User login
Fivefold Increase in Vaping During Adolescent Pregnancies
TOPLINE:
, according to research published online on December 13 in JAMA Network Open.
METHODOLOGY:
- Researchers analyzed data from the 2016-2021 Pregnancy Risk Assessment Monitoring System.
- They focused on 10,428 adolescents aged 10-19 years who had had a singleton birth and provided information about their use of e-cigarettes or cigarettes.
TAKEAWAY:
- Whereas the researchers found a roughly fivefold increase in the exclusive use of e-cigarettes, the percentage of patients using only cigarettes decreased from 9.2% in 2017 to 3.2% in 2021.
- The percentage of patients who both vaped and smoked fluctuated between 0.6% and 1.6%.
- The rate of small-for-gestational-age (SGA) births for adolescents who did not smoke or vape (12.9%) did not differ significantly from that among adolescents who exclusively used e-cigarettes (16.8%) or those who used both cigarettes and e-cigarettes (17.6%).
- The researchers found use of cigarettes only was associated with a significantly higher rate of SGA births: 24.6%.
IN PRACTICE:
“Exclusive e-cigarette use and dual use of cigarettes and e-cigarettes did not seem to be statistically significantly associated with SGA birth in our analysis, but this finding should be interpreted with caution given the low prevalence of use and the limited sample size,” the study authors wrote.
SOURCE:
Xiaozhong Wen, MD, PhD, with the Jacobs School of Medicine and Biomedical Sciences at the State University of New York at Buffalo, was the corresponding author of the study.
LIMITATIONS:
Participants may have underreported their use of e-cigarettes and cigarettes because of fears of social stigma. The researchers lacked information about vaping in the first and second trimesters, exposure to secondhand smoke, cannabis use, and diet.
DISCLOSURES:
The research was supported by the National Institute on Drug Abuse; the Food and Drug Administration Center for Tobacco Products; the National Heart, Lung, and Blood Institute; and the American Heart Association. A study coauthor has received grants from Pfizer and personal fees from Johnson & Johnson, the World Health Organization, and the Campaign for Tobacco-Free Kids.
A version of this article appeared on Medscape.com.
TOPLINE:
, according to research published online on December 13 in JAMA Network Open.
METHODOLOGY:
- Researchers analyzed data from the 2016-2021 Pregnancy Risk Assessment Monitoring System.
- They focused on 10,428 adolescents aged 10-19 years who had had a singleton birth and provided information about their use of e-cigarettes or cigarettes.
TAKEAWAY:
- Whereas the researchers found a roughly fivefold increase in the exclusive use of e-cigarettes, the percentage of patients using only cigarettes decreased from 9.2% in 2017 to 3.2% in 2021.
- The percentage of patients who both vaped and smoked fluctuated between 0.6% and 1.6%.
- The rate of small-for-gestational-age (SGA) births for adolescents who did not smoke or vape (12.9%) did not differ significantly from that among adolescents who exclusively used e-cigarettes (16.8%) or those who used both cigarettes and e-cigarettes (17.6%).
- The researchers found use of cigarettes only was associated with a significantly higher rate of SGA births: 24.6%.
IN PRACTICE:
“Exclusive e-cigarette use and dual use of cigarettes and e-cigarettes did not seem to be statistically significantly associated with SGA birth in our analysis, but this finding should be interpreted with caution given the low prevalence of use and the limited sample size,” the study authors wrote.
SOURCE:
Xiaozhong Wen, MD, PhD, with the Jacobs School of Medicine and Biomedical Sciences at the State University of New York at Buffalo, was the corresponding author of the study.
LIMITATIONS:
Participants may have underreported their use of e-cigarettes and cigarettes because of fears of social stigma. The researchers lacked information about vaping in the first and second trimesters, exposure to secondhand smoke, cannabis use, and diet.
DISCLOSURES:
The research was supported by the National Institute on Drug Abuse; the Food and Drug Administration Center for Tobacco Products; the National Heart, Lung, and Blood Institute; and the American Heart Association. A study coauthor has received grants from Pfizer and personal fees from Johnson & Johnson, the World Health Organization, and the Campaign for Tobacco-Free Kids.
A version of this article appeared on Medscape.com.
TOPLINE:
, according to research published online on December 13 in JAMA Network Open.
METHODOLOGY:
- Researchers analyzed data from the 2016-2021 Pregnancy Risk Assessment Monitoring System.
- They focused on 10,428 adolescents aged 10-19 years who had had a singleton birth and provided information about their use of e-cigarettes or cigarettes.
TAKEAWAY:
- Whereas the researchers found a roughly fivefold increase in the exclusive use of e-cigarettes, the percentage of patients using only cigarettes decreased from 9.2% in 2017 to 3.2% in 2021.
- The percentage of patients who both vaped and smoked fluctuated between 0.6% and 1.6%.
- The rate of small-for-gestational-age (SGA) births for adolescents who did not smoke or vape (12.9%) did not differ significantly from that among adolescents who exclusively used e-cigarettes (16.8%) or those who used both cigarettes and e-cigarettes (17.6%).
- The researchers found use of cigarettes only was associated with a significantly higher rate of SGA births: 24.6%.
IN PRACTICE:
“Exclusive e-cigarette use and dual use of cigarettes and e-cigarettes did not seem to be statistically significantly associated with SGA birth in our analysis, but this finding should be interpreted with caution given the low prevalence of use and the limited sample size,” the study authors wrote.
SOURCE:
Xiaozhong Wen, MD, PhD, with the Jacobs School of Medicine and Biomedical Sciences at the State University of New York at Buffalo, was the corresponding author of the study.
LIMITATIONS:
Participants may have underreported their use of e-cigarettes and cigarettes because of fears of social stigma. The researchers lacked information about vaping in the first and second trimesters, exposure to secondhand smoke, cannabis use, and diet.
DISCLOSURES:
The research was supported by the National Institute on Drug Abuse; the Food and Drug Administration Center for Tobacco Products; the National Heart, Lung, and Blood Institute; and the American Heart Association. A study coauthor has received grants from Pfizer and personal fees from Johnson & Johnson, the World Health Organization, and the Campaign for Tobacco-Free Kids.
A version of this article appeared on Medscape.com.
Researchers making strides to better understand RA-associated interstitial lung disease
SAN DIEGO — Clinically significant interstitial lung disease (ILD) is believed to occur in 5%-10% of patients with rheumatoid arthritis (RA), but robust data are lacking on how to best predict which patients face the highest risk for RA-associated ILD. However, the results of several studies presented at the American College of Rheumatology annual meeting indicate that researchers are making strides in this field of rheumatologic care.
Adding Genetic Factors Improves ILD Risk Prediction
In the realm of risk stratification, Austin M. Wheeler, MD, a rheumatology fellow at the University of Nebraska Medical Center, Omaha, discussed the development and validation of a combined clinical and genetic risk score for ILD. “There is clear and well documented phenotypic and genetic overlap of ILD with idiopathic pulmonary fibrosis (IPF),” Dr. Wheeler said. “A number of clinical risk factors have been described for RA-ILD, including older age, male sex, smoking history, higher disease activity, and seropositivity. There are also well-documented genetic risk factors for RA-ILD. The MUC5B genetic variant is the strongest risk factor for IPF, and it’s been described in RA-ILD as well.”
A recently published study indicated that a genetic risk score without the MUC5B variant improved predictive ability for IPF and interstitial lung abnormalities better than using the MUC5B variant alone, “but no prior attempts have been made at developing a composite genetic risk score in RA-ILD” using both genetic and clinical risk factors, he said.
For the current study, Dr. Wheeler and colleagues drew from 2,386 participants in the Veterans Affairs Rheumatoid Arthritis (VARA) Registry, a multicenter, prospective cohort of US veterans with rheumatologist-diagnosed RA and who fulfilled the 1987 ACR classification criteria. The researchers validated ILD through a systematic review of medical records, including clinical diagnosis of ILD plus either imaging or lung biopsy findings, and collected whole genome data that included 12 single nucleotide polymorphisms (SNPs) previously identified to be associated with risk for RA-ILD. They then used a meta-analytic approach to create pooled associations for each of those respective SNPs using data from the VARA registry participants as well as participants from the past study where the SNPs were first identified. “Those pooled associations were what we used for our effects size within the genetic risk score,” which ended up using five of the SNPs, Dr. Wheeler explained. Next, he and his colleagues combined the genetic risk score with clinical risk factors including age, sex, smoking history, disease activity, and rheumatoid factor (RF) positivity to create their combined risk score.
The mean age of the cohort was 70 years, 89% were male, 78% had a smoking history, and 78% were anti–cyclic citrullinated peptide (CCP) antibody positive. Of the 2,386 participants, 224 (9.4%) had RA-ILD. The full composite risk score had the highest area under the receiver operating curve (AUC) of 0.67, compared with an AUC of 0.623 using the clinical factors alone, 0.651 using the clinical factors plus only the MUC5B variant, and 0.654 using the composite score minus only the MUC5B variant. These AUCs show that “the combined risk score performs better than clinical factors even without the inclusion of the MUC5B variant in the score, which is notable because it supports the importance of further investigation into polygenic risk scores in RA-ILD as there is clearly more at play in a patient’s overall genetic risk,” Dr. Wheeler said.
As an example of the composite score’s ability to discriminate between people with and without RA-ILD, a cutpoint of 0.05 gave a sensitivity of 90.2% and would have eliminated about 25% of the cohort from unnecessary high-resolution CT scans and pulmonary function tests, he said.
“This study demonstrates the potential utility of genetic risk scores in RA-ILD identification and supports further investigation into individual risk stratification and screening,” he concluded. “This isn’t ready for clinical applicability by any means, but I think it serves as a proof of concept of the idea of a genetic risk score in RA-ILD.”
Biomarker Score Investigated
In a separate abstract, Brent Luedders, MD, assistant professor of rheumatology and immunology at the University of Nebraska Medical Center, and colleagues set out to determine if a previously derived biomarker score is associated with prevalent and incident ILD in the same VARA Registry cohort. An abstract presented at the ACR 2022 annual meeting found that a panel derived from IPF peripheral biomarkers was significantly associated with RA-ILD, including matrix metalloproteinase (MMP)-2, -7, and -9, eotaxin, macrophage-derived chemokine (MDC), monocyte chemoattractant protein-1 (MCP-1), fms-like tyrosine kinase 3 ligand (Flt3L) and interleukin-8 (IL-8). For the current analysis, Dr. Luedders and colleagues measured the concentrations of seven biomarkers (MMP-7, MMP-9, eotaxin, MDC, MCP-1, Flt3L, IL-8) from serum/plasma samples collected from VARA’s participants at enrollment to develop a score based on the concentrations of each biomarker.
Baseline characteristics were similar between the groups, although those with prevalent RA-ILD were slightly older than those without ILD, and those who developed incident ILD during follow-up had slightly higher RA disease activity at the time of enrollment. When the researchers examined the association of the biomarker score with prevalent RA-ILD as a continuous measure, they found an adjusted OR of 1.08 for prevalent RA-ILD for each 1-point increase in the biomarker score. “When this was divided into quartiles, we found that the highest quartile of the biomarker score was associated with an adjusted odds ratio of 2.31 for prevalent RA-ILD,” Dr. Luedders said. “We saw a significant P for trend of < .001, suggesting a dose-response relationship, in which higher scores had higher risk.” Similar associations were observed for incident RA-ILD, in which participants with the highest quartile had an adjusted hazard ratio of 2.26 for incident RA-ILD.
The AUC of 0.653 that was obtained with clinical factors did not significantly improve with inclusion of the biomarker score, rising to only 0.669. “In receiver operating characteristic analysis, the addition of the biomarker score to clinical variables (age, sex, race, smoking status, anti-CCP positivity, and RA disease activity by DAS28) did not lead to a significant increase in the area under the curve. Therefore, further work is needed to identify combinations of clinical, biomarker, and other factors to accurately predict which people with RA will develop ILD,” he said.
Dr. Luedders acknowledged certain limitations of the results, including the fact that MMP-2 was not measured in this cohort and thus not included in the score. “This was an observational study with usual care; therefore, the absence of systemic evaluation for ILD may miss early or mild RA-ILD cases,” he added. “Similarly, a male predominance may limit the generalizability, and we have limited information on the RA-ILD pattern.” He concluded that the study results “support the shared pathogenesis of IPF and RA-ILD. However, we found that this score has limited discriminative performance, compared to clinical risk factors alone.”
Drilling Down on ILD Subtypes
In a poster abstract presentation at the meeting, Gregory Campbell McDermott, MD, MPH, a rheumatologist at Brigham and Women’s Hospital, Boston, highlighted results from a study that investigated differences in demographic, serologic, and lifestyle factors for RA-ILD and the major subtypes of RA-ILD: usual interstitial pneumonia (UIP) and nonspecific interstitial pneumonia (NSIP). “Historically, RA-ILD has been studied as a single entity, even though we increasingly recognized that there are lots of different subtypes that fall under the umbrella of RA-ILD,” Dr. McDermott said in an interview. “We are also learning that the different subtypes probably have both prognostic and potentially therapeutic implications. For example, the UIP subtype, which is the most fibrotic subtype, has the worst prognosis but also may be a potential target for antifibrotic therapies. We’ve been trying to see if we can identify factors that are associated with specific subtypes, in particular the UIP subtype which has the worst prognosis.”
He and his colleagues examined 208 patients with RA-ILD with a mean age of 51 years and 547 patients with RA but no ILD with a mean age of 49 years from two RA cohorts comprising 3,328 patients: the Mass General Brigham Biobank RA Cohort and the Brigham RA Sequential Study (BRASS). Of the 208 RA-ILD cases, nearly half (48%) were RA-UIP, 18% were RA-NSIP, 8% were organizing pneumonia, 3% were respiratory bronchiolitis-ILD, and 23% were other/indeterminate. After conducting multivariable adjusted analyses, the researchers found that RA-ILD was associated with male sex (OR, 1.58; 95% CI, 1.09-2.23), seropositivity for RF and/or anti-CCP (OR, 2.22; 95% CI, 1.51-3.24) and being an ever smoker (OR, 1.70; 95% CI, 1.13-2.54). Having all three of these risk factors was strongly associated with RA-ILD (OR, 6.04; 95% CI, 2.92-12.47) and with RA-UIP in particular (OR, 7.1). “We found that a lot of the traditional RA-ILD risk factors like male sex, history of smoking, and seropositive status were most strongly associated with a UIP pattern,” Dr. McDermott said. “We think this is a first step in trying to understand how these different ILD subtypes may have different risk factors, pathogenesis, and potentially different treatments, prevention, and screening strategies.”
While clinicians wait for guidelines on systemic autoimmune rheumatic disease-associated ILD that are expected to be published by the ACR in 2024, he added that “we probably shouldn’t screen every single person with RA for ILD, but we need to identify people who have symptoms or findings on clinical exam. This study wasn’t designed to look specifically at who is at high risk, but I think we are moving toward that question: Who is high risk, and who’s asymptomatic [but] may need more screening?”
He pointed out limitations of the study, including its retrospective design and the fact that imaging was done for clinical purposes, “so it’s probably a higher risk group to begin with than the whole RA population,” he said. “We also didn’t have data on RA disease activity or erosions, some of these other measures that we think are important for understanding the full RA disease phenotype in these patients.”
Dr. Wheeler reported having no disclosures. Dr. Luedders reported that his study was supported by the VA, the Rheumatology Research Foundation, and the University of Nebraska Medical Center Mentored Scholars Program. Dr. McDermott reported that his study was supported by the Rheumatology Research Foundation.
SAN DIEGO — Clinically significant interstitial lung disease (ILD) is believed to occur in 5%-10% of patients with rheumatoid arthritis (RA), but robust data are lacking on how to best predict which patients face the highest risk for RA-associated ILD. However, the results of several studies presented at the American College of Rheumatology annual meeting indicate that researchers are making strides in this field of rheumatologic care.
Adding Genetic Factors Improves ILD Risk Prediction
In the realm of risk stratification, Austin M. Wheeler, MD, a rheumatology fellow at the University of Nebraska Medical Center, Omaha, discussed the development and validation of a combined clinical and genetic risk score for ILD. “There is clear and well documented phenotypic and genetic overlap of ILD with idiopathic pulmonary fibrosis (IPF),” Dr. Wheeler said. “A number of clinical risk factors have been described for RA-ILD, including older age, male sex, smoking history, higher disease activity, and seropositivity. There are also well-documented genetic risk factors for RA-ILD. The MUC5B genetic variant is the strongest risk factor for IPF, and it’s been described in RA-ILD as well.”
A recently published study indicated that a genetic risk score without the MUC5B variant improved predictive ability for IPF and interstitial lung abnormalities better than using the MUC5B variant alone, “but no prior attempts have been made at developing a composite genetic risk score in RA-ILD” using both genetic and clinical risk factors, he said.
For the current study, Dr. Wheeler and colleagues drew from 2,386 participants in the Veterans Affairs Rheumatoid Arthritis (VARA) Registry, a multicenter, prospective cohort of US veterans with rheumatologist-diagnosed RA and who fulfilled the 1987 ACR classification criteria. The researchers validated ILD through a systematic review of medical records, including clinical diagnosis of ILD plus either imaging or lung biopsy findings, and collected whole genome data that included 12 single nucleotide polymorphisms (SNPs) previously identified to be associated with risk for RA-ILD. They then used a meta-analytic approach to create pooled associations for each of those respective SNPs using data from the VARA registry participants as well as participants from the past study where the SNPs were first identified. “Those pooled associations were what we used for our effects size within the genetic risk score,” which ended up using five of the SNPs, Dr. Wheeler explained. Next, he and his colleagues combined the genetic risk score with clinical risk factors including age, sex, smoking history, disease activity, and rheumatoid factor (RF) positivity to create their combined risk score.
The mean age of the cohort was 70 years, 89% were male, 78% had a smoking history, and 78% were anti–cyclic citrullinated peptide (CCP) antibody positive. Of the 2,386 participants, 224 (9.4%) had RA-ILD. The full composite risk score had the highest area under the receiver operating curve (AUC) of 0.67, compared with an AUC of 0.623 using the clinical factors alone, 0.651 using the clinical factors plus only the MUC5B variant, and 0.654 using the composite score minus only the MUC5B variant. These AUCs show that “the combined risk score performs better than clinical factors even without the inclusion of the MUC5B variant in the score, which is notable because it supports the importance of further investigation into polygenic risk scores in RA-ILD as there is clearly more at play in a patient’s overall genetic risk,” Dr. Wheeler said.
As an example of the composite score’s ability to discriminate between people with and without RA-ILD, a cutpoint of 0.05 gave a sensitivity of 90.2% and would have eliminated about 25% of the cohort from unnecessary high-resolution CT scans and pulmonary function tests, he said.
“This study demonstrates the potential utility of genetic risk scores in RA-ILD identification and supports further investigation into individual risk stratification and screening,” he concluded. “This isn’t ready for clinical applicability by any means, but I think it serves as a proof of concept of the idea of a genetic risk score in RA-ILD.”
Biomarker Score Investigated
In a separate abstract, Brent Luedders, MD, assistant professor of rheumatology and immunology at the University of Nebraska Medical Center, and colleagues set out to determine if a previously derived biomarker score is associated with prevalent and incident ILD in the same VARA Registry cohort. An abstract presented at the ACR 2022 annual meeting found that a panel derived from IPF peripheral biomarkers was significantly associated with RA-ILD, including matrix metalloproteinase (MMP)-2, -7, and -9, eotaxin, macrophage-derived chemokine (MDC), monocyte chemoattractant protein-1 (MCP-1), fms-like tyrosine kinase 3 ligand (Flt3L) and interleukin-8 (IL-8). For the current analysis, Dr. Luedders and colleagues measured the concentrations of seven biomarkers (MMP-7, MMP-9, eotaxin, MDC, MCP-1, Flt3L, IL-8) from serum/plasma samples collected from VARA’s participants at enrollment to develop a score based on the concentrations of each biomarker.
