User login
Ticks use static electricity to latch onto hosts: Study
It turns out that some people really are tick magnets.
Researchers have discovered that ticks can defy gravity in their quest to latch onto people and animals. The key is static electricity, just like when someone rubs a balloon and things stick to it.
The study was published in the journal Current Biology. In the first phase of the research, scientists exposed ticks to furry rabbit feet and to acrylic surfaces that each had electrostatic charges.
“Ticks were readily attracted across air gaps of up to several millimeters or centimeters onto these statically charged surfaces,” the authors wrote.
In a second part of the study, the researchers created computer models simulating the electrostatic charges that exist in environments where both ticks and mammals are found. In one simulation, the researchers observed that the body parts of a cow with the most electric charge were the nose, tail, and legs, which are the body parts most likely to be encountered by a tick. They also found that the vegetation near the animal had a strong electric field that is just a few millimeters wide.
In a final phase of the study, the researchers conducted laboratory experiments in which they re-created the electric field conditions from the computer model and successfully lifted some ticks across an air gap, although some ticks did not make the full leap if they were observed to be resisting.
The authors noted that their findings could be applied to developing new tick prevention strategies, such as designing clothing that resists electrostatic charges or spraying livestock.
The study authors reported that they had no conflicts of interest.
A version of this article first appeared on WebMD.com.
It turns out that some people really are tick magnets.
Researchers have discovered that ticks can defy gravity in their quest to latch onto people and animals. The key is static electricity, just like when someone rubs a balloon and things stick to it.
The study was published in the journal Current Biology. In the first phase of the research, scientists exposed ticks to furry rabbit feet and to acrylic surfaces that each had electrostatic charges.
“Ticks were readily attracted across air gaps of up to several millimeters or centimeters onto these statically charged surfaces,” the authors wrote.
In a second part of the study, the researchers created computer models simulating the electrostatic charges that exist in environments where both ticks and mammals are found. In one simulation, the researchers observed that the body parts of a cow with the most electric charge were the nose, tail, and legs, which are the body parts most likely to be encountered by a tick. They also found that the vegetation near the animal had a strong electric field that is just a few millimeters wide.
In a final phase of the study, the researchers conducted laboratory experiments in which they re-created the electric field conditions from the computer model and successfully lifted some ticks across an air gap, although some ticks did not make the full leap if they were observed to be resisting.
The authors noted that their findings could be applied to developing new tick prevention strategies, such as designing clothing that resists electrostatic charges or spraying livestock.
The study authors reported that they had no conflicts of interest.
A version of this article first appeared on WebMD.com.
It turns out that some people really are tick magnets.
Researchers have discovered that ticks can defy gravity in their quest to latch onto people and animals. The key is static electricity, just like when someone rubs a balloon and things stick to it.
The study was published in the journal Current Biology. In the first phase of the research, scientists exposed ticks to furry rabbit feet and to acrylic surfaces that each had electrostatic charges.
“Ticks were readily attracted across air gaps of up to several millimeters or centimeters onto these statically charged surfaces,” the authors wrote.
In a second part of the study, the researchers created computer models simulating the electrostatic charges that exist in environments where both ticks and mammals are found. In one simulation, the researchers observed that the body parts of a cow with the most electric charge were the nose, tail, and legs, which are the body parts most likely to be encountered by a tick. They also found that the vegetation near the animal had a strong electric field that is just a few millimeters wide.
In a final phase of the study, the researchers conducted laboratory experiments in which they re-created the electric field conditions from the computer model and successfully lifted some ticks across an air gap, although some ticks did not make the full leap if they were observed to be resisting.
The authors noted that their findings could be applied to developing new tick prevention strategies, such as designing clothing that resists electrostatic charges or spraying livestock.
The study authors reported that they had no conflicts of interest.
A version of this article first appeared on WebMD.com.
FROM CURRENT BIOLOGY
Risk threshold may help providers decide on rabies PEP
The model, reported in JAMA Network Open, could help clinicians, particularly those in primary care settings, to more rationally prescribe PEP to people concerned about a potential exposure to the rabies virus (RABV). In the United States, rabies PEP often is given without a comprehensive assessment that considers regional factors as well as species, nature of an attack, and the health and vaccination status of the animal.
Providers err on the side of caution, as rabies infection has a fatality rate near 100%. When exposures are low-risk, however, patients can rack up substantial out-of-pocket expenses or experience unnecessary adverse effects from the series of shots. Those can include injection site reactions, hypersensitivity reactions, and neurological complications.
The authors write that an estimated 55,000 people per year in the United States were treated for potential exposure to RABV in 2017 and 2018, at an estimated cost of more than $3,800 per person treated.
Researchers calculate risk threshold
The researchers, led by Kelly Charniga, PhD, MPH, an infectious disease epidemiologist with the U.S. Centers for Disease Control and Prevention in Atlanta, calculated positivity rates using more than 900,000 animal samples tested for RABV between 2011 and 2020. Other parameters were estimated from surveillance data and the literature and probabilities were estimated using Bayes’ rule.
A convenience sample of state public health officials in all states (excluding Hawaii) plus Washington and Puerto Rico was used to help determine a risk threshold for recommending PEP. Respondents were asked whether they would recommend PEP given 24 standardized exposure scenarios while accounting for local rabies epidemiology.
Their model establishes a risk threshold of 0.0004 for PEP administration, which represents the probability that an animal would test positive for RABV given that a person was exposed, and the probability that a person would die from rabies after exposure to a suspect rabid animal and no PEP. PEP should not be recommended with any value lower than that cutoff.
Alfred DeMaria, DPH, a consultant to the Massachusetts Department of Public Health in Boston, who was not involved with the study, said the work will be particularly helpful for primary care physicians, giving them confidence to not recommend PEP when infection is statistically highly unlikely and thereby to reduce unnecessary and costly measures.
“Concern about rabies is often based on a very unlikely scenario,” Dr. DeMaria said. He gave the example of people coming into primary care worried that they might have been exposed after comforting their dog who had been bitten in a fight with a wild animal.
“Has that ever happened in the history of the human species? Not that we know of,” he said.
Many people also think dogs and other domestic animals are a likely source of rabies, which is not the case in the United States, Dr. DeMaria said.
“In most cases, it is exposure to a raccoon, a skunk, or a bat,” he said. “Most calls are for potential bat exposure, especially in the summer when young bats are flying around and are not very savvy about avoiding humans.”
The authors note the difference between the animals likely to bite and the species that carry RABV: “The most common mammals involved in bite events in the U.S. are dogs, cats, and small rodents. These species, when healthy and provoked into biting, represent some of the lowest risk exposures evaluated in this model.”
The canine rabies variant virus was eliminated in the United States in 2004.
The study authors note that their model should not be used in other countries because “most rabies deaths globally are caused by domestic dogs.”
Health department consultation can reduce inappropriate treatment
Dr. DeMaria said the paper may also convince physicians to consult with their health department for a final recommendation.
The authors note that a 2020 study in Cook County, Ill., found patients who received PEP were about 90% less likely to receive inappropriate treatment if their clinician had consulted with a health department.
“Anything that puts the risk in a context, like this paper does, is helpful,” he said.
Most physicians in the United States will never see a patient with rabies, the authors write, but animal bites are common – resulting in hundreds of thousands of primary care and emergency department visits each year when physicians must decide whether to administer PEP.
The study authors and Dr. DeMaria report no relevant financial relationships.
The model, reported in JAMA Network Open, could help clinicians, particularly those in primary care settings, to more rationally prescribe PEP to people concerned about a potential exposure to the rabies virus (RABV). In the United States, rabies PEP often is given without a comprehensive assessment that considers regional factors as well as species, nature of an attack, and the health and vaccination status of the animal.
Providers err on the side of caution, as rabies infection has a fatality rate near 100%. When exposures are low-risk, however, patients can rack up substantial out-of-pocket expenses or experience unnecessary adverse effects from the series of shots. Those can include injection site reactions, hypersensitivity reactions, and neurological complications.
The authors write that an estimated 55,000 people per year in the United States were treated for potential exposure to RABV in 2017 and 2018, at an estimated cost of more than $3,800 per person treated.
Researchers calculate risk threshold
The researchers, led by Kelly Charniga, PhD, MPH, an infectious disease epidemiologist with the U.S. Centers for Disease Control and Prevention in Atlanta, calculated positivity rates using more than 900,000 animal samples tested for RABV between 2011 and 2020. Other parameters were estimated from surveillance data and the literature and probabilities were estimated using Bayes’ rule.
A convenience sample of state public health officials in all states (excluding Hawaii) plus Washington and Puerto Rico was used to help determine a risk threshold for recommending PEP. Respondents were asked whether they would recommend PEP given 24 standardized exposure scenarios while accounting for local rabies epidemiology.
Their model establishes a risk threshold of 0.0004 for PEP administration, which represents the probability that an animal would test positive for RABV given that a person was exposed, and the probability that a person would die from rabies after exposure to a suspect rabid animal and no PEP. PEP should not be recommended with any value lower than that cutoff.
Alfred DeMaria, DPH, a consultant to the Massachusetts Department of Public Health in Boston, who was not involved with the study, said the work will be particularly helpful for primary care physicians, giving them confidence to not recommend PEP when infection is statistically highly unlikely and thereby to reduce unnecessary and costly measures.
“Concern about rabies is often based on a very unlikely scenario,” Dr. DeMaria said. He gave the example of people coming into primary care worried that they might have been exposed after comforting their dog who had been bitten in a fight with a wild animal.
“Has that ever happened in the history of the human species? Not that we know of,” he said.
Many people also think dogs and other domestic animals are a likely source of rabies, which is not the case in the United States, Dr. DeMaria said.
“In most cases, it is exposure to a raccoon, a skunk, or a bat,” he said. “Most calls are for potential bat exposure, especially in the summer when young bats are flying around and are not very savvy about avoiding humans.”
The authors note the difference between the animals likely to bite and the species that carry RABV: “The most common mammals involved in bite events in the U.S. are dogs, cats, and small rodents. These species, when healthy and provoked into biting, represent some of the lowest risk exposures evaluated in this model.”
The canine rabies variant virus was eliminated in the United States in 2004.
The study authors note that their model should not be used in other countries because “most rabies deaths globally are caused by domestic dogs.”
Health department consultation can reduce inappropriate treatment
Dr. DeMaria said the paper may also convince physicians to consult with their health department for a final recommendation.
The authors note that a 2020 study in Cook County, Ill., found patients who received PEP were about 90% less likely to receive inappropriate treatment if their clinician had consulted with a health department.
“Anything that puts the risk in a context, like this paper does, is helpful,” he said.
Most physicians in the United States will never see a patient with rabies, the authors write, but animal bites are common – resulting in hundreds of thousands of primary care and emergency department visits each year when physicians must decide whether to administer PEP.
The study authors and Dr. DeMaria report no relevant financial relationships.
The model, reported in JAMA Network Open, could help clinicians, particularly those in primary care settings, to more rationally prescribe PEP to people concerned about a potential exposure to the rabies virus (RABV). In the United States, rabies PEP often is given without a comprehensive assessment that considers regional factors as well as species, nature of an attack, and the health and vaccination status of the animal.
Providers err on the side of caution, as rabies infection has a fatality rate near 100%. When exposures are low-risk, however, patients can rack up substantial out-of-pocket expenses or experience unnecessary adverse effects from the series of shots. Those can include injection site reactions, hypersensitivity reactions, and neurological complications.
The authors write that an estimated 55,000 people per year in the United States were treated for potential exposure to RABV in 2017 and 2018, at an estimated cost of more than $3,800 per person treated.
Researchers calculate risk threshold
The researchers, led by Kelly Charniga, PhD, MPH, an infectious disease epidemiologist with the U.S. Centers for Disease Control and Prevention in Atlanta, calculated positivity rates using more than 900,000 animal samples tested for RABV between 2011 and 2020. Other parameters were estimated from surveillance data and the literature and probabilities were estimated using Bayes’ rule.
A convenience sample of state public health officials in all states (excluding Hawaii) plus Washington and Puerto Rico was used to help determine a risk threshold for recommending PEP. Respondents were asked whether they would recommend PEP given 24 standardized exposure scenarios while accounting for local rabies epidemiology.
Their model establishes a risk threshold of 0.0004 for PEP administration, which represents the probability that an animal would test positive for RABV given that a person was exposed, and the probability that a person would die from rabies after exposure to a suspect rabid animal and no PEP. PEP should not be recommended with any value lower than that cutoff.
Alfred DeMaria, DPH, a consultant to the Massachusetts Department of Public Health in Boston, who was not involved with the study, said the work will be particularly helpful for primary care physicians, giving them confidence to not recommend PEP when infection is statistically highly unlikely and thereby to reduce unnecessary and costly measures.
“Concern about rabies is often based on a very unlikely scenario,” Dr. DeMaria said. He gave the example of people coming into primary care worried that they might have been exposed after comforting their dog who had been bitten in a fight with a wild animal.
“Has that ever happened in the history of the human species? Not that we know of,” he said.
Many people also think dogs and other domestic animals are a likely source of rabies, which is not the case in the United States, Dr. DeMaria said.
“In most cases, it is exposure to a raccoon, a skunk, or a bat,” he said. “Most calls are for potential bat exposure, especially in the summer when young bats are flying around and are not very savvy about avoiding humans.”
The authors note the difference between the animals likely to bite and the species that carry RABV: “The most common mammals involved in bite events in the U.S. are dogs, cats, and small rodents. These species, when healthy and provoked into biting, represent some of the lowest risk exposures evaluated in this model.”
The canine rabies variant virus was eliminated in the United States in 2004.
The study authors note that their model should not be used in other countries because “most rabies deaths globally are caused by domestic dogs.”
Health department consultation can reduce inappropriate treatment
Dr. DeMaria said the paper may also convince physicians to consult with their health department for a final recommendation.
The authors note that a 2020 study in Cook County, Ill., found patients who received PEP were about 90% less likely to receive inappropriate treatment if their clinician had consulted with a health department.
“Anything that puts the risk in a context, like this paper does, is helpful,” he said.
Most physicians in the United States will never see a patient with rabies, the authors write, but animal bites are common – resulting in hundreds of thousands of primary care and emergency department visits each year when physicians must decide whether to administer PEP.
The study authors and Dr. DeMaria report no relevant financial relationships.
FROM JAMA NETWORK
Rabies: How to respond to parents’ questions
When most families hear the word rabies, they envision a dog foaming at the mouth and think about receiving multiple painful, often intra-abdominal injections. However, the epidemiology of rabies has changed in the United States. Postexposure prophylaxis (PEP) may not always be indicated and for certain persons preexposure prophylaxis (PrEP) is available and recommended.
Rabies is a Lyssavirus that is transmitted through saliva most often from the bite or scratch of an infected animal. Sometimes it’s via direct contact with mucous membranes. Although rare, cases have been described in which an undiagnosed donor passed the virus via transplant to recipients and four cases of aerosolized transmission were documented in two spelunkers and two laboratory technicians working with the virus. Worldwide it’s estimated that rabies causes 59,000 deaths annually.
Most cases (98%) are secondary to canine rabies. Prior to 1960, dogs were the major reservoir in the United States; however, after introduction of leash laws and animal vaccination in 1947, there was a drastic decline in cases caused by the canine rabies virus variant (CRVV). By 2004, CRVV was eliminated in the United States.
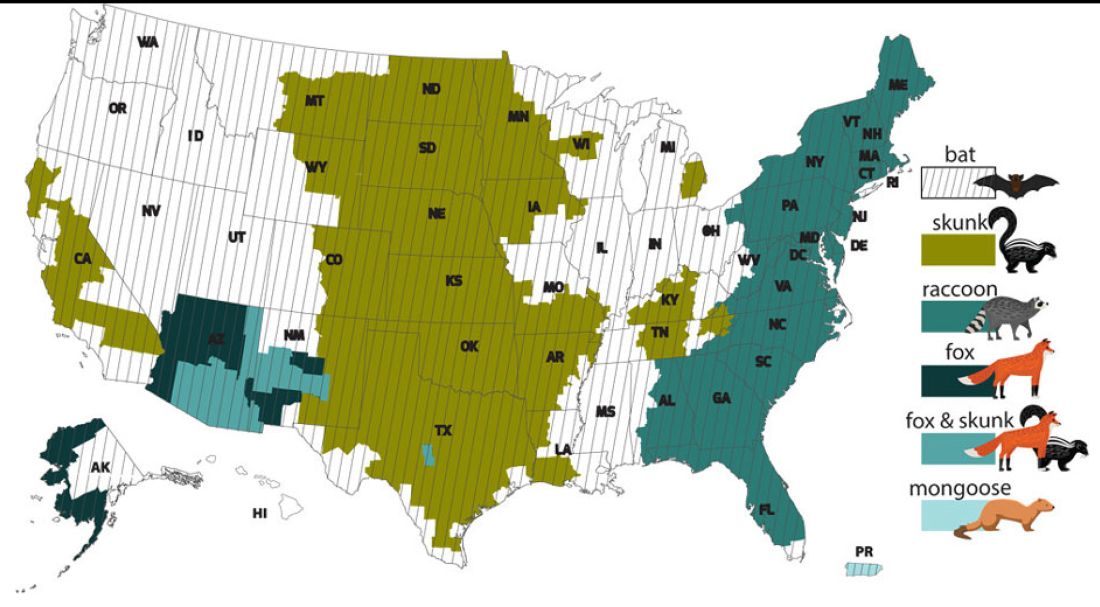
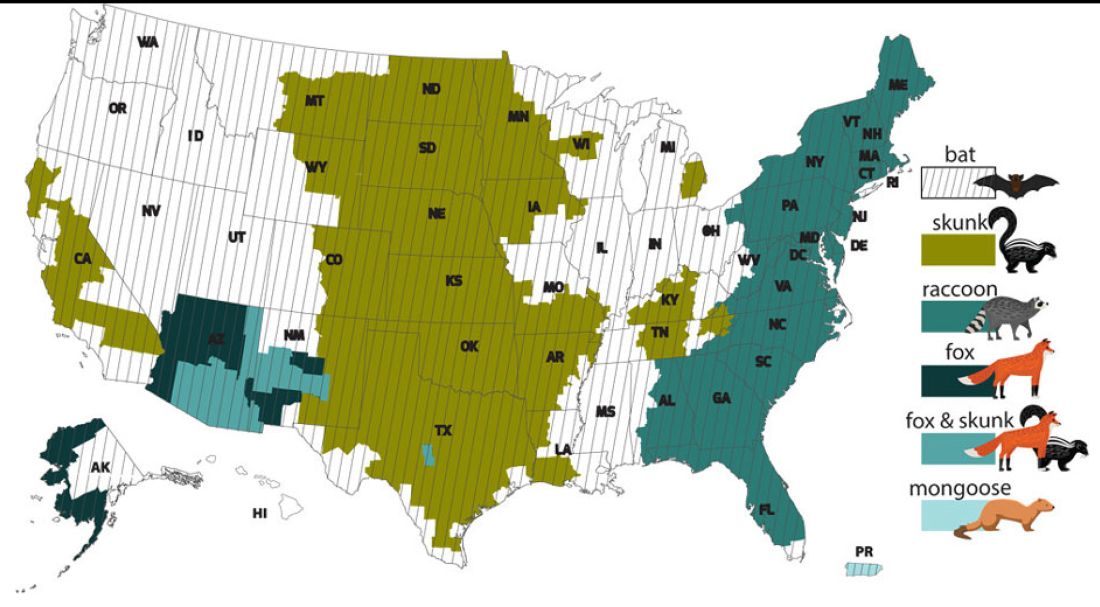
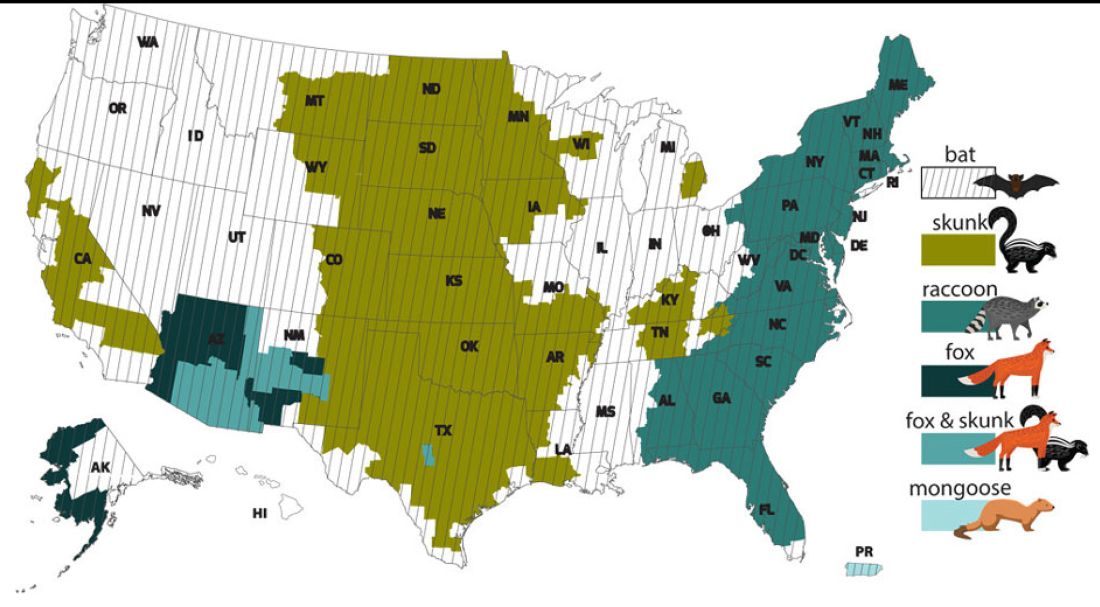
However, the proportion of strains associated with wildlife including raccoons, skunks, foxes, bats, coyotes, and mongoose now account for most of the cases in humans. Wildlife rabies is found in all states except Hawaii. Between 1960 and 2018, 89 cases were acquired in the United States and 62 (70%) were from bat exposure. Dog bites acquired during international travel were the cause of 36 cases.
