User login
Demand for COVID vaccines expected to get heated – and fast
Americans have made no secret of their skepticism of COVID-19 vaccines this year, with fears of political interference and a “warp speed” timeline blunting confidence in the shots. As recently as September, nearly half of U.S. adults said they didn’t intend to be inoculated.
But with two promising vaccines primed for release, likely within weeks, experts in ethics and immunization behavior say they expect attitudes to shift quickly from widespread hesitancy to urgent, even heated demand.
“People talk about the antivaccine people being able to kind of squelch uptake. I don’t see that happening,” Dr. Paul Offit, MD, a vaccinologist with Children’s Hospital of Philadelphia, told viewers of a recent JAMA Network webinar. “This, to me, is more like the Beanie Baby phenomenon. The attractiveness of a limited edition.”
Reports that vaccines produced by drugmakers Pfizer and BioNTech and Moderna appear to be safe and effective, along with the deliberate emphasis on science-based guidance from the incoming Biden administration, are likely to reverse uncertainty in a big way, said Arthur Caplan, PhD, director of the division of medical ethics at New York University.
“I think that’s going to flip the trust issue,” he said.
The shift is already apparent. A new poll by the Pew Research Center found that by the end of November 60% of Americans said they would get a vaccine for the coronavirus. This month, even as a federal advisory group met to hash out guidelines for vaccine distribution, a long list of advocacy groups – from those representing home-based health workers and community health centers to patients with kidney disease – were lobbying state and federal officials in hopes their constituents would be prioritized for the first scarce doses.
“As we get closer to the vaccine being a reality, there’s a lot of jockeying, to be sure,” said Katie Smith Sloan, chief executive of LeadingAge, a nonprofit organization pushing for staff and patients at long-term care centers to be included in the highest-priority category.
Certainly, some consumers remain wary, said Rupali Limaye, PhD, a social and behavioral health scientist at the Johns Hopkins Bloomberg School of Public Health, Baltimore. Fears that drugmakers and regulators might cut corners to speed a vaccine linger, even as details of the trials become public and the review process is made more transparent. Some health care workers, who are at the front of the line for the shots, are not eager to go first.
“There will be people who will say, ‘I will wait a little bit more for safety data,” Dr. Limaye said.
But those doubts likely will recede once the vaccines are approved for use and begin to circulate broadly, said Dr. Offit, who sits on the Food and Drug Administration advisory panel set to review the requests for emergency authorization Pfizer and Moderna have submitted.
He predicted demand for the COVID vaccines could rival the clamor that occurred in 2004, when production problems caused a severe shortage of flu shots just as influenza season began. That led to long lines, rationed doses and ethical debates over distribution.
“That was a highly desired vaccine,” Dr. Offit said. “I think in many ways that might happen here.”
Initially, vaccine supplies will be tight, with federal officials planning to ship 6.4 million doses within 24 hours of FDA authorization and up to 40 million doses by the end of the year. The CDC panel recommended that the first shots go to the 21 million health care workers in the United States and 3 million nursing home staff and residents, before being rolled out to other groups based on a hierarchy of risk factors.
Even before any vaccine is available, some people are trying to boost their chances of access, said Allison Kempe, MD, a professor of pediatrics at the University of Coloradoat Denver, Aurora, and expert in vaccine dissemination. “People have called me and said, ‘How can I get the vaccine?’” she said. “I think that not everyone will be happy to wait, that’s for sure. I don’t think there will be rioting in the streets, but there may be pressure brought to bear.”
That likely will include emotional debates over how, when, and to whom next doses should be distributed, said Dr. Caplan. Under the CDC recommendations, vulnerable groups next in line include 87 million workers whose jobs are deemed “essential” – a broad and ill-defined category – as well as 53 million adults age 65 and older.
“We’re going to have some fights about high-risk groups,” Dr. Caplan said.
The conversations will be complicated. Should prisoners, who have little control over their COVID exposure, get vaccine priority? How about professional sports teams, whose performance could bolster society’s overall morale? And what about residents of facilities providing care for people with intellectual and developmental disabilities, who are three times more likely to die from COVID-19 than the general population?
Control over vaccination allocation rests with the states, so that’s where the biggest conflicts will occur, Dr. Caplan said. “It’s a short fight, I hope, in the sense in which it gets done in a few months, but I think it will be pretty vocal.”
Once vaccine supplies become more plentiful, perhaps by May or June, another consideration is sure to boost demand: requirements for proof of COVID vaccination for work and travel.
“It’s inevitable that you’re going to see immunity passports or that you’re required to show a certificate on the train, airplane, bus, or subway,” Dr. Caplan predicted. “Probably also to enter certain hospitals, probably to enter certain restaurants and government facilities.”
But with a grueling winter surge ahead, and new predictions that COVID-19 will fell as many as 450,000 Americans by February, the tragic reality of the disease will no doubt fuel ample demand for vaccination.
“People now know someone who has gotten COVID, who has been hospitalized or has unfortunately died,” Dr. Limaye said.
“We’re all seeing this now,” said Dr. Kempe. “Even deniers are beginning to see what this illness can do.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Americans have made no secret of their skepticism of COVID-19 vaccines this year, with fears of political interference and a “warp speed” timeline blunting confidence in the shots. As recently as September, nearly half of U.S. adults said they didn’t intend to be inoculated.
But with two promising vaccines primed for release, likely within weeks, experts in ethics and immunization behavior say they expect attitudes to shift quickly from widespread hesitancy to urgent, even heated demand.
“People talk about the antivaccine people being able to kind of squelch uptake. I don’t see that happening,” Dr. Paul Offit, MD, a vaccinologist with Children’s Hospital of Philadelphia, told viewers of a recent JAMA Network webinar. “This, to me, is more like the Beanie Baby phenomenon. The attractiveness of a limited edition.”
Reports that vaccines produced by drugmakers Pfizer and BioNTech and Moderna appear to be safe and effective, along with the deliberate emphasis on science-based guidance from the incoming Biden administration, are likely to reverse uncertainty in a big way, said Arthur Caplan, PhD, director of the division of medical ethics at New York University.
“I think that’s going to flip the trust issue,” he said.
The shift is already apparent. A new poll by the Pew Research Center found that by the end of November 60% of Americans said they would get a vaccine for the coronavirus. This month, even as a federal advisory group met to hash out guidelines for vaccine distribution, a long list of advocacy groups – from those representing home-based health workers and community health centers to patients with kidney disease – were lobbying state and federal officials in hopes their constituents would be prioritized for the first scarce doses.
“As we get closer to the vaccine being a reality, there’s a lot of jockeying, to be sure,” said Katie Smith Sloan, chief executive of LeadingAge, a nonprofit organization pushing for staff and patients at long-term care centers to be included in the highest-priority category.
Certainly, some consumers remain wary, said Rupali Limaye, PhD, a social and behavioral health scientist at the Johns Hopkins Bloomberg School of Public Health, Baltimore. Fears that drugmakers and regulators might cut corners to speed a vaccine linger, even as details of the trials become public and the review process is made more transparent. Some health care workers, who are at the front of the line for the shots, are not eager to go first.
“There will be people who will say, ‘I will wait a little bit more for safety data,” Dr. Limaye said.
But those doubts likely will recede once the vaccines are approved for use and begin to circulate broadly, said Dr. Offit, who sits on the Food and Drug Administration advisory panel set to review the requests for emergency authorization Pfizer and Moderna have submitted.
He predicted demand for the COVID vaccines could rival the clamor that occurred in 2004, when production problems caused a severe shortage of flu shots just as influenza season began. That led to long lines, rationed doses and ethical debates over distribution.
“That was a highly desired vaccine,” Dr. Offit said. “I think in many ways that might happen here.”
Initially, vaccine supplies will be tight, with federal officials planning to ship 6.4 million doses within 24 hours of FDA authorization and up to 40 million doses by the end of the year. The CDC panel recommended that the first shots go to the 21 million health care workers in the United States and 3 million nursing home staff and residents, before being rolled out to other groups based on a hierarchy of risk factors.
Even before any vaccine is available, some people are trying to boost their chances of access, said Allison Kempe, MD, a professor of pediatrics at the University of Coloradoat Denver, Aurora, and expert in vaccine dissemination. “People have called me and said, ‘How can I get the vaccine?’” she said. “I think that not everyone will be happy to wait, that’s for sure. I don’t think there will be rioting in the streets, but there may be pressure brought to bear.”
That likely will include emotional debates over how, when, and to whom next doses should be distributed, said Dr. Caplan. Under the CDC recommendations, vulnerable groups next in line include 87 million workers whose jobs are deemed “essential” – a broad and ill-defined category – as well as 53 million adults age 65 and older.
“We’re going to have some fights about high-risk groups,” Dr. Caplan said.
The conversations will be complicated. Should prisoners, who have little control over their COVID exposure, get vaccine priority? How about professional sports teams, whose performance could bolster society’s overall morale? And what about residents of facilities providing care for people with intellectual and developmental disabilities, who are three times more likely to die from COVID-19 than the general population?
Control over vaccination allocation rests with the states, so that’s where the biggest conflicts will occur, Dr. Caplan said. “It’s a short fight, I hope, in the sense in which it gets done in a few months, but I think it will be pretty vocal.”
Once vaccine supplies become more plentiful, perhaps by May or June, another consideration is sure to boost demand: requirements for proof of COVID vaccination for work and travel.
“It’s inevitable that you’re going to see immunity passports or that you’re required to show a certificate on the train, airplane, bus, or subway,” Dr. Caplan predicted. “Probably also to enter certain hospitals, probably to enter certain restaurants and government facilities.”
But with a grueling winter surge ahead, and new predictions that COVID-19 will fell as many as 450,000 Americans by February, the tragic reality of the disease will no doubt fuel ample demand for vaccination.
“People now know someone who has gotten COVID, who has been hospitalized or has unfortunately died,” Dr. Limaye said.
“We’re all seeing this now,” said Dr. Kempe. “Even deniers are beginning to see what this illness can do.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Americans have made no secret of their skepticism of COVID-19 vaccines this year, with fears of political interference and a “warp speed” timeline blunting confidence in the shots. As recently as September, nearly half of U.S. adults said they didn’t intend to be inoculated.
But with two promising vaccines primed for release, likely within weeks, experts in ethics and immunization behavior say they expect attitudes to shift quickly from widespread hesitancy to urgent, even heated demand.
“People talk about the antivaccine people being able to kind of squelch uptake. I don’t see that happening,” Dr. Paul Offit, MD, a vaccinologist with Children’s Hospital of Philadelphia, told viewers of a recent JAMA Network webinar. “This, to me, is more like the Beanie Baby phenomenon. The attractiveness of a limited edition.”
Reports that vaccines produced by drugmakers Pfizer and BioNTech and Moderna appear to be safe and effective, along with the deliberate emphasis on science-based guidance from the incoming Biden administration, are likely to reverse uncertainty in a big way, said Arthur Caplan, PhD, director of the division of medical ethics at New York University.
“I think that’s going to flip the trust issue,” he said.
The shift is already apparent. A new poll by the Pew Research Center found that by the end of November 60% of Americans said they would get a vaccine for the coronavirus. This month, even as a federal advisory group met to hash out guidelines for vaccine distribution, a long list of advocacy groups – from those representing home-based health workers and community health centers to patients with kidney disease – were lobbying state and federal officials in hopes their constituents would be prioritized for the first scarce doses.
“As we get closer to the vaccine being a reality, there’s a lot of jockeying, to be sure,” said Katie Smith Sloan, chief executive of LeadingAge, a nonprofit organization pushing for staff and patients at long-term care centers to be included in the highest-priority category.
Certainly, some consumers remain wary, said Rupali Limaye, PhD, a social and behavioral health scientist at the Johns Hopkins Bloomberg School of Public Health, Baltimore. Fears that drugmakers and regulators might cut corners to speed a vaccine linger, even as details of the trials become public and the review process is made more transparent. Some health care workers, who are at the front of the line for the shots, are not eager to go first.
“There will be people who will say, ‘I will wait a little bit more for safety data,” Dr. Limaye said.
But those doubts likely will recede once the vaccines are approved for use and begin to circulate broadly, said Dr. Offit, who sits on the Food and Drug Administration advisory panel set to review the requests for emergency authorization Pfizer and Moderna have submitted.
He predicted demand for the COVID vaccines could rival the clamor that occurred in 2004, when production problems caused a severe shortage of flu shots just as influenza season began. That led to long lines, rationed doses and ethical debates over distribution.
“That was a highly desired vaccine,” Dr. Offit said. “I think in many ways that might happen here.”
Initially, vaccine supplies will be tight, with federal officials planning to ship 6.4 million doses within 24 hours of FDA authorization and up to 40 million doses by the end of the year. The CDC panel recommended that the first shots go to the 21 million health care workers in the United States and 3 million nursing home staff and residents, before being rolled out to other groups based on a hierarchy of risk factors.
Even before any vaccine is available, some people are trying to boost their chances of access, said Allison Kempe, MD, a professor of pediatrics at the University of Coloradoat Denver, Aurora, and expert in vaccine dissemination. “People have called me and said, ‘How can I get the vaccine?’” she said. “I think that not everyone will be happy to wait, that’s for sure. I don’t think there will be rioting in the streets, but there may be pressure brought to bear.”
That likely will include emotional debates over how, when, and to whom next doses should be distributed, said Dr. Caplan. Under the CDC recommendations, vulnerable groups next in line include 87 million workers whose jobs are deemed “essential” – a broad and ill-defined category – as well as 53 million adults age 65 and older.
“We’re going to have some fights about high-risk groups,” Dr. Caplan said.
The conversations will be complicated. Should prisoners, who have little control over their COVID exposure, get vaccine priority? How about professional sports teams, whose performance could bolster society’s overall morale? And what about residents of facilities providing care for people with intellectual and developmental disabilities, who are three times more likely to die from COVID-19 than the general population?
Control over vaccination allocation rests with the states, so that’s where the biggest conflicts will occur, Dr. Caplan said. “It’s a short fight, I hope, in the sense in which it gets done in a few months, but I think it will be pretty vocal.”
Once vaccine supplies become more plentiful, perhaps by May or June, another consideration is sure to boost demand: requirements for proof of COVID vaccination for work and travel.
“It’s inevitable that you’re going to see immunity passports or that you’re required to show a certificate on the train, airplane, bus, or subway,” Dr. Caplan predicted. “Probably also to enter certain hospitals, probably to enter certain restaurants and government facilities.”
But with a grueling winter surge ahead, and new predictions that COVID-19 will fell as many as 450,000 Americans by February, the tragic reality of the disease will no doubt fuel ample demand for vaccination.
“People now know someone who has gotten COVID, who has been hospitalized or has unfortunately died,” Dr. Limaye said.
“We’re all seeing this now,” said Dr. Kempe. “Even deniers are beginning to see what this illness can do.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Obesity, hypoxia predict severity in children with COVID-19
based on data from 281 patients at 8 locations.
Manifestations of COVID-19 in children include respiratory disease similar to that seen in adults, but the full spectrum of disease in children has been studied mainly in single settings or with a focus on one clinical manifestation, wrote Danielle M. Fernandes, MD, of Albert Einstein College of Medicine, New York, and colleagues.
In a study published in the Journal of Pediatrics, the researchers identified 281 children hospitalized with COVID-19 and/or multisystem inflammatory syndrome in children (MIS-C) at 8 sites in Connecticut, New Jersey, and New York. A total of 143 (51%) had respiratory disease, 69 (25%) had MIS-C, and 69 (25%) had other manifestations of illness including 32 patients with gastrointestinal problems, 21 infants with fever, 6 cases of neurologic disease, 6 cases of diabetic ketoacidosis, and 4 patients with other indications. The median age of the patients was 10 years, 60% were male, 51% were Hispanic, and 23% were non-Hispanic Black. The most common comorbidities were obesity (34%) and asthma (14%).
Independent predictors of disease severity in children found
After controlling for multiple variables, obesity and hypoxia at hospital admission were significant independent predictors of severe respiratory disease, with odds ratios of 3.39 and 4.01, respectively. In addition, lower absolute lymphocyte count (OR, 8.33 per unit decrease in 109 cells/L) and higher C-reactive protein (OR, 1.06 per unit increase in mg/dL) were significantly predictive of severe MIS-C (P = .001 and P = .017, respectively).
