User login
Cardiology News is an independent news source that provides cardiologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on cardiology and the cardiologist's practice. Cardiology News Digital Network is the online destination and multimedia properties of Cardiology News, the independent news publication for cardiologists. Cardiology news is the leading source of news and commentary about clinical developments in cardiology as well as health care policy and regulations that affect the cardiologist's practice. Cardiology News Digital Network is owned by Frontline Medical Communications.
A Portrait of the Patient
Most of my writing starts on paper. I’ve stacks of Docket Gold legal pads, yellow and college ruled, filled with Sharpie S-Gel black ink. There are many scratch-outs and arrows, but no doodles. I’m genetically not a doodler. The draft of this essay however was interrupted by a graphic. It is a round figure with stick arms and legs. Somewhat centered are two intense scribbles, which represent eyes. A few loopy curls rest on top. It looks like a Mr. Potato Head, with owl eyes.
“Ah, art!” I say when I flip up the page and discover this spontaneous self-portrait of my 4-year-old. Using the media she had on hand, she let free her stored creative energy, an energy we all seem to have. “Tell me about what you’ve drawn here,” I say. She’s eager to share. Art is a natural way to connect.
My patients have shown me many similar self-portraits. Last week, the artist was a 71-year-old woman. She came with her friend, a 73-year-old woman, who is also my patient. They accompany each other on all their visits. She chose a small realtor pad with a color photo of a blonde with her arms folded and back against a graphic of a house. My patient managed to fit her sketch on the small, lined space, noting with tiny scribbles the lesions she wanted me to check. Although unnecessary, she added eyes, nose, and mouth.
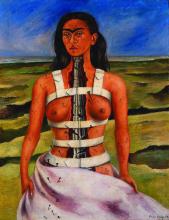
Another drawing was from a middle-aged white man. He has a look that suggests he rises early. His was on white printer paper, which he withdrew from a folder. He drew both a front and back view indicating with precision where I might find the spots he had mapped on his portrait. A retired teacher brought hers with a notably proportional anatomy and uniform tick marks on her face, arms, and legs. It reminded me of a self-portrait by the artist Frida Kahlo’s “The Broken Column.”
Kahlo was born with polio and suffered a severe bus accident as a young woman. She is one of many artists who shared their suffering through their art. “The Broken Column” depicts her with nails running from her face down her right short, weak leg. They look like the ticks my patient had added to her own self-portrait.
I remember in my neurology rotation asking patients to draw a clock. Stroke patients leave a whole half missing. Patients with dementia often crunch all the numbers into a little corner of the circle or forget to add the hands. Some of my dermatology patient self-portraits looked like that. I sometimes wonder if they also need a neurologist.
These pieces of patient art are utilitarian, drawn to narrate the story of what brought them to see me. Yet patients often add superfluous detail, demonstrating that utility and aesthetics are inseparable. I hold their drawings in the best light and notice the features and attributes. It helps me see their concerns from their point of view and primes me to notice other details during the physical exam. Viewing patients’ drawings can help build something called narrative competence the “ability to acknowledge, absorb, interpret, and act on the stories and plights of others.” Like Kahlo, patients are trying to share something with us, universal and recognizable. Art is how we connect to each other.
A few months ago, I walked in a room to see a consult. A white man in his 30s, he had prematurely graying hair and 80s-hip frames for glasses. He explained he was there for a skin screening and stood without warning, taking a step toward me. Like Michelangelo on wet plaster, he had grabbed a purple surgical marker to draw a self-portrait on the exam paper, the table set to just the right height and pitch to be an easel. It was the ginger-bread-man-type portrait with thick arms and legs and frosting-like dots marking the spots of concern. He marked L and R on the sheet, which were opposite what they would be if he was sitting facing me. But this was a self-portrait and he was drawing as it was with him facing the canvas, of course. “Ah, art!” I thought, and said, “Delightful! Tell me about what you’ve drawn here.” And so he did. A faint shadow of his portrait remains on that exam table to this day for every patient to see.
Benabio is chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at dermnews@mdedge.com.
Most of my writing starts on paper. I’ve stacks of Docket Gold legal pads, yellow and college ruled, filled with Sharpie S-Gel black ink. There are many scratch-outs and arrows, but no doodles. I’m genetically not a doodler. The draft of this essay however was interrupted by a graphic. It is a round figure with stick arms and legs. Somewhat centered are two intense scribbles, which represent eyes. A few loopy curls rest on top. It looks like a Mr. Potato Head, with owl eyes.
“Ah, art!” I say when I flip up the page and discover this spontaneous self-portrait of my 4-year-old. Using the media she had on hand, she let free her stored creative energy, an energy we all seem to have. “Tell me about what you’ve drawn here,” I say. She’s eager to share. Art is a natural way to connect.
My patients have shown me many similar self-portraits. Last week, the artist was a 71-year-old woman. She came with her friend, a 73-year-old woman, who is also my patient. They accompany each other on all their visits. She chose a small realtor pad with a color photo of a blonde with her arms folded and back against a graphic of a house. My patient managed to fit her sketch on the small, lined space, noting with tiny scribbles the lesions she wanted me to check. Although unnecessary, she added eyes, nose, and mouth.
Another drawing was from a middle-aged white man. He has a look that suggests he rises early. His was on white printer paper, which he withdrew from a folder. He drew both a front and back view indicating with precision where I might find the spots he had mapped on his portrait. A retired teacher brought hers with a notably proportional anatomy and uniform tick marks on her face, arms, and legs. It reminded me of a self-portrait by the artist Frida Kahlo’s “The Broken Column.”
Kahlo was born with polio and suffered a severe bus accident as a young woman. She is one of many artists who shared their suffering through their art. “The Broken Column” depicts her with nails running from her face down her right short, weak leg. They look like the ticks my patient had added to her own self-portrait.
I remember in my neurology rotation asking patients to draw a clock. Stroke patients leave a whole half missing. Patients with dementia often crunch all the numbers into a little corner of the circle or forget to add the hands. Some of my dermatology patient self-portraits looked like that. I sometimes wonder if they also need a neurologist.
These pieces of patient art are utilitarian, drawn to narrate the story of what brought them to see me. Yet patients often add superfluous detail, demonstrating that utility and aesthetics are inseparable. I hold their drawings in the best light and notice the features and attributes. It helps me see their concerns from their point of view and primes me to notice other details during the physical exam. Viewing patients’ drawings can help build something called narrative competence the “ability to acknowledge, absorb, interpret, and act on the stories and plights of others.” Like Kahlo, patients are trying to share something with us, universal and recognizable. Art is how we connect to each other.
A few months ago, I walked in a room to see a consult. A white man in his 30s, he had prematurely graying hair and 80s-hip frames for glasses. He explained he was there for a skin screening and stood without warning, taking a step toward me. Like Michelangelo on wet plaster, he had grabbed a purple surgical marker to draw a self-portrait on the exam paper, the table set to just the right height and pitch to be an easel. It was the ginger-bread-man-type portrait with thick arms and legs and frosting-like dots marking the spots of concern. He marked L and R on the sheet, which were opposite what they would be if he was sitting facing me. But this was a self-portrait and he was drawing as it was with him facing the canvas, of course. “Ah, art!” I thought, and said, “Delightful! Tell me about what you’ve drawn here.” And so he did. A faint shadow of his portrait remains on that exam table to this day for every patient to see.
Benabio is chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at dermnews@mdedge.com.
Most of my writing starts on paper. I’ve stacks of Docket Gold legal pads, yellow and college ruled, filled with Sharpie S-Gel black ink. There are many scratch-outs and arrows, but no doodles. I’m genetically not a doodler. The draft of this essay however was interrupted by a graphic. It is a round figure with stick arms and legs. Somewhat centered are two intense scribbles, which represent eyes. A few loopy curls rest on top. It looks like a Mr. Potato Head, with owl eyes.
“Ah, art!” I say when I flip up the page and discover this spontaneous self-portrait of my 4-year-old. Using the media she had on hand, she let free her stored creative energy, an energy we all seem to have. “Tell me about what you’ve drawn here,” I say. She’s eager to share. Art is a natural way to connect.
My patients have shown me many similar self-portraits. Last week, the artist was a 71-year-old woman. She came with her friend, a 73-year-old woman, who is also my patient. They accompany each other on all their visits. She chose a small realtor pad with a color photo of a blonde with her arms folded and back against a graphic of a house. My patient managed to fit her sketch on the small, lined space, noting with tiny scribbles the lesions she wanted me to check. Although unnecessary, she added eyes, nose, and mouth.
Another drawing was from a middle-aged white man. He has a look that suggests he rises early. His was on white printer paper, which he withdrew from a folder. He drew both a front and back view indicating with precision where I might find the spots he had mapped on his portrait. A retired teacher brought hers with a notably proportional anatomy and uniform tick marks on her face, arms, and legs. It reminded me of a self-portrait by the artist Frida Kahlo’s “The Broken Column.”
Kahlo was born with polio and suffered a severe bus accident as a young woman. She is one of many artists who shared their suffering through their art. “The Broken Column” depicts her with nails running from her face down her right short, weak leg. They look like the ticks my patient had added to her own self-portrait.
I remember in my neurology rotation asking patients to draw a clock. Stroke patients leave a whole half missing. Patients with dementia often crunch all the numbers into a little corner of the circle or forget to add the hands. Some of my dermatology patient self-portraits looked like that. I sometimes wonder if they also need a neurologist.
These pieces of patient art are utilitarian, drawn to narrate the story of what brought them to see me. Yet patients often add superfluous detail, demonstrating that utility and aesthetics are inseparable. I hold their drawings in the best light and notice the features and attributes. It helps me see their concerns from their point of view and primes me to notice other details during the physical exam. Viewing patients’ drawings can help build something called narrative competence the “ability to acknowledge, absorb, interpret, and act on the stories and plights of others.” Like Kahlo, patients are trying to share something with us, universal and recognizable. Art is how we connect to each other.
A few months ago, I walked in a room to see a consult. A white man in his 30s, he had prematurely graying hair and 80s-hip frames for glasses. He explained he was there for a skin screening and stood without warning, taking a step toward me. Like Michelangelo on wet plaster, he had grabbed a purple surgical marker to draw a self-portrait on the exam paper, the table set to just the right height and pitch to be an easel. It was the ginger-bread-man-type portrait with thick arms and legs and frosting-like dots marking the spots of concern. He marked L and R on the sheet, which were opposite what they would be if he was sitting facing me. But this was a self-portrait and he was drawing as it was with him facing the canvas, of course. “Ah, art!” I thought, and said, “Delightful! Tell me about what you’ve drawn here.” And so he did. A faint shadow of his portrait remains on that exam table to this day for every patient to see.
Benabio is chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at dermnews@mdedge.com.
Post COVID-19, Long-term Risk for Autoimmune, Autoinflammatory Skin Disorders Increased, Study Finds
In addition, the authors reported that COVID-19 vaccination appears to reduce these risks.
The study was published in JAMA Dermatology.
‘Compelling Evidence’
“This well-executed study by Heo et al provides compelling evidence to support an association between COVID-19 infection and the development of subsequent autoimmune and autoinflammatory skin diseases,” wrote authors led by Lisa M. Arkin, MD, of the Department of Dermatology, University of Wisconsin School of Medicine and Public Health in Madison, in an accompanying editorial.
Using databases from Korea’s National Health Insurance Service and the Korea Disease Control and Prevention Agency, investigators led by Yeon-Woo Heo, MD, a dermatology resident at Yonsei University Wonju College of Medicine, Wonju, Republic of Korea, compared 3.1 million people who had COVID-19 with 3.8 million controls, all with at least 180 days’ follow-up through December 31, 2022.
At a mean follow-up of 287 days in both cohorts, authors found significantly elevated risks for AA and vitiligo (adjusted hazard ratio [aHR], 1.11 for both), AT (aHR, 1.24), Behçet disease (aHR, 1.45), and BP (aHR, 1.62) in the post–COVID-19 cohort. The infection also raised the risk for other conditions such as systemic lupus erythematosus (aHR, 1.14) and Crohn’s disease (aHR, 1.35).
In subgroup analyses, demographic factors were associated with diverse effects: COVID-19 infection was associated with significantly higher odds of developing AA (for both men and women), vitiligo (men), Behçet disease (men and women), Crohn’s disease (men), ulcerative colitis (men), rheumatoid arthritis (men and women), systemic lupus erythematosus (men), ankylosing spondylitis (men), AT (women), and BP (women) than controls.
Those aged under 40 years were more likely to develop AA, primary cicatricial alopecia, Behçet disease, and ulcerative colitis, while those aged 40 years or older were more likely to develop AA, AT, vitiligo, Behçet disease, Crohn’s disease, rheumatoid arthritis, systemic lupus erythematosus, Sjögren’s syndrome, ankylosing spondylitis, and BP.
Additionally, severe COVID-19 requiring intensive care unit admission was associated with a significantly increased risk for autoimmune diseases, including AA, psoriasis, BP, and sarcoidosis. By timeframe, risks for AA, AT, and psoriasis were significantly higher during the initial Delta-dominant period.
Vaccination Effect
Moreover, vaccinated individuals were less likely to develop AA, AT, psoriasis, Behçet disease, and various nondermatologic conditions than were those who were unvaccinated. This finding, wrote Heo and colleagues, “may provide evidence to support the hypothesis that COVID-19 vaccines can help prevent autoimmune diseases.”
“That’s the part we all need to take into our offices tomorrow,” said Brett King, MD, PhD, a Fairfield, Connecticut–based dermatologist in private practice. He was not involved with the study but was asked to comment.
Overall, King said, the study carries two main messages. “The first is that COVID-19 infection increases the likelihood of developing an autoimmune or autoinflammatory disease in a large population.” The second and very important message is that being vaccinated against COVID-19 provides protection against developing an autoimmune or autoinflammatory disease.
“My concern is that the popular media highlights the first part,” said King, “and everybody who develops alopecia areata, vitiligo, or sarcoidosis blames COVID-19. That’s not what this work says.”
The foregoing distinction is especially important during the fall and winter, he added, when people getting influenza vaccines are routinely offered COVID-19 vaccines. “Many patients have said, ‘I got the COVID vaccine and developed alopecia areata 6 months later.’ Nearly everybody who has developed a new or worsening health condition in the last almost 5 years has had the perfect fall guy — the COVID vaccine or infection.”
With virtually all patients asking if they should get an updated COVID-19 vaccine or booster, he added, many report having heard that such vaccines cause AA, vitiligo, or other diseases. “To anchor these conversations in real data and not just anecdotes from a blog or Facebook is very useful,” said King, “and now we have very good data saying that the COVID vaccine is protective against these disorders.”
George Han, MD, PhD, associate professor of dermatology at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York, applauds investigators’ use of a large, robust database but suggests interpreting results cautiously. He was not involved with the study but was asked to comment.
“You could do a large, well-done study,” Han said, “but it could still not necessarily be generalizable. These autoimmune conditions they’re looking at have clear ethnic and racial biases.” Heo and colleagues acknowledged shortcomings including their study population’s monomorphic nature.
Additional issues that limit the study’s impact, said Han, include the difficulty of conceptualizing a 10%-20% increase in conditions that at baseline are rare. And many of the findings reflected natural patterns, he said. For instance, BP more commonly affects older people, COVID-19 notwithstanding.
Han said that for him, the study’s main value going forward is helping to explain a rash of worsening inflammatory skin disease that many dermatologists saw early in the pandemic. “We would regularly see patients who were well controlled with, for example, psoriasis or eczema. But after COVID-19 infection or a vaccine (usually mRNA-type), in some cases they would come in flaring badly.” This happened at least a dozen times during the first year of post-shutdown appointments, he said.
“We’ve seen patients who have flared multiple times — they get the booster, then flare again,” Han added. Similar patterns occurred with pyoderma gangrenosum and other inflammatory skin diseases, he said.
Given the modest effect sizes of the associations reported in the Korean study, Arkin and colleagues wrote in their JAMA Dermatology editorial that surveillance for autoimmune disease is probably not warranted without new examination findings or symptoms. “For certain,” King said, “we should not go hunting for things that aren’t obviously there.”
Rather, Arkin and colleagues wrote, the higher autoimmunity rates seen among the unvaccinated, as well as during the Delta phase (when patients were sicker and hospitalizations were more likely) and in patients requiring intensive care, suggest that “interventions that reduce disease severity could also potentially reduce long-term risk of subsequent autoimmune sequelae.”
Future research addressing whether people with preexisting autoimmune conditions are at greater risk for flares or developing new autoimmune diseases following COVID-19 infection “would help to frame an evidence-based approach for patients with autoimmune disorders who develop COVID-19 infection, including the role for antiviral treatments,” they added.
