User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
What’s next for COVID? Here’s what to know
As holiday celebrations wind down in the United States, COVID is on the rise.
Will there be another winter surge? If so, can we minimize it? How big a role might the boosters play in that? Are more mandates coming, along with a return to closed offices and businesses? Read on for a look at the latest info.
Cases, hospitalizations, deaths
As of Dec. 27, the latest statistics, the Centers for Disease Control and Prevention reports more than 487,000 weekly cases, compared to about 265,000 for the week ending Oct. 12. On average, 4,938 people were admitted to the hospital daily from Dec. 19 to 25, down about 6% from the 5,257 admitted daily the week before.
Deaths totaled 2,952 weekly as of Dec. 21, up from 2,699 on Dec. 14.
“What’s sobering overall is still seeing about 400 deaths a day in the U.S.,” said Peter Chin-Hong, MD, professor of medicine and infectious disease specialist at the University of California, San Francisco. “It’s still very high.”
As of Dec. 17, the variants predominating are BQ.1, BQ.1.1, and XBB. Experts said they are paying close attention to XBB, which is increasing quickly in the Northeast.
Predicting a winter surge
Experts tracking the pandemic agree there will be a surge.
“We are in the midst of it now,” said Eric Topol, MD, founder and director of the Scripps Research Translational Institute, La Jolla, Calif., and editor-in-chief of Medscape (MDedge’s sister site). “It’s not nearly like what we’ve had in Omicron or other waves; it’s not as severe. But it’s being particularly felt by seniors.”
One bit of good news: “Outside of that group it doesn’t look like – so far – it is going to be as bad a wave [as in the past],” Dr. Topol said.
Predicting the extent of the post-holiday surge “is the billion-dollar question right now,” said Katelyn Jetelina, PhD, a San Diego epidemiologist and author of the newsletter Your Local Epidemiologist.
“Much of these waves are not being driven by subvariants of concern but rather behavior,” she said.
People are opening up their social networks to gather for celebrations and family time. That’s unique to this winter, she said.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
Others point out that the surge doesn’t involve just COVID.
“We are expecting a Christmas surge and we are concerned it might be a triple surge,” said William Schaffner, MD, professor of infectious diseases at Vanderbilt University, Nashville, Tenn., referring to the rising cases of flu and RSV (respiratory syncytial virus).
Dr. Jetelina shares that concern, worrying that those illnesses may be what overwhelms hospital capacity.
Another wild card is the situation in China. With the easing of China’s “zero COVID” policies, cases there are rising dramatically. Some models are predicting up to 1 million COVID deaths could occur in China in 2023. (The United States is now requiring travelers from China to show a negative COVID test before entering. Italy and Japan have taken similar measures.)
“The suffering that is going to occur in China is not good news at all,” Dr. Topol said. “We are going to be seeing that for many weeks if not months ahead.”
Theoretically, uncontained spread such as what is expected there could generate a whole new family of variants, he said. But “the main hit is going to be in China,” he predicted. “But it’s hard to project with accuracy.”
“China is 20% of the global population, so we can’t ignore it,” Dr. Jetelina said. “The question is, what’s the probability of a subvariant of concern coming from China? I think the probability is pretty low, but the possibility is there.”
What happens with cases in China may “throw a wrench” in the transition from pandemic to endemic, Dr. Chin-Hong said. But even if the rising cases in China do result in a new variant, “there’s so much T cell and B cell immunity [here], your average person is still not going to get seriously ill, even if the variant looks really scary.”
Minimizing the damage
Experts echo the same advice on stemming the surge, especially for adults who are 65 or older: Get the bivalent booster, and get it now.
“The same with the influenza vaccine,” Dr. Schaffner said.
Both the booster vaccine and the flu vaccine have been underused this year, he said. “It’s part of the general vaccine fatigue.”
The low uptake of the booster vaccine is concerning, Dr. Topol said, especially among adults aged 65 and older, the age group most vulnerable to severe disease. Just 35.7% of U.S. adults 65 and older have gotten the booster, according to the CDC. Dr. Topol calls that a tragedy.
Younger people have not taken to the booster, either. Overall, only 14.1% of people aged 5 and up have gotten an updated booster dose, according to the CDC.
Recent studies find value in the boosters. One study looked only at adults age 65 or older, finding that the bivalent booster reduced the risk of hospitalization by 84% compared to someone not vaccinated, and 73% compared to someone who had received only the monovalent vaccine. Another study of adults found those who had gotten the bivalent were less likely to need COVID-related emergency room care or urgent care.
In a Dec. 21 report in the New England Journal of Medicine, researchers took plasma samples from people who had gotten either one or two monovalent boosters or the bivalent to determine how well they worked against the circulating Omicron subvariants BA.1, BA.5, BA.2.75.2, BQ.1.1, and XBB. The bivalent worked better than the monovalent against all the Omicron subvariants, but especially against BA.2.75.2, BQ.1.1, and XBB.
Rapid testing can help minimize transmission. On Dec. 15, the Biden administration announced its Winter Preparedness Plan, urging Americans to test before and after travel as well as indoor visiting with vulnerable individuals, providing another round of free at-home tests, continuing to make community testing available and continuing to provide vaccines.
Besides the general precautions, Dr. Schaffner suggested: “Look at yourself. Who are you? If you are older than 65, or have underlying illness or are immunocompromised, or are pregnant, please put your mask back on. And think about social distancing. It might be time to worship at home and stream a movie,” instead of going to the theaters, he said.
Back to mandates?
On Dec. 9, the New York City Commissioner of Health and Mental Hygiene urged a return to masking indoors, saying people “should” mask up, including in schools, stores, offices, and when in crowded outdoor settings.
On the same date, the County of Los Angeles Public Health urged a return to masking for everyone aged 2 and older when indoors, including at schools, in transit, or in work sites when around others.
While the CDC order requiring masks on public transportation is no longer in effect, the agency continues to recommend that those using public transportation do so.
