User login
Tips, contraindications for superficial chemical peels reviewed
CHICAGO – Heather Woolery-Lloyd, MD, says she’s generally “risk averse,” but when it comes to superficial chemical peels, she’s in her comfort zone.
Superficial peeling is “one of the most common cosmetic procedures that I do,” Dr. Woolery-Lloyd, director of the skin of color division in the dermatology department at the University of Miami, said at the Pigmentary Disorders Exchange Symposium.
In her practice, .
Contraindications are an active bacterial infection, open wounds, and active herpes simplex virus. “If someone looks like they even have a remnant of a cold sore, I tell them to come back,” she said.
Setting expectations for patients is critical, Dr. Woolery-Lloyd said, as a series of superficial peels is needed before the desired results are evident.
The peel she uses most is salicylic acid, a beta-hydroxy acid, at a strength of 20%-30%. “It’s very effective on our acne patients,” she said at the meeting, provided by MedscapeLIVE! “If you’re just starting with peels, I think this is a very safe one. You don’t have to time it, and you don’t have to neutralize it,” and at lower concentrations, is “very safe.”
Dr. Woolery-Lloyd provided these other tips during her presentation:
- Even superficial peels can be uncomfortable, she noted, so she keeps a fan nearby to use when needed to help with discomfort.
- Find the peel you’re comfortable with, master that peel, and don’t jump from peel to peel. Get familiar with the side effects and how to predict results.
- Stop retinoids up to 7 days before a peel. Consider placing the patient on hydroquinone before the chemical peel to decrease the risk of hyperpigmentation.
- Before the procedure, prep the skin with acetone or alcohol. Applying petrolatum helps protect around the eyes, alar crease, and other sensitive areas, “or anywhere you’re concerned about the depth of the peel.”
- Application with rough gauze helps avoid the waste that comes with makeup sponges soaking up the product. It also helps add exfoliation.
- Have everything ready before starting the procedure, including (depending on the peel), a neutralizer or soapless cleanser. Although peels are generally safe, you want to be able to remove one quickly, if needed, without having to leave the room.
- Start with the lowest concentration (salicylic acid or glycolic acid) then titrate up. Ask patients about any reactions they experienced with the previous peel before making the decision on the next concentration.
- For a peel to treat hyperpigmentation, she recommends one peel about every 4 weeks for a series of 5-6 peels.
- After a peel, the patient should use a mineral sunscreen; chemical sunscreens will sting.
Know your comfort zone
Conference chair Pearl Grimes, MD, director of The Vitiligo & Pigmentation Institute of Southern California in Los Angeles, said superficial peels are best for dermatologists new to peeling until they gain comfort with experience.
Superficial and medium-depth peels work well for mild to moderate photoaging, she said at the meeting.
“We know that in darker skin we have more intrinsic aging rather than photoaging. We have more textural changes, hyperpigmentation,” Dr. Grimes said.
For Fitzpatrick skin types I-III, she said, “you can do superficial, medium, and deep peels.” For darker skin types, “I typically stay in the superficial, medium range.”
She said that she uses retinoids to exfoliate before a superficial peel but added, “you’ve got to stop them early because retinoids can make a superficial peel a medium-depth peel.”
Taking photos is important before any procedure, she said, as is spending time with patients clarifying their outcome expectations.
“I love peeling,” Dr. Grimes said. “And it’s cost effective. If you don’t want to spend a ton of money, it’s amazing what you can achieve with chemical peeling.”
When asked by a member of the audience whether they avoid superficial peels in women who are pregnant or breastfeeding, both Dr. Woolery-Lloyd and Dr. Grimes said they do avoid them in those patients.
Dr. Grimes said she tells her patients, especially in the first trimester, “I am the most conservative woman on the planet. I do nothing during the first trimester.”
Dr. Woolery-Lloyd has been a speaker for Ortho Dermatologics, Loreal and EPI, and has done research for Pfizer, Galderma, Allergan, Arcutis, Vyne, Merz, and Eirion. She has been on advisory boards for Loreal, Allergan, Ortho Dermatologics, Pfize,r and Merz. Dr. Grimes reports grant/research Support from Clinuvel Pharmaceuticals, Incyte, Johnson & Johnson, LASEROPTEK, L’Oréal USA, Pfizer, Procter & Gamble, skinbetter science, and Versicolor Technologies, and is on the speakers bureau/receives honoraria for non-CME for Incyte and Procter & Gamble; and is a consultant or is on the advisory board for L’Oréal USA and Procter & Gamble. She has stock options in Versicolor Technologies.
CHICAGO – Heather Woolery-Lloyd, MD, says she’s generally “risk averse,” but when it comes to superficial chemical peels, she’s in her comfort zone.
Superficial peeling is “one of the most common cosmetic procedures that I do,” Dr. Woolery-Lloyd, director of the skin of color division in the dermatology department at the University of Miami, said at the Pigmentary Disorders Exchange Symposium.
In her practice, .
Contraindications are an active bacterial infection, open wounds, and active herpes simplex virus. “If someone looks like they even have a remnant of a cold sore, I tell them to come back,” she said.
Setting expectations for patients is critical, Dr. Woolery-Lloyd said, as a series of superficial peels is needed before the desired results are evident.
The peel she uses most is salicylic acid, a beta-hydroxy acid, at a strength of 20%-30%. “It’s very effective on our acne patients,” she said at the meeting, provided by MedscapeLIVE! “If you’re just starting with peels, I think this is a very safe one. You don’t have to time it, and you don’t have to neutralize it,” and at lower concentrations, is “very safe.”
Dr. Woolery-Lloyd provided these other tips during her presentation:
- Even superficial peels can be uncomfortable, she noted, so she keeps a fan nearby to use when needed to help with discomfort.
- Find the peel you’re comfortable with, master that peel, and don’t jump from peel to peel. Get familiar with the side effects and how to predict results.
- Stop retinoids up to 7 days before a peel. Consider placing the patient on hydroquinone before the chemical peel to decrease the risk of hyperpigmentation.
- Before the procedure, prep the skin with acetone or alcohol. Applying petrolatum helps protect around the eyes, alar crease, and other sensitive areas, “or anywhere you’re concerned about the depth of the peel.”
- Application with rough gauze helps avoid the waste that comes with makeup sponges soaking up the product. It also helps add exfoliation.
- Have everything ready before starting the procedure, including (depending on the peel), a neutralizer or soapless cleanser. Although peels are generally safe, you want to be able to remove one quickly, if needed, without having to leave the room.
- Start with the lowest concentration (salicylic acid or glycolic acid) then titrate up. Ask patients about any reactions they experienced with the previous peel before making the decision on the next concentration.
- For a peel to treat hyperpigmentation, she recommends one peel about every 4 weeks for a series of 5-6 peels.
- After a peel, the patient should use a mineral sunscreen; chemical sunscreens will sting.
Know your comfort zone
Conference chair Pearl Grimes, MD, director of The Vitiligo & Pigmentation Institute of Southern California in Los Angeles, said superficial peels are best for dermatologists new to peeling until they gain comfort with experience.
Superficial and medium-depth peels work well for mild to moderate photoaging, she said at the meeting.
“We know that in darker skin we have more intrinsic aging rather than photoaging. We have more textural changes, hyperpigmentation,” Dr. Grimes said.
For Fitzpatrick skin types I-III, she said, “you can do superficial, medium, and deep peels.” For darker skin types, “I typically stay in the superficial, medium range.”
She said that she uses retinoids to exfoliate before a superficial peel but added, “you’ve got to stop them early because retinoids can make a superficial peel a medium-depth peel.”
Taking photos is important before any procedure, she said, as is spending time with patients clarifying their outcome expectations.
“I love peeling,” Dr. Grimes said. “And it’s cost effective. If you don’t want to spend a ton of money, it’s amazing what you can achieve with chemical peeling.”
When asked by a member of the audience whether they avoid superficial peels in women who are pregnant or breastfeeding, both Dr. Woolery-Lloyd and Dr. Grimes said they do avoid them in those patients.
Dr. Grimes said she tells her patients, especially in the first trimester, “I am the most conservative woman on the planet. I do nothing during the first trimester.”
Dr. Woolery-Lloyd has been a speaker for Ortho Dermatologics, Loreal and EPI, and has done research for Pfizer, Galderma, Allergan, Arcutis, Vyne, Merz, and Eirion. She has been on advisory boards for Loreal, Allergan, Ortho Dermatologics, Pfize,r and Merz. Dr. Grimes reports grant/research Support from Clinuvel Pharmaceuticals, Incyte, Johnson & Johnson, LASEROPTEK, L’Oréal USA, Pfizer, Procter & Gamble, skinbetter science, and Versicolor Technologies, and is on the speakers bureau/receives honoraria for non-CME for Incyte and Procter & Gamble; and is a consultant or is on the advisory board for L’Oréal USA and Procter & Gamble. She has stock options in Versicolor Technologies.
CHICAGO – Heather Woolery-Lloyd, MD, says she’s generally “risk averse,” but when it comes to superficial chemical peels, she’s in her comfort zone.
Superficial peeling is “one of the most common cosmetic procedures that I do,” Dr. Woolery-Lloyd, director of the skin of color division in the dermatology department at the University of Miami, said at the Pigmentary Disorders Exchange Symposium.
In her practice, .
Contraindications are an active bacterial infection, open wounds, and active herpes simplex virus. “If someone looks like they even have a remnant of a cold sore, I tell them to come back,” she said.
Setting expectations for patients is critical, Dr. Woolery-Lloyd said, as a series of superficial peels is needed before the desired results are evident.
The peel she uses most is salicylic acid, a beta-hydroxy acid, at a strength of 20%-30%. “It’s very effective on our acne patients,” she said at the meeting, provided by MedscapeLIVE! “If you’re just starting with peels, I think this is a very safe one. You don’t have to time it, and you don’t have to neutralize it,” and at lower concentrations, is “very safe.”
Dr. Woolery-Lloyd provided these other tips during her presentation:
- Even superficial peels can be uncomfortable, she noted, so she keeps a fan nearby to use when needed to help with discomfort.
- Find the peel you’re comfortable with, master that peel, and don’t jump from peel to peel. Get familiar with the side effects and how to predict results.
- Stop retinoids up to 7 days before a peel. Consider placing the patient on hydroquinone before the chemical peel to decrease the risk of hyperpigmentation.
- Before the procedure, prep the skin with acetone or alcohol. Applying petrolatum helps protect around the eyes, alar crease, and other sensitive areas, “or anywhere you’re concerned about the depth of the peel.”
- Application with rough gauze helps avoid the waste that comes with makeup sponges soaking up the product. It also helps add exfoliation.
- Have everything ready before starting the procedure, including (depending on the peel), a neutralizer or soapless cleanser. Although peels are generally safe, you want to be able to remove one quickly, if needed, without having to leave the room.
- Start with the lowest concentration (salicylic acid or glycolic acid) then titrate up. Ask patients about any reactions they experienced with the previous peel before making the decision on the next concentration.
- For a peel to treat hyperpigmentation, she recommends one peel about every 4 weeks for a series of 5-6 peels.
- After a peel, the patient should use a mineral sunscreen; chemical sunscreens will sting.
Know your comfort zone
Conference chair Pearl Grimes, MD, director of The Vitiligo & Pigmentation Institute of Southern California in Los Angeles, said superficial peels are best for dermatologists new to peeling until they gain comfort with experience.
Superficial and medium-depth peels work well for mild to moderate photoaging, she said at the meeting.
“We know that in darker skin we have more intrinsic aging rather than photoaging. We have more textural changes, hyperpigmentation,” Dr. Grimes said.
For Fitzpatrick skin types I-III, she said, “you can do superficial, medium, and deep peels.” For darker skin types, “I typically stay in the superficial, medium range.”
She said that she uses retinoids to exfoliate before a superficial peel but added, “you’ve got to stop them early because retinoids can make a superficial peel a medium-depth peel.”
Taking photos is important before any procedure, she said, as is spending time with patients clarifying their outcome expectations.
“I love peeling,” Dr. Grimes said. “And it’s cost effective. If you don’t want to spend a ton of money, it’s amazing what you can achieve with chemical peeling.”
When asked by a member of the audience whether they avoid superficial peels in women who are pregnant or breastfeeding, both Dr. Woolery-Lloyd and Dr. Grimes said they do avoid them in those patients.
Dr. Grimes said she tells her patients, especially in the first trimester, “I am the most conservative woman on the planet. I do nothing during the first trimester.”
Dr. Woolery-Lloyd has been a speaker for Ortho Dermatologics, Loreal and EPI, and has done research for Pfizer, Galderma, Allergan, Arcutis, Vyne, Merz, and Eirion. She has been on advisory boards for Loreal, Allergan, Ortho Dermatologics, Pfize,r and Merz. Dr. Grimes reports grant/research Support from Clinuvel Pharmaceuticals, Incyte, Johnson & Johnson, LASEROPTEK, L’Oréal USA, Pfizer, Procter & Gamble, skinbetter science, and Versicolor Technologies, and is on the speakers bureau/receives honoraria for non-CME for Incyte and Procter & Gamble; and is a consultant or is on the advisory board for L’Oréal USA and Procter & Gamble. She has stock options in Versicolor Technologies.
AT THE MEDSCAPE LIVE! PIGMENTARY DISORDERS SYMPOSIUM
Men underrepresented in clinical trials of laser hair removal, review finds
PHOENIX – .
To characterize the sex of patients in trials evaluating hair removal with energy-based devices, Dr. Lee, an internal medicine intern at Beth Israel Deaconess Medical Center, Boston, and Jessica Labadie, MD, director of lasers and cosmetic surgery at the Icahn School of Medicine at Mount Sinai, New York, conducted a systematic review using PubMed with the search query hair AND laser AND removal AND (dermatology OR skin OR cutaneous). They limited the analysis to English-language clinical trials that investigated a laser and light-based therapy as an intervention and if hair reduction was an outcome, and excluded studies that did not include the face as a treatment area and laser hair removal for diseases with disproportionate occurrence in females or males, such as polycystic ovarian syndrome or pseudofolliculitis barbae.
Of 121 articles identified from the PubMed search, 28 studies involving 3,882 patients treated with lasers or intense pulsed light (IPL) for hair removal were included in the final analysis. Of these 28 articles, 22 (79%) reported the sex of trial participants. The population of these 22 studies included 3,104 (88.7%) females, 384 (11.0%) males, and 11 (0.003%) nonbinary identifying patients. None of the studies evaluated laser hair removal outcomes by sex.
“This study adds to the current knowledge of laser hair removal as a part of gender-affirming care by characterizing the representation of assigned sexes of patients in clinical trials evaluating the effectiveness of laser hair removal,” Dr. Lee told this news organization. “It highlights the underrepresentation of people assigned to male sex at birth in these clinical trials, despite this population’s potential interest in laser hair removal as a part of gender-affirming care.”
She acknowledged certain limitations of the review, including the absence of reporting on sex in the demographic sections of many trials and the exclusion of trials that did not include treatment of the face. “Clinicians need to be aware of the underrepresentation of men in clinical trials evaluating laser hair removal, and this may limit their understanding of treatment outcomes in this particular cohort,” she concluded. “Clinicians should emphasize inclusivity in future laser hair removal clinical trials and include outcomes by sex.”
The study “looks at an important aspect of clinical trials in the device-based space,” said Omar A. Ibrahimi, MD, PhD, medical director of the Connecticut Skin Institute, Stamford, who was not involved in the study and was asked to comment on the results. “Laser hair removal is the most commonly performed procedure in aesthetic energy-based device dermatology. While these trials are often very small compared to drug trials, it highlights that men are a very underrepresented cohort in laser hair removal trials,” he said. “More recently, there is an increased interest in gender-affirming procedures, and this has highlighted the need to ensure we include a diverse spectrum of patients in devices-based research studies. This is a very challenging mandate but certainly one we should strive for to make efforts to be more inclusive when designing these clinical studies so that the information we gain from these studies is more broadly applicable.”
The researchers reported having no financial disclosures. Dr. Ibrahimi disclosed that he is a member of the advisory board for Accure Acne, AbbVie, Cutera, Lutronic, Blueberry Therapeutics, Cytrellis, and Quthero, and holds stock in many device and pharmaceutical companies.
PHOENIX – .
To characterize the sex of patients in trials evaluating hair removal with energy-based devices, Dr. Lee, an internal medicine intern at Beth Israel Deaconess Medical Center, Boston, and Jessica Labadie, MD, director of lasers and cosmetic surgery at the Icahn School of Medicine at Mount Sinai, New York, conducted a systematic review using PubMed with the search query hair AND laser AND removal AND (dermatology OR skin OR cutaneous). They limited the analysis to English-language clinical trials that investigated a laser and light-based therapy as an intervention and if hair reduction was an outcome, and excluded studies that did not include the face as a treatment area and laser hair removal for diseases with disproportionate occurrence in females or males, such as polycystic ovarian syndrome or pseudofolliculitis barbae.
Of 121 articles identified from the PubMed search, 28 studies involving 3,882 patients treated with lasers or intense pulsed light (IPL) for hair removal were included in the final analysis. Of these 28 articles, 22 (79%) reported the sex of trial participants. The population of these 22 studies included 3,104 (88.7%) females, 384 (11.0%) males, and 11 (0.003%) nonbinary identifying patients. None of the studies evaluated laser hair removal outcomes by sex.
“This study adds to the current knowledge of laser hair removal as a part of gender-affirming care by characterizing the representation of assigned sexes of patients in clinical trials evaluating the effectiveness of laser hair removal,” Dr. Lee told this news organization. “It highlights the underrepresentation of people assigned to male sex at birth in these clinical trials, despite this population’s potential interest in laser hair removal as a part of gender-affirming care.”
