User login
American Urogynecologic Society (AUGS): Annual Scientific Meeting
Urinary tract injury incidence during laparoscopic hysterectomy pegged at 1.3%
LAS VEGAS – Urinary tract injury occurs in an estimated 1.3% of laparoscopic hysterectomies, with ureteral injuries about as common as bladder injuries, results from large analysis of HMO patients showed.
"Given the rising popularity of minimally invasive surgery, laparoscopic hysterectomy has emerged as one of the modalities of choice for benign gynecologic hysterectomies," Dr. Jasmine Tan-Kim said in a poster presented at the annual meeting of the American Urogynecologic Society. "This increase in popularity is largely attributable to the decreased pain, length of hospital stay, and shorter postoperative recovery when compared to abdominal hysterectomy."
In an effort to evaluate the incidence, detection, and characteristics of urinary tract injury with total laparoscopic hysterectomy and laparoscopic supracervical hysterectomy, Dr. Kim and her associates retrospectively analyzed data from 3,523 patients who underwent laparoscopic hysterectomy at Kaiser Permanente San Diego Medical Center from 2001 to 2012. They collected demographic characteristics, surgical techniques, and intra- and post-operative complications, using multivariable logistic regression to assess the independent risk factors for ureteral or bladder injury.
The mean age of patients was 46 years, their median body mass index was 29 kg/m2, and 20% had intraoperative cystoscopy.
The overall incidence of urinary tract injury was 1.3%. Of the 46 injuries, 19 (0.54%) were ureteral, 25 (0.71%) were bladder injuries, and two (0.06%) were both, reported Dr. Kim of the division of female pelvic medicine and reconstructive surgery at Kaiser Permanente, San Diego.
In more than half (57%) of urinary tract injury cases, the repair was performed by gynecologists, gynecologic oncologists, or urogynecologists, while the remainder (43%) were performed by urologists. There was no difference between total laparoscopic hysterectomy and laparoscopic supracervical hysterectomy in terms of risk of ureteral or bladder injury, Dr. Kim said.
Of the 21 ureteral injuries, 71% were diagnosed postoperatively and 29% were diagnosed intraoperatively. Of the 27 bladder injuries, 85% were identified intraoperatively and 15% were identified postoperatively.
The regression analysis revealed that risk factors significantly associated with ureteral injury were a BMI of 26-30 kg/m2 (odds ratio, 4.07) and African American ethnicity (OR, 3.14). Risk factors significantly associated with bladder injury were BMI less than 26 kg/m2 (OR, 3.86), presence of endometriosis (OR, 2.85), and nulliparity (OR, 0.27 for no deliveries vs. two deliveries and OR, 0.11 for no deliveries vs. three or more deliveries).
The researchers stated that they had no relevant financial disclosures.
LAS VEGAS – Urinary tract injury occurs in an estimated 1.3% of laparoscopic hysterectomies, with ureteral injuries about as common as bladder injuries, results from large analysis of HMO patients showed.
"Given the rising popularity of minimally invasive surgery, laparoscopic hysterectomy has emerged as one of the modalities of choice for benign gynecologic hysterectomies," Dr. Jasmine Tan-Kim said in a poster presented at the annual meeting of the American Urogynecologic Society. "This increase in popularity is largely attributable to the decreased pain, length of hospital stay, and shorter postoperative recovery when compared to abdominal hysterectomy."
In an effort to evaluate the incidence, detection, and characteristics of urinary tract injury with total laparoscopic hysterectomy and laparoscopic supracervical hysterectomy, Dr. Kim and her associates retrospectively analyzed data from 3,523 patients who underwent laparoscopic hysterectomy at Kaiser Permanente San Diego Medical Center from 2001 to 2012. They collected demographic characteristics, surgical techniques, and intra- and post-operative complications, using multivariable logistic regression to assess the independent risk factors for ureteral or bladder injury.
The mean age of patients was 46 years, their median body mass index was 29 kg/m2, and 20% had intraoperative cystoscopy.
The overall incidence of urinary tract injury was 1.3%. Of the 46 injuries, 19 (0.54%) were ureteral, 25 (0.71%) were bladder injuries, and two (0.06%) were both, reported Dr. Kim of the division of female pelvic medicine and reconstructive surgery at Kaiser Permanente, San Diego.
In more than half (57%) of urinary tract injury cases, the repair was performed by gynecologists, gynecologic oncologists, or urogynecologists, while the remainder (43%) were performed by urologists. There was no difference between total laparoscopic hysterectomy and laparoscopic supracervical hysterectomy in terms of risk of ureteral or bladder injury, Dr. Kim said.
Of the 21 ureteral injuries, 71% were diagnosed postoperatively and 29% were diagnosed intraoperatively. Of the 27 bladder injuries, 85% were identified intraoperatively and 15% were identified postoperatively.
The regression analysis revealed that risk factors significantly associated with ureteral injury were a BMI of 26-30 kg/m2 (odds ratio, 4.07) and African American ethnicity (OR, 3.14). Risk factors significantly associated with bladder injury were BMI less than 26 kg/m2 (OR, 3.86), presence of endometriosis (OR, 2.85), and nulliparity (OR, 0.27 for no deliveries vs. two deliveries and OR, 0.11 for no deliveries vs. three or more deliveries).
The researchers stated that they had no relevant financial disclosures.
LAS VEGAS – Urinary tract injury occurs in an estimated 1.3% of laparoscopic hysterectomies, with ureteral injuries about as common as bladder injuries, results from large analysis of HMO patients showed.
"Given the rising popularity of minimally invasive surgery, laparoscopic hysterectomy has emerged as one of the modalities of choice for benign gynecologic hysterectomies," Dr. Jasmine Tan-Kim said in a poster presented at the annual meeting of the American Urogynecologic Society. "This increase in popularity is largely attributable to the decreased pain, length of hospital stay, and shorter postoperative recovery when compared to abdominal hysterectomy."
In an effort to evaluate the incidence, detection, and characteristics of urinary tract injury with total laparoscopic hysterectomy and laparoscopic supracervical hysterectomy, Dr. Kim and her associates retrospectively analyzed data from 3,523 patients who underwent laparoscopic hysterectomy at Kaiser Permanente San Diego Medical Center from 2001 to 2012. They collected demographic characteristics, surgical techniques, and intra- and post-operative complications, using multivariable logistic regression to assess the independent risk factors for ureteral or bladder injury.
The mean age of patients was 46 years, their median body mass index was 29 kg/m2, and 20% had intraoperative cystoscopy.
The overall incidence of urinary tract injury was 1.3%. Of the 46 injuries, 19 (0.54%) were ureteral, 25 (0.71%) were bladder injuries, and two (0.06%) were both, reported Dr. Kim of the division of female pelvic medicine and reconstructive surgery at Kaiser Permanente, San Diego.
In more than half (57%) of urinary tract injury cases, the repair was performed by gynecologists, gynecologic oncologists, or urogynecologists, while the remainder (43%) were performed by urologists. There was no difference between total laparoscopic hysterectomy and laparoscopic supracervical hysterectomy in terms of risk of ureteral or bladder injury, Dr. Kim said.
Of the 21 ureteral injuries, 71% were diagnosed postoperatively and 29% were diagnosed intraoperatively. Of the 27 bladder injuries, 85% were identified intraoperatively and 15% were identified postoperatively.
The regression analysis revealed that risk factors significantly associated with ureteral injury were a BMI of 26-30 kg/m2 (odds ratio, 4.07) and African American ethnicity (OR, 3.14). Risk factors significantly associated with bladder injury were BMI less than 26 kg/m2 (OR, 3.86), presence of endometriosis (OR, 2.85), and nulliparity (OR, 0.27 for no deliveries vs. two deliveries and OR, 0.11 for no deliveries vs. three or more deliveries).
The researchers stated that they had no relevant financial disclosures.
AT THE AUGS ANNUAL MEETING
Major finding: Among 3,523 laparoscopic hysterectomies performed from 2001 to 2012, the incidence of urinary tract injury was 1.3%.
Data source: A review of patients who underwent laparoscopic hysterectomy at Kaiser Permanente San Diego Medical Center.
Disclosures: The researchers stated that they had no relevant financial disclosures.
Lower urinary tract symptoms bother obese women more than obese men
LAS VEGAS – Obese women report significantly greater lower urinary tract symptoms and worse overall quality of life than do obese men, results from a single-center study showed.
"Over one-third of U.S. adults are obese and 60% are considered overweight," Dr. Margarita M. Aponte said in a poster presented during the annual meeting of the American Urogynecologic Society. "In women, obesity is an independent risk factor for pelvic floor disorders, and in men, obesity has been associated with an increase in storage symptoms and benign prostatic hypertrophy."
Dr. Aponte and her associates at New York University Langone Medical Center recruited 134 men and women who were planning to undergo laparoscopic-assisted gastric banding (LAGB). They collected demographic information and clinical data, and administered validated questionnaires preoperatively, including the Overactive Bladder Questionnaire (OAB-q), the International Consultation on Incontinence Questionnaire–Short Form (ICIQ-SF), the Medical, Epidemiologic and Social aspects of Aging (MESA) scale, and the International Prostate Symptom Score (IPSS), to evaluate lower urinary tract symptoms. The investigators also evaluated quality of life preoperatively with the King’s Health Questionnaire (KHQ). The purpose was to characterize and differentiate baseline lower urinary tract symptoms and quality of life scores in obese men and women who were undergoing LAGB.
Of the 134 patients, 92 (69%) were women and their mean age was 42 years. The researchers reported that on the OAB-Q, women had higher scores in symptom severity (P = .036), concern (P = .002), and health-related quality of life (P = .028) than did men. Increasing body mass index (BMI) was associated with greater concern (P = .024), social effects (P = .021), and total health-related quality of life scores (P = .051). Increasing age and having diabetes were associated with higher scores in almost all OAB-Q domains.
Compared with men, women also had a higher total International Consultation on Incontinence Questionnaire–Short Form score (P = .000) and International Prostate Symptom Score (P = .008), and increasing BMI was associated with incontinence severity in the ICIQ (P = .01).
On the King’s Health Questionnaire, women had higher scores in incontinence impact (P = .045), role limitations (P = .016), and severity (P = .000). Increasing BMI was associated with poor general health perception (P = .006), increased role limitations (P = .005), and severity (P = .002). In men, no association was observed between obesity, age, or the presence of diabetes and any of the KHQ domains.
The researchers said they had no relevant financial disclosures.
LAS VEGAS – Obese women report significantly greater lower urinary tract symptoms and worse overall quality of life than do obese men, results from a single-center study showed.
"Over one-third of U.S. adults are obese and 60% are considered overweight," Dr. Margarita M. Aponte said in a poster presented during the annual meeting of the American Urogynecologic Society. "In women, obesity is an independent risk factor for pelvic floor disorders, and in men, obesity has been associated with an increase in storage symptoms and benign prostatic hypertrophy."
Dr. Aponte and her associates at New York University Langone Medical Center recruited 134 men and women who were planning to undergo laparoscopic-assisted gastric banding (LAGB). They collected demographic information and clinical data, and administered validated questionnaires preoperatively, including the Overactive Bladder Questionnaire (OAB-q), the International Consultation on Incontinence Questionnaire–Short Form (ICIQ-SF), the Medical, Epidemiologic and Social aspects of Aging (MESA) scale, and the International Prostate Symptom Score (IPSS), to evaluate lower urinary tract symptoms. The investigators also evaluated quality of life preoperatively with the King’s Health Questionnaire (KHQ). The purpose was to characterize and differentiate baseline lower urinary tract symptoms and quality of life scores in obese men and women who were undergoing LAGB.