But some are taking that further. In Philadelphia, for example, School Superintendent Tony B. Watlington Sr., EdD, announced before the winter break that indoor masking would be required for all students and staff for the first 2 weeks of school return, through Jan. 13, citing guidance from the Philadelphia Department of Public Health.
Universal masking in schools does reduce COVID transmission, as a study published in late November suggests. After Massachusetts dropped the statewide universal masking policy in public schools in February 2022, researchers compared the incidence of COVID in 70 school districts there that dropped the mandate with two school districts that kept it. In the 15 weeks after the policy was rescinded, the lifting of the mandate was linked with an additional 44.9 cases of COVID per 1,000 students and staff. That corresponded to an estimated 11,901 cases and to nearly 30% of the cases in all districts during that time.
That said, experts see mandates as the exception rather than the rule, at least for now, citing public backlash against mandates to mask or follow other restrictions.
“Mandating, we know, it shuts people off,” Dr. Topol said. “It’s unenforceable. If you have a very strong recommendation, that’s probably as good as you’re going to be able to do right now.”
There may be communities where mandates go over better than others, Dr. Schaffner said, such as communities where people have confidence in their public health authorities.
Glimmers of hope
Despite uncertainties, experts offered some not-so-dismal perspectives as well.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
A version of this article first appeared on WebMD.com.
As holiday celebrations wind down in the United States, COVID is on the rise.
Will there be another winter surge? If so, can we minimize it? How big a role might the boosters play in that? Are more mandates coming, along with a return to closed offices and businesses? Read on for a look at the latest info.
Cases, hospitalizations, deaths
As of Dec. 27, the latest statistics, the Centers for Disease Control and Prevention reports more than 487,000 weekly cases, compared to about 265,000 for the week ending Oct. 12. On average, 4,938 people were admitted to the hospital daily from Dec. 19 to 25, down about 6% from the 5,257 admitted daily the week before.
Deaths totaled 2,952 weekly as of Dec. 21, up from 2,699 on Dec. 14.
“What’s sobering overall is still seeing about 400 deaths a day in the U.S.,” said Peter Chin-Hong, MD, professor of medicine and infectious disease specialist at the University of California, San Francisco. “It’s still very high.”
As of Dec. 17, the variants predominating are BQ.1, BQ.1.1, and XBB. Experts said they are paying close attention to XBB, which is increasing quickly in the Northeast.
Predicting a winter surge
Experts tracking the pandemic agree there will be a surge.
“We are in the midst of it now,” said Eric Topol, MD, founder and director of the Scripps Research Translational Institute, La Jolla, Calif., and editor-in-chief of Medscape (MDedge’s sister site). “It’s not nearly like what we’ve had in Omicron or other waves; it’s not as severe. But it’s being particularly felt by seniors.”
One bit of good news: “Outside of that group it doesn’t look like – so far – it is going to be as bad a wave [as in the past],” Dr. Topol said.
Predicting the extent of the post-holiday surge “is the billion-dollar question right now,” said Katelyn Jetelina, PhD, a San Diego epidemiologist and author of the newsletter Your Local Epidemiologist.
“Much of these waves are not being driven by subvariants of concern but rather behavior,” she said.
People are opening up their social networks to gather for celebrations and family time. That’s unique to this winter, she said.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
Others point out that the surge doesn’t involve just COVID.
“We are expecting a Christmas surge and we are concerned it might be a triple surge,” said William Schaffner, MD, professor of infectious diseases at Vanderbilt University, Nashville, Tenn., referring to the rising cases of flu and RSV (respiratory syncytial virus).
Dr. Jetelina shares that concern, worrying that those illnesses may be what overwhelms hospital capacity.
Another wild card is the situation in China. With the easing of China’s “zero COVID” policies, cases there are rising dramatically. Some models are predicting up to 1 million COVID deaths could occur in China in 2023. (The United States is now requiring travelers from China to show a negative COVID test before entering. Italy and Japan have taken similar measures.)
“The suffering that is going to occur in China is not good news at all,” Dr. Topol said. “We are going to be seeing that for many weeks if not months ahead.”
Theoretically, uncontained spread such as what is expected there could generate a whole new family of variants, he said. But “the main hit is going to be in China,” he predicted. “But it’s hard to project with accuracy.”
“China is 20% of the global population, so we can’t ignore it,” Dr. Jetelina said. “The question is, what’s the probability of a subvariant of concern coming from China? I think the probability is pretty low, but the possibility is there.”
What happens with cases in China may “throw a wrench” in the transition from pandemic to endemic, Dr. Chin-Hong said. But even if the rising cases in China do result in a new variant, “there’s so much T cell and B cell immunity [here], your average person is still not going to get seriously ill, even if the variant looks really scary.”
Minimizing the damage
Experts echo the same advice on stemming the surge, especially for adults who are 65 or older: Get the bivalent booster, and get it now.
“The same with the influenza vaccine,” Dr. Schaffner said.
Both the booster vaccine and the flu vaccine have been underused this year, he said. “It’s part of the general vaccine fatigue.”
The low uptake of the booster vaccine is concerning, Dr. Topol said, especially among adults aged 65 and older, the age group most vulnerable to severe disease. Just 35.7% of U.S. adults 65 and older have gotten the booster, according to the CDC. Dr. Topol calls that a tragedy.
Younger people have not taken to the booster, either. Overall, only 14.1% of people aged 5 and up have gotten an updated booster dose, according to the CDC.
Recent studies find value in the boosters. One study looked only at adults age 65 or older, finding that the bivalent booster reduced the risk of hospitalization by 84% compared to someone not vaccinated, and 73% compared to someone who had received only the monovalent vaccine. Another study of adults found those who had gotten the bivalent were less likely to need COVID-related emergency room care or urgent care.
