User login
The Supreme Court 2020‒2021: What will affect ObGyns?
The Supreme Court’s usual processes were disrupted this term. The COVID-19 pandemic required audio hearings rather than in-person, and it resulted in a number of emergency legal appeals. As the Court began its regular sessions on October 5, 2020, there were only 8 justices—Justice Ruth Bader Ginsburg had passed away and Amy Coney Barrett had not yet been confirmed by the Senate. The Court decided many important cases this term, including dealing with the delivery of drugs to induce abortions, a Centers for Disease Control and Prevention (CDC) moratorium on housing evictions, yet another case on the Affordable Care Act, state laws concerning pharmacy benefit managers, and the Hologic and Minerva endometrial ablation systems patents. After considering these cases, we also will briefly look at other cases of general interest.
Abortion
Patient access to mifepristone
In May 2020, the American College of Obstetricians and Gynecologists (ACOG) was the named plaintiff in a lawsuit against the US Food and Drug Administration (FDA) regarding the drugs mifepristone and misoprostol that are used to induce medical abortions.1 The case was filed by the American Civil Liberties Union on behalf of ACOG and others2,3 and raised the issue of patients’ access to these medications. The basic claim of the case was that during the pandemic, the FDA’s regulation of mifepristone was unconstitutional in that they imposed an undue burden on the decision of women to have an abortion.4 (Although misoprostol is a part of the medical abortion regimen, it is not subject to special regulation and was not part of the litigation.)
The FDA regulation of mifepristone, begun in 2000 but modified since then, includes 3 elements to assure safe use:
- prescribers must have special training or certification
- the drug can be dispensed to patients only in a hospital, clinic, or medical office under the supervision of a certified health care provider (known as the “in-person dispensing requirement” because retail pharmacy or mail distribution are prohibited)
- the health care provider must review a “patient agreement form” with the patient and have the patient sign the consent form in the provider’s presence.5
The pandemic made fulfilling these requirements substantially more burdensome and difficult. The question was whether the FDA was constitutionally required to modify its regulations during a pandemic to take account of the undue burden of the regulation created by the pandemic. That is, the question was not whether the FDA could have or should have chosen to make the modification, but whether it was required to do so.
In July 2020, a federal district court in Maryland held that the FDA regulation was an unconstitutional burden on the abortion rights of women during the pandemic and issued a preliminary injunction to stop the FDA from enforcing the in-person dispensing and signature rules. The district judge applied the injunction to Maryland, but also made it a nationwide injunction. (The issue of district court nationwide injunctions is considered in, “District court ‘nationwide injunctions’”).
The FDA asked the Fourth Circuit Court of Appeals to stay the enforcement of the injunction, which the appeals court denied. The FDA then appealed to the Supreme Court, asking it to stay the injunction. In October 2020, the Court announced that it was holding the FDA’s request “in abeyance” to allow the district court to consider a motion by the FDA to dissolve or change the injunction. It gave the district court 40 days in which to act. That decision by the Court was in the “Shadow Docket” (see sidebar on page XX), so the exact vote of the Court in October is not clear, but 2 Justices (Alito and Thomas) dissented and would have stayed the injunction.6 Over the next 40 days, the district court did not withdraw its nationwide injunction.
Thus, on January 12, 2021, the case was again before the Supreme Court, which let the FDA’s regulations regarding mifepristone remain in place by lifting the district court’s injunction. Most of the justices supporting the stay did not write to explain their decision, although their dissent in the earlier cases may have served that purpose. (Maryland was permitting many kinds of activity that were more risky than visiting a clinic—indoor dining, with open hair salons, gyms, and casinos.)7 Chief Justice Roberts wrote a concurrence to indicate that, in his view, the issue was not whether the FDA’s regulations placed an undue burden on a right to an abortion generally, but that “My view is that courts owe significant deference” to the public health authorities (here meaning the FDA). Justices Sotomayor and Kagan dissented, saying that the issue was the undue burden on women, given the difficulties of the pandemic, particularly going to medical facilities during the COVID-19 pandemic.8
The injunction, sought by ACOG and others, was issued by the district court and was in effect for several months before it was dissolved by the Supreme Court. Following the change in presidential administrations, in April 2021 the FDA announced that it was going to “exercise enforcement discretion with respect to the in-person dispensing requirement…during the COVID-19 public health emergency.”9
Continue to: The Texas abortion case...
The Texas abortion case
The Court, on September 1, 2021, declined to block a Texas abortion statute from taking effect.10 This law precludes abortions after a fetal heartbeat is present at about 6 weeks of gestation. The Fifth Circuit declined to grant an injunction delaying implementation of the Texas law, and the Court did not reverse that decision.
Over the years, a variety of states have placed limitations on abortion, and those almost always have been enjoined by federal courts before they went into effect. However, the Texas statute, which undoubtedly is unconstitutional, was creatively constructed to avoid an early injunction.11 The statute does not allow state officials to enforce the new law, but rather it allows almost any private citizen to seek monetary damages from anyone performing an abortion or who “aids and abets” an abortion. Thus, it is difficult to tailor a lawsuit before this law is enforced. First, courts do not enjoin laws; they usually enjoin individuals from enforcing the law, and in this case it is difficult to know which individuals will be enforcing the laws and what their decisions might be. There also are some questions about the degree to which federal courts can enjoin state courts from deciding lawsuits under state law. For these procedural reasons, the majority of the Court found that those attacking the Texas law had not met their burden of showing that that they would win their case.
Even 3 of the dissenting justices said the defendants may be right that “existing doctrines preclude judicial intervention,” but that the consequences are such that the Court should delay the law until there is time for briefing and argument. The other 3 dissenting justices thought there would be ways of getting around the clever roadblock Texas had erected for the federal courts.
There has been some commentary that this case portends the abandonment of Roe v Wade and Casey,12 but that conclusion does not seem warranted by this case. The Court has accepted a Mississippi abortion law to be heard next term.13 In addition, the Texas statute is likely to be back in federal court once a private individual has filed a claim for money from an abortion provider (and likely even before that).
COVID-19 cases
The Supreme Court decided several cases related to COVID-19, including adjustments to election procedures, church services, and CDC eviction moratoria. As a general matter early in the pandemic, the Court deferred to government authorities, generally upholding government actions. Chief Justice Roberts emphasized the importance of the Court deferring to government officials in emergencies. As the pandemic progressed into 2021, however, the Court became less and less sympathetic to government actions that were not consistent, permitted by existing law, or reasonably necessary. For example, regulations of churches that were inconsistent with the regulation of similar organizations were struck down.14
Among the most interesting of the summer 2021 cases was the CDC eviction moratorium that essentially prohibited landlords nationwide from evicting tenants for nonpayment of rent. When the challenges to these CDC regulations first reached the Court, the moratorium was about to expire; in a 5-4 decision, the Court did not enjoin the CDC from continuing that policy. Justice Kavanaugh (the fifth vote) warned that “clear and specific congressional authorization…would be necessary to extend the moratorium past July 31.”15 Despite telling the Court that the moratorium would expire on July 31, just 3 days after the expiration and without any congressional authorization, the CDC reinstated what was practically the same moratorium.16 On August 26, the Court struck down the reinstated regulation, probably by a 6-3 margin. (Because this case arose in the “Shadow Docket,” the vote of some justices is not certain).17
Continue to: The Affordable Care Act...
The Affordable Care Act
The Affordable Care Act was challenged in the Court for the third time.18 In this term’s case, several states argued that when Congress essentially eliminated the penalty/tax for not purchasing insurance coverage, there was no longer a constitutional basis for the individual mandate. With that centerpiece gone, they claimed, the whole statute should be declared unconstitutional.
Along with many other specialty groups, ACOG joined an amicus curiae brief sponsored by the American Medical Association (AMA).19 An amicus brief is one not filed by the parties to the case, but by organizations or individuals who have information that may be of use to the Court in considering the case. Among other things, the filing of an amicus brief indicates the interest of the organization in the outcome of the case. In this case, the crux of the amicus was that even if the individual mandate currently is not constitutional, the Court should sever that provision and retain the rest of the ACA.
Despite some wild predictions about what the Court might do, it did not decide any substantive issue. Rather, it found that none of the parties to the case had “standing” to challenge the constitutionality of the ACA. Therefore, in effect, the Court dismissed the case without deciding the substantive legal issues.
Pharmacy Benefit Managers
The powerful Pharmacy Benefit Managers (PBMs) are a hidden part of the health care system; however, in recent years there has been increasing regulatory attention paid to them. Some states have begun regulating aspects of PBMs. In this term, the Court considered an Arkansas law that sought to protect local pharmacies from PBM pricing practices.20 The AMA filed an amicus brief in the case which made legal arguments, most of which had been made by the parties to the litigation.21
PBMs generally tell pharmacies how much they will reimburse the pharmacy for filling a prescription for a particular drug. In some instances, PBMs will set a reimbursement price that is lower than the wholesale price at which local pharmacies can purchase the drug. The Arkansas law prohibited PBMs in the state from reimbursing pharmacies for less than the wholesale cost the pharmacy paid for the drug.
The claim of the PBMs was that the Arkansas law violated the Employee Retirement Income Security Act (ERISA). In part, this act preempts state law that relates to fringe benefit plans. States have the authority to regulate insurance, but ERISA limits what they can do when the insurance relates to fringe benefits. The Court held that ERISA does not preempt the Arkansas law or similar state laws in other states. Because the state law was not preempted by the state law, the Arkansas regulation was upheld. The fact that this was a unanimous decision (8-0, because Justice Barrett was not on the Court when the case was heard) suggests that states may have leeway in additional regulations of PBMs, and it would not be surprising to see more of that state regulation in the future.
Continue to: Patent uncertainty...
Patent uncertainty
Csaba Truckai invented and patented the NovaSure System ablation device with a “moisture permeable” head. He sold his company and the related patents, which eventually were purchased by Hologic. Over time, Hologic added claims to the original patent. In the meantime, Truckai went on to invent another device, the Minerva Endometrial Ablation System (MEAS), which had a “moisture impermeable” head. (Note that the “Minerva Surgical, Inc.” involved in this case is not related to the company “Minerva Industries,” which some identified as a “patent troll.”)22
Hologic sued Minerva, claiming that Truckai’s second device (MEAS) infringed on its patent for the first device (NovaSure). Truckai’s defense was that the patent on NovaSure was invalid. Hologic felt that since Truckai had obtained that patent and then sold it, it was improper for him now to claim it was invalid. There is a doctrine for that: assignor estoppel—the person who sold (assigned) the patent is prevented from later claiming it was invalid. The question in this case was whether assignor estoppel is part of the patent law of the United States. It is not in the patent statutes, so it is a court-determined part of the law.
In a 5-4 decision this Term, the Court held that assignor estoppel is recognized, but that it is narrow.23 The Court identified several exceptions to assignor estoppel, notably for this case, including the situation in which the purchaser of the patent, after the purchase, returns to the Patent and Trademark Office to expand (amend) the patent’s claims. In that case, the seller could not be estopped by the amended terms of the patent. Minerva claimed that it was attacking the expanded patent that included changes made after it sold the patent. The Court, therefore, returned the case to the Federal Circuit to apply the principles it laid out about assignor estoppel.
Biotech and other fast-moving fields frequently have new technology building on slightly earlier technology. The current patent system often leaves uncertainty about who owns which part of a valid patent. This uncertainty is a drag on innovation, and the patent system is supposed to spur innovation. Assignor estoppel is likely to create additional complexity and uncertainty in some patents, which is regrettable.
Review of the Term
In addition to the other disruptions of the Term, during the first part of the Term, Amy Coney Barrett was not yet confirmed by the Senate, so there were only 8 justices until October 27. She did not participate in those cases that were heard before she joined the Court. The consensus is that the Court heard 67 cases: 57 were formally briefed and argued along with 8 summary reversals and 2 religious cases in the Shadow Docket. In my opinion, this undercounts both the number and the importance of the Shadow Docket cases, but the following data use the 67 case convention.24
The Court was unanimous in 43% of the cases, including some of the most divisive issues. That unanimity reflects very narrow decisions. There were (by conventional count) only eight 5-4 opinions (12%), an unusually low number. Justice Kavanaugh is viewed as the “median” justice. He was in the majority in 97% of all cases. Chief Justice Roberts and Justice Barrett were in the majority 91%, and Justice Gorsuch 90%. As for the other justices, they were in the majority (all cases) most of the time: Justice Alito, 83%; Justice Thomas, 81%; Justice Breyer, 76%; Justice Kagan, 75%; and Justice Sotomayor, 69%. In “divided cases” (when unanimous cases are removed), the percentages are: Justice Kavanaugh, 95%; Chief Justice Roberts and Justice Barrett, 84%; Justice Gorsuch, 82%; Justice Alito, 70%; Justice Thomas, 66%; Justice Breyer, 58%; Justice Kagan, 55%; and Justice Sotomayor, 45%.
When the term began, many Court watchers expected a relatively uninteresting term, dealing with many technical legal details. In fact, it turned out to be more interesting and important than expected, even with narrow holdings in important cases. Part of the secret of the term was that a lot of the real action was in the Shadow Docket. The end of the term is sometimes the moment when a justice announces a plan to retire. Many commentators expected Justice Breyer might announce—he has been under pressure to do so, to allow President Biden to nominate and a Democratic Senate to confirm a progressive justice. However, he did not do so. It is possible that he will announce his retirement to be effective when his successor is confirmed, but that is pure speculation.
Continue to: Next Term...
Next Term
The next term began on Monday, October 4, 2021. With the considerable current activity in the Shadow Docket, there was not much of a summer break. The coming term looks extraordinary. The headline case is an abortion case from Mississippi, Dobbs v Jackson Women’s Health Organization.25 The legal question is the constitutionality of Mississippi law that prohibits most abortions after 15 weeks of gestation. The Texas abortion law will also be back before the Court. As we saw this term, big cases may produce very narrow results, but this case has the potential for being a notable abortion decision.
In a different case the Court will decide whether a state attorney general can step in to defend an abortion law when the state health secretary does not do so.26
The Court also has accepted 3 cases dealing with reimbursement for health services. One deals with whether or not the Department of Health and Human Services can set reimbursement rates without good survey data regarding costs,27 another involves the calculation of additional payments for hospitals that serve a “disproportionate number of low-income patients,”28 and the third whether state Medicaid programs can take funds from an injured beneficiary’s tort recovery to cover future Medicaid costs.29
In other cases, the Court will review a gun control law from New York. The Court’s earlier Second Amendment cases involved guns in the home used for self-defense, but this case raises the question of whether a state can practically preclude “concealed-carry licenses.”30 Many experts believe the Court will accept a case dealing with racial preferences in college admissions, perhaps the Harvard case in which the claim is discrimination against Asian Americans.31
The ACOG mifepristone case was interesting, in part because the federal district court issued a nationwide injunction against the Americans with Disabilities Act, enforcing its rules anywhere in the country. The effect of these orders is for a single district judge to create the “law of the land,” at least until that is reviewed—which can take months. The advantage of the nationwide injunction is that it avoids having to repeatedly litigate the same issues in multiple courts around the country. The downside is that plaintiffs can seek out a nonrepresentative judge or circuit and receive an injunction that would be granted by few other circuits. In addition, a nationwide injunction can apply to specific circumstances that are not before the court issuing the injunction. In the mifepristone case, for example, 10 states requested to intervene in the ACOG case. The court rejected the request, but the nationwide injunction applied to those states.1
Although federal judges have had the authority to issue nationwide injunctions for years, they are becoming much more common. One reason is the ease of forum shopping noted earlier—organizations can cherry-pick district courts and circuits sympathetic to their views. Both left- and right-leaning organizations have learned this lesson, so left-leaning groups are likely to file in specific districts in the Ninth Circuit, and right-leaning groups to districts in the Fifth Circuit.
If the current trend of increasing nationwide injunctions continues, either the rules for the federal courts or congressional action may be required to reduce some of the abuses by both sides of the political spectrum.
The ACOG mifepristone case was interesting, in part because the federal district court issued a nationwide injunction against the Americans with Disabilities Act, enforcing its rules anywhere in the country. The effect of these orders is for a single district judge to create the “law of the land,” at least until that is reviewed—which can take months. The advantage of the nationwide injunction is that it avoids having to repeatedly litigate the same issues in multiple courts around the country. The downside is that plaintiffs can seek out a nonrepresentative judge or circuit and receive an injunction that would be granted by few other circuits. In addition, a nationwide injunction can apply to specific circumstances that are not before the court issuing the injunction. In the mifepristone case, for example, 10 states requested to intervene in the ACOG case. The court rejected the request, but the nationwide injunction applied to those states.1
Although federal judges have had the authority to issue nationwide injunctions for years, they are becoming much more common. One reason is the ease of forum shopping noted earlier—organizations can cherry-pick district courts and circuits sympathetic to their views. Both left- and right-leaning organizations have learned this lesson, so left-leaning groups are likely to file in specific districts in the Ninth Circuit, and right-leaning groups to districts in the Fifth Circuit.
If the current trend of increasing nationwide injunctions continues, either the rules for the federal courts or congressional action may be required to reduce some of the abuses by both sides of the political spectrum. Reference Am. Coll. of Obstetricians & Gynecologists v. United States FDA, 467 F. Supp. 3d 282, 284 (D. Md. 2020).
Reference
1. Am. Coll. of Obstetricians & Gynecologists v. United States FDA, 467 F. Supp. 3d 282, 284 (D. Md. 2020).
The “Shadow Docket”
The ACOG mifepristone decisions do not appear on the Supreme Court’s “Court Opinions” website.1 They appear in what has become known in recent years as “The Shadow Docket,” an informal term that includes many orders of the Court and statements of individual justices regarding some cases.2 There are hundreds of orders by the Court each Term, there is nothing particularly shadowy about any of these items—they are all publicly available on the Court’s website and later in paper format. It is, however, a little harder to find and much harder to sort through than the major opinions. In some cases, it is not possible to tell what the vote was, how each justice voted, and what the reasoning of the Court was. In a few cases it is difficult to know exactly what the Court was holding or otherwise leaves some confusion about what the law actually is.3
The part of the Shadow Docket that is most intriguing for commentators, and where the ACOG cases appear, is the “Opinions Relating to Orders.”4 These are a variety of opinions, some written by the Court and many by individual justices. It also includes the action of the Court in some cases in which there was not full briefing or oral argument. The statements by justices often are to dissent from the denial of cert of decisions of the Court. These opinions have become much more common over the years. In this past term, there were approximately 60 such opinions related to about 50 cases. In part, this relates to the number of pandemic cases that could not wait for a Court decision going through the extended ordinary process. Although the Shadow Docket has been of interest to academic observers and Court watchers for years, this year it has attracted the attention of Congress.5
References
1. Opinions of the Court. Supreme Court website. https://www.supremecourt.gov/opinions/slipopinion/20#list. Accessed October 10, 2021.
2. Baude W. Foreword: the Supreme Court’s Shadow Docket, 9 N.Y.U. J.L. & Liberty 1 (2015).
3. Vladeck SI. The Solicitor General and the Shadow Docket, 133 Harvard Law Review. 123 (2019).
4. Opinions relating to orders. Supreme Court website. https://www.supremecourt.gov/opinions/relatingtoorders/20#list. Accessed October 10, 2021.
5. The Supreme Court’s Shadow Docket: Hearing Before the Subcommittee on Courts, Intellectual Property and the Internet of the H. Committee on the Judiciary, 117th Congress (2021).
- American College of Obstetricians & Gynecologists v. United States FDA, 472 F. Supp. 3d 183 (D. Md. 2020).
- Michael Kunzelman, Doctors Sue to Block FDA Abortion Pill Rule During Pandemic, (May 29, 2020).
- ACLU, American College Of Obstetricians And Gynecologists V. U.S. Food And Drug Administration, https://www.aclu.org/cases/american-college-obstetricians-and-gynecologists-v-us-food-and-drug-administration. Updated February 12, 2021. Accessed August 27, 2021.
- Whole Woman’s Health v Hellerstedt, 579 US ___ (2016), 136 S Ct 2292.
- 2016 Clinical Review at 39, 47, 49, Opp’n Mot. PI Ex. 19, ECF No. 62-11.
- American College of Obstetricians and Gynecologists v FDA (I), decided October 8, 2020.
- October 8, 2020, dissenting opinion by Justice Alito.
- January 12, 2021, dissenting opinion by Justice Sotomayor.
- Questions and answers on Mifeprex. U.S. Food and Drug Administration website. Published April 13, 2021. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/questions-and-answers-mifeprex. Accessed October 9, 2021.
- Whole Woman’s Health v Jackson, decided September 1, 2021.
- Texas Senate Bill 8, relating to abortion, including abortions after detection of unborn child’s heartbeat; authorizing a private civil right of action. LegiScan website. https://legiscan.com/TX/text/SB8/id/2395961. Accessed October 9, 2021.
- Planned Parenthood of Southeastern Pennsylvania v Casey, 505 U. S. 833 (1992); Roe v Wade, 410 U. S. 113 (1973).
- Dobbs v Jackson Women’s Health Organization, No. 19-1392.
- Roman Catholic Diocese of Brooklyn v Cuomo, decided November 25, 2020.
- Alabama Association of Realtors v Department of Health and Human Services, decided June 29, 2021.
- Temporary halt in residential evictions in communities with substantial or high levels of community transmission of COVID-19 to prevent the further spread of COVID-19. August 6, 2021. https://www.federalregister.gov/documents/2021/08/06/2021-16945/temporary-halt-in-residential-evictions-in-communities-with-substantial-or-high-transmission-of.
- Alabama Association of Realtors v Department of Health and Human Services, decided August 26, 2021.
- California v Texas, decided June 17, 2021.
- Brief of Amici Curiae American Medical Association, American Academy of Allergy, Asthma and Immunology, Aerospace Medical Association, American Academy of Family Physicians, American Academy of Pediatrics, American College of Cardiology, American College of Emergency Physicians, American College of Medical Genetics and Genomics, American College of Obstetricians and Gynecologists, American College of Physicians, American College of Radiation Oncology, American College of Radiology, American Psychiatric Association, American Society of Gastrointestinal Endoscopy, American Society of Hematology, American Society of Metabolic and Bariatric Surgery, Endocrine Society, GLMA: Health Professionals Advancing LGBTQ Equality, Renal Physicians Association, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology in Support of Petitioners, in California v. Texas. May 13, 2020. https://www.supremecourt.gov/DocketPDF/19/19-840/143469/20200513150051995_19-840%20Amici%20Brief%20AMA.pdf. Accessed October 9, 2021.
- Rutledge v Pharmaceutical Care Management Association, decided December 10, 2020.
- Brief of the American Medical Association, The Arkansas Medical Society, and The Litigation Center of the American Medical Association and the State Medical Societies as Amici Curiae in Support of Petitioner in Rutledge v Pharmaceutical Care Management Association. March 2, 2020. https://www.supremecourt.gov/DocketPDF/18/18-540/134670/20200302163622018_Rutledge%20v.%20PCMA%20Amicus%20Brief%20of%20AMA%20et%20al.pdf. Accessed October 9, 2021.
- Apple quietly settles patent lawsuit, promptly gets hit with another one. TechCrunch website. Published July 30, 2010. https://techcrunch.com/2010/07/30/apple-minerva-emblaze/. Accessed October 9, 2021.
- Minerva Surgical, Inc. v Hologic, Inc., decided June 29, 2021.
- Stat pack. SCOTUS Blog website. Published July 6, 2021. https://www.scotusblog.com/wp-content/uploads/2021/07/Final-Stat-Pack-7.6.21.pdf. Accessed October 9, 2021.
- Dobbs v Jackson Women’s Health Organization, No. 19-1392.
- Cameron v. EMW Women’s Surgical Center, https://www.scotusblog.com/case-files/cases/cameron-v-emw-womens-surgical-center-p-s-c/. Accessed August 28, 2021.
- American Hospital Association v Becerra, No. 20-1114.
- Becerra v Empire Health Foundation, No. 20-1312.
- Gallardo v Marstiller, No. 20-1263.
- New York State Rifle & Pistol Association Inc. v Corlett, No. 20-843.
- Students for Fair Admissions v President & Fellows of Harvard College, No. 20-1199.
The Supreme Court’s usual processes were disrupted this term. The COVID-19 pandemic required audio hearings rather than in-person, and it resulted in a number of emergency legal appeals. As the Court began its regular sessions on October 5, 2020, there were only 8 justices—Justice Ruth Bader Ginsburg had passed away and Amy Coney Barrett had not yet been confirmed by the Senate. The Court decided many important cases this term, including dealing with the delivery of drugs to induce abortions, a Centers for Disease Control and Prevention (CDC) moratorium on housing evictions, yet another case on the Affordable Care Act, state laws concerning pharmacy benefit managers, and the Hologic and Minerva endometrial ablation systems patents. After considering these cases, we also will briefly look at other cases of general interest.
Abortion
Patient access to mifepristone
In May 2020, the American College of Obstetricians and Gynecologists (ACOG) was the named plaintiff in a lawsuit against the US Food and Drug Administration (FDA) regarding the drugs mifepristone and misoprostol that are used to induce medical abortions.1 The case was filed by the American Civil Liberties Union on behalf of ACOG and others2,3 and raised the issue of patients’ access to these medications. The basic claim of the case was that during the pandemic, the FDA’s regulation of mifepristone was unconstitutional in that they imposed an undue burden on the decision of women to have an abortion.4 (Although misoprostol is a part of the medical abortion regimen, it is not subject to special regulation and was not part of the litigation.)
The FDA regulation of mifepristone, begun in 2000 but modified since then, includes 3 elements to assure safe use:
- prescribers must have special training or certification
- the drug can be dispensed to patients only in a hospital, clinic, or medical office under the supervision of a certified health care provider (known as the “in-person dispensing requirement” because retail pharmacy or mail distribution are prohibited)
- the health care provider must review a “patient agreement form” with the patient and have the patient sign the consent form in the provider’s presence.5
The pandemic made fulfilling these requirements substantially more burdensome and difficult. The question was whether the FDA was constitutionally required to modify its regulations during a pandemic to take account of the undue burden of the regulation created by the pandemic. That is, the question was not whether the FDA could have or should have chosen to make the modification, but whether it was required to do so.
In July 2020, a federal district court in Maryland held that the FDA regulation was an unconstitutional burden on the abortion rights of women during the pandemic and issued a preliminary injunction to stop the FDA from enforcing the in-person dispensing and signature rules. The district judge applied the injunction to Maryland, but also made it a nationwide injunction. (The issue of district court nationwide injunctions is considered in, “District court ‘nationwide injunctions’”).
The FDA asked the Fourth Circuit Court of Appeals to stay the enforcement of the injunction, which the appeals court denied. The FDA then appealed to the Supreme Court, asking it to stay the injunction. In October 2020, the Court announced that it was holding the FDA’s request “in abeyance” to allow the district court to consider a motion by the FDA to dissolve or change the injunction. It gave the district court 40 days in which to act. That decision by the Court was in the “Shadow Docket” (see sidebar on page XX), so the exact vote of the Court in October is not clear, but 2 Justices (Alito and Thomas) dissented and would have stayed the injunction.6 Over the next 40 days, the district court did not withdraw its nationwide injunction.
Thus, on January 12, 2021, the case was again before the Supreme Court, which let the FDA’s regulations regarding mifepristone remain in place by lifting the district court’s injunction. Most of the justices supporting the stay did not write to explain their decision, although their dissent in the earlier cases may have served that purpose. (Maryland was permitting many kinds of activity that were more risky than visiting a clinic—indoor dining, with open hair salons, gyms, and casinos.)7 Chief Justice Roberts wrote a concurrence to indicate that, in his view, the issue was not whether the FDA’s regulations placed an undue burden on a right to an abortion generally, but that “My view is that courts owe significant deference” to the public health authorities (here meaning the FDA). Justices Sotomayor and Kagan dissented, saying that the issue was the undue burden on women, given the difficulties of the pandemic, particularly going to medical facilities during the COVID-19 pandemic.8
The injunction, sought by ACOG and others, was issued by the district court and was in effect for several months before it was dissolved by the Supreme Court. Following the change in presidential administrations, in April 2021 the FDA announced that it was going to “exercise enforcement discretion with respect to the in-person dispensing requirement…during the COVID-19 public health emergency.”9
Continue to: The Texas abortion case...
The Texas abortion case
The Court, on September 1, 2021, declined to block a Texas abortion statute from taking effect.10 This law precludes abortions after a fetal heartbeat is present at about 6 weeks of gestation. The Fifth Circuit declined to grant an injunction delaying implementation of the Texas law, and the Court did not reverse that decision.
Over the years, a variety of states have placed limitations on abortion, and those almost always have been enjoined by federal courts before they went into effect. However, the Texas statute, which undoubtedly is unconstitutional, was creatively constructed to avoid an early injunction.11 The statute does not allow state officials to enforce the new law, but rather it allows almost any private citizen to seek monetary damages from anyone performing an abortion or who “aids and abets” an abortion. Thus, it is difficult to tailor a lawsuit before this law is enforced. First, courts do not enjoin laws; they usually enjoin individuals from enforcing the law, and in this case it is difficult to know which individuals will be enforcing the laws and what their decisions might be. There also are some questions about the degree to which federal courts can enjoin state courts from deciding lawsuits under state law. For these procedural reasons, the majority of the Court found that those attacking the Texas law had not met their burden of showing that that they would win their case.
Even 3 of the dissenting justices said the defendants may be right that “existing doctrines preclude judicial intervention,” but that the consequences are such that the Court should delay the law until there is time for briefing and argument. The other 3 dissenting justices thought there would be ways of getting around the clever roadblock Texas had erected for the federal courts.
There has been some commentary that this case portends the abandonment of Roe v Wade and Casey,12 but that conclusion does not seem warranted by this case. The Court has accepted a Mississippi abortion law to be heard next term.13 In addition, the Texas statute is likely to be back in federal court once a private individual has filed a claim for money from an abortion provider (and likely even before that).
COVID-19 cases
The Supreme Court decided several cases related to COVID-19, including adjustments to election procedures, church services, and CDC eviction moratoria. As a general matter early in the pandemic, the Court deferred to government authorities, generally upholding government actions. Chief Justice Roberts emphasized the importance of the Court deferring to government officials in emergencies. As the pandemic progressed into 2021, however, the Court became less and less sympathetic to government actions that were not consistent, permitted by existing law, or reasonably necessary. For example, regulations of churches that were inconsistent with the regulation of similar organizations were struck down.14
Among the most interesting of the summer 2021 cases was the CDC eviction moratorium that essentially prohibited landlords nationwide from evicting tenants for nonpayment of rent. When the challenges to these CDC regulations first reached the Court, the moratorium was about to expire; in a 5-4 decision, the Court did not enjoin the CDC from continuing that policy. Justice Kavanaugh (the fifth vote) warned that “clear and specific congressional authorization…would be necessary to extend the moratorium past July 31.”15 Despite telling the Court that the moratorium would expire on July 31, just 3 days after the expiration and without any congressional authorization, the CDC reinstated what was practically the same moratorium.16 On August 26, the Court struck down the reinstated regulation, probably by a 6-3 margin. (Because this case arose in the “Shadow Docket,” the vote of some justices is not certain).17
Continue to: The Affordable Care Act...
The Affordable Care Act
The Affordable Care Act was challenged in the Court for the third time.18 In this term’s case, several states argued that when Congress essentially eliminated the penalty/tax for not purchasing insurance coverage, there was no longer a constitutional basis for the individual mandate. With that centerpiece gone, they claimed, the whole statute should be declared unconstitutional.
Along with many other specialty groups, ACOG joined an amicus curiae brief sponsored by the American Medical Association (AMA).19 An amicus brief is one not filed by the parties to the case, but by organizations or individuals who have information that may be of use to the Court in considering the case. Among other things, the filing of an amicus brief indicates the interest of the organization in the outcome of the case. In this case, the crux of the amicus was that even if the individual mandate currently is not constitutional, the Court should sever that provision and retain the rest of the ACA.
Despite some wild predictions about what the Court might do, it did not decide any substantive issue. Rather, it found that none of the parties to the case had “standing” to challenge the constitutionality of the ACA. Therefore, in effect, the Court dismissed the case without deciding the substantive legal issues.