Of the 134 patients, 92 (69%) were women and their mean age was 42 years. The researchers reported that on the OAB-Q, women had higher scores in symptom severity (P = .036), concern (P = .002), and health-related quality of life (P = .028) than did men. Increasing body mass index (BMI) was associated with greater concern (P = .024), social effects (P = .021), and total health-related quality of life scores (P = .051). Increasing age and having diabetes were associated with higher scores in almost all OAB-Q domains.
Compared with men, women also had a higher total International Consultation on Incontinence Questionnaire–Short Form score (P = .000) and International Prostate Symptom Score (P = .008), and increasing BMI was associated with incontinence severity in the ICIQ (P = .01).
On the King’s Health Questionnaire, women had higher scores in incontinence impact (P = .045), role limitations (P = .016), and severity (P = .000). Increasing BMI was associated with poor general health perception (P = .006), increased role limitations (P = .005), and severity (P = .002). In men, no association was observed between obesity, age, or the presence of diabetes and any of the KHQ domains.
The researchers said they had no relevant financial disclosures.
LAS VEGAS – Obese women report significantly greater lower urinary tract symptoms and worse overall quality of life than do obese men, results from a single-center study showed.
"Over one-third of U.S. adults are obese and 60% are considered overweight," Dr. Margarita M. Aponte said in a poster presented during the annual meeting of the American Urogynecologic Society. "In women, obesity is an independent risk factor for pelvic floor disorders, and in men, obesity has been associated with an increase in storage symptoms and benign prostatic hypertrophy."
Dr. Aponte and her associates at New York University Langone Medical Center recruited 134 men and women who were planning to undergo laparoscopic-assisted gastric banding (LAGB). They collected demographic information and clinical data, and administered validated questionnaires preoperatively, including the Overactive Bladder Questionnaire (OAB-q), the International Consultation on Incontinence Questionnaire–Short Form (ICIQ-SF), the Medical, Epidemiologic and Social aspects of Aging (MESA) scale, and the International Prostate Symptom Score (IPSS), to evaluate lower urinary tract symptoms. The investigators also evaluated quality of life preoperatively with the King’s Health Questionnaire (KHQ). The purpose was to characterize and differentiate baseline lower urinary tract symptoms and quality of life scores in obese men and women who were undergoing LAGB.
Of the 134 patients, 92 (69%) were women and their mean age was 42 years. The researchers reported that on the OAB-Q, women had higher scores in symptom severity (P = .036), concern (P = .002), and health-related quality of life (P = .028) than did men. Increasing body mass index (BMI) was associated with greater concern (P = .024), social effects (P = .021), and total health-related quality of life scores (P = .051). Increasing age and having diabetes were associated with higher scores in almost all OAB-Q domains.
Compared with men, women also had a higher total International Consultation on Incontinence Questionnaire–Short Form score (P = .000) and International Prostate Symptom Score (P = .008), and increasing BMI was associated with incontinence severity in the ICIQ (P = .01).
On the King’s Health Questionnaire, women had higher scores in incontinence impact (P = .045), role limitations (P = .016), and severity (P = .000). Increasing BMI was associated with poor general health perception (P = .006), increased role limitations (P = .005), and severity (P = .002). In men, no association was observed between obesity, age, or the presence of diabetes and any of the KHQ domains.
The researchers said they had no relevant financial disclosures.
AT THE AUGS ANNUAL MEETING
Major finding: On the Overactive Bladder Questionnaire, more obese women than obese men had higher scores in symptom severity (P = .036), concern (P = 0.002), and health-related quality of life (P =.028).
Data source: A study of baseline data from134 men and women who were planning to undergo laparoscopic-assisted gastric banding.
Disclosures: The researchers said they had no relevant financial disclosures.
Application of estrogen cream before hysterectomy thickened tissue
LAS VEGAS – Application of vaginal estrogen cream 6 weeks before undergoing hysterectomy resulted in increased thickness of both the vaginal epithelium and the muscularis, results of a randomized trial showed.
"Surgical repair remains the mainstay treatment for symptomatic prolapse," Dr. David D. Rahn said at the annual meeting of the American Urogynecologic Society. "Despite advances in surgical techniques, reoperation for recurrent prolapse is common. Clearly, there are significant trade-offs to adding graft material to surgical repairs. Given that our population is aging, there will be more women requiring surgical management of prolapse. Therefore, there’s a need to identify adjuncts to native tissue prolapse repairs that may minimize recurrent disease or lessen the likelihood of graft-associated complications."
Both basic science and clinical investigations indicate that estrogen plays an important role in the function of supportive connective tissues at the pelvic floor, said Dr. Rahn of the department of obstetrics and gynecology at the University of Texas Southwestern Medical Center, Dallas. However, clinical research regarding the effects of systemic hormone therapy on prevention or treatment of prolapse "has led to contradictory findings, with some studies suggesting a protective effect while others demonstrating either no difference or perhaps higher rates of prolapse in women using hormone therapy."
To determine the effects of vaginal estrogen on collagen synthesis in connective tissues of the vaginal muscularis and mucosa in postmenopausal women, Dr. Rahn and his associates enrolled 30 women who were 1-10 year postmenopausal with at least stage 2 anterior or apical prolapse planning total hysterectomy as part of a surgical repair. They excluded women with a body mass index of greater than 35 kg/m2, current users of tobacco or steroids, and those with a vaginal infection. Of the 30 patients, 15 were randomized to receive Premarin, a conjugated estrogens cream, while the remaining 15 received placebo cream. "They were instructed to apply 1 g using the plastic applicator nightly for 2 weeks and then twice weekly for 4 more weeks until surgery," Dr. Rahn said. "A computer-generated randomization table was used to allocate patients to one of the treatment groups. Only the pharmacist remained unblinded to treatment allocation."
The researchers performed histomorphology, quantitative polymerase chain reaction, hydroxyproline assays, and immunoblot analyses to evaluate vaginal epithelium and muscularis from standardized full thickness anterior vaginal cuff biopsies obtained at the time of surgery. Zymography was used to assess matrix metalloproteinase (MMP) activity.
Full biopsy data were available from 12 patients in each arm. Dr. Rahn reported that their mean age was 57 years, slightly more than half (57%) were Hispanic, and their mean BMI was 30.5 kg/m2. On histological assessment, the epithelial and the muscularis layer were thicker among samples from women treated with estrogen. Specifically, mean epithelial thickness was increased 1.8-fold in the estrogen group, while the muscularis thickness was increased 2.7-fold.
To determine if these estrogen-induced increases in muscularis thickness were associated with increased collagen synthesis, relative messenger RNA levels of collagen type I, alpha-1, type I, alpha-2, and collagen type III mRNA were quantified in the muscularis samples from both groups. Collagen I, alpha-1 was increased sixfold in the vaginal muscularis in the estrogen group, while collagen type I, alpha-2 and collagen type III mRNA were increased 1.8- and 2.5-fold, respectively.
Immunoblot analysis was completed in four patients in each treatment group who had sufficient tissue for protein analysis. Collagen type 1a monomers, dimers, and trimers were all increased 10-fold in the muscularis from samples of women treated with estrogen. In contrast, differences in collagen 3 protein were not significant. Further, with respect to matrix degradation, in patients adherent with local estrogen, human macrophage elastase mRNA was suppressed in the vaginal mucosa from estrogen-treated participants, and MMP-9 activity was decreased 6-fold in the mucosa and 4-fold in the muscularis. There was no change in expression of several protease inhibitors.
"Our findings from this trial suggest that 6 weeks of preoperative vaginal estrogen in postmenopausal women with prolapse may improve the substrate for suture placement at the time of repair while mitigating surgical induction of several degradative enzymes," Dr. Rahn concluded.
The study was funded by an Astellas Research Award/AUGS Foundation grant. Dr. Rahn said that he had no relevant financial conflicts to disclose.
LAS VEGAS – Application of vaginal estrogen cream 6 weeks before undergoing hysterectomy resulted in increased thickness of both the vaginal epithelium and the muscularis, results of a randomized trial showed.
"Surgical repair remains the mainstay treatment for symptomatic prolapse," Dr. David D. Rahn said at the annual meeting of the American Urogynecologic Society. "Despite advances in surgical techniques, reoperation for recurrent prolapse is common. Clearly, there are significant trade-offs to adding graft material to surgical repairs. Given that our population is aging, there will be more women requiring surgical management of prolapse. Therefore, there’s a need to identify adjuncts to native tissue prolapse repairs that may minimize recurrent disease or lessen the likelihood of graft-associated complications."
Both basic science and clinical investigations indicate that estrogen plays an important role in the function of supportive connective tissues at the pelvic floor, said Dr. Rahn of the department of obstetrics and gynecology at the University of Texas Southwestern Medical Center, Dallas. However, clinical research regarding the effects of systemic hormone therapy on prevention or treatment of prolapse "has led to contradictory findings, with some studies suggesting a protective effect while others demonstrating either no difference or perhaps higher rates of prolapse in women using hormone therapy."
To determine the effects of vaginal estrogen on collagen synthesis in connective tissues of the vaginal muscularis and mucosa in postmenopausal women, Dr. Rahn and his associates enrolled 30 women who were 1-10 year postmenopausal with at least stage 2 anterior or apical prolapse planning total hysterectomy as part of a surgical repair. They excluded women with a body mass index of greater than 35 kg/m2, current users of tobacco or steroids, and those with a vaginal infection. Of the 30 patients, 15 were randomized to receive Premarin, a conjugated estrogens cream, while the remaining 15 received placebo cream. "They were instructed to apply 1 g using the plastic applicator nightly for 2 weeks and then twice weekly for 4 more weeks until surgery," Dr. Rahn said. "A computer-generated randomization table was used to allocate patients to one of the treatment groups. Only the pharmacist remained unblinded to treatment allocation."
The researchers performed histomorphology, quantitative polymerase chain reaction, hydroxyproline assays, and immunoblot analyses to evaluate vaginal epithelium and muscularis from standardized full thickness anterior vaginal cuff biopsies obtained at the time of surgery. Zymography was used to assess matrix metalloproteinase (MMP) activity.
Full biopsy data were available from 12 patients in each arm. Dr. Rahn reported that their mean age was 57 years, slightly more than half (57%) were Hispanic, and their mean BMI was 30.5 kg/m2. On histological assessment, the epithelial and the muscularis layer were thicker among samples from women treated with estrogen. Specifically, mean epithelial thickness was increased 1.8-fold in the estrogen group, while the muscularis thickness was increased 2.7-fold.
To determine if these estrogen-induced increases in muscularis thickness were associated with increased collagen synthesis, relative messenger RNA levels of collagen type I, alpha-1, type I, alpha-2, and collagen type III mRNA were quantified in the muscularis samples from both groups. Collagen I, alpha-1 was increased sixfold in the vaginal muscularis in the estrogen group, while collagen type I, alpha-2 and collagen type III mRNA were increased 1.8- and 2.5-fold, respectively.
Immunoblot analysis was completed in four patients in each treatment group who had sufficient tissue for protein analysis. Collagen type 1a monomers, dimers, and trimers were all increased 10-fold in the muscularis from samples of women treated with estrogen. In contrast, differences in collagen 3 protein were not significant. Further, with respect to matrix degradation, in patients adherent with local estrogen, human macrophage elastase mRNA was suppressed in the vaginal mucosa from estrogen-treated participants, and MMP-9 activity was decreased 6-fold in the mucosa and 4-fold in the muscularis. There was no change in expression of several protease inhibitors.
"Our findings from this trial suggest that 6 weeks of preoperative vaginal estrogen in postmenopausal women with prolapse may improve the substrate for suture placement at the time of repair while mitigating surgical induction of several degradative enzymes," Dr. Rahn concluded.
