurred in 60 patients (1.2%) in the thrombectomy group and 36 (0.7%) in the PCI-alone group, for an increase in risk of 66% (P = .015).
The findings were simultaneously published online (Lancet 2015 Oct 13 doi: 10.1016/ S0140-6736[15]00448-1).
“Based on these endpoints, manual thrombectomy can no longer be recommended as a primary strategy in these patients,” Dr. Jolly said at the meeting, which was sponsored by the Cardiovascular Research Foundation.
Despite the unequivocal findings, it’s unclear when clinicians will completely embrace TOTAL’s results, noted Dr. Jolly of McMaster University, Hamilton, Ont.
“Unfortunately, practice has not changed with these findings. It often takes time for new evidence to get translated into the clinic, although some of my colleagues have told me that the results are giving them pause, causing them to use less thrombus aspiration. But interventional cardiologists are very visually driven. If we see something, we want to take it out. So it may take some time for these to be adopted,” he said.
The Thromwbectomy With PCI Versus PCI Alone in Patients With STEMI (TOTAL) trial randomized 10,723 patients to percutaneous coronary intervention with or without routine manual thrombectomy. The primary outcome was a composite of death from cardiovascular causes, recurrent myocardial infarction, cardiogenic shock, or New York Heart Association class IV heart failure within 180 days. The key safety outcome was stroke within 30 days.
The TOTAL results showed no difference in the primary outcome between thrombectomy and PCI patients (6.9% vs. 7%) (N Engl J Med. 2015 Apr 9;372[15]:1389-98).
Rates of cardiovascular death were similar (3% in each group) as were those for a combination of the primary outcome plus stent thrombosis or revascularization (10% in each group). Patients who had a thrombectomy were twice as likely to have a stroke within 30 days, although the absolute numbers were small (0.7% vs. 0.3%; HR, 2.06).
The 1-year follow-up study provided important perspective about the long-term risks and benefits of the two strategies.
There was no difference in the rate of the composite endpoint, which occurred in 7.8% of each group. Cardiovascular death occurred in 3.6% of the thrombectomy group and 3.8% of the PCI-alone group. There were similar rates of recurrent heart attack (2.5% vs. 2.3%), cardiogenic shock (1.9% vs. 2.1%), and class IV heart failure (2.1% vs. 1.9%).
The finding of significantly elevated stroke risk at 30 days was also present at 1 year, occurring in 1.2% of the thrombectomy patients and 0.7% of the PCI-alone patients (HR, 1.66; P = .015). The risk of a combination of stroke or transient ischemic attack was also increased significantly, by 65%, occurring in 1.4% and 0.9%, respectively (HR, 1.65; P = .008).
To further confirm the findings, Dr. Jolly also presented a meta-analysis of all-cause mortality in 20,352 patients involved in 16 studies comparing PCI plus thrombectomy with PCI alone. The meta-analysis also found that routine thrombectomy conferred no mortality benefit over PCI.
It did, however, confirm a 43% increased risk of stroke in PCI plus thrombectomy vs. PCI alone, at 0.9% and 0.6% (P = .03).
TOTAL was funded by the Canadian Institutes of Health Research, the Canadian Network and Centre for Trials Internationally, and Medtronic. Dr. Jolly received grants from Medtronic during the study.
On Twitter @Alz_Gal
Routine manual thrombectomy during percutaneous coronary intervention offers no significant long-term benefit over PCI alone for patients with acute ST-segment–elevation myocardial infarction.
In fact, thrombectomy was associated with a 66% increase in stroke risk in the year following a heart attack, Dr. Sanjit Jolly reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
A 1-year analysis of the TOTAL trial confirmed the study’s recently published 1-month findings: Routine thrombectomy isn’t any better than PCI alone in the clinical outcomes of cardiovascular death, myocardial infarction, cardiogenic shock, or heart failure.
As it was at 1 month, however, stroke at 1 year was significantly more common; it occurred in 60 patients (1.2%) in the thrombectomy group and 36 (0.7%) in the PCI-alone group, for an increase in risk of 66% (P = .015).
The findings were simultaneously published online (Lancet 2015 Oct 13 doi: 10.1016/ S0140-6736[15]00448-1).
“Based on these endpoints, manual thrombectomy can no longer be recommended as a primary strategy in these patients,” Dr. Jolly said at the meeting, which was sponsored by the Cardiovascular Research Foundation.
Despite the unequivocal findings, it’s unclear when clinicians will completely embrace TOTAL’s results, noted Dr. Jolly of McMaster University, Hamilton, Ont.
“Unfortunately, practice has not changed with these findings. It often takes time for new evidence to get translated into the clinic, although some of my colleagues have told me that the results are giving them pause, causing them to use less thrombus aspiration. But interventional cardiologists are very visually driven. If we see something, we want to take it out. So it may take some time for these to be adopted,” he said.
The Thromwbectomy With PCI Versus PCI Alone in Patients With STEMI (TOTAL) trial randomized 10,723 patients to percutaneous coronary intervention with or without routine manual thrombectomy. The primary outcome was a composite of death from cardiovascular causes, recurrent myocardial infarction, cardiogenic shock, or New York Heart Association class IV heart failure within 180 days. The key safety outcome was stroke within 30 days.
