User login
For MD-IQ use only
SNP chips deemed ‘extremely unreliable’ for identifying rare variants
In fact, SNP chips are “extremely unreliable for genotyping very rare pathogenic variants,” and a positive result for such a variant “is more likely to be wrong than right,” researchers reported in the BMJ.
The authors explained that SNP chips are “DNA microarrays that test genetic variation at many hundreds of thousands of specific locations across the genome.” Although SNP chips have proven accurate in identifying common variants, past reports have suggested that SNP chips perform poorly for genotyping rare variants.
To gain more insight, Caroline Wright, PhD, of the University of Exeter (England) and colleagues conducted a large study.
The researchers analyzed data on 49,908 people from the UK Biobank who had SNP chip and next-generation sequencing results, as well as an additional 21 people who purchased consumer genetic tests and shared their data online via the Personal Genome Project.
The researchers compared the SNP chip and sequencing results. They also selected rare pathogenic variants in BRCA1 and BRCA2 for detailed analysis of clinically actionable variants in the UK Biobank, and they assessed BRCA-related cancers in participants using cancer registry data.
Largest evaluation of SNP chips
SNP chips performed well for common variants, the researchers found. Sensitivity, specificity, positive-predictive value, and negative-predictive value all exceeded 99% for 108,574 common variants.
For rare variants, SNP chips performed poorly, with a positive-predictive value of 16% for variants with a frequency below 0.001% in the UK Biobank.
“The study provides the largest evaluation of the performance of SNP chips for genotyping genetic variants at different frequencies in the population, particularly focusing on very rare variants,” Dr. Wright said. “The biggest surprise was how poorly the SNP chips we evaluated performed for rare variants.”
Dr. Wright noted that there is an inherent problem built into using SNP chip technology to genotype very rare variants.
“The SNP chip technology relies on clustering data from multiple individuals in order to determine what genotype each individual has at a specific position in their genome,” Dr. Wright explained. “Although this method works very well for common variants, the rarer the variant, the harder it is to distinguish from experimental noise.”
False positives and cancer: ‘Don’t trust the results’
The researchers found that, for rare BRCA variants (frequency below 0.01%), SNP chips had a sensitivity of 34.6%, specificity of 98.3%, negative-predictive value of 99.9%, and positive-predictive value of 4.2%.
Rates of BRCA-related cancers in patients with positive SNP chip results were similar to rates in age-matched control subjects because “the vast majority of variants were false positives,” the researchers noted.
“If these variants are incorrectly genotyped – that is, false positives detected – a woman could be offered screening or even prophylactic surgery inappropriately when she is more likely to be at population background risk [for BRCA-related cancers],” Dr. Wright said.
“For very-rare-disease–causing genetic variants, don’t trust the results from SNP chips; for example, those from direct-to-consumer genetic tests. Never use them to guide clinical action without diagnostic validation,” she added.
Heather Hampel, a genetic counselor and researcher at the Ohio State University Comprehensive Cancer Center in Columbus, agreed.
“Positive results on SNP-based tests need to be confirmed by medical-grade genetic testing using a sequencing technology,” she said. “Negative results on an SNP- based test cannot be considered to rule out mutations in BRCA1/2 or other cancer-susceptibility genes, so individuals with strong personal and family histories of cancer should be seen by a genetic counselor to consider medical-grade genetic testing using a sequencing technology.”
Practicing oncologists can trust patients’ prior germline genetic test results if the testing was performed in a cancer genetics clinic, which uses sequencing-based technologies, Ms. Hampel noted.
“If the test was performed before 2013, there are likely new genes that have been discovered for which their patient was not tested, and repeat testing may be warranted,” Ms. Hampel said. “A referral to a cancer genetic counselor would be appropriate.”
Ms. Hampel disclosed relationships with Genome Medical, GI OnDemand, Invitae Genetics, and Promega. Dr. Wright and her coauthors disclosed no conflicts of interest. The group’s research was conducted using the UK Biobank and the University of Exeter High-Performance Computing, with funding from the Wellcome Trust and the National Institute for Health Research.
In fact, SNP chips are “extremely unreliable for genotyping very rare pathogenic variants,” and a positive result for such a variant “is more likely to be wrong than right,” researchers reported in the BMJ.
The authors explained that SNP chips are “DNA microarrays that test genetic variation at many hundreds of thousands of specific locations across the genome.” Although SNP chips have proven accurate in identifying common variants, past reports have suggested that SNP chips perform poorly for genotyping rare variants.
To gain more insight, Caroline Wright, PhD, of the University of Exeter (England) and colleagues conducted a large study.
The researchers analyzed data on 49,908 people from the UK Biobank who had SNP chip and next-generation sequencing results, as well as an additional 21 people who purchased consumer genetic tests and shared their data online via the Personal Genome Project.
The researchers compared the SNP chip and sequencing results. They also selected rare pathogenic variants in BRCA1 and BRCA2 for detailed analysis of clinically actionable variants in the UK Biobank, and they assessed BRCA-related cancers in participants using cancer registry data.
Largest evaluation of SNP chips
SNP chips performed well for common variants, the researchers found. Sensitivity, specificity, positive-predictive value, and negative-predictive value all exceeded 99% for 108,574 common variants.
For rare variants, SNP chips performed poorly, with a positive-predictive value of 16% for variants with a frequency below 0.001% in the UK Biobank.
“The study provides the largest evaluation of the performance of SNP chips for genotyping genetic variants at different frequencies in the population, particularly focusing on very rare variants,” Dr. Wright said. “The biggest surprise was how poorly the SNP chips we evaluated performed for rare variants.”
Dr. Wright noted that there is an inherent problem built into using SNP chip technology to genotype very rare variants.
“The SNP chip technology relies on clustering data from multiple individuals in order to determine what genotype each individual has at a specific position in their genome,” Dr. Wright explained. “Although this method works very well for common variants, the rarer the variant, the harder it is to distinguish from experimental noise.”
False positives and cancer: ‘Don’t trust the results’
The researchers found that, for rare BRCA variants (frequency below 0.01%), SNP chips had a sensitivity of 34.6%, specificity of 98.3%, negative-predictive value of 99.9%, and positive-predictive value of 4.2%.
Rates of BRCA-related cancers in patients with positive SNP chip results were similar to rates in age-matched control subjects because “the vast majority of variants were false positives,” the researchers noted.
“If these variants are incorrectly genotyped – that is, false positives detected – a woman could be offered screening or even prophylactic surgery inappropriately when she is more likely to be at population background risk [for BRCA-related cancers],” Dr. Wright said.
“For very-rare-disease–causing genetic variants, don’t trust the results from SNP chips; for example, those from direct-to-consumer genetic tests. Never use them to guide clinical action without diagnostic validation,” she added.
Heather Hampel, a genetic counselor and researcher at the Ohio State University Comprehensive Cancer Center in Columbus, agreed.
“Positive results on SNP-based tests need to be confirmed by medical-grade genetic testing using a sequencing technology,” she said. “Negative results on an SNP- based test cannot be considered to rule out mutations in BRCA1/2 or other cancer-susceptibility genes, so individuals with strong personal and family histories of cancer should be seen by a genetic counselor to consider medical-grade genetic testing using a sequencing technology.”
Practicing oncologists can trust patients’ prior germline genetic test results if the testing was performed in a cancer genetics clinic, which uses sequencing-based technologies, Ms. Hampel noted.
“If the test was performed before 2013, there are likely new genes that have been discovered for which their patient was not tested, and repeat testing may be warranted,” Ms. Hampel said. “A referral to a cancer genetic counselor would be appropriate.”
Ms. Hampel disclosed relationships with Genome Medical, GI OnDemand, Invitae Genetics, and Promega. Dr. Wright and her coauthors disclosed no conflicts of interest. The group’s research was conducted using the UK Biobank and the University of Exeter High-Performance Computing, with funding from the Wellcome Trust and the National Institute for Health Research.
In fact, SNP chips are “extremely unreliable for genotyping very rare pathogenic variants,” and a positive result for such a variant “is more likely to be wrong than right,” researchers reported in the BMJ.
The authors explained that SNP chips are “DNA microarrays that test genetic variation at many hundreds of thousands of specific locations across the genome.” Although SNP chips have proven accurate in identifying common variants, past reports have suggested that SNP chips perform poorly for genotyping rare variants.
To gain more insight, Caroline Wright, PhD, of the University of Exeter (England) and colleagues conducted a large study.
The researchers analyzed data on 49,908 people from the UK Biobank who had SNP chip and next-generation sequencing results, as well as an additional 21 people who purchased consumer genetic tests and shared their data online via the Personal Genome Project.
The researchers compared the SNP chip and sequencing results. They also selected rare pathogenic variants in BRCA1 and BRCA2 for detailed analysis of clinically actionable variants in the UK Biobank, and they assessed BRCA-related cancers in participants using cancer registry data.
Largest evaluation of SNP chips
SNP chips performed well for common variants, the researchers found. Sensitivity, specificity, positive-predictive value, and negative-predictive value all exceeded 99% for 108,574 common variants.
For rare variants, SNP chips performed poorly, with a positive-predictive value of 16% for variants with a frequency below 0.001% in the UK Biobank.
“The study provides the largest evaluation of the performance of SNP chips for genotyping genetic variants at different frequencies in the population, particularly focusing on very rare variants,” Dr. Wright said. “The biggest surprise was how poorly the SNP chips we evaluated performed for rare variants.”
Dr. Wright noted that there is an inherent problem built into using SNP chip technology to genotype very rare variants.
“The SNP chip technology relies on clustering data from multiple individuals in order to determine what genotype each individual has at a specific position in their genome,” Dr. Wright explained. “Although this method works very well for common variants, the rarer the variant, the harder it is to distinguish from experimental noise.”
False positives and cancer: ‘Don’t trust the results’
The researchers found that, for rare BRCA variants (frequency below 0.01%), SNP chips had a sensitivity of 34.6%, specificity of 98.3%, negative-predictive value of 99.9%, and positive-predictive value of 4.2%.
Rates of BRCA-related cancers in patients with positive SNP chip results were similar to rates in age-matched control subjects because “the vast majority of variants were false positives,” the researchers noted.
“If these variants are incorrectly genotyped – that is, false positives detected – a woman could be offered screening or even prophylactic surgery inappropriately when she is more likely to be at population background risk [for BRCA-related cancers],” Dr. Wright said.
“For very-rare-disease–causing genetic variants, don’t trust the results from SNP chips; for example, those from direct-to-consumer genetic tests. Never use them to guide clinical action without diagnostic validation,” she added.
Heather Hampel, a genetic counselor and researcher at the Ohio State University Comprehensive Cancer Center in Columbus, agreed.
“Positive results on SNP-based tests need to be confirmed by medical-grade genetic testing using a sequencing technology,” she said. “Negative results on an SNP- based test cannot be considered to rule out mutations in BRCA1/2 or other cancer-susceptibility genes, so individuals with strong personal and family histories of cancer should be seen by a genetic counselor to consider medical-grade genetic testing using a sequencing technology.”
Practicing oncologists can trust patients’ prior germline genetic test results if the testing was performed in a cancer genetics clinic, which uses sequencing-based technologies, Ms. Hampel noted.
“If the test was performed before 2013, there are likely new genes that have been discovered for which their patient was not tested, and repeat testing may be warranted,” Ms. Hampel said. “A referral to a cancer genetic counselor would be appropriate.”
Ms. Hampel disclosed relationships with Genome Medical, GI OnDemand, Invitae Genetics, and Promega. Dr. Wright and her coauthors disclosed no conflicts of interest. The group’s research was conducted using the UK Biobank and the University of Exeter High-Performance Computing, with funding from the Wellcome Trust and the National Institute for Health Research.
FROM BMJ
The skill set of the ‘pluripotent’ hospitalist
Editor’s note: National Hospitalist Day occurs the first Thursday in March annually, and serves to celebrate the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape. On National Hospitalist Day in 2021, SHM convened a virtual roundtable with a diverse group of hospitalists to discuss skill set, wellness, and other key issues for hospitalists. To listen to the entire roundtable discussion, visit this Explore The Space podcast episode.
A hospitalist isn’t just a physician who happens to work in a hospital. They are medical professionals with a robust skill set that they use both inside and outside the hospital setting. But what skill sets do hospitalists need to become successful in their careers? And what skill sets does a “pluripotent” hospitalist need in their armamentarium?
These were the issues discussed by participants of a virtual roundtable discussion on National Hospitalist Day – March 4, 2021 – as part of a joint effort of the Society of Hospital Medicine and the Explore the Space podcast.
Maylyn S. Martinez, MD, clinician-researcher and clinical associate at the University of Chicago, sees her hospitalist and research skill sets as two “buckets” of skills she can sort through, with diagnostic, knowledge-based care coordination, and interpersonal skills as lanes where she can focus and improve. “I’m always trying to work in, and sharpen, and find ways to get better at something in each of those every day,” she said.
For Anika Kumar, MD, FHM, pediatric editor of the Hospitalist and clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine, much of her work is focused on problem solving. “I approach that as: ‘How do I come up with my differential diagnosis, and how do I diagnose the patient?’ I think that the lanes are a little bit different, but there is some overlap.”
Adaptability is another important part of the skill set for the hospitalist, Ndidi Unaka, MD, MEd, associate professor in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center, said during the discussion. “I think we all really value teamwork, and we take on the role of being the coordinator and making sure things are getting done in a seamless and thoughtful manner. Communicating with families, communicating with our research team, communicating with primary care physicians. I think that is something we’re very used to doing, and I think we do it well. I think we don’t shy away from difficult conversations with consultants. And I think that’s what makes being a hospitalist so amazing.”
Achieving wellness as a hospitalist
Another topic discussed during the roundtable was “comprehensive care for the hospitalist” and how they can achieve a sense of wellness for themselves. Gurpreet Dhaliwal, MD, clinician-educator and professor of medicine at the University of California, San Francisco, said long-term satisfaction in one’s career is less about compensation and more about autonomy, mastery, and purpose.
“Autonomy is shrinking a little bit in health care. But if we connect to our purpose – ‘what are we doing here and how do we connect?’ – it’s either learning about patients and their stories, being with a team of people that you work with, that really builds that purpose,” he said.
Regarding mastery, there’s “tremendous joy if you’re in an environment where people value your mastery, whether it is working in a team or communicating or diagnosing or doing a procedure. If you think of setting up the work environment and those things are in place, I think a lot of wellness can actually happen at work, even though another component, of course, is balancing your life outside of work,” Dr. Dhaliwal said.
This may seem out of reach during COVID-19, but wellness is still achievable during the pandemic, Dr. Martinez said. Her time is spent 75% as a researcher and 25% as a clinician, which is her ideal balance. “I enjoy doing my research, doing my own statistics and writing grants and just learning about this problem that I’ve developed an interest in,” she said. “I just think that’s an important piece for people to focus on as far as health care for the hospitalist, is that there’s no no-one-size-fits-all, that’s for sure.”
Dr. Kumar noted that her clinical time gives her energy for nonclinical work. “I love my clinical time. It’s one of my favorite things that I do,” she said. Although she is tired at the end of the week, “I feel like I am not only giving back to my patients and my team, but I’m also giving back to myself and reminding myself why it is I do what I do every day,” she said.
Wellness for Dr. Unaka meant remembering what drew her to medicine. “It was definitely the opportunity to build strong relationships with patients and families,” she said. While these encounters can sometimes be heavy and stay with a hospitalist, “the fact that we’re in it with them is something that gives a lot of us purpose. I think that when I reflect on all of those things, I’m so happy that I’m in the role that I am.”
Unique skills during COVID-19
Mark Shapiro, MD, hospitalist and host of the roundtable and the Explore the Space podcast, also asked the panelists what skills they unexpectedly leveraged during the pandemic. Communication – with colleagues and with the community they serve – was a universal answer among the panelists.
“I learned – really from seeing some of our senior leaders here do it so well – the importance of being visible, particularly at a time when people were not together and more isolated,” Dr. Unaka said. “I think being able to be visible when you can, in order to deliver really complicated or tough news or communicate about uncertainty, for instance. Being here for our residents – many of our interns moved here sight unseen. I think they needed to feel like they had some sense of normalcy and a sense of community. I really learned how important it was to be visible, and available, and how important the little things mattered.”
Dr. Martinez said that worrying about her patients with COVID-19 in the hospital and the uncertainty around the disease kept her up at night. “I think we always have a hard time leaving work at work and getting a good night’s sleep. I just could not let go of worrying about these patients and having terrible insomnia, trying to leave work at work and I couldn’t – even after they were discharged.”
Dr. Shapiro said the skill he most needed to work on during the pandemic was his courage. “I remember the first time I took care of COVID patients. I was scared. I have no problems saying that out loud. That was a scary experience.”
The demeanor of the nurses on his unit, who had already seen patients with COVID-19, helped ground him during those moments and gave him the courage to move forward. “They’d already been doing it and they were the same. Same affect, same jokes, same everything,” he said. “That actually really helped, and I’ve leaned on that every time I’ve been back on our COVID service.”
Importance of mental health
The COVID-19 pandemic has also shined a light on the importance of mental health. “I think it is important to acknowledge that as hospitalists who have been out on the bleeding edge for a year, mental health is critically important, and we know that we face shortages in that space for the public at large and also for our profession,” Dr. Shapiro said.
When asked about what mental health and self-care looks like for her, Dr. Kumar referenced the need for exercise, meditation, and yoga. “My mental health was better knowing that the people closest to me – whether they be colleagues or friends or family – their mental health was also in a good place and they were also in a good place. And that helped to build me up,” she said.
Dr. Unaka called attention to the stigma around mental health, particularly among physicians, and the lack of resources to address the issue. “It’s a real problem,” she said. “I think it’s at a point where we as a profession need to advocate on behalf of each other and on behalf of our trainees. And honestly, I think we need to view mental health as just ‘health’ and stop separating it out in order for us to move to a place where people feel like they can access what they need without feeling shame about it.”
Editor’s note: National Hospitalist Day occurs the first Thursday in March annually, and serves to celebrate the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape. On National Hospitalist Day in 2021, SHM convened a virtual roundtable with a diverse group of hospitalists to discuss skill set, wellness, and other key issues for hospitalists. To listen to the entire roundtable discussion, visit this Explore The Space podcast episode.
A hospitalist isn’t just a physician who happens to work in a hospital. They are medical professionals with a robust skill set that they use both inside and outside the hospital setting. But what skill sets do hospitalists need to become successful in their careers? And what skill sets does a “pluripotent” hospitalist need in their armamentarium?
These were the issues discussed by participants of a virtual roundtable discussion on National Hospitalist Day – March 4, 2021 – as part of a joint effort of the Society of Hospital Medicine and the Explore the Space podcast.
Maylyn S. Martinez, MD, clinician-researcher and clinical associate at the University of Chicago, sees her hospitalist and research skill sets as two “buckets” of skills she can sort through, with diagnostic, knowledge-based care coordination, and interpersonal skills as lanes where she can focus and improve. “I’m always trying to work in, and sharpen, and find ways to get better at something in each of those every day,” she said.
For Anika Kumar, MD, FHM, pediatric editor of the Hospitalist and clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine, much of her work is focused on problem solving. “I approach that as: ‘How do I come up with my differential diagnosis, and how do I diagnose the patient?’ I think that the lanes are a little bit different, but there is some overlap.”
Adaptability is another important part of the skill set for the hospitalist, Ndidi Unaka, MD, MEd, associate professor in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center, said during the discussion. “I think we all really value teamwork, and we take on the role of being the coordinator and making sure things are getting done in a seamless and thoughtful manner. Communicating with families, communicating with our research team, communicating with primary care physicians. I think that is something we’re very used to doing, and I think we do it well. I think we don’t shy away from difficult conversations with consultants. And I think that’s what makes being a hospitalist so amazing.”
Achieving wellness as a hospitalist
Another topic discussed during the roundtable was “comprehensive care for the hospitalist” and how they can achieve a sense of wellness for themselves. Gurpreet Dhaliwal, MD, clinician-educator and professor of medicine at the University of California, San Francisco, said long-term satisfaction in one’s career is less about compensation and more about autonomy, mastery, and purpose.
“Autonomy is shrinking a little bit in health care. But if we connect to our purpose – ‘what are we doing here and how do we connect?’ – it’s either learning about patients and their stories, being with a team of people that you work with, that really builds that purpose,” he said.
Regarding mastery, there’s “tremendous joy if you’re in an environment where people value your mastery, whether it is working in a team or communicating or diagnosing or doing a procedure. If you think of setting up the work environment and those things are in place, I think a lot of wellness can actually happen at work, even though another component, of course, is balancing your life outside of work,” Dr. Dhaliwal said.
This may seem out of reach during COVID-19, but wellness is still achievable during the pandemic, Dr. Martinez said. Her time is spent 75% as a researcher and 25% as a clinician, which is her ideal balance. “I enjoy doing my research, doing my own statistics and writing grants and just learning about this problem that I’ve developed an interest in,” she said. “I just think that’s an important piece for people to focus on as far as health care for the hospitalist, is that there’s no no-one-size-fits-all, that’s for sure.”
