User login
Preventing suicide: What should clinicians do differently?
“Suicide rates are increasing,” Dr. Igor Galynker said, “and I believe they will continue to rise. These are deaths of despair, and despair is increasing in our society.”
That said, I listened with interest to the May 16 MDedge Psychcast, “Approach assesses imminent suicide risk,” an interview with Igor Galynker, MD, PhD, author of “The Suicidal Crisis” and director of the Galynker Suicide Research Laboratory at the Icahn School of Medicine at Mount Sinai in New York. In the podcast, Dr. Galynker talked about techniques for identifying those at risk for suicide among the patients psychiatrists see for evaluation and treatment.
“Using suicidal ideation as a risk factor is flawed,” he contended. “Asking about suicidal thoughts leaves us to miss 75% of people who go on to die by suicide.” Dr. Galynker noted that suicidal thoughts are often absent or not endorsed at all and clinicians should view other factors – such as the patient’s sense of being entrapped and the clinician’s own emotional responses to the patient – as more sensitive measures of elevated suicide risk.
This informative podcast left me with more questions, so I called Dr. Galynker. Suicide remains a rare phenomenon, and most psychiatrists will have limited experience with completed suicide during the course of a career. Dr. Galynker’s interest in suicide as an area of research began after he had a patient die the year after he finished residency training. Since then, he’s had one more patient suicide, and he’s aware of eight people who have died after leaving his care. “It can be devastating,” he said.
I wanted to know what psychiatrists should be doing differently after we have identified a patient at risk. While it seems obvious that a depressed patient should be treated for major depression, it also seems obvious that our interventions are imprecisely targeted and not fully successful.
We talked about the role of hospitalization in preventing suicide. Dr. Galynker has mixed opinions on this. He noted that suicide rates skyrocket in the time right after psychiatric hospitalization. “For women, the rate is 250 times higher at the time of hospital discharge; for men it’s 100 times higher. But hospitalization may help someone to survive a transitional period and to gather their support systems.”
Dr. Galynker noted that since the podcast in May aired, the Centers for Disease Control and Prevention published findings on suicide rates in the United States. He summarized some of the key points from the findings.
“Suicide rates were going down until 1999. From 2000 to 2006, suicide rates increased by 1% per year. From 2006 until 2016, rates have increased by 2% per year. Most people who die by suicide don’t have a diagnosis of a mental illness. And finally – and what has gone unnoticed – most people who die by suicide do not express suicidal intent. In fact, in that study, suicide intent was disclosed by less than a quarter of persons both with and without known mental health conditions.”
Dr. Galynker talked about safety plans and emphasized means restriction as ways to prevent suicide, including limiting access to firearms, placing netting under bridges, and providing medications in smaller containers.
“Suicidal ideation comes late; it may happen 15 minutes before a suicidal act or attempt. We need to alert people that there are certainly things that put them at risk, and we need to look at the drivers.
“Sometimes, people die for trivial reasons.” He noted instances where a susceptible person might attempt or complete suicide after an argument or perceived slight. Work is being done to look at outreach interventions to those at risk, including phone contacts and postcards.
“We don’t have a suicide-specific diagnosis ... and people die for other reasons besides mental illness. Final romantic rejection, terminal illness, and humiliating failures in business all place people at elevated risk. We need to work to change the suicidal narrative for people away from one where life has no future; we need to help them open doors.”
Dr. Miller is the coauthor of “Committed: The Battle Over Involuntary Psychiatric Care,” (Baltimore: Johns Hopkins University Press, 2016).
“Suicide rates are increasing,” Dr. Igor Galynker said, “and I believe they will continue to rise. These are deaths of despair, and despair is increasing in our society.”
That said, I listened with interest to the May 16 MDedge Psychcast, “Approach assesses imminent suicide risk,” an interview with Igor Galynker, MD, PhD, author of “The Suicidal Crisis” and director of the Galynker Suicide Research Laboratory at the Icahn School of Medicine at Mount Sinai in New York. In the podcast, Dr. Galynker talked about techniques for identifying those at risk for suicide among the patients psychiatrists see for evaluation and treatment.
“Using suicidal ideation as a risk factor is flawed,” he contended. “Asking about suicidal thoughts leaves us to miss 75% of people who go on to die by suicide.” Dr. Galynker noted that suicidal thoughts are often absent or not endorsed at all and clinicians should view other factors – such as the patient’s sense of being entrapped and the clinician’s own emotional responses to the patient – as more sensitive measures of elevated suicide risk.
This informative podcast left me with more questions, so I called Dr. Galynker. Suicide remains a rare phenomenon, and most psychiatrists will have limited experience with completed suicide during the course of a career. Dr. Galynker’s interest in suicide as an area of research began after he had a patient die the year after he finished residency training. Since then, he’s had one more patient suicide, and he’s aware of eight people who have died after leaving his care. “It can be devastating,” he said.
I wanted to know what psychiatrists should be doing differently after we have identified a patient at risk. While it seems obvious that a depressed patient should be treated for major depression, it also seems obvious that our interventions are imprecisely targeted and not fully successful.
We talked about the role of hospitalization in preventing suicide. Dr. Galynker has mixed opinions on this. He noted that suicide rates skyrocket in the time right after psychiatric hospitalization. “For women, the rate is 250 times higher at the time of hospital discharge; for men it’s 100 times higher. But hospitalization may help someone to survive a transitional period and to gather their support systems.”
Dr. Galynker noted that since the podcast in May aired, the Centers for Disease Control and Prevention published findings on suicide rates in the United States. He summarized some of the key points from the findings.
“Suicide rates were going down until 1999. From 2000 to 2006, suicide rates increased by 1% per year. From 2006 until 2016, rates have increased by 2% per year. Most people who die by suicide don’t have a diagnosis of a mental illness. And finally – and what has gone unnoticed – most people who die by suicide do not express suicidal intent. In fact, in that study, suicide intent was disclosed by less than a quarter of persons both with and without known mental health conditions.”
Dr. Galynker talked about safety plans and emphasized means restriction as ways to prevent suicide, including limiting access to firearms, placing netting under bridges, and providing medications in smaller containers.
“Suicidal ideation comes late; it may happen 15 minutes before a suicidal act or attempt. We need to alert people that there are certainly things that put them at risk, and we need to look at the drivers.
“Sometimes, people die for trivial reasons.” He noted instances where a susceptible person might attempt or complete suicide after an argument or perceived slight. Work is being done to look at outreach interventions to those at risk, including phone contacts and postcards.
“We don’t have a suicide-specific diagnosis ... and people die for other reasons besides mental illness. Final romantic rejection, terminal illness, and humiliating failures in business all place people at elevated risk. We need to work to change the suicidal narrative for people away from one where life has no future; we need to help them open doors.”
Dr. Miller is the coauthor of “Committed: The Battle Over Involuntary Psychiatric Care,” (Baltimore: Johns Hopkins University Press, 2016).
“Suicide rates are increasing,” Dr. Igor Galynker said, “and I believe they will continue to rise. These are deaths of despair, and despair is increasing in our society.”
That said, I listened with interest to the May 16 MDedge Psychcast, “Approach assesses imminent suicide risk,” an interview with Igor Galynker, MD, PhD, author of “The Suicidal Crisis” and director of the Galynker Suicide Research Laboratory at the Icahn School of Medicine at Mount Sinai in New York. In the podcast, Dr. Galynker talked about techniques for identifying those at risk for suicide among the patients psychiatrists see for evaluation and treatment.
“Using suicidal ideation as a risk factor is flawed,” he contended. “Asking about suicidal thoughts leaves us to miss 75% of people who go on to die by suicide.” Dr. Galynker noted that suicidal thoughts are often absent or not endorsed at all and clinicians should view other factors – such as the patient’s sense of being entrapped and the clinician’s own emotional responses to the patient – as more sensitive measures of elevated suicide risk.
This informative podcast left me with more questions, so I called Dr. Galynker. Suicide remains a rare phenomenon, and most psychiatrists will have limited experience with completed suicide during the course of a career. Dr. Galynker’s interest in suicide as an area of research began after he had a patient die the year after he finished residency training. Since then, he’s had one more patient suicide, and he’s aware of eight people who have died after leaving his care. “It can be devastating,” he said.
I wanted to know what psychiatrists should be doing differently after we have identified a patient at risk. While it seems obvious that a depressed patient should be treated for major depression, it also seems obvious that our interventions are imprecisely targeted and not fully successful.
We talked about the role of hospitalization in preventing suicide. Dr. Galynker has mixed opinions on this. He noted that suicide rates skyrocket in the time right after psychiatric hospitalization. “For women, the rate is 250 times higher at the time of hospital discharge; for men it’s 100 times higher. But hospitalization may help someone to survive a transitional period and to gather their support systems.”
Dr. Galynker noted that since the podcast in May aired, the Centers for Disease Control and Prevention published findings on suicide rates in the United States. He summarized some of the key points from the findings.
“Suicide rates were going down until 1999. From 2000 to 2006, suicide rates increased by 1% per year. From 2006 until 2016, rates have increased by 2% per year. Most people who die by suicide don’t have a diagnosis of a mental illness. And finally – and what has gone unnoticed – most people who die by suicide do not express suicidal intent. In fact, in that study, suicide intent was disclosed by less than a quarter of persons both with and without known mental health conditions.”
Dr. Galynker talked about safety plans and emphasized means restriction as ways to prevent suicide, including limiting access to firearms, placing netting under bridges, and providing medications in smaller containers.
“Suicidal ideation comes late; it may happen 15 minutes before a suicidal act or attempt. We need to alert people that there are certainly things that put them at risk, and we need to look at the drivers.
“Sometimes, people die for trivial reasons.” He noted instances where a susceptible person might attempt or complete suicide after an argument or perceived slight. Work is being done to look at outreach interventions to those at risk, including phone contacts and postcards.
“We don’t have a suicide-specific diagnosis ... and people die for other reasons besides mental illness. Final romantic rejection, terminal illness, and humiliating failures in business all place people at elevated risk. We need to work to change the suicidal narrative for people away from one where life has no future; we need to help them open doors.”
Dr. Miller is the coauthor of “Committed: The Battle Over Involuntary Psychiatric Care,” (Baltimore: Johns Hopkins University Press, 2016).
Universal depression screening for adolescents not without controversy
When 14-year-old Ryan saw his pediatrician for his annual physical this past August, he was asked a few quick questions about whether he was having any problems, if he was feeling depressed or anxious, and if there was anything he wanted to discuss. Ryan said no to each question, then the doctor examined him, reminded him to get a flu shot, and signed off on the forms he needed to play team sports in high school. The doctor assured Ryan’s mother that he was healthy, and the visit was over. Next August, Ryan’s exam will likely include a more detailed look at his mental health.
In February 2018, the American Academy of Pediatrics updated its guidelines on screening for depression in adolescents in primary care settings. The guidelines address the problem of undiagnosed and untreated psychiatric illness in children over the age of 10 years, the shortage of available mental health professionals, and techniques primary care physicians might use to address psychiatric needs in adolescents. The AAP guidelines include a new recommendation for universal screening with an assessment tool: “Adolescent patients ages 12 years and older should be screened annually for depression [MDD or depressive disorders] with a formal self-report screening tool either on paper or electronically.”
Dr. Liu noted that some of his patients drive 4-5 hours each way to see him in Omaha, then spend the night before making the return trip. “There is a dire shortage of pediatric mental health services in every state. This shifts the responsibility for care to pediatricians, teachers, and parents who often lack the resources to keep kids safe and well. It’s an unconscionable gap in care.”
Dr. Doran’s practice has not yet implemented the use of a written screening tool for all adolescents. He anticipates doing this soon because of the new guidelines, but he was not enthusiastic about the prospect. “ We are already loaded down with administrative tasks and screening requirements.” Of note, in Dr. Doran’s 35 years in clinical practice, no child under his care has died of suicide.
Dr. Miller is the coauthor of “Committed: The Battle Over Involuntary Psychiatric Care,” (Baltimore: Johns Hopkins University Press, 2016).
When 14-year-old Ryan saw his pediatrician for his annual physical this past August, he was asked a few quick questions about whether he was having any problems, if he was feeling depressed or anxious, and if there was anything he wanted to discuss. Ryan said no to each question, then the doctor examined him, reminded him to get a flu shot, and signed off on the forms he needed to play team sports in high school. The doctor assured Ryan’s mother that he was healthy, and the visit was over. Next August, Ryan’s exam will likely include a more detailed look at his mental health.
In February 2018, the American Academy of Pediatrics updated its guidelines on screening for depression in adolescents in primary care settings. The guidelines address the problem of undiagnosed and untreated psychiatric illness in children over the age of 10 years, the shortage of available mental health professionals, and techniques primary care physicians might use to address psychiatric needs in adolescents. The AAP guidelines include a new recommendation for universal screening with an assessment tool: “Adolescent patients ages 12 years and older should be screened annually for depression [MDD or depressive disorders] with a formal self-report screening tool either on paper or electronically.”
Dr. Liu noted that some of his patients drive 4-5 hours each way to see him in Omaha, then spend the night before making the return trip. “There is a dire shortage of pediatric mental health services in every state. This shifts the responsibility for care to pediatricians, teachers, and parents who often lack the resources to keep kids safe and well. It’s an unconscionable gap in care.”
Dr. Doran’s practice has not yet implemented the use of a written screening tool for all adolescents. He anticipates doing this soon because of the new guidelines, but he was not enthusiastic about the prospect. “ We are already loaded down with administrative tasks and screening requirements.” Of note, in Dr. Doran’s 35 years in clinical practice, no child under his care has died of suicide.
Dr. Miller is the coauthor of “Committed: The Battle Over Involuntary Psychiatric Care,” (Baltimore: Johns Hopkins University Press, 2016).
When 14-year-old Ryan saw his pediatrician for his annual physical this past August, he was asked a few quick questions about whether he was having any problems, if he was feeling depressed or anxious, and if there was anything he wanted to discuss. Ryan said no to each question, then the doctor examined him, reminded him to get a flu shot, and signed off on the forms he needed to play team sports in high school. The doctor assured Ryan’s mother that he was healthy, and the visit was over. Next August, Ryan’s exam will likely include a more detailed look at his mental health.
In February 2018, the American Academy of Pediatrics updated its guidelines on screening for depression in adolescents in primary care settings. The guidelines address the problem of undiagnosed and untreated psychiatric illness in children over the age of 10 years, the shortage of available mental health professionals, and techniques primary care physicians might use to address psychiatric needs in adolescents. The AAP guidelines include a new recommendation for universal screening with an assessment tool: “Adolescent patients ages 12 years and older should be screened annually for depression [MDD or depressive disorders] with a formal self-report screening tool either on paper or electronically.”
Dr. Liu noted that some of his patients drive 4-5 hours each way to see him in Omaha, then spend the night before making the return trip. “There is a dire shortage of pediatric mental health services in every state. This shifts the responsibility for care to pediatricians, teachers, and parents who often lack the resources to keep kids safe and well. It’s an unconscionable gap in care.”
Dr. Doran’s practice has not yet implemented the use of a written screening tool for all adolescents. He anticipates doing this soon because of the new guidelines, but he was not enthusiastic about the prospect. “ We are already loaded down with administrative tasks and screening requirements.” Of note, in Dr. Doran’s 35 years in clinical practice, no child under his care has died of suicide.
Dr. Miller is the coauthor of “Committed: The Battle Over Involuntary Psychiatric Care,” (Baltimore: Johns Hopkins University Press, 2016).
