User login
The Hospitalist only
Hospitalist well-being during the COVID-19 crisis
The outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and the spread of COVID-19, is overwhelming for many people. Health care workers in the United States and around the world are leading the battle on the front lines of the pandemic. Thus, they experience a higher level of stress, fear, and anxiety during this crisis.
Over the course of weeks, hospitalists have reviewed articles, attended webinars, and discussed institutional strategies to respond to COVID-19. They follow the most up-to-date clinical information about the approach to patient care, conserving personal protective equipment (PPE), and guidance on how to talk to patients and families during crisis situations. The safety of hospitalists has been underscored with persistent advocacy from multiple organizations, for PPE, access to testing supplies, and decreasing any unnecessary exposure.
While it is agreed that the safety and well-being of hospital medicine teams is crucial to our society’s victory over COVID-19, very little has been discussed with regards to the “hospitalist” well-being and wellness during this pandemic.
The well-being of providers is essential to the success of a health care system. Many hospitalists already experience moral injury and showed evidence of provider burnout before COVID-19. With the onset of the pandemic, this will only get worse and burnout will accelerate if nothing is done to stop it. We cannot wait for the dust to settle to help our colleagues, we must act now.
Many providers have expressed similar pandemic fears, including, uncertainty about screening and testing capability, fear of the PPE shortage, fear of being exposed and underprepared, and fear of bringing the virus home and making family members sick. This list is not exclusive, and there are so many other factors that providers are internally processing, all while continuing their commitment to patient care and safety.
Practicing medicine comes with the heaviest of responsibilities, including the defense of the health of humanity. Therefore, it is easy to understand that, while providers are on the battlefield of this pandemic as they defend the health of humanity, they are not thinking of their own wellness or well-being. Moral injury describes the mental, emotional, and spiritual distress people feel after “perpetrating, failing to prevent, or bearing witness to acts that transgress deeply held moral beliefs and expectations.” This is already happening, with many hospitals in various cities running out of ventilators, lacking basic supplies for provider safety and leaving providers in survival mode on the front lines without their “suits of armor.” However, many providers will never recognize moral injury or burnout because they are focused on saving as many lives as possible with very limited resources.
While many websites can aid patient and community members on wellness during COVID-19, there is no specific forum or outlet for providers. We must give all hospital medicine team members a multimedia platform to address the fear, anxiety, and uncertainty of COVID-19. We must also provide them with techniques for resilience, coping strategies, and develop a network of support as the situation evolves, in real time.
We must remind hospitalists, “You may be scared, you may feel anxious, and that is okay. It is normal to have these feelings and it is healthy to acknowledge them. Fear serves as an important role in keeping us safe, but if left unchecked it can be horrifying and crippling. However, to conquer it we must face our fears together, with strategy, knowledge, and advocacy. This is the way to rebuild the current health care climate with confidence and trust.”
Although the world may seem foreign and dangerous, it is in adversity that we will find our strength as a hospital medicine community. We go to work every day because that is what we do. Your courage to come to work every day, in spite of any danger that it may present to you, is an inspiration to the world. The battle is not lost, and as individuals and as a community we must build resilience, inspire hope, and empower each other. We are stronger together than we are alone. As hospitalists around the country, and throughout the world, we must agree to uphold the moral integrity of medicine without sacrificing ourselves.
Dr. Williams is the vice-president of the Hampton Roads chapter of the Society of Hospital Medicine. She is a hospitalist at Sentara Careplex Hospital in Hampton, Va., where she also serves as the vice-president of the Medical Executive Committee.
Resource
Dean, Wendy; Talbot, Simon; and Dean, Austin. Reframing clinician distress: Moral injury not burnout. Fed Pract. 2019 Sept;36(9):400-2.
The outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and the spread of COVID-19, is overwhelming for many people. Health care workers in the United States and around the world are leading the battle on the front lines of the pandemic. Thus, they experience a higher level of stress, fear, and anxiety during this crisis.
Over the course of weeks, hospitalists have reviewed articles, attended webinars, and discussed institutional strategies to respond to COVID-19. They follow the most up-to-date clinical information about the approach to patient care, conserving personal protective equipment (PPE), and guidance on how to talk to patients and families during crisis situations. The safety of hospitalists has been underscored with persistent advocacy from multiple organizations, for PPE, access to testing supplies, and decreasing any unnecessary exposure.
While it is agreed that the safety and well-being of hospital medicine teams is crucial to our society’s victory over COVID-19, very little has been discussed with regards to the “hospitalist” well-being and wellness during this pandemic.
The well-being of providers is essential to the success of a health care system. Many hospitalists already experience moral injury and showed evidence of provider burnout before COVID-19. With the onset of the pandemic, this will only get worse and burnout will accelerate if nothing is done to stop it. We cannot wait for the dust to settle to help our colleagues, we must act now.
Many providers have expressed similar pandemic fears, including, uncertainty about screening and testing capability, fear of the PPE shortage, fear of being exposed and underprepared, and fear of bringing the virus home and making family members sick. This list is not exclusive, and there are so many other factors that providers are internally processing, all while continuing their commitment to patient care and safety.
Practicing medicine comes with the heaviest of responsibilities, including the defense of the health of humanity. Therefore, it is easy to understand that, while providers are on the battlefield of this pandemic as they defend the health of humanity, they are not thinking of their own wellness or well-being. Moral injury describes the mental, emotional, and spiritual distress people feel after “perpetrating, failing to prevent, or bearing witness to acts that transgress deeply held moral beliefs and expectations.” This is already happening, with many hospitals in various cities running out of ventilators, lacking basic supplies for provider safety and leaving providers in survival mode on the front lines without their “suits of armor.” However, many providers will never recognize moral injury or burnout because they are focused on saving as many lives as possible with very limited resources.
While many websites can aid patient and community members on wellness during COVID-19, there is no specific forum or outlet for providers. We must give all hospital medicine team members a multimedia platform to address the fear, anxiety, and uncertainty of COVID-19. We must also provide them with techniques for resilience, coping strategies, and develop a network of support as the situation evolves, in real time.
We must remind hospitalists, “You may be scared, you may feel anxious, and that is okay. It is normal to have these feelings and it is healthy to acknowledge them. Fear serves as an important role in keeping us safe, but if left unchecked it can be horrifying and crippling. However, to conquer it we must face our fears together, with strategy, knowledge, and advocacy. This is the way to rebuild the current health care climate with confidence and trust.”
Although the world may seem foreign and dangerous, it is in adversity that we will find our strength as a hospital medicine community. We go to work every day because that is what we do. Your courage to come to work every day, in spite of any danger that it may present to you, is an inspiration to the world. The battle is not lost, and as individuals and as a community we must build resilience, inspire hope, and empower each other. We are stronger together than we are alone. As hospitalists around the country, and throughout the world, we must agree to uphold the moral integrity of medicine without sacrificing ourselves.
Dr. Williams is the vice-president of the Hampton Roads chapter of the Society of Hospital Medicine. She is a hospitalist at Sentara Careplex Hospital in Hampton, Va., where she also serves as the vice-president of the Medical Executive Committee.
Resource
Dean, Wendy; Talbot, Simon; and Dean, Austin. Reframing clinician distress: Moral injury not burnout. Fed Pract. 2019 Sept;36(9):400-2.
The outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and the spread of COVID-19, is overwhelming for many people. Health care workers in the United States and around the world are leading the battle on the front lines of the pandemic. Thus, they experience a higher level of stress, fear, and anxiety during this crisis.
Over the course of weeks, hospitalists have reviewed articles, attended webinars, and discussed institutional strategies to respond to COVID-19. They follow the most up-to-date clinical information about the approach to patient care, conserving personal protective equipment (PPE), and guidance on how to talk to patients and families during crisis situations. The safety of hospitalists has been underscored with persistent advocacy from multiple organizations, for PPE, access to testing supplies, and decreasing any unnecessary exposure.
While it is agreed that the safety and well-being of hospital medicine teams is crucial to our society’s victory over COVID-19, very little has been discussed with regards to the “hospitalist” well-being and wellness during this pandemic.
The well-being of providers is essential to the success of a health care system. Many hospitalists already experience moral injury and showed evidence of provider burnout before COVID-19. With the onset of the pandemic, this will only get worse and burnout will accelerate if nothing is done to stop it. We cannot wait for the dust to settle to help our colleagues, we must act now.
Many providers have expressed similar pandemic fears, including, uncertainty about screening and testing capability, fear of the PPE shortage, fear of being exposed and underprepared, and fear of bringing the virus home and making family members sick. This list is not exclusive, and there are so many other factors that providers are internally processing, all while continuing their commitment to patient care and safety.
Practicing medicine comes with the heaviest of responsibilities, including the defense of the health of humanity. Therefore, it is easy to understand that, while providers are on the battlefield of this pandemic as they defend the health of humanity, they are not thinking of their own wellness or well-being. Moral injury describes the mental, emotional, and spiritual distress people feel after “perpetrating, failing to prevent, or bearing witness to acts that transgress deeply held moral beliefs and expectations.” This is already happening, with many hospitals in various cities running out of ventilators, lacking basic supplies for provider safety and leaving providers in survival mode on the front lines without their “suits of armor.” However, many providers will never recognize moral injury or burnout because they are focused on saving as many lives as possible with very limited resources.
While many websites can aid patient and community members on wellness during COVID-19, there is no specific forum or outlet for providers. We must give all hospital medicine team members a multimedia platform to address the fear, anxiety, and uncertainty of COVID-19. We must also provide them with techniques for resilience, coping strategies, and develop a network of support as the situation evolves, in real time.
We must remind hospitalists, “You may be scared, you may feel anxious, and that is okay. It is normal to have these feelings and it is healthy to acknowledge them. Fear serves as an important role in keeping us safe, but if left unchecked it can be horrifying and crippling. However, to conquer it we must face our fears together, with strategy, knowledge, and advocacy. This is the way to rebuild the current health care climate with confidence and trust.”
Although the world may seem foreign and dangerous, it is in adversity that we will find our strength as a hospital medicine community. We go to work every day because that is what we do. Your courage to come to work every day, in spite of any danger that it may present to you, is an inspiration to the world. The battle is not lost, and as individuals and as a community we must build resilience, inspire hope, and empower each other. We are stronger together than we are alone. As hospitalists around the country, and throughout the world, we must agree to uphold the moral integrity of medicine without sacrificing ourselves.
Dr. Williams is the vice-president of the Hampton Roads chapter of the Society of Hospital Medicine. She is a hospitalist at Sentara Careplex Hospital in Hampton, Va., where she also serves as the vice-president of the Medical Executive Committee.
Resource
Dean, Wendy; Talbot, Simon; and Dean, Austin. Reframing clinician distress: Moral injury not burnout. Fed Pract. 2019 Sept;36(9):400-2.
Call for volunteers for palliative care in COVID-19
While working in health care has never been easy, the COVID-19 pandemic has brought on an entirely new dimension to the challenges that clinicians face. Many of the daily concerns we once had now pale in comparison with the weight of this historic pandemic. Anxiety about the survival of our patients is compounded by our own physical and emotional exhaustion, concern for our loved ones, and fear for our own safety while on the front lines. Through this seemingly insurmountable array of challenges, survival mode kicks in. We come into the hospital every day, put on our mask and gowns, and focus on providing the care we’ve been trained for. That’s what we do best – keeping on.
However, the sheer volume of patients grows by the day, including those who are critically ill and ventilated. With hundreds of deaths every day in New York City, and ICUs filled beyond three times capacity, our frontline clinicians are overstretched, exhausted, and in need of additional help. Emergency codes are called overhead at staggering frequencies. Our colleagues on the front lines are unfortunately becoming sick themselves, and those who are healthy are working extra shifts, at a pace they can only keep up for so long.
The heartbreaking reality of this pandemic is that our connection with our patients and families is fading amid the chaos. Many infection prevention policies prohibit families from physically visiting the hospitals. The scariest parts of a hospitalization – gasping for air, before intubation, and the final moments before death – are tragically occurring alone. The support we are able to give occurs behind masks and fogged goggles. There’s not a clinician I know who doesn’t want better for patients and families – and we can mobilize to do so.
At NYC Health + Hospitals, the largest public health system in the United States, and a hot zone of the COVID-19 pandemic, we’ve taken major steps to mitigate this tragedy. Our palliative care clinicians have stepped up to help reconnect the patients with their families. We secured hundreds of tablets to enable video calls, and improved inpatient work flows to facilitate updates to families. We bolstered support from our palliative care clinicians to our ICU teams and are expanding capacity to initiate goals of care conversations earlier, through automatic triggers and proactive discussions with our hospitalist teams. Last but certainly not least, we are calling out across the country for our willing colleagues who can volunteer their time remotely via telehealth to support our patients, families, and staff here in NYC Health + Hospitals.
We have been encouraged by the resolve and commitment of our friends and colleagues from all corners of the country. NYC Health + Hospitals is receiving many brave volunteers who are rising to the call and assisting in whatever way they can. If you are proficient in goals-of-care conversations and/or trained in palliative care and willing, please sign up here to volunteer remotely via telemedicine. We are still in the beginning of this war; this struggle will continue for months even after public eye has turned away. Our patients and frontline staff need your help.
Thank you and stay safe.
Dr. Cho is chief value officer at NYC Health + Hospitals, and clinical associate professor of medicine at New York University. He is a member of the Hospitalist’s editorial advisory board. Ms. Israilov is the inaugural Quality and Safety Student Scholar at NYC Health + Hospitals. She is an MD candidate at the Icahn School of Medicine at Mount Sinai, New York.
While working in health care has never been easy, the COVID-19 pandemic has brought on an entirely new dimension to the challenges that clinicians face. Many of the daily concerns we once had now pale in comparison with the weight of this historic pandemic. Anxiety about the survival of our patients is compounded by our own physical and emotional exhaustion, concern for our loved ones, and fear for our own safety while on the front lines. Through this seemingly insurmountable array of challenges, survival mode kicks in. We come into the hospital every day, put on our mask and gowns, and focus on providing the care we’ve been trained for. That’s what we do best – keeping on.
However, the sheer volume of patients grows by the day, including those who are critically ill and ventilated. With hundreds of deaths every day in New York City, and ICUs filled beyond three times capacity, our frontline clinicians are overstretched, exhausted, and in need of additional help. Emergency codes are called overhead at staggering frequencies. Our colleagues on the front lines are unfortunately becoming sick themselves, and those who are healthy are working extra shifts, at a pace they can only keep up for so long.
The heartbreaking reality of this pandemic is that our connection with our patients and families is fading amid the chaos. Many infection prevention policies prohibit families from physically visiting the hospitals. The scariest parts of a hospitalization – gasping for air, before intubation, and the final moments before death – are tragically occurring alone. The support we are able to give occurs behind masks and fogged goggles. There’s not a clinician I know who doesn’t want better for patients and families – and we can mobilize to do so.
At NYC Health + Hospitals, the largest public health system in the United States, and a hot zone of the COVID-19 pandemic, we’ve taken major steps to mitigate this tragedy. Our palliative care clinicians have stepped up to help reconnect the patients with their families. We secured hundreds of tablets to enable video calls, and improved inpatient work flows to facilitate updates to families. We bolstered support from our palliative care clinicians to our ICU teams and are expanding capacity to initiate goals of care conversations earlier, through automatic triggers and proactive discussions with our hospitalist teams. Last but certainly not least, we are calling out across the country for our willing colleagues who can volunteer their time remotely via telehealth to support our patients, families, and staff here in NYC Health + Hospitals.
We have been encouraged by the resolve and commitment of our friends and colleagues from all corners of the country. NYC Health + Hospitals is receiving many brave volunteers who are rising to the call and assisting in whatever way they can. If you are proficient in goals-of-care conversations and/or trained in palliative care and willing, please sign up here to volunteer remotely via telemedicine. We are still in the beginning of this war; this struggle will continue for months even after public eye has turned away. Our patients and frontline staff need your help.
Thank you and stay safe.
Dr. Cho is chief value officer at NYC Health + Hospitals, and clinical associate professor of medicine at New York University. He is a member of the Hospitalist’s editorial advisory board. Ms. Israilov is the inaugural Quality and Safety Student Scholar at NYC Health + Hospitals. She is an MD candidate at the Icahn School of Medicine at Mount Sinai, New York.
While working in health care has never been easy, the COVID-19 pandemic has brought on an entirely new dimension to the challenges that clinicians face. Many of the daily concerns we once had now pale in comparison with the weight of this historic pandemic. Anxiety about the survival of our patients is compounded by our own physical and emotional exhaustion, concern for our loved ones, and fear for our own safety while on the front lines. Through this seemingly insurmountable array of challenges, survival mode kicks in. We come into the hospital every day, put on our mask and gowns, and focus on providing the care we’ve been trained for. That’s what we do best – keeping on.
However, the sheer volume of patients grows by the day, including those who are critically ill and ventilated. With hundreds of deaths every day in New York City, and ICUs filled beyond three times capacity, our frontline clinicians are overstretched, exhausted, and in need of additional help. Emergency codes are called overhead at staggering frequencies. Our colleagues on the front lines are unfortunately becoming sick themselves, and those who are healthy are working extra shifts, at a pace they can only keep up for so long.
The heartbreaking reality of this pandemic is that our connection with our patients and families is fading amid the chaos. Many infection prevention policies prohibit families from physically visiting the hospitals. The scariest parts of a hospitalization – gasping for air, before intubation, and the final moments before death – are tragically occurring alone. The support we are able to give occurs behind masks and fogged goggles. There’s not a clinician I know who doesn’t want better for patients and families – and we can mobilize to do so.
At NYC Health + Hospitals, the largest public health system in the United States, and a hot zone of the COVID-19 pandemic, we’ve taken major steps to mitigate this tragedy. Our palliative care clinicians have stepped up to help reconnect the patients with their families. We secured hundreds of tablets to enable video calls, and improved inpatient work flows to facilitate updates to families. We bolstered support from our palliative care clinicians to our ICU teams and are expanding capacity to initiate goals of care conversations earlier, through automatic triggers and proactive discussions with our hospitalist teams. Last but certainly not least, we are calling out across the country for our willing colleagues who can volunteer their time remotely via telehealth to support our patients, families, and staff here in NYC Health + Hospitals.
We have been encouraged by the resolve and commitment of our friends and colleagues from all corners of the country. NYC Health + Hospitals is receiving many brave volunteers who are rising to the call and assisting in whatever way they can. If you are proficient in goals-of-care conversations and/or trained in palliative care and willing, please sign up here to volunteer remotely via telemedicine. We are still in the beginning of this war; this struggle will continue for months even after public eye has turned away. Our patients and frontline staff need your help.
Thank you and stay safe.
Dr. Cho is chief value officer at NYC Health + Hospitals, and clinical associate professor of medicine at New York University. He is a member of the Hospitalist’s editorial advisory board. Ms. Israilov is the inaugural Quality and Safety Student Scholar at NYC Health + Hospitals. She is an MD candidate at the Icahn School of Medicine at Mount Sinai, New York.
Social distancing comes to the medicine wards
As the coronavirus pandemic has swept across America, so have advisories for social distancing. As of April 2, stay-at-home orders had been given in 38 states and parts of 7 more, affecting about 300 million people. Most of these people have been asked to maintain 6 feet of separation to anyone outside their immediate family and to avoid all avoidable contacts.
Typical hospital medicine patients at an academic hospital, however, traditionally receive visits from their hospitalist, an intern, a resident, and sometimes several medical students, pharmacists, and case managers. At University of California, San Diego, Health, many of these visits would occur during Focused Interdisciplinary Team rounds, with providers moving together in close proximity.
Asymptomatic and presymptomatic spread of coronavirus have been documented, which means distancing is a good idea for everyone. The risks of traditional patient visits during the coronavirus pandemic include spread to both patients (at high risk of complications) and staff (taken out of the workforce during surge times). Even if coronavirus were not a risk, visits to isolation rooms consume PPE, which is in short supply.
In response to the pandemic, UCSD Hospital Medicine drafted guidelines for the reduction of patient contacts. Our slide presentations and written guidelines were then distributed to physicians, nurses, pharmacists, and other staff by our pandemic response command center. Key points include the following:
- Target one in-person MD visit per day for stable patients. This means that attending reexaminations of patients seen by residents, nurse practitioners, physician assistants, and so on would not be done for billing or teaching purposes, only when clinically necessary.
- Use phone or video conferencing for follow-up discussions unless direct patient contact is needed.
- Consider skipping daily exams on patients who do not require them, such as patients awaiting placement or stably receiving long courses of antibiotics. Interview them remotely or from the door instead.
- Conduct team rounds, patient discussions, and handoffs with all members 6 feet apart or by telephone or video. Avoid shared work rooms. Substitute video conferences for in-person meetings. Use EMR embedded messaging to reduce face-to-face discussions.
- Check if a patient is ready for a visit before donning PPE to avoid waste.
