User login
Palliative care underused in pulmonary arterial hypertension
of more than 30,000 hospital admissions has found.
“Specialty palliative care services (PCS) are present in the vast majority of hospitals with more than 300 beds, and PCS use for patients who are facing serious illness with potentially life-limiting prognoses increasingly is becoming the standard of care,” wrote Vidhu Anand, MD, of the Mayo Clinic, Rochester, Minn., and colleagues. But despite experts recommending PCS in pulmonary arterial hypertension (PAH), data on the use of palliative care referrals for PAH patients are limited, they added.
In a study published in Chest, the researchers used the National (Nationwide) Inpatient Sample to identify 30,495 admissions with a primary diagnosis of PAH between 2001 through 2017. The primary outcome was the use of PCS in these patients.
Overall, inpatient use of PCS was 2.2%, but that figure increased from 0.5% in 2001 to 7.6% in 2017, representing a fivefold increase over the study period, with a significant increase after 2009. The reason for this notable increase remains unclear; however, “it may be related to recognition of palliative care and hospice as a medical subspecialty with board certification in 2008 or identification of palliative care by the National Priorities Partnership as one of six priority areas in 2008,” the researchers said.
Incorporating palliative care in a treatment strategy
The perception of PCS as an element of treatment plans for patients with severe lung disease, and not only as end-of-life care, has certainly increased in recent years, Sachin Gupta, MD, FCCP, said in an interview.
Dr. Gupta is a pulmonologist practicing in the San Francisco Bay area, and he did not take part in the study. He recommended early integration of PCS treating patients with PAH. “I have frequently asked PCS to aid early on during inpatient admission with PAH patients for pain management, as well as for aiding in POLST [Physician Orders for Life-Sustaining Treatment] paperwork to be completed. Increased age and comorbidities are certainly risk factors themselves for a longer hospital course and worse outcomes; in addition, in center-based PAH care there are more means available by which to give a patient with right heart failure that ‘one last shot’ – an opportunity for a longer life. I truly think it is a relationship with the patient, built from the outpatient pulmonary hypertension clinic, that allows the treating physician to have a better sense of a patient’s quality of life longitudinally, and to have the candid conversation when things begin to decline.”
Which patients receive PCS?
The study found that socioeconomic factors, and the severity of illness, are the drivers of PCS referrals. In a multivariate analysis, independent predictors of PCS use included white race, private insurance, and higher socioeconomic status. Additional independent predictors of PCS use included increased comorbidities, admission to an urban hospital, admission to a small hospital, presence of heart failure and cardiogenic shock, acute noncardiac organ failure, and use of extracorporeal membrane oxygenation and noninvasive mechanical ventilation, the researchers noted.
Patients who received PCS consultation were significantly more likely than those not receiving PCS to have DNR status (46.2% vs. 1.8%), longer length of hospital stay (12.9 days vs. 7.2 days), higher hospitalization costs $130,434 vs. $56,499), and higher in-hospital mortality (52.8% vs. 6.4%; P < .001 for all).
Some patients refuse PCS and others are not offered PCS. Dr. Gupta noted that it should be no surprise that not all patients are comfortable with the idea of a PCS referral. “Fear, misunderstanding, and cultural beliefs may be individually or together at the root of resistance to PCS. Their reluctance may be due to a ‘false narrative’ of the purpose of palliative care. The conception of PCS being for end-of-life care may be the result of personal experiences or experience with loved ones. Occasionally, a patient equates PCS with access to narcotics (‘knock me out’), which they may or may not want. I try to reassure patients that there will be no coercion for anything they do not want, and at the end of the day, the medical team is the main driver of their care, not the palliative service.”
Actively drug-abusing PAH patients are a particular challenge, said Dr. Gupta. These patients often refuse palliative care referral both as inpatients and outpatients. “Such patients are an enigma for many PAH-treating physicians as they may survive to discharge, despite a terrible prognosis predicted by their testing.”
In addition, patients in whom organ transplantation is being pursued may not receive timely PCS, he said. “It can be an absolute challenge to bring such patients to the finish line (transplantation), and the timing of PCS referral is often deferred. Arguably, for better or worse, such patients refuse, or more often are not offered, PCS as inpatients while there is still a chance organ transplantation is a viable option for them.”
The use of PCS in less than 10% of PAH admissions is similar to previous studies showing low use of PCS for patients with acute myocardial infarction, heart failure, and COPD, the researchers noted. However, “Given the high morbidity and mortality associated with PAH even after hospitalization, hospital admissions without PCS use represent a missed opportunity,” the investigators wrote.
Early warning on the need for PCS
Increasing PCS referrals for PAH patients requires clinicians to be proactive, Dr. Gupta stressed. “Pulmonologists, especially those managing pulmonary hypertension outpatients without the aid of a PAH center, should remain vigilant at all routine visits to calculate a patient’s risk score (i.e. REVEAL 2.0 risk calculator) to stratify their risk of 1-year mortality. Based on this assessment, shared decision making can help guide next steps including early outpatient PCS involvement for those at high risk. I also calculate a patient’s risk score, based on the data I have, when PAH patients are admitted to the hospital. Occasionally, a patient who I initially think is moderate risk turns out to be high risk when I calculate their risk score. In such high-risk patients, PCS consultation should certainly be considered early on.”
The study findings were limited by several factors including the possible coding errors associated with use of discharge diagnosis, lack of data on medication and the cause of PAH, and lack of information on the reasons for PCS referrals, the researchers noted. However, the results “addressed an important knowledge gap highlighting the national use of PCS in PAH,” they said. Further research is needed to address disparities and the integration of PCS into PAH care protocols, they added.
The researchers had no financial conflicts to disclose. The study received no outside funding; one coauthor disclosed support from the National Center for Advancing Translational Sciences Clinical and Translational Science.
of more than 30,000 hospital admissions has found.
“Specialty palliative care services (PCS) are present in the vast majority of hospitals with more than 300 beds, and PCS use for patients who are facing serious illness with potentially life-limiting prognoses increasingly is becoming the standard of care,” wrote Vidhu Anand, MD, of the Mayo Clinic, Rochester, Minn., and colleagues. But despite experts recommending PCS in pulmonary arterial hypertension (PAH), data on the use of palliative care referrals for PAH patients are limited, they added.
In a study published in Chest, the researchers used the National (Nationwide) Inpatient Sample to identify 30,495 admissions with a primary diagnosis of PAH between 2001 through 2017. The primary outcome was the use of PCS in these patients.
Overall, inpatient use of PCS was 2.2%, but that figure increased from 0.5% in 2001 to 7.6% in 2017, representing a fivefold increase over the study period, with a significant increase after 2009. The reason for this notable increase remains unclear; however, “it may be related to recognition of palliative care and hospice as a medical subspecialty with board certification in 2008 or identification of palliative care by the National Priorities Partnership as one of six priority areas in 2008,” the researchers said.
Incorporating palliative care in a treatment strategy
The perception of PCS as an element of treatment plans for patients with severe lung disease, and not only as end-of-life care, has certainly increased in recent years, Sachin Gupta, MD, FCCP, said in an interview.
Dr. Gupta is a pulmonologist practicing in the San Francisco Bay area, and he did not take part in the study. He recommended early integration of PCS treating patients with PAH. “I have frequently asked PCS to aid early on during inpatient admission with PAH patients for pain management, as well as for aiding in POLST [Physician Orders for Life-Sustaining Treatment] paperwork to be completed. Increased age and comorbidities are certainly risk factors themselves for a longer hospital course and worse outcomes; in addition, in center-based PAH care there are more means available by which to give a patient with right heart failure that ‘one last shot’ – an opportunity for a longer life. I truly think it is a relationship with the patient, built from the outpatient pulmonary hypertension clinic, that allows the treating physician to have a better sense of a patient’s quality of life longitudinally, and to have the candid conversation when things begin to decline.”
Which patients receive PCS?
The study found that socioeconomic factors, and the severity of illness, are the drivers of PCS referrals. In a multivariate analysis, independent predictors of PCS use included white race, private insurance, and higher socioeconomic status. Additional independent predictors of PCS use included increased comorbidities, admission to an urban hospital, admission to a small hospital, presence of heart failure and cardiogenic shock, acute noncardiac organ failure, and use of extracorporeal membrane oxygenation and noninvasive mechanical ventilation, the researchers noted.
Patients who received PCS consultation were significantly more likely than those not receiving PCS to have DNR status (46.2% vs. 1.8%), longer length of hospital stay (12.9 days vs. 7.2 days), higher hospitalization costs $130,434 vs. $56,499), and higher in-hospital mortality (52.8% vs. 6.4%; P < .001 for all).
Some patients refuse PCS and others are not offered PCS. Dr. Gupta noted that it should be no surprise that not all patients are comfortable with the idea of a PCS referral. “Fear, misunderstanding, and cultural beliefs may be individually or together at the root of resistance to PCS. Their reluctance may be due to a ‘false narrative’ of the purpose of palliative care. The conception of PCS being for end-of-life care may be the result of personal experiences or experience with loved ones. Occasionally, a patient equates PCS with access to narcotics (‘knock me out’), which they may or may not want. I try to reassure patients that there will be no coercion for anything they do not want, and at the end of the day, the medical team is the main driver of their care, not the palliative service.”
Actively drug-abusing PAH patients are a particular challenge, said Dr. Gupta. These patients often refuse palliative care referral both as inpatients and outpatients. “Such patients are an enigma for many PAH-treating physicians as they may survive to discharge, despite a terrible prognosis predicted by their testing.”
In addition, patients in whom organ transplantation is being pursued may not receive timely PCS, he said. “It can be an absolute challenge to bring such patients to the finish line (transplantation), and the timing of PCS referral is often deferred. Arguably, for better or worse, such patients refuse, or more often are not offered, PCS as inpatients while there is still a chance organ transplantation is a viable option for them.”
The use of PCS in less than 10% of PAH admissions is similar to previous studies showing low use of PCS for patients with acute myocardial infarction, heart failure, and COPD, the researchers noted. However, “Given the high morbidity and mortality associated with PAH even after hospitalization, hospital admissions without PCS use represent a missed opportunity,” the investigators wrote.
Early warning on the need for PCS
Increasing PCS referrals for PAH patients requires clinicians to be proactive, Dr. Gupta stressed. “Pulmonologists, especially those managing pulmonary hypertension outpatients without the aid of a PAH center, should remain vigilant at all routine visits to calculate a patient’s risk score (i.e. REVEAL 2.0 risk calculator) to stratify their risk of 1-year mortality. Based on this assessment, shared decision making can help guide next steps including early outpatient PCS involvement for those at high risk. I also calculate a patient’s risk score, based on the data I have, when PAH patients are admitted to the hospital. Occasionally, a patient who I initially think is moderate risk turns out to be high risk when I calculate their risk score. In such high-risk patients, PCS consultation should certainly be considered early on.”
The study findings were limited by several factors including the possible coding errors associated with use of discharge diagnosis, lack of data on medication and the cause of PAH, and lack of information on the reasons for PCS referrals, the researchers noted. However, the results “addressed an important knowledge gap highlighting the national use of PCS in PAH,” they said. Further research is needed to address disparities and the integration of PCS into PAH care protocols, they added.
The researchers had no financial conflicts to disclose. The study received no outside funding; one coauthor disclosed support from the National Center for Advancing Translational Sciences Clinical and Translational Science.
of more than 30,000 hospital admissions has found.
“Specialty palliative care services (PCS) are present in the vast majority of hospitals with more than 300 beds, and PCS use for patients who are facing serious illness with potentially life-limiting prognoses increasingly is becoming the standard of care,” wrote Vidhu Anand, MD, of the Mayo Clinic, Rochester, Minn., and colleagues. But despite experts recommending PCS in pulmonary arterial hypertension (PAH), data on the use of palliative care referrals for PAH patients are limited, they added.
In a study published in Chest, the researchers used the National (Nationwide) Inpatient Sample to identify 30,495 admissions with a primary diagnosis of PAH between 2001 through 2017. The primary outcome was the use of PCS in these patients.
Overall, inpatient use of PCS was 2.2%, but that figure increased from 0.5% in 2001 to 7.6% in 2017, representing a fivefold increase over the study period, with a significant increase after 2009. The reason for this notable increase remains unclear; however, “it may be related to recognition of palliative care and hospice as a medical subspecialty with board certification in 2008 or identification of palliative care by the National Priorities Partnership as one of six priority areas in 2008,” the researchers said.
Incorporating palliative care in a treatment strategy
The perception of PCS as an element of treatment plans for patients with severe lung disease, and not only as end-of-life care, has certainly increased in recent years, Sachin Gupta, MD, FCCP, said in an interview.
Dr. Gupta is a pulmonologist practicing in the San Francisco Bay area, and he did not take part in the study. He recommended early integration of PCS treating patients with PAH. “I have frequently asked PCS to aid early on during inpatient admission with PAH patients for pain management, as well as for aiding in POLST [Physician Orders for Life-Sustaining Treatment] paperwork to be completed. Increased age and comorbidities are certainly risk factors themselves for a longer hospital course and worse outcomes; in addition, in center-based PAH care there are more means available by which to give a patient with right heart failure that ‘one last shot’ – an opportunity for a longer life. I truly think it is a relationship with the patient, built from the outpatient pulmonary hypertension clinic, that allows the treating physician to have a better sense of a patient’s quality of life longitudinally, and to have the candid conversation when things begin to decline.”
Which patients receive PCS?
The study found that socioeconomic factors, and the severity of illness, are the drivers of PCS referrals. In a multivariate analysis, independent predictors of PCS use included white race, private insurance, and higher socioeconomic status. Additional independent predictors of PCS use included increased comorbidities, admission to an urban hospital, admission to a small hospital, presence of heart failure and cardiogenic shock, acute noncardiac organ failure, and use of extracorporeal membrane oxygenation and noninvasive mechanical ventilation, the researchers noted.
Patients who received PCS consultation were significantly more likely than those not receiving PCS to have DNR status (46.2% vs. 1.8%), longer length of hospital stay (12.9 days vs. 7.2 days), higher hospitalization costs $130,434 vs. $56,499), and higher in-hospital mortality (52.8% vs. 6.4%; P < .001 for all).
Some patients refuse PCS and others are not offered PCS. Dr. Gupta noted that it should be no surprise that not all patients are comfortable with the idea of a PCS referral. “Fear, misunderstanding, and cultural beliefs may be individually or together at the root of resistance to PCS. Their reluctance may be due to a ‘false narrative’ of the purpose of palliative care. The conception of PCS being for end-of-life care may be the result of personal experiences or experience with loved ones. Occasionally, a patient equates PCS with access to narcotics (‘knock me out’), which they may or may not want. I try to reassure patients that there will be no coercion for anything they do not want, and at the end of the day, the medical team is the main driver of their care, not the palliative service.”
Actively drug-abusing PAH patients are a particular challenge, said Dr. Gupta. These patients often refuse palliative care referral both as inpatients and outpatients. “Such patients are an enigma for many PAH-treating physicians as they may survive to discharge, despite a terrible prognosis predicted by their testing.”
In addition, patients in whom organ transplantation is being pursued may not receive timely PCS, he said. “It can be an absolute challenge to bring such patients to the finish line (transplantation), and the timing of PCS referral is often deferred. Arguably, for better or worse, such patients refuse, or more often are not offered, PCS as inpatients while there is still a chance organ transplantation is a viable option for them.”
The use of PCS in less than 10% of PAH admissions is similar to previous studies showing low use of PCS for patients with acute myocardial infarction, heart failure, and COPD, the researchers noted. However, “Given the high morbidity and mortality associated with PAH even after hospitalization, hospital admissions without PCS use represent a missed opportunity,” the investigators wrote.
Early warning on the need for PCS
Increasing PCS referrals for PAH patients requires clinicians to be proactive, Dr. Gupta stressed. “Pulmonologists, especially those managing pulmonary hypertension outpatients without the aid of a PAH center, should remain vigilant at all routine visits to calculate a patient’s risk score (i.e. REVEAL 2.0 risk calculator) to stratify their risk of 1-year mortality. Based on this assessment, shared decision making can help guide next steps including early outpatient PCS involvement for those at high risk. I also calculate a patient’s risk score, based on the data I have, when PAH patients are admitted to the hospital. Occasionally, a patient who I initially think is moderate risk turns out to be high risk when I calculate their risk score. In such high-risk patients, PCS consultation should certainly be considered early on.”
The study findings were limited by several factors including the possible coding errors associated with use of discharge diagnosis, lack of data on medication and the cause of PAH, and lack of information on the reasons for PCS referrals, the researchers noted. However, the results “addressed an important knowledge gap highlighting the national use of PCS in PAH,” they said. Further research is needed to address disparities and the integration of PCS into PAH care protocols, they added.
The researchers had no financial conflicts to disclose. The study received no outside funding; one coauthor disclosed support from the National Center for Advancing Translational Sciences Clinical and Translational Science.
FROM CHEST
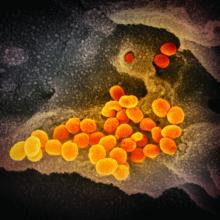
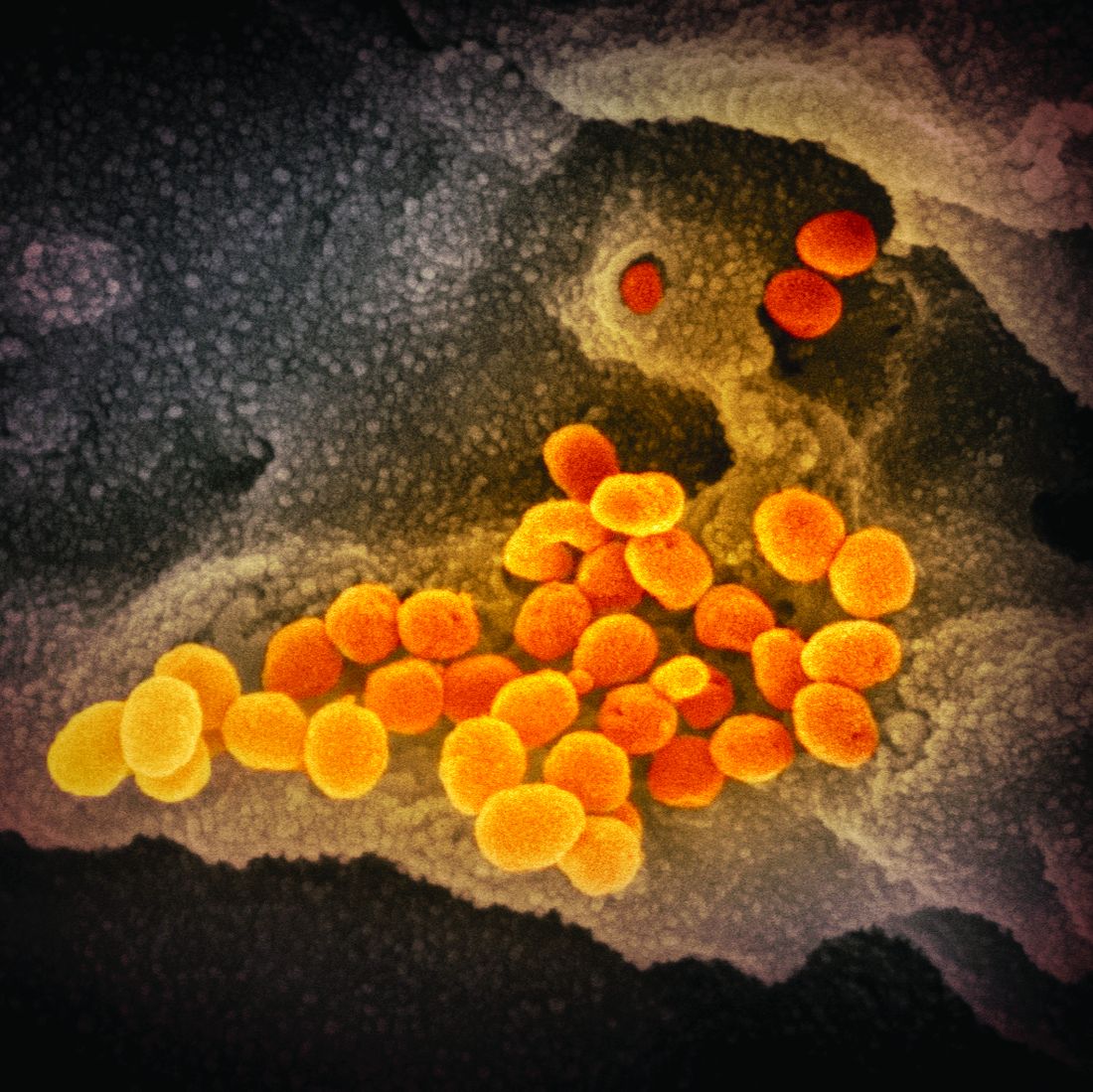
What we know and don’t know about virus variants and vaccines
About 20 states across the country have detected the more transmissible B.1.1.7 SARS-CoV-2 variant to date. Given the unknowns of the emerging situation, experts with the Infectious Diseases Society of America addressed vaccine effectiveness, how well equipped the United States is to track new mutations, and shared their impressions of President Joe Biden’s COVID-19 executive orders.
One of the major concerns remains the ability of COVID-19 vaccines to work on new strains. “All of our vaccines target the spike protein and try to elicit neutralizing antibodies that bind to that protein,” Mirella Salvatore, MD, assistant professor of medicine and population health sciences at Weill Cornell Medicine, New York, said during an IDSA press briefing on Thursday.
The B.1.1.7 mutation occurs in the “very important” spike protein, a component of the SARS-CoV-2 virus necessary for binding, which allows the virus to enter cells, added Dr. Salvatore, an IDSA fellow.
The evidence suggests that SARS-CoV-2 should be capable of producing one or two mutations per month. However, the B.1.1.7 variant surprised investigators in the United Kingdom when they first discovered the strain had 17 mutations, Dr. Salvatore said.
It’s still unknown why this particular strain is more transmissible, but Dr. Salvatore speculated that the mutation gives the virus an advantage and increases binding, allowing it to enter cells more easily. She added that the mutations might have arisen among immunocompromised people infected with SARS-CoV-2, but “that is just a hypothesis.”
On a positive note, Kathryn M. Edwards, MD, another IDSA fellow, explained at the briefing that the existing vaccines target more than one location on the virus’ spike protein. Therefore, “if there is a mutation that changes one structure of the spike protein, there will be other areas where the binding can occur.”
This polyclonal response “is why the vaccine can still be effective against this virus,” added Dr. Edwards, scientific director of the Vanderbilt Vaccine Research Program and professor of pediatrics at Vanderbilt University, Nashville, Tenn.
Dr. Salvatore emphasized that, although the new variant is more transmissible, it doesn’t appear to be more lethal. “This might affect overall mortality but not for the individual who gets the infection.”
Staying one step ahead
When asked for assurance that COVID-19 vaccines will work against emerging variants, Dr. Edwards said, “It may be we will have to change the vaccine so it is more responsive to new variants, but at this point that does not seem to be the case.”
Should the vaccines require an update, the messenger RNA vaccines have an advantage – researchers can rapidly revise them. “All you need to do is put all the little nucleotides together,” Dr. Edwards said.
“A number of us are looking at how this will work, and we look to influenza,” she added. Dr. Edwards drew an analogy to choosing – and sometimes updating – the influenza strains each year for the annual flu vaccine. With appropriate funding, the same system could be replicated to address any evolving changes to SARS-CoV-2.
On funding, Dr. Salvatore said more money would be required to optimize the surveillance system for emerging strains in the United States.
“We actually have this system – there is a wonderful network that sequences the influenza strains,” she said. “The structure exists, we just need the funding.”
“The CDC is getting the system tooled up to get more viruses to be sequenced,” Dr. Edwards said.
Both experts praised the CDC for its website with up-to-date surveillance information on emerging strains of SARS-CoV-2.
President Biden’s backing of science
A reporter asked each infectious disease expert to share their impression of President Biden’s newly signed COVID-19 executive orders.
“The biggest takeaway is the role of science and the lessons we’ve learned from masks, handwashing, and distancing,” Dr. Edwards said. “We need to heed the advice ... [especially] with a variant that is more contagious.
“It is encouraging that science will be listened to – that is the overall message,” she added.
Dr. Salvatore agreed, saying that the orders give “the feeling that we can now act by following science.”
“We have plenty of papers that show the effectiveness of masking,” for example, she said. Dr. Salvatore acknowledged that there are “a lot of contrasting ideas about masking” across the United States but stressed their importance.
“We should follow measures that we know work,” she said.
Both experts said more research is needed to stay ahead of this evolving scenario. “We still need a lot of basic science showing how this virus replicates in the cell,” Dr. Salvatore said. “We need to really characterize all these mutations and their functions.”
“We need to be concerned, do follow-up studies,” she added, “but we don’t need to panic.”
This article was based on an Infectious Diseases Society of America Media Briefing on Jan. 21, 2021. Dr. Salvatore disclosed that she is a site principal investigator on a study from Verily Life Sciences/Brin Foundation on Predictors of Severe COVID-19 Outcomes and principal investigator for an investigator-initiated study sponsored by Genentech on combination therapy in influenza. Dr. Edwards disclosed National Institutes of Health and Centers for Disease Control and Prevention grants; consulting for Bionet and IBM; and being a member of data safety and monitoring committees for Sanofi, X-4 Pharma, Seqirus, Moderna, Pfizer, and Merck.
A version of this article first appeared on Medscape.com.
About 20 states across the country have detected the more transmissible B.1.1.7 SARS-CoV-2 variant to date. Given the unknowns of the emerging situation, experts with the Infectious Diseases Society of America addressed vaccine effectiveness, how well equipped the United States is to track new mutations, and shared their impressions of President Joe Biden’s COVID-19 executive orders.
One of the major concerns remains the ability of COVID-19 vaccines to work on new strains. “All of our vaccines target the spike protein and try to elicit neutralizing antibodies that bind to that protein,” Mirella Salvatore, MD, assistant professor of medicine and population health sciences at Weill Cornell Medicine, New York, said during an IDSA press briefing on Thursday.
