User login
Metacognitive training an effective, durable treatment for schizophrenia
Metacognitive training (MCT) is effective in reducing positive and negative symptoms of schizophrenia, new research suggests.
MCT for psychosis is a brief intervention that “combines psychoeducation, cognitive bias modification, and strategy teaching but does not directly target psychosis symptoms.”
Additionally, MCT led to improvement in self-esteem and functioning, and all benefits were maintained up to 1 year post intervention.
“Our study demonstrates the effectiveness and durability of a brief, nonconfrontational intervention in the reduction of serious and debilitating symptoms of schizophrenia,” study investigator Danielle Penney, a doctoral candidate at the University of Montreal, told this news organization.
“Our results were observed in several treatment contexts and suggest that MCT can be successfully delivered by a variety of mental health practitioners [and] provide solid evidence to consider MCT in international treatment guidelines for schizophrenia spectrum disorders,” Ms. Penney said.
The findings were published online in JAMA Psychiatry.
‘Novel contribution’
MCT is a brief intervention consisting of eight to 16 modules that can be delivered in a group setting or on an individual basis. Instead of directly targeting psychotic symptoms, it uses an “indirect approach by promoting awareness of cognitive biases,” the investigators note.
Such biases include maladaptive thinking styles common to psychosis, such as jumping to conclusions, belief inflexibility, and overconfidence in judgments.
It is hypothesized that these biases “contribute to the formation and maintenance of positive symptoms, particularly delusions,” the researchers write.
MCT “aims to plant doubt in delusional beliefs through raising awareness of cognitive biases and aims to raise service engagement by proposing work on this less-confrontational objective first, which is likely to facilitate the therapeutic alliance and more direct work on psychotic symptoms,” they add.
Previous studies of MCT for psychosis yielded inconsistent results. Of the eight previous meta-analyses that analyzed MCT for psychosis, “none investigated the long-term effects of the intervention on directly targeted treatment outcomes,” such as delusions and cognitive biases, Ms. Penney said.
She added that “to our knowledge, no meta-analysis has examined the effectiveness of important indirectly targeted outcomes,” including self-esteem and functioning.
“These important gaps in the literature,” along with a large increase in recently conducted MCT efficacy trials, “provided the motivation for the current study,” said Ms. Penney.
To investigate, the researchers searched 11 databases, beginning with data from 2007, which was when the first report of MCT was published. Studies included participants with schizophrenia spectrum and related psychotic disorders.
Outcomes for the current review and meta-analysis were organized according to a “proximal-distal framework.” Proximal outcomes were those directly targeted by MCT, while distal outcomes were those not directly targeted by MCT but that were associated with improvement in proximal outcomes, either directly or indirectly.
The investigators examined these outcomes quantitatively and qualitatively from preintervention to postintervention and follow-up, “which, to our knowledge, is a novel contribution,” they write.
The review included 43 studies, of which 30 (70%) were randomized controlled trials (RCTs), 11 (25%) were non-RCTs, and two (5%) were quantitative descriptive studies. Of these, 40 reports (n = 1,816 participants) were included in the meta-analysis, and six were included in the narrative review.
Transdiagnostic treatment?
Results showed a “small to moderate” effect size (ES) in global proximal outcomes (g = .39; 95% confidence interval, .25-.53; P < .001; 38 reports).
When proximal outcomes were analyzed separately, the largest ES was found for delusions; smaller ES values were found for hallucinations and cognitive biases.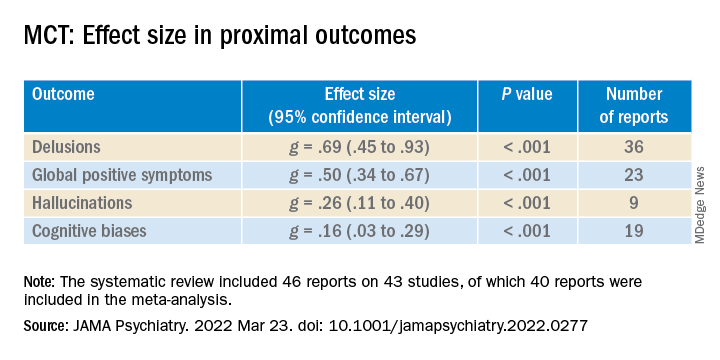
Newer studies reported higher ES values for hallucinations, compared with older studies (β = .04; 95% CI, .00-.07).
ES was small to moderate for distal outcomes (g = .31; 95% CI, .19-.44; P < .001; 26 reports). “Small but significant” ES values were shown for self-esteem and negative symptoms, small to moderate for functioning, and small but nonsignificant for quality of life (QOL).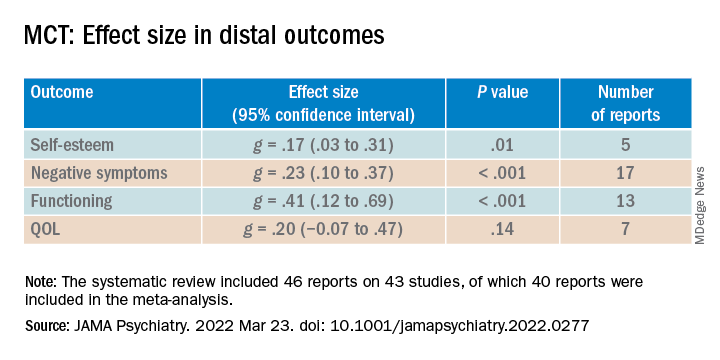
The researchers also analyzed RCTs by comparing differences between the treatment and control groups in scores from follow-up to post-treatment. Although the therapeutic gains made by the experimental group were “steadily maintained, the ES values were “small” and nonsignificant.
When the difference in scores between follow-up and baseline were compared in both groups, small to moderate ES values were found for proximal as well as distal outcomes.
“These results further indicate that net therapeutic gains remain significant even 1 year following MCT,” the investigators note.
Lower-quality studies showed significantly lower ES values for distal (between-group comparison, P = .05) but not proximal outcomes.
Overall, the findings suggest that MCT is a “beneficial and durable low-threshold intervention that can be flexibly delivered at minimal cost in a variety of contexts to individuals with psychotic disorders,” the researchers write.
They note that MCT has also been associated with positive outcomes in other patient populations, including patients with borderline personality disorder, depression, and obsessive-compulsive disorder. Future research “might consider investigating MCT as a transdiagnostic treatment,” they add.
Consistent beneficial effects
Commenting on the study, Philip Harvey, PhD, Leonard M. Miller Professor of Psychiatry and Behavioral Sciences and director of the Division of Psychology, University of Miami Miller School of Medicine, noted that self-awareness and self-assessment are critically important features in patients with serious mental illness.
Impairments in these areas “can actually have a greater impact on everyday functioning than cognitive deficits,” said Dr. Harvey, who is also the editor-in-chief of Schizophrenia Research: Cognition. He was not involved with the current meta-analysis.
He noted that the current results show that “MCT has consistent beneficial effects.”
“This is an intervention that should be considered for most people with serious mental illness, with a specific focus on those with specific types of delusions and more global challenges in self-assessment,” Dr. Harvey concluded.
Funding was provided by the Canada First Research Excellence Fund, awarded through the Healthy Brains, Healthy Lives initiative at McGill University. Ms. Penney reported no relevant financial relationships. Disclosures for the other investigators are listed in the original article. Dr. Harvey reported being a reviewer of the article but that he was not involved in its authorship.
A version of this article first appeared on Medscape.com.
Metacognitive training (MCT) is effective in reducing positive and negative symptoms of schizophrenia, new research suggests.
MCT for psychosis is a brief intervention that “combines psychoeducation, cognitive bias modification, and strategy teaching but does not directly target psychosis symptoms.”
Additionally, MCT led to improvement in self-esteem and functioning, and all benefits were maintained up to 1 year post intervention.
“Our study demonstrates the effectiveness and durability of a brief, nonconfrontational intervention in the reduction of serious and debilitating symptoms of schizophrenia,” study investigator Danielle Penney, a doctoral candidate at the University of Montreal, told this news organization.
“Our results were observed in several treatment contexts and suggest that MCT can be successfully delivered by a variety of mental health practitioners [and] provide solid evidence to consider MCT in international treatment guidelines for schizophrenia spectrum disorders,” Ms. Penney said.
The findings were published online in JAMA Psychiatry.
‘Novel contribution’
MCT is a brief intervention consisting of eight to 16 modules that can be delivered in a group setting or on an individual basis. Instead of directly targeting psychotic symptoms, it uses an “indirect approach by promoting awareness of cognitive biases,” the investigators note.
Such biases include maladaptive thinking styles common to psychosis, such as jumping to conclusions, belief inflexibility, and overconfidence in judgments.
It is hypothesized that these biases “contribute to the formation and maintenance of positive symptoms, particularly delusions,” the researchers write.
MCT “aims to plant doubt in delusional beliefs through raising awareness of cognitive biases and aims to raise service engagement by proposing work on this less-confrontational objective first, which is likely to facilitate the therapeutic alliance and more direct work on psychotic symptoms,” they add.
Previous studies of MCT for psychosis yielded inconsistent results. Of the eight previous meta-analyses that analyzed MCT for psychosis, “none investigated the long-term effects of the intervention on directly targeted treatment outcomes,” such as delusions and cognitive biases, Ms. Penney said.
She added that “to our knowledge, no meta-analysis has examined the effectiveness of important indirectly targeted outcomes,” including self-esteem and functioning.
“These important gaps in the literature,” along with a large increase in recently conducted MCT efficacy trials, “provided the motivation for the current study,” said Ms. Penney.
To investigate, the researchers searched 11 databases, beginning with data from 2007, which was when the first report of MCT was published. Studies included participants with schizophrenia spectrum and related psychotic disorders.
Outcomes for the current review and meta-analysis were organized according to a “proximal-distal framework.” Proximal outcomes were those directly targeted by MCT, while distal outcomes were those not directly targeted by MCT but that were associated with improvement in proximal outcomes, either directly or indirectly.
The investigators examined these outcomes quantitatively and qualitatively from preintervention to postintervention and follow-up, “which, to our knowledge, is a novel contribution,” they write.
The review included 43 studies, of which 30 (70%) were randomized controlled trials (RCTs), 11 (25%) were non-RCTs, and two (5%) were quantitative descriptive studies. Of these, 40 reports (n = 1,816 participants) were included in the meta-analysis, and six were included in the narrative review.
Transdiagnostic treatment?
Results showed a “small to moderate” effect size (ES) in global proximal outcomes (g = .39; 95% confidence interval, .25-.53; P < .001; 38 reports).
When proximal outcomes were analyzed separately, the largest ES was found for delusions; smaller ES values were found for hallucinations and cognitive biases.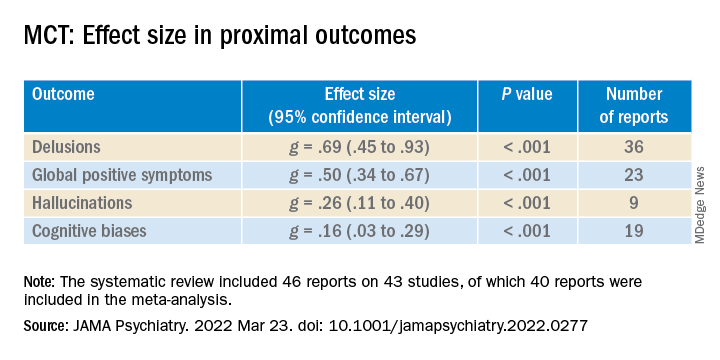
Newer studies reported higher ES values for hallucinations, compared with older studies (β = .04; 95% CI, .00-.07).
ES was small to moderate for distal outcomes (g = .31; 95% CI, .19-.44; P < .001; 26 reports). “Small but significant” ES values were shown for self-esteem and negative symptoms, small to moderate for functioning, and small but nonsignificant for quality of life (QOL).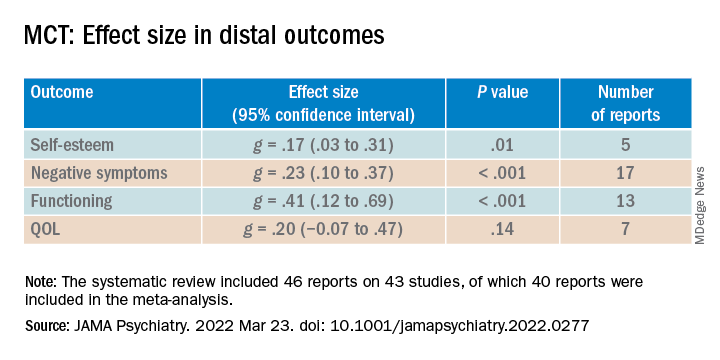
The researchers also analyzed RCTs by comparing differences between the treatment and control groups in scores from follow-up to post-treatment. Although the therapeutic gains made by the experimental group were “steadily maintained, the ES values were “small” and nonsignificant.
When the difference in scores between follow-up and baseline were compared in both groups, small to moderate ES values were found for proximal as well as distal outcomes.
“These results further indicate that net therapeutic gains remain significant even 1 year following MCT,” the investigators note.
Lower-quality studies showed significantly lower ES values for distal (between-group comparison, P = .05) but not proximal outcomes.
Overall, the findings suggest that MCT is a “beneficial and durable low-threshold intervention that can be flexibly delivered at minimal cost in a variety of contexts to individuals with psychotic disorders,” the researchers write.
They note that MCT has also been associated with positive outcomes in other patient populations, including patients with borderline personality disorder, depression, and obsessive-compulsive disorder. Future research “might consider investigating MCT as a transdiagnostic treatment,” they add.
Consistent beneficial effects
Commenting on the study, Philip Harvey, PhD, Leonard M. Miller Professor of Psychiatry and Behavioral Sciences and director of the Division of Psychology, University of Miami Miller School of Medicine, noted that self-awareness and self-assessment are critically important features in patients with serious mental illness.
Impairments in these areas “can actually have a greater impact on everyday functioning than cognitive deficits,” said Dr. Harvey, who is also the editor-in-chief of Schizophrenia Research: Cognition. He was not involved with the current meta-analysis.
He noted that the current results show that “MCT has consistent beneficial effects.”
“This is an intervention that should be considered for most people with serious mental illness, with a specific focus on those with specific types of delusions and more global challenges in self-assessment,” Dr. Harvey concluded.
Funding was provided by the Canada First Research Excellence Fund, awarded through the Healthy Brains, Healthy Lives initiative at McGill University. Ms. Penney reported no relevant financial relationships. Disclosures for the other investigators are listed in the original article. Dr. Harvey reported being a reviewer of the article but that he was not involved in its authorship.
A version of this article first appeared on Medscape.com.
Metacognitive training (MCT) is effective in reducing positive and negative symptoms of schizophrenia, new research suggests.
MCT for psychosis is a brief intervention that “combines psychoeducation, cognitive bias modification, and strategy teaching but does not directly target psychosis symptoms.”
Additionally, MCT led to improvement in self-esteem and functioning, and all benefits were maintained up to 1 year post intervention.
“Our study demonstrates the effectiveness and durability of a brief, nonconfrontational intervention in the reduction of serious and debilitating symptoms of schizophrenia,” study investigator Danielle Penney, a doctoral candidate at the University of Montreal, told this news organization.
“Our results were observed in several treatment contexts and suggest that MCT can be successfully delivered by a variety of mental health practitioners [and] provide solid evidence to consider MCT in international treatment guidelines for schizophrenia spectrum disorders,” Ms. Penney said.
The findings were published online in JAMA Psychiatry.
‘Novel contribution’
MCT is a brief intervention consisting of eight to 16 modules that can be delivered in a group setting or on an individual basis. Instead of directly targeting psychotic symptoms, it uses an “indirect approach by promoting awareness of cognitive biases,” the investigators note.
Such biases include maladaptive thinking styles common to psychosis, such as jumping to conclusions, belief inflexibility, and overconfidence in judgments.
It is hypothesized that these biases “contribute to the formation and maintenance of positive symptoms, particularly delusions,” the researchers write.
MCT “aims to plant doubt in delusional beliefs through raising awareness of cognitive biases and aims to raise service engagement by proposing work on this less-confrontational objective first, which is likely to facilitate the therapeutic alliance and more direct work on psychotic symptoms,” they add.
Previous studies of MCT for psychosis yielded inconsistent results. Of the eight previous meta-analyses that analyzed MCT for psychosis, “none investigated the long-term effects of the intervention on directly targeted treatment outcomes,” such as delusions and cognitive biases, Ms. Penney said.
She added that “to our knowledge, no meta-analysis has examined the effectiveness of important indirectly targeted outcomes,” including self-esteem and functioning.
“These important gaps in the literature,” along with a large increase in recently conducted MCT efficacy trials, “provided the motivation for the current study,” said Ms. Penney.
To investigate, the researchers searched 11 databases, beginning with data from 2007, which was when the first report of MCT was published. Studies included participants with schizophrenia spectrum and related psychotic disorders.
Outcomes for the current review and meta-analysis were organized according to a “proximal-distal framework.” Proximal outcomes were those directly targeted by MCT, while distal outcomes were those not directly targeted by MCT but that were associated with improvement in proximal outcomes, either directly or indirectly.
The investigators examined these outcomes quantitatively and qualitatively from preintervention to postintervention and follow-up, “which, to our knowledge, is a novel contribution,” they write.
The review included 43 studies, of which 30 (70%) were randomized controlled trials (RCTs), 11 (25%) were non-RCTs, and two (5%) were quantitative descriptive studies. Of these, 40 reports (n = 1,816 participants) were included in the meta-analysis, and six were included in the narrative review.
Transdiagnostic treatment?
Results showed a “small to moderate” effect size (ES) in global proximal outcomes (g = .39; 95% confidence interval, .25-.53; P < .001; 38 reports).
When proximal outcomes were analyzed separately, the largest ES was found for delusions; smaller ES values were found for hallucinations and cognitive biases.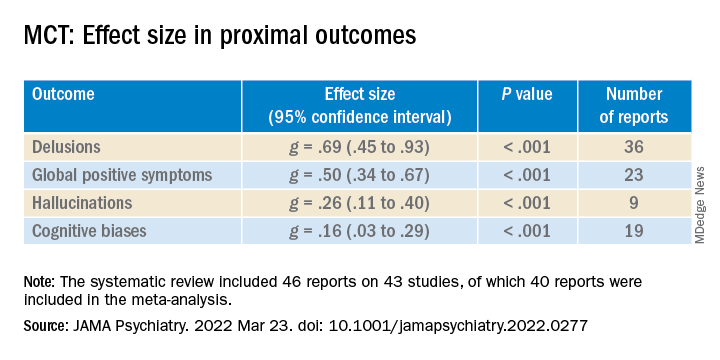
Newer studies reported higher ES values for hallucinations, compared with older studies (β = .04; 95% CI, .00-.07).