- Explain to patients that distancing is being conducted to protect them. In our experience, when patients are asked about distancing, they welcome the changes.
We have also considered that most patient visits are generated by nurses and assistants. To increase distancing and reduce PPE waste, we have encouraged nurses and pharmacists to maximize their use of remote communication with patients and to suggest changes to care plans and come up with creative solutions to reduce traffic. We specifically suggested the following changes to routine care:
- Reduce frequency of taking vital signs, such as just daily or as needed, in stable patients (for example, those awaiting placement).
- Reduce checks for alcohol withdrawal and neurologic status as soon as possible, and stop fingersticks in patients with well-controlled diabetes not receiving insulin.
- Substitute less frequently administered medications where appropriate if doing so would reduce room traffic (such as enoxaparin for heparin, ceftriaxone for cefazolin, naproxen for ibuprofen, or patient-controlled analgesia for as needed morphine).
- Place intravenous pumps in halls if needed – luckily, our situation has not required these measures in San Diego.
- Explore the possibility of increased patient self-management (self-dosed insulin or inhalers) where medically appropriate.
- Eliminate food service and janitorial trips to isolation rooms unless requested by registered nurse.
There are clear downsides to medical distancing for hospital medicine patients. Patients might have delayed diagnosis of new conditions or inadequate management of conditions requiring frequent assessment, such as alcohol withdrawal. Opportunities for miscommunication (either patient-provider or provider-provider) may be increased with distancing. Isolation also comes with emotional costs such as stress and feelings of isolation or abandonment. Given the dynamic nature of the pandemic response, we are continually reevaluating our distancing guidelines to administer the safest and most effective hospital care possible as we approach California’s expected peak coronavirus infection period.
Dr. Jenkins is professor and chair of the Patient Safety Committee in the Division of Hospital Medicine at UCSD. Dr. Seymann is clinical professor and vice chief for academic affairs, UCSD division of hospital medicine. Dr. Horman and Dr. Bell are hospitalists and associate professors of medicine at UC San Diego Health.
As the coronavirus pandemic has swept across America, so have advisories for social distancing. As of April 2, stay-at-home orders had been given in 38 states and parts of 7 more, affecting about 300 million people. Most of these people have been asked to maintain 6 feet of separation to anyone outside their immediate family and to avoid all avoidable contacts.
Typical hospital medicine patients at an academic hospital, however, traditionally receive visits from their hospitalist, an intern, a resident, and sometimes several medical students, pharmacists, and case managers. At University of California, San Diego, Health, many of these visits would occur during Focused Interdisciplinary Team rounds, with providers moving together in close proximity.
Asymptomatic and presymptomatic spread of coronavirus have been documented, which means distancing is a good idea for everyone. The risks of traditional patient visits during the coronavirus pandemic include spread to both patients (at high risk of complications) and staff (taken out of the workforce during surge times). Even if coronavirus were not a risk, visits to isolation rooms consume PPE, which is in short supply.
In response to the pandemic, UCSD Hospital Medicine drafted guidelines for the reduction of patient contacts. Our slide presentations and written guidelines were then distributed to physicians, nurses, pharmacists, and other staff by our pandemic response command center. Key points include the following:
- Target one in-person MD visit per day for stable patients. This means that attending reexaminations of patients seen by residents, nurse practitioners, physician assistants, and so on would not be done for billing or teaching purposes, only when clinically necessary.
- Use phone or video conferencing for follow-up discussions unless direct patient contact is needed.
- Consider skipping daily exams on patients who do not require them, such as patients awaiting placement or stably receiving long courses of antibiotics. Interview them remotely or from the door instead.
- Conduct team rounds, patient discussions, and handoffs with all members 6 feet apart or by telephone or video. Avoid shared work rooms. Substitute video conferences for in-person meetings. Use EMR embedded messaging to reduce face-to-face discussions.
- Check if a patient is ready for a visit before donning PPE to avoid waste.
- Explain to patients that distancing is being conducted to protect them. In our experience, when patients are asked about distancing, they welcome the changes.
We have also considered that most patient visits are generated by nurses and assistants. To increase distancing and reduce PPE waste, we have encouraged nurses and pharmacists to maximize their use of remote communication with patients and to suggest changes to care plans and come up with creative solutions to reduce traffic. We specifically suggested the following changes to routine care:
- Reduce frequency of taking vital signs, such as just daily or as needed, in stable patients (for example, those awaiting placement).
- Reduce checks for alcohol withdrawal and neurologic status as soon as possible, and stop fingersticks in patients with well-controlled diabetes not receiving insulin.
- Substitute less frequently administered medications where appropriate if doing so would reduce room traffic (such as enoxaparin for heparin, ceftriaxone for cefazolin, naproxen for ibuprofen, or patient-controlled analgesia for as needed morphine).
- Place intravenous pumps in halls if needed – luckily, our situation has not required these measures in San Diego.
- Explore the possibility of increased patient self-management (self-dosed insulin or inhalers) where medically appropriate.
- Eliminate food service and janitorial trips to isolation rooms unless requested by registered nurse.
There are clear downsides to medical distancing for hospital medicine patients. Patients might have delayed diagnosis of new conditions or inadequate management of conditions requiring frequent assessment, such as alcohol withdrawal. Opportunities for miscommunication (either patient-provider or provider-provider) may be increased with distancing. Isolation also comes with emotional costs such as stress and feelings of isolation or abandonment. Given the dynamic nature of the pandemic response, we are continually reevaluating our distancing guidelines to administer the safest and most effective hospital care possible as we approach California’s expected peak coronavirus infection period.
Dr. Jenkins is professor and chair of the Patient Safety Committee in the Division of Hospital Medicine at UCSD. Dr. Seymann is clinical professor and vice chief for academic affairs, UCSD division of hospital medicine. Dr. Horman and Dr. Bell are hospitalists and associate professors of medicine at UC San Diego Health.
As the coronavirus pandemic has swept across America, so have advisories for social distancing. As of April 2, stay-at-home orders had been given in 38 states and parts of 7 more, affecting about 300 million people. Most of these people have been asked to maintain 6 feet of separation to anyone outside their immediate family and to avoid all avoidable contacts.
Typical hospital medicine patients at an academic hospital, however, traditionally receive visits from their hospitalist, an intern, a resident, and sometimes several medical students, pharmacists, and case managers. At University of California, San Diego, Health, many of these visits would occur during Focused Interdisciplinary Team rounds, with providers moving together in close proximity.
Asymptomatic and presymptomatic spread of coronavirus have been documented, which means distancing is a good idea for everyone. The risks of traditional patient visits during the coronavirus pandemic include spread to both patients (at high risk of complications) and staff (taken out of the workforce during surge times). Even if coronavirus were not a risk, visits to isolation rooms consume PPE, which is in short supply.
In response to the pandemic, UCSD Hospital Medicine drafted guidelines for the reduction of patient contacts. Our slide presentations and written guidelines were then distributed to physicians, nurses, pharmacists, and other staff by our pandemic response command center. Key points include the following:
- Target one in-person MD visit per day for stable patients. This means that attending reexaminations of patients seen by residents, nurse practitioners, physician assistants, and so on would not be done for billing or teaching purposes, only when clinically necessary.
- Use phone or video conferencing for follow-up discussions unless direct patient contact is needed.
- Consider skipping daily exams on patients who do not require them, such as patients awaiting placement or stably receiving long courses of antibiotics. Interview them remotely or from the door instead.
- Conduct team rounds, patient discussions, and handoffs with all members 6 feet apart or by telephone or video. Avoid shared work rooms. Substitute video conferences for in-person meetings. Use EMR embedded messaging to reduce face-to-face discussions.
- Check if a patient is ready for a visit before donning PPE to avoid waste.
- Explain to patients that distancing is being conducted to protect them. In our experience, when patients are asked about distancing, they welcome the changes.
We have also considered that most patient visits are generated by nurses and assistants. To increase distancing and reduce PPE waste, we have encouraged nurses and pharmacists to maximize their use of remote communication with patients and to suggest changes to care plans and come up with creative solutions to reduce traffic. We specifically suggested the following changes to routine care:
- Reduce frequency of taking vital signs, such as just daily or as needed, in stable patients (for example, those awaiting placement).
- Reduce checks for alcohol withdrawal and neurologic status as soon as possible, and stop fingersticks in patients with well-controlled diabetes not receiving insulin.
- Substitute less frequently administered medications where appropriate if doing so would reduce room traffic (such as enoxaparin for heparin, ceftriaxone for cefazolin, naproxen for ibuprofen, or patient-controlled analgesia for as needed morphine).
- Place intravenous pumps in halls if needed – luckily, our situation has not required these measures in San Diego.
- Explore the possibility of increased patient self-management (self-dosed insulin or inhalers) where medically appropriate.
- Eliminate food service and janitorial trips to isolation rooms unless requested by registered nurse.
There are clear downsides to medical distancing for hospital medicine patients. Patients might have delayed diagnosis of new conditions or inadequate management of conditions requiring frequent assessment, such as alcohol withdrawal. Opportunities for miscommunication (either patient-provider or provider-provider) may be increased with distancing. Isolation also comes with emotional costs such as stress and feelings of isolation or abandonment. Given the dynamic nature of the pandemic response, we are continually reevaluating our distancing guidelines to administer the safest and most effective hospital care possible as we approach California’s expected peak coronavirus infection period.
Dr. Jenkins is professor and chair of the Patient Safety Committee in the Division of Hospital Medicine at UCSD. Dr. Seymann is clinical professor and vice chief for academic affairs, UCSD division of hospital medicine. Dr. Horman and Dr. Bell are hospitalists and associate professors of medicine at UC San Diego Health.
AMA asks HHS for ‘immediate’ aid to ease clinicians’ COVID-19 ‘financial peril’
The American Medical Association (AMA) along with scores of specialty and state medical societies are asking the Trump administration to help the nation’s clinicians out with an immediate cash infusion that they say they need to sustain their practices, many of which have been crippled by the COVID-19 crisis.
In an April 7 letter to Secretary of US Department of Health and Human Services (HHS) Alex Azar, the AMA, backed by 137 medical groups, made the case for “immediate financial assistance” from the government for all US physicians and nurse practitioners and physician assistants enrolled in Medicare or Medicaid. These payments would be equal to roughly 1 month’s worth of prepandemic revenue from all payers.
Under the methodology laid out in the letter, HHS would use an individual clinician’s average monthly Medicare payment from October to December 2019 to determine their precrisis monthly revenue.
Because Medicare business generates an average of 35% of practice revenue in most specialties, the letter suggests that HHS triple the monthly Medicare payment to calculate the amount of emergency funding it should provide to each clinician.
The letter acknowledges that this approach wouldn’t work for certain specialties, such as psychiatry, allergy/immunology, obstetrics/gynecology, and pediatrics, which derive far less revenue from Medicare than other specialties do. These physicians’ payouts “should be adjusted upward accordingly,” the letter states.
“Physicians are continuing to put their patients’ needs first to combat this unprecedented public health emergency,” the AMA writes. “We urge you to support them against financial peril while they put their lives and businesses at risk.”
Other Emergency Funding Programs
These disbursements would be separate from the $30 billion in direct provider payments announced on April 7 by Seema Verma, the administrator of the Centers for Medicare and Medicaid Services (CMS). Because these payments are based on Medicare volume, the vast majority of this money is expected to go to hospitals.
The government is also providing financial support to hospitals, physicians, and other clinicians affected by the pandemic through CMS’s accelerated/advance payment program, as reported by Medscape Medical News. Physician practices can apply to receive upfront payments equal to 3 months’ worth of their historical Medicare payments, but they must pay back these loans, starting at 120 days after receiving them.
In addition, providers with less than 500 employees can apply for Small Business Administration (SBA) loans that were authorized by the CURES Act. If they use at least 75% of this money to cover payroll costs, the loans will be forgiven.
Medical leaders defended their request for direct physician relief in excess of what these three government programs are offering.
“From the very beginning, the AMA has been advocating for [financial] support for physician practices,” AMA President Patrice Harris, MD, told Medscape Medical News. “It’s not an either/or, it’s not a choice between hospitals or physician practices, it’s both.”
She made it clear that this applied not only to the direct payments that the CURES Act allocated to healthcare providers, but also to the SBA loans.
“We’ve been pleased to see support through the Small Business Administration, and we know that many practices have applied for loans,” Harris said. “We’ll review this, because physician practices have to be included.”
Thus far, she added, “I haven’t heard of anyone [in a medical practice] who has actually received a loan. We’ll be monitoring that, because that will be key.”
Likewise, Robert Doherty, senior vice president of governmental affairs and public policy for the American College of Physicians (ACP), said he hadn’t heard of any practices receiving SBA loans, although many have applied.
What he has heard is that “people couldn’t even get through the SBA process and the website was freezing up. They also have to find a lender, submit documentation and get approved by the lender. And they’re competing with all the other small businesses” for a finite amount of money.
Doherty said it was unclear how many practices have received advance payments from CMS so far. CMS said it disbursed $34 billion in these payments in the first week of the program. These went to over 17,000 of the more than 25,000 applicants, CMS noted.
The ACP – which joined the AMA in its request to HHS – supports the advanced-payment program, Doherty added, but “a loan is a loan. You have to repay it. It brings in cash now, but it means you don’t have cash a few months from now. That’s different from what we’re recommending, which is an infusion of cash to practices that wouldn’t have to be repaid.”
Another advantage of the AMA-led proposal, he said, is its simplicity. It’s based on data that CMS already has, and it doesn’t require physicians to fill out forms or provide documents.
In contrast, he said, “We don’t think HHS would have the ability to process applications from thousands and thousands of physicians [for direct payments]. To create a situation where they’d have to review applications from physicians for funding out of that [CARES Act] emergency fund is probably almost impossible for HHS to administer effectively.”
Most Practices Need Help
While the medical societies’ letter makes a strong pitch for supporting physicians who are combating COVID-19, Harris and Doherty noted that physicians in all kinds of practice situations desperately need this help.
“We’ve heard from many physician practices that they have trouble making payroll,” Doherty said. “Many of them are not seeking any money out of the practices for themselves right now. They’re just trying to keep their staff employed. And some will shut their doors, unless there’s a significant and immediate infusion of money to them. From a healthcare capacity viewpoint, it’s not going to be to anyone’s benefit to see a substantial number of practices laying off staff or closing up entirely because they don’t have the money coming in to keep the doors open,” he said.
Harris agreed. “We’re hearing from practices large and small all over the country, including solo practices. Even the larger practices are losing revenue,” she pointed out. “They appropriately shut down their offices or reduced their hours. They didn’t want to contribute to the further spread of COVID-19.”
Rural practices and those launched by young physicians are facing especially difficult challenges, Harris added, and some may not make it.
It’s also important for policy makers to look ahead to what lies after the pandemic, she said. “We will come out of this, but when we come out of it there will be a lot of pent-up or unmet need where folks delayed necessary visits. Physicians and practices will have to be ready to go. If practices have to furlough some staff, it’s going to take time to ramp that up. So we’re glad to see support of physician practices so the infrastructure is strong when we start again.”
What happens if HHS turns down the medical societies’ request? “We’re hopeful that the [HHS] secretary will agree to what we’re asking,” Doherty said. While it’s always possible to ask Congress to intervene in the next stimulus bill, he said, that wouldn’t happen fast enough to get the money to physicians when they really need it.
This article first appeared on Medscape.com.
The American Medical Association (AMA) along with scores of specialty and state medical societies are asking the Trump administration to help the nation’s clinicians out with an immediate cash infusion that they say they need to sustain their practices, many of which have been crippled by the COVID-19 crisis.
In an April 7 letter to Secretary of US Department of Health and Human Services (HHS) Alex Azar, the AMA, backed by 137 medical groups, made the case for “immediate financial assistance” from the government for all US physicians and nurse practitioners and physician assistants enrolled in Medicare or Medicaid. These payments would be equal to roughly 1 month’s worth of prepandemic revenue from all payers.
Under the methodology laid out in the letter, HHS would use an individual clinician’s average monthly Medicare payment from October to December 2019 to determine their precrisis monthly revenue.
Because Medicare business generates an average of 35% of practice revenue in most specialties, the letter suggests that HHS triple the monthly Medicare payment to calculate the amount of emergency funding it should provide to each clinician.
The letter acknowledges that this approach wouldn’t work for certain specialties, such as psychiatry, allergy/immunology, obstetrics/gynecology, and pediatrics, which derive far less revenue from Medicare than other specialties do. These physicians’ payouts “should be adjusted upward accordingly,” the letter states.
“Physicians are continuing to put their patients’ needs first to combat this unprecedented public health emergency,” the AMA writes. “We urge you to support them against financial peril while they put their lives and businesses at risk.”
Other Emergency Funding Programs
These disbursements would be separate from the $30 billion in direct provider payments announced on April 7 by Seema Verma, the administrator of the Centers for Medicare and Medicaid Services (CMS). Because these payments are based on Medicare volume, the vast majority of this money is expected to go to hospitals.
The government is also providing financial support to hospitals, physicians, and other clinicians affected by the pandemic through CMS’s accelerated/advance payment program, as reported by Medscape Medical News. Physician practices can apply to receive upfront payments equal to 3 months’ worth of their historical Medicare payments, but they must pay back these loans, starting at 120 days after receiving them.
In addition, providers with less than 500 employees can apply for Small Business Administration (SBA) loans that were authorized by the CURES Act. If they use at least 75% of this money to cover payroll costs, the loans will be forgiven.
Medical leaders defended their request for direct physician relief in excess of what these three government programs are offering.
“From the very beginning, the AMA has been advocating for [financial] support for physician practices,” AMA President Patrice Harris, MD, told Medscape Medical News. “It’s not an either/or, it’s not a choice between hospitals or physician practices, it’s both.”
She made it clear that this applied not only to the direct payments that the CURES Act allocated to healthcare providers, but also to the SBA loans.
“We’ve been pleased to see support through the Small Business Administration, and we know that many practices have applied for loans,” Harris said. “We’ll review this, because physician practices have to be included.”
Thus far, she added, “I haven’t heard of anyone [in a medical practice] who has actually received a loan. We’ll be monitoring that, because that will be key.”
Likewise, Robert Doherty, senior vice president of governmental affairs and public policy for the American College of Physicians (ACP), said he hadn’t heard of any practices receiving SBA loans, although many have applied.
What he has heard is that “people couldn’t even get through the SBA process and the website was freezing up. They also have to find a lender, submit documentation and get approved by the lender. And they’re competing with all the other small businesses” for a finite amount of money.
Doherty said it was unclear how many practices have received advance payments from CMS so far. CMS said it disbursed $34 billion in these payments in the first week of the program. These went to over 17,000 of the more than 25,000 applicants, CMS noted.
The ACP – which joined the AMA in its request to HHS – supports the advanced-payment program, Doherty added, but “a loan is a loan. You have to repay it. It brings in cash now, but it means you don’t have cash a few months from now. That’s different from what we’re recommending, which is an infusion of cash to practices that wouldn’t have to be repaid.”
Another advantage of the AMA-led proposal, he said, is its simplicity. It’s based on data that CMS already has, and it doesn’t require physicians to fill out forms or provide documents.
In contrast, he said, “We don’t think HHS would have the ability to process applications from thousands and thousands of physicians [for direct payments]. To create a situation where they’d have to review applications from physicians for funding out of that [CARES Act] emergency fund is probably almost impossible for HHS to administer effectively.”
Most Practices Need Help
While the medical societies’ letter makes a strong pitch for supporting physicians who are combating COVID-19, Harris and Doherty noted that physicians in all kinds of practice situations desperately need this help.
“We’ve heard from many physician practices that they have trouble making payroll,” Doherty said. “Many of them are not seeking any money out of the practices for themselves right now. They’re just trying to keep their staff employed. And some will shut their doors, unless there’s a significant and immediate infusion of money to them. From a healthcare capacity viewpoint, it’s not going to be to anyone’s benefit to see a substantial number of practices laying off staff or closing up entirely because they don’t have the money coming in to keep the doors open,” he said.
Harris agreed. “We’re hearing from practices large and small all over the country, including solo practices. Even the larger practices are losing revenue,” she pointed out. “They appropriately shut down their offices or reduced their hours. They didn’t want to contribute to the further spread of COVID-19.”
Rural practices and those launched by young physicians are facing especially difficult challenges, Harris added, and some may not make it.
It’s also important for policy makers to look ahead to what lies after the pandemic, she said. “We will come out of this, but when we come out of it there will be a lot of pent-up or unmet need where folks delayed necessary visits. Physicians and practices will have to be ready to go. If practices have to furlough some staff, it’s going to take time to ramp that up. So we’re glad to see support of physician practices so the infrastructure is strong when we start again.”