The TOTAL results showed no difference in the primary outcome between thrombectomy and PCI patients (6.9% vs. 7%) (N Engl J Med. 2015 Apr 9;372[15]:1389-98).
Rates of cardiovascular death were similar (3% in each group) as were those for a combination of the primary outcome plus stent thrombosis or revascularization (10% in each group). Patients who had a thrombectomy were twice as likely to have a stroke within 30 days, although the absolute numbers were small (0.7% vs. 0.3%; HR, 2.06).
The 1-year follow-up study provided important perspective about the long-term risks and benefits of the two strategies.
There was no difference in the rate of the composite endpoint, which occurred in 7.8% of each group. Cardiovascular death occurred in 3.6% of the thrombectomy group and 3.8% of the PCI-alone group. There were similar rates of recurrent heart attack (2.5% vs. 2.3%), cardiogenic shock (1.9% vs. 2.1%), and class IV heart failure (2.1% vs. 1.9%).
The finding of significantly elevated stroke risk at 30 days was also present at 1 year, occurring in 1.2% of the thrombectomy patients and 0.7% of the PCI-alone patients (HR, 1.66; P = .015). The risk of a combination of stroke or transient ischemic attack was also increased significantly, by 65%, occurring in 1.4% and 0.9%, respectively (HR, 1.65; P = .008).
To further confirm the findings, Dr. Jolly also presented a meta-analysis of all-cause mortality in 20,352 patients involved in 16 studies comparing PCI plus thrombectomy with PCI alone. The meta-analysis also found that routine thrombectomy conferred no mortality benefit over PCI.
It did, however, confirm a 43% increased risk of stroke in PCI plus thrombectomy vs. PCI alone, at 0.9% and 0.6% (P = .03).
TOTAL was funded by the Canadian Institutes of Health Research, the Canadian Network and Centre for Trials Internationally, and Medtronic. Dr. Jolly received grants from Medtronic during the study.
On Twitter @Alz_Gal
AT TCT 2015
Key clinical point: Adding routine thrombectomy to PCI doesn’t improve outcomes; in fact, it increases the risk of stroke by 66% at 1 year.
Major finding: At 1 year, thrombectomy didn’t improve cardiovascular outcomes over PCI alone for patients with STEMI; in fact, it increased the risk of stroke by 66%.
Data source: The TOTAL trial randomizing 10,732 patients with STEMI to either PCI plus manual thrombectomy or PCI alone.
Disclosures: TOTAL was funded by the Canadian Institutes of Health Research, the Canadian Network and Centre for Trials Internationally, and Medtronic. Dr. Jolly received grants from Medtronic during the study.
Endovascular treatment of acute IVC thrombosis found effective
Endovascular treatment of acute thrombosis of the inferior vena cava is safe and effective with excellent short-term results, according to the results of a 10-year retrospective review reported by Dr. Khanjan H. Nagarsheth and his colleagues at the Staten Island University (N.Y.) Hospital.
Dr. Nagarsheth and his colleagues assessed 25 patients (44% men) with a mean age of 50.3 years, who underwent catheter-directed treatment in either the operating room or the angiography suite for acute (existing for less than 2 weeks) symptomatic IVC thrombosis (Annals Vasc Surg. 2015; 29:1373-9).
All patients had a prior history of deep vein thrombosis; 21 patients had an IVC filter at presentation.
Endovascular treatment was successful in all 25 patients. The greater majority of patients (22, 88%) received both catheter-directed thrombolysis (CDT) and pharmacomechanical thrombectomy; the remaining 3 patients received CDT alone.
Significant (greater than 50% luminal gain) angiographic resolution of the venous thromboembolism was achieved in all patients, with 23 (92%) reporting moderate to complete symptomatic improvement immediately after the procedure. At the median follow-up of 54.3 weeks, symptomatic improvement was noted in all patients, and complete symptom resolution was seen in 16 (89%). None of the IVC filters were removed and 67% of patients had a patent IVC at last follow-up.
“An aggressive endovascular approach to treatment of [acute thrombosis of the] IVC is warranted even in the presence of a thrombosed caval filter,” the authors concluded.
The authors did not indicate the existence of any conflicts.
Read the full study online in the Annals of Vascular Surgery.
Endovascular treatment of acute thrombosis of the inferior vena cava is safe and effective with excellent short-term results, according to the results of a 10-year retrospective review reported by Dr. Khanjan H. Nagarsheth and his colleagues at the Staten Island University (N.Y.) Hospital.
Dr. Nagarsheth and his colleagues assessed 25 patients (44% men) with a mean age of 50.3 years, who underwent catheter-directed treatment in either the operating room or the angiography suite for acute (existing for less than 2 weeks) symptomatic IVC thrombosis (Annals Vasc Surg. 2015; 29:1373-9).
All patients had a prior history of deep vein thrombosis; 21 patients had an IVC filter at presentation.
Endovascular treatment was successful in all 25 patients. The greater majority of patients (22, 88%) received both catheter-directed thrombolysis (CDT) and pharmacomechanical thrombectomy; the remaining 3 patients received CDT alone.
