User login
Add-on azithromycin cuts asthma exacerbations
Adults with persistent symptomatic asthma who took azithromycin as an add-on therapy experienced fewer exacerbations and had improved quality of life, compared with their peers who took a placebo, a multicenter, randomized trial demonstrated.
“Macrolide antibiotics have antibacterial, antiviral, and anti-inflammatory effects, and are reported to be beneficial in both eosinophilic and noneosinophilic subtypes,” a group of Australian researchers wrote online July 4 in The Lancet (doi: org/10.1016/S0140-6736[17]31281-3). “Systematic reviews of randomized, controlled trials report benefits of macrolides on asthma symptoms but [we] are unable to draw conclusions about the effects on other endpoints, including exacerbations, due to lack of data, heterogeneity of results, and inadequate study design and sample size.”
The researchers observed a significant reduction in the incidence of total asthma exacerbations in the azithromycin-treated group: 1.07/patient-year, compared with 1.86/patient year in the placebo group, which translated into an incidence rate ratio of 0.59 (P less than .0001). Specifically, 127 patients in the placebo group (61%) experienced at least one asthma exacerbation compared with 94 patients in the azithromycin group (44%; P less than .0001). A significant improvement in asthma-related quality of life was also seen among patients in the azithromycin group (adjusted mean difference of 0.36; P = .001).
Though the mechanism of the antiviral effect of macrolides is not yet determined, Dr. Gibson and his associates noted that respiratory viral infection is associated with severe exacerbations in eosinophilic asthma and causes most respiratory infections. “There is a known interaction between eosinophilic airway inflammation, exacerbation rate, and impaired innate antiviral immunity,” they wrote. “Since we observed a benefit of azithromycin on both asthma exacerbations and respiratory infections, we speculate that azithromycin might be acting to prevent viral-induced episodes in asthma.”
“Given the major impact of asthma exacerbations on patients and the community and the ongoing risk posed by these events in patients who remain symptomatic on maintenance therapy, we consider that azithromycin is a valuable addition to existing regimens for treating asthma,” the researchers concluded. “The long-term effects of this therapy on community microbial resistance require further evaluation.”
The overall rates and types of serious adverse events seen in both groups were not significantly different from each other, with serious adverse events having occurred in 16 (8%) patients treated with azithromycin and 26 (13%) patients given the placebo.
The study was funded by the National Health and Medical Research Council of Australia and the John Hunter Hospital Charitable Trust. The authors reported having no financial conflicts directly related to the study.
Since microbial resistance is a well known side effect of antibiotic use, add-on therapy with azithromycin in asthma needs to be restricted to those patients with the highest unmet medical need (for example, frequent exacerbators) and to time periods with the greatest risk of exacerbations (such as winter). Biomarkers that predict the therapeutic response to macrolides might facilitate optimal patient selection. Further research is needed to elucidate the most important mechanism of action of these pleiotropic drugs. Macrolides have anti-inflammatory, antibacterial, and antiviral effects. However, the authors did not observe a reduction in inflammatory cell counts in sputum to support a definite anti-inflammatory effect. Azithromycin also was effective in patients with and without potentially pathogenic microorganisms in sputum cultures at baseline. Since azithromycin reduced both asthma exacerbations and respiratory infections, the benefits of azithromycin might be caused by preventing viral-induced attacks in asthma. Azithromycin stimulates phagocytosis of microbes and dead cells by macrophages (i.e., efferocytosis), an effect that is likely to be independent of the nature of the accompanying neutrophilic or eosinophilic airway inflammation.
Gibson and colleagues have clearly shown that add-on therapy with azithromycin is effective and safe in adult patients with uncontrolled asthma despite treatment with inhaled corticosteroids and long-acting beta-agonists. Azithromycin benefited patients with both eosinophilic and noneosinophilic asthma. However, the effects of long-term therapy with macrolides on community microbial resistance remain a public health concern. Future studies with potentially safer nonantibiotic macrolides in uncontrolled severe asthma are warranted. Since the antimicrobial effects probably contribute to the overall efficacy of macrolides, the beneficial effects of nonantibiotic macrolides might be intermediate between macrolide antibiotics and placebo.
This text is excerpted from a commentary published online July 4 in The Lancet (doi. org/10.1016/S0140-6736[17]31547-7). Guy Brusselle, MD, is with the department of respiratory medicine at Ghent (Belgium) University Hospital and Ian Pavord, MD, is with the University of Oxford’s Nuffield Department of Medicine, England. Both authors disclosed having received honoraria and other financial support from numerous pharmaceutical companies.
Since microbial resistance is a well known side effect of antibiotic use, add-on therapy with azithromycin in asthma needs to be restricted to those patients with the highest unmet medical need (for example, frequent exacerbators) and to time periods with the greatest risk of exacerbations (such as winter). Biomarkers that predict the therapeutic response to macrolides might facilitate optimal patient selection. Further research is needed to elucidate the most important mechanism of action of these pleiotropic drugs. Macrolides have anti-inflammatory, antibacterial, and antiviral effects. However, the authors did not observe a reduction in inflammatory cell counts in sputum to support a definite anti-inflammatory effect. Azithromycin also was effective in patients with and without potentially pathogenic microorganisms in sputum cultures at baseline. Since azithromycin reduced both asthma exacerbations and respiratory infections, the benefits of azithromycin might be caused by preventing viral-induced attacks in asthma. Azithromycin stimulates phagocytosis of microbes and dead cells by macrophages (i.e., efferocytosis), an effect that is likely to be independent of the nature of the accompanying neutrophilic or eosinophilic airway inflammation.
Gibson and colleagues have clearly shown that add-on therapy with azithromycin is effective and safe in adult patients with uncontrolled asthma despite treatment with inhaled corticosteroids and long-acting beta-agonists. Azithromycin benefited patients with both eosinophilic and noneosinophilic asthma. However, the effects of long-term therapy with macrolides on community microbial resistance remain a public health concern. Future studies with potentially safer nonantibiotic macrolides in uncontrolled severe asthma are warranted. Since the antimicrobial effects probably contribute to the overall efficacy of macrolides, the beneficial effects of nonantibiotic macrolides might be intermediate between macrolide antibiotics and placebo.
This text is excerpted from a commentary published online July 4 in The Lancet (doi. org/10.1016/S0140-6736[17]31547-7). Guy Brusselle, MD, is with the department of respiratory medicine at Ghent (Belgium) University Hospital and Ian Pavord, MD, is with the University of Oxford’s Nuffield Department of Medicine, England. Both authors disclosed having received honoraria and other financial support from numerous pharmaceutical companies.
Since microbial resistance is a well known side effect of antibiotic use, add-on therapy with azithromycin in asthma needs to be restricted to those patients with the highest unmet medical need (for example, frequent exacerbators) and to time periods with the greatest risk of exacerbations (such as winter). Biomarkers that predict the therapeutic response to macrolides might facilitate optimal patient selection. Further research is needed to elucidate the most important mechanism of action of these pleiotropic drugs. Macrolides have anti-inflammatory, antibacterial, and antiviral effects. However, the authors did not observe a reduction in inflammatory cell counts in sputum to support a definite anti-inflammatory effect. Azithromycin also was effective in patients with and without potentially pathogenic microorganisms in sputum cultures at baseline. Since azithromycin reduced both asthma exacerbations and respiratory infections, the benefits of azithromycin might be caused by preventing viral-induced attacks in asthma. Azithromycin stimulates phagocytosis of microbes and dead cells by macrophages (i.e., efferocytosis), an effect that is likely to be independent of the nature of the accompanying neutrophilic or eosinophilic airway inflammation.
Gibson and colleagues have clearly shown that add-on therapy with azithromycin is effective and safe in adult patients with uncontrolled asthma despite treatment with inhaled corticosteroids and long-acting beta-agonists. Azithromycin benefited patients with both eosinophilic and noneosinophilic asthma. However, the effects of long-term therapy with macrolides on community microbial resistance remain a public health concern. Future studies with potentially safer nonantibiotic macrolides in uncontrolled severe asthma are warranted. Since the antimicrobial effects probably contribute to the overall efficacy of macrolides, the beneficial effects of nonantibiotic macrolides might be intermediate between macrolide antibiotics and placebo.
This text is excerpted from a commentary published online July 4 in The Lancet (doi. org/10.1016/S0140-6736[17]31547-7). Guy Brusselle, MD, is with the department of respiratory medicine at Ghent (Belgium) University Hospital and Ian Pavord, MD, is with the University of Oxford’s Nuffield Department of Medicine, England. Both authors disclosed having received honoraria and other financial support from numerous pharmaceutical companies.
Adults with persistent symptomatic asthma who took azithromycin as an add-on therapy experienced fewer exacerbations and had improved quality of life, compared with their peers who took a placebo, a multicenter, randomized trial demonstrated.
“Macrolide antibiotics have antibacterial, antiviral, and anti-inflammatory effects, and are reported to be beneficial in both eosinophilic and noneosinophilic subtypes,” a group of Australian researchers wrote online July 4 in The Lancet (doi: org/10.1016/S0140-6736[17]31281-3). “Systematic reviews of randomized, controlled trials report benefits of macrolides on asthma symptoms but [we] are unable to draw conclusions about the effects on other endpoints, including exacerbations, due to lack of data, heterogeneity of results, and inadequate study design and sample size.”
The researchers observed a significant reduction in the incidence of total asthma exacerbations in the azithromycin-treated group: 1.07/patient-year, compared with 1.86/patient year in the placebo group, which translated into an incidence rate ratio of 0.59 (P less than .0001). Specifically, 127 patients in the placebo group (61%) experienced at least one asthma exacerbation compared with 94 patients in the azithromycin group (44%; P less than .0001). A significant improvement in asthma-related quality of life was also seen among patients in the azithromycin group (adjusted mean difference of 0.36; P = .001).
Though the mechanism of the antiviral effect of macrolides is not yet determined, Dr. Gibson and his associates noted that respiratory viral infection is associated with severe exacerbations in eosinophilic asthma and causes most respiratory infections. “There is a known interaction between eosinophilic airway inflammation, exacerbation rate, and impaired innate antiviral immunity,” they wrote. “Since we observed a benefit of azithromycin on both asthma exacerbations and respiratory infections, we speculate that azithromycin might be acting to prevent viral-induced episodes in asthma.”
“Given the major impact of asthma exacerbations on patients and the community and the ongoing risk posed by these events in patients who remain symptomatic on maintenance therapy, we consider that azithromycin is a valuable addition to existing regimens for treating asthma,” the researchers concluded. “The long-term effects of this therapy on community microbial resistance require further evaluation.”
The overall rates and types of serious adverse events seen in both groups were not significantly different from each other, with serious adverse events having occurred in 16 (8%) patients treated with azithromycin and 26 (13%) patients given the placebo.
The study was funded by the National Health and Medical Research Council of Australia and the John Hunter Hospital Charitable Trust. The authors reported having no financial conflicts directly related to the study.
Adults with persistent symptomatic asthma who took azithromycin as an add-on therapy experienced fewer exacerbations and had improved quality of life, compared with their peers who took a placebo, a multicenter, randomized trial demonstrated.
“Macrolide antibiotics have antibacterial, antiviral, and anti-inflammatory effects, and are reported to be beneficial in both eosinophilic and noneosinophilic subtypes,” a group of Australian researchers wrote online July 4 in The Lancet (doi: org/10.1016/S0140-6736[17]31281-3). “Systematic reviews of randomized, controlled trials report benefits of macrolides on asthma symptoms but [we] are unable to draw conclusions about the effects on other endpoints, including exacerbations, due to lack of data, heterogeneity of results, and inadequate study design and sample size.”
The researchers observed a significant reduction in the incidence of total asthma exacerbations in the azithromycin-treated group: 1.07/patient-year, compared with 1.86/patient year in the placebo group, which translated into an incidence rate ratio of 0.59 (P less than .0001). Specifically, 127 patients in the placebo group (61%) experienced at least one asthma exacerbation compared with 94 patients in the azithromycin group (44%; P less than .0001). A significant improvement in asthma-related quality of life was also seen among patients in the azithromycin group (adjusted mean difference of 0.36; P = .001).