She acknowledged certain limitations of the review, including the absence of reporting on sex in the demographic sections of many trials and the exclusion of trials that did not include treatment of the face. “Clinicians need to be aware of the underrepresentation of men in clinical trials evaluating laser hair removal, and this may limit their understanding of treatment outcomes in this particular cohort,” she concluded. “Clinicians should emphasize inclusivity in future laser hair removal clinical trials and include outcomes by sex.”
The study “looks at an important aspect of clinical trials in the device-based space,” said Omar A. Ibrahimi, MD, PhD, medical director of the Connecticut Skin Institute, Stamford, who was not involved in the study and was asked to comment on the results. “Laser hair removal is the most commonly performed procedure in aesthetic energy-based device dermatology. While these trials are often very small compared to drug trials, it highlights that men are a very underrepresented cohort in laser hair removal trials,” he said. “More recently, there is an increased interest in gender-affirming procedures, and this has highlighted the need to ensure we include a diverse spectrum of patients in devices-based research studies. This is a very challenging mandate but certainly one we should strive for to make efforts to be more inclusive when designing these clinical studies so that the information we gain from these studies is more broadly applicable.”
The researchers reported having no financial disclosures. Dr. Ibrahimi disclosed that he is a member of the advisory board for Accure Acne, AbbVie, Cutera, Lutronic, Blueberry Therapeutics, Cytrellis, and Quthero, and holds stock in many device and pharmaceutical companies.
PHOENIX – .
To characterize the sex of patients in trials evaluating hair removal with energy-based devices, Dr. Lee, an internal medicine intern at Beth Israel Deaconess Medical Center, Boston, and Jessica Labadie, MD, director of lasers and cosmetic surgery at the Icahn School of Medicine at Mount Sinai, New York, conducted a systematic review using PubMed with the search query hair AND laser AND removal AND (dermatology OR skin OR cutaneous). They limited the analysis to English-language clinical trials that investigated a laser and light-based therapy as an intervention and if hair reduction was an outcome, and excluded studies that did not include the face as a treatment area and laser hair removal for diseases with disproportionate occurrence in females or males, such as polycystic ovarian syndrome or pseudofolliculitis barbae.
Of 121 articles identified from the PubMed search, 28 studies involving 3,882 patients treated with lasers or intense pulsed light (IPL) for hair removal were included in the final analysis. Of these 28 articles, 22 (79%) reported the sex of trial participants. The population of these 22 studies included 3,104 (88.7%) females, 384 (11.0%) males, and 11 (0.003%) nonbinary identifying patients. None of the studies evaluated laser hair removal outcomes by sex.
“This study adds to the current knowledge of laser hair removal as a part of gender-affirming care by characterizing the representation of assigned sexes of patients in clinical trials evaluating the effectiveness of laser hair removal,” Dr. Lee told this news organization. “It highlights the underrepresentation of people assigned to male sex at birth in these clinical trials, despite this population’s potential interest in laser hair removal as a part of gender-affirming care.”
She acknowledged certain limitations of the review, including the absence of reporting on sex in the demographic sections of many trials and the exclusion of trials that did not include treatment of the face. “Clinicians need to be aware of the underrepresentation of men in clinical trials evaluating laser hair removal, and this may limit their understanding of treatment outcomes in this particular cohort,” she concluded. “Clinicians should emphasize inclusivity in future laser hair removal clinical trials and include outcomes by sex.”
The study “looks at an important aspect of clinical trials in the device-based space,” said Omar A. Ibrahimi, MD, PhD, medical director of the Connecticut Skin Institute, Stamford, who was not involved in the study and was asked to comment on the results. “Laser hair removal is the most commonly performed procedure in aesthetic energy-based device dermatology. While these trials are often very small compared to drug trials, it highlights that men are a very underrepresented cohort in laser hair removal trials,” he said. “More recently, there is an increased interest in gender-affirming procedures, and this has highlighted the need to ensure we include a diverse spectrum of patients in devices-based research studies. This is a very challenging mandate but certainly one we should strive for to make efforts to be more inclusive when designing these clinical studies so that the information we gain from these studies is more broadly applicable.”
The researchers reported having no financial disclosures. Dr. Ibrahimi disclosed that he is a member of the advisory board for Accure Acne, AbbVie, Cutera, Lutronic, Blueberry Therapeutics, Cytrellis, and Quthero, and holds stock in many device and pharmaceutical companies.
AT ASLMS 2023
Picosecond laser applications continue to expand
PHOENIX – Ever since PicoSure became the first picosecond laser cleared by the Food and Drug Administration for the treatment of unwanted tattoos and pigmented lesions in 2012, new uses for this technology continue to expand.
Now, These include PicoWay, PicoSure, Enlighten, PicoPlus, PiQo4, and Quanta Pico, among others.
“PicoWay technology has integrated nicely into my practice in Houston, the most ethnically diverse city in the country, with its ability to safely treat a number of various benign, congenital, and acquired epidermal and dermal pigmented lesions with ultrashort pulse duration and low thermal impact, which greatly reduces the risk of postinflammatory hyperpigmentation even in darker skin types,” Paul M. Friedman, MD, director of the Dermatology and Laser Surgery Center, Houston, said at the annual conference of the American Society for Laser Medicine and Surgery.
He emphasized the importance of therapeutic clinical endpoints, noting that with q-switched lasers, “you’re looking for immediate whitening, whereas with picosecond lasers, your endpoint is slight whitening or slight darkening depending on wavelength, indication, and skin type. The ability to fractionate picosecond pulses has also allowed us to utilize this technology for photoaging as well as acne scarring.”
The PicoWay system includes a 730-nm picosecond titanium sapphire handpiece, which is FDA cleared for treatment of benign pigmented lesions and blue and green tattoo removal. Dr. Friedman said that he has seen good clinical results using the handpiece for café-au-lait macules, particularly in skin of color.
In an abstract presented at the ASLMS meeting, he and his colleagues presented a retrospective review of 12 patients with café-au-lait macules with Fitzpatrick skin types III-VI who were treated with the PicoWay 730 nm handpiece between April 2021 and January 2023. Patients received a mean of 3.1 treatments at intervals that ranged from 5 to 40 weeks. Clinical photographs were graded by three board-certified dermatologists using a 5-point visual analogue scale.
Overall, patients were rated to have a mean improvement of 26%-50%. Two patients achieved 100% clearance after four to five treatment sessions. “Café-au-lait macules with smooth borders responded less well to laser treatment, confirming prior studies at our center,” he said. “We often educate parents that café-au-lait macules may recur over time, especially with repeated sun exposure.”
Treating melasma
Dr. Friedman’s go-to devices for melasma include the low-density, low-energy 1,927-nm fractional diode laser; the 1,064 nm picosecond Nd:YAG, the low-fluence 1,064 nm Q-switched Nd:YAG with a nanosecond pulse duration, and the 595-nm pulsed dye laser for lesions exhibiting underlying vascularity. He said that combining therapies that target pigment and vasculature may be ideal to prevent relapses. “Melasma is a multifactorial condition so by improving patient education and expectation alongside advances in laser treatment of melasma, we have ultimately improved our ability to treat this condition,” he said.
“We’re approaching it from all angles, with ultraviolet photography and spectrocolorimetry, behavioral modifications, topical skin-lightening agents, broad spectrum sunscreens with protection against visible light, and oral tranexamic acid in advanced cases. Then, we intervene with these energy-based modalities, and the bottom line is, less energy and density is more, with lengthened treatment intervals. In 2023, we’re better than we’ve ever been in terms of our ability to safely and effectively improve melasma.”
Novel lasers
Dr. Friedman also described the UltraClear, a novel ablative fractional 2,910-nm erbium-doped glass fiber laser that delivers a customized blend of ablation and coagulation based on the patient’s condition, skin type, and tolerability for down time. He provided an overview of the versatility of what he described as highly customizable technology for conditions such as photoaging and dyschromia in patients of various skin types, making it a very versatile platform in his practice.
The AVAVA MIRIA system is a “next generation” laser “where you’re able to use a focal point. Basically, you’re treating the skin from the inside out in a 3D manner and you’re able to focus intradermally up to 1 mm with high energy 1,064 nm or 1,550 nm,” he said. “It’s a unique conical geometry that spares the epidermis, combined with sapphire tip cooling and images the skin at the same time with the potential for personalized treatments of dyschromia and photoaging in all skin types. It’s truly remarkable where the technology is heading.”
Dr. Friedman disclosed that he has received consulting fees from Allergan, Galderma, Acclaro, Merz Aesthetics, Solta Medical, and Cytrellis. He has conducted contracted research for Sofwave and is a member of the speakers bureau for Solta Medical and Candela.
PHOENIX – Ever since PicoSure became the first picosecond laser cleared by the Food and Drug Administration for the treatment of unwanted tattoos and pigmented lesions in 2012, new uses for this technology continue to expand.
Now, These include PicoWay, PicoSure, Enlighten, PicoPlus, PiQo4, and Quanta Pico, among others.
“PicoWay technology has integrated nicely into my practice in Houston, the most ethnically diverse city in the country, with its ability to safely treat a number of various benign, congenital, and acquired epidermal and dermal pigmented lesions with ultrashort pulse duration and low thermal impact, which greatly reduces the risk of postinflammatory hyperpigmentation even in darker skin types,” Paul M. Friedman, MD, director of the Dermatology and Laser Surgery Center, Houston, said at the annual conference of the American Society for Laser Medicine and Surgery.
He emphasized the importance of therapeutic clinical endpoints, noting that with q-switched lasers, “you’re looking for immediate whitening, whereas with picosecond lasers, your endpoint is slight whitening or slight darkening depending on wavelength, indication, and skin type. The ability to fractionate picosecond pulses has also allowed us to utilize this technology for photoaging as well as acne scarring.”
The PicoWay system includes a 730-nm picosecond titanium sapphire handpiece, which is FDA cleared for treatment of benign pigmented lesions and blue and green tattoo removal. Dr. Friedman said that he has seen good clinical results using the handpiece for café-au-lait macules, particularly in skin of color.
In an abstract presented at the ASLMS meeting, he and his colleagues presented a retrospective review of 12 patients with café-au-lait macules with Fitzpatrick skin types III-VI who were treated with the PicoWay 730 nm handpiece between April 2021 and January 2023. Patients received a mean of 3.1 treatments at intervals that ranged from 5 to 40 weeks. Clinical photographs were graded by three board-certified dermatologists using a 5-point visual analogue scale.
Overall, patients were rated to have a mean improvement of 26%-50%. Two patients achieved 100% clearance after four to five treatment sessions. “Café-au-lait macules with smooth borders responded less well to laser treatment, confirming prior studies at our center,” he said. “We often educate parents that café-au-lait macules may recur over time, especially with repeated sun exposure.”
Treating melasma
Dr. Friedman’s go-to devices for melasma include the low-density, low-energy 1,927-nm fractional diode laser; the 1,064 nm picosecond Nd:YAG, the low-fluence 1,064 nm Q-switched Nd:YAG with a nanosecond pulse duration, and the 595-nm pulsed dye laser for lesions exhibiting underlying vascularity. He said that combining therapies that target pigment and vasculature may be ideal to prevent relapses. “Melasma is a multifactorial condition so by improving patient education and expectation alongside advances in laser treatment of melasma, we have ultimately improved our ability to treat this condition,” he said.
“We’re approaching it from all angles, with ultraviolet photography and spectrocolorimetry, behavioral modifications, topical skin-lightening agents, broad spectrum sunscreens with protection against visible light, and oral tranexamic acid in advanced cases. Then, we intervene with these energy-based modalities, and the bottom line is, less energy and density is more, with lengthened treatment intervals. In 2023, we’re better than we’ve ever been in terms of our ability to safely and effectively improve melasma.”
Novel lasers
Dr. Friedman also described the UltraClear, a novel ablative fractional 2,910-nm erbium-doped glass fiber laser that delivers a customized blend of ablation and coagulation based on the patient’s condition, skin type, and tolerability for down time. He provided an overview of the versatility of what he described as highly customizable technology for conditions such as photoaging and dyschromia in patients of various skin types, making it a very versatile platform in his practice.
The AVAVA MIRIA system is a “next generation” laser “where you’re able to use a focal point. Basically, you’re treating the skin from the inside out in a 3D manner and you’re able to focus intradermally up to 1 mm with high energy 1,064 nm or 1,550 nm,” he said. “It’s a unique conical geometry that spares the epidermis, combined with sapphire tip cooling and images the skin at the same time with the potential for personalized treatments of dyschromia and photoaging in all skin types. It’s truly remarkable where the technology is heading.”
Dr. Friedman disclosed that he has received consulting fees from Allergan, Galderma, Acclaro, Merz Aesthetics, Solta Medical, and Cytrellis. He has conducted contracted research for Sofwave and is a member of the speakers bureau for Solta Medical and Candela.
PHOENIX – Ever since PicoSure became the first picosecond laser cleared by the Food and Drug Administration for the treatment of unwanted tattoos and pigmented lesions in 2012, new uses for this technology continue to expand.
Now, These include PicoWay, PicoSure, Enlighten, PicoPlus, PiQo4, and Quanta Pico, among others.
“PicoWay technology has integrated nicely into my practice in Houston, the most ethnically diverse city in the country, with its ability to safely treat a number of various benign, congenital, and acquired epidermal and dermal pigmented lesions with ultrashort pulse duration and low thermal impact, which greatly reduces the risk of postinflammatory hyperpigmentation even in darker skin types,” Paul M. Friedman, MD, director of the Dermatology and Laser Surgery Center, Houston, said at the annual conference of the American Society for Laser Medicine and Surgery.
He emphasized the importance of therapeutic clinical endpoints, noting that with q-switched lasers, “you’re looking for immediate whitening, whereas with picosecond lasers, your endpoint is slight whitening or slight darkening depending on wavelength, indication, and skin type. The ability to fractionate picosecond pulses has also allowed us to utilize this technology for photoaging as well as acne scarring.”
The PicoWay system includes a 730-nm picosecond titanium sapphire handpiece, which is FDA cleared for treatment of benign pigmented lesions and blue and green tattoo removal. Dr. Friedman said that he has seen good clinical results using the handpiece for café-au-lait macules, particularly in skin of color.
In an abstract presented at the ASLMS meeting, he and his colleagues presented a retrospective review of 12 patients with café-au-lait macules with Fitzpatrick skin types III-VI who were treated with the PicoWay 730 nm handpiece between April 2021 and January 2023. Patients received a mean of 3.1 treatments at intervals that ranged from 5 to 40 weeks. Clinical photographs were graded by three board-certified dermatologists using a 5-point visual analogue scale.
Overall, patients were rated to have a mean improvement of 26%-50%. Two patients achieved 100% clearance after four to five treatment sessions. “Café-au-lait macules with smooth borders responded less well to laser treatment, confirming prior studies at our center,” he said. “We often educate parents that café-au-lait macules may recur over time, especially with repeated sun exposure.”
Treating melasma
Dr. Friedman’s go-to devices for melasma include the low-density, low-energy 1,927-nm fractional diode laser; the 1,064 nm picosecond Nd:YAG, the low-fluence 1,064 nm Q-switched Nd:YAG with a nanosecond pulse duration, and the 595-nm pulsed dye laser for lesions exhibiting underlying vascularity. He said that combining therapies that target pigment and vasculature may be ideal to prevent relapses. “Melasma is a multifactorial condition so by improving patient education and expectation alongside advances in laser treatment of melasma, we have ultimately improved our ability to treat this condition,” he said.
“We’re approaching it from all angles, with ultraviolet photography and spectrocolorimetry, behavioral modifications, topical skin-lightening agents, broad spectrum sunscreens with protection against visible light, and oral tranexamic acid in advanced cases. Then, we intervene with these energy-based modalities, and the bottom line is, less energy and density is more, with lengthened treatment intervals. In 2023, we’re better than we’ve ever been in terms of our ability to safely and effectively improve melasma.”
Novel lasers
Dr. Friedman also described the UltraClear, a novel ablative fractional 2,910-nm erbium-doped glass fiber laser that delivers a customized blend of ablation and coagulation based on the patient’s condition, skin type, and tolerability for down time. He provided an overview of the versatility of what he described as highly customizable technology for conditions such as photoaging and dyschromia in patients of various skin types, making it a very versatile platform in his practice.
The AVAVA MIRIA system is a “next generation” laser “where you’re able to use a focal point. Basically, you’re treating the skin from the inside out in a 3D manner and you’re able to focus intradermally up to 1 mm with high energy 1,064 nm or 1,550 nm,” he said. “It’s a unique conical geometry that spares the epidermis, combined with sapphire tip cooling and images the skin at the same time with the potential for personalized treatments of dyschromia and photoaging in all skin types. It’s truly remarkable where the technology is heading.”
Dr. Friedman disclosed that he has received consulting fees from Allergan, Galderma, Acclaro, Merz Aesthetics, Solta Medical, and Cytrellis. He has conducted contracted research for Sofwave and is a member of the speakers bureau for Solta Medical and Candela.