Experts explore issues, controversies around medical marijuana use
I live and work in Maryland, where medical marijuana dispensaries are just beginning to open. So far, my patients have been content to smoke illegal marijuana, even after my admonishments. Last week, however, a patient who suffers from chronic pain told me that one of her doctors suggested she try medical marijuana. What did I think? The patient is in her 70s, and she has not tolerated opiates. She lives an active life, and she drives. I didn’t know what to think and was left to tell her that I had no experience and would not object if she wanted to try it. The timing was right for “Issues and Controversies Around Marijuana Use: What’s the Buzz?” at the American Psychiatric Association’s annual meeting in New York this week.
William Iacono, PhD, a professor of psychiatry at the University of Minnesota, Minneapolis, started with a session called “Does Adolescent Marijuana Use Cause Cognitive Decline?” Dr. Iacono and all the speakers who followed him pointed out how difficult it is to research these issues. The research is largely retrospective, and the questions are complex. The degree of use is determined by self-report, and there are questions about acute versus chronic use, whether cognitive decline is temporary or permanent, whether the age of initiating drug use is important, and finally, which tests are used to measure cognitive abilities. Dr. Iacono noted that results are inconsistent and mentioned a large population study done in Dunedin, New Zealand, which measured a decrease in verbal IQ and vocabulary measures at age 38 years if the user began smoking cannabis as an adolescent. Dr. Iacono’s twin studies showed that marijuana users scored lower on these measures in childhood, well before they began smoking, and poor academic performance predisposes to marijuana use.
“Adolescents who use cannabis are not the same as those who don’t,” Dr. Iacono said, “and heavy or daily use does not cause cognitive decline in those who begin smoking as adults.”
Dr. Pearlson introduced the second speaker by saying, “It’s easier to get funding to show the ill effects of cannabis than to show medicinal effects.” Sue Sisley, MD, director of Midtown Roots, a medical marijuana dispensary in Phoenix, conducts cannabis trials for the treatment of PTSD in veterans and noted that she has had a long and difficult road with marijuana research, and hers is the only controlled trial on cannabis for PTSD. When her Schedule I license was approved by the Food and Drug Administration, she was able to receive marijuana from the National Institute on Drug Abuse that was grown by the University of Mississippi in Oxford – the only federal growing facility. The marijuana was delivered by FedEx, and the drug was the consistency of talcum powder. It was a challenge to find a lab that could verify the components of the test drug, and when she did, she found the tetrahydrocannabinol content was considerably lower than marijuana sold on the black market. Also, the product contained both mold and lead. “As a physician, how do you hand out mold weed to our veterans?”
Her trials are still in progress, and more veterans are needed. Anecdotally, she says, a decrease has been seen in the use of both opiates and Viagra by the research subjects.
Michael Stevens, PhD, adjunct professor of psychiatry at Yale University, New Haven, Conn., discussed the risk of motor vehicle accidents in marijuana smokers and the logistical issues enforcement poses for law enforcement officials. “There is evidence that marijuana increases the risk for accidents.” Dr. Stevens went on to say that the elevated risk is notably less than that associated with the use of alcohol or stimulants. Studying the effects of marijuana on driving is difficult, as driving simulators do not necessarily reflect on-road experiences, and cognitive testing does not always translate into impairment. “We can’t give marijuana to teens and test them, and you can’t tell people who smoke every day that you’ll check in with them in a few years and check their driving records.”
In terms of law enforcement issues, roadside sobriety tests have not been validated for marijuana use, and plasma levels of the drug drop within minutes of use. “The alcohol model works well with alcohol, but cannabis is not alcohol.”
Deborah Hasin, PhD, professor of epidemiology (psychiatry) at Columbia University, New York, talked about trends of cannabis use in the United States. “Looking at states before and after legalization, we see that there is an increase in both cannabis use and cannabis disorders in adults.” Adolescents, however, are not smoking more, and “Kids are just not socializing; they are in their bedrooms with their smartphones. Depression is increasing in teens, but substance abuse is not.”
The last speaker was Deepak Cyril D’Souza, MD, a professor of psychiatry at Yale University, who talked about cannabis and psychosis. He defined three distinct relationships: acute transient psychosis that resolves fairly quickly, acute persistent psychosis that takes days or weeks to resolve, and psychotic reactions that are associated with recurrent psychotic symptoms. Studies suggest that those who have a psychotic reaction to marijuana are at elevated risk of being diagnosed with schizophrenia later, and that timing of exposure to marijuana may be important.
With regard to the important question of whether marijuana causes schizophrenia, Dr. D’Souza noted that “it’s neither a necessary nor sufficient component, but it does appear it hastens psychosis in schizophrenia and earlier symptoms are associated with a worse prognosis.”
I’ll see what happens with my patient. A Canadian physician in the audience noted that he has treated thousands of patients, and most find medical marijuana to be helpful. In our country, marijuana continues to be a controversial topic with strong opinions about its usefulness and a conversation that is limited by our lack of research.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care,” (Baltimore: Johns Hopkins University Press, 2016). She practices in Baltimore.
I live and work in Maryland, where medical marijuana dispensaries are just beginning to open. So far, my patients have been content to smoke illegal marijuana, even after my admonishments. Last week, however, a patient who suffers from chronic pain told me that one of her doctors suggested she try medical marijuana. What did I think? The patient is in her 70s, and she has not tolerated opiates. She lives an active life, and she drives. I didn’t know what to think and was left to tell her that I had no experience and would not object if she wanted to try it. The timing was right for “Issues and Controversies Around Marijuana Use: What’s the Buzz?” at the American Psychiatric Association’s annual meeting in New York this week.
William Iacono, PhD, a professor of psychiatry at the University of Minnesota, Minneapolis, started with a session called “Does Adolescent Marijuana Use Cause Cognitive Decline?” Dr. Iacono and all the speakers who followed him pointed out how difficult it is to research these issues. The research is largely retrospective, and the questions are complex. The degree of use is determined by self-report, and there are questions about acute versus chronic use, whether cognitive decline is temporary or permanent, whether the age of initiating drug use is important, and finally, which tests are used to measure cognitive abilities. Dr. Iacono noted that results are inconsistent and mentioned a large population study done in Dunedin, New Zealand, which measured a decrease in verbal IQ and vocabulary measures at age 38 years if the user began smoking cannabis as an adolescent. Dr. Iacono’s twin studies showed that marijuana users scored lower on these measures in childhood, well before they began smoking, and poor academic performance predisposes to marijuana use.
“Adolescents who use cannabis are not the same as those who don’t,” Dr. Iacono said, “and heavy or daily use does not cause cognitive decline in those who begin smoking as adults.”
Dr. Pearlson introduced the second speaker by saying, “It’s easier to get funding to show the ill effects of cannabis than to show medicinal effects.” Sue Sisley, MD, director of Midtown Roots, a medical marijuana dispensary in Phoenix, conducts cannabis trials for the treatment of PTSD in veterans and noted that she has had a long and difficult road with marijuana research, and hers is the only controlled trial on cannabis for PTSD. When her Schedule I license was approved by the Food and Drug Administration, she was able to receive marijuana from the National Institute on Drug Abuse that was grown by the University of Mississippi in Oxford – the only federal growing facility. The marijuana was delivered by FedEx, and the drug was the consistency of talcum powder. It was a challenge to find a lab that could verify the components of the test drug, and when she did, she found the tetrahydrocannabinol content was considerably lower than marijuana sold on the black market. Also, the product contained both mold and lead. “As a physician, how do you hand out mold weed to our veterans?”
Her trials are still in progress, and more veterans are needed. Anecdotally, she says, a decrease has been seen in the use of both opiates and Viagra by the research subjects.
Michael Stevens, PhD, adjunct professor of psychiatry at Yale University, New Haven, Conn., discussed the risk of motor vehicle accidents in marijuana smokers and the logistical issues enforcement poses for law enforcement officials. “There is evidence that marijuana increases the risk for accidents.” Dr. Stevens went on to say that the elevated risk is notably less than that associated with the use of alcohol or stimulants. Studying the effects of marijuana on driving is difficult, as driving simulators do not necessarily reflect on-road experiences, and cognitive testing does not always translate into impairment. “We can’t give marijuana to teens and test them, and you can’t tell people who smoke every day that you’ll check in with them in a few years and check their driving records.”
In terms of law enforcement issues, roadside sobriety tests have not been validated for marijuana use, and plasma levels of the drug drop within minutes of use. “The alcohol model works well with alcohol, but cannabis is not alcohol.”
Deborah Hasin, PhD, professor of epidemiology (psychiatry) at Columbia University, New York, talked about trends of cannabis use in the United States. “Looking at states before and after legalization, we see that there is an increase in both cannabis use and cannabis disorders in adults.” Adolescents, however, are not smoking more, and “Kids are just not socializing; they are in their bedrooms with their smartphones. Depression is increasing in teens, but substance abuse is not.”
The last speaker was Deepak Cyril D’Souza, MD, a professor of psychiatry at Yale University, who talked about cannabis and psychosis. He defined three distinct relationships: acute transient psychosis that resolves fairly quickly, acute persistent psychosis that takes days or weeks to resolve, and psychotic reactions that are associated with recurrent psychotic symptoms. Studies suggest that those who have a psychotic reaction to marijuana are at elevated risk of being diagnosed with schizophrenia later, and that timing of exposure to marijuana may be important.
With regard to the important question of whether marijuana causes schizophrenia, Dr. D’Souza noted that “it’s neither a necessary nor sufficient component, but it does appear it hastens psychosis in schizophrenia and earlier symptoms are associated with a worse prognosis.”
I’ll see what happens with my patient. A Canadian physician in the audience noted that he has treated thousands of patients, and most find medical marijuana to be helpful. In our country, marijuana continues to be a controversial topic with strong opinions about its usefulness and a conversation that is limited by our lack of research.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care,” (Baltimore: Johns Hopkins University Press, 2016). She practices in Baltimore.
I live and work in Maryland, where medical marijuana dispensaries are just beginning to open. So far, my patients have been content to smoke illegal marijuana, even after my admonishments. Last week, however, a patient who suffers from chronic pain told me that one of her doctors suggested she try medical marijuana. What did I think? The patient is in her 70s, and she has not tolerated opiates. She lives an active life, and she drives. I didn’t know what to think and was left to tell her that I had no experience and would not object if she wanted to try it. The timing was right for “Issues and Controversies Around Marijuana Use: What’s the Buzz?” at the American Psychiatric Association’s annual meeting in New York this week.
William Iacono, PhD, a professor of psychiatry at the University of Minnesota, Minneapolis, started with a session called “Does Adolescent Marijuana Use Cause Cognitive Decline?” Dr. Iacono and all the speakers who followed him pointed out how difficult it is to research these issues. The research is largely retrospective, and the questions are complex. The degree of use is determined by self-report, and there are questions about acute versus chronic use, whether cognitive decline is temporary or permanent, whether the age of initiating drug use is important, and finally, which tests are used to measure cognitive abilities. Dr. Iacono noted that results are inconsistent and mentioned a large population study done in Dunedin, New Zealand, which measured a decrease in verbal IQ and vocabulary measures at age 38 years if the user began smoking cannabis as an adolescent. Dr. Iacono’s twin studies showed that marijuana users scored lower on these measures in childhood, well before they began smoking, and poor academic performance predisposes to marijuana use.
“Adolescents who use cannabis are not the same as those who don’t,” Dr. Iacono said, “and heavy or daily use does not cause cognitive decline in those who begin smoking as adults.”
Dr. Pearlson introduced the second speaker by saying, “It’s easier to get funding to show the ill effects of cannabis than to show medicinal effects.” Sue Sisley, MD, director of Midtown Roots, a medical marijuana dispensary in Phoenix, conducts cannabis trials for the treatment of PTSD in veterans and noted that she has had a long and difficult road with marijuana research, and hers is the only controlled trial on cannabis for PTSD. When her Schedule I license was approved by the Food and Drug Administration, she was able to receive marijuana from the National Institute on Drug Abuse that was grown by the University of Mississippi in Oxford – the only federal growing facility. The marijuana was delivered by FedEx, and the drug was the consistency of talcum powder. It was a challenge to find a lab that could verify the components of the test drug, and when she did, she found the tetrahydrocannabinol content was considerably lower than marijuana sold on the black market. Also, the product contained both mold and lead. “As a physician, how do you hand out mold weed to our veterans?”
Her trials are still in progress, and more veterans are needed. Anecdotally, she says, a decrease has been seen in the use of both opiates and Viagra by the research subjects.
Michael Stevens, PhD, adjunct professor of psychiatry at Yale University, New Haven, Conn., discussed the risk of motor vehicle accidents in marijuana smokers and the logistical issues enforcement poses for law enforcement officials. “There is evidence that marijuana increases the risk for accidents.” Dr. Stevens went on to say that the elevated risk is notably less than that associated with the use of alcohol or stimulants. Studying the effects of marijuana on driving is difficult, as driving simulators do not necessarily reflect on-road experiences, and cognitive testing does not always translate into impairment. “We can’t give marijuana to teens and test them, and you can’t tell people who smoke every day that you’ll check in with them in a few years and check their driving records.”
In terms of law enforcement issues, roadside sobriety tests have not been validated for marijuana use, and plasma levels of the drug drop within minutes of use. “The alcohol model works well with alcohol, but cannabis is not alcohol.”
Deborah Hasin, PhD, professor of epidemiology (psychiatry) at Columbia University, New York, talked about trends of cannabis use in the United States. “Looking at states before and after legalization, we see that there is an increase in both cannabis use and cannabis disorders in adults.” Adolescents, however, are not smoking more, and “Kids are just not socializing; they are in their bedrooms with their smartphones. Depression is increasing in teens, but substance abuse is not.”
The last speaker was Deepak Cyril D’Souza, MD, a professor of psychiatry at Yale University, who talked about cannabis and psychosis. He defined three distinct relationships: acute transient psychosis that resolves fairly quickly, acute persistent psychosis that takes days or weeks to resolve, and psychotic reactions that are associated with recurrent psychotic symptoms. Studies suggest that those who have a psychotic reaction to marijuana are at elevated risk of being diagnosed with schizophrenia later, and that timing of exposure to marijuana may be important.
With regard to the important question of whether marijuana causes schizophrenia, Dr. D’Souza noted that “it’s neither a necessary nor sufficient component, but it does appear it hastens psychosis in schizophrenia and earlier symptoms are associated with a worse prognosis.”
I’ll see what happens with my patient. A Canadian physician in the audience noted that he has treated thousands of patients, and most find medical marijuana to be helpful. In our country, marijuana continues to be a controversial topic with strong opinions about its usefulness and a conversation that is limited by our lack of research.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care,” (Baltimore: Johns Hopkins University Press, 2016). She practices in Baltimore.
Why isn’t smart gun technology on Parkland activists’ agenda?
The evening before the March For Our Lives rally in Washington, I was hard at work on my sign. Making a statement is important, but at the Women’s March last January, I discovered that a sign was invaluable for keeping friends together in a crowd. Since my Women’s March sign read “Make America Kind Again,” I opted to keep with the theme, and I created a “Make America Safe Again” sign for gun control. My daughter looked at my sign skeptically. “It’s too vague and nondirective,” she declared. Now challenged, I added the following directives: “Universal Background Checks,” “Ban Assault Weapons,” and “Smart Guns.” My sign was now complete.
