User login
How to ‘cybersecure’ your practice
The health care sector is not immune from cybersecurity attacks (malicious attempts to access or damage a computer or network system). Between October 2019 and October 2021, 857 data breaches were reported to the United States Department of Health and Human Services.1 The 3 main types of breaches reported were theft, hacking/IT incident, or unauthorized access/disclosure.1 Health care has become a common target due to the availability of valuable patient information (health, personal, and financial), the industry’s financial stability and resource capacity, and network susceptibility.2 The top 2 cybersecurity threats facing physician practices are:
- ransomware attacks, in which an external party uses a type of malicious software (malware) that prevents you from accessing your computer files, systems, or networks, and demands you pay a ransom for their return.
- employee-related threats, such as the theft or destruction of sensitive information by a disgruntled employee.3
The financial implications of health care–related cybersecurity threats coupled with exposure to potential litigation associated with breaches of confidentiality result in a need to “cybersecure” your practice.2 In this article, I outline steps to take to protect your practice against such threats. Although the recommendations I provide will increase your practice’s cybersecurity fortification, they are not exhaustive, and you may need to consult with an IT specialist to help protect your data and network.
Improve your network protection. A broadband internet connection is always operating, which makes it continuously susceptible to cybersecurity attacks. Install a firewall (a network security system that monitors and controls network traffic and permits or blocks traffic based on a defined set of rules) between your practice’s internal computer network and the internet.4 For maximum protection, enable all available firewall settings in your operating software.2 Prevent unauthorized access by ensuring that all network passwords are strong (ie, they include a combination of uppercase and lowercase letters, numbers, and symbols). Consider using different networks for online communication and for storing sensitive information.2 Create separate Wi-Fi networks for your practice and for your patients, and use unique passwords for each that are not easily guessed.4 If you or your employees use a virtual private network (VPN) to remotely access your practice’s network, ensure that all devices used to do so (cell phones, tablets, etc) are encrypted and secured with strong passwords.
Reduce employee-related threats. Not every employee in your practice will need to access to your patients’ clinical or financial data. Limiting employee access to sensitive clinical or financial data can reduce the risks of employee-related cybersecurity threats.3 In addition, restrict an employee’s ability to install software on computers and other devices that belong to your practice.2
Frequently incorporate cybersecurity training, such as teaching your employees about the risks of clicking on links and attachments in emails and how to identify phishing attacks (in which an individual sends a fraudulent communication that appears to come from a reputable source in order to trick the recipient into revealing financial information, system credentials, or other sensitive data).2,3 Use multifactor authentication to verify an employee’s login identity, and change passwords often. Reinforce these policies at staff meetings and educate new employees about this process.3 If you need to fire an employee, consider deploying cybersurveillance software to monitor the behavior of all employees before the employee is terminated.3 Once the employee has been terminated, change all logins and passwords.
1. U.S. Department of Health and Human Services. Office for Civil Rights. Breach portal: Notice to the Secretary of HHS breach of unsecured protected health information. Accessed December 26, 2021. https://ocrportal.hhs.gov/ocr/breach/breach_report.jsf
2. Umali G. How to safeguard your practice from cybersecurity threats. Psychiatric News. 2021;56(12):23.
3. Cryts A. Top two cybersecurity threats facing physician practices. Physicians Practice. March 13, 2020. Accessed December 26, 2021. https://www.physicianspractice.com/view/top-two-cybersecurity-threats-facing-physician-practices
4. American Medical Association. Protect your practice and patients from cybersecurity threats. 2017. Accessed December 26, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/government/advocacy/network-security.pdf
The health care sector is not immune from cybersecurity attacks (malicious attempts to access or damage a computer or network system). Between October 2019 and October 2021, 857 data breaches were reported to the United States Department of Health and Human Services.1 The 3 main types of breaches reported were theft, hacking/IT incident, or unauthorized access/disclosure.1 Health care has become a common target due to the availability of valuable patient information (health, personal, and financial), the industry’s financial stability and resource capacity, and network susceptibility.2 The top 2 cybersecurity threats facing physician practices are:
- ransomware attacks, in which an external party uses a type of malicious software (malware) that prevents you from accessing your computer files, systems, or networks, and demands you pay a ransom for their return.
- employee-related threats, such as the theft or destruction of sensitive information by a disgruntled employee.3
The financial implications of health care–related cybersecurity threats coupled with exposure to potential litigation associated with breaches of confidentiality result in a need to “cybersecure” your practice.2 In this article, I outline steps to take to protect your practice against such threats. Although the recommendations I provide will increase your practice’s cybersecurity fortification, they are not exhaustive, and you may need to consult with an IT specialist to help protect your data and network.
Improve your network protection. A broadband internet connection is always operating, which makes it continuously susceptible to cybersecurity attacks. Install a firewall (a network security system that monitors and controls network traffic and permits or blocks traffic based on a defined set of rules) between your practice’s internal computer network and the internet.4 For maximum protection, enable all available firewall settings in your operating software.2 Prevent unauthorized access by ensuring that all network passwords are strong (ie, they include a combination of uppercase and lowercase letters, numbers, and symbols). Consider using different networks for online communication and for storing sensitive information.2 Create separate Wi-Fi networks for your practice and for your patients, and use unique passwords for each that are not easily guessed.4 If you or your employees use a virtual private network (VPN) to remotely access your practice’s network, ensure that all devices used to do so (cell phones, tablets, etc) are encrypted and secured with strong passwords.
Reduce employee-related threats. Not every employee in your practice will need to access to your patients’ clinical or financial data. Limiting employee access to sensitive clinical or financial data can reduce the risks of employee-related cybersecurity threats.3 In addition, restrict an employee’s ability to install software on computers and other devices that belong to your practice.2
Frequently incorporate cybersecurity training, such as teaching your employees about the risks of clicking on links and attachments in emails and how to identify phishing attacks (in which an individual sends a fraudulent communication that appears to come from a reputable source in order to trick the recipient into revealing financial information, system credentials, or other sensitive data).2,3 Use multifactor authentication to verify an employee’s login identity, and change passwords often. Reinforce these policies at staff meetings and educate new employees about this process.3 If you need to fire an employee, consider deploying cybersurveillance software to monitor the behavior of all employees before the employee is terminated.3 Once the employee has been terminated, change all logins and passwords.
The health care sector is not immune from cybersecurity attacks (malicious attempts to access or damage a computer or network system). Between October 2019 and October 2021, 857 data breaches were reported to the United States Department of Health and Human Services.1 The 3 main types of breaches reported were theft, hacking/IT incident, or unauthorized access/disclosure.1 Health care has become a common target due to the availability of valuable patient information (health, personal, and financial), the industry’s financial stability and resource capacity, and network susceptibility.2 The top 2 cybersecurity threats facing physician practices are:
- ransomware attacks, in which an external party uses a type of malicious software (malware) that prevents you from accessing your computer files, systems, or networks, and demands you pay a ransom for their return.
- employee-related threats, such as the theft or destruction of sensitive information by a disgruntled employee.3
The financial implications of health care–related cybersecurity threats coupled with exposure to potential litigation associated with breaches of confidentiality result in a need to “cybersecure” your practice.2 In this article, I outline steps to take to protect your practice against such threats. Although the recommendations I provide will increase your practice’s cybersecurity fortification, they are not exhaustive, and you may need to consult with an IT specialist to help protect your data and network.
Improve your network protection. A broadband internet connection is always operating, which makes it continuously susceptible to cybersecurity attacks. Install a firewall (a network security system that monitors and controls network traffic and permits or blocks traffic based on a defined set of rules) between your practice’s internal computer network and the internet.4 For maximum protection, enable all available firewall settings in your operating software.2 Prevent unauthorized access by ensuring that all network passwords are strong (ie, they include a combination of uppercase and lowercase letters, numbers, and symbols). Consider using different networks for online communication and for storing sensitive information.2 Create separate Wi-Fi networks for your practice and for your patients, and use unique passwords for each that are not easily guessed.4 If you or your employees use a virtual private network (VPN) to remotely access your practice’s network, ensure that all devices used to do so (cell phones, tablets, etc) are encrypted and secured with strong passwords.
Reduce employee-related threats. Not every employee in your practice will need to access to your patients’ clinical or financial data. Limiting employee access to sensitive clinical or financial data can reduce the risks of employee-related cybersecurity threats.3 In addition, restrict an employee’s ability to install software on computers and other devices that belong to your practice.2
Frequently incorporate cybersecurity training, such as teaching your employees about the risks of clicking on links and attachments in emails and how to identify phishing attacks (in which an individual sends a fraudulent communication that appears to come from a reputable source in order to trick the recipient into revealing financial information, system credentials, or other sensitive data).2,3 Use multifactor authentication to verify an employee’s login identity, and change passwords often. Reinforce these policies at staff meetings and educate new employees about this process.3 If you need to fire an employee, consider deploying cybersurveillance software to monitor the behavior of all employees before the employee is terminated.3 Once the employee has been terminated, change all logins and passwords.
1. U.S. Department of Health and Human Services. Office for Civil Rights. Breach portal: Notice to the Secretary of HHS breach of unsecured protected health information. Accessed December 26, 2021. https://ocrportal.hhs.gov/ocr/breach/breach_report.jsf
2. Umali G. How to safeguard your practice from cybersecurity threats. Psychiatric News. 2021;56(12):23.
3. Cryts A. Top two cybersecurity threats facing physician practices. Physicians Practice. March 13, 2020. Accessed December 26, 2021. https://www.physicianspractice.com/view/top-two-cybersecurity-threats-facing-physician-practices
4. American Medical Association. Protect your practice and patients from cybersecurity threats. 2017. Accessed December 26, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/government/advocacy/network-security.pdf
1. U.S. Department of Health and Human Services. Office for Civil Rights. Breach portal: Notice to the Secretary of HHS breach of unsecured protected health information. Accessed December 26, 2021. https://ocrportal.hhs.gov/ocr/breach/breach_report.jsf
2. Umali G. How to safeguard your practice from cybersecurity threats. Psychiatric News. 2021;56(12):23.
3. Cryts A. Top two cybersecurity threats facing physician practices. Physicians Practice. March 13, 2020. Accessed December 26, 2021. https://www.physicianspractice.com/view/top-two-cybersecurity-threats-facing-physician-practices
4. American Medical Association. Protect your practice and patients from cybersecurity threats. 2017. Accessed December 26, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/government/advocacy/network-security.pdf
Suing patients: Medical, ethical, and legal considerations
Although it is common to read about patients suing their hospitals, there has been increasing public and political attention given to hospitals suing their patients to collect unpaid hospital bills. KH’s story began with an emergency appendectomy. She did not have health insurance to cover the $14,000 hospital bill. The family was unable to pay the bill, and the nonprofit hospital sued them for that bill, plus some additional expenses (totaling about $17,000), plus interest was accumulating at 9% per year. The hospital won a judgment, and it garnished the husband’s pay (10% of after-taxes pay, in this case) and placed a lien on the family’s home. Years later—because of interest and additional hospital bills—the family had paid $20,000, but still owed $26,000.1
The extent of the problem
This is neither a hypothetical case nor a rare event. Studies and press reports have noted dozens of examples of hospital collection excesses. One study found that unpaid medical bill lawsuits increased by 37% in Wisconsin between 2001 and 2018, with 5% of hospitals accounting for 25% of the lawsuits.2 Another report found almost “31,000 civil cases filed by 139 hospitals in 26 New York counties from 2015 to 2019.”3 Similar to the Wisconsin report, a small number of health care providers accounted for the majority of lawsuits. In another example, one Missouri nonprofit hospital, Heartland (rebranded “Mosaic”), created its own for-profit debt collection agency (Northwest Financial Services), which filed 11,000 lawsuits from 2009 to 2013, resulting in 6,000 wage garnishments.1 The Wall Street Journal, among others, has reported for years on the difficulties created by lawsuits against patients.4 Axios and Johns Hopkins reported that “medical debt comprises 58% of all debt collections in the United States.” And although some collection actions declined early in the pandemic, it did not appear to last.5,6
Inconsistent collection policies. Collection policies vary greatly from hospital to hospital, with an increasing number of hospitals demanding up-front payments (before services). Many of these health care institutions persuade patients to put medical debt on their credit cards, sometimes as part of an up-front (before service) process.7 If using a standard credit card, this comes with a very high interest rate. There are some special health-related credit cards, such as CareCredit, that generally have better interest rates. These cards offer no-interest short-term loans, with significant interest for longer-term loans. Thus, failure to repay the full amount when due means that the “deferred interest” (about 27%) must be paid.8 Also any of the problems patients have repaying a credit card (or other loan), of course, are no longer directly related to the hospital. These “indirect collections” still burden patients with medical debt.
Where you go matters. Because there is no common collection policy or practice among hospitals, choosing the wrong hospital may result in a lawsuit. A careful study of lawsuits for medical debt or garnishments related to that debt in 2017 in Virginia showed how being treated at certain hospitals dramatically changed the odds of wage garnishment for unpaid bills.9 It revealed that 29,286 hospital lawsuits were filed to collect medical debt—9,232 of which were wage garnishments (the most aggressive form of debt collection). Five hospitals alone accounted for the majority of garnishments in the state. Notably, nonprofit hospitals accounted for 71% of the garnishment cases. On the other hand, about 50% of the hospitals in the study did not file any lawsuits to garnish wages for medical debt.9
Why is there so much hospital debt?
One would think the Affordable Care Act (ACA) and other reforms would mean fewer people do not have health insurance—and the problems experienced by the patient in the case above. Indeed, the number of insured has increased in the United States, including through the expansion of Medicaid. Nonetheless, in 2020, the Census Bureau reported that 28 million people did not have health insurance for any part of the year; that figure would be higher if those who had insurance for only part of the year were included.10
One reason for medical debt is the very high level of “under” insurance—that is, even with health insurance, copays for significant medical bills exceed what the patient can pay. Nearly half of adults (excluding the elderly) were enrolled in high-deductible health plans (in 2017).11 Among most employment-based plans, deductibles and co-pays have been going up for a decade.12 Overall, 20% of employer-provided plans had deductibles in excess of $3,000 ($5,000 for families).13 Of course, many families do not have anywhere near the resources to pay high deductibles, and that represents likely medical debt. The more modest copays of Medicare (often 20%) can be enough to push some elderly individuals beyond their capacity to pay.
“Out-of-network” care also may result in large hospital charges—and debt. Emergency care, for example, may be sought from the closest provider, even though out of network, and the insurance company may refuse to pay the charges. Another surprise form of billing is when a health care insurance company tentatively approves coverage and then after the patient receives care, determines it was unnecessary. In that case, even in-network charges may be denied, with the patient left to pay all the charges.
Continue to: How medical debt affects patients...
How medical debt affects patients
For patients, medical debt places pressure on their financial circumstances. Bankruptcy has a profound financial impact, and approximately two-thirds of bankruptcies are related to medical care costs and debt, including “indirect collection.”14 Even when the financial effect is not so devastating, it is often substantial, as the above case demonstrated. In a 2018 survey, almost 30% of those with health insurance had medical debts in some form of collection action, and 25% of those individuals said they did not know they owed the money.15 The same survey found that 20% of respondents had medical debt that adversely affected their credit scores and access to credit.15
At work, although employers are not supposed to treat employees adversely because of garnishment, some employers may not adhere to that rule. Furthermore, employees may believe or be concerned that the very existence of garnishment may penalize them at their current job or make it difficult to move to a better one.16
Lastly, patients with medical debt may be reluctant to seek needed medical care. They may be concerned about adding more medical debt or embarrassed or afraid that they would not be welcome at the hospital where they owe money.7
Public perception of hospitals
Lawsuits against patients also have a negative effect on hospitals—and it is not limited to the relatively few institutions that file many of these lawsuits each year. Press reports about lawsuits against patients garner great public interest and anger, and this tarnishes the image of heath care facilities in general because many people often do not distinguish the actions of a few institutions.
The sensitivity of health care organizations to bad publicity from debt collection practices was seen in a follow-up study of the previously discussed Virginia data. In the year following this report, there was a 59% decrease in the number of lawsuits filed, including a 66% decrease in garnishments.17 Eleven hospitals in the state that had been filing debt lawsuits stopped doing so.17
Medical debt: The obligation of nonprofit hospitals
The response seen in the Virginia follow-up study may also reflect well-founded concern from board members about political consequences and even taxation problems. The majority of hospitals, including those in these studies, are nonprofit institutions with an Internal Revenue Service (IRS) 501(c)(3) “tax-exempt” status. (Note, “nonprofit” does not mean that the organization does not make a profit, but that the profit does not accrue to individuals.) The “nonprofit” status is usually granted by states, but the federal tax-exempt status is granted by the IRS. This status exempts the institutions from paying most federal taxes, and (perhaps most importantly) qualifies donors to receive tax deductions (and similar benefits) for donations made to these hospitals. This important tax treatment is granted based on the theory that their services are so valuable to the public that advancing their work through the tax exemption ultimately benefits the public more than the tax revenue would.
In return for these benefits, the organization has obligations to work in the public interest. For years, hospitals have been criticized for not providing sufficient public benefits (compared, for example, with for-profit hospitals) to justify the tax exemption. That criticism caused the IRS to begin requiring a special Form 990, Schedule H, which is attached to the usual 501(c)(3) informational tax return, “to provide information on the activities and policies of, and community benefit provided by, its hospital facilities and other non-hospital health care facilities.”18 Part III of Schedule H asks, in part, about bad debt and collection practices.
Then the ACA Section 501(r) enhanced the obligation of nonprofit health facilities to provide charitable care in two ways. First, they must have, and make available, policies to provide free and discounted care; and second, they cannot sue for payment until they make an individualized determination as to whether the patient should have received discounted care or financial assistance.19
Thus aggressive collection practices (which should include “indirect collection”) invite special scrutiny by local officials and the IRS. In the longer-term, concern that tax-exempt hospitals are not truly operating in the public interest is undoubtedly amplified by these aggressive debt collection practices. How can a hospital claim it is truly operating in the public interest when it sues dozens of modest-income individuals each year?
Regulating medical debt and its collection
The No Surprises Act
In December 2020, Congress adopted the No Surprises Act to address some of the problems of patient debt.20 Among other things, the act protects patients “from receiving surprise medical bills when they receive most emergency services,” or when they are in an in-network hospital but receive services from out-of-network providers (such as anesthesia and radiology).21 Several states also have similar legislation, so the federal law specifically states that where state laws are more protective of patients, the state’s higher protections apply, and vice versa. The act took effect on January 1, 2022, though there is an “interim final” regulation that will be subject to change, and there is already litigation over those regulations.22 The real complexity of the rules will arise through the regulations, which are likely to change several times over the next few years. To help with this, the American Medical Association has an extensive toolkit for health care providers.23
Continue to: Additional regulations...
Additional regulations
Both the federal government and most states are likely to take additional action to reduce hospital debt lawsuits. Some proposals sound simple enough but would have significant complications. For example, governments could prohibit all lawsuits that collect hospital debt.7 Such a regulation would mean that paying hospital debts would essentially become optional. Imagine the millionaire who does not want to pay a $25,000 hospital charge; or patients with other debts who would pay those off before the hospital debt. The regulation might have income or asset limits on debt collection lawsuits and the like, but it quickly becomes complicated. Furthermore, to protect themselves, hospitals would undoubtedly become much more aggressive about requiring up-front payments—which would force the debt or prepayment onto credit cards or similar debt obligations that are not subject to the no collection lawsuit rule.
Public reporting. The follow-up study in Virginia17 suggests that requiring public reporting of the number of cases filed by or on behalf of (directly or indirectly) each hospital may help. Hospitals would, of course, have incentives to make their figures look better, perhaps by selling the debt to an agency that would be able to file suit in its name rather than the hospital’s name. These might be little more than indirect collections. For reporting purposes, any form of transferring debt might be considered filing a lawsuit. The problem, noted earlier, about requiring prepayment or credit cards would also exist.
Get the board involved. A different approach would be to ensure that a hospital’s board of trustees is involved in setting and overseeing debt collection policies. For example, the law might require boards to annually consider and adopt specific debt collection practices—including indirect collection efforts. Boards should already be doing something similar to this, but regulation might be an inexpensive way to ensure it is done—and in a manner consistent with the organization’s values. Another suggestion is to require the board to approve any legal action against specific patients.7 By making sure this is not just another item on the consent agenda, the oversight would probably reduce automatic debt collection processes.
Expand IRS reporting requirements for nonprofits. Indeed, for nonprofit hospitals with 501(c)(3) obligations, the Form 990, Schedule H already provides some information about collection actions and uncompensated care, and this is enhanced by the ACA Section 501(r). These could be expanded and perhaps include “indirect” collections. The IRS could “flag” hospitals with high total litigation and similar collection actions, and ask the hospital to provide a detailed explanation for each action and how it was consistent with the obligation to serve the public (thereby justifying the exempt taxation status, an idea proposed by the US Government Accountability Office in 2020).24
Ensure the hospital’s actions reflect their mission and values
Hospitals are created to provide medical care for people and to improve the human condition. Those who lead them should, and generally do, share that purpose. The apparent collection policies that have garnered negative public attention suggest that some of these institutions have lost focus of their ultimate mission and values. The boards and executives of these health care institutions, as well as the medical professionals and attorneys who serve them, should be continuously guided by those values.
Important decisions—including collection and prepayment processes—reflect the values of the institution. Failure to ensure these procedures are in line with the organization’s mission is an embarrassment to all health care facilities, including the majority of hospitals that do not engage in these aggressive collection practices. Not addressing these issues will likely result in political and legal action—blunt and inefficient instruments—to limit what the public sees as wrongdoing. ●
- Kiel P. From the E.R. to the courtroom: how nonprofit hospitals are seizing patients’ wages. ProPublica. December 19, 2014. Accessed March 21, 2022. https://www.propublica.org/article/how-nonprofit-hospitals-are-seizing-patients-wages
- Cooper Z, Han J, Mahoney N. Hospital lawsuits over unpaid bills increased by 37 percent in Wisconsin from 2001 to 2018. Health Affairs. 2021;40:1830-1835. Accessed March 21, 2022. https://www.healthaffairs.org/doi/full/10.1377 /hlthaff.2021.01130
- LaMantia J. New York hospitals have filed thousands of lawsuits against patients. Modern Healthcare. March 13, 2020. Accessed March 21, 2022. https://www.modernhealthcare .com/legal/new-york-hospitals-have-filed-thousands -lawsuits-against-patients
- Armour S. When patients can’t pay, many hospitals are suing. Wall Street Journal. June 25, 2019. Accessed March 21, 2022. https://www.wsj.com/articles/nonprofit-hospitals-criticized-for-debt-collection-tactics-11561467600
- McGhee M, Chase W. How America’s top hospitals hound patients with predatory billing. Axios. Accessed March 21, 2022. https://www.axios.com/hospital-billing
- Owens C. Public spotlight on hospital lawsuits may slow them down. June 14, 2021. Accessed March 22, 2022. https:// www.axios.com/hospital-lawsuits-slowing-down-media -35ce395a-9fe3-4b23-b815-d7b06cce2773.html
- Buck ID. When hospitals sue patients. Hastings L.J. 2022;73:191-232, at 209-211. Accessed March 21, 2022. https:// repository.uchastings.edu/cgi/viewcontent.cgi?article =3961&context=hastings_law_journal
- Lagasse J. Healthcare turns to zero-interest loans to give patients a better reason to pay. Healthcare Finance. May 3, 2017. Accessed March 21, 2022. https://www.healthcarefinancenews.com/news/healthcare-turns-zero-interest-loans-give-patients-better-reason-pay#:~:text=Zero%2Dinterest%20loans%20are%20finding,of%20the%20patient%2Dprovider%20relationship.
- Bruhn WE, Rutkow L, Wang P, et al. Prevalence and characteristics of Virginia hospitals suing patients and garnishing wages for unpaid medical bills. JAMA. 2019;322:691-692. doi:10.1001/jama.2019.9144
- Keisler-Starkey K, Bunch LN. Health insurance coverage in the United States: 2020. September 14, 2021. United States Census Bureau Current Population Reports, P60-274. US Government Publishing Office; September 2021. Accessed March 21, 2022. https://www.census.gov/content/dam /Census/library/publications/2021/demo/p60-274.pdf
- Cohen RA, Zammitti EP. High-deductible health plan enrollment among adults aged 18-64 with employment-based insurance coverage. NCHS Data Brief, No. 317. August 2018. Accessed March 21, 2022. https://www.cdc.gov/nchs/data/databriefs/db317.pdf
- Kaiser Family Foundation. Employer health benefits: 2020 summary of findings. Accessed March 21, 2022. https://www.kff.org/report-section/ehbs-2020-summary-of-findings/
- Picchi A. Higher health insurance deductibles a sickening trend for Americans. CBS NEWS. June 13, 2019. Accessed March 21, 2022. https://www.cbsnews.com/news/high-health-insurance-deductibles-a-sickening-trend-thats -causing-financial-hardship/
- Himmelstein DU, Lawless RM, Thorne D, Foohey P, Woolhandler S. Medical bankruptcy: still common despite the Affordable Care Act. Am J Public Health. 2019;109:431-433. doi:10.2105/AJPH.2018.304901
- Rosato D. What medical debt does to your credit score. Consumer Reports. July 26, 2018. Accessed March 21, 2022. https://www.consumerreports.org/credit-scores-reports/what-medical-debt-does-to-your-credit-score/
- State laws on wage garnishments. Nolo web site. https://www.nolo.com/legal-encyclopedia/free-books/employee-rights-book/chapter2-9.html. Accessed April 1, 2022.
- Patruzo JGR, Hashim F, Dun C, et al. Trends in hospital lawsuits filed against patients for unpaid bills following published research about their activity. JAMA Network Open. 2021;4:e2121926. doi:10.1001/jamanetworkopen.2021.21926
- About Schedule H (Form 990), hospitals. IRS. Updated June 10, 2021. Accessed March 21, 2022. https://www.irs.gov/forms-pubs/about-schedule-h-form-990
- Requirements for 501(c)(3) hospitals under the Affordable Care Act – Section 501(r). Updated September 9, 2021. Accessed March 21, 2022. https://www.irs.gov/charities-non-profits/charitable-organizations/requirements-for-501c3-hospitals-under-the-affordable-care-act-section-501r
- Pub. L. No. 116-260, 134 Stat. 1182, Division BB, § 109.
- Fact sheet. No Surprises: understand your rights against surprise medical bills. Centers for Medicare and Medicaid Services. January 3, 2022. Accessed March 21, 2022. https://www.cms.gov/newsroom/fact-sheets/no-surprises-understand-your-rights-against-surprise-medical-bills
- Implementation of the No Surprises Act. Accessed March 21, 2022. https://www.ama-assn.org/delivering-care/patient-support-advocacy/implementation-no-surprises-act
- American Medical Association. Toolkit for physicians: preparing for implementation of the No Surprises Act. January 2022. Accessed March 21, 2022. https://www.ama-assn.org/system/files/ama-nsa-toolkit.pdf
- US Government Accountability Office. Tax administration: opportunities exist to improve oversight of hospitals’ taxexempt status. September 2020. Accessed March 21, 2022. https://www.gao.gov/assets/gao-20-679.pdf
Although it is common to read about patients suing their hospitals, there has been increasing public and political attention given to hospitals suing their patients to collect unpaid hospital bills. KH’s story began with an emergency appendectomy. She did not have health insurance to cover the $14,000 hospital bill. The family was unable to pay the bill, and the nonprofit hospital sued them for that bill, plus some additional expenses (totaling about $17,000), plus interest was accumulating at 9% per year. The hospital won a judgment, and it garnished the husband’s pay (10% of after-taxes pay, in this case) and placed a lien on the family’s home. Years later—because of interest and additional hospital bills—the family had paid $20,000, but still owed $26,000.1
The extent of the problem
This is neither a hypothetical case nor a rare event. Studies and press reports have noted dozens of examples of hospital collection excesses. One study found that unpaid medical bill lawsuits increased by 37% in Wisconsin between 2001 and 2018, with 5% of hospitals accounting for 25% of the lawsuits.2 Another report found almost “31,000 civil cases filed by 139 hospitals in 26 New York counties from 2015 to 2019.”3 Similar to the Wisconsin report, a small number of health care providers accounted for the majority of lawsuits. In another example, one Missouri nonprofit hospital, Heartland (rebranded “Mosaic”), created its own for-profit debt collection agency (Northwest Financial Services), which filed 11,000 lawsuits from 2009 to 2013, resulting in 6,000 wage garnishments.1 The Wall Street Journal, among others, has reported for years on the difficulties created by lawsuits against patients.4 Axios and Johns Hopkins reported that “medical debt comprises 58% of all debt collections in the United States.” And although some collection actions declined early in the pandemic, it did not appear to last.5,6
Inconsistent collection policies. Collection policies vary greatly from hospital to hospital, with an increasing number of hospitals demanding up-front payments (before services). Many of these health care institutions persuade patients to put medical debt on their credit cards, sometimes as part of an up-front (before service) process.7 If using a standard credit card, this comes with a very high interest rate. There are some special health-related credit cards, such as CareCredit, that generally have better interest rates. These cards offer no-interest short-term loans, with significant interest for longer-term loans. Thus, failure to repay the full amount when due means that the “deferred interest” (about 27%) must be paid.8 Also any of the problems patients have repaying a credit card (or other loan), of course, are no longer directly related to the hospital. These “indirect collections” still burden patients with medical debt.
Where you go matters. Because there is no common collection policy or practice among hospitals, choosing the wrong hospital may result in a lawsuit. A careful study of lawsuits for medical debt or garnishments related to that debt in 2017 in Virginia showed how being treated at certain hospitals dramatically changed the odds of wage garnishment for unpaid bills.9 It revealed that 29,286 hospital lawsuits were filed to collect medical debt—9,232 of which were wage garnishments (the most aggressive form of debt collection). Five hospitals alone accounted for the majority of garnishments in the state. Notably, nonprofit hospitals accounted for 71% of the garnishment cases. On the other hand, about 50% of the hospitals in the study did not file any lawsuits to garnish wages for medical debt.9
Why is there so much hospital debt?