In a Dec. 21 report in the New England Journal of Medicine, researchers took plasma samples from people who had gotten either one or two monovalent boosters or the bivalent to determine how well they worked against the circulating Omicron subvariants BA.1, BA.5, BA.2.75.2, BQ.1.1, and XBB. The bivalent worked better than the monovalent against all the Omicron subvariants, but especially against BA.2.75.2, BQ.1.1, and XBB.
Rapid testing can help minimize transmission. On Dec. 15, the Biden administration announced its Winter Preparedness Plan, urging Americans to test before and after travel as well as indoor visiting with vulnerable individuals, providing another round of free at-home tests, continuing to make community testing available and continuing to provide vaccines.
Besides the general precautions, Dr. Schaffner suggested: “Look at yourself. Who are you? If you are older than 65, or have underlying illness or are immunocompromised, or are pregnant, please put your mask back on. And think about social distancing. It might be time to worship at home and stream a movie,” instead of going to the theaters, he said.
Back to mandates?
On Dec. 9, the New York City Commissioner of Health and Mental Hygiene urged a return to masking indoors, saying people “should” mask up, including in schools, stores, offices, and when in crowded outdoor settings.
On the same date, the County of Los Angeles Public Health urged a return to masking for everyone aged 2 and older when indoors, including at schools, in transit, or in work sites when around others.
While the CDC order requiring masks on public transportation is no longer in effect, the agency continues to recommend that those using public transportation do so.
But some are taking that further. In Philadelphia, for example, School Superintendent Tony B. Watlington Sr., EdD, announced before the winter break that indoor masking would be required for all students and staff for the first 2 weeks of school return, through Jan. 13, citing guidance from the Philadelphia Department of Public Health.
Universal masking in schools does reduce COVID transmission, as a study published in late November suggests. After Massachusetts dropped the statewide universal masking policy in public schools in February 2022, researchers compared the incidence of COVID in 70 school districts there that dropped the mandate with two school districts that kept it. In the 15 weeks after the policy was rescinded, the lifting of the mandate was linked with an additional 44.9 cases of COVID per 1,000 students and staff. That corresponded to an estimated 11,901 cases and to nearly 30% of the cases in all districts during that time.
That said, experts see mandates as the exception rather than the rule, at least for now, citing public backlash against mandates to mask or follow other restrictions.
“Mandating, we know, it shuts people off,” Dr. Topol said. “It’s unenforceable. If you have a very strong recommendation, that’s probably as good as you’re going to be able to do right now.”
There may be communities where mandates go over better than others, Dr. Schaffner said, such as communities where people have confidence in their public health authorities.
Glimmers of hope
Despite uncertainties, experts offered some not-so-dismal perspectives as well.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
A version of this article first appeared on WebMD.com.
As holiday celebrations wind down in the United States, COVID is on the rise.
Will there be another winter surge? If so, can we minimize it? How big a role might the boosters play in that? Are more mandates coming, along with a return to closed offices and businesses? Read on for a look at the latest info.
Cases, hospitalizations, deaths
As of Dec. 27, the latest statistics, the Centers for Disease Control and Prevention reports more than 487,000 weekly cases, compared to about 265,000 for the week ending Oct. 12. On average, 4,938 people were admitted to the hospital daily from Dec. 19 to 25, down about 6% from the 5,257 admitted daily the week before.
Deaths totaled 2,952 weekly as of Dec. 21, up from 2,699 on Dec. 14.
“What’s sobering overall is still seeing about 400 deaths a day in the U.S.,” said Peter Chin-Hong, MD, professor of medicine and infectious disease specialist at the University of California, San Francisco. “It’s still very high.”
As of Dec. 17, the variants predominating are BQ.1, BQ.1.1, and XBB. Experts said they are paying close attention to XBB, which is increasing quickly in the Northeast.
Predicting a winter surge
Experts tracking the pandemic agree there will be a surge.
“We are in the midst of it now,” said Eric Topol, MD, founder and director of the Scripps Research Translational Institute, La Jolla, Calif., and editor-in-chief of Medscape (MDedge’s sister site). “It’s not nearly like what we’ve had in Omicron or other waves; it’s not as severe. But it’s being particularly felt by seniors.”
One bit of good news: “Outside of that group it doesn’t look like – so far – it is going to be as bad a wave [as in the past],” Dr. Topol said.
Predicting the extent of the post-holiday surge “is the billion-dollar question right now,” said Katelyn Jetelina, PhD, a San Diego epidemiologist and author of the newsletter Your Local Epidemiologist.
“Much of these waves are not being driven by subvariants of concern but rather behavior,” she said.
People are opening up their social networks to gather for celebrations and family time. That’s unique to this winter, she said.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
Others point out that the surge doesn’t involve just COVID.
“We are expecting a Christmas surge and we are concerned it might be a triple surge,” said William Schaffner, MD, professor of infectious diseases at Vanderbilt University, Nashville, Tenn., referring to the rising cases of flu and RSV (respiratory syncytial virus).
Dr. Jetelina shares that concern, worrying that those illnesses may be what overwhelms hospital capacity.
Another wild card is the situation in China. With the easing of China’s “zero COVID” policies, cases there are rising dramatically. Some models are predicting up to 1 million COVID deaths could occur in China in 2023. (The United States is now requiring travelers from China to show a negative COVID test before entering. Italy and Japan have taken similar measures.)
“The suffering that is going to occur in China is not good news at all,” Dr. Topol said. “We are going to be seeing that for many weeks if not months ahead.”
Theoretically, uncontained spread such as what is expected there could generate a whole new family of variants, he said. But “the main hit is going to be in China,” he predicted. “But it’s hard to project with accuracy.”
“China is 20% of the global population, so we can’t ignore it,” Dr. Jetelina said. “The question is, what’s the probability of a subvariant of concern coming from China? I think the probability is pretty low, but the possibility is there.”