I was surprised when my daughter – our family Jeopardy! whiz – asked, “What’s a smart gun?” When we arrived to join friends, their daughter – a doctoral student – also looked at the sign and asked me what a smart gun is. I explained to both young women that a smart gun – like an iPhone – relies on a biometric such as a fingerprint so that it can be used only by authorized users. This technology would reduce the flow of firearms to illegal owners, prevent accidental discharge by children, protect rightful owners and law enforcement officers from having their own weapons used against them by criminals, and decrease the number of suicides by family members of gun owners. In my state of Maryland, there have been two school shootings, one as recently as March 20, and both were committed by boys who took a parent’s firearm to school.
We arrived at the rally and found a spot in front of the Newseum, with two jumbotrons in sight, right in the middle of the crowd. The young people who spoke were inspirational. Regardless of one’s political views or thoughts on gun control, they were bright, articulate, fearless, passionate, and determined. The show was stolen by Naomi Wadler, a precocious 11-year-old girl who is destined to be a member of Congress (if not president) one day, and by Dr. Martin Luther King Jr.’s 9-year-old granddaughter, Yolanda Renee King.
The rest of the speakers were teenagers, all of whom had lost someone to gunfire. There were speakers from Parkland, Fla., who talked about the raw losses they were feeling, and the student who wasn’t celebrating his 18th birthday on March 24. Matthew Soto from Newtown, Conn., talked about losing his sister, a first-grade teacher, in the Sandy Hook shooting.
But the rally wasn’t just about mass murders and school shootings: Zion Kelly talked about the death of his twin, a teen who was killed when he stopped at a convenience store on the way home from school in Washington, only to have his promising life snuffed out during a holdup. We heard about shootings in the bullet-riddled streets of Chicago and Los Angeles and the toll they have taken. The losses to gun violence have been felt most strongly in communities of color. While it was mentioned that the majority of gun deaths are suicides, there were no speakers from families of people who died from suicide. The final speaker was Emma Gonzalez, a young woman from Parkland who took the stage for 6 minutes and 20 seconds - the duration of the shooter’s rampage - and closed with a powerful moment of silence.* The rally closed with a performance of Bob Dylan’s “The Times They Are a-Changin’ ” by Jennifer Hudson, whose mother, brother, and nephew were murdered by a gunman.
The teens talked about what changes they wanted to see enacted. They talked about closing loopholes to background checks, and I was pleased that one young man specifically mentioned keeping guns from those who are violent, but did not mention mental illness as a reason to block gun ownership. A call to resume a ban on assault weapons was made repeatedly as was a call to raise the age (to 21) at which an individual can purchase a gun. Military-style weapons are not necessary for hunting or self-defense, and they enable the rapid-fire assassinations we have seen in mass shootings, so they remain an easy target of gun control advocacy. But in terms of numbers, these firearms are responsible for a small fraction of gun deaths. I was surprised, but the teens did not mention “smart gun” legislation as a way to reduce gun deaths.
Guns, and gun deaths, are a part of American society. While the majority of Americans favor stronger regulation of gun ownership, legislation that would end gun ownership is not likely to go anywhere. Smart guns, however, are different. Forty percent of polled gun owners have said they would swap their firearm for a smart firearm. So given the appeal of a firearm that can’t be diverted or stolen, used against the owner, discharged accidentally by a child, or used for suicide or homicide by a distressed family member, why don’t these weapons exist for use by the American people? . People want these guns and the protections they offer, yet they have never been produced and made available to either the American public or to our law enforcement officers.
So where are these firearms, and why aren’t our Parkland teens asking for them? The answer to the first part of that question lies with the National Rifle Association (NRA) and the state of New Jersey. In 2003, New Jersey passed the Childproof Handgun bill, which requires that all guns sold in the state be smart guns within 3 years of their availability. The NRA has vigorously opposed any legislation that would require all guns to be smart guns. Because the availability of these weapons would trigger the New Jersey bill, California and Maryland have been prevented from importing smart firearms from a German company. Perhaps, however, New Jersey does not need to bear all the blame; in 1999, 4 years before the passage of the bill, the NRA and its members boycotted Smith & Wesson when the gun manufacturer revealed plans to develop a smart gun for the government. The NRA’s public stance is that it does not oppose smart guns for those who want them, but it opposes legislation that would eliminate the sale of conventional firearms. The organization has voiced concerns that technology fails and that it potentially slows down firing the weapon. It doesn’t talk about dead toddlers, or about police officers who’ve been killed when their weapons were taken from them.
As for the Parkland students, I don’t know why they aren’t asking for smart gun technology while they have the attention of the country. Perhaps they, like the young women I was with, don’t know it’s an option. Perhaps it’s too removed from the issue of mass murders and an assault weapon ban feels more attainable. Or perhaps the NRA’s mission has too much of a stronghold in Florida. I don’t know why they aren’t asking for smart gun production, but I know they should be.
*Correction, 3/27/2018: An earlier version of this story misstated the duration of Emma Gonzalez's moment of silence.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press), 2016. She practices in Baltimore.
The evening before the March For Our Lives rally in Washington, I was hard at work on my sign. Making a statement is important, but at the Women’s March last January, I discovered that a sign was invaluable for keeping friends together in a crowd. Since my Women’s March sign read “Make America Kind Again,” I opted to keep with the theme, and I created a “Make America Safe Again” sign for gun control. My daughter looked at my sign skeptically. “It’s too vague and nondirective,” she declared. Now challenged, I added the following directives: “Universal Background Checks,” “Ban Assault Weapons,” and “Smart Guns.” My sign was now complete.
I was surprised when my daughter – our family Jeopardy! whiz – asked, “What’s a smart gun?” When we arrived to join friends, their daughter – a doctoral student – also looked at the sign and asked me what a smart gun is. I explained to both young women that a smart gun – like an iPhone – relies on a biometric such as a fingerprint so that it can be used only by authorized users. This technology would reduce the flow of firearms to illegal owners, prevent accidental discharge by children, protect rightful owners and law enforcement officers from having their own weapons used against them by criminals, and decrease the number of suicides by family members of gun owners. In my state of Maryland, there have been two school shootings, one as recently as March 20, and both were committed by boys who took a parent’s firearm to school.
We arrived at the rally and found a spot in front of the Newseum, with two jumbotrons in sight, right in the middle of the crowd. The young people who spoke were inspirational. Regardless of one’s political views or thoughts on gun control, they were bright, articulate, fearless, passionate, and determined. The show was stolen by Naomi Wadler, a precocious 11-year-old girl who is destined to be a member of Congress (if not president) one day, and by Dr. Martin Luther King Jr.’s 9-year-old granddaughter, Yolanda Renee King.
The rest of the speakers were teenagers, all of whom had lost someone to gunfire. There were speakers from Parkland, Fla., who talked about the raw losses they were feeling, and the student who wasn’t celebrating his 18th birthday on March 24. Matthew Soto from Newtown, Conn., talked about losing his sister, a first-grade teacher, in the Sandy Hook shooting.
But the rally wasn’t just about mass murders and school shootings: Zion Kelly talked about the death of his twin, a teen who was killed when he stopped at a convenience store on the way home from school in Washington, only to have his promising life snuffed out during a holdup. We heard about shootings in the bullet-riddled streets of Chicago and Los Angeles and the toll they have taken. The losses to gun violence have been felt most strongly in communities of color. While it was mentioned that the majority of gun deaths are suicides, there were no speakers from families of people who died from suicide. The final speaker was Emma Gonzalez, a young woman from Parkland who took the stage for 6 minutes and 20 seconds - the duration of the shooter’s rampage - and closed with a powerful moment of silence.* The rally closed with a performance of Bob Dylan’s “The Times They Are a-Changin’ ” by Jennifer Hudson, whose mother, brother, and nephew were murdered by a gunman.
The teens talked about what changes they wanted to see enacted. They talked about closing loopholes to background checks, and I was pleased that one young man specifically mentioned keeping guns from those who are violent, but did not mention mental illness as a reason to block gun ownership. A call to resume a ban on assault weapons was made repeatedly as was a call to raise the age (to 21) at which an individual can purchase a gun. Military-style weapons are not necessary for hunting or self-defense, and they enable the rapid-fire assassinations we have seen in mass shootings, so they remain an easy target of gun control advocacy. But in terms of numbers, these firearms are responsible for a small fraction of gun deaths. I was surprised, but the teens did not mention “smart gun” legislation as a way to reduce gun deaths.
Guns, and gun deaths, are a part of American society. While the majority of Americans favor stronger regulation of gun ownership, legislation that would end gun ownership is not likely to go anywhere. Smart guns, however, are different. Forty percent of polled gun owners have said they would swap their firearm for a smart firearm. So given the appeal of a firearm that can’t be diverted or stolen, used against the owner, discharged accidentally by a child, or used for suicide or homicide by a distressed family member, why don’t these weapons exist for use by the American people? . People want these guns and the protections they offer, yet they have never been produced and made available to either the American public or to our law enforcement officers.
So where are these firearms, and why aren’t our Parkland teens asking for them? The answer to the first part of that question lies with the National Rifle Association (NRA) and the state of New Jersey. In 2003, New Jersey passed the Childproof Handgun bill, which requires that all guns sold in the state be smart guns within 3 years of their availability. The NRA has vigorously opposed any legislation that would require all guns to be smart guns. Because the availability of these weapons would trigger the New Jersey bill, California and Maryland have been prevented from importing smart firearms from a German company. Perhaps, however, New Jersey does not need to bear all the blame; in 1999, 4 years before the passage of the bill, the NRA and its members boycotted Smith & Wesson when the gun manufacturer revealed plans to develop a smart gun for the government. The NRA’s public stance is that it does not oppose smart guns for those who want them, but it opposes legislation that would eliminate the sale of conventional firearms. The organization has voiced concerns that technology fails and that it potentially slows down firing the weapon. It doesn’t talk about dead toddlers, or about police officers who’ve been killed when their weapons were taken from them.
As for the Parkland students, I don’t know why they aren’t asking for smart gun technology while they have the attention of the country. Perhaps they, like the young women I was with, don’t know it’s an option. Perhaps it’s too removed from the issue of mass murders and an assault weapon ban feels more attainable. Or perhaps the NRA’s mission has too much of a stronghold in Florida. I don’t know why they aren’t asking for smart gun production, but I know they should be.
*Correction, 3/27/2018: An earlier version of this story misstated the duration of Emma Gonzalez's moment of silence.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press), 2016. She practices in Baltimore.
The evening before the March For Our Lives rally in Washington, I was hard at work on my sign. Making a statement is important, but at the Women’s March last January, I discovered that a sign was invaluable for keeping friends together in a crowd. Since my Women’s March sign read “Make America Kind Again,” I opted to keep with the theme, and I created a “Make America Safe Again” sign for gun control. My daughter looked at my sign skeptically. “It’s too vague and nondirective,” she declared. Now challenged, I added the following directives: “Universal Background Checks,” “Ban Assault Weapons,” and “Smart Guns.” My sign was now complete.
I was surprised when my daughter – our family Jeopardy! whiz – asked, “What’s a smart gun?” When we arrived to join friends, their daughter – a doctoral student – also looked at the sign and asked me what a smart gun is. I explained to both young women that a smart gun – like an iPhone – relies on a biometric such as a fingerprint so that it can be used only by authorized users. This technology would reduce the flow of firearms to illegal owners, prevent accidental discharge by children, protect rightful owners and law enforcement officers from having their own weapons used against them by criminals, and decrease the number of suicides by family members of gun owners. In my state of Maryland, there have been two school shootings, one as recently as March 20, and both were committed by boys who took a parent’s firearm to school.
We arrived at the rally and found a spot in front of the Newseum, with two jumbotrons in sight, right in the middle of the crowd. The young people who spoke were inspirational. Regardless of one’s political views or thoughts on gun control, they were bright, articulate, fearless, passionate, and determined. The show was stolen by Naomi Wadler, a precocious 11-year-old girl who is destined to be a member of Congress (if not president) one day, and by Dr. Martin Luther King Jr.’s 9-year-old granddaughter, Yolanda Renee King.
The rest of the speakers were teenagers, all of whom had lost someone to gunfire. There were speakers from Parkland, Fla., who talked about the raw losses they were feeling, and the student who wasn’t celebrating his 18th birthday on March 24. Matthew Soto from Newtown, Conn., talked about losing his sister, a first-grade teacher, in the Sandy Hook shooting.
But the rally wasn’t just about mass murders and school shootings: Zion Kelly talked about the death of his twin, a teen who was killed when he stopped at a convenience store on the way home from school in Washington, only to have his promising life snuffed out during a holdup. We heard about shootings in the bullet-riddled streets of Chicago and Los Angeles and the toll they have taken. The losses to gun violence have been felt most strongly in communities of color. While it was mentioned that the majority of gun deaths are suicides, there were no speakers from families of people who died from suicide. The final speaker was Emma Gonzalez, a young woman from Parkland who took the stage for 6 minutes and 20 seconds - the duration of the shooter’s rampage - and closed with a powerful moment of silence.* The rally closed with a performance of Bob Dylan’s “The Times They Are a-Changin’ ” by Jennifer Hudson, whose mother, brother, and nephew were murdered by a gunman.
The teens talked about what changes they wanted to see enacted. They talked about closing loopholes to background checks, and I was pleased that one young man specifically mentioned keeping guns from those who are violent, but did not mention mental illness as a reason to block gun ownership. A call to resume a ban on assault weapons was made repeatedly as was a call to raise the age (to 21) at which an individual can purchase a gun. Military-style weapons are not necessary for hunting or self-defense, and they enable the rapid-fire assassinations we have seen in mass shootings, so they remain an easy target of gun control advocacy. But in terms of numbers, these firearms are responsible for a small fraction of gun deaths. I was surprised, but the teens did not mention “smart gun” legislation as a way to reduce gun deaths.
Guns, and gun deaths, are a part of American society. While the majority of Americans favor stronger regulation of gun ownership, legislation that would end gun ownership is not likely to go anywhere. Smart guns, however, are different. Forty percent of polled gun owners have said they would swap their firearm for a smart firearm. So given the appeal of a firearm that can’t be diverted or stolen, used against the owner, discharged accidentally by a child, or used for suicide or homicide by a distressed family member, why don’t these weapons exist for use by the American people? . People want these guns and the protections they offer, yet they have never been produced and made available to either the American public or to our law enforcement officers.
So where are these firearms, and why aren’t our Parkland teens asking for them? The answer to the first part of that question lies with the National Rifle Association (NRA) and the state of New Jersey. In 2003, New Jersey passed the Childproof Handgun bill, which requires that all guns sold in the state be smart guns within 3 years of their availability. The NRA has vigorously opposed any legislation that would require all guns to be smart guns. Because the availability of these weapons would trigger the New Jersey bill, California and Maryland have been prevented from importing smart firearms from a German company. Perhaps, however, New Jersey does not need to bear all the blame; in 1999, 4 years before the passage of the bill, the NRA and its members boycotted Smith & Wesson when the gun manufacturer revealed plans to develop a smart gun for the government. The NRA’s public stance is that it does not oppose smart guns for those who want them, but it opposes legislation that would eliminate the sale of conventional firearms. The organization has voiced concerns that technology fails and that it potentially slows down firing the weapon. It doesn’t talk about dead toddlers, or about police officers who’ve been killed when their weapons were taken from them.
As for the Parkland students, I don’t know why they aren’t asking for smart gun technology while they have the attention of the country. Perhaps they, like the young women I was with, don’t know it’s an option. Perhaps it’s too removed from the issue of mass murders and an assault weapon ban feels more attainable. Or perhaps the NRA’s mission has too much of a stronghold in Florida. I don’t know why they aren’t asking for smart gun production, but I know they should be.
