User login
Sign‐Out within the Electronic Medical Record
The delivery of safe, high‐quality care to hospitalized patients depends on effective communication among providers.1, 2 Inpatients may receive care from a number of specialists in addition to their primary hospital physicians, and each provider may practice in a group that transfers care of individual patients among its members. This issue is exacerbated in teaching hospitals because fellows, residents, and interns make frequent transfers of care because of work‐hour rules.3, 4 Finally, teams of physician providers making management decisions must effectively communicate with other members of the care team, such as nurses, dieticians, and social workers, who also may be part of a group practice involving transfers. A patient hospitalized for just a few days in a modern hospital may receive care from dozens of providers and be the subject of multiple transfers of care, or handoffs, that require effective communication. Therefore, as part of its 2006 National Patient Safety Goals,5 the Joint Commission on Accreditation of Health Care Organizations (JCAHO) now requires that each hospital implement a standardized, structured approach to transfers of care.
Transfers of care have been shown to be a source of medical errors and adverse patient outcomes.2, 6, 7 In many cases, the critical information necessary to avert medical errors exists but is not available in real time to providers.6
Traditionally, provider teams have relied on the patient chart, in concert with direct patient evaluation, to provide the information to guide decision making during a hospitalization. Unfortunately, the structure of the chart in most hospitals has evolved little over the past 80 years810 and remains organized so that information is more easily filed than retrieved, read, or summarized.811 Typically, electronic medical records (EMRs) mimic the appearance of paper records and include similar organizational flaws.12 As a result, many providers have created ad hoc informational systems, separate from the chart, designed to track a patient's progress over time and to facilitate transfers of care. These sign‐out systems, which are intended to complement verbal sign‐out between providers,1315 range in complexity from simple handwritten index cards16 to adapted spreadsheets, PDA systems,17, 18 and more complex data systems (eg, FileMaker Pro)19 and often contain crucial information not found elsewhere in the medical record.20, 21
Although sign‐out systems are crucial to patient safety, they have several drawbacks. First, ad‐hoc informational systems may not be standardized, resulting in content and accuracy that vary among providers.22 These systems may fail to identify critical elements of a patient's condition, promoting ineffective communication and placing the patient at increased risk of adverse events.7, 13, 23
These observations underscore the need for a standardized patient‐tracking instrument that can distill crucial patient information, enhance communication, support transfers, improve efficiency, and enhance continuity of patient care.
We aimed to develop an integrated, problem‐based patient‐tracking tool as part of our hospital's EMR. The tool, SynopSIS, supports patient tracking, transfers of care (ie, sign‐outs), and daily rounds.
METHODS
Setting
The study took place at a 547‐bed adult and pediatric tertiary‐care university‐based teaching hospital with 2 campuses at the University of California, San Francisco, Medical Center (UCSFMC).
PROGRAM DESCRIPTION
Development and Design
A multidisciplinary team of practicing residents and attending physicians, information technology leaders, software engineers, and experts in medical communication and sign‐out developed the SynopSIS tool. We reviewed the literature to incorporate key design elements of other successfully implemented information transfer systems.24, 25
We conducted a formal review of existing patient‐tracking and sign‐out systems at our hospital to characterize provider work practices, with an emphasis on the specific information requirements of different specialties. A needs assessment of current sign‐out processes at UCSFMC was conducted by personal interviews with a chief resident or representative of each of the 18 Accreditation Council of Graduate Medical Education (ACGME) accredited residency programs through the dean's office of Graduate Medical Education. This needs assessment revealed that the majority of the programs did not have a standardized mechanism for sign‐out. Although most did use a written format for sign‐out, the actual type of written format varied from handwritten cards to databases using a variety of programs including Filemaker Pro, Microsoft Excel, and Microsoft Word. When asked what could improve the sign‐out system for their program, they most often responded that it would be having a standardized computerized sign‐out system in the hospital.26
During the design and pilot phase, we presented each SynopSIS function to an advisory committee of more than 50 trainees in medical, surgical, and pediatric general and subspecialty fields. Their input shaped the information content and presentation of our tool. In addition, we discussed the tool with the attending‐physician advisory group that oversees the implementation of clinical information systems in our hospital system.
Conceptual Model
We developed this conceptual model by integrating existing scholarship and input from stakeholders at our institution. First, we reviewed existing literature on documentation and transfers of care. Next, we conducted several focus group sessions with our EMR Residents' Advisory Group to conceptualize work flow and handoff needs for hospital physicians across specialties. We arrived at this model after several iterations of feedback from providers.
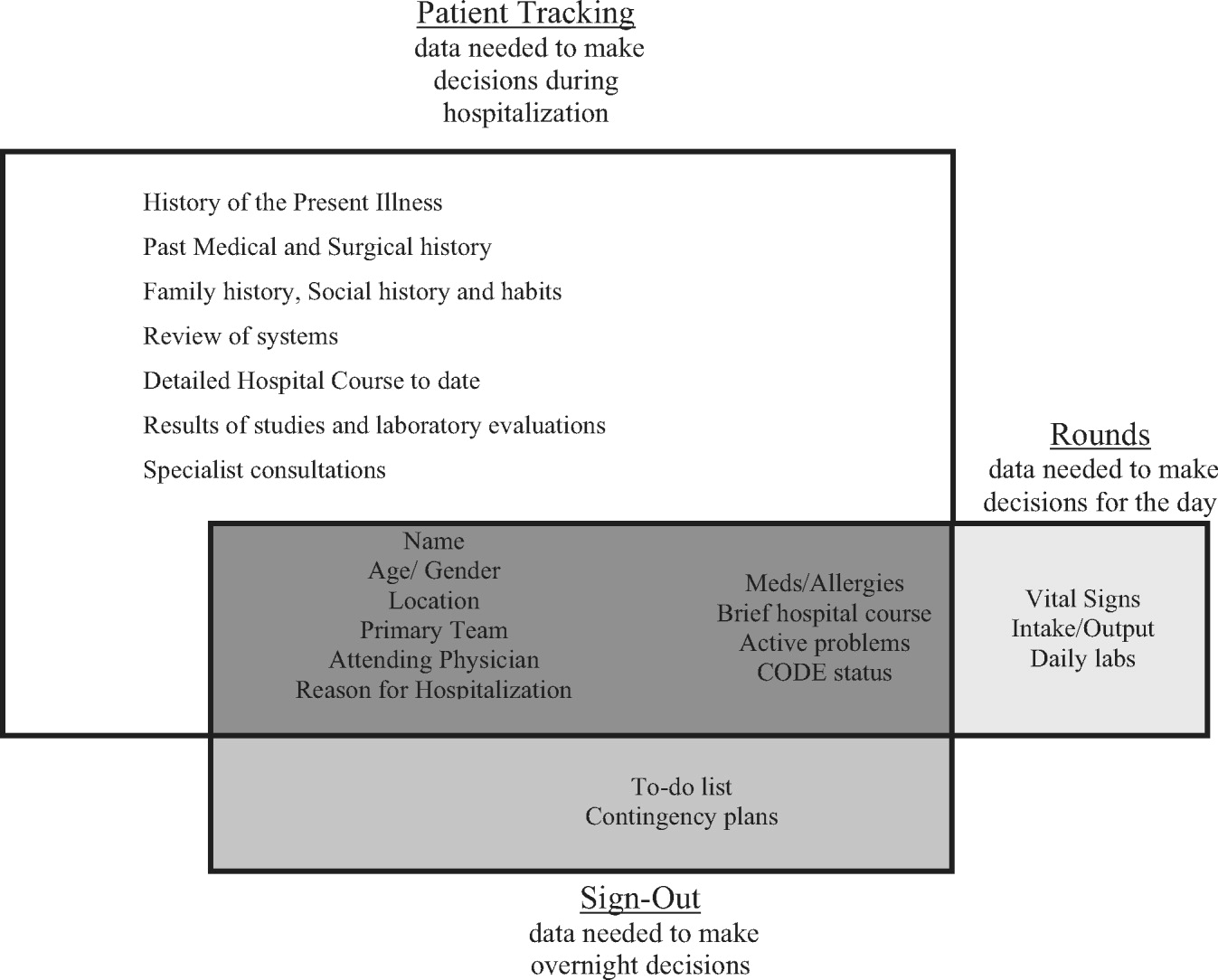
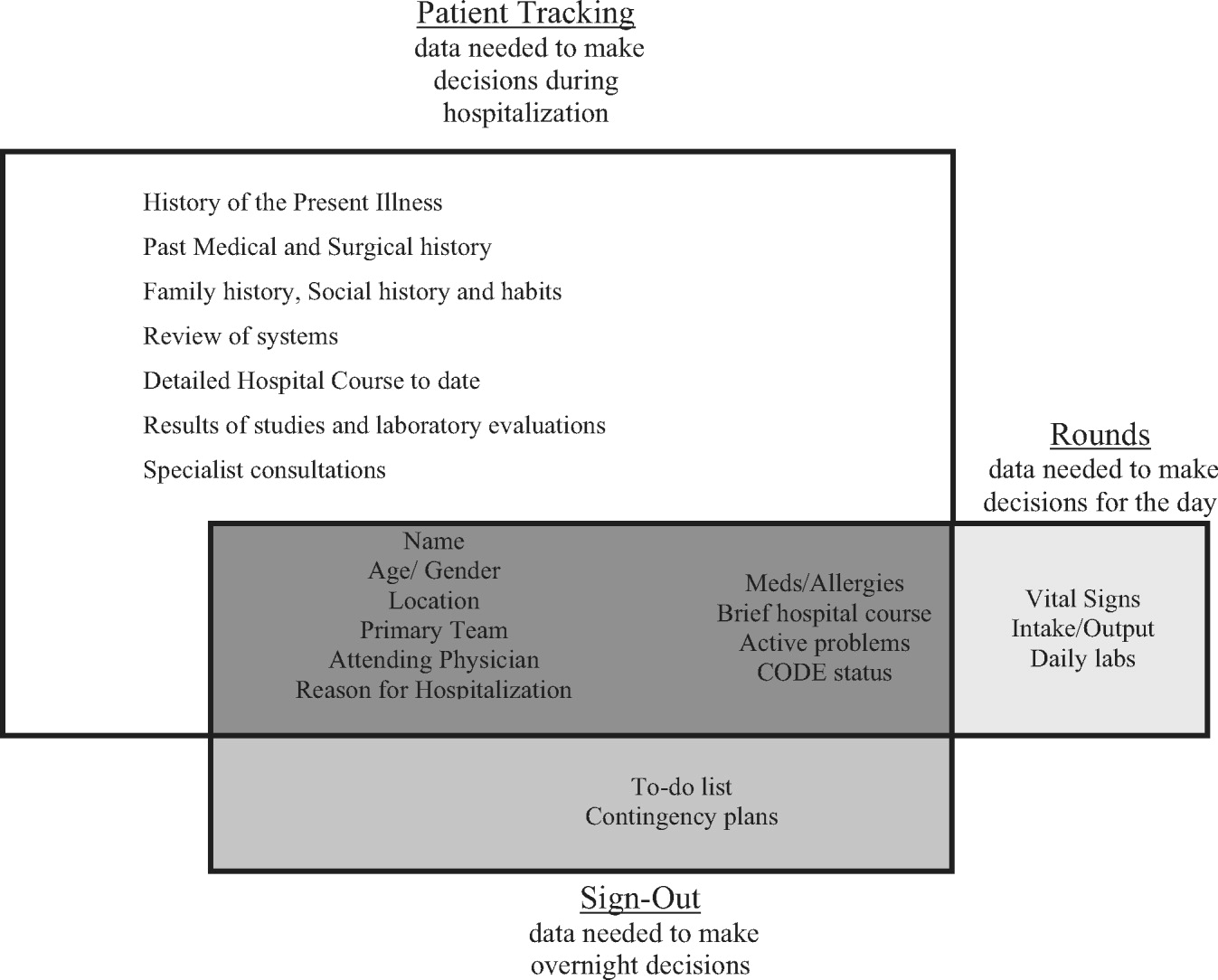
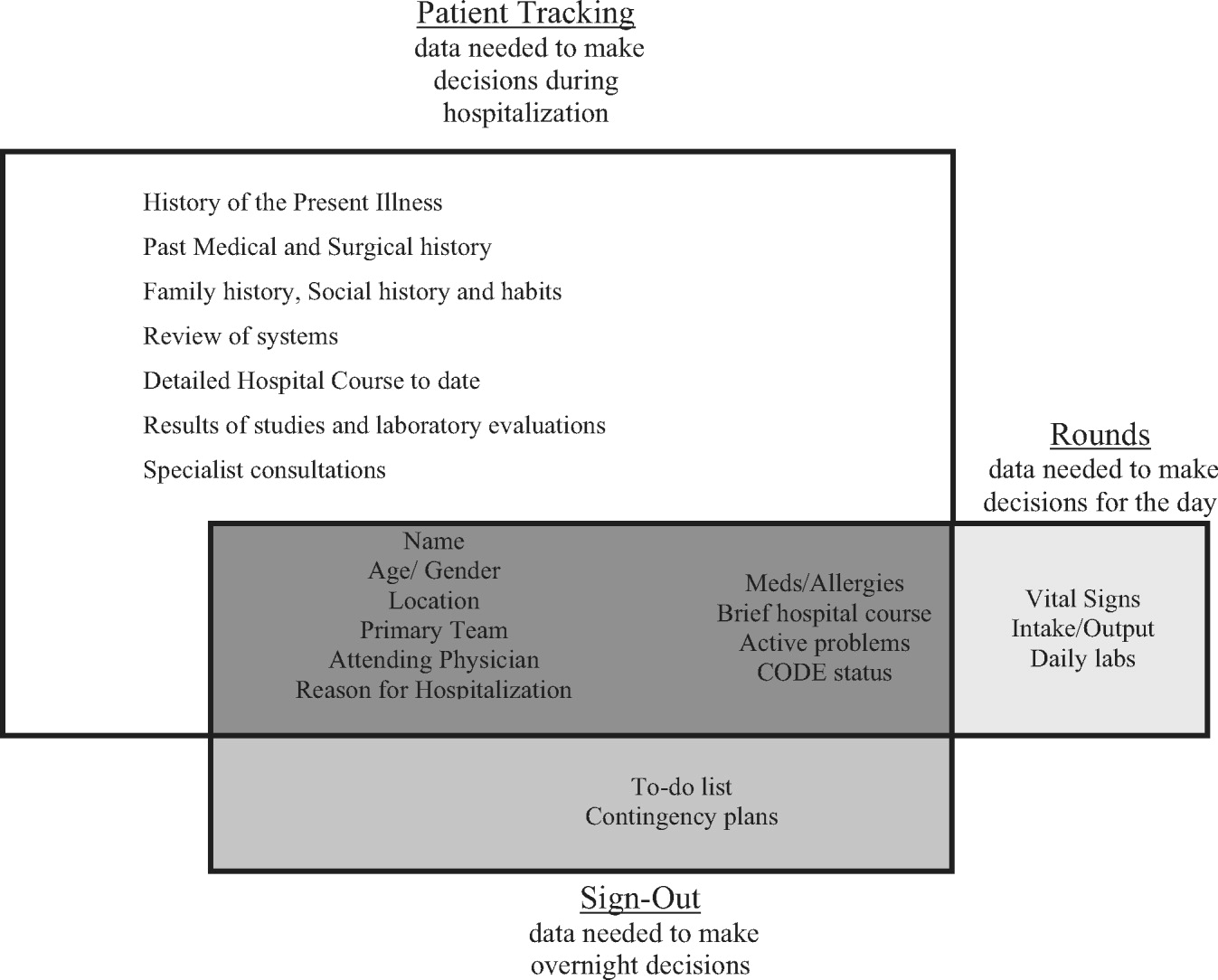
SynopSIS maps patient data available in the EMR to each of the 3 main functions according to type of clinical decisions supported by that function (Fig. 1). For example, data needed for effective patient tracking, such as likely functional status, are required to make decisions over the course of a patient's hospitalization. Similarly, data needed for sign‐out are used to make decisions over the course of a shift, typically overnight; and data needed for morning rounds are used to make decisions for the day. Although the information required for each function overlaps considerably, there are specialized data elements unique to each function.
Description of Functionality
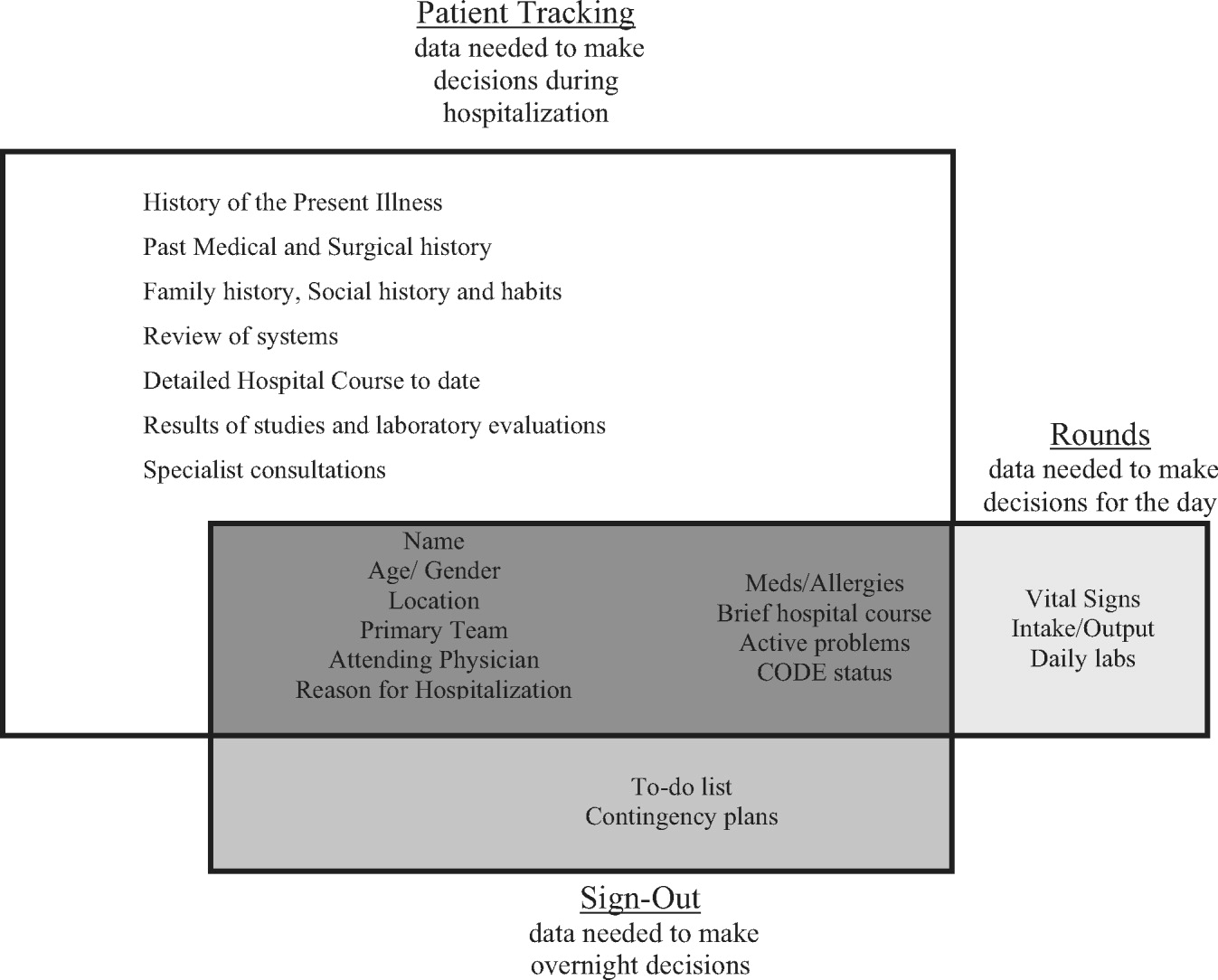
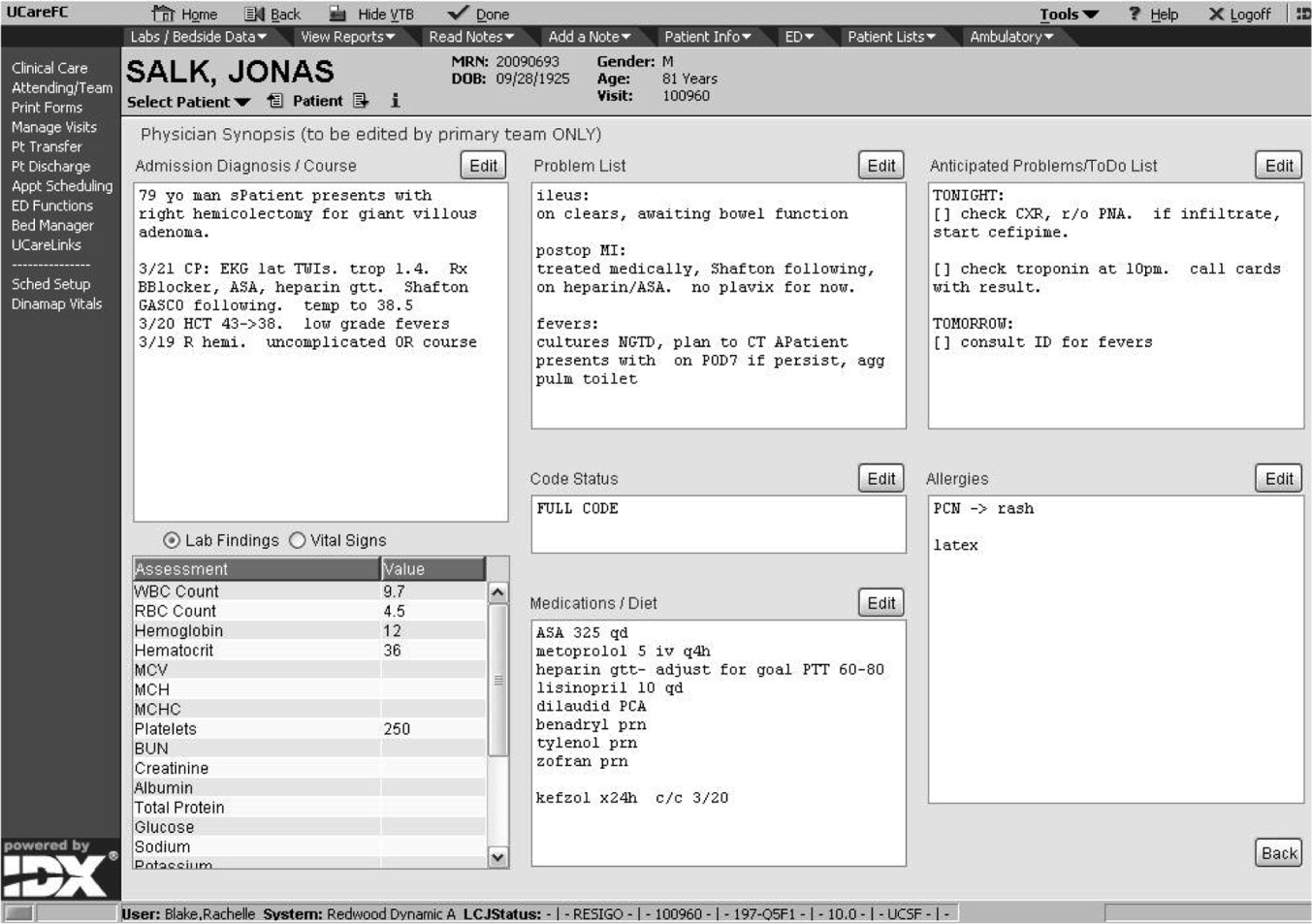
SynopSIS is integrated with our hospital's EMR, General Electric (GE) Centricity Enterprise. The physician interface for SynopSIS is shown in Figure 2. After selecting a patient from a list corresponding to a given inpatient service (eg, Medicine Team B), the user selects the menu option to view the SynopSIS screen, which provides an at a glance overview of the patient's current condition. Different fields on the screen support each of SynopSIS's 3 main functions. At the top, the patient's demographic and registration information is displayed, including name, location, age, medical record number, and attending physician. Below are fields viewable and editable by users of the EMR. The Admission Diagnosis/Course and Problem List fields support patient tracking and allow a receiving physician to understand the reason for the patient's admission, the overall course of the illness, and the current active problems. The problem list is entered by the primary hospital physician. The Anticipated Problems/To Do List field supports the sign‐out function from which providers can coordinate care‐related activities and make contingency plans for anticipated events. The patients' most recent laboratory results and vital signs are displayed on the lower left of the screen for easy reference during face‐to‐face physician sign‐outs. Finally, the CODE status, Allergies, and Medications fields allow efficient tracking of information. Temporarily, until the pharmacy component of the EMR goes into use, the primary hospital physician will enter and update the medications. When the pharmacy is linked to the EMR, medications will be added directly from the inpatient pharmacy records to the EMR‐linked sign‐out tool.
This on‐screen SynopSIS view is distinct from the summary screen typically seen in EMRs, including vendor‐based and the Veterans' Affairs systems. For instance, the Veterans' Affairs summary screen incorporates clinical and nonclinical data, including demographic and payment information, upcoming appointments, and patient‐specific information such as allergies. Moreover, it is not editable by primary hospital physicians. Unlike a summary screen, which collates select patient information from other parts of the EMR, SynopSIS is specific to the current acute hospitalization and includes information not found elsewhere in the medical record.
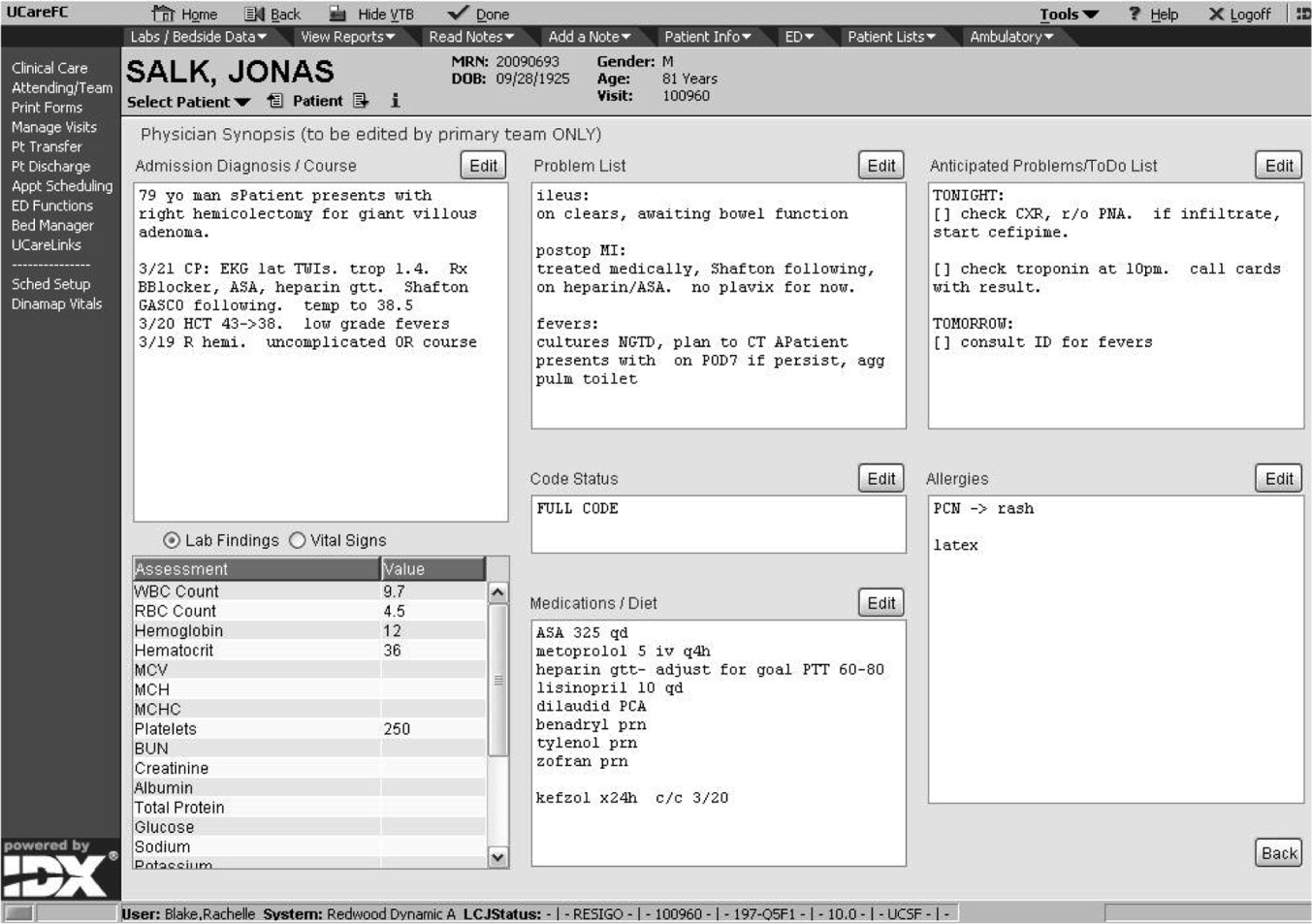
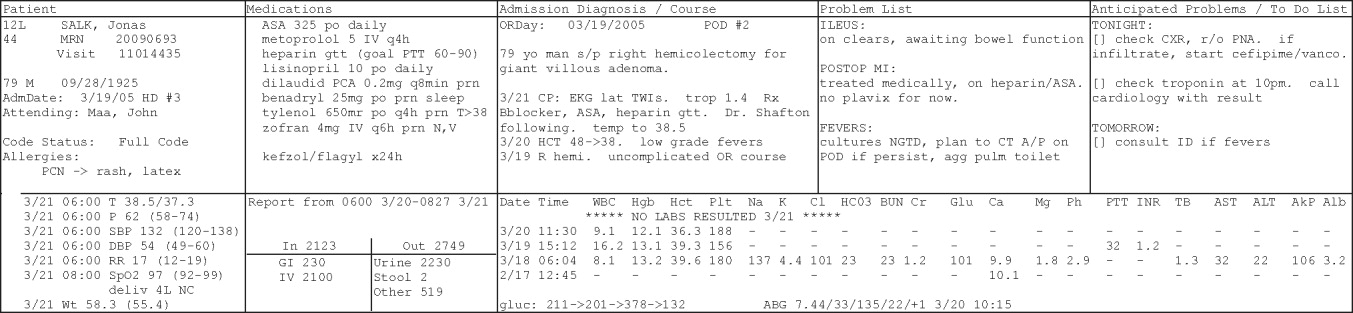
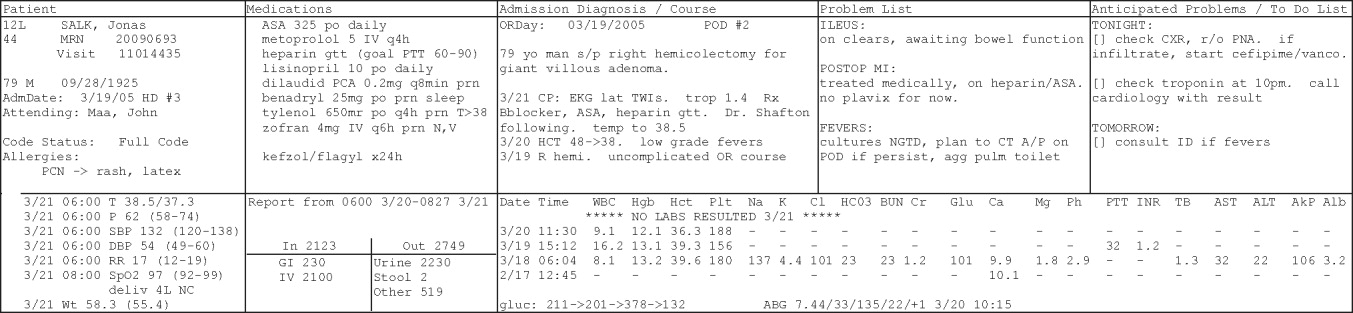
To support rounding, SynopSIS gathers and presents data from the EMR in a printed Rounds Report (Fig. 3). The report is generated for all patients assigned to an inpatient service (eg, Medicine Team B) and emphasizes clarity and brevity using a format validated in the medical literature.24, 25 Each patient's report covers one fourth of a standard 8‐by‐11‐inch landscape‐printed page. The top half of each of these quarter‐page patient reports displays data stored in SynopSIS's interface and summarizes the patient's illness and the course of that illness. The lower half displays vital signs, intake/output, and laboratory data over the 24 hours from the time of printing. The most recent value and the range over the previous 24 hours of all vital signs are displayed. Intake/output totals are listed together with a structured breakdown. Laboratory results for the past 24 hours are listed with the most immediate prior values, allowing providers to discern trends. We envision providers obtaining a rounds report on arrival each day before examining their patients.
Importantly, although SynopSIS is part of the patient's medical record, physician users may change or overwrite the data in any field. This ability is a critical feature of the toolthe focus is on providing an interpretable snapshot of the patient. Data may be removed as their importance lessens or as the patient's condition changes, which contrasts with unchangeable documentation geared for alternative purposes, such as billing or medical‐legal requirements. Deleted data are saved in the medical record and are viewable by audit.
Program Evaluation
We have planned a postimplementation evaluation for SynopSIS. Each of the 3 functions (patient tracking, rounding, and care transitions) will be assessed separately. We will explore rounding efficiency and quality by survey and through direct observation. We plan to assess the percentage of time spent on direct patient care versus gathering patient data during morning rounds. We adapted elements of SynopSIS from UWCores, an existing sign‐out application in place at the University of Washington.24, 25 In a randomized trial, UWCores was shown to improve indicators of quality of care (more time spent with patients on rounds, fewer patients missed on rounds) and rounding efficiency (less time prerounding and rounding).25 For evaluation, we plan to use a previously published instrument25 in an online survey of SynopSIS users to assess perceived changes in the quality of sign‐out, providerprovider communication, and patient continuity of care. We intend to measure daily use of SynopSIS by primary providers, covering providers, and consulting physicians in order to assess its impact on each patient's care plan. We hypothesize that primary hospital physicians will access SynopSIS at least 3 times daily: on arrival at the hospital, after rounding, and prior to handoffs. We also plan to investigate whether consulting physicians will view SynopSIS daily rather than obtaining patient data such as labs and vital signs from separate parts of the EMR. Finally, we hypothesize that SynopSIS may facilitate initiation of appropriate discharge planning earlier in a patient's hospital course because it is viewable by nursing, care management, and social work personnel. Importantly, we will implement SynopSIS after the EMR gains universal use at our hospital. We will then wait for a washout following the EMR implementation in order to avoid confounding with the effects of the EMR. We will then be able to separate the effects of this tool from the effects of the EMR. Our EMR does not offer a function comparable to the rounds report or sign‐out tool in SynopSIS.
In addition to this quantitative evaluation process, we plan to solicit feedback from SynopSIS users in focus groups, including physicians at all levels of training as well as nonphysicians. We will use this information to revise SynopSIS according to the users' needs and to tailor the application to diverse specialty services.
DISCUSSION
Several systems have been developed to enhance communication among providers and to support the transfer of care of hospitalized patients.13, 14, 16, 19, 24, 25 We have developed a tool to support patient tracking, sign‐out, and rounding that incorporates key elements of previously designed systems and may improve communication among providers. SynopSIS helps to fulfill the 2006 JCAHO accreditation requirement for standardized communication for transfers of care when used with appropriate verbal communication, including an opportunity to ask and respond to questions.5 Research from other safety‐oriented industries recommends standardized information transfer, which SynopSIS will provide.20 What is innovative about SynopSIS is that it is not a stand‐alone system, but an integrated part of the EMR.
Currently, fewer than 5% of hospitals have an electronic sign‐out tool linked to hospital information systems27; therefore, SynopSIS has great potential for dissemination. In technical terms, this tool was coded by GE and could be readily adopted by any other GE Centricity Enterprise customer. Moreover, the conceptual model, the design strategy, and the critical system elements should be relevant to effective patient tracking, sign‐out, and rounding across different IT platforms.
Despite its strengths, the SynopSIS system has several limitations. First, appropriate transfer of care is a learned process that incorporates well‐described provider and system elements.15, 21, 2830 This tool cannot perform sign‐out; it makes up one part of an effective sign‐out process. As our institution implements SynopSIS, we will also proceed with educational efforts and infrastructure to improve the sign‐out process. Second, although data can be overwritten, prior screen versions are archived in the database. Because SynopSIS is part of the medical record, users may omit sensitive or clinically useful information because of medical‐legal concerns, such as sensitive family dynamics or patient behavioral issues that providers may be reluctant to document in the patient chart. Currently, such information is conveyed verbally during sign‐out. Third, as information gathering and transfer become more automated, informal person‐to‐person interactions among providers (eg, physicians and nurses) may erode. However, we expect that SynopSIS actually will enhance the quality of this communication because it places them on the same page. Finally, SynopSIS generates paper reports that must be disposed of in accordance with standards of patient confidentiality.
We believe that SynopSIS will improve the quality of care through several mechanisms. Because this single‐screen summary will be available to all members of a patients' care team, it is possible that SynopSIS will enable providers to share management plans more readily. Although nursing and care management do not use SynopSIS for their own handoffs, they have clamored for the ability to view it. In addition, rotating providers can readily assume care of an unfamiliar patient. By automating data‐gathering tasks, SynopSIS may foster efficiency and increase time with patients during rounds. For trainee providers in particular, such increased efficiency should allow more time for education and alleviate some of the pressures of duty‐hour compliance. Most important, SynopSIS frees the EMR from emulating the historic paper chart as its method of supporting clinical work flow and communication. That paradigm does not harness the power of today's EMR databases and integration capabilities31 and creates extra work through interruptive work flow and redundant effort.32 With SynopSIS reengineering, instead of providers having to serve the needs of the chart, the chart serves the needs of providers and patients.
Future clinical documentation and EMR systems should focus on provider work flow to improve quality and efficiency in patient care. Moreover, involving providers, including residents, in system design fosters innovation and optimally applies information technology to supporting clinical practice.
Acknowledgements
The authors acknowledge Harry Wong, Chutima Assapimonwait, and Vern Rogers for programming the application. Deborah G. Airo edited the manuscript.
- ,,.Crew resource managment and its applications in medicine. Making health care safer: A critical analysis of patient safety practices. Evidence report/technology assessment2001. AHRQ publication 01‐E058(43).
- ,.Internal Bleeding: The Truth behind America's Terrifying Epidemic of Medical Mistakes.New York, NY:Rugged Land;2004.
- ,,.New requirements for resident duty hours.JAMA.2002;288:1112–1124.
- ,,,.The impact of a regulation restricting medical house staff working hours on the quality of patient care.JAMA.1993;269:374–378.
- Joint Commission 2006 National Patient Safety Goals Implementation Expectations.2005. Available at: http://www.jcaho.org/accredited+organizations/patient+safety/06_npsg_ie.pdf.
- ,,.Gaps in the continuity of care and progress on patient safety.BMJ.2000;320:791–794.
- ,,,,.Does housestaff discontinuity of care increase the risk for preventable adverse events?Ann Intern Med.1994;121:866–872.
- .The problem‐oriented record—its organizing principles and its structure.League Exch.1975 (103):3–6.
- .The problem oriented record as a basic tool in medical education, patient care and clinical research.Ann Clin Res.1971;3(3):131–134.
- .Medical records, patient care, and medical education.Ir J Med Sci.1964;17:271–282.
- ,,, et al.Creating a note classification scheme for a multi‐institutional electronic medical record.AMIA Annu Symp Proc.2003:968.
- ,,,,,.Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians.J Am Med Inform Assoc.2004;11:300–309.
- ,,,,.Using a computerized sign‐out program to improve continuity of inpatient care and prevent adverse events.Jt Comm J Qual Improv.1998;24(2):77–87.
- ,.Signing out patients for off‐hours coverage: comparison of manual and computer‐aided methods.Proc Annu Symp Comput Appl Med Care.1992:114–118.
- ,,,,.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1:257–266.
- ,,.Utility of a standardized sign‐out card for new medical interns.J Gen Intern Med.1996;11:753–755.
- ,,.The potential role of IT in supporting the work of junior doctors.J R Coll Physicians Lond.2000;34:366–370.
- ,,,.Electronic Sign‐out using a personal digital assistant.Psychiatr Serv.2001;52(2):173–174.
- .“Doctor's notes”: a computerized method for managing inpatient care.Fam Med.1988;20:223–224.
- ,,,,.Handoff strategies in settings with high consequences for failure: lessons for health care operations.Int J Qual Health Care.2004;16(2):125–132.
- ,,, et al.Understanding patient‐centered care in the context of total quality management and continuous quality improvement.Jt Comm J Qual Improv.1994;20(3):152–161.
- ,,.Utility of a standardized sign‐out card for new medical interns.J Gen Intern Med.1996;11:753–755.
- ,,,.Post‐call transfer of resident responsibility: its effect on patient care.J Gen Intern Med.1990;5:501–505.
- ,,,.Organizing the transfer of patient care information: the development of a computerized resident sign‐out system.Surgery.2004;136(1):5–13.
- ,,,,.A randomized, controlled trial evaluating the impact of a computerized rounding and sign‐out system on continuity of care and resident work hours.J Am Coll Surg.2005;200:538–545.
- .UCSFMC sign‐out needs assessment [personal communication].2007.
- ,.Is 80 the cost of saving lives? Reduced duty hours, errors, and cost.J Gen Intern Med.2005;20:969–970.
- ,,.Intern curriculum: the impact of a focused training program on the process and content of sign‐out out patients. Harvard Medical School Education Day2004.
- .When conversation is better than computation.J Am Med Inform Assoc.2000;7:277–286.
- ,.Communication behaviours in a hospital setting: an observational study.BMJ.1998;316:673–676.
- ,,,.Integration and beyond: linking information from disparate sources and into workflow.J Am Med Inform Assoc.2000;7(2):135–145.
- .Update on the electronic medical record.Otolaryngol Clin North Am.2002;35:1223–1236, vii.
The delivery of safe, high‐quality care to hospitalized patients depends on effective communication among providers.1, 2 Inpatients may receive care from a number of specialists in addition to their primary hospital physicians, and each provider may practice in a group that transfers care of individual patients among its members. This issue is exacerbated in teaching hospitals because fellows, residents, and interns make frequent transfers of care because of work‐hour rules.3, 4 Finally, teams of physician providers making management decisions must effectively communicate with other members of the care team, such as nurses, dieticians, and social workers, who also may be part of a group practice involving transfers. A patient hospitalized for just a few days in a modern hospital may receive care from dozens of providers and be the subject of multiple transfers of care, or handoffs, that require effective communication. Therefore, as part of its 2006 National Patient Safety Goals,5 the Joint Commission on Accreditation of Health Care Organizations (JCAHO) now requires that each hospital implement a standardized, structured approach to transfers of care.
Transfers of care have been shown to be a source of medical errors and adverse patient outcomes.2, 6, 7 In many cases, the critical information necessary to avert medical errors exists but is not available in real time to providers.6
Traditionally, provider teams have relied on the patient chart, in concert with direct patient evaluation, to provide the information to guide decision making during a hospitalization. Unfortunately, the structure of the chart in most hospitals has evolved little over the past 80 years810 and remains organized so that information is more easily filed than retrieved, read, or summarized.811 Typically, electronic medical records (EMRs) mimic the appearance of paper records and include similar organizational flaws.12 As a result, many providers have created ad hoc informational systems, separate from the chart, designed to track a patient's progress over time and to facilitate transfers of care. These sign‐out systems, which are intended to complement verbal sign‐out between providers,1315 range in complexity from simple handwritten index cards16 to adapted spreadsheets, PDA systems,17, 18 and more complex data systems (eg, FileMaker Pro)19 and often contain crucial information not found elsewhere in the medical record.20, 21
Although sign‐out systems are crucial to patient safety, they have several drawbacks. First, ad‐hoc informational systems may not be standardized, resulting in content and accuracy that vary among providers.22 These systems may fail to identify critical elements of a patient's condition, promoting ineffective communication and placing the patient at increased risk of adverse events.7, 13, 23
These observations underscore the need for a standardized patient‐tracking instrument that can distill crucial patient information, enhance communication, support transfers, improve efficiency, and enhance continuity of patient care.
We aimed to develop an integrated, problem‐based patient‐tracking tool as part of our hospital's EMR. The tool, SynopSIS, supports patient tracking, transfers of care (ie, sign‐outs), and daily rounds.
METHODS
Setting
The study took place at a 547‐bed adult and pediatric tertiary‐care university‐based teaching hospital with 2 campuses at the University of California, San Francisco, Medical Center (UCSFMC).
PROGRAM DESCRIPTION
Development and Design
A multidisciplinary team of practicing residents and attending physicians, information technology leaders, software engineers, and experts in medical communication and sign‐out developed the SynopSIS tool. We reviewed the literature to incorporate key design elements of other successfully implemented information transfer systems.24, 25
We conducted a formal review of existing patient‐tracking and sign‐out systems at our hospital to characterize provider work practices, with an emphasis on the specific information requirements of different specialties. A needs assessment of current sign‐out processes at UCSFMC was conducted by personal interviews with a chief resident or representative of each of the 18 Accreditation Council of Graduate Medical Education (ACGME) accredited residency programs through the dean's office of Graduate Medical Education. This needs assessment revealed that the majority of the programs did not have a standardized mechanism for sign‐out. Although most did use a written format for sign‐out, the actual type of written format varied from handwritten cards to databases using a variety of programs including Filemaker Pro, Microsoft Excel, and Microsoft Word. When asked what could improve the sign‐out system for their program, they most often responded that it would be having a standardized computerized sign‐out system in the hospital.26
During the design and pilot phase, we presented each SynopSIS function to an advisory committee of more than 50 trainees in medical, surgical, and pediatric general and subspecialty fields. Their input shaped the information content and presentation of our tool. In addition, we discussed the tool with the attending‐physician advisory group that oversees the implementation of clinical information systems in our hospital system.
Conceptual Model
We developed this conceptual model by integrating existing scholarship and input from stakeholders at our institution. First, we reviewed existing literature on documentation and transfers of care. Next, we conducted several focus group sessions with our EMR Residents' Advisory Group to conceptualize work flow and handoff needs for hospital physicians across specialties. We arrived at this model after several iterations of feedback from providers.
SynopSIS maps patient data available in the EMR to each of the 3 main functions according to type of clinical decisions supported by that function (Fig. 1). For example, data needed for effective patient tracking, such as likely functional status, are required to make decisions over the course of a patient's hospitalization. Similarly, data needed for sign‐out are used to make decisions over the course of a shift, typically overnight; and data needed for morning rounds are used to make decisions for the day. Although the information required for each function overlaps considerably, there are specialized data elements unique to each function.