What happens if HHS turns down the medical societies’ request? “We’re hopeful that the [HHS] secretary will agree to what we’re asking,” Doherty said. While it’s always possible to ask Congress to intervene in the next stimulus bill, he said, that wouldn’t happen fast enough to get the money to physicians when they really need it.
This article first appeared on Medscape.com.
The American Medical Association (AMA) along with scores of specialty and state medical societies are asking the Trump administration to help the nation’s clinicians out with an immediate cash infusion that they say they need to sustain their practices, many of which have been crippled by the COVID-19 crisis.
In an April 7 letter to Secretary of US Department of Health and Human Services (HHS) Alex Azar, the AMA, backed by 137 medical groups, made the case for “immediate financial assistance” from the government for all US physicians and nurse practitioners and physician assistants enrolled in Medicare or Medicaid. These payments would be equal to roughly 1 month’s worth of prepandemic revenue from all payers.
Under the methodology laid out in the letter, HHS would use an individual clinician’s average monthly Medicare payment from October to December 2019 to determine their precrisis monthly revenue.
Because Medicare business generates an average of 35% of practice revenue in most specialties, the letter suggests that HHS triple the monthly Medicare payment to calculate the amount of emergency funding it should provide to each clinician.
The letter acknowledges that this approach wouldn’t work for certain specialties, such as psychiatry, allergy/immunology, obstetrics/gynecology, and pediatrics, which derive far less revenue from Medicare than other specialties do. These physicians’ payouts “should be adjusted upward accordingly,” the letter states.
“Physicians are continuing to put their patients’ needs first to combat this unprecedented public health emergency,” the AMA writes. “We urge you to support them against financial peril while they put their lives and businesses at risk.”
Other Emergency Funding Programs
These disbursements would be separate from the $30 billion in direct provider payments announced on April 7 by Seema Verma, the administrator of the Centers for Medicare and Medicaid Services (CMS). Because these payments are based on Medicare volume, the vast majority of this money is expected to go to hospitals.
The government is also providing financial support to hospitals, physicians, and other clinicians affected by the pandemic through CMS’s accelerated/advance payment program, as reported by Medscape Medical News. Physician practices can apply to receive upfront payments equal to 3 months’ worth of their historical Medicare payments, but they must pay back these loans, starting at 120 days after receiving them.
In addition, providers with less than 500 employees can apply for Small Business Administration (SBA) loans that were authorized by the CURES Act. If they use at least 75% of this money to cover payroll costs, the loans will be forgiven.
Medical leaders defended their request for direct physician relief in excess of what these three government programs are offering.
“From the very beginning, the AMA has been advocating for [financial] support for physician practices,” AMA President Patrice Harris, MD, told Medscape Medical News. “It’s not an either/or, it’s not a choice between hospitals or physician practices, it’s both.”
She made it clear that this applied not only to the direct payments that the CURES Act allocated to healthcare providers, but also to the SBA loans.
“We’ve been pleased to see support through the Small Business Administration, and we know that many practices have applied for loans,” Harris said. “We’ll review this, because physician practices have to be included.”
Thus far, she added, “I haven’t heard of anyone [in a medical practice] who has actually received a loan. We’ll be monitoring that, because that will be key.”
Likewise, Robert Doherty, senior vice president of governmental affairs and public policy for the American College of Physicians (ACP), said he hadn’t heard of any practices receiving SBA loans, although many have applied.
What he has heard is that “people couldn’t even get through the SBA process and the website was freezing up. They also have to find a lender, submit documentation and get approved by the lender. And they’re competing with all the other small businesses” for a finite amount of money.
Doherty said it was unclear how many practices have received advance payments from CMS so far. CMS said it disbursed $34 billion in these payments in the first week of the program. These went to over 17,000 of the more than 25,000 applicants, CMS noted.
The ACP – which joined the AMA in its request to HHS – supports the advanced-payment program, Doherty added, but “a loan is a loan. You have to repay it. It brings in cash now, but it means you don’t have cash a few months from now. That’s different from what we’re recommending, which is an infusion of cash to practices that wouldn’t have to be repaid.”
Another advantage of the AMA-led proposal, he said, is its simplicity. It’s based on data that CMS already has, and it doesn’t require physicians to fill out forms or provide documents.
In contrast, he said, “We don’t think HHS would have the ability to process applications from thousands and thousands of physicians [for direct payments]. To create a situation where they’d have to review applications from physicians for funding out of that [CARES Act] emergency fund is probably almost impossible for HHS to administer effectively.”
Most Practices Need Help
While the medical societies’ letter makes a strong pitch for supporting physicians who are combating COVID-19, Harris and Doherty noted that physicians in all kinds of practice situations desperately need this help.
“We’ve heard from many physician practices that they have trouble making payroll,” Doherty said. “Many of them are not seeking any money out of the practices for themselves right now. They’re just trying to keep their staff employed. And some will shut their doors, unless there’s a significant and immediate infusion of money to them. From a healthcare capacity viewpoint, it’s not going to be to anyone’s benefit to see a substantial number of practices laying off staff or closing up entirely because they don’t have the money coming in to keep the doors open,” he said.
Harris agreed. “We’re hearing from practices large and small all over the country, including solo practices. Even the larger practices are losing revenue,” she pointed out. “They appropriately shut down their offices or reduced their hours. They didn’t want to contribute to the further spread of COVID-19.”
Rural practices and those launched by young physicians are facing especially difficult challenges, Harris added, and some may not make it.
It’s also important for policy makers to look ahead to what lies after the pandemic, she said. “We will come out of this, but when we come out of it there will be a lot of pent-up or unmet need where folks delayed necessary visits. Physicians and practices will have to be ready to go. If practices have to furlough some staff, it’s going to take time to ramp that up. So we’re glad to see support of physician practices so the infrastructure is strong when we start again.”
What happens if HHS turns down the medical societies’ request? “We’re hopeful that the [HHS] secretary will agree to what we’re asking,” Doherty said. While it’s always possible to ask Congress to intervene in the next stimulus bill, he said, that wouldn’t happen fast enough to get the money to physicians when they really need it.
This article first appeared on Medscape.com.
CMS loosens clinician scope-of-practice, telehealth rules for COVID-19 crisis
To boost the capacity of frontline clinicians and facilities to fight COVID-19, the Centers for Medicare & Medicaid Services (CMS) on Thursday announced it is temporarily suspending rules to allow physicians to provide telehealth services across state lines, and will permit midlevel practitioners to provide as much care as their state licenses allow.
Physicians can now care for patients at rural hospitals across state lines via phone, radio, or online communications without having to be physically present.
“Remotely located physicians, coordinating with nurse practitioners at rural hospitals, will provide staffs at such facilities additional flexibility to meet the needs of their patients,” a CMS news release said.
At skilled nursing facilities, nurse practitioners will now be able to perform some medical exams that doctors normally conduct on Medicare patients, whether they are COVID-19-related or not, CMS said.
Occupational therapists from home health agencies can now perform initial assessments on certain homebound patients, allowing home health services to start sooner and freeing home health nurses to do more direct patient care.
In addition, hospice nurses will be relieved of hospice aide in-service training tasks so they can spend more time with patients.
“It’s all hands on deck during this crisis,” said CMS Administrator Seema Verma in the press release. “All frontline medical professionals need to be able to work at the highest level they were trained for. CMS is making sure there are no regulatory obstacles to increasing the medical workforce to handle the patient surge during the COVID-19 pandemic.”
The announcement did not directly address the question of whether CMS’ new telemedicine and scope-of-practice policies override state laws. The agency said, “CMS sets and enforces essential quality and safety standards that supplement state scope-of-practice and licensure laws for healthcare workers. CMS has continuously examined its regulations to identify areas where federal requirements may be more stringent than state laws and requirements.”
On March 20, Vice President Pence announced that physicians would be allowed to practice across state lines during the COVID-19 crisis, as reported by Medscape Medical News. Until now, however, CMS had not changed its regulations to allow doctors to conduct telehealth consultations in states other than the ones in which they are licensed.
Other Changes
As part of other rule changes to support the healthcare workforce, CMS said on March 30 that it will pay for more than 80 additional services when furnished via telehealth.
These include emergency department visits, initial skilled nursing facility and discharge visits, and home visits. In addition, the agency said it would cover phone visits with Medicare beneficiaries.
Moreover, while virtual “check-in” visits had previously been limited to established patients, CMS said that doctors would be able to provide these services to both new and established patients.
Among its other regulatory changes in recent weeks, CMS has also temporarily:
- Permitted physicians whose privileges will expire to continue practicing at a hospital, and allowed new physicians to begin working prior to full hospital medical staff/governing body review and approval
- Lifted regulatory requirements regarding hospital personnel qualified to perform specific respiratory care procedures, allowing these professionals to operate to the fullest extent of their licensure
- Waived federal minimum personnel qualifications for clinical nurse specialists, nurse practitioners, and physician assistants so they can work at rural hospitals as long as they meet state licensure requirements
- Allowed physicians and nonphysician practitioners to use telehealth to care for patients at long-term care facilities, rather than having to treat patients at those facilities in person
This article first appeared on Medscape.com.
To boost the capacity of frontline clinicians and facilities to fight COVID-19, the Centers for Medicare & Medicaid Services (CMS) on Thursday announced it is temporarily suspending rules to allow physicians to provide telehealth services across state lines, and will permit midlevel practitioners to provide as much care as their state licenses allow.
Physicians can now care for patients at rural hospitals across state lines via phone, radio, or online communications without having to be physically present.
“Remotely located physicians, coordinating with nurse practitioners at rural hospitals, will provide staffs at such facilities additional flexibility to meet the needs of their patients,” a CMS news release said.
At skilled nursing facilities, nurse practitioners will now be able to perform some medical exams that doctors normally conduct on Medicare patients, whether they are COVID-19-related or not, CMS said.
Occupational therapists from home health agencies can now perform initial assessments on certain homebound patients, allowing home health services to start sooner and freeing home health nurses to do more direct patient care.
In addition, hospice nurses will be relieved of hospice aide in-service training tasks so they can spend more time with patients.
“It’s all hands on deck during this crisis,” said CMS Administrator Seema Verma in the press release. “All frontline medical professionals need to be able to work at the highest level they were trained for. CMS is making sure there are no regulatory obstacles to increasing the medical workforce to handle the patient surge during the COVID-19 pandemic.”
The announcement did not directly address the question of whether CMS’ new telemedicine and scope-of-practice policies override state laws. The agency said, “CMS sets and enforces essential quality and safety standards that supplement state scope-of-practice and licensure laws for healthcare workers. CMS has continuously examined its regulations to identify areas where federal requirements may be more stringent than state laws and requirements.”
On March 20, Vice President Pence announced that physicians would be allowed to practice across state lines during the COVID-19 crisis, as reported by Medscape Medical News. Until now, however, CMS had not changed its regulations to allow doctors to conduct telehealth consultations in states other than the ones in which they are licensed.
Other Changes
As part of other rule changes to support the healthcare workforce, CMS said on March 30 that it will pay for more than 80 additional services when furnished via telehealth.
These include emergency department visits, initial skilled nursing facility and discharge visits, and home visits. In addition, the agency said it would cover phone visits with Medicare beneficiaries.
Moreover, while virtual “check-in” visits had previously been limited to established patients, CMS said that doctors would be able to provide these services to both new and established patients.
Among its other regulatory changes in recent weeks, CMS has also temporarily:
- Permitted physicians whose privileges will expire to continue practicing at a hospital, and allowed new physicians to begin working prior to full hospital medical staff/governing body review and approval
- Lifted regulatory requirements regarding hospital personnel qualified to perform specific respiratory care procedures, allowing these professionals to operate to the fullest extent of their licensure
- Waived federal minimum personnel qualifications for clinical nurse specialists, nurse practitioners, and physician assistants so they can work at rural hospitals as long as they meet state licensure requirements
- Allowed physicians and nonphysician practitioners to use telehealth to care for patients at long-term care facilities, rather than having to treat patients at those facilities in person
This article first appeared on Medscape.com.
To boost the capacity of frontline clinicians and facilities to fight COVID-19, the Centers for Medicare & Medicaid Services (CMS) on Thursday announced it is temporarily suspending rules to allow physicians to provide telehealth services across state lines, and will permit midlevel practitioners to provide as much care as their state licenses allow.
Physicians can now care for patients at rural hospitals across state lines via phone, radio, or online communications without having to be physically present.
“Remotely located physicians, coordinating with nurse practitioners at rural hospitals, will provide staffs at such facilities additional flexibility to meet the needs of their patients,” a CMS news release said.
At skilled nursing facilities, nurse practitioners will now be able to perform some medical exams that doctors normally conduct on Medicare patients, whether they are COVID-19-related or not, CMS said.
Occupational therapists from home health agencies can now perform initial assessments on certain homebound patients, allowing home health services to start sooner and freeing home health nurses to do more direct patient care.
In addition, hospice nurses will be relieved of hospice aide in-service training tasks so they can spend more time with patients.
“It’s all hands on deck during this crisis,” said CMS Administrator Seema Verma in the press release. “All frontline medical professionals need to be able to work at the highest level they were trained for. CMS is making sure there are no regulatory obstacles to increasing the medical workforce to handle the patient surge during the COVID-19 pandemic.”
The announcement did not directly address the question of whether CMS’ new telemedicine and scope-of-practice policies override state laws. The agency said, “CMS sets and enforces essential quality and safety standards that supplement state scope-of-practice and licensure laws for healthcare workers. CMS has continuously examined its regulations to identify areas where federal requirements may be more stringent than state laws and requirements.”
On March 20, Vice President Pence announced that physicians would be allowed to practice across state lines during the COVID-19 crisis, as reported by Medscape Medical News. Until now, however, CMS had not changed its regulations to allow doctors to conduct telehealth consultations in states other than the ones in which they are licensed.
Other Changes
As part of other rule changes to support the healthcare workforce, CMS said on March 30 that it will pay for more than 80 additional services when furnished via telehealth.
These include emergency department visits, initial skilled nursing facility and discharge visits, and home visits. In addition, the agency said it would cover phone visits with Medicare beneficiaries.
Moreover, while virtual “check-in” visits had previously been limited to established patients, CMS said that doctors would be able to provide these services to both new and established patients.
Among its other regulatory changes in recent weeks, CMS has also temporarily:
- Permitted physicians whose privileges will expire to continue practicing at a hospital, and allowed new physicians to begin working prior to full hospital medical staff/governing body review and approval
- Lifted regulatory requirements regarding hospital personnel qualified to perform specific respiratory care procedures, allowing these professionals to operate to the fullest extent of their licensure
- Waived federal minimum personnel qualifications for clinical nurse specialists, nurse practitioners, and physician assistants so they can work at rural hospitals as long as they meet state licensure requirements
- Allowed physicians and nonphysician practitioners to use telehealth to care for patients at long-term care facilities, rather than having to treat patients at those facilities in person
This article first appeared on Medscape.com.
COVID-19: Managing resource crunch and ethical challenges
COVID-19 has been a watershed event in medical history of epic proportions. With this fast-spreading pandemic stretching resources at health care institutions, practical considerations for management of a disease about which we are still learning has been a huge challenge.
Although many guidelines have been made available by medical societies and experts worldwide, there appear to be very few which throw light on management in a resource-poor setup. The hospitalist, as a front-line provider, is likely expected to lead the planning and management of resources in order to deliver appropriate care.
As per American Hospital Association data, there are 2,704 community hospitals that can deliver ICU care in the United States. There are 534,964 acute care beds with 96,596 ICU beds. Additionally, there are 25,157 step-down beds and 1,183 burn unit beds. Of the 2,704 hospitals, 74% are in metropolitan areas (> 50,000 population), 17% (464) are in micropolitan areas (10,000-49,999 population), and the remaining 9% (244) are in rural areas. Only 7% (36,453) of hospital beds and 5% (4715) of ICU beds are in micropolitan areas. Two percent of acute care hospital beds and 1% of ICU beds are in rural areas. Although the US has the highest per capita number of ICU beds in the world, this may not be sufficient as these are concentrated in highly populated metropolitan areas.
Infrastructure and human power resource augmentation will be important. Infrastructure can be ramped up by:
- Canceling elective procedures
- Using the operating room and perioperative room ventilators and beds
- Servicing and using older functioning hospitals, medical wards, and ventilators.
As ventilators are expected to be in short supply, while far from ideal, other resources may include using ventilators from the Strategic National Stockpile, renting from vendors, and using state-owned stockpiles. Use of non-invasive ventilators, such as CPAP (continuous positive airway pressure), BiPAP (bi-level positive airway pressure), and HFNC (high-flow nasal cannula) may be considered in addition to full-featured ventilators. Rapidly manufacturing new ventilators with government direction is also being undertaken.
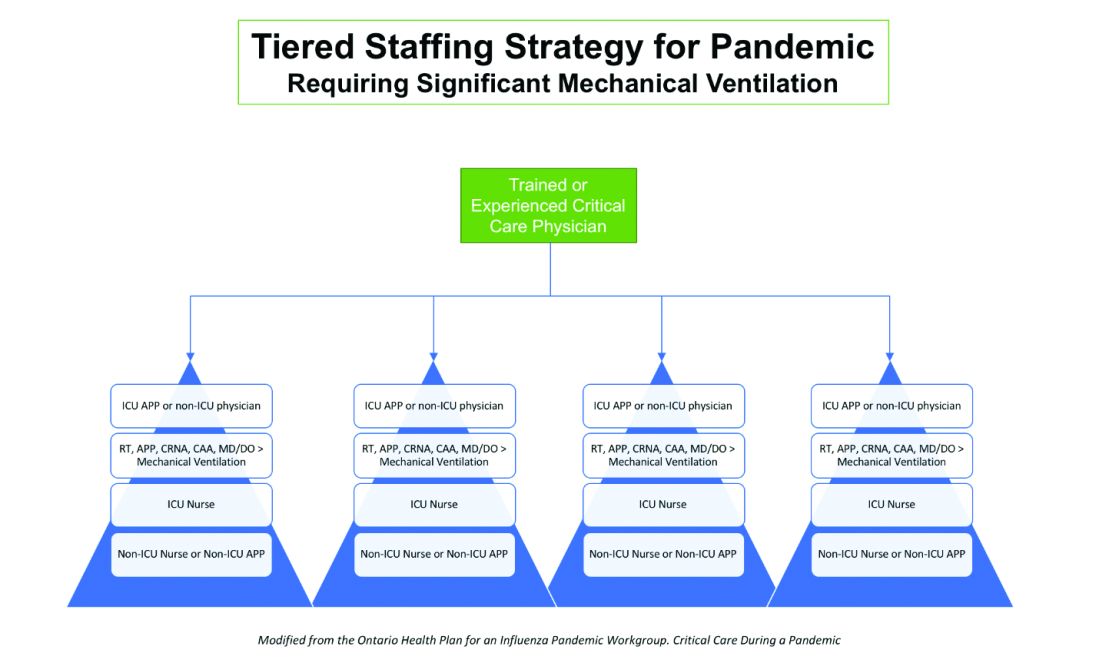
Although estimates vary based on the model used, about 1 million people are expected to need ventilatory support. However, in addition to infrastructural shortcomings, trained persons to care for these patients are lacking. Approximately 48% of acute care hospitals have no intensivists, and there are only 28,808 intensivists as per 2015 AHA data. In order to increase the amount of skilled manpower needed to staff ICUs, a model from the Society of Critical Care Medicine’s Fundamental Disaster Management Program can be adopted. This involves an intensivist overseeing four different teams, with each team caring for 24 patients. Each team is led by a non-ICU physician or an ICU advanced practice provider (APP) who in turn cares for the patient with respiratory therapists, pharmacists, ICU nurses, and other non-ICU health professionals.
It is essential that infrastructure and human power be augmented and optimized, as well as contingency plans, including triage based on ethical and legal considerations, put in place if demand overwhelms capacity.
Lack of PPE and fear among health care staff
There have been widespread reports in the media, and several anecdotal reports, about severe shortages of personal protective equipment (PPE), and as a result, an increase in fear and anxiety among frontline health care workers.
In addition, there also have been reports about hospital administrators disciplining medical and nursing staff for voicing their concerns about PPE shortages to the general public and the media. This likely stems from the narrow “optics” and public relations concerns of health care facilities.
It is evident that the size and magnitude of the COVID-19 pandemic was grossly underestimated, and preparations were inadequate. But according to past surveys of health care workers, a good number of them believe that medical and nursing staff have a duty to deliver care to sick people even if it exposes them to personal danger.
Given the special skills and privileges that health care professionals possess, they do have a moral and ethical responsibility to take care of sick patients even if a danger to themselves exists. However, society also has a responsibility to provide for the safety of these health care workers by supplying them with appropriate safety gear. Given the unprecedented nature of this pandemic, it is obvious that federal and state governments, public health officials, and hospital administrators (along with health care professionals) are still learning how to appropriately respond to the challenge.