One would think the Affordable Care Act (ACA) and other reforms would mean fewer people do not have health insurance—and the problems experienced by the patient in the case above. Indeed, the number of insured has increased in the United States, including through the expansion of Medicaid. Nonetheless, in 2020, the Census Bureau reported that 28 million people did not have health insurance for any part of the year; that figure would be higher if those who had insurance for only part of the year were included.10
One reason for medical debt is the very high level of “under” insurance—that is, even with health insurance, copays for significant medical bills exceed what the patient can pay. Nearly half of adults (excluding the elderly) were enrolled in high-deductible health plans (in 2017).11 Among most employment-based plans, deductibles and co-pays have been going up for a decade.12 Overall, 20% of employer-provided plans had deductibles in excess of $3,000 ($5,000 for families).13 Of course, many families do not have anywhere near the resources to pay high deductibles, and that represents likely medical debt. The more modest copays of Medicare (often 20%) can be enough to push some elderly individuals beyond their capacity to pay.
“Out-of-network” care also may result in large hospital charges—and debt. Emergency care, for example, may be sought from the closest provider, even though out of network, and the insurance company may refuse to pay the charges. Another surprise form of billing is when a health care insurance company tentatively approves coverage and then after the patient receives care, determines it was unnecessary. In that case, even in-network charges may be denied, with the patient left to pay all the charges.
Continue to: How medical debt affects patients...
How medical debt affects patients
For patients, medical debt places pressure on their financial circumstances. Bankruptcy has a profound financial impact, and approximately two-thirds of bankruptcies are related to medical care costs and debt, including “indirect collection.”14 Even when the financial effect is not so devastating, it is often substantial, as the above case demonstrated. In a 2018 survey, almost 30% of those with health insurance had medical debts in some form of collection action, and 25% of those individuals said they did not know they owed the money.15 The same survey found that 20% of respondents had medical debt that adversely affected their credit scores and access to credit.15
At work, although employers are not supposed to treat employees adversely because of garnishment, some employers may not adhere to that rule. Furthermore, employees may believe or be concerned that the very existence of garnishment may penalize them at their current job or make it difficult to move to a better one.16
Lastly, patients with medical debt may be reluctant to seek needed medical care. They may be concerned about adding more medical debt or embarrassed or afraid that they would not be welcome at the hospital where they owe money.7
Public perception of hospitals
Lawsuits against patients also have a negative effect on hospitals—and it is not limited to the relatively few institutions that file many of these lawsuits each year. Press reports about lawsuits against patients garner great public interest and anger, and this tarnishes the image of heath care facilities in general because many people often do not distinguish the actions of a few institutions.
The sensitivity of health care organizations to bad publicity from debt collection practices was seen in a follow-up study of the previously discussed Virginia data. In the year following this report, there was a 59% decrease in the number of lawsuits filed, including a 66% decrease in garnishments.17 Eleven hospitals in the state that had been filing debt lawsuits stopped doing so.17
Medical debt: The obligation of nonprofit hospitals
The response seen in the Virginia follow-up study may also reflect well-founded concern from board members about political consequences and even taxation problems. The majority of hospitals, including those in these studies, are nonprofit institutions with an Internal Revenue Service (IRS) 501(c)(3) “tax-exempt” status. (Note, “nonprofit” does not mean that the organization does not make a profit, but that the profit does not accrue to individuals.) The “nonprofit” status is usually granted by states, but the federal tax-exempt status is granted by the IRS. This status exempts the institutions from paying most federal taxes, and (perhaps most importantly) qualifies donors to receive tax deductions (and similar benefits) for donations made to these hospitals. This important tax treatment is granted based on the theory that their services are so valuable to the public that advancing their work through the tax exemption ultimately benefits the public more than the tax revenue would.
In return for these benefits, the organization has obligations to work in the public interest. For years, hospitals have been criticized for not providing sufficient public benefits (compared, for example, with for-profit hospitals) to justify the tax exemption. That criticism caused the IRS to begin requiring a special Form 990, Schedule H, which is attached to the usual 501(c)(3) informational tax return, “to provide information on the activities and policies of, and community benefit provided by, its hospital facilities and other non-hospital health care facilities.”18 Part III of Schedule H asks, in part, about bad debt and collection practices.
Then the ACA Section 501(r) enhanced the obligation of nonprofit health facilities to provide charitable care in two ways. First, they must have, and make available, policies to provide free and discounted care; and second, they cannot sue for payment until they make an individualized determination as to whether the patient should have received discounted care or financial assistance.19
Thus aggressive collection practices (which should include “indirect collection”) invite special scrutiny by local officials and the IRS. In the longer-term, concern that tax-exempt hospitals are not truly operating in the public interest is undoubtedly amplified by these aggressive debt collection practices. How can a hospital claim it is truly operating in the public interest when it sues dozens of modest-income individuals each year?
Regulating medical debt and its collection
The No Surprises Act
In December 2020, Congress adopted the No Surprises Act to address some of the problems of patient debt.20 Among other things, the act protects patients “from receiving surprise medical bills when they receive most emergency services,” or when they are in an in-network hospital but receive services from out-of-network providers (such as anesthesia and radiology).21 Several states also have similar legislation, so the federal law specifically states that where state laws are more protective of patients, the state’s higher protections apply, and vice versa. The act took effect on January 1, 2022, though there is an “interim final” regulation that will be subject to change, and there is already litigation over those regulations.22 The real complexity of the rules will arise through the regulations, which are likely to change several times over the next few years. To help with this, the American Medical Association has an extensive toolkit for health care providers.23
Continue to: Additional regulations...
Additional regulations
Both the federal government and most states are likely to take additional action to reduce hospital debt lawsuits. Some proposals sound simple enough but would have significant complications. For example, governments could prohibit all lawsuits that collect hospital debt.7 Such a regulation would mean that paying hospital debts would essentially become optional. Imagine the millionaire who does not want to pay a $25,000 hospital charge; or patients with other debts who would pay those off before the hospital debt. The regulation might have income or asset limits on debt collection lawsuits and the like, but it quickly becomes complicated. Furthermore, to protect themselves, hospitals would undoubtedly become much more aggressive about requiring up-front payments—which would force the debt or prepayment onto credit cards or similar debt obligations that are not subject to the no collection lawsuit rule.
Public reporting. The follow-up study in Virginia17 suggests that requiring public reporting of the number of cases filed by or on behalf of (directly or indirectly) each hospital may help. Hospitals would, of course, have incentives to make their figures look better, perhaps by selling the debt to an agency that would be able to file suit in its name rather than the hospital’s name. These might be little more than indirect collections. For reporting purposes, any form of transferring debt might be considered filing a lawsuit. The problem, noted earlier, about requiring prepayment or credit cards would also exist.
Get the board involved. A different approach would be to ensure that a hospital’s board of trustees is involved in setting and overseeing debt collection policies. For example, the law might require boards to annually consider and adopt specific debt collection practices—including indirect collection efforts. Boards should already be doing something similar to this, but regulation might be an inexpensive way to ensure it is done—and in a manner consistent with the organization’s values. Another suggestion is to require the board to approve any legal action against specific patients.7 By making sure this is not just another item on the consent agenda, the oversight would probably reduce automatic debt collection processes.
Expand IRS reporting requirements for nonprofits. Indeed, for nonprofit hospitals with 501(c)(3) obligations, the Form 990, Schedule H already provides some information about collection actions and uncompensated care, and this is enhanced by the ACA Section 501(r). These could be expanded and perhaps include “indirect” collections. The IRS could “flag” hospitals with high total litigation and similar collection actions, and ask the hospital to provide a detailed explanation for each action and how it was consistent with the obligation to serve the public (thereby justifying the exempt taxation status, an idea proposed by the US Government Accountability Office in 2020).24
Ensure the hospital’s actions reflect their mission and values
Hospitals are created to provide medical care for people and to improve the human condition. Those who lead them should, and generally do, share that purpose. The apparent collection policies that have garnered negative public attention suggest that some of these institutions have lost focus of their ultimate mission and values. The boards and executives of these health care institutions, as well as the medical professionals and attorneys who serve them, should be continuously guided by those values.
Important decisions—including collection and prepayment processes—reflect the values of the institution. Failure to ensure these procedures are in line with the organization’s mission is an embarrassment to all health care facilities, including the majority of hospitals that do not engage in these aggressive collection practices. Not addressing these issues will likely result in political and legal action—blunt and inefficient instruments—to limit what the public sees as wrongdoing. ●
Although it is common to read about patients suing their hospitals, there has been increasing public and political attention given to hospitals suing their patients to collect unpaid hospital bills. KH’s story began with an emergency appendectomy. She did not have health insurance to cover the $14,000 hospital bill. The family was unable to pay the bill, and the nonprofit hospital sued them for that bill, plus some additional expenses (totaling about $17,000), plus interest was accumulating at 9% per year. The hospital won a judgment, and it garnished the husband’s pay (10% of after-taxes pay, in this case) and placed a lien on the family’s home. Years later—because of interest and additional hospital bills—the family had paid $20,000, but still owed $26,000.1
The extent of the problem
This is neither a hypothetical case nor a rare event. Studies and press reports have noted dozens of examples of hospital collection excesses. One study found that unpaid medical bill lawsuits increased by 37% in Wisconsin between 2001 and 2018, with 5% of hospitals accounting for 25% of the lawsuits.2 Another report found almost “31,000 civil cases filed by 139 hospitals in 26 New York counties from 2015 to 2019.”3 Similar to the Wisconsin report, a small number of health care providers accounted for the majority of lawsuits. In another example, one Missouri nonprofit hospital, Heartland (rebranded “Mosaic”), created its own for-profit debt collection agency (Northwest Financial Services), which filed 11,000 lawsuits from 2009 to 2013, resulting in 6,000 wage garnishments.1 The Wall Street Journal, among others, has reported for years on the difficulties created by lawsuits against patients.4 Axios and Johns Hopkins reported that “medical debt comprises 58% of all debt collections in the United States.” And although some collection actions declined early in the pandemic, it did not appear to last.5,6
Inconsistent collection policies. Collection policies vary greatly from hospital to hospital, with an increasing number of hospitals demanding up-front payments (before services). Many of these health care institutions persuade patients to put medical debt on their credit cards, sometimes as part of an up-front (before service) process.7 If using a standard credit card, this comes with a very high interest rate. There are some special health-related credit cards, such as CareCredit, that generally have better interest rates. These cards offer no-interest short-term loans, with significant interest for longer-term loans. Thus, failure to repay the full amount when due means that the “deferred interest” (about 27%) must be paid.8 Also any of the problems patients have repaying a credit card (or other loan), of course, are no longer directly related to the hospital. These “indirect collections” still burden patients with medical debt.
Where you go matters. Because there is no common collection policy or practice among hospitals, choosing the wrong hospital may result in a lawsuit. A careful study of lawsuits for medical debt or garnishments related to that debt in 2017 in Virginia showed how being treated at certain hospitals dramatically changed the odds of wage garnishment for unpaid bills.9 It revealed that 29,286 hospital lawsuits were filed to collect medical debt—9,232 of which were wage garnishments (the most aggressive form of debt collection). Five hospitals alone accounted for the majority of garnishments in the state. Notably, nonprofit hospitals accounted for 71% of the garnishment cases. On the other hand, about 50% of the hospitals in the study did not file any lawsuits to garnish wages for medical debt.9
Why is there so much hospital debt?
One would think the Affordable Care Act (ACA) and other reforms would mean fewer people do not have health insurance—and the problems experienced by the patient in the case above. Indeed, the number of insured has increased in the United States, including through the expansion of Medicaid. Nonetheless, in 2020, the Census Bureau reported that 28 million people did not have health insurance for any part of the year; that figure would be higher if those who had insurance for only part of the year were included.10
One reason for medical debt is the very high level of “under” insurance—that is, even with health insurance, copays for significant medical bills exceed what the patient can pay. Nearly half of adults (excluding the elderly) were enrolled in high-deductible health plans (in 2017).11 Among most employment-based plans, deductibles and co-pays have been going up for a decade.12 Overall, 20% of employer-provided plans had deductibles in excess of $3,000 ($5,000 for families).13 Of course, many families do not have anywhere near the resources to pay high deductibles, and that represents likely medical debt. The more modest copays of Medicare (often 20%) can be enough to push some elderly individuals beyond their capacity to pay.
“Out-of-network” care also may result in large hospital charges—and debt. Emergency care, for example, may be sought from the closest provider, even though out of network, and the insurance company may refuse to pay the charges. Another surprise form of billing is when a health care insurance company tentatively approves coverage and then after the patient receives care, determines it was unnecessary. In that case, even in-network charges may be denied, with the patient left to pay all the charges.
Continue to: How medical debt affects patients...
How medical debt affects patients
For patients, medical debt places pressure on their financial circumstances. Bankruptcy has a profound financial impact, and approximately two-thirds of bankruptcies are related to medical care costs and debt, including “indirect collection.”14 Even when the financial effect is not so devastating, it is often substantial, as the above case demonstrated. In a 2018 survey, almost 30% of those with health insurance had medical debts in some form of collection action, and 25% of those individuals said they did not know they owed the money.15 The same survey found that 20% of respondents had medical debt that adversely affected their credit scores and access to credit.15
At work, although employers are not supposed to treat employees adversely because of garnishment, some employers may not adhere to that rule. Furthermore, employees may believe or be concerned that the very existence of garnishment may penalize them at their current job or make it difficult to move to a better one.16
Lastly, patients with medical debt may be reluctant to seek needed medical care. They may be concerned about adding more medical debt or embarrassed or afraid that they would not be welcome at the hospital where they owe money.7
Public perception of hospitals
Lawsuits against patients also have a negative effect on hospitals—and it is not limited to the relatively few institutions that file many of these lawsuits each year. Press reports about lawsuits against patients garner great public interest and anger, and this tarnishes the image of heath care facilities in general because many people often do not distinguish the actions of a few institutions.
The sensitivity of health care organizations to bad publicity from debt collection practices was seen in a follow-up study of the previously discussed Virginia data. In the year following this report, there was a 59% decrease in the number of lawsuits filed, including a 66% decrease in garnishments.17 Eleven hospitals in the state that had been filing debt lawsuits stopped doing so.17
Medical debt: The obligation of nonprofit hospitals
The response seen in the Virginia follow-up study may also reflect well-founded concern from board members about political consequences and even taxation problems. The majority of hospitals, including those in these studies, are nonprofit institutions with an Internal Revenue Service (IRS) 501(c)(3) “tax-exempt” status. (Note, “nonprofit” does not mean that the organization does not make a profit, but that the profit does not accrue to individuals.) The “nonprofit” status is usually granted by states, but the federal tax-exempt status is granted by the IRS. This status exempts the institutions from paying most federal taxes, and (perhaps most importantly) qualifies donors to receive tax deductions (and similar benefits) for donations made to these hospitals. This important tax treatment is granted based on the theory that their services are so valuable to the public that advancing their work through the tax exemption ultimately benefits the public more than the tax revenue would.
In return for these benefits, the organization has obligations to work in the public interest. For years, hospitals have been criticized for not providing sufficient public benefits (compared, for example, with for-profit hospitals) to justify the tax exemption. That criticism caused the IRS to begin requiring a special Form 990, Schedule H, which is attached to the usual 501(c)(3) informational tax return, “to provide information on the activities and policies of, and community benefit provided by, its hospital facilities and other non-hospital health care facilities.”18 Part III of Schedule H asks, in part, about bad debt and collection practices.
Then the ACA Section 501(r) enhanced the obligation of nonprofit health facilities to provide charitable care in two ways. First, they must have, and make available, policies to provide free and discounted care; and second, they cannot sue for payment until they make an individualized determination as to whether the patient should have received discounted care or financial assistance.19
Thus aggressive collection practices (which should include “indirect collection”) invite special scrutiny by local officials and the IRS. In the longer-term, concern that tax-exempt hospitals are not truly operating in the public interest is undoubtedly amplified by these aggressive debt collection practices. How can a hospital claim it is truly operating in the public interest when it sues dozens of modest-income individuals each year?
Regulating medical debt and its collection
The No Surprises Act
In December 2020, Congress adopted the No Surprises Act to address some of the problems of patient debt.20 Among other things, the act protects patients “from receiving surprise medical bills when they receive most emergency services,” or when they are in an in-network hospital but receive services from out-of-network providers (such as anesthesia and radiology).21 Several states also have similar legislation, so the federal law specifically states that where state laws are more protective of patients, the state’s higher protections apply, and vice versa. The act took effect on January 1, 2022, though there is an “interim final” regulation that will be subject to change, and there is already litigation over those regulations.22 The real complexity of the rules will arise through the regulations, which are likely to change several times over the next few years. To help with this, the American Medical Association has an extensive toolkit for health care providers.23
Continue to: Additional regulations...
Additional regulations
Both the federal government and most states are likely to take additional action to reduce hospital debt lawsuits. Some proposals sound simple enough but would have significant complications. For example, governments could prohibit all lawsuits that collect hospital debt.7 Such a regulation would mean that paying hospital debts would essentially become optional. Imagine the millionaire who does not want to pay a $25,000 hospital charge; or patients with other debts who would pay those off before the hospital debt. The regulation might have income or asset limits on debt collection lawsuits and the like, but it quickly becomes complicated. Furthermore, to protect themselves, hospitals would undoubtedly become much more aggressive about requiring up-front payments—which would force the debt or prepayment onto credit cards or similar debt obligations that are not subject to the no collection lawsuit rule.
Public reporting. The follow-up study in Virginia17 suggests that requiring public reporting of the number of cases filed by or on behalf of (directly or indirectly) each hospital may help. Hospitals would, of course, have incentives to make their figures look better, perhaps by selling the debt to an agency that would be able to file suit in its name rather than the hospital’s name. These might be little more than indirect collections. For reporting purposes, any form of transferring debt might be considered filing a lawsuit. The problem, noted earlier, about requiring prepayment or credit cards would also exist.
Get the board involved. A different approach would be to ensure that a hospital’s board of trustees is involved in setting and overseeing debt collection policies. For example, the law might require boards to annually consider and adopt specific debt collection practices—including indirect collection efforts. Boards should already be doing something similar to this, but regulation might be an inexpensive way to ensure it is done—and in a manner consistent with the organization’s values. Another suggestion is to require the board to approve any legal action against specific patients.7 By making sure this is not just another item on the consent agenda, the oversight would probably reduce automatic debt collection processes.
Expand IRS reporting requirements for nonprofits. Indeed, for nonprofit hospitals with 501(c)(3) obligations, the Form 990, Schedule H already provides some information about collection actions and uncompensated care, and this is enhanced by the ACA Section 501(r). These could be expanded and perhaps include “indirect” collections. The IRS could “flag” hospitals with high total litigation and similar collection actions, and ask the hospital to provide a detailed explanation for each action and how it was consistent with the obligation to serve the public (thereby justifying the exempt taxation status, an idea proposed by the US Government Accountability Office in 2020).24
Ensure the hospital’s actions reflect their mission and values
Hospitals are created to provide medical care for people and to improve the human condition. Those who lead them should, and generally do, share that purpose. The apparent collection policies that have garnered negative public attention suggest that some of these institutions have lost focus of their ultimate mission and values. The boards and executives of these health care institutions, as well as the medical professionals and attorneys who serve them, should be continuously guided by those values.
Important decisions—including collection and prepayment processes—reflect the values of the institution. Failure to ensure these procedures are in line with the organization’s mission is an embarrassment to all health care facilities, including the majority of hospitals that do not engage in these aggressive collection practices. Not addressing these issues will likely result in political and legal action—blunt and inefficient instruments—to limit what the public sees as wrongdoing. ●
- Kiel P. From the E.R. to the courtroom: how nonprofit hospitals are seizing patients’ wages. ProPublica. December 19, 2014. Accessed March 21, 2022. https://www.propublica.org/article/how-nonprofit-hospitals-are-seizing-patients-wages
- Cooper Z, Han J, Mahoney N. Hospital lawsuits over unpaid bills increased by 37 percent in Wisconsin from 2001 to 2018. Health Affairs. 2021;40:1830-1835. Accessed March 21, 2022. https://www.healthaffairs.org/doi/full/10.1377 /hlthaff.2021.01130
- LaMantia J. New York hospitals have filed thousands of lawsuits against patients. Modern Healthcare. March 13, 2020. Accessed March 21, 2022. https://www.modernhealthcare .com/legal/new-york-hospitals-have-filed-thousands -lawsuits-against-patients
- Armour S. When patients can’t pay, many hospitals are suing. Wall Street Journal. June 25, 2019. Accessed March 21, 2022. https://www.wsj.com/articles/nonprofit-hospitals-criticized-for-debt-collection-tactics-11561467600
- McGhee M, Chase W. How America’s top hospitals hound patients with predatory billing. Axios. Accessed March 21, 2022. https://www.axios.com/hospital-billing
- Owens C. Public spotlight on hospital lawsuits may slow them down. June 14, 2021. Accessed March 22, 2022. https:// www.axios.com/hospital-lawsuits-slowing-down-media -35ce395a-9fe3-4b23-b815-d7b06cce2773.html
- Buck ID. When hospitals sue patients. Hastings L.J. 2022;73:191-232, at 209-211. Accessed March 21, 2022. https:// repository.uchastings.edu/cgi/viewcontent.cgi?article =3961&context=hastings_law_journal
- Lagasse J. Healthcare turns to zero-interest loans to give patients a better reason to pay. Healthcare Finance. May 3, 2017. Accessed March 21, 2022. https://www.healthcarefinancenews.com/news/healthcare-turns-zero-interest-loans-give-patients-better-reason-pay#:~:text=Zero%2Dinterest%20loans%20are%20finding,of%20the%20patient%2Dprovider%20relationship.
- Bruhn WE, Rutkow L, Wang P, et al. Prevalence and characteristics of Virginia hospitals suing patients and garnishing wages for unpaid medical bills. JAMA. 2019;322:691-692. doi:10.1001/jama.2019.9144
- Keisler-Starkey K, Bunch LN. Health insurance coverage in the United States: 2020. September 14, 2021. United States Census Bureau Current Population Reports, P60-274. US Government Publishing Office; September 2021. Accessed March 21, 2022. https://www.census.gov/content/dam /Census/library/publications/2021/demo/p60-274.pdf
- Cohen RA, Zammitti EP. High-deductible health plan enrollment among adults aged 18-64 with employment-based insurance coverage. NCHS Data Brief, No. 317. August 2018. Accessed March 21, 2022. https://www.cdc.gov/nchs/data/databriefs/db317.pdf
- Kaiser Family Foundation. Employer health benefits: 2020 summary of findings. Accessed March 21, 2022. https://www.kff.org/report-section/ehbs-2020-summary-of-findings/
- Picchi A. Higher health insurance deductibles a sickening trend for Americans. CBS NEWS. June 13, 2019. Accessed March 21, 2022. https://www.cbsnews.com/news/high-health-insurance-deductibles-a-sickening-trend-thats -causing-financial-hardship/
- Himmelstein DU, Lawless RM, Thorne D, Foohey P, Woolhandler S. Medical bankruptcy: still common despite the Affordable Care Act. Am J Public Health. 2019;109:431-433. doi:10.2105/AJPH.2018.304901
- Rosato D. What medical debt does to your credit score. Consumer Reports. July 26, 2018. Accessed March 21, 2022. https://www.consumerreports.org/credit-scores-reports/what-medical-debt-does-to-your-credit-score/
- State laws on wage garnishments. Nolo web site. https://www.nolo.com/legal-encyclopedia/free-books/employee-rights-book/chapter2-9.html. Accessed April 1, 2022.
- Patruzo JGR, Hashim F, Dun C, et al. Trends in hospital lawsuits filed against patients for unpaid bills following published research about their activity. JAMA Network Open. 2021;4:e2121926. doi:10.1001/jamanetworkopen.2021.21926
- About Schedule H (Form 990), hospitals. IRS. Updated June 10, 2021. Accessed March 21, 2022. https://www.irs.gov/forms-pubs/about-schedule-h-form-990
- Requirements for 501(c)(3) hospitals under the Affordable Care Act – Section 501(r). Updated September 9, 2021. Accessed March 21, 2022. https://www.irs.gov/charities-non-profits/charitable-organizations/requirements-for-501c3-hospitals-under-the-affordable-care-act-section-501r
- Pub. L. No. 116-260, 134 Stat. 1182, Division BB, § 109.
- Fact sheet. No Surprises: understand your rights against surprise medical bills. Centers for Medicare and Medicaid Services. January 3, 2022. Accessed March 21, 2022. https://www.cms.gov/newsroom/fact-sheets/no-surprises-understand-your-rights-against-surprise-medical-bills
- Implementation of the No Surprises Act. Accessed March 21, 2022. https://www.ama-assn.org/delivering-care/patient-support-advocacy/implementation-no-surprises-act
- American Medical Association. Toolkit for physicians: preparing for implementation of the No Surprises Act. January 2022. Accessed March 21, 2022. https://www.ama-assn.org/system/files/ama-nsa-toolkit.pdf
- US Government Accountability Office. Tax administration: opportunities exist to improve oversight of hospitals’ taxexempt status. September 2020. Accessed March 21, 2022. https://www.gao.gov/assets/gao-20-679.pdf
- Kiel P. From the E.R. to the courtroom: how nonprofit hospitals are seizing patients’ wages. ProPublica. December 19, 2014. Accessed March 21, 2022. https://www.propublica.org/article/how-nonprofit-hospitals-are-seizing-patients-wages
- Cooper Z, Han J, Mahoney N. Hospital lawsuits over unpaid bills increased by 37 percent in Wisconsin from 2001 to 2018. Health Affairs. 2021;40:1830-1835. Accessed March 21, 2022. https://www.healthaffairs.org/doi/full/10.1377 /hlthaff.2021.01130
- LaMantia J. New York hospitals have filed thousands of lawsuits against patients. Modern Healthcare. March 13, 2020. Accessed March 21, 2022. https://www.modernhealthcare .com/legal/new-york-hospitals-have-filed-thousands -lawsuits-against-patients
- Armour S. When patients can’t pay, many hospitals are suing. Wall Street Journal. June 25, 2019. Accessed March 21, 2022. https://www.wsj.com/articles/nonprofit-hospitals-criticized-for-debt-collection-tactics-11561467600
- McGhee M, Chase W. How America’s top hospitals hound patients with predatory billing. Axios. Accessed March 21, 2022. https://www.axios.com/hospital-billing
- Owens C. Public spotlight on hospital lawsuits may slow them down. June 14, 2021. Accessed March 22, 2022. https:// www.axios.com/hospital-lawsuits-slowing-down-media -35ce395a-9fe3-4b23-b815-d7b06cce2773.html
- Buck ID. When hospitals sue patients. Hastings L.J. 2022;73:191-232, at 209-211. Accessed March 21, 2022. https:// repository.uchastings.edu/cgi/viewcontent.cgi?article =3961&context=hastings_law_journal
- Lagasse J. Healthcare turns to zero-interest loans to give patients a better reason to pay. Healthcare Finance. May 3, 2017. Accessed March 21, 2022. https://www.healthcarefinancenews.com/news/healthcare-turns-zero-interest-loans-give-patients-better-reason-pay#:~:text=Zero%2Dinterest%20loans%20are%20finding,of%20the%20patient%2Dprovider%20relationship.
- Bruhn WE, Rutkow L, Wang P, et al. Prevalence and characteristics of Virginia hospitals suing patients and garnishing wages for unpaid medical bills. JAMA. 2019;322:691-692. doi:10.1001/jama.2019.9144
- Keisler-Starkey K, Bunch LN. Health insurance coverage in the United States: 2020. September 14, 2021. United States Census Bureau Current Population Reports, P60-274. US Government Publishing Office; September 2021. Accessed March 21, 2022. https://www.census.gov/content/dam /Census/library/publications/2021/demo/p60-274.pdf
- Cohen RA, Zammitti EP. High-deductible health plan enrollment among adults aged 18-64 with employment-based insurance coverage. NCHS Data Brief, No. 317. August 2018. Accessed March 21, 2022. https://www.cdc.gov/nchs/data/databriefs/db317.pdf
- Kaiser Family Foundation. Employer health benefits: 2020 summary of findings. Accessed March 21, 2022. https://www.kff.org/report-section/ehbs-2020-summary-of-findings/
- Picchi A. Higher health insurance deductibles a sickening trend for Americans. CBS NEWS. June 13, 2019. Accessed March 21, 2022. https://www.cbsnews.com/news/high-health-insurance-deductibles-a-sickening-trend-thats -causing-financial-hardship/
- Himmelstein DU, Lawless RM, Thorne D, Foohey P, Woolhandler S. Medical bankruptcy: still common despite the Affordable Care Act. Am J Public Health. 2019;109:431-433. doi:10.2105/AJPH.2018.304901
- Rosato D. What medical debt does to your credit score. Consumer Reports. July 26, 2018. Accessed March 21, 2022. https://www.consumerreports.org/credit-scores-reports/what-medical-debt-does-to-your-credit-score/
- State laws on wage garnishments. Nolo web site. https://www.nolo.com/legal-encyclopedia/free-books/employee-rights-book/chapter2-9.html. Accessed April 1, 2022.
- Patruzo JGR, Hashim F, Dun C, et al. Trends in hospital lawsuits filed against patients for unpaid bills following published research about their activity. JAMA Network Open. 2021;4:e2121926. doi:10.1001/jamanetworkopen.2021.21926
- About Schedule H (Form 990), hospitals. IRS. Updated June 10, 2021. Accessed March 21, 2022. https://www.irs.gov/forms-pubs/about-schedule-h-form-990
- Requirements for 501(c)(3) hospitals under the Affordable Care Act – Section 501(r). Updated September 9, 2021. Accessed March 21, 2022. https://www.irs.gov/charities-non-profits/charitable-organizations/requirements-for-501c3-hospitals-under-the-affordable-care-act-section-501r
- Pub. L. No. 116-260, 134 Stat. 1182, Division BB, § 109.
