User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Online support tool improves AD self-management
MONTREAL – for up to 1 year, according to two randomized controlled trials presented at the annual meeting of the International Society of Atopic Dermatitis.
The intervention, directed either at parents of children with AD or young adults with AD, “is very low cost, evidence based, easily accessible, and free from possible commercial bias,” said investigator Kim Thomas, MD, professor of applied dermatology research and codirector of the Centre of Evidence Based Dermatology, faculty of medicine & health sciences, University of Nottingham (England).
The main focus of the intervention, along with general education, is “getting control” of the condition with flare-control creams and “keeping control” with regular emollient use.
Efficacy of the intervention, available free online, was compared with “usual eczema care” in 340 parents of children with AD up to age 12 and 337 young patients with AD aged 13-25. Participants were randomized to the intervention plus usual care or usual care alone. The primary outcome was the Patient-Oriented Eczema Measure(POEM) at 24 weeks, with a further measurement at 52 weeks.
In the parent group, about half were women and 83% were White, and the median age of their children was 4 years. About 50% of parents had a university degree, making them “possibly better educated than we might want our target audience for this type of intervention,” Dr. Thomas commented. Most of the children had moderate AD.
In the young patient group, the mean age was 19 years, more than three-quarters were female, 83% were White, and most had moderate AD.
At 24 weeks, both intervention groups had improved POEM scores, compared with controls, with a mean difference of 1.5 points in the parent group (P = .002) and 1.7 points in the young patient group (P = .04). “A small difference, but statistically significant and sustained,” Dr. Thomas said, adding that this difference was sustained up to 52 weeks.
In terms of mechanism of action, a secondary outcome looked at the concept of enablement, “which again, seemed to be improved in the intervention group, which suggests it’s something to do with being able to understand and cope with their disease better,” she said. The tool is targeted to “people who wouldn’t normally get to a dermatologist and certainly wouldn’t get access to group interventions.”
An additional aim of the intervention was “to provide a single, consistent message received from every point of contact that people might engage with ... [from] community doctors, pharmacists, dermatologists, and importantly, eczema charities all signposting [the intervention] and sharing a consistent message.”
While the intervention is free and available to patients anywhere, Dr. Thomas emphasized that it is tailored to the U.K. health care system. “If people would like to get in touch and help work with us to maybe adapt it slightly to make it more suitable for your own health care systems, that’s something we’d be very happy to look at with you.”
Asked for comment, Natalie Cunningham, MD, panel moderator, was lukewarm about the tool. “It can be a supplement, but you can never replace the one-on-one patient–health care provider interaction,” she told this news organization. “That could be provided by a nondermatologist and supplemented by an online component,” said Dr. Cunningham, from the Izaak Walton Killam Hospital for Children in Halifax, N.S.
“First-line treatment for eczema, no matter what kind of eczema, is topical steroids, and that is something that requires a lot of education – and something you want to do one on one in person because everyone comes to it with a different experience, baggage, or understanding,” she said. “We need to figure out what the barrier is so that you can do the right education.”
In addition, with systemic AD therapies currently approved for children, parents and young patients need to be able to advocate for specialist care to access these medications, she noted.
Dr. Thomas and Dr. Cunningham reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MONTREAL – for up to 1 year, according to two randomized controlled trials presented at the annual meeting of the International Society of Atopic Dermatitis.
The intervention, directed either at parents of children with AD or young adults with AD, “is very low cost, evidence based, easily accessible, and free from possible commercial bias,” said investigator Kim Thomas, MD, professor of applied dermatology research and codirector of the Centre of Evidence Based Dermatology, faculty of medicine & health sciences, University of Nottingham (England).
The main focus of the intervention, along with general education, is “getting control” of the condition with flare-control creams and “keeping control” with regular emollient use.
Efficacy of the intervention, available free online, was compared with “usual eczema care” in 340 parents of children with AD up to age 12 and 337 young patients with AD aged 13-25. Participants were randomized to the intervention plus usual care or usual care alone. The primary outcome was the Patient-Oriented Eczema Measure(POEM) at 24 weeks, with a further measurement at 52 weeks.
In the parent group, about half were women and 83% were White, and the median age of their children was 4 years. About 50% of parents had a university degree, making them “possibly better educated than we might want our target audience for this type of intervention,” Dr. Thomas commented. Most of the children had moderate AD.
In the young patient group, the mean age was 19 years, more than three-quarters were female, 83% were White, and most had moderate AD.
At 24 weeks, both intervention groups had improved POEM scores, compared with controls, with a mean difference of 1.5 points in the parent group (P = .002) and 1.7 points in the young patient group (P = .04). “A small difference, but statistically significant and sustained,” Dr. Thomas said, adding that this difference was sustained up to 52 weeks.
In terms of mechanism of action, a secondary outcome looked at the concept of enablement, “which again, seemed to be improved in the intervention group, which suggests it’s something to do with being able to understand and cope with their disease better,” she said. The tool is targeted to “people who wouldn’t normally get to a dermatologist and certainly wouldn’t get access to group interventions.”
An additional aim of the intervention was “to provide a single, consistent message received from every point of contact that people might engage with ... [from] community doctors, pharmacists, dermatologists, and importantly, eczema charities all signposting [the intervention] and sharing a consistent message.”
While the intervention is free and available to patients anywhere, Dr. Thomas emphasized that it is tailored to the U.K. health care system. “If people would like to get in touch and help work with us to maybe adapt it slightly to make it more suitable for your own health care systems, that’s something we’d be very happy to look at with you.”
Asked for comment, Natalie Cunningham, MD, panel moderator, was lukewarm about the tool. “It can be a supplement, but you can never replace the one-on-one patient–health care provider interaction,” she told this news organization. “That could be provided by a nondermatologist and supplemented by an online component,” said Dr. Cunningham, from the Izaak Walton Killam Hospital for Children in Halifax, N.S.
“First-line treatment for eczema, no matter what kind of eczema, is topical steroids, and that is something that requires a lot of education – and something you want to do one on one in person because everyone comes to it with a different experience, baggage, or understanding,” she said. “We need to figure out what the barrier is so that you can do the right education.”
In addition, with systemic AD therapies currently approved for children, parents and young patients need to be able to advocate for specialist care to access these medications, she noted.
Dr. Thomas and Dr. Cunningham reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MONTREAL – for up to 1 year, according to two randomized controlled trials presented at the annual meeting of the International Society of Atopic Dermatitis.
The intervention, directed either at parents of children with AD or young adults with AD, “is very low cost, evidence based, easily accessible, and free from possible commercial bias,” said investigator Kim Thomas, MD, professor of applied dermatology research and codirector of the Centre of Evidence Based Dermatology, faculty of medicine & health sciences, University of Nottingham (England).
The main focus of the intervention, along with general education, is “getting control” of the condition with flare-control creams and “keeping control” with regular emollient use.
Efficacy of the intervention, available free online, was compared with “usual eczema care” in 340 parents of children with AD up to age 12 and 337 young patients with AD aged 13-25. Participants were randomized to the intervention plus usual care or usual care alone. The primary outcome was the Patient-Oriented Eczema Measure(POEM) at 24 weeks, with a further measurement at 52 weeks.
In the parent group, about half were women and 83% were White, and the median age of their children was 4 years. About 50% of parents had a university degree, making them “possibly better educated than we might want our target audience for this type of intervention,” Dr. Thomas commented. Most of the children had moderate AD.
In the young patient group, the mean age was 19 years, more than three-quarters were female, 83% were White, and most had moderate AD.
At 24 weeks, both intervention groups had improved POEM scores, compared with controls, with a mean difference of 1.5 points in the parent group (P = .002) and 1.7 points in the young patient group (P = .04). “A small difference, but statistically significant and sustained,” Dr. Thomas said, adding that this difference was sustained up to 52 weeks.
In terms of mechanism of action, a secondary outcome looked at the concept of enablement, “which again, seemed to be improved in the intervention group, which suggests it’s something to do with being able to understand and cope with their disease better,” she said. The tool is targeted to “people who wouldn’t normally get to a dermatologist and certainly wouldn’t get access to group interventions.”
An additional aim of the intervention was “to provide a single, consistent message received from every point of contact that people might engage with ... [from] community doctors, pharmacists, dermatologists, and importantly, eczema charities all signposting [the intervention] and sharing a consistent message.”
While the intervention is free and available to patients anywhere, Dr. Thomas emphasized that it is tailored to the U.K. health care system. “If people would like to get in touch and help work with us to maybe adapt it slightly to make it more suitable for your own health care systems, that’s something we’d be very happy to look at with you.”
Asked for comment, Natalie Cunningham, MD, panel moderator, was lukewarm about the tool. “It can be a supplement, but you can never replace the one-on-one patient–health care provider interaction,” she told this news organization. “That could be provided by a nondermatologist and supplemented by an online component,” said Dr. Cunningham, from the Izaak Walton Killam Hospital for Children in Halifax, N.S.
“First-line treatment for eczema, no matter what kind of eczema, is topical steroids, and that is something that requires a lot of education – and something you want to do one on one in person because everyone comes to it with a different experience, baggage, or understanding,” she said. “We need to figure out what the barrier is so that you can do the right education.”
In addition, with systemic AD therapies currently approved for children, parents and young patients need to be able to advocate for specialist care to access these medications, she noted.
Dr. Thomas and Dr. Cunningham reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ISAD 2022
AHA 2022 to recapture in-person vibe but preserve global reach
That a bustling medical conference can have global reach as it unfolds is one of the COVID pandemic’s many lessons for science. Hybrid meetings such as the American Heart Association scientific sessions, getting underway Nov. 5 in Chicago and cyberspace, are one of its legacies.
The conference is set to recapture the magic of the in-person Scientific Sessions last experienced in Philadelphia in 2019. But planners are mindful of a special responsibility to younger clinicians and scientists who entered the field knowing only the virtual format and who may not know “what it’s like in a room when major science is presented or to present posters and have people come by for conversations,” Manesh R. Patel, MD, chair of the AHA 2022 Scientific Sessions program committee, told this news organization.
Still, the pandemic has underlined the value of live streaming for the great many who can’t attend in person, Dr. Patel said. At AHA 2022, virtual access doesn’t mean only late breaking and featured presentations; more than 70 full sessions will be streamed from Friday through Monday.
Overall, the conference has more than 800 sessions on the schedule, about a third are panels or invited lectures and two-thirds are original reports on the latest research. At the core of the research offerings, 78 studies and analyses are slated across 18 Late-Breaking Science (LBS) and Featured Science (FS) sessions from Saturday through Monday. At least 30 presentations and abstracts will enter the peer-reviewed literature right away with their simultaneous online publication, Dr. Patel said.
More a meet-and-greet than a presentation, the Puppy Snuggles Booth will make a return appearance in Chicago after earning rave reviews at the 2019 Sessions in Philadelphia. All are invited to take a breather from their schedules to pet, cuddle, and play with a passel of pups, all in need of homes and available for adoption. The experience’s favorable effect on blood pressure is almost guaranteed.
LBS and FS highlights
“It’s an amazing year for Late Breaking Science and Featured Science at the Scientific Sessions,” Dr. Patel said of the presentations selected for special attention after a rigorous review process. “We have science that is as broad and as deep as we’ve seen in years.”
Saturday’s two LBS sessions kick off the series with studies looking at agents long available in heart failure and hypertension but lacking solid supporting evidence, “pretty large randomized trials that are, we think, going to affect clinical practice as soon as they are presented,” Dr. Patel said.
They include TRANSFORM-HF, a comparison of the loop diuretics furosemide and torsemide in patients hospitalized with heart failure. And the Diuretic Comparison Project (DCP), with more than 13,000 patients with hypertension assigned to the diuretics chlorthalidone or hydrochlorothiazide, “is going to immediately impact how people think about blood pressure management,” Dr. Patel said.
Other highlights in the hypertension arena include the CRHCP trial, the MB-BP study, the Rich Life Project, and the polypill efficacy and safety trial QUARTET-USA, all in Sunday’s LBS-4; and the FRESH, PRECISION, and BrigHTN trials, all in LBS-9 on Monday.
Other heart failure trials joining TRANSFORM-HF in the line-up include IRONMAN, which revisited IV iron therapy in iron-deficient patients, in LBS-2 on Saturday and, in FS-4 on Monday, BETA3LVH and STRONG-HF, the latter a timely randomized test of pre- and post-discharge biomarker-driven uptitration of guideline-directed heart failure meds.
STRONG-HF was halted early, the trial’s nonprofit sponsor announced only weeks ago, after patients following the intensive uptitration strategy versus usual care showed a reduced risk of death or heart failure readmission; few other details were given.
Several sessions will be devoted to a rare breed of randomized trial, one that tests the efficacy of traditional herbal meds or nonprescription supplements against proven medications. “These are going to get a lot of people’s interest, one can imagine, because they are on common questions that patients bring to the clinic every day,” Dr. Patel said.
Such studies include CTS-AMI, which explored the traditional Chinese herbal medicine tongxinluo in ST-segment elevation myocardial infarction, in LBS-3 on Sunday, and SPORT in Sunday’s LBS-5, a small randomized comparison of low-dose rosuvastatin, cinnamon, garlic, turmeric, an omega-3 fish-oil supplement, a plant sterol, red yeast rice, and placebo for any effects on LDL-C levels.
Other novel approaches to dyslipidemia management are to be covered in RESPECT-EPA and OCEAN(a)-DOSE, both in LBS-5 on Sunday, and all five presentations in Monday’s FS-9, including ARCHES-2, SHASTA-2, FOURIER-OLE, and ORION-3.
The interplay of antiplatelets and coronary interventions will be explored in presentations called OPTION, in LBS-6 on Sunday, and HOST-EXAM and TWILIGHT, in FS-6 on Monday.
Coronary and peripheral-vascular interventions are center stage in reports on RAPCO in LBS-3 and BRIGHT-4 in LBS-6, both on Sunday, and BEST-CLI in LBS-7 and the After-80 Study in FS-6, both on Monday.
Several Monday reports will cover comorbidities and complications associated with COVID-19, including PREVENT-HD in LBS-7, and PANAMO, FERMIN, COVID-NET, and a secondary analysis of the DELIVER trial in FS-5.
Rebroadcasts for the Pacific Rim
The sessions will also feature several evening rebroadcasts of earlier LBS sessions that meeting planners scored highly for scientific merit and potential clinical impact but also for their “regional pull,” primarily for our colleagues in Asia, Dr. Patel said.
The first two LBS sessions presented live during the day in Chicago will be rebroadcast that evening as, for example, Sunday morning and afternoon fare in Tokyo and Singapore. And LBS-5 live Sunday afternoon will rebroadcast that night as a Monday mid-morning session in, say, Hong Kong or Seoul.
This year’s AHA meeting spans the range of cardiovascular care, from precision therapies, such as gene editing or specific drugs, to broad strategies that consider, for example, social determinants of health, Dr. Patel said. “I think people, when they leave the Scientific Sessions, will feel very engaged in the larger conversation about how you impact very common conditions globally.”
A version of this article first appeared on Medscape.com.
That a bustling medical conference can have global reach as it unfolds is one of the COVID pandemic’s many lessons for science. Hybrid meetings such as the American Heart Association scientific sessions, getting underway Nov. 5 in Chicago and cyberspace, are one of its legacies.
The conference is set to recapture the magic of the in-person Scientific Sessions last experienced in Philadelphia in 2019. But planners are mindful of a special responsibility to younger clinicians and scientists who entered the field knowing only the virtual format and who may not know “what it’s like in a room when major science is presented or to present posters and have people come by for conversations,” Manesh R. Patel, MD, chair of the AHA 2022 Scientific Sessions program committee, told this news organization.
Still, the pandemic has underlined the value of live streaming for the great many who can’t attend in person, Dr. Patel said. At AHA 2022, virtual access doesn’t mean only late breaking and featured presentations; more than 70 full sessions will be streamed from Friday through Monday.
Overall, the conference has more than 800 sessions on the schedule, about a third are panels or invited lectures and two-thirds are original reports on the latest research. At the core of the research offerings, 78 studies and analyses are slated across 18 Late-Breaking Science (LBS) and Featured Science (FS) sessions from Saturday through Monday. At least 30 presentations and abstracts will enter the peer-reviewed literature right away with their simultaneous online publication, Dr. Patel said.