What happens with cases in China may “throw a wrench” in the transition from pandemic to endemic, Dr. Chin-Hong said. But even if the rising cases in China do result in a new variant, “there’s so much T cell and B cell immunity [here], your average person is still not going to get seriously ill, even if the variant looks really scary.”
Minimizing the damage
Experts echo the same advice on stemming the surge, especially for adults who are 65 or older: Get the bivalent booster, and get it now.
“The same with the influenza vaccine,” Dr. Schaffner said.
Both the booster vaccine and the flu vaccine have been underused this year, he said. “It’s part of the general vaccine fatigue.”
The low uptake of the booster vaccine is concerning, Dr. Topol said, especially among adults aged 65 and older, the age group most vulnerable to severe disease. Just 35.7% of U.S. adults 65 and older have gotten the booster, according to the CDC. Dr. Topol calls that a tragedy.
Younger people have not taken to the booster, either. Overall, only 14.1% of people aged 5 and up have gotten an updated booster dose, according to the CDC.
Recent studies find value in the boosters. One study looked only at adults age 65 or older, finding that the bivalent booster reduced the risk of hospitalization by 84% compared to someone not vaccinated, and 73% compared to someone who had received only the monovalent vaccine. Another study of adults found those who had gotten the bivalent were less likely to need COVID-related emergency room care or urgent care.
In a Dec. 21 report in the New England Journal of Medicine, researchers took plasma samples from people who had gotten either one or two monovalent boosters or the bivalent to determine how well they worked against the circulating Omicron subvariants BA.1, BA.5, BA.2.75.2, BQ.1.1, and XBB. The bivalent worked better than the monovalent against all the Omicron subvariants, but especially against BA.2.75.2, BQ.1.1, and XBB.
Rapid testing can help minimize transmission. On Dec. 15, the Biden administration announced its Winter Preparedness Plan, urging Americans to test before and after travel as well as indoor visiting with vulnerable individuals, providing another round of free at-home tests, continuing to make community testing available and continuing to provide vaccines.
Besides the general precautions, Dr. Schaffner suggested: “Look at yourself. Who are you? If you are older than 65, or have underlying illness or are immunocompromised, or are pregnant, please put your mask back on. And think about social distancing. It might be time to worship at home and stream a movie,” instead of going to the theaters, he said.
Back to mandates?
On Dec. 9, the New York City Commissioner of Health and Mental Hygiene urged a return to masking indoors, saying people “should” mask up, including in schools, stores, offices, and when in crowded outdoor settings.
On the same date, the County of Los Angeles Public Health urged a return to masking for everyone aged 2 and older when indoors, including at schools, in transit, or in work sites when around others.
While the CDC order requiring masks on public transportation is no longer in effect, the agency continues to recommend that those using public transportation do so.
But some are taking that further. In Philadelphia, for example, School Superintendent Tony B. Watlington Sr., EdD, announced before the winter break that indoor masking would be required for all students and staff for the first 2 weeks of school return, through Jan. 13, citing guidance from the Philadelphia Department of Public Health.
Universal masking in schools does reduce COVID transmission, as a study published in late November suggests. After Massachusetts dropped the statewide universal masking policy in public schools in February 2022, researchers compared the incidence of COVID in 70 school districts there that dropped the mandate with two school districts that kept it. In the 15 weeks after the policy was rescinded, the lifting of the mandate was linked with an additional 44.9 cases of COVID per 1,000 students and staff. That corresponded to an estimated 11,901 cases and to nearly 30% of the cases in all districts during that time.
That said, experts see mandates as the exception rather than the rule, at least for now, citing public backlash against mandates to mask or follow other restrictions.
“Mandating, we know, it shuts people off,” Dr. Topol said. “It’s unenforceable. If you have a very strong recommendation, that’s probably as good as you’re going to be able to do right now.”
There may be communities where mandates go over better than others, Dr. Schaffner said, such as communities where people have confidence in their public health authorities.
Glimmers of hope
Despite uncertainties, experts offered some not-so-dismal perspectives as well.
“I think our numbers will continue to go up, but certainly not like 2021 or 2020,” Dr. Chin-Hong said.
A version of this article first appeared on WebMD.com.
Medical practice gave 8,000 patients cancer for Christmas
We wish you a merry Christmas and a happy heart failure
Does anyone really like it when places of business send out cards or messages for the holidays? A card from a truly small family business is one thing, but when you start getting emails from multibillion dollar corporations, it feels a bit dishonest. And that’s not even mentioning the potential blowback when things go wrong.
Now, you may wonder how a company could possibly mess up something so simple. “We wish you a merry Christmas and a happy New Year.” Not that difficult. Unless you’re Askern Medical Practice in Doncaster, England. Instead of expressing a simple expression of joy for the holiday season, Askern informed all 8,000 of its patients that they had aggressive lung cancer with metastases and they needed to fill out a DS1500 form, which entitles terminal patients to certain benefits.
It only took an hour for Askern to recognize its mistake and send a second text apologizing and adding in the appropriate season’s greetings, but obviously the damage was done. Presumably patients who were last at the doctor to have their cold treated were able to shrug off the text, or simply didn’t see it before the correction came through, but obviously many patients had concerns directly related to cancer and panicked. They called in but were by and large unable to reach anyone at the practice. Some patients close by even went to center itself to clear things up.
One patient, Mr. Carl Chegwin, raised an excellent point about the debacle: “What if that message was meant for someone, and then they are told it’s a Christmas message, then again told, ‘Oh no, that was actually meant for you?’ ” The old double backtrack into yes, you actually do have cancer has got to be a candidate for worst Christmas gift of all. Yes, even worse than socks.
Genes know it: You are when you eat
There’s been a lot of recent research on intermittent fasting and what it can and can’t do for one’s health. Much of it has focused on participants’ metabolic rates, but a study just published in Cell Metabolism shows how time-restricted feeding (TRF) has an impact on gene expression, the process through which genes are activated and respond to their environment by creating proteins.