The study was supported by grants from the Research Program of the Korea Medical Institute, the Korea Health Industry Development Institute, and the National Research Foundation of Korea. Han and King reported no relevant financial relationships. Arkin disclosed receiving research grants to her institution from Amgen and Eli Lilly, personal fees from Sanofi/Regeneron for consulting, and personal consulting fees from Merck outside the submitted work. Another author reported personal consulting fees from Dexcel Pharma and Honeydew outside the submitted work. No other disclosures were reported.
A version of this article appeared on Medscape.com.
In addition, the authors reported that COVID-19 vaccination appears to reduce these risks.
The study was published in JAMA Dermatology.
‘Compelling Evidence’
“This well-executed study by Heo et al provides compelling evidence to support an association between COVID-19 infection and the development of subsequent autoimmune and autoinflammatory skin diseases,” wrote authors led by Lisa M. Arkin, MD, of the Department of Dermatology, University of Wisconsin School of Medicine and Public Health in Madison, in an accompanying editorial.
Using databases from Korea’s National Health Insurance Service and the Korea Disease Control and Prevention Agency, investigators led by Yeon-Woo Heo, MD, a dermatology resident at Yonsei University Wonju College of Medicine, Wonju, Republic of Korea, compared 3.1 million people who had COVID-19 with 3.8 million controls, all with at least 180 days’ follow-up through December 31, 2022.
At a mean follow-up of 287 days in both cohorts, authors found significantly elevated risks for AA and vitiligo (adjusted hazard ratio [aHR], 1.11 for both), AT (aHR, 1.24), Behçet disease (aHR, 1.45), and BP (aHR, 1.62) in the post–COVID-19 cohort. The infection also raised the risk for other conditions such as systemic lupus erythematosus (aHR, 1.14) and Crohn’s disease (aHR, 1.35).
In subgroup analyses, demographic factors were associated with diverse effects: COVID-19 infection was associated with significantly higher odds of developing AA (for both men and women), vitiligo (men), Behçet disease (men and women), Crohn’s disease (men), ulcerative colitis (men), rheumatoid arthritis (men and women), systemic lupus erythematosus (men), ankylosing spondylitis (men), AT (women), and BP (women) than controls.
Those aged under 40 years were more likely to develop AA, primary cicatricial alopecia, Behçet disease, and ulcerative colitis, while those aged 40 years or older were more likely to develop AA, AT, vitiligo, Behçet disease, Crohn’s disease, rheumatoid arthritis, systemic lupus erythematosus, Sjögren’s syndrome, ankylosing spondylitis, and BP.
Additionally, severe COVID-19 requiring intensive care unit admission was associated with a significantly increased risk for autoimmune diseases, including AA, psoriasis, BP, and sarcoidosis. By timeframe, risks for AA, AT, and psoriasis were significantly higher during the initial Delta-dominant period.
Vaccination Effect
Moreover, vaccinated individuals were less likely to develop AA, AT, psoriasis, Behçet disease, and various nondermatologic conditions than were those who were unvaccinated. This finding, wrote Heo and colleagues, “may provide evidence to support the hypothesis that COVID-19 vaccines can help prevent autoimmune diseases.”
“That’s the part we all need to take into our offices tomorrow,” said Brett King, MD, PhD, a Fairfield, Connecticut–based dermatologist in private practice. He was not involved with the study but was asked to comment.
Overall, King said, the study carries two main messages. “The first is that COVID-19 infection increases the likelihood of developing an autoimmune or autoinflammatory disease in a large population.” The second and very important message is that being vaccinated against COVID-19 provides protection against developing an autoimmune or autoinflammatory disease.
“My concern is that the popular media highlights the first part,” said King, “and everybody who develops alopecia areata, vitiligo, or sarcoidosis blames COVID-19. That’s not what this work says.”
The foregoing distinction is especially important during the fall and winter, he added, when people getting influenza vaccines are routinely offered COVID-19 vaccines. “Many patients have said, ‘I got the COVID vaccine and developed alopecia areata 6 months later.’ Nearly everybody who has developed a new or worsening health condition in the last almost 5 years has had the perfect fall guy — the COVID vaccine or infection.”
With virtually all patients asking if they should get an updated COVID-19 vaccine or booster, he added, many report having heard that such vaccines cause AA, vitiligo, or other diseases. “To anchor these conversations in real data and not just anecdotes from a blog or Facebook is very useful,” said King, “and now we have very good data saying that the COVID vaccine is protective against these disorders.”
George Han, MD, PhD, associate professor of dermatology at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York, applauds investigators’ use of a large, robust database but suggests interpreting results cautiously. He was not involved with the study but was asked to comment.
“You could do a large, well-done study,” Han said, “but it could still not necessarily be generalizable. These autoimmune conditions they’re looking at have clear ethnic and racial biases.” Heo and colleagues acknowledged shortcomings including their study population’s monomorphic nature.
Additional issues that limit the study’s impact, said Han, include the difficulty of conceptualizing a 10%-20% increase in conditions that at baseline are rare. And many of the findings reflected natural patterns, he said. For instance, BP more commonly affects older people, COVID-19 notwithstanding.
Han said that for him, the study’s main value going forward is helping to explain a rash of worsening inflammatory skin disease that many dermatologists saw early in the pandemic. “We would regularly see patients who were well controlled with, for example, psoriasis or eczema. But after COVID-19 infection or a vaccine (usually mRNA-type), in some cases they would come in flaring badly.” This happened at least a dozen times during the first year of post-shutdown appointments, he said.
“We’ve seen patients who have flared multiple times — they get the booster, then flare again,” Han added. Similar patterns occurred with pyoderma gangrenosum and other inflammatory skin diseases, he said.
Given the modest effect sizes of the associations reported in the Korean study, Arkin and colleagues wrote in their JAMA Dermatology editorial that surveillance for autoimmune disease is probably not warranted without new examination findings or symptoms. “For certain,” King said, “we should not go hunting for things that aren’t obviously there.”
Rather, Arkin and colleagues wrote, the higher autoimmunity rates seen among the unvaccinated, as well as during the Delta phase (when patients were sicker and hospitalizations were more likely) and in patients requiring intensive care, suggest that “interventions that reduce disease severity could also potentially reduce long-term risk of subsequent autoimmune sequelae.”
Future research addressing whether people with preexisting autoimmune conditions are at greater risk for flares or developing new autoimmune diseases following COVID-19 infection “would help to frame an evidence-based approach for patients with autoimmune disorders who develop COVID-19 infection, including the role for antiviral treatments,” they added.
The study was supported by grants from the Research Program of the Korea Medical Institute, the Korea Health Industry Development Institute, and the National Research Foundation of Korea. Han and King reported no relevant financial relationships. Arkin disclosed receiving research grants to her institution from Amgen and Eli Lilly, personal fees from Sanofi/Regeneron for consulting, and personal consulting fees from Merck outside the submitted work. Another author reported personal consulting fees from Dexcel Pharma and Honeydew outside the submitted work. No other disclosures were reported.
A version of this article appeared on Medscape.com.
In addition, the authors reported that COVID-19 vaccination appears to reduce these risks.
The study was published in JAMA Dermatology.
‘Compelling Evidence’
“This well-executed study by Heo et al provides compelling evidence to support an association between COVID-19 infection and the development of subsequent autoimmune and autoinflammatory skin diseases,” wrote authors led by Lisa M. Arkin, MD, of the Department of Dermatology, University of Wisconsin School of Medicine and Public Health in Madison, in an accompanying editorial.
Using databases from Korea’s National Health Insurance Service and the Korea Disease Control and Prevention Agency, investigators led by Yeon-Woo Heo, MD, a dermatology resident at Yonsei University Wonju College of Medicine, Wonju, Republic of Korea, compared 3.1 million people who had COVID-19 with 3.8 million controls, all with at least 180 days’ follow-up through December 31, 2022.
At a mean follow-up of 287 days in both cohorts, authors found significantly elevated risks for AA and vitiligo (adjusted hazard ratio [aHR], 1.11 for both), AT (aHR, 1.24), Behçet disease (aHR, 1.45), and BP (aHR, 1.62) in the post–COVID-19 cohort. The infection also raised the risk for other conditions such as systemic lupus erythematosus (aHR, 1.14) and Crohn’s disease (aHR, 1.35).
In subgroup analyses, demographic factors were associated with diverse effects: COVID-19 infection was associated with significantly higher odds of developing AA (for both men and women), vitiligo (men), Behçet disease (men and women), Crohn’s disease (men), ulcerative colitis (men), rheumatoid arthritis (men and women), systemic lupus erythematosus (men), ankylosing spondylitis (men), AT (women), and BP (women) than controls.
Those aged under 40 years were more likely to develop AA, primary cicatricial alopecia, Behçet disease, and ulcerative colitis, while those aged 40 years or older were more likely to develop AA, AT, vitiligo, Behçet disease, Crohn’s disease, rheumatoid arthritis, systemic lupus erythematosus, Sjögren’s syndrome, ankylosing spondylitis, and BP.
Additionally, severe COVID-19 requiring intensive care unit admission was associated with a significantly increased risk for autoimmune diseases, including AA, psoriasis, BP, and sarcoidosis. By timeframe, risks for AA, AT, and psoriasis were significantly higher during the initial Delta-dominant period.
Vaccination Effect
Moreover, vaccinated individuals were less likely to develop AA, AT, psoriasis, Behçet disease, and various nondermatologic conditions than were those who were unvaccinated. This finding, wrote Heo and colleagues, “may provide evidence to support the hypothesis that COVID-19 vaccines can help prevent autoimmune diseases.”
“That’s the part we all need to take into our offices tomorrow,” said Brett King, MD, PhD, a Fairfield, Connecticut–based dermatologist in private practice. He was not involved with the study but was asked to comment.
Overall, King said, the study carries two main messages. “The first is that COVID-19 infection increases the likelihood of developing an autoimmune or autoinflammatory disease in a large population.” The second and very important message is that being vaccinated against COVID-19 provides protection against developing an autoimmune or autoinflammatory disease.
“My concern is that the popular media highlights the first part,” said King, “and everybody who develops alopecia areata, vitiligo, or sarcoidosis blames COVID-19. That’s not what this work says.”
The foregoing distinction is especially important during the fall and winter, he added, when people getting influenza vaccines are routinely offered COVID-19 vaccines. “Many patients have said, ‘I got the COVID vaccine and developed alopecia areata 6 months later.’ Nearly everybody who has developed a new or worsening health condition in the last almost 5 years has had the perfect fall guy — the COVID vaccine or infection.”
With virtually all patients asking if they should get an updated COVID-19 vaccine or booster, he added, many report having heard that such vaccines cause AA, vitiligo, or other diseases. “To anchor these conversations in real data and not just anecdotes from a blog or Facebook is very useful,” said King, “and now we have very good data saying that the COVID vaccine is protective against these disorders.”
George Han, MD, PhD, associate professor of dermatology at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York, applauds investigators’ use of a large, robust database but suggests interpreting results cautiously. He was not involved with the study but was asked to comment.
“You could do a large, well-done study,” Han said, “but it could still not necessarily be generalizable. These autoimmune conditions they’re looking at have clear ethnic and racial biases.” Heo and colleagues acknowledged shortcomings including their study population’s monomorphic nature.
Additional issues that limit the study’s impact, said Han, include the difficulty of conceptualizing a 10%-20% increase in conditions that at baseline are rare. And many of the findings reflected natural patterns, he said. For instance, BP more commonly affects older people, COVID-19 notwithstanding.
Han said that for him, the study’s main value going forward is helping to explain a rash of worsening inflammatory skin disease that many dermatologists saw early in the pandemic. “We would regularly see patients who were well controlled with, for example, psoriasis or eczema. But after COVID-19 infection or a vaccine (usually mRNA-type), in some cases they would come in flaring badly.” This happened at least a dozen times during the first year of post-shutdown appointments, he said.
“We’ve seen patients who have flared multiple times — they get the booster, then flare again,” Han added. Similar patterns occurred with pyoderma gangrenosum and other inflammatory skin diseases, he said.
Given the modest effect sizes of the associations reported in the Korean study, Arkin and colleagues wrote in their JAMA Dermatology editorial that surveillance for autoimmune disease is probably not warranted without new examination findings or symptoms. “For certain,” King said, “we should not go hunting for things that aren’t obviously there.”
Rather, Arkin and colleagues wrote, the higher autoimmunity rates seen among the unvaccinated, as well as during the Delta phase (when patients were sicker and hospitalizations were more likely) and in patients requiring intensive care, suggest that “interventions that reduce disease severity could also potentially reduce long-term risk of subsequent autoimmune sequelae.”
Future research addressing whether people with preexisting autoimmune conditions are at greater risk for flares or developing new autoimmune diseases following COVID-19 infection “would help to frame an evidence-based approach for patients with autoimmune disorders who develop COVID-19 infection, including the role for antiviral treatments,” they added.
The study was supported by grants from the Research Program of the Korea Medical Institute, the Korea Health Industry Development Institute, and the National Research Foundation of Korea. Han and King reported no relevant financial relationships. Arkin disclosed receiving research grants to her institution from Amgen and Eli Lilly, personal fees from Sanofi/Regeneron for consulting, and personal consulting fees from Merck outside the submitted work. Another author reported personal consulting fees from Dexcel Pharma and Honeydew outside the submitted work. No other disclosures were reported.
A version of this article appeared on Medscape.com.
FROM JAMA DERMATOLOGY
Sitting for More Than 10 Hours Daily Ups Heart Disease Risk
TOPLINE:
Sedentary time exceeding 10.6 h/d is linked to an increased risk for atrial fibrillation, heart failure, myocardial infarction, and cardiovascular (CV) mortality, researchers found. The risk persists even in individuals who meet recommended physical activity levels.
METHODOLOGY:
- Researchers used a validated machine learning approach to investigate the relationships between sedentary behavior and the future risks for CV illness and mortality in 89,530 middle-aged and older adults (mean age, 62 years; 56% women) from the UK Biobank.
- Participants provided data from a wrist-worn triaxial accelerometer that recorded their movements over a period of 7 days.
- Machine learning algorithms classified accelerometer signals into four classes of activities: Sleep, sedentary behavior, light physical activity, and moderate to vigorous physical activity.
- Participants were followed up for a median of 8 years through linkage to national health-related datasets in England, Scotland, and Wales.
- The median sedentary time was 9.4 h/d.
TAKEAWAY:
- During the follow-up period, 3638 individuals (4.9%) experienced incident atrial fibrillation, 1854 (2.09%) developed incident heart failure, 1610 (1.84%) experienced incident myocardial infarction, and 846 (0.94%) died from cardiovascular causes.
- The risks for atrial fibrillation and myocardial infarction increased steadily with an increase in sedentary time, with sedentary time greater than 10.6 h/d showing a modest increase in risk for atrial fibrillation (hazard ratio [HR], 1.11; 95% CI, 1.01-1.21).
- The risks for heart failure and CV mortality were low until sedentary time surpassed approximately 10.6 h/d, after which they rose by 45% (HR, 1.45; 95% CI, 1.28-1.65) and 62% (HR, 1.62; 95% CI, 1.34-1.96), respectively.
- The associations were attenuated but remained significant for CV mortality (HR, 1.33; 95% CI: 1.07-1.64) in individuals who met the recommended levels for physical activity yet were sedentary for more than 10.6 h/d. Reallocating 30 minutes of sedentary time to other activities reduced the risk for heart failure (HR, 0.93; 95% CI, 0.90-0.96) among those who were sedentary more than 10.6 h/d.
IN PRACTICE:
The study “highlights a complex interplay between sedentary behavior and physical activity, ultimately suggesting that sedentary behavior remains relevant for CV disease risk even among individuals meeting sufficient” levels of activity, the researchers reported.
“Individuals should move more and be less sedentary to reduce CV risk. ... Being a ‘weekend warrior’ and meeting guideline levels of [moderate to vigorous physical activity] of 150 minutes/week will not completely abolish the deleterious effects of extended sedentary time of > 10.6 hours per day,” Charles B. Eaton, MD, MS, of the Warren Alpert Medical School of Brown University in Providence, Rhode Island, wrote in an editorial accompanying the journal article.
SOURCE:
The study was led by Ezimamaka Ajufo, MD, of Brigham and Women’s Hospital in Boston. It was published online on November 15, 2024, in the Journal of the American College of Cardiology.
LIMITATIONS:
Wrist-based accelerometers cannot assess specific contexts for sedentary behavior and may misclassify standing time as sedentary time, and these limitations may have affected the findings. Physical activity was measured for 1 week only, which might not have fully represented habitual activity patterns. The sample included predominantly White participants and was enriched for health and socioeconomic status, which may have limited the generalizability of the findings.
DISCLOSURES:
The authors disclosed receiving research support, grants, and research fellowships and collaborations from various institutions and pharmaceutical companies, as well as serving on their advisory boards.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Sedentary time exceeding 10.6 h/d is linked to an increased risk for atrial fibrillation, heart failure, myocardial infarction, and cardiovascular (CV) mortality, researchers found. The risk persists even in individuals who meet recommended physical activity levels.