ES was small to moderate for distal outcomes (g = .31; 95% CI, .19-.44; P < .001; 26 reports). “Small but significant” ES values were shown for self-esteem and negative symptoms, small to moderate for functioning, and small but nonsignificant for quality of life (QOL).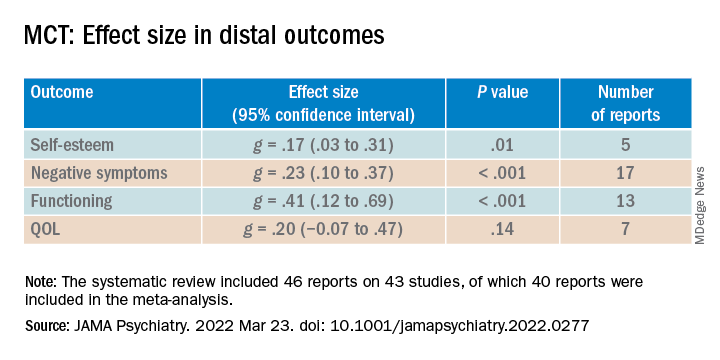
The researchers also analyzed RCTs by comparing differences between the treatment and control groups in scores from follow-up to post-treatment. Although the therapeutic gains made by the experimental group were “steadily maintained, the ES values were “small” and nonsignificant.
When the difference in scores between follow-up and baseline were compared in both groups, small to moderate ES values were found for proximal as well as distal outcomes.
“These results further indicate that net therapeutic gains remain significant even 1 year following MCT,” the investigators note.
Lower-quality studies showed significantly lower ES values for distal (between-group comparison, P = .05) but not proximal outcomes.
Overall, the findings suggest that MCT is a “beneficial and durable low-threshold intervention that can be flexibly delivered at minimal cost in a variety of contexts to individuals with psychotic disorders,” the researchers write.
They note that MCT has also been associated with positive outcomes in other patient populations, including patients with borderline personality disorder, depression, and obsessive-compulsive disorder. Future research “might consider investigating MCT as a transdiagnostic treatment,” they add.
Consistent beneficial effects
Commenting on the study, Philip Harvey, PhD, Leonard M. Miller Professor of Psychiatry and Behavioral Sciences and director of the Division of Psychology, University of Miami Miller School of Medicine, noted that self-awareness and self-assessment are critically important features in patients with serious mental illness.
Impairments in these areas “can actually have a greater impact on everyday functioning than cognitive deficits,” said Dr. Harvey, who is also the editor-in-chief of Schizophrenia Research: Cognition. He was not involved with the current meta-analysis.
He noted that the current results show that “MCT has consistent beneficial effects.”
“This is an intervention that should be considered for most people with serious mental illness, with a specific focus on those with specific types of delusions and more global challenges in self-assessment,” Dr. Harvey concluded.
Funding was provided by the Canada First Research Excellence Fund, awarded through the Healthy Brains, Healthy Lives initiative at McGill University. Ms. Penney reported no relevant financial relationships. Disclosures for the other investigators are listed in the original article. Dr. Harvey reported being a reviewer of the article but that he was not involved in its authorship.
A version of this article first appeared on Medscape.com.
Psychotropic med use tied to ‘striking’ post-COVID dementia risk
, new research suggests.
Results from a large study of more than 1,700 patients who had been hospitalized with COVID showed a greater than twofold increased risk for post-COVID dementia in those taking antipsychotics and mood stabilizers/anticonvulsants – medications often used to treat schizophrenia, psychosis, bipolar disorder, and seizures.
“We know that pre-existing psychiatric illness is associated with poor COVID-19 outcomes, but our study is the first to show an association with certain psychiatric medications and dementia,” co-investigator Liron Sinvani, MD, the Feinstein Institutes for Medical Research, Manhasset, New York, said in an interview.
“Our study highlights the potential interaction between baseline neuropsychiatric disease, psychotropic medications, COVID-19, and dementia,” Dr. Sinvani added.
The findings were published online March 18 in Frontiers in Medicine.
‘Striking’ dementia rate
Using electronic health records, the researchers evaluated pre-COVID psychotropic medication use and post-COVID dementia onset in 1,755 adults aged 65 and older. All were hospitalized with COVID-19 at Northwell Health between March 1 and April 20, 2020.
A “striking” 13% of the participants (n = 223) developed dementia within 1-year of follow-up, the investigators report.
Among the 438 patients (25%) exposed to at least one psychotropic medication before COVID-19, 105 (24%) developed dementia in the year following COVID versus 118 of 1,317 (9%) patients with no pre-COVID exposure to psychotropic medication (odds ratio, 3.2; 95% confidence interval, 2.37-4.32).
Both pre-COVID psychotropic medication use (OR, 2.7; 95% CI, 1.8-4.0, P < .001) and delirium (OR, 3.0; 95% CI, 1.9-4.6, P < .001) were significantly associated with post-COVID dementia at 1 year.
In a sensitivity analysis in the subset of 423 patients with at least one documented neurologic or psychiatric diagnosis at the time of COVID admission, and after adjusting for confounding factors, pre-COVID psychotropic medication use remained significantly linked to post-COVID dementia onset (OR, 3.09; 95% CI, 1.5-6.6, P = .002).
Drug classes most strongly associated with 1-year post-COVID dementia onset were antipsychotics (OR, 2.8, 95% CI, 1.7-4.4, P < .001) and mood stabilizers/anticonvulsants (OR, 2.4, 95% CI, 1.39-4.02, P = .001).
In a further exploratory analysis, the psychotropics valproic acid (multiple brands) and haloperidol (Haldol) had the largest association with post-COVID dementia.
Antidepressants as a class were not associated with post-COVID dementia, but the potential effects of two commonly prescribed antidepressants in older adults, mirtazapine (Remeron) and escitalopram (Lexapro), “warrant further investigation,” the researchers note.
Predictive risk marker?
“This research shows that psychotropic medications can be considered a predictive risk marker for post-COVID dementia. In patients taking psychotropic medications, COVID-19 could have accelerated progression of dementia after hospitalization,” lead author Yun Freudenberg-Hua, MD, the Feinstein Institutes, said in a news release.
It is unclear why psychotropic medications may raise the risk for dementia onset after COVID, the investigators note.
“It is intuitive that psychotropic medications indicate pre-existing neuropsychiatric conditions in which COVID-19 occurs. It is possible that psychotropic medications may potentiate the neurostructural changes that have been found in the brain of those who have recovered from COVID-19,” they write.
The sensitivity analysis in patients with documented neurologic and psychiatric diagnoses supports this interpretation.
COVID-19 may also accelerate the underlying brain disorders for which psychotropic medications were prescribed, leading to the greater incidence of post-COVID dementia, the researchers write.
“It is important to note that this study is in no way recommending people should stop taking antipsychotics but simply that clinicians need to factor in a patient’s medication history while considering post-COVID aftereffects,” Dr. Freudenberg-Hua said.
“Given that the number of patients with dementia is projected to triple in the next 30 years, these findings have significant public health implications,” Dr. Sinvani added.
She noted that “care partners and health care professionals” should look for early signs of dementia, such as forgetfulness and depressive symptoms, in their patients.
“Future studies must continue to evaluate these associations, which are key for potential future interventions to prevent dementia,” Dr. Sinvani said.
The study was funded by the National Institutes of Health. Dr. Freudenberg-Hua co-owns stock and stock options from Regeneron Pharmaceuticals. Dr. Sinvani has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
Results from a large study of more than 1,700 patients who had been hospitalized with COVID showed a greater than twofold increased risk for post-COVID dementia in those taking antipsychotics and mood stabilizers/anticonvulsants – medications often used to treat schizophrenia, psychosis, bipolar disorder, and seizures.
“We know that pre-existing psychiatric illness is associated with poor COVID-19 outcomes, but our study is the first to show an association with certain psychiatric medications and dementia,” co-investigator Liron Sinvani, MD, the Feinstein Institutes for Medical Research, Manhasset, New York, said in an interview.
“Our study highlights the potential interaction between baseline neuropsychiatric disease, psychotropic medications, COVID-19, and dementia,” Dr. Sinvani added.
The findings were published online March 18 in Frontiers in Medicine.
‘Striking’ dementia rate
Using electronic health records, the researchers evaluated pre-COVID psychotropic medication use and post-COVID dementia onset in 1,755 adults aged 65 and older. All were hospitalized with COVID-19 at Northwell Health between March 1 and April 20, 2020.
A “striking” 13% of the participants (n = 223) developed dementia within 1-year of follow-up, the investigators report.
Among the 438 patients (25%) exposed to at least one psychotropic medication before COVID-19, 105 (24%) developed dementia in the year following COVID versus 118 of 1,317 (9%) patients with no pre-COVID exposure to psychotropic medication (odds ratio, 3.2; 95% confidence interval, 2.37-4.32).
Both pre-COVID psychotropic medication use (OR, 2.7; 95% CI, 1.8-4.0, P < .001) and delirium (OR, 3.0; 95% CI, 1.9-4.6, P < .001) were significantly associated with post-COVID dementia at 1 year.
In a sensitivity analysis in the subset of 423 patients with at least one documented neurologic or psychiatric diagnosis at the time of COVID admission, and after adjusting for confounding factors, pre-COVID psychotropic medication use remained significantly linked to post-COVID dementia onset (OR, 3.09; 95% CI, 1.5-6.6, P = .002).
Drug classes most strongly associated with 1-year post-COVID dementia onset were antipsychotics (OR, 2.8, 95% CI, 1.7-4.4, P < .001) and mood stabilizers/anticonvulsants (OR, 2.4, 95% CI, 1.39-4.02, P = .001).
In a further exploratory analysis, the psychotropics valproic acid (multiple brands) and haloperidol (Haldol) had the largest association with post-COVID dementia.
Antidepressants as a class were not associated with post-COVID dementia, but the potential effects of two commonly prescribed antidepressants in older adults, mirtazapine (Remeron) and escitalopram (Lexapro), “warrant further investigation,” the researchers note.
Predictive risk marker?
“This research shows that psychotropic medications can be considered a predictive risk marker for post-COVID dementia. In patients taking psychotropic medications, COVID-19 could have accelerated progression of dementia after hospitalization,” lead author Yun Freudenberg-Hua, MD, the Feinstein Institutes, said in a news release.
It is unclear why psychotropic medications may raise the risk for dementia onset after COVID, the investigators note.
“It is intuitive that psychotropic medications indicate pre-existing neuropsychiatric conditions in which COVID-19 occurs. It is possible that psychotropic medications may potentiate the neurostructural changes that have been found in the brain of those who have recovered from COVID-19,” they write.
The sensitivity analysis in patients with documented neurologic and psychiatric diagnoses supports this interpretation.
COVID-19 may also accelerate the underlying brain disorders for which psychotropic medications were prescribed, leading to the greater incidence of post-COVID dementia, the researchers write.
“It is important to note that this study is in no way recommending people should stop taking antipsychotics but simply that clinicians need to factor in a patient’s medication history while considering post-COVID aftereffects,” Dr. Freudenberg-Hua said.
“Given that the number of patients with dementia is projected to triple in the next 30 years, these findings have significant public health implications,” Dr. Sinvani added.
She noted that “care partners and health care professionals” should look for early signs of dementia, such as forgetfulness and depressive symptoms, in their patients.
“Future studies must continue to evaluate these associations, which are key for potential future interventions to prevent dementia,” Dr. Sinvani said.
The study was funded by the National Institutes of Health. Dr. Freudenberg-Hua co-owns stock and stock options from Regeneron Pharmaceuticals. Dr. Sinvani has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
Results from a large study of more than 1,700 patients who had been hospitalized with COVID showed a greater than twofold increased risk for post-COVID dementia in those taking antipsychotics and mood stabilizers/anticonvulsants – medications often used to treat schizophrenia, psychosis, bipolar disorder, and seizures.
“We know that pre-existing psychiatric illness is associated with poor COVID-19 outcomes, but our study is the first to show an association with certain psychiatric medications and dementia,” co-investigator Liron Sinvani, MD, the Feinstein Institutes for Medical Research, Manhasset, New York, said in an interview.
“Our study highlights the potential interaction between baseline neuropsychiatric disease, psychotropic medications, COVID-19, and dementia,” Dr. Sinvani added.
The findings were published online March 18 in Frontiers in Medicine.
‘Striking’ dementia rate
Using electronic health records, the researchers evaluated pre-COVID psychotropic medication use and post-COVID dementia onset in 1,755 adults aged 65 and older. All were hospitalized with COVID-19 at Northwell Health between March 1 and April 20, 2020.
A “striking” 13% of the participants (n = 223) developed dementia within 1-year of follow-up, the investigators report.
Among the 438 patients (25%) exposed to at least one psychotropic medication before COVID-19, 105 (24%) developed dementia in the year following COVID versus 118 of 1,317 (9%) patients with no pre-COVID exposure to psychotropic medication (odds ratio, 3.2; 95% confidence interval, 2.37-4.32).
Both pre-COVID psychotropic medication use (OR, 2.7; 95% CI, 1.8-4.0, P < .001) and delirium (OR, 3.0; 95% CI, 1.9-4.6, P < .001) were significantly associated with post-COVID dementia at 1 year.
In a sensitivity analysis in the subset of 423 patients with at least one documented neurologic or psychiatric diagnosis at the time of COVID admission, and after adjusting for confounding factors, pre-COVID psychotropic medication use remained significantly linked to post-COVID dementia onset (OR, 3.09; 95% CI, 1.5-6.6, P = .002).
Drug classes most strongly associated with 1-year post-COVID dementia onset were antipsychotics (OR, 2.8, 95% CI, 1.7-4.4, P < .001) and mood stabilizers/anticonvulsants (OR, 2.4, 95% CI, 1.39-4.02, P = .001).
In a further exploratory analysis, the psychotropics valproic acid (multiple brands) and haloperidol (Haldol) had the largest association with post-COVID dementia.
Antidepressants as a class were not associated with post-COVID dementia, but the potential effects of two commonly prescribed antidepressants in older adults, mirtazapine (Remeron) and escitalopram (Lexapro), “warrant further investigation,” the researchers note.
Predictive risk marker?
“This research shows that psychotropic medications can be considered a predictive risk marker for post-COVID dementia. In patients taking psychotropic medications, COVID-19 could have accelerated progression of dementia after hospitalization,” lead author Yun Freudenberg-Hua, MD, the Feinstein Institutes, said in a news release.
It is unclear why psychotropic medications may raise the risk for dementia onset after COVID, the investigators note.
“It is intuitive that psychotropic medications indicate pre-existing neuropsychiatric conditions in which COVID-19 occurs. It is possible that psychotropic medications may potentiate the neurostructural changes that have been found in the brain of those who have recovered from COVID-19,” they write.
The sensitivity analysis in patients with documented neurologic and psychiatric diagnoses supports this interpretation.
COVID-19 may also accelerate the underlying brain disorders for which psychotropic medications were prescribed, leading to the greater incidence of post-COVID dementia, the researchers write.
“It is important to note that this study is in no way recommending people should stop taking antipsychotics but simply that clinicians need to factor in a patient’s medication history while considering post-COVID aftereffects,” Dr. Freudenberg-Hua said.
“Given that the number of patients with dementia is projected to triple in the next 30 years, these findings have significant public health implications,” Dr. Sinvani added.
She noted that “care partners and health care professionals” should look for early signs of dementia, such as forgetfulness and depressive symptoms, in their patients.
“Future studies must continue to evaluate these associations, which are key for potential future interventions to prevent dementia,” Dr. Sinvani said.
The study was funded by the National Institutes of Health. Dr. Freudenberg-Hua co-owns stock and stock options from Regeneron Pharmaceuticals. Dr. Sinvani has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM FRONTIERS IN MEDICINE
Older adults with schizophrenia need ‘person-centered’ care
For example, individuals in a group characterized by substance use disorders (SUDs) had a depression prevalence of about 60% and relatively high death rates from unintentional injury and hepatitis.
“The health care needs of older adults with schizophrenia can vary widely, so aging persons with schizophrenia can’t be considered a uniform population,” study investigator Alison Hwong, MD, PhD, University of California, San Francisco, National Clinicians Scholars Program and San Francisco Veterans Affairs, told this news organization.
“For patients with multiple chronic conditions, we need to be proactive in coordinating specialty care. At the same time, we need novel models of person-centered care to help aging adults with schizophrenia live longer, healthier lives,” Dr. Hwong added.
The findings were presented as part of the American Association for Geriatric Psychiatry annual meeting.
Widening mortality gap
The life expectancy of patients with schizophrenia is lower by 8-15 years, compared with those without schizophrenia and this “mortality gap” has widened in recent years, Dr. Hwong noted. Those with schizophrenia also have high rates of health care utilization and high direct and indirect health care costs.
Most previous research looking at illness in schizophrenia focused on a single medical condition, “but by midlife, adults with schizophrenia may have multiple medical conditions,” said Dr. Hwong. “Little is known about multimorbidity in aging adults with schizophrenia and how that could be related to mortality outcomes.”
The study included 82,858 U.S. veterans aged 50 years and older who had at least one inpatient or two outpatient encounters associated with a diagnosis of schizophrenia in the previous 2 years. The study period ran from 2012 to 2018.
Using health care records and data linkages, researchers examined 20 common medical and psychiatric conditions other than schizophrenia that required medical attention. The investigators used the “latent class analysis” statistical model to assess differences across classes.
The study included three distinct patient classes: minimal morbidity (43% of the cohort), depression and medical comorbidity (34.2%), and SUDs and related conditions (22.8%).
The SUD group tended to be younger, with a mean age of 57.9 years versus 60.4 years for the minimal comorbidity group and 65.9 years for the depression group.
The SUD group was also less likely to be female (4.8% vs. 6.7% and 6%, respectively), less likely to be White, and more likely to be Black. This group was also less likely to be married and more likely to have a history of homelessness.
Disease prevalence rates
Results showed the minimal morbidity group had prevalence rates of less than 10% for all major conditions, except for tobacco dependence, which had a rate of 11.8%.
The depression and medical comorbidity group had very high prevalence rates (more than 20%) for heart attack, heart failure, stroke, cancer, dementia, arthritis, renal disease, sleep disorders, depression, and tobacco dependence. In addition, the rate was 60% for chronic obstructive pulmonary disease.