Pharmacy Benefit Managers
The powerful Pharmacy Benefit Managers (PBMs) are a hidden part of the health care system; however, in recent years there has been increasing regulatory attention paid to them. Some states have begun regulating aspects of PBMs. In this term, the Court considered an Arkansas law that sought to protect local pharmacies from PBM pricing practices.20 The AMA filed an amicus brief in the case which made legal arguments, most of which had been made by the parties to the litigation.21
PBMs generally tell pharmacies how much they will reimburse the pharmacy for filling a prescription for a particular drug. In some instances, PBMs will set a reimbursement price that is lower than the wholesale price at which local pharmacies can purchase the drug. The Arkansas law prohibited PBMs in the state from reimbursing pharmacies for less than the wholesale cost the pharmacy paid for the drug.
The claim of the PBMs was that the Arkansas law violated the Employee Retirement Income Security Act (ERISA). In part, this act preempts state law that relates to fringe benefit plans. States have the authority to regulate insurance, but ERISA limits what they can do when the insurance relates to fringe benefits. The Court held that ERISA does not preempt the Arkansas law or similar state laws in other states. Because the state law was not preempted by the state law, the Arkansas regulation was upheld. The fact that this was a unanimous decision (8-0, because Justice Barrett was not on the Court when the case was heard) suggests that states may have leeway in additional regulations of PBMs, and it would not be surprising to see more of that state regulation in the future.
Continue to: Patent uncertainty...
Patent uncertainty
Csaba Truckai invented and patented the NovaSure System ablation device with a “moisture permeable” head. He sold his company and the related patents, which eventually were purchased by Hologic. Over time, Hologic added claims to the original patent. In the meantime, Truckai went on to invent another device, the Minerva Endometrial Ablation System (MEAS), which had a “moisture impermeable” head. (Note that the “Minerva Surgical, Inc.” involved in this case is not related to the company “Minerva Industries,” which some identified as a “patent troll.”)22
Hologic sued Minerva, claiming that Truckai’s second device (MEAS) infringed on its patent for the first device (NovaSure). Truckai’s defense was that the patent on NovaSure was invalid. Hologic felt that since Truckai had obtained that patent and then sold it, it was improper for him now to claim it was invalid. There is a doctrine for that: assignor estoppel—the person who sold (assigned) the patent is prevented from later claiming it was invalid. The question in this case was whether assignor estoppel is part of the patent law of the United States. It is not in the patent statutes, so it is a court-determined part of the law.
In a 5-4 decision this Term, the Court held that assignor estoppel is recognized, but that it is narrow.23 The Court identified several exceptions to assignor estoppel, notably for this case, including the situation in which the purchaser of the patent, after the purchase, returns to the Patent and Trademark Office to expand (amend) the patent’s claims. In that case, the seller could not be estopped by the amended terms of the patent. Minerva claimed that it was attacking the expanded patent that included changes made after it sold the patent. The Court, therefore, returned the case to the Federal Circuit to apply the principles it laid out about assignor estoppel.
Biotech and other fast-moving fields frequently have new technology building on slightly earlier technology. The current patent system often leaves uncertainty about who owns which part of a valid patent. This uncertainty is a drag on innovation, and the patent system is supposed to spur innovation. Assignor estoppel is likely to create additional complexity and uncertainty in some patents, which is regrettable.
Review of the Term
In addition to the other disruptions of the Term, during the first part of the Term, Amy Coney Barrett was not yet confirmed by the Senate, so there were only 8 justices until October 27. She did not participate in those cases that were heard before she joined the Court. The consensus is that the Court heard 67 cases: 57 were formally briefed and argued along with 8 summary reversals and 2 religious cases in the Shadow Docket. In my opinion, this undercounts both the number and the importance of the Shadow Docket cases, but the following data use the 67 case convention.24
The Court was unanimous in 43% of the cases, including some of the most divisive issues. That unanimity reflects very narrow decisions. There were (by conventional count) only eight 5-4 opinions (12%), an unusually low number. Justice Kavanaugh is viewed as the “median” justice. He was in the majority in 97% of all cases. Chief Justice Roberts and Justice Barrett were in the majority 91%, and Justice Gorsuch 90%. As for the other justices, they were in the majority (all cases) most of the time: Justice Alito, 83%; Justice Thomas, 81%; Justice Breyer, 76%; Justice Kagan, 75%; and Justice Sotomayor, 69%. In “divided cases” (when unanimous cases are removed), the percentages are: Justice Kavanaugh, 95%; Chief Justice Roberts and Justice Barrett, 84%; Justice Gorsuch, 82%; Justice Alito, 70%; Justice Thomas, 66%; Justice Breyer, 58%; Justice Kagan, 55%; and Justice Sotomayor, 45%.
When the term began, many Court watchers expected a relatively uninteresting term, dealing with many technical legal details. In fact, it turned out to be more interesting and important than expected, even with narrow holdings in important cases. Part of the secret of the term was that a lot of the real action was in the Shadow Docket. The end of the term is sometimes the moment when a justice announces a plan to retire. Many commentators expected Justice Breyer might announce—he has been under pressure to do so, to allow President Biden to nominate and a Democratic Senate to confirm a progressive justice. However, he did not do so. It is possible that he will announce his retirement to be effective when his successor is confirmed, but that is pure speculation.
Continue to: Next Term...
Next Term
The next term began on Monday, October 4, 2021. With the considerable current activity in the Shadow Docket, there was not much of a summer break. The coming term looks extraordinary. The headline case is an abortion case from Mississippi, Dobbs v Jackson Women’s Health Organization.25 The legal question is the constitutionality of Mississippi law that prohibits most abortions after 15 weeks of gestation. The Texas abortion law will also be back before the Court. As we saw this term, big cases may produce very narrow results, but this case has the potential for being a notable abortion decision.
In a different case the Court will decide whether a state attorney general can step in to defend an abortion law when the state health secretary does not do so.26
The Court also has accepted 3 cases dealing with reimbursement for health services. One deals with whether or not the Department of Health and Human Services can set reimbursement rates without good survey data regarding costs,27 another involves the calculation of additional payments for hospitals that serve a “disproportionate number of low-income patients,”28 and the third whether state Medicaid programs can take funds from an injured beneficiary’s tort recovery to cover future Medicaid costs.29
In other cases, the Court will review a gun control law from New York. The Court’s earlier Second Amendment cases involved guns in the home used for self-defense, but this case raises the question of whether a state can practically preclude “concealed-carry licenses.”30 Many experts believe the Court will accept a case dealing with racial preferences in college admissions, perhaps the Harvard case in which the claim is discrimination against Asian Americans.31
The ACOG mifepristone case was interesting, in part because the federal district court issued a nationwide injunction against the Americans with Disabilities Act, enforcing its rules anywhere in the country. The effect of these orders is for a single district judge to create the “law of the land,” at least until that is reviewed—which can take months. The advantage of the nationwide injunction is that it avoids having to repeatedly litigate the same issues in multiple courts around the country. The downside is that plaintiffs can seek out a nonrepresentative judge or circuit and receive an injunction that would be granted by few other circuits. In addition, a nationwide injunction can apply to specific circumstances that are not before the court issuing the injunction. In the mifepristone case, for example, 10 states requested to intervene in the ACOG case. The court rejected the request, but the nationwide injunction applied to those states.1
Although federal judges have had the authority to issue nationwide injunctions for years, they are becoming much more common. One reason is the ease of forum shopping noted earlier—organizations can cherry-pick district courts and circuits sympathetic to their views. Both left- and right-leaning organizations have learned this lesson, so left-leaning groups are likely to file in specific districts in the Ninth Circuit, and right-leaning groups to districts in the Fifth Circuit.
If the current trend of increasing nationwide injunctions continues, either the rules for the federal courts or congressional action may be required to reduce some of the abuses by both sides of the political spectrum.
The ACOG mifepristone case was interesting, in part because the federal district court issued a nationwide injunction against the Americans with Disabilities Act, enforcing its rules anywhere in the country. The effect of these orders is for a single district judge to create the “law of the land,” at least until that is reviewed—which can take months. The advantage of the nationwide injunction is that it avoids having to repeatedly litigate the same issues in multiple courts around the country. The downside is that plaintiffs can seek out a nonrepresentative judge or circuit and receive an injunction that would be granted by few other circuits. In addition, a nationwide injunction can apply to specific circumstances that are not before the court issuing the injunction. In the mifepristone case, for example, 10 states requested to intervene in the ACOG case. The court rejected the request, but the nationwide injunction applied to those states.1
Although federal judges have had the authority to issue nationwide injunctions for years, they are becoming much more common. One reason is the ease of forum shopping noted earlier—organizations can cherry-pick district courts and circuits sympathetic to their views. Both left- and right-leaning organizations have learned this lesson, so left-leaning groups are likely to file in specific districts in the Ninth Circuit, and right-leaning groups to districts in the Fifth Circuit.
If the current trend of increasing nationwide injunctions continues, either the rules for the federal courts or congressional action may be required to reduce some of the abuses by both sides of the political spectrum. Reference Am. Coll. of Obstetricians & Gynecologists v. United States FDA, 467 F. Supp. 3d 282, 284 (D. Md. 2020).
Reference
1. Am. Coll. of Obstetricians & Gynecologists v. United States FDA, 467 F. Supp. 3d 282, 284 (D. Md. 2020).
The “Shadow Docket”
The ACOG mifepristone decisions do not appear on the Supreme Court’s “Court Opinions” website.1 They appear in what has become known in recent years as “The Shadow Docket,” an informal term that includes many orders of the Court and statements of individual justices regarding some cases.2 There are hundreds of orders by the Court each Term, there is nothing particularly shadowy about any of these items—they are all publicly available on the Court’s website and later in paper format. It is, however, a little harder to find and much harder to sort through than the major opinions. In some cases, it is not possible to tell what the vote was, how each justice voted, and what the reasoning of the Court was. In a few cases it is difficult to know exactly what the Court was holding or otherwise leaves some confusion about what the law actually is.3
The part of the Shadow Docket that is most intriguing for commentators, and where the ACOG cases appear, is the “Opinions Relating to Orders.”4 These are a variety of opinions, some written by the Court and many by individual justices. It also includes the action of the Court in some cases in which there was not full briefing or oral argument. The statements by justices often are to dissent from the denial of cert of decisions of the Court. These opinions have become much more common over the years. In this past term, there were approximately 60 such opinions related to about 50 cases. In part, this relates to the number of pandemic cases that could not wait for a Court decision going through the extended ordinary process. Although the Shadow Docket has been of interest to academic observers and Court watchers for years, this year it has attracted the attention of Congress.5
References
1. Opinions of the Court. Supreme Court website. https://www.supremecourt.gov/opinions/slipopinion/20#list. Accessed October 10, 2021.
2. Baude W. Foreword: the Supreme Court’s Shadow Docket, 9 N.Y.U. J.L. & Liberty 1 (2015).
3. Vladeck SI. The Solicitor General and the Shadow Docket, 133 Harvard Law Review. 123 (2019).
4. Opinions relating to orders. Supreme Court website. https://www.supremecourt.gov/opinions/relatingtoorders/20#list. Accessed October 10, 2021.
5. The Supreme Court’s Shadow Docket: Hearing Before the Subcommittee on Courts, Intellectual Property and the Internet of the H. Committee on the Judiciary, 117th Congress (2021).
The Supreme Court’s usual processes were disrupted this term. The COVID-19 pandemic required audio hearings rather than in-person, and it resulted in a number of emergency legal appeals. As the Court began its regular sessions on October 5, 2020, there were only 8 justices—Justice Ruth Bader Ginsburg had passed away and Amy Coney Barrett had not yet been confirmed by the Senate. The Court decided many important cases this term, including dealing with the delivery of drugs to induce abortions, a Centers for Disease Control and Prevention (CDC) moratorium on housing evictions, yet another case on the Affordable Care Act, state laws concerning pharmacy benefit managers, and the Hologic and Minerva endometrial ablation systems patents. After considering these cases, we also will briefly look at other cases of general interest.
Abortion
Patient access to mifepristone
In May 2020, the American College of Obstetricians and Gynecologists (ACOG) was the named plaintiff in a lawsuit against the US Food and Drug Administration (FDA) regarding the drugs mifepristone and misoprostol that are used to induce medical abortions.1 The case was filed by the American Civil Liberties Union on behalf of ACOG and others2,3 and raised the issue of patients’ access to these medications. The basic claim of the case was that during the pandemic, the FDA’s regulation of mifepristone was unconstitutional in that they imposed an undue burden on the decision of women to have an abortion.4 (Although misoprostol is a part of the medical abortion regimen, it is not subject to special regulation and was not part of the litigation.)
The FDA regulation of mifepristone, begun in 2000 but modified since then, includes 3 elements to assure safe use:
- prescribers must have special training or certification
- the drug can be dispensed to patients only in a hospital, clinic, or medical office under the supervision of a certified health care provider (known as the “in-person dispensing requirement” because retail pharmacy or mail distribution are prohibited)
- the health care provider must review a “patient agreement form” with the patient and have the patient sign the consent form in the provider’s presence.5
The pandemic made fulfilling these requirements substantially more burdensome and difficult. The question was whether the FDA was constitutionally required to modify its regulations during a pandemic to take account of the undue burden of the regulation created by the pandemic. That is, the question was not whether the FDA could have or should have chosen to make the modification, but whether it was required to do so.
In July 2020, a federal district court in Maryland held that the FDA regulation was an unconstitutional burden on the abortion rights of women during the pandemic and issued a preliminary injunction to stop the FDA from enforcing the in-person dispensing and signature rules. The district judge applied the injunction to Maryland, but also made it a nationwide injunction. (The issue of district court nationwide injunctions is considered in, “District court ‘nationwide injunctions’”).
The FDA asked the Fourth Circuit Court of Appeals to stay the enforcement of the injunction, which the appeals court denied. The FDA then appealed to the Supreme Court, asking it to stay the injunction. In October 2020, the Court announced that it was holding the FDA’s request “in abeyance” to allow the district court to consider a motion by the FDA to dissolve or change the injunction. It gave the district court 40 days in which to act. That decision by the Court was in the “Shadow Docket” (see sidebar on page XX), so the exact vote of the Court in October is not clear, but 2 Justices (Alito and Thomas) dissented and would have stayed the injunction.6 Over the next 40 days, the district court did not withdraw its nationwide injunction.
Thus, on January 12, 2021, the case was again before the Supreme Court, which let the FDA’s regulations regarding mifepristone remain in place by lifting the district court’s injunction. Most of the justices supporting the stay did not write to explain their decision, although their dissent in the earlier cases may have served that purpose. (Maryland was permitting many kinds of activity that were more risky than visiting a clinic—indoor dining, with open hair salons, gyms, and casinos.)7 Chief Justice Roberts wrote a concurrence to indicate that, in his view, the issue was not whether the FDA’s regulations placed an undue burden on a right to an abortion generally, but that “My view is that courts owe significant deference” to the public health authorities (here meaning the FDA). Justices Sotomayor and Kagan dissented, saying that the issue was the undue burden on women, given the difficulties of the pandemic, particularly going to medical facilities during the COVID-19 pandemic.8
The injunction, sought by ACOG and others, was issued by the district court and was in effect for several months before it was dissolved by the Supreme Court. Following the change in presidential administrations, in April 2021 the FDA announced that it was going to “exercise enforcement discretion with respect to the in-person dispensing requirement…during the COVID-19 public health emergency.”9
Continue to: The Texas abortion case...
The Texas abortion case
The Court, on September 1, 2021, declined to block a Texas abortion statute from taking effect.10 This law precludes abortions after a fetal heartbeat is present at about 6 weeks of gestation. The Fifth Circuit declined to grant an injunction delaying implementation of the Texas law, and the Court did not reverse that decision.
Over the years, a variety of states have placed limitations on abortion, and those almost always have been enjoined by federal courts before they went into effect. However, the Texas statute, which undoubtedly is unconstitutional, was creatively constructed to avoid an early injunction.11 The statute does not allow state officials to enforce the new law, but rather it allows almost any private citizen to seek monetary damages from anyone performing an abortion or who “aids and abets” an abortion. Thus, it is difficult to tailor a lawsuit before this law is enforced. First, courts do not enjoin laws; they usually enjoin individuals from enforcing the law, and in this case it is difficult to know which individuals will be enforcing the laws and what their decisions might be. There also are some questions about the degree to which federal courts can enjoin state courts from deciding lawsuits under state law. For these procedural reasons, the majority of the Court found that those attacking the Texas law had not met their burden of showing that that they would win their case.
Even 3 of the dissenting justices said the defendants may be right that “existing doctrines preclude judicial intervention,” but that the consequences are such that the Court should delay the law until there is time for briefing and argument. The other 3 dissenting justices thought there would be ways of getting around the clever roadblock Texas had erected for the federal courts.
There has been some commentary that this case portends the abandonment of Roe v Wade and Casey,12 but that conclusion does not seem warranted by this case. The Court has accepted a Mississippi abortion law to be heard next term.13 In addition, the Texas statute is likely to be back in federal court once a private individual has filed a claim for money from an abortion provider (and likely even before that).
COVID-19 cases
The Supreme Court decided several cases related to COVID-19, including adjustments to election procedures, church services, and CDC eviction moratoria. As a general matter early in the pandemic, the Court deferred to government authorities, generally upholding government actions. Chief Justice Roberts emphasized the importance of the Court deferring to government officials in emergencies. As the pandemic progressed into 2021, however, the Court became less and less sympathetic to government actions that were not consistent, permitted by existing law, or reasonably necessary. For example, regulations of churches that were inconsistent with the regulation of similar organizations were struck down.14
Among the most interesting of the summer 2021 cases was the CDC eviction moratorium that essentially prohibited landlords nationwide from evicting tenants for nonpayment of rent. When the challenges to these CDC regulations first reached the Court, the moratorium was about to expire; in a 5-4 decision, the Court did not enjoin the CDC from continuing that policy. Justice Kavanaugh (the fifth vote) warned that “clear and specific congressional authorization…would be necessary to extend the moratorium past July 31.”15 Despite telling the Court that the moratorium would expire on July 31, just 3 days after the expiration and without any congressional authorization, the CDC reinstated what was practically the same moratorium.16 On August 26, the Court struck down the reinstated regulation, probably by a 6-3 margin. (Because this case arose in the “Shadow Docket,” the vote of some justices is not certain).17
Continue to: The Affordable Care Act...
The Affordable Care Act
The Affordable Care Act was challenged in the Court for the third time.18 In this term’s case, several states argued that when Congress essentially eliminated the penalty/tax for not purchasing insurance coverage, there was no longer a constitutional basis for the individual mandate. With that centerpiece gone, they claimed, the whole statute should be declared unconstitutional.
Along with many other specialty groups, ACOG joined an amicus curiae brief sponsored by the American Medical Association (AMA).19 An amicus brief is one not filed by the parties to the case, but by organizations or individuals who have information that may be of use to the Court in considering the case. Among other things, the filing of an amicus brief indicates the interest of the organization in the outcome of the case. In this case, the crux of the amicus was that even if the individual mandate currently is not constitutional, the Court should sever that provision and retain the rest of the ACA.
Despite some wild predictions about what the Court might do, it did not decide any substantive issue. Rather, it found that none of the parties to the case had “standing” to challenge the constitutionality of the ACA. Therefore, in effect, the Court dismissed the case without deciding the substantive legal issues.
Pharmacy Benefit Managers
The powerful Pharmacy Benefit Managers (PBMs) are a hidden part of the health care system; however, in recent years there has been increasing regulatory attention paid to them. Some states have begun regulating aspects of PBMs. In this term, the Court considered an Arkansas law that sought to protect local pharmacies from PBM pricing practices.20 The AMA filed an amicus brief in the case which made legal arguments, most of which had been made by the parties to the litigation.21
PBMs generally tell pharmacies how much they will reimburse the pharmacy for filling a prescription for a particular drug. In some instances, PBMs will set a reimbursement price that is lower than the wholesale price at which local pharmacies can purchase the drug. The Arkansas law prohibited PBMs in the state from reimbursing pharmacies for less than the wholesale cost the pharmacy paid for the drug.
The claim of the PBMs was that the Arkansas law violated the Employee Retirement Income Security Act (ERISA). In part, this act preempts state law that relates to fringe benefit plans. States have the authority to regulate insurance, but ERISA limits what they can do when the insurance relates to fringe benefits. The Court held that ERISA does not preempt the Arkansas law or similar state laws in other states. Because the state law was not preempted by the state law, the Arkansas regulation was upheld. The fact that this was a unanimous decision (8-0, because Justice Barrett was not on the Court when the case was heard) suggests that states may have leeway in additional regulations of PBMs, and it would not be surprising to see more of that state regulation in the future.
Continue to: Patent uncertainty...
Patent uncertainty
Csaba Truckai invented and patented the NovaSure System ablation device with a “moisture permeable” head. He sold his company and the related patents, which eventually were purchased by Hologic. Over time, Hologic added claims to the original patent. In the meantime, Truckai went on to invent another device, the Minerva Endometrial Ablation System (MEAS), which had a “moisture impermeable” head. (Note that the “Minerva Surgical, Inc.” involved in this case is not related to the company “Minerva Industries,” which some identified as a “patent troll.”)22
Hologic sued Minerva, claiming that Truckai’s second device (MEAS) infringed on its patent for the first device (NovaSure). Truckai’s defense was that the patent on NovaSure was invalid. Hologic felt that since Truckai had obtained that patent and then sold it, it was improper for him now to claim it was invalid. There is a doctrine for that: assignor estoppel—the person who sold (assigned) the patent is prevented from later claiming it was invalid. The question in this case was whether assignor estoppel is part of the patent law of the United States. It is not in the patent statutes, so it is a court-determined part of the law.
In a 5-4 decision this Term, the Court held that assignor estoppel is recognized, but that it is narrow.23 The Court identified several exceptions to assignor estoppel, notably for this case, including the situation in which the purchaser of the patent, after the purchase, returns to the Patent and Trademark Office to expand (amend) the patent’s claims. In that case, the seller could not be estopped by the amended terms of the patent. Minerva claimed that it was attacking the expanded patent that included changes made after it sold the patent. The Court, therefore, returned the case to the Federal Circuit to apply the principles it laid out about assignor estoppel.
Biotech and other fast-moving fields frequently have new technology building on slightly earlier technology. The current patent system often leaves uncertainty about who owns which part of a valid patent. This uncertainty is a drag on innovation, and the patent system is supposed to spur innovation. Assignor estoppel is likely to create additional complexity and uncertainty in some patents, which is regrettable.
Review of the Term
In addition to the other disruptions of the Term, during the first part of the Term, Amy Coney Barrett was not yet confirmed by the Senate, so there were only 8 justices until October 27. She did not participate in those cases that were heard before she joined the Court. The consensus is that the Court heard 67 cases: 57 were formally briefed and argued along with 8 summary reversals and 2 religious cases in the Shadow Docket. In my opinion, this undercounts both the number and the importance of the Shadow Docket cases, but the following data use the 67 case convention.24
The Court was unanimous in 43% of the cases, including some of the most divisive issues. That unanimity reflects very narrow decisions. There were (by conventional count) only eight 5-4 opinions (12%), an unusually low number. Justice Kavanaugh is viewed as the “median” justice. He was in the majority in 97% of all cases. Chief Justice Roberts and Justice Barrett were in the majority 91%, and Justice Gorsuch 90%. As for the other justices, they were in the majority (all cases) most of the time: Justice Alito, 83%; Justice Thomas, 81%; Justice Breyer, 76%; Justice Kagan, 75%; and Justice Sotomayor, 69%. In “divided cases” (when unanimous cases are removed), the percentages are: Justice Kavanaugh, 95%; Chief Justice Roberts and Justice Barrett, 84%; Justice Gorsuch, 82%; Justice Alito, 70%; Justice Thomas, 66%; Justice Breyer, 58%; Justice Kagan, 55%; and Justice Sotomayor, 45%.
When the term began, many Court watchers expected a relatively uninteresting term, dealing with many technical legal details. In fact, it turned out to be more interesting and important than expected, even with narrow holdings in important cases. Part of the secret of the term was that a lot of the real action was in the Shadow Docket. The end of the term is sometimes the moment when a justice announces a plan to retire. Many commentators expected Justice Breyer might announce—he has been under pressure to do so, to allow President Biden to nominate and a Democratic Senate to confirm a progressive justice. However, he did not do so. It is possible that he will announce his retirement to be effective when his successor is confirmed, but that is pure speculation.
Continue to: Next Term...
Next Term
The next term began on Monday, October 4, 2021. With the considerable current activity in the Shadow Docket, there was not much of a summer break. The coming term looks extraordinary. The headline case is an abortion case from Mississippi, Dobbs v Jackson Women’s Health Organization.25 The legal question is the constitutionality of Mississippi law that prohibits most abortions after 15 weeks of gestation. The Texas abortion law will also be back before the Court. As we saw this term, big cases may produce very narrow results, but this case has the potential for being a notable abortion decision.
In a different case the Court will decide whether a state attorney general can step in to defend an abortion law when the state health secretary does not do so.26
The Court also has accepted 3 cases dealing with reimbursement for health services. One deals with whether or not the Department of Health and Human Services can set reimbursement rates without good survey data regarding costs,27 another involves the calculation of additional payments for hospitals that serve a “disproportionate number of low-income patients,”28 and the third whether state Medicaid programs can take funds from an injured beneficiary’s tort recovery to cover future Medicaid costs.29
In other cases, the Court will review a gun control law from New York. The Court’s earlier Second Amendment cases involved guns in the home used for self-defense, but this case raises the question of whether a state can practically preclude “concealed-carry licenses.”30 Many experts believe the Court will accept a case dealing with racial preferences in college admissions, perhaps the Harvard case in which the claim is discrimination against Asian Americans.31
The ACOG mifepristone case was interesting, in part because the federal district court issued a nationwide injunction against the Americans with Disabilities Act, enforcing its rules anywhere in the country. The effect of these orders is for a single district judge to create the “law of the land,” at least until that is reviewed—which can take months. The advantage of the nationwide injunction is that it avoids having to repeatedly litigate the same issues in multiple courts around the country. The downside is that plaintiffs can seek out a nonrepresentative judge or circuit and receive an injunction that would be granted by few other circuits. In addition, a nationwide injunction can apply to specific circumstances that are not before the court issuing the injunction. In the mifepristone case, for example, 10 states requested to intervene in the ACOG case. The court rejected the request, but the nationwide injunction applied to those states.1
Although federal judges have had the authority to issue nationwide injunctions for years, they are becoming much more common. One reason is the ease of forum shopping noted earlier—organizations can cherry-pick district courts and circuits sympathetic to their views. Both left- and right-leaning organizations have learned this lesson, so left-leaning groups are likely to file in specific districts in the Ninth Circuit, and right-leaning groups to districts in the Fifth Circuit.
If the current trend of increasing nationwide injunctions continues, either the rules for the federal courts or congressional action may be required to reduce some of the abuses by both sides of the political spectrum.
The ACOG mifepristone case was interesting, in part because the federal district court issued a nationwide injunction against the Americans with Disabilities Act, enforcing its rules anywhere in the country. The effect of these orders is for a single district judge to create the “law of the land,” at least until that is reviewed—which can take months. The advantage of the nationwide injunction is that it avoids having to repeatedly litigate the same issues in multiple courts around the country. The downside is that plaintiffs can seek out a nonrepresentative judge or circuit and receive an injunction that would be granted by few other circuits. In addition, a nationwide injunction can apply to specific circumstances that are not before the court issuing the injunction. In the mifepristone case, for example, 10 states requested to intervene in the ACOG case. The court rejected the request, but the nationwide injunction applied to those states.1
Although federal judges have had the authority to issue nationwide injunctions for years, they are becoming much more common. One reason is the ease of forum shopping noted earlier—organizations can cherry-pick district courts and circuits sympathetic to their views. Both left- and right-leaning organizations have learned this lesson, so left-leaning groups are likely to file in specific districts in the Ninth Circuit, and right-leaning groups to districts in the Fifth Circuit.
If the current trend of increasing nationwide injunctions continues, either the rules for the federal courts or congressional action may be required to reduce some of the abuses by both sides of the political spectrum. Reference Am. Coll. of Obstetricians & Gynecologists v. United States FDA, 467 F. Supp. 3d 282, 284 (D. Md. 2020).
Reference
1. Am. Coll. of Obstetricians & Gynecologists v. United States FDA, 467 F. Supp. 3d 282, 284 (D. Md. 2020).
The “Shadow Docket”
The ACOG mifepristone decisions do not appear on the Supreme Court’s “Court Opinions” website.1 They appear in what has become known in recent years as “The Shadow Docket,” an informal term that includes many orders of the Court and statements of individual justices regarding some cases.2 There are hundreds of orders by the Court each Term, there is nothing particularly shadowy about any of these items—they are all publicly available on the Court’s website and later in paper format. It is, however, a little harder to find and much harder to sort through than the major opinions. In some cases, it is not possible to tell what the vote was, how each justice voted, and what the reasoning of the Court was. In a few cases it is difficult to know exactly what the Court was holding or otherwise leaves some confusion about what the law actually is.3
The part of the Shadow Docket that is most intriguing for commentators, and where the ACOG cases appear, is the “Opinions Relating to Orders.”4 These are a variety of opinions, some written by the Court and many by individual justices. It also includes the action of the Court in some cases in which there was not full briefing or oral argument. The statements by justices often are to dissent from the denial of cert of decisions of the Court. These opinions have become much more common over the years. In this past term, there were approximately 60 such opinions related to about 50 cases. In part, this relates to the number of pandemic cases that could not wait for a Court decision going through the extended ordinary process. Although the Shadow Docket has been of interest to academic observers and Court watchers for years, this year it has attracted the attention of Congress.5
References
1. Opinions of the Court. Supreme Court website. https://www.supremecourt.gov/opinions/slipopinion/20#list. Accessed October 10, 2021.
2. Baude W. Foreword: the Supreme Court’s Shadow Docket, 9 N.Y.U. J.L. & Liberty 1 (2015).
3. Vladeck SI. The Solicitor General and the Shadow Docket, 133 Harvard Law Review. 123 (2019).
4. Opinions relating to orders. Supreme Court website. https://www.supremecourt.gov/opinions/relatingtoorders/20#list. Accessed October 10, 2021.
5. The Supreme Court’s Shadow Docket: Hearing Before the Subcommittee on Courts, Intellectual Property and the Internet of the H. Committee on the Judiciary, 117th Congress (2021).
- American College of Obstetricians & Gynecologists v. United States FDA, 472 F. Supp. 3d 183 (D. Md. 2020).
- Michael Kunzelman, Doctors Sue to Block FDA Abortion Pill Rule During Pandemic, (May 29, 2020).
- ACLU, American College Of Obstetricians And Gynecologists V. U.S. Food And Drug Administration, https://www.aclu.org/cases/american-college-obstetricians-and-gynecologists-v-us-food-and-drug-administration. Updated February 12, 2021. Accessed August 27, 2021.
- Whole Woman’s Health v Hellerstedt, 579 US ___ (2016), 136 S Ct 2292.
- 2016 Clinical Review at 39, 47, 49, Opp’n Mot. PI Ex. 19, ECF No. 62-11.
- American College of Obstetricians and Gynecologists v FDA (I), decided October 8, 2020.
- October 8, 2020, dissenting opinion by Justice Alito.
- January 12, 2021, dissenting opinion by Justice Sotomayor.
- Questions and answers on Mifeprex. U.S. Food and Drug Administration website. Published April 13, 2021. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/questions-and-answers-mifeprex. Accessed October 9, 2021.
- Whole Woman’s Health v Jackson, decided September 1, 2021.
- Texas Senate Bill 8, relating to abortion, including abortions after detection of unborn child’s heartbeat; authorizing a private civil right of action. LegiScan website. https://legiscan.com/TX/text/SB8/id/2395961. Accessed October 9, 2021.
- Planned Parenthood of Southeastern Pennsylvania v Casey, 505 U. S. 833 (1992); Roe v Wade, 410 U. S. 113 (1973).
- Dobbs v Jackson Women’s Health Organization, No. 19-1392.