“The association between weight and severe respiratory COVID-19 is consistent with the adult literature; however, the mechanisms of this association require further study,” Dr. Fernandes and associates noted.
Overall, children with MIS-C were significantly more likely to be non-Hispanic Black, compared with children with respiratory disease, an 18% difference. However, neither race/ethnicity nor socioeconomic status were significant predictors of disease severity, the researchers wrote.
During the study period, 7 patients (2%) died and 114 (41%) were admitted to the ICU.
“We found a wide array of clinical manifestations in children and youth hospitalized with SARS-CoV-2,” Dr. Fernandes and associates wrote. Notably, gastrointestinal symptoms, ocular symptoms, and dermatologic symptoms have rarely been noted in adults with COVID-19, but occurred in more than 30% of the pediatric patients.
“We also found that SARS-CoV-2 can be an incidental finding in a substantial number of hospitalized pediatric patients,” the researchers said.
The findings were limited by several factors including a population of patients only from Connecticut, New Jersey, and New York, and the possibility that decisions on hospital and ICU admission may have varied by location, the researchers said. In addition, approaches may have varied in the absence of data on the optimal treatment of MIS-C.
“This study builds on the growing body of evidence showing that mortality in hospitalized pediatric patients is low, compared with adults,” Dr. Fernandes and associates said. “However, it highlights that the young population is not universally spared from morbidity, and that even previously healthy children and youth can develop severe disease requiring supportive therapy.”
Findings confirm other clinical experience
The study was important to show that, “although most children are spared severe illness from COVID-19, some children are hospitalized both with acute COVID-19 respiratory disease, with MIS-C and with a range of other complications,” Adrienne Randolph, MD, of Boston Children’s Hospital and Harvard Medical School, Boston, said in an interview.
Dr. Randolph said she was not surprised by the study findings, “as we are also seeing these types of complications at Boston Children’s Hospital where I work.”
Additional research is needed on the outcomes of these patients, “especially the longer-term sequelae of having COVID-19 or MIS-C early in life,” she emphasized.
The take-home message to clinicians from the findings at this time is to be aware that children and adolescents can become severely ill from COVID-19–related complications, said Dr. Randolph. “Some of the laboratory values on presentation appear to be associated with disease severity.”
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Randolph disclosed funding from the Centers for Disease Control and Prevention to lead the Overcoming COVID-19 Study in U.S. Children and Adults.
SOURCE: Fernandes DM et al. J Pediatr. 2020 Nov 13. doi: 10.1016/j.jpeds.2020.11.016.
based on data from 281 patients at 8 locations.
Manifestations of COVID-19 in children include respiratory disease similar to that seen in adults, but the full spectrum of disease in children has been studied mainly in single settings or with a focus on one clinical manifestation, wrote Danielle M. Fernandes, MD, of Albert Einstein College of Medicine, New York, and colleagues.
In a study published in the Journal of Pediatrics, the researchers identified 281 children hospitalized with COVID-19 and/or multisystem inflammatory syndrome in children (MIS-C) at 8 sites in Connecticut, New Jersey, and New York. A total of 143 (51%) had respiratory disease, 69 (25%) had MIS-C, and 69 (25%) had other manifestations of illness including 32 patients with gastrointestinal problems, 21 infants with fever, 6 cases of neurologic disease, 6 cases of diabetic ketoacidosis, and 4 patients with other indications. The median age of the patients was 10 years, 60% were male, 51% were Hispanic, and 23% were non-Hispanic Black. The most common comorbidities were obesity (34%) and asthma (14%).
Independent predictors of disease severity in children found
After controlling for multiple variables, obesity and hypoxia at hospital admission were significant independent predictors of severe respiratory disease, with odds ratios of 3.39 and 4.01, respectively. In addition, lower absolute lymphocyte count (OR, 8.33 per unit decrease in 109 cells/L) and higher C-reactive protein (OR, 1.06 per unit increase in mg/dL) were significantly predictive of severe MIS-C (P = .001 and P = .017, respectively).
“The association between weight and severe respiratory COVID-19 is consistent with the adult literature; however, the mechanisms of this association require further study,” Dr. Fernandes and associates noted.
Overall, children with MIS-C were significantly more likely to be non-Hispanic Black, compared with children with respiratory disease, an 18% difference. However, neither race/ethnicity nor socioeconomic status were significant predictors of disease severity, the researchers wrote.
During the study period, 7 patients (2%) died and 114 (41%) were admitted to the ICU.
“We found a wide array of clinical manifestations in children and youth hospitalized with SARS-CoV-2,” Dr. Fernandes and associates wrote. Notably, gastrointestinal symptoms, ocular symptoms, and dermatologic symptoms have rarely been noted in adults with COVID-19, but occurred in more than 30% of the pediatric patients.
“We also found that SARS-CoV-2 can be an incidental finding in a substantial number of hospitalized pediatric patients,” the researchers said.
The findings were limited by several factors including a population of patients only from Connecticut, New Jersey, and New York, and the possibility that decisions on hospital and ICU admission may have varied by location, the researchers said. In addition, approaches may have varied in the absence of data on the optimal treatment of MIS-C.
“This study builds on the growing body of evidence showing that mortality in hospitalized pediatric patients is low, compared with adults,” Dr. Fernandes and associates said. “However, it highlights that the young population is not universally spared from morbidity, and that even previously healthy children and youth can develop severe disease requiring supportive therapy.”
Findings confirm other clinical experience
The study was important to show that, “although most children are spared severe illness from COVID-19, some children are hospitalized both with acute COVID-19 respiratory disease, with MIS-C and with a range of other complications,” Adrienne Randolph, MD, of Boston Children’s Hospital and Harvard Medical School, Boston, said in an interview.
Dr. Randolph said she was not surprised by the study findings, “as we are also seeing these types of complications at Boston Children’s Hospital where I work.”
Additional research is needed on the outcomes of these patients, “especially the longer-term sequelae of having COVID-19 or MIS-C early in life,” she emphasized.
The take-home message to clinicians from the findings at this time is to be aware that children and adolescents can become severely ill from COVID-19–related complications, said Dr. Randolph. “Some of the laboratory values on presentation appear to be associated with disease severity.”
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Randolph disclosed funding from the Centers for Disease Control and Prevention to lead the Overcoming COVID-19 Study in U.S. Children and Adults.
SOURCE: Fernandes DM et al. J Pediatr. 2020 Nov 13. doi: 10.1016/j.jpeds.2020.11.016.
based on data from 281 patients at 8 locations.
Manifestations of COVID-19 in children include respiratory disease similar to that seen in adults, but the full spectrum of disease in children has been studied mainly in single settings or with a focus on one clinical manifestation, wrote Danielle M. Fernandes, MD, of Albert Einstein College of Medicine, New York, and colleagues.
In a study published in the Journal of Pediatrics, the researchers identified 281 children hospitalized with COVID-19 and/or multisystem inflammatory syndrome in children (MIS-C) at 8 sites in Connecticut, New Jersey, and New York. A total of 143 (51%) had respiratory disease, 69 (25%) had MIS-C, and 69 (25%) had other manifestations of illness including 32 patients with gastrointestinal problems, 21 infants with fever, 6 cases of neurologic disease, 6 cases of diabetic ketoacidosis, and 4 patients with other indications. The median age of the patients was 10 years, 60% were male, 51% were Hispanic, and 23% were non-Hispanic Black. The most common comorbidities were obesity (34%) and asthma (14%).
Independent predictors of disease severity in children found
After controlling for multiple variables, obesity and hypoxia at hospital admission were significant independent predictors of severe respiratory disease, with odds ratios of 3.39 and 4.01, respectively. In addition, lower absolute lymphocyte count (OR, 8.33 per unit decrease in 109 cells/L) and higher C-reactive protein (OR, 1.06 per unit increase in mg/dL) were significantly predictive of severe MIS-C (P = .001 and P = .017, respectively).
“The association between weight and severe respiratory COVID-19 is consistent with the adult literature; however, the mechanisms of this association require further study,” Dr. Fernandes and associates noted.
Overall, children with MIS-C were significantly more likely to be non-Hispanic Black, compared with children with respiratory disease, an 18% difference. However, neither race/ethnicity nor socioeconomic status were significant predictors of disease severity, the researchers wrote.
During the study period, 7 patients (2%) died and 114 (41%) were admitted to the ICU.
“We found a wide array of clinical manifestations in children and youth hospitalized with SARS-CoV-2,” Dr. Fernandes and associates wrote. Notably, gastrointestinal symptoms, ocular symptoms, and dermatologic symptoms have rarely been noted in adults with COVID-19, but occurred in more than 30% of the pediatric patients.
“We also found that SARS-CoV-2 can be an incidental finding in a substantial number of hospitalized pediatric patients,” the researchers said.
The findings were limited by several factors including a population of patients only from Connecticut, New Jersey, and New York, and the possibility that decisions on hospital and ICU admission may have varied by location, the researchers said. In addition, approaches may have varied in the absence of data on the optimal treatment of MIS-C.
“This study builds on the growing body of evidence showing that mortality in hospitalized pediatric patients is low, compared with adults,” Dr. Fernandes and associates said. “However, it highlights that the young population is not universally spared from morbidity, and that even previously healthy children and youth can develop severe disease requiring supportive therapy.”
Findings confirm other clinical experience
The study was important to show that, “although most children are spared severe illness from COVID-19, some children are hospitalized both with acute COVID-19 respiratory disease, with MIS-C and with a range of other complications,” Adrienne Randolph, MD, of Boston Children’s Hospital and Harvard Medical School, Boston, said in an interview.
Dr. Randolph said she was not surprised by the study findings, “as we are also seeing these types of complications at Boston Children’s Hospital where I work.”
Additional research is needed on the outcomes of these patients, “especially the longer-term sequelae of having COVID-19 or MIS-C early in life,” she emphasized.
The take-home message to clinicians from the findings at this time is to be aware that children and adolescents can become severely ill from COVID-19–related complications, said Dr. Randolph. “Some of the laboratory values on presentation appear to be associated with disease severity.”
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Randolph disclosed funding from the Centers for Disease Control and Prevention to lead the Overcoming COVID-19 Study in U.S. Children and Adults.
SOURCE: Fernandes DM et al. J Pediatr. 2020 Nov 13. doi: 10.1016/j.jpeds.2020.11.016.
FROM THE JOURNAL OF PEDIATRICS
Liquid oxygen recommended for mobile patients with lung disease
People with chronic lung disease who need significant amounts of oxygen should be able to take it in liquid form when they are able to leave home, according to a new guideline from the American Thoracic Society.
“For those patients, often the other types of devices either can’t supply enough oxygen or are not portable enough,” said Anne Holland, PT, PhD, a professor of physiotherapy at Monash University and Alfred Hospital in Melbourne. “They’re heavy and cumbersome to use.”
Dr. Holland and colleagues also gave a more general recommendation to prescribe ambulatory oxygen – though not necessarily in liquid form – for adults with chronic obstructive pulmonary disease (COPD) or interstitial lung disease (ILD) who have severe exertional room air hypoxemia.
They published the recommendations as part of the ATS’ first-ever guideline on home oxygen therapy for adults with chronic lung disease in the American Journal of Respiratory and Critical Care Medicine.
The ATS identified the need for an updated guideline because of new research, and because an online survey of almost 2,000 U.S. oxygen users showed they were having problems accessing and using oxygen.
For long-term oxygen therapy, the guideline reinforces what most practitioners are already doing, Dr. Holland said. It recommends that adults with COPD or ILD who have severe chronic resting room air hypoxemia receive oxygen therapy at least 15 hours per day.
On the other hand, in adults with COPD who have moderate chronic resting room-air hypoxemia, the guideline recommends against long-term oxygen therapy.
The recommendation to prescribe ambulatory oxygen for people with severe exertional room-air hypoxemia may have more effect on practice, Dr. Holland said. Laboratory-based tests have suggested oxygen can improve exercise capacity, but clinical trials used during daily life have had inconsistent results.
The evidence is particularly lacking for patients with ILD, Dr. Holland said in an interview. “It’s such an important part of practice to maintain oxygen therapy that it’s ethically very difficult to conduct such a trial. So, we did have to make use of indirect evidence from patients with COPD” for the guidelines.
The portable equipment comes with burdens, including managing its weight and bulk, social stigma, fear of cylinders running out, and equipment noise.
“We tried to clearly set out both the benefits and burdens of that therapy and made a conditional recommendation, and also a really strong call for shared decision-making with patients and health professionals,” Dr. Holland said.
In addition to looking at the evidence, the panel took into consideration the concerns identified by patients. This included the challenge of figuring out how to use the equipment. “All the oxygen equipment was ‘dumped’ on me,” wrote one oxygen user quoted in the guideline. “I knew nothing and was in a daze. I am sure that the delivery guy gave me some instructions when it was delivered but I retained nothing.”
For this reason, the guideline describes instruction and training on the use and maintenance of the equipment, including smoking cessation, fire prevention, and tripping hazards, as a “best practice.”
Nothing about the guideline is surprising, said MeiLan K. Han, MD, a spokesperson for the American Lung Association and professor of pulmonary and critical care medicine at the University of Michigan Health System in Ann Arbor. “I don’t think they’ve actually come to any new conclusion,” she said in an interview. “This is pretty much how I practice already.”
But the guideline could have an effect on policy, she said. The panel noted research showing that lower Medicare reimbursement to durable medical equipment companies since 2011 has forced many patients to switch from small, easily portable liquid oxygen to home-fill oxygen systems that include heavy cylinders.
“The impact of this decline in the availability and adequacy of portable oxygen devices in the United States has been profound,” Dr. Holland and colleagues wrote. “Supplemental oxygen users reported numerous problems, with the overarching theme being restricted mobility and isolation due to inadequate portable options.”
For this reason, the guideline recommends liquid oxygen for patients with chronic lung disease who are mobile outside of the home and require continuous oxygen flow rates of >3 L/min during exertion.
Many of Dr. Han’s patients have struggled with this problem, she said. “The clunkiest, most painful form of ‘ambulatory oxygen’ are these really large metal cylinders. They’re huge. And you have to carry them on a cart. It’s portable in theory only.”
Some of her patients have resorted to buying their own equipment on eBay, she said.
The authors report multiple disclosures including serving as advisory board members to foundations and pharmaceutical companies, and some are company employees or stockholders.
A version of this article originally appeared on Medscape.com.
People with chronic lung disease who need significant amounts of oxygen should be able to take it in liquid form when they are able to leave home, according to a new guideline from the American Thoracic Society.
“For those patients, often the other types of devices either can’t supply enough oxygen or are not portable enough,” said Anne Holland, PT, PhD, a professor of physiotherapy at Monash University and Alfred Hospital in Melbourne. “They’re heavy and cumbersome to use.”
Dr. Holland and colleagues also gave a more general recommendation to prescribe ambulatory oxygen – though not necessarily in liquid form – for adults with chronic obstructive pulmonary disease (COPD) or interstitial lung disease (ILD) who have severe exertional room air hypoxemia.
They published the recommendations as part of the ATS’ first-ever guideline on home oxygen therapy for adults with chronic lung disease in the American Journal of Respiratory and Critical Care Medicine.
The ATS identified the need for an updated guideline because of new research, and because an online survey of almost 2,000 U.S. oxygen users showed they were having problems accessing and using oxygen.
For long-term oxygen therapy, the guideline reinforces what most practitioners are already doing, Dr. Holland said. It recommends that adults with COPD or ILD who have severe chronic resting room air hypoxemia receive oxygen therapy at least 15 hours per day.
On the other hand, in adults with COPD who have moderate chronic resting room-air hypoxemia, the guideline recommends against long-term oxygen therapy.
The recommendation to prescribe ambulatory oxygen for people with severe exertional room-air hypoxemia may have more effect on practice, Dr. Holland said. Laboratory-based tests have suggested oxygen can improve exercise capacity, but clinical trials used during daily life have had inconsistent results.
The evidence is particularly lacking for patients with ILD, Dr. Holland said in an interview. “It’s such an important part of practice to maintain oxygen therapy that it’s ethically very difficult to conduct such a trial. So, we did have to make use of indirect evidence from patients with COPD” for the guidelines.
The portable equipment comes with burdens, including managing its weight and bulk, social stigma, fear of cylinders running out, and equipment noise.