FROM ASLMS 2023
Papular Reticulated Rash
The Diagnosis: Prurigo Pigmentosa
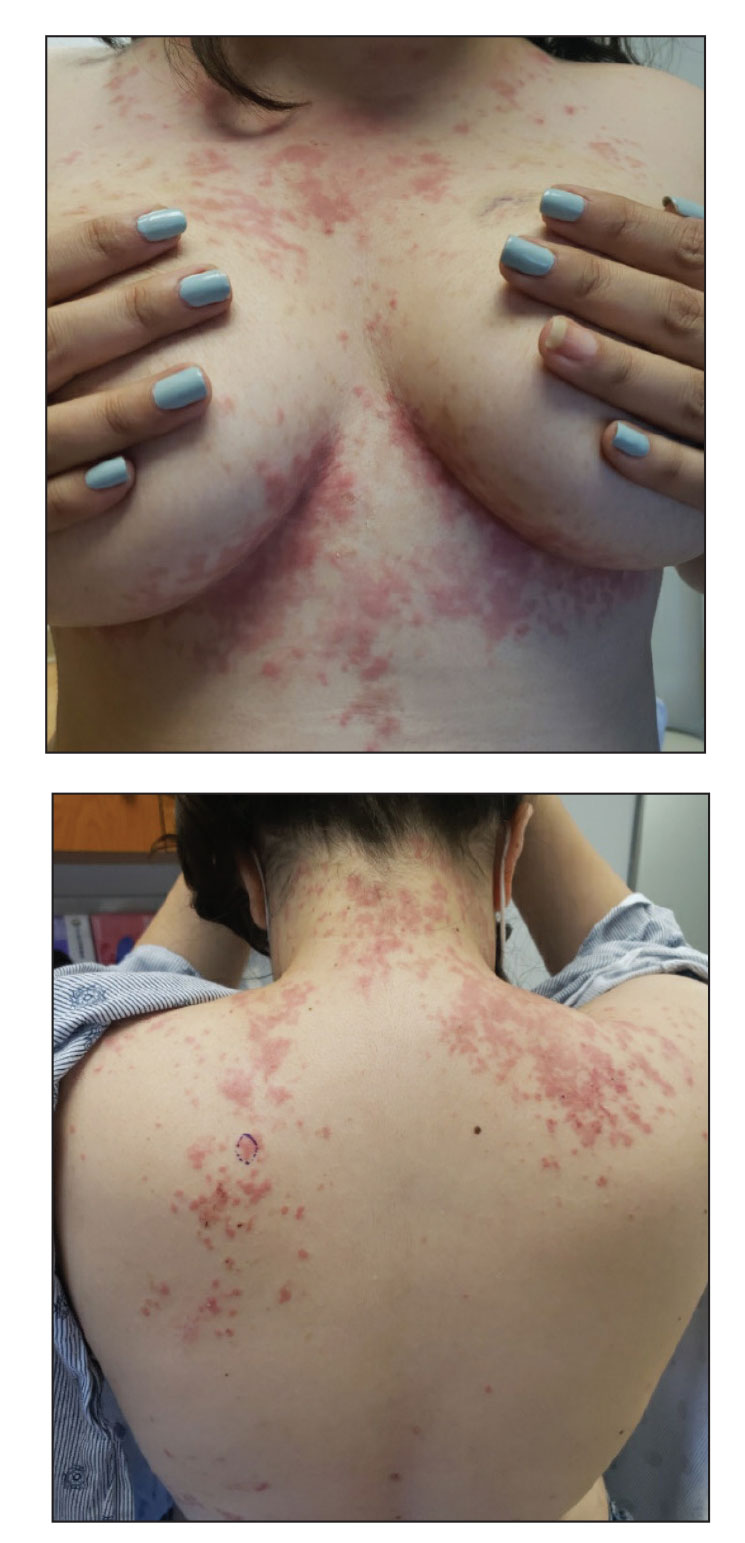
Histopathology of the punch biopsy revealed subcorneal collections of neutrophils flanked by a spongiotic epidermis with neutrophil and eosinophil exocytosis. Rare dyskeratotic keratinocytes were identified at the dermoepidermal junction, and grampositive bacterial organisms were seen in a follicular infundibulum with purulent inflammation. The dermis demonstrated a mildly dense superficial perivascular and interstitial infiltrate composed of lymphocytes, histiocytes, scattered neutrophils, and eosinophils (Figure).

Given the combination of clinical and histologic findings, a diagnosis of prurigo pigmentosa (PP) was rendered and a urinalysis was ordered, which confirmed ketonuria. The patient was started on minocycline 100 mg twice daily and was advised to reintroduce carbohydrates into her diet. Resolution of the inflammatory component of the rash was achieved at 3-week follow-up, with residual reticulated postinflammatory hyperpigmentation.
Prurigo pigmentosa is a rare, albeit globally underrecognized, inflammatory dermatosis characterized by pruritic, symmetric, erythematous papules and plaques on the chest, back, neck, and rarely the arms and forehead that subsequently involute, leaving reticular postinflammatory hyperpigmentation.1 Prurigo pigmentosa is predominant in females (2.6:1 ratio). The mean age at presentation is 24.4 years, and it most commonly has been documented among populations in Asian countries, though it is unclear if a genetic predilection exists, as reports of PP are increasing globally with improved clinical awareness.1,2
The etiology of PP remains unknown; however, associations are well documented between PP and a ketogenic state secondary to uncontrolled diabetes, a low-carbohydrate diet, anorexia nervosa, or bariatric surgery.3 It is theorized that high serum ketones lead to perivascular ketone deposition, which induces neutrophil migration and chemotaxis,4 as substantiated by evidence of rash resolution with correction of the ketogenic state and improvement after administration of tetracyclines, a drug class known for neutrophil chemotaxis inhibition.5 Improvement of PP via these treatment mechanisms suggests that ketone bodies may play a role in the pathogenesis of PP.
Interestingly, Kafle et al6 reported that patients with PP commonly have bacterial colonies and associated inflammatory sequelae at the level of the hair follicles, which suggests that follicular involvement plays a role in the pathogenesis of PP. These findings are consistent with our patient’s histopathology consisting of gram-positive organisms and purulent inflammation at the infundibulum. The histopathologic features of PP are stage specific.1 Early stages are characterized by a superficial perivascular infiltrate of neutrophils that then spread to dermal papillae. Neutrophils then quickly sweep through the epidermis, causing spongiosis, ballooning, necrotic keratocytes, and consequent surface epithelium abscess formation. Over time, the dermal infiltrate assumes a lichenoid pattern as eosinophils and lymphocytes invade and predominate over neutrophils. Eventually, melanophages appear in the dermis as the epidermis undergoes hyperplasia, parakeratosis, and hyperpigmentation.1 The histologic differential diagnosis for PP is broad and varies based on the stage-specific progression of clinical and histopathologic findings.
Similar to PP, subacute cutaneous lupus erythematosus has a female predominance and resolves with subsequent dyspigmentation; however, it initially is characterized by annular plaques with central clearing or papulosquamous lesions restricted to sun-exposed skin. Photosensitivity is a prominent feature, and roughly 50% of patients meet diagnostic criteria for systemic lupus erythematosus.7 Histopathology shows interface changes with increased dermal mucin and a perivascular lymphoplasmacytic inflammatory infiltrate.
Papular pityriasis rosea can present as a pruritic papular rash on the back and chest; however, it most commonly is associated with a herald patch and typically follows a flulike prodrome.8 Biopsy reveals mounds of parakeratosis with mild spongiosis, perivascular inflammation, and extravasated erythrocytes.
Galli-Galli disease can present as a pruritic rash with follicular papules under the breasts and other flexural areas but histopathologically shows elongated rete ridges with dermal melanosis and acantholysis.9
Hailey-Hailey disease commonly presents in the third decade of life and can manifest as painful, pruritic, vesicular lesions on erythematous skin distributed on the back, neck, and inframammary region, as seen in our case; however, it is histopathologically associated with widespread epidermal acantholysis unlike the findings seen in our patient.10
First-line treatment of PP includes antibiotics such as minocycline, doxycycline, and dapsone due to their anti-inflammatory properties and ability to inhibit neutrophil chemotaxis. In patients with nutritional deficiencies or ketosis, reintroduction of carbohydrates alone has been effective.5,11
Prurigo pigmentosa is an underrecognized inflammatory dermatosis with a complex stage-dependent clinicopathologic presentation. Clinicians should be aware of the etiologic and histopathologic patterns of this unique dermatosis. Rash presentation in the context of a low-carbohydrate diet should prompt biopsy as well as treatment with antibiotics and dietary reintroduction of carbohydrates.
- Böer A, Misago N, Wolter M, et al. Prurigo pigmentosa: a distinctive inflammatory disease of the skin. Am J Dermatopathol. 2003;25:117-129. doi:10.1097/00000372-200304000-00005
- de Sousa Vargas TJ, Abreu Raposo CM, Lima RB, et al. Prurigo pigmentosa: report of 3 cases from Brazil and literature review. Am J Dermatopathol. 2017;39:267-274. doi:10.1097/DAD.0000000000000643
- Mufti A, Mirali S, Abduelmula A, et al. Clinical manifestations and treatment outcomes in prurigo pigmentosa (Nagashima disease): a systematic review of the literature. JAAD Int. 2021;3:79. doi:10.1016/J .JDIN.2021.03.003
- Beutler BD, Cohen PR, Lee RA. Prurigo pigmentosa: literature review. Am J Clin Dermatol. 2015;16:533-543. doi:10.1007/S40257-015-0154-4
- Chiam LYT, Goh BK, Lim KS, et al. Prurigo pigmentosa: a report of two cases that responded to minocycline. Clin Exp Dermatol. 2009;34. doi:10.1111/J.1365-2230.2009.03253.X
- Kafle SU, Swe SM, Hsiao PF, et al. Folliculitis in prurigo pigmentosa: a proposed pathogenesis based on clinical and pathological observation. J Cutan Pathol. 2017;44:20-27. doi:10.1111/CUP.12829
- Sontheimer RD. Subacute cutaneous lupus erythematosus: 25-year evolution of a prototypic subset (subphenotype) of lupus erythematosus defined by characteristic cutaneous, pathological, immunological, and genetic findings. Autoimmun Rev. 2005;4:253-263. doi:10.1016/J .AUTREV.2004.10.00
- Leung AKC, Lam JM, Leong KF, et al. Pityriasis rosea: an updated review. Curr Pediatr Rev. 2021;17:201-211. doi:10.2174/15733963166662 00923161330
- Sprecher E, Indelman M, Khamaysi Z, et al. Galli-Galli disease is an acantholytic variant of Dowling-Degos disease. Br J Dermatol. 2007;156:572-574. doi:10.1111/J.1365-2133.2006.07703.X
- Burge SM. Hailey-Hailey disease: the clinical features, response to treatment and prognosis. Br J Dermatol. 1992;126:275-282. doi:10.1111/J.1365-2133.1992.TB00658
- Lu L-Y, Chen C-B. Keto rash: ketoacidosis-induced prurigo pigmentosa. Mayo Clin Proc. 2022;97:20-21. doi:10.1016/j.mayocp.2021.11.019
The Diagnosis: Prurigo Pigmentosa
Histopathology of the punch biopsy revealed subcorneal collections of neutrophils flanked by a spongiotic epidermis with neutrophil and eosinophil exocytosis. Rare dyskeratotic keratinocytes were identified at the dermoepidermal junction, and grampositive bacterial organisms were seen in a follicular infundibulum with purulent inflammation. The dermis demonstrated a mildly dense superficial perivascular and interstitial infiltrate composed of lymphocytes, histiocytes, scattered neutrophils, and eosinophils (Figure).

Given the combination of clinical and histologic findings, a diagnosis of prurigo pigmentosa (PP) was rendered and a urinalysis was ordered, which confirmed ketonuria. The patient was started on minocycline 100 mg twice daily and was advised to reintroduce carbohydrates into her diet. Resolution of the inflammatory component of the rash was achieved at 3-week follow-up, with residual reticulated postinflammatory hyperpigmentation.
Prurigo pigmentosa is a rare, albeit globally underrecognized, inflammatory dermatosis characterized by pruritic, symmetric, erythematous papules and plaques on the chest, back, neck, and rarely the arms and forehead that subsequently involute, leaving reticular postinflammatory hyperpigmentation.1 Prurigo pigmentosa is predominant in females (2.6:1 ratio). The mean age at presentation is 24.4 years, and it most commonly has been documented among populations in Asian countries, though it is unclear if a genetic predilection exists, as reports of PP are increasing globally with improved clinical awareness.1,2
The etiology of PP remains unknown; however, associations are well documented between PP and a ketogenic state secondary to uncontrolled diabetes, a low-carbohydrate diet, anorexia nervosa, or bariatric surgery.3 It is theorized that high serum ketones lead to perivascular ketone deposition, which induces neutrophil migration and chemotaxis,4 as substantiated by evidence of rash resolution with correction of the ketogenic state and improvement after administration of tetracyclines, a drug class known for neutrophil chemotaxis inhibition.5 Improvement of PP via these treatment mechanisms suggests that ketone bodies may play a role in the pathogenesis of PP.
Interestingly, Kafle et al6 reported that patients with PP commonly have bacterial colonies and associated inflammatory sequelae at the level of the hair follicles, which suggests that follicular involvement plays a role in the pathogenesis of PP. These findings are consistent with our patient’s histopathology consisting of gram-positive organisms and purulent inflammation at the infundibulum. The histopathologic features of PP are stage specific.1 Early stages are characterized by a superficial perivascular infiltrate of neutrophils that then spread to dermal papillae. Neutrophils then quickly sweep through the epidermis, causing spongiosis, ballooning, necrotic keratocytes, and consequent surface epithelium abscess formation. Over time, the dermal infiltrate assumes a lichenoid pattern as eosinophils and lymphocytes invade and predominate over neutrophils. Eventually, melanophages appear in the dermis as the epidermis undergoes hyperplasia, parakeratosis, and hyperpigmentation.1 The histologic differential diagnosis for PP is broad and varies based on the stage-specific progression of clinical and histopathologic findings.
Similar to PP, subacute cutaneous lupus erythematosus has a female predominance and resolves with subsequent dyspigmentation; however, it initially is characterized by annular plaques with central clearing or papulosquamous lesions restricted to sun-exposed skin. Photosensitivity is a prominent feature, and roughly 50% of patients meet diagnostic criteria for systemic lupus erythematosus.7 Histopathology shows interface changes with increased dermal mucin and a perivascular lymphoplasmacytic inflammatory infiltrate.
Papular pityriasis rosea can present as a pruritic papular rash on the back and chest; however, it most commonly is associated with a herald patch and typically follows a flulike prodrome.8 Biopsy reveals mounds of parakeratosis with mild spongiosis, perivascular inflammation, and extravasated erythrocytes.
Galli-Galli disease can present as a pruritic rash with follicular papules under the breasts and other flexural areas but histopathologically shows elongated rete ridges with dermal melanosis and acantholysis.9
Hailey-Hailey disease commonly presents in the third decade of life and can manifest as painful, pruritic, vesicular lesions on erythematous skin distributed on the back, neck, and inframammary region, as seen in our case; however, it is histopathologically associated with widespread epidermal acantholysis unlike the findings seen in our patient.10
First-line treatment of PP includes antibiotics such as minocycline, doxycycline, and dapsone due to their anti-inflammatory properties and ability to inhibit neutrophil chemotaxis. In patients with nutritional deficiencies or ketosis, reintroduction of carbohydrates alone has been effective.5,11
Prurigo pigmentosa is an underrecognized inflammatory dermatosis with a complex stage-dependent clinicopathologic presentation. Clinicians should be aware of the etiologic and histopathologic patterns of this unique dermatosis. Rash presentation in the context of a low-carbohydrate diet should prompt biopsy as well as treatment with antibiotics and dietary reintroduction of carbohydrates.
The Diagnosis: Prurigo Pigmentosa
Histopathology of the punch biopsy revealed subcorneal collections of neutrophils flanked by a spongiotic epidermis with neutrophil and eosinophil exocytosis. Rare dyskeratotic keratinocytes were identified at the dermoepidermal junction, and grampositive bacterial organisms were seen in a follicular infundibulum with purulent inflammation. The dermis demonstrated a mildly dense superficial perivascular and interstitial infiltrate composed of lymphocytes, histiocytes, scattered neutrophils, and eosinophils (Figure).

Given the combination of clinical and histologic findings, a diagnosis of prurigo pigmentosa (PP) was rendered and a urinalysis was ordered, which confirmed ketonuria. The patient was started on minocycline 100 mg twice daily and was advised to reintroduce carbohydrates into her diet. Resolution of the inflammatory component of the rash was achieved at 3-week follow-up, with residual reticulated postinflammatory hyperpigmentation.
Prurigo pigmentosa is a rare, albeit globally underrecognized, inflammatory dermatosis characterized by pruritic, symmetric, erythematous papules and plaques on the chest, back, neck, and rarely the arms and forehead that subsequently involute, leaving reticular postinflammatory hyperpigmentation.1 Prurigo pigmentosa is predominant in females (2.6:1 ratio). The mean age at presentation is 24.4 years, and it most commonly has been documented among populations in Asian countries, though it is unclear if a genetic predilection exists, as reports of PP are increasing globally with improved clinical awareness.1,2
The etiology of PP remains unknown; however, associations are well documented between PP and a ketogenic state secondary to uncontrolled diabetes, a low-carbohydrate diet, anorexia nervosa, or bariatric surgery.3 It is theorized that high serum ketones lead to perivascular ketone deposition, which induces neutrophil migration and chemotaxis,4 as substantiated by evidence of rash resolution with correction of the ketogenic state and improvement after administration of tetracyclines, a drug class known for neutrophil chemotaxis inhibition.5 Improvement of PP via these treatment mechanisms suggests that ketone bodies may play a role in the pathogenesis of PP.
Interestingly, Kafle et al6 reported that patients with PP commonly have bacterial colonies and associated inflammatory sequelae at the level of the hair follicles, which suggests that follicular involvement plays a role in the pathogenesis of PP. These findings are consistent with our patient’s histopathology consisting of gram-positive organisms and purulent inflammation at the infundibulum. The histopathologic features of PP are stage specific.1 Early stages are characterized by a superficial perivascular infiltrate of neutrophils that then spread to dermal papillae. Neutrophils then quickly sweep through the epidermis, causing spongiosis, ballooning, necrotic keratocytes, and consequent surface epithelium abscess formation. Over time, the dermal infiltrate assumes a lichenoid pattern as eosinophils and lymphocytes invade and predominate over neutrophils. Eventually, melanophages appear in the dermis as the epidermis undergoes hyperplasia, parakeratosis, and hyperpigmentation.1 The histologic differential diagnosis for PP is broad and varies based on the stage-specific progression of clinical and histopathologic findings.