Though the mechanism of the antiviral effect of macrolides is not yet determined, Dr. Gibson and his associates noted that respiratory viral infection is associated with severe exacerbations in eosinophilic asthma and causes most respiratory infections. “There is a known interaction between eosinophilic airway inflammation, exacerbation rate, and impaired innate antiviral immunity,” they wrote. “Since we observed a benefit of azithromycin on both asthma exacerbations and respiratory infections, we speculate that azithromycin might be acting to prevent viral-induced episodes in asthma.”
“Given the major impact of asthma exacerbations on patients and the community and the ongoing risk posed by these events in patients who remain symptomatic on maintenance therapy, we consider that azithromycin is a valuable addition to existing regimens for treating asthma,” the researchers concluded. “The long-term effects of this therapy on community microbial resistance require further evaluation.”
The overall rates and types of serious adverse events seen in both groups were not significantly different from each other, with serious adverse events having occurred in 16 (8%) patients treated with azithromycin and 26 (13%) patients given the placebo.
The study was funded by the National Health and Medical Research Council of Australia and the John Hunter Hospital Charitable Trust. The authors reported having no financial conflicts directly related to the study.
FROM THE LANCET
Key clinical point:
Major finding: Azithromycin reduced the incidence of total asthma exacerbations, compared with placebo (1.07/patient-year vs. 1.86/patient-year, respectively, for an incidence rate ratio of 0.59; P less than .0001).
Data source: A randomized, placebo-controlled, multicenter trial of 420 adults with persistent, uncontrolled asthma.
Disclosures: The study was funded by the National Health and Medical Research Council of Australia and the John Hunter Hospital Charitable Trust. The authors reported having no financial conflicts directly related to the study.
New tool predicts antimicrobial resistance in sepsis
Use of a clinical decision tree predicted antibiotic resistance in sepsis patients infected with gram-negative bacteria, based on data from 1,618 patients.
Increasing rates of bacterial resistance have “contributed to the unwarranted empiric administration of broad-spectrum antibiotics, further promoting resistance emergence across microbial species,” said M. Cristina Vazquez Guillamet, MD, of the University of New Mexico, Albuquerque, and her colleagues (Clin Infect Dis. cix612. 2017 Jul 10. doi: 10.1093/cid/cix612).
The researchers identified adults with sepsis or septic shock caused by bloodstream infections who were treated at a single center between 2008 and 2015. They developed clinical decision trees using the CHAID algorithm (Chi squared Automatic Interaction Detection) to analyze risk factors for resistance associated with three antibiotics: piperacillin-tazobactam (PT), cefepime (CE), and meropenem (ME).
Overall, resistance rates to PT, CE, and ME were 29%, 22%, and 9%, respectively, and 6.6% of the isolates were resistant to all three antibiotics.
Factors associated with increased resistance risk included residence in a nursing home, transfer from an outside hospital, and prior antibiotics use. Resistance to ME was associated with infection with Pseudomonas or Acinetobacter spp, the researchers noted, and resistance to PT was associated with central nervous system and central venous catheter infections.
Clinical decision trees were able to separate patients at low risk for resistance to PT and CE, as well as those with a risk greater than 30% of resistance to PT, CE, or ME. “We also found good overall agreement between the accuracies of the [multivariable logistic regression] models and the decision tree analyses for predicting antibiotic resistance,” the researchers said.
The findings were limited by several factors, including the use of data from a single center and incomplete reporting of previous antibiotic exposure, the researchers noted. However, the results “provide a framework for how empiric antibiotics can be tailored according to decision tree patient clusters,” they said.
Combining user-friendly clinical decision trees and multivariable logistic regression models may offer the best opportunities for hospitals to derive local models to help with antimicrobial prescription.
The researchers had no financial conflicts to disclose.
Use of a clinical decision tree predicted antibiotic resistance in sepsis patients infected with gram-negative bacteria, based on data from 1,618 patients.
Increasing rates of bacterial resistance have “contributed to the unwarranted empiric administration of broad-spectrum antibiotics, further promoting resistance emergence across microbial species,” said M. Cristina Vazquez Guillamet, MD, of the University of New Mexico, Albuquerque, and her colleagues (Clin Infect Dis. cix612. 2017 Jul 10. doi: 10.1093/cid/cix612).
The researchers identified adults with sepsis or septic shock caused by bloodstream infections who were treated at a single center between 2008 and 2015. They developed clinical decision trees using the CHAID algorithm (Chi squared Automatic Interaction Detection) to analyze risk factors for resistance associated with three antibiotics: piperacillin-tazobactam (PT), cefepime (CE), and meropenem (ME).
Overall, resistance rates to PT, CE, and ME were 29%, 22%, and 9%, respectively, and 6.6% of the isolates were resistant to all three antibiotics.
Factors associated with increased resistance risk included residence in a nursing home, transfer from an outside hospital, and prior antibiotics use. Resistance to ME was associated with infection with Pseudomonas or Acinetobacter spp, the researchers noted, and resistance to PT was associated with central nervous system and central venous catheter infections.
Clinical decision trees were able to separate patients at low risk for resistance to PT and CE, as well as those with a risk greater than 30% of resistance to PT, CE, or ME. “We also found good overall agreement between the accuracies of the [multivariable logistic regression] models and the decision tree analyses for predicting antibiotic resistance,” the researchers said.
The findings were limited by several factors, including the use of data from a single center and incomplete reporting of previous antibiotic exposure, the researchers noted. However, the results “provide a framework for how empiric antibiotics can be tailored according to decision tree patient clusters,” they said.
Combining user-friendly clinical decision trees and multivariable logistic regression models may offer the best opportunities for hospitals to derive local models to help with antimicrobial prescription.
The researchers had no financial conflicts to disclose.
Use of a clinical decision tree predicted antibiotic resistance in sepsis patients infected with gram-negative bacteria, based on data from 1,618 patients.
Increasing rates of bacterial resistance have “contributed to the unwarranted empiric administration of broad-spectrum antibiotics, further promoting resistance emergence across microbial species,” said M. Cristina Vazquez Guillamet, MD, of the University of New Mexico, Albuquerque, and her colleagues (Clin Infect Dis. cix612. 2017 Jul 10. doi: 10.1093/cid/cix612).
The researchers identified adults with sepsis or septic shock caused by bloodstream infections who were treated at a single center between 2008 and 2015. They developed clinical decision trees using the CHAID algorithm (Chi squared Automatic Interaction Detection) to analyze risk factors for resistance associated with three antibiotics: piperacillin-tazobactam (PT), cefepime (CE), and meropenem (ME).
Overall, resistance rates to PT, CE, and ME were 29%, 22%, and 9%, respectively, and 6.6% of the isolates were resistant to all three antibiotics.
Factors associated with increased resistance risk included residence in a nursing home, transfer from an outside hospital, and prior antibiotics use. Resistance to ME was associated with infection with Pseudomonas or Acinetobacter spp, the researchers noted, and resistance to PT was associated with central nervous system and central venous catheter infections.
Clinical decision trees were able to separate patients at low risk for resistance to PT and CE, as well as those with a risk greater than 30% of resistance to PT, CE, or ME. “We also found good overall agreement between the accuracies of the [multivariable logistic regression] models and the decision tree analyses for predicting antibiotic resistance,” the researchers said.
The findings were limited by several factors, including the use of data from a single center and incomplete reporting of previous antibiotic exposure, the researchers noted. However, the results “provide a framework for how empiric antibiotics can be tailored according to decision tree patient clusters,” they said.
Combining user-friendly clinical decision trees and multivariable logistic regression models may offer the best opportunities for hospitals to derive local models to help with antimicrobial prescription.
The researchers had no financial conflicts to disclose.
FROM CLINICAL INFECTIOUS DISEASES
Key clinical point:
Major finding: The model found prevalence rates for resistance to piperacillin-tazobactam, cefepime, and meropenem of 28.6%, 21.8%, and 8.5%, respectively.
Data source: A review of 1,618 adults with sepsis.
Disclosures: The researchers had no financial conflicts to disclose.
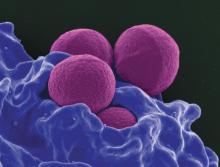
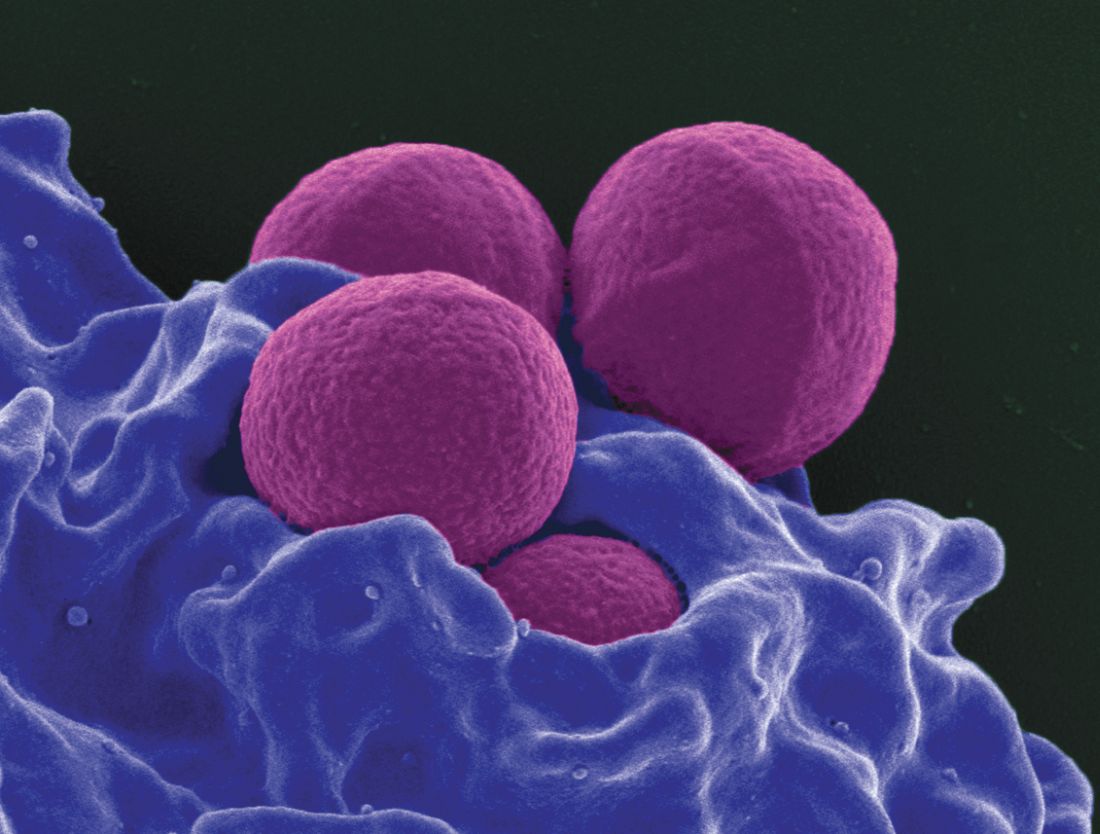
Adding cefepime to vancomycin improved MRSA bacteremia outcomes
NEW ORLEANS – Compared with vancomycin monotherapy, vancomycin combined with cefepime improved some outcomes for patients with methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infections, a retrospective study of 109 patients revealed.
A lower likelihood of microbiological failure and fewer bloodstream infections persisting 7 days or more were the notable differences between treatment groups.
All patients had at least 72 hours of vancomycin therapy to treat MRSA bacteremia confirmed by blood culture. During 2008-2015, 38 adults received vancomycin monotherapy and 71 received vancomycin plus 24 hours or more of cefepime.
Compared with monotherapy, the combination treatment was associated with a nonsignificant reduction in the primary composite treatment failure outcome of 30-day all-cause mortality, in bacteremia duration of 7 days or more, and in 60-day bloodstream-infection recurrence: 55% for monotherapy versus 42% for combination therapy (P = .195). The difference was primarily associated with decreased duration of sepsis and fewer MRSA bloodstream infections persisting 7 days or more in the combination cohort.
Rates of bacteremia duration of 7 days or more were 42% in monotherapy patients and 20% in combination patients (P = .013). Differences in 60-day bloodstream-infection recurrence were nonsignificant, 8% versus 4%, respectively (P = .42).
Thirty-day mortality, however, was lower among monotherapy patients than combination patients – 13% vs. 25% – although the difference was nonsignificant (P = .21).
“From what I see here … it seems like they will have a lower duration of bacteremia, which is always great,” Ms. Atwan said. “You want to decrease length of stay in the hospital,” which will cut down on costs and on patients’ risks of getting more infections.