The study was funded by an Astellas Research Award/AUGS Foundation grant. Dr. Rahn said that he had no relevant financial conflicts to disclose.
LAS VEGAS – Application of vaginal estrogen cream 6 weeks before undergoing hysterectomy resulted in increased thickness of both the vaginal epithelium and the muscularis, results of a randomized trial showed.
"Surgical repair remains the mainstay treatment for symptomatic prolapse," Dr. David D. Rahn said at the annual meeting of the American Urogynecologic Society. "Despite advances in surgical techniques, reoperation for recurrent prolapse is common. Clearly, there are significant trade-offs to adding graft material to surgical repairs. Given that our population is aging, there will be more women requiring surgical management of prolapse. Therefore, there’s a need to identify adjuncts to native tissue prolapse repairs that may minimize recurrent disease or lessen the likelihood of graft-associated complications."
Both basic science and clinical investigations indicate that estrogen plays an important role in the function of supportive connective tissues at the pelvic floor, said Dr. Rahn of the department of obstetrics and gynecology at the University of Texas Southwestern Medical Center, Dallas. However, clinical research regarding the effects of systemic hormone therapy on prevention or treatment of prolapse "has led to contradictory findings, with some studies suggesting a protective effect while others demonstrating either no difference or perhaps higher rates of prolapse in women using hormone therapy."
To determine the effects of vaginal estrogen on collagen synthesis in connective tissues of the vaginal muscularis and mucosa in postmenopausal women, Dr. Rahn and his associates enrolled 30 women who were 1-10 year postmenopausal with at least stage 2 anterior or apical prolapse planning total hysterectomy as part of a surgical repair. They excluded women with a body mass index of greater than 35 kg/m2, current users of tobacco or steroids, and those with a vaginal infection. Of the 30 patients, 15 were randomized to receive Premarin, a conjugated estrogens cream, while the remaining 15 received placebo cream. "They were instructed to apply 1 g using the plastic applicator nightly for 2 weeks and then twice weekly for 4 more weeks until surgery," Dr. Rahn said. "A computer-generated randomization table was used to allocate patients to one of the treatment groups. Only the pharmacist remained unblinded to treatment allocation."
The researchers performed histomorphology, quantitative polymerase chain reaction, hydroxyproline assays, and immunoblot analyses to evaluate vaginal epithelium and muscularis from standardized full thickness anterior vaginal cuff biopsies obtained at the time of surgery. Zymography was used to assess matrix metalloproteinase (MMP) activity.
Full biopsy data were available from 12 patients in each arm. Dr. Rahn reported that their mean age was 57 years, slightly more than half (57%) were Hispanic, and their mean BMI was 30.5 kg/m2. On histological assessment, the epithelial and the muscularis layer were thicker among samples from women treated with estrogen. Specifically, mean epithelial thickness was increased 1.8-fold in the estrogen group, while the muscularis thickness was increased 2.7-fold.
To determine if these estrogen-induced increases in muscularis thickness were associated with increased collagen synthesis, relative messenger RNA levels of collagen type I, alpha-1, type I, alpha-2, and collagen type III mRNA were quantified in the muscularis samples from both groups. Collagen I, alpha-1 was increased sixfold in the vaginal muscularis in the estrogen group, while collagen type I, alpha-2 and collagen type III mRNA were increased 1.8- and 2.5-fold, respectively.
Immunoblot analysis was completed in four patients in each treatment group who had sufficient tissue for protein analysis. Collagen type 1a monomers, dimers, and trimers were all increased 10-fold in the muscularis from samples of women treated with estrogen. In contrast, differences in collagen 3 protein were not significant. Further, with respect to matrix degradation, in patients adherent with local estrogen, human macrophage elastase mRNA was suppressed in the vaginal mucosa from estrogen-treated participants, and MMP-9 activity was decreased 6-fold in the mucosa and 4-fold in the muscularis. There was no change in expression of several protease inhibitors.
"Our findings from this trial suggest that 6 weeks of preoperative vaginal estrogen in postmenopausal women with prolapse may improve the substrate for suture placement at the time of repair while mitigating surgical induction of several degradative enzymes," Dr. Rahn concluded.
The study was funded by an Astellas Research Award/AUGS Foundation grant. Dr. Rahn said that he had no relevant financial conflicts to disclose.
AT THE AUGS ANNUAL MEETING
Major finding: On histological assessment, mean epithelial thickness among women in the estrogen group was increased by 1.8-fold while the muscularis thickness was increased by 2.7-fold.
Data source: Results from a study of 30 postmenopausal women who, 6 weeks prior to undergoing hysterectomy, were randomized to estrogen cream or placebo in an effort to determine the vaginal effects of estrogen.
Disclosures: The study was funded by an Astellas Research Award/AUGS Foundation grant. Dr. Rahn said that he had no relevant financial conflicts to disclose.
Combined factors predicted risk of de novo stress urinary incontinence
LAS VEGAS – A prediction model of seven combined risk factors provides a validated, individualized way to determine a patient’s risk for developing de novo stress urinary incontinence following pelvic prolapse surgery, a novel study showed.
"In women without stress urinary incontinence symptoms, prolapse surgery may cause de novo SUI in 16%-51% of patients," Dr. J. Eric Jelovsek said at the annual meeting of the American Urogynecologic Society.
"Recent studies have demonstrated effective prevention strategies, including prophylactic incontinence surgery such as concomitant midurethral sling or Burch urethropexy, and provided refined estimates of the average patient’s risk. While these studies have advanced our knowledge of the overall prevalence of de novo SUI, the risk prediction for a specific patient varies based on individual characteristics. A prediction model that more accurately predicts an individual’s risk may further help customize the shared decision-making process that occurs between a patient and her physician when planning for a concomitant continence operation," Dr. Jelovsek said.
In order to develop and validate a model to predict an individual’s risk of de novo SUI within 12 months of prolapse surgery, Dr. Jelovsek and his associates with the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s Pelvic Floor Disorders Network used data from the OPUS (Outcomes Following Vaginal Prolapse Repair and Midurethral Sling) trial.
To externally validate the model, they also used data from the CARE (Colpopexy and Urinary Reduction Efforts) trial. The investigators identified 12 original preoperative patient and test characteristics commonly used to predict the risk of de novo SUI following surgery from the available data sets. They were increased age, white race, higher vaginal parity, higher body mass index (BMI), current smoker, current diagnosis of diabetes, strenuous physical activity, baseline urgency urinary incontinence symptoms, higher preoperative Pelvic Organ Prolapse Quantification (POP-Q) stage, higher POP-Q point Aa measure, positive preoperative prolapse reduction stress test, and performance of a concomitant retropubic midurethral sling.
"We hypothesized that all risk factors except for the performance of a concomitant [retropubic midurethral sling] would increase the risk of de novo SUI," said Dr. Jelovsek, who is director of the Cleveland Clinic Multidisciplinary Simulation Center. The outcome of the prediction model was defined as development of de novo SUI as determined by the response of "somewhat," "moderately," or "quite a bit" on the Pelvic Floor Distress Inventory (PFDI) questions 20-22, as these responses have been shown to be highly relevant outcomes to patients.
Of the 465 women in the OPUS trial, 457 had SUI data available 12 months after surgery. Of the 12 original risk factors hypothesized to predict de novo SUI, 7 final risk factors were identified that when combined together accurately predicted de novo SUI. They were decreased age, higher vaginal parity, higher BMI, current diagnosis of diabetes, baseline urgency urinary incontinence symptoms, positive preoperative prolapse reduction stress test, and performance of a concomitant retropubic midurethral sling.
"Contrary to our original hypothesis, as age increased, a participant’s risk of experiencing de novo SUI decreased when combined with other factors," Dr. Jelovsek said. The researchers created a calculator using the variables from the model for making predictions in a clinical setting.
He went on to report that the prediction model had useful discrimination between women who ultimately did or did not experience de novo SUI, with a concordance index of 0.73. The accuracy of the model on the entire CARE data set was also significantly better than that of random chance (a concordance index of 0.62) as well as that of using the preoperative prolapse reduction stress test alone (a concordance index of 0.54).
"Our model demonstrates good predictive accuracy, with a concordance index of 0.72 in women undergoing transvaginal prolapse surgery," Dr. Jelovsek said. "This compares favorably to the National Cancer Institute Gail Model for Breast Cancer (a concordance index of 0.59), and the Framingham Cardiovascular Risk Model (a concordance index of 0.72)."
He acknowledged certain limitations of the study, including the fact that although the model was better than random chance in predicting the probability of SUI after abdominal sacral colpopexy and Burch urethropexy in the CARE population, the accuracy was lower. "This may have been because women in the OPUS data set underwent sling with vaginal surgery for prolapse, while those in CARE underwent a Burch procedure and abdominal surgery," he explained.
"It is also possible that abdominal sacral colpopexy places a different amount of risk of de novo stress urinary incontinence on individuals than does vaginal surgery for pelvic organ prolapse. Despite this, a concordance index of 0.62 suggests that the model is also a valuable adjunct for shared decision-making between the clinician and patients prior to abdominal sacral colpopexy with Burch urethropexy surgery."
He said that future studies should include populations of women undergoing minimally invasive colpopexy.
Dr. Jelovsek said he had no relevant financial disclosures.
LAS VEGAS – A prediction model of seven combined risk factors provides a validated, individualized way to determine a patient’s risk for developing de novo stress urinary incontinence following pelvic prolapse surgery, a novel study showed.
"In women without stress urinary incontinence symptoms, prolapse surgery may cause de novo SUI in 16%-51% of patients," Dr. J. Eric Jelovsek said at the annual meeting of the American Urogynecologic Society.
"Recent studies have demonstrated effective prevention strategies, including prophylactic incontinence surgery such as concomitant midurethral sling or Burch urethropexy, and provided refined estimates of the average patient’s risk. While these studies have advanced our knowledge of the overall prevalence of de novo SUI, the risk prediction for a specific patient varies based on individual characteristics. A prediction model that more accurately predicts an individual’s risk may further help customize the shared decision-making process that occurs between a patient and her physician when planning for a concomitant continence operation," Dr. Jelovsek said.
In order to develop and validate a model to predict an individual’s risk of de novo SUI within 12 months of prolapse surgery, Dr. Jelovsek and his associates with the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s Pelvic Floor Disorders Network used data from the OPUS (Outcomes Following Vaginal Prolapse Repair and Midurethral Sling) trial.
To externally validate the model, they also used data from the CARE (Colpopexy and Urinary Reduction Efforts) trial. The investigators identified 12 original preoperative patient and test characteristics commonly used to predict the risk of de novo SUI following surgery from the available data sets. They were increased age, white race, higher vaginal parity, higher body mass index (BMI), current smoker, current diagnosis of diabetes, strenuous physical activity, baseline urgency urinary incontinence symptoms, higher preoperative Pelvic Organ Prolapse Quantification (POP-Q) stage, higher POP-Q point Aa measure, positive preoperative prolapse reduction stress test, and performance of a concomitant retropubic midurethral sling.
"We hypothesized that all risk factors except for the performance of a concomitant [retropubic midurethral sling] would increase the risk of de novo SUI," said Dr. Jelovsek, who is director of the Cleveland Clinic Multidisciplinary Simulation Center. The outcome of the prediction model was defined as development of de novo SUI as determined by the response of "somewhat," "moderately," or "quite a bit" on the Pelvic Floor Distress Inventory (PFDI) questions 20-22, as these responses have been shown to be highly relevant outcomes to patients.