- Roman Catholic Diocese of Brooklyn v Cuomo, decided November 25, 2020.
- Alabama Association of Realtors v Department of Health and Human Services, decided June 29, 2021.
- Temporary halt in residential evictions in communities with substantial or high levels of community transmission of COVID-19 to prevent the further spread of COVID-19. August 6, 2021. https://www.federalregister.gov/documents/2021/08/06/2021-16945/temporary-halt-in-residential-evictions-in-communities-with-substantial-or-high-transmission-of.
- Alabama Association of Realtors v Department of Health and Human Services, decided August 26, 2021.
- California v Texas, decided June 17, 2021.
- Brief of Amici Curiae American Medical Association, American Academy of Allergy, Asthma and Immunology, Aerospace Medical Association, American Academy of Family Physicians, American Academy of Pediatrics, American College of Cardiology, American College of Emergency Physicians, American College of Medical Genetics and Genomics, American College of Obstetricians and Gynecologists, American College of Physicians, American College of Radiation Oncology, American College of Radiology, American Psychiatric Association, American Society of Gastrointestinal Endoscopy, American Society of Hematology, American Society of Metabolic and Bariatric Surgery, Endocrine Society, GLMA: Health Professionals Advancing LGBTQ Equality, Renal Physicians Association, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology in Support of Petitioners, in California v. Texas. May 13, 2020. https://www.supremecourt.gov/DocketPDF/19/19-840/143469/20200513150051995_19-840%20Amici%20Brief%20AMA.pdf. Accessed October 9, 2021.
- Rutledge v Pharmaceutical Care Management Association, decided December 10, 2020.
- Brief of the American Medical Association, The Arkansas Medical Society, and The Litigation Center of the American Medical Association and the State Medical Societies as Amici Curiae in Support of Petitioner in Rutledge v Pharmaceutical Care Management Association. March 2, 2020. https://www.supremecourt.gov/DocketPDF/18/18-540/134670/20200302163622018_Rutledge%20v.%20PCMA%20Amicus%20Brief%20of%20AMA%20et%20al.pdf. Accessed October 9, 2021.
- Apple quietly settles patent lawsuit, promptly gets hit with another one. TechCrunch website. Published July 30, 2010. https://techcrunch.com/2010/07/30/apple-minerva-emblaze/. Accessed October 9, 2021.
- Minerva Surgical, Inc. v Hologic, Inc., decided June 29, 2021.
- Stat pack. SCOTUS Blog website. Published July 6, 2021. https://www.scotusblog.com/wp-content/uploads/2021/07/Final-Stat-Pack-7.6.21.pdf. Accessed October 9, 2021.
- Dobbs v Jackson Women’s Health Organization, No. 19-1392.
- Cameron v. EMW Women’s Surgical Center, https://www.scotusblog.com/case-files/cases/cameron-v-emw-womens-surgical-center-p-s-c/. Accessed August 28, 2021.
- American Hospital Association v Becerra, No. 20-1114.
- Becerra v Empire Health Foundation, No. 20-1312.
- Gallardo v Marstiller, No. 20-1263.
- New York State Rifle & Pistol Association Inc. v Corlett, No. 20-843.
- Students for Fair Admissions v President & Fellows of Harvard College, No. 20-1199.
- American College of Obstetricians & Gynecologists v. United States FDA, 472 F. Supp. 3d 183 (D. Md. 2020).
- Michael Kunzelman, Doctors Sue to Block FDA Abortion Pill Rule During Pandemic, (May 29, 2020).
- ACLU, American College Of Obstetricians And Gynecologists V. U.S. Food And Drug Administration, https://www.aclu.org/cases/american-college-obstetricians-and-gynecologists-v-us-food-and-drug-administration. Updated February 12, 2021. Accessed August 27, 2021.
- Whole Woman’s Health v Hellerstedt, 579 US ___ (2016), 136 S Ct 2292.
- 2016 Clinical Review at 39, 47, 49, Opp’n Mot. PI Ex. 19, ECF No. 62-11.
- American College of Obstetricians and Gynecologists v FDA (I), decided October 8, 2020.
- October 8, 2020, dissenting opinion by Justice Alito.
- January 12, 2021, dissenting opinion by Justice Sotomayor.
- Questions and answers on Mifeprex. U.S. Food and Drug Administration website. Published April 13, 2021. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/questions-and-answers-mifeprex. Accessed October 9, 2021.
- Whole Woman’s Health v Jackson, decided September 1, 2021.
- Texas Senate Bill 8, relating to abortion, including abortions after detection of unborn child’s heartbeat; authorizing a private civil right of action. LegiScan website. https://legiscan.com/TX/text/SB8/id/2395961. Accessed October 9, 2021.
- Planned Parenthood of Southeastern Pennsylvania v Casey, 505 U. S. 833 (1992); Roe v Wade, 410 U. S. 113 (1973).
- Dobbs v Jackson Women’s Health Organization, No. 19-1392.
- Roman Catholic Diocese of Brooklyn v Cuomo, decided November 25, 2020.
- Alabama Association of Realtors v Department of Health and Human Services, decided June 29, 2021.
- Temporary halt in residential evictions in communities with substantial or high levels of community transmission of COVID-19 to prevent the further spread of COVID-19. August 6, 2021. https://www.federalregister.gov/documents/2021/08/06/2021-16945/temporary-halt-in-residential-evictions-in-communities-with-substantial-or-high-transmission-of.
- Alabama Association of Realtors v Department of Health and Human Services, decided August 26, 2021.
- California v Texas, decided June 17, 2021.
- Brief of Amici Curiae American Medical Association, American Academy of Allergy, Asthma and Immunology, Aerospace Medical Association, American Academy of Family Physicians, American Academy of Pediatrics, American College of Cardiology, American College of Emergency Physicians, American College of Medical Genetics and Genomics, American College of Obstetricians and Gynecologists, American College of Physicians, American College of Radiation Oncology, American College of Radiology, American Psychiatric Association, American Society of Gastrointestinal Endoscopy, American Society of Hematology, American Society of Metabolic and Bariatric Surgery, Endocrine Society, GLMA: Health Professionals Advancing LGBTQ Equality, Renal Physicians Association, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology in Support of Petitioners, in California v. Texas. May 13, 2020. https://www.supremecourt.gov/DocketPDF/19/19-840/143469/20200513150051995_19-840%20Amici%20Brief%20AMA.pdf. Accessed October 9, 2021.
- Rutledge v Pharmaceutical Care Management Association, decided December 10, 2020.
- Brief of the American Medical Association, The Arkansas Medical Society, and The Litigation Center of the American Medical Association and the State Medical Societies as Amici Curiae in Support of Petitioner in Rutledge v Pharmaceutical Care Management Association. March 2, 2020. https://www.supremecourt.gov/DocketPDF/18/18-540/134670/20200302163622018_Rutledge%20v.%20PCMA%20Amicus%20Brief%20of%20AMA%20et%20al.pdf. Accessed October 9, 2021.
- Apple quietly settles patent lawsuit, promptly gets hit with another one. TechCrunch website. Published July 30, 2010. https://techcrunch.com/2010/07/30/apple-minerva-emblaze/. Accessed October 9, 2021.
- Minerva Surgical, Inc. v Hologic, Inc., decided June 29, 2021.
- Stat pack. SCOTUS Blog website. Published July 6, 2021. https://www.scotusblog.com/wp-content/uploads/2021/07/Final-Stat-Pack-7.6.21.pdf. Accessed October 9, 2021.
- Dobbs v Jackson Women’s Health Organization, No. 19-1392.
- Cameron v. EMW Women’s Surgical Center, https://www.scotusblog.com/case-files/cases/cameron-v-emw-womens-surgical-center-p-s-c/. Accessed August 28, 2021.
- American Hospital Association v Becerra, No. 20-1114.
- Becerra v Empire Health Foundation, No. 20-1312.
- Gallardo v Marstiller, No. 20-1263.
- New York State Rifle & Pistol Association Inc. v Corlett, No. 20-843.
- Students for Fair Admissions v President & Fellows of Harvard College, No. 20-1199.
Service animals and emotional support animals: Should you write that letter?

For centuries, animals, especially dogs, have assisted humans in a variety of ways in their daily lives. Animals that assist people with disabilities fall into 2 broad categories: disability service animals, and emotional support animals (ESAs). Often there is confusion in how these categories differ because of the animal’s role and the laws related to them.
This article describes the differences between disability service animals and ESAs, and outlines the forensic and ethical concerns you should consider before agreeing to write a letter for a patient outlining their need for a disability service animal or ESA. A letter may protect a patient and their service animal or ESA in situations where laws and regulations typically prohibit animals, such as on a flight or when renting an apartment or house. Note that a description of how to conduct the formal patient evaluation before writing a verification letter is beyond the scope of this article.
The differences between disability service animals and ESAs
Purpose and training. Disability service animals, or service animals, are dogs of any breed (and in some cases miniature horses) that are specially trained to perform tasks for an individual with a disability (physical, sensory, psychiatric, intellectual, or other mental disability).1-3 These tasks must be directly related to the individual’s disability.1,2 On the other hand, ESAs, which can be any species of animal, provide support and minimize the impact of an individual’s emotional or psychological disability based on their presence alone. Unlike disability service animals, ESAs are not trained to perform a specific task or duty.2,3
There is no legal requirement for service animals to know specific commands, and professional training is not required—individuals can train the animals themselves.1 Service animals, mainly dogs, can be trained to perform numerous tasks, including4:
- attending to an individual’s mobility and activities of daily living
- guiding an individual who is deaf or hearing impaired
- helping to remind an individual to take their medications
- assisting an individual during and/or after a seizure
- alerting individuals with diabetes in advance of low or high blood sugar episodes
- supporting an individual with autism
- assisting an individual with a psychiatric or mental disability
- applying sensory commands such as lying on the person or resting their head on the individual’s lap to help the individual regain behavioral control.
Service dog verification works via an honor system, which can be problematic, especially in the case of psychiatric service dogs, whose handlers may not have a visible disability (Box 11,5).
Box 1
In the United States, there is no national service dog certification program—meaning there is no official test that a dog has to pass in order to obtain formal recognition as a service animal—nor is there a central and mandatory service dog registry.5 Instead, service dog verification works through an honor system, which can be problematic.5 In many states, misrepresenting one’s dog as a service dog is considered a misdemeanor.5 Unfortunately, other than the guidance set forth by the Americans with Disabilities Act, there are no criteria by which one can recognize a genuine service dog vs one being passed off as a service dog.5
In situations in public settings where it is not obvious or there’s doubt that the dog is a service animal (such as when a person visits a restaurant or store), employees are not allowed to request documentation for the dog, require the dog demonstrate its task, or inquire about the nature of the person’s disability.1
However, they can ask 2 questions1:
1. Is the animal required because of a disability?
2. What work or task has the animal been trained to perform?
Legal protections. Under the Americans with Disabilities Act (ADA), individuals with disabilities can bring their service animals into buildings or facilities where members of the public, program participants, clients, customers, patrons, or invitees are allowed.2 This does not include private clubs, religious organizations, or places of worship that are not open to the public.6,7 ESAs do not qualify as service animals under the ADA and are not given the same legal accommodations as service animals.1,3 Although ESAs were initially covered by the Air Carrier Access Act, they are no longer allowed in aircraft cabins after the US Department of Transportation revised this Act’s regulations in December 2020. ESAs are covered under the Fair Housing Act. Box 21-3,6-15 further discusses these laws and protections.
Evidence.
Due to the difficulty in reconciling inconsistent definitions for ESAs, there is limited high-quality data pertaining to the potential benefits and risks of ESAs.9 Currently, ESAs are not an evidence-based treatment for psychiatric disorders. To date, a handful of small studies have focused on ESAs. However, data from actual tests of the clinical risks and benefits of ESAs do not exist.9 In practice, ESAs are equivalent to pets. It stands to reason that similar to pets, ESAs could reduce loneliness, improve life satisfaction, and provide a sense of well-being.9 A systematic review suggested that pets provide benefits to patients with mental health conditions “through the intensity of connectivity with their owners and the contribution they make to emotional support in times of crises together with their ability to help manage symptoms when they arise.”18 In response to a congressional mandate, the US Department of Veterans Affairs launched a multi-site study from December 2014 to June 2019 to examine how limitations on activity and quality of life in veterans with posttraumatic stress disorder are impacted by the provision of a service dog vs an emotional support dog.19 As of October 14, 2021, results had not been published.19
Continue to: What’s in a disability service animal/ESA letter?
What’s in a disability service animal/ESA letter?
If you decide to write a letter advocating for your patient to have a service animal or ESA, the letter should appear on letterhead, be written by a licensed mental health professional, and include the following2,20:
- statement that the letter is being written at the patient’s request and is being given directly to the patient for use as the patient sees fit
- confirmation of the patient’s DSM-5 mental health diagnosis
- explanation of how the animal helps alleviate symptoms of the patient’s condition, briefly describing any interaction(s) between the animal and patient that you may have observed, and if applicable, a mention of any training the animal may have received from a qualified trainer if applicable
- explanation of the possible negative effects of the patient not having the animal with him or her
- statement that you are not vouching for the animal’s behavior
- verification of your involvement in your patient’s treatment and your assessment of the patient as their licensed mental health professional (including details such as date and type of license you have and the state/other jurisdiction where it was issued).
In a letter for a service animal, also indicate that your patient is psychiatrically disabled to the extent that your patient is not able to perform at least one major life task without the daily assistance of a service animal.2Should you write your patient a letter?
Writing a letter advocating for a patient to have a service animal or ESA may appear innocuous, but doing so may have serious ramifications. Writing a letter certifying a dog as a service animal does not make that animal a service animal; the dog must be specifically trained for a task or tasks directly related to that individual’s disability. There are no current standards for conducting evaluations to determine the need a patient has for a service animal or ESA. How to conduct such evaluations is beyond the scope of this article. There are meager opportunities for formal education and training on how to conduct these evaluations.9 Online resources may be incomplete or inaccurate, and this information is often produced by lay animal enthusiasts and organizations, which can lead to a biased depiction of these animals.9
If you decide to write a letter for your patient, consider the following forensic and ethical concerns.
Remain objective. As an advocate for your patient, you may find it difficult to remain neutral and objective when asked to determine if your patient has a disability, the severity of the disability, the impact of the disability on your patient’s life, and the need for a service animal or ESA. Ensure that your advocacy for your patient does not impair your objectivity; if that is difficult, consider referring your patient to a third party who can conduct an objective evaluation.
Understand the risks. If you make written recommendations for special accommodations in a letter and those recommendations are disputed by an agency, that agency could initiate legal action and you may be called to justify your recommendations in a deposition or open court.9,21 Before writing the letter, ask yourself, “Can I defend my determination that my patient is disabled by a DSM-5 disorder and that this disability requires the presence of an animal in exception to existing policy?”21 Be prepared to state in a legal proceeding that the presence of a service animal or ESA is necessary. If you are unwilling to risk exposure to a legal action, then you should likely refrain from writing the letter. It is a crime to fraudulently certify an animal as a service animal in some jurisdictions, and such conduct could result in disciplinary action by your licensing board.21
Conduct a systematic examination. When you write a letter for your patient, you are explicitly declaring your patient has a disability or condition. Comprehensive disability determinations are complex and are best conducted by assessing for objective evidence of psychiatric disorders and impairment through the use of standard, systematic examination methods.22 Unstandardized measures (eg, asking patients open-ended questions and then relying on your clinical judgement and interpretation in arriving at conclusions) are not as effective.22 In addition, consider the possibility that your patient may malinger their symptoms in an effort to obtain a letter supporting a service animal or ESA. Assessing for malingering is essential to making a disability determination, especially if a disability claim is based primarily on self-report.22
Anticipate pushback. Problems can arise when a patient wants a letter that you cannot or will not provide due to your scope of practice. Consider how you would resolve the situation when you do not believe your patient has a disability that requires the presence of a service animal or ESA—or you believe that your patient no longer needs a service animal or ESA—and the patient disagrees.21 Disagreeing with your patient’s assessment could result in a conflict of interest that could damage the therapeutic relationship.21
Box 2
The Americans with Disabilities Act (ADA) of 1990, as amended by the ADA Amendments Act of 2008, prohibits discrimination on the basis of disability in several areas, including state and local governments (under Title II of the ADA) and places of public accommodations, commercial facilities, and private entities (under Title III of the ADA).6,7 Thus, individuals with disabilities can bring their service animals into the building or facility where members of the public, program participants, clients, customers, patrons, or invitees are allowed.2 This does not include private clubs not open to the public, religious organizations, or places of worship.6,7
Service animals. Although the ADA recognizes miniature horses as service animals, only dogs are recognized as service animals in regards to Title II and Title III protections under the ADA as of March 15, 2011.2 Federal agencies do not have to comply with the ADA1; however, Section 504 of the Rehabilitation Act of 1973 is the federal law that protects the rights of people with disabilities to participate in federal programs and services.1,8 It states that no qualified individual with a disability shall be excluded from, denied the benefits of, or be subjected to discrimination under any program or activity that receives federal funding or is conducted by federal agencies.8 Courts have strived to interpret the Rehabilitation Act and the ADA in a consistent manner, specifically applying the ADA regulations regarding service animals (including its narrow definition regarding specifically trained tasks and emotional support) to the Rehabilitation Act.9-11
Similarly, commercial airlines do not have to comply with the ADA1 ; however, the Air Carrier Access Act (ACAA) of 1986 is the federal law that protects the rights of people with disabilities in air travel.1,12 On December 2, 2020, the US Department of Transportation announced that it was revising its ACAA regulation regarding service animals on aircraft (this final rule will be effective 30 days after date of publication in the Federal Register).13 Among the many revisions, the US Department of Transportation narrowed the definition of service animals to only dogs that were individually trained to work or perform tasks for the benefits of a person with a disability.13 It requires airlines to treat psychiatric service animals the same as other service animals.13 Although the US Department of Transportation has chosen to closely align its ACAA service animal definition with US Department of Justice service animal definition under the ADA, the substantive requirements in this final rule differ from US Department of Justice’s requirements for service animals under the ADA in various areas (for example, by allowing airlines to require service animal documentation and prohibiting the use of voice control over a service animal).13
Emotional support animals. Regulations regarding ESAs are primarily set by individual states1,3; however, ESAs may qualify for a waiver of a no-pet rule or a pet deposit under the Fair Housing Amendments Act (FHAA) of 1988.2,14 Under the FHAA, if an individual has a disability, as defined by the ADA, that requires the presence of an ESA, or if they have symptoms that are ameliorated by the presence of an ESA, the landlord must comply with this request and allow the animal into the facility without charging pet fees.15
Bottom Line
Disability service animals and emotional support animals (ESAs) differ in their roles and legal protections. Before writing a letter in support of a patient’s request for a service animal or ESA, take into account the forensic and ethical implications of doing so.
Related Resources
- US Department of Justice. Civil Rights Division. Disability Rights Section. ADA requirements. Service animals. Updated February 24, 2020. https://www.ada.gov/service_ animals_2010.htm
American Veterinary Medical Association. Service, emotional support and therapy animals. https://www. avma.org/resources-tools/animal-health-welfare/ service-emotional-support-and-therapy-animals
US Department of Transportation. US Department of Transportation announces final rule on traveling by air with service animals. https://www.transportation.gov/briefingroom/us-department-transportation-announces-finalrule-traveling-air-service-animals
1. US Department of Justice. Frequently asked questions about service animals and the ADA. Published July 20, 2015. Accessed on July 28, 2021. https://www.ada.gov/regs2010/service_animal_qa.pdf
2. ADA National Network. Service animals and emotional support animals: where are they allowed and under what conditions? Published 2014. Accessed July 28, 2021. https://adata.org/sites/adata.org/files/files/Service_Animal_Booklet_2014(2).pdf
3. Huben-Kearney A. What to do if patients want service or emotional support animals. Psychiatric News. Published September 28, 2020. Accessed July 28, 2021. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2020.10a24
4. Fine AH. The role of therapy and service animals in the lives of persons with disabilities. Rev Sci Tech. 2018;37(1):141-149.
5. Wlodarczyk J. When pigs fly: emotional support animals, service dogs and the politics of legitimacy across species boundaries. Med Humanit. 2019;45(1):82-91.
6. Americans with Disabilities Act of 1990. Pub L. 101-336, 104 Stat. 327.
7. ADA Amendments Act of 2008. Pub L. 110-325.
8. Rehabilitation Act of 1973. Pub L. 93-112, 87 Stat 355.
9. Carroll JD, Mohlenhoff BS, Kersten CM, et al. Laws and ethics related to emotional support animals. J Am Acad Psychiatry Law. 2020;48(4):509-518.
10. Sanchez v US Dept of Energy. 870 F3d 1185 (10th Circuit 2017).
11. Berardelli v Allied Services Inst. of Rehab. Med., 900 F3d 104 (3rd Circuit 2018).
12. Air Carrier Access Act of 1986. 49 USC §41705.
13. US Department of Transportation. US Department of Transportation announces final rule on traveling by air with service animals. Published December 2, 2020. Accessed July 28, 2021. https://www.transportation.gov/briefing-room/us-department-transportation-announces-final-rule-traveling-air-service-animals
14. Fair Housing Amendments Act of 1988. Pub. L. 100-430. https://www.govinfo.gov/content/pkg/STATUTE-102/pdf/STATUTE-102-Pg1619.pdf
15. Boness CL, Younggren JN, Frumkin IB. The certification of emotional support animals: difference between clinical and forensic mental health practitioners. Professional Psychology: Research and Practice. 2017;48(3):216-223.
16. Lane DR, McNicholas J, Collis GM. Dogs for the disabled: benefits to recipients and welfare of the dog. Applied Animal Behaviour Science. 1998;59(1-3):49-60.
17. Hall SS, MacMichael J, Turner A, et al. A survey of the impact of owning a service dog on quality of life for individuals with physical and hearing disability: a pilot study. Health Qual Life Outcomes. 2017;15(1):59. doi:10.1186/s12955-017-0640-x
18. Brooks HL, Rushton K, Lovell K, et al. The power of support from companion animals for people living with mental health problems: a systematic review and narrative synthesis of the evidence. BMC Psychiatry. 2018;18(1):31. doi: 10.1186/s12888-018-1613-2
19. US National Library of Medicine: ClinicalTrials.gov. Can service dogs improve activity and quality of life in veterans with PTSD? (SDPTSD). Updated August 15, 2019. Accessed October 14, 2021. https://clinicaltrials.gov/ct2/show/study/NCT02039843
20. Clay RA. Is that a pet or therapeutic aid? American Psychological Association. 2016;47(8):38. https://www.apa.org/monitor/2016/09/pet-aid
21. Younggren JN, Boisvert JA, Boness CL. Examining emotional support animals and role conflicts in professional psychology. Prof Psychol Res Pr. 2016;47(4):255-260.
22. Gold LH, Anfang SA, Drukteinis AM, et al. AAPL practice guideline for the forensic evaluation of psychiatric disability. J Am Acad Psychiatry Law. 2008;36(4 Suppl):S3-S50. https://www.aapl.org/docs/pdf/Evaluation%20of%20Psychiatric%20Disability.pdf

For centuries, animals, especially dogs, have assisted humans in a variety of ways in their daily lives. Animals that assist people with disabilities fall into 2 broad categories: disability service animals, and emotional support animals (ESAs). Often there is confusion in how these categories differ because of the animal’s role and the laws related to them.
This article describes the differences between disability service animals and ESAs, and outlines the forensic and ethical concerns you should consider before agreeing to write a letter for a patient outlining their need for a disability service animal or ESA. A letter may protect a patient and their service animal or ESA in situations where laws and regulations typically prohibit animals, such as on a flight or when renting an apartment or house. Note that a description of how to conduct the formal patient evaluation before writing a verification letter is beyond the scope of this article.
The differences between disability service animals and ESAs
Purpose and training. Disability service animals, or service animals, are dogs of any breed (and in some cases miniature horses) that are specially trained to perform tasks for an individual with a disability (physical, sensory, psychiatric, intellectual, or other mental disability).1-3 These tasks must be directly related to the individual’s disability.1,2 On the other hand, ESAs, which can be any species of animal, provide support and minimize the impact of an individual’s emotional or psychological disability based on their presence alone. Unlike disability service animals, ESAs are not trained to perform a specific task or duty.2,3
There is no legal requirement for service animals to know specific commands, and professional training is not required—individuals can train the animals themselves.1 Service animals, mainly dogs, can be trained to perform numerous tasks, including4:
- attending to an individual’s mobility and activities of daily living
- guiding an individual who is deaf or hearing impaired
- helping to remind an individual to take their medications
- assisting an individual during and/or after a seizure
- alerting individuals with diabetes in advance of low or high blood sugar episodes
- supporting an individual with autism
- assisting an individual with a psychiatric or mental disability
- applying sensory commands such as lying on the person or resting their head on the individual’s lap to help the individual regain behavioral control.
Service dog verification works via an honor system, which can be problematic, especially in the case of psychiatric service dogs, whose handlers may not have a visible disability (Box 11,5).
Box 1
In the United States, there is no national service dog certification program—meaning there is no official test that a dog has to pass in order to obtain formal recognition as a service animal—nor is there a central and mandatory service dog registry.5 Instead, service dog verification works through an honor system, which can be problematic.5 In many states, misrepresenting one’s dog as a service dog is considered a misdemeanor.5 Unfortunately, other than the guidance set forth by the Americans with Disabilities Act, there are no criteria by which one can recognize a genuine service dog vs one being passed off as a service dog.5
In situations in public settings where it is not obvious or there’s doubt that the dog is a service animal (such as when a person visits a restaurant or store), employees are not allowed to request documentation for the dog, require the dog demonstrate its task, or inquire about the nature of the person’s disability.1
However, they can ask 2 questions1:
1. Is the animal required because of a disability?
2. What work or task has the animal been trained to perform?
Legal protections. Under the Americans with Disabilities Act (ADA), individuals with disabilities can bring their service animals into buildings or facilities where members of the public, program participants, clients, customers, patrons, or invitees are allowed.2 This does not include private clubs, religious organizations, or places of worship that are not open to the public.6,7 ESAs do not qualify as service animals under the ADA and are not given the same legal accommodations as service animals.1,3 Although ESAs were initially covered by the Air Carrier Access Act, they are no longer allowed in aircraft cabins after the US Department of Transportation revised this Act’s regulations in December 2020. ESAs are covered under the Fair Housing Act. Box 21-3,6-15 further discusses these laws and protections.
Evidence.
Due to the difficulty in reconciling inconsistent definitions for ESAs, there is limited high-quality data pertaining to the potential benefits and risks of ESAs.9 Currently, ESAs are not an evidence-based treatment for psychiatric disorders. To date, a handful of small studies have focused on ESAs. However, data from actual tests of the clinical risks and benefits of ESAs do not exist.9 In practice, ESAs are equivalent to pets. It stands to reason that similar to pets, ESAs could reduce loneliness, improve life satisfaction, and provide a sense of well-being.9 A systematic review suggested that pets provide benefits to patients with mental health conditions “through the intensity of connectivity with their owners and the contribution they make to emotional support in times of crises together with their ability to help manage symptoms when they arise.”18 In response to a congressional mandate, the US Department of Veterans Affairs launched a multi-site study from December 2014 to June 2019 to examine how limitations on activity and quality of life in veterans with posttraumatic stress disorder are impacted by the provision of a service dog vs an emotional support dog.19 As of October 14, 2021, results had not been published.19
Continue to: What’s in a disability service animal/ESA letter?
What’s in a disability service animal/ESA letter?
If you decide to write a letter advocating for your patient to have a service animal or ESA, the letter should appear on letterhead, be written by a licensed mental health professional, and include the following2,20:
- statement that the letter is being written at the patient’s request and is being given directly to the patient for use as the patient sees fit
- confirmation of the patient’s DSM-5 mental health diagnosis
- explanation of how the animal helps alleviate symptoms of the patient’s condition, briefly describing any interaction(s) between the animal and patient that you may have observed, and if applicable, a mention of any training the animal may have received from a qualified trainer if applicable
- explanation of the possible negative effects of the patient not having the animal with him or her
- statement that you are not vouching for the animal’s behavior
- verification of your involvement in your patient’s treatment and your assessment of the patient as their licensed mental health professional (including details such as date and type of license you have and the state/other jurisdiction where it was issued).
In a letter for a service animal, also indicate that your patient is psychiatrically disabled to the extent that your patient is not able to perform at least one major life task without the daily assistance of a service animal.2Should you write your patient a letter?
Writing a letter advocating for a patient to have a service animal or ESA may appear innocuous, but doing so may have serious ramifications. Writing a letter certifying a dog as a service animal does not make that animal a service animal; the dog must be specifically trained for a task or tasks directly related to that individual’s disability. There are no current standards for conducting evaluations to determine the need a patient has for a service animal or ESA. How to conduct such evaluations is beyond the scope of this article. There are meager opportunities for formal education and training on how to conduct these evaluations.9 Online resources may be incomplete or inaccurate, and this information is often produced by lay animal enthusiasts and organizations, which can lead to a biased depiction of these animals.9
If you decide to write a letter for your patient, consider the following forensic and ethical concerns.
Remain objective. As an advocate for your patient, you may find it difficult to remain neutral and objective when asked to determine if your patient has a disability, the severity of the disability, the impact of the disability on your patient’s life, and the need for a service animal or ESA. Ensure that your advocacy for your patient does not impair your objectivity; if that is difficult, consider referring your patient to a third party who can conduct an objective evaluation.
Understand the risks. If you make written recommendations for special accommodations in a letter and those recommendations are disputed by an agency, that agency could initiate legal action and you may be called to justify your recommendations in a deposition or open court.9,21 Before writing the letter, ask yourself, “Can I defend my determination that my patient is disabled by a DSM-5 disorder and that this disability requires the presence of an animal in exception to existing policy?”21 Be prepared to state in a legal proceeding that the presence of a service animal or ESA is necessary. If you are unwilling to risk exposure to a legal action, then you should likely refrain from writing the letter. It is a crime to fraudulently certify an animal as a service animal in some jurisdictions, and such conduct could result in disciplinary action by your licensing board.21
Conduct a systematic examination. When you write a letter for your patient, you are explicitly declaring your patient has a disability or condition. Comprehensive disability determinations are complex and are best conducted by assessing for objective evidence of psychiatric disorders and impairment through the use of standard, systematic examination methods.22 Unstandardized measures (eg, asking patients open-ended questions and then relying on your clinical judgement and interpretation in arriving at conclusions) are not as effective.22 In addition, consider the possibility that your patient may malinger their symptoms in an effort to obtain a letter supporting a service animal or ESA. Assessing for malingering is essential to making a disability determination, especially if a disability claim is based primarily on self-report.22
Anticipate pushback. Problems can arise when a patient wants a letter that you cannot or will not provide due to your scope of practice. Consider how you would resolve the situation when you do not believe your patient has a disability that requires the presence of a service animal or ESA—or you believe that your patient no longer needs a service animal or ESA—and the patient disagrees.21 Disagreeing with your patient’s assessment could result in a conflict of interest that could damage the therapeutic relationship.21
Box 2
The Americans with Disabilities Act (ADA) of 1990, as amended by the ADA Amendments Act of 2008, prohibits discrimination on the basis of disability in several areas, including state and local governments (under Title II of the ADA) and places of public accommodations, commercial facilities, and private entities (under Title III of the ADA).6,7 Thus, individuals with disabilities can bring their service animals into the building or facility where members of the public, program participants, clients, customers, patrons, or invitees are allowed.2 This does not include private clubs not open to the public, religious organizations, or places of worship.6,7
Service animals. Although the ADA recognizes miniature horses as service animals, only dogs are recognized as service animals in regards to Title II and Title III protections under the ADA as of March 15, 2011.2 Federal agencies do not have to comply with the ADA1; however, Section 504 of the Rehabilitation Act of 1973 is the federal law that protects the rights of people with disabilities to participate in federal programs and services.1,8 It states that no qualified individual with a disability shall be excluded from, denied the benefits of, or be subjected to discrimination under any program or activity that receives federal funding or is conducted by federal agencies.8 Courts have strived to interpret the Rehabilitation Act and the ADA in a consistent manner, specifically applying the ADA regulations regarding service animals (including its narrow definition regarding specifically trained tasks and emotional support) to the Rehabilitation Act.9-11
Similarly, commercial airlines do not have to comply with the ADA1 ; however, the Air Carrier Access Act (ACAA) of 1986 is the federal law that protects the rights of people with disabilities in air travel.1,12 On December 2, 2020, the US Department of Transportation announced that it was revising its ACAA regulation regarding service animals on aircraft (this final rule will be effective 30 days after date of publication in the Federal Register).13 Among the many revisions, the US Department of Transportation narrowed the definition of service animals to only dogs that were individually trained to work or perform tasks for the benefits of a person with a disability.13 It requires airlines to treat psychiatric service animals the same as other service animals.13 Although the US Department of Transportation has chosen to closely align its ACAA service animal definition with US Department of Justice service animal definition under the ADA, the substantive requirements in this final rule differ from US Department of Justice’s requirements for service animals under the ADA in various areas (for example, by allowing airlines to require service animal documentation and prohibiting the use of voice control over a service animal).13
Emotional support animals. Regulations regarding ESAs are primarily set by individual states1,3; however, ESAs may qualify for a waiver of a no-pet rule or a pet deposit under the Fair Housing Amendments Act (FHAA) of 1988.2,14 Under the FHAA, if an individual has a disability, as defined by the ADA, that requires the presence of an ESA, or if they have symptoms that are ameliorated by the presence of an ESA, the landlord must comply with this request and allow the animal into the facility without charging pet fees.15
Bottom Line
Disability service animals and emotional support animals (ESAs) differ in their roles and legal protections. Before writing a letter in support of a patient’s request for a service animal or ESA, take into account the forensic and ethical implications of doing so.