Description of Functionality
SynopSIS is integrated with our hospital's EMR, General Electric (GE) Centricity Enterprise. The physician interface for SynopSIS is shown in Figure 2. After selecting a patient from a list corresponding to a given inpatient service (eg, Medicine Team B), the user selects the menu option to view the SynopSIS screen, which provides an at a glance overview of the patient's current condition. Different fields on the screen support each of SynopSIS's 3 main functions. At the top, the patient's demographic and registration information is displayed, including name, location, age, medical record number, and attending physician. Below are fields viewable and editable by users of the EMR. The Admission Diagnosis/Course and Problem List fields support patient tracking and allow a receiving physician to understand the reason for the patient's admission, the overall course of the illness, and the current active problems. The problem list is entered by the primary hospital physician. The Anticipated Problems/To Do List field supports the sign‐out function from which providers can coordinate care‐related activities and make contingency plans for anticipated events. The patients' most recent laboratory results and vital signs are displayed on the lower left of the screen for easy reference during face‐to‐face physician sign‐outs. Finally, the CODE status, Allergies, and Medications fields allow efficient tracking of information. Temporarily, until the pharmacy component of the EMR goes into use, the primary hospital physician will enter and update the medications. When the pharmacy is linked to the EMR, medications will be added directly from the inpatient pharmacy records to the EMR‐linked sign‐out tool.
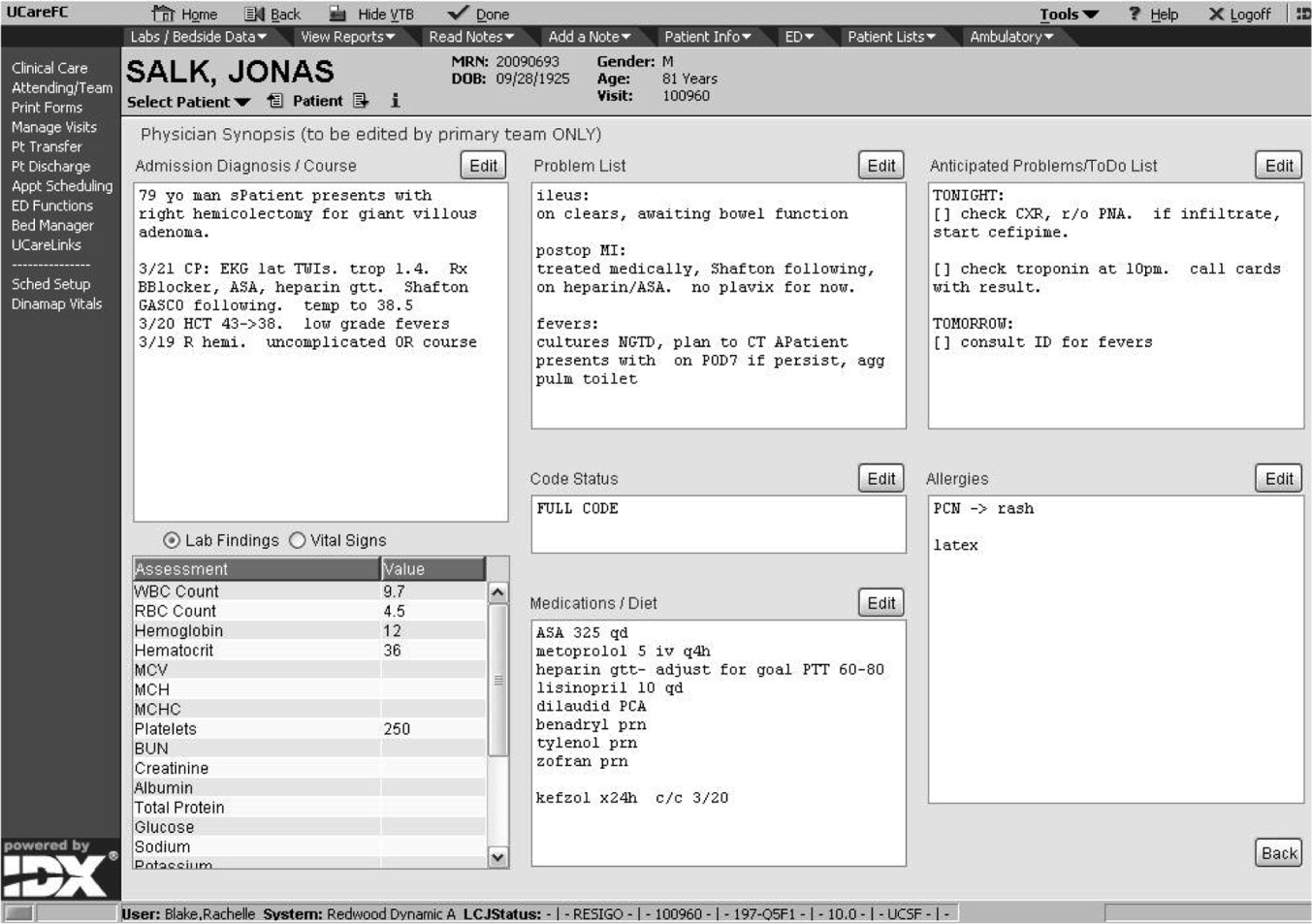
This on‐screen SynopSIS view is distinct from the summary screen typically seen in EMRs, including vendor‐based and the Veterans' Affairs systems. For instance, the Veterans' Affairs summary screen incorporates clinical and nonclinical data, including demographic and payment information, upcoming appointments, and patient‐specific information such as allergies. Moreover, it is not editable by primary hospital physicians. Unlike a summary screen, which collates select patient information from other parts of the EMR, SynopSIS is specific to the current acute hospitalization and includes information not found elsewhere in the medical record.
To support rounding, SynopSIS gathers and presents data from the EMR in a printed Rounds Report (Fig. 3). The report is generated for all patients assigned to an inpatient service (eg, Medicine Team B) and emphasizes clarity and brevity using a format validated in the medical literature.24, 25 Each patient's report covers one fourth of a standard 8‐by‐11‐inch landscape‐printed page. The top half of each of these quarter‐page patient reports displays data stored in SynopSIS's interface and summarizes the patient's illness and the course of that illness. The lower half displays vital signs, intake/output, and laboratory data over the 24 hours from the time of printing. The most recent value and the range over the previous 24 hours of all vital signs are displayed. Intake/output totals are listed together with a structured breakdown. Laboratory results for the past 24 hours are listed with the most immediate prior values, allowing providers to discern trends. We envision providers obtaining a rounds report on arrival each day before examining their patients.
Importantly, although SynopSIS is part of the patient's medical record, physician users may change or overwrite the data in any field. This ability is a critical feature of the toolthe focus is on providing an interpretable snapshot of the patient. Data may be removed as their importance lessens or as the patient's condition changes, which contrasts with unchangeable documentation geared for alternative purposes, such as billing or medical‐legal requirements. Deleted data are saved in the medical record and are viewable by audit.
Program Evaluation
We have planned a postimplementation evaluation for SynopSIS. Each of the 3 functions (patient tracking, rounding, and care transitions) will be assessed separately. We will explore rounding efficiency and quality by survey and through direct observation. We plan to assess the percentage of time spent on direct patient care versus gathering patient data during morning rounds. We adapted elements of SynopSIS from UWCores, an existing sign‐out application in place at the University of Washington.24, 25 In a randomized trial, UWCores was shown to improve indicators of quality of care (more time spent with patients on rounds, fewer patients missed on rounds) and rounding efficiency (less time prerounding and rounding).25 For evaluation, we plan to use a previously published instrument25 in an online survey of SynopSIS users to assess perceived changes in the quality of sign‐out, providerprovider communication, and patient continuity of care. We intend to measure daily use of SynopSIS by primary providers, covering providers, and consulting physicians in order to assess its impact on each patient's care plan. We hypothesize that primary hospital physicians will access SynopSIS at least 3 times daily: on arrival at the hospital, after rounding, and prior to handoffs. We also plan to investigate whether consulting physicians will view SynopSIS daily rather than obtaining patient data such as labs and vital signs from separate parts of the EMR. Finally, we hypothesize that SynopSIS may facilitate initiation of appropriate discharge planning earlier in a patient's hospital course because it is viewable by nursing, care management, and social work personnel. Importantly, we will implement SynopSIS after the EMR gains universal use at our hospital. We will then wait for a washout following the EMR implementation in order to avoid confounding with the effects of the EMR. We will then be able to separate the effects of this tool from the effects of the EMR. Our EMR does not offer a function comparable to the rounds report or sign‐out tool in SynopSIS.
In addition to this quantitative evaluation process, we plan to solicit feedback from SynopSIS users in focus groups, including physicians at all levels of training as well as nonphysicians. We will use this information to revise SynopSIS according to the users' needs and to tailor the application to diverse specialty services.
DISCUSSION
Several systems have been developed to enhance communication among providers and to support the transfer of care of hospitalized patients.13, 14, 16, 19, 24, 25 We have developed a tool to support patient tracking, sign‐out, and rounding that incorporates key elements of previously designed systems and may improve communication among providers. SynopSIS helps to fulfill the 2006 JCAHO accreditation requirement for standardized communication for transfers of care when used with appropriate verbal communication, including an opportunity to ask and respond to questions.5 Research from other safety‐oriented industries recommends standardized information transfer, which SynopSIS will provide.20 What is innovative about SynopSIS is that it is not a stand‐alone system, but an integrated part of the EMR.
Currently, fewer than 5% of hospitals have an electronic sign‐out tool linked to hospital information systems27; therefore, SynopSIS has great potential for dissemination. In technical terms, this tool was coded by GE and could be readily adopted by any other GE Centricity Enterprise customer. Moreover, the conceptual model, the design strategy, and the critical system elements should be relevant to effective patient tracking, sign‐out, and rounding across different IT platforms.
Despite its strengths, the SynopSIS system has several limitations. First, appropriate transfer of care is a learned process that incorporates well‐described provider and system elements.15, 21, 2830 This tool cannot perform sign‐out; it makes up one part of an effective sign‐out process. As our institution implements SynopSIS, we will also proceed with educational efforts and infrastructure to improve the sign‐out process. Second, although data can be overwritten, prior screen versions are archived in the database. Because SynopSIS is part of the medical record, users may omit sensitive or clinically useful information because of medical‐legal concerns, such as sensitive family dynamics or patient behavioral issues that providers may be reluctant to document in the patient chart. Currently, such information is conveyed verbally during sign‐out. Third, as information gathering and transfer become more automated, informal person‐to‐person interactions among providers (eg, physicians and nurses) may erode. However, we expect that SynopSIS actually will enhance the quality of this communication because it places them on the same page. Finally, SynopSIS generates paper reports that must be disposed of in accordance with standards of patient confidentiality.
We believe that SynopSIS will improve the quality of care through several mechanisms. Because this single‐screen summary will be available to all members of a patients' care team, it is possible that SynopSIS will enable providers to share management plans more readily. Although nursing and care management do not use SynopSIS for their own handoffs, they have clamored for the ability to view it. In addition, rotating providers can readily assume care of an unfamiliar patient. By automating data‐gathering tasks, SynopSIS may foster efficiency and increase time with patients during rounds. For trainee providers in particular, such increased efficiency should allow more time for education and alleviate some of the pressures of duty‐hour compliance. Most important, SynopSIS frees the EMR from emulating the historic paper chart as its method of supporting clinical work flow and communication. That paradigm does not harness the power of today's EMR databases and integration capabilities31 and creates extra work through interruptive work flow and redundant effort.32 With SynopSIS reengineering, instead of providers having to serve the needs of the chart, the chart serves the needs of providers and patients.
Future clinical documentation and EMR systems should focus on provider work flow to improve quality and efficiency in patient care. Moreover, involving providers, including residents, in system design fosters innovation and optimally applies information technology to supporting clinical practice.
Acknowledgements
The authors acknowledge Harry Wong, Chutima Assapimonwait, and Vern Rogers for programming the application. Deborah G. Airo edited the manuscript.
The delivery of safe, high‐quality care to hospitalized patients depends on effective communication among providers.1, 2 Inpatients may receive care from a number of specialists in addition to their primary hospital physicians, and each provider may practice in a group that transfers care of individual patients among its members. This issue is exacerbated in teaching hospitals because fellows, residents, and interns make frequent transfers of care because of work‐hour rules.3, 4 Finally, teams of physician providers making management decisions must effectively communicate with other members of the care team, such as nurses, dieticians, and social workers, who also may be part of a group practice involving transfers. A patient hospitalized for just a few days in a modern hospital may receive care from dozens of providers and be the subject of multiple transfers of care, or handoffs, that require effective communication. Therefore, as part of its 2006 National Patient Safety Goals,5 the Joint Commission on Accreditation of Health Care Organizations (JCAHO) now requires that each hospital implement a standardized, structured approach to transfers of care.
Transfers of care have been shown to be a source of medical errors and adverse patient outcomes.2, 6, 7 In many cases, the critical information necessary to avert medical errors exists but is not available in real time to providers.6
Traditionally, provider teams have relied on the patient chart, in concert with direct patient evaluation, to provide the information to guide decision making during a hospitalization. Unfortunately, the structure of the chart in most hospitals has evolved little over the past 80 years810 and remains organized so that information is more easily filed than retrieved, read, or summarized.811 Typically, electronic medical records (EMRs) mimic the appearance of paper records and include similar organizational flaws.12 As a result, many providers have created ad hoc informational systems, separate from the chart, designed to track a patient's progress over time and to facilitate transfers of care. These sign‐out systems, which are intended to complement verbal sign‐out between providers,1315 range in complexity from simple handwritten index cards16 to adapted spreadsheets, PDA systems,17, 18 and more complex data systems (eg, FileMaker Pro)19 and often contain crucial information not found elsewhere in the medical record.20, 21
Although sign‐out systems are crucial to patient safety, they have several drawbacks. First, ad‐hoc informational systems may not be standardized, resulting in content and accuracy that vary among providers.22 These systems may fail to identify critical elements of a patient's condition, promoting ineffective communication and placing the patient at increased risk of adverse events.7, 13, 23
These observations underscore the need for a standardized patient‐tracking instrument that can distill crucial patient information, enhance communication, support transfers, improve efficiency, and enhance continuity of patient care.
We aimed to develop an integrated, problem‐based patient‐tracking tool as part of our hospital's EMR. The tool, SynopSIS, supports patient tracking, transfers of care (ie, sign‐outs), and daily rounds.
METHODS
Setting
The study took place at a 547‐bed adult and pediatric tertiary‐care university‐based teaching hospital with 2 campuses at the University of California, San Francisco, Medical Center (UCSFMC).
PROGRAM DESCRIPTION
Development and Design
A multidisciplinary team of practicing residents and attending physicians, information technology leaders, software engineers, and experts in medical communication and sign‐out developed the SynopSIS tool. We reviewed the literature to incorporate key design elements of other successfully implemented information transfer systems.24, 25
We conducted a formal review of existing patient‐tracking and sign‐out systems at our hospital to characterize provider work practices, with an emphasis on the specific information requirements of different specialties. A needs assessment of current sign‐out processes at UCSFMC was conducted by personal interviews with a chief resident or representative of each of the 18 Accreditation Council of Graduate Medical Education (ACGME) accredited residency programs through the dean's office of Graduate Medical Education. This needs assessment revealed that the majority of the programs did not have a standardized mechanism for sign‐out. Although most did use a written format for sign‐out, the actual type of written format varied from handwritten cards to databases using a variety of programs including Filemaker Pro, Microsoft Excel, and Microsoft Word. When asked what could improve the sign‐out system for their program, they most often responded that it would be having a standardized computerized sign‐out system in the hospital.26
During the design and pilot phase, we presented each SynopSIS function to an advisory committee of more than 50 trainees in medical, surgical, and pediatric general and subspecialty fields. Their input shaped the information content and presentation of our tool. In addition, we discussed the tool with the attending‐physician advisory group that oversees the implementation of clinical information systems in our hospital system.
Conceptual Model
We developed this conceptual model by integrating existing scholarship and input from stakeholders at our institution. First, we reviewed existing literature on documentation and transfers of care. Next, we conducted several focus group sessions with our EMR Residents' Advisory Group to conceptualize work flow and handoff needs for hospital physicians across specialties. We arrived at this model after several iterations of feedback from providers.
SynopSIS maps patient data available in the EMR to each of the 3 main functions according to type of clinical decisions supported by that function (Fig. 1). For example, data needed for effective patient tracking, such as likely functional status, are required to make decisions over the course of a patient's hospitalization. Similarly, data needed for sign‐out are used to make decisions over the course of a shift, typically overnight; and data needed for morning rounds are used to make decisions for the day. Although the information required for each function overlaps considerably, there are specialized data elements unique to each function.
Description of Functionality
SynopSIS is integrated with our hospital's EMR, General Electric (GE) Centricity Enterprise. The physician interface for SynopSIS is shown in Figure 2. After selecting a patient from a list corresponding to a given inpatient service (eg, Medicine Team B), the user selects the menu option to view the SynopSIS screen, which provides an at a glance overview of the patient's current condition. Different fields on the screen support each of SynopSIS's 3 main functions. At the top, the patient's demographic and registration information is displayed, including name, location, age, medical record number, and attending physician. Below are fields viewable and editable by users of the EMR. The Admission Diagnosis/Course and Problem List fields support patient tracking and allow a receiving physician to understand the reason for the patient's admission, the overall course of the illness, and the current active problems. The problem list is entered by the primary hospital physician. The Anticipated Problems/To Do List field supports the sign‐out function from which providers can coordinate care‐related activities and make contingency plans for anticipated events. The patients' most recent laboratory results and vital signs are displayed on the lower left of the screen for easy reference during face‐to‐face physician sign‐outs. Finally, the CODE status, Allergies, and Medications fields allow efficient tracking of information. Temporarily, until the pharmacy component of the EMR goes into use, the primary hospital physician will enter and update the medications. When the pharmacy is linked to the EMR, medications will be added directly from the inpatient pharmacy records to the EMR‐linked sign‐out tool.
This on‐screen SynopSIS view is distinct from the summary screen typically seen in EMRs, including vendor‐based and the Veterans' Affairs systems. For instance, the Veterans' Affairs summary screen incorporates clinical and nonclinical data, including demographic and payment information, upcoming appointments, and patient‐specific information such as allergies. Moreover, it is not editable by primary hospital physicians. Unlike a summary screen, which collates select patient information from other parts of the EMR, SynopSIS is specific to the current acute hospitalization and includes information not found elsewhere in the medical record.
To support rounding, SynopSIS gathers and presents data from the EMR in a printed Rounds Report (Fig. 3). The report is generated for all patients assigned to an inpatient service (eg, Medicine Team B) and emphasizes clarity and brevity using a format validated in the medical literature.24, 25 Each patient's report covers one fourth of a standard 8‐by‐11‐inch landscape‐printed page. The top half of each of these quarter‐page patient reports displays data stored in SynopSIS's interface and summarizes the patient's illness and the course of that illness. The lower half displays vital signs, intake/output, and laboratory data over the 24 hours from the time of printing. The most recent value and the range over the previous 24 hours of all vital signs are displayed. Intake/output totals are listed together with a structured breakdown. Laboratory results for the past 24 hours are listed with the most immediate prior values, allowing providers to discern trends. We envision providers obtaining a rounds report on arrival each day before examining their patients.
Importantly, although SynopSIS is part of the patient's medical record, physician users may change or overwrite the data in any field. This ability is a critical feature of the toolthe focus is on providing an interpretable snapshot of the patient. Data may be removed as their importance lessens or as the patient's condition changes, which contrasts with unchangeable documentation geared for alternative purposes, such as billing or medical‐legal requirements. Deleted data are saved in the medical record and are viewable by audit.
Program Evaluation
We have planned a postimplementation evaluation for SynopSIS. Each of the 3 functions (patient tracking, rounding, and care transitions) will be assessed separately. We will explore rounding efficiency and quality by survey and through direct observation. We plan to assess the percentage of time spent on direct patient care versus gathering patient data during morning rounds. We adapted elements of SynopSIS from UWCores, an existing sign‐out application in place at the University of Washington.24, 25 In a randomized trial, UWCores was shown to improve indicators of quality of care (more time spent with patients on rounds, fewer patients missed on rounds) and rounding efficiency (less time prerounding and rounding).25 For evaluation, we plan to use a previously published instrument25 in an online survey of SynopSIS users to assess perceived changes in the quality of sign‐out, providerprovider communication, and patient continuity of care. We intend to measure daily use of SynopSIS by primary providers, covering providers, and consulting physicians in order to assess its impact on each patient's care plan. We hypothesize that primary hospital physicians will access SynopSIS at least 3 times daily: on arrival at the hospital, after rounding, and prior to handoffs. We also plan to investigate whether consulting physicians will view SynopSIS daily rather than obtaining patient data such as labs and vital signs from separate parts of the EMR. Finally, we hypothesize that SynopSIS may facilitate initiation of appropriate discharge planning earlier in a patient's hospital course because it is viewable by nursing, care management, and social work personnel. Importantly, we will implement SynopSIS after the EMR gains universal use at our hospital. We will then wait for a washout following the EMR implementation in order to avoid confounding with the effects of the EMR. We will then be able to separate the effects of this tool from the effects of the EMR. Our EMR does not offer a function comparable to the rounds report or sign‐out tool in SynopSIS.
In addition to this quantitative evaluation process, we plan to solicit feedback from SynopSIS users in focus groups, including physicians at all levels of training as well as nonphysicians. We will use this information to revise SynopSIS according to the users' needs and to tailor the application to diverse specialty services.
DISCUSSION
Several systems have been developed to enhance communication among providers and to support the transfer of care of hospitalized patients.13, 14, 16, 19, 24, 25 We have developed a tool to support patient tracking, sign‐out, and rounding that incorporates key elements of previously designed systems and may improve communication among providers. SynopSIS helps to fulfill the 2006 JCAHO accreditation requirement for standardized communication for transfers of care when used with appropriate verbal communication, including an opportunity to ask and respond to questions.5 Research from other safety‐oriented industries recommends standardized information transfer, which SynopSIS will provide.20 What is innovative about SynopSIS is that it is not a stand‐alone system, but an integrated part of the EMR.
Currently, fewer than 5% of hospitals have an electronic sign‐out tool linked to hospital information systems27; therefore, SynopSIS has great potential for dissemination. In technical terms, this tool was coded by GE and could be readily adopted by any other GE Centricity Enterprise customer. Moreover, the conceptual model, the design strategy, and the critical system elements should be relevant to effective patient tracking, sign‐out, and rounding across different IT platforms.
Despite its strengths, the SynopSIS system has several limitations. First, appropriate transfer of care is a learned process that incorporates well‐described provider and system elements.15, 21, 2830 This tool cannot perform sign‐out; it makes up one part of an effective sign‐out process. As our institution implements SynopSIS, we will also proceed with educational efforts and infrastructure to improve the sign‐out process. Second, although data can be overwritten, prior screen versions are archived in the database. Because SynopSIS is part of the medical record, users may omit sensitive or clinically useful information because of medical‐legal concerns, such as sensitive family dynamics or patient behavioral issues that providers may be reluctant to document in the patient chart. Currently, such information is conveyed verbally during sign‐out. Third, as information gathering and transfer become more automated, informal person‐to‐person interactions among providers (eg, physicians and nurses) may erode. However, we expect that SynopSIS actually will enhance the quality of this communication because it places them on the same page. Finally, SynopSIS generates paper reports that must be disposed of in accordance with standards of patient confidentiality.
We believe that SynopSIS will improve the quality of care through several mechanisms. Because this single‐screen summary will be available to all members of a patients' care team, it is possible that SynopSIS will enable providers to share management plans more readily. Although nursing and care management do not use SynopSIS for their own handoffs, they have clamored for the ability to view it. In addition, rotating providers can readily assume care of an unfamiliar patient. By automating data‐gathering tasks, SynopSIS may foster efficiency and increase time with patients during rounds. For trainee providers in particular, such increased efficiency should allow more time for education and alleviate some of the pressures of duty‐hour compliance. Most important, SynopSIS frees the EMR from emulating the historic paper chart as its method of supporting clinical work flow and communication. That paradigm does not harness the power of today's EMR databases and integration capabilities31 and creates extra work through interruptive work flow and redundant effort.32 With SynopSIS reengineering, instead of providers having to serve the needs of the chart, the chart serves the needs of providers and patients.
Future clinical documentation and EMR systems should focus on provider work flow to improve quality and efficiency in patient care. Moreover, involving providers, including residents, in system design fosters innovation and optimally applies information technology to supporting clinical practice.
Acknowledgements
The authors acknowledge Harry Wong, Chutima Assapimonwait, and Vern Rogers for programming the application. Deborah G. Airo edited the manuscript.
- ,,.Crew resource managment and its applications in medicine. Making health care safer: A critical analysis of patient safety practices. Evidence report/technology assessment2001. AHRQ publication 01‐E058(43).
- ,.Internal Bleeding: The Truth behind America's Terrifying Epidemic of Medical Mistakes.New York, NY:Rugged Land;2004.
- ,,.New requirements for resident duty hours.JAMA.2002;288:1112–1124.
- ,,,.The impact of a regulation restricting medical house staff working hours on the quality of patient care.JAMA.1993;269:374–378.
- Joint Commission 2006 National Patient Safety Goals Implementation Expectations.2005. Available at: http://www.jcaho.org/accredited+organizations/patient+safety/06_npsg_ie.pdf.
- ,,.Gaps in the continuity of care and progress on patient safety.BMJ.2000;320:791–794.
- ,,,,.Does housestaff discontinuity of care increase the risk for preventable adverse events?Ann Intern Med.1994;121:866–872.
- .The problem‐oriented record—its organizing principles and its structure.League Exch.1975 (103):3–6.
- .The problem oriented record as a basic tool in medical education, patient care and clinical research.Ann Clin Res.1971;3(3):131–134.
- .Medical records, patient care, and medical education.Ir J Med Sci.1964;17:271–282.
- ,,, et al.Creating a note classification scheme for a multi‐institutional electronic medical record.AMIA Annu Symp Proc.2003:968.
- ,,,,,.Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians.J Am Med Inform Assoc.2004;11:300–309.
- ,,,,.Using a computerized sign‐out program to improve continuity of inpatient care and prevent adverse events.Jt Comm J Qual Improv.1998;24(2):77–87.
- ,.Signing out patients for off‐hours coverage: comparison of manual and computer‐aided methods.Proc Annu Symp Comput Appl Med Care.1992:114–118.
- ,,,,.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1:257–266.
- ,,.Utility of a standardized sign‐out card for new medical interns.J Gen Intern Med.1996;11:753–755.
- ,,.The potential role of IT in supporting the work of junior doctors.J R Coll Physicians Lond.2000;34:366–370.
- ,,,.Electronic Sign‐out using a personal digital assistant.Psychiatr Serv.2001;52(2):173–174.
- .“Doctor's notes”: a computerized method for managing inpatient care.Fam Med.1988;20:223–224.
- ,,,,.Handoff strategies in settings with high consequences for failure: lessons for health care operations.Int J Qual Health Care.2004;16(2):125–132.
- ,,, et al.Understanding patient‐centered care in the context of total quality management and continuous quality improvement.Jt Comm J Qual Improv.1994;20(3):152–161.
- ,,.Utility of a standardized sign‐out card for new medical interns.J Gen Intern Med.1996;11:753–755.
- ,,,.Post‐call transfer of resident responsibility: its effect on patient care.J Gen Intern Med.1990;5:501–505.
- ,,,.Organizing the transfer of patient care information: the development of a computerized resident sign‐out system.Surgery.2004;136(1):5–13.
- ,,,,.A randomized, controlled trial evaluating the impact of a computerized rounding and sign‐out system on continuity of care and resident work hours.J Am Coll Surg.2005;200:538–545.
- .UCSFMC sign‐out needs assessment [personal communication].2007.
- ,.Is 80 the cost of saving lives? Reduced duty hours, errors, and cost.J Gen Intern Med.2005;20:969–970.
- ,,.Intern curriculum: the impact of a focused training program on the process and content of sign‐out out patients. Harvard Medical School Education Day2004.
- .When conversation is better than computation.J Am Med Inform Assoc.2000;7:277–286.
- ,.Communication behaviours in a hospital setting: an observational study.BMJ.1998;316:673–676.
- ,,,.Integration and beyond: linking information from disparate sources and into workflow.J Am Med Inform Assoc.2000;7(2):135–145.
- .Update on the electronic medical record.Otolaryngol Clin North Am.2002;35:1223–1236, vii.
- ,,.Crew resource managment and its applications in medicine. Making health care safer: A critical analysis of patient safety practices. Evidence report/technology assessment2001. AHRQ publication 01‐E058(43).
- ,.Internal Bleeding: The Truth behind America's Terrifying Epidemic of Medical Mistakes.New York, NY:Rugged Land;2004.
- ,,.New requirements for resident duty hours.JAMA.2002;288:1112–1124.
- ,,,.The impact of a regulation restricting medical house staff working hours on the quality of patient care.JAMA.1993;269:374–378.
- Joint Commission 2006 National Patient Safety Goals Implementation Expectations.2005. Available at: http://www.jcaho.org/accredited+organizations/patient+safety/06_npsg_ie.pdf.
- ,,.Gaps in the continuity of care and progress on patient safety.BMJ.2000;320:791–794.
- ,,,,.Does housestaff discontinuity of care increase the risk for preventable adverse events?Ann Intern Med.1994;121:866–872.
- .The problem‐oriented record—its organizing principles and its structure.League Exch.1975 (103):3–6.
- .The problem oriented record as a basic tool in medical education, patient care and clinical research.Ann Clin Res.1971;3(3):131–134.
- .Medical records, patient care, and medical education.Ir J Med Sci.1964;17:271–282.
- ,,, et al.Creating a note classification scheme for a multi‐institutional electronic medical record.AMIA Annu Symp Proc.2003:968.
- ,,,,,.Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians.J Am Med Inform Assoc.2004;11:300–309.
- ,,,,.Using a computerized sign‐out program to improve continuity of inpatient care and prevent adverse events.Jt Comm J Qual Improv.1998;24(2):77–87.
- ,.Signing out patients for off‐hours coverage: comparison of manual and computer‐aided methods.Proc Annu Symp Comput Appl Med Care.1992:114–118.
- ,,,,.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1:257–266.
- ,,.Utility of a standardized sign‐out card for new medical interns.J Gen Intern Med.1996;11:753–755.
- ,,.The potential role of IT in supporting the work of junior doctors.J R Coll Physicians Lond.2000;34:366–370.
- ,,,.Electronic Sign‐out using a personal digital assistant.Psychiatr Serv.2001;52(2):173–174.
- .“Doctor's notes”: a computerized method for managing inpatient care.Fam Med.1988;20:223–224.
- ,,,,.Handoff strategies in settings with high consequences for failure: lessons for health care operations.Int J Qual Health Care.2004;16(2):125–132.
- ,,, et al.Understanding patient‐centered care in the context of total quality management and continuous quality improvement.Jt Comm J Qual Improv.1994;20(3):152–161.
- ,,.Utility of a standardized sign‐out card for new medical interns.J Gen Intern Med.1996;11:753–755.
- ,,,.Post‐call transfer of resident responsibility: its effect on patient care.J Gen Intern Med.1990;5:501–505.
- ,,,.Organizing the transfer of patient care information: the development of a computerized resident sign‐out system.Surgery.2004;136(1):5–13.
- ,,,,.A randomized, controlled trial evaluating the impact of a computerized rounding and sign‐out system on continuity of care and resident work hours.J Am Coll Surg.2005;200:538–545.
- .UCSFMC sign‐out needs assessment [personal communication].2007.
- ,.Is 80 the cost of saving lives? Reduced duty hours, errors, and cost.J Gen Intern Med.2005;20:969–970.
- ,,.Intern curriculum: the impact of a focused training program on the process and content of sign‐out out patients. Harvard Medical School Education Day2004.
- .When conversation is better than computation.J Am Med Inform Assoc.2000;7:277–286.
- ,.Communication behaviours in a hospital setting: an observational study.BMJ.1998;316:673–676.
- ,,,.Integration and beyond: linking information from disparate sources and into workflow.J Am Med Inform Assoc.2000;7(2):135–145.
- .Update on the electronic medical record.Otolaryngol Clin North Am.2002;35:1223–1236, vii.
Barriers to Mobility During Hospitalization
Institute of Medicine (IOM) reports1, 2 have estimated that between 44,000 and 98,000 patients die every year in hospitals because of iatrogenic errors of omission and commission. More people die in a year from medical errors than from car accidents (43,458), breast cancer (42,297), or AIDS (16,515).3 The IOM report recommended a goal of a 50% reduction in errors over the next 5 years.4 Since publication of these reports, a great deal of interest has been focused on how to make our hospitals safer.5, 6 Times of transitions in care (eg, from home to hospital, from emergency department to hospital, from the intensive care unit to the general ward) have been identified as opportune times to improve continuity and thus to decrease errors.
The hospital discharge process is often nonstandardized and frequently marked by poor quality.7 One in five hospital discharges is complicated by adverse events within 30 days, many of which lead to visits to emergency departments (EDs) and rehospitalization.810 Nationally, approximately 25% of hospitalized patients are readmitted within 90 days, often because of errors resulting from discontinuity and fragmentation of care at discharge, which exposes patients to iatrogenic risk and raises costs.11, 12 Low health literacy rates, lack of coordination in the handoff from the hospital to community care, gaps in social supports, and the absence of physician follow‐up after discharge place patients at high risk of rehospitalization.1315 Increasingly, as hospitalists provide more inpatient care, it is difficult for primary care physicians to be aware of all the complexities of a hospitalization.16
Studying the hospital discharge process provides an opportunity to learn more about its complexities,17 which could then be used to standardize the process and focus on those interventions that reduce the number of medical errors and resulting adverse events. However, to date, few studies have described the essential components of the discharge process, and no studies have focused on the discharge process from the point of view of the hospitalized patient. Therefore, a qualitative study was conducted in order to understand the phenomenon of frequent rehospitalization from the perspective of the discharged patient and to determine if activities at the time of discharge could be designed to reduce the number of adverse events and rehospitalizations.
METHODS
The larger study of which this work is a part examined the transition from inpatient service at a large inner‐city hospital to community care in order to lead to the development of an intervention to improve the discharge process. Qualitative research stresses the socially constructed nature of reality, and qualitative researchers seek to answer questions that stress how social experience is created and given meaning.18 Qualitative interviewing permits the researcher to understand the world as seen by the respondent within the context of the respondent's everyday life.19 Learning from the experiences of patients hospitalized more than once in a 6‐month period will help to identify their perceptions and beliefs about their disease and discharge instructions and assist additional interventions that could prevent rehospitalization.
Sample
Semistructured, open‐ended interviews were conducted with 21 patients during their hospital stay at Boston Medical Center. To be eligible for the study, a patient had to receive medical care through a health center affiliated with Boston Health Net, a network of community health centers serving primarily low‐income patients, and had to have been hospitalized on at least 1 additional occasion in the previous 6 months. Each day during the interview period the Boston Health Net nurse identified all patients previously admitted within 6 months and contacted the interviewer with the names and room numbers of those patients. The interviewer (M.S.) approached potential participants in their hospital rooms and obtained informed consent at the time of the interview. If the patient agreed, the interview was conducted at that time. If the patient was not available at that time, the interviewer made at least 2 attempts to visit the patient at a convenient time. The interviews were conducted on 17 days of a 4‐month period with no more than 2 interviews completed a day. The participants ranged in age from 18 to 79; 10 respondents were male, and 11 were female. All were English speaking. The mean age of the 20 patients who provided demographic information was 45.55 years, and the median age was 47 years. Nine of the participants reported their racial or ethnic identities as white (5 male, 3 female), 3 as black (2 male, 1 female), 4 as African American (1 male, 3 female); 1 as Latina; 1 as Hispanic (male), 1 as Spanish (male), and 1 as mixed (female). One male and 1 female participant provided no race or ethnic identity. Two participants were excluded from the study because they did not speak English, and 2 were excluded because they were unable to speak due to their medical conditions. Interviews were audiotaped, but full names were not used on the tape. Only subject code numbers were used to identify respondents. The discharge records of each participant were reviewed for consistency with that participant's descriptions of his or her condition. The study was approved by the Institutional Review Board of Boston University Medical Center.
Interview Guide
To help assure collection of comparable qualitative data, an interview guide listed specific questions and topics to be covered in a particular order in the interview. Questions were drawn in part from a pilot test of interviewing patients on the inpatient service rehospitalized within 90 days of the previous admission.17 Interviews assessed continuity of care after discharge, need for and availability of social support, and the participant's ability to obtain follow‐up medical care. The interview script consisted of open‐ended questions about events leading up to the current hospitalization, previous hospitalizations, instructions received the last time discharged, home situation, and ability to attend medical appointments, and participant feedback on the discharge process was requested. Follow‐up questions were asked based on a patient's responses to these questions. Interviews lasted between 20 and 45 minutes.
Analysis
The interview tapes were transcribed by a subcontracted transcriber, and the transcripts were checked for accuracy by the interviewer. Each interview was evaluated according to a set of thematic codes developed by 2 qualitative researchers (L.S. and M.S.). The codes represent categories or themes found in the data, and the appropriate codes were attached to their corresponding sections of text. To improve interrater reliability in coding, the 2 qualitative researchers coded 3 interviews, reviewed the codes, and, once it was clear that they both understood the coding scheme, coded the interviews. They resolved any problem cases and checked each other's work throughout the coding process to ensure that each interview was coded correctly. The findings were analyzed to explore whether there were linkages between and among particular themes. The discharge records of all patients were reviewed in order to compare the discharge notes about each patient's condition with that patient's own description of his or her condition and treatment.
RESULTS
All the patients who participated in this study were able to describe their medical condition and the reasons they were admitted to the hospital. Almost all, 20 of the 21 participants, were rehospitalized for the same primary diagnosis. For 5 of these 20 participants, length of time since the last hospitalization was 5‐6 months (4 for diabetes control, 1 for a lupus erythematosus flare); for 4 participants time since last hospitalization was between 6 weeks and 2 months (1 because of a fall, 1 because of seizures, 1 with hypertension, and 1 with SOB); for 8 participants time since last hospitalization was between 3 weeks and 1 month (2 with kidney disease, 2 with seizures, and 1 each with chronic obstructive pulmonary disease, sickle cell disease, PVD, and alcoholic gastritis), and for 3 participants time since last hospitalization was 1‐2 weeks (1 each with abdominal pain, alcohol intoxication, and lower gastrointestinal bleed). The principal diagnosis in a patient's discharge records matched that participant's description. Participants also described the discharge instructions they received. Although some did not report the brand names of the medications they were taking, all reports of the types of medications being taken or the conditions for which the medications were prescribed were consistent with discharge summaries. Although none of the participants incorrectly reported a medication or condition to the interviewer, a few did not provide information about every medication or condition. In 1 case the discharge summary noted medications for bipolar disorder and mental illness; in 2 cases medications were prescribed for depression. None of these participants mentioned these conditions or medications to the interviewer. One patient talked about stress and depression, but nothing was written about these issues in the discharge record.
For participants in this study, difficult life circumstances posed a greater barrier to recuperation than did lack of medical knowledge. The interviews conducted in this study illustrate the personal and social impact of disease that resulted in rehospitalization.
Discharge and Medical Knowledge
During discharge, transition care processes can fail at many points.20 These include: communication of the care plan, reconciliation of current and initial medication regimens, transportation of the patient, follow‐up care with a provider, and preparation of patient and caregiver for maintaining the patient's regimen.4, 2022 Participants in this study identified some of these and other factors as constituting barriers to effective care transitions.
At discharge, 7 participants were advised by physicians to change their diets or refrain from tobacco or alcohol use. Participants clearly understood the instructions and could give detailed accounts of diet changes they were supposed to make or explain the reasons tobacco or alcohol use caused or exacerbated their diseases. A diabetic whose discharge instructions included diet change listed sweet ones, starchy oneswith a lot of carbohydrates as foods she is not supposed to eat, wherease others described the links between alcohol use and adverse health: In my mind, I think that alcohol is a way out.But I know that it, that it's not.And so, the pancreatitis develops.
Lack of understanding about their medical condition or of knowledge about procedures to be followed was not evident in this population. Instead, recuperation was compromised by factors such as distress, substance use, support for medical and basic needs, and limitations in the availability of transportation to medical appointments. Many participants reported not receiving necessary rest as a result of needing to work or care for young children.
Crises and Coping: Distress
Despite understanding needed behavior changes, almost half the participants explained how difficult life circumstances and gaps in ongoing care or support made it impossible for them to follow medical advice.
Almost half the participants described themselves as being stressed, sad, or depressed. Their explanations indicate a relationship between distress and subsequent behaviors that exacerbated their conditions.
Of 3 self‐described alcoholics, one, a 52‐year‐old white man rehospitalized for alcohol related seizures, had relapsed after the deaths of his mother and his girlfriend. He explained, Well, after my girlfriend died, I really started to hit the bottle. Another, an unemployed 45‐year‐old black woman, lacked stable housing and at the time of the interview lived with a heavy drinker. She said that when I get stressed out, the first thing I want to do is go run to the [liquor] store. The third self‐described alcoholic, a 62‐year‐old white man, reported drinking because of lack of regular treatment for chronic depression:
My problem is has to do with stress and depression, which is what I'm gonna try to deal with this time. 'Cause that'scontributed to me getting so depressed I justjust started drinking again. I justnext time it'll kill me. So. That's almosta kind of a suicide wish, I guess.I know it's gonna kill me if I keep drinking.I think I need to get into something. Butthere'sI don't know if you call it substance abuse, butI think it's related todeep depression, which is not necessarily substance abuse, but it canI'm sure there's some relationship.
Similarly, the experiences of participants with diabetes illustrate clearly how depression contributed to undermining their ability to follow their doctors' recommendations. For example, an 18‐year‐old African American teenager rehospitalized for diabetes control discussed her inability to maintain her physician‐recommended diet:
Like when I'm stressed out.I get depressed and, umI give up. Just don't wanna do it anymore. It's not [that] I don't want to, I can't. I just can't do it I, when I got home, I actually did good! I actually really did good. I was eating salads. I did go on a diet. I ate salads, grilled food, and things like that. I took my medicine. I started loggin', like writin' everything down in a book. I wrote down what I ate every day, what my blood sugar was, and how much medicine I took. I was doin' good. But then I got depressed, and I stopped doin' it.
Continuity of Condition Management
Participants expressed a need after discharge for help at home, although in most cases, the help they reported needing did not require medical knowledge or technical skills.
Skilled Care
Few participants reported needing and/or receiving visiting nurse services; even in these cases, some of the responsibility for care fell to family members. Their health suffered because they lacked sufficient access to visiting nurse services or other needed support. A 42‐year‐old Latina diabetic with kidney infection described a visiting nurse's unsuccessful attempt to teach her husband how to change her catheter:
They try to show, 'cause before? I don't got the catheter, they're comin' in my house, in the morning? You know, put the catheter into my bladder, and they come back before me go to sleep, they try to show my husband how to do it, but he can't [CHUCKLES LIGHTLY], you know, he can't.So thethe doctor decide to leave the catheter there.
Basic Need Care
For most participants, the posthospital assistance needed did not require medical expertise. In the period after their last hospitalization, most participants needed assistance with daily chores such as cleaning, cooking, child care, and driving; they turned to friends and family members to meet these needs. However, because no family member was capable of providing full‐time care during recuperation, some participants were unable to follow advice from physicians about resting or refraining from certain activities. A 67‐year‐old African American man whose foot ulcers kept him from walking explained that during his recuperation he had to stay in the same place for 8 hours while his brother worked:
Oh, maybe if I had to go to the bathroom or something, I can'tbut for the most part, I guess I had things set upwhere I didn't, you know, where I didn't moveI just set my things up to keep me from movin' all day. I'd set my food up and everything else, little sandwich and all that. So, there wasn't anything aboutyou know, worrying about movin'or getting hungry, I guess.
None of the participants were able to pay for support services such as housecleaning or in‐home care, and all relied on busy friends and family members to meet their needs.
The experiences of 3 single mothers with health conditions characterized by debilitating chronic pain illustrate how very different access to supportive family members affected their ability to seek care and follow medical instructions as well as how child care responsibilities compromised their recuperation. One, a 20‐year‐old African American woman hospitalized for polycystic kidney disease, described situations during which the intensity of the pain did not permit her to do basic household chores. At those times she relied on her 5‐year‐old son:
Hehe actually knows how to sweep, he knows how to wash dishes. At 5 and a half, he surprised me, but [CHUCKLES] he can wash dishes, so. He has to get up on a chair, but he can wash 'em.
As a result of needing more care than was available, she traveled south to stay with her mother, who was unable to leave work to come to Boston:
I took the bus because my son has sickle cell trait, so they told me from day one it's not really good for him to fly on a plane? So, I had to take himit took like 20 hoursyou know, stoppin' here, stoppin' there, like, pullin' my bags and stuff, so it put me in more pain than I was in.
Another, a 24‐year‐old of mixed background chronically hospitalized with sickle cell pain crises, delayed medical treatment because of lack of child care:
There's been times that I have had to wait till I could find somebody to watch my kids, to even come to the hospital.There's been times thatuh, it'd be a while before I could get anybody, so instead of me coming to the hospital, I have to wait at home, in a lot of pain.I would have to waitany time between 5 hours to 2 days before I could find somebody to watch my kids.
This pattern of child care interfering with recovery continued after leaving the hospital:
The minute I get home it'd be nice to have somebody to watch the kids, so I could at least recuperate for like 24 hours before I have to take care of thingsI would have to usually just go home and just get right to it.
The experience of a third, a 29‐year‐old African American woman with systemic lupus erythematosus, illustrates the ways in which family support can ease the burden of illness. This participant relocated to be close to her mother, aunt, and cousins, all of whom cared for her children when she is in the hospital:
When I was in [NEIGHBORING STATE] it was terrible'cause my, my kids wasn't goin' to school, 'cause I couldn't get up to get them dressed and wake them up. My daughter almost got kept back and stuff. It was real hardand it wasn't good, you know, that they could justrun through the house rampant, do whatever they want and not be supervised.So that was very dangerous, too. And then, it put like, it put a strain on my oldest, my daughter
She contrasted this with her current situation in which family members cared for her children when she is in the hospital or sick at home:
Like, this morningthey took the kids to school for me and everything. Made 'em breakfast, made sure they was dressed right this morningMy mother picked them up from school this afternoon.
Transportation to Appointments
Travel to follow‐up appointments was difficult for many participants. Almost half reported taking public transportation to appointments; the others either drove themselves, were driven by relatives or friends, or paid for taxis. Those relying on public transportation were more likely than others to miss appointments because of transportation issues if they did not feel well:
Depending how I feel. If I feel all right, I'll take the bus; if not, I'll get a taxi or I'll just won't show up. I would borrow a bus pass or somethin', you know, from [HIS NAME] is Joebecause I would make, like, evening appointments. Um, because my sickle cell tends to act up if it's coldSo, if it's really cold, I don't go.
As one 55‐year‐old white woman who has seizures summed up the matter of traveling by bus when not feeling well, You do what you have to do!