Once signs and symptoms of disease develop there is no treatment. Regardless of the species variant, rabies virus infection is fatal in over 99% of cases. However, disease can be prevented with prompt initiation of PEP, which includes administration of rabies immune globulin (RIG) and rabies vaccine. Let’s look at a few different scenarios.
1. A delivery person is bitten by your neighbor’s dog while making a delivery. He was told to get rabies vaccine. What should we advise?
Canine rabies has been eliminated in the United States. However, unvaccinated canines can acquire rabies from wildlife. In this situation, you can determine the immunization status of the dog. Contact your local/state health department to assist with enforcement and management. Bites by cats and ferrets should be managed similarly.
Healthy dog:
1. Observe for 10 days.
2. PEP is not indicated unless the animal develops signs/symptoms of rabies. Then euthanize and begin PEP.
Dog appears rabid or suspected to be rabid:
1. Begin PEP.
2. Animal should be euthanized. If immunofluorescent test is negative discontinue PEP.
Dog unavailable:
Contact local/state health department. They are more familiar with rabies surveillance data.
2. Patient relocating to Malaysia for 3-4 years. Rabies PrEP was recommended but the family wants your opinion before receiving the vaccine. What would you advise?
Canine rabies is felt to be the primary cause of rabies outside of the United States. Canines are not routinely vaccinated in many foreign destinations, and the availability of RIG and rabies vaccine is not guaranteed in developing countries. As noted above, dog bites during international travel accounted for 28% of U.S. cases between 1960 and 2018.
In May 2022 recommendations for a modified two-dose PrEP schedule was published that identifies five risk groups and includes specific timing for checking rabies titers. The third rabies dose can now be administered up until year 3 (Morb Mortal Wkly Rep. 2022 May 6;71[18]:619-27). For individuals relocating to countries where CRVV is present, I prefer the traditional three-dose PrEP schedule administered between 21 and 28 days. However, we now have options. If exposure occurs any time after completion of a three-dose PrEP series or within 3 years after completion of a two-dose PrEP series, RIG would not be required. All patients would receive two doses of rabies vaccine (days 0, 3). If exposure occurs after 3 years in a person who received two doses of PrEP who did not have documentation of a protective rabies titer (> 5 IU/mL), treatment will include RIG plus four doses of vaccine (days 0, 3, 7, 14).
For this relocating patient, supporting PrEP would be strongly recommended.
3. A mother tells you she sees bats flying around her home at night and a few have even gotten into the home. This morning she saw one in her child’s room. He was still sleeping. Is there anything she needs to do?
Bats have become the predominant source of rabies in the United States. In addition to the cases noted above, three fatal cases occurred between Sept. 28 and Nov. 10, 2021, after bat exposures in August 2021 (MMWR Morb Mortal Wkly Rep. 2022 Jan 7;71:31-2). All had recognized contact with a bat 3-7 weeks prior to onset of symptoms and died 2-3 weeks after symptom onset. One declined PEP and the other two did not realize the risk for rabies from their exposure or did not notice a scratch or bite. Bites from bats may be small and unnoticed. Exposure to a bat in a closed room while sleeping is considered an exposure. Hawaii is the only state not reporting rabid bats.
PEP is recommended for her child. She should identify potential areas bats may enter the home and seal them in addition to removal of any bat roosts.
4. A parent realizes a house guest has been feeding raccoons in the backyard. What’s your response?
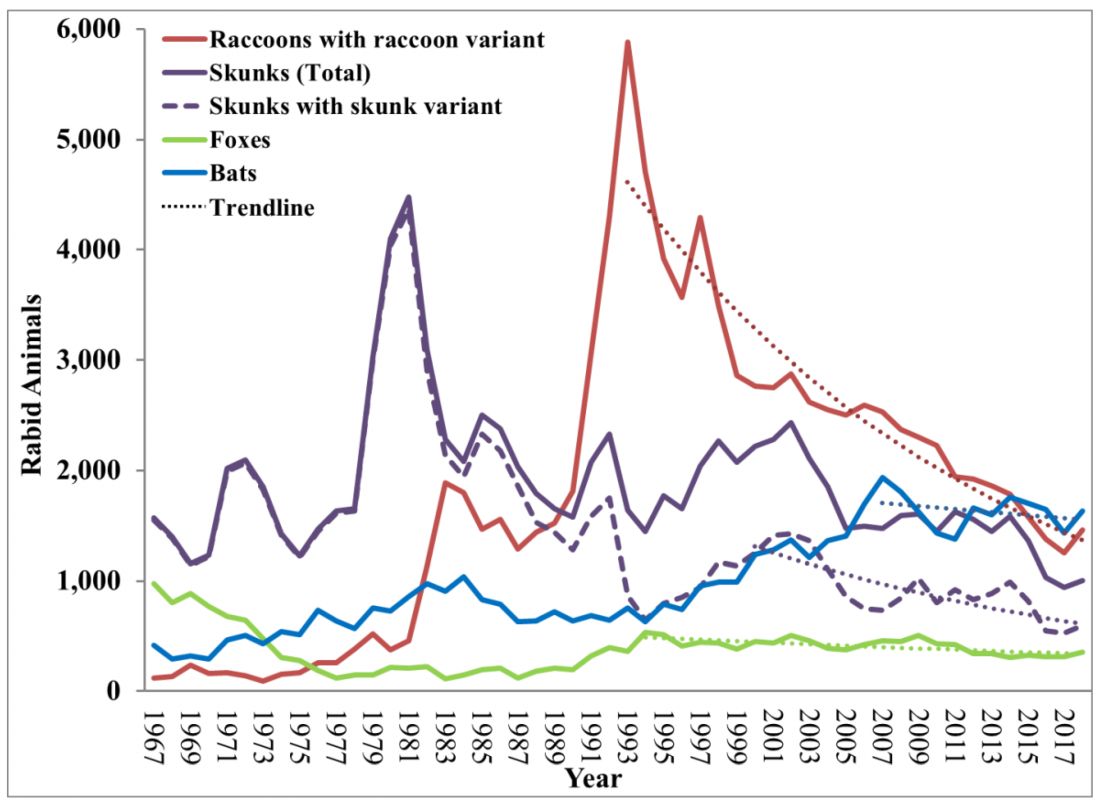
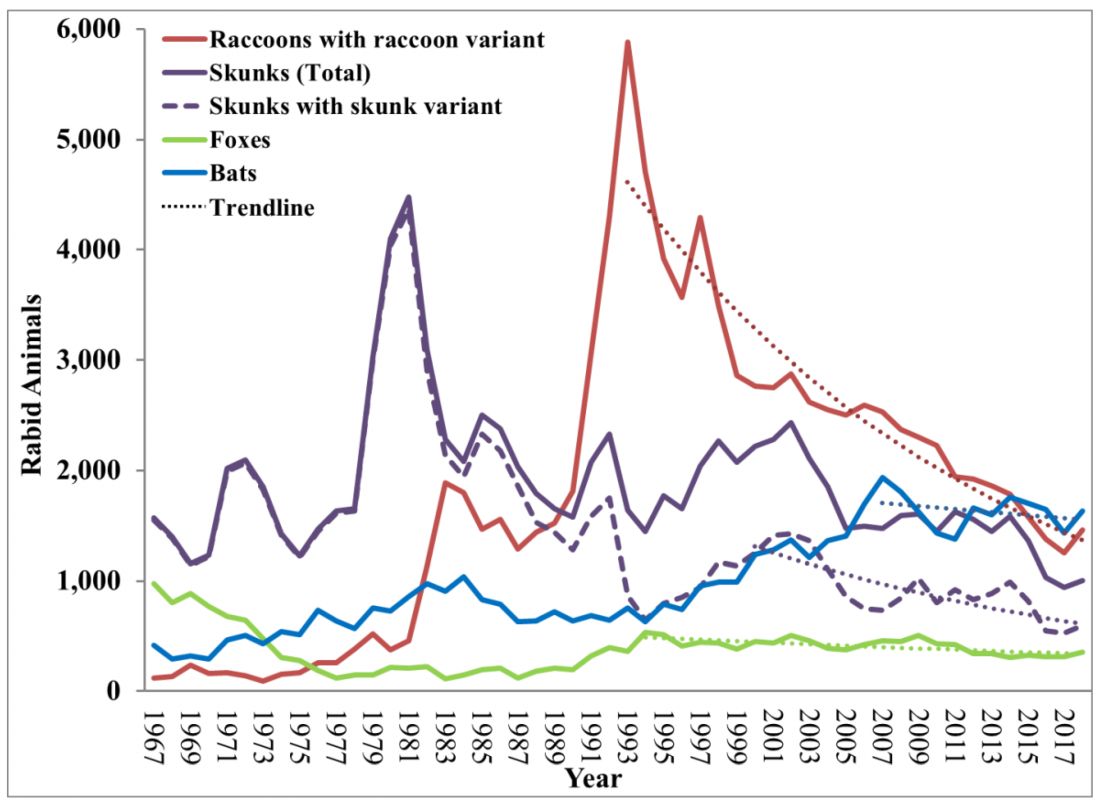
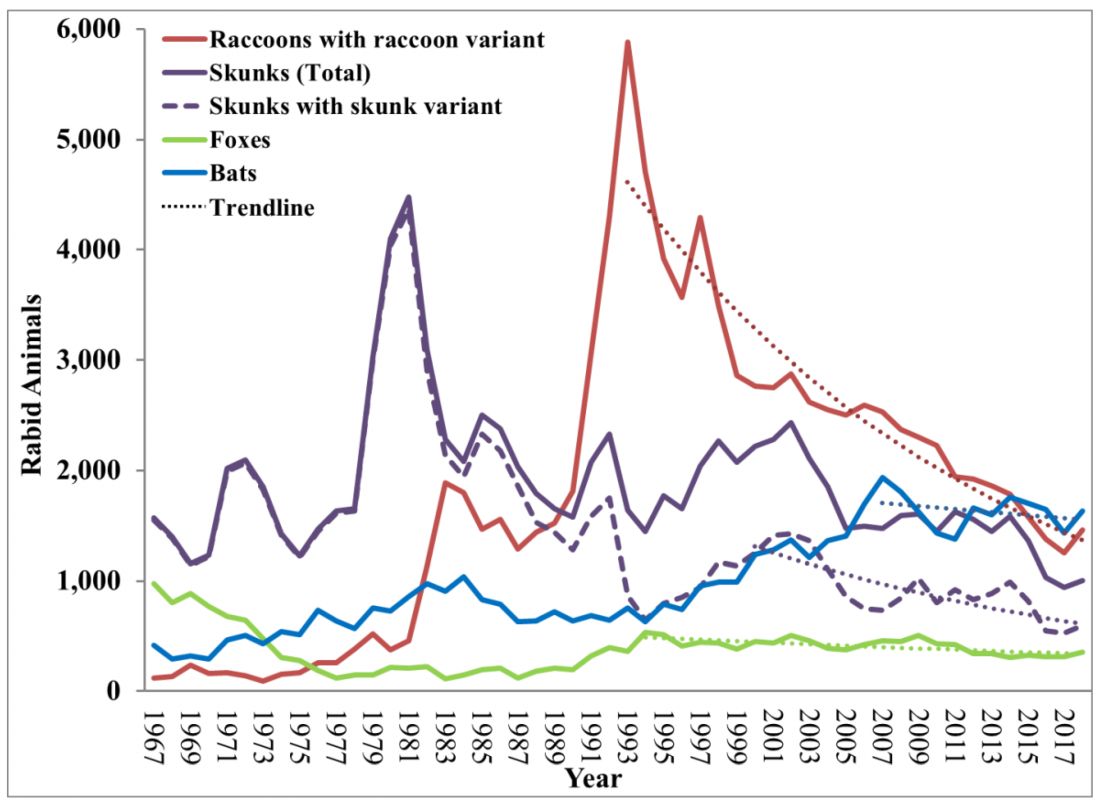
While bat rabies is the predominant variant associated with disease in the United States, as illustrated in Figure 1, other species of wildlife including raccoons are a major source of rabies. The geographic spread of the raccoon variant of rabies has been limited by oral vaccination via bait. In the situation noted here, the raccoons have returned because food was being offered thus increasing the families chance of a potential rabies exposure. Wildlife including skunks, raccoons, coyotes, foxes, and mongooses are always considered rabid until proven negative by laboratory testing.
You recommend to stop feeding wildlife and never to approach them. Have them contact the local rabies control unit and/or state wildlife services to assist with removal of the raccoons. Depending on the locale, pest control may be required at the owners expense. Inform the family to seek PEP if anyone is bitten or scratched by the raccoons.
As per the Centers for Disease Control and Prevention, about 55,000 residents receive PEP annually with health-associated expenditures including diagnostics, prevention, and control estimated between $245 and $510 million annually. Rabies is one of the most fatal diseases that can be prevented by avoiding contact with wild animals, maintenance of high immunization rates in pets, and keeping people informed of potential sources including bats. One can’t determine if an animal has rabies by looking at it. Rabies remains an urgent disease that we have to remember to address with our patients and their families. For additional information go to www.CDC.gov/rabies.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She has no relevant financial disclosures.
When most families hear the word rabies, they envision a dog foaming at the mouth and think about receiving multiple painful, often intra-abdominal injections. However, the epidemiology of rabies has changed in the United States. Postexposure prophylaxis (PEP) may not always be indicated and for certain persons preexposure prophylaxis (PrEP) is available and recommended.
Rabies is a Lyssavirus that is transmitted through saliva most often from the bite or scratch of an infected animal. Sometimes it’s via direct contact with mucous membranes. Although rare, cases have been described in which an undiagnosed donor passed the virus via transplant to recipients and four cases of aerosolized transmission were documented in two spelunkers and two laboratory technicians working with the virus. Worldwide it’s estimated that rabies causes 59,000 deaths annually.
Most cases (98%) are secondary to canine rabies. Prior to 1960, dogs were the major reservoir in the United States; however, after introduction of leash laws and animal vaccination in 1947, there was a drastic decline in cases caused by the canine rabies virus variant (CRVV). By 2004, CRVV was eliminated in the United States.
However, the proportion of strains associated with wildlife including raccoons, skunks, foxes, bats, coyotes, and mongoose now account for most of the cases in humans. Wildlife rabies is found in all states except Hawaii. Between 1960 and 2018, 89 cases were acquired in the United States and 62 (70%) were from bat exposure. Dog bites acquired during international travel were the cause of 36 cases.
Once signs and symptoms of disease develop there is no treatment. Regardless of the species variant, rabies virus infection is fatal in over 99% of cases. However, disease can be prevented with prompt initiation of PEP, which includes administration of rabies immune globulin (RIG) and rabies vaccine. Let’s look at a few different scenarios.
1. A delivery person is bitten by your neighbor’s dog while making a delivery. He was told to get rabies vaccine. What should we advise?
Canine rabies has been eliminated in the United States. However, unvaccinated canines can acquire rabies from wildlife. In this situation, you can determine the immunization status of the dog. Contact your local/state health department to assist with enforcement and management. Bites by cats and ferrets should be managed similarly.
Healthy dog:
1. Observe for 10 days.
2. PEP is not indicated unless the animal develops signs/symptoms of rabies. Then euthanize and begin PEP.
Dog appears rabid or suspected to be rabid:
1. Begin PEP.
2. Animal should be euthanized. If immunofluorescent test is negative discontinue PEP.
Dog unavailable:
Contact local/state health department. They are more familiar with rabies surveillance data.
2. Patient relocating to Malaysia for 3-4 years. Rabies PrEP was recommended but the family wants your opinion before receiving the vaccine. What would you advise?
Canine rabies is felt to be the primary cause of rabies outside of the United States. Canines are not routinely vaccinated in many foreign destinations, and the availability of RIG and rabies vaccine is not guaranteed in developing countries. As noted above, dog bites during international travel accounted for 28% of U.S. cases between 1960 and 2018.
In May 2022 recommendations for a modified two-dose PrEP schedule was published that identifies five risk groups and includes specific timing for checking rabies titers. The third rabies dose can now be administered up until year 3 (Morb Mortal Wkly Rep. 2022 May 6;71[18]:619-27). For individuals relocating to countries where CRVV is present, I prefer the traditional three-dose PrEP schedule administered between 21 and 28 days. However, we now have options. If exposure occurs any time after completion of a three-dose PrEP series or within 3 years after completion of a two-dose PrEP series, RIG would not be required. All patients would receive two doses of rabies vaccine (days 0, 3). If exposure occurs after 3 years in a person who received two doses of PrEP who did not have documentation of a protective rabies titer (> 5 IU/mL), treatment will include RIG plus four doses of vaccine (days 0, 3, 7, 14).