METHODOLOGY:
- Researchers used a validated machine learning approach to investigate the relationships between sedentary behavior and the future risks for CV illness and mortality in 89,530 middle-aged and older adults (mean age, 62 years; 56% women) from the UK Biobank.
- Participants provided data from a wrist-worn triaxial accelerometer that recorded their movements over a period of 7 days.
- Machine learning algorithms classified accelerometer signals into four classes of activities: Sleep, sedentary behavior, light physical activity, and moderate to vigorous physical activity.
- Participants were followed up for a median of 8 years through linkage to national health-related datasets in England, Scotland, and Wales.
- The median sedentary time was 9.4 h/d.
TAKEAWAY:
- During the follow-up period, 3638 individuals (4.9%) experienced incident atrial fibrillation, 1854 (2.09%) developed incident heart failure, 1610 (1.84%) experienced incident myocardial infarction, and 846 (0.94%) died from cardiovascular causes.
- The risks for atrial fibrillation and myocardial infarction increased steadily with an increase in sedentary time, with sedentary time greater than 10.6 h/d showing a modest increase in risk for atrial fibrillation (hazard ratio [HR], 1.11; 95% CI, 1.01-1.21).
- The risks for heart failure and CV mortality were low until sedentary time surpassed approximately 10.6 h/d, after which they rose by 45% (HR, 1.45; 95% CI, 1.28-1.65) and 62% (HR, 1.62; 95% CI, 1.34-1.96), respectively.
- The associations were attenuated but remained significant for CV mortality (HR, 1.33; 95% CI: 1.07-1.64) in individuals who met the recommended levels for physical activity yet were sedentary for more than 10.6 h/d. Reallocating 30 minutes of sedentary time to other activities reduced the risk for heart failure (HR, 0.93; 95% CI, 0.90-0.96) among those who were sedentary more than 10.6 h/d.
IN PRACTICE:
The study “highlights a complex interplay between sedentary behavior and physical activity, ultimately suggesting that sedentary behavior remains relevant for CV disease risk even among individuals meeting sufficient” levels of activity, the researchers reported.
“Individuals should move more and be less sedentary to reduce CV risk. ... Being a ‘weekend warrior’ and meeting guideline levels of [moderate to vigorous physical activity] of 150 minutes/week will not completely abolish the deleterious effects of extended sedentary time of > 10.6 hours per day,” Charles B. Eaton, MD, MS, of the Warren Alpert Medical School of Brown University in Providence, Rhode Island, wrote in an editorial accompanying the journal article.
SOURCE:
The study was led by Ezimamaka Ajufo, MD, of Brigham and Women’s Hospital in Boston. It was published online on November 15, 2024, in the Journal of the American College of Cardiology.
LIMITATIONS:
Wrist-based accelerometers cannot assess specific contexts for sedentary behavior and may misclassify standing time as sedentary time, and these limitations may have affected the findings. Physical activity was measured for 1 week only, which might not have fully represented habitual activity patterns. The sample included predominantly White participants and was enriched for health and socioeconomic status, which may have limited the generalizability of the findings.
DISCLOSURES:
The authors disclosed receiving research support, grants, and research fellowships and collaborations from various institutions and pharmaceutical companies, as well as serving on their advisory boards.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Sedentary time exceeding 10.6 h/d is linked to an increased risk for atrial fibrillation, heart failure, myocardial infarction, and cardiovascular (CV) mortality, researchers found. The risk persists even in individuals who meet recommended physical activity levels.
METHODOLOGY:
- Researchers used a validated machine learning approach to investigate the relationships between sedentary behavior and the future risks for CV illness and mortality in 89,530 middle-aged and older adults (mean age, 62 years; 56% women) from the UK Biobank.
- Participants provided data from a wrist-worn triaxial accelerometer that recorded their movements over a period of 7 days.
- Machine learning algorithms classified accelerometer signals into four classes of activities: Sleep, sedentary behavior, light physical activity, and moderate to vigorous physical activity.
- Participants were followed up for a median of 8 years through linkage to national health-related datasets in England, Scotland, and Wales.
- The median sedentary time was 9.4 h/d.
TAKEAWAY:
- During the follow-up period, 3638 individuals (4.9%) experienced incident atrial fibrillation, 1854 (2.09%) developed incident heart failure, 1610 (1.84%) experienced incident myocardial infarction, and 846 (0.94%) died from cardiovascular causes.
- The risks for atrial fibrillation and myocardial infarction increased steadily with an increase in sedentary time, with sedentary time greater than 10.6 h/d showing a modest increase in risk for atrial fibrillation (hazard ratio [HR], 1.11; 95% CI, 1.01-1.21).
- The risks for heart failure and CV mortality were low until sedentary time surpassed approximately 10.6 h/d, after which they rose by 45% (HR, 1.45; 95% CI, 1.28-1.65) and 62% (HR, 1.62; 95% CI, 1.34-1.96), respectively.
- The associations were attenuated but remained significant for CV mortality (HR, 1.33; 95% CI: 1.07-1.64) in individuals who met the recommended levels for physical activity yet were sedentary for more than 10.6 h/d. Reallocating 30 minutes of sedentary time to other activities reduced the risk for heart failure (HR, 0.93; 95% CI, 0.90-0.96) among those who were sedentary more than 10.6 h/d.
IN PRACTICE:
The study “highlights a complex interplay between sedentary behavior and physical activity, ultimately suggesting that sedentary behavior remains relevant for CV disease risk even among individuals meeting sufficient” levels of activity, the researchers reported.
“Individuals should move more and be less sedentary to reduce CV risk. ... Being a ‘weekend warrior’ and meeting guideline levels of [moderate to vigorous physical activity] of 150 minutes/week will not completely abolish the deleterious effects of extended sedentary time of > 10.6 hours per day,” Charles B. Eaton, MD, MS, of the Warren Alpert Medical School of Brown University in Providence, Rhode Island, wrote in an editorial accompanying the journal article.
SOURCE:
The study was led by Ezimamaka Ajufo, MD, of Brigham and Women’s Hospital in Boston. It was published online on November 15, 2024, in the Journal of the American College of Cardiology.
LIMITATIONS:
Wrist-based accelerometers cannot assess specific contexts for sedentary behavior and may misclassify standing time as sedentary time, and these limitations may have affected the findings. Physical activity was measured for 1 week only, which might not have fully represented habitual activity patterns. The sample included predominantly White participants and was enriched for health and socioeconomic status, which may have limited the generalizability of the findings.
DISCLOSURES:
The authors disclosed receiving research support, grants, and research fellowships and collaborations from various institutions and pharmaceutical companies, as well as serving on their advisory boards.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
In IBD Patients, No Increased Risk for MACE Seen for JAK Inhibitors vs Anti-TNF
PHILADELPHIA — according to a study presented at the American College of Gastroenterology (ACG) 2024 Annual Scientific Meeting.
In particular, 1.76% of patients taking JAKi and 1.94% of patients taking anti-TNF developed MACE. There also weren’t significant differences when comparing ulcerative colitis with Crohn’s disease, upadacitinib with tofacitinib, or JAKi with infliximab.
“IBD is associated with an increased risk of cardiovascular diseases, and with the emergence of JAK inhibitors and anti-TNF therapies, there is a concern about the increased risk of MACE,” said lead author Saqr Alsakarneh, MD, an internal medicine resident at the University of Missouri–Kansas City School of Medicine.
Previous randomized controlled trials have indicated increased risks of MACE with JAKi and anti-TNF agents, compared with placebo, but researchers haven’t conducted a head-to-head comparison, he said.
“A potential explanation for previous associations could be linked to immune modulation and inflammation that can increase coagulation risk, as well as fluctuation in disease severity while patients are on the medications, which can impact cardiovascular risk factors,” he added.
Alsakarneh and colleagues conducted a retrospective cohort study using the TriNetX database to identify adult patients with IBD who were treated with JAKi or anti-TNF therapy after diagnosis. After matching patients in the JAKi cohort with patients in the anti-TNF cohort, the research team looked for MACE and VTE within a year of medication initiation, as well as associations by age, sex, and IBD type.
Overall, 3740 patients in the JAKi cohort had a mean age of 43.1 and were 48.9% women and 75.3% White individuals, while 3,740 patients in the anti-TNF cohort had a mean age of 43 and were 48.9% women and 75.3% White individuals.
After excluding those with a history of a prior cardiovascular event, 57 patients (1.76%) in the JAKi cohort developed MACE, compared with 63 patients (1.94%) in the anti-TNF cohort. There weren’t significant differences between the groups in MACE (adjusted hazard ratio [aHR], 0.99) or VTE (aHR, 0.9).
Among patients aged ≥ 65, 25 patients (5.3%) in the JAKi cohort developed MACE, as compared with 30 patients (6.4%) in the anti-TNF cohort. There weren’t significant differences between the groups in MACE (aHR, 0.83) or VTE (aHR, 0.77).
In addition, there were no differences when comparing Crohn’s disease with ulcerative colitis for MACE (aHR, 1.69) or VTE (aHR, 0.85); upadacitinib with tofacitinib for MACE (aHR, 1.1) or VTE (aHR, 1.13); or JAKi medications with infliximab for MACE (aHR, 0.85) or VTE (aHR, 0.8).
Patients in the JAKi group were more likely to undergo intestinal resection surgery (aHR, 1.32), but there wasn’t a statistically significant difference in systematic corticosteroid use (aHR, 0.99).
The study limitations included the inability to assess for disease severity, dose-dependent risk for MACE or VTE, or long-term outcomes among the two cohorts, Alsakarneh said. Prospective controlled trials are needed to confirm findings.
“This is a wonderful study and nice to see. We presented the same thing at Digestive Disease Week that’s being confirmed in this data,” said Miguel Regueiro, MD, AGAF, chief of Cleveland Clinic’s Digestive Disease Institute in Ohio. Regueiro, who wasn’t involved with the study, attended the conference session.
“Looking ahead, all of us are wondering if the regulatory guidance by the FDA [Food and Drug Administration] is going to change the label so we don’t need to step through a TNF,” he said. “I think we’re seeing study after study showing safety or at least not an increased risk with JAK.”
The study was awarded an ACG Noteworthy Abstract. Alsakarneh and Regueiro reported no relevant disclosures.
A version of this article appeared on Medscape.com.
PHILADELPHIA — according to a study presented at the American College of Gastroenterology (ACG) 2024 Annual Scientific Meeting.
In particular, 1.76% of patients taking JAKi and 1.94% of patients taking anti-TNF developed MACE. There also weren’t significant differences when comparing ulcerative colitis with Crohn’s disease, upadacitinib with tofacitinib, or JAKi with infliximab.
“IBD is associated with an increased risk of cardiovascular diseases, and with the emergence of JAK inhibitors and anti-TNF therapies, there is a concern about the increased risk of MACE,” said lead author Saqr Alsakarneh, MD, an internal medicine resident at the University of Missouri–Kansas City School of Medicine.
Previous randomized controlled trials have indicated increased risks of MACE with JAKi and anti-TNF agents, compared with placebo, but researchers haven’t conducted a head-to-head comparison, he said.
“A potential explanation for previous associations could be linked to immune modulation and inflammation that can increase coagulation risk, as well as fluctuation in disease severity while patients are on the medications, which can impact cardiovascular risk factors,” he added.
Alsakarneh and colleagues conducted a retrospective cohort study using the TriNetX database to identify adult patients with IBD who were treated with JAKi or anti-TNF therapy after diagnosis. After matching patients in the JAKi cohort with patients in the anti-TNF cohort, the research team looked for MACE and VTE within a year of medication initiation, as well as associations by age, sex, and IBD type.
Overall, 3740 patients in the JAKi cohort had a mean age of 43.1 and were 48.9% women and 75.3% White individuals, while 3,740 patients in the anti-TNF cohort had a mean age of 43 and were 48.9% women and 75.3% White individuals.
After excluding those with a history of a prior cardiovascular event, 57 patients (1.76%) in the JAKi cohort developed MACE, compared with 63 patients (1.94%) in the anti-TNF cohort. There weren’t significant differences between the groups in MACE (adjusted hazard ratio [aHR], 0.99) or VTE (aHR, 0.9).
Among patients aged ≥ 65, 25 patients (5.3%) in the JAKi cohort developed MACE, as compared with 30 patients (6.4%) in the anti-TNF cohort. There weren’t significant differences between the groups in MACE (aHR, 0.83) or VTE (aHR, 0.77).
In addition, there were no differences when comparing Crohn’s disease with ulcerative colitis for MACE (aHR, 1.69) or VTE (aHR, 0.85); upadacitinib with tofacitinib for MACE (aHR, 1.1) or VTE (aHR, 1.13); or JAKi medications with infliximab for MACE (aHR, 0.85) or VTE (aHR, 0.8).
Patients in the JAKi group were more likely to undergo intestinal resection surgery (aHR, 1.32), but there wasn’t a statistically significant difference in systematic corticosteroid use (aHR, 0.99).
The study limitations included the inability to assess for disease severity, dose-dependent risk for MACE or VTE, or long-term outcomes among the two cohorts, Alsakarneh said. Prospective controlled trials are needed to confirm findings.
“This is a wonderful study and nice to see. We presented the same thing at Digestive Disease Week that’s being confirmed in this data,” said Miguel Regueiro, MD, AGAF, chief of Cleveland Clinic’s Digestive Disease Institute in Ohio. Regueiro, who wasn’t involved with the study, attended the conference session.
“Looking ahead, all of us are wondering if the regulatory guidance by the FDA [Food and Drug Administration] is going to change the label so we don’t need to step through a TNF,” he said. “I think we’re seeing study after study showing safety or at least not an increased risk with JAK.”
The study was awarded an ACG Noteworthy Abstract. Alsakarneh and Regueiro reported no relevant disclosures.
A version of this article appeared on Medscape.com.
PHILADELPHIA — according to a study presented at the American College of Gastroenterology (ACG) 2024 Annual Scientific Meeting.
In particular, 1.76% of patients taking JAKi and 1.94% of patients taking anti-TNF developed MACE. There also weren’t significant differences when comparing ulcerative colitis with Crohn’s disease, upadacitinib with tofacitinib, or JAKi with infliximab.
“IBD is associated with an increased risk of cardiovascular diseases, and with the emergence of JAK inhibitors and anti-TNF therapies, there is a concern about the increased risk of MACE,” said lead author Saqr Alsakarneh, MD, an internal medicine resident at the University of Missouri–Kansas City School of Medicine.
Previous randomized controlled trials have indicated increased risks of MACE with JAKi and anti-TNF agents, compared with placebo, but researchers haven’t conducted a head-to-head comparison, he said.
“A potential explanation for previous associations could be linked to immune modulation and inflammation that can increase coagulation risk, as well as fluctuation in disease severity while patients are on the medications, which can impact cardiovascular risk factors,” he added.
Alsakarneh and colleagues conducted a retrospective cohort study using the TriNetX database to identify adult patients with IBD who were treated with JAKi or anti-TNF therapy after diagnosis. After matching patients in the JAKi cohort with patients in the anti-TNF cohort, the research team looked for MACE and VTE within a year of medication initiation, as well as associations by age, sex, and IBD type.
Overall, 3740 patients in the JAKi cohort had a mean age of 43.1 and were 48.9% women and 75.3% White individuals, while 3,740 patients in the anti-TNF cohort had a mean age of 43 and were 48.9% women and 75.3% White individuals.
After excluding those with a history of a prior cardiovascular event, 57 patients (1.76%) in the JAKi cohort developed MACE, compared with 63 patients (1.94%) in the anti-TNF cohort. There weren’t significant differences between the groups in MACE (adjusted hazard ratio [aHR], 0.99) or VTE (aHR, 0.9).
Among patients aged ≥ 65, 25 patients (5.3%) in the JAKi cohort developed MACE, as compared with 30 patients (6.4%) in the anti-TNF cohort. There weren’t significant differences between the groups in MACE (aHR, 0.83) or VTE (aHR, 0.77).
In addition, there were no differences when comparing Crohn’s disease with ulcerative colitis for MACE (aHR, 1.69) or VTE (aHR, 0.85); upadacitinib with tofacitinib for MACE (aHR, 1.1) or VTE (aHR, 1.13); or JAKi medications with infliximab for MACE (aHR, 0.85) or VTE (aHR, 0.8).
Patients in the JAKi group were more likely to undergo intestinal resection surgery (aHR, 1.32), but there wasn’t a statistically significant difference in systematic corticosteroid use (aHR, 0.99).
The study limitations included the inability to assess for disease severity, dose-dependent risk for MACE or VTE, or long-term outcomes among the two cohorts, Alsakarneh said. Prospective controlled trials are needed to confirm findings.
“This is a wonderful study and nice to see. We presented the same thing at Digestive Disease Week that’s being confirmed in this data,” said Miguel Regueiro, MD, AGAF, chief of Cleveland Clinic’s Digestive Disease Institute in Ohio. Regueiro, who wasn’t involved with the study, attended the conference session.