*Correction, 3/27/2018: An earlier version of this story misstated the duration of Emma Gonzalez's moment of silence.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press), 2016. She practices in Baltimore.
Trauma surgeon shares story of involuntary commitment, redemption
Over the last few years, I have spoken to many people about their experiences with involuntary psychiatric hospitalizations. While the stories I’ve heard are anecdotes, often from people who have reached out to me, and not randomized, controlled studies, I’ve taken the liberty of coming to a few conclusions. First, involuntary hospitalizations help people. Most people say that they left the hospital with fewer symptoms than they had when they entered. Second, many of those people, helped though they may have been, are angry about the treatment they received. An unknown percentage feel traumatized by their psychiatric treatment, and years later they dwell on a perception of injustice and injury.
It’s perplexing that this negative residue remains given that involuntary psychiatric care often helps people to escape from the torment of psychosis or from soul-crushing depressions. While many feel it should be easier to involuntarily treat psychiatric disorders, there are no groups of patients asking for easier access to involuntary care. One group, Mad in America – formed by journalist Robert Whitaker – takes the position that psychiatric medications don’t just harm people, but that psychotropic medications actually cause psychiatric disorders in people who would have fared better without them. It now offers CME activities through its conferences and website!
“In the middle of elective inpatient electroconvulsive therapy for treatment-resistant depression, he had become profoundly depressed, delirious, and hopeless. He’d lost faith in treatment and in reasons to live. He withdrew to bed and would not get up or eat. He had to be committed for his own safety. Several security guards had to forcefully remove him from his bed.”
The patient, he noted, was injected with haloperidol and placed in restraints in a seclusion room. By the third paragraph, Weinstein switches to a first-person narrative and reveals that he is that patient. He goes on to talk about the stresses of life as a trauma surgeon, and describes both classic physician burnout and severe major depression. The essay includes an element of catharsis. The author shares his painful story, with all the gore of amputating the limbs of others to the agony of feeling that those he loves might be better off without him. Post-hospitalization, Weinstein’s message is clear: He wants to help others break free from the stigma of silent shame and let them know that help is available. “You would not be reading this today were it not for the love of my wife, my children, my mother and sister, and so many others, including the guards and doctors who ‘locked me up’ against my will. They kept me from crossing into the abyss,” he writes.
The essay (N Engl J Med. 2018;378:793-5) surprised me, because I have never heard a patient who has been forcibly medicated and placed in restraints and seclusion talk about the experience with gratitude. I contacted Dr. Weinstein and asked if he would speak with me about his experiences as a committed patient back in early 2016. In fact, he said that he had only recently begun to speak of his experiences with his therapist, and he spoke openly about what he remembered of those events.
Dr. Weinstein told me his story in more detail – it was a long and tumultuous journey from the depth of depression to where he is now. “I’m in a much better place than I’ve ever been. I’ve developed tools for resilience and I’ve found joy.” His gratitude was real, and his purpose in sharing his story remains a positive and hopeful vision for others who suffer. Clearly, he was not traumatized by his treatment. I approached him with the question of what psychiatrists could learn from his experiences. The story that followed had the texture of those I was used to hearing from people who had been involuntarily treated.
Like many people I’ve spoken with, Dr. Weinstein assumed he was officially committed to the locked unit, but he did not recall a legal hearing. In fact, many of those I’ve talked with had actually signed themselves in, and Dr. Weinstein thought that was possible.
“When I wrote the New England Journal piece, it originated from a place of anger. I was voluntarily admitted to a private, self-pay psychiatric unit, and I was getting ECT. I was getting worse, not better. I was in a scary place, and I was deeply depressed. The day before, I had gone for a walk without telling the staff or following the sign-out procedure. They decided I needed to be in a locked unit, and when they told me, I was lying in bed.”
Upon hearing that he would be transferred, Dr. Weinstein became combative. He was medicated and taken to a locked unit in the hospital, placed in restraints, and put into a seclusion room.
“I’ve wondered if this could have been done another way. Maybe if they had given me a chance to process the information, perhaps I would have gone more willingly without guards carrying me through the facility. I wondered if the way the information was delivered didn’t escalate things, if it could have been done differently.” Listening to him, I wondered as well, though Dr. Weinstein was well aware that the actions of his treatment team came with the best of intentions to help him. I pointed out that the treatment team may have felt fearful when he disappeared from the unit, and as they watched him decline further, they may well have felt a bit desperate and fearful of their ability to keep him safe on an unlocked unit. None of this surprised him.
Was Dr. Weinstein open to returning to a psychiatric unit if his depression recurs?
“A few months after I left, I became even more depressed and suicidal. I didn’t go back, and I really hope I’ll never have to be in a hospital again.” Instead,. “They changed my perspective.”
Dr. Weinstein also questions if he should have agreed to ECT. “I was better when I left the hospital, but the treatment itself was crude, and I still wonder if it affects my memory now.”
I wanted to know what psychiatrists might learn from his experiences with involuntary care. Weinstein hesitated. “It wasn’t the best experience, and I felt there had to be a better way, but I know everyone was trying to help me, and I want my overall message to be one of hope. I don’t want to complain, because I’ve ended up in a much better place, I’m back at work, enjoying my family, and I feel joy now.”
For psychiatrists, this is the best outcome from a story such as Dr. Weinstein’s. He’s much better, in a scenario where he could have just as easily have died, and he wasn’t traumatized by his care. However, he avoided returning to inpatient care at a precarious time, and he’s left asking if there weren’t a gentler way this could have transpired. These questions are easier to look at from the perspective of a Monday morning quarterback than they are to look at from the perspective of a treatment team dealing with a very sick and combative patient. Still, I hope we all continue to question patients about their experiences and ask if there might be better ways.
Dr. Miller, who practices in Baltimore, is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Care” (Baltimore: Johns Hopkins University Press, 2016).
Over the last few years, I have spoken to many people about their experiences with involuntary psychiatric hospitalizations. While the stories I’ve heard are anecdotes, often from people who have reached out to me, and not randomized, controlled studies, I’ve taken the liberty of coming to a few conclusions. First, involuntary hospitalizations help people. Most people say that they left the hospital with fewer symptoms than they had when they entered. Second, many of those people, helped though they may have been, are angry about the treatment they received. An unknown percentage feel traumatized by their psychiatric treatment, and years later they dwell on a perception of injustice and injury.
It’s perplexing that this negative residue remains given that involuntary psychiatric care often helps people to escape from the torment of psychosis or from soul-crushing depressions. While many feel it should be easier to involuntarily treat psychiatric disorders, there are no groups of patients asking for easier access to involuntary care. One group, Mad in America – formed by journalist Robert Whitaker – takes the position that psychiatric medications don’t just harm people, but that psychotropic medications actually cause psychiatric disorders in people who would have fared better without them. It now offers CME activities through its conferences and website!
“In the middle of elective inpatient electroconvulsive therapy for treatment-resistant depression, he had become profoundly depressed, delirious, and hopeless. He’d lost faith in treatment and in reasons to live. He withdrew to bed and would not get up or eat. He had to be committed for his own safety. Several security guards had to forcefully remove him from his bed.”
The patient, he noted, was injected with haloperidol and placed in restraints in a seclusion room. By the third paragraph, Weinstein switches to a first-person narrative and reveals that he is that patient. He goes on to talk about the stresses of life as a trauma surgeon, and describes both classic physician burnout and severe major depression. The essay includes an element of catharsis. The author shares his painful story, with all the gore of amputating the limbs of others to the agony of feeling that those he loves might be better off without him. Post-hospitalization, Weinstein’s message is clear: He wants to help others break free from the stigma of silent shame and let them know that help is available. “You would not be reading this today were it not for the love of my wife, my children, my mother and sister, and so many others, including the guards and doctors who ‘locked me up’ against my will. They kept me from crossing into the abyss,” he writes.
The essay (N Engl J Med. 2018;378:793-5) surprised me, because I have never heard a patient who has been forcibly medicated and placed in restraints and seclusion talk about the experience with gratitude. I contacted Dr. Weinstein and asked if he would speak with me about his experiences as a committed patient back in early 2016. In fact, he said that he had only recently begun to speak of his experiences with his therapist, and he spoke openly about what he remembered of those events.
Dr. Weinstein told me his story in more detail – it was a long and tumultuous journey from the depth of depression to where he is now. “I’m in a much better place than I’ve ever been. I’ve developed tools for resilience and I’ve found joy.” His gratitude was real, and his purpose in sharing his story remains a positive and hopeful vision for others who suffer. Clearly, he was not traumatized by his treatment. I approached him with the question of what psychiatrists could learn from his experiences. The story that followed had the texture of those I was used to hearing from people who had been involuntarily treated.
Like many people I’ve spoken with, Dr. Weinstein assumed he was officially committed to the locked unit, but he did not recall a legal hearing. In fact, many of those I’ve talked with had actually signed themselves in, and Dr. Weinstein thought that was possible.
“When I wrote the New England Journal piece, it originated from a place of anger. I was voluntarily admitted to a private, self-pay psychiatric unit, and I was getting ECT. I was getting worse, not better. I was in a scary place, and I was deeply depressed. The day before, I had gone for a walk without telling the staff or following the sign-out procedure. They decided I needed to be in a locked unit, and when they told me, I was lying in bed.”
Upon hearing that he would be transferred, Dr. Weinstein became combative. He was medicated and taken to a locked unit in the hospital, placed in restraints, and put into a seclusion room.
“I’ve wondered if this could have been done another way. Maybe if they had given me a chance to process the information, perhaps I would have gone more willingly without guards carrying me through the facility. I wondered if the way the information was delivered didn’t escalate things, if it could have been done differently.” Listening to him, I wondered as well, though Dr. Weinstein was well aware that the actions of his treatment team came with the best of intentions to help him. I pointed out that the treatment team may have felt fearful when he disappeared from the unit, and as they watched him decline further, they may well have felt a bit desperate and fearful of their ability to keep him safe on an unlocked unit. None of this surprised him.
Was Dr. Weinstein open to returning to a psychiatric unit if his depression recurs?
“A few months after I left, I became even more depressed and suicidal. I didn’t go back, and I really hope I’ll never have to be in a hospital again.” Instead,. “They changed my perspective.”
Dr. Weinstein also questions if he should have agreed to ECT. “I was better when I left the hospital, but the treatment itself was crude, and I still wonder if it affects my memory now.”
I wanted to know what psychiatrists might learn from his experiences with involuntary care. Weinstein hesitated. “It wasn’t the best experience, and I felt there had to be a better way, but I know everyone was trying to help me, and I want my overall message to be one of hope. I don’t want to complain, because I’ve ended up in a much better place, I’m back at work, enjoying my family, and I feel joy now.”
For psychiatrists, this is the best outcome from a story such as Dr. Weinstein’s. He’s much better, in a scenario where he could have just as easily have died, and he wasn’t traumatized by his care. However, he avoided returning to inpatient care at a precarious time, and he’s left asking if there weren’t a gentler way this could have transpired. These questions are easier to look at from the perspective of a Monday morning quarterback than they are to look at from the perspective of a treatment team dealing with a very sick and combative patient. Still, I hope we all continue to question patients about their experiences and ask if there might be better ways.
Dr. Miller, who practices in Baltimore, is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Care” (Baltimore: Johns Hopkins University Press, 2016).
Over the last few years, I have spoken to many people about their experiences with involuntary psychiatric hospitalizations. While the stories I’ve heard are anecdotes, often from people who have reached out to me, and not randomized, controlled studies, I’ve taken the liberty of coming to a few conclusions. First, involuntary hospitalizations help people. Most people say that they left the hospital with fewer symptoms than they had when they entered. Second, many of those people, helped though they may have been, are angry about the treatment they received. An unknown percentage feel traumatized by their psychiatric treatment, and years later they dwell on a perception of injustice and injury.
It’s perplexing that this negative residue remains given that involuntary psychiatric care often helps people to escape from the torment of psychosis or from soul-crushing depressions. While many feel it should be easier to involuntarily treat psychiatric disorders, there are no groups of patients asking for easier access to involuntary care. One group, Mad in America – formed by journalist Robert Whitaker – takes the position that psychiatric medications don’t just harm people, but that psychotropic medications actually cause psychiatric disorders in people who would have fared better without them. It now offers CME activities through its conferences and website!
“In the middle of elective inpatient electroconvulsive therapy for treatment-resistant depression, he had become profoundly depressed, delirious, and hopeless. He’d lost faith in treatment and in reasons to live. He withdrew to bed and would not get up or eat. He had to be committed for his own safety. Several security guards had to forcefully remove him from his bed.”
The patient, he noted, was injected with haloperidol and placed in restraints in a seclusion room. By the third paragraph, Weinstein switches to a first-person narrative and reveals that he is that patient. He goes on to talk about the stresses of life as a trauma surgeon, and describes both classic physician burnout and severe major depression. The essay includes an element of catharsis. The author shares his painful story, with all the gore of amputating the limbs of others to the agony of feeling that those he loves might be better off without him. Post-hospitalization, Weinstein’s message is clear: He wants to help others break free from the stigma of silent shame and let them know that help is available. “You would not be reading this today were it not for the love of my wife, my children, my mother and sister, and so many others, including the guards and doctors who ‘locked me up’ against my will. They kept me from crossing into the abyss,” he writes.
The essay (N Engl J Med. 2018;378:793-5) surprised me, because I have never heard a patient who has been forcibly medicated and placed in restraints and seclusion talk about the experience with gratitude. I contacted Dr. Weinstein and asked if he would speak with me about his experiences as a committed patient back in early 2016. In fact, he said that he had only recently begun to speak of his experiences with his therapist, and he spoke openly about what he remembered of those events.
Dr. Weinstein told me his story in more detail – it was a long and tumultuous journey from the depth of depression to where he is now. “I’m in a much better place than I’ve ever been. I’ve developed tools for resilience and I’ve found joy.” His gratitude was real, and his purpose in sharing his story remains a positive and hopeful vision for others who suffer. Clearly, he was not traumatized by his treatment. I approached him with the question of what psychiatrists could learn from his experiences. The story that followed had the texture of those I was used to hearing from people who had been involuntarily treated.
Like many people I’ve spoken with, Dr. Weinstein assumed he was officially committed to the locked unit, but he did not recall a legal hearing. In fact, many of those I’ve talked with had actually signed themselves in, and Dr. Weinstein thought that was possible.
“When I wrote the New England Journal piece, it originated from a place of anger. I was voluntarily admitted to a private, self-pay psychiatric unit, and I was getting ECT. I was getting worse, not better. I was in a scary place, and I was deeply depressed. The day before, I had gone for a walk without telling the staff or following the sign-out procedure. They decided I needed to be in a locked unit, and when they told me, I was lying in bed.”
Upon hearing that he would be transferred, Dr. Weinstein became combative. He was medicated and taken to a locked unit in the hospital, placed in restraints, and put into a seclusion room.
“I’ve wondered if this could have been done another way. Maybe if they had given me a chance to process the information, perhaps I would have gone more willingly without guards carrying me through the facility. I wondered if the way the information was delivered didn’t escalate things, if it could have been done differently.” Listening to him, I wondered as well, though Dr. Weinstein was well aware that the actions of his treatment team came with the best of intentions to help him. I pointed out that the treatment team may have felt fearful when he disappeared from the unit, and as they watched him decline further, they may well have felt a bit desperate and fearful of their ability to keep him safe on an unlocked unit. None of this surprised him.