The research conducted by Satchidananda Panda, PhD, of the Salk Institute and his team involved two groups of mice, one with free access to food and the other with a daily 9-hour feeding window. Analysis of tissue samples collected from 22 organ groups revealed that nearly 80% of mouse genes responded to TRF. Interestingly, 40% of the genes in the hypothalamus, adrenal gland, and pancreas, which handle hormone regulation, were affected, suggesting that TRF could potentially aid in diabetes and stress disorder management, the investigators said in a written statement.
The researchers also found that TRF aligned the circadian rhythms of multiple organs of the body, which brings sleep into the picture. “Time-restricted eating synchronized the circadian rhythms to have two major waves: one during fasting, and another just after eating. We suspect this allows the body to coordinate different processes,” said Dr. Panda, whose previous research looked at TRF in firefighters, who typically work on shift schedules.
Time-restricted eating, it appears, affects gene expression throughout the body and allows interconnected organ systems to work smoothly. It’s not just about eating. Go figure.
This group practice reduced stress for everyone
It’s been awhile since we checked in on the good folks at Maharishi International University in Fairfield, Iowa – fictional home of the Fighting Transcendentalists [MAHARISHI RULES!] – but we just have to mention their long-term effort to reduce the national stress.
Way back in the year 2000, a group from MIU began practicing transcendental meditation. The size of the group increased over the next few years and eventually reached 1,725 in 2006. That number is important because it represents the square root of 1% of the U.S. population. When that “transition threshold was achieved,” the university explained in a written statement, “all stress indicators immediately started decreasing.”
By stress indicators they mean the U.S. stress index, the mean of eight variables – murder, rape, assault, robbery, infant mortality, drug deaths, vehicle fatalities, and child deaths by injuries – that the study investigators used to track the effectiveness of the meditation program, they said in the World Journal of Social Science.
After 2011, “when the size of the group size began to decline the rate of decrease in stress slowed and then it reversed and began to increase,” MIU reported.
Coauthor Dr. Kenneth Cavanaugh of MIU explained the process: “This study used state-of-the-art methods of time series regression analysis for eliminating potential alternative explanations due to intrinsic preexisting trends and fluctuations in the data. We carefully studied potential alternative explanations in terms of changes in economic conditions, political leadership, population demographics, and policing strategies. None of these factors could account for the results.”
Since we here at LOTME are serious professional journalists, the use of quotes means we are not making this up. Here’s one more thing in quotes: “A grant for 75 million dollars from the Howard and Alice Settle Foundation provided stipends for participants to be in the group and provided funding to bring several hundred visiting [meditation] experts from India to further augment the MIU group.”
Who needs to make up stuff? Not us.
We wish you a merry Christmas and a happy heart failure
Does anyone really like it when places of business send out cards or messages for the holidays? A card from a truly small family business is one thing, but when you start getting emails from multibillion dollar corporations, it feels a bit dishonest. And that’s not even mentioning the potential blowback when things go wrong.
Now, you may wonder how a company could possibly mess up something so simple. “We wish you a merry Christmas and a happy New Year.” Not that difficult. Unless you’re Askern Medical Practice in Doncaster, England. Instead of expressing a simple expression of joy for the holiday season, Askern informed all 8,000 of its patients that they had aggressive lung cancer with metastases and they needed to fill out a DS1500 form, which entitles terminal patients to certain benefits.
It only took an hour for Askern to recognize its mistake and send a second text apologizing and adding in the appropriate season’s greetings, but obviously the damage was done. Presumably patients who were last at the doctor to have their cold treated were able to shrug off the text, or simply didn’t see it before the correction came through, but obviously many patients had concerns directly related to cancer and panicked. They called in but were by and large unable to reach anyone at the practice. Some patients close by even went to center itself to clear things up.
One patient, Mr. Carl Chegwin, raised an excellent point about the debacle: “What if that message was meant for someone, and then they are told it’s a Christmas message, then again told, ‘Oh no, that was actually meant for you?’ ” The old double backtrack into yes, you actually do have cancer has got to be a candidate for worst Christmas gift of all. Yes, even worse than socks.
Genes know it: You are when you eat
There’s been a lot of recent research on intermittent fasting and what it can and can’t do for one’s health. Much of it has focused on participants’ metabolic rates, but a study just published in Cell Metabolism shows how time-restricted feeding (TRF) has an impact on gene expression, the process through which genes are activated and respond to their environment by creating proteins.
The research conducted by Satchidananda Panda, PhD, of the Salk Institute and his team involved two groups of mice, one with free access to food and the other with a daily 9-hour feeding window. Analysis of tissue samples collected from 22 organ groups revealed that nearly 80% of mouse genes responded to TRF. Interestingly, 40% of the genes in the hypothalamus, adrenal gland, and pancreas, which handle hormone regulation, were affected, suggesting that TRF could potentially aid in diabetes and stress disorder management, the investigators said in a written statement.
The researchers also found that TRF aligned the circadian rhythms of multiple organs of the body, which brings sleep into the picture. “Time-restricted eating synchronized the circadian rhythms to have two major waves: one during fasting, and another just after eating. We suspect this allows the body to coordinate different processes,” said Dr. Panda, whose previous research looked at TRF in firefighters, who typically work on shift schedules.
Time-restricted eating, it appears, affects gene expression throughout the body and allows interconnected organ systems to work smoothly. It’s not just about eating. Go figure.
This group practice reduced stress for everyone
It’s been awhile since we checked in on the good folks at Maharishi International University in Fairfield, Iowa – fictional home of the Fighting Transcendentalists [MAHARISHI RULES!] – but we just have to mention their long-term effort to reduce the national stress.
Way back in the year 2000, a group from MIU began practicing transcendental meditation. The size of the group increased over the next few years and eventually reached 1,725 in 2006. That number is important because it represents the square root of 1% of the U.S. population. When that “transition threshold was achieved,” the university explained in a written statement, “all stress indicators immediately started decreasing.”