Similar to PP, subacute cutaneous lupus erythematosus has a female predominance and resolves with subsequent dyspigmentation; however, it initially is characterized by annular plaques with central clearing or papulosquamous lesions restricted to sun-exposed skin. Photosensitivity is a prominent feature, and roughly 50% of patients meet diagnostic criteria for systemic lupus erythematosus.7 Histopathology shows interface changes with increased dermal mucin and a perivascular lymphoplasmacytic inflammatory infiltrate.
Papular pityriasis rosea can present as a pruritic papular rash on the back and chest; however, it most commonly is associated with a herald patch and typically follows a flulike prodrome.8 Biopsy reveals mounds of parakeratosis with mild spongiosis, perivascular inflammation, and extravasated erythrocytes.
Galli-Galli disease can present as a pruritic rash with follicular papules under the breasts and other flexural areas but histopathologically shows elongated rete ridges with dermal melanosis and acantholysis.9
Hailey-Hailey disease commonly presents in the third decade of life and can manifest as painful, pruritic, vesicular lesions on erythematous skin distributed on the back, neck, and inframammary region, as seen in our case; however, it is histopathologically associated with widespread epidermal acantholysis unlike the findings seen in our patient.10
First-line treatment of PP includes antibiotics such as minocycline, doxycycline, and dapsone due to their anti-inflammatory properties and ability to inhibit neutrophil chemotaxis. In patients with nutritional deficiencies or ketosis, reintroduction of carbohydrates alone has been effective.5,11
Prurigo pigmentosa is an underrecognized inflammatory dermatosis with a complex stage-dependent clinicopathologic presentation. Clinicians should be aware of the etiologic and histopathologic patterns of this unique dermatosis. Rash presentation in the context of a low-carbohydrate diet should prompt biopsy as well as treatment with antibiotics and dietary reintroduction of carbohydrates.
- Böer A, Misago N, Wolter M, et al. Prurigo pigmentosa: a distinctive inflammatory disease of the skin. Am J Dermatopathol. 2003;25:117-129. doi:10.1097/00000372-200304000-00005
- de Sousa Vargas TJ, Abreu Raposo CM, Lima RB, et al. Prurigo pigmentosa: report of 3 cases from Brazil and literature review. Am J Dermatopathol. 2017;39:267-274. doi:10.1097/DAD.0000000000000643
- Mufti A, Mirali S, Abduelmula A, et al. Clinical manifestations and treatment outcomes in prurigo pigmentosa (Nagashima disease): a systematic review of the literature. JAAD Int. 2021;3:79. doi:10.1016/J .JDIN.2021.03.003
- Beutler BD, Cohen PR, Lee RA. Prurigo pigmentosa: literature review. Am J Clin Dermatol. 2015;16:533-543. doi:10.1007/S40257-015-0154-4
- Chiam LYT, Goh BK, Lim KS, et al. Prurigo pigmentosa: a report of two cases that responded to minocycline. Clin Exp Dermatol. 2009;34. doi:10.1111/J.1365-2230.2009.03253.X
- Kafle SU, Swe SM, Hsiao PF, et al. Folliculitis in prurigo pigmentosa: a proposed pathogenesis based on clinical and pathological observation. J Cutan Pathol. 2017;44:20-27. doi:10.1111/CUP.12829
- Sontheimer RD. Subacute cutaneous lupus erythematosus: 25-year evolution of a prototypic subset (subphenotype) of lupus erythematosus defined by characteristic cutaneous, pathological, immunological, and genetic findings. Autoimmun Rev. 2005;4:253-263. doi:10.1016/J .AUTREV.2004.10.00
- Leung AKC, Lam JM, Leong KF, et al. Pityriasis rosea: an updated review. Curr Pediatr Rev. 2021;17:201-211. doi:10.2174/15733963166662 00923161330
- Sprecher E, Indelman M, Khamaysi Z, et al. Galli-Galli disease is an acantholytic variant of Dowling-Degos disease. Br J Dermatol. 2007;156:572-574. doi:10.1111/J.1365-2133.2006.07703.X
- Burge SM. Hailey-Hailey disease: the clinical features, response to treatment and prognosis. Br J Dermatol. 1992;126:275-282. doi:10.1111/J.1365-2133.1992.TB00658
- Lu L-Y, Chen C-B. Keto rash: ketoacidosis-induced prurigo pigmentosa. Mayo Clin Proc. 2022;97:20-21. doi:10.1016/j.mayocp.2021.11.019
- Böer A, Misago N, Wolter M, et al. Prurigo pigmentosa: a distinctive inflammatory disease of the skin. Am J Dermatopathol. 2003;25:117-129. doi:10.1097/00000372-200304000-00005
- de Sousa Vargas TJ, Abreu Raposo CM, Lima RB, et al. Prurigo pigmentosa: report of 3 cases from Brazil and literature review. Am J Dermatopathol. 2017;39:267-274. doi:10.1097/DAD.0000000000000643
- Mufti A, Mirali S, Abduelmula A, et al. Clinical manifestations and treatment outcomes in prurigo pigmentosa (Nagashima disease): a systematic review of the literature. JAAD Int. 2021;3:79. doi:10.1016/J .JDIN.2021.03.003
- Beutler BD, Cohen PR, Lee RA. Prurigo pigmentosa: literature review. Am J Clin Dermatol. 2015;16:533-543. doi:10.1007/S40257-015-0154-4
- Chiam LYT, Goh BK, Lim KS, et al. Prurigo pigmentosa: a report of two cases that responded to minocycline. Clin Exp Dermatol. 2009;34. doi:10.1111/J.1365-2230.2009.03253.X
- Kafle SU, Swe SM, Hsiao PF, et al. Folliculitis in prurigo pigmentosa: a proposed pathogenesis based on clinical and pathological observation. J Cutan Pathol. 2017;44:20-27. doi:10.1111/CUP.12829
- Sontheimer RD. Subacute cutaneous lupus erythematosus: 25-year evolution of a prototypic subset (subphenotype) of lupus erythematosus defined by characteristic cutaneous, pathological, immunological, and genetic findings. Autoimmun Rev. 2005;4:253-263. doi:10.1016/J .AUTREV.2004.10.00
- Leung AKC, Lam JM, Leong KF, et al. Pityriasis rosea: an updated review. Curr Pediatr Rev. 2021;17:201-211. doi:10.2174/15733963166662 00923161330
- Sprecher E, Indelman M, Khamaysi Z, et al. Galli-Galli disease is an acantholytic variant of Dowling-Degos disease. Br J Dermatol. 2007;156:572-574. doi:10.1111/J.1365-2133.2006.07703.X
- Burge SM. Hailey-Hailey disease: the clinical features, response to treatment and prognosis. Br J Dermatol. 1992;126:275-282. doi:10.1111/J.1365-2133.1992.TB00658
- Lu L-Y, Chen C-B. Keto rash: ketoacidosis-induced prurigo pigmentosa. Mayo Clin Proc. 2022;97:20-21. doi:10.1016/j.mayocp.2021.11.019
An otherwise healthy 22-year-old woman presented with a painful eruption with burning and pruritus that had been slowly worsening as it spread over the last 4 weeks. The rash first appeared on the lower chest and inframammary folds (top) and spread to the upper chest, neck, back (bottom), arms, and lower face. Physical examination revealed multiple illdefined, erythematous papules, patches, and plaques on the chest, back, neck, and upper abdomen. Individual lesions coalesced into plaques that displayed a reticular configuration. There were no lesions in the axillae. The patient had been following a low-carbohydrate diet for 4 months. A punch biopsy was performed.
Gray hair and aging: Could ‘stuck’ stem cells be to blame?
New evidence points more to a cycle wherein undifferentiated stem cells mature to perform their hair-coloring duties and then transform back to their primitive form. To accomplish this, they need to stay on the move.
When these special stem cells get “stuck” in the follicle, gray hair is the result, according to a new study reported online in Nature.
The regeneration cycle of melanocyte stem cells (McSCs) to melanocytes and back again can last for years. However, McSCs die sooner than do other cells nearby, such as hair follicle stem cells. This difference can explain why people go gray but still grow hair.
“It was thought that melanocyte stem cells are maintained in an undifferentiated state, instead of repeating differentiation and de-differentiation,” said the study’s senior investigator Mayumi Ito, PhD, professor in the departments of dermatology and cell biology at NYU Langone Health, New York.
The process involves different compartments in the hair follicle – the germ area is where the stem cells regenerate; the follicle bulge is where they get stuck. A different microenvironment in each location dictates how they change. This “chameleon-like” property surprised researchers.
Now that investigators figured out how gray hair might get started, a next step will be to search for a way to stop it.
The research has been performed in mice to date but could translate to humans. “Because the structure of the hair follicle is similar between mice and humans, we speculate that human melanocytes may also demonstrate the plasticity during hair regeneration,” Dr. Ito told this news organization.
Future findings could also lead to new therapies. “Our study suggests that moving melanocytes to a proper location within the hair follicle may help prevent gray hair,” Dr. Ito said.
Given the known effects of ultraviolet B (UVB) radiation on melanocytes, Dr. Ito and colleagues wanted to see what effect it might have on this cycle. So in the study, they exposed hair follicles of mice to UVB radiation and report it speeds up the process for McSCs to transform to color-producing melanocytes. They found that these McSCs can regenerate or change back to undifferentiated stem cells, so UVB radiation does not interrupt the process.
A melanoma clue?
The study also could have implications for melanoma. Unlike other tumors, melanocytes that cause cancer can self-renew even from a fully differentiated, pigmented form, the researchers note.
This makes melanomas more difficult to eliminate.
“Our study suggests normal melanocytes are very plastic and can reverse a differentiation state. Melanoma cells are known to be very plastic,” Dr. Ito said. “We consider this feature of melanoma may be related to the high plasticity of original melanocytes.”
The finding that melanocyte stem cells “are more plastic than maybe previously given credit for … certainly has implications in melanoma,” agreed Melissa Harris, PhD, associate professor, department of biology at the University of Alabama, Birmingham, when asked to comment on the study.
Small technology, big insights?
The advanced technology used by Dr. Ito and colleagues in the study included 3D-intravital imaging and single-cell RNA sequencing to track the stem cells in almost real time as they aged and moved within each hair follicle.
“This paper uses a nice mix of classic and modern techniques to help answer a question that many in the field of pigmentation biology have suspected for a long time. Not all dormant melanocyte stem cells are created equal,” Dr. Harris said.
“The one question not answered in this paper is how to reverse the dysfunction of the melanocyte stem cell ‘stuck’ in the hair bulge,” Dr. Harris added. “There are numerous clinical case studies in humans showing medicine-induced hair repigmentation, and perhaps these cases are examples of dysfunctional melanocyte stem cells becoming ‘unstuck.’ ”
‘Very interesting’ findings
The study and its results “are very interesting from a mechanistic perspective and basic science view,” said Anthony M. Rossi, MD, a private practice dermatologist and assistant attending dermatologist at Memorial Sloan Kettering Cancer Center in New York, when asked to comment on the results.
The research provides another view of how melanocyte stem cells can pigment the hair shaft, Dr. Rossi added. “It gives insight into the behavior of stem cells and how they can travel and change state, something not well-known before.”
Dr. Rossi cautioned that other mechanisms are likely taking place. He pointed out that graying of hair can actually occur after a sudden stress event, as well as with vitamin B12 deficiency, thyroid disease, vitiligo-related autoimmune destruction, neurofibromatosis, tuberous sclerosis, and alopecia areata.
The “standout concept” in this paper is that the melanocyte stem cells are stranded and are not getting the right signal from the microenvironment to amplify and appropriately migrate to provide pigment to the hair shaft, said Paradi Mirmirani, MD, a private practice dermatologist in Vallejo, Calif.
It could be challenging to find the right signaling to reverse the graying process, Dr. Mirmirani added. “But the first step is always to understand the underlying basic mechanism. It would be interesting to see if other factors such as smoking, stress … influence the melanocyte stem cells in the same way.”
Grants from the National Institutes of Health and the Department of Defense supported the study. Dr. Ito, Dr. Harris, Dr. Mirmirani, and Dr. Rossi had no relevant disclosures.
A version of this article first appeared on Medscape.com.
New evidence points more to a cycle wherein undifferentiated stem cells mature to perform their hair-coloring duties and then transform back to their primitive form. To accomplish this, they need to stay on the move.
When these special stem cells get “stuck” in the follicle, gray hair is the result, according to a new study reported online in Nature.
The regeneration cycle of melanocyte stem cells (McSCs) to melanocytes and back again can last for years. However, McSCs die sooner than do other cells nearby, such as hair follicle stem cells. This difference can explain why people go gray but still grow hair.
“It was thought that melanocyte stem cells are maintained in an undifferentiated state, instead of repeating differentiation and de-differentiation,” said the study’s senior investigator Mayumi Ito, PhD, professor in the departments of dermatology and cell biology at NYU Langone Health, New York.
The process involves different compartments in the hair follicle – the germ area is where the stem cells regenerate; the follicle bulge is where they get stuck. A different microenvironment in each location dictates how they change. This “chameleon-like” property surprised researchers.
Now that investigators figured out how gray hair might get started, a next step will be to search for a way to stop it.
The research has been performed in mice to date but could translate to humans. “Because the structure of the hair follicle is similar between mice and humans, we speculate that human melanocytes may also demonstrate the plasticity during hair regeneration,” Dr. Ito told this news organization.
Future findings could also lead to new therapies. “Our study suggests that moving melanocytes to a proper location within the hair follicle may help prevent gray hair,” Dr. Ito said.
Given the known effects of ultraviolet B (UVB) radiation on melanocytes, Dr. Ito and colleagues wanted to see what effect it might have on this cycle. So in the study, they exposed hair follicles of mice to UVB radiation and report it speeds up the process for McSCs to transform to color-producing melanocytes. They found that these McSCs can regenerate or change back to undifferentiated stem cells, so UVB radiation does not interrupt the process.
A melanoma clue?
The study also could have implications for melanoma. Unlike other tumors, melanocytes that cause cancer can self-renew even from a fully differentiated, pigmented form, the researchers note.
This makes melanomas more difficult to eliminate.
“Our study suggests normal melanocytes are very plastic and can reverse a differentiation state. Melanoma cells are known to be very plastic,” Dr. Ito said. “We consider this feature of melanoma may be related to the high plasticity of original melanocytes.”
The finding that melanocyte stem cells “are more plastic than maybe previously given credit for … certainly has implications in melanoma,” agreed Melissa Harris, PhD, associate professor, department of biology at the University of Alabama, Birmingham, when asked to comment on the study.
Small technology, big insights?
The advanced technology used by Dr. Ito and colleagues in the study included 3D-intravital imaging and single-cell RNA sequencing to track the stem cells in almost real time as they aged and moved within each hair follicle.
“This paper uses a nice mix of classic and modern techniques to help answer a question that many in the field of pigmentation biology have suspected for a long time. Not all dormant melanocyte stem cells are created equal,” Dr. Harris said.
“The one question not answered in this paper is how to reverse the dysfunction of the melanocyte stem cell ‘stuck’ in the hair bulge,” Dr. Harris added. “There are numerous clinical case studies in humans showing medicine-induced hair repigmentation, and perhaps these cases are examples of dysfunctional melanocyte stem cells becoming ‘unstuck.’ ”
‘Very interesting’ findings
The study and its results “are very interesting from a mechanistic perspective and basic science view,” said Anthony M. Rossi, MD, a private practice dermatologist and assistant attending dermatologist at Memorial Sloan Kettering Cancer Center in New York, when asked to comment on the results.
The research provides another view of how melanocyte stem cells can pigment the hair shaft, Dr. Rossi added. “It gives insight into the behavior of stem cells and how they can travel and change state, something not well-known before.”
Dr. Rossi cautioned that other mechanisms are likely taking place. He pointed out that graying of hair can actually occur after a sudden stress event, as well as with vitamin B12 deficiency, thyroid disease, vitiligo-related autoimmune destruction, neurofibromatosis, tuberous sclerosis, and alopecia areata.
The “standout concept” in this paper is that the melanocyte stem cells are stranded and are not getting the right signal from the microenvironment to amplify and appropriately migrate to provide pigment to the hair shaft, said Paradi Mirmirani, MD, a private practice dermatologist in Vallejo, Calif.
It could be challenging to find the right signaling to reverse the graying process, Dr. Mirmirani added. “But the first step is always to understand the underlying basic mechanism. It would be interesting to see if other factors such as smoking, stress … influence the melanocyte stem cells in the same way.”
Grants from the National Institutes of Health and the Department of Defense supported the study. Dr. Ito, Dr. Harris, Dr. Mirmirani, and Dr. Rossi had no relevant disclosures.
A version of this article first appeared on Medscape.com.
New evidence points more to a cycle wherein undifferentiated stem cells mature to perform their hair-coloring duties and then transform back to their primitive form. To accomplish this, they need to stay on the move.
When these special stem cells get “stuck” in the follicle, gray hair is the result, according to a new study reported online in Nature.
The regeneration cycle of melanocyte stem cells (McSCs) to melanocytes and back again can last for years. However, McSCs die sooner than do other cells nearby, such as hair follicle stem cells. This difference can explain why people go gray but still grow hair.
“It was thought that melanocyte stem cells are maintained in an undifferentiated state, instead of repeating differentiation and de-differentiation,” said the study’s senior investigator Mayumi Ito, PhD, professor in the departments of dermatology and cell biology at NYU Langone Health, New York.
The process involves different compartments in the hair follicle – the germ area is where the stem cells regenerate; the follicle bulge is where they get stuck. A different microenvironment in each location dictates how they change. This “chameleon-like” property surprised researchers.
Now that investigators figured out how gray hair might get started, a next step will be to search for a way to stop it.
The research has been performed in mice to date but could translate to humans. “Because the structure of the hair follicle is similar between mice and humans, we speculate that human melanocytes may also demonstrate the plasticity during hair regeneration,” Dr. Ito told this news organization.