Of the 465 women in the OPUS trial, 457 had SUI data available 12 months after surgery. Of the 12 original risk factors hypothesized to predict de novo SUI, 7 final risk factors were identified that when combined together accurately predicted de novo SUI. They were decreased age, higher vaginal parity, higher BMI, current diagnosis of diabetes, baseline urgency urinary incontinence symptoms, positive preoperative prolapse reduction stress test, and performance of a concomitant retropubic midurethral sling.
"Contrary to our original hypothesis, as age increased, a participant’s risk of experiencing de novo SUI decreased when combined with other factors," Dr. Jelovsek said. The researchers created a calculator using the variables from the model for making predictions in a clinical setting.
He went on to report that the prediction model had useful discrimination between women who ultimately did or did not experience de novo SUI, with a concordance index of 0.73. The accuracy of the model on the entire CARE data set was also significantly better than that of random chance (a concordance index of 0.62) as well as that of using the preoperative prolapse reduction stress test alone (a concordance index of 0.54).
"Our model demonstrates good predictive accuracy, with a concordance index of 0.72 in women undergoing transvaginal prolapse surgery," Dr. Jelovsek said. "This compares favorably to the National Cancer Institute Gail Model for Breast Cancer (a concordance index of 0.59), and the Framingham Cardiovascular Risk Model (a concordance index of 0.72)."
He acknowledged certain limitations of the study, including the fact that although the model was better than random chance in predicting the probability of SUI after abdominal sacral colpopexy and Burch urethropexy in the CARE population, the accuracy was lower. "This may have been because women in the OPUS data set underwent sling with vaginal surgery for prolapse, while those in CARE underwent a Burch procedure and abdominal surgery," he explained.
"It is also possible that abdominal sacral colpopexy places a different amount of risk of de novo stress urinary incontinence on individuals than does vaginal surgery for pelvic organ prolapse. Despite this, a concordance index of 0.62 suggests that the model is also a valuable adjunct for shared decision-making between the clinician and patients prior to abdominal sacral colpopexy with Burch urethropexy surgery."
He said that future studies should include populations of women undergoing minimally invasive colpopexy.
Dr. Jelovsek said he had no relevant financial disclosures.
LAS VEGAS – A prediction model of seven combined risk factors provides a validated, individualized way to determine a patient’s risk for developing de novo stress urinary incontinence following pelvic prolapse surgery, a novel study showed.
"In women without stress urinary incontinence symptoms, prolapse surgery may cause de novo SUI in 16%-51% of patients," Dr. J. Eric Jelovsek said at the annual meeting of the American Urogynecologic Society.
"Recent studies have demonstrated effective prevention strategies, including prophylactic incontinence surgery such as concomitant midurethral sling or Burch urethropexy, and provided refined estimates of the average patient’s risk. While these studies have advanced our knowledge of the overall prevalence of de novo SUI, the risk prediction for a specific patient varies based on individual characteristics. A prediction model that more accurately predicts an individual’s risk may further help customize the shared decision-making process that occurs between a patient and her physician when planning for a concomitant continence operation," Dr. Jelovsek said.
In order to develop and validate a model to predict an individual’s risk of de novo SUI within 12 months of prolapse surgery, Dr. Jelovsek and his associates with the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s Pelvic Floor Disorders Network used data from the OPUS (Outcomes Following Vaginal Prolapse Repair and Midurethral Sling) trial.
To externally validate the model, they also used data from the CARE (Colpopexy and Urinary Reduction Efforts) trial. The investigators identified 12 original preoperative patient and test characteristics commonly used to predict the risk of de novo SUI following surgery from the available data sets. They were increased age, white race, higher vaginal parity, higher body mass index (BMI), current smoker, current diagnosis of diabetes, strenuous physical activity, baseline urgency urinary incontinence symptoms, higher preoperative Pelvic Organ Prolapse Quantification (POP-Q) stage, higher POP-Q point Aa measure, positive preoperative prolapse reduction stress test, and performance of a concomitant retropubic midurethral sling.
"We hypothesized that all risk factors except for the performance of a concomitant [retropubic midurethral sling] would increase the risk of de novo SUI," said Dr. Jelovsek, who is director of the Cleveland Clinic Multidisciplinary Simulation Center. The outcome of the prediction model was defined as development of de novo SUI as determined by the response of "somewhat," "moderately," or "quite a bit" on the Pelvic Floor Distress Inventory (PFDI) questions 20-22, as these responses have been shown to be highly relevant outcomes to patients.
Of the 465 women in the OPUS trial, 457 had SUI data available 12 months after surgery. Of the 12 original risk factors hypothesized to predict de novo SUI, 7 final risk factors were identified that when combined together accurately predicted de novo SUI. They were decreased age, higher vaginal parity, higher BMI, current diagnosis of diabetes, baseline urgency urinary incontinence symptoms, positive preoperative prolapse reduction stress test, and performance of a concomitant retropubic midurethral sling.
"Contrary to our original hypothesis, as age increased, a participant’s risk of experiencing de novo SUI decreased when combined with other factors," Dr. Jelovsek said. The researchers created a calculator using the variables from the model for making predictions in a clinical setting.
He went on to report that the prediction model had useful discrimination between women who ultimately did or did not experience de novo SUI, with a concordance index of 0.73. The accuracy of the model on the entire CARE data set was also significantly better than that of random chance (a concordance index of 0.62) as well as that of using the preoperative prolapse reduction stress test alone (a concordance index of 0.54).
"Our model demonstrates good predictive accuracy, with a concordance index of 0.72 in women undergoing transvaginal prolapse surgery," Dr. Jelovsek said. "This compares favorably to the National Cancer Institute Gail Model for Breast Cancer (a concordance index of 0.59), and the Framingham Cardiovascular Risk Model (a concordance index of 0.72)."
He acknowledged certain limitations of the study, including the fact that although the model was better than random chance in predicting the probability of SUI after abdominal sacral colpopexy and Burch urethropexy in the CARE population, the accuracy was lower. "This may have been because women in the OPUS data set underwent sling with vaginal surgery for prolapse, while those in CARE underwent a Burch procedure and abdominal surgery," he explained.
"It is also possible that abdominal sacral colpopexy places a different amount of risk of de novo stress urinary incontinence on individuals than does vaginal surgery for pelvic organ prolapse. Despite this, a concordance index of 0.62 suggests that the model is also a valuable adjunct for shared decision-making between the clinician and patients prior to abdominal sacral colpopexy with Burch urethropexy surgery."
He said that future studies should include populations of women undergoing minimally invasive colpopexy.
Dr. Jelovsek said he had no relevant financial disclosures.
AT THE AUGS ANNUAL MEETING
Major finding: Of the 12 original risk factors hypothesized to predict de novo SUI, 7 final risk factors were identified that when combined together accurately predicted de novo SUI in patients following pelvic prolapse surgery.
Data source: A study of 457 patients in the OPUS (Outcomes Following Vaginal Prolapse Repair and Midurethral Sling) trial.
Disclosures: Dr. Jelovsek said he had no relevant financial disclosures.
Distribution of female pelvic medicine fellowships varied
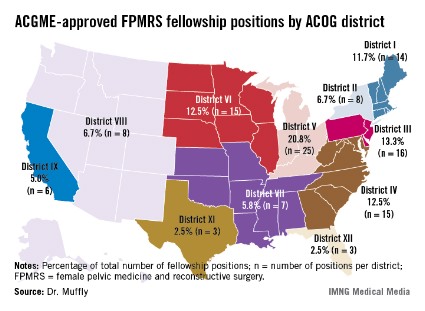
LAS VEGAS – The geographic distribution of female pelvic medicine and reconstructive surgery fellowships approved by the Accreditation Council for Graduate Medical Education varies widely in the United States, results from an analysis demonstrated.
Such variation "may limit the choices for residents wishing to pursue further training in female pelvic medicine and reconstructive surgery," Dr. Tyler Muffly said in an interview during a poster session at the annual meeting of the American Urogynecologic Society. "It also means that patients in some areas are going to have to travel further to get to a referral center."
In an effort to determine the distribution of first-year female pelvic medicine and reconstructive surgery (FPMRS) fellowship positions according to population within states and within districts of the American Congress of Obstetrics and Gynecology, Dr. Muffly and his associates used data from the 2010 U.S. Census and from the number of 2012 female pelvic medicine and reconstructive surgery fellowship positions available through the match, which were obtained from the Accreditation Council for Graduate Medical Education (ACGME). They rounded off population data to the nearest 1,000 persons.
Dr. Muffly of the division of female pelvic medicine and reconstructive surgery (FPMRS) at the University of Colorado, Aurora, reported that there was a mean of 9.6 FPMRS fellowship positions per ACOG district and a mean of 2.3 FPMRS programs per ACOG district. More than two-thirds of fellowship programs were located east of the Mississippi River (67.5% vs. 32.5% west of that spot), with the greatest number clustered in ACOG District V, which consists of Michigan, Indiana, Ohio, and Kentucky (20.8%).
The researchers observed a significant difference between ACOG districts based on the number of FPMRS fellowship programs (P = .04) as well as a difference in total population between districts (P less than .0001). Specifically, Florida (ACOG District XII) had the highest proportion of women overall (P = .001) while California (ACOG District IX) had the highest proportion of postmenopausal women (P less than .001).
When Dr. Muffly and his associates analyzed the distribution of FPMRS fellowship positions within ACOG districts, a statistically significant difference was observed in the number of FPMRS fellowship positions per district (P = .03). For example, there were only 8 positions in ACOG District VIII (Arizona, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming), compared with 16 positions in ACOG District III (Delaware, New Jersey, and Pennsylvania).
"The findings suggest that future FPMRS fellowships might be started in the West or in high-density states like Florida or California where there are many postmenopausal women," Dr. Muffly concluded. "There are fellowships in all 11 ACOG districts. Physicians in the West or in the high plains states might have to look a little harder for a fellowship or a referral center for female pelvic medicine and reconstructive surgery."
Dr. Muffly said he had no relevant financial disclosures.
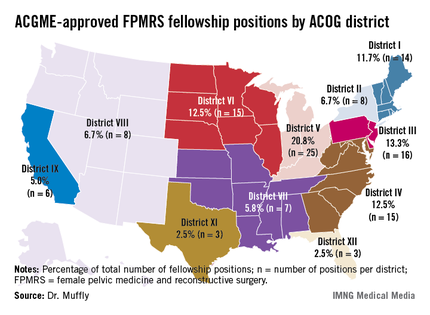
LAS VEGAS – The geographic distribution of female pelvic medicine and reconstructive surgery fellowships approved by the Accreditation Council for Graduate Medical Education varies widely in the United States, results from an analysis demonstrated.
Such variation "may limit the choices for residents wishing to pursue further training in female pelvic medicine and reconstructive surgery," Dr. Tyler Muffly said in an interview during a poster session at the annual meeting of the American Urogynecologic Society. "It also means that patients in some areas are going to have to travel further to get to a referral center."
In an effort to determine the distribution of first-year female pelvic medicine and reconstructive surgery (FPMRS) fellowship positions according to population within states and within districts of the American Congress of Obstetrics and Gynecology, Dr. Muffly and his associates used data from the 2010 U.S. Census and from the number of 2012 female pelvic medicine and reconstructive surgery fellowship positions available through the match, which were obtained from the Accreditation Council for Graduate Medical Education (ACGME). They rounded off population data to the nearest 1,000 persons.
Dr. Muffly of the division of female pelvic medicine and reconstructive surgery (FPMRS) at the University of Colorado, Aurora, reported that there was a mean of 9.6 FPMRS fellowship positions per ACOG district and a mean of 2.3 FPMRS programs per ACOG district. More than two-thirds of fellowship programs were located east of the Mississippi River (67.5% vs. 32.5% west of that spot), with the greatest number clustered in ACOG District V, which consists of Michigan, Indiana, Ohio, and Kentucky (20.8%).