Significant (greater than 50% luminal gain) angiographic resolution of the venous thromboembolism was achieved in all patients, with 23 (92%) reporting moderate to complete symptomatic improvement immediately after the procedure. At the median follow-up of 54.3 weeks, symptomatic improvement was noted in all patients, and complete symptom resolution was seen in 16 (89%). None of the IVC filters were removed and 67% of patients had a patent IVC at last follow-up.
“An aggressive endovascular approach to treatment of [acute thrombosis of the] IVC is warranted even in the presence of a thrombosed caval filter,” the authors concluded.
The authors did not indicate the existence of any conflicts.
Read the full study online in the Annals of Vascular Surgery.
Endovascular treatment of acute thrombosis of the inferior vena cava is safe and effective with excellent short-term results, according to the results of a 10-year retrospective review reported by Dr. Khanjan H. Nagarsheth and his colleagues at the Staten Island University (N.Y.) Hospital.
Dr. Nagarsheth and his colleagues assessed 25 patients (44% men) with a mean age of 50.3 years, who underwent catheter-directed treatment in either the operating room or the angiography suite for acute (existing for less than 2 weeks) symptomatic IVC thrombosis (Annals Vasc Surg. 2015; 29:1373-9).
All patients had a prior history of deep vein thrombosis; 21 patients had an IVC filter at presentation.
Endovascular treatment was successful in all 25 patients. The greater majority of patients (22, 88%) received both catheter-directed thrombolysis (CDT) and pharmacomechanical thrombectomy; the remaining 3 patients received CDT alone.
Significant (greater than 50% luminal gain) angiographic resolution of the venous thromboembolism was achieved in all patients, with 23 (92%) reporting moderate to complete symptomatic improvement immediately after the procedure. At the median follow-up of 54.3 weeks, symptomatic improvement was noted in all patients, and complete symptom resolution was seen in 16 (89%). None of the IVC filters were removed and 67% of patients had a patent IVC at last follow-up.
“An aggressive endovascular approach to treatment of [acute thrombosis of the] IVC is warranted even in the presence of a thrombosed caval filter,” the authors concluded.
The authors did not indicate the existence of any conflicts.
Read the full study online in the Annals of Vascular Surgery.
FROM THE ANNALS OF VASCULAR SURGERY
ESC model predicts recurrent VTE risk
Recurrent venous thromboembolism was significantly associated with a higher European Society of Cardiology (ESC) pulmonary embolism score. This association was independent of other factors such as age, sex, and body mass index, according to a long-term, prospective follow-up study of 627 patients with a first episode of pulmonary embolism.
In addition, unprovoked PE and varicose veins of the lower limbs also increased recurrence risk, while longer anticoagulation treatment reduced it (Intnl J Cardiol. 2016;202:275-81).
Dr. Shuai Zhang of the Beijing Institute of Respiratory Medicine and coauthors categorized their patients into three groups according to the ESC risk stratification model (Eur Heart J. 2008;29:2276-315). These were low-, intermediate-, and high-risk groups. Of the 627 patients, 84 had suspected VTE recurrence, 68 of whom had this confirmed by imaging diagnosis and were designated as the recurrent group. The 1-, 2-, and 5-year cumulative incidences of recurrent VTE were 4.5%. 7.3%, and 13.9%, respectively.
The researchers compared the 68 recurrent to the 559 nonrecurrent patients; all patients had had a first episode of PE.
Compared with nonrecurrent VTE patients, the recurrent group had significantly more high-risk and intermediate-risk patients, and the high-risk and intermediate-risk patients overall had significantly more cumulative recurrent events than the low-risk group. Multivariate analysis confirmed the association between higher risk in ESC stratification and VTE recurrence independent of age, sex, and body mass index.
Based on these results, the authors stated that, “The severity of disease should be considered in determining the initial treatment and duration of follow-up anticoagulation.”
“These finding support the notion that optimized therapy based on risk stratification is valuable while treating PE patients,” they concluded.
The authors reported having no conflicts of interest.
Read the full study online in the International Journal of Cardiology.
Recurrent venous thromboembolism was significantly associated with a higher European Society of Cardiology (ESC) pulmonary embolism score. This association was independent of other factors such as age, sex, and body mass index, according to a long-term, prospective follow-up study of 627 patients with a first episode of pulmonary embolism.
In addition, unprovoked PE and varicose veins of the lower limbs also increased recurrence risk, while longer anticoagulation treatment reduced it (Intnl J Cardiol. 2016;202:275-81).
Dr. Shuai Zhang of the Beijing Institute of Respiratory Medicine and coauthors categorized their patients into three groups according to the ESC risk stratification model (Eur Heart J. 2008;29:2276-315). These were low-, intermediate-, and high-risk groups. Of the 627 patients, 84 had suspected VTE recurrence, 68 of whom had this confirmed by imaging diagnosis and were designated as the recurrent group. The 1-, 2-, and 5-year cumulative incidences of recurrent VTE were 4.5%. 7.3%, and 13.9%, respectively.
The researchers compared the 68 recurrent to the 559 nonrecurrent patients; all patients had had a first episode of PE.
Compared with nonrecurrent VTE patients, the recurrent group had significantly more high-risk and intermediate-risk patients, and the high-risk and intermediate-risk patients overall had significantly more cumulative recurrent events than the low-risk group. Multivariate analysis confirmed the association between higher risk in ESC stratification and VTE recurrence independent of age, sex, and body mass index.