DISCUSSION AND CONCLUSIONS
The hospital discharge process has been identified as a time when sources of error occur that result in rehospitalization. Many factors that adversely affect care transitions apply to the hospital discharge process, including preparation of the patient and caregiver, communication of the care plan, changes in the medication regimen, transportation of the patient, scheduling of follow‐up care, and availability of advance care directives.20 Patients with low socioeconomic status have been found to be especially vulnerable after discharge. A 1989 telephone survey of 6455 patients recently discharged from hospitals in the United States found that low socioeconomic status and poor patient health were independent predictors of patient problems after discharge.21 A nationwide telephone survey of 1800 recently discharged patients and their care partners also revealed that low socioeconomic status and poor patient health status were associated with problems experienced by care partners.22
High rates of unnecessary rehospitalization have been shown to be related to poorly managed discharge processes.23 Although some factors identified in other studies of care transition did influence the rehospitalization of participants in this study; others did not. Transportation and follow‐up care greatly affected rehospitalization, whereas health literacy had a minimal effect. Fifteen of 20 participants were readmitted within weeks up to 2 months for the same primary diagnosis, yet they understood their medical conditions and knew the procedures to be followed. Having a chronic illness may have affected their understanding of their disease because they had received teaching over time. However, for most participants in this studyinner‐city, minority, low‐income patientsfactors beyond the discharge process affected their rehospitalization. Difficult life circumstances and gaps in ongoing care or support resulted in distress and behavior that exacerbated their conditions. Participants lacked social and emotional support that would have enabled them to prioritize maintaining their health.
Although there is not a universally accepted definition of the concept of social support, it is generally understood that it involves emotional connection and caring24 and occurs in a relationship in which the person providing the support is equipped to respond to a wide variety of needs ranging from practical assistance to counseling and encouragement based on the concerns or life circumstances of the patient. Qualitative studies of social support interventions demonstrate the ways in which having a dependable person to whom a patient can turn for encouragement, information, and practical assistance improves the patient's ability to maintain health regimens and manage chronic pain. An intervention in which nurses made weekly telephone contact with low‐income pregnant smokers helped these patients manage numerous stressors and, in some cases, reduce their tobacco use.25 A support group for women with chronic pain helped participants learn practical strategies for reducing pain and reduced isolation and emotional distress about their conditions.26 A study of consumer experiences of transition care27 found that the most valued institutions were those in which providers from one facility thoroughly communicated a patient's medical and treatment history to providers in another; also important was involving the consumer in medical decision making, preparing the consumer to actively participate in his or her own care, and attending to individual needs and preferences.
This study had several limitations, including reliance on participants' reports of their conditions and experiences with medical staff at a time when they were rehospitalized. In the vulnerable position of being hospitalized, participants may have been reluctant to have complaints about their hospital experiences tape‐recorded. All participants reported positive experiences with hospital staff during the formal interview. Two participants reported negative experiences with hospital staff after the audio‐recorder was turned off and the interview concluded. Other limitations of the hospital setting include limited privacy. Either a roommate was present during the interview or the interview was interrupted by a visit from a hospital staff person or a telephone call. Participants were asked to recall events that for some had occurred several months before the interview, introducing the possibility of inaccurate recall. To address these limitations, we compared interview transcripts to discharge summaries in order to assess any inconsistencies that may have resulted from this lack of privacy. The differences between summaries and patient self‐reports were that 2 participants did not report illicit substance use and 2 did not report psychiatric conditions. Despite these limitations, conducting this study in a hospital setting allowed investigators access to a highly vulnerable population that would be most affected by improvements in the discharge process. Given the difficulties many participants reported in getting to appointments, it is unlikely that a study conducted outside the hospital setting would have effectively reached this population.
These results support the findings in this study that life circumstances outside the hospital can be as important to recovery as institutional coordination of medical care. Although the stresses described by the low‐income patients in this study may not directly cause subsequent illness, their experiences clearly demonstrate the ways in which stresses make it difficult or impossible to attain sufficient rest to heal, maintain the behavioral change necessary to improve health, and follow instructions given by clinicians at the time of discharge. Interventions targeting low‐income patients thus are more likely to succeed if they include provisions for social support and assist patients in easing the burden of daily responsibilities. Effective transition care includes support that may not be explicitly medical, but without which participants lack the stability to fully recuperate. Without the possibility of taking a break from household or parenting responsibilities, it is difficult to rest enough to truly recover. The descriptions of extreme measures taken in order to obtain needed support illustrate how recuperation was compromised by both family responsibilities and lack of flexibility in caregiver work schedules. Distress, particularly depression, further contributed to poor health and undermined the ability to follow doctors' recommendations and discharge plans.
Discharge interventions that explicitly assess requirements for social support and connect patients with agencies or volunteer groups that call or visit those recuperating, provide meals on wheels, or offer other services such as light cleaning or shopping can address the complex circumstances that result in poor health and chronic rehospitalization. This study has identified the crucial role social support plays in getting and staying well.
Acknowledgements
The authors thank Maria Rizzo DePaoli MSW and Cornelia Walsh RN for assistance with logistics of the study.
- ,.Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization.JAMA.2003;290:1868–1874.
- ,,,Institute of Medicine (U.S.).Committee on Quality of Health Care in America.To Err Is Human: Building a Safer Health System.Washington, DC:National Academy Press:2000.
- Centers for Disease Control and Prevention (National Center for Health Statistics).Births and deaths: preliminary data for 1998.Nat Vit Stat Rep.1999:47.
- Institute of Medicine (U.S.).Committee on Quality of Health Care in America.Crossing the Quality Chasm: a New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- AHRQ's Patient Safety Initiative: Building Foundations, Reducing Risk. Interim Report to the Senate Committee on Appropriations, AHRQ Publication No. 04‐RG005.Rockville, MD:Agency for Healthcare Research and Quality;2003. Available at: http://www.ahrq.gov/qual/pscongrpt/.
- ,,,,,.Patient safety at time of discharge—an example of a multifaceted process evaluation. In:Henriksen K,Battles JB,Marks ES,Lewin DI, editors. Advances in Patient Safety: from Research to Implementation. Vol.2,Concepts and methodology. AHRQ Publication No. 05‐0021‐2.Rockville, MD:Agency for Healthcare Research and Quality;2005.
- ,,.Dissemination of discharge summaries. Not reaching follow‐up physicians.Can Fam Physician.2002;48:737–742.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138(3):161–167.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,, et al.Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients.BMJ.2004;329:15–19.
- and.Hospital readmissions in the Medicare population.N Engl J Med.1984;311:1349–1353.
- and.Factors predicting readmission of older general medicine patients.J Gen Intern Med.1991;6:389–393.
- ,,,.Delayed access to health care: risk factors, reasons and consequences.Ann Intern Med.1991;114:325–331.
- ,,,,,.Impact of socioeconomic status on hospital use in New York City.Health Aff (Millwood).1993 Spring;12(1):162–173.
- ,,.The impact of patient socioeconomic status and other social factors on readmission: a prospective study in four Massachusetts hospitals.Inquiry.1994;31(2):163–172.
- ,,,.Primary care physician attitudes regarding communication with hospitalists.Dis Mon.2002;48(4):218–229.
- ,,,,,.Patient safety at time of discharge: an example of a multifaceted process evaluation.Washington, DC:AHRQ Patient Safety 2 Volume Site;2004.
- ,.Entering the field of qualitative research. In:Denzin NK,Lincoln YS, eds.Handbook of Qualitative Research.Newbury Park, CA:Sage;1994.
- ,.The workers' compensation system: worker friend or foe?Am J Ind Med.2004;45:338–345.
- .Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs.J Am Geriatr Soc.2003;51:549–555.
- ,,,,.Carepartner experiences with hospital care.Med Care.1999;37:33–38.
- ,,.Patients' and caregivers' transition from hospital to home. Needs and recommendations.Home Health Care Serv Q.1998;17:27–48.
- ,,, et al.Patients evaluate their hospital care: A national survey.Health Aff.1991;10:254.
- ,,.Defining social support in context: a necessary step in improving research, intervention, and practice.Qual Health Res.2004;14:942–960.
- .Telephone social support or nursing presence? Analysis of a nursing intervention.Qual Health Res.2005;15(1):19–29.
- ...Encountering the continuing challenges for women with chronic pain: recovery through recognition.Qual Health Res.2003;13:491–509.
- ,.Understanding coordination of care from the consumer's perspective in a regional health system.Health Serv Res.2002;37:1031–1054.
Institute of Medicine (IOM) reports1, 2 have estimated that between 44,000 and 98,000 patients die every year in hospitals because of iatrogenic errors of omission and commission. More people die in a year from medical errors than from car accidents (43,458), breast cancer (42,297), or AIDS (16,515).3 The IOM report recommended a goal of a 50% reduction in errors over the next 5 years.4 Since publication of these reports, a great deal of interest has been focused on how to make our hospitals safer.5, 6 Times of transitions in care (eg, from home to hospital, from emergency department to hospital, from the intensive care unit to the general ward) have been identified as opportune times to improve continuity and thus to decrease errors.
The hospital discharge process is often nonstandardized and frequently marked by poor quality.7 One in five hospital discharges is complicated by adverse events within 30 days, many of which lead to visits to emergency departments (EDs) and rehospitalization.810 Nationally, approximately 25% of hospitalized patients are readmitted within 90 days, often because of errors resulting from discontinuity and fragmentation of care at discharge, which exposes patients to iatrogenic risk and raises costs.11, 12 Low health literacy rates, lack of coordination in the handoff from the hospital to community care, gaps in social supports, and the absence of physician follow‐up after discharge place patients at high risk of rehospitalization.1315 Increasingly, as hospitalists provide more inpatient care, it is difficult for primary care physicians to be aware of all the complexities of a hospitalization.16
Studying the hospital discharge process provides an opportunity to learn more about its complexities,17 which could then be used to standardize the process and focus on those interventions that reduce the number of medical errors and resulting adverse events. However, to date, few studies have described the essential components of the discharge process, and no studies have focused on the discharge process from the point of view of the hospitalized patient. Therefore, a qualitative study was conducted in order to understand the phenomenon of frequent rehospitalization from the perspective of the discharged patient and to determine if activities at the time of discharge could be designed to reduce the number of adverse events and rehospitalizations.
METHODS
The larger study of which this work is a part examined the transition from inpatient service at a large inner‐city hospital to community care in order to lead to the development of an intervention to improve the discharge process. Qualitative research stresses the socially constructed nature of reality, and qualitative researchers seek to answer questions that stress how social experience is created and given meaning.18 Qualitative interviewing permits the researcher to understand the world as seen by the respondent within the context of the respondent's everyday life.19 Learning from the experiences of patients hospitalized more than once in a 6‐month period will help to identify their perceptions and beliefs about their disease and discharge instructions and assist additional interventions that could prevent rehospitalization.
Sample
Semistructured, open‐ended interviews were conducted with 21 patients during their hospital stay at Boston Medical Center. To be eligible for the study, a patient had to receive medical care through a health center affiliated with Boston Health Net, a network of community health centers serving primarily low‐income patients, and had to have been hospitalized on at least 1 additional occasion in the previous 6 months. Each day during the interview period the Boston Health Net nurse identified all patients previously admitted within 6 months and contacted the interviewer with the names and room numbers of those patients. The interviewer (M.S.) approached potential participants in their hospital rooms and obtained informed consent at the time of the interview. If the patient agreed, the interview was conducted at that time. If the patient was not available at that time, the interviewer made at least 2 attempts to visit the patient at a convenient time. The interviews were conducted on 17 days of a 4‐month period with no more than 2 interviews completed a day. The participants ranged in age from 18 to 79; 10 respondents were male, and 11 were female. All were English speaking. The mean age of the 20 patients who provided demographic information was 45.55 years, and the median age was 47 years. Nine of the participants reported their racial or ethnic identities as white (5 male, 3 female), 3 as black (2 male, 1 female), 4 as African American (1 male, 3 female); 1 as Latina; 1 as Hispanic (male), 1 as Spanish (male), and 1 as mixed (female). One male and 1 female participant provided no race or ethnic identity. Two participants were excluded from the study because they did not speak English, and 2 were excluded because they were unable to speak due to their medical conditions. Interviews were audiotaped, but full names were not used on the tape. Only subject code numbers were used to identify respondents. The discharge records of each participant were reviewed for consistency with that participant's descriptions of his or her condition. The study was approved by the Institutional Review Board of Boston University Medical Center.
Interview Guide
To help assure collection of comparable qualitative data, an interview guide listed specific questions and topics to be covered in a particular order in the interview. Questions were drawn in part from a pilot test of interviewing patients on the inpatient service rehospitalized within 90 days of the previous admission.17 Interviews assessed continuity of care after discharge, need for and availability of social support, and the participant's ability to obtain follow‐up medical care. The interview script consisted of open‐ended questions about events leading up to the current hospitalization, previous hospitalizations, instructions received the last time discharged, home situation, and ability to attend medical appointments, and participant feedback on the discharge process was requested. Follow‐up questions were asked based on a patient's responses to these questions. Interviews lasted between 20 and 45 minutes.
Analysis
The interview tapes were transcribed by a subcontracted transcriber, and the transcripts were checked for accuracy by the interviewer. Each interview was evaluated according to a set of thematic codes developed by 2 qualitative researchers (L.S. and M.S.). The codes represent categories or themes found in the data, and the appropriate codes were attached to their corresponding sections of text. To improve interrater reliability in coding, the 2 qualitative researchers coded 3 interviews, reviewed the codes, and, once it was clear that they both understood the coding scheme, coded the interviews. They resolved any problem cases and checked each other's work throughout the coding process to ensure that each interview was coded correctly. The findings were analyzed to explore whether there were linkages between and among particular themes. The discharge records of all patients were reviewed in order to compare the discharge notes about each patient's condition with that patient's own description of his or her condition and treatment.
RESULTS
All the patients who participated in this study were able to describe their medical condition and the reasons they were admitted to the hospital. Almost all, 20 of the 21 participants, were rehospitalized for the same primary diagnosis. For 5 of these 20 participants, length of time since the last hospitalization was 5‐6 months (4 for diabetes control, 1 for a lupus erythematosus flare); for 4 participants time since last hospitalization was between 6 weeks and 2 months (1 because of a fall, 1 because of seizures, 1 with hypertension, and 1 with SOB); for 8 participants time since last hospitalization was between 3 weeks and 1 month (2 with kidney disease, 2 with seizures, and 1 each with chronic obstructive pulmonary disease, sickle cell disease, PVD, and alcoholic gastritis), and for 3 participants time since last hospitalization was 1‐2 weeks (1 each with abdominal pain, alcohol intoxication, and lower gastrointestinal bleed). The principal diagnosis in a patient's discharge records matched that participant's description. Participants also described the discharge instructions they received. Although some did not report the brand names of the medications they were taking, all reports of the types of medications being taken or the conditions for which the medications were prescribed were consistent with discharge summaries. Although none of the participants incorrectly reported a medication or condition to the interviewer, a few did not provide information about every medication or condition. In 1 case the discharge summary noted medications for bipolar disorder and mental illness; in 2 cases medications were prescribed for depression. None of these participants mentioned these conditions or medications to the interviewer. One patient talked about stress and depression, but nothing was written about these issues in the discharge record.
For participants in this study, difficult life circumstances posed a greater barrier to recuperation than did lack of medical knowledge. The interviews conducted in this study illustrate the personal and social impact of disease that resulted in rehospitalization.
Discharge and Medical Knowledge
During discharge, transition care processes can fail at many points.20 These include: communication of the care plan, reconciliation of current and initial medication regimens, transportation of the patient, follow‐up care with a provider, and preparation of patient and caregiver for maintaining the patient's regimen.4, 2022 Participants in this study identified some of these and other factors as constituting barriers to effective care transitions.
At discharge, 7 participants were advised by physicians to change their diets or refrain from tobacco or alcohol use. Participants clearly understood the instructions and could give detailed accounts of diet changes they were supposed to make or explain the reasons tobacco or alcohol use caused or exacerbated their diseases. A diabetic whose discharge instructions included diet change listed sweet ones, starchy oneswith a lot of carbohydrates as foods she is not supposed to eat, wherease others described the links between alcohol use and adverse health: In my mind, I think that alcohol is a way out.But I know that it, that it's not.And so, the pancreatitis develops.
Lack of understanding about their medical condition or of knowledge about procedures to be followed was not evident in this population. Instead, recuperation was compromised by factors such as distress, substance use, support for medical and basic needs, and limitations in the availability of transportation to medical appointments. Many participants reported not receiving necessary rest as a result of needing to work or care for young children.
Crises and Coping: Distress
Despite understanding needed behavior changes, almost half the participants explained how difficult life circumstances and gaps in ongoing care or support made it impossible for them to follow medical advice.
Almost half the participants described themselves as being stressed, sad, or depressed. Their explanations indicate a relationship between distress and subsequent behaviors that exacerbated their conditions.
Of 3 self‐described alcoholics, one, a 52‐year‐old white man rehospitalized for alcohol related seizures, had relapsed after the deaths of his mother and his girlfriend. He explained, Well, after my girlfriend died, I really started to hit the bottle. Another, an unemployed 45‐year‐old black woman, lacked stable housing and at the time of the interview lived with a heavy drinker. She said that when I get stressed out, the first thing I want to do is go run to the [liquor] store. The third self‐described alcoholic, a 62‐year‐old white man, reported drinking because of lack of regular treatment for chronic depression:
My problem is has to do with stress and depression, which is what I'm gonna try to deal with this time. 'Cause that'scontributed to me getting so depressed I justjust started drinking again. I justnext time it'll kill me. So. That's almosta kind of a suicide wish, I guess.I know it's gonna kill me if I keep drinking.I think I need to get into something. Butthere'sI don't know if you call it substance abuse, butI think it's related todeep depression, which is not necessarily substance abuse, but it canI'm sure there's some relationship.
Similarly, the experiences of participants with diabetes illustrate clearly how depression contributed to undermining their ability to follow their doctors' recommendations. For example, an 18‐year‐old African American teenager rehospitalized for diabetes control discussed her inability to maintain her physician‐recommended diet:
Like when I'm stressed out.I get depressed and, umI give up. Just don't wanna do it anymore. It's not [that] I don't want to, I can't. I just can't do it I, when I got home, I actually did good! I actually really did good. I was eating salads. I did go on a diet. I ate salads, grilled food, and things like that. I took my medicine. I started loggin', like writin' everything down in a book. I wrote down what I ate every day, what my blood sugar was, and how much medicine I took. I was doin' good. But then I got depressed, and I stopped doin' it.
Continuity of Condition Management
Participants expressed a need after discharge for help at home, although in most cases, the help they reported needing did not require medical knowledge or technical skills.
Skilled Care
Few participants reported needing and/or receiving visiting nurse services; even in these cases, some of the responsibility for care fell to family members. Their health suffered because they lacked sufficient access to visiting nurse services or other needed support. A 42‐year‐old Latina diabetic with kidney infection described a visiting nurse's unsuccessful attempt to teach her husband how to change her catheter:
They try to show, 'cause before? I don't got the catheter, they're comin' in my house, in the morning? You know, put the catheter into my bladder, and they come back before me go to sleep, they try to show my husband how to do it, but he can't [CHUCKLES LIGHTLY], you know, he can't.So thethe doctor decide to leave the catheter there.
Basic Need Care
For most participants, the posthospital assistance needed did not require medical expertise. In the period after their last hospitalization, most participants needed assistance with daily chores such as cleaning, cooking, child care, and driving; they turned to friends and family members to meet these needs. However, because no family member was capable of providing full‐time care during recuperation, some participants were unable to follow advice from physicians about resting or refraining from certain activities. A 67‐year‐old African American man whose foot ulcers kept him from walking explained that during his recuperation he had to stay in the same place for 8 hours while his brother worked:
Oh, maybe if I had to go to the bathroom or something, I can'tbut for the most part, I guess I had things set upwhere I didn't, you know, where I didn't moveI just set my things up to keep me from movin' all day. I'd set my food up and everything else, little sandwich and all that. So, there wasn't anything aboutyou know, worrying about movin'or getting hungry, I guess.
None of the participants were able to pay for support services such as housecleaning or in‐home care, and all relied on busy friends and family members to meet their needs.
The experiences of 3 single mothers with health conditions characterized by debilitating chronic pain illustrate how very different access to supportive family members affected their ability to seek care and follow medical instructions as well as how child care responsibilities compromised their recuperation. One, a 20‐year‐old African American woman hospitalized for polycystic kidney disease, described situations during which the intensity of the pain did not permit her to do basic household chores. At those times she relied on her 5‐year‐old son:
Hehe actually knows how to sweep, he knows how to wash dishes. At 5 and a half, he surprised me, but [CHUCKLES] he can wash dishes, so. He has to get up on a chair, but he can wash 'em.
As a result of needing more care than was available, she traveled south to stay with her mother, who was unable to leave work to come to Boston:
I took the bus because my son has sickle cell trait, so they told me from day one it's not really good for him to fly on a plane? So, I had to take himit took like 20 hoursyou know, stoppin' here, stoppin' there, like, pullin' my bags and stuff, so it put me in more pain than I was in.
Another, a 24‐year‐old of mixed background chronically hospitalized with sickle cell pain crises, delayed medical treatment because of lack of child care:
There's been times that I have had to wait till I could find somebody to watch my kids, to even come to the hospital.There's been times thatuh, it'd be a while before I could get anybody, so instead of me coming to the hospital, I have to wait at home, in a lot of pain.I would have to waitany time between 5 hours to 2 days before I could find somebody to watch my kids.
This pattern of child care interfering with recovery continued after leaving the hospital:
The minute I get home it'd be nice to have somebody to watch the kids, so I could at least recuperate for like 24 hours before I have to take care of thingsI would have to usually just go home and just get right to it.
The experience of a third, a 29‐year‐old African American woman with systemic lupus erythematosus, illustrates the ways in which family support can ease the burden of illness. This participant relocated to be close to her mother, aunt, and cousins, all of whom cared for her children when she is in the hospital:
When I was in [NEIGHBORING STATE] it was terrible'cause my, my kids wasn't goin' to school, 'cause I couldn't get up to get them dressed and wake them up. My daughter almost got kept back and stuff. It was real hardand it wasn't good, you know, that they could justrun through the house rampant, do whatever they want and not be supervised.So that was very dangerous, too. And then, it put like, it put a strain on my oldest, my daughter
She contrasted this with her current situation in which family members cared for her children when she is in the hospital or sick at home:
Like, this morningthey took the kids to school for me and everything. Made 'em breakfast, made sure they was dressed right this morningMy mother picked them up from school this afternoon.
Transportation to Appointments
Travel to follow‐up appointments was difficult for many participants. Almost half reported taking public transportation to appointments; the others either drove themselves, were driven by relatives or friends, or paid for taxis. Those relying on public transportation were more likely than others to miss appointments because of transportation issues if they did not feel well:
Depending how I feel. If I feel all right, I'll take the bus; if not, I'll get a taxi or I'll just won't show up. I would borrow a bus pass or somethin', you know, from [HIS NAME] is Joebecause I would make, like, evening appointments. Um, because my sickle cell tends to act up if it's coldSo, if it's really cold, I don't go.
As one 55‐year‐old white woman who has seizures summed up the matter of traveling by bus when not feeling well, You do what you have to do!
DISCUSSION AND CONCLUSIONS
The hospital discharge process has been identified as a time when sources of error occur that result in rehospitalization. Many factors that adversely affect care transitions apply to the hospital discharge process, including preparation of the patient and caregiver, communication of the care plan, changes in the medication regimen, transportation of the patient, scheduling of follow‐up care, and availability of advance care directives.20 Patients with low socioeconomic status have been found to be especially vulnerable after discharge. A 1989 telephone survey of 6455 patients recently discharged from hospitals in the United States found that low socioeconomic status and poor patient health were independent predictors of patient problems after discharge.21 A nationwide telephone survey of 1800 recently discharged patients and their care partners also revealed that low socioeconomic status and poor patient health status were associated with problems experienced by care partners.22
High rates of unnecessary rehospitalization have been shown to be related to poorly managed discharge processes.23 Although some factors identified in other studies of care transition did influence the rehospitalization of participants in this study; others did not. Transportation and follow‐up care greatly affected rehospitalization, whereas health literacy had a minimal effect. Fifteen of 20 participants were readmitted within weeks up to 2 months for the same primary diagnosis, yet they understood their medical conditions and knew the procedures to be followed. Having a chronic illness may have affected their understanding of their disease because they had received teaching over time. However, for most participants in this studyinner‐city, minority, low‐income patientsfactors beyond the discharge process affected their rehospitalization. Difficult life circumstances and gaps in ongoing care or support resulted in distress and behavior that exacerbated their conditions. Participants lacked social and emotional support that would have enabled them to prioritize maintaining their health.
Although there is not a universally accepted definition of the concept of social support, it is generally understood that it involves emotional connection and caring24 and occurs in a relationship in which the person providing the support is equipped to respond to a wide variety of needs ranging from practical assistance to counseling and encouragement based on the concerns or life circumstances of the patient. Qualitative studies of social support interventions demonstrate the ways in which having a dependable person to whom a patient can turn for encouragement, information, and practical assistance improves the patient's ability to maintain health regimens and manage chronic pain. An intervention in which nurses made weekly telephone contact with low‐income pregnant smokers helped these patients manage numerous stressors and, in some cases, reduce their tobacco use.25 A support group for women with chronic pain helped participants learn practical strategies for reducing pain and reduced isolation and emotional distress about their conditions.26 A study of consumer experiences of transition care27 found that the most valued institutions were those in which providers from one facility thoroughly communicated a patient's medical and treatment history to providers in another; also important was involving the consumer in medical decision making, preparing the consumer to actively participate in his or her own care, and attending to individual needs and preferences.
This study had several limitations, including reliance on participants' reports of their conditions and experiences with medical staff at a time when they were rehospitalized. In the vulnerable position of being hospitalized, participants may have been reluctant to have complaints about their hospital experiences tape‐recorded. All participants reported positive experiences with hospital staff during the formal interview. Two participants reported negative experiences with hospital staff after the audio‐recorder was turned off and the interview concluded. Other limitations of the hospital setting include limited privacy. Either a roommate was present during the interview or the interview was interrupted by a visit from a hospital staff person or a telephone call. Participants were asked to recall events that for some had occurred several months before the interview, introducing the possibility of inaccurate recall. To address these limitations, we compared interview transcripts to discharge summaries in order to assess any inconsistencies that may have resulted from this lack of privacy. The differences between summaries and patient self‐reports were that 2 participants did not report illicit substance use and 2 did not report psychiatric conditions. Despite these limitations, conducting this study in a hospital setting allowed investigators access to a highly vulnerable population that would be most affected by improvements in the discharge process. Given the difficulties many participants reported in getting to appointments, it is unlikely that a study conducted outside the hospital setting would have effectively reached this population.
These results support the findings in this study that life circumstances outside the hospital can be as important to recovery as institutional coordination of medical care. Although the stresses described by the low‐income patients in this study may not directly cause subsequent illness, their experiences clearly demonstrate the ways in which stresses make it difficult or impossible to attain sufficient rest to heal, maintain the behavioral change necessary to improve health, and follow instructions given by clinicians at the time of discharge. Interventions targeting low‐income patients thus are more likely to succeed if they include provisions for social support and assist patients in easing the burden of daily responsibilities. Effective transition care includes support that may not be explicitly medical, but without which participants lack the stability to fully recuperate. Without the possibility of taking a break from household or parenting responsibilities, it is difficult to rest enough to truly recover. The descriptions of extreme measures taken in order to obtain needed support illustrate how recuperation was compromised by both family responsibilities and lack of flexibility in caregiver work schedules. Distress, particularly depression, further contributed to poor health and undermined the ability to follow doctors' recommendations and discharge plans.
Discharge interventions that explicitly assess requirements for social support and connect patients with agencies or volunteer groups that call or visit those recuperating, provide meals on wheels, or offer other services such as light cleaning or shopping can address the complex circumstances that result in poor health and chronic rehospitalization. This study has identified the crucial role social support plays in getting and staying well.
Acknowledgements
The authors thank Maria Rizzo DePaoli MSW and Cornelia Walsh RN for assistance with logistics of the study.
Institute of Medicine (IOM) reports1, 2 have estimated that between 44,000 and 98,000 patients die every year in hospitals because of iatrogenic errors of omission and commission. More people die in a year from medical errors than from car accidents (43,458), breast cancer (42,297), or AIDS (16,515).3 The IOM report recommended a goal of a 50% reduction in errors over the next 5 years.4 Since publication of these reports, a great deal of interest has been focused on how to make our hospitals safer.5, 6 Times of transitions in care (eg, from home to hospital, from emergency department to hospital, from the intensive care unit to the general ward) have been identified as opportune times to improve continuity and thus to decrease errors.
The hospital discharge process is often nonstandardized and frequently marked by poor quality.7 One in five hospital discharges is complicated by adverse events within 30 days, many of which lead to visits to emergency departments (EDs) and rehospitalization.810 Nationally, approximately 25% of hospitalized patients are readmitted within 90 days, often because of errors resulting from discontinuity and fragmentation of care at discharge, which exposes patients to iatrogenic risk and raises costs.11, 12 Low health literacy rates, lack of coordination in the handoff from the hospital to community care, gaps in social supports, and the absence of physician follow‐up after discharge place patients at high risk of rehospitalization.1315 Increasingly, as hospitalists provide more inpatient care, it is difficult for primary care physicians to be aware of all the complexities of a hospitalization.16
Studying the hospital discharge process provides an opportunity to learn more about its complexities,17 which could then be used to standardize the process and focus on those interventions that reduce the number of medical errors and resulting adverse events. However, to date, few studies have described the essential components of the discharge process, and no studies have focused on the discharge process from the point of view of the hospitalized patient. Therefore, a qualitative study was conducted in order to understand the phenomenon of frequent rehospitalization from the perspective of the discharged patient and to determine if activities at the time of discharge could be designed to reduce the number of adverse events and rehospitalizations.
METHODS
The larger study of which this work is a part examined the transition from inpatient service at a large inner‐city hospital to community care in order to lead to the development of an intervention to improve the discharge process. Qualitative research stresses the socially constructed nature of reality, and qualitative researchers seek to answer questions that stress how social experience is created and given meaning.18 Qualitative interviewing permits the researcher to understand the world as seen by the respondent within the context of the respondent's everyday life.19 Learning from the experiences of patients hospitalized more than once in a 6‐month period will help to identify their perceptions and beliefs about their disease and discharge instructions and assist additional interventions that could prevent rehospitalization.
Sample
Semistructured, open‐ended interviews were conducted with 21 patients during their hospital stay at Boston Medical Center. To be eligible for the study, a patient had to receive medical care through a health center affiliated with Boston Health Net, a network of community health centers serving primarily low‐income patients, and had to have been hospitalized on at least 1 additional occasion in the previous 6 months. Each day during the interview period the Boston Health Net nurse identified all patients previously admitted within 6 months and contacted the interviewer with the names and room numbers of those patients. The interviewer (M.S.) approached potential participants in their hospital rooms and obtained informed consent at the time of the interview. If the patient agreed, the interview was conducted at that time. If the patient was not available at that time, the interviewer made at least 2 attempts to visit the patient at a convenient time. The interviews were conducted on 17 days of a 4‐month period with no more than 2 interviews completed a day. The participants ranged in age from 18 to 79; 10 respondents were male, and 11 were female. All were English speaking. The mean age of the 20 patients who provided demographic information was 45.55 years, and the median age was 47 years. Nine of the participants reported their racial or ethnic identities as white (5 male, 3 female), 3 as black (2 male, 1 female), 4 as African American (1 male, 3 female); 1 as Latina; 1 as Hispanic (male), 1 as Spanish (male), and 1 as mixed (female). One male and 1 female participant provided no race or ethnic identity. Two participants were excluded from the study because they did not speak English, and 2 were excluded because they were unable to speak due to their medical conditions. Interviews were audiotaped, but full names were not used on the tape. Only subject code numbers were used to identify respondents. The discharge records of each participant were reviewed for consistency with that participant's descriptions of his or her condition. The study was approved by the Institutional Review Board of Boston University Medical Center.
Interview Guide
To help assure collection of comparable qualitative data, an interview guide listed specific questions and topics to be covered in a particular order in the interview. Questions were drawn in part from a pilot test of interviewing patients on the inpatient service rehospitalized within 90 days of the previous admission.17 Interviews assessed continuity of care after discharge, need for and availability of social support, and the participant's ability to obtain follow‐up medical care. The interview script consisted of open‐ended questions about events leading up to the current hospitalization, previous hospitalizations, instructions received the last time discharged, home situation, and ability to attend medical appointments, and participant feedback on the discharge process was requested. Follow‐up questions were asked based on a patient's responses to these questions. Interviews lasted between 20 and 45 minutes.
Analysis
The interview tapes were transcribed by a subcontracted transcriber, and the transcripts were checked for accuracy by the interviewer. Each interview was evaluated according to a set of thematic codes developed by 2 qualitative researchers (L.S. and M.S.). The codes represent categories or themes found in the data, and the appropriate codes were attached to their corresponding sections of text. To improve interrater reliability in coding, the 2 qualitative researchers coded 3 interviews, reviewed the codes, and, once it was clear that they both understood the coding scheme, coded the interviews. They resolved any problem cases and checked each other's work throughout the coding process to ensure that each interview was coded correctly. The findings were analyzed to explore whether there were linkages between and among particular themes. The discharge records of all patients were reviewed in order to compare the discharge notes about each patient's condition with that patient's own description of his or her condition and treatment.
RESULTS
All the patients who participated in this study were able to describe their medical condition and the reasons they were admitted to the hospital. Almost all, 20 of the 21 participants, were rehospitalized for the same primary diagnosis. For 5 of these 20 participants, length of time since the last hospitalization was 5‐6 months (4 for diabetes control, 1 for a lupus erythematosus flare); for 4 participants time since last hospitalization was between 6 weeks and 2 months (1 because of a fall, 1 because of seizures, 1 with hypertension, and 1 with SOB); for 8 participants time since last hospitalization was between 3 weeks and 1 month (2 with kidney disease, 2 with seizures, and 1 each with chronic obstructive pulmonary disease, sickle cell disease, PVD, and alcoholic gastritis), and for 3 participants time since last hospitalization was 1‐2 weeks (1 each with abdominal pain, alcohol intoxication, and lower gastrointestinal bleed). The principal diagnosis in a patient's discharge records matched that participant's description. Participants also described the discharge instructions they received. Although some did not report the brand names of the medications they were taking, all reports of the types of medications being taken or the conditions for which the medications were prescribed were consistent with discharge summaries. Although none of the participants incorrectly reported a medication or condition to the interviewer, a few did not provide information about every medication or condition. In 1 case the discharge summary noted medications for bipolar disorder and mental illness; in 2 cases medications were prescribed for depression. None of these participants mentioned these conditions or medications to the interviewer. One patient talked about stress and depression, but nothing was written about these issues in the discharge record.
For participants in this study, difficult life circumstances posed a greater barrier to recuperation than did lack of medical knowledge. The interviews conducted in this study illustrate the personal and social impact of disease that resulted in rehospitalization.
Discharge and Medical Knowledge
During discharge, transition care processes can fail at many points.20 These include: communication of the care plan, reconciliation of current and initial medication regimens, transportation of the patient, follow‐up care with a provider, and preparation of patient and caregiver for maintaining the patient's regimen.4, 2022 Participants in this study identified some of these and other factors as constituting barriers to effective care transitions.
At discharge, 7 participants were advised by physicians to change their diets or refrain from tobacco or alcohol use. Participants clearly understood the instructions and could give detailed accounts of diet changes they were supposed to make or explain the reasons tobacco or alcohol use caused or exacerbated their diseases. A diabetic whose discharge instructions included diet change listed sweet ones, starchy oneswith a lot of carbohydrates as foods she is not supposed to eat, wherease others described the links between alcohol use and adverse health: In my mind, I think that alcohol is a way out.But I know that it, that it's not.And so, the pancreatitis develops.
Lack of understanding about their medical condition or of knowledge about procedures to be followed was not evident in this population. Instead, recuperation was compromised by factors such as distress, substance use, support for medical and basic needs, and limitations in the availability of transportation to medical appointments. Many participants reported not receiving necessary rest as a result of needing to work or care for young children.
Crises and Coping: Distress
Despite understanding needed behavior changes, almost half the participants explained how difficult life circumstances and gaps in ongoing care or support made it impossible for them to follow medical advice.
Almost half the participants described themselves as being stressed, sad, or depressed. Their explanations indicate a relationship between distress and subsequent behaviors that exacerbated their conditions.
Of 3 self‐described alcoholics, one, a 52‐year‐old white man rehospitalized for alcohol related seizures, had relapsed after the deaths of his mother and his girlfriend. He explained, Well, after my girlfriend died, I really started to hit the bottle. Another, an unemployed 45‐year‐old black woman, lacked stable housing and at the time of the interview lived with a heavy drinker. She said that when I get stressed out, the first thing I want to do is go run to the [liquor] store. The third self‐described alcoholic, a 62‐year‐old white man, reported drinking because of lack of regular treatment for chronic depression:
My problem is has to do with stress and depression, which is what I'm gonna try to deal with this time. 'Cause that'scontributed to me getting so depressed I justjust started drinking again. I justnext time it'll kill me. So. That's almosta kind of a suicide wish, I guess.I know it's gonna kill me if I keep drinking.I think I need to get into something. Butthere'sI don't know if you call it substance abuse, butI think it's related todeep depression, which is not necessarily substance abuse, but it canI'm sure there's some relationship.
Similarly, the experiences of participants with diabetes illustrate clearly how depression contributed to undermining their ability to follow their doctors' recommendations. For example, an 18‐year‐old African American teenager rehospitalized for diabetes control discussed her inability to maintain her physician‐recommended diet:
Like when I'm stressed out.I get depressed and, umI give up. Just don't wanna do it anymore. It's not [that] I don't want to, I can't. I just can't do it I, when I got home, I actually did good! I actually really did good. I was eating salads. I did go on a diet. I ate salads, grilled food, and things like that. I took my medicine. I started loggin', like writin' everything down in a book. I wrote down what I ate every day, what my blood sugar was, and how much medicine I took. I was doin' good. But then I got depressed, and I stopped doin' it.
Continuity of Condition Management
Participants expressed a need after discharge for help at home, although in most cases, the help they reported needing did not require medical knowledge or technical skills.
Skilled Care
Few participants reported needing and/or receiving visiting nurse services; even in these cases, some of the responsibility for care fell to family members. Their health suffered because they lacked sufficient access to visiting nurse services or other needed support. A 42‐year‐old Latina diabetic with kidney infection described a visiting nurse's unsuccessful attempt to teach her husband how to change her catheter:
They try to show, 'cause before? I don't got the catheter, they're comin' in my house, in the morning? You know, put the catheter into my bladder, and they come back before me go to sleep, they try to show my husband how to do it, but he can't [CHUCKLES LIGHTLY], you know, he can't.So thethe doctor decide to leave the catheter there.
Basic Need Care
For most participants, the posthospital assistance needed did not require medical expertise. In the period after their last hospitalization, most participants needed assistance with daily chores such as cleaning, cooking, child care, and driving; they turned to friends and family members to meet these needs. However, because no family member was capable of providing full‐time care during recuperation, some participants were unable to follow advice from physicians about resting or refraining from certain activities. A 67‐year‐old African American man whose foot ulcers kept him from walking explained that during his recuperation he had to stay in the same place for 8 hours while his brother worked:
Oh, maybe if I had to go to the bathroom or something, I can'tbut for the most part, I guess I had things set upwhere I didn't, you know, where I didn't moveI just set my things up to keep me from movin' all day. I'd set my food up and everything else, little sandwich and all that. So, there wasn't anything aboutyou know, worrying about movin'or getting hungry, I guess.
None of the participants were able to pay for support services such as housecleaning or in‐home care, and all relied on busy friends and family members to meet their needs.
The experiences of 3 single mothers with health conditions characterized by debilitating chronic pain illustrate how very different access to supportive family members affected their ability to seek care and follow medical instructions as well as how child care responsibilities compromised their recuperation. One, a 20‐year‐old African American woman hospitalized for polycystic kidney disease, described situations during which the intensity of the pain did not permit her to do basic household chores. At those times she relied on her 5‐year‐old son:
Hehe actually knows how to sweep, he knows how to wash dishes. At 5 and a half, he surprised me, but [CHUCKLES] he can wash dishes, so. He has to get up on a chair, but he can wash 'em.
As a result of needing more care than was available, she traveled south to stay with her mother, who was unable to leave work to come to Boston:
I took the bus because my son has sickle cell trait, so they told me from day one it's not really good for him to fly on a plane? So, I had to take himit took like 20 hoursyou know, stoppin' here, stoppin' there, like, pullin' my bags and stuff, so it put me in more pain than I was in.
Another, a 24‐year‐old of mixed background chronically hospitalized with sickle cell pain crises, delayed medical treatment because of lack of child care:
There's been times that I have had to wait till I could find somebody to watch my kids, to even come to the hospital.There's been times thatuh, it'd be a while before I could get anybody, so instead of me coming to the hospital, I have to wait at home, in a lot of pain.I would have to waitany time between 5 hours to 2 days before I could find somebody to watch my kids.
This pattern of child care interfering with recovery continued after leaving the hospital:
The minute I get home it'd be nice to have somebody to watch the kids, so I could at least recuperate for like 24 hours before I have to take care of thingsI would have to usually just go home and just get right to it.
The experience of a third, a 29‐year‐old African American woman with systemic lupus erythematosus, illustrates the ways in which family support can ease the burden of illness. This participant relocated to be close to her mother, aunt, and cousins, all of whom cared for her children when she is in the hospital:
When I was in [NEIGHBORING STATE] it was terrible'cause my, my kids wasn't goin' to school, 'cause I couldn't get up to get them dressed and wake them up. My daughter almost got kept back and stuff. It was real hardand it wasn't good, you know, that they could justrun through the house rampant, do whatever they want and not be supervised.So that was very dangerous, too. And then, it put like, it put a strain on my oldest, my daughter
She contrasted this with her current situation in which family members cared for her children when she is in the hospital or sick at home:
Like, this morningthey took the kids to school for me and everything. Made 'em breakfast, made sure they was dressed right this morningMy mother picked them up from school this afternoon.
Transportation to Appointments
Travel to follow‐up appointments was difficult for many participants. Almost half reported taking public transportation to appointments; the others either drove themselves, were driven by relatives or friends, or paid for taxis. Those relying on public transportation were more likely than others to miss appointments because of transportation issues if they did not feel well:
Depending how I feel. If I feel all right, I'll take the bus; if not, I'll get a taxi or I'll just won't show up. I would borrow a bus pass or somethin', you know, from [HIS NAME] is Joebecause I would make, like, evening appointments. Um, because my sickle cell tends to act up if it's coldSo, if it's really cold, I don't go.
As one 55‐year‐old white woman who has seizures summed up the matter of traveling by bus when not feeling well, You do what you have to do!
DISCUSSION AND CONCLUSIONS
The hospital discharge process has been identified as a time when sources of error occur that result in rehospitalization. Many factors that adversely affect care transitions apply to the hospital discharge process, including preparation of the patient and caregiver, communication of the care plan, changes in the medication regimen, transportation of the patient, scheduling of follow‐up care, and availability of advance care directives.20 Patients with low socioeconomic status have been found to be especially vulnerable after discharge. A 1989 telephone survey of 6455 patients recently discharged from hospitals in the United States found that low socioeconomic status and poor patient health were independent predictors of patient problems after discharge.21 A nationwide telephone survey of 1800 recently discharged patients and their care partners also revealed that low socioeconomic status and poor patient health status were associated with problems experienced by care partners.22
High rates of unnecessary rehospitalization have been shown to be related to poorly managed discharge processes.23 Although some factors identified in other studies of care transition did influence the rehospitalization of participants in this study; others did not. Transportation and follow‐up care greatly affected rehospitalization, whereas health literacy had a minimal effect. Fifteen of 20 participants were readmitted within weeks up to 2 months for the same primary diagnosis, yet they understood their medical conditions and knew the procedures to be followed. Having a chronic illness may have affected their understanding of their disease because they had received teaching over time. However, for most participants in this studyinner‐city, minority, low‐income patientsfactors beyond the discharge process affected their rehospitalization. Difficult life circumstances and gaps in ongoing care or support resulted in distress and behavior that exacerbated their conditions. Participants lacked social and emotional support that would have enabled them to prioritize maintaining their health.
Although there is not a universally accepted definition of the concept of social support, it is generally understood that it involves emotional connection and caring24 and occurs in a relationship in which the person providing the support is equipped to respond to a wide variety of needs ranging from practical assistance to counseling and encouragement based on the concerns or life circumstances of the patient. Qualitative studies of social support interventions demonstrate the ways in which having a dependable person to whom a patient can turn for encouragement, information, and practical assistance improves the patient's ability to maintain health regimens and manage chronic pain. An intervention in which nurses made weekly telephone contact with low‐income pregnant smokers helped these patients manage numerous stressors and, in some cases, reduce their tobacco use.25 A support group for women with chronic pain helped participants learn practical strategies for reducing pain and reduced isolation and emotional distress about their conditions.26 A study of consumer experiences of transition care27 found that the most valued institutions were those in which providers from one facility thoroughly communicated a patient's medical and treatment history to providers in another; also important was involving the consumer in medical decision making, preparing the consumer to actively participate in his or her own care, and attending to individual needs and preferences.
This study had several limitations, including reliance on participants' reports of their conditions and experiences with medical staff at a time when they were rehospitalized. In the vulnerable position of being hospitalized, participants may have been reluctant to have complaints about their hospital experiences tape‐recorded. All participants reported positive experiences with hospital staff during the formal interview. Two participants reported negative experiences with hospital staff after the audio‐recorder was turned off and the interview concluded. Other limitations of the hospital setting include limited privacy. Either a roommate was present during the interview or the interview was interrupted by a visit from a hospital staff person or a telephone call. Participants were asked to recall events that for some had occurred several months before the interview, introducing the possibility of inaccurate recall. To address these limitations, we compared interview transcripts to discharge summaries in order to assess any inconsistencies that may have resulted from this lack of privacy. The differences between summaries and patient self‐reports were that 2 participants did not report illicit substance use and 2 did not report psychiatric conditions. Despite these limitations, conducting this study in a hospital setting allowed investigators access to a highly vulnerable population that would be most affected by improvements in the discharge process. Given the difficulties many participants reported in getting to appointments, it is unlikely that a study conducted outside the hospital setting would have effectively reached this population.
These results support the findings in this study that life circumstances outside the hospital can be as important to recovery as institutional coordination of medical care. Although the stresses described by the low‐income patients in this study may not directly cause subsequent illness, their experiences clearly demonstrate the ways in which stresses make it difficult or impossible to attain sufficient rest to heal, maintain the behavioral change necessary to improve health, and follow instructions given by clinicians at the time of discharge. Interventions targeting low‐income patients thus are more likely to succeed if they include provisions for social support and assist patients in easing the burden of daily responsibilities. Effective transition care includes support that may not be explicitly medical, but without which participants lack the stability to fully recuperate. Without the possibility of taking a break from household or parenting responsibilities, it is difficult to rest enough to truly recover. The descriptions of extreme measures taken in order to obtain needed support illustrate how recuperation was compromised by both family responsibilities and lack of flexibility in caregiver work schedules. Distress, particularly depression, further contributed to poor health and undermined the ability to follow doctors' recommendations and discharge plans.
Discharge interventions that explicitly assess requirements for social support and connect patients with agencies or volunteer groups that call or visit those recuperating, provide meals on wheels, or offer other services such as light cleaning or shopping can address the complex circumstances that result in poor health and chronic rehospitalization. This study has identified the crucial role social support plays in getting and staying well.
Acknowledgements
The authors thank Maria Rizzo DePaoli MSW and Cornelia Walsh RN for assistance with logistics of the study.