Participants in the SUD and related conditions group had rates of more than 70% for alcohol use disorder, other drug use disorders, and tobacco dependence. They also had high rates of COPD, hepatitis C, chronic pain, sleep disorders, depression, and PTSD.
On average, the SUD group was younger and may explain why they were less likely to have heart failure and renal disease, Dr. Hwong noted. These results may help inform treatment approaches, she added.
“For the group with largely substance use–related conditions, perhaps we can better address their needs with, for example, specific addiction and infectious disease services instead of a one-size-fits-all model,” said Dr. Hwong.
The investigators also examined mortality rates. Those in the depression and morbidity group had the highest rate of overall mortality; 47.5% of this class died during the observation period, compared with 27.2% of the SUD group.
More research is needed to understand why the mortality rate is so high in the depression and morbidity group, she said.
High rates of accidental death
The SUD group had the highest rates of death from accidents, possibly from overdoses, suicide, hepatitis C, and alcohol use–related deaths. “Their risks are very specific and appear largely related to substance use,” Dr. Hwong said.
The minimal comorbidity group showed the lowest rates of overall mortality rate (18%) and of cause-specific mortality for most of the included conditions.
Dr. Hwong noted she would like to study this class further. “I’m interested to know who are the people with schizophrenia who are thriving and are successfully aging – to learn what is going well for them.”
The researchers also plan to examine the subgroups in more detail to understand differences in treatments, health care utilization, and outcomes across groups. They are also interested in assessing other predictors of mortality outcomes in addition to multimorbidity.
One limitation of the study is that its cohort consisted of male veterans, so the findings may not be generalizable to other populations. In addition, these were observational data and so the results do not imply causality, Dr. Hwong said.
Dr. Hwong reported no relevant financial relationships, but she is supported by the VA and the UCSF National Clinician Scholars Program.
A version of this article first appeared on Medscape.com.
For example, individuals in a group characterized by substance use disorders (SUDs) had a depression prevalence of about 60% and relatively high death rates from unintentional injury and hepatitis.
“The health care needs of older adults with schizophrenia can vary widely, so aging persons with schizophrenia can’t be considered a uniform population,” study investigator Alison Hwong, MD, PhD, University of California, San Francisco, National Clinicians Scholars Program and San Francisco Veterans Affairs, told this news organization.
“For patients with multiple chronic conditions, we need to be proactive in coordinating specialty care. At the same time, we need novel models of person-centered care to help aging adults with schizophrenia live longer, healthier lives,” Dr. Hwong added.
The findings were presented as part of the American Association for Geriatric Psychiatry annual meeting.
Widening mortality gap
The life expectancy of patients with schizophrenia is lower by 8-15 years, compared with those without schizophrenia and this “mortality gap” has widened in recent years, Dr. Hwong noted. Those with schizophrenia also have high rates of health care utilization and high direct and indirect health care costs.
Most previous research looking at illness in schizophrenia focused on a single medical condition, “but by midlife, adults with schizophrenia may have multiple medical conditions,” said Dr. Hwong. “Little is known about multimorbidity in aging adults with schizophrenia and how that could be related to mortality outcomes.”
The study included 82,858 U.S. veterans aged 50 years and older who had at least one inpatient or two outpatient encounters associated with a diagnosis of schizophrenia in the previous 2 years. The study period ran from 2012 to 2018.
Using health care records and data linkages, researchers examined 20 common medical and psychiatric conditions other than schizophrenia that required medical attention. The investigators used the “latent class analysis” statistical model to assess differences across classes.
The study included three distinct patient classes: minimal morbidity (43% of the cohort), depression and medical comorbidity (34.2%), and SUDs and related conditions (22.8%).
The SUD group tended to be younger, with a mean age of 57.9 years versus 60.4 years for the minimal comorbidity group and 65.9 years for the depression group.
The SUD group was also less likely to be female (4.8% vs. 6.7% and 6%, respectively), less likely to be White, and more likely to be Black. This group was also less likely to be married and more likely to have a history of homelessness.
Disease prevalence rates
Results showed the minimal morbidity group had prevalence rates of less than 10% for all major conditions, except for tobacco dependence, which had a rate of 11.8%.
The depression and medical comorbidity group had very high prevalence rates (more than 20%) for heart attack, heart failure, stroke, cancer, dementia, arthritis, renal disease, sleep disorders, depression, and tobacco dependence. In addition, the rate was 60% for chronic obstructive pulmonary disease.
Participants in the SUD and related conditions group had rates of more than 70% for alcohol use disorder, other drug use disorders, and tobacco dependence. They also had high rates of COPD, hepatitis C, chronic pain, sleep disorders, depression, and PTSD.
On average, the SUD group was younger and may explain why they were less likely to have heart failure and renal disease, Dr. Hwong noted. These results may help inform treatment approaches, she added.
“For the group with largely substance use–related conditions, perhaps we can better address their needs with, for example, specific addiction and infectious disease services instead of a one-size-fits-all model,” said Dr. Hwong.
The investigators also examined mortality rates. Those in the depression and morbidity group had the highest rate of overall mortality; 47.5% of this class died during the observation period, compared with 27.2% of the SUD group.
More research is needed to understand why the mortality rate is so high in the depression and morbidity group, she said.
High rates of accidental death
The SUD group had the highest rates of death from accidents, possibly from overdoses, suicide, hepatitis C, and alcohol use–related deaths. “Their risks are very specific and appear largely related to substance use,” Dr. Hwong said.
The minimal comorbidity group showed the lowest rates of overall mortality rate (18%) and of cause-specific mortality for most of the included conditions.
Dr. Hwong noted she would like to study this class further. “I’m interested to know who are the people with schizophrenia who are thriving and are successfully aging – to learn what is going well for them.”
The researchers also plan to examine the subgroups in more detail to understand differences in treatments, health care utilization, and outcomes across groups. They are also interested in assessing other predictors of mortality outcomes in addition to multimorbidity.
One limitation of the study is that its cohort consisted of male veterans, so the findings may not be generalizable to other populations. In addition, these were observational data and so the results do not imply causality, Dr. Hwong said.
Dr. Hwong reported no relevant financial relationships, but she is supported by the VA and the UCSF National Clinician Scholars Program.
A version of this article first appeared on Medscape.com.
For example, individuals in a group characterized by substance use disorders (SUDs) had a depression prevalence of about 60% and relatively high death rates from unintentional injury and hepatitis.
“The health care needs of older adults with schizophrenia can vary widely, so aging persons with schizophrenia can’t be considered a uniform population,” study investigator Alison Hwong, MD, PhD, University of California, San Francisco, National Clinicians Scholars Program and San Francisco Veterans Affairs, told this news organization.
“For patients with multiple chronic conditions, we need to be proactive in coordinating specialty care. At the same time, we need novel models of person-centered care to help aging adults with schizophrenia live longer, healthier lives,” Dr. Hwong added.
The findings were presented as part of the American Association for Geriatric Psychiatry annual meeting.
Widening mortality gap
The life expectancy of patients with schizophrenia is lower by 8-15 years, compared with those without schizophrenia and this “mortality gap” has widened in recent years, Dr. Hwong noted. Those with schizophrenia also have high rates of health care utilization and high direct and indirect health care costs.
Most previous research looking at illness in schizophrenia focused on a single medical condition, “but by midlife, adults with schizophrenia may have multiple medical conditions,” said Dr. Hwong. “Little is known about multimorbidity in aging adults with schizophrenia and how that could be related to mortality outcomes.”
The study included 82,858 U.S. veterans aged 50 years and older who had at least one inpatient or two outpatient encounters associated with a diagnosis of schizophrenia in the previous 2 years. The study period ran from 2012 to 2018.
Using health care records and data linkages, researchers examined 20 common medical and psychiatric conditions other than schizophrenia that required medical attention. The investigators used the “latent class analysis” statistical model to assess differences across classes.
The study included three distinct patient classes: minimal morbidity (43% of the cohort), depression and medical comorbidity (34.2%), and SUDs and related conditions (22.8%).
The SUD group tended to be younger, with a mean age of 57.9 years versus 60.4 years for the minimal comorbidity group and 65.9 years for the depression group.
The SUD group was also less likely to be female (4.8% vs. 6.7% and 6%, respectively), less likely to be White, and more likely to be Black. This group was also less likely to be married and more likely to have a history of homelessness.
Disease prevalence rates
Results showed the minimal morbidity group had prevalence rates of less than 10% for all major conditions, except for tobacco dependence, which had a rate of 11.8%.
The depression and medical comorbidity group had very high prevalence rates (more than 20%) for heart attack, heart failure, stroke, cancer, dementia, arthritis, renal disease, sleep disorders, depression, and tobacco dependence. In addition, the rate was 60% for chronic obstructive pulmonary disease.
Participants in the SUD and related conditions group had rates of more than 70% for alcohol use disorder, other drug use disorders, and tobacco dependence. They also had high rates of COPD, hepatitis C, chronic pain, sleep disorders, depression, and PTSD.
On average, the SUD group was younger and may explain why they were less likely to have heart failure and renal disease, Dr. Hwong noted. These results may help inform treatment approaches, she added.
“For the group with largely substance use–related conditions, perhaps we can better address their needs with, for example, specific addiction and infectious disease services instead of a one-size-fits-all model,” said Dr. Hwong.
The investigators also examined mortality rates. Those in the depression and morbidity group had the highest rate of overall mortality; 47.5% of this class died during the observation period, compared with 27.2% of the SUD group.
More research is needed to understand why the mortality rate is so high in the depression and morbidity group, she said.
High rates of accidental death
The SUD group had the highest rates of death from accidents, possibly from overdoses, suicide, hepatitis C, and alcohol use–related deaths. “Their risks are very specific and appear largely related to substance use,” Dr. Hwong said.
The minimal comorbidity group showed the lowest rates of overall mortality rate (18%) and of cause-specific mortality for most of the included conditions.
Dr. Hwong noted she would like to study this class further. “I’m interested to know who are the people with schizophrenia who are thriving and are successfully aging – to learn what is going well for them.”
The researchers also plan to examine the subgroups in more detail to understand differences in treatments, health care utilization, and outcomes across groups. They are also interested in assessing other predictors of mortality outcomes in addition to multimorbidity.
One limitation of the study is that its cohort consisted of male veterans, so the findings may not be generalizable to other populations. In addition, these were observational data and so the results do not imply causality, Dr. Hwong said.
Dr. Hwong reported no relevant financial relationships, but she is supported by the VA and the UCSF National Clinician Scholars Program.
A version of this article first appeared on Medscape.com.
FROM AAGP 2022
Schizophrenia risk lower for people with access to green space
The investigators, led by Martin Rotenberg, MD, of Centre for Addiction and Mental Health and the University of Toronto, found individuals living in areas with the lowest levels of green space were 24% more likely to develop schizophrenia.
This study contributes to a growing body of evidence showing the importance of exposure to green space to mental health.
“These findings contribute to a growing evidence base that environmental factors may play a role in the etiology of schizophrenia,” the researchers write.
The study was published online Feb. 4 in the Canadian Journal of Psychiatry.
Underlying mechanism unknown
For the study, researchers used a retrospective population-based cohort of 649,020 individuals between ages 14 and 40 years from different neighborhoods in Toronto.
Green space was calculated using geospatial data of all public parks and green spaces in the city; data were drawn from the Urban Health Equity Assessment and Response Tool.
Over a 10-year period, 4,841 participants were diagnosed with schizophrenia.
Those who lived in neighborhoods with the least amount of green space were significantly more likely to develop schizophrenia than those who lived in areas with the most green space, even after adjusting for age, sex, and neighborhood-level marginalization (adjusted incidence rate ratio, 1.24; 95% confidence interval, 1.06-1.45).
Overall, schizophrenia risk was also elevated in men vs. women (adjusted IRR, 1.59; 95% CI, 1.50-1.68). Those living in areas with moderate amounts of green space did not have an increased schizophrenia risk.
“We found that residing in an area with the lowest amount of green space was associated with an increased risk of developing schizophrenia, independent of other sociodemographic and socioenvironmental factors,” the researchers note. “The underlying mechanism at play is unknown and requires further study.”
One possibility, they added, is that exposure to green space may reduce the risk of air pollution, which other studies have suggested may be associated with increased schizophrenia risk.
The new study builds on a 2018 report from Denmark that showed a 52% increased risk of psychotic disorders in adulthood among people who spent their childhood in neighborhoods with little green space.
Important, longitudinal data
Commenting on the findings, John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, said the study provides important longitudinal data.
“The 10-year duration of the study and large sample size make the results very compelling and help confirm what has been thought about green space and risk of schizophrenia,” Dr. Torous said.
“Often, we think of green space at a very macro level,” he added. “This study is important because it shows us that green space matters on a block-by-block level just as much.”
The study was unfunded. The authors and Dr. Torous have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The investigators, led by Martin Rotenberg, MD, of Centre for Addiction and Mental Health and the University of Toronto, found individuals living in areas with the lowest levels of green space were 24% more likely to develop schizophrenia.
This study contributes to a growing body of evidence showing the importance of exposure to green space to mental health.
“These findings contribute to a growing evidence base that environmental factors may play a role in the etiology of schizophrenia,” the researchers write.
The study was published online Feb. 4 in the Canadian Journal of Psychiatry.
Underlying mechanism unknown
For the study, researchers used a retrospective population-based cohort of 649,020 individuals between ages 14 and 40 years from different neighborhoods in Toronto.
Green space was calculated using geospatial data of all public parks and green spaces in the city; data were drawn from the Urban Health Equity Assessment and Response Tool.
Over a 10-year period, 4,841 participants were diagnosed with schizophrenia.
Those who lived in neighborhoods with the least amount of green space were significantly more likely to develop schizophrenia than those who lived in areas with the most green space, even after adjusting for age, sex, and neighborhood-level marginalization (adjusted incidence rate ratio, 1.24; 95% confidence interval, 1.06-1.45).
Overall, schizophrenia risk was also elevated in men vs. women (adjusted IRR, 1.59; 95% CI, 1.50-1.68). Those living in areas with moderate amounts of green space did not have an increased schizophrenia risk.
“We found that residing in an area with the lowest amount of green space was associated with an increased risk of developing schizophrenia, independent of other sociodemographic and socioenvironmental factors,” the researchers note. “The underlying mechanism at play is unknown and requires further study.”
One possibility, they added, is that exposure to green space may reduce the risk of air pollution, which other studies have suggested may be associated with increased schizophrenia risk.
The new study builds on a 2018 report from Denmark that showed a 52% increased risk of psychotic disorders in adulthood among people who spent their childhood in neighborhoods with little green space.
Important, longitudinal data
Commenting on the findings, John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, said the study provides important longitudinal data.
“The 10-year duration of the study and large sample size make the results very compelling and help confirm what has been thought about green space and risk of schizophrenia,” Dr. Torous said.
“Often, we think of green space at a very macro level,” he added. “This study is important because it shows us that green space matters on a block-by-block level just as much.”
The study was unfunded. The authors and Dr. Torous have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The investigators, led by Martin Rotenberg, MD, of Centre for Addiction and Mental Health and the University of Toronto, found individuals living in areas with the lowest levels of green space were 24% more likely to develop schizophrenia.
This study contributes to a growing body of evidence showing the importance of exposure to green space to mental health.
“These findings contribute to a growing evidence base that environmental factors may play a role in the etiology of schizophrenia,” the researchers write.
The study was published online Feb. 4 in the Canadian Journal of Psychiatry.
Underlying mechanism unknown
For the study, researchers used a retrospective population-based cohort of 649,020 individuals between ages 14 and 40 years from different neighborhoods in Toronto.
Green space was calculated using geospatial data of all public parks and green spaces in the city; data were drawn from the Urban Health Equity Assessment and Response Tool.
Over a 10-year period, 4,841 participants were diagnosed with schizophrenia.
Those who lived in neighborhoods with the least amount of green space were significantly more likely to develop schizophrenia than those who lived in areas with the most green space, even after adjusting for age, sex, and neighborhood-level marginalization (adjusted incidence rate ratio, 1.24; 95% confidence interval, 1.06-1.45).
Overall, schizophrenia risk was also elevated in men vs. women (adjusted IRR, 1.59; 95% CI, 1.50-1.68). Those living in areas with moderate amounts of green space did not have an increased schizophrenia risk.
“We found that residing in an area with the lowest amount of green space was associated with an increased risk of developing schizophrenia, independent of other sociodemographic and socioenvironmental factors,” the researchers note. “The underlying mechanism at play is unknown and requires further study.”
One possibility, they added, is that exposure to green space may reduce the risk of air pollution, which other studies have suggested may be associated with increased schizophrenia risk.
The new study builds on a 2018 report from Denmark that showed a 52% increased risk of psychotic disorders in adulthood among people who spent their childhood in neighborhoods with little green space.
Important, longitudinal data
Commenting on the findings, John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, said the study provides important longitudinal data.
“The 10-year duration of the study and large sample size make the results very compelling and help confirm what has been thought about green space and risk of schizophrenia,” Dr. Torous said.
“Often, we think of green space at a very macro level,” he added. “This study is important because it shows us that green space matters on a block-by-block level just as much.”
The study was unfunded. The authors and Dr. Torous have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CANADIAN JOURNAL OF PSYCHIATRY
Common eye disorder in children tied to mental illness
Misaligned eyes in children are associated with an increased prevalence of mental illness, results of a large study suggest.
“Psychiatrists who have a patient with depression or anxiety and notice that patient also has strabismus might think about the link between those two conditions and refer that patient,” study investigator Stacy L. Pineles, MD, professor, department of ophthalmology, University of California, Los Angeles, told this news organization.
The study was published online March 10 in JAMA Ophthalmology.
A common condition
Strabismus, a condition in which the eyes don’t line up or are “crossed,” is one of the most common eye diseases in children, with some estimates suggesting it affects more than 1.5 million American youth.
Patients with strabismus have problems making eye contact and are affected socially and functionally, said Dr. Pineles. They’re often met with a negative bias, as shown by children’s responses to pictures of faces with and without strabismus, she said.
There is a signal from previous research suggesting that strabismus is linked to a higher risk of mental illness. However, most of these studies were small and had relatively homogenous populations, said Dr. Pineles.
The new study includes over 12 million children (mean age, 8.0 years) from a private health insurance claims database that represents diverse races and ethnicities as well as geographic regions across the United States.
