User login
Two regenerative techniques prove comparable for repairing knee cartilage
When it comes to repairing knee cartilage, a new study found no significant differences between autologous matrix-induced chondrogenesis (AMIC) and autologous chondrocyte implantation with a collagen membrane (ACI-C) as treatment options.
“If the conclusion of the present study stands and is confirmed by further clinical trials, AMIC could be considered an equal alternative to techniques based on chondrocyte transplantation for treatment of cartilage defects of the knee,” wrote Vegard Fossum, MD, of University Hospital of North Norway, Tromsø, and coauthors, adding that cost and comparative ease might actually make AMIC the preferred choice. The study was published in the Orthopaedic Journal of Sports Medicine.
To evaluate outcomes of the two procedures, the researchers initiated a clinical trial of 41 patients with at least one chondral or osteochondral defect of the distal femur or patella. They were split into two groups: those treated with ACI-C (n = 21) and those treated with AMIC (n = 20). At 1- and 2-year follow-up, patients were assessed via improvements in Knee Injury and Osteoarthritis Outcome Score (KOOS), compared with baseline, along with Lysholm and visual analog scale (VAS) pain scores.
After 1 and 2 years, both groups saw improvements from baseline. At 2 years, the AMIC group had an 18.1 change in KOOS, compared with 10.3 in the ACI-C group (P = .17). Two-year improvements on the Lysholm score (19.7 in AMIC, compared with 17.0 in ACI-C, P = .66) and VAS pain score (30.6 in AMIC versus 19.6 in ACI-C, P = .19) were not significantly different. Two patients in the AMIC group had undergone total knee replacement after 2 years, compared with zero in the ACI-C group.
The authors noted their study’s potential limitations, including the small number of patients in each group – the initial plan was to include 80 total – and its broad inclusion criteria. However, since the aim was to compare treatment results and not evaluate effectiveness, they did not consider the broad criteria “a major limitation.”
The authors reported no conflicts of interest.
SOURCE: Fossum V et al. Orthop J Sports Med. 2019 Sept 17. doi: 10.1177/2325967119868212.
When it comes to repairing knee cartilage, a new study found no significant differences between autologous matrix-induced chondrogenesis (AMIC) and autologous chondrocyte implantation with a collagen membrane (ACI-C) as treatment options.
“If the conclusion of the present study stands and is confirmed by further clinical trials, AMIC could be considered an equal alternative to techniques based on chondrocyte transplantation for treatment of cartilage defects of the knee,” wrote Vegard Fossum, MD, of University Hospital of North Norway, Tromsø, and coauthors, adding that cost and comparative ease might actually make AMIC the preferred choice. The study was published in the Orthopaedic Journal of Sports Medicine.
To evaluate outcomes of the two procedures, the researchers initiated a clinical trial of 41 patients with at least one chondral or osteochondral defect of the distal femur or patella. They were split into two groups: those treated with ACI-C (n = 21) and those treated with AMIC (n = 20). At 1- and 2-year follow-up, patients were assessed via improvements in Knee Injury and Osteoarthritis Outcome Score (KOOS), compared with baseline, along with Lysholm and visual analog scale (VAS) pain scores.
After 1 and 2 years, both groups saw improvements from baseline. At 2 years, the AMIC group had an 18.1 change in KOOS, compared with 10.3 in the ACI-C group (P = .17). Two-year improvements on the Lysholm score (19.7 in AMIC, compared with 17.0 in ACI-C, P = .66) and VAS pain score (30.6 in AMIC versus 19.6 in ACI-C, P = .19) were not significantly different. Two patients in the AMIC group had undergone total knee replacement after 2 years, compared with zero in the ACI-C group.
The authors noted their study’s potential limitations, including the small number of patients in each group – the initial plan was to include 80 total – and its broad inclusion criteria. However, since the aim was to compare treatment results and not evaluate effectiveness, they did not consider the broad criteria “a major limitation.”
The authors reported no conflicts of interest.
SOURCE: Fossum V et al. Orthop J Sports Med. 2019 Sept 17. doi: 10.1177/2325967119868212.
When it comes to repairing knee cartilage, a new study found no significant differences between autologous matrix-induced chondrogenesis (AMIC) and autologous chondrocyte implantation with a collagen membrane (ACI-C) as treatment options.
“If the conclusion of the present study stands and is confirmed by further clinical trials, AMIC could be considered an equal alternative to techniques based on chondrocyte transplantation for treatment of cartilage defects of the knee,” wrote Vegard Fossum, MD, of University Hospital of North Norway, Tromsø, and coauthors, adding that cost and comparative ease might actually make AMIC the preferred choice. The study was published in the Orthopaedic Journal of Sports Medicine.
To evaluate outcomes of the two procedures, the researchers initiated a clinical trial of 41 patients with at least one chondral or osteochondral defect of the distal femur or patella. They were split into two groups: those treated with ACI-C (n = 21) and those treated with AMIC (n = 20). At 1- and 2-year follow-up, patients were assessed via improvements in Knee Injury and Osteoarthritis Outcome Score (KOOS), compared with baseline, along with Lysholm and visual analog scale (VAS) pain scores.
After 1 and 2 years, both groups saw improvements from baseline. At 2 years, the AMIC group had an 18.1 change in KOOS, compared with 10.3 in the ACI-C group (P = .17). Two-year improvements on the Lysholm score (19.7 in AMIC, compared with 17.0 in ACI-C, P = .66) and VAS pain score (30.6 in AMIC versus 19.6 in ACI-C, P = .19) were not significantly different. Two patients in the AMIC group had undergone total knee replacement after 2 years, compared with zero in the ACI-C group.
The authors noted their study’s potential limitations, including the small number of patients in each group – the initial plan was to include 80 total – and its broad inclusion criteria. However, since the aim was to compare treatment results and not evaluate effectiveness, they did not consider the broad criteria “a major limitation.”
The authors reported no conflicts of interest.
SOURCE: Fossum V et al. Orthop J Sports Med. 2019 Sept 17. doi: 10.1177/2325967119868212.
FROM THE ORTHOPAEDIC JOURNAL OF SPORTS MEDICINE
No infection increase seen with biologics in older psoriasis patients
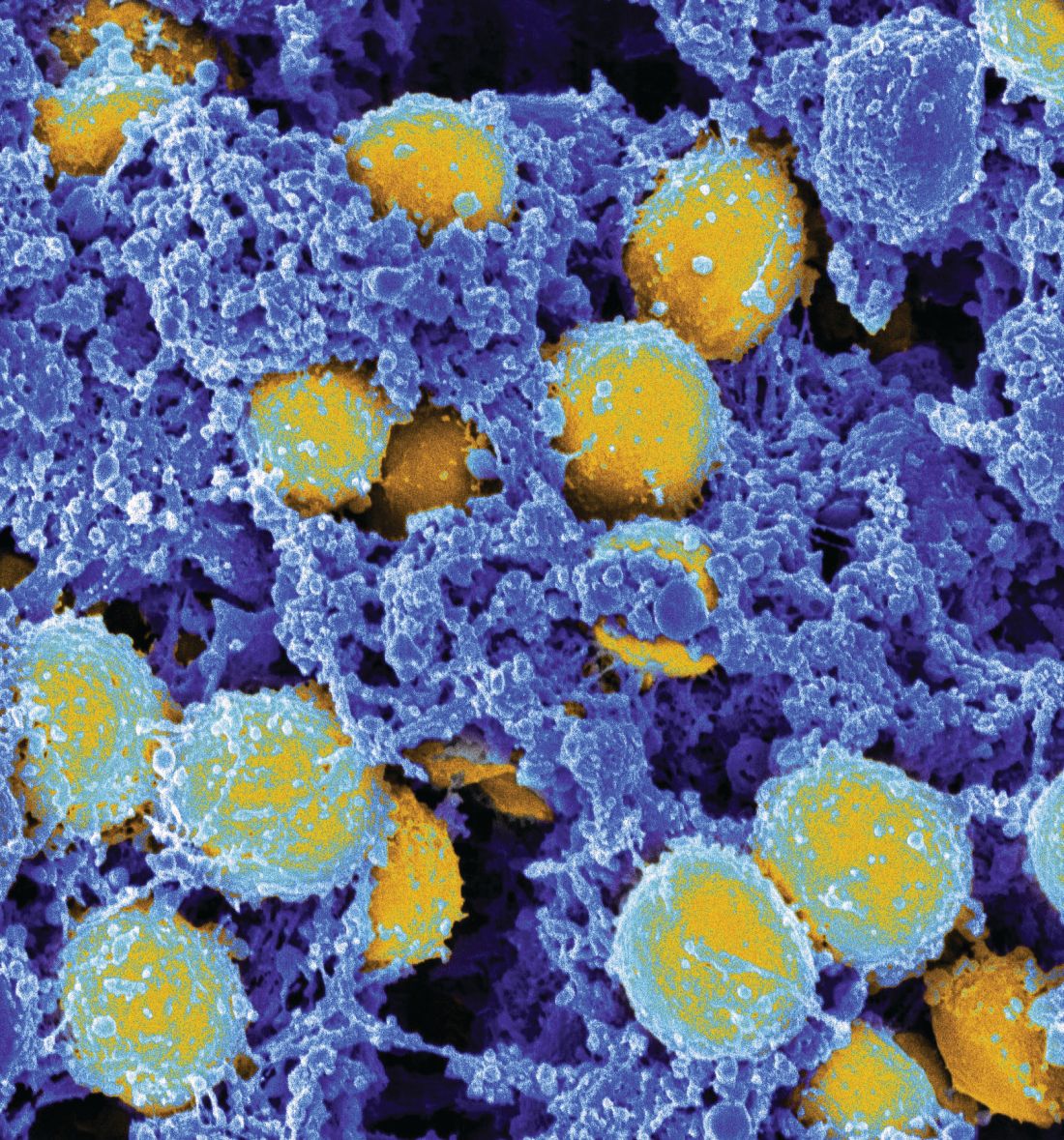
MADRID – Psoriasis patients aged 65 years and older are at more than twice the risk of serious bacterial and opportunistic infections, compared with younger patients, but that risk is not further elevated by being on biologic agents, Joseph F. Merola, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
He presented a large, The study implications, he said, are clear: When moderate to severe psoriasis warrants consideration of highly effective biologic therapies, that therapeutic option shouldn’t be taken off the table on the basis of a mistaken belief that biologics pose a greater infection risk just because the affected patient is over age 65 years.
“We really think that older patients should be offered treatments at the same level of disease control as all the rest of our psoriasis patients, in the context of shared decision making,” said Dr. Merola, a dermatologist and rheumatologist who is the director of the Center for Skin and Related Musculoskeletal Diseases at Brigham and Women’s Hospital, Boston.