Based on these results, the authors stated that, “The severity of disease should be considered in determining the initial treatment and duration of follow-up anticoagulation.”
“These finding support the notion that optimized therapy based on risk stratification is valuable while treating PE patients,” they concluded.
The authors reported having no conflicts of interest.
Read the full study online in the International Journal of Cardiology.
Recurrent venous thromboembolism was significantly associated with a higher European Society of Cardiology (ESC) pulmonary embolism score. This association was independent of other factors such as age, sex, and body mass index, according to a long-term, prospective follow-up study of 627 patients with a first episode of pulmonary embolism.
In addition, unprovoked PE and varicose veins of the lower limbs also increased recurrence risk, while longer anticoagulation treatment reduced it (Intnl J Cardiol. 2016;202:275-81).
Dr. Shuai Zhang of the Beijing Institute of Respiratory Medicine and coauthors categorized their patients into three groups according to the ESC risk stratification model (Eur Heart J. 2008;29:2276-315). These were low-, intermediate-, and high-risk groups. Of the 627 patients, 84 had suspected VTE recurrence, 68 of whom had this confirmed by imaging diagnosis and were designated as the recurrent group. The 1-, 2-, and 5-year cumulative incidences of recurrent VTE were 4.5%. 7.3%, and 13.9%, respectively.
The researchers compared the 68 recurrent to the 559 nonrecurrent patients; all patients had had a first episode of PE.
Compared with nonrecurrent VTE patients, the recurrent group had significantly more high-risk and intermediate-risk patients, and the high-risk and intermediate-risk patients overall had significantly more cumulative recurrent events than the low-risk group. Multivariate analysis confirmed the association between higher risk in ESC stratification and VTE recurrence independent of age, sex, and body mass index.
Based on these results, the authors stated that, “The severity of disease should be considered in determining the initial treatment and duration of follow-up anticoagulation.”
“These finding support the notion that optimized therapy based on risk stratification is valuable while treating PE patients,” they concluded.
The authors reported having no conflicts of interest.
Read the full study online in the International Journal of Cardiology.
FROM THE INTERNATIONAL JOURNAL OF CARDIOLOGY
EASD: Diabetes doubles death risk from many causes
STOCKHOLM – Having diabetes doubles the risk for death from a multitude of causes and shortens the life span by 5-7 years, judging from evidence from the United Kingdom Prospective Studies Collaboration presented at the annual meeting of the European Association for the Study of Diabetes.
Patients with diabetes were two and a half times more likely than those without it to die from ischemic heart disease (odds ratio, 2.37; 95% confidence interval, 2.23-2.52). They were also more likely to die from ischemic stroke (OR, 2.75; 95% CI, 2.29-3.31) and “a surprising association with” cardiac arrhythmia (OR, 2.47; 95% CI, 1.80-3.38) was found, said the presenting author, Dr. Louisa Gnatiuc of the clinical trial service unit and epidemiological studies unit at Oxford (England) University. She noted, however, that diabetes was more weakly associated with death from nonischemic causes (OR, 1.57; 95% CI, 1.34-1.85).
In addition, diabetic individuals were almost twice as likely as those with no diabetes to die from renal (OR, 1.90; 95% CI, 1.40-2.58) or hepatic (OR, 1.75; 95% CI, 1.36-2.26) causes, and there was a 13% increase in the overall risk for death from cancer (OR, 1.13; 95% CI, 1.06-1.21). The small increased risk for cancer death was largely due to deaths from oral (OR, 1.81; 95% CI, 1.17-2.81), liver (OR, 1.80; 95% CI, 1.26-2.58), and pancreatic (OR, 1.57; 95% CI, 1.21-2.03) cancers, Dr. Gnatiuc observed. Diabetic individuals were also more likely to die from respiratory causes than their nondiabetic counterparts (OR, 1.59; 95% CI, 1.37-1.83).
These data provide further insight into the risk for death from a multitude of causes in patients with diabetes, said Dr. Naveed Sattar, who was not involved in the analysis, in an interview. “While it is pretty much a replication of the Emerging Risk Factor Paper that was published in the New England Journal of Medicine, there is a little bit of new information here, such as the relative risks in women versus men and by age as well,” he observed.
The odds ratio for death from ischemic heart disease was higher among women aged 35-39 years with diabetes versus those with no diabetes than in men aged 35-39 years with diabetes versus no diabetes, at 5.61 (95% CI, 4.08-7.72) and 2.49 (95% CI, 2.16-2.85), respectively. Similar finding were seen at other age ranges, with around a twofold increase in men aged 60-69 years (OR, 2.26; 95% CI, 2.01-2.53) and 70-89 years (OR, 1.89; 95% CI, 1.70-2.11), but a two- to fourfold increase in women aged 60-69 years (OR, 4.15; 95% CI, 3.38-5.10) and 70-79 years (OR, 2.45, 95% CI, 2.11-2.84).
“So it looks like if you develop diabetes younger, your risk for mortality’s higher,” said Dr. Sattar, professor of metabolic medicine at the Institute of Cardiovascular and Medical Sciences, University of Glasgow (Scotland). “That makes sense,” he added, “because if you develop type 2 diabetes at the age of 30, it must be a much more malignant type of diabetes than, say, if you developed diabetes at age 80, and there are other data that now confirm that is the case as well.”