More a meet-and-greet than a presentation, the Puppy Snuggles Booth will make a return appearance in Chicago after earning rave reviews at the 2019 Sessions in Philadelphia. All are invited to take a breather from their schedules to pet, cuddle, and play with a passel of pups, all in need of homes and available for adoption. The experience’s favorable effect on blood pressure is almost guaranteed.
LBS and FS highlights
“It’s an amazing year for Late Breaking Science and Featured Science at the Scientific Sessions,” Dr. Patel said of the presentations selected for special attention after a rigorous review process. “We have science that is as broad and as deep as we’ve seen in years.”
Saturday’s two LBS sessions kick off the series with studies looking at agents long available in heart failure and hypertension but lacking solid supporting evidence, “pretty large randomized trials that are, we think, going to affect clinical practice as soon as they are presented,” Dr. Patel said.
They include TRANSFORM-HF, a comparison of the loop diuretics furosemide and torsemide in patients hospitalized with heart failure. And the Diuretic Comparison Project (DCP), with more than 13,000 patients with hypertension assigned to the diuretics chlorthalidone or hydrochlorothiazide, “is going to immediately impact how people think about blood pressure management,” Dr. Patel said.
Other highlights in the hypertension arena include the CRHCP trial, the MB-BP study, the Rich Life Project, and the polypill efficacy and safety trial QUARTET-USA, all in Sunday’s LBS-4; and the FRESH, PRECISION, and BrigHTN trials, all in LBS-9 on Monday.
Other heart failure trials joining TRANSFORM-HF in the line-up include IRONMAN, which revisited IV iron therapy in iron-deficient patients, in LBS-2 on Saturday and, in FS-4 on Monday, BETA3LVH and STRONG-HF, the latter a timely randomized test of pre- and post-discharge biomarker-driven uptitration of guideline-directed heart failure meds.
STRONG-HF was halted early, the trial’s nonprofit sponsor announced only weeks ago, after patients following the intensive uptitration strategy versus usual care showed a reduced risk of death or heart failure readmission; few other details were given.
Several sessions will be devoted to a rare breed of randomized trial, one that tests the efficacy of traditional herbal meds or nonprescription supplements against proven medications. “These are going to get a lot of people’s interest, one can imagine, because they are on common questions that patients bring to the clinic every day,” Dr. Patel said.
Such studies include CTS-AMI, which explored the traditional Chinese herbal medicine tongxinluo in ST-segment elevation myocardial infarction, in LBS-3 on Sunday, and SPORT in Sunday’s LBS-5, a small randomized comparison of low-dose rosuvastatin, cinnamon, garlic, turmeric, an omega-3 fish-oil supplement, a plant sterol, red yeast rice, and placebo for any effects on LDL-C levels.
Other novel approaches to dyslipidemia management are to be covered in RESPECT-EPA and OCEAN(a)-DOSE, both in LBS-5 on Sunday, and all five presentations in Monday’s FS-9, including ARCHES-2, SHASTA-2, FOURIER-OLE, and ORION-3.
The interplay of antiplatelets and coronary interventions will be explored in presentations called OPTION, in LBS-6 on Sunday, and HOST-EXAM and TWILIGHT, in FS-6 on Monday.
Coronary and peripheral-vascular interventions are center stage in reports on RAPCO in LBS-3 and BRIGHT-4 in LBS-6, both on Sunday, and BEST-CLI in LBS-7 and the After-80 Study in FS-6, both on Monday.
Several Monday reports will cover comorbidities and complications associated with COVID-19, including PREVENT-HD in LBS-7, and PANAMO, FERMIN, COVID-NET, and a secondary analysis of the DELIVER trial in FS-5.
Rebroadcasts for the Pacific Rim
The sessions will also feature several evening rebroadcasts of earlier LBS sessions that meeting planners scored highly for scientific merit and potential clinical impact but also for their “regional pull,” primarily for our colleagues in Asia, Dr. Patel said.
The first two LBS sessions presented live during the day in Chicago will be rebroadcast that evening as, for example, Sunday morning and afternoon fare in Tokyo and Singapore. And LBS-5 live Sunday afternoon will rebroadcast that night as a Monday mid-morning session in, say, Hong Kong or Seoul.
This year’s AHA meeting spans the range of cardiovascular care, from precision therapies, such as gene editing or specific drugs, to broad strategies that consider, for example, social determinants of health, Dr. Patel said. “I think people, when they leave the Scientific Sessions, will feel very engaged in the larger conversation about how you impact very common conditions globally.”
A version of this article first appeared on Medscape.com.
That a bustling medical conference can have global reach as it unfolds is one of the COVID pandemic’s many lessons for science. Hybrid meetings such as the American Heart Association scientific sessions, getting underway Nov. 5 in Chicago and cyberspace, are one of its legacies.
The conference is set to recapture the magic of the in-person Scientific Sessions last experienced in Philadelphia in 2019. But planners are mindful of a special responsibility to younger clinicians and scientists who entered the field knowing only the virtual format and who may not know “what it’s like in a room when major science is presented or to present posters and have people come by for conversations,” Manesh R. Patel, MD, chair of the AHA 2022 Scientific Sessions program committee, told this news organization.
Still, the pandemic has underlined the value of live streaming for the great many who can’t attend in person, Dr. Patel said. At AHA 2022, virtual access doesn’t mean only late breaking and featured presentations; more than 70 full sessions will be streamed from Friday through Monday.
Overall, the conference has more than 800 sessions on the schedule, about a third are panels or invited lectures and two-thirds are original reports on the latest research. At the core of the research offerings, 78 studies and analyses are slated across 18 Late-Breaking Science (LBS) and Featured Science (FS) sessions from Saturday through Monday. At least 30 presentations and abstracts will enter the peer-reviewed literature right away with their simultaneous online publication, Dr. Patel said.
More a meet-and-greet than a presentation, the Puppy Snuggles Booth will make a return appearance in Chicago after earning rave reviews at the 2019 Sessions in Philadelphia. All are invited to take a breather from their schedules to pet, cuddle, and play with a passel of pups, all in need of homes and available for adoption. The experience’s favorable effect on blood pressure is almost guaranteed.
LBS and FS highlights
“It’s an amazing year for Late Breaking Science and Featured Science at the Scientific Sessions,” Dr. Patel said of the presentations selected for special attention after a rigorous review process. “We have science that is as broad and as deep as we’ve seen in years.”
Saturday’s two LBS sessions kick off the series with studies looking at agents long available in heart failure and hypertension but lacking solid supporting evidence, “pretty large randomized trials that are, we think, going to affect clinical practice as soon as they are presented,” Dr. Patel said.
They include TRANSFORM-HF, a comparison of the loop diuretics furosemide and torsemide in patients hospitalized with heart failure. And the Diuretic Comparison Project (DCP), with more than 13,000 patients with hypertension assigned to the diuretics chlorthalidone or hydrochlorothiazide, “is going to immediately impact how people think about blood pressure management,” Dr. Patel said.
Other highlights in the hypertension arena include the CRHCP trial, the MB-BP study, the Rich Life Project, and the polypill efficacy and safety trial QUARTET-USA, all in Sunday’s LBS-4; and the FRESH, PRECISION, and BrigHTN trials, all in LBS-9 on Monday.
Other heart failure trials joining TRANSFORM-HF in the line-up include IRONMAN, which revisited IV iron therapy in iron-deficient patients, in LBS-2 on Saturday and, in FS-4 on Monday, BETA3LVH and STRONG-HF, the latter a timely randomized test of pre- and post-discharge biomarker-driven uptitration of guideline-directed heart failure meds.
STRONG-HF was halted early, the trial’s nonprofit sponsor announced only weeks ago, after patients following the intensive uptitration strategy versus usual care showed a reduced risk of death or heart failure readmission; few other details were given.
Several sessions will be devoted to a rare breed of randomized trial, one that tests the efficacy of traditional herbal meds or nonprescription supplements against proven medications. “These are going to get a lot of people’s interest, one can imagine, because they are on common questions that patients bring to the clinic every day,” Dr. Patel said.
Such studies include CTS-AMI, which explored the traditional Chinese herbal medicine tongxinluo in ST-segment elevation myocardial infarction, in LBS-3 on Sunday, and SPORT in Sunday’s LBS-5, a small randomized comparison of low-dose rosuvastatin, cinnamon, garlic, turmeric, an omega-3 fish-oil supplement, a plant sterol, red yeast rice, and placebo for any effects on LDL-C levels.
Other novel approaches to dyslipidemia management are to be covered in RESPECT-EPA and OCEAN(a)-DOSE, both in LBS-5 on Sunday, and all five presentations in Monday’s FS-9, including ARCHES-2, SHASTA-2, FOURIER-OLE, and ORION-3.
The interplay of antiplatelets and coronary interventions will be explored in presentations called OPTION, in LBS-6 on Sunday, and HOST-EXAM and TWILIGHT, in FS-6 on Monday.
Coronary and peripheral-vascular interventions are center stage in reports on RAPCO in LBS-3 and BRIGHT-4 in LBS-6, both on Sunday, and BEST-CLI in LBS-7 and the After-80 Study in FS-6, both on Monday.
Several Monday reports will cover comorbidities and complications associated with COVID-19, including PREVENT-HD in LBS-7, and PANAMO, FERMIN, COVID-NET, and a secondary analysis of the DELIVER trial in FS-5.
Rebroadcasts for the Pacific Rim
The sessions will also feature several evening rebroadcasts of earlier LBS sessions that meeting planners scored highly for scientific merit and potential clinical impact but also for their “regional pull,” primarily for our colleagues in Asia, Dr. Patel said.
The first two LBS sessions presented live during the day in Chicago will be rebroadcast that evening as, for example, Sunday morning and afternoon fare in Tokyo and Singapore. And LBS-5 live Sunday afternoon will rebroadcast that night as a Monday mid-morning session in, say, Hong Kong or Seoul.
This year’s AHA meeting spans the range of cardiovascular care, from precision therapies, such as gene editing or specific drugs, to broad strategies that consider, for example, social determinants of health, Dr. Patel said. “I think people, when they leave the Scientific Sessions, will feel very engaged in the larger conversation about how you impact very common conditions globally.”
A version of this article first appeared on Medscape.com.
Children and COVID: Weekly cases can’t sustain downward trend
New COVID-19 cases in children inched up in late October, just 1 week after dipping to their lowest level in more than a year, and some measures of pediatric emergency visits and hospital admissions rose as well.
There was an 8% increase in the number of cases for the week of Oct. 21-27, compared with the previous week, but this week’s total was still below 25,000, and the overall trend since the beginning of September is still one of decline, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.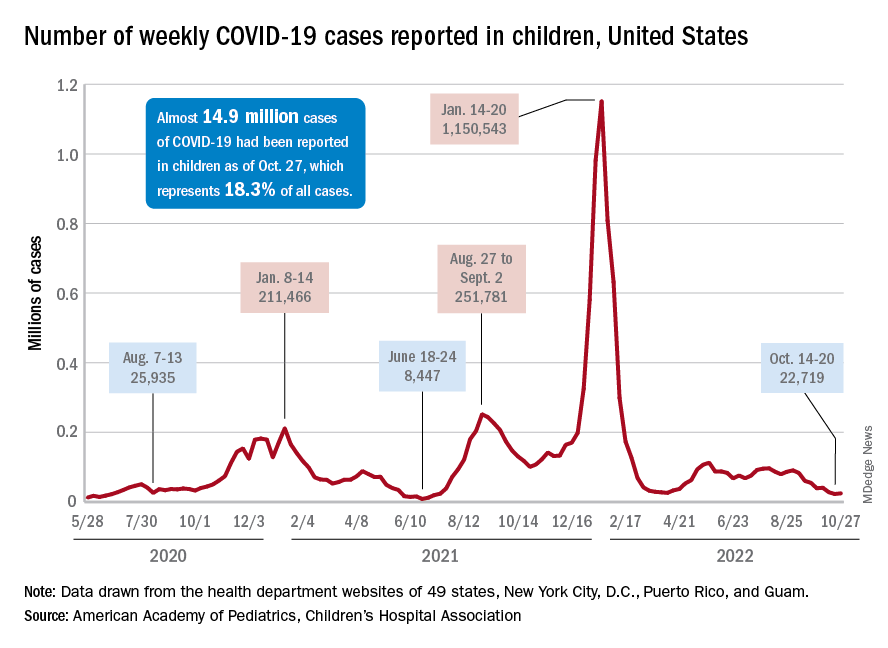
A similar increase can be seen for hospitalizations with confirmed COVID. The rate for children aged 0-17 years fell from 0.44 admissions per 100,000 population at the end of August to 0.16 per 100,000 on Oct. 23. Hospitalizations have since ticked up to 0.17 per 100,000, according to the Centers for Disease Control and Prevention.
Emergency department visits with diagnosed COVID among children aged 16-17 years, as a percentage of all ED visits, rose from 0.6% on Oct. 21 to 0.8% on Oct. 26. ED visits for 12- to 15-year-olds rose from 0.6% to 0.7% at about the same time, with both increases coming after declines that started in late August. No such increase has occurred yet among children aged 0-11 years, the CDC reported on its COVID Data Tracker.
One small milestone reached in the past week involved the proportion of all COVID cases that have occurred in children. The total number of child cases as of Oct. 27 was almost 14.9 million, which represents 18.3% of cases in all Americans, according to the AAP and CHA. That figure had been sitting at 18.4% since mid-August after reaching as high as 19.0% during the spring.
The CDC puts total COVID-related hospital admissions for children aged 0-17 at 163,588 since Aug. 1, 2020, which is 3.0% of all U.S. admissions. Total pediatric deaths number 1,843, or just about 0.2% of all COVID-related fatalities since the start of the pandemic, the CDC data show.
The latest vaccination figures show that 71.3% of children aged 12-17 years have received at least one dose, as have 38.8% of 5- to 11-year-olds, 8.4% of 2- to 4-year-olds, and 5.5% of those under age 2. Full vaccination by age group looks like this: 60.9% (12-17 years), 31.7% (5-11 years), 3.7% (2-4 years), and 2.1% (<2 years), the CDC reported. Almost 30% of children aged 12-17 have gotten a first booster dose, as have 16% of 5- to 11-year-olds.
New COVID-19 cases in children inched up in late October, just 1 week after dipping to their lowest level in more than a year, and some measures of pediatric emergency visits and hospital admissions rose as well.
There was an 8% increase in the number of cases for the week of Oct. 21-27, compared with the previous week, but this week’s total was still below 25,000, and the overall trend since the beginning of September is still one of decline, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.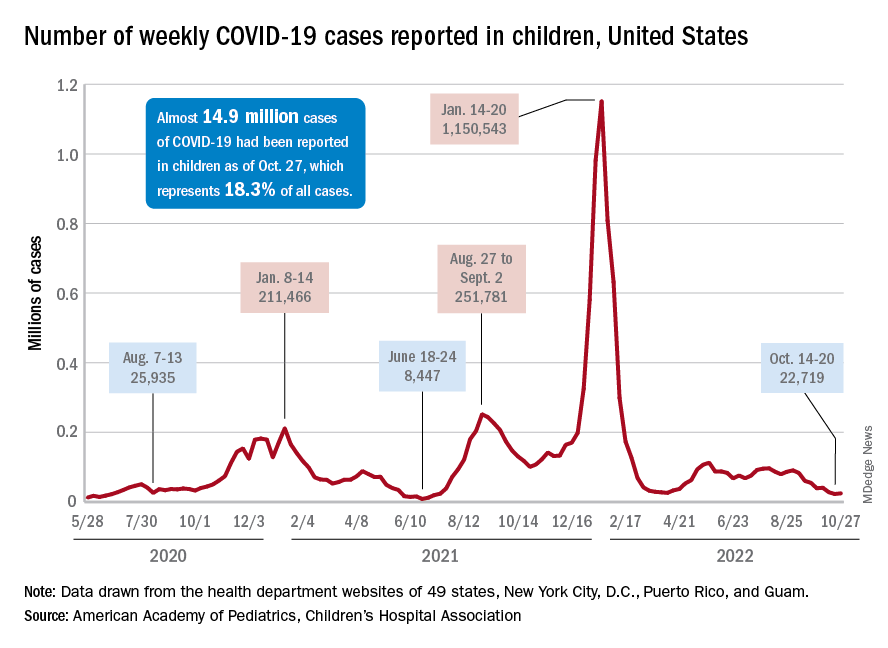
A similar increase can be seen for hospitalizations with confirmed COVID. The rate for children aged 0-17 years fell from 0.44 admissions per 100,000 population at the end of August to 0.16 per 100,000 on Oct. 23. Hospitalizations have since ticked up to 0.17 per 100,000, according to the Centers for Disease Control and Prevention.