The study utilized longitudinal claims data from a very large U.S. database covering the years 2003-2017. Among the 185 million covered lives were 1.1 million individuals with psoriasis, including 150,000 aged 65 years or older. After excluding older psoriasis patients with comorbid cancer or autoimmune disease, the investigators were left with 11,218 older psoriasis patients initiating systemic therapy for the first time and therefore eligible for propensity score matching using a highly accurate proprietary platform. The final study population consisted of 2,795 older psoriasis patients newly initiating biologic therapy, 2,795 others newly initiating nonbiologic systemic agents, and 2,529 seniors starting phototherapy. The matching was based upon factors including age, sex, prior infections, comorbid psoriatic arthritis, diabetes, and obesity.
The primary study endpoint was the rate of serious bacterial or opportunistic infections requiring hospitalization during the first 6 months of treatment. The bottom line: The rates were closely similar across all three groups, with the most common serious infections being pneumonia and cellulitis.
In contrast, among a population of 115,047 senior psoriasis patients who never used systemic therapy, the risk of serious infection was 12.2 events per 1,000 patients over 6 months, compared with 5.3 events in 120,174 matched controls without psoriasis. That translates to a 2.24-fold increased risk.
One audience member commented that a limitation of the study was that all biologics were lumped together. He would expect that the tumor necrosis factor inhibitors, for example, would be associated with a significantly higher serious infection risk than biologics with other targets.
Dr. Merola conceded the point, adding that the investigators are trying to reanalyze the data in a more granular way to address that shortcoming. Other study limitations included an inability to access the specific doses of systemic treatments used or to stratify patients by disease severity.
Another audience member noted that dermatologists often reassure surgeons that there’s no increased risk of infection associated with psoriasis when in fact there is increased risk in older psoriasis patients, according to these new data.
“We’re not trying to send a message to surgeons to withhold a knee transplant because of a psoriasis plaque over the knee,” Dr. Merola replied. “I think we’ve all been there; we’ve all fought that battle.” Based on the data, he said, he would advise that “our patients who need to be on systemics should remain appropriately on systemics as we see fit.”
The study was entirely funded by Brigham and Women’s Hospital. Dr. Merola reported serving as a consultant to and/or recipient of research grants from nearly two dozen pharmaceutical companies.
MADRID – Psoriasis patients aged 65 years and older are at more than twice the risk of serious bacterial and opportunistic infections, compared with younger patients, but that risk is not further elevated by being on biologic agents, Joseph F. Merola, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
He presented a large, The study implications, he said, are clear: When moderate to severe psoriasis warrants consideration of highly effective biologic therapies, that therapeutic option shouldn’t be taken off the table on the basis of a mistaken belief that biologics pose a greater infection risk just because the affected patient is over age 65 years.
“We really think that older patients should be offered treatments at the same level of disease control as all the rest of our psoriasis patients, in the context of shared decision making,” said Dr. Merola, a dermatologist and rheumatologist who is the director of the Center for Skin and Related Musculoskeletal Diseases at Brigham and Women’s Hospital, Boston.
The study utilized longitudinal claims data from a very large U.S. database covering the years 2003-2017. Among the 185 million covered lives were 1.1 million individuals with psoriasis, including 150,000 aged 65 years or older. After excluding older psoriasis patients with comorbid cancer or autoimmune disease, the investigators were left with 11,218 older psoriasis patients initiating systemic therapy for the first time and therefore eligible for propensity score matching using a highly accurate proprietary platform. The final study population consisted of 2,795 older psoriasis patients newly initiating biologic therapy, 2,795 others newly initiating nonbiologic systemic agents, and 2,529 seniors starting phototherapy. The matching was based upon factors including age, sex, prior infections, comorbid psoriatic arthritis, diabetes, and obesity.
The primary study endpoint was the rate of serious bacterial or opportunistic infections requiring hospitalization during the first 6 months of treatment. The bottom line: The rates were closely similar across all three groups, with the most common serious infections being pneumonia and cellulitis.
In contrast, among a population of 115,047 senior psoriasis patients who never used systemic therapy, the risk of serious infection was 12.2 events per 1,000 patients over 6 months, compared with 5.3 events in 120,174 matched controls without psoriasis. That translates to a 2.24-fold increased risk.
One audience member commented that a limitation of the study was that all biologics were lumped together. He would expect that the tumor necrosis factor inhibitors, for example, would be associated with a significantly higher serious infection risk than biologics with other targets.
Dr. Merola conceded the point, adding that the investigators are trying to reanalyze the data in a more granular way to address that shortcoming. Other study limitations included an inability to access the specific doses of systemic treatments used or to stratify patients by disease severity.
Another audience member noted that dermatologists often reassure surgeons that there’s no increased risk of infection associated with psoriasis when in fact there is increased risk in older psoriasis patients, according to these new data.
“We’re not trying to send a message to surgeons to withhold a knee transplant because of a psoriasis plaque over the knee,” Dr. Merola replied. “I think we’ve all been there; we’ve all fought that battle.” Based on the data, he said, he would advise that “our patients who need to be on systemics should remain appropriately on systemics as we see fit.”
The study was entirely funded by Brigham and Women’s Hospital. Dr. Merola reported serving as a consultant to and/or recipient of research grants from nearly two dozen pharmaceutical companies.
MADRID – Psoriasis patients aged 65 years and older are at more than twice the risk of serious bacterial and opportunistic infections, compared with younger patients, but that risk is not further elevated by being on biologic agents, Joseph F. Merola, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
He presented a large, The study implications, he said, are clear: When moderate to severe psoriasis warrants consideration of highly effective biologic therapies, that therapeutic option shouldn’t be taken off the table on the basis of a mistaken belief that biologics pose a greater infection risk just because the affected patient is over age 65 years.
“We really think that older patients should be offered treatments at the same level of disease control as all the rest of our psoriasis patients, in the context of shared decision making,” said Dr. Merola, a dermatologist and rheumatologist who is the director of the Center for Skin and Related Musculoskeletal Diseases at Brigham and Women’s Hospital, Boston.
The study utilized longitudinal claims data from a very large U.S. database covering the years 2003-2017. Among the 185 million covered lives were 1.1 million individuals with psoriasis, including 150,000 aged 65 years or older. After excluding older psoriasis patients with comorbid cancer or autoimmune disease, the investigators were left with 11,218 older psoriasis patients initiating systemic therapy for the first time and therefore eligible for propensity score matching using a highly accurate proprietary platform. The final study population consisted of 2,795 older psoriasis patients newly initiating biologic therapy, 2,795 others newly initiating nonbiologic systemic agents, and 2,529 seniors starting phototherapy. The matching was based upon factors including age, sex, prior infections, comorbid psoriatic arthritis, diabetes, and obesity.
The primary study endpoint was the rate of serious bacterial or opportunistic infections requiring hospitalization during the first 6 months of treatment. The bottom line: The rates were closely similar across all three groups, with the most common serious infections being pneumonia and cellulitis.
In contrast, among a population of 115,047 senior psoriasis patients who never used systemic therapy, the risk of serious infection was 12.2 events per 1,000 patients over 6 months, compared with 5.3 events in 120,174 matched controls without psoriasis. That translates to a 2.24-fold increased risk.
One audience member commented that a limitation of the study was that all biologics were lumped together. He would expect that the tumor necrosis factor inhibitors, for example, would be associated with a significantly higher serious infection risk than biologics with other targets.
Dr. Merola conceded the point, adding that the investigators are trying to reanalyze the data in a more granular way to address that shortcoming. Other study limitations included an inability to access the specific doses of systemic treatments used or to stratify patients by disease severity.
Another audience member noted that dermatologists often reassure surgeons that there’s no increased risk of infection associated with psoriasis when in fact there is increased risk in older psoriasis patients, according to these new data.
“We’re not trying to send a message to surgeons to withhold a knee transplant because of a psoriasis plaque over the knee,” Dr. Merola replied. “I think we’ve all been there; we’ve all fought that battle.” Based on the data, he said, he would advise that “our patients who need to be on systemics should remain appropriately on systemics as we see fit.”
The study was entirely funded by Brigham and Women’s Hospital. Dr. Merola reported serving as a consultant to and/or recipient of research grants from nearly two dozen pharmaceutical companies.
REPORTING FROM EADV 2019
Preop IV dexamethasone conveys relief after total knee surgery
Patients given a single preoperative dose of intravenous dexamethasone had significantly less pain after total knee arthroplasty than did those given a placebo in a randomized controlled study of 100 adults.
“Corticosteroids were introduced several years ago for relieving postoperative pain in total joint replacement but, unfortunately, are not widely used due to surgeons’ concerns and the limited supporting evidence,” wrote Nattapol Tammachote, MD, of Thammasat University, Khlong Luang, Pathumthani, Thailand, and colleagues.
In a study published in the Journal of Arthroplasty, the researchers randomized 50 adults undergoing unilateral total knee surgery to a preoperative IV dexamethasone dose of 0.15 mg/kg diluted with normal saline or saline placebo. Patients, who were aged 50-85 years, were assessed every 3 hours after surgery, up to 48 hours; the primary outcomes were pain level, using the visual analog pain scale (VAS), and morphine use.
Overall, patients in the treatment group reported significant reductions on the VAS in mean pain scores of 11 points at rest and 15 points with knee movement. No significant differences in morphine use were noted between groups overall or at 12-hour intervals post-surgery.
In the first 24-48 hours after surgery dexamethasone was associated with a significantly lower rate of nausea and vomiting vs. placebo (58% vs. 84%), and a lower average C-reactive protein level (89 mg/L vs. 167 mg/L) at 48 hours after surgery. Hospital stays averaged 3 days for both groups, and no wound infections were reported.
Scores on tests of knee function using the modified Western Ontario and McMaster University Osteoarthritis Index scores and range of motion of the knee at three months were similar between the groups.
The study findings were limited by several factors, including the small sample size and use of multimodal pain control that may have impacted morphine use, a lack of data on hyperglycemia, and variation in doses of ketorolac given to patients in both groups, the researchers noted.
The results nevertheless support the potential of preoperative dexamethasone as “a promising approach in postoperative pain management and may be suitable for patients with contraindication to multimodal pain regimens,” they concluded.
The researchers reported no financial conflicts.
SOURCE: Tammachote N et al. J Arthroplasty. 2019. doi: https://doi.org/10.1016/ j.arth.2019.09.002.