Baseline characteristics were similar between the groups, although those with prevalent RA-ILD were slightly older than those without ILD, and those who developed incident ILD during follow-up had slightly higher RA disease activity at the time of enrollment. When the researchers examined the association of the biomarker score with prevalent RA-ILD as a continuous measure, they found an adjusted OR of 1.08 for prevalent RA-ILD for each 1-point increase in the biomarker score. “When this was divided into quartiles, we found that the highest quartile of the biomarker score was associated with an adjusted odds ratio of 2.31 for prevalent RA-ILD,” Dr. Luedders said. “We saw a significant P for trend of < .001, suggesting a dose-response relationship, in which higher scores had higher risk.” Similar associations were observed for incident RA-ILD, in which participants with the highest quartile had an adjusted hazard ratio of 2.26 for incident RA-ILD.
The AUC of 0.653 that was obtained with clinical factors did not significantly improve with inclusion of the biomarker score, rising to only 0.669. “In receiver operating characteristic analysis, the addition of the biomarker score to clinical variables (age, sex, race, smoking status, anti-CCP positivity, and RA disease activity by DAS28) did not lead to a significant increase in the area under the curve. Therefore, further work is needed to identify combinations of clinical, biomarker, and other factors to accurately predict which people with RA will develop ILD,” he said.
Dr. Luedders acknowledged certain limitations of the results, including the fact that MMP-2 was not measured in this cohort and thus not included in the score. “This was an observational study with usual care; therefore, the absence of systemic evaluation for ILD may miss early or mild RA-ILD cases,” he added. “Similarly, a male predominance may limit the generalizability, and we have limited information on the RA-ILD pattern.” He concluded that the study results “support the shared pathogenesis of IPF and RA-ILD. However, we found that this score has limited discriminative performance, compared to clinical risk factors alone.”
Drilling Down on ILD Subtypes
In a poster abstract presentation at the meeting, Gregory Campbell McDermott, MD, MPH, a rheumatologist at Brigham and Women’s Hospital, Boston, highlighted results from a study that investigated differences in demographic, serologic, and lifestyle factors for RA-ILD and the major subtypes of RA-ILD: usual interstitial pneumonia (UIP) and nonspecific interstitial pneumonia (NSIP). “Historically, RA-ILD has been studied as a single entity, even though we increasingly recognized that there are lots of different subtypes that fall under the umbrella of RA-ILD,” Dr. McDermott said in an interview. “We are also learning that the different subtypes probably have both prognostic and potentially therapeutic implications. For example, the UIP subtype, which is the most fibrotic subtype, has the worst prognosis but also may be a potential target for antifibrotic therapies. We’ve been trying to see if we can identify factors that are associated with specific subtypes, in particular the UIP subtype which has the worst prognosis.”
He and his colleagues examined 208 patients with RA-ILD with a mean age of 51 years and 547 patients with RA but no ILD with a mean age of 49 years from two RA cohorts comprising 3,328 patients: the Mass General Brigham Biobank RA Cohort and the Brigham RA Sequential Study (BRASS). Of the 208 RA-ILD cases, nearly half (48%) were RA-UIP, 18% were RA-NSIP, 8% were organizing pneumonia, 3% were respiratory bronchiolitis-ILD, and 23% were other/indeterminate. After conducting multivariable adjusted analyses, the researchers found that RA-ILD was associated with male sex (OR, 1.58; 95% CI, 1.09-2.23), seropositivity for RF and/or anti-CCP (OR, 2.22; 95% CI, 1.51-3.24) and being an ever smoker (OR, 1.70; 95% CI, 1.13-2.54). Having all three of these risk factors was strongly associated with RA-ILD (OR, 6.04; 95% CI, 2.92-12.47) and with RA-UIP in particular (OR, 7.1). “We found that a lot of the traditional RA-ILD risk factors like male sex, history of smoking, and seropositive status were most strongly associated with a UIP pattern,” Dr. McDermott said. “We think this is a first step in trying to understand how these different ILD subtypes may have different risk factors, pathogenesis, and potentially different treatments, prevention, and screening strategies.”
While clinicians wait for guidelines on systemic autoimmune rheumatic disease-associated ILD that are expected to be published by the ACR in 2024, he added that “we probably shouldn’t screen every single person with RA for ILD, but we need to identify people who have symptoms or findings on clinical exam. This study wasn’t designed to look specifically at who is at high risk, but I think we are moving toward that question: Who is high risk, and who’s asymptomatic [but] may need more screening?”
He pointed out limitations of the study, including its retrospective design and the fact that imaging was done for clinical purposes, “so it’s probably a higher risk group to begin with than the whole RA population,” he said. “We also didn’t have data on RA disease activity or erosions, some of these other measures that we think are important for understanding the full RA disease phenotype in these patients.”
Dr. Wheeler reported having no disclosures. Dr. Luedders reported that his study was supported by the VA, the Rheumatology Research Foundation, and the University of Nebraska Medical Center Mentored Scholars Program. Dr. McDermott reported that his study was supported by the Rheumatology Research Foundation.
SAN DIEGO — Clinically significant interstitial lung disease (ILD) is believed to occur in 5%-10% of patients with rheumatoid arthritis (RA), but robust data are lacking on how to best predict which patients face the highest risk for RA-associated ILD. However, the results of several studies presented at the American College of Rheumatology annual meeting indicate that researchers are making strides in this field of rheumatologic care.
Adding Genetic Factors Improves ILD Risk Prediction
In the realm of risk stratification, Austin M. Wheeler, MD, a rheumatology fellow at the University of Nebraska Medical Center, Omaha, discussed the development and validation of a combined clinical and genetic risk score for ILD. “There is clear and well documented phenotypic and genetic overlap of ILD with idiopathic pulmonary fibrosis (IPF),” Dr. Wheeler said. “A number of clinical risk factors have been described for RA-ILD, including older age, male sex, smoking history, higher disease activity, and seropositivity. There are also well-documented genetic risk factors for RA-ILD. The MUC5B genetic variant is the strongest risk factor for IPF, and it’s been described in RA-ILD as well.”
A recently published study indicated that a genetic risk score without the MUC5B variant improved predictive ability for IPF and interstitial lung abnormalities better than using the MUC5B variant alone, “but no prior attempts have been made at developing a composite genetic risk score in RA-ILD” using both genetic and clinical risk factors, he said.
For the current study, Dr. Wheeler and colleagues drew from 2,386 participants in the Veterans Affairs Rheumatoid Arthritis (VARA) Registry, a multicenter, prospective cohort of US veterans with rheumatologist-diagnosed RA and who fulfilled the 1987 ACR classification criteria. The researchers validated ILD through a systematic review of medical records, including clinical diagnosis of ILD plus either imaging or lung biopsy findings, and collected whole genome data that included 12 single nucleotide polymorphisms (SNPs) previously identified to be associated with risk for RA-ILD. They then used a meta-analytic approach to create pooled associations for each of those respective SNPs using data from the VARA registry participants as well as participants from the past study where the SNPs were first identified. “Those pooled associations were what we used for our effects size within the genetic risk score,” which ended up using five of the SNPs, Dr. Wheeler explained. Next, he and his colleagues combined the genetic risk score with clinical risk factors including age, sex, smoking history, disease activity, and rheumatoid factor (RF) positivity to create their combined risk score.
The mean age of the cohort was 70 years, 89% were male, 78% had a smoking history, and 78% were anti–cyclic citrullinated peptide (CCP) antibody positive. Of the 2,386 participants, 224 (9.4%) had RA-ILD. The full composite risk score had the highest area under the receiver operating curve (AUC) of 0.67, compared with an AUC of 0.623 using the clinical factors alone, 0.651 using the clinical factors plus only the MUC5B variant, and 0.654 using the composite score minus only the MUC5B variant. These AUCs show that “the combined risk score performs better than clinical factors even without the inclusion of the MUC5B variant in the score, which is notable because it supports the importance of further investigation into polygenic risk scores in RA-ILD as there is clearly more at play in a patient’s overall genetic risk,” Dr. Wheeler said.
As an example of the composite score’s ability to discriminate between people with and without RA-ILD, a cutpoint of 0.05 gave a sensitivity of 90.2% and would have eliminated about 25% of the cohort from unnecessary high-resolution CT scans and pulmonary function tests, he said.
“This study demonstrates the potential utility of genetic risk scores in RA-ILD identification and supports further investigation into individual risk stratification and screening,” he concluded. “This isn’t ready for clinical applicability by any means, but I think it serves as a proof of concept of the idea of a genetic risk score in RA-ILD.”
Biomarker Score Investigated
In a separate abstract, Brent Luedders, MD, assistant professor of rheumatology and immunology at the University of Nebraska Medical Center, and colleagues set out to determine if a previously derived biomarker score is associated with prevalent and incident ILD in the same VARA Registry cohort. An abstract presented at the ACR 2022 annual meeting found that a panel derived from IPF peripheral biomarkers was significantly associated with RA-ILD, including matrix metalloproteinase (MMP)-2, -7, and -9, eotaxin, macrophage-derived chemokine (MDC), monocyte chemoattractant protein-1 (MCP-1), fms-like tyrosine kinase 3 ligand (Flt3L) and interleukin-8 (IL-8). For the current analysis, Dr. Luedders and colleagues measured the concentrations of seven biomarkers (MMP-7, MMP-9, eotaxin, MDC, MCP-1, Flt3L, IL-8) from serum/plasma samples collected from VARA’s participants at enrollment to develop a score based on the concentrations of each biomarker.
Baseline characteristics were similar between the groups, although those with prevalent RA-ILD were slightly older than those without ILD, and those who developed incident ILD during follow-up had slightly higher RA disease activity at the time of enrollment. When the researchers examined the association of the biomarker score with prevalent RA-ILD as a continuous measure, they found an adjusted OR of 1.08 for prevalent RA-ILD for each 1-point increase in the biomarker score. “When this was divided into quartiles, we found that the highest quartile of the biomarker score was associated with an adjusted odds ratio of 2.31 for prevalent RA-ILD,” Dr. Luedders said. “We saw a significant P for trend of < .001, suggesting a dose-response relationship, in which higher scores had higher risk.” Similar associations were observed for incident RA-ILD, in which participants with the highest quartile had an adjusted hazard ratio of 2.26 for incident RA-ILD.
The AUC of 0.653 that was obtained with clinical factors did not significantly improve with inclusion of the biomarker score, rising to only 0.669. “In receiver operating characteristic analysis, the addition of the biomarker score to clinical variables (age, sex, race, smoking status, anti-CCP positivity, and RA disease activity by DAS28) did not lead to a significant increase in the area under the curve. Therefore, further work is needed to identify combinations of clinical, biomarker, and other factors to accurately predict which people with RA will develop ILD,” he said.
Dr. Luedders acknowledged certain limitations of the results, including the fact that MMP-2 was not measured in this cohort and thus not included in the score. “This was an observational study with usual care; therefore, the absence of systemic evaluation for ILD may miss early or mild RA-ILD cases,” he added. “Similarly, a male predominance may limit the generalizability, and we have limited information on the RA-ILD pattern.” He concluded that the study results “support the shared pathogenesis of IPF and RA-ILD. However, we found that this score has limited discriminative performance, compared to clinical risk factors alone.”
Drilling Down on ILD Subtypes
In a poster abstract presentation at the meeting, Gregory Campbell McDermott, MD, MPH, a rheumatologist at Brigham and Women’s Hospital, Boston, highlighted results from a study that investigated differences in demographic, serologic, and lifestyle factors for RA-ILD and the major subtypes of RA-ILD: usual interstitial pneumonia (UIP) and nonspecific interstitial pneumonia (NSIP). “Historically, RA-ILD has been studied as a single entity, even though we increasingly recognized that there are lots of different subtypes that fall under the umbrella of RA-ILD,” Dr. McDermott said in an interview. “We are also learning that the different subtypes probably have both prognostic and potentially therapeutic implications. For example, the UIP subtype, which is the most fibrotic subtype, has the worst prognosis but also may be a potential target for antifibrotic therapies. We’ve been trying to see if we can identify factors that are associated with specific subtypes, in particular the UIP subtype which has the worst prognosis.”
He and his colleagues examined 208 patients with RA-ILD with a mean age of 51 years and 547 patients with RA but no ILD with a mean age of 49 years from two RA cohorts comprising 3,328 patients: the Mass General Brigham Biobank RA Cohort and the Brigham RA Sequential Study (BRASS). Of the 208 RA-ILD cases, nearly half (48%) were RA-UIP, 18% were RA-NSIP, 8% were organizing pneumonia, 3% were respiratory bronchiolitis-ILD, and 23% were other/indeterminate. After conducting multivariable adjusted analyses, the researchers found that RA-ILD was associated with male sex (OR, 1.58; 95% CI, 1.09-2.23), seropositivity for RF and/or anti-CCP (OR, 2.22; 95% CI, 1.51-3.24) and being an ever smoker (OR, 1.70; 95% CI, 1.13-2.54). Having all three of these risk factors was strongly associated with RA-ILD (OR, 6.04; 95% CI, 2.92-12.47) and with RA-UIP in particular (OR, 7.1). “We found that a lot of the traditional RA-ILD risk factors like male sex, history of smoking, and seropositive status were most strongly associated with a UIP pattern,” Dr. McDermott said. “We think this is a first step in trying to understand how these different ILD subtypes may have different risk factors, pathogenesis, and potentially different treatments, prevention, and screening strategies.”
While clinicians wait for guidelines on systemic autoimmune rheumatic disease-associated ILD that are expected to be published by the ACR in 2024, he added that “we probably shouldn’t screen every single person with RA for ILD, but we need to identify people who have symptoms or findings on clinical exam. This study wasn’t designed to look specifically at who is at high risk, but I think we are moving toward that question: Who is high risk, and who’s asymptomatic [but] may need more screening?”
He pointed out limitations of the study, including its retrospective design and the fact that imaging was done for clinical purposes, “so it’s probably a higher risk group to begin with than the whole RA population,” he said. “We also didn’t have data on RA disease activity or erosions, some of these other measures that we think are important for understanding the full RA disease phenotype in these patients.”
Dr. Wheeler reported having no disclosures. Dr. Luedders reported that his study was supported by the VA, the Rheumatology Research Foundation, and the University of Nebraska Medical Center Mentored Scholars Program. Dr. McDermott reported that his study was supported by the Rheumatology Research Foundation.
FROM ACR 2023
Sotatercept Endorsed for PAH by ICER
In a new report, the Midwest Institute for Clinical and Economic Review’s (ICER) Comparative Effectiveness Public Advisory Council concluded that the Merck drug sotatercept, currently under review by the US Food and Drug Administration (FDA), has a high certainty of at least a small net health benefit to patients with pulmonary arterial hypertension (PAH) when added to background therapy. The limited availability of evidence means that the benefit could range from minimal to substantial, according to the authors.
Sotatercept, administered by injection every 3 weeks, is a first-in-class activin signaling inhibitor. It counters cell proliferation and decreases inflammation in vessel walls, which may lead to improved pulmonary blood flow. The US FDA is considering it for approval through a biologics license application, with a decision expected by March 26, 2024.
There remains a great deal of uncertainty surrounding the long-term benefits of sotatercept. It’s possible that the drug is disease-modifying, but there isn’t yet any proof, according to Greg Curfman, MD, who attended a virtual ICER public meeting on December 1 that summarized the report and accepted public comments. “I’m still wondering the extent to which disease-modifying issue here is more aspirational at this point than really documented,” said Dr. Curfman, who is an associated professor of medicine at Harvard Medical School and executive editor of the Journal of the American Medical Association.
Current PAH treatment consists of vasodilators, including phosphodiesterase-5 inhibitors (PDE5i), guanylate cyclase stimulators, endothelin receptor antagonists (ERA), prostacyclin analogues (prostanoids), and a prostacyclin receptor agonist. The 2022 European Society of Cardiology and the European Respiratory Society clinical practice guideline recommends that low- and intermediate-risk patients should be started on ERA/PDE5i combination therapy, while high-risk patients should also be given an intravenous or subcutaneous prostacyclin analogue, referred to as triple therapy.
Sotatercept’s regulatory approval hinges on the phase 3 STELLAR trial, which included 323 patients with World Health Organization functional class (WHO-FC) II and III PAH who were randomized to 0.75 mg/kg sotatercept in addition to background double or triple therapy, or background therapy alone. The mean age was 48 years, and the mean time since diagnosis was 8.8 years. About 40% received infused prostacyclin therapy at baseline. At 24 weeks, the median change in 6-min walking distance (6mWD) was 40.8 m longer in the sotatercept group. More patients in the sotatercept group experienced WHO-FC improvement (29.4% vs 13.8%). Those in the sotatercept group also experienced an 84% reduction in risk for clinical worsening or death. PAH-specific quality of life scales did not show a difference between the two groups. Open-label extension trials have shown that benefits are maintained for up to 2 years. Adverse events likely related to sotatercept included telangiectasias, increased hemoglobin levels, and bleeding events.
Along with its benefits, the report authors suggest that the subcutaneous delivery of sotatercept may be less burdensome to patients than some other PAH treatments, especially inhaled and intravenous prostanoids. “However, uncertainty remains about sotatercept’s efficacy in sicker populations and in those with connective tissue disease, and about the durability of effect,” the authors wrote.
A lack of long-term data leaves open the question of its effect on mortality and unknown adverse effects.
Using a de novo decision analytic model, the authors estimated that sotatercept treatment would lead to a longer time without symptoms at rest and more quality-adjusted life years, life years, and equal value life years. They determined the health benefit price benchmark for sotatercept to be between $18,700 and $36,200 per year. “The long-term conventional cost-effectiveness of sotatercept is largely dependent on the long-term effect of sotatercept on improving functional class and slowing the worsening in functional class; however, controlled trial evidence for sotatercept is limited to 24 weeks. Long-term data are necessary to reduce the uncertainty in sotatercept’s long-term effect on improving functional class and slowing the worsening in functional class,” the authors wrote.
During the online meeting, Dr. Curfman took note of the fact that the STELLAR trial reported a median value of increase in 6mWD, rather than a mean, and the 40-m improvement is close to the value accepted as clinically meaningful. “So that tells us that half the patients had less than a clinically important improvement in the six-minute walk distance. We should be putting that in perspective,” said Dr. Curfman.
Another attendee pointed out that the open-label PULSAR extension trial showed that the proportion of patients in the sotatercept arm who were functional class I rose from 7.5% at the end of the trial to 20.6% at the end of the open-label period and wondered if that could be a sign of disease-modifying activity. “I think that’s a remarkable piece of data. I don’t recall seeing that in any other open label [trial of a PAH therapy] — that much of an improvement in getting to our best functional status,” said Marc Simon, MD, professor of medicine and director of the Pulmonary Hypertension Center at the University of California, San Francisco, who was a coauthor of the report.
Dr. Curfman has no relevant financial disclosures. Dr. Simon has consulted for Merck.
A version of this article appeared on Medscape.com.
In a new report, the Midwest Institute for Clinical and Economic Review’s (ICER) Comparative Effectiveness Public Advisory Council concluded that the Merck drug sotatercept, currently under review by the US Food and Drug Administration (FDA), has a high certainty of at least a small net health benefit to patients with pulmonary arterial hypertension (PAH) when added to background therapy. The limited availability of evidence means that the benefit could range from minimal to substantial, according to the authors.
Sotatercept, administered by injection every 3 weeks, is a first-in-class activin signaling inhibitor. It counters cell proliferation and decreases inflammation in vessel walls, which may lead to improved pulmonary blood flow. The US FDA is considering it for approval through a biologics license application, with a decision expected by March 26, 2024.
There remains a great deal of uncertainty surrounding the long-term benefits of sotatercept. It’s possible that the drug is disease-modifying, but there isn’t yet any proof, according to Greg Curfman, MD, who attended a virtual ICER public meeting on December 1 that summarized the report and accepted public comments. “I’m still wondering the extent to which disease-modifying issue here is more aspirational at this point than really documented,” said Dr. Curfman, who is an associated professor of medicine at Harvard Medical School and executive editor of the Journal of the American Medical Association.
Current PAH treatment consists of vasodilators, including phosphodiesterase-5 inhibitors (PDE5i), guanylate cyclase stimulators, endothelin receptor antagonists (ERA), prostacyclin analogues (prostanoids), and a prostacyclin receptor agonist. The 2022 European Society of Cardiology and the European Respiratory Society clinical practice guideline recommends that low- and intermediate-risk patients should be started on ERA/PDE5i combination therapy, while high-risk patients should also be given an intravenous or subcutaneous prostacyclin analogue, referred to as triple therapy.