Emergency department visits with diagnosed COVID among children aged 16-17 years, as a percentage of all ED visits, rose from 0.6% on Oct. 21 to 0.8% on Oct. 26. ED visits for 12- to 15-year-olds rose from 0.6% to 0.7% at about the same time, with both increases coming after declines that started in late August. No such increase has occurred yet among children aged 0-11 years, the CDC reported on its COVID Data Tracker.
One small milestone reached in the past week involved the proportion of all COVID cases that have occurred in children. The total number of child cases as of Oct. 27 was almost 14.9 million, which represents 18.3% of cases in all Americans, according to the AAP and CHA. That figure had been sitting at 18.4% since mid-August after reaching as high as 19.0% during the spring.
The CDC puts total COVID-related hospital admissions for children aged 0-17 at 163,588 since Aug. 1, 2020, which is 3.0% of all U.S. admissions. Total pediatric deaths number 1,843, or just about 0.2% of all COVID-related fatalities since the start of the pandemic, the CDC data show.
The latest vaccination figures show that 71.3% of children aged 12-17 years have received at least one dose, as have 38.8% of 5- to 11-year-olds, 8.4% of 2- to 4-year-olds, and 5.5% of those under age 2. Full vaccination by age group looks like this: 60.9% (12-17 years), 31.7% (5-11 years), 3.7% (2-4 years), and 2.1% (<2 years), the CDC reported. Almost 30% of children aged 12-17 have gotten a first booster dose, as have 16% of 5- to 11-year-olds.
New COVID-19 cases in children inched up in late October, just 1 week after dipping to their lowest level in more than a year, and some measures of pediatric emergency visits and hospital admissions rose as well.
There was an 8% increase in the number of cases for the week of Oct. 21-27, compared with the previous week, but this week’s total was still below 25,000, and the overall trend since the beginning of September is still one of decline, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.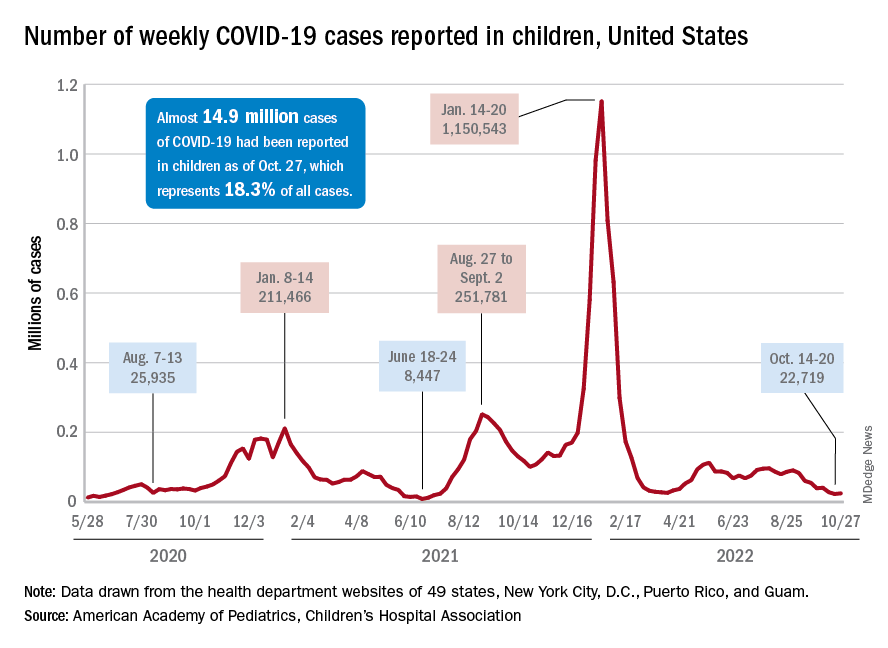
A similar increase can be seen for hospitalizations with confirmed COVID. The rate for children aged 0-17 years fell from 0.44 admissions per 100,000 population at the end of August to 0.16 per 100,000 on Oct. 23. Hospitalizations have since ticked up to 0.17 per 100,000, according to the Centers for Disease Control and Prevention.
Emergency department visits with diagnosed COVID among children aged 16-17 years, as a percentage of all ED visits, rose from 0.6% on Oct. 21 to 0.8% on Oct. 26. ED visits for 12- to 15-year-olds rose from 0.6% to 0.7% at about the same time, with both increases coming after declines that started in late August. No such increase has occurred yet among children aged 0-11 years, the CDC reported on its COVID Data Tracker.
One small milestone reached in the past week involved the proportion of all COVID cases that have occurred in children. The total number of child cases as of Oct. 27 was almost 14.9 million, which represents 18.3% of cases in all Americans, according to the AAP and CHA. That figure had been sitting at 18.4% since mid-August after reaching as high as 19.0% during the spring.
The CDC puts total COVID-related hospital admissions for children aged 0-17 at 163,588 since Aug. 1, 2020, which is 3.0% of all U.S. admissions. Total pediatric deaths number 1,843, or just about 0.2% of all COVID-related fatalities since the start of the pandemic, the CDC data show.
The latest vaccination figures show that 71.3% of children aged 12-17 years have received at least one dose, as have 38.8% of 5- to 11-year-olds, 8.4% of 2- to 4-year-olds, and 5.5% of those under age 2. Full vaccination by age group looks like this: 60.9% (12-17 years), 31.7% (5-11 years), 3.7% (2-4 years), and 2.1% (<2 years), the CDC reported. Almost 30% of children aged 12-17 have gotten a first booster dose, as have 16% of 5- to 11-year-olds.
Oral FMT on par with colonic FMT for recurrent C. difficile
A real-world analysis confirms that fecal microbiota transplantation (FMT) is highly effective for recurrent Clostridioides difficile infection (rCDI) – and there is no difference between delivery by capsule (cap-FMT) and colonoscopy (colo-FMT).
“We present one of the largest cohorts involving people who received capsule FMT. Byron Vaughn, MD, with the division of gastroenterology, hepatology, and nutrition, University of Minnesota, Minneapolis, said in an interview.
The study was published online in Clinical Gastroenterology and Hepatology.
The Food and Drug Administration allows FMT to be used for patients who have failed standard treatment for rCDI under a policy of enforcement discretion.
The past decade has seen an increase in the use of FMT in clinical practice, owing to an increase in cases of rCDI after failure of standard antibiotic therapy.
Unlike antibiotics, which perpetuate and worsen intestinal dysbiosis, FMT restores the diversity and function of host microbiota, effectively breaking the cycle of rCDI, the authors of the study noted. But it’s been unclear whether the efficacy and safety of FMT vary by route of administration.
Effective without procedural risks
To investigate, Dr. Vaughn and colleagues evaluated clinical outcomes and adverse events in 170 patients with rCDI who underwent cap-FMT and 96 peers who underwent colo-FMT.
FMT was performed using one of two standardized formulations of microbiota manufactured by the University of Minnesota microbiota therapeutics program: freeze-dried/encapsulated or frozen-thawed/liquid.
Overall, the cure rates of CDI were 86% at 1 month and 81% at 2 months. There was no statistically significant difference at either time between cap-FMT and colo-FMT.
The 1-month cure rate was 84% with cap-FMT and 91% with colo-FMT; at 2 months, the cure rates were 81% and 83%, respectively.
Cap-FMT has a safety and effectiveness profile similar to that of colo-FMT, without the procedural risks of colonoscopy, the researchers concluded.
They cautioned that, although FMT is highly effective overall, patient selection is a key factor to optimizing FMT success.
Older age and hemodialysis were associated with FMT failure by 2 months on multivariate logistic regression.
“These risk factors can help determine if a patient should receive FMT or an alternative therapy for rCDI. This is not to say FMT should be avoided in older patients or those on dialysis, but clinicians should be aware of these associations in light of other options for rCDI,” Dr. Vaughn said.
Confirming prior studies, antibiotic use after FMT was a major factor in its failure. Patient selection for FMT should include an assessment of the potential need for antibiotics after transplant, the researchers noted.
One serious adverse event (aspiration pneumonia) was related to colonoscopy; otherwise, no new safety signals were identified.
As reported in other studies, changes in bowel function, including diarrhea, constipation, gas, and bloating were common, although it’s tough to disentangle gastrointestinal symptoms related to FMT from those after CDI, the researchers said. Importantly, no transmission of an infectious agent related to FMT was identified.
Two good options
The researchers said their findings are “highly generalizable” because the population reflects all FMT use by participating institutions and contains a mix of academic centers and private practices.
Many patients included in the study would not have been eligible for a clinical trial, owing to their having many comorbid conditions, including immune compromise and inflammatory bowel disease, the authors noted.
“FMT is recommended by major gastroenterology and infectious disease society guidelines,” Dr. Vaughn said. “Our group, and others, have consistently found strategies that incorporate FMT as cost-effective strategies for treating rCDI.”
However, lack of access to FMT products often is a barrier to treatment, he said.
“A stool banking model, similar to the nonprofit blood banking model, may be a useful solution to ensure equitable access to FMT to all who need it,” Dr. Vaughn added.
Reached for comment, Majdi Osman, MD, MPH, told this news organization that the study is valuable, “as it nicely shows in a real-world setting that capsules and colonoscopy are good options for patients who need this.”
Dr. Osman is chief medical officer of OpenBiome, a nonprofit organization that operates a public stool bank and is the major FMT source in the United States. The organization has provided over 63,000 FMT treatments to over 1,200 hospitals in the United States.
“FMT has become standard of care for patients who failed antibiotic therapy, and certainly is being used widely as a treatment option for these patients who have often run out of existing options,” Dr. Osman said.
Support for the study was provided by a donation from Achieving Cures Together, a nonprofit organization dedicated to advancing microbiome-based research. Dr. Vaughn receives grant support from Takeda, Roche, Celgene, and Diasorin and has received consulting fees from Prometheus and AbbVie. Dr. Osman reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A real-world analysis confirms that fecal microbiota transplantation (FMT) is highly effective for recurrent Clostridioides difficile infection (rCDI) – and there is no difference between delivery by capsule (cap-FMT) and colonoscopy (colo-FMT).
“We present one of the largest cohorts involving people who received capsule FMT. Byron Vaughn, MD, with the division of gastroenterology, hepatology, and nutrition, University of Minnesota, Minneapolis, said in an interview.
The study was published online in Clinical Gastroenterology and Hepatology.
The Food and Drug Administration allows FMT to be used for patients who have failed standard treatment for rCDI under a policy of enforcement discretion.
The past decade has seen an increase in the use of FMT in clinical practice, owing to an increase in cases of rCDI after failure of standard antibiotic therapy.
Unlike antibiotics, which perpetuate and worsen intestinal dysbiosis, FMT restores the diversity and function of host microbiota, effectively breaking the cycle of rCDI, the authors of the study noted. But it’s been unclear whether the efficacy and safety of FMT vary by route of administration.
Effective without procedural risks
To investigate, Dr. Vaughn and colleagues evaluated clinical outcomes and adverse events in 170 patients with rCDI who underwent cap-FMT and 96 peers who underwent colo-FMT.
FMT was performed using one of two standardized formulations of microbiota manufactured by the University of Minnesota microbiota therapeutics program: freeze-dried/encapsulated or frozen-thawed/liquid.
Overall, the cure rates of CDI were 86% at 1 month and 81% at 2 months. There was no statistically significant difference at either time between cap-FMT and colo-FMT.
The 1-month cure rate was 84% with cap-FMT and 91% with colo-FMT; at 2 months, the cure rates were 81% and 83%, respectively.
Cap-FMT has a safety and effectiveness profile similar to that of colo-FMT, without the procedural risks of colonoscopy, the researchers concluded.
They cautioned that, although FMT is highly effective overall, patient selection is a key factor to optimizing FMT success.
Older age and hemodialysis were associated with FMT failure by 2 months on multivariate logistic regression.
“These risk factors can help determine if a patient should receive FMT or an alternative therapy for rCDI. This is not to say FMT should be avoided in older patients or those on dialysis, but clinicians should be aware of these associations in light of other options for rCDI,” Dr. Vaughn said.
Confirming prior studies, antibiotic use after FMT was a major factor in its failure. Patient selection for FMT should include an assessment of the potential need for antibiotics after transplant, the researchers noted.
One serious adverse event (aspiration pneumonia) was related to colonoscopy; otherwise, no new safety signals were identified.
As reported in other studies, changes in bowel function, including diarrhea, constipation, gas, and bloating were common, although it’s tough to disentangle gastrointestinal symptoms related to FMT from those after CDI, the researchers said. Importantly, no transmission of an infectious agent related to FMT was identified.
Two good options
The researchers said their findings are “highly generalizable” because the population reflects all FMT use by participating institutions and contains a mix of academic centers and private practices.
Many patients included in the study would not have been eligible for a clinical trial, owing to their having many comorbid conditions, including immune compromise and inflammatory bowel disease, the authors noted.
“FMT is recommended by major gastroenterology and infectious disease society guidelines,” Dr. Vaughn said. “Our group, and others, have consistently found strategies that incorporate FMT as cost-effective strategies for treating rCDI.”
However, lack of access to FMT products often is a barrier to treatment, he said.
“A stool banking model, similar to the nonprofit blood banking model, may be a useful solution to ensure equitable access to FMT to all who need it,” Dr. Vaughn added.
Reached for comment, Majdi Osman, MD, MPH, told this news organization that the study is valuable, “as it nicely shows in a real-world setting that capsules and colonoscopy are good options for patients who need this.”
Dr. Osman is chief medical officer of OpenBiome, a nonprofit organization that operates a public stool bank and is the major FMT source in the United States. The organization has provided over 63,000 FMT treatments to over 1,200 hospitals in the United States.
“FMT has become standard of care for patients who failed antibiotic therapy, and certainly is being used widely as a treatment option for these patients who have often run out of existing options,” Dr. Osman said.
Support for the study was provided by a donation from Achieving Cures Together, a nonprofit organization dedicated to advancing microbiome-based research. Dr. Vaughn receives grant support from Takeda, Roche, Celgene, and Diasorin and has received consulting fees from Prometheus and AbbVie. Dr. Osman reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A real-world analysis confirms that fecal microbiota transplantation (FMT) is highly effective for recurrent Clostridioides difficile infection (rCDI) – and there is no difference between delivery by capsule (cap-FMT) and colonoscopy (colo-FMT).
“We present one of the largest cohorts involving people who received capsule FMT. Byron Vaughn, MD, with the division of gastroenterology, hepatology, and nutrition, University of Minnesota, Minneapolis, said in an interview.
The study was published online in Clinical Gastroenterology and Hepatology.
The Food and Drug Administration allows FMT to be used for patients who have failed standard treatment for rCDI under a policy of enforcement discretion.
The past decade has seen an increase in the use of FMT in clinical practice, owing to an increase in cases of rCDI after failure of standard antibiotic therapy.
Unlike antibiotics, which perpetuate and worsen intestinal dysbiosis, FMT restores the diversity and function of host microbiota, effectively breaking the cycle of rCDI, the authors of the study noted. But it’s been unclear whether the efficacy and safety of FMT vary by route of administration.
Effective without procedural risks
To investigate, Dr. Vaughn and colleagues evaluated clinical outcomes and adverse events in 170 patients with rCDI who underwent cap-FMT and 96 peers who underwent colo-FMT.
FMT was performed using one of two standardized formulations of microbiota manufactured by the University of Minnesota microbiota therapeutics program: freeze-dried/encapsulated or frozen-thawed/liquid.
Overall, the cure rates of CDI were 86% at 1 month and 81% at 2 months. There was no statistically significant difference at either time between cap-FMT and colo-FMT.