The B.1.1.7 mutation occurs in the “very important” spike protein, a component of the SARS-CoV-2 virus necessary for binding, which allows the virus to enter cells, added Dr. Salvatore, an IDSA fellow.
The evidence suggests that SARS-CoV-2 should be capable of producing one or two mutations per month. However, the B.1.1.7 variant surprised investigators in the United Kingdom when they first discovered the strain had 17 mutations, Dr. Salvatore said.
It’s still unknown why this particular strain is more transmissible, but Dr. Salvatore speculated that the mutation gives the virus an advantage and increases binding, allowing it to enter cells more easily. She added that the mutations might have arisen among immunocompromised people infected with SARS-CoV-2, but “that is just a hypothesis.”
On a positive note, Kathryn M. Edwards, MD, another IDSA fellow, explained at the briefing that the existing vaccines target more than one location on the virus’ spike protein. Therefore, “if there is a mutation that changes one structure of the spike protein, there will be other areas where the binding can occur.”
This polyclonal response “is why the vaccine can still be effective against this virus,” added Dr. Edwards, scientific director of the Vanderbilt Vaccine Research Program and professor of pediatrics at Vanderbilt University, Nashville, Tenn.
Dr. Salvatore emphasized that, although the new variant is more transmissible, it doesn’t appear to be more lethal. “This might affect overall mortality but not for the individual who gets the infection.”
Staying one step ahead
When asked for assurance that COVID-19 vaccines will work against emerging variants, Dr. Edwards said, “It may be we will have to change the vaccine so it is more responsive to new variants, but at this point that does not seem to be the case.”
Should the vaccines require an update, the messenger RNA vaccines have an advantage – researchers can rapidly revise them. “All you need to do is put all the little nucleotides together,” Dr. Edwards said.
“A number of us are looking at how this will work, and we look to influenza,” she added. Dr. Edwards drew an analogy to choosing – and sometimes updating – the influenza strains each year for the annual flu vaccine. With appropriate funding, the same system could be replicated to address any evolving changes to SARS-CoV-2.
On funding, Dr. Salvatore said more money would be required to optimize the surveillance system for emerging strains in the United States.
“We actually have this system – there is a wonderful network that sequences the influenza strains,” she said. “The structure exists, we just need the funding.”
“The CDC is getting the system tooled up to get more viruses to be sequenced,” Dr. Edwards said.
Both experts praised the CDC for its website with up-to-date surveillance information on emerging strains of SARS-CoV-2.
President Biden’s backing of science
A reporter asked each infectious disease expert to share their impression of President Biden’s newly signed COVID-19 executive orders.
“The biggest takeaway is the role of science and the lessons we’ve learned from masks, handwashing, and distancing,” Dr. Edwards said. “We need to heed the advice ... [especially] with a variant that is more contagious.
“It is encouraging that science will be listened to – that is the overall message,” she added.
Dr. Salvatore agreed, saying that the orders give “the feeling that we can now act by following science.”
“We have plenty of papers that show the effectiveness of masking,” for example, she said. Dr. Salvatore acknowledged that there are “a lot of contrasting ideas about masking” across the United States but stressed their importance.
“We should follow measures that we know work,” she said.
Both experts said more research is needed to stay ahead of this evolving scenario. “We still need a lot of basic science showing how this virus replicates in the cell,” Dr. Salvatore said. “We need to really characterize all these mutations and their functions.”
“We need to be concerned, do follow-up studies,” she added, “but we don’t need to panic.”
This article was based on an Infectious Diseases Society of America Media Briefing on Jan. 21, 2021. Dr. Salvatore disclosed that she is a site principal investigator on a study from Verily Life Sciences/Brin Foundation on Predictors of Severe COVID-19 Outcomes and principal investigator for an investigator-initiated study sponsored by Genentech on combination therapy in influenza. Dr. Edwards disclosed National Institutes of Health and Centers for Disease Control and Prevention grants; consulting for Bionet and IBM; and being a member of data safety and monitoring committees for Sanofi, X-4 Pharma, Seqirus, Moderna, Pfizer, and Merck.
A version of this article first appeared on Medscape.com.
About 20 states across the country have detected the more transmissible B.1.1.7 SARS-CoV-2 variant to date. Given the unknowns of the emerging situation, experts with the Infectious Diseases Society of America addressed vaccine effectiveness, how well equipped the United States is to track new mutations, and shared their impressions of President Joe Biden’s COVID-19 executive orders.
One of the major concerns remains the ability of COVID-19 vaccines to work on new strains. “All of our vaccines target the spike protein and try to elicit neutralizing antibodies that bind to that protein,” Mirella Salvatore, MD, assistant professor of medicine and population health sciences at Weill Cornell Medicine, New York, said during an IDSA press briefing on Thursday.
The B.1.1.7 mutation occurs in the “very important” spike protein, a component of the SARS-CoV-2 virus necessary for binding, which allows the virus to enter cells, added Dr. Salvatore, an IDSA fellow.
The evidence suggests that SARS-CoV-2 should be capable of producing one or two mutations per month. However, the B.1.1.7 variant surprised investigators in the United Kingdom when they first discovered the strain had 17 mutations, Dr. Salvatore said.
It’s still unknown why this particular strain is more transmissible, but Dr. Salvatore speculated that the mutation gives the virus an advantage and increases binding, allowing it to enter cells more easily. She added that the mutations might have arisen among immunocompromised people infected with SARS-CoV-2, but “that is just a hypothesis.”
On a positive note, Kathryn M. Edwards, MD, another IDSA fellow, explained at the briefing that the existing vaccines target more than one location on the virus’ spike protein. Therefore, “if there is a mutation that changes one structure of the spike protein, there will be other areas where the binding can occur.”
This polyclonal response “is why the vaccine can still be effective against this virus,” added Dr. Edwards, scientific director of the Vanderbilt Vaccine Research Program and professor of pediatrics at Vanderbilt University, Nashville, Tenn.
Dr. Salvatore emphasized that, although the new variant is more transmissible, it doesn’t appear to be more lethal. “This might affect overall mortality but not for the individual who gets the infection.”
Staying one step ahead
When asked for assurance that COVID-19 vaccines will work against emerging variants, Dr. Edwards said, “It may be we will have to change the vaccine so it is more responsive to new variants, but at this point that does not seem to be the case.”
Should the vaccines require an update, the messenger RNA vaccines have an advantage – researchers can rapidly revise them. “All you need to do is put all the little nucleotides together,” Dr. Edwards said.
“A number of us are looking at how this will work, and we look to influenza,” she added. Dr. Edwards drew an analogy to choosing – and sometimes updating – the influenza strains each year for the annual flu vaccine. With appropriate funding, the same system could be replicated to address any evolving changes to SARS-CoV-2.
On funding, Dr. Salvatore said more money would be required to optimize the surveillance system for emerging strains in the United States.
“We actually have this system – there is a wonderful network that sequences the influenza strains,” she said. “The structure exists, we just need the funding.”
“The CDC is getting the system tooled up to get more viruses to be sequenced,” Dr. Edwards said.
Both experts praised the CDC for its website with up-to-date surveillance information on emerging strains of SARS-CoV-2.
President Biden’s backing of science
A reporter asked each infectious disease expert to share their impression of President Biden’s newly signed COVID-19 executive orders.
“The biggest takeaway is the role of science and the lessons we’ve learned from masks, handwashing, and distancing,” Dr. Edwards said. “We need to heed the advice ... [especially] with a variant that is more contagious.
“It is encouraging that science will be listened to – that is the overall message,” she added.
Dr. Salvatore agreed, saying that the orders give “the feeling that we can now act by following science.”
“We have plenty of papers that show the effectiveness of masking,” for example, she said. Dr. Salvatore acknowledged that there are “a lot of contrasting ideas about masking” across the United States but stressed their importance.
“We should follow measures that we know work,” she said.
Both experts said more research is needed to stay ahead of this evolving scenario. “We still need a lot of basic science showing how this virus replicates in the cell,” Dr. Salvatore said. “We need to really characterize all these mutations and their functions.”
“We need to be concerned, do follow-up studies,” she added, “but we don’t need to panic.”
This article was based on an Infectious Diseases Society of America Media Briefing on Jan. 21, 2021. Dr. Salvatore disclosed that she is a site principal investigator on a study from Verily Life Sciences/Brin Foundation on Predictors of Severe COVID-19 Outcomes and principal investigator for an investigator-initiated study sponsored by Genentech on combination therapy in influenza. Dr. Edwards disclosed National Institutes of Health and Centers for Disease Control and Prevention grants; consulting for Bionet and IBM; and being a member of data safety and monitoring committees for Sanofi, X-4 Pharma, Seqirus, Moderna, Pfizer, and Merck.
A version of this article first appeared on Medscape.com.
Long-haul COVID-19 cases rise as stigma of chronic fatigue taunts
When Margot Gage-Witvliet began feeling run down after her family returned from a trip to the Netherlands in late February 2020, she initially chalked up her symptoms to jet lag. Three days later, however, her situation went from concerning to alarming as she struggled to breathe. “It felt like there was an elephant sitting on my chest,” she said.
Her husband and daughters also became ill with COVID-19, but Ms. Gage-Witvliet was the only one in her family who didn’t get better. After an early improvement, a rare coronavirus-induced tonic-clonic seizure in early April sent her spiraling back down. Ms. Gage-Witvliet spent the next several weeks in bed with the curtains drawn, unable to tolerate light or sound.
Today, Ms. Gage-Witvliet’s life looks nothing like it did 6 months ago when she first got sick. As one of COVID-19’s so called long-haulers, she continues to struggle with crushing fatigue, brain fog, and headaches – symptoms that worsen when she pushes herself to do more. Across the country, as many as 1 in 10 COVID-19 patients are reporting illnesses that continue for weeks and months after their initial diagnosis. Nearly all report neurologic issues like Ms. Gage-Witvliet, as well as shortness of breath and psychiatric concerns.
For Avindra Nath, MD, a neurologist at the National Institutes of Health, the experience of these long-haul COVID-19 patients feels familiar and reminds him of myalgic encephalomyelitis, also known as chronic fatigue syndrome.
Dr. Nath has long been interested in the lingering neurologic issues connected to chronic fatigue. An estimated three-quarters of all patients with chronic fatigue syndrome report that their symptoms started after a viral infection, and they suffer unrelenting exhaustion, difficulties regulating pulse and blood pressure, aches and pains, and brain fog. When Dr. Nath first read about the novel coronavirus, he began to worry that the virus would trigger symptoms in a subset of those infected. Hearing about the experiences of long-haulers like Ms. Gage-Witvliet raised his suspicions even more.
Unlike COVID-19 long-haulers, however, many patients with chronic fatigue syndrome go at least a year with these symptoms before receiving a diagnosis, according to a British survey. That means researchers have had few opportunities to study the early stages of the syndrome. “When we see patients with myalgic encephalomyelitis, whatever infection they might have had occurred in the remote past, so there’s no way for us to know how they got infected with it, what the infection was, or what the effects of it were in that early phase. We’re seeing them 2 years afterward,” Dr. Nath said.
Dr. Nath quickly realized that studying patients like Ms. Gage-Witvliet would give physicians and scientists a unique opportunity to understand not only long-term outcomes of COVID-19 infections, but also other postviral syndromes, including chronic fatigue syndrome at their earliest stages. It’s why Dr. Nath has spent the past several months scrambling to launch two NIH studies to examine the phenomenon.
Although Dr. Nath said that the parallels between COVID-19 long-haulers and those with chronic fatigue syndrome are obvious, he cautions against assuming that they are the same phenomenon. Some long-haulers might simply be taking a much slower path to recovery, or they might have a condition that looks similar on the surface but differs from chronic fatigue syndrome on a molecular level. But even if Dr. Nath fails to see links to chronic fatigue syndrome, with more than 92.5 million documented cases of COVID-19 around the world, the work will be relevant to the substantial number of infected individuals who don’t recover quickly.
“With so many people having exposure to the same virus over a similar time period, we really have the opportunity to look at these manifestations and at the very least to understand postviral syndromes,” said Mady Hornig, MD, a psychiatrist at Columbia University, New York.
The origins of chronic fatigue syndrome date back to 1985, when the Centers for Disease Control and Prevention received a request from two physicians – Paul Cheney, MD, and Daniel Peterson, MD – to investigate a mysterious disease outbreak in Nevada. In November 1984, residents in and around the idyllic vacation spot of Incline Village, a small town tucked into the north shore of Lake Tahoe, had begun reporting flu-like symptoms that persisted for weeks, even months. The doctors had searched high and low for a cause, but they couldn’t figure out what was making their patients sick.
They reported a range of symptoms – including muscle aches and pains, low-grade fevers, sore throats, and headaches – but everyone said that crippling fatigue was the most debilitating issue. This wasn’t the kind of fatigue that could be cured by a nap or even a long holiday. No matter how much their patients slept – and some were almost completely bedbound – their fatigue didn’t abate. What’s more, the fatigue got worse whenever they tried to push themselves to do more. Puzzled, the CDC sent two epidemic intelligence service (EIS) officers to try to get to the bottom of what might be happening.
Muscle aches and pains with crippling fatigue
After their visit to Incline Village, however, the CDC was just as perplexed as Dr. Cheney and Dr. Peterson. Many of the people with the condition reported flu-like symptoms right around the time they first got sick, and the physicians’ leading hypothesis was that the outbreak and its lasting symptoms were caused by chronic Epstein-Barr virus infection. But neither the CDC nor anyone else could identify the infection or any other microbial cause. The two EIS officers duly wrote up a report for the CDC’s flagship publication, Morbidity and Mortality Weekly ReportI, titled “Chronic Fatigue Possibly Related to Epstein-Barr Virus – Nevada”.
That investigators focused on the fatigue aspect made sense, says Leonard A. Jason, PhD, professor of psychology at DePaul University and director of the Center for Community Research, both in Chicago, because it was one of the few symptoms shared by all the individuals studied and it was also the most debilitating. But that focus – and the name “chronic fatigue syndrome” – led to broad public dismissal of the condition’s severity, as did an editorial note in MMWR urging physicians to look for “more definable, and possibly treatable, conditions.” Subsequent research failed to confirm a specific link to the Epstein-Barr virus, which only added to the condition’s phony reputation. Rather than being considered a potentially disabling illness, it was disregarded as a “yuppie flu” or a fancy name for malingering.
“It’s not a surprise that patients are being dismissed because there’s already this sort of grandfathered-in sense that fatigue is not real,” said Jennifer Frankovich, MD, a pediatric rheumatologist at Stanford (Calif.) University’s Lucile Packard Children’s Hospital in Palo Alto. “I’m sure that’s frustrating for them to be tired and then to have the clinician not believe them or dismiss them or think they’re making it up. It would be more helpful to the families to say: ‘You know what, we don’t know, we do not have the answer, and we believe you.’ ”
A syndrome’s shame
As time passed, patient advocacy groups began pushing back against the negative way the condition was being perceived. This criticism came as organizations like the CDC worked to develop a set of diagnostic criteria that researchers and clinicians dealing with chronic fatigue syndrome could use. With such a heterogeneous group of patients and symptoms, the task was no small challenge. The discussions, which took place over nearly 2 decades, played a key role in helping scientists home in on the single factor that was central to chronic fatigue: postexertional malaise.
“This is quite unique for chronic fatigue syndrome. With other diseases, yes, you may have fatigue as one of the components of the disease, but postexertional fatigue is very specific,” said Alain Moreau, PhD, a molecular biologist at the University of Montreal.
Of course, plenty of people have pushed themselves too hard physically and paid the price the next day. But those with chronic fatigue syndrome weren’t running marathons. To them, exertion could be anything from getting the mail to reading a book. Nor could the resulting exhaustion be resolved by an afternoon on the couch or a long vacation.
“If they do these activities, they can crash for weeks, even months,” Dr. Moreau said. It was deep, persistent, and – for 40% of those with chronic fatigue syndrome – disabling. In 2015, a study group from the Institute of Medicine proposed renaming chronic fatigue to “systemic exercise intolerance disease” because of the centrality of this symptom. Although that effort mostly stalled, their report did bring the condition out of its historic place as a scientific backwater. What resulted was an uptick in research on chronic fatigue syndrome, which helped define some of the physiological issues that either contribute to or result from the condition.
Researchers had long known about the link between infection and fatigue, said Dr. Frankovich. Work included mysterious outbreaks like the one in Lake Tahoe and well-documented issues like the wave of encephalitis lethargica (a condition that leaves patients in an almost vegetative state) that followed the 1918 H1N1 influenza pandemic.
“As a clinician, when you see someone who comes in with a chronic infection, they’re tired. I think that’s why, in the chronic-fatigue world, people are desperately looking for the infection so we can treat it, and maybe these poor suffering people will feel better,” Dr. Frankovich added. Then the pandemic struck, giving him yet another opportunity to study postviral syndromes.
Immunologic symptoms
Given the close link between a nonspecific viral illness and the onset of symptoms in chronic fatigue syndrome, scientists like Dr. Hornig opted to focus on immunologic symptoms. In a 2015 analysis published in Science, Dr. Hornig and colleagues showed that immune problems can be found in the earliest stages of chronic fatigue syndrome, and that they change as the illness progresses. Patients who had been sick for less than 3 years showed significant increases in levels of both pro- and anti-inflammatory cytokines, and the factor most strongly correlated to this inability to regulate cytokine levels was the duration of symptoms, not their severity. A series of other studies also revealed problems with regulation of the immune system, although no one could show what might have set these problems in motion.
Other researchers found signs of mitochondrial dysfunction in those with chronic fatigue syndrome. Because mitochondria make energy for cells, it wasn’t an intellectual stretch to believe that glitches in this process could contribute to fatigue. As early as 1991, scientists had discovered signs of mitochondrial degeneration in muscle biopsies from people with chronic fatigue syndrome. Subsequent studies showed that those affected by chronic fatigue were missing segments of mitochondrial DNA and had significantly reduced levels of mitochondrial activity. Although exercise normally improves mitochondrial functioning, the opposite appears to happen in chronic fatigue.
To Dr. Nath, these dual hypotheses aren’t necessarily mutually exclusive. Some studies have hinted that infection with the common human herpesvirus–6 (HHV-6) can lead to an autoimmune condition in which the body makes antibodies against the mitochondria. Mitochondria also play a key role in the ability of the innate immune system to produce interferon and other proinflammatory cytokines. It might also be that the link between immune and mitochondrial problems is more convoluted than originally thought, or that the two systems are affected independent of one another, Dr. Nath said.
Finding answers, especially those that could lead to potential treatments, wouldn’t be easy, however. In 2016, the NIH launched an in-depth study of a small number of individuals with chronic fatigue, hoping to find clues about what the condition was and how it might be treated.
For scientists like Dr. Nath, the NIH study provided a way to get at the underlying biology of chronic fatigue syndrome. Then the pandemic struck, giving him yet another opportunity to study postviral syndromes.
Chronic post-SARS syndrome
In March 2020, retired physician Harvey Moldofsky, MD, began receiving inquiries about a 2011 study he and his colleague, John Patcai, MD, had published in BMC Neurology about something they dubbed “chronic post-SARS syndrome.” The small case-control study, which involved mainly health care workers in Toronto, received little attention when it was first published, but with COVID-19, it was suddenly relevant.
Early clusters of similar cases in Miami made local physicians desperate for Dr. Moldofsky’s expertise. Luckily, he was nearby; he had fled the frigid Canadian winter for the warmth of Sarasota, Fla.
“I had people from various countries around the world writing to me and asking what they should do. And of course I don’t have any answers,” he said. But the study contained one of the world’s only references to the syndrome.
In 2003, a woman arrived in Toronto from Hong Kong. She didn’t know it at the time, but her preairport stay at the Hotel Metropole had infected her with the first SARS (severe acute respiratory syndrome) coronavirus. Her subsequent hospitalization in Toronto sparked a city-wide outbreak of SARS in which 273 people became ill and 44 died. Many of those affected were health care workers, including nurses and respiratory therapists. Although most eventually returned to work, a subset couldn’t. They complained of energy-sapping fatigue, poor sleep, brain fog, and assorted body aches and pains that persisted for more than 18 months. The aches and pains brought them to the attention of Dr. Moldofsky, then director of the Centre for the Study of Pain at the University of Toronto.
His primary interest at the time was fibromyalgia, which caused symptoms similar to those reported by the original SARS long-haulers. Intrigued, Dr. Moldofsky agreed to take a look. Their chest x-rays were clear and the nurses showed no signs of lingering viral infection. Dr. Moldofsky could see that the nurses were ill and suffering, but no lab tests or anything else could identify what was causing their symptoms.
In 2011, Dr. Moldofsky and Dr. Patcai found a strong overlap between chronic SARS, fibromyalgia, and chronic fatigue syndrome when they compared 22 patients with long-term SARS issues with 21 who had fibromyalgia. “Their problems are exactly the same. They have strange symptoms and nobody can figure out what they’re about. And these symptoms are aches and pains, and they have trouble thinking and concentrating,” Dr. Moldofsky said. Reports of COVID-19 long-haulers didn’t surprise Dr. Moldofsky, and he immediately recognized that Nath’s intention to follow these patients could provide insights into both fibromyalgia and chronic fatigue syndrome.
That’s exactly what Dr. Nath is proposing with the two NIH studies. One will focus solely on the neurologic impacts of COVID-19, including stroke, loss of taste and smell, and brain fog. The other will bring patients who have had COVID-19 symptoms for at least 6 months to the NIH Clinical Center for an inpatient stay during which they will undergo detailed physiologic tests.
Scientists around the world are launching their own post–COVID-19 studies. Dr. Moreau’s group in Montreal has laid the groundwork for such an endeavor, and the CoroNerve group in the United Kingdom is monitoring neurologic complications from the coronavirus. Many of them have the same goals as the NIH studies: Leverage the large number of COVID-19 long-haulers to better understand the earliest stages of postviral syndrome.
“At this juncture, after all the reports that we’ve seen so far, I think it’s very unlikely that there will be no relationship whatsoever between COVID-19 and chronic fatigue syndrome,” Dr. Hornig said. “I think there certainly will be some, but again, what’s the scope, what’s the size? And then, of course, even more importantly, if it is happening, what is the mechanism and how is it happening?”
For people like Ms. Gage-Witvliet, the answers can’t come soon enough. For the first time in more than a decade, the full-time professor of epidemiology didn’t prepare to teach this year because she simply can’t. It’s too taxing for her brain to deal with impromptu student questions. Ms. Gage-Witvliet hopes that, by sharing her own experiences with post COVID-19, she can help others.
“In my work, I use data to give a voice to people who don’t have a voice,” she said. “Now, I am one of those people.”
A version of this article first appeared on Medscape.com.
When Margot Gage-Witvliet began feeling run down after her family returned from a trip to the Netherlands in late February 2020, she initially chalked up her symptoms to jet lag. Three days later, however, her situation went from concerning to alarming as she struggled to breathe. “It felt like there was an elephant sitting on my chest,” she said.
Her husband and daughters also became ill with COVID-19, but Ms. Gage-Witvliet was the only one in her family who didn’t get better. After an early improvement, a rare coronavirus-induced tonic-clonic seizure in early April sent her spiraling back down. Ms. Gage-Witvliet spent the next several weeks in bed with the curtains drawn, unable to tolerate light or sound.
Today, Ms. Gage-Witvliet’s life looks nothing like it did 6 months ago when she first got sick. As one of COVID-19’s so called long-haulers, she continues to struggle with crushing fatigue, brain fog, and headaches – symptoms that worsen when she pushes herself to do more. Across the country, as many as 1 in 10 COVID-19 patients are reporting illnesses that continue for weeks and months after their initial diagnosis. Nearly all report neurologic issues like Ms. Gage-Witvliet, as well as shortness of breath and psychiatric concerns.
For Avindra Nath, MD, a neurologist at the National Institutes of Health, the experience of these long-haul COVID-19 patients feels familiar and reminds him of myalgic encephalomyelitis, also known as chronic fatigue syndrome.
Dr. Nath has long been interested in the lingering neurologic issues connected to chronic fatigue. An estimated three-quarters of all patients with chronic fatigue syndrome report that their symptoms started after a viral infection, and they suffer unrelenting exhaustion, difficulties regulating pulse and blood pressure, aches and pains, and brain fog. When Dr. Nath first read about the novel coronavirus, he began to worry that the virus would trigger symptoms in a subset of those infected. Hearing about the experiences of long-haulers like Ms. Gage-Witvliet raised his suspicions even more.
Unlike COVID-19 long-haulers, however, many patients with chronic fatigue syndrome go at least a year with these symptoms before receiving a diagnosis, according to a British survey. That means researchers have had few opportunities to study the early stages of the syndrome. “When we see patients with myalgic encephalomyelitis, whatever infection they might have had occurred in the remote past, so there’s no way for us to know how they got infected with it, what the infection was, or what the effects of it were in that early phase. We’re seeing them 2 years afterward,” Dr. Nath said.
Dr. Nath quickly realized that studying patients like Ms. Gage-Witvliet would give physicians and scientists a unique opportunity to understand not only long-term outcomes of COVID-19 infections, but also other postviral syndromes, including chronic fatigue syndrome at their earliest stages. It’s why Dr. Nath has spent the past several months scrambling to launch two NIH studies to examine the phenomenon.
Although Dr. Nath said that the parallels between COVID-19 long-haulers and those with chronic fatigue syndrome are obvious, he cautions against assuming that they are the same phenomenon. Some long-haulers might simply be taking a much slower path to recovery, or they might have a condition that looks similar on the surface but differs from chronic fatigue syndrome on a molecular level. But even if Dr. Nath fails to see links to chronic fatigue syndrome, with more than 92.5 million documented cases of COVID-19 around the world, the work will be relevant to the substantial number of infected individuals who don’t recover quickly.
“With so many people having exposure to the same virus over a similar time period, we really have the opportunity to look at these manifestations and at the very least to understand postviral syndromes,” said Mady Hornig, MD, a psychiatrist at Columbia University, New York.