Patients given a single preoperative dose of intravenous dexamethasone had significantly less pain after total knee arthroplasty than did those given a placebo in a randomized controlled study of 100 adults.
“Corticosteroids were introduced several years ago for relieving postoperative pain in total joint replacement but, unfortunately, are not widely used due to surgeons’ concerns and the limited supporting evidence,” wrote Nattapol Tammachote, MD, of Thammasat University, Khlong Luang, Pathumthani, Thailand, and colleagues.
In a study published in the Journal of Arthroplasty, the researchers randomized 50 adults undergoing unilateral total knee surgery to a preoperative IV dexamethasone dose of 0.15 mg/kg diluted with normal saline or saline placebo. Patients, who were aged 50-85 years, were assessed every 3 hours after surgery, up to 48 hours; the primary outcomes were pain level, using the visual analog pain scale (VAS), and morphine use.
Overall, patients in the treatment group reported significant reductions on the VAS in mean pain scores of 11 points at rest and 15 points with knee movement. No significant differences in morphine use were noted between groups overall or at 12-hour intervals post-surgery.
In the first 24-48 hours after surgery dexamethasone was associated with a significantly lower rate of nausea and vomiting vs. placebo (58% vs. 84%), and a lower average C-reactive protein level (89 mg/L vs. 167 mg/L) at 48 hours after surgery. Hospital stays averaged 3 days for both groups, and no wound infections were reported.
Scores on tests of knee function using the modified Western Ontario and McMaster University Osteoarthritis Index scores and range of motion of the knee at three months were similar between the groups.
The study findings were limited by several factors, including the small sample size and use of multimodal pain control that may have impacted morphine use, a lack of data on hyperglycemia, and variation in doses of ketorolac given to patients in both groups, the researchers noted.
The results nevertheless support the potential of preoperative dexamethasone as “a promising approach in postoperative pain management and may be suitable for patients with contraindication to multimodal pain regimens,” they concluded.
The researchers reported no financial conflicts.
SOURCE: Tammachote N et al. J Arthroplasty. 2019. doi: https://doi.org/10.1016/ j.arth.2019.09.002.
Patients given a single preoperative dose of intravenous dexamethasone had significantly less pain after total knee arthroplasty than did those given a placebo in a randomized controlled study of 100 adults.
“Corticosteroids were introduced several years ago for relieving postoperative pain in total joint replacement but, unfortunately, are not widely used due to surgeons’ concerns and the limited supporting evidence,” wrote Nattapol Tammachote, MD, of Thammasat University, Khlong Luang, Pathumthani, Thailand, and colleagues.
In a study published in the Journal of Arthroplasty, the researchers randomized 50 adults undergoing unilateral total knee surgery to a preoperative IV dexamethasone dose of 0.15 mg/kg diluted with normal saline or saline placebo. Patients, who were aged 50-85 years, were assessed every 3 hours after surgery, up to 48 hours; the primary outcomes were pain level, using the visual analog pain scale (VAS), and morphine use.
Overall, patients in the treatment group reported significant reductions on the VAS in mean pain scores of 11 points at rest and 15 points with knee movement. No significant differences in morphine use were noted between groups overall or at 12-hour intervals post-surgery.
In the first 24-48 hours after surgery dexamethasone was associated with a significantly lower rate of nausea and vomiting vs. placebo (58% vs. 84%), and a lower average C-reactive protein level (89 mg/L vs. 167 mg/L) at 48 hours after surgery. Hospital stays averaged 3 days for both groups, and no wound infections were reported.
Scores on tests of knee function using the modified Western Ontario and McMaster University Osteoarthritis Index scores and range of motion of the knee at three months were similar between the groups.
The study findings were limited by several factors, including the small sample size and use of multimodal pain control that may have impacted morphine use, a lack of data on hyperglycemia, and variation in doses of ketorolac given to patients in both groups, the researchers noted.
The results nevertheless support the potential of preoperative dexamethasone as “a promising approach in postoperative pain management and may be suitable for patients with contraindication to multimodal pain regimens,” they concluded.
The researchers reported no financial conflicts.
SOURCE: Tammachote N et al. J Arthroplasty. 2019. doi: https://doi.org/10.1016/ j.arth.2019.09.002.
FROM THE JOURNAL OF ARTHROPLASTY
Cannabinoids, stem cells lack evidence for osteoarthritis, expert says
LAS VEGAS – Planned clinical trials may clarify whether they benefit patients, said Joel A. Block, MD, professor of rheumatology at Rush University in Chicago.
Cannabinoid therapy “is on everybody’s mind, including our patients,” Dr. Block said at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education. “Cannabinoid receptors are widely present in all joint tissues, and endocannabinoids are clearly present in OA joint tissue. There is good evidence that the receptors regulate pain responses and central sensitization in a variety of OA animal models.” Where cannabis is legal, many people use it for chronic noncancer pain. Side effects may include altered perception, dizziness, drowsiness, and gastrointestinal adverse events.
Cannabis in the literature
“Nonetheless, if you do a systematic review of all of the randomized clinical trials of cannabinoids in human rheumatic diseases, what you will find is there is a grand total of four,” he said. The trials included patients with rheumatoid arthritis, OA, and fibromyalgia. An analysis of aggregated data found that cannabinoids improved pain and sleep, but all of the trials had a high risk of bias, poor allocation concealment, and poor blinding, said Dr. Block (Arthritis Care Res [Hoboken]. 2016 May;68[5]:681-8.). “In OA, there is one randomized trial, and it was entirely null,” he said. “There was no positive effect on pain or on function in human OA” (Pain. 2012 Sep;153[9]:1837-46.).
ClinicalTrials.gov lists two planned randomized controlled trials of cannabinoids – one using vaporized cannabis in patients with knee OA, and one using cannabidiol for hand OA and psoriatic arthritis. “Clinical trials are still scarce as of right now, so it will take a while before we have evidence for or against,” said Dr. Block.
Stem cell injections
Intra-articular stem cell injections are widely offered in the United States and abroad, he said. “In every newspaper, wherever I go, I open it up and there are full-page ads on stem cell injections that will cure everything that you want,” he said.
A systematic review of the effect of stem cell injections on structural outcomes and pain-related behaviors in animals found that “for all outcomes, the evidence quality was either low or very low,” Dr. Block said (Osteoarthritis Cartilage. 2018 Apr;26[4]:445-61.). “Even in the animal models, it has been very hard to demonstrate any effect at all from just injecting stem cells into the joint.”
Systematic reviews of the evidence in humans have found that the data do not support the use of stem cell injections. The authors of one review concluded, “In the absence of high-level evidence, we do not recommend stem cell therapy” for knee OA (Br J Sports Med. 2017 Aug;51[15]:1125-33.).
For another recent review, researchers screened hundreds of articles and identified 5 trials that met their inclusion criteria. They concluded, “Current evidence does not support the use of intra-articular [mesenchymal stem cells] for improving cartilage repair in knee osteoarthritis” (Arch Orthop Trauma Surg. 2019 Jul;139[7]:971-80.).
Many clinical trials are planned, however. “Over the next several years, I would expect that we are going to get some real data on whether these are helpful or not,” Dr. Block said.
Meanwhile, some patients spend thousands of dollars to receive stem cell injections, and clinics report average patient satisfaction rates of 82%. “How can they be getting so much relief when there is no evidence that it is helpful? In fact, whatever evidence we have says that it is no better than placebo,” said Dr. Block. “Placebo itself is very potent....People always do what they feel helps them regardless of objective data, because placebo itself is very palliative.”
Dr. Block is a consultant for GlaxoSmithKline, Medivir, and Zynerba Pharmaceuticals. He has received royalties from Agios, Daiichi Sankyo, and Omeros. In addition, he has received grant or research support from AbbVie, Janssen, Novartis, Pfizer, and Kolon TissueGene.
Global Academy for Medical Education and this news organization are owned by the same parent company.
LAS VEGAS – Planned clinical trials may clarify whether they benefit patients, said Joel A. Block, MD, professor of rheumatology at Rush University in Chicago.
Cannabinoid therapy “is on everybody’s mind, including our patients,” Dr. Block said at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education. “Cannabinoid receptors are widely present in all joint tissues, and endocannabinoids are clearly present in OA joint tissue. There is good evidence that the receptors regulate pain responses and central sensitization in a variety of OA animal models.” Where cannabis is legal, many people use it for chronic noncancer pain. Side effects may include altered perception, dizziness, drowsiness, and gastrointestinal adverse events.
Cannabis in the literature
“Nonetheless, if you do a systematic review of all of the randomized clinical trials of cannabinoids in human rheumatic diseases, what you will find is there is a grand total of four,” he said. The trials included patients with rheumatoid arthritis, OA, and fibromyalgia. An analysis of aggregated data found that cannabinoids improved pain and sleep, but all of the trials had a high risk of bias, poor allocation concealment, and poor blinding, said Dr. Block (Arthritis Care Res [Hoboken]. 2016 May;68[5]:681-8.). “In OA, there is one randomized trial, and it was entirely null,” he said. “There was no positive effect on pain or on function in human OA” (Pain. 2012 Sep;153[9]:1837-46.).
ClinicalTrials.gov lists two planned randomized controlled trials of cannabinoids – one using vaporized cannabis in patients with knee OA, and one using cannabidiol for hand OA and psoriatic arthritis. “Clinical trials are still scarce as of right now, so it will take a while before we have evidence for or against,” said Dr. Block.
Stem cell injections
Intra-articular stem cell injections are widely offered in the United States and abroad, he said. “In every newspaper, wherever I go, I open it up and there are full-page ads on stem cell injections that will cure everything that you want,” he said.
A systematic review of the effect of stem cell injections on structural outcomes and pain-related behaviors in animals found that “for all outcomes, the evidence quality was either low or very low,” Dr. Block said (Osteoarthritis Cartilage. 2018 Apr;26[4]:445-61.). “Even in the animal models, it has been very hard to demonstrate any effect at all from just injecting stem cells into the joint.”
Systematic reviews of the evidence in humans have found that the data do not support the use of stem cell injections. The authors of one review concluded, “In the absence of high-level evidence, we do not recommend stem cell therapy” for knee OA (Br J Sports Med. 2017 Aug;51[15]:1125-33.).
For another recent review, researchers screened hundreds of articles and identified 5 trials that met their inclusion criteria. They concluded, “Current evidence does not support the use of intra-articular [mesenchymal stem cells] for improving cartilage repair in knee osteoarthritis” (Arch Orthop Trauma Surg. 2019 Jul;139[7]:971-80.).
Many clinical trials are planned, however. “Over the next several years, I would expect that we are going to get some real data on whether these are helpful or not,” Dr. Block said.