Dr. Kumar noted that her clinical time gives her energy for nonclinical work. “I love my clinical time. It’s one of my favorite things that I do,” she said. Although she is tired at the end of the week, “I feel like I am not only giving back to my patients and my team, but I’m also giving back to myself and reminding myself why it is I do what I do every day,” she said.
Wellness for Dr. Unaka meant remembering what drew her to medicine. “It was definitely the opportunity to build strong relationships with patients and families,” she said. While these encounters can sometimes be heavy and stay with a hospitalist, “the fact that we’re in it with them is something that gives a lot of us purpose. I think that when I reflect on all of those things, I’m so happy that I’m in the role that I am.”
Unique skills during COVID-19
Mark Shapiro, MD, hospitalist and host of the roundtable and the Explore the Space podcast, also asked the panelists what skills they unexpectedly leveraged during the pandemic. Communication – with colleagues and with the community they serve – was a universal answer among the panelists.
“I learned – really from seeing some of our senior leaders here do it so well – the importance of being visible, particularly at a time when people were not together and more isolated,” Dr. Unaka said. “I think being able to be visible when you can, in order to deliver really complicated or tough news or communicate about uncertainty, for instance. Being here for our residents – many of our interns moved here sight unseen. I think they needed to feel like they had some sense of normalcy and a sense of community. I really learned how important it was to be visible, and available, and how important the little things mattered.”
Dr. Martinez said that worrying about her patients with COVID-19 in the hospital and the uncertainty around the disease kept her up at night. “I think we always have a hard time leaving work at work and getting a good night’s sleep. I just could not let go of worrying about these patients and having terrible insomnia, trying to leave work at work and I couldn’t – even after they were discharged.”
Dr. Shapiro said the skill he most needed to work on during the pandemic was his courage. “I remember the first time I took care of COVID patients. I was scared. I have no problems saying that out loud. That was a scary experience.”
The demeanor of the nurses on his unit, who had already seen patients with COVID-19, helped ground him during those moments and gave him the courage to move forward. “They’d already been doing it and they were the same. Same affect, same jokes, same everything,” he said. “That actually really helped, and I’ve leaned on that every time I’ve been back on our COVID service.”
Importance of mental health
The COVID-19 pandemic has also shined a light on the importance of mental health. “I think it is important to acknowledge that as hospitalists who have been out on the bleeding edge for a year, mental health is critically important, and we know that we face shortages in that space for the public at large and also for our profession,” Dr. Shapiro said.
When asked about what mental health and self-care looks like for her, Dr. Kumar referenced the need for exercise, meditation, and yoga. “My mental health was better knowing that the people closest to me – whether they be colleagues or friends or family – their mental health was also in a good place and they were also in a good place. And that helped to build me up,” she said.
Dr. Unaka called attention to the stigma around mental health, particularly among physicians, and the lack of resources to address the issue. “It’s a real problem,” she said. “I think it’s at a point where we as a profession need to advocate on behalf of each other and on behalf of our trainees. And honestly, I think we need to view mental health as just ‘health’ and stop separating it out in order for us to move to a place where people feel like they can access what they need without feeling shame about it.”
Editor’s note: National Hospitalist Day occurs the first Thursday in March annually, and serves to celebrate the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape. On National Hospitalist Day in 2021, SHM convened a virtual roundtable with a diverse group of hospitalists to discuss skill set, wellness, and other key issues for hospitalists. To listen to the entire roundtable discussion, visit this Explore The Space podcast episode.
A hospitalist isn’t just a physician who happens to work in a hospital. They are medical professionals with a robust skill set that they use both inside and outside the hospital setting. But what skill sets do hospitalists need to become successful in their careers? And what skill sets does a “pluripotent” hospitalist need in their armamentarium?
These were the issues discussed by participants of a virtual roundtable discussion on National Hospitalist Day – March 4, 2021 – as part of a joint effort of the Society of Hospital Medicine and the Explore the Space podcast.
Maylyn S. Martinez, MD, clinician-researcher and clinical associate at the University of Chicago, sees her hospitalist and research skill sets as two “buckets” of skills she can sort through, with diagnostic, knowledge-based care coordination, and interpersonal skills as lanes where she can focus and improve. “I’m always trying to work in, and sharpen, and find ways to get better at something in each of those every day,” she said.
For Anika Kumar, MD, FHM, pediatric editor of the Hospitalist and clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine, much of her work is focused on problem solving. “I approach that as: ‘How do I come up with my differential diagnosis, and how do I diagnose the patient?’ I think that the lanes are a little bit different, but there is some overlap.”
Adaptability is another important part of the skill set for the hospitalist, Ndidi Unaka, MD, MEd, associate professor in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center, said during the discussion. “I think we all really value teamwork, and we take on the role of being the coordinator and making sure things are getting done in a seamless and thoughtful manner. Communicating with families, communicating with our research team, communicating with primary care physicians. I think that is something we’re very used to doing, and I think we do it well. I think we don’t shy away from difficult conversations with consultants. And I think that’s what makes being a hospitalist so amazing.”
Achieving wellness as a hospitalist
Another topic discussed during the roundtable was “comprehensive care for the hospitalist” and how they can achieve a sense of wellness for themselves. Gurpreet Dhaliwal, MD, clinician-educator and professor of medicine at the University of California, San Francisco, said long-term satisfaction in one’s career is less about compensation and more about autonomy, mastery, and purpose.
“Autonomy is shrinking a little bit in health care. But if we connect to our purpose – ‘what are we doing here and how do we connect?’ – it’s either learning about patients and their stories, being with a team of people that you work with, that really builds that purpose,” he said.
Regarding mastery, there’s “tremendous joy if you’re in an environment where people value your mastery, whether it is working in a team or communicating or diagnosing or doing a procedure. If you think of setting up the work environment and those things are in place, I think a lot of wellness can actually happen at work, even though another component, of course, is balancing your life outside of work,” Dr. Dhaliwal said.
This may seem out of reach during COVID-19, but wellness is still achievable during the pandemic, Dr. Martinez said. Her time is spent 75% as a researcher and 25% as a clinician, which is her ideal balance. “I enjoy doing my research, doing my own statistics and writing grants and just learning about this problem that I’ve developed an interest in,” she said. “I just think that’s an important piece for people to focus on as far as health care for the hospitalist, is that there’s no no-one-size-fits-all, that’s for sure.”
Dr. Kumar noted that her clinical time gives her energy for nonclinical work. “I love my clinical time. It’s one of my favorite things that I do,” she said. Although she is tired at the end of the week, “I feel like I am not only giving back to my patients and my team, but I’m also giving back to myself and reminding myself why it is I do what I do every day,” she said.
Wellness for Dr. Unaka meant remembering what drew her to medicine. “It was definitely the opportunity to build strong relationships with patients and families,” she said. While these encounters can sometimes be heavy and stay with a hospitalist, “the fact that we’re in it with them is something that gives a lot of us purpose. I think that when I reflect on all of those things, I’m so happy that I’m in the role that I am.”
Unique skills during COVID-19
Mark Shapiro, MD, hospitalist and host of the roundtable and the Explore the Space podcast, also asked the panelists what skills they unexpectedly leveraged during the pandemic. Communication – with colleagues and with the community they serve – was a universal answer among the panelists.
“I learned – really from seeing some of our senior leaders here do it so well – the importance of being visible, particularly at a time when people were not together and more isolated,” Dr. Unaka said. “I think being able to be visible when you can, in order to deliver really complicated or tough news or communicate about uncertainty, for instance. Being here for our residents – many of our interns moved here sight unseen. I think they needed to feel like they had some sense of normalcy and a sense of community. I really learned how important it was to be visible, and available, and how important the little things mattered.”
Dr. Martinez said that worrying about her patients with COVID-19 in the hospital and the uncertainty around the disease kept her up at night. “I think we always have a hard time leaving work at work and getting a good night’s sleep. I just could not let go of worrying about these patients and having terrible insomnia, trying to leave work at work and I couldn’t – even after they were discharged.”
Dr. Shapiro said the skill he most needed to work on during the pandemic was his courage. “I remember the first time I took care of COVID patients. I was scared. I have no problems saying that out loud. That was a scary experience.”
The demeanor of the nurses on his unit, who had already seen patients with COVID-19, helped ground him during those moments and gave him the courage to move forward. “They’d already been doing it and they were the same. Same affect, same jokes, same everything,” he said. “That actually really helped, and I’ve leaned on that every time I’ve been back on our COVID service.”
Importance of mental health
The COVID-19 pandemic has also shined a light on the importance of mental health. “I think it is important to acknowledge that as hospitalists who have been out on the bleeding edge for a year, mental health is critically important, and we know that we face shortages in that space for the public at large and also for our profession,” Dr. Shapiro said.
When asked about what mental health and self-care looks like for her, Dr. Kumar referenced the need for exercise, meditation, and yoga. “My mental health was better knowing that the people closest to me – whether they be colleagues or friends or family – their mental health was also in a good place and they were also in a good place. And that helped to build me up,” she said.
Dr. Unaka called attention to the stigma around mental health, particularly among physicians, and the lack of resources to address the issue. “It’s a real problem,” she said. “I think it’s at a point where we as a profession need to advocate on behalf of each other and on behalf of our trainees. And honestly, I think we need to view mental health as just ‘health’ and stop separating it out in order for us to move to a place where people feel like they can access what they need without feeling shame about it.”
Virtual is the new real
Why did we fall short on maximizing telehealth’s value in the COVID-19 pandemic?
The COVID-19 pandemic catalyzed the transformation of Internet-based, remotely accessible innovative technologies. Internet-based customer service delivery technology was rapidly adopted and utilized by several services industries, but health care systems in most of the countries across the world faced unique challenges in adopting the technology for the delivery of health care services. The health care ecosystem of the United States was not immune to such challenges, and several significant barriers surfaced while the pandemic was underway.
Complexly structured, fragmented, unprepared, and overly burnt-out health systems in the United States arguably have fallen short of maximizing the value of telehealth in delivering safe, easily accessible, comprehensive, and cost-effective health care services. In this essay, we examine the reasons for such a suboptimal performance and discuss a few important strategies that may be useful in maximizing the value of telehealth value in several, appropriate health care services.
Hospitals and telehealth
Are hospitalists preparing ourselves “not to see” patients in a hospital-based health care delivery setting? If you have not yet started yet, now may be the right time! Yes, a certain percentage of doctor-patient encounters in hospital settings will remain virtual forever.
A well-established telehealth infrastructure is rarely found in most U.S. hospitals, although the COVID-19 pandemic has unexpectedly boosted the rapid growth of telehealth in the country.1 Public health emergency declarations in the United States in the face of the COVID-19 crisis have facilitated two important initiatives to restore health care delivery amidst formal and informal lockdowns that brought states to a grinding halt. These extend from expansion of virtual services, including telehealth, virtual check-ins, and e-visits, to the decision by the Department of Health & Human Services Office of Civil Rights to exercise enforcement discretion and waive penalties for the use of relatively inexpensive, non–public-facing mobile and other audiovisual technology tools.2
Hospital-based care in the United States taps nearly 33% of national health expenditure. An additional 30% of national health expenditure that is related to physicians, prescriptions, and other facilities is indirectly influenced by care delivered at health care facilities.3 Studies show that about 20% of ED visits could potentially be avoided via virtual urgent care offerings.4 A rapidly changing health care ecosystem is proving formidable for most hospital systems, and a test for their resilience and agility. Not just the implementation of telehealth is challenging, but getting it right is the key success factor.
Hospital-based telehealth
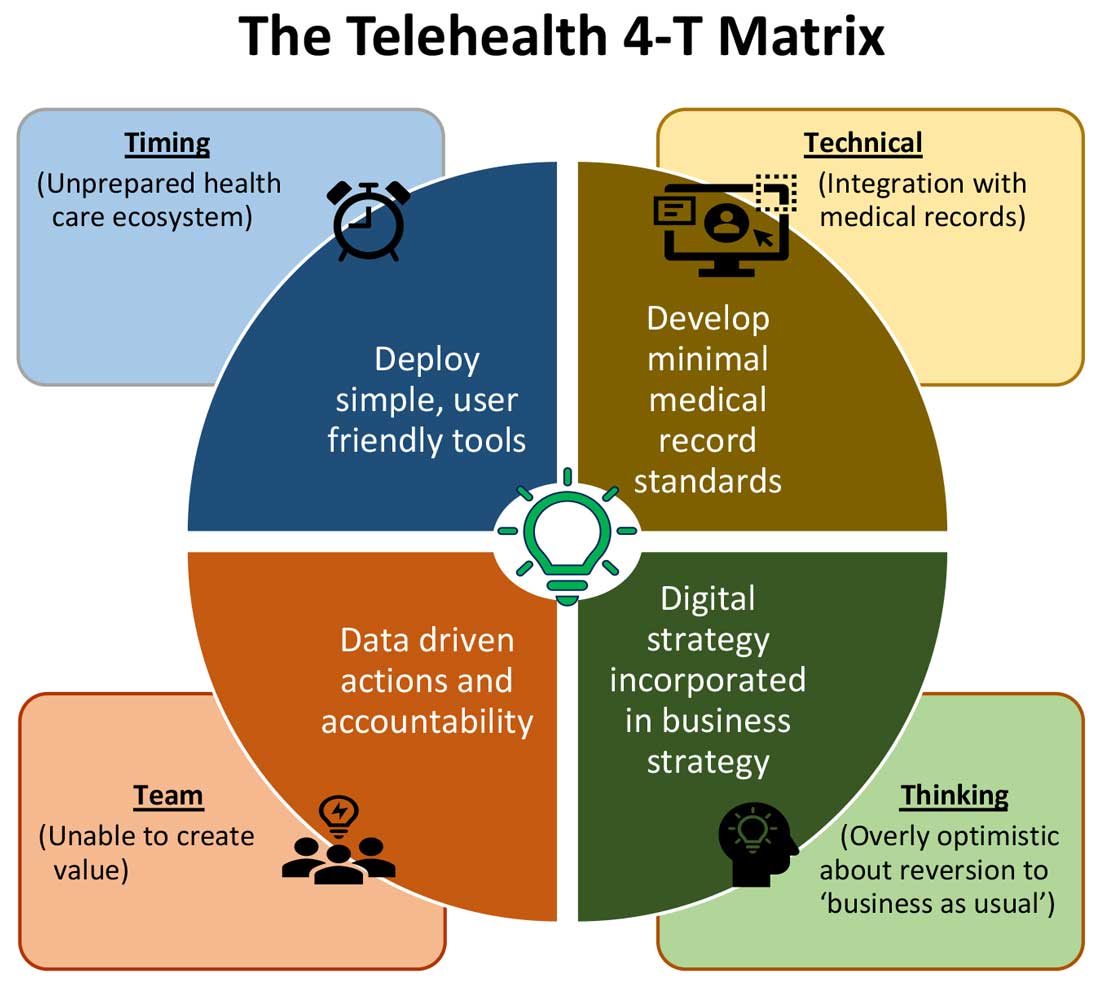
Expansion of telehealth coverage by the Centers for Medicare & Medicaid Services and most commercial payers did not quite ride the pandemic-induced momentum across the care continuum. Hospitals are lagging far behind ambulatory care in implementing telehealth. As illustrated in the “4-T Matrix” (see graphic) we would like to examine four key reasons for such a sluggish initial uptake and try to propose four important strategies that may help us to maximize the value created by telehealth technologies.
1. Timing
The health care system has always lagged far behind other service industries in terms of technology adaptation. Because of the unique nature of health care services, face-to-face interaction supersedes all other forms of communication. A rapidly evolving pandemic was not matched by simultaneous technology education for patients and providers. The enormous choice of hard-to-navigate telehealth tools; time and labor-intensive implementation; and uncertainty around payer, policy, and regulatory expectations might have precluded providers from the rapid adoption of telehealth in the hospital setting. Patients’ specific characteristics, such as the absence of technology-centered education, information, age, comorbidities, lack of technical literacy, and dependency on caregivers contributed to the suboptimal response from patients and families.
Deploying simple, ubiquitous, user-friendly, and technologically less challenging telehealth solutions may be a better approach to increase the adoption of such solutions by providers and patients. Hospitals need to develop and distribute telehealth user guides in all possible modes of communication. Provider-centric in-service sessions, workshops, and live support by “superuser teams” often work well in reducing end-user resistance.
2. Technical
Current electronic medical records vary widely in their features and offerings, and their ability to interact with third-party software and platforms. Dissatisfaction of end users with EMRs is well known, as is their likely relationship to burnout. Recent research continues to show a strong relationship between EMR usability and the odds of burnout among physicians.5 In the current climate, administrators and health informaticists have the responsibility to avoid adding increased burdens to end users.
Another issue is the limited connectivity in many remote/rural areas that would impact implementation of telehealth platforms. Studies indicate that 33% of rural Americans lack access to high-speed broadband Internet to support video visits.6 The recent successful implementation of telehealth across 530 providers in 75 ambulatory practices operated by Munson Healthcare, a rural health system in northern Michigan, sheds light on the technology’s enormous potential in providing safe access to rural populations.6,7
Privacy and safety of patient data is of paramount importance. According to a national poll on healthy aging by the University of Michigan in May 2019, targeting older adults, 47% of survey responders expressed difficulty using technology and 49% of survey responders were concerned about privacy.8 Use of certification and other tools offered by the Office of the National Coordinator for Health Information Technology would help reassure users, and the ability to capture and share images between providers would be of immense benefit in facilitating e-consults.
The need of the hour is redesigned work flow, to help providers adopt and use virtual care/telehealth efficiently. Work flow redesign must be coupled with technological advances to allow seamless integration of third-party telehealth platforms into existing EMR systems or built directly into EMRs. Use of quality metrics and analytical tools specific to telehealth would help measure the technology’s impact on patient care, outcomes, and end-user/provider experience.
3. Teams and training
Outcomes of health care interventions are often determined by the effectiveness of teams. Irrespective of how robust health care systems may have been initially, rapidly spreading infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and patients to a breaking point.5 Decentralized, uncoordinated, and siloed efforts by individual teams across the care continuum were contributing factors for the partial success of telehealth care delivery pathways. The hospital systems with telehealth-ready teams at the start of the COVID-19 pandemic were so rare that the knowledge and technical training opportunities for innovators grew severalfold during the pandemic.
As per the American Medical Association, telehealth success is massively dependent on building the right team. Core, leadership, advisory, and implementation teams comprised of clinical representatives, end users, administrative personnel, executive members of the organization, technical experts, and payment/policy experts should be put together before implementing a telehealth strategy.9 Seamless integration of hospital-based care with ambulatory care via a telehealth platform is only complete when care managers are trained and deployed to fulfill the needs of a diverse group of patients. Deriving overall value from telehealth is only possible when there is a skill development, training and mentoring team put in place.
4. Thinking
In most U.S. hospitals, inpatient health care is equally distributed between nonprocedure and procedure-based services. Hospitals resorted to suspension of nonemergent procedures to mitigate the risk of spreading COVID-19. This was further compounded by many patients’ self-selection to defer care, an abrupt reduction in the influx of patients from the referral base because of suboptimally operating ambulatory care services, leading to low hospital occupancy.
Hospitals across the nation have gone through a massive short-term financial crunch and unfavorable cash-flow forecast, which prompted a paradoxical work-force reduction. While some argue that it may be akin to strategic myopia, the authors believed that such a response is strategically imperative to keep the hospital afloat. It is reasonable to attribute the paucity of innovation to constrained resources, and health systems are simply staying overly optimistic about “weathering the storm” and reverting soon to “business as usual.” The technological framework necessary for deploying a telehealth solution often comes with a price. Financially challenged hospital systems rarely exercise any capital-intensive activities. By contrast, telehealth adoption by ambulatory care can result in quicker resumption of patient care in community settings. A lack of operational and infrastructure synchrony between ambulatory and in-hospital systems has failed to capture telehealth-driven inpatient volume. For example, direct admissions from ambulatory telehealth referrals was a missed opportunity in several places. Referrals for labs, diagnostic tests, and other allied services could have helped hospitals offset their fixed costs. Similarly, work flows related to discharge and postdischarge follow up rarely embrace telehealth tools or telehealth care pathways. A brisk change in the health care ecosystem is partly responsible for this.
Digital strategy needs to be incorporated into business strategy. For the reasons already discussed, telehealth technology is not a “nice to have” anymore, but a “must have.” At present, providers are of the opinion that about 20% of their patient services can be delivered via a telehealth platform. Similar trends are observed among patients, as a new modality of access to care is increasingly beneficial to them. Telehealth must be incorporated in standardized hospital work flows. Use of telehealth for preoperative clearance will greatly minimize same-day surgery cancellations. Given the potential shortage in resources, telehealth adoption for inpatient consultations will help systems conserve personal protective equipment, minimize the risk of staff exposure to COVID-19, and improve efficiency.