“Looking ahead, all of us are wondering if the regulatory guidance by the FDA [Food and Drug Administration] is going to change the label so we don’t need to step through a TNF,” he said. “I think we’re seeing study after study showing safety or at least not an increased risk with JAK.”
The study was awarded an ACG Noteworthy Abstract. Alsakarneh and Regueiro reported no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM ACG 2024
New Pill Successfully Lowers Lp(a) Levels
Concentrations of Lp(a) cholesterol are genetically determined and remain steady throughout life. Levels of 125 nmol/L or higher promote clotting and inflammation, significantly increasing the risk for heart attack, stroke, aortic stenosis, and peripheral artery disease. This affects about 20% of the population, particularly people of Black African and South Asian descent.
There are currently no approved therapies that lower Lp(a), said study author Stephen Nicholls, MBBS, PhD, director of the Victorian Heart Institute at Monash University in Melbourne, Australia. Several injectable therapies are currently in clinical trials, but muvalaplin is the only oral option. The new drug lowers Lp(a) levels by disrupting the bond between the two parts of the Lp(a) particle.
The KRAKEN Trial
In the KRAKEN trial, 233 adults from around the world with very high Lp(a) levels (> 175 nmol/L) were randomized either to one of three daily doses of muvalaplin — 10, 60, or 240 mg — or to placebo for 12 weeks.
The researchers measured Lp(a) levels with a standard blood test and with a novel test designed to specifically measure levels of intact Lp(a) particles in the blood. In addition to Lp(a), the standard test detects one of its components, apolipoprotein A particles, that are bound to the drug, which can lead to an underestimation of Lp(a) reductions.
Lp(a) levels were up to 70.0% lower in the muvalaplin group than in the placebo group when measured with the traditional blood test and by up to 85.5% lower when measured with the new test. Approximately 82% of participants achieved an Lp(a) level lower than 125 nmol/L when measured with the traditional blood test, and 97% achieved that level when the new test was used. Patients who received either 60 or 240 mg of muvalaplin had similar reductions in Lp(a) levels, which were greater than the reductions seen in the 10 mg group. The drug was safe and generally well tolerated.
“This is a very reassuring phase 2 result,” Nicholls said when he presented the KRAKEN findings at the American Heart Association (AHA) Scientific Sessions 2024 in Chicago, which were simultaneously published online in JAMA. “It encourages the ongoing development of this agent.”
Lp(a) levels are not affected by changes in lifestyle or diet or by traditional lipid-lowering treatments like statins, said Erin Michos, MD, a cardiologist at the Johns Hopkins University School of Medicine in Baltimore, Maryland, who was not involved in the study.
And high Lp(a) levels confer significant cardiovascular risk even when other risks are reduced. So muvalaplin is “a highly promising approach to treat a previously untreatable disorder,” she explained.
Larger and longer studies, with more diverse patient populations, are needed to confirm the results and to determine whether reducing Lp(a) also improves cardiovascular outcomes, Michos pointed out.
“While muvalaplin appears to be an effective approach to lowering Lp(a) levels, we still need to study whether Lp(a) lowering will result in fewer heart attacks and strokes,” Nicholls added.
A version of this article appeared on Medscape.com.
Concentrations of Lp(a) cholesterol are genetically determined and remain steady throughout life. Levels of 125 nmol/L or higher promote clotting and inflammation, significantly increasing the risk for heart attack, stroke, aortic stenosis, and peripheral artery disease. This affects about 20% of the population, particularly people of Black African and South Asian descent.
There are currently no approved therapies that lower Lp(a), said study author Stephen Nicholls, MBBS, PhD, director of the Victorian Heart Institute at Monash University in Melbourne, Australia. Several injectable therapies are currently in clinical trials, but muvalaplin is the only oral option. The new drug lowers Lp(a) levels by disrupting the bond between the two parts of the Lp(a) particle.
The KRAKEN Trial
In the KRAKEN trial, 233 adults from around the world with very high Lp(a) levels (> 175 nmol/L) were randomized either to one of three daily doses of muvalaplin — 10, 60, or 240 mg — or to placebo for 12 weeks.
The researchers measured Lp(a) levels with a standard blood test and with a novel test designed to specifically measure levels of intact Lp(a) particles in the blood. In addition to Lp(a), the standard test detects one of its components, apolipoprotein A particles, that are bound to the drug, which can lead to an underestimation of Lp(a) reductions.
Lp(a) levels were up to 70.0% lower in the muvalaplin group than in the placebo group when measured with the traditional blood test and by up to 85.5% lower when measured with the new test. Approximately 82% of participants achieved an Lp(a) level lower than 125 nmol/L when measured with the traditional blood test, and 97% achieved that level when the new test was used. Patients who received either 60 or 240 mg of muvalaplin had similar reductions in Lp(a) levels, which were greater than the reductions seen in the 10 mg group. The drug was safe and generally well tolerated.
“This is a very reassuring phase 2 result,” Nicholls said when he presented the KRAKEN findings at the American Heart Association (AHA) Scientific Sessions 2024 in Chicago, which were simultaneously published online in JAMA. “It encourages the ongoing development of this agent.”
Lp(a) levels are not affected by changes in lifestyle or diet or by traditional lipid-lowering treatments like statins, said Erin Michos, MD, a cardiologist at the Johns Hopkins University School of Medicine in Baltimore, Maryland, who was not involved in the study.
And high Lp(a) levels confer significant cardiovascular risk even when other risks are reduced. So muvalaplin is “a highly promising approach to treat a previously untreatable disorder,” she explained.
Larger and longer studies, with more diverse patient populations, are needed to confirm the results and to determine whether reducing Lp(a) also improves cardiovascular outcomes, Michos pointed out.
“While muvalaplin appears to be an effective approach to lowering Lp(a) levels, we still need to study whether Lp(a) lowering will result in fewer heart attacks and strokes,” Nicholls added.
A version of this article appeared on Medscape.com.
Concentrations of Lp(a) cholesterol are genetically determined and remain steady throughout life. Levels of 125 nmol/L or higher promote clotting and inflammation, significantly increasing the risk for heart attack, stroke, aortic stenosis, and peripheral artery disease. This affects about 20% of the population, particularly people of Black African and South Asian descent.
There are currently no approved therapies that lower Lp(a), said study author Stephen Nicholls, MBBS, PhD, director of the Victorian Heart Institute at Monash University in Melbourne, Australia. Several injectable therapies are currently in clinical trials, but muvalaplin is the only oral option. The new drug lowers Lp(a) levels by disrupting the bond between the two parts of the Lp(a) particle.
The KRAKEN Trial
In the KRAKEN trial, 233 adults from around the world with very high Lp(a) levels (> 175 nmol/L) were randomized either to one of three daily doses of muvalaplin — 10, 60, or 240 mg — or to placebo for 12 weeks.
The researchers measured Lp(a) levels with a standard blood test and with a novel test designed to specifically measure levels of intact Lp(a) particles in the blood. In addition to Lp(a), the standard test detects one of its components, apolipoprotein A particles, that are bound to the drug, which can lead to an underestimation of Lp(a) reductions.
Lp(a) levels were up to 70.0% lower in the muvalaplin group than in the placebo group when measured with the traditional blood test and by up to 85.5% lower when measured with the new test. Approximately 82% of participants achieved an Lp(a) level lower than 125 nmol/L when measured with the traditional blood test, and 97% achieved that level when the new test was used. Patients who received either 60 or 240 mg of muvalaplin had similar reductions in Lp(a) levels, which were greater than the reductions seen in the 10 mg group. The drug was safe and generally well tolerated.
“This is a very reassuring phase 2 result,” Nicholls said when he presented the KRAKEN findings at the American Heart Association (AHA) Scientific Sessions 2024 in Chicago, which were simultaneously published online in JAMA. “It encourages the ongoing development of this agent.”
Lp(a) levels are not affected by changes in lifestyle or diet or by traditional lipid-lowering treatments like statins, said Erin Michos, MD, a cardiologist at the Johns Hopkins University School of Medicine in Baltimore, Maryland, who was not involved in the study.
And high Lp(a) levels confer significant cardiovascular risk even when other risks are reduced. So muvalaplin is “a highly promising approach to treat a previously untreatable disorder,” she explained.
Larger and longer studies, with more diverse patient populations, are needed to confirm the results and to determine whether reducing Lp(a) also improves cardiovascular outcomes, Michos pointed out.
“While muvalaplin appears to be an effective approach to lowering Lp(a) levels, we still need to study whether Lp(a) lowering will result in fewer heart attacks and strokes,” Nicholls added.
A version of this article appeared on Medscape.com.
Lessons Learned: What Docs Wish Med Students Knew
Despite 4 years of med school and 3-7 years in residency, when you enter the workforce as a doctor, you still have much to learn. There is only so much your professors and attending physicians can pack in. Going forward, you’ll continue to learn on the job and via continuing education.
Some of that lifelong learning will involve soft skills — how to compassionately work with your patients and their families, for instance. Other lessons will get down to the business of medicine — the paperwork, the work/life balance, and the moral dilemmas you never saw coming. And still others will involve learning how to take care of yourself in the middle of seemingly endless hours on the job.
“We all have things we wish we had known upon starting our careers,” said Daniel Opris, MD, a primary care physician at Ohio-based Executive Medical Centers.
We tapped several veteran physicians and an educator to learn what they wish med students knew as they enter the workforce. We’ve compiled them here to give you a head start on the lessons ahead.
You Won’t Know Everything, and That’s Okay
When you go through your medical training, it can feel overwhelming to absorb all the knowledge your professors and attendings impart. The bottom line, said Shoshana Ungerleider, MD, an internal medicine specialist, is that you shouldn’t worry about it.
David Lenihan, PhD, CEO at Ponce Health Sciences University, agrees. “What we’ve lost in recent years, is the ability to apply your skill set and say, ‘let me take a day and get back to you,’” he said. “Doctors love it when you do that because it shows you can pitch in and work as part of a team.”
Medicine is a collaborative field, said Ungerleider, and learning from others, whether peers, nurses, or specialists, is “not a weakness.” She recommends embracing uncertainty and getting comfortable with the unknown.
You’ll Take Your Work Home With You
Doctors enter the field because they care about their patients and want to help. Successful outcomes are never guaranteed, however, no matter how much you try. The result? Some days you’ll bring home those upsetting and haunting cases, said Lenihan.
“We often believe that we should leave our work at the office, but sometimes you need to bring it home and think it through,” he said. “It can’t overwhelm you, but you should digest what happened.”
When you do, said Lenihan, you’ll come out the other end more empathetic and that helps the healthcare system in the long run. “The more you reflect on your day, the better you’ll get at reading the room and treating your patients.”
Drew Remignanti, MD, a retired emergency medicine physician from New Hampshire, agrees, but puts a different spin on bringing work home.
“We revisit the patient care decisions we made, second-guess ourselves, and worry about our patients’ welfare and outcomes,” he said. “I think it can only lead to better outcomes down the road, however, if you learn from that bad decision, preventing you from committing a similar mistake.”
Burnout Is Real — Make Self-Care a Priority
As a retired physician who spent 40 years practicing medicine, Remignanti experienced the evolution of healthcare as it has become what he calls a “consumer-provider” model. “Productivity didn’t use to be part of the equation, but now it’s the focus,” he said.
The result is burnout, a very real threat to incoming physicians. Remignanti holds that if you are aware of the risk, you can resist it. Part of avoiding burnout is self-care, according to Ungerleider. “The sooner you prioritize your mental, emotional, and physical well-being, the better,” she said. “Balancing work and life may feel impossible at times but taking care of yourself is essential to being a better physician in the long run.”
That means carving out time for exercise, hobbies, and connections outside of the medical field. It also means making sleep and nutrition a priority, even when that feels hard to accomplish. “If you don’t take care of yourself, you can’t take care of others,” added Opris. “It’s so common to lose yourself in your career, but you need to hold onto your physical, emotional, and spiritual self.”
Avoid Relying Too Heavily on Tech
Technology is invading every aspect of our lives — often for the greater good — but in medicine, it’s important to always return to your core knowledge above all else. Case in point, said Opris, the UpToDate app. While it can be a useful tool, it’s important not to become too reliant on it. “UpToDate is expert opinion-based guidance, and it’s a fantastic resource,” he said. “But you need to use your references and knowledge in every case.”
It’s key to remember that every patient is different, and their case may not line up perfectly with the guidance presented in UpToDate or other technology source. Piggybacking on that, Ungerleider added that it’s important to remember medicine is about people, not just conditions.
“It’s easy to focus on mastering the science, but the real art of medicine comes from seeing the whole person in front of you,” she said. “Your patients are more than their diagnoses — they come with complex emotions, life stories, and needs.” Being compassionate, listening carefully, and building trust should match up to your clinical skills.
Partner With Your Patients, Even When It’s Difficult
Perhaps the most difficult lesson of all is remembering that your patients may not always agree with your recommendations and choose to ignore them. After all your years spent learning, there may be times when it feels your education is going to waste.
“Remember that the landscape today is so varied, and that bleeds into medicine,” said Opris. “We go into cases with our own biases, and it’s important to take a step back to reset, every time.”
Opris reminds himself of Sir William Osler’s famous essay, “Aequanimitas,” in which he tells graduating medical students to practice with “coolness and presence of mind under all circumstances.”
Remignanti offers this advice: “Physicians need to be able to partner with their patients and jointly decide which courses of action are most effective,” he said. “Cling to the idea that you are forming a partnership with your patients — what can we together determine is the best course?”
At the same time, the path the patient chooses may not be what’s best for them — potentially even leading to a poor outcome.
“You may not always understand their choices,” said Opris. “But they do have a choice. Think of yourself almost like a consultant.”
A version of this article first appeared on Medscape.com.
Despite 4 years of med school and 3-7 years in residency, when you enter the workforce as a doctor, you still have much to learn. There is only so much your professors and attending physicians can pack in. Going forward, you’ll continue to learn on the job and via continuing education.
Some of that lifelong learning will involve soft skills — how to compassionately work with your patients and their families, for instance. Other lessons will get down to the business of medicine — the paperwork, the work/life balance, and the moral dilemmas you never saw coming. And still others will involve learning how to take care of yourself in the middle of seemingly endless hours on the job.
“We all have things we wish we had known upon starting our careers,” said Daniel Opris, MD, a primary care physician at Ohio-based Executive Medical Centers.
We tapped several veteran physicians and an educator to learn what they wish med students knew as they enter the workforce. We’ve compiled them here to give you a head start on the lessons ahead.
You Won’t Know Everything, and That’s Okay
When you go through your medical training, it can feel overwhelming to absorb all the knowledge your professors and attendings impart. The bottom line, said Shoshana Ungerleider, MD, an internal medicine specialist, is that you shouldn’t worry about it.
David Lenihan, PhD, CEO at Ponce Health Sciences University, agrees. “What we’ve lost in recent years, is the ability to apply your skill set and say, ‘let me take a day and get back to you,’” he said. “Doctors love it when you do that because it shows you can pitch in and work as part of a team.”
Medicine is a collaborative field, said Ungerleider, and learning from others, whether peers, nurses, or specialists, is “not a weakness.” She recommends embracing uncertainty and getting comfortable with the unknown.
You’ll Take Your Work Home With You
Doctors enter the field because they care about their patients and want to help. Successful outcomes are never guaranteed, however, no matter how much you try. The result? Some days you’ll bring home those upsetting and haunting cases, said Lenihan.
“We often believe that we should leave our work at the office, but sometimes you need to bring it home and think it through,” he said. “It can’t overwhelm you, but you should digest what happened.”
When you do, said Lenihan, you’ll come out the other end more empathetic and that helps the healthcare system in the long run. “The more you reflect on your day, the better you’ll get at reading the room and treating your patients.”
Drew Remignanti, MD, a retired emergency medicine physician from New Hampshire, agrees, but puts a different spin on bringing work home.
“We revisit the patient care decisions we made, second-guess ourselves, and worry about our patients’ welfare and outcomes,” he said. “I think it can only lead to better outcomes down the road, however, if you learn from that bad decision, preventing you from committing a similar mistake.”
Burnout Is Real — Make Self-Care a Priority
As a retired physician who spent 40 years practicing medicine, Remignanti experienced the evolution of healthcare as it has become what he calls a “consumer-provider” model. “Productivity didn’t use to be part of the equation, but now it’s the focus,” he said.
The result is burnout, a very real threat to incoming physicians. Remignanti holds that if you are aware of the risk, you can resist it. Part of avoiding burnout is self-care, according to Ungerleider. “The sooner you prioritize your mental, emotional, and physical well-being, the better,” she said. “Balancing work and life may feel impossible at times but taking care of yourself is essential to being a better physician in the long run.”
That means carving out time for exercise, hobbies, and connections outside of the medical field. It also means making sleep and nutrition a priority, even when that feels hard to accomplish. “If you don’t take care of yourself, you can’t take care of others,” added Opris. “It’s so common to lose yourself in your career, but you need to hold onto your physical, emotional, and spiritual self.”