Was Dr. Weinstein open to returning to a psychiatric unit if his depression recurs?
“A few months after I left, I became even more depressed and suicidal. I didn’t go back, and I really hope I’ll never have to be in a hospital again.” Instead,. “They changed my perspective.”
Dr. Weinstein also questions if he should have agreed to ECT. “I was better when I left the hospital, but the treatment itself was crude, and I still wonder if it affects my memory now.”
I wanted to know what psychiatrists might learn from his experiences with involuntary care. Weinstein hesitated. “It wasn’t the best experience, and I felt there had to be a better way, but I know everyone was trying to help me, and I want my overall message to be one of hope. I don’t want to complain, because I’ve ended up in a much better place, I’m back at work, enjoying my family, and I feel joy now.”
For psychiatrists, this is the best outcome from a story such as Dr. Weinstein’s. He’s much better, in a scenario where he could have just as easily have died, and he wasn’t traumatized by his care. However, he avoided returning to inpatient care at a precarious time, and he’s left asking if there weren’t a gentler way this could have transpired. These questions are easier to look at from the perspective of a Monday morning quarterback than they are to look at from the perspective of a treatment team dealing with a very sick and combative patient. Still, I hope we all continue to question patients about their experiences and ask if there might be better ways.
Dr. Miller, who practices in Baltimore, is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Care” (Baltimore: Johns Hopkins University Press, 2016).
Medication pricing: So this is how it works
This is the second part in a series on medication pricing.
In my last column, I looked at the tremendous variation in prices among pharmacies for two psychotropic medications, aripiprazole and modafinil. The cash price variation could be as much as 45 times more from one pharmacy to the next, which I found to be both outrageous and incomprehensible.
To learn more about pharmaceutical pricing, I contacted Doug Hirsch, the cofounder of GoodRx, a firm based in Santa Monica, Calif., that offers deep discounts on some medications. The company sends discount cards to physicians’ offices – call me if you need some, I have many boxes of GoodRx cards – and has a website (www.GoodRx.com) and an app. It advertises that it is about transparency, and if you’ve ever tried the company’s site or app, the service it offers is remarkable and simple to use.
I approached Mr. Hirsch with two simple questions. The company offers “up to 90% discount” on the cash price of medications through its app, website, or discount card – all of which can be gotten for free. I wanted to know 1) Who pays for this difference in the medication cost, and 2) How does the company, with 95 employees, make any money? Mr. Hirsch was gracious enough (and patient enough!) to spend the next hour walking me through the steps of medication pricing. It was a lively conversation, so let me share with you what I have learned.
Medications are made by a pharmaceutical company or, for generics, there may be many manufacturers. The medications are sent to a pharmaceutical distributor, such as McKesson, and it, in turn, sells and delivers the products to pharmacy chains, as well as to smaller, independent pharmacies. The pharmacies pay an acquisition cost for medications then set a price for these medications that are considerably – or even astronomically – higher than the acquisition price. This is the cash retail price, or in medicine, what is called the Usual & Customary (U&C) cost of the medication. The price may be neither usual, customary, nor reasonable, and it’s not the price the pharmacy expects to recoup on sales.
Every major insurance company contracts with a pharmacy benefits manager (for example, Caremark, Express Scripts, and Optum) to negotiate the cost of medications with each major pharmacy chain. Physicians are familiar with PBMs, who intercede by requiring preauthorization procedures for certain medications or by instituting stepwise, fail-first, requirements before they will allow pharmacy benefits toward the purchase of medications. When the PBMs negotiate with the pharmacies, they will negotiate for a discount off the pharmacy’s U&C charge for medication, perhaps a discount as much as 75% or 80%. Mr. Hirsch noted, “The discount is not negotiated on a per-medication basis but as an across-the-board average, so for one medication, the insurance price may be 2% discount from the U&C cost, and on another medicine it may be 95%. There is a dramatic variation, more than you’d ever expect.”
GoodRx gathers prices from many places, including partnerships with a number of PBMs. In addition to providing discounted prices for insured customers, the PBMs also include in their negotiations a slightly less-discounted price for cash-paying patients who present with a GoodRx card or coupon. You might be surprised to learn that discounted prices can often be less than the typical patient copay. For patients with a high deductible, for medications that are not covered at all, or for times when the copay is higher than the cost of the medication, it will often be less expensive for patients to use a GoodRx discount instead of their insurance. And whether patients uses either their insurance or a GoodRx discount, part of the cost of the prescription includes an administrative fee that goes to the PBM. When GoodRx cards are used, the PBM pays GoodRx part of that fee. I hope you are still with me, because this is the part of the conversation where I started telling Mr. Hirsch that I was getting a headache.
I went back to the enormous cost discrepancy that I had discovered a couple of years ago with Provigil (modafinil). Thirty pills cost just under $35 at Costco, while all other pharmacies were charging close to $1,000. Mr. Hirsch explained, “From what I’ve been told, Costco bases their prices on their acquisition costs and then raises them a certain percent. It’s one way to provide a fair price, but that doesn’t mean they always have the lowest price. They are also the only major pharmacy that lists their drug prices on their website.”
I wanted to know what was in it for the PBMs. Why would Express Scripts be motivated to negotiate a discount in price for cash-paying customers outside of the insurance networks, and how did partnering with GoodRx benefit them? The answer, in part, lies with the fact that the website and app allow patients to comparison shop and go to pharmacies with lower prices. If patients use their insurance, the insurance company is paying less; if they don’t use their insurance because they learned the cash cost is less, then the cost burden has shifted from the insurance company entirely to the patient.
What’s in it for the pharmacies? Why would they be willing to accept less money from a patient bearing a discount card? Mr. Hirsch explained, “Pharmacies want to honor their contracts with PBMs, and the U&C prices are set high to enable negotiation so that they still make some profit. Most people couldn’t afford to pay the high U&C, but they can’t lower them for individual cash-pay customers because that would violate their agreements with PBMs, and Medicare and Medicaid, which is a felony. With the GoodRx price, they still make a profit, and people in drugstores buy other items as well.
GoodRx has 95 employees, and I was still left wondering how they generate income. Mr. Hirsch pinned it down to three sources: the portion of the administration fees the PBMs pay GoodRx, a small amount of advertising, and finally, GoodRx provides technology for the PBMs and charges for this service.
“We started asking how we could gather prices in this bizarre marketplace and address the pricing inefficiencies,” Mr. Hirsch said, “and now I get emails every day expressing gratitude.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
This is the second part in a series on medication pricing.
In my last column, I looked at the tremendous variation in prices among pharmacies for two psychotropic medications, aripiprazole and modafinil. The cash price variation could be as much as 45 times more from one pharmacy to the next, which I found to be both outrageous and incomprehensible.
To learn more about pharmaceutical pricing, I contacted Doug Hirsch, the cofounder of GoodRx, a firm based in Santa Monica, Calif., that offers deep discounts on some medications. The company sends discount cards to physicians’ offices – call me if you need some, I have many boxes of GoodRx cards – and has a website (www.GoodRx.com) and an app. It advertises that it is about transparency, and if you’ve ever tried the company’s site or app, the service it offers is remarkable and simple to use.
I approached Mr. Hirsch with two simple questions. The company offers “up to 90% discount” on the cash price of medications through its app, website, or discount card – all of which can be gotten for free. I wanted to know 1) Who pays for this difference in the medication cost, and 2) How does the company, with 95 employees, make any money? Mr. Hirsch was gracious enough (and patient enough!) to spend the next hour walking me through the steps of medication pricing. It was a lively conversation, so let me share with you what I have learned.
Medications are made by a pharmaceutical company or, for generics, there may be many manufacturers. The medications are sent to a pharmaceutical distributor, such as McKesson, and it, in turn, sells and delivers the products to pharmacy chains, as well as to smaller, independent pharmacies. The pharmacies pay an acquisition cost for medications then set a price for these medications that are considerably – or even astronomically – higher than the acquisition price. This is the cash retail price, or in medicine, what is called the Usual & Customary (U&C) cost of the medication. The price may be neither usual, customary, nor reasonable, and it’s not the price the pharmacy expects to recoup on sales.
Every major insurance company contracts with a pharmacy benefits manager (for example, Caremark, Express Scripts, and Optum) to negotiate the cost of medications with each major pharmacy chain. Physicians are familiar with PBMs, who intercede by requiring preauthorization procedures for certain medications or by instituting stepwise, fail-first, requirements before they will allow pharmacy benefits toward the purchase of medications. When the PBMs negotiate with the pharmacies, they will negotiate for a discount off the pharmacy’s U&C charge for medication, perhaps a discount as much as 75% or 80%. Mr. Hirsch noted, “The discount is not negotiated on a per-medication basis but as an across-the-board average, so for one medication, the insurance price may be 2% discount from the U&C cost, and on another medicine it may be 95%. There is a dramatic variation, more than you’d ever expect.”
GoodRx gathers prices from many places, including partnerships with a number of PBMs. In addition to providing discounted prices for insured customers, the PBMs also include in their negotiations a slightly less-discounted price for cash-paying patients who present with a GoodRx card or coupon. You might be surprised to learn that discounted prices can often be less than the typical patient copay. For patients with a high deductible, for medications that are not covered at all, or for times when the copay is higher than the cost of the medication, it will often be less expensive for patients to use a GoodRx discount instead of their insurance. And whether patients uses either their insurance or a GoodRx discount, part of the cost of the prescription includes an administrative fee that goes to the PBM. When GoodRx cards are used, the PBM pays GoodRx part of that fee. I hope you are still with me, because this is the part of the conversation where I started telling Mr. Hirsch that I was getting a headache.
I went back to the enormous cost discrepancy that I had discovered a couple of years ago with Provigil (modafinil). Thirty pills cost just under $35 at Costco, while all other pharmacies were charging close to $1,000. Mr. Hirsch explained, “From what I’ve been told, Costco bases their prices on their acquisition costs and then raises them a certain percent. It’s one way to provide a fair price, but that doesn’t mean they always have the lowest price. They are also the only major pharmacy that lists their drug prices on their website.”
I wanted to know what was in it for the PBMs. Why would Express Scripts be motivated to negotiate a discount in price for cash-paying customers outside of the insurance networks, and how did partnering with GoodRx benefit them? The answer, in part, lies with the fact that the website and app allow patients to comparison shop and go to pharmacies with lower prices. If patients use their insurance, the insurance company is paying less; if they don’t use their insurance because they learned the cash cost is less, then the cost burden has shifted from the insurance company entirely to the patient.
What’s in it for the pharmacies? Why would they be willing to accept less money from a patient bearing a discount card? Mr. Hirsch explained, “Pharmacies want to honor their contracts with PBMs, and the U&C prices are set high to enable negotiation so that they still make some profit. Most people couldn’t afford to pay the high U&C, but they can’t lower them for individual cash-pay customers because that would violate their agreements with PBMs, and Medicare and Medicaid, which is a felony. With the GoodRx price, they still make a profit, and people in drugstores buy other items as well.
GoodRx has 95 employees, and I was still left wondering how they generate income. Mr. Hirsch pinned it down to three sources: the portion of the administration fees the PBMs pay GoodRx, a small amount of advertising, and finally, GoodRx provides technology for the PBMs and charges for this service.
“We started asking how we could gather prices in this bizarre marketplace and address the pricing inefficiencies,” Mr. Hirsch said, “and now I get emails every day expressing gratitude.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
This is the second part in a series on medication pricing.
In my last column, I looked at the tremendous variation in prices among pharmacies for two psychotropic medications, aripiprazole and modafinil. The cash price variation could be as much as 45 times more from one pharmacy to the next, which I found to be both outrageous and incomprehensible.
To learn more about pharmaceutical pricing, I contacted Doug Hirsch, the cofounder of GoodRx, a firm based in Santa Monica, Calif., that offers deep discounts on some medications. The company sends discount cards to physicians’ offices – call me if you need some, I have many boxes of GoodRx cards – and has a website (www.GoodRx.com) and an app. It advertises that it is about transparency, and if you’ve ever tried the company’s site or app, the service it offers is remarkable and simple to use.
I approached Mr. Hirsch with two simple questions. The company offers “up to 90% discount” on the cash price of medications through its app, website, or discount card – all of which can be gotten for free. I wanted to know 1) Who pays for this difference in the medication cost, and 2) How does the company, with 95 employees, make any money? Mr. Hirsch was gracious enough (and patient enough!) to spend the next hour walking me through the steps of medication pricing. It was a lively conversation, so let me share with you what I have learned.
Medications are made by a pharmaceutical company or, for generics, there may be many manufacturers. The medications are sent to a pharmaceutical distributor, such as McKesson, and it, in turn, sells and delivers the products to pharmacy chains, as well as to smaller, independent pharmacies. The pharmacies pay an acquisition cost for medications then set a price for these medications that are considerably – or even astronomically – higher than the acquisition price. This is the cash retail price, or in medicine, what is called the Usual & Customary (U&C) cost of the medication. The price may be neither usual, customary, nor reasonable, and it’s not the price the pharmacy expects to recoup on sales.
Every major insurance company contracts with a pharmacy benefits manager (for example, Caremark, Express Scripts, and Optum) to negotiate the cost of medications with each major pharmacy chain. Physicians are familiar with PBMs, who intercede by requiring preauthorization procedures for certain medications or by instituting stepwise, fail-first, requirements before they will allow pharmacy benefits toward the purchase of medications. When the PBMs negotiate with the pharmacies, they will negotiate for a discount off the pharmacy’s U&C charge for medication, perhaps a discount as much as 75% or 80%. Mr. Hirsch noted, “The discount is not negotiated on a per-medication basis but as an across-the-board average, so for one medication, the insurance price may be 2% discount from the U&C cost, and on another medicine it may be 95%. There is a dramatic variation, more than you’d ever expect.”
GoodRx gathers prices from many places, including partnerships with a number of PBMs. In addition to providing discounted prices for insured customers, the PBMs also include in their negotiations a slightly less-discounted price for cash-paying patients who present with a GoodRx card or coupon. You might be surprised to learn that discounted prices can often be less than the typical patient copay. For patients with a high deductible, for medications that are not covered at all, or for times when the copay is higher than the cost of the medication, it will often be less expensive for patients to use a GoodRx discount instead of their insurance. And whether patients uses either their insurance or a GoodRx discount, part of the cost of the prescription includes an administrative fee that goes to the PBM. When GoodRx cards are used, the PBM pays GoodRx part of that fee. I hope you are still with me, because this is the part of the conversation where I started telling Mr. Hirsch that I was getting a headache.
I went back to the enormous cost discrepancy that I had discovered a couple of years ago with Provigil (modafinil). Thirty pills cost just under $35 at Costco, while all other pharmacies were charging close to $1,000. Mr. Hirsch explained, “From what I’ve been told, Costco bases their prices on their acquisition costs and then raises them a certain percent. It’s one way to provide a fair price, but that doesn’t mean they always have the lowest price. They are also the only major pharmacy that lists their drug prices on their website.”
I wanted to know what was in it for the PBMs. Why would Express Scripts be motivated to negotiate a discount in price for cash-paying customers outside of the insurance networks, and how did partnering with GoodRx benefit them? The answer, in part, lies with the fact that the website and app allow patients to comparison shop and go to pharmacies with lower prices. If patients use their insurance, the insurance company is paying less; if they don’t use their insurance because they learned the cash cost is less, then the cost burden has shifted from the insurance company entirely to the patient.