Digital strategy also prompts the reengineering of care delivery.10 Excessive and unused physical capacity can be converted into digital care hubs. Health maintenance, prevention, health promotion, health education, and chronic disease management not only can serve a variety of patient groups but can also help address the “last-mile problem” in health care. A successful digital strategy usually has three important components – Commitment: Hospital leadership is committed to include digital transformation as a strategic objective; Cost: Digital strategy is added as a line item in the budget; and Control: Measurable metrics are put in place to monitor the performance, impact, and influence of the digital strategy.
Conclusion
For decades, most U.S. health systems occupied the periphery of technological transformation when compared to the rest of the service industry. While most health systems took a heroic approach to the adoption of telehealth during COVID-19, despite being unprepared, the need for a systematic telehealth deployment is far from being adequately fulfilled. The COVID-19 pandemic brought permanent changes to several business disciplines globally. Given the impact of the pandemic on the health and overall wellbeing of American society, the U.S. health care industry must leave no stone unturned in its quest for transformation.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark, and is cofounder/president of SHM’s Arkansas chapter. Dr. Prasad is medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. He is cochair of SHM’s IT Special Interest Group, sits on the HQPS committee, and is president of SHM’s Wisconsin chapter. Dr. Palabindala is the medical director, utilization management, and physician advisory services at the University of Mississippi Medical Center and an associate professor of medicine and academic hospitalist at the University of Mississippi, both in Jackson.
References
1. Finnegan M. “Telehealth booms amid COVID-19 crisis.” Computerworld. 2020 Apr 27. www.computerworld.com/article/3540315/telehealth-booms-amid-covid-19-crisis-virtual-care-is-here-to-stay.html. Accessed 2020 Sep 12.
2. Department of Health & Human Services. “OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency.” 2020 Mar 17. www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html. Accessed 2020 Sep 12.
3. National Center for Health Statistics. “Health Expenditures.” www.cdc.gov/nchs/fastats/health-expenditures.htm. Accessed 2020 Sep 12.
4. Bestsennyy O et al. “Telehealth: A post–COVID-19 reality?” McKinsey & Company. 2020 May 29. www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality. Accessed 2020 Sep 12.
5. Melnick ER et al. The Association Between Perceived Electronic Health Record Usability and Professional Burnout Among U.S. Physicians. Mayo Clin Proc. 2020 March;95(3):476-87.
6. Hirko KA et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Inform Assoc. 2020 Nov;27(11):1816-8. .
7. American Academy of Family Physicians. “Study Examines Telehealth, Rural Disparities in Pandemic.” 2020 July 30. www.aafp.org/news/practice-professional-issues/20200730ruraltelehealth.html. Accessed 2020 Dec 15.
8. Kurlander J et al. “Virtual Visits: Telehealth and Older Adults.” National Poll on Healthy Aging. 2019 Oct. hdl.handle.net/2027.42/151376.
9. American Medical Association. Telehealth Implementation Playbook. 2019. www.ama-assn.org/system/files/2020-04/ama-telehealth-implementation-playbook.pdf.
10. Smith AC et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020 Jun;26(5):309-13.
Why did we fall short on maximizing telehealth’s value in the COVID-19 pandemic?
Why did we fall short on maximizing telehealth’s value in the COVID-19 pandemic?
The COVID-19 pandemic catalyzed the transformation of Internet-based, remotely accessible innovative technologies. Internet-based customer service delivery technology was rapidly adopted and utilized by several services industries, but health care systems in most of the countries across the world faced unique challenges in adopting the technology for the delivery of health care services. The health care ecosystem of the United States was not immune to such challenges, and several significant barriers surfaced while the pandemic was underway.
Complexly structured, fragmented, unprepared, and overly burnt-out health systems in the United States arguably have fallen short of maximizing the value of telehealth in delivering safe, easily accessible, comprehensive, and cost-effective health care services. In this essay, we examine the reasons for such a suboptimal performance and discuss a few important strategies that may be useful in maximizing the value of telehealth value in several, appropriate health care services.
Hospitals and telehealth
Are hospitalists preparing ourselves “not to see” patients in a hospital-based health care delivery setting? If you have not yet started yet, now may be the right time! Yes, a certain percentage of doctor-patient encounters in hospital settings will remain virtual forever.
A well-established telehealth infrastructure is rarely found in most U.S. hospitals, although the COVID-19 pandemic has unexpectedly boosted the rapid growth of telehealth in the country.1 Public health emergency declarations in the United States in the face of the COVID-19 crisis have facilitated two important initiatives to restore health care delivery amidst formal and informal lockdowns that brought states to a grinding halt. These extend from expansion of virtual services, including telehealth, virtual check-ins, and e-visits, to the decision by the Department of Health & Human Services Office of Civil Rights to exercise enforcement discretion and waive penalties for the use of relatively inexpensive, non–public-facing mobile and other audiovisual technology tools.2
Hospital-based care in the United States taps nearly 33% of national health expenditure. An additional 30% of national health expenditure that is related to physicians, prescriptions, and other facilities is indirectly influenced by care delivered at health care facilities.3 Studies show that about 20% of ED visits could potentially be avoided via virtual urgent care offerings.4 A rapidly changing health care ecosystem is proving formidable for most hospital systems, and a test for their resilience and agility. Not just the implementation of telehealth is challenging, but getting it right is the key success factor.
Hospital-based telehealth
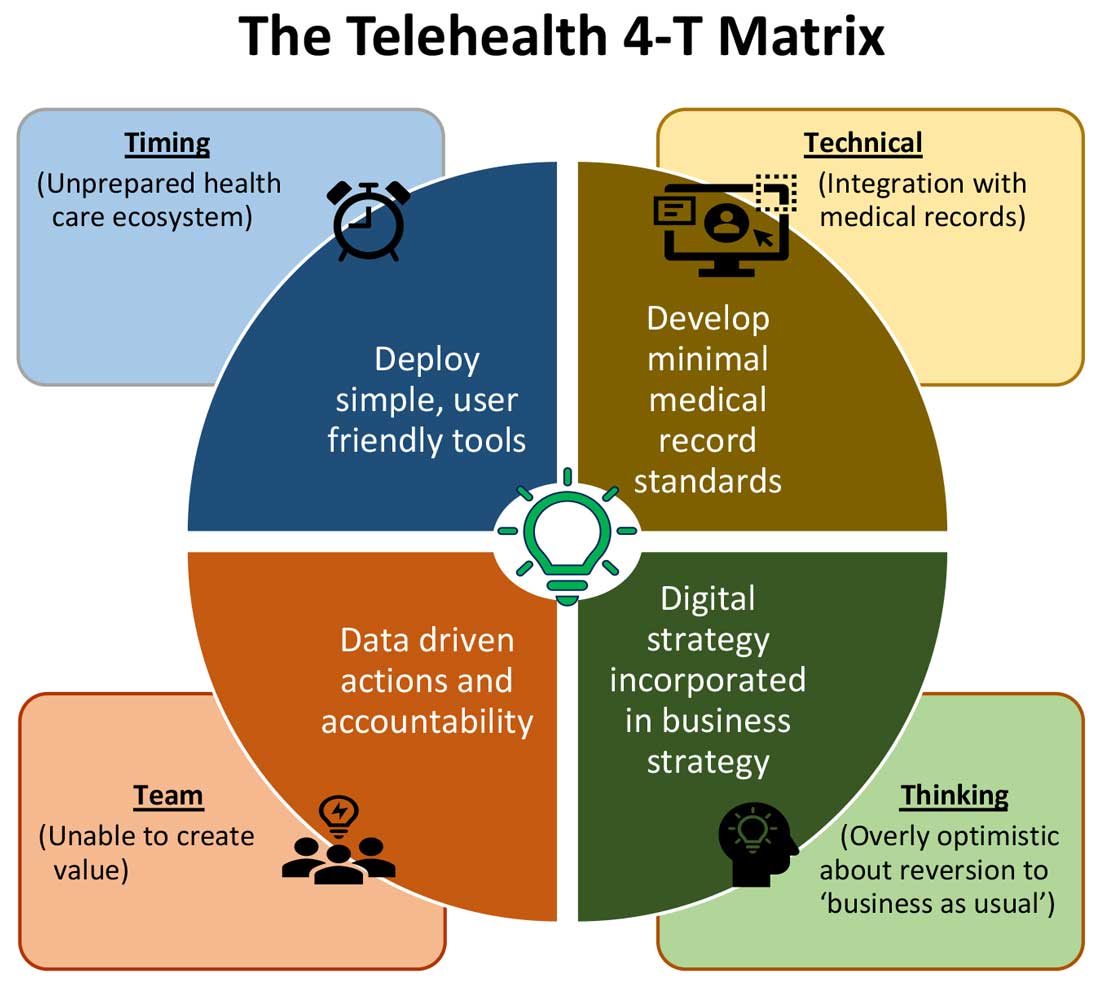
Expansion of telehealth coverage by the Centers for Medicare & Medicaid Services and most commercial payers did not quite ride the pandemic-induced momentum across the care continuum. Hospitals are lagging far behind ambulatory care in implementing telehealth. As illustrated in the “4-T Matrix” (see graphic) we would like to examine four key reasons for such a sluggish initial uptake and try to propose four important strategies that may help us to maximize the value created by telehealth technologies.
1. Timing
The health care system has always lagged far behind other service industries in terms of technology adaptation. Because of the unique nature of health care services, face-to-face interaction supersedes all other forms of communication. A rapidly evolving pandemic was not matched by simultaneous technology education for patients and providers. The enormous choice of hard-to-navigate telehealth tools; time and labor-intensive implementation; and uncertainty around payer, policy, and regulatory expectations might have precluded providers from the rapid adoption of telehealth in the hospital setting. Patients’ specific characteristics, such as the absence of technology-centered education, information, age, comorbidities, lack of technical literacy, and dependency on caregivers contributed to the suboptimal response from patients and families.
Deploying simple, ubiquitous, user-friendly, and technologically less challenging telehealth solutions may be a better approach to increase the adoption of such solutions by providers and patients. Hospitals need to develop and distribute telehealth user guides in all possible modes of communication. Provider-centric in-service sessions, workshops, and live support by “superuser teams” often work well in reducing end-user resistance.
2. Technical
Current electronic medical records vary widely in their features and offerings, and their ability to interact with third-party software and platforms. Dissatisfaction of end users with EMRs is well known, as is their likely relationship to burnout. Recent research continues to show a strong relationship between EMR usability and the odds of burnout among physicians.5 In the current climate, administrators and health informaticists have the responsibility to avoid adding increased burdens to end users.
Another issue is the limited connectivity in many remote/rural areas that would impact implementation of telehealth platforms. Studies indicate that 33% of rural Americans lack access to high-speed broadband Internet to support video visits.6 The recent successful implementation of telehealth across 530 providers in 75 ambulatory practices operated by Munson Healthcare, a rural health system in northern Michigan, sheds light on the technology’s enormous potential in providing safe access to rural populations.6,7
Privacy and safety of patient data is of paramount importance. According to a national poll on healthy aging by the University of Michigan in May 2019, targeting older adults, 47% of survey responders expressed difficulty using technology and 49% of survey responders were concerned about privacy.8 Use of certification and other tools offered by the Office of the National Coordinator for Health Information Technology would help reassure users, and the ability to capture and share images between providers would be of immense benefit in facilitating e-consults.
The need of the hour is redesigned work flow, to help providers adopt and use virtual care/telehealth efficiently. Work flow redesign must be coupled with technological advances to allow seamless integration of third-party telehealth platforms into existing EMR systems or built directly into EMRs. Use of quality metrics and analytical tools specific to telehealth would help measure the technology’s impact on patient care, outcomes, and end-user/provider experience.
3. Teams and training
Outcomes of health care interventions are often determined by the effectiveness of teams. Irrespective of how robust health care systems may have been initially, rapidly spreading infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and patients to a breaking point.5 Decentralized, uncoordinated, and siloed efforts by individual teams across the care continuum were contributing factors for the partial success of telehealth care delivery pathways. The hospital systems with telehealth-ready teams at the start of the COVID-19 pandemic were so rare that the knowledge and technical training opportunities for innovators grew severalfold during the pandemic.
As per the American Medical Association, telehealth success is massively dependent on building the right team. Core, leadership, advisory, and implementation teams comprised of clinical representatives, end users, administrative personnel, executive members of the organization, technical experts, and payment/policy experts should be put together before implementing a telehealth strategy.9 Seamless integration of hospital-based care with ambulatory care via a telehealth platform is only complete when care managers are trained and deployed to fulfill the needs of a diverse group of patients. Deriving overall value from telehealth is only possible when there is a skill development, training and mentoring team put in place.
4. Thinking
In most U.S. hospitals, inpatient health care is equally distributed between nonprocedure and procedure-based services. Hospitals resorted to suspension of nonemergent procedures to mitigate the risk of spreading COVID-19. This was further compounded by many patients’ self-selection to defer care, an abrupt reduction in the influx of patients from the referral base because of suboptimally operating ambulatory care services, leading to low hospital occupancy.
Hospitals across the nation have gone through a massive short-term financial crunch and unfavorable cash-flow forecast, which prompted a paradoxical work-force reduction. While some argue that it may be akin to strategic myopia, the authors believed that such a response is strategically imperative to keep the hospital afloat. It is reasonable to attribute the paucity of innovation to constrained resources, and health systems are simply staying overly optimistic about “weathering the storm” and reverting soon to “business as usual.” The technological framework necessary for deploying a telehealth solution often comes with a price. Financially challenged hospital systems rarely exercise any capital-intensive activities. By contrast, telehealth adoption by ambulatory care can result in quicker resumption of patient care in community settings. A lack of operational and infrastructure synchrony between ambulatory and in-hospital systems has failed to capture telehealth-driven inpatient volume. For example, direct admissions from ambulatory telehealth referrals was a missed opportunity in several places. Referrals for labs, diagnostic tests, and other allied services could have helped hospitals offset their fixed costs. Similarly, work flows related to discharge and postdischarge follow up rarely embrace telehealth tools or telehealth care pathways. A brisk change in the health care ecosystem is partly responsible for this.
Digital strategy needs to be incorporated into business strategy. For the reasons already discussed, telehealth technology is not a “nice to have” anymore, but a “must have.” At present, providers are of the opinion that about 20% of their patient services can be delivered via a telehealth platform. Similar trends are observed among patients, as a new modality of access to care is increasingly beneficial to them. Telehealth must be incorporated in standardized hospital work flows. Use of telehealth for preoperative clearance will greatly minimize same-day surgery cancellations. Given the potential shortage in resources, telehealth adoption for inpatient consultations will help systems conserve personal protective equipment, minimize the risk of staff exposure to COVID-19, and improve efficiency.
Digital strategy also prompts the reengineering of care delivery.10 Excessive and unused physical capacity can be converted into digital care hubs. Health maintenance, prevention, health promotion, health education, and chronic disease management not only can serve a variety of patient groups but can also help address the “last-mile problem” in health care. A successful digital strategy usually has three important components – Commitment: Hospital leadership is committed to include digital transformation as a strategic objective; Cost: Digital strategy is added as a line item in the budget; and Control: Measurable metrics are put in place to monitor the performance, impact, and influence of the digital strategy.
Conclusion
For decades, most U.S. health systems occupied the periphery of technological transformation when compared to the rest of the service industry. While most health systems took a heroic approach to the adoption of telehealth during COVID-19, despite being unprepared, the need for a systematic telehealth deployment is far from being adequately fulfilled. The COVID-19 pandemic brought permanent changes to several business disciplines globally. Given the impact of the pandemic on the health and overall wellbeing of American society, the U.S. health care industry must leave no stone unturned in its quest for transformation.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark, and is cofounder/president of SHM’s Arkansas chapter. Dr. Prasad is medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. He is cochair of SHM’s IT Special Interest Group, sits on the HQPS committee, and is president of SHM’s Wisconsin chapter. Dr. Palabindala is the medical director, utilization management, and physician advisory services at the University of Mississippi Medical Center and an associate professor of medicine and academic hospitalist at the University of Mississippi, both in Jackson.
References
1. Finnegan M. “Telehealth booms amid COVID-19 crisis.” Computerworld. 2020 Apr 27. www.computerworld.com/article/3540315/telehealth-booms-amid-covid-19-crisis-virtual-care-is-here-to-stay.html. Accessed 2020 Sep 12.
2. Department of Health & Human Services. “OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency.” 2020 Mar 17. www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html. Accessed 2020 Sep 12.
3. National Center for Health Statistics. “Health Expenditures.” www.cdc.gov/nchs/fastats/health-expenditures.htm. Accessed 2020 Sep 12.
4. Bestsennyy O et al. “Telehealth: A post–COVID-19 reality?” McKinsey & Company. 2020 May 29. www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality. Accessed 2020 Sep 12.
5. Melnick ER et al. The Association Between Perceived Electronic Health Record Usability and Professional Burnout Among U.S. Physicians. Mayo Clin Proc. 2020 March;95(3):476-87.
6. Hirko KA et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Inform Assoc. 2020 Nov;27(11):1816-8. .
7. American Academy of Family Physicians. “Study Examines Telehealth, Rural Disparities in Pandemic.” 2020 July 30. www.aafp.org/news/practice-professional-issues/20200730ruraltelehealth.html. Accessed 2020 Dec 15.
8. Kurlander J et al. “Virtual Visits: Telehealth and Older Adults.” National Poll on Healthy Aging. 2019 Oct. hdl.handle.net/2027.42/151376.
9. American Medical Association. Telehealth Implementation Playbook. 2019. www.ama-assn.org/system/files/2020-04/ama-telehealth-implementation-playbook.pdf.
10. Smith AC et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020 Jun;26(5):309-13.
The COVID-19 pandemic catalyzed the transformation of Internet-based, remotely accessible innovative technologies. Internet-based customer service delivery technology was rapidly adopted and utilized by several services industries, but health care systems in most of the countries across the world faced unique challenges in adopting the technology for the delivery of health care services. The health care ecosystem of the United States was not immune to such challenges, and several significant barriers surfaced while the pandemic was underway.
Complexly structured, fragmented, unprepared, and overly burnt-out health systems in the United States arguably have fallen short of maximizing the value of telehealth in delivering safe, easily accessible, comprehensive, and cost-effective health care services. In this essay, we examine the reasons for such a suboptimal performance and discuss a few important strategies that may be useful in maximizing the value of telehealth value in several, appropriate health care services.
Hospitals and telehealth
Are hospitalists preparing ourselves “not to see” patients in a hospital-based health care delivery setting? If you have not yet started yet, now may be the right time! Yes, a certain percentage of doctor-patient encounters in hospital settings will remain virtual forever.
A well-established telehealth infrastructure is rarely found in most U.S. hospitals, although the COVID-19 pandemic has unexpectedly boosted the rapid growth of telehealth in the country.1 Public health emergency declarations in the United States in the face of the COVID-19 crisis have facilitated two important initiatives to restore health care delivery amidst formal and informal lockdowns that brought states to a grinding halt. These extend from expansion of virtual services, including telehealth, virtual check-ins, and e-visits, to the decision by the Department of Health & Human Services Office of Civil Rights to exercise enforcement discretion and waive penalties for the use of relatively inexpensive, non–public-facing mobile and other audiovisual technology tools.2
Hospital-based care in the United States taps nearly 33% of national health expenditure. An additional 30% of national health expenditure that is related to physicians, prescriptions, and other facilities is indirectly influenced by care delivered at health care facilities.3 Studies show that about 20% of ED visits could potentially be avoided via virtual urgent care offerings.4 A rapidly changing health care ecosystem is proving formidable for most hospital systems, and a test for their resilience and agility. Not just the implementation of telehealth is challenging, but getting it right is the key success factor.