The origins of chronic fatigue syndrome date back to 1985, when the Centers for Disease Control and Prevention received a request from two physicians – Paul Cheney, MD, and Daniel Peterson, MD – to investigate a mysterious disease outbreak in Nevada. In November 1984, residents in and around the idyllic vacation spot of Incline Village, a small town tucked into the north shore of Lake Tahoe, had begun reporting flu-like symptoms that persisted for weeks, even months. The doctors had searched high and low for a cause, but they couldn’t figure out what was making their patients sick.
They reported a range of symptoms – including muscle aches and pains, low-grade fevers, sore throats, and headaches – but everyone said that crippling fatigue was the most debilitating issue. This wasn’t the kind of fatigue that could be cured by a nap or even a long holiday. No matter how much their patients slept – and some were almost completely bedbound – their fatigue didn’t abate. What’s more, the fatigue got worse whenever they tried to push themselves to do more. Puzzled, the CDC sent two epidemic intelligence service (EIS) officers to try to get to the bottom of what might be happening.
Muscle aches and pains with crippling fatigue
After their visit to Incline Village, however, the CDC was just as perplexed as Dr. Cheney and Dr. Peterson. Many of the people with the condition reported flu-like symptoms right around the time they first got sick, and the physicians’ leading hypothesis was that the outbreak and its lasting symptoms were caused by chronic Epstein-Barr virus infection. But neither the CDC nor anyone else could identify the infection or any other microbial cause. The two EIS officers duly wrote up a report for the CDC’s flagship publication, Morbidity and Mortality Weekly ReportI, titled “Chronic Fatigue Possibly Related to Epstein-Barr Virus – Nevada”.
That investigators focused on the fatigue aspect made sense, says Leonard A. Jason, PhD, professor of psychology at DePaul University and director of the Center for Community Research, both in Chicago, because it was one of the few symptoms shared by all the individuals studied and it was also the most debilitating. But that focus – and the name “chronic fatigue syndrome” – led to broad public dismissal of the condition’s severity, as did an editorial note in MMWR urging physicians to look for “more definable, and possibly treatable, conditions.” Subsequent research failed to confirm a specific link to the Epstein-Barr virus, which only added to the condition’s phony reputation. Rather than being considered a potentially disabling illness, it was disregarded as a “yuppie flu” or a fancy name for malingering.
“It’s not a surprise that patients are being dismissed because there’s already this sort of grandfathered-in sense that fatigue is not real,” said Jennifer Frankovich, MD, a pediatric rheumatologist at Stanford (Calif.) University’s Lucile Packard Children’s Hospital in Palo Alto. “I’m sure that’s frustrating for them to be tired and then to have the clinician not believe them or dismiss them or think they’re making it up. It would be more helpful to the families to say: ‘You know what, we don’t know, we do not have the answer, and we believe you.’ ”
A syndrome’s shame
As time passed, patient advocacy groups began pushing back against the negative way the condition was being perceived. This criticism came as organizations like the CDC worked to develop a set of diagnostic criteria that researchers and clinicians dealing with chronic fatigue syndrome could use. With such a heterogeneous group of patients and symptoms, the task was no small challenge. The discussions, which took place over nearly 2 decades, played a key role in helping scientists home in on the single factor that was central to chronic fatigue: postexertional malaise.
“This is quite unique for chronic fatigue syndrome. With other diseases, yes, you may have fatigue as one of the components of the disease, but postexertional fatigue is very specific,” said Alain Moreau, PhD, a molecular biologist at the University of Montreal.
Of course, plenty of people have pushed themselves too hard physically and paid the price the next day. But those with chronic fatigue syndrome weren’t running marathons. To them, exertion could be anything from getting the mail to reading a book. Nor could the resulting exhaustion be resolved by an afternoon on the couch or a long vacation.
“If they do these activities, they can crash for weeks, even months,” Dr. Moreau said. It was deep, persistent, and – for 40% of those with chronic fatigue syndrome – disabling. In 2015, a study group from the Institute of Medicine proposed renaming chronic fatigue to “systemic exercise intolerance disease” because of the centrality of this symptom. Although that effort mostly stalled, their report did bring the condition out of its historic place as a scientific backwater. What resulted was an uptick in research on chronic fatigue syndrome, which helped define some of the physiological issues that either contribute to or result from the condition.
Researchers had long known about the link between infection and fatigue, said Dr. Frankovich. Work included mysterious outbreaks like the one in Lake Tahoe and well-documented issues like the wave of encephalitis lethargica (a condition that leaves patients in an almost vegetative state) that followed the 1918 H1N1 influenza pandemic.
“As a clinician, when you see someone who comes in with a chronic infection, they’re tired. I think that’s why, in the chronic-fatigue world, people are desperately looking for the infection so we can treat it, and maybe these poor suffering people will feel better,” Dr. Frankovich added. Then the pandemic struck, giving him yet another opportunity to study postviral syndromes.
Immunologic symptoms
Given the close link between a nonspecific viral illness and the onset of symptoms in chronic fatigue syndrome, scientists like Dr. Hornig opted to focus on immunologic symptoms. In a 2015 analysis published in Science, Dr. Hornig and colleagues showed that immune problems can be found in the earliest stages of chronic fatigue syndrome, and that they change as the illness progresses. Patients who had been sick for less than 3 years showed significant increases in levels of both pro- and anti-inflammatory cytokines, and the factor most strongly correlated to this inability to regulate cytokine levels was the duration of symptoms, not their severity. A series of other studies also revealed problems with regulation of the immune system, although no one could show what might have set these problems in motion.
Other researchers found signs of mitochondrial dysfunction in those with chronic fatigue syndrome. Because mitochondria make energy for cells, it wasn’t an intellectual stretch to believe that glitches in this process could contribute to fatigue. As early as 1991, scientists had discovered signs of mitochondrial degeneration in muscle biopsies from people with chronic fatigue syndrome. Subsequent studies showed that those affected by chronic fatigue were missing segments of mitochondrial DNA and had significantly reduced levels of mitochondrial activity. Although exercise normally improves mitochondrial functioning, the opposite appears to happen in chronic fatigue.
To Dr. Nath, these dual hypotheses aren’t necessarily mutually exclusive. Some studies have hinted that infection with the common human herpesvirus–6 (HHV-6) can lead to an autoimmune condition in which the body makes antibodies against the mitochondria. Mitochondria also play a key role in the ability of the innate immune system to produce interferon and other proinflammatory cytokines. It might also be that the link between immune and mitochondrial problems is more convoluted than originally thought, or that the two systems are affected independent of one another, Dr. Nath said.
Finding answers, especially those that could lead to potential treatments, wouldn’t be easy, however. In 2016, the NIH launched an in-depth study of a small number of individuals with chronic fatigue, hoping to find clues about what the condition was and how it might be treated.
For scientists like Dr. Nath, the NIH study provided a way to get at the underlying biology of chronic fatigue syndrome. Then the pandemic struck, giving him yet another opportunity to study postviral syndromes.
Chronic post-SARS syndrome
In March 2020, retired physician Harvey Moldofsky, MD, began receiving inquiries about a 2011 study he and his colleague, John Patcai, MD, had published in BMC Neurology about something they dubbed “chronic post-SARS syndrome.” The small case-control study, which involved mainly health care workers in Toronto, received little attention when it was first published, but with COVID-19, it was suddenly relevant.
Early clusters of similar cases in Miami made local physicians desperate for Dr. Moldofsky’s expertise. Luckily, he was nearby; he had fled the frigid Canadian winter for the warmth of Sarasota, Fla.
“I had people from various countries around the world writing to me and asking what they should do. And of course I don’t have any answers,” he said. But the study contained one of the world’s only references to the syndrome.
In 2003, a woman arrived in Toronto from Hong Kong. She didn’t know it at the time, but her preairport stay at the Hotel Metropole had infected her with the first SARS (severe acute respiratory syndrome) coronavirus. Her subsequent hospitalization in Toronto sparked a city-wide outbreak of SARS in which 273 people became ill and 44 died. Many of those affected were health care workers, including nurses and respiratory therapists. Although most eventually returned to work, a subset couldn’t. They complained of energy-sapping fatigue, poor sleep, brain fog, and assorted body aches and pains that persisted for more than 18 months. The aches and pains brought them to the attention of Dr. Moldofsky, then director of the Centre for the Study of Pain at the University of Toronto.
His primary interest at the time was fibromyalgia, which caused symptoms similar to those reported by the original SARS long-haulers. Intrigued, Dr. Moldofsky agreed to take a look. Their chest x-rays were clear and the nurses showed no signs of lingering viral infection. Dr. Moldofsky could see that the nurses were ill and suffering, but no lab tests or anything else could identify what was causing their symptoms.
In 2011, Dr. Moldofsky and Dr. Patcai found a strong overlap between chronic SARS, fibromyalgia, and chronic fatigue syndrome when they compared 22 patients with long-term SARS issues with 21 who had fibromyalgia. “Their problems are exactly the same. They have strange symptoms and nobody can figure out what they’re about. And these symptoms are aches and pains, and they have trouble thinking and concentrating,” Dr. Moldofsky said. Reports of COVID-19 long-haulers didn’t surprise Dr. Moldofsky, and he immediately recognized that Nath’s intention to follow these patients could provide insights into both fibromyalgia and chronic fatigue syndrome.
That’s exactly what Dr. Nath is proposing with the two NIH studies. One will focus solely on the neurologic impacts of COVID-19, including stroke, loss of taste and smell, and brain fog. The other will bring patients who have had COVID-19 symptoms for at least 6 months to the NIH Clinical Center for an inpatient stay during which they will undergo detailed physiologic tests.
Scientists around the world are launching their own post–COVID-19 studies. Dr. Moreau’s group in Montreal has laid the groundwork for such an endeavor, and the CoroNerve group in the United Kingdom is monitoring neurologic complications from the coronavirus. Many of them have the same goals as the NIH studies: Leverage the large number of COVID-19 long-haulers to better understand the earliest stages of postviral syndrome.
“At this juncture, after all the reports that we’ve seen so far, I think it’s very unlikely that there will be no relationship whatsoever between COVID-19 and chronic fatigue syndrome,” Dr. Hornig said. “I think there certainly will be some, but again, what’s the scope, what’s the size? And then, of course, even more importantly, if it is happening, what is the mechanism and how is it happening?”
For people like Ms. Gage-Witvliet, the answers can’t come soon enough. For the first time in more than a decade, the full-time professor of epidemiology didn’t prepare to teach this year because she simply can’t. It’s too taxing for her brain to deal with impromptu student questions. Ms. Gage-Witvliet hopes that, by sharing her own experiences with post COVID-19, she can help others.
“In my work, I use data to give a voice to people who don’t have a voice,” she said. “Now, I am one of those people.”
A version of this article first appeared on Medscape.com.
When Margot Gage-Witvliet began feeling run down after her family returned from a trip to the Netherlands in late February 2020, she initially chalked up her symptoms to jet lag. Three days later, however, her situation went from concerning to alarming as she struggled to breathe. “It felt like there was an elephant sitting on my chest,” she said.
Her husband and daughters also became ill with COVID-19, but Ms. Gage-Witvliet was the only one in her family who didn’t get better. After an early improvement, a rare coronavirus-induced tonic-clonic seizure in early April sent her spiraling back down. Ms. Gage-Witvliet spent the next several weeks in bed with the curtains drawn, unable to tolerate light or sound.
Today, Ms. Gage-Witvliet’s life looks nothing like it did 6 months ago when she first got sick. As one of COVID-19’s so called long-haulers, she continues to struggle with crushing fatigue, brain fog, and headaches – symptoms that worsen when she pushes herself to do more. Across the country, as many as 1 in 10 COVID-19 patients are reporting illnesses that continue for weeks and months after their initial diagnosis. Nearly all report neurologic issues like Ms. Gage-Witvliet, as well as shortness of breath and psychiatric concerns.
For Avindra Nath, MD, a neurologist at the National Institutes of Health, the experience of these long-haul COVID-19 patients feels familiar and reminds him of myalgic encephalomyelitis, also known as chronic fatigue syndrome.
Dr. Nath has long been interested in the lingering neurologic issues connected to chronic fatigue. An estimated three-quarters of all patients with chronic fatigue syndrome report that their symptoms started after a viral infection, and they suffer unrelenting exhaustion, difficulties regulating pulse and blood pressure, aches and pains, and brain fog. When Dr. Nath first read about the novel coronavirus, he began to worry that the virus would trigger symptoms in a subset of those infected. Hearing about the experiences of long-haulers like Ms. Gage-Witvliet raised his suspicions even more.
Unlike COVID-19 long-haulers, however, many patients with chronic fatigue syndrome go at least a year with these symptoms before receiving a diagnosis, according to a British survey. That means researchers have had few opportunities to study the early stages of the syndrome. “When we see patients with myalgic encephalomyelitis, whatever infection they might have had occurred in the remote past, so there’s no way for us to know how they got infected with it, what the infection was, or what the effects of it were in that early phase. We’re seeing them 2 years afterward,” Dr. Nath said.
Dr. Nath quickly realized that studying patients like Ms. Gage-Witvliet would give physicians and scientists a unique opportunity to understand not only long-term outcomes of COVID-19 infections, but also other postviral syndromes, including chronic fatigue syndrome at their earliest stages. It’s why Dr. Nath has spent the past several months scrambling to launch two NIH studies to examine the phenomenon.
Although Dr. Nath said that the parallels between COVID-19 long-haulers and those with chronic fatigue syndrome are obvious, he cautions against assuming that they are the same phenomenon. Some long-haulers might simply be taking a much slower path to recovery, or they might have a condition that looks similar on the surface but differs from chronic fatigue syndrome on a molecular level. But even if Dr. Nath fails to see links to chronic fatigue syndrome, with more than 92.5 million documented cases of COVID-19 around the world, the work will be relevant to the substantial number of infected individuals who don’t recover quickly.
“With so many people having exposure to the same virus over a similar time period, we really have the opportunity to look at these manifestations and at the very least to understand postviral syndromes,” said Mady Hornig, MD, a psychiatrist at Columbia University, New York.
The origins of chronic fatigue syndrome date back to 1985, when the Centers for Disease Control and Prevention received a request from two physicians – Paul Cheney, MD, and Daniel Peterson, MD – to investigate a mysterious disease outbreak in Nevada. In November 1984, residents in and around the idyllic vacation spot of Incline Village, a small town tucked into the north shore of Lake Tahoe, had begun reporting flu-like symptoms that persisted for weeks, even months. The doctors had searched high and low for a cause, but they couldn’t figure out what was making their patients sick.
They reported a range of symptoms – including muscle aches and pains, low-grade fevers, sore throats, and headaches – but everyone said that crippling fatigue was the most debilitating issue. This wasn’t the kind of fatigue that could be cured by a nap or even a long holiday. No matter how much their patients slept – and some were almost completely bedbound – their fatigue didn’t abate. What’s more, the fatigue got worse whenever they tried to push themselves to do more. Puzzled, the CDC sent two epidemic intelligence service (EIS) officers to try to get to the bottom of what might be happening.
Muscle aches and pains with crippling fatigue
After their visit to Incline Village, however, the CDC was just as perplexed as Dr. Cheney and Dr. Peterson. Many of the people with the condition reported flu-like symptoms right around the time they first got sick, and the physicians’ leading hypothesis was that the outbreak and its lasting symptoms were caused by chronic Epstein-Barr virus infection. But neither the CDC nor anyone else could identify the infection or any other microbial cause. The two EIS officers duly wrote up a report for the CDC’s flagship publication, Morbidity and Mortality Weekly ReportI, titled “Chronic Fatigue Possibly Related to Epstein-Barr Virus – Nevada”.
That investigators focused on the fatigue aspect made sense, says Leonard A. Jason, PhD, professor of psychology at DePaul University and director of the Center for Community Research, both in Chicago, because it was one of the few symptoms shared by all the individuals studied and it was also the most debilitating. But that focus – and the name “chronic fatigue syndrome” – led to broad public dismissal of the condition’s severity, as did an editorial note in MMWR urging physicians to look for “more definable, and possibly treatable, conditions.” Subsequent research failed to confirm a specific link to the Epstein-Barr virus, which only added to the condition’s phony reputation. Rather than being considered a potentially disabling illness, it was disregarded as a “yuppie flu” or a fancy name for malingering.
“It’s not a surprise that patients are being dismissed because there’s already this sort of grandfathered-in sense that fatigue is not real,” said Jennifer Frankovich, MD, a pediatric rheumatologist at Stanford (Calif.) University’s Lucile Packard Children’s Hospital in Palo Alto. “I’m sure that’s frustrating for them to be tired and then to have the clinician not believe them or dismiss them or think they’re making it up. It would be more helpful to the families to say: ‘You know what, we don’t know, we do not have the answer, and we believe you.’ ”
A syndrome’s shame
As time passed, patient advocacy groups began pushing back against the negative way the condition was being perceived. This criticism came as organizations like the CDC worked to develop a set of diagnostic criteria that researchers and clinicians dealing with chronic fatigue syndrome could use. With such a heterogeneous group of patients and symptoms, the task was no small challenge. The discussions, which took place over nearly 2 decades, played a key role in helping scientists home in on the single factor that was central to chronic fatigue: postexertional malaise.
“This is quite unique for chronic fatigue syndrome. With other diseases, yes, you may have fatigue as one of the components of the disease, but postexertional fatigue is very specific,” said Alain Moreau, PhD, a molecular biologist at the University of Montreal.
Of course, plenty of people have pushed themselves too hard physically and paid the price the next day. But those with chronic fatigue syndrome weren’t running marathons. To them, exertion could be anything from getting the mail to reading a book. Nor could the resulting exhaustion be resolved by an afternoon on the couch or a long vacation.
“If they do these activities, they can crash for weeks, even months,” Dr. Moreau said. It was deep, persistent, and – for 40% of those with chronic fatigue syndrome – disabling. In 2015, a study group from the Institute of Medicine proposed renaming chronic fatigue to “systemic exercise intolerance disease” because of the centrality of this symptom. Although that effort mostly stalled, their report did bring the condition out of its historic place as a scientific backwater. What resulted was an uptick in research on chronic fatigue syndrome, which helped define some of the physiological issues that either contribute to or result from the condition.
Researchers had long known about the link between infection and fatigue, said Dr. Frankovich. Work included mysterious outbreaks like the one in Lake Tahoe and well-documented issues like the wave of encephalitis lethargica (a condition that leaves patients in an almost vegetative state) that followed the 1918 H1N1 influenza pandemic.
“As a clinician, when you see someone who comes in with a chronic infection, they’re tired. I think that’s why, in the chronic-fatigue world, people are desperately looking for the infection so we can treat it, and maybe these poor suffering people will feel better,” Dr. Frankovich added. Then the pandemic struck, giving him yet another opportunity to study postviral syndromes.
Immunologic symptoms
Given the close link between a nonspecific viral illness and the onset of symptoms in chronic fatigue syndrome, scientists like Dr. Hornig opted to focus on immunologic symptoms. In a 2015 analysis published in Science, Dr. Hornig and colleagues showed that immune problems can be found in the earliest stages of chronic fatigue syndrome, and that they change as the illness progresses. Patients who had been sick for less than 3 years showed significant increases in levels of both pro- and anti-inflammatory cytokines, and the factor most strongly correlated to this inability to regulate cytokine levels was the duration of symptoms, not their severity. A series of other studies also revealed problems with regulation of the immune system, although no one could show what might have set these problems in motion.
Other researchers found signs of mitochondrial dysfunction in those with chronic fatigue syndrome. Because mitochondria make energy for cells, it wasn’t an intellectual stretch to believe that glitches in this process could contribute to fatigue. As early as 1991, scientists had discovered signs of mitochondrial degeneration in muscle biopsies from people with chronic fatigue syndrome. Subsequent studies showed that those affected by chronic fatigue were missing segments of mitochondrial DNA and had significantly reduced levels of mitochondrial activity. Although exercise normally improves mitochondrial functioning, the opposite appears to happen in chronic fatigue.
To Dr. Nath, these dual hypotheses aren’t necessarily mutually exclusive. Some studies have hinted that infection with the common human herpesvirus–6 (HHV-6) can lead to an autoimmune condition in which the body makes antibodies against the mitochondria. Mitochondria also play a key role in the ability of the innate immune system to produce interferon and other proinflammatory cytokines. It might also be that the link between immune and mitochondrial problems is more convoluted than originally thought, or that the two systems are affected independent of one another, Dr. Nath said.
Finding answers, especially those that could lead to potential treatments, wouldn’t be easy, however. In 2016, the NIH launched an in-depth study of a small number of individuals with chronic fatigue, hoping to find clues about what the condition was and how it might be treated.
For scientists like Dr. Nath, the NIH study provided a way to get at the underlying biology of chronic fatigue syndrome. Then the pandemic struck, giving him yet another opportunity to study postviral syndromes.
Chronic post-SARS syndrome
In March 2020, retired physician Harvey Moldofsky, MD, began receiving inquiries about a 2011 study he and his colleague, John Patcai, MD, had published in BMC Neurology about something they dubbed “chronic post-SARS syndrome.” The small case-control study, which involved mainly health care workers in Toronto, received little attention when it was first published, but with COVID-19, it was suddenly relevant.
Early clusters of similar cases in Miami made local physicians desperate for Dr. Moldofsky’s expertise. Luckily, he was nearby; he had fled the frigid Canadian winter for the warmth of Sarasota, Fla.
“I had people from various countries around the world writing to me and asking what they should do. And of course I don’t have any answers,” he said. But the study contained one of the world’s only references to the syndrome.
In 2003, a woman arrived in Toronto from Hong Kong. She didn’t know it at the time, but her preairport stay at the Hotel Metropole had infected her with the first SARS (severe acute respiratory syndrome) coronavirus. Her subsequent hospitalization in Toronto sparked a city-wide outbreak of SARS in which 273 people became ill and 44 died. Many of those affected were health care workers, including nurses and respiratory therapists. Although most eventually returned to work, a subset couldn’t. They complained of energy-sapping fatigue, poor sleep, brain fog, and assorted body aches and pains that persisted for more than 18 months. The aches and pains brought them to the attention of Dr. Moldofsky, then director of the Centre for the Study of Pain at the University of Toronto.
His primary interest at the time was fibromyalgia, which caused symptoms similar to those reported by the original SARS long-haulers. Intrigued, Dr. Moldofsky agreed to take a look. Their chest x-rays were clear and the nurses showed no signs of lingering viral infection. Dr. Moldofsky could see that the nurses were ill and suffering, but no lab tests or anything else could identify what was causing their symptoms.
In 2011, Dr. Moldofsky and Dr. Patcai found a strong overlap between chronic SARS, fibromyalgia, and chronic fatigue syndrome when they compared 22 patients with long-term SARS issues with 21 who had fibromyalgia. “Their problems are exactly the same. They have strange symptoms and nobody can figure out what they’re about. And these symptoms are aches and pains, and they have trouble thinking and concentrating,” Dr. Moldofsky said. Reports of COVID-19 long-haulers didn’t surprise Dr. Moldofsky, and he immediately recognized that Nath’s intention to follow these patients could provide insights into both fibromyalgia and chronic fatigue syndrome.
That’s exactly what Dr. Nath is proposing with the two NIH studies. One will focus solely on the neurologic impacts of COVID-19, including stroke, loss of taste and smell, and brain fog. The other will bring patients who have had COVID-19 symptoms for at least 6 months to the NIH Clinical Center for an inpatient stay during which they will undergo detailed physiologic tests.
Scientists around the world are launching their own post–COVID-19 studies. Dr. Moreau’s group in Montreal has laid the groundwork for such an endeavor, and the CoroNerve group in the United Kingdom is monitoring neurologic complications from the coronavirus. Many of them have the same goals as the NIH studies: Leverage the large number of COVID-19 long-haulers to better understand the earliest stages of postviral syndrome.
“At this juncture, after all the reports that we’ve seen so far, I think it’s very unlikely that there will be no relationship whatsoever between COVID-19 and chronic fatigue syndrome,” Dr. Hornig said. “I think there certainly will be some, but again, what’s the scope, what’s the size? And then, of course, even more importantly, if it is happening, what is the mechanism and how is it happening?”
For people like Ms. Gage-Witvliet, the answers can’t come soon enough. For the first time in more than a decade, the full-time professor of epidemiology didn’t prepare to teach this year because she simply can’t. It’s too taxing for her brain to deal with impromptu student questions. Ms. Gage-Witvliet hopes that, by sharing her own experiences with post COVID-19, she can help others.
“In my work, I use data to give a voice to people who don’t have a voice,” she said. “Now, I am one of those people.”
A version of this article first appeared on Medscape.com.
U.S. hits 20 million cases as COVID variant spreads
The United States started 2021 they way it ended 2020: Setting new records amidst the coronavirus pandemic.
The country passed the 20 million mark for coronavirus cases on Friday, setting the mark sometime around noon, according to Johns Hopkins University’s COVID-19 tracker. The total is nearly twice as many as the next worst country – India, which has 10.28 million cases.
Along with the case count, more than 346,000 Americans have now died of COVID-19, the disease caused by the coronavirus. That is 77% more fatalities than Brazil, which ranks second globally with 194,949 deaths.
More than 125,370 coronavirus patients were hospitalized on Thursday, the fourth record-setting day in a row, according to the COVID Tracking Project.
Going by official tallies, it took 292 days for the United States to reach its first 10 million cases, and just 54 more days to double it, CNN reported.
Meanwhile, 12.41 million doses of COVID-19 vaccines have been distributed in the United States as of Wednesday, according to the Centers for Disease Control and Prevention. Yet only 2.8 million people have received the first of a two-shot regimen.
The slower-than-hoped-for rollout of the Pfizer and Moderna vaccines comes as a new variant of the coronavirus has emerged in a third state. Florida officials announced a confirmed case of the new variant – believed to have originated in the United Kingdom – in Martin County in southeast Florida.
The state health department said on Twitter that the patient is a man in his 20s with no history of travel. The department said it is working with the CDC to investigate.
The variant has also been confirmed in cases in Colorado and California. It is believed to be more contagious. The BBC reported that the new variant increases the reproduction, or “R number,” by 0.4 and 0.7. The UK’s most recent R number has been estimated at 1.1-1.3, meaning anyone who has the coronavirus could be assumed to spread it to up to 1.3 people.