- Fact sheet. No Surprises: understand your rights against surprise medical bills. Centers for Medicare and Medicaid Services. January 3, 2022. Accessed March 21, 2022. https://www.cms.gov/newsroom/fact-sheets/no-surprises-understand-your-rights-against-surprise-medical-bills
- Implementation of the No Surprises Act. Accessed March 21, 2022. https://www.ama-assn.org/delivering-care/patient-support-advocacy/implementation-no-surprises-act
- American Medical Association. Toolkit for physicians: preparing for implementation of the No Surprises Act. January 2022. Accessed March 21, 2022. https://www.ama-assn.org/system/files/ama-nsa-toolkit.pdf
- US Government Accountability Office. Tax administration: opportunities exist to improve oversight of hospitals’ taxexempt status. September 2020. Accessed March 21, 2022. https://www.gao.gov/assets/gao-20-679.pdf
Embryo mix-up debacles: Is there liability?
CASE Embryo mix-up with 2 couples
A lawsuit was recently filed in California by a couple after the woman carried and gave birth to “the wrong child.” This was the second full-term pregnancy for the couple. The couple had undergone an unsuccessful in vitro fertilization (IVF) cycle in October 2018. The next IVF cycle in 2019 led to the birth of a daughter on September 24, 2019, who is the subject of this case.1
At the time of birth, the couple suspected something was wrong because the baby had “jet-black hair and a complexion that was darker” than their complexions. The couple eventually obtained a DNA test, which confirmed in November 2019 that this was not their biological child.1
A few weeks later, they learned that another woman who went to the same IVF clinic gave birth to a female baby 1 week after their daughter was born. Similarly, that baby did not resemble the parents, and DNA testing confirmed the baby belonged to the first couple. The couples ultimately exchanged the babies.1
The legal claim filed against the IVF center and its owner (an obstetrician) was for breach of contract, medical malpractice, and infliction of emotional distress, including experiencing “disassociation” on the part of the couple(s). Each couple felt they did not get to experience the birth of their biological child, and, of course there was considerable distress in the process of learning that the child was not theirs and exchanging the birth child for the biological child. In addition, the couple who filed the suit had another child (now age 7 years), who begged them to keep the baby to whom they gave birth. The couple also reported experiencing panic attacks as a result of the events.1
Medical considerations
As of 2018, more than 8 million IVF babies had been born, with the first in 1978 in the United Kingdom.2 Advances in science and technology have improved the process. Storage tanks now have alarms and several safeguards to monitor the level of liquid nitrogen and immediately notify key personnel if levels are low (FIGURES 1 and 2). Preimplantation genetic testing is also readily available to assess the embryo prior to transfer into the uterus and identify various genetic problems.


Guidelines for embryo straw labelling are provided by the College of American Pathologists and the Centers for Disease Control and Prevention. The American Society for Reproductive Medicine (ASRM) also provides guidelines. When an error occurs, disclosure is recommended and ethical and legal counsel should be involved. Failing to disclose can lead to professional penalties.4
Unfortunately, despite these advances and guidelines, embryo mix-ups like the one in the above case do occur and receive public notice (See “Cross country embryo mix-up cases”).5,6 A report from the University of Nevada assessed liability for embryo mix-ups in US fertility practices from 2000 to 2020.7 They evaluated 184,015 IVF cycles with 176 claims. Payments were made to plaintiffs in 21 cases, resulting in $15 million of awarded damages (average award was $199,188).7 The most common problem was in the embryology laboratory with an overall incidence of 0.03% of the total number of IVF cycles.7 To avoid damages, the authors emphasized the importance of following labeling guidelines when storing embryos, considering a 2-step read-back method prior to embryo transfer, and offering genetic testing when a discrepancy is noted in the record (TABLE).7

Other medical liability considerations
Embryo mix-ups are not the only source of problems and potential liability in IVF. At the 2021 Association of Sexual and Reproductive Medicine Annual Meeting, Applebaum et al presented results from a comprehensive review of malpractice litigation involving IVF in the United States.8 Using the legal database NEXIS Uni they identified 50 cases between 1986 and 2020 (32% of which were filed in New York state). Common thematic elements among patient allegations were embryology errors (eg, lost or destroyed embryos or incorrect sperm or egg donor), errors in preimplantation genetics, surgical or medical errors/complications, or misdiagnosis (eg, sexually transmitted disease screening or malignancy).8 Overall, the most common plaintiff complaint was negligence (26 cases) due to informed consent–related issues (9 cases), wrongful life or birth (9 cases), or negligent or intentional infliction of emotional distress (5 cases).8
In 48% of cases, the verdict was in favor of the defendant; it was for the plaintiff in 36% of cases and ongoing proceedings or partial judgement accounted for the remaining cases.8 Damages ranged from $4,171.45 to $50 million. The authors emphasized specific defense strategies, including the importance of careful labeling and handling of embryos, prompt disclosure when an error does occur, and awareness of the specific state statute(s) of limitations for medical malpractice claims.8
Continue to: Legal considerations...
Legal considerations
The case at the beginning of this article is a “mix-up” case, in which an IVF center implanted the wrong embryo, resulting in the birth parents not being the biological parents.1 As in that case, there may be (but are not always)6,9 2 mix-ups, so that 2 couples have each other’s biological children. These cases may go unnoticed by the birth parent if the physical appearance is not unexpected and the parents never do genetic testing, or if the IVF center does not discover the error and inform the parents. Infrequently the cases make the news or the courts.10,11
News accounts are not trials, and we do not suggest that all the facts discussed in news reports on the case described here are complete—or even accurate in the details reported. They are generally 1-sided, so there are other perspectives. To consider the legal issues, however, we will assume for discussion only that the facts are as they have been reported in the news coverage—with the understanding that the discovery and trial processes would undoubtedly bring to light many other important facts or corrections.
Negligence
Although there are several potential bases for liability (ie, contract or warranty claims, a form of product liability/defect) in mix-up and other artificial reproductive technology (ART), negligence or malpractice seem most likely.12 “Negligence” here is intended to be simple negligence but may also include gross negligence or recklessness.
Although the incidence of errors in ART is unknown, there is limited evidence that suggests it is not a rare event. One study suggested >20% of fertility clinics knew of errors in processing or handling donor samples and embryos for implantation.13 Another study in the United Kingdom found that 1 in 1,000 IVF embryos were implanted in the wrong woman.14
Was there negligence? The first question in a malpractice or negligence-type action is, was there a professional relationship between the plaintiff who is claiming harm and the professional or organization defendant? The next question is whether the defendant was reasonably careful given the circumstances—that is, did the physician meet the “standard of care”? This is sometimes described as whether the professional’s actions would be acceptable (ie, reasonably prudent within the profession or specialty). If there was negligence, then the next question is, did that negligence cause an injury to the plaintiff?15
Determining the standard of care. The nature of the expected standard of care is dependent, in part, on the potential consequences of an error. For example, the care required when there is a significant risk of death from an error would be considerably more cautious than for an error that might result in small property damage. In this case study, a mix-up error is likely to be less severe than death, but is very substantial in terms of emotional harm and disruption. Thus, considerable care and attention would be expected to avoid these errors. They should be a “never” event. Institutions and physicians should give considerable attention to their processes and procedures to avoid the possibility of a mix-up error.16
Where did the negligence occur? There is an old tort doctrine “Res ipsa loquitor” (RIL) that means, “The thing speaks for itself.” Although there are several technical rules around the application of RIL as a presumption of negligence, it comes down to the proposition that some injuries do not occur without negligence. A traditional medical example is the sponge left in a patient during surgery—ordinarily that does not happen without some negligence. For RIL to be applied, usually the mechanism by which the injury occurred had to be under the control of the defendant (or the agents of the defendant).
The “mix-up” of embryos is an example of the kind of error that would not likely occur without negligence.17 But the embryo may not be in the exclusive control of any 1 institution. For example, the mistake could be made by the IVF center (or its employees), a separate facility that has processed or cryogenically stored the genetic materials, and independent physicians (not employees or agents of the center). Therefore, it is necessary to pinpoint where the negligence occurred and who is legally responsible. In some cases, a health care provider must take steps to ensure that its contractors have sufficient safeguards to avoid unnecessary harms. For example, an IVF center that uses an external cryogenic storage facility may have some obligation to know that the genetic material returned to the center is the same material that the center provided the storage facility in the first place and is properly identified.18
Assessing damages
From the facts as we have them, it appears that there must have been negligence that caused the mix-up of the embryos in the original case. It also appears reasonably clear that the negligence resulted in harm to both sets of parents and their families. This would suggest that the families should recover substantial damages. But that, somewhat surprisingly, may not be the case.19 Several legal principles may limit the availability or size of damages in mix-up cases. Also, it is worth remembering that there are differences in how states treat the different types of damages in these cases. Although the case was filed in California, we’ll take a more national view of the damages issue.
Not all harm is treated as equal. The first problem facing plaintiffs in mix-up cases may be the fact that they have suffered only emotional harm, without any physical injury. Traditionally, the courts have been reluctant to allow recovery in negligence for purely emotional injuries. Also “intentional” infliction of emotional distress does permit financial recovery, but generally “negligent” infliction of emotional harm traditionally has not. In part, this was because of the fear of unwarranted (and difficult-to-assess) claims of emotional harm that are not related to a physical harm. Some states developed a “zone of danger” exception (eg, where someone was almost hit by a car) or allowed some emotional injury recovery if there were “physical manifestations” of the emotional harm. In short, depending on the state’s rules, negligence that causes purely emotional harm may not be compensable.20
State-based malpractice “caps.” Another limitation on emotional injuries is the “caps” on malpractice damages enacted by several states (including California, where this mix-up case occurred). Therefore, if a mix-up case is determined to be a malpractice case under state law, emotional suffering damages (which are non-economic damages) may be limited to the cap—$250,000 in California, for example—even if the state allows damages for emotional injuries without physical injuries.
The rare exception. Very careless labeling or handling of the identity of the embryo could at the extreme be considered gross negligence or recklessness. There are relatively inexpensive and easy procedures that could easily avoid what is likely to be significant harm to families (including emotional upset).21 Institutions that callously fail to use those procedures might be seen by some courts as reckless, or in outrageous cases, even intentional. An example would be the University of California Irvine Center for Reproductive Health case, in which physicians intentionally (without consent) used patients’ ova, fertilized them, and then implanted them in other patients, with at least 15 births, many lawsuits, and multimillion dollar settlements.22 In “intentional” cases, limitations on emotional injuries would usually not be major barriers to recovery of damages. However, those are legal stretches, and recovery is the exception rather than the rule.23
Continue to: Additional legal concerns with IVF...
Additional legal concerns with IVF
Reproduction negligence cases include a large range of errors and injuries—not just embryo mix-ups. Courts have struggled with when it is appropriate to allow damages, even when there have been clear injuries. For the most part courts have been reluctant to find liability in many areas of new IVF technology.12 One problem in determining how to assess damages is determining how incidental benefits should be used to offset some or all of the damages. For example, how should the joy of having a child offset the costs of raising the child?
There are more than a dozen kinds of current and likely future claims arising from problems with ART. It is tempting to conclude, “Oh, what a tangled legal web we weave when first we practice to artificially conceive.” There are various groupings of such claims, with several examples of cases presented in this article. It is not possible to consider those in detail in this article. As a general proposition, however, “our legal system treats wrongfully disrupted plans concerning reproduction like one of those life adversities that people are expected to abide without remedy.”24
This is not to say, however, that there is no compensation for IVF-related injuries. Applebaum and colleagues found more than 100 cases in the 35 years covered by the study (1984-2020).8 However, only 50 of those cases fit the criteria for inclusion in their data. The successful cases for the plaintiffs involved medical or surgical error, while it appeared that various forms of wrongful life or birth were much less successful. It would be a mistake to conclude from these data that there are not, and will not be, meaningful risks of liability in the areas of IVF and ART more generally.
First, claims that fit with existing legal doctrine are producing liability. About half of the claims (25 over the 34 years) examined by Applebaum et al resulted in liability. Admittedly, that number was small because ART use was increasing. Where the claims fit well-recognized legal forms of damages and forms of action (primarily negligence), the liability could be substantial. A remarkable example of this is the case of Wuth v Lab. Corp (see “Liability for genetic testing errors”),25 which was the largest verdict ($50 million) in the Applebaum and colleagues’ study.8 The large verdict was due to the failure of the testing company and a medical center to properly perform and assess a genetic test, which resulted in the birth of a child with an unbalanced chromosome translocation.8,25 The child’s serious disabilities would require a great deal of expensive care. Although the jury held the testing laboratory and medical center liable, they did not find liability against the physician.25 Ultimately, this case would be considered a failure of genetic testing rather than an IVF case.
More than 2 couples
In a second case from California, a couples’ son was born to another couple in New York—along with another boy from a third couple. The woman in New York thought she had carried biological twins but genetic testing confirmed the twins were not related to the couple or to each other (the second couple filed a separate medical malpractice and negligence lawsuit in New York). All 3 couples had sought care at the same IVF clinic. The babies were eventually returned to their biological parents.1
Different races
In a New York case, a Korean couple had twin White boys after consenting to a single embryo transfer. Meanwhile a couple in Los Angeles who went to the same in vitro fertilization clinic gave birth to a child that did not match their appearance. Both couples had undergone embryo transfers on the same day. The court arranged for the Korean couple to surrender their twins to their biological parents when they were 6 months of age in exchange for their biological child.2
References
1. Couple claims clinic implanted their embryo in wrong woman. Associated Press. July 10, 2019. https://apnews.com/article/de32d537c6e34808b28834c23f00e272. Accessed January 6, 2022.
2. In the matter of accusation against Steven L. Katz. Case no. 03-20001-122617.OAH no. N2004080093. Sacramento, CA. Medical Board of California Department of Consumer Affairs 2005.
Future challenges
The future is likely to bring substantially expanded IVF/ART liability for several reasons. ART is becoming more common. Although courts have struggled with how to apply existing liability rules to the new technologies and related novel legal claims, the absence of established legal principles into which IVF injuries fit will not last forever. The legal system eventually finds ways of adjusting old rules or adopting new ones to cover injuries from new technology.
Although IVF injuries that most people feel deserve compensation currently are not cognizable in law, that will undoubtedly change. Either the courts will find new ways of assessing ART claims, or state legislatures and Congress will step in with legislation. To date, Congress has been relatively “hands off” on the ART processes, with the Fertility Clinic Success Rate and Certification Act of 1992 being a notable exception.24 This law requires ART programs to report success rates and directs the Centers for Disease Control and Prevention (CDC) to publish reported success rates and laboratory incidents. It also establishes a model state laboratory certification program.24 The CDC has an outline of the work under the statute,26 as well as state-specific data regarding ART27 and lists of publications in key areas.28 In addition there are various state laws related to recordkeeping, donor qualifications, licensing, and family law issues.29 Ultimately, physicians, scientists, and legal professionals can perform a valuable role in helping to fashion IVF liability principles that are workable and reasonable, that will not interfere with the progress of medicine, and that will ensure that those injured through carelessness or bad medicine receive compensation. ●
Although not technically an in vitro fertilization (IVF) case, Wuth v Lab. Corp. involved an infant born through IVF with a translocation defect chromosome 2 (ie, deleted material) and extra chromatin on 9. The father’s family history included birth defects, including a female cousin with profound developmental disabilities, seizures, and antisocial behavior. He had undergone genetic testing that revealed an asymptomatic balanced, 2;9 translocation. As part of the IVF process, the couple had a genetic consultation and were told there was a 50% chance that the fetus would have an unbalanced 2;9 translocation given the father’s family history and that chorionic villus sampling or amniocentesis could detect this in the fetus.1
Amniocentesis had been performed, with the specimen sent to Lab. Corp. The result was “normal male karyotype.” However, when the baby was born, it was immediately apparent that he had severe physical defects and subsequently cognitive defects. Genetic testing of the child revealed an unbalanced 2;9 translocation. The couple filed a suit for wrongful birth and wrongful life, which went to a jury. The child was awarded $25 million and the parents/family were awarded another $25 million in general damages. The verdict reflected errors in genetic (laboratory) testing.
Reference
1. Wuth v Lab. Corp. of Am., 189 Wash. App. 660, 359 P.3d 841 (2015).
- Mark J. California couple sues fertility clinic following IVF embryo mix-up. Washington Post. November 9, 2021. https://www.washingtonpost.com/nation/2021/11/09/in-vitro-fertilization-ivf-mix-up-daphna-cardinale. Accessed January 5, 2022.
- More than 8 million babies born from IVF since the world’s first in 1978. Science Daily. July 3, 2018. https://www.sciencedaily.com/releases/2018/07/180703084127.htm. Accessed January 11, 2022.
- ESCO Medical. In vitro fertilization (IVF) as fertility treatment. https://www.esco-medical.com/resource/in-vitro-fertilization-ivf-as-fertility-treatment.
- Vigdor N. “We had their baby, and they had our baby”: couple sues over embryo “mix-up.” NY Times. November 9, 2021. https://www.nytimes.com/2021/11/09/us/fertility-clinic-embryo-mixup.html. Accessed January 11, 2022.
- Couple claims clinic implanted their embryo in wrong woman. Associated Press. July 10, 2019. https://apnews.com/article/de32d537c6e34808b28834c23f00e2728. Accessed January 6, 2022.
- In the matter of accusation against Steven L. Katz. Case no. 03-20001-122617.OAH no. N2004080093. Sacramento, CA. Medical Board of California Department of Consumer Affairs 2005
- Rasouli MA, Moutos CP, Phelps JY. Liability for embryo mix-ups in fertility practices in the USA. J Assist Reprod Genet. 2021;38:1101-1107. doi:10.1007/s10815-021-02108-1
- Applebaum J, Berger D, O’Neill K. Can a reproductive endocrinologist be sued for 50 million dollars? A comprehensive review of malpractice litigation involving in vitro fertilization in the U.S. Fertil Steril. 2021;116(3s):e19. doi:10.1016/j.fertnstert.2021.07.059
- Andrews v Keltz, 838 N.Y.S.2d 363, 365 (Sup. Ct. 2007).
- Chichi DV. In vitro fertilization, fertility frustrations, and the lack of regulation. Hofstra L Rev. 2021;49:535-568. https://www.hofstralawreview.org/wp-content/uploads/2021/04/bb.2.chichi.pdf. Accessed January 11, 2022.
- Lewin T. Sperm banks accused of losing samples and lying about donors. NY Times. July 21, 2016. https://www.nytimes.com/2016/07/22/us/sperm-banks-accused-of-losing-samples-and-lying-about-donors.html. Accessed January 11, 2022.
- Bender L. To err is human ART mix-ups: labor-based, relational proposal. J Gender Race Justice. 2006;9:443-508. https://surface.syr.edu/cgi/viewcontent.cgi?article=1050&context=lawpub. Accessed January 11, 2022.
- Baruch S, Kaufman D, Hudson KL. Genetic testing of embryos: practices and perspectives of U.S. in vitro fertilization clinics. Fertil Steril. 2007;89:1053-1058. doi:10.1016/j.fertnstert.2007.05.048
- Liebler R. Are you my parent? Are you my child? The role of genetics and race in defining relationships after reproductive technological mistakes. DePaul J Health Care Law. 2002;5:15-56. https://via.library.depaul.edu/cgi/viewcontent.cgi?article=1202&context=jhcl. Accessed January 11, 2022.
- Crockin SL, Altman AB, Edmonds MA. The history and future trends of art medicine and law. Fam Court Rev. 2021;59:22-45. doi:10.1111/fcre.12550
- Fernandes JS. Perfecting pregnancy via preimplantation genetic screening: the quest for an elusive standard of care. UC Irvine L Rev. 2014;4:1295-1326. https://www.law.uci.edu/lawreview/vol4/no4/Fernandes.pdf. Accessed January 11, 2022.
- VanGessel MM. Wrongful surrogacy: the need for right of action in cases of clear negligence. U Toledo L Rev. 2015;46:681-706.
- Reich J, Swink D. Outsourcing human reproduction: embryos and surrogacy services in the cyberprocreation era. J Health Care L Policy. 2011;14:241-298. https://core.ac.uk/download/pdf/217156567.pdf. Accessed January 11, 2022.
- Strasser M. Prenatal tort slippage. Health Matrix. 2021;31:221-262. https://scholarlycommons.law.case.edu/healthmatrix/vol31/iss1/9. Accessed January 11, 2022.
- Heide IH. Negligence in the creation of healthy babies: negligent infliction of emotional distress in cases of alternative reproductive technology malpractice without physical injury. J Med L. 2005;9:55-94.
- Novo S, Nogués C, Penon O, et al. Barcode tagging of human oocytes and embryos to prevent mix-ups in assisted reproduction technologies. Hum Reprod. 2014;29:18-28. doi: 10.1093/humrep/det409
- Yoshino K. UCI Settles Dozens of Fertility Suits. LA Times. September 11, 2009. https://www.latimes.com/archives/la-xpm-2009-sep-11-me-uci-fertility11-story.html. Accessed January 11, 2022.
- Fox D. Reproductive negligence. Columbia L Rev. 2017;117:149-242. https://columbialawreview.org/wp-content/uploads/2017/01/149.pdf. Accessed January 11, 2022.
- 42 U.S.C.S. §263a-1-263a-7; Public Law 102-493. https://www.govinfo.gov/content/pkg/STATUTE-106/pdf/STATUTE-106-Pg3146.pdf. Accessed January 11, 2022.
- Wuth v Lab. Corp. of Am., 189 Wash. App. 660, 359 P.3d 841 (2015).
- Centers for Disease Control and Prevention. The Fertility Clinic Success Rate and Certification Act. December 14, 2020. https://www.cdc.gov/art/nass/policy.html#act. Accessed January 11, 2022.
- Centers for Disease Control and Prevention. State-specific assisted reproductive technology surveillance. December 17, 2020. https://www.cdc.gov/art/state-specific-surveillance/index.html. Accessed January 11, 2022.
- Centers for Disease Control and Prevention. Key findings. March 12, 2021. https://www.cdc.gov/art/key-findings/index.html. Accessed January 11, 2022.
- Cohen EN. 5 Treatise on Health Care Law §22.04, (ed. Hooper, Lundy & Bookman, & Robert W. Lundy, Jr. RW.) (Matthew Bender-LexisNexis)
CASE Embryo mix-up with 2 couples
A lawsuit was recently filed in California by a couple after the woman carried and gave birth to “the wrong child.” This was the second full-term pregnancy for the couple. The couple had undergone an unsuccessful in vitro fertilization (IVF) cycle in October 2018. The next IVF cycle in 2019 led to the birth of a daughter on September 24, 2019, who is the subject of this case.1
At the time of birth, the couple suspected something was wrong because the baby had “jet-black hair and a complexion that was darker” than their complexions. The couple eventually obtained a DNA test, which confirmed in November 2019 that this was not their biological child.1
A few weeks later, they learned that another woman who went to the same IVF clinic gave birth to a female baby 1 week after their daughter was born. Similarly, that baby did not resemble the parents, and DNA testing confirmed the baby belonged to the first couple. The couples ultimately exchanged the babies.1
The legal claim filed against the IVF center and its owner (an obstetrician) was for breach of contract, medical malpractice, and infliction of emotional distress, including experiencing “disassociation” on the part of the couple(s). Each couple felt they did not get to experience the birth of their biological child, and, of course there was considerable distress in the process of learning that the child was not theirs and exchanging the birth child for the biological child. In addition, the couple who filed the suit had another child (now age 7 years), who begged them to keep the baby to whom they gave birth. The couple also reported experiencing panic attacks as a result of the events.1
Medical considerations
As of 2018, more than 8 million IVF babies had been born, with the first in 1978 in the United Kingdom.2 Advances in science and technology have improved the process. Storage tanks now have alarms and several safeguards to monitor the level of liquid nitrogen and immediately notify key personnel if levels are low (FIGURES 1 and 2). Preimplantation genetic testing is also readily available to assess the embryo prior to transfer into the uterus and identify various genetic problems.


Guidelines for embryo straw labelling are provided by the College of American Pathologists and the Centers for Disease Control and Prevention. The American Society for Reproductive Medicine (ASRM) also provides guidelines. When an error occurs, disclosure is recommended and ethical and legal counsel should be involved. Failing to disclose can lead to professional penalties.4
Unfortunately, despite these advances and guidelines, embryo mix-ups like the one in the above case do occur and receive public notice (See “Cross country embryo mix-up cases”).5,6 A report from the University of Nevada assessed liability for embryo mix-ups in US fertility practices from 2000 to 2020.7 They evaluated 184,015 IVF cycles with 176 claims. Payments were made to plaintiffs in 21 cases, resulting in $15 million of awarded damages (average award was $199,188).7 The most common problem was in the embryology laboratory with an overall incidence of 0.03% of the total number of IVF cycles.7 To avoid damages, the authors emphasized the importance of following labeling guidelines when storing embryos, considering a 2-step read-back method prior to embryo transfer, and offering genetic testing when a discrepancy is noted in the record (TABLE).7

Other medical liability considerations
Embryo mix-ups are not the only source of problems and potential liability in IVF. At the 2021 Association of Sexual and Reproductive Medicine Annual Meeting, Applebaum et al presented results from a comprehensive review of malpractice litigation involving IVF in the United States.8 Using the legal database NEXIS Uni they identified 50 cases between 1986 and 2020 (32% of which were filed in New York state). Common thematic elements among patient allegations were embryology errors (eg, lost or destroyed embryos or incorrect sperm or egg donor), errors in preimplantation genetics, surgical or medical errors/complications, or misdiagnosis (eg, sexually transmitted disease screening or malignancy).8 Overall, the most common plaintiff complaint was negligence (26 cases) due to informed consent–related issues (9 cases), wrongful life or birth (9 cases), or negligent or intentional infliction of emotional distress (5 cases).8
In 48% of cases, the verdict was in favor of the defendant; it was for the plaintiff in 36% of cases and ongoing proceedings or partial judgement accounted for the remaining cases.8 Damages ranged from $4,171.45 to $50 million. The authors emphasized specific defense strategies, including the importance of careful labeling and handling of embryos, prompt disclosure when an error does occur, and awareness of the specific state statute(s) of limitations for medical malpractice claims.8
Continue to: Legal considerations...
Legal considerations
The case at the beginning of this article is a “mix-up” case, in which an IVF center implanted the wrong embryo, resulting in the birth parents not being the biological parents.1 As in that case, there may be (but are not always)6,9 2 mix-ups, so that 2 couples have each other’s biological children. These cases may go unnoticed by the birth parent if the physical appearance is not unexpected and the parents never do genetic testing, or if the IVF center does not discover the error and inform the parents. Infrequently the cases make the news or the courts.10,11
News accounts are not trials, and we do not suggest that all the facts discussed in news reports on the case described here are complete—or even accurate in the details reported. They are generally 1-sided, so there are other perspectives. To consider the legal issues, however, we will assume for discussion only that the facts are as they have been reported in the news coverage—with the understanding that the discovery and trial processes would undoubtedly bring to light many other important facts or corrections.
Negligence
Although there are several potential bases for liability (ie, contract or warranty claims, a form of product liability/defect) in mix-up and other artificial reproductive technology (ART), negligence or malpractice seem most likely.12 “Negligence” here is intended to be simple negligence but may also include gross negligence or recklessness.
Although the incidence of errors in ART is unknown, there is limited evidence that suggests it is not a rare event. One study suggested >20% of fertility clinics knew of errors in processing or handling donor samples and embryos for implantation.13 Another study in the United Kingdom found that 1 in 1,000 IVF embryos were implanted in the wrong woman.14
Was there negligence? The first question in a malpractice or negligence-type action is, was there a professional relationship between the plaintiff who is claiming harm and the professional or organization defendant? The next question is whether the defendant was reasonably careful given the circumstances—that is, did the physician meet the “standard of care”? This is sometimes described as whether the professional’s actions would be acceptable (ie, reasonably prudent within the profession or specialty). If there was negligence, then the next question is, did that negligence cause an injury to the plaintiff?15
Determining the standard of care. The nature of the expected standard of care is dependent, in part, on the potential consequences of an error. For example, the care required when there is a significant risk of death from an error would be considerably more cautious than for an error that might result in small property damage. In this case study, a mix-up error is likely to be less severe than death, but is very substantial in terms of emotional harm and disruption. Thus, considerable care and attention would be expected to avoid these errors. They should be a “never” event. Institutions and physicians should give considerable attention to their processes and procedures to avoid the possibility of a mix-up error.16
Where did the negligence occur? There is an old tort doctrine “Res ipsa loquitor” (RIL) that means, “The thing speaks for itself.” Although there are several technical rules around the application of RIL as a presumption of negligence, it comes down to the proposition that some injuries do not occur without negligence. A traditional medical example is the sponge left in a patient during surgery—ordinarily that does not happen without some negligence. For RIL to be applied, usually the mechanism by which the injury occurred had to be under the control of the defendant (or the agents of the defendant).
The “mix-up” of embryos is an example of the kind of error that would not likely occur without negligence.17 But the embryo may not be in the exclusive control of any 1 institution. For example, the mistake could be made by the IVF center (or its employees), a separate facility that has processed or cryogenically stored the genetic materials, and independent physicians (not employees or agents of the center). Therefore, it is necessary to pinpoint where the negligence occurred and who is legally responsible. In some cases, a health care provider must take steps to ensure that its contractors have sufficient safeguards to avoid unnecessary harms. For example, an IVF center that uses an external cryogenic storage facility may have some obligation to know that the genetic material returned to the center is the same material that the center provided the storage facility in the first place and is properly identified.18
Assessing damages
From the facts as we have them, it appears that there must have been negligence that caused the mix-up of the embryos in the original case. It also appears reasonably clear that the negligence resulted in harm to both sets of parents and their families. This would suggest that the families should recover substantial damages. But that, somewhat surprisingly, may not be the case.19 Several legal principles may limit the availability or size of damages in mix-up cases. Also, it is worth remembering that there are differences in how states treat the different types of damages in these cases. Although the case was filed in California, we’ll take a more national view of the damages issue.