The researchers observed a significant difference between ACOG districts based on the number of FPMRS fellowship programs (P = .04) as well as a difference in total population between districts (P less than .0001). Specifically, Florida (ACOG District XII) had the highest proportion of women overall (P = .001) while California (ACOG District IX) had the highest proportion of postmenopausal women (P less than .001).
When Dr. Muffly and his associates analyzed the distribution of FPMRS fellowship positions within ACOG districts, a statistically significant difference was observed in the number of FPMRS fellowship positions per district (P = .03). For example, there were only 8 positions in ACOG District VIII (Arizona, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming), compared with 16 positions in ACOG District III (Delaware, New Jersey, and Pennsylvania).
"The findings suggest that future FPMRS fellowships might be started in the West or in high-density states like Florida or California where there are many postmenopausal women," Dr. Muffly concluded. "There are fellowships in all 11 ACOG districts. Physicians in the West or in the high plains states might have to look a little harder for a fellowship or a referral center for female pelvic medicine and reconstructive surgery."
Dr. Muffly said he had no relevant financial disclosures.
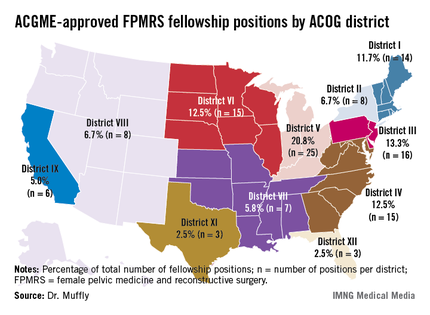
LAS VEGAS – The geographic distribution of female pelvic medicine and reconstructive surgery fellowships approved by the Accreditation Council for Graduate Medical Education varies widely in the United States, results from an analysis demonstrated.
Such variation "may limit the choices for residents wishing to pursue further training in female pelvic medicine and reconstructive surgery," Dr. Tyler Muffly said in an interview during a poster session at the annual meeting of the American Urogynecologic Society. "It also means that patients in some areas are going to have to travel further to get to a referral center."
In an effort to determine the distribution of first-year female pelvic medicine and reconstructive surgery (FPMRS) fellowship positions according to population within states and within districts of the American Congress of Obstetrics and Gynecology, Dr. Muffly and his associates used data from the 2010 U.S. Census and from the number of 2012 female pelvic medicine and reconstructive surgery fellowship positions available through the match, which were obtained from the Accreditation Council for Graduate Medical Education (ACGME). They rounded off population data to the nearest 1,000 persons.
Dr. Muffly of the division of female pelvic medicine and reconstructive surgery (FPMRS) at the University of Colorado, Aurora, reported that there was a mean of 9.6 FPMRS fellowship positions per ACOG district and a mean of 2.3 FPMRS programs per ACOG district. More than two-thirds of fellowship programs were located east of the Mississippi River (67.5% vs. 32.5% west of that spot), with the greatest number clustered in ACOG District V, which consists of Michigan, Indiana, Ohio, and Kentucky (20.8%).
The researchers observed a significant difference between ACOG districts based on the number of FPMRS fellowship programs (P = .04) as well as a difference in total population between districts (P less than .0001). Specifically, Florida (ACOG District XII) had the highest proportion of women overall (P = .001) while California (ACOG District IX) had the highest proportion of postmenopausal women (P less than .001).
When Dr. Muffly and his associates analyzed the distribution of FPMRS fellowship positions within ACOG districts, a statistically significant difference was observed in the number of FPMRS fellowship positions per district (P = .03). For example, there were only 8 positions in ACOG District VIII (Arizona, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming), compared with 16 positions in ACOG District III (Delaware, New Jersey, and Pennsylvania).
"The findings suggest that future FPMRS fellowships might be started in the West or in high-density states like Florida or California where there are many postmenopausal women," Dr. Muffly concluded. "There are fellowships in all 11 ACOG districts. Physicians in the West or in the high plains states might have to look a little harder for a fellowship or a referral center for female pelvic medicine and reconstructive surgery."
Dr. Muffly said he had no relevant financial disclosures.
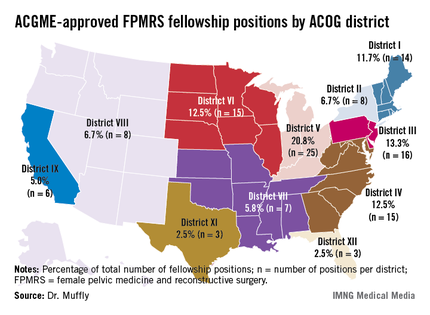
AT THE AUGS ANNUAL MEETING
Major finding: More than two-thirds of fellowship programs in female pelvic medicine and reconstructive surgery were located east of the Mississippi River (67.5% vs. 32.5% west of that spot), with the greatest number clustered in American Congress of Obstetrics and Gynecology District V, which consists of Michigan, Indiana, Ohio, and Kentucky (20.8%).
Data source: An analysis of data from the 2010 U.S. Census and from the number of 2012 female pelvic medicine and reconstructive surgery fellowship positions available through the match.
Disclosures: Dr. Muffly said he had no relevant financial disclosures.
Surgical treatments for failed midurethral sling compared
LAS VEGAS – In a study of patients who experienced a failed midurethral sling, urethral bulking injection was associated with a greater than threefold increased risk of failure compared with a repeat midurethral sling procedure, a retrospective analysis showed.
In addition, the diagnosis of intrinsic sphincter deficiency conferred a greater than fourfold risk of failure compared with patients without the diagnosis, regardless of which procedure was performed.
Those are findings from the largest cohort study to date evaluating failure of midurethral sling (MUS), and the only one to include both repeat MUS procedures and urethral bulking injections.
"This study provides important baseline data for surgeons when faced with MUS failure," Dr. Anthony Gaddi said at the annual meeting of the American Urogynecologic Society. "Prospective, randomized data with validated subjective and objective outcomes is warranted."
In an effort to compare the efficacy and safety of a repeat MUS procedure with urethral bulking injection after failed primary MUS, Dr. Gaddi and his associates performed an electronic chart review of patients from the Southern California Permanente Medical Group who underwent MUS for stress urinary incontinence (SUI) between 2008 and 2011.
The primary outcome was a measure of subjective failure, defined as a complaint of SUI, or objective failure, defined as documentation of a positive cough stress test, urodynamic stress incontinence, or reoperation for SUI, said Dr. Gaddi of the department of obstetrics and gynecology at the University of California, Irvine. Secondary outcomes included perioperative complications and adverse events.
For the 7,412 MUS procedures performed between 2008 and 2011, there were 165 repeat procedures for sling failure. Of these, 98 were repeat MUS procedures and 67 were urethral bulking injections. The mean age of patients was 58 years, their mean body mass index was 29.3 kg/m2, 65% were menopausal, and 59% were white.
Dr. Gaddi reported that there were 11 failures in the MUS group (11.2%), compared with 26 failures in the bulking group (38.8%), a difference that reached significance (P less than .01).
In multivariable logistic regression analysis, patients who underwent urethral bulking injections experienced a 3.7-fold increased risk of failure compared with those in the repeat MUS group. In addition, patients with a preoperative diagnosis of intrinsic sphincter deficiency experienced a 4.45-fold higher risk of failure compared with those who had no such deficiency, regardless of which procedure was performed.
Perioperative complications were similar between the two groups, "suggesting that both are safe options in this cohort," Dr. Gaddi said.
He acknowledged certain limitations of the study, including its retrospective design, and "difficulty standardizing our definition of failure. The low number of complications among our repeat procedures limits conclusions that can be made about safety."
Dr. Gaddi said that he had no relevant financial conflicts to disclose.
LAS VEGAS – In a study of patients who experienced a failed midurethral sling, urethral bulking injection was associated with a greater than threefold increased risk of failure compared with a repeat midurethral sling procedure, a retrospective analysis showed.
In addition, the diagnosis of intrinsic sphincter deficiency conferred a greater than fourfold risk of failure compared with patients without the diagnosis, regardless of which procedure was performed.
Those are findings from the largest cohort study to date evaluating failure of midurethral sling (MUS), and the only one to include both repeat MUS procedures and urethral bulking injections.
"This study provides important baseline data for surgeons when faced with MUS failure," Dr. Anthony Gaddi said at the annual meeting of the American Urogynecologic Society. "Prospective, randomized data with validated subjective and objective outcomes is warranted."
In an effort to compare the efficacy and safety of a repeat MUS procedure with urethral bulking injection after failed primary MUS, Dr. Gaddi and his associates performed an electronic chart review of patients from the Southern California Permanente Medical Group who underwent MUS for stress urinary incontinence (SUI) between 2008 and 2011.
The primary outcome was a measure of subjective failure, defined as a complaint of SUI, or objective failure, defined as documentation of a positive cough stress test, urodynamic stress incontinence, or reoperation for SUI, said Dr. Gaddi of the department of obstetrics and gynecology at the University of California, Irvine. Secondary outcomes included perioperative complications and adverse events.
For the 7,412 MUS procedures performed between 2008 and 2011, there were 165 repeat procedures for sling failure. Of these, 98 were repeat MUS procedures and 67 were urethral bulking injections. The mean age of patients was 58 years, their mean body mass index was 29.3 kg/m2, 65% were menopausal, and 59% were white.
Dr. Gaddi reported that there were 11 failures in the MUS group (11.2%), compared with 26 failures in the bulking group (38.8%), a difference that reached significance (P less than .01).
In multivariable logistic regression analysis, patients who underwent urethral bulking injections experienced a 3.7-fold increased risk of failure compared with those in the repeat MUS group. In addition, patients with a preoperative diagnosis of intrinsic sphincter deficiency experienced a 4.45-fold higher risk of failure compared with those who had no such deficiency, regardless of which procedure was performed.
Perioperative complications were similar between the two groups, "suggesting that both are safe options in this cohort," Dr. Gaddi said.
He acknowledged certain limitations of the study, including its retrospective design, and "difficulty standardizing our definition of failure. The low number of complications among our repeat procedures limits conclusions that can be made about safety."
Dr. Gaddi said that he had no relevant financial conflicts to disclose.
LAS VEGAS – In a study of patients who experienced a failed midurethral sling, urethral bulking injection was associated with a greater than threefold increased risk of failure compared with a repeat midurethral sling procedure, a retrospective analysis showed.
In addition, the diagnosis of intrinsic sphincter deficiency conferred a greater than fourfold risk of failure compared with patients without the diagnosis, regardless of which procedure was performed.
Those are findings from the largest cohort study to date evaluating failure of midurethral sling (MUS), and the only one to include both repeat MUS procedures and urethral bulking injections.
"This study provides important baseline data for surgeons when faced with MUS failure," Dr. Anthony Gaddi said at the annual meeting of the American Urogynecologic Society. "Prospective, randomized data with validated subjective and objective outcomes is warranted."
In an effort to compare the efficacy and safety of a repeat MUS procedure with urethral bulking injection after failed primary MUS, Dr. Gaddi and his associates performed an electronic chart review of patients from the Southern California Permanente Medical Group who underwent MUS for stress urinary incontinence (SUI) between 2008 and 2011.
The primary outcome was a measure of subjective failure, defined as a complaint of SUI, or objective failure, defined as documentation of a positive cough stress test, urodynamic stress incontinence, or reoperation for SUI, said Dr. Gaddi of the department of obstetrics and gynecology at the University of California, Irvine. Secondary outcomes included perioperative complications and adverse events.