Avoid Relying Too Heavily on Tech
Technology is invading every aspect of our lives — often for the greater good — but in medicine, it’s important to always return to your core knowledge above all else. Case in point, said Opris, the UpToDate app. While it can be a useful tool, it’s important not to become too reliant on it. “UpToDate is expert opinion-based guidance, and it’s a fantastic resource,” he said. “But you need to use your references and knowledge in every case.”
It’s key to remember that every patient is different, and their case may not line up perfectly with the guidance presented in UpToDate or other technology source. Piggybacking on that, Ungerleider added that it’s important to remember medicine is about people, not just conditions.
“It’s easy to focus on mastering the science, but the real art of medicine comes from seeing the whole person in front of you,” she said. “Your patients are more than their diagnoses — they come with complex emotions, life stories, and needs.” Being compassionate, listening carefully, and building trust should match up to your clinical skills.
Partner With Your Patients, Even When It’s Difficult
Perhaps the most difficult lesson of all is remembering that your patients may not always agree with your recommendations and choose to ignore them. After all your years spent learning, there may be times when it feels your education is going to waste.
“Remember that the landscape today is so varied, and that bleeds into medicine,” said Opris. “We go into cases with our own biases, and it’s important to take a step back to reset, every time.”
Opris reminds himself of Sir William Osler’s famous essay, “Aequanimitas,” in which he tells graduating medical students to practice with “coolness and presence of mind under all circumstances.”
Remignanti offers this advice: “Physicians need to be able to partner with their patients and jointly decide which courses of action are most effective,” he said. “Cling to the idea that you are forming a partnership with your patients — what can we together determine is the best course?”
At the same time, the path the patient chooses may not be what’s best for them — potentially even leading to a poor outcome.
“You may not always understand their choices,” said Opris. “But they do have a choice. Think of yourself almost like a consultant.”
A version of this article first appeared on Medscape.com.
Despite 4 years of med school and 3-7 years in residency, when you enter the workforce as a doctor, you still have much to learn. There is only so much your professors and attending physicians can pack in. Going forward, you’ll continue to learn on the job and via continuing education.
Some of that lifelong learning will involve soft skills — how to compassionately work with your patients and their families, for instance. Other lessons will get down to the business of medicine — the paperwork, the work/life balance, and the moral dilemmas you never saw coming. And still others will involve learning how to take care of yourself in the middle of seemingly endless hours on the job.
“We all have things we wish we had known upon starting our careers,” said Daniel Opris, MD, a primary care physician at Ohio-based Executive Medical Centers.
We tapped several veteran physicians and an educator to learn what they wish med students knew as they enter the workforce. We’ve compiled them here to give you a head start on the lessons ahead.
You Won’t Know Everything, and That’s Okay
When you go through your medical training, it can feel overwhelming to absorb all the knowledge your professors and attendings impart. The bottom line, said Shoshana Ungerleider, MD, an internal medicine specialist, is that you shouldn’t worry about it.
David Lenihan, PhD, CEO at Ponce Health Sciences University, agrees. “What we’ve lost in recent years, is the ability to apply your skill set and say, ‘let me take a day and get back to you,’” he said. “Doctors love it when you do that because it shows you can pitch in and work as part of a team.”
Medicine is a collaborative field, said Ungerleider, and learning from others, whether peers, nurses, or specialists, is “not a weakness.” She recommends embracing uncertainty and getting comfortable with the unknown.
You’ll Take Your Work Home With You
Doctors enter the field because they care about their patients and want to help. Successful outcomes are never guaranteed, however, no matter how much you try. The result? Some days you’ll bring home those upsetting and haunting cases, said Lenihan.
“We often believe that we should leave our work at the office, but sometimes you need to bring it home and think it through,” he said. “It can’t overwhelm you, but you should digest what happened.”
When you do, said Lenihan, you’ll come out the other end more empathetic and that helps the healthcare system in the long run. “The more you reflect on your day, the better you’ll get at reading the room and treating your patients.”
Drew Remignanti, MD, a retired emergency medicine physician from New Hampshire, agrees, but puts a different spin on bringing work home.
“We revisit the patient care decisions we made, second-guess ourselves, and worry about our patients’ welfare and outcomes,” he said. “I think it can only lead to better outcomes down the road, however, if you learn from that bad decision, preventing you from committing a similar mistake.”
Burnout Is Real — Make Self-Care a Priority
As a retired physician who spent 40 years practicing medicine, Remignanti experienced the evolution of healthcare as it has become what he calls a “consumer-provider” model. “Productivity didn’t use to be part of the equation, but now it’s the focus,” he said.
The result is burnout, a very real threat to incoming physicians. Remignanti holds that if you are aware of the risk, you can resist it. Part of avoiding burnout is self-care, according to Ungerleider. “The sooner you prioritize your mental, emotional, and physical well-being, the better,” she said. “Balancing work and life may feel impossible at times but taking care of yourself is essential to being a better physician in the long run.”
That means carving out time for exercise, hobbies, and connections outside of the medical field. It also means making sleep and nutrition a priority, even when that feels hard to accomplish. “If you don’t take care of yourself, you can’t take care of others,” added Opris. “It’s so common to lose yourself in your career, but you need to hold onto your physical, emotional, and spiritual self.”
Avoid Relying Too Heavily on Tech
Technology is invading every aspect of our lives — often for the greater good — but in medicine, it’s important to always return to your core knowledge above all else. Case in point, said Opris, the UpToDate app. While it can be a useful tool, it’s important not to become too reliant on it. “UpToDate is expert opinion-based guidance, and it’s a fantastic resource,” he said. “But you need to use your references and knowledge in every case.”
It’s key to remember that every patient is different, and their case may not line up perfectly with the guidance presented in UpToDate or other technology source. Piggybacking on that, Ungerleider added that it’s important to remember medicine is about people, not just conditions.
“It’s easy to focus on mastering the science, but the real art of medicine comes from seeing the whole person in front of you,” she said. “Your patients are more than their diagnoses — they come with complex emotions, life stories, and needs.” Being compassionate, listening carefully, and building trust should match up to your clinical skills.
Partner With Your Patients, Even When It’s Difficult
Perhaps the most difficult lesson of all is remembering that your patients may not always agree with your recommendations and choose to ignore them. After all your years spent learning, there may be times when it feels your education is going to waste.
“Remember that the landscape today is so varied, and that bleeds into medicine,” said Opris. “We go into cases with our own biases, and it’s important to take a step back to reset, every time.”
Opris reminds himself of Sir William Osler’s famous essay, “Aequanimitas,” in which he tells graduating medical students to practice with “coolness and presence of mind under all circumstances.”
Remignanti offers this advice: “Physicians need to be able to partner with their patients and jointly decide which courses of action are most effective,” he said. “Cling to the idea that you are forming a partnership with your patients — what can we together determine is the best course?”
At the same time, the path the patient chooses may not be what’s best for them — potentially even leading to a poor outcome.
“You may not always understand their choices,” said Opris. “But they do have a choice. Think of yourself almost like a consultant.”
A version of this article first appeared on Medscape.com.
Gout and SGLT2 Inhibitors: Evidence Points to Reduced Need for ULT, Flare Drugs
WASHINGTON — Use of sodium-glucose cotransporter 2 inhibitors (SGLT2i) reduced the need for urate-lowering therapy (ULT) and gout flare therapies in people who had both type 2 diabetes (T2D) and gout, new research has found.
Data from a large US claims database showed that SGLT2i use was associated with a 31% lower rate of initiation of ULT. “This provides further support for the use of SLGT2i therapy in patients with gout, particularly those with high-risk multimorbidity and polypharmacy,” Greg Challener, MD, a postdoctoral fellow at the Rheumatology and Allergy Clinical Epidemiology Research Center, Massachusetts General Hospital, Boston, said in his presentation of the data at the annual meeting of the American College of Rheumatology.
The first agent of the SGLT2i class, dapagliflozin, was initially approved in the United States a decade ago for treating T2D. Since then, several other “flozins” have become available, and some have also received additional indications for heart failure and albuminuric chronic kidney disease. Several prior studies have linked SGLT2i use with lower rates of gout flares as well as lower likelihood of developing gout in the first place, although not all studies have found this benefit.
Asked about the clinical implications of the new data, Challener said in an interview that “I don’t think we’re quite at the point where this is changing gout management per se, but this just helps us understand that [SGT2is] may have a role at some point, maybe as a combination on top of another agent. Or, in some patients, it really may be enough if they’re already on an SGLT2i where we don’t need to jump to adding allopurinol. Maybe they have tophi, but they were just started on an SGLT2i and they’re not flaring. Typically, you would start those patients on allopurinol, but you could potentially just monitor them if they were just started on one of those [SGLT2i] agents.”
Asked to comment, session moderator J. Antonio Aviña-Zubieta, MD, PhD, head of the Division of Rheumatology at the University of British Columbia, Vancouver, Canada, and senior scientist at Arthritis Research Canada, said in an interview: “What I can see possibly happening when there’s more evidence is that SGLT2is may be used or even become standard of care as an adjuvant therapy to decrease flares, and by that, decrease the risk of complications.”
Reductions in ULT, Flares, and Healthcare Visits
The new study used administrative health data from the multicenter TriNetX Diamond network of electronic medical record and claims data from 92 healthcare sites with 212 million patients. Among those with both T2D and gout who were not taking ULT at baseline, a total of 16,104 initiated SGLT2is and 16,046 initiated glucagon-like peptide 1 receptor agonists (GLP-1 RA).
Propensity score matching was conducted for demographics including age, race, and sex; comorbidities; use of emergency, inpatient, and critical care services; medications; labs; and body mass index. That yielded 11,800 individuals each in the SGLT2i and GLP-1 RA groups.
Over 5 years, 9.9% of the SGLT2i group vs 13.4% of those using GLP-1 RA had initiated ULT, a significant difference with a hazard ratio (HR) of 0.69 (95% CI, 0.64-0.75). The risk for initiation of colchicine for gout flares was 4.7% with SGLT2i vs 6.0% for GLP-1 RA — also a significant difference with an HR of 0.74 (0.65-0.83).
Medical visits for gout occurred in 28.0% vs 28.4% of patients, which also reached statistical significance (HR, 0.94; 95% CI, 0.89-0.99).
Aviña-Zubieta, an author of one of the previous studies finding a reduction in gout flares with SGLT2i, said, “many patients do not want to start gout therapy until they start having more acute attacks. ... So, for a lot of people, it’s a burden taking another pill to prevent one attack. But, if you don’t treat it over time, the attacks come more often. So, can we still delay the initiation of therapy? If you’re not having that many flares, you’re decreasing the burden of the disease and polypharmacy, which I think is the potential benefit in the long run if you already have an indication for the therapy for diabetes. ... These data are supporting that.”
Indeed, Challener said these data can help in counseling patients. “Taking your SGLT2i for your heart failure and your diabetes is also providing some benefit for your gout, and we know that there is also cardiac benefit when gout is controlled.”
Challener and Aviña-Zubieta had no disclosures.
A version of this article first appeared on Medscape.com.
WASHINGTON — Use of sodium-glucose cotransporter 2 inhibitors (SGLT2i) reduced the need for urate-lowering therapy (ULT) and gout flare therapies in people who had both type 2 diabetes (T2D) and gout, new research has found.
Data from a large US claims database showed that SGLT2i use was associated with a 31% lower rate of initiation of ULT. “This provides further support for the use of SLGT2i therapy in patients with gout, particularly those with high-risk multimorbidity and polypharmacy,” Greg Challener, MD, a postdoctoral fellow at the Rheumatology and Allergy Clinical Epidemiology Research Center, Massachusetts General Hospital, Boston, said in his presentation of the data at the annual meeting of the American College of Rheumatology.
The first agent of the SGLT2i class, dapagliflozin, was initially approved in the United States a decade ago for treating T2D. Since then, several other “flozins” have become available, and some have also received additional indications for heart failure and albuminuric chronic kidney disease. Several prior studies have linked SGLT2i use with lower rates of gout flares as well as lower likelihood of developing gout in the first place, although not all studies have found this benefit.
Asked about the clinical implications of the new data, Challener said in an interview that “I don’t think we’re quite at the point where this is changing gout management per se, but this just helps us understand that [SGT2is] may have a role at some point, maybe as a combination on top of another agent. Or, in some patients, it really may be enough if they’re already on an SGLT2i where we don’t need to jump to adding allopurinol. Maybe they have tophi, but they were just started on an SGLT2i and they’re not flaring. Typically, you would start those patients on allopurinol, but you could potentially just monitor them if they were just started on one of those [SGLT2i] agents.”
Asked to comment, session moderator J. Antonio Aviña-Zubieta, MD, PhD, head of the Division of Rheumatology at the University of British Columbia, Vancouver, Canada, and senior scientist at Arthritis Research Canada, said in an interview: “What I can see possibly happening when there’s more evidence is that SGLT2is may be used or even become standard of care as an adjuvant therapy to decrease flares, and by that, decrease the risk of complications.”
Reductions in ULT, Flares, and Healthcare Visits
The new study used administrative health data from the multicenter TriNetX Diamond network of electronic medical record and claims data from 92 healthcare sites with 212 million patients. Among those with both T2D and gout who were not taking ULT at baseline, a total of 16,104 initiated SGLT2is and 16,046 initiated glucagon-like peptide 1 receptor agonists (GLP-1 RA).
Propensity score matching was conducted for demographics including age, race, and sex; comorbidities; use of emergency, inpatient, and critical care services; medications; labs; and body mass index. That yielded 11,800 individuals each in the SGLT2i and GLP-1 RA groups.
Over 5 years, 9.9% of the SGLT2i group vs 13.4% of those using GLP-1 RA had initiated ULT, a significant difference with a hazard ratio (HR) of 0.69 (95% CI, 0.64-0.75). The risk for initiation of colchicine for gout flares was 4.7% with SGLT2i vs 6.0% for GLP-1 RA — also a significant difference with an HR of 0.74 (0.65-0.83).
Medical visits for gout occurred in 28.0% vs 28.4% of patients, which also reached statistical significance (HR, 0.94; 95% CI, 0.89-0.99).
Aviña-Zubieta, an author of one of the previous studies finding a reduction in gout flares with SGLT2i, said, “many patients do not want to start gout therapy until they start having more acute attacks. ... So, for a lot of people, it’s a burden taking another pill to prevent one attack. But, if you don’t treat it over time, the attacks come more often. So, can we still delay the initiation of therapy? If you’re not having that many flares, you’re decreasing the burden of the disease and polypharmacy, which I think is the potential benefit in the long run if you already have an indication for the therapy for diabetes. ... These data are supporting that.”
Indeed, Challener said these data can help in counseling patients. “Taking your SGLT2i for your heart failure and your diabetes is also providing some benefit for your gout, and we know that there is also cardiac benefit when gout is controlled.”
Challener and Aviña-Zubieta had no disclosures.
A version of this article first appeared on Medscape.com.
WASHINGTON — Use of sodium-glucose cotransporter 2 inhibitors (SGLT2i) reduced the need for urate-lowering therapy (ULT) and gout flare therapies in people who had both type 2 diabetes (T2D) and gout, new research has found.
Data from a large US claims database showed that SGLT2i use was associated with a 31% lower rate of initiation of ULT. “This provides further support for the use of SLGT2i therapy in patients with gout, particularly those with high-risk multimorbidity and polypharmacy,” Greg Challener, MD, a postdoctoral fellow at the Rheumatology and Allergy Clinical Epidemiology Research Center, Massachusetts General Hospital, Boston, said in his presentation of the data at the annual meeting of the American College of Rheumatology.
The first agent of the SGLT2i class, dapagliflozin, was initially approved in the United States a decade ago for treating T2D. Since then, several other “flozins” have become available, and some have also received additional indications for heart failure and albuminuric chronic kidney disease. Several prior studies have linked SGLT2i use with lower rates of gout flares as well as lower likelihood of developing gout in the first place, although not all studies have found this benefit.
Asked about the clinical implications of the new data, Challener said in an interview that “I don’t think we’re quite at the point where this is changing gout management per se, but this just helps us understand that [SGT2is] may have a role at some point, maybe as a combination on top of another agent. Or, in some patients, it really may be enough if they’re already on an SGLT2i where we don’t need to jump to adding allopurinol. Maybe they have tophi, but they were just started on an SGLT2i and they’re not flaring. Typically, you would start those patients on allopurinol, but you could potentially just monitor them if they were just started on one of those [SGLT2i] agents.”
Asked to comment, session moderator J. Antonio Aviña-Zubieta, MD, PhD, head of the Division of Rheumatology at the University of British Columbia, Vancouver, Canada, and senior scientist at Arthritis Research Canada, said in an interview: “What I can see possibly happening when there’s more evidence is that SGLT2is may be used or even become standard of care as an adjuvant therapy to decrease flares, and by that, decrease the risk of complications.”