“We tried to clearly set out both the benefits and burdens of that therapy and made a conditional recommendation, and also a really strong call for shared decision-making with patients and health professionals,” Dr. Holland said.
In addition to looking at the evidence, the panel took into consideration the concerns identified by patients. This included the challenge of figuring out how to use the equipment. “All the oxygen equipment was ‘dumped’ on me,” wrote one oxygen user quoted in the guideline. “I knew nothing and was in a daze. I am sure that the delivery guy gave me some instructions when it was delivered but I retained nothing.”
For this reason, the guideline describes instruction and training on the use and maintenance of the equipment, including smoking cessation, fire prevention, and tripping hazards, as a “best practice.”
Nothing about the guideline is surprising, said MeiLan K. Han, MD, a spokesperson for the American Lung Association and professor of pulmonary and critical care medicine at the University of Michigan Health System in Ann Arbor. “I don’t think they’ve actually come to any new conclusion,” she said in an interview. “This is pretty much how I practice already.”
But the guideline could have an effect on policy, she said. The panel noted research showing that lower Medicare reimbursement to durable medical equipment companies since 2011 has forced many patients to switch from small, easily portable liquid oxygen to home-fill oxygen systems that include heavy cylinders.
“The impact of this decline in the availability and adequacy of portable oxygen devices in the United States has been profound,” Dr. Holland and colleagues wrote. “Supplemental oxygen users reported numerous problems, with the overarching theme being restricted mobility and isolation due to inadequate portable options.”
For this reason, the guideline recommends liquid oxygen for patients with chronic lung disease who are mobile outside of the home and require continuous oxygen flow rates of >3 L/min during exertion.
Many of Dr. Han’s patients have struggled with this problem, she said. “The clunkiest, most painful form of ‘ambulatory oxygen’ are these really large metal cylinders. They’re huge. And you have to carry them on a cart. It’s portable in theory only.”
Some of her patients have resorted to buying their own equipment on eBay, she said.
The authors report multiple disclosures including serving as advisory board members to foundations and pharmaceutical companies, and some are company employees or stockholders.
A version of this article originally appeared on Medscape.com.
People with chronic lung disease who need significant amounts of oxygen should be able to take it in liquid form when they are able to leave home, according to a new guideline from the American Thoracic Society.
“For those patients, often the other types of devices either can’t supply enough oxygen or are not portable enough,” said Anne Holland, PT, PhD, a professor of physiotherapy at Monash University and Alfred Hospital in Melbourne. “They’re heavy and cumbersome to use.”
Dr. Holland and colleagues also gave a more general recommendation to prescribe ambulatory oxygen – though not necessarily in liquid form – for adults with chronic obstructive pulmonary disease (COPD) or interstitial lung disease (ILD) who have severe exertional room air hypoxemia.
They published the recommendations as part of the ATS’ first-ever guideline on home oxygen therapy for adults with chronic lung disease in the American Journal of Respiratory and Critical Care Medicine.
The ATS identified the need for an updated guideline because of new research, and because an online survey of almost 2,000 U.S. oxygen users showed they were having problems accessing and using oxygen.
For long-term oxygen therapy, the guideline reinforces what most practitioners are already doing, Dr. Holland said. It recommends that adults with COPD or ILD who have severe chronic resting room air hypoxemia receive oxygen therapy at least 15 hours per day.
On the other hand, in adults with COPD who have moderate chronic resting room-air hypoxemia, the guideline recommends against long-term oxygen therapy.
The recommendation to prescribe ambulatory oxygen for people with severe exertional room-air hypoxemia may have more effect on practice, Dr. Holland said. Laboratory-based tests have suggested oxygen can improve exercise capacity, but clinical trials used during daily life have had inconsistent results.
The evidence is particularly lacking for patients with ILD, Dr. Holland said in an interview. “It’s such an important part of practice to maintain oxygen therapy that it’s ethically very difficult to conduct such a trial. So, we did have to make use of indirect evidence from patients with COPD” for the guidelines.
The portable equipment comes with burdens, including managing its weight and bulk, social stigma, fear of cylinders running out, and equipment noise.
“We tried to clearly set out both the benefits and burdens of that therapy and made a conditional recommendation, and also a really strong call for shared decision-making with patients and health professionals,” Dr. Holland said.
In addition to looking at the evidence, the panel took into consideration the concerns identified by patients. This included the challenge of figuring out how to use the equipment. “All the oxygen equipment was ‘dumped’ on me,” wrote one oxygen user quoted in the guideline. “I knew nothing and was in a daze. I am sure that the delivery guy gave me some instructions when it was delivered but I retained nothing.”
For this reason, the guideline describes instruction and training on the use and maintenance of the equipment, including smoking cessation, fire prevention, and tripping hazards, as a “best practice.”
Nothing about the guideline is surprising, said MeiLan K. Han, MD, a spokesperson for the American Lung Association and professor of pulmonary and critical care medicine at the University of Michigan Health System in Ann Arbor. “I don’t think they’ve actually come to any new conclusion,” she said in an interview. “This is pretty much how I practice already.”
But the guideline could have an effect on policy, she said. The panel noted research showing that lower Medicare reimbursement to durable medical equipment companies since 2011 has forced many patients to switch from small, easily portable liquid oxygen to home-fill oxygen systems that include heavy cylinders.
“The impact of this decline in the availability and adequacy of portable oxygen devices in the United States has been profound,” Dr. Holland and colleagues wrote. “Supplemental oxygen users reported numerous problems, with the overarching theme being restricted mobility and isolation due to inadequate portable options.”
For this reason, the guideline recommends liquid oxygen for patients with chronic lung disease who are mobile outside of the home and require continuous oxygen flow rates of >3 L/min during exertion.
Many of Dr. Han’s patients have struggled with this problem, she said. “The clunkiest, most painful form of ‘ambulatory oxygen’ are these really large metal cylinders. They’re huge. And you have to carry them on a cart. It’s portable in theory only.”
Some of her patients have resorted to buying their own equipment on eBay, she said.
The authors report multiple disclosures including serving as advisory board members to foundations and pharmaceutical companies, and some are company employees or stockholders.
A version of this article originally appeared on Medscape.com.
Telehealth finds acceptance among patients with CF, clinicians
(CF) and the physicians who treat them, according to three new studies. The surveys examined attitudes during the COVID-19 pandemic, which complicates interpretation of the survey, but the results nevertheless bode well for telehealth’s future in the management of CF.
“Patients could be responding positively just because they could have a visit during the pandemic,” said Andrew NeSmith, during a presentation of a survey of adults with CF at the virtual North American Cystic Fibrosis Conference. Mr. NeSmith is the clinical data coordinator at the University of Alabama at Birmingham Cystic Fibrosis Center.
Other posters at the conference examined attitudes among pediatric populations and treating physicians, with generally positive results, which has generated optimism that telehealth could become an important element of care after the pandemic fades. “This data suggests that telehealth could be integrated into routine follow-up care in the CF chronic care model,” said Mr. NeSmith.
His team collected responses from 119 individuals at the University of Alabama at Birmingham; Boston Children’s Hospital; Brigham and Women’s Hospital, Boston; Virginia Commonwealth University, Richmond; and West Virginia University, Morgantown. A total of 28% had conducted a prior telehealth visit before the study; 92% of visits were conducted with a medical doctor. Only 13% reported experiencing difficulties with their first telehealth visit. Eighty-five percent rated convenience, and 77% rated their satisfaction with telehealth as “high.” Most (92%) said they were able to see their desired disciplines, 95% felt all of their issues had been addressed, and 83% strongly agreed that telehealth visits were of adequate length.
Not everything was rosy. A total of 48% of participants expressed at least moderate concern over a lack of pulmonary function test or throat/sputum culture. There were much fewer concerns over missing vital signs or weight measurements.
The overall results weren’t surprising to Robert Giusti, MD, clinical professor of pediatrics at New York University and director of the Pediatric Cystic Fibrosis Center, New York, who was not involved in the study. “I was expecting that patients were going to like it. It makes their life easier,” he said in an interview.
A survey of families of pediatric individuals with CF at seven centers found similar levels of satisfaction. A total of 23% had used telehealth previously; 96% rated convenience, and 93% rated satisfaction as “high.” Almost all (99%) felt that all concerns were met, 98% said that sessions were adequately long, and 87% had no trouble connecting to the visit.
Some participants in this survey had concerns about what might be missing with a televisit. Half (52%) had at least a moderate concern over lack of pulmonary function tests, 45% over lack of vital signs, 29% about lack of weight measurements, and 64% about the need for throat/sputum culture. Despite those issues, 69% preferred that “some” and 22% preferred that “most” future visits be conducted by telehealth.
A survey of physicians who used telehealth with CF patients also found broad support. They reported some challenges, with 70% saying they experienced technical difficulty, and 77% saying it “took time” to resolve a visit with only 18% reporting that visits were “quickly resolved.” Most (86%) said they were satisfied with telehealth for care delivery, and 78% said it was appropriate for most patients. Most said telehealth improved the patient-physician relationship, and they believed visits were more efficient when conducted via telehealth than in person. A majority (81%) endorsed using telehealth for some visits, and 12% for most visits.
A key question will be how telehealth affects patient outcomes, according to Ryan Perkins, MD, who was a coauthor of the survey of physicians. “If they’re not doing as well from an outcomes perspective, that would be a huge limitation to our patients,” said Dr. Perkins, who is a pediatric and adult pulmonary fellow at Boston Children’s Hospital and Brigham and Women’s Hospital.
Although the study examined only models of care that were entirely virtual, Dr. Perkins noted that hybrid in-person/virtual care models are also possible. “Do we have better outcomes doing it that way? Is there higher patient satisfaction? I’m sure that will be a hot topic moving forward.”
Dr. Perkins noted that patients expressed concern about not being able to get sputum cultures and spirometry recordings during telehealth sessions. “That’s not really surprising to me, but I think it raises the question as we’re imagining care models for the future – how can we implement those components into future care delivery?”
Another hurdle will be insurance coverage. “My fear is that insurance companies are going to cut down the amount of reimbursement for telehealth visits in the future and just going to make it more complicated,” said Dr. Giusti. “Certainly, though, I think telehealth is an important outreach that we’d like to continue with our patients.”
Mr. NeSmith, Dr. Giusti, and Dr. Perkins reported no relevant financial disclosures.
SOURCE: NeSmith A et al. NACFC 2020, Abstracts 797, 799, 810.
(CF) and the physicians who treat them, according to three new studies. The surveys examined attitudes during the COVID-19 pandemic, which complicates interpretation of the survey, but the results nevertheless bode well for telehealth’s future in the management of CF.
“Patients could be responding positively just because they could have a visit during the pandemic,” said Andrew NeSmith, during a presentation of a survey of adults with CF at the virtual North American Cystic Fibrosis Conference. Mr. NeSmith is the clinical data coordinator at the University of Alabama at Birmingham Cystic Fibrosis Center.
Other posters at the conference examined attitudes among pediatric populations and treating physicians, with generally positive results, which has generated optimism that telehealth could become an important element of care after the pandemic fades. “This data suggests that telehealth could be integrated into routine follow-up care in the CF chronic care model,” said Mr. NeSmith.
His team collected responses from 119 individuals at the University of Alabama at Birmingham; Boston Children’s Hospital; Brigham and Women’s Hospital, Boston; Virginia Commonwealth University, Richmond; and West Virginia University, Morgantown. A total of 28% had conducted a prior telehealth visit before the study; 92% of visits were conducted with a medical doctor. Only 13% reported experiencing difficulties with their first telehealth visit. Eighty-five percent rated convenience, and 77% rated their satisfaction with telehealth as “high.” Most (92%) said they were able to see their desired disciplines, 95% felt all of their issues had been addressed, and 83% strongly agreed that telehealth visits were of adequate length.
Not everything was rosy. A total of 48% of participants expressed at least moderate concern over a lack of pulmonary function test or throat/sputum culture. There were much fewer concerns over missing vital signs or weight measurements.
The overall results weren’t surprising to Robert Giusti, MD, clinical professor of pediatrics at New York University and director of the Pediatric Cystic Fibrosis Center, New York, who was not involved in the study. “I was expecting that patients were going to like it. It makes their life easier,” he said in an interview.
A survey of families of pediatric individuals with CF at seven centers found similar levels of satisfaction. A total of 23% had used telehealth previously; 96% rated convenience, and 93% rated satisfaction as “high.” Almost all (99%) felt that all concerns were met, 98% said that sessions were adequately long, and 87% had no trouble connecting to the visit.
Some participants in this survey had concerns about what might be missing with a televisit. Half (52%) had at least a moderate concern over lack of pulmonary function tests, 45% over lack of vital signs, 29% about lack of weight measurements, and 64% about the need for throat/sputum culture. Despite those issues, 69% preferred that “some” and 22% preferred that “most” future visits be conducted by telehealth.
A survey of physicians who used telehealth with CF patients also found broad support. They reported some challenges, with 70% saying they experienced technical difficulty, and 77% saying it “took time” to resolve a visit with only 18% reporting that visits were “quickly resolved.” Most (86%) said they were satisfied with telehealth for care delivery, and 78% said it was appropriate for most patients. Most said telehealth improved the patient-physician relationship, and they believed visits were more efficient when conducted via telehealth than in person. A majority (81%) endorsed using telehealth for some visits, and 12% for most visits.
A key question will be how telehealth affects patient outcomes, according to Ryan Perkins, MD, who was a coauthor of the survey of physicians. “If they’re not doing as well from an outcomes perspective, that would be a huge limitation to our patients,” said Dr. Perkins, who is a pediatric and adult pulmonary fellow at Boston Children’s Hospital and Brigham and Women’s Hospital.
Although the study examined only models of care that were entirely virtual, Dr. Perkins noted that hybrid in-person/virtual care models are also possible. “Do we have better outcomes doing it that way? Is there higher patient satisfaction? I’m sure that will be a hot topic moving forward.”
Dr. Perkins noted that patients expressed concern about not being able to get sputum cultures and spirometry recordings during telehealth sessions. “That’s not really surprising to me, but I think it raises the question as we’re imagining care models for the future – how can we implement those components into future care delivery?”
Another hurdle will be insurance coverage. “My fear is that insurance companies are going to cut down the amount of reimbursement for telehealth visits in the future and just going to make it more complicated,” said Dr. Giusti. “Certainly, though, I think telehealth is an important outreach that we’d like to continue with our patients.”
Mr. NeSmith, Dr. Giusti, and Dr. Perkins reported no relevant financial disclosures.
SOURCE: NeSmith A et al. NACFC 2020, Abstracts 797, 799, 810.
(CF) and the physicians who treat them, according to three new studies. The surveys examined attitudes during the COVID-19 pandemic, which complicates interpretation of the survey, but the results nevertheless bode well for telehealth’s future in the management of CF.
“Patients could be responding positively just because they could have a visit during the pandemic,” said Andrew NeSmith, during a presentation of a survey of adults with CF at the virtual North American Cystic Fibrosis Conference. Mr. NeSmith is the clinical data coordinator at the University of Alabama at Birmingham Cystic Fibrosis Center.
Other posters at the conference examined attitudes among pediatric populations and treating physicians, with generally positive results, which has generated optimism that telehealth could become an important element of care after the pandemic fades. “This data suggests that telehealth could be integrated into routine follow-up care in the CF chronic care model,” said Mr. NeSmith.
His team collected responses from 119 individuals at the University of Alabama at Birmingham; Boston Children’s Hospital; Brigham and Women’s Hospital, Boston; Virginia Commonwealth University, Richmond; and West Virginia University, Morgantown. A total of 28% had conducted a prior telehealth visit before the study; 92% of visits were conducted with a medical doctor. Only 13% reported experiencing difficulties with their first telehealth visit. Eighty-five percent rated convenience, and 77% rated their satisfaction with telehealth as “high.” Most (92%) said they were able to see their desired disciplines, 95% felt all of their issues had been addressed, and 83% strongly agreed that telehealth visits were of adequate length.
Not everything was rosy. A total of 48% of participants expressed at least moderate concern over a lack of pulmonary function test or throat/sputum culture. There were much fewer concerns over missing vital signs or weight measurements.