The R number needs to be below 1.0 for the spread of the virus to fall.
“There is a huge difference in how easily the variant virus spreads,” Professor Axel Gandy of London’s Imperial College told BBC News. “This is the most serious change in the virus since the epidemic began.”
A version of this article first appeared on WebMD.com.
The United States started 2021 they way it ended 2020: Setting new records amidst the coronavirus pandemic.
The country passed the 20 million mark for coronavirus cases on Friday, setting the mark sometime around noon, according to Johns Hopkins University’s COVID-19 tracker. The total is nearly twice as many as the next worst country – India, which has 10.28 million cases.
Along with the case count, more than 346,000 Americans have now died of COVID-19, the disease caused by the coronavirus. That is 77% more fatalities than Brazil, which ranks second globally with 194,949 deaths.
More than 125,370 coronavirus patients were hospitalized on Thursday, the fourth record-setting day in a row, according to the COVID Tracking Project.
Going by official tallies, it took 292 days for the United States to reach its first 10 million cases, and just 54 more days to double it, CNN reported.
Meanwhile, 12.41 million doses of COVID-19 vaccines have been distributed in the United States as of Wednesday, according to the Centers for Disease Control and Prevention. Yet only 2.8 million people have received the first of a two-shot regimen.
The slower-than-hoped-for rollout of the Pfizer and Moderna vaccines comes as a new variant of the coronavirus has emerged in a third state. Florida officials announced a confirmed case of the new variant – believed to have originated in the United Kingdom – in Martin County in southeast Florida.
The state health department said on Twitter that the patient is a man in his 20s with no history of travel. The department said it is working with the CDC to investigate.
The variant has also been confirmed in cases in Colorado and California. It is believed to be more contagious. The BBC reported that the new variant increases the reproduction, or “R number,” by 0.4 and 0.7. The UK’s most recent R number has been estimated at 1.1-1.3, meaning anyone who has the coronavirus could be assumed to spread it to up to 1.3 people.
The R number needs to be below 1.0 for the spread of the virus to fall.
“There is a huge difference in how easily the variant virus spreads,” Professor Axel Gandy of London’s Imperial College told BBC News. “This is the most serious change in the virus since the epidemic began.”
A version of this article first appeared on WebMD.com.
The United States started 2021 they way it ended 2020: Setting new records amidst the coronavirus pandemic.
The country passed the 20 million mark for coronavirus cases on Friday, setting the mark sometime around noon, according to Johns Hopkins University’s COVID-19 tracker. The total is nearly twice as many as the next worst country – India, which has 10.28 million cases.
Along with the case count, more than 346,000 Americans have now died of COVID-19, the disease caused by the coronavirus. That is 77% more fatalities than Brazil, which ranks second globally with 194,949 deaths.
More than 125,370 coronavirus patients were hospitalized on Thursday, the fourth record-setting day in a row, according to the COVID Tracking Project.
Going by official tallies, it took 292 days for the United States to reach its first 10 million cases, and just 54 more days to double it, CNN reported.
Meanwhile, 12.41 million doses of COVID-19 vaccines have been distributed in the United States as of Wednesday, according to the Centers for Disease Control and Prevention. Yet only 2.8 million people have received the first of a two-shot regimen.
The slower-than-hoped-for rollout of the Pfizer and Moderna vaccines comes as a new variant of the coronavirus has emerged in a third state. Florida officials announced a confirmed case of the new variant – believed to have originated in the United Kingdom – in Martin County in southeast Florida.
The state health department said on Twitter that the patient is a man in his 20s with no history of travel. The department said it is working with the CDC to investigate.
The variant has also been confirmed in cases in Colorado and California. It is believed to be more contagious. The BBC reported that the new variant increases the reproduction, or “R number,” by 0.4 and 0.7. The UK’s most recent R number has been estimated at 1.1-1.3, meaning anyone who has the coronavirus could be assumed to spread it to up to 1.3 people.
The R number needs to be below 1.0 for the spread of the virus to fall.
“There is a huge difference in how easily the variant virus spreads,” Professor Axel Gandy of London’s Imperial College told BBC News. “This is the most serious change in the virus since the epidemic began.”
A version of this article first appeared on WebMD.com.
Does daily inhaler monitoring improve asthma outcomes in children?
Among children with moderate or severe persistent asthma, a randomized trial suggests.
But the intervention also may lead to more ED visits and increased hospitalization rates.
“We improved asthma symptom control but did not reduce health care use,” Ruchi S. Gupta, MD, MPH, and colleagues, wrote in a study published in Pediatrics.
The monitoring system alerted clinicians when a patient used a short-acting beta-agonist more than four times in a day. It could be that the “alerts enabled providers to detect asthma exacerbation virtually and refer for clinically appropriate care that included directing children to the ED,” the authors suggested. It also is possible that the intervention led caregivers to be more vigilant about symptoms and more empowered to seek care.
Adherence to preventive regimens
Many patients with asthma need to use preventive medications such as daily inhaled corticosteroids to control symptoms. Researchers have developed sensor-based inhaler monitoring interventions to improve treatment adherence, but the effectiveness of these interventions in improving asthma outcomes in urban and minority populations is unclear.
To assess the effectiveness of a clinically integrated, sensor-based inhaler monitoring intervention on improving asthma symptom control and related outcomes in children, Dr. Gupta, of Northwestern University and Ann & Robert H. Lurie Children’s Hospital of Chicago, and colleagues conducted a randomized, unblinded study, known as the Improving Technology-Assisted Recording of Asthma Control in Children (iTRACC) trial. They included 252 children: 127 in the control group and 125 in the intervention group.
Patients in the intervention group received Propeller Health’s Food and Drug Administration–cleared inhaler sensors for inhaled corticosteroids and short-acting beta-agonists. Caregivers could use a mobile application and clinicians could use a Web portal to track patients’ medication use. The app featured personalized insights, educational content, encouragement, surveys, and care team services.
Researchers recruited caregivers and children from five Chicago clinics for the study, which was conducted between 2016 and 2018. They included children aged 4-17 years who had a prescription for daily inhaled corticosteroids for at least 1 year before enrollment. In addition, participants had at least 1 exacerbation requiring oral corticosteroids in the previous year. They excluded children with other respiratory conditions. They also excluded participants who did not speak English because the app was available only in English.
“Sensors monitored inhaled medication use, capturing the date, time, and number of uses, and transmitted this information via Bluetooth to a paired smartphone and the provider portal in real-time,” the authors said.
Clinicians were alerted to call participants if a patient missed inhaled corticosteroid doses for 4 continuous days or used more than 4 short-acting beta-agonist doses per day. Clinicians could help guide asthma management, schedule an appointment, refill medications, and address technical difficulties with the sensors.
The intervention and control groups had similar baseline characteristics. About one-third of the patients were female, and the mean age was 9.3 years. In the control group, 28% identified as Hispanic, and 33% identified as non-Hispanic Black. In the intervention group, 40% identified as Hispanic, and 23% identified as non-Hispanic Black. About 59% reported Medicaid insurance. The intervention and control arms completed electronic surveys at 1, 3, 6, 9, and 12 months.
Average Asthma Control Test score increased from 19 to 22 in the intervention group, compared with an increase from 19 to 20 in the control group. Adjusted rates of emergency department visits and hospitalizations were greater in the intervention group (incidence rate ratios, 2.2 and 3.4, respectively). A measure of caregiver quality of life was greater in the intervention group, although the difference was not significant.
During the trial, more caregivers in the intervention group reported asthma attacks for which steroids were prescribed by a medical office (73% vs. 35%).
Some participants had to manually enter the number of daily puffs into the app because their inhalers were incompatible with the sensors. In addition, some data were missing because of incomplete or missing survey responses and sensor failure over time. “The number of intervention participants with actively transmitting sensors decreased from 102 at baseline to 56 at 12 months,” Dr. Gupta and associates noted.
Important area of research
“One interesting finding of this study is the increase in health care use in the intervention group to nearly twice as many emergency department (ED) visits and three times as many hospitalizations as the control group over 12 months,” Rachelle R. Ramsey, PhD, and Theresa W. Guilbert, MD, MS, of the University of Cincinnati, wrote in a related commentary. “Although it is plausible that, as the authors suggest, greater asthma knowledge and monitoring may have led to increased vigilance of asthma symptoms, it seems that this would have only led to an increase in ED visits but not hospitalizations.”
The mixture of objective electronic monitoring and subjective self-reported adherence may complicate interpretation of the results, they added.
“Overall, this article underscores the feasibility and importance of sensor-based electronic monitoring of adherence in pediatric asthma and encourages future research in this area,” Dr. Ramsey and Dr. Guilbert said.
The trial was supported by the UnitedHealth Group. Dr. Gupta has received grants from the National Institutes of Health, Rho, and other organizations, and has served as a medical consultant and adviser for a variety of companies. Dr. Ramsey is supported by the NIH. Dr. Guilbert reported fees from the American Board of Pediatrics, the Pediatric Pulmonary Subboard, and some pharmaceutical companies, plus grants from the NIH, grants and personal fees from Sanofi, Regeneron, and AstraZeneca, and royalties from UpToDate.
SOURCE: Gupta RS et al. Pediatrics. 2020 Dec 22. doi: 10.1542/peds.2020-1330.
Among children with moderate or severe persistent asthma, a randomized trial suggests.
But the intervention also may lead to more ED visits and increased hospitalization rates.
“We improved asthma symptom control but did not reduce health care use,” Ruchi S. Gupta, MD, MPH, and colleagues, wrote in a study published in Pediatrics.
The monitoring system alerted clinicians when a patient used a short-acting beta-agonist more than four times in a day. It could be that the “alerts enabled providers to detect asthma exacerbation virtually and refer for clinically appropriate care that included directing children to the ED,” the authors suggested. It also is possible that the intervention led caregivers to be more vigilant about symptoms and more empowered to seek care.
Adherence to preventive regimens
Many patients with asthma need to use preventive medications such as daily inhaled corticosteroids to control symptoms. Researchers have developed sensor-based inhaler monitoring interventions to improve treatment adherence, but the effectiveness of these interventions in improving asthma outcomes in urban and minority populations is unclear.
To assess the effectiveness of a clinically integrated, sensor-based inhaler monitoring intervention on improving asthma symptom control and related outcomes in children, Dr. Gupta, of Northwestern University and Ann & Robert H. Lurie Children’s Hospital of Chicago, and colleagues conducted a randomized, unblinded study, known as the Improving Technology-Assisted Recording of Asthma Control in Children (iTRACC) trial. They included 252 children: 127 in the control group and 125 in the intervention group.
Patients in the intervention group received Propeller Health’s Food and Drug Administration–cleared inhaler sensors for inhaled corticosteroids and short-acting beta-agonists. Caregivers could use a mobile application and clinicians could use a Web portal to track patients’ medication use. The app featured personalized insights, educational content, encouragement, surveys, and care team services.
Researchers recruited caregivers and children from five Chicago clinics for the study, which was conducted between 2016 and 2018. They included children aged 4-17 years who had a prescription for daily inhaled corticosteroids for at least 1 year before enrollment. In addition, participants had at least 1 exacerbation requiring oral corticosteroids in the previous year. They excluded children with other respiratory conditions. They also excluded participants who did not speak English because the app was available only in English.
“Sensors monitored inhaled medication use, capturing the date, time, and number of uses, and transmitted this information via Bluetooth to a paired smartphone and the provider portal in real-time,” the authors said.
Clinicians were alerted to call participants if a patient missed inhaled corticosteroid doses for 4 continuous days or used more than 4 short-acting beta-agonist doses per day. Clinicians could help guide asthma management, schedule an appointment, refill medications, and address technical difficulties with the sensors.
The intervention and control groups had similar baseline characteristics. About one-third of the patients were female, and the mean age was 9.3 years. In the control group, 28% identified as Hispanic, and 33% identified as non-Hispanic Black. In the intervention group, 40% identified as Hispanic, and 23% identified as non-Hispanic Black. About 59% reported Medicaid insurance. The intervention and control arms completed electronic surveys at 1, 3, 6, 9, and 12 months.
Average Asthma Control Test score increased from 19 to 22 in the intervention group, compared with an increase from 19 to 20 in the control group. Adjusted rates of emergency department visits and hospitalizations were greater in the intervention group (incidence rate ratios, 2.2 and 3.4, respectively). A measure of caregiver quality of life was greater in the intervention group, although the difference was not significant.
During the trial, more caregivers in the intervention group reported asthma attacks for which steroids were prescribed by a medical office (73% vs. 35%).
Some participants had to manually enter the number of daily puffs into the app because their inhalers were incompatible with the sensors. In addition, some data were missing because of incomplete or missing survey responses and sensor failure over time. “The number of intervention participants with actively transmitting sensors decreased from 102 at baseline to 56 at 12 months,” Dr. Gupta and associates noted.
Important area of research
“One interesting finding of this study is the increase in health care use in the intervention group to nearly twice as many emergency department (ED) visits and three times as many hospitalizations as the control group over 12 months,” Rachelle R. Ramsey, PhD, and Theresa W. Guilbert, MD, MS, of the University of Cincinnati, wrote in a related commentary. “Although it is plausible that, as the authors suggest, greater asthma knowledge and monitoring may have led to increased vigilance of asthma symptoms, it seems that this would have only led to an increase in ED visits but not hospitalizations.”
The mixture of objective electronic monitoring and subjective self-reported adherence may complicate interpretation of the results, they added.
“Overall, this article underscores the feasibility and importance of sensor-based electronic monitoring of adherence in pediatric asthma and encourages future research in this area,” Dr. Ramsey and Dr. Guilbert said.
The trial was supported by the UnitedHealth Group. Dr. Gupta has received grants from the National Institutes of Health, Rho, and other organizations, and has served as a medical consultant and adviser for a variety of companies. Dr. Ramsey is supported by the NIH. Dr. Guilbert reported fees from the American Board of Pediatrics, the Pediatric Pulmonary Subboard, and some pharmaceutical companies, plus grants from the NIH, grants and personal fees from Sanofi, Regeneron, and AstraZeneca, and royalties from UpToDate.
SOURCE: Gupta RS et al. Pediatrics. 2020 Dec 22. doi: 10.1542/peds.2020-1330.
Among children with moderate or severe persistent asthma, a randomized trial suggests.
But the intervention also may lead to more ED visits and increased hospitalization rates.
“We improved asthma symptom control but did not reduce health care use,” Ruchi S. Gupta, MD, MPH, and colleagues, wrote in a study published in Pediatrics.
The monitoring system alerted clinicians when a patient used a short-acting beta-agonist more than four times in a day. It could be that the “alerts enabled providers to detect asthma exacerbation virtually and refer for clinically appropriate care that included directing children to the ED,” the authors suggested. It also is possible that the intervention led caregivers to be more vigilant about symptoms and more empowered to seek care.
Adherence to preventive regimens
Many patients with asthma need to use preventive medications such as daily inhaled corticosteroids to control symptoms. Researchers have developed sensor-based inhaler monitoring interventions to improve treatment adherence, but the effectiveness of these interventions in improving asthma outcomes in urban and minority populations is unclear.
To assess the effectiveness of a clinically integrated, sensor-based inhaler monitoring intervention on improving asthma symptom control and related outcomes in children, Dr. Gupta, of Northwestern University and Ann & Robert H. Lurie Children’s Hospital of Chicago, and colleagues conducted a randomized, unblinded study, known as the Improving Technology-Assisted Recording of Asthma Control in Children (iTRACC) trial. They included 252 children: 127 in the control group and 125 in the intervention group.
Patients in the intervention group received Propeller Health’s Food and Drug Administration–cleared inhaler sensors for inhaled corticosteroids and short-acting beta-agonists. Caregivers could use a mobile application and clinicians could use a Web portal to track patients’ medication use. The app featured personalized insights, educational content, encouragement, surveys, and care team services.
Researchers recruited caregivers and children from five Chicago clinics for the study, which was conducted between 2016 and 2018. They included children aged 4-17 years who had a prescription for daily inhaled corticosteroids for at least 1 year before enrollment. In addition, participants had at least 1 exacerbation requiring oral corticosteroids in the previous year. They excluded children with other respiratory conditions. They also excluded participants who did not speak English because the app was available only in English.
“Sensors monitored inhaled medication use, capturing the date, time, and number of uses, and transmitted this information via Bluetooth to a paired smartphone and the provider portal in real-time,” the authors said.
Clinicians were alerted to call participants if a patient missed inhaled corticosteroid doses for 4 continuous days or used more than 4 short-acting beta-agonist doses per day. Clinicians could help guide asthma management, schedule an appointment, refill medications, and address technical difficulties with the sensors.
The intervention and control groups had similar baseline characteristics. About one-third of the patients were female, and the mean age was 9.3 years. In the control group, 28% identified as Hispanic, and 33% identified as non-Hispanic Black. In the intervention group, 40% identified as Hispanic, and 23% identified as non-Hispanic Black. About 59% reported Medicaid insurance. The intervention and control arms completed electronic surveys at 1, 3, 6, 9, and 12 months.
Average Asthma Control Test score increased from 19 to 22 in the intervention group, compared with an increase from 19 to 20 in the control group. Adjusted rates of emergency department visits and hospitalizations were greater in the intervention group (incidence rate ratios, 2.2 and 3.4, respectively). A measure of caregiver quality of life was greater in the intervention group, although the difference was not significant.
During the trial, more caregivers in the intervention group reported asthma attacks for which steroids were prescribed by a medical office (73% vs. 35%).
Some participants had to manually enter the number of daily puffs into the app because their inhalers were incompatible with the sensors. In addition, some data were missing because of incomplete or missing survey responses and sensor failure over time. “The number of intervention participants with actively transmitting sensors decreased from 102 at baseline to 56 at 12 months,” Dr. Gupta and associates noted.
Important area of research
“One interesting finding of this study is the increase in health care use in the intervention group to nearly twice as many emergency department (ED) visits and three times as many hospitalizations as the control group over 12 months,” Rachelle R. Ramsey, PhD, and Theresa W. Guilbert, MD, MS, of the University of Cincinnati, wrote in a related commentary. “Although it is plausible that, as the authors suggest, greater asthma knowledge and monitoring may have led to increased vigilance of asthma symptoms, it seems that this would have only led to an increase in ED visits but not hospitalizations.”
The mixture of objective electronic monitoring and subjective self-reported adherence may complicate interpretation of the results, they added.
“Overall, this article underscores the feasibility and importance of sensor-based electronic monitoring of adherence in pediatric asthma and encourages future research in this area,” Dr. Ramsey and Dr. Guilbert said.
The trial was supported by the UnitedHealth Group. Dr. Gupta has received grants from the National Institutes of Health, Rho, and other organizations, and has served as a medical consultant and adviser for a variety of companies. Dr. Ramsey is supported by the NIH. Dr. Guilbert reported fees from the American Board of Pediatrics, the Pediatric Pulmonary Subboard, and some pharmaceutical companies, plus grants from the NIH, grants and personal fees from Sanofi, Regeneron, and AstraZeneca, and royalties from UpToDate.
SOURCE: Gupta RS et al. Pediatrics. 2020 Dec 22. doi: 10.1542/peds.2020-1330.
FROM PEDIATRICS
COVID-19–induced drop in first measles vaccinations sparks resurgence concerns
Widespread use of the MMR vaccine is not only crucial for protecting the community against infectious outbreaks, but also serves as the overall pacesetter for preventive services, said Sara M. Bode, MD and colleagues at Nationwide Children’s Hospital in Columbus.
As part of a bivariate logistic regression analysis, Dr. Bode and colleagues sought to evaluate changes in measles vaccination rates across 12 clinic sites of the Nationwide Children’s Hospital pediatric primary care network in Columbus among 23,534 children aged 16 months. The study period targeted the time between April and May 2020, when clinic access and appointment attendance declined following the start of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, until the June-to-August 2020 time period, when clinical care was allowed to return.
The need for the study was prompted by Centers for Disease Control and Prevention reporting on a state-specific precipitous decline in MMR vaccination rates shortly after the onset of COVID-19 in May 2020. Citing the results of one study, such reductions in vaccination have raised concerns over the possibility of a measles resurgence, noted Dr. Bode and associates.
MMR vaccination rates begin to drop with onset of COVID-19 pandemic.
From March 2017 to March 2020, the average rate of MMR vaccination in 16-month-olds was 72%. It subsequently decreased to 67% from April to May 2020, and then dropped further to 62% during the period June to August, 2020 (P = .001). Those without insurance were less likely to be vaccinated than were those carrying private insurance or Medicaid.
Among patients who had not attended a preventive care visit after 12 months of age, the proportion who received vaccines declined during the same time periods, from 10% before the pandemic to 6% at the start of the pandemic and 3% during the summer months of 2020.
“Given the baseline low vaccination rates even before the pandemic and the subsequent decline, we face a critical need to improve timely vaccination and provide catch-up opportunities” in areas with the highest incidence of COVID-19, observed Dr. Bode and colleagues.
Innovative approaches are needed to encourage families to seek preventive care.
In response, the researchers announced the implementation of new community-based vaccination approaches in Ohio, including pop-up vaccine clinics, mobile clinics, and school-based clinics to provide families, who are reluctant to visit health care facilities over COVID-19 related concerns, with safe alternatives. “We believe that it is critical to develop innovative approaches to have families return for preventive care,” they added.
In a separate interview, Herschel Lessin, MD, a private practice pediatrician in Poughkeepsie, N.Y., noted: “This study confirms the anecdotal experience of pediatricians around the country, and our greatest fear that the pandemic will interfere with herd immunity of children for vaccine-preventable illness. Although the study was of urban offices with a primarily Medicaid population, I believe the results to be very worrisome should they prove to be generalizable to the country, as a whole. The significant reduction of well-child visits due to COVID-19 (and fear of COVID-19) seriously impaired the vaccination status of a standard required vaccine in a large population. What is even more worrisome is that the rates continued to fall even after the initial closure of many offices and well into their reopening, despite concerted efforts to try to catch up these missed visits and immunizations.”
Measles is an intensely contagious illness that has not been eradicated, as evidenced by the enormous measles outbreak stemming from Disneyland in 2014-2015, and again with the possible exposure of hundreds to an infected Disneyland visitor last fall, where coverage rates were even higher than in this study, added Dr. Lessin. “This phenomenon, unless forcefully remedied, could easily result in large outbreaks of other vaccine-preventable illness besides COVID-19,” he cautioned.
Dr. Bode and colleagues as well as Dr. Lessin had no conflicts of interest and no relevant financial disclosures.
SOURCE: Bode SM et al. Pediatrics. 2021. doi: 10.1542/peds.2020-035576.
Widespread use of the MMR vaccine is not only crucial for protecting the community against infectious outbreaks, but also serves as the overall pacesetter for preventive services, said Sara M. Bode, MD and colleagues at Nationwide Children’s Hospital in Columbus.
As part of a bivariate logistic regression analysis, Dr. Bode and colleagues sought to evaluate changes in measles vaccination rates across 12 clinic sites of the Nationwide Children’s Hospital pediatric primary care network in Columbus among 23,534 children aged 16 months. The study period targeted the time between April and May 2020, when clinic access and appointment attendance declined following the start of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, until the June-to-August 2020 time period, when clinical care was allowed to return.
The need for the study was prompted by Centers for Disease Control and Prevention reporting on a state-specific precipitous decline in MMR vaccination rates shortly after the onset of COVID-19 in May 2020. Citing the results of one study, such reductions in vaccination have raised concerns over the possibility of a measles resurgence, noted Dr. Bode and associates.
MMR vaccination rates begin to drop with onset of COVID-19 pandemic.
From March 2017 to March 2020, the average rate of MMR vaccination in 16-month-olds was 72%. It subsequently decreased to 67% from April to May 2020, and then dropped further to 62% during the period June to August, 2020 (P = .001). Those without insurance were less likely to be vaccinated than were those carrying private insurance or Medicaid.
Among patients who had not attended a preventive care visit after 12 months of age, the proportion who received vaccines declined during the same time periods, from 10% before the pandemic to 6% at the start of the pandemic and 3% during the summer months of 2020.
“Given the baseline low vaccination rates even before the pandemic and the subsequent decline, we face a critical need to improve timely vaccination and provide catch-up opportunities” in areas with the highest incidence of COVID-19, observed Dr. Bode and colleagues.
Innovative approaches are needed to encourage families to seek preventive care.
In response, the researchers announced the implementation of new community-based vaccination approaches in Ohio, including pop-up vaccine clinics, mobile clinics, and school-based clinics to provide families, who are reluctant to visit health care facilities over COVID-19 related concerns, with safe alternatives. “We believe that it is critical to develop innovative approaches to have families return for preventive care,” they added.
In a separate interview, Herschel Lessin, MD, a private practice pediatrician in Poughkeepsie, N.Y., noted: “This study confirms the anecdotal experience of pediatricians around the country, and our greatest fear that the pandemic will interfere with herd immunity of children for vaccine-preventable illness. Although the study was of urban offices with a primarily Medicaid population, I believe the results to be very worrisome should they prove to be generalizable to the country, as a whole. The significant reduction of well-child visits due to COVID-19 (and fear of COVID-19) seriously impaired the vaccination status of a standard required vaccine in a large population. What is even more worrisome is that the rates continued to fall even after the initial closure of many offices and well into their reopening, despite concerted efforts to try to catch up these missed visits and immunizations.”
Measles is an intensely contagious illness that has not been eradicated, as evidenced by the enormous measles outbreak stemming from Disneyland in 2014-2015, and again with the possible exposure of hundreds to an infected Disneyland visitor last fall, where coverage rates were even higher than in this study, added Dr. Lessin. “This phenomenon, unless forcefully remedied, could easily result in large outbreaks of other vaccine-preventable illness besides COVID-19,” he cautioned.
Dr. Bode and colleagues as well as Dr. Lessin had no conflicts of interest and no relevant financial disclosures.
SOURCE: Bode SM et al. Pediatrics. 2021. doi: 10.1542/peds.2020-035576.