The 1-month cure rate was 84% with cap-FMT and 91% with colo-FMT; at 2 months, the cure rates were 81% and 83%, respectively.
Cap-FMT has a safety and effectiveness profile similar to that of colo-FMT, without the procedural risks of colonoscopy, the researchers concluded.
They cautioned that, although FMT is highly effective overall, patient selection is a key factor to optimizing FMT success.
Older age and hemodialysis were associated with FMT failure by 2 months on multivariate logistic regression.
“These risk factors can help determine if a patient should receive FMT or an alternative therapy for rCDI. This is not to say FMT should be avoided in older patients or those on dialysis, but clinicians should be aware of these associations in light of other options for rCDI,” Dr. Vaughn said.
Confirming prior studies, antibiotic use after FMT was a major factor in its failure. Patient selection for FMT should include an assessment of the potential need for antibiotics after transplant, the researchers noted.
One serious adverse event (aspiration pneumonia) was related to colonoscopy; otherwise, no new safety signals were identified.
As reported in other studies, changes in bowel function, including diarrhea, constipation, gas, and bloating were common, although it’s tough to disentangle gastrointestinal symptoms related to FMT from those after CDI, the researchers said. Importantly, no transmission of an infectious agent related to FMT was identified.
Two good options
The researchers said their findings are “highly generalizable” because the population reflects all FMT use by participating institutions and contains a mix of academic centers and private practices.
Many patients included in the study would not have been eligible for a clinical trial, owing to their having many comorbid conditions, including immune compromise and inflammatory bowel disease, the authors noted.
“FMT is recommended by major gastroenterology and infectious disease society guidelines,” Dr. Vaughn said. “Our group, and others, have consistently found strategies that incorporate FMT as cost-effective strategies for treating rCDI.”
However, lack of access to FMT products often is a barrier to treatment, he said.
“A stool banking model, similar to the nonprofit blood banking model, may be a useful solution to ensure equitable access to FMT to all who need it,” Dr. Vaughn added.
Reached for comment, Majdi Osman, MD, MPH, told this news organization that the study is valuable, “as it nicely shows in a real-world setting that capsules and colonoscopy are good options for patients who need this.”
Dr. Osman is chief medical officer of OpenBiome, a nonprofit organization that operates a public stool bank and is the major FMT source in the United States. The organization has provided over 63,000 FMT treatments to over 1,200 hospitals in the United States.
“FMT has become standard of care for patients who failed antibiotic therapy, and certainly is being used widely as a treatment option for these patients who have often run out of existing options,” Dr. Osman said.
Support for the study was provided by a donation from Achieving Cures Together, a nonprofit organization dedicated to advancing microbiome-based research. Dr. Vaughn receives grant support from Takeda, Roche, Celgene, and Diasorin and has received consulting fees from Prometheus and AbbVie. Dr. Osman reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Multiple menopause symptoms linked to increased cardiovascular risk
Up to 10 different menopausal symptoms were linked to an increased risk of cardiovascular disease when they were moderate to severe in women who initially had no evidence of cardiovascular disease, according to research presented at the North American Menopause Society annual meeting in Atlanta.
“The take-home message is that severe menopausal symptoms may increase the risk of cardiovascular disease,” Matthew Nudy, MD, an assistant professor of medicine at the Heart and Vascular Institute at Penn State University, Hershey, said in an interview about his findings. “Physicians and patients should be aware of this association. Women with severe symptoms may be more likely to see their physician, and this would be an ideal time to have their cardiovascular risk assessed.”
Margaret Nachtigall, MD, a clinical associate professor of obstetrics and gynecology at New York University and at NYU Langone Health, noted that these findings lined up with other studies showing an increased risk of cardiovascular disease in patients who have more symptoms, especially hot flashes.
“Other recent studies showed that an increase in severity of hot flush is associated with worse blood vessel function, leading to heart disease,” Dr. Nachtigall, who was not involved with the study, said in an interview. “The next step that makes sense is to try to eliminate these symptoms and hope that, in turn, would lower cardiovascular disease and improve survival.”
The researchers compared menopausal symptoms with cardiovascular outcomes and all-cause mortality in an observational cohort of 80,278 postmenopausal women for a median 8.2 years of follow-up. None of the women, all enrolled in the Women’s Health Initiative, had known cardiovascular disease at baseline. They had an average age of 63 years and average body mass index (BMI) of 25.9 at baseline. Most participants were White (86.7%), with 7% being Black and 4.1% Hispanic. Cardiovascular disease was a composite outcome that included hospitalized myocardial infarction, definite silent myocardial infarction, coronary death, stroke, congestive heart failure, angina, peripheral vascular disease, carotid artery disease, and coronary revascularization.
The researchers used a four-item Likert scale (0-3) to assess the severity of 15 symptoms experienced within the past 4 weeks at baseline: “night sweats, hot flashes, waking up several times at night, joint pain or stiffness, headaches or migraines, vaginal or genital dryness, heart racing or skipping beats, breast tenderness, dizziness, tremors (shakes), feeling tired, forgetfulness, mood swings, [feeling] restless or fidgety, and difficulty concentrating.”
The associations were adjusted for the following covariates: race/ethnicity, blood pressure, education, smoking status, bilateral oophorectomy, menopausal hormone therapy use (never/past/current), sleep duration, statin use, history of high cholesterol, aspirin use, use of antihypertensives, treated diabetes, and family history of heart attack. Continuous variables included age, age at menopause, BMI, blood pressure, and physical activity levels. Because of the high number of multiple comparisons, the researchers also used a Bonferroni correction to reduce the risk of spurious statistical significance.
The researchers found some clustering of symptoms. Among women who had at least two moderate or severe menopausal symptoms, more than half frequently woke up at night, had joint pain, or felt tired, the researchers reported. Those symptoms were also the most commonly reported ones overall. Younger women, between ages 50 and 59, were more likely than older women (60-79 years old) to experience vasomotor symptoms and all cognitive affective symptoms except forgetfulness.
The researchers identified 10 symptoms whose severity was significantly associated with cardiovascular disease. Compared to having no symptoms at all, the following moderate or severe symptoms were associated with an increased risk of a cardiovascular event after adjustment for covariates and corrected for multiple comparisons: night sweats – a 19% increased risk (P = .03), waking up several times at night – 11% increased risk (P = .05), joint pain or stiffness – 27% increased risk (P < .001), heart racing or skipping beats – 55% increased risk (P < .001), dizziness – 34% increased risk (P < .001), feeling tired – 35% increased risk (P < .001), forgetfulness – 25% increased risk (P < .001), mood swings – 21% increased risk (P = .02), feeling restless or fidgety – 29% increased risk (P < .001), and difficulty concentrating – 31% increased risk (P < .001)
In addition, all-cause mortality was associated with these symptoms when they were moderate or severe: heart racing or skipping beats (32% increased risk of all-cause mortality; hazard ratio, 1.32; P =.006), dizziness (HR, 1.58; P < .001), tremors (HR, 1.44; P < .001), feeling tired (HR, 1.26; P < .001), forgetfulness (HR, 1.29; P = .01), mood swings (HR, 1.35; P = .02), feeling restless or fidgety (HR, 1.35; P < .001), and difficulty concentrating (HR, 1.47; P < .001).
The symptom with the greatest association with all-cause mortality was dizziness, which was associated with an increased risk of 58% when rated moderate or severe. Any dizziness at all was linked to a 12% increased risk of cardiovascular disease, compared with no dizziness. Machine learning with the LASSO method determined that the symptoms most predictive of cardiovascular disease were dizziness, heart racing, feeling tired, and joint pain. The symptoms most associated with all-cause mortality, based on the machine learning algorithm, were dizziness, tremors, and feeling tired.
Dr. Nudy said that their study did not look at mitigation strategies. “Women should discuss with their physician the best methods for cardiovascular risk reduction,” he said. He also cautioned that severe menopausal symptoms can also indicate other health conditions that may require investigation.
“It is certainly possible some symptoms may represent other medical conditions we were unable to control for and may not be directly related to menopause,” such as autoimmune diseases, endocrine abnormalities, or subclinical cardiovascular disease, he said. Additional limitations of the study included an older cohort and retrospective assessment of menopausal symptoms only at baseline. In addition, ”we did not assess the cardiovascular risk among women whose symptoms persisted versus resolved during the study period,” Dr. Nudy said.
Dr. Nachtigall said a key message is that people who are experiencing these symptoms should try to get treatment for them and attempt to alleviate them, hopefully reducing the risk of heart disease and death.
”Estrogen treatment is one excellent option for some individuals and should be considered in the appropriate person,” Dr. Nachtigall said. “If estrogen treatment is to be considered, it should be given closer to menopause, within the first 10 years after menopause and in younger individuals (under 59) at start.”
Dr. Nachtigall referred to the NAMS 2022 position statement concluding that, for healthy women within 10 years of menopause who have bothersome menopause symptoms, “the benefits of hormone therapy outweigh its risks, with fewer cardiovascular events in younger versus older women.”
”Menopause and having menopausal symptoms is an opportunity for clinicians and patients to have a conversation about appropriate individualized management options,” Dr. Nachtigall said.
Women may also be able to mitigate their cardiovascular risk with regular exercise, eating a healthy diet, not smoking, and getting adequate sleep, Dr. Nachtigall said. But these healthy behaviors may not adequately treat moderate or severe menopausal symptoms.
“Some health care providers have said that because menopause happens naturally, individuals should just accept the symptoms and try to wait it out and not get treatment, but this study, as well as others, makes it clear that it actually may be beneficial to treat the symptoms,” Dr. Nachtigall said.
The research used no external funding. Dr. Nudy and Dr. Nachtigall had no disclosures.
Up to 10 different menopausal symptoms were linked to an increased risk of cardiovascular disease when they were moderate to severe in women who initially had no evidence of cardiovascular disease, according to research presented at the North American Menopause Society annual meeting in Atlanta.
“The take-home message is that severe menopausal symptoms may increase the risk of cardiovascular disease,” Matthew Nudy, MD, an assistant professor of medicine at the Heart and Vascular Institute at Penn State University, Hershey, said in an interview about his findings. “Physicians and patients should be aware of this association. Women with severe symptoms may be more likely to see their physician, and this would be an ideal time to have their cardiovascular risk assessed.”
Margaret Nachtigall, MD, a clinical associate professor of obstetrics and gynecology at New York University and at NYU Langone Health, noted that these findings lined up with other studies showing an increased risk of cardiovascular disease in patients who have more symptoms, especially hot flashes.
“Other recent studies showed that an increase in severity of hot flush is associated with worse blood vessel function, leading to heart disease,” Dr. Nachtigall, who was not involved with the study, said in an interview. “The next step that makes sense is to try to eliminate these symptoms and hope that, in turn, would lower cardiovascular disease and improve survival.”
The researchers compared menopausal symptoms with cardiovascular outcomes and all-cause mortality in an observational cohort of 80,278 postmenopausal women for a median 8.2 years of follow-up. None of the women, all enrolled in the Women’s Health Initiative, had known cardiovascular disease at baseline. They had an average age of 63 years and average body mass index (BMI) of 25.9 at baseline. Most participants were White (86.7%), with 7% being Black and 4.1% Hispanic. Cardiovascular disease was a composite outcome that included hospitalized myocardial infarction, definite silent myocardial infarction, coronary death, stroke, congestive heart failure, angina, peripheral vascular disease, carotid artery disease, and coronary revascularization.
The researchers used a four-item Likert scale (0-3) to assess the severity of 15 symptoms experienced within the past 4 weeks at baseline: “night sweats, hot flashes, waking up several times at night, joint pain or stiffness, headaches or migraines, vaginal or genital dryness, heart racing or skipping beats, breast tenderness, dizziness, tremors (shakes), feeling tired, forgetfulness, mood swings, [feeling] restless or fidgety, and difficulty concentrating.”
The associations were adjusted for the following covariates: race/ethnicity, blood pressure, education, smoking status, bilateral oophorectomy, menopausal hormone therapy use (never/past/current), sleep duration, statin use, history of high cholesterol, aspirin use, use of antihypertensives, treated diabetes, and family history of heart attack. Continuous variables included age, age at menopause, BMI, blood pressure, and physical activity levels. Because of the high number of multiple comparisons, the researchers also used a Bonferroni correction to reduce the risk of spurious statistical significance.
The researchers found some clustering of symptoms. Among women who had at least two moderate or severe menopausal symptoms, more than half frequently woke up at night, had joint pain, or felt tired, the researchers reported. Those symptoms were also the most commonly reported ones overall. Younger women, between ages 50 and 59, were more likely than older women (60-79 years old) to experience vasomotor symptoms and all cognitive affective symptoms except forgetfulness.
The researchers identified 10 symptoms whose severity was significantly associated with cardiovascular disease. Compared to having no symptoms at all, the following moderate or severe symptoms were associated with an increased risk of a cardiovascular event after adjustment for covariates and corrected for multiple comparisons: night sweats – a 19% increased risk (P = .03), waking up several times at night – 11% increased risk (P = .05), joint pain or stiffness – 27% increased risk (P < .001), heart racing or skipping beats – 55% increased risk (P < .001), dizziness – 34% increased risk (P < .001), feeling tired – 35% increased risk (P < .001), forgetfulness – 25% increased risk (P < .001), mood swings – 21% increased risk (P = .02), feeling restless or fidgety – 29% increased risk (P < .001), and difficulty concentrating – 31% increased risk (P < .001)
In addition, all-cause mortality was associated with these symptoms when they were moderate or severe: heart racing or skipping beats (32% increased risk of all-cause mortality; hazard ratio, 1.32; P =.006), dizziness (HR, 1.58; P < .001), tremors (HR, 1.44; P < .001), feeling tired (HR, 1.26; P < .001), forgetfulness (HR, 1.29; P = .01), mood swings (HR, 1.35; P = .02), feeling restless or fidgety (HR, 1.35; P < .001), and difficulty concentrating (HR, 1.47; P < .001).
The symptom with the greatest association with all-cause mortality was dizziness, which was associated with an increased risk of 58% when rated moderate or severe. Any dizziness at all was linked to a 12% increased risk of cardiovascular disease, compared with no dizziness. Machine learning with the LASSO method determined that the symptoms most predictive of cardiovascular disease were dizziness, heart racing, feeling tired, and joint pain. The symptoms most associated with all-cause mortality, based on the machine learning algorithm, were dizziness, tremors, and feeling tired.
Dr. Nudy said that their study did not look at mitigation strategies. “Women should discuss with their physician the best methods for cardiovascular risk reduction,” he said. He also cautioned that severe menopausal symptoms can also indicate other health conditions that may require investigation.
“It is certainly possible some symptoms may represent other medical conditions we were unable to control for and may not be directly related to menopause,” such as autoimmune diseases, endocrine abnormalities, or subclinical cardiovascular disease, he said. Additional limitations of the study included an older cohort and retrospective assessment of menopausal symptoms only at baseline. In addition, ”we did not assess the cardiovascular risk among women whose symptoms persisted versus resolved during the study period,” Dr. Nudy said.
Dr. Nachtigall said a key message is that people who are experiencing these symptoms should try to get treatment for them and attempt to alleviate them, hopefully reducing the risk of heart disease and death.
”Estrogen treatment is one excellent option for some individuals and should be considered in the appropriate person,” Dr. Nachtigall said. “If estrogen treatment is to be considered, it should be given closer to menopause, within the first 10 years after menopause and in younger individuals (under 59) at start.”
Dr. Nachtigall referred to the NAMS 2022 position statement concluding that, for healthy women within 10 years of menopause who have bothersome menopause symptoms, “the benefits of hormone therapy outweigh its risks, with fewer cardiovascular events in younger versus older women.”
”Menopause and having menopausal symptoms is an opportunity for clinicians and patients to have a conversation about appropriate individualized management options,” Dr. Nachtigall said.
Women may also be able to mitigate their cardiovascular risk with regular exercise, eating a healthy diet, not smoking, and getting adequate sleep, Dr. Nachtigall said. But these healthy behaviors may not adequately treat moderate or severe menopausal symptoms.