The overall results weren’t surprising to Robert Giusti, MD, clinical professor of pediatrics at New York University and director of the Pediatric Cystic Fibrosis Center, New York, who was not involved in the study. “I was expecting that patients were going to like it. It makes their life easier,” he said in an interview.
A survey of families of pediatric individuals with CF at seven centers found similar levels of satisfaction. A total of 23% had used telehealth previously; 96% rated convenience, and 93% rated satisfaction as “high.” Almost all (99%) felt that all concerns were met, 98% said that sessions were adequately long, and 87% had no trouble connecting to the visit.
Some participants in this survey had concerns about what might be missing with a televisit. Half (52%) had at least a moderate concern over lack of pulmonary function tests, 45% over lack of vital signs, 29% about lack of weight measurements, and 64% about the need for throat/sputum culture. Despite those issues, 69% preferred that “some” and 22% preferred that “most” future visits be conducted by telehealth.
A survey of physicians who used telehealth with CF patients also found broad support. They reported some challenges, with 70% saying they experienced technical difficulty, and 77% saying it “took time” to resolve a visit with only 18% reporting that visits were “quickly resolved.” Most (86%) said they were satisfied with telehealth for care delivery, and 78% said it was appropriate for most patients. Most said telehealth improved the patient-physician relationship, and they believed visits were more efficient when conducted via telehealth than in person. A majority (81%) endorsed using telehealth for some visits, and 12% for most visits.
A key question will be how telehealth affects patient outcomes, according to Ryan Perkins, MD, who was a coauthor of the survey of physicians. “If they’re not doing as well from an outcomes perspective, that would be a huge limitation to our patients,” said Dr. Perkins, who is a pediatric and adult pulmonary fellow at Boston Children’s Hospital and Brigham and Women’s Hospital.
Although the study examined only models of care that were entirely virtual, Dr. Perkins noted that hybrid in-person/virtual care models are also possible. “Do we have better outcomes doing it that way? Is there higher patient satisfaction? I’m sure that will be a hot topic moving forward.”
Dr. Perkins noted that patients expressed concern about not being able to get sputum cultures and spirometry recordings during telehealth sessions. “That’s not really surprising to me, but I think it raises the question as we’re imagining care models for the future – how can we implement those components into future care delivery?”
Another hurdle will be insurance coverage. “My fear is that insurance companies are going to cut down the amount of reimbursement for telehealth visits in the future and just going to make it more complicated,” said Dr. Giusti. “Certainly, though, I think telehealth is an important outreach that we’d like to continue with our patients.”
Mr. NeSmith, Dr. Giusti, and Dr. Perkins reported no relevant financial disclosures.
SOURCE: NeSmith A et al. NACFC 2020, Abstracts 797, 799, 810.
FROM NACFC 2020
Pfizer’s COVID-19 vaccine 95% effective in final phase 3 results
After initial promising interim results on Nov. 9, Pfizer and BioNTech today announced that their mRNA vaccine, in development to prevent COVID-19, is 95% effective.
Final analysis of the randomized, phase 3 study of more than 43,000 people yielded 170 confirmed cases of COVID-19 – with 162 positive cases in the placebo group versus 8 in the BNT162b2 vaccine group.
Researchers reported 10 severe cases of COVID-19 in the trial, 9 of which occurred in the placebo group.
The study was ethnically diverse, and results were consistent across gender and age groups, with a 94% efficacy reported among participants aged older than 65 years.
Pfizer plans to file for an emergency-use authorization with the Food and Drug Administration “within days,” having now met all the FDA data endpoints, according to a news release from the two companies.
The vaccine was well tolerated with no serious safety concerns, the company stated. Two grade 3 adverse events were reported – fatigue in 3.8% of participants and headache in 2%.
The 95% efficacy places the Pfizer vaccine in the same neighborhood as the interim results of the Moderna vaccine, reported at 94.5%. Both products are two-dose mRNA vaccines.
As of Nov. 13, of 43,661 total participants in the Pfizer vaccine phase 3 trial, 41,135 received a second dose. The final results are based on two outcomes measured 7 days after the second dose: vaccine efficacy in people without prior SARS-CoV-2 infection as well as a secondary outcome in people both with and without prior SARS-CoV-2 infection.
The 95% vaccine efficacy was statistically significant, compared with placebo (P < .0001).
‘Historic 8-month journey’
The BNT162b2 vaccine candidate is a joint effort between Pfizer and BioNTech. “The study results mark an important step in this historic 8-month journey to bring forward a vaccine capable of helping to end this devastating pandemic,” Albert Bourla, DVM, PhD, Pfizer chairman and CEO, said in a statement. “With hundreds of thousands of people around the globe infected every day, we urgently need to get a safe and effective vaccine to the world.”
Ugur Sahin, MD, PhD, cofounder and CEO of BioNTech, added, “we are grateful that the first global trial to reach the final efficacy analysis mark indicates that a high rate of protection against COVID-19 can be achieved very fast after the first 30-mcg dose, underscoring the power of BNT162 in providing early protection.”
The two companies expect to produce up to 50 million vaccine doses in 2020 for global distribution. Projections for 2021 include up to 1.3 billion doses.
The companies also designed temperature-controlled thermal shipping containers with dry ice to maintain the required, approximate –70° C (–94° F) conditions. Clinicians can use the containers as temporary storage units for up to 15 days by replacing the dry ice.
This article first appeared on Medscape.com.
After initial promising interim results on Nov. 9, Pfizer and BioNTech today announced that their mRNA vaccine, in development to prevent COVID-19, is 95% effective.
Final analysis of the randomized, phase 3 study of more than 43,000 people yielded 170 confirmed cases of COVID-19 – with 162 positive cases in the placebo group versus 8 in the BNT162b2 vaccine group.
Researchers reported 10 severe cases of COVID-19 in the trial, 9 of which occurred in the placebo group.
The study was ethnically diverse, and results were consistent across gender and age groups, with a 94% efficacy reported among participants aged older than 65 years.
Pfizer plans to file for an emergency-use authorization with the Food and Drug Administration “within days,” having now met all the FDA data endpoints, according to a news release from the two companies.
The vaccine was well tolerated with no serious safety concerns, the company stated. Two grade 3 adverse events were reported – fatigue in 3.8% of participants and headache in 2%.
The 95% efficacy places the Pfizer vaccine in the same neighborhood as the interim results of the Moderna vaccine, reported at 94.5%. Both products are two-dose mRNA vaccines.
As of Nov. 13, of 43,661 total participants in the Pfizer vaccine phase 3 trial, 41,135 received a second dose. The final results are based on two outcomes measured 7 days after the second dose: vaccine efficacy in people without prior SARS-CoV-2 infection as well as a secondary outcome in people both with and without prior SARS-CoV-2 infection.
The 95% vaccine efficacy was statistically significant, compared with placebo (P < .0001).
‘Historic 8-month journey’
The BNT162b2 vaccine candidate is a joint effort between Pfizer and BioNTech. “The study results mark an important step in this historic 8-month journey to bring forward a vaccine capable of helping to end this devastating pandemic,” Albert Bourla, DVM, PhD, Pfizer chairman and CEO, said in a statement. “With hundreds of thousands of people around the globe infected every day, we urgently need to get a safe and effective vaccine to the world.”
Ugur Sahin, MD, PhD, cofounder and CEO of BioNTech, added, “we are grateful that the first global trial to reach the final efficacy analysis mark indicates that a high rate of protection against COVID-19 can be achieved very fast after the first 30-mcg dose, underscoring the power of BNT162 in providing early protection.”
The two companies expect to produce up to 50 million vaccine doses in 2020 for global distribution. Projections for 2021 include up to 1.3 billion doses.
The companies also designed temperature-controlled thermal shipping containers with dry ice to maintain the required, approximate –70° C (–94° F) conditions. Clinicians can use the containers as temporary storage units for up to 15 days by replacing the dry ice.
This article first appeared on Medscape.com.
After initial promising interim results on Nov. 9, Pfizer and BioNTech today announced that their mRNA vaccine, in development to prevent COVID-19, is 95% effective.
Final analysis of the randomized, phase 3 study of more than 43,000 people yielded 170 confirmed cases of COVID-19 – with 162 positive cases in the placebo group versus 8 in the BNT162b2 vaccine group.
Researchers reported 10 severe cases of COVID-19 in the trial, 9 of which occurred in the placebo group.
The study was ethnically diverse, and results were consistent across gender and age groups, with a 94% efficacy reported among participants aged older than 65 years.
Pfizer plans to file for an emergency-use authorization with the Food and Drug Administration “within days,” having now met all the FDA data endpoints, according to a news release from the two companies.
The vaccine was well tolerated with no serious safety concerns, the company stated. Two grade 3 adverse events were reported – fatigue in 3.8% of participants and headache in 2%.
The 95% efficacy places the Pfizer vaccine in the same neighborhood as the interim results of the Moderna vaccine, reported at 94.5%. Both products are two-dose mRNA vaccines.
As of Nov. 13, of 43,661 total participants in the Pfizer vaccine phase 3 trial, 41,135 received a second dose. The final results are based on two outcomes measured 7 days after the second dose: vaccine efficacy in people without prior SARS-CoV-2 infection as well as a secondary outcome in people both with and without prior SARS-CoV-2 infection.
The 95% vaccine efficacy was statistically significant, compared with placebo (P < .0001).
‘Historic 8-month journey’
The BNT162b2 vaccine candidate is a joint effort between Pfizer and BioNTech. “The study results mark an important step in this historic 8-month journey to bring forward a vaccine capable of helping to end this devastating pandemic,” Albert Bourla, DVM, PhD, Pfizer chairman and CEO, said in a statement. “With hundreds of thousands of people around the globe infected every day, we urgently need to get a safe and effective vaccine to the world.”
Ugur Sahin, MD, PhD, cofounder and CEO of BioNTech, added, “we are grateful that the first global trial to reach the final efficacy analysis mark indicates that a high rate of protection against COVID-19 can be achieved very fast after the first 30-mcg dose, underscoring the power of BNT162 in providing early protection.”
The two companies expect to produce up to 50 million vaccine doses in 2020 for global distribution. Projections for 2021 include up to 1.3 billion doses.
The companies also designed temperature-controlled thermal shipping containers with dry ice to maintain the required, approximate –70° C (–94° F) conditions. Clinicians can use the containers as temporary storage units for up to 15 days by replacing the dry ice.
This article first appeared on Medscape.com.
One-third of critical illness survivors emerge from ICU with functional deterioration
More patients are surviving critical illnesses requiring ICU care but many emerge with physical debility that may or may not eventually resolve.
Over the past decade, functional status deterioration after critical illness has become more common and of greater magnitude, despite concurrent efforts to reduce post–intensive care syndrome, based on a retrospective analysis of more than 100,000 patients.
Almost one-third of patients who survived nonsurgical ICU admission had evidence of functional status decline, reported lead author Nicholas E. Ingraham, MD, of the University of Minnesota, Minneapolis, and colleagues.
“Increasing capacity and decreasing mortality have created an evolving and diverse population of ICU survivors,” the investigators wrote in Critical Care Medicine. “Today’s survivors of critical illness are increasingly burdened by extensive physical and psychological comorbidities, often resulting in reduced quality of life.”
To determine trends in post–intensive care syndrome from 2008 to 2016, Dr. Ingraham and colleagues analyzed data from the Cerner Acute Physiology and Chronic Health Evaluation outcomes database, a national prospective cohort. Out of 202,786 adult patients admitted to the ICU, 129,917 were eligible for the study. Patients were excluded because of surgical admission, death, lack of functional status documentation, or inadequate hospital size or duration of participation. The final dataset had a median age of 63 years, with a slight predominance of male patients (54.0%). Most patients (80.9%) were White.
The primary outcome was defined as presence or absence of functional status deterioration, based on functional status at admission versus time of discharge. The secondary outcome was magnitude of deterioration over time.
The analysis, which controlled for age and severity of illness, revealed concerning trends for both outcomes.
Across the entire cohort 38,116 patients (29.3%) had functional status deterioration, with a 15% increase in prevalence over the course of the decade that spanned all disease categories (prevalence rate ratio, 1.15; 95% confidence interval, 1.13-1.17; P < .001). The magnitude of functional status decline also increased by 4% (odds ratio, 1.04; P < .001), with all but nonsurgical trauma patients showing greater deterioration over time.
“However, despite the decreasing magnitude of functional status deterioration in nonsurgical trauma, many admission diagnoses in this category remain in the top quartile of higher risk for functional status deterioration,” the investigators noted.
Functional status decline was most common among patients with head and polytrauma (OR, 3.39), followed closely by chest and spine trauma (OR, 3.38), and spine trauma (OR, 3.19). The top quartile of categories for prevalence of deterioration included nonsurgical trauma, neurologic, pulmonary, and gastrointestinal diseases.
Functional status decline was least common among patients diagnosed with diabetic ketoacidosis (OR, 0.27) or asthma (OR, 0.35).
“We believe our study provides important information that can be used in beginning to identify patients at high risk of functional status decline,” the investigators concluded. “Improving the identification of these patients and targeting appropriate interventions to mitigate this decline will be important directions for future studies in this area.”
According to David L. Bowton, MD, FCCP, professor emeritus, section on critical care, Wake Forest Baptist Health, Winston-Salem, N.C., the findings show just how common functional decline is after critical illness, and may actually underestimate prevalence.
“Because the authors employed a course evaluation tool employing only three categories of ability/disability and abstracted the level of disability from the medical record, they likely underestimated the frequency of clinically important, though not detected, disability at the time of hospital discharge,” Dr. Bowton said. “The study did not address cognitive impairment which can be detected in half of patients at 3 months following critical illness, and which significantly affects patients’ quality of life (Am J Respir Crit Care Med. 2020;202[2]:193-201).”
Dr. Bowton suggested that evidence-based methods of preventing post–intensive care syndrome are limited.
“Current efforts to improve post-ICU functional and cognitive outcomes suffer from the lack of proven effective interventions (Crit Care Med. 2019;47[11]:1607-18),” he said. “Observational data indicates that compliance with the ABCDEF bundle decreases the duration and incidence of delirium, ICU length of stay, duration of mechanical ventilation, and mortality (Crit Care Med. 2019;47[1]:3-14). However, the implications of these improvements on postdischarge functional outcomes are unknown as area the relative importance of individual elements of the bundle. Early mobility and patient and family diaries appear to improve functional status at discharge and postdischarge anxiety and depression, though the evidence supporting this is thin.”
Appropriate intervention may be especially challenging during the COVID-19 pandemic, he added.
“The impact of COVID on ICU staffing adequacy and stress is significant and the impact on quality bundle compliance and the availability of support services is currently not clear, but likely to be detrimental, especially to support services such as physical therapy that are already commonly understaffed,” Dr. Bowton said.
The study was supported by grants from the University of Minnesota’s Critical Care Research and Programmatic Development Program; the National Heart, Lung, and Blood Institute; and the University of Minnesota Clinical and Translational Science via the National Center for Advancing Translational Sciences. The investigators reported financial relationships with no other relevant organizations. Dr. Bowton reported no conflicts of interest.
SOURCE: Ingraham NE et al. Crit Care Med. 2020 Nov. doi: 10.1097/CCM.0000000000004524.
More patients are surviving critical illnesses requiring ICU care but many emerge with physical debility that may or may not eventually resolve.
Over the past decade, functional status deterioration after critical illness has become more common and of greater magnitude, despite concurrent efforts to reduce post–intensive care syndrome, based on a retrospective analysis of more than 100,000 patients.
Almost one-third of patients who survived nonsurgical ICU admission had evidence of functional status decline, reported lead author Nicholas E. Ingraham, MD, of the University of Minnesota, Minneapolis, and colleagues.
“Increasing capacity and decreasing mortality have created an evolving and diverse population of ICU survivors,” the investigators wrote in Critical Care Medicine. “Today’s survivors of critical illness are increasingly burdened by extensive physical and psychological comorbidities, often resulting in reduced quality of life.”
To determine trends in post–intensive care syndrome from 2008 to 2016, Dr. Ingraham and colleagues analyzed data from the Cerner Acute Physiology and Chronic Health Evaluation outcomes database, a national prospective cohort. Out of 202,786 adult patients admitted to the ICU, 129,917 were eligible for the study. Patients were excluded because of surgical admission, death, lack of functional status documentation, or inadequate hospital size or duration of participation. The final dataset had a median age of 63 years, with a slight predominance of male patients (54.0%). Most patients (80.9%) were White.