Not all harm is treated as equal. The first problem facing plaintiffs in mix-up cases may be the fact that they have suffered only emotional harm, without any physical injury. Traditionally, the courts have been reluctant to allow recovery in negligence for purely emotional injuries. Also “intentional” infliction of emotional distress does permit financial recovery, but generally “negligent” infliction of emotional harm traditionally has not. In part, this was because of the fear of unwarranted (and difficult-to-assess) claims of emotional harm that are not related to a physical harm. Some states developed a “zone of danger” exception (eg, where someone was almost hit by a car) or allowed some emotional injury recovery if there were “physical manifestations” of the emotional harm. In short, depending on the state’s rules, negligence that causes purely emotional harm may not be compensable.20
State-based malpractice “caps.” Another limitation on emotional injuries is the “caps” on malpractice damages enacted by several states (including California, where this mix-up case occurred). Therefore, if a mix-up case is determined to be a malpractice case under state law, emotional suffering damages (which are non-economic damages) may be limited to the cap—$250,000 in California, for example—even if the state allows damages for emotional injuries without physical injuries.
The rare exception. Very careless labeling or handling of the identity of the embryo could at the extreme be considered gross negligence or recklessness. There are relatively inexpensive and easy procedures that could easily avoid what is likely to be significant harm to families (including emotional upset).21 Institutions that callously fail to use those procedures might be seen by some courts as reckless, or in outrageous cases, even intentional. An example would be the University of California Irvine Center for Reproductive Health case, in which physicians intentionally (without consent) used patients’ ova, fertilized them, and then implanted them in other patients, with at least 15 births, many lawsuits, and multimillion dollar settlements.22 In “intentional” cases, limitations on emotional injuries would usually not be major barriers to recovery of damages. However, those are legal stretches, and recovery is the exception rather than the rule.23
Continue to: Additional legal concerns with IVF...
Additional legal concerns with IVF
Reproduction negligence cases include a large range of errors and injuries—not just embryo mix-ups. Courts have struggled with when it is appropriate to allow damages, even when there have been clear injuries. For the most part courts have been reluctant to find liability in many areas of new IVF technology.12 One problem in determining how to assess damages is determining how incidental benefits should be used to offset some or all of the damages. For example, how should the joy of having a child offset the costs of raising the child?
There are more than a dozen kinds of current and likely future claims arising from problems with ART. It is tempting to conclude, “Oh, what a tangled legal web we weave when first we practice to artificially conceive.” There are various groupings of such claims, with several examples of cases presented in this article. It is not possible to consider those in detail in this article. As a general proposition, however, “our legal system treats wrongfully disrupted plans concerning reproduction like one of those life adversities that people are expected to abide without remedy.”24
This is not to say, however, that there is no compensation for IVF-related injuries. Applebaum and colleagues found more than 100 cases in the 35 years covered by the study (1984-2020).8 However, only 50 of those cases fit the criteria for inclusion in their data. The successful cases for the plaintiffs involved medical or surgical error, while it appeared that various forms of wrongful life or birth were much less successful. It would be a mistake to conclude from these data that there are not, and will not be, meaningful risks of liability in the areas of IVF and ART more generally.
First, claims that fit with existing legal doctrine are producing liability. About half of the claims (25 over the 34 years) examined by Applebaum et al resulted in liability. Admittedly, that number was small because ART use was increasing. Where the claims fit well-recognized legal forms of damages and forms of action (primarily negligence), the liability could be substantial. A remarkable example of this is the case of Wuth v Lab. Corp (see “Liability for genetic testing errors”),25 which was the largest verdict ($50 million) in the Applebaum and colleagues’ study.8 The large verdict was due to the failure of the testing company and a medical center to properly perform and assess a genetic test, which resulted in the birth of a child with an unbalanced chromosome translocation.8,25 The child’s serious disabilities would require a great deal of expensive care. Although the jury held the testing laboratory and medical center liable, they did not find liability against the physician.25 Ultimately, this case would be considered a failure of genetic testing rather than an IVF case.
More than 2 couples
In a second case from California, a couples’ son was born to another couple in New York—along with another boy from a third couple. The woman in New York thought she had carried biological twins but genetic testing confirmed the twins were not related to the couple or to each other (the second couple filed a separate medical malpractice and negligence lawsuit in New York). All 3 couples had sought care at the same IVF clinic. The babies were eventually returned to their biological parents.1
Different races
In a New York case, a Korean couple had twin White boys after consenting to a single embryo transfer. Meanwhile a couple in Los Angeles who went to the same in vitro fertilization clinic gave birth to a child that did not match their appearance. Both couples had undergone embryo transfers on the same day. The court arranged for the Korean couple to surrender their twins to their biological parents when they were 6 months of age in exchange for their biological child.2
References
1. Couple claims clinic implanted their embryo in wrong woman. Associated Press. July 10, 2019. https://apnews.com/article/de32d537c6e34808b28834c23f00e272. Accessed January 6, 2022.
2. In the matter of accusation against Steven L. Katz. Case no. 03-20001-122617.OAH no. N2004080093. Sacramento, CA. Medical Board of California Department of Consumer Affairs 2005.
Future challenges
The future is likely to bring substantially expanded IVF/ART liability for several reasons. ART is becoming more common. Although courts have struggled with how to apply existing liability rules to the new technologies and related novel legal claims, the absence of established legal principles into which IVF injuries fit will not last forever. The legal system eventually finds ways of adjusting old rules or adopting new ones to cover injuries from new technology.
Although IVF injuries that most people feel deserve compensation currently are not cognizable in law, that will undoubtedly change. Either the courts will find new ways of assessing ART claims, or state legislatures and Congress will step in with legislation. To date, Congress has been relatively “hands off” on the ART processes, with the Fertility Clinic Success Rate and Certification Act of 1992 being a notable exception.24 This law requires ART programs to report success rates and directs the Centers for Disease Control and Prevention (CDC) to publish reported success rates and laboratory incidents. It also establishes a model state laboratory certification program.24 The CDC has an outline of the work under the statute,26 as well as state-specific data regarding ART27 and lists of publications in key areas.28 In addition there are various state laws related to recordkeeping, donor qualifications, licensing, and family law issues.29 Ultimately, physicians, scientists, and legal professionals can perform a valuable role in helping to fashion IVF liability principles that are workable and reasonable, that will not interfere with the progress of medicine, and that will ensure that those injured through carelessness or bad medicine receive compensation. ●
Although not technically an in vitro fertilization (IVF) case, Wuth v Lab. Corp. involved an infant born through IVF with a translocation defect chromosome 2 (ie, deleted material) and extra chromatin on 9. The father’s family history included birth defects, including a female cousin with profound developmental disabilities, seizures, and antisocial behavior. He had undergone genetic testing that revealed an asymptomatic balanced, 2;9 translocation. As part of the IVF process, the couple had a genetic consultation and were told there was a 50% chance that the fetus would have an unbalanced 2;9 translocation given the father’s family history and that chorionic villus sampling or amniocentesis could detect this in the fetus.1
Amniocentesis had been performed, with the specimen sent to Lab. Corp. The result was “normal male karyotype.” However, when the baby was born, it was immediately apparent that he had severe physical defects and subsequently cognitive defects. Genetic testing of the child revealed an unbalanced 2;9 translocation. The couple filed a suit for wrongful birth and wrongful life, which went to a jury. The child was awarded $25 million and the parents/family were awarded another $25 million in general damages. The verdict reflected errors in genetic (laboratory) testing.
Reference
1. Wuth v Lab. Corp. of Am., 189 Wash. App. 660, 359 P.3d 841 (2015).
CASE Embryo mix-up with 2 couples
A lawsuit was recently filed in California by a couple after the woman carried and gave birth to “the wrong child.” This was the second full-term pregnancy for the couple. The couple had undergone an unsuccessful in vitro fertilization (IVF) cycle in October 2018. The next IVF cycle in 2019 led to the birth of a daughter on September 24, 2019, who is the subject of this case.1
At the time of birth, the couple suspected something was wrong because the baby had “jet-black hair and a complexion that was darker” than their complexions. The couple eventually obtained a DNA test, which confirmed in November 2019 that this was not their biological child.1
A few weeks later, they learned that another woman who went to the same IVF clinic gave birth to a female baby 1 week after their daughter was born. Similarly, that baby did not resemble the parents, and DNA testing confirmed the baby belonged to the first couple. The couples ultimately exchanged the babies.1
The legal claim filed against the IVF center and its owner (an obstetrician) was for breach of contract, medical malpractice, and infliction of emotional distress, including experiencing “disassociation” on the part of the couple(s). Each couple felt they did not get to experience the birth of their biological child, and, of course there was considerable distress in the process of learning that the child was not theirs and exchanging the birth child for the biological child. In addition, the couple who filed the suit had another child (now age 7 years), who begged them to keep the baby to whom they gave birth. The couple also reported experiencing panic attacks as a result of the events.1
Medical considerations
As of 2018, more than 8 million IVF babies had been born, with the first in 1978 in the United Kingdom.2 Advances in science and technology have improved the process. Storage tanks now have alarms and several safeguards to monitor the level of liquid nitrogen and immediately notify key personnel if levels are low (FIGURES 1 and 2). Preimplantation genetic testing is also readily available to assess the embryo prior to transfer into the uterus and identify various genetic problems.


Guidelines for embryo straw labelling are provided by the College of American Pathologists and the Centers for Disease Control and Prevention. The American Society for Reproductive Medicine (ASRM) also provides guidelines. When an error occurs, disclosure is recommended and ethical and legal counsel should be involved. Failing to disclose can lead to professional penalties.4
Unfortunately, despite these advances and guidelines, embryo mix-ups like the one in the above case do occur and receive public notice (See “Cross country embryo mix-up cases”).5,6 A report from the University of Nevada assessed liability for embryo mix-ups in US fertility practices from 2000 to 2020.7 They evaluated 184,015 IVF cycles with 176 claims. Payments were made to plaintiffs in 21 cases, resulting in $15 million of awarded damages (average award was $199,188).7 The most common problem was in the embryology laboratory with an overall incidence of 0.03% of the total number of IVF cycles.7 To avoid damages, the authors emphasized the importance of following labeling guidelines when storing embryos, considering a 2-step read-back method prior to embryo transfer, and offering genetic testing when a discrepancy is noted in the record (TABLE).7

Other medical liability considerations
Embryo mix-ups are not the only source of problems and potential liability in IVF. At the 2021 Association of Sexual and Reproductive Medicine Annual Meeting, Applebaum et al presented results from a comprehensive review of malpractice litigation involving IVF in the United States.8 Using the legal database NEXIS Uni they identified 50 cases between 1986 and 2020 (32% of which were filed in New York state). Common thematic elements among patient allegations were embryology errors (eg, lost or destroyed embryos or incorrect sperm or egg donor), errors in preimplantation genetics, surgical or medical errors/complications, or misdiagnosis (eg, sexually transmitted disease screening or malignancy).8 Overall, the most common plaintiff complaint was negligence (26 cases) due to informed consent–related issues (9 cases), wrongful life or birth (9 cases), or negligent or intentional infliction of emotional distress (5 cases).8
In 48% of cases, the verdict was in favor of the defendant; it was for the plaintiff in 36% of cases and ongoing proceedings or partial judgement accounted for the remaining cases.8 Damages ranged from $4,171.45 to $50 million. The authors emphasized specific defense strategies, including the importance of careful labeling and handling of embryos, prompt disclosure when an error does occur, and awareness of the specific state statute(s) of limitations for medical malpractice claims.8
Continue to: Legal considerations...
Legal considerations
The case at the beginning of this article is a “mix-up” case, in which an IVF center implanted the wrong embryo, resulting in the birth parents not being the biological parents.1 As in that case, there may be (but are not always)6,9 2 mix-ups, so that 2 couples have each other’s biological children. These cases may go unnoticed by the birth parent if the physical appearance is not unexpected and the parents never do genetic testing, or if the IVF center does not discover the error and inform the parents. Infrequently the cases make the news or the courts.10,11
News accounts are not trials, and we do not suggest that all the facts discussed in news reports on the case described here are complete—or even accurate in the details reported. They are generally 1-sided, so there are other perspectives. To consider the legal issues, however, we will assume for discussion only that the facts are as they have been reported in the news coverage—with the understanding that the discovery and trial processes would undoubtedly bring to light many other important facts or corrections.
Negligence
Although there are several potential bases for liability (ie, contract or warranty claims, a form of product liability/defect) in mix-up and other artificial reproductive technology (ART), negligence or malpractice seem most likely.12 “Negligence” here is intended to be simple negligence but may also include gross negligence or recklessness.
Although the incidence of errors in ART is unknown, there is limited evidence that suggests it is not a rare event. One study suggested >20% of fertility clinics knew of errors in processing or handling donor samples and embryos for implantation.13 Another study in the United Kingdom found that 1 in 1,000 IVF embryos were implanted in the wrong woman.14
Was there negligence? The first question in a malpractice or negligence-type action is, was there a professional relationship between the plaintiff who is claiming harm and the professional or organization defendant? The next question is whether the defendant was reasonably careful given the circumstances—that is, did the physician meet the “standard of care”? This is sometimes described as whether the professional’s actions would be acceptable (ie, reasonably prudent within the profession or specialty). If there was negligence, then the next question is, did that negligence cause an injury to the plaintiff?15
Determining the standard of care. The nature of the expected standard of care is dependent, in part, on the potential consequences of an error. For example, the care required when there is a significant risk of death from an error would be considerably more cautious than for an error that might result in small property damage. In this case study, a mix-up error is likely to be less severe than death, but is very substantial in terms of emotional harm and disruption. Thus, considerable care and attention would be expected to avoid these errors. They should be a “never” event. Institutions and physicians should give considerable attention to their processes and procedures to avoid the possibility of a mix-up error.16
Where did the negligence occur? There is an old tort doctrine “Res ipsa loquitor” (RIL) that means, “The thing speaks for itself.” Although there are several technical rules around the application of RIL as a presumption of negligence, it comes down to the proposition that some injuries do not occur without negligence. A traditional medical example is the sponge left in a patient during surgery—ordinarily that does not happen without some negligence. For RIL to be applied, usually the mechanism by which the injury occurred had to be under the control of the defendant (or the agents of the defendant).
The “mix-up” of embryos is an example of the kind of error that would not likely occur without negligence.17 But the embryo may not be in the exclusive control of any 1 institution. For example, the mistake could be made by the IVF center (or its employees), a separate facility that has processed or cryogenically stored the genetic materials, and independent physicians (not employees or agents of the center). Therefore, it is necessary to pinpoint where the negligence occurred and who is legally responsible. In some cases, a health care provider must take steps to ensure that its contractors have sufficient safeguards to avoid unnecessary harms. For example, an IVF center that uses an external cryogenic storage facility may have some obligation to know that the genetic material returned to the center is the same material that the center provided the storage facility in the first place and is properly identified.18
Assessing damages
From the facts as we have them, it appears that there must have been negligence that caused the mix-up of the embryos in the original case. It also appears reasonably clear that the negligence resulted in harm to both sets of parents and their families. This would suggest that the families should recover substantial damages. But that, somewhat surprisingly, may not be the case.19 Several legal principles may limit the availability or size of damages in mix-up cases. Also, it is worth remembering that there are differences in how states treat the different types of damages in these cases. Although the case was filed in California, we’ll take a more national view of the damages issue.
Not all harm is treated as equal. The first problem facing plaintiffs in mix-up cases may be the fact that they have suffered only emotional harm, without any physical injury. Traditionally, the courts have been reluctant to allow recovery in negligence for purely emotional injuries. Also “intentional” infliction of emotional distress does permit financial recovery, but generally “negligent” infliction of emotional harm traditionally has not. In part, this was because of the fear of unwarranted (and difficult-to-assess) claims of emotional harm that are not related to a physical harm. Some states developed a “zone of danger” exception (eg, where someone was almost hit by a car) or allowed some emotional injury recovery if there were “physical manifestations” of the emotional harm. In short, depending on the state’s rules, negligence that causes purely emotional harm may not be compensable.20
State-based malpractice “caps.” Another limitation on emotional injuries is the “caps” on malpractice damages enacted by several states (including California, where this mix-up case occurred). Therefore, if a mix-up case is determined to be a malpractice case under state law, emotional suffering damages (which are non-economic damages) may be limited to the cap—$250,000 in California, for example—even if the state allows damages for emotional injuries without physical injuries.
The rare exception. Very careless labeling or handling of the identity of the embryo could at the extreme be considered gross negligence or recklessness. There are relatively inexpensive and easy procedures that could easily avoid what is likely to be significant harm to families (including emotional upset).21 Institutions that callously fail to use those procedures might be seen by some courts as reckless, or in outrageous cases, even intentional. An example would be the University of California Irvine Center for Reproductive Health case, in which physicians intentionally (without consent) used patients’ ova, fertilized them, and then implanted them in other patients, with at least 15 births, many lawsuits, and multimillion dollar settlements.22 In “intentional” cases, limitations on emotional injuries would usually not be major barriers to recovery of damages. However, those are legal stretches, and recovery is the exception rather than the rule.23
Continue to: Additional legal concerns with IVF...
Additional legal concerns with IVF
Reproduction negligence cases include a large range of errors and injuries—not just embryo mix-ups. Courts have struggled with when it is appropriate to allow damages, even when there have been clear injuries. For the most part courts have been reluctant to find liability in many areas of new IVF technology.12 One problem in determining how to assess damages is determining how incidental benefits should be used to offset some or all of the damages. For example, how should the joy of having a child offset the costs of raising the child?
There are more than a dozen kinds of current and likely future claims arising from problems with ART. It is tempting to conclude, “Oh, what a tangled legal web we weave when first we practice to artificially conceive.” There are various groupings of such claims, with several examples of cases presented in this article. It is not possible to consider those in detail in this article. As a general proposition, however, “our legal system treats wrongfully disrupted plans concerning reproduction like one of those life adversities that people are expected to abide without remedy.”24
This is not to say, however, that there is no compensation for IVF-related injuries. Applebaum and colleagues found more than 100 cases in the 35 years covered by the study (1984-2020).8 However, only 50 of those cases fit the criteria for inclusion in their data. The successful cases for the plaintiffs involved medical or surgical error, while it appeared that various forms of wrongful life or birth were much less successful. It would be a mistake to conclude from these data that there are not, and will not be, meaningful risks of liability in the areas of IVF and ART more generally.
First, claims that fit with existing legal doctrine are producing liability. About half of the claims (25 over the 34 years) examined by Applebaum et al resulted in liability. Admittedly, that number was small because ART use was increasing. Where the claims fit well-recognized legal forms of damages and forms of action (primarily negligence), the liability could be substantial. A remarkable example of this is the case of Wuth v Lab. Corp (see “Liability for genetic testing errors”),25 which was the largest verdict ($50 million) in the Applebaum and colleagues’ study.8 The large verdict was due to the failure of the testing company and a medical center to properly perform and assess a genetic test, which resulted in the birth of a child with an unbalanced chromosome translocation.8,25 The child’s serious disabilities would require a great deal of expensive care. Although the jury held the testing laboratory and medical center liable, they did not find liability against the physician.25 Ultimately, this case would be considered a failure of genetic testing rather than an IVF case.
More than 2 couples
In a second case from California, a couples’ son was born to another couple in New York—along with another boy from a third couple. The woman in New York thought she had carried biological twins but genetic testing confirmed the twins were not related to the couple or to each other (the second couple filed a separate medical malpractice and negligence lawsuit in New York). All 3 couples had sought care at the same IVF clinic. The babies were eventually returned to their biological parents.1
Different races
In a New York case, a Korean couple had twin White boys after consenting to a single embryo transfer. Meanwhile a couple in Los Angeles who went to the same in vitro fertilization clinic gave birth to a child that did not match their appearance. Both couples had undergone embryo transfers on the same day. The court arranged for the Korean couple to surrender their twins to their biological parents when they were 6 months of age in exchange for their biological child.2
References
1. Couple claims clinic implanted their embryo in wrong woman. Associated Press. July 10, 2019. https://apnews.com/article/de32d537c6e34808b28834c23f00e272. Accessed January 6, 2022.
2. In the matter of accusation against Steven L. Katz. Case no. 03-20001-122617.OAH no. N2004080093. Sacramento, CA. Medical Board of California Department of Consumer Affairs 2005.
Future challenges
The future is likely to bring substantially expanded IVF/ART liability for several reasons. ART is becoming more common. Although courts have struggled with how to apply existing liability rules to the new technologies and related novel legal claims, the absence of established legal principles into which IVF injuries fit will not last forever. The legal system eventually finds ways of adjusting old rules or adopting new ones to cover injuries from new technology.
Although IVF injuries that most people feel deserve compensation currently are not cognizable in law, that will undoubtedly change. Either the courts will find new ways of assessing ART claims, or state legislatures and Congress will step in with legislation. To date, Congress has been relatively “hands off” on the ART processes, with the Fertility Clinic Success Rate and Certification Act of 1992 being a notable exception.24 This law requires ART programs to report success rates and directs the Centers for Disease Control and Prevention (CDC) to publish reported success rates and laboratory incidents. It also establishes a model state laboratory certification program.24 The CDC has an outline of the work under the statute,26 as well as state-specific data regarding ART27 and lists of publications in key areas.28 In addition there are various state laws related to recordkeeping, donor qualifications, licensing, and family law issues.29 Ultimately, physicians, scientists, and legal professionals can perform a valuable role in helping to fashion IVF liability principles that are workable and reasonable, that will not interfere with the progress of medicine, and that will ensure that those injured through carelessness or bad medicine receive compensation. ●
Although not technically an in vitro fertilization (IVF) case, Wuth v Lab. Corp. involved an infant born through IVF with a translocation defect chromosome 2 (ie, deleted material) and extra chromatin on 9. The father’s family history included birth defects, including a female cousin with profound developmental disabilities, seizures, and antisocial behavior. He had undergone genetic testing that revealed an asymptomatic balanced, 2;9 translocation. As part of the IVF process, the couple had a genetic consultation and were told there was a 50% chance that the fetus would have an unbalanced 2;9 translocation given the father’s family history and that chorionic villus sampling or amniocentesis could detect this in the fetus.1
Amniocentesis had been performed, with the specimen sent to Lab. Corp. The result was “normal male karyotype.” However, when the baby was born, it was immediately apparent that he had severe physical defects and subsequently cognitive defects. Genetic testing of the child revealed an unbalanced 2;9 translocation. The couple filed a suit for wrongful birth and wrongful life, which went to a jury. The child was awarded $25 million and the parents/family were awarded another $25 million in general damages. The verdict reflected errors in genetic (laboratory) testing.
Reference
1. Wuth v Lab. Corp. of Am., 189 Wash. App. 660, 359 P.3d 841 (2015).
- Mark J. California couple sues fertility clinic following IVF embryo mix-up. Washington Post. November 9, 2021. https://www.washingtonpost.com/nation/2021/11/09/in-vitro-fertilization-ivf-mix-up-daphna-cardinale. Accessed January 5, 2022.
- More than 8 million babies born from IVF since the world’s first in 1978. Science Daily. July 3, 2018. https://www.sciencedaily.com/releases/2018/07/180703084127.htm. Accessed January 11, 2022.
- ESCO Medical. In vitro fertilization (IVF) as fertility treatment. https://www.esco-medical.com/resource/in-vitro-fertilization-ivf-as-fertility-treatment.
- Vigdor N. “We had their baby, and they had our baby”: couple sues over embryo “mix-up.” NY Times. November 9, 2021. https://www.nytimes.com/2021/11/09/us/fertility-clinic-embryo-mixup.html. Accessed January 11, 2022.
- Couple claims clinic implanted their embryo in wrong woman. Associated Press. July 10, 2019. https://apnews.com/article/de32d537c6e34808b28834c23f00e2728. Accessed January 6, 2022.
- In the matter of accusation against Steven L. Katz. Case no. 03-20001-122617.OAH no. N2004080093. Sacramento, CA. Medical Board of California Department of Consumer Affairs 2005
- Rasouli MA, Moutos CP, Phelps JY. Liability for embryo mix-ups in fertility practices in the USA. J Assist Reprod Genet. 2021;38:1101-1107. doi:10.1007/s10815-021-02108-1
- Applebaum J, Berger D, O’Neill K. Can a reproductive endocrinologist be sued for 50 million dollars? A comprehensive review of malpractice litigation involving in vitro fertilization in the U.S. Fertil Steril. 2021;116(3s):e19. doi:10.1016/j.fertnstert.2021.07.059
- Andrews v Keltz, 838 N.Y.S.2d 363, 365 (Sup. Ct. 2007).
- Chichi DV. In vitro fertilization, fertility frustrations, and the lack of regulation. Hofstra L Rev. 2021;49:535-568. https://www.hofstralawreview.org/wp-content/uploads/2021/04/bb.2.chichi.pdf. Accessed January 11, 2022.
- Lewin T. Sperm banks accused of losing samples and lying about donors. NY Times. July 21, 2016. https://www.nytimes.com/2016/07/22/us/sperm-banks-accused-of-losing-samples-and-lying-about-donors.html. Accessed January 11, 2022.
- Bender L. To err is human ART mix-ups: labor-based, relational proposal. J Gender Race Justice. 2006;9:443-508. https://surface.syr.edu/cgi/viewcontent.cgi?article=1050&context=lawpub. Accessed January 11, 2022.
- Baruch S, Kaufman D, Hudson KL. Genetic testing of embryos: practices and perspectives of U.S. in vitro fertilization clinics. Fertil Steril. 2007;89:1053-1058. doi:10.1016/j.fertnstert.2007.05.048
- Liebler R. Are you my parent? Are you my child? The role of genetics and race in defining relationships after reproductive technological mistakes. DePaul J Health Care Law. 2002;5:15-56. https://via.library.depaul.edu/cgi/viewcontent.cgi?article=1202&context=jhcl. Accessed January 11, 2022.
- Crockin SL, Altman AB, Edmonds MA. The history and future trends of art medicine and law. Fam Court Rev. 2021;59:22-45. doi:10.1111/fcre.12550
- Fernandes JS. Perfecting pregnancy via preimplantation genetic screening: the quest for an elusive standard of care. UC Irvine L Rev. 2014;4:1295-1326. https://www.law.uci.edu/lawreview/vol4/no4/Fernandes.pdf. Accessed January 11, 2022.
- VanGessel MM. Wrongful surrogacy: the need for right of action in cases of clear negligence. U Toledo L Rev. 2015;46:681-706.
- Reich J, Swink D. Outsourcing human reproduction: embryos and surrogacy services in the cyberprocreation era. J Health Care L Policy. 2011;14:241-298. https://core.ac.uk/download/pdf/217156567.pdf. Accessed January 11, 2022.
- Strasser M. Prenatal tort slippage. Health Matrix. 2021;31:221-262. https://scholarlycommons.law.case.edu/healthmatrix/vol31/iss1/9. Accessed January 11, 2022.
- Heide IH. Negligence in the creation of healthy babies: negligent infliction of emotional distress in cases of alternative reproductive technology malpractice without physical injury. J Med L. 2005;9:55-94.
- Novo S, Nogués C, Penon O, et al. Barcode tagging of human oocytes and embryos to prevent mix-ups in assisted reproduction technologies. Hum Reprod. 2014;29:18-28. doi: 10.1093/humrep/det409
- Yoshino K. UCI Settles Dozens of Fertility Suits. LA Times. September 11, 2009. https://www.latimes.com/archives/la-xpm-2009-sep-11-me-uci-fertility11-story.html. Accessed January 11, 2022.
- Fox D. Reproductive negligence. Columbia L Rev. 2017;117:149-242. https://columbialawreview.org/wp-content/uploads/2017/01/149.pdf. Accessed January 11, 2022.
- 42 U.S.C.S. §263a-1-263a-7; Public Law 102-493. https://www.govinfo.gov/content/pkg/STATUTE-106/pdf/STATUTE-106-Pg3146.pdf. Accessed January 11, 2022.
- Wuth v Lab. Corp. of Am., 189 Wash. App. 660, 359 P.3d 841 (2015).
- Centers for Disease Control and Prevention. The Fertility Clinic Success Rate and Certification Act. December 14, 2020. https://www.cdc.gov/art/nass/policy.html#act. Accessed January 11, 2022.
- Centers for Disease Control and Prevention. State-specific assisted reproductive technology surveillance. December 17, 2020. https://www.cdc.gov/art/state-specific-surveillance/index.html. Accessed January 11, 2022.
- Centers for Disease Control and Prevention. Key findings. March 12, 2021. https://www.cdc.gov/art/key-findings/index.html. Accessed January 11, 2022.
- Cohen EN. 5 Treatise on Health Care Law §22.04, (ed. Hooper, Lundy & Bookman, & Robert W. Lundy, Jr. RW.) (Matthew Bender-LexisNexis)
- Mark J. California couple sues fertility clinic following IVF embryo mix-up. Washington Post. November 9, 2021. https://www.washingtonpost.com/nation/2021/11/09/in-vitro-fertilization-ivf-mix-up-daphna-cardinale. Accessed January 5, 2022.
- More than 8 million babies born from IVF since the world’s first in 1978. Science Daily. July 3, 2018. https://www.sciencedaily.com/releases/2018/07/180703084127.htm. Accessed January 11, 2022.
- ESCO Medical. In vitro fertilization (IVF) as fertility treatment. https://www.esco-medical.com/resource/in-vitro-fertilization-ivf-as-fertility-treatment.