Hospital-based telehealth
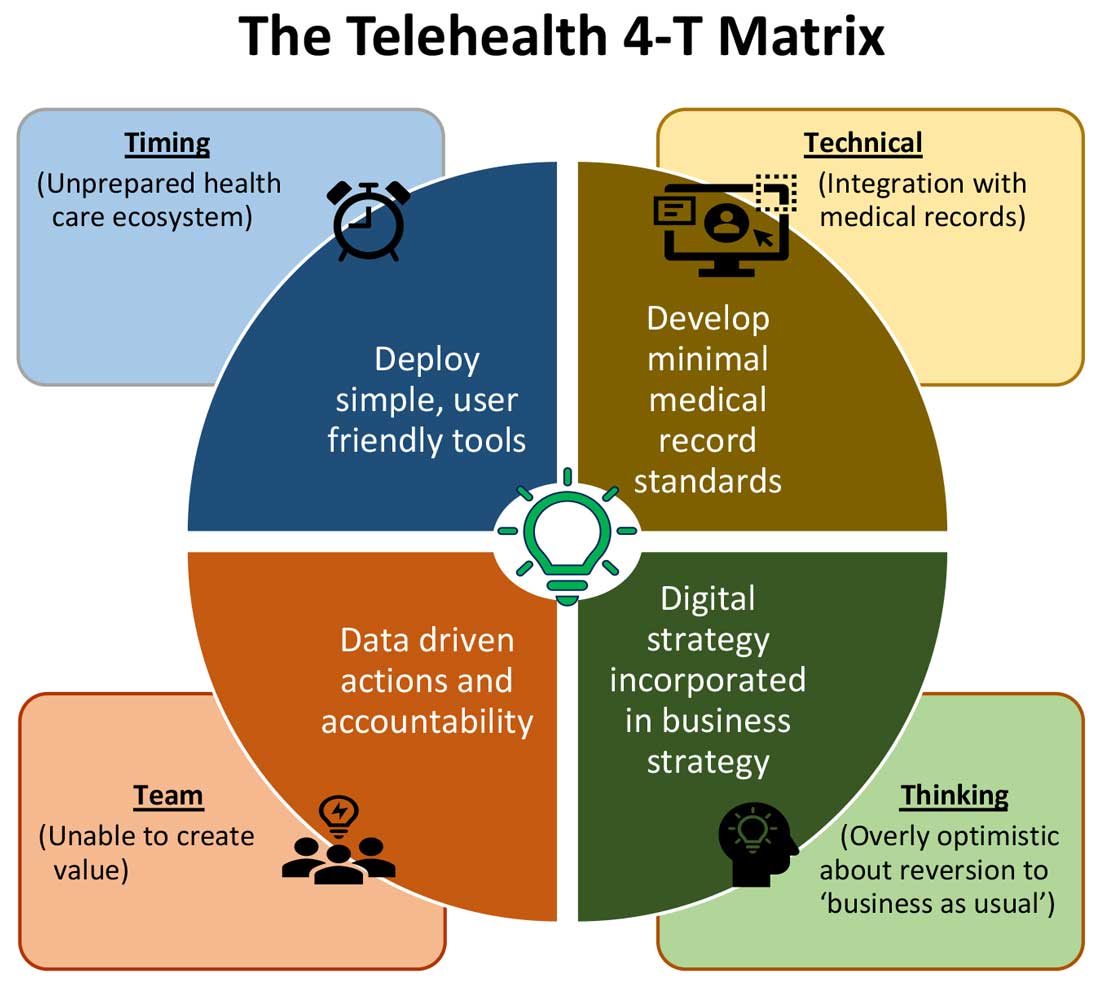
Expansion of telehealth coverage by the Centers for Medicare & Medicaid Services and most commercial payers did not quite ride the pandemic-induced momentum across the care continuum. Hospitals are lagging far behind ambulatory care in implementing telehealth. As illustrated in the “4-T Matrix” (see graphic) we would like to examine four key reasons for such a sluggish initial uptake and try to propose four important strategies that may help us to maximize the value created by telehealth technologies.
1. Timing
The health care system has always lagged far behind other service industries in terms of technology adaptation. Because of the unique nature of health care services, face-to-face interaction supersedes all other forms of communication. A rapidly evolving pandemic was not matched by simultaneous technology education for patients and providers. The enormous choice of hard-to-navigate telehealth tools; time and labor-intensive implementation; and uncertainty around payer, policy, and regulatory expectations might have precluded providers from the rapid adoption of telehealth in the hospital setting. Patients’ specific characteristics, such as the absence of technology-centered education, information, age, comorbidities, lack of technical literacy, and dependency on caregivers contributed to the suboptimal response from patients and families.
Deploying simple, ubiquitous, user-friendly, and technologically less challenging telehealth solutions may be a better approach to increase the adoption of such solutions by providers and patients. Hospitals need to develop and distribute telehealth user guides in all possible modes of communication. Provider-centric in-service sessions, workshops, and live support by “superuser teams” often work well in reducing end-user resistance.
2. Technical
Current electronic medical records vary widely in their features and offerings, and their ability to interact with third-party software and platforms. Dissatisfaction of end users with EMRs is well known, as is their likely relationship to burnout. Recent research continues to show a strong relationship between EMR usability and the odds of burnout among physicians.5 In the current climate, administrators and health informaticists have the responsibility to avoid adding increased burdens to end users.
Another issue is the limited connectivity in many remote/rural areas that would impact implementation of telehealth platforms. Studies indicate that 33% of rural Americans lack access to high-speed broadband Internet to support video visits.6 The recent successful implementation of telehealth across 530 providers in 75 ambulatory practices operated by Munson Healthcare, a rural health system in northern Michigan, sheds light on the technology’s enormous potential in providing safe access to rural populations.6,7
Privacy and safety of patient data is of paramount importance. According to a national poll on healthy aging by the University of Michigan in May 2019, targeting older adults, 47% of survey responders expressed difficulty using technology and 49% of survey responders were concerned about privacy.8 Use of certification and other tools offered by the Office of the National Coordinator for Health Information Technology would help reassure users, and the ability to capture and share images between providers would be of immense benefit in facilitating e-consults.
The need of the hour is redesigned work flow, to help providers adopt and use virtual care/telehealth efficiently. Work flow redesign must be coupled with technological advances to allow seamless integration of third-party telehealth platforms into existing EMR systems or built directly into EMRs. Use of quality metrics and analytical tools specific to telehealth would help measure the technology’s impact on patient care, outcomes, and end-user/provider experience.
3. Teams and training
Outcomes of health care interventions are often determined by the effectiveness of teams. Irrespective of how robust health care systems may have been initially, rapidly spreading infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and patients to a breaking point.5 Decentralized, uncoordinated, and siloed efforts by individual teams across the care continuum were contributing factors for the partial success of telehealth care delivery pathways. The hospital systems with telehealth-ready teams at the start of the COVID-19 pandemic were so rare that the knowledge and technical training opportunities for innovators grew severalfold during the pandemic.
As per the American Medical Association, telehealth success is massively dependent on building the right team. Core, leadership, advisory, and implementation teams comprised of clinical representatives, end users, administrative personnel, executive members of the organization, technical experts, and payment/policy experts should be put together before implementing a telehealth strategy.9 Seamless integration of hospital-based care with ambulatory care via a telehealth platform is only complete when care managers are trained and deployed to fulfill the needs of a diverse group of patients. Deriving overall value from telehealth is only possible when there is a skill development, training and mentoring team put in place.
4. Thinking
In most U.S. hospitals, inpatient health care is equally distributed between nonprocedure and procedure-based services. Hospitals resorted to suspension of nonemergent procedures to mitigate the risk of spreading COVID-19. This was further compounded by many patients’ self-selection to defer care, an abrupt reduction in the influx of patients from the referral base because of suboptimally operating ambulatory care services, leading to low hospital occupancy.
Hospitals across the nation have gone through a massive short-term financial crunch and unfavorable cash-flow forecast, which prompted a paradoxical work-force reduction. While some argue that it may be akin to strategic myopia, the authors believed that such a response is strategically imperative to keep the hospital afloat. It is reasonable to attribute the paucity of innovation to constrained resources, and health systems are simply staying overly optimistic about “weathering the storm” and reverting soon to “business as usual.” The technological framework necessary for deploying a telehealth solution often comes with a price. Financially challenged hospital systems rarely exercise any capital-intensive activities. By contrast, telehealth adoption by ambulatory care can result in quicker resumption of patient care in community settings. A lack of operational and infrastructure synchrony between ambulatory and in-hospital systems has failed to capture telehealth-driven inpatient volume. For example, direct admissions from ambulatory telehealth referrals was a missed opportunity in several places. Referrals for labs, diagnostic tests, and other allied services could have helped hospitals offset their fixed costs. Similarly, work flows related to discharge and postdischarge follow up rarely embrace telehealth tools or telehealth care pathways. A brisk change in the health care ecosystem is partly responsible for this.
Digital strategy needs to be incorporated into business strategy. For the reasons already discussed, telehealth technology is not a “nice to have” anymore, but a “must have.” At present, providers are of the opinion that about 20% of their patient services can be delivered via a telehealth platform. Similar trends are observed among patients, as a new modality of access to care is increasingly beneficial to them. Telehealth must be incorporated in standardized hospital work flows. Use of telehealth for preoperative clearance will greatly minimize same-day surgery cancellations. Given the potential shortage in resources, telehealth adoption for inpatient consultations will help systems conserve personal protective equipment, minimize the risk of staff exposure to COVID-19, and improve efficiency.
Digital strategy also prompts the reengineering of care delivery.10 Excessive and unused physical capacity can be converted into digital care hubs. Health maintenance, prevention, health promotion, health education, and chronic disease management not only can serve a variety of patient groups but can also help address the “last-mile problem” in health care. A successful digital strategy usually has three important components – Commitment: Hospital leadership is committed to include digital transformation as a strategic objective; Cost: Digital strategy is added as a line item in the budget; and Control: Measurable metrics are put in place to monitor the performance, impact, and influence of the digital strategy.
Conclusion
For decades, most U.S. health systems occupied the periphery of technological transformation when compared to the rest of the service industry. While most health systems took a heroic approach to the adoption of telehealth during COVID-19, despite being unprepared, the need for a systematic telehealth deployment is far from being adequately fulfilled. The COVID-19 pandemic brought permanent changes to several business disciplines globally. Given the impact of the pandemic on the health and overall wellbeing of American society, the U.S. health care industry must leave no stone unturned in its quest for transformation.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark, and is cofounder/president of SHM’s Arkansas chapter. Dr. Prasad is medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. He is cochair of SHM’s IT Special Interest Group, sits on the HQPS committee, and is president of SHM’s Wisconsin chapter. Dr. Palabindala is the medical director, utilization management, and physician advisory services at the University of Mississippi Medical Center and an associate professor of medicine and academic hospitalist at the University of Mississippi, both in Jackson.
References
1. Finnegan M. “Telehealth booms amid COVID-19 crisis.” Computerworld. 2020 Apr 27. www.computerworld.com/article/3540315/telehealth-booms-amid-covid-19-crisis-virtual-care-is-here-to-stay.html. Accessed 2020 Sep 12.
2. Department of Health & Human Services. “OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency.” 2020 Mar 17. www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html. Accessed 2020 Sep 12.
3. National Center for Health Statistics. “Health Expenditures.” www.cdc.gov/nchs/fastats/health-expenditures.htm. Accessed 2020 Sep 12.
4. Bestsennyy O et al. “Telehealth: A post–COVID-19 reality?” McKinsey & Company. 2020 May 29. www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality. Accessed 2020 Sep 12.
5. Melnick ER et al. The Association Between Perceived Electronic Health Record Usability and Professional Burnout Among U.S. Physicians. Mayo Clin Proc. 2020 March;95(3):476-87.
6. Hirko KA et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Inform Assoc. 2020 Nov;27(11):1816-8. .
7. American Academy of Family Physicians. “Study Examines Telehealth, Rural Disparities in Pandemic.” 2020 July 30. www.aafp.org/news/practice-professional-issues/20200730ruraltelehealth.html. Accessed 2020 Dec 15.
8. Kurlander J et al. “Virtual Visits: Telehealth and Older Adults.” National Poll on Healthy Aging. 2019 Oct. hdl.handle.net/2027.42/151376.
9. American Medical Association. Telehealth Implementation Playbook. 2019. www.ama-assn.org/system/files/2020-04/ama-telehealth-implementation-playbook.pdf.
10. Smith AC et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020 Jun;26(5):309-13.
‘Major update’ of BP guidance for kidney disease; treat to 120 mm Hg
The new 2021 Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guideline for blood pressure management for adults with chronic kidney disease (CKD) who are not receiving dialysis advises treating to a target systolic blood pressure of less than 120 mm Hg, provided measurements are “standardized” and that blood pressure is “measured properly.”
This blood pressure target – largely based on evidence from the Systolic Blood Pressure Intervention Trial (SPRINT) – represents “a major update” from the 2012 KDIGO guideline, which advised clinicians to treat to a target blood pressure of less than or equal to 130/80 mm Hg for patients with albuminuria or less than or equal to 140/90 mm Hg for patients without albuminuria.
The new goal is also lower than the less than 130/80 mm Hg target in the 2017 American College of Cardiology/American Heart Association guideline.
In a study of the public health implications of the guideline, Kathryn Foti, PhD, and colleagues determined that 70% of U.S. adults with CKD would now be eligible for treatment to lower blood pressure, as opposed to 50% under the previous KDIGO guideline and 56% under the ACC/AHA guideline.
“This is a major update of an influential set of guidelines for chronic kidney disease patients” at a time when blood pressure control is worsening in the United States, Dr. Foti, a postdoctoral researcher in the department of epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, said in a statement from her institution.
The 2021 KDIGO blood pressure guideline and executive summary and the public health implications study are published online in Kidney International.
First, ‘take blood pressure well’
The cochair of the new KDIGO guidelines, Alfred K. Cheung, MD, from the University of Utah, Salt Lake City, said in an interview that the guideline has “two important points.”
First, “take that blood pressure well,” he said. “That has a lot to do with patient preparation rather than any fancy instrument,” he emphasized.
Second, the guideline proposes a systolic blood pressure target of less than 120 mm Hg for most people with CKD not receiving dialysis, except for children and kidney transplant recipients. This target is “contingent on ‘standardized’ blood pressure measurement.”
The document provides a checklist for obtaining a standardized blood pressure measurement, adapted from the 2017 ACC/AHA blood pressure guidelines. It starts with the patient relaxed and sitting on a chair for more than 5 minutes.
In contrast to this measurement, a “routine” or “casual” office blood pressure measurement could be off by plus or minus 10 mm Hg, Dr. Cheung noted.
In a typical scenario, he continued, a patient cannot find a place to park, rushes into the clinic, and has his or her blood pressure checked right away, which would provide a “totally unreliable” reading. Adding a “fudge factor” (correction factor) would not provide an accurate reading.
Clinicians “would not settle for a potassium measurement that is 5.0 mmol/L plus or minus a few decimal points” to guide treatment, he pointed out.
Second, target 120, properly measured
“The very first chapter of the guidelines is devoted to blood pressure measurement, because we recognize if we’re going to do 120 [mm Hg] – the emphasis is on 120 measured properly – so we try to drive that point home,” Tara I. Chang, MD, guideline second author and a coauthor of the public health implications study, pointed out in an interview.
“There are a lot of other things that we base clinical decisions on where we really require some degree of precision, and blood pressure is important enough that to us it’s kind of in the same boat,” said Dr. Chang, from Stanford (Calif.) University.
“In SPRINT, people were randomized to less than less than 120 vs. less than 140 (they weren’t randomized to <130),” she noted.
“The recommendation should be widely adopted in clinical practice,” the guideline authors write, “since accurate measurements will ensure that proper guidance is being applied to the management of BP, as it is to the management of other risk factors.”
Still need individual treatment
Nevertheless, patients still need individualized treatment, the document stresses. “Not every patient with CKD will be appropriate to target to less than 120,” Dr. Chang said. However, “we want people to at least consider less than 120,” she added, to avoid therapeutic inertia.
“If you take the blood pressure in a standardized manner – such as in the ACCORD trial and in the SPRINT trial – even patients over 75 years old, or people over 80 years old, they have very little side effects,” Dr. Cheung noted.
“In the overall cohort,” he continued, “they do not have a significant increase in serious adverse events, do not have adverse events of postural hypotension, syncope, bradycardia, injurious falls – so people are worried about it, but it’s not borne out by the data.
“That said, I have two cautions,” Dr. Cheung noted. “One. If you drop somebody’s blood pressure rapidly over a week, you may be more likely to get in trouble. If you drop the blood pressure gradually over several weeks, several months, you’re much less likely to get into trouble.”
“Two. If the patient is old, you know the patient has carotid stenosis and already has postural dizziness, you may not want to try on that patient – but just because the patient is old is not the reason not to target 120.”
ACE inhibitors and ARBs beneficial in albuminuria, underused
“How do you get to less than 120? The short answer is, use whatever medications you need to – there is no necessarily right cocktail,” Dr. Chang said.
“We’ve known that angiotensin-converting enzyme (ACE) inhibitors and ARBs [angiotensin II receptor blockers] are beneficial in patients with CKD and in particular those with heavier albuminuria,” she continued. “We’ve known this for over 20 years.”
Yet, the study identified underutilization – “a persistent gap, just like blood pressure control and awareness,” she noted. “We’re just not making much headway.
“We are not recommending ACE inhibitors or ARBs for all the patients,” Dr. Cheung clarified. “If you are diabetic and have heavy proteinuria, that’s when the use of ACE inhibitors and ARBs are most indicated.”
Public health implications
SPRINT showed that treating to a systolic blood pressure of less than 120 mm Hg vs. less than 140 mm Hg reduced the risk for cardiovascular disease by 25% and all-cause mortality by 27% for participants with and those without CKD, Dr. Foti and colleagues stress.
They aimed to estimate how the new guideline would affect (1) the number of U.S. patients with CKD who would be eligible for blood pressure lowering treatment, and (2) the proportion of those with albuminuria who would be eligible for an ACE inhibitor or an ARB.
The researchers analyzed data from 1,699 adults with CKD (estimated glomerular filtration rate, 15-59 mL/min/1.73 m2 or a urinary albumin-to-creatinine ratio of ≥30 mg/g) who participated in the 2015-2018 National Health and Nutrition Examination Survey.
Both the 2021 and 2012 KDIGO guidelines recommend that patients with albuminuria and blood pressure higher than the target value who are not kidney transplant recipients should be treated with an ACE inhibitor or an ARB.
On the basis of the new target, 78% of patients with CKD and albuminuria were eligible for ACE inhibitor/ARB treatment by the 2021 KDIGO guideline, compared with 71% by the 2012 KDIGO guideline. However, only 39% were taking one of these drugs.
These findings show that “with the new guideline and with the lower blood pressure target, you potentially have an even larger pool of people who have blood pressure that’s not under control, and a potential larger group of people who may benefit from ACE inhibitors and ARBs,” Dr. Chang said.
“Our paper is not the only one to show that we haven’t made a whole lot of progress,” she said, “and now that the bar has been lowered, there [have] to be some renewed efforts on controlling blood pressure, because we know that blood pressure control is such an important risk factor for cardiovascular outcomes.”
Dr. Foti is supported by an NIH/National Heart, Lung, and Blood Institute grant. Dr. Cheung has received consultancy fees from Amgen, Bard, Boehringer Ingelheim, Calliditas, Tricida, and UpToDate, and grant/research support from the National Institutes of Health for SPRINT (monies paid to institution). Dr. Chang has received consultancy fees from Bayer, Gilead, Janssen Research and Development, Novo Nordisk, Tricida, and Vascular Dynamics; grant/research support from AstraZeneca and Satellite Healthcare (monies paid to institution), the NIH, and the American Heart Association; is on advisory boards for AstraZeneca and Fresenius Medical Care Renal Therapies Group; and has received workshop honoraria from Fresenius. Disclosures of relevant financial relationships of the other authors are listed in the original articles.
A version of this article first appeared on Medscape.com.
The new 2021 Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guideline for blood pressure management for adults with chronic kidney disease (CKD) who are not receiving dialysis advises treating to a target systolic blood pressure of less than 120 mm Hg, provided measurements are “standardized” and that blood pressure is “measured properly.”
This blood pressure target – largely based on evidence from the Systolic Blood Pressure Intervention Trial (SPRINT) – represents “a major update” from the 2012 KDIGO guideline, which advised clinicians to treat to a target blood pressure of less than or equal to 130/80 mm Hg for patients with albuminuria or less than or equal to 140/90 mm Hg for patients without albuminuria.
The new goal is also lower than the less than 130/80 mm Hg target in the 2017 American College of Cardiology/American Heart Association guideline.
In a study of the public health implications of the guideline, Kathryn Foti, PhD, and colleagues determined that 70% of U.S. adults with CKD would now be eligible for treatment to lower blood pressure, as opposed to 50% under the previous KDIGO guideline and 56% under the ACC/AHA guideline.
“This is a major update of an influential set of guidelines for chronic kidney disease patients” at a time when blood pressure control is worsening in the United States, Dr. Foti, a postdoctoral researcher in the department of epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, said in a statement from her institution.
The 2021 KDIGO blood pressure guideline and executive summary and the public health implications study are published online in Kidney International.
First, ‘take blood pressure well’
The cochair of the new KDIGO guidelines, Alfred K. Cheung, MD, from the University of Utah, Salt Lake City, said in an interview that the guideline has “two important points.”
First, “take that blood pressure well,” he said. “That has a lot to do with patient preparation rather than any fancy instrument,” he emphasized.
Second, the guideline proposes a systolic blood pressure target of less than 120 mm Hg for most people with CKD not receiving dialysis, except for children and kidney transplant recipients. This target is “contingent on ‘standardized’ blood pressure measurement.”
The document provides a checklist for obtaining a standardized blood pressure measurement, adapted from the 2017 ACC/AHA blood pressure guidelines. It starts with the patient relaxed and sitting on a chair for more than 5 minutes.
In contrast to this measurement, a “routine” or “casual” office blood pressure measurement could be off by plus or minus 10 mm Hg, Dr. Cheung noted.
In a typical scenario, he continued, a patient cannot find a place to park, rushes into the clinic, and has his or her blood pressure checked right away, which would provide a “totally unreliable” reading. Adding a “fudge factor” (correction factor) would not provide an accurate reading.
Clinicians “would not settle for a potassium measurement that is 5.0 mmol/L plus or minus a few decimal points” to guide treatment, he pointed out.