For the 7,412 MUS procedures performed between 2008 and 2011, there were 165 repeat procedures for sling failure. Of these, 98 were repeat MUS procedures and 67 were urethral bulking injections. The mean age of patients was 58 years, their mean body mass index was 29.3 kg/m2, 65% were menopausal, and 59% were white.
Dr. Gaddi reported that there were 11 failures in the MUS group (11.2%), compared with 26 failures in the bulking group (38.8%), a difference that reached significance (P less than .01).
In multivariable logistic regression analysis, patients who underwent urethral bulking injections experienced a 3.7-fold increased risk of failure compared with those in the repeat MUS group. In addition, patients with a preoperative diagnosis of intrinsic sphincter deficiency experienced a 4.45-fold higher risk of failure compared with those who had no such deficiency, regardless of which procedure was performed.
Perioperative complications were similar between the two groups, "suggesting that both are safe options in this cohort," Dr. Gaddi said.
He acknowledged certain limitations of the study, including its retrospective design, and "difficulty standardizing our definition of failure. The low number of complications among our repeat procedures limits conclusions that can be made about safety."
Dr. Gaddi said that he had no relevant financial conflicts to disclose.
AT THE AUGS ANNUAL MEETING
Major finding: In multivariable logistic regression analysis, patients who underwent urethral bulking injections for a failed midurethral sling experienced a 3.7-fold increased risk of failure, compared with those who underwent a repeat midurethral sling procedure.
Data source: A single-center study of 165 repeat procedures for midurethral sling failure performed between 2008 and 2011.
Disclosures: Dr. Gaddi said that he had no relevant financial conflicts to disclose.
Cost of Botox vs. anticholinergics for urge urinary incontinence
LAS VEGAS – Onabotulinum toxin A and anticholinergic medications have similar cost effectiveness in the first 6 months of treatment for urge urinary incontinence, results from a multicenter randomized trial showed.
However, if costs and outcomes are considered through 9 months, Botox has significantly lower costs than anticholinergics but similar urge urinary incontinence (UUI) control, Dr. Anthony G. Visco reported at the annual meeting of the American Urogynecologic Society.
On behalf of the National Institute of Child Health and Human Development–funded Pelvic Floor Disorders Network, Dr. Visco presented findings from an analysis of 231 women who participated in the ABC trial, which directly compared the safety and efficacy of a 6-month regimen of anticholinergic medications (solifenacin or trospium) to a single 100-U injection of Botox (N. Engl. J. Med. 2012;367:1803-13).
The current study sought to compare the cost effectiveness of anticholinergic medications and Botox for the management of urge urinary incontinence (UUI). The researchers adopted a societal cost perspective and included both direct costs such as physician visits/procedures and medication costs, as well as indirect costs such as incontinence pads, laundry use, and time lost from work.
Patients were randomized to one of the two groups and were followed for 6 months. At each month the researchers obtained bladder diaries, including the Overactive Bladder Questionnaire (OABq) and the Patient Global Symptom Control instrument (PGSC). At 6 months, all anticholinergic pills were stopped. Dr. Visco and his associates followed the patients up to an additional 6 months "to look at the effect of Botox using the PGSC scores to determine the duration of adequate symptom control," he said.
The researchers adopted two different measures of efficacy. In the first 6 months, efficacy outcome was the average reduction in UUI episodes, and utilities were obtained from the OABq completed at baseline through 6 months; quality-adjusted life-years were calculated and annualized from 6 months to a full year.
Between 6 and 9 months, the efficacy outcome was adequate symptom control as measured by the PGSC. "We chose 9 months because that was a period of time when half the participants in the Botox group still had adequate symptom control," explained Dr. Visco, chief of urogynecology and female pelvic medicine and reconstructive surgery at Duke University, Durham, N.C.
Cost analyses assumed that Botox patients incurred no additional costs between months 6 and 9 while those on anticholinergics incurred an additional 3 months of medication costs.
At 6 months the direct medical costs were similar between the anticholinergic and Botox groups ($1,339 vs. $1,266), as were the indirect costs ($150 vs. $106). Both treatments decreased the amount of UUI episodes by 3.3 per day. Both groups also had improvements in total quality-adjusted life-years (0.702 vs. 0.707) and in the annualized cost per quality-adjusted life-year ($57,890 vs. $55,869).
Dr. Visco noted that 74% of study participants who received Botox had adequate symptom control at 6 months. That decreased to 55% at the 9-month mark.
The cost-effectiveness analysis through 9 months revealed that anticholinergics cost $1,942 while Botox cost $1,266. Months of symptom control also were similar between the groups (a mean of 6.36 vs. 6.13, respectively), but in the analysis of cost per month of adequate symptom control, anticholinergics were significantly more expensive: $305 vs. $207 for Botox (P value less than .0001).
Dr. Visco acknowledged certain limitations of the study, including the fact that true cost data were not available beyond 6 months and that the researchers evaluated only solifenacin or trospium. In addition, "quality-adjusted life-year data were limited to the first 6 months, and we are unable to comment on the cost effectiveness of multiple injections," he said. "Anticholinergic assumptions were also made between 6 and 9 months."
Dr. Visco said he had no relevant financial disclosures.
LAS VEGAS – Onabotulinum toxin A and anticholinergic medications have similar cost effectiveness in the first 6 months of treatment for urge urinary incontinence, results from a multicenter randomized trial showed.
However, if costs and outcomes are considered through 9 months, Botox has significantly lower costs than anticholinergics but similar urge urinary incontinence (UUI) control, Dr. Anthony G. Visco reported at the annual meeting of the American Urogynecologic Society.
On behalf of the National Institute of Child Health and Human Development–funded Pelvic Floor Disorders Network, Dr. Visco presented findings from an analysis of 231 women who participated in the ABC trial, which directly compared the safety and efficacy of a 6-month regimen of anticholinergic medications (solifenacin or trospium) to a single 100-U injection of Botox (N. Engl. J. Med. 2012;367:1803-13).
The current study sought to compare the cost effectiveness of anticholinergic medications and Botox for the management of urge urinary incontinence (UUI). The researchers adopted a societal cost perspective and included both direct costs such as physician visits/procedures and medication costs, as well as indirect costs such as incontinence pads, laundry use, and time lost from work.
Patients were randomized to one of the two groups and were followed for 6 months. At each month the researchers obtained bladder diaries, including the Overactive Bladder Questionnaire (OABq) and the Patient Global Symptom Control instrument (PGSC). At 6 months, all anticholinergic pills were stopped. Dr. Visco and his associates followed the patients up to an additional 6 months "to look at the effect of Botox using the PGSC scores to determine the duration of adequate symptom control," he said.
The researchers adopted two different measures of efficacy. In the first 6 months, efficacy outcome was the average reduction in UUI episodes, and utilities were obtained from the OABq completed at baseline through 6 months; quality-adjusted life-years were calculated and annualized from 6 months to a full year.
Between 6 and 9 months, the efficacy outcome was adequate symptom control as measured by the PGSC. "We chose 9 months because that was a period of time when half the participants in the Botox group still had adequate symptom control," explained Dr. Visco, chief of urogynecology and female pelvic medicine and reconstructive surgery at Duke University, Durham, N.C.
Cost analyses assumed that Botox patients incurred no additional costs between months 6 and 9 while those on anticholinergics incurred an additional 3 months of medication costs.
At 6 months the direct medical costs were similar between the anticholinergic and Botox groups ($1,339 vs. $1,266), as were the indirect costs ($150 vs. $106). Both treatments decreased the amount of UUI episodes by 3.3 per day. Both groups also had improvements in total quality-adjusted life-years (0.702 vs. 0.707) and in the annualized cost per quality-adjusted life-year ($57,890 vs. $55,869).
Dr. Visco noted that 74% of study participants who received Botox had adequate symptom control at 6 months. That decreased to 55% at the 9-month mark.
The cost-effectiveness analysis through 9 months revealed that anticholinergics cost $1,942 while Botox cost $1,266. Months of symptom control also were similar between the groups (a mean of 6.36 vs. 6.13, respectively), but in the analysis of cost per month of adequate symptom control, anticholinergics were significantly more expensive: $305 vs. $207 for Botox (P value less than .0001).
Dr. Visco acknowledged certain limitations of the study, including the fact that true cost data were not available beyond 6 months and that the researchers evaluated only solifenacin or trospium. In addition, "quality-adjusted life-year data were limited to the first 6 months, and we are unable to comment on the cost effectiveness of multiple injections," he said. "Anticholinergic assumptions were also made between 6 and 9 months."
Dr. Visco said he had no relevant financial disclosures.
LAS VEGAS – Onabotulinum toxin A and anticholinergic medications have similar cost effectiveness in the first 6 months of treatment for urge urinary incontinence, results from a multicenter randomized trial showed.
However, if costs and outcomes are considered through 9 months, Botox has significantly lower costs than anticholinergics but similar urge urinary incontinence (UUI) control, Dr. Anthony G. Visco reported at the annual meeting of the American Urogynecologic Society.
On behalf of the National Institute of Child Health and Human Development–funded Pelvic Floor Disorders Network, Dr. Visco presented findings from an analysis of 231 women who participated in the ABC trial, which directly compared the safety and efficacy of a 6-month regimen of anticholinergic medications (solifenacin or trospium) to a single 100-U injection of Botox (N. Engl. J. Med. 2012;367:1803-13).
The current study sought to compare the cost effectiveness of anticholinergic medications and Botox for the management of urge urinary incontinence (UUI). The researchers adopted a societal cost perspective and included both direct costs such as physician visits/procedures and medication costs, as well as indirect costs such as incontinence pads, laundry use, and time lost from work.
Patients were randomized to one of the two groups and were followed for 6 months. At each month the researchers obtained bladder diaries, including the Overactive Bladder Questionnaire (OABq) and the Patient Global Symptom Control instrument (PGSC). At 6 months, all anticholinergic pills were stopped. Dr. Visco and his associates followed the patients up to an additional 6 months "to look at the effect of Botox using the PGSC scores to determine the duration of adequate symptom control," he said.
The researchers adopted two different measures of efficacy. In the first 6 months, efficacy outcome was the average reduction in UUI episodes, and utilities were obtained from the OABq completed at baseline through 6 months; quality-adjusted life-years were calculated and annualized from 6 months to a full year.
Between 6 and 9 months, the efficacy outcome was adequate symptom control as measured by the PGSC. "We chose 9 months because that was a period of time when half the participants in the Botox group still had adequate symptom control," explained Dr. Visco, chief of urogynecology and female pelvic medicine and reconstructive surgery at Duke University, Durham, N.C.
Cost analyses assumed that Botox patients incurred no additional costs between months 6 and 9 while those on anticholinergics incurred an additional 3 months of medication costs.
At 6 months the direct medical costs were similar between the anticholinergic and Botox groups ($1,339 vs. $1,266), as were the indirect costs ($150 vs. $106). Both treatments decreased the amount of UUI episodes by 3.3 per day. Both groups also had improvements in total quality-adjusted life-years (0.702 vs. 0.707) and in the annualized cost per quality-adjusted life-year ($57,890 vs. $55,869).
Dr. Visco noted that 74% of study participants who received Botox had adequate symptom control at 6 months. That decreased to 55% at the 9-month mark.
The cost-effectiveness analysis through 9 months revealed that anticholinergics cost $1,942 while Botox cost $1,266. Months of symptom control also were similar between the groups (a mean of 6.36 vs. 6.13, respectively), but in the analysis of cost per month of adequate symptom control, anticholinergics were significantly more expensive: $305 vs. $207 for Botox (P value less than .0001).
Dr. Visco acknowledged certain limitations of the study, including the fact that true cost data were not available beyond 6 months and that the researchers evaluated only solifenacin or trospium. In addition, "quality-adjusted life-year data were limited to the first 6 months, and we are unable to comment on the cost effectiveness of multiple injections," he said. "Anticholinergic assumptions were also made between 6 and 9 months."