Sotatercept’s regulatory approval hinges on the phase 3 STELLAR trial, which included 323 patients with World Health Organization functional class (WHO-FC) II and III PAH who were randomized to 0.75 mg/kg sotatercept in addition to background double or triple therapy, or background therapy alone. The mean age was 48 years, and the mean time since diagnosis was 8.8 years. About 40% received infused prostacyclin therapy at baseline. At 24 weeks, the median change in 6-min walking distance (6mWD) was 40.8 m longer in the sotatercept group. More patients in the sotatercept group experienced WHO-FC improvement (29.4% vs 13.8%). Those in the sotatercept group also experienced an 84% reduction in risk for clinical worsening or death. PAH-specific quality of life scales did not show a difference between the two groups. Open-label extension trials have shown that benefits are maintained for up to 2 years. Adverse events likely related to sotatercept included telangiectasias, increased hemoglobin levels, and bleeding events.
Along with its benefits, the report authors suggest that the subcutaneous delivery of sotatercept may be less burdensome to patients than some other PAH treatments, especially inhaled and intravenous prostanoids. “However, uncertainty remains about sotatercept’s efficacy in sicker populations and in those with connective tissue disease, and about the durability of effect,” the authors wrote.
A lack of long-term data leaves open the question of its effect on mortality and unknown adverse effects.
Using a de novo decision analytic model, the authors estimated that sotatercept treatment would lead to a longer time without symptoms at rest and more quality-adjusted life years, life years, and equal value life years. They determined the health benefit price benchmark for sotatercept to be between $18,700 and $36,200 per year. “The long-term conventional cost-effectiveness of sotatercept is largely dependent on the long-term effect of sotatercept on improving functional class and slowing the worsening in functional class; however, controlled trial evidence for sotatercept is limited to 24 weeks. Long-term data are necessary to reduce the uncertainty in sotatercept’s long-term effect on improving functional class and slowing the worsening in functional class,” the authors wrote.
During the online meeting, Dr. Curfman took note of the fact that the STELLAR trial reported a median value of increase in 6mWD, rather than a mean, and the 40-m improvement is close to the value accepted as clinically meaningful. “So that tells us that half the patients had less than a clinically important improvement in the six-minute walk distance. We should be putting that in perspective,” said Dr. Curfman.
Another attendee pointed out that the open-label PULSAR extension trial showed that the proportion of patients in the sotatercept arm who were functional class I rose from 7.5% at the end of the trial to 20.6% at the end of the open-label period and wondered if that could be a sign of disease-modifying activity. “I think that’s a remarkable piece of data. I don’t recall seeing that in any other open label [trial of a PAH therapy] — that much of an improvement in getting to our best functional status,” said Marc Simon, MD, professor of medicine and director of the Pulmonary Hypertension Center at the University of California, San Francisco, who was a coauthor of the report.
Dr. Curfman has no relevant financial disclosures. Dr. Simon has consulted for Merck.
A version of this article appeared on Medscape.com.
In a new report, the Midwest Institute for Clinical and Economic Review’s (ICER) Comparative Effectiveness Public Advisory Council concluded that the Merck drug sotatercept, currently under review by the US Food and Drug Administration (FDA), has a high certainty of at least a small net health benefit to patients with pulmonary arterial hypertension (PAH) when added to background therapy. The limited availability of evidence means that the benefit could range from minimal to substantial, according to the authors.
Sotatercept, administered by injection every 3 weeks, is a first-in-class activin signaling inhibitor. It counters cell proliferation and decreases inflammation in vessel walls, which may lead to improved pulmonary blood flow. The US FDA is considering it for approval through a biologics license application, with a decision expected by March 26, 2024.
There remains a great deal of uncertainty surrounding the long-term benefits of sotatercept. It’s possible that the drug is disease-modifying, but there isn’t yet any proof, according to Greg Curfman, MD, who attended a virtual ICER public meeting on December 1 that summarized the report and accepted public comments. “I’m still wondering the extent to which disease-modifying issue here is more aspirational at this point than really documented,” said Dr. Curfman, who is an associated professor of medicine at Harvard Medical School and executive editor of the Journal of the American Medical Association.
Current PAH treatment consists of vasodilators, including phosphodiesterase-5 inhibitors (PDE5i), guanylate cyclase stimulators, endothelin receptor antagonists (ERA), prostacyclin analogues (prostanoids), and a prostacyclin receptor agonist. The 2022 European Society of Cardiology and the European Respiratory Society clinical practice guideline recommends that low- and intermediate-risk patients should be started on ERA/PDE5i combination therapy, while high-risk patients should also be given an intravenous or subcutaneous prostacyclin analogue, referred to as triple therapy.
Sotatercept’s regulatory approval hinges on the phase 3 STELLAR trial, which included 323 patients with World Health Organization functional class (WHO-FC) II and III PAH who were randomized to 0.75 mg/kg sotatercept in addition to background double or triple therapy, or background therapy alone. The mean age was 48 years, and the mean time since diagnosis was 8.8 years. About 40% received infused prostacyclin therapy at baseline. At 24 weeks, the median change in 6-min walking distance (6mWD) was 40.8 m longer in the sotatercept group. More patients in the sotatercept group experienced WHO-FC improvement (29.4% vs 13.8%). Those in the sotatercept group also experienced an 84% reduction in risk for clinical worsening or death. PAH-specific quality of life scales did not show a difference between the two groups. Open-label extension trials have shown that benefits are maintained for up to 2 years. Adverse events likely related to sotatercept included telangiectasias, increased hemoglobin levels, and bleeding events.
Along with its benefits, the report authors suggest that the subcutaneous delivery of sotatercept may be less burdensome to patients than some other PAH treatments, especially inhaled and intravenous prostanoids. “However, uncertainty remains about sotatercept’s efficacy in sicker populations and in those with connective tissue disease, and about the durability of effect,” the authors wrote.
A lack of long-term data leaves open the question of its effect on mortality and unknown adverse effects.
Using a de novo decision analytic model, the authors estimated that sotatercept treatment would lead to a longer time without symptoms at rest and more quality-adjusted life years, life years, and equal value life years. They determined the health benefit price benchmark for sotatercept to be between $18,700 and $36,200 per year. “The long-term conventional cost-effectiveness of sotatercept is largely dependent on the long-term effect of sotatercept on improving functional class and slowing the worsening in functional class; however, controlled trial evidence for sotatercept is limited to 24 weeks. Long-term data are necessary to reduce the uncertainty in sotatercept’s long-term effect on improving functional class and slowing the worsening in functional class,” the authors wrote.
During the online meeting, Dr. Curfman took note of the fact that the STELLAR trial reported a median value of increase in 6mWD, rather than a mean, and the 40-m improvement is close to the value accepted as clinically meaningful. “So that tells us that half the patients had less than a clinically important improvement in the six-minute walk distance. We should be putting that in perspective,” said Dr. Curfman.
Another attendee pointed out that the open-label PULSAR extension trial showed that the proportion of patients in the sotatercept arm who were functional class I rose from 7.5% at the end of the trial to 20.6% at the end of the open-label period and wondered if that could be a sign of disease-modifying activity. “I think that’s a remarkable piece of data. I don’t recall seeing that in any other open label [trial of a PAH therapy] — that much of an improvement in getting to our best functional status,” said Marc Simon, MD, professor of medicine and director of the Pulmonary Hypertension Center at the University of California, San Francisco, who was a coauthor of the report.
Dr. Curfman has no relevant financial disclosures. Dr. Simon has consulted for Merck.
A version of this article appeared on Medscape.com.
New COVID variant JN.1 could disrupt holiday plans
No one planning holiday gatherings or travel wants to hear this, but the rise of a new COVID-19 variant, JN.1, is concerning experts, who say it may threaten those good times.
The good news is recent research suggests the 2023-2024 COVID-19 vaccine appears to work against this newest variant. But so few people have gotten the latest vaccine — less than 16% of U.S. adults — that some experts suggest it’s time for the CDC to urge the public who haven’t it to do so now, so the antibodies can kick in before the festivities.
“A significant wave [of JN.1] has started here and could be blunted with a high booster rate and mitigation measures,” said Eric Topol, MD, professor and executive vice president of Scripps Research in La Jolla, CA, and editor-in-chief of Medscape, a sister site of this news organization.
COVID metrics, meanwhile, have started to climb again. Nearly 10,000 people were hospitalized for COVID in the U.S. for the week ending Nov. 25, the CDC said, a 10% increase over the previous week.
Who’s Who in the Family Tree
JN.1, an Omicron subvariant, was first detected in the U.S. in September and is termed “a notable descendent lineage” of Omicron subvariant BA.2.86 by the World Health Organization. When BA.2.86, also known as Pirola, was first identified in August, it appeared very different from other variants, the CDC said. That triggered concerns it might be more infectious than previous ones, even for people with immunity from vaccination and previous infections.
“JN.1 is Pirola’s kid,” said Rajendram Rajnarayanan, PhD, assistant dean of research and associate professor at the New York Institute of Technology at Arkansas State University, who maintains a COVID-19 variant database. The variant BA.2.86 and offspring are worrisome due to the mutations, he said.
How Widespread Is JN.1?
As of Nov. 27, the CDC says, BA.2.86 is projected to comprise 5%-15% of circulating variants in the U.S. “The expected public health risk of this variant, including its offshoot JN.1, is low,” the agency said.
Currently, JN.1 is reported more often in Europe, Dr. Rajnarayanan said, but some countries have better reporting data than others. “It has probably spread to every country tracking COVID,’’ he said, due to the mutations in the spike protein that make it easier for it to bind and infect.
Wastewater data suggest the variant’s rise is helping to fuel a wave, Dr. Topol said.
Vaccine Effectiveness Against JN.1, Other New Variants
The new XBB.1.5 monovalent vaccine, protects against XBB.1.5, another Omicron subvariant, but also JN.1 and other “emergent” viruses, a team of researchers reported Nov. 26 in a study on bioRxiv that has not yet been certified by peer review.
The updated vaccine, when given to uninfected people, boosted antibodies about 27-fold against XBB.1.5 and about 13- to 27-fold against JN.1 and other emergent viruses, the researchers reported.
While even primary doses of the COVID vaccine will likely help protect against the new JN.1 subvariant, “if you got the XBB.1.5 booster, it is going to be protecting you better against this new variant,” Dr. Rajnarayanan said.
2023-2024 Vaccine Uptake Low
In November, the CDC posted the first detailed estimates of who did. As of Nov. 18, less than 16% of U.S. adults had, with nearly 15% saying they planned to get it.
Coverage among children is lower, with just 6.3% of children up to date on the newest vaccine and 19% of parents saying they planned to get the 2023-2024 vaccine for their children.
Predictions, Mitigation
While some experts say a peak due to JN.1 is expected in the weeks ahead, Dr. Topol said it’s impossible to predict exactly how JN.1 will play out.
“It’s not going to be a repeat of November 2021,” when Omicron surfaced, Dr. Rajnarayanan predicted. Within 4 weeks of the World Health Organization declaring Omicron as a virus of concern, it spread around the world.
Mitigation measures can help, Dr. Rajnarayanan said. He suggested:
Get the new vaccine, and especially encourage vulnerable family and friends to do so.
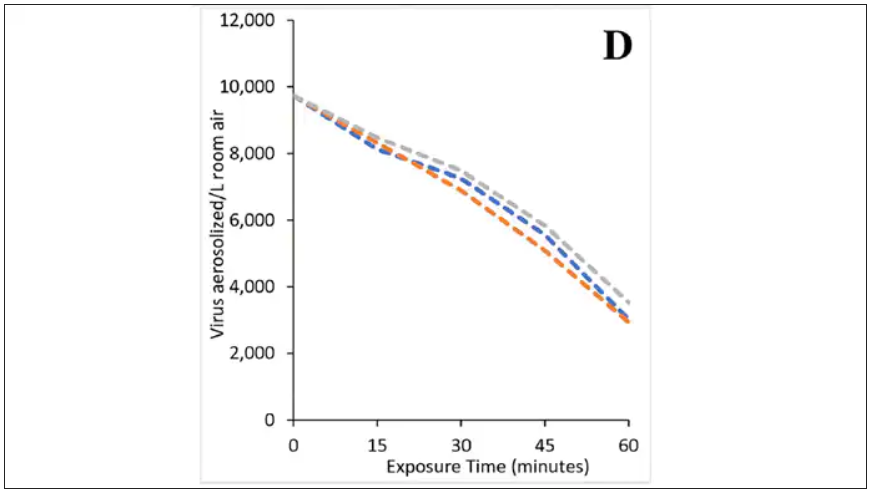
If you are gathering inside for holiday festivities, improve circulation in the house, if possible.
Wear masks in airports and on planes and other public transportation.
A version of this article appeared on WebMD.com.
No one planning holiday gatherings or travel wants to hear this, but the rise of a new COVID-19 variant, JN.1, is concerning experts, who say it may threaten those good times.
The good news is recent research suggests the 2023-2024 COVID-19 vaccine appears to work against this newest variant. But so few people have gotten the latest vaccine — less than 16% of U.S. adults — that some experts suggest it’s time for the CDC to urge the public who haven’t it to do so now, so the antibodies can kick in before the festivities.
“A significant wave [of JN.1] has started here and could be blunted with a high booster rate and mitigation measures,” said Eric Topol, MD, professor and executive vice president of Scripps Research in La Jolla, CA, and editor-in-chief of Medscape, a sister site of this news organization.
COVID metrics, meanwhile, have started to climb again. Nearly 10,000 people were hospitalized for COVID in the U.S. for the week ending Nov. 25, the CDC said, a 10% increase over the previous week.
Who’s Who in the Family Tree
JN.1, an Omicron subvariant, was first detected in the U.S. in September and is termed “a notable descendent lineage” of Omicron subvariant BA.2.86 by the World Health Organization. When BA.2.86, also known as Pirola, was first identified in August, it appeared very different from other variants, the CDC said. That triggered concerns it might be more infectious than previous ones, even for people with immunity from vaccination and previous infections.
“JN.1 is Pirola’s kid,” said Rajendram Rajnarayanan, PhD, assistant dean of research and associate professor at the New York Institute of Technology at Arkansas State University, who maintains a COVID-19 variant database. The variant BA.2.86 and offspring are worrisome due to the mutations, he said.
How Widespread Is JN.1?
As of Nov. 27, the CDC says, BA.2.86 is projected to comprise 5%-15% of circulating variants in the U.S. “The expected public health risk of this variant, including its offshoot JN.1, is low,” the agency said.
Currently, JN.1 is reported more often in Europe, Dr. Rajnarayanan said, but some countries have better reporting data than others. “It has probably spread to every country tracking COVID,’’ he said, due to the mutations in the spike protein that make it easier for it to bind and infect.
Wastewater data suggest the variant’s rise is helping to fuel a wave, Dr. Topol said.
Vaccine Effectiveness Against JN.1, Other New Variants
The new XBB.1.5 monovalent vaccine, protects against XBB.1.5, another Omicron subvariant, but also JN.1 and other “emergent” viruses, a team of researchers reported Nov. 26 in a study on bioRxiv that has not yet been certified by peer review.
The updated vaccine, when given to uninfected people, boosted antibodies about 27-fold against XBB.1.5 and about 13- to 27-fold against JN.1 and other emergent viruses, the researchers reported.
While even primary doses of the COVID vaccine will likely help protect against the new JN.1 subvariant, “if you got the XBB.1.5 booster, it is going to be protecting you better against this new variant,” Dr. Rajnarayanan said.
2023-2024 Vaccine Uptake Low
In November, the CDC posted the first detailed estimates of who did. As of Nov. 18, less than 16% of U.S. adults had, with nearly 15% saying they planned to get it.
Coverage among children is lower, with just 6.3% of children up to date on the newest vaccine and 19% of parents saying they planned to get the 2023-2024 vaccine for their children.
Predictions, Mitigation
While some experts say a peak due to JN.1 is expected in the weeks ahead, Dr. Topol said it’s impossible to predict exactly how JN.1 will play out.
“It’s not going to be a repeat of November 2021,” when Omicron surfaced, Dr. Rajnarayanan predicted. Within 4 weeks of the World Health Organization declaring Omicron as a virus of concern, it spread around the world.
Mitigation measures can help, Dr. Rajnarayanan said. He suggested:
Get the new vaccine, and especially encourage vulnerable family and friends to do so.
If you are gathering inside for holiday festivities, improve circulation in the house, if possible.
Wear masks in airports and on planes and other public transportation.
A version of this article appeared on WebMD.com.
No one planning holiday gatherings or travel wants to hear this, but the rise of a new COVID-19 variant, JN.1, is concerning experts, who say it may threaten those good times.
The good news is recent research suggests the 2023-2024 COVID-19 vaccine appears to work against this newest variant. But so few people have gotten the latest vaccine — less than 16% of U.S. adults — that some experts suggest it’s time for the CDC to urge the public who haven’t it to do so now, so the antibodies can kick in before the festivities.
“A significant wave [of JN.1] has started here and could be blunted with a high booster rate and mitigation measures,” said Eric Topol, MD, professor and executive vice president of Scripps Research in La Jolla, CA, and editor-in-chief of Medscape, a sister site of this news organization.
COVID metrics, meanwhile, have started to climb again. Nearly 10,000 people were hospitalized for COVID in the U.S. for the week ending Nov. 25, the CDC said, a 10% increase over the previous week.
Who’s Who in the Family Tree
JN.1, an Omicron subvariant, was first detected in the U.S. in September and is termed “a notable descendent lineage” of Omicron subvariant BA.2.86 by the World Health Organization. When BA.2.86, also known as Pirola, was first identified in August, it appeared very different from other variants, the CDC said. That triggered concerns it might be more infectious than previous ones, even for people with immunity from vaccination and previous infections.
“JN.1 is Pirola’s kid,” said Rajendram Rajnarayanan, PhD, assistant dean of research and associate professor at the New York Institute of Technology at Arkansas State University, who maintains a COVID-19 variant database. The variant BA.2.86 and offspring are worrisome due to the mutations, he said.
How Widespread Is JN.1?
As of Nov. 27, the CDC says, BA.2.86 is projected to comprise 5%-15% of circulating variants in the U.S. “The expected public health risk of this variant, including its offshoot JN.1, is low,” the agency said.
Currently, JN.1 is reported more often in Europe, Dr. Rajnarayanan said, but some countries have better reporting data than others. “It has probably spread to every country tracking COVID,’’ he said, due to the mutations in the spike protein that make it easier for it to bind and infect.
Wastewater data suggest the variant’s rise is helping to fuel a wave, Dr. Topol said.
Vaccine Effectiveness Against JN.1, Other New Variants
The new XBB.1.5 monovalent vaccine, protects against XBB.1.5, another Omicron subvariant, but also JN.1 and other “emergent” viruses, a team of researchers reported Nov. 26 in a study on bioRxiv that has not yet been certified by peer review.
The updated vaccine, when given to uninfected people, boosted antibodies about 27-fold against XBB.1.5 and about 13- to 27-fold against JN.1 and other emergent viruses, the researchers reported.
While even primary doses of the COVID vaccine will likely help protect against the new JN.1 subvariant, “if you got the XBB.1.5 booster, it is going to be protecting you better against this new variant,” Dr. Rajnarayanan said.
2023-2024 Vaccine Uptake Low
In November, the CDC posted the first detailed estimates of who did. As of Nov. 18, less than 16% of U.S. adults had, with nearly 15% saying they planned to get it.
Coverage among children is lower, with just 6.3% of children up to date on the newest vaccine and 19% of parents saying they planned to get the 2023-2024 vaccine for their children.
Predictions, Mitigation
While some experts say a peak due to JN.1 is expected in the weeks ahead, Dr. Topol said it’s impossible to predict exactly how JN.1 will play out.
“It’s not going to be a repeat of November 2021,” when Omicron surfaced, Dr. Rajnarayanan predicted. Within 4 weeks of the World Health Organization declaring Omicron as a virus of concern, it spread around the world.