Although the primary outcome was a composite endpoint, “when we looked at them separately, we found the patients in the combination group had more mortality,” Ms. Atwan said at the annual meeting of the American Society for Microbiology. “That surprised me initially. But those patients are sicker and more likely to get dual coverage.”
The investigators confirmed the association between the severity of MRSA bacteremia and combination therapy by looking at Acute Physiology and Chronic Health Evaluation (APACHE II) scores. The median APACHE score was 23 in the combination group, compared with 13.5 in the monotherapy group (P = 0003). Higher APACHE scores were associated with greater odds of meeting the composite failure endpoint (adjusted odds ratio, 1.08) and of developing endocarditis (aOR, 3.6) in multivariate analyses.
More patients in the combination group had pneumonia as the primary source of infection than did patients in the monotherapy group: 54% vs. 29% (P = .016). Further, more of them had skin or soft tissue infections as the primary infection source: 29% vs. 13% (P = .036).
Although the exact mechanism remains unknown, synergy between the two agents could be caused by an increase in penicillin-binding proteins, Ms. Atwan said.
The study is still ongoing; Ms. Atwan hopes additional patients and data will lead to statistically significant differences between the outcomes of combination therapy and vancomycin monotherapy.
“I want to say that combination therapy is something you will always want to go to when you have a sicker patient, but I can’t really tell you that combination therapy is going to cause better outcomes for your patient,” she cautioned. “Hopefully, I can by the end of the study.”
In the meantime, “it looks like vancomycin and beta-lactams could be beneficial for MRSA bacteremia,” she added.
The researchers noted that although vancomycin monotherapy is a mainstay of treatment for MRSA bloodstream infections, emergence of reduced susceptibility and treatment failures warrants other therapeutic strategies.
Ms. Atwan had no relevant financial disclosures.
NEW ORLEANS – Compared with vancomycin monotherapy, vancomycin combined with cefepime improved some outcomes for patients with methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infections, a retrospective study of 109 patients revealed.
A lower likelihood of microbiological failure and fewer bloodstream infections persisting 7 days or more were the notable differences between treatment groups.
All patients had at least 72 hours of vancomycin therapy to treat MRSA bacteremia confirmed by blood culture. During 2008-2015, 38 adults received vancomycin monotherapy and 71 received vancomycin plus 24 hours or more of cefepime.
Compared with monotherapy, the combination treatment was associated with a nonsignificant reduction in the primary composite treatment failure outcome of 30-day all-cause mortality, in bacteremia duration of 7 days or more, and in 60-day bloodstream-infection recurrence: 55% for monotherapy versus 42% for combination therapy (P = .195). The difference was primarily associated with decreased duration of sepsis and fewer MRSA bloodstream infections persisting 7 days or more in the combination cohort.
Rates of bacteremia duration of 7 days or more were 42% in monotherapy patients and 20% in combination patients (P = .013). Differences in 60-day bloodstream-infection recurrence were nonsignificant, 8% versus 4%, respectively (P = .42).
Thirty-day mortality, however, was lower among monotherapy patients than combination patients – 13% vs. 25% – although the difference was nonsignificant (P = .21).
“From what I see here … it seems like they will have a lower duration of bacteremia, which is always great,” Ms. Atwan said. “You want to decrease length of stay in the hospital,” which will cut down on costs and on patients’ risks of getting more infections.
Although the primary outcome was a composite endpoint, “when we looked at them separately, we found the patients in the combination group had more mortality,” Ms. Atwan said at the annual meeting of the American Society for Microbiology. “That surprised me initially. But those patients are sicker and more likely to get dual coverage.”
The investigators confirmed the association between the severity of MRSA bacteremia and combination therapy by looking at Acute Physiology and Chronic Health Evaluation (APACHE II) scores. The median APACHE score was 23 in the combination group, compared with 13.5 in the monotherapy group (P = 0003). Higher APACHE scores were associated with greater odds of meeting the composite failure endpoint (adjusted odds ratio, 1.08) and of developing endocarditis (aOR, 3.6) in multivariate analyses.
More patients in the combination group had pneumonia as the primary source of infection than did patients in the monotherapy group: 54% vs. 29% (P = .016). Further, more of them had skin or soft tissue infections as the primary infection source: 29% vs. 13% (P = .036).
Although the exact mechanism remains unknown, synergy between the two agents could be caused by an increase in penicillin-binding proteins, Ms. Atwan said.
The study is still ongoing; Ms. Atwan hopes additional patients and data will lead to statistically significant differences between the outcomes of combination therapy and vancomycin monotherapy.
“I want to say that combination therapy is something you will always want to go to when you have a sicker patient, but I can’t really tell you that combination therapy is going to cause better outcomes for your patient,” she cautioned. “Hopefully, I can by the end of the study.”
In the meantime, “it looks like vancomycin and beta-lactams could be beneficial for MRSA bacteremia,” she added.
The researchers noted that although vancomycin monotherapy is a mainstay of treatment for MRSA bloodstream infections, emergence of reduced susceptibility and treatment failures warrants other therapeutic strategies.
Ms. Atwan had no relevant financial disclosures.
NEW ORLEANS – Compared with vancomycin monotherapy, vancomycin combined with cefepime improved some outcomes for patients with methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infections, a retrospective study of 109 patients revealed.
A lower likelihood of microbiological failure and fewer bloodstream infections persisting 7 days or more were the notable differences between treatment groups.
All patients had at least 72 hours of vancomycin therapy to treat MRSA bacteremia confirmed by blood culture. During 2008-2015, 38 adults received vancomycin monotherapy and 71 received vancomycin plus 24 hours or more of cefepime.
Compared with monotherapy, the combination treatment was associated with a nonsignificant reduction in the primary composite treatment failure outcome of 30-day all-cause mortality, in bacteremia duration of 7 days or more, and in 60-day bloodstream-infection recurrence: 55% for monotherapy versus 42% for combination therapy (P = .195). The difference was primarily associated with decreased duration of sepsis and fewer MRSA bloodstream infections persisting 7 days or more in the combination cohort.
Rates of bacteremia duration of 7 days or more were 42% in monotherapy patients and 20% in combination patients (P = .013). Differences in 60-day bloodstream-infection recurrence were nonsignificant, 8% versus 4%, respectively (P = .42).
Thirty-day mortality, however, was lower among monotherapy patients than combination patients – 13% vs. 25% – although the difference was nonsignificant (P = .21).
“From what I see here … it seems like they will have a lower duration of bacteremia, which is always great,” Ms. Atwan said. “You want to decrease length of stay in the hospital,” which will cut down on costs and on patients’ risks of getting more infections.
Although the primary outcome was a composite endpoint, “when we looked at them separately, we found the patients in the combination group had more mortality,” Ms. Atwan said at the annual meeting of the American Society for Microbiology. “That surprised me initially. But those patients are sicker and more likely to get dual coverage.”
The investigators confirmed the association between the severity of MRSA bacteremia and combination therapy by looking at Acute Physiology and Chronic Health Evaluation (APACHE II) scores. The median APACHE score was 23 in the combination group, compared with 13.5 in the monotherapy group (P = 0003). Higher APACHE scores were associated with greater odds of meeting the composite failure endpoint (adjusted odds ratio, 1.08) and of developing endocarditis (aOR, 3.6) in multivariate analyses.
More patients in the combination group had pneumonia as the primary source of infection than did patients in the monotherapy group: 54% vs. 29% (P = .016). Further, more of them had skin or soft tissue infections as the primary infection source: 29% vs. 13% (P = .036).
Although the exact mechanism remains unknown, synergy between the two agents could be caused by an increase in penicillin-binding proteins, Ms. Atwan said.
The study is still ongoing; Ms. Atwan hopes additional patients and data will lead to statistically significant differences between the outcomes of combination therapy and vancomycin monotherapy.
“I want to say that combination therapy is something you will always want to go to when you have a sicker patient, but I can’t really tell you that combination therapy is going to cause better outcomes for your patient,” she cautioned. “Hopefully, I can by the end of the study.”
In the meantime, “it looks like vancomycin and beta-lactams could be beneficial for MRSA bacteremia,” she added.
The researchers noted that although vancomycin monotherapy is a mainstay of treatment for MRSA bloodstream infections, emergence of reduced susceptibility and treatment failures warrants other therapeutic strategies.
Ms. Atwan had no relevant financial disclosures.
AT ASM MICROBE 2017
Key clinical point:
Major finding: Median duration of MRSA bacteremia was 4 days with combination therapy, versus 6 days with vancomycin alone.
Data source: A retrospective, single-center comparison of 109 patients treated with either vancomycin plus cefepime or vancomycin alone.
Disclosures: Safana M. Atwan had no relevant financial disclosures.
The burden of health care–associated C. difficile infection in a nonmetropolitan setting
Clostridium difficile infection (CDI) remains a major cause of health care–associated diarrhea in industrialized countries and is a common target of antimicrobial stewardship programs (ASPs).
While the burden of CDI has been well described in tertiary metropolitan hospitals, there is a lack of published evidence from regional and rural hospitals. Our recent study published in the Journal of Hospital Infection explores the effect of an ASP on health care–associated CDI rates and the impact of CDI on length of stay and hospital costs.
The ASP functioned alongside infection control practices, including isolation of patients with antimicrobial-resistant organisms (including C. difficile), hand hygiene, personal protective equipment, and terminal cleaning. Timely feedback emails to medical officers contained information on patient-specific risk factors for CDI, current and prior antimicrobials, and suggestions for CDI treatment. The effect of health care–associated CDI on length of stay and hospital costs was investigated using a group of matched controls, identified retrospectively using hospital performance data. Prior antimicrobial and proton pump inhibitor use were also measured and compared with background use.
The results of our study demonstrated a stable health care–associated CDI rate of around four cases per 10,000 occupied bed days over a 5-year period, similar to the average Australian rate. The length of time over which CDI rates could be effectively examined prior to the intervention was limited by changes to C. difficile stool testing methods. Median length of stay was 11 days greater, and median hospital costs were AU$11,361 higher for patients with health care–associated CDI (n = 91) than for their matched controls (n = 172). It is likely that the increase in costs was associated with additional length of stay but also with increased investigation and treatment costs. Among the group of patients with severe disease (n = 8), only four received oral vancomycin according to Australian guidelines, possibly because of under-recognition of severity criteria. The response rate to emails was low at 19%, showing that other methods are additionally necessary to communicate CDI case feedback.
Third generation cephalosporins and beta-lactamase inhibitor combinations were over-represented in the health care–associated CDI group, where narrower spectrum antimicrobials such as beta-lactamase sensitive penicillins were under represented. Rates of prior antimicrobial use and proton pump inhibitor use were broadly in agreement with the literature.
Our study demonstrated that, in the Australian nonmetropolitan setting, there was a high burden of health care–associated CDI in terms of hospital costs and length of stay, even though our health district experienced CDI rates that were similar to the Australian average. Challenges associated with the study included maintenance of consistent data collection across multiple hospital sites without comprehensive electronic medical records, provision of timely email feedback, and dissemination of study results.
Analysis of prior antimicrobial use has allowed us to identify targets for ongoing antimicrobial stewardship activities, and we also intend to provide further education on recognition of severity criteria. These activities can be supported through daily antimicrobial stewardship ward rounds. Future research could involve application of appropriateness criteria to prior and current antimicrobial use in CDI patients in order to identify avoidable cases and use of more advanced statistical techniques such as multistate modeling to determine differences in outcomes between cases and controls.
Stuart Bond, BPharm, DipPharmPrac, is an antimicrobial stewardship pharmacist based at Wollongong Hospital in New South Wales, Australia.
Clostridium difficile infection (CDI) remains a major cause of health care–associated diarrhea in industrialized countries and is a common target of antimicrobial stewardship programs (ASPs).
While the burden of CDI has been well described in tertiary metropolitan hospitals, there is a lack of published evidence from regional and rural hospitals. Our recent study published in the Journal of Hospital Infection explores the effect of an ASP on health care–associated CDI rates and the impact of CDI on length of stay and hospital costs.
The ASP functioned alongside infection control practices, including isolation of patients with antimicrobial-resistant organisms (including C. difficile), hand hygiene, personal protective equipment, and terminal cleaning. Timely feedback emails to medical officers contained information on patient-specific risk factors for CDI, current and prior antimicrobials, and suggestions for CDI treatment. The effect of health care–associated CDI on length of stay and hospital costs was investigated using a group of matched controls, identified retrospectively using hospital performance data. Prior antimicrobial and proton pump inhibitor use were also measured and compared with background use.