Dr. Visco said he had no relevant financial disclosures.
AT THE AUGS ANNUAL MEETING
Major finding: In an analysis of cost per month of adequate symptom control for urge urinary incontinence through 9 months of treatment, anticholinergics were significantly more expensive than Botox ($305 vs. $207; P value less than .0001).
Data source: A study of 231 women who participated in the ABC trial, which directly compared the safety and efficacy of a 6-month regimen of anticholinergic medications (solifenacin or trospium) to a single 100-U injection of Botox.
Disclosures: Dr. Visco said he had no relevant financial disclosures.
One in five women undergoes urogynecologic surgery
LAS VEGAS – Among women with private health insurance in this country, the lifetime risk of surgery for either stress urinary incontinence or pelvic organ prolapse stands at 20.2%, results from a large analysis demonstrated.
"This means that one out of every five women in the United States will undergo a urogynecologic procedure by the age of 80," Dr. Jennifer M. Wu said at the annual meeting of the American Urogynecologic Society. "This high rate highlights the public health burden of pelvic floor disorders, exposes the need for improved prevention strategies, and underscores the importance of effective long-term surgical interventions."
A commonly referenced statistic is that the lifetime risk of surgery for either stress urinary incontinence (SUI) or pelvic organ prolapse (POP) is 11%, but this was based on a study of 395 patients who underwent surgery in 1995 in the Northwest (Obstet. Gynecol. 1997;89:501-6).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Since 1995, several factors may have increased this risk. These include "the integration of midurethral slings and vaginal mesh prolapse procedures, regional differences in surgery rates, and the greater number of elderly women," explained Dr. Wu of the department of obstetrics and gynecology and the Center for Women’s Health Research at the University of North Carolina at Chapel Hill. "Thus, the objective of our study was to estimate the cumulative risk of SUI or POP surgery over a woman’s lifetime until the age of 80."
The researchers used the Market Scan Commercial Claims and Encounters database with the Medicare Supplemental, which contains de-identified inpatient and outpatient claims data from about 100 employer-based insurance plans in the United States. They included women aged 18 years and older and identified any SUI or POP surgery performed between 2007 and 2011 based on CPT codes. This resulted in a study population of 51.8 million women. Of these, 311,070 underwent surgery for either SUI or POP.
To estimate age-specific incidence rates for each age between 18 and 80 years, Dr. Wu and her associates multiplied age-specific prevalence rates by the proportion of cases that were incident. To estimate the proportion of all procedures that were repeat surgeries, they evaluated women who had a SUI or POP surgery in 2011 and "looked back" 5 years to identify prior surgeries. Finally, they used Monte Carlo simulations to determine the cumulative lifetime risk of either incontinence or prolapse surgery with 95% confidence intervals.
Dr. Wu reported that the cumulative lifetime risk of either SUI or POP surgery was 20.2% (95% CI, 19.2%-21.1%). The cumulative lifetime risk of SUI was 14.5% (95% CI, 13.4%-15.5%), and the risk of POP surgery was 13.7% (95% CI, 12.6%-14.8%). The cumulative lifetime risk for SUI or POP surgery increased with age in a stepwise fashion, from 11.4% by age 60 years to 15.9% by age 70 and 20.2% by age 80, she noted.
To place the risk of any primary surgery for SUI or POP in perspective, Dr. Wu drew a comparison with the lifetime risk estimates for colon cancer (4.8%), lung cancer (6.3%), breast cancer (14.8%), and any type of cancer (41.3%). "Granted, incontinence and prolapse are not life-threatening conditions, but this 20% risk highlights how common surgeries are for pelvic floor disorders, despite the fact that they’re widely underrecognized," she noted.
She acknowledged certain limitations of the study, including the fact that she and her associates were unable to review actual medical records to confirm the rate of prior surgeries. "In addition, we assumed a closed cohort and no competing risks such that all women live until the age of 80," she said. "Also, these results reflect women with private insurance and may not be generalizable to those who are uninsured or underinsured."
Dr. Wu disclosed that she is a consultant for Procter & Gamble.
Dr. David M. Jaspan comments: Direct to consumer advertising has enabled more women to feel comfortable discussing incontinence with their health care providers, which is great. Industry had inundated general ob.gyn. offices with the opportunity to attend short courses to learn "mesh procedures," which may not have been great. Therefore, I am not surprised that the numbers of women with private insurance undergoing urogynecologic surgery are so high.
These advanced procedures should be undertaken by those surgeons with sufficient training and experience to properly counsel women about the risk and benefit of a native tissue repair, compared with a graft placement. In addition, surgeons should have a volume of experience and training that qualifies them to provide this detailed counseling and should perform an appropriate preoperative evaluation to determine the absolute need for a procedure. More procedures may have brought more risk to women.
I applaud the American College of Obstetricians and Gynecologists for the 2011 ACOG Committee Opinion #513, which says, "Surgeons performing complex pelvic floor reconstructive surgery should have adequate experience and training in native tissue repairs as well as repairs using mesh augmentation specific to each device, should have a thorough understanding of pelvic anatomy, and should be able to counsel patients regarding the risk/benefit ratio on the use of mesh compared with native tissue repairs" (Obstet. Gynecol. 2011;118:1459-64).
In its 2011 Safety Communication, the Food and Drug Administration said that transvaginal placement of surgical mesh for POP is of "continuing serious concern." In the document, the FDA restated its 2008 recommendation that health care providers "inform patients about the potential for serious complications and the effect on quality of life, including pain during sexual intercourse, scarring, and narrowing of the vaginal wall in POP repair using surgical mesh; and provide a copy of the patient labeling from the surgical mesh manufacturer if available."
The FDA also made several new recommendations for health care providers in its report:
- Surgeons should recognize that, in most cases, POP can be treated successfully without mesh, thus avoiding the risk of mesh-related complications.
- Surgeons should choose mesh surgery only after weighing the risks and benefits of surgery with mesh versus all surgical and nonsurgical alternatives.
- Removal of mesh may involve multiple surgical procedures and significantly impair the patient's quality of life. Complete removal of mesh may not be possible and may not result in complete resolution of complications, including pain.
Patient counseling needs to include discussion of alternative native tissue repair and the fact that synthetic mesh is permanent, according to ACOG. Other issues to discuss include that vaginal bleeding, pain, and dyspareunia may be related to vaginal mesh; Patients reporting such symptoms should undergo a thorough vaginal exam, including an exam under anesthesia if necessary.
Dr. David M. Jaspan is chairman of ob.gyn. for the Einstein Health Care Network in Philadelphia. He was asked to comment on Dr. Wu's study. Dr. Jaspan said that he had no financial disclosures.
Remember to ask about pelvic floor issues
Dr. Meadow Maze Good comments: This is a well done and important study that highlights the magnitude of pelvic floor disorders in women. Previous studies indicate that women delay or do not seek care for pelvic floor disorders and incorrectly think that these problems are a normal result of aging.
These data presented at the American Urogynecologic Society meeting by Dr. Wu and her colleagues reinforce the need for increased public awareness and education regarding pelvic floor disorders as well as available treatment options, including nonsurgical and surgical options. Additionally, this study points out that the physicians treating women of all ages including the primary care provider (family practice physicians and obstetrician/gynecologists) should query women about possible pelvic floor symptoms, including incontinence, prolapse, and sexual function.
It is especially important for the ob.gyn. to ask their patient about these symptoms if there is planning underway for a hysterectomy for other causes. This is an exciting time for the newly board-certifiable field of female pelvic medicine and reconstructive surgery. As the aging population of women with prolapse and incontinence increases, fellowship programs are graduating physicians knowledgeable in this specific field who are dedicated to taking care of women with these treatable conditions.
Meadow Maze Good, D.O., is a fellow in female pelvic medicine and reconstructive surgery at the University of Texas Southwestern Medical Center, Dallas. Dr. Good, who is also the chair of the Junior Fellow Congress Advisory Council of the American Congress of Obstetricians and Gynecologists, was asked to comment on Dr. Wu's study. She said she had no relevant financial disclosures.
Dr. David M. Jaspan comments: Direct to consumer advertising has enabled more women to feel comfortable discussing incontinence with their health care providers, which is great. Industry had inundated general ob.gyn. offices with the opportunity to attend short courses to learn "mesh procedures," which may not have been great. Therefore, I am not surprised that the numbers of women with private insurance undergoing urogynecologic surgery are so high.
These advanced procedures should be undertaken by those surgeons with sufficient training and experience to properly counsel women about the risk and benefit of a native tissue repair, compared with a graft placement. In addition, surgeons should have a volume of experience and training that qualifies them to provide this detailed counseling and should perform an appropriate preoperative evaluation to determine the absolute need for a procedure. More procedures may have brought more risk to women.
I applaud the American College of Obstetricians and Gynecologists for the 2011 ACOG Committee Opinion #513, which says, "Surgeons performing complex pelvic floor reconstructive surgery should have adequate experience and training in native tissue repairs as well as repairs using mesh augmentation specific to each device, should have a thorough understanding of pelvic anatomy, and should be able to counsel patients regarding the risk/benefit ratio on the use of mesh compared with native tissue repairs" (Obstet. Gynecol. 2011;118:1459-64).
In its 2011 Safety Communication, the Food and Drug Administration said that transvaginal placement of surgical mesh for POP is of "continuing serious concern." In the document, the FDA restated its 2008 recommendation that health care providers "inform patients about the potential for serious complications and the effect on quality of life, including pain during sexual intercourse, scarring, and narrowing of the vaginal wall in POP repair using surgical mesh; and provide a copy of the patient labeling from the surgical mesh manufacturer if available."
The FDA also made several new recommendations for health care providers in its report:
- Surgeons should recognize that, in most cases, POP can be treated successfully without mesh, thus avoiding the risk of mesh-related complications.
- Surgeons should choose mesh surgery only after weighing the risks and benefits of surgery with mesh versus all surgical and nonsurgical alternatives.
- Removal of mesh may involve multiple surgical procedures and significantly impair the patient's quality of life. Complete removal of mesh may not be possible and may not result in complete resolution of complications, including pain.
Patient counseling needs to include discussion of alternative native tissue repair and the fact that synthetic mesh is permanent, according to ACOG. Other issues to discuss include that vaginal bleeding, pain, and dyspareunia may be related to vaginal mesh; Patients reporting such symptoms should undergo a thorough vaginal exam, including an exam under anesthesia if necessary.
Dr. David M. Jaspan is chairman of ob.gyn. for the Einstein Health Care Network in Philadelphia. He was asked to comment on Dr. Wu's study. Dr. Jaspan said that he had no financial disclosures.
Remember to ask about pelvic floor issues
Dr. Meadow Maze Good comments: This is a well done and important study that highlights the magnitude of pelvic floor disorders in women. Previous studies indicate that women delay or do not seek care for pelvic floor disorders and incorrectly think that these problems are a normal result of aging.
These data presented at the American Urogynecologic Society meeting by Dr. Wu and her colleagues reinforce the need for increased public awareness and education regarding pelvic floor disorders as well as available treatment options, including nonsurgical and surgical options. Additionally, this study points out that the physicians treating women of all ages including the primary care provider (family practice physicians and obstetrician/gynecologists) should query women about possible pelvic floor symptoms, including incontinence, prolapse, and sexual function.
It is especially important for the ob.gyn. to ask their patient about these symptoms if there is planning underway for a hysterectomy for other causes. This is an exciting time for the newly board-certifiable field of female pelvic medicine and reconstructive surgery. As the aging population of women with prolapse and incontinence increases, fellowship programs are graduating physicians knowledgeable in this specific field who are dedicated to taking care of women with these treatable conditions.