Reductions in ULT, Flares, and Healthcare Visits
The new study used administrative health data from the multicenter TriNetX Diamond network of electronic medical record and claims data from 92 healthcare sites with 212 million patients. Among those with both T2D and gout who were not taking ULT at baseline, a total of 16,104 initiated SGLT2is and 16,046 initiated glucagon-like peptide 1 receptor agonists (GLP-1 RA).
Propensity score matching was conducted for demographics including age, race, and sex; comorbidities; use of emergency, inpatient, and critical care services; medications; labs; and body mass index. That yielded 11,800 individuals each in the SGLT2i and GLP-1 RA groups.
Over 5 years, 9.9% of the SGLT2i group vs 13.4% of those using GLP-1 RA had initiated ULT, a significant difference with a hazard ratio (HR) of 0.69 (95% CI, 0.64-0.75). The risk for initiation of colchicine for gout flares was 4.7% with SGLT2i vs 6.0% for GLP-1 RA — also a significant difference with an HR of 0.74 (0.65-0.83).
Medical visits for gout occurred in 28.0% vs 28.4% of patients, which also reached statistical significance (HR, 0.94; 95% CI, 0.89-0.99).
Aviña-Zubieta, an author of one of the previous studies finding a reduction in gout flares with SGLT2i, said, “many patients do not want to start gout therapy until they start having more acute attacks. ... So, for a lot of people, it’s a burden taking another pill to prevent one attack. But, if you don’t treat it over time, the attacks come more often. So, can we still delay the initiation of therapy? If you’re not having that many flares, you’re decreasing the burden of the disease and polypharmacy, which I think is the potential benefit in the long run if you already have an indication for the therapy for diabetes. ... These data are supporting that.”
Indeed, Challener said these data can help in counseling patients. “Taking your SGLT2i for your heart failure and your diabetes is also providing some benefit for your gout, and we know that there is also cardiac benefit when gout is controlled.”
Challener and Aviña-Zubieta had no disclosures.
A version of this article first appeared on Medscape.com.
FROM ACR 2024
An Epidemiologist’s Guide to Debunking Nutritional Research
You’re invited to a dinner party but you struggle to make small talk. Do not worry; that will invariably crop up over cocktails. Because all journalism has been reduced to listicles, here are four ways to seem clever at dinner parties.
1. The Predinner Cocktails: A Lesson in Reverse Causation
Wine connoisseurs sniff, swirl, and gently swish the wine in their mouths before spitting out and cleansing their palates to better appreciate the subtlety of each vintage. If you’re not an oenophile, no matter. Whenever somebody claims that moderate amounts of alcohol are good for your heart, this is your moment to pounce. Interject yourself in the conversation and tell everybody about reverse causation.
Reverse causation, also known as protopathic bias, involves misinterpreting the directionality of an association. You assume that X leads to Y, when in fact Y leads to X. Temporal paradoxes are useful plot devices in science fiction movies, but they have no place in medical research. In our bland world, cause must precede effect. As such, smoking leads to lung cancer; lung cancer doesn’t make you smoke more.
But with alcohol, directionality is less obvious. Many studies of alcohol and cardiovascular disease have demonstrated a U-shaped association, with risk being lowest among those who drink moderate amounts of alcohol (usually one to two drinks per day) and higher in those who drink more and also those who drink very little.
But one must ask why some people drink little or no alcohol. There is an important difference between former drinkers and never drinkers. Former drinkers cut back for a reason. More likely than not, the reason for this newfound sobriety was medical. A new cancer diagnosis, the emergence of atrial fibrillation, the development of diabetes, or rising blood pressure are all good reasons to reduce or eliminate alcohol. A cross-sectional study will fail to capture that alcohol consumption changes over time — people who now don’t drink may have imbibed alcohol in years past. It was not abstinence that led to an increased risk for heart disease; it was the increased risk for heart disease that led to abstinence.
You see the same phenomenon with the so-called obesity paradox. The idea that being a little overweight is good for you may appeal when you no longer fit into last year’s pants. But people who are underweight are so for a reason. Malnutrition, cachexia from cancer, or some other cause is almost certainly driving up the risk at the left-hand side of the U-shaped curve that makes the middle part seem better than it actually is.
Food consumption changes over time. A cross-sectional survey at one point in time cannot accurately capture past habits and distant exposures, especially for diseases such as heart disease and cancer that develop slowly over time. Studies on alcohol that try to overcome these shortcomings by eliminating former drinkers, or by using Mendelian randomization to better account for past exposure, do not show a cardiovascular benefit for moderate red wine drinking.
2. The Hors D’oeuvres — The Importance of RCTs
Now that you have made yourself the center of attention, it is time to cement your newfound reputation as a font of scientific knowledge. Most self-respecting hosts will serve smoked salmon as an amuse-bouche before the main meal. When someone mentions the health benefits of fish oils, you should take the opportunity to teach them about confounding.
Fish, especially cold-water fish from northern climates, have relatively high amounts of omega-3 fatty acids. Despite the plethora of observational studies suggesting a cardiovascular benefit, it’s now relatively clear that fish oil or omega-3 supplements have no medical benefit.
This will probably come as a shock to the worried well, but many studies, including VITAL and ASCEND, have demonstrated no cardiovascular or cancer benefit to supplementation with omega-3s. The reason is straightforward and explains why hormone replacement therapy, vitamin D, and myriad purported game-changers never panned out. Confounding is hard to overcome in observational research.
Prior to the publication of the Women’s Health Initiative (WHI) Study, hormone replacement therapy was routinely prescribed to postmenopausal women because numerous observational studies suggested a cardiovascular benefit. But with the publication of the WHI study, it became clear that much of that “benefit” was due to confounding. The women choosing to take hormones were more health conscious at baseline and healthier overall.
A similar phenomenon occurred during COVID. Patients with low serum vitamin D levels had worse outcomes, prompting many to suggest vitamin D supplementation as a possible treatment. Trials did not support the intervention because we’d overlooked the obvious. People with vitamin D deficiency have underlying health problems that contribute to the vitamin D deficiency. They are probably older, frailer, possibly with a poorer diet. No amount of statistical adjustment can account for all those differences, and some degree of residual confounding will always persist.
The only way to overcome confounding is with randomization. When patients are randomly assigned to one group or another, their baseline differences largely balance out if the randomization was performed properly and the groups were large enough. There is a role for observational research, such as in situations where ethics, cost, and practicality do not allow for a randomized controlled trial. But randomized controlled trials have largely put to rest the purported health benefits of over-the-counter fish oils, omega-3s, and vitamin D.
3. The Main Course — Absolute vs Relative Risk
When you get to the main course, all eyes will now be on you. You will almost certainly be called upon to pronounce on the harms or benefits of red meat consumption. Begin by regaling your guests with a little trivia. Ask them if they know the definition of red meat and white meat. When someone says pork is white meat, you can reveal that “pork, the other white meat,” was a marketing slogan with no scientific underpinning. Now that everyone is lulled into a stupefied silence, tell them that red meat comes from mammals and white meat comes from birds. As they process this revelation, you can now launch into the deeply mathematical concept of absolute vs relative risk.
Many etiquette books will caution against bringing up math at a dinner party. These books are wrong. Everyone finds math interesting if they are primed properly. For example, you can point to a study claiming that berries reduce cardiovascular risk in women. Even if true — and there is reason to be cautious, given the observational nature of the research — we need to understand what the authors meant by a 32% risk reduction. (Side note: It was a reduction in hazard, with a hazard ratio of 0.68 (95% CI, 0.49-0.96), but we won’t dwell on the difference between hazard ratios and risk ratios right now.)
This relative risk reduction has to be interpreted carefully. The authors divided the population into quintiles based on their consumption of anthocyanins (the antioxidant in blueberries and strawberries) and compared the bottom fifth (average consumption, 2.5 mg/d) with the top fifth (average consumption, 25 mg/d). The bottom quintile had 126 myocardial infarctions (MIs) over 324,793 patient-years compared with 59 MIs over 332,143 patient-years. Some quick math shows an approximate reduction from 39 to 18 MIs per 100,000 patient-years. Or to put it another way, you must get 4762 women to increase their berry consumption 10-fold for 1 year to prevent one heart attack. Feel free to show people how you calculated this number. They will be impressed by your head for numbers. It is nothing more than 39 minus 18, divided by 100,000, to get the absolute risk reduction. Take the reciprocal of this (ie, 1 divided by this number) to get the number needed to treat.
Describing risks in absolute terms or using number needed to treat (or harm) can help conceptualize statistics that are sometimes hard to wrap your head around.
4. Dessert — Funding
By the time the coffee is served, everyone will be hanging on to your every word. This is as it should be, and you should not be afraid of your newfound power and influence.
Dessert will probably involve some form of chocolate, possibly in cake format. (Anyone who serves fruit as dessert is not someone you should associate with.) Take the opportunity to tell your follow diners that chocolate is not actually good for you and will not boost brain performance.
The health benefits of chocolate are often repeated but rarely scrutinized. In fact, much of the scientific research purporting to show that chocolate is good for you did not actually study chocolate. It usually involved a cocoa bean extract because the chocolate manufacturing process destroys the supposedly health-promoting antioxidants in the cocoa bean. It is true that dark chocolate has more antioxidants than milk chocolate, and that the addition of milk to chocolate further inactivates the potentially healthy antioxidants. But the amount of sugar and fat that has to be added to chocolate to make it palatable precludes any serious consideration about health benefits. Dark chocolate may have less fat and sugar than milk chocolate, but it still has a lot.
But even the cocoa bean extract doesn’t seem to do much for your heart or your brain. The long-awaited COSMOS study was published with surprisingly little fanfare. The largest randomized controlled trial of chocolate (or rather cocoa bean extract) was supposed to settle the issue definitively.
COSMOS showed no cardiovascular or neurocognitive benefit to the cocoa bean extract. But the health halo of chocolate continues to be bolstered by many studies funded by chocolate manufacturers.
We are appropriately critical of the pharmaceutical industry’s involvement in drug research. However, we should not forget that any private entity is prone to the same self-interest regardless of its product’s tastiness. How many of you knew that there was an avocado lobby funding research? No matter how many industry-funded observational studies using surrogate endpoints are out there telling you that chocolate is healthy, a randomized trial with hard clinical endpoints such as COSMOS should generally win the day.
The Final Goodbyes — Summarizing Your Case
As the party slowly winds down and everyone is saddened that you will soon take your leave, synthesize everything you have taught them over the evening. Like movies, not all studies are good. Some are just bad. They can be prone to reverse causation or confounding, and they may report relative risks when absolute risks would be more telling. Reading research studies critically is essential for separating the wheat from the chaff. With the knowledge you have now imparted to your friends, they will be much better consumers of medical news, especially when it comes to food.
And they will no doubt thank you for it by never inviting you to another dinner party!
Labos, a cardiologist at Hôpital, Notre-Dame, Montreal, Quebec, Canada, has disclosed no relevant financial relationships. He has a degree in epidemiology.
A version of this article appeared on Medscape.com.
You’re invited to a dinner party but you struggle to make small talk. Do not worry; that will invariably crop up over cocktails. Because all journalism has been reduced to listicles, here are four ways to seem clever at dinner parties.
1. The Predinner Cocktails: A Lesson in Reverse Causation
Wine connoisseurs sniff, swirl, and gently swish the wine in their mouths before spitting out and cleansing their palates to better appreciate the subtlety of each vintage. If you’re not an oenophile, no matter. Whenever somebody claims that moderate amounts of alcohol are good for your heart, this is your moment to pounce. Interject yourself in the conversation and tell everybody about reverse causation.
Reverse causation, also known as protopathic bias, involves misinterpreting the directionality of an association. You assume that X leads to Y, when in fact Y leads to X. Temporal paradoxes are useful plot devices in science fiction movies, but they have no place in medical research. In our bland world, cause must precede effect. As such, smoking leads to lung cancer; lung cancer doesn’t make you smoke more.
But with alcohol, directionality is less obvious. Many studies of alcohol and cardiovascular disease have demonstrated a U-shaped association, with risk being lowest among those who drink moderate amounts of alcohol (usually one to two drinks per day) and higher in those who drink more and also those who drink very little.
But one must ask why some people drink little or no alcohol. There is an important difference between former drinkers and never drinkers. Former drinkers cut back for a reason. More likely than not, the reason for this newfound sobriety was medical. A new cancer diagnosis, the emergence of atrial fibrillation, the development of diabetes, or rising blood pressure are all good reasons to reduce or eliminate alcohol. A cross-sectional study will fail to capture that alcohol consumption changes over time — people who now don’t drink may have imbibed alcohol in years past. It was not abstinence that led to an increased risk for heart disease; it was the increased risk for heart disease that led to abstinence.
You see the same phenomenon with the so-called obesity paradox. The idea that being a little overweight is good for you may appeal when you no longer fit into last year’s pants. But people who are underweight are so for a reason. Malnutrition, cachexia from cancer, or some other cause is almost certainly driving up the risk at the left-hand side of the U-shaped curve that makes the middle part seem better than it actually is.
Food consumption changes over time. A cross-sectional survey at one point in time cannot accurately capture past habits and distant exposures, especially for diseases such as heart disease and cancer that develop slowly over time. Studies on alcohol that try to overcome these shortcomings by eliminating former drinkers, or by using Mendelian randomization to better account for past exposure, do not show a cardiovascular benefit for moderate red wine drinking.
2. The Hors D’oeuvres — The Importance of RCTs
Now that you have made yourself the center of attention, it is time to cement your newfound reputation as a font of scientific knowledge. Most self-respecting hosts will serve smoked salmon as an amuse-bouche before the main meal. When someone mentions the health benefits of fish oils, you should take the opportunity to teach them about confounding.
Fish, especially cold-water fish from northern climates, have relatively high amounts of omega-3 fatty acids. Despite the plethora of observational studies suggesting a cardiovascular benefit, it’s now relatively clear that fish oil or omega-3 supplements have no medical benefit.
This will probably come as a shock to the worried well, but many studies, including VITAL and ASCEND, have demonstrated no cardiovascular or cancer benefit to supplementation with omega-3s. The reason is straightforward and explains why hormone replacement therapy, vitamin D, and myriad purported game-changers never panned out. Confounding is hard to overcome in observational research.
Prior to the publication of the Women’s Health Initiative (WHI) Study, hormone replacement therapy was routinely prescribed to postmenopausal women because numerous observational studies suggested a cardiovascular benefit. But with the publication of the WHI study, it became clear that much of that “benefit” was due to confounding. The women choosing to take hormones were more health conscious at baseline and healthier overall.
A similar phenomenon occurred during COVID. Patients with low serum vitamin D levels had worse outcomes, prompting many to suggest vitamin D supplementation as a possible treatment. Trials did not support the intervention because we’d overlooked the obvious. People with vitamin D deficiency have underlying health problems that contribute to the vitamin D deficiency. They are probably older, frailer, possibly with a poorer diet. No amount of statistical adjustment can account for all those differences, and some degree of residual confounding will always persist.
The only way to overcome confounding is with randomization. When patients are randomly assigned to one group or another, their baseline differences largely balance out if the randomization was performed properly and the groups were large enough. There is a role for observational research, such as in situations where ethics, cost, and practicality do not allow for a randomized controlled trial. But randomized controlled trials have largely put to rest the purported health benefits of over-the-counter fish oils, omega-3s, and vitamin D.
3. The Main Course — Absolute vs Relative Risk
When you get to the main course, all eyes will now be on you. You will almost certainly be called upon to pronounce on the harms or benefits of red meat consumption. Begin by regaling your guests with a little trivia. Ask them if they know the definition of red meat and white meat. When someone says pork is white meat, you can reveal that “pork, the other white meat,” was a marketing slogan with no scientific underpinning. Now that everyone is lulled into a stupefied silence, tell them that red meat comes from mammals and white meat comes from birds. As they process this revelation, you can now launch into the deeply mathematical concept of absolute vs relative risk.
Many etiquette books will caution against bringing up math at a dinner party. These books are wrong. Everyone finds math interesting if they are primed properly. For example, you can point to a study claiming that berries reduce cardiovascular risk in women. Even if true — and there is reason to be cautious, given the observational nature of the research — we need to understand what the authors meant by a 32% risk reduction. (Side note: It was a reduction in hazard, with a hazard ratio of 0.68 (95% CI, 0.49-0.96), but we won’t dwell on the difference between hazard ratios and risk ratios right now.)
This relative risk reduction has to be interpreted carefully. The authors divided the population into quintiles based on their consumption of anthocyanins (the antioxidant in blueberries and strawberries) and compared the bottom fifth (average consumption, 2.5 mg/d) with the top fifth (average consumption, 25 mg/d). The bottom quintile had 126 myocardial infarctions (MIs) over 324,793 patient-years compared with 59 MIs over 332,143 patient-years. Some quick math shows an approximate reduction from 39 to 18 MIs per 100,000 patient-years. Or to put it another way, you must get 4762 women to increase their berry consumption 10-fold for 1 year to prevent one heart attack. Feel free to show people how you calculated this number. They will be impressed by your head for numbers. It is nothing more than 39 minus 18, divided by 100,000, to get the absolute risk reduction. Take the reciprocal of this (ie, 1 divided by this number) to get the number needed to treat.