It would be reasonable and appropriate for everyone concerned to understand and acknowledge that there is a shortage of PPE, and while arranging for this to be replenished, undertake and implement measures that maximize the safety of all health care workers. An open forum, mutually agreed-upon policy and procedures, along with mechanisms to address concerns should be formulated.
In addition, health care workers who test positive for COVID-19 can be a source of infection for other health care workers and non-infected patients. Therefore, health care workers have the responsibility of reporting their symptoms, the right to have themselves tested, and they must follow agreed-upon procedures that would limit their ability to infect other people, including mandated absenteeism from work. Every individual has a right to safety at the workplace and this right cannot be compromised, as otherwise this will lead to a suboptimal response to the pandemic. The government, hospital administrators, and health care workers will need to come together and work cohesively.
Ethical issues surrounding resource allocation
At the time of hospital admission, any suspected or confirmed COVID-19 patient should have his or her wishes recorded with the admitting team regarding the goals of care and code status. During any critical illness, goals evolve depending on discussions, reflections of the patient with family, and clinical response to therapy. A patient who does not want any kind of life support obviously should not be offered an ICU level of care.
On the other hand, in the event of resources becoming overwhelmed by demand as can be expected during this pandemic, careful ethical considerations will need to be applied.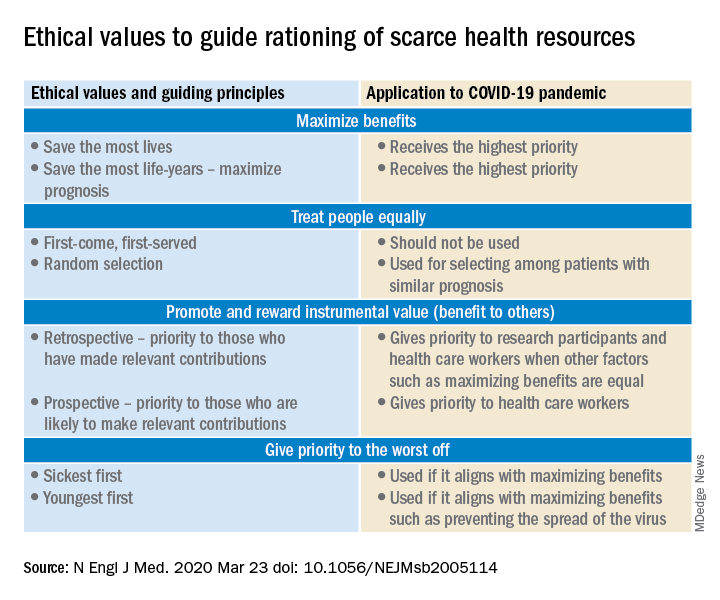
A carefully crafted transparent ethical framework, with a clear understanding of the decision-making process, that involves all stakeholders – including government entities, public health officials, health care workers, ethics specialists, and members of the community – is essential. Ideally, allocation of resources should be made according to a well-written plan, by a triage team that can include a nontreating physician, bioethicists, legal personnel, and religious representatives. It should not be left to the front-line treating physician, who is unlikely to be trained to make these decisions and who has an ethical responsibility to advocate for the patient under his care.
Ethical principles that deserve consideration
The “principle of utility” provides the maximum possible benefit to the maximum number of people. It should not only save the greatest number of lives but also maximize improvements in individuals’ posttreatment length of life.
The “principle of equity” requires that resources are allocated on a nondiscriminatory basis with a fair distribution of benefits and burdens. When conflicts arise between these two principles, a balanced approach likely will help when handled with a transparent decision-making process, with decisions to be applied consistently. Most experts would agree on not only saving more lives but also in preserving more years of life.
The distribution of medical resources should not be based on age or disability. Frailty and functional status are important considerations; however, priority is to be given to sicker patients who have lesser comorbidities and are also likely to survive longer. This could entail that younger, healthier patients will access scarce resources based on the principle of maximizing benefits.
Another consideration is “preservation of functioning of the society.” Those individuals who are important for providing important public services, health care services, and the functioning of other key aspects of society can be considered for prioritization of resources. While this may not satisfy the classic utilitarian principle of doing maximum good to the maximum number of people, it will help to continue augmenting the fight against the pandemic because of the critical role that such individuals play.
For patients with a similar prognosis, the principle of equality comes into play, and distribution should be done by way of random allocation, like a lottery. Distribution based on the principle of “first come, first served” is unlikely to be a fair process, as it would likely discriminate against patients based on their ability to access care.
Care should also be taken not to discriminate among people who have COVID-19 and non–COVID-19 health conditions that require medical care. Distribution should never be done based on an individual’s political influence, celebrity, or financial status, as occurred in the early days of the pandemic regarding access to testing.
Resuscitation or not?
Should a COVID-19 positive patient be offered CPR in case of cardiac arrest? The concern is that CPR is a high-level aerosolizing procedure and PPE is in short supply with the worsening of the pandemic. This will depend more on local policies and resource availability, along with goals of care that have to be determined at the time of admission and subsequent conversations.
The American Hospital Association has issued a general guideline and as more data become available, we can have more informed discussions with patients and families. At this point, all due precautions that prevent the infection of health care personnel are applicable.
Ethical considerations often do not have answers that are a universal fit, and the challenge is always to promote the best interest of the patient with a balance of judiciously utilizing scarce community resources.
Although many states have had discussions and some even have written policies, they have never been implemented. The organization and application of a judicious ethical “crisis level of care” is extremely challenging and likely to test the foundation and fabric of the society.
Dr. Jain is senior associate consultant, hospital & critical care medicine, at Mayo Clinic in Mankato, Minn. He is a board-certified internal medicine, pulmonary, and critical care physician, and has special interests in rural medicine and ethical issues involving critical care medicine. Dr. Tirupathi is the medical director of keystone infectious diseases/HIV in Chambersburg and is currently chair of infection prevention at Wellspan Chambersburg and Waynesboro Hospitals, all in Pennsylvania. Dr. Palabindala is hospital medicine division chief at the University of Mississippi Medical Center, Jackson, and a member of the editorial advisory board for The Hospitalist.
Sources
1. United States Resource Availability for COVID-19. SCCM Blog.
2. Intensive care medicine: Triage in case of bottlenecks. l
3. Interim Guidance for Healthcare Providers during COVID-19 Outbreak.
4. Emanuel EJ et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med 2020 Mar 23.doi: 10.1056/NEJMsb2005114.
5. Devnani M et al. Planning and response to the influenza A (H1N1) pandemic: Ethics, equity and justice. Indian J Med Ethics. 2011 Oct-Dec;8(4):237-40.
6. Alexander C and Wynia M. Ready and willing? Physicians’ sense of preparedness for bioterrorism. Health Aff (Millwood). 2003 Sep-Oct;22(5):189-97.
7. Damery S et al. Healthcare workers’ perceptions of the duty to work during an influenza pandemic. J Med Ethics. 2010 Jan;36(1):12-8.
COVID-19 has been a watershed event in medical history of epic proportions. With this fast-spreading pandemic stretching resources at health care institutions, practical considerations for management of a disease about which we are still learning has been a huge challenge.
Although many guidelines have been made available by medical societies and experts worldwide, there appear to be very few which throw light on management in a resource-poor setup. The hospitalist, as a front-line provider, is likely expected to lead the planning and management of resources in order to deliver appropriate care.
As per American Hospital Association data, there are 2,704 community hospitals that can deliver ICU care in the United States. There are 534,964 acute care beds with 96,596 ICU beds. Additionally, there are 25,157 step-down beds and 1,183 burn unit beds. Of the 2,704 hospitals, 74% are in metropolitan areas (> 50,000 population), 17% (464) are in micropolitan areas (10,000-49,999 population), and the remaining 9% (244) are in rural areas. Only 7% (36,453) of hospital beds and 5% (4715) of ICU beds are in micropolitan areas. Two percent of acute care hospital beds and 1% of ICU beds are in rural areas. Although the US has the highest per capita number of ICU beds in the world, this may not be sufficient as these are concentrated in highly populated metropolitan areas.
Infrastructure and human power resource augmentation will be important. Infrastructure can be ramped up by:
- Canceling elective procedures
- Using the operating room and perioperative room ventilators and beds
- Servicing and using older functioning hospitals, medical wards, and ventilators.
As ventilators are expected to be in short supply, while far from ideal, other resources may include using ventilators from the Strategic National Stockpile, renting from vendors, and using state-owned stockpiles. Use of non-invasive ventilators, such as CPAP (continuous positive airway pressure), BiPAP (bi-level positive airway pressure), and HFNC (high-flow nasal cannula) may be considered in addition to full-featured ventilators. Rapidly manufacturing new ventilators with government direction is also being undertaken.
Although estimates vary based on the model used, about 1 million people are expected to need ventilatory support. However, in addition to infrastructural shortcomings, trained persons to care for these patients are lacking. Approximately 48% of acute care hospitals have no intensivists, and there are only 28,808 intensivists as per 2015 AHA data. In order to increase the amount of skilled manpower needed to staff ICUs, a model from the Society of Critical Care Medicine’s Fundamental Disaster Management Program can be adopted. This involves an intensivist overseeing four different teams, with each team caring for 24 patients. Each team is led by a non-ICU physician or an ICU advanced practice provider (APP) who in turn cares for the patient with respiratory therapists, pharmacists, ICU nurses, and other non-ICU health professionals.
It is essential that infrastructure and human power be augmented and optimized, as well as contingency plans, including triage based on ethical and legal considerations, put in place if demand overwhelms capacity.
Lack of PPE and fear among health care staff
There have been widespread reports in the media, and several anecdotal reports, about severe shortages of personal protective equipment (PPE), and as a result, an increase in fear and anxiety among frontline health care workers.
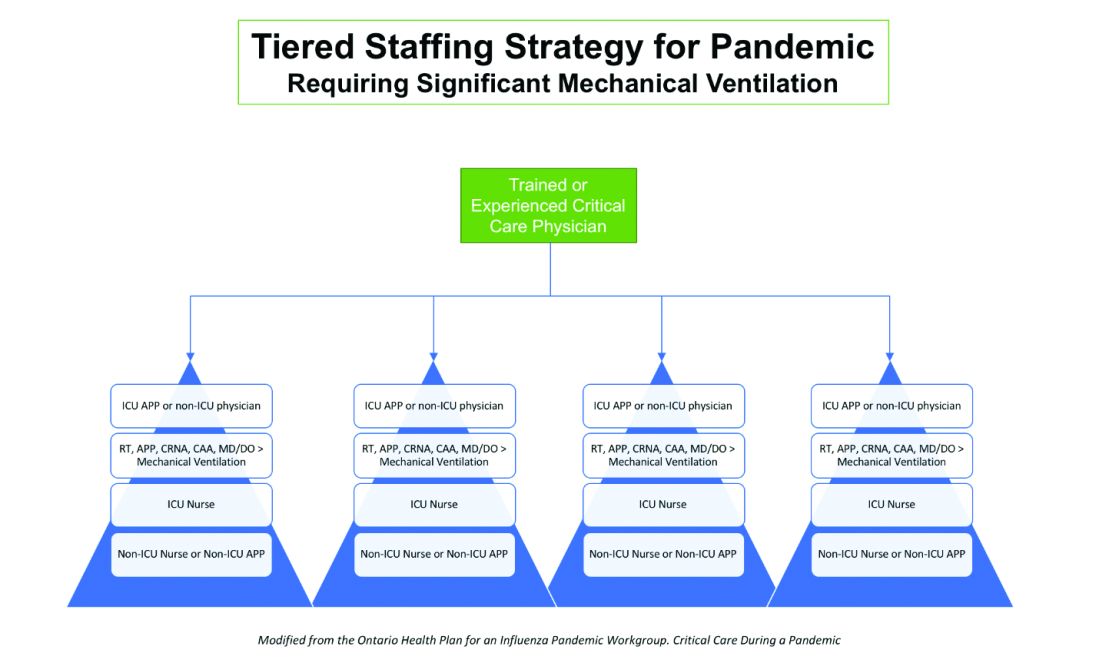
In addition, there also have been reports about hospital administrators disciplining medical and nursing staff for voicing their concerns about PPE shortages to the general public and the media. This likely stems from the narrow “optics” and public relations concerns of health care facilities.
It is evident that the size and magnitude of the COVID-19 pandemic was grossly underestimated, and preparations were inadequate. But according to past surveys of health care workers, a good number of them believe that medical and nursing staff have a duty to deliver care to sick people even if it exposes them to personal danger.
Given the special skills and privileges that health care professionals possess, they do have a moral and ethical responsibility to take care of sick patients even if a danger to themselves exists. However, society also has a responsibility to provide for the safety of these health care workers by supplying them with appropriate safety gear. Given the unprecedented nature of this pandemic, it is obvious that federal and state governments, public health officials, and hospital administrators (along with health care professionals) are still learning how to appropriately respond to the challenge.
It would be reasonable and appropriate for everyone concerned to understand and acknowledge that there is a shortage of PPE, and while arranging for this to be replenished, undertake and implement measures that maximize the safety of all health care workers. An open forum, mutually agreed-upon policy and procedures, along with mechanisms to address concerns should be formulated.
In addition, health care workers who test positive for COVID-19 can be a source of infection for other health care workers and non-infected patients. Therefore, health care workers have the responsibility of reporting their symptoms, the right to have themselves tested, and they must follow agreed-upon procedures that would limit their ability to infect other people, including mandated absenteeism from work. Every individual has a right to safety at the workplace and this right cannot be compromised, as otherwise this will lead to a suboptimal response to the pandemic. The government, hospital administrators, and health care workers will need to come together and work cohesively.
Ethical issues surrounding resource allocation
At the time of hospital admission, any suspected or confirmed COVID-19 patient should have his or her wishes recorded with the admitting team regarding the goals of care and code status. During any critical illness, goals evolve depending on discussions, reflections of the patient with family, and clinical response to therapy. A patient who does not want any kind of life support obviously should not be offered an ICU level of care.
On the other hand, in the event of resources becoming overwhelmed by demand as can be expected during this pandemic, careful ethical considerations will need to be applied.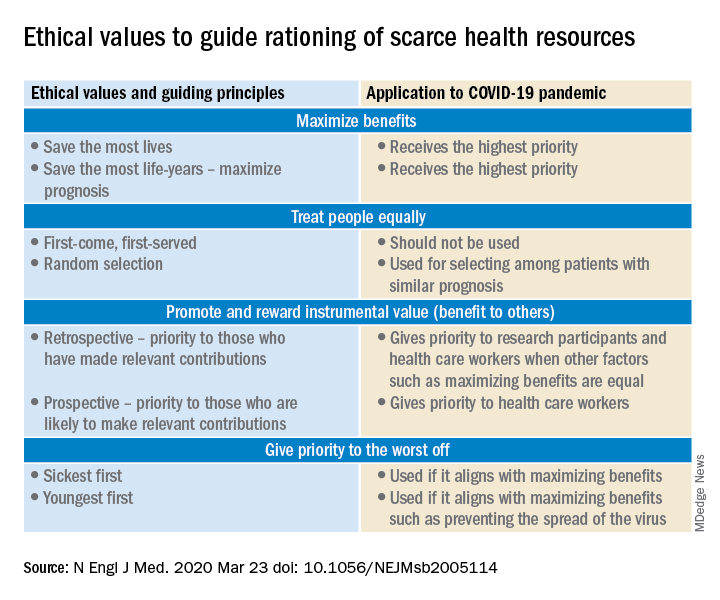
A carefully crafted transparent ethical framework, with a clear understanding of the decision-making process, that involves all stakeholders – including government entities, public health officials, health care workers, ethics specialists, and members of the community – is essential. Ideally, allocation of resources should be made according to a well-written plan, by a triage team that can include a nontreating physician, bioethicists, legal personnel, and religious representatives. It should not be left to the front-line treating physician, who is unlikely to be trained to make these decisions and who has an ethical responsibility to advocate for the patient under his care.
Ethical principles that deserve consideration
The “principle of utility” provides the maximum possible benefit to the maximum number of people. It should not only save the greatest number of lives but also maximize improvements in individuals’ posttreatment length of life.
The “principle of equity” requires that resources are allocated on a nondiscriminatory basis with a fair distribution of benefits and burdens. When conflicts arise between these two principles, a balanced approach likely will help when handled with a transparent decision-making process, with decisions to be applied consistently. Most experts would agree on not only saving more lives but also in preserving more years of life.
The distribution of medical resources should not be based on age or disability. Frailty and functional status are important considerations; however, priority is to be given to sicker patients who have lesser comorbidities and are also likely to survive longer. This could entail that younger, healthier patients will access scarce resources based on the principle of maximizing benefits.
Another consideration is “preservation of functioning of the society.” Those individuals who are important for providing important public services, health care services, and the functioning of other key aspects of society can be considered for prioritization of resources. While this may not satisfy the classic utilitarian principle of doing maximum good to the maximum number of people, it will help to continue augmenting the fight against the pandemic because of the critical role that such individuals play.
For patients with a similar prognosis, the principle of equality comes into play, and distribution should be done by way of random allocation, like a lottery. Distribution based on the principle of “first come, first served” is unlikely to be a fair process, as it would likely discriminate against patients based on their ability to access care.
Care should also be taken not to discriminate among people who have COVID-19 and non–COVID-19 health conditions that require medical care. Distribution should never be done based on an individual’s political influence, celebrity, or financial status, as occurred in the early days of the pandemic regarding access to testing.
Resuscitation or not?
Should a COVID-19 positive patient be offered CPR in case of cardiac arrest? The concern is that CPR is a high-level aerosolizing procedure and PPE is in short supply with the worsening of the pandemic. This will depend more on local policies and resource availability, along with goals of care that have to be determined at the time of admission and subsequent conversations.
The American Hospital Association has issued a general guideline and as more data become available, we can have more informed discussions with patients and families. At this point, all due precautions that prevent the infection of health care personnel are applicable.
Ethical considerations often do not have answers that are a universal fit, and the challenge is always to promote the best interest of the patient with a balance of judiciously utilizing scarce community resources.
Although many states have had discussions and some even have written policies, they have never been implemented. The organization and application of a judicious ethical “crisis level of care” is extremely challenging and likely to test the foundation and fabric of the society.
Dr. Jain is senior associate consultant, hospital & critical care medicine, at Mayo Clinic in Mankato, Minn. He is a board-certified internal medicine, pulmonary, and critical care physician, and has special interests in rural medicine and ethical issues involving critical care medicine. Dr. Tirupathi is the medical director of keystone infectious diseases/HIV in Chambersburg and is currently chair of infection prevention at Wellspan Chambersburg and Waynesboro Hospitals, all in Pennsylvania. Dr. Palabindala is hospital medicine division chief at the University of Mississippi Medical Center, Jackson, and a member of the editorial advisory board for The Hospitalist.
Sources
1. United States Resource Availability for COVID-19. SCCM Blog.
2. Intensive care medicine: Triage in case of bottlenecks. l
3. Interim Guidance for Healthcare Providers during COVID-19 Outbreak.
4. Emanuel EJ et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med 2020 Mar 23.doi: 10.1056/NEJMsb2005114.
5. Devnani M et al. Planning and response to the influenza A (H1N1) pandemic: Ethics, equity and justice. Indian J Med Ethics. 2011 Oct-Dec;8(4):237-40.
6. Alexander C and Wynia M. Ready and willing? Physicians’ sense of preparedness for bioterrorism. Health Aff (Millwood). 2003 Sep-Oct;22(5):189-97.
7. Damery S et al. Healthcare workers’ perceptions of the duty to work during an influenza pandemic. J Med Ethics. 2010 Jan;36(1):12-8.
COVID-19 has been a watershed event in medical history of epic proportions. With this fast-spreading pandemic stretching resources at health care institutions, practical considerations for management of a disease about which we are still learning has been a huge challenge.
Although many guidelines have been made available by medical societies and experts worldwide, there appear to be very few which throw light on management in a resource-poor setup. The hospitalist, as a front-line provider, is likely expected to lead the planning and management of resources in order to deliver appropriate care.
As per American Hospital Association data, there are 2,704 community hospitals that can deliver ICU care in the United States. There are 534,964 acute care beds with 96,596 ICU beds. Additionally, there are 25,157 step-down beds and 1,183 burn unit beds. Of the 2,704 hospitals, 74% are in metropolitan areas (> 50,000 population), 17% (464) are in micropolitan areas (10,000-49,999 population), and the remaining 9% (244) are in rural areas. Only 7% (36,453) of hospital beds and 5% (4715) of ICU beds are in micropolitan areas. Two percent of acute care hospital beds and 1% of ICU beds are in rural areas. Although the US has the highest per capita number of ICU beds in the world, this may not be sufficient as these are concentrated in highly populated metropolitan areas.
Infrastructure and human power resource augmentation will be important. Infrastructure can be ramped up by:
- Canceling elective procedures
- Using the operating room and perioperative room ventilators and beds
- Servicing and using older functioning hospitals, medical wards, and ventilators.