For this relocating patient, supporting PrEP would be strongly recommended.
3. A mother tells you she sees bats flying around her home at night and a few have even gotten into the home. This morning she saw one in her child’s room. He was still sleeping. Is there anything she needs to do?
Bats have become the predominant source of rabies in the United States. In addition to the cases noted above, three fatal cases occurred between Sept. 28 and Nov. 10, 2021, after bat exposures in August 2021 (MMWR Morb Mortal Wkly Rep. 2022 Jan 7;71:31-2). All had recognized contact with a bat 3-7 weeks prior to onset of symptoms and died 2-3 weeks after symptom onset. One declined PEP and the other two did not realize the risk for rabies from their exposure or did not notice a scratch or bite. Bites from bats may be small and unnoticed. Exposure to a bat in a closed room while sleeping is considered an exposure. Hawaii is the only state not reporting rabid bats.
PEP is recommended for her child. She should identify potential areas bats may enter the home and seal them in addition to removal of any bat roosts.
4. A parent realizes a house guest has been feeding raccoons in the backyard. What’s your response?
While bat rabies is the predominant variant associated with disease in the United States, as illustrated in Figure 1, other species of wildlife including raccoons are a major source of rabies. The geographic spread of the raccoon variant of rabies has been limited by oral vaccination via bait. In the situation noted here, the raccoons have returned because food was being offered thus increasing the families chance of a potential rabies exposure. Wildlife including skunks, raccoons, coyotes, foxes, and mongooses are always considered rabid until proven negative by laboratory testing.
You recommend to stop feeding wildlife and never to approach them. Have them contact the local rabies control unit and/or state wildlife services to assist with removal of the raccoons. Depending on the locale, pest control may be required at the owners expense. Inform the family to seek PEP if anyone is bitten or scratched by the raccoons.
As per the Centers for Disease Control and Prevention, about 55,000 residents receive PEP annually with health-associated expenditures including diagnostics, prevention, and control estimated between $245 and $510 million annually. Rabies is one of the most fatal diseases that can be prevented by avoiding contact with wild animals, maintenance of high immunization rates in pets, and keeping people informed of potential sources including bats. One can’t determine if an animal has rabies by looking at it. Rabies remains an urgent disease that we have to remember to address with our patients and their families. For additional information go to www.CDC.gov/rabies.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She has no relevant financial disclosures.
When most families hear the word rabies, they envision a dog foaming at the mouth and think about receiving multiple painful, often intra-abdominal injections. However, the epidemiology of rabies has changed in the United States. Postexposure prophylaxis (PEP) may not always be indicated and for certain persons preexposure prophylaxis (PrEP) is available and recommended.
Rabies is a Lyssavirus that is transmitted through saliva most often from the bite or scratch of an infected animal. Sometimes it’s via direct contact with mucous membranes. Although rare, cases have been described in which an undiagnosed donor passed the virus via transplant to recipients and four cases of aerosolized transmission were documented in two spelunkers and two laboratory technicians working with the virus. Worldwide it’s estimated that rabies causes 59,000 deaths annually.
Most cases (98%) are secondary to canine rabies. Prior to 1960, dogs were the major reservoir in the United States; however, after introduction of leash laws and animal vaccination in 1947, there was a drastic decline in cases caused by the canine rabies virus variant (CRVV). By 2004, CRVV was eliminated in the United States.
However, the proportion of strains associated with wildlife including raccoons, skunks, foxes, bats, coyotes, and mongoose now account for most of the cases in humans. Wildlife rabies is found in all states except Hawaii. Between 1960 and 2018, 89 cases were acquired in the United States and 62 (70%) were from bat exposure. Dog bites acquired during international travel were the cause of 36 cases.
Once signs and symptoms of disease develop there is no treatment. Regardless of the species variant, rabies virus infection is fatal in over 99% of cases. However, disease can be prevented with prompt initiation of PEP, which includes administration of rabies immune globulin (RIG) and rabies vaccine. Let’s look at a few different scenarios.
1. A delivery person is bitten by your neighbor’s dog while making a delivery. He was told to get rabies vaccine. What should we advise?
Canine rabies has been eliminated in the United States. However, unvaccinated canines can acquire rabies from wildlife. In this situation, you can determine the immunization status of the dog. Contact your local/state health department to assist with enforcement and management. Bites by cats and ferrets should be managed similarly.
Healthy dog:
1. Observe for 10 days.
2. PEP is not indicated unless the animal develops signs/symptoms of rabies. Then euthanize and begin PEP.
Dog appears rabid or suspected to be rabid:
1. Begin PEP.
2. Animal should be euthanized. If immunofluorescent test is negative discontinue PEP.
Dog unavailable:
Contact local/state health department. They are more familiar with rabies surveillance data.
2. Patient relocating to Malaysia for 3-4 years. Rabies PrEP was recommended but the family wants your opinion before receiving the vaccine. What would you advise?
Canine rabies is felt to be the primary cause of rabies outside of the United States. Canines are not routinely vaccinated in many foreign destinations, and the availability of RIG and rabies vaccine is not guaranteed in developing countries. As noted above, dog bites during international travel accounted for 28% of U.S. cases between 1960 and 2018.
In May 2022 recommendations for a modified two-dose PrEP schedule was published that identifies five risk groups and includes specific timing for checking rabies titers. The third rabies dose can now be administered up until year 3 (Morb Mortal Wkly Rep. 2022 May 6;71[18]:619-27). For individuals relocating to countries where CRVV is present, I prefer the traditional three-dose PrEP schedule administered between 21 and 28 days. However, we now have options. If exposure occurs any time after completion of a three-dose PrEP series or within 3 years after completion of a two-dose PrEP series, RIG would not be required. All patients would receive two doses of rabies vaccine (days 0, 3). If exposure occurs after 3 years in a person who received two doses of PrEP who did not have documentation of a protective rabies titer (> 5 IU/mL), treatment will include RIG plus four doses of vaccine (days 0, 3, 7, 14).
For this relocating patient, supporting PrEP would be strongly recommended.
3. A mother tells you she sees bats flying around her home at night and a few have even gotten into the home. This morning she saw one in her child’s room. He was still sleeping. Is there anything she needs to do?
Bats have become the predominant source of rabies in the United States. In addition to the cases noted above, three fatal cases occurred between Sept. 28 and Nov. 10, 2021, after bat exposures in August 2021 (MMWR Morb Mortal Wkly Rep. 2022 Jan 7;71:31-2). All had recognized contact with a bat 3-7 weeks prior to onset of symptoms and died 2-3 weeks after symptom onset. One declined PEP and the other two did not realize the risk for rabies from their exposure or did not notice a scratch or bite. Bites from bats may be small and unnoticed. Exposure to a bat in a closed room while sleeping is considered an exposure. Hawaii is the only state not reporting rabid bats.
PEP is recommended for her child. She should identify potential areas bats may enter the home and seal them in addition to removal of any bat roosts.
4. A parent realizes a house guest has been feeding raccoons in the backyard. What’s your response?
While bat rabies is the predominant variant associated with disease in the United States, as illustrated in Figure 1, other species of wildlife including raccoons are a major source of rabies. The geographic spread of the raccoon variant of rabies has been limited by oral vaccination via bait. In the situation noted here, the raccoons have returned because food was being offered thus increasing the families chance of a potential rabies exposure. Wildlife including skunks, raccoons, coyotes, foxes, and mongooses are always considered rabid until proven negative by laboratory testing.
You recommend to stop feeding wildlife and never to approach them. Have them contact the local rabies control unit and/or state wildlife services to assist with removal of the raccoons. Depending on the locale, pest control may be required at the owners expense. Inform the family to seek PEP if anyone is bitten or scratched by the raccoons.
As per the Centers for Disease Control and Prevention, about 55,000 residents receive PEP annually with health-associated expenditures including diagnostics, prevention, and control estimated between $245 and $510 million annually. Rabies is one of the most fatal diseases that can be prevented by avoiding contact with wild animals, maintenance of high immunization rates in pets, and keeping people informed of potential sources including bats. One can’t determine if an animal has rabies by looking at it. Rabies remains an urgent disease that we have to remember to address with our patients and their families. For additional information go to www.CDC.gov/rabies.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She has no relevant financial disclosures.
Can particles in dairy and beef cause cancer and MS?
In Western diets, dairy and beef are ubiquitous: Milk goes with coffee, melted cheese with pizza, and chili with rice. But what if dairy products and beef contained a new kind of pathogen that could infect you as a child and trigger cancer or multiple sclerosis (MS) 40-70 years later?
However, in two joint statements, the German Federal Institute for Risk Assessment (BfR) and the Max Rubner Institute (MRI) have rejected such theories.
In 2008, Harald zur Hausen, MD, DSc, received the Nobel Prize in Medicine for his discovery that human papillomaviruses cause cervical cancer. His starting point was the observation that sexually abstinent women, such as nuns, rarely develop this cancer. So it was possible to draw the conclusion that pathogens are transmitted during sexual intercourse, explain Dr. zur Hausen and his wife Ethel-Michele de Villiers, PhD, both of DKFZ Heidelberg.
Papillomaviruses, as well as human herpes and Epstein-Barr viruses (EBV), polyomaviruses, and retroviruses, cause cancer in a direct way: by inserting their genes into the DNA of human cells. With a latency of a few years to a few decades, the proteins formed through expression stimulate malignant growth by altering the regulating host gene.
Acid radicals
However, viruses – just like bacteria and parasites – can also indirectly trigger cancer. One mechanism for this triggering is the disruption of immune defenses, as shown by the sometimes drastically increased tumor incidence with AIDS or with immunosuppressants after transplants. Chronic inflammation is a second mechanism that generates acid radicals and thereby causes random mutations in replicating cells. Examples include stomach cancer caused by Helicobacter pylori and liver cancer caused by Schistosoma, liver fluke, and hepatitis B and C viruses.
According to Dr. de Villiers and Dr. zur Hausen, there are good reasons to believe that other pathogens could cause chronic inflammation and thereby lead to cancer. Epidemiologic data suggest that dairy and meat products from European cows (Bos taurus) are a potential source. This is because colon cancer and breast cancer commonly occur in places where these foods are heavily consumed (that is, in North America, Argentina, Europe, and Australia). In contrast, the rate is low in India, where cows are revered as holy animals. Also noteworthy is that women with a lactose intolerance rarely develop breast cancer.
Viral progeny
In fact, the researchers found single-stranded DNA rings that originated in viruses, which they named bovine meat and milk factors (BMMF), in the intestines of patients with colon cancer. They reported, “This new class of pathogen deserves, in our opinion at least, to become the focus of cancer development and further chronic diseases.” They also detected elevated levels of acid radicals in these areas (that is, oxidative stress), which is typical for chronic inflammation.
The researchers assume that infants, whose immune system is not yet fully matured, ingest the BMMF as soon as they have dairy. Therefore, there is no need for adults to avoid dairy or beef because everyone is infected anyway, said Dr. zur Hausen.
‘Breast milk is healthy’
Dr. De Villiers and Dr. zur Hausen outlined more evidence of cancer-triggering pathogens. Mothers who have breastfed are less likely, especially after multiple pregnancies, to develop tumors in various organs or to have MS and type 2 diabetes. The authors attribute the protective effect to oligosaccharides in breast milk, which begin to be formed midway through the pregnancy. They bind to lectin receptors and, in so doing, mask the terminal molecule onto which the viruses need to dock. As a result, their port of entry into the cells is blocked.
The oligosaccharides also protect the baby against life-threatening infections by blocking access by rotaviruses and noroviruses. In this way, especially if breastfeeding lasts a long time – around 1 year – the period of incomplete immunocompetence is bridged.
Colon cancer
To date, it has been assumed that around 20% of all cancerous diseases globally are caused by infections, said the researchers. But if the suspected BMMF cases are included, this figure rises to 50%, even to around 80%, for colon cancer. If the suspicion is confirmed, the consequences for prevention and therapy would be significant.
The voice of a Nobel prize winner undoubtedly carries weight, but at the time, Dr. zur Hausen still had to convince a host of skeptics with his discovery that a viral infection is a major cause of cervical cancer. Nonetheless, some indicators suggest that he and his wife have found a dead end this time.
Institutional skepticism
When his working group made the results public in February 2019, the DKFZ felt the need to give an all-clear signal in response to alarmed press reports. There is no reason to see dairy and meat consumption as something negative. Similarly, in their first joint statement, the BfR and the MRI judged the data to be insufficient and called for further studies. Multiple research teams began to focus on BMMF as a result. In what foods can they be found? Are they more common in patients with cancer than in healthy people? Are they infectious? Do they cause inflammation and cancer?
The findings presented in a second statement by the BfR and MRI at the end of November 2022 contradicted the claims made by the DKFZ scientists across the board. In no way do BMMF represent new pathogens. They are variants of already known DNA sequences. In addition, they are present in numerous animal-based and plant-based foods, including pork, fish, fruit, vegetables, and nuts.
BMMF do not possess the ability to infect human cells, the institutes said. The proof that they are damaging to one’s health was also absent. It is true that the incidence of intestinal tumors correlates positively with the consumption of red and processed meat – which in no way signifies causality – but dairy products are linked to a reduced risk. On the other hand, breast cancer cannot be associated with the consumption of beef or dairy.
Therefore, both institutes recommend continuing to use these products as supplementary diet for infants because of their micronutrients. They further stated that the products are safe for people of all ages.
Association with MS?
Unperturbed, Dr. de Villiers and Dr. zur Hausen went one step further in their current article. They posited that MS is also associated with the consumption of dairy products and beef. Here too geographic distribution prompted the idea to look for BMMF in the brain lesions of patients with MS. The researchers isolated ring-shaped DNA molecules that proved to be closely related to BMMF from dairy and cattle blood. “The result was electrifying for us.”
However, there are several other factors to consider, such as vitamin D3 deficiency. This is because the incidence of MS decreases the further you travel from the poles toward the equator (that is, as solar radiation increases). Also, EBV clearly plays a role because patients with MS display increased titers of EBV antibodies. One study also showed that people in Antarctica excreted reactivated EBV in their saliva during winter and that vitamin D3 stopped the viral secretion.
Under these conditions, the researchers hypothesized that MS is caused by a double infection of brain cells by EBV and BMMF. EBV is reactivated by a lack of vitamin D3, and the BMMF multiply and are eventually converted into proteins. A focal immunoreaction causes the Schwann cells and oligodendrocytes to malfunction, which leads to the destruction of the myelin sheaths around the nerve fibers.
This article was translated from the Medscape German Edition. A version appeared on Medscape.com.
In Western diets, dairy and beef are ubiquitous: Milk goes with coffee, melted cheese with pizza, and chili with rice. But what if dairy products and beef contained a new kind of pathogen that could infect you as a child and trigger cancer or multiple sclerosis (MS) 40-70 years later?
However, in two joint statements, the German Federal Institute for Risk Assessment (BfR) and the Max Rubner Institute (MRI) have rejected such theories.
In 2008, Harald zur Hausen, MD, DSc, received the Nobel Prize in Medicine for his discovery that human papillomaviruses cause cervical cancer. His starting point was the observation that sexually abstinent women, such as nuns, rarely develop this cancer. So it was possible to draw the conclusion that pathogens are transmitted during sexual intercourse, explain Dr. zur Hausen and his wife Ethel-Michele de Villiers, PhD, both of DKFZ Heidelberg.
Papillomaviruses, as well as human herpes and Epstein-Barr viruses (EBV), polyomaviruses, and retroviruses, cause cancer in a direct way: by inserting their genes into the DNA of human cells. With a latency of a few years to a few decades, the proteins formed through expression stimulate malignant growth by altering the regulating host gene.
Acid radicals
However, viruses – just like bacteria and parasites – can also indirectly trigger cancer. One mechanism for this triggering is the disruption of immune defenses, as shown by the sometimes drastically increased tumor incidence with AIDS or with immunosuppressants after transplants. Chronic inflammation is a second mechanism that generates acid radicals and thereby causes random mutations in replicating cells. Examples include stomach cancer caused by Helicobacter pylori and liver cancer caused by Schistosoma, liver fluke, and hepatitis B and C viruses.
According to Dr. de Villiers and Dr. zur Hausen, there are good reasons to believe that other pathogens could cause chronic inflammation and thereby lead to cancer. Epidemiologic data suggest that dairy and meat products from European cows (Bos taurus) are a potential source. This is because colon cancer and breast cancer commonly occur in places where these foods are heavily consumed (that is, in North America, Argentina, Europe, and Australia). In contrast, the rate is low in India, where cows are revered as holy animals. Also noteworthy is that women with a lactose intolerance rarely develop breast cancer.
Viral progeny
In fact, the researchers found single-stranded DNA rings that originated in viruses, which they named bovine meat and milk factors (BMMF), in the intestines of patients with colon cancer. They reported, “This new class of pathogen deserves, in our opinion at least, to become the focus of cancer development and further chronic diseases.” They also detected elevated levels of acid radicals in these areas (that is, oxidative stress), which is typical for chronic inflammation.
The researchers assume that infants, whose immune system is not yet fully matured, ingest the BMMF as soon as they have dairy. Therefore, there is no need for adults to avoid dairy or beef because everyone is infected anyway, said Dr. zur Hausen.
‘Breast milk is healthy’
Dr. De Villiers and Dr. zur Hausen outlined more evidence of cancer-triggering pathogens. Mothers who have breastfed are less likely, especially after multiple pregnancies, to develop tumors in various organs or to have MS and type 2 diabetes. The authors attribute the protective effect to oligosaccharides in breast milk, which begin to be formed midway through the pregnancy. They bind to lectin receptors and, in so doing, mask the terminal molecule onto which the viruses need to dock. As a result, their port of entry into the cells is blocked.
The oligosaccharides also protect the baby against life-threatening infections by blocking access by rotaviruses and noroviruses. In this way, especially if breastfeeding lasts a long time – around 1 year – the period of incomplete immunocompetence is bridged.
Colon cancer
To date, it has been assumed that around 20% of all cancerous diseases globally are caused by infections, said the researchers. But if the suspected BMMF cases are included, this figure rises to 50%, even to around 80%, for colon cancer. If the suspicion is confirmed, the consequences for prevention and therapy would be significant.
The voice of a Nobel prize winner undoubtedly carries weight, but at the time, Dr. zur Hausen still had to convince a host of skeptics with his discovery that a viral infection is a major cause of cervical cancer. Nonetheless, some indicators suggest that he and his wife have found a dead end this time.
Institutional skepticism
When his working group made the results public in February 2019, the DKFZ felt the need to give an all-clear signal in response to alarmed press reports. There is no reason to see dairy and meat consumption as something negative. Similarly, in their first joint statement, the BfR and the MRI judged the data to be insufficient and called for further studies. Multiple research teams began to focus on BMMF as a result. In what foods can they be found? Are they more common in patients with cancer than in healthy people? Are they infectious? Do they cause inflammation and cancer?