The sample included 352,636 children with strabismus and 11,652,553 children with no diagnosed eye disease who served as controls. Most participants were White (51.6%), came from a family with an annual household income of $40,000 or more (51.0%), had point-of-service insurance (68.7%), and had at least one comorbid condition (64.5%).
The study evaluated five mental illness diagnoses. These included anxiety disorder, depressive disorder, substance use or addictive disorder, bipolar disorder, and schizophrenia.
Overall, children with strabismus had a higher prevalence of all these illnesses, with the exception of substance use disorder.
After adjusting for age, sex, race and ethnicity, census region, education level of caregiver, family net worth, and presence of at least one comorbid condition, the odds ratios among those with versus without strabismus were: 2.01 (95% confidence interval, 1.99-2.04; P < .001) for anxiety disorder, 1.83 (95% CI, 1.76-1.90; P < .001) for schizophrenia, 1.64 (95% CI, 1.59-1.70; P < .001) for bipolar disorder, and 1.61 (95% CI, 1.59-1.63; P < .001) for depressive disorder.
Substance use disorder had a negative unadjusted association with strabismus, but after adjustment for confounders, the association was not significant (OR, 0.99; 95% CI, 0.97-1.02; P = .48).
Dr. Pineles noted that the study participants, who were all under age 19, may be too young to have substance use disorders.
The results for substance use disorders provided something of an “internal control” and reaffirmed results for the other four conditions, said Dr. Pineles.
“When you do research on such a large database, you’re very likely to find significant associations; the dataset is so large that even very small differences become statistically significant. It was interesting that not everything gave us a positive association.”
Researchers divided the strabismus group into those with esotropia, where the eyes turn inward (52.2%), exotropia, where they turn outward (46.3%), and hypertropia, where one eye wanders upward (12.5%). Investigators found that all three conditions were associated with increased risk of anxiety disorder, depressive disorder, bipolar disorders, and schizophrenia.
Investigators note that rates in the current study were lower than in previous studies, which showed that children with congenital esotropia were 2.6 times more likely to receive a mental health diagnosis, and children with intermittent exotropia were 2.7 times more likely to receive a mental health diagnosis.
“It is probable that our study found a lower risk than these studies, because our study was cross-sectional and claims based, whereas these studies observed the children to early adulthood and were based on medical records,” the investigators note.
It’s impossible to determine from this study how strabismus is connected to mental illness. However, Dr. Pineles believes depression and anxiety might be tied to strabismus via teasing, which affects self-esteem, although genetics could also play a role. For conditions such as schizophrenia, a shared genetic link with strabismus might be more likely, she added.
“Schizophrenia is a pretty severe diagnosis, so just being teased or having poor self-esteem is probably not enough” to develop schizophrenia.
Based on her clinical experience, Dr. Pineles said that realigning the eyes of patients with milder forms of depression or anxiety “definitely anecdotally helps these patients a lot.”
Dr. Pineles and colleagues have another paper in press that examines mental illnesses and other serious eye disorders in children and shows similar findings, she said.
Implications for insurance coverage?
In an accompanying editorial, experts, led by S. Grace Prakalapakorn, MD, department of ophthalmology and pediatrics, Duke University Medical Center, Durham, N.C., noted the exclusion of children covered under government insurance or without insurance is an important study limitation, largely because socioeconomic status is a risk factor for poor mental health.
The editorialists point to studies showing that surgical correction of ocular misalignments may be associated with reduced anxiety and depression. However, health insurance coverage for such surgical correction “may not be available owing to a misconception that these conditions are ‘cosmetic’.”
Evidence of the broader association of strabismus with physical and mental health “may play an important role in shifting policy to promote insurance coverage for timely strabismus care,” they write.
As many mental health disorders begin in childhood or adolescence, “it is paramount to identify, address, and, if possible, prevent mental health disorders at a young age, because failure to intervene in a timely fashion can have lifelong health consequences,” say Dr. Prakalapakorn and colleagues.
With mental health conditions and disorders increasing worldwide, compounded by the stressors of the COVID-19 pandemic, additional studies are needed to explore the causal relationships between ocular and psychiatric phenomena, their treatment, and outcomes, they add.
The study was supported by a grant from the National Eye Institute and an unrestricted grant from Research to Prevent Blindness. Dr. Pineles has reported no relevant conflicts of interest. Commentary author Manpreet K. Singh, MD, has reported receiving research support from Stanford’s Maternal Child Health Research Institute and Stanford’s Department of Psychiatry and Behavioral Sciences, the National Institute of Mental Health, the National Institute on Aging, the Patient-Centered Outcomes Research Institute, Johnson & Johnson, Allergan, and the Brain and Behavior Research Foundation; serving on the advisory board for Sunovion and Skyland Trail; serving as a consultant for Johnson & Johnson; previously serving as a consultant for X, the moonshot factory, Alphabet, and Limbix Health; receiving honoraria from the American Academy of Child and Adolescent Psychiatry; and receiving royalties from American Psychiatric Association Publishing and Thrive Global. Commentary author Nathan Congdon, MD, has reported receiving personal fees from Belkin Vision outside the submitted work.
A version of this article first appeared on Medscape.com.
Misaligned eyes in children are associated with an increased prevalence of mental illness, results of a large study suggest.
“Psychiatrists who have a patient with depression or anxiety and notice that patient also has strabismus might think about the link between those two conditions and refer that patient,” study investigator Stacy L. Pineles, MD, professor, department of ophthalmology, University of California, Los Angeles, told this news organization.
The study was published online March 10 in JAMA Ophthalmology.
A common condition
Strabismus, a condition in which the eyes don’t line up or are “crossed,” is one of the most common eye diseases in children, with some estimates suggesting it affects more than 1.5 million American youth.
Patients with strabismus have problems making eye contact and are affected socially and functionally, said Dr. Pineles. They’re often met with a negative bias, as shown by children’s responses to pictures of faces with and without strabismus, she said.
There is a signal from previous research suggesting that strabismus is linked to a higher risk of mental illness. However, most of these studies were small and had relatively homogenous populations, said Dr. Pineles.
The new study includes over 12 million children (mean age, 8.0 years) from a private health insurance claims database that represents diverse races and ethnicities as well as geographic regions across the United States.
The sample included 352,636 children with strabismus and 11,652,553 children with no diagnosed eye disease who served as controls. Most participants were White (51.6%), came from a family with an annual household income of $40,000 or more (51.0%), had point-of-service insurance (68.7%), and had at least one comorbid condition (64.5%).
The study evaluated five mental illness diagnoses. These included anxiety disorder, depressive disorder, substance use or addictive disorder, bipolar disorder, and schizophrenia.
Overall, children with strabismus had a higher prevalence of all these illnesses, with the exception of substance use disorder.
After adjusting for age, sex, race and ethnicity, census region, education level of caregiver, family net worth, and presence of at least one comorbid condition, the odds ratios among those with versus without strabismus were: 2.01 (95% confidence interval, 1.99-2.04; P < .001) for anxiety disorder, 1.83 (95% CI, 1.76-1.90; P < .001) for schizophrenia, 1.64 (95% CI, 1.59-1.70; P < .001) for bipolar disorder, and 1.61 (95% CI, 1.59-1.63; P < .001) for depressive disorder.
Substance use disorder had a negative unadjusted association with strabismus, but after adjustment for confounders, the association was not significant (OR, 0.99; 95% CI, 0.97-1.02; P = .48).
Dr. Pineles noted that the study participants, who were all under age 19, may be too young to have substance use disorders.
The results for substance use disorders provided something of an “internal control” and reaffirmed results for the other four conditions, said Dr. Pineles.
“When you do research on such a large database, you’re very likely to find significant associations; the dataset is so large that even very small differences become statistically significant. It was interesting that not everything gave us a positive association.”
Researchers divided the strabismus group into those with esotropia, where the eyes turn inward (52.2%), exotropia, where they turn outward (46.3%), and hypertropia, where one eye wanders upward (12.5%). Investigators found that all three conditions were associated with increased risk of anxiety disorder, depressive disorder, bipolar disorders, and schizophrenia.
Investigators note that rates in the current study were lower than in previous studies, which showed that children with congenital esotropia were 2.6 times more likely to receive a mental health diagnosis, and children with intermittent exotropia were 2.7 times more likely to receive a mental health diagnosis.
“It is probable that our study found a lower risk than these studies, because our study was cross-sectional and claims based, whereas these studies observed the children to early adulthood and were based on medical records,” the investigators note.
It’s impossible to determine from this study how strabismus is connected to mental illness. However, Dr. Pineles believes depression and anxiety might be tied to strabismus via teasing, which affects self-esteem, although genetics could also play a role. For conditions such as schizophrenia, a shared genetic link with strabismus might be more likely, she added.
“Schizophrenia is a pretty severe diagnosis, so just being teased or having poor self-esteem is probably not enough” to develop schizophrenia.
Based on her clinical experience, Dr. Pineles said that realigning the eyes of patients with milder forms of depression or anxiety “definitely anecdotally helps these patients a lot.”
Dr. Pineles and colleagues have another paper in press that examines mental illnesses and other serious eye disorders in children and shows similar findings, she said.
Implications for insurance coverage?
In an accompanying editorial, experts, led by S. Grace Prakalapakorn, MD, department of ophthalmology and pediatrics, Duke University Medical Center, Durham, N.C., noted the exclusion of children covered under government insurance or without insurance is an important study limitation, largely because socioeconomic status is a risk factor for poor mental health.
The editorialists point to studies showing that surgical correction of ocular misalignments may be associated with reduced anxiety and depression. However, health insurance coverage for such surgical correction “may not be available owing to a misconception that these conditions are ‘cosmetic’.”
Evidence of the broader association of strabismus with physical and mental health “may play an important role in shifting policy to promote insurance coverage for timely strabismus care,” they write.
As many mental health disorders begin in childhood or adolescence, “it is paramount to identify, address, and, if possible, prevent mental health disorders at a young age, because failure to intervene in a timely fashion can have lifelong health consequences,” say Dr. Prakalapakorn and colleagues.
With mental health conditions and disorders increasing worldwide, compounded by the stressors of the COVID-19 pandemic, additional studies are needed to explore the causal relationships between ocular and psychiatric phenomena, their treatment, and outcomes, they add.
The study was supported by a grant from the National Eye Institute and an unrestricted grant from Research to Prevent Blindness. Dr. Pineles has reported no relevant conflicts of interest. Commentary author Manpreet K. Singh, MD, has reported receiving research support from Stanford’s Maternal Child Health Research Institute and Stanford’s Department of Psychiatry and Behavioral Sciences, the National Institute of Mental Health, the National Institute on Aging, the Patient-Centered Outcomes Research Institute, Johnson & Johnson, Allergan, and the Brain and Behavior Research Foundation; serving on the advisory board for Sunovion and Skyland Trail; serving as a consultant for Johnson & Johnson; previously serving as a consultant for X, the moonshot factory, Alphabet, and Limbix Health; receiving honoraria from the American Academy of Child and Adolescent Psychiatry; and receiving royalties from American Psychiatric Association Publishing and Thrive Global. Commentary author Nathan Congdon, MD, has reported receiving personal fees from Belkin Vision outside the submitted work.
A version of this article first appeared on Medscape.com.
Misaligned eyes in children are associated with an increased prevalence of mental illness, results of a large study suggest.
“Psychiatrists who have a patient with depression or anxiety and notice that patient also has strabismus might think about the link between those two conditions and refer that patient,” study investigator Stacy L. Pineles, MD, professor, department of ophthalmology, University of California, Los Angeles, told this news organization.
The study was published online March 10 in JAMA Ophthalmology.
A common condition
Strabismus, a condition in which the eyes don’t line up or are “crossed,” is one of the most common eye diseases in children, with some estimates suggesting it affects more than 1.5 million American youth.
Patients with strabismus have problems making eye contact and are affected socially and functionally, said Dr. Pineles. They’re often met with a negative bias, as shown by children’s responses to pictures of faces with and without strabismus, she said.
There is a signal from previous research suggesting that strabismus is linked to a higher risk of mental illness. However, most of these studies were small and had relatively homogenous populations, said Dr. Pineles.
The new study includes over 12 million children (mean age, 8.0 years) from a private health insurance claims database that represents diverse races and ethnicities as well as geographic regions across the United States.
The sample included 352,636 children with strabismus and 11,652,553 children with no diagnosed eye disease who served as controls. Most participants were White (51.6%), came from a family with an annual household income of $40,000 or more (51.0%), had point-of-service insurance (68.7%), and had at least one comorbid condition (64.5%).
The study evaluated five mental illness diagnoses. These included anxiety disorder, depressive disorder, substance use or addictive disorder, bipolar disorder, and schizophrenia.
Overall, children with strabismus had a higher prevalence of all these illnesses, with the exception of substance use disorder.
After adjusting for age, sex, race and ethnicity, census region, education level of caregiver, family net worth, and presence of at least one comorbid condition, the odds ratios among those with versus without strabismus were: 2.01 (95% confidence interval, 1.99-2.04; P < .001) for anxiety disorder, 1.83 (95% CI, 1.76-1.90; P < .001) for schizophrenia, 1.64 (95% CI, 1.59-1.70; P < .001) for bipolar disorder, and 1.61 (95% CI, 1.59-1.63; P < .001) for depressive disorder.
Substance use disorder had a negative unadjusted association with strabismus, but after adjustment for confounders, the association was not significant (OR, 0.99; 95% CI, 0.97-1.02; P = .48).
Dr. Pineles noted that the study participants, who were all under age 19, may be too young to have substance use disorders.
The results for substance use disorders provided something of an “internal control” and reaffirmed results for the other four conditions, said Dr. Pineles.
“When you do research on such a large database, you’re very likely to find significant associations; the dataset is so large that even very small differences become statistically significant. It was interesting that not everything gave us a positive association.”
Researchers divided the strabismus group into those with esotropia, where the eyes turn inward (52.2%), exotropia, where they turn outward (46.3%), and hypertropia, where one eye wanders upward (12.5%). Investigators found that all three conditions were associated with increased risk of anxiety disorder, depressive disorder, bipolar disorders, and schizophrenia.
Investigators note that rates in the current study were lower than in previous studies, which showed that children with congenital esotropia were 2.6 times more likely to receive a mental health diagnosis, and children with intermittent exotropia were 2.7 times more likely to receive a mental health diagnosis.
“It is probable that our study found a lower risk than these studies, because our study was cross-sectional and claims based, whereas these studies observed the children to early adulthood and were based on medical records,” the investigators note.
It’s impossible to determine from this study how strabismus is connected to mental illness. However, Dr. Pineles believes depression and anxiety might be tied to strabismus via teasing, which affects self-esteem, although genetics could also play a role. For conditions such as schizophrenia, a shared genetic link with strabismus might be more likely, she added.
“Schizophrenia is a pretty severe diagnosis, so just being teased or having poor self-esteem is probably not enough” to develop schizophrenia.
Based on her clinical experience, Dr. Pineles said that realigning the eyes of patients with milder forms of depression or anxiety “definitely anecdotally helps these patients a lot.”
Dr. Pineles and colleagues have another paper in press that examines mental illnesses and other serious eye disorders in children and shows similar findings, she said.
Implications for insurance coverage?
In an accompanying editorial, experts, led by S. Grace Prakalapakorn, MD, department of ophthalmology and pediatrics, Duke University Medical Center, Durham, N.C., noted the exclusion of children covered under government insurance or without insurance is an important study limitation, largely because socioeconomic status is a risk factor for poor mental health.
The editorialists point to studies showing that surgical correction of ocular misalignments may be associated with reduced anxiety and depression. However, health insurance coverage for such surgical correction “may not be available owing to a misconception that these conditions are ‘cosmetic’.”
Evidence of the broader association of strabismus with physical and mental health “may play an important role in shifting policy to promote insurance coverage for timely strabismus care,” they write.
As many mental health disorders begin in childhood or adolescence, “it is paramount to identify, address, and, if possible, prevent mental health disorders at a young age, because failure to intervene in a timely fashion can have lifelong health consequences,” say Dr. Prakalapakorn and colleagues.
With mental health conditions and disorders increasing worldwide, compounded by the stressors of the COVID-19 pandemic, additional studies are needed to explore the causal relationships between ocular and psychiatric phenomena, their treatment, and outcomes, they add.
The study was supported by a grant from the National Eye Institute and an unrestricted grant from Research to Prevent Blindness. Dr. Pineles has reported no relevant conflicts of interest. Commentary author Manpreet K. Singh, MD, has reported receiving research support from Stanford’s Maternal Child Health Research Institute and Stanford’s Department of Psychiatry and Behavioral Sciences, the National Institute of Mental Health, the National Institute on Aging, the Patient-Centered Outcomes Research Institute, Johnson & Johnson, Allergan, and the Brain and Behavior Research Foundation; serving on the advisory board for Sunovion and Skyland Trail; serving as a consultant for Johnson & Johnson; previously serving as a consultant for X, the moonshot factory, Alphabet, and Limbix Health; receiving honoraria from the American Academy of Child and Adolescent Psychiatry; and receiving royalties from American Psychiatric Association Publishing and Thrive Global. Commentary author Nathan Congdon, MD, has reported receiving personal fees from Belkin Vision outside the submitted work.
A version of this article first appeared on Medscape.com.
The context of our lives
Neuroscience expands our knowledge of relational and social worlds
Psychiatry may be emerging from the era of psychopharmacology and entering the era of the brain, but these reductionist, jingoistic labels do little justice to the need to acknowledge and incorporate the context of our lives into our theories and treatments. Yet psychiatrists who embrace context have much to celebrate in evolving neuroscience research.
One aptly named article – ’Families that fire together smile together’ – illustrates the fundamental connection between parent and child.1 In the functional MRIs (fMRIs) taken of these parent-child dyads (n = 76), the dyads with similar resting state connectomes also have similar day-to-day emotional states, as reflected in their diary entries. Their empathic states were identified in the multivoxel patterns in the fusiform face area of the brain.2 Another study of fMRIs and parent-child dyads (n = 93) found that the parental functional connectomes (fbc) predicted their children’s externalizing and internalizing problems. The maternal fbcs were correlated with the daughter-mother relationship, and to the daughter’s internalizing problems, suggesting a potential future focus on gendered relationships.3
The implications for psychotherapy are clear: These studies show that empathic connection between parent and child results in a better outcome for the child. Patient and psychotherapist can choose from a range of psychotherapeutic interventions that promote empathy, from providing behavioral tasks that support connection between parent and child to more in-depth family interventions. Family interventions that promote empathy include increasing the family’s understanding of the importance of empathic connection and providing a safe space to help establish empathic connection.