Related Resources
- US Department of Justice. Civil Rights Division. Disability Rights Section. ADA requirements. Service animals. Updated February 24, 2020. https://www.ada.gov/service_ animals_2010.htm
American Veterinary Medical Association. Service, emotional support and therapy animals. https://www. avma.org/resources-tools/animal-health-welfare/ service-emotional-support-and-therapy-animals
US Department of Transportation. US Department of Transportation announces final rule on traveling by air with service animals. https://www.transportation.gov/briefingroom/us-department-transportation-announces-finalrule-traveling-air-service-animals

For centuries, animals, especially dogs, have assisted humans in a variety of ways in their daily lives. Animals that assist people with disabilities fall into 2 broad categories: disability service animals, and emotional support animals (ESAs). Often there is confusion in how these categories differ because of the animal’s role and the laws related to them.
This article describes the differences between disability service animals and ESAs, and outlines the forensic and ethical concerns you should consider before agreeing to write a letter for a patient outlining their need for a disability service animal or ESA. A letter may protect a patient and their service animal or ESA in situations where laws and regulations typically prohibit animals, such as on a flight or when renting an apartment or house. Note that a description of how to conduct the formal patient evaluation before writing a verification letter is beyond the scope of this article.
The differences between disability service animals and ESAs
Purpose and training. Disability service animals, or service animals, are dogs of any breed (and in some cases miniature horses) that are specially trained to perform tasks for an individual with a disability (physical, sensory, psychiatric, intellectual, or other mental disability).1-3 These tasks must be directly related to the individual’s disability.1,2 On the other hand, ESAs, which can be any species of animal, provide support and minimize the impact of an individual’s emotional or psychological disability based on their presence alone. Unlike disability service animals, ESAs are not trained to perform a specific task or duty.2,3
There is no legal requirement for service animals to know specific commands, and professional training is not required—individuals can train the animals themselves.1 Service animals, mainly dogs, can be trained to perform numerous tasks, including4:
- attending to an individual’s mobility and activities of daily living
- guiding an individual who is deaf or hearing impaired
- helping to remind an individual to take their medications
- assisting an individual during and/or after a seizure
- alerting individuals with diabetes in advance of low or high blood sugar episodes
- supporting an individual with autism
- assisting an individual with a psychiatric or mental disability
- applying sensory commands such as lying on the person or resting their head on the individual’s lap to help the individual regain behavioral control.
Service dog verification works via an honor system, which can be problematic, especially in the case of psychiatric service dogs, whose handlers may not have a visible disability (Box 11,5).
Box 1
In the United States, there is no national service dog certification program—meaning there is no official test that a dog has to pass in order to obtain formal recognition as a service animal—nor is there a central and mandatory service dog registry.5 Instead, service dog verification works through an honor system, which can be problematic.5 In many states, misrepresenting one’s dog as a service dog is considered a misdemeanor.5 Unfortunately, other than the guidance set forth by the Americans with Disabilities Act, there are no criteria by which one can recognize a genuine service dog vs one being passed off as a service dog.5
In situations in public settings where it is not obvious or there’s doubt that the dog is a service animal (such as when a person visits a restaurant or store), employees are not allowed to request documentation for the dog, require the dog demonstrate its task, or inquire about the nature of the person’s disability.1
However, they can ask 2 questions1:
1. Is the animal required because of a disability?
2. What work or task has the animal been trained to perform?
Legal protections. Under the Americans with Disabilities Act (ADA), individuals with disabilities can bring their service animals into buildings or facilities where members of the public, program participants, clients, customers, patrons, or invitees are allowed.2 This does not include private clubs, religious organizations, or places of worship that are not open to the public.6,7 ESAs do not qualify as service animals under the ADA and are not given the same legal accommodations as service animals.1,3 Although ESAs were initially covered by the Air Carrier Access Act, they are no longer allowed in aircraft cabins after the US Department of Transportation revised this Act’s regulations in December 2020. ESAs are covered under the Fair Housing Act. Box 21-3,6-15 further discusses these laws and protections.
Evidence.
Due to the difficulty in reconciling inconsistent definitions for ESAs, there is limited high-quality data pertaining to the potential benefits and risks of ESAs.9 Currently, ESAs are not an evidence-based treatment for psychiatric disorders. To date, a handful of small studies have focused on ESAs. However, data from actual tests of the clinical risks and benefits of ESAs do not exist.9 In practice, ESAs are equivalent to pets. It stands to reason that similar to pets, ESAs could reduce loneliness, improve life satisfaction, and provide a sense of well-being.9 A systematic review suggested that pets provide benefits to patients with mental health conditions “through the intensity of connectivity with their owners and the contribution they make to emotional support in times of crises together with their ability to help manage symptoms when they arise.”18 In response to a congressional mandate, the US Department of Veterans Affairs launched a multi-site study from December 2014 to June 2019 to examine how limitations on activity and quality of life in veterans with posttraumatic stress disorder are impacted by the provision of a service dog vs an emotional support dog.19 As of October 14, 2021, results had not been published.19
Continue to: What’s in a disability service animal/ESA letter?
What’s in a disability service animal/ESA letter?
If you decide to write a letter advocating for your patient to have a service animal or ESA, the letter should appear on letterhead, be written by a licensed mental health professional, and include the following2,20:
- statement that the letter is being written at the patient’s request and is being given directly to the patient for use as the patient sees fit
- confirmation of the patient’s DSM-5 mental health diagnosis
- explanation of how the animal helps alleviate symptoms of the patient’s condition, briefly describing any interaction(s) between the animal and patient that you may have observed, and if applicable, a mention of any training the animal may have received from a qualified trainer if applicable
- explanation of the possible negative effects of the patient not having the animal with him or her
- statement that you are not vouching for the animal’s behavior
- verification of your involvement in your patient’s treatment and your assessment of the patient as their licensed mental health professional (including details such as date and type of license you have and the state/other jurisdiction where it was issued).
In a letter for a service animal, also indicate that your patient is psychiatrically disabled to the extent that your patient is not able to perform at least one major life task without the daily assistance of a service animal.2Should you write your patient a letter?
Writing a letter advocating for a patient to have a service animal or ESA may appear innocuous, but doing so may have serious ramifications. Writing a letter certifying a dog as a service animal does not make that animal a service animal; the dog must be specifically trained for a task or tasks directly related to that individual’s disability. There are no current standards for conducting evaluations to determine the need a patient has for a service animal or ESA. How to conduct such evaluations is beyond the scope of this article. There are meager opportunities for formal education and training on how to conduct these evaluations.9 Online resources may be incomplete or inaccurate, and this information is often produced by lay animal enthusiasts and organizations, which can lead to a biased depiction of these animals.9
If you decide to write a letter for your patient, consider the following forensic and ethical concerns.
Remain objective. As an advocate for your patient, you may find it difficult to remain neutral and objective when asked to determine if your patient has a disability, the severity of the disability, the impact of the disability on your patient’s life, and the need for a service animal or ESA. Ensure that your advocacy for your patient does not impair your objectivity; if that is difficult, consider referring your patient to a third party who can conduct an objective evaluation.
Understand the risks. If you make written recommendations for special accommodations in a letter and those recommendations are disputed by an agency, that agency could initiate legal action and you may be called to justify your recommendations in a deposition or open court.9,21 Before writing the letter, ask yourself, “Can I defend my determination that my patient is disabled by a DSM-5 disorder and that this disability requires the presence of an animal in exception to existing policy?”21 Be prepared to state in a legal proceeding that the presence of a service animal or ESA is necessary. If you are unwilling to risk exposure to a legal action, then you should likely refrain from writing the letter. It is a crime to fraudulently certify an animal as a service animal in some jurisdictions, and such conduct could result in disciplinary action by your licensing board.21
Conduct a systematic examination. When you write a letter for your patient, you are explicitly declaring your patient has a disability or condition. Comprehensive disability determinations are complex and are best conducted by assessing for objective evidence of psychiatric disorders and impairment through the use of standard, systematic examination methods.22 Unstandardized measures (eg, asking patients open-ended questions and then relying on your clinical judgement and interpretation in arriving at conclusions) are not as effective.22 In addition, consider the possibility that your patient may malinger their symptoms in an effort to obtain a letter supporting a service animal or ESA. Assessing for malingering is essential to making a disability determination, especially if a disability claim is based primarily on self-report.22
Anticipate pushback. Problems can arise when a patient wants a letter that you cannot or will not provide due to your scope of practice. Consider how you would resolve the situation when you do not believe your patient has a disability that requires the presence of a service animal or ESA—or you believe that your patient no longer needs a service animal or ESA—and the patient disagrees.21 Disagreeing with your patient’s assessment could result in a conflict of interest that could damage the therapeutic relationship.21
Box 2
The Americans with Disabilities Act (ADA) of 1990, as amended by the ADA Amendments Act of 2008, prohibits discrimination on the basis of disability in several areas, including state and local governments (under Title II of the ADA) and places of public accommodations, commercial facilities, and private entities (under Title III of the ADA).6,7 Thus, individuals with disabilities can bring their service animals into the building or facility where members of the public, program participants, clients, customers, patrons, or invitees are allowed.2 This does not include private clubs not open to the public, religious organizations, or places of worship.6,7
Service animals. Although the ADA recognizes miniature horses as service animals, only dogs are recognized as service animals in regards to Title II and Title III protections under the ADA as of March 15, 2011.2 Federal agencies do not have to comply with the ADA1; however, Section 504 of the Rehabilitation Act of 1973 is the federal law that protects the rights of people with disabilities to participate in federal programs and services.1,8 It states that no qualified individual with a disability shall be excluded from, denied the benefits of, or be subjected to discrimination under any program or activity that receives federal funding or is conducted by federal agencies.8 Courts have strived to interpret the Rehabilitation Act and the ADA in a consistent manner, specifically applying the ADA regulations regarding service animals (including its narrow definition regarding specifically trained tasks and emotional support) to the Rehabilitation Act.9-11
Similarly, commercial airlines do not have to comply with the ADA1 ; however, the Air Carrier Access Act (ACAA) of 1986 is the federal law that protects the rights of people with disabilities in air travel.1,12 On December 2, 2020, the US Department of Transportation announced that it was revising its ACAA regulation regarding service animals on aircraft (this final rule will be effective 30 days after date of publication in the Federal Register).13 Among the many revisions, the US Department of Transportation narrowed the definition of service animals to only dogs that were individually trained to work or perform tasks for the benefits of a person with a disability.13 It requires airlines to treat psychiatric service animals the same as other service animals.13 Although the US Department of Transportation has chosen to closely align its ACAA service animal definition with US Department of Justice service animal definition under the ADA, the substantive requirements in this final rule differ from US Department of Justice’s requirements for service animals under the ADA in various areas (for example, by allowing airlines to require service animal documentation and prohibiting the use of voice control over a service animal).13
Emotional support animals. Regulations regarding ESAs are primarily set by individual states1,3; however, ESAs may qualify for a waiver of a no-pet rule or a pet deposit under the Fair Housing Amendments Act (FHAA) of 1988.2,14 Under the FHAA, if an individual has a disability, as defined by the ADA, that requires the presence of an ESA, or if they have symptoms that are ameliorated by the presence of an ESA, the landlord must comply with this request and allow the animal into the facility without charging pet fees.15
Bottom Line
Disability service animals and emotional support animals (ESAs) differ in their roles and legal protections. Before writing a letter in support of a patient’s request for a service animal or ESA, take into account the forensic and ethical implications of doing so.
Related Resources
- US Department of Justice. Civil Rights Division. Disability Rights Section. ADA requirements. Service animals. Updated February 24, 2020. https://www.ada.gov/service_ animals_2010.htm
American Veterinary Medical Association. Service, emotional support and therapy animals. https://www. avma.org/resources-tools/animal-health-welfare/ service-emotional-support-and-therapy-animals
US Department of Transportation. US Department of Transportation announces final rule on traveling by air with service animals. https://www.transportation.gov/briefingroom/us-department-transportation-announces-finalrule-traveling-air-service-animals
1. US Department of Justice. Frequently asked questions about service animals and the ADA. Published July 20, 2015. Accessed on July 28, 2021. https://www.ada.gov/regs2010/service_animal_qa.pdf
2. ADA National Network. Service animals and emotional support animals: where are they allowed and under what conditions? Published 2014. Accessed July 28, 2021. https://adata.org/sites/adata.org/files/files/Service_Animal_Booklet_2014(2).pdf
3. Huben-Kearney A. What to do if patients want service or emotional support animals. Psychiatric News. Published September 28, 2020. Accessed July 28, 2021. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2020.10a24
4. Fine AH. The role of therapy and service animals in the lives of persons with disabilities. Rev Sci Tech. 2018;37(1):141-149.
5. Wlodarczyk J. When pigs fly: emotional support animals, service dogs and the politics of legitimacy across species boundaries. Med Humanit. 2019;45(1):82-91.
6. Americans with Disabilities Act of 1990. Pub L. 101-336, 104 Stat. 327.
7. ADA Amendments Act of 2008. Pub L. 110-325.
8. Rehabilitation Act of 1973. Pub L. 93-112, 87 Stat 355.
9. Carroll JD, Mohlenhoff BS, Kersten CM, et al. Laws and ethics related to emotional support animals. J Am Acad Psychiatry Law. 2020;48(4):509-518.
10. Sanchez v US Dept of Energy. 870 F3d 1185 (10th Circuit 2017).
11. Berardelli v Allied Services Inst. of Rehab. Med., 900 F3d 104 (3rd Circuit 2018).
12. Air Carrier Access Act of 1986. 49 USC §41705.
13. US Department of Transportation. US Department of Transportation announces final rule on traveling by air with service animals. Published December 2, 2020. Accessed July 28, 2021. https://www.transportation.gov/briefing-room/us-department-transportation-announces-final-rule-traveling-air-service-animals
14. Fair Housing Amendments Act of 1988. Pub. L. 100-430. https://www.govinfo.gov/content/pkg/STATUTE-102/pdf/STATUTE-102-Pg1619.pdf
15. Boness CL, Younggren JN, Frumkin IB. The certification of emotional support animals: difference between clinical and forensic mental health practitioners. Professional Psychology: Research and Practice. 2017;48(3):216-223.
16. Lane DR, McNicholas J, Collis GM. Dogs for the disabled: benefits to recipients and welfare of the dog. Applied Animal Behaviour Science. 1998;59(1-3):49-60.
17. Hall SS, MacMichael J, Turner A, et al. A survey of the impact of owning a service dog on quality of life for individuals with physical and hearing disability: a pilot study. Health Qual Life Outcomes. 2017;15(1):59. doi:10.1186/s12955-017-0640-x
18. Brooks HL, Rushton K, Lovell K, et al. The power of support from companion animals for people living with mental health problems: a systematic review and narrative synthesis of the evidence. BMC Psychiatry. 2018;18(1):31. doi: 10.1186/s12888-018-1613-2
19. US National Library of Medicine: ClinicalTrials.gov. Can service dogs improve activity and quality of life in veterans with PTSD? (SDPTSD). Updated August 15, 2019. Accessed October 14, 2021. https://clinicaltrials.gov/ct2/show/study/NCT02039843
20. Clay RA. Is that a pet or therapeutic aid? American Psychological Association. 2016;47(8):38. https://www.apa.org/monitor/2016/09/pet-aid
21. Younggren JN, Boisvert JA, Boness CL. Examining emotional support animals and role conflicts in professional psychology. Prof Psychol Res Pr. 2016;47(4):255-260.
22. Gold LH, Anfang SA, Drukteinis AM, et al. AAPL practice guideline for the forensic evaluation of psychiatric disability. J Am Acad Psychiatry Law. 2008;36(4 Suppl):S3-S50. https://www.aapl.org/docs/pdf/Evaluation%20of%20Psychiatric%20Disability.pdf
1. US Department of Justice. Frequently asked questions about service animals and the ADA. Published July 20, 2015. Accessed on July 28, 2021. https://www.ada.gov/regs2010/service_animal_qa.pdf
2. ADA National Network. Service animals and emotional support animals: where are they allowed and under what conditions? Published 2014. Accessed July 28, 2021. https://adata.org/sites/adata.org/files/files/Service_Animal_Booklet_2014(2).pdf
3. Huben-Kearney A. What to do if patients want service or emotional support animals. Psychiatric News. Published September 28, 2020. Accessed July 28, 2021. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2020.10a24
4. Fine AH. The role of therapy and service animals in the lives of persons with disabilities. Rev Sci Tech. 2018;37(1):141-149.
5. Wlodarczyk J. When pigs fly: emotional support animals, service dogs and the politics of legitimacy across species boundaries. Med Humanit. 2019;45(1):82-91.
6. Americans with Disabilities Act of 1990. Pub L. 101-336, 104 Stat. 327.
7. ADA Amendments Act of 2008. Pub L. 110-325.
8. Rehabilitation Act of 1973. Pub L. 93-112, 87 Stat 355.
9. Carroll JD, Mohlenhoff BS, Kersten CM, et al. Laws and ethics related to emotional support animals. J Am Acad Psychiatry Law. 2020;48(4):509-518.
10. Sanchez v US Dept of Energy. 870 F3d 1185 (10th Circuit 2017).
11. Berardelli v Allied Services Inst. of Rehab. Med., 900 F3d 104 (3rd Circuit 2018).
12. Air Carrier Access Act of 1986. 49 USC §41705.
13. US Department of Transportation. US Department of Transportation announces final rule on traveling by air with service animals. Published December 2, 2020. Accessed July 28, 2021. https://www.transportation.gov/briefing-room/us-department-transportation-announces-final-rule-traveling-air-service-animals
14. Fair Housing Amendments Act of 1988. Pub. L. 100-430. https://www.govinfo.gov/content/pkg/STATUTE-102/pdf/STATUTE-102-Pg1619.pdf
15. Boness CL, Younggren JN, Frumkin IB. The certification of emotional support animals: difference between clinical and forensic mental health practitioners. Professional Psychology: Research and Practice. 2017;48(3):216-223.
16. Lane DR, McNicholas J, Collis GM. Dogs for the disabled: benefits to recipients and welfare of the dog. Applied Animal Behaviour Science. 1998;59(1-3):49-60.
17. Hall SS, MacMichael J, Turner A, et al. A survey of the impact of owning a service dog on quality of life for individuals with physical and hearing disability: a pilot study. Health Qual Life Outcomes. 2017;15(1):59. doi:10.1186/s12955-017-0640-x
18. Brooks HL, Rushton K, Lovell K, et al. The power of support from companion animals for people living with mental health problems: a systematic review and narrative synthesis of the evidence. BMC Psychiatry. 2018;18(1):31. doi: 10.1186/s12888-018-1613-2
19. US National Library of Medicine: ClinicalTrials.gov. Can service dogs improve activity and quality of life in veterans with PTSD? (SDPTSD). Updated August 15, 2019. Accessed October 14, 2021. https://clinicaltrials.gov/ct2/show/study/NCT02039843
20. Clay RA. Is that a pet or therapeutic aid? American Psychological Association. 2016;47(8):38. https://www.apa.org/monitor/2016/09/pet-aid
21. Younggren JN, Boisvert JA, Boness CL. Examining emotional support animals and role conflicts in professional psychology. Prof Psychol Res Pr. 2016;47(4):255-260.
22. Gold LH, Anfang SA, Drukteinis AM, et al. AAPL practice guideline for the forensic evaluation of psychiatric disability. J Am Acad Psychiatry Law. 2008;36(4 Suppl):S3-S50. https://www.aapl.org/docs/pdf/Evaluation%20of%20Psychiatric%20Disability.pdf
Confidentiality and privilege: What you don’t know can hurt you
Mrs. W, age 35, presents to your clinic seeking treatment for anxiety and depression. She has no psychiatric history but reports feeling sad, overwhelmed, and stressed. Mrs. W has been married for 10 years, has 2 young children, and is currently pregnant. She recently discovered that her husband has been having an affair. Mrs. W tells you that she feels her marriage is unsalvageable and would like to ask her husband for a divorce, but worries that he will “put up a fight” and demand full custody of their children. When you ask why, she states that her husband is “pretty narcissistic” and tends to become combative when criticized or threatened, such as a recent discussion they had about his affair that ended with him concluding that if she were “sexier and more confident” he would not have cheated on her.
As Mrs. W is talking, you recall a conversation you recently overheard at a continuing medical education event. Two clinicians were discussing how their records had been subpoenaed in a child custody case, even though the patient’s mental health was not contested. You realize that Mrs. W’s situation may also fit under this exception to confidentiality or privilege. You wonder if you should have disclosed this possibility to her at the outset of your session and wonder what you should say now, because she is clearly in distress and in need of psychiatric treatment. On the other hand, you want her to be fully informed of the potential repercussions if she continues with treatment.
Confidentiality and privilege allow our patients to disclose sensitive details in a safe space. The psychiatrist’s duty is to keep the patient’s information confidential, except in limited circumstances. The patient’s privilege is their right to prevent someone in a special confidential relationship from testifying against them or releasing their private records. In certain instances, a patient may waive or be forced to waive privilege, and a psychiatrist may be compelled to testify or release treatment records to a court. This article reviews exceptions to confidentiality and privilege, focusing specifically on a little-known exception to privilege that arises in divorce and child custody cases. We discuss relevant legislation and provide recommendations for psychiatrists to better understand how to discuss these legal realities with patients who are or may go through a divorce or child custody case.
Understanding confidentiality and privilege
Confidentiality and privilege are related but distinct concepts. Confidentiality relates to the overall trusting relationship created between 2 parties, such as a physician and their patient, and the duty on the part of the trusted individual to keep information private. Privilege refers to a person’s specific legal right to prevent someone in that confidential, trusting relationship from testifying against them in court or releasing confidential records. Privilege is owned by the patient and must be asserted or waived by the patient in legal proceedings. The concepts of confidentiality and privilege are crucial in creating an open, candid therapeutic environment. Many courts, including the US Supreme Court,1 have recognized the importance of confidentiality and privilege in establishing a positive therapeutic relationship between a psychotherapist and a patient. Without confidentiality and privilege, patients would be less likely to share sensitive yet clinically important information.
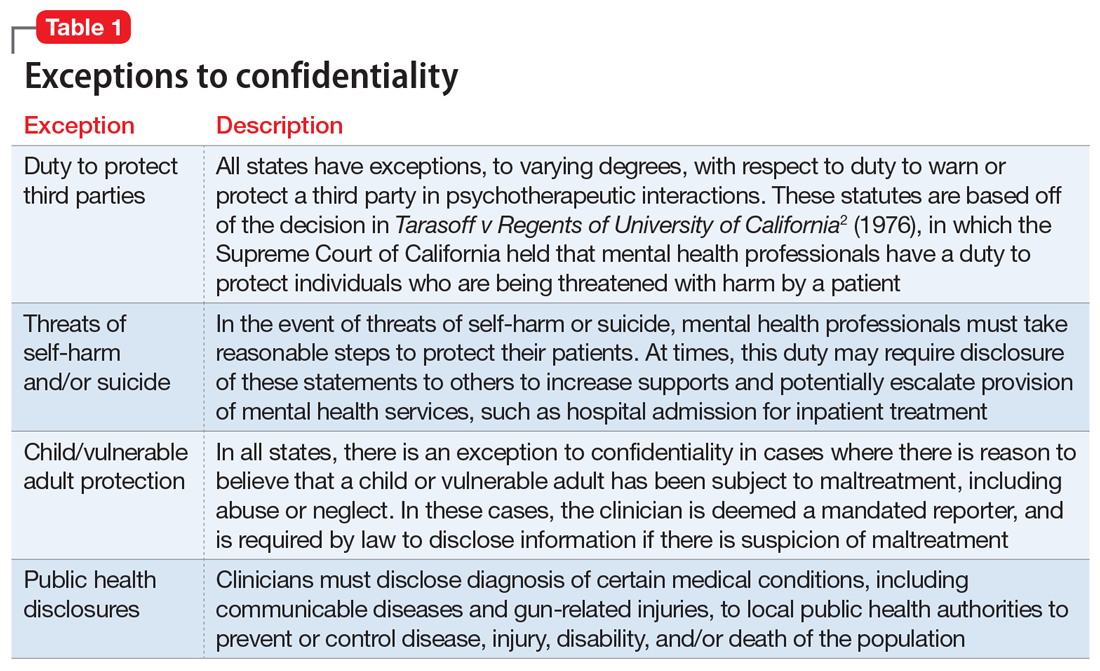
Commonly encountered exceptions to confidentiality (Table 12) and privilege (Table 2) exist in medical practice. Psychiatrists should discuss these exceptions with patients at the outset of clinical treatment. A little-known exception to privilege that may compel a psychiatrist to disclose confidential records can occur in child custody proceedings. In certain states, the mere filing of a child custody claim constitutes an exception to physician-patient privilege. In these states, the parent filing for divorce and custody may automatically waive privilege and thus compel disclosure of psychiatric records, even if their mental health is not in question. The following recent Ohio Supreme Court case illustrates this exception.
Friedenberg v Friedenberg (2020)
Friedenberg v Friedenberg3 addressed the issue of privilege and release of mental health treatment records in custody disputes. Belinda Torres Friedenberg and Keith Friedenberg were married with 4 minor children. Mrs. Friedenberg filed for divorce in 2016, requesting custody of the children and spousal support. In response, Mr. Friedenberg also filed a complaint seeking custody. Mr. Friedenberg subpoenaed mental health treatment records for Mrs. Friedenberg, who responded by filing a request to prevent the release of these records given physician-patient privilege. Mr. Friedenberg argued that Mrs. Friedenberg had placed her physical and mental health at issue when she filed for divorce and custody. At no point did Mr. Friedenberg allege that Mrs. Friedenberg’s mental health made her an unfit parent. The court agreed with Mr. Friedenberg and compelled disclosure of Mrs. Friedenberg’s psychiatric records, stating it is “hard to imagine a scenario where the mental health records of a parent would not be relevant to issues around custody and the best interests of the children.” The judge reviewed Mrs. Friedenberg’s psychiatric records privately and released records deemed relevant to the custody proceedings. On appeal, the Ohio Supreme Court agreed with this approach, holding that a parent’s mental fitness is always an issue in child custody cases, even if not asserted by either party. The court further held that unnecessary disclosure of sensitive information was prevented by the judge’s private review of records before deciding which records to release to the opposing spouse.
Waiver of physician-patient privilege
Waiver of physician-patient privilege in custody and divorce proceedings varies by state (Table 33-6). The Friedenberg decision highlights the most restrictive approach, where the mere filing of a divorce and child custody request automatically waives privilege. Some states, such as Indiana,4 follow a similar scheme to Ohio. Other states are silent on this issue or explicitly prohibit a waiver of privilege, asserting that custody disputes alone do not trigger disclosure without additional justifications, such as aberrant parental behaviors or other historical information concerning for abuse, neglect, or lack of parental fitness, or if a parent places their mental health at issue.7
Continue to: Once privilege is waived...
Once privilege is waived, the next step is to determine who should examine psychiatric records, deem relevance, and disclose sensitive information to the court and the opposing party. A judge may make this determination, as in the Friedenberg case. Alternatively, an independent psychiatric examiner may be appointed by the court to examine one or both parties; to obtain collateral information, including psychiatric records; and to submit a report to the court with medicolegal opinions regarding parental fitness. For example, in Maryland,6 the mere filing of a custody suit does not waive privilege. If a parent’s mental health is questioned, the judge may order an independent psychiatric examination to determine the parent’s fitness, thus balancing the best interests of the child with the parent’s right to physician-patient privilege.
The problem with automatic waivers
The foundation of the physician-patient relationship is trust and confidentiality. While this holds true for every specialty, perhaps it is even more important in psychiatry, where our patients routinely disclose sensitive, personal information in hopes of healing. Patients may not be aware of exceptions to confidentiality, or only be aware of the most well-known exceptions, such as the clinician’s duty to report abuse, or to warn a third party about risk of harm by a patient. Furthermore, clinicians and patients alike may not be aware of less-common exceptions to privilege, such as those that may occur in custody proceedings. This is critically important in light of the high number of patients who are or may be seeking divorce and custody of their children.
As psychiatric clinicians, it is highly likely that we will see patients going through divorce and custody proceedings. In 2018, there were 2.24 marriages for every divorce,8 and in 2014, 27% of all American children were living with a custodial parent, with the other parent living elsewhere.9 Divorce can be a profoundly stressful time; thus, it would be expected that many individuals going through divorce would seek psychiatric treatment and support.
Our concern is that the Friedenberg approach, which results in automatic disclosure of sensitive mental health information when a party files for divorce and custody, could deter patients from seeking psychiatric treatment, especially those anticipating divorce. Importantly, because women are nearly twice as likely as men to experience depression and anxiety10 and are more likely to seek treatment, this approach could disproportionately impact them.11 In general, an automatic waiver policy may create an additional obstacle for individuals who are already reticent to seek treatment.
How to handle these situations
As a psychiatrist, you should be familiar with your state’s laws regarding exceptions to patient-physician privilege, and should discuss exceptions at the outset of treatment. However, you will need to weigh the potential negative impacts of this information on the therapeutic relationship, including possible early termination. Furthermore, this information may impact a patient’s willingness to disclose all relevant information to mental health treatment if there is concern for later court disclosure. How should you balance these concerns? First, encourage patients to ask questions and raise concerns about confidentiality and privilege.12 In addition, you may direct the patient to other resources, such as a family law attorney, if they have questions about how certain information may be used in a legal proceeding.
Continue to: Second, you should be...
Second, you should be transparent regarding documentation of psychiatric visits. While documentation must meet ethical, legal, and billing requirements, you should take care to include only relevant information needed to make a diagnosis and provide indicated treatment while maintaining a neutral tone and avoiding medical jargon.13 For instance, we frequently use the term “denied” in medical documentation, as in “Mr. X denied cough, sore throat, fever or chills.” However, in psychiatric notes, if a patient “denied alcohol use,” the colloquial interpretation of this word could imply a tone of distrust toward the patient. A more sensitive way to document this might be: “When screened, reported no alcohol use.” If a patient divulges information and then asks you to omit this from their chart, but you do not feel comfortable doing so, explain what and why you must include the information in the chart.14
Third, if you receive a subpoena or other document requesting privileged information, first contact the patient and inform them of the request, and then seek legal consultation through your employer or malpractice insurer.15 Not all subpoenas are valid and enforceable, so it is important for an attorney to examine the subpoena; in addition, the patient’s attorney may choose to challenge the subpoena and limit the disclosure of privileged information.