- Vigdor N. “We had their baby, and they had our baby”: couple sues over embryo “mix-up.” NY Times. November 9, 2021. https://www.nytimes.com/2021/11/09/us/fertility-clinic-embryo-mixup.html. Accessed January 11, 2022.
- Couple claims clinic implanted their embryo in wrong woman. Associated Press. July 10, 2019. https://apnews.com/article/de32d537c6e34808b28834c23f00e2728. Accessed January 6, 2022.
- In the matter of accusation against Steven L. Katz. Case no. 03-20001-122617.OAH no. N2004080093. Sacramento, CA. Medical Board of California Department of Consumer Affairs 2005
- Rasouli MA, Moutos CP, Phelps JY. Liability for embryo mix-ups in fertility practices in the USA. J Assist Reprod Genet. 2021;38:1101-1107. doi:10.1007/s10815-021-02108-1
- Applebaum J, Berger D, O’Neill K. Can a reproductive endocrinologist be sued for 50 million dollars? A comprehensive review of malpractice litigation involving in vitro fertilization in the U.S. Fertil Steril. 2021;116(3s):e19. doi:10.1016/j.fertnstert.2021.07.059
- Andrews v Keltz, 838 N.Y.S.2d 363, 365 (Sup. Ct. 2007).
- Chichi DV. In vitro fertilization, fertility frustrations, and the lack of regulation. Hofstra L Rev. 2021;49:535-568. https://www.hofstralawreview.org/wp-content/uploads/2021/04/bb.2.chichi.pdf. Accessed January 11, 2022.
- Lewin T. Sperm banks accused of losing samples and lying about donors. NY Times. July 21, 2016. https://www.nytimes.com/2016/07/22/us/sperm-banks-accused-of-losing-samples-and-lying-about-donors.html. Accessed January 11, 2022.
- Bender L. To err is human ART mix-ups: labor-based, relational proposal. J Gender Race Justice. 2006;9:443-508. https://surface.syr.edu/cgi/viewcontent.cgi?article=1050&context=lawpub. Accessed January 11, 2022.
- Baruch S, Kaufman D, Hudson KL. Genetic testing of embryos: practices and perspectives of U.S. in vitro fertilization clinics. Fertil Steril. 2007;89:1053-1058. doi:10.1016/j.fertnstert.2007.05.048
- Liebler R. Are you my parent? Are you my child? The role of genetics and race in defining relationships after reproductive technological mistakes. DePaul J Health Care Law. 2002;5:15-56. https://via.library.depaul.edu/cgi/viewcontent.cgi?article=1202&context=jhcl. Accessed January 11, 2022.
- Crockin SL, Altman AB, Edmonds MA. The history and future trends of art medicine and law. Fam Court Rev. 2021;59:22-45. doi:10.1111/fcre.12550
- Fernandes JS. Perfecting pregnancy via preimplantation genetic screening: the quest for an elusive standard of care. UC Irvine L Rev. 2014;4:1295-1326. https://www.law.uci.edu/lawreview/vol4/no4/Fernandes.pdf. Accessed January 11, 2022.
- VanGessel MM. Wrongful surrogacy: the need for right of action in cases of clear negligence. U Toledo L Rev. 2015;46:681-706.
- Reich J, Swink D. Outsourcing human reproduction: embryos and surrogacy services in the cyberprocreation era. J Health Care L Policy. 2011;14:241-298. https://core.ac.uk/download/pdf/217156567.pdf. Accessed January 11, 2022.
- Strasser M. Prenatal tort slippage. Health Matrix. 2021;31:221-262. https://scholarlycommons.law.case.edu/healthmatrix/vol31/iss1/9. Accessed January 11, 2022.
- Heide IH. Negligence in the creation of healthy babies: negligent infliction of emotional distress in cases of alternative reproductive technology malpractice without physical injury. J Med L. 2005;9:55-94.
- Novo S, Nogués C, Penon O, et al. Barcode tagging of human oocytes and embryos to prevent mix-ups in assisted reproduction technologies. Hum Reprod. 2014;29:18-28. doi: 10.1093/humrep/det409
- Yoshino K. UCI Settles Dozens of Fertility Suits. LA Times. September 11, 2009. https://www.latimes.com/archives/la-xpm-2009-sep-11-me-uci-fertility11-story.html. Accessed January 11, 2022.
- Fox D. Reproductive negligence. Columbia L Rev. 2017;117:149-242. https://columbialawreview.org/wp-content/uploads/2017/01/149.pdf. Accessed January 11, 2022.
- 42 U.S.C.S. §263a-1-263a-7; Public Law 102-493. https://www.govinfo.gov/content/pkg/STATUTE-106/pdf/STATUTE-106-Pg3146.pdf. Accessed January 11, 2022.
- Wuth v Lab. Corp. of Am., 189 Wash. App. 660, 359 P.3d 841 (2015).
- Centers for Disease Control and Prevention. The Fertility Clinic Success Rate and Certification Act. December 14, 2020. https://www.cdc.gov/art/nass/policy.html#act. Accessed January 11, 2022.
- Centers for Disease Control and Prevention. State-specific assisted reproductive technology surveillance. December 17, 2020. https://www.cdc.gov/art/state-specific-surveillance/index.html. Accessed January 11, 2022.
- Centers for Disease Control and Prevention. Key findings. March 12, 2021. https://www.cdc.gov/art/key-findings/index.html. Accessed January 11, 2022.
- Cohen EN. 5 Treatise on Health Care Law §22.04, (ed. Hooper, Lundy & Bookman, & Robert W. Lundy, Jr. RW.) (Matthew Bender-LexisNexis)
Honor thy parents? Understanding parricide and associated spree killings
Mr. B, age 37, presents to a community mental health center for an appointment following a recent emergency department visit. He is diagnosed with schizophrenia, and has been treated for approximately 1 year. Six months ago, Mr. B stopped taking his antipsychotic due to its adverse effects. Despite compliance with another agent, he has become increasingly disorganized and paranoid.
He now believes that his mother, with whom he has lived all his life and who serves as his guardian, is poisoning his food and trying to kill him. She is an employee at a local grocery store, and Mr. B has expressed concern that her coworkers are assisting her in the plot to kill him.
Following a home visit, Mr. B’s case manager indicates that the patient showed them the collection of weapons he is amassing to “defend” himself. This leads to a concern for the safety of the patient, his mother, and others.
Although parricide—killing one’s parent—is a relatively rare event, its sensationalistic nature has long captured the attention of headline writers and the general public. This article discusses the diagnostic and demographic factors that may be seen among individuals who kill their parents, with an emphasis on those who commit matricide (murder of one’s mother) and associated spree killings, where an individual kills multiple people within a single brief but contiguous time period. Understanding these characteristics can help clinicians identify and more safely manage patients who may be at risk of harming their parents in addition to others.
Characteristics of perpetrators of parricide
Worldwide, approximately 2% to 4% of homicides involve parricide, or killing one’s parent.1,2 Most offenders are men in early adulthood, though a proportion are adolescents and some are women.1,3 They are often single, unemployed, and live with the parent prior to the killing.1 Patricide occurs more frequently than matricide.4 In the United States, approximately 150 fathers and 100 mothers are killed by their child each year.5
In a study of all homicides in England and Wales between 1997 and 2014, two-thirds of parricide offenders had previously been diagnosed with a mental disorder.1 One-third were diagnosed with schizophrenia.1 In a Canadian study focusing on 43 adult perpetrators found not criminally responsible,6 most were experiencing psychotic symptoms at the time of parricide; symptoms of a personality disorder were the second-most prevalent symptoms. Similarly, Bourget et al4 studied Canadian coroner records for 64 parents killed by their children. Of the children involved in those parricides, 15% attempted suicide after the killing. Two-thirds of the male offenders evidenced delusional thinking, and/or excessive violence (overkill) was common. Some cases (16%) followed an argument, and some of those perpetrators were intoxicated or psychotic. From our clinical experience, when there are identifiable nonpsychotic triggers, they often can be small things such as an argument over food, smoking, or video games. Often, the perpetrator was financially dependent on their parents and were “trapped in a difficult/hostile/dependence/love relationship” with that parent.6 Adolescent males who kill their parents may not have psychosis7; however, they may be victims of longstanding serious abuse at the hands of their parents. These perpetrators often express relief rather than remorse after committing murder.
Three categories to classify the perpetrators of parricide have been proposed: severely abused, severely mentally ill, and “dangerously antisocial.”3 While severe mental illness was most common in adult defendants, severe abuse was most common in adolescent offenders. There may be significant commonalities between adolescent and adult perpetrators. A more recent latent class analysis by Bojanic et al1 indicated 3 unique types of parricide offenders (Table 1).
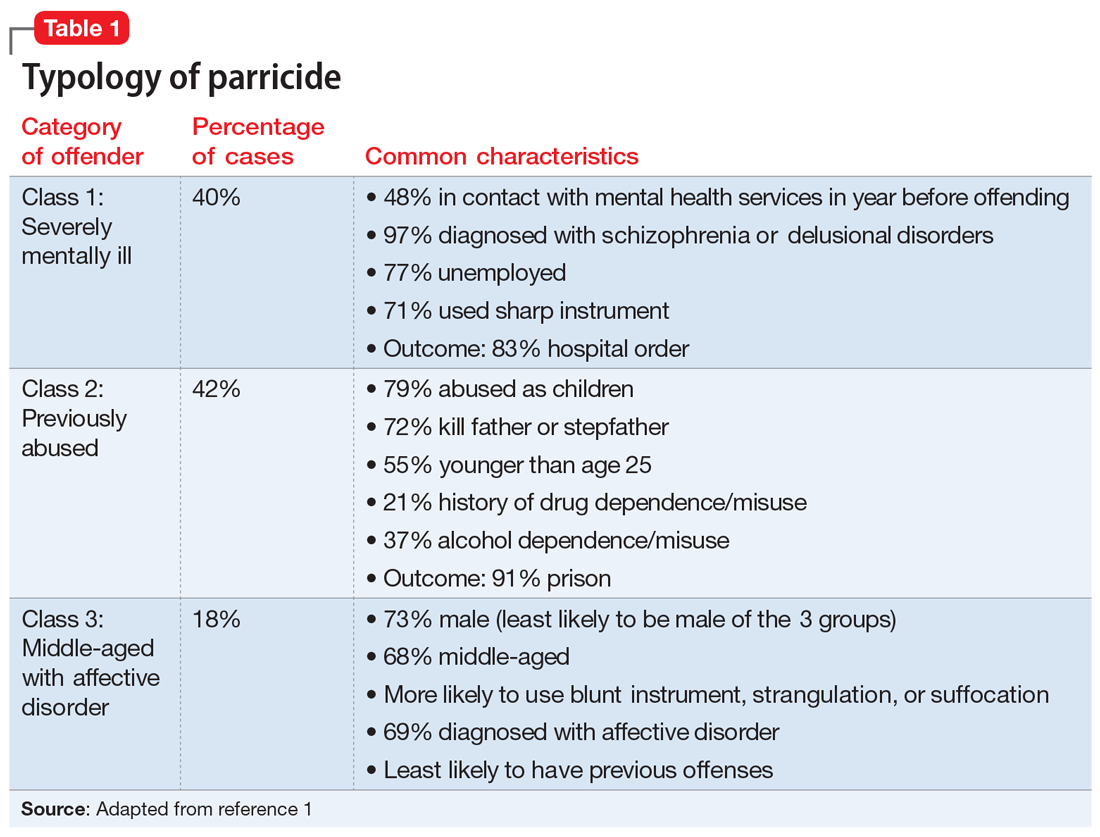
Continue to: Matricide: A closer look...
Matricide: A closer look
Though multiple studies have found a higher rate of psychosis among perpetrators of matricide, it is important to note that most people with psychotic disorders would never kill their mother. These events, however, tend to grab headlines and may be highly focused upon by the general population. In addition, matricide may be part of a larger crime that draws additional attention. For example, the 1966 University of Texas Bell Tower shooter and the 2012 Sandy Hook Elementary school shooter both killed their mothers before engaging in mass homicide. Often in cases of matricide, a longer-term dysfunctional relationship existed between the mother and the child. The mother is frequently described as controlling and intrusive and the (often adult) child as overly dependent, while the father may be absent or ineffectual. Hostility and mutual dependence are usual hallmarks of these relationships.8
However, in some cases where an individual with a psychotic disorder kills their mother, there may have been a traditional nurturing relationship.8 Alternative motivations unrelated to psychosis must be considered, including crimes motivated by money/inheritance or those perpetrated out of nonpsychotic anger. Green8 described motive categories for matricide that include paranoid and persecutory, altruistic, and other. In the “paranoid and persecutory” group, delusional beliefs about the mother occur; for example, the perpetrator may believe their mother was the devil. Sexual elements are found in some cases.8 Alternatively, the “altruistic” group demonstrated rather selfless reasons for killing, such as altruistic infanticide cases, or killing out of love.9 The altruistic matricide perpetrator may believe their mother is unwell, which may be a delusion or actually true. Finally, the “other” category contains cases related to jealousy, rage, and impulsivity.
In a study of 15 matricidal men in New York conducted by Campion et al,10 individuals seen by forensic psychiatric services for the crime of matricide included those with schizophrenia, substance-induced psychosis, and impulse control disorders. The authors noted there was often “a serious chronic derangement in the relationships of most matricidal men and their mothers.” Psychometric testing in these cases indicated feelings of dependency, weakness, and difficulty accepting an adult role separate from their mother. Some had conceptualized their mothers as a threat to their masculinity, while others had become enraged at their mothers.
Prevention requires addressing underlying issues
As described above, several factors are common among individuals who commit parricide, and these can be used to develop prevention strategies that focus on addressing underlying issues (Table 2). It is important to consider the relationship dynamics between the potential victim and perpetrator, as well as the motive, rather than focusing solely on mental illness or substance misuse.2
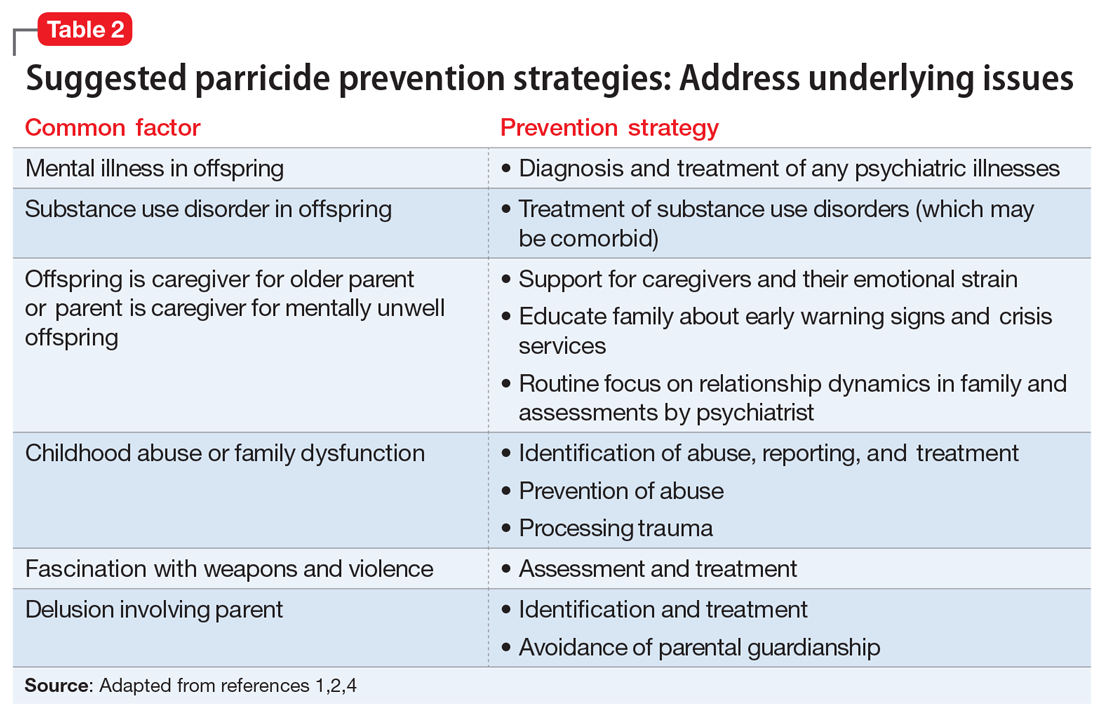
Spree killings that start as parricide
Although spree killing is a relatively rare event, a subset of spree killings involve parricide. One infamous recent event occurred in 2012 at Sandy Hook Elementary School, where the gunman killed his mother before going to the school and killing 26 additional people, many of whom were children.11,12 Because such events are rare, and because in these cases there is a high likelihood that the perpetrator is deceased (eg, died by suicide or killed by the police), much remains unknown about specific motivations and causative factors.
Information is often pieced together from postmortem reviews, which can be hampered by hindsight/recall bias and lack of contemporaneous documentation. Even worse, when these events occur, they may lead to a bias that all parricides or mass murders follow the pattern of the most recent case. This can result in overgeneralization of an individual’s history as being actionable risk violence factors for all potential parricide cases both by the public (eg, “My sister’s son has autism, and the Sandy Hook shooter was reported to have autism—should I be worried for my sister?”) and professionals (eg, “Will I be blamed for the next Sandy Hook by not taking more aggressive action even though I am not sure it is clinically warranted?”).
To identify trends for individuals committing parricide who engage in mass murder events (such as spree killing), we reviewed the 2000-2019 FBI active shooter list.12 Of the 333 events identified, 46 could be classified as domestic violence situations (eg, the perpetrator was in a romantic or familial relationship/former relationship and engaged in an active shooting incident involving at least 1 person from that relationship). We classified 11 of those 46 cases as parricide. Ten of those 11 parricides involved a child killing a parent (Table 3), and the other involved a grandchild killing a grandfather who served as their primary caregiver. Of the 11 incidents, mothers were involved (killed or wounded) in 4, and father figures (including the grandfather serving as a father and a stepfather) were killed in 9, with 2 incidents involving both parents. In 4 of the 11 parricides, other family members were killed in addition to the parent (including siblings, grandparents, or extended family). When considering spree shooters who committed parricide, 4 alleged perpetrators died by suicide, 1 was killed at the scene, and the rest were apprehended. The most common active shooting site endangering the public was an educational location (5), followed by commerce locations (4), with 2 involving open spaces. Eight of the 11 parricides occurred before the event was designated as an active shooting. The mean age for a parricide plus spree shooter was 23, once the oldest (age 61) and youngest (age 14) were removed from the calculation. The majority of the cases fell into the age range of 16 to 25 (n = 6), followed by 3 individuals who were age 26 to 31 (n = 3). All suspected individuals were male.
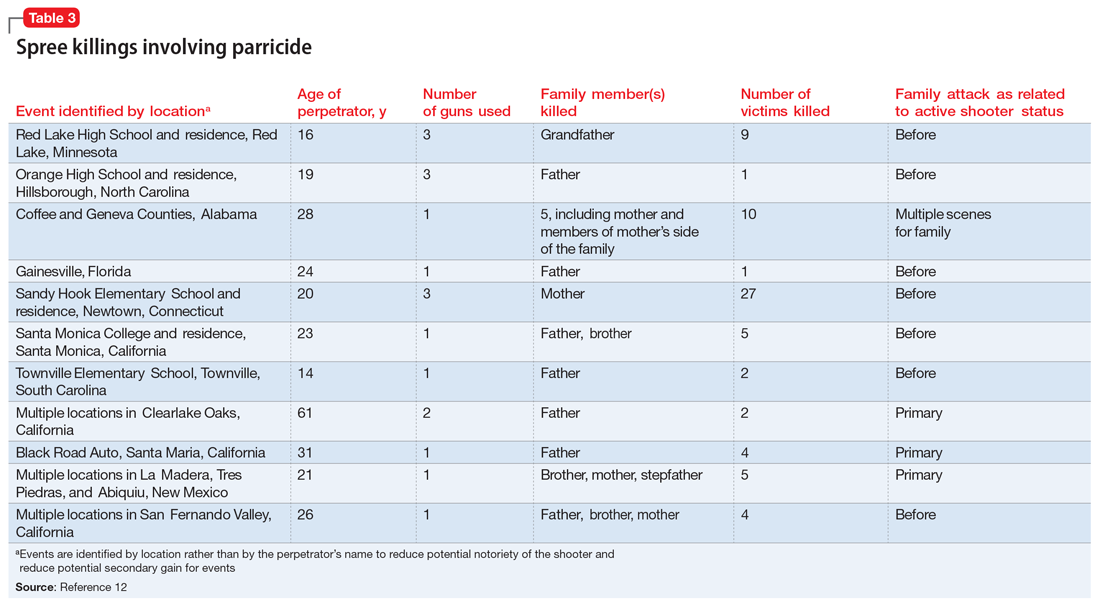
It is difficult to ascertain the existence of prior mental health care because perpetrators’ medical records may be confidential, juvenile court records may be sealed, and there may not even be a trial due to death or suicide (leading to limited forensic psychiatry examination or public testimony). Among those apprehended, many individuals raise some form of mental health defense, but the validity of their diagnosis may be undermined by concerns of possible malingering, especially in cases where the individual did not have a history of psychiatric treatment prior to the event.11 In summary, based on FBI data,12 spree shooters who committed parricide were usually male, in their late adolescence or early 20s, and more frequently targeted father figures. They often committed the parricide first and at a different location from later “active” shootings. Police were usually not aware of the parricide until after the spree is over.
Continue to: Parricide and society...
Parricide and society
For centuries, mothers and fathers have been honored and revered. Therefore, it is not surprising that killing of one’s mother or father attracts a great deal of macabre interest. Examples of parricide are present throughout popular culture, in mythology, comic books, movies, and television. As all psychiatrists know, Oedipus killed his father and married his mother. Other popular culture examples include: Grant Morrison’s Arkham Asylum: A Serious House on Serious Earth, Alfred Hitchcock’s Psycho, Oliver Stone’s Natural Born Killers, Peter Jackson’s Heavenly Creatures, The Affair drama series, and Star Wars: The Force Awakens.13,14
CASE CONTINUED
In Mr. B’s case, it is imperative for the treatment team to inquire about his history of violence, paying particular attention to prior violent acts towards his mother. His clinicians should consider hospitalization with the guardian’s consent if the danger appears imminent, especially considering the presence of weapons at home. They should attempt to stabilize Mr. B on effective, tolerable medications to ameliorate his psychosis, and to refer him for long-term psychotherapy to address difficult dynamic issues in the family relationship and encourage compliance with treatment. These steps may help avert a tragedy.
Bottom Line
Individuals who commit parricide often have a history of psychosis, a mood disorder, childhood abuse, and/or difficult relationship dynamics with the parent they kill. Some go on a spree killing in the community. Through careful consideration of individual risk factors, psychiatrists may help prevent some cases of parent murder by a child and possibly more tragedy in the community.
1. Bojanié L, Flynn S, Gianatsi M, et al. The typology of parricide and the role of mental illness: data-driven approach. Aggress Behav. 2020;46(6):516-522.
2. Pinals DS. Parricide. In Friedman SH, ed. Family Murder: Pathologies of Love and Hate. American Psychiatric Publishing; 2019:113-138.
3. Heide KM. Matricide and stepmatricide victims and offenders: an empirical analysis of US arrest data. Behav Sci Law. 2013;31(2):203-214.
4. Bourget D, Gagné P, Labelle ME. Parricide: a comparative study of matricide versus patricide. J Am Acad Psychiatry Law. 2007;35(3):306-312.
5. Heide KM, Frei A. Matricide: a critique of the literature. Trauma Violence Abuse. 2010;11(1):3-17.
6. Marleau JD, Auclair N, Millaud F. Comparison of factors associated with parricide in adults and adolescents. J Fam Viol. 2006;21:321-325.
7. West SG, Feldsher M. Parricide: characteristics of sons and daughters who kill their parents. Current Psychiatry. 2010;9(11):20-38.
8. Green CM. Matricide by sons. Med Sci Law. 1981;21(3):207-214.
9. Friedman SH. Conclusions. In Friedman SH, ed. Family Murder: Pathologies of Love and Hate. American Psychiatric Publishing; 2019:161-164.
10. Campion J, Cravens JM, Rotholc A, et al. A study of 15 matricidal men. Am J Psychiatry. 1985;142(3):312-317.
11. Hall RCW, Friedman SH, Sorrentino R, et al. The myth of school shooters and psychotropic medications. Behav Sci Law. 2019;37(5):540-558.
12. Department of Justice Federal Bureau of Investigation. Active Shooter Incidents: 20-Year Review, 2000-2019. June 1, 2021. Accessed October 12, 2021. https://www.fbi.gov/file-repository/active-shooter-incidents-20-year-review-2000-2019-060121.pdf/view
13. Friedman SH, Hall RCW. Star Wars: The Force Awakens, forensic teaching about matricide. J Am Acad Psychiatry Law. 2017;45(1):128-130.
14. Friedman SH, Hall RCW. Deadly and dysfunctional family dynamics: when fiction mirrors fact. In: Packer S, Fredrick DR, eds. Welcome to Arkham Asylum: Essays on Psychiatry and the Gotham City Institution. McFarland; 2019:65-75.
Mr. B, age 37, presents to a community mental health center for an appointment following a recent emergency department visit. He is diagnosed with schizophrenia, and has been treated for approximately 1 year. Six months ago, Mr. B stopped taking his antipsychotic due to its adverse effects. Despite compliance with another agent, he has become increasingly disorganized and paranoid.
He now believes that his mother, with whom he has lived all his life and who serves as his guardian, is poisoning his food and trying to kill him. She is an employee at a local grocery store, and Mr. B has expressed concern that her coworkers are assisting her in the plot to kill him.
Following a home visit, Mr. B’s case manager indicates that the patient showed them the collection of weapons he is amassing to “defend” himself. This leads to a concern for the safety of the patient, his mother, and others.
Although parricide—killing one’s parent—is a relatively rare event, its sensationalistic nature has long captured the attention of headline writers and the general public. This article discusses the diagnostic and demographic factors that may be seen among individuals who kill their parents, with an emphasis on those who commit matricide (murder of one’s mother) and associated spree killings, where an individual kills multiple people within a single brief but contiguous time period. Understanding these characteristics can help clinicians identify and more safely manage patients who may be at risk of harming their parents in addition to others.
Characteristics of perpetrators of parricide
Worldwide, approximately 2% to 4% of homicides involve parricide, or killing one’s parent.1,2 Most offenders are men in early adulthood, though a proportion are adolescents and some are women.1,3 They are often single, unemployed, and live with the parent prior to the killing.1 Patricide occurs more frequently than matricide.4 In the United States, approximately 150 fathers and 100 mothers are killed by their child each year.5
In a study of all homicides in England and Wales between 1997 and 2014, two-thirds of parricide offenders had previously been diagnosed with a mental disorder.1 One-third were diagnosed with schizophrenia.1 In a Canadian study focusing on 43 adult perpetrators found not criminally responsible,6 most were experiencing psychotic symptoms at the time of parricide; symptoms of a personality disorder were the second-most prevalent symptoms. Similarly, Bourget et al4 studied Canadian coroner records for 64 parents killed by their children. Of the children involved in those parricides, 15% attempted suicide after the killing. Two-thirds of the male offenders evidenced delusional thinking, and/or excessive violence (overkill) was common. Some cases (16%) followed an argument, and some of those perpetrators were intoxicated or psychotic. From our clinical experience, when there are identifiable nonpsychotic triggers, they often can be small things such as an argument over food, smoking, or video games. Often, the perpetrator was financially dependent on their parents and were “trapped in a difficult/hostile/dependence/love relationship” with that parent.6 Adolescent males who kill their parents may not have psychosis7; however, they may be victims of longstanding serious abuse at the hands of their parents. These perpetrators often express relief rather than remorse after committing murder.
Three categories to classify the perpetrators of parricide have been proposed: severely abused, severely mentally ill, and “dangerously antisocial.”3 While severe mental illness was most common in adult defendants, severe abuse was most common in adolescent offenders. There may be significant commonalities between adolescent and adult perpetrators. A more recent latent class analysis by Bojanic et al1 indicated 3 unique types of parricide offenders (Table 1).
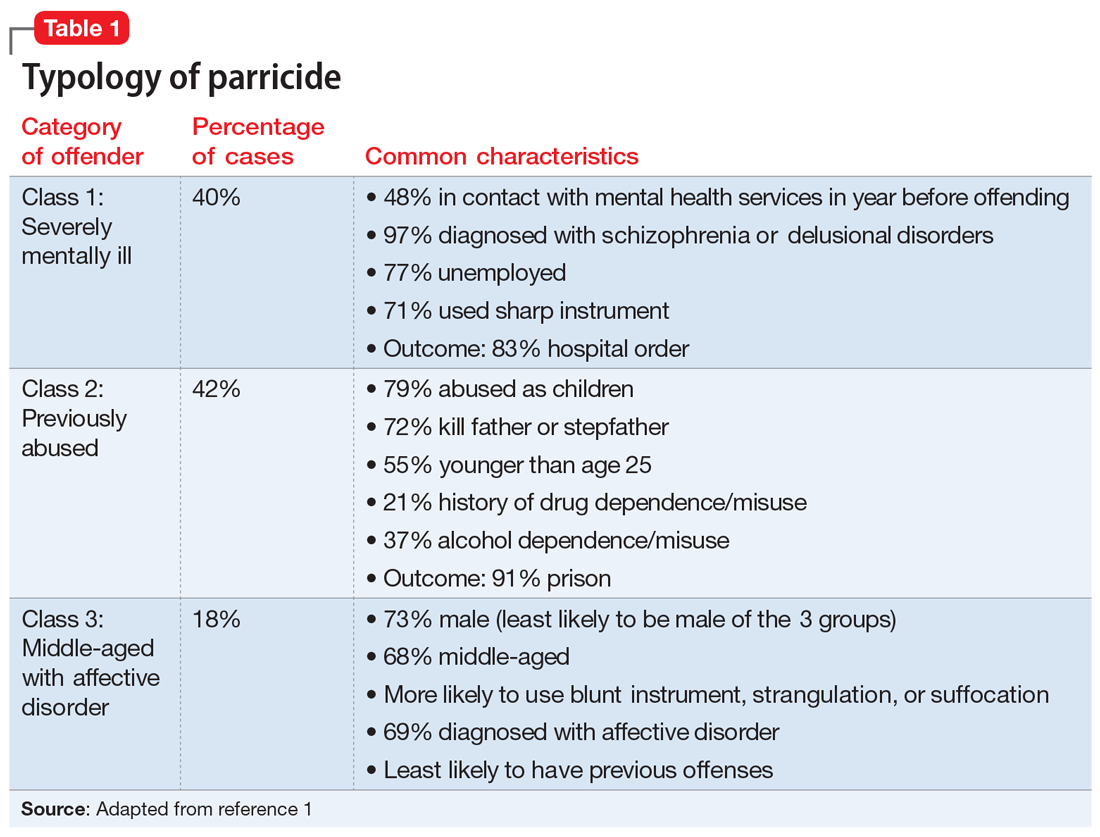
Continue to: Matricide: A closer look...