- ,.Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization.JAMA.2003;290:1868–1874.
- ,,,Institute of Medicine (U.S.).Committee on Quality of Health Care in America.To Err Is Human: Building a Safer Health System.Washington, DC:National Academy Press:2000.
- Centers for Disease Control and Prevention (National Center for Health Statistics).Births and deaths: preliminary data for 1998.Nat Vit Stat Rep.1999:47.
- Institute of Medicine (U.S.).Committee on Quality of Health Care in America.Crossing the Quality Chasm: a New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- AHRQ's Patient Safety Initiative: Building Foundations, Reducing Risk. Interim Report to the Senate Committee on Appropriations, AHRQ Publication No. 04‐RG005.Rockville, MD:Agency for Healthcare Research and Quality;2003. Available at: http://www.ahrq.gov/qual/pscongrpt/.
- ,,,,,.Patient safety at time of discharge—an example of a multifaceted process evaluation. In:Henriksen K,Battles JB,Marks ES,Lewin DI, editors. Advances in Patient Safety: from Research to Implementation. Vol.2,Concepts and methodology. AHRQ Publication No. 05‐0021‐2.Rockville, MD:Agency for Healthcare Research and Quality;2005.
- ,,.Dissemination of discharge summaries. Not reaching follow‐up physicians.Can Fam Physician.2002;48:737–742.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138(3):161–167.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,, et al.Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients.BMJ.2004;329:15–19.
- and.Hospital readmissions in the Medicare population.N Engl J Med.1984;311:1349–1353.
- and.Factors predicting readmission of older general medicine patients.J Gen Intern Med.1991;6:389–393.
- ,,,.Delayed access to health care: risk factors, reasons and consequences.Ann Intern Med.1991;114:325–331.
- ,,,,,.Impact of socioeconomic status on hospital use in New York City.Health Aff (Millwood).1993 Spring;12(1):162–173.
- ,,.The impact of patient socioeconomic status and other social factors on readmission: a prospective study in four Massachusetts hospitals.Inquiry.1994;31(2):163–172.
- ,,,.Primary care physician attitudes regarding communication with hospitalists.Dis Mon.2002;48(4):218–229.
- ,,,,,.Patient safety at time of discharge: an example of a multifaceted process evaluation.Washington, DC:AHRQ Patient Safety 2 Volume Site;2004.
- ,.Entering the field of qualitative research. In:Denzin NK,Lincoln YS, eds.Handbook of Qualitative Research.Newbury Park, CA:Sage;1994.
- ,.The workers' compensation system: worker friend or foe?Am J Ind Med.2004;45:338–345.
- .Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs.J Am Geriatr Soc.2003;51:549–555.
- ,,,,.Carepartner experiences with hospital care.Med Care.1999;37:33–38.
- ,,.Patients' and caregivers' transition from hospital to home. Needs and recommendations.Home Health Care Serv Q.1998;17:27–48.
- ,,, et al.Patients evaluate their hospital care: A national survey.Health Aff.1991;10:254.
- ,,.Defining social support in context: a necessary step in improving research, intervention, and practice.Qual Health Res.2004;14:942–960.
- .Telephone social support or nursing presence? Analysis of a nursing intervention.Qual Health Res.2005;15(1):19–29.
- ...Encountering the continuing challenges for women with chronic pain: recovery through recognition.Qual Health Res.2003;13:491–509.
- ,.Understanding coordination of care from the consumer's perspective in a regional health system.Health Serv Res.2002;37:1031–1054.
- ,.Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization.JAMA.2003;290:1868–1874.
- ,,,Institute of Medicine (U.S.).Committee on Quality of Health Care in America.To Err Is Human: Building a Safer Health System.Washington, DC:National Academy Press:2000.
- Centers for Disease Control and Prevention (National Center for Health Statistics).Births and deaths: preliminary data for 1998.Nat Vit Stat Rep.1999:47.
- Institute of Medicine (U.S.).Committee on Quality of Health Care in America.Crossing the Quality Chasm: a New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- AHRQ's Patient Safety Initiative: Building Foundations, Reducing Risk. Interim Report to the Senate Committee on Appropriations, AHRQ Publication No. 04‐RG005.Rockville, MD:Agency for Healthcare Research and Quality;2003. Available at: http://www.ahrq.gov/qual/pscongrpt/.
- ,,,,,.Patient safety at time of discharge—an example of a multifaceted process evaluation. In:Henriksen K,Battles JB,Marks ES,Lewin DI, editors. Advances in Patient Safety: from Research to Implementation. Vol.2,Concepts and methodology. AHRQ Publication No. 05‐0021‐2.Rockville, MD:Agency for Healthcare Research and Quality;2005.
- ,,.Dissemination of discharge summaries. Not reaching follow‐up physicians.Can Fam Physician.2002;48:737–742.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138(3):161–167.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,, et al.Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients.BMJ.2004;329:15–19.
- and.Hospital readmissions in the Medicare population.N Engl J Med.1984;311:1349–1353.
- and.Factors predicting readmission of older general medicine patients.J Gen Intern Med.1991;6:389–393.
- ,,,.Delayed access to health care: risk factors, reasons and consequences.Ann Intern Med.1991;114:325–331.
- ,,,,,.Impact of socioeconomic status on hospital use in New York City.Health Aff (Millwood).1993 Spring;12(1):162–173.
- ,,.The impact of patient socioeconomic status and other social factors on readmission: a prospective study in four Massachusetts hospitals.Inquiry.1994;31(2):163–172.
- ,,,.Primary care physician attitudes regarding communication with hospitalists.Dis Mon.2002;48(4):218–229.
- ,,,,,.Patient safety at time of discharge: an example of a multifaceted process evaluation.Washington, DC:AHRQ Patient Safety 2 Volume Site;2004.
- ,.Entering the field of qualitative research. In:Denzin NK,Lincoln YS, eds.Handbook of Qualitative Research.Newbury Park, CA:Sage;1994.
- ,.The workers' compensation system: worker friend or foe?Am J Ind Med.2004;45:338–345.
- .Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs.J Am Geriatr Soc.2003;51:549–555.
- ,,,,.Carepartner experiences with hospital care.Med Care.1999;37:33–38.
- ,,.Patients' and caregivers' transition from hospital to home. Needs and recommendations.Home Health Care Serv Q.1998;17:27–48.
- ,,, et al.Patients evaluate their hospital care: A national survey.Health Aff.1991;10:254.
- ,,.Defining social support in context: a necessary step in improving research, intervention, and practice.Qual Health Res.2004;14:942–960.
- .Telephone social support or nursing presence? Analysis of a nursing intervention.Qual Health Res.2005;15(1):19–29.
- ...Encountering the continuing challenges for women with chronic pain: recovery through recognition.Qual Health Res.2003;13:491–509.
- ,.Understanding coordination of care from the consumer's perspective in a regional health system.Health Serv Res.2002;37:1031–1054.
Copyright © 2007 Society of Hospital Medicine
Transitions of Care at Hospital Discharge
As the counterpart to hospital admission, hospital discharge is a necessary process experienced by each living patient. For all patients except those being transferred to a continuing care facility, discharge is a period of transition from hospital to home that involves a transfer in responsibility from the inpatient provider or hospitalist to the patient and primary care physician (PCP).1 Prescription medications are commonly altered at this transition point, with patients asked to discontinue some medications, switch to a new dosage schedule of others, or begin new treatments.2, 3 Self‐care responsibilities also increase in number and importance, presenting new challenges for patients and their families as they return home.4 Under these circumstances, ineffective planning and coordination of care can undermine patient satisfaction, facilitate adverse events, and contribute to more frequent hospital readmissions.58
Following hospital discharge nearly half (49%) of hospitalized patients experience at least 1 medical error in medication continuity, diagnostic workup, or test follow‐up.7 It has been reported that 19%23% of patients suffer an adverse event, most frequently an adverse drug event (ADE).911 Half of ADEs are considered preventable or ameliorable (ie, their severity or duration could have been decreased). Most errors and adverse events in this setting result from a breakdown in communication between the hospital team and the patient or primary care physician.10
To promote more effective care transitions, The Joint Commission now requires accredited facilities to accurately and completely reconcile medications across the continuum of care.12 The Society of Hospital Medicine recently published recommendations for the discharge of elderly patients.13 The joint Society of Hospital MedicineSociety of General Internal Medicine Continuity of Care Task Force also recently published a systematic review with recommendations for improving the handoff of patient information at discharge.14 Apart from these reports, however, it is uncommon to find evidence‐based recommendations for hospital discharge applicable to a broad range of patients.15 This review highlights several important challenges for physicians who seek to provide high‐quality care during hospital discharge and the subsequent period of transition. Based on the best available evidence, recommendations are also provided for how to improve communication and facilitate the care transition for adult inpatients returning home.
INPATIENTOUTPATIENT PHYSICIAN DISCONTINUITY
Traditionally, primary care physicians have admitted their own patients, provided hospital care (in addition to seeing outpatients during the day), and followed patients after discharge. Under this model, continuity of care has been preserved; however, this method of care has faltered under the weight of inpatients and outpatients with more severe illnesses, rapid technological advancements, managed care pressuring outpatient physicians to see more patients, and a thrust toward reduced hospital costs and length of stay.16 Increases in the efficiency and quality of hospital care have accompanied a new reliance on the field of hospital medicine, while allowing PCPs to focus on outpatient care.1719 With more than 14,000 hospitalists currently practicing in the United States and 25,000 anticipated to be practicing by 2010, transfer of care from hospital‐based providers to PCPs has become increasingly common at discharge.20
Patient discharge summaries are the most common means of communication between inpatient and outpatient providers. However, numerous studies have shown that discharge summaries often fail to provide important administrative and medical information, such as the primary diagnosis, results of abnormal diagnostics, details about the hospital course, follow‐up plans, whether laboratory test results are pending, and patient or family counseling.14 Summaries also may not arrive in a timely manner and sometimes may not reach the PCP at all.2123
At the time patients first follow up with their PCPs after hospitalization, discharge summaries have not yet arrived about 75% of the time,22, 24, 25 restricting the PCPs' ability to provide adequate follow‐up care in 24% of hospital follow‐up visits, according to one study.26 In another investigation, PCPs reported being unaware of 62% of the pending test results that returned after discharge, of which 37% were considered actionable.27
Improving Physician Information Transfer and Continuity
To improve information transfer from hospitalist to PCP, attention must be paid to the content, format, and timely delivery of discharge information (Table 1).14 Surveys of primary care physicians suggest the following information should be included in discharge summaries: diagnoses, abnormal physical findings, important test results, discharge medications, follow‐up arrangements made and appointments that still need to be made, counseling provided to the patient and family, and tests still pending at discharge.24, 2833 These domains are consistent with Joint Commission guidelines for discharge summaries,34 and the inclusion of a detailed medication list and pending test results also has implications for patient safety.911, 27
| Challenge | Recommended approaches |
|---|---|
| Inpatientoutpatient physician discontinuity | When possible, involve the primary care physician (PCP) in discharge planning and work together to develop a follow‐up plan |
| At minimum, communicate the following to the PCP on the day of discharge: diagnoses, medications, results of procedures, pending tests, follow‐up arrangements, and suggested next steps | |
| Provide the PCP with a detailed discharge summary within 1 week | |
| In discharge summaries include: diagnoses, abnormal physical findings, important test results, discharge medications with rationale for new or changed medications, follow‐up arrangements made, counseling provided to the patient and family, and tasks to be completed (eg, appointments that still need to be made and tests that require follow‐up) | |
| Follow a structured template with subheadings in discharge communications | |
| When possible, use health information technology to create and disseminate discharge summaries | |
| Changes and discrepancies in medication regimen | Obtain a complete medication history by asking patients about: medications taken at different times of day; medications prescribed by different physicians; nonoral medications; over‐the‐counter products; dosage, indication, length of therapy, and timing of last dose of all drugs; allergies; and adherence |
| Compare and reconcile medication information obtained from patient and caregiver reports, patient lists, prescription bottles, medical records, and pharmacy records | |
| Display preadmission medication list prominently in the chart | |
| Reconcile medications at all care transitions, including admission, intrahospital transfer, and discharge | |
| Communicate complete and accurate medication information to the next provider at discharge, including indications for new medications and reasons for any changes | |
| When possible, partner with clinical pharmacists to manage medication information and reconciliation, especially for high‐risk patients | |
| Self‐care responsibilities and social support | Use multidisciplinary discharge planning teams to assess the needs of patients and their families |
| Arrange a specific follow‐up appointment prior to discharge | |
| Contact patients by telephone a few days after discharge to assess questions, symptoms, and medication‐related issues | |
| Order home health services when indicated | |
| Consider home visits for frail elderly patients | |
| Ineffective physicianpatient communication | Focus discharge counseling on informing patients of major diagnoses, medication changes, dates of follow‐up appointments, self‐care instructions, and who to contact if problems develop |
| Ensure that staff members communicate consistent instructions | |
| For high‐volume conditions, consider using audiovisual recordings for discharge education, combined with an opportunity for additional counseling and questions | |
| Use trained interpreters when a language gap exists | |
| Provide simply written materials that include illustrations when possible to reinforce verbal instructions | |
| Ensure patients and family members comprehend key points by asking them to teach back the information in their own words and demonstrate any self‐care behaviors | |
| Encourage patients and family members to ask questions through an open‐ended invitation like, What questions do you have? instead of Do you have any questions? |
Because many patients follow up with their PCPs within a few days of discharge, it becomes important to provide the PCPs with some information about the hospitalization on the day of discharge. This can be accomplished via a quick telephone call, fax, or e‐mail update to the PCP.24, 35 Important things to include in this communiqu are the discharge diagnosis, medications, results of procedures, pending test results, follow‐up arrangements, and suggested next steps. Within 1 week, a detailed discharge summary should have been received.26, 33, 36 As electronic medical records become more widely available, computer‐generated summaries offer a way to more quickly and completely highlight the key elements of the hospitalization, and they are ready for delivery sooner than traditional dictated summaries.37 Additionally, all forms of discharge summariescomputer‐generated, handwritten, and dictatedshould include subheadings to better organize and present the information instead of unstructured narrative summaries.38
There is increasing interest in moving away from the traditional 1‐way transfer of information about a hospitalization toward a 2‐way dialogue between hospitalist and primary care physician.39 Preferences about how to do this will vary among physicians. One strategy might be to provide the PCP with the hospitalist's contact information and encouraging questions about the hospitalization. Another approach would involve contacting the PCP during the discharge planning process to exchange information about the patient, provide an opportunity for the PCP to ask questions about the hospitalization, and formulate a cohesive plan for follow‐up, particularly about contingency planning (ie, what is most likely to go wrong and what should be done about it) and specific follow‐up needs (ie, what tasks should be accomplished at the first postdischarge visit).
CHANGES AND DISCREPANCIES IN THE MEDICATION REGIMEN
Medication errors make up a large portion of the adverse events patients may experience in the period following hospital discharge.7 In fact, errors during the ordering of admission or discharge medications make up almost half of all hospital medication errors.4043 At transition points such as admission and discharge, errors are often associated with changes in the medication regimen, including discrepancies between the new set of medication orders and what the patient was taking previously. In 2 recent studies, 54% of patients experienced at least 1 unintended medication discrepancy on admission to the hospital, and 39%‐45% of these discrepancies were considered a potential threat to the patient.44, 45
At discharge, differences between the prescribed medication regimen and the prehospital regimen may exist for several reasons. First, physicians may not obtain a comprehensive and accurate medication history at the time of admission.46 The medication history elicited from the patient at hospital admission is often affected by health literacy, language barriers, current health status, medication‐history interviewing skills, and time constraints.47 Physicians may not consult other important sources of medication information, including family members, prescription lists or bottles, and community pharmacy records. The most common error in the admission medication history is omitting a medication taken at home.46 Additionally, several providers, including a physician, a nurse, and an inpatient pharmacist, may independently take medication histories for the same patient. These multiple accounts lead to discrepancies that are rarely recognized or corrected.
Second, a patient's medication regimen can be significantly altered several times during a hospitalization. Acute illness may cause physicians to hold certain medications, discontinue others, or change prescribed doses during hospitalization.48 In addition, at most hospitals closed drug formularies necessitate automatic substitution of 1 medication for another drug in the same class during the patient's hospital stay.49 Changes from long‐acting to short‐acting medications are also routinely made in the name of tighter control (eg, of blood pressure). One study of hospitalized elders found that 40% of all admission medications had been discontinued by discharge and that 45% of all discharge medications were newly started during the hospitalization.3
Finally, at discharge, the current medication regimen needs to be reconciled with the preadmission medication regimen in a thoughtful manner.2 This includes resuming medications held or modified at admission for clinical reasons, resuming medications that were substituted in the hospital for formulary or pharmacokinetic reasons, and stopping newly started medications that were only required during the hospitalization (eg, for prevention of venous thromboembolism or stress ulcers).50 It is difficult, even in hospitals with advanced electronic health information systems, to prompt physicians to make these necessary changes. In a recent study, unexplained discrepancies between the preadmission medication list and discharge medication orders were noted in 49% of hospital discharges.51 Errors in discharge medication reconciliation may subsequently increase the risk of postdischarge ADEs.51
Medication Reconciliation and Education
An optimal strategy for obtaining a complete medication history may include asking patients about the following: a typical day and what medications are taken at different times of day; whether prescriptions come from more than 1 doctor; medications not taken orally (eg, inhalers, patches); dosages and indications for all medications; length of therapy and timing of last dose; over‐the‐counter products, herbals, vitamins, and supplements used and vaccinations received; allergies; and number of doses missed in the last week (Table 1).5254 Forms are also available to help patients maintain a list of current medications.5557
Ideally, the process of obtaining a medication history involves integration of information from several sources, including patient and caregiver recollections, patient‐provided lists of medications, prescription bottles, outpatient medical records, and prescription refill information from community pharmacies.58, 59 Any discrepancies in the information obtained should be explicitly resolved with the patient and/or caregiver. Assistance from a pharmacist or the patient's PCP may also be required.
Once the preadmission medication regimen is confirmed, it should be entered on a standardized form and placed in a prominent place in the chart. This list should then be compared against the patient's medication orders at admission, throughout the hospital stay, and at discharge.12 The planned action for each of these medications (eg, continue at same dose/route/frequency, substitute) should be made explicit. At discharge, this preadmission list also needs to be compared with the current hospital medications in order to create a coherent set of discharge orders.
Staff responsibilities for obtaining and documenting an accurate list of preadmission medications and reconciling medications at admission, transfer, and discharge should be well defined and based on the resources available at each institution. Redundant work (eg, multiple personnel independently taking a medication history) should be replaced by interdisciplinary communication (ie, a member of the team confirming the accuracy of a list obtained by another member of the team). When discrepancies are found (eg, between preadmission and discharge medications), reconciliation requires correction of unintentional discrepancies and appropriate documentation of intentional changes.60
Because a patient's medications change frequently during the transitions of admission, intrahospital transfer, and discharge, reconciliation is an active and ongoing process that aims to ensure the patient is receiving the correct medication regimen at all times. Reconciliation also allows for a review of the safety and appropriateness of the regimen and discontinuation of any unsuitable or needless medications.61, 62
Finally, a comprehensive list of a patient's medications should be reported to the next service provider when the patient is referred or transferred to another setting, service, practitioner, or level of care within or outside the organization. Avoiding overarching orders such as continue home medications and resume all medications becomes crucial to patient safety during transitions in care. At discharge, physicians should provide patients with a complete list of medications to be taken at home with indications and instructions for administration written in everyday language. Physicians should also highlight the results of medication reconciliation by pointing out any changes from the preadmission regimen, especially medications that are at home but should no longer be taken.
Ultimately, physicians have the duty to ensure that correct and complete medication information is provided. However, to achieve optimal results, physicians should partner with clinical pharmacists when possible. Pharmacists have been formally educated about and are experienced at taking medication histories, which may make them the ideal individuals to interview newly admitted patients about their medication histories.63 Unfortunately, according to a recent survey, pharmacists perform admission drug histories in only 5% of U.S. hospitals and provide drug therapy counseling in just 49% of U.S. hospitals.64 Patients who are elderly, have limited literacy skills, take more than 5 medications daily, or take high‐risk medications such as insulin, warfarin, cardiovascular drugs (including antiarrhythmics), inhalers, antiseizure medications, eye medications, analgesics, oral hypoglycemics, oral methotrexate, and immunosuppressants may require additional counseling or pharmacist involvement for effective reconciliation.10, 65, 66
Although the evidence supporting medication reconciliation is limited, it is convincing enough to support carrying out such reconciliations. In 1 investigation, when the nursing staff obtained and pharmacists verified orders for home medications, the accuracy of admission medication orders increased from 40% to 95%.67 In another work, in which there was pharmacist‐led medication reconciliation, significant discrepancies were found in approximately 25% of patients' medication histories and admission orders.45 In the absence of pharmacist intervention, the authors predicted that 22% of the discrepancies could have caused some form of patient harm during hospitalization and that 59% of the discrepancies might have contributed to an adverse event if the error continued after discharge.45 Others report that orders were changed as a result of reconciliation for 94% of patients being transferred out of the intensive care unit.2 Finally, in a randomized controlled trial of a pharmacist intervention at discharge in which medication reconciliation was the most common action performed, after 30 days preventable ADEs were detected in 11% of control patients and 1% of intervention patients. Medication discrepancy was the cause of half the preventable ADEs in the control group.51
SELF‐CARE RESPONSIBILITIES AND SOCIAL SUPPORT
Compounding the difficulties at discharge are the economic pressures on our health care system, causing patients to be released from the hospital quicker and sicker than ever before.68 The scope of care provided to patients also undergoes a major shift at discharge. Multidisciplinary providers no longer continually review the health status and needs of patients; instead, patients must follow up with their outpatient physician over a period of days to weeks. In the interim, the patients themselves are responsible for administering new medications, participating in physical therapy, and tracking their own symptoms to see if they are worsening. For many patients, sufficient social and family support is not available to help perform these activities effectively. Unfortunately, hospital personnel often inaccurately assess patients' functional status and overestimate patients' knowledge of required self‐care activities.69
Providing Adequate Medical and Social Support
A multidisciplinary discharge planning team can facilitate proper assessments of the social needs of patients and their families (Table 1).7072 This team is often composed of a nurse case manager and a social worker but may also include a physical therapist, an occupational therapist, a pharmacist, and other health care providers. Following discussion with a patient and the patient's family, the team may suggest home health services during the transition home to supplement available medical support,73 or they may decide that discharge to a rehabilitation or skilled nursing facility is more appropriate.
In addition, follow‐up should be arranged prior to discharge. Patients who are given a set appointment are more likely to show up for their follow‐up visits than are those who are simply asked to call and arrange their own visits.74 Typically, follow‐up with the PCP should be conducted within 2 weeks of hospital discharge. However, depending on a patient's functional status, pending test results, and need for medication monitoring or follow‐up testing, this may need to take place sooner. Interestingly, research indicates that follow‐up appointments with the inpatient provider can result in a lower combined rate of readmission and 30‐day mortality.75 Thus, hospitalists may consider operating a hospitalist‐staffed follow‐up clinic, especially for patients without a regular PCP.
Telephone follow‐up conducted a few days after discharge can also be an effective means of bridging the inpatientoutpatient transition.35 Such follow‐up provides a chance to attend to any patient questions, new or concerning symptoms, and medication‐related issues (eg, not filling the discharge medications or difficulty comprehending the new medication regimen).76 A physician, physician assistant, advanced practice nurse, registered nurse, pharmacist, or care manager can effectively carry out this telephone follow‐up. No matter who telephones, the caller must be aware of the patient's recent course of events as well as the care plan decided at discharge. Published evidence indicates that telephone follow‐up fosters patient satisfaction, increases medication adherence, decreases preventable ADEs, and decreases the number of subsequent emergency room visits and hospital readmissions,51, 77, 78 although not all evaluations have demonstrated benefit.79 As with medication histories performed by pharmacists, limited resources may mean that such follow‐up be restricted to those patients at highest risk for readmission.
Home visits may be appropriate for certain patient populations, such as the frail elderly.80 Home visits enable a patient's daily needs and safety (eg, fall risk) to be assessed. They can also be a means of assessing medication safety and adherence by reviewing all prescription and over‐the‐counter products in the household.81 Close follow‐up of at‐risk or elderly patients after discharge can help to minimize hospital readmission and total health care costs.4, 8285
INEFFECTIVE PHYSICIANPATIENT COMMUNICATION
Physicianpatient communication is fundamental to the practice of medicine and is crucially important at discharge. However, several studies have demonstrated a disconnect between physician information giving and patient understanding.76, 9690 When providing instructions, physicians commonly use medical jargon and attempt to cover a wealth of information in a limited amount of time.69, 87 They also tend to rely on verbal instructions and fail to provide supplementary audiovisual materials (eg, educational handouts or videos) that could aid patient comprehension. Physicians may not point out important self‐care tasks that patients should carry out at home. The entire interaction may be rushed or seem rushed. Moreover, when physicians solicit questions from patients, they may only allow for yes/no responses by using statements like Any questions? or Do you have any questions? that make it easy for patients to simply respond, No. The encounter usually comes to an end without true confirmation of a patient's level of understanding or assessment of a patient's ability to perform the self‐care activities and medication management required on returning home.81
Adding to the challenges of effective physicianpatient communication is the large number of adult Americans (more than 90 million) who have limited functional literacy skills.91, 92 Such patients typically have difficulty reading and understanding medical instructions, medication labels, and appointment slips.9396 Not surprisingly, patients with limited literacy skills know less about their chronic illnesses and how to manage their diseases.97 Having low literacy is also linked to increased use of emergency department services, a higher risk of hospitalization, and higher health care costs.9799 Patients with limited English proficiency have similar or even greater challenges and also have longer stays in the hospital.100
More Effective PhysicianPatient Communication
Discharge counseling should concentrate on the few key points that are of the greatest interest and the most importance to patients: major diagnoses, medication changes, dates of follow‐up appointments, self‐care instructions, and who to contact if problems develop (Table 1).101 Furthermore, these key instructions should be reinforced by other hospital staff, including nurses and pharmacists. For common conditions (eg, high‐volume cardiac procedures), offering standardized audiovisual instructions can be both efficient and worthwhile if used in conjunction with questionanswer sessions.102 In the event that physicians and hospital staff cannot fluently communicate in a patient's language, it is essential to engage trained interpreters, not rely on rudimentary language skills, the patient's family, or other ad hoc ways to communicate.103
Because patients are unlikely to fully remember verbal instructions at discharge, it is helpful to provide patients and family members with written materials to take home in order to reinforce important self‐care instructions.76, 87 These materials, written at a 5th‐ to 8th‐grade reading level, should outline key information in a simple format with little or no medical jargon. Illustrated materials are often better comprehended and subsequently remembered by patients.104, 105 If preprinted illustrated materials are not on hand, then physicians can convey key points by drawing simple pictures.
Confirming patient comprehension with the teach‐back method is perhaps the most important step in effectively communicating discharge instructions.106 With this method, patients are asked to repeat back what they understand from the discharge instructions. Application of this simple technique is advocated as one of the most effective means of improving patient safety.107, 108 Patients should also be asked to demonstrate any new self‐care tasks that they will be required to carry out at home, such as using an inhaler or administering a subcutaneous injection.
Last, The Joint Commission recently created a National Patent Safety Goal to encourage the active involvement of patients and their families in the patient's own care.12 This charge requires that physicians offer ample time for patients and their family members to ask questions. Physicians should avoid questions with yes/no responses and instead invite patient and family member questions in a more open‐ended manner (eg, What questions do you have?) to help ensure comprehension and comfort with the care plan.
CONCLUSIONS
The transition from hospital to home is a vulnerable period of discontinuity and potential adverse events. Hospitalists and other inpatient providers should not view discharge as an end to their obligation to patients but rather should attempt to promote a safe and efficient transition of care. Hospitalists can play an important role in bridging the gap between inpatient and outpatient care through appropriate discharge planning and effective communication with patients, their family members, and outpatient physicians.
Acknowledgements
The authors thank Marra Katz for her editorial assistance in the preparation of this manuscript
- .Whither continuity of care?N Engl J Med.1999;340:1362–1363.
- ,,, et al.Medication reconciliation: a practical tool to reduce the risk of medication errors.J Crit Care.2003;18(4):201–205.
- ,,,.Influence of hospitalization on drug therapy in the elderly.J Am Geriatr Soc.1989;37:679–683.
- ,,,,,.Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention.J Am Geriatr Soc.2004;52:1817–1825.
- ,,.Predictors of elder and family caregiver satisfaction with discharge planning.J Cardiovasc Nurs.2000;14(3):76–87.
- ,.Discharge planning and continuity of care for aged people: indicators of satisfaction and implications for practice.Aust J Adv Nurs.1998;16(1):7–13.
- ,,,.Medical errors related to discontinuity of care from an inpatient to an outpatient setting.J Gen Intern Med.2003;18:646–651.
- ,,.Assessing the quality of preparation for posthospital care from the patient's perspective: the care transitions measure.Med Care.2005;43(3):246–255.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20:317–323.
- The Joint Commission. Joint Commission National Patient Safety Goals. Available at: http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/. Accessed July 17,2006.
- ,,, et al.Transition of care for hospitalized elderly patients ‐ Development of a discharge checklist for hospitalists.J Hosp Med.2006;1:354–360.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297:831–841.
- Agency for Healthcare Research and Quality. National Guideline Clearinghouse. Available at: http://www.guideline.gov. Accessed January 3,2007.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .Hospitalists in the United States—mission accomplished or work in progress?N Engl J Med.2004;350:1935–1936.
- .The evolution of the hospitalist model in the United States.Med Clin North Am2002;86(4):687–706.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- Society of Hospital Medicine. Growth of hospital medicine nationwide. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Media/GrowthofHospitalMedicineNationwide/Growth_of_Hospital_M.htm. Accessed July 17,2006.
- ,,,,.Quality assessment of discharge letters in a French university hospital.Int J Health Care Qual Assur Inc Leadersh Health Serv.1998;11(2‐3):90–95.
- ,,.Dissemination of discharge summaries. Not reaching follow‐up physicians.Can Fam Physician.2002;48:737–742.
- ,.Quality assessment of a discharge summary system.CMAJ.1995;152:1437–1442.
- ,,,.Primary care physician attitudes regarding communication with hospitalists.Am J Med.2001;111(9B):15S–20S.
- ,,,.Effect of discharge summary availability during post‐discharge visits on hospital readmission.J Gen Intern Med.2002;17(3):186–192.
- .Study of discharge communications from hospital doctors to an inner London general practice.J R Coll Gen Pract.1987;37:494–495.
- ,,, et al.Patient safety concerns arising from test results that return after hospital discharge.Ann Intern Med.2005;143(2):121–128.
- ,,.Communication between general practitioners and consultants: what should their letters contain?BMJ1992;304(6830):821–824.
- ,,,.Written communication from specialists to general practitioners in cancer care. What are the expectations and how are they met?Scand J Prim Health Care.1998;16(3):154–159.
- ,.Improving the continuity of care between general practitioners and public hospitals.Med J Aust.1994;161:656–659.
- ,.Towards better discharge summaries: brevity and structure.West Engl Med J.1991;106(2):40–41,55.
- ,,.Content of a discharge summary from a medical ward: views of general practitioners and hospital doctors.J R Coll Physicians Lond.1995;29:307–310.
- ,.What is necessary for high‐quality discharge summaries?Am J Med Qual.1999;14(4):160–169.
- The Joint Commission.Standard IM.6.10. Hospital Accreditation Standards.Oakbrook Terrace, IL:The Joint Commission;2006:338–340.
- .The importance of postdischarge telephone follow‐up for hospitalists: a view from the trenches.Am J Med.2001;111(9B):43S–44S.
- ,,,.The quality of communication between hospitals and general practitioners: an assessment.J Qual Clin Pract.1998;18:241–247.
- ,,,.Dictated versus database‐generated discharge summaries: a randomized clinical trial.CMAJ.1999;160:319–326.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,.Moving from information transfer to information exchange in health and health care.Soc Sci Med.2003;56:449–464.
- ,,, et al.The costs of adverse drug events in hospitalized patients.Adverse Drug Events Prevention Study Group.JAMA.1997;277:307–311.
- ,,, et al.Systems analysis of adverse drug events.ADE Prevention Study Group.JAMA.1995;274(1):35–43.
- ,,, et al.Incidence of adverse drug events and potential adverse drug events. Implications for prevention.ADE Prevention Study Group.JAMA.1995;274(1):29–34.
- ,.Medication errors in hospitalized cardiovascular patients.Arch Intern Med.2003;163:1461–1466.
- ,,, et al.Unintended medication discrepancies at the time of hospital admission.Arch Intern Med.2005;165:424–429.
- ,,,,,.Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.Am J Health Syst Pharm.2004;61:1689–1695.
- ,,,,,.Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review.CMAJ.2005;173:510–515.
- ,,,,.Medication reconciliation in the acute care setting: opportunity and challenge for nursing.J Nurs Care Qual.2005;20(2):95–98.
- ,,.The adverse effects of hospitalization on drug regimens.Arch Intern Med.1991;151:1562–1564.
- ,,,,.Prevalence and cost savings of therapeutic interchange among U.S. hospitals.Am J Health Syst Pharm.2002;59:529–533.
- ,,, et al.Medication reconciliation: are we meeting the requirements?JCOM.2006;13:441–444.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166:565–571.
- ,.Effectiveness of a pharmacist‐acquired medication history in promoting patient safety.Am J Health Syst Pharm.2002;59:2221–2225.
- .Ensuring continuity of care and accuracy of patients' medication history on hospital admission.Am J Health Syst Pharm.2002;59:1054–1055.
- ,,,.Current methods used to teach the medication history interview to doctor of pharmacy students.Am J Pharm Educ.2002;66(Summer):103–107.
- AARP. My Personal Medication Record. Available at: http://assets.aarp.org/www.aarp.org_/articles/learntech/wellbeing/medication‐record.pdf. Accessed October 20,2006.
- AARP. Mi registro de medicacion. Available at: http://assets.aarp.org/www.aarp.org_/articles/health/docs/PersonalMedRecordSP.pdf. Accessed October 20,2006.
- Institute for Safe Medication Practices. Available at: http://www.ismp.org. Accessed September 8,2006.
- ,,.Parents as partners in obtaining the medication history.J Am Med Inform Assoc.2005;12:299–305.
- ,,.Medication history on internal medicine wards: assessment of extra information collected from second drug interviews and GP lists.Pharmacoepidemiology Drug Saf.2003;12:491–498.
- Medication Discrepancy Tool. Available at: http://www.caretransitions.org. Accessed July 28,2005.
- ,,,,,.Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts.Arch Intern Med.2003;163:2716–2724.
- .Using the NO TEARS tool for medication review.BMJ2004;329(7463):434.
- ,,,.Clinical pharmacists and inpatient medical care: a systematic review.Arch Intern Med.2006;166:955–964.
- ,.Clinical pharmacy services, pharmacy staffing, and adverse drug reactions in United States hospitals.Pharmacotherapy.2006;26:735–747.
- ,,, et al.Adverse drug events in ambulatory care.N Engl J Med.2003;348:1556–1564.
- MA Coalition for the Prevention of Medical Errors. Reconciling medications. Recommended practices. Available at: http://www.macoalition.org/documents/RecMedPractices.pdf. Accessed July 27,2005.
- ,.OSF healthcare's journey in patient safety.Qual Manag Health Care.2004;13(1):53–59.
- ,,, et al.Prospective payment system and impairment at discharge. The ‘quicker‐and‐sicker’ story revisited.JAMA.1990;264:1980–1983.
- ,,,,,.Discharge planning: comparison of patients and nurses' perceptions of patients following hospital discharge.Image J Nurs Sch.1996;28(2):143–147.
- ,,,.The Care Transitions Intervention: results of a randomized controlled trial.Arch Intern Med.2006;166:1822–1828.
- ,,,,,.Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta‐analysis.JAMA.2004;291:1358–1367.
- ,,,.Discharge planning from hospital to home.Cochrane Database Syst Rev.2006;4.
- .Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs.J Am Geriatr Soc.2003;51:549–555.
- .The best way to improve emergency department follow‐up is actually to give the patient a specific appointment.J Gen Intern Med.2006;21:398; author reply398.
- ,,,.Continuity of care and patient outcomes after hospital discharge.J Gen Intern Med.2004;19:624–631.
- ,.Patients' understanding of their treatment plans and diagnosis at discharge.Mayo Clin Proc.2005;80:991–994.
- ,,,.The impact of follow‐up telephone calls to patients after hospitalization.Am J Med.2001;111(9B):26S–30S.
- ,.The impact of clinical pharmacists' consultations on geriatric patients' compliance and medical care use: a randomized controlled trial.Gerontologist.1994;34:307–315.
- ,.Telephone follow‐up, initiated by a hospital‐based health professional, for postdischarge problems in patients discharged from hospital to home.Cochrane Database Syst Rev.2007;1.
- ,,, et al.Geriatric home assessment after hospital discharge.J Am Geriatr Soc.1994;42:1229–1234.
- ,.Uncovering a multitude of sins: medication management in the home post acute hospitalisation among the chronically ill.Aust N Z J Med.1999;29(2):220–227.
- ,,, et al.Comprehensive discharge planning and home follow‐up of hospitalized elders: a randomized clinical trial.JAMA.1999;281:613–620.
- ,,,.The cost‐effectiveness of intensive postdischarge care. A randomized trial.Med Care.1988;26:1092–1102.
- ,,,,.The effects of aftercare on chronic patients and frail elderly patients when discharged from hospital: a systematic review.J Adv Nurs.1998;27:1076–1086.
- ,,,,,.A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure.N Engl J Med.1995;333:1190–1195.
- ,,.Medication education of acutely hospitalized older patients.J Gen Intern Med.1999;14:610–616.
- ,,, et al.Patient‐physician communication at hospital discharge and patients' understanding of the postdischarge treatment plan.Arch Intern Med.1997;157:1026–1030.
- ,,.Patient understanding of commonly used medical vocabulary.J Fam Pract.1987;25:176–178.
- .The understanding of medical terminology used in printed health education materials.Heal Educ J.1979;38:111–121.
- ,,,,.The gap between patient reading comprehension and the readability of patient education materials.J Fam Pract.1990;31:533–538.
- ,,. National Assessment of Adult Literacy (NAAL). A first look at the literacy of America's adults in the 21st century. Available at: http://nces.ed.gov/naal. Accessed May 2,2006.
- ,,,.Adult Literacy in America: A First Look at the Findings of the National Adult Literacy Survey.Washington, DC:National Center for Education Statistics, U.S. Department of Education;1993.
- ,,,.The role of health literacy in patient‐physician communication.Fam Med.2002;34:383–389.
- American Medical Association Council on Scientific Affairs.Health literacy.JAMA.1999;281:552–557.
- National Work Group on Literacy and Health.Communicating with patients who have limited literacy skills.J Fam Pract.1998;46:168–176.
- ,.Communicating with patients who cannot read.N Engl J Med.1997;337:272–274.
- ,,,,.Literacy and health outcomes: a systematic review of the literature.J Gen Intern Med.2004;19:1129–1139.
- ,,.The impact of low health literacy on the medical costs of Medicare managed care enrollees.Am J Med.2005;118:371–377.
- ,,,.Health literacy and the risk of hospital admission.J Gen Intern Med.1998;13:791–798.
- ,,, et al.The effect of English language proficiency on length of stay and in‐hospital mortality.J Gen Intern Med.2004;19(3):221–228.
- ,,, et al.Effects of a structured patient‐centered discharge interview on patients' knowledge about their medications.Am J Med.2004;117:563–568.
- ,,.Effects of a videotape information intervention at discharge on diet and exercise compliance after coronary artery bypass surgery.J Cardiopulm Rehab.1999;19(3):170–177.
- .The impact of medical interpreter services on the quality of health care: a systematic review.Med Care Res Rev.2005;62(3):255–299.
- ,,.Use of pictorial aids in medication instructions: a review of the literature.Am J Health Syst Pharm.2006;63:2391–2397.
- ,,,.The role of pictures in improving health communication: A review of research on attention, comprehension, recall, and adherence.Patient Educ Couns.2006;61(2):173–190.
- ,,, et al.Closing the loop. Physician communication with diabetic patients who have low health literacy.Arch Intern Med.2003;163:83–90.
- National Quality Forum.Safe Practices for Better Healthcare,2003; Washington, DC.
- Shojania KG, Duncan BW, McDonald KM, Wachter RM, eds.Making Healthcare Safer: A Critical Analysis of Patient Safety Practices. Evidence Report No. 43 from the Agency for Healthcare Research and Quality. AHRQ Publication No. 01‐E058;2001.
As the counterpart to hospital admission, hospital discharge is a necessary process experienced by each living patient. For all patients except those being transferred to a continuing care facility, discharge is a period of transition from hospital to home that involves a transfer in responsibility from the inpatient provider or hospitalist to the patient and primary care physician (PCP).1 Prescription medications are commonly altered at this transition point, with patients asked to discontinue some medications, switch to a new dosage schedule of others, or begin new treatments.2, 3 Self‐care responsibilities also increase in number and importance, presenting new challenges for patients and their families as they return home.4 Under these circumstances, ineffective planning and coordination of care can undermine patient satisfaction, facilitate adverse events, and contribute to more frequent hospital readmissions.58
Following hospital discharge nearly half (49%) of hospitalized patients experience at least 1 medical error in medication continuity, diagnostic workup, or test follow‐up.7 It has been reported that 19%23% of patients suffer an adverse event, most frequently an adverse drug event (ADE).911 Half of ADEs are considered preventable or ameliorable (ie, their severity or duration could have been decreased). Most errors and adverse events in this setting result from a breakdown in communication between the hospital team and the patient or primary care physician.10
To promote more effective care transitions, The Joint Commission now requires accredited facilities to accurately and completely reconcile medications across the continuum of care.12 The Society of Hospital Medicine recently published recommendations for the discharge of elderly patients.13 The joint Society of Hospital MedicineSociety of General Internal Medicine Continuity of Care Task Force also recently published a systematic review with recommendations for improving the handoff of patient information at discharge.14 Apart from these reports, however, it is uncommon to find evidence‐based recommendations for hospital discharge applicable to a broad range of patients.15 This review highlights several important challenges for physicians who seek to provide high‐quality care during hospital discharge and the subsequent period of transition. Based on the best available evidence, recommendations are also provided for how to improve communication and facilitate the care transition for adult inpatients returning home.
INPATIENTOUTPATIENT PHYSICIAN DISCONTINUITY
Traditionally, primary care physicians have admitted their own patients, provided hospital care (in addition to seeing outpatients during the day), and followed patients after discharge. Under this model, continuity of care has been preserved; however, this method of care has faltered under the weight of inpatients and outpatients with more severe illnesses, rapid technological advancements, managed care pressuring outpatient physicians to see more patients, and a thrust toward reduced hospital costs and length of stay.16 Increases in the efficiency and quality of hospital care have accompanied a new reliance on the field of hospital medicine, while allowing PCPs to focus on outpatient care.1719 With more than 14,000 hospitalists currently practicing in the United States and 25,000 anticipated to be practicing by 2010, transfer of care from hospital‐based providers to PCPs has become increasingly common at discharge.20
Patient discharge summaries are the most common means of communication between inpatient and outpatient providers. However, numerous studies have shown that discharge summaries often fail to provide important administrative and medical information, such as the primary diagnosis, results of abnormal diagnostics, details about the hospital course, follow‐up plans, whether laboratory test results are pending, and patient or family counseling.14 Summaries also may not arrive in a timely manner and sometimes may not reach the PCP at all.2123
At the time patients first follow up with their PCPs after hospitalization, discharge summaries have not yet arrived about 75% of the time,22, 24, 25 restricting the PCPs' ability to provide adequate follow‐up care in 24% of hospital follow‐up visits, according to one study.26 In another investigation, PCPs reported being unaware of 62% of the pending test results that returned after discharge, of which 37% were considered actionable.27
Improving Physician Information Transfer and Continuity
To improve information transfer from hospitalist to PCP, attention must be paid to the content, format, and timely delivery of discharge information (Table 1).14 Surveys of primary care physicians suggest the following information should be included in discharge summaries: diagnoses, abnormal physical findings, important test results, discharge medications, follow‐up arrangements made and appointments that still need to be made, counseling provided to the patient and family, and tests still pending at discharge.24, 2833 These domains are consistent with Joint Commission guidelines for discharge summaries,34 and the inclusion of a detailed medication list and pending test results also has implications for patient safety.911, 27
| Challenge | Recommended approaches |
|---|---|
| Inpatientoutpatient physician discontinuity | When possible, involve the primary care physician (PCP) in discharge planning and work together to develop a follow‐up plan |
| At minimum, communicate the following to the PCP on the day of discharge: diagnoses, medications, results of procedures, pending tests, follow‐up arrangements, and suggested next steps | |
| Provide the PCP with a detailed discharge summary within 1 week | |
| In discharge summaries include: diagnoses, abnormal physical findings, important test results, discharge medications with rationale for new or changed medications, follow‐up arrangements made, counseling provided to the patient and family, and tasks to be completed (eg, appointments that still need to be made and tests that require follow‐up) | |
| Follow a structured template with subheadings in discharge communications | |
| When possible, use health information technology to create and disseminate discharge summaries | |
| Changes and discrepancies in medication regimen | Obtain a complete medication history by asking patients about: medications taken at different times of day; medications prescribed by different physicians; nonoral medications; over‐the‐counter products; dosage, indication, length of therapy, and timing of last dose of all drugs; allergies; and adherence |
| Compare and reconcile medication information obtained from patient and caregiver reports, patient lists, prescription bottles, medical records, and pharmacy records | |
| Display preadmission medication list prominently in the chart | |
| Reconcile medications at all care transitions, including admission, intrahospital transfer, and discharge | |
| Communicate complete and accurate medication information to the next provider at discharge, including indications for new medications and reasons for any changes | |
| When possible, partner with clinical pharmacists to manage medication information and reconciliation, especially for high‐risk patients | |
| Self‐care responsibilities and social support | Use multidisciplinary discharge planning teams to assess the needs of patients and their families |
| Arrange a specific follow‐up appointment prior to discharge | |
| Contact patients by telephone a few days after discharge to assess questions, symptoms, and medication‐related issues | |
| Order home health services when indicated | |
| Consider home visits for frail elderly patients | |
| Ineffective physicianpatient communication | Focus discharge counseling on informing patients of major diagnoses, medication changes, dates of follow‐up appointments, self‐care instructions, and who to contact if problems develop |
| Ensure that staff members communicate consistent instructions | |
| For high‐volume conditions, consider using audiovisual recordings for discharge education, combined with an opportunity for additional counseling and questions | |
| Use trained interpreters when a language gap exists | |
| Provide simply written materials that include illustrations when possible to reinforce verbal instructions | |
| Ensure patients and family members comprehend key points by asking them to teach back the information in their own words and demonstrate any self‐care behaviors | |
| Encourage patients and family members to ask questions through an open‐ended invitation like, What questions do you have? instead of Do you have any questions? |
Because many patients follow up with their PCPs within a few days of discharge, it becomes important to provide the PCPs with some information about the hospitalization on the day of discharge. This can be accomplished via a quick telephone call, fax, or e‐mail update to the PCP.24, 35 Important things to include in this communiqu are the discharge diagnosis, medications, results of procedures, pending test results, follow‐up arrangements, and suggested next steps. Within 1 week, a detailed discharge summary should have been received.26, 33, 36 As electronic medical records become more widely available, computer‐generated summaries offer a way to more quickly and completely highlight the key elements of the hospitalization, and they are ready for delivery sooner than traditional dictated summaries.37 Additionally, all forms of discharge summariescomputer‐generated, handwritten, and dictatedshould include subheadings to better organize and present the information instead of unstructured narrative summaries.38
There is increasing interest in moving away from the traditional 1‐way transfer of information about a hospitalization toward a 2‐way dialogue between hospitalist and primary care physician.39 Preferences about how to do this will vary among physicians. One strategy might be to provide the PCP with the hospitalist's contact information and encouraging questions about the hospitalization. Another approach would involve contacting the PCP during the discharge planning process to exchange information about the patient, provide an opportunity for the PCP to ask questions about the hospitalization, and formulate a cohesive plan for follow‐up, particularly about contingency planning (ie, what is most likely to go wrong and what should be done about it) and specific follow‐up needs (ie, what tasks should be accomplished at the first postdischarge visit).