Studying prosocial behavior, Lukas Lengersdorff and colleagues found that fMRIs of male participants (n = 96) reflected stronger activity when they were acting on behalf of the other, rather than when acting for themselves.4 During this prosocial learning fMRI study, there was stronger engagement of the ventromedial prefrontal cortex (PFC) and higher connectivity between the ventromedial PFC and the right temporoparietal junction (rTPJ). Protecting others from harm appears to be associated with neural mechanisms that support self-relevant learning, but with the added recruitment of structures associated with the social brain. This study shows what we already know – that our brains are wired for social context. This research supports psychotherapeutic interventions aimed at creating interpersonal connection, not just at an intimate level, but also at the prosocial level, such as caring and helping others.
When social interactions are coded, the default mode network (DMN) shows increased activity. Participants (n = 11) in another study had heightened medial PFC–rTPJ connectivity, not only during rest that followed the experimental social encoding, but also during rest that followed a subsequent, nonsocial task.5 Engaging portions of the DMN during live social interactions when actively decoding the social environment, and later engaging these regions when relaxing after the social interaction, appears to facilitate social functioning. Our brains are wired to respond to context. This research underscores the positive impact of interventions such as group therapy and support groups, two underutilized modalities.
Neuroscience evaluation of our relationships provides depth to studies that fall under the medical paradigm of the gene/environment interaction. One of the most elegant in psychiatry is the Finnish study of a sample of offspring of mothers with schizophrenia who gave their children up for adoption.6 This sample of index offspring (n = 155) was compared blindly with matched controls (n = 186) of adopted/away offspring of parents without schizophrenia. The genetic effect manifested only as a psychiatric disorder in the presence of a disturbed family environment. We can now extrapolate certain possible mechanisms from the studies mentioned above: That the deficits lie in the activity or lack of activity in the DMN and associated areas, and in the generation of connectomes responsible for empathic connections.
Neuroscience expands our knowledge of our relational and social worlds, but can psychiatry make the case for inclusion of context in our conceptualization of psychiatric distress? From time to time, inroads are made, for example, the Global Assessment of Relational Functioning was incorporated into the DSM-IV-R and the Cultural Formulation Interview is in the DSM-5. However, without a sustained paradigm shift that places the gene/environment paradigm at the core of psychiatry, these efforts will rise and fall as the pioneers in these fields rise and fall.
A major barrier to moving the gene/environment paradigm more centrally in psychiatry is the prominence of individualism as an American ideal. As the neuroscience of context develops, we will be able to argue more robustly for a contextual approach to patient care.
A second barrier is the difficulty of teaching and learning about complexity. It is easy to learn how to use the DSM to make a diagnosis, to understand when and how to prescribe medications, but it is much more difficult to understand how to incorporate the complexity of life and the context within which we live, into our lexicon of psychiatric theories and treatments. As Tanya Luhrmann, PhD, points out in her study of the process of psychiatric training, residents are intimidated by the need to learn the many psychological theories and their practice; learning about medications is much simpler and takes much less time and effort.7
Nevertheless, context is embraced by several psychiatric subspecialties. Family psychiatrists recognize the power of relational dynamics in the family, and their role in shaping the individual. From understanding family communication patterns, to understanding how roles in the family get allocated, family psychiatry has well established tools for assessment and many evidence-based treatments that focus on changing relational dynamics. Social and community psychiatrists emphasize the role of race, poverty, and access, and support the assessment and treatment of the underprivileged. Cultural psychiatrists recognize that each culture has its own way of constructing identities and shaping our experiences, its own conceptualization of illness and specific idioms of distress. Cultural psychiatrists focus on sensitizing the general psychiatrist to these nuances. Child psychiatrists involve parents, and geriatric psychiatrists involve guardians. General psychiatrists understand context when, for example, understanding the role of trauma in the development of an individual, recognizing that its impact is contingent on the context within which the trauma occurs.
Neuroscience clarifies the neural pathways involved in the development of empathic and social behaviors. Our psychological theories and practice must reflect this advancement. We can teach the relevant neuroscience along with basic concepts such as child-parent relationships. We must assess an individual’s degree of fit within their family and community. Apart from asking relational questions, such as who in your world is important to you, we can use well recognized tools to help us bring context to the forefront. An easy tool is the three generational genogram, or an ecomap, which allows each individual to see where they sit in the context of their world.8 Cultural influences, societal, religious, and family influences can be drawn on the genogram, highlighting both formal and hidden family narratives. In addition, we can share how the brain works with our patients; the science of empathy and social behaviors shows us that our need for interpersonal connection is hardwired.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
References
1. Lee TH et al. Families that fire together smile together: Resting state connectome similarity and daily emotional synchrony in parent-child dyads. Neuroimage. 2017 May 15;152:31-37. doi: 10.1016/j.neuroimage.2017.02.078.
2. Lee TH et al. Love flows downstream: Mothers’ and children’s neural representation similarity in perceiving distress of self and family. Soc Cogn Affect Neurosci. 2017 Dec 1;12(12):1916-27. doi: 10.1093/scan/nsx125.
3. Itahashi T et al. Functional connectomes linking child-parent relationships with psychological problems in adolescence. Neuroimage. 2020 Oct 1;219:117013. doi: 10.1016/j.neuroimage.2020.117013.
4. Lengersdorff LL et al. When implicit prosociality trumps selfishness: The neural valuation system underpins more optimal choices when learning to avoid harm to others than to oneself. J Neurosci. 2020 Sep 16;40(38):7286-99. doi: 10.1523/JNEUROSCI.0842-20.2020.
5. Meyer ML et al. Evidence that default network connectivity during rest consolidates social information. Cereb Cortex. 2019 May 1;29(5):1910-20. doi: 10.1093/cercor/bhy071.
6. Tienari P et al. The Finnish adoptive family study of schizophrenia. Implications for family research. Br J Psychiatry Suppl. 1994 Apr;(23):20-6.
7. Luhrmann, TM. Of two minds: The growing disorder in American psychiatry. New York, NY: Alfred A. Knopf, 2000.
8. Libbon R et al. Family skills for the resident toolbox: The 10-min. Genogram, Ecomap, and Prescribing Homework. Acad Psychiatry. 2019 Aug;43(4):435-439. doi: 10.1007/s40596-019-01054-6.
Neuroscience expands our knowledge of relational and social worlds
Neuroscience expands our knowledge of relational and social worlds
Psychiatry may be emerging from the era of psychopharmacology and entering the era of the brain, but these reductionist, jingoistic labels do little justice to the need to acknowledge and incorporate the context of our lives into our theories and treatments. Yet psychiatrists who embrace context have much to celebrate in evolving neuroscience research.
One aptly named article – ’Families that fire together smile together’ – illustrates the fundamental connection between parent and child.1 In the functional MRIs (fMRIs) taken of these parent-child dyads (n = 76), the dyads with similar resting state connectomes also have similar day-to-day emotional states, as reflected in their diary entries. Their empathic states were identified in the multivoxel patterns in the fusiform face area of the brain.2 Another study of fMRIs and parent-child dyads (n = 93) found that the parental functional connectomes (fbc) predicted their children’s externalizing and internalizing problems. The maternal fbcs were correlated with the daughter-mother relationship, and to the daughter’s internalizing problems, suggesting a potential future focus on gendered relationships.3
The implications for psychotherapy are clear: These studies show that empathic connection between parent and child results in a better outcome for the child. Patient and psychotherapist can choose from a range of psychotherapeutic interventions that promote empathy, from providing behavioral tasks that support connection between parent and child to more in-depth family interventions. Family interventions that promote empathy include increasing the family’s understanding of the importance of empathic connection and providing a safe space to help establish empathic connection.
Studying prosocial behavior, Lukas Lengersdorff and colleagues found that fMRIs of male participants (n = 96) reflected stronger activity when they were acting on behalf of the other, rather than when acting for themselves.4 During this prosocial learning fMRI study, there was stronger engagement of the ventromedial prefrontal cortex (PFC) and higher connectivity between the ventromedial PFC and the right temporoparietal junction (rTPJ). Protecting others from harm appears to be associated with neural mechanisms that support self-relevant learning, but with the added recruitment of structures associated with the social brain. This study shows what we already know – that our brains are wired for social context. This research supports psychotherapeutic interventions aimed at creating interpersonal connection, not just at an intimate level, but also at the prosocial level, such as caring and helping others.
When social interactions are coded, the default mode network (DMN) shows increased activity. Participants (n = 11) in another study had heightened medial PFC–rTPJ connectivity, not only during rest that followed the experimental social encoding, but also during rest that followed a subsequent, nonsocial task.5 Engaging portions of the DMN during live social interactions when actively decoding the social environment, and later engaging these regions when relaxing after the social interaction, appears to facilitate social functioning. Our brains are wired to respond to context. This research underscores the positive impact of interventions such as group therapy and support groups, two underutilized modalities.
Neuroscience evaluation of our relationships provides depth to studies that fall under the medical paradigm of the gene/environment interaction. One of the most elegant in psychiatry is the Finnish study of a sample of offspring of mothers with schizophrenia who gave their children up for adoption.6 This sample of index offspring (n = 155) was compared blindly with matched controls (n = 186) of adopted/away offspring of parents without schizophrenia. The genetic effect manifested only as a psychiatric disorder in the presence of a disturbed family environment. We can now extrapolate certain possible mechanisms from the studies mentioned above: That the deficits lie in the activity or lack of activity in the DMN and associated areas, and in the generation of connectomes responsible for empathic connections.
Neuroscience expands our knowledge of our relational and social worlds, but can psychiatry make the case for inclusion of context in our conceptualization of psychiatric distress? From time to time, inroads are made, for example, the Global Assessment of Relational Functioning was incorporated into the DSM-IV-R and the Cultural Formulation Interview is in the DSM-5. However, without a sustained paradigm shift that places the gene/environment paradigm at the core of psychiatry, these efforts will rise and fall as the pioneers in these fields rise and fall.
A major barrier to moving the gene/environment paradigm more centrally in psychiatry is the prominence of individualism as an American ideal. As the neuroscience of context develops, we will be able to argue more robustly for a contextual approach to patient care.
A second barrier is the difficulty of teaching and learning about complexity. It is easy to learn how to use the DSM to make a diagnosis, to understand when and how to prescribe medications, but it is much more difficult to understand how to incorporate the complexity of life and the context within which we live, into our lexicon of psychiatric theories and treatments. As Tanya Luhrmann, PhD, points out in her study of the process of psychiatric training, residents are intimidated by the need to learn the many psychological theories and their practice; learning about medications is much simpler and takes much less time and effort.7
Nevertheless, context is embraced by several psychiatric subspecialties. Family psychiatrists recognize the power of relational dynamics in the family, and their role in shaping the individual. From understanding family communication patterns, to understanding how roles in the family get allocated, family psychiatry has well established tools for assessment and many evidence-based treatments that focus on changing relational dynamics. Social and community psychiatrists emphasize the role of race, poverty, and access, and support the assessment and treatment of the underprivileged. Cultural psychiatrists recognize that each culture has its own way of constructing identities and shaping our experiences, its own conceptualization of illness and specific idioms of distress. Cultural psychiatrists focus on sensitizing the general psychiatrist to these nuances. Child psychiatrists involve parents, and geriatric psychiatrists involve guardians. General psychiatrists understand context when, for example, understanding the role of trauma in the development of an individual, recognizing that its impact is contingent on the context within which the trauma occurs.
Neuroscience clarifies the neural pathways involved in the development of empathic and social behaviors. Our psychological theories and practice must reflect this advancement. We can teach the relevant neuroscience along with basic concepts such as child-parent relationships. We must assess an individual’s degree of fit within their family and community. Apart from asking relational questions, such as who in your world is important to you, we can use well recognized tools to help us bring context to the forefront. An easy tool is the three generational genogram, or an ecomap, which allows each individual to see where they sit in the context of their world.8 Cultural influences, societal, religious, and family influences can be drawn on the genogram, highlighting both formal and hidden family narratives. In addition, we can share how the brain works with our patients; the science of empathy and social behaviors shows us that our need for interpersonal connection is hardwired.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
References
1. Lee TH et al. Families that fire together smile together: Resting state connectome similarity and daily emotional synchrony in parent-child dyads. Neuroimage. 2017 May 15;152:31-37. doi: 10.1016/j.neuroimage.2017.02.078.
2. Lee TH et al. Love flows downstream: Mothers’ and children’s neural representation similarity in perceiving distress of self and family. Soc Cogn Affect Neurosci. 2017 Dec 1;12(12):1916-27. doi: 10.1093/scan/nsx125.
3. Itahashi T et al. Functional connectomes linking child-parent relationships with psychological problems in adolescence. Neuroimage. 2020 Oct 1;219:117013. doi: 10.1016/j.neuroimage.2020.117013.
4. Lengersdorff LL et al. When implicit prosociality trumps selfishness: The neural valuation system underpins more optimal choices when learning to avoid harm to others than to oneself. J Neurosci. 2020 Sep 16;40(38):7286-99. doi: 10.1523/JNEUROSCI.0842-20.2020.
5. Meyer ML et al. Evidence that default network connectivity during rest consolidates social information. Cereb Cortex. 2019 May 1;29(5):1910-20. doi: 10.1093/cercor/bhy071.
6. Tienari P et al. The Finnish adoptive family study of schizophrenia. Implications for family research. Br J Psychiatry Suppl. 1994 Apr;(23):20-6.
7. Luhrmann, TM. Of two minds: The growing disorder in American psychiatry. New York, NY: Alfred A. Knopf, 2000.
8. Libbon R et al. Family skills for the resident toolbox: The 10-min. Genogram, Ecomap, and Prescribing Homework. Acad Psychiatry. 2019 Aug;43(4):435-439. doi: 10.1007/s40596-019-01054-6.
Psychiatry may be emerging from the era of psychopharmacology and entering the era of the brain, but these reductionist, jingoistic labels do little justice to the need to acknowledge and incorporate the context of our lives into our theories and treatments. Yet psychiatrists who embrace context have much to celebrate in evolving neuroscience research.
One aptly named article – ’Families that fire together smile together’ – illustrates the fundamental connection between parent and child.1 In the functional MRIs (fMRIs) taken of these parent-child dyads (n = 76), the dyads with similar resting state connectomes also have similar day-to-day emotional states, as reflected in their diary entries. Their empathic states were identified in the multivoxel patterns in the fusiform face area of the brain.2 Another study of fMRIs and parent-child dyads (n = 93) found that the parental functional connectomes (fbc) predicted their children’s externalizing and internalizing problems. The maternal fbcs were correlated with the daughter-mother relationship, and to the daughter’s internalizing problems, suggesting a potential future focus on gendered relationships.3
The implications for psychotherapy are clear: These studies show that empathic connection between parent and child results in a better outcome for the child. Patient and psychotherapist can choose from a range of psychotherapeutic interventions that promote empathy, from providing behavioral tasks that support connection between parent and child to more in-depth family interventions. Family interventions that promote empathy include increasing the family’s understanding of the importance of empathic connection and providing a safe space to help establish empathic connection.
Studying prosocial behavior, Lukas Lengersdorff and colleagues found that fMRIs of male participants (n = 96) reflected stronger activity when they were acting on behalf of the other, rather than when acting for themselves.4 During this prosocial learning fMRI study, there was stronger engagement of the ventromedial prefrontal cortex (PFC) and higher connectivity between the ventromedial PFC and the right temporoparietal junction (rTPJ). Protecting others from harm appears to be associated with neural mechanisms that support self-relevant learning, but with the added recruitment of structures associated with the social brain. This study shows what we already know – that our brains are wired for social context. This research supports psychotherapeutic interventions aimed at creating interpersonal connection, not just at an intimate level, but also at the prosocial level, such as caring and helping others.
When social interactions are coded, the default mode network (DMN) shows increased activity. Participants (n = 11) in another study had heightened medial PFC–rTPJ connectivity, not only during rest that followed the experimental social encoding, but also during rest that followed a subsequent, nonsocial task.5 Engaging portions of the DMN during live social interactions when actively decoding the social environment, and later engaging these regions when relaxing after the social interaction, appears to facilitate social functioning. Our brains are wired to respond to context. This research underscores the positive impact of interventions such as group therapy and support groups, two underutilized modalities.
Neuroscience evaluation of our relationships provides depth to studies that fall under the medical paradigm of the gene/environment interaction. One of the most elegant in psychiatry is the Finnish study of a sample of offspring of mothers with schizophrenia who gave their children up for adoption.6 This sample of index offspring (n = 155) was compared blindly with matched controls (n = 186) of adopted/away offspring of parents without schizophrenia. The genetic effect manifested only as a psychiatric disorder in the presence of a disturbed family environment. We can now extrapolate certain possible mechanisms from the studies mentioned above: That the deficits lie in the activity or lack of activity in the DMN and associated areas, and in the generation of connectomes responsible for empathic connections.
Neuroscience expands our knowledge of our relational and social worlds, but can psychiatry make the case for inclusion of context in our conceptualization of psychiatric distress? From time to time, inroads are made, for example, the Global Assessment of Relational Functioning was incorporated into the DSM-IV-R and the Cultural Formulation Interview is in the DSM-5. However, without a sustained paradigm shift that places the gene/environment paradigm at the core of psychiatry, these efforts will rise and fall as the pioneers in these fields rise and fall.
A major barrier to moving the gene/environment paradigm more centrally in psychiatry is the prominence of individualism as an American ideal. As the neuroscience of context develops, we will be able to argue more robustly for a contextual approach to patient care.
A second barrier is the difficulty of teaching and learning about complexity. It is easy to learn how to use the DSM to make a diagnosis, to understand when and how to prescribe medications, but it is much more difficult to understand how to incorporate the complexity of life and the context within which we live, into our lexicon of psychiatric theories and treatments. As Tanya Luhrmann, PhD, points out in her study of the process of psychiatric training, residents are intimidated by the need to learn the many psychological theories and their practice; learning about medications is much simpler and takes much less time and effort.7
Nevertheless, context is embraced by several psychiatric subspecialties. Family psychiatrists recognize the power of relational dynamics in the family, and their role in shaping the individual. From understanding family communication patterns, to understanding how roles in the family get allocated, family psychiatry has well established tools for assessment and many evidence-based treatments that focus on changing relational dynamics. Social and community psychiatrists emphasize the role of race, poverty, and access, and support the assessment and treatment of the underprivileged. Cultural psychiatrists recognize that each culture has its own way of constructing identities and shaping our experiences, its own conceptualization of illness and specific idioms of distress. Cultural psychiatrists focus on sensitizing the general psychiatrist to these nuances. Child psychiatrists involve parents, and geriatric psychiatrists involve guardians. General psychiatrists understand context when, for example, understanding the role of trauma in the development of an individual, recognizing that its impact is contingent on the context within which the trauma occurs.