“Some health care providers have said that because menopause happens naturally, individuals should just accept the symptoms and try to wait it out and not get treatment, but this study, as well as others, makes it clear that it actually may be beneficial to treat the symptoms,” Dr. Nachtigall said.
The research used no external funding. Dr. Nudy and Dr. Nachtigall had no disclosures.
Up to 10 different menopausal symptoms were linked to an increased risk of cardiovascular disease when they were moderate to severe in women who initially had no evidence of cardiovascular disease, according to research presented at the North American Menopause Society annual meeting in Atlanta.
“The take-home message is that severe menopausal symptoms may increase the risk of cardiovascular disease,” Matthew Nudy, MD, an assistant professor of medicine at the Heart and Vascular Institute at Penn State University, Hershey, said in an interview about his findings. “Physicians and patients should be aware of this association. Women with severe symptoms may be more likely to see their physician, and this would be an ideal time to have their cardiovascular risk assessed.”
Margaret Nachtigall, MD, a clinical associate professor of obstetrics and gynecology at New York University and at NYU Langone Health, noted that these findings lined up with other studies showing an increased risk of cardiovascular disease in patients who have more symptoms, especially hot flashes.
“Other recent studies showed that an increase in severity of hot flush is associated with worse blood vessel function, leading to heart disease,” Dr. Nachtigall, who was not involved with the study, said in an interview. “The next step that makes sense is to try to eliminate these symptoms and hope that, in turn, would lower cardiovascular disease and improve survival.”
The researchers compared menopausal symptoms with cardiovascular outcomes and all-cause mortality in an observational cohort of 80,278 postmenopausal women for a median 8.2 years of follow-up. None of the women, all enrolled in the Women’s Health Initiative, had known cardiovascular disease at baseline. They had an average age of 63 years and average body mass index (BMI) of 25.9 at baseline. Most participants were White (86.7%), with 7% being Black and 4.1% Hispanic. Cardiovascular disease was a composite outcome that included hospitalized myocardial infarction, definite silent myocardial infarction, coronary death, stroke, congestive heart failure, angina, peripheral vascular disease, carotid artery disease, and coronary revascularization.
The researchers used a four-item Likert scale (0-3) to assess the severity of 15 symptoms experienced within the past 4 weeks at baseline: “night sweats, hot flashes, waking up several times at night, joint pain or stiffness, headaches or migraines, vaginal or genital dryness, heart racing or skipping beats, breast tenderness, dizziness, tremors (shakes), feeling tired, forgetfulness, mood swings, [feeling] restless or fidgety, and difficulty concentrating.”
The associations were adjusted for the following covariates: race/ethnicity, blood pressure, education, smoking status, bilateral oophorectomy, menopausal hormone therapy use (never/past/current), sleep duration, statin use, history of high cholesterol, aspirin use, use of antihypertensives, treated diabetes, and family history of heart attack. Continuous variables included age, age at menopause, BMI, blood pressure, and physical activity levels. Because of the high number of multiple comparisons, the researchers also used a Bonferroni correction to reduce the risk of spurious statistical significance.
The researchers found some clustering of symptoms. Among women who had at least two moderate or severe menopausal symptoms, more than half frequently woke up at night, had joint pain, or felt tired, the researchers reported. Those symptoms were also the most commonly reported ones overall. Younger women, between ages 50 and 59, were more likely than older women (60-79 years old) to experience vasomotor symptoms and all cognitive affective symptoms except forgetfulness.
The researchers identified 10 symptoms whose severity was significantly associated with cardiovascular disease. Compared to having no symptoms at all, the following moderate or severe symptoms were associated with an increased risk of a cardiovascular event after adjustment for covariates and corrected for multiple comparisons: night sweats – a 19% increased risk (P = .03), waking up several times at night – 11% increased risk (P = .05), joint pain or stiffness – 27% increased risk (P < .001), heart racing or skipping beats – 55% increased risk (P < .001), dizziness – 34% increased risk (P < .001), feeling tired – 35% increased risk (P < .001), forgetfulness – 25% increased risk (P < .001), mood swings – 21% increased risk (P = .02), feeling restless or fidgety – 29% increased risk (P < .001), and difficulty concentrating – 31% increased risk (P < .001)
In addition, all-cause mortality was associated with these symptoms when they were moderate or severe: heart racing or skipping beats (32% increased risk of all-cause mortality; hazard ratio, 1.32; P =.006), dizziness (HR, 1.58; P < .001), tremors (HR, 1.44; P < .001), feeling tired (HR, 1.26; P < .001), forgetfulness (HR, 1.29; P = .01), mood swings (HR, 1.35; P = .02), feeling restless or fidgety (HR, 1.35; P < .001), and difficulty concentrating (HR, 1.47; P < .001).
The symptom with the greatest association with all-cause mortality was dizziness, which was associated with an increased risk of 58% when rated moderate or severe. Any dizziness at all was linked to a 12% increased risk of cardiovascular disease, compared with no dizziness. Machine learning with the LASSO method determined that the symptoms most predictive of cardiovascular disease were dizziness, heart racing, feeling tired, and joint pain. The symptoms most associated with all-cause mortality, based on the machine learning algorithm, were dizziness, tremors, and feeling tired.
Dr. Nudy said that their study did not look at mitigation strategies. “Women should discuss with their physician the best methods for cardiovascular risk reduction,” he said. He also cautioned that severe menopausal symptoms can also indicate other health conditions that may require investigation.
“It is certainly possible some symptoms may represent other medical conditions we were unable to control for and may not be directly related to menopause,” such as autoimmune diseases, endocrine abnormalities, or subclinical cardiovascular disease, he said. Additional limitations of the study included an older cohort and retrospective assessment of menopausal symptoms only at baseline. In addition, ”we did not assess the cardiovascular risk among women whose symptoms persisted versus resolved during the study period,” Dr. Nudy said.
Dr. Nachtigall said a key message is that people who are experiencing these symptoms should try to get treatment for them and attempt to alleviate them, hopefully reducing the risk of heart disease and death.
”Estrogen treatment is one excellent option for some individuals and should be considered in the appropriate person,” Dr. Nachtigall said. “If estrogen treatment is to be considered, it should be given closer to menopause, within the first 10 years after menopause and in younger individuals (under 59) at start.”
Dr. Nachtigall referred to the NAMS 2022 position statement concluding that, for healthy women within 10 years of menopause who have bothersome menopause symptoms, “the benefits of hormone therapy outweigh its risks, with fewer cardiovascular events in younger versus older women.”
”Menopause and having menopausal symptoms is an opportunity for clinicians and patients to have a conversation about appropriate individualized management options,” Dr. Nachtigall said.
Women may also be able to mitigate their cardiovascular risk with regular exercise, eating a healthy diet, not smoking, and getting adequate sleep, Dr. Nachtigall said. But these healthy behaviors may not adequately treat moderate or severe menopausal symptoms.
“Some health care providers have said that because menopause happens naturally, individuals should just accept the symptoms and try to wait it out and not get treatment, but this study, as well as others, makes it clear that it actually may be beneficial to treat the symptoms,” Dr. Nachtigall said.
The research used no external funding. Dr. Nudy and Dr. Nachtigall had no disclosures.
FROM NAMS 2022
Best anticoagulant for minimizing bleeding risk identified
A commonly prescribed direct oral anticoagulant (DOAC) has the lowest risk of bleeding, say researchers. Used to prevent strokes in those with atrial fibrillation (AFib), DOACs have recently become more common than warfarin, the previous standard treatment, as they do not require as much follow-up monitoring – which was “particularly valuable” during the COVID-19 pandemic – and have “less risk” of side effects, highlighted the authors of a new study, published in Annals of Internal Medicine.
However, the authors explained that, although current guidelines recommend using DOACs over warfarin in patients with AFib, “head-to-head trial data do not exist to guide the choice of DOAC.” So, they set out to try and fill this evidence gap by doing a large-scale comparison between all DOACs – apixaban, dabigatran, edoxaban, and rivaroxaban – in routine clinical practice.
Wallis Lau, PhD, University College London, and co–lead author, said: “Direct oral anticoagulants have been prescribed with increasing frequency worldwide in recent years, but evidence comparing them directly has been limited.”
One drug stood out
For the multinational population-based cohort study the researchers compared the efficacy and risk of side effects for the four most common DOACs. They reviewed data – from five standardized electronic health care databases that covered 221 million people in the United Kingdom, France, Germany, and the United States – of 527,226 patients who had been newly diagnosed with AFib between 2010 and 2019, and who had received a new DOAC prescription. The study included 281,320 apixaban users, 61,008 dabigatran users, 12,722 edoxaban users, and 172,176 rivaroxaban users.
Database-specific hazard ratios of ischemic stroke or systemic embolism, intracranial hemorrhage, gastrointestinal bleeding, and all-cause mortality between DOACs were estimated using a Cox regression model stratified by propensity score and pooled using a random-effects model.
In total, 9,530 ischemic stroke or systemic embolism events, 841 intercranial hemorrhage events, 8,319 gastrointestinal bleeding events, and 1,476 deaths were identified over the study follow-up. The researchers found that all four drugs were comparable on outcomes for ischemic stroke, intercranial hemorrhage, and all-cause mortality.
However, they identified a difference in the risk of gastrointestinal bleeding, which they highlighted “is one of the most common and concerning side effects of DOACs.”
“Apixaban stood out as having lower risk of gastrointestinal bleeding,” said the authors, with a 19%-28% lower risk when compared directly with each of the other three DOACs. Specifically, apixaban use was associated with lower risk for gastrointestinal bleeding than use of dabigatran (HR, 0.81; 95% confidence interval, 0.70-0.94), edoxaban (HR, 0.77; 95% CI, 0.66-0.91), or rivaroxaban (HR, 0.72; 95% CI, 0.66-0.79).
The researchers also highlighted that their findings held true when looking at data only from those aged over 80, and those with chronic kidney disease, two groups that are “often underrepresented” in clinical trials.
Apixaban may be preferable
The researchers concluded that, compared with dabigatran, edoxaban, and rivaroxaban.
“Our results indicate that apixaban may be preferable to other blood thinners because of the lower rate of gastrointestinal bleeding and similar rates of stroke, a finding that we hope will be supported by randomized controlled trials,” said Dr. Lau.
However, he emphasized that, “as with all medications, potential risks and benefits can differ between people, so considering the full spectrum of outcomes and side effects will still be necessary for each individual patient.”
The authors all declared no conflicting interests.
A version of this article first appeared on Medscape UK.
A commonly prescribed direct oral anticoagulant (DOAC) has the lowest risk of bleeding, say researchers. Used to prevent strokes in those with atrial fibrillation (AFib), DOACs have recently become more common than warfarin, the previous standard treatment, as they do not require as much follow-up monitoring – which was “particularly valuable” during the COVID-19 pandemic – and have “less risk” of side effects, highlighted the authors of a new study, published in Annals of Internal Medicine.
However, the authors explained that, although current guidelines recommend using DOACs over warfarin in patients with AFib, “head-to-head trial data do not exist to guide the choice of DOAC.” So, they set out to try and fill this evidence gap by doing a large-scale comparison between all DOACs – apixaban, dabigatran, edoxaban, and rivaroxaban – in routine clinical practice.
Wallis Lau, PhD, University College London, and co–lead author, said: “Direct oral anticoagulants have been prescribed with increasing frequency worldwide in recent years, but evidence comparing them directly has been limited.”
One drug stood out
For the multinational population-based cohort study the researchers compared the efficacy and risk of side effects for the four most common DOACs. They reviewed data – from five standardized electronic health care databases that covered 221 million people in the United Kingdom, France, Germany, and the United States – of 527,226 patients who had been newly diagnosed with AFib between 2010 and 2019, and who had received a new DOAC prescription. The study included 281,320 apixaban users, 61,008 dabigatran users, 12,722 edoxaban users, and 172,176 rivaroxaban users.
Database-specific hazard ratios of ischemic stroke or systemic embolism, intracranial hemorrhage, gastrointestinal bleeding, and all-cause mortality between DOACs were estimated using a Cox regression model stratified by propensity score and pooled using a random-effects model.
In total, 9,530 ischemic stroke or systemic embolism events, 841 intercranial hemorrhage events, 8,319 gastrointestinal bleeding events, and 1,476 deaths were identified over the study follow-up. The researchers found that all four drugs were comparable on outcomes for ischemic stroke, intercranial hemorrhage, and all-cause mortality.
However, they identified a difference in the risk of gastrointestinal bleeding, which they highlighted “is one of the most common and concerning side effects of DOACs.”
“Apixaban stood out as having lower risk of gastrointestinal bleeding,” said the authors, with a 19%-28% lower risk when compared directly with each of the other three DOACs. Specifically, apixaban use was associated with lower risk for gastrointestinal bleeding than use of dabigatran (HR, 0.81; 95% confidence interval, 0.70-0.94), edoxaban (HR, 0.77; 95% CI, 0.66-0.91), or rivaroxaban (HR, 0.72; 95% CI, 0.66-0.79).
The researchers also highlighted that their findings held true when looking at data only from those aged over 80, and those with chronic kidney disease, two groups that are “often underrepresented” in clinical trials.
Apixaban may be preferable
The researchers concluded that, compared with dabigatran, edoxaban, and rivaroxaban.
“Our results indicate that apixaban may be preferable to other blood thinners because of the lower rate of gastrointestinal bleeding and similar rates of stroke, a finding that we hope will be supported by randomized controlled trials,” said Dr. Lau.
However, he emphasized that, “as with all medications, potential risks and benefits can differ between people, so considering the full spectrum of outcomes and side effects will still be necessary for each individual patient.”
The authors all declared no conflicting interests.
A version of this article first appeared on Medscape UK.
A commonly prescribed direct oral anticoagulant (DOAC) has the lowest risk of bleeding, say researchers. Used to prevent strokes in those with atrial fibrillation (AFib), DOACs have recently become more common than warfarin, the previous standard treatment, as they do not require as much follow-up monitoring – which was “particularly valuable” during the COVID-19 pandemic – and have “less risk” of side effects, highlighted the authors of a new study, published in Annals of Internal Medicine.
However, the authors explained that, although current guidelines recommend using DOACs over warfarin in patients with AFib, “head-to-head trial data do not exist to guide the choice of DOAC.” So, they set out to try and fill this evidence gap by doing a large-scale comparison between all DOACs – apixaban, dabigatran, edoxaban, and rivaroxaban – in routine clinical practice.
Wallis Lau, PhD, University College London, and co–lead author, said: “Direct oral anticoagulants have been prescribed with increasing frequency worldwide in recent years, but evidence comparing them directly has been limited.”
One drug stood out
For the multinational population-based cohort study the researchers compared the efficacy and risk of side effects for the four most common DOACs. They reviewed data – from five standardized electronic health care databases that covered 221 million people in the United Kingdom, France, Germany, and the United States – of 527,226 patients who had been newly diagnosed with AFib between 2010 and 2019, and who had received a new DOAC prescription. The study included 281,320 apixaban users, 61,008 dabigatran users, 12,722 edoxaban users, and 172,176 rivaroxaban users.
Database-specific hazard ratios of ischemic stroke or systemic embolism, intracranial hemorrhage, gastrointestinal bleeding, and all-cause mortality between DOACs were estimated using a Cox regression model stratified by propensity score and pooled using a random-effects model.
In total, 9,530 ischemic stroke or systemic embolism events, 841 intercranial hemorrhage events, 8,319 gastrointestinal bleeding events, and 1,476 deaths were identified over the study follow-up. The researchers found that all four drugs were comparable on outcomes for ischemic stroke, intercranial hemorrhage, and all-cause mortality.
However, they identified a difference in the risk of gastrointestinal bleeding, which they highlighted “is one of the most common and concerning side effects of DOACs.”
“Apixaban stood out as having lower risk of gastrointestinal bleeding,” said the authors, with a 19%-28% lower risk when compared directly with each of the other three DOACs. Specifically, apixaban use was associated with lower risk for gastrointestinal bleeding than use of dabigatran (HR, 0.81; 95% confidence interval, 0.70-0.94), edoxaban (HR, 0.77; 95% CI, 0.66-0.91), or rivaroxaban (HR, 0.72; 95% CI, 0.66-0.79).