Second, target 120, properly measured
“The very first chapter of the guidelines is devoted to blood pressure measurement, because we recognize if we’re going to do 120 [mm Hg] – the emphasis is on 120 measured properly – so we try to drive that point home,” Tara I. Chang, MD, guideline second author and a coauthor of the public health implications study, pointed out in an interview.
“There are a lot of other things that we base clinical decisions on where we really require some degree of precision, and blood pressure is important enough that to us it’s kind of in the same boat,” said Dr. Chang, from Stanford (Calif.) University.
“In SPRINT, people were randomized to less than less than 120 vs. less than 140 (they weren’t randomized to <130),” she noted.
“The recommendation should be widely adopted in clinical practice,” the guideline authors write, “since accurate measurements will ensure that proper guidance is being applied to the management of BP, as it is to the management of other risk factors.”
Still need individual treatment
Nevertheless, patients still need individualized treatment, the document stresses. “Not every patient with CKD will be appropriate to target to less than 120,” Dr. Chang said. However, “we want people to at least consider less than 120,” she added, to avoid therapeutic inertia.
“If you take the blood pressure in a standardized manner – such as in the ACCORD trial and in the SPRINT trial – even patients over 75 years old, or people over 80 years old, they have very little side effects,” Dr. Cheung noted.
“In the overall cohort,” he continued, “they do not have a significant increase in serious adverse events, do not have adverse events of postural hypotension, syncope, bradycardia, injurious falls – so people are worried about it, but it’s not borne out by the data.
“That said, I have two cautions,” Dr. Cheung noted. “One. If you drop somebody’s blood pressure rapidly over a week, you may be more likely to get in trouble. If you drop the blood pressure gradually over several weeks, several months, you’re much less likely to get into trouble.”
“Two. If the patient is old, you know the patient has carotid stenosis and already has postural dizziness, you may not want to try on that patient – but just because the patient is old is not the reason not to target 120.”
ACE inhibitors and ARBs beneficial in albuminuria, underused
“How do you get to less than 120? The short answer is, use whatever medications you need to – there is no necessarily right cocktail,” Dr. Chang said.
“We’ve known that angiotensin-converting enzyme (ACE) inhibitors and ARBs [angiotensin II receptor blockers] are beneficial in patients with CKD and in particular those with heavier albuminuria,” she continued. “We’ve known this for over 20 years.”
Yet, the study identified underutilization – “a persistent gap, just like blood pressure control and awareness,” she noted. “We’re just not making much headway.
“We are not recommending ACE inhibitors or ARBs for all the patients,” Dr. Cheung clarified. “If you are diabetic and have heavy proteinuria, that’s when the use of ACE inhibitors and ARBs are most indicated.”
Public health implications
SPRINT showed that treating to a systolic blood pressure of less than 120 mm Hg vs. less than 140 mm Hg reduced the risk for cardiovascular disease by 25% and all-cause mortality by 27% for participants with and those without CKD, Dr. Foti and colleagues stress.
They aimed to estimate how the new guideline would affect (1) the number of U.S. patients with CKD who would be eligible for blood pressure lowering treatment, and (2) the proportion of those with albuminuria who would be eligible for an ACE inhibitor or an ARB.
The researchers analyzed data from 1,699 adults with CKD (estimated glomerular filtration rate, 15-59 mL/min/1.73 m2 or a urinary albumin-to-creatinine ratio of ≥30 mg/g) who participated in the 2015-2018 National Health and Nutrition Examination Survey.
Both the 2021 and 2012 KDIGO guidelines recommend that patients with albuminuria and blood pressure higher than the target value who are not kidney transplant recipients should be treated with an ACE inhibitor or an ARB.
On the basis of the new target, 78% of patients with CKD and albuminuria were eligible for ACE inhibitor/ARB treatment by the 2021 KDIGO guideline, compared with 71% by the 2012 KDIGO guideline. However, only 39% were taking one of these drugs.
These findings show that “with the new guideline and with the lower blood pressure target, you potentially have an even larger pool of people who have blood pressure that’s not under control, and a potential larger group of people who may benefit from ACE inhibitors and ARBs,” Dr. Chang said.
“Our paper is not the only one to show that we haven’t made a whole lot of progress,” she said, “and now that the bar has been lowered, there [have] to be some renewed efforts on controlling blood pressure, because we know that blood pressure control is such an important risk factor for cardiovascular outcomes.”
Dr. Foti is supported by an NIH/National Heart, Lung, and Blood Institute grant. Dr. Cheung has received consultancy fees from Amgen, Bard, Boehringer Ingelheim, Calliditas, Tricida, and UpToDate, and grant/research support from the National Institutes of Health for SPRINT (monies paid to institution). Dr. Chang has received consultancy fees from Bayer, Gilead, Janssen Research and Development, Novo Nordisk, Tricida, and Vascular Dynamics; grant/research support from AstraZeneca and Satellite Healthcare (monies paid to institution), the NIH, and the American Heart Association; is on advisory boards for AstraZeneca and Fresenius Medical Care Renal Therapies Group; and has received workshop honoraria from Fresenius. Disclosures of relevant financial relationships of the other authors are listed in the original articles.
A version of this article first appeared on Medscape.com.
The new 2021 Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guideline for blood pressure management for adults with chronic kidney disease (CKD) who are not receiving dialysis advises treating to a target systolic blood pressure of less than 120 mm Hg, provided measurements are “standardized” and that blood pressure is “measured properly.”
This blood pressure target – largely based on evidence from the Systolic Blood Pressure Intervention Trial (SPRINT) – represents “a major update” from the 2012 KDIGO guideline, which advised clinicians to treat to a target blood pressure of less than or equal to 130/80 mm Hg for patients with albuminuria or less than or equal to 140/90 mm Hg for patients without albuminuria.
The new goal is also lower than the less than 130/80 mm Hg target in the 2017 American College of Cardiology/American Heart Association guideline.
In a study of the public health implications of the guideline, Kathryn Foti, PhD, and colleagues determined that 70% of U.S. adults with CKD would now be eligible for treatment to lower blood pressure, as opposed to 50% under the previous KDIGO guideline and 56% under the ACC/AHA guideline.
“This is a major update of an influential set of guidelines for chronic kidney disease patients” at a time when blood pressure control is worsening in the United States, Dr. Foti, a postdoctoral researcher in the department of epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, said in a statement from her institution.
The 2021 KDIGO blood pressure guideline and executive summary and the public health implications study are published online in Kidney International.
First, ‘take blood pressure well’
The cochair of the new KDIGO guidelines, Alfred K. Cheung, MD, from the University of Utah, Salt Lake City, said in an interview that the guideline has “two important points.”
First, “take that blood pressure well,” he said. “That has a lot to do with patient preparation rather than any fancy instrument,” he emphasized.
Second, the guideline proposes a systolic blood pressure target of less than 120 mm Hg for most people with CKD not receiving dialysis, except for children and kidney transplant recipients. This target is “contingent on ‘standardized’ blood pressure measurement.”
The document provides a checklist for obtaining a standardized blood pressure measurement, adapted from the 2017 ACC/AHA blood pressure guidelines. It starts with the patient relaxed and sitting on a chair for more than 5 minutes.
In contrast to this measurement, a “routine” or “casual” office blood pressure measurement could be off by plus or minus 10 mm Hg, Dr. Cheung noted.
In a typical scenario, he continued, a patient cannot find a place to park, rushes into the clinic, and has his or her blood pressure checked right away, which would provide a “totally unreliable” reading. Adding a “fudge factor” (correction factor) would not provide an accurate reading.
Clinicians “would not settle for a potassium measurement that is 5.0 mmol/L plus or minus a few decimal points” to guide treatment, he pointed out.
Second, target 120, properly measured
“The very first chapter of the guidelines is devoted to blood pressure measurement, because we recognize if we’re going to do 120 [mm Hg] – the emphasis is on 120 measured properly – so we try to drive that point home,” Tara I. Chang, MD, guideline second author and a coauthor of the public health implications study, pointed out in an interview.
“There are a lot of other things that we base clinical decisions on where we really require some degree of precision, and blood pressure is important enough that to us it’s kind of in the same boat,” said Dr. Chang, from Stanford (Calif.) University.
“In SPRINT, people were randomized to less than less than 120 vs. less than 140 (they weren’t randomized to <130),” she noted.
“The recommendation should be widely adopted in clinical practice,” the guideline authors write, “since accurate measurements will ensure that proper guidance is being applied to the management of BP, as it is to the management of other risk factors.”
Still need individual treatment
Nevertheless, patients still need individualized treatment, the document stresses. “Not every patient with CKD will be appropriate to target to less than 120,” Dr. Chang said. However, “we want people to at least consider less than 120,” she added, to avoid therapeutic inertia.
“If you take the blood pressure in a standardized manner – such as in the ACCORD trial and in the SPRINT trial – even patients over 75 years old, or people over 80 years old, they have very little side effects,” Dr. Cheung noted.
“In the overall cohort,” he continued, “they do not have a significant increase in serious adverse events, do not have adverse events of postural hypotension, syncope, bradycardia, injurious falls – so people are worried about it, but it’s not borne out by the data.
“That said, I have two cautions,” Dr. Cheung noted. “One. If you drop somebody’s blood pressure rapidly over a week, you may be more likely to get in trouble. If you drop the blood pressure gradually over several weeks, several months, you’re much less likely to get into trouble.”
“Two. If the patient is old, you know the patient has carotid stenosis and already has postural dizziness, you may not want to try on that patient – but just because the patient is old is not the reason not to target 120.”
ACE inhibitors and ARBs beneficial in albuminuria, underused
“How do you get to less than 120? The short answer is, use whatever medications you need to – there is no necessarily right cocktail,” Dr. Chang said.
“We’ve known that angiotensin-converting enzyme (ACE) inhibitors and ARBs [angiotensin II receptor blockers] are beneficial in patients with CKD and in particular those with heavier albuminuria,” she continued. “We’ve known this for over 20 years.”
Yet, the study identified underutilization – “a persistent gap, just like blood pressure control and awareness,” she noted. “We’re just not making much headway.
“We are not recommending ACE inhibitors or ARBs for all the patients,” Dr. Cheung clarified. “If you are diabetic and have heavy proteinuria, that’s when the use of ACE inhibitors and ARBs are most indicated.”
Public health implications
SPRINT showed that treating to a systolic blood pressure of less than 120 mm Hg vs. less than 140 mm Hg reduced the risk for cardiovascular disease by 25% and all-cause mortality by 27% for participants with and those without CKD, Dr. Foti and colleagues stress.
They aimed to estimate how the new guideline would affect (1) the number of U.S. patients with CKD who would be eligible for blood pressure lowering treatment, and (2) the proportion of those with albuminuria who would be eligible for an ACE inhibitor or an ARB.
The researchers analyzed data from 1,699 adults with CKD (estimated glomerular filtration rate, 15-59 mL/min/1.73 m2 or a urinary albumin-to-creatinine ratio of ≥30 mg/g) who participated in the 2015-2018 National Health and Nutrition Examination Survey.
Both the 2021 and 2012 KDIGO guidelines recommend that patients with albuminuria and blood pressure higher than the target value who are not kidney transplant recipients should be treated with an ACE inhibitor or an ARB.
On the basis of the new target, 78% of patients with CKD and albuminuria were eligible for ACE inhibitor/ARB treatment by the 2021 KDIGO guideline, compared with 71% by the 2012 KDIGO guideline. However, only 39% were taking one of these drugs.
These findings show that “with the new guideline and with the lower blood pressure target, you potentially have an even larger pool of people who have blood pressure that’s not under control, and a potential larger group of people who may benefit from ACE inhibitors and ARBs,” Dr. Chang said.
“Our paper is not the only one to show that we haven’t made a whole lot of progress,” she said, “and now that the bar has been lowered, there [have] to be some renewed efforts on controlling blood pressure, because we know that blood pressure control is such an important risk factor for cardiovascular outcomes.”
Dr. Foti is supported by an NIH/National Heart, Lung, and Blood Institute grant. Dr. Cheung has received consultancy fees from Amgen, Bard, Boehringer Ingelheim, Calliditas, Tricida, and UpToDate, and grant/research support from the National Institutes of Health for SPRINT (monies paid to institution). Dr. Chang has received consultancy fees from Bayer, Gilead, Janssen Research and Development, Novo Nordisk, Tricida, and Vascular Dynamics; grant/research support from AstraZeneca and Satellite Healthcare (monies paid to institution), the NIH, and the American Heart Association; is on advisory boards for AstraZeneca and Fresenius Medical Care Renal Therapies Group; and has received workshop honoraria from Fresenius. Disclosures of relevant financial relationships of the other authors are listed in the original articles.
A version of this article first appeared on Medscape.com.
Hospitalist movers and shakers – March 2021
Vivek H. Murthy, MD, was named by President Joe Biden as his selection for Surgeon General of the United States. Dr. Murthy filled the same role from 2014-17 during President Barack Obama’s administration.
Dr. Murthy was a hospitalist and an instructor at Brigham and Women’s Hospital at Harvard Medical School prior to becoming surgeon general the first time. He also is the founder of Doctors for America.
David Tupponce, MD, recently was named the new president of Allegheny Health Network’s Grove City (Pa.) Medical Center. He takes over for interim president Allan Klapper, MD, who filled the position since August 2020.
Dr. Tupponce comes to Grove City Medical Center after a successful tenure as president of Central Maine Medical Center (Lewiston, Maine), where he grew its physician group and fine-tuned the hospital quality program. Prior to that, he was chief executive officer at Tenet Healthcare’s Abrazo Scottsdale (Ariz.) Campus and CEO at Paradise Valley Hospital (Phoenix, Ariz.).
Dr. Tupponce is familiar with western Pennsylvania, having earned a master’s degree in medical management from Carnegie Mellon University in Pittsburgh. He also was chief resident at the University of Pittsburgh Medical Center.
Malcolm Mar Fan, MD, has been elevated to medical director of the Hospitalist Group at Evangelical Community Hospital (Lewisburg, Pa.). In the newly established position, Dr. Mar Fan will oversee all operations for the facility’s hospitalist program.
Dr. Mar Fan has been a hospitalist at Evangelical since 2014 after completing his internist residency at Albert Einstein Medical Center in Philadelphia. He has played a major role on Evangelical’s Peri-operative Glucose Management Committee and its Informatics Committee for Impatient and Outpatient Electronic Health Records.
Lyon County (Kansas) recently announced that Ladun Oyenuga, MD, has been appointed as public health officer for the county. She began her tenure on January 1.
Dr. Oyenuga is a hospitalist at Newman Regional Health (Emporia, Kan.). She is a native of Nigeria and did her residency at Harlem (N.Y.) Hospital Center. She has been with Newman since 2017.
Cherese Mari Laulhere BirthCare Center (Long Beach, Calif.) recently announced the addition of an OB hospitalist program at Miller Children’s & Women’s Hospital. OB hospitalists, or laborists, care for women with obstetrical issues while in the hospital.
At Cherese Mari Laulhere, OB hospitalists will be on hand 24 hours a day to assist patients’ OB/GYNs or to fill in if the personal physician cannot get to the hospital quickly.
Hospitalists at Nationwide Children’s (Columbus, Ohio) are now providing care for children who are hospitalized at Adena Regional Medical Center (Chillicothe, Ohio).
It is an expansion of an ongoing partnership between the two hospitals. Adena and Nationwide Children’s have been working together in helping to care for children in the south central and southern Ohio region since 2011. Nationwide Children’s hospitalists will round in special care and the well-baby nursery at Adena, as well as provide education programs for Adena providers and staff.
MultiCare Health System (Tacoma, Wash.) has announced that it will expand its hospitalist program partnership with Sound Physicians, also based in Tacoma, to create a region-wide, cohesive group of providers. The goal is to help ensure efficient management of inpatient populations as a region instead of at the individual hospital level, and will allow MultiCare to implement standard tools, processes and regionwide best practices.
The hospitalist programs at Tacoma General Hospital, Allenmore Hospital and Covington Medical Center will transition to Sound Physicians on April 5, 2021. Sound hospitalists are already working at three other MultiCare facilities – Tacoma General Hospital, Allenmore Hospital, and Covington Medical Center.
Vivek H. Murthy, MD, was named by President Joe Biden as his selection for Surgeon General of the United States. Dr. Murthy filled the same role from 2014-17 during President Barack Obama’s administration.
Dr. Murthy was a hospitalist and an instructor at Brigham and Women’s Hospital at Harvard Medical School prior to becoming surgeon general the first time. He also is the founder of Doctors for America.
David Tupponce, MD, recently was named the new president of Allegheny Health Network’s Grove City (Pa.) Medical Center. He takes over for interim president Allan Klapper, MD, who filled the position since August 2020.
Dr. Tupponce comes to Grove City Medical Center after a successful tenure as president of Central Maine Medical Center (Lewiston, Maine), where he grew its physician group and fine-tuned the hospital quality program. Prior to that, he was chief executive officer at Tenet Healthcare’s Abrazo Scottsdale (Ariz.) Campus and CEO at Paradise Valley Hospital (Phoenix, Ariz.).
Dr. Tupponce is familiar with western Pennsylvania, having earned a master’s degree in medical management from Carnegie Mellon University in Pittsburgh. He also was chief resident at the University of Pittsburgh Medical Center.
Malcolm Mar Fan, MD, has been elevated to medical director of the Hospitalist Group at Evangelical Community Hospital (Lewisburg, Pa.). In the newly established position, Dr. Mar Fan will oversee all operations for the facility’s hospitalist program.
Dr. Mar Fan has been a hospitalist at Evangelical since 2014 after completing his internist residency at Albert Einstein Medical Center in Philadelphia. He has played a major role on Evangelical’s Peri-operative Glucose Management Committee and its Informatics Committee for Impatient and Outpatient Electronic Health Records.
Lyon County (Kansas) recently announced that Ladun Oyenuga, MD, has been appointed as public health officer for the county. She began her tenure on January 1.
Dr. Oyenuga is a hospitalist at Newman Regional Health (Emporia, Kan.). She is a native of Nigeria and did her residency at Harlem (N.Y.) Hospital Center. She has been with Newman since 2017.
Cherese Mari Laulhere BirthCare Center (Long Beach, Calif.) recently announced the addition of an OB hospitalist program at Miller Children’s & Women’s Hospital. OB hospitalists, or laborists, care for women with obstetrical issues while in the hospital.
At Cherese Mari Laulhere, OB hospitalists will be on hand 24 hours a day to assist patients’ OB/GYNs or to fill in if the personal physician cannot get to the hospital quickly.
Hospitalists at Nationwide Children’s (Columbus, Ohio) are now providing care for children who are hospitalized at Adena Regional Medical Center (Chillicothe, Ohio).
It is an expansion of an ongoing partnership between the two hospitals. Adena and Nationwide Children’s have been working together in helping to care for children in the south central and southern Ohio region since 2011. Nationwide Children’s hospitalists will round in special care and the well-baby nursery at Adena, as well as provide education programs for Adena providers and staff.
MultiCare Health System (Tacoma, Wash.) has announced that it will expand its hospitalist program partnership with Sound Physicians, also based in Tacoma, to create a region-wide, cohesive group of providers. The goal is to help ensure efficient management of inpatient populations as a region instead of at the individual hospital level, and will allow MultiCare to implement standard tools, processes and regionwide best practices.
The hospitalist programs at Tacoma General Hospital, Allenmore Hospital and Covington Medical Center will transition to Sound Physicians on April 5, 2021. Sound hospitalists are already working at three other MultiCare facilities – Tacoma General Hospital, Allenmore Hospital, and Covington Medical Center.
Vivek H. Murthy, MD, was named by President Joe Biden as his selection for Surgeon General of the United States. Dr. Murthy filled the same role from 2014-17 during President Barack Obama’s administration.
Dr. Murthy was a hospitalist and an instructor at Brigham and Women’s Hospital at Harvard Medical School prior to becoming surgeon general the first time. He also is the founder of Doctors for America.
David Tupponce, MD, recently was named the new president of Allegheny Health Network’s Grove City (Pa.) Medical Center. He takes over for interim president Allan Klapper, MD, who filled the position since August 2020.
Dr. Tupponce comes to Grove City Medical Center after a successful tenure as president of Central Maine Medical Center (Lewiston, Maine), where he grew its physician group and fine-tuned the hospital quality program. Prior to that, he was chief executive officer at Tenet Healthcare’s Abrazo Scottsdale (Ariz.) Campus and CEO at Paradise Valley Hospital (Phoenix, Ariz.).
Dr. Tupponce is familiar with western Pennsylvania, having earned a master’s degree in medical management from Carnegie Mellon University in Pittsburgh. He also was chief resident at the University of Pittsburgh Medical Center.
Malcolm Mar Fan, MD, has been elevated to medical director of the Hospitalist Group at Evangelical Community Hospital (Lewisburg, Pa.). In the newly established position, Dr. Mar Fan will oversee all operations for the facility’s hospitalist program.
Dr. Mar Fan has been a hospitalist at Evangelical since 2014 after completing his internist residency at Albert Einstein Medical Center in Philadelphia. He has played a major role on Evangelical’s Peri-operative Glucose Management Committee and its Informatics Committee for Impatient and Outpatient Electronic Health Records.