Future findings could also lead to new therapies. “Our study suggests that moving melanocytes to a proper location within the hair follicle may help prevent gray hair,” Dr. Ito said.
Given the known effects of ultraviolet B (UVB) radiation on melanocytes, Dr. Ito and colleagues wanted to see what effect it might have on this cycle. So in the study, they exposed hair follicles of mice to UVB radiation and report it speeds up the process for McSCs to transform to color-producing melanocytes. They found that these McSCs can regenerate or change back to undifferentiated stem cells, so UVB radiation does not interrupt the process.
A melanoma clue?
The study also could have implications for melanoma. Unlike other tumors, melanocytes that cause cancer can self-renew even from a fully differentiated, pigmented form, the researchers note.
This makes melanomas more difficult to eliminate.
“Our study suggests normal melanocytes are very plastic and can reverse a differentiation state. Melanoma cells are known to be very plastic,” Dr. Ito said. “We consider this feature of melanoma may be related to the high plasticity of original melanocytes.”
The finding that melanocyte stem cells “are more plastic than maybe previously given credit for … certainly has implications in melanoma,” agreed Melissa Harris, PhD, associate professor, department of biology at the University of Alabama, Birmingham, when asked to comment on the study.
Small technology, big insights?
The advanced technology used by Dr. Ito and colleagues in the study included 3D-intravital imaging and single-cell RNA sequencing to track the stem cells in almost real time as they aged and moved within each hair follicle.
“This paper uses a nice mix of classic and modern techniques to help answer a question that many in the field of pigmentation biology have suspected for a long time. Not all dormant melanocyte stem cells are created equal,” Dr. Harris said.
“The one question not answered in this paper is how to reverse the dysfunction of the melanocyte stem cell ‘stuck’ in the hair bulge,” Dr. Harris added. “There are numerous clinical case studies in humans showing medicine-induced hair repigmentation, and perhaps these cases are examples of dysfunctional melanocyte stem cells becoming ‘unstuck.’ ”
‘Very interesting’ findings
The study and its results “are very interesting from a mechanistic perspective and basic science view,” said Anthony M. Rossi, MD, a private practice dermatologist and assistant attending dermatologist at Memorial Sloan Kettering Cancer Center in New York, when asked to comment on the results.
The research provides another view of how melanocyte stem cells can pigment the hair shaft, Dr. Rossi added. “It gives insight into the behavior of stem cells and how they can travel and change state, something not well-known before.”
Dr. Rossi cautioned that other mechanisms are likely taking place. He pointed out that graying of hair can actually occur after a sudden stress event, as well as with vitamin B12 deficiency, thyroid disease, vitiligo-related autoimmune destruction, neurofibromatosis, tuberous sclerosis, and alopecia areata.
The “standout concept” in this paper is that the melanocyte stem cells are stranded and are not getting the right signal from the microenvironment to amplify and appropriately migrate to provide pigment to the hair shaft, said Paradi Mirmirani, MD, a private practice dermatologist in Vallejo, Calif.
It could be challenging to find the right signaling to reverse the graying process, Dr. Mirmirani added. “But the first step is always to understand the underlying basic mechanism. It would be interesting to see if other factors such as smoking, stress … influence the melanocyte stem cells in the same way.”
Grants from the National Institutes of Health and the Department of Defense supported the study. Dr. Ito, Dr. Harris, Dr. Mirmirani, and Dr. Rossi had no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM NATURE
Best practices document outlines genitourinary applications of lasers and energy-based devices
PHOENIX –
“Even a cursory review of PubMed today yields over 100,000 results” on this topic, Macrene R. Alexiades, MD, PhD, associate clinical professor of dermatology at Yale University, New Haven, Conn., said at the annual conference of the American Society for Laser Medicine and Surgery. “Add to that radiofrequency and various diagnoses, the number of publications has skyrocketed, particularly over the last 10 years.”
What has been missing from this hot research topic all these years, she continued, is that no one has distilled this pile of data into a practical guide for office-based clinicians who use lasers and energy-based devices for genitourinary conditions – until now. Working with experts in gynecology and urogynecology, Dr. Alexiades spearheaded a 2-year-long effort to assemble a document on optimal protocols and best practices for genitourinary application of lasers and energy-based devices. The document, published soon after the ASLMS meeting in Lasers in Medicine and Surgery, includes a table that lists the current Food and Drug Administration approval status of devices in genitourinary applications, as well as individual sections dedicated to fractional lasers, radiofrequency (RF) devices, and high-intensity focused electromagnetic technology. It concludes with a section on the current status of clearances and future pathways.
“The work we did was exhaustive,” said Dr. Alexiades, who is also founder and director of Dermatology & Laser Surgery Center of New York. “We went through all the clinical trial data and compiled the parameters that, as a consensus, we agree are best practices for each technology for which we had rigorous published data.”
The document contains a brief background on the history of the devices used for genitourinary issues and it addresses core topics for each technology, such as conditions treated, contraindications, preoperative physical assessment and preparation, perioperative protocols, and postoperative care.
Contraindications to the genitourinary use of lasers and energy-based devices are numerous and include use of an intrauterine device, active urinary tract or genital infection, vaginal bleeding, current pregnancy, active or recent malignancy, having an electrical implant anywhere in the body, significant concurrent illness, and an anticoagulative or thromboembolic condition or taking anticoagulant medications 1 week prior to the procedure. Another condition to screen for is advanced prolapse, which was considered a contraindication in all clinical trials, she added. “It’s important that you’re able to do the speculum exam and stage the prolapse” so that a patient with this contraindication is not treated.
Dr. Alexiades shared the following highlights from the document’s section related to the use of fractional CO2 lasers:
Preoperative management. Schedule the treatment one week after the patient’s menstrual period. Patients should avoid blood thinners for 7 days and avoid intercourse the night before the procedure. Reschedule in the case of fever, chills, or vaginal bleeding or discharge.
Preoperative physical exam and testing. A normal speculum exam and a recent negative PAP smear are required. For those of child-bearing potential, a pregnancy test is warranted. Obtain written and verbal consent, including discussion of all treatment options, risks, and benefits. No topical or local anesthesia is necessary internally. “Externally, we sometimes apply topical lidocaine gel, but I have found that’s not necessary in most cases,” Dr. Alexiades said. “The treatment is so quick.”
Peri-operative management. In general, device settings are provided by the manufacturer. “For most of the studies that had successful outcomes and no adverse events, researchers adhered to the mild or moderate settings on the technology,” she said. Energy settings were between 15 and 30 watts, delivered at a laser fluence of about 250-300 mJ/cm2 with a spacing of microbeams 1 mm apart. Typically, three treatments are done at 1-month intervals and maintenance treatments are recommended at 6 and 12 months based on duration of the outcomes.
Vulvovaginal postoperative management. A 3-day recovery time is recommended with avoidance of intercourse during this period, because “re-epithelialization is usually complete in 3 days, so we want to give the opportunity for the lining to heal prior to introducing any friction, Dr. Alexiades said.” Rarely, spotting or discharge may occur and there should be no discomfort. “Any severe discomfort or burning may potentially signify infection and should prompt evaluation and possibly vaginal cultures. The patient can shower, but we recommend avoiding seated baths to decrease any introduction of infectious agents.”
Patients should be followed up monthly until three treatments are completed, and a maintenance treatment is considered appropriate between 6 and 12 months. “I do recommend doing a 1-month follow-up following the final treatment, unless it’s a patient who has already had a series of three treatments and is coming in for maintenance,” she said.
In a study from her own practice, Dr. Alexiades evaluated a series of three fractional CO2 laser treatments to the vulva and vagina with a 1-year follow-up in postmenopausal patients. She used the Vaginal Health Index (VHI) to assess changes in vaginal elasticity, fluid volume, vaginal pH, epithelial integrity, and moisture. She and her colleagues discovered that there was improvement in every VHI category after treatment and during the follow-up interval up to 6 months.
“Between 6 and 12 months, we started to see a return a bit toward baseline on all of these parameters,” she said. “The serendipitous discovery that I made during the course of that study was that early intervention improves outcomes. I observed that the younger, most recently postmenopausal cohort seemed to attain normal or near normal VHI quicker than the more extended postmenopausal cohorts.”
In an editorial published in 2020, Dr. Alexiades reviewed the effects of fractional CO2 laser treatment of vulvar skin on vaginal pH and referred to a study she conducted that found that the mean baseline pH pretreatment was 6.32 in the cohort of postmenopausal patients, and was reduced after 3 treatments. “Postmenopausally, the normal acidic pH becomes alkaline,” she said. But she did not expect to see an additional reduction in pH following the treatment out to 6 months. “This indicates that, whatever the wound healing and other restorative effects of these devices are, they seem to continue out to 6 months, at which point it turns around and moves toward baseline [levels].”
Dr. Alexiades highlighted two published meta-analyses of studies related to the genitourinary use of lasers and energy-based devices. One included 59 studies of 3,609 women treated for vaginal rejuvenation using either radiofrequency or fractional ablative laser therapy. The studies reported improvements in symptoms of GSM/VVA and sexual function, high patient satisfaction, with minor adverse events, including treatment-associated vaginal swelling or vaginal discharge.
“Further research needs to be completed to determine which specific pathologies can be treated, if maintenance treatment is necessary, and long-term safety concerns,” the authors concluded.
In another review, researchers analyzed 64 studies related to vaginal laser therapy for GSM. Of these, 47 were before and after studies without a control group, 10 were controlled intervention studies, and 7 were observational cohort and cross-sectional studies.
Vaginal laser treatment “seems to improve scores on the visual analogue scale, Female Sexual Function Index, and the Vaginal Health Index over the short term,” the authors wrote. “Safety outcomes are underreported and short term. Further well-designed clinical trials with sham-laser control groups and evaluating objective variables are needed to provide the best evidence on efficacy.”
“Lasers and energy-based devices are now considered alternative therapeutic modalities for genitourinary conditions,” Dr. Alexiades concluded. “The shortcomings in the literature with respect to lasers and device treatments demonstrate the need for the consensus on best practices and protocols.”
During a separate presentation at the meeting, Michael Gold, MD, highlighted data from Grand View Research, a market research database, which estimated that the global women’s health and wellness market is valued at more than $31 billion globally and is expected to grow at a compound annual growth rate of 4.8% from 2022 to 2030.
“Sales of women’s health energy-based devices continue to grow as new technologies are developed,” said Dr. Gold, a Nashville, Tenn.–based dermatologist and cosmetic surgeon who is also editor-in-chief of the Journal of Cosmetic Dermatology. “Evolving societal norms have made discussions about feminine health issues acceptable. Suffering in silence is no longer necessary or advocated.”
Dr. Alexiades disclosed that she has conducted research for Candela Lasers, Lumenis, Allergan/AbbVie, InMode, and Endymed. She is also the founder and CEO of Macrene Actives. Dr. Gold disclosed that he is a consultant to and/or an investigator and a speaker for Joylux, InMode, and Alma Lasers.
PHOENIX –
“Even a cursory review of PubMed today yields over 100,000 results” on this topic, Macrene R. Alexiades, MD, PhD, associate clinical professor of dermatology at Yale University, New Haven, Conn., said at the annual conference of the American Society for Laser Medicine and Surgery. “Add to that radiofrequency and various diagnoses, the number of publications has skyrocketed, particularly over the last 10 years.”
What has been missing from this hot research topic all these years, she continued, is that no one has distilled this pile of data into a practical guide for office-based clinicians who use lasers and energy-based devices for genitourinary conditions – until now. Working with experts in gynecology and urogynecology, Dr. Alexiades spearheaded a 2-year-long effort to assemble a document on optimal protocols and best practices for genitourinary application of lasers and energy-based devices. The document, published soon after the ASLMS meeting in Lasers in Medicine and Surgery, includes a table that lists the current Food and Drug Administration approval status of devices in genitourinary applications, as well as individual sections dedicated to fractional lasers, radiofrequency (RF) devices, and high-intensity focused electromagnetic technology. It concludes with a section on the current status of clearances and future pathways.
“The work we did was exhaustive,” said Dr. Alexiades, who is also founder and director of Dermatology & Laser Surgery Center of New York. “We went through all the clinical trial data and compiled the parameters that, as a consensus, we agree are best practices for each technology for which we had rigorous published data.”
The document contains a brief background on the history of the devices used for genitourinary issues and it addresses core topics for each technology, such as conditions treated, contraindications, preoperative physical assessment and preparation, perioperative protocols, and postoperative care.
Contraindications to the genitourinary use of lasers and energy-based devices are numerous and include use of an intrauterine device, active urinary tract or genital infection, vaginal bleeding, current pregnancy, active or recent malignancy, having an electrical implant anywhere in the body, significant concurrent illness, and an anticoagulative or thromboembolic condition or taking anticoagulant medications 1 week prior to the procedure. Another condition to screen for is advanced prolapse, which was considered a contraindication in all clinical trials, she added. “It’s important that you’re able to do the speculum exam and stage the prolapse” so that a patient with this contraindication is not treated.
Dr. Alexiades shared the following highlights from the document’s section related to the use of fractional CO2 lasers:
Preoperative management. Schedule the treatment one week after the patient’s menstrual period. Patients should avoid blood thinners for 7 days and avoid intercourse the night before the procedure. Reschedule in the case of fever, chills, or vaginal bleeding or discharge.
Preoperative physical exam and testing. A normal speculum exam and a recent negative PAP smear are required. For those of child-bearing potential, a pregnancy test is warranted. Obtain written and verbal consent, including discussion of all treatment options, risks, and benefits. No topical or local anesthesia is necessary internally. “Externally, we sometimes apply topical lidocaine gel, but I have found that’s not necessary in most cases,” Dr. Alexiades said. “The treatment is so quick.”
Peri-operative management. In general, device settings are provided by the manufacturer. “For most of the studies that had successful outcomes and no adverse events, researchers adhered to the mild or moderate settings on the technology,” she said. Energy settings were between 15 and 30 watts, delivered at a laser fluence of about 250-300 mJ/cm2 with a spacing of microbeams 1 mm apart. Typically, three treatments are done at 1-month intervals and maintenance treatments are recommended at 6 and 12 months based on duration of the outcomes.
Vulvovaginal postoperative management. A 3-day recovery time is recommended with avoidance of intercourse during this period, because “re-epithelialization is usually complete in 3 days, so we want to give the opportunity for the lining to heal prior to introducing any friction, Dr. Alexiades said.” Rarely, spotting or discharge may occur and there should be no discomfort. “Any severe discomfort or burning may potentially signify infection and should prompt evaluation and possibly vaginal cultures. The patient can shower, but we recommend avoiding seated baths to decrease any introduction of infectious agents.”
Patients should be followed up monthly until three treatments are completed, and a maintenance treatment is considered appropriate between 6 and 12 months. “I do recommend doing a 1-month follow-up following the final treatment, unless it’s a patient who has already had a series of three treatments and is coming in for maintenance,” she said.
In a study from her own practice, Dr. Alexiades evaluated a series of three fractional CO2 laser treatments to the vulva and vagina with a 1-year follow-up in postmenopausal patients. She used the Vaginal Health Index (VHI) to assess changes in vaginal elasticity, fluid volume, vaginal pH, epithelial integrity, and moisture. She and her colleagues discovered that there was improvement in every VHI category after treatment and during the follow-up interval up to 6 months.
“Between 6 and 12 months, we started to see a return a bit toward baseline on all of these parameters,” she said. “The serendipitous discovery that I made during the course of that study was that early intervention improves outcomes. I observed that the younger, most recently postmenopausal cohort seemed to attain normal or near normal VHI quicker than the more extended postmenopausal cohorts.”
In an editorial published in 2020, Dr. Alexiades reviewed the effects of fractional CO2 laser treatment of vulvar skin on vaginal pH and referred to a study she conducted that found that the mean baseline pH pretreatment was 6.32 in the cohort of postmenopausal patients, and was reduced after 3 treatments. “Postmenopausally, the normal acidic pH becomes alkaline,” she said. But she did not expect to see an additional reduction in pH following the treatment out to 6 months. “This indicates that, whatever the wound healing and other restorative effects of these devices are, they seem to continue out to 6 months, at which point it turns around and moves toward baseline [levels].”
Dr. Alexiades highlighted two published meta-analyses of studies related to the genitourinary use of lasers and energy-based devices. One included 59 studies of 3,609 women treated for vaginal rejuvenation using either radiofrequency or fractional ablative laser therapy. The studies reported improvements in symptoms of GSM/VVA and sexual function, high patient satisfaction, with minor adverse events, including treatment-associated vaginal swelling or vaginal discharge.
“Further research needs to be completed to determine which specific pathologies can be treated, if maintenance treatment is necessary, and long-term safety concerns,” the authors concluded.
In another review, researchers analyzed 64 studies related to vaginal laser therapy for GSM. Of these, 47 were before and after studies without a control group, 10 were controlled intervention studies, and 7 were observational cohort and cross-sectional studies.
Vaginal laser treatment “seems to improve scores on the visual analogue scale, Female Sexual Function Index, and the Vaginal Health Index over the short term,” the authors wrote. “Safety outcomes are underreported and short term. Further well-designed clinical trials with sham-laser control groups and evaluating objective variables are needed to provide the best evidence on efficacy.”
“Lasers and energy-based devices are now considered alternative therapeutic modalities for genitourinary conditions,” Dr. Alexiades concluded. “The shortcomings in the literature with respect to lasers and device treatments demonstrate the need for the consensus on best practices and protocols.”
During a separate presentation at the meeting, Michael Gold, MD, highlighted data from Grand View Research, a market research database, which estimated that the global women’s health and wellness market is valued at more than $31 billion globally and is expected to grow at a compound annual growth rate of 4.8% from 2022 to 2030.