What’s in it for the pharmacies? Why would they be willing to accept less money from a patient bearing a discount card? Mr. Hirsch explained, “Pharmacies want to honor their contracts with PBMs, and the U&C prices are set high to enable negotiation so that they still make some profit. Most people couldn’t afford to pay the high U&C, but they can’t lower them for individual cash-pay customers because that would violate their agreements with PBMs, and Medicare and Medicaid, which is a felony. With the GoodRx price, they still make a profit, and people in drugstores buy other items as well.
GoodRx has 95 employees, and I was still left wondering how they generate income. Mr. Hirsch pinned it down to three sources: the portion of the administration fees the PBMs pay GoodRx, a small amount of advertising, and finally, GoodRx provides technology for the PBMs and charges for this service.
“We started asking how we could gather prices in this bizarre marketplace and address the pricing inefficiencies,” Mr. Hirsch said, “and now I get emails every day expressing gratitude.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
You paid how much for that medicine?
This is the first article in a series on the cost of medications.
While it’s not news that some pharmaceuticals are exorbitantly expensive and therefore unavailable to our patients, I have learned that there are ways around the obstacle of cost for at least some medications. I want to tell you what I’ve learned about the high cost of two medications: aripiprazole, the generic of Abilify, and modafinil, the generic of Provigil, but the lessons learned may apply to other psychotropics – and Smokey Robinson and the Miracles said it best in a line from their 1960 hit song, “You’d better shop around.”
Over the past few years, the price of aripiprazole has come down considerably, or so I believed. A patient recently complained that his copay after insurance for a 1-month supply of 2-mg tablets was hundreds of dollars, and he showed me a bill where the cost before insurance was more than $2,000! Another patient, also someone with commercial insurance, said he couldn’t afford aripiprazole and asked me to phone in a prescription to healthwarehouse.com. The medication was mailed to him for about $35 a month. Finally, a third patient with Medicare used an online service called Blink Health. He explained that he paid for the medicine online with a credit card – about $80, far less than the price quoted by the pharmacy. He was then given some type of code to present to the pharmacist, who then supplied the medications. In this case, the same pills, the same pharmacy, at a fraction of the cost. With that, I called several pharmacies and asked about the price of generic Abilify, 5 mg, 30 tablets.
I also wrote a column about the tremendous difficulty I had trying to get preauthorization for modafinil, in “Preauthorization of medications: Who oversees the placement of the hoops?” In that case, I spent weeks trying to get approval for the medication, and in the end, it was not approved, and the patient was not able to get it. Soon after, I learned on a Psychiatry Network Facebook discussion that generic Provigil is not expensive at all! Once again, I fired up my phone and called around. Those prices and those I found for Abilify are listed in the chart.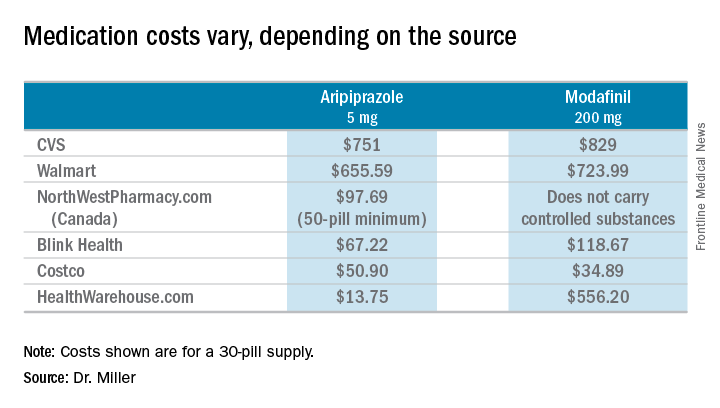
So these are cash prices; they do not take into account the cost with insurance. My patients have educated me after they could not afford the insurance copays. I wondered about my own coverage, and signed on to my pharmacy benefits manager account to look up the cost of both Abilify and Provigil. I’m sorry to say that I can’t report back: With my health insurance, Empire Blue Cross and Express Scripts, both medications require Coverage Review. It was also noted that Abilify requires Step treatment; I must first fail other medications. Should I ever need either of these medications, you’ll know where to find me: in line at the Costco pharmacy. I’ll be the one dancing to Smokey Robinson and the Miracles. https://www.youtube.com/watch?v=AQGXa3FiXKM
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
This is the first article in a series on the cost of medications.
While it’s not news that some pharmaceuticals are exorbitantly expensive and therefore unavailable to our patients, I have learned that there are ways around the obstacle of cost for at least some medications. I want to tell you what I’ve learned about the high cost of two medications: aripiprazole, the generic of Abilify, and modafinil, the generic of Provigil, but the lessons learned may apply to other psychotropics – and Smokey Robinson and the Miracles said it best in a line from their 1960 hit song, “You’d better shop around.”
Over the past few years, the price of aripiprazole has come down considerably, or so I believed. A patient recently complained that his copay after insurance for a 1-month supply of 2-mg tablets was hundreds of dollars, and he showed me a bill where the cost before insurance was more than $2,000! Another patient, also someone with commercial insurance, said he couldn’t afford aripiprazole and asked me to phone in a prescription to healthwarehouse.com. The medication was mailed to him for about $35 a month. Finally, a third patient with Medicare used an online service called Blink Health. He explained that he paid for the medicine online with a credit card – about $80, far less than the price quoted by the pharmacy. He was then given some type of code to present to the pharmacist, who then supplied the medications. In this case, the same pills, the same pharmacy, at a fraction of the cost. With that, I called several pharmacies and asked about the price of generic Abilify, 5 mg, 30 tablets.
I also wrote a column about the tremendous difficulty I had trying to get preauthorization for modafinil, in “Preauthorization of medications: Who oversees the placement of the hoops?” In that case, I spent weeks trying to get approval for the medication, and in the end, it was not approved, and the patient was not able to get it. Soon after, I learned on a Psychiatry Network Facebook discussion that generic Provigil is not expensive at all! Once again, I fired up my phone and called around. Those prices and those I found for Abilify are listed in the chart.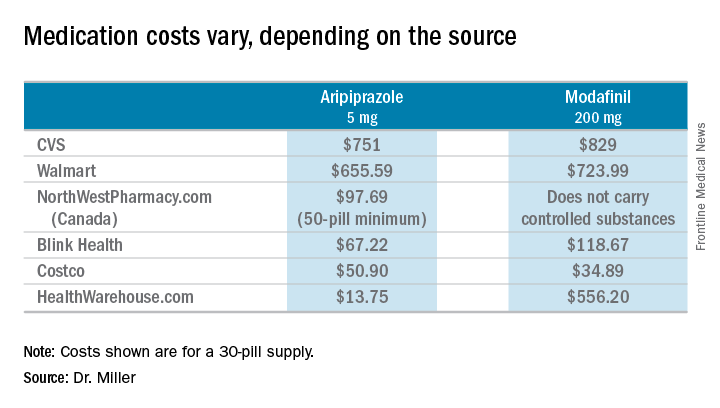
So these are cash prices; they do not take into account the cost with insurance. My patients have educated me after they could not afford the insurance copays. I wondered about my own coverage, and signed on to my pharmacy benefits manager account to look up the cost of both Abilify and Provigil. I’m sorry to say that I can’t report back: With my health insurance, Empire Blue Cross and Express Scripts, both medications require Coverage Review. It was also noted that Abilify requires Step treatment; I must first fail other medications. Should I ever need either of these medications, you’ll know where to find me: in line at the Costco pharmacy. I’ll be the one dancing to Smokey Robinson and the Miracles. https://www.youtube.com/watch?v=AQGXa3FiXKM
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
This is the first article in a series on the cost of medications.
While it’s not news that some pharmaceuticals are exorbitantly expensive and therefore unavailable to our patients, I have learned that there are ways around the obstacle of cost for at least some medications. I want to tell you what I’ve learned about the high cost of two medications: aripiprazole, the generic of Abilify, and modafinil, the generic of Provigil, but the lessons learned may apply to other psychotropics – and Smokey Robinson and the Miracles said it best in a line from their 1960 hit song, “You’d better shop around.”
Over the past few years, the price of aripiprazole has come down considerably, or so I believed. A patient recently complained that his copay after insurance for a 1-month supply of 2-mg tablets was hundreds of dollars, and he showed me a bill where the cost before insurance was more than $2,000! Another patient, also someone with commercial insurance, said he couldn’t afford aripiprazole and asked me to phone in a prescription to healthwarehouse.com. The medication was mailed to him for about $35 a month. Finally, a third patient with Medicare used an online service called Blink Health. He explained that he paid for the medicine online with a credit card – about $80, far less than the price quoted by the pharmacy. He was then given some type of code to present to the pharmacist, who then supplied the medications. In this case, the same pills, the same pharmacy, at a fraction of the cost. With that, I called several pharmacies and asked about the price of generic Abilify, 5 mg, 30 tablets.
I also wrote a column about the tremendous difficulty I had trying to get preauthorization for modafinil, in “Preauthorization of medications: Who oversees the placement of the hoops?” In that case, I spent weeks trying to get approval for the medication, and in the end, it was not approved, and the patient was not able to get it. Soon after, I learned on a Psychiatry Network Facebook discussion that generic Provigil is not expensive at all! Once again, I fired up my phone and called around. Those prices and those I found for Abilify are listed in the chart.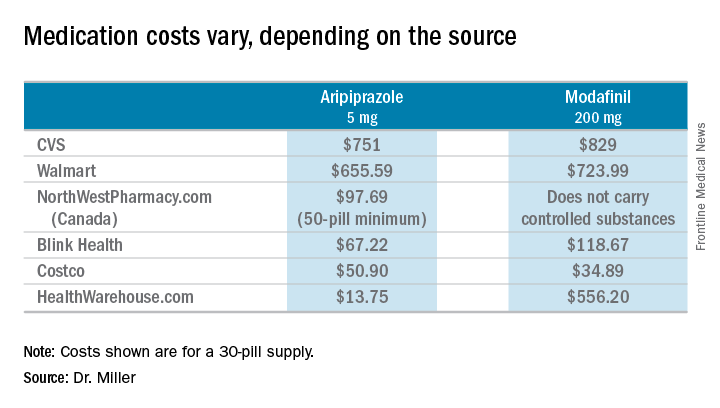
So these are cash prices; they do not take into account the cost with insurance. My patients have educated me after they could not afford the insurance copays. I wondered about my own coverage, and signed on to my pharmacy benefits manager account to look up the cost of both Abilify and Provigil. I’m sorry to say that I can’t report back: With my health insurance, Empire Blue Cross and Express Scripts, both medications require Coverage Review. It was also noted that Abilify requires Step treatment; I must first fail other medications. Should I ever need either of these medications, you’ll know where to find me: in line at the Costco pharmacy. I’ll be the one dancing to Smokey Robinson and the Miracles. https://www.youtube.com/watch?v=AQGXa3FiXKM
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
Massachusetts and the opioid crisis: Can involuntary holds work?
My son played on a neighborhood little league team for several years. I have such sweet memories of little boys in baseball uniforms lined up on the bench singing cheers while they waited their turns to go to bat. The two devoted dads who worked together coaching the team were a gentle presence in the background of my family’s life every spring for years. One might hope that the love and attention those fathers invested in their sons and their teammates might confer some special protection from life’s tragedies, but the opioid epidemic spares no hostages, and last year, one of those singing little boys from so many years ago – the son of one of the coaches – died of a drug overdose.
President Trump has punted on how to stop the epidemic, one he finally deemed a national public health emergency in October, with no clear addition of federal resources. States have varied in their responses, and Massachusetts, in particular, has been aggressive with new legislation and funding. The laws in Massachusetts allow for involuntary rehab for substance abusers if a family member petitions the court under the state’s decades-old section 35. The irony is that much of this “involuntary” treatment is voluntary: People will ask family members to apply for them as a way of getting into treatment and as a way of bypassing the cost. Section 35 admissions are funded by the state, not by the individual or by health insurance.
As a Boston Globe article (“Mass. governor aims to expand battle against opioid addiction,” Nov. 15, 2017) explains, “Two years ago, Baker stirred controversy with a proposal to hold addicted patients for 72 hours against their will in emergency departments. That idea was rejected by the Legislature. The new bill takes a different approach to the 72-hour hold, enabling doctors to transfer patients with addiction to a treatment facility, much as they would with a person deemed a danger because of mental illness.”
The issues with involuntary care are complicated and nuanced in psychiatric disorders, and perhaps even more so with substance abuse. The time frame of 72 hours for mental health conditions allows for assessment and sometimes for the start of treatment. In some states, a hearing must be held for continued involuntary detention; in other states, a decision must be made as to whether further inpatient care will be pursued, and the actual hearing takes place days to weeks later, depending on the state. For the purposes of allowing someone to clear from an opioid intoxication, then persuading them to engage in voluntary substance abuse treatment, it seems that 72 hours could be the exact wrong time period.
Ideally, a patient would be placed in a comfortable inpatient unit, begun on medication-assisted withdrawal, and offered a high quality of care for those 72 hours so that continuing with treatment might be a palatable option. But would that actually happen? Does Massachusetts have the means and facilities for all its overdose patients? Massachusetts has, in fact, been aggressive with funding. Since 2015, the state has added 1,100 new treatment beds. The efforts to fund and offer novel treatments are commendable. My concern remains that without adequate treatment or a positive experience – a difficult target in the best of circumstances for a patient who is 72 hours into opioid withdrawal – patients would leave only to resume their substance abuse. In a disastrous scenario, patients who have overdosed and fear being detained might not call for help, and the death rate could actually rise.
John A. Renner Jr., MD, is the past president of the American Academy of Addiction Psychiatry and coeditor of Office-Based Buprenorphine Treatment of Opioid Use Disorder (American Psychiatric Association Publishing, 2018). Dr. Renner, who is a professor at Boston University, said, “I would like to see some evidence and research to be sure there were not unintended harms before we go this route.”
Eric C. Strain, MD, director of the Johns Hopkins Center for Substance Abuse Treatment and Research, Baltimore, noted: “Simply holding someone for 3 days, especially against their will, doesn’t make a lot of sense. They are certainly not going to be all better either from a physiological or psychological standpoint. It might, however, be possible to get a person who was not interested in treatment engaged in treatment, and that would be a success.”
Despite the increased numbers of beds and aggressive, thoughtful interventions, Massachusetts still had 1,450 overdose deaths in the first 9 months of 2017, a decrease of only 10% from the year before, according to the Globe article. For the sake of the former Little League players in Maryland, and all the other victims of this lethal nationwide epidemic, it is imperative that any untested treatments be the source of new research. If these measures are implemented, it is essential that Massachusetts follow the people who are the beneficiaries of interventions and create the data that allow other states to either follow suit if these efforts are successful, or allocate resources to other treatments if they are not.
Dr. Miller is coauthor with Annette Hanson, MD, of Committed: The Battle Over Involuntary Psychiatry Care (Baltimore: Johns Hopkins University Press, 2016).
My son played on a neighborhood little league team for several years. I have such sweet memories of little boys in baseball uniforms lined up on the bench singing cheers while they waited their turns to go to bat. The two devoted dads who worked together coaching the team were a gentle presence in the background of my family’s life every spring for years. One might hope that the love and attention those fathers invested in their sons and their teammates might confer some special protection from life’s tragedies, but the opioid epidemic spares no hostages, and last year, one of those singing little boys from so many years ago – the son of one of the coaches – died of a drug overdose.