The results of our study demonstrated a stable health care–associated CDI rate of around four cases per 10,000 occupied bed days over a 5-year period, similar to the average Australian rate. The length of time over which CDI rates could be effectively examined prior to the intervention was limited by changes to C. difficile stool testing methods. Median length of stay was 11 days greater, and median hospital costs were AU$11,361 higher for patients with health care–associated CDI (n = 91) than for their matched controls (n = 172). It is likely that the increase in costs was associated with additional length of stay but also with increased investigation and treatment costs. Among the group of patients with severe disease (n = 8), only four received oral vancomycin according to Australian guidelines, possibly because of under-recognition of severity criteria. The response rate to emails was low at 19%, showing that other methods are additionally necessary to communicate CDI case feedback.
Third generation cephalosporins and beta-lactamase inhibitor combinations were over-represented in the health care–associated CDI group, where narrower spectrum antimicrobials such as beta-lactamase sensitive penicillins were under represented. Rates of prior antimicrobial use and proton pump inhibitor use were broadly in agreement with the literature.
Our study demonstrated that, in the Australian nonmetropolitan setting, there was a high burden of health care–associated CDI in terms of hospital costs and length of stay, even though our health district experienced CDI rates that were similar to the Australian average. Challenges associated with the study included maintenance of consistent data collection across multiple hospital sites without comprehensive electronic medical records, provision of timely email feedback, and dissemination of study results.
Analysis of prior antimicrobial use has allowed us to identify targets for ongoing antimicrobial stewardship activities, and we also intend to provide further education on recognition of severity criteria. These activities can be supported through daily antimicrobial stewardship ward rounds. Future research could involve application of appropriateness criteria to prior and current antimicrobial use in CDI patients in order to identify avoidable cases and use of more advanced statistical techniques such as multistate modeling to determine differences in outcomes between cases and controls.
Stuart Bond, BPharm, DipPharmPrac, is an antimicrobial stewardship pharmacist based at Wollongong Hospital in New South Wales, Australia.
Clostridium difficile infection (CDI) remains a major cause of health care–associated diarrhea in industrialized countries and is a common target of antimicrobial stewardship programs (ASPs).
While the burden of CDI has been well described in tertiary metropolitan hospitals, there is a lack of published evidence from regional and rural hospitals. Our recent study published in the Journal of Hospital Infection explores the effect of an ASP on health care–associated CDI rates and the impact of CDI on length of stay and hospital costs.
The ASP functioned alongside infection control practices, including isolation of patients with antimicrobial-resistant organisms (including C. difficile), hand hygiene, personal protective equipment, and terminal cleaning. Timely feedback emails to medical officers contained information on patient-specific risk factors for CDI, current and prior antimicrobials, and suggestions for CDI treatment. The effect of health care–associated CDI on length of stay and hospital costs was investigated using a group of matched controls, identified retrospectively using hospital performance data. Prior antimicrobial and proton pump inhibitor use were also measured and compared with background use.
The results of our study demonstrated a stable health care–associated CDI rate of around four cases per 10,000 occupied bed days over a 5-year period, similar to the average Australian rate. The length of time over which CDI rates could be effectively examined prior to the intervention was limited by changes to C. difficile stool testing methods. Median length of stay was 11 days greater, and median hospital costs were AU$11,361 higher for patients with health care–associated CDI (n = 91) than for their matched controls (n = 172). It is likely that the increase in costs was associated with additional length of stay but also with increased investigation and treatment costs. Among the group of patients with severe disease (n = 8), only four received oral vancomycin according to Australian guidelines, possibly because of under-recognition of severity criteria. The response rate to emails was low at 19%, showing that other methods are additionally necessary to communicate CDI case feedback.
Third generation cephalosporins and beta-lactamase inhibitor combinations were over-represented in the health care–associated CDI group, where narrower spectrum antimicrobials such as beta-lactamase sensitive penicillins were under represented. Rates of prior antimicrobial use and proton pump inhibitor use were broadly in agreement with the literature.
Our study demonstrated that, in the Australian nonmetropolitan setting, there was a high burden of health care–associated CDI in terms of hospital costs and length of stay, even though our health district experienced CDI rates that were similar to the Australian average. Challenges associated with the study included maintenance of consistent data collection across multiple hospital sites without comprehensive electronic medical records, provision of timely email feedback, and dissemination of study results.
Analysis of prior antimicrobial use has allowed us to identify targets for ongoing antimicrobial stewardship activities, and we also intend to provide further education on recognition of severity criteria. These activities can be supported through daily antimicrobial stewardship ward rounds. Future research could involve application of appropriateness criteria to prior and current antimicrobial use in CDI patients in order to identify avoidable cases and use of more advanced statistical techniques such as multistate modeling to determine differences in outcomes between cases and controls.
Stuart Bond, BPharm, DipPharmPrac, is an antimicrobial stewardship pharmacist based at Wollongong Hospital in New South Wales, Australia.
Increased risk of death even in lower-risk PPI users
Proton pump inhibitors (PPIs) are associated with a significantly higher risk of death than are H2 receptor antagonists, according to a 5-year longitudinal cohort study.
The study, published online in BMJ Open, found that increased risk of death was evident even in people without gastrointestinal conditions, and it increased with longer duration of use.
Yan Xie, PhD, of the VA Saint Louis Health Care System and coauthors, wrote that PPIs are linked to a range of serious adverse outcomes – such as acute interstitial nephritis, chronic kidney disease, incident dementia, and Clostridium difficile infection – each of which is associated with higher risk of mortality.
“Whether PPI use is associated with excess risk of death is not known and has not been examined in large epidemiological studies spanning a sufficiently long duration of follow-up.”
In this study, a cohort of 349,312 veterans initiated on acid-suppression therapy was followed for a mean duration of 5.71 years (BMJ Open 2017. July 4;7:e015735. doi: 10.1136/bmjopen-2016-015735).
Researchers saw a 25% higher risk of death in the 275,977 participants treated with PPIs, compared with that in those who were treated with H2 receptor antagonists (95% confidence interval, 1.23-1.28), after adjusting for factors such as estimated glomerular filtration rate, age, hospitalizations, and a range of comorbidities, including gastrointestinal disorders.
When PPI use was compared with no PPI use, there was a 15% increase in the risk of death (95% CI, 1.14-1.15). When compared with no known exposure to any acid suppression therapy, the increased risk of death was 23% (95% CI, 1.22-1.24).
In an attempt to look at the risk of death in a lower-risk cohort, the researchers analyzed a subgroup of participants who did not have the conditions for which PPIs are normally prescribed, such as gastroesophageal reflux disease, upper gastrointestinal tract bleeding, ulcer disease, Helicobacter pylori infection, and Barrett’s esophagus.
However, even in this lower-risk cohort, the study still showed a 24% increase in the risk of death with PPIs, compared with that in H2 receptor antagonists (95% CI, 1.21-1.27); a 19% increase with PPIs, compared with no PPIs; and a 22% increase with PPIs, compared with no acid suppression.
Duration of exposure to PPIs was also associated with increasing risk of death. Participants who had taken PPIs for fewer than 90 days in total only had a 5% increase in risk, while those taking them for 361-720 days had a 51% increased risk of death.
“Although our results should not deter prescription and use of PPIs where medically indicated, they may be used to encourage and promote pharmacovigilance and emphasize the need to exercise judicious use of PPIs and limit use and duration of therapy to instances where there is a clear medical indication and where benefit outweighs potential risk,” the authors wrote.
“Standardized guidelines for initiating PPI prescription may lead to reduced overuse [and] regular review of prescription and over-the-counter medications, and deprescription, where a medical indication for PPI treatment ceases to exist, may be a meritorious approach.”
Examining possible physiologic mechanisms to explain the increased risk of death, the authors noted that animal studies suggested PPIs may limit the liver’s capacity to regenerate.
PPIs are also associated with increased activity of the heme oxygenase-1 enzyme in gastric and endothelial cells and impairment of lysosomal acidification and proteostasis and may alter gene expression in the cellular retinol metabolism pathway and the complement and coagulation cascades pathway.
However, the clinical mediator of the heightened risk of death was likely one of the adverse events linked to PPI use, they said.
No conflicts of interest were declared.
Proton pump inhibitors (PPIs) are associated with a significantly higher risk of death than are H2 receptor antagonists, according to a 5-year longitudinal cohort study.
The study, published online in BMJ Open, found that increased risk of death was evident even in people without gastrointestinal conditions, and it increased with longer duration of use.
Yan Xie, PhD, of the VA Saint Louis Health Care System and coauthors, wrote that PPIs are linked to a range of serious adverse outcomes – such as acute interstitial nephritis, chronic kidney disease, incident dementia, and Clostridium difficile infection – each of which is associated with higher risk of mortality.
“Whether PPI use is associated with excess risk of death is not known and has not been examined in large epidemiological studies spanning a sufficiently long duration of follow-up.”
In this study, a cohort of 349,312 veterans initiated on acid-suppression therapy was followed for a mean duration of 5.71 years (BMJ Open 2017. July 4;7:e015735. doi: 10.1136/bmjopen-2016-015735).
Researchers saw a 25% higher risk of death in the 275,977 participants treated with PPIs, compared with that in those who were treated with H2 receptor antagonists (95% confidence interval, 1.23-1.28), after adjusting for factors such as estimated glomerular filtration rate, age, hospitalizations, and a range of comorbidities, including gastrointestinal disorders.
When PPI use was compared with no PPI use, there was a 15% increase in the risk of death (95% CI, 1.14-1.15). When compared with no known exposure to any acid suppression therapy, the increased risk of death was 23% (95% CI, 1.22-1.24).
In an attempt to look at the risk of death in a lower-risk cohort, the researchers analyzed a subgroup of participants who did not have the conditions for which PPIs are normally prescribed, such as gastroesophageal reflux disease, upper gastrointestinal tract bleeding, ulcer disease, Helicobacter pylori infection, and Barrett’s esophagus.
However, even in this lower-risk cohort, the study still showed a 24% increase in the risk of death with PPIs, compared with that in H2 receptor antagonists (95% CI, 1.21-1.27); a 19% increase with PPIs, compared with no PPIs; and a 22% increase with PPIs, compared with no acid suppression.
Duration of exposure to PPIs was also associated with increasing risk of death. Participants who had taken PPIs for fewer than 90 days in total only had a 5% increase in risk, while those taking them for 361-720 days had a 51% increased risk of death.
“Although our results should not deter prescription and use of PPIs where medically indicated, they may be used to encourage and promote pharmacovigilance and emphasize the need to exercise judicious use of PPIs and limit use and duration of therapy to instances where there is a clear medical indication and where benefit outweighs potential risk,” the authors wrote.
“Standardized guidelines for initiating PPI prescription may lead to reduced overuse [and] regular review of prescription and over-the-counter medications, and deprescription, where a medical indication for PPI treatment ceases to exist, may be a meritorious approach.”
Examining possible physiologic mechanisms to explain the increased risk of death, the authors noted that animal studies suggested PPIs may limit the liver’s capacity to regenerate.
PPIs are also associated with increased activity of the heme oxygenase-1 enzyme in gastric and endothelial cells and impairment of lysosomal acidification and proteostasis and may alter gene expression in the cellular retinol metabolism pathway and the complement and coagulation cascades pathway.
However, the clinical mediator of the heightened risk of death was likely one of the adverse events linked to PPI use, they said.
No conflicts of interest were declared.
Proton pump inhibitors (PPIs) are associated with a significantly higher risk of death than are H2 receptor antagonists, according to a 5-year longitudinal cohort study.
The study, published online in BMJ Open, found that increased risk of death was evident even in people without gastrointestinal conditions, and it increased with longer duration of use.
Yan Xie, PhD, of the VA Saint Louis Health Care System and coauthors, wrote that PPIs are linked to a range of serious adverse outcomes – such as acute interstitial nephritis, chronic kidney disease, incident dementia, and Clostridium difficile infection – each of which is associated with higher risk of mortality.
“Whether PPI use is associated with excess risk of death is not known and has not been examined in large epidemiological studies spanning a sufficiently long duration of follow-up.”