As ventilators are expected to be in short supply, while far from ideal, other resources may include using ventilators from the Strategic National Stockpile, renting from vendors, and using state-owned stockpiles. Use of non-invasive ventilators, such as CPAP (continuous positive airway pressure), BiPAP (bi-level positive airway pressure), and HFNC (high-flow nasal cannula) may be considered in addition to full-featured ventilators. Rapidly manufacturing new ventilators with government direction is also being undertaken.
Although estimates vary based on the model used, about 1 million people are expected to need ventilatory support. However, in addition to infrastructural shortcomings, trained persons to care for these patients are lacking. Approximately 48% of acute care hospitals have no intensivists, and there are only 28,808 intensivists as per 2015 AHA data. In order to increase the amount of skilled manpower needed to staff ICUs, a model from the Society of Critical Care Medicine’s Fundamental Disaster Management Program can be adopted. This involves an intensivist overseeing four different teams, with each team caring for 24 patients. Each team is led by a non-ICU physician or an ICU advanced practice provider (APP) who in turn cares for the patient with respiratory therapists, pharmacists, ICU nurses, and other non-ICU health professionals.
It is essential that infrastructure and human power be augmented and optimized, as well as contingency plans, including triage based on ethical and legal considerations, put in place if demand overwhelms capacity.
Lack of PPE and fear among health care staff
There have been widespread reports in the media, and several anecdotal reports, about severe shortages of personal protective equipment (PPE), and as a result, an increase in fear and anxiety among frontline health care workers.
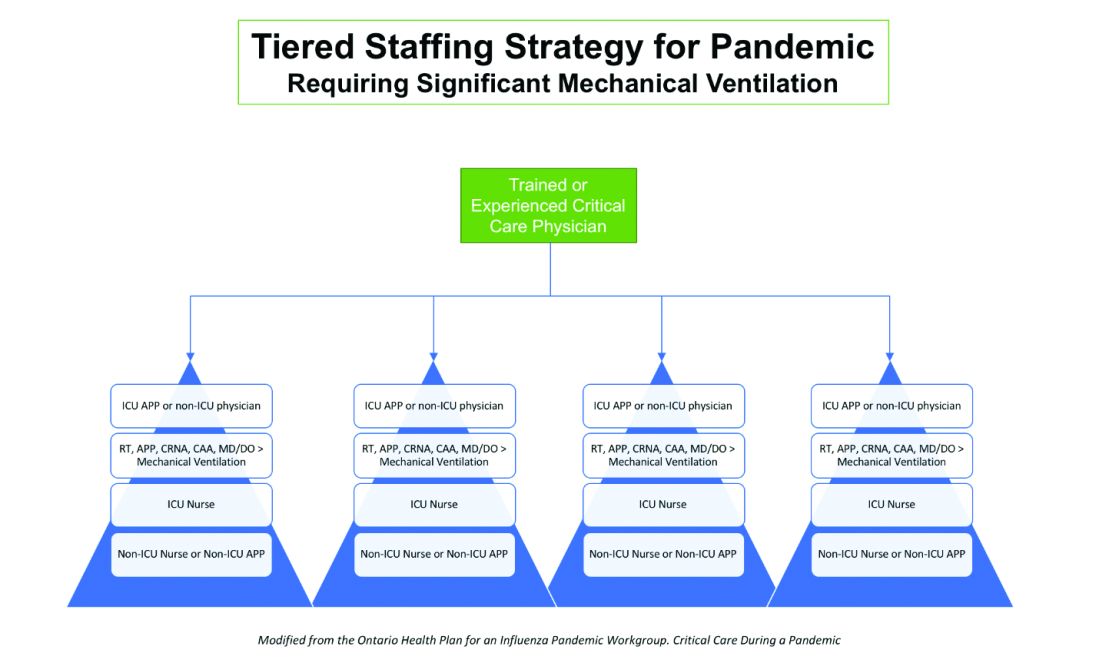
In addition, there also have been reports about hospital administrators disciplining medical and nursing staff for voicing their concerns about PPE shortages to the general public and the media. This likely stems from the narrow “optics” and public relations concerns of health care facilities.
It is evident that the size and magnitude of the COVID-19 pandemic was grossly underestimated, and preparations were inadequate. But according to past surveys of health care workers, a good number of them believe that medical and nursing staff have a duty to deliver care to sick people even if it exposes them to personal danger.
Given the special skills and privileges that health care professionals possess, they do have a moral and ethical responsibility to take care of sick patients even if a danger to themselves exists. However, society also has a responsibility to provide for the safety of these health care workers by supplying them with appropriate safety gear. Given the unprecedented nature of this pandemic, it is obvious that federal and state governments, public health officials, and hospital administrators (along with health care professionals) are still learning how to appropriately respond to the challenge.
It would be reasonable and appropriate for everyone concerned to understand and acknowledge that there is a shortage of PPE, and while arranging for this to be replenished, undertake and implement measures that maximize the safety of all health care workers. An open forum, mutually agreed-upon policy and procedures, along with mechanisms to address concerns should be formulated.
In addition, health care workers who test positive for COVID-19 can be a source of infection for other health care workers and non-infected patients. Therefore, health care workers have the responsibility of reporting their symptoms, the right to have themselves tested, and they must follow agreed-upon procedures that would limit their ability to infect other people, including mandated absenteeism from work. Every individual has a right to safety at the workplace and this right cannot be compromised, as otherwise this will lead to a suboptimal response to the pandemic. The government, hospital administrators, and health care workers will need to come together and work cohesively.
Ethical issues surrounding resource allocation
At the time of hospital admission, any suspected or confirmed COVID-19 patient should have his or her wishes recorded with the admitting team regarding the goals of care and code status. During any critical illness, goals evolve depending on discussions, reflections of the patient with family, and clinical response to therapy. A patient who does not want any kind of life support obviously should not be offered an ICU level of care.
On the other hand, in the event of resources becoming overwhelmed by demand as can be expected during this pandemic, careful ethical considerations will need to be applied.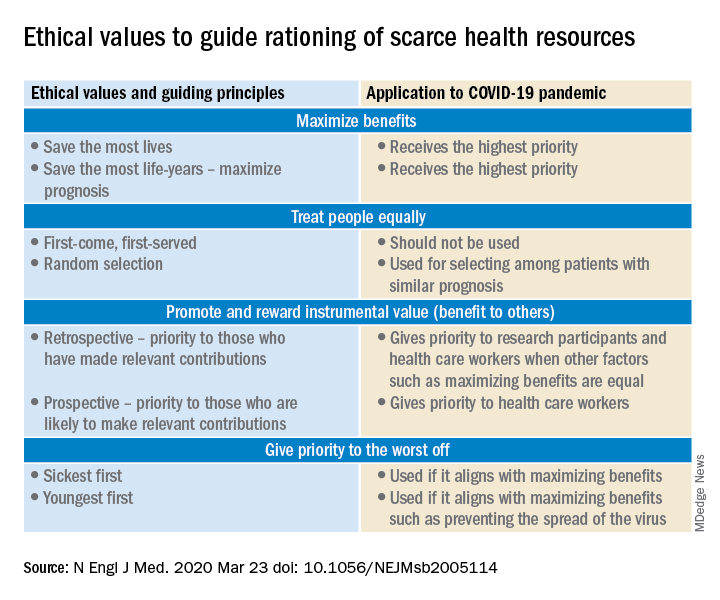
A carefully crafted transparent ethical framework, with a clear understanding of the decision-making process, that involves all stakeholders – including government entities, public health officials, health care workers, ethics specialists, and members of the community – is essential. Ideally, allocation of resources should be made according to a well-written plan, by a triage team that can include a nontreating physician, bioethicists, legal personnel, and religious representatives. It should not be left to the front-line treating physician, who is unlikely to be trained to make these decisions and who has an ethical responsibility to advocate for the patient under his care.
Ethical principles that deserve consideration
The “principle of utility” provides the maximum possible benefit to the maximum number of people. It should not only save the greatest number of lives but also maximize improvements in individuals’ posttreatment length of life.
The “principle of equity” requires that resources are allocated on a nondiscriminatory basis with a fair distribution of benefits and burdens. When conflicts arise between these two principles, a balanced approach likely will help when handled with a transparent decision-making process, with decisions to be applied consistently. Most experts would agree on not only saving more lives but also in preserving more years of life.
The distribution of medical resources should not be based on age or disability. Frailty and functional status are important considerations; however, priority is to be given to sicker patients who have lesser comorbidities and are also likely to survive longer. This could entail that younger, healthier patients will access scarce resources based on the principle of maximizing benefits.
Another consideration is “preservation of functioning of the society.” Those individuals who are important for providing important public services, health care services, and the functioning of other key aspects of society can be considered for prioritization of resources. While this may not satisfy the classic utilitarian principle of doing maximum good to the maximum number of people, it will help to continue augmenting the fight against the pandemic because of the critical role that such individuals play.
For patients with a similar prognosis, the principle of equality comes into play, and distribution should be done by way of random allocation, like a lottery. Distribution based on the principle of “first come, first served” is unlikely to be a fair process, as it would likely discriminate against patients based on their ability to access care.
Care should also be taken not to discriminate among people who have COVID-19 and non–COVID-19 health conditions that require medical care. Distribution should never be done based on an individual’s political influence, celebrity, or financial status, as occurred in the early days of the pandemic regarding access to testing.
Resuscitation or not?
Should a COVID-19 positive patient be offered CPR in case of cardiac arrest? The concern is that CPR is a high-level aerosolizing procedure and PPE is in short supply with the worsening of the pandemic. This will depend more on local policies and resource availability, along with goals of care that have to be determined at the time of admission and subsequent conversations.
The American Hospital Association has issued a general guideline and as more data become available, we can have more informed discussions with patients and families. At this point, all due precautions that prevent the infection of health care personnel are applicable.
Ethical considerations often do not have answers that are a universal fit, and the challenge is always to promote the best interest of the patient with a balance of judiciously utilizing scarce community resources.
Although many states have had discussions and some even have written policies, they have never been implemented. The organization and application of a judicious ethical “crisis level of care” is extremely challenging and likely to test the foundation and fabric of the society.
Dr. Jain is senior associate consultant, hospital & critical care medicine, at Mayo Clinic in Mankato, Minn. He is a board-certified internal medicine, pulmonary, and critical care physician, and has special interests in rural medicine and ethical issues involving critical care medicine. Dr. Tirupathi is the medical director of keystone infectious diseases/HIV in Chambersburg and is currently chair of infection prevention at Wellspan Chambersburg and Waynesboro Hospitals, all in Pennsylvania. Dr. Palabindala is hospital medicine division chief at the University of Mississippi Medical Center, Jackson, and a member of the editorial advisory board for The Hospitalist.
Sources
1. United States Resource Availability for COVID-19. SCCM Blog.
2. Intensive care medicine: Triage in case of bottlenecks. l
3. Interim Guidance for Healthcare Providers during COVID-19 Outbreak.
4. Emanuel EJ et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med 2020 Mar 23.doi: 10.1056/NEJMsb2005114.
5. Devnani M et al. Planning and response to the influenza A (H1N1) pandemic: Ethics, equity and justice. Indian J Med Ethics. 2011 Oct-Dec;8(4):237-40.
6. Alexander C and Wynia M. Ready and willing? Physicians’ sense of preparedness for bioterrorism. Health Aff (Millwood). 2003 Sep-Oct;22(5):189-97.
7. Damery S et al. Healthcare workers’ perceptions of the duty to work during an influenza pandemic. J Med Ethics. 2010 Jan;36(1):12-8.
ABIM grants MOC extension
Physicians will not lose their certification if they are unable to complete maintenance of certification requirements in 2020, the American Board of Internal Medicine announced.
ABIM President Richard Baron, MD, said in a letter sent to all diplomates.
Additionally, physicians “currently in their grace year will also be afforded an additional grace year in 2021,” the letter continued.
ABIM noted that many assessments were planned for the fall of 2020 and the organization will continue to offer them as planned for physicians who are able to take them. It added that more assessment dates for 2020 and 2021 will be sent out later this year.
“The next few weeks and months will challenge our health care system and country like never before,” Dr. Baron stated. “Our many internal medicine colleagues – and the clinical teams that support them – have been heroic in their response, often selflessly putting their own personal safety at risk while using their superb skills to provide care for others. They have inspired all of us.”
Physicians will not lose their certification if they are unable to complete maintenance of certification requirements in 2020, the American Board of Internal Medicine announced.
ABIM President Richard Baron, MD, said in a letter sent to all diplomates.
Additionally, physicians “currently in their grace year will also be afforded an additional grace year in 2021,” the letter continued.
ABIM noted that many assessments were planned for the fall of 2020 and the organization will continue to offer them as planned for physicians who are able to take them. It added that more assessment dates for 2020 and 2021 will be sent out later this year.
“The next few weeks and months will challenge our health care system and country like never before,” Dr. Baron stated. “Our many internal medicine colleagues – and the clinical teams that support them – have been heroic in their response, often selflessly putting their own personal safety at risk while using their superb skills to provide care for others. They have inspired all of us.”
Physicians will not lose their certification if they are unable to complete maintenance of certification requirements in 2020, the American Board of Internal Medicine announced.
ABIM President Richard Baron, MD, said in a letter sent to all diplomates.
Additionally, physicians “currently in their grace year will also be afforded an additional grace year in 2021,” the letter continued.
ABIM noted that many assessments were planned for the fall of 2020 and the organization will continue to offer them as planned for physicians who are able to take them. It added that more assessment dates for 2020 and 2021 will be sent out later this year.
“The next few weeks and months will challenge our health care system and country like never before,” Dr. Baron stated. “Our many internal medicine colleagues – and the clinical teams that support them – have been heroic in their response, often selflessly putting their own personal safety at risk while using their superb skills to provide care for others. They have inspired all of us.”
The wide-ranging impact of hospital closures
Clinicians struggle to balance priorities
On June 26, 2019, American Academic Health System and Philadelphia Academic Health System announced that Hahnemann University Hospital, a 496-bed tertiary care center in North Philadelphia in operation for over 170 years, would close that September.
The emergency department closed 52 days after the announcement, leaving little time for physicians and staff to coordinate care for patients and secure new employment. The announcement was also made right at the beginning of the new academic year, which meant residents and fellows were forced to find new training programs. In total, 2,500 workers at Hahnemann, including more than 570 hospitalists and physicians training as residents and fellows, were displaced as the hospital closed – the largest such closing in U.S. history.
For most of its existence, Hahnemann was a teaching hospital. While trainees were all eventually placed in new programs thanks to efforts from the Accreditation Council for Graduate Medical Education (ACGME), some of the permanent staff at Hahnemann weren’t so lucky. A month after the announcement, Drexel University’s president told university employees that 40% of the staff who worked at Hahnemann would be cut as a result of the closing. Drexel, also based in Philadelphia, had long had an academic affiliation agreement for training Drexel’s medical school students as a primary academic partner. Overall, Drexel’s entire clinical staff at Hahnemann was let go, and Tower Health Medical Group is expected to hire about 60% of the former Hahnemann staff.
Kevin D’Mello, MD, FACP, FHM, a hospitalist and assistant professor of medicine at Drexel University, said residents during Hahnemann’s closure were essentially teaching themselves how to swim. “There were just no laws, no rules,” he said.
The vast majority of programs accepting applications from residents at Hahnemann were sympathetic and accommodating, he said, but a few programs applied “pressure tactics” to some of the residents offered a transfer position, despite graduate medical education rules in place to prevent such a situation from happening. “The resident says: ‘Oh, well, I’m waiting to hear from this other program,’ ” said Dr. D’Mello. “They’d say: ‘Okay, well, we’re giving you a position now. You have 12 hours to answer.’ ”
Decision makers at the hospital also were not very forthcoming with information to residents, fellows and program directors, according to a recent paper written by Thomas J. Nasca, MD, current president and CEO of ACGME, and colleagues in the journal Academic Medicine (Nasca T et al. Acad Med. 2019 Dec 17. doi: 10.1097/ACM.0000000000003133). When Dr. Nasca and colleagues went to investigate the situation at Hahnemann firsthand, “the team found that residents, fellows, and program directors alike considered their voices to have been ignored in decision making and deemed themselves ‘out of the loop’ of important information that would affect their career transitions.”
While the hospital closed in September 2019, the effects are still being felt. In Pennsylvania, the Medical Care Availability and Reduction of Error Act requires that hospitals and providers have malpractice insurance, including tail insurance for when a doctor’s insurance policy expires. American Academic announced it would not be paying tail insurance for claims made while physicians were at Hahnemann. This meant residents, fellows and physicians who worked at Hahnemann during the closure would be on the hook for paying their own malpractice insurance.
“On one hand, the risk is very low for the house staff. Lawsuits that come up later for house staff are generally dropped at some point,” said William W. Pinsky, MD, FAAP, FACC, president and CEO of the Educational Commission for Foreign Medical Graduates (ECFMG). “But who wants to take that risk going forward? It’s an issue that’s still not resolved.”
The American Medical Association, Association of American Medical Colleges (AAMC), the Philadelphia County Medical Society, and other medical societies have collectively put pressure on Hahnemann’s owners to pay for tail coverage. Beyond a Feb. 10, 2020 deadline, former Hahnemann physicians were still expected to cover their own tail insurance.
To further complicate matters, American Academic attempted to auction more than 570 residency slots at Hahnemann. The slots were sold to a consortium of six health systems in the area – Thomas Jefferson University Hospitals, Einstein Healthcare Network, Temple University Health System, Main Line Health, Cooper University Health Care, and Christiana Care Health System – for $55 million. The Centers for Medicare & Medicaid Services opposed the sale, arguing that the slots are a contract that hospitals enter into with CMS, rather than an asset to be sold. An appeal is currently pending.
The case is being watched by former physicians at Hahnemann. “American Academic said, ‘If we don’t get this $55 million, we’re not going to be able to cover this tail insurance.’ They’re kind of linking the two things,” said Dr. D’Mello. “To me, it’s almost like putting pressure to allow the sale to happen.”
Urban hospital closures disrupt health system balance
When an urban hospital like Hahnemann University Hospital closes, there is a major disruption to patient care. Patients need to relocate to other nearby centers, and they may not always be able to follow their physician to the next health center.
If patients have comorbidities, are being tracked across multiple care points, or change physicians during a hospital closure, details can be missed and care can become more complicated for physicians who end up seeing the patient at a new center. For example, a patient receiving obstetrics care at a hospital that closes will have to reschedule their delivery at another health center, noted Dr. Pinsky.
“Where patients get lost is when there’s not a physician or an individual can keep track of all that, coordinate, and help to be sure that the patient follows through,” he said.
Patients at a closing hospital need to go somewhere else for care, and patient volume naturally increases at other nearby centers, potentially causing problems for systems without the resources to handle the spike in traffic.
“I’m a service director of quality improvement and patient safety for Drexel internal medicine. I know that those sort of jumps and volumes are what increases medical errors and potentially could create some adverse outcomes,” said Dr. D’Mello. “That’s something I’m particularly worried about.”
Physicians are also reconciling their own personal situations during a hospital closure, attempting to figure out their next step while at the same time helping patients figure out theirs. In the case of international medical graduates on J-1 or H1-B visas, who are dependent on hospital positions and training programs to remain in the United States, the situation can be even more dire.
During Hahnemann’s closure, Dr. Pinsky said that the ECFMG, which represents 11,000 individuals with J-1 visas across the country, reached out to the 55 individuals on J-1 visas at the hospital and offered them assistance, including working with the Department of State to ensure they aren’t in jeopardy of deportation before they secure another training program position.
The ECFMG, AMA, AAMC, and ACGME also offered funding to help J-1 visa holders who needed to relocate outside Philadelphia. “Many of them spent a lot of their money or all their money just coming over here,” said Dr. Pinsky. “This was a way to help defray some immediate costs that they might have.”
Education and research, of which hospitalists and residents play a large role, are likewise affected during a hospital closure, Dr. Pinsky said. “Education and research in the hospital is an important contributor to the community, health care and medical education nationally overall. When it’s not considered, there can be a significant asset that is lost in the process, which is hard to ever regain.
“The hospitalists have an integral role in medical education. In most hospitals where there is graduate medical education, particularly in internal medicine or pediatrics, and where there is a hospitalist program, it’s the hospitalists that do the majority of the in-hospital or inpatient training and education,” he added.
Rural hospital closures affect access to care
Since 2005, 163 rural hospitals have closed in the United States. When rural hospitals close, the situation for hospitalists and other physicians is different. In communities where a larger health system owns a hospital, such as when Vidant Health closed Pungo District Hospital in Belhaven, N.C., in 2014 before reopening a nonemergency clinic in the area in 2016, health care services for the community may have limited interruption.