President Trump has punted on how to stop the epidemic, one he finally deemed a national public health emergency in October, with no clear addition of federal resources. States have varied in their responses, and Massachusetts, in particular, has been aggressive with new legislation and funding. The laws in Massachusetts allow for involuntary rehab for substance abusers if a family member petitions the court under the state’s decades-old section 35. The irony is that much of this “involuntary” treatment is voluntary: People will ask family members to apply for them as a way of getting into treatment and as a way of bypassing the cost. Section 35 admissions are funded by the state, not by the individual or by health insurance.
As a Boston Globe article (“Mass. governor aims to expand battle against opioid addiction,” Nov. 15, 2017) explains, “Two years ago, Baker stirred controversy with a proposal to hold addicted patients for 72 hours against their will in emergency departments. That idea was rejected by the Legislature. The new bill takes a different approach to the 72-hour hold, enabling doctors to transfer patients with addiction to a treatment facility, much as they would with a person deemed a danger because of mental illness.”
The issues with involuntary care are complicated and nuanced in psychiatric disorders, and perhaps even more so with substance abuse. The time frame of 72 hours for mental health conditions allows for assessment and sometimes for the start of treatment. In some states, a hearing must be held for continued involuntary detention; in other states, a decision must be made as to whether further inpatient care will be pursued, and the actual hearing takes place days to weeks later, depending on the state. For the purposes of allowing someone to clear from an opioid intoxication, then persuading them to engage in voluntary substance abuse treatment, it seems that 72 hours could be the exact wrong time period.
Ideally, a patient would be placed in a comfortable inpatient unit, begun on medication-assisted withdrawal, and offered a high quality of care for those 72 hours so that continuing with treatment might be a palatable option. But would that actually happen? Does Massachusetts have the means and facilities for all its overdose patients? Massachusetts has, in fact, been aggressive with funding. Since 2015, the state has added 1,100 new treatment beds. The efforts to fund and offer novel treatments are commendable. My concern remains that without adequate treatment or a positive experience – a difficult target in the best of circumstances for a patient who is 72 hours into opioid withdrawal – patients would leave only to resume their substance abuse. In a disastrous scenario, patients who have overdosed and fear being detained might not call for help, and the death rate could actually rise.
John A. Renner Jr., MD, is the past president of the American Academy of Addiction Psychiatry and coeditor of Office-Based Buprenorphine Treatment of Opioid Use Disorder (American Psychiatric Association Publishing, 2018). Dr. Renner, who is a professor at Boston University, said, “I would like to see some evidence and research to be sure there were not unintended harms before we go this route.”
Eric C. Strain, MD, director of the Johns Hopkins Center for Substance Abuse Treatment and Research, Baltimore, noted: “Simply holding someone for 3 days, especially against their will, doesn’t make a lot of sense. They are certainly not going to be all better either from a physiological or psychological standpoint. It might, however, be possible to get a person who was not interested in treatment engaged in treatment, and that would be a success.”
Despite the increased numbers of beds and aggressive, thoughtful interventions, Massachusetts still had 1,450 overdose deaths in the first 9 months of 2017, a decrease of only 10% from the year before, according to the Globe article. For the sake of the former Little League players in Maryland, and all the other victims of this lethal nationwide epidemic, it is imperative that any untested treatments be the source of new research. If these measures are implemented, it is essential that Massachusetts follow the people who are the beneficiaries of interventions and create the data that allow other states to either follow suit if these efforts are successful, or allocate resources to other treatments if they are not.
Dr. Miller is coauthor with Annette Hanson, MD, of Committed: The Battle Over Involuntary Psychiatry Care (Baltimore: Johns Hopkins University Press, 2016).
My son played on a neighborhood little league team for several years. I have such sweet memories of little boys in baseball uniforms lined up on the bench singing cheers while they waited their turns to go to bat. The two devoted dads who worked together coaching the team were a gentle presence in the background of my family’s life every spring for years. One might hope that the love and attention those fathers invested in their sons and their teammates might confer some special protection from life’s tragedies, but the opioid epidemic spares no hostages, and last year, one of those singing little boys from so many years ago – the son of one of the coaches – died of a drug overdose.
President Trump has punted on how to stop the epidemic, one he finally deemed a national public health emergency in October, with no clear addition of federal resources. States have varied in their responses, and Massachusetts, in particular, has been aggressive with new legislation and funding. The laws in Massachusetts allow for involuntary rehab for substance abusers if a family member petitions the court under the state’s decades-old section 35. The irony is that much of this “involuntary” treatment is voluntary: People will ask family members to apply for them as a way of getting into treatment and as a way of bypassing the cost. Section 35 admissions are funded by the state, not by the individual or by health insurance.
As a Boston Globe article (“Mass. governor aims to expand battle against opioid addiction,” Nov. 15, 2017) explains, “Two years ago, Baker stirred controversy with a proposal to hold addicted patients for 72 hours against their will in emergency departments. That idea was rejected by the Legislature. The new bill takes a different approach to the 72-hour hold, enabling doctors to transfer patients with addiction to a treatment facility, much as they would with a person deemed a danger because of mental illness.”
The issues with involuntary care are complicated and nuanced in psychiatric disorders, and perhaps even more so with substance abuse. The time frame of 72 hours for mental health conditions allows for assessment and sometimes for the start of treatment. In some states, a hearing must be held for continued involuntary detention; in other states, a decision must be made as to whether further inpatient care will be pursued, and the actual hearing takes place days to weeks later, depending on the state. For the purposes of allowing someone to clear from an opioid intoxication, then persuading them to engage in voluntary substance abuse treatment, it seems that 72 hours could be the exact wrong time period.
Ideally, a patient would be placed in a comfortable inpatient unit, begun on medication-assisted withdrawal, and offered a high quality of care for those 72 hours so that continuing with treatment might be a palatable option. But would that actually happen? Does Massachusetts have the means and facilities for all its overdose patients? Massachusetts has, in fact, been aggressive with funding. Since 2015, the state has added 1,100 new treatment beds. The efforts to fund and offer novel treatments are commendable. My concern remains that without adequate treatment or a positive experience – a difficult target in the best of circumstances for a patient who is 72 hours into opioid withdrawal – patients would leave only to resume their substance abuse. In a disastrous scenario, patients who have overdosed and fear being detained might not call for help, and the death rate could actually rise.
John A. Renner Jr., MD, is the past president of the American Academy of Addiction Psychiatry and coeditor of Office-Based Buprenorphine Treatment of Opioid Use Disorder (American Psychiatric Association Publishing, 2018). Dr. Renner, who is a professor at Boston University, said, “I would like to see some evidence and research to be sure there were not unintended harms before we go this route.”
Eric C. Strain, MD, director of the Johns Hopkins Center for Substance Abuse Treatment and Research, Baltimore, noted: “Simply holding someone for 3 days, especially against their will, doesn’t make a lot of sense. They are certainly not going to be all better either from a physiological or psychological standpoint. It might, however, be possible to get a person who was not interested in treatment engaged in treatment, and that would be a success.”
Despite the increased numbers of beds and aggressive, thoughtful interventions, Massachusetts still had 1,450 overdose deaths in the first 9 months of 2017, a decrease of only 10% from the year before, according to the Globe article. For the sake of the former Little League players in Maryland, and all the other victims of this lethal nationwide epidemic, it is imperative that any untested treatments be the source of new research. If these measures are implemented, it is essential that Massachusetts follow the people who are the beneficiaries of interventions and create the data that allow other states to either follow suit if these efforts are successful, or allocate resources to other treatments if they are not.
Dr. Miller is coauthor with Annette Hanson, MD, of Committed: The Battle Over Involuntary Psychiatry Care (Baltimore: Johns Hopkins University Press, 2016).
Physician health programs: ‘Diagnosing for dollars’?
As medicine struggles with rising rates of physician burnout, dissatisfaction, depression, and suicide, one solution comes in the form of Physician Health Programs, or PHPs. These organizations were originally started by volunteer physicians, often doctors in recovery, and funded by medical societies, as a way of providing help while maintaining confidentiality. Now, they are run by independent corporations, by medical societies in some states, and sometimes by hospitals or health systems. The services they offer vary by PHP, and they may have relationships with state licensing boards. While they can provide a gateway to help for a troubled doctor, there has also been concern about the services that are being provided.
Louise Andrew, MD, JD, served as the liaison from the American College of Emergency Physicians (ACEP) to the the Federation of State Medical Boards from 2006 to 2014. In an online forum called Collective Wisdom, Andrew talked about the benefits of Physician Health Programs as entities that are helpful to stuggling doctors and urged her colleagues to use them as a safe alternative to suffering in silence.
More recently, Dr. Andrew has become concerned that PHPs may have taken on the role of what is more akin to “diagnosing for dollars.” In her May, 2016 column in Emergency Physician’s Monthly, Andrew noted, “A decade later, and my convictions have changed dramatically. Horror stories that colleagues related to me while I chaired ACEP’s Personal and Professional WellBeing Committee cannot all be isolated events. For example, physicians who self-referred to the PHP for management of stress and depression were reportedly railroaded into incredibly expensive and inconvenient out-of-state drug and alcohol treatment programs, even when there was no coexisting drug or alcohol problem.”
Dr. Andrew is not the only one voicing concerns about PHPs. In “Physician Health Programs: More harm than good?” (Medscape, Aug. 19, 2015), Pauline Anderson wrote about a several problems that have surfaced. In North Carolina, the state audited the PHPs after complaints that they were mandating physicians to lengthy and expensive inpatient programs. The complaints asserted that the physicians had no recourse and were not able to see their records. “The state auditor’s report found no abuse by North Carolina’s PHP. However, there was a caveat – the report determined that abuse could occur and potentially go undetected.
“It also found that the North Carolina PHP created the appearance of conflicts of interest by allowing the centers to provide both patient evaluation and treatments and that procedures did not ensure that physicians receive quality evaluations and treatment because the PHP had no documented criteria for selecting treatment centers and did not adequately monitor them.”
Finally, in a Florida Fox4News story, “Are FL doctors and nurses being sent to rehab unnecessarily? Accusations: Overdiagnosing; overcharging” (Nov. 16, 2017), reporters Katie Lagrone and Matthew Apthorp wrote about financial incentives for evaluators to refer doctors to inpatient substance abuse facilities.
The American Psychiatric Association has made it a priority to address physician burnout and mental health. Richard F. Summers, MD, APA Trustee-at-Large noted: “State PHPs are an essential resource for physicians, but there is a tremendous diversity in quality and approach. It is critical that these programs include attention to mental health problems as well as addiction, and that they support individual physicians’ treatment and journey toward well-being. They need to be accessible, private, and high quality, and they should be staffed by excellent psychiatrists and other mental health professionals.”
PHPs provide a much-needed and wanted service. But if the goal is to provide mental health and substance abuse services to physicians who are struggling – to prevent physicians from burning out, leaving medicine, and dying of suicide – then any whiff of corruption and any fear of professional repercussions become a reason not to use these services. If they are to be helpful, physicians must feel safe using them.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
As medicine struggles with rising rates of physician burnout, dissatisfaction, depression, and suicide, one solution comes in the form of Physician Health Programs, or PHPs. These organizations were originally started by volunteer physicians, often doctors in recovery, and funded by medical societies, as a way of providing help while maintaining confidentiality. Now, they are run by independent corporations, by medical societies in some states, and sometimes by hospitals or health systems. The services they offer vary by PHP, and they may have relationships with state licensing boards. While they can provide a gateway to help for a troubled doctor, there has also been concern about the services that are being provided.
Louise Andrew, MD, JD, served as the liaison from the American College of Emergency Physicians (ACEP) to the the Federation of State Medical Boards from 2006 to 2014. In an online forum called Collective Wisdom, Andrew talked about the benefits of Physician Health Programs as entities that are helpful to stuggling doctors and urged her colleagues to use them as a safe alternative to suffering in silence.
More recently, Dr. Andrew has become concerned that PHPs may have taken on the role of what is more akin to “diagnosing for dollars.” In her May, 2016 column in Emergency Physician’s Monthly, Andrew noted, “A decade later, and my convictions have changed dramatically. Horror stories that colleagues related to me while I chaired ACEP’s Personal and Professional WellBeing Committee cannot all be isolated events. For example, physicians who self-referred to the PHP for management of stress and depression were reportedly railroaded into incredibly expensive and inconvenient out-of-state drug and alcohol treatment programs, even when there was no coexisting drug or alcohol problem.”
Dr. Andrew is not the only one voicing concerns about PHPs. In “Physician Health Programs: More harm than good?” (Medscape, Aug. 19, 2015), Pauline Anderson wrote about a several problems that have surfaced. In North Carolina, the state audited the PHPs after complaints that they were mandating physicians to lengthy and expensive inpatient programs. The complaints asserted that the physicians had no recourse and were not able to see their records. “The state auditor’s report found no abuse by North Carolina’s PHP. However, there was a caveat – the report determined that abuse could occur and potentially go undetected.
“It also found that the North Carolina PHP created the appearance of conflicts of interest by allowing the centers to provide both patient evaluation and treatments and that procedures did not ensure that physicians receive quality evaluations and treatment because the PHP had no documented criteria for selecting treatment centers and did not adequately monitor them.”
Finally, in a Florida Fox4News story, “Are FL doctors and nurses being sent to rehab unnecessarily? Accusations: Overdiagnosing; overcharging” (Nov. 16, 2017), reporters Katie Lagrone and Matthew Apthorp wrote about financial incentives for evaluators to refer doctors to inpatient substance abuse facilities.
The American Psychiatric Association has made it a priority to address physician burnout and mental health. Richard F. Summers, MD, APA Trustee-at-Large noted: “State PHPs are an essential resource for physicians, but there is a tremendous diversity in quality and approach. It is critical that these programs include attention to mental health problems as well as addiction, and that they support individual physicians’ treatment and journey toward well-being. They need to be accessible, private, and high quality, and they should be staffed by excellent psychiatrists and other mental health professionals.”
PHPs provide a much-needed and wanted service. But if the goal is to provide mental health and substance abuse services to physicians who are struggling – to prevent physicians from burning out, leaving medicine, and dying of suicide – then any whiff of corruption and any fear of professional repercussions become a reason not to use these services. If they are to be helpful, physicians must feel safe using them.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
As medicine struggles with rising rates of physician burnout, dissatisfaction, depression, and suicide, one solution comes in the form of Physician Health Programs, or PHPs. These organizations were originally started by volunteer physicians, often doctors in recovery, and funded by medical societies, as a way of providing help while maintaining confidentiality. Now, they are run by independent corporations, by medical societies in some states, and sometimes by hospitals or health systems. The services they offer vary by PHP, and they may have relationships with state licensing boards. While they can provide a gateway to help for a troubled doctor, there has also been concern about the services that are being provided.
Louise Andrew, MD, JD, served as the liaison from the American College of Emergency Physicians (ACEP) to the the Federation of State Medical Boards from 2006 to 2014. In an online forum called Collective Wisdom, Andrew talked about the benefits of Physician Health Programs as entities that are helpful to stuggling doctors and urged her colleagues to use them as a safe alternative to suffering in silence.
More recently, Dr. Andrew has become concerned that PHPs may have taken on the role of what is more akin to “diagnosing for dollars.” In her May, 2016 column in Emergency Physician’s Monthly, Andrew noted, “A decade later, and my convictions have changed dramatically. Horror stories that colleagues related to me while I chaired ACEP’s Personal and Professional WellBeing Committee cannot all be isolated events. For example, physicians who self-referred to the PHP for management of stress and depression were reportedly railroaded into incredibly expensive and inconvenient out-of-state drug and alcohol treatment programs, even when there was no coexisting drug or alcohol problem.”