Lyon County (Kansas) recently announced that Ladun Oyenuga, MD, has been appointed as public health officer for the county. She began her tenure on January 1.
Dr. Oyenuga is a hospitalist at Newman Regional Health (Emporia, Kan.). She is a native of Nigeria and did her residency at Harlem (N.Y.) Hospital Center. She has been with Newman since 2017.
Cherese Mari Laulhere BirthCare Center (Long Beach, Calif.) recently announced the addition of an OB hospitalist program at Miller Children’s & Women’s Hospital. OB hospitalists, or laborists, care for women with obstetrical issues while in the hospital.
At Cherese Mari Laulhere, OB hospitalists will be on hand 24 hours a day to assist patients’ OB/GYNs or to fill in if the personal physician cannot get to the hospital quickly.
Hospitalists at Nationwide Children’s (Columbus, Ohio) are now providing care for children who are hospitalized at Adena Regional Medical Center (Chillicothe, Ohio).
It is an expansion of an ongoing partnership between the two hospitals. Adena and Nationwide Children’s have been working together in helping to care for children in the south central and southern Ohio region since 2011. Nationwide Children’s hospitalists will round in special care and the well-baby nursery at Adena, as well as provide education programs for Adena providers and staff.
MultiCare Health System (Tacoma, Wash.) has announced that it will expand its hospitalist program partnership with Sound Physicians, also based in Tacoma, to create a region-wide, cohesive group of providers. The goal is to help ensure efficient management of inpatient populations as a region instead of at the individual hospital level, and will allow MultiCare to implement standard tools, processes and regionwide best practices.
The hospitalist programs at Tacoma General Hospital, Allenmore Hospital and Covington Medical Center will transition to Sound Physicians on April 5, 2021. Sound hospitalists are already working at three other MultiCare facilities – Tacoma General Hospital, Allenmore Hospital, and Covington Medical Center.
Liver stiffness predicts hepatic events in NAFLD
Among patients with nonalcoholic fatty liver disease (NAFLD) and compensated advanced chronic liver disease, liver stiffness measurements (LSMs) are associated with risks of hepatic events, according to a retrospective analysis of more than 1,000 patients.
“[N]oninvasive markers that can predict liver disease severity and outcomes in patients with NAFLD and advanced fibrosis are a major unmet need,” wrote lead author Salvatore Petta, MD, of the University of Palermo, Italy, and colleagues. Their report is in Clinical Gastroenterology and Hepatology. “Data about the accuracy of LSM in the prediction of events in NAFLD, and especially in patients with NAFLD and F3-F4 fibrosis, are scarce.”
To address this knowledge gap, the investigators retrospectively analyzed data from 1,039 consecutive patients with NAFLD who had baseline LSMs of more than 10 kPa and/or histologically diagnosed F3-F4 fibrosis. Patients were prospectively recruited at 10 centers in 6 countries, then followed for a median of 35 months, ranging from 19 to 63 months.
All patients had their liver stiffness measured with an M or XL probe at baseline. In addition, approximately half of the patients (n = 533) had a follow-up measurement using the same method, generating a subgroup with changes in liver stiffness. “Improved” liver stiffness was defined as a decrease in LSM greater than 20% from baseline, “impaired” liver stiffness was defined as an increase in LSM greater than 20% from baseline, and “stable” liver stiffness was defined as a change falling between 20% lower and 20% higher than baseline.
At baseline, mean LSM was 17.6 kPa. Cox regression analysis revealed that baseline LSM was independently associated with HCC (hazard ratio, 1.03; 95% confidence interval, 1.00-1.04; P = .003), liver decompensation (HR, 1.03; 95% CI, 1.02-1.04; P < .001), and liver-related death (HR, 1.02; 95% CI, 1.00-1.03; P = .005), but not extrahepatic events.
According to the investigators, the association between LSM at baseline and risk of liver decompensation was maintained after adjustment for the severity of liver disease and for surrogate markers of portal hypertension, they noted. Furthermore, patients with a baseline LSM of at least 21 kPa – which indicates high risk of clinically significant portal hypertension (CSPH) – were at greater risk of liver decompensation than were those with an LSM less than 21 kPa (HR, 3.71; 95% CI, 1.89-6.78; P = .04).
In the subgroup with follow-up measurements, approximately half of the patients had an improved LSM (53.3%), while 27.2% had a stable LSM, and 19.5% had an impaired LSM, a pattern that was significantly associated with diabetes at baseline (P = .01).
“These data agree with the available literature identifying diabetes as a risk factor for liver disease progression and liver-related complications,” the investigators wrote.
Cox regression showed that, among those with follow-up LSM, changes in LSM were independently associated with HCC (HR, 1.72; 95% CI, 1.01-3.02; P = .04), liver decompensation (HR, 1.56; 95% CI, 1.05-2.51; P = . 04), liver-related mortality (HR, 1.96; 95% CI, 1.10-3.38; P = .02), and mortality of any cause (HR, 1.73; 95% CI, 1.11-2.69; P = .01).
These risks could be further stratified by level of change in liver stiffness, with greater impairment predicting greater risk: The crude rate of liver decompensation was 14.4% among those with impaired LSM, compared with 6.2% among those with stable LSM and 3.8% among those with LSM improvement. That said, the categories of changes in LSM were not predictive of decompensation among patients with high risk of CSPH at baseline; however, they remained predictive among those with low risk of CSPH at baseline.
“[T]his study … showed that an integrated assessment of baseline LSM or [changes in LSM] can help in stratifying the risk of development of liver-related complications and of both hepatic and overall mortality,” the investigators concluded. “These data, if further validated, could help personalize prognosis and follow-up in NAFLD with [compensated advanced chronic liver disease].”
The investigators disclosed relationships with AbbVie, Novo Nordisk, Gilead, and others.
Among patients with nonalcoholic fatty liver disease (NAFLD) and compensated advanced chronic liver disease, liver stiffness measurements (LSMs) are associated with risks of hepatic events, according to a retrospective analysis of more than 1,000 patients.
“[N]oninvasive markers that can predict liver disease severity and outcomes in patients with NAFLD and advanced fibrosis are a major unmet need,” wrote lead author Salvatore Petta, MD, of the University of Palermo, Italy, and colleagues. Their report is in Clinical Gastroenterology and Hepatology. “Data about the accuracy of LSM in the prediction of events in NAFLD, and especially in patients with NAFLD and F3-F4 fibrosis, are scarce.”
To address this knowledge gap, the investigators retrospectively analyzed data from 1,039 consecutive patients with NAFLD who had baseline LSMs of more than 10 kPa and/or histologically diagnosed F3-F4 fibrosis. Patients were prospectively recruited at 10 centers in 6 countries, then followed for a median of 35 months, ranging from 19 to 63 months.
All patients had their liver stiffness measured with an M or XL probe at baseline. In addition, approximately half of the patients (n = 533) had a follow-up measurement using the same method, generating a subgroup with changes in liver stiffness. “Improved” liver stiffness was defined as a decrease in LSM greater than 20% from baseline, “impaired” liver stiffness was defined as an increase in LSM greater than 20% from baseline, and “stable” liver stiffness was defined as a change falling between 20% lower and 20% higher than baseline.
At baseline, mean LSM was 17.6 kPa. Cox regression analysis revealed that baseline LSM was independently associated with HCC (hazard ratio, 1.03; 95% confidence interval, 1.00-1.04; P = .003), liver decompensation (HR, 1.03; 95% CI, 1.02-1.04; P < .001), and liver-related death (HR, 1.02; 95% CI, 1.00-1.03; P = .005), but not extrahepatic events.
According to the investigators, the association between LSM at baseline and risk of liver decompensation was maintained after adjustment for the severity of liver disease and for surrogate markers of portal hypertension, they noted. Furthermore, patients with a baseline LSM of at least 21 kPa – which indicates high risk of clinically significant portal hypertension (CSPH) – were at greater risk of liver decompensation than were those with an LSM less than 21 kPa (HR, 3.71; 95% CI, 1.89-6.78; P = .04).
In the subgroup with follow-up measurements, approximately half of the patients had an improved LSM (53.3%), while 27.2% had a stable LSM, and 19.5% had an impaired LSM, a pattern that was significantly associated with diabetes at baseline (P = .01).
“These data agree with the available literature identifying diabetes as a risk factor for liver disease progression and liver-related complications,” the investigators wrote.
Cox regression showed that, among those with follow-up LSM, changes in LSM were independently associated with HCC (HR, 1.72; 95% CI, 1.01-3.02; P = .04), liver decompensation (HR, 1.56; 95% CI, 1.05-2.51; P = . 04), liver-related mortality (HR, 1.96; 95% CI, 1.10-3.38; P = .02), and mortality of any cause (HR, 1.73; 95% CI, 1.11-2.69; P = .01).
These risks could be further stratified by level of change in liver stiffness, with greater impairment predicting greater risk: The crude rate of liver decompensation was 14.4% among those with impaired LSM, compared with 6.2% among those with stable LSM and 3.8% among those with LSM improvement. That said, the categories of changes in LSM were not predictive of decompensation among patients with high risk of CSPH at baseline; however, they remained predictive among those with low risk of CSPH at baseline.
“[T]his study … showed that an integrated assessment of baseline LSM or [changes in LSM] can help in stratifying the risk of development of liver-related complications and of both hepatic and overall mortality,” the investigators concluded. “These data, if further validated, could help personalize prognosis and follow-up in NAFLD with [compensated advanced chronic liver disease].”
The investigators disclosed relationships with AbbVie, Novo Nordisk, Gilead, and others.
Among patients with nonalcoholic fatty liver disease (NAFLD) and compensated advanced chronic liver disease, liver stiffness measurements (LSMs) are associated with risks of hepatic events, according to a retrospective analysis of more than 1,000 patients.
“[N]oninvasive markers that can predict liver disease severity and outcomes in patients with NAFLD and advanced fibrosis are a major unmet need,” wrote lead author Salvatore Petta, MD, of the University of Palermo, Italy, and colleagues. Their report is in Clinical Gastroenterology and Hepatology. “Data about the accuracy of LSM in the prediction of events in NAFLD, and especially in patients with NAFLD and F3-F4 fibrosis, are scarce.”
To address this knowledge gap, the investigators retrospectively analyzed data from 1,039 consecutive patients with NAFLD who had baseline LSMs of more than 10 kPa and/or histologically diagnosed F3-F4 fibrosis. Patients were prospectively recruited at 10 centers in 6 countries, then followed for a median of 35 months, ranging from 19 to 63 months.
All patients had their liver stiffness measured with an M or XL probe at baseline. In addition, approximately half of the patients (n = 533) had a follow-up measurement using the same method, generating a subgroup with changes in liver stiffness. “Improved” liver stiffness was defined as a decrease in LSM greater than 20% from baseline, “impaired” liver stiffness was defined as an increase in LSM greater than 20% from baseline, and “stable” liver stiffness was defined as a change falling between 20% lower and 20% higher than baseline.
At baseline, mean LSM was 17.6 kPa. Cox regression analysis revealed that baseline LSM was independently associated with HCC (hazard ratio, 1.03; 95% confidence interval, 1.00-1.04; P = .003), liver decompensation (HR, 1.03; 95% CI, 1.02-1.04; P < .001), and liver-related death (HR, 1.02; 95% CI, 1.00-1.03; P = .005), but not extrahepatic events.
According to the investigators, the association between LSM at baseline and risk of liver decompensation was maintained after adjustment for the severity of liver disease and for surrogate markers of portal hypertension, they noted. Furthermore, patients with a baseline LSM of at least 21 kPa – which indicates high risk of clinically significant portal hypertension (CSPH) – were at greater risk of liver decompensation than were those with an LSM less than 21 kPa (HR, 3.71; 95% CI, 1.89-6.78; P = .04).
In the subgroup with follow-up measurements, approximately half of the patients had an improved LSM (53.3%), while 27.2% had a stable LSM, and 19.5% had an impaired LSM, a pattern that was significantly associated with diabetes at baseline (P = .01).
“These data agree with the available literature identifying diabetes as a risk factor for liver disease progression and liver-related complications,” the investigators wrote.
Cox regression showed that, among those with follow-up LSM, changes in LSM were independently associated with HCC (HR, 1.72; 95% CI, 1.01-3.02; P = .04), liver decompensation (HR, 1.56; 95% CI, 1.05-2.51; P = . 04), liver-related mortality (HR, 1.96; 95% CI, 1.10-3.38; P = .02), and mortality of any cause (HR, 1.73; 95% CI, 1.11-2.69; P = .01).
These risks could be further stratified by level of change in liver stiffness, with greater impairment predicting greater risk: The crude rate of liver decompensation was 14.4% among those with impaired LSM, compared with 6.2% among those with stable LSM and 3.8% among those with LSM improvement. That said, the categories of changes in LSM were not predictive of decompensation among patients with high risk of CSPH at baseline; however, they remained predictive among those with low risk of CSPH at baseline.
“[T]his study … showed that an integrated assessment of baseline LSM or [changes in LSM] can help in stratifying the risk of development of liver-related complications and of both hepatic and overall mortality,” the investigators concluded. “These data, if further validated, could help personalize prognosis and follow-up in NAFLD with [compensated advanced chronic liver disease].”
The investigators disclosed relationships with AbbVie, Novo Nordisk, Gilead, and others.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Close joint health monitoring essential with new hemophilia therapies
Novel therapies have transformed the treatment of hemophilia in recent decades, but these new approaches also raise new challenges for clinicians who monitor joint health in persons with hemophilia, a specialist said.
“Patient-reported outcomes should be combined with other, more objective outcome measures for joint health monitoring, and joint ultrasound is a promising tool for objective joint health monitoring, although, due to its relatively recent introduction in clinical practice, we lack objective data and standardization,” said Roberta Gualtierotti, MD, PhD, from the Università Degli Studi of Milan.
She reviewed the challenges and approaches to monitoring joint health in persons with hemophilia during the annual congress of the European Association for Haemophilia and Allied Disorders.
Over the last decades the target of hemophilia treatment has shifted from prolonging survival to improving joint health and quality of life, and care has improved with the introduction of novel therapies such as extended half-life replacement products, nonreplacement therapies, and gene therapy, she noted.
However, “due to different pharmacodynamics and pharmacokinetics profiles, the currently available therapies cannot be compared to each other on several levels,” Dr. Gualtierotti said.
Laboratory monitoring of replacement therapies with standard coagulation assays may be unreliable, and depending on the mechanism of action and type of administration of nonreplacement agents, patients may experience breakthrough bleeding, especially after traumatic injury, she said.
Until the specific noncoagulatory effects of factor VIII on bone and joint health is better understood, close monitoring of patients will be required, she added.
Outcome measures
Subjective measures of joint health include patient-reported bleeding rates and health-related quality of life. These are practical for home management, but patients may not be able to distinguish symptoms of acute joint bleeding from chronic arthritis pain, with the potential for either under- or overtreatment, and subjective reporting is likely to miss subclinical bleeding that can occur even when patients are on prophylaxis.
Health-related quality of life tools, whether generic or specific for hemophilia, are not sensitive to small improvements, and they are not always used in routine clinical practice.
Objective measures include physical examination with scoring according to the World Federation of Hemophilia (Gilbert Scale) score or Hemophilia Joint Health Score, but these measures have limited ability to identify early or subclinical joint abnormalities.
“Therefore, joint physical examination on its own is not a sufficient measure of treatment efficacy, and it should be used in combination with other tools more objective, such as imaging,” Dr. Gualtierotti said.
Get the picture?
Imaging with x-rays, MRI, and, recently in some centers, point-of-care ultrasound can provide clinicians with important real-time information about the joint stability and health.
Point-of-care ultrasound in particular offers promise as a practical tool, with no ionizing radiation and high sensitivity for synovial hyperplasia subclinical joint effusion. It’s relatively inexpensive, can be used to image multiple joints, and allows for ease of follow-up, she said. The technique requires specialized training, however, and there is a lack of prospective data about its utility in hemophilia.
Various ultrasound scoring systems have been proposed, and home-based ultrasound is currently being explored in several clinical trials, Dr. Gualtierotti noted.
Other avenues for remote joint health monitoring under consideration are serum or synovial biomarkers for joint bleeding and arthropathy that could be employed at bedside or at home, smartphone apps for breakthrough bleeding and patient-reported outcomes, and sensors for detecting abnormalities in gait that may signal joint dysfunction, she said.
Best practice
In the question-and-answer session following the talk, Fernando Zikan, MD, from the Federal University of Rio de Janeiro noted that, “in underdeveloped countries, we still find it very difficult to guide good practices for joint health control by the patient and family members. Which strategy do you think is fundamental for the patient to feel safe to notice changes in his body?”
“It would be useful to educate patients to come to the center whenever the patient has trauma and whenever an increase in his physical activity occurs. If this is far, a bedside ultrasound evaluation by the general practitioner could help avoid joint damage. Finally, a correct rehabilitation is fundamental,” Dr. Gualtierotti replied.
Asked by several others whether she used ultrasound in her daily practice, Dr. Gualtierotti said that “we use joint ultrasound in our clinical practice in the regular annual check-up examination and whenever the patient suspects and reports hemarthrosis.”
Dr. Gualtierotti reported participation in advisory boards for Biomarin, Pfizer, Bayer, and Takeda, and in educational seminars sponsored by Pfizer, Sobi, and Roche. She has received support for congress travel and/or attendance by Bayer and Pfizer. Dr. Zikan reported no relevant disclosures.
Novel therapies have transformed the treatment of hemophilia in recent decades, but these new approaches also raise new challenges for clinicians who monitor joint health in persons with hemophilia, a specialist said.
“Patient-reported outcomes should be combined with other, more objective outcome measures for joint health monitoring, and joint ultrasound is a promising tool for objective joint health monitoring, although, due to its relatively recent introduction in clinical practice, we lack objective data and standardization,” said Roberta Gualtierotti, MD, PhD, from the Università Degli Studi of Milan.
She reviewed the challenges and approaches to monitoring joint health in persons with hemophilia during the annual congress of the European Association for Haemophilia and Allied Disorders.
Over the last decades the target of hemophilia treatment has shifted from prolonging survival to improving joint health and quality of life, and care has improved with the introduction of novel therapies such as extended half-life replacement products, nonreplacement therapies, and gene therapy, she noted.
However, “due to different pharmacodynamics and pharmacokinetics profiles, the currently available therapies cannot be compared to each other on several levels,” Dr. Gualtierotti said.
Laboratory monitoring of replacement therapies with standard coagulation assays may be unreliable, and depending on the mechanism of action and type of administration of nonreplacement agents, patients may experience breakthrough bleeding, especially after traumatic injury, she said.
Until the specific noncoagulatory effects of factor VIII on bone and joint health is better understood, close monitoring of patients will be required, she added.
Outcome measures
Subjective measures of joint health include patient-reported bleeding rates and health-related quality of life. These are practical for home management, but patients may not be able to distinguish symptoms of acute joint bleeding from chronic arthritis pain, with the potential for either under- or overtreatment, and subjective reporting is likely to miss subclinical bleeding that can occur even when patients are on prophylaxis.
Health-related quality of life tools, whether generic or specific for hemophilia, are not sensitive to small improvements, and they are not always used in routine clinical practice.
Objective measures include physical examination with scoring according to the World Federation of Hemophilia (Gilbert Scale) score or Hemophilia Joint Health Score, but these measures have limited ability to identify early or subclinical joint abnormalities.
“Therefore, joint physical examination on its own is not a sufficient measure of treatment efficacy, and it should be used in combination with other tools more objective, such as imaging,” Dr. Gualtierotti said.
Get the picture?
Imaging with x-rays, MRI, and, recently in some centers, point-of-care ultrasound can provide clinicians with important real-time information about the joint stability and health.
Point-of-care ultrasound in particular offers promise as a practical tool, with no ionizing radiation and high sensitivity for synovial hyperplasia subclinical joint effusion. It’s relatively inexpensive, can be used to image multiple joints, and allows for ease of follow-up, she said. The technique requires specialized training, however, and there is a lack of prospective data about its utility in hemophilia.
Various ultrasound scoring systems have been proposed, and home-based ultrasound is currently being explored in several clinical trials, Dr. Gualtierotti noted.
Other avenues for remote joint health monitoring under consideration are serum or synovial biomarkers for joint bleeding and arthropathy that could be employed at bedside or at home, smartphone apps for breakthrough bleeding and patient-reported outcomes, and sensors for detecting abnormalities in gait that may signal joint dysfunction, she said.
Best practice
In the question-and-answer session following the talk, Fernando Zikan, MD, from the Federal University of Rio de Janeiro noted that, “in underdeveloped countries, we still find it very difficult to guide good practices for joint health control by the patient and family members. Which strategy do you think is fundamental for the patient to feel safe to notice changes in his body?”
“It would be useful to educate patients to come to the center whenever the patient has trauma and whenever an increase in his physical activity occurs. If this is far, a bedside ultrasound evaluation by the general practitioner could help avoid joint damage. Finally, a correct rehabilitation is fundamental,” Dr. Gualtierotti replied.