Meanwhile, some patients spend thousands of dollars to receive stem cell injections, and clinics report average patient satisfaction rates of 82%. “How can they be getting so much relief when there is no evidence that it is helpful? In fact, whatever evidence we have says that it is no better than placebo,” said Dr. Block. “Placebo itself is very potent....People always do what they feel helps them regardless of objective data, because placebo itself is very palliative.”
Dr. Block is a consultant for GlaxoSmithKline, Medivir, and Zynerba Pharmaceuticals. He has received royalties from Agios, Daiichi Sankyo, and Omeros. In addition, he has received grant or research support from AbbVie, Janssen, Novartis, Pfizer, and Kolon TissueGene.
Global Academy for Medical Education and this news organization are owned by the same parent company.
LAS VEGAS – Planned clinical trials may clarify whether they benefit patients, said Joel A. Block, MD, professor of rheumatology at Rush University in Chicago.
Cannabinoid therapy “is on everybody’s mind, including our patients,” Dr. Block said at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education. “Cannabinoid receptors are widely present in all joint tissues, and endocannabinoids are clearly present in OA joint tissue. There is good evidence that the receptors regulate pain responses and central sensitization in a variety of OA animal models.” Where cannabis is legal, many people use it for chronic noncancer pain. Side effects may include altered perception, dizziness, drowsiness, and gastrointestinal adverse events.
Cannabis in the literature
“Nonetheless, if you do a systematic review of all of the randomized clinical trials of cannabinoids in human rheumatic diseases, what you will find is there is a grand total of four,” he said. The trials included patients with rheumatoid arthritis, OA, and fibromyalgia. An analysis of aggregated data found that cannabinoids improved pain and sleep, but all of the trials had a high risk of bias, poor allocation concealment, and poor blinding, said Dr. Block (Arthritis Care Res [Hoboken]. 2016 May;68[5]:681-8.). “In OA, there is one randomized trial, and it was entirely null,” he said. “There was no positive effect on pain or on function in human OA” (Pain. 2012 Sep;153[9]:1837-46.).
ClinicalTrials.gov lists two planned randomized controlled trials of cannabinoids – one using vaporized cannabis in patients with knee OA, and one using cannabidiol for hand OA and psoriatic arthritis. “Clinical trials are still scarce as of right now, so it will take a while before we have evidence for or against,” said Dr. Block.
Stem cell injections
Intra-articular stem cell injections are widely offered in the United States and abroad, he said. “In every newspaper, wherever I go, I open it up and there are full-page ads on stem cell injections that will cure everything that you want,” he said.
A systematic review of the effect of stem cell injections on structural outcomes and pain-related behaviors in animals found that “for all outcomes, the evidence quality was either low or very low,” Dr. Block said (Osteoarthritis Cartilage. 2018 Apr;26[4]:445-61.). “Even in the animal models, it has been very hard to demonstrate any effect at all from just injecting stem cells into the joint.”
Systematic reviews of the evidence in humans have found that the data do not support the use of stem cell injections. The authors of one review concluded, “In the absence of high-level evidence, we do not recommend stem cell therapy” for knee OA (Br J Sports Med. 2017 Aug;51[15]:1125-33.).
For another recent review, researchers screened hundreds of articles and identified 5 trials that met their inclusion criteria. They concluded, “Current evidence does not support the use of intra-articular [mesenchymal stem cells] for improving cartilage repair in knee osteoarthritis” (Arch Orthop Trauma Surg. 2019 Jul;139[7]:971-80.).
Many clinical trials are planned, however. “Over the next several years, I would expect that we are going to get some real data on whether these are helpful or not,” Dr. Block said.
Meanwhile, some patients spend thousands of dollars to receive stem cell injections, and clinics report average patient satisfaction rates of 82%. “How can they be getting so much relief when there is no evidence that it is helpful? In fact, whatever evidence we have says that it is no better than placebo,” said Dr. Block. “Placebo itself is very potent....People always do what they feel helps them regardless of objective data, because placebo itself is very palliative.”
Dr. Block is a consultant for GlaxoSmithKline, Medivir, and Zynerba Pharmaceuticals. He has received royalties from Agios, Daiichi Sankyo, and Omeros. In addition, he has received grant or research support from AbbVie, Janssen, Novartis, Pfizer, and Kolon TissueGene.
Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM PRD 2019
Preop pain perceptions drive outcomes after knee surgery
Adult athletes who underwent knee surgery and had higher levels of preoperative pain catastrophizing were significantly less likely to return to preinjury activity, based on data from 101 individuals.
Pain is highly subjective, and pain perception can play a role in postsurgical outcomes, but the relationships among preoperative pain perception and short-term outcomes including returning to sports have not been well-studied, wrote Joshua S. Everhart, MD, of The Ohio State University Wexner Medical Center, Columbus, and colleagues.
In a study published in the Journal of Science and Medicine in Sport, the researchers assessed 101 adult athletes who underwent knee surgery at a single center. The average age of the patients was 33 years, and 49 were women.
Pain perception and coping were assessed via the McGill Pain questionnaire (SF-MPQ), Pain Catastrophizing Scale (PCS), Pain Coping Measure (PCM), and the brief COPE subscales of acceptance, denial, positive reframing, and use of instrumental support.
Patients who were severe pain catastrophizers (defined as scores greater than 36 on the Pain Catastrophizing Scale) had increased odds of not returning to a similar level of sport (OR 11.3).
Higher scores on the brief COPE subscale of “use of instrumental support” (instruments designed to help patients cope with pain) had a protective effect on returning to preinjury activity (OR 0.72 per point increase). However, higher COPE-denial scores were significantly associated with lower odds of improvement in kinesiophobia (OR 0.43).
Patients with greater levels of problem-focused coping had significantly greater improvement in International Knee Documentation Committee (IKDC) scores, as did patients who were older and more active.
“Specific coping strategies appear to moderate the effect of pain perceptions on postoperative outcomes, with some coping strategies being protective and others being harmful,” the researchers said.
The findings were limited by several factors including the use of multiple comparisons, the inability to assess the impact of pain perception after knee rehabilitation independent of surgery, and the small number of some uncommon procedures, the researchers noted.
However, the results suggest that “recognition of pain perception and coping styles early on in treatment may help sports medicine providers identify patients at risk for an unsatisfactory subjective outcome,” they concluded.
The researchers had no financial conflicts to disclose.
SOURCE: Everhart JS et al. J Sci Med Sport. 2019. doi: 10.1016/j.jsams.2019.09.011.
Adult athletes who underwent knee surgery and had higher levels of preoperative pain catastrophizing were significantly less likely to return to preinjury activity, based on data from 101 individuals.
Pain is highly subjective, and pain perception can play a role in postsurgical outcomes, but the relationships among preoperative pain perception and short-term outcomes including returning to sports have not been well-studied, wrote Joshua S. Everhart, MD, of The Ohio State University Wexner Medical Center, Columbus, and colleagues.
In a study published in the Journal of Science and Medicine in Sport, the researchers assessed 101 adult athletes who underwent knee surgery at a single center. The average age of the patients was 33 years, and 49 were women.
Pain perception and coping were assessed via the McGill Pain questionnaire (SF-MPQ), Pain Catastrophizing Scale (PCS), Pain Coping Measure (PCM), and the brief COPE subscales of acceptance, denial, positive reframing, and use of instrumental support.
Patients who were severe pain catastrophizers (defined as scores greater than 36 on the Pain Catastrophizing Scale) had increased odds of not returning to a similar level of sport (OR 11.3).
Higher scores on the brief COPE subscale of “use of instrumental support” (instruments designed to help patients cope with pain) had a protective effect on returning to preinjury activity (OR 0.72 per point increase). However, higher COPE-denial scores were significantly associated with lower odds of improvement in kinesiophobia (OR 0.43).
Patients with greater levels of problem-focused coping had significantly greater improvement in International Knee Documentation Committee (IKDC) scores, as did patients who were older and more active.
“Specific coping strategies appear to moderate the effect of pain perceptions on postoperative outcomes, with some coping strategies being protective and others being harmful,” the researchers said.
The findings were limited by several factors including the use of multiple comparisons, the inability to assess the impact of pain perception after knee rehabilitation independent of surgery, and the small number of some uncommon procedures, the researchers noted.
However, the results suggest that “recognition of pain perception and coping styles early on in treatment may help sports medicine providers identify patients at risk for an unsatisfactory subjective outcome,” they concluded.
The researchers had no financial conflicts to disclose.
SOURCE: Everhart JS et al. J Sci Med Sport. 2019. doi: 10.1016/j.jsams.2019.09.011.
Adult athletes who underwent knee surgery and had higher levels of preoperative pain catastrophizing were significantly less likely to return to preinjury activity, based on data from 101 individuals.
Pain is highly subjective, and pain perception can play a role in postsurgical outcomes, but the relationships among preoperative pain perception and short-term outcomes including returning to sports have not been well-studied, wrote Joshua S. Everhart, MD, of The Ohio State University Wexner Medical Center, Columbus, and colleagues.
In a study published in the Journal of Science and Medicine in Sport, the researchers assessed 101 adult athletes who underwent knee surgery at a single center. The average age of the patients was 33 years, and 49 were women.
Pain perception and coping were assessed via the McGill Pain questionnaire (SF-MPQ), Pain Catastrophizing Scale (PCS), Pain Coping Measure (PCM), and the brief COPE subscales of acceptance, denial, positive reframing, and use of instrumental support.
Patients who were severe pain catastrophizers (defined as scores greater than 36 on the Pain Catastrophizing Scale) had increased odds of not returning to a similar level of sport (OR 11.3).
Higher scores on the brief COPE subscale of “use of instrumental support” (instruments designed to help patients cope with pain) had a protective effect on returning to preinjury activity (OR 0.72 per point increase). However, higher COPE-denial scores were significantly associated with lower odds of improvement in kinesiophobia (OR 0.43).
Patients with greater levels of problem-focused coping had significantly greater improvement in International Knee Documentation Committee (IKDC) scores, as did patients who were older and more active.
“Specific coping strategies appear to moderate the effect of pain perceptions on postoperative outcomes, with some coping strategies being protective and others being harmful,” the researchers said.
The findings were limited by several factors including the use of multiple comparisons, the inability to assess the impact of pain perception after knee rehabilitation independent of surgery, and the small number of some uncommon procedures, the researchers noted.
However, the results suggest that “recognition of pain perception and coping styles early on in treatment may help sports medicine providers identify patients at risk for an unsatisfactory subjective outcome,” they concluded.
The researchers had no financial conflicts to disclose.