CHANGES AND DISCREPANCIES IN THE MEDICATION REGIMEN
Medication errors make up a large portion of the adverse events patients may experience in the period following hospital discharge.7 In fact, errors during the ordering of admission or discharge medications make up almost half of all hospital medication errors.4043 At transition points such as admission and discharge, errors are often associated with changes in the medication regimen, including discrepancies between the new set of medication orders and what the patient was taking previously. In 2 recent studies, 54% of patients experienced at least 1 unintended medication discrepancy on admission to the hospital, and 39%‐45% of these discrepancies were considered a potential threat to the patient.44, 45
At discharge, differences between the prescribed medication regimen and the prehospital regimen may exist for several reasons. First, physicians may not obtain a comprehensive and accurate medication history at the time of admission.46 The medication history elicited from the patient at hospital admission is often affected by health literacy, language barriers, current health status, medication‐history interviewing skills, and time constraints.47 Physicians may not consult other important sources of medication information, including family members, prescription lists or bottles, and community pharmacy records. The most common error in the admission medication history is omitting a medication taken at home.46 Additionally, several providers, including a physician, a nurse, and an inpatient pharmacist, may independently take medication histories for the same patient. These multiple accounts lead to discrepancies that are rarely recognized or corrected.
Second, a patient's medication regimen can be significantly altered several times during a hospitalization. Acute illness may cause physicians to hold certain medications, discontinue others, or change prescribed doses during hospitalization.48 In addition, at most hospitals closed drug formularies necessitate automatic substitution of 1 medication for another drug in the same class during the patient's hospital stay.49 Changes from long‐acting to short‐acting medications are also routinely made in the name of tighter control (eg, of blood pressure). One study of hospitalized elders found that 40% of all admission medications had been discontinued by discharge and that 45% of all discharge medications were newly started during the hospitalization.3
Finally, at discharge, the current medication regimen needs to be reconciled with the preadmission medication regimen in a thoughtful manner.2 This includes resuming medications held or modified at admission for clinical reasons, resuming medications that were substituted in the hospital for formulary or pharmacokinetic reasons, and stopping newly started medications that were only required during the hospitalization (eg, for prevention of venous thromboembolism or stress ulcers).50 It is difficult, even in hospitals with advanced electronic health information systems, to prompt physicians to make these necessary changes. In a recent study, unexplained discrepancies between the preadmission medication list and discharge medication orders were noted in 49% of hospital discharges.51 Errors in discharge medication reconciliation may subsequently increase the risk of postdischarge ADEs.51
Medication Reconciliation and Education
An optimal strategy for obtaining a complete medication history may include asking patients about the following: a typical day and what medications are taken at different times of day; whether prescriptions come from more than 1 doctor; medications not taken orally (eg, inhalers, patches); dosages and indications for all medications; length of therapy and timing of last dose; over‐the‐counter products, herbals, vitamins, and supplements used and vaccinations received; allergies; and number of doses missed in the last week (Table 1).5254 Forms are also available to help patients maintain a list of current medications.5557
Ideally, the process of obtaining a medication history involves integration of information from several sources, including patient and caregiver recollections, patient‐provided lists of medications, prescription bottles, outpatient medical records, and prescription refill information from community pharmacies.58, 59 Any discrepancies in the information obtained should be explicitly resolved with the patient and/or caregiver. Assistance from a pharmacist or the patient's PCP may also be required.
Once the preadmission medication regimen is confirmed, it should be entered on a standardized form and placed in a prominent place in the chart. This list should then be compared against the patient's medication orders at admission, throughout the hospital stay, and at discharge.12 The planned action for each of these medications (eg, continue at same dose/route/frequency, substitute) should be made explicit. At discharge, this preadmission list also needs to be compared with the current hospital medications in order to create a coherent set of discharge orders.
Staff responsibilities for obtaining and documenting an accurate list of preadmission medications and reconciling medications at admission, transfer, and discharge should be well defined and based on the resources available at each institution. Redundant work (eg, multiple personnel independently taking a medication history) should be replaced by interdisciplinary communication (ie, a member of the team confirming the accuracy of a list obtained by another member of the team). When discrepancies are found (eg, between preadmission and discharge medications), reconciliation requires correction of unintentional discrepancies and appropriate documentation of intentional changes.60
Because a patient's medications change frequently during the transitions of admission, intrahospital transfer, and discharge, reconciliation is an active and ongoing process that aims to ensure the patient is receiving the correct medication regimen at all times. Reconciliation also allows for a review of the safety and appropriateness of the regimen and discontinuation of any unsuitable or needless medications.61, 62
Finally, a comprehensive list of a patient's medications should be reported to the next service provider when the patient is referred or transferred to another setting, service, practitioner, or level of care within or outside the organization. Avoiding overarching orders such as continue home medications and resume all medications becomes crucial to patient safety during transitions in care. At discharge, physicians should provide patients with a complete list of medications to be taken at home with indications and instructions for administration written in everyday language. Physicians should also highlight the results of medication reconciliation by pointing out any changes from the preadmission regimen, especially medications that are at home but should no longer be taken.
Ultimately, physicians have the duty to ensure that correct and complete medication information is provided. However, to achieve optimal results, physicians should partner with clinical pharmacists when possible. Pharmacists have been formally educated about and are experienced at taking medication histories, which may make them the ideal individuals to interview newly admitted patients about their medication histories.63 Unfortunately, according to a recent survey, pharmacists perform admission drug histories in only 5% of U.S. hospitals and provide drug therapy counseling in just 49% of U.S. hospitals.64 Patients who are elderly, have limited literacy skills, take more than 5 medications daily, or take high‐risk medications such as insulin, warfarin, cardiovascular drugs (including antiarrhythmics), inhalers, antiseizure medications, eye medications, analgesics, oral hypoglycemics, oral methotrexate, and immunosuppressants may require additional counseling or pharmacist involvement for effective reconciliation.10, 65, 66
Although the evidence supporting medication reconciliation is limited, it is convincing enough to support carrying out such reconciliations. In 1 investigation, when the nursing staff obtained and pharmacists verified orders for home medications, the accuracy of admission medication orders increased from 40% to 95%.67 In another work, in which there was pharmacist‐led medication reconciliation, significant discrepancies were found in approximately 25% of patients' medication histories and admission orders.45 In the absence of pharmacist intervention, the authors predicted that 22% of the discrepancies could have caused some form of patient harm during hospitalization and that 59% of the discrepancies might have contributed to an adverse event if the error continued after discharge.45 Others report that orders were changed as a result of reconciliation for 94% of patients being transferred out of the intensive care unit.2 Finally, in a randomized controlled trial of a pharmacist intervention at discharge in which medication reconciliation was the most common action performed, after 30 days preventable ADEs were detected in 11% of control patients and 1% of intervention patients. Medication discrepancy was the cause of half the preventable ADEs in the control group.51
SELF‐CARE RESPONSIBILITIES AND SOCIAL SUPPORT
Compounding the difficulties at discharge are the economic pressures on our health care system, causing patients to be released from the hospital quicker and sicker than ever before.68 The scope of care provided to patients also undergoes a major shift at discharge. Multidisciplinary providers no longer continually review the health status and needs of patients; instead, patients must follow up with their outpatient physician over a period of days to weeks. In the interim, the patients themselves are responsible for administering new medications, participating in physical therapy, and tracking their own symptoms to see if they are worsening. For many patients, sufficient social and family support is not available to help perform these activities effectively. Unfortunately, hospital personnel often inaccurately assess patients' functional status and overestimate patients' knowledge of required self‐care activities.69
Providing Adequate Medical and Social Support
A multidisciplinary discharge planning team can facilitate proper assessments of the social needs of patients and their families (Table 1).7072 This team is often composed of a nurse case manager and a social worker but may also include a physical therapist, an occupational therapist, a pharmacist, and other health care providers. Following discussion with a patient and the patient's family, the team may suggest home health services during the transition home to supplement available medical support,73 or they may decide that discharge to a rehabilitation or skilled nursing facility is more appropriate.
In addition, follow‐up should be arranged prior to discharge. Patients who are given a set appointment are more likely to show up for their follow‐up visits than are those who are simply asked to call and arrange their own visits.74 Typically, follow‐up with the PCP should be conducted within 2 weeks of hospital discharge. However, depending on a patient's functional status, pending test results, and need for medication monitoring or follow‐up testing, this may need to take place sooner. Interestingly, research indicates that follow‐up appointments with the inpatient provider can result in a lower combined rate of readmission and 30‐day mortality.75 Thus, hospitalists may consider operating a hospitalist‐staffed follow‐up clinic, especially for patients without a regular PCP.
Telephone follow‐up conducted a few days after discharge can also be an effective means of bridging the inpatientoutpatient transition.35 Such follow‐up provides a chance to attend to any patient questions, new or concerning symptoms, and medication‐related issues (eg, not filling the discharge medications or difficulty comprehending the new medication regimen).76 A physician, physician assistant, advanced practice nurse, registered nurse, pharmacist, or care manager can effectively carry out this telephone follow‐up. No matter who telephones, the caller must be aware of the patient's recent course of events as well as the care plan decided at discharge. Published evidence indicates that telephone follow‐up fosters patient satisfaction, increases medication adherence, decreases preventable ADEs, and decreases the number of subsequent emergency room visits and hospital readmissions,51, 77, 78 although not all evaluations have demonstrated benefit.79 As with medication histories performed by pharmacists, limited resources may mean that such follow‐up be restricted to those patients at highest risk for readmission.
Home visits may be appropriate for certain patient populations, such as the frail elderly.80 Home visits enable a patient's daily needs and safety (eg, fall risk) to be assessed. They can also be a means of assessing medication safety and adherence by reviewing all prescription and over‐the‐counter products in the household.81 Close follow‐up of at‐risk or elderly patients after discharge can help to minimize hospital readmission and total health care costs.4, 8285
INEFFECTIVE PHYSICIANPATIENT COMMUNICATION
Physicianpatient communication is fundamental to the practice of medicine and is crucially important at discharge. However, several studies have demonstrated a disconnect between physician information giving and patient understanding.76, 9690 When providing instructions, physicians commonly use medical jargon and attempt to cover a wealth of information in a limited amount of time.69, 87 They also tend to rely on verbal instructions and fail to provide supplementary audiovisual materials (eg, educational handouts or videos) that could aid patient comprehension. Physicians may not point out important self‐care tasks that patients should carry out at home. The entire interaction may be rushed or seem rushed. Moreover, when physicians solicit questions from patients, they may only allow for yes/no responses by using statements like Any questions? or Do you have any questions? that make it easy for patients to simply respond, No. The encounter usually comes to an end without true confirmation of a patient's level of understanding or assessment of a patient's ability to perform the self‐care activities and medication management required on returning home.81
Adding to the challenges of effective physicianpatient communication is the large number of adult Americans (more than 90 million) who have limited functional literacy skills.91, 92 Such patients typically have difficulty reading and understanding medical instructions, medication labels, and appointment slips.9396 Not surprisingly, patients with limited literacy skills know less about their chronic illnesses and how to manage their diseases.97 Having low literacy is also linked to increased use of emergency department services, a higher risk of hospitalization, and higher health care costs.9799 Patients with limited English proficiency have similar or even greater challenges and also have longer stays in the hospital.100
More Effective PhysicianPatient Communication
Discharge counseling should concentrate on the few key points that are of the greatest interest and the most importance to patients: major diagnoses, medication changes, dates of follow‐up appointments, self‐care instructions, and who to contact if problems develop (Table 1).101 Furthermore, these key instructions should be reinforced by other hospital staff, including nurses and pharmacists. For common conditions (eg, high‐volume cardiac procedures), offering standardized audiovisual instructions can be both efficient and worthwhile if used in conjunction with questionanswer sessions.102 In the event that physicians and hospital staff cannot fluently communicate in a patient's language, it is essential to engage trained interpreters, not rely on rudimentary language skills, the patient's family, or other ad hoc ways to communicate.103
Because patients are unlikely to fully remember verbal instructions at discharge, it is helpful to provide patients and family members with written materials to take home in order to reinforce important self‐care instructions.76, 87 These materials, written at a 5th‐ to 8th‐grade reading level, should outline key information in a simple format with little or no medical jargon. Illustrated materials are often better comprehended and subsequently remembered by patients.104, 105 If preprinted illustrated materials are not on hand, then physicians can convey key points by drawing simple pictures.
Confirming patient comprehension with the teach‐back method is perhaps the most important step in effectively communicating discharge instructions.106 With this method, patients are asked to repeat back what they understand from the discharge instructions. Application of this simple technique is advocated as one of the most effective means of improving patient safety.107, 108 Patients should also be asked to demonstrate any new self‐care tasks that they will be required to carry out at home, such as using an inhaler or administering a subcutaneous injection.
Last, The Joint Commission recently created a National Patent Safety Goal to encourage the active involvement of patients and their families in the patient's own care.12 This charge requires that physicians offer ample time for patients and their family members to ask questions. Physicians should avoid questions with yes/no responses and instead invite patient and family member questions in a more open‐ended manner (eg, What questions do you have?) to help ensure comprehension and comfort with the care plan.
CONCLUSIONS
The transition from hospital to home is a vulnerable period of discontinuity and potential adverse events. Hospitalists and other inpatient providers should not view discharge as an end to their obligation to patients but rather should attempt to promote a safe and efficient transition of care. Hospitalists can play an important role in bridging the gap between inpatient and outpatient care through appropriate discharge planning and effective communication with patients, their family members, and outpatient physicians.
Acknowledgements
The authors thank Marra Katz for her editorial assistance in the preparation of this manuscript
As the counterpart to hospital admission, hospital discharge is a necessary process experienced by each living patient. For all patients except those being transferred to a continuing care facility, discharge is a period of transition from hospital to home that involves a transfer in responsibility from the inpatient provider or hospitalist to the patient and primary care physician (PCP).1 Prescription medications are commonly altered at this transition point, with patients asked to discontinue some medications, switch to a new dosage schedule of others, or begin new treatments.2, 3 Self‐care responsibilities also increase in number and importance, presenting new challenges for patients and their families as they return home.4 Under these circumstances, ineffective planning and coordination of care can undermine patient satisfaction, facilitate adverse events, and contribute to more frequent hospital readmissions.58
Following hospital discharge nearly half (49%) of hospitalized patients experience at least 1 medical error in medication continuity, diagnostic workup, or test follow‐up.7 It has been reported that 19%23% of patients suffer an adverse event, most frequently an adverse drug event (ADE).911 Half of ADEs are considered preventable or ameliorable (ie, their severity or duration could have been decreased). Most errors and adverse events in this setting result from a breakdown in communication between the hospital team and the patient or primary care physician.10
To promote more effective care transitions, The Joint Commission now requires accredited facilities to accurately and completely reconcile medications across the continuum of care.12 The Society of Hospital Medicine recently published recommendations for the discharge of elderly patients.13 The joint Society of Hospital MedicineSociety of General Internal Medicine Continuity of Care Task Force also recently published a systematic review with recommendations for improving the handoff of patient information at discharge.14 Apart from these reports, however, it is uncommon to find evidence‐based recommendations for hospital discharge applicable to a broad range of patients.15 This review highlights several important challenges for physicians who seek to provide high‐quality care during hospital discharge and the subsequent period of transition. Based on the best available evidence, recommendations are also provided for how to improve communication and facilitate the care transition for adult inpatients returning home.
INPATIENTOUTPATIENT PHYSICIAN DISCONTINUITY
Traditionally, primary care physicians have admitted their own patients, provided hospital care (in addition to seeing outpatients during the day), and followed patients after discharge. Under this model, continuity of care has been preserved; however, this method of care has faltered under the weight of inpatients and outpatients with more severe illnesses, rapid technological advancements, managed care pressuring outpatient physicians to see more patients, and a thrust toward reduced hospital costs and length of stay.16 Increases in the efficiency and quality of hospital care have accompanied a new reliance on the field of hospital medicine, while allowing PCPs to focus on outpatient care.1719 With more than 14,000 hospitalists currently practicing in the United States and 25,000 anticipated to be practicing by 2010, transfer of care from hospital‐based providers to PCPs has become increasingly common at discharge.20
Patient discharge summaries are the most common means of communication between inpatient and outpatient providers. However, numerous studies have shown that discharge summaries often fail to provide important administrative and medical information, such as the primary diagnosis, results of abnormal diagnostics, details about the hospital course, follow‐up plans, whether laboratory test results are pending, and patient or family counseling.14 Summaries also may not arrive in a timely manner and sometimes may not reach the PCP at all.2123
At the time patients first follow up with their PCPs after hospitalization, discharge summaries have not yet arrived about 75% of the time,22, 24, 25 restricting the PCPs' ability to provide adequate follow‐up care in 24% of hospital follow‐up visits, according to one study.26 In another investigation, PCPs reported being unaware of 62% of the pending test results that returned after discharge, of which 37% were considered actionable.27
Improving Physician Information Transfer and Continuity
To improve information transfer from hospitalist to PCP, attention must be paid to the content, format, and timely delivery of discharge information (Table 1).14 Surveys of primary care physicians suggest the following information should be included in discharge summaries: diagnoses, abnormal physical findings, important test results, discharge medications, follow‐up arrangements made and appointments that still need to be made, counseling provided to the patient and family, and tests still pending at discharge.24, 2833 These domains are consistent with Joint Commission guidelines for discharge summaries,34 and the inclusion of a detailed medication list and pending test results also has implications for patient safety.911, 27
| Challenge | Recommended approaches |
|---|---|
| Inpatientoutpatient physician discontinuity | When possible, involve the primary care physician (PCP) in discharge planning and work together to develop a follow‐up plan |
| At minimum, communicate the following to the PCP on the day of discharge: diagnoses, medications, results of procedures, pending tests, follow‐up arrangements, and suggested next steps | |
| Provide the PCP with a detailed discharge summary within 1 week | |
| In discharge summaries include: diagnoses, abnormal physical findings, important test results, discharge medications with rationale for new or changed medications, follow‐up arrangements made, counseling provided to the patient and family, and tasks to be completed (eg, appointments that still need to be made and tests that require follow‐up) | |
| Follow a structured template with subheadings in discharge communications | |
| When possible, use health information technology to create and disseminate discharge summaries | |
| Changes and discrepancies in medication regimen | Obtain a complete medication history by asking patients about: medications taken at different times of day; medications prescribed by different physicians; nonoral medications; over‐the‐counter products; dosage, indication, length of therapy, and timing of last dose of all drugs; allergies; and adherence |
| Compare and reconcile medication information obtained from patient and caregiver reports, patient lists, prescription bottles, medical records, and pharmacy records | |
| Display preadmission medication list prominently in the chart | |
| Reconcile medications at all care transitions, including admission, intrahospital transfer, and discharge | |
| Communicate complete and accurate medication information to the next provider at discharge, including indications for new medications and reasons for any changes | |
| When possible, partner with clinical pharmacists to manage medication information and reconciliation, especially for high‐risk patients | |
| Self‐care responsibilities and social support | Use multidisciplinary discharge planning teams to assess the needs of patients and their families |
| Arrange a specific follow‐up appointment prior to discharge | |
| Contact patients by telephone a few days after discharge to assess questions, symptoms, and medication‐related issues | |
| Order home health services when indicated | |
| Consider home visits for frail elderly patients | |
| Ineffective physicianpatient communication | Focus discharge counseling on informing patients of major diagnoses, medication changes, dates of follow‐up appointments, self‐care instructions, and who to contact if problems develop |
| Ensure that staff members communicate consistent instructions | |
| For high‐volume conditions, consider using audiovisual recordings for discharge education, combined with an opportunity for additional counseling and questions | |
| Use trained interpreters when a language gap exists | |
| Provide simply written materials that include illustrations when possible to reinforce verbal instructions | |
| Ensure patients and family members comprehend key points by asking them to teach back the information in their own words and demonstrate any self‐care behaviors | |
| Encourage patients and family members to ask questions through an open‐ended invitation like, What questions do you have? instead of Do you have any questions? |
Because many patients follow up with their PCPs within a few days of discharge, it becomes important to provide the PCPs with some information about the hospitalization on the day of discharge. This can be accomplished via a quick telephone call, fax, or e‐mail update to the PCP.24, 35 Important things to include in this communiqu are the discharge diagnosis, medications, results of procedures, pending test results, follow‐up arrangements, and suggested next steps. Within 1 week, a detailed discharge summary should have been received.26, 33, 36 As electronic medical records become more widely available, computer‐generated summaries offer a way to more quickly and completely highlight the key elements of the hospitalization, and they are ready for delivery sooner than traditional dictated summaries.37 Additionally, all forms of discharge summariescomputer‐generated, handwritten, and dictatedshould include subheadings to better organize and present the information instead of unstructured narrative summaries.38
There is increasing interest in moving away from the traditional 1‐way transfer of information about a hospitalization toward a 2‐way dialogue between hospitalist and primary care physician.39 Preferences about how to do this will vary among physicians. One strategy might be to provide the PCP with the hospitalist's contact information and encouraging questions about the hospitalization. Another approach would involve contacting the PCP during the discharge planning process to exchange information about the patient, provide an opportunity for the PCP to ask questions about the hospitalization, and formulate a cohesive plan for follow‐up, particularly about contingency planning (ie, what is most likely to go wrong and what should be done about it) and specific follow‐up needs (ie, what tasks should be accomplished at the first postdischarge visit).
CHANGES AND DISCREPANCIES IN THE MEDICATION REGIMEN
Medication errors make up a large portion of the adverse events patients may experience in the period following hospital discharge.7 In fact, errors during the ordering of admission or discharge medications make up almost half of all hospital medication errors.4043 At transition points such as admission and discharge, errors are often associated with changes in the medication regimen, including discrepancies between the new set of medication orders and what the patient was taking previously. In 2 recent studies, 54% of patients experienced at least 1 unintended medication discrepancy on admission to the hospital, and 39%‐45% of these discrepancies were considered a potential threat to the patient.44, 45
At discharge, differences between the prescribed medication regimen and the prehospital regimen may exist for several reasons. First, physicians may not obtain a comprehensive and accurate medication history at the time of admission.46 The medication history elicited from the patient at hospital admission is often affected by health literacy, language barriers, current health status, medication‐history interviewing skills, and time constraints.47 Physicians may not consult other important sources of medication information, including family members, prescription lists or bottles, and community pharmacy records. The most common error in the admission medication history is omitting a medication taken at home.46 Additionally, several providers, including a physician, a nurse, and an inpatient pharmacist, may independently take medication histories for the same patient. These multiple accounts lead to discrepancies that are rarely recognized or corrected.
Second, a patient's medication regimen can be significantly altered several times during a hospitalization. Acute illness may cause physicians to hold certain medications, discontinue others, or change prescribed doses during hospitalization.48 In addition, at most hospitals closed drug formularies necessitate automatic substitution of 1 medication for another drug in the same class during the patient's hospital stay.49 Changes from long‐acting to short‐acting medications are also routinely made in the name of tighter control (eg, of blood pressure). One study of hospitalized elders found that 40% of all admission medications had been discontinued by discharge and that 45% of all discharge medications were newly started during the hospitalization.3
Finally, at discharge, the current medication regimen needs to be reconciled with the preadmission medication regimen in a thoughtful manner.2 This includes resuming medications held or modified at admission for clinical reasons, resuming medications that were substituted in the hospital for formulary or pharmacokinetic reasons, and stopping newly started medications that were only required during the hospitalization (eg, for prevention of venous thromboembolism or stress ulcers).50 It is difficult, even in hospitals with advanced electronic health information systems, to prompt physicians to make these necessary changes. In a recent study, unexplained discrepancies between the preadmission medication list and discharge medication orders were noted in 49% of hospital discharges.51 Errors in discharge medication reconciliation may subsequently increase the risk of postdischarge ADEs.51
Medication Reconciliation and Education
An optimal strategy for obtaining a complete medication history may include asking patients about the following: a typical day and what medications are taken at different times of day; whether prescriptions come from more than 1 doctor; medications not taken orally (eg, inhalers, patches); dosages and indications for all medications; length of therapy and timing of last dose; over‐the‐counter products, herbals, vitamins, and supplements used and vaccinations received; allergies; and number of doses missed in the last week (Table 1).5254 Forms are also available to help patients maintain a list of current medications.5557
Ideally, the process of obtaining a medication history involves integration of information from several sources, including patient and caregiver recollections, patient‐provided lists of medications, prescription bottles, outpatient medical records, and prescription refill information from community pharmacies.58, 59 Any discrepancies in the information obtained should be explicitly resolved with the patient and/or caregiver. Assistance from a pharmacist or the patient's PCP may also be required.
Once the preadmission medication regimen is confirmed, it should be entered on a standardized form and placed in a prominent place in the chart. This list should then be compared against the patient's medication orders at admission, throughout the hospital stay, and at discharge.12 The planned action for each of these medications (eg, continue at same dose/route/frequency, substitute) should be made explicit. At discharge, this preadmission list also needs to be compared with the current hospital medications in order to create a coherent set of discharge orders.
Staff responsibilities for obtaining and documenting an accurate list of preadmission medications and reconciling medications at admission, transfer, and discharge should be well defined and based on the resources available at each institution. Redundant work (eg, multiple personnel independently taking a medication history) should be replaced by interdisciplinary communication (ie, a member of the team confirming the accuracy of a list obtained by another member of the team). When discrepancies are found (eg, between preadmission and discharge medications), reconciliation requires correction of unintentional discrepancies and appropriate documentation of intentional changes.60
Because a patient's medications change frequently during the transitions of admission, intrahospital transfer, and discharge, reconciliation is an active and ongoing process that aims to ensure the patient is receiving the correct medication regimen at all times. Reconciliation also allows for a review of the safety and appropriateness of the regimen and discontinuation of any unsuitable or needless medications.61, 62
Finally, a comprehensive list of a patient's medications should be reported to the next service provider when the patient is referred or transferred to another setting, service, practitioner, or level of care within or outside the organization. Avoiding overarching orders such as continue home medications and resume all medications becomes crucial to patient safety during transitions in care. At discharge, physicians should provide patients with a complete list of medications to be taken at home with indications and instructions for administration written in everyday language. Physicians should also highlight the results of medication reconciliation by pointing out any changes from the preadmission regimen, especially medications that are at home but should no longer be taken.
Ultimately, physicians have the duty to ensure that correct and complete medication information is provided. However, to achieve optimal results, physicians should partner with clinical pharmacists when possible. Pharmacists have been formally educated about and are experienced at taking medication histories, which may make them the ideal individuals to interview newly admitted patients about their medication histories.63 Unfortunately, according to a recent survey, pharmacists perform admission drug histories in only 5% of U.S. hospitals and provide drug therapy counseling in just 49% of U.S. hospitals.64 Patients who are elderly, have limited literacy skills, take more than 5 medications daily, or take high‐risk medications such as insulin, warfarin, cardiovascular drugs (including antiarrhythmics), inhalers, antiseizure medications, eye medications, analgesics, oral hypoglycemics, oral methotrexate, and immunosuppressants may require additional counseling or pharmacist involvement for effective reconciliation.10, 65, 66
Although the evidence supporting medication reconciliation is limited, it is convincing enough to support carrying out such reconciliations. In 1 investigation, when the nursing staff obtained and pharmacists verified orders for home medications, the accuracy of admission medication orders increased from 40% to 95%.67 In another work, in which there was pharmacist‐led medication reconciliation, significant discrepancies were found in approximately 25% of patients' medication histories and admission orders.45 In the absence of pharmacist intervention, the authors predicted that 22% of the discrepancies could have caused some form of patient harm during hospitalization and that 59% of the discrepancies might have contributed to an adverse event if the error continued after discharge.45 Others report that orders were changed as a result of reconciliation for 94% of patients being transferred out of the intensive care unit.2 Finally, in a randomized controlled trial of a pharmacist intervention at discharge in which medication reconciliation was the most common action performed, after 30 days preventable ADEs were detected in 11% of control patients and 1% of intervention patients. Medication discrepancy was the cause of half the preventable ADEs in the control group.51
SELF‐CARE RESPONSIBILITIES AND SOCIAL SUPPORT
Compounding the difficulties at discharge are the economic pressures on our health care system, causing patients to be released from the hospital quicker and sicker than ever before.68 The scope of care provided to patients also undergoes a major shift at discharge. Multidisciplinary providers no longer continually review the health status and needs of patients; instead, patients must follow up with their outpatient physician over a period of days to weeks. In the interim, the patients themselves are responsible for administering new medications, participating in physical therapy, and tracking their own symptoms to see if they are worsening. For many patients, sufficient social and family support is not available to help perform these activities effectively. Unfortunately, hospital personnel often inaccurately assess patients' functional status and overestimate patients' knowledge of required self‐care activities.69
Providing Adequate Medical and Social Support
A multidisciplinary discharge planning team can facilitate proper assessments of the social needs of patients and their families (Table 1).7072 This team is often composed of a nurse case manager and a social worker but may also include a physical therapist, an occupational therapist, a pharmacist, and other health care providers. Following discussion with a patient and the patient's family, the team may suggest home health services during the transition home to supplement available medical support,73 or they may decide that discharge to a rehabilitation or skilled nursing facility is more appropriate.
In addition, follow‐up should be arranged prior to discharge. Patients who are given a set appointment are more likely to show up for their follow‐up visits than are those who are simply asked to call and arrange their own visits.74 Typically, follow‐up with the PCP should be conducted within 2 weeks of hospital discharge. However, depending on a patient's functional status, pending test results, and need for medication monitoring or follow‐up testing, this may need to take place sooner. Interestingly, research indicates that follow‐up appointments with the inpatient provider can result in a lower combined rate of readmission and 30‐day mortality.75 Thus, hospitalists may consider operating a hospitalist‐staffed follow‐up clinic, especially for patients without a regular PCP.
Telephone follow‐up conducted a few days after discharge can also be an effective means of bridging the inpatientoutpatient transition.35 Such follow‐up provides a chance to attend to any patient questions, new or concerning symptoms, and medication‐related issues (eg, not filling the discharge medications or difficulty comprehending the new medication regimen).76 A physician, physician assistant, advanced practice nurse, registered nurse, pharmacist, or care manager can effectively carry out this telephone follow‐up. No matter who telephones, the caller must be aware of the patient's recent course of events as well as the care plan decided at discharge. Published evidence indicates that telephone follow‐up fosters patient satisfaction, increases medication adherence, decreases preventable ADEs, and decreases the number of subsequent emergency room visits and hospital readmissions,51, 77, 78 although not all evaluations have demonstrated benefit.79 As with medication histories performed by pharmacists, limited resources may mean that such follow‐up be restricted to those patients at highest risk for readmission.
Home visits may be appropriate for certain patient populations, such as the frail elderly.80 Home visits enable a patient's daily needs and safety (eg, fall risk) to be assessed. They can also be a means of assessing medication safety and adherence by reviewing all prescription and over‐the‐counter products in the household.81 Close follow‐up of at‐risk or elderly patients after discharge can help to minimize hospital readmission and total health care costs.4, 8285
INEFFECTIVE PHYSICIANPATIENT COMMUNICATION
Physicianpatient communication is fundamental to the practice of medicine and is crucially important at discharge. However, several studies have demonstrated a disconnect between physician information giving and patient understanding.76, 9690 When providing instructions, physicians commonly use medical jargon and attempt to cover a wealth of information in a limited amount of time.69, 87 They also tend to rely on verbal instructions and fail to provide supplementary audiovisual materials (eg, educational handouts or videos) that could aid patient comprehension. Physicians may not point out important self‐care tasks that patients should carry out at home. The entire interaction may be rushed or seem rushed. Moreover, when physicians solicit questions from patients, they may only allow for yes/no responses by using statements like Any questions? or Do you have any questions? that make it easy for patients to simply respond, No. The encounter usually comes to an end without true confirmation of a patient's level of understanding or assessment of a patient's ability to perform the self‐care activities and medication management required on returning home.81
Adding to the challenges of effective physicianpatient communication is the large number of adult Americans (more than 90 million) who have limited functional literacy skills.91, 92 Such patients typically have difficulty reading and understanding medical instructions, medication labels, and appointment slips.9396 Not surprisingly, patients with limited literacy skills know less about their chronic illnesses and how to manage their diseases.97 Having low literacy is also linked to increased use of emergency department services, a higher risk of hospitalization, and higher health care costs.9799 Patients with limited English proficiency have similar or even greater challenges and also have longer stays in the hospital.100
More Effective PhysicianPatient Communication
Discharge counseling should concentrate on the few key points that are of the greatest interest and the most importance to patients: major diagnoses, medication changes, dates of follow‐up appointments, self‐care instructions, and who to contact if problems develop (Table 1).101 Furthermore, these key instructions should be reinforced by other hospital staff, including nurses and pharmacists. For common conditions (eg, high‐volume cardiac procedures), offering standardized audiovisual instructions can be both efficient and worthwhile if used in conjunction with questionanswer sessions.102 In the event that physicians and hospital staff cannot fluently communicate in a patient's language, it is essential to engage trained interpreters, not rely on rudimentary language skills, the patient's family, or other ad hoc ways to communicate.103
Because patients are unlikely to fully remember verbal instructions at discharge, it is helpful to provide patients and family members with written materials to take home in order to reinforce important self‐care instructions.76, 87 These materials, written at a 5th‐ to 8th‐grade reading level, should outline key information in a simple format with little or no medical jargon. Illustrated materials are often better comprehended and subsequently remembered by patients.104, 105 If preprinted illustrated materials are not on hand, then physicians can convey key points by drawing simple pictures.
Confirming patient comprehension with the teach‐back method is perhaps the most important step in effectively communicating discharge instructions.106 With this method, patients are asked to repeat back what they understand from the discharge instructions. Application of this simple technique is advocated as one of the most effective means of improving patient safety.107, 108 Patients should also be asked to demonstrate any new self‐care tasks that they will be required to carry out at home, such as using an inhaler or administering a subcutaneous injection.
Last, The Joint Commission recently created a National Patent Safety Goal to encourage the active involvement of patients and their families in the patient's own care.12 This charge requires that physicians offer ample time for patients and their family members to ask questions. Physicians should avoid questions with yes/no responses and instead invite patient and family member questions in a more open‐ended manner (eg, What questions do you have?) to help ensure comprehension and comfort with the care plan.
CONCLUSIONS
The transition from hospital to home is a vulnerable period of discontinuity and potential adverse events. Hospitalists and other inpatient providers should not view discharge as an end to their obligation to patients but rather should attempt to promote a safe and efficient transition of care. Hospitalists can play an important role in bridging the gap between inpatient and outpatient care through appropriate discharge planning and effective communication with patients, their family members, and outpatient physicians.
Acknowledgements
The authors thank Marra Katz for her editorial assistance in the preparation of this manuscript
- .Whither continuity of care?N Engl J Med.1999;340:1362–1363.
- ,,, et al.Medication reconciliation: a practical tool to reduce the risk of medication errors.J Crit Care.2003;18(4):201–205.
- ,,,.Influence of hospitalization on drug therapy in the elderly.J Am Geriatr Soc.1989;37:679–683.
- ,,,,,.Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention.J Am Geriatr Soc.2004;52:1817–1825.
- ,,.Predictors of elder and family caregiver satisfaction with discharge planning.J Cardiovasc Nurs.2000;14(3):76–87.
- ,.Discharge planning and continuity of care for aged people: indicators of satisfaction and implications for practice.Aust J Adv Nurs.1998;16(1):7–13.
- ,,,.Medical errors related to discontinuity of care from an inpatient to an outpatient setting.J Gen Intern Med.2003;18:646–651.
- ,,.Assessing the quality of preparation for posthospital care from the patient's perspective: the care transitions measure.Med Care.2005;43(3):246–255.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20:317–323.
- The Joint Commission. Joint Commission National Patient Safety Goals. Available at: http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/. Accessed July 17,2006.
- ,,, et al.Transition of care for hospitalized elderly patients ‐ Development of a discharge checklist for hospitalists.J Hosp Med.2006;1:354–360.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297:831–841.
- Agency for Healthcare Research and Quality. National Guideline Clearinghouse. Available at: http://www.guideline.gov. Accessed January 3,2007.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .Hospitalists in the United States—mission accomplished or work in progress?N Engl J Med.2004;350:1935–1936.
- .The evolution of the hospitalist model in the United States.Med Clin North Am2002;86(4):687–706.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- Society of Hospital Medicine. Growth of hospital medicine nationwide. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Media/GrowthofHospitalMedicineNationwide/Growth_of_Hospital_M.htm. Accessed July 17,2006.
- ,,,,.Quality assessment of discharge letters in a French university hospital.Int J Health Care Qual Assur Inc Leadersh Health Serv.1998;11(2‐3):90–95.
- ,,.Dissemination of discharge summaries. Not reaching follow‐up physicians.Can Fam Physician.2002;48:737–742.
- ,.Quality assessment of a discharge summary system.CMAJ.1995;152:1437–1442.
- ,,,.Primary care physician attitudes regarding communication with hospitalists.Am J Med.2001;111(9B):15S–20S.
- ,,,.Effect of discharge summary availability during post‐discharge visits on hospital readmission.J Gen Intern Med.2002;17(3):186–192.
- .Study of discharge communications from hospital doctors to an inner London general practice.J R Coll Gen Pract.1987;37:494–495.
- ,,, et al.Patient safety concerns arising from test results that return after hospital discharge.Ann Intern Med.2005;143(2):121–128.
- ,,.Communication between general practitioners and consultants: what should their letters contain?BMJ1992;304(6830):821–824.
- ,,,.Written communication from specialists to general practitioners in cancer care. What are the expectations and how are they met?Scand J Prim Health Care.1998;16(3):154–159.
- ,.Improving the continuity of care between general practitioners and public hospitals.Med J Aust.1994;161:656–659.
- ,.Towards better discharge summaries: brevity and structure.West Engl Med J.1991;106(2):40–41,55.
- ,,.Content of a discharge summary from a medical ward: views of general practitioners and hospital doctors.J R Coll Physicians Lond.1995;29:307–310.
- ,.What is necessary for high‐quality discharge summaries?Am J Med Qual.1999;14(4):160–169.
- The Joint Commission.Standard IM.6.10. Hospital Accreditation Standards.Oakbrook Terrace, IL:The Joint Commission;2006:338–340.
- .The importance of postdischarge telephone follow‐up for hospitalists: a view from the trenches.Am J Med.2001;111(9B):43S–44S.
- ,,,.The quality of communication between hospitals and general practitioners: an assessment.J Qual Clin Pract.1998;18:241–247.
- ,,,.Dictated versus database‐generated discharge summaries: a randomized clinical trial.CMAJ.1999;160:319–326.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,.Moving from information transfer to information exchange in health and health care.Soc Sci Med.2003;56:449–464.
- ,,, et al.The costs of adverse drug events in hospitalized patients.Adverse Drug Events Prevention Study Group.JAMA.1997;277:307–311.
- ,,, et al.Systems analysis of adverse drug events.ADE Prevention Study Group.JAMA.1995;274(1):35–43.
- ,,, et al.Incidence of adverse drug events and potential adverse drug events. Implications for prevention.ADE Prevention Study Group.JAMA.1995;274(1):29–34.
- ,.Medication errors in hospitalized cardiovascular patients.Arch Intern Med.2003;163:1461–1466.
- ,,, et al.Unintended medication discrepancies at the time of hospital admission.Arch Intern Med.2005;165:424–429.
- ,,,,,.Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.Am J Health Syst Pharm.2004;61:1689–1695.
- ,,,,,.Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review.CMAJ.2005;173:510–515.
- ,,,,.Medication reconciliation in the acute care setting: opportunity and challenge for nursing.J Nurs Care Qual.2005;20(2):95–98.
- ,,.The adverse effects of hospitalization on drug regimens.Arch Intern Med.1991;151:1562–1564.
- ,,,,.Prevalence and cost savings of therapeutic interchange among U.S. hospitals.Am J Health Syst Pharm.2002;59:529–533.
- ,,, et al.Medication reconciliation: are we meeting the requirements?JCOM.2006;13:441–444.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166:565–571.
- ,.Effectiveness of a pharmacist‐acquired medication history in promoting patient safety.Am J Health Syst Pharm.2002;59:2221–2225.
- .Ensuring continuity of care and accuracy of patients' medication history on hospital admission.Am J Health Syst Pharm.2002;59:1054–1055.
- ,,,.Current methods used to teach the medication history interview to doctor of pharmacy students.Am J Pharm Educ.2002;66(Summer):103–107.
- AARP. My Personal Medication Record. Available at: http://assets.aarp.org/www.aarp.org_/articles/learntech/wellbeing/medication‐record.pdf. Accessed October 20,2006.
- AARP. Mi registro de medicacion. Available at: http://assets.aarp.org/www.aarp.org_/articles/health/docs/PersonalMedRecordSP.pdf. Accessed October 20,2006.
- Institute for Safe Medication Practices. Available at: http://www.ismp.org. Accessed September 8,2006.
- ,,.Parents as partners in obtaining the medication history.J Am Med Inform Assoc.2005;12:299–305.
- ,,.Medication history on internal medicine wards: assessment of extra information collected from second drug interviews and GP lists.Pharmacoepidemiology Drug Saf.2003;12:491–498.
- Medication Discrepancy Tool. Available at: http://www.caretransitions.org. Accessed July 28,2005.
- ,,,,,.Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts.Arch Intern Med.2003;163:2716–2724.
- .Using the NO TEARS tool for medication review.BMJ2004;329(7463):434.
- ,,,.Clinical pharmacists and inpatient medical care: a systematic review.Arch Intern Med.2006;166:955–964.
- ,.Clinical pharmacy services, pharmacy staffing, and adverse drug reactions in United States hospitals.Pharmacotherapy.2006;26:735–747.
- ,,, et al.Adverse drug events in ambulatory care.N Engl J Med.2003;348:1556–1564.
- MA Coalition for the Prevention of Medical Errors. Reconciling medications. Recommended practices. Available at: http://www.macoalition.org/documents/RecMedPractices.pdf. Accessed July 27,2005.
- ,.OSF healthcare's journey in patient safety.Qual Manag Health Care.2004;13(1):53–59.
- ,,, et al.Prospective payment system and impairment at discharge. The ‘quicker‐and‐sicker’ story revisited.JAMA.1990;264:1980–1983.
- ,,,,,.Discharge planning: comparison of patients and nurses' perceptions of patients following hospital discharge.Image J Nurs Sch.1996;28(2):143–147.
- ,,,.The Care Transitions Intervention: results of a randomized controlled trial.Arch Intern Med.2006;166:1822–1828.
- ,,,,,.Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta‐analysis.JAMA.2004;291:1358–1367.
- ,,,.Discharge planning from hospital to home.Cochrane Database Syst Rev.2006;4.
- .Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs.J Am Geriatr Soc.2003;51:549–555.
- .The best way to improve emergency department follow‐up is actually to give the patient a specific appointment.J Gen Intern Med.2006;21:398; author reply398.
- ,,,.Continuity of care and patient outcomes after hospital discharge.J Gen Intern Med.2004;19:624–631.
- ,.Patients' understanding of their treatment plans and diagnosis at discharge.Mayo Clin Proc.2005;80:991–994.
- ,,,.The impact of follow‐up telephone calls to patients after hospitalization.Am J Med.2001;111(9B):26S–30S.
- ,.The impact of clinical pharmacists' consultations on geriatric patients' compliance and medical care use: a randomized controlled trial.Gerontologist.1994;34:307–315.
- ,.Telephone follow‐up, initiated by a hospital‐based health professional, for postdischarge problems in patients discharged from hospital to home.Cochrane Database Syst Rev.2007;1.
- ,,, et al.Geriatric home assessment after hospital discharge.J Am Geriatr Soc.1994;42:1229–1234.
- ,.Uncovering a multitude of sins: medication management in the home post acute hospitalisation among the chronically ill.Aust N Z J Med.1999;29(2):220–227.
- ,,, et al.Comprehensive discharge planning and home follow‐up of hospitalized elders: a randomized clinical trial.JAMA.1999;281:613–620.
- ,,,.The cost‐effectiveness of intensive postdischarge care. A randomized trial.Med Care.1988;26:1092–1102.
- ,,,,.The effects of aftercare on chronic patients and frail elderly patients when discharged from hospital: a systematic review.J Adv Nurs.1998;27:1076–1086.
- ,,,,,.A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure.N Engl J Med.1995;333:1190–1195.
- ,,.Medication education of acutely hospitalized older patients.J Gen Intern Med.1999;14:610–616.
- ,,, et al.Patient‐physician communication at hospital discharge and patients' understanding of the postdischarge treatment plan.Arch Intern Med.1997;157:1026–1030.
- ,,.Patient understanding of commonly used medical vocabulary.J Fam Pract.1987;25:176–178.
- .The understanding of medical terminology used in printed health education materials.Heal Educ J.1979;38:111–121.
- ,,,,.The gap between patient reading comprehension and the readability of patient education materials.J Fam Pract.1990;31:533–538.
- ,,. National Assessment of Adult Literacy (NAAL). A first look at the literacy of America's adults in the 21st century. Available at: http://nces.ed.gov/naal. Accessed May 2,2006.
- ,,,.Adult Literacy in America: A First Look at the Findings of the National Adult Literacy Survey.Washington, DC:National Center for Education Statistics, U.S. Department of Education;1993.
- ,,,.The role of health literacy in patient‐physician communication.Fam Med.2002;34:383–389.
- American Medical Association Council on Scientific Affairs.Health literacy.JAMA.1999;281:552–557.
- National Work Group on Literacy and Health.Communicating with patients who have limited literacy skills.J Fam Pract.1998;46:168–176.
- ,.Communicating with patients who cannot read.N Engl J Med.1997;337:272–274.
- ,,,,.Literacy and health outcomes: a systematic review of the literature.J Gen Intern Med.2004;19:1129–1139.
- ,,.The impact of low health literacy on the medical costs of Medicare managed care enrollees.Am J Med.2005;118:371–377.
- ,,,.Health literacy and the risk of hospital admission.J Gen Intern Med.1998;13:791–798.
- ,,, et al.The effect of English language proficiency on length of stay and in‐hospital mortality.J Gen Intern Med.2004;19(3):221–228.
- ,,, et al.Effects of a structured patient‐centered discharge interview on patients' knowledge about their medications.Am J Med.2004;117:563–568.