In this study, a cohort of 349,312 veterans initiated on acid-suppression therapy was followed for a mean duration of 5.71 years (BMJ Open 2017. July 4;7:e015735. doi: 10.1136/bmjopen-2016-015735).
Researchers saw a 25% higher risk of death in the 275,977 participants treated with PPIs, compared with that in those who were treated with H2 receptor antagonists (95% confidence interval, 1.23-1.28), after adjusting for factors such as estimated glomerular filtration rate, age, hospitalizations, and a range of comorbidities, including gastrointestinal disorders.
When PPI use was compared with no PPI use, there was a 15% increase in the risk of death (95% CI, 1.14-1.15). When compared with no known exposure to any acid suppression therapy, the increased risk of death was 23% (95% CI, 1.22-1.24).
In an attempt to look at the risk of death in a lower-risk cohort, the researchers analyzed a subgroup of participants who did not have the conditions for which PPIs are normally prescribed, such as gastroesophageal reflux disease, upper gastrointestinal tract bleeding, ulcer disease, Helicobacter pylori infection, and Barrett’s esophagus.
However, even in this lower-risk cohort, the study still showed a 24% increase in the risk of death with PPIs, compared with that in H2 receptor antagonists (95% CI, 1.21-1.27); a 19% increase with PPIs, compared with no PPIs; and a 22% increase with PPIs, compared with no acid suppression.
Duration of exposure to PPIs was also associated with increasing risk of death. Participants who had taken PPIs for fewer than 90 days in total only had a 5% increase in risk, while those taking them for 361-720 days had a 51% increased risk of death.
“Although our results should not deter prescription and use of PPIs where medically indicated, they may be used to encourage and promote pharmacovigilance and emphasize the need to exercise judicious use of PPIs and limit use and duration of therapy to instances where there is a clear medical indication and where benefit outweighs potential risk,” the authors wrote.
“Standardized guidelines for initiating PPI prescription may lead to reduced overuse [and] regular review of prescription and over-the-counter medications, and deprescription, where a medical indication for PPI treatment ceases to exist, may be a meritorious approach.”
Examining possible physiologic mechanisms to explain the increased risk of death, the authors noted that animal studies suggested PPIs may limit the liver’s capacity to regenerate.
PPIs are also associated with increased activity of the heme oxygenase-1 enzyme in gastric and endothelial cells and impairment of lysosomal acidification and proteostasis and may alter gene expression in the cellular retinol metabolism pathway and the complement and coagulation cascades pathway.
However, the clinical mediator of the heightened risk of death was likely one of the adverse events linked to PPI use, they said.
No conflicts of interest were declared.
FROM BMJ OPEN
Key clinical point: Proton pump inhibitors are associated with a significantly higher risk of death, even among people without the gastrointestinal conditions for which the drugs are normally prescribed.
Major finding: People taking PPIs have a 25% higher risk of death, compared with those taking H2 receptor antagonists.
Data source: A longitudinal cohort study in 349,312 veterans.
Disclosures: No conflicts of interest were declared.
Ceftaroline shortens duration of MRSA bacteremia
NEW ORLEANS – Ceftaroline fosamil reduced the median duration of methicillin-resistant Staphylococcus aureus (MRSA) bacteremia by 2 days in Veterans Administration patients, a retrospective study showed.
Investigators identified 219 patients with MRSA within the Veterans Affairs (VA) medical system nationwide from 2011 to 2015. All patients received at least 48 hours of ceftaroline fosamil (Teflaro) therapy to treat MRSA bacteremia. “We know it has good activity against MRSA in vitro. We use it in bacteremia, but we don’t have a lot of clinical data to support or refute its use,” said Nicholas S. Britt, PharmD, a PGY2 infectious diseases resident at Barnes-Jewish Hospital in St. Louis.
“Ceftaroline was primarily used as second-line or salvage therapy … which is basically what we expected, based on how it’s used in clinical practice,” Dr. Britt said.
Treatment failures
A total of 88 of the 219 (40%) patients experienced treatment failure. This rate “seems kind of high, but, if you look at some of the other MRSA agents for bacteremia (vancomycin, for example), it usually has a treatment failure rate around 60%,” Dr. Britt said. “The outcomes were not as poor as I would expect with [patients] using it for second- and third-line therapy.”
Hospital-acquired infection (odds ratio, 2.11; P = .013), ICU admission (OR, 3.95; P less than .001) and infective endocarditis (OR, 4.77; P = .002) were significantly associated with treatment failure in a univariate analysis. “Admissions to the ICU and endocarditis were the big ones, factors you would associate with failure for most antibiotics,” Dr. Britt said. In a multivariate analysis, only ICU admission remained significantly associated with treatment failure (adjusted OR, 2.24; P = .028).
The investigators also looked at treatment failure with ceftaroline monotherapy, compared with its use in combination. There is in vitro data showing synergy when you add ceftaroline to daptomycin, vancomycin, or some of these other agents,” Dr. Britt said. However, he added, “We didn’t find any significant difference in outcomes when you added another agent.” Treatment failure with monotherapy was 35%, versus 46%, with combination treatment (P = .107).
“This could be because the sicker patients are the ones getting combination therapy.”
No observed differences by dosing
Dr. Britt and his colleagues also looked for any differences by dosing interval, “which hasn’t been evaluated extensively.”
The Food and Drug Administration labeled it for use every 12 hours, but treatment of MRSA bacteremia is an off-label use, Dr. Britt explained. Dosing every 8 hours instead improves the achievement of pharmacokinetic and pharmacodynamic parameters in in vitro studies. “Clinically, we’re almost always using it q8. They’re sick patients, so you don’t want to under-dose them. And ceftaroline is pretty well tolerated overall.”
“But, we didn’t really see any difference between the q8 and the q12” in terms of treatment failure. The rates were 36% and 42%, respectively, and not significantly different (P = .440). “Granted, patients who are sicker are probably going to get treated more aggressively,” Dr. Britt added.
The current research only focused on outcomes associated with ceftaroline. Going forward, Dr. Britt said, “We’re hoping to use this data to compare ceftaroline to other agents as well, probably as second-line therapy, since that’s how it’s used most often.”
Dr. Britt had no relevant financial disclosures.
NEW ORLEANS – Ceftaroline fosamil reduced the median duration of methicillin-resistant Staphylococcus aureus (MRSA) bacteremia by 2 days in Veterans Administration patients, a retrospective study showed.
Investigators identified 219 patients with MRSA within the Veterans Affairs (VA) medical system nationwide from 2011 to 2015. All patients received at least 48 hours of ceftaroline fosamil (Teflaro) therapy to treat MRSA bacteremia. “We know it has good activity against MRSA in vitro. We use it in bacteremia, but we don’t have a lot of clinical data to support or refute its use,” said Nicholas S. Britt, PharmD, a PGY2 infectious diseases resident at Barnes-Jewish Hospital in St. Louis.
“Ceftaroline was primarily used as second-line or salvage therapy … which is basically what we expected, based on how it’s used in clinical practice,” Dr. Britt said.
Treatment failures
A total of 88 of the 219 (40%) patients experienced treatment failure. This rate “seems kind of high, but, if you look at some of the other MRSA agents for bacteremia (vancomycin, for example), it usually has a treatment failure rate around 60%,” Dr. Britt said. “The outcomes were not as poor as I would expect with [patients] using it for second- and third-line therapy.”
Hospital-acquired infection (odds ratio, 2.11; P = .013), ICU admission (OR, 3.95; P less than .001) and infective endocarditis (OR, 4.77; P = .002) were significantly associated with treatment failure in a univariate analysis. “Admissions to the ICU and endocarditis were the big ones, factors you would associate with failure for most antibiotics,” Dr. Britt said. In a multivariate analysis, only ICU admission remained significantly associated with treatment failure (adjusted OR, 2.24; P = .028).
The investigators also looked at treatment failure with ceftaroline monotherapy, compared with its use in combination. There is in vitro data showing synergy when you add ceftaroline to daptomycin, vancomycin, or some of these other agents,” Dr. Britt said. However, he added, “We didn’t find any significant difference in outcomes when you added another agent.” Treatment failure with monotherapy was 35%, versus 46%, with combination treatment (P = .107).
“This could be because the sicker patients are the ones getting combination therapy.”
No observed differences by dosing
Dr. Britt and his colleagues also looked for any differences by dosing interval, “which hasn’t been evaluated extensively.”
The Food and Drug Administration labeled it for use every 12 hours, but treatment of MRSA bacteremia is an off-label use, Dr. Britt explained. Dosing every 8 hours instead improves the achievement of pharmacokinetic and pharmacodynamic parameters in in vitro studies. “Clinically, we’re almost always using it q8. They’re sick patients, so you don’t want to under-dose them. And ceftaroline is pretty well tolerated overall.”
“But, we didn’t really see any difference between the q8 and the q12” in terms of treatment failure. The rates were 36% and 42%, respectively, and not significantly different (P = .440). “Granted, patients who are sicker are probably going to get treated more aggressively,” Dr. Britt added.
The current research only focused on outcomes associated with ceftaroline. Going forward, Dr. Britt said, “We’re hoping to use this data to compare ceftaroline to other agents as well, probably as second-line therapy, since that’s how it’s used most often.”
Dr. Britt had no relevant financial disclosures.
NEW ORLEANS – Ceftaroline fosamil reduced the median duration of methicillin-resistant Staphylococcus aureus (MRSA) bacteremia by 2 days in Veterans Administration patients, a retrospective study showed.
Investigators identified 219 patients with MRSA within the Veterans Affairs (VA) medical system nationwide from 2011 to 2015. All patients received at least 48 hours of ceftaroline fosamil (Teflaro) therapy to treat MRSA bacteremia. “We know it has good activity against MRSA in vitro. We use it in bacteremia, but we don’t have a lot of clinical data to support or refute its use,” said Nicholas S. Britt, PharmD, a PGY2 infectious diseases resident at Barnes-Jewish Hospital in St. Louis.
“Ceftaroline was primarily used as second-line or salvage therapy … which is basically what we expected, based on how it’s used in clinical practice,” Dr. Britt said.
Treatment failures
A total of 88 of the 219 (40%) patients experienced treatment failure. This rate “seems kind of high, but, if you look at some of the other MRSA agents for bacteremia (vancomycin, for example), it usually has a treatment failure rate around 60%,” Dr. Britt said. “The outcomes were not as poor as I would expect with [patients] using it for second- and third-line therapy.”
Hospital-acquired infection (odds ratio, 2.11; P = .013), ICU admission (OR, 3.95; P less than .001) and infective endocarditis (OR, 4.77; P = .002) were significantly associated with treatment failure in a univariate analysis. “Admissions to the ICU and endocarditis were the big ones, factors you would associate with failure for most antibiotics,” Dr. Britt said. In a multivariate analysis, only ICU admission remained significantly associated with treatment failure (adjusted OR, 2.24; P = .028).
The investigators also looked at treatment failure with ceftaroline monotherapy, compared with its use in combination. There is in vitro data showing synergy when you add ceftaroline to daptomycin, vancomycin, or some of these other agents,” Dr. Britt said. However, he added, “We didn’t find any significant difference in outcomes when you added another agent.” Treatment failure with monotherapy was 35%, versus 46%, with combination treatment (P = .107).
“This could be because the sicker patients are the ones getting combination therapy.”
No observed differences by dosing
Dr. Britt and his colleagues also looked for any differences by dosing interval, “which hasn’t been evaluated extensively.”
The Food and Drug Administration labeled it for use every 12 hours, but treatment of MRSA bacteremia is an off-label use, Dr. Britt explained. Dosing every 8 hours instead improves the achievement of pharmacokinetic and pharmacodynamic parameters in in vitro studies. “Clinically, we’re almost always using it q8. They’re sick patients, so you don’t want to under-dose them. And ceftaroline is pretty well tolerated overall.”
“But, we didn’t really see any difference between the q8 and the q12” in terms of treatment failure. The rates were 36% and 42%, respectively, and not significantly different (P = .440). “Granted, patients who are sicker are probably going to get treated more aggressively,” Dr. Britt added.
The current research only focused on outcomes associated with ceftaroline. Going forward, Dr. Britt said, “We’re hoping to use this data to compare ceftaroline to other agents as well, probably as second-line therapy, since that’s how it’s used most often.”
Dr. Britt had no relevant financial disclosures.