Describing risks in absolute terms or using number needed to treat (or harm) can help conceptualize statistics that are sometimes hard to wrap your head around.
4. Dessert — Funding
By the time the coffee is served, everyone will be hanging on to your every word. This is as it should be, and you should not be afraid of your newfound power and influence.
Dessert will probably involve some form of chocolate, possibly in cake format. (Anyone who serves fruit as dessert is not someone you should associate with.) Take the opportunity to tell your follow diners that chocolate is not actually good for you and will not boost brain performance.
The health benefits of chocolate are often repeated but rarely scrutinized. In fact, much of the scientific research purporting to show that chocolate is good for you did not actually study chocolate. It usually involved a cocoa bean extract because the chocolate manufacturing process destroys the supposedly health-promoting antioxidants in the cocoa bean. It is true that dark chocolate has more antioxidants than milk chocolate, and that the addition of milk to chocolate further inactivates the potentially healthy antioxidants. But the amount of sugar and fat that has to be added to chocolate to make it palatable precludes any serious consideration about health benefits. Dark chocolate may have less fat and sugar than milk chocolate, but it still has a lot.
But even the cocoa bean extract doesn’t seem to do much for your heart or your brain. The long-awaited COSMOS study was published with surprisingly little fanfare. The largest randomized controlled trial of chocolate (or rather cocoa bean extract) was supposed to settle the issue definitively.
COSMOS showed no cardiovascular or neurocognitive benefit to the cocoa bean extract. But the health halo of chocolate continues to be bolstered by many studies funded by chocolate manufacturers.
We are appropriately critical of the pharmaceutical industry’s involvement in drug research. However, we should not forget that any private entity is prone to the same self-interest regardless of its product’s tastiness. How many of you knew that there was an avocado lobby funding research? No matter how many industry-funded observational studies using surrogate endpoints are out there telling you that chocolate is healthy, a randomized trial with hard clinical endpoints such as COSMOS should generally win the day.
The Final Goodbyes — Summarizing Your Case
As the party slowly winds down and everyone is saddened that you will soon take your leave, synthesize everything you have taught them over the evening. Like movies, not all studies are good. Some are just bad. They can be prone to reverse causation or confounding, and they may report relative risks when absolute risks would be more telling. Reading research studies critically is essential for separating the wheat from the chaff. With the knowledge you have now imparted to your friends, they will be much better consumers of medical news, especially when it comes to food.
And they will no doubt thank you for it by never inviting you to another dinner party!
Labos, a cardiologist at Hôpital, Notre-Dame, Montreal, Quebec, Canada, has disclosed no relevant financial relationships. He has a degree in epidemiology.
A version of this article appeared on Medscape.com.
You’re invited to a dinner party but you struggle to make small talk. Do not worry; that will invariably crop up over cocktails. Because all journalism has been reduced to listicles, here are four ways to seem clever at dinner parties.
1. The Predinner Cocktails: A Lesson in Reverse Causation
Wine connoisseurs sniff, swirl, and gently swish the wine in their mouths before spitting out and cleansing their palates to better appreciate the subtlety of each vintage. If you’re not an oenophile, no matter. Whenever somebody claims that moderate amounts of alcohol are good for your heart, this is your moment to pounce. Interject yourself in the conversation and tell everybody about reverse causation.
Reverse causation, also known as protopathic bias, involves misinterpreting the directionality of an association. You assume that X leads to Y, when in fact Y leads to X. Temporal paradoxes are useful plot devices in science fiction movies, but they have no place in medical research. In our bland world, cause must precede effect. As such, smoking leads to lung cancer; lung cancer doesn’t make you smoke more.
But with alcohol, directionality is less obvious. Many studies of alcohol and cardiovascular disease have demonstrated a U-shaped association, with risk being lowest among those who drink moderate amounts of alcohol (usually one to two drinks per day) and higher in those who drink more and also those who drink very little.
But one must ask why some people drink little or no alcohol. There is an important difference between former drinkers and never drinkers. Former drinkers cut back for a reason. More likely than not, the reason for this newfound sobriety was medical. A new cancer diagnosis, the emergence of atrial fibrillation, the development of diabetes, or rising blood pressure are all good reasons to reduce or eliminate alcohol. A cross-sectional study will fail to capture that alcohol consumption changes over time — people who now don’t drink may have imbibed alcohol in years past. It was not abstinence that led to an increased risk for heart disease; it was the increased risk for heart disease that led to abstinence.
You see the same phenomenon with the so-called obesity paradox. The idea that being a little overweight is good for you may appeal when you no longer fit into last year’s pants. But people who are underweight are so for a reason. Malnutrition, cachexia from cancer, or some other cause is almost certainly driving up the risk at the left-hand side of the U-shaped curve that makes the middle part seem better than it actually is.
Food consumption changes over time. A cross-sectional survey at one point in time cannot accurately capture past habits and distant exposures, especially for diseases such as heart disease and cancer that develop slowly over time. Studies on alcohol that try to overcome these shortcomings by eliminating former drinkers, or by using Mendelian randomization to better account for past exposure, do not show a cardiovascular benefit for moderate red wine drinking.
2. The Hors D’oeuvres — The Importance of RCTs
Now that you have made yourself the center of attention, it is time to cement your newfound reputation as a font of scientific knowledge. Most self-respecting hosts will serve smoked salmon as an amuse-bouche before the main meal. When someone mentions the health benefits of fish oils, you should take the opportunity to teach them about confounding.
Fish, especially cold-water fish from northern climates, have relatively high amounts of omega-3 fatty acids. Despite the plethora of observational studies suggesting a cardiovascular benefit, it’s now relatively clear that fish oil or omega-3 supplements have no medical benefit.
This will probably come as a shock to the worried well, but many studies, including VITAL and ASCEND, have demonstrated no cardiovascular or cancer benefit to supplementation with omega-3s. The reason is straightforward and explains why hormone replacement therapy, vitamin D, and myriad purported game-changers never panned out. Confounding is hard to overcome in observational research.
Prior to the publication of the Women’s Health Initiative (WHI) Study, hormone replacement therapy was routinely prescribed to postmenopausal women because numerous observational studies suggested a cardiovascular benefit. But with the publication of the WHI study, it became clear that much of that “benefit” was due to confounding. The women choosing to take hormones were more health conscious at baseline and healthier overall.
A similar phenomenon occurred during COVID. Patients with low serum vitamin D levels had worse outcomes, prompting many to suggest vitamin D supplementation as a possible treatment. Trials did not support the intervention because we’d overlooked the obvious. People with vitamin D deficiency have underlying health problems that contribute to the vitamin D deficiency. They are probably older, frailer, possibly with a poorer diet. No amount of statistical adjustment can account for all those differences, and some degree of residual confounding will always persist.
The only way to overcome confounding is with randomization. When patients are randomly assigned to one group or another, their baseline differences largely balance out if the randomization was performed properly and the groups were large enough. There is a role for observational research, such as in situations where ethics, cost, and practicality do not allow for a randomized controlled trial. But randomized controlled trials have largely put to rest the purported health benefits of over-the-counter fish oils, omega-3s, and vitamin D.
3. The Main Course — Absolute vs Relative Risk
When you get to the main course, all eyes will now be on you. You will almost certainly be called upon to pronounce on the harms or benefits of red meat consumption. Begin by regaling your guests with a little trivia. Ask them if they know the definition of red meat and white meat. When someone says pork is white meat, you can reveal that “pork, the other white meat,” was a marketing slogan with no scientific underpinning. Now that everyone is lulled into a stupefied silence, tell them that red meat comes from mammals and white meat comes from birds. As they process this revelation, you can now launch into the deeply mathematical concept of absolute vs relative risk.
Many etiquette books will caution against bringing up math at a dinner party. These books are wrong. Everyone finds math interesting if they are primed properly. For example, you can point to a study claiming that berries reduce cardiovascular risk in women. Even if true — and there is reason to be cautious, given the observational nature of the research — we need to understand what the authors meant by a 32% risk reduction. (Side note: It was a reduction in hazard, with a hazard ratio of 0.68 (95% CI, 0.49-0.96), but we won’t dwell on the difference between hazard ratios and risk ratios right now.)
This relative risk reduction has to be interpreted carefully. The authors divided the population into quintiles based on their consumption of anthocyanins (the antioxidant in blueberries and strawberries) and compared the bottom fifth (average consumption, 2.5 mg/d) with the top fifth (average consumption, 25 mg/d). The bottom quintile had 126 myocardial infarctions (MIs) over 324,793 patient-years compared with 59 MIs over 332,143 patient-years. Some quick math shows an approximate reduction from 39 to 18 MIs per 100,000 patient-years. Or to put it another way, you must get 4762 women to increase their berry consumption 10-fold for 1 year to prevent one heart attack. Feel free to show people how you calculated this number. They will be impressed by your head for numbers. It is nothing more than 39 minus 18, divided by 100,000, to get the absolute risk reduction. Take the reciprocal of this (ie, 1 divided by this number) to get the number needed to treat.
Describing risks in absolute terms or using number needed to treat (or harm) can help conceptualize statistics that are sometimes hard to wrap your head around.
4. Dessert — Funding
By the time the coffee is served, everyone will be hanging on to your every word. This is as it should be, and you should not be afraid of your newfound power and influence.
Dessert will probably involve some form of chocolate, possibly in cake format. (Anyone who serves fruit as dessert is not someone you should associate with.) Take the opportunity to tell your follow diners that chocolate is not actually good for you and will not boost brain performance.
The health benefits of chocolate are often repeated but rarely scrutinized. In fact, much of the scientific research purporting to show that chocolate is good for you did not actually study chocolate. It usually involved a cocoa bean extract because the chocolate manufacturing process destroys the supposedly health-promoting antioxidants in the cocoa bean. It is true that dark chocolate has more antioxidants than milk chocolate, and that the addition of milk to chocolate further inactivates the potentially healthy antioxidants. But the amount of sugar and fat that has to be added to chocolate to make it palatable precludes any serious consideration about health benefits. Dark chocolate may have less fat and sugar than milk chocolate, but it still has a lot.
But even the cocoa bean extract doesn’t seem to do much for your heart or your brain. The long-awaited COSMOS study was published with surprisingly little fanfare. The largest randomized controlled trial of chocolate (or rather cocoa bean extract) was supposed to settle the issue definitively.
COSMOS showed no cardiovascular or neurocognitive benefit to the cocoa bean extract. But the health halo of chocolate continues to be bolstered by many studies funded by chocolate manufacturers.
We are appropriately critical of the pharmaceutical industry’s involvement in drug research. However, we should not forget that any private entity is prone to the same self-interest regardless of its product’s tastiness. How many of you knew that there was an avocado lobby funding research? No matter how many industry-funded observational studies using surrogate endpoints are out there telling you that chocolate is healthy, a randomized trial with hard clinical endpoints such as COSMOS should generally win the day.
The Final Goodbyes — Summarizing Your Case
As the party slowly winds down and everyone is saddened that you will soon take your leave, synthesize everything you have taught them over the evening. Like movies, not all studies are good. Some are just bad. They can be prone to reverse causation or confounding, and they may report relative risks when absolute risks would be more telling. Reading research studies critically is essential for separating the wheat from the chaff. With the knowledge you have now imparted to your friends, they will be much better consumers of medical news, especially when it comes to food.
And they will no doubt thank you for it by never inviting you to another dinner party!
Labos, a cardiologist at Hôpital, Notre-Dame, Montreal, Quebec, Canada, has disclosed no relevant financial relationships. He has a degree in epidemiology.
A version of this article appeared on Medscape.com.
Vitamin D May Lower Blood Pressure in Seniors With Overweight
TOPLINE:
Supplementation with vitamin D and calcium can reduce systolic and diastolic blood pressure in older individuals with overweight, particularly in those with a body mass index (BMI) > 30 and those diagnosed with hypertension.
METHODOLOGY:
- Large cohort data have provided epidemiologic evidence linking vitamin D deficiency to a higher risk for cardiovascular disorders, including hypertension; however, evidence on the beneficial effects of vitamin D supplementation on blood pressure outcomes remains inconclusive.
- A post hoc analysis of a randomized controlled trial was conducted to investigate the effect of two doses of cholecalciferol (vitamin D3) on blood pressure in individuals aged 65 years or older with a BMI > 25 and serum vitamin D levels of 10-30 ng/mL.
- A total of 221 participants were recruited through outpatient departments, clinics, and advertisements in the greater Beirut area and received calcium supplementation in combination with either a low dose (600 IU/d, as recommended by the Institute of Medicine [IOM]) or a high dose (3750 IU/d) of vitamin D3.
- Blood pressure measurements were taken at baseline, 6 months, and 12 months using a SureSigns VS3 monitor.
- Participants were also stratified by BMI and hypertension status to assess the effects of vitamin D and calcium on blood pressure.
TAKEAWAY:
- Systolic and diastolic blood pressures were significantly reduced with vitamin D supplementation in the overall cohort (mean difference, 3.5 and 2.8 mm Hg, respectively; P = .005 and P = .002, respectively), with the effect more prominent in those in the high-dose vitamin D group.
- Participants with a BMI > 30 experienced reductions in both systolic and diastolic blood pressures in the overall cohort (P < .0001 and P = .01, respectively); although the systolic blood pressure was significantly reduced with both high- and low-dose vitamin D, the diastolic blood pressure decreased in the high-dose group only.
- Patients with hypertension benefited from all doses of vitamin D, regardless of the BMI.
- Systolic blood pressure at 6 and 12 months was significantly predicted by BMI and baseline systolic blood pressure measurements, although not by the dose of vitamin D received.
IN PRACTICE:
“Our study found vitamin D supplementation may decrease blood pressure in specific subgroups such as older people, people with obesity, and possibly those with low vitamin D levels,” said study author Ghada El-Hajj Fuleihan, MD, MPH, of the American University of Beirut Medical Center in Beirut, Lebanon, said in a news release. “High vitamin D doses compared to the IOM’s recommended daily dose did not provide additional health benefits.”
SOURCE:
This study was led by Maya Rahme, Department of Internal Medicine, Division of Endocrinology, Calcium Metabolism and Osteoporosis Program, World Health Organization Collaborating Center for Metabolic Bone Disorders, American University of Beirut Medical Center in Beirut, Lebanon. It was published online in Journal of the Endocrine Society.
LIMITATIONS:
This study’s limitations included the exploratory nature of the analyses and the low power of the subgroup analyses. Additionally, the study focused on older individuals who were sedentary and had overweight, many of whom had prediabetes — conditions known to influence blood pressure. The possible effect of calcium alone on blood pressure reduction was also unclear.
DISCLOSURES:
This study was supported by grants from the American University of Beirut, St Joseph University, and the Lebanese Council for National Scientific Research. No relevant conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.
TOPLINE:
Supplementation with vitamin D and calcium can reduce systolic and diastolic blood pressure in older individuals with overweight, particularly in those with a body mass index (BMI) > 30 and those diagnosed with hypertension.
METHODOLOGY:
- Large cohort data have provided epidemiologic evidence linking vitamin D deficiency to a higher risk for cardiovascular disorders, including hypertension; however, evidence on the beneficial effects of vitamin D supplementation on blood pressure outcomes remains inconclusive.
- A post hoc analysis of a randomized controlled trial was conducted to investigate the effect of two doses of cholecalciferol (vitamin D3) on blood pressure in individuals aged 65 years or older with a BMI > 25 and serum vitamin D levels of 10-30 ng/mL.
- A total of 221 participants were recruited through outpatient departments, clinics, and advertisements in the greater Beirut area and received calcium supplementation in combination with either a low dose (600 IU/d, as recommended by the Institute of Medicine [IOM]) or a high dose (3750 IU/d) of vitamin D3.
- Blood pressure measurements were taken at baseline, 6 months, and 12 months using a SureSigns VS3 monitor.
- Participants were also stratified by BMI and hypertension status to assess the effects of vitamin D and calcium on blood pressure.
TAKEAWAY:
- Systolic and diastolic blood pressures were significantly reduced with vitamin D supplementation in the overall cohort (mean difference, 3.5 and 2.8 mm Hg, respectively; P = .005 and P = .002, respectively), with the effect more prominent in those in the high-dose vitamin D group.
- Participants with a BMI > 30 experienced reductions in both systolic and diastolic blood pressures in the overall cohort (P < .0001 and P = .01, respectively); although the systolic blood pressure was significantly reduced with both high- and low-dose vitamin D, the diastolic blood pressure decreased in the high-dose group only.
- Patients with hypertension benefited from all doses of vitamin D, regardless of the BMI.