The analysis was based on data from 44 prospective studies that recorded 55,855 deaths in 690,700 adults who had no prior vascular or other chronic diseases at baseline. Men accounted for 60% of the study population, with a mean age of 48 years. During the postpresentation discussion, Dr. Gnatiuc noted that it was difficult to standardize the definition of diabetes used in the study and that all 25,000 cases of diabetes included in the study had been self-reported. It is likely that most cases were type 2. No information on the duration of diabetes was available, but she noted that this should not matter given the prospective nature of the analysis.
During 13 million patient-years of follow up the most common cause of death was ischemic heart disease, accounting for 17,218 deaths, followed by cancer (18,658 deaths). There were 5,466 strokes of which 1,353 were ischemic (OR, 2.75; 95% CI 2.29-3.31), 1,124 hemorrhagic (OR, 1.59; 95% CI 1.26-2.01), 2,563 that were unspecified (OR, 2.30; 95% CI 1.99-2.66), and 626 classed as subarachnoid hemorrhage (OR, 0.62; 95% CI, 0.36-1.08). Vascular causes of death included inflammatory heart disease, sudden death, and atherosclerosis, among others, which were all increased in diabetic versus nondiabetic subjects.
Dr. Gnatiuc noted that the risk for ischemic heart disease increased with increasing age, systolic blood pressure, and total cholesterol in diabetics and in nondiabetics, although it was much higher in those with diabetes than in those without. “Controlling blood pressure, cholesterol, and obesity are particularly important to reduce absolute mortality rates in those with diabetes, she suggested.
The differences between the sexes in terms of ischemic heart disease need further study, she suggested, noting that improved understanding of the sex differences may help better understand and thus reduce the excess mortality seen.
Premature mortality of up to 5 years in men and 7 years in women was observed. “At the age of 70 a man with diabetes would have about 10% less probability to survive up to the age of 90 as compared to their nondiabetic counterparts,” Dr. Gnatiuc said. Women would have about a 30% decrease in survival probability from age 70-90, she added.
STOCKHOLM – Having diabetes doubles the risk for death from a multitude of causes and shortens the life span by 5-7 years, judging from evidence from the United Kingdom Prospective Studies Collaboration presented at the annual meeting of the European Association for the Study of Diabetes.
Patients with diabetes were two and a half times more likely than those without it to die from ischemic heart disease (odds ratio, 2.37; 95% confidence interval, 2.23-2.52). They were also more likely to die from ischemic stroke (OR, 2.75; 95% CI, 2.29-3.31) and “a surprising association with” cardiac arrhythmia (OR, 2.47; 95% CI, 1.80-3.38) was found, said the presenting author, Dr. Louisa Gnatiuc of the clinical trial service unit and epidemiological studies unit at Oxford (England) University. She noted, however, that diabetes was more weakly associated with death from nonischemic causes (OR, 1.57; 95% CI, 1.34-1.85).
In addition, diabetic individuals were almost twice as likely as those with no diabetes to die from renal (OR, 1.90; 95% CI, 1.40-2.58) or hepatic (OR, 1.75; 95% CI, 1.36-2.26) causes, and there was a 13% increase in the overall risk for death from cancer (OR, 1.13; 95% CI, 1.06-1.21). The small increased risk for cancer death was largely due to deaths from oral (OR, 1.81; 95% CI, 1.17-2.81), liver (OR, 1.80; 95% CI, 1.26-2.58), and pancreatic (OR, 1.57; 95% CI, 1.21-2.03) cancers, Dr. Gnatiuc observed. Diabetic individuals were also more likely to die from respiratory causes than their nondiabetic counterparts (OR, 1.59; 95% CI, 1.37-1.83).
These data provide further insight into the risk for death from a multitude of causes in patients with diabetes, said Dr. Naveed Sattar, who was not involved in the analysis, in an interview. “While it is pretty much a replication of the Emerging Risk Factor Paper that was published in the New England Journal of Medicine, there is a little bit of new information here, such as the relative risks in women versus men and by age as well,” he observed.
The odds ratio for death from ischemic heart disease was higher among women aged 35-39 years with diabetes versus those with no diabetes than in men aged 35-39 years with diabetes versus no diabetes, at 5.61 (95% CI, 4.08-7.72) and 2.49 (95% CI, 2.16-2.85), respectively. Similar finding were seen at other age ranges, with around a twofold increase in men aged 60-69 years (OR, 2.26; 95% CI, 2.01-2.53) and 70-89 years (OR, 1.89; 95% CI, 1.70-2.11), but a two- to fourfold increase in women aged 60-69 years (OR, 4.15; 95% CI, 3.38-5.10) and 70-79 years (OR, 2.45, 95% CI, 2.11-2.84).
“So it looks like if you develop diabetes younger, your risk for mortality’s higher,” said Dr. Sattar, professor of metabolic medicine at the Institute of Cardiovascular and Medical Sciences, University of Glasgow (Scotland). “That makes sense,” he added, “because if you develop type 2 diabetes at the age of 30, it must be a much more malignant type of diabetes than, say, if you developed diabetes at age 80, and there are other data that now confirm that is the case as well.”