Widespread use of the MMR vaccine is not only crucial for protecting the community against infectious outbreaks, but also serves as the overall pacesetter for preventive services, said Sara M. Bode, MD and colleagues at Nationwide Children’s Hospital in Columbus.
As part of a bivariate logistic regression analysis, Dr. Bode and colleagues sought to evaluate changes in measles vaccination rates across 12 clinic sites of the Nationwide Children’s Hospital pediatric primary care network in Columbus among 23,534 children aged 16 months. The study period targeted the time between April and May 2020, when clinic access and appointment attendance declined following the start of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, until the June-to-August 2020 time period, when clinical care was allowed to return.
The need for the study was prompted by Centers for Disease Control and Prevention reporting on a state-specific precipitous decline in MMR vaccination rates shortly after the onset of COVID-19 in May 2020. Citing the results of one study, such reductions in vaccination have raised concerns over the possibility of a measles resurgence, noted Dr. Bode and associates.
MMR vaccination rates begin to drop with onset of COVID-19 pandemic.
From March 2017 to March 2020, the average rate of MMR vaccination in 16-month-olds was 72%. It subsequently decreased to 67% from April to May 2020, and then dropped further to 62% during the period June to August, 2020 (P = .001). Those without insurance were less likely to be vaccinated than were those carrying private insurance or Medicaid.
Among patients who had not attended a preventive care visit after 12 months of age, the proportion who received vaccines declined during the same time periods, from 10% before the pandemic to 6% at the start of the pandemic and 3% during the summer months of 2020.
“Given the baseline low vaccination rates even before the pandemic and the subsequent decline, we face a critical need to improve timely vaccination and provide catch-up opportunities” in areas with the highest incidence of COVID-19, observed Dr. Bode and colleagues.
Innovative approaches are needed to encourage families to seek preventive care.
In response, the researchers announced the implementation of new community-based vaccination approaches in Ohio, including pop-up vaccine clinics, mobile clinics, and school-based clinics to provide families, who are reluctant to visit health care facilities over COVID-19 related concerns, with safe alternatives. “We believe that it is critical to develop innovative approaches to have families return for preventive care,” they added.
In a separate interview, Herschel Lessin, MD, a private practice pediatrician in Poughkeepsie, N.Y., noted: “This study confirms the anecdotal experience of pediatricians around the country, and our greatest fear that the pandemic will interfere with herd immunity of children for vaccine-preventable illness. Although the study was of urban offices with a primarily Medicaid population, I believe the results to be very worrisome should they prove to be generalizable to the country, as a whole. The significant reduction of well-child visits due to COVID-19 (and fear of COVID-19) seriously impaired the vaccination status of a standard required vaccine in a large population. What is even more worrisome is that the rates continued to fall even after the initial closure of many offices and well into their reopening, despite concerted efforts to try to catch up these missed visits and immunizations.”
Measles is an intensely contagious illness that has not been eradicated, as evidenced by the enormous measles outbreak stemming from Disneyland in 2014-2015, and again with the possible exposure of hundreds to an infected Disneyland visitor last fall, where coverage rates were even higher than in this study, added Dr. Lessin. “This phenomenon, unless forcefully remedied, could easily result in large outbreaks of other vaccine-preventable illness besides COVID-19,” he cautioned.
Dr. Bode and colleagues as well as Dr. Lessin had no conflicts of interest and no relevant financial disclosures.
SOURCE: Bode SM et al. Pediatrics. 2021. doi: 10.1542/peds.2020-035576.
FROM PEDIATRICS
COVID-19 vaccine found effective but doctors watching for reactions, adverse events
The Pfizer COVID-19 vaccine was shown to be highly effective in a large trial, but clinicians will be waiting and watching for reactions and adverse events in their vaccinated patients.
A two-dose regimen of the BNT162b2 mRNA COVID-19 vaccine was found to be safe and 95% effective in preventing SARS-CoV-2 infection in persons aged 16 years and older, according to an ongoing phase 2/3 trial. Pfizer and BioNTech published safety and efficacy results from the landmark global phase 1/2/3 trial of their COVID-19 vaccine candidate in the New England Journal of Medicine .
“We previously reported phase 1 safety and immunogenicity results from clinical trials of the vaccine candidate BNT162b2,” lead author Fernando P. Polack, MD, of Vanderbilt University, Nashville, Tenn., and colleagues wrote. “This data set and [present] trial results are the basis for an application for emergency-use authorization,” they explained.
The BNT162b2 vaccine trial
Among 43,448 individuals aged 16 years and older, the efficacy, safety, and immunogenicity of the BNT162b2 vaccine candidate was evaluated in a continuous phase 1/2/3 study. Participants were randomly assigned (1:1) to receive two injections of either 30 mcg of BNT162b2 (n = 21,720) or saline placebo (n = 21,728) administered intramuscularly 21 days apart. The safety evaluation, where subjects were monitored 30 minutes post vaccination for acute reactions, was observer blinded.
Eligibility criteria included healthy individuals or those with stable chronic medical conditions, including viral hepatitis B and C, as well as human immunodeficiency virus. Persons with a diagnosis of an immunocompromising condition, those receiving immunosuppressive therapy, and individuals with a medical history of COVID-19 were excluded.
The first primary endpoint was efficacy of BNT162b2 against laboratory-confirmed COVID-19 with onset at least 7 days following the second dose. The primary safety endpoint was local and systemic reactions occurring within 7 days post injection of BNT162b2 or placebo.
Safety
“At the data cutoff date of Oct. 9, a total of 37,706 participants had a median of at least 2 months of safety data available after the second dose and contributed to the main safety data set,” the authors wrote.
Among these participants, 83% were White, 28% were Hispanic or Latinx, and 9% were Black or African American; 49% of subjects were female and the median age was 52 years, with 42% over aged 55 years.
Overall, BNT162b2 had a favorable safety profile. Mild to moderate pain at the injection site within 7 days after the injection was the most frequently reported local reaction (<1% across all age groups reported severe pain). Most local reactions resolved within 1-2 days and no grade 4 reactions were reported.
The investigators reported: “Fever (temperature, ≥38° C) was reported after the second dose by 16% of younger vaccine recipients and by 11% of older recipients. Only 0.2% of vaccine recipients and 0.1% of placebo recipients reported fever (temperature, 38.9-40° C) after the first dose, as compared with 0.8% and 0.1%, respectively, after the second dose.”
BNT162b2 recipients had more injection-site pain than those receiving the placebo. After the first and second doses, younger recipients (under 55 years) had more pain at the injection site (83 vs. 14 and 78 vs. 12 events, respectively), redness (5 vs. 1 and 6 vs. 1), and swelling (6 vs. 0 and 6 vs. 0), compared with placebo recipients.
The same trend was observed for patients aged over 55 years, with vaccine recipients reporting more pain at the injection site (71 vs. 9 and 66 vs. 8 events, respectively), redness (5 vs. 1 and 7 vs. 1), and swelling (7 vs. 1 and 7 vs. 1) than placebo recipients.
Pain was less common overall among vaccine recipients aged over 55 years (71% reported pain after the first dose; 66% post second dose) than among younger vaccine recipients (83% post first dose; 78% post second dose).
The most common systemic events following the second dose were fatigue and headache, which occurred in 59% and 52% of younger vaccine recipients and 51% and 39% of older vaccine recipients, respectively. But fatigue and headache were also reported by participants in the placebo group (23% and 24%, respectively, post second dose, among younger vaccine recipients; 17% and 14% among older recipients).
The incidence of serious adverse events was low and similar in the vaccine (0.6%) and placebo (0.5%) arms. Severe systemic events occurred in 2% or less of vaccine recipients following either dose, except for fatigue (3.8%) and headache (2.0%) post second dose. No deaths were considered to be vaccine or placebo related.
“The safety appears comparable to other vaccines, but the relatively short period of observation, 2 months, and the relatively small number of subjects who have received the vaccine (less than 30,000), compared to the hundreds of millions likely to ultimately receive the vaccine, precludes conclusions regarding the potential for rare long term adverse effects,” David L. Bowton, MD, FCCP, a pulmonologist and professor emeritus of critical care anesthesiology at Wake Forest University, Winston-Salem, N.C., said in an interview. “Clinicians should be aware of the risk of anaphylactic reactions and discuss it with their patients [who have] a history of these reactions.”
Efficacy
Among 36,523 subjects without evidence of existing or prior COVID-19 infection, 8 cases of COVID-19 with onset at least 7 days after the second dose were seen among vaccine recipients and 162 among placebo recipients, corresponding to 95.0% vaccine efficacy (95% credible interval, 90.3%-97.6%).
“Supplemental analyses indicated that vaccine efficacy among subgroups defined by age, sex, race, ethnicity, obesity, and presence of a coexisting condition was generally consistent with that observed in the overall population,” the authors wrote.
Between the first and second doses, 39 cases of COVID-19 were observed among BNT162b2 recipients and 82 cases among placebo recipients, corresponding to 52% vaccine efficacy during the 21-day interval (95% CI, 29.5%-68.4%) suggesting early protection may begin as soon as 12 days after the first injection.
“This is an incredible achievement given that an effective vaccine has never been developed and approved for use in such a short timeframe,” Dr. Bowton explained. “That the vaccine is highly effective in reducing the incidence of symptomatic COVID-19 seems incontrovertible.”
“This vaccine has shockingly amazing efficacy and is well tolerated, and the results are beyond even optimistic projections,” Douglas S. Paauw, MD, of the University of Washington, Seattle, said in an interview.
Questions remain
“It is not yet known if the vaccine prevents asymptomatic infections, with their attendant risk of contagion, as rates of seroconversion of trial participants against betacoronavirus nucleoproteins not included in the vaccine has not been reported,” Dr. Bowton commented.
“Common questions our patients will ask us remain unanswered for now, [including] how long will the protection last, is it safe in pregnant women, and does it prevent asymptomatic infection,” Dr. Paauw explained. “We do not know everything about longer term side effects, but the benefits of this vaccine appear to outweigh the risks of the vaccine.”
The researchers noted these and other limitations in their report, acknowledging that longer follow-up is needed to evaluate long-term safety of the vaccine.
This study was supported by BioNTech and Pfizer. Several authors disclosed financial relationships with Pfizer and other pharmaceutical companies outside the submitted work. Dr. Bowton and Dr. Paauw had no conflicts to disclose.
SOURCE: Polack FP et al. N Engl J Med. 2020 Dec 10. doi: 10.1056/NEJMoa2034577
The Pfizer COVID-19 vaccine was shown to be highly effective in a large trial, but clinicians will be waiting and watching for reactions and adverse events in their vaccinated patients.
A two-dose regimen of the BNT162b2 mRNA COVID-19 vaccine was found to be safe and 95% effective in preventing SARS-CoV-2 infection in persons aged 16 years and older, according to an ongoing phase 2/3 trial. Pfizer and BioNTech published safety and efficacy results from the landmark global phase 1/2/3 trial of their COVID-19 vaccine candidate in the New England Journal of Medicine .
“We previously reported phase 1 safety and immunogenicity results from clinical trials of the vaccine candidate BNT162b2,” lead author Fernando P. Polack, MD, of Vanderbilt University, Nashville, Tenn., and colleagues wrote. “This data set and [present] trial results are the basis for an application for emergency-use authorization,” they explained.
The BNT162b2 vaccine trial
Among 43,448 individuals aged 16 years and older, the efficacy, safety, and immunogenicity of the BNT162b2 vaccine candidate was evaluated in a continuous phase 1/2/3 study. Participants were randomly assigned (1:1) to receive two injections of either 30 mcg of BNT162b2 (n = 21,720) or saline placebo (n = 21,728) administered intramuscularly 21 days apart. The safety evaluation, where subjects were monitored 30 minutes post vaccination for acute reactions, was observer blinded.
Eligibility criteria included healthy individuals or those with stable chronic medical conditions, including viral hepatitis B and C, as well as human immunodeficiency virus. Persons with a diagnosis of an immunocompromising condition, those receiving immunosuppressive therapy, and individuals with a medical history of COVID-19 were excluded.
The first primary endpoint was efficacy of BNT162b2 against laboratory-confirmed COVID-19 with onset at least 7 days following the second dose. The primary safety endpoint was local and systemic reactions occurring within 7 days post injection of BNT162b2 or placebo.
Safety
“At the data cutoff date of Oct. 9, a total of 37,706 participants had a median of at least 2 months of safety data available after the second dose and contributed to the main safety data set,” the authors wrote.
Among these participants, 83% were White, 28% were Hispanic or Latinx, and 9% were Black or African American; 49% of subjects were female and the median age was 52 years, with 42% over aged 55 years.
Overall, BNT162b2 had a favorable safety profile. Mild to moderate pain at the injection site within 7 days after the injection was the most frequently reported local reaction (<1% across all age groups reported severe pain). Most local reactions resolved within 1-2 days and no grade 4 reactions were reported.
The investigators reported: “Fever (temperature, ≥38° C) was reported after the second dose by 16% of younger vaccine recipients and by 11% of older recipients. Only 0.2% of vaccine recipients and 0.1% of placebo recipients reported fever (temperature, 38.9-40° C) after the first dose, as compared with 0.8% and 0.1%, respectively, after the second dose.”
BNT162b2 recipients had more injection-site pain than those receiving the placebo. After the first and second doses, younger recipients (under 55 years) had more pain at the injection site (83 vs. 14 and 78 vs. 12 events, respectively), redness (5 vs. 1 and 6 vs. 1), and swelling (6 vs. 0 and 6 vs. 0), compared with placebo recipients.
The same trend was observed for patients aged over 55 years, with vaccine recipients reporting more pain at the injection site (71 vs. 9 and 66 vs. 8 events, respectively), redness (5 vs. 1 and 7 vs. 1), and swelling (7 vs. 1 and 7 vs. 1) than placebo recipients.
Pain was less common overall among vaccine recipients aged over 55 years (71% reported pain after the first dose; 66% post second dose) than among younger vaccine recipients (83% post first dose; 78% post second dose).
The most common systemic events following the second dose were fatigue and headache, which occurred in 59% and 52% of younger vaccine recipients and 51% and 39% of older vaccine recipients, respectively. But fatigue and headache were also reported by participants in the placebo group (23% and 24%, respectively, post second dose, among younger vaccine recipients; 17% and 14% among older recipients).
The incidence of serious adverse events was low and similar in the vaccine (0.6%) and placebo (0.5%) arms. Severe systemic events occurred in 2% or less of vaccine recipients following either dose, except for fatigue (3.8%) and headache (2.0%) post second dose. No deaths were considered to be vaccine or placebo related.
“The safety appears comparable to other vaccines, but the relatively short period of observation, 2 months, and the relatively small number of subjects who have received the vaccine (less than 30,000), compared to the hundreds of millions likely to ultimately receive the vaccine, precludes conclusions regarding the potential for rare long term adverse effects,” David L. Bowton, MD, FCCP, a pulmonologist and professor emeritus of critical care anesthesiology at Wake Forest University, Winston-Salem, N.C., said in an interview. “Clinicians should be aware of the risk of anaphylactic reactions and discuss it with their patients [who have] a history of these reactions.”
Efficacy
Among 36,523 subjects without evidence of existing or prior COVID-19 infection, 8 cases of COVID-19 with onset at least 7 days after the second dose were seen among vaccine recipients and 162 among placebo recipients, corresponding to 95.0% vaccine efficacy (95% credible interval, 90.3%-97.6%).
“Supplemental analyses indicated that vaccine efficacy among subgroups defined by age, sex, race, ethnicity, obesity, and presence of a coexisting condition was generally consistent with that observed in the overall population,” the authors wrote.
Between the first and second doses, 39 cases of COVID-19 were observed among BNT162b2 recipients and 82 cases among placebo recipients, corresponding to 52% vaccine efficacy during the 21-day interval (95% CI, 29.5%-68.4%) suggesting early protection may begin as soon as 12 days after the first injection.
“This is an incredible achievement given that an effective vaccine has never been developed and approved for use in such a short timeframe,” Dr. Bowton explained. “That the vaccine is highly effective in reducing the incidence of symptomatic COVID-19 seems incontrovertible.”
“This vaccine has shockingly amazing efficacy and is well tolerated, and the results are beyond even optimistic projections,” Douglas S. Paauw, MD, of the University of Washington, Seattle, said in an interview.
Questions remain
“It is not yet known if the vaccine prevents asymptomatic infections, with their attendant risk of contagion, as rates of seroconversion of trial participants against betacoronavirus nucleoproteins not included in the vaccine has not been reported,” Dr. Bowton commented.
“Common questions our patients will ask us remain unanswered for now, [including] how long will the protection last, is it safe in pregnant women, and does it prevent asymptomatic infection,” Dr. Paauw explained. “We do not know everything about longer term side effects, but the benefits of this vaccine appear to outweigh the risks of the vaccine.”
The researchers noted these and other limitations in their report, acknowledging that longer follow-up is needed to evaluate long-term safety of the vaccine.
This study was supported by BioNTech and Pfizer. Several authors disclosed financial relationships with Pfizer and other pharmaceutical companies outside the submitted work. Dr. Bowton and Dr. Paauw had no conflicts to disclose.
SOURCE: Polack FP et al. N Engl J Med. 2020 Dec 10. doi: 10.1056/NEJMoa2034577
The Pfizer COVID-19 vaccine was shown to be highly effective in a large trial, but clinicians will be waiting and watching for reactions and adverse events in their vaccinated patients.
A two-dose regimen of the BNT162b2 mRNA COVID-19 vaccine was found to be safe and 95% effective in preventing SARS-CoV-2 infection in persons aged 16 years and older, according to an ongoing phase 2/3 trial. Pfizer and BioNTech published safety and efficacy results from the landmark global phase 1/2/3 trial of their COVID-19 vaccine candidate in the New England Journal of Medicine .
“We previously reported phase 1 safety and immunogenicity results from clinical trials of the vaccine candidate BNT162b2,” lead author Fernando P. Polack, MD, of Vanderbilt University, Nashville, Tenn., and colleagues wrote. “This data set and [present] trial results are the basis for an application for emergency-use authorization,” they explained.
The BNT162b2 vaccine trial
Among 43,448 individuals aged 16 years and older, the efficacy, safety, and immunogenicity of the BNT162b2 vaccine candidate was evaluated in a continuous phase 1/2/3 study. Participants were randomly assigned (1:1) to receive two injections of either 30 mcg of BNT162b2 (n = 21,720) or saline placebo (n = 21,728) administered intramuscularly 21 days apart. The safety evaluation, where subjects were monitored 30 minutes post vaccination for acute reactions, was observer blinded.
Eligibility criteria included healthy individuals or those with stable chronic medical conditions, including viral hepatitis B and C, as well as human immunodeficiency virus. Persons with a diagnosis of an immunocompromising condition, those receiving immunosuppressive therapy, and individuals with a medical history of COVID-19 were excluded.
The first primary endpoint was efficacy of BNT162b2 against laboratory-confirmed COVID-19 with onset at least 7 days following the second dose. The primary safety endpoint was local and systemic reactions occurring within 7 days post injection of BNT162b2 or placebo.
Safety
“At the data cutoff date of Oct. 9, a total of 37,706 participants had a median of at least 2 months of safety data available after the second dose and contributed to the main safety data set,” the authors wrote.
Among these participants, 83% were White, 28% were Hispanic or Latinx, and 9% were Black or African American; 49% of subjects were female and the median age was 52 years, with 42% over aged 55 years.
Overall, BNT162b2 had a favorable safety profile. Mild to moderate pain at the injection site within 7 days after the injection was the most frequently reported local reaction (<1% across all age groups reported severe pain). Most local reactions resolved within 1-2 days and no grade 4 reactions were reported.
The investigators reported: “Fever (temperature, ≥38° C) was reported after the second dose by 16% of younger vaccine recipients and by 11% of older recipients. Only 0.2% of vaccine recipients and 0.1% of placebo recipients reported fever (temperature, 38.9-40° C) after the first dose, as compared with 0.8% and 0.1%, respectively, after the second dose.”
BNT162b2 recipients had more injection-site pain than those receiving the placebo. After the first and second doses, younger recipients (under 55 years) had more pain at the injection site (83 vs. 14 and 78 vs. 12 events, respectively), redness (5 vs. 1 and 6 vs. 1), and swelling (6 vs. 0 and 6 vs. 0), compared with placebo recipients.
The same trend was observed for patients aged over 55 years, with vaccine recipients reporting more pain at the injection site (71 vs. 9 and 66 vs. 8 events, respectively), redness (5 vs. 1 and 7 vs. 1), and swelling (7 vs. 1 and 7 vs. 1) than placebo recipients.
Pain was less common overall among vaccine recipients aged over 55 years (71% reported pain after the first dose; 66% post second dose) than among younger vaccine recipients (83% post first dose; 78% post second dose).
The most common systemic events following the second dose were fatigue and headache, which occurred in 59% and 52% of younger vaccine recipients and 51% and 39% of older vaccine recipients, respectively. But fatigue and headache were also reported by participants in the placebo group (23% and 24%, respectively, post second dose, among younger vaccine recipients; 17% and 14% among older recipients).
The incidence of serious adverse events was low and similar in the vaccine (0.6%) and placebo (0.5%) arms. Severe systemic events occurred in 2% or less of vaccine recipients following either dose, except for fatigue (3.8%) and headache (2.0%) post second dose. No deaths were considered to be vaccine or placebo related.
“The safety appears comparable to other vaccines, but the relatively short period of observation, 2 months, and the relatively small number of subjects who have received the vaccine (less than 30,000), compared to the hundreds of millions likely to ultimately receive the vaccine, precludes conclusions regarding the potential for rare long term adverse effects,” David L. Bowton, MD, FCCP, a pulmonologist and professor emeritus of critical care anesthesiology at Wake Forest University, Winston-Salem, N.C., said in an interview. “Clinicians should be aware of the risk of anaphylactic reactions and discuss it with their patients [who have] a history of these reactions.”
Efficacy
Among 36,523 subjects without evidence of existing or prior COVID-19 infection, 8 cases of COVID-19 with onset at least 7 days after the second dose were seen among vaccine recipients and 162 among placebo recipients, corresponding to 95.0% vaccine efficacy (95% credible interval, 90.3%-97.6%).
“Supplemental analyses indicated that vaccine efficacy among subgroups defined by age, sex, race, ethnicity, obesity, and presence of a coexisting condition was generally consistent with that observed in the overall population,” the authors wrote.
Between the first and second doses, 39 cases of COVID-19 were observed among BNT162b2 recipients and 82 cases among placebo recipients, corresponding to 52% vaccine efficacy during the 21-day interval (95% CI, 29.5%-68.4%) suggesting early protection may begin as soon as 12 days after the first injection.
“This is an incredible achievement given that an effective vaccine has never been developed and approved for use in such a short timeframe,” Dr. Bowton explained. “That the vaccine is highly effective in reducing the incidence of symptomatic COVID-19 seems incontrovertible.”
“This vaccine has shockingly amazing efficacy and is well tolerated, and the results are beyond even optimistic projections,” Douglas S. Paauw, MD, of the University of Washington, Seattle, said in an interview.
Questions remain
“It is not yet known if the vaccine prevents asymptomatic infections, with their attendant risk of contagion, as rates of seroconversion of trial participants against betacoronavirus nucleoproteins not included in the vaccine has not been reported,” Dr. Bowton commented.
“Common questions our patients will ask us remain unanswered for now, [including] how long will the protection last, is it safe in pregnant women, and does it prevent asymptomatic infection,” Dr. Paauw explained. “We do not know everything about longer term side effects, but the benefits of this vaccine appear to outweigh the risks of the vaccine.”
The researchers noted these and other limitations in their report, acknowledging that longer follow-up is needed to evaluate long-term safety of the vaccine.
This study was supported by BioNTech and Pfizer. Several authors disclosed financial relationships with Pfizer and other pharmaceutical companies outside the submitted work. Dr. Bowton and Dr. Paauw had no conflicts to disclose.
SOURCE: Polack FP et al. N Engl J Med. 2020 Dec 10. doi: 10.1056/NEJMoa2034577
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
To vape or not to vape: Is that really a question?
All pediatricians are relieved that the rates of children smoking cigarettes has dropped steadily since 2011. This decline seems to be associated with education on the dangers of cigarettes and fewer parents smoking. Perhaps less modeling of cigarette use in movies (although it increased again from 2010 to 2019) and lawsuits against advertisements targeting children also has helped.
“Whew,” we may have said, “we can relax our efforts to convince children to avoid smoking.” But, as is commonly true in medicine, the next threat was right around the corner – in this case vaping or e-cigarettes, also called vapes, e-hookahs, vape pens, tank systems, mods, and electronic nicotine delivery systems. And the size of the problem is huge – over 20% of high school students report using e-cigarettes – and immediate, as vaping can kill in the short term as well as causing long-term harm.
“E-cigarette, or vaping, product use–associated Lung Injury” – EVALI for short – has killed 68 vapers and hospitalized thousands. EVALI is thought to be caused by a vitamin E acetate additive used when vaping marijuana, particularly from informal sources like friends, family, or in-person or online dealers.
Vaping increases the risk of severe COVID-19 disease
While EVALI deaths dropped in months after being explained, the COVID-19 epidemic is now a much greater threat to vapers. Vaping increases risk of severe COVID-19 disease because of its immediate paralysis of lung cilia. Sharing vape devices and touching one’s lips while using also increase the risk of virus transmission. Vaping and smoking increase the number of ACE2 receptors to which the SARS-CoV-2 virus attaches causing the characteristic cell damage, and suppresses macrophages and neutrophils, resulting in more smokers testing positive, being twice as likely to develop a severe illness and get hospitalized because of pneumonia from COVID-19, and being less likely to recover. Unfortunately, addressing this new threat to the immediate and long-term health of our patients appears to be more complicated than for addressing smoking tobacco. First of all, vaping is much more difficult to detect than smelly cigarettes sending smoke signals from behind the garage or in the school bathrooms. Many, if not most, adults do not recognize the vaping devices when they see them, as many are tiny and some look like computer thumb drives. The aerosol emitted when in use, while containing dangerous toxins, has less odor than tobacco smoke. Vaping equipment and ads have been designed to attract youth, including linking them to sports and music events. Vaping has been advertised as a way to wean off nicotine addiction, a claim that has some scientific evidence in adults, but at a lower dose of nicotine. Warning children about the dangers of marijuana vaping has been made less credible by the rapid expansion of legalization of marijuana around the United States, eliciting “I told you it was fine” reactions from youth. And the person vaping does not know what or how much of the psychoactive components are being delivered into their bodies. One Juul pod, for example, has the equivalent in nicotine of an entire pack of 20 cigarettes. They are highly addictive, especially to the developing brain, such that youth who vape are more likely to become addicted and to smoke cigarettes in the future.