The primary outcome was defined as presence or absence of functional status deterioration, based on functional status at admission versus time of discharge. The secondary outcome was magnitude of deterioration over time.
The analysis, which controlled for age and severity of illness, revealed concerning trends for both outcomes.
Across the entire cohort 38,116 patients (29.3%) had functional status deterioration, with a 15% increase in prevalence over the course of the decade that spanned all disease categories (prevalence rate ratio, 1.15; 95% confidence interval, 1.13-1.17; P < .001). The magnitude of functional status decline also increased by 4% (odds ratio, 1.04; P < .001), with all but nonsurgical trauma patients showing greater deterioration over time.
“However, despite the decreasing magnitude of functional status deterioration in nonsurgical trauma, many admission diagnoses in this category remain in the top quartile of higher risk for functional status deterioration,” the investigators noted.
Functional status decline was most common among patients with head and polytrauma (OR, 3.39), followed closely by chest and spine trauma (OR, 3.38), and spine trauma (OR, 3.19). The top quartile of categories for prevalence of deterioration included nonsurgical trauma, neurologic, pulmonary, and gastrointestinal diseases.
Functional status decline was least common among patients diagnosed with diabetic ketoacidosis (OR, 0.27) or asthma (OR, 0.35).
“We believe our study provides important information that can be used in beginning to identify patients at high risk of functional status decline,” the investigators concluded. “Improving the identification of these patients and targeting appropriate interventions to mitigate this decline will be important directions for future studies in this area.”
According to David L. Bowton, MD, FCCP, professor emeritus, section on critical care, Wake Forest Baptist Health, Winston-Salem, N.C., the findings show just how common functional decline is after critical illness, and may actually underestimate prevalence.
“Because the authors employed a course evaluation tool employing only three categories of ability/disability and abstracted the level of disability from the medical record, they likely underestimated the frequency of clinically important, though not detected, disability at the time of hospital discharge,” Dr. Bowton said. “The study did not address cognitive impairment which can be detected in half of patients at 3 months following critical illness, and which significantly affects patients’ quality of life (Am J Respir Crit Care Med. 2020;202[2]:193-201).”
Dr. Bowton suggested that evidence-based methods of preventing post–intensive care syndrome are limited.
“Current efforts to improve post-ICU functional and cognitive outcomes suffer from the lack of proven effective interventions (Crit Care Med. 2019;47[11]:1607-18),” he said. “Observational data indicates that compliance with the ABCDEF bundle decreases the duration and incidence of delirium, ICU length of stay, duration of mechanical ventilation, and mortality (Crit Care Med. 2019;47[1]:3-14). However, the implications of these improvements on postdischarge functional outcomes are unknown as area the relative importance of individual elements of the bundle. Early mobility and patient and family diaries appear to improve functional status at discharge and postdischarge anxiety and depression, though the evidence supporting this is thin.”
Appropriate intervention may be especially challenging during the COVID-19 pandemic, he added.
“The impact of COVID on ICU staffing adequacy and stress is significant and the impact on quality bundle compliance and the availability of support services is currently not clear, but likely to be detrimental, especially to support services such as physical therapy that are already commonly understaffed,” Dr. Bowton said.
The study was supported by grants from the University of Minnesota’s Critical Care Research and Programmatic Development Program; the National Heart, Lung, and Blood Institute; and the University of Minnesota Clinical and Translational Science via the National Center for Advancing Translational Sciences. The investigators reported financial relationships with no other relevant organizations. Dr. Bowton reported no conflicts of interest.
SOURCE: Ingraham NE et al. Crit Care Med. 2020 Nov. doi: 10.1097/CCM.0000000000004524.
More patients are surviving critical illnesses requiring ICU care but many emerge with physical debility that may or may not eventually resolve.
Over the past decade, functional status deterioration after critical illness has become more common and of greater magnitude, despite concurrent efforts to reduce post–intensive care syndrome, based on a retrospective analysis of more than 100,000 patients.
Almost one-third of patients who survived nonsurgical ICU admission had evidence of functional status decline, reported lead author Nicholas E. Ingraham, MD, of the University of Minnesota, Minneapolis, and colleagues.
“Increasing capacity and decreasing mortality have created an evolving and diverse population of ICU survivors,” the investigators wrote in Critical Care Medicine. “Today’s survivors of critical illness are increasingly burdened by extensive physical and psychological comorbidities, often resulting in reduced quality of life.”
To determine trends in post–intensive care syndrome from 2008 to 2016, Dr. Ingraham and colleagues analyzed data from the Cerner Acute Physiology and Chronic Health Evaluation outcomes database, a national prospective cohort. Out of 202,786 adult patients admitted to the ICU, 129,917 were eligible for the study. Patients were excluded because of surgical admission, death, lack of functional status documentation, or inadequate hospital size or duration of participation. The final dataset had a median age of 63 years, with a slight predominance of male patients (54.0%). Most patients (80.9%) were White.
The primary outcome was defined as presence or absence of functional status deterioration, based on functional status at admission versus time of discharge. The secondary outcome was magnitude of deterioration over time.
The analysis, which controlled for age and severity of illness, revealed concerning trends for both outcomes.
Across the entire cohort 38,116 patients (29.3%) had functional status deterioration, with a 15% increase in prevalence over the course of the decade that spanned all disease categories (prevalence rate ratio, 1.15; 95% confidence interval, 1.13-1.17; P < .001). The magnitude of functional status decline also increased by 4% (odds ratio, 1.04; P < .001), with all but nonsurgical trauma patients showing greater deterioration over time.
“However, despite the decreasing magnitude of functional status deterioration in nonsurgical trauma, many admission diagnoses in this category remain in the top quartile of higher risk for functional status deterioration,” the investigators noted.
Functional status decline was most common among patients with head and polytrauma (OR, 3.39), followed closely by chest and spine trauma (OR, 3.38), and spine trauma (OR, 3.19). The top quartile of categories for prevalence of deterioration included nonsurgical trauma, neurologic, pulmonary, and gastrointestinal diseases.
Functional status decline was least common among patients diagnosed with diabetic ketoacidosis (OR, 0.27) or asthma (OR, 0.35).
“We believe our study provides important information that can be used in beginning to identify patients at high risk of functional status decline,” the investigators concluded. “Improving the identification of these patients and targeting appropriate interventions to mitigate this decline will be important directions for future studies in this area.”
According to David L. Bowton, MD, FCCP, professor emeritus, section on critical care, Wake Forest Baptist Health, Winston-Salem, N.C., the findings show just how common functional decline is after critical illness, and may actually underestimate prevalence.
“Because the authors employed a course evaluation tool employing only three categories of ability/disability and abstracted the level of disability from the medical record, they likely underestimated the frequency of clinically important, though not detected, disability at the time of hospital discharge,” Dr. Bowton said. “The study did not address cognitive impairment which can be detected in half of patients at 3 months following critical illness, and which significantly affects patients’ quality of life (Am J Respir Crit Care Med. 2020;202[2]:193-201).”
Dr. Bowton suggested that evidence-based methods of preventing post–intensive care syndrome are limited.
“Current efforts to improve post-ICU functional and cognitive outcomes suffer from the lack of proven effective interventions (Crit Care Med. 2019;47[11]:1607-18),” he said. “Observational data indicates that compliance with the ABCDEF bundle decreases the duration and incidence of delirium, ICU length of stay, duration of mechanical ventilation, and mortality (Crit Care Med. 2019;47[1]:3-14). However, the implications of these improvements on postdischarge functional outcomes are unknown as area the relative importance of individual elements of the bundle. Early mobility and patient and family diaries appear to improve functional status at discharge and postdischarge anxiety and depression, though the evidence supporting this is thin.”
Appropriate intervention may be especially challenging during the COVID-19 pandemic, he added.
“The impact of COVID on ICU staffing adequacy and stress is significant and the impact on quality bundle compliance and the availability of support services is currently not clear, but likely to be detrimental, especially to support services such as physical therapy that are already commonly understaffed,” Dr. Bowton said.
The study was supported by grants from the University of Minnesota’s Critical Care Research and Programmatic Development Program; the National Heart, Lung, and Blood Institute; and the University of Minnesota Clinical and Translational Science via the National Center for Advancing Translational Sciences. The investigators reported financial relationships with no other relevant organizations. Dr. Bowton reported no conflicts of interest.
SOURCE: Ingraham NE et al. Crit Care Med. 2020 Nov. doi: 10.1097/CCM.0000000000004524.
FROM CRITICAL CARE MEDICINE
COVID-19 burdens follow patients after discharge
COVID-19 patients who survive their hospitalization don’t leave the disease behind upon discharge, as a significant percentage died within 60 days of discharge, with an ICU admission heightening the risk, according to an observational study of 38 Michigan hospitals. What’s more, many of them were burdened with health and emotional challenges ranging from hospital readmission to job loss and financial problems.
“These data confirm that the toll of COVID-19 extends well beyond hospitalization, a finding consistent with long-term sequelae from sepsis and other severe respiratory viral illnesses,” wrote lead author Vineet Chopra, MBBS, of the University of Michigan, Ann Arbor, and colleagues (Ann Intern Med. 2020 Nov 11: doi: 10.7326/M20-5661)
The researchers found that 29.2% of all patients hospitalized for COVID-19 from March 16 to July 1 died. The observational cohort study included 1,648 COVID-19 patients hospitalized at 38 Michigan hospitals participating in a statewide collaborative.
The bulk of those deaths occurred during hospitalization: 24.2% of patients (n = 398). Of the 1,250 patients discharged, 78% (n = 975) went home and 12.6% (n = 158) went to a skilled nursing facility, with the remainder unaccounted for. Within 60 days of discharge, 6.7% (n = 84) of hospitalized survivors had died and 15.2% (n = 189) were readmitted. The researchers gathered 60-day postdischarge data via a telephone survey, contacting 41.8% (n = 488) of discharged patients.
Outcomes were even worse for discharged patients who spent time in the ICU. The death rate among this group was 10.4% (17 of 165) after discharge. That resulted in an overall study death rate of 63.5% (n = 257) for the 405 patients who were in the ICU.
While the study data were in the first wave of the novel coronavirus, the findings have relevance today, said Mary Jo Farmer, MD, PhD, FCCP, directory of pulmonary hypertension services at Baystate Health in Springfield, Mass.
“This is the best information we have to date,” she said. “We have to continue to have an open mind and expect that this information may change as the virus possibly mutates as it spreads, and we should continue doing these types of outcomes studies at 90 days, 120 days, etc.”
The median age of study patients was 62, with a range of 50-72. The three leading comorbidities among discharged patients were hypertension (n = 800, 64%), diabetes (34.9%, n = 436), and cardiovascular disease (24.1%, n = 301).
Poor postdischarge outcomes weren’t limited to mortality and readmission. Almost 19% (n = 92) reported new or worsening cardiopulmonary symptoms such as cough and dyspnea, 13.3% had a persistent loss of taste or smell, and 12% (n = 58) reported more difficulty with daily living tasks.
The after-effects were not only physical. Nearly half of discharged patients (48.7%, n = 238) reported emotional effects and almost 6% (n = 28) sought mental health care. Among the 40% (n = 195) employed before they were hospitalized, 36% (n = 78) couldn’t return to work because of health issues or layoffs. Sixty percent (n = 117) of the pre-employed discharged patients did return to work, but 25% (n = 30) did so with reduced hours or modified job duties because of health problems.
Financial problems were also a burden. More than a third, 36.7% (n = 179), reported some financial impact from their hospitalization. About 10% (n = 47) said they used most or all of their savings, and 7% (n = 35) said they resorted to rationing necessities such as food or medications.
The researchers noted that one in five patients had no primary care follow-up at 2 months post discharge. “Collectively, these findings suggest that better models to support COVID-19 survivors are necessary,” said Dr. Chopra and colleagues.
The postdischarge course for patients involves two humps, said Sachin Gupta, MD, FCCP a pulmonary and critical care specialist at Alameda Health System in Oakland, Calif.: Getting over the hospitalization itself and the recovery phase. “As you look at the median age of the survivors, elderly patients who survive a hospital stay are still going to have a period of recovery, and like any viral illness that leads to someone being hospitalized, when you have an elderly patient with comorbidities, not all of them can make it over that final hump.”
He echoed the study authors’ call for better postdischarge support for COVID-19 patients. “There’s typically, although not at every hospital, a one-size-fits-all discharge planning process,” Dr. Gupta said. “For older patients, particularly with comorbid conditions, close follow-up after discharge is important.”
Dr. Farmer noted that one challenge in discharge support may be a matter of personnel. “The providers of this care might be fearful of patients who have had COVID-19 – Do the patients remain contagious? What if symptoms of COVID-19 return such as dry cough, fever? – and of contracting the disease themselves,” she said.
The findings regarding the emotional status of discharged patients should factor into discharge planning, she added. “Providers of posthospital care need to be educated in the emotional impact of this disease (e.g., the patients may feel ostracized or that no one wants to be around them) to assist in their recovery.”
Dr. Chopra and Dr. Farmer have no financial relationships to disclose. Dr. Gupta is an employee and shareholder of Genentech.
SOURCE: Chopra V et al. Ann Intern Med. 2020 Nov 11. doi: 10.7326/M20-5661.
COVID-19 patients who survive their hospitalization don’t leave the disease behind upon discharge, as a significant percentage died within 60 days of discharge, with an ICU admission heightening the risk, according to an observational study of 38 Michigan hospitals. What’s more, many of them were burdened with health and emotional challenges ranging from hospital readmission to job loss and financial problems.
“These data confirm that the toll of COVID-19 extends well beyond hospitalization, a finding consistent with long-term sequelae from sepsis and other severe respiratory viral illnesses,” wrote lead author Vineet Chopra, MBBS, of the University of Michigan, Ann Arbor, and colleagues (Ann Intern Med. 2020 Nov 11: doi: 10.7326/M20-5661)
The researchers found that 29.2% of all patients hospitalized for COVID-19 from March 16 to July 1 died. The observational cohort study included 1,648 COVID-19 patients hospitalized at 38 Michigan hospitals participating in a statewide collaborative.
The bulk of those deaths occurred during hospitalization: 24.2% of patients (n = 398). Of the 1,250 patients discharged, 78% (n = 975) went home and 12.6% (n = 158) went to a skilled nursing facility, with the remainder unaccounted for. Within 60 days of discharge, 6.7% (n = 84) of hospitalized survivors had died and 15.2% (n = 189) were readmitted. The researchers gathered 60-day postdischarge data via a telephone survey, contacting 41.8% (n = 488) of discharged patients.
Outcomes were even worse for discharged patients who spent time in the ICU. The death rate among this group was 10.4% (17 of 165) after discharge. That resulted in an overall study death rate of 63.5% (n = 257) for the 405 patients who were in the ICU.
While the study data were in the first wave of the novel coronavirus, the findings have relevance today, said Mary Jo Farmer, MD, PhD, FCCP, directory of pulmonary hypertension services at Baystate Health in Springfield, Mass.
“This is the best information we have to date,” she said. “We have to continue to have an open mind and expect that this information may change as the virus possibly mutates as it spreads, and we should continue doing these types of outcomes studies at 90 days, 120 days, etc.”
The median age of study patients was 62, with a range of 50-72. The three leading comorbidities among discharged patients were hypertension (n = 800, 64%), diabetes (34.9%, n = 436), and cardiovascular disease (24.1%, n = 301).
Poor postdischarge outcomes weren’t limited to mortality and readmission. Almost 19% (n = 92) reported new or worsening cardiopulmonary symptoms such as cough and dyspnea, 13.3% had a persistent loss of taste or smell, and 12% (n = 58) reported more difficulty with daily living tasks.
The after-effects were not only physical. Nearly half of discharged patients (48.7%, n = 238) reported emotional effects and almost 6% (n = 28) sought mental health care. Among the 40% (n = 195) employed before they were hospitalized, 36% (n = 78) couldn’t return to work because of health issues or layoffs. Sixty percent (n = 117) of the pre-employed discharged patients did return to work, but 25% (n = 30) did so with reduced hours or modified job duties because of health problems.