Mitigation measures can help, Dr. Rajnarayanan said. He suggested:
Get the new vaccine, and especially encourage vulnerable family and friends to do so.
If you are gathering inside for holiday festivities, improve circulation in the house, if possible.
Wear masks in airports and on planes and other public transportation.
A version of this article appeared on WebMD.com.
Pulmonary arterial hypertension: Promising results for investigational agents and catheter-based denervation
PHILADELPHIA — Promise that the unmet need for more effective pulmonary artery hypertension treatments may soon be met was in strong evidence in research into three strategies presented at this year’s recent American Heart Association scientific sessions; one was based on an ancient Chinese herb epimedium (yin yang huo or horny goat weed) commonly used for treating sexual dysfunction and directly related to the phosphodiesterase inhibitors sildenafil, vardenafil, and tadalafil (sold as Viagra, Levitra, and Cialis). A second studied sotatercept, an investigational, potential first-in-class activin signaling inhibitor biologic, and a third evaluated physically ablating the baroreceptor nerves that stimulate vasoconstriction of the pulmonary artery via catheter-based techniques.
Until as recently as the late 1970s, a pulmonary arterial hypertension diagnosis was a uniformly fatal one.1 While associated with pulmonary and right ventricle remodeling, and leads toward heart failure and death. The complex underlying pathogenesis was divided into six groups by the 6th World Symposium on Pulmonary Hypertension (WSPH) in 2018, and includes as its most common features pulmonary artery endothelial cell dysfunction, pulmonary artery smooth muscle cell proliferation and migration, and dysregulated fibroblast activity leading to dysregulated vasoconstriction, micro and in-situ vascular thrombosis, vascular fibrosis and pathogenic remodeling of pulmonary vessels.1 The threshold mean arterial pressure (mPAP) for pulmonary arterial hypertension was defined by the 6th [WSPH] at mPAP ≥ 20 mm Hg, twice the upper limit of a normal mPAP of 14.0 ± 3.3 mm Hg as reported by Kovacs et al. in 2018.2
Pathways for current therapies
Current drugs for pulmonary arterial hypertension focus on three signaling pathways, including the endothelin receptor, prostacyclin and nitric oxide pathways, stated Zhi-Cheng Jing, MD, professor of medicine, head of the cardiology department at Peking Union Medical College Hospital, Peking, China. While the phosphodiesterase 5 inhibitors sildenafil and tadalafil, which target the nitric oxide pathway, came into wide use after Food and Drug Administration approval, the need for higher PDE5-selectivity remains, Dr. Jing said. Structurally modified from the active ingredient in epimedium, TPN171H is an investigational PDE5 inhibitor which has shown several favorable features: a greater PDE5 selectivity than both sildenafil and tadalafil in vitro, an ability to decrease right ventricular systolic pressure and alleviate arterial remodeling in animal studies, and safety and tolerability in healthy human subjects.
The current randomized, double-blind, placebo-and active-controlled phase IIa study assessed the hemodynamic impact of a single oral dose of TPN171H in 60 pulmonary arterial hypertension patients (mean age ~34 years, 83.3% female), all with negative vasodilation test results and in WHO class 2 or 3. Only patients aged 18-75 years with group 1 pulmonary arterial hypertension of idiopathic, connective tissue disorder, or repaired congenital heart defects etiology were included. Patients were divided into six groups: placebo, TPN171H at 2.5, 5, and 10 milligrams, and tadalafil at 20 and 40 milligrams.
For the primary endpoint of maximum decrease in pulmonary vascular resistance (PVR), significant reductions vs. placebo were found only for the TPN171H 5-mg group (–41.2% vs. –24.4%; P = .008) and for the 20-mg (–39.8%) and 40-mg (–37.6%) tadalafil groups (both P < .05). What was not seen in the tadalafil groups, but was evident in the TPN171H 5-mg group, was a significant reduction in the secondary endpoint of PVR/SVR (systolic vascular resistance) at 2, 3, and 5 hours (all P < .05). “As we know,” Dr. Jing said in an interview, “the PDE5 inhibitor functions as a vasodilator, having an impact on both pulmonary circulation and systemic circulation. So, to evaluate the selectivity for pulmonary circulation is crucial when exploring a novel drug for pulmonary arterial hypertension. The change of PVR/SVR ratio from baseline is an indicator for selectivity for pulmonary circulation and implies that TPN171H has good PDE5 selectivity in the pulmonary vasculature,” Dr. Jing said.
TPN171H was well tolerated with no serious adverse effects (vomiting 10% and headache 10% were most common with no discontinuations).
TGF-signaling pathway
A meta-analysis of randomized controlled trials of sotatercept, an investigational fusion protein under priority FDA review that modulates the TGF-beta superfamily signaling pathway, looked at PVR, pulmonary arterial pressure (PAP), right arterial pressure (RAP) and N-terminal pro-brain natriuretic peptide (NT-proBNP). A literature search by corresponding author Vamsikalyan Borra, MD, Knapp Medical Center, Weslaco, Texas, and colleagues identified two trials (STELLAR and PULSAR) comprising 429 patients with pulmonary arterial hypertension. The experimental arms (sotatercept) had 237 patients (mean age ~49 years, ~82% female) and the placebo arm had 192 patients (mean age ~47 years, ~80% female).
A pooled analysis showed significant reductions with sotatercept in PVR (standardization mean difference [SMD] = –1.00, 95% confidence interval [CI] = –1.2, –.79, P < .001), PAP (SMD = –1.34, 95% CI = 1.6, –1.08, P < .001), RAP (SMD = –0.66, 95% CI = –0.93, –0.39, P < .001), and the levels of NT-proBNP (SMD = –0.64, 95% CI = –1.01, –0.27, P < .001) at 24 weeks from baseline. The sotatercept safety profile was favorable, with lower overall incidence of adverse events (84.8% vs. 87.5%) and fewer adverse events leading to death (0.4% vs. 3.1%) compared with placebo. Further investigation is needed, however, according to Dr. Borra, into the higher frequency of reported thrombocytopenia (71.7% vs. 20.8%) with sotatercept. “Our findings,” Dr. Borra said in a poster session, “suggest that sotatercept is an effective treatment option for pulmonary arterial hypertension, with the potential to improve both pulmonary and cardiac function.”
Denervation technique
Catheter-based ablation techniques, most commonly using thermal energy, target the afferent and efferent fibers of the baroreceptor reflex in the main pulmonary artery trunk and bifurcation involved in elevated pulmonary artery pressure. Mounica Vorla, MD, Carle Foundation Hospital, Urbana, Illinois, and colleagues conducted an updated systematic review and meta-analysis of the safety and efficacy of pulmonary artery denervation (PADN) for pulmonary arterial hypertension in seven clinical trials with 506 patients with moderate-severe pulmonary arterial hypertension conducted from 2013 to 2022.
Compared with placebo, PADN treatment was associated with a significant reduction in mean pulmonary artery pressure (weighted mean difference [WMD] = –6.9 mm Hg; 95% CI = –9.7, –4.1; P < .01; I2 = 61) and pulmonary vascular resistance (WMD = –3.2; 95% CI = –5.4, –0.9; P = .005). PADN improvements in cardiac output were also statistically significant (WMD = 0.3; 95% CI = 0.07, 0.6; P = .012), with numerical improvement in 6-minute walking distance (WMD = 67.7; 95% CI = –3.73, 139.2; P = .06) in the PADN group. Side effects were less common in the PADN group as compared with the placebo group, Dr. Vorla reported. She concluded, “This updated meta-analysis supports PADN as a safe and efficacious therapy for severe pulmonary arterial hypertension.” The authors noted limitations imposed by the small sample size, large data heterogeneity, and medium-quality literature. Larger randomized, controlled trials with clinical endpoints comparing PADN with optimal medical therapy are needed, they stated.
References
1. Shah AJ et al. New Drugs and Therapies in Pulmonary Arterial Hypertension. Int J Mol Sci. 2023 Mar 19;24(6):5850. doi: 10.3390/ijms24065850. PMID: 36982922; PMCID: PMC10058689.
2. Kovacs G et al. Pulmonary Vascular Involvement in Chronic Obstructive Pulmonary Disease. Is There a Pulmonary Vascular Phenotype? Am J Respir Crit Care Med. 2018 Oct 15;198(8):1000-11. doi: 10.1164/rccm.201801-0095PP. PMID: 29746142.
PHILADELPHIA — Promise that the unmet need for more effective pulmonary artery hypertension treatments may soon be met was in strong evidence in research into three strategies presented at this year’s recent American Heart Association scientific sessions; one was based on an ancient Chinese herb epimedium (yin yang huo or horny goat weed) commonly used for treating sexual dysfunction and directly related to the phosphodiesterase inhibitors sildenafil, vardenafil, and tadalafil (sold as Viagra, Levitra, and Cialis). A second studied sotatercept, an investigational, potential first-in-class activin signaling inhibitor biologic, and a third evaluated physically ablating the baroreceptor nerves that stimulate vasoconstriction of the pulmonary artery via catheter-based techniques.
Until as recently as the late 1970s, a pulmonary arterial hypertension diagnosis was a uniformly fatal one.1 While associated with pulmonary and right ventricle remodeling, and leads toward heart failure and death. The complex underlying pathogenesis was divided into six groups by the 6th World Symposium on Pulmonary Hypertension (WSPH) in 2018, and includes as its most common features pulmonary artery endothelial cell dysfunction, pulmonary artery smooth muscle cell proliferation and migration, and dysregulated fibroblast activity leading to dysregulated vasoconstriction, micro and in-situ vascular thrombosis, vascular fibrosis and pathogenic remodeling of pulmonary vessels.1 The threshold mean arterial pressure (mPAP) for pulmonary arterial hypertension was defined by the 6th [WSPH] at mPAP ≥ 20 mm Hg, twice the upper limit of a normal mPAP of 14.0 ± 3.3 mm Hg as reported by Kovacs et al. in 2018.2
Pathways for current therapies
Current drugs for pulmonary arterial hypertension focus on three signaling pathways, including the endothelin receptor, prostacyclin and nitric oxide pathways, stated Zhi-Cheng Jing, MD, professor of medicine, head of the cardiology department at Peking Union Medical College Hospital, Peking, China. While the phosphodiesterase 5 inhibitors sildenafil and tadalafil, which target the nitric oxide pathway, came into wide use after Food and Drug Administration approval, the need for higher PDE5-selectivity remains, Dr. Jing said. Structurally modified from the active ingredient in epimedium, TPN171H is an investigational PDE5 inhibitor which has shown several favorable features: a greater PDE5 selectivity than both sildenafil and tadalafil in vitro, an ability to decrease right ventricular systolic pressure and alleviate arterial remodeling in animal studies, and safety and tolerability in healthy human subjects.
The current randomized, double-blind, placebo-and active-controlled phase IIa study assessed the hemodynamic impact of a single oral dose of TPN171H in 60 pulmonary arterial hypertension patients (mean age ~34 years, 83.3% female), all with negative vasodilation test results and in WHO class 2 or 3. Only patients aged 18-75 years with group 1 pulmonary arterial hypertension of idiopathic, connective tissue disorder, or repaired congenital heart defects etiology were included. Patients were divided into six groups: placebo, TPN171H at 2.5, 5, and 10 milligrams, and tadalafil at 20 and 40 milligrams.
For the primary endpoint of maximum decrease in pulmonary vascular resistance (PVR), significant reductions vs. placebo were found only for the TPN171H 5-mg group (–41.2% vs. –24.4%; P = .008) and for the 20-mg (–39.8%) and 40-mg (–37.6%) tadalafil groups (both P < .05). What was not seen in the tadalafil groups, but was evident in the TPN171H 5-mg group, was a significant reduction in the secondary endpoint of PVR/SVR (systolic vascular resistance) at 2, 3, and 5 hours (all P < .05). “As we know,” Dr. Jing said in an interview, “the PDE5 inhibitor functions as a vasodilator, having an impact on both pulmonary circulation and systemic circulation. So, to evaluate the selectivity for pulmonary circulation is crucial when exploring a novel drug for pulmonary arterial hypertension. The change of PVR/SVR ratio from baseline is an indicator for selectivity for pulmonary circulation and implies that TPN171H has good PDE5 selectivity in the pulmonary vasculature,” Dr. Jing said.
TPN171H was well tolerated with no serious adverse effects (vomiting 10% and headache 10% were most common with no discontinuations).
TGF-signaling pathway
A meta-analysis of randomized controlled trials of sotatercept, an investigational fusion protein under priority FDA review that modulates the TGF-beta superfamily signaling pathway, looked at PVR, pulmonary arterial pressure (PAP), right arterial pressure (RAP) and N-terminal pro-brain natriuretic peptide (NT-proBNP). A literature search by corresponding author Vamsikalyan Borra, MD, Knapp Medical Center, Weslaco, Texas, and colleagues identified two trials (STELLAR and PULSAR) comprising 429 patients with pulmonary arterial hypertension. The experimental arms (sotatercept) had 237 patients (mean age ~49 years, ~82% female) and the placebo arm had 192 patients (mean age ~47 years, ~80% female).
A pooled analysis showed significant reductions with sotatercept in PVR (standardization mean difference [SMD] = –1.00, 95% confidence interval [CI] = –1.2, –.79, P < .001), PAP (SMD = –1.34, 95% CI = 1.6, –1.08, P < .001), RAP (SMD = –0.66, 95% CI = –0.93, –0.39, P < .001), and the levels of NT-proBNP (SMD = –0.64, 95% CI = –1.01, –0.27, P < .001) at 24 weeks from baseline. The sotatercept safety profile was favorable, with lower overall incidence of adverse events (84.8% vs. 87.5%) and fewer adverse events leading to death (0.4% vs. 3.1%) compared with placebo. Further investigation is needed, however, according to Dr. Borra, into the higher frequency of reported thrombocytopenia (71.7% vs. 20.8%) with sotatercept. “Our findings,” Dr. Borra said in a poster session, “suggest that sotatercept is an effective treatment option for pulmonary arterial hypertension, with the potential to improve both pulmonary and cardiac function.”
Denervation technique
Catheter-based ablation techniques, most commonly using thermal energy, target the afferent and efferent fibers of the baroreceptor reflex in the main pulmonary artery trunk and bifurcation involved in elevated pulmonary artery pressure. Mounica Vorla, MD, Carle Foundation Hospital, Urbana, Illinois, and colleagues conducted an updated systematic review and meta-analysis of the safety and efficacy of pulmonary artery denervation (PADN) for pulmonary arterial hypertension in seven clinical trials with 506 patients with moderate-severe pulmonary arterial hypertension conducted from 2013 to 2022.
Compared with placebo, PADN treatment was associated with a significant reduction in mean pulmonary artery pressure (weighted mean difference [WMD] = –6.9 mm Hg; 95% CI = –9.7, –4.1; P < .01; I2 = 61) and pulmonary vascular resistance (WMD = –3.2; 95% CI = –5.4, –0.9; P = .005). PADN improvements in cardiac output were also statistically significant (WMD = 0.3; 95% CI = 0.07, 0.6; P = .012), with numerical improvement in 6-minute walking distance (WMD = 67.7; 95% CI = –3.73, 139.2; P = .06) in the PADN group. Side effects were less common in the PADN group as compared with the placebo group, Dr. Vorla reported. She concluded, “This updated meta-analysis supports PADN as a safe and efficacious therapy for severe pulmonary arterial hypertension.” The authors noted limitations imposed by the small sample size, large data heterogeneity, and medium-quality literature. Larger randomized, controlled trials with clinical endpoints comparing PADN with optimal medical therapy are needed, they stated.
References
1. Shah AJ et al. New Drugs and Therapies in Pulmonary Arterial Hypertension. Int J Mol Sci. 2023 Mar 19;24(6):5850. doi: 10.3390/ijms24065850. PMID: 36982922; PMCID: PMC10058689.
2. Kovacs G et al. Pulmonary Vascular Involvement in Chronic Obstructive Pulmonary Disease. Is There a Pulmonary Vascular Phenotype? Am J Respir Crit Care Med. 2018 Oct 15;198(8):1000-11. doi: 10.1164/rccm.201801-0095PP. PMID: 29746142.
PHILADELPHIA — Promise that the unmet need for more effective pulmonary artery hypertension treatments may soon be met was in strong evidence in research into three strategies presented at this year’s recent American Heart Association scientific sessions; one was based on an ancient Chinese herb epimedium (yin yang huo or horny goat weed) commonly used for treating sexual dysfunction and directly related to the phosphodiesterase inhibitors sildenafil, vardenafil, and tadalafil (sold as Viagra, Levitra, and Cialis). A second studied sotatercept, an investigational, potential first-in-class activin signaling inhibitor biologic, and a third evaluated physically ablating the baroreceptor nerves that stimulate vasoconstriction of the pulmonary artery via catheter-based techniques.
Until as recently as the late 1970s, a pulmonary arterial hypertension diagnosis was a uniformly fatal one.1 While associated with pulmonary and right ventricle remodeling, and leads toward heart failure and death. The complex underlying pathogenesis was divided into six groups by the 6th World Symposium on Pulmonary Hypertension (WSPH) in 2018, and includes as its most common features pulmonary artery endothelial cell dysfunction, pulmonary artery smooth muscle cell proliferation and migration, and dysregulated fibroblast activity leading to dysregulated vasoconstriction, micro and in-situ vascular thrombosis, vascular fibrosis and pathogenic remodeling of pulmonary vessels.1 The threshold mean arterial pressure (mPAP) for pulmonary arterial hypertension was defined by the 6th [WSPH] at mPAP ≥ 20 mm Hg, twice the upper limit of a normal mPAP of 14.0 ± 3.3 mm Hg as reported by Kovacs et al. in 2018.2
Pathways for current therapies
Current drugs for pulmonary arterial hypertension focus on three signaling pathways, including the endothelin receptor, prostacyclin and nitric oxide pathways, stated Zhi-Cheng Jing, MD, professor of medicine, head of the cardiology department at Peking Union Medical College Hospital, Peking, China. While the phosphodiesterase 5 inhibitors sildenafil and tadalafil, which target the nitric oxide pathway, came into wide use after Food and Drug Administration approval, the need for higher PDE5-selectivity remains, Dr. Jing said. Structurally modified from the active ingredient in epimedium, TPN171H is an investigational PDE5 inhibitor which has shown several favorable features: a greater PDE5 selectivity than both sildenafil and tadalafil in vitro, an ability to decrease right ventricular systolic pressure and alleviate arterial remodeling in animal studies, and safety and tolerability in healthy human subjects.
The current randomized, double-blind, placebo-and active-controlled phase IIa study assessed the hemodynamic impact of a single oral dose of TPN171H in 60 pulmonary arterial hypertension patients (mean age ~34 years, 83.3% female), all with negative vasodilation test results and in WHO class 2 or 3. Only patients aged 18-75 years with group 1 pulmonary arterial hypertension of idiopathic, connective tissue disorder, or repaired congenital heart defects etiology were included. Patients were divided into six groups: placebo, TPN171H at 2.5, 5, and 10 milligrams, and tadalafil at 20 and 40 milligrams.
For the primary endpoint of maximum decrease in pulmonary vascular resistance (PVR), significant reductions vs. placebo were found only for the TPN171H 5-mg group (–41.2% vs. –24.4%; P = .008) and for the 20-mg (–39.8%) and 40-mg (–37.6%) tadalafil groups (both P < .05). What was not seen in the tadalafil groups, but was evident in the TPN171H 5-mg group, was a significant reduction in the secondary endpoint of PVR/SVR (systolic vascular resistance) at 2, 3, and 5 hours (all P < .05). “As we know,” Dr. Jing said in an interview, “the PDE5 inhibitor functions as a vasodilator, having an impact on both pulmonary circulation and systemic circulation. So, to evaluate the selectivity for pulmonary circulation is crucial when exploring a novel drug for pulmonary arterial hypertension. The change of PVR/SVR ratio from baseline is an indicator for selectivity for pulmonary circulation and implies that TPN171H has good PDE5 selectivity in the pulmonary vasculature,” Dr. Jing said.
TPN171H was well tolerated with no serious adverse effects (vomiting 10% and headache 10% were most common with no discontinuations).