Asked by several others whether she used ultrasound in her daily practice, Dr. Gualtierotti said that “we use joint ultrasound in our clinical practice in the regular annual check-up examination and whenever the patient suspects and reports hemarthrosis.”
Dr. Gualtierotti reported participation in advisory boards for Biomarin, Pfizer, Bayer, and Takeda, and in educational seminars sponsored by Pfizer, Sobi, and Roche. She has received support for congress travel and/or attendance by Bayer and Pfizer. Dr. Zikan reported no relevant disclosures.
Novel therapies have transformed the treatment of hemophilia in recent decades, but these new approaches also raise new challenges for clinicians who monitor joint health in persons with hemophilia, a specialist said.
“Patient-reported outcomes should be combined with other, more objective outcome measures for joint health monitoring, and joint ultrasound is a promising tool for objective joint health monitoring, although, due to its relatively recent introduction in clinical practice, we lack objective data and standardization,” said Roberta Gualtierotti, MD, PhD, from the Università Degli Studi of Milan.
She reviewed the challenges and approaches to monitoring joint health in persons with hemophilia during the annual congress of the European Association for Haemophilia and Allied Disorders.
Over the last decades the target of hemophilia treatment has shifted from prolonging survival to improving joint health and quality of life, and care has improved with the introduction of novel therapies such as extended half-life replacement products, nonreplacement therapies, and gene therapy, she noted.
However, “due to different pharmacodynamics and pharmacokinetics profiles, the currently available therapies cannot be compared to each other on several levels,” Dr. Gualtierotti said.
Laboratory monitoring of replacement therapies with standard coagulation assays may be unreliable, and depending on the mechanism of action and type of administration of nonreplacement agents, patients may experience breakthrough bleeding, especially after traumatic injury, she said.
Until the specific noncoagulatory effects of factor VIII on bone and joint health is better understood, close monitoring of patients will be required, she added.
Outcome measures
Subjective measures of joint health include patient-reported bleeding rates and health-related quality of life. These are practical for home management, but patients may not be able to distinguish symptoms of acute joint bleeding from chronic arthritis pain, with the potential for either under- or overtreatment, and subjective reporting is likely to miss subclinical bleeding that can occur even when patients are on prophylaxis.
Health-related quality of life tools, whether generic or specific for hemophilia, are not sensitive to small improvements, and they are not always used in routine clinical practice.
Objective measures include physical examination with scoring according to the World Federation of Hemophilia (Gilbert Scale) score or Hemophilia Joint Health Score, but these measures have limited ability to identify early or subclinical joint abnormalities.
“Therefore, joint physical examination on its own is not a sufficient measure of treatment efficacy, and it should be used in combination with other tools more objective, such as imaging,” Dr. Gualtierotti said.
Get the picture?
Imaging with x-rays, MRI, and, recently in some centers, point-of-care ultrasound can provide clinicians with important real-time information about the joint stability and health.
Point-of-care ultrasound in particular offers promise as a practical tool, with no ionizing radiation and high sensitivity for synovial hyperplasia subclinical joint effusion. It’s relatively inexpensive, can be used to image multiple joints, and allows for ease of follow-up, she said. The technique requires specialized training, however, and there is a lack of prospective data about its utility in hemophilia.
Various ultrasound scoring systems have been proposed, and home-based ultrasound is currently being explored in several clinical trials, Dr. Gualtierotti noted.
Other avenues for remote joint health monitoring under consideration are serum or synovial biomarkers for joint bleeding and arthropathy that could be employed at bedside or at home, smartphone apps for breakthrough bleeding and patient-reported outcomes, and sensors for detecting abnormalities in gait that may signal joint dysfunction, she said.
Best practice
In the question-and-answer session following the talk, Fernando Zikan, MD, from the Federal University of Rio de Janeiro noted that, “in underdeveloped countries, we still find it very difficult to guide good practices for joint health control by the patient and family members. Which strategy do you think is fundamental for the patient to feel safe to notice changes in his body?”
“It would be useful to educate patients to come to the center whenever the patient has trauma and whenever an increase in his physical activity occurs. If this is far, a bedside ultrasound evaluation by the general practitioner could help avoid joint damage. Finally, a correct rehabilitation is fundamental,” Dr. Gualtierotti replied.
Asked by several others whether she used ultrasound in her daily practice, Dr. Gualtierotti said that “we use joint ultrasound in our clinical practice in the regular annual check-up examination and whenever the patient suspects and reports hemarthrosis.”
Dr. Gualtierotti reported participation in advisory boards for Biomarin, Pfizer, Bayer, and Takeda, and in educational seminars sponsored by Pfizer, Sobi, and Roche. She has received support for congress travel and/or attendance by Bayer and Pfizer. Dr. Zikan reported no relevant disclosures.
FROM EAHAD 2021
Vaginal pH may predict CIN 2 progression in HIV-positive women
Elevated vaginal pH at the time of cervical intraepithelial neoplasia 2 diagnosis may be a useful marker of CIN 2 persistence/progression, as well as the rate of persistence/progression in HIV-positive women, new research suggests.
“We analyzed data from the Women’s Interagency HIV Study [WIHS], an observational, longitudinal cohort of women with and without HIV to determine factors that may influence CIN 2 natural history,” said Kate Michel, PhD, MPH, of Georgetown University, Washington. She presented the results at the Conference on Retroviruses and Opportunistic Infections.
As previous data have shown a high incidence of CIN 2 progression among women with HIV, the researchers evaluated the role of human papillomavirus (HPV) type, local immune response, and markers of the cervicovaginal microbiome on the risk of CIN 2 persistence/progression.
Within the cohort, follow-up visits occur every 6 months, and clinical data is collected via questionnaires, physical and gynecologic exams, and biological samples. As no specific treatment is offered in the WIHS, treatment for cervical abnormalities is abstracted from medical records.
In the present study, Dr. Michel and colleagues selected up to four banked cervicovaginal lavage (CVL) samples per woman, with the first sample selected 6-12 months prior to CIN 2 diagnosis, the second at CIN 2 diagnosis, the third between CIN 2 diagnosis and outcome, and the fourth at the outcome visit.
The investigators performed HPV typing and muiltiplex immune mediator testing on each CVL sample. Lab results from WIHS core testing were also extracted, including plasma CD4+ T-cell count and HIV viral load, as well as vaginal pH and Nugent’s score.
Study outcomes included persistence/progression and regression, defined as a subsequent CIN 2 or CIN 3 diagnosis and subsequent CIN 1 or normal diagnosis, respectively. Logistic regression models were used to determine CIN 2 regression versus persistence/progression.
Results
A total of 337 samples were obtained and 94 women were included in the analysis. Key demographic and behavioral factor were similar at CIN 2 diagnosis.
The majority of participants were African American (53.2%) and on antiretroviral therapy (66.0%). The most prevalent high-risk types were HPV-58 (18.4%) and HPV-16 (17.5%).
After a median 12.5 years of follow-up, 33 participants (35.1%) with incident CIN 2 had a subsequent CIN 2/CIN 3 diagnosis and those who regressed had a higher CD4 T-cell count at CIN 2 diagnosis (P = .02).
Each subsequent high-risk HPV type identified at the pre–CIN 2 visit was associated with higher odds of CIN2 persistence/progression (odds ratio, 2.27; 95% confidence interval, 1.15-4.50).
Bacterial vaginosis (adjusted OR, 5.08; 95% CI, 1.30-19.94) and vaginal pH (aOR, 2.27; 95% CI, 1.15-4.50) at the CIN 2 diagnosis visit were each associated with increased odds of CIN 2 persistence/progression.
Vaginal pH greater than 4.5 at CIN 2 diagnosis was also associated with unadjusted time to CIN 2 persistence/progression (log rank P = .002) and an increased rate of CIN 2 persistence/progression (adjusted hazard ratio, 3.37; 95% CI, 1.26-8.99).
Furthermore, among participants who did not receive CIN 2 treatment, vaginal pH remained associated with greater odds of CIN 2 persistence/progression (OR, 2.46; 95% CI, 1.19-5.13). Cervicovaginal immune mediator levels were not associated with CIN 2 persistence/progression.
“The most striking finding from this work was that vaginal pH was associated with higher odds of, quicker time to, and increased hazard of CIN 2 persistence/progression,” Dr. Michel said. “We postulate this effect is mediated by the cervical microbiome, but more work is needed to establish the exact mechanism.”
“It would be interesting to test whether this association might be explained by different vaginal cleaning techniques, such as douching,” said moderator Ronald T. Mitsuyasu, MD, of the University of California, Los Angeles.
“We’re currently working on an analysis of cervicovaginal bacterial species to explore the microbiome in more detail,” Dr. Michel concluded.
Dr. Michel disclosed no conflicts of interest. The study was supported by multiple sources, including the National Institute of Allergy and Infectious Diseases, the National Cancer Institute, and the Georgetown-Howard Universities Center for Clinical and Translational Science.
Elevated vaginal pH at the time of cervical intraepithelial neoplasia 2 diagnosis may be a useful marker of CIN 2 persistence/progression, as well as the rate of persistence/progression in HIV-positive women, new research suggests.
“We analyzed data from the Women’s Interagency HIV Study [WIHS], an observational, longitudinal cohort of women with and without HIV to determine factors that may influence CIN 2 natural history,” said Kate Michel, PhD, MPH, of Georgetown University, Washington. She presented the results at the Conference on Retroviruses and Opportunistic Infections.
As previous data have shown a high incidence of CIN 2 progression among women with HIV, the researchers evaluated the role of human papillomavirus (HPV) type, local immune response, and markers of the cervicovaginal microbiome on the risk of CIN 2 persistence/progression.
Within the cohort, follow-up visits occur every 6 months, and clinical data is collected via questionnaires, physical and gynecologic exams, and biological samples. As no specific treatment is offered in the WIHS, treatment for cervical abnormalities is abstracted from medical records.
In the present study, Dr. Michel and colleagues selected up to four banked cervicovaginal lavage (CVL) samples per woman, with the first sample selected 6-12 months prior to CIN 2 diagnosis, the second at CIN 2 diagnosis, the third between CIN 2 diagnosis and outcome, and the fourth at the outcome visit.
The investigators performed HPV typing and muiltiplex immune mediator testing on each CVL sample. Lab results from WIHS core testing were also extracted, including plasma CD4+ T-cell count and HIV viral load, as well as vaginal pH and Nugent’s score.
Study outcomes included persistence/progression and regression, defined as a subsequent CIN 2 or CIN 3 diagnosis and subsequent CIN 1 or normal diagnosis, respectively. Logistic regression models were used to determine CIN 2 regression versus persistence/progression.
Results
A total of 337 samples were obtained and 94 women were included in the analysis. Key demographic and behavioral factor were similar at CIN 2 diagnosis.
The majority of participants were African American (53.2%) and on antiretroviral therapy (66.0%). The most prevalent high-risk types were HPV-58 (18.4%) and HPV-16 (17.5%).
After a median 12.5 years of follow-up, 33 participants (35.1%) with incident CIN 2 had a subsequent CIN 2/CIN 3 diagnosis and those who regressed had a higher CD4 T-cell count at CIN 2 diagnosis (P = .02).
Each subsequent high-risk HPV type identified at the pre–CIN 2 visit was associated with higher odds of CIN2 persistence/progression (odds ratio, 2.27; 95% confidence interval, 1.15-4.50).
Bacterial vaginosis (adjusted OR, 5.08; 95% CI, 1.30-19.94) and vaginal pH (aOR, 2.27; 95% CI, 1.15-4.50) at the CIN 2 diagnosis visit were each associated with increased odds of CIN 2 persistence/progression.
Vaginal pH greater than 4.5 at CIN 2 diagnosis was also associated with unadjusted time to CIN 2 persistence/progression (log rank P = .002) and an increased rate of CIN 2 persistence/progression (adjusted hazard ratio, 3.37; 95% CI, 1.26-8.99).
Furthermore, among participants who did not receive CIN 2 treatment, vaginal pH remained associated with greater odds of CIN 2 persistence/progression (OR, 2.46; 95% CI, 1.19-5.13). Cervicovaginal immune mediator levels were not associated with CIN 2 persistence/progression.
“The most striking finding from this work was that vaginal pH was associated with higher odds of, quicker time to, and increased hazard of CIN 2 persistence/progression,” Dr. Michel said. “We postulate this effect is mediated by the cervical microbiome, but more work is needed to establish the exact mechanism.”
“It would be interesting to test whether this association might be explained by different vaginal cleaning techniques, such as douching,” said moderator Ronald T. Mitsuyasu, MD, of the University of California, Los Angeles.
“We’re currently working on an analysis of cervicovaginal bacterial species to explore the microbiome in more detail,” Dr. Michel concluded.
Dr. Michel disclosed no conflicts of interest. The study was supported by multiple sources, including the National Institute of Allergy and Infectious Diseases, the National Cancer Institute, and the Georgetown-Howard Universities Center for Clinical and Translational Science.
Elevated vaginal pH at the time of cervical intraepithelial neoplasia 2 diagnosis may be a useful marker of CIN 2 persistence/progression, as well as the rate of persistence/progression in HIV-positive women, new research suggests.
“We analyzed data from the Women’s Interagency HIV Study [WIHS], an observational, longitudinal cohort of women with and without HIV to determine factors that may influence CIN 2 natural history,” said Kate Michel, PhD, MPH, of Georgetown University, Washington. She presented the results at the Conference on Retroviruses and Opportunistic Infections.
As previous data have shown a high incidence of CIN 2 progression among women with HIV, the researchers evaluated the role of human papillomavirus (HPV) type, local immune response, and markers of the cervicovaginal microbiome on the risk of CIN 2 persistence/progression.
Within the cohort, follow-up visits occur every 6 months, and clinical data is collected via questionnaires, physical and gynecologic exams, and biological samples. As no specific treatment is offered in the WIHS, treatment for cervical abnormalities is abstracted from medical records.
In the present study, Dr. Michel and colleagues selected up to four banked cervicovaginal lavage (CVL) samples per woman, with the first sample selected 6-12 months prior to CIN 2 diagnosis, the second at CIN 2 diagnosis, the third between CIN 2 diagnosis and outcome, and the fourth at the outcome visit.
The investigators performed HPV typing and muiltiplex immune mediator testing on each CVL sample. Lab results from WIHS core testing were also extracted, including plasma CD4+ T-cell count and HIV viral load, as well as vaginal pH and Nugent’s score.
Study outcomes included persistence/progression and regression, defined as a subsequent CIN 2 or CIN 3 diagnosis and subsequent CIN 1 or normal diagnosis, respectively. Logistic regression models were used to determine CIN 2 regression versus persistence/progression.
Results
A total of 337 samples were obtained and 94 women were included in the analysis. Key demographic and behavioral factor were similar at CIN 2 diagnosis.
The majority of participants were African American (53.2%) and on antiretroviral therapy (66.0%). The most prevalent high-risk types were HPV-58 (18.4%) and HPV-16 (17.5%).
After a median 12.5 years of follow-up, 33 participants (35.1%) with incident CIN 2 had a subsequent CIN 2/CIN 3 diagnosis and those who regressed had a higher CD4 T-cell count at CIN 2 diagnosis (P = .02).
Each subsequent high-risk HPV type identified at the pre–CIN 2 visit was associated with higher odds of CIN2 persistence/progression (odds ratio, 2.27; 95% confidence interval, 1.15-4.50).
Bacterial vaginosis (adjusted OR, 5.08; 95% CI, 1.30-19.94) and vaginal pH (aOR, 2.27; 95% CI, 1.15-4.50) at the CIN 2 diagnosis visit were each associated with increased odds of CIN 2 persistence/progression.
Vaginal pH greater than 4.5 at CIN 2 diagnosis was also associated with unadjusted time to CIN 2 persistence/progression (log rank P = .002) and an increased rate of CIN 2 persistence/progression (adjusted hazard ratio, 3.37; 95% CI, 1.26-8.99).
Furthermore, among participants who did not receive CIN 2 treatment, vaginal pH remained associated with greater odds of CIN 2 persistence/progression (OR, 2.46; 95% CI, 1.19-5.13). Cervicovaginal immune mediator levels were not associated with CIN 2 persistence/progression.
“The most striking finding from this work was that vaginal pH was associated with higher odds of, quicker time to, and increased hazard of CIN 2 persistence/progression,” Dr. Michel said. “We postulate this effect is mediated by the cervical microbiome, but more work is needed to establish the exact mechanism.”
“It would be interesting to test whether this association might be explained by different vaginal cleaning techniques, such as douching,” said moderator Ronald T. Mitsuyasu, MD, of the University of California, Los Angeles.
“We’re currently working on an analysis of cervicovaginal bacterial species to explore the microbiome in more detail,” Dr. Michel concluded.
Dr. Michel disclosed no conflicts of interest. The study was supported by multiple sources, including the National Institute of Allergy and Infectious Diseases, the National Cancer Institute, and the Georgetown-Howard Universities Center for Clinical and Translational Science.
FROM CROI 2021
JAMA editor resigns over controversial podcast
JAMA editor in chief Howard Bauchner, MD, apologized to JAMA staff and stakeholders and asked for and received Dr. Livingston’s resignation, according to a statement from AMA CEO James Madara.
More than 2,000 people have signed a petition on Change.org calling for an investigation at JAMA over the podcast, called “Structural Racism for Doctors: What Is It?”
It appears they are now getting their wish. Dr. Bauchner announced that the journal’s oversight committee is investigating how the podcast and a tweet promoting the episode were developed, reviewed, and ultimately posted.
“This investigation and report of its findings will be thorough and completed rapidly,” Dr. Bauchner said.
Dr. Livingston, the host of the podcast, has been heavily criticized across social media. During the podcast, Dr. Livingston, who is White, said: “Structural racism is an unfortunate term. Personally, I think taking racism out of the conversation will help. Many of us are offended by the concept that we are racist.”
The audio of the podcast has been deleted from JAMA’s website. In its place is audio of a statement from Dr. Bauchner. In his statement, which he released last week, he said the comments in the podcast, which also featured Mitch Katz, MD, were “inaccurate, offensive, hurtful, and inconsistent with the standards of JAMA.”
Dr. Katz is an editor at JAMA Internal Medicine and CEO of NYC Health + Hospitals in New York.
Also deleted was a JAMA tweet promoting the podcast episode. The tweet said: “No physician is racist, so how can there be structural racism in health care? An explanation of the idea by doctors for doctors in this user-friendly podcast.”
The incident was met with anger and confusion in the medical community.
Herbert C. Smitherman, MD, vice dean of diversity and community affairs at Wayne State University, Detroit, noted after hearing the podcast that it was a symptom of a much larger problem.
“At its core, this podcast had racist tendencies. Those attitudes are why you don’t have as many articles by Black and Brown people in JAMA,” he said. “People’s attitudes, whether conscious or unconscious, are what drive the policies and practices which create the structural racism.”
Dr. Katz responded to the backlash last week with the following statement: “Systemic racism exists in our country. The disparate effects of the pandemic have made this painfully clear in New York City and across the country.
“As clinicians, we must understand how these structures and policies have a direct impact on the health outcomes of the patients and communities we serve. It is woefully naive to say that no physician is a racist just because the Civil Rights Act of 1964 forbade it, or that we should avoid the term ‘systematic racism’ because it makes people uncomfortable. We must and can do better.”
JAMA, an independent arm of the AMA, is taking other steps to address concerns. Its executive publisher, Thomas Easley, held an employee town hall this week, and said JAMA acknowledges that “structural racism is real, pernicious, and pervasive in health care.” The journal is also starting an “end-to-end review” of all editorial processes across all JAMA publications. Finally, the journal will also create a new associate editor’s position who will provide “insight and counsel” on racism and structural racism in health care.
A version of this article first appeared on WebMD.com .
JAMA editor in chief Howard Bauchner, MD, apologized to JAMA staff and stakeholders and asked for and received Dr. Livingston’s resignation, according to a statement from AMA CEO James Madara.
More than 2,000 people have signed a petition on Change.org calling for an investigation at JAMA over the podcast, called “Structural Racism for Doctors: What Is It?”
It appears they are now getting their wish. Dr. Bauchner announced that the journal’s oversight committee is investigating how the podcast and a tweet promoting the episode were developed, reviewed, and ultimately posted.
“This investigation and report of its findings will be thorough and completed rapidly,” Dr. Bauchner said.
Dr. Livingston, the host of the podcast, has been heavily criticized across social media. During the podcast, Dr. Livingston, who is White, said: “Structural racism is an unfortunate term. Personally, I think taking racism out of the conversation will help. Many of us are offended by the concept that we are racist.”
The audio of the podcast has been deleted from JAMA’s website. In its place is audio of a statement from Dr. Bauchner. In his statement, which he released last week, he said the comments in the podcast, which also featured Mitch Katz, MD, were “inaccurate, offensive, hurtful, and inconsistent with the standards of JAMA.”
Dr. Katz is an editor at JAMA Internal Medicine and CEO of NYC Health + Hospitals in New York.
Also deleted was a JAMA tweet promoting the podcast episode. The tweet said: “No physician is racist, so how can there be structural racism in health care? An explanation of the idea by doctors for doctors in this user-friendly podcast.”