Help from federal regulation has been weak
While all 50 states ban sales to youth, adults can still buy. Food and Drug Administration limitations on kid-friendly ads, and use of sweet, fruity, and mint flavorings that are most preferred by children, apply only to new producers. The FDA does not yet regulate content of vaping solutions.
So we pediatricians are on the front line for this new threat to prevent vaping or convince youth to cut down or quit. The first step in addressing vaping is being knowledgeable about its many known and emerging health risks. It may seem obvious that the dangers of vaping microscopic particles depends on the contents. Water vapor alone is not dangerous; in fact, we prescribe it in nebulizers. Unfortunately, the contents of different vaping products vary and are not well defined in different vape products. The process of using an electric current to vaporize a substance can make it more toxic than the precursor, and teens have little idea about the substances they are inhaling. The psychoactive components vary from nicotine to tetrahydrocannabinol in varying amounts. These have the well known effects of stimulation or a high, but also the potential adverse effects of poor concentration, agitation, and even psychosis. Most e-cigarettes contain nicotine, which is highly addictive and can harm adolescent brain development, which continues into the early- to mid-20s. About two-thirds of Juul users aged 15-24 years did not know that it always contains nicotine, as do 99% of all vape solutions (Centers for Disease Control and Prevention, 2020). Earlier use of nicotine is more highly associated with later addiction to tobacco products that cause lung damage, acid reflux, insulin resistance, harm to the testes, harm to fetuses, cancer, and heart disease.
E-cigarette aerosols also contain dozens of other harmful substances besides nicotine ranging from acetone, propylene glycol, and metals to formaldehyde and ethyl benzene. These same chemicals are part of familiar toxic substances such as antifreeze, paint thinner, and pesticides. These cause ear, eye and throat irritation, and impairments in the cardiovascular system reducing athletic ability – at the least. Some flavorings in vape fluids also are toxic. Even the residual left on furniture and floors is harmful to those coming in contact, including pets.
How to encourage teens not to vaping
Trying to scare youth about health hazards is not generally effective in stopping risk behaviors since adolescence is a time of perceived singularity (it does not apply to me) and even a sense of immortality. Teens also see peers who vape as being unaffected and decide on using based on this small personal sample instead of valid statistics.
But teens do pay some attention to peer models or influencers saying why they do not use. One source of such testimony you can refer to is videos of inspiring athletes, musicians, and other “cool” young adults found on the naturalhigh.org website. You may know other examples of community teens desisting you can reference.
Parent rules, and less so advice, against smoking have been shown to be effective in deterring youth cigarette smoking. Because parents are less aware of vaping and its dangers, another step we can take is educating parents in our practices about vaping, its variable forms, its effects, and dangers, supplying authoritative materials, and advising them to talk with their children. Other steps the American Academy of Pediatrics recommends regarding smoking is for parents to be a role model of not using or try to quit, designate the house and car as smoking free, avoid children viewing smoking in media, tell their children about the side effects, and encourage their children who use to quit. Parents also can encourage schools to teach and have rules about smoking and vaping (e.g., med.stanford.edu/tobaccopreventiontoolkit.html).
Another approach we have been using is to not only screen for all substance use, but also to gather information about the teen’s strengths, activities, and life goals both to enhance rapport and to reference during motivational interviewing as reasons to avoid, reduce, or quit vaping. Motivational interviewing has been shown to help patients make healthier lifestyle choices by nonjudgmentally exploring their pros and cons in a conversation that takes into account readiness to change. This fits well with the stage of developing autonomy when teens want above all to make their own decisions. The cons of using can be discussed as including the effects and side effects of vaping interfering with their favored activities and moving towards their identified goals. Praising abstinence and asking them to show you how they could decline offers to vape are valuable reinforcement you can provide.
Finally, we all know that teens hate being manipulated. Vaping education we provide can make it clear that youth are being tricked by companies – most being large cigarette producers who know the dangers of vaping – into getting addicted so these companies can get rich on their money.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She has no other relevant disclosures. Dr. Howard’s contribution to this publication is as a paid expert to MDedge News. Email her at pdnews@mdedge.com.
All pediatricians are relieved that the rates of children smoking cigarettes has dropped steadily since 2011. This decline seems to be associated with education on the dangers of cigarettes and fewer parents smoking. Perhaps less modeling of cigarette use in movies (although it increased again from 2010 to 2019) and lawsuits against advertisements targeting children also has helped.
“Whew,” we may have said, “we can relax our efforts to convince children to avoid smoking.” But, as is commonly true in medicine, the next threat was right around the corner – in this case vaping or e-cigarettes, also called vapes, e-hookahs, vape pens, tank systems, mods, and electronic nicotine delivery systems. And the size of the problem is huge – over 20% of high school students report using e-cigarettes – and immediate, as vaping can kill in the short term as well as causing long-term harm.
“E-cigarette, or vaping, product use–associated Lung Injury” – EVALI for short – has killed 68 vapers and hospitalized thousands. EVALI is thought to be caused by a vitamin E acetate additive used when vaping marijuana, particularly from informal sources like friends, family, or in-person or online dealers.
Vaping increases the risk of severe COVID-19 disease
While EVALI deaths dropped in months after being explained, the COVID-19 epidemic is now a much greater threat to vapers. Vaping increases risk of severe COVID-19 disease because of its immediate paralysis of lung cilia. Sharing vape devices and touching one’s lips while using also increase the risk of virus transmission. Vaping and smoking increase the number of ACE2 receptors to which the SARS-CoV-2 virus attaches causing the characteristic cell damage, and suppresses macrophages and neutrophils, resulting in more smokers testing positive, being twice as likely to develop a severe illness and get hospitalized because of pneumonia from COVID-19, and being less likely to recover. Unfortunately, addressing this new threat to the immediate and long-term health of our patients appears to be more complicated than for addressing smoking tobacco. First of all, vaping is much more difficult to detect than smelly cigarettes sending smoke signals from behind the garage or in the school bathrooms. Many, if not most, adults do not recognize the vaping devices when they see them, as many are tiny and some look like computer thumb drives. The aerosol emitted when in use, while containing dangerous toxins, has less odor than tobacco smoke. Vaping equipment and ads have been designed to attract youth, including linking them to sports and music events. Vaping has been advertised as a way to wean off nicotine addiction, a claim that has some scientific evidence in adults, but at a lower dose of nicotine. Warning children about the dangers of marijuana vaping has been made less credible by the rapid expansion of legalization of marijuana around the United States, eliciting “I told you it was fine” reactions from youth. And the person vaping does not know what or how much of the psychoactive components are being delivered into their bodies. One Juul pod, for example, has the equivalent in nicotine of an entire pack of 20 cigarettes. They are highly addictive, especially to the developing brain, such that youth who vape are more likely to become addicted and to smoke cigarettes in the future.
Help from federal regulation has been weak
While all 50 states ban sales to youth, adults can still buy. Food and Drug Administration limitations on kid-friendly ads, and use of sweet, fruity, and mint flavorings that are most preferred by children, apply only to new producers. The FDA does not yet regulate content of vaping solutions.
So we pediatricians are on the front line for this new threat to prevent vaping or convince youth to cut down or quit. The first step in addressing vaping is being knowledgeable about its many known and emerging health risks. It may seem obvious that the dangers of vaping microscopic particles depends on the contents. Water vapor alone is not dangerous; in fact, we prescribe it in nebulizers. Unfortunately, the contents of different vaping products vary and are not well defined in different vape products. The process of using an electric current to vaporize a substance can make it more toxic than the precursor, and teens have little idea about the substances they are inhaling. The psychoactive components vary from nicotine to tetrahydrocannabinol in varying amounts. These have the well known effects of stimulation or a high, but also the potential adverse effects of poor concentration, agitation, and even psychosis. Most e-cigarettes contain nicotine, which is highly addictive and can harm adolescent brain development, which continues into the early- to mid-20s. About two-thirds of Juul users aged 15-24 years did not know that it always contains nicotine, as do 99% of all vape solutions (Centers for Disease Control and Prevention, 2020). Earlier use of nicotine is more highly associated with later addiction to tobacco products that cause lung damage, acid reflux, insulin resistance, harm to the testes, harm to fetuses, cancer, and heart disease.
E-cigarette aerosols also contain dozens of other harmful substances besides nicotine ranging from acetone, propylene glycol, and metals to formaldehyde and ethyl benzene. These same chemicals are part of familiar toxic substances such as antifreeze, paint thinner, and pesticides. These cause ear, eye and throat irritation, and impairments in the cardiovascular system reducing athletic ability – at the least. Some flavorings in vape fluids also are toxic. Even the residual left on furniture and floors is harmful to those coming in contact, including pets.
How to encourage teens not to vaping
Trying to scare youth about health hazards is not generally effective in stopping risk behaviors since adolescence is a time of perceived singularity (it does not apply to me) and even a sense of immortality. Teens also see peers who vape as being unaffected and decide on using based on this small personal sample instead of valid statistics.
But teens do pay some attention to peer models or influencers saying why they do not use. One source of such testimony you can refer to is videos of inspiring athletes, musicians, and other “cool” young adults found on the naturalhigh.org website. You may know other examples of community teens desisting you can reference.
Parent rules, and less so advice, against smoking have been shown to be effective in deterring youth cigarette smoking. Because parents are less aware of vaping and its dangers, another step we can take is educating parents in our practices about vaping, its variable forms, its effects, and dangers, supplying authoritative materials, and advising them to talk with their children. Other steps the American Academy of Pediatrics recommends regarding smoking is for parents to be a role model of not using or try to quit, designate the house and car as smoking free, avoid children viewing smoking in media, tell their children about the side effects, and encourage their children who use to quit. Parents also can encourage schools to teach and have rules about smoking and vaping (e.g., med.stanford.edu/tobaccopreventiontoolkit.html).
Another approach we have been using is to not only screen for all substance use, but also to gather information about the teen’s strengths, activities, and life goals both to enhance rapport and to reference during motivational interviewing as reasons to avoid, reduce, or quit vaping. Motivational interviewing has been shown to help patients make healthier lifestyle choices by nonjudgmentally exploring their pros and cons in a conversation that takes into account readiness to change. This fits well with the stage of developing autonomy when teens want above all to make their own decisions. The cons of using can be discussed as including the effects and side effects of vaping interfering with their favored activities and moving towards their identified goals. Praising abstinence and asking them to show you how they could decline offers to vape are valuable reinforcement you can provide.
Finally, we all know that teens hate being manipulated. Vaping education we provide can make it clear that youth are being tricked by companies – most being large cigarette producers who know the dangers of vaping – into getting addicted so these companies can get rich on their money.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She has no other relevant disclosures. Dr. Howard’s contribution to this publication is as a paid expert to MDedge News. Email her at pdnews@mdedge.com.
All pediatricians are relieved that the rates of children smoking cigarettes has dropped steadily since 2011. This decline seems to be associated with education on the dangers of cigarettes and fewer parents smoking. Perhaps less modeling of cigarette use in movies (although it increased again from 2010 to 2019) and lawsuits against advertisements targeting children also has helped.
“Whew,” we may have said, “we can relax our efforts to convince children to avoid smoking.” But, as is commonly true in medicine, the next threat was right around the corner – in this case vaping or e-cigarettes, also called vapes, e-hookahs, vape pens, tank systems, mods, and electronic nicotine delivery systems. And the size of the problem is huge – over 20% of high school students report using e-cigarettes – and immediate, as vaping can kill in the short term as well as causing long-term harm.
“E-cigarette, or vaping, product use–associated Lung Injury” – EVALI for short – has killed 68 vapers and hospitalized thousands. EVALI is thought to be caused by a vitamin E acetate additive used when vaping marijuana, particularly from informal sources like friends, family, or in-person or online dealers.
Vaping increases the risk of severe COVID-19 disease
While EVALI deaths dropped in months after being explained, the COVID-19 epidemic is now a much greater threat to vapers. Vaping increases risk of severe COVID-19 disease because of its immediate paralysis of lung cilia. Sharing vape devices and touching one’s lips while using also increase the risk of virus transmission. Vaping and smoking increase the number of ACE2 receptors to which the SARS-CoV-2 virus attaches causing the characteristic cell damage, and suppresses macrophages and neutrophils, resulting in more smokers testing positive, being twice as likely to develop a severe illness and get hospitalized because of pneumonia from COVID-19, and being less likely to recover. Unfortunately, addressing this new threat to the immediate and long-term health of our patients appears to be more complicated than for addressing smoking tobacco. First of all, vaping is much more difficult to detect than smelly cigarettes sending smoke signals from behind the garage or in the school bathrooms. Many, if not most, adults do not recognize the vaping devices when they see them, as many are tiny and some look like computer thumb drives. The aerosol emitted when in use, while containing dangerous toxins, has less odor than tobacco smoke. Vaping equipment and ads have been designed to attract youth, including linking them to sports and music events. Vaping has been advertised as a way to wean off nicotine addiction, a claim that has some scientific evidence in adults, but at a lower dose of nicotine. Warning children about the dangers of marijuana vaping has been made less credible by the rapid expansion of legalization of marijuana around the United States, eliciting “I told you it was fine” reactions from youth. And the person vaping does not know what or how much of the psychoactive components are being delivered into their bodies. One Juul pod, for example, has the equivalent in nicotine of an entire pack of 20 cigarettes. They are highly addictive, especially to the developing brain, such that youth who vape are more likely to become addicted and to smoke cigarettes in the future.
Help from federal regulation has been weak
While all 50 states ban sales to youth, adults can still buy. Food and Drug Administration limitations on kid-friendly ads, and use of sweet, fruity, and mint flavorings that are most preferred by children, apply only to new producers. The FDA does not yet regulate content of vaping solutions.
So we pediatricians are on the front line for this new threat to prevent vaping or convince youth to cut down or quit. The first step in addressing vaping is being knowledgeable about its many known and emerging health risks. It may seem obvious that the dangers of vaping microscopic particles depends on the contents. Water vapor alone is not dangerous; in fact, we prescribe it in nebulizers. Unfortunately, the contents of different vaping products vary and are not well defined in different vape products. The process of using an electric current to vaporize a substance can make it more toxic than the precursor, and teens have little idea about the substances they are inhaling. The psychoactive components vary from nicotine to tetrahydrocannabinol in varying amounts. These have the well known effects of stimulation or a high, but also the potential adverse effects of poor concentration, agitation, and even psychosis. Most e-cigarettes contain nicotine, which is highly addictive and can harm adolescent brain development, which continues into the early- to mid-20s. About two-thirds of Juul users aged 15-24 years did not know that it always contains nicotine, as do 99% of all vape solutions (Centers for Disease Control and Prevention, 2020). Earlier use of nicotine is more highly associated with later addiction to tobacco products that cause lung damage, acid reflux, insulin resistance, harm to the testes, harm to fetuses, cancer, and heart disease.
E-cigarette aerosols also contain dozens of other harmful substances besides nicotine ranging from acetone, propylene glycol, and metals to formaldehyde and ethyl benzene. These same chemicals are part of familiar toxic substances such as antifreeze, paint thinner, and pesticides. These cause ear, eye and throat irritation, and impairments in the cardiovascular system reducing athletic ability – at the least. Some flavorings in vape fluids also are toxic. Even the residual left on furniture and floors is harmful to those coming in contact, including pets.
How to encourage teens not to vaping
Trying to scare youth about health hazards is not generally effective in stopping risk behaviors since adolescence is a time of perceived singularity (it does not apply to me) and even a sense of immortality. Teens also see peers who vape as being unaffected and decide on using based on this small personal sample instead of valid statistics.
But teens do pay some attention to peer models or influencers saying why they do not use. One source of such testimony you can refer to is videos of inspiring athletes, musicians, and other “cool” young adults found on the naturalhigh.org website. You may know other examples of community teens desisting you can reference.
Parent rules, and less so advice, against smoking have been shown to be effective in deterring youth cigarette smoking. Because parents are less aware of vaping and its dangers, another step we can take is educating parents in our practices about vaping, its variable forms, its effects, and dangers, supplying authoritative materials, and advising them to talk with their children. Other steps the American Academy of Pediatrics recommends regarding smoking is for parents to be a role model of not using or try to quit, designate the house and car as smoking free, avoid children viewing smoking in media, tell their children about the side effects, and encourage their children who use to quit. Parents also can encourage schools to teach and have rules about smoking and vaping (e.g., med.stanford.edu/tobaccopreventiontoolkit.html).
Another approach we have been using is to not only screen for all substance use, but also to gather information about the teen’s strengths, activities, and life goals both to enhance rapport and to reference during motivational interviewing as reasons to avoid, reduce, or quit vaping. Motivational interviewing has been shown to help patients make healthier lifestyle choices by nonjudgmentally exploring their pros and cons in a conversation that takes into account readiness to change. This fits well with the stage of developing autonomy when teens want above all to make their own decisions. The cons of using can be discussed as including the effects and side effects of vaping interfering with their favored activities and moving towards their identified goals. Praising abstinence and asking them to show you how they could decline offers to vape are valuable reinforcement you can provide.
Finally, we all know that teens hate being manipulated. Vaping education we provide can make it clear that youth are being tricked by companies – most being large cigarette producers who know the dangers of vaping – into getting addicted so these companies can get rich on their money.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She has no other relevant disclosures. Dr. Howard’s contribution to this publication is as a paid expert to MDedge News. Email her at pdnews@mdedge.com.
Understanding messenger RNA and other SARS-CoV-2 vaccines
In mid-November, Pfizer/BioNTech were the first with surprising positive protection interim data for their coronavirus vaccine, BNT162b2. A week later, Moderna released interim efficacy results showing its coronavirus vaccine, mRNA-1273, also protected patients from developing SARS-CoV-2 infections. Both studies included mostly healthy adults. A diverse ethnic and racial vaccinated population was included. A reasonable number of persons aged over 65 years, and persons with stable compromising medical conditions were included. Adolescents aged 16 years and over were included. Younger adolescents have been vaccinated or such studies are in the planning or early implementation stage as 2020 came to a close.
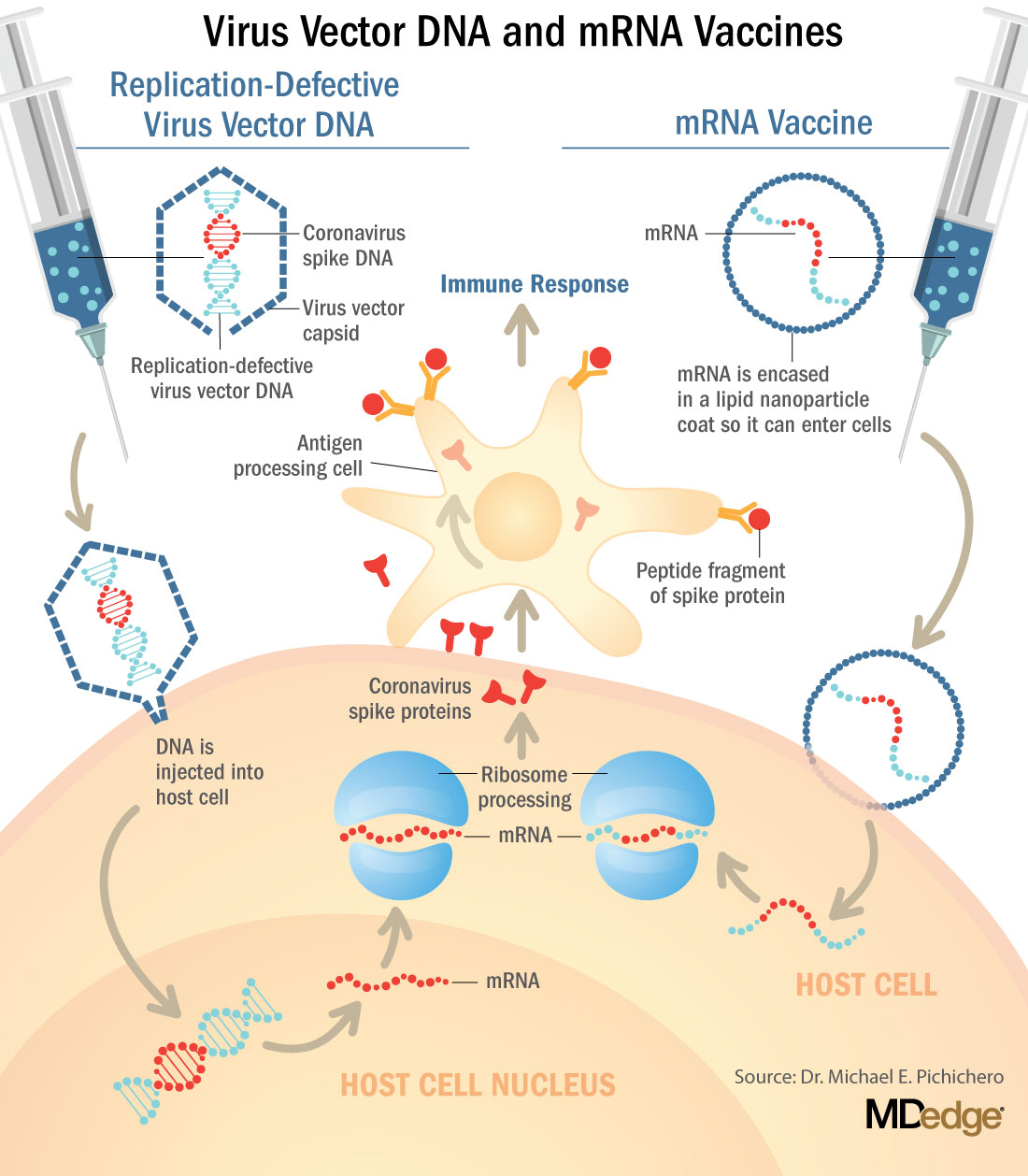
These are new and revolutionary vaccines, although the ability to inject mRNA into animals dates back to 1990, technological advances today make it a reality.1 Traditional vaccines typically involve injection with antigens such as purified proteins or polysaccharides or inactivated/attenuated viruses. In the case of Pfizer’s and Moderna’s vaccines, the mRNA provides the genetic information to synthesize the spike protein that the SARS-CoV-2 virus uses to attach to and infect human cells. Each type of vaccine is packaged in proprietary lipid nanoparticles to protect the mRNA from rapid degradation, and the nanoparticles serve as an adjuvant to attract immune cells to the site of injection. (The properties of the respective lipid nanoparticle packaging may be the factor that impacts storage requirements discussed below.) When injected into muscle (myocyte), the lipid nanoparticles containing the mRNA inside are taken into muscle cells, where the cytoplasmic ribosomes detect and decode the mRNA resulting in the production of the spike protein antigen. It should be noted that the mRNA does not enter the nucleus, where the genetic information (DNA) of a cell is located, and can’t be reproduced or integrated into the DNA. The antigen is exported to the myocyte cell surface where the immune system’s antigen presenting cells detect the protein, ingest it, and take it to regional lymph nodes where interactions with T cells and B cells results in antibodies, T cell–mediated immunity, and generation of immune memory T cells and B cells. A particular subset of T cells – cytotoxic or killer T cells – destroy cells that have been infected by a pathogen. The SARS-CoV-2 mRNA vaccine from Pfizer was reported to induce powerful cytotoxic T-cell responses. Results for Moderna’s vaccine had not been reported at the time this column was prepared, but I anticipate the same positive results.
The revolutionary aspect of mRNA vaccines is the speed at which they can be designed and produced. This is why they lead the pack among the SARS-CoV-2 vaccine candidates and why the National Institute of Allergy and Infectious Diseases provided financial, technical, and/or clinical support. Indeed, once the amino acid sequence of a protein can be determined (a relatively easy task these days) it’s straightforward to synthesize mRNA in the lab – and it can be done incredibly fast. It is reported that the mRNA code for the vaccine by Moderna was made in 2 days and production development was completed in about 2 months.2
A 2007 World Health Organization report noted that infectious diseases are emerging at “the historically unprecedented rate of one per year.”3 Severe acute respiratory syndrome (SARS), Zika, Ebola, and avian and swine flu are recent examples. For most vaccines against emerging diseases, the challenge is about speed: developing and manufacturing a vaccine and getting it to persons who need it as quickly as possible. The current seasonal flu vaccine takes about 6 months to develop; it takes years for most of the traditional vaccines. That’s why once the infrastructure is in place, mRNA vaccines may prove to offer a big advantage as vaccines against emerging pathogens.
Early efficacy results have been surprising
Both vaccines were reported to produce about 95% efficacy in the final analysis. That was unexpectedly high because most vaccines for respiratory illness achieve efficacy of 60%-80%, e.g., flu vaccines. However, the efficacy rate may drop as time goes by because stimulation of short-term immunity would be in the earliest reported results.
Preventing SARS-CoV-2 cases is an important aspect of a coronavirus vaccine, but preventing severe illness is especially important considering that severe cases can result in prolonged intubation/artificial ventilation, prolonged disability and death. Pfizer/BioNTech had not released any data on the breakdown of severe cases as this column was finalized. In Moderna’s clinical trial, a secondary endpoint analyzed severe cases of COVID-19 and included 30 severe cases (as defined in the study protocol) in this analysis. All 30 cases occurred in the placebo group and none in the mRNA-1273–vaccinated group. In the Pfizer/BioNTech trial there were too few cases of severe illness to calculate efficacy.
Duration of immunity and need to revaccinate after initial primary vaccination are unknowns. Study of induction of B- and T-cell memory and levels of long-term protection have not been reported thus far.