Finally, inform legislatures and courts about the potential harm of automatic waivers in custody proceedings. A judge’s examination of the psychiatric records, as in Friedenberg, is not an adequate safeguard. A judge is not a trained mental health professional and may deem “relevant” information to be nearly everything: a history of abuse, remote drug or alcohol use, disclosure of a past crime, or financial troubles. We advocate for courts to follow the Maryland model, where a spouse does not automatically waive privilege if filing for divorce or custody. If mental health becomes an issue in a case, then the court may seek an independent psychiatric examination. The independent examiner will have access to patient records but will be in a better position to determine which details are relevant in determining diagnosis and parental fitness, and to render an opinion to the court.
CASE CONTINUED
You inform Mrs. W about a possible exception to privilege in divorce and custody cases. She decides to first talk with a family law attorney before proceeding with treatment. You defer your diagnosis and wait to see if she wants to proceed with treatment. Unfortunately, she does not return to your office.
Bottom Line
Some states limit the confidentiality and privilege of parents who are in psychiatric treatment and also involved in divorce and child custody cases. Psychiatrists should be mindful of these exceptions, and discuss them with patients at the onset of treatment.
Related Resources
- Legal Information Institute. Child custody: an overview. www.law.cornell.edu/wex/child_custody
- Melton GB, Petrila J, Poythress NG, et al. Child custody in divorce. In: Melton GB, Petrila J, Poythress NG, et al. Psychological evaluations for the courts. Guilford Press; 2018:530-533.
1. Jaffee v Redmond, 518 US 1 (1996).
2. Tarasoff v Regents of the University of California, 118 Cal Rptr 129 (Cal 1974); modified by Tarasoff v Regents of the Univ. of Cal., 551 P.2d 334 (Cal 1976).
3. Friedenberg v Friedenberg, No. 2019-0416 (Ohio 2020).
4. Owen v Owen, 563 NE 2d 605 (Ind 1991).
5. People ex. Rel. Hickox v Hickox, 410 NY S 2d 81 (NY App Div 1978).
6. Laznovsky v Laznovsky, 745 A 2d 1054 (Md 2000).
7. Eykel I, Miskel E. The mental health privilege in divorce and custody cases. Journal of the American Academy of Matrimonial Lawyers. 2012;25(2):453-476.
8. Center for Disease Control and Prevention. FastStats: Family life. Marriage and divorce. Published May 2020. Accessed July 29, 2021. www.cdc.gov/nchs/fastats/marriage-divorce.htm
9. The United States Census Bureau. Current population reports: custodial mothers and fathers and their child support: 2013. Published January 2016. Accessed July 29, 2021. https://www.census.gov/content/dam/Census/library/publications/2016/demo/P60-255.pdf
10. World Health Organization. Gender and mental health. Published June 2002. Accessed August 2, 2021. https://www.who.int/gender/other_health/genderMH.pdf
11. Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):629-640.
12. Younggren J, Harris E. Can you keep a secret? Confidentiality in psychotherapy. J Clin Psychol. 2008;64(5):589-600.
13. The Committee on Psychiatry and Law. Confidentiality and privilege communication in the practice of psychiatry. Report no. 45. Group for the Advancement of Psychiatry; 1960.
14. Wiger D. Ethical considerations in documentation. In: Wiger D. The psychotherapy documentation primer. 3rd ed. Wiley; 2013:35-45.
15. Stansbury CD. Accessibility to a parent’s psychotherapy records in custody disputes: how can the competing interests be balanced? Behav Sci Law. 2010;28(4):522-541.
Mrs. W, age 35, presents to your clinic seeking treatment for anxiety and depression. She has no psychiatric history but reports feeling sad, overwhelmed, and stressed. Mrs. W has been married for 10 years, has 2 young children, and is currently pregnant. She recently discovered that her husband has been having an affair. Mrs. W tells you that she feels her marriage is unsalvageable and would like to ask her husband for a divorce, but worries that he will “put up a fight” and demand full custody of their children. When you ask why, she states that her husband is “pretty narcissistic” and tends to become combative when criticized or threatened, such as a recent discussion they had about his affair that ended with him concluding that if she were “sexier and more confident” he would not have cheated on her.
As Mrs. W is talking, you recall a conversation you recently overheard at a continuing medical education event. Two clinicians were discussing how their records had been subpoenaed in a child custody case, even though the patient’s mental health was not contested. You realize that Mrs. W’s situation may also fit under this exception to confidentiality or privilege. You wonder if you should have disclosed this possibility to her at the outset of your session and wonder what you should say now, because she is clearly in distress and in need of psychiatric treatment. On the other hand, you want her to be fully informed of the potential repercussions if she continues with treatment.
Confidentiality and privilege allow our patients to disclose sensitive details in a safe space. The psychiatrist’s duty is to keep the patient’s information confidential, except in limited circumstances. The patient’s privilege is their right to prevent someone in a special confidential relationship from testifying against them or releasing their private records. In certain instances, a patient may waive or be forced to waive privilege, and a psychiatrist may be compelled to testify or release treatment records to a court. This article reviews exceptions to confidentiality and privilege, focusing specifically on a little-known exception to privilege that arises in divorce and child custody cases. We discuss relevant legislation and provide recommendations for psychiatrists to better understand how to discuss these legal realities with patients who are or may go through a divorce or child custody case.
Understanding confidentiality and privilege
Confidentiality and privilege are related but distinct concepts. Confidentiality relates to the overall trusting relationship created between 2 parties, such as a physician and their patient, and the duty on the part of the trusted individual to keep information private. Privilege refers to a person’s specific legal right to prevent someone in that confidential, trusting relationship from testifying against them in court or releasing confidential records. Privilege is owned by the patient and must be asserted or waived by the patient in legal proceedings. The concepts of confidentiality and privilege are crucial in creating an open, candid therapeutic environment. Many courts, including the US Supreme Court,1 have recognized the importance of confidentiality and privilege in establishing a positive therapeutic relationship between a psychotherapist and a patient. Without confidentiality and privilege, patients would be less likely to share sensitive yet clinically important information.
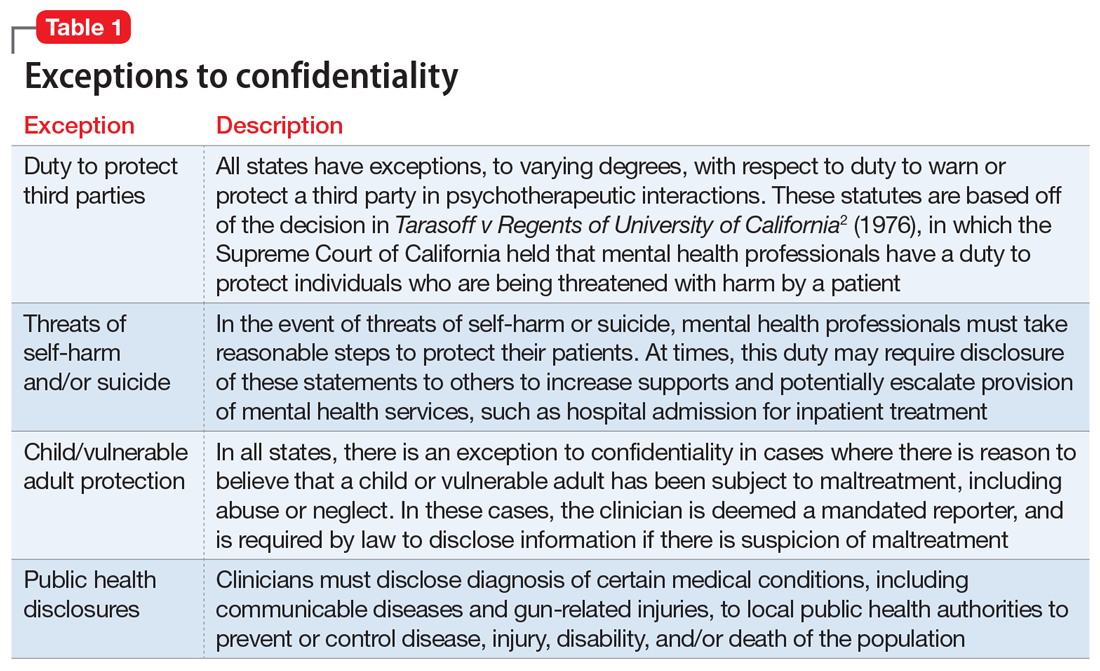
Commonly encountered exceptions to confidentiality (Table 12) and privilege (Table 2) exist in medical practice. Psychiatrists should discuss these exceptions with patients at the outset of clinical treatment. A little-known exception to privilege that may compel a psychiatrist to disclose confidential records can occur in child custody proceedings. In certain states, the mere filing of a child custody claim constitutes an exception to physician-patient privilege. In these states, the parent filing for divorce and custody may automatically waive privilege and thus compel disclosure of psychiatric records, even if their mental health is not in question. The following recent Ohio Supreme Court case illustrates this exception.
Friedenberg v Friedenberg (2020)
Friedenberg v Friedenberg3 addressed the issue of privilege and release of mental health treatment records in custody disputes. Belinda Torres Friedenberg and Keith Friedenberg were married with 4 minor children. Mrs. Friedenberg filed for divorce in 2016, requesting custody of the children and spousal support. In response, Mr. Friedenberg also filed a complaint seeking custody. Mr. Friedenberg subpoenaed mental health treatment records for Mrs. Friedenberg, who responded by filing a request to prevent the release of these records given physician-patient privilege. Mr. Friedenberg argued that Mrs. Friedenberg had placed her physical and mental health at issue when she filed for divorce and custody. At no point did Mr. Friedenberg allege that Mrs. Friedenberg’s mental health made her an unfit parent. The court agreed with Mr. Friedenberg and compelled disclosure of Mrs. Friedenberg’s psychiatric records, stating it is “hard to imagine a scenario where the mental health records of a parent would not be relevant to issues around custody and the best interests of the children.” The judge reviewed Mrs. Friedenberg’s psychiatric records privately and released records deemed relevant to the custody proceedings. On appeal, the Ohio Supreme Court agreed with this approach, holding that a parent’s mental fitness is always an issue in child custody cases, even if not asserted by either party. The court further held that unnecessary disclosure of sensitive information was prevented by the judge’s private review of records before deciding which records to release to the opposing spouse.
Waiver of physician-patient privilege
Waiver of physician-patient privilege in custody and divorce proceedings varies by state (Table 33-6). The Friedenberg decision highlights the most restrictive approach, where the mere filing of a divorce and child custody request automatically waives privilege. Some states, such as Indiana,4 follow a similar scheme to Ohio. Other states are silent on this issue or explicitly prohibit a waiver of privilege, asserting that custody disputes alone do not trigger disclosure without additional justifications, such as aberrant parental behaviors or other historical information concerning for abuse, neglect, or lack of parental fitness, or if a parent places their mental health at issue.7
Continue to: Once privilege is waived...
Once privilege is waived, the next step is to determine who should examine psychiatric records, deem relevance, and disclose sensitive information to the court and the opposing party. A judge may make this determination, as in the Friedenberg case. Alternatively, an independent psychiatric examiner may be appointed by the court to examine one or both parties; to obtain collateral information, including psychiatric records; and to submit a report to the court with medicolegal opinions regarding parental fitness. For example, in Maryland,6 the mere filing of a custody suit does not waive privilege. If a parent’s mental health is questioned, the judge may order an independent psychiatric examination to determine the parent’s fitness, thus balancing the best interests of the child with the parent’s right to physician-patient privilege.
The problem with automatic waivers
The foundation of the physician-patient relationship is trust and confidentiality. While this holds true for every specialty, perhaps it is even more important in psychiatry, where our patients routinely disclose sensitive, personal information in hopes of healing. Patients may not be aware of exceptions to confidentiality, or only be aware of the most well-known exceptions, such as the clinician’s duty to report abuse, or to warn a third party about risk of harm by a patient. Furthermore, clinicians and patients alike may not be aware of less-common exceptions to privilege, such as those that may occur in custody proceedings. This is critically important in light of the high number of patients who are or may be seeking divorce and custody of their children.
As psychiatric clinicians, it is highly likely that we will see patients going through divorce and custody proceedings. In 2018, there were 2.24 marriages for every divorce,8 and in 2014, 27% of all American children were living with a custodial parent, with the other parent living elsewhere.9 Divorce can be a profoundly stressful time; thus, it would be expected that many individuals going through divorce would seek psychiatric treatment and support.
Our concern is that the Friedenberg approach, which results in automatic disclosure of sensitive mental health information when a party files for divorce and custody, could deter patients from seeking psychiatric treatment, especially those anticipating divorce. Importantly, because women are nearly twice as likely as men to experience depression and anxiety10 and are more likely to seek treatment, this approach could disproportionately impact them.11 In general, an automatic waiver policy may create an additional obstacle for individuals who are already reticent to seek treatment.
How to handle these situations
As a psychiatrist, you should be familiar with your state’s laws regarding exceptions to patient-physician privilege, and should discuss exceptions at the outset of treatment. However, you will need to weigh the potential negative impacts of this information on the therapeutic relationship, including possible early termination. Furthermore, this information may impact a patient’s willingness to disclose all relevant information to mental health treatment if there is concern for later court disclosure. How should you balance these concerns? First, encourage patients to ask questions and raise concerns about confidentiality and privilege.12 In addition, you may direct the patient to other resources, such as a family law attorney, if they have questions about how certain information may be used in a legal proceeding.
Continue to: Second, you should be...
Second, you should be transparent regarding documentation of psychiatric visits. While documentation must meet ethical, legal, and billing requirements, you should take care to include only relevant information needed to make a diagnosis and provide indicated treatment while maintaining a neutral tone and avoiding medical jargon.13 For instance, we frequently use the term “denied” in medical documentation, as in “Mr. X denied cough, sore throat, fever or chills.” However, in psychiatric notes, if a patient “denied alcohol use,” the colloquial interpretation of this word could imply a tone of distrust toward the patient. A more sensitive way to document this might be: “When screened, reported no alcohol use.” If a patient divulges information and then asks you to omit this from their chart, but you do not feel comfortable doing so, explain what and why you must include the information in the chart.14
Third, if you receive a subpoena or other document requesting privileged information, first contact the patient and inform them of the request, and then seek legal consultation through your employer or malpractice insurer.15 Not all subpoenas are valid and enforceable, so it is important for an attorney to examine the subpoena; in addition, the patient’s attorney may choose to challenge the subpoena and limit the disclosure of privileged information.
Finally, inform legislatures and courts about the potential harm of automatic waivers in custody proceedings. A judge’s examination of the psychiatric records, as in Friedenberg, is not an adequate safeguard. A judge is not a trained mental health professional and may deem “relevant” information to be nearly everything: a history of abuse, remote drug or alcohol use, disclosure of a past crime, or financial troubles. We advocate for courts to follow the Maryland model, where a spouse does not automatically waive privilege if filing for divorce or custody. If mental health becomes an issue in a case, then the court may seek an independent psychiatric examination. The independent examiner will have access to patient records but will be in a better position to determine which details are relevant in determining diagnosis and parental fitness, and to render an opinion to the court.
CASE CONTINUED
You inform Mrs. W about a possible exception to privilege in divorce and custody cases. She decides to first talk with a family law attorney before proceeding with treatment. You defer your diagnosis and wait to see if she wants to proceed with treatment. Unfortunately, she does not return to your office.
Bottom Line
Some states limit the confidentiality and privilege of parents who are in psychiatric treatment and also involved in divorce and child custody cases. Psychiatrists should be mindful of these exceptions, and discuss them with patients at the onset of treatment.
Related Resources
- Legal Information Institute. Child custody: an overview. www.law.cornell.edu/wex/child_custody
- Melton GB, Petrila J, Poythress NG, et al. Child custody in divorce. In: Melton GB, Petrila J, Poythress NG, et al. Psychological evaluations for the courts. Guilford Press; 2018:530-533.
Mrs. W, age 35, presents to your clinic seeking treatment for anxiety and depression. She has no psychiatric history but reports feeling sad, overwhelmed, and stressed. Mrs. W has been married for 10 years, has 2 young children, and is currently pregnant. She recently discovered that her husband has been having an affair. Mrs. W tells you that she feels her marriage is unsalvageable and would like to ask her husband for a divorce, but worries that he will “put up a fight” and demand full custody of their children. When you ask why, she states that her husband is “pretty narcissistic” and tends to become combative when criticized or threatened, such as a recent discussion they had about his affair that ended with him concluding that if she were “sexier and more confident” he would not have cheated on her.
As Mrs. W is talking, you recall a conversation you recently overheard at a continuing medical education event. Two clinicians were discussing how their records had been subpoenaed in a child custody case, even though the patient’s mental health was not contested. You realize that Mrs. W’s situation may also fit under this exception to confidentiality or privilege. You wonder if you should have disclosed this possibility to her at the outset of your session and wonder what you should say now, because she is clearly in distress and in need of psychiatric treatment. On the other hand, you want her to be fully informed of the potential repercussions if she continues with treatment.
Confidentiality and privilege allow our patients to disclose sensitive details in a safe space. The psychiatrist’s duty is to keep the patient’s information confidential, except in limited circumstances. The patient’s privilege is their right to prevent someone in a special confidential relationship from testifying against them or releasing their private records. In certain instances, a patient may waive or be forced to waive privilege, and a psychiatrist may be compelled to testify or release treatment records to a court. This article reviews exceptions to confidentiality and privilege, focusing specifically on a little-known exception to privilege that arises in divorce and child custody cases. We discuss relevant legislation and provide recommendations for psychiatrists to better understand how to discuss these legal realities with patients who are or may go through a divorce or child custody case.
Understanding confidentiality and privilege
Confidentiality and privilege are related but distinct concepts. Confidentiality relates to the overall trusting relationship created between 2 parties, such as a physician and their patient, and the duty on the part of the trusted individual to keep information private. Privilege refers to a person’s specific legal right to prevent someone in that confidential, trusting relationship from testifying against them in court or releasing confidential records. Privilege is owned by the patient and must be asserted or waived by the patient in legal proceedings. The concepts of confidentiality and privilege are crucial in creating an open, candid therapeutic environment. Many courts, including the US Supreme Court,1 have recognized the importance of confidentiality and privilege in establishing a positive therapeutic relationship between a psychotherapist and a patient. Without confidentiality and privilege, patients would be less likely to share sensitive yet clinically important information.
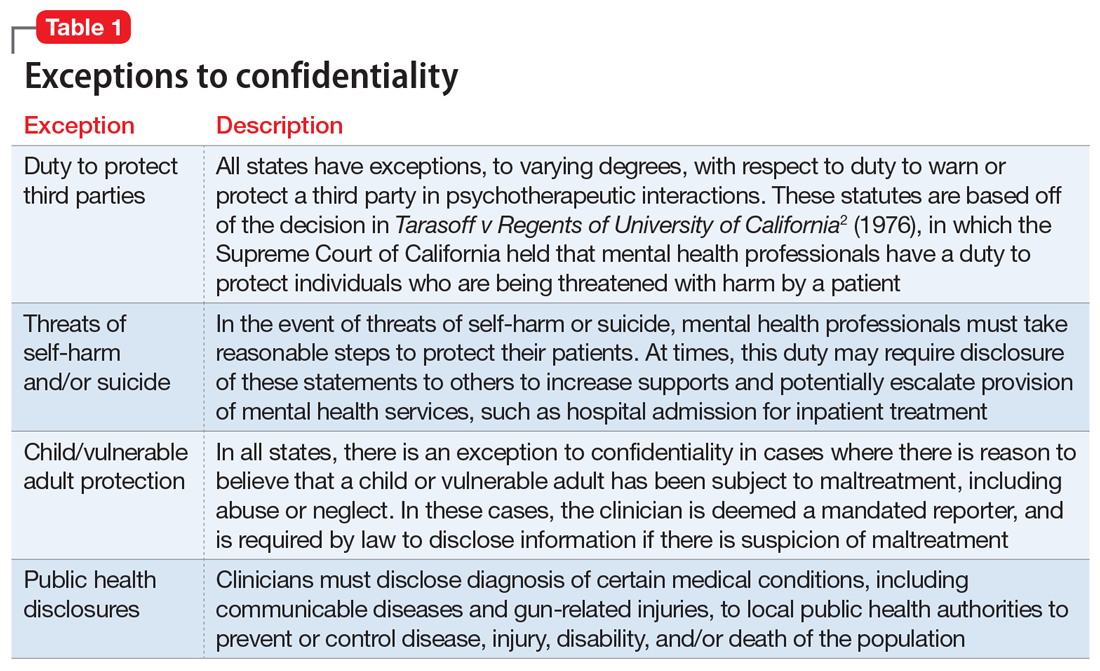
Commonly encountered exceptions to confidentiality (Table 12) and privilege (Table 2) exist in medical practice. Psychiatrists should discuss these exceptions with patients at the outset of clinical treatment. A little-known exception to privilege that may compel a psychiatrist to disclose confidential records can occur in child custody proceedings. In certain states, the mere filing of a child custody claim constitutes an exception to physician-patient privilege. In these states, the parent filing for divorce and custody may automatically waive privilege and thus compel disclosure of psychiatric records, even if their mental health is not in question. The following recent Ohio Supreme Court case illustrates this exception.
Friedenberg v Friedenberg (2020)
Friedenberg v Friedenberg3 addressed the issue of privilege and release of mental health treatment records in custody disputes. Belinda Torres Friedenberg and Keith Friedenberg were married with 4 minor children. Mrs. Friedenberg filed for divorce in 2016, requesting custody of the children and spousal support. In response, Mr. Friedenberg also filed a complaint seeking custody. Mr. Friedenberg subpoenaed mental health treatment records for Mrs. Friedenberg, who responded by filing a request to prevent the release of these records given physician-patient privilege. Mr. Friedenberg argued that Mrs. Friedenberg had placed her physical and mental health at issue when she filed for divorce and custody. At no point did Mr. Friedenberg allege that Mrs. Friedenberg’s mental health made her an unfit parent. The court agreed with Mr. Friedenberg and compelled disclosure of Mrs. Friedenberg’s psychiatric records, stating it is “hard to imagine a scenario where the mental health records of a parent would not be relevant to issues around custody and the best interests of the children.” The judge reviewed Mrs. Friedenberg’s psychiatric records privately and released records deemed relevant to the custody proceedings. On appeal, the Ohio Supreme Court agreed with this approach, holding that a parent’s mental fitness is always an issue in child custody cases, even if not asserted by either party. The court further held that unnecessary disclosure of sensitive information was prevented by the judge’s private review of records before deciding which records to release to the opposing spouse.
Waiver of physician-patient privilege
Waiver of physician-patient privilege in custody and divorce proceedings varies by state (Table 33-6). The Friedenberg decision highlights the most restrictive approach, where the mere filing of a divorce and child custody request automatically waives privilege. Some states, such as Indiana,4 follow a similar scheme to Ohio. Other states are silent on this issue or explicitly prohibit a waiver of privilege, asserting that custody disputes alone do not trigger disclosure without additional justifications, such as aberrant parental behaviors or other historical information concerning for abuse, neglect, or lack of parental fitness, or if a parent places their mental health at issue.7
Continue to: Once privilege is waived...
Once privilege is waived, the next step is to determine who should examine psychiatric records, deem relevance, and disclose sensitive information to the court and the opposing party. A judge may make this determination, as in the Friedenberg case. Alternatively, an independent psychiatric examiner may be appointed by the court to examine one or both parties; to obtain collateral information, including psychiatric records; and to submit a report to the court with medicolegal opinions regarding parental fitness. For example, in Maryland,6 the mere filing of a custody suit does not waive privilege. If a parent’s mental health is questioned, the judge may order an independent psychiatric examination to determine the parent’s fitness, thus balancing the best interests of the child with the parent’s right to physician-patient privilege.
The problem with automatic waivers
The foundation of the physician-patient relationship is trust and confidentiality. While this holds true for every specialty, perhaps it is even more important in psychiatry, where our patients routinely disclose sensitive, personal information in hopes of healing. Patients may not be aware of exceptions to confidentiality, or only be aware of the most well-known exceptions, such as the clinician’s duty to report abuse, or to warn a third party about risk of harm by a patient. Furthermore, clinicians and patients alike may not be aware of less-common exceptions to privilege, such as those that may occur in custody proceedings. This is critically important in light of the high number of patients who are or may be seeking divorce and custody of their children.
As psychiatric clinicians, it is highly likely that we will see patients going through divorce and custody proceedings. In 2018, there were 2.24 marriages for every divorce,8 and in 2014, 27% of all American children were living with a custodial parent, with the other parent living elsewhere.9 Divorce can be a profoundly stressful time; thus, it would be expected that many individuals going through divorce would seek psychiatric treatment and support.
Our concern is that the Friedenberg approach, which results in automatic disclosure of sensitive mental health information when a party files for divorce and custody, could deter patients from seeking psychiatric treatment, especially those anticipating divorce. Importantly, because women are nearly twice as likely as men to experience depression and anxiety10 and are more likely to seek treatment, this approach could disproportionately impact them.11 In general, an automatic waiver policy may create an additional obstacle for individuals who are already reticent to seek treatment.
How to handle these situations
As a psychiatrist, you should be familiar with your state’s laws regarding exceptions to patient-physician privilege, and should discuss exceptions at the outset of treatment. However, you will need to weigh the potential negative impacts of this information on the therapeutic relationship, including possible early termination. Furthermore, this information may impact a patient’s willingness to disclose all relevant information to mental health treatment if there is concern for later court disclosure. How should you balance these concerns? First, encourage patients to ask questions and raise concerns about confidentiality and privilege.12 In addition, you may direct the patient to other resources, such as a family law attorney, if they have questions about how certain information may be used in a legal proceeding.
Continue to: Second, you should be...
Second, you should be transparent regarding documentation of psychiatric visits. While documentation must meet ethical, legal, and billing requirements, you should take care to include only relevant information needed to make a diagnosis and provide indicated treatment while maintaining a neutral tone and avoiding medical jargon.13 For instance, we frequently use the term “denied” in medical documentation, as in “Mr. X denied cough, sore throat, fever or chills.” However, in psychiatric notes, if a patient “denied alcohol use,” the colloquial interpretation of this word could imply a tone of distrust toward the patient. A more sensitive way to document this might be: “When screened, reported no alcohol use.” If a patient divulges information and then asks you to omit this from their chart, but you do not feel comfortable doing so, explain what and why you must include the information in the chart.14
Third, if you receive a subpoena or other document requesting privileged information, first contact the patient and inform them of the request, and then seek legal consultation through your employer or malpractice insurer.15 Not all subpoenas are valid and enforceable, so it is important for an attorney to examine the subpoena; in addition, the patient’s attorney may choose to challenge the subpoena and limit the disclosure of privileged information.
Finally, inform legislatures and courts about the potential harm of automatic waivers in custody proceedings. A judge’s examination of the psychiatric records, as in Friedenberg, is not an adequate safeguard. A judge is not a trained mental health professional and may deem “relevant” information to be nearly everything: a history of abuse, remote drug or alcohol use, disclosure of a past crime, or financial troubles. We advocate for courts to follow the Maryland model, where a spouse does not automatically waive privilege if filing for divorce or custody. If mental health becomes an issue in a case, then the court may seek an independent psychiatric examination. The independent examiner will have access to patient records but will be in a better position to determine which details are relevant in determining diagnosis and parental fitness, and to render an opinion to the court.
CASE CONTINUED
You inform Mrs. W about a possible exception to privilege in divorce and custody cases. She decides to first talk with a family law attorney before proceeding with treatment. You defer your diagnosis and wait to see if she wants to proceed with treatment. Unfortunately, she does not return to your office.
Bottom Line
Some states limit the confidentiality and privilege of parents who are in psychiatric treatment and also involved in divorce and child custody cases. Psychiatrists should be mindful of these exceptions, and discuss them with patients at the onset of treatment.
Related Resources
- Legal Information Institute. Child custody: an overview. www.law.cornell.edu/wex/child_custody
- Melton GB, Petrila J, Poythress NG, et al. Child custody in divorce. In: Melton GB, Petrila J, Poythress NG, et al. Psychological evaluations for the courts. Guilford Press; 2018:530-533.
1. Jaffee v Redmond, 518 US 1 (1996).
2. Tarasoff v Regents of the University of California, 118 Cal Rptr 129 (Cal 1974); modified by Tarasoff v Regents of the Univ. of Cal., 551 P.2d 334 (Cal 1976).
3. Friedenberg v Friedenberg, No. 2019-0416 (Ohio 2020).
4. Owen v Owen, 563 NE 2d 605 (Ind 1991).
5. People ex. Rel. Hickox v Hickox, 410 NY S 2d 81 (NY App Div 1978).
6. Laznovsky v Laznovsky, 745 A 2d 1054 (Md 2000).
7. Eykel I, Miskel E. The mental health privilege in divorce and custody cases. Journal of the American Academy of Matrimonial Lawyers. 2012;25(2):453-476.
8. Center for Disease Control and Prevention. FastStats: Family life. Marriage and divorce. Published May 2020. Accessed July 29, 2021. www.cdc.gov/nchs/fastats/marriage-divorce.htm
9. The United States Census Bureau. Current population reports: custodial mothers and fathers and their child support: 2013. Published January 2016. Accessed July 29, 2021. https://www.census.gov/content/dam/Census/library/publications/2016/demo/P60-255.pdf
10. World Health Organization. Gender and mental health. Published June 2002. Accessed August 2, 2021. https://www.who.int/gender/other_health/genderMH.pdf
11. Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):629-640.
12. Younggren J, Harris E. Can you keep a secret? Confidentiality in psychotherapy. J Clin Psychol. 2008;64(5):589-600.
13. The Committee on Psychiatry and Law. Confidentiality and privilege communication in the practice of psychiatry. Report no. 45. Group for the Advancement of Psychiatry; 1960.
14. Wiger D. Ethical considerations in documentation. In: Wiger D. The psychotherapy documentation primer. 3rd ed. Wiley; 2013:35-45.
15. Stansbury CD. Accessibility to a parent’s psychotherapy records in custody disputes: how can the competing interests be balanced? Behav Sci Law. 2010;28(4):522-541.
1. Jaffee v Redmond, 518 US 1 (1996).
2. Tarasoff v Regents of the University of California, 118 Cal Rptr 129 (Cal 1974); modified by Tarasoff v Regents of the Univ. of Cal., 551 P.2d 334 (Cal 1976).
3. Friedenberg v Friedenberg, No. 2019-0416 (Ohio 2020).
4. Owen v Owen, 563 NE 2d 605 (Ind 1991).
5. People ex. Rel. Hickox v Hickox, 410 NY S 2d 81 (NY App Div 1978).
6. Laznovsky v Laznovsky, 745 A 2d 1054 (Md 2000).
7. Eykel I, Miskel E. The mental health privilege in divorce and custody cases. Journal of the American Academy of Matrimonial Lawyers. 2012;25(2):453-476.
8. Center for Disease Control and Prevention. FastStats: Family life. Marriage and divorce. Published May 2020. Accessed July 29, 2021. www.cdc.gov/nchs/fastats/marriage-divorce.htm
9. The United States Census Bureau. Current population reports: custodial mothers and fathers and their child support: 2013. Published January 2016. Accessed July 29, 2021. https://www.census.gov/content/dam/Census/library/publications/2016/demo/P60-255.pdf
10. World Health Organization. Gender and mental health. Published June 2002. Accessed August 2, 2021. https://www.who.int/gender/other_health/genderMH.pdf
11. Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):629-640.
12. Younggren J, Harris E. Can you keep a secret? Confidentiality in psychotherapy. J Clin Psychol. 2008;64(5):589-600.
13. The Committee on Psychiatry and Law. Confidentiality and privilege communication in the practice of psychiatry. Report no. 45. Group for the Advancement of Psychiatry; 1960.
14. Wiger D. Ethical considerations in documentation. In: Wiger D. The psychotherapy documentation primer. 3rd ed. Wiley; 2013:35-45.
15. Stansbury CD. Accessibility to a parent’s psychotherapy records in custody disputes: how can the competing interests be balanced? Behav Sci Law. 2010;28(4):522-541.