SOURCE: Everhart JS et al. J Sci Med Sport. 2019. doi: 10.1016/j.jsams.2019.09.011.
FROM THE JOURNAL OF SCIENCE AND MEDICINE IN SPORT
Consider centralized pain in patients with rheumatic disease
Las Vegas – A fibromyalgia survey may provide important information about the degree to which patients with rheumatic disease experience centralized pain. This information may guide treatment decisions, said Daniel J. Clauw, MD, professor of anesthesiology, rheumatology, and psychiatry and director of the Chronic Pain and Fatigue Research Center at the University of Michigan in Ann Arbor.
The questionnaire that Dr. Clauw uses is a patient self-report survey for the assessment of fibromyalgia based on criteria in the 2011 modification of the American College of Rheumatology preliminary diagnostic criteria for fibromyalgia. In it, he asks patients to report where they experience pain throughout the body and symptoms such as fatigue, sleep problems, and memory problems. The survey predicts outcomes of surgery for osteoarthritis better than x-rays, MRI scans, or psychological factors do, he said.
Physicians should ask every patient with chronic pain, including patients with OA, rheumatoid arthritis, or lupus, to complete the survey, Dr. Clauw said at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education. “This score will tell you the degree to which their central nervous system is augmenting or amplifying what is going on in their body,” he said. “And the higher their score is, the more you should treat them like you would someone with fibromyalgia, even if their underlying disease might be an autoimmune disease.”
Physicians should not use a cutoff of 13 points on the fibromyalgia measure to define whether a patient has the disease, as has been done in the past, he said. The threshold is arbitrary, he said. “We should not think about fibromyalgia as ‘yes’ or ‘no.’ We should think of the degree of fibromyalgia that people have.”
A poor relationship between pain and imaging
Some patients who have severe knee OA on imaging walk without pain. Other patients have normal x-rays, but severe pain. “There is a terrible relationship between what you see on a knee x-ray or an MRI and whether someone has pain,” Dr. Clauw said. Furthermore, the poor relationship between imaging and pain is common across chronic pain conditions, he said.
This phenomenon may occur because pain manifests in different ways, similar to there being multiple ways to adjust the volume of an electric guitar, he said. How hard the strings are strummed affects the volume. But so does the amplifier setting. “In these centralized pain conditions, the problem is an amplifier problem, not a guitar problem,” he said. “The amplifier, i.e., the central nervous system, is set too high.”
Researchers have found that people who have severe OA of the knee on x-ray but do not experience pain “have a very low amplifier setting,” he said. That is, they are nontender and less sensitive to pain. Most of these patients are men. “On average, men have a much lower amplifier setting than women,” he said. “This is also why ... women have 1.5 to 2 times the rate of any type of chronic pain than men, because on average women have a higher amplifier setting. ... In OA, at any given age, men and women have the exact same percentage of radiographic OA. But if you look at the clinical condition of OA, it is always two-thirds women, one-third men.”
Opioid responsiveness
To examine whether fibromyalgia survey results correlate with outcomes after knee and hip arthroplasty, Dr. Clauw and colleagues conducted a prospective, observational cohort study that included approximately 500 people. Patients completed the questionnaire on the day of surgery.
Patients with higher levels of fibromyalgia were less responsive to opioids. “For each 1-point increase in the fibromyalgia score, people needed about one more hydrocodone tablet in the first 24-48 hours to control their pain,” he said (Anesthesiology. 2013 Dec;119[6]:1434-43). In addition, each 1-point increase in the fibromyalgia score made people about 25% less likely to have a 50% improvement in knee pain level after 6 months (Arthritis Rheumatol. 2015 May;67[5]:1386-94). The correlations were independent of psychological factors. In addition, the associations were linear. “There was nothing magical about a fibromyalgia score of 13,” Dr. Clauw said.
Dr. Clauw is a coauthor of a study to be presented at the 2019 American College of Rheumatology/Association of Rheumatology Professionals annual meeting that found pain centralization in patients with RA is associated with poor response to disease-modifying antirheumatic drugs (DMARDs).
Prior studies in patients with RA have found that the degree of fibromyalgia is a better predictor of pain and disability than erythrocyte sedimentation rate or the number of swollen joints.
Diagnosed cases are the “tip of the iceberg”
Researchers at Dr. Clauw’s institution have identified dozens of patients undergoing knee surgery who met criteria for fibromyalgia but had not received the diagnosis. “This is at the University of Michigan, which is the epicenter for fibromyalgia research. If we are not seeing fibromyalgia superimposed on OA in our patients, no one is seeing it,” he said.
Patients with diagnosed fibromyalgia are “the tip of the iceberg,” he said. “There are far greater numbers of individuals whose primary diagnosis is OA, RA, lupus, ankylosing spondylitis, cancer pain, or sickle cell disease that have the same fundamental problem as fibromyalgia patients. But you do not see it because you label them as having an autoimmune disease or osteoarthritis. And that is at your peril and at their peril. Because treating that individual as if all of their pain and other symptoms are due to a problem out on the periphery will not make that person better.”
Patients with high levels of centralized pain may be less responsive to peripherally directed therapies such as surgery or injections, Dr. Clauw said. Pharmacologic options for patients with centralized pain include gabapentinoids (e.g., pregabalin and gabapentin), serotonin-norepinephrine reuptake inhibitors (e.g., duloxetine and milnacipran), and tricyclic compounds (e.g., amitriptyline and cyclobenzaprine), he said. “Opioids are going to be quite unlikely to help these individuals,” he said. “In fact, it is likely that opioids will make this kind of pain worse.”
Dr. Clauw is a consultant for Aptinyx, Daiichi Sankyo, Eli Lilly, Intec Pharma, Pfizer, Samumed, Theravance, Tonix, and Zynerba Pharma. He has received grant or research support from Aptinyx and Pfizer and is an expert witness.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Las Vegas – A fibromyalgia survey may provide important information about the degree to which patients with rheumatic disease experience centralized pain. This information may guide treatment decisions, said Daniel J. Clauw, MD, professor of anesthesiology, rheumatology, and psychiatry and director of the Chronic Pain and Fatigue Research Center at the University of Michigan in Ann Arbor.
The questionnaire that Dr. Clauw uses is a patient self-report survey for the assessment of fibromyalgia based on criteria in the 2011 modification of the American College of Rheumatology preliminary diagnostic criteria for fibromyalgia. In it, he asks patients to report where they experience pain throughout the body and symptoms such as fatigue, sleep problems, and memory problems. The survey predicts outcomes of surgery for osteoarthritis better than x-rays, MRI scans, or psychological factors do, he said.
Physicians should ask every patient with chronic pain, including patients with OA, rheumatoid arthritis, or lupus, to complete the survey, Dr. Clauw said at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education. “This score will tell you the degree to which their central nervous system is augmenting or amplifying what is going on in their body,” he said. “And the higher their score is, the more you should treat them like you would someone with fibromyalgia, even if their underlying disease might be an autoimmune disease.”
Physicians should not use a cutoff of 13 points on the fibromyalgia measure to define whether a patient has the disease, as has been done in the past, he said. The threshold is arbitrary, he said. “We should not think about fibromyalgia as ‘yes’ or ‘no.’ We should think of the degree of fibromyalgia that people have.”
A poor relationship between pain and imaging
Some patients who have severe knee OA on imaging walk without pain. Other patients have normal x-rays, but severe pain. “There is a terrible relationship between what you see on a knee x-ray or an MRI and whether someone has pain,” Dr. Clauw said. Furthermore, the poor relationship between imaging and pain is common across chronic pain conditions, he said.
This phenomenon may occur because pain manifests in different ways, similar to there being multiple ways to adjust the volume of an electric guitar, he said. How hard the strings are strummed affects the volume. But so does the amplifier setting. “In these centralized pain conditions, the problem is an amplifier problem, not a guitar problem,” he said. “The amplifier, i.e., the central nervous system, is set too high.”
Researchers have found that people who have severe OA of the knee on x-ray but do not experience pain “have a very low amplifier setting,” he said. That is, they are nontender and less sensitive to pain. Most of these patients are men. “On average, men have a much lower amplifier setting than women,” he said. “This is also why ... women have 1.5 to 2 times the rate of any type of chronic pain than men, because on average women have a higher amplifier setting. ... In OA, at any given age, men and women have the exact same percentage of radiographic OA. But if you look at the clinical condition of OA, it is always two-thirds women, one-third men.”
Opioid responsiveness
To examine whether fibromyalgia survey results correlate with outcomes after knee and hip arthroplasty, Dr. Clauw and colleagues conducted a prospective, observational cohort study that included approximately 500 people. Patients completed the questionnaire on the day of surgery.
Patients with higher levels of fibromyalgia were less responsive to opioids. “For each 1-point increase in the fibromyalgia score, people needed about one more hydrocodone tablet in the first 24-48 hours to control their pain,” he said (Anesthesiology. 2013 Dec;119[6]:1434-43). In addition, each 1-point increase in the fibromyalgia score made people about 25% less likely to have a 50% improvement in knee pain level after 6 months (Arthritis Rheumatol. 2015 May;67[5]:1386-94). The correlations were independent of psychological factors. In addition, the associations were linear. “There was nothing magical about a fibromyalgia score of 13,” Dr. Clauw said.
Dr. Clauw is a coauthor of a study to be presented at the 2019 American College of Rheumatology/Association of Rheumatology Professionals annual meeting that found pain centralization in patients with RA is associated with poor response to disease-modifying antirheumatic drugs (DMARDs).
Prior studies in patients with RA have found that the degree of fibromyalgia is a better predictor of pain and disability than erythrocyte sedimentation rate or the number of swollen joints.
Diagnosed cases are the “tip of the iceberg”
Researchers at Dr. Clauw’s institution have identified dozens of patients undergoing knee surgery who met criteria for fibromyalgia but had not received the diagnosis. “This is at the University of Michigan, which is the epicenter for fibromyalgia research. If we are not seeing fibromyalgia superimposed on OA in our patients, no one is seeing it,” he said.
Patients with diagnosed fibromyalgia are “the tip of the iceberg,” he said. “There are far greater numbers of individuals whose primary diagnosis is OA, RA, lupus, ankylosing spondylitis, cancer pain, or sickle cell disease that have the same fundamental problem as fibromyalgia patients. But you do not see it because you label them as having an autoimmune disease or osteoarthritis. And that is at your peril and at their peril. Because treating that individual as if all of their pain and other symptoms are due to a problem out on the periphery will not make that person better.”