The analysis was based on data from 44 prospective studies that recorded 55,855 deaths in 690,700 adults who had no prior vascular or other chronic diseases at baseline. Men accounted for 60% of the study population, with a mean age of 48 years. During the postpresentation discussion, Dr. Gnatiuc noted that it was difficult to standardize the definition of diabetes used in the study and that all 25,000 cases of diabetes included in the study had been self-reported. It is likely that most cases were type 2. No information on the duration of diabetes was available, but she noted that this should not matter given the prospective nature of the analysis.
During 13 million patient-years of follow up the most common cause of death was ischemic heart disease, accounting for 17,218 deaths, followed by cancer (18,658 deaths). There were 5,466 strokes of which 1,353 were ischemic (OR, 2.75; 95% CI 2.29-3.31), 1,124 hemorrhagic (OR, 1.59; 95% CI 1.26-2.01), 2,563 that were unspecified (OR, 2.30; 95% CI 1.99-2.66), and 626 classed as subarachnoid hemorrhage (OR, 0.62; 95% CI, 0.36-1.08). Vascular causes of death included inflammatory heart disease, sudden death, and atherosclerosis, among others, which were all increased in diabetic versus nondiabetic subjects.
Dr. Gnatiuc noted that the risk for ischemic heart disease increased with increasing age, systolic blood pressure, and total cholesterol in diabetics and in nondiabetics, although it was much higher in those with diabetes than in those without. “Controlling blood pressure, cholesterol, and obesity are particularly important to reduce absolute mortality rates in those with diabetes, she suggested.
The differences between the sexes in terms of ischemic heart disease need further study, she suggested, noting that improved understanding of the sex differences may help better understand and thus reduce the excess mortality seen.
Premature mortality of up to 5 years in men and 7 years in women was observed. “At the age of 70 a man with diabetes would have about 10% less probability to survive up to the age of 90 as compared to their nondiabetic counterparts,” Dr. Gnatiuc said. Women would have about a 30% decrease in survival probability from age 70-90, she added.
STOCKHOLM – Having diabetes doubles the risk for death from a multitude of causes and shortens the life span by 5-7 years, judging from evidence from the United Kingdom Prospective Studies Collaboration presented at the annual meeting of the European Association for the Study of Diabetes.
Patients with diabetes were two and a half times more likely than those without it to die from ischemic heart disease (odds ratio, 2.37; 95% confidence interval, 2.23-2.52). They were also more likely to die from ischemic stroke (OR, 2.75; 95% CI, 2.29-3.31) and “a surprising association with” cardiac arrhythmia (OR, 2.47; 95% CI, 1.80-3.38) was found, said the presenting author, Dr. Louisa Gnatiuc of the clinical trial service unit and epidemiological studies unit at Oxford (England) University. She noted, however, that diabetes was more weakly associated with death from nonischemic causes (OR, 1.57; 95% CI, 1.34-1.85).
In addition, diabetic individuals were almost twice as likely as those with no diabetes to die from renal (OR, 1.90; 95% CI, 1.40-2.58) or hepatic (OR, 1.75; 95% CI, 1.36-2.26) causes, and there was a 13% increase in the overall risk for death from cancer (OR, 1.13; 95% CI, 1.06-1.21). The small increased risk for cancer death was largely due to deaths from oral (OR, 1.81; 95% CI, 1.17-2.81), liver (OR, 1.80; 95% CI, 1.26-2.58), and pancreatic (OR, 1.57; 95% CI, 1.21-2.03) cancers, Dr. Gnatiuc observed. Diabetic individuals were also more likely to die from respiratory causes than their nondiabetic counterparts (OR, 1.59; 95% CI, 1.37-1.83).
These data provide further insight into the risk for death from a multitude of causes in patients with diabetes, said Dr. Naveed Sattar, who was not involved in the analysis, in an interview. “While it is pretty much a replication of the Emerging Risk Factor Paper that was published in the New England Journal of Medicine, there is a little bit of new information here, such as the relative risks in women versus men and by age as well,” he observed.
The odds ratio for death from ischemic heart disease was higher among women aged 35-39 years with diabetes versus those with no diabetes than in men aged 35-39 years with diabetes versus no diabetes, at 5.61 (95% CI, 4.08-7.72) and 2.49 (95% CI, 2.16-2.85), respectively. Similar finding were seen at other age ranges, with around a twofold increase in men aged 60-69 years (OR, 2.26; 95% CI, 2.01-2.53) and 70-89 years (OR, 1.89; 95% CI, 1.70-2.11), but a two- to fourfold increase in women aged 60-69 years (OR, 4.15; 95% CI, 3.38-5.10) and 70-79 years (OR, 2.45, 95% CI, 2.11-2.84).
“So it looks like if you develop diabetes younger, your risk for mortality’s higher,” said Dr. Sattar, professor of metabolic medicine at the Institute of Cardiovascular and Medical Sciences, University of Glasgow (Scotland). “That makes sense,” he added, “because if you develop type 2 diabetes at the age of 30, it must be a much more malignant type of diabetes than, say, if you developed diabetes at age 80, and there are other data that now confirm that is the case as well.”