Avoiding malpractice while treating depression in pregnant women
Many physicians have seen advertisements that encourage women who took an antidepressant while they were pregnant and had a negative outcome to contact a law firm. These ads could make patients more reluctant to take prescribed antidepressants, and psychiatrists more hesitant to prescribe necessary medications during pregnancy—which is a disservice to the mother and child.
More recently, several headline-grabbing studies appeared to suggest that there is an increased risk to infants who are exposed to antidepressants prenatally. Unfortunately, many patients do not understand that replication of these studies is often lacking, and methodological and confounding issues abound. All of this makes it difficult for patients and their families to know if they should take an antidepressant during pregnancy, and for psychiatrists to know what to discuss about the risks and benefits of various antidepressants during pregnancy. This article reviews the rationale for treatment of depression in pregnancy; the risks of untreated depression in pregnancy, as well as the potential risks of medication; ethical issues in the treatment of depression in pregnancy; the limitations of available research; and best approaches for practice.
Risks of untreated depression in pregnancy
Pregnant women may have misconceptions about treatment during pregnancy, and psychiatrists often are hesitant to treat pregnant women. However, the risks of untreated depression during pregnancy are even greater than the risks of untreated depression at other points in a woman’s life. In addition to general psychiatric risks seen in depression, pregnant women may experience other issues, such as preeclampsia and liver metabolism changes.1-2 Risks to the fetus related to untreated or partially treated mental health concerns include poor prenatal care related to poor self-care, an increased risk of exposure to illicit substances or alcohol related to “self-medication,” preterm delivery, and low birthweight (Table 13-8). Further risks for an infant of a mother with untreated depression include decreased cognitive performance and poor bonding with poor stress adaptation.5,6 Thus, appropriate treatment of depression is even more important during pregnancy than at other times of life.
Potential risks of treating depression in pregnancy
When prescribing psychotropic medications to a pregnant woman, there are several naturally occurring adverse outcomes to consider. For example, miscarriages, stillbirths, and congenital malformations can occur without explanation in the general population. In addition, also consider the specific health history of the mother and the available research literature regarding the specific psychotropic agent (keeping in mind that there are ethical issues associated with conducting prospective research in pregnant women, such as it being unethical to withhold treatment to pregnant women who are depressed in order to have a control group, and that retrospective research is often confounded by recall bias). Potential risks to be aware of include miscarriage (spontaneous abortion), malformation (teratogenesis, birth defects), preterm delivery, neonatal adaptation syndrome, and behavioral teratogenesis (Table 13-8).
Selective serotonin reuptake inhibitors (SSRIs), the usual medication treatment of choice for depression, have at times been implicated in adverse pregnancy outcomes, but no strong evidence suggests they increase the miscarriage rate. Overall data are reassuring regarding the risk of malformation associated with SSRI use. Of note, the FDA had switched paroxetine from a Class C drug to a Class D drug after early reports of a potential 1.5% to 2% risk of fetal cardiac malformations compared with a 1% baseline risk in the general population (these FDA pregnancy risk letter categories have since been phased out).9,10 Nevertheless, the absolute risk remains small. Another large study found that there was no substantial increased risk of cardiac malformations attributable to antidepressant use during the first trimester.11
Lessons from a class action suit
Since we last reviewed pregnancy and antidepressants in 2013,8 several class action lawsuits against the manufacturers of psychotropic medications have been heard. Product liability actions brought against manufacturers are different from medical malpractice suits brought against individual physicians, which may result from lack of informed consent, suicide, or homicide.
One of the largest class action suits was against Zoloft (specifically Zoloft and Pfizer, since the brand manufacturer is responsible for the product insert information.)12,13 At the time, sertraline was already commonly prescribed due to the relatively safe reproductive profile.
Continue to: Many of the more than 300...
Many of the more than 300 federal claims were united in a multi-district litigation (MDL) suit under the United States District Court of Eastern Pennsylvania (MDL 2342). Pfizer issued Daubert challenges (efforts to exclude the introduction of “junk science” into the courtroom) against the plaintiffs’ experts’ scientific methods and results.12,13 The plaintiffs (those suing Pfizer) had to prove that the medications caused the negative outcome, not that they were merely temporally associated. Subsequently, 2 plaintiff experts—a PharmD and a biostatistician—were removed. Pfizer successfully challenged the methodological soundness of the plaintiffs’ experts’ testimony (Table 212,13), and the case was dismissed. In general, the courts identified the Bradford Hill criteria as often being important (though not definitive) methodology for determining causation (Table 312,13).
A concept raised in prior psychotropic lawsuits was the “learned intermediary doctrine,” in which pharmaceutical companies stated that once a risk is known, it is the responsibility of the prescribing physician to assess risks vs benefits and inform the patient.8 Many aspects of the larger class action lawsuits related to failure of the company to do adequate research to identify risks and appropriately inform the public and the medical community of these risks.14
Challenges in interpreting the literature
Some of the difficulties in interpreting the literature on the association of antidepressants and birth defects can be seen in a 2020 study by Anderson et al.15 This study was published in JAMA Psychiatry, received widespread coverage in the media, and was discussed on the CDC’s website.16 Anderson et al15 compared a large cohort of 30,630 infants with birth defects from the multicenter case-control National Birth Defects Prevention Study with 11,478 randomly selected controls with no defects. Three primary study groups were women whose pregnancies resulted in:
- birth defects with no antidepressant exposure (n = 28,719)
- birth defects with exposure to an antidepressant (n = 1,911)
- no birth defect control group (n = 10,886 no antidepressant exposure, n = 592 antidepressant exposure).
This study reported there were “some associations between maternal antidepressant use and specific birth defects” and “Venlafaxine was associated with more birth defects than other antidepressants, which needs confirmation.”15 However, in an accompanying editorial, Wisner et al17 discussed potential problems and limitations with this study and research of this nature in general (Table 417). In addition, Anderson et al15 used certain “controversial” statistical practices.18 For example, “[T]o align with American Statistical Association guidelines to consider effect sizes when interpreting results instead of statistical significance, we noted associations as meaningfully elevated if [adjusted odds ratios] were 2.0 or greater and lower confidence interval bounds were 0.8 or greater.”15
Those who read only abstracts or news stories may believe this study of >40,000 participants included a large number of women who were receiving venlafaxine. However, the number of pregnant women who were prescribed venlafaxine was actually very small—112 who took venlafaxine experienced a birth defect. In addition, the authors noted “Venlafaxine was associated with many of the same defects across the samples (data not shown).”15 As discussed above, historically one of the areas the courts have considered was whether or not appropriate methodology was applied, and whether the results could be replicated with the data provided.
Continue to: Further, new studies...
Further, new studies need to be considered in context of the literature as a whole and collective clinical experience. A recent systematic review found that among 3,186 infants exposed to venlafaxine during the first trimester, there were 107 major malformations.19 This indicated a relative risk estimate of 1.12, with a 95% CI of 0.92 to 1.35. The authors concluded that venlafaxine exposure in the first trimester was not associated with an increased risk of malformations.
Expectant parents may come across a headline that implies a specific antidepressant causes problems, but have not read the study or know how to interpret it. Often it is best for a physician to find out what the basis of the concern is, and if possible, review the study with the patient to make sure it is in the right context, and if it applies to the individual patient’s situation.
Consider the ethical issues
In addition to preventive ethics, other critical ethical issues in pregnancy include omission bias, beneficence, and autonomy.4,20-24 Omission bias occurs when physicians are more concerned about acts of commission (in which treatment leads to a negative outcome) than they are about acts of omission, which involve not treating the patient’s illness. To address this, it is important to discuss with the patient both the risks of treating and the risks of not treating maternal depression, so that the mother can make the best decision for her own specific set of circumstances.
Regarding beneficence (promoting the patient’s best interest), consider both the mother’s and the infant’s best interest, which usually are quite closely related. Women may feel guilty about taking a medication that they perceive is harmful for the fetus but good for their own mental health. Physicians can help with this by providing education about the benefits of treating depression for the fetus’ benefit as well. The fetus is completely dependent on the environment that the mother places them in, not merely the medication effects (eg, psychologic/physiologic stress effects, poor diet, lack of exercise, risk of “self-medication”).
Regarding autonomy (a woman’s own decision-making), Coverdale et al21 discussed strategies that can enhance a pregnant patient’s autonomy—including discussing treatment options and counselling about the effects of depression itself in pregnancy, as well as considering the effects of depression on the process of decision-making. For example, a woman with depression may see the world through a negative lens or may have difficulty concentrating. Patients may also require education about the concept of relative risk in comparison to absolute risk—especially in light of attention-grabbing headlines.
Continue to: Finally, as part of...
Finally, as part of preventative ethics, anticipate the ethical dilemmas before the common situation of pregnancy. Almost one-half of pregnancies are unplanned.25 Many women thus expose their fetus to medication during the critical early period of organogenesis, before noticing they were pregnant. Therefore, even if a patient of childbearing age insists that she is not sexually active, the prudent psychiatrist should still begin discussions about medications in pregnancy.
An outline of best practices
Best practice includes preventive ethics, and when treating any woman of childbearing age, psychiatrists should consider prescribing medications that are known to be relatively safe in pregnancy rather than risky in pregnancy. Therefore, any psychiatrist whose practice includes women of childbearing age should have a working knowledge of which agents are relatively safe in pregnancy. After a woman is pregnant, careful decision-making about medication should continue. Consult with reproductive psychiatry colleagues where necessary.
A patient with depression would usually merit closer follow-up during the pregnancy. In some cases, psychotherapy alone can be effective in depression. However, approximately 6% to 13% of women are prescribed antidepressants during pregnancy, and this has been increasing.26 Women who discontinue their antidepressant while pregnant are more likely to relapse than those who continue their medication,27 thus exposing their fetus to negative effects of depression as well as medication (prior to discontinuation).
When possible, monotherapy (one agent) in the lowest effective dose is often the judicious approach to treatment. For a patient prescribed pre-existing polypharmacy at time of pregnancy, a risk-benefit analysis of which medications should remain, which should be stopped, and a plan for taper, if needed, should be discussed and documented. Using too little of an antidepressant dose would expose the fetus to both depression and medication, whereas using a maximum dose when not needed would expose the fetus to more medication than is necessary to treat the mother’s symptoms. This discussion with the mother (and her partner, if available) should be documented in the chart. The mother should understand both the risk of untreated illness and the potential risks of medications, as well as the benefits of medications and alternatives. It is important for the mother to realize that there is no risk-free option, and that malformations can occur in the general population as well as in individuals with untreated depression, separate from any medication exposure. In fact, most malformations do not have a known cause, and overall approximately 3% of pregnancies result in a birth defect.28
If possible, discuss the treatment plan with the patient’s obstetrician, or ask the mother to discuss the plan with her obstetrician, so that everyone is on the same page. This discussion can help attenuate patient anxiety that results from hearing different things from different clinicians. Communication with other treating professionals (eg, OB/GYNs, pediatricians) can be beneficial and reduce liability if multiple physicians have agreed on a treatment plan—even if there is a negative outcome. With malpractice, a clinician is not necessarily at fault for a bad outcome or adverse effect, but is at fault for lack of informed consent or negligence (deviation from standard of care), which is harder for an attorney to demonstrate if there is deliberation, communication, and a plan that multiple doctors agree upon.
Continue to: Be aware that informed consent...
Be aware that informed consent is an ongoing process, and a woman may need to be reminded or informed of potential risks at varying stages of her life (eg, when starting a new relationship, getting married, etc.). Documentation can include that the clinician has discussed the risks, benefits, adverse effects, and alternatives of various medications, and a description of any patient-specific or medication-specific issues. In addition to verbal discussions, giving patients printed information can be helpful, as can directing them to appropriate websites (see Related Resources). Some physicians require patients to sign a form to indicate that they are aware of known risks.
Similar to being proactive before your patient becomes pregnant, think proactively regarding the postpartum period. Is your patient planning to breastfeed? Is the medication compatible with breastfeeding, or is bottle feeding the best option considering the mother’s specific circumstances? For example, developing severe symptoms, experiencing insomnia, needing to take a contraindicated medication, or having a vulnerable infant might sway a mother towards not breastfeeding. The expectant mother (and her partner, where possible) should be educated about postpartum risks and the importance of sleep in preventing postpartum depression.
Bottom Line
Concerns about being sued should not prevent appropriate care of depression in a woman who is pregnant. Discuss with your patient both the risk of untreated mental illness and the risk of medications to ensure she understands that avoiding antidepressants does not guarantee a safe or healthy pregnancy.
Related Resources
- MotherToBaby. www.mothertobaby.org/
- Centers for Disease Control and Prevention. Treating for two: medicine and pregnancy. www.cdc.gov/pregnancy/meds/treatingfortwo/index.html
- MGH Center for Women’s Mental Health. Reproductive psychiatry resource and information center. www.womensmentalhealth.org/
Drug Brand Names
Paroxetine • Paxil
Sertraline • Zoloft
Venlafaxine • Effexor
1. Palmsten K, Setoguchi S, Margulis AV, et al. Elevated risk of preeclampsia in pregnant women with depression: depression or antidepressants? Am J Epidemiol. 2012;175(10):988-997.
2. Sit DK, Perel JM, Helsel JC, et al. Changes in antidepressant metabolism and dosing across pregnancy and early postpartum. J Clin Psychiatry. 2008;69(4):652-658.
3. Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012-1024.
4. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
5. Friedman SH, Resnick PJ. Postpartum depression: an update. Women’s Health. 2009;5(3):287-295.
6. Liu Y, Kaaya S, Chai J, et al. Maternal depressive symptoms and early childhood cognitive development: a meta-analysis. Psychol Med. 2017;47(4):680-689.
7. Wisner KL, Sit DK, Hanusa BH, et al. Major depression and antidepressant treatment: impact on pregnancy and neonatal outcomes. Am J Psychiatry. 2009; 166(5):557-566.
8. Friedman SH, Hall RCW. Antidepressant use during pregnancy: How to avoid clinical and legal pitfalls. Current Psychiatry. 2013;12(2):21-25.
9. Bar-Oz B, Einarson T, Einarson A, et al. Paroxetine and congenital malformations: meta-analysis and consideration of potential confounding factors. Clin Ther. 2007;29(5):918-926.
10. Einarson A, Pistelli A, DeSantis M, et al. Evaluation of the risk of congenital cardiovascular defects associated with use of paroxetine during pregnancy. Am J Psychiatry. 2008;165(6):749-752.
11. Huybrechts KF, Palmsten K, Avorn J, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370(25):2397-2407.
12. In re: Zoloft (sertraline hydrochloride) products liability litigation. MDL No. 2342. No. 12-md-2342. United States District Court, E.D. Pennsylvania. June 27, 2014.
13. In re: Zoloft (sertraline hydrocloride) products liability litigation. MDL No. 2342. United States District Court, E.D. Pennsylvania. December 2, 2015.
14. Kirsch N, Pacheco LD, Hossain A, et al. Medicolegal review: perinatal Effexor lawsuits and legal strategies adverse to prescribing obstetric providers. AJP Rep. 2019;9(1):e88-e91.
15. Anderson KN, Lind JN, Simeone RM, et al. Maternal use of specific antidepressant medications during early pregnancy and the risk of selected birth defects. JAMA Psychiatry. 2020;77(12):1246-1255.
16. Centers for Disease Control and Prevention. Use of the antidepressant venlafaxine during early pregnancy may be linked to specific birth defects. Published October 28, 2020. Accessed October 29, 2020. https://www.cdc.gov/ncbddd/birthdefects/features/venlafaxine-during-pregnancy.html
17. Wisner KL, Oberlander TF, Huybrechts KF. The association between antidepressant exposure and birth defects--are we there yet? JAMA Psychiatry. 2020;77(12):1215-1216.
18. Wasserstein RL, Lazar NA. The ASA statement on p-values: context, process, and purpose. American Statistician. 2016;70(2):129-133.
19. Lassen D, Ennis ZN, Damkier P. First-trimester pregnancy exposure to venlafaxine or duloxetine and risk of major congenital malformations: a systematic review. Basic Clin Pharmacol Toxicol. 2016;118(1):32-36.
20. Miller LJ. Ethical issues in perinatal mental health. Psychiatr Clin North Am. 2009;32(2):259-270.
21. Coverdale JH, McCullough JB, Chervenak FA. Enhancing decision-making by depressed pregnant patients. J Perinat Med. 2002;30(4):349-351.
22. Coverdale JH, McCullough LB, Chervenak FA, et al. Clinical implications of respect for autonomy in the psychiatric treatment of pregnant patients with depression. Psychiatr Serv. 1997;48:209-212.
23. Coverdale JH, Chervenak FA, McCullough LB, et al. Ethically justified clinically comprehensive guidelines for the management of the depressed pregnant patient. Am J Obstet Gynecol. 1996;174(1):169-173.
24. Wisner KL, Zarin DA, Holmboe ES, et al. Risk-benefit decision making for treatment of depression during pregnancy. Am J Psychiatry. 2000;157(12):1933-1940.
25. Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84(5):478-485.
26. Cooper WO, Willy ME, Pont SJ, et al. Increasing use of antidepressants in pregnancy. Am J Obstet Gynecol. 2007;196(6):544.e1-5.
27. Cohen LS, Altshuler LL, Harlow BL, et al. Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. JAMA. 2006;295(5):499-507.
28. Centers for Disease Control and Prevention. Update on overall prevalence of major birth defects--Atlanta, Georgia, 1978-2005. MMWR Morb Mortal Wkly Rep. 2008;57(1):1-5.
Many physicians have seen advertisements that encourage women who took an antidepressant while they were pregnant and had a negative outcome to contact a law firm. These ads could make patients more reluctant to take prescribed antidepressants, and psychiatrists more hesitant to prescribe necessary medications during pregnancy—which is a disservice to the mother and child.
More recently, several headline-grabbing studies appeared to suggest that there is an increased risk to infants who are exposed to antidepressants prenatally. Unfortunately, many patients do not understand that replication of these studies is often lacking, and methodological and confounding issues abound. All of this makes it difficult for patients and their families to know if they should take an antidepressant during pregnancy, and for psychiatrists to know what to discuss about the risks and benefits of various antidepressants during pregnancy. This article reviews the rationale for treatment of depression in pregnancy; the risks of untreated depression in pregnancy, as well as the potential risks of medication; ethical issues in the treatment of depression in pregnancy; the limitations of available research; and best approaches for practice.
Risks of untreated depression in pregnancy
Pregnant women may have misconceptions about treatment during pregnancy, and psychiatrists often are hesitant to treat pregnant women. However, the risks of untreated depression during pregnancy are even greater than the risks of untreated depression at other points in a woman’s life. In addition to general psychiatric risks seen in depression, pregnant women may experience other issues, such as preeclampsia and liver metabolism changes.1-2 Risks to the fetus related to untreated or partially treated mental health concerns include poor prenatal care related to poor self-care, an increased risk of exposure to illicit substances or alcohol related to “self-medication,” preterm delivery, and low birthweight (Table 13-8). Further risks for an infant of a mother with untreated depression include decreased cognitive performance and poor bonding with poor stress adaptation.5,6 Thus, appropriate treatment of depression is even more important during pregnancy than at other times of life.
Potential risks of treating depression in pregnancy
When prescribing psychotropic medications to a pregnant woman, there are several naturally occurring adverse outcomes to consider. For example, miscarriages, stillbirths, and congenital malformations can occur without explanation in the general population. In addition, also consider the specific health history of the mother and the available research literature regarding the specific psychotropic agent (keeping in mind that there are ethical issues associated with conducting prospective research in pregnant women, such as it being unethical to withhold treatment to pregnant women who are depressed in order to have a control group, and that retrospective research is often confounded by recall bias). Potential risks to be aware of include miscarriage (spontaneous abortion), malformation (teratogenesis, birth defects), preterm delivery, neonatal adaptation syndrome, and behavioral teratogenesis (Table 13-8).
Selective serotonin reuptake inhibitors (SSRIs), the usual medication treatment of choice for depression, have at times been implicated in adverse pregnancy outcomes, but no strong evidence suggests they increase the miscarriage rate. Overall data are reassuring regarding the risk of malformation associated with SSRI use. Of note, the FDA had switched paroxetine from a Class C drug to a Class D drug after early reports of a potential 1.5% to 2% risk of fetal cardiac malformations compared with a 1% baseline risk in the general population (these FDA pregnancy risk letter categories have since been phased out).9,10 Nevertheless, the absolute risk remains small. Another large study found that there was no substantial increased risk of cardiac malformations attributable to antidepressant use during the first trimester.11
Lessons from a class action suit
Since we last reviewed pregnancy and antidepressants in 2013,8 several class action lawsuits against the manufacturers of psychotropic medications have been heard. Product liability actions brought against manufacturers are different from medical malpractice suits brought against individual physicians, which may result from lack of informed consent, suicide, or homicide.
One of the largest class action suits was against Zoloft (specifically Zoloft and Pfizer, since the brand manufacturer is responsible for the product insert information.)12,13 At the time, sertraline was already commonly prescribed due to the relatively safe reproductive profile.
Continue to: Many of the more than 300...
Many of the more than 300 federal claims were united in a multi-district litigation (MDL) suit under the United States District Court of Eastern Pennsylvania (MDL 2342). Pfizer issued Daubert challenges (efforts to exclude the introduction of “junk science” into the courtroom) against the plaintiffs’ experts’ scientific methods and results.12,13 The plaintiffs (those suing Pfizer) had to prove that the medications caused the negative outcome, not that they were merely temporally associated. Subsequently, 2 plaintiff experts—a PharmD and a biostatistician—were removed. Pfizer successfully challenged the methodological soundness of the plaintiffs’ experts’ testimony (Table 212,13), and the case was dismissed. In general, the courts identified the Bradford Hill criteria as often being important (though not definitive) methodology for determining causation (Table 312,13).
A concept raised in prior psychotropic lawsuits was the “learned intermediary doctrine,” in which pharmaceutical companies stated that once a risk is known, it is the responsibility of the prescribing physician to assess risks vs benefits and inform the patient.8 Many aspects of the larger class action lawsuits related to failure of the company to do adequate research to identify risks and appropriately inform the public and the medical community of these risks.14
Challenges in interpreting the literature
Some of the difficulties in interpreting the literature on the association of antidepressants and birth defects can be seen in a 2020 study by Anderson et al.15 This study was published in JAMA Psychiatry, received widespread coverage in the media, and was discussed on the CDC’s website.16 Anderson et al15 compared a large cohort of 30,630 infants with birth defects from the multicenter case-control National Birth Defects Prevention Study with 11,478 randomly selected controls with no defects. Three primary study groups were women whose pregnancies resulted in:
- birth defects with no antidepressant exposure (n = 28,719)
- birth defects with exposure to an antidepressant (n = 1,911)
- no birth defect control group (n = 10,886 no antidepressant exposure, n = 592 antidepressant exposure).
This study reported there were “some associations between maternal antidepressant use and specific birth defects” and “Venlafaxine was associated with more birth defects than other antidepressants, which needs confirmation.”15 However, in an accompanying editorial, Wisner et al17 discussed potential problems and limitations with this study and research of this nature in general (Table 417). In addition, Anderson et al15 used certain “controversial” statistical practices.18 For example, “[T]o align with American Statistical Association guidelines to consider effect sizes when interpreting results instead of statistical significance, we noted associations as meaningfully elevated if [adjusted odds ratios] were 2.0 or greater and lower confidence interval bounds were 0.8 or greater.”15
Those who read only abstracts or news stories may believe this study of >40,000 participants included a large number of women who were receiving venlafaxine. However, the number of pregnant women who were prescribed venlafaxine was actually very small—112 who took venlafaxine experienced a birth defect. In addition, the authors noted “Venlafaxine was associated with many of the same defects across the samples (data not shown).”15 As discussed above, historically one of the areas the courts have considered was whether or not appropriate methodology was applied, and whether the results could be replicated with the data provided.
Continue to: Further, new studies...
Further, new studies need to be considered in context of the literature as a whole and collective clinical experience. A recent systematic review found that among 3,186 infants exposed to venlafaxine during the first trimester, there were 107 major malformations.19 This indicated a relative risk estimate of 1.12, with a 95% CI of 0.92 to 1.35. The authors concluded that venlafaxine exposure in the first trimester was not associated with an increased risk of malformations.
Expectant parents may come across a headline that implies a specific antidepressant causes problems, but have not read the study or know how to interpret it. Often it is best for a physician to find out what the basis of the concern is, and if possible, review the study with the patient to make sure it is in the right context, and if it applies to the individual patient’s situation.
Consider the ethical issues
In addition to preventive ethics, other critical ethical issues in pregnancy include omission bias, beneficence, and autonomy.4,20-24 Omission bias occurs when physicians are more concerned about acts of commission (in which treatment leads to a negative outcome) than they are about acts of omission, which involve not treating the patient’s illness. To address this, it is important to discuss with the patient both the risks of treating and the risks of not treating maternal depression, so that the mother can make the best decision for her own specific set of circumstances.
Regarding beneficence (promoting the patient’s best interest), consider both the mother’s and the infant’s best interest, which usually are quite closely related. Women may feel guilty about taking a medication that they perceive is harmful for the fetus but good for their own mental health. Physicians can help with this by providing education about the benefits of treating depression for the fetus’ benefit as well. The fetus is completely dependent on the environment that the mother places them in, not merely the medication effects (eg, psychologic/physiologic stress effects, poor diet, lack of exercise, risk of “self-medication”).
Regarding autonomy (a woman’s own decision-making), Coverdale et al21 discussed strategies that can enhance a pregnant patient’s autonomy—including discussing treatment options and counselling about the effects of depression itself in pregnancy, as well as considering the effects of depression on the process of decision-making. For example, a woman with depression may see the world through a negative lens or may have difficulty concentrating. Patients may also require education about the concept of relative risk in comparison to absolute risk—especially in light of attention-grabbing headlines.
Continue to: Finally, as part of...
Finally, as part of preventative ethics, anticipate the ethical dilemmas before the common situation of pregnancy. Almost one-half of pregnancies are unplanned.25 Many women thus expose their fetus to medication during the critical early period of organogenesis, before noticing they were pregnant. Therefore, even if a patient of childbearing age insists that she is not sexually active, the prudent psychiatrist should still begin discussions about medications in pregnancy.
An outline of best practices
Best practice includes preventive ethics, and when treating any woman of childbearing age, psychiatrists should consider prescribing medications that are known to be relatively safe in pregnancy rather than risky in pregnancy. Therefore, any psychiatrist whose practice includes women of childbearing age should have a working knowledge of which agents are relatively safe in pregnancy. After a woman is pregnant, careful decision-making about medication should continue. Consult with reproductive psychiatry colleagues where necessary.
A patient with depression would usually merit closer follow-up during the pregnancy. In some cases, psychotherapy alone can be effective in depression. However, approximately 6% to 13% of women are prescribed antidepressants during pregnancy, and this has been increasing.26 Women who discontinue their antidepressant while pregnant are more likely to relapse than those who continue their medication,27 thus exposing their fetus to negative effects of depression as well as medication (prior to discontinuation).
When possible, monotherapy (one agent) in the lowest effective dose is often the judicious approach to treatment. For a patient prescribed pre-existing polypharmacy at time of pregnancy, a risk-benefit analysis of which medications should remain, which should be stopped, and a plan for taper, if needed, should be discussed and documented. Using too little of an antidepressant dose would expose the fetus to both depression and medication, whereas using a maximum dose when not needed would expose the fetus to more medication than is necessary to treat the mother’s symptoms. This discussion with the mother (and her partner, if available) should be documented in the chart. The mother should understand both the risk of untreated illness and the potential risks of medications, as well as the benefits of medications and alternatives. It is important for the mother to realize that there is no risk-free option, and that malformations can occur in the general population as well as in individuals with untreated depression, separate from any medication exposure. In fact, most malformations do not have a known cause, and overall approximately 3% of pregnancies result in a birth defect.28
If possible, discuss the treatment plan with the patient’s obstetrician, or ask the mother to discuss the plan with her obstetrician, so that everyone is on the same page. This discussion can help attenuate patient anxiety that results from hearing different things from different clinicians. Communication with other treating professionals (eg, OB/GYNs, pediatricians) can be beneficial and reduce liability if multiple physicians have agreed on a treatment plan—even if there is a negative outcome. With malpractice, a clinician is not necessarily at fault for a bad outcome or adverse effect, but is at fault for lack of informed consent or negligence (deviation from standard of care), which is harder for an attorney to demonstrate if there is deliberation, communication, and a plan that multiple doctors agree upon.
Continue to: Be aware that informed consent...
Be aware that informed consent is an ongoing process, and a woman may need to be reminded or informed of potential risks at varying stages of her life (eg, when starting a new relationship, getting married, etc.). Documentation can include that the clinician has discussed the risks, benefits, adverse effects, and alternatives of various medications, and a description of any patient-specific or medication-specific issues. In addition to verbal discussions, giving patients printed information can be helpful, as can directing them to appropriate websites (see Related Resources). Some physicians require patients to sign a form to indicate that they are aware of known risks.
Similar to being proactive before your patient becomes pregnant, think proactively regarding the postpartum period. Is your patient planning to breastfeed? Is the medication compatible with breastfeeding, or is bottle feeding the best option considering the mother’s specific circumstances? For example, developing severe symptoms, experiencing insomnia, needing to take a contraindicated medication, or having a vulnerable infant might sway a mother towards not breastfeeding. The expectant mother (and her partner, where possible) should be educated about postpartum risks and the importance of sleep in preventing postpartum depression.
Bottom Line
Concerns about being sued should not prevent appropriate care of depression in a woman who is pregnant. Discuss with your patient both the risk of untreated mental illness and the risk of medications to ensure she understands that avoiding antidepressants does not guarantee a safe or healthy pregnancy.
Related Resources
- MotherToBaby. www.mothertobaby.org/
- Centers for Disease Control and Prevention. Treating for two: medicine and pregnancy. www.cdc.gov/pregnancy/meds/treatingfortwo/index.html
- MGH Center for Women’s Mental Health. Reproductive psychiatry resource and information center. www.womensmentalhealth.org/
Drug Brand Names
Paroxetine • Paxil
Sertraline • Zoloft
Venlafaxine • Effexor
Many physicians have seen advertisements that encourage women who took an antidepressant while they were pregnant and had a negative outcome to contact a law firm. These ads could make patients more reluctant to take prescribed antidepressants, and psychiatrists more hesitant to prescribe necessary medications during pregnancy—which is a disservice to the mother and child.
More recently, several headline-grabbing studies appeared to suggest that there is an increased risk to infants who are exposed to antidepressants prenatally. Unfortunately, many patients do not understand that replication of these studies is often lacking, and methodological and confounding issues abound. All of this makes it difficult for patients and their families to know if they should take an antidepressant during pregnancy, and for psychiatrists to know what to discuss about the risks and benefits of various antidepressants during pregnancy. This article reviews the rationale for treatment of depression in pregnancy; the risks of untreated depression in pregnancy, as well as the potential risks of medication; ethical issues in the treatment of depression in pregnancy; the limitations of available research; and best approaches for practice.
Risks of untreated depression in pregnancy
Pregnant women may have misconceptions about treatment during pregnancy, and psychiatrists often are hesitant to treat pregnant women. However, the risks of untreated depression during pregnancy are even greater than the risks of untreated depression at other points in a woman’s life. In addition to general psychiatric risks seen in depression, pregnant women may experience other issues, such as preeclampsia and liver metabolism changes.1-2 Risks to the fetus related to untreated or partially treated mental health concerns include poor prenatal care related to poor self-care, an increased risk of exposure to illicit substances or alcohol related to “self-medication,” preterm delivery, and low birthweight (Table 13-8). Further risks for an infant of a mother with untreated depression include decreased cognitive performance and poor bonding with poor stress adaptation.5,6 Thus, appropriate treatment of depression is even more important during pregnancy than at other times of life.
Potential risks of treating depression in pregnancy
When prescribing psychotropic medications to a pregnant woman, there are several naturally occurring adverse outcomes to consider. For example, miscarriages, stillbirths, and congenital malformations can occur without explanation in the general population. In addition, also consider the specific health history of the mother and the available research literature regarding the specific psychotropic agent (keeping in mind that there are ethical issues associated with conducting prospective research in pregnant women, such as it being unethical to withhold treatment to pregnant women who are depressed in order to have a control group, and that retrospective research is often confounded by recall bias). Potential risks to be aware of include miscarriage (spontaneous abortion), malformation (teratogenesis, birth defects), preterm delivery, neonatal adaptation syndrome, and behavioral teratogenesis (Table 13-8).