Patients with high levels of centralized pain may be less responsive to peripherally directed therapies such as surgery or injections, Dr. Clauw said. Pharmacologic options for patients with centralized pain include gabapentinoids (e.g., pregabalin and gabapentin), serotonin-norepinephrine reuptake inhibitors (e.g., duloxetine and milnacipran), and tricyclic compounds (e.g., amitriptyline and cyclobenzaprine), he said. “Opioids are going to be quite unlikely to help these individuals,” he said. “In fact, it is likely that opioids will make this kind of pain worse.”
Dr. Clauw is a consultant for Aptinyx, Daiichi Sankyo, Eli Lilly, Intec Pharma, Pfizer, Samumed, Theravance, Tonix, and Zynerba Pharma. He has received grant or research support from Aptinyx and Pfizer and is an expert witness.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Las Vegas – A fibromyalgia survey may provide important information about the degree to which patients with rheumatic disease experience centralized pain. This information may guide treatment decisions, said Daniel J. Clauw, MD, professor of anesthesiology, rheumatology, and psychiatry and director of the Chronic Pain and Fatigue Research Center at the University of Michigan in Ann Arbor.
The questionnaire that Dr. Clauw uses is a patient self-report survey for the assessment of fibromyalgia based on criteria in the 2011 modification of the American College of Rheumatology preliminary diagnostic criteria for fibromyalgia. In it, he asks patients to report where they experience pain throughout the body and symptoms such as fatigue, sleep problems, and memory problems. The survey predicts outcomes of surgery for osteoarthritis better than x-rays, MRI scans, or psychological factors do, he said.
Physicians should ask every patient with chronic pain, including patients with OA, rheumatoid arthritis, or lupus, to complete the survey, Dr. Clauw said at the annual Perspectives in Rheumatic Diseases held by Global Academy for Medical Education. “This score will tell you the degree to which their central nervous system is augmenting or amplifying what is going on in their body,” he said. “And the higher their score is, the more you should treat them like you would someone with fibromyalgia, even if their underlying disease might be an autoimmune disease.”
Physicians should not use a cutoff of 13 points on the fibromyalgia measure to define whether a patient has the disease, as has been done in the past, he said. The threshold is arbitrary, he said. “We should not think about fibromyalgia as ‘yes’ or ‘no.’ We should think of the degree of fibromyalgia that people have.”
A poor relationship between pain and imaging
Some patients who have severe knee OA on imaging walk without pain. Other patients have normal x-rays, but severe pain. “There is a terrible relationship between what you see on a knee x-ray or an MRI and whether someone has pain,” Dr. Clauw said. Furthermore, the poor relationship between imaging and pain is common across chronic pain conditions, he said.
This phenomenon may occur because pain manifests in different ways, similar to there being multiple ways to adjust the volume of an electric guitar, he said. How hard the strings are strummed affects the volume. But so does the amplifier setting. “In these centralized pain conditions, the problem is an amplifier problem, not a guitar problem,” he said. “The amplifier, i.e., the central nervous system, is set too high.”
Researchers have found that people who have severe OA of the knee on x-ray but do not experience pain “have a very low amplifier setting,” he said. That is, they are nontender and less sensitive to pain. Most of these patients are men. “On average, men have a much lower amplifier setting than women,” he said. “This is also why ... women have 1.5 to 2 times the rate of any type of chronic pain than men, because on average women have a higher amplifier setting. ... In OA, at any given age, men and women have the exact same percentage of radiographic OA. But if you look at the clinical condition of OA, it is always two-thirds women, one-third men.”
Opioid responsiveness
To examine whether fibromyalgia survey results correlate with outcomes after knee and hip arthroplasty, Dr. Clauw and colleagues conducted a prospective, observational cohort study that included approximately 500 people. Patients completed the questionnaire on the day of surgery.
Patients with higher levels of fibromyalgia were less responsive to opioids. “For each 1-point increase in the fibromyalgia score, people needed about one more hydrocodone tablet in the first 24-48 hours to control their pain,” he said (Anesthesiology. 2013 Dec;119[6]:1434-43). In addition, each 1-point increase in the fibromyalgia score made people about 25% less likely to have a 50% improvement in knee pain level after 6 months (Arthritis Rheumatol. 2015 May;67[5]:1386-94). The correlations were independent of psychological factors. In addition, the associations were linear. “There was nothing magical about a fibromyalgia score of 13,” Dr. Clauw said.
Dr. Clauw is a coauthor of a study to be presented at the 2019 American College of Rheumatology/Association of Rheumatology Professionals annual meeting that found pain centralization in patients with RA is associated with poor response to disease-modifying antirheumatic drugs (DMARDs).
Prior studies in patients with RA have found that the degree of fibromyalgia is a better predictor of pain and disability than erythrocyte sedimentation rate or the number of swollen joints.
Diagnosed cases are the “tip of the iceberg”
Researchers at Dr. Clauw’s institution have identified dozens of patients undergoing knee surgery who met criteria for fibromyalgia but had not received the diagnosis. “This is at the University of Michigan, which is the epicenter for fibromyalgia research. If we are not seeing fibromyalgia superimposed on OA in our patients, no one is seeing it,” he said.
Patients with diagnosed fibromyalgia are “the tip of the iceberg,” he said. “There are far greater numbers of individuals whose primary diagnosis is OA, RA, lupus, ankylosing spondylitis, cancer pain, or sickle cell disease that have the same fundamental problem as fibromyalgia patients. But you do not see it because you label them as having an autoimmune disease or osteoarthritis. And that is at your peril and at their peril. Because treating that individual as if all of their pain and other symptoms are due to a problem out on the periphery will not make that person better.”
Patients with high levels of centralized pain may be less responsive to peripherally directed therapies such as surgery or injections, Dr. Clauw said. Pharmacologic options for patients with centralized pain include gabapentinoids (e.g., pregabalin and gabapentin), serotonin-norepinephrine reuptake inhibitors (e.g., duloxetine and milnacipran), and tricyclic compounds (e.g., amitriptyline and cyclobenzaprine), he said. “Opioids are going to be quite unlikely to help these individuals,” he said. “In fact, it is likely that opioids will make this kind of pain worse.”
Dr. Clauw is a consultant for Aptinyx, Daiichi Sankyo, Eli Lilly, Intec Pharma, Pfizer, Samumed, Theravance, Tonix, and Zynerba Pharma. He has received grant or research support from Aptinyx and Pfizer and is an expert witness.
Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM PRD 2019
Tranexamic acid does not increase complications in high-risk joint replacement surgery patients
A study has found that administering tranexamic acid (TXA) to high-risk patients undergoing total joint arthroplasty (TJA) does not increase their odds of adverse outcomes.
“The inclusion of high-risk patients in our study increases the generalizability of our findings and is consistent with the previous studies that showed no increase in complications when TXA is administered to TJA patients,” wrote Steven B. Porter, MD, of the Mayo Clinic in Jacksonville, Fla., and coauthors. The study was published in the Journal of Arthroplasty.
To determine the safety of TXA in patients at risk for thrombotic complications, the researchers investigated 38,220 patients who underwent total knee or total hip arthroplasty between 2011 and 2017 at the Mayo Clinic. Of those patients, 20,501 (54%) patients received TXA during their operation and 17,719 (46%) did not. Overall, 8,877 were classified as “high-risk” cases, which meant they had one or more cardiovascular disease or thromboembolic event before surgery.
After multivariable analysis, high risk-patients who received TXA had no significant difference in adverse outcome odds, compared with high-risk patients who did not receive TXA (odds ratio, 1.00; 95% confidence interval, 0.85-1.18). After 90 days, high-risk patients who did not receive TXA were more likely than those who received TXA to experience deep vein thrombosis (2.3% vs 0.8%, P less than .001), pulmonary embolism (1.7% vs 1.0%, P less than .001), cerebrovascular accident (0.8% vs. 0.4%, P less than .001), or death (0.5% vs. 0.4%, P less than .001).
The authors noted their study’s limitations, including a higher baseline incidence of risk factors in high-risk patients who did not receive TXA, compared with high-risk patients who did, which could have led to that group being “self-selected” to not receive TXA. In addition, all medical histories and rates of complications were based on ICD codes, which may have been inaccurate and therefore led to mischaracterized risk or miscoded postoperative complications.
The study was funded by the Mayo Clinic’s Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery. No conflicts of interest were reported.
SOURCE: Porter SB et al. J Arthroplasty. 2019 Aug 17. doi: 10.1016/j.arth.2019.08.015.
A study has found that administering tranexamic acid (TXA) to high-risk patients undergoing total joint arthroplasty (TJA) does not increase their odds of adverse outcomes.
“The inclusion of high-risk patients in our study increases the generalizability of our findings and is consistent with the previous studies that showed no increase in complications when TXA is administered to TJA patients,” wrote Steven B. Porter, MD, of the Mayo Clinic in Jacksonville, Fla., and coauthors. The study was published in the Journal of Arthroplasty.
To determine the safety of TXA in patients at risk for thrombotic complications, the researchers investigated 38,220 patients who underwent total knee or total hip arthroplasty between 2011 and 2017 at the Mayo Clinic. Of those patients, 20,501 (54%) patients received TXA during their operation and 17,719 (46%) did not. Overall, 8,877 were classified as “high-risk” cases, which meant they had one or more cardiovascular disease or thromboembolic event before surgery.
After multivariable analysis, high risk-patients who received TXA had no significant difference in adverse outcome odds, compared with high-risk patients who did not receive TXA (odds ratio, 1.00; 95% confidence interval, 0.85-1.18). After 90 days, high-risk patients who did not receive TXA were more likely than those who received TXA to experience deep vein thrombosis (2.3% vs 0.8%, P less than .001), pulmonary embolism (1.7% vs 1.0%, P less than .001), cerebrovascular accident (0.8% vs. 0.4%, P less than .001), or death (0.5% vs. 0.4%, P less than .001).
The authors noted their study’s limitations, including a higher baseline incidence of risk factors in high-risk patients who did not receive TXA, compared with high-risk patients who did, which could have led to that group being “self-selected” to not receive TXA. In addition, all medical histories and rates of complications were based on ICD codes, which may have been inaccurate and therefore led to mischaracterized risk or miscoded postoperative complications.
The study was funded by the Mayo Clinic’s Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery. No conflicts of interest were reported.
SOURCE: Porter SB et al. J Arthroplasty. 2019 Aug 17. doi: 10.1016/j.arth.2019.08.015.
A study has found that administering tranexamic acid (TXA) to high-risk patients undergoing total joint arthroplasty (TJA) does not increase their odds of adverse outcomes.