By stress indicators they mean the U.S. stress index, the mean of eight variables – murder, rape, assault, robbery, infant mortality, drug deaths, vehicle fatalities, and child deaths by injuries – that the study investigators used to track the effectiveness of the meditation program, they said in the World Journal of Social Science.
After 2011, “when the size of the group size began to decline the rate of decrease in stress slowed and then it reversed and began to increase,” MIU reported.
Coauthor Dr. Kenneth Cavanaugh of MIU explained the process: “This study used state-of-the-art methods of time series regression analysis for eliminating potential alternative explanations due to intrinsic preexisting trends and fluctuations in the data. We carefully studied potential alternative explanations in terms of changes in economic conditions, political leadership, population demographics, and policing strategies. None of these factors could account for the results.”
Since we here at LOTME are serious professional journalists, the use of quotes means we are not making this up. Here’s one more thing in quotes: “A grant for 75 million dollars from the Howard and Alice Settle Foundation provided stipends for participants to be in the group and provided funding to bring several hundred visiting [meditation] experts from India to further augment the MIU group.”
Who needs to make up stuff? Not us.
We wish you a merry Christmas and a happy heart failure
Does anyone really like it when places of business send out cards or messages for the holidays? A card from a truly small family business is one thing, but when you start getting emails from multibillion dollar corporations, it feels a bit dishonest. And that’s not even mentioning the potential blowback when things go wrong.
Now, you may wonder how a company could possibly mess up something so simple. “We wish you a merry Christmas and a happy New Year.” Not that difficult. Unless you’re Askern Medical Practice in Doncaster, England. Instead of expressing a simple expression of joy for the holiday season, Askern informed all 8,000 of its patients that they had aggressive lung cancer with metastases and they needed to fill out a DS1500 form, which entitles terminal patients to certain benefits.
It only took an hour for Askern to recognize its mistake and send a second text apologizing and adding in the appropriate season’s greetings, but obviously the damage was done. Presumably patients who were last at the doctor to have their cold treated were able to shrug off the text, or simply didn’t see it before the correction came through, but obviously many patients had concerns directly related to cancer and panicked. They called in but were by and large unable to reach anyone at the practice. Some patients close by even went to center itself to clear things up.
One patient, Mr. Carl Chegwin, raised an excellent point about the debacle: “What if that message was meant for someone, and then they are told it’s a Christmas message, then again told, ‘Oh no, that was actually meant for you?’ ” The old double backtrack into yes, you actually do have cancer has got to be a candidate for worst Christmas gift of all. Yes, even worse than socks.
Genes know it: You are when you eat
There’s been a lot of recent research on intermittent fasting and what it can and can’t do for one’s health. Much of it has focused on participants’ metabolic rates, but a study just published in Cell Metabolism shows how time-restricted feeding (TRF) has an impact on gene expression, the process through which genes are activated and respond to their environment by creating proteins.
The research conducted by Satchidananda Panda, PhD, of the Salk Institute and his team involved two groups of mice, one with free access to food and the other with a daily 9-hour feeding window. Analysis of tissue samples collected from 22 organ groups revealed that nearly 80% of mouse genes responded to TRF. Interestingly, 40% of the genes in the hypothalamus, adrenal gland, and pancreas, which handle hormone regulation, were affected, suggesting that TRF could potentially aid in diabetes and stress disorder management, the investigators said in a written statement.
The researchers also found that TRF aligned the circadian rhythms of multiple organs of the body, which brings sleep into the picture. “Time-restricted eating synchronized the circadian rhythms to have two major waves: one during fasting, and another just after eating. We suspect this allows the body to coordinate different processes,” said Dr. Panda, whose previous research looked at TRF in firefighters, who typically work on shift schedules.
Time-restricted eating, it appears, affects gene expression throughout the body and allows interconnected organ systems to work smoothly. It’s not just about eating. Go figure.
This group practice reduced stress for everyone
It’s been awhile since we checked in on the good folks at Maharishi International University in Fairfield, Iowa – fictional home of the Fighting Transcendentalists [MAHARISHI RULES!] – but we just have to mention their long-term effort to reduce the national stress.
Way back in the year 2000, a group from MIU began practicing transcendental meditation. The size of the group increased over the next few years and eventually reached 1,725 in 2006. That number is important because it represents the square root of 1% of the U.S. population. When that “transition threshold was achieved,” the university explained in a written statement, “all stress indicators immediately started decreasing.”
By stress indicators they mean the U.S. stress index, the mean of eight variables – murder, rape, assault, robbery, infant mortality, drug deaths, vehicle fatalities, and child deaths by injuries – that the study investigators used to track the effectiveness of the meditation program, they said in the World Journal of Social Science.
After 2011, “when the size of the group size began to decline the rate of decrease in stress slowed and then it reversed and began to increase,” MIU reported.
Coauthor Dr. Kenneth Cavanaugh of MIU explained the process: “This study used state-of-the-art methods of time series regression analysis for eliminating potential alternative explanations due to intrinsic preexisting trends and fluctuations in the data. We carefully studied potential alternative explanations in terms of changes in economic conditions, political leadership, population demographics, and policing strategies. None of these factors could account for the results.”
Since we here at LOTME are serious professional journalists, the use of quotes means we are not making this up. Here’s one more thing in quotes: “A grant for 75 million dollars from the Howard and Alice Settle Foundation provided stipends for participants to be in the group and provided funding to bring several hundred visiting [meditation] experts from India to further augment the MIU group.”
Who needs to make up stuff? Not us.