TGF-signaling pathway
A meta-analysis of randomized controlled trials of sotatercept, an investigational fusion protein under priority FDA review that modulates the TGF-beta superfamily signaling pathway, looked at PVR, pulmonary arterial pressure (PAP), right arterial pressure (RAP) and N-terminal pro-brain natriuretic peptide (NT-proBNP). A literature search by corresponding author Vamsikalyan Borra, MD, Knapp Medical Center, Weslaco, Texas, and colleagues identified two trials (STELLAR and PULSAR) comprising 429 patients with pulmonary arterial hypertension. The experimental arms (sotatercept) had 237 patients (mean age ~49 years, ~82% female) and the placebo arm had 192 patients (mean age ~47 years, ~80% female).
A pooled analysis showed significant reductions with sotatercept in PVR (standardization mean difference [SMD] = –1.00, 95% confidence interval [CI] = –1.2, –.79, P < .001), PAP (SMD = –1.34, 95% CI = 1.6, –1.08, P < .001), RAP (SMD = –0.66, 95% CI = –0.93, –0.39, P < .001), and the levels of NT-proBNP (SMD = –0.64, 95% CI = –1.01, –0.27, P < .001) at 24 weeks from baseline. The sotatercept safety profile was favorable, with lower overall incidence of adverse events (84.8% vs. 87.5%) and fewer adverse events leading to death (0.4% vs. 3.1%) compared with placebo. Further investigation is needed, however, according to Dr. Borra, into the higher frequency of reported thrombocytopenia (71.7% vs. 20.8%) with sotatercept. “Our findings,” Dr. Borra said in a poster session, “suggest that sotatercept is an effective treatment option for pulmonary arterial hypertension, with the potential to improve both pulmonary and cardiac function.”
Denervation technique
Catheter-based ablation techniques, most commonly using thermal energy, target the afferent and efferent fibers of the baroreceptor reflex in the main pulmonary artery trunk and bifurcation involved in elevated pulmonary artery pressure. Mounica Vorla, MD, Carle Foundation Hospital, Urbana, Illinois, and colleagues conducted an updated systematic review and meta-analysis of the safety and efficacy of pulmonary artery denervation (PADN) for pulmonary arterial hypertension in seven clinical trials with 506 patients with moderate-severe pulmonary arterial hypertension conducted from 2013 to 2022.
Compared with placebo, PADN treatment was associated with a significant reduction in mean pulmonary artery pressure (weighted mean difference [WMD] = –6.9 mm Hg; 95% CI = –9.7, –4.1; P < .01; I2 = 61) and pulmonary vascular resistance (WMD = –3.2; 95% CI = –5.4, –0.9; P = .005). PADN improvements in cardiac output were also statistically significant (WMD = 0.3; 95% CI = 0.07, 0.6; P = .012), with numerical improvement in 6-minute walking distance (WMD = 67.7; 95% CI = –3.73, 139.2; P = .06) in the PADN group. Side effects were less common in the PADN group as compared with the placebo group, Dr. Vorla reported. She concluded, “This updated meta-analysis supports PADN as a safe and efficacious therapy for severe pulmonary arterial hypertension.” The authors noted limitations imposed by the small sample size, large data heterogeneity, and medium-quality literature. Larger randomized, controlled trials with clinical endpoints comparing PADN with optimal medical therapy are needed, they stated.
References
1. Shah AJ et al. New Drugs and Therapies in Pulmonary Arterial Hypertension. Int J Mol Sci. 2023 Mar 19;24(6):5850. doi: 10.3390/ijms24065850. PMID: 36982922; PMCID: PMC10058689.
2. Kovacs G et al. Pulmonary Vascular Involvement in Chronic Obstructive Pulmonary Disease. Is There a Pulmonary Vascular Phenotype? Am J Respir Crit Care Med. 2018 Oct 15;198(8):1000-11. doi: 10.1164/rccm.201801-0095PP. PMID: 29746142.
FROM AHA 2023
Smoking alters salivary microbiota in potential path to disease risk
TOPLINE:
Salivary microbiota changes caused by cigarette smoking may affect metabolic pathways and increase disease risk.
METHODOLOGY:
The researchers analyzed health information and data on the composition of salivary microbiota from 1601 adult participants in the Cooperative Health Research in South Tyrol (CHRIS) microbiome study (CHRISMB); CHRIS is an ongoing study in Italy.
The average age of the study population was 45 years; 53% were female, and 45% were current or former smokers.
The researchers hypothesized that changes in salivary microbial composition would be associated with smoking, with more nitrate-reducing bacteria present, and that nitrate reduction pathways would be reduced in smokers.
TAKEAWAY:
The researchers identified 44 genera that differed in the salivary microbiota of current smokers and nonsmokers. In smokers, seven genera in the phylum Proteobacteria were decreased and six in the phylum Actinobacteria were increased compared with nonsmokers; these phyla contain primarily aerobic and anaerobic taxa, respectively.
Some microbiota changes were significantly associated with daily smoking intensity; genera from the classes Betaproteobacteria (Lautropia or Neisseria), Gammaproteobacteria (Cardiobacterium), and Flavobacteriia (Capnocytophaga) decreased significantly with increased grams of tobacco smoked per day, measured in 5-g increments.
Smoking was associated with changes in the salivary microbiota; the nitrate reduction pathway was significantly lower in smokers compared with nonsmokers, and these decreases were consistent with previous studies of decreased cardiovascular events in former smokers.
However, the salivary microbiota of smokers who had quit for at least 5 years resembled that of individuals who had never smoked.
IN PRACTICE:
“Decreased microbial nitrate reduction pathway abundance in smokers may provide an additional explanation for the effect of smoking on cardiovascular and periodontal diseases risk, a hypothesis which should be tested in future studies,” the researchers wrote.
SOURCE:
The lead author of the study was Giacomo Antonello, MD, of Eurac Research, Affiliated Institute of the University of Lübeck, Bolzano, Italy. The study was published online in Scientific Reports (a Nature journal) on November 2, 2023.
LIMITATIONS:
The cross-sectional design and lack of professional assessment of tooth and gum health were limiting factors, as were potential confounding factors including medication use, diet, and alcohol intake.
DISCLOSURES:
The study was supported by the Department of Innovation, Research and University of the Autonomous Province of Bolzano-South Tyrol and by the European Regional Development Fund. The CHRISMB microbiota data generation was funded by the National Institute of Dental and Craniofacial Research. The researchers had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
TOPLINE:
Salivary microbiota changes caused by cigarette smoking may affect metabolic pathways and increase disease risk.
METHODOLOGY:
The researchers analyzed health information and data on the composition of salivary microbiota from 1601 adult participants in the Cooperative Health Research in South Tyrol (CHRIS) microbiome study (CHRISMB); CHRIS is an ongoing study in Italy.
The average age of the study population was 45 years; 53% were female, and 45% were current or former smokers.
The researchers hypothesized that changes in salivary microbial composition would be associated with smoking, with more nitrate-reducing bacteria present, and that nitrate reduction pathways would be reduced in smokers.
TAKEAWAY:
The researchers identified 44 genera that differed in the salivary microbiota of current smokers and nonsmokers. In smokers, seven genera in the phylum Proteobacteria were decreased and six in the phylum Actinobacteria were increased compared with nonsmokers; these phyla contain primarily aerobic and anaerobic taxa, respectively.
Some microbiota changes were significantly associated with daily smoking intensity; genera from the classes Betaproteobacteria (Lautropia or Neisseria), Gammaproteobacteria (Cardiobacterium), and Flavobacteriia (Capnocytophaga) decreased significantly with increased grams of tobacco smoked per day, measured in 5-g increments.
Smoking was associated with changes in the salivary microbiota; the nitrate reduction pathway was significantly lower in smokers compared with nonsmokers, and these decreases were consistent with previous studies of decreased cardiovascular events in former smokers.
However, the salivary microbiota of smokers who had quit for at least 5 years resembled that of individuals who had never smoked.
IN PRACTICE:
“Decreased microbial nitrate reduction pathway abundance in smokers may provide an additional explanation for the effect of smoking on cardiovascular and periodontal diseases risk, a hypothesis which should be tested in future studies,” the researchers wrote.
SOURCE:
The lead author of the study was Giacomo Antonello, MD, of Eurac Research, Affiliated Institute of the University of Lübeck, Bolzano, Italy. The study was published online in Scientific Reports (a Nature journal) on November 2, 2023.
LIMITATIONS:
The cross-sectional design and lack of professional assessment of tooth and gum health were limiting factors, as were potential confounding factors including medication use, diet, and alcohol intake.
DISCLOSURES:
The study was supported by the Department of Innovation, Research and University of the Autonomous Province of Bolzano-South Tyrol and by the European Regional Development Fund. The CHRISMB microbiota data generation was funded by the National Institute of Dental and Craniofacial Research. The researchers had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
TOPLINE:
Salivary microbiota changes caused by cigarette smoking may affect metabolic pathways and increase disease risk.
METHODOLOGY:
The researchers analyzed health information and data on the composition of salivary microbiota from 1601 adult participants in the Cooperative Health Research in South Tyrol (CHRIS) microbiome study (CHRISMB); CHRIS is an ongoing study in Italy.
The average age of the study population was 45 years; 53% were female, and 45% were current or former smokers.
The researchers hypothesized that changes in salivary microbial composition would be associated with smoking, with more nitrate-reducing bacteria present, and that nitrate reduction pathways would be reduced in smokers.
TAKEAWAY:
The researchers identified 44 genera that differed in the salivary microbiota of current smokers and nonsmokers. In smokers, seven genera in the phylum Proteobacteria were decreased and six in the phylum Actinobacteria were increased compared with nonsmokers; these phyla contain primarily aerobic and anaerobic taxa, respectively.
Some microbiota changes were significantly associated with daily smoking intensity; genera from the classes Betaproteobacteria (Lautropia or Neisseria), Gammaproteobacteria (Cardiobacterium), and Flavobacteriia (Capnocytophaga) decreased significantly with increased grams of tobacco smoked per day, measured in 5-g increments.
Smoking was associated with changes in the salivary microbiota; the nitrate reduction pathway was significantly lower in smokers compared with nonsmokers, and these decreases were consistent with previous studies of decreased cardiovascular events in former smokers.
However, the salivary microbiota of smokers who had quit for at least 5 years resembled that of individuals who had never smoked.
IN PRACTICE:
“Decreased microbial nitrate reduction pathway abundance in smokers may provide an additional explanation for the effect of smoking on cardiovascular and periodontal diseases risk, a hypothesis which should be tested in future studies,” the researchers wrote.
SOURCE:
The lead author of the study was Giacomo Antonello, MD, of Eurac Research, Affiliated Institute of the University of Lübeck, Bolzano, Italy. The study was published online in Scientific Reports (a Nature journal) on November 2, 2023.
LIMITATIONS:
The cross-sectional design and lack of professional assessment of tooth and gum health were limiting factors, as were potential confounding factors including medication use, diet, and alcohol intake.
DISCLOSURES:
The study was supported by the Department of Innovation, Research and University of the Autonomous Province of Bolzano-South Tyrol and by the European Regional Development Fund. The CHRISMB microbiota data generation was funded by the National Institute of Dental and Craniofacial Research. The researchers had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
Discontinuation Schedule of Inhaled Corticosteroids in Patients With Chronic Obstructive Pulmonary Disease
Inhaled corticosteroids (ICSs) are frequently prescribed for the treatment of chronic obstructive pulmonary disease (COPD) to reduce exacerbations in a specific subset of patients. The long-term use of ICSs, however, is associated with several potential systemic adverse effects, including adrenal suppression, decreased bone mineral density, and immunosuppression.1 The concern for immunosuppression is particularly notable and leads to a known increased risk for developing pneumonia in patients with COPD. These patients frequently have other concurrent risk factors for pneumonia (eg, history of tobacco use, older age, and severe airway limitations) and are at higher risk for more severe outcomes in the setting of pneumonia.2,3
Primarily due to the concern of pneumonia risks, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines have recommended ICS discontinuation in patients who are less likely to receive significant benefits from therapy.4 Likely due to an anti-inflammatory mechanism of action, ICSs have been shown to reduce COPD exacerbation rates in patients with comorbid asthma or who have evidence of a strong inflammatory component to their COPD. The strongest indicator of an inflammatory component is an elevated blood eosinophil (EOS) count; those with EOS > 300 cells/µL are most likely to benefit from ICSs, whereas those with a count < 100 cells/µL are unlikely to have a significant response. In addition to the inflammatory component consideration, prior studies have shown improvements in lung function and reduction of exacerbations with ICS use in patients with frequent moderate-to-severe COPD exacerbations.5 Although the GOLD guidelines provide recommendations about who is appropriate to discontinue ICS use, clinicians have no clear guidance on the risks or the best discontinuation strategy.
Based primarily on data from a prior randomized controlled trial, the Veterans Integrated Services Network (VISN) 17, which includes the Veterans Affairs North Texas Health Care System (VANTHCS) in Dallas, established a recommended ICS de-escalation strategy.6,7 The strategy included a 12-week stepwise taper using a mometasone inhaler for all patients discontinuing a moderate or high dose ICS. The lack of substantial clinical trial data or expert consensus guideline recommendations has left open the question of whether a taper is necessary. To answer that question, this study was conducted to evaluate whether there is a difference in the rate of COPD exacerbations following abrupt discontinuation vs gradual taper of ICS therapy.
Methods
This single-center, retrospective cohort study was conducted at VANTHCS. Patient electronic health records between January 10, 2021, and September 1, 2021, were reviewed for the last documented fill date of any inhaler containing a steroid component. This time frame was chosen to coincide with a VANTHCS initiative to follow GOLD guidelines for ICS discontinuation. Patients were followed for outcomes until November 1, 2022.
To be included in this study, patients had to have active prescriptions at VANTHCS, have a documented diagnosis of COPD in their chart, and be prescribed a stable dose of ICS for ≥ 1 year prior to their latest refill. The inhaler used could contain an ICS as monotherapy, in combination with a long-acting β-agonist (LABA), or as part of triple therapy with an additional long-acting muscarinic antagonist (LAMA). The inhaler needed to be discontinued during the study period of interest.
Patients were excluded if they had a diagnosis of asthma, were aged < 40 years, had active prescriptions for multiple ICS inhalers or nebulizers, or had significant oral steroid use (≥ 5 mg/d prednisone or an equivalent steroid for > 6 weeks) within 1 year of their ICS discontinuation date. In addition, to reduce the risk of future events being misclassified as COPD exacerbations, patients were excluded if they had a congestive heart failure exacerbation up to 2 years before ICS discontinuation or a diagnosis of COVID-19 infection up to 1 year before or 6 months after ICS discontinuation. Patients with a COPD exacerbation requiring an emergency department or hospital visit within 2 years prior to ICS discontinuation were also excluded, as de-escalation of ICS therapy was likely inappropriate in these cases. Finally, patients were excluded if they were started on a different ICS immediately following the discontinuation of their first ICS.
The primary outcome for this study was COPD exacerbations requiring an emergency department visit or hospitalization within 6 months of ICS discontinuation. A secondary outcome examining the rates of COPD exacerbations within 12 months also was used. The original study design called for the use of inferential statistics to compare the rates of primary and secondary outcomes in patients whose ICS was abruptly discontinued with those who were tapered slowly. After data collection, however, the small sample size and low event rate meant that the planned statistical tests were no longer appropriate. Instead, we decided to analyze the planned outcomes using descriptive statistics and look at an additional number of post hoc outcomes to provide deeper insight into clinical practice. We examined the association between relevant demographic factors, such as age, comorbidity burden, ICS potency, duration of ICS therapy, and EOS count and the clinician decision whether to taper the ICS. These same factors were also evaluated for potential association with the increased risk of COPD exacerbations following ICS discontinuation.
Results
A total of 75 patients were included. Most patients were White race and male with a mean (SD) age of 71.6 (7.4) years. Charlson Comorbidity Index scores were calculated for all included patients with a mean (SD) score of 5.4 (2.0). Of note, scores > 5 are considered a severe comorbidity burden and have an estimated mean 10-year survival rate < 21%. The overwhelming majority of patients were receiving budesonide/formoterol as their ICS inhaler with 1 receiving mometasone monotherapy. When evaluating the steroid dose, 18 (24%) patients received a low dose ICS (200-400 µg of budesonide or 110-220 µg of mometasone), while 57 (76%) received a medium dose (400-800 µg of budesonide or 440 µg of mometasone). No patients received a high ICS dose. The mean (SD) duration of therapy before discontinuation was 4.0 (2.7) years (Table 1).
Nine (12%) patients had their ICS slowly tapered, while therapy was abruptly discontinued in the other 66 (88%) patients. A variety of taper types were used (Figure) without a strong preference for a particular dosing strategy. The primary outcome of COPD exacerbation requiring emergency department visit or hospitalization within 6 months occurred in 2 patients. When the time frame was extended to 12 months for the secondary outcome, an additional 3 patients experienced an event. The mean time to event was 172 days following ICS discontinuation. All the events occurred in patients whose ICS was discontinued without any type of taper.
In a post hoc analysis, we examined the relationship between specific variables and the clinician choice whether to taper an ICS. There was no discernable impact of age, race and ethnicity, comorbidity score, or ICS dose on whether an ICS was tapered. We observed a slight association between shorter duration of therapy and lower EOS count and use of a taper. When evaluating the relationship between these same factors and exacerbation occurrence, we saw comparable trends (Table 2). Patients with an exacerbation had a slightly longer mean duration of ICS therapy and lower mean EOS count.
Discussion
Despite facility guidance recommending tapering of therapy when discontinuing a moderate- or high-dose ICS, most patients in this study discontinued the ICS abruptly. The clinician may have been concerned with patients being able to adhere to a taper regimen, skeptical of the actual need to taper, or unaware of the VANTHCS recommendations for a specific taper method. Shared decision making with patients may have also played a role in prescribing patterns. Currently, there is not sufficient data to support the use of any one particular type of taper over another, which accounts for the variability seen in practice.
The decision to taper ICSs did not seem to be strongly associated with any specific demographic factor, although the ability to examine the impact of factors (eg, race and ethnicity) was limited due to the largely homogenous population. One may have expected a taper to be more common in older patients or in those with more comorbidities; however, this was not observed in this study. The only discernible trends seen were a lower frequency of tapering in patients who had a shorter duration of ICS therapy and those with lower EOS counts. These patients were at lower risk of repeat COPD exacerbations compared with those with longer ICS therapy duration and higher EOS counts; therefore, this finding was unexpected. This suggests that patient-specific factors may not be the primary driving force in the ICS tapering decision; instead it may be based on general clinician preferences or shared decision making with individual patients.
Overall, we noted very low rates of COPD exacerbations. As ICS discontinuation was occurring in stable patients without any recent exacerbations, lower rates of future exacerbations were expected compared with the population of patients with COPD as a whole. This suggests that ICS therapy can be safely stopped in stable patients with COPD who are not likely to receive significant benefits as defined in the GOLD guidelines. All of the exacerbations that occurred were in patients whose ICS was abruptly discontinued; however, given the small number of patients who had a taper, it is difficult to draw conclusions. The low overall rate of exacerbations suggests that a taper may not be necessary to ensure safety while stopping a low- or moderate-intensity ICS.
Several randomized controlled trials have attempted to evaluate the need for an ICS taper; however, results remain mixed. The COSMIC study showed a decline in lung function following ICS discontinuation in patients with ≥ 2 COPD exacerbations in the previous year.8 Similar results were seen in the SUNSET study with increased exacerbation rates after ICS discontinuation in patients with elevated EOS counts.9 However, these studies included patients for whom ICS discontinuation is currently not recommended. Alternatively, the INSTEAD trial looked at patients without frequent recent exacerbations and found no difference in lung function, exacerbation rates, or rescue inhaler use in patients that continued combination ICS plus bronchodilator use vs those de-escalated to bronchodilator monotherapy.10
All 3 studies chose to abruptly stop the ICS when discontinuing therapy; however, using a slow, stepwise taper similar to that used after long periods of oral steroid use may reduce the risk of worsening exacerbations. The WISDOM trial is the only major randomized trial to date that stopped ICS therapy using a stepwise withdrawal of therapy.7 In patients who were continued on triple inhaled therapy (2 bronchodilators plus ICS) vs those who were de-escalated to dual bronchodilator therapy, de-escalation was noninferior to continuation of therapy in time to first COPD exacerbation. Both the WISDOM and INSTEAD trials were consistent with the results found in our real-world retrospective evaluation.