“The inclusion of high-risk patients in our study increases the generalizability of our findings and is consistent with the previous studies that showed no increase in complications when TXA is administered to TJA patients,” wrote Steven B. Porter, MD, of the Mayo Clinic in Jacksonville, Fla., and coauthors. The study was published in the Journal of Arthroplasty.
To determine the safety of TXA in patients at risk for thrombotic complications, the researchers investigated 38,220 patients who underwent total knee or total hip arthroplasty between 2011 and 2017 at the Mayo Clinic. Of those patients, 20,501 (54%) patients received TXA during their operation and 17,719 (46%) did not. Overall, 8,877 were classified as “high-risk” cases, which meant they had one or more cardiovascular disease or thromboembolic event before surgery.
After multivariable analysis, high risk-patients who received TXA had no significant difference in adverse outcome odds, compared with high-risk patients who did not receive TXA (odds ratio, 1.00; 95% confidence interval, 0.85-1.18). After 90 days, high-risk patients who did not receive TXA were more likely than those who received TXA to experience deep vein thrombosis (2.3% vs 0.8%, P less than .001), pulmonary embolism (1.7% vs 1.0%, P less than .001), cerebrovascular accident (0.8% vs. 0.4%, P less than .001), or death (0.5% vs. 0.4%, P less than .001).
The authors noted their study’s limitations, including a higher baseline incidence of risk factors in high-risk patients who did not receive TXA, compared with high-risk patients who did, which could have led to that group being “self-selected” to not receive TXA. In addition, all medical histories and rates of complications were based on ICD codes, which may have been inaccurate and therefore led to mischaracterized risk or miscoded postoperative complications.
The study was funded by the Mayo Clinic’s Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery. No conflicts of interest were reported.
SOURCE: Porter SB et al. J Arthroplasty. 2019 Aug 17. doi: 10.1016/j.arth.2019.08.015.
FROM THE JOURNAL OF ARTHROPLASTY
Key clinical point: Administering tranexamic acid to high-risk patients undergoing joint replacement surgery does not increase the odds of adverse outcomes.
Major finding: After multivariable analysis, high-risk patients who received tranexamic acid had no significant difference in adverse outcome odds, compared with high-risk patients who did not receive tranexamic acid (odd ratio, 1.00; 95% confidence interval, 0.85-1.18).
Study details: A retrospective case-control study of 38,220 patients who underwent primary total knee or total hip arthroplasty between 2011 and 2017.
Disclosures: The study was funded by the Mayo Clinic’s Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery. No conflicts of interest were reported.
Source: Porter SB et al. J Arthroplasty. 2019 Aug 17. doi: 10.1016/j.arth.2019.08.015.
Delaying revision knee replacement increases the odds of infection
According to a study on patients undergoing revision knee replacement, a delay of more than 24 hours between hospital admission and total knee arthroplasty (TKA) for periprosthetic fracture (PPF) led to increased odds of complications such as surgical site and urinary tract infections.
“Although this association is an important finding, the confounding factors that cause delay to surgery must be elucidated in non-database studies,” wrote Venkat Boddapati, MD, of Columbia University Medical Center, New York, and coauthors. The study was published in Arthroplasty Today.
To assess the best time for revision TKA after PPF of the knee, the researchers analyzed data from 484 patients who underwent another TKA from 2005 to 2016. Of those patients, 377 (78%) had expedited surgery – defined as less than or equal to 24 hours from hospital admission – and 107 (22%) had non-expedited surgery. Non-expedited patients averaged 3.2 days from admission to surgery.
After multivariate analysis, non-expedited patients had more complications overall, compared with expedited patients (odds ratio 2.35, P = .037). They also had comparative increases in surgical site infections (OR 12.87, P = .029), urinary tract infections (OR 10.46, P = .048), non-home discharge (OR 4.27, P less than .001), and blood transfusions (OR 4.53, P less than .001). The two groups saw no statistical difference in mortality.
The authors noted their study’s limitations, including an inability to assess complications beyond 30 days after surgery, which may affect tracking longer-term outcomes such as mortality. In addition, they were only able to classify surgery as expedited or non-expedited based on when the patient was admitted to the hospital, not the time since their injury. Finally, they lacked “relevant variables that may have contributed to this analysis,” including the type of fracture and the revision implants used.
Three authors reported being paid consultants for, and receiving research support from, several medical companies. The others reported no conflicts of interest.
SOURCE: Boddapati V et al. Arthroplast Today. 2019 Sep 1. doi: 10.1016/j.artd.2019.05.002.
According to a study on patients undergoing revision knee replacement, a delay of more than 24 hours between hospital admission and total knee arthroplasty (TKA) for periprosthetic fracture (PPF) led to increased odds of complications such as surgical site and urinary tract infections.
“Although this association is an important finding, the confounding factors that cause delay to surgery must be elucidated in non-database studies,” wrote Venkat Boddapati, MD, of Columbia University Medical Center, New York, and coauthors. The study was published in Arthroplasty Today.
To assess the best time for revision TKA after PPF of the knee, the researchers analyzed data from 484 patients who underwent another TKA from 2005 to 2016. Of those patients, 377 (78%) had expedited surgery – defined as less than or equal to 24 hours from hospital admission – and 107 (22%) had non-expedited surgery. Non-expedited patients averaged 3.2 days from admission to surgery.
After multivariate analysis, non-expedited patients had more complications overall, compared with expedited patients (odds ratio 2.35, P = .037). They also had comparative increases in surgical site infections (OR 12.87, P = .029), urinary tract infections (OR 10.46, P = .048), non-home discharge (OR 4.27, P less than .001), and blood transfusions (OR 4.53, P less than .001). The two groups saw no statistical difference in mortality.
The authors noted their study’s limitations, including an inability to assess complications beyond 30 days after surgery, which may affect tracking longer-term outcomes such as mortality. In addition, they were only able to classify surgery as expedited or non-expedited based on when the patient was admitted to the hospital, not the time since their injury. Finally, they lacked “relevant variables that may have contributed to this analysis,” including the type of fracture and the revision implants used.
Three authors reported being paid consultants for, and receiving research support from, several medical companies. The others reported no conflicts of interest.
SOURCE: Boddapati V et al. Arthroplast Today. 2019 Sep 1. doi: 10.1016/j.artd.2019.05.002.
According to a study on patients undergoing revision knee replacement, a delay of more than 24 hours between hospital admission and total knee arthroplasty (TKA) for periprosthetic fracture (PPF) led to increased odds of complications such as surgical site and urinary tract infections.
“Although this association is an important finding, the confounding factors that cause delay to surgery must be elucidated in non-database studies,” wrote Venkat Boddapati, MD, of Columbia University Medical Center, New York, and coauthors. The study was published in Arthroplasty Today.
To assess the best time for revision TKA after PPF of the knee, the researchers analyzed data from 484 patients who underwent another TKA from 2005 to 2016. Of those patients, 377 (78%) had expedited surgery – defined as less than or equal to 24 hours from hospital admission – and 107 (22%) had non-expedited surgery. Non-expedited patients averaged 3.2 days from admission to surgery.
After multivariate analysis, non-expedited patients had more complications overall, compared with expedited patients (odds ratio 2.35, P = .037). They also had comparative increases in surgical site infections (OR 12.87, P = .029), urinary tract infections (OR 10.46, P = .048), non-home discharge (OR 4.27, P less than .001), and blood transfusions (OR 4.53, P less than .001). The two groups saw no statistical difference in mortality.
The authors noted their study’s limitations, including an inability to assess complications beyond 30 days after surgery, which may affect tracking longer-term outcomes such as mortality. In addition, they were only able to classify surgery as expedited or non-expedited based on when the patient was admitted to the hospital, not the time since their injury. Finally, they lacked “relevant variables that may have contributed to this analysis,” including the type of fracture and the revision implants used.
Three authors reported being paid consultants for, and receiving research support from, several medical companies. The others reported no conflicts of interest.
SOURCE: Boddapati V et al. Arthroplast Today. 2019 Sep 1. doi: 10.1016/j.artd.2019.05.002.
FROM ARTHROPLASTY TODAY
Bariatric surgery has mostly positive impact in knee arthroplasty
a large study has found.
The study, led by Yicun Wang, PhD, of Nanjing (China) University was published in the Journal of Arthroplasty. “Generally speaking, bariatric surgery decreases some postoperative complications, decreases length of stay, and lowers mortality,” the study investigators wrote, [but] anemia and blood transfusion seem to be more common in patients with prior bariatric surgery.
They analyzed the effect of bariatric surgery on subsequent arthroplasty in morbidly obese patients in the United States using Nationwide Inpatient Sample 2006-2014 data on total hip arthroplasty (THA) and total knee arthroplasty (TKA). The researchers defined morbid obese patients as those with a body mass index higher than 40 kg/m2.
Among patients who underwent TKA, the researchers compared a group of 9,803 morbidly obese patients with the same number of patients who had undergone bariatric surgery. The two groups were matched by age, sex, income, primary insurance payer, and race.
There were large differences between the bariatric surgery group vs. morbidly obese group: Pulmonary embolism was much more common in the morbid obesity group (odds ratio, 0.22; 95% confidence interval, 0.05-1.03; P = .0346) while blood transfusion was more common in the bariatric surgery group (OR, 1.76; 95% CI, 1.52-2.03; P less than .0001).
For TKA, the researchers used the same approach to analyze 2,540 matched pairs of patients. In the bariatric surgery vs. morbidly obese comparison, pulmonary embolism was more common in the morbidly obese group (OR, 0.34; 95% CI, 0.20-0.57; P less than .0001), as were respiratory complications (OR, 0.45; 95% CI, 0.26-0.78; P = .0032) and death (OR, 0.07; 95% CI, 0.01-0.50; P = .0005). But the bariatric surgery group had higher levels of blood transfusion (OR, 1.87; 95% CI, 1.71-2.04; P less than .0001) and anemia (OR, 1.16; 95% CI, 1.09-1.24; P less than .0001).
Going forward, the researchers write, “future studies on these patients should attempt to evaluate the impact of bariatric surgery on the long-term outcomes of arthroplasty.”
The study was supported by various funders including the National Natural Science Foundation of China, the Natural Science Foundation of Guangdong Province, the Project of Administration of Traditional Chinese Medicine of Guangdong Province and others. No author disclosures are reported.
SOURCE: Wang Y et al. J Arthroplasty. 2019;S0883-5403(19)30667-9.
a large study has found.
The study, led by Yicun Wang, PhD, of Nanjing (China) University was published in the Journal of Arthroplasty. “Generally speaking, bariatric surgery decreases some postoperative complications, decreases length of stay, and lowers mortality,” the study investigators wrote, [but] anemia and blood transfusion seem to be more common in patients with prior bariatric surgery.