Selective serotonin reuptake inhibitors (SSRIs), the usual medication treatment of choice for depression, have at times been implicated in adverse pregnancy outcomes, but no strong evidence suggests they increase the miscarriage rate. Overall data are reassuring regarding the risk of malformation associated with SSRI use. Of note, the FDA had switched paroxetine from a Class C drug to a Class D drug after early reports of a potential 1.5% to 2% risk of fetal cardiac malformations compared with a 1% baseline risk in the general population (these FDA pregnancy risk letter categories have since been phased out).9,10 Nevertheless, the absolute risk remains small. Another large study found that there was no substantial increased risk of cardiac malformations attributable to antidepressant use during the first trimester.11
Lessons from a class action suit
Since we last reviewed pregnancy and antidepressants in 2013,8 several class action lawsuits against the manufacturers of psychotropic medications have been heard. Product liability actions brought against manufacturers are different from medical malpractice suits brought against individual physicians, which may result from lack of informed consent, suicide, or homicide.
One of the largest class action suits was against Zoloft (specifically Zoloft and Pfizer, since the brand manufacturer is responsible for the product insert information.)12,13 At the time, sertraline was already commonly prescribed due to the relatively safe reproductive profile.
Continue to: Many of the more than 300...
Many of the more than 300 federal claims were united in a multi-district litigation (MDL) suit under the United States District Court of Eastern Pennsylvania (MDL 2342). Pfizer issued Daubert challenges (efforts to exclude the introduction of “junk science” into the courtroom) against the plaintiffs’ experts’ scientific methods and results.12,13 The plaintiffs (those suing Pfizer) had to prove that the medications caused the negative outcome, not that they were merely temporally associated. Subsequently, 2 plaintiff experts—a PharmD and a biostatistician—were removed. Pfizer successfully challenged the methodological soundness of the plaintiffs’ experts’ testimony (Table 212,13), and the case was dismissed. In general, the courts identified the Bradford Hill criteria as often being important (though not definitive) methodology for determining causation (Table 312,13).
A concept raised in prior psychotropic lawsuits was the “learned intermediary doctrine,” in which pharmaceutical companies stated that once a risk is known, it is the responsibility of the prescribing physician to assess risks vs benefits and inform the patient.8 Many aspects of the larger class action lawsuits related to failure of the company to do adequate research to identify risks and appropriately inform the public and the medical community of these risks.14
Challenges in interpreting the literature
Some of the difficulties in interpreting the literature on the association of antidepressants and birth defects can be seen in a 2020 study by Anderson et al.15 This study was published in JAMA Psychiatry, received widespread coverage in the media, and was discussed on the CDC’s website.16 Anderson et al15 compared a large cohort of 30,630 infants with birth defects from the multicenter case-control National Birth Defects Prevention Study with 11,478 randomly selected controls with no defects. Three primary study groups were women whose pregnancies resulted in:
- birth defects with no antidepressant exposure (n = 28,719)
- birth defects with exposure to an antidepressant (n = 1,911)
- no birth defect control group (n = 10,886 no antidepressant exposure, n = 592 antidepressant exposure).
This study reported there were “some associations between maternal antidepressant use and specific birth defects” and “Venlafaxine was associated with more birth defects than other antidepressants, which needs confirmation.”15 However, in an accompanying editorial, Wisner et al17 discussed potential problems and limitations with this study and research of this nature in general (Table 417). In addition, Anderson et al15 used certain “controversial” statistical practices.18 For example, “[T]o align with American Statistical Association guidelines to consider effect sizes when interpreting results instead of statistical significance, we noted associations as meaningfully elevated if [adjusted odds ratios] were 2.0 or greater and lower confidence interval bounds were 0.8 or greater.”15
Those who read only abstracts or news stories may believe this study of >40,000 participants included a large number of women who were receiving venlafaxine. However, the number of pregnant women who were prescribed venlafaxine was actually very small—112 who took venlafaxine experienced a birth defect. In addition, the authors noted “Venlafaxine was associated with many of the same defects across the samples (data not shown).”15 As discussed above, historically one of the areas the courts have considered was whether or not appropriate methodology was applied, and whether the results could be replicated with the data provided.
Continue to: Further, new studies...
Further, new studies need to be considered in context of the literature as a whole and collective clinical experience. A recent systematic review found that among 3,186 infants exposed to venlafaxine during the first trimester, there were 107 major malformations.19 This indicated a relative risk estimate of 1.12, with a 95% CI of 0.92 to 1.35. The authors concluded that venlafaxine exposure in the first trimester was not associated with an increased risk of malformations.
Expectant parents may come across a headline that implies a specific antidepressant causes problems, but have not read the study or know how to interpret it. Often it is best for a physician to find out what the basis of the concern is, and if possible, review the study with the patient to make sure it is in the right context, and if it applies to the individual patient’s situation.
Consider the ethical issues
In addition to preventive ethics, other critical ethical issues in pregnancy include omission bias, beneficence, and autonomy.4,20-24 Omission bias occurs when physicians are more concerned about acts of commission (in which treatment leads to a negative outcome) than they are about acts of omission, which involve not treating the patient’s illness. To address this, it is important to discuss with the patient both the risks of treating and the risks of not treating maternal depression, so that the mother can make the best decision for her own specific set of circumstances.
Regarding beneficence (promoting the patient’s best interest), consider both the mother’s and the infant’s best interest, which usually are quite closely related. Women may feel guilty about taking a medication that they perceive is harmful for the fetus but good for their own mental health. Physicians can help with this by providing education about the benefits of treating depression for the fetus’ benefit as well. The fetus is completely dependent on the environment that the mother places them in, not merely the medication effects (eg, psychologic/physiologic stress effects, poor diet, lack of exercise, risk of “self-medication”).
Regarding autonomy (a woman’s own decision-making), Coverdale et al21 discussed strategies that can enhance a pregnant patient’s autonomy—including discussing treatment options and counselling about the effects of depression itself in pregnancy, as well as considering the effects of depression on the process of decision-making. For example, a woman with depression may see the world through a negative lens or may have difficulty concentrating. Patients may also require education about the concept of relative risk in comparison to absolute risk—especially in light of attention-grabbing headlines.
Continue to: Finally, as part of...
Finally, as part of preventative ethics, anticipate the ethical dilemmas before the common situation of pregnancy. Almost one-half of pregnancies are unplanned.25 Many women thus expose their fetus to medication during the critical early period of organogenesis, before noticing they were pregnant. Therefore, even if a patient of childbearing age insists that she is not sexually active, the prudent psychiatrist should still begin discussions about medications in pregnancy.
An outline of best practices
Best practice includes preventive ethics, and when treating any woman of childbearing age, psychiatrists should consider prescribing medications that are known to be relatively safe in pregnancy rather than risky in pregnancy. Therefore, any psychiatrist whose practice includes women of childbearing age should have a working knowledge of which agents are relatively safe in pregnancy. After a woman is pregnant, careful decision-making about medication should continue. Consult with reproductive psychiatry colleagues where necessary.
A patient with depression would usually merit closer follow-up during the pregnancy. In some cases, psychotherapy alone can be effective in depression. However, approximately 6% to 13% of women are prescribed antidepressants during pregnancy, and this has been increasing.26 Women who discontinue their antidepressant while pregnant are more likely to relapse than those who continue their medication,27 thus exposing their fetus to negative effects of depression as well as medication (prior to discontinuation).
When possible, monotherapy (one agent) in the lowest effective dose is often the judicious approach to treatment. For a patient prescribed pre-existing polypharmacy at time of pregnancy, a risk-benefit analysis of which medications should remain, which should be stopped, and a plan for taper, if needed, should be discussed and documented. Using too little of an antidepressant dose would expose the fetus to both depression and medication, whereas using a maximum dose when not needed would expose the fetus to more medication than is necessary to treat the mother’s symptoms. This discussion with the mother (and her partner, if available) should be documented in the chart. The mother should understand both the risk of untreated illness and the potential risks of medications, as well as the benefits of medications and alternatives. It is important for the mother to realize that there is no risk-free option, and that malformations can occur in the general population as well as in individuals with untreated depression, separate from any medication exposure. In fact, most malformations do not have a known cause, and overall approximately 3% of pregnancies result in a birth defect.28
If possible, discuss the treatment plan with the patient’s obstetrician, or ask the mother to discuss the plan with her obstetrician, so that everyone is on the same page. This discussion can help attenuate patient anxiety that results from hearing different things from different clinicians. Communication with other treating professionals (eg, OB/GYNs, pediatricians) can be beneficial and reduce liability if multiple physicians have agreed on a treatment plan—even if there is a negative outcome. With malpractice, a clinician is not necessarily at fault for a bad outcome or adverse effect, but is at fault for lack of informed consent or negligence (deviation from standard of care), which is harder for an attorney to demonstrate if there is deliberation, communication, and a plan that multiple doctors agree upon.
Continue to: Be aware that informed consent...
Be aware that informed consent is an ongoing process, and a woman may need to be reminded or informed of potential risks at varying stages of her life (eg, when starting a new relationship, getting married, etc.). Documentation can include that the clinician has discussed the risks, benefits, adverse effects, and alternatives of various medications, and a description of any patient-specific or medication-specific issues. In addition to verbal discussions, giving patients printed information can be helpful, as can directing them to appropriate websites (see Related Resources). Some physicians require patients to sign a form to indicate that they are aware of known risks.
Similar to being proactive before your patient becomes pregnant, think proactively regarding the postpartum period. Is your patient planning to breastfeed? Is the medication compatible with breastfeeding, or is bottle feeding the best option considering the mother’s specific circumstances? For example, developing severe symptoms, experiencing insomnia, needing to take a contraindicated medication, or having a vulnerable infant might sway a mother towards not breastfeeding. The expectant mother (and her partner, where possible) should be educated about postpartum risks and the importance of sleep in preventing postpartum depression.
Bottom Line
Concerns about being sued should not prevent appropriate care of depression in a woman who is pregnant. Discuss with your patient both the risk of untreated mental illness and the risk of medications to ensure she understands that avoiding antidepressants does not guarantee a safe or healthy pregnancy.
Related Resources
- MotherToBaby. www.mothertobaby.org/
- Centers for Disease Control and Prevention. Treating for two: medicine and pregnancy. www.cdc.gov/pregnancy/meds/treatingfortwo/index.html
- MGH Center for Women’s Mental Health. Reproductive psychiatry resource and information center. www.womensmentalhealth.org/
Drug Brand Names
Paroxetine • Paxil
Sertraline • Zoloft
Venlafaxine • Effexor
1. Palmsten K, Setoguchi S, Margulis AV, et al. Elevated risk of preeclampsia in pregnant women with depression: depression or antidepressants? Am J Epidemiol. 2012;175(10):988-997.
2. Sit DK, Perel JM, Helsel JC, et al. Changes in antidepressant metabolism and dosing across pregnancy and early postpartum. J Clin Psychiatry. 2008;69(4):652-658.
3. Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012-1024.
4. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
5. Friedman SH, Resnick PJ. Postpartum depression: an update. Women’s Health. 2009;5(3):287-295.
6. Liu Y, Kaaya S, Chai J, et al. Maternal depressive symptoms and early childhood cognitive development: a meta-analysis. Psychol Med. 2017;47(4):680-689.
7. Wisner KL, Sit DK, Hanusa BH, et al. Major depression and antidepressant treatment: impact on pregnancy and neonatal outcomes. Am J Psychiatry. 2009; 166(5):557-566.
8. Friedman SH, Hall RCW. Antidepressant use during pregnancy: How to avoid clinical and legal pitfalls. Current Psychiatry. 2013;12(2):21-25.
9. Bar-Oz B, Einarson T, Einarson A, et al. Paroxetine and congenital malformations: meta-analysis and consideration of potential confounding factors. Clin Ther. 2007;29(5):918-926.
10. Einarson A, Pistelli A, DeSantis M, et al. Evaluation of the risk of congenital cardiovascular defects associated with use of paroxetine during pregnancy. Am J Psychiatry. 2008;165(6):749-752.
11. Huybrechts KF, Palmsten K, Avorn J, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370(25):2397-2407.
12. In re: Zoloft (sertraline hydrochloride) products liability litigation. MDL No. 2342. No. 12-md-2342. United States District Court, E.D. Pennsylvania. June 27, 2014.
13. In re: Zoloft (sertraline hydrocloride) products liability litigation. MDL No. 2342. United States District Court, E.D. Pennsylvania. December 2, 2015.
14. Kirsch N, Pacheco LD, Hossain A, et al. Medicolegal review: perinatal Effexor lawsuits and legal strategies adverse to prescribing obstetric providers. AJP Rep. 2019;9(1):e88-e91.
15. Anderson KN, Lind JN, Simeone RM, et al. Maternal use of specific antidepressant medications during early pregnancy and the risk of selected birth defects. JAMA Psychiatry. 2020;77(12):1246-1255.
16. Centers for Disease Control and Prevention. Use of the antidepressant venlafaxine during early pregnancy may be linked to specific birth defects. Published October 28, 2020. Accessed October 29, 2020. https://www.cdc.gov/ncbddd/birthdefects/features/venlafaxine-during-pregnancy.html
17. Wisner KL, Oberlander TF, Huybrechts KF. The association between antidepressant exposure and birth defects--are we there yet? JAMA Psychiatry. 2020;77(12):1215-1216.
18. Wasserstein RL, Lazar NA. The ASA statement on p-values: context, process, and purpose. American Statistician. 2016;70(2):129-133.
19. Lassen D, Ennis ZN, Damkier P. First-trimester pregnancy exposure to venlafaxine or duloxetine and risk of major congenital malformations: a systematic review. Basic Clin Pharmacol Toxicol. 2016;118(1):32-36.
20. Miller LJ. Ethical issues in perinatal mental health. Psychiatr Clin North Am. 2009;32(2):259-270.
21. Coverdale JH, McCullough JB, Chervenak FA. Enhancing decision-making by depressed pregnant patients. J Perinat Med. 2002;30(4):349-351.
22. Coverdale JH, McCullough LB, Chervenak FA, et al. Clinical implications of respect for autonomy in the psychiatric treatment of pregnant patients with depression. Psychiatr Serv. 1997;48:209-212.
23. Coverdale JH, Chervenak FA, McCullough LB, et al. Ethically justified clinically comprehensive guidelines for the management of the depressed pregnant patient. Am J Obstet Gynecol. 1996;174(1):169-173.
24. Wisner KL, Zarin DA, Holmboe ES, et al. Risk-benefit decision making for treatment of depression during pregnancy. Am J Psychiatry. 2000;157(12):1933-1940.
25. Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84(5):478-485.
26. Cooper WO, Willy ME, Pont SJ, et al. Increasing use of antidepressants in pregnancy. Am J Obstet Gynecol. 2007;196(6):544.e1-5.
27. Cohen LS, Altshuler LL, Harlow BL, et al. Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. JAMA. 2006;295(5):499-507.
28. Centers for Disease Control and Prevention. Update on overall prevalence of major birth defects--Atlanta, Georgia, 1978-2005. MMWR Morb Mortal Wkly Rep. 2008;57(1):1-5.
1. Palmsten K, Setoguchi S, Margulis AV, et al. Elevated risk of preeclampsia in pregnant women with depression: depression or antidepressants? Am J Epidemiol. 2012;175(10):988-997.
2. Sit DK, Perel JM, Helsel JC, et al. Changes in antidepressant metabolism and dosing across pregnancy and early postpartum. J Clin Psychiatry. 2008;69(4):652-658.
3. Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012-1024.
4. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
5. Friedman SH, Resnick PJ. Postpartum depression: an update. Women’s Health. 2009;5(3):287-295.
6. Liu Y, Kaaya S, Chai J, et al. Maternal depressive symptoms and early childhood cognitive development: a meta-analysis. Psychol Med. 2017;47(4):680-689.
7. Wisner KL, Sit DK, Hanusa BH, et al. Major depression and antidepressant treatment: impact on pregnancy and neonatal outcomes. Am J Psychiatry. 2009; 166(5):557-566.
8. Friedman SH, Hall RCW. Antidepressant use during pregnancy: How to avoid clinical and legal pitfalls. Current Psychiatry. 2013;12(2):21-25.
9. Bar-Oz B, Einarson T, Einarson A, et al. Paroxetine and congenital malformations: meta-analysis and consideration of potential confounding factors. Clin Ther. 2007;29(5):918-926.
10. Einarson A, Pistelli A, DeSantis M, et al. Evaluation of the risk of congenital cardiovascular defects associated with use of paroxetine during pregnancy. Am J Psychiatry. 2008;165(6):749-752.
11. Huybrechts KF, Palmsten K, Avorn J, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370(25):2397-2407.
12. In re: Zoloft (sertraline hydrochloride) products liability litigation. MDL No. 2342. No. 12-md-2342. United States District Court, E.D. Pennsylvania. June 27, 2014.
13. In re: Zoloft (sertraline hydrocloride) products liability litigation. MDL No. 2342. United States District Court, E.D. Pennsylvania. December 2, 2015.
14. Kirsch N, Pacheco LD, Hossain A, et al. Medicolegal review: perinatal Effexor lawsuits and legal strategies adverse to prescribing obstetric providers. AJP Rep. 2019;9(1):e88-e91.
15. Anderson KN, Lind JN, Simeone RM, et al. Maternal use of specific antidepressant medications during early pregnancy and the risk of selected birth defects. JAMA Psychiatry. 2020;77(12):1246-1255.
16. Centers for Disease Control and Prevention. Use of the antidepressant venlafaxine during early pregnancy may be linked to specific birth defects. Published October 28, 2020. Accessed October 29, 2020. https://www.cdc.gov/ncbddd/birthdefects/features/venlafaxine-during-pregnancy.html
17. Wisner KL, Oberlander TF, Huybrechts KF. The association between antidepressant exposure and birth defects--are we there yet? JAMA Psychiatry. 2020;77(12):1215-1216.
18. Wasserstein RL, Lazar NA. The ASA statement on p-values: context, process, and purpose. American Statistician. 2016;70(2):129-133.
19. Lassen D, Ennis ZN, Damkier P. First-trimester pregnancy exposure to venlafaxine or duloxetine and risk of major congenital malformations: a systematic review. Basic Clin Pharmacol Toxicol. 2016;118(1):32-36.
20. Miller LJ. Ethical issues in perinatal mental health. Psychiatr Clin North Am. 2009;32(2):259-270.
21. Coverdale JH, McCullough JB, Chervenak FA. Enhancing decision-making by depressed pregnant patients. J Perinat Med. 2002;30(4):349-351.
22. Coverdale JH, McCullough LB, Chervenak FA, et al. Clinical implications of respect for autonomy in the psychiatric treatment of pregnant patients with depression. Psychiatr Serv. 1997;48:209-212.
23. Coverdale JH, Chervenak FA, McCullough LB, et al. Ethically justified clinically comprehensive guidelines for the management of the depressed pregnant patient. Am J Obstet Gynecol. 1996;174(1):169-173.
24. Wisner KL, Zarin DA, Holmboe ES, et al. Risk-benefit decision making for treatment of depression during pregnancy. Am J Psychiatry. 2000;157(12):1933-1940.
25. Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84(5):478-485.
26. Cooper WO, Willy ME, Pont SJ, et al. Increasing use of antidepressants in pregnancy. Am J Obstet Gynecol. 2007;196(6):544.e1-5.
27. Cohen LS, Altshuler LL, Harlow BL, et al. Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. JAMA. 2006;295(5):499-507.
28. Centers for Disease Control and Prevention. Update on overall prevalence of major birth defects--Atlanta, Georgia, 1978-2005. MMWR Morb Mortal Wkly Rep. 2008;57(1):1-5.
Liability protection when practicing during a disaster: How the laws work
Disasters—both natural and human-caused—can strike at any time, causing severe trauma for those impacted. Disasters may create circumstances where the need for mental health resources could exceed capacity, and hospitals and clinics would be unable to meet the needs of the affected communities. As psychiatric clinicians, we may want to provide our services in such situations; however, we are still at risk for civil, criminal, or constitutional liability claims against us if we fail to meet our legal obligations related to psychiatric practice. Ideally, whether we live and work in an area affected by a disaster or volunteer from other states, we should be able to care for patients without fear of facing unreasonable liability risks. Although an exhaustive list of all relevant federal and state laws and regulations is beyond the scope of this article, here I discuss some of the federal and state laws and regulations that could provide protection from these risks, and some limitations of liability protection.
A familiar list of liability concerns
From a liability perspective, what should we be aware of when practicing during disasters? The same liability concerns we have during our day-to-day practice also exist during disasters, especially when there are suboptimal or adverse outcomes.
Box
During disasters, changes in the usual standard of practice may be necessary to save as many lives as possible, and when resources are scarce, the focus of mental health services could shift from individualized patient care to those who are most in need. Examples of potential liability concerns clinicians may face in such situations include:
Negligence. Clinicians may have to provide emergent care for patients that may result in an adverse outcome. Examples include applying a tourniquet to a patient’s badly injured limb without their consent, and then that patient loses their limb, or administering the COVID-19 vaccine to a patient because of significant clinician shortages, and then that patient develops complications. These scenarios could possibly give rise to ordinary negligence claims of practicing outside the usual scope of practice, especially for a clinician who does not have liability protections.
Practicing without the proper state medical license. When out-of-state clinicians come to a facility that needs emergency assistance, they can face liability concerns for practicing without a properly recognized state medical license.1 Because care is deemed to have been provided where the patient was physically present when services were provided, liability can occur when providing services to patients in a state where the psychiatrist does not have a medical license. An example of this would be a psychiatrist in South Carolina who provides telehealth services to patients in a Florida community ravaged by a hurricane when the psychiatrist does not have a Florida medical license.
Abandonment. When we take a confirmatory step to provide care to an individual, it may create a clinician-patient relationship and a duty on behalf of the clinician within the applicable standard of care.2 With disasters, the customary expectations and parameters associated with clinician-patient relationships can change. We may have to cease treating some patients so that we can focus our time or resources elsewhere, which could open up liability concerns regarding claims of abandonment.1 At times, we may refuse to treat patients outright, creating conflicts with the Emergency Medical Treatment & Active Labor Act (EMTALA) and its state counterparts.
Liability protections
There are no comprehensive national liability protections for all practitioners during disasters.1 Limited immunity is often provided through a patchwork of federal and state laws and regulations, which can be complex and are often modified. This immunity depends on several factors, such as applicable regulations, the type of services that are provided, and whether the clinicians are volunteering their services (ie, they are not being paid for providing services).2 There is usually no immunity due to willful or wanton acts, gross negligence, providing care while intoxicated, or criminal acts.2
Federal laws and regulations
Most of the federal laws that provide liability protections are activated once a disaster is declared. However, some laws provide liability protections without requiring such declarations. Additional federal laws and regulations that provide additional liability protections, especially to volunteers, can be enacted after disasters occur.
Federal Tort Claims Act
The Federal Tort Claims Act (FTCA)3 protects federal government employees from tort liability by substituting the federal government as the defendant in certain types of suits brought against the federal government. These suits may involve injury, loss of personal property, personal injury, or death by the negligent or wrongful act or omission of any federal government employees while acting in the scope of their office or employment.3,4 It does not require that an emergency be declared before immunity is conferred. FTCA covers all federal government employees, including volunteers.4 In the context of an emergency response, volunteers can assert the liability protections afforded to federal employees if they are designated as unpaid employees of the federal government.4 Federal employees are immune from suit under state tort law.4
Volunteer Protection Act
The Volunteer Protection Act (VPA) of 19975 provides liability protections to uncompensated volunteer health professionals (VHPs) who perform services for nonprofit organizations or government entities against claims of ordinary negligence committed within the scope of their volunteer responsibilities.4 It does not require that an emergency be declared before immunity is conferred. Although VHPs are not liable for economic damages caused by providing medical care within the scope of their volunteer responsibilities, this exemption does not extend to non-economic damages, such as losses for suffering and mental anguish.5 VPA does not protect VHPs working in businesses (including for-profit hospitals) and organizational entities of any type (including nonprofit or governmental organizations) that use VHPs.4
VPA only protects VHPs practicing with a license as required by law in the state where the harm occurred, unless state authorities allow for licensure exceptions. VPA overrides state laws that are inconsistent with VPA, unless those state laws provide greater liability protection for VHPs.4 However, VPA protections are limited. VPA protects only volunteers, not clinicians working in their regular nonemergency roles and capacities.6 A nonprofit or government agent can still bring civil claims against VHPs.6 VPA does not override certain state laws that put conditions on volunteers, such as risk management requirements, vicarious liability, and a financially secure form of recovery for intended victims.6
Continue to: Health Insurance Portability and Accountability Act
Health Insurance Portability and Accountability Act
The Health Insurance Portability and Accountability Act (HIPAA) of 1996,7 specifically Section 194, extends eligibility for FTCA liability protections to VHPs at qualifying free clinics, provided the clinic sponsors the VHPs by applying to the Health Resources and Services Administration.8 It does not require that an emergency be declared before immunity is conferred.
Public Readiness and Emergency Preparedness Act
The Public Readiness and Emergency Preparedness (PREP) Act of 20059 authorizes the US Department of Health and Human Services (HHS) Secretary to issue a declaration that provides immunity to VHPs from tort liability for claims of loss caused by the use of authorized countermeasures (eg, vaccines) against diseases or other threats of public health emergencies.4 A separate emergency determination under Public Health Service Act Section 319 or another statute is not required for PREP Act immunities to take effect.4 The PREP Act covers individual persons and entities involved in the manufacture, testing, distribution, administration, and use of covered countermeasures.4
PREP Act immunity is not absolute and does not protect against claims of willful misconduct, violation of the Americans with Disabilities Act (ADA), or other civil rights violations.4 Liability protection under the PREP Act is limited to a specific emergency and includes only the countermeasures and other conditions listed in the PREP Act declaration by the HHS Secretary.4
State laws and regulations
States have a variety of standing liability protections that could apply to VHPs who provide care in an emergency. Some states have crafted executive orders to be put into effect during a disaster. Most of these executive orders, which can include extending liability protections, are similar to what other states have done by adopting model acts such as Model State Emergency Health Powers Act.6 These orders are not actually laws; they only become effective when the governor signs them at the time of the disaster. These orders also are time-limited and must be reissued in subsequent disasters.
State tort claims acts and state claims acts
Similar to the federal government, some states have waived sovereign immunity in certain circumstances through state tort claims or state claims acts.
Continue to: State tort claims act
State tort claims acts either abolish state sovereign immunity generally and provide immunity only in specific circumstances, or preserve sovereign immunity generally but identify certain exceptions in which immunity is waived.4
State claims acts limit state sovereign immunity by establishing procedures for making claims against the state.4 These acts typically immunize state government employees from tort liability for acts or omissions committed within the scope of their employment.4 Some states extend these protections to volunteers, and some states declare volunteers to be unpaid state employees during an emergency, which allows volunteers to assert the liability protections afforded of state employees.4
Emergency power statutes
State emergency laws can trigger additional powers, suspend certain administrative requirements, and provide or enhance liability protections to specified groups of volunteers and other responders upon a gubernatorial declaration of emergency.4 These statutes can extend the rights and immunities provided to governmental employees to volunteers performing work that is eligible for coverage under governmental immunity and state tort claims acts.4 There is a wide range in the types and degrees of coverage provided to volunteers under emergency powers statutes, and these provisions can be broad or duplicative of other provisions in state law.4
State volunteer protection statutes
All states have some statutory provisions for volunteers. Similar to the VPA, these state volunteer protection statutes generally do not require that an emergency be declared, apply to uncompensated individual volunteers for nonprofit and government entities only, and apply only to individuals and not to organizations.4 Many states have adopted specific liability protections for VHPs in addition to or to supplement their emergency powers and general volunteer protection statutes.4 These statutes confer immunity from civil liability provided that certain conditions are met and are not dependent on the declaration of an emergency.4 Each state statute differs in regard to who receives immunity, which acts are immune from liability, and what liability protections are available.
Good Samaritan laws
All 50 states and the District of Columbia have enacted Good Samaritan laws. These laws, which do not need an official declaration of an emergency in order to be applicable, generally protect VHPs from liability when volunteering in good faith and without compensation at the scene of an emergency.2 Good Samaritan protections may also apply to care provided by VHPs in a hospital if the VHP is not on duty and does not charge a fee.2 However, the effect and scope of Good Samaritan laws vary dramatically from state to state. Some states include hospital settings as an emergency scene in their statutes, while others expressly exclude hospitals from their statutes.6 Some state statutes only include declared emergencies, while others are drawn to broadly cover all emergency situations.6
Continue to: Limitations
Limitations. Many Good Samaritan statutes apply only to volunteers, and not all states have statutes that allow clinicians to be designated as such,6 so receiving compensation would take a clinician outside the scope of the statute. Further, most states only shield action taken at the scene of an accident, and immunity would not extend to a hospital emergency department, or in the aftermath of an emergency as normal conditions slowly return.6 Therefore, Good Samaritan liability protection would apply to the common scenario of assisting at the scene of a car crash, but not necessarily to treating individuals in the emergency department after a hurricane or during a pandemic.6 State laws vary considerably on what constitutes “good faith” and “without compensation,” which would determine whether protection applies for a clinician who is otherwise salaried in a regular job.1
Mutual aid agreements
Mutual aid agreements are mechanisms through which jurisdictions can aid other jurisdictions during emergencies.4 These agreements also include provisions for reimbursing expenses, providing liability protections to governmental employees and volunteers who provide aid, and awarding compensation for injuries to personnel deployed under the agreement.4 These protections are not automatic and are limited in their applicability.
The Emergency Management Assistance Compact (EMAC), the most widely adopted mutual aid agreement in the United States, has been adopted by all 50 states, the District of Columbia, and some territories.10 It only becomes effective once an emergency has been declared. EMAC provides immunity to officers from the state that is rendering aid to the state requesting aid, in which officers are considered agents of the requesting state for tort liability and immunity purposes.8 These individuals, who must be properly dispatched in response to an EMAC request, are not to be held liable for acts or omissions rendered in good faith; however, EMAC does not provide liability protection for actions constituting willful misconduct, gross negligence, or recklessness.6 EMAC also provides reciprocity for individuals who are properly dispatched in response to an EMAC request who hold medical licenses to practice medicine in the receiving state, subject to any limitations imposed by the receiving state.4 Clinicians can familiarize themselves with a state’s medical licensing requirements by reviewing that state’s medical board website. For EMAC protections to apply, a state must make a request to another/other state(s) through EMAC, and such requests must be formally accepted by the rendering state.8 EMAC does not require participating states to actually provide aid.10
Non-volunteer health care clinicians
Non-volunteer (salaried or paid) health care clinicians are more likely to bear the brunt of providing care during a disaster, especially in the early stages before VHPs arrive; however, most legislation does not address the associated disproportionate liability risk burden of non-volunteer health care clinicians.1,11 As opposed to VHPs and government employees, non-volunteer health care clinicians performing their regular job duties during a disaster are generally not provided immunity from negligence by most legislation.1,6 One exception is the PREP Act, which provides immunity for all clinicians from claims that may arise from dispensing a specific countermeasure during a declared public health emergency.1,9 Some states have enacted the Model State Emergency Health Powers Act, which may offer immunity from negligence if the non-volunteer clinician is rendering care under contract with or at the request of a state1; however, non-volunteer clinicians who practice from their office or a local hospital will not receive protection through these laws.1 Good Samaritan laws may not apply unless care is provided at a scene of an emergency.
A few states have attempted to narrow this legislative gap by enacting laws that provide immunity more broadly for clinicians, regardless of their volunteer or compensation status.1 Elements of these states’ laws include acting in response to a declared emergency or disaster in which there is a recognized depletion of resources attributable to the disaster, at express or implied request of the state government, and consistent with emergency plans.1
Continue to: Bottom Line
Bottom Line
There are potential liability risks when treating patients during a disaster. Statutory protections that limit liability may be enacted when the US President or a state Governor declares an official state of emergency. Although some federal and state laws and regulations provide liability protections during these situations, there is a discrepancy in the protections offered to non-volunteer vs volunteer clinicians.