- ,,.Effects of a videotape information intervention at discharge on diet and exercise compliance after coronary artery bypass surgery.J Cardiopulm Rehab.1999;19(3):170–177.
- .The impact of medical interpreter services on the quality of health care: a systematic review.Med Care Res Rev.2005;62(3):255–299.
- ,,.Use of pictorial aids in medication instructions: a review of the literature.Am J Health Syst Pharm.2006;63:2391–2397.
- ,,,.The role of pictures in improving health communication: A review of research on attention, comprehension, recall, and adherence.Patient Educ Couns.2006;61(2):173–190.
- ,,, et al.Closing the loop. Physician communication with diabetic patients who have low health literacy.Arch Intern Med.2003;163:83–90.
- National Quality Forum.Safe Practices for Better Healthcare,2003; Washington, DC.
- Shojania KG, Duncan BW, McDonald KM, Wachter RM, eds.Making Healthcare Safer: A Critical Analysis of Patient Safety Practices. Evidence Report No. 43 from the Agency for Healthcare Research and Quality. AHRQ Publication No. 01‐E058;2001.
- .Whither continuity of care?N Engl J Med.1999;340:1362–1363.
- ,,, et al.Medication reconciliation: a practical tool to reduce the risk of medication errors.J Crit Care.2003;18(4):201–205.
- ,,,.Influence of hospitalization on drug therapy in the elderly.J Am Geriatr Soc.1989;37:679–683.
- ,,,,,.Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention.J Am Geriatr Soc.2004;52:1817–1825.
- ,,.Predictors of elder and family caregiver satisfaction with discharge planning.J Cardiovasc Nurs.2000;14(3):76–87.
- ,.Discharge planning and continuity of care for aged people: indicators of satisfaction and implications for practice.Aust J Adv Nurs.1998;16(1):7–13.
- ,,,.Medical errors related to discontinuity of care from an inpatient to an outpatient setting.J Gen Intern Med.2003;18:646–651.
- ,,.Assessing the quality of preparation for posthospital care from the patient's perspective: the care transitions measure.Med Care.2005;43(3):246–255.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20:317–323.
- The Joint Commission. Joint Commission National Patient Safety Goals. Available at: http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/. Accessed July 17,2006.
- ,,, et al.Transition of care for hospitalized elderly patients ‐ Development of a discharge checklist for hospitalists.J Hosp Med.2006;1:354–360.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care.JAMA.2007;297:831–841.
- Agency for Healthcare Research and Quality. National Guideline Clearinghouse. Available at: http://www.guideline.gov. Accessed January 3,2007.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .Hospitalists in the United States—mission accomplished or work in progress?N Engl J Med.2004;350:1935–1936.
- .The evolution of the hospitalist model in the United States.Med Clin North Am2002;86(4):687–706.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- Society of Hospital Medicine. Growth of hospital medicine nationwide. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Media/GrowthofHospitalMedicineNationwide/Growth_of_Hospital_M.htm. Accessed July 17,2006.
- ,,,,.Quality assessment of discharge letters in a French university hospital.Int J Health Care Qual Assur Inc Leadersh Health Serv.1998;11(2‐3):90–95.
- ,,.Dissemination of discharge summaries. Not reaching follow‐up physicians.Can Fam Physician.2002;48:737–742.
- ,.Quality assessment of a discharge summary system.CMAJ.1995;152:1437–1442.
- ,,,.Primary care physician attitudes regarding communication with hospitalists.Am J Med.2001;111(9B):15S–20S.
- ,,,.Effect of discharge summary availability during post‐discharge visits on hospital readmission.J Gen Intern Med.2002;17(3):186–192.
- .Study of discharge communications from hospital doctors to an inner London general practice.J R Coll Gen Pract.1987;37:494–495.
- ,,, et al.Patient safety concerns arising from test results that return after hospital discharge.Ann Intern Med.2005;143(2):121–128.
- ,,.Communication between general practitioners and consultants: what should their letters contain?BMJ1992;304(6830):821–824.
- ,,,.Written communication from specialists to general practitioners in cancer care. What are the expectations and how are they met?Scand J Prim Health Care.1998;16(3):154–159.
- ,.Improving the continuity of care between general practitioners and public hospitals.Med J Aust.1994;161:656–659.
- ,.Towards better discharge summaries: brevity and structure.West Engl Med J.1991;106(2):40–41,55.
- ,,.Content of a discharge summary from a medical ward: views of general practitioners and hospital doctors.J R Coll Physicians Lond.1995;29:307–310.
- ,.What is necessary for high‐quality discharge summaries?Am J Med Qual.1999;14(4):160–169.
- The Joint Commission.Standard IM.6.10. Hospital Accreditation Standards.Oakbrook Terrace, IL:The Joint Commission;2006:338–340.
- .The importance of postdischarge telephone follow‐up for hospitalists: a view from the trenches.Am J Med.2001;111(9B):43S–44S.
- ,,,.The quality of communication between hospitals and general practitioners: an assessment.J Qual Clin Pract.1998;18:241–247.
- ,,,.Dictated versus database‐generated discharge summaries: a randomized clinical trial.CMAJ.1999;160:319–326.
- ,,,.Standardized or narrative discharge summaries. Which do family physicians prefer?Can Fam Physician.1998;44:62–69.
- ,.Moving from information transfer to information exchange in health and health care.Soc Sci Med.2003;56:449–464.
- ,,, et al.The costs of adverse drug events in hospitalized patients.Adverse Drug Events Prevention Study Group.JAMA.1997;277:307–311.
- ,,, et al.Systems analysis of adverse drug events.ADE Prevention Study Group.JAMA.1995;274(1):35–43.
- ,,, et al.Incidence of adverse drug events and potential adverse drug events. Implications for prevention.ADE Prevention Study Group.JAMA.1995;274(1):29–34.
- ,.Medication errors in hospitalized cardiovascular patients.Arch Intern Med.2003;163:1461–1466.
- ,,, et al.Unintended medication discrepancies at the time of hospital admission.Arch Intern Med.2005;165:424–429.
- ,,,,,.Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.Am J Health Syst Pharm.2004;61:1689–1695.
- ,,,,,.Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review.CMAJ.2005;173:510–515.
- ,,,,.Medication reconciliation in the acute care setting: opportunity and challenge for nursing.J Nurs Care Qual.2005;20(2):95–98.
- ,,.The adverse effects of hospitalization on drug regimens.Arch Intern Med.1991;151:1562–1564.
- ,,,,.Prevalence and cost savings of therapeutic interchange among U.S. hospitals.Am J Health Syst Pharm.2002;59:529–533.
- ,,, et al.Medication reconciliation: are we meeting the requirements?JCOM.2006;13:441–444.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166:565–571.
- ,.Effectiveness of a pharmacist‐acquired medication history in promoting patient safety.Am J Health Syst Pharm.2002;59:2221–2225.
- .Ensuring continuity of care and accuracy of patients' medication history on hospital admission.Am J Health Syst Pharm.2002;59:1054–1055.
- ,,,.Current methods used to teach the medication history interview to doctor of pharmacy students.Am J Pharm Educ.2002;66(Summer):103–107.
- AARP. My Personal Medication Record. Available at: http://assets.aarp.org/www.aarp.org_/articles/learntech/wellbeing/medication‐record.pdf. Accessed October 20,2006.
- AARP. Mi registro de medicacion. Available at: http://assets.aarp.org/www.aarp.org_/articles/health/docs/PersonalMedRecordSP.pdf. Accessed October 20,2006.
- Institute for Safe Medication Practices. Available at: http://www.ismp.org. Accessed September 8,2006.
- ,,.Parents as partners in obtaining the medication history.J Am Med Inform Assoc.2005;12:299–305.
- ,,.Medication history on internal medicine wards: assessment of extra information collected from second drug interviews and GP lists.Pharmacoepidemiology Drug Saf.2003;12:491–498.
- Medication Discrepancy Tool. Available at: http://www.caretransitions.org. Accessed July 28,2005.
- ,,,,,.Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts.Arch Intern Med.2003;163:2716–2724.
- .Using the NO TEARS tool for medication review.BMJ2004;329(7463):434.
- ,,,.Clinical pharmacists and inpatient medical care: a systematic review.Arch Intern Med.2006;166:955–964.
- ,.Clinical pharmacy services, pharmacy staffing, and adverse drug reactions in United States hospitals.Pharmacotherapy.2006;26:735–747.
- ,,, et al.Adverse drug events in ambulatory care.N Engl J Med.2003;348:1556–1564.
- MA Coalition for the Prevention of Medical Errors. Reconciling medications. Recommended practices. Available at: http://www.macoalition.org/documents/RecMedPractices.pdf. Accessed July 27,2005.
- ,.OSF healthcare's journey in patient safety.Qual Manag Health Care.2004;13(1):53–59.
- ,,, et al.Prospective payment system and impairment at discharge. The ‘quicker‐and‐sicker’ story revisited.JAMA.1990;264:1980–1983.
- ,,,,,.Discharge planning: comparison of patients and nurses' perceptions of patients following hospital discharge.Image J Nurs Sch.1996;28(2):143–147.
- ,,,.The Care Transitions Intervention: results of a randomized controlled trial.Arch Intern Med.2006;166:1822–1828.
- ,,,,,.Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta‐analysis.JAMA.2004;291:1358–1367.
- ,,,.Discharge planning from hospital to home.Cochrane Database Syst Rev.2006;4.
- .Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs.J Am Geriatr Soc.2003;51:549–555.
- .The best way to improve emergency department follow‐up is actually to give the patient a specific appointment.J Gen Intern Med.2006;21:398; author reply398.
- ,,,.Continuity of care and patient outcomes after hospital discharge.J Gen Intern Med.2004;19:624–631.
- ,.Patients' understanding of their treatment plans and diagnosis at discharge.Mayo Clin Proc.2005;80:991–994.
- ,,,.The impact of follow‐up telephone calls to patients after hospitalization.Am J Med.2001;111(9B):26S–30S.
- ,.The impact of clinical pharmacists' consultations on geriatric patients' compliance and medical care use: a randomized controlled trial.Gerontologist.1994;34:307–315.
- ,.Telephone follow‐up, initiated by a hospital‐based health professional, for postdischarge problems in patients discharged from hospital to home.Cochrane Database Syst Rev.2007;1.
- ,,, et al.Geriatric home assessment after hospital discharge.J Am Geriatr Soc.1994;42:1229–1234.
- ,.Uncovering a multitude of sins: medication management in the home post acute hospitalisation among the chronically ill.Aust N Z J Med.1999;29(2):220–227.
- ,,, et al.Comprehensive discharge planning and home follow‐up of hospitalized elders: a randomized clinical trial.JAMA.1999;281:613–620.
- ,,,.The cost‐effectiveness of intensive postdischarge care. A randomized trial.Med Care.1988;26:1092–1102.
- ,,,,.The effects of aftercare on chronic patients and frail elderly patients when discharged from hospital: a systematic review.J Adv Nurs.1998;27:1076–1086.
- ,,,,,.A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure.N Engl J Med.1995;333:1190–1195.
- ,,.Medication education of acutely hospitalized older patients.J Gen Intern Med.1999;14:610–616.
- ,,, et al.Patient‐physician communication at hospital discharge and patients' understanding of the postdischarge treatment plan.Arch Intern Med.1997;157:1026–1030.
- ,,.Patient understanding of commonly used medical vocabulary.J Fam Pract.1987;25:176–178.
- .The understanding of medical terminology used in printed health education materials.Heal Educ J.1979;38:111–121.
- ,,,,.The gap between patient reading comprehension and the readability of patient education materials.J Fam Pract.1990;31:533–538.
- ,,. National Assessment of Adult Literacy (NAAL). A first look at the literacy of America's adults in the 21st century. Available at: http://nces.ed.gov/naal. Accessed May 2,2006.
- ,,,.Adult Literacy in America: A First Look at the Findings of the National Adult Literacy Survey.Washington, DC:National Center for Education Statistics, U.S. Department of Education;1993.
- ,,,.The role of health literacy in patient‐physician communication.Fam Med.2002;34:383–389.
- American Medical Association Council on Scientific Affairs.Health literacy.JAMA.1999;281:552–557.
- National Work Group on Literacy and Health.Communicating with patients who have limited literacy skills.J Fam Pract.1998;46:168–176.
- ,.Communicating with patients who cannot read.N Engl J Med.1997;337:272–274.
- ,,,,.Literacy and health outcomes: a systematic review of the literature.J Gen Intern Med.2004;19:1129–1139.
- ,,.The impact of low health literacy on the medical costs of Medicare managed care enrollees.Am J Med.2005;118:371–377.
- ,,,.Health literacy and the risk of hospital admission.J Gen Intern Med.1998;13:791–798.
- ,,, et al.The effect of English language proficiency on length of stay and in‐hospital mortality.J Gen Intern Med.2004;19(3):221–228.
- ,,, et al.Effects of a structured patient‐centered discharge interview on patients' knowledge about their medications.Am J Med.2004;117:563–568.
- ,,.Effects of a videotape information intervention at discharge on diet and exercise compliance after coronary artery bypass surgery.J Cardiopulm Rehab.1999;19(3):170–177.
- .The impact of medical interpreter services on the quality of health care: a systematic review.Med Care Res Rev.2005;62(3):255–299.
- ,,.Use of pictorial aids in medication instructions: a review of the literature.Am J Health Syst Pharm.2006;63:2391–2397.
- ,,,.The role of pictures in improving health communication: A review of research on attention, comprehension, recall, and adherence.Patient Educ Couns.2006;61(2):173–190.
- ,,, et al.Closing the loop. Physician communication with diabetic patients who have low health literacy.Arch Intern Med.2003;163:83–90.
- National Quality Forum.Safe Practices for Better Healthcare,2003; Washington, DC.
- Shojania KG, Duncan BW, McDonald KM, Wachter RM, eds.Making Healthcare Safer: A Critical Analysis of Patient Safety Practices. Evidence Report No. 43 from the Agency for Healthcare Research and Quality. AHRQ Publication No. 01‐E058;2001.
Editorial
As a hospital practitioner, you have undoubtedly experienced the frustration of witnessing how easily the excellent care you provide can unravel as the patient goes out the door. Patients are admitted acutely ill, and largely attributed to your clinical acumen, they are discharged tuned up and stable to return home. Days later, however, you may learn that your best‐laid discharge plans were not properly executed, and the patient returned with yet another exacerbation. Clearly this scenario represents a major setback for the patient and family caregivers. Possibly dismissed as another episode of patient noncompliance, such readmissions are now being recognized as system failures and reflect a discharge process that has been described as random events connected to highly variable actions with only a remote possibility of meeting implied expectations (Roger Resar, MD, Senior Fellow, Institute for Healthcare Improvement).
Once an area that received relatively little attention, transitions out of the hospital has been identified as a priority area in need of action by a confluence of recent research and national activities. Recognizing the expanding evidence for lapses in quality and safety, many esteemed organizations, including the Joint Commission, the Centers for Medicare and Medicaid Services and their accompanying Quality Improvement Organizations, the Institute for Healthcare Improvement, the Institute of Medicine, National Quality Forum, the Medicare Payment Advisory Committee, the American Board of Internal Medicine Foundation, the National Transitions of Care Coalition, the American College of Physicians, the Society for General Medicine, and the Society for Hospital Medicine, are currently focusing their efforts on how to optimize transitions. All have articulated the need for further clinical investigation that can offer greater insight into the nature of the problems that arise during this vulnerable period and what the potential solutions are.
In this edition of the Journal of Hospital Medicine, 3 teams of investigators have responded to this need, making timely, important, and unique contributions to advance the field.13 Specifically, each of these articles further raises awareness that a patient's transition out of the hospital often unfolds quickly in a fast‐paced, chaotic manner, placing many competing demands on clinicians, patients, and family caregivers. Not surprisingly, such competing demands can contribute to deficits in quality and safety. The authors of these studies all directly identify the central role of communication among clinicians as well as between patients and clinicians in ensuring successful handoffs, further affirming the Joint Commission's finding that inadequate communication is the leading cause of sentinel events.4 In this respect, communication is more than simply the transfer of information; rather, it involves the need to ensure comprehension and provide an opportunity to have a 2‐way dialogue. Importantly, these articles share a common approach in fostering our understanding of the perspective of patients and family caregivers with a particular focus on disadvantaged populations.
Kripalani and colleagues conducted a comprehensive review of the state of the science for those key hospital discharge issues that pertain to hospitalists. They identified a number of challenges including communication between hospital‐ and ambulatory‐based clinicians, medication reconciliation, timely hospital follow‐up, and engaging patients in self‐care. For each of these priority areas, the authors provide pragmatic recommendations for improving care that could be implemented within the current state of practice, either individually or as a bundle of interventions.
Recognizing that patients are often the only common thread across different sites of care, Strunin and colleagues demonstrate the value of including the voice of the patient in helping clinicians to understand the challenges and larger context in which they attempt to follow through with discharge instructions. Strunin et al. found that among a range of factors that contribute to adherence problems, many were nonmedical. Fortunately, a number of these are modifiable and point to the need to both prioritize recommendations to patients and to simplify them whenever possible. The authors' findings resonate with a growing literature that examines the hospital discharge process from the patient's perspective.510
Flacker and colleagues surveyed older patients to gain greater insights into their information needs at discharge. From a process standpoint, they demonstrated that a posthospital survey was feasible and acceptable to older patients. In and of itself, this finding has important implications in the context of national efforts aimed at implementing performance measurement and accompanying public reporting. It also may reflect patients' eagerness to be contacted after discharge; hospitalization is a major event in patients' lives, and attentive follow‐up is appreciated. The authors found that more than half of patients did not recall being asked about how they would care for themselves on returning home from the hospital. Although there may be a variety of explanations for this finding, it nevertheless points to an immediate area for intervention.
Collectively, these 3 articles set the stage for a proposed clinical investigation agenda aimed at optimizing transitions out of the hospital (see Table 1).
| 1. Greater recognition of the integral role of family caregivers |
| 2. Empirically define the appropriate follow‐up interval |
| 3. Define physician accountability for patients referred to home health on hospital discharge |
| 4. Delineate the role of the hospitalist in the advanced medical home |
| 5. Develop the ability to examine episodes of care |
These 5 recommendations have the potential to ensure that the gains patients make in our hospitals are maintained long after discharge.
-
Greater Recognition for the Integral Role of Family Caregivers. The patient and family caregivers should be integrated into health care professionals' efforts to improve care coordination across settings. Family caregivers have been silent partners in health care delivery, functioning as de facto care coordinators. During care handoffs, family caregivers make important contributions to ensuring quality, safety, and adherence to patient preferences; their role needs to be formally recognized and supported. An important initial step would be standardizing the approach to defining the types and intensity of the roles family caregivers play to facilitate improved communication. One proposed working definition is the FACED classification developed by one of the authors (E.C.). Modeled after the TNM system used in cancer, each letter of FACED refers to a different contribution made by a family caregiver: F = Financial; A = Advocacy; C = Care coordination; E = Emotional support; and D = Direct care provision. A simple numeric rating system could be developed whereby 0 = does not contribute in this area and 3 = makes significant contribution to this area. Such a straightforward approach would readily inform all members of the health care team about the caregivers' roles and capabilities and how they can optimally collaborate in the care plan.
-
Empirically Define Appropriate Follow‐Up Interval. At present, patients are given rather arbitrary and generic instructions for when to obtain follow‐up with their outpatient primary care physician or specialist. Surgical patients are often instructed to follow up with their surgeon, and yet most of the readmissions of these patients are attributable to medical conditions (personal communication, Steven Jencks, MD, Centers for Medicare and Medicaid Services). Furthermore, a significant number of discharged medical and surgical patients are readmitted to the hospital within 30 days without any outpatient contact with a health professional. One may envision an evidence‐based tiered approach whereby patients are assigned a hospital readmission risk score at the time of discharge that then determines the timing of their follow‐up appointment. Using this framework, the highest‐risk patients may be encouraged to receive follow‐up within 2472 hours, whereas lower‐risk patients may be able to wait 1421 days. Of course, there will need to be sufficient access to outpatient physicians, who will need to be available, to ensure the success of this strategy.
-
Define Physician Accountability for Patients Referred to Home Health on Hospital Discharge. Communication problems between the hospital and the home health care agency are a source of aggravation for both parties, not to mention patients. Typically, a hospitalist provides the initial order for services and then expects subsequent home care coordination to be managed by an outpatient physician. Unfortunately, in some cases the patient may not have an outpatient physician or the patient's primary physician may be unaware of the recent hospitalization and thus unwilling to assume management of an unfamiliar care plan. As a result, home care nurses often cannot identify a physician to respond to their questions or concerns. At the center of this problem lies a lack of understanding of where the responsibility of the ordering hospitalist ends and the outpatient physician assuming care begins. Recognizing the profound costs of failed home health care leading to hospital readmission, the nation's Quality Improvement Organizations launched a national campaign in 2006 to address this problem. Hospitalists should engage in this effort and not punt the entire responsibility to home health agenciesimagine if hospitals and hospitalists were financially penalized if a patient was readmitted.
-
Delineate the Role of the Hospitalist in the Advanced Medical Home. Modeled after a concept with origins in pediatrics, the American College of Physicians and American Academy of Family Physicians are promoting the advanced medical home as a new care model that aims to provide comprehensive ambulatory care with an explicit focus on care coordination.11 The Centers for Medicare and Medicaid Services is planning to initiate a demonstration of this approach. What has not been adequately underscored is how the advanced medical home will communicate essential clinical information with the hospitalist and what, if any, will be the role of the hospitalist in relation to a patient's medical home? Ideally, the medical home approach will alleviate many of the current access problems that impede timely follow‐up.
-
Develop Ability to Examine Episodes of Care. Patients with complex conditions often require care from different practitioners in multiple settings. From the vantage point of health care professionals, these may appear to occur as merely a string of individual interactions, including hospital admissions and discharges. However from the patient's perspective, the experience is more appropriately characterized as a journey across an aggregated episode of care. The National Quality Forum is currently exploring how to measure quality of care delivered across such an episode of care. Additionally, the Centers for Medicare and Medicaid Services is developing a new assessment tool that will transcend acute and postacute care settings, the Continuity Assessment Record and Evaluation (CARE). This tool will potentially enhance our ability to measure care across a predefined episode. Measurement can further pave the way for payment reform designed to align incentives toward higher‐quality care transitions. Currently, professional fees for coronary artery bypass grafting surgery are bundled across an episode, including hospital and posthospital care settings. Extending this approach to a wider array of conditions and services could encourage new perspectives on the timing of discharge and the use of posthospital care venues. For example, under bundled payment, incentives might support a plan to keep a patient in the hospital an extra 1 or 2 days in order to obviate a transfer to a skilled nursing facility and the concomitant risks of transfer‐related problems. Further, bundled payment may allow for the provision of additional services not currently covered, including transportation, as identified by Strunin and colleagues.3
Hospitalists are well positioned to offer leadership in these high‐leverage areas and thereby make a unique contribution to the quality and safety of care transitions. By so doing, they are poised to reaffirm their professionalism,12 ensuring that the excellent care that they provide in the hospital is sustained well into the future.
- ,,.Discharge information and older patients: do they get what they need?J Hosp Med.2007;2:291–296.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2:314–323.
- ,,.Understanding rehospitalization risk: can the hospital discharge be modified to impact recurrent hospitalization.J Hosp Med.2007;2:297–304.
- The Joint Commission. Sentinel event statistics. Available at: http://www.jointcommission.org/SentinelEvents/Statistics/. Accessed August 7,2007.
- ,,.Patients' and caregivers' transition from hospital to home: needs and recommendations.Home Health Care Serv Q.1998;17:27–48.
- ,,,,.Carepartner experiences with hospital care.Med Care.1999;37:33–38.
- ,.Understanding coordination of care from the consumer's perspective in a regional health system.Health Serv Res.2002;37:1031–1054.
- ,,, et al.Development and testing of a measure designed to assess the quality of care transitions.Int J Integrated Care.2002;2:e02.
- .Rough crossings: family caregivers odysseys through the health care system.New York:United Hospital Fund of New York;1998.
- ,.Facilitating the transition out of the hospital. In:Gerteis M,Edgman‐Levitan S,Daley J,Delbanco T, editors.Through the Patient's Eyes: Understanding and Promoting Patient‐Centered Care.San Francisco:Jossey‐Bass;1993:204–223.
- ,,American College of Physicians. The advanced medical home: a patient‐centered, physician‐guided model of health care. p. 1–22. http://www.acponline.org/hpp/adv_med.pdf Accessed August 7,2007.
- Project of the ABIM Foundation A‐AFaEFoIM.Medical professionalism in the new millennium: a physician charter.Ann Intern Med.2002;136:243–246.
As a hospital practitioner, you have undoubtedly experienced the frustration of witnessing how easily the excellent care you provide can unravel as the patient goes out the door. Patients are admitted acutely ill, and largely attributed to your clinical acumen, they are discharged tuned up and stable to return home. Days later, however, you may learn that your best‐laid discharge plans were not properly executed, and the patient returned with yet another exacerbation. Clearly this scenario represents a major setback for the patient and family caregivers. Possibly dismissed as another episode of patient noncompliance, such readmissions are now being recognized as system failures and reflect a discharge process that has been described as random events connected to highly variable actions with only a remote possibility of meeting implied expectations (Roger Resar, MD, Senior Fellow, Institute for Healthcare Improvement).
Once an area that received relatively little attention, transitions out of the hospital has been identified as a priority area in need of action by a confluence of recent research and national activities. Recognizing the expanding evidence for lapses in quality and safety, many esteemed organizations, including the Joint Commission, the Centers for Medicare and Medicaid Services and their accompanying Quality Improvement Organizations, the Institute for Healthcare Improvement, the Institute of Medicine, National Quality Forum, the Medicare Payment Advisory Committee, the American Board of Internal Medicine Foundation, the National Transitions of Care Coalition, the American College of Physicians, the Society for General Medicine, and the Society for Hospital Medicine, are currently focusing their efforts on how to optimize transitions. All have articulated the need for further clinical investigation that can offer greater insight into the nature of the problems that arise during this vulnerable period and what the potential solutions are.
In this edition of the Journal of Hospital Medicine, 3 teams of investigators have responded to this need, making timely, important, and unique contributions to advance the field.13 Specifically, each of these articles further raises awareness that a patient's transition out of the hospital often unfolds quickly in a fast‐paced, chaotic manner, placing many competing demands on clinicians, patients, and family caregivers. Not surprisingly, such competing demands can contribute to deficits in quality and safety. The authors of these studies all directly identify the central role of communication among clinicians as well as between patients and clinicians in ensuring successful handoffs, further affirming the Joint Commission's finding that inadequate communication is the leading cause of sentinel events.4 In this respect, communication is more than simply the transfer of information; rather, it involves the need to ensure comprehension and provide an opportunity to have a 2‐way dialogue. Importantly, these articles share a common approach in fostering our understanding of the perspective of patients and family caregivers with a particular focus on disadvantaged populations.
Kripalani and colleagues conducted a comprehensive review of the state of the science for those key hospital discharge issues that pertain to hospitalists. They identified a number of challenges including communication between hospital‐ and ambulatory‐based clinicians, medication reconciliation, timely hospital follow‐up, and engaging patients in self‐care. For each of these priority areas, the authors provide pragmatic recommendations for improving care that could be implemented within the current state of practice, either individually or as a bundle of interventions.
Recognizing that patients are often the only common thread across different sites of care, Strunin and colleagues demonstrate the value of including the voice of the patient in helping clinicians to understand the challenges and larger context in which they attempt to follow through with discharge instructions. Strunin et al. found that among a range of factors that contribute to adherence problems, many were nonmedical. Fortunately, a number of these are modifiable and point to the need to both prioritize recommendations to patients and to simplify them whenever possible. The authors' findings resonate with a growing literature that examines the hospital discharge process from the patient's perspective.510
Flacker and colleagues surveyed older patients to gain greater insights into their information needs at discharge. From a process standpoint, they demonstrated that a posthospital survey was feasible and acceptable to older patients. In and of itself, this finding has important implications in the context of national efforts aimed at implementing performance measurement and accompanying public reporting. It also may reflect patients' eagerness to be contacted after discharge; hospitalization is a major event in patients' lives, and attentive follow‐up is appreciated. The authors found that more than half of patients did not recall being asked about how they would care for themselves on returning home from the hospital. Although there may be a variety of explanations for this finding, it nevertheless points to an immediate area for intervention.
Collectively, these 3 articles set the stage for a proposed clinical investigation agenda aimed at optimizing transitions out of the hospital (see Table 1).
| 1. Greater recognition of the integral role of family caregivers |
| 2. Empirically define the appropriate follow‐up interval |
| 3. Define physician accountability for patients referred to home health on hospital discharge |
| 4. Delineate the role of the hospitalist in the advanced medical home |
| 5. Develop the ability to examine episodes of care |
These 5 recommendations have the potential to ensure that the gains patients make in our hospitals are maintained long after discharge.
-
Greater Recognition for the Integral Role of Family Caregivers. The patient and family caregivers should be integrated into health care professionals' efforts to improve care coordination across settings. Family caregivers have been silent partners in health care delivery, functioning as de facto care coordinators. During care handoffs, family caregivers make important contributions to ensuring quality, safety, and adherence to patient preferences; their role needs to be formally recognized and supported. An important initial step would be standardizing the approach to defining the types and intensity of the roles family caregivers play to facilitate improved communication. One proposed working definition is the FACED classification developed by one of the authors (E.C.). Modeled after the TNM system used in cancer, each letter of FACED refers to a different contribution made by a family caregiver: F = Financial; A = Advocacy; C = Care coordination; E = Emotional support; and D = Direct care provision. A simple numeric rating system could be developed whereby 0 = does not contribute in this area and 3 = makes significant contribution to this area. Such a straightforward approach would readily inform all members of the health care team about the caregivers' roles and capabilities and how they can optimally collaborate in the care plan.
-
Empirically Define Appropriate Follow‐Up Interval. At present, patients are given rather arbitrary and generic instructions for when to obtain follow‐up with their outpatient primary care physician or specialist. Surgical patients are often instructed to follow up with their surgeon, and yet most of the readmissions of these patients are attributable to medical conditions (personal communication, Steven Jencks, MD, Centers for Medicare and Medicaid Services). Furthermore, a significant number of discharged medical and surgical patients are readmitted to the hospital within 30 days without any outpatient contact with a health professional. One may envision an evidence‐based tiered approach whereby patients are assigned a hospital readmission risk score at the time of discharge that then determines the timing of their follow‐up appointment. Using this framework, the highest‐risk patients may be encouraged to receive follow‐up within 2472 hours, whereas lower‐risk patients may be able to wait 1421 days. Of course, there will need to be sufficient access to outpatient physicians, who will need to be available, to ensure the success of this strategy.
-
Define Physician Accountability for Patients Referred to Home Health on Hospital Discharge. Communication problems between the hospital and the home health care agency are a source of aggravation for both parties, not to mention patients. Typically, a hospitalist provides the initial order for services and then expects subsequent home care coordination to be managed by an outpatient physician. Unfortunately, in some cases the patient may not have an outpatient physician or the patient's primary physician may be unaware of the recent hospitalization and thus unwilling to assume management of an unfamiliar care plan. As a result, home care nurses often cannot identify a physician to respond to their questions or concerns. At the center of this problem lies a lack of understanding of where the responsibility of the ordering hospitalist ends and the outpatient physician assuming care begins. Recognizing the profound costs of failed home health care leading to hospital readmission, the nation's Quality Improvement Organizations launched a national campaign in 2006 to address this problem. Hospitalists should engage in this effort and not punt the entire responsibility to home health agenciesimagine if hospitals and hospitalists were financially penalized if a patient was readmitted.
-
Delineate the Role of the Hospitalist in the Advanced Medical Home. Modeled after a concept with origins in pediatrics, the American College of Physicians and American Academy of Family Physicians are promoting the advanced medical home as a new care model that aims to provide comprehensive ambulatory care with an explicit focus on care coordination.11 The Centers for Medicare and Medicaid Services is planning to initiate a demonstration of this approach. What has not been adequately underscored is how the advanced medical home will communicate essential clinical information with the hospitalist and what, if any, will be the role of the hospitalist in relation to a patient's medical home? Ideally, the medical home approach will alleviate many of the current access problems that impede timely follow‐up.
-
Develop Ability to Examine Episodes of Care. Patients with complex conditions often require care from different practitioners in multiple settings. From the vantage point of health care professionals, these may appear to occur as merely a string of individual interactions, including hospital admissions and discharges. However from the patient's perspective, the experience is more appropriately characterized as a journey across an aggregated episode of care. The National Quality Forum is currently exploring how to measure quality of care delivered across such an episode of care. Additionally, the Centers for Medicare and Medicaid Services is developing a new assessment tool that will transcend acute and postacute care settings, the Continuity Assessment Record and Evaluation (CARE). This tool will potentially enhance our ability to measure care across a predefined episode. Measurement can further pave the way for payment reform designed to align incentives toward higher‐quality care transitions. Currently, professional fees for coronary artery bypass grafting surgery are bundled across an episode, including hospital and posthospital care settings. Extending this approach to a wider array of conditions and services could encourage new perspectives on the timing of discharge and the use of posthospital care venues. For example, under bundled payment, incentives might support a plan to keep a patient in the hospital an extra 1 or 2 days in order to obviate a transfer to a skilled nursing facility and the concomitant risks of transfer‐related problems. Further, bundled payment may allow for the provision of additional services not currently covered, including transportation, as identified by Strunin and colleagues.3
Hospitalists are well positioned to offer leadership in these high‐leverage areas and thereby make a unique contribution to the quality and safety of care transitions. By so doing, they are poised to reaffirm their professionalism,12 ensuring that the excellent care that they provide in the hospital is sustained well into the future.
As a hospital practitioner, you have undoubtedly experienced the frustration of witnessing how easily the excellent care you provide can unravel as the patient goes out the door. Patients are admitted acutely ill, and largely attributed to your clinical acumen, they are discharged tuned up and stable to return home. Days later, however, you may learn that your best‐laid discharge plans were not properly executed, and the patient returned with yet another exacerbation. Clearly this scenario represents a major setback for the patient and family caregivers. Possibly dismissed as another episode of patient noncompliance, such readmissions are now being recognized as system failures and reflect a discharge process that has been described as random events connected to highly variable actions with only a remote possibility of meeting implied expectations (Roger Resar, MD, Senior Fellow, Institute for Healthcare Improvement).
Once an area that received relatively little attention, transitions out of the hospital has been identified as a priority area in need of action by a confluence of recent research and national activities. Recognizing the expanding evidence for lapses in quality and safety, many esteemed organizations, including the Joint Commission, the Centers for Medicare and Medicaid Services and their accompanying Quality Improvement Organizations, the Institute for Healthcare Improvement, the Institute of Medicine, National Quality Forum, the Medicare Payment Advisory Committee, the American Board of Internal Medicine Foundation, the National Transitions of Care Coalition, the American College of Physicians, the Society for General Medicine, and the Society for Hospital Medicine, are currently focusing their efforts on how to optimize transitions. All have articulated the need for further clinical investigation that can offer greater insight into the nature of the problems that arise during this vulnerable period and what the potential solutions are.
In this edition of the Journal of Hospital Medicine, 3 teams of investigators have responded to this need, making timely, important, and unique contributions to advance the field.13 Specifically, each of these articles further raises awareness that a patient's transition out of the hospital often unfolds quickly in a fast‐paced, chaotic manner, placing many competing demands on clinicians, patients, and family caregivers. Not surprisingly, such competing demands can contribute to deficits in quality and safety. The authors of these studies all directly identify the central role of communication among clinicians as well as between patients and clinicians in ensuring successful handoffs, further affirming the Joint Commission's finding that inadequate communication is the leading cause of sentinel events.4 In this respect, communication is more than simply the transfer of information; rather, it involves the need to ensure comprehension and provide an opportunity to have a 2‐way dialogue. Importantly, these articles share a common approach in fostering our understanding of the perspective of patients and family caregivers with a particular focus on disadvantaged populations.
Kripalani and colleagues conducted a comprehensive review of the state of the science for those key hospital discharge issues that pertain to hospitalists. They identified a number of challenges including communication between hospital‐ and ambulatory‐based clinicians, medication reconciliation, timely hospital follow‐up, and engaging patients in self‐care. For each of these priority areas, the authors provide pragmatic recommendations for improving care that could be implemented within the current state of practice, either individually or as a bundle of interventions.
Recognizing that patients are often the only common thread across different sites of care, Strunin and colleagues demonstrate the value of including the voice of the patient in helping clinicians to understand the challenges and larger context in which they attempt to follow through with discharge instructions. Strunin et al. found that among a range of factors that contribute to adherence problems, many were nonmedical. Fortunately, a number of these are modifiable and point to the need to both prioritize recommendations to patients and to simplify them whenever possible. The authors' findings resonate with a growing literature that examines the hospital discharge process from the patient's perspective.510
Flacker and colleagues surveyed older patients to gain greater insights into their information needs at discharge. From a process standpoint, they demonstrated that a posthospital survey was feasible and acceptable to older patients. In and of itself, this finding has important implications in the context of national efforts aimed at implementing performance measurement and accompanying public reporting. It also may reflect patients' eagerness to be contacted after discharge; hospitalization is a major event in patients' lives, and attentive follow‐up is appreciated. The authors found that more than half of patients did not recall being asked about how they would care for themselves on returning home from the hospital. Although there may be a variety of explanations for this finding, it nevertheless points to an immediate area for intervention.
Collectively, these 3 articles set the stage for a proposed clinical investigation agenda aimed at optimizing transitions out of the hospital (see Table 1).
| 1. Greater recognition of the integral role of family caregivers |
| 2. Empirically define the appropriate follow‐up interval |
| 3. Define physician accountability for patients referred to home health on hospital discharge |
| 4. Delineate the role of the hospitalist in the advanced medical home |
| 5. Develop the ability to examine episodes of care |
These 5 recommendations have the potential to ensure that the gains patients make in our hospitals are maintained long after discharge.
-
Greater Recognition for the Integral Role of Family Caregivers. The patient and family caregivers should be integrated into health care professionals' efforts to improve care coordination across settings. Family caregivers have been silent partners in health care delivery, functioning as de facto care coordinators. During care handoffs, family caregivers make important contributions to ensuring quality, safety, and adherence to patient preferences; their role needs to be formally recognized and supported. An important initial step would be standardizing the approach to defining the types and intensity of the roles family caregivers play to facilitate improved communication. One proposed working definition is the FACED classification developed by one of the authors (E.C.). Modeled after the TNM system used in cancer, each letter of FACED refers to a different contribution made by a family caregiver: F = Financial; A = Advocacy; C = Care coordination; E = Emotional support; and D = Direct care provision. A simple numeric rating system could be developed whereby 0 = does not contribute in this area and 3 = makes significant contribution to this area. Such a straightforward approach would readily inform all members of the health care team about the caregivers' roles and capabilities and how they can optimally collaborate in the care plan.
-
Empirically Define Appropriate Follow‐Up Interval. At present, patients are given rather arbitrary and generic instructions for when to obtain follow‐up with their outpatient primary care physician or specialist. Surgical patients are often instructed to follow up with their surgeon, and yet most of the readmissions of these patients are attributable to medical conditions (personal communication, Steven Jencks, MD, Centers for Medicare and Medicaid Services). Furthermore, a significant number of discharged medical and surgical patients are readmitted to the hospital within 30 days without any outpatient contact with a health professional. One may envision an evidence‐based tiered approach whereby patients are assigned a hospital readmission risk score at the time of discharge that then determines the timing of their follow‐up appointment. Using this framework, the highest‐risk patients may be encouraged to receive follow‐up within 2472 hours, whereas lower‐risk patients may be able to wait 1421 days. Of course, there will need to be sufficient access to outpatient physicians, who will need to be available, to ensure the success of this strategy.
-
Define Physician Accountability for Patients Referred to Home Health on Hospital Discharge. Communication problems between the hospital and the home health care agency are a source of aggravation for both parties, not to mention patients. Typically, a hospitalist provides the initial order for services and then expects subsequent home care coordination to be managed by an outpatient physician. Unfortunately, in some cases the patient may not have an outpatient physician or the patient's primary physician may be unaware of the recent hospitalization and thus unwilling to assume management of an unfamiliar care plan. As a result, home care nurses often cannot identify a physician to respond to their questions or concerns. At the center of this problem lies a lack of understanding of where the responsibility of the ordering hospitalist ends and the outpatient physician assuming care begins. Recognizing the profound costs of failed home health care leading to hospital readmission, the nation's Quality Improvement Organizations launched a national campaign in 2006 to address this problem. Hospitalists should engage in this effort and not punt the entire responsibility to home health agenciesimagine if hospitals and hospitalists were financially penalized if a patient was readmitted.
-
Delineate the Role of the Hospitalist in the Advanced Medical Home. Modeled after a concept with origins in pediatrics, the American College of Physicians and American Academy of Family Physicians are promoting the advanced medical home as a new care model that aims to provide comprehensive ambulatory care with an explicit focus on care coordination.11 The Centers for Medicare and Medicaid Services is planning to initiate a demonstration of this approach. What has not been adequately underscored is how the advanced medical home will communicate essential clinical information with the hospitalist and what, if any, will be the role of the hospitalist in relation to a patient's medical home? Ideally, the medical home approach will alleviate many of the current access problems that impede timely follow‐up.
-
Develop Ability to Examine Episodes of Care. Patients with complex conditions often require care from different practitioners in multiple settings. From the vantage point of health care professionals, these may appear to occur as merely a string of individual interactions, including hospital admissions and discharges. However from the patient's perspective, the experience is more appropriately characterized as a journey across an aggregated episode of care. The National Quality Forum is currently exploring how to measure quality of care delivered across such an episode of care. Additionally, the Centers for Medicare and Medicaid Services is developing a new assessment tool that will transcend acute and postacute care settings, the Continuity Assessment Record and Evaluation (CARE). This tool will potentially enhance our ability to measure care across a predefined episode. Measurement can further pave the way for payment reform designed to align incentives toward higher‐quality care transitions. Currently, professional fees for coronary artery bypass grafting surgery are bundled across an episode, including hospital and posthospital care settings. Extending this approach to a wider array of conditions and services could encourage new perspectives on the timing of discharge and the use of posthospital care venues. For example, under bundled payment, incentives might support a plan to keep a patient in the hospital an extra 1 or 2 days in order to obviate a transfer to a skilled nursing facility and the concomitant risks of transfer‐related problems. Further, bundled payment may allow for the provision of additional services not currently covered, including transportation, as identified by Strunin and colleagues.3
Hospitalists are well positioned to offer leadership in these high‐leverage areas and thereby make a unique contribution to the quality and safety of care transitions. By so doing, they are poised to reaffirm their professionalism,12 ensuring that the excellent care that they provide in the hospital is sustained well into the future.
- ,,.Discharge information and older patients: do they get what they need?J Hosp Med.2007;2:291–296.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2:314–323.
- ,,.Understanding rehospitalization risk: can the hospital discharge be modified to impact recurrent hospitalization.J Hosp Med.2007;2:297–304.
- The Joint Commission. Sentinel event statistics. Available at: http://www.jointcommission.org/SentinelEvents/Statistics/. Accessed August 7,2007.
- ,,.Patients' and caregivers' transition from hospital to home: needs and recommendations.Home Health Care Serv Q.1998;17:27–48.
- ,,,,.Carepartner experiences with hospital care.Med Care.1999;37:33–38.
- ,.Understanding coordination of care from the consumer's perspective in a regional health system.Health Serv Res.2002;37:1031–1054.
- ,,, et al.Development and testing of a measure designed to assess the quality of care transitions.Int J Integrated Care.2002;2:e02.
- .Rough crossings: family caregivers odysseys through the health care system.New York:United Hospital Fund of New York;1998.
- ,.Facilitating the transition out of the hospital. In:Gerteis M,Edgman‐Levitan S,Daley J,Delbanco T, editors.Through the Patient's Eyes: Understanding and Promoting Patient‐Centered Care.San Francisco:Jossey‐Bass;1993:204–223.
- ,,American College of Physicians. The advanced medical home: a patient‐centered, physician‐guided model of health care. p. 1–22. http://www.acponline.org/hpp/adv_med.pdf Accessed August 7,2007.
- Project of the ABIM Foundation A‐AFaEFoIM.Medical professionalism in the new millennium: a physician charter.Ann Intern Med.2002;136:243–246.
- ,,.Discharge information and older patients: do they get what they need?J Hosp Med.2007;2:291–296.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2:314–323.
- ,,.Understanding rehospitalization risk: can the hospital discharge be modified to impact recurrent hospitalization.J Hosp Med.2007;2:297–304.
- The Joint Commission. Sentinel event statistics. Available at: http://www.jointcommission.org/SentinelEvents/Statistics/. Accessed August 7,2007.
- ,,.Patients' and caregivers' transition from hospital to home: needs and recommendations.Home Health Care Serv Q.1998;17:27–48.
- ,,,,.Carepartner experiences with hospital care.Med Care.1999;37:33–38.
- ,.Understanding coordination of care from the consumer's perspective in a regional health system.Health Serv Res.2002;37:1031–1054.
- ,,, et al.Development and testing of a measure designed to assess the quality of care transitions.Int J Integrated Care.2002;2:e02.
- .Rough crossings: family caregivers odysseys through the health care system.New York:United Hospital Fund of New York;1998.
- ,.Facilitating the transition out of the hospital. In:Gerteis M,Edgman‐Levitan S,Daley J,Delbanco T, editors.Through the Patient's Eyes: Understanding and Promoting Patient‐Centered Care.San Francisco:Jossey‐Bass;1993:204–223.
- ,,American College of Physicians. The advanced medical home: a patient‐centered, physician‐guided model of health care. p. 1–22. http://www.acponline.org/hpp/adv_med.pdf Accessed August 7,2007.
- Project of the ABIM Foundation A‐AFaEFoIM.Medical professionalism in the new millennium: a physician charter.Ann Intern Med.2002;136:243–246.
FDA clears first rapid test to screen for bacterial contamination in platelets
The US Food and Drug Administration (FDA) has cleared for marketing the first rapid test to detect bacterial contamination in leukoreduced apheresis platelets prior to transfusion.
The platelet pan genera detection (PGD) test system is a disposable test strip for use in a hospital transfusion service setting.
It is intended to supplement current quality control testing methods of platelets following collection.
The clearance of this test is a significant advancement in detecting bacterial contamination of platelets, according to Jesse L. Goodman, MD, MPH, director of the FDA’s Center for Biologics Evaluation and Research.
“In half an hour, a sample is prepared, processed, and read, providing an additional assurance that the product is free from harmful bacteria,” Dr Goodman said.
Bacterial contamination of platelets is the leading infectious cause of transfusion-related patient fatalities. The risk of a patient receiving a transfusion contaminated with bacteria is 1 in 5,000, far greater than the risk of transmitting hepatitis C (1 in 1.6 million) or HIV (1 in 1.9 million).
To reduce the risk of transfusing contaminated platelets, blood centers culture samples of the platelets 24 hours after the donation. The culture is read within 48 hours of donation, and contaminated units are discarded.
However, there is a possibility that the number of bacteria present at the time of culture may be so low that bacteria are not detected due to sampling limitations.