Neuroscience clarifies the neural pathways involved in the development of empathic and social behaviors. Our psychological theories and practice must reflect this advancement. We can teach the relevant neuroscience along with basic concepts such as child-parent relationships. We must assess an individual’s degree of fit within their family and community. Apart from asking relational questions, such as who in your world is important to you, we can use well recognized tools to help us bring context to the forefront. An easy tool is the three generational genogram, or an ecomap, which allows each individual to see where they sit in the context of their world.8 Cultural influences, societal, religious, and family influences can be drawn on the genogram, highlighting both formal and hidden family narratives. In addition, we can share how the brain works with our patients; the science of empathy and social behaviors shows us that our need for interpersonal connection is hardwired.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
References
1. Lee TH et al. Families that fire together smile together: Resting state connectome similarity and daily emotional synchrony in parent-child dyads. Neuroimage. 2017 May 15;152:31-37. doi: 10.1016/j.neuroimage.2017.02.078.
2. Lee TH et al. Love flows downstream: Mothers’ and children’s neural representation similarity in perceiving distress of self and family. Soc Cogn Affect Neurosci. 2017 Dec 1;12(12):1916-27. doi: 10.1093/scan/nsx125.
3. Itahashi T et al. Functional connectomes linking child-parent relationships with psychological problems in adolescence. Neuroimage. 2020 Oct 1;219:117013. doi: 10.1016/j.neuroimage.2020.117013.
4. Lengersdorff LL et al. When implicit prosociality trumps selfishness: The neural valuation system underpins more optimal choices when learning to avoid harm to others than to oneself. J Neurosci. 2020 Sep 16;40(38):7286-99. doi: 10.1523/JNEUROSCI.0842-20.2020.
5. Meyer ML et al. Evidence that default network connectivity during rest consolidates social information. Cereb Cortex. 2019 May 1;29(5):1910-20. doi: 10.1093/cercor/bhy071.
6. Tienari P et al. The Finnish adoptive family study of schizophrenia. Implications for family research. Br J Psychiatry Suppl. 1994 Apr;(23):20-6.
7. Luhrmann, TM. Of two minds: The growing disorder in American psychiatry. New York, NY: Alfred A. Knopf, 2000.
8. Libbon R et al. Family skills for the resident toolbox: The 10-min. Genogram, Ecomap, and Prescribing Homework. Acad Psychiatry. 2019 Aug;43(4):435-439. doi: 10.1007/s40596-019-01054-6.
Schizophrenia and HIV: missed opportunities for care
“People don’t think about schizophrenia when they think about HIV,” Christina Mangurian, MD, professor of clinical psychiatry and vice chair for diversity and health equity at the University of California, San Francisco (UCSF), told this news organization.
The problem is complicated. According to the Centers for Disease Control and Prevention and National Institutes of Health, roughly 6% of people with serious mental illness are living with HIV, a rate that is about 10 times higher than the general U.S. population (0.4%). However, findings from a study by Dr. Mangurian and her team, published online in the journal AIDS, demonstrated that half of Medicaid patients with schizophrenia and HIV admitted to inpatient units in New York State were not coded as such upon discharge.
These data raise the question: , lack of social support, and under-recognition by practitioners that a problem even exists?
Lost in the care continuum
Dr. Mangurian and her research team examined documentation of pre-existing HIV/AIDS diagnoses and absence of ICD-9-CM HIV/AIDS coding at psychiatric discharge among 14,602 adults (aged 18-64 years) admitted to hospital inpatient units in New York State between Jan. 1, 2012, and Dec. 31, 2013. HIV diagnoses were defined as recent (within 30 days of admission) or distant (within 30-366 days of admission), and first admission was used as the index in people with multiple hospitalizations.
People living with HIV comprised 5.1% (741) of the overall dataset; 34% were diagnosed with schizophrenia and 27.9% with bipolar disorders. Overall, 54.5% were male and 50.7% were non-Hispanic Black. Furthermore, 58.3% were discharged without HIV/AIDS ICD-9 coding, reinforcing the likelihood that they were lost in the care continuum.
Dr. Mangurian explained that this break in the chain of care upon discharge can have an important impact on efforts to break the cycle of HIV transmission.
“There’s data that people with serious mental illnesses like schizophrenia are less likely to have sex, but when they do they’re more likely to engage in risky sexual behaviors, including sex for money [and] unprotected sex with partners who use injection drugs or who have HIV,” she said.
Although the majority of patients – both with and without prior HIV diagnoses – were older, adjusted models demonstrated that people aged 18-24 years had more than twice the odds of having their HIV/AIDS undocumented at discharge, compared with older adults aged 55-64 years (adjusted odds ratio, 2.37; P = .038), as were those aged 25-34 years (aOR, 2.17; P = .003). Individuals with more distant HIV diagnoses had three times the odds for an undocumented HIV/AIDS discharge, compared with more recent diagnoses (aOR, 3.25; P < .001).
Additional factors contributing to the lack of ICD-9 discharge coding included shorter lengths of stay (0-3 days vs. 15-30 days; aOR, 0.03; P = .01) and fewer HIV claims for HIV/AIDS services before hospitalization (1-2 vs. 3-9; aOR, 0.34; P < .01). Hospitals serving medium or high levels of Medicaid patients were also less likely to document HIV/AIDS before discharge (medium aOR, 1.69, P = .01; high aOR, 1.71, P = .03).
The study is not without limitations. For example, the 10-year-old dataset might not entirely reflect more recent structural or systemic changes for improving HIV detection on inpatient psychiatric units. Moreover, there was no comparator group without psychiatric inpatient admission.
Still, “[if these patients] didn’t have a discharge diagnosis, then it’s possible that they were not managed for their HIV, or their HIV was not addressed while they were in the hospital,” Sarah Andrews, MD, assistant professor of psychiatry and behavioral sciences and AIDS psychiatrist at Johns Hopkins School of Medicine, Baltimore, explained.
Dr. Andrews, who was not involved in the study, noted that this omission is significant. “A psychiatric admission or medical admission in general is a great opportunity to further manage and treat comorbidities. When we have a patient who comes in with HIV and they haven’t been on an antiviral prior to admission, we try to get infectious disease to give us recommendations of what to start, what labs to draw, to help them re-establish care,” she said.
Severe mental health an HIV disparity
Despite the burden of HIV among patient populations with serious mental health issues and data suggesting that these populations are over-represented among new HIV infections, the study findings point to an important missed opportunity for meeting several key outcomes on the HIV/AIDS care continuum, especially linkage to and retention in care.
The challenge is multifactorial.
In an earlier publication appearing in April 2021 in The Lancet HIV, Dr. Mangurian and colleagues explore a concept known as the “purview paradox,” which refers to a practitioner’s belief about who should be responsible for offering patients a particular intervention.
Structural and systemic issues also abound, as psychiatry records are often kept separate from the rest of the medical system due to insurer billing issues. “The true integration of all psychiatric and medical care has to happen to make sure that all of our patients receive the care that they deserve,” explained Dr. Mangurian.
Dr. Andrews agrees. “HIV care, as well as psychiatry, case management, pharmacy ... putting them together really helps decrease the risk of falling through the cracks and being able to refer appropriately for mental health,” she said.
Aside from changing practitioner attitudes and awareness and changing systems to include the wrap-around care model, current guidelines also need to reflect the role that patients with HIV and psychiatric comorbidities play in HIV transmission. Dr. Andrews and Dr. Mangurian agree: Routine screening in psychiatric inpatient units might be a good start.
The study was independently supported. Dr. Mangurian has reported grant funding from Genentech Charitable Foundation. Dr. Andrews has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“People don’t think about schizophrenia when they think about HIV,” Christina Mangurian, MD, professor of clinical psychiatry and vice chair for diversity and health equity at the University of California, San Francisco (UCSF), told this news organization.
The problem is complicated. According to the Centers for Disease Control and Prevention and National Institutes of Health, roughly 6% of people with serious mental illness are living with HIV, a rate that is about 10 times higher than the general U.S. population (0.4%). However, findings from a study by Dr. Mangurian and her team, published online in the journal AIDS, demonstrated that half of Medicaid patients with schizophrenia and HIV admitted to inpatient units in New York State were not coded as such upon discharge.
These data raise the question: , lack of social support, and under-recognition by practitioners that a problem even exists?
Lost in the care continuum
Dr. Mangurian and her research team examined documentation of pre-existing HIV/AIDS diagnoses and absence of ICD-9-CM HIV/AIDS coding at psychiatric discharge among 14,602 adults (aged 18-64 years) admitted to hospital inpatient units in New York State between Jan. 1, 2012, and Dec. 31, 2013. HIV diagnoses were defined as recent (within 30 days of admission) or distant (within 30-366 days of admission), and first admission was used as the index in people with multiple hospitalizations.
People living with HIV comprised 5.1% (741) of the overall dataset; 34% were diagnosed with schizophrenia and 27.9% with bipolar disorders. Overall, 54.5% were male and 50.7% were non-Hispanic Black. Furthermore, 58.3% were discharged without HIV/AIDS ICD-9 coding, reinforcing the likelihood that they were lost in the care continuum.
Dr. Mangurian explained that this break in the chain of care upon discharge can have an important impact on efforts to break the cycle of HIV transmission.
“There’s data that people with serious mental illnesses like schizophrenia are less likely to have sex, but when they do they’re more likely to engage in risky sexual behaviors, including sex for money [and] unprotected sex with partners who use injection drugs or who have HIV,” she said.
Although the majority of patients – both with and without prior HIV diagnoses – were older, adjusted models demonstrated that people aged 18-24 years had more than twice the odds of having their HIV/AIDS undocumented at discharge, compared with older adults aged 55-64 years (adjusted odds ratio, 2.37; P = .038), as were those aged 25-34 years (aOR, 2.17; P = .003). Individuals with more distant HIV diagnoses had three times the odds for an undocumented HIV/AIDS discharge, compared with more recent diagnoses (aOR, 3.25; P < .001).
Additional factors contributing to the lack of ICD-9 discharge coding included shorter lengths of stay (0-3 days vs. 15-30 days; aOR, 0.03; P = .01) and fewer HIV claims for HIV/AIDS services before hospitalization (1-2 vs. 3-9; aOR, 0.34; P < .01). Hospitals serving medium or high levels of Medicaid patients were also less likely to document HIV/AIDS before discharge (medium aOR, 1.69, P = .01; high aOR, 1.71, P = .03).
The study is not without limitations. For example, the 10-year-old dataset might not entirely reflect more recent structural or systemic changes for improving HIV detection on inpatient psychiatric units. Moreover, there was no comparator group without psychiatric inpatient admission.
Still, “[if these patients] didn’t have a discharge diagnosis, then it’s possible that they were not managed for their HIV, or their HIV was not addressed while they were in the hospital,” Sarah Andrews, MD, assistant professor of psychiatry and behavioral sciences and AIDS psychiatrist at Johns Hopkins School of Medicine, Baltimore, explained.
Dr. Andrews, who was not involved in the study, noted that this omission is significant. “A psychiatric admission or medical admission in general is a great opportunity to further manage and treat comorbidities. When we have a patient who comes in with HIV and they haven’t been on an antiviral prior to admission, we try to get infectious disease to give us recommendations of what to start, what labs to draw, to help them re-establish care,” she said.
Severe mental health an HIV disparity
Despite the burden of HIV among patient populations with serious mental health issues and data suggesting that these populations are over-represented among new HIV infections, the study findings point to an important missed opportunity for meeting several key outcomes on the HIV/AIDS care continuum, especially linkage to and retention in care.
The challenge is multifactorial.
In an earlier publication appearing in April 2021 in The Lancet HIV, Dr. Mangurian and colleagues explore a concept known as the “purview paradox,” which refers to a practitioner’s belief about who should be responsible for offering patients a particular intervention.
Structural and systemic issues also abound, as psychiatry records are often kept separate from the rest of the medical system due to insurer billing issues. “The true integration of all psychiatric and medical care has to happen to make sure that all of our patients receive the care that they deserve,” explained Dr. Mangurian.
Dr. Andrews agrees. “HIV care, as well as psychiatry, case management, pharmacy ... putting them together really helps decrease the risk of falling through the cracks and being able to refer appropriately for mental health,” she said.
Aside from changing practitioner attitudes and awareness and changing systems to include the wrap-around care model, current guidelines also need to reflect the role that patients with HIV and psychiatric comorbidities play in HIV transmission. Dr. Andrews and Dr. Mangurian agree: Routine screening in psychiatric inpatient units might be a good start.
The study was independently supported. Dr. Mangurian has reported grant funding from Genentech Charitable Foundation. Dr. Andrews has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“People don’t think about schizophrenia when they think about HIV,” Christina Mangurian, MD, professor of clinical psychiatry and vice chair for diversity and health equity at the University of California, San Francisco (UCSF), told this news organization.
The problem is complicated. According to the Centers for Disease Control and Prevention and National Institutes of Health, roughly 6% of people with serious mental illness are living with HIV, a rate that is about 10 times higher than the general U.S. population (0.4%). However, findings from a study by Dr. Mangurian and her team, published online in the journal AIDS, demonstrated that half of Medicaid patients with schizophrenia and HIV admitted to inpatient units in New York State were not coded as such upon discharge.
These data raise the question: , lack of social support, and under-recognition by practitioners that a problem even exists?
Lost in the care continuum
Dr. Mangurian and her research team examined documentation of pre-existing HIV/AIDS diagnoses and absence of ICD-9-CM HIV/AIDS coding at psychiatric discharge among 14,602 adults (aged 18-64 years) admitted to hospital inpatient units in New York State between Jan. 1, 2012, and Dec. 31, 2013. HIV diagnoses were defined as recent (within 30 days of admission) or distant (within 30-366 days of admission), and first admission was used as the index in people with multiple hospitalizations.
People living with HIV comprised 5.1% (741) of the overall dataset; 34% were diagnosed with schizophrenia and 27.9% with bipolar disorders. Overall, 54.5% were male and 50.7% were non-Hispanic Black. Furthermore, 58.3% were discharged without HIV/AIDS ICD-9 coding, reinforcing the likelihood that they were lost in the care continuum.
Dr. Mangurian explained that this break in the chain of care upon discharge can have an important impact on efforts to break the cycle of HIV transmission.
“There’s data that people with serious mental illnesses like schizophrenia are less likely to have sex, but when they do they’re more likely to engage in risky sexual behaviors, including sex for money [and] unprotected sex with partners who use injection drugs or who have HIV,” she said.
Although the majority of patients – both with and without prior HIV diagnoses – were older, adjusted models demonstrated that people aged 18-24 years had more than twice the odds of having their HIV/AIDS undocumented at discharge, compared with older adults aged 55-64 years (adjusted odds ratio, 2.37; P = .038), as were those aged 25-34 years (aOR, 2.17; P = .003). Individuals with more distant HIV diagnoses had three times the odds for an undocumented HIV/AIDS discharge, compared with more recent diagnoses (aOR, 3.25; P < .001).
Additional factors contributing to the lack of ICD-9 discharge coding included shorter lengths of stay (0-3 days vs. 15-30 days; aOR, 0.03; P = .01) and fewer HIV claims for HIV/AIDS services before hospitalization (1-2 vs. 3-9; aOR, 0.34; P < .01). Hospitals serving medium or high levels of Medicaid patients were also less likely to document HIV/AIDS before discharge (medium aOR, 1.69, P = .01; high aOR, 1.71, P = .03).
The study is not without limitations. For example, the 10-year-old dataset might not entirely reflect more recent structural or systemic changes for improving HIV detection on inpatient psychiatric units. Moreover, there was no comparator group without psychiatric inpatient admission.
Still, “[if these patients] didn’t have a discharge diagnosis, then it’s possible that they were not managed for their HIV, or their HIV was not addressed while they were in the hospital,” Sarah Andrews, MD, assistant professor of psychiatry and behavioral sciences and AIDS psychiatrist at Johns Hopkins School of Medicine, Baltimore, explained.
Dr. Andrews, who was not involved in the study, noted that this omission is significant. “A psychiatric admission or medical admission in general is a great opportunity to further manage and treat comorbidities. When we have a patient who comes in with HIV and they haven’t been on an antiviral prior to admission, we try to get infectious disease to give us recommendations of what to start, what labs to draw, to help them re-establish care,” she said.
Severe mental health an HIV disparity
Despite the burden of HIV among patient populations with serious mental health issues and data suggesting that these populations are over-represented among new HIV infections, the study findings point to an important missed opportunity for meeting several key outcomes on the HIV/AIDS care continuum, especially linkage to and retention in care.
The challenge is multifactorial.
In an earlier publication appearing in April 2021 in The Lancet HIV, Dr. Mangurian and colleagues explore a concept known as the “purview paradox,” which refers to a practitioner’s belief about who should be responsible for offering patients a particular intervention.
Structural and systemic issues also abound, as psychiatry records are often kept separate from the rest of the medical system due to insurer billing issues. “The true integration of all psychiatric and medical care has to happen to make sure that all of our patients receive the care that they deserve,” explained Dr. Mangurian.
Dr. Andrews agrees. “HIV care, as well as psychiatry, case management, pharmacy ... putting them together really helps decrease the risk of falling through the cracks and being able to refer appropriately for mental health,” she said.
Aside from changing practitioner attitudes and awareness and changing systems to include the wrap-around care model, current guidelines also need to reflect the role that patients with HIV and psychiatric comorbidities play in HIV transmission. Dr. Andrews and Dr. Mangurian agree: Routine screening in psychiatric inpatient units might be a good start.
The study was independently supported. Dr. Mangurian has reported grant funding from Genentech Charitable Foundation. Dr. Andrews has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cat ownership in childhood linked ‘conditionally’ to psychosis in adult males
Owning an outdoor cat as a child is associated with an increased risk of psychotic experiences in adulthood – but only in males, new research suggests.
Investigators found
The suspected culprit is not the cat itself but rather exposure to Toxoplasma gondii, a common parasite carried by rodents and sometimes found in cat feces. The study adds to a growing evidence showing exposure to T. gondii may be a risk factor for schizophrenia and other psychotic disorders.