“Sales of women’s health energy-based devices continue to grow as new technologies are developed,” said Dr. Gold, a Nashville, Tenn.–based dermatologist and cosmetic surgeon who is also editor-in-chief of the Journal of Cosmetic Dermatology. “Evolving societal norms have made discussions about feminine health issues acceptable. Suffering in silence is no longer necessary or advocated.”
Dr. Alexiades disclosed that she has conducted research for Candela Lasers, Lumenis, Allergan/AbbVie, InMode, and Endymed. She is also the founder and CEO of Macrene Actives. Dr. Gold disclosed that he is a consultant to and/or an investigator and a speaker for Joylux, InMode, and Alma Lasers.
PHOENIX –
“Even a cursory review of PubMed today yields over 100,000 results” on this topic, Macrene R. Alexiades, MD, PhD, associate clinical professor of dermatology at Yale University, New Haven, Conn., said at the annual conference of the American Society for Laser Medicine and Surgery. “Add to that radiofrequency and various diagnoses, the number of publications has skyrocketed, particularly over the last 10 years.”
What has been missing from this hot research topic all these years, she continued, is that no one has distilled this pile of data into a practical guide for office-based clinicians who use lasers and energy-based devices for genitourinary conditions – until now. Working with experts in gynecology and urogynecology, Dr. Alexiades spearheaded a 2-year-long effort to assemble a document on optimal protocols and best practices for genitourinary application of lasers and energy-based devices. The document, published soon after the ASLMS meeting in Lasers in Medicine and Surgery, includes a table that lists the current Food and Drug Administration approval status of devices in genitourinary applications, as well as individual sections dedicated to fractional lasers, radiofrequency (RF) devices, and high-intensity focused electromagnetic technology. It concludes with a section on the current status of clearances and future pathways.
“The work we did was exhaustive,” said Dr. Alexiades, who is also founder and director of Dermatology & Laser Surgery Center of New York. “We went through all the clinical trial data and compiled the parameters that, as a consensus, we agree are best practices for each technology for which we had rigorous published data.”
The document contains a brief background on the history of the devices used for genitourinary issues and it addresses core topics for each technology, such as conditions treated, contraindications, preoperative physical assessment and preparation, perioperative protocols, and postoperative care.
Contraindications to the genitourinary use of lasers and energy-based devices are numerous and include use of an intrauterine device, active urinary tract or genital infection, vaginal bleeding, current pregnancy, active or recent malignancy, having an electrical implant anywhere in the body, significant concurrent illness, and an anticoagulative or thromboembolic condition or taking anticoagulant medications 1 week prior to the procedure. Another condition to screen for is advanced prolapse, which was considered a contraindication in all clinical trials, she added. “It’s important that you’re able to do the speculum exam and stage the prolapse” so that a patient with this contraindication is not treated.
Dr. Alexiades shared the following highlights from the document’s section related to the use of fractional CO2 lasers:
Preoperative management. Schedule the treatment one week after the patient’s menstrual period. Patients should avoid blood thinners for 7 days and avoid intercourse the night before the procedure. Reschedule in the case of fever, chills, or vaginal bleeding or discharge.
Preoperative physical exam and testing. A normal speculum exam and a recent negative PAP smear are required. For those of child-bearing potential, a pregnancy test is warranted. Obtain written and verbal consent, including discussion of all treatment options, risks, and benefits. No topical or local anesthesia is necessary internally. “Externally, we sometimes apply topical lidocaine gel, but I have found that’s not necessary in most cases,” Dr. Alexiades said. “The treatment is so quick.”
Peri-operative management. In general, device settings are provided by the manufacturer. “For most of the studies that had successful outcomes and no adverse events, researchers adhered to the mild or moderate settings on the technology,” she said. Energy settings were between 15 and 30 watts, delivered at a laser fluence of about 250-300 mJ/cm2 with a spacing of microbeams 1 mm apart. Typically, three treatments are done at 1-month intervals and maintenance treatments are recommended at 6 and 12 months based on duration of the outcomes.
Vulvovaginal postoperative management. A 3-day recovery time is recommended with avoidance of intercourse during this period, because “re-epithelialization is usually complete in 3 days, so we want to give the opportunity for the lining to heal prior to introducing any friction, Dr. Alexiades said.” Rarely, spotting or discharge may occur and there should be no discomfort. “Any severe discomfort or burning may potentially signify infection and should prompt evaluation and possibly vaginal cultures. The patient can shower, but we recommend avoiding seated baths to decrease any introduction of infectious agents.”
Patients should be followed up monthly until three treatments are completed, and a maintenance treatment is considered appropriate between 6 and 12 months. “I do recommend doing a 1-month follow-up following the final treatment, unless it’s a patient who has already had a series of three treatments and is coming in for maintenance,” she said.
In a study from her own practice, Dr. Alexiades evaluated a series of three fractional CO2 laser treatments to the vulva and vagina with a 1-year follow-up in postmenopausal patients. She used the Vaginal Health Index (VHI) to assess changes in vaginal elasticity, fluid volume, vaginal pH, epithelial integrity, and moisture. She and her colleagues discovered that there was improvement in every VHI category after treatment and during the follow-up interval up to 6 months.
“Between 6 and 12 months, we started to see a return a bit toward baseline on all of these parameters,” she said. “The serendipitous discovery that I made during the course of that study was that early intervention improves outcomes. I observed that the younger, most recently postmenopausal cohort seemed to attain normal or near normal VHI quicker than the more extended postmenopausal cohorts.”
In an editorial published in 2020, Dr. Alexiades reviewed the effects of fractional CO2 laser treatment of vulvar skin on vaginal pH and referred to a study she conducted that found that the mean baseline pH pretreatment was 6.32 in the cohort of postmenopausal patients, and was reduced after 3 treatments. “Postmenopausally, the normal acidic pH becomes alkaline,” she said. But she did not expect to see an additional reduction in pH following the treatment out to 6 months. “This indicates that, whatever the wound healing and other restorative effects of these devices are, they seem to continue out to 6 months, at which point it turns around and moves toward baseline [levels].”
Dr. Alexiades highlighted two published meta-analyses of studies related to the genitourinary use of lasers and energy-based devices. One included 59 studies of 3,609 women treated for vaginal rejuvenation using either radiofrequency or fractional ablative laser therapy. The studies reported improvements in symptoms of GSM/VVA and sexual function, high patient satisfaction, with minor adverse events, including treatment-associated vaginal swelling or vaginal discharge.
“Further research needs to be completed to determine which specific pathologies can be treated, if maintenance treatment is necessary, and long-term safety concerns,” the authors concluded.
In another review, researchers analyzed 64 studies related to vaginal laser therapy for GSM. Of these, 47 were before and after studies without a control group, 10 were controlled intervention studies, and 7 were observational cohort and cross-sectional studies.
Vaginal laser treatment “seems to improve scores on the visual analogue scale, Female Sexual Function Index, and the Vaginal Health Index over the short term,” the authors wrote. “Safety outcomes are underreported and short term. Further well-designed clinical trials with sham-laser control groups and evaluating objective variables are needed to provide the best evidence on efficacy.”
“Lasers and energy-based devices are now considered alternative therapeutic modalities for genitourinary conditions,” Dr. Alexiades concluded. “The shortcomings in the literature with respect to lasers and device treatments demonstrate the need for the consensus on best practices and protocols.”
During a separate presentation at the meeting, Michael Gold, MD, highlighted data from Grand View Research, a market research database, which estimated that the global women’s health and wellness market is valued at more than $31 billion globally and is expected to grow at a compound annual growth rate of 4.8% from 2022 to 2030.
“Sales of women’s health energy-based devices continue to grow as new technologies are developed,” said Dr. Gold, a Nashville, Tenn.–based dermatologist and cosmetic surgeon who is also editor-in-chief of the Journal of Cosmetic Dermatology. “Evolving societal norms have made discussions about feminine health issues acceptable. Suffering in silence is no longer necessary or advocated.”
Dr. Alexiades disclosed that she has conducted research for Candela Lasers, Lumenis, Allergan/AbbVie, InMode, and Endymed. She is also the founder and CEO of Macrene Actives. Dr. Gold disclosed that he is a consultant to and/or an investigator and a speaker for Joylux, InMode, and Alma Lasers.
AT ASLMS 2023
FDA approves injectable treatment for cheek lines, wrinkles
The treatment, marketed as Sculptra, is the first FDA-approved PLLA collagen stimulator that, “when injected into the cheek area, helps stimulate natural collagen production to smooth wrinkles and improve skin quality such as firmness and glow,” according to a press release from the manufacturer, Galderma. Sculptra was first approved for aesthetic use in 2009 in the United States and is now available in more than 40 countries.
With this expanded approval, PLLA-SCA is now indicated for use in people with healthy immune systems for correcting shallow to deep nasolabial fold contour deficiencies, fine lines, and wrinkles in the cheeks and other facial areas.
94% have enduring improvement at 2 years
In a clinical trial, PLLA-SCA achieved the primary efficacy endpoint of at least a 1-grade improvement in wrinkles on both cheeks concurrently at rest and its secondary endpoint of improving cheek wrinkles when smiling for up to 2 years, the company states.
According to Galderma, patients showed aesthetic improvement in cheek wrinkles throughout the study; 96% showed improvement at 3 months, 94% showed improvement at 1 year, and 94% showed improvement at 2 years.
The most common side effects after initial treatment are injection site swelling, tenderness, redness, pain, bruising, bleeding, itching, and lumps, according to the company. Other side effects may include small lumps under the skin that are sometimes noticeable when pressing on the treated area.
PLLA-SCA is available only through a licensed practitioner and should not be used by people allergic to any ingredient of the product or who have a history of keloid formation or hypertrophic scarring. The company notes that safety has not been established in patients who are pregnant, lactating, breastfeeding, or younger than 18.
In its instruction to clinicians, the company warns the treatment should not be injected into the blood vessels “as it may cause vascular occlusion, infarction, or embolic phenomena.”
Skin sores, cysts, pimples, rashes, hives, or infection should be healed completely before injecting the treatment, the company cautions. PLLA-SCA should not be injected into the red area of the lip or in the periorbital area.
A version of this article first appeared on Medscape.com.
The treatment, marketed as Sculptra, is the first FDA-approved PLLA collagen stimulator that, “when injected into the cheek area, helps stimulate natural collagen production to smooth wrinkles and improve skin quality such as firmness and glow,” according to a press release from the manufacturer, Galderma. Sculptra was first approved for aesthetic use in 2009 in the United States and is now available in more than 40 countries.
With this expanded approval, PLLA-SCA is now indicated for use in people with healthy immune systems for correcting shallow to deep nasolabial fold contour deficiencies, fine lines, and wrinkles in the cheeks and other facial areas.
94% have enduring improvement at 2 years
In a clinical trial, PLLA-SCA achieved the primary efficacy endpoint of at least a 1-grade improvement in wrinkles on both cheeks concurrently at rest and its secondary endpoint of improving cheek wrinkles when smiling for up to 2 years, the company states.
According to Galderma, patients showed aesthetic improvement in cheek wrinkles throughout the study; 96% showed improvement at 3 months, 94% showed improvement at 1 year, and 94% showed improvement at 2 years.
The most common side effects after initial treatment are injection site swelling, tenderness, redness, pain, bruising, bleeding, itching, and lumps, according to the company. Other side effects may include small lumps under the skin that are sometimes noticeable when pressing on the treated area.
PLLA-SCA is available only through a licensed practitioner and should not be used by people allergic to any ingredient of the product or who have a history of keloid formation or hypertrophic scarring. The company notes that safety has not been established in patients who are pregnant, lactating, breastfeeding, or younger than 18.
In its instruction to clinicians, the company warns the treatment should not be injected into the blood vessels “as it may cause vascular occlusion, infarction, or embolic phenomena.”
Skin sores, cysts, pimples, rashes, hives, or infection should be healed completely before injecting the treatment, the company cautions. PLLA-SCA should not be injected into the red area of the lip or in the periorbital area.
A version of this article first appeared on Medscape.com.
The treatment, marketed as Sculptra, is the first FDA-approved PLLA collagen stimulator that, “when injected into the cheek area, helps stimulate natural collagen production to smooth wrinkles and improve skin quality such as firmness and glow,” according to a press release from the manufacturer, Galderma. Sculptra was first approved for aesthetic use in 2009 in the United States and is now available in more than 40 countries.
With this expanded approval, PLLA-SCA is now indicated for use in people with healthy immune systems for correcting shallow to deep nasolabial fold contour deficiencies, fine lines, and wrinkles in the cheeks and other facial areas.
94% have enduring improvement at 2 years
In a clinical trial, PLLA-SCA achieved the primary efficacy endpoint of at least a 1-grade improvement in wrinkles on both cheeks concurrently at rest and its secondary endpoint of improving cheek wrinkles when smiling for up to 2 years, the company states.
According to Galderma, patients showed aesthetic improvement in cheek wrinkles throughout the study; 96% showed improvement at 3 months, 94% showed improvement at 1 year, and 94% showed improvement at 2 years.
The most common side effects after initial treatment are injection site swelling, tenderness, redness, pain, bruising, bleeding, itching, and lumps, according to the company. Other side effects may include small lumps under the skin that are sometimes noticeable when pressing on the treated area.
PLLA-SCA is available only through a licensed practitioner and should not be used by people allergic to any ingredient of the product or who have a history of keloid formation or hypertrophic scarring. The company notes that safety has not been established in patients who are pregnant, lactating, breastfeeding, or younger than 18.
In its instruction to clinicians, the company warns the treatment should not be injected into the blood vessels “as it may cause vascular occlusion, infarction, or embolic phenomena.”
Skin sores, cysts, pimples, rashes, hives, or infection should be healed completely before injecting the treatment, the company cautions. PLLA-SCA should not be injected into the red area of the lip or in the periorbital area.
A version of this article first appeared on Medscape.com.
Could combining topical antioxidants with a nonablative laser prevent acne scars?
PHOENIX – lesions, results from a prospective, single-center study showed.
“Acne vulgaris is the most common inflammatory dermatosis worldwide, often resulting in sequelae such as scarring, PIE, and PIH,” presenting author Jamie Hu, MD, said at the annual conference of the American Society for Laser Medicine and Surgery, where the study results were presented during an abstract session. “This dyschromia can cause greater psychological distress than the original acne lesions, and disproportionately affects skin of color patients.”
Blemish-prone skin is known to have higher levels of sebum and lower levels of antioxidants, leading to lipid peroxidation and oxidative stress, resulting in proliferation of Cutibacterium acnes and an inflammatory cascade that has recently been implicated in postinflammatory dyschromia and the development of PIE and PIH, noted Dr. Hu, a dermatology resident at the University of Miami. “Therefore, the use of antioxidants presents an opportunity to disrupt blemish and dyschromia,” she said.
One such antioxidant is silymarin, which is derived from the milk thistle plant. Recent studies have demonstrated that silymarin reduces proinflammatory mediators, prevents lipid peroxidation, and presents a new way to target the treatment of both acne and postinflammatory dyschromia.
Dr. Hu’s mentor, Jill S. Waibel, MD, owner and medical director of the Miami Dermatology and Laser Institute, hypothesized that nonablative laser therapy followed by topical application of silymarin would improve acne-associated postinflammatory dyschromia. To test her hunch, she conducted a 12-week, prospective trial in which 24 patients with PIE and/or PIH were randomized to one of two treatment arms: laser treatment with topical antioxidants or laser treatment with vehicle control. Patients received three laser treatments, each 1 month apart. The topical antioxidant used was Silymarin CF, a serum that contains 0.5% silymarin, 0.5% salicylic acid, 15% L-ascorbic acid, and 0.5% ferulic acid. (The study was sponsored by SkinCeuticals, the manufacturer of the serum.)
Laser selection was made primarily on the type of dyschromia, with PIE patients receiving treatment with the pulsed dye laser and PIH patients receiving treatment with the 1,927-nm thulium laser. Patients were treated on days 0, 28, and 56 of the 12-week study, followed by immediate application of topical antioxidants or vehicle control. They were also instructed to apply the assigned topical twice daily for the duration of the study. Patients ranged in age from 21 to 61 years, and 20 had skin types III-IV.
To evaluate efficacy, the researchers conducted blinded clinical assessments with the postacne hyperpigmentation index (PAHPI) and the Global Aesthetic Improvement Scale (GAIS), instrumentation with the Mexameter, a device that captures erythema and melanin index values, and visual diagnostics with optical coherence tomography (OCT).
Dr. Hu reported that at week 12, the PAHPI in the silymarin-plus-laser treatment group fell from an average of 3.18 to 1.74 (a decrease of 1.44), which suggested an improvement trend, compared with the laser treatment–only group, whose PAHPI fell from an average of 3.25 to 1.97 (a decrease of 1.28).
As for the GAIS, a one-time score assessed at the end of the trial, the average score for all patients was 3.24, which translated to “much improved/very much improved.” Patients in the silymarin-plus-laser treatment group had higher average scores compared with patients in the laser treatment–only group (3.35 vs. 3.10, respectively), but the differences did not reach statistical significance.
According to results of the Mexameter assessment, paired t-tests showed that the levels of intralesional melanin decreased significantly for patients in the silymarin-plus-laser treatment group, compared with the laser treatment–only group (P < .05). OCT assessments demonstrated an increase in dermal brightness in both groups, corresponding to an increase in dermal collagen, as well as an increase in blood vessel density.
In an interview at the meeting, Dr. Waibel, subsection chief of dermatology at Baptist Hospital of Miami, said that future studies will focus on long-term follow-up to determine if acne scars can be prevented by combining silymarin with lasers to prevent PIH and PIE. “That would be priceless,” she said. “I believe that the PIH is what causes damage to the collagen, and that damage to the collagen is what causes the scarring. So, if we can prevent or treat PIH, we may be able to prevent scarring.”