The researchers also highlighted that their findings held true when looking at data only from those aged over 80, and those with chronic kidney disease, two groups that are “often underrepresented” in clinical trials.
Apixaban may be preferable
The researchers concluded that, compared with dabigatran, edoxaban, and rivaroxaban.
“Our results indicate that apixaban may be preferable to other blood thinners because of the lower rate of gastrointestinal bleeding and similar rates of stroke, a finding that we hope will be supported by randomized controlled trials,” said Dr. Lau.
However, he emphasized that, “as with all medications, potential risks and benefits can differ between people, so considering the full spectrum of outcomes and side effects will still be necessary for each individual patient.”
The authors all declared no conflicting interests.
A version of this article first appeared on Medscape UK.
FROM ANNALS OF INTERNAL MEDICINE
Guide eases prayer for Muslims with knee osteoarthritis
For devout Muslims, praying multiple times a day is a lifelong observance and a core aspect of their faith. But osteoarthritis of the knee (KOA) can make kneeling and prostration challenging. To address this problem in an aging U.S. Muslim population, a multicenter team developed literature-based guidelines published online in Arthritis & Rheumatology.
In an interview, corresponding author Mahfujul Z. Haque, a medical student at Michigan State University, Grand Rapids, discussed the guide, which he assembled with Marina N. Magrey, MD, the Ronald Moskowitz Professor of Rheumatology at Case Western Reserve University, Cleveland, and orthopedic surgeon Karl C. Roberts, MD, president of West Michigan Orthopaedics in Grand Rapids, among others.
Could you detail the clinical and cultural context for these recommendations?
Mr. Haque: Muslims currently make up 1.1% of the U.S. population, or 3.45 million people. This guidance provides advice to Muslim patients with KOA in a culturally sensitive manner that can supplement standard care. Prayer, or Salah, is a religious obligation typically performed in 17-48 daily repetitions of squatting, floor sitting, full-knee flexion, and kneeling. For patients with KOA, prayer can be painful, and a few studies have found a link between these repeated movements and KOA progression.
Yet recommending stopping or limiting prayer is insensitive, so our group did a thorough literature search to identify easily implemented and culturally appropriate ways to ease praying.
Is there a traditional preference for praying on a hard surface?
Mr. Haque: Prayer can be performed on any surface that is clean and free from impurities. Cushioned and carpeted surfaces are permissible if the surface is somewhat firm and supportive for when worshippers prostrate themselves and put their faces on the ground. For example, compacted snow that wouldn’t allow the face to sink into it is permissible, but snow that is soft and would allow the face to sink in is not.
Have an increasing number of older patients raised the issue of knee pain during prayers?
Mr. Haque: We found no research on this in the literature. Anecdotally, however, two of our authors lead prayer in large Muslim communities in Detroit, and people often share with them that they feel discomfort during prayer and ask if there is anything they can do to limit this.
It is important to dispel the common myth that after total knee replacement one cannot kneel. About 20% of patients have some anterior knee discomfort after total knee arthroplasty, which can be exacerbated by kneeling, but kneeling causes no harm and can be done safely.
Could you outline the main recommendations?
Mr. Haque: These fall under three main categories: prayer surface, mechanics, and lifestyle modifications. The surface recommendations essentially advise using prayer rugs that provide cushioning or using cushioned kneepads.
The mechanics recommendations involve bracing with the palms down, standing up using the hands and knees, and guiding prayer motions with the hands. Chairs may be used as well.
Lifestyle recommendations outline home-exercise programs tailored to KOA and suggest the use of ice and compression during acute exacerbations.
Could these recommendations benefit other arthritic joints such as the wrists?
Mr. Haque: Anecdotally, our authors do not hear about pain in joints except for the knee and spine. To a limited extent, some of these recommendations may help patients with spinal arthritis as well.
What do you see as the greatest obstacle to implementation?
Mr. Haque: These recommendations, although permissible in the Muslim faith, are not part of traditional ritual and thus patients may simply forget to implement them. We advise physicians to ask patients which recommendations they are most likely to follow and to monitor how these have worked for them.
What is your best overall advice for broaching this issue with patients?
Mr. Haque: Holistic, functional, and culturally sensitive recommendations will be highly appreciated. Physicians are therefore encouraged to share this guidance with Muslim patients while using terms such as Salah, pronounced saa-laah, and Sajdah, pronounced sajduh and meaning prostration, and engage in a healthy dialogue.
These guidelines received no funding. The authors disclosed no competing interests relevant to their recommendations, but Dr. Magrey reported consulting and research relationships with private-sector companies outside of this work.
For devout Muslims, praying multiple times a day is a lifelong observance and a core aspect of their faith. But osteoarthritis of the knee (KOA) can make kneeling and prostration challenging. To address this problem in an aging U.S. Muslim population, a multicenter team developed literature-based guidelines published online in Arthritis & Rheumatology.
In an interview, corresponding author Mahfujul Z. Haque, a medical student at Michigan State University, Grand Rapids, discussed the guide, which he assembled with Marina N. Magrey, MD, the Ronald Moskowitz Professor of Rheumatology at Case Western Reserve University, Cleveland, and orthopedic surgeon Karl C. Roberts, MD, president of West Michigan Orthopaedics in Grand Rapids, among others.
Could you detail the clinical and cultural context for these recommendations?
Mr. Haque: Muslims currently make up 1.1% of the U.S. population, or 3.45 million people. This guidance provides advice to Muslim patients with KOA in a culturally sensitive manner that can supplement standard care. Prayer, or Salah, is a religious obligation typically performed in 17-48 daily repetitions of squatting, floor sitting, full-knee flexion, and kneeling. For patients with KOA, prayer can be painful, and a few studies have found a link between these repeated movements and KOA progression.
Yet recommending stopping or limiting prayer is insensitive, so our group did a thorough literature search to identify easily implemented and culturally appropriate ways to ease praying.
Is there a traditional preference for praying on a hard surface?
Mr. Haque: Prayer can be performed on any surface that is clean and free from impurities. Cushioned and carpeted surfaces are permissible if the surface is somewhat firm and supportive for when worshippers prostrate themselves and put their faces on the ground. For example, compacted snow that wouldn’t allow the face to sink into it is permissible, but snow that is soft and would allow the face to sink in is not.
Have an increasing number of older patients raised the issue of knee pain during prayers?
Mr. Haque: We found no research on this in the literature. Anecdotally, however, two of our authors lead prayer in large Muslim communities in Detroit, and people often share with them that they feel discomfort during prayer and ask if there is anything they can do to limit this.
It is important to dispel the common myth that after total knee replacement one cannot kneel. About 20% of patients have some anterior knee discomfort after total knee arthroplasty, which can be exacerbated by kneeling, but kneeling causes no harm and can be done safely.
Could you outline the main recommendations?
Mr. Haque: These fall under three main categories: prayer surface, mechanics, and lifestyle modifications. The surface recommendations essentially advise using prayer rugs that provide cushioning or using cushioned kneepads.
The mechanics recommendations involve bracing with the palms down, standing up using the hands and knees, and guiding prayer motions with the hands. Chairs may be used as well.
Lifestyle recommendations outline home-exercise programs tailored to KOA and suggest the use of ice and compression during acute exacerbations.
Could these recommendations benefit other arthritic joints such as the wrists?
Mr. Haque: Anecdotally, our authors do not hear about pain in joints except for the knee and spine. To a limited extent, some of these recommendations may help patients with spinal arthritis as well.
What do you see as the greatest obstacle to implementation?
Mr. Haque: These recommendations, although permissible in the Muslim faith, are not part of traditional ritual and thus patients may simply forget to implement them. We advise physicians to ask patients which recommendations they are most likely to follow and to monitor how these have worked for them.
What is your best overall advice for broaching this issue with patients?
Mr. Haque: Holistic, functional, and culturally sensitive recommendations will be highly appreciated. Physicians are therefore encouraged to share this guidance with Muslim patients while using terms such as Salah, pronounced saa-laah, and Sajdah, pronounced sajduh and meaning prostration, and engage in a healthy dialogue.
These guidelines received no funding. The authors disclosed no competing interests relevant to their recommendations, but Dr. Magrey reported consulting and research relationships with private-sector companies outside of this work.
For devout Muslims, praying multiple times a day is a lifelong observance and a core aspect of their faith. But osteoarthritis of the knee (KOA) can make kneeling and prostration challenging. To address this problem in an aging U.S. Muslim population, a multicenter team developed literature-based guidelines published online in Arthritis & Rheumatology.
In an interview, corresponding author Mahfujul Z. Haque, a medical student at Michigan State University, Grand Rapids, discussed the guide, which he assembled with Marina N. Magrey, MD, the Ronald Moskowitz Professor of Rheumatology at Case Western Reserve University, Cleveland, and orthopedic surgeon Karl C. Roberts, MD, president of West Michigan Orthopaedics in Grand Rapids, among others.
Could you detail the clinical and cultural context for these recommendations?
Mr. Haque: Muslims currently make up 1.1% of the U.S. population, or 3.45 million people. This guidance provides advice to Muslim patients with KOA in a culturally sensitive manner that can supplement standard care. Prayer, or Salah, is a religious obligation typically performed in 17-48 daily repetitions of squatting, floor sitting, full-knee flexion, and kneeling. For patients with KOA, prayer can be painful, and a few studies have found a link between these repeated movements and KOA progression.
Yet recommending stopping or limiting prayer is insensitive, so our group did a thorough literature search to identify easily implemented and culturally appropriate ways to ease praying.
Is there a traditional preference for praying on a hard surface?
Mr. Haque: Prayer can be performed on any surface that is clean and free from impurities. Cushioned and carpeted surfaces are permissible if the surface is somewhat firm and supportive for when worshippers prostrate themselves and put their faces on the ground. For example, compacted snow that wouldn’t allow the face to sink into it is permissible, but snow that is soft and would allow the face to sink in is not.
Have an increasing number of older patients raised the issue of knee pain during prayers?
Mr. Haque: We found no research on this in the literature. Anecdotally, however, two of our authors lead prayer in large Muslim communities in Detroit, and people often share with them that they feel discomfort during prayer and ask if there is anything they can do to limit this.
It is important to dispel the common myth that after total knee replacement one cannot kneel. About 20% of patients have some anterior knee discomfort after total knee arthroplasty, which can be exacerbated by kneeling, but kneeling causes no harm and can be done safely.
Could you outline the main recommendations?
Mr. Haque: These fall under three main categories: prayer surface, mechanics, and lifestyle modifications. The surface recommendations essentially advise using prayer rugs that provide cushioning or using cushioned kneepads.
The mechanics recommendations involve bracing with the palms down, standing up using the hands and knees, and guiding prayer motions with the hands. Chairs may be used as well.
Lifestyle recommendations outline home-exercise programs tailored to KOA and suggest the use of ice and compression during acute exacerbations.
Could these recommendations benefit other arthritic joints such as the wrists?
Mr. Haque: Anecdotally, our authors do not hear about pain in joints except for the knee and spine. To a limited extent, some of these recommendations may help patients with spinal arthritis as well.
What do you see as the greatest obstacle to implementation?
Mr. Haque: These recommendations, although permissible in the Muslim faith, are not part of traditional ritual and thus patients may simply forget to implement them. We advise physicians to ask patients which recommendations they are most likely to follow and to monitor how these have worked for them.
What is your best overall advice for broaching this issue with patients?
Mr. Haque: Holistic, functional, and culturally sensitive recommendations will be highly appreciated. Physicians are therefore encouraged to share this guidance with Muslim patients while using terms such as Salah, pronounced saa-laah, and Sajdah, pronounced sajduh and meaning prostration, and engage in a healthy dialogue.
These guidelines received no funding. The authors disclosed no competing interests relevant to their recommendations, but Dr. Magrey reported consulting and research relationships with private-sector companies outside of this work.
FROM ARTHRITIS & RHEUMATOLOGY
Metabolites may distinguish severe subtypes of PAH
, based on data from approximately 1,500 individuals.
The overall prognosis and therapeutic response for patients with pulmonary arterial hypertension associated with systemic sclerosis (SSc-PAH) tends to be worse than for patients with other types of PAH, such as idiopathic pulmonary arterial hypertension (IPAH), but the impact of different metabolite profiles among subtypes of disease has not been explored, wrote Mona Alotaibi, MD, of the University of California, San Diego, and colleagues.
“Recently, metabolic dysregulation has been proposed as a key mechanism by which IPAH and SSc-PAH differ and could control such disparities,” they noted. Clarifying the molecular mechanisms of SSc-PAH could inform management and treatment, they added.
In a study published in the journal Chest, the researchers sought to identify a bioactive lipid signature unique to SSc-PAH. They identified 400 patients with SSc-PAH and 1,082 with IPAH. An additional 100 patients with scleroderma but no PH and 44 patients with scleroderma who had PH were included for external validation. The mean ages of the patients with IPAH and SSc-PAH in the discovery and validation cohorts ranged from approximately 51 to 65 years; more than 75% of patients across the groups were women.
The researchers tested more than 700 bioactive lipid metabolites using liquid chromatography/mass spectrometry. They found five metabolites that distinguished SSc-PAH and IPAH that were significantly associated with markers of disease severity: 17-beta estradiol, novel Eic, nervonic acid, fatty acid esters of hydroxy fatty acids, and prostaglandin F2 alpha (PGF 2 alpha).
The biomarkers were increased in SSc-PAH patients compared to patients with SSC alone, which suggests that the biomarkers are related to PAH and not to scleroderma alone, the researchers noted.
In particular, nervonic acid was associated with worse functional capacity, in SSc-PAH patients, as were higher levels of 17-beta estradiol and prostaglandin F2 alpha. Also, 17-beta estradiol was associated with lower cardiac impairment (CI) and stroke volume index (SVI) in SSc-PAH patients, but higher SVI in IPAH patients. PGF 2 alpha was associated with lower CI and SVI and higher pulmonary vascular resistance in SSc-PAH and IPAH combined.
The study findings were limited by several factors including the inability to adjust for all potential confounders between IPAH and SSc-PAH, and the fact that a clear causal relationship could not be determined, the researchers noted. Inadequate statistical power to analyze SSc-PAH data was another limitation, and studies with detailed scleroderma phenotypes are needed to validate the results, they said.
However, the current study provides insight on the metabolic differences in SSc-PAH and the potential impact on disease pathology that may inform diagnosis, prognosis, and treatment strategies for SSc-PAH patients, they concluded.
The study was supported by the National Institutes of Health. Several individual investigators received support from organizations including the American Heart Association and the Chest Foundation, and from companies including Livanova, Equillium, Corvus, Bayer, and Actelion, but the authors had no relevant financial conflicts to disclose.
, based on data from approximately 1,500 individuals.
The overall prognosis and therapeutic response for patients with pulmonary arterial hypertension associated with systemic sclerosis (SSc-PAH) tends to be worse than for patients with other types of PAH, such as idiopathic pulmonary arterial hypertension (IPAH), but the impact of different metabolite profiles among subtypes of disease has not been explored, wrote Mona Alotaibi, MD, of the University of California, San Diego, and colleagues.
“Recently, metabolic dysregulation has been proposed as a key mechanism by which IPAH and SSc-PAH differ and could control such disparities,” they noted. Clarifying the molecular mechanisms of SSc-PAH could inform management and treatment, they added.
In a study published in the journal Chest, the researchers sought to identify a bioactive lipid signature unique to SSc-PAH. They identified 400 patients with SSc-PAH and 1,082 with IPAH. An additional 100 patients with scleroderma but no PH and 44 patients with scleroderma who had PH were included for external validation. The mean ages of the patients with IPAH and SSc-PAH in the discovery and validation cohorts ranged from approximately 51 to 65 years; more than 75% of patients across the groups were women.
The researchers tested more than 700 bioactive lipid metabolites using liquid chromatography/mass spectrometry. They found five metabolites that distinguished SSc-PAH and IPAH that were significantly associated with markers of disease severity: 17-beta estradiol, novel Eic, nervonic acid, fatty acid esters of hydroxy fatty acids, and prostaglandin F2 alpha (PGF 2 alpha).
The biomarkers were increased in SSc-PAH patients compared to patients with SSC alone, which suggests that the biomarkers are related to PAH and not to scleroderma alone, the researchers noted.