Matricide: A closer look
Though multiple studies have found a higher rate of psychosis among perpetrators of matricide, it is important to note that most people with psychotic disorders would never kill their mother. These events, however, tend to grab headlines and may be highly focused upon by the general population. In addition, matricide may be part of a larger crime that draws additional attention. For example, the 1966 University of Texas Bell Tower shooter and the 2012 Sandy Hook Elementary school shooter both killed their mothers before engaging in mass homicide. Often in cases of matricide, a longer-term dysfunctional relationship existed between the mother and the child. The mother is frequently described as controlling and intrusive and the (often adult) child as overly dependent, while the father may be absent or ineffectual. Hostility and mutual dependence are usual hallmarks of these relationships.8
However, in some cases where an individual with a psychotic disorder kills their mother, there may have been a traditional nurturing relationship.8 Alternative motivations unrelated to psychosis must be considered, including crimes motivated by money/inheritance or those perpetrated out of nonpsychotic anger. Green8 described motive categories for matricide that include paranoid and persecutory, altruistic, and other. In the “paranoid and persecutory” group, delusional beliefs about the mother occur; for example, the perpetrator may believe their mother was the devil. Sexual elements are found in some cases.8 Alternatively, the “altruistic” group demonstrated rather selfless reasons for killing, such as altruistic infanticide cases, or killing out of love.9 The altruistic matricide perpetrator may believe their mother is unwell, which may be a delusion or actually true. Finally, the “other” category contains cases related to jealousy, rage, and impulsivity.
In a study of 15 matricidal men in New York conducted by Campion et al,10 individuals seen by forensic psychiatric services for the crime of matricide included those with schizophrenia, substance-induced psychosis, and impulse control disorders. The authors noted there was often “a serious chronic derangement in the relationships of most matricidal men and their mothers.” Psychometric testing in these cases indicated feelings of dependency, weakness, and difficulty accepting an adult role separate from their mother. Some had conceptualized their mothers as a threat to their masculinity, while others had become enraged at their mothers.
Prevention requires addressing underlying issues
As described above, several factors are common among individuals who commit parricide, and these can be used to develop prevention strategies that focus on addressing underlying issues (Table 2). It is important to consider the relationship dynamics between the potential victim and perpetrator, as well as the motive, rather than focusing solely on mental illness or substance misuse.2
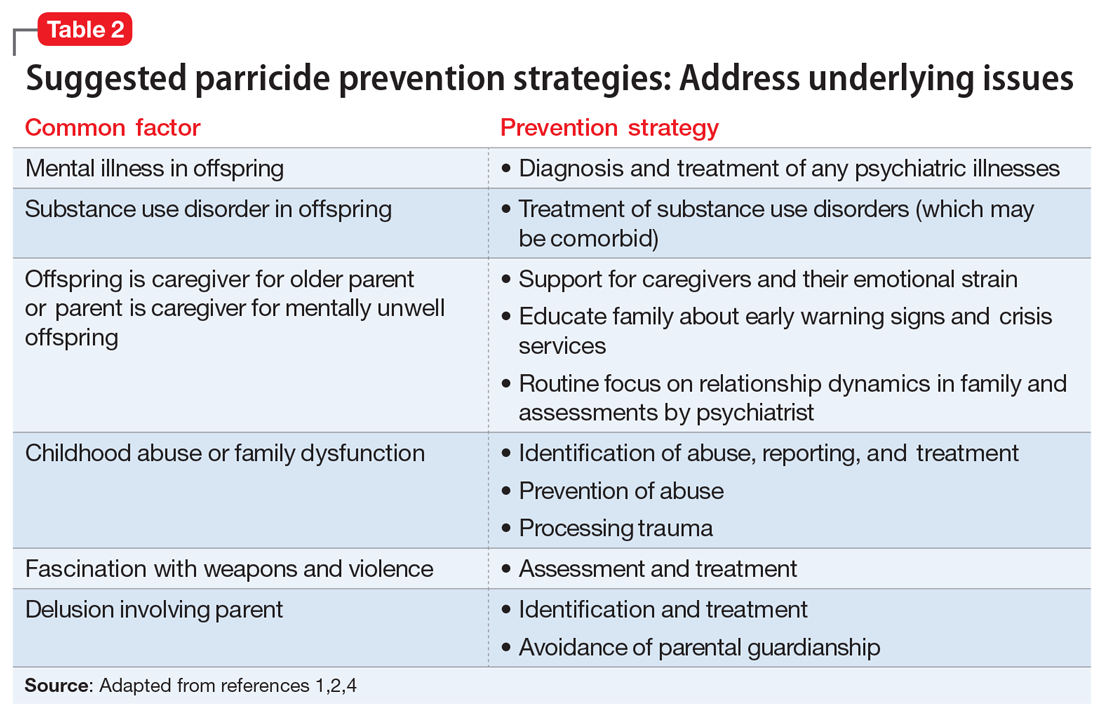
Spree killings that start as parricide
Although spree killing is a relatively rare event, a subset of spree killings involve parricide. One infamous recent event occurred in 2012 at Sandy Hook Elementary School, where the gunman killed his mother before going to the school and killing 26 additional people, many of whom were children.11,12 Because such events are rare, and because in these cases there is a high likelihood that the perpetrator is deceased (eg, died by suicide or killed by the police), much remains unknown about specific motivations and causative factors.
Information is often pieced together from postmortem reviews, which can be hampered by hindsight/recall bias and lack of contemporaneous documentation. Even worse, when these events occur, they may lead to a bias that all parricides or mass murders follow the pattern of the most recent case. This can result in overgeneralization of an individual’s history as being actionable risk violence factors for all potential parricide cases both by the public (eg, “My sister’s son has autism, and the Sandy Hook shooter was reported to have autism—should I be worried for my sister?”) and professionals (eg, “Will I be blamed for the next Sandy Hook by not taking more aggressive action even though I am not sure it is clinically warranted?”).
To identify trends for individuals committing parricide who engage in mass murder events (such as spree killing), we reviewed the 2000-2019 FBI active shooter list.12 Of the 333 events identified, 46 could be classified as domestic violence situations (eg, the perpetrator was in a romantic or familial relationship/former relationship and engaged in an active shooting incident involving at least 1 person from that relationship). We classified 11 of those 46 cases as parricide. Ten of those 11 parricides involved a child killing a parent (Table 3), and the other involved a grandchild killing a grandfather who served as their primary caregiver. Of the 11 incidents, mothers were involved (killed or wounded) in 4, and father figures (including the grandfather serving as a father and a stepfather) were killed in 9, with 2 incidents involving both parents. In 4 of the 11 parricides, other family members were killed in addition to the parent (including siblings, grandparents, or extended family). When considering spree shooters who committed parricide, 4 alleged perpetrators died by suicide, 1 was killed at the scene, and the rest were apprehended. The most common active shooting site endangering the public was an educational location (5), followed by commerce locations (4), with 2 involving open spaces. Eight of the 11 parricides occurred before the event was designated as an active shooting. The mean age for a parricide plus spree shooter was 23, once the oldest (age 61) and youngest (age 14) were removed from the calculation. The majority of the cases fell into the age range of 16 to 25 (n = 6), followed by 3 individuals who were age 26 to 31 (n = 3). All suspected individuals were male.
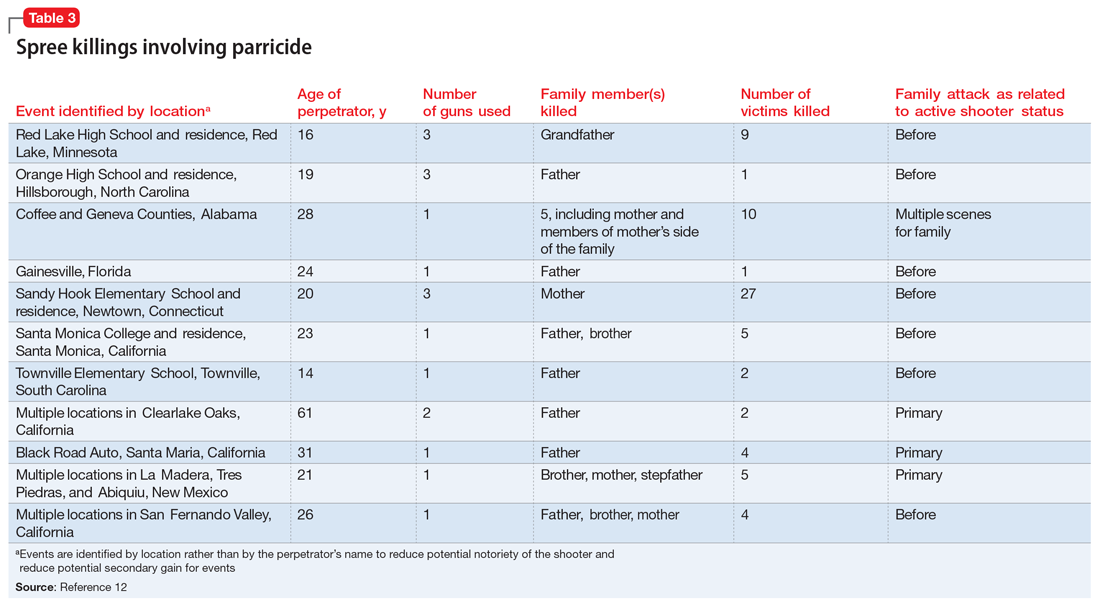
It is difficult to ascertain the existence of prior mental health care because perpetrators’ medical records may be confidential, juvenile court records may be sealed, and there may not even be a trial due to death or suicide (leading to limited forensic psychiatry examination or public testimony). Among those apprehended, many individuals raise some form of mental health defense, but the validity of their diagnosis may be undermined by concerns of possible malingering, especially in cases where the individual did not have a history of psychiatric treatment prior to the event.11 In summary, based on FBI data,12 spree shooters who committed parricide were usually male, in their late adolescence or early 20s, and more frequently targeted father figures. They often committed the parricide first and at a different location from later “active” shootings. Police were usually not aware of the parricide until after the spree is over.
Continue to: Parricide and society...
Parricide and society
For centuries, mothers and fathers have been honored and revered. Therefore, it is not surprising that killing of one’s mother or father attracts a great deal of macabre interest. Examples of parricide are present throughout popular culture, in mythology, comic books, movies, and television. As all psychiatrists know, Oedipus killed his father and married his mother. Other popular culture examples include: Grant Morrison’s Arkham Asylum: A Serious House on Serious Earth, Alfred Hitchcock’s Psycho, Oliver Stone’s Natural Born Killers, Peter Jackson’s Heavenly Creatures, The Affair drama series, and Star Wars: The Force Awakens.13,14
CASE CONTINUED
In Mr. B’s case, it is imperative for the treatment team to inquire about his history of violence, paying particular attention to prior violent acts towards his mother. His clinicians should consider hospitalization with the guardian’s consent if the danger appears imminent, especially considering the presence of weapons at home. They should attempt to stabilize Mr. B on effective, tolerable medications to ameliorate his psychosis, and to refer him for long-term psychotherapy to address difficult dynamic issues in the family relationship and encourage compliance with treatment. These steps may help avert a tragedy.
Bottom Line
Individuals who commit parricide often have a history of psychosis, a mood disorder, childhood abuse, and/or difficult relationship dynamics with the parent they kill. Some go on a spree killing in the community. Through careful consideration of individual risk factors, psychiatrists may help prevent some cases of parent murder by a child and possibly more tragedy in the community.
Mr. B, age 37, presents to a community mental health center for an appointment following a recent emergency department visit. He is diagnosed with schizophrenia, and has been treated for approximately 1 year. Six months ago, Mr. B stopped taking his antipsychotic due to its adverse effects. Despite compliance with another agent, he has become increasingly disorganized and paranoid.
He now believes that his mother, with whom he has lived all his life and who serves as his guardian, is poisoning his food and trying to kill him. She is an employee at a local grocery store, and Mr. B has expressed concern that her coworkers are assisting her in the plot to kill him.
Following a home visit, Mr. B’s case manager indicates that the patient showed them the collection of weapons he is amassing to “defend” himself. This leads to a concern for the safety of the patient, his mother, and others.
Although parricide—killing one’s parent—is a relatively rare event, its sensationalistic nature has long captured the attention of headline writers and the general public. This article discusses the diagnostic and demographic factors that may be seen among individuals who kill their parents, with an emphasis on those who commit matricide (murder of one’s mother) and associated spree killings, where an individual kills multiple people within a single brief but contiguous time period. Understanding these characteristics can help clinicians identify and more safely manage patients who may be at risk of harming their parents in addition to others.
Characteristics of perpetrators of parricide
Worldwide, approximately 2% to 4% of homicides involve parricide, or killing one’s parent.1,2 Most offenders are men in early adulthood, though a proportion are adolescents and some are women.1,3 They are often single, unemployed, and live with the parent prior to the killing.1 Patricide occurs more frequently than matricide.4 In the United States, approximately 150 fathers and 100 mothers are killed by their child each year.5
In a study of all homicides in England and Wales between 1997 and 2014, two-thirds of parricide offenders had previously been diagnosed with a mental disorder.1 One-third were diagnosed with schizophrenia.1 In a Canadian study focusing on 43 adult perpetrators found not criminally responsible,6 most were experiencing psychotic symptoms at the time of parricide; symptoms of a personality disorder were the second-most prevalent symptoms. Similarly, Bourget et al4 studied Canadian coroner records for 64 parents killed by their children. Of the children involved in those parricides, 15% attempted suicide after the killing. Two-thirds of the male offenders evidenced delusional thinking, and/or excessive violence (overkill) was common. Some cases (16%) followed an argument, and some of those perpetrators were intoxicated or psychotic. From our clinical experience, when there are identifiable nonpsychotic triggers, they often can be small things such as an argument over food, smoking, or video games. Often, the perpetrator was financially dependent on their parents and were “trapped in a difficult/hostile/dependence/love relationship” with that parent.6 Adolescent males who kill their parents may not have psychosis7; however, they may be victims of longstanding serious abuse at the hands of their parents. These perpetrators often express relief rather than remorse after committing murder.
Three categories to classify the perpetrators of parricide have been proposed: severely abused, severely mentally ill, and “dangerously antisocial.”3 While severe mental illness was most common in adult defendants, severe abuse was most common in adolescent offenders. There may be significant commonalities between adolescent and adult perpetrators. A more recent latent class analysis by Bojanic et al1 indicated 3 unique types of parricide offenders (Table 1).
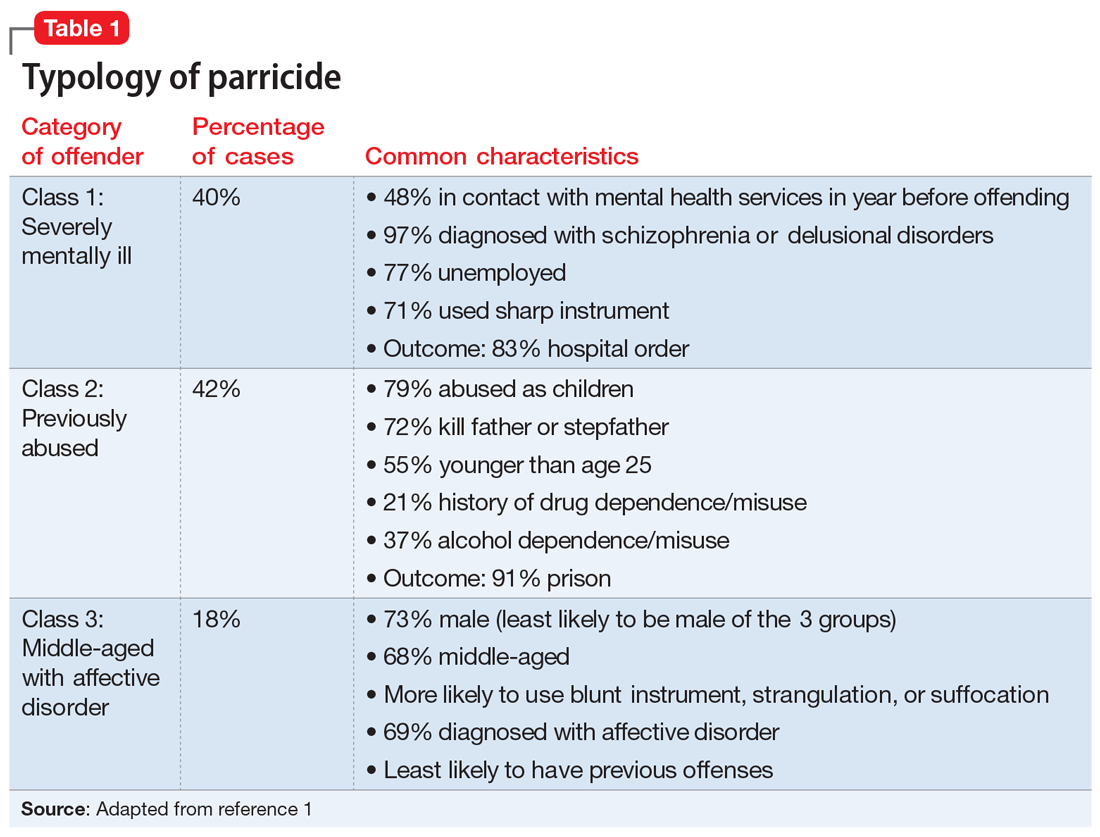
Continue to: Matricide: A closer look...
Matricide: A closer look
Though multiple studies have found a higher rate of psychosis among perpetrators of matricide, it is important to note that most people with psychotic disorders would never kill their mother. These events, however, tend to grab headlines and may be highly focused upon by the general population. In addition, matricide may be part of a larger crime that draws additional attention. For example, the 1966 University of Texas Bell Tower shooter and the 2012 Sandy Hook Elementary school shooter both killed their mothers before engaging in mass homicide. Often in cases of matricide, a longer-term dysfunctional relationship existed between the mother and the child. The mother is frequently described as controlling and intrusive and the (often adult) child as overly dependent, while the father may be absent or ineffectual. Hostility and mutual dependence are usual hallmarks of these relationships.8
However, in some cases where an individual with a psychotic disorder kills their mother, there may have been a traditional nurturing relationship.8 Alternative motivations unrelated to psychosis must be considered, including crimes motivated by money/inheritance or those perpetrated out of nonpsychotic anger. Green8 described motive categories for matricide that include paranoid and persecutory, altruistic, and other. In the “paranoid and persecutory” group, delusional beliefs about the mother occur; for example, the perpetrator may believe their mother was the devil. Sexual elements are found in some cases.8 Alternatively, the “altruistic” group demonstrated rather selfless reasons for killing, such as altruistic infanticide cases, or killing out of love.9 The altruistic matricide perpetrator may believe their mother is unwell, which may be a delusion or actually true. Finally, the “other” category contains cases related to jealousy, rage, and impulsivity.
In a study of 15 matricidal men in New York conducted by Campion et al,10 individuals seen by forensic psychiatric services for the crime of matricide included those with schizophrenia, substance-induced psychosis, and impulse control disorders. The authors noted there was often “a serious chronic derangement in the relationships of most matricidal men and their mothers.” Psychometric testing in these cases indicated feelings of dependency, weakness, and difficulty accepting an adult role separate from their mother. Some had conceptualized their mothers as a threat to their masculinity, while others had become enraged at their mothers.
Prevention requires addressing underlying issues
As described above, several factors are common among individuals who commit parricide, and these can be used to develop prevention strategies that focus on addressing underlying issues (Table 2). It is important to consider the relationship dynamics between the potential victim and perpetrator, as well as the motive, rather than focusing solely on mental illness or substance misuse.2
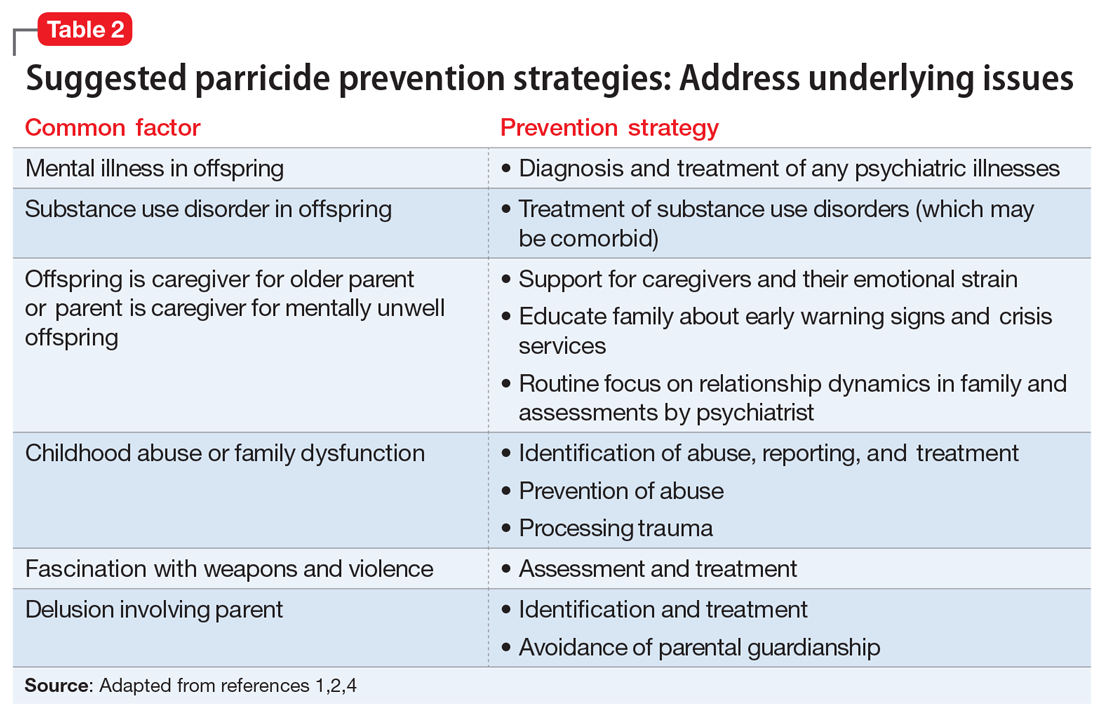
Spree killings that start as parricide
Although spree killing is a relatively rare event, a subset of spree killings involve parricide. One infamous recent event occurred in 2012 at Sandy Hook Elementary School, where the gunman killed his mother before going to the school and killing 26 additional people, many of whom were children.11,12 Because such events are rare, and because in these cases there is a high likelihood that the perpetrator is deceased (eg, died by suicide or killed by the police), much remains unknown about specific motivations and causative factors.
Information is often pieced together from postmortem reviews, which can be hampered by hindsight/recall bias and lack of contemporaneous documentation. Even worse, when these events occur, they may lead to a bias that all parricides or mass murders follow the pattern of the most recent case. This can result in overgeneralization of an individual’s history as being actionable risk violence factors for all potential parricide cases both by the public (eg, “My sister’s son has autism, and the Sandy Hook shooter was reported to have autism—should I be worried for my sister?”) and professionals (eg, “Will I be blamed for the next Sandy Hook by not taking more aggressive action even though I am not sure it is clinically warranted?”).
To identify trends for individuals committing parricide who engage in mass murder events (such as spree killing), we reviewed the 2000-2019 FBI active shooter list.12 Of the 333 events identified, 46 could be classified as domestic violence situations (eg, the perpetrator was in a romantic or familial relationship/former relationship and engaged in an active shooting incident involving at least 1 person from that relationship). We classified 11 of those 46 cases as parricide. Ten of those 11 parricides involved a child killing a parent (Table 3), and the other involved a grandchild killing a grandfather who served as their primary caregiver. Of the 11 incidents, mothers were involved (killed or wounded) in 4, and father figures (including the grandfather serving as a father and a stepfather) were killed in 9, with 2 incidents involving both parents. In 4 of the 11 parricides, other family members were killed in addition to the parent (including siblings, grandparents, or extended family). When considering spree shooters who committed parricide, 4 alleged perpetrators died by suicide, 1 was killed at the scene, and the rest were apprehended. The most common active shooting site endangering the public was an educational location (5), followed by commerce locations (4), with 2 involving open spaces. Eight of the 11 parricides occurred before the event was designated as an active shooting. The mean age for a parricide plus spree shooter was 23, once the oldest (age 61) and youngest (age 14) were removed from the calculation. The majority of the cases fell into the age range of 16 to 25 (n = 6), followed by 3 individuals who were age 26 to 31 (n = 3). All suspected individuals were male.
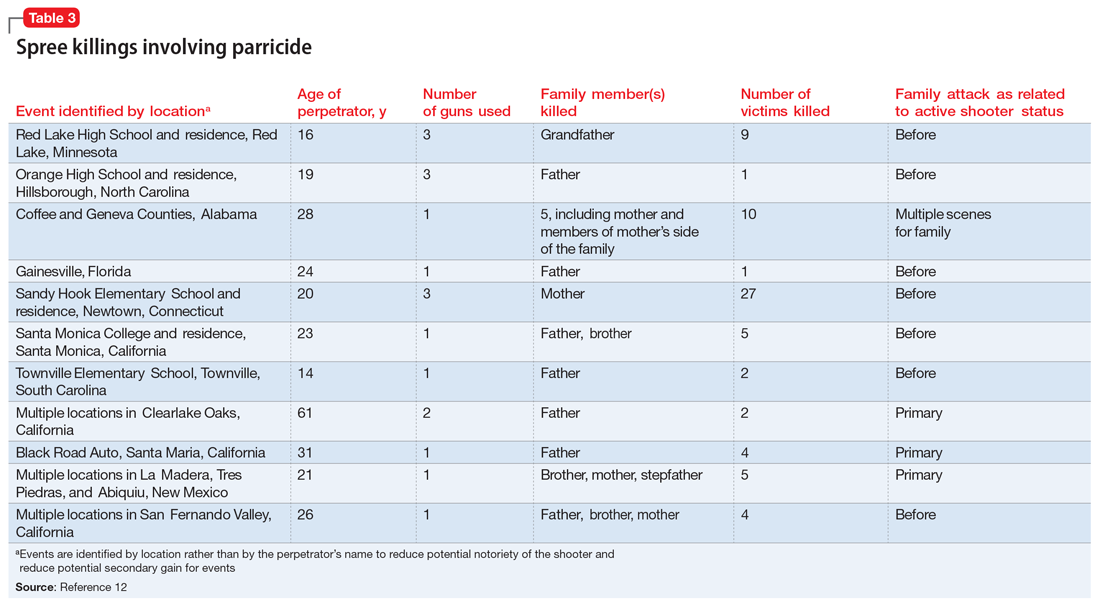
It is difficult to ascertain the existence of prior mental health care because perpetrators’ medical records may be confidential, juvenile court records may be sealed, and there may not even be a trial due to death or suicide (leading to limited forensic psychiatry examination or public testimony). Among those apprehended, many individuals raise some form of mental health defense, but the validity of their diagnosis may be undermined by concerns of possible malingering, especially in cases where the individual did not have a history of psychiatric treatment prior to the event.11 In summary, based on FBI data,12 spree shooters who committed parricide were usually male, in their late adolescence or early 20s, and more frequently targeted father figures. They often committed the parricide first and at a different location from later “active” shootings. Police were usually not aware of the parricide until after the spree is over.
Continue to: Parricide and society...
Parricide and society
For centuries, mothers and fathers have been honored and revered. Therefore, it is not surprising that killing of one’s mother or father attracts a great deal of macabre interest. Examples of parricide are present throughout popular culture, in mythology, comic books, movies, and television. As all psychiatrists know, Oedipus killed his father and married his mother. Other popular culture examples include: Grant Morrison’s Arkham Asylum: A Serious House on Serious Earth, Alfred Hitchcock’s Psycho, Oliver Stone’s Natural Born Killers, Peter Jackson’s Heavenly Creatures, The Affair drama series, and Star Wars: The Force Awakens.13,14
CASE CONTINUED
In Mr. B’s case, it is imperative for the treatment team to inquire about his history of violence, paying particular attention to prior violent acts towards his mother. His clinicians should consider hospitalization with the guardian’s consent if the danger appears imminent, especially considering the presence of weapons at home. They should attempt to stabilize Mr. B on effective, tolerable medications to ameliorate his psychosis, and to refer him for long-term psychotherapy to address difficult dynamic issues in the family relationship and encourage compliance with treatment. These steps may help avert a tragedy.
Bottom Line
Individuals who commit parricide often have a history of psychosis, a mood disorder, childhood abuse, and/or difficult relationship dynamics with the parent they kill. Some go on a spree killing in the community. Through careful consideration of individual risk factors, psychiatrists may help prevent some cases of parent murder by a child and possibly more tragedy in the community.
1. Bojanié L, Flynn S, Gianatsi M, et al. The typology of parricide and the role of mental illness: data-driven approach. Aggress Behav. 2020;46(6):516-522.