This approach, she added, “would decrease the pharmaceutical cost because I think there are many dermatologists who are treating PEI and PIH as active acne. You really have to have a keen eye for understanding the differences and you really have to be looking, because PIE and PIH are flat, whereas active acne consists of either comedones or nodules.”
She noted that in skin of color patients, she has seen PIH persist for 9 or 10 months after treatment with isotretinoin. “It’s not the isotretinoin causing the scars, or even the acne, it’s the prolonged inflammation,” she said.
Catherine M. DiGiorgio, MD, a Boston-based laser and cosmetic dermatologist who was asked to comment on the study, said that patients and dermatologists frequently seek alternatives to hydroquinone for unwanted hyperpigmentation.
“This topical contains an active ingredient – silymarin – obtained from the milk thistle plant along with several already well known topicals used for the treatment of acne and PIH,” said Dr. DiGiorgio, program co-chair of the 2023 ASLMS conference. “Further and larger studies are needed to demonstrate and support the effectiveness of this product and silymarin for PIH and/or PIE.”
Also commenting on the results, Ray Jalian, MD, a Los Angeles–based laser and cosmetic dermatologist, told this news organization that the study findings demonstrate the power of combining topical and laser treatment for more effective improvement in acne-related PIH.
“While the study failed to show statistically significant improvement in postinflammatory erythema with concomitant laser and topical therapy versus laser alone, the promising data supporting concurrent use of topicals and fractional lasers for treatment of PIH, particularly in dark skin phototypes, is a clinically impactful contribution to our daily practice,” he said.
Dr. Waibel disclosed that she has conducted clinical trials for many device and pharmaceutical companies including SkinCeuticals. Dr. Hu, Dr. DiGiorgio, and Dr. Jalian were not involved with the study and reported having no relevant disclosures.
PHOENIX – lesions, results from a prospective, single-center study showed.
“Acne vulgaris is the most common inflammatory dermatosis worldwide, often resulting in sequelae such as scarring, PIE, and PIH,” presenting author Jamie Hu, MD, said at the annual conference of the American Society for Laser Medicine and Surgery, where the study results were presented during an abstract session. “This dyschromia can cause greater psychological distress than the original acne lesions, and disproportionately affects skin of color patients.”
Blemish-prone skin is known to have higher levels of sebum and lower levels of antioxidants, leading to lipid peroxidation and oxidative stress, resulting in proliferation of Cutibacterium acnes and an inflammatory cascade that has recently been implicated in postinflammatory dyschromia and the development of PIE and PIH, noted Dr. Hu, a dermatology resident at the University of Miami. “Therefore, the use of antioxidants presents an opportunity to disrupt blemish and dyschromia,” she said.
One such antioxidant is silymarin, which is derived from the milk thistle plant. Recent studies have demonstrated that silymarin reduces proinflammatory mediators, prevents lipid peroxidation, and presents a new way to target the treatment of both acne and postinflammatory dyschromia.
Dr. Hu’s mentor, Jill S. Waibel, MD, owner and medical director of the Miami Dermatology and Laser Institute, hypothesized that nonablative laser therapy followed by topical application of silymarin would improve acne-associated postinflammatory dyschromia. To test her hunch, she conducted a 12-week, prospective trial in which 24 patients with PIE and/or PIH were randomized to one of two treatment arms: laser treatment with topical antioxidants or laser treatment with vehicle control. Patients received three laser treatments, each 1 month apart. The topical antioxidant used was Silymarin CF, a serum that contains 0.5% silymarin, 0.5% salicylic acid, 15% L-ascorbic acid, and 0.5% ferulic acid. (The study was sponsored by SkinCeuticals, the manufacturer of the serum.)
Laser selection was made primarily on the type of dyschromia, with PIE patients receiving treatment with the pulsed dye laser and PIH patients receiving treatment with the 1,927-nm thulium laser. Patients were treated on days 0, 28, and 56 of the 12-week study, followed by immediate application of topical antioxidants or vehicle control. They were also instructed to apply the assigned topical twice daily for the duration of the study. Patients ranged in age from 21 to 61 years, and 20 had skin types III-IV.
To evaluate efficacy, the researchers conducted blinded clinical assessments with the postacne hyperpigmentation index (PAHPI) and the Global Aesthetic Improvement Scale (GAIS), instrumentation with the Mexameter, a device that captures erythema and melanin index values, and visual diagnostics with optical coherence tomography (OCT).
Dr. Hu reported that at week 12, the PAHPI in the silymarin-plus-laser treatment group fell from an average of 3.18 to 1.74 (a decrease of 1.44), which suggested an improvement trend, compared with the laser treatment–only group, whose PAHPI fell from an average of 3.25 to 1.97 (a decrease of 1.28).
As for the GAIS, a one-time score assessed at the end of the trial, the average score for all patients was 3.24, which translated to “much improved/very much improved.” Patients in the silymarin-plus-laser treatment group had higher average scores compared with patients in the laser treatment–only group (3.35 vs. 3.10, respectively), but the differences did not reach statistical significance.
According to results of the Mexameter assessment, paired t-tests showed that the levels of intralesional melanin decreased significantly for patients in the silymarin-plus-laser treatment group, compared with the laser treatment–only group (P < .05). OCT assessments demonstrated an increase in dermal brightness in both groups, corresponding to an increase in dermal collagen, as well as an increase in blood vessel density.
In an interview at the meeting, Dr. Waibel, subsection chief of dermatology at Baptist Hospital of Miami, said that future studies will focus on long-term follow-up to determine if acne scars can be prevented by combining silymarin with lasers to prevent PIH and PIE. “That would be priceless,” she said. “I believe that the PIH is what causes damage to the collagen, and that damage to the collagen is what causes the scarring. So, if we can prevent or treat PIH, we may be able to prevent scarring.”
This approach, she added, “would decrease the pharmaceutical cost because I think there are many dermatologists who are treating PEI and PIH as active acne. You really have to have a keen eye for understanding the differences and you really have to be looking, because PIE and PIH are flat, whereas active acne consists of either comedones or nodules.”
She noted that in skin of color patients, she has seen PIH persist for 9 or 10 months after treatment with isotretinoin. “It’s not the isotretinoin causing the scars, or even the acne, it’s the prolonged inflammation,” she said.
Catherine M. DiGiorgio, MD, a Boston-based laser and cosmetic dermatologist who was asked to comment on the study, said that patients and dermatologists frequently seek alternatives to hydroquinone for unwanted hyperpigmentation.
“This topical contains an active ingredient – silymarin – obtained from the milk thistle plant along with several already well known topicals used for the treatment of acne and PIH,” said Dr. DiGiorgio, program co-chair of the 2023 ASLMS conference. “Further and larger studies are needed to demonstrate and support the effectiveness of this product and silymarin for PIH and/or PIE.”
Also commenting on the results, Ray Jalian, MD, a Los Angeles–based laser and cosmetic dermatologist, told this news organization that the study findings demonstrate the power of combining topical and laser treatment for more effective improvement in acne-related PIH.
“While the study failed to show statistically significant improvement in postinflammatory erythema with concomitant laser and topical therapy versus laser alone, the promising data supporting concurrent use of topicals and fractional lasers for treatment of PIH, particularly in dark skin phototypes, is a clinically impactful contribution to our daily practice,” he said.
Dr. Waibel disclosed that she has conducted clinical trials for many device and pharmaceutical companies including SkinCeuticals. Dr. Hu, Dr. DiGiorgio, and Dr. Jalian were not involved with the study and reported having no relevant disclosures.
PHOENIX – lesions, results from a prospective, single-center study showed.
“Acne vulgaris is the most common inflammatory dermatosis worldwide, often resulting in sequelae such as scarring, PIE, and PIH,” presenting author Jamie Hu, MD, said at the annual conference of the American Society for Laser Medicine and Surgery, where the study results were presented during an abstract session. “This dyschromia can cause greater psychological distress than the original acne lesions, and disproportionately affects skin of color patients.”
Blemish-prone skin is known to have higher levels of sebum and lower levels of antioxidants, leading to lipid peroxidation and oxidative stress, resulting in proliferation of Cutibacterium acnes and an inflammatory cascade that has recently been implicated in postinflammatory dyschromia and the development of PIE and PIH, noted Dr. Hu, a dermatology resident at the University of Miami. “Therefore, the use of antioxidants presents an opportunity to disrupt blemish and dyschromia,” she said.
One such antioxidant is silymarin, which is derived from the milk thistle plant. Recent studies have demonstrated that silymarin reduces proinflammatory mediators, prevents lipid peroxidation, and presents a new way to target the treatment of both acne and postinflammatory dyschromia.
Dr. Hu’s mentor, Jill S. Waibel, MD, owner and medical director of the Miami Dermatology and Laser Institute, hypothesized that nonablative laser therapy followed by topical application of silymarin would improve acne-associated postinflammatory dyschromia. To test her hunch, she conducted a 12-week, prospective trial in which 24 patients with PIE and/or PIH were randomized to one of two treatment arms: laser treatment with topical antioxidants or laser treatment with vehicle control. Patients received three laser treatments, each 1 month apart. The topical antioxidant used was Silymarin CF, a serum that contains 0.5% silymarin, 0.5% salicylic acid, 15% L-ascorbic acid, and 0.5% ferulic acid. (The study was sponsored by SkinCeuticals, the manufacturer of the serum.)
Laser selection was made primarily on the type of dyschromia, with PIE patients receiving treatment with the pulsed dye laser and PIH patients receiving treatment with the 1,927-nm thulium laser. Patients were treated on days 0, 28, and 56 of the 12-week study, followed by immediate application of topical antioxidants or vehicle control. They were also instructed to apply the assigned topical twice daily for the duration of the study. Patients ranged in age from 21 to 61 years, and 20 had skin types III-IV.
To evaluate efficacy, the researchers conducted blinded clinical assessments with the postacne hyperpigmentation index (PAHPI) and the Global Aesthetic Improvement Scale (GAIS), instrumentation with the Mexameter, a device that captures erythema and melanin index values, and visual diagnostics with optical coherence tomography (OCT).
Dr. Hu reported that at week 12, the PAHPI in the silymarin-plus-laser treatment group fell from an average of 3.18 to 1.74 (a decrease of 1.44), which suggested an improvement trend, compared with the laser treatment–only group, whose PAHPI fell from an average of 3.25 to 1.97 (a decrease of 1.28).
As for the GAIS, a one-time score assessed at the end of the trial, the average score for all patients was 3.24, which translated to “much improved/very much improved.” Patients in the silymarin-plus-laser treatment group had higher average scores compared with patients in the laser treatment–only group (3.35 vs. 3.10, respectively), but the differences did not reach statistical significance.
According to results of the Mexameter assessment, paired t-tests showed that the levels of intralesional melanin decreased significantly for patients in the silymarin-plus-laser treatment group, compared with the laser treatment–only group (P < .05). OCT assessments demonstrated an increase in dermal brightness in both groups, corresponding to an increase in dermal collagen, as well as an increase in blood vessel density.
In an interview at the meeting, Dr. Waibel, subsection chief of dermatology at Baptist Hospital of Miami, said that future studies will focus on long-term follow-up to determine if acne scars can be prevented by combining silymarin with lasers to prevent PIH and PIE. “That would be priceless,” she said. “I believe that the PIH is what causes damage to the collagen, and that damage to the collagen is what causes the scarring. So, if we can prevent or treat PIH, we may be able to prevent scarring.”
This approach, she added, “would decrease the pharmaceutical cost because I think there are many dermatologists who are treating PEI and PIH as active acne. You really have to have a keen eye for understanding the differences and you really have to be looking, because PIE and PIH are flat, whereas active acne consists of either comedones or nodules.”
She noted that in skin of color patients, she has seen PIH persist for 9 or 10 months after treatment with isotretinoin. “It’s not the isotretinoin causing the scars, or even the acne, it’s the prolonged inflammation,” she said.
Catherine M. DiGiorgio, MD, a Boston-based laser and cosmetic dermatologist who was asked to comment on the study, said that patients and dermatologists frequently seek alternatives to hydroquinone for unwanted hyperpigmentation.
“This topical contains an active ingredient – silymarin – obtained from the milk thistle plant along with several already well known topicals used for the treatment of acne and PIH,” said Dr. DiGiorgio, program co-chair of the 2023 ASLMS conference. “Further and larger studies are needed to demonstrate and support the effectiveness of this product and silymarin for PIH and/or PIE.”
Also commenting on the results, Ray Jalian, MD, a Los Angeles–based laser and cosmetic dermatologist, told this news organization that the study findings demonstrate the power of combining topical and laser treatment for more effective improvement in acne-related PIH.
“While the study failed to show statistically significant improvement in postinflammatory erythema with concomitant laser and topical therapy versus laser alone, the promising data supporting concurrent use of topicals and fractional lasers for treatment of PIH, particularly in dark skin phototypes, is a clinically impactful contribution to our daily practice,” he said.
Dr. Waibel disclosed that she has conducted clinical trials for many device and pharmaceutical companies including SkinCeuticals. Dr. Hu, Dr. DiGiorgio, and Dr. Jalian were not involved with the study and reported having no relevant disclosures.
AT ASLMS 2023
Branding tattoo removal helps sex trafficking survivor close door on painful past
PHOENIX – When Kathy Givens walked onstage during a plenary session at the annual conference of the American Society for Laser Medicine and Surgery to reflect on her 9-month ordeal being sex trafficked in Texas more than 20 years ago, you could hear a pin drop.
“One of the scariest things about the life of sex trafficking is not knowing who’s going to be on the other side,” said Ms. Givens, who now lives in Houston. “There was some violence. There were some horrible things that happened. But you know what was really scary? When I got out. People may ask, ‘How’s that so? You escaped your trafficker. The past is behind you. Why were you afraid?’ I was afraid because I didn’t know that I had community. I didn’t know that community or that society would care about someone like me.”
She said that she found herself immobilized by fear of being shamed in society and labeled a sex trafficking victim, and wondered if she could overcome that fear and if anyone would view her as human again. Once free from her trafficker, she began a “healing journey,” which included getting married, raising four children, and re-enrolling in college with hopes of becoming a social worker. In 2020, she and her husband founded Twelve 11 Partners, an organization committed to supporting human trafficking survivors.
“I was working in the anti-trafficking field helping other survivors ... who have experienced this horrific crime,” she said. “I thought I was on my way.” But one “stain” from her sex trafficking past remained: The name of her trafficker was tattooed on her skin, “a reminder of what I’d gone through.”
Ms. Givens was eventually introduced to Paul M. Friedman, MD, the current ASLMS president and one of the that was formed in 2022. According to a survey that Dr. Friedman and colleagues presented at the 2022 annual ASLMS conference, an estimated 1 in 2 sex trafficking survivors have branding tattoos, and at least 1,000 survivors a year could benefit from removal of those tattoos.
“To date, 87 physicians in the U.S. and one in Canada have stepped forward to volunteer their services to be part of this program,” Dr. Friedman, who directs the Dermatology and Laser Surgery Center in Houston, said at this year’s meeting. “My goal is to double this number by the next annual conference,” he added, noting that trauma-informed training is part of the program, “to support the survivor experience during the treatment process.”
ASLMS is also working on this issue in partnership with the American Academy of Dermatology (AAD) Ad Hoc Task Force on Dermatological Resources for the Intervention and Prevention of Human Trafficking, which is headed by Boston dermatologist Shadi Kourosh, MD.
“Dermatologists are uniquely positioned to aid in efforts to assist those experiences in trafficking with our training to recognize and diagnose relevant signs on the skin and to assist patients with certain aspects of care and recovery including the treatment of the disease of scars and tattoos,” Dr. Friedman said. “Ultimately, we hope to create a database together to improve recognition of branding tattoos to aid in identifying sex trafficking victims.”
Ms. Givens, who sits on the U.S. Advisory Council on Human Trafficking, said that she was able to truly close the door on her sex trafficking past thanks to the tattoo removal Dr. Friedman performed as part of New Beginnings. “It means the world to me to know that I can now be an advocate for other individuals who have experienced human trafficking,” she told meeting attendees.
“Again, one of the scariest things is not knowing that you have community. I was scared of losing hope, but I’m standing here today. I have all the hope that I need. You have the power to change lives.”
PHOENIX – When Kathy Givens walked onstage during a plenary session at the annual conference of the American Society for Laser Medicine and Surgery to reflect on her 9-month ordeal being sex trafficked in Texas more than 20 years ago, you could hear a pin drop.
“One of the scariest things about the life of sex trafficking is not knowing who’s going to be on the other side,” said Ms. Givens, who now lives in Houston. “There was some violence. There were some horrible things that happened. But you know what was really scary? When I got out. People may ask, ‘How’s that so? You escaped your trafficker. The past is behind you. Why were you afraid?’ I was afraid because I didn’t know that I had community. I didn’t know that community or that society would care about someone like me.”
She said that she found herself immobilized by fear of being shamed in society and labeled a sex trafficking victim, and wondered if she could overcome that fear and if anyone would view her as human again. Once free from her trafficker, she began a “healing journey,” which included getting married, raising four children, and re-enrolling in college with hopes of becoming a social worker. In 2020, she and her husband founded Twelve 11 Partners, an organization committed to supporting human trafficking survivors.
“I was working in the anti-trafficking field helping other survivors ... who have experienced this horrific crime,” she said. “I thought I was on my way.” But one “stain” from her sex trafficking past remained: The name of her trafficker was tattooed on her skin, “a reminder of what I’d gone through.”
Ms. Givens was eventually introduced to Paul M. Friedman, MD, the current ASLMS president and one of the that was formed in 2022. According to a survey that Dr. Friedman and colleagues presented at the 2022 annual ASLMS conference, an estimated 1 in 2 sex trafficking survivors have branding tattoos, and at least 1,000 survivors a year could benefit from removal of those tattoos.