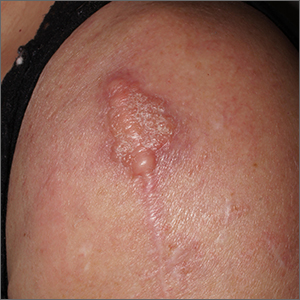
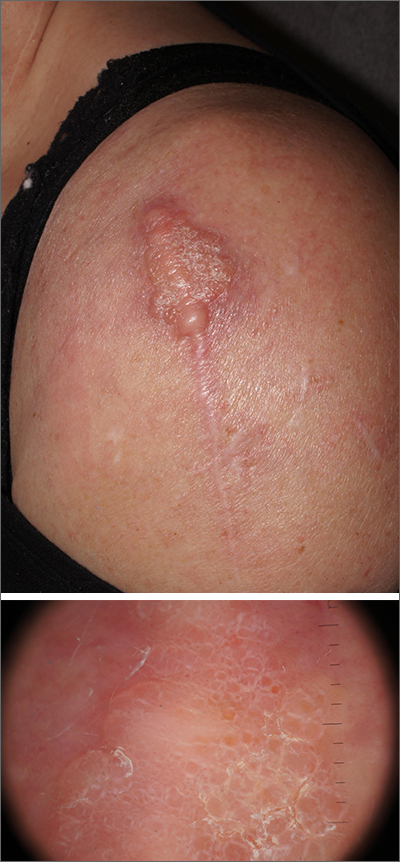
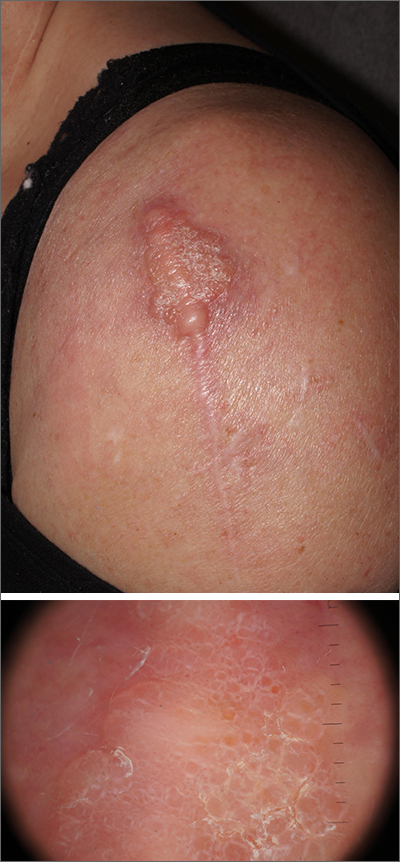
Scar overgrowth
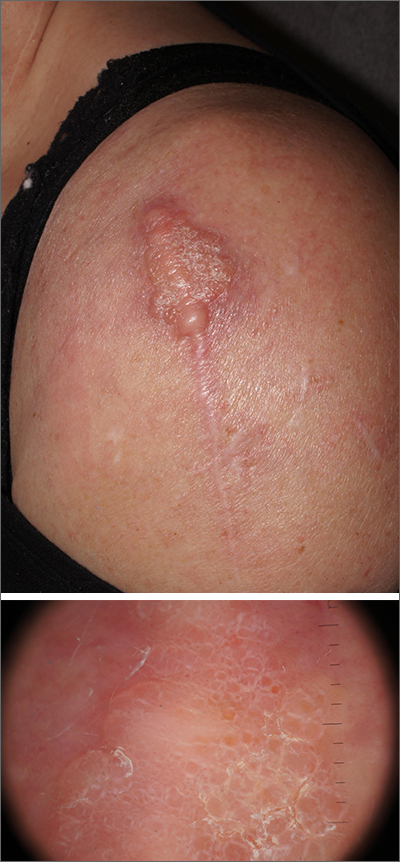
Dermatopathology was consistent with a diagnosis of cutaneous myxoma (CM). There are very few dermoscopic descriptions of CM in the literature, so diagnostic features are not established. However, the absence of more diagnostic features of basal cell carcinoma or squamous cell carcinoma (SCC) increases the likelihood of a rare diagnosis, such as CM.
CMs are rare benign neoplasms that manifest most commonly in young adults as small (< 1 cm) flesh-colored to blue papules on the head, neck, and trunk. The size of this particular CM was an outlier. CMs may be associated with Carney Complex (CNC), a rare inherited syndrome that has been linked to multiple endocrine neoplasias—namely, pituitary adenomas, testicular Sertoli cell tumors, thyroid tumors, and cardiac atrial myxomas.1 Additionally, in CNC, lentigines and multiple blue nevi develop on the skin and mucosal surfaces.
The differential diagnosis for a large, pink to flesh-colored nodule of this size includes benign histiocytoma, SCC, CM, and dermatofibrosarcoma protuberans. Benign histiocytomas and SCCs are much more common than CM. Clinical features only hint at the correct diagnosis, which must be made histologically.
Patients with CMs benefit from ongoing dermatology surveillance to monitor for the development of atypical nevi or new CMs. In this case, a wide excision with generous margins was planned with plastic surgery. (CMs have been reported to recur after surgery, which is why wide margins are essential.)
Additionally, 2 factors prompted an echocardiogram: the association between CMs and possible cardiac tumors and the patient’s need to undergo future orthopedic surgery under general anesthesia. No cardiac tumors were visible on echocardiogram. Thyroid imaging and genetic evaluation were planned but not completed.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Zou Y, Billings SD. Myxoid cutaneous tumors: a review. J Cutan Pathol. 2016;43:903-18. doi: 10.1111/cup.12749.
Dermatopathology was consistent with a diagnosis of cutaneous myxoma (CM). There are very few dermoscopic descriptions of CM in the literature, so diagnostic features are not established. However, the absence of more diagnostic features of basal cell carcinoma or squamous cell carcinoma (SCC) increases the likelihood of a rare diagnosis, such as CM.
CMs are rare benign neoplasms that manifest most commonly in young adults as small (< 1 cm) flesh-colored to blue papules on the head, neck, and trunk. The size of this particular CM was an outlier. CMs may be associated with Carney Complex (CNC), a rare inherited syndrome that has been linked to multiple endocrine neoplasias—namely, pituitary adenomas, testicular Sertoli cell tumors, thyroid tumors, and cardiac atrial myxomas.1 Additionally, in CNC, lentigines and multiple blue nevi develop on the skin and mucosal surfaces.