Related Resources
- Federal Emergency Management Agency. https://www.fema.gov/
- Federation of State Medical Boards. https://www.fsmb.org
1. Altman RL, Santucci KA, Anderson MR, et al. American Academy of Pediatrics Committee on Medical Liability and Risk Management. Understanding liability risks and protections for pediatric providers during disasters. Pediatrics. 2019;143(3):e20183893. doi.org/10.1542/peds.2018-3892
2. Lambert K, Wertheimer M. American Professional Agency: Risk management in disaster response. Published September 2017. Accessed May 25, 2021. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/disaster/resource_group/resources/orgs/RMDisasterResp.pdf
3. Federal Torts Claims Act, as amended. Codified at 28 USC. §1346 (1946).
4. Association of State and Territorial Health Officials (ASTHO). Liability, immunity, and workers’ compensation issue in public health emergencies. Published 2012. Accessed May 25, 2021. https://www.astho.org/Programs/Preparedness/Public-Health-Emergency-Law/Emergency-Authority-and-Immunity-Toolkit/Liability,-Immunity,-and-Workers%E2%80%99-Compensation-Issues-in-Public-Health-Emergencies-Issue-Brief/
5. Volunteer Protection Act of 1997. Pub. L. 105-19, 111 Stat. 221.
6. Pope TM, Palazzo MF. Legal briefing: crisis standards of care and legal protections during disasters and emergencies. J Clin Ethics. 2010;21(4):358-367.
7. Health Insurance Portability and Accountability Act of 1996. Pub. L. 104-191, 110 Stat. 1936. https://www.congress.gov/104/plaws/publ191/PLAW-104publ191.pdf
8. American Medical Association. Liability protections for health care professionals during COVID-19. Updated April 8, 2020. Accessed May 25, 2021. https://www.ama-assn.org/practice-management/sustainability/liability-protections-health-care-professionals-during-covid-19
9. Public Readiness and Emergency Preparedness Act of 2005. Pub. L. 109-148, 119 Stat. 2818. https://www.govinfo.gov/content/pkg/PLAW-109publ148/html/PLAW-109publ148.htm
10. Emergency Management Assistance Compact (EMAC). Accessed May 25, 2021. https://www.emacweb.org/
11. Hodge JG, Garcia AM, Anderson ED, et al. Emergency legal preparedness for hospitals and health care personnel. Disaster Med Public Health Prep. 2009;3(2 Supplement):S37-S44. doi: 10.1097/DMP.0b013e31819d977c
Disasters—both natural and human-caused—can strike at any time, causing severe trauma for those impacted. Disasters may create circumstances where the need for mental health resources could exceed capacity, and hospitals and clinics would be unable to meet the needs of the affected communities. As psychiatric clinicians, we may want to provide our services in such situations; however, we are still at risk for civil, criminal, or constitutional liability claims against us if we fail to meet our legal obligations related to psychiatric practice. Ideally, whether we live and work in an area affected by a disaster or volunteer from other states, we should be able to care for patients without fear of facing unreasonable liability risks. Although an exhaustive list of all relevant federal and state laws and regulations is beyond the scope of this article, here I discuss some of the federal and state laws and regulations that could provide protection from these risks, and some limitations of liability protection.
A familiar list of liability concerns
From a liability perspective, what should we be aware of when practicing during disasters? The same liability concerns we have during our day-to-day practice also exist during disasters, especially when there are suboptimal or adverse outcomes.
Box
During disasters, changes in the usual standard of practice may be necessary to save as many lives as possible, and when resources are scarce, the focus of mental health services could shift from individualized patient care to those who are most in need. Examples of potential liability concerns clinicians may face in such situations include:
Negligence. Clinicians may have to provide emergent care for patients that may result in an adverse outcome. Examples include applying a tourniquet to a patient’s badly injured limb without their consent, and then that patient loses their limb, or administering the COVID-19 vaccine to a patient because of significant clinician shortages, and then that patient develops complications. These scenarios could possibly give rise to ordinary negligence claims of practicing outside the usual scope of practice, especially for a clinician who does not have liability protections.
Practicing without the proper state medical license. When out-of-state clinicians come to a facility that needs emergency assistance, they can face liability concerns for practicing without a properly recognized state medical license.1 Because care is deemed to have been provided where the patient was physically present when services were provided, liability can occur when providing services to patients in a state where the psychiatrist does not have a medical license. An example of this would be a psychiatrist in South Carolina who provides telehealth services to patients in a Florida community ravaged by a hurricane when the psychiatrist does not have a Florida medical license.
Abandonment. When we take a confirmatory step to provide care to an individual, it may create a clinician-patient relationship and a duty on behalf of the clinician within the applicable standard of care.2 With disasters, the customary expectations and parameters associated with clinician-patient relationships can change. We may have to cease treating some patients so that we can focus our time or resources elsewhere, which could open up liability concerns regarding claims of abandonment.1 At times, we may refuse to treat patients outright, creating conflicts with the Emergency Medical Treatment & Active Labor Act (EMTALA) and its state counterparts.
Liability protections
There are no comprehensive national liability protections for all practitioners during disasters.1 Limited immunity is often provided through a patchwork of federal and state laws and regulations, which can be complex and are often modified. This immunity depends on several factors, such as applicable regulations, the type of services that are provided, and whether the clinicians are volunteering their services (ie, they are not being paid for providing services).2 There is usually no immunity due to willful or wanton acts, gross negligence, providing care while intoxicated, or criminal acts.2
Federal laws and regulations
Most of the federal laws that provide liability protections are activated once a disaster is declared. However, some laws provide liability protections without requiring such declarations. Additional federal laws and regulations that provide additional liability protections, especially to volunteers, can be enacted after disasters occur.
Federal Tort Claims Act
The Federal Tort Claims Act (FTCA)3 protects federal government employees from tort liability by substituting the federal government as the defendant in certain types of suits brought against the federal government. These suits may involve injury, loss of personal property, personal injury, or death by the negligent or wrongful act or omission of any federal government employees while acting in the scope of their office or employment.3,4 It does not require that an emergency be declared before immunity is conferred. FTCA covers all federal government employees, including volunteers.4 In the context of an emergency response, volunteers can assert the liability protections afforded to federal employees if they are designated as unpaid employees of the federal government.4 Federal employees are immune from suit under state tort law.4
Volunteer Protection Act
The Volunteer Protection Act (VPA) of 19975 provides liability protections to uncompensated volunteer health professionals (VHPs) who perform services for nonprofit organizations or government entities against claims of ordinary negligence committed within the scope of their volunteer responsibilities.4 It does not require that an emergency be declared before immunity is conferred. Although VHPs are not liable for economic damages caused by providing medical care within the scope of their volunteer responsibilities, this exemption does not extend to non-economic damages, such as losses for suffering and mental anguish.5 VPA does not protect VHPs working in businesses (including for-profit hospitals) and organizational entities of any type (including nonprofit or governmental organizations) that use VHPs.4
VPA only protects VHPs practicing with a license as required by law in the state where the harm occurred, unless state authorities allow for licensure exceptions. VPA overrides state laws that are inconsistent with VPA, unless those state laws provide greater liability protection for VHPs.4 However, VPA protections are limited. VPA protects only volunteers, not clinicians working in their regular nonemergency roles and capacities.6 A nonprofit or government agent can still bring civil claims against VHPs.6 VPA does not override certain state laws that put conditions on volunteers, such as risk management requirements, vicarious liability, and a financially secure form of recovery for intended victims.6
Continue to: Health Insurance Portability and Accountability Act
Health Insurance Portability and Accountability Act
The Health Insurance Portability and Accountability Act (HIPAA) of 1996,7 specifically Section 194, extends eligibility for FTCA liability protections to VHPs at qualifying free clinics, provided the clinic sponsors the VHPs by applying to the Health Resources and Services Administration.8 It does not require that an emergency be declared before immunity is conferred.
Public Readiness and Emergency Preparedness Act
The Public Readiness and Emergency Preparedness (PREP) Act of 20059 authorizes the US Department of Health and Human Services (HHS) Secretary to issue a declaration that provides immunity to VHPs from tort liability for claims of loss caused by the use of authorized countermeasures (eg, vaccines) against diseases or other threats of public health emergencies.4 A separate emergency determination under Public Health Service Act Section 319 or another statute is not required for PREP Act immunities to take effect.4 The PREP Act covers individual persons and entities involved in the manufacture, testing, distribution, administration, and use of covered countermeasures.4
PREP Act immunity is not absolute and does not protect against claims of willful misconduct, violation of the Americans with Disabilities Act (ADA), or other civil rights violations.4 Liability protection under the PREP Act is limited to a specific emergency and includes only the countermeasures and other conditions listed in the PREP Act declaration by the HHS Secretary.4
State laws and regulations
States have a variety of standing liability protections that could apply to VHPs who provide care in an emergency. Some states have crafted executive orders to be put into effect during a disaster. Most of these executive orders, which can include extending liability protections, are similar to what other states have done by adopting model acts such as Model State Emergency Health Powers Act.6 These orders are not actually laws; they only become effective when the governor signs them at the time of the disaster. These orders also are time-limited and must be reissued in subsequent disasters.
State tort claims acts and state claims acts
Similar to the federal government, some states have waived sovereign immunity in certain circumstances through state tort claims or state claims acts.
Continue to: State tort claims act
State tort claims acts either abolish state sovereign immunity generally and provide immunity only in specific circumstances, or preserve sovereign immunity generally but identify certain exceptions in which immunity is waived.4
State claims acts limit state sovereign immunity by establishing procedures for making claims against the state.4 These acts typically immunize state government employees from tort liability for acts or omissions committed within the scope of their employment.4 Some states extend these protections to volunteers, and some states declare volunteers to be unpaid state employees during an emergency, which allows volunteers to assert the liability protections afforded of state employees.4
Emergency power statutes
State emergency laws can trigger additional powers, suspend certain administrative requirements, and provide or enhance liability protections to specified groups of volunteers and other responders upon a gubernatorial declaration of emergency.4 These statutes can extend the rights and immunities provided to governmental employees to volunteers performing work that is eligible for coverage under governmental immunity and state tort claims acts.4 There is a wide range in the types and degrees of coverage provided to volunteers under emergency powers statutes, and these provisions can be broad or duplicative of other provisions in state law.4
State volunteer protection statutes
All states have some statutory provisions for volunteers. Similar to the VPA, these state volunteer protection statutes generally do not require that an emergency be declared, apply to uncompensated individual volunteers for nonprofit and government entities only, and apply only to individuals and not to organizations.4 Many states have adopted specific liability protections for VHPs in addition to or to supplement their emergency powers and general volunteer protection statutes.4 These statutes confer immunity from civil liability provided that certain conditions are met and are not dependent on the declaration of an emergency.4 Each state statute differs in regard to who receives immunity, which acts are immune from liability, and what liability protections are available.
Good Samaritan laws
All 50 states and the District of Columbia have enacted Good Samaritan laws. These laws, which do not need an official declaration of an emergency in order to be applicable, generally protect VHPs from liability when volunteering in good faith and without compensation at the scene of an emergency.2 Good Samaritan protections may also apply to care provided by VHPs in a hospital if the VHP is not on duty and does not charge a fee.2 However, the effect and scope of Good Samaritan laws vary dramatically from state to state. Some states include hospital settings as an emergency scene in their statutes, while others expressly exclude hospitals from their statutes.6 Some state statutes only include declared emergencies, while others are drawn to broadly cover all emergency situations.6
Continue to: Limitations
Limitations. Many Good Samaritan statutes apply only to volunteers, and not all states have statutes that allow clinicians to be designated as such,6 so receiving compensation would take a clinician outside the scope of the statute. Further, most states only shield action taken at the scene of an accident, and immunity would not extend to a hospital emergency department, or in the aftermath of an emergency as normal conditions slowly return.6 Therefore, Good Samaritan liability protection would apply to the common scenario of assisting at the scene of a car crash, but not necessarily to treating individuals in the emergency department after a hurricane or during a pandemic.6 State laws vary considerably on what constitutes “good faith” and “without compensation,” which would determine whether protection applies for a clinician who is otherwise salaried in a regular job.1
Mutual aid agreements
Mutual aid agreements are mechanisms through which jurisdictions can aid other jurisdictions during emergencies.4 These agreements also include provisions for reimbursing expenses, providing liability protections to governmental employees and volunteers who provide aid, and awarding compensation for injuries to personnel deployed under the agreement.4 These protections are not automatic and are limited in their applicability.
The Emergency Management Assistance Compact (EMAC), the most widely adopted mutual aid agreement in the United States, has been adopted by all 50 states, the District of Columbia, and some territories.10 It only becomes effective once an emergency has been declared. EMAC provides immunity to officers from the state that is rendering aid to the state requesting aid, in which officers are considered agents of the requesting state for tort liability and immunity purposes.8 These individuals, who must be properly dispatched in response to an EMAC request, are not to be held liable for acts or omissions rendered in good faith; however, EMAC does not provide liability protection for actions constituting willful misconduct, gross negligence, or recklessness.6 EMAC also provides reciprocity for individuals who are properly dispatched in response to an EMAC request who hold medical licenses to practice medicine in the receiving state, subject to any limitations imposed by the receiving state.4 Clinicians can familiarize themselves with a state’s medical licensing requirements by reviewing that state’s medical board website. For EMAC protections to apply, a state must make a request to another/other state(s) through EMAC, and such requests must be formally accepted by the rendering state.8 EMAC does not require participating states to actually provide aid.10
Non-volunteer health care clinicians
Non-volunteer (salaried or paid) health care clinicians are more likely to bear the brunt of providing care during a disaster, especially in the early stages before VHPs arrive; however, most legislation does not address the associated disproportionate liability risk burden of non-volunteer health care clinicians.1,11 As opposed to VHPs and government employees, non-volunteer health care clinicians performing their regular job duties during a disaster are generally not provided immunity from negligence by most legislation.1,6 One exception is the PREP Act, which provides immunity for all clinicians from claims that may arise from dispensing a specific countermeasure during a declared public health emergency.1,9 Some states have enacted the Model State Emergency Health Powers Act, which may offer immunity from negligence if the non-volunteer clinician is rendering care under contract with or at the request of a state1; however, non-volunteer clinicians who practice from their office or a local hospital will not receive protection through these laws.1 Good Samaritan laws may not apply unless care is provided at a scene of an emergency.
A few states have attempted to narrow this legislative gap by enacting laws that provide immunity more broadly for clinicians, regardless of their volunteer or compensation status.1 Elements of these states’ laws include acting in response to a declared emergency or disaster in which there is a recognized depletion of resources attributable to the disaster, at express or implied request of the state government, and consistent with emergency plans.1
Continue to: Bottom Line
Bottom Line
There are potential liability risks when treating patients during a disaster. Statutory protections that limit liability may be enacted when the US President or a state Governor declares an official state of emergency. Although some federal and state laws and regulations provide liability protections during these situations, there is a discrepancy in the protections offered to non-volunteer vs volunteer clinicians.
Related Resources
- Federal Emergency Management Agency. https://www.fema.gov/
- Federation of State Medical Boards. https://www.fsmb.org
Disasters—both natural and human-caused—can strike at any time, causing severe trauma for those impacted. Disasters may create circumstances where the need for mental health resources could exceed capacity, and hospitals and clinics would be unable to meet the needs of the affected communities. As psychiatric clinicians, we may want to provide our services in such situations; however, we are still at risk for civil, criminal, or constitutional liability claims against us if we fail to meet our legal obligations related to psychiatric practice. Ideally, whether we live and work in an area affected by a disaster or volunteer from other states, we should be able to care for patients without fear of facing unreasonable liability risks. Although an exhaustive list of all relevant federal and state laws and regulations is beyond the scope of this article, here I discuss some of the federal and state laws and regulations that could provide protection from these risks, and some limitations of liability protection.
A familiar list of liability concerns
From a liability perspective, what should we be aware of when practicing during disasters? The same liability concerns we have during our day-to-day practice also exist during disasters, especially when there are suboptimal or adverse outcomes.
Box
During disasters, changes in the usual standard of practice may be necessary to save as many lives as possible, and when resources are scarce, the focus of mental health services could shift from individualized patient care to those who are most in need. Examples of potential liability concerns clinicians may face in such situations include:
Negligence. Clinicians may have to provide emergent care for patients that may result in an adverse outcome. Examples include applying a tourniquet to a patient’s badly injured limb without their consent, and then that patient loses their limb, or administering the COVID-19 vaccine to a patient because of significant clinician shortages, and then that patient develops complications. These scenarios could possibly give rise to ordinary negligence claims of practicing outside the usual scope of practice, especially for a clinician who does not have liability protections.
Practicing without the proper state medical license. When out-of-state clinicians come to a facility that needs emergency assistance, they can face liability concerns for practicing without a properly recognized state medical license.1 Because care is deemed to have been provided where the patient was physically present when services were provided, liability can occur when providing services to patients in a state where the psychiatrist does not have a medical license. An example of this would be a psychiatrist in South Carolina who provides telehealth services to patients in a Florida community ravaged by a hurricane when the psychiatrist does not have a Florida medical license.
Abandonment. When we take a confirmatory step to provide care to an individual, it may create a clinician-patient relationship and a duty on behalf of the clinician within the applicable standard of care.2 With disasters, the customary expectations and parameters associated with clinician-patient relationships can change. We may have to cease treating some patients so that we can focus our time or resources elsewhere, which could open up liability concerns regarding claims of abandonment.1 At times, we may refuse to treat patients outright, creating conflicts with the Emergency Medical Treatment & Active Labor Act (EMTALA) and its state counterparts.
Liability protections
There are no comprehensive national liability protections for all practitioners during disasters.1 Limited immunity is often provided through a patchwork of federal and state laws and regulations, which can be complex and are often modified. This immunity depends on several factors, such as applicable regulations, the type of services that are provided, and whether the clinicians are volunteering their services (ie, they are not being paid for providing services).2 There is usually no immunity due to willful or wanton acts, gross negligence, providing care while intoxicated, or criminal acts.2
Federal laws and regulations
Most of the federal laws that provide liability protections are activated once a disaster is declared. However, some laws provide liability protections without requiring such declarations. Additional federal laws and regulations that provide additional liability protections, especially to volunteers, can be enacted after disasters occur.
Federal Tort Claims Act
The Federal Tort Claims Act (FTCA)3 protects federal government employees from tort liability by substituting the federal government as the defendant in certain types of suits brought against the federal government. These suits may involve injury, loss of personal property, personal injury, or death by the negligent or wrongful act or omission of any federal government employees while acting in the scope of their office or employment.3,4 It does not require that an emergency be declared before immunity is conferred. FTCA covers all federal government employees, including volunteers.4 In the context of an emergency response, volunteers can assert the liability protections afforded to federal employees if they are designated as unpaid employees of the federal government.4 Federal employees are immune from suit under state tort law.4
Volunteer Protection Act
The Volunteer Protection Act (VPA) of 19975 provides liability protections to uncompensated volunteer health professionals (VHPs) who perform services for nonprofit organizations or government entities against claims of ordinary negligence committed within the scope of their volunteer responsibilities.4 It does not require that an emergency be declared before immunity is conferred. Although VHPs are not liable for economic damages caused by providing medical care within the scope of their volunteer responsibilities, this exemption does not extend to non-economic damages, such as losses for suffering and mental anguish.5 VPA does not protect VHPs working in businesses (including for-profit hospitals) and organizational entities of any type (including nonprofit or governmental organizations) that use VHPs.4
VPA only protects VHPs practicing with a license as required by law in the state where the harm occurred, unless state authorities allow for licensure exceptions. VPA overrides state laws that are inconsistent with VPA, unless those state laws provide greater liability protection for VHPs.4 However, VPA protections are limited. VPA protects only volunteers, not clinicians working in their regular nonemergency roles and capacities.6 A nonprofit or government agent can still bring civil claims against VHPs.6 VPA does not override certain state laws that put conditions on volunteers, such as risk management requirements, vicarious liability, and a financially secure form of recovery for intended victims.6
Continue to: Health Insurance Portability and Accountability Act
Health Insurance Portability and Accountability Act
The Health Insurance Portability and Accountability Act (HIPAA) of 1996,7 specifically Section 194, extends eligibility for FTCA liability protections to VHPs at qualifying free clinics, provided the clinic sponsors the VHPs by applying to the Health Resources and Services Administration.8 It does not require that an emergency be declared before immunity is conferred.
Public Readiness and Emergency Preparedness Act
The Public Readiness and Emergency Preparedness (PREP) Act of 20059 authorizes the US Department of Health and Human Services (HHS) Secretary to issue a declaration that provides immunity to VHPs from tort liability for claims of loss caused by the use of authorized countermeasures (eg, vaccines) against diseases or other threats of public health emergencies.4 A separate emergency determination under Public Health Service Act Section 319 or another statute is not required for PREP Act immunities to take effect.4 The PREP Act covers individual persons and entities involved in the manufacture, testing, distribution, administration, and use of covered countermeasures.4
PREP Act immunity is not absolute and does not protect against claims of willful misconduct, violation of the Americans with Disabilities Act (ADA), or other civil rights violations.4 Liability protection under the PREP Act is limited to a specific emergency and includes only the countermeasures and other conditions listed in the PREP Act declaration by the HHS Secretary.4
State laws and regulations
States have a variety of standing liability protections that could apply to VHPs who provide care in an emergency. Some states have crafted executive orders to be put into effect during a disaster. Most of these executive orders, which can include extending liability protections, are similar to what other states have done by adopting model acts such as Model State Emergency Health Powers Act.6 These orders are not actually laws; they only become effective when the governor signs them at the time of the disaster. These orders also are time-limited and must be reissued in subsequent disasters.
State tort claims acts and state claims acts
Similar to the federal government, some states have waived sovereign immunity in certain circumstances through state tort claims or state claims acts.
Continue to: State tort claims act
State tort claims acts either abolish state sovereign immunity generally and provide immunity only in specific circumstances, or preserve sovereign immunity generally but identify certain exceptions in which immunity is waived.4
State claims acts limit state sovereign immunity by establishing procedures for making claims against the state.4 These acts typically immunize state government employees from tort liability for acts or omissions committed within the scope of their employment.4 Some states extend these protections to volunteers, and some states declare volunteers to be unpaid state employees during an emergency, which allows volunteers to assert the liability protections afforded of state employees.4
Emergency power statutes
State emergency laws can trigger additional powers, suspend certain administrative requirements, and provide or enhance liability protections to specified groups of volunteers and other responders upon a gubernatorial declaration of emergency.4 These statutes can extend the rights and immunities provided to governmental employees to volunteers performing work that is eligible for coverage under governmental immunity and state tort claims acts.4 There is a wide range in the types and degrees of coverage provided to volunteers under emergency powers statutes, and these provisions can be broad or duplicative of other provisions in state law.4
State volunteer protection statutes
All states have some statutory provisions for volunteers. Similar to the VPA, these state volunteer protection statutes generally do not require that an emergency be declared, apply to uncompensated individual volunteers for nonprofit and government entities only, and apply only to individuals and not to organizations.4 Many states have adopted specific liability protections for VHPs in addition to or to supplement their emergency powers and general volunteer protection statutes.4 These statutes confer immunity from civil liability provided that certain conditions are met and are not dependent on the declaration of an emergency.4 Each state statute differs in regard to who receives immunity, which acts are immune from liability, and what liability protections are available.
Good Samaritan laws
All 50 states and the District of Columbia have enacted Good Samaritan laws. These laws, which do not need an official declaration of an emergency in order to be applicable, generally protect VHPs from liability when volunteering in good faith and without compensation at the scene of an emergency.2 Good Samaritan protections may also apply to care provided by VHPs in a hospital if the VHP is not on duty and does not charge a fee.2 However, the effect and scope of Good Samaritan laws vary dramatically from state to state. Some states include hospital settings as an emergency scene in their statutes, while others expressly exclude hospitals from their statutes.6 Some state statutes only include declared emergencies, while others are drawn to broadly cover all emergency situations.6
Continue to: Limitations
Limitations. Many Good Samaritan statutes apply only to volunteers, and not all states have statutes that allow clinicians to be designated as such,6 so receiving compensation would take a clinician outside the scope of the statute. Further, most states only shield action taken at the scene of an accident, and immunity would not extend to a hospital emergency department, or in the aftermath of an emergency as normal conditions slowly return.6 Therefore, Good Samaritan liability protection would apply to the common scenario of assisting at the scene of a car crash, but not necessarily to treating individuals in the emergency department after a hurricane or during a pandemic.6 State laws vary considerably on what constitutes “good faith” and “without compensation,” which would determine whether protection applies for a clinician who is otherwise salaried in a regular job.1
Mutual aid agreements
Mutual aid agreements are mechanisms through which jurisdictions can aid other jurisdictions during emergencies.4 These agreements also include provisions for reimbursing expenses, providing liability protections to governmental employees and volunteers who provide aid, and awarding compensation for injuries to personnel deployed under the agreement.4 These protections are not automatic and are limited in their applicability.
The Emergency Management Assistance Compact (EMAC), the most widely adopted mutual aid agreement in the United States, has been adopted by all 50 states, the District of Columbia, and some territories.10 It only becomes effective once an emergency has been declared. EMAC provides immunity to officers from the state that is rendering aid to the state requesting aid, in which officers are considered agents of the requesting state for tort liability and immunity purposes.8 These individuals, who must be properly dispatched in response to an EMAC request, are not to be held liable for acts or omissions rendered in good faith; however, EMAC does not provide liability protection for actions constituting willful misconduct, gross negligence, or recklessness.6 EMAC also provides reciprocity for individuals who are properly dispatched in response to an EMAC request who hold medical licenses to practice medicine in the receiving state, subject to any limitations imposed by the receiving state.4 Clinicians can familiarize themselves with a state’s medical licensing requirements by reviewing that state’s medical board website. For EMAC protections to apply, a state must make a request to another/other state(s) through EMAC, and such requests must be formally accepted by the rendering state.8 EMAC does not require participating states to actually provide aid.10
Non-volunteer health care clinicians
Non-volunteer (salaried or paid) health care clinicians are more likely to bear the brunt of providing care during a disaster, especially in the early stages before VHPs arrive; however, most legislation does not address the associated disproportionate liability risk burden of non-volunteer health care clinicians.1,11 As opposed to VHPs and government employees, non-volunteer health care clinicians performing their regular job duties during a disaster are generally not provided immunity from negligence by most legislation.1,6 One exception is the PREP Act, which provides immunity for all clinicians from claims that may arise from dispensing a specific countermeasure during a declared public health emergency.1,9 Some states have enacted the Model State Emergency Health Powers Act, which may offer immunity from negligence if the non-volunteer clinician is rendering care under contract with or at the request of a state1; however, non-volunteer clinicians who practice from their office or a local hospital will not receive protection through these laws.1 Good Samaritan laws may not apply unless care is provided at a scene of an emergency.
A few states have attempted to narrow this legislative gap by enacting laws that provide immunity more broadly for clinicians, regardless of their volunteer or compensation status.1 Elements of these states’ laws include acting in response to a declared emergency or disaster in which there is a recognized depletion of resources attributable to the disaster, at express or implied request of the state government, and consistent with emergency plans.1
Continue to: Bottom Line
Bottom Line
There are potential liability risks when treating patients during a disaster. Statutory protections that limit liability may be enacted when the US President or a state Governor declares an official state of emergency. Although some federal and state laws and regulations provide liability protections during these situations, there is a discrepancy in the protections offered to non-volunteer vs volunteer clinicians.
Related Resources
- Federal Emergency Management Agency. https://www.fema.gov/
- Federation of State Medical Boards. https://www.fsmb.org
1. Altman RL, Santucci KA, Anderson MR, et al. American Academy of Pediatrics Committee on Medical Liability and Risk Management. Understanding liability risks and protections for pediatric providers during disasters. Pediatrics. 2019;143(3):e20183893. doi.org/10.1542/peds.2018-3892
2. Lambert K, Wertheimer M. American Professional Agency: Risk management in disaster response. Published September 2017. Accessed May 25, 2021. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/disaster/resource_group/resources/orgs/RMDisasterResp.pdf
3. Federal Torts Claims Act, as amended. Codified at 28 USC. §1346 (1946).
4. Association of State and Territorial Health Officials (ASTHO). Liability, immunity, and workers’ compensation issue in public health emergencies. Published 2012. Accessed May 25, 2021. https://www.astho.org/Programs/Preparedness/Public-Health-Emergency-Law/Emergency-Authority-and-Immunity-Toolkit/Liability,-Immunity,-and-Workers%E2%80%99-Compensation-Issues-in-Public-Health-Emergencies-Issue-Brief/
5. Volunteer Protection Act of 1997. Pub. L. 105-19, 111 Stat. 221.
6. Pope TM, Palazzo MF. Legal briefing: crisis standards of care and legal protections during disasters and emergencies. J Clin Ethics. 2010;21(4):358-367.
7. Health Insurance Portability and Accountability Act of 1996. Pub. L. 104-191, 110 Stat. 1936. https://www.congress.gov/104/plaws/publ191/PLAW-104publ191.pdf
8. American Medical Association. Liability protections for health care professionals during COVID-19. Updated April 8, 2020. Accessed May 25, 2021. https://www.ama-assn.org/practice-management/sustainability/liability-protections-health-care-professionals-during-covid-19
9. Public Readiness and Emergency Preparedness Act of 2005. Pub. L. 109-148, 119 Stat. 2818. https://www.govinfo.gov/content/pkg/PLAW-109publ148/html/PLAW-109publ148.htm
10. Emergency Management Assistance Compact (EMAC). Accessed May 25, 2021. https://www.emacweb.org/
11. Hodge JG, Garcia AM, Anderson ED, et al. Emergency legal preparedness for hospitals and health care personnel. Disaster Med Public Health Prep. 2009;3(2 Supplement):S37-S44. doi: 10.1097/DMP.0b013e31819d977c
1. Altman RL, Santucci KA, Anderson MR, et al. American Academy of Pediatrics Committee on Medical Liability and Risk Management. Understanding liability risks and protections for pediatric providers during disasters. Pediatrics. 2019;143(3):e20183893. doi.org/10.1542/peds.2018-3892
2. Lambert K, Wertheimer M. American Professional Agency: Risk management in disaster response. Published September 2017. Accessed May 25, 2021. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/disaster/resource_group/resources/orgs/RMDisasterResp.pdf
3. Federal Torts Claims Act, as amended. Codified at 28 USC. §1346 (1946).
4. Association of State and Territorial Health Officials (ASTHO). Liability, immunity, and workers’ compensation issue in public health emergencies. Published 2012. Accessed May 25, 2021. https://www.astho.org/Programs/Preparedness/Public-Health-Emergency-Law/Emergency-Authority-and-Immunity-Toolkit/Liability,-Immunity,-and-Workers%E2%80%99-Compensation-Issues-in-Public-Health-Emergencies-Issue-Brief/
5. Volunteer Protection Act of 1997. Pub. L. 105-19, 111 Stat. 221.
6. Pope TM, Palazzo MF. Legal briefing: crisis standards of care and legal protections during disasters and emergencies. J Clin Ethics. 2010;21(4):358-367.
7. Health Insurance Portability and Accountability Act of 1996. Pub. L. 104-191, 110 Stat. 1936. https://www.congress.gov/104/plaws/publ191/PLAW-104publ191.pdf
8. American Medical Association. Liability protections for health care professionals during COVID-19. Updated April 8, 2020. Accessed May 25, 2021. https://www.ama-assn.org/practice-management/sustainability/liability-protections-health-care-professionals-during-covid-19
9. Public Readiness and Emergency Preparedness Act of 2005. Pub. L. 109-148, 119 Stat. 2818. https://www.govinfo.gov/content/pkg/PLAW-109publ148/html/PLAW-109publ148.htm
10. Emergency Management Assistance Compact (EMAC). Accessed May 25, 2021. https://www.emacweb.org/
11. Hodge JG, Garcia AM, Anderson ED, et al. Emergency legal preparedness for hospitals and health care personnel. Disaster Med Public Health Prep. 2009;3(2 Supplement):S37-S44. doi: 10.1097/DMP.0b013e31819d977c