In particular, nervonic acid was associated with worse functional capacity, in SSc-PAH patients, as were higher levels of 17-beta estradiol and prostaglandin F2 alpha. Also, 17-beta estradiol was associated with lower cardiac impairment (CI) and stroke volume index (SVI) in SSc-PAH patients, but higher SVI in IPAH patients. PGF 2 alpha was associated with lower CI and SVI and higher pulmonary vascular resistance in SSc-PAH and IPAH combined.
The study findings were limited by several factors including the inability to adjust for all potential confounders between IPAH and SSc-PAH, and the fact that a clear causal relationship could not be determined, the researchers noted. Inadequate statistical power to analyze SSc-PAH data was another limitation, and studies with detailed scleroderma phenotypes are needed to validate the results, they said.
However, the current study provides insight on the metabolic differences in SSc-PAH and the potential impact on disease pathology that may inform diagnosis, prognosis, and treatment strategies for SSc-PAH patients, they concluded.
The study was supported by the National Institutes of Health. Several individual investigators received support from organizations including the American Heart Association and the Chest Foundation, and from companies including Livanova, Equillium, Corvus, Bayer, and Actelion, but the authors had no relevant financial conflicts to disclose.
, based on data from approximately 1,500 individuals.
The overall prognosis and therapeutic response for patients with pulmonary arterial hypertension associated with systemic sclerosis (SSc-PAH) tends to be worse than for patients with other types of PAH, such as idiopathic pulmonary arterial hypertension (IPAH), but the impact of different metabolite profiles among subtypes of disease has not been explored, wrote Mona Alotaibi, MD, of the University of California, San Diego, and colleagues.
“Recently, metabolic dysregulation has been proposed as a key mechanism by which IPAH and SSc-PAH differ and could control such disparities,” they noted. Clarifying the molecular mechanisms of SSc-PAH could inform management and treatment, they added.
In a study published in the journal Chest, the researchers sought to identify a bioactive lipid signature unique to SSc-PAH. They identified 400 patients with SSc-PAH and 1,082 with IPAH. An additional 100 patients with scleroderma but no PH and 44 patients with scleroderma who had PH were included for external validation. The mean ages of the patients with IPAH and SSc-PAH in the discovery and validation cohorts ranged from approximately 51 to 65 years; more than 75% of patients across the groups were women.
The researchers tested more than 700 bioactive lipid metabolites using liquid chromatography/mass spectrometry. They found five metabolites that distinguished SSc-PAH and IPAH that were significantly associated with markers of disease severity: 17-beta estradiol, novel Eic, nervonic acid, fatty acid esters of hydroxy fatty acids, and prostaglandin F2 alpha (PGF 2 alpha).
The biomarkers were increased in SSc-PAH patients compared to patients with SSC alone, which suggests that the biomarkers are related to PAH and not to scleroderma alone, the researchers noted.
In particular, nervonic acid was associated with worse functional capacity, in SSc-PAH patients, as were higher levels of 17-beta estradiol and prostaglandin F2 alpha. Also, 17-beta estradiol was associated with lower cardiac impairment (CI) and stroke volume index (SVI) in SSc-PAH patients, but higher SVI in IPAH patients. PGF 2 alpha was associated with lower CI and SVI and higher pulmonary vascular resistance in SSc-PAH and IPAH combined.
The study findings were limited by several factors including the inability to adjust for all potential confounders between IPAH and SSc-PAH, and the fact that a clear causal relationship could not be determined, the researchers noted. Inadequate statistical power to analyze SSc-PAH data was another limitation, and studies with detailed scleroderma phenotypes are needed to validate the results, they said.
However, the current study provides insight on the metabolic differences in SSc-PAH and the potential impact on disease pathology that may inform diagnosis, prognosis, and treatment strategies for SSc-PAH patients, they concluded.
The study was supported by the National Institutes of Health. Several individual investigators received support from organizations including the American Heart Association and the Chest Foundation, and from companies including Livanova, Equillium, Corvus, Bayer, and Actelion, but the authors had no relevant financial conflicts to disclose.
FROM CHEST
Nicotine blocks estrogen production in women’s brains
VIENNA – The production of estrogen in the thalamus appears to be curtailed by just one dose of nicotine, equivalent to that in a cigarette, reveals a whole brain analysis of healthy women in the first study of its kind.
The findings were presented at the 35th European College of Neuropsychopharmacology (ECNP) Congress.
The researchers performed both MRI and positron emission tomography (PET) scans in 10 healthy women using a tracer that binds to aromatase, also known as estrogen synthase.
They found that, following an intranasal spray delivering 1 mg of nicotine, there was a significant reduction in estrogen synthase in both the right and left thalamus.
“For the first time, we can see that nicotine works to shut down the estrogen production mechanism in the brains of women,” said lead researcher Erika Comasco, PhD, department of neuroscience, Uppsala University, Sweden, in a release.
“We were surprised to see that this effect could be seen even with a single dose of nicotine, equivalent to just one cigarette, showing how powerful the effects of smoking are on a woman’s brain.”
Emphasizing the preliminary nature of the study and the need for a larger sample, she added: “We’re still not sure what the behavioral or cognitive outcomes are, only that nicotine acts on this area of the brain.
“However, we note that the affected brain system is a target for addictive drugs, such as nicotine.”
Previous research has revealed that women are less successful at quitting smoking than men, and appear to be more resistant to nicotine replacement therapy, and experience more relapses.
There is evidence to suggest that there is a complex interaction between sex and steroid hormones and the reward effect of nicotine, modulated by the dopaminergic system.
Moreover, women who smoke enter menopause earlier than nonsmokers, and have lower plasma estrogen levels, Dr. Camasco told this news organization.
Dr. Comasco explained that “besides its role in reproductive function and sexual behavior, estrogen has an impact on the brain wherever there are receptors, which is basically regions that are related to emotional regulation, cognitive function, and so on.”
Estrogen, she continued, has two main mechanisms of action, via dopaminergic and serotonergic signaling. However, levels of the hormone cannot be measured directly in the brain.
The researchers therefore turned to estrogen synthase, which regulates the synthesis of estrogen, and is highly expressed in the limbic system, a brain region associated with addiction.
Moreover, estrogen synthase levels can be measured in vivo, and previous animal studies have indicated that nicotine inhibits estrogen synthase.
To investigate its impact in humans, the researchers performed structural MRI and two 11C-cetrozole PET scans in 10 healthy women.
The assessments were performed before and after the nasal administration of 1 mg of nicotine, the dose contained in one cigarette, via two sprays of a nasal spray each containing 0.5 mg of nicotine.
A whole brain analysis was then used to determine changes in nondisplaceable binding potential of 11C-cetrozole to estrogen synthase between the two scans to indicate the availability of the enzyme at the two time points.
The results showed that, at baseline, high availability of estrogen synthase was observed in the thalamus, hypothalamus, and amygdala, with the highest levels in the right and left thalamus.
However, nicotine exposure was associated with a significant reduction in estrogen binding bilaterally in the thalamus when averaged across the participants (P < .01).
Region-of-interest analysis using within-individual voxel-wise comparison confirmed reduced estrogen synthase levels in both the right and left thalamus (P < .05), as well as in the subthalamic area.
Next, Dr. Comasco would like to test the impact of nicotine on estrogen synthase in men.
While men have lower levels of estrogen then women, “the reaction will take place anyway,” she said, although the “impact would be different.”
She would also like to look at the behavioral effects of reductions in estrogen synthase, and look at the effect of nicotine from a functional point of view.
Wim van den Brink, MD, PhD, professor of psychiatry and addiction at the Academic Medical Center, University of Amsterdam, commented that this is an “important first finding.”
“Smoking has many adverse effects in men and in women, but this particular effect of nicotine on the reduction of estrogen production in women was not known before,” he added in the release.
However, he underlined that tobacco addition is a “complex disorder” and it is “unlikely that this specific effect of nicotine on the thalamus explains all the observed differences in the development, treatment, and outcomes between male and female smokers.”
“It is still a long way from a nicotine-induced reduction in estrogen production to a reduced risk of nicotine addiction and negative effects of treatment and relapse in female cigarette smokers, but this work merits further investigation,” Dr. van den Brink said.
The study was funded by the Science for Life Laboratory/Uppsala University.
No relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
VIENNA – The production of estrogen in the thalamus appears to be curtailed by just one dose of nicotine, equivalent to that in a cigarette, reveals a whole brain analysis of healthy women in the first study of its kind.
The findings were presented at the 35th European College of Neuropsychopharmacology (ECNP) Congress.
The researchers performed both MRI and positron emission tomography (PET) scans in 10 healthy women using a tracer that binds to aromatase, also known as estrogen synthase.
They found that, following an intranasal spray delivering 1 mg of nicotine, there was a significant reduction in estrogen synthase in both the right and left thalamus.
“For the first time, we can see that nicotine works to shut down the estrogen production mechanism in the brains of women,” said lead researcher Erika Comasco, PhD, department of neuroscience, Uppsala University, Sweden, in a release.
“We were surprised to see that this effect could be seen even with a single dose of nicotine, equivalent to just one cigarette, showing how powerful the effects of smoking are on a woman’s brain.”
Emphasizing the preliminary nature of the study and the need for a larger sample, she added: “We’re still not sure what the behavioral or cognitive outcomes are, only that nicotine acts on this area of the brain.
“However, we note that the affected brain system is a target for addictive drugs, such as nicotine.”
Previous research has revealed that women are less successful at quitting smoking than men, and appear to be more resistant to nicotine replacement therapy, and experience more relapses.
There is evidence to suggest that there is a complex interaction between sex and steroid hormones and the reward effect of nicotine, modulated by the dopaminergic system.
Moreover, women who smoke enter menopause earlier than nonsmokers, and have lower plasma estrogen levels, Dr. Camasco told this news organization.
Dr. Comasco explained that “besides its role in reproductive function and sexual behavior, estrogen has an impact on the brain wherever there are receptors, which is basically regions that are related to emotional regulation, cognitive function, and so on.”
Estrogen, she continued, has two main mechanisms of action, via dopaminergic and serotonergic signaling. However, levels of the hormone cannot be measured directly in the brain.
The researchers therefore turned to estrogen synthase, which regulates the synthesis of estrogen, and is highly expressed in the limbic system, a brain region associated with addiction.
Moreover, estrogen synthase levels can be measured in vivo, and previous animal studies have indicated that nicotine inhibits estrogen synthase.
To investigate its impact in humans, the researchers performed structural MRI and two 11C-cetrozole PET scans in 10 healthy women.
The assessments were performed before and after the nasal administration of 1 mg of nicotine, the dose contained in one cigarette, via two sprays of a nasal spray each containing 0.5 mg of nicotine.
A whole brain analysis was then used to determine changes in nondisplaceable binding potential of 11C-cetrozole to estrogen synthase between the two scans to indicate the availability of the enzyme at the two time points.
The results showed that, at baseline, high availability of estrogen synthase was observed in the thalamus, hypothalamus, and amygdala, with the highest levels in the right and left thalamus.
However, nicotine exposure was associated with a significant reduction in estrogen binding bilaterally in the thalamus when averaged across the participants (P < .01).
Region-of-interest analysis using within-individual voxel-wise comparison confirmed reduced estrogen synthase levels in both the right and left thalamus (P < .05), as well as in the subthalamic area.
Next, Dr. Comasco would like to test the impact of nicotine on estrogen synthase in men.
While men have lower levels of estrogen then women, “the reaction will take place anyway,” she said, although the “impact would be different.”
She would also like to look at the behavioral effects of reductions in estrogen synthase, and look at the effect of nicotine from a functional point of view.
Wim van den Brink, MD, PhD, professor of psychiatry and addiction at the Academic Medical Center, University of Amsterdam, commented that this is an “important first finding.”
“Smoking has many adverse effects in men and in women, but this particular effect of nicotine on the reduction of estrogen production in women was not known before,” he added in the release.
However, he underlined that tobacco addition is a “complex disorder” and it is “unlikely that this specific effect of nicotine on the thalamus explains all the observed differences in the development, treatment, and outcomes between male and female smokers.”
“It is still a long way from a nicotine-induced reduction in estrogen production to a reduced risk of nicotine addiction and negative effects of treatment and relapse in female cigarette smokers, but this work merits further investigation,” Dr. van den Brink said.
The study was funded by the Science for Life Laboratory/Uppsala University.
No relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
VIENNA – The production of estrogen in the thalamus appears to be curtailed by just one dose of nicotine, equivalent to that in a cigarette, reveals a whole brain analysis of healthy women in the first study of its kind.
The findings were presented at the 35th European College of Neuropsychopharmacology (ECNP) Congress.
The researchers performed both MRI and positron emission tomography (PET) scans in 10 healthy women using a tracer that binds to aromatase, also known as estrogen synthase.
They found that, following an intranasal spray delivering 1 mg of nicotine, there was a significant reduction in estrogen synthase in both the right and left thalamus.
“For the first time, we can see that nicotine works to shut down the estrogen production mechanism in the brains of women,” said lead researcher Erika Comasco, PhD, department of neuroscience, Uppsala University, Sweden, in a release.
“We were surprised to see that this effect could be seen even with a single dose of nicotine, equivalent to just one cigarette, showing how powerful the effects of smoking are on a woman’s brain.”
Emphasizing the preliminary nature of the study and the need for a larger sample, she added: “We’re still not sure what the behavioral or cognitive outcomes are, only that nicotine acts on this area of the brain.
“However, we note that the affected brain system is a target for addictive drugs, such as nicotine.”
Previous research has revealed that women are less successful at quitting smoking than men, and appear to be more resistant to nicotine replacement therapy, and experience more relapses.
There is evidence to suggest that there is a complex interaction between sex and steroid hormones and the reward effect of nicotine, modulated by the dopaminergic system.
Moreover, women who smoke enter menopause earlier than nonsmokers, and have lower plasma estrogen levels, Dr. Camasco told this news organization.
Dr. Comasco explained that “besides its role in reproductive function and sexual behavior, estrogen has an impact on the brain wherever there are receptors, which is basically regions that are related to emotional regulation, cognitive function, and so on.”
Estrogen, she continued, has two main mechanisms of action, via dopaminergic and serotonergic signaling. However, levels of the hormone cannot be measured directly in the brain.
The researchers therefore turned to estrogen synthase, which regulates the synthesis of estrogen, and is highly expressed in the limbic system, a brain region associated with addiction.
Moreover, estrogen synthase levels can be measured in vivo, and previous animal studies have indicated that nicotine inhibits estrogen synthase.
To investigate its impact in humans, the researchers performed structural MRI and two 11C-cetrozole PET scans in 10 healthy women.
The assessments were performed before and after the nasal administration of 1 mg of nicotine, the dose contained in one cigarette, via two sprays of a nasal spray each containing 0.5 mg of nicotine.
A whole brain analysis was then used to determine changes in nondisplaceable binding potential of 11C-cetrozole to estrogen synthase between the two scans to indicate the availability of the enzyme at the two time points.
The results showed that, at baseline, high availability of estrogen synthase was observed in the thalamus, hypothalamus, and amygdala, with the highest levels in the right and left thalamus.
However, nicotine exposure was associated with a significant reduction in estrogen binding bilaterally in the thalamus when averaged across the participants (P < .01).
Region-of-interest analysis using within-individual voxel-wise comparison confirmed reduced estrogen synthase levels in both the right and left thalamus (P < .05), as well as in the subthalamic area.
Next, Dr. Comasco would like to test the impact of nicotine on estrogen synthase in men.
While men have lower levels of estrogen then women, “the reaction will take place anyway,” she said, although the “impact would be different.”
She would also like to look at the behavioral effects of reductions in estrogen synthase, and look at the effect of nicotine from a functional point of view.
Wim van den Brink, MD, PhD, professor of psychiatry and addiction at the Academic Medical Center, University of Amsterdam, commented that this is an “important first finding.”
“Smoking has many adverse effects in men and in women, but this particular effect of nicotine on the reduction of estrogen production in women was not known before,” he added in the release.
However, he underlined that tobacco addition is a “complex disorder” and it is “unlikely that this specific effect of nicotine on the thalamus explains all the observed differences in the development, treatment, and outcomes between male and female smokers.”