The findings presented in a second statement by the BfR and MRI at the end of November 2022 contradicted the claims made by the DKFZ scientists across the board. In no way do BMMF represent new pathogens. They are variants of already known DNA sequences. In addition, they are present in numerous animal-based and plant-based foods, including pork, fish, fruit, vegetables, and nuts.
BMMF do not possess the ability to infect human cells, the institutes said. The proof that they are damaging to one’s health was also absent. It is true that the incidence of intestinal tumors correlates positively with the consumption of red and processed meat – which in no way signifies causality – but dairy products are linked to a reduced risk. On the other hand, breast cancer cannot be associated with the consumption of beef or dairy.
Therefore, both institutes recommend continuing to use these products as supplementary diet for infants because of their micronutrients. They further stated that the products are safe for people of all ages.
Association with MS?
Unperturbed, Dr. de Villiers and Dr. zur Hausen went one step further in their current article. They posited that MS is also associated with the consumption of dairy products and beef. Here too geographic distribution prompted the idea to look for BMMF in the brain lesions of patients with MS. The researchers isolated ring-shaped DNA molecules that proved to be closely related to BMMF from dairy and cattle blood. “The result was electrifying for us.”
However, there are several other factors to consider, such as vitamin D3 deficiency. This is because the incidence of MS decreases the further you travel from the poles toward the equator (that is, as solar radiation increases). Also, EBV clearly plays a role because patients with MS display increased titers of EBV antibodies. One study also showed that people in Antarctica excreted reactivated EBV in their saliva during winter and that vitamin D3 stopped the viral secretion.
Under these conditions, the researchers hypothesized that MS is caused by a double infection of brain cells by EBV and BMMF. EBV is reactivated by a lack of vitamin D3, and the BMMF multiply and are eventually converted into proteins. A focal immunoreaction causes the Schwann cells and oligodendrocytes to malfunction, which leads to the destruction of the myelin sheaths around the nerve fibers.
This article was translated from the Medscape German Edition. A version appeared on Medscape.com.
In Western diets, dairy and beef are ubiquitous: Milk goes with coffee, melted cheese with pizza, and chili with rice. But what if dairy products and beef contained a new kind of pathogen that could infect you as a child and trigger cancer or multiple sclerosis (MS) 40-70 years later?
However, in two joint statements, the German Federal Institute for Risk Assessment (BfR) and the Max Rubner Institute (MRI) have rejected such theories.
In 2008, Harald zur Hausen, MD, DSc, received the Nobel Prize in Medicine for his discovery that human papillomaviruses cause cervical cancer. His starting point was the observation that sexually abstinent women, such as nuns, rarely develop this cancer. So it was possible to draw the conclusion that pathogens are transmitted during sexual intercourse, explain Dr. zur Hausen and his wife Ethel-Michele de Villiers, PhD, both of DKFZ Heidelberg.
Papillomaviruses, as well as human herpes and Epstein-Barr viruses (EBV), polyomaviruses, and retroviruses, cause cancer in a direct way: by inserting their genes into the DNA of human cells. With a latency of a few years to a few decades, the proteins formed through expression stimulate malignant growth by altering the regulating host gene.
Acid radicals
However, viruses – just like bacteria and parasites – can also indirectly trigger cancer. One mechanism for this triggering is the disruption of immune defenses, as shown by the sometimes drastically increased tumor incidence with AIDS or with immunosuppressants after transplants. Chronic inflammation is a second mechanism that generates acid radicals and thereby causes random mutations in replicating cells. Examples include stomach cancer caused by Helicobacter pylori and liver cancer caused by Schistosoma, liver fluke, and hepatitis B and C viruses.
According to Dr. de Villiers and Dr. zur Hausen, there are good reasons to believe that other pathogens could cause chronic inflammation and thereby lead to cancer. Epidemiologic data suggest that dairy and meat products from European cows (Bos taurus) are a potential source. This is because colon cancer and breast cancer commonly occur in places where these foods are heavily consumed (that is, in North America, Argentina, Europe, and Australia). In contrast, the rate is low in India, where cows are revered as holy animals. Also noteworthy is that women with a lactose intolerance rarely develop breast cancer.
Viral progeny
In fact, the researchers found single-stranded DNA rings that originated in viruses, which they named bovine meat and milk factors (BMMF), in the intestines of patients with colon cancer. They reported, “This new class of pathogen deserves, in our opinion at least, to become the focus of cancer development and further chronic diseases.” They also detected elevated levels of acid radicals in these areas (that is, oxidative stress), which is typical for chronic inflammation.
The researchers assume that infants, whose immune system is not yet fully matured, ingest the BMMF as soon as they have dairy. Therefore, there is no need for adults to avoid dairy or beef because everyone is infected anyway, said Dr. zur Hausen.
‘Breast milk is healthy’
Dr. De Villiers and Dr. zur Hausen outlined more evidence of cancer-triggering pathogens. Mothers who have breastfed are less likely, especially after multiple pregnancies, to develop tumors in various organs or to have MS and type 2 diabetes. The authors attribute the protective effect to oligosaccharides in breast milk, which begin to be formed midway through the pregnancy. They bind to lectin receptors and, in so doing, mask the terminal molecule onto which the viruses need to dock. As a result, their port of entry into the cells is blocked.
The oligosaccharides also protect the baby against life-threatening infections by blocking access by rotaviruses and noroviruses. In this way, especially if breastfeeding lasts a long time – around 1 year – the period of incomplete immunocompetence is bridged.
Colon cancer
To date, it has been assumed that around 20% of all cancerous diseases globally are caused by infections, said the researchers. But if the suspected BMMF cases are included, this figure rises to 50%, even to around 80%, for colon cancer. If the suspicion is confirmed, the consequences for prevention and therapy would be significant.
The voice of a Nobel prize winner undoubtedly carries weight, but at the time, Dr. zur Hausen still had to convince a host of skeptics with his discovery that a viral infection is a major cause of cervical cancer. Nonetheless, some indicators suggest that he and his wife have found a dead end this time.
Institutional skepticism
When his working group made the results public in February 2019, the DKFZ felt the need to give an all-clear signal in response to alarmed press reports. There is no reason to see dairy and meat consumption as something negative. Similarly, in their first joint statement, the BfR and the MRI judged the data to be insufficient and called for further studies. Multiple research teams began to focus on BMMF as a result. In what foods can they be found? Are they more common in patients with cancer than in healthy people? Are they infectious? Do they cause inflammation and cancer?
The findings presented in a second statement by the BfR and MRI at the end of November 2022 contradicted the claims made by the DKFZ scientists across the board. In no way do BMMF represent new pathogens. They are variants of already known DNA sequences. In addition, they are present in numerous animal-based and plant-based foods, including pork, fish, fruit, vegetables, and nuts.
BMMF do not possess the ability to infect human cells, the institutes said. The proof that they are damaging to one’s health was also absent. It is true that the incidence of intestinal tumors correlates positively with the consumption of red and processed meat – which in no way signifies causality – but dairy products are linked to a reduced risk. On the other hand, breast cancer cannot be associated with the consumption of beef or dairy.
Therefore, both institutes recommend continuing to use these products as supplementary diet for infants because of their micronutrients. They further stated that the products are safe for people of all ages.
Association with MS?
Unperturbed, Dr. de Villiers and Dr. zur Hausen went one step further in their current article. They posited that MS is also associated with the consumption of dairy products and beef. Here too geographic distribution prompted the idea to look for BMMF in the brain lesions of patients with MS. The researchers isolated ring-shaped DNA molecules that proved to be closely related to BMMF from dairy and cattle blood. “The result was electrifying for us.”
However, there are several other factors to consider, such as vitamin D3 deficiency. This is because the incidence of MS decreases the further you travel from the poles toward the equator (that is, as solar radiation increases). Also, EBV clearly plays a role because patients with MS display increased titers of EBV antibodies. One study also showed that people in Antarctica excreted reactivated EBV in their saliva during winter and that vitamin D3 stopped the viral secretion.
Under these conditions, the researchers hypothesized that MS is caused by a double infection of brain cells by EBV and BMMF. EBV is reactivated by a lack of vitamin D3, and the BMMF multiply and are eventually converted into proteins. A focal immunoreaction causes the Schwann cells and oligodendrocytes to malfunction, which leads to the destruction of the myelin sheaths around the nerve fibers.
This article was translated from the Medscape German Edition. A version appeared on Medscape.com.
Will a one-dose drug mean the end of sleeping sickness?
A single dose of oral acoziborole resulted in a greater than 95% cure or probable cure rate for human African trypanosomiasis (HAT), also known as sleeping sickness, according to results from a clinical trial testing a one-dose experimental drug.
The drug has “the potential to revolutionize treatment” for the disease, which remains endemic in sub-Saharan Africa, said Antoine Tarral, MD, head of the human African trypanosomiasis clinical program at the Drugs for Neglected Diseases initiative, based in Geneva, and senior author of the study, in a press release.
he told this news organization. “It’s the first drug we can use without hospitalization. ... All the previous medications needed hospitalization, and therefore we could not treat the population early before they started expressing symptoms.”
The World Health Organization “has been working for decades for such a possibility to implement a new strategy for this disease,” Dr. Tarral said.
Current (2019) WHO guidelines recommend oral fexinidazole as first-line treatment for any stage of the disease. The 10-day course often requires hospitalization and skilled staff. Previous recommendations required disease-staging with cerebrospinal fluid (CSF) sampling and 7 days of intramuscular pentamidine for early-stage disease or nifurtimox-eflornithine combination therapy (NECT) with hospitalization for late-stage disease.
By contrast, acoziborole, which was codeveloped by the DND initiative and Sanofi, “is administered in a single dose and is effective across every stage of the disease, thereby eliminating the many barriers currently in place for people most vulnerable to the diseases, such as invasive treatments and long travel distances to a hospital or clinic, and opening the door to screen-and-treat approaches at the village level,” Dr. Tarral said in the statement.
“Today, and in the future, we will have less and less support to do this long and costly diagnostic process and treatment in the hospital,” he said in an interview. “This development means we can go for a simple test and a simple treatment, which means we can meet the WHO 2030 goal for ending transmission of this disease.”
Results from the multicenter, prospective, open-label, single-arm, noncomparative, phase 2/3 study were published in The Lancet.
Pragmatic study design
Sleeping sickness is caused by Trypanosoma brucei gambiense (gambiense HAT). It is transmitted by the tsetse fly and mostly fatal when left untreated.
The study enrolled 208 adults and adolescents (167 with late-stage, and 41 with early-stage or intermediate-stage disease) from 10 hospitals in the Democratic Republic of the Congo and Guinea. All patients were treated with acoziborole 960 mg – an unusual study design.
“Due to the substantial decline in incidence, enrolling patients with gambiense HAT into clinical trials is challenging,” the authors wrote. “Following advice from the European Medicines Agency, this study was designed as an open-label, single-arm trial with no comparator or control group.”
After 18 months of follow-up, treatment success, defined as absence of trypanosomes and less than 20 white blood cells per mcL of CSF, occurred in 159 (95.2%) of the late-stage patients, and 100% of the early- and intermediate-stage patients, “which was similar to the estimated historical results for NECT,” the authors noted.
Serious treatment-emergent adverse events were reported in 21 (10%) of patients, “but none of these events were considered drug-related,” they added.
The DND initiative and the WHO are currently nearing completion of a much larger, double-blind, placebo-controlled trial of acoziborole to “increase the safety database,” Dr. Tarral explained.
“Purists will say that acoziborole has not been evaluated according to current standards, because the study was not a randomized trial, there was no control group, and the number of participants was small,” said Jacques Pépin, MD, from the University of Sherbrooke (Que.), in a linked commentary.
“But these were difficult challenges to overcome, considering the drastic reduction in the number of patients with HAT and dispersion over a vast territory, particularly in the Democratic Republic of the Congo. For these reasons, the authors took a pragmatic approach instead,” he wrote.
A potential new tool for eradication of sleeping sickness
“This is really an exciting development, which will be useful in the drive for eradication/interruption of transmission of this disease,” Dr. Pépin told this news organization.
Dr. Pépin treated around 1,000 trypanosomiasis patients during an outbreak in Zaire in the early 1980s. Because the asymptomatic incubation period for the disease can be several months or even years, “the core strategy for controlling the disease is active screening,” he said in an interview.
“You try to convince the whole population of endemic villages to show up on a given day, and then you have a mobile team of nurses who examine everybody, trying to find those with early trypanosomiasis. This includes physical examination for lymph nodes in the neck, but also a blood test whose results are available within minutes,” he said.
“Until now, these persons with a positive serology would undergo additional and labor-intensive examinations of blood to try to find trypanosomes and prove that they have the disease. So far those with a positive serology and negative parasitological assays (‘serological suspects’) were left untreated, because the treatments were toxic and cumbersome, and because a substantial but unknown proportion of these ‘suspects’ just have a false positive of their serological test, without having the disease,” Dr. Pépin said.
“Now with acoziborole, which seems to have little serious toxicity ... and can be given as a single-dose oral med, it might be reasonable to treat the ‘serological suspects,’ ” he said.
“Take it one step further, it might be possible to do the serological test only and treat all individuals with a positive serology without bothering to do parasitological assays. This is what they call ‘test-and-treat’ strategy. It would make sense, provided that we are sure that the drug is very well tolerated.”
Dr. Pépin added that he is “just slightly worried” about three patients described in the paper who had psychiatric adverse events 3 months after treatment. “If that happens to patients who indeed have trypanosomiasis, that’s a reasonable price to pay considering the toxicity of other drugs,” he said. “If that happens to serological suspects, many of whom don’t have any disease, this becomes a preoccupation.”
But Dr. Tarral said, “We have no indication that the drug can provoke psychiatric symptoms. In fact, the psychiatric symptoms did not emerge – they re-emerged after 3 months due to some patients’ refusal to be followed up.”
“We included patients in very advanced stages of the disease, and these symptoms are considered disease sequelae,” Dr. Tarral said. “The majority of patients who have such psychiatric symptoms need follow-up after treatment. If not, they can relapse very early. There were a lot of patients who had such symptoms and the investigators proposed they should be followed by a psychiatrist and some of them refused. And due to that only three of our patients had this relapse, and they were cured after psychiatric support.”
The study was funded through the DND initiative and was supported by grants from the Bill & Melinda Gates Foundation; UK Aid; the Federal Ministry of Education and Research through Kreditanstalt für Wiederaufbau, Germany; the Swiss Agency for Development and Cooperation; Médecins Sans Frontières; the Dutch Ministry of Foreign Affairs; the Norwegian Agency for Development Cooperation; the Stavros Niarchos Foundation; the Spanish Agency for International Development Cooperation; and the Banco Bilbao Vizcaya Argentaria Foundation.
A number of study investigators, including Dr. Tarral, report employment at the DND initiative. Other investigators report fees from the DND initiative for the statistical report, consulting fees from CEMAG, D&A Pharma, Inventiva, and OT4B Pharma. The Swiss Tropical and Public Health Institute acted as a service provider for the DND initiative by monitoring the study sites. Dr. Pépin declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A single dose of oral acoziborole resulted in a greater than 95% cure or probable cure rate for human African trypanosomiasis (HAT), also known as sleeping sickness, according to results from a clinical trial testing a one-dose experimental drug.
The drug has “the potential to revolutionize treatment” for the disease, which remains endemic in sub-Saharan Africa, said Antoine Tarral, MD, head of the human African trypanosomiasis clinical program at the Drugs for Neglected Diseases initiative, based in Geneva, and senior author of the study, in a press release.
he told this news organization. “It’s the first drug we can use without hospitalization. ... All the previous medications needed hospitalization, and therefore we could not treat the population early before they started expressing symptoms.”
The World Health Organization “has been working for decades for such a possibility to implement a new strategy for this disease,” Dr. Tarral said.
Current (2019) WHO guidelines recommend oral fexinidazole as first-line treatment for any stage of the disease. The 10-day course often requires hospitalization and skilled staff. Previous recommendations required disease-staging with cerebrospinal fluid (CSF) sampling and 7 days of intramuscular pentamidine for early-stage disease or nifurtimox-eflornithine combination therapy (NECT) with hospitalization for late-stage disease.
By contrast, acoziborole, which was codeveloped by the DND initiative and Sanofi, “is administered in a single dose and is effective across every stage of the disease, thereby eliminating the many barriers currently in place for people most vulnerable to the diseases, such as invasive treatments and long travel distances to a hospital or clinic, and opening the door to screen-and-treat approaches at the village level,” Dr. Tarral said in the statement.
“Today, and in the future, we will have less and less support to do this long and costly diagnostic process and treatment in the hospital,” he said in an interview. “This development means we can go for a simple test and a simple treatment, which means we can meet the WHO 2030 goal for ending transmission of this disease.”
Results from the multicenter, prospective, open-label, single-arm, noncomparative, phase 2/3 study were published in The Lancet.
Pragmatic study design
Sleeping sickness is caused by Trypanosoma brucei gambiense (gambiense HAT). It is transmitted by the tsetse fly and mostly fatal when left untreated.
The study enrolled 208 adults and adolescents (167 with late-stage, and 41 with early-stage or intermediate-stage disease) from 10 hospitals in the Democratic Republic of the Congo and Guinea. All patients were treated with acoziborole 960 mg – an unusual study design.
“Due to the substantial decline in incidence, enrolling patients with gambiense HAT into clinical trials is challenging,” the authors wrote. “Following advice from the European Medicines Agency, this study was designed as an open-label, single-arm trial with no comparator or control group.”
After 18 months of follow-up, treatment success, defined as absence of trypanosomes and less than 20 white blood cells per mcL of CSF, occurred in 159 (95.2%) of the late-stage patients, and 100% of the early- and intermediate-stage patients, “which was similar to the estimated historical results for NECT,” the authors noted.
Serious treatment-emergent adverse events were reported in 21 (10%) of patients, “but none of these events were considered drug-related,” they added.
The DND initiative and the WHO are currently nearing completion of a much larger, double-blind, placebo-controlled trial of acoziborole to “increase the safety database,” Dr. Tarral explained.
“Purists will say that acoziborole has not been evaluated according to current standards, because the study was not a randomized trial, there was no control group, and the number of participants was small,” said Jacques Pépin, MD, from the University of Sherbrooke (Que.), in a linked commentary.
“But these were difficult challenges to overcome, considering the drastic reduction in the number of patients with HAT and dispersion over a vast territory, particularly in the Democratic Republic of the Congo. For these reasons, the authors took a pragmatic approach instead,” he wrote.
A potential new tool for eradication of sleeping sickness
“This is really an exciting development, which will be useful in the drive for eradication/interruption of transmission of this disease,” Dr. Pépin told this news organization.
Dr. Pépin treated around 1,000 trypanosomiasis patients during an outbreak in Zaire in the early 1980s. Because the asymptomatic incubation period for the disease can be several months or even years, “the core strategy for controlling the disease is active screening,” he said in an interview.
“You try to convince the whole population of endemic villages to show up on a given day, and then you have a mobile team of nurses who examine everybody, trying to find those with early trypanosomiasis. This includes physical examination for lymph nodes in the neck, but also a blood test whose results are available within minutes,” he said.