Financial problems were also a burden. More than a third, 36.7% (n = 179), reported some financial impact from their hospitalization. About 10% (n = 47) said they used most or all of their savings, and 7% (n = 35) said they resorted to rationing necessities such as food or medications.
The researchers noted that one in five patients had no primary care follow-up at 2 months post discharge. “Collectively, these findings suggest that better models to support COVID-19 survivors are necessary,” said Dr. Chopra and colleagues.
The postdischarge course for patients involves two humps, said Sachin Gupta, MD, FCCP a pulmonary and critical care specialist at Alameda Health System in Oakland, Calif.: Getting over the hospitalization itself and the recovery phase. “As you look at the median age of the survivors, elderly patients who survive a hospital stay are still going to have a period of recovery, and like any viral illness that leads to someone being hospitalized, when you have an elderly patient with comorbidities, not all of them can make it over that final hump.”
He echoed the study authors’ call for better postdischarge support for COVID-19 patients. “There’s typically, although not at every hospital, a one-size-fits-all discharge planning process,” Dr. Gupta said. “For older patients, particularly with comorbid conditions, close follow-up after discharge is important.”
Dr. Farmer noted that one challenge in discharge support may be a matter of personnel. “The providers of this care might be fearful of patients who have had COVID-19 – Do the patients remain contagious? What if symptoms of COVID-19 return such as dry cough, fever? – and of contracting the disease themselves,” she said.
The findings regarding the emotional status of discharged patients should factor into discharge planning, she added. “Providers of posthospital care need to be educated in the emotional impact of this disease (e.g., the patients may feel ostracized or that no one wants to be around them) to assist in their recovery.”
Dr. Chopra and Dr. Farmer have no financial relationships to disclose. Dr. Gupta is an employee and shareholder of Genentech.
SOURCE: Chopra V et al. Ann Intern Med. 2020 Nov 11. doi: 10.7326/M20-5661.
COVID-19 patients who survive their hospitalization don’t leave the disease behind upon discharge, as a significant percentage died within 60 days of discharge, with an ICU admission heightening the risk, according to an observational study of 38 Michigan hospitals. What’s more, many of them were burdened with health and emotional challenges ranging from hospital readmission to job loss and financial problems.
“These data confirm that the toll of COVID-19 extends well beyond hospitalization, a finding consistent with long-term sequelae from sepsis and other severe respiratory viral illnesses,” wrote lead author Vineet Chopra, MBBS, of the University of Michigan, Ann Arbor, and colleagues (Ann Intern Med. 2020 Nov 11: doi: 10.7326/M20-5661)
The researchers found that 29.2% of all patients hospitalized for COVID-19 from March 16 to July 1 died. The observational cohort study included 1,648 COVID-19 patients hospitalized at 38 Michigan hospitals participating in a statewide collaborative.
The bulk of those deaths occurred during hospitalization: 24.2% of patients (n = 398). Of the 1,250 patients discharged, 78% (n = 975) went home and 12.6% (n = 158) went to a skilled nursing facility, with the remainder unaccounted for. Within 60 days of discharge, 6.7% (n = 84) of hospitalized survivors had died and 15.2% (n = 189) were readmitted. The researchers gathered 60-day postdischarge data via a telephone survey, contacting 41.8% (n = 488) of discharged patients.
Outcomes were even worse for discharged patients who spent time in the ICU. The death rate among this group was 10.4% (17 of 165) after discharge. That resulted in an overall study death rate of 63.5% (n = 257) for the 405 patients who were in the ICU.
While the study data were in the first wave of the novel coronavirus, the findings have relevance today, said Mary Jo Farmer, MD, PhD, FCCP, directory of pulmonary hypertension services at Baystate Health in Springfield, Mass.
“This is the best information we have to date,” she said. “We have to continue to have an open mind and expect that this information may change as the virus possibly mutates as it spreads, and we should continue doing these types of outcomes studies at 90 days, 120 days, etc.”
The median age of study patients was 62, with a range of 50-72. The three leading comorbidities among discharged patients were hypertension (n = 800, 64%), diabetes (34.9%, n = 436), and cardiovascular disease (24.1%, n = 301).
Poor postdischarge outcomes weren’t limited to mortality and readmission. Almost 19% (n = 92) reported new or worsening cardiopulmonary symptoms such as cough and dyspnea, 13.3% had a persistent loss of taste or smell, and 12% (n = 58) reported more difficulty with daily living tasks.
The after-effects were not only physical. Nearly half of discharged patients (48.7%, n = 238) reported emotional effects and almost 6% (n = 28) sought mental health care. Among the 40% (n = 195) employed before they were hospitalized, 36% (n = 78) couldn’t return to work because of health issues or layoffs. Sixty percent (n = 117) of the pre-employed discharged patients did return to work, but 25% (n = 30) did so with reduced hours or modified job duties because of health problems.
Financial problems were also a burden. More than a third, 36.7% (n = 179), reported some financial impact from their hospitalization. About 10% (n = 47) said they used most or all of their savings, and 7% (n = 35) said they resorted to rationing necessities such as food or medications.
The researchers noted that one in five patients had no primary care follow-up at 2 months post discharge. “Collectively, these findings suggest that better models to support COVID-19 survivors are necessary,” said Dr. Chopra and colleagues.
The postdischarge course for patients involves two humps, said Sachin Gupta, MD, FCCP a pulmonary and critical care specialist at Alameda Health System in Oakland, Calif.: Getting over the hospitalization itself and the recovery phase. “As you look at the median age of the survivors, elderly patients who survive a hospital stay are still going to have a period of recovery, and like any viral illness that leads to someone being hospitalized, when you have an elderly patient with comorbidities, not all of them can make it over that final hump.”
He echoed the study authors’ call for better postdischarge support for COVID-19 patients. “There’s typically, although not at every hospital, a one-size-fits-all discharge planning process,” Dr. Gupta said. “For older patients, particularly with comorbid conditions, close follow-up after discharge is important.”
Dr. Farmer noted that one challenge in discharge support may be a matter of personnel. “The providers of this care might be fearful of patients who have had COVID-19 – Do the patients remain contagious? What if symptoms of COVID-19 return such as dry cough, fever? – and of contracting the disease themselves,” she said.
The findings regarding the emotional status of discharged patients should factor into discharge planning, she added. “Providers of posthospital care need to be educated in the emotional impact of this disease (e.g., the patients may feel ostracized or that no one wants to be around them) to assist in their recovery.”
Dr. Chopra and Dr. Farmer have no financial relationships to disclose. Dr. Gupta is an employee and shareholder of Genentech.
SOURCE: Chopra V et al. Ann Intern Med. 2020 Nov 11. doi: 10.7326/M20-5661.
FROM ANNALS OF INTERNAL MEDICINE
FDA-approved peanut immunotherapy protocol comes with a cost
Peanut allergy immunotherapy now comes with approval from the US Food and Drug Administration (FDA), but it also comes with protocols, standards, and paperwork. Whether it will be widely adopted has yet to be determined.
A few dozen allergists around the world have been offering food allergy immunotherapy for many years, having developed their own measuring techniques using store-bought food.
But the vast majority of allergists are not interested in developing home-grown treatments, not only because it involves research and development, but also because it comes with legal risks.
“Finally we have another treatment option,” said Edwin Kim, MD, from the UNC Allergy and Immunology Clinic in Chapel Hill, N.C. “This is what we were waiting for. It’s not cowboy stuff; this works.”
In January, the FDA approved peanut allergen powder (Palforzia) for patients 4-17 years of age, as reported by Medscape Medical News.
The pill contains measured doses of peanut flour and comes with a protocol that will allow allergists to bring patients to a peanut tolerance of 300 mg (about one peanut) and a black-box warning about anaphylaxis risk.
And before allergists can prescribe it, they must take a Risk Evaluation and Mitigation Strategy course to learn about dosing and the allergic reaction protocol.
“That may scare some away,” said Dr. Kim, who discussed the FDA-approved option during his presentation at the American College of Allergy, Asthma & Immunology 2020 Annual Scientific Meeting.
Allergic reaction, including the potential for anaphylaxis, has always been an issue with immunotherapy.
“People make the argument that there is a difference” between an expected allergic reaction – such as one that occurs after the administration of immunotherapy – and an unexpected reaction, he said. Because an expected reaction can be treated quickly, “some feel these expected reactions don’t matter so much.”
“Others say a reaction is a reaction” and argue that if, a treatment causes reaction, then it doesn’t make sense, he explained.
It comes down to patients – they must be willing to take a risk to develop tolerance and improve their quality of life – and the allergists willing to treat them.
The peanut powder involves paperwork, preauthorization forms, denials of care, a higher price tag, regimented procedures, and a prerequisite number of visits with patients. “Not everyone will want to do this,” said Dr. Kim.
The regimen involves three phases. During initial dose escalation, five doses are administered in the office on day 1. Then, over the next 6 months, updoses are administered during 11 in-office sessions and a 300-mg tolerance is achieved. Finally, to maintain tolerance to one peanut, daily doses are administered at home.
The drug cost alone is about $4,200 a year, according to Institute for Clinical and Economic Review. Peanut flour from the grocery store is cheaper, but comes with the risk of bacteria or other contamination.
“This product offers some reassurance, and that matters,” Dr. Kim said.
It’s good to have more options for food allergy treatment. “We need a more proactive way to treat food allergy; avoidance is not good enough,” he explained. “And presumably, at some point, the patient will be able to eat a grocery-store peanut instead of buying the pills.”
The art of medicine
But not all allergists will be able to make the protocol work. And it’s not clear whether there is room to alter treatment and offer patients with a higher tolerance a higher starting dose. What we do know, though, is that “the product leaves little room for ‘the art of medicine,’ ” Kim said.
That art is practiced by Arnon Elizur, MD, from the Shamir Medical Center in Tzrifin, Israel, but it’s backed by a rigid home-grown protocol.
Since 2010, he has treated 1,800 patients for peanut allergy, updosing slowly to a tolerance of 3,000 mg of peanut, the equivalent of 10 peanuts. He keeps the maintenance dose at four peanuts (1,200 mg). His center takes a personalized approach, starting patients on the highest dose they can tolerate and working up, with daily patient check-ins from home and a staff available around the clock to answer questions and deal with reactions.
“We aim for full sensitization,” Dr. Elizur said in an interview.
The peanut pill is “a big step forward” for immunotherapy, he said. It is “a standardized product, checked for bacteria and allergen content, which is available to a wide community of physicians.”
But, he pointed out, “it’s expensive.” And it’s only for peanut. “There are millions of food-allergic patients around the world dying from adverse reactions to many different kinds of food. We don’t want to wait for years for a product for all of them. We can use the actual food.”
He questions the lifelong maintenance protocol with a daily 300-mg pill. “If you can’t eat a peanut, why would you buy a drug that’s a peanut?” he asked.
He also said he’s disappointed that the product is not indicated for adults.
At the Shamir clinic, reactions are closely monitored. “Some are mild, others we treat with autoinjectors, epinephrine,” he reported. “Those are the most undesirable.”
Data from his center show that reactions occur in about 15% of patients. But his treatment success rates are good. In an average of 8 months, he is able to get 80% of his adult patients to full sensitization.
But it’s not for all patients or for all clinics, he acknowledged. “We continue to look at this balance in quality of life throughout the process. Our goal is to improve the quality of life threshold.”
Treatment that involves “native food” is “a lot of work” and requires “a lot of investment,” Dr. Elizur said. His center uses a web reporting system to maintain a 24/7 dialogue with patients, “and we look at the reports every day.” They also have a physician on call at all times. “Not everyone can commit to providing care throughout the day and night.”
His center charges the equivalent of $US3,000 per food allergy treated. “That’s whether it takes 6 months or 2 years,” he said.
There are more than 1,000 people on his 3-year waiting list.
“This is the first year that the American College of Allergy, Asthma, and Immunology is not hosting a pro–con debate on oral immunotherapy,” Dr. Kim pointed out. “We have a therapy now.”
However, the pandemic has slowed treatment uptake. “Immunotherapy is not easy to do, whether it’s FDA approved or not,” he explained. With at least 11 doctor visits in the first 6 months – each visit is between 30 minutes and 2-3 hours long – it hasn’t been possible to set up this year. “It’s not ideal.”
It will be interesting to see “how this will roll out and how it will be adopted,” Dr. Kim said. “From a food allergy point of view, the next 12 months are going to be very interesting.”
Dr. Kim reports receiving consulting honorarium from Aimmune, the maker of Palforzia; being on the clinical medical advisory board for DBV Technologies; and consulting for Aimmune, Allakos, Allergenis, DBV, Duke Clinical Research Institute, Ukko Incorporated, Vibrant America, and Kenota Health. Dr. Elizur has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Peanut allergy immunotherapy now comes with approval from the US Food and Drug Administration (FDA), but it also comes with protocols, standards, and paperwork. Whether it will be widely adopted has yet to be determined.
A few dozen allergists around the world have been offering food allergy immunotherapy for many years, having developed their own measuring techniques using store-bought food.
But the vast majority of allergists are not interested in developing home-grown treatments, not only because it involves research and development, but also because it comes with legal risks.
“Finally we have another treatment option,” said Edwin Kim, MD, from the UNC Allergy and Immunology Clinic in Chapel Hill, N.C. “This is what we were waiting for. It’s not cowboy stuff; this works.”
In January, the FDA approved peanut allergen powder (Palforzia) for patients 4-17 years of age, as reported by Medscape Medical News.
The pill contains measured doses of peanut flour and comes with a protocol that will allow allergists to bring patients to a peanut tolerance of 300 mg (about one peanut) and a black-box warning about anaphylaxis risk.
And before allergists can prescribe it, they must take a Risk Evaluation and Mitigation Strategy course to learn about dosing and the allergic reaction protocol.
“That may scare some away,” said Dr. Kim, who discussed the FDA-approved option during his presentation at the American College of Allergy, Asthma & Immunology 2020 Annual Scientific Meeting.
Allergic reaction, including the potential for anaphylaxis, has always been an issue with immunotherapy.
“People make the argument that there is a difference” between an expected allergic reaction – such as one that occurs after the administration of immunotherapy – and an unexpected reaction, he said. Because an expected reaction can be treated quickly, “some feel these expected reactions don’t matter so much.”
“Others say a reaction is a reaction” and argue that if, a treatment causes reaction, then it doesn’t make sense, he explained.
It comes down to patients – they must be willing to take a risk to develop tolerance and improve their quality of life – and the allergists willing to treat them.
The peanut powder involves paperwork, preauthorization forms, denials of care, a higher price tag, regimented procedures, and a prerequisite number of visits with patients. “Not everyone will want to do this,” said Dr. Kim.
The regimen involves three phases. During initial dose escalation, five doses are administered in the office on day 1. Then, over the next 6 months, updoses are administered during 11 in-office sessions and a 300-mg tolerance is achieved. Finally, to maintain tolerance to one peanut, daily doses are administered at home.
The drug cost alone is about $4,200 a year, according to Institute for Clinical and Economic Review. Peanut flour from the grocery store is cheaper, but comes with the risk of bacteria or other contamination.
“This product offers some reassurance, and that matters,” Dr. Kim said.
It’s good to have more options for food allergy treatment. “We need a more proactive way to treat food allergy; avoidance is not good enough,” he explained. “And presumably, at some point, the patient will be able to eat a grocery-store peanut instead of buying the pills.”
The art of medicine
But not all allergists will be able to make the protocol work. And it’s not clear whether there is room to alter treatment and offer patients with a higher tolerance a higher starting dose. What we do know, though, is that “the product leaves little room for ‘the art of medicine,’ ” Kim said.
That art is practiced by Arnon Elizur, MD, from the Shamir Medical Center in Tzrifin, Israel, but it’s backed by a rigid home-grown protocol.
Since 2010, he has treated 1,800 patients for peanut allergy, updosing slowly to a tolerance of 3,000 mg of peanut, the equivalent of 10 peanuts. He keeps the maintenance dose at four peanuts (1,200 mg). His center takes a personalized approach, starting patients on the highest dose they can tolerate and working up, with daily patient check-ins from home and a staff available around the clock to answer questions and deal with reactions.
“We aim for full sensitization,” Dr. Elizur said in an interview.
The peanut pill is “a big step forward” for immunotherapy, he said. It is “a standardized product, checked for bacteria and allergen content, which is available to a wide community of physicians.”