Could mRNA COVID-19 vaccines be dangerous in the long term?
These will be the first-ever mRNA vaccines brought to market for humans. In order to receive Food and Drug Administration approval, the companies had to prove there were no immediate or short-term negative adverse effects from the vaccines. The companies reported that their independent data-monitoring committees hadn’t “reported any serious safety concerns.” However, fairly significant local reactions at the site of injection, fever, malaise, and fatigue occur with modest frequency following vaccinations with these products, reportedly in 10%-15% of vaccinees. Overall, the immediate reaction profile appears to be more severe than what occurs following seasonal influenza vaccination. When mass inoculations with these completely new and revolutionary vaccines begins, we will know virtually nothing about their long-term side effects. The possibility of systemic inflammatory responses that could lead to autoimmune conditions, persistence of the induced immunogen expression, development of autoreactive antibodies, and toxic effects of delivery components have been raised as theoretical concerns.4-6 None of these theoretical risks have been observed to date and postmarketing phase 4 safety monitoring studies are in place from the Centers for Disease Control and Prevention and the companies that produce the vaccines. This is a risk public health authorities are willing to take because the risk to benefit calculation strongly favors taking theoretical risks, compared with clear benefits in preventing severe illnesses and death.
What about availability?
Pfizer/BioNTech expects to be able to produce up to 50 million vaccine doses in 2020 and up to 1.3 billion doses in 2021. Moderna expects to produce 20 million doses by the end of 2020, and 500 million to 1 billion doses in 2021. Storage requirements are inherent to the composition of the vaccines with their differing lipid nanoparticle delivery systems. Pfizer/BioNTech’s BNT162b2 has to be stored and transported at –80° C, which requires specialized freezers, which most doctors’ offices and pharmacies are unlikely to have on site, or dry ice containers. Once the vaccine is thawed, it can only remain in the refrigerator for 24 hours. Moderna’s mRNA-1273 will be much easier to distribute. The vaccine is stable in a standard freezer at –20° C for up to 6 months, in a refrigerator for up to 30 days within that 6-month shelf life, and at room temperature for up to 12 hours.
Timelines and testing other vaccines
Strong efficacy data from the two leading SARS-CoV-2 vaccines and emergency-use authorization Food and Drug Administration approval suggest the window for testing additional vaccine candidates in the United States could soon start to close. Of the more than 200 vaccines in development for SARS-CoV-2, at least 7 have a chance of gathering pivotal data before the front-runners become broadly available.
Testing diverse vaccine candidates, based on different technologies, is important for ensuring sufficient supply and could lead to products with tolerability and safety profiles that make them better suited, or more attractive, to subsets of the population. Different vaccine antigens and technologies also may yield different durations of protection, a question that will not be answered until long after the first products are on the market.
AstraZeneca enrolled about 23,000 subjects into its two phase 3 trials of AZD1222 (ChAdOx1 nCoV-19): a 40,000-subject U.S. trial and a 10,000-subject study in Brazil. AstraZeneca’s AZD1222, developed with the University of Oxford (England), uses a replication defective simian adenovirus vector called ChAdOx1.AZD1222 which encodes the SARS-CoV-2 spike protein. After injection, the viral vector delivers recombinant DNA that is decoded to mRNA, followed by mRNA decoding to become a protein. A serendipitous manufacturing error for the first 3,000 doses resulted in a half dose for those subjects before the error was discovered. Full doses were given to those subjects on second injections and those subjects showed 90% efficacy. Subjects who received 2 full doses showed 62% efficacy. A vaccine cannot be licensed based on 3,000 subjects so AstraZeneca has started a new phase 3 trial involving many more subjects to receive the combination lower dose followed by the full dose.
Johnson and Johnson (J&J) started its phase 3 trial evaluating a single dose of JNJ-78436735 in September. Phase 3 data may be reported by the end of2020. In November, J&J announced it was starting a second phase 3 trial to test two doses of the candidate. J&J’s JNJ-78436735 encodes the SARS-CoV-2 spike protein in an adenovirus serotype 26 (Ad26) vector, which is one of the two adenovirus vectors used in Sputnik V, the Russian vaccine reported to have 90% efficacy at an early interim analysis.
Sanofi and Novavax are both developing protein-based vaccines, a proven modality. Sanofi, in partnership with GlaxoSmithKline started a phase 1/2 clinical trial in the Fall 2020 with plans to commence a phase 3 trial in late December. Sanofi developed the protein ingredients and GlaxoSmithKline added one of their novel adjuvants. Novavax expects data from a U.K. phase 3 trial of NVX-CoV2373 in early 2021 and began a U.S. phase 3 study in late November. NVX-CoV2373 was created using Novavax’ recombinant nanoparticle technology to generate antigen derived from the coronavirus spike protein and contains Novavax’s patented saponin-based Matrix-M adjuvant.
Inovio Pharmaceuticals was gearing up to start a U.S. phase 2/3 trial of DNA vaccine INO-4800 by the end of 2020.
After Moderna and Pfizer-BioNTech, CureVac has the next most advanced mRNA vaccine. It was planned that a phase 2b/3 trial of CVnCoV would be conducted in Europe, Latin America, Africa, and Asia. Sanofi is also developing a mRNA vaccine as a second product in addition to its protein vaccine.
Vaxxinity planned to begin phase 3 testing of UB-612, a multitope peptide–based vaccine, in Brazil by the end of 2020.
However, emergency-use authorizations for the Pfizer and Moderna vaccines could hinder trial recruitment in at least two ways. Given the gravity of the pandemic, some stakeholders believe it would be ethical to unblind ongoing trials to give subjects the opportunity to switch to a vaccine proven to be effective. Even if unblinding doesn’t occur, as the two authorized vaccines start to become widely available, volunteering for clinical trials may become less attractive.
Dr. Pichichero is a specialist in pediatric infectious diseases, and director of the Research Institute at Rochester (N.Y.) General Hospital. He said he has no relevant financial disclosures. Email Dr. Pichichero at pdnews@mdedge.com.
References
1. Wolff JA et al. Science. 1990 Mar 23. doi: 10.1126/science.1690918.
2. Jackson LA et al. N Engl J Med. 2020 Nov 12. doi: 10.1056/NEJMoa2022483.
3. Prentice T and Reinders LT. The world health report 2007. (Geneva Switzerland: World Health Organization, 2007).
4. Peck KM and Lauring AS. J Virol. 2018. doi: 10.1128/JVI.01031-17.
5. Pepini T et al. J Immunol. 2017 May 15. doi: 10.4049/jimmunol.1601877.
6. Theofilopoulos AN et al. Annu Rev Immunol. 2005. doi: 10.1146/annurev.immunol.23.021704.115843.
In mid-November, Pfizer/BioNTech were the first with surprising positive protection interim data for their coronavirus vaccine, BNT162b2. A week later, Moderna released interim efficacy results showing its coronavirus vaccine, mRNA-1273, also protected patients from developing SARS-CoV-2 infections. Both studies included mostly healthy adults. A diverse ethnic and racial vaccinated population was included. A reasonable number of persons aged over 65 years, and persons with stable compromising medical conditions were included. Adolescents aged 16 years and over were included. Younger adolescents have been vaccinated or such studies are in the planning or early implementation stage as 2020 came to a close.
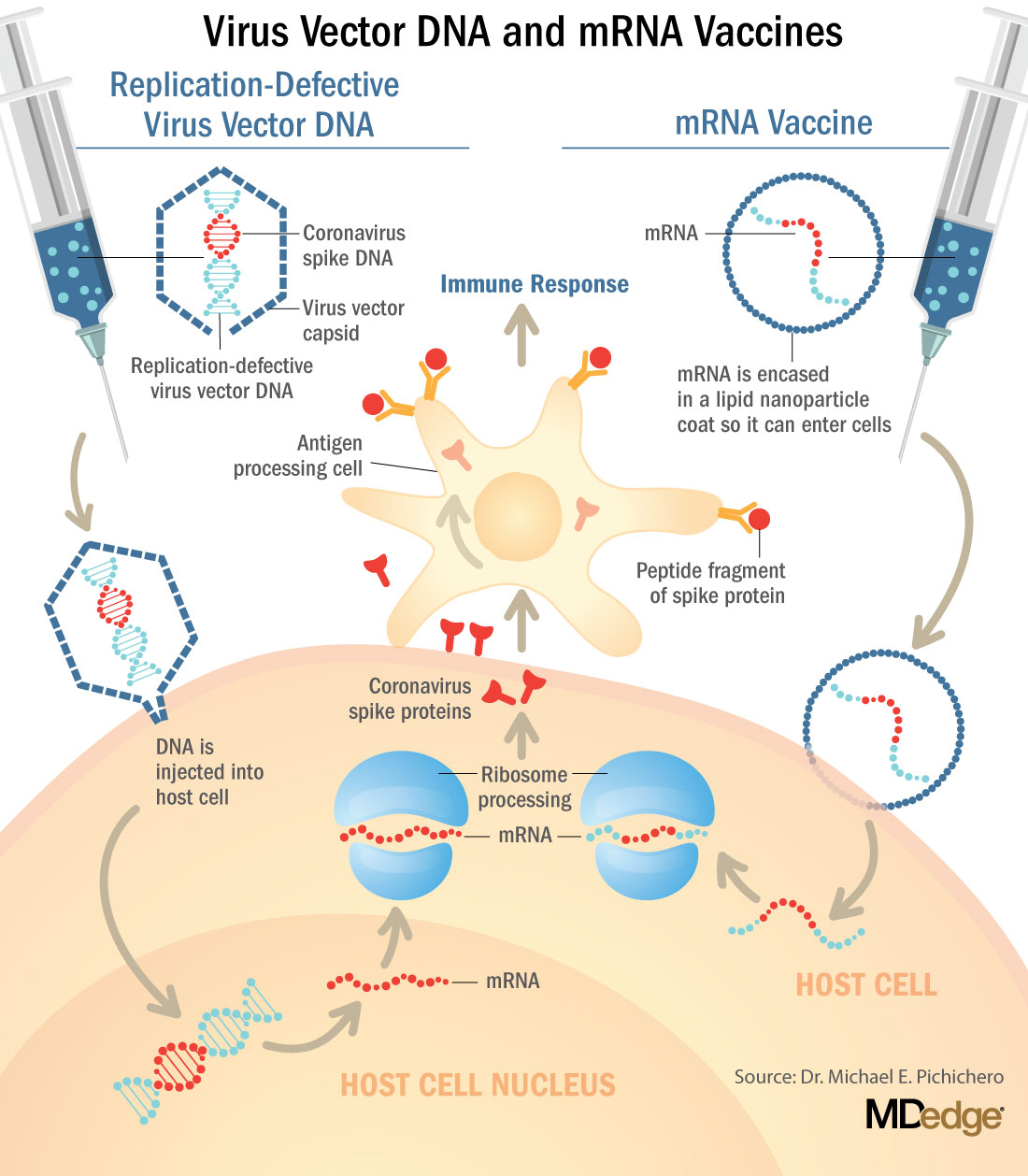
These are new and revolutionary vaccines, although the ability to inject mRNA into animals dates back to 1990, technological advances today make it a reality.1 Traditional vaccines typically involve injection with antigens such as purified proteins or polysaccharides or inactivated/attenuated viruses. In the case of Pfizer’s and Moderna’s vaccines, the mRNA provides the genetic information to synthesize the spike protein that the SARS-CoV-2 virus uses to attach to and infect human cells. Each type of vaccine is packaged in proprietary lipid nanoparticles to protect the mRNA from rapid degradation, and the nanoparticles serve as an adjuvant to attract immune cells to the site of injection. (The properties of the respective lipid nanoparticle packaging may be the factor that impacts storage requirements discussed below.) When injected into muscle (myocyte), the lipid nanoparticles containing the mRNA inside are taken into muscle cells, where the cytoplasmic ribosomes detect and decode the mRNA resulting in the production of the spike protein antigen. It should be noted that the mRNA does not enter the nucleus, where the genetic information (DNA) of a cell is located, and can’t be reproduced or integrated into the DNA. The antigen is exported to the myocyte cell surface where the immune system’s antigen presenting cells detect the protein, ingest it, and take it to regional lymph nodes where interactions with T cells and B cells results in antibodies, T cell–mediated immunity, and generation of immune memory T cells and B cells. A particular subset of T cells – cytotoxic or killer T cells – destroy cells that have been infected by a pathogen. The SARS-CoV-2 mRNA vaccine from Pfizer was reported to induce powerful cytotoxic T-cell responses. Results for Moderna’s vaccine had not been reported at the time this column was prepared, but I anticipate the same positive results.
The revolutionary aspect of mRNA vaccines is the speed at which they can be designed and produced. This is why they lead the pack among the SARS-CoV-2 vaccine candidates and why the National Institute of Allergy and Infectious Diseases provided financial, technical, and/or clinical support. Indeed, once the amino acid sequence of a protein can be determined (a relatively easy task these days) it’s straightforward to synthesize mRNA in the lab – and it can be done incredibly fast. It is reported that the mRNA code for the vaccine by Moderna was made in 2 days and production development was completed in about 2 months.2
A 2007 World Health Organization report noted that infectious diseases are emerging at “the historically unprecedented rate of one per year.”3 Severe acute respiratory syndrome (SARS), Zika, Ebola, and avian and swine flu are recent examples. For most vaccines against emerging diseases, the challenge is about speed: developing and manufacturing a vaccine and getting it to persons who need it as quickly as possible. The current seasonal flu vaccine takes about 6 months to develop; it takes years for most of the traditional vaccines. That’s why once the infrastructure is in place, mRNA vaccines may prove to offer a big advantage as vaccines against emerging pathogens.
Early efficacy results have been surprising
Both vaccines were reported to produce about 95% efficacy in the final analysis. That was unexpectedly high because most vaccines for respiratory illness achieve efficacy of 60%-80%, e.g., flu vaccines. However, the efficacy rate may drop as time goes by because stimulation of short-term immunity would be in the earliest reported results.
Preventing SARS-CoV-2 cases is an important aspect of a coronavirus vaccine, but preventing severe illness is especially important considering that severe cases can result in prolonged intubation/artificial ventilation, prolonged disability and death. Pfizer/BioNTech had not released any data on the breakdown of severe cases as this column was finalized. In Moderna’s clinical trial, a secondary endpoint analyzed severe cases of COVID-19 and included 30 severe cases (as defined in the study protocol) in this analysis. All 30 cases occurred in the placebo group and none in the mRNA-1273–vaccinated group. In the Pfizer/BioNTech trial there were too few cases of severe illness to calculate efficacy.
Duration of immunity and need to revaccinate after initial primary vaccination are unknowns. Study of induction of B- and T-cell memory and levels of long-term protection have not been reported thus far.
Could mRNA COVID-19 vaccines be dangerous in the long term?
These will be the first-ever mRNA vaccines brought to market for humans. In order to receive Food and Drug Administration approval, the companies had to prove there were no immediate or short-term negative adverse effects from the vaccines. The companies reported that their independent data-monitoring committees hadn’t “reported any serious safety concerns.” However, fairly significant local reactions at the site of injection, fever, malaise, and fatigue occur with modest frequency following vaccinations with these products, reportedly in 10%-15% of vaccinees. Overall, the immediate reaction profile appears to be more severe than what occurs following seasonal influenza vaccination. When mass inoculations with these completely new and revolutionary vaccines begins, we will know virtually nothing about their long-term side effects. The possibility of systemic inflammatory responses that could lead to autoimmune conditions, persistence of the induced immunogen expression, development of autoreactive antibodies, and toxic effects of delivery components have been raised as theoretical concerns.4-6 None of these theoretical risks have been observed to date and postmarketing phase 4 safety monitoring studies are in place from the Centers for Disease Control and Prevention and the companies that produce the vaccines. This is a risk public health authorities are willing to take because the risk to benefit calculation strongly favors taking theoretical risks, compared with clear benefits in preventing severe illnesses and death.
What about availability?
Pfizer/BioNTech expects to be able to produce up to 50 million vaccine doses in 2020 and up to 1.3 billion doses in 2021. Moderna expects to produce 20 million doses by the end of 2020, and 500 million to 1 billion doses in 2021. Storage requirements are inherent to the composition of the vaccines with their differing lipid nanoparticle delivery systems. Pfizer/BioNTech’s BNT162b2 has to be stored and transported at –80° C, which requires specialized freezers, which most doctors’ offices and pharmacies are unlikely to have on site, or dry ice containers. Once the vaccine is thawed, it can only remain in the refrigerator for 24 hours. Moderna’s mRNA-1273 will be much easier to distribute. The vaccine is stable in a standard freezer at –20° C for up to 6 months, in a refrigerator for up to 30 days within that 6-month shelf life, and at room temperature for up to 12 hours.
Timelines and testing other vaccines
Strong efficacy data from the two leading SARS-CoV-2 vaccines and emergency-use authorization Food and Drug Administration approval suggest the window for testing additional vaccine candidates in the United States could soon start to close. Of the more than 200 vaccines in development for SARS-CoV-2, at least 7 have a chance of gathering pivotal data before the front-runners become broadly available.
Testing diverse vaccine candidates, based on different technologies, is important for ensuring sufficient supply and could lead to products with tolerability and safety profiles that make them better suited, or more attractive, to subsets of the population. Different vaccine antigens and technologies also may yield different durations of protection, a question that will not be answered until long after the first products are on the market.
AstraZeneca enrolled about 23,000 subjects into its two phase 3 trials of AZD1222 (ChAdOx1 nCoV-19): a 40,000-subject U.S. trial and a 10,000-subject study in Brazil. AstraZeneca’s AZD1222, developed with the University of Oxford (England), uses a replication defective simian adenovirus vector called ChAdOx1.AZD1222 which encodes the SARS-CoV-2 spike protein. After injection, the viral vector delivers recombinant DNA that is decoded to mRNA, followed by mRNA decoding to become a protein. A serendipitous manufacturing error for the first 3,000 doses resulted in a half dose for those subjects before the error was discovered. Full doses were given to those subjects on second injections and those subjects showed 90% efficacy. Subjects who received 2 full doses showed 62% efficacy. A vaccine cannot be licensed based on 3,000 subjects so AstraZeneca has started a new phase 3 trial involving many more subjects to receive the combination lower dose followed by the full dose.
Johnson and Johnson (J&J) started its phase 3 trial evaluating a single dose of JNJ-78436735 in September. Phase 3 data may be reported by the end of2020. In November, J&J announced it was starting a second phase 3 trial to test two doses of the candidate. J&J’s JNJ-78436735 encodes the SARS-CoV-2 spike protein in an adenovirus serotype 26 (Ad26) vector, which is one of the two adenovirus vectors used in Sputnik V, the Russian vaccine reported to have 90% efficacy at an early interim analysis.
Sanofi and Novavax are both developing protein-based vaccines, a proven modality. Sanofi, in partnership with GlaxoSmithKline started a phase 1/2 clinical trial in the Fall 2020 with plans to commence a phase 3 trial in late December. Sanofi developed the protein ingredients and GlaxoSmithKline added one of their novel adjuvants. Novavax expects data from a U.K. phase 3 trial of NVX-CoV2373 in early 2021 and began a U.S. phase 3 study in late November. NVX-CoV2373 was created using Novavax’ recombinant nanoparticle technology to generate antigen derived from the coronavirus spike protein and contains Novavax’s patented saponin-based Matrix-M adjuvant.
Inovio Pharmaceuticals was gearing up to start a U.S. phase 2/3 trial of DNA vaccine INO-4800 by the end of 2020.
After Moderna and Pfizer-BioNTech, CureVac has the next most advanced mRNA vaccine. It was planned that a phase 2b/3 trial of CVnCoV would be conducted in Europe, Latin America, Africa, and Asia. Sanofi is also developing a mRNA vaccine as a second product in addition to its protein vaccine.
Vaxxinity planned to begin phase 3 testing of UB-612, a multitope peptide–based vaccine, in Brazil by the end of 2020.
However, emergency-use authorizations for the Pfizer and Moderna vaccines could hinder trial recruitment in at least two ways. Given the gravity of the pandemic, some stakeholders believe it would be ethical to unblind ongoing trials to give subjects the opportunity to switch to a vaccine proven to be effective. Even if unblinding doesn’t occur, as the two authorized vaccines start to become widely available, volunteering for clinical trials may become less attractive.
Dr. Pichichero is a specialist in pediatric infectious diseases, and director of the Research Institute at Rochester (N.Y.) General Hospital. He said he has no relevant financial disclosures. Email Dr. Pichichero at pdnews@mdedge.com.
References
1. Wolff JA et al. Science. 1990 Mar 23. doi: 10.1126/science.1690918.
2. Jackson LA et al. N Engl J Med. 2020 Nov 12. doi: 10.1056/NEJMoa2022483.
3. Prentice T and Reinders LT. The world health report 2007. (Geneva Switzerland: World Health Organization, 2007).
4. Peck KM and Lauring AS. J Virol. 2018. doi: 10.1128/JVI.01031-17.
5. Pepini T et al. J Immunol. 2017 May 15. doi: 10.4049/jimmunol.1601877.
6. Theofilopoulos AN et al. Annu Rev Immunol. 2005. doi: 10.1146/annurev.immunol.23.021704.115843.
In mid-November, Pfizer/BioNTech were the first with surprising positive protection interim data for their coronavirus vaccine, BNT162b2. A week later, Moderna released interim efficacy results showing its coronavirus vaccine, mRNA-1273, also protected patients from developing SARS-CoV-2 infections. Both studies included mostly healthy adults. A diverse ethnic and racial vaccinated population was included. A reasonable number of persons aged over 65 years, and persons with stable compromising medical conditions were included. Adolescents aged 16 years and over were included. Younger adolescents have been vaccinated or such studies are in the planning or early implementation stage as 2020 came to a close.
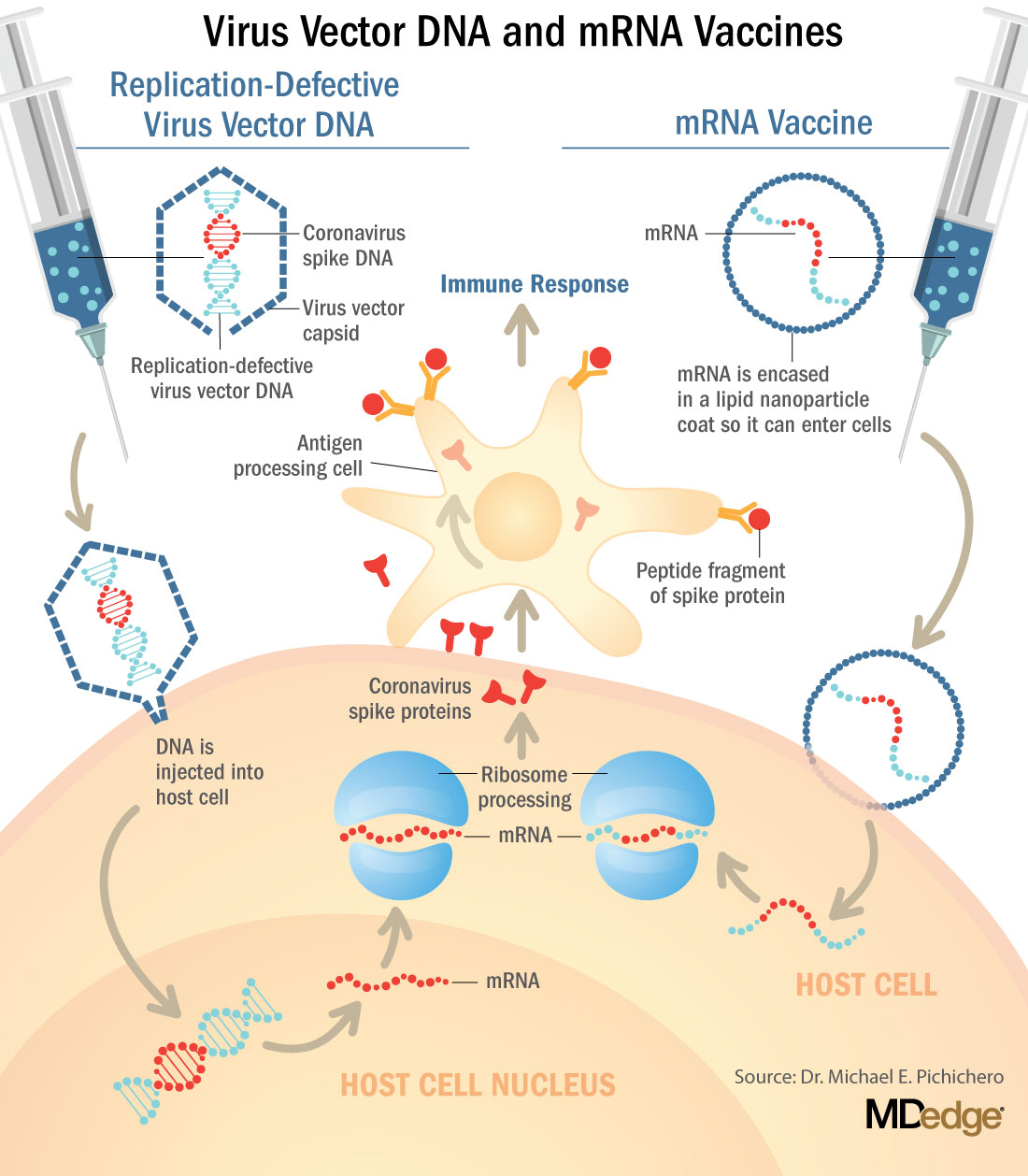
These are new and revolutionary vaccines, although the ability to inject mRNA into animals dates back to 1990, technological advances today make it a reality.1 Traditional vaccines typically involve injection with antigens such as purified proteins or polysaccharides or inactivated/attenuated viruses. In the case of Pfizer’s and Moderna’s vaccines, the mRNA provides the genetic information to synthesize the spike protein that the SARS-CoV-2 virus uses to attach to and infect human cells. Each type of vaccine is packaged in proprietary lipid nanoparticles to protect the mRNA from rapid degradation, and the nanoparticles serve as an adjuvant to attract immune cells to the site of injection. (The properties of the respective lipid nanoparticle packaging may be the factor that impacts storage requirements discussed below.) When injected into muscle (myocyte), the lipid nanoparticles containing the mRNA inside are taken into muscle cells, where the cytoplasmic ribosomes detect and decode the mRNA resulting in the production of the spike protein antigen. It should be noted that the mRNA does not enter the nucleus, where the genetic information (DNA) of a cell is located, and can’t be reproduced or integrated into the DNA. The antigen is exported to the myocyte cell surface where the immune system’s antigen presenting cells detect the protein, ingest it, and take it to regional lymph nodes where interactions with T cells and B cells results in antibodies, T cell–mediated immunity, and generation of immune memory T cells and B cells. A particular subset of T cells – cytotoxic or killer T cells – destroy cells that have been infected by a pathogen. The SARS-CoV-2 mRNA vaccine from Pfizer was reported to induce powerful cytotoxic T-cell responses. Results for Moderna’s vaccine had not been reported at the time this column was prepared, but I anticipate the same positive results.