“To date, 87 physicians in the U.S. and one in Canada have stepped forward to volunteer their services to be part of this program,” Dr. Friedman, who directs the Dermatology and Laser Surgery Center in Houston, said at this year’s meeting. “My goal is to double this number by the next annual conference,” he added, noting that trauma-informed training is part of the program, “to support the survivor experience during the treatment process.”
ASLMS is also working on this issue in partnership with the American Academy of Dermatology (AAD) Ad Hoc Task Force on Dermatological Resources for the Intervention and Prevention of Human Trafficking, which is headed by Boston dermatologist Shadi Kourosh, MD.
“Dermatologists are uniquely positioned to aid in efforts to assist those experiences in trafficking with our training to recognize and diagnose relevant signs on the skin and to assist patients with certain aspects of care and recovery including the treatment of the disease of scars and tattoos,” Dr. Friedman said. “Ultimately, we hope to create a database together to improve recognition of branding tattoos to aid in identifying sex trafficking victims.”
Ms. Givens, who sits on the U.S. Advisory Council on Human Trafficking, said that she was able to truly close the door on her sex trafficking past thanks to the tattoo removal Dr. Friedman performed as part of New Beginnings. “It means the world to me to know that I can now be an advocate for other individuals who have experienced human trafficking,” she told meeting attendees.
“Again, one of the scariest things is not knowing that you have community. I was scared of losing hope, but I’m standing here today. I have all the hope that I need. You have the power to change lives.”
PHOENIX – When Kathy Givens walked onstage during a plenary session at the annual conference of the American Society for Laser Medicine and Surgery to reflect on her 9-month ordeal being sex trafficked in Texas more than 20 years ago, you could hear a pin drop.
“One of the scariest things about the life of sex trafficking is not knowing who’s going to be on the other side,” said Ms. Givens, who now lives in Houston. “There was some violence. There were some horrible things that happened. But you know what was really scary? When I got out. People may ask, ‘How’s that so? You escaped your trafficker. The past is behind you. Why were you afraid?’ I was afraid because I didn’t know that I had community. I didn’t know that community or that society would care about someone like me.”
She said that she found herself immobilized by fear of being shamed in society and labeled a sex trafficking victim, and wondered if she could overcome that fear and if anyone would view her as human again. Once free from her trafficker, she began a “healing journey,” which included getting married, raising four children, and re-enrolling in college with hopes of becoming a social worker. In 2020, she and her husband founded Twelve 11 Partners, an organization committed to supporting human trafficking survivors.
“I was working in the anti-trafficking field helping other survivors ... who have experienced this horrific crime,” she said. “I thought I was on my way.” But one “stain” from her sex trafficking past remained: The name of her trafficker was tattooed on her skin, “a reminder of what I’d gone through.”
Ms. Givens was eventually introduced to Paul M. Friedman, MD, the current ASLMS president and one of the that was formed in 2022. According to a survey that Dr. Friedman and colleagues presented at the 2022 annual ASLMS conference, an estimated 1 in 2 sex trafficking survivors have branding tattoos, and at least 1,000 survivors a year could benefit from removal of those tattoos.
“To date, 87 physicians in the U.S. and one in Canada have stepped forward to volunteer their services to be part of this program,” Dr. Friedman, who directs the Dermatology and Laser Surgery Center in Houston, said at this year’s meeting. “My goal is to double this number by the next annual conference,” he added, noting that trauma-informed training is part of the program, “to support the survivor experience during the treatment process.”
ASLMS is also working on this issue in partnership with the American Academy of Dermatology (AAD) Ad Hoc Task Force on Dermatological Resources for the Intervention and Prevention of Human Trafficking, which is headed by Boston dermatologist Shadi Kourosh, MD.
“Dermatologists are uniquely positioned to aid in efforts to assist those experiences in trafficking with our training to recognize and diagnose relevant signs on the skin and to assist patients with certain aspects of care and recovery including the treatment of the disease of scars and tattoos,” Dr. Friedman said. “Ultimately, we hope to create a database together to improve recognition of branding tattoos to aid in identifying sex trafficking victims.”
Ms. Givens, who sits on the U.S. Advisory Council on Human Trafficking, said that she was able to truly close the door on her sex trafficking past thanks to the tattoo removal Dr. Friedman performed as part of New Beginnings. “It means the world to me to know that I can now be an advocate for other individuals who have experienced human trafficking,” she told meeting attendees.
“Again, one of the scariest things is not knowing that you have community. I was scared of losing hope, but I’m standing here today. I have all the hope that I need. You have the power to change lives.”
AT ASLMS 2023
Small study finds IPL-radiofrequency combination effective for dry eye disease
PHOENIX – and improved meibum quality in both upper and lower eyelids, results from an ongoing, novel study showed.
Dry eye disease affects a large proportion of people in the United States “and the factors that contribute to that are certainly not going away,” lead study author James G. Chelnis MD, said at the annual conference of the American Society for Laser Medicine and Surgery, where he presented the results during an abstract session. “Prepandemic, we used to have meetings in person; now most are on a computer screen,” a common risk factor for worsening dry eyes, he said. Telltale dry eye symptoms include blurry vision, irritation, and corneal damage – mostly caused by meibomian gland dysfunction – which impacts the quality and quantity of meibum secreted. Common treatments include warm compresses, doxycycline, and artificial tears.
While some studies have shown IPL is helpful in treating dry eye disease caused by meibomian gland dysfunction, little information is available on its use alone or in combination with topical RF to preserve and improve the function of meibomian glands, said Dr. Chelnis, an ophthalmic plastic surgeon in New York City. “The theory here is that the radiofrequency would be able to vibrate the water molecules inside the meibomian glands, which would allow you to turn over the meibum faster, as well as improve the blink reflex response by building supporting collagen,” he said. “Our novel study explores the ability of this combined modality treatment to improve upon meibomian gland health.”
Study design, results
Dr. Chelnis and his colleagues enrolled 11 individuals with a previous diagnosis of dry eye disease and meibomian gland dysfunction with Ocular Surface Disease Index (OSDI) survey scores higher than 23, which indicate at least moderate dry eye symptoms. Inclusion criteria were being 22 years of age or older, signs of meibomian gland dysfunction as detected by biomicroscopy, a modified meibomian gland score over 12 in the lower eyelid of at least one eye, and type I-IV skin.
All patients received four treatments (each 2 weeks apart) of IPL to the lower eyelid, surrounding malar region, and nose, followed by 7 minutes of topical RF treatments at 1 MHz and 4 MHz extending to the inferior, lateral, and superior orbital rim. Evaluation of meibomian gland expression and quality of meibum upon expression was conducted following each treatment session, with a final evaluation 4 weeks after the final treatment session.
Meibum quality was evaluated on a scale of 0-3 representing clear (0), cloudy (1), inspissated (2), and blocked (3) meibum, respectively.
Following treatment, meibomian gland expression and meibum quality improved in all eyelids in all 11 patients. Specifically, in the right eye, the number of upper lid expressible glands increased from an average of 13 to 27.9 and the number of lower lid expressible glands increased from an average of 14.6 to 28.2; and in the left eye, the number of upper lid expressible glands increased from an average of 13.3 to 27.3 and the number of lower lid expressible glands increased from an average of 14.8 to 26.8 (P < .001 for all associations).
The overall percentage improvement in meibomian gland expression in the right eye was 82.7% for the upper lids and 136.6% for the lower lids, and in the left eye, 82.9% for the upper lids, and 112.2% for the lower lids.
When comparing upper against lower lids, meibomian gland expression increased 124.4% and 82.8%, respectively. Meibum quality improved in all four eyelids, although upper eyelids displayed a superior improvement compared with lower eyelids.
“We are finding that combining IPL plus RF produces a more complete and comprehensive improvement in the quality of their meibomian gland health, and as such, their dry eyes,” with “a large decrease in their symptom profile,” he concluded.
More patients to be studied
Dr. Chelnis acknowledged certain limitations of the study, including the small number of patients, but he and his colleagues have added an additional clinical site to expand the sample size. “Larger scale studies are needed to evaluate long-term effectiveness of IPL plus RF as well as a comparison with other treatment options.”
During a question-and-answer session Mathew M. Avram, MD, JD, director of laser, cosmetics, and dermatologic surgery at Massachusetts General Hospital, Boston, who served as one of the abstract session moderators, asked Dr. Chelnis to comment on what the mechanism of action of the IPL-RF combination in improving meibomian gland health.
“It’s not fully understood, but part of it is improved vascularity at the lid margin,” said Dr. Chelnis, who holds a faculty position in the department of ophthalmology at Icahn School of Medicine at Mount Sinai, New York. “Your ocular surface is sort of like your screen door; it catches everything that’s in the environment. An increase in vascularity and immunologic cytokines occurs in response to that. If you’re looking at the eye with a slit lamp, you can see a lot of vascularity that occurs at the lid margin and crowds the meibomian glands. When you decrease that crowding and immunogenic response, you move towards a normally functioning lid margin.”
Dr. Chelnis disclosed that he is a consultant to or an adviser for Lumenis, Horizon Therapeutics, and Soniquence.
PHOENIX – and improved meibum quality in both upper and lower eyelids, results from an ongoing, novel study showed.
Dry eye disease affects a large proportion of people in the United States “and the factors that contribute to that are certainly not going away,” lead study author James G. Chelnis MD, said at the annual conference of the American Society for Laser Medicine and Surgery, where he presented the results during an abstract session. “Prepandemic, we used to have meetings in person; now most are on a computer screen,” a common risk factor for worsening dry eyes, he said. Telltale dry eye symptoms include blurry vision, irritation, and corneal damage – mostly caused by meibomian gland dysfunction – which impacts the quality and quantity of meibum secreted. Common treatments include warm compresses, doxycycline, and artificial tears.
While some studies have shown IPL is helpful in treating dry eye disease caused by meibomian gland dysfunction, little information is available on its use alone or in combination with topical RF to preserve and improve the function of meibomian glands, said Dr. Chelnis, an ophthalmic plastic surgeon in New York City. “The theory here is that the radiofrequency would be able to vibrate the water molecules inside the meibomian glands, which would allow you to turn over the meibum faster, as well as improve the blink reflex response by building supporting collagen,” he said. “Our novel study explores the ability of this combined modality treatment to improve upon meibomian gland health.”
Study design, results
Dr. Chelnis and his colleagues enrolled 11 individuals with a previous diagnosis of dry eye disease and meibomian gland dysfunction with Ocular Surface Disease Index (OSDI) survey scores higher than 23, which indicate at least moderate dry eye symptoms. Inclusion criteria were being 22 years of age or older, signs of meibomian gland dysfunction as detected by biomicroscopy, a modified meibomian gland score over 12 in the lower eyelid of at least one eye, and type I-IV skin.
All patients received four treatments (each 2 weeks apart) of IPL to the lower eyelid, surrounding malar region, and nose, followed by 7 minutes of topical RF treatments at 1 MHz and 4 MHz extending to the inferior, lateral, and superior orbital rim. Evaluation of meibomian gland expression and quality of meibum upon expression was conducted following each treatment session, with a final evaluation 4 weeks after the final treatment session.
Meibum quality was evaluated on a scale of 0-3 representing clear (0), cloudy (1), inspissated (2), and blocked (3) meibum, respectively.
Following treatment, meibomian gland expression and meibum quality improved in all eyelids in all 11 patients. Specifically, in the right eye, the number of upper lid expressible glands increased from an average of 13 to 27.9 and the number of lower lid expressible glands increased from an average of 14.6 to 28.2; and in the left eye, the number of upper lid expressible glands increased from an average of 13.3 to 27.3 and the number of lower lid expressible glands increased from an average of 14.8 to 26.8 (P < .001 for all associations).
The overall percentage improvement in meibomian gland expression in the right eye was 82.7% for the upper lids and 136.6% for the lower lids, and in the left eye, 82.9% for the upper lids, and 112.2% for the lower lids.
When comparing upper against lower lids, meibomian gland expression increased 124.4% and 82.8%, respectively. Meibum quality improved in all four eyelids, although upper eyelids displayed a superior improvement compared with lower eyelids.
“We are finding that combining IPL plus RF produces a more complete and comprehensive improvement in the quality of their meibomian gland health, and as such, their dry eyes,” with “a large decrease in their symptom profile,” he concluded.
More patients to be studied
Dr. Chelnis acknowledged certain limitations of the study, including the small number of patients, but he and his colleagues have added an additional clinical site to expand the sample size. “Larger scale studies are needed to evaluate long-term effectiveness of IPL plus RF as well as a comparison with other treatment options.”
During a question-and-answer session Mathew M. Avram, MD, JD, director of laser, cosmetics, and dermatologic surgery at Massachusetts General Hospital, Boston, who served as one of the abstract session moderators, asked Dr. Chelnis to comment on what the mechanism of action of the IPL-RF combination in improving meibomian gland health.
“It’s not fully understood, but part of it is improved vascularity at the lid margin,” said Dr. Chelnis, who holds a faculty position in the department of ophthalmology at Icahn School of Medicine at Mount Sinai, New York. “Your ocular surface is sort of like your screen door; it catches everything that’s in the environment. An increase in vascularity and immunologic cytokines occurs in response to that. If you’re looking at the eye with a slit lamp, you can see a lot of vascularity that occurs at the lid margin and crowds the meibomian glands. When you decrease that crowding and immunogenic response, you move towards a normally functioning lid margin.”
Dr. Chelnis disclosed that he is a consultant to or an adviser for Lumenis, Horizon Therapeutics, and Soniquence.
PHOENIX – and improved meibum quality in both upper and lower eyelids, results from an ongoing, novel study showed.
Dry eye disease affects a large proportion of people in the United States “and the factors that contribute to that are certainly not going away,” lead study author James G. Chelnis MD, said at the annual conference of the American Society for Laser Medicine and Surgery, where he presented the results during an abstract session. “Prepandemic, we used to have meetings in person; now most are on a computer screen,” a common risk factor for worsening dry eyes, he said. Telltale dry eye symptoms include blurry vision, irritation, and corneal damage – mostly caused by meibomian gland dysfunction – which impacts the quality and quantity of meibum secreted. Common treatments include warm compresses, doxycycline, and artificial tears.
While some studies have shown IPL is helpful in treating dry eye disease caused by meibomian gland dysfunction, little information is available on its use alone or in combination with topical RF to preserve and improve the function of meibomian glands, said Dr. Chelnis, an ophthalmic plastic surgeon in New York City. “The theory here is that the radiofrequency would be able to vibrate the water molecules inside the meibomian glands, which would allow you to turn over the meibum faster, as well as improve the blink reflex response by building supporting collagen,” he said. “Our novel study explores the ability of this combined modality treatment to improve upon meibomian gland health.”
Study design, results
Dr. Chelnis and his colleagues enrolled 11 individuals with a previous diagnosis of dry eye disease and meibomian gland dysfunction with Ocular Surface Disease Index (OSDI) survey scores higher than 23, which indicate at least moderate dry eye symptoms. Inclusion criteria were being 22 years of age or older, signs of meibomian gland dysfunction as detected by biomicroscopy, a modified meibomian gland score over 12 in the lower eyelid of at least one eye, and type I-IV skin.
All patients received four treatments (each 2 weeks apart) of IPL to the lower eyelid, surrounding malar region, and nose, followed by 7 minutes of topical RF treatments at 1 MHz and 4 MHz extending to the inferior, lateral, and superior orbital rim. Evaluation of meibomian gland expression and quality of meibum upon expression was conducted following each treatment session, with a final evaluation 4 weeks after the final treatment session.
Meibum quality was evaluated on a scale of 0-3 representing clear (0), cloudy (1), inspissated (2), and blocked (3) meibum, respectively.
Following treatment, meibomian gland expression and meibum quality improved in all eyelids in all 11 patients. Specifically, in the right eye, the number of upper lid expressible glands increased from an average of 13 to 27.9 and the number of lower lid expressible glands increased from an average of 14.6 to 28.2; and in the left eye, the number of upper lid expressible glands increased from an average of 13.3 to 27.3 and the number of lower lid expressible glands increased from an average of 14.8 to 26.8 (P < .001 for all associations).
The overall percentage improvement in meibomian gland expression in the right eye was 82.7% for the upper lids and 136.6% for the lower lids, and in the left eye, 82.9% for the upper lids, and 112.2% for the lower lids.
When comparing upper against lower lids, meibomian gland expression increased 124.4% and 82.8%, respectively. Meibum quality improved in all four eyelids, although upper eyelids displayed a superior improvement compared with lower eyelids.
“We are finding that combining IPL plus RF produces a more complete and comprehensive improvement in the quality of their meibomian gland health, and as such, their dry eyes,” with “a large decrease in their symptom profile,” he concluded.
More patients to be studied
Dr. Chelnis acknowledged certain limitations of the study, including the small number of patients, but he and his colleagues have added an additional clinical site to expand the sample size. “Larger scale studies are needed to evaluate long-term effectiveness of IPL plus RF as well as a comparison with other treatment options.”
During a question-and-answer session Mathew M. Avram, MD, JD, director of laser, cosmetics, and dermatologic surgery at Massachusetts General Hospital, Boston, who served as one of the abstract session moderators, asked Dr. Chelnis to comment on what the mechanism of action of the IPL-RF combination in improving meibomian gland health.
“It’s not fully understood, but part of it is improved vascularity at the lid margin,” said Dr. Chelnis, who holds a faculty position in the department of ophthalmology at Icahn School of Medicine at Mount Sinai, New York. “Your ocular surface is sort of like your screen door; it catches everything that’s in the environment. An increase in vascularity and immunologic cytokines occurs in response to that. If you’re looking at the eye with a slit lamp, you can see a lot of vascularity that occurs at the lid margin and crowds the meibomian glands. When you decrease that crowding and immunogenic response, you move towards a normally functioning lid margin.”
Dr. Chelnis disclosed that he is a consultant to or an adviser for Lumenis, Horizon Therapeutics, and Soniquence.
AT ASLMS 2023




