The incident was met with anger and confusion in the medical community.
Herbert C. Smitherman, MD, vice dean of diversity and community affairs at Wayne State University, Detroit, noted after hearing the podcast that it was a symptom of a much larger problem.
“At its core, this podcast had racist tendencies. Those attitudes are why you don’t have as many articles by Black and Brown people in JAMA,” he said. “People’s attitudes, whether conscious or unconscious, are what drive the policies and practices which create the structural racism.”
Dr. Katz responded to the backlash last week with the following statement: “Systemic racism exists in our country. The disparate effects of the pandemic have made this painfully clear in New York City and across the country.
“As clinicians, we must understand how these structures and policies have a direct impact on the health outcomes of the patients and communities we serve. It is woefully naive to say that no physician is a racist just because the Civil Rights Act of 1964 forbade it, or that we should avoid the term ‘systematic racism’ because it makes people uncomfortable. We must and can do better.”
JAMA, an independent arm of the AMA, is taking other steps to address concerns. Its executive publisher, Thomas Easley, held an employee town hall this week, and said JAMA acknowledges that “structural racism is real, pernicious, and pervasive in health care.” The journal is also starting an “end-to-end review” of all editorial processes across all JAMA publications. Finally, the journal will also create a new associate editor’s position who will provide “insight and counsel” on racism and structural racism in health care.
A version of this article first appeared on WebMD.com .
JAMA editor in chief Howard Bauchner, MD, apologized to JAMA staff and stakeholders and asked for and received Dr. Livingston’s resignation, according to a statement from AMA CEO James Madara.
More than 2,000 people have signed a petition on Change.org calling for an investigation at JAMA over the podcast, called “Structural Racism for Doctors: What Is It?”
It appears they are now getting their wish. Dr. Bauchner announced that the journal’s oversight committee is investigating how the podcast and a tweet promoting the episode were developed, reviewed, and ultimately posted.
“This investigation and report of its findings will be thorough and completed rapidly,” Dr. Bauchner said.
Dr. Livingston, the host of the podcast, has been heavily criticized across social media. During the podcast, Dr. Livingston, who is White, said: “Structural racism is an unfortunate term. Personally, I think taking racism out of the conversation will help. Many of us are offended by the concept that we are racist.”
The audio of the podcast has been deleted from JAMA’s website. In its place is audio of a statement from Dr. Bauchner. In his statement, which he released last week, he said the comments in the podcast, which also featured Mitch Katz, MD, were “inaccurate, offensive, hurtful, and inconsistent with the standards of JAMA.”
Dr. Katz is an editor at JAMA Internal Medicine and CEO of NYC Health + Hospitals in New York.
Also deleted was a JAMA tweet promoting the podcast episode. The tweet said: “No physician is racist, so how can there be structural racism in health care? An explanation of the idea by doctors for doctors in this user-friendly podcast.”
The incident was met with anger and confusion in the medical community.
Herbert C. Smitherman, MD, vice dean of diversity and community affairs at Wayne State University, Detroit, noted after hearing the podcast that it was a symptom of a much larger problem.
“At its core, this podcast had racist tendencies. Those attitudes are why you don’t have as many articles by Black and Brown people in JAMA,” he said. “People’s attitudes, whether conscious or unconscious, are what drive the policies and practices which create the structural racism.”
Dr. Katz responded to the backlash last week with the following statement: “Systemic racism exists in our country. The disparate effects of the pandemic have made this painfully clear in New York City and across the country.
“As clinicians, we must understand how these structures and policies have a direct impact on the health outcomes of the patients and communities we serve. It is woefully naive to say that no physician is a racist just because the Civil Rights Act of 1964 forbade it, or that we should avoid the term ‘systematic racism’ because it makes people uncomfortable. We must and can do better.”
JAMA, an independent arm of the AMA, is taking other steps to address concerns. Its executive publisher, Thomas Easley, held an employee town hall this week, and said JAMA acknowledges that “structural racism is real, pernicious, and pervasive in health care.” The journal is also starting an “end-to-end review” of all editorial processes across all JAMA publications. Finally, the journal will also create a new associate editor’s position who will provide “insight and counsel” on racism and structural racism in health care.
A version of this article first appeared on WebMD.com .
Benefits of bremelanotide to women with HSDD questioned in analysis paper
Dr. Spielmans, professor of psychology at Metropolitan State University in Saint Paul, Minn., examined data from the FDA application for bremelanotide, clinicaltrials.gov entries for two phase 3 trials of the drug, and a 2019 article published in Obstetrics & Gynecology that described results from the 24-week trials.
In Dr. Speilman’s analysis, which was published online March 7 in the Journal of Sex Research, he notes that 42.1% of trial participants who received bremelanotide did not complete the trial, compared with 20.48% of participants who received placebo.
Of those who completed the study, 87.22% who received placebo wanted to continue treatment in an open-label extension, compared with 69.97% who received bremelanotide, he wrote.
Women “should be aware of the small degree of bremelanotide’s efficacy, that the protocol-specified outcomes of bremelanotide are mostly unknown, and that participants would rather take a placebo than bremelanotide,” Dr. Spielmans said.
Anita H. Clayton, MD, an author of the Obstetrics & Gynecology paper addressed in Dr. Spielmans’ analysis, says the Journal of Sex Research article does not provide new information and is a disservice to women because it questions accurate scientific data.
Measuring outcomes in HSDD is an evolving field, Dr. Clayton, a psychiatrist at the University of Virginia in Charlottesville, said in an interview. Initial FDA guidance relied on satisfying sexual events as an outcome measure, but this measure was derived from erectile dysfunction studies and is not necessarily adequate for assessing HSDD, she said. The FDA and drug developers agreed to use the desire subscale of the Female Sexual Function Index (FSFI-D) as a coprimary outcome measure instead, she noted.
Dr. Spielmans’ critique of Obstetrics & Gynecology paper
The article published in Obstetrics & Gynecology reporting bremelanotide trial results was noteworthy, although the various issues involved can be seen in reports about other drug trials, Dr. Spielmans said in an interview.
“It is well-established that journal articles reporting clinical trial data overstate benefits and understate harms,” he continued. In this case, “the very incomplete data reporting, reliance on many post-hoc measures of questionable validity, hiding the concerning number of dropouts due to adverse events, and putting a positive spin on efficacy and tolerability is both remarkable and highly problematic,” Dr. Spielmans said.
Dr. Clayton’s reaction
Data about dropout rates due to adverse events have been reported and presented at national meetings, she said in an interview. In addition, a questionnaire found that bremelanotide was superior to placebo in terms of patients feeling that the treatment had provided clinically meaningful benefit, Dr. Clayton said.
The available information enables patients to make informed treatment decisions, Dr. Clayton continued. “There is really this sexist attitude of women needing protection from their own decisions,” she said.
Diagnosing and treating HSDD
Eight of 11 efficacy outcomes in the clinicaltrials.gov study protocols for bremelanotide were not reported in the Obstetrics & Gynecology article in a way that was consistent with the protocols, Dr. Spielmans said. Changing a coprimary outcome to the key secondary outcome “occurred over a year after the trials had begun,” and the authors of the journal article “did not mention that this change occurred,” Dr. Spielmans wrote.
For the coprimary outcome measures of mean change on FSFI-D and Female Sexual Distress Scale–Desire/Arousal/Orgasm #13, “bremelanotide offers modest benefits over placebo,” Dr. Spielmans reported.
In addition to outlining his concerns about transparency in the reporting of trial data and raising questions about the outcome measures used in the Obstetrics & Gynecology article, Dr. Spielmans wrote that the diagnosis of HSDD is problematic.
“The lack of specifying symptom duration, questionable validity for the lack of sexual fantasies as a diagnostic criterion, difficulty in disentangling individual sexual problems from relational problems, and the failure to consider cultural influence (including the pressure on women to satisfy the sexual desires of their male partners) in the experience of sexuality all render HSDD as a problematic entity,” Dr. Spielmans wrote.
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders replaced HSDD and female sexual arousal disorder with the combined condition female sexual interest/arousal disorder. HSDD is in the 11th edition of the International Classification of Diseases and can be applied to men or women, Dr. Spielmans said.
FDA acknowledged HSDD as an unmet medical need
Dr. Clayton pointed out that HSDD was described decades ago and the FDA acknowledged it as an unmet medical need, and she expressed dissatisfaction with the fact the hypoactive sexual desire disorder appears with quotation marks around it in the title of Dr. Spielmans’ article. This way of presenting HSDD indicates that “the author has no concept of sexual health or sexual dysfunction,” Dr. Clayton said. “Basically this is sort of a dramatic tool, I think, to act like this is not a real disorder,” she added.
Carl Spana, PhD, CEO and president of Palatin Technologies, the developer of bremelanotide, defined the article in the Journal of Sex Research as a “retrospective meta-analysis, and not a re-analysis of the data.
“As a meta-analysis, it is open to various interpretations and reflects the author’s interpretations, which appear to have clear biases,” Dr. Spana said in an interview. “We believe several of this author’s interpretations are contrary to the FDA’s positive assessment that led to Vyleesi’s approval as a safe and effective treatment for women suffering from hypoactive sexual desire disorder.”
The author is unaware of the validation that was conducted at the direction of the FDA to establish clinically meaningful cutoffs for patient-reported outcomes and to establish metrics that define clinical benefit, Dr. Spana said
“Vyleesi was approved by the FDA after a thorough analysis of data from two well-controlled phase 3 clinical studies and multiple clinical and preclinical safety studies,” he said. “The analyses in the New Drug Application were prespecified and conducted according to a statistical analysis plan that the sponsor and FDA agreed to prior to database lock.”
Dr. Spielmans disclosed holdings in Vanguard Healthcare, a mutual fund that invests in pharmaceutical firms. Dr. Clayton has received financial support from Palatin and AMAG Pharmaceuticals, the companies that developed bremelanotide, in previous years.
Dr. Spielmans, professor of psychology at Metropolitan State University in Saint Paul, Minn., examined data from the FDA application for bremelanotide, clinicaltrials.gov entries for two phase 3 trials of the drug, and a 2019 article published in Obstetrics & Gynecology that described results from the 24-week trials.
In Dr. Speilman’s analysis, which was published online March 7 in the Journal of Sex Research, he notes that 42.1% of trial participants who received bremelanotide did not complete the trial, compared with 20.48% of participants who received placebo.
Of those who completed the study, 87.22% who received placebo wanted to continue treatment in an open-label extension, compared with 69.97% who received bremelanotide, he wrote.
Women “should be aware of the small degree of bremelanotide’s efficacy, that the protocol-specified outcomes of bremelanotide are mostly unknown, and that participants would rather take a placebo than bremelanotide,” Dr. Spielmans said.
Anita H. Clayton, MD, an author of the Obstetrics & Gynecology paper addressed in Dr. Spielmans’ analysis, says the Journal of Sex Research article does not provide new information and is a disservice to women because it questions accurate scientific data.
Measuring outcomes in HSDD is an evolving field, Dr. Clayton, a psychiatrist at the University of Virginia in Charlottesville, said in an interview. Initial FDA guidance relied on satisfying sexual events as an outcome measure, but this measure was derived from erectile dysfunction studies and is not necessarily adequate for assessing HSDD, she said. The FDA and drug developers agreed to use the desire subscale of the Female Sexual Function Index (FSFI-D) as a coprimary outcome measure instead, she noted.
Dr. Spielmans’ critique of Obstetrics & Gynecology paper
The article published in Obstetrics & Gynecology reporting bremelanotide trial results was noteworthy, although the various issues involved can be seen in reports about other drug trials, Dr. Spielmans said in an interview.
“It is well-established that journal articles reporting clinical trial data overstate benefits and understate harms,” he continued. In this case, “the very incomplete data reporting, reliance on many post-hoc measures of questionable validity, hiding the concerning number of dropouts due to adverse events, and putting a positive spin on efficacy and tolerability is both remarkable and highly problematic,” Dr. Spielmans said.
Dr. Clayton’s reaction
Data about dropout rates due to adverse events have been reported and presented at national meetings, she said in an interview. In addition, a questionnaire found that bremelanotide was superior to placebo in terms of patients feeling that the treatment had provided clinically meaningful benefit, Dr. Clayton said.
The available information enables patients to make informed treatment decisions, Dr. Clayton continued. “There is really this sexist attitude of women needing protection from their own decisions,” she said.
Diagnosing and treating HSDD
Eight of 11 efficacy outcomes in the clinicaltrials.gov study protocols for bremelanotide were not reported in the Obstetrics & Gynecology article in a way that was consistent with the protocols, Dr. Spielmans said. Changing a coprimary outcome to the key secondary outcome “occurred over a year after the trials had begun,” and the authors of the journal article “did not mention that this change occurred,” Dr. Spielmans wrote.
For the coprimary outcome measures of mean change on FSFI-D and Female Sexual Distress Scale–Desire/Arousal/Orgasm #13, “bremelanotide offers modest benefits over placebo,” Dr. Spielmans reported.
In addition to outlining his concerns about transparency in the reporting of trial data and raising questions about the outcome measures used in the Obstetrics & Gynecology article, Dr. Spielmans wrote that the diagnosis of HSDD is problematic.
“The lack of specifying symptom duration, questionable validity for the lack of sexual fantasies as a diagnostic criterion, difficulty in disentangling individual sexual problems from relational problems, and the failure to consider cultural influence (including the pressure on women to satisfy the sexual desires of their male partners) in the experience of sexuality all render HSDD as a problematic entity,” Dr. Spielmans wrote.
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders replaced HSDD and female sexual arousal disorder with the combined condition female sexual interest/arousal disorder. HSDD is in the 11th edition of the International Classification of Diseases and can be applied to men or women, Dr. Spielmans said.
FDA acknowledged HSDD as an unmet medical need
Dr. Clayton pointed out that HSDD was described decades ago and the FDA acknowledged it as an unmet medical need, and she expressed dissatisfaction with the fact the hypoactive sexual desire disorder appears with quotation marks around it in the title of Dr. Spielmans’ article. This way of presenting HSDD indicates that “the author has no concept of sexual health or sexual dysfunction,” Dr. Clayton said. “Basically this is sort of a dramatic tool, I think, to act like this is not a real disorder,” she added.
Carl Spana, PhD, CEO and president of Palatin Technologies, the developer of bremelanotide, defined the article in the Journal of Sex Research as a “retrospective meta-analysis, and not a re-analysis of the data.
“As a meta-analysis, it is open to various interpretations and reflects the author’s interpretations, which appear to have clear biases,” Dr. Spana said in an interview. “We believe several of this author’s interpretations are contrary to the FDA’s positive assessment that led to Vyleesi’s approval as a safe and effective treatment for women suffering from hypoactive sexual desire disorder.”
The author is unaware of the validation that was conducted at the direction of the FDA to establish clinically meaningful cutoffs for patient-reported outcomes and to establish metrics that define clinical benefit, Dr. Spana said
“Vyleesi was approved by the FDA after a thorough analysis of data from two well-controlled phase 3 clinical studies and multiple clinical and preclinical safety studies,” he said. “The analyses in the New Drug Application were prespecified and conducted according to a statistical analysis plan that the sponsor and FDA agreed to prior to database lock.”
Dr. Spielmans disclosed holdings in Vanguard Healthcare, a mutual fund that invests in pharmaceutical firms. Dr. Clayton has received financial support from Palatin and AMAG Pharmaceuticals, the companies that developed bremelanotide, in previous years.
Dr. Spielmans, professor of psychology at Metropolitan State University in Saint Paul, Minn., examined data from the FDA application for bremelanotide, clinicaltrials.gov entries for two phase 3 trials of the drug, and a 2019 article published in Obstetrics & Gynecology that described results from the 24-week trials.
In Dr. Speilman’s analysis, which was published online March 7 in the Journal of Sex Research, he notes that 42.1% of trial participants who received bremelanotide did not complete the trial, compared with 20.48% of participants who received placebo.
Of those who completed the study, 87.22% who received placebo wanted to continue treatment in an open-label extension, compared with 69.97% who received bremelanotide, he wrote.
Women “should be aware of the small degree of bremelanotide’s efficacy, that the protocol-specified outcomes of bremelanotide are mostly unknown, and that participants would rather take a placebo than bremelanotide,” Dr. Spielmans said.
Anita H. Clayton, MD, an author of the Obstetrics & Gynecology paper addressed in Dr. Spielmans’ analysis, says the Journal of Sex Research article does not provide new information and is a disservice to women because it questions accurate scientific data.
Measuring outcomes in HSDD is an evolving field, Dr. Clayton, a psychiatrist at the University of Virginia in Charlottesville, said in an interview. Initial FDA guidance relied on satisfying sexual events as an outcome measure, but this measure was derived from erectile dysfunction studies and is not necessarily adequate for assessing HSDD, she said. The FDA and drug developers agreed to use the desire subscale of the Female Sexual Function Index (FSFI-D) as a coprimary outcome measure instead, she noted.
Dr. Spielmans’ critique of Obstetrics & Gynecology paper
The article published in Obstetrics & Gynecology reporting bremelanotide trial results was noteworthy, although the various issues involved can be seen in reports about other drug trials, Dr. Spielmans said in an interview.
“It is well-established that journal articles reporting clinical trial data overstate benefits and understate harms,” he continued. In this case, “the very incomplete data reporting, reliance on many post-hoc measures of questionable validity, hiding the concerning number of dropouts due to adverse events, and putting a positive spin on efficacy and tolerability is both remarkable and highly problematic,” Dr. Spielmans said.
Dr. Clayton’s reaction
Data about dropout rates due to adverse events have been reported and presented at national meetings, she said in an interview. In addition, a questionnaire found that bremelanotide was superior to placebo in terms of patients feeling that the treatment had provided clinically meaningful benefit, Dr. Clayton said.
The available information enables patients to make informed treatment decisions, Dr. Clayton continued. “There is really this sexist attitude of women needing protection from their own decisions,” she said.
Diagnosing and treating HSDD
Eight of 11 efficacy outcomes in the clinicaltrials.gov study protocols for bremelanotide were not reported in the Obstetrics & Gynecology article in a way that was consistent with the protocols, Dr. Spielmans said. Changing a coprimary outcome to the key secondary outcome “occurred over a year after the trials had begun,” and the authors of the journal article “did not mention that this change occurred,” Dr. Spielmans wrote.
For the coprimary outcome measures of mean change on FSFI-D and Female Sexual Distress Scale–Desire/Arousal/Orgasm #13, “bremelanotide offers modest benefits over placebo,” Dr. Spielmans reported.
In addition to outlining his concerns about transparency in the reporting of trial data and raising questions about the outcome measures used in the Obstetrics & Gynecology article, Dr. Spielmans wrote that the diagnosis of HSDD is problematic.
“The lack of specifying symptom duration, questionable validity for the lack of sexual fantasies as a diagnostic criterion, difficulty in disentangling individual sexual problems from relational problems, and the failure to consider cultural influence (including the pressure on women to satisfy the sexual desires of their male partners) in the experience of sexuality all render HSDD as a problematic entity,” Dr. Spielmans wrote.
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders replaced HSDD and female sexual arousal disorder with the combined condition female sexual interest/arousal disorder. HSDD is in the 11th edition of the International Classification of Diseases and can be applied to men or women, Dr. Spielmans said.
FDA acknowledged HSDD as an unmet medical need
Dr. Clayton pointed out that HSDD was described decades ago and the FDA acknowledged it as an unmet medical need, and she expressed dissatisfaction with the fact the hypoactive sexual desire disorder appears with quotation marks around it in the title of Dr. Spielmans’ article. This way of presenting HSDD indicates that “the author has no concept of sexual health or sexual dysfunction,” Dr. Clayton said. “Basically this is sort of a dramatic tool, I think, to act like this is not a real disorder,” she added.
Carl Spana, PhD, CEO and president of Palatin Technologies, the developer of bremelanotide, defined the article in the Journal of Sex Research as a “retrospective meta-analysis, and not a re-analysis of the data.
“As a meta-analysis, it is open to various interpretations and reflects the author’s interpretations, which appear to have clear biases,” Dr. Spana said in an interview. “We believe several of this author’s interpretations are contrary to the FDA’s positive assessment that led to Vyleesi’s approval as a safe and effective treatment for women suffering from hypoactive sexual desire disorder.”
The author is unaware of the validation that was conducted at the direction of the FDA to establish clinically meaningful cutoffs for patient-reported outcomes and to establish metrics that define clinical benefit, Dr. Spana said
“Vyleesi was approved by the FDA after a thorough analysis of data from two well-controlled phase 3 clinical studies and multiple clinical and preclinical safety studies,” he said. “The analyses in the New Drug Application were prespecified and conducted according to a statistical analysis plan that the sponsor and FDA agreed to prior to database lock.”
Dr. Spielmans disclosed holdings in Vanguard Healthcare, a mutual fund that invests in pharmaceutical firms. Dr. Clayton has received financial support from Palatin and AMAG Pharmaceuticals, the companies that developed bremelanotide, in previous years.
FROM THE JOURNAL OF SEX RESEARCH