Rapid testing of platelets using the platelet PGD test system permits units of platelets to be retested at a time closer to their use. Although the test system is less sensitive than standard cultures, it is done later in storage when bacteria, if present, have multiplied and are therefore easier to detect.
The platelet PGD test system was developed by Verax Biomedica Inc., Worcester, Massachusetts. ![]()
The US Food and Drug Administration (FDA) has cleared for marketing the first rapid test to detect bacterial contamination in leukoreduced apheresis platelets prior to transfusion.
The platelet pan genera detection (PGD) test system is a disposable test strip for use in a hospital transfusion service setting.
It is intended to supplement current quality control testing methods of platelets following collection.
The clearance of this test is a significant advancement in detecting bacterial contamination of platelets, according to Jesse L. Goodman, MD, MPH, director of the FDA’s Center for Biologics Evaluation and Research.
“In half an hour, a sample is prepared, processed, and read, providing an additional assurance that the product is free from harmful bacteria,” Dr Goodman said.
Bacterial contamination of platelets is the leading infectious cause of transfusion-related patient fatalities. The risk of a patient receiving a transfusion contaminated with bacteria is 1 in 5,000, far greater than the risk of transmitting hepatitis C (1 in 1.6 million) or HIV (1 in 1.9 million).
To reduce the risk of transfusing contaminated platelets, blood centers culture samples of the platelets 24 hours after the donation. The culture is read within 48 hours of donation, and contaminated units are discarded.
However, there is a possibility that the number of bacteria present at the time of culture may be so low that bacteria are not detected due to sampling limitations.
Rapid testing of platelets using the platelet PGD test system permits units of platelets to be retested at a time closer to their use. Although the test system is less sensitive than standard cultures, it is done later in storage when bacteria, if present, have multiplied and are therefore easier to detect.
The platelet PGD test system was developed by Verax Biomedica Inc., Worcester, Massachusetts. ![]()
The US Food and Drug Administration (FDA) has cleared for marketing the first rapid test to detect bacterial contamination in leukoreduced apheresis platelets prior to transfusion.
The platelet pan genera detection (PGD) test system is a disposable test strip for use in a hospital transfusion service setting.
It is intended to supplement current quality control testing methods of platelets following collection.
The clearance of this test is a significant advancement in detecting bacterial contamination of platelets, according to Jesse L. Goodman, MD, MPH, director of the FDA’s Center for Biologics Evaluation and Research.
“In half an hour, a sample is prepared, processed, and read, providing an additional assurance that the product is free from harmful bacteria,” Dr Goodman said.
Bacterial contamination of platelets is the leading infectious cause of transfusion-related patient fatalities. The risk of a patient receiving a transfusion contaminated with bacteria is 1 in 5,000, far greater than the risk of transmitting hepatitis C (1 in 1.6 million) or HIV (1 in 1.9 million).
To reduce the risk of transfusing contaminated platelets, blood centers culture samples of the platelets 24 hours after the donation. The culture is read within 48 hours of donation, and contaminated units are discarded.
However, there is a possibility that the number of bacteria present at the time of culture may be so low that bacteria are not detected due to sampling limitations.
Rapid testing of platelets using the platelet PGD test system permits units of platelets to be retested at a time closer to their use. Although the test system is less sensitive than standard cultures, it is done later in storage when bacteria, if present, have multiplied and are therefore easier to detect.
The platelet PGD test system was developed by Verax Biomedica Inc., Worcester, Massachusetts. ![]()
The Boutique Lure
The Boutique Lure
Question: I recently received a brochure in the mail about a hospital that caters only to cardiac patients. While I think this job sounds intriguing, I’m concerned that this may be a boutique hospital. What do you think of the movement toward boutique hospitals? Do you think they are ethical?
Curious in Boston
Dr. Hospitalist responds: Boutique or specialty hospitals have been hotly debated among healthcare policymakers over the past few years. Compared with the number of general hospitals, the numbers of specialty hospitals—typically those that focus on cardiac, orthopedic, surgical, and women’s procedures—are small.
A Government Accounting Office (GAO) report in 2003 identified 100 such hospitals in the country. More than two-thirds of the hospitals are in seven states (Arizona, California, Kansas, Oklahoma, Louisiana, South Dakota, and Texas).
The GAO found that compared with general hospitals, specialty hospitals are “much less likely to have emergency departments, treated smaller percentages of Medicaid patients and derived a smaller share of their revenues from inpatient services.” Although small, this is a growing segment of the healthcare industry.
Specialty hospitals are controversial because many are for-profit and often owned by some of the physicians who work at the hospital. Specialty hospital supporters believe competition between specialty and general hospitals for services can lower costs and improve care.
A 2005 Medicare Payment Advisory Commission study found that physician-owned specialty hospitals decreased lengths of stay but didn’t lower costs for Medicare patients.
In general, specialty hospitals treated less-severe cases and tended to have lower numbers of Medicaid patients than community hospitals.
Specialty care hospital critics are concerned that specialty hospitals take care of the most profitable patients (those who are less ill) and leave the general hospital with the sicker patients who incur higher costs.
They fear growing numbers of specialty hospitals will make it financially difficult for general hospitals to meet all of a community’s needs, including charity care and emergency services.
Critics are also concerned that physician ownership of specialty hospitals could affect physicians’ clinical behavior by driving inappropriate referrals.
You may remember that the federal Stark law (named after Rep. Peter Stark, D-Calif.) generally prohibits physicians from referring Medicare patients for healthcare services to facilities where they have financial interests.
This law was enacted after several studies demonstrated that physicians with ownership interest in clinical laboratories, diagnostic imaging centers, and physical therapy providers made more referrals to these centers and ordered more services at higher costs.
The Stark law lets physicians who have an ownership interest in an entire hospital and are authorized to perform services there to refer patients to that hospital.
As you consider this opportunity, further investigate the risks, benefits, and potential effect of the specialty hospital on your community and our healthcare system.
Holiday Dilemma
Question: I just took over scheduling for our hospitalist group. I’ve been practicing nearly two years and am wondering how to staff holidays. I’m finding it difficult handling the multiple requests for Thanksgiving, Christmas, and New Year’s Eve. Do you know of any innovative scheduling techniques?
Schedule Grinch in Philadelphia
Dr. Hospitalist responds: Congratulations on your new responsibility! I write this with my tongue firmly planted in my cheek. As you now realize, completing the schedule is not easy.
Unfortunately, most hospitalists don’t recognize the enormous challenge one faces in filling the schedule until they are given the task.
Unless you were a chief medical resident, you probably didn’t learn or practice scheduling in the course of your medical training. Inevitably, everyone wants and expects to get their choice of days off. Of course, that is rarely possible.
How do you make everyone happy? It is important to recognize that making everyone happy every time is not possible. But it is possible and important to be fair to everyone all the time. There are some steps you can take to ensure the scheduling process is fair.
The first step is to set appropriate expectations. It is critical for the group leader and the staff member making the schedule to help each group member understand the enormous challenges that come with scheduling.
Providers who understand the difficulties of scheduling will be more understanding and accommodating in their requests.
The second step is to establish and clearly state the rules of engagement. For example, be explicit in explaining the rules for submitting requests and the deadline for requests. Avoid misconceptions by stating when the final schedule will be revealed.
The last step is to clearly state how to handle requests for schedule changes. Many hospitalist groups keep track of who works which holidays so the distribution of work on holidays is fair from year to year.
I have one last suggestion. Consider rotating the job of scheduling so everyone understands firsthand the challenges of the job. To entice people to assume this responsibility, the job should come with remuneration—either salary support and/or preference in choosing their own holiday schedule.
Of course, recognize that not everyone will want the job or be good at it. An effective group leader helps individuals identify opportunities and helps them succeed.
Foreign Medical Grads
Question: What’s your opinion on the effect of foreign medical graduates in the U.S.?
IMG in Cincinnati
Dr. Hospitalist responds: The U.S. healthcare system would be quite different without foreign (aka international) medical graduates (IMGs), who play important clinical, educational, administrative, and research roles.
Some physicians and patients believe medical education outside this country is inferior. In some cases, they are correct—in others, they could not be more wrong. Medical education outside this country varies in standards and curricula.
Many people are not aware that IMGs who wish to enter an Accreditation Council for Graduate Medical Education residency of fellowship program in the United States must have Educational Commission for Foreign Medical Graduates (ECFMG) certification. ECFMG certification requires the applicant to pass a series of examinations, including United States Medical Licensing Examination (USMLE) Steps 1 and 2.
ECFMG certification is also required before an applicant can take Step 3 of the USMLE and is required before a physician can obtain an unrestricted license to practice medicine in the United States.
I suspect some IMGs face discrimination in this country because some may speak with an accent. But truth be told, the United States healthcare system could not exist without the contributions made by IMGs. TH
The Boutique Lure
Question: I recently received a brochure in the mail about a hospital that caters only to cardiac patients. While I think this job sounds intriguing, I’m concerned that this may be a boutique hospital. What do you think of the movement toward boutique hospitals? Do you think they are ethical?
Curious in Boston
Dr. Hospitalist responds: Boutique or specialty hospitals have been hotly debated among healthcare policymakers over the past few years. Compared with the number of general hospitals, the numbers of specialty hospitals—typically those that focus on cardiac, orthopedic, surgical, and women’s procedures—are small.
A Government Accounting Office (GAO) report in 2003 identified 100 such hospitals in the country. More than two-thirds of the hospitals are in seven states (Arizona, California, Kansas, Oklahoma, Louisiana, South Dakota, and Texas).
The GAO found that compared with general hospitals, specialty hospitals are “much less likely to have emergency departments, treated smaller percentages of Medicaid patients and derived a smaller share of their revenues from inpatient services.” Although small, this is a growing segment of the healthcare industry.
Specialty hospitals are controversial because many are for-profit and often owned by some of the physicians who work at the hospital. Specialty hospital supporters believe competition between specialty and general hospitals for services can lower costs and improve care.
A 2005 Medicare Payment Advisory Commission study found that physician-owned specialty hospitals decreased lengths of stay but didn’t lower costs for Medicare patients.
In general, specialty hospitals treated less-severe cases and tended to have lower numbers of Medicaid patients than community hospitals.
Specialty care hospital critics are concerned that specialty hospitals take care of the most profitable patients (those who are less ill) and leave the general hospital with the sicker patients who incur higher costs.
They fear growing numbers of specialty hospitals will make it financially difficult for general hospitals to meet all of a community’s needs, including charity care and emergency services.
Critics are also concerned that physician ownership of specialty hospitals could affect physicians’ clinical behavior by driving inappropriate referrals.
You may remember that the federal Stark law (named after Rep. Peter Stark, D-Calif.) generally prohibits physicians from referring Medicare patients for healthcare services to facilities where they have financial interests.
This law was enacted after several studies demonstrated that physicians with ownership interest in clinical laboratories, diagnostic imaging centers, and physical therapy providers made more referrals to these centers and ordered more services at higher costs.
The Stark law lets physicians who have an ownership interest in an entire hospital and are authorized to perform services there to refer patients to that hospital.
As you consider this opportunity, further investigate the risks, benefits, and potential effect of the specialty hospital on your community and our healthcare system.
Holiday Dilemma
Question: I just took over scheduling for our hospitalist group. I’ve been practicing nearly two years and am wondering how to staff holidays. I’m finding it difficult handling the multiple requests for Thanksgiving, Christmas, and New Year’s Eve. Do you know of any innovative scheduling techniques?
Schedule Grinch in Philadelphia
Dr. Hospitalist responds: Congratulations on your new responsibility! I write this with my tongue firmly planted in my cheek. As you now realize, completing the schedule is not easy.
Unfortunately, most hospitalists don’t recognize the enormous challenge one faces in filling the schedule until they are given the task.
Unless you were a chief medical resident, you probably didn’t learn or practice scheduling in the course of your medical training. Inevitably, everyone wants and expects to get their choice of days off. Of course, that is rarely possible.
How do you make everyone happy? It is important to recognize that making everyone happy every time is not possible. But it is possible and important to be fair to everyone all the time. There are some steps you can take to ensure the scheduling process is fair.
The first step is to set appropriate expectations. It is critical for the group leader and the staff member making the schedule to help each group member understand the enormous challenges that come with scheduling.
Providers who understand the difficulties of scheduling will be more understanding and accommodating in their requests.
The second step is to establish and clearly state the rules of engagement. For example, be explicit in explaining the rules for submitting requests and the deadline for requests. Avoid misconceptions by stating when the final schedule will be revealed.
The last step is to clearly state how to handle requests for schedule changes. Many hospitalist groups keep track of who works which holidays so the distribution of work on holidays is fair from year to year.
I have one last suggestion. Consider rotating the job of scheduling so everyone understands firsthand the challenges of the job. To entice people to assume this responsibility, the job should come with remuneration—either salary support and/or preference in choosing their own holiday schedule.
Of course, recognize that not everyone will want the job or be good at it. An effective group leader helps individuals identify opportunities and helps them succeed.
Foreign Medical Grads
Question: What’s your opinion on the effect of foreign medical graduates in the U.S.?
IMG in Cincinnati
Dr. Hospitalist responds: The U.S. healthcare system would be quite different without foreign (aka international) medical graduates (IMGs), who play important clinical, educational, administrative, and research roles.
Some physicians and patients believe medical education outside this country is inferior. In some cases, they are correct—in others, they could not be more wrong. Medical education outside this country varies in standards and curricula.
Many people are not aware that IMGs who wish to enter an Accreditation Council for Graduate Medical Education residency of fellowship program in the United States must have Educational Commission for Foreign Medical Graduates (ECFMG) certification. ECFMG certification requires the applicant to pass a series of examinations, including United States Medical Licensing Examination (USMLE) Steps 1 and 2.
ECFMG certification is also required before an applicant can take Step 3 of the USMLE and is required before a physician can obtain an unrestricted license to practice medicine in the United States.
I suspect some IMGs face discrimination in this country because some may speak with an accent. But truth be told, the United States healthcare system could not exist without the contributions made by IMGs. TH
The Boutique Lure
Question: I recently received a brochure in the mail about a hospital that caters only to cardiac patients. While I think this job sounds intriguing, I’m concerned that this may be a boutique hospital. What do you think of the movement toward boutique hospitals? Do you think they are ethical?
Curious in Boston
Dr. Hospitalist responds: Boutique or specialty hospitals have been hotly debated among healthcare policymakers over the past few years. Compared with the number of general hospitals, the numbers of specialty hospitals—typically those that focus on cardiac, orthopedic, surgical, and women’s procedures—are small.
A Government Accounting Office (GAO) report in 2003 identified 100 such hospitals in the country. More than two-thirds of the hospitals are in seven states (Arizona, California, Kansas, Oklahoma, Louisiana, South Dakota, and Texas).
The GAO found that compared with general hospitals, specialty hospitals are “much less likely to have emergency departments, treated smaller percentages of Medicaid patients and derived a smaller share of their revenues from inpatient services.” Although small, this is a growing segment of the healthcare industry.
Specialty hospitals are controversial because many are for-profit and often owned by some of the physicians who work at the hospital. Specialty hospital supporters believe competition between specialty and general hospitals for services can lower costs and improve care.
A 2005 Medicare Payment Advisory Commission study found that physician-owned specialty hospitals decreased lengths of stay but didn’t lower costs for Medicare patients.
In general, specialty hospitals treated less-severe cases and tended to have lower numbers of Medicaid patients than community hospitals.
Specialty care hospital critics are concerned that specialty hospitals take care of the most profitable patients (those who are less ill) and leave the general hospital with the sicker patients who incur higher costs.
They fear growing numbers of specialty hospitals will make it financially difficult for general hospitals to meet all of a community’s needs, including charity care and emergency services.
Critics are also concerned that physician ownership of specialty hospitals could affect physicians’ clinical behavior by driving inappropriate referrals.
You may remember that the federal Stark law (named after Rep. Peter Stark, D-Calif.) generally prohibits physicians from referring Medicare patients for healthcare services to facilities where they have financial interests.
This law was enacted after several studies demonstrated that physicians with ownership interest in clinical laboratories, diagnostic imaging centers, and physical therapy providers made more referrals to these centers and ordered more services at higher costs.
The Stark law lets physicians who have an ownership interest in an entire hospital and are authorized to perform services there to refer patients to that hospital.
As you consider this opportunity, further investigate the risks, benefits, and potential effect of the specialty hospital on your community and our healthcare system.
Holiday Dilemma
Question: I just took over scheduling for our hospitalist group. I’ve been practicing nearly two years and am wondering how to staff holidays. I’m finding it difficult handling the multiple requests for Thanksgiving, Christmas, and New Year’s Eve. Do you know of any innovative scheduling techniques?
Schedule Grinch in Philadelphia
Dr. Hospitalist responds: Congratulations on your new responsibility! I write this with my tongue firmly planted in my cheek. As you now realize, completing the schedule is not easy.
Unfortunately, most hospitalists don’t recognize the enormous challenge one faces in filling the schedule until they are given the task.
Unless you were a chief medical resident, you probably didn’t learn or practice scheduling in the course of your medical training. Inevitably, everyone wants and expects to get their choice of days off. Of course, that is rarely possible.
How do you make everyone happy? It is important to recognize that making everyone happy every time is not possible. But it is possible and important to be fair to everyone all the time. There are some steps you can take to ensure the scheduling process is fair.
The first step is to set appropriate expectations. It is critical for the group leader and the staff member making the schedule to help each group member understand the enormous challenges that come with scheduling.
Providers who understand the difficulties of scheduling will be more understanding and accommodating in their requests.
The second step is to establish and clearly state the rules of engagement. For example, be explicit in explaining the rules for submitting requests and the deadline for requests. Avoid misconceptions by stating when the final schedule will be revealed.
The last step is to clearly state how to handle requests for schedule changes. Many hospitalist groups keep track of who works which holidays so the distribution of work on holidays is fair from year to year.
I have one last suggestion. Consider rotating the job of scheduling so everyone understands firsthand the challenges of the job. To entice people to assume this responsibility, the job should come with remuneration—either salary support and/or preference in choosing their own holiday schedule.
Of course, recognize that not everyone will want the job or be good at it. An effective group leader helps individuals identify opportunities and helps them succeed.
Foreign Medical Grads
Question: What’s your opinion on the effect of foreign medical graduates in the U.S.?
IMG in Cincinnati
Dr. Hospitalist responds: The U.S. healthcare system would be quite different without foreign (aka international) medical graduates (IMGs), who play important clinical, educational, administrative, and research roles.
Some physicians and patients believe medical education outside this country is inferior. In some cases, they are correct—in others, they could not be more wrong. Medical education outside this country varies in standards and curricula.
Many people are not aware that IMGs who wish to enter an Accreditation Council for Graduate Medical Education residency of fellowship program in the United States must have Educational Commission for Foreign Medical Graduates (ECFMG) certification. ECFMG certification requires the applicant to pass a series of examinations, including United States Medical Licensing Examination (USMLE) Steps 1 and 2.
ECFMG certification is also required before an applicant can take Step 3 of the USMLE and is required before a physician can obtain an unrestricted license to practice medicine in the United States.
I suspect some IMGs face discrimination in this country because some may speak with an accent. But truth be told, the United States healthcare system could not exist without the contributions made by IMGs. TH
Haggle With the Hospital
Negotiating support from the hospital where you practice is one of the most critical skills you can learn. I am often asked, “How can our group prove our value to the hospital so we can get the support we need?” The best approach is the same whether you are a practice employed by the hospital or a separate legal entity that contracts with the hospital.
There are many valuable sources of guidance regarding the best way to negotiate any important agreement, including a book I recommend, Getting to Yes. I suggest you read such a book if you want to be a better negotiator. But here I want to highlight some features of negotiations between a hospital medicine practice and a hospital that such sources won’t specifically address.
Clearly this is complicated, and different situations call for different strategies. These are generalizations worth thinking about in any situation.
Know what is important to the hospital. I often hear hospitalists say, “We want to attend to the things that are important to the hospital, but we don’t know what those things are.” If that is really the case, the communication between the hospital and hospitalists must be awfully poor—and there is an opportunity for the hospitalists to improve it. It is worth the time and energy required to know what is on the mind of the hospital’s leadership. It may be as simple as having a person-to-person conversation with one or more hospital leaders about what they see as the institution’s most important goals—and how your practice could help achieve them. You need to be sure and understand the particulars at your hospital, but the topics below are on the mind of most executives.
Propose using additional funding to ensure adequate staffing, not raises for existing doctors. In the current environment of difficult recruiting, hospital executives are usually far more inclined to pay for increased staffing than worry about whether you need a raise just because you deserve it. So it is usually much more effective to tell the hospital, “Our practice needs more money so we can add doctors and more fully meet the demand for our services.” Much less effective is saying, “We [existing hospitalists] are working so hard that if we don’t get more money we’re going to quit.”
While the latter may be true, a hospital executive is much more likely to respond positively to paying for increased manpower so the existing doctors won’t have to continue working at unreasonably high workloads, rather than to providing money to support a raise for doctors already working unreasonably hard.
Propose additional resources to support quality improvement, and consider sharing some financial risk. Most hospital executives care about their hospital’s performance on quality measures and are willing to provide money to improve it. You might win more financial support if it is contingent on your group improving performance on quality measures.
You could propose that the hospital make additional money available to encourage and reward improved performance. You could even put existing financial support at risk and ask the hospital to match it. In other words, you could say you will contribute $5,000 or $10,000 of the money currently provided annually by the hospital per full-time equivalent hospitalist into a pool matched dollar for dollar (or some other ratio) by the hospital. Your group would get less total financial support (i.e., lose the funds put at risk) if quality doesn’t improve, but get more support if performance improved by an agreed-upon amount. A willingness to share financial risk demonstrates your commitment to success and can be compelling to the hospital.
Know your data. Hard data are far more effective than anecdotes when trying to convince the hospital of your practice’s value. Trumpet your successes, but remember that same executive will probably hear from 10 others in the same week that spending huge sums of money on their product or service will dramatically improve the hospital’s bottom line. If you’re trying to convince the hospital that every dollar spent to support your practice will provide an attractive return on investment, you need hard data to prove it.
It would be best if you could independently collect this data. But in most cases, you will have to rely on data the hospital has collected. It’s worthwhile to insist on routine reports (e.g., monthly, or no less than quarterly) from the hospital summarizing your group’s performance on quality and financial metrics (CMS core measures, patient satisfaction, cost per case). This data will be critical to you when you negotiate financial support from the hospital.
You should also have data about other hospitalist practices, such as results from the 2005-06 “SHM Survey of Hospitalist Productivity and Compensation” and other sources I discussed in a recent column (July 2007, p. 73). And if you’re able to get reliable data about other practices in your local marketplace (i.e., something more significant than just what you heard through the grapevine), be sure to share that information as well.
Agree to conditions carefully. Don’t agree to do things you would be unhappy doing just because it might help get more financial support from the hospital. Executives know it is bad business to pay people more money to get them to keep doing something they don’t want to do. Such an agreement usually leads to the hospitalists asking for more money each year to continue providing the service—and the quality of the service is often sub par if it’s something the hospitalists really don’t want to do (even if paid well to do it).
Stay focused on hospital performance—even in areas not specifically governed by your contractual relationship. Many or most hospitals that employ hospitalists assume all the financial risk for the practice. That is, the hospital agrees to make up the difference between collected professional fee revenue and the cost of operating the practice.
If the doctors underdocument and downcode, or are not compulsive about ensuring that their charges get to the billing agent, fee collections will suffer—and the hospital will end up having to pay more to support the practice.
If you are in such a situation, you should ensure that you’re helping to support optimal documentation, coding, billing, and collection practices—even if it won’t increase your paycheck but simply saves the hospital money. This will increase your chance of getting the hospital to increase financial support of your practice.
Remember your financial support isn’t a one-time negotiation; it is part of an ongoing relationship. In some negotiations, such as buying a car from a stranger, it seems reasonable to use any leverage most favorable for you. After all, you’re unlikely to ever interact with that person again. A hospitalist practice might compel the hospital to provide more support by threatening to quit suddenly. Yet it is usually a bad idea to do this because it can severely damage the long-term relationship.
Further, if you make it clear you’re going to quit unless you get more money, the hospital is in a tough spot. While the hospital may not want to lose you, any executive will realize that by making such a threat you probably aren’t committed to staying long even if you do get more financial support. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management-consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Negotiating support from the hospital where you practice is one of the most critical skills you can learn. I am often asked, “How can our group prove our value to the hospital so we can get the support we need?” The best approach is the same whether you are a practice employed by the hospital or a separate legal entity that contracts with the hospital.
There are many valuable sources of guidance regarding the best way to negotiate any important agreement, including a book I recommend, Getting to Yes. I suggest you read such a book if you want to be a better negotiator. But here I want to highlight some features of negotiations between a hospital medicine practice and a hospital that such sources won’t specifically address.
Clearly this is complicated, and different situations call for different strategies. These are generalizations worth thinking about in any situation.
Know what is important to the hospital. I often hear hospitalists say, “We want to attend to the things that are important to the hospital, but we don’t know what those things are.” If that is really the case, the communication between the hospital and hospitalists must be awfully poor—and there is an opportunity for the hospitalists to improve it. It is worth the time and energy required to know what is on the mind of the hospital’s leadership. It may be as simple as having a person-to-person conversation with one or more hospital leaders about what they see as the institution’s most important goals—and how your practice could help achieve them. You need to be sure and understand the particulars at your hospital, but the topics below are on the mind of most executives.
Propose using additional funding to ensure adequate staffing, not raises for existing doctors. In the current environment of difficult recruiting, hospital executives are usually far more inclined to pay for increased staffing than worry about whether you need a raise just because you deserve it. So it is usually much more effective to tell the hospital, “Our practice needs more money so we can add doctors and more fully meet the demand for our services.” Much less effective is saying, “We [existing hospitalists] are working so hard that if we don’t get more money we’re going to quit.”
While the latter may be true, a hospital executive is much more likely to respond positively to paying for increased manpower so the existing doctors won’t have to continue working at unreasonably high workloads, rather than to providing money to support a raise for doctors already working unreasonably hard.
Propose additional resources to support quality improvement, and consider sharing some financial risk. Most hospital executives care about their hospital’s performance on quality measures and are willing to provide money to improve it. You might win more financial support if it is contingent on your group improving performance on quality measures.
You could propose that the hospital make additional money available to encourage and reward improved performance. You could even put existing financial support at risk and ask the hospital to match it. In other words, you could say you will contribute $5,000 or $10,000 of the money currently provided annually by the hospital per full-time equivalent hospitalist into a pool matched dollar for dollar (or some other ratio) by the hospital. Your group would get less total financial support (i.e., lose the funds put at risk) if quality doesn’t improve, but get more support if performance improved by an agreed-upon amount. A willingness to share financial risk demonstrates your commitment to success and can be compelling to the hospital.
Know your data. Hard data are far more effective than anecdotes when trying to convince the hospital of your practice’s value. Trumpet your successes, but remember that same executive will probably hear from 10 others in the same week that spending huge sums of money on their product or service will dramatically improve the hospital’s bottom line. If you’re trying to convince the hospital that every dollar spent to support your practice will provide an attractive return on investment, you need hard data to prove it.
It would be best if you could independently collect this data. But in most cases, you will have to rely on data the hospital has collected. It’s worthwhile to insist on routine reports (e.g., monthly, or no less than quarterly) from the hospital summarizing your group’s performance on quality and financial metrics (CMS core measures, patient satisfaction, cost per case). This data will be critical to you when you negotiate financial support from the hospital.
You should also have data about other hospitalist practices, such as results from the 2005-06 “SHM Survey of Hospitalist Productivity and Compensation” and other sources I discussed in a recent column (July 2007, p. 73). And if you’re able to get reliable data about other practices in your local marketplace (i.e., something more significant than just what you heard through the grapevine), be sure to share that information as well.
Agree to conditions carefully. Don’t agree to do things you would be unhappy doing just because it might help get more financial support from the hospital. Executives know it is bad business to pay people more money to get them to keep doing something they don’t want to do. Such an agreement usually leads to the hospitalists asking for more money each year to continue providing the service—and the quality of the service is often sub par if it’s something the hospitalists really don’t want to do (even if paid well to do it).
Stay focused on hospital performance—even in areas not specifically governed by your contractual relationship. Many or most hospitals that employ hospitalists assume all the financial risk for the practice. That is, the hospital agrees to make up the difference between collected professional fee revenue and the cost of operating the practice.
If the doctors underdocument and downcode, or are not compulsive about ensuring that their charges get to the billing agent, fee collections will suffer—and the hospital will end up having to pay more to support the practice.
If you are in such a situation, you should ensure that you’re helping to support optimal documentation, coding, billing, and collection practices—even if it won’t increase your paycheck but simply saves the hospital money. This will increase your chance of getting the hospital to increase financial support of your practice.
Remember your financial support isn’t a one-time negotiation; it is part of an ongoing relationship. In some negotiations, such as buying a car from a stranger, it seems reasonable to use any leverage most favorable for you. After all, you’re unlikely to ever interact with that person again. A hospitalist practice might compel the hospital to provide more support by threatening to quit suddenly. Yet it is usually a bad idea to do this because it can severely damage the long-term relationship.
Further, if you make it clear you’re going to quit unless you get more money, the hospital is in a tough spot. While the hospital may not want to lose you, any executive will realize that by making such a threat you probably aren’t committed to staying long even if you do get more financial support. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management-consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
Negotiating support from the hospital where you practice is one of the most critical skills you can learn. I am often asked, “How can our group prove our value to the hospital so we can get the support we need?” The best approach is the same whether you are a practice employed by the hospital or a separate legal entity that contracts with the hospital.
There are many valuable sources of guidance regarding the best way to negotiate any important agreement, including a book I recommend, Getting to Yes. I suggest you read such a book if you want to be a better negotiator. But here I want to highlight some features of negotiations between a hospital medicine practice and a hospital that such sources won’t specifically address.
Clearly this is complicated, and different situations call for different strategies. These are generalizations worth thinking about in any situation.
Know what is important to the hospital. I often hear hospitalists say, “We want to attend to the things that are important to the hospital, but we don’t know what those things are.” If that is really the case, the communication between the hospital and hospitalists must be awfully poor—and there is an opportunity for the hospitalists to improve it. It is worth the time and energy required to know what is on the mind of the hospital’s leadership. It may be as simple as having a person-to-person conversation with one or more hospital leaders about what they see as the institution’s most important goals—and how your practice could help achieve them. You need to be sure and understand the particulars at your hospital, but the topics below are on the mind of most executives.
Propose using additional funding to ensure adequate staffing, not raises for existing doctors. In the current environment of difficult recruiting, hospital executives are usually far more inclined to pay for increased staffing than worry about whether you need a raise just because you deserve it. So it is usually much more effective to tell the hospital, “Our practice needs more money so we can add doctors and more fully meet the demand for our services.” Much less effective is saying, “We [existing hospitalists] are working so hard that if we don’t get more money we’re going to quit.”
While the latter may be true, a hospital executive is much more likely to respond positively to paying for increased manpower so the existing doctors won’t have to continue working at unreasonably high workloads, rather than to providing money to support a raise for doctors already working unreasonably hard.
Propose additional resources to support quality improvement, and consider sharing some financial risk. Most hospital executives care about their hospital’s performance on quality measures and are willing to provide money to improve it. You might win more financial support if it is contingent on your group improving performance on quality measures.
You could propose that the hospital make additional money available to encourage and reward improved performance. You could even put existing financial support at risk and ask the hospital to match it. In other words, you could say you will contribute $5,000 or $10,000 of the money currently provided annually by the hospital per full-time equivalent hospitalist into a pool matched dollar for dollar (or some other ratio) by the hospital. Your group would get less total financial support (i.e., lose the funds put at risk) if quality doesn’t improve, but get more support if performance improved by an agreed-upon amount. A willingness to share financial risk demonstrates your commitment to success and can be compelling to the hospital.
Know your data. Hard data are far more effective than anecdotes when trying to convince the hospital of your practice’s value. Trumpet your successes, but remember that same executive will probably hear from 10 others in the same week that spending huge sums of money on their product or service will dramatically improve the hospital’s bottom line. If you’re trying to convince the hospital that every dollar spent to support your practice will provide an attractive return on investment, you need hard data to prove it.
It would be best if you could independently collect this data. But in most cases, you will have to rely on data the hospital has collected. It’s worthwhile to insist on routine reports (e.g., monthly, or no less than quarterly) from the hospital summarizing your group’s performance on quality and financial metrics (CMS core measures, patient satisfaction, cost per case). This data will be critical to you when you negotiate financial support from the hospital.
You should also have data about other hospitalist practices, such as results from the 2005-06 “SHM Survey of Hospitalist Productivity and Compensation” and other sources I discussed in a recent column (July 2007, p. 73). And if you’re able to get reliable data about other practices in your local marketplace (i.e., something more significant than just what you heard through the grapevine), be sure to share that information as well.
Agree to conditions carefully. Don’t agree to do things you would be unhappy doing just because it might help get more financial support from the hospital. Executives know it is bad business to pay people more money to get them to keep doing something they don’t want to do. Such an agreement usually leads to the hospitalists asking for more money each year to continue providing the service—and the quality of the service is often sub par if it’s something the hospitalists really don’t want to do (even if paid well to do it).
Stay focused on hospital performance—even in areas not specifically governed by your contractual relationship. Many or most hospitals that employ hospitalists assume all the financial risk for the practice. That is, the hospital agrees to make up the difference between collected professional fee revenue and the cost of operating the practice.
If the doctors underdocument and downcode, or are not compulsive about ensuring that their charges get to the billing agent, fee collections will suffer—and the hospital will end up having to pay more to support the practice.
If you are in such a situation, you should ensure that you’re helping to support optimal documentation, coding, billing, and collection practices—even if it won’t increase your paycheck but simply saves the hospital money. This will increase your chance of getting the hospital to increase financial support of your practice.
Remember your financial support isn’t a one-time negotiation; it is part of an ongoing relationship. In some negotiations, such as buying a car from a stranger, it seems reasonable to use any leverage most favorable for you. After all, you’re unlikely to ever interact with that person again. A hospitalist practice might compel the hospital to provide more support by threatening to quit suddenly. Yet it is usually a bad idea to do this because it can severely damage the long-term relationship.
Further, if you make it clear you’re going to quit unless you get more money, the hospital is in a tough spot. While the hospital may not want to lose you, any executive will realize that by making such a threat you probably aren’t committed to staying long even if you do get more financial support. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management-consulting firm. This column represents his views and is not intended to reflect an official position of SHM.
End-of-Life Predictions
The July 26 New England Journal of Medicine contained several articles of interest for hospitalists: A trial of steroids for bronchiolitis, mortality associated with type B aortic dissections, cardiovascular outcomes in patients using rofecoxib, implications of our social networks on obesity, and a terrific review of methicillin-resistant Staph aureus in soft-tissue infections.
But all these were trumped in the media by Oscar the cat.1
National Public Radio, CNN, Fox, and the BBC all covered the story about the cantankerous cat that could predict death in a community nursing home’s third-floor dementia unit with Grim Reaper-like proficiency. The 2-year-old cat was adopted and raised from kittenhood by staff members at the Steere House Nursing and Rehabilitation Center in Providence, R.I.
Nursing staff began noticing that Oscar would curl up in bed next to patients who had only hours to live. Oscar was so adept at predicting death that the nursing staff began using his prophesies to alert family members of an impending demise. Oscar rounds daily, waiting for closed doors to open when necessary and employing somewhat less-sophisticated methods than his human colleagues—namely observing and sniffing. However, this “cat scan” appears to serve as an unprecedented augur, accurately predicting the death of 25 nursing home residents.
Why all the fuss about this predictive puss in boots? To be sure it’s an intriguing story. But why does the public care so much that Oscar the cat can now be found in Wikipedia—and why should the average hospitalist care about a prognosticating cat?
The answer lies in the medical profession’s dreadful lack of ability to predict patients’ survival at the end of life. Multiple studies have shown physicians are terrible at predicting survival, most often in an overly optimistic manner. A paper in the British Medical Journal examined the ability of 343 doctors to estimate the survival of 468 patients at the time of referral to hospice.2 Only 20% of physicians were able to accurately prognosticate the time of death to within 33% of the actual survival. While median survival was 24 days doctors, on average, predicted patients would live 5.3 times longer than they did. Interestingly, the longer the doctor knew the patient the more likely they were to predict wrongly.
Most seriously ill patients value prognostic information more than they do information about therapeutic options. It is a central determinant in how patients and families make end-of-life decisions. The fact that we seem to systematically provide overly optimistic predictions has several important downstream effects.
Unduly optimistic predictions likely delay referral to palliative care providers and hospice. Doctors generally believe patients should receive hospice care for several months before death. However, patients typically receive this care for less than a month and in many cases only a few hours. Our inability to realistically predict survival most likely plays into this discrepancy and negatively affects our patients’ quality of life.
Second, our consistently overestimated predictions likely translate into patients making inappropriate or counterproductive end-of-life decisions.
We’ve all experienced the patient who continues to push for obviously futile care despite our attempts to nudge them toward a palliative approach. Yet it’s easy to see why patients who believe they have six months to live would push for more aggressive treatments. If they knew they had six weeks to live, they might choose more palliative options.
Finally, hospitalists are increasingly under the gun to decrease length of stay (LOS) and contain costs. It is estimated that more than 25% of Medicare costs (approximately $88 billion a year) are associated with care in the last year of life, much of it in the hospital. While several studies have shown that early palliative care intervention reduces LOS and cost of care, overly optimistic predictions make it less likely these timely referrals will be made.
The development of the hospitalist model, with its fractured approach to care, might provide an opportunity to improve end-of-life prognostication. Having a strong, long-lasting relationship with a patient appears to be an important predictor of inaccurate prognosis. It isn’t hard to imagine that a provider with a long relationship with a patient might have a more difficult time acknowledging a patient’s poor outcome or unwittingly be less likely to squelch a patient’s hope with a poor prognosis.
We can take advantage of the inherent discontinuities of the hospitalist model as well as the severity and immediacy of the patient’s acute illness to not only proffer an end-of-life prediction but contextualize it for the patient. This, of course, needs to be done in a sensitive manner that recognizes our brief role in their care and, as such, is most often best managed in concert with the patient’s primary care provider.
The promise of the hospital medicine movement is that we can do it better and cheaper. This is a tall order indeed. While the hospitalist model has improved efficiency and quality, future improvements will require us to adopt and develop new efficiencies and better systems of care.
It is in this vein that I believe we can and should be able to improve end-of-life care. An early salvo in this front can be a dedicated and systematic push to improve end-of-life prognostication and its myriad downstream effects. This will require a conscientious effort, more formal education, and better predictive tools. As hospitalists, we are perfectly positioned to lead these efforts. The other alternative may be to adopt more cats into our multidisciplinary team. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver and Health Sciences Center, where he serves as director of the Hospital Medicine Program, Inpatient Clinical Services in the Department of Medicine, and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Dosa DA. A day in the life of Oscar the cat. N Engl J Med. 2007;357(4):328-329.
- Christakis NA, Lamont EB. Extent and determinants of error in doctors’ prognoses in terminally ill patients: prospective cohort study. BMJ. 2000;320:469-472.
The July 26 New England Journal of Medicine contained several articles of interest for hospitalists: A trial of steroids for bronchiolitis, mortality associated with type B aortic dissections, cardiovascular outcomes in patients using rofecoxib, implications of our social networks on obesity, and a terrific review of methicillin-resistant Staph aureus in soft-tissue infections.
But all these were trumped in the media by Oscar the cat.1
National Public Radio, CNN, Fox, and the BBC all covered the story about the cantankerous cat that could predict death in a community nursing home’s third-floor dementia unit with Grim Reaper-like proficiency. The 2-year-old cat was adopted and raised from kittenhood by staff members at the Steere House Nursing and Rehabilitation Center in Providence, R.I.
Nursing staff began noticing that Oscar would curl up in bed next to patients who had only hours to live. Oscar was so adept at predicting death that the nursing staff began using his prophesies to alert family members of an impending demise. Oscar rounds daily, waiting for closed doors to open when necessary and employing somewhat less-sophisticated methods than his human colleagues—namely observing and sniffing. However, this “cat scan” appears to serve as an unprecedented augur, accurately predicting the death of 25 nursing home residents.
Why all the fuss about this predictive puss in boots? To be sure it’s an intriguing story. But why does the public care so much that Oscar the cat can now be found in Wikipedia—and why should the average hospitalist care about a prognosticating cat?
The answer lies in the medical profession’s dreadful lack of ability to predict patients’ survival at the end of life. Multiple studies have shown physicians are terrible at predicting survival, most often in an overly optimistic manner. A paper in the British Medical Journal examined the ability of 343 doctors to estimate the survival of 468 patients at the time of referral to hospice.2 Only 20% of physicians were able to accurately prognosticate the time of death to within 33% of the actual survival. While median survival was 24 days doctors, on average, predicted patients would live 5.3 times longer than they did. Interestingly, the longer the doctor knew the patient the more likely they were to predict wrongly.
Most seriously ill patients value prognostic information more than they do information about therapeutic options. It is a central determinant in how patients and families make end-of-life decisions. The fact that we seem to systematically provide overly optimistic predictions has several important downstream effects.
Unduly optimistic predictions likely delay referral to palliative care providers and hospice. Doctors generally believe patients should receive hospice care for several months before death. However, patients typically receive this care for less than a month and in many cases only a few hours. Our inability to realistically predict survival most likely plays into this discrepancy and negatively affects our patients’ quality of life.
Second, our consistently overestimated predictions likely translate into patients making inappropriate or counterproductive end-of-life decisions.
We’ve all experienced the patient who continues to push for obviously futile care despite our attempts to nudge them toward a palliative approach. Yet it’s easy to see why patients who believe they have six months to live would push for more aggressive treatments. If they knew they had six weeks to live, they might choose more palliative options.
Finally, hospitalists are increasingly under the gun to decrease length of stay (LOS) and contain costs. It is estimated that more than 25% of Medicare costs (approximately $88 billion a year) are associated with care in the last year of life, much of it in the hospital. While several studies have shown that early palliative care intervention reduces LOS and cost of care, overly optimistic predictions make it less likely these timely referrals will be made.
The development of the hospitalist model, with its fractured approach to care, might provide an opportunity to improve end-of-life prognostication. Having a strong, long-lasting relationship with a patient appears to be an important predictor of inaccurate prognosis. It isn’t hard to imagine that a provider with a long relationship with a patient might have a more difficult time acknowledging a patient’s poor outcome or unwittingly be less likely to squelch a patient’s hope with a poor prognosis.
We can take advantage of the inherent discontinuities of the hospitalist model as well as the severity and immediacy of the patient’s acute illness to not only proffer an end-of-life prediction but contextualize it for the patient. This, of course, needs to be done in a sensitive manner that recognizes our brief role in their care and, as such, is most often best managed in concert with the patient’s primary care provider.
The promise of the hospital medicine movement is that we can do it better and cheaper. This is a tall order indeed. While the hospitalist model has improved efficiency and quality, future improvements will require us to adopt and develop new efficiencies and better systems of care.
It is in this vein that I believe we can and should be able to improve end-of-life care. An early salvo in this front can be a dedicated and systematic push to improve end-of-life prognostication and its myriad downstream effects. This will require a conscientious effort, more formal education, and better predictive tools. As hospitalists, we are perfectly positioned to lead these efforts. The other alternative may be to adopt more cats into our multidisciplinary team. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver and Health Sciences Center, where he serves as director of the Hospital Medicine Program, Inpatient Clinical Services in the Department of Medicine, and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Dosa DA. A day in the life of Oscar the cat. N Engl J Med. 2007;357(4):328-329.
- Christakis NA, Lamont EB. Extent and determinants of error in doctors’ prognoses in terminally ill patients: prospective cohort study. BMJ. 2000;320:469-472.
The July 26 New England Journal of Medicine contained several articles of interest for hospitalists: A trial of steroids for bronchiolitis, mortality associated with type B aortic dissections, cardiovascular outcomes in patients using rofecoxib, implications of our social networks on obesity, and a terrific review of methicillin-resistant Staph aureus in soft-tissue infections.
But all these were trumped in the media by Oscar the cat.1
National Public Radio, CNN, Fox, and the BBC all covered the story about the cantankerous cat that could predict death in a community nursing home’s third-floor dementia unit with Grim Reaper-like proficiency. The 2-year-old cat was adopted and raised from kittenhood by staff members at the Steere House Nursing and Rehabilitation Center in Providence, R.I.
Nursing staff began noticing that Oscar would curl up in bed next to patients who had only hours to live. Oscar was so adept at predicting death that the nursing staff began using his prophesies to alert family members of an impending demise. Oscar rounds daily, waiting for closed doors to open when necessary and employing somewhat less-sophisticated methods than his human colleagues—namely observing and sniffing. However, this “cat scan” appears to serve as an unprecedented augur, accurately predicting the death of 25 nursing home residents.
Why all the fuss about this predictive puss in boots? To be sure it’s an intriguing story. But why does the public care so much that Oscar the cat can now be found in Wikipedia—and why should the average hospitalist care about a prognosticating cat?
The answer lies in the medical profession’s dreadful lack of ability to predict patients’ survival at the end of life. Multiple studies have shown physicians are terrible at predicting survival, most often in an overly optimistic manner. A paper in the British Medical Journal examined the ability of 343 doctors to estimate the survival of 468 patients at the time of referral to hospice.2 Only 20% of physicians were able to accurately prognosticate the time of death to within 33% of the actual survival. While median survival was 24 days doctors, on average, predicted patients would live 5.3 times longer than they did. Interestingly, the longer the doctor knew the patient the more likely they were to predict wrongly.
Most seriously ill patients value prognostic information more than they do information about therapeutic options. It is a central determinant in how patients and families make end-of-life decisions. The fact that we seem to systematically provide overly optimistic predictions has several important downstream effects.
Unduly optimistic predictions likely delay referral to palliative care providers and hospice. Doctors generally believe patients should receive hospice care for several months before death. However, patients typically receive this care for less than a month and in many cases only a few hours. Our inability to realistically predict survival most likely plays into this discrepancy and negatively affects our patients’ quality of life.
Second, our consistently overestimated predictions likely translate into patients making inappropriate or counterproductive end-of-life decisions.
We’ve all experienced the patient who continues to push for obviously futile care despite our attempts to nudge them toward a palliative approach. Yet it’s easy to see why patients who believe they have six months to live would push for more aggressive treatments. If they knew they had six weeks to live, they might choose more palliative options.
Finally, hospitalists are increasingly under the gun to decrease length of stay (LOS) and contain costs. It is estimated that more than 25% of Medicare costs (approximately $88 billion a year) are associated with care in the last year of life, much of it in the hospital. While several studies have shown that early palliative care intervention reduces LOS and cost of care, overly optimistic predictions make it less likely these timely referrals will be made.
The development of the hospitalist model, with its fractured approach to care, might provide an opportunity to improve end-of-life prognostication. Having a strong, long-lasting relationship with a patient appears to be an important predictor of inaccurate prognosis. It isn’t hard to imagine that a provider with a long relationship with a patient might have a more difficult time acknowledging a patient’s poor outcome or unwittingly be less likely to squelch a patient’s hope with a poor prognosis.