“Until now, these persons with a positive serology would undergo additional and labor-intensive examinations of blood to try to find trypanosomes and prove that they have the disease. So far those with a positive serology and negative parasitological assays (‘serological suspects’) were left untreated, because the treatments were toxic and cumbersome, and because a substantial but unknown proportion of these ‘suspects’ just have a false positive of their serological test, without having the disease,” Dr. Pépin said.
“Now with acoziborole, which seems to have little serious toxicity ... and can be given as a single-dose oral med, it might be reasonable to treat the ‘serological suspects,’ ” he said.
“Take it one step further, it might be possible to do the serological test only and treat all individuals with a positive serology without bothering to do parasitological assays. This is what they call ‘test-and-treat’ strategy. It would make sense, provided that we are sure that the drug is very well tolerated.”
Dr. Pépin added that he is “just slightly worried” about three patients described in the paper who had psychiatric adverse events 3 months after treatment. “If that happens to patients who indeed have trypanosomiasis, that’s a reasonable price to pay considering the toxicity of other drugs,” he said. “If that happens to serological suspects, many of whom don’t have any disease, this becomes a preoccupation.”
But Dr. Tarral said, “We have no indication that the drug can provoke psychiatric symptoms. In fact, the psychiatric symptoms did not emerge – they re-emerged after 3 months due to some patients’ refusal to be followed up.”
“We included patients in very advanced stages of the disease, and these symptoms are considered disease sequelae,” Dr. Tarral said. “The majority of patients who have such psychiatric symptoms need follow-up after treatment. If not, they can relapse very early. There were a lot of patients who had such symptoms and the investigators proposed they should be followed by a psychiatrist and some of them refused. And due to that only three of our patients had this relapse, and they were cured after psychiatric support.”
The study was funded through the DND initiative and was supported by grants from the Bill & Melinda Gates Foundation; UK Aid; the Federal Ministry of Education and Research through Kreditanstalt für Wiederaufbau, Germany; the Swiss Agency for Development and Cooperation; Médecins Sans Frontières; the Dutch Ministry of Foreign Affairs; the Norwegian Agency for Development Cooperation; the Stavros Niarchos Foundation; the Spanish Agency for International Development Cooperation; and the Banco Bilbao Vizcaya Argentaria Foundation.
A number of study investigators, including Dr. Tarral, report employment at the DND initiative. Other investigators report fees from the DND initiative for the statistical report, consulting fees from CEMAG, D&A Pharma, Inventiva, and OT4B Pharma. The Swiss Tropical and Public Health Institute acted as a service provider for the DND initiative by monitoring the study sites. Dr. Pépin declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A single dose of oral acoziborole resulted in a greater than 95% cure or probable cure rate for human African trypanosomiasis (HAT), also known as sleeping sickness, according to results from a clinical trial testing a one-dose experimental drug.
The drug has “the potential to revolutionize treatment” for the disease, which remains endemic in sub-Saharan Africa, said Antoine Tarral, MD, head of the human African trypanosomiasis clinical program at the Drugs for Neglected Diseases initiative, based in Geneva, and senior author of the study, in a press release.
he told this news organization. “It’s the first drug we can use without hospitalization. ... All the previous medications needed hospitalization, and therefore we could not treat the population early before they started expressing symptoms.”
The World Health Organization “has been working for decades for such a possibility to implement a new strategy for this disease,” Dr. Tarral said.
Current (2019) WHO guidelines recommend oral fexinidazole as first-line treatment for any stage of the disease. The 10-day course often requires hospitalization and skilled staff. Previous recommendations required disease-staging with cerebrospinal fluid (CSF) sampling and 7 days of intramuscular pentamidine for early-stage disease or nifurtimox-eflornithine combination therapy (NECT) with hospitalization for late-stage disease.
By contrast, acoziborole, which was codeveloped by the DND initiative and Sanofi, “is administered in a single dose and is effective across every stage of the disease, thereby eliminating the many barriers currently in place for people most vulnerable to the diseases, such as invasive treatments and long travel distances to a hospital or clinic, and opening the door to screen-and-treat approaches at the village level,” Dr. Tarral said in the statement.
“Today, and in the future, we will have less and less support to do this long and costly diagnostic process and treatment in the hospital,” he said in an interview. “This development means we can go for a simple test and a simple treatment, which means we can meet the WHO 2030 goal for ending transmission of this disease.”
Results from the multicenter, prospective, open-label, single-arm, noncomparative, phase 2/3 study were published in The Lancet.
Pragmatic study design
Sleeping sickness is caused by Trypanosoma brucei gambiense (gambiense HAT). It is transmitted by the tsetse fly and mostly fatal when left untreated.
The study enrolled 208 adults and adolescents (167 with late-stage, and 41 with early-stage or intermediate-stage disease) from 10 hospitals in the Democratic Republic of the Congo and Guinea. All patients were treated with acoziborole 960 mg – an unusual study design.
“Due to the substantial decline in incidence, enrolling patients with gambiense HAT into clinical trials is challenging,” the authors wrote. “Following advice from the European Medicines Agency, this study was designed as an open-label, single-arm trial with no comparator or control group.”
After 18 months of follow-up, treatment success, defined as absence of trypanosomes and less than 20 white blood cells per mcL of CSF, occurred in 159 (95.2%) of the late-stage patients, and 100% of the early- and intermediate-stage patients, “which was similar to the estimated historical results for NECT,” the authors noted.
Serious treatment-emergent adverse events were reported in 21 (10%) of patients, “but none of these events were considered drug-related,” they added.
The DND initiative and the WHO are currently nearing completion of a much larger, double-blind, placebo-controlled trial of acoziborole to “increase the safety database,” Dr. Tarral explained.
“Purists will say that acoziborole has not been evaluated according to current standards, because the study was not a randomized trial, there was no control group, and the number of participants was small,” said Jacques Pépin, MD, from the University of Sherbrooke (Que.), in a linked commentary.
“But these were difficult challenges to overcome, considering the drastic reduction in the number of patients with HAT and dispersion over a vast territory, particularly in the Democratic Republic of the Congo. For these reasons, the authors took a pragmatic approach instead,” he wrote.
A potential new tool for eradication of sleeping sickness
“This is really an exciting development, which will be useful in the drive for eradication/interruption of transmission of this disease,” Dr. Pépin told this news organization.
Dr. Pépin treated around 1,000 trypanosomiasis patients during an outbreak in Zaire in the early 1980s. Because the asymptomatic incubation period for the disease can be several months or even years, “the core strategy for controlling the disease is active screening,” he said in an interview.
“You try to convince the whole population of endemic villages to show up on a given day, and then you have a mobile team of nurses who examine everybody, trying to find those with early trypanosomiasis. This includes physical examination for lymph nodes in the neck, but also a blood test whose results are available within minutes,” he said.
“Until now, these persons with a positive serology would undergo additional and labor-intensive examinations of blood to try to find trypanosomes and prove that they have the disease. So far those with a positive serology and negative parasitological assays (‘serological suspects’) were left untreated, because the treatments were toxic and cumbersome, and because a substantial but unknown proportion of these ‘suspects’ just have a false positive of their serological test, without having the disease,” Dr. Pépin said.
“Now with acoziborole, which seems to have little serious toxicity ... and can be given as a single-dose oral med, it might be reasonable to treat the ‘serological suspects,’ ” he said.
“Take it one step further, it might be possible to do the serological test only and treat all individuals with a positive serology without bothering to do parasitological assays. This is what they call ‘test-and-treat’ strategy. It would make sense, provided that we are sure that the drug is very well tolerated.”
Dr. Pépin added that he is “just slightly worried” about three patients described in the paper who had psychiatric adverse events 3 months after treatment. “If that happens to patients who indeed have trypanosomiasis, that’s a reasonable price to pay considering the toxicity of other drugs,” he said. “If that happens to serological suspects, many of whom don’t have any disease, this becomes a preoccupation.”
But Dr. Tarral said, “We have no indication that the drug can provoke psychiatric symptoms. In fact, the psychiatric symptoms did not emerge – they re-emerged after 3 months due to some patients’ refusal to be followed up.”
“We included patients in very advanced stages of the disease, and these symptoms are considered disease sequelae,” Dr. Tarral said. “The majority of patients who have such psychiatric symptoms need follow-up after treatment. If not, they can relapse very early. There were a lot of patients who had such symptoms and the investigators proposed they should be followed by a psychiatrist and some of them refused. And due to that only three of our patients had this relapse, and they were cured after psychiatric support.”
The study was funded through the DND initiative and was supported by grants from the Bill & Melinda Gates Foundation; UK Aid; the Federal Ministry of Education and Research through Kreditanstalt für Wiederaufbau, Germany; the Swiss Agency for Development and Cooperation; Médecins Sans Frontières; the Dutch Ministry of Foreign Affairs; the Norwegian Agency for Development Cooperation; the Stavros Niarchos Foundation; the Spanish Agency for International Development Cooperation; and the Banco Bilbao Vizcaya Argentaria Foundation.
A number of study investigators, including Dr. Tarral, report employment at the DND initiative. Other investigators report fees from the DND initiative for the statistical report, consulting fees from CEMAG, D&A Pharma, Inventiva, and OT4B Pharma. The Swiss Tropical and Public Health Institute acted as a service provider for the DND initiative by monitoring the study sites. Dr. Pépin declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Lyme disease may cost U.S. nearly $970 million per year
The annual cost of Lyme disease in the United States could be nearly $970 million, according to new research. But not all cases of Lyme disease are equally costly. Costs for patients with disseminated Lyme disease were more than twice as high as those for patients with localized disease.
“These findings emphasize the importance of early and accurate diagnosis to reduce both illness and its associated personal and societal costs,” the study’s authors write. The analysis was published in Emerging Infectious Diseases. The authors are from the Centers for Disease Control and Prevention, the Yale School of Public Health, and the Departments of Health of Minnesota, Maryland, and New York State.
Lyme disease is the most reported vector-borne disease in the United States; an estimated 476,000 Americans are diagnosed with the infection every year. Though the highest incidences are in the Northeast and in Minnesota and Wisconsin, the CDC has recorded cases in all 50 states. Over the past 20 years, estimates of the total cost of treating Lyme disease have varied from $203 million to nearly $1.3 billion. A major limitation to these studies, however, is that they may not accurately identify patients with Lyme disease or capture many of the nonmedical costs associated with treatment, the authors write, such as costs associated with time taken off work and travel to appointments.
To better capture the comprehensive cost of Lyme disease in the United States, researchers conducted a prospective study from September 2014 to January 2016 and followed reported cases in four states with high rates of Lyme disease: Connecticut, Maryland, Minnesota, and New York. The team conducted monthly patient surveys and queried billing codes from participants’ clinicians to estimate both the personal expenses and societal costs – such as total costs to the health care system – of Lyme disease.
Participants were variously assigned to one of three categories: those with confirmed local disease (such as patients with erythema migrans); those with confirmed disseminated disease, with symptoms including arthritis, lymphocytic meningitis, and encephalomyelitis; and those with probable cases with reported symptoms.
The researchers surveyed 901 participants with clinician-diagnosed Lyme disease: 402 with localized disease, 238 with disseminated disease, and 261 with probable cases. Nearly all participants (94%) were White, 57% were men, and 71% had an annual household income above $60,000. About 28% of participants were younger than 18 years, 16% were aged 18-45 years, 36% were aged 46-65, and 19% were older than 65 years. For most participants (68%), complete medical cost data were available. Those data were used to calculate societal costs.
Costs per patient varied dramatically, from $0.46 to $30,628. On average, patients spent $1,252 during the study period on expenses related to Lyme disease treatment, including expenses associated with travel and time taken off work. The median cost to patients was notably smaller, at $244. Patients with disseminated disease had the highest median ($358) and mean ($1,692) costs, followed by participants with probable disease (median, $315; mean, $1,277). Participants with localized disease had the lowest median ($170) and mean ($1,070) costs.
Societal costs ranged from $54 to $122,766 per patient; the median was $690, and the mean was $2,032. Multiplying these numbers by the estimated cases diagnosed nationally each year, researchers determined that the total cost of Lyme disease in the United States is between $345 million and $968 million.
The study “pointed out the tremendous variability in costs” associated with Lyme disease treatment, Brian Fallon, MD, MPH, director of the Lyme and Tick-Borne Diseases Research Center at the Columbia University Irving Medical Center, New York, told this news organization. He was not involved with the research. Some patients continued having health expenses after the end of the study, which means their costs would be even higher, he noted. Though most patients fully recovered after 1 year, about 4% still reported symptoms, and 3% were still incurring costs.
And while the calculated total cost is “significant,” it is likely an underestimate, said John Aucott, MD, director of the Johns Hopkins Lyme Disease Clinical Research Center, Baltimore, in an interview. Dr. Aucott is also unaffiliated with the work. The researchers included confirmed or probable Lyme disease cases, he said, but that does not capture patients who may have had Lyme disease but were initially misdiagnosed. “Those poor patients end up going to see many different doctors to try to figure out what their diagnosis is,” added Dr. Fallon. “If they do have Lyme, they may not get started on treatment until much later than those who had the classic manifestations [of the disease].” These patients are more likely to have relapsing symptoms, he said, and their cost of care would be much higher, as highlighted in the research findings.
“The take-home point is that the cost to the patient and society is much less if you make an early diagnosis,” Dr. Aucott said. “It highlights the need for rapid diagnosis and rapid identification,” added Dr. Fallon, “as well as the potential importance and value of better means of prevention.”
A version of this article first appeared on Medscape.com.
The annual cost of Lyme disease in the United States could be nearly $970 million, according to new research. But not all cases of Lyme disease are equally costly. Costs for patients with disseminated Lyme disease were more than twice as high as those for patients with localized disease.
“These findings emphasize the importance of early and accurate diagnosis to reduce both illness and its associated personal and societal costs,” the study’s authors write. The analysis was published in Emerging Infectious Diseases. The authors are from the Centers for Disease Control and Prevention, the Yale School of Public Health, and the Departments of Health of Minnesota, Maryland, and New York State.
Lyme disease is the most reported vector-borne disease in the United States; an estimated 476,000 Americans are diagnosed with the infection every year. Though the highest incidences are in the Northeast and in Minnesota and Wisconsin, the CDC has recorded cases in all 50 states. Over the past 20 years, estimates of the total cost of treating Lyme disease have varied from $203 million to nearly $1.3 billion. A major limitation to these studies, however, is that they may not accurately identify patients with Lyme disease or capture many of the nonmedical costs associated with treatment, the authors write, such as costs associated with time taken off work and travel to appointments.
To better capture the comprehensive cost of Lyme disease in the United States, researchers conducted a prospective study from September 2014 to January 2016 and followed reported cases in four states with high rates of Lyme disease: Connecticut, Maryland, Minnesota, and New York. The team conducted monthly patient surveys and queried billing codes from participants’ clinicians to estimate both the personal expenses and societal costs – such as total costs to the health care system – of Lyme disease.
Participants were variously assigned to one of three categories: those with confirmed local disease (such as patients with erythema migrans); those with confirmed disseminated disease, with symptoms including arthritis, lymphocytic meningitis, and encephalomyelitis; and those with probable cases with reported symptoms.
The researchers surveyed 901 participants with clinician-diagnosed Lyme disease: 402 with localized disease, 238 with disseminated disease, and 261 with probable cases. Nearly all participants (94%) were White, 57% were men, and 71% had an annual household income above $60,000. About 28% of participants were younger than 18 years, 16% were aged 18-45 years, 36% were aged 46-65, and 19% were older than 65 years. For most participants (68%), complete medical cost data were available. Those data were used to calculate societal costs.
Costs per patient varied dramatically, from $0.46 to $30,628. On average, patients spent $1,252 during the study period on expenses related to Lyme disease treatment, including expenses associated with travel and time taken off work. The median cost to patients was notably smaller, at $244. Patients with disseminated disease had the highest median ($358) and mean ($1,692) costs, followed by participants with probable disease (median, $315; mean, $1,277). Participants with localized disease had the lowest median ($170) and mean ($1,070) costs.
Societal costs ranged from $54 to $122,766 per patient; the median was $690, and the mean was $2,032. Multiplying these numbers by the estimated cases diagnosed nationally each year, researchers determined that the total cost of Lyme disease in the United States is between $345 million and $968 million.
The study “pointed out the tremendous variability in costs” associated with Lyme disease treatment, Brian Fallon, MD, MPH, director of the Lyme and Tick-Borne Diseases Research Center at the Columbia University Irving Medical Center, New York, told this news organization. He was not involved with the research. Some patients continued having health expenses after the end of the study, which means their costs would be even higher, he noted. Though most patients fully recovered after 1 year, about 4% still reported symptoms, and 3% were still incurring costs.
And while the calculated total cost is “significant,” it is likely an underestimate, said John Aucott, MD, director of the Johns Hopkins Lyme Disease Clinical Research Center, Baltimore, in an interview. Dr. Aucott is also unaffiliated with the work. The researchers included confirmed or probable Lyme disease cases, he said, but that does not capture patients who may have had Lyme disease but were initially misdiagnosed. “Those poor patients end up going to see many different doctors to try to figure out what their diagnosis is,” added Dr. Fallon. “If they do have Lyme, they may not get started on treatment until much later than those who had the classic manifestations [of the disease].” These patients are more likely to have relapsing symptoms, he said, and their cost of care would be much higher, as highlighted in the research findings.
“The take-home point is that the cost to the patient and society is much less if you make an early diagnosis,” Dr. Aucott said. “It highlights the need for rapid diagnosis and rapid identification,” added Dr. Fallon, “as well as the potential importance and value of better means of prevention.”
A version of this article first appeared on Medscape.com.
The annual cost of Lyme disease in the United States could be nearly $970 million, according to new research. But not all cases of Lyme disease are equally costly. Costs for patients with disseminated Lyme disease were more than twice as high as those for patients with localized disease.
“These findings emphasize the importance of early and accurate diagnosis to reduce both illness and its associated personal and societal costs,” the study’s authors write. The analysis was published in Emerging Infectious Diseases. The authors are from the Centers for Disease Control and Prevention, the Yale School of Public Health, and the Departments of Health of Minnesota, Maryland, and New York State.
Lyme disease is the most reported vector-borne disease in the United States; an estimated 476,000 Americans are diagnosed with the infection every year. Though the highest incidences are in the Northeast and in Minnesota and Wisconsin, the CDC has recorded cases in all 50 states. Over the past 20 years, estimates of the total cost of treating Lyme disease have varied from $203 million to nearly $1.3 billion. A major limitation to these studies, however, is that they may not accurately identify patients with Lyme disease or capture many of the nonmedical costs associated with treatment, the authors write, such as costs associated with time taken off work and travel to appointments.
To better capture the comprehensive cost of Lyme disease in the United States, researchers conducted a prospective study from September 2014 to January 2016 and followed reported cases in four states with high rates of Lyme disease: Connecticut, Maryland, Minnesota, and New York. The team conducted monthly patient surveys and queried billing codes from participants’ clinicians to estimate both the personal expenses and societal costs – such as total costs to the health care system – of Lyme disease.
Participants were variously assigned to one of three categories: those with confirmed local disease (such as patients with erythema migrans); those with confirmed disseminated disease, with symptoms including arthritis, lymphocytic meningitis, and encephalomyelitis; and those with probable cases with reported symptoms.