There did not seem to be an increased exacerbation risk following ICS discontinuation in any patient subpopulation based on sex, age, race and ethnicity, or comorbidity burden. We noted a trend toward more exacerbations in patients with a longer duration of ICS therapy, suggesting that additional caution may be needed when stopping ICS therapy for these patients. We also noted a trend toward more exacerbations in patients with a lower mean EOS count; however, given the low event rate and wide variability in observed patient EOS counts, this is likely a spurious finding.
Limitations
The small sample size, resulting from the strict exclusion criteria, limits the generalizability of the results. Although the low number of events seen in this study supports safety in ICS discontinuation, there may have been higher rates observed in a larger population. The most common reason for patient exclusion was the initiation of another ICS immediately following discontinuation of the original ICS. During the study period, VANTHCS underwent a change to its formulary: Fluticasone/salmeterol replaced budesonide/formoterol as the preferred ICS/LABA combination. As a result, many patients had their budesonide/formoterol discontinued during the study period solely to initiate fluticasone/salmeterol therapy. As these patients did not truly have their ICS discontinued or have a significant period without ICS therapy, they were not included in the results, and the total patient population available to analyze was relatively limited.
The low event rate also limits the ability to compare various factors influencing exacerbation risk, particularly taper vs abrupt ICS discontinuation. This is further compounded by the small number of patients who had a taper performed and the lack of consistency in the method of tapering used. Statistical significance could not be determined for any outcome, and all findings were purely hypothesis generating. Finally, data were only collected for moderate or severe COPD exacerbations that resulted in an emergency department visit or hospitalization, so there may have been mild exacerbations treated in the outpatient setting that were not captured.
Despite these limitations, this study adds data to an area of COPD management that currently lacks strong clinical guidance. Since investigators had access to clinician notes, we were able to capture ICS tapers even if patients did not receive a prescription with specific taper instructions. The extended follow-up period of 12 months evaluated a longer potential time to impact of ICS discontinuation than is done in most COPD clinical trials.
Conclusions
Overall, very low rates of COPD exacerbations occurred following ICS discontinuation, regardless of whether a taper
1. Yang IA, Clarke MS, Sim EH, Fong KM. Inhaled corticosteroids for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;7(7):CD002991. doi:10.1002/14651858.CD002991.pub3
2. Crim C, Dransfield MT, Bourbeau J, et al. Pneumonia risk with inhaled fluticasone furoate and vilanterol compared with vilanterol alone in patients with COPD. Ann Am Thorac Soc. 2015;12(1):27-34. doi:10.1513/AnnalsATS.201409-413OC
3. Crim C, Calverley PMA, Anderson JA, et al. Pneumonia risk with inhaled fluticasone furoate and vilanterol in COPD patients with moderate airflow limitation: The SUMMIT trial. Respir Med. 2017;131:27-34. doi:10.1016/j.rmed.2017.07.060
4. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2023 Report). Accessed November 3, 2023. https://goldcopd.org/wp-content/uploads/2023/03/GOLD-2023-ver-1.3-17Feb2023_WMV.pdf
5. Nannini LJ, Lasserson TJ, Poole P. Combined corticosteroid and long-acting beta(2)-agonist in one inhaler versus long-acting beta(2)-agonists for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;9(9):CD006829. doi:10.1002/14651858.CD006826.pub2
6. Kaplan AG. Applying the wisdom of stepping down inhaled corticosteroids in patients with COPD: a proposed algorithm for clinical practice. Int J Chron Obstruct Pulmon Dis. 2015;10:2535-2548. doi:10.2147/COPD.S93321
7. Magnussen H, Disse B, Rodriguez-Roisin R, et al; WISDOM Investigators. Withdrawal of inhaled glucocorticoids and exacerbations of COPD. N Engl J Med. 2014;371(14):1285-1294. doi:10.1056/NEJMoa1407154
8. Wouters EFM, Postma DS, Fokkens B. COSMIC (COPD and Seretide: a Multi-Center Intervention and Characterization) Study Group. Withdrawal of fluticasone propionate from combined salmeterol/fluticasone treatment in patients with COPD causes immediate and sustained disease deterioration: a randomized controlled trial. Thorax. 2005;60(6):480-487. doi:10.1136/thx.2004.034280
9. Chapman KR, Hurst JR, Frent S-M, et al. Long-term triple therapy de-escalation to indacaterol/glycopyrronium in patients with chronic obstructive pulmonary disease (SUNSET): a randomized, double-blind, triple-dummy clinical trial. Am J Respir Crit Care Med. 2018;198(3):329-339. doi:10.1164/rccm.201803-0405OC
10. Rossi A, van der Molen T, del Olmo R, et al. INSTEAD: a randomized switch trial of indacaterol versus salmeterol/fluticasone in moderate COPD. Eur Respir J. 2014;44(6):1548-1556. doi:10.1183/09031936.00126814
Inhaled corticosteroids (ICSs) are frequently prescribed for the treatment of chronic obstructive pulmonary disease (COPD) to reduce exacerbations in a specific subset of patients. The long-term use of ICSs, however, is associated with several potential systemic adverse effects, including adrenal suppression, decreased bone mineral density, and immunosuppression.1 The concern for immunosuppression is particularly notable and leads to a known increased risk for developing pneumonia in patients with COPD. These patients frequently have other concurrent risk factors for pneumonia (eg, history of tobacco use, older age, and severe airway limitations) and are at higher risk for more severe outcomes in the setting of pneumonia.2,3
Primarily due to the concern of pneumonia risks, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines have recommended ICS discontinuation in patients who are less likely to receive significant benefits from therapy.4 Likely due to an anti-inflammatory mechanism of action, ICSs have been shown to reduce COPD exacerbation rates in patients with comorbid asthma or who have evidence of a strong inflammatory component to their COPD. The strongest indicator of an inflammatory component is an elevated blood eosinophil (EOS) count; those with EOS > 300 cells/µL are most likely to benefit from ICSs, whereas those with a count < 100 cells/µL are unlikely to have a significant response. In addition to the inflammatory component consideration, prior studies have shown improvements in lung function and reduction of exacerbations with ICS use in patients with frequent moderate-to-severe COPD exacerbations.5 Although the GOLD guidelines provide recommendations about who is appropriate to discontinue ICS use, clinicians have no clear guidance on the risks or the best discontinuation strategy.
Based primarily on data from a prior randomized controlled trial, the Veterans Integrated Services Network (VISN) 17, which includes the Veterans Affairs North Texas Health Care System (VANTHCS) in Dallas, established a recommended ICS de-escalation strategy.6,7 The strategy included a 12-week stepwise taper using a mometasone inhaler for all patients discontinuing a moderate or high dose ICS. The lack of substantial clinical trial data or expert consensus guideline recommendations has left open the question of whether a taper is necessary. To answer that question, this study was conducted to evaluate whether there is a difference in the rate of COPD exacerbations following abrupt discontinuation vs gradual taper of ICS therapy.
Methods
This single-center, retrospective cohort study was conducted at VANTHCS. Patient electronic health records between January 10, 2021, and September 1, 2021, were reviewed for the last documented fill date of any inhaler containing a steroid component. This time frame was chosen to coincide with a VANTHCS initiative to follow GOLD guidelines for ICS discontinuation. Patients were followed for outcomes until November 1, 2022.
To be included in this study, patients had to have active prescriptions at VANTHCS, have a documented diagnosis of COPD in their chart, and be prescribed a stable dose of ICS for ≥ 1 year prior to their latest refill. The inhaler used could contain an ICS as monotherapy, in combination with a long-acting β-agonist (LABA), or as part of triple therapy with an additional long-acting muscarinic antagonist (LAMA). The inhaler needed to be discontinued during the study period of interest.
Patients were excluded if they had a diagnosis of asthma, were aged < 40 years, had active prescriptions for multiple ICS inhalers or nebulizers, or had significant oral steroid use (≥ 5 mg/d prednisone or an equivalent steroid for > 6 weeks) within 1 year of their ICS discontinuation date. In addition, to reduce the risk of future events being misclassified as COPD exacerbations, patients were excluded if they had a congestive heart failure exacerbation up to 2 years before ICS discontinuation or a diagnosis of COVID-19 infection up to 1 year before or 6 months after ICS discontinuation. Patients with a COPD exacerbation requiring an emergency department or hospital visit within 2 years prior to ICS discontinuation were also excluded, as de-escalation of ICS therapy was likely inappropriate in these cases. Finally, patients were excluded if they were started on a different ICS immediately following the discontinuation of their first ICS.
The primary outcome for this study was COPD exacerbations requiring an emergency department visit or hospitalization within 6 months of ICS discontinuation. A secondary outcome examining the rates of COPD exacerbations within 12 months also was used. The original study design called for the use of inferential statistics to compare the rates of primary and secondary outcomes in patients whose ICS was abruptly discontinued with those who were tapered slowly. After data collection, however, the small sample size and low event rate meant that the planned statistical tests were no longer appropriate. Instead, we decided to analyze the planned outcomes using descriptive statistics and look at an additional number of post hoc outcomes to provide deeper insight into clinical practice. We examined the association between relevant demographic factors, such as age, comorbidity burden, ICS potency, duration of ICS therapy, and EOS count and the clinician decision whether to taper the ICS. These same factors were also evaluated for potential association with the increased risk of COPD exacerbations following ICS discontinuation.
Results
A total of 75 patients were included. Most patients were White race and male with a mean (SD) age of 71.6 (7.4) years. Charlson Comorbidity Index scores were calculated for all included patients with a mean (SD) score of 5.4 (2.0). Of note, scores > 5 are considered a severe comorbidity burden and have an estimated mean 10-year survival rate < 21%. The overwhelming majority of patients were receiving budesonide/formoterol as their ICS inhaler with 1 receiving mometasone monotherapy. When evaluating the steroid dose, 18 (24%) patients received a low dose ICS (200-400 µg of budesonide or 110-220 µg of mometasone), while 57 (76%) received a medium dose (400-800 µg of budesonide or 440 µg of mometasone). No patients received a high ICS dose. The mean (SD) duration of therapy before discontinuation was 4.0 (2.7) years (Table 1).
Nine (12%) patients had their ICS slowly tapered, while therapy was abruptly discontinued in the other 66 (88%) patients. A variety of taper types were used (Figure) without a strong preference for a particular dosing strategy. The primary outcome of COPD exacerbation requiring emergency department visit or hospitalization within 6 months occurred in 2 patients. When the time frame was extended to 12 months for the secondary outcome, an additional 3 patients experienced an event. The mean time to event was 172 days following ICS discontinuation. All the events occurred in patients whose ICS was discontinued without any type of taper.
In a post hoc analysis, we examined the relationship between specific variables and the clinician choice whether to taper an ICS. There was no discernable impact of age, race and ethnicity, comorbidity score, or ICS dose on whether an ICS was tapered. We observed a slight association between shorter duration of therapy and lower EOS count and use of a taper. When evaluating the relationship between these same factors and exacerbation occurrence, we saw comparable trends (Table 2). Patients with an exacerbation had a slightly longer mean duration of ICS therapy and lower mean EOS count.
Discussion
Despite facility guidance recommending tapering of therapy when discontinuing a moderate- or high-dose ICS, most patients in this study discontinued the ICS abruptly. The clinician may have been concerned with patients being able to adhere to a taper regimen, skeptical of the actual need to taper, or unaware of the VANTHCS recommendations for a specific taper method. Shared decision making with patients may have also played a role in prescribing patterns. Currently, there is not sufficient data to support the use of any one particular type of taper over another, which accounts for the variability seen in practice.
The decision to taper ICSs did not seem to be strongly associated with any specific demographic factor, although the ability to examine the impact of factors (eg, race and ethnicity) was limited due to the largely homogenous population. One may have expected a taper to be more common in older patients or in those with more comorbidities; however, this was not observed in this study. The only discernible trends seen were a lower frequency of tapering in patients who had a shorter duration of ICS therapy and those with lower EOS counts. These patients were at lower risk of repeat COPD exacerbations compared with those with longer ICS therapy duration and higher EOS counts; therefore, this finding was unexpected. This suggests that patient-specific factors may not be the primary driving force in the ICS tapering decision; instead it may be based on general clinician preferences or shared decision making with individual patients.
Overall, we noted very low rates of COPD exacerbations. As ICS discontinuation was occurring in stable patients without any recent exacerbations, lower rates of future exacerbations were expected compared with the population of patients with COPD as a whole. This suggests that ICS therapy can be safely stopped in stable patients with COPD who are not likely to receive significant benefits as defined in the GOLD guidelines. All of the exacerbations that occurred were in patients whose ICS was abruptly discontinued; however, given the small number of patients who had a taper, it is difficult to draw conclusions. The low overall rate of exacerbations suggests that a taper may not be necessary to ensure safety while stopping a low- or moderate-intensity ICS.
Several randomized controlled trials have attempted to evaluate the need for an ICS taper; however, results remain mixed. The COSMIC study showed a decline in lung function following ICS discontinuation in patients with ≥ 2 COPD exacerbations in the previous year.8 Similar results were seen in the SUNSET study with increased exacerbation rates after ICS discontinuation in patients with elevated EOS counts.9 However, these studies included patients for whom ICS discontinuation is currently not recommended. Alternatively, the INSTEAD trial looked at patients without frequent recent exacerbations and found no difference in lung function, exacerbation rates, or rescue inhaler use in patients that continued combination ICS plus bronchodilator use vs those de-escalated to bronchodilator monotherapy.10
All 3 studies chose to abruptly stop the ICS when discontinuing therapy; however, using a slow, stepwise taper similar to that used after long periods of oral steroid use may reduce the risk of worsening exacerbations. The WISDOM trial is the only major randomized trial to date that stopped ICS therapy using a stepwise withdrawal of therapy.7 In patients who were continued on triple inhaled therapy (2 bronchodilators plus ICS) vs those who were de-escalated to dual bronchodilator therapy, de-escalation was noninferior to continuation of therapy in time to first COPD exacerbation. Both the WISDOM and INSTEAD trials were consistent with the results found in our real-world retrospective evaluation.
There did not seem to be an increased exacerbation risk following ICS discontinuation in any patient subpopulation based on sex, age, race and ethnicity, or comorbidity burden. We noted a trend toward more exacerbations in patients with a longer duration of ICS therapy, suggesting that additional caution may be needed when stopping ICS therapy for these patients. We also noted a trend toward more exacerbations in patients with a lower mean EOS count; however, given the low event rate and wide variability in observed patient EOS counts, this is likely a spurious finding.
Limitations
The small sample size, resulting from the strict exclusion criteria, limits the generalizability of the results. Although the low number of events seen in this study supports safety in ICS discontinuation, there may have been higher rates observed in a larger population. The most common reason for patient exclusion was the initiation of another ICS immediately following discontinuation of the original ICS. During the study period, VANTHCS underwent a change to its formulary: Fluticasone/salmeterol replaced budesonide/formoterol as the preferred ICS/LABA combination. As a result, many patients had their budesonide/formoterol discontinued during the study period solely to initiate fluticasone/salmeterol therapy. As these patients did not truly have their ICS discontinued or have a significant period without ICS therapy, they were not included in the results, and the total patient population available to analyze was relatively limited.
The low event rate also limits the ability to compare various factors influencing exacerbation risk, particularly taper vs abrupt ICS discontinuation. This is further compounded by the small number of patients who had a taper performed and the lack of consistency in the method of tapering used. Statistical significance could not be determined for any outcome, and all findings were purely hypothesis generating. Finally, data were only collected for moderate or severe COPD exacerbations that resulted in an emergency department visit or hospitalization, so there may have been mild exacerbations treated in the outpatient setting that were not captured.
Despite these limitations, this study adds data to an area of COPD management that currently lacks strong clinical guidance. Since investigators had access to clinician notes, we were able to capture ICS tapers even if patients did not receive a prescription with specific taper instructions. The extended follow-up period of 12 months evaluated a longer potential time to impact of ICS discontinuation than is done in most COPD clinical trials.
Conclusions
Overall, very low rates of COPD exacerbations occurred following ICS discontinuation, regardless of whether a taper
Inhaled corticosteroids (ICSs) are frequently prescribed for the treatment of chronic obstructive pulmonary disease (COPD) to reduce exacerbations in a specific subset of patients. The long-term use of ICSs, however, is associated with several potential systemic adverse effects, including adrenal suppression, decreased bone mineral density, and immunosuppression.1 The concern for immunosuppression is particularly notable and leads to a known increased risk for developing pneumonia in patients with COPD. These patients frequently have other concurrent risk factors for pneumonia (eg, history of tobacco use, older age, and severe airway limitations) and are at higher risk for more severe outcomes in the setting of pneumonia.2,3
Primarily due to the concern of pneumonia risks, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines have recommended ICS discontinuation in patients who are less likely to receive significant benefits from therapy.4 Likely due to an anti-inflammatory mechanism of action, ICSs have been shown to reduce COPD exacerbation rates in patients with comorbid asthma or who have evidence of a strong inflammatory component to their COPD. The strongest indicator of an inflammatory component is an elevated blood eosinophil (EOS) count; those with EOS > 300 cells/µL are most likely to benefit from ICSs, whereas those with a count < 100 cells/µL are unlikely to have a significant response. In addition to the inflammatory component consideration, prior studies have shown improvements in lung function and reduction of exacerbations with ICS use in patients with frequent moderate-to-severe COPD exacerbations.5 Although the GOLD guidelines provide recommendations about who is appropriate to discontinue ICS use, clinicians have no clear guidance on the risks or the best discontinuation strategy.
Based primarily on data from a prior randomized controlled trial, the Veterans Integrated Services Network (VISN) 17, which includes the Veterans Affairs North Texas Health Care System (VANTHCS) in Dallas, established a recommended ICS de-escalation strategy.6,7 The strategy included a 12-week stepwise taper using a mometasone inhaler for all patients discontinuing a moderate or high dose ICS. The lack of substantial clinical trial data or expert consensus guideline recommendations has left open the question of whether a taper is necessary. To answer that question, this study was conducted to evaluate whether there is a difference in the rate of COPD exacerbations following abrupt discontinuation vs gradual taper of ICS therapy.
Methods
This single-center, retrospective cohort study was conducted at VANTHCS. Patient electronic health records between January 10, 2021, and September 1, 2021, were reviewed for the last documented fill date of any inhaler containing a steroid component. This time frame was chosen to coincide with a VANTHCS initiative to follow GOLD guidelines for ICS discontinuation. Patients were followed for outcomes until November 1, 2022.
To be included in this study, patients had to have active prescriptions at VANTHCS, have a documented diagnosis of COPD in their chart, and be prescribed a stable dose of ICS for ≥ 1 year prior to their latest refill. The inhaler used could contain an ICS as monotherapy, in combination with a long-acting β-agonist (LABA), or as part of triple therapy with an additional long-acting muscarinic antagonist (LAMA). The inhaler needed to be discontinued during the study period of interest.
Patients were excluded if they had a diagnosis of asthma, were aged < 40 years, had active prescriptions for multiple ICS inhalers or nebulizers, or had significant oral steroid use (≥ 5 mg/d prednisone or an equivalent steroid for > 6 weeks) within 1 year of their ICS discontinuation date. In addition, to reduce the risk of future events being misclassified as COPD exacerbations, patients were excluded if they had a congestive heart failure exacerbation up to 2 years before ICS discontinuation or a diagnosis of COVID-19 infection up to 1 year before or 6 months after ICS discontinuation. Patients with a COPD exacerbation requiring an emergency department or hospital visit within 2 years prior to ICS discontinuation were also excluded, as de-escalation of ICS therapy was likely inappropriate in these cases. Finally, patients were excluded if they were started on a different ICS immediately following the discontinuation of their first ICS.