AT ASM MICROBE 2017
Key clinical point:
Major finding: Median duration of MRSA bacteremia dropped from 2.79 days before to 1.18 days after initiation of ceftaroline (P less than .001).
Data source: A retrospective study of 219 hospitalized VA patients initiating ceftaroline for MRSA bacteremia.
Disclosures: Dr. Britt had no relevant financial disclosures.
Carbapenem-resistant sepsis risk factors vary significantly
NEW ORLEANS – Investigators discovered significant differences in risk factors when comparing 603 people hospitalized with carbapenem-resistant Gram-negative sepsis with either Enterobacteriaceae-caused or non-Enterobacteriaceae–caused infection.
“We know some of the virulence factors and the resistance mechanisms can differ between those two groups. We really wanted to see if that would influence outcomes,” said Nicholas S. Britt, PharmD, a PGY2 infectious disease resident at Barnes-Jewish Hospital in St. Louis. Mortality rates, however, did not differ significantly.
“Patients who had Enterobacteriaceae infections were more likely to have urinary tract infections, to be older patients, and to have higher APACHE (Acute Physiologic Assessment and Chronic Health Evaluation) II scores,” Dr. Britt said at the annual meeting of the American Society for Microbiology. These differences all were statistically significant, compared with those of the CRNE group (P less than .05).
In contrast, the non-Enterobacteriaceae patients tended to have more respiratory infections and more frequent central venous catheter use. This group also was more likely to have a history of carbapenem use and more frequent antimicrobial exposures overall and to present after solid organ transplantation. “The cystic fibrosis patients were more likely to get non-Enterobacteriaceae infections as well,” Dr. Britt added. These differences also were statistically significant (all P less than .05).
“I think the biggest takeaway from this study, honestly, is the number of patients infected with CRE, versus CRNE,” Dr. Britt said. “We know CRE are a serious public health threat, one of the biggest threats out there, but, if you look at the burden on carbapenem-resistant disease, it’s primarily the non-Enterobacteriaceae.”
In fact, more than three-quarters of the patient studied (78%) had CRNE infections, and Pseudomonas was a major driver, he added. “Carbapenem resistance in this group of patients is something we should be focusing on – not only the CRE – because we’re seeing more of the non-CRE clinically.”
Patient age, presence of bloodstream infection, and use of mechanical ventilation, vasopressors, and immunosuppression was associated with hospital mortality in the study. After adjusting for potential confounders, however, CRNE infection was not associated with increased hospital mortality, compared with CRE cases (adjusted odds ratio, 0.97; P = .917).
“Our mortality rate was 16%, which is comparable to [that of] other studies,” Dr. Britt said. “There doesn’t seem to be any difference in this outcome between the two groups.” Mortality was 16.4% in the CRE cohort, versus 16.5% in the CRNE cohort (P = 0.965).
NEW ORLEANS – Investigators discovered significant differences in risk factors when comparing 603 people hospitalized with carbapenem-resistant Gram-negative sepsis with either Enterobacteriaceae-caused or non-Enterobacteriaceae–caused infection.
“We know some of the virulence factors and the resistance mechanisms can differ between those two groups. We really wanted to see if that would influence outcomes,” said Nicholas S. Britt, PharmD, a PGY2 infectious disease resident at Barnes-Jewish Hospital in St. Louis. Mortality rates, however, did not differ significantly.
“Patients who had Enterobacteriaceae infections were more likely to have urinary tract infections, to be older patients, and to have higher APACHE (Acute Physiologic Assessment and Chronic Health Evaluation) II scores,” Dr. Britt said at the annual meeting of the American Society for Microbiology. These differences all were statistically significant, compared with those of the CRNE group (P less than .05).
In contrast, the non-Enterobacteriaceae patients tended to have more respiratory infections and more frequent central venous catheter use. This group also was more likely to have a history of carbapenem use and more frequent antimicrobial exposures overall and to present after solid organ transplantation. “The cystic fibrosis patients were more likely to get non-Enterobacteriaceae infections as well,” Dr. Britt added. These differences also were statistically significant (all P less than .05).
“I think the biggest takeaway from this study, honestly, is the number of patients infected with CRE, versus CRNE,” Dr. Britt said. “We know CRE are a serious public health threat, one of the biggest threats out there, but, if you look at the burden on carbapenem-resistant disease, it’s primarily the non-Enterobacteriaceae.”
In fact, more than three-quarters of the patient studied (78%) had CRNE infections, and Pseudomonas was a major driver, he added. “Carbapenem resistance in this group of patients is something we should be focusing on – not only the CRE – because we’re seeing more of the non-CRE clinically.”
Patient age, presence of bloodstream infection, and use of mechanical ventilation, vasopressors, and immunosuppression was associated with hospital mortality in the study. After adjusting for potential confounders, however, CRNE infection was not associated with increased hospital mortality, compared with CRE cases (adjusted odds ratio, 0.97; P = .917).
“Our mortality rate was 16%, which is comparable to [that of] other studies,” Dr. Britt said. “There doesn’t seem to be any difference in this outcome between the two groups.” Mortality was 16.4% in the CRE cohort, versus 16.5% in the CRNE cohort (P = 0.965).
NEW ORLEANS – Investigators discovered significant differences in risk factors when comparing 603 people hospitalized with carbapenem-resistant Gram-negative sepsis with either Enterobacteriaceae-caused or non-Enterobacteriaceae–caused infection.
“We know some of the virulence factors and the resistance mechanisms can differ between those two groups. We really wanted to see if that would influence outcomes,” said Nicholas S. Britt, PharmD, a PGY2 infectious disease resident at Barnes-Jewish Hospital in St. Louis. Mortality rates, however, did not differ significantly.
“Patients who had Enterobacteriaceae infections were more likely to have urinary tract infections, to be older patients, and to have higher APACHE (Acute Physiologic Assessment and Chronic Health Evaluation) II scores,” Dr. Britt said at the annual meeting of the American Society for Microbiology. These differences all were statistically significant, compared with those of the CRNE group (P less than .05).
In contrast, the non-Enterobacteriaceae patients tended to have more respiratory infections and more frequent central venous catheter use. This group also was more likely to have a history of carbapenem use and more frequent antimicrobial exposures overall and to present after solid organ transplantation. “The cystic fibrosis patients were more likely to get non-Enterobacteriaceae infections as well,” Dr. Britt added. These differences also were statistically significant (all P less than .05).
“I think the biggest takeaway from this study, honestly, is the number of patients infected with CRE, versus CRNE,” Dr. Britt said. “We know CRE are a serious public health threat, one of the biggest threats out there, but, if you look at the burden on carbapenem-resistant disease, it’s primarily the non-Enterobacteriaceae.”
In fact, more than three-quarters of the patient studied (78%) had CRNE infections, and Pseudomonas was a major driver, he added. “Carbapenem resistance in this group of patients is something we should be focusing on – not only the CRE – because we’re seeing more of the non-CRE clinically.”
Patient age, presence of bloodstream infection, and use of mechanical ventilation, vasopressors, and immunosuppression was associated with hospital mortality in the study. After adjusting for potential confounders, however, CRNE infection was not associated with increased hospital mortality, compared with CRE cases (adjusted odds ratio, 0.97; P = .917).
“Our mortality rate was 16%, which is comparable to [that of] other studies,” Dr. Britt said. “There doesn’t seem to be any difference in this outcome between the two groups.” Mortality was 16.4% in the CRE cohort, versus 16.5% in the CRNE cohort (P = 0.965).
AT ASM MICROBE 2017
Key clinical point:
Major finding: Hospital mortality was 16% overall and did not differ significantly between Enterobacteriaceae and non-Enterobacteriaceae infections (16.5% vs. 16.4%; P = 0.965).
Data source: A retrospective cohort study of 603 patients with Gram-negative sepsis at a tertiary academic medical center from 2012 to 2016.
Disclosures: Dr. Britt did not have any relevant financial disclosures.
New drug choices emerging to battle antibiotic resistance
SAN FRANCISCO – When the Infectious Diseases Society of America released the “Bad Bugs, No Drugs” report in 2004, its authors warned that effective antibiotics may not be available to treat seriously ill patients in the near future.
It also proposed legislative, regulatory, and funding solutions with a goal of developing and licensing 10 new antibiotics by the year 2020.
One such advancement was the Generating Antibiotics Incentives Now Act, which was signed into law in 2012 and created a designation for new antibiotics that are used to treat serious and/or life-threatening diseases due to certain pathogens. It also extends the patent life of these antibiotics and allows for fast-track Food and Drug Administration approval.
According to Dr. Erlich, chief of staff and medical director of infection control and antibiotic stewardship at Mills Peninsula Medical Center, Burlingame, Calif., increasingly common antibiotic-resistant pathogens besides MRSA and VRE include penicillin-resistant Streptococcus pneumoniae, extended-spectrum beta-lactamase–producing gram-negative rods, carbapenem-resistant Enterobacteriaceae (CRE), multidrug-resistant Mycobacterium tuberculosis, Salmonella enterica serotype Typhimurium DT 104, and drug-resistant Candida species.
Since 2010, several new antibiotics have been introduced to the market, including three second-generation lipoglycopeptide antibiotics with gram-positive coverage that are approved primarily for skin and soft tissue infections: dalbavancin (Dalvance), telavancin (Vibativ), and oritavancin (Orbactiv).
Compared with vancomycin, these new agents have more convenient dosing and a longer half life, “but they’re also more expensive,” said Dr. Erlich. Dalbavancin can be dosed once a week intravenously, telavancin can be dosed once daily intravenously, and oritavancin requires just one dose.
Another new agent is tedizolid phosphate (Sivextro), a second-generation oxazolidinone that is in the same drug class as linezolid (Zyvox). Tedizolid phosphate has gram-positive coverage including MRSA, but it is not approved for VRE. “It’s FDA approved for skin and soft-tissue infections (SSTI) but can be used for other locations as well,” Dr. Erlich said. “It features once-daily dosing IV or PO.”
Ceftaroline fosamil (Teflaro), ceftolozane/tazobactam (Zerbaxa), and ceftazidime/avibactam (Avycaz) are broad-spectrum cephalosporins with or without beta-lactamase inhibitors resulting in extended gram-negative coverage. FDA-approved indications include complicated urinary tract infections, complicated abdominal infections, SSTI, and pneumonia.
The primary advantage of these drugs, compared with other agents, is for multidrug-resistant gram-negative bacteria such as extended-spectrum beta-lactamase producers and CRE. “We’re not using a lot of these drugs in clinical practice, but they are available for patients with multidrug-resistant gram-negative rods who have no other options,” Dr. Erlich said.
Practical ways that clinicians can prevent antibiotic resistance include prescribing antibiotics only when necessary. “Be aware of local resistance patterns, avoid antibiotics for probable viral infections, use narrow-spectrum choices when possible, use shorter durations when appropriate, and consult published guidelines for optimal empiric antibiotic therapy,” Dr. Erlich advised.
In addition, “advocate infection control measures to keep patients from developing infections, including proper wound care, hand washing, respiratory etiquette, vaccinations, and social isolation for symptomatic individuals,” he noted.
Dr. Erlich reported having no relevant financial disclosures.
SAN FRANCISCO – When the Infectious Diseases Society of America released the “Bad Bugs, No Drugs” report in 2004, its authors warned that effective antibiotics may not be available to treat seriously ill patients in the near future.
It also proposed legislative, regulatory, and funding solutions with a goal of developing and licensing 10 new antibiotics by the year 2020.
One such advancement was the Generating Antibiotics Incentives Now Act, which was signed into law in 2012 and created a designation for new antibiotics that are used to treat serious and/or life-threatening diseases due to certain pathogens. It also extends the patent life of these antibiotics and allows for fast-track Food and Drug Administration approval.
According to Dr. Erlich, chief of staff and medical director of infection control and antibiotic stewardship at Mills Peninsula Medical Center, Burlingame, Calif., increasingly common antibiotic-resistant pathogens besides MRSA and VRE include penicillin-resistant Streptococcus pneumoniae, extended-spectrum beta-lactamase–producing gram-negative rods, carbapenem-resistant Enterobacteriaceae (CRE), multidrug-resistant Mycobacterium tuberculosis, Salmonella enterica serotype Typhimurium DT 104, and drug-resistant Candida species.
Since 2010, several new antibiotics have been introduced to the market, including three second-generation lipoglycopeptide antibiotics with gram-positive coverage that are approved primarily for skin and soft tissue infections: dalbavancin (Dalvance), telavancin (Vibativ), and oritavancin (Orbactiv).