Meadow Maze Good, D.O., is a fellow in female pelvic medicine and reconstructive surgery at the University of Texas Southwestern Medical Center, Dallas. Dr. Good, who is also the chair of the Junior Fellow Congress Advisory Council of the American Congress of Obstetricians and Gynecologists, was asked to comment on Dr. Wu's study. She said she had no relevant financial disclosures.
Dr. David M. Jaspan comments: Direct to consumer advertising has enabled more women to feel comfortable discussing incontinence with their health care providers, which is great. Industry had inundated general ob.gyn. offices with the opportunity to attend short courses to learn "mesh procedures," which may not have been great. Therefore, I am not surprised that the numbers of women with private insurance undergoing urogynecologic surgery are so high.
These advanced procedures should be undertaken by those surgeons with sufficient training and experience to properly counsel women about the risk and benefit of a native tissue repair, compared with a graft placement. In addition, surgeons should have a volume of experience and training that qualifies them to provide this detailed counseling and should perform an appropriate preoperative evaluation to determine the absolute need for a procedure. More procedures may have brought more risk to women.
I applaud the American College of Obstetricians and Gynecologists for the 2011 ACOG Committee Opinion #513, which says, "Surgeons performing complex pelvic floor reconstructive surgery should have adequate experience and training in native tissue repairs as well as repairs using mesh augmentation specific to each device, should have a thorough understanding of pelvic anatomy, and should be able to counsel patients regarding the risk/benefit ratio on the use of mesh compared with native tissue repairs" (Obstet. Gynecol. 2011;118:1459-64).
In its 2011 Safety Communication, the Food and Drug Administration said that transvaginal placement of surgical mesh for POP is of "continuing serious concern." In the document, the FDA restated its 2008 recommendation that health care providers "inform patients about the potential for serious complications and the effect on quality of life, including pain during sexual intercourse, scarring, and narrowing of the vaginal wall in POP repair using surgical mesh; and provide a copy of the patient labeling from the surgical mesh manufacturer if available."
The FDA also made several new recommendations for health care providers in its report:
- Surgeons should recognize that, in most cases, POP can be treated successfully without mesh, thus avoiding the risk of mesh-related complications.
- Surgeons should choose mesh surgery only after weighing the risks and benefits of surgery with mesh versus all surgical and nonsurgical alternatives.
- Removal of mesh may involve multiple surgical procedures and significantly impair the patient's quality of life. Complete removal of mesh may not be possible and may not result in complete resolution of complications, including pain.
Patient counseling needs to include discussion of alternative native tissue repair and the fact that synthetic mesh is permanent, according to ACOG. Other issues to discuss include that vaginal bleeding, pain, and dyspareunia may be related to vaginal mesh; Patients reporting such symptoms should undergo a thorough vaginal exam, including an exam under anesthesia if necessary.
Dr. David M. Jaspan is chairman of ob.gyn. for the Einstein Health Care Network in Philadelphia. He was asked to comment on Dr. Wu's study. Dr. Jaspan said that he had no financial disclosures.
Remember to ask about pelvic floor issues
Dr. Meadow Maze Good comments: This is a well done and important study that highlights the magnitude of pelvic floor disorders in women. Previous studies indicate that women delay or do not seek care for pelvic floor disorders and incorrectly think that these problems are a normal result of aging.
These data presented at the American Urogynecologic Society meeting by Dr. Wu and her colleagues reinforce the need for increased public awareness and education regarding pelvic floor disorders as well as available treatment options, including nonsurgical and surgical options. Additionally, this study points out that the physicians treating women of all ages including the primary care provider (family practice physicians and obstetrician/gynecologists) should query women about possible pelvic floor symptoms, including incontinence, prolapse, and sexual function.
It is especially important for the ob.gyn. to ask their patient about these symptoms if there is planning underway for a hysterectomy for other causes. This is an exciting time for the newly board-certifiable field of female pelvic medicine and reconstructive surgery. As the aging population of women with prolapse and incontinence increases, fellowship programs are graduating physicians knowledgeable in this specific field who are dedicated to taking care of women with these treatable conditions.
Meadow Maze Good, D.O., is a fellow in female pelvic medicine and reconstructive surgery at the University of Texas Southwestern Medical Center, Dallas. Dr. Good, who is also the chair of the Junior Fellow Congress Advisory Council of the American Congress of Obstetricians and Gynecologists, was asked to comment on Dr. Wu's study. She said she had no relevant financial disclosures.
LAS VEGAS – Among women with private health insurance in this country, the lifetime risk of surgery for either stress urinary incontinence or pelvic organ prolapse stands at 20.2%, results from a large analysis demonstrated.
"This means that one out of every five women in the United States will undergo a urogynecologic procedure by the age of 80," Dr. Jennifer M. Wu said at the annual meeting of the American Urogynecologic Society. "This high rate highlights the public health burden of pelvic floor disorders, exposes the need for improved prevention strategies, and underscores the importance of effective long-term surgical interventions."
A commonly referenced statistic is that the lifetime risk of surgery for either stress urinary incontinence (SUI) or pelvic organ prolapse (POP) is 11%, but this was based on a study of 395 patients who underwent surgery in 1995 in the Northwest (Obstet. Gynecol. 1997;89:501-6).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Since 1995, several factors may have increased this risk. These include "the integration of midurethral slings and vaginal mesh prolapse procedures, regional differences in surgery rates, and the greater number of elderly women," explained Dr. Wu of the department of obstetrics and gynecology and the Center for Women’s Health Research at the University of North Carolina at Chapel Hill. "Thus, the objective of our study was to estimate the cumulative risk of SUI or POP surgery over a woman’s lifetime until the age of 80."
The researchers used the Market Scan Commercial Claims and Encounters database with the Medicare Supplemental, which contains de-identified inpatient and outpatient claims data from about 100 employer-based insurance plans in the United States. They included women aged 18 years and older and identified any SUI or POP surgery performed between 2007 and 2011 based on CPT codes. This resulted in a study population of 51.8 million women. Of these, 311,070 underwent surgery for either SUI or POP.
To estimate age-specific incidence rates for each age between 18 and 80 years, Dr. Wu and her associates multiplied age-specific prevalence rates by the proportion of cases that were incident. To estimate the proportion of all procedures that were repeat surgeries, they evaluated women who had a SUI or POP surgery in 2011 and "looked back" 5 years to identify prior surgeries. Finally, they used Monte Carlo simulations to determine the cumulative lifetime risk of either incontinence or prolapse surgery with 95% confidence intervals.
Dr. Wu reported that the cumulative lifetime risk of either SUI or POP surgery was 20.2% (95% CI, 19.2%-21.1%). The cumulative lifetime risk of SUI was 14.5% (95% CI, 13.4%-15.5%), and the risk of POP surgery was 13.7% (95% CI, 12.6%-14.8%). The cumulative lifetime risk for SUI or POP surgery increased with age in a stepwise fashion, from 11.4% by age 60 years to 15.9% by age 70 and 20.2% by age 80, she noted.
To place the risk of any primary surgery for SUI or POP in perspective, Dr. Wu drew a comparison with the lifetime risk estimates for colon cancer (4.8%), lung cancer (6.3%), breast cancer (14.8%), and any type of cancer (41.3%). "Granted, incontinence and prolapse are not life-threatening conditions, but this 20% risk highlights how common surgeries are for pelvic floor disorders, despite the fact that they’re widely underrecognized," she noted.
She acknowledged certain limitations of the study, including the fact that she and her associates were unable to review actual medical records to confirm the rate of prior surgeries. "In addition, we assumed a closed cohort and no competing risks such that all women live until the age of 80," she said. "Also, these results reflect women with private insurance and may not be generalizable to those who are uninsured or underinsured."
Dr. Wu disclosed that she is a consultant for Procter & Gamble.
LAS VEGAS – Among women with private health insurance in this country, the lifetime risk of surgery for either stress urinary incontinence or pelvic organ prolapse stands at 20.2%, results from a large analysis demonstrated.
"This means that one out of every five women in the United States will undergo a urogynecologic procedure by the age of 80," Dr. Jennifer M. Wu said at the annual meeting of the American Urogynecologic Society. "This high rate highlights the public health burden of pelvic floor disorders, exposes the need for improved prevention strategies, and underscores the importance of effective long-term surgical interventions."
A commonly referenced statistic is that the lifetime risk of surgery for either stress urinary incontinence (SUI) or pelvic organ prolapse (POP) is 11%, but this was based on a study of 395 patients who underwent surgery in 1995 in the Northwest (Obstet. Gynecol. 1997;89:501-6).
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Since 1995, several factors may have increased this risk. These include "the integration of midurethral slings and vaginal mesh prolapse procedures, regional differences in surgery rates, and the greater number of elderly women," explained Dr. Wu of the department of obstetrics and gynecology and the Center for Women’s Health Research at the University of North Carolina at Chapel Hill. "Thus, the objective of our study was to estimate the cumulative risk of SUI or POP surgery over a woman’s lifetime until the age of 80."
The researchers used the Market Scan Commercial Claims and Encounters database with the Medicare Supplemental, which contains de-identified inpatient and outpatient claims data from about 100 employer-based insurance plans in the United States. They included women aged 18 years and older and identified any SUI or POP surgery performed between 2007 and 2011 based on CPT codes. This resulted in a study population of 51.8 million women. Of these, 311,070 underwent surgery for either SUI or POP.
To estimate age-specific incidence rates for each age between 18 and 80 years, Dr. Wu and her associates multiplied age-specific prevalence rates by the proportion of cases that were incident. To estimate the proportion of all procedures that were repeat surgeries, they evaluated women who had a SUI or POP surgery in 2011 and "looked back" 5 years to identify prior surgeries. Finally, they used Monte Carlo simulations to determine the cumulative lifetime risk of either incontinence or prolapse surgery with 95% confidence intervals.
Dr. Wu reported that the cumulative lifetime risk of either SUI or POP surgery was 20.2% (95% CI, 19.2%-21.1%). The cumulative lifetime risk of SUI was 14.5% (95% CI, 13.4%-15.5%), and the risk of POP surgery was 13.7% (95% CI, 12.6%-14.8%). The cumulative lifetime risk for SUI or POP surgery increased with age in a stepwise fashion, from 11.4% by age 60 years to 15.9% by age 70 and 20.2% by age 80, she noted.
To place the risk of any primary surgery for SUI or POP in perspective, Dr. Wu drew a comparison with the lifetime risk estimates for colon cancer (4.8%), lung cancer (6.3%), breast cancer (14.8%), and any type of cancer (41.3%). "Granted, incontinence and prolapse are not life-threatening conditions, but this 20% risk highlights how common surgeries are for pelvic floor disorders, despite the fact that they’re widely underrecognized," she noted.
She acknowledged certain limitations of the study, including the fact that she and her associates were unable to review actual medical records to confirm the rate of prior surgeries. "In addition, we assumed a closed cohort and no competing risks such that all women live until the age of 80," she said. "Also, these results reflect women with private insurance and may not be generalizable to those who are uninsured or underinsured."
Dr. Wu disclosed that she is a consultant for Procter & Gamble.
AT THE AUGS ANNUAL MEETING
Major finding: The cumulative lifetime risk of surgery for either stress urinary incontinence (SUI) or pelvic organ prolapse (POP) was 20.2% (95%CI 19.2%, 21.1%).
Data source: Claims data from 311,070 women in the United States who underwent any SUI or POP surgery between 2007 and 2011.
Disclosures: Dr. Wu disclosed that she is a consultant for Procter & Gamble.