2. Pinals DS. Parricide. In Friedman SH, ed. Family Murder: Pathologies of Love and Hate. American Psychiatric Publishing; 2019:113-138.
3. Heide KM. Matricide and stepmatricide victims and offenders: an empirical analysis of US arrest data. Behav Sci Law. 2013;31(2):203-214.
4. Bourget D, Gagné P, Labelle ME. Parricide: a comparative study of matricide versus patricide. J Am Acad Psychiatry Law. 2007;35(3):306-312.
5. Heide KM, Frei A. Matricide: a critique of the literature. Trauma Violence Abuse. 2010;11(1):3-17.
6. Marleau JD, Auclair N, Millaud F. Comparison of factors associated with parricide in adults and adolescents. J Fam Viol. 2006;21:321-325.
7. West SG, Feldsher M. Parricide: characteristics of sons and daughters who kill their parents. Current Psychiatry. 2010;9(11):20-38.
8. Green CM. Matricide by sons. Med Sci Law. 1981;21(3):207-214.
9. Friedman SH. Conclusions. In Friedman SH, ed. Family Murder: Pathologies of Love and Hate. American Psychiatric Publishing; 2019:161-164.
10. Campion J, Cravens JM, Rotholc A, et al. A study of 15 matricidal men. Am J Psychiatry. 1985;142(3):312-317.
11. Hall RCW, Friedman SH, Sorrentino R, et al. The myth of school shooters and psychotropic medications. Behav Sci Law. 2019;37(5):540-558.
12. Department of Justice Federal Bureau of Investigation. Active Shooter Incidents: 20-Year Review, 2000-2019. June 1, 2021. Accessed October 12, 2021. https://www.fbi.gov/file-repository/active-shooter-incidents-20-year-review-2000-2019-060121.pdf/view
13. Friedman SH, Hall RCW. Star Wars: The Force Awakens, forensic teaching about matricide. J Am Acad Psychiatry Law. 2017;45(1):128-130.
14. Friedman SH, Hall RCW. Deadly and dysfunctional family dynamics: when fiction mirrors fact. In: Packer S, Fredrick DR, eds. Welcome to Arkham Asylum: Essays on Psychiatry and the Gotham City Institution. McFarland; 2019:65-75.
1. Bojanié L, Flynn S, Gianatsi M, et al. The typology of parricide and the role of mental illness: data-driven approach. Aggress Behav. 2020;46(6):516-522.
2. Pinals DS. Parricide. In Friedman SH, ed. Family Murder: Pathologies of Love and Hate. American Psychiatric Publishing; 2019:113-138.
3. Heide KM. Matricide and stepmatricide victims and offenders: an empirical analysis of US arrest data. Behav Sci Law. 2013;31(2):203-214.
4. Bourget D, Gagné P, Labelle ME. Parricide: a comparative study of matricide versus patricide. J Am Acad Psychiatry Law. 2007;35(3):306-312.
5. Heide KM, Frei A. Matricide: a critique of the literature. Trauma Violence Abuse. 2010;11(1):3-17.
6. Marleau JD, Auclair N, Millaud F. Comparison of factors associated with parricide in adults and adolescents. J Fam Viol. 2006;21:321-325.
7. West SG, Feldsher M. Parricide: characteristics of sons and daughters who kill their parents. Current Psychiatry. 2010;9(11):20-38.
8. Green CM. Matricide by sons. Med Sci Law. 1981;21(3):207-214.
9. Friedman SH. Conclusions. In Friedman SH, ed. Family Murder: Pathologies of Love and Hate. American Psychiatric Publishing; 2019:161-164.
10. Campion J, Cravens JM, Rotholc A, et al. A study of 15 matricidal men. Am J Psychiatry. 1985;142(3):312-317.
11. Hall RCW, Friedman SH, Sorrentino R, et al. The myth of school shooters and psychotropic medications. Behav Sci Law. 2019;37(5):540-558.
12. Department of Justice Federal Bureau of Investigation. Active Shooter Incidents: 20-Year Review, 2000-2019. June 1, 2021. Accessed October 12, 2021. https://www.fbi.gov/file-repository/active-shooter-incidents-20-year-review-2000-2019-060121.pdf/view
13. Friedman SH, Hall RCW. Star Wars: The Force Awakens, forensic teaching about matricide. J Am Acad Psychiatry Law. 2017;45(1):128-130.
14. Friedman SH, Hall RCW. Deadly and dysfunctional family dynamics: when fiction mirrors fact. In: Packer S, Fredrick DR, eds. Welcome to Arkham Asylum: Essays on Psychiatry and the Gotham City Institution. McFarland; 2019:65-75.
The Supreme Court and reproductive rights

There is now great interest in the Supreme Court’s handling of cases that involve a woman’s ability to have an abortion. Recent decisions, and those planned in the next few months will be the source of intense scrutiny. But the Court’s involvement in reproductive rights did not begin with abortion. In fact, the Supreme Court has a long history of controversial decisions dealing with reproductive rights.
Involuntary sterilization
A notable, even infamous, case was Buck v Bell (1927)—later discredited—in which the Court reviewed a state law that provided for the involuntary sterilization of the “feeble minded.”1 The 8-1 decision was that the state could choose to have such a law to protect the so-called genetic health of the state. The law was based on a theory of eugenics. The opinion by the highly respected Justice Oliver Wendell Holmes included the unfortunate conclusion, “Three generations of imbeciles are enough.”2 As mentioned, the law has since been thoroughly discredited. In 1942, the Court did come to a different result, holding in Skinner v Oklahoma that it was unconstitutional for a state to involuntarily sterilize “habitual criminals.”3
Contraception
Forty years after Buck, in Griswold v Connecticut, the Court reviewed a state law that prohibited the distribution of any drug or device used for contraception (even for married couples).4 In a 7-2 decision, the Supreme Court struck down the state law as violating a marital right of privacy. Beyond its specific holding, Griswold was important in several ways. First, a physician was raising the rights of patients (not specifically his own rights). This is notable because, ordinarily in court, litigants may argue their own rights, not the rights of others. This has been important in later reproductive rights cases because often it has been physicians raising and arguing the rights of patients.
A second interesting part of Griswold was the source of this constitutional right of privacy. The Constitution contains no express privacy provision. In Griswold, the Court found that the 1st, 3rd, 4th, and 9th Amendments create the right to privacy in marital relations. Writing for the majority, Justice Douglas found that “emanations” from these amendments have “penumbras” that create a right of marital privacy.
Although Griswold was based on marital privacy, a few years later, in 1972, the Court essentially converted that right to one of reproductive privacy (“the decision whether to bear or beget a child.”) In Eisenstadt v Baird, the Court held that it was a violation of equal protection (the 14th Amendment) for a state to allow contraception to the married but deny it to an unmarried person.5
Continue to: Abortion...
Abortion
In 1971, the Court had heard arguments in 2 cases that raised issues regarding whether state laws prohibiting abortion were constitutional. The first oral argument in Roe v Wade is widely considered one of the worst oral arguments in modern history, and for several reasons the Court set the case for rehearing the following Term (October 1972). In January 1973, the Court decided Roe v Wade.6 The 7-2 decision was written by Justice Blackmun, who had at one point been the attorney for the Mayo Clinic and might be considered one of the first “health lawyers.” The Court held that the Constitution (perhaps in the 14th or 9th Amendment) includes a right of privacy that includes the right of a woman to choose to have, or not to have, an abortion. In implementing the right, the Court held that a state may impose only modest medical safeguards for the mother (eg, requiring that abortions be performed by a licensed physician). In the second trimester, to the point of viability, a state could impose only limitations on abortion that were reasonably directed to ensure the health of the mother. After a fetus was viable (could live outside the mother’s body), the state was free to regulate or prohibit abortions and protect the fetus. At the time, viability was approximately the beginning of the third trimester.6
The clear majority of the Court in Roe (7-2) may have suggested that there was not strong opposition to the decision. That, of course, was not the case. Legal and political conflict surrounding the case has been, and remains, intense. Since 1973, the Court has been called upon to decide many abortion cases, and each case seems to beget more controversy and still more cases.
Some of the legal objections to Roe and other abortion decisions are that the constitutional basis for the decision remains unclear—a specific right of privacy is not contained in the text of the Constitution. Several locations of a possible right of privacy have been mentioned by various justices, but “substantive due process” became the common constitutional basis for the right. Critics note that “substantive” due process (as opposed to procedural due process) is not mentioned in the Constitution, and it is short on clear guiding principles. Beyond those jurisprudential issues, of course, there were strong religious and philosophical objections to abortion. What followed Roe has been a long series of efforts to limit or discourage access to abortion, and the Supreme Court has had to decide a great many abortion cases (and a few contraception cases) over the last 50 years. Most years (except from 2008‒2013) the Court has heard, on average, at least one abortion case.
By way of examples, here are some of the issues related to abortion that the Court has decided:
- Payment and facilities. States and the federal government are not required to pay for abortions for women who cannot afford them or to provide facilities for abortion.7-10
- Informed consent. Some states’ special informed consent requirements for abortion were upheld, but complex consents that required the father’s participation were not.
- Ability to advertise. Prohibitions on advertisement of abortion services were struck down.
- Location. Requirements for hospital-only abortions (or similar regulations) were struck down.
- Anti-abortion protests. Several cases addressed guidelines involving demonstrations near abortion clinics.
Of particular importance was the case of Planned Parenthood of Southeastern Pennsylvania v Casey—“Casey.”11 In 1992 that case reaffirmed the “essential” holding of Roe v Wade. A plurality in that case de-emphasized the trimester framework and applied an “undue burden” test on limitations on abortion. In the more recent cases argued before the Court, Casey is frequently referred to as specifically reaffirming, and therefore solidifying, Roe.
Consent for minors
There have been several cases since 1973 that involved contraceptives or abortions and “minors” (generally, adolescents aged <18 years, although there are some state-defined exceptions). These cases typically involve 2 issues: the right of minors to consent to treatment and the obligation of the physician to provide information to parents about treatment to their minor daughter. In 1977 the Court struck down a New York law that prohibited the distribution of contraceptives to minors.12 However, abortion issues involving minors have been more complicated. While the Court has struck down “2-parent” consent statutes,13 it has generally upheld 1-parent consent statutes, but only if those statutes contain a “judicial bypass” provision and an emergency medical provision.11,14,15 (This bypass allows a minor to “bypass” parental consent to abortion in some circumstances, and instead seek judicial authorization for an abortion.) Generally, the Court has upheld parental notification for abortions, with exceptions where it would be harmful to the minor who is seeking the abortion.16-19
Continue to: Who can perform an abortion...
Who can perform an abortion
Over the years there have also been several cases raising questions about the professionals who can perform abortions, their hospital privileges, and what facilities can perform abortions. Two of those cases in recent years have, for example, seen the Court strike down state statutes that required the physicians who perform abortions to have admitting privileges at least in 1 nearby hospital.20,21 The basis for these decisions is that the admitting qualification is an “undue burden” because it serves almost no health purpose, while significantly limiting the number of professionals who can perform abortions.
Cases this Term
The current Term of the Court (officially the “October 2021 Term”) may be one of the most significant for reproductive rights in recent history. The Court accepted 6 abortion-related cases to hear. It dismissed 3 of those cases, which had become “moot” because the Biden administration changed the rules that had been legally challenged.22-24 It has heard arguments in the 3 (technically 4) remaining cases, in which decisions will be announced over the next several months.
The first of these cases (involving the Texas Heartbeat Act) raises very important, but vexing, procedural issues about a Texas abortion law. The second (Whole Woman’s Health v Jackson) is a direct challenge to Roe v Wade. The third case (Cameron v EMW Women’s Surgical Center) involves the narrow question of whether a state attorney general can intervene in a case to uphold a state abortion law when another state official refuses to defend the law.25 It is worthwhile taking a look at the first 2 of these cases.
Texas Heartbeat Act
In the first case (technically, it is 2 cases, as we will see), the Texas legislature adopted a law that prohibits abortions after there is a discernable heartbeat (around 6 weeks of pregnancy). The law precludes state officials from enforcing the law. Instead, it allows almost any private citizen to seek monetary damages ($10,000 plus fees) from anyone who performs an abortion or “aids and abets” an abortion. (This is in some ways similar to “private attorney general” actions found in the False Claims Act, and in some civil rights and labor laws.) This statute is clearly inconsistent with Roe in that it prohibits abortions before the end of the second trimester. If it were a usual law—a Texas law being enforced by state officials—federal courts would issue injunctions to state officials against enforcing the law. The difficulty with the Texas law (and its very purpose) is that there are procedural limitations in federal law that make it very difficult to find a path for federal courts to review the Texas statute quickly. For example, would federal courts enjoin every private citizen of the state? There is a longstanding Constitutional doctrine that precludes federal courts from enjoining state courts.26 Therefore, it is difficult to challenge the law before someone performing or aiding an abortion has been ordered to pay the private citizen who is enforcing it. In the interim, which could be months or even years, health care providers face uncertainty about continuing to provide abortion services. Some providers would stop providing abortion services, reducing the availability of those services.
Two cases challenge this Texas procedure. In the first, Whole Woman’s Health v Jackson, 27 abortion providers seek to find some way through the procedural thicket to allow an immediate challenge to the statute. It is important because this technique of exclusive private enforcement could be used in any number of ways by the state to chill important constitutional rights (beyond abortion—to speech, to bear arms). In the second case involving the Texas law, U.S. v Texas, the federal government seeks to intervene in the case, which is another unusual procedure.28 The Court found these questions so important and difficult that it allowed 3 hours of argument (and 4 sets of lawyers). It seems likely that the Court will find a mechanism for allowing some early federal court review of individual enforcement of state laws, while minimizing harm to the state-national federalism that is at the heart of the Constitution.
For the recent procedural decisions in the Texas cases, see the “Current Court Decisions” box below.
On December 10, 2021, the Court handed down two decisions in reproductive freedom (abortion) cases, both involving the Texas abortion law (which prohibits most abortions after a fetal heartbeat can be detected and allows only private individuals to enforce the law). The more significant of the two cases, Whole Woman’s Health v Jackson,1 was the request of abortion providers (and others) to allow them to challenge the constitutionality of the Texas law by suing various state officials or a private individual, before the enforcement of the new Texas law.
The decision of the Court was somewhat complex because of the split among justices. Overall:
- The Court held 8-1 that before the law is enforced, providers have the ability to sue executives of medical licensing boards. This was based on the possibility that there could be licensure discipline for professionals who violate the new abortion law. Only Justice Thomas dissented from this part of the decision, which was written by Justice Gorsuch.
- The Court unanimously held that state-court judges could not be sued to stop enforcement of the law, and dismissed them from the suit.
- In a 5-4 split the Court held that state court clerks (and the state attorney general) could not be brought into federal court as a way of challenging the law. This was based on the 11th Amendment, sovereign immunity, and an important precedent from 1908.2 Chief Justice Roberts wrote from the justices who were essentially in dissent (Justices Bryer, Kagan, and Sotomayor). Justice Sotomayor also wrote a dissent (joined by Justices Breyer and Kagan) urging that there should be some way for providers to test the constitutionality of the law before enforcement. Allowing an action against state court clerks would be a good way to do that. She also expressly noted the problem of the Texas law approach being used by other states to attack any number of constitutional rights.
- The Court unanimously dismissed (for lack of standing) the one private citizen who had been sued. He had signed a sworn statement that he did not intend to seek the damages against abortion providers under the Texas law.
- The Court declined again to stay the Texas law while it is being challenged. That is, it left standing the 5th Circuit order allowing the law to go into effect.
- In a second, related case, the Court dismissed, without deciding, the Biden administration’s request to become a party in the Texas abortion case.3
References
- Whole Woman’s Health v Jackson, No. 21–463 (Dec. 10, 2021). https://www.supremecourt.gov /opinions/21pdf/21-463_new_8o6b.pdf.
- Ex parte Young, 209 U.S. 123 (1908).
- U.S. v Texas, 21-588 (Dec. 10, 2021). https://www.supremecourt.gov/opinions/21pdf/21-588 _c07d.pdf
Continue to: Re-evaluating the viability standard...
Re-evaluating the viability standard
The substantive abortion issue in Dobbs v Jackson Women’s Health Organization is the constitutionality of the Mississippi Gestational Age Act, which allows abortions after 15 weeks of pregnancy only for medical emergencies or severe fetal abnormality.29 This case is likely the most watched and controversial case of the Term. Many medical organizations have filed amicus curiae briefs, including the American College of Obstetricians and Gynecologists joined by the American Medical Association,30 the International Federation of Gynecology and Obstetrics,31 and the American Association of Pro-Life Obstetricians and Gynecologists.32 The reason for all this attention is that the Court has accepted to resolve “whether all pre-viability prohibitions on elective abortions are unconstitutional.” Thus, it represents a direct challenge to the trimester/viability structure of Roe.
It appears that there are 3 justices ready to outright overrule Roe, 3 that would uphold it as is, and 3 who are not in favor of Roe, but feel bound by precedent or are not in favor of a traumatic move. For that reason, there may be a narrow decision in this case. For example, the Court might find a procedural way to avoid directly deciding the abortion issue in this case, or it might uphold the right to abortion but change the viability standard. It is also true that predicting what the Court will do in controversial cases is a fool’s errand.
The complexity of reproductive rights and the ObGyn practice
These cases and policies affect the day-to-day practice of obstetrics. It is the most legally complex area of medical practice for several reasons. The law varies considerably from state to state. The clinician who practices both in California and across the border in Arizona will face substantially different laws, especially regarding the treatment of adolescents. And the reproductive rights laws in many states are a complicated mix of state statutes and state court decisions, with an overlay of federal statutes and court decisions, and a series of both state and federal regulations. This article demonstrates an additional complexity for practitioners—the continuous change in the law surrounding reproductive rights—and practice involving adolescent patients is especially difficult.
There are some good state-by-state reviews of laws related to abortion and contraception. We find the Guttmacher Institute particularly helpful. (See “State-by-state reviews of laws related to abortion and contraception”.) Although these are good resources, they are not the basis for legal practice with the current law in a state. The complexity and ever-changing nature of reproductive rights is one of the reasons we believe that it is important that anyone in active ObGyn practice maintain an ongoing professional relationship with a lawyer with expertise in this area of practice. This relationship should establish and update policies and procedures consistent with local law, consent and other forms, reporting of possible child abuse, and the like. An annual legal checkup may be as important for physicians as a physical checkup is for their patients.
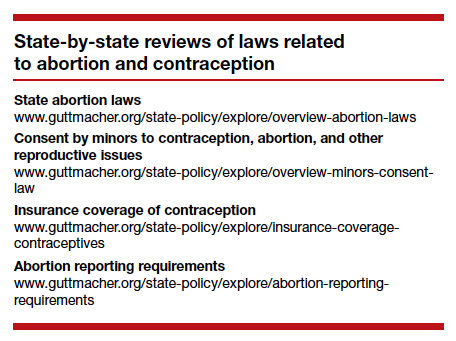
Future outcomes
At the end of the Term, we will review the outcome of the cases noted above—and the possibility of follow-on cases. Whatever the Court does this Term, it will not be the end of the legal and political struggles over abortion and other reproductive issues. These questions deeply divide our society, and the cases and controversies reflect that continuing division. ●
- Buck v Bell, 274 U.S. 200 (1927).
- Id. at 207.
- Skinner v State of Oklahoma, ex rel. Williamson, 316 U.S. 535 (1942).
- Griswold v Connecticut, 381 U.S. 479 (1965)
- Eisenstadt v Baird, 405 U.S. 438 (1972).
- Roe v Wade, 410 U.S. 113 (1973).
- Harris v McRae, 448 U.S. 297 (1980).
- Williams v Zbaraz, 448 U.S 358 (1980).
- Webster v Reproductive Health Services, 492 U.S. 490 (1989).
- Rust v Sullivan, 500 U.S. 173 (1991).
- Planned Parenthood of Southeastern Pennsylvania v Casey, 505 U.S. 833 (1992).
- Carey v Population Services, 431 U.S. 678 (1977).
- Bellotti v Baird, 443 U.S. 622 (1979).
- Planned Parenthood of Kansas City v Ashcroft, 462 U.S. 476 (1983).
- Planned Parenthood of Northern New England v Ayotte, 546 U.S. 320 (2006).
- H.L. v Matheson, 450 U.S. 398 (1981).
- Hodgson v Minnesota, 497 U.S. 417 (1990).
- Ohio v Akron Center for Reproductive Health, 497 U.S. 502 (1990).
- Lambert v Wicklund, 520 U.S. 292 (1997).
- June Medical Services v Russo, 591 U.S. ___ (2020), https:// www.supremecourt.gov/opinions/19pdf/18-1323_c07d.pdf.
- Whole Woman’s Health v Hellerstedt, 579 U.S. 582 (2016).
- AMA v Becerra, dismissed May 17, 2021, https://www .scotusblog.com/case-files/cases/american-medical -association-v-cochran.
- Becerra v Baltimore, dismissed May 17, 2021, https://www .scotusblog.com/case-files/cases/cochran-v-mayor-and-city-council-of-baltimore.
- Oregon v Becerra, dismissed May 17, 2021, https://www .scotusblog.com/case-files/cases/oregon-v-cochran.
- Cameron v EMW Women’s Surgical Center, 20-601. https:// www.scotusblog.com/case-files/cases/cameron-v-emw -womens-surgical-center-p-s-c.
- Ex parte Young, 209 U.S. 123 (1908).
- Whole Woman’s Health v Jackson, 21-463. https://www .scotusblog.com/case-files/cases/whole-womans-health-v -jackson.
- U.S. v Texas, 21-588. https://www.scotusblog.com/case-files /cases/united-states-v-texas-3.
- Dobbs v Jackson Women’s Health Organization, 19-1392. https://www.scotusblog.com/case-files/cases/dobbs-v -jackson-womens-health-organization.
- Brief of Amici Curiae American College of Obstetricians and Gynecologists et al., Dobbs v Jackson Women’s Health Organization (Sep. 2021). https://www.acog.org/ -/media/project/acog/acogorg/files/advocacy/amicus -briefs/2021/20210920-dobbs-v-jwho-amicus-brief.pdf?la=e n&hash=717DFDD07A03B93A04490E66835BB8C5.
- Brief Amicus Curiae of International Federation of Gynecology and Obstetrics, Dobbs v Jackson Women’s Health Organization (Sep. 20, 2021). https://www.supremecourt. gov/DocketPDF/19/19-1392/193019/20210920155508744 _41426%20pdf%20Chen.pdf.
- Brief Amicus Curiae of American Association of Pro-Life Obstetricians and Gynecologists. Dobbs v Jackson Women’s Health Organization (Sep. 2021). https://www.supremecourt .gov/DocketPDF/19/19-1392/185350/20210729163532595 _No.%2019-1392%20-%20American%20Association %20of%20Pro-Life%20Obstetricians%20and%20 Gynecologists%20-%20Amicus%20Brief%20in%20Support %20of%20Petitioner%20-%207-29-21.pdf.

There is now great interest in the Supreme Court’s handling of cases that involve a woman’s ability to have an abortion. Recent decisions, and those planned in the next few months will be the source of intense scrutiny. But the Court’s involvement in reproductive rights did not begin with abortion. In fact, the Supreme Court has a long history of controversial decisions dealing with reproductive rights.
Involuntary sterilization
A notable, even infamous, case was Buck v Bell (1927)—later discredited—in which the Court reviewed a state law that provided for the involuntary sterilization of the “feeble minded.”1 The 8-1 decision was that the state could choose to have such a law to protect the so-called genetic health of the state. The law was based on a theory of eugenics. The opinion by the highly respected Justice Oliver Wendell Holmes included the unfortunate conclusion, “Three generations of imbeciles are enough.”2 As mentioned, the law has since been thoroughly discredited. In 1942, the Court did come to a different result, holding in Skinner v Oklahoma that it was unconstitutional for a state to involuntarily sterilize “habitual criminals.”3
Contraception
Forty years after Buck, in Griswold v Connecticut, the Court reviewed a state law that prohibited the distribution of any drug or device used for contraception (even for married couples).4 In a 7-2 decision, the Supreme Court struck down the state law as violating a marital right of privacy. Beyond its specific holding, Griswold was important in several ways. First, a physician was raising the rights of patients (not specifically his own rights). This is notable because, ordinarily in court, litigants may argue their own rights, not the rights of others. This has been important in later reproductive rights cases because often it has been physicians raising and arguing the rights of patients.
A second interesting part of Griswold was the source of this constitutional right of privacy. The Constitution contains no express privacy provision. In Griswold, the Court found that the 1st, 3rd, 4th, and 9th Amendments create the right to privacy in marital relations. Writing for the majority, Justice Douglas found that “emanations” from these amendments have “penumbras” that create a right of marital privacy.
Although Griswold was based on marital privacy, a few years later, in 1972, the Court essentially converted that right to one of reproductive privacy (“the decision whether to bear or beget a child.”) In Eisenstadt v Baird, the Court held that it was a violation of equal protection (the 14th Amendment) for a state to allow contraception to the married but deny it to an unmarried person.5
Continue to: Abortion...
Abortion
In 1971, the Court had heard arguments in 2 cases that raised issues regarding whether state laws prohibiting abortion were constitutional. The first oral argument in Roe v Wade is widely considered one of the worst oral arguments in modern history, and for several reasons the Court set the case for rehearing the following Term (October 1972). In January 1973, the Court decided Roe v Wade.6 The 7-2 decision was written by Justice Blackmun, who had at one point been the attorney for the Mayo Clinic and might be considered one of the first “health lawyers.” The Court held that the Constitution (perhaps in the 14th or 9th Amendment) includes a right of privacy that includes the right of a woman to choose to have, or not to have, an abortion. In implementing the right, the Court held that a state may impose only modest medical safeguards for the mother (eg, requiring that abortions be performed by a licensed physician). In the second trimester, to the point of viability, a state could impose only limitations on abortion that were reasonably directed to ensure the health of the mother. After a fetus was viable (could live outside the mother’s body), the state was free to regulate or prohibit abortions and protect the fetus. At the time, viability was approximately the beginning of the third trimester.6
The clear majority of the Court in Roe (7-2) may have suggested that there was not strong opposition to the decision. That, of course, was not the case. Legal and political conflict surrounding the case has been, and remains, intense. Since 1973, the Court has been called upon to decide many abortion cases, and each case seems to beget more controversy and still more cases.
Some of the legal objections to Roe and other abortion decisions are that the constitutional basis for the decision remains unclear—a specific right of privacy is not contained in the text of the Constitution. Several locations of a possible right of privacy have been mentioned by various justices, but “substantive due process” became the common constitutional basis for the right. Critics note that “substantive” due process (as opposed to procedural due process) is not mentioned in the Constitution, and it is short on clear guiding principles. Beyond those jurisprudential issues, of course, there were strong religious and philosophical objections to abortion. What followed Roe has been a long series of efforts to limit or discourage access to abortion, and the Supreme Court has had to decide a great many abortion cases (and a few contraception cases) over the last 50 years. Most years (except from 2008‒2013) the Court has heard, on average, at least one abortion case.
By way of examples, here are some of the issues related to abortion that the Court has decided:
- Payment and facilities. States and the federal government are not required to pay for abortions for women who cannot afford them or to provide facilities for abortion.7-10
- Informed consent. Some states’ special informed consent requirements for abortion were upheld, but complex consents that required the father’s participation were not.
- Ability to advertise. Prohibitions on advertisement of abortion services were struck down.
- Location. Requirements for hospital-only abortions (or similar regulations) were struck down.
- Anti-abortion protests. Several cases addressed guidelines involving demonstrations near abortion clinics.
Of particular importance was the case of Planned Parenthood of Southeastern Pennsylvania v Casey—“Casey.”11 In 1992 that case reaffirmed the “essential” holding of Roe v Wade. A plurality in that case de-emphasized the trimester framework and applied an “undue burden” test on limitations on abortion. In the more recent cases argued before the Court, Casey is frequently referred to as specifically reaffirming, and therefore solidifying, Roe.
Consent for minors
There have been several cases since 1973 that involved contraceptives or abortions and “minors” (generally, adolescents aged <18 years, although there are some state-defined exceptions). These cases typically involve 2 issues: the right of minors to consent to treatment and the obligation of the physician to provide information to parents about treatment to their minor daughter. In 1977 the Court struck down a New York law that prohibited the distribution of contraceptives to minors.12 However, abortion issues involving minors have been more complicated. While the Court has struck down “2-parent” consent statutes,13 it has generally upheld 1-parent consent statutes, but only if those statutes contain a “judicial bypass” provision and an emergency medical provision.11,14,15 (This bypass allows a minor to “bypass” parental consent to abortion in some circumstances, and instead seek judicial authorization for an abortion.) Generally, the Court has upheld parental notification for abortions, with exceptions where it would be harmful to the minor who is seeking the abortion.16-19
Continue to: Who can perform an abortion...
Who can perform an abortion
Over the years there have also been several cases raising questions about the professionals who can perform abortions, their hospital privileges, and what facilities can perform abortions. Two of those cases in recent years have, for example, seen the Court strike down state statutes that required the physicians who perform abortions to have admitting privileges at least in 1 nearby hospital.20,21 The basis for these decisions is that the admitting qualification is an “undue burden” because it serves almost no health purpose, while significantly limiting the number of professionals who can perform abortions.
Cases this Term
The current Term of the Court (officially the “October 2021 Term”) may be one of the most significant for reproductive rights in recent history. The Court accepted 6 abortion-related cases to hear. It dismissed 3 of those cases, which had become “moot” because the Biden administration changed the rules that had been legally challenged.22-24 It has heard arguments in the 3 (technically 4) remaining cases, in which decisions will be announced over the next several months.