“These are small pieces of evidence but it’s interesting to consider that there might be combinations of risk factors at play,” lead author Vincent Paquin, MD, psychiatry resident at McGill University, Montreal, said in an interview.
“And even if the magnitude of the risk is small at the individual level,” he added, “cats and Toxoplasma gondii are so present in our society that if we add up all these small potential effects then it becomes a potential public health question.”
The study was published online Jan. 30, 2022, in the Journal of Psychiatric Research.
Inconsistent evidence
T. gondii infects about 30% of the human population and is usually transmitted by cats. Most infections are asymptomatic, but T. gondii can cause toxoplasmosis in humans, which has been linked to increased risk of schizophrenia, suicide attempts, and more recently, mild cognitive impairment.
Although some studies show an association between cat ownership and increased risk of mental illness, the research findings have been inconsistent.
“The evidence has been mixed about the association between cat ownership and psychosis expression, so our approach was to consider whether specific factors or combinations of factors could explain this mixed evidence,” Dr. Paquin said.
For the study, 2206 individuals aged 18-40 years completed the Community Assessment of Psychic Experiences (CAPE-42) and a questionnaire to gather information about cat ownership at any time between birth and age 13 and if the cats lived exclusively indoors (nonhunting) or if they were allowed outside (rodent hunting).
Participants were also asked about the number of residential moves between birth and age 15, date and place of birth, lifetime history of head trauma, and tobacco smoking history.
Rodent-hunting cat ownership was associated with higher risk of psychosis in male participants, compared with owning no cat or a nonhunting cat. When the investigators added head trauma and residential moves to rodent-hunting cat ownership, psychosis risk was elevated in both men and women.
Independent of cat ownership, younger age, moving more than three times as a child, a history of head trauma, and being a smoker were all associated with higher psychosis risk.
The study wasn’t designed to explore potential biological mechanisms to explain the sex differences in psychosis risk seen among rodent-hunting cat owners, but “one possible explanation based on the animal model literature is that the neurobiological effects of parasitic exposure may be greater with male sex,” senior author Suzanne King, PhD, professor of psychiatry at McGill, said in an interview.
The new study is part of a larger, long-term project called EnviroGen, led by Dr. King, examining the environmental and genetic risk factors for schizophrenia.
Need for replication
Commenting on the findings, E. Fuller Torrey, MD, who was among the first researchers to identify a link between cat ownership, T. gondii infection, and schizophrenia, said the study is “an interesting addition to the studies of cat ownership in childhood as a risk factor for psychosis.”
Of the approximately 10 published studies on the topic, about half suggest a link between cat ownership and psychosis later in life, said Dr. Torrey, associate director for research at the Stanley Medical Research Institute in Rockville, Md.
“The Canadian study is interesting in that it is the first study that separates exposure to permanently indoor cats from cats that are allowed to go outdoors, and the results were positive only for outdoor cats,” Dr. Torrey said.
The study has limitations, Dr. Torrey added, including its retrospective design and the use of a self-report questionnaire to assess psychotic experiences in adulthood.
Also commenting on findings, James Kirkbride, PhD, professor of psychiatric and social epidemiology, University College London, noted the same limitations.
Dr. Kirkbride is the lead author of a 2017 study that showed no link between cat ownership and serious mental illness that included nearly 5,000 people born in 1991 or 1992 and followed until age 18. In this study, there was no link between psychosis and cat ownership during pregnancy or at ages 4 or 10 years.
“Researchers have long been fascinated with the idea that cat ownership may affect mental health. This paper may have them chasing their own tail,” Dr. Kirkbride said.
“Evidence of any association is limited to certain subgroups without a strong theoretical basis for why this may be the case,” he added. “The retrospective and cross-sectional nature of the survey also raise the possibility that the results are impacted by differential recall bias, as well as the broader issues of chance and unobserved confounding.”
Dr. King noted that recall bias is a limitation the researchers highlighted in their study, but “considering the exposures are relatively objective and factual, we do not believe the potential for recall bias is substantial.”
“Nonetheless, we strongly believe that replication of our results in prospective, population-representative cohorts will be crucial to making firmer conclusions,” he added.
The study was funded by grants from the Quebec Health Research Fund. The study authors and Dr. Kirkbride disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Owning an outdoor cat as a child is associated with an increased risk of psychotic experiences in adulthood – but only in males, new research suggests.
Investigators found
The suspected culprit is not the cat itself but rather exposure to Toxoplasma gondii, a common parasite carried by rodents and sometimes found in cat feces. The study adds to a growing evidence showing exposure to T. gondii may be a risk factor for schizophrenia and other psychotic disorders.
“These are small pieces of evidence but it’s interesting to consider that there might be combinations of risk factors at play,” lead author Vincent Paquin, MD, psychiatry resident at McGill University, Montreal, said in an interview.
“And even if the magnitude of the risk is small at the individual level,” he added, “cats and Toxoplasma gondii are so present in our society that if we add up all these small potential effects then it becomes a potential public health question.”
The study was published online Jan. 30, 2022, in the Journal of Psychiatric Research.
Inconsistent evidence
T. gondii infects about 30% of the human population and is usually transmitted by cats. Most infections are asymptomatic, but T. gondii can cause toxoplasmosis in humans, which has been linked to increased risk of schizophrenia, suicide attempts, and more recently, mild cognitive impairment.
Although some studies show an association between cat ownership and increased risk of mental illness, the research findings have been inconsistent.
“The evidence has been mixed about the association between cat ownership and psychosis expression, so our approach was to consider whether specific factors or combinations of factors could explain this mixed evidence,” Dr. Paquin said.
For the study, 2206 individuals aged 18-40 years completed the Community Assessment of Psychic Experiences (CAPE-42) and a questionnaire to gather information about cat ownership at any time between birth and age 13 and if the cats lived exclusively indoors (nonhunting) or if they were allowed outside (rodent hunting).
Participants were also asked about the number of residential moves between birth and age 15, date and place of birth, lifetime history of head trauma, and tobacco smoking history.
Rodent-hunting cat ownership was associated with higher risk of psychosis in male participants, compared with owning no cat or a nonhunting cat. When the investigators added head trauma and residential moves to rodent-hunting cat ownership, psychosis risk was elevated in both men and women.
Independent of cat ownership, younger age, moving more than three times as a child, a history of head trauma, and being a smoker were all associated with higher psychosis risk.
The study wasn’t designed to explore potential biological mechanisms to explain the sex differences in psychosis risk seen among rodent-hunting cat owners, but “one possible explanation based on the animal model literature is that the neurobiological effects of parasitic exposure may be greater with male sex,” senior author Suzanne King, PhD, professor of psychiatry at McGill, said in an interview.
The new study is part of a larger, long-term project called EnviroGen, led by Dr. King, examining the environmental and genetic risk factors for schizophrenia.
Need for replication
Commenting on the findings, E. Fuller Torrey, MD, who was among the first researchers to identify a link between cat ownership, T. gondii infection, and schizophrenia, said the study is “an interesting addition to the studies of cat ownership in childhood as a risk factor for psychosis.”
Of the approximately 10 published studies on the topic, about half suggest a link between cat ownership and psychosis later in life, said Dr. Torrey, associate director for research at the Stanley Medical Research Institute in Rockville, Md.
“The Canadian study is interesting in that it is the first study that separates exposure to permanently indoor cats from cats that are allowed to go outdoors, and the results were positive only for outdoor cats,” Dr. Torrey said.
The study has limitations, Dr. Torrey added, including its retrospective design and the use of a self-report questionnaire to assess psychotic experiences in adulthood.
Also commenting on findings, James Kirkbride, PhD, professor of psychiatric and social epidemiology, University College London, noted the same limitations.
Dr. Kirkbride is the lead author of a 2017 study that showed no link between cat ownership and serious mental illness that included nearly 5,000 people born in 1991 or 1992 and followed until age 18. In this study, there was no link between psychosis and cat ownership during pregnancy or at ages 4 or 10 years.
“Researchers have long been fascinated with the idea that cat ownership may affect mental health. This paper may have them chasing their own tail,” Dr. Kirkbride said.
“Evidence of any association is limited to certain subgroups without a strong theoretical basis for why this may be the case,” he added. “The retrospective and cross-sectional nature of the survey also raise the possibility that the results are impacted by differential recall bias, as well as the broader issues of chance and unobserved confounding.”
Dr. King noted that recall bias is a limitation the researchers highlighted in their study, but “considering the exposures are relatively objective and factual, we do not believe the potential for recall bias is substantial.”
“Nonetheless, we strongly believe that replication of our results in prospective, population-representative cohorts will be crucial to making firmer conclusions,” he added.
The study was funded by grants from the Quebec Health Research Fund. The study authors and Dr. Kirkbride disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Owning an outdoor cat as a child is associated with an increased risk of psychotic experiences in adulthood – but only in males, new research suggests.
Investigators found
The suspected culprit is not the cat itself but rather exposure to Toxoplasma gondii, a common parasite carried by rodents and sometimes found in cat feces. The study adds to a growing evidence showing exposure to T. gondii may be a risk factor for schizophrenia and other psychotic disorders.
“These are small pieces of evidence but it’s interesting to consider that there might be combinations of risk factors at play,” lead author Vincent Paquin, MD, psychiatry resident at McGill University, Montreal, said in an interview.
“And even if the magnitude of the risk is small at the individual level,” he added, “cats and Toxoplasma gondii are so present in our society that if we add up all these small potential effects then it becomes a potential public health question.”
The study was published online Jan. 30, 2022, in the Journal of Psychiatric Research.
Inconsistent evidence
T. gondii infects about 30% of the human population and is usually transmitted by cats. Most infections are asymptomatic, but T. gondii can cause toxoplasmosis in humans, which has been linked to increased risk of schizophrenia, suicide attempts, and more recently, mild cognitive impairment.
Although some studies show an association between cat ownership and increased risk of mental illness, the research findings have been inconsistent.
“The evidence has been mixed about the association between cat ownership and psychosis expression, so our approach was to consider whether specific factors or combinations of factors could explain this mixed evidence,” Dr. Paquin said.
For the study, 2206 individuals aged 18-40 years completed the Community Assessment of Psychic Experiences (CAPE-42) and a questionnaire to gather information about cat ownership at any time between birth and age 13 and if the cats lived exclusively indoors (nonhunting) or if they were allowed outside (rodent hunting).
Participants were also asked about the number of residential moves between birth and age 15, date and place of birth, lifetime history of head trauma, and tobacco smoking history.
Rodent-hunting cat ownership was associated with higher risk of psychosis in male participants, compared with owning no cat or a nonhunting cat. When the investigators added head trauma and residential moves to rodent-hunting cat ownership, psychosis risk was elevated in both men and women.
Independent of cat ownership, younger age, moving more than three times as a child, a history of head trauma, and being a smoker were all associated with higher psychosis risk.
The study wasn’t designed to explore potential biological mechanisms to explain the sex differences in psychosis risk seen among rodent-hunting cat owners, but “one possible explanation based on the animal model literature is that the neurobiological effects of parasitic exposure may be greater with male sex,” senior author Suzanne King, PhD, professor of psychiatry at McGill, said in an interview.
The new study is part of a larger, long-term project called EnviroGen, led by Dr. King, examining the environmental and genetic risk factors for schizophrenia.
Need for replication
Commenting on the findings, E. Fuller Torrey, MD, who was among the first researchers to identify a link between cat ownership, T. gondii infection, and schizophrenia, said the study is “an interesting addition to the studies of cat ownership in childhood as a risk factor for psychosis.”
Of the approximately 10 published studies on the topic, about half suggest a link between cat ownership and psychosis later in life, said Dr. Torrey, associate director for research at the Stanley Medical Research Institute in Rockville, Md.
“The Canadian study is interesting in that it is the first study that separates exposure to permanently indoor cats from cats that are allowed to go outdoors, and the results were positive only for outdoor cats,” Dr. Torrey said.
The study has limitations, Dr. Torrey added, including its retrospective design and the use of a self-report questionnaire to assess psychotic experiences in adulthood.
Also commenting on findings, James Kirkbride, PhD, professor of psychiatric and social epidemiology, University College London, noted the same limitations.
Dr. Kirkbride is the lead author of a 2017 study that showed no link between cat ownership and serious mental illness that included nearly 5,000 people born in 1991 or 1992 and followed until age 18. In this study, there was no link between psychosis and cat ownership during pregnancy or at ages 4 or 10 years.
“Researchers have long been fascinated with the idea that cat ownership may affect mental health. This paper may have them chasing their own tail,” Dr. Kirkbride said.
“Evidence of any association is limited to certain subgroups without a strong theoretical basis for why this may be the case,” he added. “The retrospective and cross-sectional nature of the survey also raise the possibility that the results are impacted by differential recall bias, as well as the broader issues of chance and unobserved confounding.”
Dr. King noted that recall bias is a limitation the researchers highlighted in their study, but “considering the exposures are relatively objective and factual, we do not believe the potential for recall bias is substantial.”
“Nonetheless, we strongly believe that replication of our results in prospective, population-representative cohorts will be crucial to making firmer conclusions,” he added.
The study was funded by grants from the Quebec Health Research Fund. The study authors and Dr. Kirkbride disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF PSYCHIATRIC RESEARCH
Clozapine interrupted: APA, others seek FDA forum on REMS
In a Feb. 14 letter, the groups asked the FDA to reconsider its new risk evaluation and mitigation strategy (REMS) for clozapine because of concerns it had the potential to cause abrupt discontinuation of the medication.
The groups cite an Institute for Safe Medication Practices (ISMP) report of a 40-year-old woman who was a long-time clozapine user, had a cardiac arrest, and died after she stopped taking the drug because her psychiatrist was unable to register for the updated version of the REMS.
“It is unacceptable for a REMS with unproven effectiveness at meeting its goal to carry risks of interruptions that can result in rehospitalization, acute exacerbation of psychosis, increased risk of suicide, and potentially fatal orthostatic hypotension/bradycardic syndromes associated with incorrect restarts,” the groups said in the letter.
“We feel certain that this case reported in the literature is not the only serious adverse outcome from the REMS and the transition,” they added.
The letter was signed by the American Psychiatric Association, the American Association for Community Psychiatry, the American Psychiatric Nurses Association, the College of Psychiatric and Neurologic Pharmacists, the National Alliance on Mental Illness, the National Association of State Mental Health Program Directors, and the National Council for Mental Wellbeing.
Clozapine can decrease the neutrophil count, which can lead to severe neutropenia, serious infection, and death. Consequently, the FDA put additional safety measures in place governing clozapine prescribing.
In 2015, a centralized clozapine REMS replaced separate prescribing registries that the drug manufacturers maintained. There were technical issues with the 2015 start-up of that website, including data migration problems and long call wait times, the FDA said.
Subsequently, the drug’s manufacturers then decided to change the REMS platform, which created new issues that led to high call volume and long wait times for clinicians and pharmacists who were trying to enroll.
Maintaining access
In November 2021, the FDA announced it would put some aspects of a planned switch on hold. A month later, the agency made further modifications to its plan.
The FDA said it would exercise “enforcement discretion” to try to maintain access to clozapine amid hitches with the REMS transition efforts. The agency also said at the time that it would not object if pharmacists dispensed clozapine without the usual authorization. In addition, wholesalers could ship the drug to pharmacies and health care settings without confirming REMS enrollment.
The FDA also held two December meetings to allow various stakeholders to air concerns.
In their letter, the APA and other groups asked if the FDA intends to continue with accommodations, such as allowing pharmacies to order clozapine from wholesalers without restriction.
“We do not feel the issues are resolved,” the groups said.
A version of this article first appeared on Medscape.com.
In a Feb. 14 letter, the groups asked the FDA to reconsider its new risk evaluation and mitigation strategy (REMS) for clozapine because of concerns it had the potential to cause abrupt discontinuation of the medication.
The groups cite an Institute for Safe Medication Practices (ISMP) report of a 40-year-old woman who was a long-time clozapine user, had a cardiac arrest, and died after she stopped taking the drug because her psychiatrist was unable to register for the updated version of the REMS.
“It is unacceptable for a REMS with unproven effectiveness at meeting its goal to carry risks of interruptions that can result in rehospitalization, acute exacerbation of psychosis, increased risk of suicide, and potentially fatal orthostatic hypotension/bradycardic syndromes associated with incorrect restarts,” the groups said in the letter.
“We feel certain that this case reported in the literature is not the only serious adverse outcome from the REMS and the transition,” they added.
The letter was signed by the American Psychiatric Association, the American Association for Community Psychiatry, the American Psychiatric Nurses Association, the College of Psychiatric and Neurologic Pharmacists, the National Alliance on Mental Illness, the National Association of State Mental Health Program Directors, and the National Council for Mental Wellbeing.
Clozapine can decrease the neutrophil count, which can lead to severe neutropenia, serious infection, and death. Consequently, the FDA put additional safety measures in place governing clozapine prescribing.
In 2015, a centralized clozapine REMS replaced separate prescribing registries that the drug manufacturers maintained. There were technical issues with the 2015 start-up of that website, including data migration problems and long call wait times, the FDA said.
Subsequently, the drug’s manufacturers then decided to change the REMS platform, which created new issues that led to high call volume and long wait times for clinicians and pharmacists who were trying to enroll.
Maintaining access
In November 2021, the FDA announced it would put some aspects of a planned switch on hold. A month later, the agency made further modifications to its plan.
The FDA said it would exercise “enforcement discretion” to try to maintain access to clozapine amid hitches with the REMS transition efforts. The agency also said at the time that it would not object if pharmacists dispensed clozapine without the usual authorization. In addition, wholesalers could ship the drug to pharmacies and health care settings without confirming REMS enrollment.
The FDA also held two December meetings to allow various stakeholders to air concerns.
In their letter, the APA and other groups asked if the FDA intends to continue with accommodations, such as allowing pharmacies to order clozapine from wholesalers without restriction.
“We do not feel the issues are resolved,” the groups said.
A version of this article first appeared on Medscape.com.
In a Feb. 14 letter, the groups asked the FDA to reconsider its new risk evaluation and mitigation strategy (REMS) for clozapine because of concerns it had the potential to cause abrupt discontinuation of the medication.
The groups cite an Institute for Safe Medication Practices (ISMP) report of a 40-year-old woman who was a long-time clozapine user, had a cardiac arrest, and died after she stopped taking the drug because her psychiatrist was unable to register for the updated version of the REMS.
“It is unacceptable for a REMS with unproven effectiveness at meeting its goal to carry risks of interruptions that can result in rehospitalization, acute exacerbation of psychosis, increased risk of suicide, and potentially fatal orthostatic hypotension/bradycardic syndromes associated with incorrect restarts,” the groups said in the letter.