The primary outcome for this study was COPD exacerbations requiring an emergency department visit or hospitalization within 6 months of ICS discontinuation. A secondary outcome examining the rates of COPD exacerbations within 12 months also was used. The original study design called for the use of inferential statistics to compare the rates of primary and secondary outcomes in patients whose ICS was abruptly discontinued with those who were tapered slowly. After data collection, however, the small sample size and low event rate meant that the planned statistical tests were no longer appropriate. Instead, we decided to analyze the planned outcomes using descriptive statistics and look at an additional number of post hoc outcomes to provide deeper insight into clinical practice. We examined the association between relevant demographic factors, such as age, comorbidity burden, ICS potency, duration of ICS therapy, and EOS count and the clinician decision whether to taper the ICS. These same factors were also evaluated for potential association with the increased risk of COPD exacerbations following ICS discontinuation.
Results
A total of 75 patients were included. Most patients were White race and male with a mean (SD) age of 71.6 (7.4) years. Charlson Comorbidity Index scores were calculated for all included patients with a mean (SD) score of 5.4 (2.0). Of note, scores > 5 are considered a severe comorbidity burden and have an estimated mean 10-year survival rate < 21%. The overwhelming majority of patients were receiving budesonide/formoterol as their ICS inhaler with 1 receiving mometasone monotherapy. When evaluating the steroid dose, 18 (24%) patients received a low dose ICS (200-400 µg of budesonide or 110-220 µg of mometasone), while 57 (76%) received a medium dose (400-800 µg of budesonide or 440 µg of mometasone). No patients received a high ICS dose. The mean (SD) duration of therapy before discontinuation was 4.0 (2.7) years (Table 1).
Nine (12%) patients had their ICS slowly tapered, while therapy was abruptly discontinued in the other 66 (88%) patients. A variety of taper types were used (Figure) without a strong preference for a particular dosing strategy. The primary outcome of COPD exacerbation requiring emergency department visit or hospitalization within 6 months occurred in 2 patients. When the time frame was extended to 12 months for the secondary outcome, an additional 3 patients experienced an event. The mean time to event was 172 days following ICS discontinuation. All the events occurred in patients whose ICS was discontinued without any type of taper.
In a post hoc analysis, we examined the relationship between specific variables and the clinician choice whether to taper an ICS. There was no discernable impact of age, race and ethnicity, comorbidity score, or ICS dose on whether an ICS was tapered. We observed a slight association between shorter duration of therapy and lower EOS count and use of a taper. When evaluating the relationship between these same factors and exacerbation occurrence, we saw comparable trends (Table 2). Patients with an exacerbation had a slightly longer mean duration of ICS therapy and lower mean EOS count.
Discussion
Despite facility guidance recommending tapering of therapy when discontinuing a moderate- or high-dose ICS, most patients in this study discontinued the ICS abruptly. The clinician may have been concerned with patients being able to adhere to a taper regimen, skeptical of the actual need to taper, or unaware of the VANTHCS recommendations for a specific taper method. Shared decision making with patients may have also played a role in prescribing patterns. Currently, there is not sufficient data to support the use of any one particular type of taper over another, which accounts for the variability seen in practice.
The decision to taper ICSs did not seem to be strongly associated with any specific demographic factor, although the ability to examine the impact of factors (eg, race and ethnicity) was limited due to the largely homogenous population. One may have expected a taper to be more common in older patients or in those with more comorbidities; however, this was not observed in this study. The only discernible trends seen were a lower frequency of tapering in patients who had a shorter duration of ICS therapy and those with lower EOS counts. These patients were at lower risk of repeat COPD exacerbations compared with those with longer ICS therapy duration and higher EOS counts; therefore, this finding was unexpected. This suggests that patient-specific factors may not be the primary driving force in the ICS tapering decision; instead it may be based on general clinician preferences or shared decision making with individual patients.
Overall, we noted very low rates of COPD exacerbations. As ICS discontinuation was occurring in stable patients without any recent exacerbations, lower rates of future exacerbations were expected compared with the population of patients with COPD as a whole. This suggests that ICS therapy can be safely stopped in stable patients with COPD who are not likely to receive significant benefits as defined in the GOLD guidelines. All of the exacerbations that occurred were in patients whose ICS was abruptly discontinued; however, given the small number of patients who had a taper, it is difficult to draw conclusions. The low overall rate of exacerbations suggests that a taper may not be necessary to ensure safety while stopping a low- or moderate-intensity ICS.
Several randomized controlled trials have attempted to evaluate the need for an ICS taper; however, results remain mixed. The COSMIC study showed a decline in lung function following ICS discontinuation in patients with ≥ 2 COPD exacerbations in the previous year.8 Similar results were seen in the SUNSET study with increased exacerbation rates after ICS discontinuation in patients with elevated EOS counts.9 However, these studies included patients for whom ICS discontinuation is currently not recommended. Alternatively, the INSTEAD trial looked at patients without frequent recent exacerbations and found no difference in lung function, exacerbation rates, or rescue inhaler use in patients that continued combination ICS plus bronchodilator use vs those de-escalated to bronchodilator monotherapy.10
All 3 studies chose to abruptly stop the ICS when discontinuing therapy; however, using a slow, stepwise taper similar to that used after long periods of oral steroid use may reduce the risk of worsening exacerbations. The WISDOM trial is the only major randomized trial to date that stopped ICS therapy using a stepwise withdrawal of therapy.7 In patients who were continued on triple inhaled therapy (2 bronchodilators plus ICS) vs those who were de-escalated to dual bronchodilator therapy, de-escalation was noninferior to continuation of therapy in time to first COPD exacerbation. Both the WISDOM and INSTEAD trials were consistent with the results found in our real-world retrospective evaluation.
There did not seem to be an increased exacerbation risk following ICS discontinuation in any patient subpopulation based on sex, age, race and ethnicity, or comorbidity burden. We noted a trend toward more exacerbations in patients with a longer duration of ICS therapy, suggesting that additional caution may be needed when stopping ICS therapy for these patients. We also noted a trend toward more exacerbations in patients with a lower mean EOS count; however, given the low event rate and wide variability in observed patient EOS counts, this is likely a spurious finding.
Limitations
The small sample size, resulting from the strict exclusion criteria, limits the generalizability of the results. Although the low number of events seen in this study supports safety in ICS discontinuation, there may have been higher rates observed in a larger population. The most common reason for patient exclusion was the initiation of another ICS immediately following discontinuation of the original ICS. During the study period, VANTHCS underwent a change to its formulary: Fluticasone/salmeterol replaced budesonide/formoterol as the preferred ICS/LABA combination. As a result, many patients had their budesonide/formoterol discontinued during the study period solely to initiate fluticasone/salmeterol therapy. As these patients did not truly have their ICS discontinued or have a significant period without ICS therapy, they were not included in the results, and the total patient population available to analyze was relatively limited.
The low event rate also limits the ability to compare various factors influencing exacerbation risk, particularly taper vs abrupt ICS discontinuation. This is further compounded by the small number of patients who had a taper performed and the lack of consistency in the method of tapering used. Statistical significance could not be determined for any outcome, and all findings were purely hypothesis generating. Finally, data were only collected for moderate or severe COPD exacerbations that resulted in an emergency department visit or hospitalization, so there may have been mild exacerbations treated in the outpatient setting that were not captured.
Despite these limitations, this study adds data to an area of COPD management that currently lacks strong clinical guidance. Since investigators had access to clinician notes, we were able to capture ICS tapers even if patients did not receive a prescription with specific taper instructions. The extended follow-up period of 12 months evaluated a longer potential time to impact of ICS discontinuation than is done in most COPD clinical trials.
Conclusions
Overall, very low rates of COPD exacerbations occurred following ICS discontinuation, regardless of whether a taper
1. Yang IA, Clarke MS, Sim EH, Fong KM. Inhaled corticosteroids for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;7(7):CD002991. doi:10.1002/14651858.CD002991.pub3
2. Crim C, Dransfield MT, Bourbeau J, et al. Pneumonia risk with inhaled fluticasone furoate and vilanterol compared with vilanterol alone in patients with COPD. Ann Am Thorac Soc. 2015;12(1):27-34. doi:10.1513/AnnalsATS.201409-413OC
3. Crim C, Calverley PMA, Anderson JA, et al. Pneumonia risk with inhaled fluticasone furoate and vilanterol in COPD patients with moderate airflow limitation: The SUMMIT trial. Respir Med. 2017;131:27-34. doi:10.1016/j.rmed.2017.07.060
4. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2023 Report). Accessed November 3, 2023. https://goldcopd.org/wp-content/uploads/2023/03/GOLD-2023-ver-1.3-17Feb2023_WMV.pdf
5. Nannini LJ, Lasserson TJ, Poole P. Combined corticosteroid and long-acting beta(2)-agonist in one inhaler versus long-acting beta(2)-agonists for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;9(9):CD006829. doi:10.1002/14651858.CD006826.pub2
6. Kaplan AG. Applying the wisdom of stepping down inhaled corticosteroids in patients with COPD: a proposed algorithm for clinical practice. Int J Chron Obstruct Pulmon Dis. 2015;10:2535-2548. doi:10.2147/COPD.S93321
7. Magnussen H, Disse B, Rodriguez-Roisin R, et al; WISDOM Investigators. Withdrawal of inhaled glucocorticoids and exacerbations of COPD. N Engl J Med. 2014;371(14):1285-1294. doi:10.1056/NEJMoa1407154
8. Wouters EFM, Postma DS, Fokkens B. COSMIC (COPD and Seretide: a Multi-Center Intervention and Characterization) Study Group. Withdrawal of fluticasone propionate from combined salmeterol/fluticasone treatment in patients with COPD causes immediate and sustained disease deterioration: a randomized controlled trial. Thorax. 2005;60(6):480-487. doi:10.1136/thx.2004.034280
9. Chapman KR, Hurst JR, Frent S-M, et al. Long-term triple therapy de-escalation to indacaterol/glycopyrronium in patients with chronic obstructive pulmonary disease (SUNSET): a randomized, double-blind, triple-dummy clinical trial. Am J Respir Crit Care Med. 2018;198(3):329-339. doi:10.1164/rccm.201803-0405OC
10. Rossi A, van der Molen T, del Olmo R, et al. INSTEAD: a randomized switch trial of indacaterol versus salmeterol/fluticasone in moderate COPD. Eur Respir J. 2014;44(6):1548-1556. doi:10.1183/09031936.00126814
1. Yang IA, Clarke MS, Sim EH, Fong KM. Inhaled corticosteroids for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;7(7):CD002991. doi:10.1002/14651858.CD002991.pub3
2. Crim C, Dransfield MT, Bourbeau J, et al. Pneumonia risk with inhaled fluticasone furoate and vilanterol compared with vilanterol alone in patients with COPD. Ann Am Thorac Soc. 2015;12(1):27-34. doi:10.1513/AnnalsATS.201409-413OC
3. Crim C, Calverley PMA, Anderson JA, et al. Pneumonia risk with inhaled fluticasone furoate and vilanterol in COPD patients with moderate airflow limitation: The SUMMIT trial. Respir Med. 2017;131:27-34. doi:10.1016/j.rmed.2017.07.060
4. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2023 Report). Accessed November 3, 2023. https://goldcopd.org/wp-content/uploads/2023/03/GOLD-2023-ver-1.3-17Feb2023_WMV.pdf
5. Nannini LJ, Lasserson TJ, Poole P. Combined corticosteroid and long-acting beta(2)-agonist in one inhaler versus long-acting beta(2)-agonists for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;9(9):CD006829. doi:10.1002/14651858.CD006826.pub2
6. Kaplan AG. Applying the wisdom of stepping down inhaled corticosteroids in patients with COPD: a proposed algorithm for clinical practice. Int J Chron Obstruct Pulmon Dis. 2015;10:2535-2548. doi:10.2147/COPD.S93321
7. Magnussen H, Disse B, Rodriguez-Roisin R, et al; WISDOM Investigators. Withdrawal of inhaled glucocorticoids and exacerbations of COPD. N Engl J Med. 2014;371(14):1285-1294. doi:10.1056/NEJMoa1407154
8. Wouters EFM, Postma DS, Fokkens B. COSMIC (COPD and Seretide: a Multi-Center Intervention and Characterization) Study Group. Withdrawal of fluticasone propionate from combined salmeterol/fluticasone treatment in patients with COPD causes immediate and sustained disease deterioration: a randomized controlled trial. Thorax. 2005;60(6):480-487. doi:10.1136/thx.2004.034280
9. Chapman KR, Hurst JR, Frent S-M, et al. Long-term triple therapy de-escalation to indacaterol/glycopyrronium in patients with chronic obstructive pulmonary disease (SUNSET): a randomized, double-blind, triple-dummy clinical trial. Am J Respir Crit Care Med. 2018;198(3):329-339. doi:10.1164/rccm.201803-0405OC
10. Rossi A, van der Molen T, del Olmo R, et al. INSTEAD: a randomized switch trial of indacaterol versus salmeterol/fluticasone in moderate COPD. Eur Respir J. 2014;44(6):1548-1556. doi:10.1183/09031936.00126814
Secondhand smoke exposure linked to migraine, severe headache
TOPLINE:
, with effects of exposure varying depending on body mass index (BMI) and level of physical activity, new research shows.
METHODOLOGY:
Investigators analyzed data on 4,560 participants (median age, 43 years; 60% female; 71.5% White) from the 1999-2004 National Health and Nutrition Examination Survey.
Participants were aged 20 years or older and had never smoked.
Migraine headache status was determined by asking whether participants experienced severe headaches or migraines during the previous 3 months.
SHS exposure was categorized as unexposed (serum cotinine levels <0.05 ng/mL and no smoker in the home), low (0.05 ng/mL ≤ serum cotinine level <1 ng/mL), or heavy (1 ng/mL ≤ serum cotinine level ≤ 10 ng/mL).
TAKEAWAY:
In all, 919 (20%) participants had severe headaches or migraines.
After adjustment for demographic and lifestyle factors (including medication use), heavy SHS exposure was positively associated with severe headache or migraine (adjusted odds ratio [aOR], 2.02; 95% CI, 1.19-3.43).
No significant association was found between low SHS exposure and severe headaches or migraine (aOR, 1.15; 95% CI, 0.91-1.47).
In participants who were sedentary (P=.016) and those with a BMI <25 (P=.001), significant associations between SHS and severe headache or migraine were observed.
IN PRACTICE:
Noting a linear dose-response relationship between cotinine and severe headaches or migraine, the investigators write, “These findings underscore the need for stronger regulation of tobacco exposure, particularly in homes and public places.”
SOURCE:
Junpeng Wu, MMc, and Haitang Wang, MD, of Southern Medical University in Guangzhou, China, and their colleagues conducted the study. It was published online in Headache.
LIMITATIONS:
The study could not establish causal relationships between SHS and migraine or severe headache. In addition, the half-life of serum cotinine is 15-40 hours and thus this measure can reflect only recent SHS exposure.
DISCLOSURES:
The study was not funded. The investigators reported no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
, with effects of exposure varying depending on body mass index (BMI) and level of physical activity, new research shows.
METHODOLOGY:
Investigators analyzed data on 4,560 participants (median age, 43 years; 60% female; 71.5% White) from the 1999-2004 National Health and Nutrition Examination Survey.
Participants were aged 20 years or older and had never smoked.
Migraine headache status was determined by asking whether participants experienced severe headaches or migraines during the previous 3 months.
SHS exposure was categorized as unexposed (serum cotinine levels <0.05 ng/mL and no smoker in the home), low (0.05 ng/mL ≤ serum cotinine level <1 ng/mL), or heavy (1 ng/mL ≤ serum cotinine level ≤ 10 ng/mL).
TAKEAWAY:
In all, 919 (20%) participants had severe headaches or migraines.
After adjustment for demographic and lifestyle factors (including medication use), heavy SHS exposure was positively associated with severe headache or migraine (adjusted odds ratio [aOR], 2.02; 95% CI, 1.19-3.43).
No significant association was found between low SHS exposure and severe headaches or migraine (aOR, 1.15; 95% CI, 0.91-1.47).
In participants who were sedentary (P=.016) and those with a BMI <25 (P=.001), significant associations between SHS and severe headache or migraine were observed.
IN PRACTICE:
Noting a linear dose-response relationship between cotinine and severe headaches or migraine, the investigators write, “These findings underscore the need for stronger regulation of tobacco exposure, particularly in homes and public places.”
SOURCE:
Junpeng Wu, MMc, and Haitang Wang, MD, of Southern Medical University in Guangzhou, China, and their colleagues conducted the study. It was published online in Headache.
LIMITATIONS:
The study could not establish causal relationships between SHS and migraine or severe headache. In addition, the half-life of serum cotinine is 15-40 hours and thus this measure can reflect only recent SHS exposure.
DISCLOSURES:
The study was not funded. The investigators reported no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
, with effects of exposure varying depending on body mass index (BMI) and level of physical activity, new research shows.
METHODOLOGY:
Investigators analyzed data on 4,560 participants (median age, 43 years; 60% female; 71.5% White) from the 1999-2004 National Health and Nutrition Examination Survey.
Participants were aged 20 years or older and had never smoked.
Migraine headache status was determined by asking whether participants experienced severe headaches or migraines during the previous 3 months.
SHS exposure was categorized as unexposed (serum cotinine levels <0.05 ng/mL and no smoker in the home), low (0.05 ng/mL ≤ serum cotinine level <1 ng/mL), or heavy (1 ng/mL ≤ serum cotinine level ≤ 10 ng/mL).
TAKEAWAY:
In all, 919 (20%) participants had severe headaches or migraines.
After adjustment for demographic and lifestyle factors (including medication use), heavy SHS exposure was positively associated with severe headache or migraine (adjusted odds ratio [aOR], 2.02; 95% CI, 1.19-3.43).
No significant association was found between low SHS exposure and severe headaches or migraine (aOR, 1.15; 95% CI, 0.91-1.47).
In participants who were sedentary (P=.016) and those with a BMI <25 (P=.001), significant associations between SHS and severe headache or migraine were observed.
IN PRACTICE:
Noting a linear dose-response relationship between cotinine and severe headaches or migraine, the investigators write, “These findings underscore the need for stronger regulation of tobacco exposure, particularly in homes and public places.”
SOURCE:
Junpeng Wu, MMc, and Haitang Wang, MD, of Southern Medical University in Guangzhou, China, and their colleagues conducted the study. It was published online in Headache.
LIMITATIONS:
The study could not establish causal relationships between SHS and migraine or severe headache. In addition, the half-life of serum cotinine is 15-40 hours and thus this measure can reflect only recent SHS exposure.
DISCLOSURES:
The study was not funded. The investigators reported no disclosures.
A version of this article appeared on Medscape.com.
All-oral regimen succeeds for rifampin-resistant tuberculosis
A combination oral-only therapy of bedaquiline, pretomanid, and linezolid was significantly more effective than standard care in preventing unfavorable outcomes in patients with treatment-resistant tuberculosis, based on data from more than 500 individuals.
, and data on the use of new and repurposed drug combinations are lacking, wrote Bern-Thomas Nyang’wa, MBBS, of Médecins Sans Frontières, Amsterdam, and colleagues.
In a study known as the TB-PRACTECAL trial, the researchers enrolled 552 pulmonary rifampin-resistant tuberculosis patients aged 15 years and older to examine several new and repurposed drug combinations. The participants were randomized in a 1:1:1:1 ratio to treatment with 36-80 weeks of standard care; 24-week oral bedaquiline, pretomanid, and linezolid (BPaL); BPaL plus clofazimine (BPaLC); or BPaL plus moxifloxacin (BPaLM) . This was followed by stage two of the trial, in which participants were randomized 1:1 to receive standard care or BPaLM. The current study, published in The Lancet Respiratory Medicine, reported the stage two findings; the primary outcome was a composite of unfavorable outcomes at 72 weeks including death, treatment failure, treatment discontinuation, recurrence of tuberculosis, or loss to follow-up.
The modified intent-to-treat population included 138 patients in the BPaLM group and 137 patients in the standard care group. In this population, 56 (41%) of 137 participants in the standard care group and 16 (12%) of 137 participants in the BPaLM group met criteria for the unfavorable outcome at 72 weeks; noninferiority and superiority were significantly greater in the BPaLM group (P < .0001).