The analysis was based on data from 44 prospective studies that recorded 55,855 deaths in 690,700 adults who had no prior vascular or other chronic diseases at baseline. Men accounted for 60% of the study population, with a mean age of 48 years. During the postpresentation discussion, Dr. Gnatiuc noted that it was difficult to standardize the definition of diabetes used in the study and that all 25,000 cases of diabetes included in the study had been self-reported. It is likely that most cases were type 2. No information on the duration of diabetes was available, but she noted that this should not matter given the prospective nature of the analysis.
During 13 million patient-years of follow up the most common cause of death was ischemic heart disease, accounting for 17,218 deaths, followed by cancer (18,658 deaths). There were 5,466 strokes of which 1,353 were ischemic (OR, 2.75; 95% CI 2.29-3.31), 1,124 hemorrhagic (OR, 1.59; 95% CI 1.26-2.01), 2,563 that were unspecified (OR, 2.30; 95% CI 1.99-2.66), and 626 classed as subarachnoid hemorrhage (OR, 0.62; 95% CI, 0.36-1.08). Vascular causes of death included inflammatory heart disease, sudden death, and atherosclerosis, among others, which were all increased in diabetic versus nondiabetic subjects.
Dr. Gnatiuc noted that the risk for ischemic heart disease increased with increasing age, systolic blood pressure, and total cholesterol in diabetics and in nondiabetics, although it was much higher in those with diabetes than in those without. “Controlling blood pressure, cholesterol, and obesity are particularly important to reduce absolute mortality rates in those with diabetes, she suggested.
The differences between the sexes in terms of ischemic heart disease need further study, she suggested, noting that improved understanding of the sex differences may help better understand and thus reduce the excess mortality seen.
Premature mortality of up to 5 years in men and 7 years in women was observed. “At the age of 70 a man with diabetes would have about 10% less probability to survive up to the age of 90 as compared to their nondiabetic counterparts,” Dr. Gnatiuc said. Women would have about a 30% decrease in survival probability from age 70-90, she added.
AT EASD 2015
Key clinical point:Women with diabetes were more likely to die from ischemic heart disease than men with diabetes when compared to those without diabetes.
Major finding: Women with diabetes were more likely to die from ischemic heart disease than men with diabetes when compared to those without diabetes.
Data source: United Kingdom Prospective Studies Collaboration analysis of 44 prospective studies that recorded 55,855 deaths in 690,700 adults who had no prior vascular or other chronic diseases at baseline.
Disclosures: The study was funded by research grants from the British Heart Foundation, UK Medical Research Council, The National Institutes of Health (UK), Cancer Research UK, and the Clinical Trial Service Unit and Epidemiological Studies Unit at Oxford University, UK. Dr. Gnatiuc did not report any personal disclosures.
New composite measure improves warfarin anticoagulation monitoring
A new composite measure that incorporates both time in therapeutic range and international normalized ratio variability appears to be more accurate than either of these tests alone at monitoring warfarin anticoagulation, according to a report published online Sept. 29 in Circulation: Cardiovascular Quality and Outcomes.
Time in therapeutic range (TTR) and international normalized ratio (INR) variability track two different aspects of anticoagulation control. TTR measures the percentage of time that patients spend within the therapeutic range while taking warfarin, which reflects the amount of time that treatment intensity was appropriate. INR variability measures variations in the stability of warfarin’s anticoagulation effects over time. Most clinicians monitor their patients using one or the other of these measures, usually TTR. A composite measure that combines the two “would encourage providers to focus on all components of anticoagulation control, not just those measured by the current standard of care, TTR,” said Dr. Zayd Razouki of the Center for Health Services Research in Primary Care, Durham (N.C.) Veterans Affairs Medical Center, and his associates.
It is important to note that a substantial number of patients taking warfarin could be classified as having poor control of anticoagulation by one of these measures, but good control by the other. Combining TTR with INR variability would ensure that both appropriate intensity and appropriate stability of warfarin therapy were being used to judge each patient’s anticoagulation control, they noted.
The investigators devised such a measure, a summary score they called WCM (warfarin composite measure). They then compared the performance of all three measures at predicting major warfarin-related complications, using as a sample population 40,404 participants in the Veterans Affairs Study to Improve Anticoagulation (VARIA). These study subjects were aged 65 years or older (mean age 76), had been taking warfarin for at least 6 months to treat atrial fibrillation, and were followed for an average of 14 months for the development of ischemic stroke, major bleeding, and fatal bleeding.
A total of 3.1% of these patients developed ischemic stroke, 6.4% developed major bleeding, and 0.9% developed fatal bleeding while taking warfarin. After the data were adjusted to account for numerous potential confounding factors, WCM correlated most closely with risk for adverse warfarin-related clinical events, Dr. Razouki and his associates wrote (Circ Cardiovasc Qual Outcomes. 2015 Sep 29. doi:10.1161/circoutcomes.115.001789).
Their findings also indicate that WCM may be a more accurate measure of a clinic’s or a medical system’s performance at monitoring anticoagulation than either their average TTR or INR variability alone.
The study results may not be generalizable to all populations, because this VA sample was overwhelmingly male (98%), the investigators added.
A new composite measure that incorporates both time in therapeutic range and international normalized ratio variability appears to be more accurate than either of these tests alone at monitoring warfarin anticoagulation, according to a report published online Sept. 29 in Circulation: Cardiovascular Quality and Outcomes.