“It is still a long way from a nicotine-induced reduction in estrogen production to a reduced risk of nicotine addiction and negative effects of treatment and relapse in female cigarette smokers, but this work merits further investigation,” Dr. van den Brink said.
The study was funded by the Science for Life Laboratory/Uppsala University.
No relevant financial relationships were declared.
A version of this article first appeared on Medscape.com.
AT ECNP 2022
ObesityWeek 2022: What’s stopping effective treatment of obesity?
ObesityWeek 2022 is the largest international conference on obesity, with over 100 sessions, and coincides with the 40th anniversary of the Obesity Society. Being held Nov. 1-4, it is a hybrid meeting that participants can attend onsite in sunny San Diego or virtually.
“The meeting offers a wide perspective, from basic science, all the way to public policy on studies of treatment and prevention of obesity,” program planning chair for ObesityWeek, Kelly C. Allison, PhD, said in an interview.
The Presidential Plenary session on Nov. 1 will kick off the meeting with “a series of 10-minute rapid talks on cutting-edge topics in the field,” noted Dr. Allison, who is also director, Center for Weight and Eating Disorders, Hospital of the University of Pennsylvania, and professor of psychiatry, University of Pennsylvania, both in Philadelphia.
Among others, Ania M. Jastreboff, MD, PhD, will speak about “New developments in anti-obesity pharmacotherapy,” and Theodore K. Kyle, RPh, MBA, will discuss “Reducing barriers to treatment: Insurance coverage.”
“We’re seeing some pretty effective antiobesity medication, but still they are not being covered by many insurances,” said Dr. Allison. Some clinicians might be hesitant to prescribe antiobesity medications, remembering older drugs that were pulled from the market for health concerns, and some patients may also have concerns, she speculated. There is a need for greater education about the current antiobesity drugs.
In his presidential address, Dan Bessesen, MD, professor of medicine at the University of Colorado at Denver, Aurora, will discuss “Regulation of body weight and adaptive responses to weight loss.”
Pediatric obesity is a major focus of this year›s conference too, Allison noted.
At 8 a.m on Nov. 3, The Obesity Society, the World Obesity Federation, the European Association for the Study of Obesity, and Obesity Canada will present a joint symposium, “International innovations in pediatric obesity,” with speakers from Canada, Australia, and Ireland discussing ongoing paradigm shifts in the prevention and treatment of pediatric obesity.
Two hours later, at a joint symposium by the American Academy of Pediatrics/The Obesity Society, attendees will get a behind-the-scenes look at the making of the new AAP Obesity Clinical Practice Guideline for children and adolescents with obesity.
The conference tracks reflect the broad scope of this event: Track 1: Metabolism and Integrative Physiology; Track 2: Neuroscience; Track 3: Interventional and Clinical Studies; Track 4: Population Health; Track 5: Clinical/Professional Practice; Track 6: Policy/Public Health, and a subtrack: Eradicating Treatment Barriers.
Dr. Allison highlighted the following oral presentations and posters about antiobesity drugs:
- “Once-weekly subcutaneous semaglutide 2.4 mg in adolescents with overweight or obesity,” with an extended Q&A session, Nov. 2.
- “Clinical outcomes with medication use in tertiary pediatric weight management program,” by Enayet and colleagues. Poster 030.
- “The metabolically healthy obese paradigm and liver fat content in the Fels longitudinal study,” by Garza and colleagues Oral 055, Nov. 2.
- “Phase 3 clinical trial of metformin for treatment of COVID-19 in adults with overweight and obesity,” by Bramante and colleagues. Oral 067, Nov. 3. This trial was published in the (N Engl J Med. 2022;387:599-610).
- “Glucagon/GLP-1 receptor dual agonist BI 456906 reduces bodyweight in patients with type 2 diabetes,” by Rosenstock and colleagues. Oral-063, Nov. 3.
- “A randomized controlled trial of naltrexone and bupropion and behavior therapy for binge-eating disorder,” by Grilo and colleagues. Oral 066, Nov. 3.
And on Nov. 4, researchers will present four oral abstracts about the dual glucose-dependent insulinotropic polypeptide and glucagonlike peptide–1 (GLP-1) receptor agonist tirzepatide (Mounjaro), which is approved for type 2 diabetes and now has fast track designation for weight loss from the Food and Drug Administration. Oral abstracts 109, 110, 111, and 112 cover weight loss with tirzepatide across different age groups, body mass indexes, and comorbidities, as well as quality of life.
Dr. Allison also highlighted the following presentations that cover other diverse topics:
- Family-based treatment: “Pilot study to inform a randomized controlled trial of HeLP: Obesity prevention & treatment for the entire Hispanic family,” by Haemer and colleagues. Oral 029. November 2.
- Bariatric surgery: “Long-term outcomes of laparoscopic sleeve gastrectomy from 2010-2016: A nationwide cohort study,” Oral 014. Nov. 2.
- Prevention/public health: “Impact of positive and negative front-of-package food labels in a randomized experiment,” by Grummon and colleagues. Oral 068. Nov. 3.
- Time-restricted eating: “Effects of 8-hour time restricted eating for weight loss over 12 months,” by Gabel and colleagues. Oral 102. Nov. 4.
- Patient management: “Identifying interprofessional drivers of practice gaps in the management of patients with obesity,” by Robinson and colleagues. Poster 055.
On Nov. 4, researchers will present five winning papers that will be published in the December issue of the Obesity journal about GLP-1 agonists versus bariatric surgery; monoacylglycerol O-acyltransferase 1 in mice; a behavioral weight-loss intervention; the Canberra Obesity Management Service; and macronutrient (im)balance in an obesogenic environment.
“I’m always excited to hear some talks that are outside of my comfort area to understand the mechanisms of obesity better,” concluded Dr. Allison.
A version of this article first appeared on Medscape.com.
ObesityWeek 2022 is the largest international conference on obesity, with over 100 sessions, and coincides with the 40th anniversary of the Obesity Society. Being held Nov. 1-4, it is a hybrid meeting that participants can attend onsite in sunny San Diego or virtually.
“The meeting offers a wide perspective, from basic science, all the way to public policy on studies of treatment and prevention of obesity,” program planning chair for ObesityWeek, Kelly C. Allison, PhD, said in an interview.
The Presidential Plenary session on Nov. 1 will kick off the meeting with “a series of 10-minute rapid talks on cutting-edge topics in the field,” noted Dr. Allison, who is also director, Center for Weight and Eating Disorders, Hospital of the University of Pennsylvania, and professor of psychiatry, University of Pennsylvania, both in Philadelphia.
Among others, Ania M. Jastreboff, MD, PhD, will speak about “New developments in anti-obesity pharmacotherapy,” and Theodore K. Kyle, RPh, MBA, will discuss “Reducing barriers to treatment: Insurance coverage.”
“We’re seeing some pretty effective antiobesity medication, but still they are not being covered by many insurances,” said Dr. Allison. Some clinicians might be hesitant to prescribe antiobesity medications, remembering older drugs that were pulled from the market for health concerns, and some patients may also have concerns, she speculated. There is a need for greater education about the current antiobesity drugs.
In his presidential address, Dan Bessesen, MD, professor of medicine at the University of Colorado at Denver, Aurora, will discuss “Regulation of body weight and adaptive responses to weight loss.”
Pediatric obesity is a major focus of this year›s conference too, Allison noted.
At 8 a.m on Nov. 3, The Obesity Society, the World Obesity Federation, the European Association for the Study of Obesity, and Obesity Canada will present a joint symposium, “International innovations in pediatric obesity,” with speakers from Canada, Australia, and Ireland discussing ongoing paradigm shifts in the prevention and treatment of pediatric obesity.
Two hours later, at a joint symposium by the American Academy of Pediatrics/The Obesity Society, attendees will get a behind-the-scenes look at the making of the new AAP Obesity Clinical Practice Guideline for children and adolescents with obesity.
The conference tracks reflect the broad scope of this event: Track 1: Metabolism and Integrative Physiology; Track 2: Neuroscience; Track 3: Interventional and Clinical Studies; Track 4: Population Health; Track 5: Clinical/Professional Practice; Track 6: Policy/Public Health, and a subtrack: Eradicating Treatment Barriers.
Dr. Allison highlighted the following oral presentations and posters about antiobesity drugs:
- “Once-weekly subcutaneous semaglutide 2.4 mg in adolescents with overweight or obesity,” with an extended Q&A session, Nov. 2.
- “Clinical outcomes with medication use in tertiary pediatric weight management program,” by Enayet and colleagues. Poster 030.
- “The metabolically healthy obese paradigm and liver fat content in the Fels longitudinal study,” by Garza and colleagues Oral 055, Nov. 2.
- “Phase 3 clinical trial of metformin for treatment of COVID-19 in adults with overweight and obesity,” by Bramante and colleagues. Oral 067, Nov. 3. This trial was published in the (N Engl J Med. 2022;387:599-610).
- “Glucagon/GLP-1 receptor dual agonist BI 456906 reduces bodyweight in patients with type 2 diabetes,” by Rosenstock and colleagues. Oral-063, Nov. 3.
- “A randomized controlled trial of naltrexone and bupropion and behavior therapy for binge-eating disorder,” by Grilo and colleagues. Oral 066, Nov. 3.
And on Nov. 4, researchers will present four oral abstracts about the dual glucose-dependent insulinotropic polypeptide and glucagonlike peptide–1 (GLP-1) receptor agonist tirzepatide (Mounjaro), which is approved for type 2 diabetes and now has fast track designation for weight loss from the Food and Drug Administration. Oral abstracts 109, 110, 111, and 112 cover weight loss with tirzepatide across different age groups, body mass indexes, and comorbidities, as well as quality of life.
Dr. Allison also highlighted the following presentations that cover other diverse topics:
- Family-based treatment: “Pilot study to inform a randomized controlled trial of HeLP: Obesity prevention & treatment for the entire Hispanic family,” by Haemer and colleagues. Oral 029. November 2.
- Bariatric surgery: “Long-term outcomes of laparoscopic sleeve gastrectomy from 2010-2016: A nationwide cohort study,” Oral 014. Nov. 2.
- Prevention/public health: “Impact of positive and negative front-of-package food labels in a randomized experiment,” by Grummon and colleagues. Oral 068. Nov. 3.
- Time-restricted eating: “Effects of 8-hour time restricted eating for weight loss over 12 months,” by Gabel and colleagues. Oral 102. Nov. 4.
- Patient management: “Identifying interprofessional drivers of practice gaps in the management of patients with obesity,” by Robinson and colleagues. Poster 055.
On Nov. 4, researchers will present five winning papers that will be published in the December issue of the Obesity journal about GLP-1 agonists versus bariatric surgery; monoacylglycerol O-acyltransferase 1 in mice; a behavioral weight-loss intervention; the Canberra Obesity Management Service; and macronutrient (im)balance in an obesogenic environment.
“I’m always excited to hear some talks that are outside of my comfort area to understand the mechanisms of obesity better,” concluded Dr. Allison.
A version of this article first appeared on Medscape.com.
ObesityWeek 2022 is the largest international conference on obesity, with over 100 sessions, and coincides with the 40th anniversary of the Obesity Society. Being held Nov. 1-4, it is a hybrid meeting that participants can attend onsite in sunny San Diego or virtually.
“The meeting offers a wide perspective, from basic science, all the way to public policy on studies of treatment and prevention of obesity,” program planning chair for ObesityWeek, Kelly C. Allison, PhD, said in an interview.
The Presidential Plenary session on Nov. 1 will kick off the meeting with “a series of 10-minute rapid talks on cutting-edge topics in the field,” noted Dr. Allison, who is also director, Center for Weight and Eating Disorders, Hospital of the University of Pennsylvania, and professor of psychiatry, University of Pennsylvania, both in Philadelphia.
Among others, Ania M. Jastreboff, MD, PhD, will speak about “New developments in anti-obesity pharmacotherapy,” and Theodore K. Kyle, RPh, MBA, will discuss “Reducing barriers to treatment: Insurance coverage.”
“We’re seeing some pretty effective antiobesity medication, but still they are not being covered by many insurances,” said Dr. Allison. Some clinicians might be hesitant to prescribe antiobesity medications, remembering older drugs that were pulled from the market for health concerns, and some patients may also have concerns, she speculated. There is a need for greater education about the current antiobesity drugs.
In his presidential address, Dan Bessesen, MD, professor of medicine at the University of Colorado at Denver, Aurora, will discuss “Regulation of body weight and adaptive responses to weight loss.”
Pediatric obesity is a major focus of this year›s conference too, Allison noted.
At 8 a.m on Nov. 3, The Obesity Society, the World Obesity Federation, the European Association for the Study of Obesity, and Obesity Canada will present a joint symposium, “International innovations in pediatric obesity,” with speakers from Canada, Australia, and Ireland discussing ongoing paradigm shifts in the prevention and treatment of pediatric obesity.
Two hours later, at a joint symposium by the American Academy of Pediatrics/The Obesity Society, attendees will get a behind-the-scenes look at the making of the new AAP Obesity Clinical Practice Guideline for children and adolescents with obesity.
The conference tracks reflect the broad scope of this event: Track 1: Metabolism and Integrative Physiology; Track 2: Neuroscience; Track 3: Interventional and Clinical Studies; Track 4: Population Health; Track 5: Clinical/Professional Practice; Track 6: Policy/Public Health, and a subtrack: Eradicating Treatment Barriers.
Dr. Allison highlighted the following oral presentations and posters about antiobesity drugs:
- “Once-weekly subcutaneous semaglutide 2.4 mg in adolescents with overweight or obesity,” with an extended Q&A session, Nov. 2.
- “Clinical outcomes with medication use in tertiary pediatric weight management program,” by Enayet and colleagues. Poster 030.
- “The metabolically healthy obese paradigm and liver fat content in the Fels longitudinal study,” by Garza and colleagues Oral 055, Nov. 2.
- “Phase 3 clinical trial of metformin for treatment of COVID-19 in adults with overweight and obesity,” by Bramante and colleagues. Oral 067, Nov. 3. This trial was published in the (N Engl J Med. 2022;387:599-610).
- “Glucagon/GLP-1 receptor dual agonist BI 456906 reduces bodyweight in patients with type 2 diabetes,” by Rosenstock and colleagues. Oral-063, Nov. 3.
- “A randomized controlled trial of naltrexone and bupropion and behavior therapy for binge-eating disorder,” by Grilo and colleagues. Oral 066, Nov. 3.
And on Nov. 4, researchers will present four oral abstracts about the dual glucose-dependent insulinotropic polypeptide and glucagonlike peptide–1 (GLP-1) receptor agonist tirzepatide (Mounjaro), which is approved for type 2 diabetes and now has fast track designation for weight loss from the Food and Drug Administration. Oral abstracts 109, 110, 111, and 112 cover weight loss with tirzepatide across different age groups, body mass indexes, and comorbidities, as well as quality of life.
Dr. Allison also highlighted the following presentations that cover other diverse topics:
- Family-based treatment: “Pilot study to inform a randomized controlled trial of HeLP: Obesity prevention & treatment for the entire Hispanic family,” by Haemer and colleagues. Oral 029. November 2.
- Bariatric surgery: “Long-term outcomes of laparoscopic sleeve gastrectomy from 2010-2016: A nationwide cohort study,” Oral 014. Nov. 2.
- Prevention/public health: “Impact of positive and negative front-of-package food labels in a randomized experiment,” by Grummon and colleagues. Oral 068. Nov. 3.
- Time-restricted eating: “Effects of 8-hour time restricted eating for weight loss over 12 months,” by Gabel and colleagues. Oral 102. Nov. 4.
- Patient management: “Identifying interprofessional drivers of practice gaps in the management of patients with obesity,” by Robinson and colleagues. Poster 055.
On Nov. 4, researchers will present five winning papers that will be published in the December issue of the Obesity journal about GLP-1 agonists versus bariatric surgery; monoacylglycerol O-acyltransferase 1 in mice; a behavioral weight-loss intervention; the Canberra Obesity Management Service; and macronutrient (im)balance in an obesogenic environment.
“I’m always excited to hear some talks that are outside of my comfort area to understand the mechanisms of obesity better,” concluded Dr. Allison.
A version of this article first appeared on Medscape.com.