However, if there isn’t a nearby system to join, many doctors will end up leaving the area. More than half of rural hospitals that close end up not providing any kind of supplementary health care service, according to the NC Rural Health Research Program.
“A lot of the hospitals that have closed have not been owned by a system,” said George H. Pink, PhD, deputy director of the NC Rural Health Research Program at the University of North Carolina at Chapel Hill. “They’ve been independent, freestanding, and that perhaps is one of the reasons why they’re closing, is because they haven’t been able to find a system that would buy them out and inject capital into the community.”
This can also have an effect on the number of health care providers in the area, Dr. Pink said. “Their ability to refer patients and treat patients locally may be affected. That’s why, in many towns where hospitals have closed, we see a drop in the number of providers, particularly primary care doctors who actually live in the community.”
Politicians and federal entities have proposed a number of solutions to help protect rural hospitals from closure. Sen. Charles Grassley (R-Iowa), Sen. Amy Klobuchar (D-Minn.), and Sen. Cory Gardener (R-Colo.) have sponsored bills in the Senate, while Rep. Sam Graves (R-Mo.) has introduced legislation in the House. The Medicare Payment Advisory Commission has proposed two models of rural hospital care, and there are additional models proposed by the Kansas Hospital Association. A pilot program in Pennsylvania, the Pennsylvania Rural Health Model, is testing how a global budget by CMS for all inpatient and hospital-based outcomes might help rural hospitals.
“What we haven’t had a lot of action on is actually testing these models out and seeing whether they will work, and in what kinds of communities they will work,” Dr. Pink said.
Hospitalists as community advocates
Dr. D’Mello, who wrote an article for the Journal of Hospital Medicine on Hahnemann’s ownership by a private equity firm (doi: 10.12788/jhm.3378), said that the inherent nature of a for-profit entity trying to make a hospital profitable is a bad sign for a hospital and not necessarily what is in the best interest for an academic institution or for doctors who train there.
“I don’t know if I could blame the private equity firm completely, but in retrospect, the private equity firms stepping in was like the death knell of the hospital,” he said of Hahnemann’s closure.
“I think what the community needs to know – what the health care community, patient community, the hospitalist community need to know – is that there’s got to be more attention paid to these types of issues during mergers and acquisitions to prevent this from happening,” Dr. Pinsky said.
One larger issue was Hahnemann’s position as a safety net hospital, which partly played into American Academic’s lack of success in making the hospital as profitable as they wanted it to be, Dr. D’Mello noted. Hahnemann’s patient population consisted mostly of minority patients on Medicare, Medicaid, and charity care insurance, while recent studies have shown that hospitals are more likely to succeed when they have a larger proportion of patients with private insurance.
“Studies show that, to [make more] money from private insurance, you really have to have this huge footprint, because then you’ve got a better ability to negotiate with these private insurance companies,” Dr. D’Mello said. “Whether that’s actually good for health care is a different issue.”
Despite their own situations, it is not unusual for hospitalists and hospital physicians to step up during a hospital closure and advocate for their patients on behalf of the community, Dr. Pink said.
“When hospitals are in financial difficulty and there’s the risk of closure, typically, the medical staff are among the first to step up and warn the community: ‘We’re at risk of losing our service. We need some help,’ ” he said. “Generally speaking, the local physicians have been at the forefront of helping to keep access to hospital care available in some of these small communities – unfortunately, not always successfully.”
Dr. D’Mello, Dr. Pinsky, and Dr. Pink report no relevant conflicts of interest.
Clinicians struggle to balance priorities
Clinicians struggle to balance priorities
On June 26, 2019, American Academic Health System and Philadelphia Academic Health System announced that Hahnemann University Hospital, a 496-bed tertiary care center in North Philadelphia in operation for over 170 years, would close that September.
The emergency department closed 52 days after the announcement, leaving little time for physicians and staff to coordinate care for patients and secure new employment. The announcement was also made right at the beginning of the new academic year, which meant residents and fellows were forced to find new training programs. In total, 2,500 workers at Hahnemann, including more than 570 hospitalists and physicians training as residents and fellows, were displaced as the hospital closed – the largest such closing in U.S. history.
For most of its existence, Hahnemann was a teaching hospital. While trainees were all eventually placed in new programs thanks to efforts from the Accreditation Council for Graduate Medical Education (ACGME), some of the permanent staff at Hahnemann weren’t so lucky. A month after the announcement, Drexel University’s president told university employees that 40% of the staff who worked at Hahnemann would be cut as a result of the closing. Drexel, also based in Philadelphia, had long had an academic affiliation agreement for training Drexel’s medical school students as a primary academic partner. Overall, Drexel’s entire clinical staff at Hahnemann was let go, and Tower Health Medical Group is expected to hire about 60% of the former Hahnemann staff.
Kevin D’Mello, MD, FACP, FHM, a hospitalist and assistant professor of medicine at Drexel University, said residents during Hahnemann’s closure were essentially teaching themselves how to swim. “There were just no laws, no rules,” he said.
The vast majority of programs accepting applications from residents at Hahnemann were sympathetic and accommodating, he said, but a few programs applied “pressure tactics” to some of the residents offered a transfer position, despite graduate medical education rules in place to prevent such a situation from happening. “The resident says: ‘Oh, well, I’m waiting to hear from this other program,’ ” said Dr. D’Mello. “They’d say: ‘Okay, well, we’re giving you a position now. You have 12 hours to answer.’ ”
Decision makers at the hospital also were not very forthcoming with information to residents, fellows and program directors, according to a recent paper written by Thomas J. Nasca, MD, current president and CEO of ACGME, and colleagues in the journal Academic Medicine (Nasca T et al. Acad Med. 2019 Dec 17. doi: 10.1097/ACM.0000000000003133). When Dr. Nasca and colleagues went to investigate the situation at Hahnemann firsthand, “the team found that residents, fellows, and program directors alike considered their voices to have been ignored in decision making and deemed themselves ‘out of the loop’ of important information that would affect their career transitions.”
While the hospital closed in September 2019, the effects are still being felt. In Pennsylvania, the Medical Care Availability and Reduction of Error Act requires that hospitals and providers have malpractice insurance, including tail insurance for when a doctor’s insurance policy expires. American Academic announced it would not be paying tail insurance for claims made while physicians were at Hahnemann. This meant residents, fellows and physicians who worked at Hahnemann during the closure would be on the hook for paying their own malpractice insurance.
“On one hand, the risk is very low for the house staff. Lawsuits that come up later for house staff are generally dropped at some point,” said William W. Pinsky, MD, FAAP, FACC, president and CEO of the Educational Commission for Foreign Medical Graduates (ECFMG). “But who wants to take that risk going forward? It’s an issue that’s still not resolved.”
The American Medical Association, Association of American Medical Colleges (AAMC), the Philadelphia County Medical Society, and other medical societies have collectively put pressure on Hahnemann’s owners to pay for tail coverage. Beyond a Feb. 10, 2020 deadline, former Hahnemann physicians were still expected to cover their own tail insurance.
To further complicate matters, American Academic attempted to auction more than 570 residency slots at Hahnemann. The slots were sold to a consortium of six health systems in the area – Thomas Jefferson University Hospitals, Einstein Healthcare Network, Temple University Health System, Main Line Health, Cooper University Health Care, and Christiana Care Health System – for $55 million. The Centers for Medicare & Medicaid Services opposed the sale, arguing that the slots are a contract that hospitals enter into with CMS, rather than an asset to be sold. An appeal is currently pending.
The case is being watched by former physicians at Hahnemann. “American Academic said, ‘If we don’t get this $55 million, we’re not going to be able to cover this tail insurance.’ They’re kind of linking the two things,” said Dr. D’Mello. “To me, it’s almost like putting pressure to allow the sale to happen.”
Urban hospital closures disrupt health system balance
When an urban hospital like Hahnemann University Hospital closes, there is a major disruption to patient care. Patients need to relocate to other nearby centers, and they may not always be able to follow their physician to the next health center.
If patients have comorbidities, are being tracked across multiple care points, or change physicians during a hospital closure, details can be missed and care can become more complicated for physicians who end up seeing the patient at a new center. For example, a patient receiving obstetrics care at a hospital that closes will have to reschedule their delivery at another health center, noted Dr. Pinsky.
“Where patients get lost is when there’s not a physician or an individual can keep track of all that, coordinate, and help to be sure that the patient follows through,” he said.
Patients at a closing hospital need to go somewhere else for care, and patient volume naturally increases at other nearby centers, potentially causing problems for systems without the resources to handle the spike in traffic.
“I’m a service director of quality improvement and patient safety for Drexel internal medicine. I know that those sort of jumps and volumes are what increases medical errors and potentially could create some adverse outcomes,” said Dr. D’Mello. “That’s something I’m particularly worried about.”
Physicians are also reconciling their own personal situations during a hospital closure, attempting to figure out their next step while at the same time helping patients figure out theirs. In the case of international medical graduates on J-1 or H1-B visas, who are dependent on hospital positions and training programs to remain in the United States, the situation can be even more dire.
During Hahnemann’s closure, Dr. Pinsky said that the ECFMG, which represents 11,000 individuals with J-1 visas across the country, reached out to the 55 individuals on J-1 visas at the hospital and offered them assistance, including working with the Department of State to ensure they aren’t in jeopardy of deportation before they secure another training program position.
The ECFMG, AMA, AAMC, and ACGME also offered funding to help J-1 visa holders who needed to relocate outside Philadelphia. “Many of them spent a lot of their money or all their money just coming over here,” said Dr. Pinsky. “This was a way to help defray some immediate costs that they might have.”
Education and research, of which hospitalists and residents play a large role, are likewise affected during a hospital closure, Dr. Pinsky said. “Education and research in the hospital is an important contributor to the community, health care and medical education nationally overall. When it’s not considered, there can be a significant asset that is lost in the process, which is hard to ever regain.
“The hospitalists have an integral role in medical education. In most hospitals where there is graduate medical education, particularly in internal medicine or pediatrics, and where there is a hospitalist program, it’s the hospitalists that do the majority of the in-hospital or inpatient training and education,” he added.
Rural hospital closures affect access to care
Since 2005, 163 rural hospitals have closed in the United States. When rural hospitals close, the situation for hospitalists and other physicians is different. In communities where a larger health system owns a hospital, such as when Vidant Health closed Pungo District Hospital in Belhaven, N.C., in 2014 before reopening a nonemergency clinic in the area in 2016, health care services for the community may have limited interruption.
However, if there isn’t a nearby system to join, many doctors will end up leaving the area. More than half of rural hospitals that close end up not providing any kind of supplementary health care service, according to the NC Rural Health Research Program.
“A lot of the hospitals that have closed have not been owned by a system,” said George H. Pink, PhD, deputy director of the NC Rural Health Research Program at the University of North Carolina at Chapel Hill. “They’ve been independent, freestanding, and that perhaps is one of the reasons why they’re closing, is because they haven’t been able to find a system that would buy them out and inject capital into the community.”
This can also have an effect on the number of health care providers in the area, Dr. Pink said. “Their ability to refer patients and treat patients locally may be affected. That’s why, in many towns where hospitals have closed, we see a drop in the number of providers, particularly primary care doctors who actually live in the community.”
Politicians and federal entities have proposed a number of solutions to help protect rural hospitals from closure. Sen. Charles Grassley (R-Iowa), Sen. Amy Klobuchar (D-Minn.), and Sen. Cory Gardener (R-Colo.) have sponsored bills in the Senate, while Rep. Sam Graves (R-Mo.) has introduced legislation in the House. The Medicare Payment Advisory Commission has proposed two models of rural hospital care, and there are additional models proposed by the Kansas Hospital Association. A pilot program in Pennsylvania, the Pennsylvania Rural Health Model, is testing how a global budget by CMS for all inpatient and hospital-based outcomes might help rural hospitals.
“What we haven’t had a lot of action on is actually testing these models out and seeing whether they will work, and in what kinds of communities they will work,” Dr. Pink said.
Hospitalists as community advocates
Dr. D’Mello, who wrote an article for the Journal of Hospital Medicine on Hahnemann’s ownership by a private equity firm (doi: 10.12788/jhm.3378), said that the inherent nature of a for-profit entity trying to make a hospital profitable is a bad sign for a hospital and not necessarily what is in the best interest for an academic institution or for doctors who train there.
“I don’t know if I could blame the private equity firm completely, but in retrospect, the private equity firms stepping in was like the death knell of the hospital,” he said of Hahnemann’s closure.
“I think what the community needs to know – what the health care community, patient community, the hospitalist community need to know – is that there’s got to be more attention paid to these types of issues during mergers and acquisitions to prevent this from happening,” Dr. Pinsky said.
One larger issue was Hahnemann’s position as a safety net hospital, which partly played into American Academic’s lack of success in making the hospital as profitable as they wanted it to be, Dr. D’Mello noted. Hahnemann’s patient population consisted mostly of minority patients on Medicare, Medicaid, and charity care insurance, while recent studies have shown that hospitals are more likely to succeed when they have a larger proportion of patients with private insurance.
“Studies show that, to [make more] money from private insurance, you really have to have this huge footprint, because then you’ve got a better ability to negotiate with these private insurance companies,” Dr. D’Mello said. “Whether that’s actually good for health care is a different issue.”
Despite their own situations, it is not unusual for hospitalists and hospital physicians to step up during a hospital closure and advocate for their patients on behalf of the community, Dr. Pink said.
“When hospitals are in financial difficulty and there’s the risk of closure, typically, the medical staff are among the first to step up and warn the community: ‘We’re at risk of losing our service. We need some help,’ ” he said. “Generally speaking, the local physicians have been at the forefront of helping to keep access to hospital care available in some of these small communities – unfortunately, not always successfully.”
Dr. D’Mello, Dr. Pinsky, and Dr. Pink report no relevant conflicts of interest.
On June 26, 2019, American Academic Health System and Philadelphia Academic Health System announced that Hahnemann University Hospital, a 496-bed tertiary care center in North Philadelphia in operation for over 170 years, would close that September.
The emergency department closed 52 days after the announcement, leaving little time for physicians and staff to coordinate care for patients and secure new employment. The announcement was also made right at the beginning of the new academic year, which meant residents and fellows were forced to find new training programs. In total, 2,500 workers at Hahnemann, including more than 570 hospitalists and physicians training as residents and fellows, were displaced as the hospital closed – the largest such closing in U.S. history.
For most of its existence, Hahnemann was a teaching hospital. While trainees were all eventually placed in new programs thanks to efforts from the Accreditation Council for Graduate Medical Education (ACGME), some of the permanent staff at Hahnemann weren’t so lucky. A month after the announcement, Drexel University’s president told university employees that 40% of the staff who worked at Hahnemann would be cut as a result of the closing. Drexel, also based in Philadelphia, had long had an academic affiliation agreement for training Drexel’s medical school students as a primary academic partner. Overall, Drexel’s entire clinical staff at Hahnemann was let go, and Tower Health Medical Group is expected to hire about 60% of the former Hahnemann staff.
Kevin D’Mello, MD, FACP, FHM, a hospitalist and assistant professor of medicine at Drexel University, said residents during Hahnemann’s closure were essentially teaching themselves how to swim. “There were just no laws, no rules,” he said.
The vast majority of programs accepting applications from residents at Hahnemann were sympathetic and accommodating, he said, but a few programs applied “pressure tactics” to some of the residents offered a transfer position, despite graduate medical education rules in place to prevent such a situation from happening. “The resident says: ‘Oh, well, I’m waiting to hear from this other program,’ ” said Dr. D’Mello. “They’d say: ‘Okay, well, we’re giving you a position now. You have 12 hours to answer.’ ”
Decision makers at the hospital also were not very forthcoming with information to residents, fellows and program directors, according to a recent paper written by Thomas J. Nasca, MD, current president and CEO of ACGME, and colleagues in the journal Academic Medicine (Nasca T et al. Acad Med. 2019 Dec 17. doi: 10.1097/ACM.0000000000003133). When Dr. Nasca and colleagues went to investigate the situation at Hahnemann firsthand, “the team found that residents, fellows, and program directors alike considered their voices to have been ignored in decision making and deemed themselves ‘out of the loop’ of important information that would affect their career transitions.”
While the hospital closed in September 2019, the effects are still being felt. In Pennsylvania, the Medical Care Availability and Reduction of Error Act requires that hospitals and providers have malpractice insurance, including tail insurance for when a doctor’s insurance policy expires. American Academic announced it would not be paying tail insurance for claims made while physicians were at Hahnemann. This meant residents, fellows and physicians who worked at Hahnemann during the closure would be on the hook for paying their own malpractice insurance.
“On one hand, the risk is very low for the house staff. Lawsuits that come up later for house staff are generally dropped at some point,” said William W. Pinsky, MD, FAAP, FACC, president and CEO of the Educational Commission for Foreign Medical Graduates (ECFMG). “But who wants to take that risk going forward? It’s an issue that’s still not resolved.”
The American Medical Association, Association of American Medical Colleges (AAMC), the Philadelphia County Medical Society, and other medical societies have collectively put pressure on Hahnemann’s owners to pay for tail coverage. Beyond a Feb. 10, 2020 deadline, former Hahnemann physicians were still expected to cover their own tail insurance.
To further complicate matters, American Academic attempted to auction more than 570 residency slots at Hahnemann. The slots were sold to a consortium of six health systems in the area – Thomas Jefferson University Hospitals, Einstein Healthcare Network, Temple University Health System, Main Line Health, Cooper University Health Care, and Christiana Care Health System – for $55 million. The Centers for Medicare & Medicaid Services opposed the sale, arguing that the slots are a contract that hospitals enter into with CMS, rather than an asset to be sold. An appeal is currently pending.
The case is being watched by former physicians at Hahnemann. “American Academic said, ‘If we don’t get this $55 million, we’re not going to be able to cover this tail insurance.’ They’re kind of linking the two things,” said Dr. D’Mello. “To me, it’s almost like putting pressure to allow the sale to happen.”
Urban hospital closures disrupt health system balance
When an urban hospital like Hahnemann University Hospital closes, there is a major disruption to patient care. Patients need to relocate to other nearby centers, and they may not always be able to follow their physician to the next health center.
If patients have comorbidities, are being tracked across multiple care points, or change physicians during a hospital closure, details can be missed and care can become more complicated for physicians who end up seeing the patient at a new center. For example, a patient receiving obstetrics care at a hospital that closes will have to reschedule their delivery at another health center, noted Dr. Pinsky.
“Where patients get lost is when there’s not a physician or an individual can keep track of all that, coordinate, and help to be sure that the patient follows through,” he said.
Patients at a closing hospital need to go somewhere else for care, and patient volume naturally increases at other nearby centers, potentially causing problems for systems without the resources to handle the spike in traffic.
“I’m a service director of quality improvement and patient safety for Drexel internal medicine. I know that those sort of jumps and volumes are what increases medical errors and potentially could create some adverse outcomes,” said Dr. D’Mello. “That’s something I’m particularly worried about.”
Physicians are also reconciling their own personal situations during a hospital closure, attempting to figure out their next step while at the same time helping patients figure out theirs. In the case of international medical graduates on J-1 or H1-B visas, who are dependent on hospital positions and training programs to remain in the United States, the situation can be even more dire.
During Hahnemann’s closure, Dr. Pinsky said that the ECFMG, which represents 11,000 individuals with J-1 visas across the country, reached out to the 55 individuals on J-1 visas at the hospital and offered them assistance, including working with the Department of State to ensure they aren’t in jeopardy of deportation before they secure another training program position.
The ECFMG, AMA, AAMC, and ACGME also offered funding to help J-1 visa holders who needed to relocate outside Philadelphia. “Many of them spent a lot of their money or all their money just coming over here,” said Dr. Pinsky. “This was a way to help defray some immediate costs that they might have.”
Education and research, of which hospitalists and residents play a large role, are likewise affected during a hospital closure, Dr. Pinsky said. “Education and research in the hospital is an important contributor to the community, health care and medical education nationally overall. When it’s not considered, there can be a significant asset that is lost in the process, which is hard to ever regain.
“The hospitalists have an integral role in medical education. In most hospitals where there is graduate medical education, particularly in internal medicine or pediatrics, and where there is a hospitalist program, it’s the hospitalists that do the majority of the in-hospital or inpatient training and education,” he added.
Rural hospital closures affect access to care
Since 2005, 163 rural hospitals have closed in the United States. When rural hospitals close, the situation for hospitalists and other physicians is different. In communities where a larger health system owns a hospital, such as when Vidant Health closed Pungo District Hospital in Belhaven, N.C., in 2014 before reopening a nonemergency clinic in the area in 2016, health care services for the community may have limited interruption.
However, if there isn’t a nearby system to join, many doctors will end up leaving the area. More than half of rural hospitals that close end up not providing any kind of supplementary health care service, according to the NC Rural Health Research Program.