Compared with vancomycin, these new agents have more convenient dosing and a longer half life, “but they’re also more expensive,” said Dr. Erlich. Dalbavancin can be dosed once a week intravenously, telavancin can be dosed once daily intravenously, and oritavancin requires just one dose.
Another new agent is tedizolid phosphate (Sivextro), a second-generation oxazolidinone that is in the same drug class as linezolid (Zyvox). Tedizolid phosphate has gram-positive coverage including MRSA, but it is not approved for VRE. “It’s FDA approved for skin and soft-tissue infections (SSTI) but can be used for other locations as well,” Dr. Erlich said. “It features once-daily dosing IV or PO.”
Ceftaroline fosamil (Teflaro), ceftolozane/tazobactam (Zerbaxa), and ceftazidime/avibactam (Avycaz) are broad-spectrum cephalosporins with or without beta-lactamase inhibitors resulting in extended gram-negative coverage. FDA-approved indications include complicated urinary tract infections, complicated abdominal infections, SSTI, and pneumonia.
The primary advantage of these drugs, compared with other agents, is for multidrug-resistant gram-negative bacteria such as extended-spectrum beta-lactamase producers and CRE. “We’re not using a lot of these drugs in clinical practice, but they are available for patients with multidrug-resistant gram-negative rods who have no other options,” Dr. Erlich said.
Practical ways that clinicians can prevent antibiotic resistance include prescribing antibiotics only when necessary. “Be aware of local resistance patterns, avoid antibiotics for probable viral infections, use narrow-spectrum choices when possible, use shorter durations when appropriate, and consult published guidelines for optimal empiric antibiotic therapy,” Dr. Erlich advised.
In addition, “advocate infection control measures to keep patients from developing infections, including proper wound care, hand washing, respiratory etiquette, vaccinations, and social isolation for symptomatic individuals,” he noted.
Dr. Erlich reported having no relevant financial disclosures.
SAN FRANCISCO – When the Infectious Diseases Society of America released the “Bad Bugs, No Drugs” report in 2004, its authors warned that effective antibiotics may not be available to treat seriously ill patients in the near future.
It also proposed legislative, regulatory, and funding solutions with a goal of developing and licensing 10 new antibiotics by the year 2020.
One such advancement was the Generating Antibiotics Incentives Now Act, which was signed into law in 2012 and created a designation for new antibiotics that are used to treat serious and/or life-threatening diseases due to certain pathogens. It also extends the patent life of these antibiotics and allows for fast-track Food and Drug Administration approval.
According to Dr. Erlich, chief of staff and medical director of infection control and antibiotic stewardship at Mills Peninsula Medical Center, Burlingame, Calif., increasingly common antibiotic-resistant pathogens besides MRSA and VRE include penicillin-resistant Streptococcus pneumoniae, extended-spectrum beta-lactamase–producing gram-negative rods, carbapenem-resistant Enterobacteriaceae (CRE), multidrug-resistant Mycobacterium tuberculosis, Salmonella enterica serotype Typhimurium DT 104, and drug-resistant Candida species.
Since 2010, several new antibiotics have been introduced to the market, including three second-generation lipoglycopeptide antibiotics with gram-positive coverage that are approved primarily for skin and soft tissue infections: dalbavancin (Dalvance), telavancin (Vibativ), and oritavancin (Orbactiv).
Compared with vancomycin, these new agents have more convenient dosing and a longer half life, “but they’re also more expensive,” said Dr. Erlich. Dalbavancin can be dosed once a week intravenously, telavancin can be dosed once daily intravenously, and oritavancin requires just one dose.
Another new agent is tedizolid phosphate (Sivextro), a second-generation oxazolidinone that is in the same drug class as linezolid (Zyvox). Tedizolid phosphate has gram-positive coverage including MRSA, but it is not approved for VRE. “It’s FDA approved for skin and soft-tissue infections (SSTI) but can be used for other locations as well,” Dr. Erlich said. “It features once-daily dosing IV or PO.”
Ceftaroline fosamil (Teflaro), ceftolozane/tazobactam (Zerbaxa), and ceftazidime/avibactam (Avycaz) are broad-spectrum cephalosporins with or without beta-lactamase inhibitors resulting in extended gram-negative coverage. FDA-approved indications include complicated urinary tract infections, complicated abdominal infections, SSTI, and pneumonia.
The primary advantage of these drugs, compared with other agents, is for multidrug-resistant gram-negative bacteria such as extended-spectrum beta-lactamase producers and CRE. “We’re not using a lot of these drugs in clinical practice, but they are available for patients with multidrug-resistant gram-negative rods who have no other options,” Dr. Erlich said.
Practical ways that clinicians can prevent antibiotic resistance include prescribing antibiotics only when necessary. “Be aware of local resistance patterns, avoid antibiotics for probable viral infections, use narrow-spectrum choices when possible, use shorter durations when appropriate, and consult published guidelines for optimal empiric antibiotic therapy,” Dr. Erlich advised.
In addition, “advocate infection control measures to keep patients from developing infections, including proper wound care, hand washing, respiratory etiquette, vaccinations, and social isolation for symptomatic individuals,” he noted.
Dr. Erlich reported having no relevant financial disclosures.
AT THE ANNUAL ADVANCES IN INTERNAL MEDICINE
Hospital antibiograms may not apply to emergency department patients
NEW ORLEANS – Patients seen in the emergency department present with a wider range of risk for resistant infections than do hospitalized patients overall, and as a result, hospital-wide antibiograms that dictate empiric therapy may not translate well to the ED setting, a study showed.
Instead, investigators suggested that clinicians choose empiric antimicrobial therapy in the emergency department based on factors associated with differences in susceptibility.
The study researchers compared common antibiotics to treat Escherichia coli between adults treated at their institution overall versus the emergency department, and by sex, patient age, and whether people came to the ED from home versus a long-term care setting. They found some significant differences that could guide empiric treatment in the ED setting.
“Our ED pharmacist observed a lot of broad-spectrum antibiotic prescribing for UTIs,” lead investigator Sarah Jorgensen, PharmD, said at the annual meeting of the American Society for Microbiology. “Also, we’ve had a culture follow-up program in place for the last 5 years, and they had to intervene on a lot of postdischarge antibiotic mismatches.”
E. coli was the most common urinary pathogen detected in this study of 500 randomly selected ED patients with ICD-9/ICD-10 diagnostic codes for urinary tract infection. Investigators found E. coli in 64% of the 226 culture-positive patients presenting to the ED at Huntington Hospital in Pasadena, Calif., between July 2015 and June 2016.
“What was surprising for us, because our enrollment was based on ICD codes for a UTI, is that only about 50% had a positive urine culture,” said Dr. Jorgensen, a pharmacy resident at the University of Southern California in Los Angeles. “Urinalysis was positive in about 99% of the population.”
Dr. Jorgensen and her colleagues found overall low susceptibilities of 71% for ciprofloxacin, 66% for trimethoprim/sulfamethoxazole, and 67% for cefazolin susceptibilities in the ED. They also found that 8% of isolates were positive for extended-spectrum beta-lactamase isolates, as were 1% of E. coli isolates.
The 67% cefazolin susceptibility was significantly lower in the ED, compared with the 86% susceptibility in the institutional antibiogram (P less than .001).
The investigators found E. coli susceptibility to ciprofloxacin was lower in men, at 55%, compared with 74% among women, but the difference was not statistically significant (P = .14). A similar pattern emerged with cefazolin – 55% susceptibility among men and 69% among women (P = .26). In contrast, trimethoprim/sulfamethoxazole susceptibility trended higher in men, at 73%, vs. 64% among women in the ED (P = .63).
When they divided patients by age 50 years and younger versus those older than 50, the investigators found ampicillin susceptibilities were lower in the younger group, at 30%, compared with 51% among those in the older cohort (P = .03). Similarly, gentamicin susceptibilities were 80% in the younger group, compared with 92% in the older group (P = .04).
Ciprofloxacin susceptibility was significantly lower among people coming to the ED from a long-term care facility than among those coming from home – 35% vs. 77% (P less than .001). Differences in ciprofloxacin susceptibility between admitted and discharged patients was less striking – 63% vs. 78% (P = .04).
Nitrofurantoin was the only oral agent with susceptibility greater than 80% in all patient groups, with susceptibility ranging from 88% to 100%.
Because it typically takes 2-3 days to get the susceptibility results back at Huntington Hospital, many patients are discharged on empiric therapy, noted Mira Zurayk, PharmD, a resident at Huntington Hospital. That can present multiple challenges, particularly with homeless patients who are difficult to find and provide follow-up for, Dr. Jorgensen added.
Based partly on the study findings, the investigators developed a clinical algorithm specifically to address UTI antimicrobial prescriptions in the ED. The algorithm incorporates different recommendations for different groups of patients because of their different resistance trends.
“I think that is a good way to tailor empiric therapy when you don’t have culture results up front,” Dr. Jorgensen said. “We just implemented the algorithm, and I’m now analyzing the outcomes.”
Having more data on outcomes will help the clinicians target lowering the rate of “drug-bug mismatches,” as well as UTI-related revisits to the ED. In addition, the work could help expand the antibiotic stewardship program in the hospital to the ED for the first time, Dr. Jorgensen said.
Dr. Jorgensen and Dr. Zurayk had no relevant financial disclosures. One of the study coauthors, Annie Wong-Beringer, PharmD, receives grant funding from Merck.
NEW ORLEANS – Patients seen in the emergency department present with a wider range of risk for resistant infections than do hospitalized patients overall, and as a result, hospital-wide antibiograms that dictate empiric therapy may not translate well to the ED setting, a study showed.
Instead, investigators suggested that clinicians choose empiric antimicrobial therapy in the emergency department based on factors associated with differences in susceptibility.
The study researchers compared common antibiotics to treat Escherichia coli between adults treated at their institution overall versus the emergency department, and by sex, patient age, and whether people came to the ED from home versus a long-term care setting. They found some significant differences that could guide empiric treatment in the ED setting.
“Our ED pharmacist observed a lot of broad-spectrum antibiotic prescribing for UTIs,” lead investigator Sarah Jorgensen, PharmD, said at the annual meeting of the American Society for Microbiology. “Also, we’ve had a culture follow-up program in place for the last 5 years, and they had to intervene on a lot of postdischarge antibiotic mismatches.”
E. coli was the most common urinary pathogen detected in this study of 500 randomly selected ED patients with ICD-9/ICD-10 diagnostic codes for urinary tract infection. Investigators found E. coli in 64% of the 226 culture-positive patients presenting to the ED at Huntington Hospital in Pasadena, Calif., between July 2015 and June 2016.
“What was surprising for us, because our enrollment was based on ICD codes for a UTI, is that only about 50% had a positive urine culture,” said Dr. Jorgensen, a pharmacy resident at the University of Southern California in Los Angeles. “Urinalysis was positive in about 99% of the population.”
Dr. Jorgensen and her colleagues found overall low susceptibilities of 71% for ciprofloxacin, 66% for trimethoprim/sulfamethoxazole, and 67% for cefazolin susceptibilities in the ED. They also found that 8% of isolates were positive for extended-spectrum beta-lactamase isolates, as were 1% of E. coli isolates.
The 67% cefazolin susceptibility was significantly lower in the ED, compared with the 86% susceptibility in the institutional antibiogram (P less than .001).
The investigators found E. coli susceptibility to ciprofloxacin was lower in men, at 55%, compared with 74% among women, but the difference was not statistically significant (P = .14). A similar pattern emerged with cefazolin – 55% susceptibility among men and 69% among women (P = .26). In contrast, trimethoprim/sulfamethoxazole susceptibility trended higher in men, at 73%, vs. 64% among women in the ED (P = .63).
When they divided patients by age 50 years and younger versus those older than 50, the investigators found ampicillin susceptibilities were lower in the younger group, at 30%, compared with 51% among those in the older cohort (P = .03). Similarly, gentamicin susceptibilities were 80% in the younger group, compared with 92% in the older group (P = .04).
Ciprofloxacin susceptibility was significantly lower among people coming to the ED from a long-term care facility than among those coming from home – 35% vs. 77% (P less than .001). Differences in ciprofloxacin susceptibility between admitted and discharged patients was less striking – 63% vs. 78% (P = .04).