They analyzed the effect of bariatric surgery on subsequent arthroplasty in morbidly obese patients in the United States using Nationwide Inpatient Sample 2006-2014 data on total hip arthroplasty (THA) and total knee arthroplasty (TKA). The researchers defined morbid obese patients as those with a body mass index higher than 40 kg/m2.
Among patients who underwent TKA, the researchers compared a group of 9,803 morbidly obese patients with the same number of patients who had undergone bariatric surgery. The two groups were matched by age, sex, income, primary insurance payer, and race.
There were large differences between the bariatric surgery group vs. morbidly obese group: Pulmonary embolism was much more common in the morbid obesity group (odds ratio, 0.22; 95% confidence interval, 0.05-1.03; P = .0346) while blood transfusion was more common in the bariatric surgery group (OR, 1.76; 95% CI, 1.52-2.03; P less than .0001).
For TKA, the researchers used the same approach to analyze 2,540 matched pairs of patients. In the bariatric surgery vs. morbidly obese comparison, pulmonary embolism was more common in the morbidly obese group (OR, 0.34; 95% CI, 0.20-0.57; P less than .0001), as were respiratory complications (OR, 0.45; 95% CI, 0.26-0.78; P = .0032) and death (OR, 0.07; 95% CI, 0.01-0.50; P = .0005). But the bariatric surgery group had higher levels of blood transfusion (OR, 1.87; 95% CI, 1.71-2.04; P less than .0001) and anemia (OR, 1.16; 95% CI, 1.09-1.24; P less than .0001).
Going forward, the researchers write, “future studies on these patients should attempt to evaluate the impact of bariatric surgery on the long-term outcomes of arthroplasty.”
The study was supported by various funders including the National Natural Science Foundation of China, the Natural Science Foundation of Guangdong Province, the Project of Administration of Traditional Chinese Medicine of Guangdong Province and others. No author disclosures are reported.
SOURCE: Wang Y et al. J Arthroplasty. 2019;S0883-5403(19)30667-9.
a large study has found.
The study, led by Yicun Wang, PhD, of Nanjing (China) University was published in the Journal of Arthroplasty. “Generally speaking, bariatric surgery decreases some postoperative complications, decreases length of stay, and lowers mortality,” the study investigators wrote, [but] anemia and blood transfusion seem to be more common in patients with prior bariatric surgery.
They analyzed the effect of bariatric surgery on subsequent arthroplasty in morbidly obese patients in the United States using Nationwide Inpatient Sample 2006-2014 data on total hip arthroplasty (THA) and total knee arthroplasty (TKA). The researchers defined morbid obese patients as those with a body mass index higher than 40 kg/m2.
Among patients who underwent TKA, the researchers compared a group of 9,803 morbidly obese patients with the same number of patients who had undergone bariatric surgery. The two groups were matched by age, sex, income, primary insurance payer, and race.
There were large differences between the bariatric surgery group vs. morbidly obese group: Pulmonary embolism was much more common in the morbid obesity group (odds ratio, 0.22; 95% confidence interval, 0.05-1.03; P = .0346) while blood transfusion was more common in the bariatric surgery group (OR, 1.76; 95% CI, 1.52-2.03; P less than .0001).
For TKA, the researchers used the same approach to analyze 2,540 matched pairs of patients. In the bariatric surgery vs. morbidly obese comparison, pulmonary embolism was more common in the morbidly obese group (OR, 0.34; 95% CI, 0.20-0.57; P less than .0001), as were respiratory complications (OR, 0.45; 95% CI, 0.26-0.78; P = .0032) and death (OR, 0.07; 95% CI, 0.01-0.50; P = .0005). But the bariatric surgery group had higher levels of blood transfusion (OR, 1.87; 95% CI, 1.71-2.04; P less than .0001) and anemia (OR, 1.16; 95% CI, 1.09-1.24; P less than .0001).
Going forward, the researchers write, “future studies on these patients should attempt to evaluate the impact of bariatric surgery on the long-term outcomes of arthroplasty.”
The study was supported by various funders including the National Natural Science Foundation of China, the Natural Science Foundation of Guangdong Province, the Project of Administration of Traditional Chinese Medicine of Guangdong Province and others. No author disclosures are reported.
SOURCE: Wang Y et al. J Arthroplasty. 2019;S0883-5403(19)30667-9.
FROM THE JOURNAL OF ARTHROPLASTY
Be alert to deep SSI risk after knee surgery
Deep surgical-site infections (SSIs) and septic arthritis are not uncommon after the surgeries for periarticular knee fractures, a meta-analysis of existing research found.
A smaller analysis of 1,567 patients found that 2.4% had septic arthritis. “Surgeons managing periarticular knee fractures should be vigilant when wounds are not pristine,” the investigators recommended.
The report, which appeared in JAMA Network Open, was led by premed student Grayson R. Norris of High Point (N.C.) University.
The researchers noted that there are widely variable statistics regarding SSI after surgery for periarticular knee fractures. A better understanding of the risk would help orthopedic surgeons, given the mortality risk and extra costs associated with postoperative deep SSIs.
For the analysis, the researchers reviewed 117 studies with 11,432 patients who had fractures in the tibial plateau (61% of studies), distal femur (14%), proximal tibia (11%), patella (9%), and multiple sites (6%). More than two-thirds of the studies were retrospective.
Overall, 5.7% of patients suffered deep SSIs, with the highest percentage in the proximal tibia group (6.4%).
A total of 20 studies examined septic arthritis and found that 2.4% of patients in those studies suffered from the condition. Of 182 cases of deep SSIs with bacterial culture results, methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-susceptible S. aureus were the most common bacteria.
“Considering that MRSA was the most common pathogen in our study and that this pathogen is increasing in prevalence, health care practitioners should revisit the use of specific and appropriate prophylactic antibiotics,” the researchers wrote. “Risk factors, such as open fractures, diabetes, smoking, and, most importantly, compartment syndrome, should alert the treating surgeon to an increased risk. Further work is needed to mitigate the association of these conditions with SSI risk in periarticular knee fractures.”
The researchers added that many of the studies in their analysis were of poor quality. “Authors in orthopedic traumatology should strive to conduct higher-quality research, such as randomized clinical trials and case-control or cohort studies,” they noted.
One author reported receiving grants from Zimmer Biomet and DePuy Synthes outside the submitted work. No other disclosures were reported. No study funding was reported.
SOURCE: Norris GR et al. JAMA Netw Open. 2019;2(8):e199951.
Deep surgical-site infections (SSIs) and septic arthritis are not uncommon after the surgeries for periarticular knee fractures, a meta-analysis of existing research found.
A smaller analysis of 1,567 patients found that 2.4% had septic arthritis. “Surgeons managing periarticular knee fractures should be vigilant when wounds are not pristine,” the investigators recommended.
The report, which appeared in JAMA Network Open, was led by premed student Grayson R. Norris of High Point (N.C.) University.
The researchers noted that there are widely variable statistics regarding SSI after surgery for periarticular knee fractures. A better understanding of the risk would help orthopedic surgeons, given the mortality risk and extra costs associated with postoperative deep SSIs.
For the analysis, the researchers reviewed 117 studies with 11,432 patients who had fractures in the tibial plateau (61% of studies), distal femur (14%), proximal tibia (11%), patella (9%), and multiple sites (6%). More than two-thirds of the studies were retrospective.
Overall, 5.7% of patients suffered deep SSIs, with the highest percentage in the proximal tibia group (6.4%).
A total of 20 studies examined septic arthritis and found that 2.4% of patients in those studies suffered from the condition. Of 182 cases of deep SSIs with bacterial culture results, methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-susceptible S. aureus were the most common bacteria.
“Considering that MRSA was the most common pathogen in our study and that this pathogen is increasing in prevalence, health care practitioners should revisit the use of specific and appropriate prophylactic antibiotics,” the researchers wrote. “Risk factors, such as open fractures, diabetes, smoking, and, most importantly, compartment syndrome, should alert the treating surgeon to an increased risk. Further work is needed to mitigate the association of these conditions with SSI risk in periarticular knee fractures.”
The researchers added that many of the studies in their analysis were of poor quality. “Authors in orthopedic traumatology should strive to conduct higher-quality research, such as randomized clinical trials and case-control or cohort studies,” they noted.
One author reported receiving grants from Zimmer Biomet and DePuy Synthes outside the submitted work. No other disclosures were reported. No study funding was reported.
SOURCE: Norris GR et al. JAMA Netw Open. 2019;2(8):e199951.
Deep surgical-site infections (SSIs) and septic arthritis are not uncommon after the surgeries for periarticular knee fractures, a meta-analysis of existing research found.
A smaller analysis of 1,567 patients found that 2.4% had septic arthritis. “Surgeons managing periarticular knee fractures should be vigilant when wounds are not pristine,” the investigators recommended.
The report, which appeared in JAMA Network Open, was led by premed student Grayson R. Norris of High Point (N.C.) University.
The researchers noted that there are widely variable statistics regarding SSI after surgery for periarticular knee fractures. A better understanding of the risk would help orthopedic surgeons, given the mortality risk and extra costs associated with postoperative deep SSIs.
For the analysis, the researchers reviewed 117 studies with 11,432 patients who had fractures in the tibial plateau (61% of studies), distal femur (14%), proximal tibia (11%), patella (9%), and multiple sites (6%). More than two-thirds of the studies were retrospective.
Overall, 5.7% of patients suffered deep SSIs, with the highest percentage in the proximal tibia group (6.4%).
A total of 20 studies examined septic arthritis and found that 2.4% of patients in those studies suffered from the condition. Of 182 cases of deep SSIs with bacterial culture results, methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-susceptible S. aureus were the most common bacteria.
“Considering that MRSA was the most common pathogen in our study and that this pathogen is increasing in prevalence, health care practitioners should revisit the use of specific and appropriate prophylactic antibiotics,” the researchers wrote. “Risk factors, such as open fractures, diabetes, smoking, and, most importantly, compartment syndrome, should alert the treating surgeon to an increased risk. Further work is needed to mitigate the association of these conditions with SSI risk in periarticular knee fractures.”
The researchers added that many of the studies in their analysis were of poor quality. “Authors in orthopedic traumatology should strive to conduct higher-quality research, such as randomized clinical trials and case-control or cohort studies,” they noted.
One author reported receiving grants from Zimmer Biomet and DePuy Synthes outside the submitted work. No other disclosures were reported. No study funding was reported.
SOURCE: Norris GR et al. JAMA Netw Open. 2019;2(8):e199951.
FROM JAMA NETWORK OPEN