“A lot of the hospitals that have closed have not been owned by a system,” said George H. Pink, PhD, deputy director of the NC Rural Health Research Program at the University of North Carolina at Chapel Hill. “They’ve been independent, freestanding, and that perhaps is one of the reasons why they’re closing, is because they haven’t been able to find a system that would buy them out and inject capital into the community.”
This can also have an effect on the number of health care providers in the area, Dr. Pink said. “Their ability to refer patients and treat patients locally may be affected. That’s why, in many towns where hospitals have closed, we see a drop in the number of providers, particularly primary care doctors who actually live in the community.”
Politicians and federal entities have proposed a number of solutions to help protect rural hospitals from closure. Sen. Charles Grassley (R-Iowa), Sen. Amy Klobuchar (D-Minn.), and Sen. Cory Gardener (R-Colo.) have sponsored bills in the Senate, while Rep. Sam Graves (R-Mo.) has introduced legislation in the House. The Medicare Payment Advisory Commission has proposed two models of rural hospital care, and there are additional models proposed by the Kansas Hospital Association. A pilot program in Pennsylvania, the Pennsylvania Rural Health Model, is testing how a global budget by CMS for all inpatient and hospital-based outcomes might help rural hospitals.
“What we haven’t had a lot of action on is actually testing these models out and seeing whether they will work, and in what kinds of communities they will work,” Dr. Pink said.
Hospitalists as community advocates
Dr. D’Mello, who wrote an article for the Journal of Hospital Medicine on Hahnemann’s ownership by a private equity firm (doi: 10.12788/jhm.3378), said that the inherent nature of a for-profit entity trying to make a hospital profitable is a bad sign for a hospital and not necessarily what is in the best interest for an academic institution or for doctors who train there.
“I don’t know if I could blame the private equity firm completely, but in retrospect, the private equity firms stepping in was like the death knell of the hospital,” he said of Hahnemann’s closure.
“I think what the community needs to know – what the health care community, patient community, the hospitalist community need to know – is that there’s got to be more attention paid to these types of issues during mergers and acquisitions to prevent this from happening,” Dr. Pinsky said.
One larger issue was Hahnemann’s position as a safety net hospital, which partly played into American Academic’s lack of success in making the hospital as profitable as they wanted it to be, Dr. D’Mello noted. Hahnemann’s patient population consisted mostly of minority patients on Medicare, Medicaid, and charity care insurance, while recent studies have shown that hospitals are more likely to succeed when they have a larger proportion of patients with private insurance.
“Studies show that, to [make more] money from private insurance, you really have to have this huge footprint, because then you’ve got a better ability to negotiate with these private insurance companies,” Dr. D’Mello said. “Whether that’s actually good for health care is a different issue.”
Despite their own situations, it is not unusual for hospitalists and hospital physicians to step up during a hospital closure and advocate for their patients on behalf of the community, Dr. Pink said.
“When hospitals are in financial difficulty and there’s the risk of closure, typically, the medical staff are among the first to step up and warn the community: ‘We’re at risk of losing our service. We need some help,’ ” he said. “Generally speaking, the local physicians have been at the forefront of helping to keep access to hospital care available in some of these small communities – unfortunately, not always successfully.”
Dr. D’Mello, Dr. Pinsky, and Dr. Pink report no relevant conflicts of interest.
COVID-19: A guide to making telepsychiatry work
Changes prompted by social distancing could last beyond the pandemic
As the coronavirus pandemic persists, insurers and the federal government are making it easier for mental health professionals to deliver safe and effective psychiatric services to patients via Zoom, FaceTime, and other conferencing tools. Many psychiatrists, meanwhile, are embracing telepsychiatry for the first time – in some cases with urgency.
Jay H. Shore, MD, MPH, said in an interview that mental health providers at his medical center have gone entirely virtual in recent weeks.
“The genie is out of the bottle on this,” said Dr. Shore, director of telemedicine at the Helen and Arthur E. Johnson Depression Center and director of telemedicine programming for the department of psychiatry at the University of Colorado at Denver, Aurora. He thinks this is the beginning of a new era that will last beyond the pandemic. “There’s going to be a much wider and diffuse acceptance of telemedicine as we go forward,” he added.
Dr. Shore and several colleagues from across the country offered several tips about factors to consider while learning to use telepsychiatry as a treatment tool.
To start, Dr. Shore advised reviewing the American Psychiatric Association’s Telepsychiatry Practice Guidelines and its Telepsychiatry Toolkit, which include dozens of brief videos about topics such as room lighting and managing the content process.
Another resource is the joint APA–American Academy of Child and Adolescent Psychiatry Telepsychiatry Toolkit, said Shabana Khan, MD, an assistant professor and director of telemedicine for the department of child and adolescent psychiatry at New York University Langone Health.
One of the challenges is managing emergencies long distance. If a patient experiences a mental health emergency in a psychiatrist’s office, the clinician can call 911 or direct staff to seek help. “When they’re at their house,” said Dr. Shore, “it’s a little different.”
Staff members are not present at home offices, for example, and the patient might live in a different city and therefore have a different 911 system. “It’s important to know your protocol about how you plan to handle these emergencies before you start working with the patient,” Dr. Shore said.
Another tip is to ask staff to perform a test session to work out the technical kinks before the first patient appointment. “They can make the connection and make sure there’s a video signal with adequate quality,” Dr. Shore said. Failing to conduct a test run can lead to spending several minutes of a session trying to help patients figure out how to make video conferencing work properly.
“You can spend a lot of time acting as IT support,” he said.
It is important to ensure that virtual visits are not interrupted by technical glitches, Daniel Bristow, MD, said in an interview. If possible, hardwire your laptop or computer to an ethernet cable, said Dr. Bristow, president of the Oregon Psychiatric Physicians Association, the state’s branch of the APA. “This will lead to fewer fluctuations that you could see by using wifi,” said Dr. Bristow, who practices in Portland.
“Initially, I assumed that those with psychotic symptoms might struggle more. But I have been surprised at how well some patients have done,” said Andrew J. McLean, MD, MPH, clinical professor and chair of the department of psychiatry and behavioral science at the University of North Dakota, Grand Forks.
However, it might help to provide additional coaching to those patients, said Dr. Bristow. He offers a warning to these patients: “If you feel like you’re getting messages over the TV, my talking to you may make you feel worse.” However, “in every case, the patient was able to say, ‘I know you’re real.’ One patient even said: ‘I’ve heard these voices from my TV for years. But I know you’re a doctor, and you’re in an office trying to help me.’ ”
Dr. Shore thinks that video meetings have the potential to help psychiatrists and patients form better personal connections than in-person meetings. Patients with anxiety or PTSD, for example, “may feel safer since they’re in their own space, and they have a greater sense of control over the session than being in somebody’s office,” he said.
Dr. Khan agreed. “Some children, such as those with a significant trauma history or with significant anxiety, may feel more comfortable with this modality and may open up more during video sessions,” she said. In addition, “the distance that telepsychiatry provides may also enhance feelings of confidentiality and reduce potential stigma that may be associated with seeking mental health care.”
When it comes to using videoconferencing to treat children, take advantage of interactive features that are available, said Katherine Nguyen Williams, PhD. Zoom’s HIPAA-compliant health care software, for example, offers a “share screen” capability. “It allows for easy interactive activities,” said Dr. Nguyen Williams, director of strategic development and clinical innovation at Rady Children’s Hospital’s department of psychiatry at the University of California, San Diego. “Clinicians can play tic-tac-toe on the screen with the young patients, and they can work on cognitive-behavioral therapy worksheets together on the digital screen. Clinicians can even show a mindfulness video to the patient while actively coaching and giving feedback to the patient as they practice diaphragmatic breathing while viewing the video.
“There are so many more options for making virtual therapy as interactive as face-to-face therapy,” said Dr. Nguyen Williams, who also is an associate clinical professor at the university. “This is the key to getting and keeping the patient engaged in telepsychiatry.”
Despite the many positive aspects of using telepsychiatry as a treatment tool, some negative factors must be considered. “You lose some of the nuances, subtleties in terms of expression, movement, smell, etc.,” said Dr. McLean. “Also, there are rare instances where a part of a physical examination would be appropriate, which also is precluded.”
Videoconferencing software might allow the clinician to zoom in to take a closer look at a patient to look for subtle movements and tremors, Dr. McLean said. And, he added, he has asked nursing staff to check for particular signs and symptoms during visits and to describe them to him. “Still,” Dr. McLean said, “this does not take the place of being there.”
Dr. Shore suggested several other practical considerations. For example, while on a screen, keep the home environment as professional as the office would be, he said. Be clear with family members about the importance of not interrupting and make sure that privacy is maintained. The message should be: “I’m working from home, and I’m not available during these hours,” Dr. Shore said. “You need to be aware that, during this time, I need this for clinical work.”
Dr. Shore reported serving as chief medical officer of AccessCare Services, and receiving royalties from American Psychiatric Association Publishing and Springer. He also is coauthor with Peter Yellowlees, MD, of “Telepsychiatry and Health Technologies: A Guide for Mental Health Professionals” (Arlington, Va.: American Psychiatric Association Publishing, 2018). Dr. Khan and Dr. McLean reported no relevant disclosures. Dr. Bristow reported relationships with MCG Health and Insight + Regroup Telehealth.
For more details about using telepsychiatry in the time of COVID-19, listen to the April 8 Psychcast Masterclass lecture by Dr. Shore.
Changes prompted by social distancing could last beyond the pandemic
Changes prompted by social distancing could last beyond the pandemic
As the coronavirus pandemic persists, insurers and the federal government are making it easier for mental health professionals to deliver safe and effective psychiatric services to patients via Zoom, FaceTime, and other conferencing tools. Many psychiatrists, meanwhile, are embracing telepsychiatry for the first time – in some cases with urgency.
Jay H. Shore, MD, MPH, said in an interview that mental health providers at his medical center have gone entirely virtual in recent weeks.
“The genie is out of the bottle on this,” said Dr. Shore, director of telemedicine at the Helen and Arthur E. Johnson Depression Center and director of telemedicine programming for the department of psychiatry at the University of Colorado at Denver, Aurora. He thinks this is the beginning of a new era that will last beyond the pandemic. “There’s going to be a much wider and diffuse acceptance of telemedicine as we go forward,” he added.
Dr. Shore and several colleagues from across the country offered several tips about factors to consider while learning to use telepsychiatry as a treatment tool.
To start, Dr. Shore advised reviewing the American Psychiatric Association’s Telepsychiatry Practice Guidelines and its Telepsychiatry Toolkit, which include dozens of brief videos about topics such as room lighting and managing the content process.
Another resource is the joint APA–American Academy of Child and Adolescent Psychiatry Telepsychiatry Toolkit, said Shabana Khan, MD, an assistant professor and director of telemedicine for the department of child and adolescent psychiatry at New York University Langone Health.
One of the challenges is managing emergencies long distance. If a patient experiences a mental health emergency in a psychiatrist’s office, the clinician can call 911 or direct staff to seek help. “When they’re at their house,” said Dr. Shore, “it’s a little different.”
Staff members are not present at home offices, for example, and the patient might live in a different city and therefore have a different 911 system. “It’s important to know your protocol about how you plan to handle these emergencies before you start working with the patient,” Dr. Shore said.
Another tip is to ask staff to perform a test session to work out the technical kinks before the first patient appointment. “They can make the connection and make sure there’s a video signal with adequate quality,” Dr. Shore said. Failing to conduct a test run can lead to spending several minutes of a session trying to help patients figure out how to make video conferencing work properly.
“You can spend a lot of time acting as IT support,” he said.
It is important to ensure that virtual visits are not interrupted by technical glitches, Daniel Bristow, MD, said in an interview. If possible, hardwire your laptop or computer to an ethernet cable, said Dr. Bristow, president of the Oregon Psychiatric Physicians Association, the state’s branch of the APA. “This will lead to fewer fluctuations that you could see by using wifi,” said Dr. Bristow, who practices in Portland.
“Initially, I assumed that those with psychotic symptoms might struggle more. But I have been surprised at how well some patients have done,” said Andrew J. McLean, MD, MPH, clinical professor and chair of the department of psychiatry and behavioral science at the University of North Dakota, Grand Forks.
However, it might help to provide additional coaching to those patients, said Dr. Bristow. He offers a warning to these patients: “If you feel like you’re getting messages over the TV, my talking to you may make you feel worse.” However, “in every case, the patient was able to say, ‘I know you’re real.’ One patient even said: ‘I’ve heard these voices from my TV for years. But I know you’re a doctor, and you’re in an office trying to help me.’ ”
Dr. Shore thinks that video meetings have the potential to help psychiatrists and patients form better personal connections than in-person meetings. Patients with anxiety or PTSD, for example, “may feel safer since they’re in their own space, and they have a greater sense of control over the session than being in somebody’s office,” he said.
Dr. Khan agreed. “Some children, such as those with a significant trauma history or with significant anxiety, may feel more comfortable with this modality and may open up more during video sessions,” she said. In addition, “the distance that telepsychiatry provides may also enhance feelings of confidentiality and reduce potential stigma that may be associated with seeking mental health care.”
When it comes to using videoconferencing to treat children, take advantage of interactive features that are available, said Katherine Nguyen Williams, PhD. Zoom’s HIPAA-compliant health care software, for example, offers a “share screen” capability. “It allows for easy interactive activities,” said Dr. Nguyen Williams, director of strategic development and clinical innovation at Rady Children’s Hospital’s department of psychiatry at the University of California, San Diego. “Clinicians can play tic-tac-toe on the screen with the young patients, and they can work on cognitive-behavioral therapy worksheets together on the digital screen. Clinicians can even show a mindfulness video to the patient while actively coaching and giving feedback to the patient as they practice diaphragmatic breathing while viewing the video.
“There are so many more options for making virtual therapy as interactive as face-to-face therapy,” said Dr. Nguyen Williams, who also is an associate clinical professor at the university. “This is the key to getting and keeping the patient engaged in telepsychiatry.”
Despite the many positive aspects of using telepsychiatry as a treatment tool, some negative factors must be considered. “You lose some of the nuances, subtleties in terms of expression, movement, smell, etc.,” said Dr. McLean. “Also, there are rare instances where a part of a physical examination would be appropriate, which also is precluded.”
Videoconferencing software might allow the clinician to zoom in to take a closer look at a patient to look for subtle movements and tremors, Dr. McLean said. And, he added, he has asked nursing staff to check for particular signs and symptoms during visits and to describe them to him. “Still,” Dr. McLean said, “this does not take the place of being there.”
Dr. Shore suggested several other practical considerations. For example, while on a screen, keep the home environment as professional as the office would be, he said. Be clear with family members about the importance of not interrupting and make sure that privacy is maintained. The message should be: “I’m working from home, and I’m not available during these hours,” Dr. Shore said. “You need to be aware that, during this time, I need this for clinical work.”
Dr. Shore reported serving as chief medical officer of AccessCare Services, and receiving royalties from American Psychiatric Association Publishing and Springer. He also is coauthor with Peter Yellowlees, MD, of “Telepsychiatry and Health Technologies: A Guide for Mental Health Professionals” (Arlington, Va.: American Psychiatric Association Publishing, 2018). Dr. Khan and Dr. McLean reported no relevant disclosures. Dr. Bristow reported relationships with MCG Health and Insight + Regroup Telehealth.
For more details about using telepsychiatry in the time of COVID-19, listen to the April 8 Psychcast Masterclass lecture by Dr. Shore.
As the coronavirus pandemic persists, insurers and the federal government are making it easier for mental health professionals to deliver safe and effective psychiatric services to patients via Zoom, FaceTime, and other conferencing tools. Many psychiatrists, meanwhile, are embracing telepsychiatry for the first time – in some cases with urgency.
Jay H. Shore, MD, MPH, said in an interview that mental health providers at his medical center have gone entirely virtual in recent weeks.
“The genie is out of the bottle on this,” said Dr. Shore, director of telemedicine at the Helen and Arthur E. Johnson Depression Center and director of telemedicine programming for the department of psychiatry at the University of Colorado at Denver, Aurora. He thinks this is the beginning of a new era that will last beyond the pandemic. “There’s going to be a much wider and diffuse acceptance of telemedicine as we go forward,” he added.
Dr. Shore and several colleagues from across the country offered several tips about factors to consider while learning to use telepsychiatry as a treatment tool.
To start, Dr. Shore advised reviewing the American Psychiatric Association’s Telepsychiatry Practice Guidelines and its Telepsychiatry Toolkit, which include dozens of brief videos about topics such as room lighting and managing the content process.
Another resource is the joint APA–American Academy of Child and Adolescent Psychiatry Telepsychiatry Toolkit, said Shabana Khan, MD, an assistant professor and director of telemedicine for the department of child and adolescent psychiatry at New York University Langone Health.
One of the challenges is managing emergencies long distance. If a patient experiences a mental health emergency in a psychiatrist’s office, the clinician can call 911 or direct staff to seek help. “When they’re at their house,” said Dr. Shore, “it’s a little different.”
Staff members are not present at home offices, for example, and the patient might live in a different city and therefore have a different 911 system. “It’s important to know your protocol about how you plan to handle these emergencies before you start working with the patient,” Dr. Shore said.
Another tip is to ask staff to perform a test session to work out the technical kinks before the first patient appointment. “They can make the connection and make sure there’s a video signal with adequate quality,” Dr. Shore said. Failing to conduct a test run can lead to spending several minutes of a session trying to help patients figure out how to make video conferencing work properly.
“You can spend a lot of time acting as IT support,” he said.
It is important to ensure that virtual visits are not interrupted by technical glitches, Daniel Bristow, MD, said in an interview. If possible, hardwire your laptop or computer to an ethernet cable, said Dr. Bristow, president of the Oregon Psychiatric Physicians Association, the state’s branch of the APA. “This will lead to fewer fluctuations that you could see by using wifi,” said Dr. Bristow, who practices in Portland.
“Initially, I assumed that those with psychotic symptoms might struggle more. But I have been surprised at how well some patients have done,” said Andrew J. McLean, MD, MPH, clinical professor and chair of the department of psychiatry and behavioral science at the University of North Dakota, Grand Forks.
However, it might help to provide additional coaching to those patients, said Dr. Bristow. He offers a warning to these patients: “If you feel like you’re getting messages over the TV, my talking to you may make you feel worse.” However, “in every case, the patient was able to say, ‘I know you’re real.’ One patient even said: ‘I’ve heard these voices from my TV for years. But I know you’re a doctor, and you’re in an office trying to help me.’ ”
Dr. Shore thinks that video meetings have the potential to help psychiatrists and patients form better personal connections than in-person meetings. Patients with anxiety or PTSD, for example, “may feel safer since they’re in their own space, and they have a greater sense of control over the session than being in somebody’s office,” he said.
Dr. Khan agreed. “Some children, such as those with a significant trauma history or with significant anxiety, may feel more comfortable with this modality and may open up more during video sessions,” she said. In addition, “the distance that telepsychiatry provides may also enhance feelings of confidentiality and reduce potential stigma that may be associated with seeking mental health care.”
When it comes to using videoconferencing to treat children, take advantage of interactive features that are available, said Katherine Nguyen Williams, PhD. Zoom’s HIPAA-compliant health care software, for example, offers a “share screen” capability. “It allows for easy interactive activities,” said Dr. Nguyen Williams, director of strategic development and clinical innovation at Rady Children’s Hospital’s department of psychiatry at the University of California, San Diego. “Clinicians can play tic-tac-toe on the screen with the young patients, and they can work on cognitive-behavioral therapy worksheets together on the digital screen. Clinicians can even show a mindfulness video to the patient while actively coaching and giving feedback to the patient as they practice diaphragmatic breathing while viewing the video.
“There are so many more options for making virtual therapy as interactive as face-to-face therapy,” said Dr. Nguyen Williams, who also is an associate clinical professor at the university. “This is the key to getting and keeping the patient engaged in telepsychiatry.”
Despite the many positive aspects of using telepsychiatry as a treatment tool, some negative factors must be considered. “You lose some of the nuances, subtleties in terms of expression, movement, smell, etc.,” said Dr. McLean. “Also, there are rare instances where a part of a physical examination would be appropriate, which also is precluded.”
Videoconferencing software might allow the clinician to zoom in to take a closer look at a patient to look for subtle movements and tremors, Dr. McLean said. And, he added, he has asked nursing staff to check for particular signs and symptoms during visits and to describe them to him. “Still,” Dr. McLean said, “this does not take the place of being there.”
Dr. Shore suggested several other practical considerations. For example, while on a screen, keep the home environment as professional as the office would be, he said. Be clear with family members about the importance of not interrupting and make sure that privacy is maintained. The message should be: “I’m working from home, and I’m not available during these hours,” Dr. Shore said. “You need to be aware that, during this time, I need this for clinical work.”