Nitrofurantoin was the only oral agent with susceptibility greater than 80% in all patient groups, with susceptibility ranging from 88% to 100%.
Because it typically takes 2-3 days to get the susceptibility results back at Huntington Hospital, many patients are discharged on empiric therapy, noted Mira Zurayk, PharmD, a resident at Huntington Hospital. That can present multiple challenges, particularly with homeless patients who are difficult to find and provide follow-up for, Dr. Jorgensen added.
Based partly on the study findings, the investigators developed a clinical algorithm specifically to address UTI antimicrobial prescriptions in the ED. The algorithm incorporates different recommendations for different groups of patients because of their different resistance trends.
“I think that is a good way to tailor empiric therapy when you don’t have culture results up front,” Dr. Jorgensen said. “We just implemented the algorithm, and I’m now analyzing the outcomes.”
Having more data on outcomes will help the clinicians target lowering the rate of “drug-bug mismatches,” as well as UTI-related revisits to the ED. In addition, the work could help expand the antibiotic stewardship program in the hospital to the ED for the first time, Dr. Jorgensen said.
Dr. Jorgensen and Dr. Zurayk had no relevant financial disclosures. One of the study coauthors, Annie Wong-Beringer, PharmD, receives grant funding from Merck.
NEW ORLEANS – Patients seen in the emergency department present with a wider range of risk for resistant infections than do hospitalized patients overall, and as a result, hospital-wide antibiograms that dictate empiric therapy may not translate well to the ED setting, a study showed.
Instead, investigators suggested that clinicians choose empiric antimicrobial therapy in the emergency department based on factors associated with differences in susceptibility.
The study researchers compared common antibiotics to treat Escherichia coli between adults treated at their institution overall versus the emergency department, and by sex, patient age, and whether people came to the ED from home versus a long-term care setting. They found some significant differences that could guide empiric treatment in the ED setting.
“Our ED pharmacist observed a lot of broad-spectrum antibiotic prescribing for UTIs,” lead investigator Sarah Jorgensen, PharmD, said at the annual meeting of the American Society for Microbiology. “Also, we’ve had a culture follow-up program in place for the last 5 years, and they had to intervene on a lot of postdischarge antibiotic mismatches.”
E. coli was the most common urinary pathogen detected in this study of 500 randomly selected ED patients with ICD-9/ICD-10 diagnostic codes for urinary tract infection. Investigators found E. coli in 64% of the 226 culture-positive patients presenting to the ED at Huntington Hospital in Pasadena, Calif., between July 2015 and June 2016.
“What was surprising for us, because our enrollment was based on ICD codes for a UTI, is that only about 50% had a positive urine culture,” said Dr. Jorgensen, a pharmacy resident at the University of Southern California in Los Angeles. “Urinalysis was positive in about 99% of the population.”
Dr. Jorgensen and her colleagues found overall low susceptibilities of 71% for ciprofloxacin, 66% for trimethoprim/sulfamethoxazole, and 67% for cefazolin susceptibilities in the ED. They also found that 8% of isolates were positive for extended-spectrum beta-lactamase isolates, as were 1% of E. coli isolates.
The 67% cefazolin susceptibility was significantly lower in the ED, compared with the 86% susceptibility in the institutional antibiogram (P less than .001).
The investigators found E. coli susceptibility to ciprofloxacin was lower in men, at 55%, compared with 74% among women, but the difference was not statistically significant (P = .14). A similar pattern emerged with cefazolin – 55% susceptibility among men and 69% among women (P = .26). In contrast, trimethoprim/sulfamethoxazole susceptibility trended higher in men, at 73%, vs. 64% among women in the ED (P = .63).
When they divided patients by age 50 years and younger versus those older than 50, the investigators found ampicillin susceptibilities were lower in the younger group, at 30%, compared with 51% among those in the older cohort (P = .03). Similarly, gentamicin susceptibilities were 80% in the younger group, compared with 92% in the older group (P = .04).
Ciprofloxacin susceptibility was significantly lower among people coming to the ED from a long-term care facility than among those coming from home – 35% vs. 77% (P less than .001). Differences in ciprofloxacin susceptibility between admitted and discharged patients was less striking – 63% vs. 78% (P = .04).
Nitrofurantoin was the only oral agent with susceptibility greater than 80% in all patient groups, with susceptibility ranging from 88% to 100%.
Because it typically takes 2-3 days to get the susceptibility results back at Huntington Hospital, many patients are discharged on empiric therapy, noted Mira Zurayk, PharmD, a resident at Huntington Hospital. That can present multiple challenges, particularly with homeless patients who are difficult to find and provide follow-up for, Dr. Jorgensen added.
Based partly on the study findings, the investigators developed a clinical algorithm specifically to address UTI antimicrobial prescriptions in the ED. The algorithm incorporates different recommendations for different groups of patients because of their different resistance trends.
“I think that is a good way to tailor empiric therapy when you don’t have culture results up front,” Dr. Jorgensen said. “We just implemented the algorithm, and I’m now analyzing the outcomes.”
Having more data on outcomes will help the clinicians target lowering the rate of “drug-bug mismatches,” as well as UTI-related revisits to the ED. In addition, the work could help expand the antibiotic stewardship program in the hospital to the ED for the first time, Dr. Jorgensen said.
Dr. Jorgensen and Dr. Zurayk had no relevant financial disclosures. One of the study coauthors, Annie Wong-Beringer, PharmD, receives grant funding from Merck.
AT ASM MICROBE 2017
Key clinical point: Escherichia coli susceptibility to common antibiotics in the emergency department varies by age, sex, and admitted versus discharge status.
Major finding: The only oral antimicrobial with greater than 80% susceptibility across all groups was nitrofurantoin.
Data source: A study of 500 randomly selected adults who presented to the ED with a urinary tract infection, based on ICD-9 or ICD-10 codes.
Disclosures: Dr. Jorgensen and Dr. Zurayk had no relevant financial disclosures. One study coauthor, Annie Wong-Beringer, PharmD, receives grant funding from Merck.
Study shows that 20% of inpatients given antibiotics develop adverse reactions
Twenty percent of hospitalized adults given antibiotics develop adverse drug events, including GI, nephrotoxic, hematologic, cardiac, and neurotoxic effects, according to a report in JAMA Internal Medicine.
This high frequency of adverse reactions “may not be recognized by clinicians because [these events] have varied manifestations, clinicians may be unaware of the risks associated with specific antibiotic agents, or because they occur after patients are discharged from the hospital,” said Pranita D. Tamma, MD, of the division of pediatric infectious diseases, Johns Hopkins University, Baltimore, and her associates.
They assessed antibiotic-associated adverse drug events in all 1,488 adults admitted to four general medicine services at a single medical center during a 9-month period and given at least 24 hours of any antibiotic therapy. The most common indications for antibiotics were urinary tract infections (12%), skin and soft-tissue infections (8%), and community-acquired pneumonia (7%).
Perhaps as important, the researchers noted, 19% of these adverse drug events were attributed to unnecessary antibiotics – drugs given for conditions for which they were not clinically indicated according to the hospital’s own antibiotic guidelines. These included asymptomatic bacteriuria, aspiration pneumonitis, and heart failure (JAMA Intern. Med. 2017 June 12. doi: 10.1001/jamainternmed.2017.1938).
The most common adverse reactions that developed within 30 days were GI, renal, and hematologic abnormalities. Neurotoxic effects included encephalopathy and seizures; cardiotoxic effects included QTc prolongation. Less frequent adverse events included anaphylaxis, daptomycin-associated myositis, trimethoprim/sulfamethoxazole-associated pancreatitis, linezolid-associated neuropathy, and ciprofloxacin-related tendinitis. The most common adverse reactions that developed within 90 days were C. difficile infections and infections involving multidrug-resistant organisms.
“Our findings underscore the importance of avoiding unnecessary antibiotic prescribing to reduce the harm that can result from antibiotic-associated adverse drug events,” Dr. Tamma and her associates said.
Twenty percent of hospitalized adults given antibiotics develop adverse drug events, including GI, nephrotoxic, hematologic, cardiac, and neurotoxic effects, according to a report in JAMA Internal Medicine.
This high frequency of adverse reactions “may not be recognized by clinicians because [these events] have varied manifestations, clinicians may be unaware of the risks associated with specific antibiotic agents, or because they occur after patients are discharged from the hospital,” said Pranita D. Tamma, MD, of the division of pediatric infectious diseases, Johns Hopkins University, Baltimore, and her associates.
They assessed antibiotic-associated adverse drug events in all 1,488 adults admitted to four general medicine services at a single medical center during a 9-month period and given at least 24 hours of any antibiotic therapy. The most common indications for antibiotics were urinary tract infections (12%), skin and soft-tissue infections (8%), and community-acquired pneumonia (7%).
Perhaps as important, the researchers noted, 19% of these adverse drug events were attributed to unnecessary antibiotics – drugs given for conditions for which they were not clinically indicated according to the hospital’s own antibiotic guidelines. These included asymptomatic bacteriuria, aspiration pneumonitis, and heart failure (JAMA Intern. Med. 2017 June 12. doi: 10.1001/jamainternmed.2017.1938).
The most common adverse reactions that developed within 30 days were GI, renal, and hematologic abnormalities. Neurotoxic effects included encephalopathy and seizures; cardiotoxic effects included QTc prolongation. Less frequent adverse events included anaphylaxis, daptomycin-associated myositis, trimethoprim/sulfamethoxazole-associated pancreatitis, linezolid-associated neuropathy, and ciprofloxacin-related tendinitis. The most common adverse reactions that developed within 90 days were C. difficile infections and infections involving multidrug-resistant organisms.
“Our findings underscore the importance of avoiding unnecessary antibiotic prescribing to reduce the harm that can result from antibiotic-associated adverse drug events,” Dr. Tamma and her associates said.
Twenty percent of hospitalized adults given antibiotics develop adverse drug events, including GI, nephrotoxic, hematologic, cardiac, and neurotoxic effects, according to a report in JAMA Internal Medicine.
This high frequency of adverse reactions “may not be recognized by clinicians because [these events] have varied manifestations, clinicians may be unaware of the risks associated with specific antibiotic agents, or because they occur after patients are discharged from the hospital,” said Pranita D. Tamma, MD, of the division of pediatric infectious diseases, Johns Hopkins University, Baltimore, and her associates.
They assessed antibiotic-associated adverse drug events in all 1,488 adults admitted to four general medicine services at a single medical center during a 9-month period and given at least 24 hours of any antibiotic therapy. The most common indications for antibiotics were urinary tract infections (12%), skin and soft-tissue infections (8%), and community-acquired pneumonia (7%).
Perhaps as important, the researchers noted, 19% of these adverse drug events were attributed to unnecessary antibiotics – drugs given for conditions for which they were not clinically indicated according to the hospital’s own antibiotic guidelines. These included asymptomatic bacteriuria, aspiration pneumonitis, and heart failure (JAMA Intern. Med. 2017 June 12. doi: 10.1001/jamainternmed.2017.1938).
The most common adverse reactions that developed within 30 days were GI, renal, and hematologic abnormalities. Neurotoxic effects included encephalopathy and seizures; cardiotoxic effects included QTc prolongation. Less frequent adverse events included anaphylaxis, daptomycin-associated myositis, trimethoprim/sulfamethoxazole-associated pancreatitis, linezolid-associated neuropathy, and ciprofloxacin-related tendinitis. The most common adverse reactions that developed within 90 days were C. difficile infections and infections involving multidrug-resistant organisms.
“Our findings underscore the importance of avoiding unnecessary antibiotic prescribing to reduce the harm that can result from antibiotic-associated adverse drug events,” Dr. Tamma and her associates said.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Among hospitalized adults given antibiotics, 20% develop adverse reactions, including GI, nephrotoxic, hematologic, cardiac, and neurotoxic effects.
Major finding: Among 1,488 patients, 298 (20%) developed 324 adverse reactions to antibiotics – 73% during hospitalization and 27% after discharge – requiring prolonged hospitalization; a subsequent hospitalization; an ED visit; or additional lab tests, ECGs, or imaging studies.
Data source: A single-center retrospective cohort study involving all 1,488 general medicine inpatients admitted during a 9-month period who received any antibiotic for at least 24 hours.
Disclosures: This study was supported by Pfizer Independent Grants for Learning and Change and the Joint Commission. Dr. Tamma and her associates reported having no relevant financial disclosures.