- Systolic blood pressure at 6 and 12 months was significantly predicted by BMI and baseline systolic blood pressure measurements, although not by the dose of vitamin D received.
IN PRACTICE:
“Our study found vitamin D supplementation may decrease blood pressure in specific subgroups such as older people, people with obesity, and possibly those with low vitamin D levels,” said study author Ghada El-Hajj Fuleihan, MD, MPH, of the American University of Beirut Medical Center in Beirut, Lebanon, said in a news release. “High vitamin D doses compared to the IOM’s recommended daily dose did not provide additional health benefits.”
SOURCE:
This study was led by Maya Rahme, Department of Internal Medicine, Division of Endocrinology, Calcium Metabolism and Osteoporosis Program, World Health Organization Collaborating Center for Metabolic Bone Disorders, American University of Beirut Medical Center in Beirut, Lebanon. It was published online in Journal of the Endocrine Society.
LIMITATIONS:
This study’s limitations included the exploratory nature of the analyses and the low power of the subgroup analyses. Additionally, the study focused on older individuals who were sedentary and had overweight, many of whom had prediabetes — conditions known to influence blood pressure. The possible effect of calcium alone on blood pressure reduction was also unclear.
DISCLOSURES:
This study was supported by grants from the American University of Beirut, St Joseph University, and the Lebanese Council for National Scientific Research. No relevant conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.
TOPLINE:
Supplementation with vitamin D and calcium can reduce systolic and diastolic blood pressure in older individuals with overweight, particularly in those with a body mass index (BMI) > 30 and those diagnosed with hypertension.
METHODOLOGY:
- Large cohort data have provided epidemiologic evidence linking vitamin D deficiency to a higher risk for cardiovascular disorders, including hypertension; however, evidence on the beneficial effects of vitamin D supplementation on blood pressure outcomes remains inconclusive.
- A post hoc analysis of a randomized controlled trial was conducted to investigate the effect of two doses of cholecalciferol (vitamin D3) on blood pressure in individuals aged 65 years or older with a BMI > 25 and serum vitamin D levels of 10-30 ng/mL.
- A total of 221 participants were recruited through outpatient departments, clinics, and advertisements in the greater Beirut area and received calcium supplementation in combination with either a low dose (600 IU/d, as recommended by the Institute of Medicine [IOM]) or a high dose (3750 IU/d) of vitamin D3.
- Blood pressure measurements were taken at baseline, 6 months, and 12 months using a SureSigns VS3 monitor.
- Participants were also stratified by BMI and hypertension status to assess the effects of vitamin D and calcium on blood pressure.
TAKEAWAY:
- Systolic and diastolic blood pressures were significantly reduced with vitamin D supplementation in the overall cohort (mean difference, 3.5 and 2.8 mm Hg, respectively; P = .005 and P = .002, respectively), with the effect more prominent in those in the high-dose vitamin D group.
- Participants with a BMI > 30 experienced reductions in both systolic and diastolic blood pressures in the overall cohort (P < .0001 and P = .01, respectively); although the systolic blood pressure was significantly reduced with both high- and low-dose vitamin D, the diastolic blood pressure decreased in the high-dose group only.
- Patients with hypertension benefited from all doses of vitamin D, regardless of the BMI.
- Systolic blood pressure at 6 and 12 months was significantly predicted by BMI and baseline systolic blood pressure measurements, although not by the dose of vitamin D received.
IN PRACTICE:
“Our study found vitamin D supplementation may decrease blood pressure in specific subgroups such as older people, people with obesity, and possibly those with low vitamin D levels,” said study author Ghada El-Hajj Fuleihan, MD, MPH, of the American University of Beirut Medical Center in Beirut, Lebanon, said in a news release. “High vitamin D doses compared to the IOM’s recommended daily dose did not provide additional health benefits.”
SOURCE:
This study was led by Maya Rahme, Department of Internal Medicine, Division of Endocrinology, Calcium Metabolism and Osteoporosis Program, World Health Organization Collaborating Center for Metabolic Bone Disorders, American University of Beirut Medical Center in Beirut, Lebanon. It was published online in Journal of the Endocrine Society.
LIMITATIONS:
This study’s limitations included the exploratory nature of the analyses and the low power of the subgroup analyses. Additionally, the study focused on older individuals who were sedentary and had overweight, many of whom had prediabetes — conditions known to influence blood pressure. The possible effect of calcium alone on blood pressure reduction was also unclear.
DISCLOSURES:
This study was supported by grants from the American University of Beirut, St Joseph University, and the Lebanese Council for National Scientific Research. No relevant conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.
PRECISE-DAPT Score Predicts GI Bleeding Risk Among Post-PCI Patients
PHILADELPHIA — Gastrointestinal (GI) bleeding after percutaneous coronary intervention (PCI) among patients on dual antiplatelet therapy (DAPT) remains risky in terms of morbidity and mortality, but the Predicting Bleeding Complications in Patients Undergoing Stent Implantation and Subsequent Dual Antiplatelet Therapy (PRECISE-DAPT) score could help predict that risk, according to a study presented at the American College of Gastroenterology (ACG) 2024 Annual Scientific Meeting.
In a predominantly Hispanic population in Texas, 2.5% of post-PCI patients on DAPT had GI bleeding in the first year.
“Our study established that the PRECISE-DAPT score possesses a moderate predictive accuracy not only for overall bleeding risk but also specifically for gastrointestinal bleeding,” said lead author Jesus Guzman, MD, a gastroenterology fellow at the Texas Tech University Health Sciences Center El Paso.
Current guidelines from the American College of Cardiology and American Heart Association recommend DAPT for 6-12 months post-PCI, with consideration for shorter durations in patients with lower ischemic risks but higher bleeding risks.
“Interestingly, some of these patients were on DAPT for more than 2 years, which goes beyond the guidelines,” he said. “In this patient population, this has to do with them being lost to follow-up and getting reestablished, and they kept refilling their prescriptions.”
Guzman and colleagues conducted a retrospective cohort study of patients receiving DAPT after PCI from 2014 to 2021. They looked for GI bleeding rates at 1 year and across the duration of the study period, as well as endoscopic indications, findings, concurrent antiplatelet therapy, and the primary cause of bleeding.
In addition, the research team evaluated the predictive value of the PRECISE-DAPT score, which categorizes patients based on low risk (≤ 17), moderate risk (18-24), and high risk (≥ 25) for bleeding. The score aims to optimize the balance between bleeding and ischemic risks, Guzman said, by incorporating five factors: Age, creatinine clearance, hemoglobin, white blood cell count, and history of spontaneous bleeding.
Among 1067 patients, 563 (57.9%) received clopidogrel and 409 (42%) received ticagrelor. The overall cohort was 66.6% men, 77.1% Hispanic, and had a mean age of 62 years.
The GI bleeding rate was 2.5% at 1-year post-PCI among 27 patients and 3.7% for the study duration among 39 patients, with a median follow-up of 2.2 years.
Among the 39 GI bleeds, 41% were lower GI bleeds, 28% were upper GI bleeds, 15% were small bowel bleeds, and 15% were undetermined. The most frequent etiology was colon cancer, accounting for 18% of bleeds, followed by 15% for gastric ulcers, 10% for diverticular bleeds, and 10% for hemorrhoidal bleeds.
In general, analyses indicated no significant differences in GI bleeding between patients on clopidogrel (21.2%) and those on ticagrelor (19.2%).
However, the odds of GI bleeding were significantly higher in patients with high-risk PRECISE-DAPT scores (odds ratio [OR], 2.5) and moderate-risk scores (OR, 2.8) than in those with low-risk scores. The majority of patients without GI bleeding had scores < 17, whereas the majority of patients with GI bleeding had scores > 24. An optimal threshold for the PRECISE-DAPT score was identified as ≥ 19.
“When patients on DAPT present with GI bleeding, it can be a clinical conundrum for gastroenterologists and cardiologists, especially when it can be a life-or-death event, and stopping DAPT can increase risk of thrombosis,” said Jeff Taclob, MD, a hepatology fellow at The University of Tennessee Health Science Center in Memphis. Taclob, who wasn’t involved with the study, attended the conference session.
“In this population in El Paso, in particular, many patients don’t have adequate healthcare, may be lost to follow-up, and get their prescriptions filled elsewhere, such as Juárez, Mexico,” he said. “Then they come in with this life-threatening bleed, so we need to focus more on their risks.”
Paying attention to specific patient populations, cultures, and values remains important for patient communication and clinical decision-making, Taclob noted.
“In this population of older men, there’s often a macho persona where they don’t want to seek help,” he said. “DAPT criteria could differ in other populations, but here, the PRECISE-DAPT score appeared to help.”
The study was awarded the ACG Outstanding Research Award in the GI Bleeding Category (Trainee). Guzman and Taclob reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
PHILADELPHIA — Gastrointestinal (GI) bleeding after percutaneous coronary intervention (PCI) among patients on dual antiplatelet therapy (DAPT) remains risky in terms of morbidity and mortality, but the Predicting Bleeding Complications in Patients Undergoing Stent Implantation and Subsequent Dual Antiplatelet Therapy (PRECISE-DAPT) score could help predict that risk, according to a study presented at the American College of Gastroenterology (ACG) 2024 Annual Scientific Meeting.
In a predominantly Hispanic population in Texas, 2.5% of post-PCI patients on DAPT had GI bleeding in the first year.
“Our study established that the PRECISE-DAPT score possesses a moderate predictive accuracy not only for overall bleeding risk but also specifically for gastrointestinal bleeding,” said lead author Jesus Guzman, MD, a gastroenterology fellow at the Texas Tech University Health Sciences Center El Paso.
Current guidelines from the American College of Cardiology and American Heart Association recommend DAPT for 6-12 months post-PCI, with consideration for shorter durations in patients with lower ischemic risks but higher bleeding risks.
“Interestingly, some of these patients were on DAPT for more than 2 years, which goes beyond the guidelines,” he said. “In this patient population, this has to do with them being lost to follow-up and getting reestablished, and they kept refilling their prescriptions.”
Guzman and colleagues conducted a retrospective cohort study of patients receiving DAPT after PCI from 2014 to 2021. They looked for GI bleeding rates at 1 year and across the duration of the study period, as well as endoscopic indications, findings, concurrent antiplatelet therapy, and the primary cause of bleeding.
In addition, the research team evaluated the predictive value of the PRECISE-DAPT score, which categorizes patients based on low risk (≤ 17), moderate risk (18-24), and high risk (≥ 25) for bleeding. The score aims to optimize the balance between bleeding and ischemic risks, Guzman said, by incorporating five factors: Age, creatinine clearance, hemoglobin, white blood cell count, and history of spontaneous bleeding.
Among 1067 patients, 563 (57.9%) received clopidogrel and 409 (42%) received ticagrelor. The overall cohort was 66.6% men, 77.1% Hispanic, and had a mean age of 62 years.
The GI bleeding rate was 2.5% at 1-year post-PCI among 27 patients and 3.7% for the study duration among 39 patients, with a median follow-up of 2.2 years.
Among the 39 GI bleeds, 41% were lower GI bleeds, 28% were upper GI bleeds, 15% were small bowel bleeds, and 15% were undetermined. The most frequent etiology was colon cancer, accounting for 18% of bleeds, followed by 15% for gastric ulcers, 10% for diverticular bleeds, and 10% for hemorrhoidal bleeds.
In general, analyses indicated no significant differences in GI bleeding between patients on clopidogrel (21.2%) and those on ticagrelor (19.2%).
However, the odds of GI bleeding were significantly higher in patients with high-risk PRECISE-DAPT scores (odds ratio [OR], 2.5) and moderate-risk scores (OR, 2.8) than in those with low-risk scores. The majority of patients without GI bleeding had scores < 17, whereas the majority of patients with GI bleeding had scores > 24. An optimal threshold for the PRECISE-DAPT score was identified as ≥ 19.
“When patients on DAPT present with GI bleeding, it can be a clinical conundrum for gastroenterologists and cardiologists, especially when it can be a life-or-death event, and stopping DAPT can increase risk of thrombosis,” said Jeff Taclob, MD, a hepatology fellow at The University of Tennessee Health Science Center in Memphis. Taclob, who wasn’t involved with the study, attended the conference session.
“In this population in El Paso, in particular, many patients don’t have adequate healthcare, may be lost to follow-up, and get their prescriptions filled elsewhere, such as Juárez, Mexico,” he said. “Then they come in with this life-threatening bleed, so we need to focus more on their risks.”
Paying attention to specific patient populations, cultures, and values remains important for patient communication and clinical decision-making, Taclob noted.
“In this population of older men, there’s often a macho persona where they don’t want to seek help,” he said. “DAPT criteria could differ in other populations, but here, the PRECISE-DAPT score appeared to help.”
The study was awarded the ACG Outstanding Research Award in the GI Bleeding Category (Trainee). Guzman and Taclob reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
PHILADELPHIA — Gastrointestinal (GI) bleeding after percutaneous coronary intervention (PCI) among patients on dual antiplatelet therapy (DAPT) remains risky in terms of morbidity and mortality, but the Predicting Bleeding Complications in Patients Undergoing Stent Implantation and Subsequent Dual Antiplatelet Therapy (PRECISE-DAPT) score could help predict that risk, according to a study presented at the American College of Gastroenterology (ACG) 2024 Annual Scientific Meeting.
In a predominantly Hispanic population in Texas, 2.5% of post-PCI patients on DAPT had GI bleeding in the first year.
“Our study established that the PRECISE-DAPT score possesses a moderate predictive accuracy not only for overall bleeding risk but also specifically for gastrointestinal bleeding,” said lead author Jesus Guzman, MD, a gastroenterology fellow at the Texas Tech University Health Sciences Center El Paso.
Current guidelines from the American College of Cardiology and American Heart Association recommend DAPT for 6-12 months post-PCI, with consideration for shorter durations in patients with lower ischemic risks but higher bleeding risks.
“Interestingly, some of these patients were on DAPT for more than 2 years, which goes beyond the guidelines,” he said. “In this patient population, this has to do with them being lost to follow-up and getting reestablished, and they kept refilling their prescriptions.”
Guzman and colleagues conducted a retrospective cohort study of patients receiving DAPT after PCI from 2014 to 2021. They looked for GI bleeding rates at 1 year and across the duration of the study period, as well as endoscopic indications, findings, concurrent antiplatelet therapy, and the primary cause of bleeding.
In addition, the research team evaluated the predictive value of the PRECISE-DAPT score, which categorizes patients based on low risk (≤ 17), moderate risk (18-24), and high risk (≥ 25) for bleeding. The score aims to optimize the balance between bleeding and ischemic risks, Guzman said, by incorporating five factors: Age, creatinine clearance, hemoglobin, white blood cell count, and history of spontaneous bleeding.
Among 1067 patients, 563 (57.9%) received clopidogrel and 409 (42%) received ticagrelor. The overall cohort was 66.6% men, 77.1% Hispanic, and had a mean age of 62 years.
The GI bleeding rate was 2.5% at 1-year post-PCI among 27 patients and 3.7% for the study duration among 39 patients, with a median follow-up of 2.2 years.
Among the 39 GI bleeds, 41% were lower GI bleeds, 28% were upper GI bleeds, 15% were small bowel bleeds, and 15% were undetermined. The most frequent etiology was colon cancer, accounting for 18% of bleeds, followed by 15% for gastric ulcers, 10% for diverticular bleeds, and 10% for hemorrhoidal bleeds.
In general, analyses indicated no significant differences in GI bleeding between patients on clopidogrel (21.2%) and those on ticagrelor (19.2%).
However, the odds of GI bleeding were significantly higher in patients with high-risk PRECISE-DAPT scores (odds ratio [OR], 2.5) and moderate-risk scores (OR, 2.8) than in those with low-risk scores. The majority of patients without GI bleeding had scores < 17, whereas the majority of patients with GI bleeding had scores > 24. An optimal threshold for the PRECISE-DAPT score was identified as ≥ 19.
“When patients on DAPT present with GI bleeding, it can be a clinical conundrum for gastroenterologists and cardiologists, especially when it can be a life-or-death event, and stopping DAPT can increase risk of thrombosis,” said Jeff Taclob, MD, a hepatology fellow at The University of Tennessee Health Science Center in Memphis. Taclob, who wasn’t involved with the study, attended the conference session.
“In this population in El Paso, in particular, many patients don’t have adequate healthcare, may be lost to follow-up, and get their prescriptions filled elsewhere, such as Juárez, Mexico,” he said. “Then they come in with this life-threatening bleed, so we need to focus more on their risks.”
Paying attention to specific patient populations, cultures, and values remains important for patient communication and clinical decision-making, Taclob noted.
“In this population of older men, there’s often a macho persona where they don’t want to seek help,” he said. “DAPT criteria could differ in other populations, but here, the PRECISE-DAPT score appeared to help.”
The study was awarded the ACG Outstanding Research Award in the GI Bleeding Category (Trainee). Guzman and Taclob reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM ACG 2024