Early discontinuation was the main reason patients met the unfavorable outcome criteria (89% of standard care patients and 69% of BPaLM patients); adverse events accounted for 23% of discontinuations in the standard care group and 64% of discontinuations in the BPaLM group.
However, fewer patients in the BPaLM group experienced grade 3 or higher adverse events compared with the standard care group (23% vs. 48%). The most common adverse events included hepatic disorders, cardiac disorders, and anemia.
In addition, all subgroup analyses favored BPaLM over standard care at 72 weeks including subgroups based on sex, age, disease severity, re-treatment status, and smoking status.
The findings were limited by several factors including the changes to standard of care over the course of the study, potential bias because the study was stopped for efficacy, and inclusion of loss to follow-up as part of the composite unfavorable outcome, the researchers noted.
Remaining research questions include the optimal dose of linezolid, whether use of alternative fluoroquinolones would yield similar results, and whether the results would generalize to populations including children, pregnant women, and patients with extrapulmonary tuberculosis, they added.
However, the results support BPaLM as the preferred treatment for adults and adolescents with pulmonary rifampin-resistant TB, the researchers concluded.
BPaLM poised to improve TB care
Before 2020, treatment for rifampin-resistant tuberculosis was 9-20 months in duration, toxic, and inadequately effective, and new treatment regimens are urgently needed, Mary Jo Farmer, MD, a pulmonary and critical care specialist at the University of Massachusetts Baystate Health Regional Campus, Springfield, said in an interview.
“The BPaL-based regimens perform better than the 9- to 20-month standard of care, are shorter in duration, have a lower pill burden, improve quality of life, and are cost-effective,” she said. “The BPaL regimens have the potential to improve outcomes for thousands of patients with rifampin-resistant tuberculosis.”
“The 24-week oral regimen consisting of bedaquiline, pretomanid, linezolid and moxifloxacin is noninferior to standard of care for treatment of patients with pulmonary rifampin-resistant tuberculosis, and this BPaLM regimen was added to the WHO guidance for treatment of this condition in 2022,” said Dr. Farmer, who was not involved in the study. “It remains to be seen if BPaLM will become the preferred regimen for adolescents and adults with pulmonary rifampin-resistant tuberculosis,” she said.
Dr. Farmer agreed with the study authors that the optimal dose of linezolid, optimal duration of treatment, and the role of dose reduction remain unknown, and pharmacokinetic studies are needed to identify these parameters.
The study was supported by Médecins Sans Frontières. TB Alliance donated pretomanid to the study prior to its commercialization. The researchers had no financial conflicts to disclose. Dr. Farmer had no financial conflicts to disclose, but serves on the editorial advisory board of CHEST Physician.
A combination oral-only therapy of bedaquiline, pretomanid, and linezolid was significantly more effective than standard care in preventing unfavorable outcomes in patients with treatment-resistant tuberculosis, based on data from more than 500 individuals.
, and data on the use of new and repurposed drug combinations are lacking, wrote Bern-Thomas Nyang’wa, MBBS, of Médecins Sans Frontières, Amsterdam, and colleagues.
In a study known as the TB-PRACTECAL trial, the researchers enrolled 552 pulmonary rifampin-resistant tuberculosis patients aged 15 years and older to examine several new and repurposed drug combinations. The participants were randomized in a 1:1:1:1 ratio to treatment with 36-80 weeks of standard care; 24-week oral bedaquiline, pretomanid, and linezolid (BPaL); BPaL plus clofazimine (BPaLC); or BPaL plus moxifloxacin (BPaLM) . This was followed by stage two of the trial, in which participants were randomized 1:1 to receive standard care or BPaLM. The current study, published in The Lancet Respiratory Medicine, reported the stage two findings; the primary outcome was a composite of unfavorable outcomes at 72 weeks including death, treatment failure, treatment discontinuation, recurrence of tuberculosis, or loss to follow-up.
The modified intent-to-treat population included 138 patients in the BPaLM group and 137 patients in the standard care group. In this population, 56 (41%) of 137 participants in the standard care group and 16 (12%) of 137 participants in the BPaLM group met criteria for the unfavorable outcome at 72 weeks; noninferiority and superiority were significantly greater in the BPaLM group (P < .0001).
Early discontinuation was the main reason patients met the unfavorable outcome criteria (89% of standard care patients and 69% of BPaLM patients); adverse events accounted for 23% of discontinuations in the standard care group and 64% of discontinuations in the BPaLM group.
However, fewer patients in the BPaLM group experienced grade 3 or higher adverse events compared with the standard care group (23% vs. 48%). The most common adverse events included hepatic disorders, cardiac disorders, and anemia.
In addition, all subgroup analyses favored BPaLM over standard care at 72 weeks including subgroups based on sex, age, disease severity, re-treatment status, and smoking status.
The findings were limited by several factors including the changes to standard of care over the course of the study, potential bias because the study was stopped for efficacy, and inclusion of loss to follow-up as part of the composite unfavorable outcome, the researchers noted.
Remaining research questions include the optimal dose of linezolid, whether use of alternative fluoroquinolones would yield similar results, and whether the results would generalize to populations including children, pregnant women, and patients with extrapulmonary tuberculosis, they added.
However, the results support BPaLM as the preferred treatment for adults and adolescents with pulmonary rifampin-resistant TB, the researchers concluded.
BPaLM poised to improve TB care
Before 2020, treatment for rifampin-resistant tuberculosis was 9-20 months in duration, toxic, and inadequately effective, and new treatment regimens are urgently needed, Mary Jo Farmer, MD, a pulmonary and critical care specialist at the University of Massachusetts Baystate Health Regional Campus, Springfield, said in an interview.
“The BPaL-based regimens perform better than the 9- to 20-month standard of care, are shorter in duration, have a lower pill burden, improve quality of life, and are cost-effective,” she said. “The BPaL regimens have the potential to improve outcomes for thousands of patients with rifampin-resistant tuberculosis.”
“The 24-week oral regimen consisting of bedaquiline, pretomanid, linezolid and moxifloxacin is noninferior to standard of care for treatment of patients with pulmonary rifampin-resistant tuberculosis, and this BPaLM regimen was added to the WHO guidance for treatment of this condition in 2022,” said Dr. Farmer, who was not involved in the study. “It remains to be seen if BPaLM will become the preferred regimen for adolescents and adults with pulmonary rifampin-resistant tuberculosis,” she said.
Dr. Farmer agreed with the study authors that the optimal dose of linezolid, optimal duration of treatment, and the role of dose reduction remain unknown, and pharmacokinetic studies are needed to identify these parameters.
The study was supported by Médecins Sans Frontières. TB Alliance donated pretomanid to the study prior to its commercialization. The researchers had no financial conflicts to disclose. Dr. Farmer had no financial conflicts to disclose, but serves on the editorial advisory board of CHEST Physician.
A combination oral-only therapy of bedaquiline, pretomanid, and linezolid was significantly more effective than standard care in preventing unfavorable outcomes in patients with treatment-resistant tuberculosis, based on data from more than 500 individuals.
, and data on the use of new and repurposed drug combinations are lacking, wrote Bern-Thomas Nyang’wa, MBBS, of Médecins Sans Frontières, Amsterdam, and colleagues.
In a study known as the TB-PRACTECAL trial, the researchers enrolled 552 pulmonary rifampin-resistant tuberculosis patients aged 15 years and older to examine several new and repurposed drug combinations. The participants were randomized in a 1:1:1:1 ratio to treatment with 36-80 weeks of standard care; 24-week oral bedaquiline, pretomanid, and linezolid (BPaL); BPaL plus clofazimine (BPaLC); or BPaL plus moxifloxacin (BPaLM) . This was followed by stage two of the trial, in which participants were randomized 1:1 to receive standard care or BPaLM. The current study, published in The Lancet Respiratory Medicine, reported the stage two findings; the primary outcome was a composite of unfavorable outcomes at 72 weeks including death, treatment failure, treatment discontinuation, recurrence of tuberculosis, or loss to follow-up.
The modified intent-to-treat population included 138 patients in the BPaLM group and 137 patients in the standard care group. In this population, 56 (41%) of 137 participants in the standard care group and 16 (12%) of 137 participants in the BPaLM group met criteria for the unfavorable outcome at 72 weeks; noninferiority and superiority were significantly greater in the BPaLM group (P < .0001).
Early discontinuation was the main reason patients met the unfavorable outcome criteria (89% of standard care patients and 69% of BPaLM patients); adverse events accounted for 23% of discontinuations in the standard care group and 64% of discontinuations in the BPaLM group.
However, fewer patients in the BPaLM group experienced grade 3 or higher adverse events compared with the standard care group (23% vs. 48%). The most common adverse events included hepatic disorders, cardiac disorders, and anemia.
In addition, all subgroup analyses favored BPaLM over standard care at 72 weeks including subgroups based on sex, age, disease severity, re-treatment status, and smoking status.
The findings were limited by several factors including the changes to standard of care over the course of the study, potential bias because the study was stopped for efficacy, and inclusion of loss to follow-up as part of the composite unfavorable outcome, the researchers noted.
Remaining research questions include the optimal dose of linezolid, whether use of alternative fluoroquinolones would yield similar results, and whether the results would generalize to populations including children, pregnant women, and patients with extrapulmonary tuberculosis, they added.
However, the results support BPaLM as the preferred treatment for adults and adolescents with pulmonary rifampin-resistant TB, the researchers concluded.
BPaLM poised to improve TB care
Before 2020, treatment for rifampin-resistant tuberculosis was 9-20 months in duration, toxic, and inadequately effective, and new treatment regimens are urgently needed, Mary Jo Farmer, MD, a pulmonary and critical care specialist at the University of Massachusetts Baystate Health Regional Campus, Springfield, said in an interview.
“The BPaL-based regimens perform better than the 9- to 20-month standard of care, are shorter in duration, have a lower pill burden, improve quality of life, and are cost-effective,” she said. “The BPaL regimens have the potential to improve outcomes for thousands of patients with rifampin-resistant tuberculosis.”
“The 24-week oral regimen consisting of bedaquiline, pretomanid, linezolid and moxifloxacin is noninferior to standard of care for treatment of patients with pulmonary rifampin-resistant tuberculosis, and this BPaLM regimen was added to the WHO guidance for treatment of this condition in 2022,” said Dr. Farmer, who was not involved in the study. “It remains to be seen if BPaLM will become the preferred regimen for adolescents and adults with pulmonary rifampin-resistant tuberculosis,” she said.
Dr. Farmer agreed with the study authors that the optimal dose of linezolid, optimal duration of treatment, and the role of dose reduction remain unknown, and pharmacokinetic studies are needed to identify these parameters.
The study was supported by Médecins Sans Frontières. TB Alliance donated pretomanid to the study prior to its commercialization. The researchers had no financial conflicts to disclose. Dr. Farmer had no financial conflicts to disclose, but serves on the editorial advisory board of CHEST Physician.
FROM LANCET RESPIRATORY MEDICINE
Is air filtration the best public health intervention against respiratory viruses?
This transcript has been edited for clarity.
When it comes to the public health fight against respiratory viruses – COVID, flu, RSV, and so on – it has always struck me as strange how staunchly basically any intervention is opposed. Masking was, of course, the prototypical entrenched warfare of opposing ideologies, with advocates pointing to studies suggesting the efficacy of masking to prevent transmission and advocating for broad masking recommendations, and detractors citing studies that suggested masks were ineffective and characterizing masking policies as fascist overreach. I’ll admit that I was always perplexed by this a bit, as that particular intervention seemed so benign – a bit annoying, I guess, but not crazy.
I have come to appreciate what I call status quo bias, which is the tendency to reject any policy, advice, or intervention that would force you, as an individual, to change your usual behavior. We just don’t like to do that. It has made me think that the most successful public health interventions might be the ones that take the individual out of the loop. And air quality control seems an ideal fit here. Here is a potential intervention where you, the individual, have to do precisely nothing. The status quo is preserved. We just, you know, have cleaner indoor air.
But even the suggestion of air treatment systems as a bulwark against respiratory virus transmission has been met with not just skepticism but cynicism, and perhaps even defeatism. It seems that there are those out there who think there really is nothing we can do. Sickness is interpreted in a Calvinistic framework: You become ill because it is your pre-destiny. But maybe air treatment could actually work. It seems like it might, if a new paper from PLOS One is to be believed.
What we’re talking about is a study titled “Bipolar Ionization Rapidly Inactivates Real-World, Airborne Concentrations of Infective Respiratory Viruses” – a highly controlled, laboratory-based analysis of a bipolar ionization system which seems to rapidly reduce viral counts in the air.
The proposed mechanism of action is pretty simple. The ionization system – which, don’t worry, has been shown not to produce ozone – spits out positively and negatively charged particles, which float around the test chamber, designed to look like a pretty standard room that you might find in an office or a school.
Virus is then injected into the chamber through an aerosolization machine, to achieve concentrations on the order of what you might get standing within 6 feet or so of someone actively infected with COVID while they are breathing and talking.
The idea is that those ions stick to the virus particles, similar to how a balloon sticks to the wall after you rub it on your hair, and that tends to cause them to clump together and settle on surfaces more rapidly, and thus get farther away from their ports of entry to the human system: nose, mouth, and eyes. But the ions may also interfere with viruses’ ability to bind to cellular receptors, even in the air.
To quantify viral infectivity, the researchers used a biological system. Basically, you take air samples and expose a petri dish of cells to them and see how many cells die. Fewer cells dying, less infective. Under control conditions, you can see that virus infectivity does decrease over time. Time zero here is the end of a SARS-CoV-2 aerosolization.
This may simply reflect the fact that virus particles settle out of the air. But As you can see, within about an hour, you have almost no infective virus detectable. That’s fairly impressive.
Now, I’m not saying that this is a panacea, but it is certainly worth considering the use of technologies like these if we are going to revamp the infrastructure of our offices and schools. And, of course, it would be nice to see this tested in a rigorous clinical trial with actual infected people, not cells, as the outcome. But I continue to be encouraged by interventions like this which, to be honest, ask very little of us as individuals. Maybe it’s time we accept the things, or people, that we cannot change.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
When it comes to the public health fight against respiratory viruses – COVID, flu, RSV, and so on – it has always struck me as strange how staunchly basically any intervention is opposed. Masking was, of course, the prototypical entrenched warfare of opposing ideologies, with advocates pointing to studies suggesting the efficacy of masking to prevent transmission and advocating for broad masking recommendations, and detractors citing studies that suggested masks were ineffective and characterizing masking policies as fascist overreach. I’ll admit that I was always perplexed by this a bit, as that particular intervention seemed so benign – a bit annoying, I guess, but not crazy.
I have come to appreciate what I call status quo bias, which is the tendency to reject any policy, advice, or intervention that would force you, as an individual, to change your usual behavior. We just don’t like to do that. It has made me think that the most successful public health interventions might be the ones that take the individual out of the loop. And air quality control seems an ideal fit here. Here is a potential intervention where you, the individual, have to do precisely nothing. The status quo is preserved. We just, you know, have cleaner indoor air.
But even the suggestion of air treatment systems as a bulwark against respiratory virus transmission has been met with not just skepticism but cynicism, and perhaps even defeatism. It seems that there are those out there who think there really is nothing we can do. Sickness is interpreted in a Calvinistic framework: You become ill because it is your pre-destiny. But maybe air treatment could actually work. It seems like it might, if a new paper from PLOS One is to be believed.
What we’re talking about is a study titled “Bipolar Ionization Rapidly Inactivates Real-World, Airborne Concentrations of Infective Respiratory Viruses” – a highly controlled, laboratory-based analysis of a bipolar ionization system which seems to rapidly reduce viral counts in the air.
The proposed mechanism of action is pretty simple. The ionization system – which, don’t worry, has been shown not to produce ozone – spits out positively and negatively charged particles, which float around the test chamber, designed to look like a pretty standard room that you might find in an office or a school.
Virus is then injected into the chamber through an aerosolization machine, to achieve concentrations on the order of what you might get standing within 6 feet or so of someone actively infected with COVID while they are breathing and talking.
The idea is that those ions stick to the virus particles, similar to how a balloon sticks to the wall after you rub it on your hair, and that tends to cause them to clump together and settle on surfaces more rapidly, and thus get farther away from their ports of entry to the human system: nose, mouth, and eyes. But the ions may also interfere with viruses’ ability to bind to cellular receptors, even in the air.
To quantify viral infectivity, the researchers used a biological system. Basically, you take air samples and expose a petri dish of cells to them and see how many cells die. Fewer cells dying, less infective. Under control conditions, you can see that virus infectivity does decrease over time. Time zero here is the end of a SARS-CoV-2 aerosolization.
This may simply reflect the fact that virus particles settle out of the air. But As you can see, within about an hour, you have almost no infective virus detectable. That’s fairly impressive.
Now, I’m not saying that this is a panacea, but it is certainly worth considering the use of technologies like these if we are going to revamp the infrastructure of our offices and schools. And, of course, it would be nice to see this tested in a rigorous clinical trial with actual infected people, not cells, as the outcome. But I continue to be encouraged by interventions like this which, to be honest, ask very little of us as individuals. Maybe it’s time we accept the things, or people, that we cannot change.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
When it comes to the public health fight against respiratory viruses – COVID, flu, RSV, and so on – it has always struck me as strange how staunchly basically any intervention is opposed. Masking was, of course, the prototypical entrenched warfare of opposing ideologies, with advocates pointing to studies suggesting the efficacy of masking to prevent transmission and advocating for broad masking recommendations, and detractors citing studies that suggested masks were ineffective and characterizing masking policies as fascist overreach. I’ll admit that I was always perplexed by this a bit, as that particular intervention seemed so benign – a bit annoying, I guess, but not crazy.
I have come to appreciate what I call status quo bias, which is the tendency to reject any policy, advice, or intervention that would force you, as an individual, to change your usual behavior. We just don’t like to do that. It has made me think that the most successful public health interventions might be the ones that take the individual out of the loop. And air quality control seems an ideal fit here. Here is a potential intervention where you, the individual, have to do precisely nothing. The status quo is preserved. We just, you know, have cleaner indoor air.
But even the suggestion of air treatment systems as a bulwark against respiratory virus transmission has been met with not just skepticism but cynicism, and perhaps even defeatism. It seems that there are those out there who think there really is nothing we can do. Sickness is interpreted in a Calvinistic framework: You become ill because it is your pre-destiny. But maybe air treatment could actually work. It seems like it might, if a new paper from PLOS One is to be believed.
What we’re talking about is a study titled “Bipolar Ionization Rapidly Inactivates Real-World, Airborne Concentrations of Infective Respiratory Viruses” – a highly controlled, laboratory-based analysis of a bipolar ionization system which seems to rapidly reduce viral counts in the air.
The proposed mechanism of action is pretty simple. The ionization system – which, don’t worry, has been shown not to produce ozone – spits out positively and negatively charged particles, which float around the test chamber, designed to look like a pretty standard room that you might find in an office or a school.
Virus is then injected into the chamber through an aerosolization machine, to achieve concentrations on the order of what you might get standing within 6 feet or so of someone actively infected with COVID while they are breathing and talking.
The idea is that those ions stick to the virus particles, similar to how a balloon sticks to the wall after you rub it on your hair, and that tends to cause them to clump together and settle on surfaces more rapidly, and thus get farther away from their ports of entry to the human system: nose, mouth, and eyes. But the ions may also interfere with viruses’ ability to bind to cellular receptors, even in the air.
To quantify viral infectivity, the researchers used a biological system. Basically, you take air samples and expose a petri dish of cells to them and see how many cells die. Fewer cells dying, less infective. Under control conditions, you can see that virus infectivity does decrease over time. Time zero here is the end of a SARS-CoV-2 aerosolization.
This may simply reflect the fact that virus particles settle out of the air. But As you can see, within about an hour, you have almost no infective virus detectable. That’s fairly impressive.
Now, I’m not saying that this is a panacea, but it is certainly worth considering the use of technologies like these if we are going to revamp the infrastructure of our offices and schools. And, of course, it would be nice to see this tested in a rigorous clinical trial with actual infected people, not cells, as the outcome. But I continue to be encouraged by interventions like this which, to be honest, ask very little of us as individuals. Maybe it’s time we accept the things, or people, that we cannot change.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.