The revolutionary aspect of mRNA vaccines is the speed at which they can be designed and produced. This is why they lead the pack among the SARS-CoV-2 vaccine candidates and why the National Institute of Allergy and Infectious Diseases provided financial, technical, and/or clinical support. Indeed, once the amino acid sequence of a protein can be determined (a relatively easy task these days) it’s straightforward to synthesize mRNA in the lab – and it can be done incredibly fast. It is reported that the mRNA code for the vaccine by Moderna was made in 2 days and production development was completed in about 2 months.2
A 2007 World Health Organization report noted that infectious diseases are emerging at “the historically unprecedented rate of one per year.”3 Severe acute respiratory syndrome (SARS), Zika, Ebola, and avian and swine flu are recent examples. For most vaccines against emerging diseases, the challenge is about speed: developing and manufacturing a vaccine and getting it to persons who need it as quickly as possible. The current seasonal flu vaccine takes about 6 months to develop; it takes years for most of the traditional vaccines. That’s why once the infrastructure is in place, mRNA vaccines may prove to offer a big advantage as vaccines against emerging pathogens.
Early efficacy results have been surprising
Both vaccines were reported to produce about 95% efficacy in the final analysis. That was unexpectedly high because most vaccines for respiratory illness achieve efficacy of 60%-80%, e.g., flu vaccines. However, the efficacy rate may drop as time goes by because stimulation of short-term immunity would be in the earliest reported results.
Preventing SARS-CoV-2 cases is an important aspect of a coronavirus vaccine, but preventing severe illness is especially important considering that severe cases can result in prolonged intubation/artificial ventilation, prolonged disability and death. Pfizer/BioNTech had not released any data on the breakdown of severe cases as this column was finalized. In Moderna’s clinical trial, a secondary endpoint analyzed severe cases of COVID-19 and included 30 severe cases (as defined in the study protocol) in this analysis. All 30 cases occurred in the placebo group and none in the mRNA-1273–vaccinated group. In the Pfizer/BioNTech trial there were too few cases of severe illness to calculate efficacy.
Duration of immunity and need to revaccinate after initial primary vaccination are unknowns. Study of induction of B- and T-cell memory and levels of long-term protection have not been reported thus far.
Could mRNA COVID-19 vaccines be dangerous in the long term?
These will be the first-ever mRNA vaccines brought to market for humans. In order to receive Food and Drug Administration approval, the companies had to prove there were no immediate or short-term negative adverse effects from the vaccines. The companies reported that their independent data-monitoring committees hadn’t “reported any serious safety concerns.” However, fairly significant local reactions at the site of injection, fever, malaise, and fatigue occur with modest frequency following vaccinations with these products, reportedly in 10%-15% of vaccinees. Overall, the immediate reaction profile appears to be more severe than what occurs following seasonal influenza vaccination. When mass inoculations with these completely new and revolutionary vaccines begins, we will know virtually nothing about their long-term side effects. The possibility of systemic inflammatory responses that could lead to autoimmune conditions, persistence of the induced immunogen expression, development of autoreactive antibodies, and toxic effects of delivery components have been raised as theoretical concerns.4-6 None of these theoretical risks have been observed to date and postmarketing phase 4 safety monitoring studies are in place from the Centers for Disease Control and Prevention and the companies that produce the vaccines. This is a risk public health authorities are willing to take because the risk to benefit calculation strongly favors taking theoretical risks, compared with clear benefits in preventing severe illnesses and death.
What about availability?
Pfizer/BioNTech expects to be able to produce up to 50 million vaccine doses in 2020 and up to 1.3 billion doses in 2021. Moderna expects to produce 20 million doses by the end of 2020, and 500 million to 1 billion doses in 2021. Storage requirements are inherent to the composition of the vaccines with their differing lipid nanoparticle delivery systems. Pfizer/BioNTech’s BNT162b2 has to be stored and transported at –80° C, which requires specialized freezers, which most doctors’ offices and pharmacies are unlikely to have on site, or dry ice containers. Once the vaccine is thawed, it can only remain in the refrigerator for 24 hours. Moderna’s mRNA-1273 will be much easier to distribute. The vaccine is stable in a standard freezer at –20° C for up to 6 months, in a refrigerator for up to 30 days within that 6-month shelf life, and at room temperature for up to 12 hours.
Timelines and testing other vaccines
Strong efficacy data from the two leading SARS-CoV-2 vaccines and emergency-use authorization Food and Drug Administration approval suggest the window for testing additional vaccine candidates in the United States could soon start to close. Of the more than 200 vaccines in development for SARS-CoV-2, at least 7 have a chance of gathering pivotal data before the front-runners become broadly available.
Testing diverse vaccine candidates, based on different technologies, is important for ensuring sufficient supply and could lead to products with tolerability and safety profiles that make them better suited, or more attractive, to subsets of the population. Different vaccine antigens and technologies also may yield different durations of protection, a question that will not be answered until long after the first products are on the market.
AstraZeneca enrolled about 23,000 subjects into its two phase 3 trials of AZD1222 (ChAdOx1 nCoV-19): a 40,000-subject U.S. trial and a 10,000-subject study in Brazil. AstraZeneca’s AZD1222, developed with the University of Oxford (England), uses a replication defective simian adenovirus vector called ChAdOx1.AZD1222 which encodes the SARS-CoV-2 spike protein. After injection, the viral vector delivers recombinant DNA that is decoded to mRNA, followed by mRNA decoding to become a protein. A serendipitous manufacturing error for the first 3,000 doses resulted in a half dose for those subjects before the error was discovered. Full doses were given to those subjects on second injections and those subjects showed 90% efficacy. Subjects who received 2 full doses showed 62% efficacy. A vaccine cannot be licensed based on 3,000 subjects so AstraZeneca has started a new phase 3 trial involving many more subjects to receive the combination lower dose followed by the full dose.
Johnson and Johnson (J&J) started its phase 3 trial evaluating a single dose of JNJ-78436735 in September. Phase 3 data may be reported by the end of2020. In November, J&J announced it was starting a second phase 3 trial to test two doses of the candidate. J&J’s JNJ-78436735 encodes the SARS-CoV-2 spike protein in an adenovirus serotype 26 (Ad26) vector, which is one of the two adenovirus vectors used in Sputnik V, the Russian vaccine reported to have 90% efficacy at an early interim analysis.
Sanofi and Novavax are both developing protein-based vaccines, a proven modality. Sanofi, in partnership with GlaxoSmithKline started a phase 1/2 clinical trial in the Fall 2020 with plans to commence a phase 3 trial in late December. Sanofi developed the protein ingredients and GlaxoSmithKline added one of their novel adjuvants. Novavax expects data from a U.K. phase 3 trial of NVX-CoV2373 in early 2021 and began a U.S. phase 3 study in late November. NVX-CoV2373 was created using Novavax’ recombinant nanoparticle technology to generate antigen derived from the coronavirus spike protein and contains Novavax’s patented saponin-based Matrix-M adjuvant.
Inovio Pharmaceuticals was gearing up to start a U.S. phase 2/3 trial of DNA vaccine INO-4800 by the end of 2020.
After Moderna and Pfizer-BioNTech, CureVac has the next most advanced mRNA vaccine. It was planned that a phase 2b/3 trial of CVnCoV would be conducted in Europe, Latin America, Africa, and Asia. Sanofi is also developing a mRNA vaccine as a second product in addition to its protein vaccine.
Vaxxinity planned to begin phase 3 testing of UB-612, a multitope peptide–based vaccine, in Brazil by the end of 2020.
However, emergency-use authorizations for the Pfizer and Moderna vaccines could hinder trial recruitment in at least two ways. Given the gravity of the pandemic, some stakeholders believe it would be ethical to unblind ongoing trials to give subjects the opportunity to switch to a vaccine proven to be effective. Even if unblinding doesn’t occur, as the two authorized vaccines start to become widely available, volunteering for clinical trials may become less attractive.
Dr. Pichichero is a specialist in pediatric infectious diseases, and director of the Research Institute at Rochester (N.Y.) General Hospital. He said he has no relevant financial disclosures. Email Dr. Pichichero at pdnews@mdedge.com.
References
1. Wolff JA et al. Science. 1990 Mar 23. doi: 10.1126/science.1690918.
2. Jackson LA et al. N Engl J Med. 2020 Nov 12. doi: 10.1056/NEJMoa2022483.
3. Prentice T and Reinders LT. The world health report 2007. (Geneva Switzerland: World Health Organization, 2007).
4. Peck KM and Lauring AS. J Virol. 2018. doi: 10.1128/JVI.01031-17.
5. Pepini T et al. J Immunol. 2017 May 15. doi: 10.4049/jimmunol.1601877.
6. Theofilopoulos AN et al. Annu Rev Immunol. 2005. doi: 10.1146/annurev.immunol.23.021704.115843.
Prioritize COVID-19 vaccination in both types of diabetes, say docs
The risk for increased COVID-19 severity in people with type 1 diabetes appears similar to that of type 2 diabetes, contrary to some official advice from the Centers for Disease Control and Prevention. The new finding indicates that people with both types should be priority for receiving a vaccine, investigators say.
The study is the first to prospectively evaluate both inpatients and outpatients and to examine COVID-19 severity factors in addition to death in people with type 1 and type 2 diabetes separately, and was published online Dec. 2 in Diabetes Care.
Among the patients, who were seen at Vanderbilt University Medical Center in Nashville, Tenn., between March and August of 2020, those with both type 1 and type 2 diabetes had between a three- and fourfold greater risk for COVID-19 hospitalization and greater illness severity compared with people without diabetes after adjustments for age, race, and a number of other risk factors.
This finding is important since as of Dec. 1, 2020, the CDC has classified the diabetes types differently in terms of underlying medical conditions that increase the risk for severe COVID-19.
Adults of any age with type 2 diabetes are considered “at increased risk of severe illness” from the virus that causes COVID-19 whereas the CDC says those with type 1 “might be at an increased risk.”
Lead author of the new paper Justin M. Gregory, MD, said in an interview: “I think this needs revision based on the current evidence. I think the data presented in our study and that of Barron et al. in Lancet Endocrinology 2020 indicate the need to place type 1 diabetes at parity with type 2 diabetes.
“These studies indicate both conditions carry an adjusted odds ratio of three to four when compared with people without diabetes for hospitalization, illness severity, and mortality,” he stressed.
Vaccines look promising for patients with diabetes
There were no phase 3 vaccine data available for the vaccine at the time that Dr. Gregory, of the Ian M. Burr Division of Pediatric Endocrinology and Diabetes, Vanderbilt University, Nashville, Tenn., and colleagues were writing their manuscript in late summer, so the article does not mention this.
But now, Dr. Gregory said, “Based on the initial press releases from Pfizer and Moderna, I am now optimistic that these vaccines might mitigate the excess morbidity and mortality from COVID-19 experienced by patients with diabetes.
“I am eager to see what we learn on December 10 and 17 [the scheduled dates for the meetings of the Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee to review the Pfizer and Moderna vaccines, respectively].”
But with the winter pandemic surge in the meantime, “Our investigation suggests that as COVID-19 hospitalizations rise, patients with both type 1 and 2 diabetes will comprise a disproportionately higher number of those admissions and, once hospitalized, demonstrate a greater degree of illness severity,” he and his colleagues said.
“In light of these data, we call on our colleagues to emphasize the importance of social distancing measures and hand hygiene, with particular emphasis on patients with diabetes, including those in the most vulnerable communities whom our study affirms will face the most severe impact.”
After adjustments, excess severity risk similar for both diabetes types
The new study data came from electronic health records at Vanderbilt University Medical Center, comprising 137 primary care, urgent care, and hospital facilities where patients were tested for SARS-CoV-2 regardless of the reason for their visit.
Between March 17 and August 7, 2020, 6,451 patients tested positive for COVID-19. Of those, 273 had type 2 diabetes and 40 had type 1 diabetes.
Children younger than 18 years accounted for 20% of those with type 1 diabetes and 9.4% of those without diabetes, but none of the type 2 group. The group with type 2 diabetes was considerably older than the type 1 diabetes and no-diabetes groups, 58 years versus 37 and 33 years, respectively.
Before adjustment for baseline characteristics that differed between groups, patients with type 1 diabetes appeared to have a risk for hospitalization and greater illness severity that was intermediate between the group with no diabetes and the group with type 2 diabetes, the researchers said.
But after adjustment for age, race, sex, hypertension, smoking, and body mass index, people with type 1 diabetes had odds ratios of 3.90 for hospitalization and 3.35 for greater illness severity, which was similar to risk in type 2 diabetes (3.36 and 3.42, respectively), compared to those without diabetes.
Deep dive explores COVID-19 severity risk factors in type 1 diabetes
The investigators then conducted a detailed chart review for 37 of the 40 patients with type 1 diabetes and phone surveys with 15 of them.
The majority (28) had not been hospitalized, and only one was hospitalized for diabetic ketoacidosis (DKA) within 14 days of positive SARS-CoV-2 testing.
This contrasts with a report from the T1D Exchange, in which nearly half of 33 patients with type 1 diabetes and COVID-19 had been hospitalized with DKA. The reason for the discrepancy may be that more severe patients would more likely be referred to the T1D Exchange Registry, Dr. Gregory and colleagues hypothesized.
Clinical factors associated with COVID-19 severity (P < .05) in their study included a prior hypertension diagnosis, higher hemoglobin A1c, at least one prior DKA admission in the past year, and not using a continuous glucose monitor (CGM).
Hospitalizations were twice as likely and illness severity nearly twice as great among those with type 1 diabetes who were Black versus White. Just 8% of those with private insurance were hospitalized, compared with 60% of those with public insurance and 67% with no insurance (P = .001).
“Whereas previous reports have indicated proportionally higher rates of hospitalizations from COVID-19 among Black patients and those with public insurance, this study is the first to show a similar finding in the population with type 1 diabetes,” Dr. Gregory and colleagues wrote.
Only 9% of patients using a CGM were hospitalized versus 47% who used blood glucose meters (P < .016). Similarly, hospitalizations occurred in 6% using an insulin pump versus 33% using multiple daily injections (P < .085).
“Our analysis cannot exclude the possibility that greater amounts of diabetes technology use are a surrogate for higher socioeconomic status,” they noted.
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, JDRF, and the Appleby Foundation. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The risk for increased COVID-19 severity in people with type 1 diabetes appears similar to that of type 2 diabetes, contrary to some official advice from the Centers for Disease Control and Prevention. The new finding indicates that people with both types should be priority for receiving a vaccine, investigators say.
The study is the first to prospectively evaluate both inpatients and outpatients and to examine COVID-19 severity factors in addition to death in people with type 1 and type 2 diabetes separately, and was published online Dec. 2 in Diabetes Care.
Among the patients, who were seen at Vanderbilt University Medical Center in Nashville, Tenn., between March and August of 2020, those with both type 1 and type 2 diabetes had between a three- and fourfold greater risk for COVID-19 hospitalization and greater illness severity compared with people without diabetes after adjustments for age, race, and a number of other risk factors.
This finding is important since as of Dec. 1, 2020, the CDC has classified the diabetes types differently in terms of underlying medical conditions that increase the risk for severe COVID-19.
Adults of any age with type 2 diabetes are considered “at increased risk of severe illness” from the virus that causes COVID-19 whereas the CDC says those with type 1 “might be at an increased risk.”
Lead author of the new paper Justin M. Gregory, MD, said in an interview: “I think this needs revision based on the current evidence. I think the data presented in our study and that of Barron et al. in Lancet Endocrinology 2020 indicate the need to place type 1 diabetes at parity with type 2 diabetes.
“These studies indicate both conditions carry an adjusted odds ratio of three to four when compared with people without diabetes for hospitalization, illness severity, and mortality,” he stressed.
Vaccines look promising for patients with diabetes
There were no phase 3 vaccine data available for the vaccine at the time that Dr. Gregory, of the Ian M. Burr Division of Pediatric Endocrinology and Diabetes, Vanderbilt University, Nashville, Tenn., and colleagues were writing their manuscript in late summer, so the article does not mention this.
But now, Dr. Gregory said, “Based on the initial press releases from Pfizer and Moderna, I am now optimistic that these vaccines might mitigate the excess morbidity and mortality from COVID-19 experienced by patients with diabetes.
“I am eager to see what we learn on December 10 and 17 [the scheduled dates for the meetings of the Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee to review the Pfizer and Moderna vaccines, respectively].”
But with the winter pandemic surge in the meantime, “Our investigation suggests that as COVID-19 hospitalizations rise, patients with both type 1 and 2 diabetes will comprise a disproportionately higher number of those admissions and, once hospitalized, demonstrate a greater degree of illness severity,” he and his colleagues said.
“In light of these data, we call on our colleagues to emphasize the importance of social distancing measures and hand hygiene, with particular emphasis on patients with diabetes, including those in the most vulnerable communities whom our study affirms will face the most severe impact.”
After adjustments, excess severity risk similar for both diabetes types
The new study data came from electronic health records at Vanderbilt University Medical Center, comprising 137 primary care, urgent care, and hospital facilities where patients were tested for SARS-CoV-2 regardless of the reason for their visit.
Between March 17 and August 7, 2020, 6,451 patients tested positive for COVID-19. Of those, 273 had type 2 diabetes and 40 had type 1 diabetes.
Children younger than 18 years accounted for 20% of those with type 1 diabetes and 9.4% of those without diabetes, but none of the type 2 group. The group with type 2 diabetes was considerably older than the type 1 diabetes and no-diabetes groups, 58 years versus 37 and 33 years, respectively.
Before adjustment for baseline characteristics that differed between groups, patients with type 1 diabetes appeared to have a risk for hospitalization and greater illness severity that was intermediate between the group with no diabetes and the group with type 2 diabetes, the researchers said.
But after adjustment for age, race, sex, hypertension, smoking, and body mass index, people with type 1 diabetes had odds ratios of 3.90 for hospitalization and 3.35 for greater illness severity, which was similar to risk in type 2 diabetes (3.36 and 3.42, respectively), compared to those without diabetes.
Deep dive explores COVID-19 severity risk factors in type 1 diabetes
The investigators then conducted a detailed chart review for 37 of the 40 patients with type 1 diabetes and phone surveys with 15 of them.
The majority (28) had not been hospitalized, and only one was hospitalized for diabetic ketoacidosis (DKA) within 14 days of positive SARS-CoV-2 testing.
This contrasts with a report from the T1D Exchange, in which nearly half of 33 patients with type 1 diabetes and COVID-19 had been hospitalized with DKA. The reason for the discrepancy may be that more severe patients would more likely be referred to the T1D Exchange Registry, Dr. Gregory and colleagues hypothesized.
Clinical factors associated with COVID-19 severity (P < .05) in their study included a prior hypertension diagnosis, higher hemoglobin A1c, at least one prior DKA admission in the past year, and not using a continuous glucose monitor (CGM).
Hospitalizations were twice as likely and illness severity nearly twice as great among those with type 1 diabetes who were Black versus White. Just 8% of those with private insurance were hospitalized, compared with 60% of those with public insurance and 67% with no insurance (P = .001).
“Whereas previous reports have indicated proportionally higher rates of hospitalizations from COVID-19 among Black patients and those with public insurance, this study is the first to show a similar finding in the population with type 1 diabetes,” Dr. Gregory and colleagues wrote.
Only 9% of patients using a CGM were hospitalized versus 47% who used blood glucose meters (P < .016). Similarly, hospitalizations occurred in 6% using an insulin pump versus 33% using multiple daily injections (P < .085).
“Our analysis cannot exclude the possibility that greater amounts of diabetes technology use are a surrogate for higher socioeconomic status,” they noted.
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, JDRF, and the Appleby Foundation. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The risk for increased COVID-19 severity in people with type 1 diabetes appears similar to that of type 2 diabetes, contrary to some official advice from the Centers for Disease Control and Prevention. The new finding indicates that people with both types should be priority for receiving a vaccine, investigators say.
The study is the first to prospectively evaluate both inpatients and outpatients and to examine COVID-19 severity factors in addition to death in people with type 1 and type 2 diabetes separately, and was published online Dec. 2 in Diabetes Care.
Among the patients, who were seen at Vanderbilt University Medical Center in Nashville, Tenn., between March and August of 2020, those with both type 1 and type 2 diabetes had between a three- and fourfold greater risk for COVID-19 hospitalization and greater illness severity compared with people without diabetes after adjustments for age, race, and a number of other risk factors.
This finding is important since as of Dec. 1, 2020, the CDC has classified the diabetes types differently in terms of underlying medical conditions that increase the risk for severe COVID-19.
Adults of any age with type 2 diabetes are considered “at increased risk of severe illness” from the virus that causes COVID-19 whereas the CDC says those with type 1 “might be at an increased risk.”
Lead author of the new paper Justin M. Gregory, MD, said in an interview: “I think this needs revision based on the current evidence. I think the data presented in our study and that of Barron et al. in Lancet Endocrinology 2020 indicate the need to place type 1 diabetes at parity with type 2 diabetes.
“These studies indicate both conditions carry an adjusted odds ratio of three to four when compared with people without diabetes for hospitalization, illness severity, and mortality,” he stressed.
Vaccines look promising for patients with diabetes
There were no phase 3 vaccine data available for the vaccine at the time that Dr. Gregory, of the Ian M. Burr Division of Pediatric Endocrinology and Diabetes, Vanderbilt University, Nashville, Tenn., and colleagues were writing their manuscript in late summer, so the article does not mention this.
But now, Dr. Gregory said, “Based on the initial press releases from Pfizer and Moderna, I am now optimistic that these vaccines might mitigate the excess morbidity and mortality from COVID-19 experienced by patients with diabetes.
“I am eager to see what we learn on December 10 and 17 [the scheduled dates for the meetings of the Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee to review the Pfizer and Moderna vaccines, respectively].”
But with the winter pandemic surge in the meantime, “Our investigation suggests that as COVID-19 hospitalizations rise, patients with both type 1 and 2 diabetes will comprise a disproportionately higher number of those admissions and, once hospitalized, demonstrate a greater degree of illness severity,” he and his colleagues said.
“In light of these data, we call on our colleagues to emphasize the importance of social distancing measures and hand hygiene, with particular emphasis on patients with diabetes, including those in the most vulnerable communities whom our study affirms will face the most severe impact.”
After adjustments, excess severity risk similar for both diabetes types
The new study data came from electronic health records at Vanderbilt University Medical Center, comprising 137 primary care, urgent care, and hospital facilities where patients were tested for SARS-CoV-2 regardless of the reason for their visit.
Between March 17 and August 7, 2020, 6,451 patients tested positive for COVID-19. Of those, 273 had type 2 diabetes and 40 had type 1 diabetes.
Children younger than 18 years accounted for 20% of those with type 1 diabetes and 9.4% of those without diabetes, but none of the type 2 group. The group with type 2 diabetes was considerably older than the type 1 diabetes and no-diabetes groups, 58 years versus 37 and 33 years, respectively.
Before adjustment for baseline characteristics that differed between groups, patients with type 1 diabetes appeared to have a risk for hospitalization and greater illness severity that was intermediate between the group with no diabetes and the group with type 2 diabetes, the researchers said.
But after adjustment for age, race, sex, hypertension, smoking, and body mass index, people with type 1 diabetes had odds ratios of 3.90 for hospitalization and 3.35 for greater illness severity, which was similar to risk in type 2 diabetes (3.36 and 3.42, respectively), compared to those without diabetes.
Deep dive explores COVID-19 severity risk factors in type 1 diabetes
The investigators then conducted a detailed chart review for 37 of the 40 patients with type 1 diabetes and phone surveys with 15 of them.
The majority (28) had not been hospitalized, and only one was hospitalized for diabetic ketoacidosis (DKA) within 14 days of positive SARS-CoV-2 testing.
This contrasts with a report from the T1D Exchange, in which nearly half of 33 patients with type 1 diabetes and COVID-19 had been hospitalized with DKA. The reason for the discrepancy may be that more severe patients would more likely be referred to the T1D Exchange Registry, Dr. Gregory and colleagues hypothesized.
Clinical factors associated with COVID-19 severity (P < .05) in their study included a prior hypertension diagnosis, higher hemoglobin A1c, at least one prior DKA admission in the past year, and not using a continuous glucose monitor (CGM).
Hospitalizations were twice as likely and illness severity nearly twice as great among those with type 1 diabetes who were Black versus White. Just 8% of those with private insurance were hospitalized, compared with 60% of those with public insurance and 67% with no insurance (P = .001).
“Whereas previous reports have indicated proportionally higher rates of hospitalizations from COVID-19 among Black patients and those with public insurance, this study is the first to show a similar finding in the population with type 1 diabetes,” Dr. Gregory and colleagues wrote.
Only 9% of patients using a CGM were hospitalized versus 47% who used blood glucose meters (P < .016). Similarly, hospitalizations occurred in 6% using an insulin pump versus 33% using multiple daily injections (P < .085).
“Our analysis cannot exclude the possibility that greater amounts of diabetes technology use are a surrogate for higher socioeconomic status,” they noted.
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, JDRF, and the Appleby Foundation. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.