The researchers surveyed 901 participants with clinician-diagnosed Lyme disease: 402 with localized disease, 238 with disseminated disease, and 261 with probable cases. Nearly all participants (94%) were White, 57% were men, and 71% had an annual household income above $60,000. About 28% of participants were younger than 18 years, 16% were aged 18-45 years, 36% were aged 46-65, and 19% were older than 65 years. For most participants (68%), complete medical cost data were available. Those data were used to calculate societal costs.
Costs per patient varied dramatically, from $0.46 to $30,628. On average, patients spent $1,252 during the study period on expenses related to Lyme disease treatment, including expenses associated with travel and time taken off work. The median cost to patients was notably smaller, at $244. Patients with disseminated disease had the highest median ($358) and mean ($1,692) costs, followed by participants with probable disease (median, $315; mean, $1,277). Participants with localized disease had the lowest median ($170) and mean ($1,070) costs.
Societal costs ranged from $54 to $122,766 per patient; the median was $690, and the mean was $2,032. Multiplying these numbers by the estimated cases diagnosed nationally each year, researchers determined that the total cost of Lyme disease in the United States is between $345 million and $968 million.
The study “pointed out the tremendous variability in costs” associated with Lyme disease treatment, Brian Fallon, MD, MPH, director of the Lyme and Tick-Borne Diseases Research Center at the Columbia University Irving Medical Center, New York, told this news organization. He was not involved with the research. Some patients continued having health expenses after the end of the study, which means their costs would be even higher, he noted. Though most patients fully recovered after 1 year, about 4% still reported symptoms, and 3% were still incurring costs.
And while the calculated total cost is “significant,” it is likely an underestimate, said John Aucott, MD, director of the Johns Hopkins Lyme Disease Clinical Research Center, Baltimore, in an interview. Dr. Aucott is also unaffiliated with the work. The researchers included confirmed or probable Lyme disease cases, he said, but that does not capture patients who may have had Lyme disease but were initially misdiagnosed. “Those poor patients end up going to see many different doctors to try to figure out what their diagnosis is,” added Dr. Fallon. “If they do have Lyme, they may not get started on treatment until much later than those who had the classic manifestations [of the disease].” These patients are more likely to have relapsing symptoms, he said, and their cost of care would be much higher, as highlighted in the research findings.
“The take-home point is that the cost to the patient and society is much less if you make an early diagnosis,” Dr. Aucott said. “It highlights the need for rapid diagnosis and rapid identification,” added Dr. Fallon, “as well as the potential importance and value of better means of prevention.”
A version of this article first appeared on Medscape.com.
FROM EMERGING INFECTIOUS DISEASES
Malaria: Testing parasite DNA in travelers’ blood may help predict drug resistance
Testing the DNA of antimicrobial-resistant Plasmodium falciparum in the blood of travelers from malaria-endemic regions may help researchers monitor how drug resistance changes over time, a study from Canada reports.
“Malaria remains the deadliest vector-borne infectious disease worldwide. Plasmodium spp., most commonly P. falciparum, are responsible for [approximately] 229 million cases and 500,000 deaths from malaria annually,” the authors write in Emerging Infectious Diseases.
“Our findings demonstrate an absence of genetic markers of resistance to the most powerful antimalarials on the planet – the artemisinins – in potentially deadly malaria imported primarily from sub-Saharan Africa over time. This is good news,” senior study author Andrea K. Boggild, MD, MSc, DTMH, told this news organization.
“We also showed that over 90% of falciparum malaria imports were resistant to the proguanil component of the fixed drug combination atovaquone-proguanil, a popular oral antimalarial that is first-line treatment for uncomplicated malaria in Canada,” Dr. Boggild, an associate professor in the department of medicine at the University of Toronto, Canada, added in an email. “We documented no genetic markers of atovaquone resistance.”
Search for global patterns of emerging drug resistance
Dr. Boggild, the medical director of the tropical disease unit at Toronto General Hospital, and colleagues analyzed 243 whole-blood specimens that contained P. falciparum and no other Plasmodium species from the malaria biobank at the Public Health Ontario Laboratory in Toronto. They analyzed specimens from the years 2008-2009, 2013-2014, and 2017-2018 from patients ranging in age from 3 to 88 years. Of the 186 patients with a documented travel history, 81 had traveled in West Africa, the most common region, and 40 in Nigeria, the most common country. Five specimens came from travelers to Southeast Asia, and one came from a traveler to the Caribbean.
The researchers extracted DNA from whole blood and detected the parasite’s DNA by real-time quantitative polymerase chain reaction (qPCR). They analyzed 23 different single-nucleotide polymorphisms (SNPs) in six genes, and quantified the prevalence of resistance markers, including genes that provoke resistance to the most common antimalarial drugs: chloroquine, mefloquine, atovaquone/proguanil, and the artemisinins.
They analyzed SNPs at atpase6 (pfATPase6), pfcrt (chloroquine resistance transporter, cytb (cytochrome b), dhfr (dihydrofolate reductase), dhps (dihydropteroate synthetase), mdr1 (multidrug resistance protein) and mdr1 copy number, and kelch13 (kelch protein gene on chromosome 13).
Over time, they detected increasing mutant genotypes for dhfr S108N (P = .001) and dhps A613T (P = .029) but decreasing mutant genotypes for mdr1 N86Y (P < .001), D1246Y (P = .003), pfcrt K76T (P = .011), and pfcrt 74-75 (P = .014). They found no kelch13 mutations. They detected fewer mutations indicating chloroquine resistance over time, suggesting less chloroquine pressure in specimens from travelers to Africa, but mutations that provided proguanil resistance increased.
“Antimalarial resistance – particularly resistance to the powerful artemisinins – continues to expand globally, and it is important to conduct routine surveillance for resistant parasites in order to inform appropriate prevention and treatment guidelines,” Dr. Boggild explained. “It cannot be presumed that a drug’s efficacy will be durable over time given the global landscape of antimalarial resistance.”
Dr. Boggild acknowledged limitations to the study, including incomplete travel history in about half of the patients, relatively few patients from Southeast Asia, and the small sample set.
“Clinicians caring for travelers before or after travel should familiarize themselves with the options for malaria prevention and treatment and understand the risk–benefit profile of each drug,” Dr. Boggild advised.
“Resistance to proguanil means that we are reliant on the partner drug atovaquone for the antimalarial action of this formulation, which is effective only when taken with food,” she added.
Anne N. Cowell, MD, MPH, of the division of infectious diseases at the University of California, San Diego, was not surprised by the findings.
“The study demonstrates how quickly malaria parasites adapt and evolve to survive changes in malaria treatment,” Dr. Cowell, who was not involved in the study, told this news organization.
“These changes reflect changing malaria treatment and thus drug pressure during the time period,” she said in an email. “Because the majority of the clinical samples with a known travel history came from West Africa, and there was no clear evidence of artemisinin resistance in the area during the final time period studied, it is not surprising that they did not find kelch13 resistance mutations.
“The increase in mutations associated with proguanil resistance is concerning because atovaquone-proguanil is frequently used for prophylaxis during travel,” Dr. Cowell added. “There is no widespread evidence of resistance in travelers at this time, but it warrants monitoring.”
Sean C. Murphy, MD, PhD, an associate professor of laboratory medicine and the director of the malaria molecular diagnostic laboratory at the University of Washington in Seattle, also was not surprised by the study’s results.
“It may be just a matter of time before evidence of artemisinin resistance crops up among returning travelers,” he said in an email. “When that happens, we may lose the opportunity to easily use common go-to drugs like atovaquone/proguanil to treat these patients.
“The biggest takeaway of this study is the reminder that drug-resistant malaria (including the future potential for artemisinin-resistant malaria) is just an airplane flight or two away from nonendemic places like Canada and the United States,” Dr. Murphy noted. He was not involved with this Canadian study.
“Continued investment is needed to support malaria control, drug resistance monitoring, and vaccine efforts in order to fight this relentless, terrible parasite,” he urged.
The Project Initiation Fund of Public Health Ontario funded the study. The study authors, Dr. Cowell, and Dr. Murphy have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Testing the DNA of antimicrobial-resistant Plasmodium falciparum in the blood of travelers from malaria-endemic regions may help researchers monitor how drug resistance changes over time, a study from Canada reports.
“Malaria remains the deadliest vector-borne infectious disease worldwide. Plasmodium spp., most commonly P. falciparum, are responsible for [approximately] 229 million cases and 500,000 deaths from malaria annually,” the authors write in Emerging Infectious Diseases.
“Our findings demonstrate an absence of genetic markers of resistance to the most powerful antimalarials on the planet – the artemisinins – in potentially deadly malaria imported primarily from sub-Saharan Africa over time. This is good news,” senior study author Andrea K. Boggild, MD, MSc, DTMH, told this news organization.
“We also showed that over 90% of falciparum malaria imports were resistant to the proguanil component of the fixed drug combination atovaquone-proguanil, a popular oral antimalarial that is first-line treatment for uncomplicated malaria in Canada,” Dr. Boggild, an associate professor in the department of medicine at the University of Toronto, Canada, added in an email. “We documented no genetic markers of atovaquone resistance.”
Search for global patterns of emerging drug resistance
Dr. Boggild, the medical director of the tropical disease unit at Toronto General Hospital, and colleagues analyzed 243 whole-blood specimens that contained P. falciparum and no other Plasmodium species from the malaria biobank at the Public Health Ontario Laboratory in Toronto. They analyzed specimens from the years 2008-2009, 2013-2014, and 2017-2018 from patients ranging in age from 3 to 88 years. Of the 186 patients with a documented travel history, 81 had traveled in West Africa, the most common region, and 40 in Nigeria, the most common country. Five specimens came from travelers to Southeast Asia, and one came from a traveler to the Caribbean.
The researchers extracted DNA from whole blood and detected the parasite’s DNA by real-time quantitative polymerase chain reaction (qPCR). They analyzed 23 different single-nucleotide polymorphisms (SNPs) in six genes, and quantified the prevalence of resistance markers, including genes that provoke resistance to the most common antimalarial drugs: chloroquine, mefloquine, atovaquone/proguanil, and the artemisinins.
They analyzed SNPs at atpase6 (pfATPase6), pfcrt (chloroquine resistance transporter, cytb (cytochrome b), dhfr (dihydrofolate reductase), dhps (dihydropteroate synthetase), mdr1 (multidrug resistance protein) and mdr1 copy number, and kelch13 (kelch protein gene on chromosome 13).
Over time, they detected increasing mutant genotypes for dhfr S108N (P = .001) and dhps A613T (P = .029) but decreasing mutant genotypes for mdr1 N86Y (P < .001), D1246Y (P = .003), pfcrt K76T (P = .011), and pfcrt 74-75 (P = .014). They found no kelch13 mutations. They detected fewer mutations indicating chloroquine resistance over time, suggesting less chloroquine pressure in specimens from travelers to Africa, but mutations that provided proguanil resistance increased.
“Antimalarial resistance – particularly resistance to the powerful artemisinins – continues to expand globally, and it is important to conduct routine surveillance for resistant parasites in order to inform appropriate prevention and treatment guidelines,” Dr. Boggild explained. “It cannot be presumed that a drug’s efficacy will be durable over time given the global landscape of antimalarial resistance.”
Dr. Boggild acknowledged limitations to the study, including incomplete travel history in about half of the patients, relatively few patients from Southeast Asia, and the small sample set.
“Clinicians caring for travelers before or after travel should familiarize themselves with the options for malaria prevention and treatment and understand the risk–benefit profile of each drug,” Dr. Boggild advised.
“Resistance to proguanil means that we are reliant on the partner drug atovaquone for the antimalarial action of this formulation, which is effective only when taken with food,” she added.
Anne N. Cowell, MD, MPH, of the division of infectious diseases at the University of California, San Diego, was not surprised by the findings.
“The study demonstrates how quickly malaria parasites adapt and evolve to survive changes in malaria treatment,” Dr. Cowell, who was not involved in the study, told this news organization.
“These changes reflect changing malaria treatment and thus drug pressure during the time period,” she said in an email. “Because the majority of the clinical samples with a known travel history came from West Africa, and there was no clear evidence of artemisinin resistance in the area during the final time period studied, it is not surprising that they did not find kelch13 resistance mutations.
“The increase in mutations associated with proguanil resistance is concerning because atovaquone-proguanil is frequently used for prophylaxis during travel,” Dr. Cowell added. “There is no widespread evidence of resistance in travelers at this time, but it warrants monitoring.”
Sean C. Murphy, MD, PhD, an associate professor of laboratory medicine and the director of the malaria molecular diagnostic laboratory at the University of Washington in Seattle, also was not surprised by the study’s results.
“It may be just a matter of time before evidence of artemisinin resistance crops up among returning travelers,” he said in an email. “When that happens, we may lose the opportunity to easily use common go-to drugs like atovaquone/proguanil to treat these patients.
“The biggest takeaway of this study is the reminder that drug-resistant malaria (including the future potential for artemisinin-resistant malaria) is just an airplane flight or two away from nonendemic places like Canada and the United States,” Dr. Murphy noted. He was not involved with this Canadian study.
“Continued investment is needed to support malaria control, drug resistance monitoring, and vaccine efforts in order to fight this relentless, terrible parasite,” he urged.
The Project Initiation Fund of Public Health Ontario funded the study. The study authors, Dr. Cowell, and Dr. Murphy have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Testing the DNA of antimicrobial-resistant Plasmodium falciparum in the blood of travelers from malaria-endemic regions may help researchers monitor how drug resistance changes over time, a study from Canada reports.
“Malaria remains the deadliest vector-borne infectious disease worldwide. Plasmodium spp., most commonly P. falciparum, are responsible for [approximately] 229 million cases and 500,000 deaths from malaria annually,” the authors write in Emerging Infectious Diseases.
“Our findings demonstrate an absence of genetic markers of resistance to the most powerful antimalarials on the planet – the artemisinins – in potentially deadly malaria imported primarily from sub-Saharan Africa over time. This is good news,” senior study author Andrea K. Boggild, MD, MSc, DTMH, told this news organization.
“We also showed that over 90% of falciparum malaria imports were resistant to the proguanil component of the fixed drug combination atovaquone-proguanil, a popular oral antimalarial that is first-line treatment for uncomplicated malaria in Canada,” Dr. Boggild, an associate professor in the department of medicine at the University of Toronto, Canada, added in an email. “We documented no genetic markers of atovaquone resistance.”
Search for global patterns of emerging drug resistance
Dr. Boggild, the medical director of the tropical disease unit at Toronto General Hospital, and colleagues analyzed 243 whole-blood specimens that contained P. falciparum and no other Plasmodium species from the malaria biobank at the Public Health Ontario Laboratory in Toronto. They analyzed specimens from the years 2008-2009, 2013-2014, and 2017-2018 from patients ranging in age from 3 to 88 years. Of the 186 patients with a documented travel history, 81 had traveled in West Africa, the most common region, and 40 in Nigeria, the most common country. Five specimens came from travelers to Southeast Asia, and one came from a traveler to the Caribbean.
The researchers extracted DNA from whole blood and detected the parasite’s DNA by real-time quantitative polymerase chain reaction (qPCR). They analyzed 23 different single-nucleotide polymorphisms (SNPs) in six genes, and quantified the prevalence of resistance markers, including genes that provoke resistance to the most common antimalarial drugs: chloroquine, mefloquine, atovaquone/proguanil, and the artemisinins.
They analyzed SNPs at atpase6 (pfATPase6), pfcrt (chloroquine resistance transporter, cytb (cytochrome b), dhfr (dihydrofolate reductase), dhps (dihydropteroate synthetase), mdr1 (multidrug resistance protein) and mdr1 copy number, and kelch13 (kelch protein gene on chromosome 13).
Over time, they detected increasing mutant genotypes for dhfr S108N (P = .001) and dhps A613T (P = .029) but decreasing mutant genotypes for mdr1 N86Y (P < .001), D1246Y (P = .003), pfcrt K76T (P = .011), and pfcrt 74-75 (P = .014). They found no kelch13 mutations. They detected fewer mutations indicating chloroquine resistance over time, suggesting less chloroquine pressure in specimens from travelers to Africa, but mutations that provided proguanil resistance increased.
“Antimalarial resistance – particularly resistance to the powerful artemisinins – continues to expand globally, and it is important to conduct routine surveillance for resistant parasites in order to inform appropriate prevention and treatment guidelines,” Dr. Boggild explained. “It cannot be presumed that a drug’s efficacy will be durable over time given the global landscape of antimalarial resistance.”
Dr. Boggild acknowledged limitations to the study, including incomplete travel history in about half of the patients, relatively few patients from Southeast Asia, and the small sample set.
“Clinicians caring for travelers before or after travel should familiarize themselves with the options for malaria prevention and treatment and understand the risk–benefit profile of each drug,” Dr. Boggild advised.
“Resistance to proguanil means that we are reliant on the partner drug atovaquone for the antimalarial action of this formulation, which is effective only when taken with food,” she added.
Anne N. Cowell, MD, MPH, of the division of infectious diseases at the University of California, San Diego, was not surprised by the findings.
“The study demonstrates how quickly malaria parasites adapt and evolve to survive changes in malaria treatment,” Dr. Cowell, who was not involved in the study, told this news organization.
“These changes reflect changing malaria treatment and thus drug pressure during the time period,” she said in an email. “Because the majority of the clinical samples with a known travel history came from West Africa, and there was no clear evidence of artemisinin resistance in the area during the final time period studied, it is not surprising that they did not find kelch13 resistance mutations.
“The increase in mutations associated with proguanil resistance is concerning because atovaquone-proguanil is frequently used for prophylaxis during travel,” Dr. Cowell added. “There is no widespread evidence of resistance in travelers at this time, but it warrants monitoring.”
Sean C. Murphy, MD, PhD, an associate professor of laboratory medicine and the director of the malaria molecular diagnostic laboratory at the University of Washington in Seattle, also was not surprised by the study’s results.
“It may be just a matter of time before evidence of artemisinin resistance crops up among returning travelers,” he said in an email. “When that happens, we may lose the opportunity to easily use common go-to drugs like atovaquone/proguanil to treat these patients.
“The biggest takeaway of this study is the reminder that drug-resistant malaria (including the future potential for artemisinin-resistant malaria) is just an airplane flight or two away from nonendemic places like Canada and the United States,” Dr. Murphy noted. He was not involved with this Canadian study.
“Continued investment is needed to support malaria control, drug resistance monitoring, and vaccine efforts in order to fight this relentless, terrible parasite,” he urged.
The Project Initiation Fund of Public Health Ontario funded the study. The study authors, Dr. Cowell, and Dr. Murphy have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM EMERGING INFECTIOUS DISEASES
Cat ownership in childhood linked ‘conditionally’ to psychosis in adult males
Owning an outdoor cat as a child is associated with an increased risk of psychotic experiences in adulthood – but only in males, new research suggests.
Investigators found
The suspected culprit is not the cat itself but rather exposure to Toxoplasma gondii, a common parasite carried by rodents and sometimes found in cat feces. The study adds to a growing evidence showing exposure to T. gondii may be a risk factor for schizophrenia and other psychotic disorders.