But, he pointed out, “it’s expensive.” And it’s only for peanut. “There are millions of food-allergic patients around the world dying from adverse reactions to many different kinds of food. We don’t want to wait for years for a product for all of them. We can use the actual food.”
He questions the lifelong maintenance protocol with a daily 300-mg pill. “If you can’t eat a peanut, why would you buy a drug that’s a peanut?” he asked.
He also said he’s disappointed that the product is not indicated for adults.
At the Shamir clinic, reactions are closely monitored. “Some are mild, others we treat with autoinjectors, epinephrine,” he reported. “Those are the most undesirable.”
Data from his center show that reactions occur in about 15% of patients. But his treatment success rates are good. In an average of 8 months, he is able to get 80% of his adult patients to full sensitization.
But it’s not for all patients or for all clinics, he acknowledged. “We continue to look at this balance in quality of life throughout the process. Our goal is to improve the quality of life threshold.”
Treatment that involves “native food” is “a lot of work” and requires “a lot of investment,” Dr. Elizur said. His center uses a web reporting system to maintain a 24/7 dialogue with patients, “and we look at the reports every day.” They also have a physician on call at all times. “Not everyone can commit to providing care throughout the day and night.”
His center charges the equivalent of $US3,000 per food allergy treated. “That’s whether it takes 6 months or 2 years,” he said.
There are more than 1,000 people on his 3-year waiting list.
“This is the first year that the American College of Allergy, Asthma, and Immunology is not hosting a pro–con debate on oral immunotherapy,” Dr. Kim pointed out. “We have a therapy now.”
However, the pandemic has slowed treatment uptake. “Immunotherapy is not easy to do, whether it’s FDA approved or not,” he explained. With at least 11 doctor visits in the first 6 months – each visit is between 30 minutes and 2-3 hours long – it hasn’t been possible to set up this year. “It’s not ideal.”
It will be interesting to see “how this will roll out and how it will be adopted,” Dr. Kim said. “From a food allergy point of view, the next 12 months are going to be very interesting.”
Dr. Kim reports receiving consulting honorarium from Aimmune, the maker of Palforzia; being on the clinical medical advisory board for DBV Technologies; and consulting for Aimmune, Allakos, Allergenis, DBV, Duke Clinical Research Institute, Ukko Incorporated, Vibrant America, and Kenota Health. Dr. Elizur has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Peanut allergy immunotherapy now comes with approval from the US Food and Drug Administration (FDA), but it also comes with protocols, standards, and paperwork. Whether it will be widely adopted has yet to be determined.
A few dozen allergists around the world have been offering food allergy immunotherapy for many years, having developed their own measuring techniques using store-bought food.
But the vast majority of allergists are not interested in developing home-grown treatments, not only because it involves research and development, but also because it comes with legal risks.
“Finally we have another treatment option,” said Edwin Kim, MD, from the UNC Allergy and Immunology Clinic in Chapel Hill, N.C. “This is what we were waiting for. It’s not cowboy stuff; this works.”
In January, the FDA approved peanut allergen powder (Palforzia) for patients 4-17 years of age, as reported by Medscape Medical News.
The pill contains measured doses of peanut flour and comes with a protocol that will allow allergists to bring patients to a peanut tolerance of 300 mg (about one peanut) and a black-box warning about anaphylaxis risk.
And before allergists can prescribe it, they must take a Risk Evaluation and Mitigation Strategy course to learn about dosing and the allergic reaction protocol.
“That may scare some away,” said Dr. Kim, who discussed the FDA-approved option during his presentation at the American College of Allergy, Asthma & Immunology 2020 Annual Scientific Meeting.
Allergic reaction, including the potential for anaphylaxis, has always been an issue with immunotherapy.
“People make the argument that there is a difference” between an expected allergic reaction – such as one that occurs after the administration of immunotherapy – and an unexpected reaction, he said. Because an expected reaction can be treated quickly, “some feel these expected reactions don’t matter so much.”
“Others say a reaction is a reaction” and argue that if, a treatment causes reaction, then it doesn’t make sense, he explained.
It comes down to patients – they must be willing to take a risk to develop tolerance and improve their quality of life – and the allergists willing to treat them.
The peanut powder involves paperwork, preauthorization forms, denials of care, a higher price tag, regimented procedures, and a prerequisite number of visits with patients. “Not everyone will want to do this,” said Dr. Kim.
The regimen involves three phases. During initial dose escalation, five doses are administered in the office on day 1. Then, over the next 6 months, updoses are administered during 11 in-office sessions and a 300-mg tolerance is achieved. Finally, to maintain tolerance to one peanut, daily doses are administered at home.
The drug cost alone is about $4,200 a year, according to Institute for Clinical and Economic Review. Peanut flour from the grocery store is cheaper, but comes with the risk of bacteria or other contamination.
“This product offers some reassurance, and that matters,” Dr. Kim said.
It’s good to have more options for food allergy treatment. “We need a more proactive way to treat food allergy; avoidance is not good enough,” he explained. “And presumably, at some point, the patient will be able to eat a grocery-store peanut instead of buying the pills.”
The art of medicine
But not all allergists will be able to make the protocol work. And it’s not clear whether there is room to alter treatment and offer patients with a higher tolerance a higher starting dose. What we do know, though, is that “the product leaves little room for ‘the art of medicine,’ ” Kim said.
That art is practiced by Arnon Elizur, MD, from the Shamir Medical Center in Tzrifin, Israel, but it’s backed by a rigid home-grown protocol.
Since 2010, he has treated 1,800 patients for peanut allergy, updosing slowly to a tolerance of 3,000 mg of peanut, the equivalent of 10 peanuts. He keeps the maintenance dose at four peanuts (1,200 mg). His center takes a personalized approach, starting patients on the highest dose they can tolerate and working up, with daily patient check-ins from home and a staff available around the clock to answer questions and deal with reactions.
“We aim for full sensitization,” Dr. Elizur said in an interview.
The peanut pill is “a big step forward” for immunotherapy, he said. It is “a standardized product, checked for bacteria and allergen content, which is available to a wide community of physicians.”
But, he pointed out, “it’s expensive.” And it’s only for peanut. “There are millions of food-allergic patients around the world dying from adverse reactions to many different kinds of food. We don’t want to wait for years for a product for all of them. We can use the actual food.”
He questions the lifelong maintenance protocol with a daily 300-mg pill. “If you can’t eat a peanut, why would you buy a drug that’s a peanut?” he asked.
He also said he’s disappointed that the product is not indicated for adults.
At the Shamir clinic, reactions are closely monitored. “Some are mild, others we treat with autoinjectors, epinephrine,” he reported. “Those are the most undesirable.”
Data from his center show that reactions occur in about 15% of patients. But his treatment success rates are good. In an average of 8 months, he is able to get 80% of his adult patients to full sensitization.
But it’s not for all patients or for all clinics, he acknowledged. “We continue to look at this balance in quality of life throughout the process. Our goal is to improve the quality of life threshold.”
Treatment that involves “native food” is “a lot of work” and requires “a lot of investment,” Dr. Elizur said. His center uses a web reporting system to maintain a 24/7 dialogue with patients, “and we look at the reports every day.” They also have a physician on call at all times. “Not everyone can commit to providing care throughout the day and night.”
His center charges the equivalent of $US3,000 per food allergy treated. “That’s whether it takes 6 months or 2 years,” he said.
There are more than 1,000 people on his 3-year waiting list.
“This is the first year that the American College of Allergy, Asthma, and Immunology is not hosting a pro–con debate on oral immunotherapy,” Dr. Kim pointed out. “We have a therapy now.”
However, the pandemic has slowed treatment uptake. “Immunotherapy is not easy to do, whether it’s FDA approved or not,” he explained. With at least 11 doctor visits in the first 6 months – each visit is between 30 minutes and 2-3 hours long – it hasn’t been possible to set up this year. “It’s not ideal.”
It will be interesting to see “how this will roll out and how it will be adopted,” Dr. Kim said. “From a food allergy point of view, the next 12 months are going to be very interesting.”
Dr. Kim reports receiving consulting honorarium from Aimmune, the maker of Palforzia; being on the clinical medical advisory board for DBV Technologies; and consulting for Aimmune, Allakos, Allergenis, DBV, Duke Clinical Research Institute, Ukko Incorporated, Vibrant America, and Kenota Health. Dr. Elizur has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Moderna: Interim data show 94.5% efficacy for COVID-19 vaccine, will seek FDA EUA
The Moderna mRNA-1273 vaccine, in development to prevent COVID-19, yielded 94.5% efficacy in early results and is generally well tolerated, the company announced early Monday. The product can be stored at refrigeration temperatures common to many physician offices, pharmacies, and hospitals.
The first interim results of the phase 3 COVE trial included 95 participants with confirmed COVID-19. An independent data safety monitoring board, which was appointed by the National Institutes of Health, informed Moderna that 90 of the patients who were positive for COVID-19 were in a placebo group and that 5 patients were in the mRNA-1273 vaccine group, resulting in a vaccine efficacy of 94.5% (P < .0001).
Interim data included 11 patients with severe COVID-19, all of whom were in the placebo group.
“This positive interim analysis from our phase 3 study has given us the first clinical validation that our vaccine can prevent COVID-19 disease, including severe disease,” said Stéphane Bancel, CEO of Moderna, said in a statement.
The vaccine met its primary study endpoint, which was based on adjudicated data that were collected starting 2 weeks after the second dose of mRNA-1273. The interim study population included people who could be at higher risk for COVID-19, including 15 adults aged 65 years and older and 20 participants from diverse communities.
Safety data
The DSMB also reviewed safety data for the COVE study interim results. The vaccine was generally safe and well tolerated, as determined on the basis of solicited adverse events. Most adverse events were mild to moderate and were generally short-lived, according to a company news release.
Injection-site pain was reported in 2.7% of participants after the first dose. After the second dose, 9.7% of participants reported fatigue, 8.9% reported myalgia, 5.2% reported arthralgia, 4.5% reported headache, 4.1% reported pain, and 2.0% reported erythema or redness at the injection site.
Moderna plans to request emergency-use authorization (EUA) from the Food and Drug Administration in the coming weeks. The company expects that the EUA will be based on more data from the COVE study, including a final analysis of 151 patients with a median follow-up of more than 2 months. Moderna also plans to seek authorizations from global regulatory agencies.
The company expects to have approximately 20 million doses of mRNA-1273 ready to ship in the United States by the end of the year. In addition, the company says it remains on track to manufacture between 500 million and 1 billion doses globally in 2021.
Moderna is developing distribution plans in conjunction with the Centers for Disease Control and Prevention, the federal government’s Operation Warp Speed, and McKesson, a COVID-19 vaccine distributor contracted by the U.S. government.
Refrigeration requirements
The mRNA-1273 vaccine can be shipped and stored for up to 6 months at –20° C (about –4° F), a temperature maintained in most home or medical freezers, according to Moderna. The company expects that, after the product thaws, it will remain stable at standard refrigerator temperatures of 2°-8° C (36°-46° F) for up to 30 days within the 6-month shelf life.
Because the mRNA-1273 vaccine is stable at these refrigerator temperatures, it can be stored at most physicians’ offices, pharmacies, and hospitals, the company noted. In contrast, the similar Pfizer BTN162b2 vaccine – early results for which showed a 90% efficacy rate – requires shipment and storage at “deep-freeze” conditions of –70° C or –80° C, which is more challenging from a logistic point of view.
Moderna’s mRNA-1273 can be kept at room temperature for up to 12 hours after removal from a refrigerator for patient administration. The vaccine will not require dilution prior to use.
More than 30,000 people aged older than 18 years in the United States are enrolled in the COVE study. The research is being conducted in collaboration with the National Institute of Allergy and Infectious Diseases and the Biomedical Advanced Research and Development Authority, part of the Office of the Assistant Secretary for Preparedness and Response at the Department of Health & Human Services.
A version of this article originally appeared on Medscape.com.
The Moderna mRNA-1273 vaccine, in development to prevent COVID-19, yielded 94.5% efficacy in early results and is generally well tolerated, the company announced early Monday. The product can be stored at refrigeration temperatures common to many physician offices, pharmacies, and hospitals.
The first interim results of the phase 3 COVE trial included 95 participants with confirmed COVID-19. An independent data safety monitoring board, which was appointed by the National Institutes of Health, informed Moderna that 90 of the patients who were positive for COVID-19 were in a placebo group and that 5 patients were in the mRNA-1273 vaccine group, resulting in a vaccine efficacy of 94.5% (P < .0001).
Interim data included 11 patients with severe COVID-19, all of whom were in the placebo group.
“This positive interim analysis from our phase 3 study has given us the first clinical validation that our vaccine can prevent COVID-19 disease, including severe disease,” said Stéphane Bancel, CEO of Moderna, said in a statement.
The vaccine met its primary study endpoint, which was based on adjudicated data that were collected starting 2 weeks after the second dose of mRNA-1273. The interim study population included people who could be at higher risk for COVID-19, including 15 adults aged 65 years and older and 20 participants from diverse communities.
Safety data
The DSMB also reviewed safety data for the COVE study interim results. The vaccine was generally safe and well tolerated, as determined on the basis of solicited adverse events. Most adverse events were mild to moderate and were generally short-lived, according to a company news release.
Injection-site pain was reported in 2.7% of participants after the first dose. After the second dose, 9.7% of participants reported fatigue, 8.9% reported myalgia, 5.2% reported arthralgia, 4.5% reported headache, 4.1% reported pain, and 2.0% reported erythema or redness at the injection site.
Moderna plans to request emergency-use authorization (EUA) from the Food and Drug Administration in the coming weeks. The company expects that the EUA will be based on more data from the COVE study, including a final analysis of 151 patients with a median follow-up of more than 2 months. Moderna also plans to seek authorizations from global regulatory agencies.
The company expects to have approximately 20 million doses of mRNA-1273 ready to ship in the United States by the end of the year. In addition, the company says it remains on track to manufacture between 500 million and 1 billion doses globally in 2021.
Moderna is developing distribution plans in conjunction with the Centers for Disease Control and Prevention, the federal government’s Operation Warp Speed, and McKesson, a COVID-19 vaccine distributor contracted by the U.S. government.
Refrigeration requirements
The mRNA-1273 vaccine can be shipped and stored for up to 6 months at –20° C (about –4° F), a temperature maintained in most home or medical freezers, according to Moderna. The company expects that, after the product thaws, it will remain stable at standard refrigerator temperatures of 2°-8° C (36°-46° F) for up to 30 days within the 6-month shelf life.
Because the mRNA-1273 vaccine is stable at these refrigerator temperatures, it can be stored at most physicians’ offices, pharmacies, and hospitals, the company noted. In contrast, the similar Pfizer BTN162b2 vaccine – early results for which showed a 90% efficacy rate – requires shipment and storage at “deep-freeze” conditions of –70° C or –80° C, which is more challenging from a logistic point of view.
Moderna’s mRNA-1273 can be kept at room temperature for up to 12 hours after removal from a refrigerator for patient administration. The vaccine will not require dilution prior to use.
More than 30,000 people aged older than 18 years in the United States are enrolled in the COVE study. The research is being conducted in collaboration with the National Institute of Allergy and Infectious Diseases and the Biomedical Advanced Research and Development Authority, part of the Office of the Assistant Secretary for Preparedness and Response at the Department of Health & Human Services.
A version of this article originally appeared on Medscape.com.
The Moderna mRNA-1273 vaccine, in development to prevent COVID-19, yielded 94.5% efficacy in early results and is generally well tolerated, the company announced early Monday. The product can be stored at refrigeration temperatures common to many physician offices, pharmacies, and hospitals.
The first interim results of the phase 3 COVE trial included 95 participants with confirmed COVID-19. An independent data safety monitoring board, which was appointed by the National Institutes of Health, informed Moderna that 90 of the patients who were positive for COVID-19 were in a placebo group and that 5 patients were in the mRNA-1273 vaccine group, resulting in a vaccine efficacy of 94.5% (P < .0001).
Interim data included 11 patients with severe COVID-19, all of whom were in the placebo group.
“This positive interim analysis from our phase 3 study has given us the first clinical validation that our vaccine can prevent COVID-19 disease, including severe disease,” said Stéphane Bancel, CEO of Moderna, said in a statement.