“We feel certain that this case reported in the literature is not the only serious adverse outcome from the REMS and the transition,” they added.
The letter was signed by the American Psychiatric Association, the American Association for Community Psychiatry, the American Psychiatric Nurses Association, the College of Psychiatric and Neurologic Pharmacists, the National Alliance on Mental Illness, the National Association of State Mental Health Program Directors, and the National Council for Mental Wellbeing.
Clozapine can decrease the neutrophil count, which can lead to severe neutropenia, serious infection, and death. Consequently, the FDA put additional safety measures in place governing clozapine prescribing.
In 2015, a centralized clozapine REMS replaced separate prescribing registries that the drug manufacturers maintained. There were technical issues with the 2015 start-up of that website, including data migration problems and long call wait times, the FDA said.
Subsequently, the drug’s manufacturers then decided to change the REMS platform, which created new issues that led to high call volume and long wait times for clinicians and pharmacists who were trying to enroll.
Maintaining access
In November 2021, the FDA announced it would put some aspects of a planned switch on hold. A month later, the agency made further modifications to its plan.
The FDA said it would exercise “enforcement discretion” to try to maintain access to clozapine amid hitches with the REMS transition efforts. The agency also said at the time that it would not object if pharmacists dispensed clozapine without the usual authorization. In addition, wholesalers could ship the drug to pharmacies and health care settings without confirming REMS enrollment.
The FDA also held two December meetings to allow various stakeholders to air concerns.
In their letter, the APA and other groups asked if the FDA intends to continue with accommodations, such as allowing pharmacies to order clozapine from wholesalers without restriction.
“We do not feel the issues are resolved,” the groups said.
A version of this article first appeared on Medscape.com.
Routine pharmacogenetic testing in psychiatry not indicated
LAS VEGAS –
“It’s misleading to rely on results of genetic tests to drive clinical treatment,” Dr. Nurmi, a child and adolescent psychiatrist in the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles, said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “There’s a lot of hope and promise there. But currently, we only know the tip of the iceberg about how drugs work and the genetics influencing these effects. Current testing is probably a very poor reflection of the complexity of drug effects.”
According to Dr. Nurmi, there are at least 165 Food and Drug Administration–approved drugs with pharmacogenetic information on 64 different biomarkers – 37% with CYP p450 notations. Of these, 32 psychiatric drugs have pharmacogenetic information, and most of them are dosing recommendations based on whether a patient has the variant. However, there is wide public acceptance of genetic testing in preventing the wrong drug from being used, in selecting the best drug dose, and avoiding side effects (Pharmacogenomics 2012;12[3]:197-204). “Most people have a lot of hope [for genetic testing in psychiatry],” Dr. Nurmi said. “But is the science really there? It doesn’t matter, because these companies are doing it, and you are being shown these reports from patients. Whether or not the science supports it, we’re going to have to interpret these reports and explain them to our patients – even if we don’t order them.”
Currently, she continued, clinicians practice trial and error prescribing where they might try one treatment in a class that they think that will work based on previous literature. If nothing works, they try another one. If that’s intolerable, they try a third treatment, and so on. “When we finally find the right treatment, it can take some time to get the dosing right,” Dr. Nurmi said. “So, it can take many months to get a child on the right medication. Precision treatment, on the other hand, would start off by taking a saliva or blood sample to get a printout that lets physicians know which drugs might be used with caution because they might lack efficacy at standard doses, which ones would likely have adverse effects at standard doses, and which are the best choices and what are the dosing recommendations for those choices. If we could get all the information to guide us, that would be a useful product, but right now, we don’t know enough to be able to make these determinations.”
Current evidence-based genetic testing supports a limited role for CYP2D6 and CYP2C19 genotyping because most psychiatric drugs are metabolized by those two enzymes. Poor metabolizers have two dysfunctional copies of the enzyme-encoding gene. This results in increased drug plasma levels with a potentially increased rate of adverse effects.
“Intermediate and extensive metabolizers usually have a normal phenotype, but you can also have ultrarapid metabolizers who have duplications or other enhancing mutations of the CYP gene,” Dr. Nurmi said. “This can result in lower bioavailability and possibly efficacy. Psychiatrists treat poor metabolizers and ultrarapid metabolizers all the time, because the variants are very common.” An estimated 10% of White people are poor metabolizers at the CYP2D6 gene while about 7% are ultrarapid metabolizers. At the same time, an estimated 20% of Asians, Africans, and Whites are poor metabolizers at the CYP2C19 gene. “So, you’re seeing a lot of this in your practice, and you’re probably changing dosing based on genetic differences in metabolism,” she said.
The only FDA pharmacodynamic treatment guideline is for the risk of Stevens-Johnson syndrome (SJS) with the use of carbamazepine. In a study of 44 patients with SJS, all were positive for the HLA-B*1502 variant, compared with 3% of carbamazepine-tolerant patients (Nature 2004;428[6982]:486). The frequency of carrying this variant is an estimated 1:10,000 among Whites and 1:1,000 among Asians. In 2007, the FDA recommended that patients of Asian ancestry should be screened for HLA-B*1502 prior to starting carbamazepine.
Genetic variation also predicts clinical outcome with atomoxetine use. “Most child psychiatrists I know think atomoxetine doesn’t work as a second-line nonstimulant medication for ADHD,” Dr. Nurmi said. “I’d like to convince you that why you think it doesn’t work is because of the genetics.” In a study published in 2019, Dr. Nurmi and colleagues reviewed medical literature and provided therapeutic recommendations for atomoxetine therapy based on CYP2D6 genotype (Clin Pharmacol Ther 2019 Jul;106[1]:94-102). They observed 10- to 30-fold plasma differences in drug exposure between normal metabolizers and poor metabolizers.
“Poor metabolizers therefore get more benefit, but they are also going to get more side effects,” she said. “FDA recommended doses are inadequate for normal metabolizers, so they had to make guidelines based on poor metabolizers because there would be too much risk for them at higher doses. One-third of individuals require doses above the FDA limit to achieve a therapeutic drug level.”
Dr. Nurmi warned that the existing evidence base for using these genetic tests in children “is really poor. There is no data in adults with any diagnosis other than depression, and even those studies are plagued by concerns. When you’re implementing decision support tools in your practice, the key factors are patient presentation, history and symptoms, your clinical skills, the evidence base, FDA recommendations, and patient autonomy. Appropriate incorporation of genetic data should include avoiding a medication with high toxicity (like SJS), titration planning (dose and titration speed adjustments), and choosing between medications in the same class with an indication or evidence base for the target disorder.” She added that while the benefit of current genetic testing is limited, it may help some patients feel more comfortable tolerating a medication. “For example, being able to tell someone with anxiety that their genetics suggests that they will not have side effects could be very powerful,” she said.
In a 2018 safety communication, the FDA warned the public about its concerns with companies making claims about how to use genetic test results to manage medication treatments that are not supported by recommendations in the FDA-approved drug labeling or other scientific evidence. The American Academy of Child and Adolescent Psychiatry also published a guide for patients and families.
Dr. Nurmi disclosed that she is an unpaid advisory board member for Myriad Genetics and the Tourette Association of America, a paid adviser for Teva Pharmaceuticals, and a recipient of research support from Emalex Pharmaceuticals. She has received research funding from the National Institutes Health, the International OCD Foundation, the Tourette Association of America, and the Brain & Behavior Research Foundation.
LAS VEGAS –
“It’s misleading to rely on results of genetic tests to drive clinical treatment,” Dr. Nurmi, a child and adolescent psychiatrist in the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles, said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “There’s a lot of hope and promise there. But currently, we only know the tip of the iceberg about how drugs work and the genetics influencing these effects. Current testing is probably a very poor reflection of the complexity of drug effects.”
According to Dr. Nurmi, there are at least 165 Food and Drug Administration–approved drugs with pharmacogenetic information on 64 different biomarkers – 37% with CYP p450 notations. Of these, 32 psychiatric drugs have pharmacogenetic information, and most of them are dosing recommendations based on whether a patient has the variant. However, there is wide public acceptance of genetic testing in preventing the wrong drug from being used, in selecting the best drug dose, and avoiding side effects (Pharmacogenomics 2012;12[3]:197-204). “Most people have a lot of hope [for genetic testing in psychiatry],” Dr. Nurmi said. “But is the science really there? It doesn’t matter, because these companies are doing it, and you are being shown these reports from patients. Whether or not the science supports it, we’re going to have to interpret these reports and explain them to our patients – even if we don’t order them.”
Currently, she continued, clinicians practice trial and error prescribing where they might try one treatment in a class that they think that will work based on previous literature. If nothing works, they try another one. If that’s intolerable, they try a third treatment, and so on. “When we finally find the right treatment, it can take some time to get the dosing right,” Dr. Nurmi said. “So, it can take many months to get a child on the right medication. Precision treatment, on the other hand, would start off by taking a saliva or blood sample to get a printout that lets physicians know which drugs might be used with caution because they might lack efficacy at standard doses, which ones would likely have adverse effects at standard doses, and which are the best choices and what are the dosing recommendations for those choices. If we could get all the information to guide us, that would be a useful product, but right now, we don’t know enough to be able to make these determinations.”
Current evidence-based genetic testing supports a limited role for CYP2D6 and CYP2C19 genotyping because most psychiatric drugs are metabolized by those two enzymes. Poor metabolizers have two dysfunctional copies of the enzyme-encoding gene. This results in increased drug plasma levels with a potentially increased rate of adverse effects.
“Intermediate and extensive metabolizers usually have a normal phenotype, but you can also have ultrarapid metabolizers who have duplications or other enhancing mutations of the CYP gene,” Dr. Nurmi said. “This can result in lower bioavailability and possibly efficacy. Psychiatrists treat poor metabolizers and ultrarapid metabolizers all the time, because the variants are very common.” An estimated 10% of White people are poor metabolizers at the CYP2D6 gene while about 7% are ultrarapid metabolizers. At the same time, an estimated 20% of Asians, Africans, and Whites are poor metabolizers at the CYP2C19 gene. “So, you’re seeing a lot of this in your practice, and you’re probably changing dosing based on genetic differences in metabolism,” she said.
The only FDA pharmacodynamic treatment guideline is for the risk of Stevens-Johnson syndrome (SJS) with the use of carbamazepine. In a study of 44 patients with SJS, all were positive for the HLA-B*1502 variant, compared with 3% of carbamazepine-tolerant patients (Nature 2004;428[6982]:486). The frequency of carrying this variant is an estimated 1:10,000 among Whites and 1:1,000 among Asians. In 2007, the FDA recommended that patients of Asian ancestry should be screened for HLA-B*1502 prior to starting carbamazepine.
Genetic variation also predicts clinical outcome with atomoxetine use. “Most child psychiatrists I know think atomoxetine doesn’t work as a second-line nonstimulant medication for ADHD,” Dr. Nurmi said. “I’d like to convince you that why you think it doesn’t work is because of the genetics.” In a study published in 2019, Dr. Nurmi and colleagues reviewed medical literature and provided therapeutic recommendations for atomoxetine therapy based on CYP2D6 genotype (Clin Pharmacol Ther 2019 Jul;106[1]:94-102). They observed 10- to 30-fold plasma differences in drug exposure between normal metabolizers and poor metabolizers.
“Poor metabolizers therefore get more benefit, but they are also going to get more side effects,” she said. “FDA recommended doses are inadequate for normal metabolizers, so they had to make guidelines based on poor metabolizers because there would be too much risk for them at higher doses. One-third of individuals require doses above the FDA limit to achieve a therapeutic drug level.”
Dr. Nurmi warned that the existing evidence base for using these genetic tests in children “is really poor. There is no data in adults with any diagnosis other than depression, and even those studies are plagued by concerns. When you’re implementing decision support tools in your practice, the key factors are patient presentation, history and symptoms, your clinical skills, the evidence base, FDA recommendations, and patient autonomy. Appropriate incorporation of genetic data should include avoiding a medication with high toxicity (like SJS), titration planning (dose and titration speed adjustments), and choosing between medications in the same class with an indication or evidence base for the target disorder.” She added that while the benefit of current genetic testing is limited, it may help some patients feel more comfortable tolerating a medication. “For example, being able to tell someone with anxiety that their genetics suggests that they will not have side effects could be very powerful,” she said.
In a 2018 safety communication, the FDA warned the public about its concerns with companies making claims about how to use genetic test results to manage medication treatments that are not supported by recommendations in the FDA-approved drug labeling or other scientific evidence. The American Academy of Child and Adolescent Psychiatry also published a guide for patients and families.
Dr. Nurmi disclosed that she is an unpaid advisory board member for Myriad Genetics and the Tourette Association of America, a paid adviser for Teva Pharmaceuticals, and a recipient of research support from Emalex Pharmaceuticals. She has received research funding from the National Institutes Health, the International OCD Foundation, the Tourette Association of America, and the Brain & Behavior Research Foundation.
LAS VEGAS –
“It’s misleading to rely on results of genetic tests to drive clinical treatment,” Dr. Nurmi, a child and adolescent psychiatrist in the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles, said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “There’s a lot of hope and promise there. But currently, we only know the tip of the iceberg about how drugs work and the genetics influencing these effects. Current testing is probably a very poor reflection of the complexity of drug effects.”
According to Dr. Nurmi, there are at least 165 Food and Drug Administration–approved drugs with pharmacogenetic information on 64 different biomarkers – 37% with CYP p450 notations. Of these, 32 psychiatric drugs have pharmacogenetic information, and most of them are dosing recommendations based on whether a patient has the variant. However, there is wide public acceptance of genetic testing in preventing the wrong drug from being used, in selecting the best drug dose, and avoiding side effects (Pharmacogenomics 2012;12[3]:197-204). “Most people have a lot of hope [for genetic testing in psychiatry],” Dr. Nurmi said. “But is the science really there? It doesn’t matter, because these companies are doing it, and you are being shown these reports from patients. Whether or not the science supports it, we’re going to have to interpret these reports and explain them to our patients – even if we don’t order them.”
Currently, she continued, clinicians practice trial and error prescribing where they might try one treatment in a class that they think that will work based on previous literature. If nothing works, they try another one. If that’s intolerable, they try a third treatment, and so on. “When we finally find the right treatment, it can take some time to get the dosing right,” Dr. Nurmi said. “So, it can take many months to get a child on the right medication. Precision treatment, on the other hand, would start off by taking a saliva or blood sample to get a printout that lets physicians know which drugs might be used with caution because they might lack efficacy at standard doses, which ones would likely have adverse effects at standard doses, and which are the best choices and what are the dosing recommendations for those choices. If we could get all the information to guide us, that would be a useful product, but right now, we don’t know enough to be able to make these determinations.”
Current evidence-based genetic testing supports a limited role for CYP2D6 and CYP2C19 genotyping because most psychiatric drugs are metabolized by those two enzymes. Poor metabolizers have two dysfunctional copies of the enzyme-encoding gene. This results in increased drug plasma levels with a potentially increased rate of adverse effects.
“Intermediate and extensive metabolizers usually have a normal phenotype, but you can also have ultrarapid metabolizers who have duplications or other enhancing mutations of the CYP gene,” Dr. Nurmi said. “This can result in lower bioavailability and possibly efficacy. Psychiatrists treat poor metabolizers and ultrarapid metabolizers all the time, because the variants are very common.” An estimated 10% of White people are poor metabolizers at the CYP2D6 gene while about 7% are ultrarapid metabolizers. At the same time, an estimated 20% of Asians, Africans, and Whites are poor metabolizers at the CYP2C19 gene. “So, you’re seeing a lot of this in your practice, and you’re probably changing dosing based on genetic differences in metabolism,” she said.
The only FDA pharmacodynamic treatment guideline is for the risk of Stevens-Johnson syndrome (SJS) with the use of carbamazepine. In a study of 44 patients with SJS, all were positive for the HLA-B*1502 variant, compared with 3% of carbamazepine-tolerant patients (Nature 2004;428[6982]:486). The frequency of carrying this variant is an estimated 1:10,000 among Whites and 1:1,000 among Asians. In 2007, the FDA recommended that patients of Asian ancestry should be screened for HLA-B*1502 prior to starting carbamazepine.
Genetic variation also predicts clinical outcome with atomoxetine use. “Most child psychiatrists I know think atomoxetine doesn’t work as a second-line nonstimulant medication for ADHD,” Dr. Nurmi said. “I’d like to convince you that why you think it doesn’t work is because of the genetics.” In a study published in 2019, Dr. Nurmi and colleagues reviewed medical literature and provided therapeutic recommendations for atomoxetine therapy based on CYP2D6 genotype (Clin Pharmacol Ther 2019 Jul;106[1]:94-102). They observed 10- to 30-fold plasma differences in drug exposure between normal metabolizers and poor metabolizers.
“Poor metabolizers therefore get more benefit, but they are also going to get more side effects,” she said. “FDA recommended doses are inadequate for normal metabolizers, so they had to make guidelines based on poor metabolizers because there would be too much risk for them at higher doses. One-third of individuals require doses above the FDA limit to achieve a therapeutic drug level.”
Dr. Nurmi warned that the existing evidence base for using these genetic tests in children “is really poor. There is no data in adults with any diagnosis other than depression, and even those studies are plagued by concerns. When you’re implementing decision support tools in your practice, the key factors are patient presentation, history and symptoms, your clinical skills, the evidence base, FDA recommendations, and patient autonomy. Appropriate incorporation of genetic data should include avoiding a medication with high toxicity (like SJS), titration planning (dose and titration speed adjustments), and choosing between medications in the same class with an indication or evidence base for the target disorder.” She added that while the benefit of current genetic testing is limited, it may help some patients feel more comfortable tolerating a medication. “For example, being able to tell someone with anxiety that their genetics suggests that they will not have side effects could be very powerful,” she said.
In a 2018 safety communication, the FDA warned the public about its concerns with companies making claims about how to use genetic test results to manage medication treatments that are not supported by recommendations in the FDA-approved drug labeling or other scientific evidence. The American Academy of Child and Adolescent Psychiatry also published a guide for patients and families.
Dr. Nurmi disclosed that she is an unpaid advisory board member for Myriad Genetics and the Tourette Association of America, a paid adviser for Teva Pharmaceuticals, and a recipient of research support from Emalex Pharmaceuticals. She has received research funding from the National Institutes Health, the International OCD Foundation, the Tourette Association of America, and the Brain & Behavior Research Foundation.
REPORTING FROM NPA 2022