“These are small pieces of evidence but it’s interesting to consider that there might be combinations of risk factors at play,” lead author Vincent Paquin, MD, psychiatry resident at McGill University, Montreal, said in an interview.
“And even if the magnitude of the risk is small at the individual level,” he added, “cats and Toxoplasma gondii are so present in our society that if we add up all these small potential effects then it becomes a potential public health question.”
The study was published online Jan. 30, 2022, in the Journal of Psychiatric Research.
Inconsistent evidence
T. gondii infects about 30% of the human population and is usually transmitted by cats. Most infections are asymptomatic, but T. gondii can cause toxoplasmosis in humans, which has been linked to increased risk of schizophrenia, suicide attempts, and more recently, mild cognitive impairment.
Although some studies show an association between cat ownership and increased risk of mental illness, the research findings have been inconsistent.
“The evidence has been mixed about the association between cat ownership and psychosis expression, so our approach was to consider whether specific factors or combinations of factors could explain this mixed evidence,” Dr. Paquin said.
For the study, 2206 individuals aged 18-40 years completed the Community Assessment of Psychic Experiences (CAPE-42) and a questionnaire to gather information about cat ownership at any time between birth and age 13 and if the cats lived exclusively indoors (nonhunting) or if they were allowed outside (rodent hunting).
Participants were also asked about the number of residential moves between birth and age 15, date and place of birth, lifetime history of head trauma, and tobacco smoking history.
Rodent-hunting cat ownership was associated with higher risk of psychosis in male participants, compared with owning no cat or a nonhunting cat. When the investigators added head trauma and residential moves to rodent-hunting cat ownership, psychosis risk was elevated in both men and women.
Independent of cat ownership, younger age, moving more than three times as a child, a history of head trauma, and being a smoker were all associated with higher psychosis risk.
The study wasn’t designed to explore potential biological mechanisms to explain the sex differences in psychosis risk seen among rodent-hunting cat owners, but “one possible explanation based on the animal model literature is that the neurobiological effects of parasitic exposure may be greater with male sex,” senior author Suzanne King, PhD, professor of psychiatry at McGill, said in an interview.
The new study is part of a larger, long-term project called EnviroGen, led by Dr. King, examining the environmental and genetic risk factors for schizophrenia.
Need for replication
Commenting on the findings, E. Fuller Torrey, MD, who was among the first researchers to identify a link between cat ownership, T. gondii infection, and schizophrenia, said the study is “an interesting addition to the studies of cat ownership in childhood as a risk factor for psychosis.”
Of the approximately 10 published studies on the topic, about half suggest a link between cat ownership and psychosis later in life, said Dr. Torrey, associate director for research at the Stanley Medical Research Institute in Rockville, Md.
“The Canadian study is interesting in that it is the first study that separates exposure to permanently indoor cats from cats that are allowed to go outdoors, and the results were positive only for outdoor cats,” Dr. Torrey said.
The study has limitations, Dr. Torrey added, including its retrospective design and the use of a self-report questionnaire to assess psychotic experiences in adulthood.
Also commenting on findings, James Kirkbride, PhD, professor of psychiatric and social epidemiology, University College London, noted the same limitations.
Dr. Kirkbride is the lead author of a 2017 study that showed no link between cat ownership and serious mental illness that included nearly 5,000 people born in 1991 or 1992 and followed until age 18. In this study, there was no link between psychosis and cat ownership during pregnancy or at ages 4 or 10 years.
“Researchers have long been fascinated with the idea that cat ownership may affect mental health. This paper may have them chasing their own tail,” Dr. Kirkbride said.
“Evidence of any association is limited to certain subgroups without a strong theoretical basis for why this may be the case,” he added. “The retrospective and cross-sectional nature of the survey also raise the possibility that the results are impacted by differential recall bias, as well as the broader issues of chance and unobserved confounding.”
Dr. King noted that recall bias is a limitation the researchers highlighted in their study, but “considering the exposures are relatively objective and factual, we do not believe the potential for recall bias is substantial.”
“Nonetheless, we strongly believe that replication of our results in prospective, population-representative cohorts will be crucial to making firmer conclusions,” he added.
The study was funded by grants from the Quebec Health Research Fund. The study authors and Dr. Kirkbride disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Owning an outdoor cat as a child is associated with an increased risk of psychotic experiences in adulthood – but only in males, new research suggests.
Investigators found
The suspected culprit is not the cat itself but rather exposure to Toxoplasma gondii, a common parasite carried by rodents and sometimes found in cat feces. The study adds to a growing evidence showing exposure to T. gondii may be a risk factor for schizophrenia and other psychotic disorders.
“These are small pieces of evidence but it’s interesting to consider that there might be combinations of risk factors at play,” lead author Vincent Paquin, MD, psychiatry resident at McGill University, Montreal, said in an interview.
“And even if the magnitude of the risk is small at the individual level,” he added, “cats and Toxoplasma gondii are so present in our society that if we add up all these small potential effects then it becomes a potential public health question.”
The study was published online Jan. 30, 2022, in the Journal of Psychiatric Research.
Inconsistent evidence
T. gondii infects about 30% of the human population and is usually transmitted by cats. Most infections are asymptomatic, but T. gondii can cause toxoplasmosis in humans, which has been linked to increased risk of schizophrenia, suicide attempts, and more recently, mild cognitive impairment.
Although some studies show an association between cat ownership and increased risk of mental illness, the research findings have been inconsistent.
“The evidence has been mixed about the association between cat ownership and psychosis expression, so our approach was to consider whether specific factors or combinations of factors could explain this mixed evidence,” Dr. Paquin said.
For the study, 2206 individuals aged 18-40 years completed the Community Assessment of Psychic Experiences (CAPE-42) and a questionnaire to gather information about cat ownership at any time between birth and age 13 and if the cats lived exclusively indoors (nonhunting) or if they were allowed outside (rodent hunting).
Participants were also asked about the number of residential moves between birth and age 15, date and place of birth, lifetime history of head trauma, and tobacco smoking history.
Rodent-hunting cat ownership was associated with higher risk of psychosis in male participants, compared with owning no cat or a nonhunting cat. When the investigators added head trauma and residential moves to rodent-hunting cat ownership, psychosis risk was elevated in both men and women.
Independent of cat ownership, younger age, moving more than three times as a child, a history of head trauma, and being a smoker were all associated with higher psychosis risk.
The study wasn’t designed to explore potential biological mechanisms to explain the sex differences in psychosis risk seen among rodent-hunting cat owners, but “one possible explanation based on the animal model literature is that the neurobiological effects of parasitic exposure may be greater with male sex,” senior author Suzanne King, PhD, professor of psychiatry at McGill, said in an interview.
The new study is part of a larger, long-term project called EnviroGen, led by Dr. King, examining the environmental and genetic risk factors for schizophrenia.
Need for replication
Commenting on the findings, E. Fuller Torrey, MD, who was among the first researchers to identify a link between cat ownership, T. gondii infection, and schizophrenia, said the study is “an interesting addition to the studies of cat ownership in childhood as a risk factor for psychosis.”
Of the approximately 10 published studies on the topic, about half suggest a link between cat ownership and psychosis later in life, said Dr. Torrey, associate director for research at the Stanley Medical Research Institute in Rockville, Md.
“The Canadian study is interesting in that it is the first study that separates exposure to permanently indoor cats from cats that are allowed to go outdoors, and the results were positive only for outdoor cats,” Dr. Torrey said.
The study has limitations, Dr. Torrey added, including its retrospective design and the use of a self-report questionnaire to assess psychotic experiences in adulthood.
Also commenting on findings, James Kirkbride, PhD, professor of psychiatric and social epidemiology, University College London, noted the same limitations.
Dr. Kirkbride is the lead author of a 2017 study that showed no link between cat ownership and serious mental illness that included nearly 5,000 people born in 1991 or 1992 and followed until age 18. In this study, there was no link between psychosis and cat ownership during pregnancy or at ages 4 or 10 years.
“Researchers have long been fascinated with the idea that cat ownership may affect mental health. This paper may have them chasing their own tail,” Dr. Kirkbride said.
“Evidence of any association is limited to certain subgroups without a strong theoretical basis for why this may be the case,” he added. “The retrospective and cross-sectional nature of the survey also raise the possibility that the results are impacted by differential recall bias, as well as the broader issues of chance and unobserved confounding.”
Dr. King noted that recall bias is a limitation the researchers highlighted in their study, but “considering the exposures are relatively objective and factual, we do not believe the potential for recall bias is substantial.”
“Nonetheless, we strongly believe that replication of our results in prospective, population-representative cohorts will be crucial to making firmer conclusions,” he added.
The study was funded by grants from the Quebec Health Research Fund. The study authors and Dr. Kirkbride disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Owning an outdoor cat as a child is associated with an increased risk of psychotic experiences in adulthood – but only in males, new research suggests.
Investigators found
The suspected culprit is not the cat itself but rather exposure to Toxoplasma gondii, a common parasite carried by rodents and sometimes found in cat feces. The study adds to a growing evidence showing exposure to T. gondii may be a risk factor for schizophrenia and other psychotic disorders.
“These are small pieces of evidence but it’s interesting to consider that there might be combinations of risk factors at play,” lead author Vincent Paquin, MD, psychiatry resident at McGill University, Montreal, said in an interview.
“And even if the magnitude of the risk is small at the individual level,” he added, “cats and Toxoplasma gondii are so present in our society that if we add up all these small potential effects then it becomes a potential public health question.”
The study was published online Jan. 30, 2022, in the Journal of Psychiatric Research.
Inconsistent evidence
T. gondii infects about 30% of the human population and is usually transmitted by cats. Most infections are asymptomatic, but T. gondii can cause toxoplasmosis in humans, which has been linked to increased risk of schizophrenia, suicide attempts, and more recently, mild cognitive impairment.
Although some studies show an association between cat ownership and increased risk of mental illness, the research findings have been inconsistent.
“The evidence has been mixed about the association between cat ownership and psychosis expression, so our approach was to consider whether specific factors or combinations of factors could explain this mixed evidence,” Dr. Paquin said.
For the study, 2206 individuals aged 18-40 years completed the Community Assessment of Psychic Experiences (CAPE-42) and a questionnaire to gather information about cat ownership at any time between birth and age 13 and if the cats lived exclusively indoors (nonhunting) or if they were allowed outside (rodent hunting).
Participants were also asked about the number of residential moves between birth and age 15, date and place of birth, lifetime history of head trauma, and tobacco smoking history.
Rodent-hunting cat ownership was associated with higher risk of psychosis in male participants, compared with owning no cat or a nonhunting cat. When the investigators added head trauma and residential moves to rodent-hunting cat ownership, psychosis risk was elevated in both men and women.
Independent of cat ownership, younger age, moving more than three times as a child, a history of head trauma, and being a smoker were all associated with higher psychosis risk.
The study wasn’t designed to explore potential biological mechanisms to explain the sex differences in psychosis risk seen among rodent-hunting cat owners, but “one possible explanation based on the animal model literature is that the neurobiological effects of parasitic exposure may be greater with male sex,” senior author Suzanne King, PhD, professor of psychiatry at McGill, said in an interview.
The new study is part of a larger, long-term project called EnviroGen, led by Dr. King, examining the environmental and genetic risk factors for schizophrenia.
Need for replication
Commenting on the findings, E. Fuller Torrey, MD, who was among the first researchers to identify a link between cat ownership, T. gondii infection, and schizophrenia, said the study is “an interesting addition to the studies of cat ownership in childhood as a risk factor for psychosis.”
Of the approximately 10 published studies on the topic, about half suggest a link between cat ownership and psychosis later in life, said Dr. Torrey, associate director for research at the Stanley Medical Research Institute in Rockville, Md.
“The Canadian study is interesting in that it is the first study that separates exposure to permanently indoor cats from cats that are allowed to go outdoors, and the results were positive only for outdoor cats,” Dr. Torrey said.
The study has limitations, Dr. Torrey added, including its retrospective design and the use of a self-report questionnaire to assess psychotic experiences in adulthood.
Also commenting on findings, James Kirkbride, PhD, professor of psychiatric and social epidemiology, University College London, noted the same limitations.
Dr. Kirkbride is the lead author of a 2017 study that showed no link between cat ownership and serious mental illness that included nearly 5,000 people born in 1991 or 1992 and followed until age 18. In this study, there was no link between psychosis and cat ownership during pregnancy or at ages 4 or 10 years.
“Researchers have long been fascinated with the idea that cat ownership may affect mental health. This paper may have them chasing their own tail,” Dr. Kirkbride said.
“Evidence of any association is limited to certain subgroups without a strong theoretical basis for why this may be the case,” he added. “The retrospective and cross-sectional nature of the survey also raise the possibility that the results are impacted by differential recall bias, as well as the broader issues of chance and unobserved confounding.”
Dr. King noted that recall bias is a limitation the researchers highlighted in their study, but “considering the exposures are relatively objective and factual, we do not believe the potential for recall bias is substantial.”
“Nonetheless, we strongly believe that replication of our results in prospective, population-representative cohorts will be crucial to making firmer conclusions,” he added.
The study was funded by grants from the Quebec Health Research Fund. The study authors and Dr. Kirkbride disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF PSYCHIATRIC RESEARCH
Wilderness Medical Society issues clinical guidelines for tick-borne illness
The recently published “Clinical Practice Guidelines for the Prevention and Management of Tick-Borne Illness,” from the Wilderness Medical Society, are a good compilation of treatment suggestions but are not, in fact, new recommendations, lead author Benjamin Ho, MD, of Southern Wisconsin Emergency Associates in Janesville, acknowledged in an interview.
Dr. Ho emphasized that the focus of the report was on “practitioners who practice in resource-limited settings” and are “the group’s way of solidifying a ... standard of practice” for such physicians. Dr. Ho also said that, while “a lot of the recommendations aren’t well supported, the risk-benefit ratio, we believe, supports the recommendations.”
The article first reviewed the different types of ticks and their distribution in the United States, the specific pathogen associated with each, the disease it causes, and comments about seasonal variations in biting behavior. Another table outlines the most common clinical syndromes, typical lab findings, recommended diagnostic testing, and antibiotic treatments. A third section contains images of different types of ticks and photos of ticks in various life-cycle stages and different levels of engorgement.
The authors were careful to note: “Several tick species are able to carry multiple pathogens. In one study, nearly 25% of Ixodes were coinfected with some combination of the bacteria or parasites causing Lyme disease, anaplasmosis, or babesiosis. Although TBI [tick-borne illness] diagnosis is not the focus of this [clinical practice guideline], providers should be aware of high rates of coinfection; the presence of one TBI should in many instances prompt testing for others.”
In terms of recommendations for preventing TBIs, the authors challenge the suggestion of wearing light-colored clothing. For repellents, they recommend DEET, picaridin, and permethrin. And they also give instructions for laundering clothing and removing ticks.
One recommendation is controversial: that of providing single-dose doxycycline as prophylaxis against Lyme disease. Dr. Ho stresses that this was only for “high-risk” tick bites, defined as a tick bite from an identified Ixodes vector species in which the tick was attached for at least 36 hours and that occurred in an endemic area.
The recommendation for prophylactic doxycycline originated with an article by Robert Nadelman and colleagues in the New England Journal of Medicine and has been strongly challenged by ILADS (International Lyme and Associated Diseases Society) physicians, including Daniel Cameron, MD, and others.
Sam Donta, MD, a recent member of the Department of Health & Human Services Tick-borne Working Group and a member of the Infectious Disease Society of America, said in an interview: “The problem with the one-dose doxycycline is you may not begin to develop symptoms until 2 months later.” It might mask the early symptoms of Lyme. “My impression is that the doxycycline – even the single dose – might have abrogated the ability to see an immune response. The idea, though, if you’ve had a tick bite, is to do nothing and to wait for symptoms to develop. That becomes a little bit more complex. But even then, you could choose to follow the patient and see the patient in 2 weeks and then get blood testing.”
Dr. Donta added: “I think the screening test is inadequate. So you have to go directly to the Western blot. And you have to do both the IgM and IgG” and look for specific bands.
Dr. Donta emphasized that patients should be encouraged to save any ticks that were attached and that, if at all possible, ticks should be sent to a reference lab for testing before committing a patient to a course of antibiotics. There is no harm in that brief delay, he said, and most labs can identify an array of pathogens.
The Wilderness Society guidelines on TBIs provide a good overview for clinicians practicing in limited resource settings and mirror those from the IDSA.
Dr. Ho and Dr. Donta reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The recently published “Clinical Practice Guidelines for the Prevention and Management of Tick-Borne Illness,” from the Wilderness Medical Society, are a good compilation of treatment suggestions but are not, in fact, new recommendations, lead author Benjamin Ho, MD, of Southern Wisconsin Emergency Associates in Janesville, acknowledged in an interview.
Dr. Ho emphasized that the focus of the report was on “practitioners who practice in resource-limited settings” and are “the group’s way of solidifying a ... standard of practice” for such physicians. Dr. Ho also said that, while “a lot of the recommendations aren’t well supported, the risk-benefit ratio, we believe, supports the recommendations.”
The article first reviewed the different types of ticks and their distribution in the United States, the specific pathogen associated with each, the disease it causes, and comments about seasonal variations in biting behavior. Another table outlines the most common clinical syndromes, typical lab findings, recommended diagnostic testing, and antibiotic treatments. A third section contains images of different types of ticks and photos of ticks in various life-cycle stages and different levels of engorgement.
The authors were careful to note: “Several tick species are able to carry multiple pathogens. In one study, nearly 25% of Ixodes were coinfected with some combination of the bacteria or parasites causing Lyme disease, anaplasmosis, or babesiosis. Although TBI [tick-borne illness] diagnosis is not the focus of this [clinical practice guideline], providers should be aware of high rates of coinfection; the presence of one TBI should in many instances prompt testing for others.”
In terms of recommendations for preventing TBIs, the authors challenge the suggestion of wearing light-colored clothing. For repellents, they recommend DEET, picaridin, and permethrin. And they also give instructions for laundering clothing and removing ticks.
One recommendation is controversial: that of providing single-dose doxycycline as prophylaxis against Lyme disease. Dr. Ho stresses that this was only for “high-risk” tick bites, defined as a tick bite from an identified Ixodes vector species in which the tick was attached for at least 36 hours and that occurred in an endemic area.
The recommendation for prophylactic doxycycline originated with an article by Robert Nadelman and colleagues in the New England Journal of Medicine and has been strongly challenged by ILADS (International Lyme and Associated Diseases Society) physicians, including Daniel Cameron, MD, and others.
Sam Donta, MD, a recent member of the Department of Health & Human Services Tick-borne Working Group and a member of the Infectious Disease Society of America, said in an interview: “The problem with the one-dose doxycycline is you may not begin to develop symptoms until 2 months later.” It might mask the early symptoms of Lyme. “My impression is that the doxycycline – even the single dose – might have abrogated the ability to see an immune response. The idea, though, if you’ve had a tick bite, is to do nothing and to wait for symptoms to develop. That becomes a little bit more complex. But even then, you could choose to follow the patient and see the patient in 2 weeks and then get blood testing.”
Dr. Donta added: “I think the screening test is inadequate. So you have to go directly to the Western blot. And you have to do both the IgM and IgG” and look for specific bands.