Dr. Andrew is not the only one voicing concerns about PHPs. In “Physician Health Programs: More harm than good?” (Medscape, Aug. 19, 2015), Pauline Anderson wrote about a several problems that have surfaced. In North Carolina, the state audited the PHPs after complaints that they were mandating physicians to lengthy and expensive inpatient programs. The complaints asserted that the physicians had no recourse and were not able to see their records. “The state auditor’s report found no abuse by North Carolina’s PHP. However, there was a caveat – the report determined that abuse could occur and potentially go undetected.
“It also found that the North Carolina PHP created the appearance of conflicts of interest by allowing the centers to provide both patient evaluation and treatments and that procedures did not ensure that physicians receive quality evaluations and treatment because the PHP had no documented criteria for selecting treatment centers and did not adequately monitor them.”
Finally, in a Florida Fox4News story, “Are FL doctors and nurses being sent to rehab unnecessarily? Accusations: Overdiagnosing; overcharging” (Nov. 16, 2017), reporters Katie Lagrone and Matthew Apthorp wrote about financial incentives for evaluators to refer doctors to inpatient substance abuse facilities.
The American Psychiatric Association has made it a priority to address physician burnout and mental health. Richard F. Summers, MD, APA Trustee-at-Large noted: “State PHPs are an essential resource for physicians, but there is a tremendous diversity in quality and approach. It is critical that these programs include attention to mental health problems as well as addiction, and that they support individual physicians’ treatment and journey toward well-being. They need to be accessible, private, and high quality, and they should be staffed by excellent psychiatrists and other mental health professionals.”
PHPs provide a much-needed and wanted service. But if the goal is to provide mental health and substance abuse services to physicians who are struggling – to prevent physicians from burning out, leaving medicine, and dying of suicide – then any whiff of corruption and any fear of professional repercussions become a reason not to use these services. If they are to be helpful, physicians must feel safe using them.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
#MeToo: Does it help?
I can still hear my mother saying these words: “Sticks and stones will break your bones but names will never hurt you.” It was a call for resilience, in a world that wasn’t always kind, but where the expectation was clear: I was to let insults roll off me.
We live in a different world now, one in which there are divisions between the good and the bad, where children have the right not to be called names by bullies. Our college students want safe spaces where they won’t hear offensive ideologies and trigger warnings if they are to be exposed to anything that may rekindle a past trauma.
If you’ve been following social media, then you might be familiar with the #MeToo topic that traveled after the public was made aware of the despicable, sexually aggressive behavior of acclaimed film executive Harvey Weinstein. Actress Alyssa Milano put out a call on social media: “Suggested by a friend: If all the women who have been sexually harassed or assaulted wrote ‘Me too’ as a status, we might give people a sense of the magnitude of the problem.” Others have noted that in medicine, it might well be that 100% of women have been harassed. The hashtag took off, and millions of people wrote #MeToo on their social media sites, including four female U.S. senators who told their stories.
On my personal Facebook page, I voiced a concern about the #MeToo tag. I noted that there were times when men had said some inappropriate things to me and I’d felt uncomfortable. I went on to write, “I don’t feel I was changed, harmed, or victimized by these uncomfortable advances, and I worry that by turning everyone into a victim of sexual harassment, then we detract from the stories of the women who were raped, molested, and those who were the victims of men who were maliciously taking advantage of a power differential. I don’t think we should dilute the message.” One friend (a woman) responded that if I felt uncomfortable, then I was harassed. Another friend (a man) responded that if I did not feel harmed, then I was not harassed.
With no clear definition, this does lead to the question of whether we might be turning everyone into victims and if that is good for our collective psyches. What we don’t seem to say is that if everyone is a victim of something – if not sexual assault or harassment, then something else – then doesn’t that also make everyone a perpetrator? Cam Newton, for instance, has been an advocate of kneeling to oppose institutional racism and, in terms of his own victimization, I would add that he also is the victim of a sport that now knowingly inflicts permanent and disabling brain damage on healthy young men. And now he is not just a victim, he is also a sexist perpetrator, unworthy of endorsing something as wholesome as yogurt.
Other concerns about the #MeToo campaign have also been expressed on social media. Might those who have been victimized feel pressured to publicly announce their victimization? Might the campaign trigger women to recall troubling events that were safely suppressed? While I would not personally use the terms “victimized,” “triggered,” or “harassed,” to describe myself, I would say that the campaign, like many things I see on social media, left me to think about events I had not considered in many years. That’s not necessarily bad: I like revisiting old memories, but others certainly may not. It does leave us to ask how we can live in a society where we can’t openly address our horrors for fear that the victims might be forced to relive them.
And what do we do about these issues with our patients? As a psychotherapist, I don’t live in a comfortable world. Patients often do and say things that make me personally uneasy, and I never considered the idea that I might be entitled to live without such discomfort. The mandate of psychotherapy for the patient is to talk openly about that which is on his or her mind and for the therapist to provide a safe space for thoughts that might be unacceptable in other settings. Patients talk of behaviors that make me worry for their safety. Some talk of sexual fantasies that are demeaning to others. Others are openly sexist, racist, anti-Semitic, or supportive of political ideologies that I strongly oppose. This can be hard work.
Was my mother right? Or was she dismissive? It was good that I always felt she was in my corner cheering me on. Obviously, it’s not just a saying, but a mindset that gets transmitted, sometimes successfully breeding resilience, and sometimes not. Certainly, I have seen that patients feel helped when I have validated their victimization. I have also seen people reassess their values when I have pointed out alternative ways about thinking about situations. I have not found it particularly helpful to tell people that their wounds are not so bad and others have it worse. While I don’t tell patients that sticks and stones will break their bones and names will never hurt them, I do sometimes gently tell them that I wish I could have them dipped in tin so that they would have stronger armor and so that the insensitive words of others might roll off without injuring them so. And as with all communications in our chaotic world, it’s often not the exact words that matter, but rather the context, the tone, and the intention with which they are said.
Sometimes, there really are clear victims and clear perpetrators, but in our world today, one can be both and the sides can be blurry. We are all trying to negotiate a society where words, spoken or unspoken, well-considered or not, have become weapons. Who gets to be comfortable and protected, we might ask, and who does not? Perhaps, in the end, we are left with the possibility that there are no safe spaces.
With thanks to Dr. Emile Bendit for considering the #MeToo hashtag with me.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The battle over involuntary psychiatric care” (Baltimore: Johns Hopkins University Press, 2016).
I can still hear my mother saying these words: “Sticks and stones will break your bones but names will never hurt you.” It was a call for resilience, in a world that wasn’t always kind, but where the expectation was clear: I was to let insults roll off me.
We live in a different world now, one in which there are divisions between the good and the bad, where children have the right not to be called names by bullies. Our college students want safe spaces where they won’t hear offensive ideologies and trigger warnings if they are to be exposed to anything that may rekindle a past trauma.
If you’ve been following social media, then you might be familiar with the #MeToo topic that traveled after the public was made aware of the despicable, sexually aggressive behavior of acclaimed film executive Harvey Weinstein. Actress Alyssa Milano put out a call on social media: “Suggested by a friend: If all the women who have been sexually harassed or assaulted wrote ‘Me too’ as a status, we might give people a sense of the magnitude of the problem.” Others have noted that in medicine, it might well be that 100% of women have been harassed. The hashtag took off, and millions of people wrote #MeToo on their social media sites, including four female U.S. senators who told their stories.
On my personal Facebook page, I voiced a concern about the #MeToo tag. I noted that there were times when men had said some inappropriate things to me and I’d felt uncomfortable. I went on to write, “I don’t feel I was changed, harmed, or victimized by these uncomfortable advances, and I worry that by turning everyone into a victim of sexual harassment, then we detract from the stories of the women who were raped, molested, and those who were the victims of men who were maliciously taking advantage of a power differential. I don’t think we should dilute the message.” One friend (a woman) responded that if I felt uncomfortable, then I was harassed. Another friend (a man) responded that if I did not feel harmed, then I was not harassed.
With no clear definition, this does lead to the question of whether we might be turning everyone into victims and if that is good for our collective psyches. What we don’t seem to say is that if everyone is a victim of something – if not sexual assault or harassment, then something else – then doesn’t that also make everyone a perpetrator? Cam Newton, for instance, has been an advocate of kneeling to oppose institutional racism and, in terms of his own victimization, I would add that he also is the victim of a sport that now knowingly inflicts permanent and disabling brain damage on healthy young men. And now he is not just a victim, he is also a sexist perpetrator, unworthy of endorsing something as wholesome as yogurt.
Other concerns about the #MeToo campaign have also been expressed on social media. Might those who have been victimized feel pressured to publicly announce their victimization? Might the campaign trigger women to recall troubling events that were safely suppressed? While I would not personally use the terms “victimized,” “triggered,” or “harassed,” to describe myself, I would say that the campaign, like many things I see on social media, left me to think about events I had not considered in many years. That’s not necessarily bad: I like revisiting old memories, but others certainly may not. It does leave us to ask how we can live in a society where we can’t openly address our horrors for fear that the victims might be forced to relive them.
And what do we do about these issues with our patients? As a psychotherapist, I don’t live in a comfortable world. Patients often do and say things that make me personally uneasy, and I never considered the idea that I might be entitled to live without such discomfort. The mandate of psychotherapy for the patient is to talk openly about that which is on his or her mind and for the therapist to provide a safe space for thoughts that might be unacceptable in other settings. Patients talk of behaviors that make me worry for their safety. Some talk of sexual fantasies that are demeaning to others. Others are openly sexist, racist, anti-Semitic, or supportive of political ideologies that I strongly oppose. This can be hard work.
Was my mother right? Or was she dismissive? It was good that I always felt she was in my corner cheering me on. Obviously, it’s not just a saying, but a mindset that gets transmitted, sometimes successfully breeding resilience, and sometimes not. Certainly, I have seen that patients feel helped when I have validated their victimization. I have also seen people reassess their values when I have pointed out alternative ways about thinking about situations. I have not found it particularly helpful to tell people that their wounds are not so bad and others have it worse. While I don’t tell patients that sticks and stones will break their bones and names will never hurt them, I do sometimes gently tell them that I wish I could have them dipped in tin so that they would have stronger armor and so that the insensitive words of others might roll off without injuring them so. And as with all communications in our chaotic world, it’s often not the exact words that matter, but rather the context, the tone, and the intention with which they are said.
Sometimes, there really are clear victims and clear perpetrators, but in our world today, one can be both and the sides can be blurry. We are all trying to negotiate a society where words, spoken or unspoken, well-considered or not, have become weapons. Who gets to be comfortable and protected, we might ask, and who does not? Perhaps, in the end, we are left with the possibility that there are no safe spaces.
With thanks to Dr. Emile Bendit for considering the #MeToo hashtag with me.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The battle over involuntary psychiatric care” (Baltimore: Johns Hopkins University Press, 2016).
I can still hear my mother saying these words: “Sticks and stones will break your bones but names will never hurt you.” It was a call for resilience, in a world that wasn’t always kind, but where the expectation was clear: I was to let insults roll off me.
We live in a different world now, one in which there are divisions between the good and the bad, where children have the right not to be called names by bullies. Our college students want safe spaces where they won’t hear offensive ideologies and trigger warnings if they are to be exposed to anything that may rekindle a past trauma.
If you’ve been following social media, then you might be familiar with the #MeToo topic that traveled after the public was made aware of the despicable, sexually aggressive behavior of acclaimed film executive Harvey Weinstein. Actress Alyssa Milano put out a call on social media: “Suggested by a friend: If all the women who have been sexually harassed or assaulted wrote ‘Me too’ as a status, we might give people a sense of the magnitude of the problem.” Others have noted that in medicine, it might well be that 100% of women have been harassed. The hashtag took off, and millions of people wrote #MeToo on their social media sites, including four female U.S. senators who told their stories.
On my personal Facebook page, I voiced a concern about the #MeToo tag. I noted that there were times when men had said some inappropriate things to me and I’d felt uncomfortable. I went on to write, “I don’t feel I was changed, harmed, or victimized by these uncomfortable advances, and I worry that by turning everyone into a victim of sexual harassment, then we detract from the stories of the women who were raped, molested, and those who were the victims of men who were maliciously taking advantage of a power differential. I don’t think we should dilute the message.” One friend (a woman) responded that if I felt uncomfortable, then I was harassed. Another friend (a man) responded that if I did not feel harmed, then I was not harassed.
With no clear definition, this does lead to the question of whether we might be turning everyone into victims and if that is good for our collective psyches. What we don’t seem to say is that if everyone is a victim of something – if not sexual assault or harassment, then something else – then doesn’t that also make everyone a perpetrator? Cam Newton, for instance, has been an advocate of kneeling to oppose institutional racism and, in terms of his own victimization, I would add that he also is the victim of a sport that now knowingly inflicts permanent and disabling brain damage on healthy young men. And now he is not just a victim, he is also a sexist perpetrator, unworthy of endorsing something as wholesome as yogurt.
Other concerns about the #MeToo campaign have also been expressed on social media. Might those who have been victimized feel pressured to publicly announce their victimization? Might the campaign trigger women to recall troubling events that were safely suppressed? While I would not personally use the terms “victimized,” “triggered,” or “harassed,” to describe myself, I would say that the campaign, like many things I see on social media, left me to think about events I had not considered in many years. That’s not necessarily bad: I like revisiting old memories, but others certainly may not. It does leave us to ask how we can live in a society where we can’t openly address our horrors for fear that the victims might be forced to relive them.
And what do we do about these issues with our patients? As a psychotherapist, I don’t live in a comfortable world. Patients often do and say things that make me personally uneasy, and I never considered the idea that I might be entitled to live without such discomfort. The mandate of psychotherapy for the patient is to talk openly about that which is on his or her mind and for the therapist to provide a safe space for thoughts that might be unacceptable in other settings. Patients talk of behaviors that make me worry for their safety. Some talk of sexual fantasies that are demeaning to others. Others are openly sexist, racist, anti-Semitic, or supportive of political ideologies that I strongly oppose. This can be hard work.
Was my mother right? Or was she dismissive? It was good that I always felt she was in my corner cheering me on. Obviously, it’s not just a saying, but a mindset that gets transmitted, sometimes successfully breeding resilience, and sometimes not. Certainly, I have seen that patients feel helped when I have validated their victimization. I have also seen people reassess their values when I have pointed out alternative ways about thinking about situations. I have not found it particularly helpful to tell people that their wounds are not so bad and others have it worse. While I don’t tell patients that sticks and stones will break their bones and names will never hurt them, I do sometimes gently tell them that I wish I could have them dipped in tin so that they would have stronger armor and so that the insensitive words of others might roll off without injuring them so. And as with all communications in our chaotic world, it’s often not the exact words that matter, but rather the context, the tone, and the intention with which they are said.
Sometimes, there really are clear victims and clear perpetrators, but in our world today, one can be both and the sides can be blurry. We are all trying to negotiate a society where words, spoken or unspoken, well-considered or not, have become weapons. Who gets to be comfortable and protected, we might ask, and who does not? Perhaps, in the end, we are left with the possibility that there are no safe spaces.
With thanks to Dr. Emile Bendit for considering the #MeToo hashtag with me.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The battle over involuntary psychiatric care” (Baltimore: Johns Hopkins University Press, 2016).