We can take advantage of the inherent discontinuities of the hospitalist model as well as the severity and immediacy of the patient’s acute illness to not only proffer an end-of-life prediction but contextualize it for the patient. This, of course, needs to be done in a sensitive manner that recognizes our brief role in their care and, as such, is most often best managed in concert with the patient’s primary care provider.
The promise of the hospital medicine movement is that we can do it better and cheaper. This is a tall order indeed. While the hospitalist model has improved efficiency and quality, future improvements will require us to adopt and develop new efficiencies and better systems of care.
It is in this vein that I believe we can and should be able to improve end-of-life care. An early salvo in this front can be a dedicated and systematic push to improve end-of-life prognostication and its myriad downstream effects. This will require a conscientious effort, more formal education, and better predictive tools. As hospitalists, we are perfectly positioned to lead these efforts. The other alternative may be to adopt more cats into our multidisciplinary team. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver and Health Sciences Center, where he serves as director of the Hospital Medicine Program, Inpatient Clinical Services in the Department of Medicine, and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
References
- Dosa DA. A day in the life of Oscar the cat. N Engl J Med. 2007;357(4):328-329.
- Christakis NA, Lamont EB. Extent and determinants of error in doctors’ prognoses in terminally ill patients: prospective cohort study. BMJ. 2000;320:469-472.
Information Deficits
If there is one thing most everyone in healthcare can agree on, it is that too often the information we need is not readily available.
Primary care physicians (PCP) complain that when recently hospitalized patients show up in their office—or, heaven forbid, call the first day after their hospital discharge—they don’t have their discharge information. We often hear that when hospitalists are called to admit an acutely ill patient information is sketchy or incomplete. We hear most hospitalized patients present not only as diagnostic challenges but as “unknowns” with insufficient history and medication information.
A 2006 study by the Common-wealth Fund found that in 32% of outpatient visits or referrals, crucial test results or clinical information were absent and consultation needed to be rescheduled.
In many ways the biggest knock on the hospitalist model is that, despite their better in-house availability, use of resources, or quality of care, hospitalists create another “interruption” in care coordination.
This “voltage drop” didn’t start with hospitalists. It has been around whenever patients are referred to specialists or for surgery—or most procedures, for that matter.
But hospitalists and SHM have seized on this perceived Achilles’ heel and formed coalitions to improve transitions of care and urge better care coordination. While working with many others in medicine, SHM also has had interesting discussions with key change agents not traditionally encountered in healthcare.
With grants from the John Hartford Foundation, SHM has developed state-of-the-art discharge planning tools available on the SHM Web site. And, SHM and Intel have discussed broader strategies for managing information.
In addition, I attended a recent American Hospital Association Leadership Summit and had lunch with Colin Powell, who is active at RevolutionHealth.com—the brainchild of AOL founder Steven Case.
One of RevolutionHealth.com’s projects is to create a widely used personal health record (PHR). This would be a Web database with the patient as the focal point. When a patient has a test, sees a physician, visits an ED, or is hospitalized, that information would flow into an updated record accessible by the patient or physician virtually anywhere, any time.
For hospitalists, this could be a source of complete, up-to-date medication lists, diagnoses, and test results. Hospitalists or case managers could update this PHR at discharge so it is immediately available to PCP or coverage partners, home healthcare providers, or a skilled nursing facility. This type of tool doesn’t require that every physician have an electronic medical record (EMR) and isn’t limited by interoperability issues.
Other strategies are gaining traction. At a recent conference on care coordination sponsored by the American Board of Internal Medicine Foundation (ABIM) in Montreal, Quebec, Canada, Chuck Kilo, MD, MPH, CEO of GreenField Health and The GreenField Group in Portland, Ore., showed how e-mail smoothes transitions and improves information flow.
Those in Dr. Kilo’s practice recognize that, while some professionals may have reservations about e-mails between patients and physicians, there seems less resistance to physicians and hospitals using e-mail to exchange information. With minimal expense and startup costs, PCPs can e-mail patients’ medication records, recent chart notes, and test results to a specialist for referral or a hospitalist for admission.
When the consultant or hospitalist is ready to provide information in the transition back to the PCP, e-mail is a quick solution. It’s not perfect, but it’s immediate. Certainly there are barriers to overcome: HIPAA issues are always important to resolve, and documents converted to PDFs don’t flow into an EMR. But this is a step forward.
These solutions get information to the point of decision when the patient is there and the acute need must be met. For those in the trenches this is good news—a great improvement on the hunt-and-peck paradigm.
In a broader strategic approach, SHM has advocated giving hospitalists a role in defining the standards and measures to be used in assessing performance in transitions of care. In July, SHM worked with the ABIM, the American College of Physicians, the Society of General Internal Medicine, the American Geriatrics Society, and the Agency for Healthcare Research and Quality to develop consensus on transitions-of-care standards. This group included most of the big players in the house of internal medicine as well as representatives from nursing, pharmacy, case management, home health, patients, and families. The American College of Emergency Physicians (ACEP) joined the discourse in August.
At the same time, SHM has been working with the American Medical Association’s Physician Consortium and the National Quality Forum to use standards conceived in consensus to develop measures for transitions of care. The measures would mark either stand-alone performance or performance with specific disease states (e.g., management of diabetes or acute heart failure).
Hospitalists will need resources and tools to give patients the best care and smoothest transitions (and score well on these measures). SHM has developed a Web-based quality-improvement resource room on transitions and continues to work with a broad coalition to improve the discharge process under our Hartford grant.
We add real value for our patients. But our job doesn’t end at the hospital door. Hospitalists recognize their obligation to patients as well those who will assume their care outside the hospital. Whether working on tools with Intel or RevolutionHealth or working with professional societies and organizations charged with developing performance standards and measures, hospitalists and SHM must take an active leadership role.
This is not easy stuff and can’t be solved in one meeting—or even one year.
A few years ago no one was talking much about patient safety, notes past SHM President Bob Wachter, MD, professor of medicine at the University of California, San Francisco, associate chairman of UCSF’s Department of Medicine, and chief of the Medical Service at UCSF Medical Center. That is, until the Institute of Medicine’s 2000 report “To Err Is Human: Building a Safer Health System” and some disastrous medical errors.
Transitions aren’t happening well, and care is sporadic and isolated. This is high on our agenda; SHM and hospitalists are willing to work with any group that will help all of us get closer to a solution. TH
Dr. Wellikson is the CEO of SHM.
If there is one thing most everyone in healthcare can agree on, it is that too often the information we need is not readily available.
Primary care physicians (PCP) complain that when recently hospitalized patients show up in their office—or, heaven forbid, call the first day after their hospital discharge—they don’t have their discharge information. We often hear that when hospitalists are called to admit an acutely ill patient information is sketchy or incomplete. We hear most hospitalized patients present not only as diagnostic challenges but as “unknowns” with insufficient history and medication information.
A 2006 study by the Common-wealth Fund found that in 32% of outpatient visits or referrals, crucial test results or clinical information were absent and consultation needed to be rescheduled.
In many ways the biggest knock on the hospitalist model is that, despite their better in-house availability, use of resources, or quality of care, hospitalists create another “interruption” in care coordination.
This “voltage drop” didn’t start with hospitalists. It has been around whenever patients are referred to specialists or for surgery—or most procedures, for that matter.
But hospitalists and SHM have seized on this perceived Achilles’ heel and formed coalitions to improve transitions of care and urge better care coordination. While working with many others in medicine, SHM also has had interesting discussions with key change agents not traditionally encountered in healthcare.
With grants from the John Hartford Foundation, SHM has developed state-of-the-art discharge planning tools available on the SHM Web site. And, SHM and Intel have discussed broader strategies for managing information.
In addition, I attended a recent American Hospital Association Leadership Summit and had lunch with Colin Powell, who is active at RevolutionHealth.com—the brainchild of AOL founder Steven Case.
One of RevolutionHealth.com’s projects is to create a widely used personal health record (PHR). This would be a Web database with the patient as the focal point. When a patient has a test, sees a physician, visits an ED, or is hospitalized, that information would flow into an updated record accessible by the patient or physician virtually anywhere, any time.
For hospitalists, this could be a source of complete, up-to-date medication lists, diagnoses, and test results. Hospitalists or case managers could update this PHR at discharge so it is immediately available to PCP or coverage partners, home healthcare providers, or a skilled nursing facility. This type of tool doesn’t require that every physician have an electronic medical record (EMR) and isn’t limited by interoperability issues.
Other strategies are gaining traction. At a recent conference on care coordination sponsored by the American Board of Internal Medicine Foundation (ABIM) in Montreal, Quebec, Canada, Chuck Kilo, MD, MPH, CEO of GreenField Health and The GreenField Group in Portland, Ore., showed how e-mail smoothes transitions and improves information flow.
Those in Dr. Kilo’s practice recognize that, while some professionals may have reservations about e-mails between patients and physicians, there seems less resistance to physicians and hospitals using e-mail to exchange information. With minimal expense and startup costs, PCPs can e-mail patients’ medication records, recent chart notes, and test results to a specialist for referral or a hospitalist for admission.
When the consultant or hospitalist is ready to provide information in the transition back to the PCP, e-mail is a quick solution. It’s not perfect, but it’s immediate. Certainly there are barriers to overcome: HIPAA issues are always important to resolve, and documents converted to PDFs don’t flow into an EMR. But this is a step forward.
These solutions get information to the point of decision when the patient is there and the acute need must be met. For those in the trenches this is good news—a great improvement on the hunt-and-peck paradigm.
In a broader strategic approach, SHM has advocated giving hospitalists a role in defining the standards and measures to be used in assessing performance in transitions of care. In July, SHM worked with the ABIM, the American College of Physicians, the Society of General Internal Medicine, the American Geriatrics Society, and the Agency for Healthcare Research and Quality to develop consensus on transitions-of-care standards. This group included most of the big players in the house of internal medicine as well as representatives from nursing, pharmacy, case management, home health, patients, and families. The American College of Emergency Physicians (ACEP) joined the discourse in August.
At the same time, SHM has been working with the American Medical Association’s Physician Consortium and the National Quality Forum to use standards conceived in consensus to develop measures for transitions of care. The measures would mark either stand-alone performance or performance with specific disease states (e.g., management of diabetes or acute heart failure).
Hospitalists will need resources and tools to give patients the best care and smoothest transitions (and score well on these measures). SHM has developed a Web-based quality-improvement resource room on transitions and continues to work with a broad coalition to improve the discharge process under our Hartford grant.
We add real value for our patients. But our job doesn’t end at the hospital door. Hospitalists recognize their obligation to patients as well those who will assume their care outside the hospital. Whether working on tools with Intel or RevolutionHealth or working with professional societies and organizations charged with developing performance standards and measures, hospitalists and SHM must take an active leadership role.
This is not easy stuff and can’t be solved in one meeting—or even one year.
A few years ago no one was talking much about patient safety, notes past SHM President Bob Wachter, MD, professor of medicine at the University of California, San Francisco, associate chairman of UCSF’s Department of Medicine, and chief of the Medical Service at UCSF Medical Center. That is, until the Institute of Medicine’s 2000 report “To Err Is Human: Building a Safer Health System” and some disastrous medical errors.
Transitions aren’t happening well, and care is sporadic and isolated. This is high on our agenda; SHM and hospitalists are willing to work with any group that will help all of us get closer to a solution. TH
Dr. Wellikson is the CEO of SHM.
If there is one thing most everyone in healthcare can agree on, it is that too often the information we need is not readily available.
Primary care physicians (PCP) complain that when recently hospitalized patients show up in their office—or, heaven forbid, call the first day after their hospital discharge—they don’t have their discharge information. We often hear that when hospitalists are called to admit an acutely ill patient information is sketchy or incomplete. We hear most hospitalized patients present not only as diagnostic challenges but as “unknowns” with insufficient history and medication information.
A 2006 study by the Common-wealth Fund found that in 32% of outpatient visits or referrals, crucial test results or clinical information were absent and consultation needed to be rescheduled.
In many ways the biggest knock on the hospitalist model is that, despite their better in-house availability, use of resources, or quality of care, hospitalists create another “interruption” in care coordination.
This “voltage drop” didn’t start with hospitalists. It has been around whenever patients are referred to specialists or for surgery—or most procedures, for that matter.
But hospitalists and SHM have seized on this perceived Achilles’ heel and formed coalitions to improve transitions of care and urge better care coordination. While working with many others in medicine, SHM also has had interesting discussions with key change agents not traditionally encountered in healthcare.
With grants from the John Hartford Foundation, SHM has developed state-of-the-art discharge planning tools available on the SHM Web site. And, SHM and Intel have discussed broader strategies for managing information.
In addition, I attended a recent American Hospital Association Leadership Summit and had lunch with Colin Powell, who is active at RevolutionHealth.com—the brainchild of AOL founder Steven Case.
One of RevolutionHealth.com’s projects is to create a widely used personal health record (PHR). This would be a Web database with the patient as the focal point. When a patient has a test, sees a physician, visits an ED, or is hospitalized, that information would flow into an updated record accessible by the patient or physician virtually anywhere, any time.
For hospitalists, this could be a source of complete, up-to-date medication lists, diagnoses, and test results. Hospitalists or case managers could update this PHR at discharge so it is immediately available to PCP or coverage partners, home healthcare providers, or a skilled nursing facility. This type of tool doesn’t require that every physician have an electronic medical record (EMR) and isn’t limited by interoperability issues.
Other strategies are gaining traction. At a recent conference on care coordination sponsored by the American Board of Internal Medicine Foundation (ABIM) in Montreal, Quebec, Canada, Chuck Kilo, MD, MPH, CEO of GreenField Health and The GreenField Group in Portland, Ore., showed how e-mail smoothes transitions and improves information flow.
Those in Dr. Kilo’s practice recognize that, while some professionals may have reservations about e-mails between patients and physicians, there seems less resistance to physicians and hospitals using e-mail to exchange information. With minimal expense and startup costs, PCPs can e-mail patients’ medication records, recent chart notes, and test results to a specialist for referral or a hospitalist for admission.
When the consultant or hospitalist is ready to provide information in the transition back to the PCP, e-mail is a quick solution. It’s not perfect, but it’s immediate. Certainly there are barriers to overcome: HIPAA issues are always important to resolve, and documents converted to PDFs don’t flow into an EMR. But this is a step forward.
These solutions get information to the point of decision when the patient is there and the acute need must be met. For those in the trenches this is good news—a great improvement on the hunt-and-peck paradigm.
In a broader strategic approach, SHM has advocated giving hospitalists a role in defining the standards and measures to be used in assessing performance in transitions of care. In July, SHM worked with the ABIM, the American College of Physicians, the Society of General Internal Medicine, the American Geriatrics Society, and the Agency for Healthcare Research and Quality to develop consensus on transitions-of-care standards. This group included most of the big players in the house of internal medicine as well as representatives from nursing, pharmacy, case management, home health, patients, and families. The American College of Emergency Physicians (ACEP) joined the discourse in August.
At the same time, SHM has been working with the American Medical Association’s Physician Consortium and the National Quality Forum to use standards conceived in consensus to develop measures for transitions of care. The measures would mark either stand-alone performance or performance with specific disease states (e.g., management of diabetes or acute heart failure).
Hospitalists will need resources and tools to give patients the best care and smoothest transitions (and score well on these measures). SHM has developed a Web-based quality-improvement resource room on transitions and continues to work with a broad coalition to improve the discharge process under our Hartford grant.
We add real value for our patients. But our job doesn’t end at the hospital door. Hospitalists recognize their obligation to patients as well those who will assume their care outside the hospital. Whether working on tools with Intel or RevolutionHealth or working with professional societies and organizations charged with developing performance standards and measures, hospitalists and SHM must take an active leadership role.
This is not easy stuff and can’t be solved in one meeting—or even one year.
A few years ago no one was talking much about patient safety, notes past SHM President Bob Wachter, MD, professor of medicine at the University of California, San Francisco, associate chairman of UCSF’s Department of Medicine, and chief of the Medical Service at UCSF Medical Center. That is, until the Institute of Medicine’s 2000 report “To Err Is Human: Building a Safer Health System” and some disastrous medical errors.
Transitions aren’t happening well, and care is sporadic and isolated. This is high on our agenda; SHM and hospitalists are willing to work with any group that will help all of us get closer to a solution. TH
Dr. Wellikson is the CEO of SHM.
Experts in the Elderly
The average young or middle-age person probably finds a hospital stay stressful, uncomfortable, and inconvenient. The experience can be strikingly more disruptive for a geriatric patient.
A frail elderly person can easily succumb to delirium, a fall, dehydration, polypharmacy, and deterioration in basic life skills, quickly turning even a routine hospitalization into a catastrophic downhill slide. But if a patient is lucky, she will be treated by a geriatric hospitalist—a physician who by training and temperament is uniquely suited to care for her.
Geriatric hospitalists bring heightened sensitivity and experience to treating and preventing the common syndromes that can overwhelm the elderly during hospitalizations. Fredrick Sherman, MD, FACP, medical director of Senior Health Partners and professor of geriatrics at the Mount Sinai School of Medicine in Manhattan, has been a geriatrician since the 1980s. He sees a great opportunity for hospitalist geriatricians to improve the metrics by which hospitalist programs are judged: reduced length of stay, bounceback, and morbidity. They do this, he says, with a unique blend of skills, mindset, and temperament.
“In one or two minutes at the bedside, a geriatric hospitalist can do a basic functional assessment of an elderly patient,” he says. “We can understand their ADL [activities of daily living] skills, mental status, and what resources we have to mobilize during the hospital stay and for a safe discharge plan. We don’t want to turn hospitalists into social workers, but geriatricians can teach them a body of knowledge to help them better understand and develop a holistic approach to elderly patients.”
How geriatricians work best, though, can be somewhat out of synch with hospital medicine’s fast pace. “Many hospitalists are younger and have been trained very recently,” Dr. Sherman says. “They quickly learn to take care of a 55-year-old with a [myocardial infarction], but they sometimes lack a global view of geriatric patients that is more a frame of mind than about the physician’s technical skills.”
Challenges Ahead
As hospital medicine groups integrate geriatricians into their ranks, they will have recruited major players invested in improving the care of hospitalized elderly patients. There’s a lot at stake in caring for them.
The Healthcare Cost and Utilization Project’s (HCUP) most recent figures of what hospitalizations of the elderly cost is staggering. Medicare patients account for 76% of public spending on hospital care. The costliest diagnoses for Medicare-paid hospitalizations are coronary arteriosclerosis ($44 billion), acute myocardial infarction ($31 billion), and heart failure ($29 billion). Further, 90% of elderly patients with osteoarthritis are hospitalized for elective hip or knee joint replacement therapy.
The expertise of board-certified hospitalist geriatricians will be hard to disseminate throughout the corps of hospitalists. Only a tiny fraction of the nation’s hospitalist programs claim special expertise in geriatrics. Researchers from the University of Colorado Health Sciences Center and the Mayo Clinic College of Medicine conducted a cross-sectional survey of the hospitalist community in 2003-2004 to determine the impact of the hospitalist movement on acute care geriatrics. They found:
- Out of 1,415 hospitalist programs, 11 reported geriatric innovations.
- Four developed core clinical activities, four used geriatric QI measures, three used comprehensive geriatric assessments, and two had specific protocols for elderly patients discharged to nursing facilities; and
- In terms of staffing, four had hospitalists with no special geriatric training, four employed fellowship-trained geriatricians, two had general hospitalists and geriatricians, and four used advanced practice nurses with and without geriatric training.1
Adding to the difficulty of building a cadre of geriatric hospitalists is the national paucity of geriatricians. According to the American Geriatrics Society (AGS), there were 9,000 board-certified geriatricians in 1998. A decade later there are 7,600—and the pipeline is narrow. Of 9,780 medical school graduates in 2004, only 321 were geriatricians. The AGS estimates that the United States needs 14,000 geriatricians now and 36,000 in 2030, when there will be an estimated 70 million adults 65 years and older.
But there’s hope. Hospital medicine programs, growing by leaps and bounds, offer a new career path for physicians interested in geriatrics. As the number of hospitalists continues to grow, there’s room for physicians to have an impact by staying tuned in to the special clinical, psychosocial, emotional, spiritual, and environmental needs of elderly patients.
The Breed
According to Leslie Libow, MD, distinguished clinical professor at the Jewish Home and Hospital of New York in Manhattan, physicians who pursue a career in geriatrics do so because they have the right psychological make-up to work with elderly people.
He should know. In 1968, Dr. Libow petitioned the American Board of Internal Medicine (ABIM) to recognize geriatrics as a sub-specialty of internal medicine. Shortly after ABIM recognition, Dr. Libow established a geriatric residency/fellowship at Mount Sinai—still a national leader in geriatric education.
Being a geriatric hospitalist allows physicians with a simpatico set of personality traits to thrive. One study of geriatricians who had been practicing for up to 25 years found that they shared these traits:
- Highly value enduring relationships;
- Enjoy making small but potent changes in their patients’ lives;
- Like to make a difference personally and for society;
- Prefer working in a multidisciplinary team;
- Prefer democratic, not autocratic, decision-making;
- Desire the intellectual challenges of geriatric medicine and like to teach; and
- Perceive that they have a distinct and different career path than other physicians.2
That essentially describes Purnima Joshi, chief of medicine, at Kaiser-Permanente Mid-Atlantic States at Washington Hospital Center in Washington, D.C. She directs a group of 12 hospitalists, is the group’s only geriatrician at the 800-bed tertiary care facility, and enjoys teaching residents about geriatric medicine. A family physician by trade, she was grandfathered into geriatrics in 1992 and recertified in 2002.
“I love working with the frail elderly and practicing Kaiser’s brand of medicine because I don’t do billing—I just treat patients,” Dr. Joshi says. Additionally, Kaiser simplifies record-keeping on inpatient and outpatient treatments and makes communicating with Kaiser’s outpatient doctors about post-discharge care smooth and efficient.
Dr. Joshi explains that being a geriatric hospitalist is different than specializing in general internal medicine because she customizes the approach for each patient—including tailoring therapies to life expectancy. “Guidelines and evidence-based medicine are fine and very important, and we use geriatric guidelines on our teaching service,” she says. “But geriatrics liberates your thinking as a doctor. You treat the whole person—a diabetic with three days to live, and a 90-year-old with delirium and decubitus ulcers.”
She calls herself a surrogate primary care physician, seeing 12 patients most days. She consults frequently with other hospitalists on their toughest geriatric issues and makes daily multidisciplinary rounds—with discharge planner, pharmacist, physical therapist, palliative care specialist, nurses, and resident in tow.
“We keep length of stay and guidelines in mind, but the patient is the center of my universe,” Dr. Joshi asserts. “I deliver holistic, patient-centered care and use gentle teaching tools for our residents. I have the luxury of taking time to see the patient and talk to them and their families. It’s wonderful.”
Dr. Joshi’s attitude toward her profession reflects a consistent national finding: Geriatricians rank No. 1 in nearly every study of physician career satisfaction, from the American Medical Association to the American Geriatrics Society.
Across the country, Alpesh Amin, MD, MBA, FACP, professor and chief of general internal medicine and executive director of the University of California at Irvine’s School of Medicine Hospitalist Service, is making the most of the two geriatricians on his 15-hospitalist team. Starting about eight years ago, Dr. Amin—also a member of SHM’s board of directors—turned to his hospitalist geriatricians for a host of services: geriatric assessments, co-management of psychiatric problems, perioperative consults, critical care, and palliative care consults.
“Geriatricians have such knowledge and insight into elderly patients to share with the other hospitalists,” says Dr. Amin. “That’s why they work well side by side with internal medicine and family medicine hospitalists. They keep us aware of issues in geriatrics and the literature on what works best with these patients.”
Knowing that geriatricians are scarce, Dr. Amin accesses their expertise by using a system that focuses team members’ attention on their knowledge. There are journal clubs, frequent consults, monthly meetings, teaching rounds, geriatric fellowships, and other opportunities that keep the geriatrician’s unique perspective front and center for other team members. “They are so in tune with issues related to delirium, polypharmacy, falls risk, etc.,” he says. “Our model incorporates that expertise, and it works very well. We truly work as a multidisciplinary team with ownership and accountability of the special needs of our geriatric patients.”
—Fredrick Sherman, MD, FACP, medical director of Senior Health Partners and professor of geriatrics at the Mount Sinai School of Medicine in Manhattan
A New Generation
The rapid growth of hospital medicine has encouraged new physicians to choose this career path.
Claudene George, MD, recently completed a two-year geriatric fellowship at Mount Sinai Hospital in New York City and is starting as a geriatric hospitalist at Montefiore Hospital in the Bronx. “Becoming a geriatrician sort of surprised me because I thought I’d go into internal medicine,” she says. “But I love the approach to caring for the whole person and communicating with their families.”
As part of her contract at Montefiore, she negotiated a half-day-per-week rotation at the hospital’s outpatient clinic—part of her commitment to being a well-rounded physician.
“The geriatric assessment up front is essential to find out what the patient’s and family’s goals of care are,” says Dr. George. “If they’re 80 years old and want to stay at home, we need to help them do that safely. That may mean linking them to the [visiting nurse service], a home aide, or adult day care.”
She points out that an inpatient stay also offers seniors the opportunity to be seen by subspecialists and do a lot in a short period of time. “As a hospitalist geriatrician you can see change almost immediately; you can have an impact,” she concludes.
As the hospitalist movement affords career opportunities to geriatricians, young physicians can obtain financial incentives to pursue a career in geriatrics. For instance, in 2006 South Carolina enacted a Geriatrician Loan Forgiveness program, helping physicians to repay up to $35,000 of medical school loans if they complete a geriatrics fellowship and practice in South Carolina for five years after completing medical training.
Victor Hirth, MD, medical director for the Division of Geriatric Services of Palmetto Health of Columbia, S.C., has recruited eight geriatric fellows, two of whom will be hospitalists. A recent recruit, Andres Leone, MD, went to medical school in Ecuador, recently completed a geriatric fellowship in South Carolina, and works as a hospitalist half time and at a free clinic for Hispanics half-time. “The flexibility to work as a hospitalist and in an outpatient clinic feels right to me,” says Dr. Leone.
While the number of geriatric hospitalists today is small, some predict their growing presence is inevitable.
“The baby boomers will deluge us, and they will demand so much more of hospitalists in the near future,” Dr. Sherman says. “They will have complicated issues and be very inquisitive geriatric patients.” TH
Marlene Piturro is a frequent contributor to The Hospitalist.
References
- Wald H, Huddleston J, Kramer A. Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs. J Hosp Med. 2006 Jan;1(1):29-35.
- Shah U, Aung M, Chan S, et al. Do geriatricians stay in geriatrics? Gerontol Geriatr Educ. 2006;27(1):57-65.
The average young or middle-age person probably finds a hospital stay stressful, uncomfortable, and inconvenient. The experience can be strikingly more disruptive for a geriatric patient.
A frail elderly person can easily succumb to delirium, a fall, dehydration, polypharmacy, and deterioration in basic life skills, quickly turning even a routine hospitalization into a catastrophic downhill slide. But if a patient is lucky, she will be treated by a geriatric hospitalist—a physician who by training and temperament is uniquely suited to care for her.
Geriatric hospitalists bring heightened sensitivity and experience to treating and preventing the common syndromes that can overwhelm the elderly during hospitalizations. Fredrick Sherman, MD, FACP, medical director of Senior Health Partners and professor of geriatrics at the Mount Sinai School of Medicine in Manhattan, has been a geriatrician since the 1980s. He sees a great opportunity for hospitalist geriatricians to improve the metrics by which hospitalist programs are judged: reduced length of stay, bounceback, and morbidity. They do this, he says, with a unique blend of skills, mindset, and temperament.
“In one or two minutes at the bedside, a geriatric hospitalist can do a basic functional assessment of an elderly patient,” he says. “We can understand their ADL [activities of daily living] skills, mental status, and what resources we have to mobilize during the hospital stay and for a safe discharge plan. We don’t want to turn hospitalists into social workers, but geriatricians can teach them a body of knowledge to help them better understand and develop a holistic approach to elderly patients.”
How geriatricians work best, though, can be somewhat out of synch with hospital medicine’s fast pace. “Many hospitalists are younger and have been trained very recently,” Dr. Sherman says. “They quickly learn to take care of a 55-year-old with a [myocardial infarction], but they sometimes lack a global view of geriatric patients that is more a frame of mind than about the physician’s technical skills.”
Challenges Ahead
As hospital medicine groups integrate geriatricians into their ranks, they will have recruited major players invested in improving the care of hospitalized elderly patients. There’s a lot at stake in caring for them.
The Healthcare Cost and Utilization Project’s (HCUP) most recent figures of what hospitalizations of the elderly cost is staggering. Medicare patients account for 76% of public spending on hospital care. The costliest diagnoses for Medicare-paid hospitalizations are coronary arteriosclerosis ($44 billion), acute myocardial infarction ($31 billion), and heart failure ($29 billion). Further, 90% of elderly patients with osteoarthritis are hospitalized for elective hip or knee joint replacement therapy.
The expertise of board-certified hospitalist geriatricians will be hard to disseminate throughout the corps of hospitalists. Only a tiny fraction of the nation’s hospitalist programs claim special expertise in geriatrics. Researchers from the University of Colorado Health Sciences Center and the Mayo Clinic College of Medicine conducted a cross-sectional survey of the hospitalist community in 2003-2004 to determine the impact of the hospitalist movement on acute care geriatrics. They found:
- Out of 1,415 hospitalist programs, 11 reported geriatric innovations.
- Four developed core clinical activities, four used geriatric QI measures, three used comprehensive geriatric assessments, and two had specific protocols for elderly patients discharged to nursing facilities; and
- In terms of staffing, four had hospitalists with no special geriatric training, four employed fellowship-trained geriatricians, two had general hospitalists and geriatricians, and four used advanced practice nurses with and without geriatric training.1
Adding to the difficulty of building a cadre of geriatric hospitalists is the national paucity of geriatricians. According to the American Geriatrics Society (AGS), there were 9,000 board-certified geriatricians in 1998. A decade later there are 7,600—and the pipeline is narrow. Of 9,780 medical school graduates in 2004, only 321 were geriatricians. The AGS estimates that the United States needs 14,000 geriatricians now and 36,000 in 2030, when there will be an estimated 70 million adults 65 years and older.
But there’s hope. Hospital medicine programs, growing by leaps and bounds, offer a new career path for physicians interested in geriatrics. As the number of hospitalists continues to grow, there’s room for physicians to have an impact by staying tuned in to the special clinical, psychosocial, emotional, spiritual, and environmental needs of elderly patients.
The Breed
According to Leslie Libow, MD, distinguished clinical professor at the Jewish Home and Hospital of New York in Manhattan, physicians who pursue a career in geriatrics do so because they have the right psychological make-up to work with elderly people.
He should know. In 1968, Dr. Libow petitioned the American Board of Internal Medicine (ABIM) to recognize geriatrics as a sub-specialty of internal medicine. Shortly after ABIM recognition, Dr. Libow established a geriatric residency/fellowship at Mount Sinai—still a national leader in geriatric education.
Being a geriatric hospitalist allows physicians with a simpatico set of personality traits to thrive. One study of geriatricians who had been practicing for up to 25 years found that they shared these traits:
- Highly value enduring relationships;
- Enjoy making small but potent changes in their patients’ lives;
- Like to make a difference personally and for society;
- Prefer working in a multidisciplinary team;
- Prefer democratic, not autocratic, decision-making;
- Desire the intellectual challenges of geriatric medicine and like to teach; and
- Perceive that they have a distinct and different career path than other physicians.2
That essentially describes Purnima Joshi, chief of medicine, at Kaiser-Permanente Mid-Atlantic States at Washington Hospital Center in Washington, D.C. She directs a group of 12 hospitalists, is the group’s only geriatrician at the 800-bed tertiary care facility, and enjoys teaching residents about geriatric medicine. A family physician by trade, she was grandfathered into geriatrics in 1992 and recertified in 2002.
“I love working with the frail elderly and practicing Kaiser’s brand of medicine because I don’t do billing—I just treat patients,” Dr. Joshi says. Additionally, Kaiser simplifies record-keeping on inpatient and outpatient treatments and makes communicating with Kaiser’s outpatient doctors about post-discharge care smooth and efficient.
Dr. Joshi explains that being a geriatric hospitalist is different than specializing in general internal medicine because she customizes the approach for each patient—including tailoring therapies to life expectancy. “Guidelines and evidence-based medicine are fine and very important, and we use geriatric guidelines on our teaching service,” she says. “But geriatrics liberates your thinking as a doctor. You treat the whole person—a diabetic with three days to live, and a 90-year-old with delirium and decubitus ulcers.”
She calls herself a surrogate primary care physician, seeing 12 patients most days. She consults frequently with other hospitalists on their toughest geriatric issues and makes daily multidisciplinary rounds—with discharge planner, pharmacist, physical therapist, palliative care specialist, nurses, and resident in tow.
“We keep length of stay and guidelines in mind, but the patient is the center of my universe,” Dr. Joshi asserts. “I deliver holistic, patient-centered care and use gentle teaching tools for our residents. I have the luxury of taking time to see the patient and talk to them and their families. It’s wonderful.”
Dr. Joshi’s attitude toward her profession reflects a consistent national finding: Geriatricians rank No. 1 in nearly every study of physician career satisfaction, from the American Medical Association to the American Geriatrics Society.
Across the country, Alpesh Amin, MD, MBA, FACP, professor and chief of general internal medicine and executive director of the University of California at Irvine’s School of Medicine Hospitalist Service, is making the most of the two geriatricians on his 15-hospitalist team. Starting about eight years ago, Dr. Amin—also a member of SHM’s board of directors—turned to his hospitalist geriatricians for a host of services: geriatric assessments, co-management of psychiatric problems, perioperative consults, critical care, and palliative care consults.
“Geriatricians have such knowledge and insight into elderly patients to share with the other hospitalists,” says Dr. Amin. “That’s why they work well side by side with internal medicine and family medicine hospitalists. They keep us aware of issues in geriatrics and the literature on what works best with these patients.”
Knowing that geriatricians are scarce, Dr. Amin accesses their expertise by using a system that focuses team members’ attention on their knowledge. There are journal clubs, frequent consults, monthly meetings, teaching rounds, geriatric fellowships, and other opportunities that keep the geriatrician’s unique perspective front and center for other team members. “They are so in tune with issues related to delirium, polypharmacy, falls risk, etc.,” he says. “Our model incorporates that expertise, and it works very well. We truly work as a multidisciplinary team with ownership and accountability of the special needs of our geriatric patients.”
—Fredrick Sherman, MD, FACP, medical director of Senior Health Partners and professor of geriatrics at the Mount Sinai School of Medicine in Manhattan
A New Generation
The rapid growth of hospital medicine has encouraged new physicians to choose this career path.
Claudene George, MD, recently completed a two-year geriatric fellowship at Mount Sinai Hospital in New York City and is starting as a geriatric hospitalist at Montefiore Hospital in the Bronx. “Becoming a geriatrician sort of surprised me because I thought I’d go into internal medicine,” she says. “But I love the approach to caring for the whole person and communicating with their families.”
As part of her contract at Montefiore, she negotiated a half-day-per-week rotation at the hospital’s outpatient clinic—part of her commitment to being a well-rounded physician.
“The geriatric assessment up front is essential to find out what the patient’s and family’s goals of care are,” says Dr. George. “If they’re 80 years old and want to stay at home, we need to help them do that safely. That may mean linking them to the [visiting nurse service], a home aide, or adult day care.”
She points out that an inpatient stay also offers seniors the opportunity to be seen by subspecialists and do a lot in a short period of time. “As a hospitalist geriatrician you can see change almost immediately; you can have an impact,” she concludes.
As the hospitalist movement affords career opportunities to geriatricians, young physicians can obtain financial incentives to pursue a career in geriatrics. For instance, in 2006 South Carolina enacted a Geriatrician Loan Forgiveness program, helping physicians to repay up to $35,000 of medical school loans if they complete a geriatrics fellowship and practice in South Carolina for five years after completing medical training.
Victor Hirth, MD, medical director for the Division of Geriatric Services of Palmetto Health of Columbia, S.C., has recruited eight geriatric fellows, two of whom will be hospitalists. A recent recruit, Andres Leone, MD, went to medical school in Ecuador, recently completed a geriatric fellowship in South Carolina, and works as a hospitalist half time and at a free clinic for Hispanics half-time. “The flexibility to work as a hospitalist and in an outpatient clinic feels right to me,” says Dr. Leone.
While the number of geriatric hospitalists today is small, some predict their growing presence is inevitable.
“The baby boomers will deluge us, and they will demand so much more of hospitalists in the near future,” Dr. Sherman says. “They will have complicated issues and be very inquisitive geriatric patients.” TH
Marlene Piturro is a frequent contributor to The Hospitalist.
References
- Wald H, Huddleston J, Kramer A. Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs. J Hosp Med. 2006 Jan;1(1):29-35.
- Shah U, Aung M, Chan S, et al. Do geriatricians stay in geriatrics? Gerontol Geriatr Educ. 2006;27(1):57-65.
The average young or middle-age person probably finds a hospital stay stressful, uncomfortable, and inconvenient. The experience can be strikingly more disruptive for a geriatric patient.
A frail elderly person can easily succumb to delirium, a fall, dehydration, polypharmacy, and deterioration in basic life skills, quickly turning even a routine hospitalization into a catastrophic downhill slide. But if a patient is lucky, she will be treated by a geriatric hospitalist—a physician who by training and temperament is uniquely suited to care for her.
Geriatric hospitalists bring heightened sensitivity and experience to treating and preventing the common syndromes that can overwhelm the elderly during hospitalizations. Fredrick Sherman, MD, FACP, medical director of Senior Health Partners and professor of geriatrics at the Mount Sinai School of Medicine in Manhattan, has been a geriatrician since the 1980s. He sees a great opportunity for hospitalist geriatricians to improve the metrics by which hospitalist programs are judged: reduced length of stay, bounceback, and morbidity. They do this, he says, with a unique blend of skills, mindset, and temperament.
“In one or two minutes at the bedside, a geriatric hospitalist can do a basic functional assessment of an elderly patient,” he says. “We can understand their ADL [activities of daily living] skills, mental status, and what resources we have to mobilize during the hospital stay and for a safe discharge plan. We don’t want to turn hospitalists into social workers, but geriatricians can teach them a body of knowledge to help them better understand and develop a holistic approach to elderly patients.”
How geriatricians work best, though, can be somewhat out of synch with hospital medicine’s fast pace. “Many hospitalists are younger and have been trained very recently,” Dr. Sherman says. “They quickly learn to take care of a 55-year-old with a [myocardial infarction], but they sometimes lack a global view of geriatric patients that is more a frame of mind than about the physician’s technical skills.”
Challenges Ahead
As hospital medicine groups integrate geriatricians into their ranks, they will have recruited major players invested in improving the care of hospitalized elderly patients. There’s a lot at stake in caring for them.
The Healthcare Cost and Utilization Project’s (HCUP) most recent figures of what hospitalizations of the elderly cost is staggering. Medicare patients account for 76% of public spending on hospital care. The costliest diagnoses for Medicare-paid hospitalizations are coronary arteriosclerosis ($44 billion), acute myocardial infarction ($31 billion), and heart failure ($29 billion). Further, 90% of elderly patients with osteoarthritis are hospitalized for elective hip or knee joint replacement therapy.
The expertise of board-certified hospitalist geriatricians will be hard to disseminate throughout the corps of hospitalists. Only a tiny fraction of the nation’s hospitalist programs claim special expertise in geriatrics. Researchers from the University of Colorado Health Sciences Center and the Mayo Clinic College of Medicine conducted a cross-sectional survey of the hospitalist community in 2003-2004 to determine the impact of the hospitalist movement on acute care geriatrics. They found:
- Out of 1,415 hospitalist programs, 11 reported geriatric innovations.
- Four developed core clinical activities, four used geriatric QI measures, three used comprehensive geriatric assessments, and two had specific protocols for elderly patients discharged to nursing facilities; and
- In terms of staffing, four had hospitalists with no special geriatric training, four employed fellowship-trained geriatricians, two had general hospitalists and geriatricians, and four used advanced practice nurses with and without geriatric training.1
Adding to the difficulty of building a cadre of geriatric hospitalists is the national paucity of geriatricians. According to the American Geriatrics Society (AGS), there were 9,000 board-certified geriatricians in 1998. A decade later there are 7,600—and the pipeline is narrow. Of 9,780 medical school graduates in 2004, only 321 were geriatricians. The AGS estimates that the United States needs 14,000 geriatricians now and 36,000 in 2030, when there will be an estimated 70 million adults 65 years and older.
But there’s hope. Hospital medicine programs, growing by leaps and bounds, offer a new career path for physicians interested in geriatrics. As the number of hospitalists continues to grow, there’s room for physicians to have an impact by staying tuned in to the special clinical, psychosocial, emotional, spiritual, and environmental needs of elderly patients.
The Breed
According to Leslie Libow, MD, distinguished clinical professor at the Jewish Home and Hospital of New York in Manhattan, physicians who pursue a career in geriatrics do so because they have the right psychological make-up to work with elderly people.
He should know. In 1968, Dr. Libow petitioned the American Board of Internal Medicine (ABIM) to recognize geriatrics as a sub-specialty of internal medicine. Shortly after ABIM recognition, Dr. Libow established a geriatric residency/fellowship at Mount Sinai—still a national leader in geriatric education.
Being a geriatric hospitalist allows physicians with a simpatico set of personality traits to thrive. One study of geriatricians who had been practicing for up to 25 years found that they shared these traits:
- Highly value enduring relationships;
- Enjoy making small but potent changes in their patients’ lives;
- Like to make a difference personally and for society;
- Prefer working in a multidisciplinary team;
- Prefer democratic, not autocratic, decision-making;
- Desire the intellectual challenges of geriatric medicine and like to teach; and
- Perceive that they have a distinct and different career path than other physicians.2
That essentially describes Purnima Joshi, chief of medicine, at Kaiser-Permanente Mid-Atlantic States at Washington Hospital Center in Washington, D.C. She directs a group of 12 hospitalists, is the group’s only geriatrician at the 800-bed tertiary care facility, and enjoys teaching residents about geriatric medicine. A family physician by trade, she was grandfathered into geriatrics in 1992 and recertified in 2002.
“I love working with the frail elderly and practicing Kaiser’s brand of medicine because I don’t do billing—I just treat patients,” Dr. Joshi says. Additionally, Kaiser simplifies record-keeping on inpatient and outpatient treatments and makes communicating with Kaiser’s outpatient doctors about post-discharge care smooth and efficient.
Dr. Joshi explains that being a geriatric hospitalist is different than specializing in general internal medicine because she customizes the approach for each patient—including tailoring therapies to life expectancy. “Guidelines and evidence-based medicine are fine and very important, and we use geriatric guidelines on our teaching service,” she says. “But geriatrics liberates your thinking as a doctor. You treat the whole person—a diabetic with three days to live, and a 90-year-old with delirium and decubitus ulcers.”
She calls herself a surrogate primary care physician, seeing 12 patients most days. She consults frequently with other hospitalists on their toughest geriatric issues and makes daily multidisciplinary rounds—with discharge planner, pharmacist, physical therapist, palliative care specialist, nurses, and resident in tow.
“We keep length of stay and guidelines in mind, but the patient is the center of my universe,” Dr. Joshi asserts. “I deliver holistic, patient-centered care and use gentle teaching tools for our residents. I have the luxury of taking time to see the patient and talk to them and their families. It’s wonderful.”
Dr. Joshi’s attitude toward her profession reflects a consistent national finding: Geriatricians rank No. 1 in nearly every study of physician career satisfaction, from the American Medical Association to the American Geriatrics Society.
Across the country, Alpesh Amin, MD, MBA, FACP, professor and chief of general internal medicine and executive director of the University of California at Irvine’s School of Medicine Hospitalist Service, is making the most of the two geriatricians on his 15-hospitalist team. Starting about eight years ago, Dr. Amin—also a member of SHM’s board of directors—turned to his hospitalist geriatricians for a host of services: geriatric assessments, co-management of psychiatric problems, perioperative consults, critical care, and palliative care consults.
“Geriatricians have such knowledge and insight into elderly patients to share with the other hospitalists,” says Dr. Amin. “That’s why they work well side by side with internal medicine and family medicine hospitalists. They keep us aware of issues in geriatrics and the literature on what works best with these patients.”
Knowing that geriatricians are scarce, Dr. Amin accesses their expertise by using a system that focuses team members’ attention on their knowledge. There are journal clubs, frequent consults, monthly meetings, teaching rounds, geriatric fellowships, and other opportunities that keep the geriatrician’s unique perspective front and center for other team members. “They are so in tune with issues related to delirium, polypharmacy, falls risk, etc.,” he says. “Our model incorporates that expertise, and it works very well. We truly work as a multidisciplinary team with ownership and accountability of the special needs of our geriatric patients.”
—Fredrick Sherman, MD, FACP, medical director of Senior Health Partners and professor of geriatrics at the Mount Sinai School of Medicine in Manhattan
A New Generation
The rapid growth of hospital medicine has encouraged new physicians to choose this career path.
Claudene George, MD, recently completed a two-year geriatric fellowship at Mount Sinai Hospital in New York City and is starting as a geriatric hospitalist at Montefiore Hospital in the Bronx. “Becoming a geriatrician sort of surprised me because I thought I’d go into internal medicine,” she says. “But I love the approach to caring for the whole person and communicating with their families.”
As part of her contract at Montefiore, she negotiated a half-day-per-week rotation at the hospital’s outpatient clinic—part of her commitment to being a well-rounded physician.
“The geriatric assessment up front is essential to find out what the patient’s and family’s goals of care are,” says Dr. George. “If they’re 80 years old and want to stay at home, we need to help them do that safely. That may mean linking them to the [visiting nurse service], a home aide, or adult day care.”
She points out that an inpatient stay also offers seniors the opportunity to be seen by subspecialists and do a lot in a short period of time. “As a hospitalist geriatrician you can see change almost immediately; you can have an impact,” she concludes.
As the hospitalist movement affords career opportunities to geriatricians, young physicians can obtain financial incentives to pursue a career in geriatrics. For instance, in 2006 South Carolina enacted a Geriatrician Loan Forgiveness program, helping physicians to repay up to $35,000 of medical school loans if they complete a geriatrics fellowship and practice in South Carolina for five years after completing medical training.
Victor Hirth, MD, medical director for the Division of Geriatric Services of Palmetto Health of Columbia, S.C., has recruited eight geriatric fellows, two of whom will be hospitalists. A recent recruit, Andres Leone, MD, went to medical school in Ecuador, recently completed a geriatric fellowship in South Carolina, and works as a hospitalist half time and at a free clinic for Hispanics half-time. “The flexibility to work as a hospitalist and in an outpatient clinic feels right to me,” says Dr. Leone.
While the number of geriatric hospitalists today is small, some predict their growing presence is inevitable.
“The baby boomers will deluge us, and they will demand so much more of hospitalists in the near future,” Dr. Sherman says. “They will have complicated issues and be very inquisitive geriatric patients.” TH
Marlene Piturro is a frequent contributor to The Hospitalist.
References
- Wald H, Huddleston J, Kramer A. Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs. J Hosp Med. 2006 Jan;1(1):29-35.
- Shah U, Aung M, Chan S, et al. Do geriatricians stay in geriatrics? Gerontol Geriatr Educ. 2006;27(1):57-65.