Dr. Donta emphasized that patients should be encouraged to save any ticks that were attached and that, if at all possible, ticks should be sent to a reference lab for testing before committing a patient to a course of antibiotics. There is no harm in that brief delay, he said, and most labs can identify an array of pathogens.
The Wilderness Society guidelines on TBIs provide a good overview for clinicians practicing in limited resource settings and mirror those from the IDSA.
Dr. Ho and Dr. Donta reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The recently published “Clinical Practice Guidelines for the Prevention and Management of Tick-Borne Illness,” from the Wilderness Medical Society, are a good compilation of treatment suggestions but are not, in fact, new recommendations, lead author Benjamin Ho, MD, of Southern Wisconsin Emergency Associates in Janesville, acknowledged in an interview.
Dr. Ho emphasized that the focus of the report was on “practitioners who practice in resource-limited settings” and are “the group’s way of solidifying a ... standard of practice” for such physicians. Dr. Ho also said that, while “a lot of the recommendations aren’t well supported, the risk-benefit ratio, we believe, supports the recommendations.”
The article first reviewed the different types of ticks and their distribution in the United States, the specific pathogen associated with each, the disease it causes, and comments about seasonal variations in biting behavior. Another table outlines the most common clinical syndromes, typical lab findings, recommended diagnostic testing, and antibiotic treatments. A third section contains images of different types of ticks and photos of ticks in various life-cycle stages and different levels of engorgement.
The authors were careful to note: “Several tick species are able to carry multiple pathogens. In one study, nearly 25% of Ixodes were coinfected with some combination of the bacteria or parasites causing Lyme disease, anaplasmosis, or babesiosis. Although TBI [tick-borne illness] diagnosis is not the focus of this [clinical practice guideline], providers should be aware of high rates of coinfection; the presence of one TBI should in many instances prompt testing for others.”
In terms of recommendations for preventing TBIs, the authors challenge the suggestion of wearing light-colored clothing. For repellents, they recommend DEET, picaridin, and permethrin. And they also give instructions for laundering clothing and removing ticks.
One recommendation is controversial: that of providing single-dose doxycycline as prophylaxis against Lyme disease. Dr. Ho stresses that this was only for “high-risk” tick bites, defined as a tick bite from an identified Ixodes vector species in which the tick was attached for at least 36 hours and that occurred in an endemic area.
The recommendation for prophylactic doxycycline originated with an article by Robert Nadelman and colleagues in the New England Journal of Medicine and has been strongly challenged by ILADS (International Lyme and Associated Diseases Society) physicians, including Daniel Cameron, MD, and others.
Sam Donta, MD, a recent member of the Department of Health & Human Services Tick-borne Working Group and a member of the Infectious Disease Society of America, said in an interview: “The problem with the one-dose doxycycline is you may not begin to develop symptoms until 2 months later.” It might mask the early symptoms of Lyme. “My impression is that the doxycycline – even the single dose – might have abrogated the ability to see an immune response. The idea, though, if you’ve had a tick bite, is to do nothing and to wait for symptoms to develop. That becomes a little bit more complex. But even then, you could choose to follow the patient and see the patient in 2 weeks and then get blood testing.”
Dr. Donta added: “I think the screening test is inadequate. So you have to go directly to the Western blot. And you have to do both the IgM and IgG” and look for specific bands.
Dr. Donta emphasized that patients should be encouraged to save any ticks that were attached and that, if at all possible, ticks should be sent to a reference lab for testing before committing a patient to a course of antibiotics. There is no harm in that brief delay, he said, and most labs can identify an array of pathogens.
The Wilderness Society guidelines on TBIs provide a good overview for clinicians practicing in limited resource settings and mirror those from the IDSA.
Dr. Ho and Dr. Donta reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM WILDERNESS ENVIRONMENTAL MEDICINE
Freshwater aquarium provides source for melioidosis infection
A Maryland woman came down with a severe tropical infection called melioidosis from her freshwater home aquarium, says a report in Emerging Infectious Diseases describing a new route of transmission. Melioidosis is caused by the bacteria Burkholderia pseudomallei in soil or water.
Until last year, almost all U.S. cases of melioidosis were from people who lived or traveled to disease-endemic areas. It has been a rare infection in the United States.
But this is not the first case of melioidosis from an unusual source. Earlier in 2021, CDC and state epidemiologists traced an outbreak of melioidosis in Georgia, Kansas, Minnesota, and Texas to B pseudomallei in a bottle of “Better Homes & Gardens Lavender & Chamomile Essential Oil Infused Aromatherapy Room Spray with Gemstones.”
In the aquarium case, the patient was a 56-year-old woman with diabetes and rheumatologic disease. She had been on immunosuppressives (methotrexate, azathioprine, and prednisone) until 1 month before she became symptomatic. She was hospitalized for fever and pneumonia.
Multiple blood cultures obtained on days 1-4 grew B. pseudomallei, but she had no evidence of endocarditis or intravascular seeding. Despite weeks of meropenem (Merrem), she developed evidence of a lung abscess, and trimethoprim/sulfamethoxazole (Bactrim) was added. Ultimately, the patient required a 12-week course of antibiotics.
CDC epidemiologist Patrick Dawson, PhD, first author of the report, told this news organization that although outbreak investigators always ask about pet ownership, they have not explicitly asked about fish. In this case, the patient did not volunteer exposure to the fish.
When state epidemiologists visited the patient’s home, “one of the first things they saw was a few aquariums,” Dr. Dawson said. Seeing the water and knowing “that most freshwater tropical fish in the U.S. are imported from Southeast Asia” led them to culture specifically for B. pseudomallei, which can be difficult for the microbiology lab to identify.
From there, Dr. Dawson explained, “The Maryland Department of Health sent a team to the local pet store” but did not find any of the bacteria there. (The patient had bought her fish 6 months earlier.) The investigators then worked with the national brand “to identify where they had actually sourced the fish from.”
Two retailers supply almost all of U.S. guppies and plants. While investigators could not find an exact matching isolate after so many months had elapsed, they found a positive PCR for B. pseudomallei in a water sample from imported fish in Los Angeles.
Dr. Dawson said tropical fish are imported from southeast Asia and typically come from small family fish farms. The fish import industry has “certain products that they add to the water to hopefully kill any bacteria.” He was unaware whether this included antibiotics but suggested, “we would have seen many more cases [of antibiotic resistance] by now” if it did.
In general advice for the public, Dr. Dawson said, “I would recommend washing hands before and after contact with the aquarium. If you have cuts or wounds on your hands, it’s really important to wear gloves if you have to go clean or maintain the aquarium and you’re putting your hands in the water, just for that extra layer of protection. It’s probably a strong idea to just avoid that altogether if someone’s immunocompromised. And not letting young children under 5 years old clean aquariums.” These are the “simplest things to do to protect yourself.”
Stephen A. Smith, DVM, PhD, a professor in the Aquatic Medicine Program at Virginia-Maryland College of Veterinary Medicine, Blacksburg, also stressed the importance of careful hand hygiene when caring for aquariums. He said that the filter, filter floss, biofilm, charcoal, and gravel might have exceptionally high concentrations of bacteria. Dr. Smith also recommended gloves when cleaning aquariums and not doing this task if immunocompromised.
Dr. Smith, who was not involved in the CDC study, shared a broader perspective, noting that “the reason why it’s important to federal regulators is that [B. pseudomallei] is a tier 1 select agent. And so, when that was isolated, it sent up all the red flags.” The far more common Mycobacterium marinum, or fish handler’s disease, is not reportable.
Mycobacterium marinum is another pathogen of concern that can be acquired from aquariums. These infections typically occur as nodular lesions on the arms and require months of therapy.
Dr. Smith stressed the importance of physicians eliciting a careful exposure history as the key to diagnosing zoonoses. For most exotic aquarium animals, he noted, “They’re caught in the wild wherever they are. They’re transported to a major hub to transport to the U.S., and a lot of times, we don’t have quarantine for those animals.”
Dr. Smith said.
Many infections also occur in the course of water sports – or even hiking and getting a cut or abrasion wet from a stream or lake. Aeromonas hydrophila can cause life-threatening infections. Vibrio vulnificus infections from salt-water injuries can cause sepsis and characteristic hemorrhagic bullae – large, discolored blisters filled with body fluid – during the summer. And eating contaminated shellfish has a 50%-60% death rate.
Other exposures to water-loving bacteria happen during fishing or cleaning/preparing fish. For example, Streptococcus iniae has caused cellulitis, arthritis, endocarditis, and meningitis following superficial or puncture injuries, notably from cleaning tilapia.
Other infections from contact with fish include Erysipelothrix rhusiopathiae (primarily skin infections) and gastroenteritis from Plesiomonas shigelloides, Campylobacter spp, and Salmonella spp.
Each of these zoonoses illustrates the importance of a careful exposure history when there’s an atypical presentation or an infection that is not responding promptly to empiric treatment. The aquarium case broadens the differential to include melioidosis, a serious disease from southeast Asia.
Dr. Dawson and Dr. Smith have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A Maryland woman came down with a severe tropical infection called melioidosis from her freshwater home aquarium, says a report in Emerging Infectious Diseases describing a new route of transmission. Melioidosis is caused by the bacteria Burkholderia pseudomallei in soil or water.
Until last year, almost all U.S. cases of melioidosis were from people who lived or traveled to disease-endemic areas. It has been a rare infection in the United States.
But this is not the first case of melioidosis from an unusual source. Earlier in 2021, CDC and state epidemiologists traced an outbreak of melioidosis in Georgia, Kansas, Minnesota, and Texas to B pseudomallei in a bottle of “Better Homes & Gardens Lavender & Chamomile Essential Oil Infused Aromatherapy Room Spray with Gemstones.”
In the aquarium case, the patient was a 56-year-old woman with diabetes and rheumatologic disease. She had been on immunosuppressives (methotrexate, azathioprine, and prednisone) until 1 month before she became symptomatic. She was hospitalized for fever and pneumonia.
Multiple blood cultures obtained on days 1-4 grew B. pseudomallei, but she had no evidence of endocarditis or intravascular seeding. Despite weeks of meropenem (Merrem), she developed evidence of a lung abscess, and trimethoprim/sulfamethoxazole (Bactrim) was added. Ultimately, the patient required a 12-week course of antibiotics.
CDC epidemiologist Patrick Dawson, PhD, first author of the report, told this news organization that although outbreak investigators always ask about pet ownership, they have not explicitly asked about fish. In this case, the patient did not volunteer exposure to the fish.
When state epidemiologists visited the patient’s home, “one of the first things they saw was a few aquariums,” Dr. Dawson said. Seeing the water and knowing “that most freshwater tropical fish in the U.S. are imported from Southeast Asia” led them to culture specifically for B. pseudomallei, which can be difficult for the microbiology lab to identify.
From there, Dr. Dawson explained, “The Maryland Department of Health sent a team to the local pet store” but did not find any of the bacteria there. (The patient had bought her fish 6 months earlier.) The investigators then worked with the national brand “to identify where they had actually sourced the fish from.”
Two retailers supply almost all of U.S. guppies and plants. While investigators could not find an exact matching isolate after so many months had elapsed, they found a positive PCR for B. pseudomallei in a water sample from imported fish in Los Angeles.
Dr. Dawson said tropical fish are imported from southeast Asia and typically come from small family fish farms. The fish import industry has “certain products that they add to the water to hopefully kill any bacteria.” He was unaware whether this included antibiotics but suggested, “we would have seen many more cases [of antibiotic resistance] by now” if it did.
In general advice for the public, Dr. Dawson said, “I would recommend washing hands before and after contact with the aquarium. If you have cuts or wounds on your hands, it’s really important to wear gloves if you have to go clean or maintain the aquarium and you’re putting your hands in the water, just for that extra layer of protection. It’s probably a strong idea to just avoid that altogether if someone’s immunocompromised. And not letting young children under 5 years old clean aquariums.” These are the “simplest things to do to protect yourself.”
Stephen A. Smith, DVM, PhD, a professor in the Aquatic Medicine Program at Virginia-Maryland College of Veterinary Medicine, Blacksburg, also stressed the importance of careful hand hygiene when caring for aquariums. He said that the filter, filter floss, biofilm, charcoal, and gravel might have exceptionally high concentrations of bacteria. Dr. Smith also recommended gloves when cleaning aquariums and not doing this task if immunocompromised.
Dr. Smith, who was not involved in the CDC study, shared a broader perspective, noting that “the reason why it’s important to federal regulators is that [B. pseudomallei] is a tier 1 select agent. And so, when that was isolated, it sent up all the red flags.” The far more common Mycobacterium marinum, or fish handler’s disease, is not reportable.
Mycobacterium marinum is another pathogen of concern that can be acquired from aquariums. These infections typically occur as nodular lesions on the arms and require months of therapy.
Dr. Smith stressed the importance of physicians eliciting a careful exposure history as the key to diagnosing zoonoses. For most exotic aquarium animals, he noted, “They’re caught in the wild wherever they are. They’re transported to a major hub to transport to the U.S., and a lot of times, we don’t have quarantine for those animals.”
Dr. Smith said.
Many infections also occur in the course of water sports – or even hiking and getting a cut or abrasion wet from a stream or lake. Aeromonas hydrophila can cause life-threatening infections. Vibrio vulnificus infections from salt-water injuries can cause sepsis and characteristic hemorrhagic bullae – large, discolored blisters filled with body fluid – during the summer. And eating contaminated shellfish has a 50%-60% death rate.
Other exposures to water-loving bacteria happen during fishing or cleaning/preparing fish. For example, Streptococcus iniae has caused cellulitis, arthritis, endocarditis, and meningitis following superficial or puncture injuries, notably from cleaning tilapia.
Other infections from contact with fish include Erysipelothrix rhusiopathiae (primarily skin infections) and gastroenteritis from Plesiomonas shigelloides, Campylobacter spp, and Salmonella spp.
Each of these zoonoses illustrates the importance of a careful exposure history when there’s an atypical presentation or an infection that is not responding promptly to empiric treatment. The aquarium case broadens the differential to include melioidosis, a serious disease from southeast Asia.
Dr. Dawson and Dr. Smith have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A Maryland woman came down with a severe tropical infection called melioidosis from her freshwater home aquarium, says a report in Emerging Infectious Diseases describing a new route of transmission. Melioidosis is caused by the bacteria Burkholderia pseudomallei in soil or water.
Until last year, almost all U.S. cases of melioidosis were from people who lived or traveled to disease-endemic areas. It has been a rare infection in the United States.
But this is not the first case of melioidosis from an unusual source. Earlier in 2021, CDC and state epidemiologists traced an outbreak of melioidosis in Georgia, Kansas, Minnesota, and Texas to B pseudomallei in a bottle of “Better Homes & Gardens Lavender & Chamomile Essential Oil Infused Aromatherapy Room Spray with Gemstones.”
In the aquarium case, the patient was a 56-year-old woman with diabetes and rheumatologic disease. She had been on immunosuppressives (methotrexate, azathioprine, and prednisone) until 1 month before she became symptomatic. She was hospitalized for fever and pneumonia.
Multiple blood cultures obtained on days 1-4 grew B. pseudomallei, but she had no evidence of endocarditis or intravascular seeding. Despite weeks of meropenem (Merrem), she developed evidence of a lung abscess, and trimethoprim/sulfamethoxazole (Bactrim) was added. Ultimately, the patient required a 12-week course of antibiotics.
CDC epidemiologist Patrick Dawson, PhD, first author of the report, told this news organization that although outbreak investigators always ask about pet ownership, they have not explicitly asked about fish. In this case, the patient did not volunteer exposure to the fish.
When state epidemiologists visited the patient’s home, “one of the first things they saw was a few aquariums,” Dr. Dawson said. Seeing the water and knowing “that most freshwater tropical fish in the U.S. are imported from Southeast Asia” led them to culture specifically for B. pseudomallei, which can be difficult for the microbiology lab to identify.
From there, Dr. Dawson explained, “The Maryland Department of Health sent a team to the local pet store” but did not find any of the bacteria there. (The patient had bought her fish 6 months earlier.) The investigators then worked with the national brand “to identify where they had actually sourced the fish from.”
Two retailers supply almost all of U.S. guppies and plants. While investigators could not find an exact matching isolate after so many months had elapsed, they found a positive PCR for B. pseudomallei in a water sample from imported fish in Los Angeles.
Dr. Dawson said tropical fish are imported from southeast Asia and typically come from small family fish farms. The fish import industry has “certain products that they add to the water to hopefully kill any bacteria.” He was unaware whether this included antibiotics but suggested, “we would have seen many more cases [of antibiotic resistance] by now” if it did.
In general advice for the public, Dr. Dawson said, “I would recommend washing hands before and after contact with the aquarium. If you have cuts or wounds on your hands, it’s really important to wear gloves if you have to go clean or maintain the aquarium and you’re putting your hands in the water, just for that extra layer of protection. It’s probably a strong idea to just avoid that altogether if someone’s immunocompromised. And not letting young children under 5 years old clean aquariums.” These are the “simplest things to do to protect yourself.”
Stephen A. Smith, DVM, PhD, a professor in the Aquatic Medicine Program at Virginia-Maryland College of Veterinary Medicine, Blacksburg, also stressed the importance of careful hand hygiene when caring for aquariums. He said that the filter, filter floss, biofilm, charcoal, and gravel might have exceptionally high concentrations of bacteria. Dr. Smith also recommended gloves when cleaning aquariums and not doing this task if immunocompromised.
Dr. Smith, who was not involved in the CDC study, shared a broader perspective, noting that “the reason why it’s important to federal regulators is that [B. pseudomallei] is a tier 1 select agent. And so, when that was isolated, it sent up all the red flags.” The far more common Mycobacterium marinum, or fish handler’s disease, is not reportable.
Mycobacterium marinum is another pathogen of concern that can be acquired from aquariums. These infections typically occur as nodular lesions on the arms and require months of therapy.
Dr. Smith stressed the importance of physicians eliciting a careful exposure history as the key to diagnosing zoonoses. For most exotic aquarium animals, he noted, “They’re caught in the wild wherever they are. They’re transported to a major hub to transport to the U.S., and a lot of times, we don’t have quarantine for those animals.”
Dr. Smith said.
Many infections also occur in the course of water sports – or even hiking and getting a cut or abrasion wet from a stream or lake. Aeromonas hydrophila can cause life-threatening infections. Vibrio vulnificus infections from salt-water injuries can cause sepsis and characteristic hemorrhagic bullae – large, discolored blisters filled with body fluid – during the summer. And eating contaminated shellfish has a 50%-60% death rate.
Other exposures to water-loving bacteria happen during fishing or cleaning/preparing fish. For example, Streptococcus iniae has caused cellulitis, arthritis, endocarditis, and meningitis following superficial or puncture injuries, notably from cleaning tilapia.
Other infections from contact with fish include Erysipelothrix rhusiopathiae (primarily skin infections) and gastroenteritis from Plesiomonas shigelloides, Campylobacter spp, and Salmonella spp.
Each of these zoonoses illustrates the importance of a careful exposure history when there’s an atypical presentation or an infection that is not responding promptly to empiric treatment. The aquarium case broadens the differential to include melioidosis, a serious disease from southeast Asia.
Dr. Dawson and Dr. Smith have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.