Time in therapeutic range (TTR) and international normalized ratio (INR) variability track two different aspects of anticoagulation control. TTR measures the percentage of time that patients spend within the therapeutic range while taking warfarin, which reflects the amount of time that treatment intensity was appropriate. INR variability measures variations in the stability of warfarin’s anticoagulation effects over time. Most clinicians monitor their patients using one or the other of these measures, usually TTR. A composite measure that combines the two “would encourage providers to focus on all components of anticoagulation control, not just those measured by the current standard of care, TTR,” said Dr. Zayd Razouki of the Center for Health Services Research in Primary Care, Durham (N.C.) Veterans Affairs Medical Center, and his associates.
It is important to note that a substantial number of patients taking warfarin could be classified as having poor control of anticoagulation by one of these measures, but good control by the other. Combining TTR with INR variability would ensure that both appropriate intensity and appropriate stability of warfarin therapy were being used to judge each patient’s anticoagulation control, they noted.
The investigators devised such a measure, a summary score they called WCM (warfarin composite measure). They then compared the performance of all three measures at predicting major warfarin-related complications, using as a sample population 40,404 participants in the Veterans Affairs Study to Improve Anticoagulation (VARIA). These study subjects were aged 65 years or older (mean age 76), had been taking warfarin for at least 6 months to treat atrial fibrillation, and were followed for an average of 14 months for the development of ischemic stroke, major bleeding, and fatal bleeding.
A total of 3.1% of these patients developed ischemic stroke, 6.4% developed major bleeding, and 0.9% developed fatal bleeding while taking warfarin. After the data were adjusted to account for numerous potential confounding factors, WCM correlated most closely with risk for adverse warfarin-related clinical events, Dr. Razouki and his associates wrote (Circ Cardiovasc Qual Outcomes. 2015 Sep 29. doi:10.1161/circoutcomes.115.001789).
Their findings also indicate that WCM may be a more accurate measure of a clinic’s or a medical system’s performance at monitoring anticoagulation than either their average TTR or INR variability alone.
The study results may not be generalizable to all populations, because this VA sample was overwhelmingly male (98%), the investigators added.
A new composite measure that incorporates both time in therapeutic range and international normalized ratio variability appears to be more accurate than either of these tests alone at monitoring warfarin anticoagulation, according to a report published online Sept. 29 in Circulation: Cardiovascular Quality and Outcomes.
Time in therapeutic range (TTR) and international normalized ratio (INR) variability track two different aspects of anticoagulation control. TTR measures the percentage of time that patients spend within the therapeutic range while taking warfarin, which reflects the amount of time that treatment intensity was appropriate. INR variability measures variations in the stability of warfarin’s anticoagulation effects over time. Most clinicians monitor their patients using one or the other of these measures, usually TTR. A composite measure that combines the two “would encourage providers to focus on all components of anticoagulation control, not just those measured by the current standard of care, TTR,” said Dr. Zayd Razouki of the Center for Health Services Research in Primary Care, Durham (N.C.) Veterans Affairs Medical Center, and his associates.
It is important to note that a substantial number of patients taking warfarin could be classified as having poor control of anticoagulation by one of these measures, but good control by the other. Combining TTR with INR variability would ensure that both appropriate intensity and appropriate stability of warfarin therapy were being used to judge each patient’s anticoagulation control, they noted.
The investigators devised such a measure, a summary score they called WCM (warfarin composite measure). They then compared the performance of all three measures at predicting major warfarin-related complications, using as a sample population 40,404 participants in the Veterans Affairs Study to Improve Anticoagulation (VARIA). These study subjects were aged 65 years or older (mean age 76), had been taking warfarin for at least 6 months to treat atrial fibrillation, and were followed for an average of 14 months for the development of ischemic stroke, major bleeding, and fatal bleeding.
A total of 3.1% of these patients developed ischemic stroke, 6.4% developed major bleeding, and 0.9% developed fatal bleeding while taking warfarin. After the data were adjusted to account for numerous potential confounding factors, WCM correlated most closely with risk for adverse warfarin-related clinical events, Dr. Razouki and his associates wrote (Circ Cardiovasc Qual Outcomes. 2015 Sep 29. doi:10.1161/circoutcomes.115.001789).
Their findings also indicate that WCM may be a more accurate measure of a clinic’s or a medical system’s performance at monitoring anticoagulation than either their average TTR or INR variability alone.
The study results may not be generalizable to all populations, because this VA sample was overwhelmingly male (98%), the investigators added.
FROM CIRCULATION: CARDIOVASCULAR QUALITY AND OUTCOMES
Key clinical point: A composite measure that combines TTR with INR variability appears more accurate than either of these individual tests at monitoring warfarin anticoagulation.
Major finding: Of the participants, 3.1% developed ischemic stroke, 6.4% developed major bleeding, and 0.9% developed fatal bleeding while taking warfarin.
Data source: A secondary analysis of data from the Veterans Affairs Study to Improve Anticoagulation, involving 40,404 VA patients taking warfarin for AF during a 2-year period.
Disclosures: This study was supported by the Durham VA Medical Center and VA Health Service Research and Development. Dr. Razouki and his associates reported having no relevant financial disclosures.