Dr. Shore reported serving as chief medical officer of AccessCare Services, and receiving royalties from American Psychiatric Association Publishing and Springer. He also is coauthor with Peter Yellowlees, MD, of “Telepsychiatry and Health Technologies: A Guide for Mental Health Professionals” (Arlington, Va.: American Psychiatric Association Publishing, 2018). Dr. Khan and Dr. McLean reported no relevant disclosures. Dr. Bristow reported relationships with MCG Health and Insight + Regroup Telehealth.
For more details about using telepsychiatry in the time of COVID-19, listen to the April 8 Psychcast Masterclass lecture by Dr. Shore.
COVID-19: Dramatic changes to telepsychiatry rules and regs
In the wake of the coronavirus pandemic,
Under the 1135 emergency waiver, Medicare has expanded telehealth services to include patients across the country – not just in rural areas or under other limited conditions, as was previously the case. In addition, there’s now a waiver to the Ryan Haight Act that allows the prescribing of controlled substances via telemedicine.
Peter Yellowlees, MD, from University of California, Davis, reported that outpatient service at his center was converted to an almost 100% telepsychiatry service from mid- to late March.
He and John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, led a free webinar late last month sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA).
During the hour-long event, they answered questions and offered tips on changes in licensure, patient safety, new prescribing rules, and equipment needed.
“Clinicians need to be aware of these changes so they can ensure they are reaching as many people as possible and taking advantage of the reduced barriers to offering safe and effective video visits,” Dr. Torous said in an interview.
‘This is huge’
The new 1135 waiver “basically says CMS will pay for any patient on Medicare who is seen by video by any provider who is correctly licensed in any state in this country,” Dr. Yellowlees told webinar attendees.
“You don’t need to be licensed in the state where the patient is if the patient is on Medicare. This opens up a huge number of patients we can now see on video,” he said. “And you can bill at normal Medicare rates for whatever you normally get for your in-person patients.”
Although this temporary rule only applies to Medicare and not to private insurers, or to patients on Medicaid, “these are really big changes. This is huge,” Dr. Torous said.
Previously, the “originating site” rule stated that, for the most part, clinicians had to be licensed in the state where the patient was located and not where the physician was stationed.
Asked about college students receiving mental health care who were in school in the psychiatrist’s area but are now back home in a state where the clinician doesn’t have a license, Dr. Yellowlees said that scenario could be a bit “tricky.”
“Most of those patients probably aren’t on Medicare. Legally, you [usually] can’t see them on video if they have private insurance or Medicaid. So, hopefully you can give them a 3-month supply of medication and then recommend they see a local provider,” he said.
Still, all states have their own rules, Dr. Yellowlees said. He and Dr. Torous noted that the Federation of State Medical Boards has a “very up-to-date” listing of policies at FSMB.org, all of which are organized by state. In addition, the American Psychiatric Association provides a telepsychiatry toolkit on its website.
Ryan Haight Act and prescribing
Physicians are now permitted to prescribe medication to patients assessed via telemedicine.
For those with substance use disorders, the U.S. Drug Enforcement Administration has announced a new waiver for the Ryan Haight Online Pharmacy Consumer Protection Act.
The waiver states that “practitioners in all areas of the United States may issue prescriptions for all schedule II-V controlled substances” – as long as it’s for a legitimate medical purpose; real-time, two-way interactive communication with patients has been used; and the clinician “is acting in accordance with applicable Federal and State laws.”
“It’s now possible to prescribe all the normal psychiatric drugs but also benzodiazepines, stimulants, and potentially narcotics over telepsychiatry,” even at a first visit via video, Dr. Yellowlees said.
However, he noted at this point the waiver is current for only 60 days. “This isn’t a permanent condition. It could be extended or even shortened at any given time.”
In addition, SAMHSA has relaxed some of its own regulations regarding telehealth and opioid treatment programs. An FAQ section on the organization’s website provides guidance for providing methadone and buprenorphine treatment.
“Some of the previous regulations will probably be put back in place later on, but the new changes are helpful now,” Dr. Yellowlees said.
Simple equipment needed
Regarding equipment, Dr. Yellowlees noted that the most important component is just a laptop, tablet, or smartphone – for the clinician and for the patient.
“You don’t need fancy new technology with a separate camera or microphone,” he said. However, it might be worth investing in a little better system down the line, he added.
Simple platforms that can be used to meet virtually with patients include FaceTime, Google Hangouts, and Skype.
Although some of these (such as FaceTime) are not HIPAA compliant, “that’s okay for now” under the new rules, Dr. Yellowlees said. While the health system/commercial version of Skype is compliant, the normal consumer-downloaded version is not, he noted.
“I would still strongly suggest using HIPAA-compliant video-conferencing programs in the long run,” he added.
Either way, it’s important for various safety practices to be put into place. For example, clinicians should be careful because the consumer version of Skype can show names of patients who were previously spoken with.
A business associate agreement (BAA) is something that HIPAA-compliant video systems will offer and which should be signed. It’s an agreement that “you’ll be, essentially, looking through a tunnel at the persona at the other end, and the company cannot get inside the tunnel and watch you while you’re having your interview,” said Dr. Yellowlees.
“There are multiple videoconferencing systems around that you can use,” he added. “The three major ones are from Zoom, Vidyo, and VSee, but there are probably 40 or 50 more.”
“There are a lot out there, and we’re certainly not endorsing any one of them,” Dr. Torous added.
When evaluating potential programs, Dr. Yellowlees suggested looking at Yelp-style reviews or telemedicine review sites, or talk with colleagues.
“Basically, you want systems that offer high-definition video quality and the ability to ‘lock’ and ‘unlock’ the rooms. And you want it to have an app so mobile devices can use it,” he said.
Phone vs. video
Some patients, especially older ones, may be resistant to the idea of video chats, preferring to talk via telephone instead.
“If you can use video, it’s better to do that if you can, especially when setting up the systems are relatively simple,” Dr. Yellowlees said, adding that it might just be an issue of patients needing help to get started.
However, “for some people, this is a barrier that we have to respect,” Dr. Torous said.
Either way, clinicians should check the American Medical Association’s website for information about coding for both video and phone visits.
Asked whether a clinician needs written consent from patients for conducting telepsychiatry visits, Dr. Yellowlees said it’s important to check state-by-state rules. For example, California allows a verbal consent.
In many cases, “simply jot down a note that consent was given and how” and write down the address where the patient is located at time of visit, such as for their home, he said.
If a patient wants to conduct a telehealth session while in their car, Dr. Yellowlees suggested getting the address of the parking lot. For safety, clinicians also are advised asking for the cell phone number of the patient as well as that of a loved one.
Vital signs
When it comes to checking vital signs, Dr. Yellowlees suggested asking patients to purchase an inexpensive blood pressure (BP) monitor, thermometer, etc, prior to an appointment.
“Ask them to do a BP test on video and show you the readings. For the AIMS [Abnormal Involuntary Movement Scale] test, or to check for tardive dyskinesia, instruct patients to come close to the camera to show movement.”
In addition, most psychiatric rating scales are available online, which patients can fill out before a telehealth visit. The Serious Mental Illness (SMI) Adviser mobile app also includes several of these scales, Dr. Torous noted.
Overall, “there have been dramatic changes in the rules and regulations governing [telepsychiatry] that, for the next 60 days, make it easier to offer telehealth to patients,” Dr. Torous said.
Therefore, all psychiatrists need to “get on board,” as soon as possible, Dr. Yellowlees added.
The webinar was funded in part by a grant from SAMHSA.
A version of this article originally appeared on Medscape.com.
In the wake of the coronavirus pandemic,
Under the 1135 emergency waiver, Medicare has expanded telehealth services to include patients across the country – not just in rural areas or under other limited conditions, as was previously the case. In addition, there’s now a waiver to the Ryan Haight Act that allows the prescribing of controlled substances via telemedicine.
Peter Yellowlees, MD, from University of California, Davis, reported that outpatient service at his center was converted to an almost 100% telepsychiatry service from mid- to late March.
He and John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, led a free webinar late last month sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA).
During the hour-long event, they answered questions and offered tips on changes in licensure, patient safety, new prescribing rules, and equipment needed.
“Clinicians need to be aware of these changes so they can ensure they are reaching as many people as possible and taking advantage of the reduced barriers to offering safe and effective video visits,” Dr. Torous said in an interview.
‘This is huge’
The new 1135 waiver “basically says CMS will pay for any patient on Medicare who is seen by video by any provider who is correctly licensed in any state in this country,” Dr. Yellowlees told webinar attendees.
“You don’t need to be licensed in the state where the patient is if the patient is on Medicare. This opens up a huge number of patients we can now see on video,” he said. “And you can bill at normal Medicare rates for whatever you normally get for your in-person patients.”
Although this temporary rule only applies to Medicare and not to private insurers, or to patients on Medicaid, “these are really big changes. This is huge,” Dr. Torous said.
Previously, the “originating site” rule stated that, for the most part, clinicians had to be licensed in the state where the patient was located and not where the physician was stationed.
Asked about college students receiving mental health care who were in school in the psychiatrist’s area but are now back home in a state where the clinician doesn’t have a license, Dr. Yellowlees said that scenario could be a bit “tricky.”
“Most of those patients probably aren’t on Medicare. Legally, you [usually] can’t see them on video if they have private insurance or Medicaid. So, hopefully you can give them a 3-month supply of medication and then recommend they see a local provider,” he said.
Still, all states have their own rules, Dr. Yellowlees said. He and Dr. Torous noted that the Federation of State Medical Boards has a “very up-to-date” listing of policies at FSMB.org, all of which are organized by state. In addition, the American Psychiatric Association provides a telepsychiatry toolkit on its website.
Ryan Haight Act and prescribing
Physicians are now permitted to prescribe medication to patients assessed via telemedicine.
For those with substance use disorders, the U.S. Drug Enforcement Administration has announced a new waiver for the Ryan Haight Online Pharmacy Consumer Protection Act.
The waiver states that “practitioners in all areas of the United States may issue prescriptions for all schedule II-V controlled substances” – as long as it’s for a legitimate medical purpose; real-time, two-way interactive communication with patients has been used; and the clinician “is acting in accordance with applicable Federal and State laws.”
“It’s now possible to prescribe all the normal psychiatric drugs but also benzodiazepines, stimulants, and potentially narcotics over telepsychiatry,” even at a first visit via video, Dr. Yellowlees said.
However, he noted at this point the waiver is current for only 60 days. “This isn’t a permanent condition. It could be extended or even shortened at any given time.”
In addition, SAMHSA has relaxed some of its own regulations regarding telehealth and opioid treatment programs. An FAQ section on the organization’s website provides guidance for providing methadone and buprenorphine treatment.
“Some of the previous regulations will probably be put back in place later on, but the new changes are helpful now,” Dr. Yellowlees said.
Simple equipment needed
Regarding equipment, Dr. Yellowlees noted that the most important component is just a laptop, tablet, or smartphone – for the clinician and for the patient.
“You don’t need fancy new technology with a separate camera or microphone,” he said. However, it might be worth investing in a little better system down the line, he added.
Simple platforms that can be used to meet virtually with patients include FaceTime, Google Hangouts, and Skype.
Although some of these (such as FaceTime) are not HIPAA compliant, “that’s okay for now” under the new rules, Dr. Yellowlees said. While the health system/commercial version of Skype is compliant, the normal consumer-downloaded version is not, he noted.
“I would still strongly suggest using HIPAA-compliant video-conferencing programs in the long run,” he added.
Either way, it’s important for various safety practices to be put into place. For example, clinicians should be careful because the consumer version of Skype can show names of patients who were previously spoken with.
A business associate agreement (BAA) is something that HIPAA-compliant video systems will offer and which should be signed. It’s an agreement that “you’ll be, essentially, looking through a tunnel at the persona at the other end, and the company cannot get inside the tunnel and watch you while you’re having your interview,” said Dr. Yellowlees.
“There are multiple videoconferencing systems around that you can use,” he added. “The three major ones are from Zoom, Vidyo, and VSee, but there are probably 40 or 50 more.”
“There are a lot out there, and we’re certainly not endorsing any one of them,” Dr. Torous added.
When evaluating potential programs, Dr. Yellowlees suggested looking at Yelp-style reviews or telemedicine review sites, or talk with colleagues.
“Basically, you want systems that offer high-definition video quality and the ability to ‘lock’ and ‘unlock’ the rooms. And you want it to have an app so mobile devices can use it,” he said.
Phone vs. video
Some patients, especially older ones, may be resistant to the idea of video chats, preferring to talk via telephone instead.
“If you can use video, it’s better to do that if you can, especially when setting up the systems are relatively simple,” Dr. Yellowlees said, adding that it might just be an issue of patients needing help to get started.
However, “for some people, this is a barrier that we have to respect,” Dr. Torous said.
Either way, clinicians should check the American Medical Association’s website for information about coding for both video and phone visits.
Asked whether a clinician needs written consent from patients for conducting telepsychiatry visits, Dr. Yellowlees said it’s important to check state-by-state rules. For example, California allows a verbal consent.
In many cases, “simply jot down a note that consent was given and how” and write down the address where the patient is located at time of visit, such as for their home, he said.
If a patient wants to conduct a telehealth session while in their car, Dr. Yellowlees suggested getting the address of the parking lot. For safety, clinicians also are advised asking for the cell phone number of the patient as well as that of a loved one.
Vital signs
When it comes to checking vital signs, Dr. Yellowlees suggested asking patients to purchase an inexpensive blood pressure (BP) monitor, thermometer, etc, prior to an appointment.
“Ask them to do a BP test on video and show you the readings. For the AIMS [Abnormal Involuntary Movement Scale] test, or to check for tardive dyskinesia, instruct patients to come close to the camera to show movement.”
In addition, most psychiatric rating scales are available online, which patients can fill out before a telehealth visit. The Serious Mental Illness (SMI) Adviser mobile app also includes several of these scales, Dr. Torous noted.
Overall, “there have been dramatic changes in the rules and regulations governing [telepsychiatry] that, for the next 60 days, make it easier to offer telehealth to patients,” Dr. Torous said.
Therefore, all psychiatrists need to “get on board,” as soon as possible, Dr. Yellowlees added.
The webinar was funded in part by a grant from SAMHSA.
A version of this article originally appeared on Medscape.com.
In the wake of the coronavirus pandemic,
Under the 1135 emergency waiver, Medicare has expanded telehealth services to include patients across the country – not just in rural areas or under other limited conditions, as was previously the case. In addition, there’s now a waiver to the Ryan Haight Act that allows the prescribing of controlled substances via telemedicine.
Peter Yellowlees, MD, from University of California, Davis, reported that outpatient service at his center was converted to an almost 100% telepsychiatry service from mid- to late March.
He and John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, led a free webinar late last month sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA).
During the hour-long event, they answered questions and offered tips on changes in licensure, patient safety, new prescribing rules, and equipment needed.
“Clinicians need to be aware of these changes so they can ensure they are reaching as many people as possible and taking advantage of the reduced barriers to offering safe and effective video visits,” Dr. Torous said in an interview.
‘This is huge’
The new 1135 waiver “basically says CMS will pay for any patient on Medicare who is seen by video by any provider who is correctly licensed in any state in this country,” Dr. Yellowlees told webinar attendees.
“You don’t need to be licensed in the state where the patient is if the patient is on Medicare. This opens up a huge number of patients we can now see on video,” he said. “And you can bill at normal Medicare rates for whatever you normally get for your in-person patients.”
Although this temporary rule only applies to Medicare and not to private insurers, or to patients on Medicaid, “these are really big changes. This is huge,” Dr. Torous said.
Previously, the “originating site” rule stated that, for the most part, clinicians had to be licensed in the state where the patient was located and not where the physician was stationed.
Asked about college students receiving mental health care who were in school in the psychiatrist’s area but are now back home in a state where the clinician doesn’t have a license, Dr. Yellowlees said that scenario could be a bit “tricky.”
“Most of those patients probably aren’t on Medicare. Legally, you [usually] can’t see them on video if they have private insurance or Medicaid. So, hopefully you can give them a 3-month supply of medication and then recommend they see a local provider,” he said.
Still, all states have their own rules, Dr. Yellowlees said. He and Dr. Torous noted that the Federation of State Medical Boards has a “very up-to-date” listing of policies at FSMB.org, all of which are organized by state. In addition, the American Psychiatric Association provides a telepsychiatry toolkit on its website.
Ryan Haight Act and prescribing
Physicians are now permitted to prescribe medication to patients assessed via telemedicine.
For those with substance use disorders, the U.S. Drug Enforcement Administration has announced a new waiver for the Ryan Haight Online Pharmacy Consumer Protection Act.
The waiver states that “practitioners in all areas of the United States may issue prescriptions for all schedule II-V controlled substances” – as long as it’s for a legitimate medical purpose; real-time, two-way interactive communication with patients has been used; and the clinician “is acting in accordance with applicable Federal and State laws.”
“It’s now possible to prescribe all the normal psychiatric drugs but also benzodiazepines, stimulants, and potentially narcotics over telepsychiatry,” even at a first visit via video, Dr. Yellowlees said.
However, he noted at this point the waiver is current for only 60 days. “This isn’t a permanent condition. It could be extended or even shortened at any given time.”
In addition, SAMHSA has relaxed some of its own regulations regarding telehealth and opioid treatment programs. An FAQ section on the organization’s website provides guidance for providing methadone and buprenorphine treatment.
“Some of the previous regulations will probably be put back in place later on, but the new changes are helpful now,” Dr. Yellowlees said.
Simple equipment needed
Regarding equipment, Dr. Yellowlees noted that the most important component is just a laptop, tablet, or smartphone – for the clinician and for the patient.
“You don’t need fancy new technology with a separate camera or microphone,” he said. However, it might be worth investing in a little better system down the line, he added.
Simple platforms that can be used to meet virtually with patients include FaceTime, Google Hangouts, and Skype.
Although some of these (such as FaceTime) are not HIPAA compliant, “that’s okay for now” under the new rules, Dr. Yellowlees said. While the health system/commercial version of Skype is compliant, the normal consumer-downloaded version is not, he noted.
“I would still strongly suggest using HIPAA-compliant video-conferencing programs in the long run,” he added.
Either way, it’s important for various safety practices to be put into place. For example, clinicians should be careful because the consumer version of Skype can show names of patients who were previously spoken with.
A business associate agreement (BAA) is something that HIPAA-compliant video systems will offer and which should be signed. It’s an agreement that “you’ll be, essentially, looking through a tunnel at the persona at the other end, and the company cannot get inside the tunnel and watch you while you’re having your interview,” said Dr. Yellowlees.
“There are multiple videoconferencing systems around that you can use,” he added. “The three major ones are from Zoom, Vidyo, and VSee, but there are probably 40 or 50 more.”
“There are a lot out there, and we’re certainly not endorsing any one of them,” Dr. Torous added.
When evaluating potential programs, Dr. Yellowlees suggested looking at Yelp-style reviews or telemedicine review sites, or talk with colleagues.
“Basically, you want systems that offer high-definition video quality and the ability to ‘lock’ and ‘unlock’ the rooms. And you want it to have an app so mobile devices can use it,” he said.
Phone vs. video
Some patients, especially older ones, may be resistant to the idea of video chats, preferring to talk via telephone instead.
“If you can use video, it’s better to do that if you can, especially when setting up the systems are relatively simple,” Dr. Yellowlees said, adding that it might just be an issue of patients needing help to get started.
However, “for some people, this is a barrier that we have to respect,” Dr. Torous said.
Either way, clinicians should check the American Medical Association’s website for information about coding for both video and phone visits.
Asked whether a clinician needs written consent from patients for conducting telepsychiatry visits, Dr. Yellowlees said it’s important to check state-by-state rules. For example, California allows a verbal consent.
In many cases, “simply jot down a note that consent was given and how” and write down the address where the patient is located at time of visit, such as for their home, he said.
If a patient wants to conduct a telehealth session while in their car, Dr. Yellowlees suggested getting the address of the parking lot. For safety, clinicians also are advised asking for the cell phone number of the patient as well as that of a loved one.
Vital signs
When it comes to checking vital signs, Dr. Yellowlees suggested asking patients to purchase an inexpensive blood pressure (BP) monitor, thermometer, etc, prior to an appointment.
“Ask them to do a BP test on video and show you the readings. For the AIMS [Abnormal Involuntary Movement Scale] test, or to check for tardive dyskinesia, instruct patients to come close to the camera to show movement.”
In addition, most psychiatric rating scales are available online, which patients can fill out before a telehealth visit. The Serious Mental Illness (SMI) Adviser mobile app also includes several of these scales, Dr. Torous noted.
Overall, “there have been dramatic changes in the rules and regulations governing [telepsychiatry] that, for the next 60 days, make it easier to offer telehealth to patients,” Dr. Torous said.
Therefore, all psychiatrists need to “get on board,” as soon as possible, Dr. Yellowlees added.
The webinar was funded in part by a grant from SAMHSA.
A version of this article originally appeared on Medscape.com.