The first of these cases (involving the Texas Heartbeat Act) raises very important, but vexing, procedural issues about a Texas abortion law. The second (Whole Woman’s Health v Jackson) is a direct challenge to Roe v Wade. The third case (Cameron v EMW Women’s Surgical Center) involves the narrow question of whether a state attorney general can intervene in a case to uphold a state abortion law when another state official refuses to defend the law.25 It is worthwhile taking a look at the first 2 of these cases.
Texas Heartbeat Act
In the first case (technically, it is 2 cases, as we will see), the Texas legislature adopted a law that prohibits abortions after there is a discernable heartbeat (around 6 weeks of pregnancy). The law precludes state officials from enforcing the law. Instead, it allows almost any private citizen to seek monetary damages ($10,000 plus fees) from anyone who performs an abortion or “aids and abets” an abortion. (This is in some ways similar to “private attorney general” actions found in the False Claims Act, and in some civil rights and labor laws.) This statute is clearly inconsistent with Roe in that it prohibits abortions before the end of the second trimester. If it were a usual law—a Texas law being enforced by state officials—federal courts would issue injunctions to state officials against enforcing the law. The difficulty with the Texas law (and its very purpose) is that there are procedural limitations in federal law that make it very difficult to find a path for federal courts to review the Texas statute quickly. For example, would federal courts enjoin every private citizen of the state? There is a longstanding Constitutional doctrine that precludes federal courts from enjoining state courts.26 Therefore, it is difficult to challenge the law before someone performing or aiding an abortion has been ordered to pay the private citizen who is enforcing it. In the interim, which could be months or even years, health care providers face uncertainty about continuing to provide abortion services. Some providers would stop providing abortion services, reducing the availability of those services.
Two cases challenge this Texas procedure. In the first, Whole Woman’s Health v Jackson, 27 abortion providers seek to find some way through the procedural thicket to allow an immediate challenge to the statute. It is important because this technique of exclusive private enforcement could be used in any number of ways by the state to chill important constitutional rights (beyond abortion—to speech, to bear arms). In the second case involving the Texas law, U.S. v Texas, the federal government seeks to intervene in the case, which is another unusual procedure.28 The Court found these questions so important and difficult that it allowed 3 hours of argument (and 4 sets of lawyers). It seems likely that the Court will find a mechanism for allowing some early federal court review of individual enforcement of state laws, while minimizing harm to the state-national federalism that is at the heart of the Constitution.
For the recent procedural decisions in the Texas cases, see the “Current Court Decisions” box below.
On December 10, 2021, the Court handed down two decisions in reproductive freedom (abortion) cases, both involving the Texas abortion law (which prohibits most abortions after a fetal heartbeat can be detected and allows only private individuals to enforce the law). The more significant of the two cases, Whole Woman’s Health v Jackson,1 was the request of abortion providers (and others) to allow them to challenge the constitutionality of the Texas law by suing various state officials or a private individual, before the enforcement of the new Texas law.
The decision of the Court was somewhat complex because of the split among justices. Overall:
- The Court held 8-1 that before the law is enforced, providers have the ability to sue executives of medical licensing boards. This was based on the possibility that there could be licensure discipline for professionals who violate the new abortion law. Only Justice Thomas dissented from this part of the decision, which was written by Justice Gorsuch.
- The Court unanimously held that state-court judges could not be sued to stop enforcement of the law, and dismissed them from the suit.
- In a 5-4 split the Court held that state court clerks (and the state attorney general) could not be brought into federal court as a way of challenging the law. This was based on the 11th Amendment, sovereign immunity, and an important precedent from 1908.2 Chief Justice Roberts wrote from the justices who were essentially in dissent (Justices Bryer, Kagan, and Sotomayor). Justice Sotomayor also wrote a dissent (joined by Justices Breyer and Kagan) urging that there should be some way for providers to test the constitutionality of the law before enforcement. Allowing an action against state court clerks would be a good way to do that. She also expressly noted the problem of the Texas law approach being used by other states to attack any number of constitutional rights.
- The Court unanimously dismissed (for lack of standing) the one private citizen who had been sued. He had signed a sworn statement that he did not intend to seek the damages against abortion providers under the Texas law.
- The Court declined again to stay the Texas law while it is being challenged. That is, it left standing the 5th Circuit order allowing the law to go into effect.
- In a second, related case, the Court dismissed, without deciding, the Biden administration’s request to become a party in the Texas abortion case.3
References
- Whole Woman’s Health v Jackson, No. 21–463 (Dec. 10, 2021). https://www.supremecourt.gov /opinions/21pdf/21-463_new_8o6b.pdf.
- Ex parte Young, 209 U.S. 123 (1908).
- U.S. v Texas, 21-588 (Dec. 10, 2021). https://www.supremecourt.gov/opinions/21pdf/21-588 _c07d.pdf
Continue to: Re-evaluating the viability standard...
Re-evaluating the viability standard
The substantive abortion issue in Dobbs v Jackson Women’s Health Organization is the constitutionality of the Mississippi Gestational Age Act, which allows abortions after 15 weeks of pregnancy only for medical emergencies or severe fetal abnormality.29 This case is likely the most watched and controversial case of the Term. Many medical organizations have filed amicus curiae briefs, including the American College of Obstetricians and Gynecologists joined by the American Medical Association,30 the International Federation of Gynecology and Obstetrics,31 and the American Association of Pro-Life Obstetricians and Gynecologists.32 The reason for all this attention is that the Court has accepted to resolve “whether all pre-viability prohibitions on elective abortions are unconstitutional.” Thus, it represents a direct challenge to the trimester/viability structure of Roe.
It appears that there are 3 justices ready to outright overrule Roe, 3 that would uphold it as is, and 3 who are not in favor of Roe, but feel bound by precedent or are not in favor of a traumatic move. For that reason, there may be a narrow decision in this case. For example, the Court might find a procedural way to avoid directly deciding the abortion issue in this case, or it might uphold the right to abortion but change the viability standard. It is also true that predicting what the Court will do in controversial cases is a fool’s errand.
The complexity of reproductive rights and the ObGyn practice
These cases and policies affect the day-to-day practice of obstetrics. It is the most legally complex area of medical practice for several reasons. The law varies considerably from state to state. The clinician who practices both in California and across the border in Arizona will face substantially different laws, especially regarding the treatment of adolescents. And the reproductive rights laws in many states are a complicated mix of state statutes and state court decisions, with an overlay of federal statutes and court decisions, and a series of both state and federal regulations. This article demonstrates an additional complexity for practitioners—the continuous change in the law surrounding reproductive rights—and practice involving adolescent patients is especially difficult.
There are some good state-by-state reviews of laws related to abortion and contraception. We find the Guttmacher Institute particularly helpful. (See “State-by-state reviews of laws related to abortion and contraception”.) Although these are good resources, they are not the basis for legal practice with the current law in a state. The complexity and ever-changing nature of reproductive rights is one of the reasons we believe that it is important that anyone in active ObGyn practice maintain an ongoing professional relationship with a lawyer with expertise in this area of practice. This relationship should establish and update policies and procedures consistent with local law, consent and other forms, reporting of possible child abuse, and the like. An annual legal checkup may be as important for physicians as a physical checkup is for their patients.
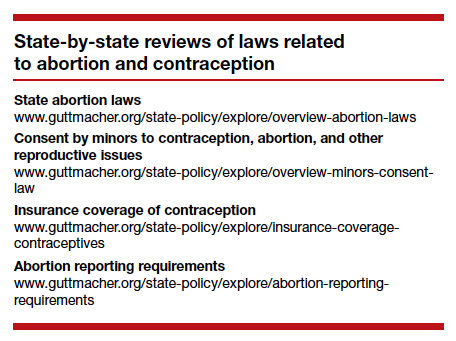
Future outcomes
At the end of the Term, we will review the outcome of the cases noted above—and the possibility of follow-on cases. Whatever the Court does this Term, it will not be the end of the legal and political struggles over abortion and other reproductive issues. These questions deeply divide our society, and the cases and controversies reflect that continuing division. ●

There is now great interest in the Supreme Court’s handling of cases that involve a woman’s ability to have an abortion. Recent decisions, and those planned in the next few months will be the source of intense scrutiny. But the Court’s involvement in reproductive rights did not begin with abortion. In fact, the Supreme Court has a long history of controversial decisions dealing with reproductive rights.
Involuntary sterilization
A notable, even infamous, case was Buck v Bell (1927)—later discredited—in which the Court reviewed a state law that provided for the involuntary sterilization of the “feeble minded.”1 The 8-1 decision was that the state could choose to have such a law to protect the so-called genetic health of the state. The law was based on a theory of eugenics. The opinion by the highly respected Justice Oliver Wendell Holmes included the unfortunate conclusion, “Three generations of imbeciles are enough.”2 As mentioned, the law has since been thoroughly discredited. In 1942, the Court did come to a different result, holding in Skinner v Oklahoma that it was unconstitutional for a state to involuntarily sterilize “habitual criminals.”3
Contraception
Forty years after Buck, in Griswold v Connecticut, the Court reviewed a state law that prohibited the distribution of any drug or device used for contraception (even for married couples).4 In a 7-2 decision, the Supreme Court struck down the state law as violating a marital right of privacy. Beyond its specific holding, Griswold was important in several ways. First, a physician was raising the rights of patients (not specifically his own rights). This is notable because, ordinarily in court, litigants may argue their own rights, not the rights of others. This has been important in later reproductive rights cases because often it has been physicians raising and arguing the rights of patients.
A second interesting part of Griswold was the source of this constitutional right of privacy. The Constitution contains no express privacy provision. In Griswold, the Court found that the 1st, 3rd, 4th, and 9th Amendments create the right to privacy in marital relations. Writing for the majority, Justice Douglas found that “emanations” from these amendments have “penumbras” that create a right of marital privacy.
Although Griswold was based on marital privacy, a few years later, in 1972, the Court essentially converted that right to one of reproductive privacy (“the decision whether to bear or beget a child.”) In Eisenstadt v Baird, the Court held that it was a violation of equal protection (the 14th Amendment) for a state to allow contraception to the married but deny it to an unmarried person.5
Continue to: Abortion...
Abortion
In 1971, the Court had heard arguments in 2 cases that raised issues regarding whether state laws prohibiting abortion were constitutional. The first oral argument in Roe v Wade is widely considered one of the worst oral arguments in modern history, and for several reasons the Court set the case for rehearing the following Term (October 1972). In January 1973, the Court decided Roe v Wade.6 The 7-2 decision was written by Justice Blackmun, who had at one point been the attorney for the Mayo Clinic and might be considered one of the first “health lawyers.” The Court held that the Constitution (perhaps in the 14th or 9th Amendment) includes a right of privacy that includes the right of a woman to choose to have, or not to have, an abortion. In implementing the right, the Court held that a state may impose only modest medical safeguards for the mother (eg, requiring that abortions be performed by a licensed physician). In the second trimester, to the point of viability, a state could impose only limitations on abortion that were reasonably directed to ensure the health of the mother. After a fetus was viable (could live outside the mother’s body), the state was free to regulate or prohibit abortions and protect the fetus. At the time, viability was approximately the beginning of the third trimester.6
The clear majority of the Court in Roe (7-2) may have suggested that there was not strong opposition to the decision. That, of course, was not the case. Legal and political conflict surrounding the case has been, and remains, intense. Since 1973, the Court has been called upon to decide many abortion cases, and each case seems to beget more controversy and still more cases.
Some of the legal objections to Roe and other abortion decisions are that the constitutional basis for the decision remains unclear—a specific right of privacy is not contained in the text of the Constitution. Several locations of a possible right of privacy have been mentioned by various justices, but “substantive due process” became the common constitutional basis for the right. Critics note that “substantive” due process (as opposed to procedural due process) is not mentioned in the Constitution, and it is short on clear guiding principles. Beyond those jurisprudential issues, of course, there were strong religious and philosophical objections to abortion. What followed Roe has been a long series of efforts to limit or discourage access to abortion, and the Supreme Court has had to decide a great many abortion cases (and a few contraception cases) over the last 50 years. Most years (except from 2008‒2013) the Court has heard, on average, at least one abortion case.
By way of examples, here are some of the issues related to abortion that the Court has decided:
- Payment and facilities. States and the federal government are not required to pay for abortions for women who cannot afford them or to provide facilities for abortion.7-10
- Informed consent. Some states’ special informed consent requirements for abortion were upheld, but complex consents that required the father’s participation were not.
- Ability to advertise. Prohibitions on advertisement of abortion services were struck down.
- Location. Requirements for hospital-only abortions (or similar regulations) were struck down.
- Anti-abortion protests. Several cases addressed guidelines involving demonstrations near abortion clinics.
Of particular importance was the case of Planned Parenthood of Southeastern Pennsylvania v Casey—“Casey.”11 In 1992 that case reaffirmed the “essential” holding of Roe v Wade. A plurality in that case de-emphasized the trimester framework and applied an “undue burden” test on limitations on abortion. In the more recent cases argued before the Court, Casey is frequently referred to as specifically reaffirming, and therefore solidifying, Roe.
Consent for minors
There have been several cases since 1973 that involved contraceptives or abortions and “minors” (generally, adolescents aged <18 years, although there are some state-defined exceptions). These cases typically involve 2 issues: the right of minors to consent to treatment and the obligation of the physician to provide information to parents about treatment to their minor daughter. In 1977 the Court struck down a New York law that prohibited the distribution of contraceptives to minors.12 However, abortion issues involving minors have been more complicated. While the Court has struck down “2-parent” consent statutes,13 it has generally upheld 1-parent consent statutes, but only if those statutes contain a “judicial bypass” provision and an emergency medical provision.11,14,15 (This bypass allows a minor to “bypass” parental consent to abortion in some circumstances, and instead seek judicial authorization for an abortion.) Generally, the Court has upheld parental notification for abortions, with exceptions where it would be harmful to the minor who is seeking the abortion.16-19
Continue to: Who can perform an abortion...
Who can perform an abortion
Over the years there have also been several cases raising questions about the professionals who can perform abortions, their hospital privileges, and what facilities can perform abortions. Two of those cases in recent years have, for example, seen the Court strike down state statutes that required the physicians who perform abortions to have admitting privileges at least in 1 nearby hospital.20,21 The basis for these decisions is that the admitting qualification is an “undue burden” because it serves almost no health purpose, while significantly limiting the number of professionals who can perform abortions.
Cases this Term
The current Term of the Court (officially the “October 2021 Term”) may be one of the most significant for reproductive rights in recent history. The Court accepted 6 abortion-related cases to hear. It dismissed 3 of those cases, which had become “moot” because the Biden administration changed the rules that had been legally challenged.22-24 It has heard arguments in the 3 (technically 4) remaining cases, in which decisions will be announced over the next several months.
The first of these cases (involving the Texas Heartbeat Act) raises very important, but vexing, procedural issues about a Texas abortion law. The second (Whole Woman’s Health v Jackson) is a direct challenge to Roe v Wade. The third case (Cameron v EMW Women’s Surgical Center) involves the narrow question of whether a state attorney general can intervene in a case to uphold a state abortion law when another state official refuses to defend the law.25 It is worthwhile taking a look at the first 2 of these cases.
Texas Heartbeat Act
In the first case (technically, it is 2 cases, as we will see), the Texas legislature adopted a law that prohibits abortions after there is a discernable heartbeat (around 6 weeks of pregnancy). The law precludes state officials from enforcing the law. Instead, it allows almost any private citizen to seek monetary damages ($10,000 plus fees) from anyone who performs an abortion or “aids and abets” an abortion. (This is in some ways similar to “private attorney general” actions found in the False Claims Act, and in some civil rights and labor laws.) This statute is clearly inconsistent with Roe in that it prohibits abortions before the end of the second trimester. If it were a usual law—a Texas law being enforced by state officials—federal courts would issue injunctions to state officials against enforcing the law. The difficulty with the Texas law (and its very purpose) is that there are procedural limitations in federal law that make it very difficult to find a path for federal courts to review the Texas statute quickly. For example, would federal courts enjoin every private citizen of the state? There is a longstanding Constitutional doctrine that precludes federal courts from enjoining state courts.26 Therefore, it is difficult to challenge the law before someone performing or aiding an abortion has been ordered to pay the private citizen who is enforcing it. In the interim, which could be months or even years, health care providers face uncertainty about continuing to provide abortion services. Some providers would stop providing abortion services, reducing the availability of those services.
Two cases challenge this Texas procedure. In the first, Whole Woman’s Health v Jackson, 27 abortion providers seek to find some way through the procedural thicket to allow an immediate challenge to the statute. It is important because this technique of exclusive private enforcement could be used in any number of ways by the state to chill important constitutional rights (beyond abortion—to speech, to bear arms). In the second case involving the Texas law, U.S. v Texas, the federal government seeks to intervene in the case, which is another unusual procedure.28 The Court found these questions so important and difficult that it allowed 3 hours of argument (and 4 sets of lawyers). It seems likely that the Court will find a mechanism for allowing some early federal court review of individual enforcement of state laws, while minimizing harm to the state-national federalism that is at the heart of the Constitution.
For the recent procedural decisions in the Texas cases, see the “Current Court Decisions” box below.
On December 10, 2021, the Court handed down two decisions in reproductive freedom (abortion) cases, both involving the Texas abortion law (which prohibits most abortions after a fetal heartbeat can be detected and allows only private individuals to enforce the law). The more significant of the two cases, Whole Woman’s Health v Jackson,1 was the request of abortion providers (and others) to allow them to challenge the constitutionality of the Texas law by suing various state officials or a private individual, before the enforcement of the new Texas law.
The decision of the Court was somewhat complex because of the split among justices. Overall:
- The Court held 8-1 that before the law is enforced, providers have the ability to sue executives of medical licensing boards. This was based on the possibility that there could be licensure discipline for professionals who violate the new abortion law. Only Justice Thomas dissented from this part of the decision, which was written by Justice Gorsuch.
- The Court unanimously held that state-court judges could not be sued to stop enforcement of the law, and dismissed them from the suit.
- In a 5-4 split the Court held that state court clerks (and the state attorney general) could not be brought into federal court as a way of challenging the law. This was based on the 11th Amendment, sovereign immunity, and an important precedent from 1908.2 Chief Justice Roberts wrote from the justices who were essentially in dissent (Justices Bryer, Kagan, and Sotomayor). Justice Sotomayor also wrote a dissent (joined by Justices Breyer and Kagan) urging that there should be some way for providers to test the constitutionality of the law before enforcement. Allowing an action against state court clerks would be a good way to do that. She also expressly noted the problem of the Texas law approach being used by other states to attack any number of constitutional rights.
- The Court unanimously dismissed (for lack of standing) the one private citizen who had been sued. He had signed a sworn statement that he did not intend to seek the damages against abortion providers under the Texas law.
- The Court declined again to stay the Texas law while it is being challenged. That is, it left standing the 5th Circuit order allowing the law to go into effect.
- In a second, related case, the Court dismissed, without deciding, the Biden administration’s request to become a party in the Texas abortion case.3
References
- Whole Woman’s Health v Jackson, No. 21–463 (Dec. 10, 2021). https://www.supremecourt.gov /opinions/21pdf/21-463_new_8o6b.pdf.
- Ex parte Young, 209 U.S. 123 (1908).
- U.S. v Texas, 21-588 (Dec. 10, 2021). https://www.supremecourt.gov/opinions/21pdf/21-588 _c07d.pdf
Continue to: Re-evaluating the viability standard...
Re-evaluating the viability standard
The substantive abortion issue in Dobbs v Jackson Women’s Health Organization is the constitutionality of the Mississippi Gestational Age Act, which allows abortions after 15 weeks of pregnancy only for medical emergencies or severe fetal abnormality.29 This case is likely the most watched and controversial case of the Term. Many medical organizations have filed amicus curiae briefs, including the American College of Obstetricians and Gynecologists joined by the American Medical Association,30 the International Federation of Gynecology and Obstetrics,31 and the American Association of Pro-Life Obstetricians and Gynecologists.32 The reason for all this attention is that the Court has accepted to resolve “whether all pre-viability prohibitions on elective abortions are unconstitutional.” Thus, it represents a direct challenge to the trimester/viability structure of Roe.
It appears that there are 3 justices ready to outright overrule Roe, 3 that would uphold it as is, and 3 who are not in favor of Roe, but feel bound by precedent or are not in favor of a traumatic move. For that reason, there may be a narrow decision in this case. For example, the Court might find a procedural way to avoid directly deciding the abortion issue in this case, or it might uphold the right to abortion but change the viability standard. It is also true that predicting what the Court will do in controversial cases is a fool’s errand.
The complexity of reproductive rights and the ObGyn practice
These cases and policies affect the day-to-day practice of obstetrics. It is the most legally complex area of medical practice for several reasons. The law varies considerably from state to state. The clinician who practices both in California and across the border in Arizona will face substantially different laws, especially regarding the treatment of adolescents. And the reproductive rights laws in many states are a complicated mix of state statutes and state court decisions, with an overlay of federal statutes and court decisions, and a series of both state and federal regulations. This article demonstrates an additional complexity for practitioners—the continuous change in the law surrounding reproductive rights—and practice involving adolescent patients is especially difficult.
There are some good state-by-state reviews of laws related to abortion and contraception. We find the Guttmacher Institute particularly helpful. (See “State-by-state reviews of laws related to abortion and contraception”.) Although these are good resources, they are not the basis for legal practice with the current law in a state. The complexity and ever-changing nature of reproductive rights is one of the reasons we believe that it is important that anyone in active ObGyn practice maintain an ongoing professional relationship with a lawyer with expertise in this area of practice. This relationship should establish and update policies and procedures consistent with local law, consent and other forms, reporting of possible child abuse, and the like. An annual legal checkup may be as important for physicians as a physical checkup is for their patients.
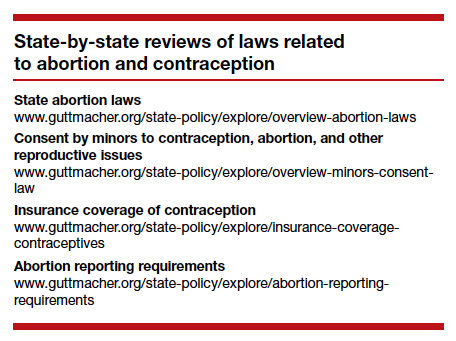
Future outcomes
At the end of the Term, we will review the outcome of the cases noted above—and the possibility of follow-on cases. Whatever the Court does this Term, it will not be the end of the legal and political struggles over abortion and other reproductive issues. These questions deeply divide our society, and the cases and controversies reflect that continuing division. ●
- Buck v Bell, 274 U.S. 200 (1927).
- Id. at 207.
- Skinner v State of Oklahoma, ex rel. Williamson, 316 U.S. 535 (1942).
- Griswold v Connecticut, 381 U.S. 479 (1965)
- Eisenstadt v Baird, 405 U.S. 438 (1972).
- Roe v Wade, 410 U.S. 113 (1973).
- Harris v McRae, 448 U.S. 297 (1980).
- Williams v Zbaraz, 448 U.S 358 (1980).
- Webster v Reproductive Health Services, 492 U.S. 490 (1989).
- Rust v Sullivan, 500 U.S. 173 (1991).
- Planned Parenthood of Southeastern Pennsylvania v Casey, 505 U.S. 833 (1992).
- Carey v Population Services, 431 U.S. 678 (1977).
- Bellotti v Baird, 443 U.S. 622 (1979).
- Planned Parenthood of Kansas City v Ashcroft, 462 U.S. 476 (1983).
- Planned Parenthood of Northern New England v Ayotte, 546 U.S. 320 (2006).
- H.L. v Matheson, 450 U.S. 398 (1981).
- Hodgson v Minnesota, 497 U.S. 417 (1990).
- Ohio v Akron Center for Reproductive Health, 497 U.S. 502 (1990).
- Lambert v Wicklund, 520 U.S. 292 (1997).
- June Medical Services v Russo, 591 U.S. ___ (2020), https:// www.supremecourt.gov/opinions/19pdf/18-1323_c07d.pdf.
- Whole Woman’s Health v Hellerstedt, 579 U.S. 582 (2016).
- AMA v Becerra, dismissed May 17, 2021, https://www .scotusblog.com/case-files/cases/american-medical -association-v-cochran.
- Becerra v Baltimore, dismissed May 17, 2021, https://www .scotusblog.com/case-files/cases/cochran-v-mayor-and-city-council-of-baltimore.
- Oregon v Becerra, dismissed May 17, 2021, https://www .scotusblog.com/case-files/cases/oregon-v-cochran.
- Cameron v EMW Women’s Surgical Center, 20-601. https:// www.scotusblog.com/case-files/cases/cameron-v-emw -womens-surgical-center-p-s-c.
- Ex parte Young, 209 U.S. 123 (1908).
- Whole Woman’s Health v Jackson, 21-463. https://www .scotusblog.com/case-files/cases/whole-womans-health-v -jackson.
- U.S. v Texas, 21-588. https://www.scotusblog.com/case-files /cases/united-states-v-texas-3.
- Dobbs v Jackson Women’s Health Organization, 19-1392. https://www.scotusblog.com/case-files/cases/dobbs-v -jackson-womens-health-organization.
- Brief of Amici Curiae American College of Obstetricians and Gynecologists et al., Dobbs v Jackson Women’s Health Organization (Sep. 2021). https://www.acog.org/ -/media/project/acog/acogorg/files/advocacy/amicus -briefs/2021/20210920-dobbs-v-jwho-amicus-brief.pdf?la=e n&hash=717DFDD07A03B93A04490E66835BB8C5.
- Brief Amicus Curiae of International Federation of Gynecology and Obstetrics, Dobbs v Jackson Women’s Health Organization (Sep. 20, 2021). https://www.supremecourt. gov/DocketPDF/19/19-1392/193019/20210920155508744 _41426%20pdf%20Chen.pdf.
- Brief Amicus Curiae of American Association of Pro-Life Obstetricians and Gynecologists. Dobbs v Jackson Women’s Health Organization (Sep. 2021). https://www.supremecourt .gov/DocketPDF/19/19-1392/185350/20210729163532595 _No.%2019-1392%20-%20American%20Association %20of%20Pro-Life%20Obstetricians%20and%20 Gynecologists%20-%20Amicus%20Brief%20in%20Support %20of%20Petitioner%20-%207-29-21.pdf.
- Buck v Bell, 274 U.S. 200 (1927).
- Id. at 207.
- Skinner v State of Oklahoma, ex rel. Williamson, 316 U.S. 535 (1942).
- Griswold v Connecticut, 381 U.S. 479 (1965)
- Eisenstadt v Baird, 405 U.S. 438 (1972).
- Roe v Wade, 410 U.S. 113 (1973).
- Harris v McRae, 448 U.S. 297 (1980).
- Williams v Zbaraz, 448 U.S 358 (1980).
- Webster v Reproductive Health Services, 492 U.S. 490 (1989).
- Rust v Sullivan, 500 U.S. 173 (1991).
- Planned Parenthood of Southeastern Pennsylvania v Casey, 505 U.S. 833 (1992).
- Carey v Population Services, 431 U.S. 678 (1977).
- Bellotti v Baird, 443 U.S. 622 (1979).
- Planned Parenthood of Kansas City v Ashcroft, 462 U.S. 476 (1983).
- Planned Parenthood of Northern New England v Ayotte, 546 U.S. 320 (2006).
- H.L. v Matheson, 450 U.S. 398 (1981).
- Hodgson v Minnesota, 497 U.S. 417 (1990).
- Ohio v Akron Center for Reproductive Health, 497 U.S. 502 (1990).
- Lambert v Wicklund, 520 U.S. 292 (1997).
- June Medical Services v Russo, 591 U.S. ___ (2020), https:// www.supremecourt.gov/opinions/19pdf/18-1323_c07d.pdf.
- Whole Woman’s Health v Hellerstedt, 579 U.S. 582 (2016).
- AMA v Becerra, dismissed May 17, 2021, https://www .scotusblog.com/case-files/cases/american-medical -association-v-cochran.
- Becerra v Baltimore, dismissed May 17, 2021, https://www .scotusblog.com/case-files/cases/cochran-v-mayor-and-city-council-of-baltimore.
- Oregon v Becerra, dismissed May 17, 2021, https://www .scotusblog.com/case-files/cases/oregon-v-cochran.
- Cameron v EMW Women’s Surgical Center, 20-601. https:// www.scotusblog.com/case-files/cases/cameron-v-emw -womens-surgical-center-p-s-c.
- Ex parte Young, 209 U.S. 123 (1908).
- Whole Woman’s Health v Jackson, 21-463. https://www .scotusblog.com/case-files/cases/whole-womans-health-v -jackson.
- U.S. v Texas, 21-588. https://www.scotusblog.com/case-files /cases/united-states-v-texas-3.
- Dobbs v Jackson Women’s Health Organization, 19-1392. https://www.scotusblog.com/case-files/cases/dobbs-v -jackson-womens-health-organization.
- Brief of Amici Curiae American College of Obstetricians and Gynecologists et al., Dobbs v Jackson Women’s Health Organization (Sep. 2021). https://www.acog.org/ -/media/project/acog/acogorg/files/advocacy/amicus -briefs/2021/20210920-dobbs-v-jwho-amicus-brief.pdf?la=e n&hash=717DFDD07A03B93A04490E66835BB8C5.
- Brief Amicus Curiae of International Federation of Gynecology and Obstetrics, Dobbs v Jackson Women’s Health Organization (Sep. 20, 2021). https://www.supremecourt. gov/DocketPDF/19/19-1392/193019/20210920155508744 _41426%20pdf%20Chen.pdf.
- Brief Amicus Curiae of American Association of Pro-Life Obstetricians and Gynecologists. Dobbs v Jackson Women’s Health Organization (Sep. 2021). https://www.supremecourt .gov/DocketPDF/19/19-1392/185350/20210729163532595 _No.%2019-1392%20-%20American%20Association %20of%20Pro-Life%20Obstetricians%20and%20 Gynecologists%20-%20Amicus%20Brief%20in%20Support %20of%20Petitioner%20-%207-29-21.pdf.