The vaccine met its primary study endpoint, which was based on adjudicated data that were collected starting 2 weeks after the second dose of mRNA-1273. The interim study population included people who could be at higher risk for COVID-19, including 15 adults aged 65 years and older and 20 participants from diverse communities.
Safety data
The DSMB also reviewed safety data for the COVE study interim results. The vaccine was generally safe and well tolerated, as determined on the basis of solicited adverse events. Most adverse events were mild to moderate and were generally short-lived, according to a company news release.
Injection-site pain was reported in 2.7% of participants after the first dose. After the second dose, 9.7% of participants reported fatigue, 8.9% reported myalgia, 5.2% reported arthralgia, 4.5% reported headache, 4.1% reported pain, and 2.0% reported erythema or redness at the injection site.
Moderna plans to request emergency-use authorization (EUA) from the Food and Drug Administration in the coming weeks. The company expects that the EUA will be based on more data from the COVE study, including a final analysis of 151 patients with a median follow-up of more than 2 months. Moderna also plans to seek authorizations from global regulatory agencies.
The company expects to have approximately 20 million doses of mRNA-1273 ready to ship in the United States by the end of the year. In addition, the company says it remains on track to manufacture between 500 million and 1 billion doses globally in 2021.
Moderna is developing distribution plans in conjunction with the Centers for Disease Control and Prevention, the federal government’s Operation Warp Speed, and McKesson, a COVID-19 vaccine distributor contracted by the U.S. government.
Refrigeration requirements
The mRNA-1273 vaccine can be shipped and stored for up to 6 months at –20° C (about –4° F), a temperature maintained in most home or medical freezers, according to Moderna. The company expects that, after the product thaws, it will remain stable at standard refrigerator temperatures of 2°-8° C (36°-46° F) for up to 30 days within the 6-month shelf life.
Because the mRNA-1273 vaccine is stable at these refrigerator temperatures, it can be stored at most physicians’ offices, pharmacies, and hospitals, the company noted. In contrast, the similar Pfizer BTN162b2 vaccine – early results for which showed a 90% efficacy rate – requires shipment and storage at “deep-freeze” conditions of –70° C or –80° C, which is more challenging from a logistic point of view.
Moderna’s mRNA-1273 can be kept at room temperature for up to 12 hours after removal from a refrigerator for patient administration. The vaccine will not require dilution prior to use.
More than 30,000 people aged older than 18 years in the United States are enrolled in the COVE study. The research is being conducted in collaboration with the National Institute of Allergy and Infectious Diseases and the Biomedical Advanced Research and Development Authority, part of the Office of the Assistant Secretary for Preparedness and Response at the Department of Health & Human Services.
A version of this article originally appeared on Medscape.com.
Poverty raises depression risk in patients with cystic fibrosis
Poor people with chronic illness have greater difficulty managing their disease than do their better-off counterparts, and a new study confirms this reality for patients with cystic fibrosis.
and anxiety symptoms, according to a new cross-sectional study. The data were drawn from the Cystic Fibrosis Foundation’s Success with Therapies Research Consortium.
“Assessing the special challenges that individuals with lower SES face, including financial barriers, is essential to understand how we can address the unique combinations of adherence barriers. In other chronic disorders, financial barriers or lower socioeconomic status is associated with nonadherence, but this relationship has not been well established in cystic fibrosis,” said Kimberly Dickinson, MD, MPH, of Johns Hopkins University, Baltimore, during her presentation of the results at the virtual North American Cystic Fibrosis Conference.
“I’ve always thought that my patients in the poorer population were doing worse, and I think this demonstrates that that’s true,” said Robert Giusti, MD, in an interview. Dr. Giusti is a clinical professor of pediatrics at the New York University and director of the Pediatric Cystic Fibrosis Center in New York. He was not involved in the study.
“These are very pertinent issues, especially if you think about the pandemic, and some of the issues related to mental health. It just highlights the importance of socioeconomic status and screening for some of the known risk factors so that we can develop interventions or programs to provide equitable care to all of our cystic fibrosis patients,” said Ryan Perkins, MD, who moderated the session where the study was presented. He is a pediatric and adult pulmonary fellow at Boston Children’s Hospital and Brigham and Women’s Hospital, also in Boston.
The researchers looked retrospectively at 1 year’s worth of pharmacy refill receipts and number of times prescriptions were refilled versus the number of times prescribed, then calculated medicinal possession ratios. This was cross-referenced with annual household income and insurance status of patients with CF at 12 pediatric and 9 adult CF care centers, for a total of 376 patients (128 pediatric and 248 adult).
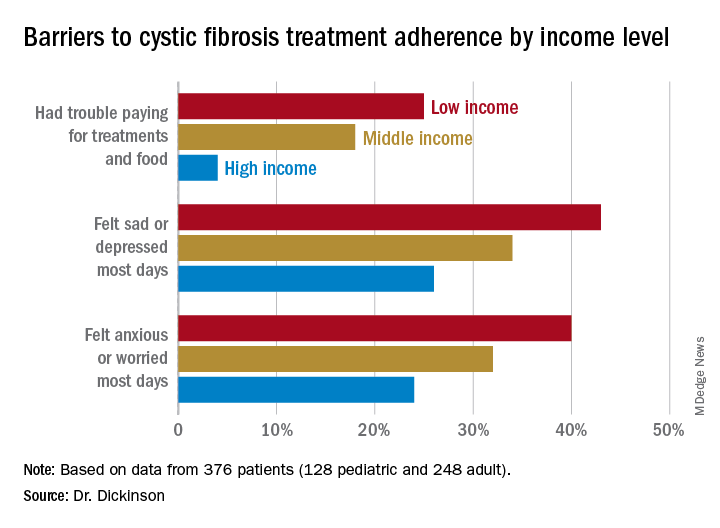
In this population, 32% of participants had public or no insurance, 68% had private or military insurance. The public/no insurance group was more likely than the private/military insurance group to report having trouble paying for treatments, food, or critical expenses related to CF care (23.3% vs. 12.1%, respectively); feeling symptoms on most days of depression (42.5% vs. 31.3%) or anxiety (40.0% vs. 28.5%); and experiencing conflict or stress with loved ones over treatments (30.0% vs. 20.3%) (P < .05 for all).
In all, 35% had a household income less than $40,000 per year, 33% between $44,000 and $100,000, and 32% higher than $100,000. The low-income group had a lower composite medication possession ratio (0.41) than the middle- (0.44) or high-income (0.52) groups, were more likely to have trouble paying for treatments, food, or treatment-related expenses (25%, 18%, 4%, respectively); were more likely most days to report symptoms of depression (43%, 34%, 26%) or anxiety (40%, 32%, 24%), and to have concerns about whether treatments were effective (42%, 27%, 29%). They were more likely to not be able to maintain a daily schedule or routine for treatments (28%, 22%, 14%).
The study showed that adherence barriers and suboptimal adherence are issues that cross all socioeconomic categories, though they were more problematic in the lowest bracket. Greater anxiety and depression among lower income individuals and those with private or no insurance was a key finding, according to Dr. Dickinson. “It highlights the importance of screening for mental health comorbidities that may impact non-adherence,” she said.
The study received funding from the Cystic Fibrosis Foundation. Dr. Dickinson, Dr. Giusti, and Dr. Perkins have no relevant financial disclosures.
Poor people with chronic illness have greater difficulty managing their disease than do their better-off counterparts, and a new study confirms this reality for patients with cystic fibrosis.
and anxiety symptoms, according to a new cross-sectional study. The data were drawn from the Cystic Fibrosis Foundation’s Success with Therapies Research Consortium.
“Assessing the special challenges that individuals with lower SES face, including financial barriers, is essential to understand how we can address the unique combinations of adherence barriers. In other chronic disorders, financial barriers or lower socioeconomic status is associated with nonadherence, but this relationship has not been well established in cystic fibrosis,” said Kimberly Dickinson, MD, MPH, of Johns Hopkins University, Baltimore, during her presentation of the results at the virtual North American Cystic Fibrosis Conference.
“I’ve always thought that my patients in the poorer population were doing worse, and I think this demonstrates that that’s true,” said Robert Giusti, MD, in an interview. Dr. Giusti is a clinical professor of pediatrics at the New York University and director of the Pediatric Cystic Fibrosis Center in New York. He was not involved in the study.
“These are very pertinent issues, especially if you think about the pandemic, and some of the issues related to mental health. It just highlights the importance of socioeconomic status and screening for some of the known risk factors so that we can develop interventions or programs to provide equitable care to all of our cystic fibrosis patients,” said Ryan Perkins, MD, who moderated the session where the study was presented. He is a pediatric and adult pulmonary fellow at Boston Children’s Hospital and Brigham and Women’s Hospital, also in Boston.
The researchers looked retrospectively at 1 year’s worth of pharmacy refill receipts and number of times prescriptions were refilled versus the number of times prescribed, then calculated medicinal possession ratios. This was cross-referenced with annual household income and insurance status of patients with CF at 12 pediatric and 9 adult CF care centers, for a total of 376 patients (128 pediatric and 248 adult).
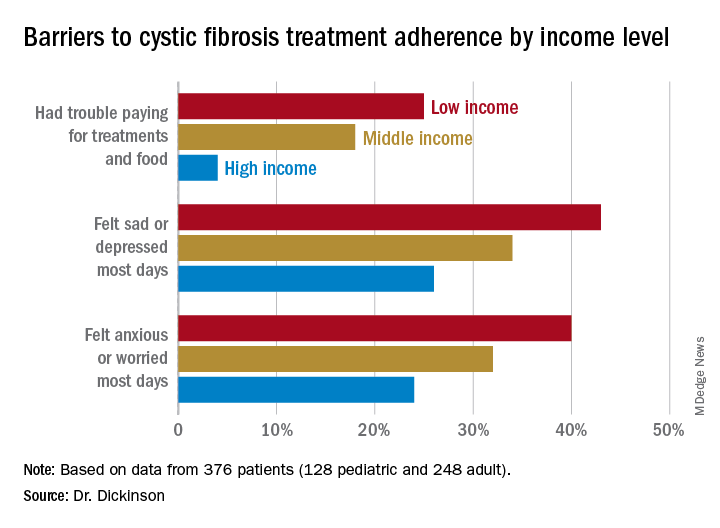
In this population, 32% of participants had public or no insurance, 68% had private or military insurance. The public/no insurance group was more likely than the private/military insurance group to report having trouble paying for treatments, food, or critical expenses related to CF care (23.3% vs. 12.1%, respectively); feeling symptoms on most days of depression (42.5% vs. 31.3%) or anxiety (40.0% vs. 28.5%); and experiencing conflict or stress with loved ones over treatments (30.0% vs. 20.3%) (P < .05 for all).
In all, 35% had a household income less than $40,000 per year, 33% between $44,000 and $100,000, and 32% higher than $100,000. The low-income group had a lower composite medication possession ratio (0.41) than the middle- (0.44) or high-income (0.52) groups, were more likely to have trouble paying for treatments, food, or treatment-related expenses (25%, 18%, 4%, respectively); were more likely most days to report symptoms of depression (43%, 34%, 26%) or anxiety (40%, 32%, 24%), and to have concerns about whether treatments were effective (42%, 27%, 29%). They were more likely to not be able to maintain a daily schedule or routine for treatments (28%, 22%, 14%).
The study showed that adherence barriers and suboptimal adherence are issues that cross all socioeconomic categories, though they were more problematic in the lowest bracket. Greater anxiety and depression among lower income individuals and those with private or no insurance was a key finding, according to Dr. Dickinson. “It highlights the importance of screening for mental health comorbidities that may impact non-adherence,” she said.
The study received funding from the Cystic Fibrosis Foundation. Dr. Dickinson, Dr. Giusti, and Dr. Perkins have no relevant financial disclosures.
Poor people with chronic illness have greater difficulty managing their disease than do their better-off counterparts, and a new study confirms this reality for patients with cystic fibrosis.
and anxiety symptoms, according to a new cross-sectional study. The data were drawn from the Cystic Fibrosis Foundation’s Success with Therapies Research Consortium.
“Assessing the special challenges that individuals with lower SES face, including financial barriers, is essential to understand how we can address the unique combinations of adherence barriers. In other chronic disorders, financial barriers or lower socioeconomic status is associated with nonadherence, but this relationship has not been well established in cystic fibrosis,” said Kimberly Dickinson, MD, MPH, of Johns Hopkins University, Baltimore, during her presentation of the results at the virtual North American Cystic Fibrosis Conference.
“I’ve always thought that my patients in the poorer population were doing worse, and I think this demonstrates that that’s true,” said Robert Giusti, MD, in an interview. Dr. Giusti is a clinical professor of pediatrics at the New York University and director of the Pediatric Cystic Fibrosis Center in New York. He was not involved in the study.
“These are very pertinent issues, especially if you think about the pandemic, and some of the issues related to mental health. It just highlights the importance of socioeconomic status and screening for some of the known risk factors so that we can develop interventions or programs to provide equitable care to all of our cystic fibrosis patients,” said Ryan Perkins, MD, who moderated the session where the study was presented. He is a pediatric and adult pulmonary fellow at Boston Children’s Hospital and Brigham and Women’s Hospital, also in Boston.
The researchers looked retrospectively at 1 year’s worth of pharmacy refill receipts and number of times prescriptions were refilled versus the number of times prescribed, then calculated medicinal possession ratios. This was cross-referenced with annual household income and insurance status of patients with CF at 12 pediatric and 9 adult CF care centers, for a total of 376 patients (128 pediatric and 248 adult).
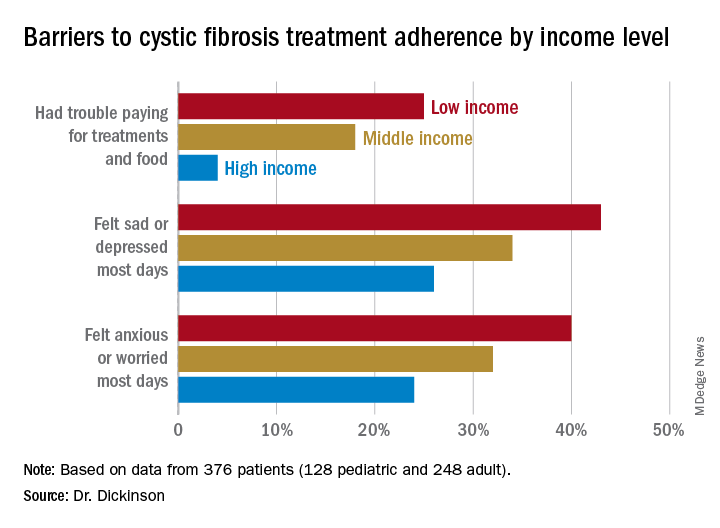
In this population, 32% of participants had public or no insurance, 68% had private or military insurance. The public/no insurance group was more likely than the private/military insurance group to report having trouble paying for treatments, food, or critical expenses related to CF care (23.3% vs. 12.1%, respectively); feeling symptoms on most days of depression (42.5% vs. 31.3%) or anxiety (40.0% vs. 28.5%); and experiencing conflict or stress with loved ones over treatments (30.0% vs. 20.3%) (P < .05 for all).
In all, 35% had a household income less than $40,000 per year, 33% between $44,000 and $100,000, and 32% higher than $100,000. The low-income group had a lower composite medication possession ratio (0.41) than the middle- (0.44) or high-income (0.52) groups, were more likely to have trouble paying for treatments, food, or treatment-related expenses (25%, 18%, 4%, respectively); were more likely most days to report symptoms of depression (43%, 34%, 26%) or anxiety (40%, 32%, 24%), and to have concerns about whether treatments were effective (42%, 27%, 29%). They were more likely to not be able to maintain a daily schedule or routine for treatments (28%, 22%, 14%).
The study showed that adherence barriers and suboptimal adherence are issues that cross all socioeconomic categories, though they were more problematic in the lowest bracket. Greater anxiety and depression among lower income individuals and those with private or no insurance was a key finding, according to Dr. Dickinson. “It highlights the importance of screening for mental health comorbidities that may impact non-adherence,” she said.
The study received funding from the Cystic Fibrosis Foundation. Dr. Dickinson, Dr. Giusti, and Dr. Perkins have no relevant financial disclosures.
FROM NACFC 2020
.