The differential diagnosis for a large, pink to flesh-colored nodule of this size includes benign histiocytoma, SCC, CM, and dermatofibrosarcoma protuberans. Benign histiocytomas and SCCs are much more common than CM. Clinical features only hint at the correct diagnosis, which must be made histologically.
Patients with CMs benefit from ongoing dermatology surveillance to monitor for the development of atypical nevi or new CMs. In this case, a wide excision with generous margins was planned with plastic surgery. (CMs have been reported to recur after surgery, which is why wide margins are essential.)
Additionally, 2 factors prompted an echocardiogram: the association between CMs and possible cardiac tumors and the patient’s need to undergo future orthopedic surgery under general anesthesia. No cardiac tumors were visible on echocardiogram. Thyroid imaging and genetic evaluation were planned but not completed.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
Dermatopathology was consistent with a diagnosis of cutaneous myxoma (CM). There are very few dermoscopic descriptions of CM in the literature, so diagnostic features are not established. However, the absence of more diagnostic features of basal cell carcinoma or squamous cell carcinoma (SCC) increases the likelihood of a rare diagnosis, such as CM.
CMs are rare benign neoplasms that manifest most commonly in young adults as small (< 1 cm) flesh-colored to blue papules on the head, neck, and trunk. The size of this particular CM was an outlier. CMs may be associated with Carney Complex (CNC), a rare inherited syndrome that has been linked to multiple endocrine neoplasias—namely, pituitary adenomas, testicular Sertoli cell tumors, thyroid tumors, and cardiac atrial myxomas.1 Additionally, in CNC, lentigines and multiple blue nevi develop on the skin and mucosal surfaces.
The differential diagnosis for a large, pink to flesh-colored nodule of this size includes benign histiocytoma, SCC, CM, and dermatofibrosarcoma protuberans. Benign histiocytomas and SCCs are much more common than CM. Clinical features only hint at the correct diagnosis, which must be made histologically.
Patients with CMs benefit from ongoing dermatology surveillance to monitor for the development of atypical nevi or new CMs. In this case, a wide excision with generous margins was planned with plastic surgery. (CMs have been reported to recur after surgery, which is why wide margins are essential.)
Additionally, 2 factors prompted an echocardiogram: the association between CMs and possible cardiac tumors and the patient’s need to undergo future orthopedic surgery under general anesthesia. No cardiac tumors were visible on echocardiogram. Thyroid imaging and genetic evaluation were planned but not completed.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Zou Y, Billings SD. Myxoid cutaneous tumors: a review. J Cutan Pathol. 2016;43:903-18. doi: 10.1111/cup.12749.
1. Zou Y, Billings SD. Myxoid cutaneous tumors: a review. J Cutan Pathol. 2016;43:903-18. doi: 10.1111/cup.12749.
Best diets in 2023: Mediterranean diet wins again
After all, weight loss usually lands one of the top spots on New Year’s resolution surveys.
And just in time, there’s guidance to pick the best plan, as U.S. News & World Report’s annual rankings of the best diet plans were released on Jan. 3.
Once again, the Mediterranean diet, which emphasizes fruits, vegetables, olive oil, and fish, got the top spot, as best diet overall. It’s the sixth consecutive year for that win. But many other diets got top marks as well.
In 2023, U.S. News, with the help of more than 30 nutritionists, doctors, and epidemiologists, ranked 24 diets in several categories to help people find a plan that meets their goals, whether it’s finding the best weight loss diet, easiest one to follow, or plans for other goals, such as managing diabetes or heart disease. Two new categories were added: Best Diets for Bone & Joint Health and Best Family-Friendly Diets.
In previous years, the publication ranked 40 diets. Even if a diet is no longer ranked, its profile with detailed information remains on the site.
“Each year we ask ourselves what we can do better or differently next time,” said Gretel Schueller, managing editor of health for U.S. News. When the publication got feedback from their experts this year, they had requests to consider sustainability of diets and whether they meet a busy family’s needs, in addition to considering many other factors.
This year’s report ranks plans in 11 categories.
The winners and the categories:
Best diets overall
After the Mediterranean diet, two others tied for second place:
- DASH (Dietary Approaches to Stop Hypertension) diet, which fights high blood pressure and emphasizes fruits, vegetables, whole grains, lean protein, and low-fat dairy.
- Flexitarian diet, which focuses on fruits, vegetables, and other healthy foods but also allows occasional meat.
Best weight-loss diets
WW, formerly known as Weight Watchers, got first place. The plan emphasizes not only weight loss but healthier eating and regular activity. The Points program, which assigns specific points to foods, with a daily Points budget, is more personalized than in the past.
- DASH got second place.
- Mayo Clinic Diet and TLC diet tied for third place. The Mayo Clinic Diet focuses on fruits, vegetables, and whole grains. It helps people improve their eating habits. The TLC diet (Therapeutic Lifestyle Changes) focuses on vegetables, fruit, lean protein, and reducing cholesterol levels.
Best fast weight-loss diets
The keto diet got first place. It’s a high-fat, low-carb diet that aims to achieve weight loss through fat burning. Four others tied for second place:
- Atkins, a diet created by the cardiologist Robert Atkins, which begins with very few carbs and then recommends progressively eating more until the weight loss goal is achieved
- Nutrisystem, a commercial program that includes prepackaged meals and focuses on high-protein, lower-glycemic foods to stabilize blood sugar levels
- Optavia, a plan focused on low-carb, low-calorie foods and including fortified meal replacements
- SlimFast Diet, a plan of shakes, smoothies, and meal bars to replace two of three meals a day
Best diets for healthy eating
- Mediterranean
- DASH
- Flexitarian
Best heart-healthy diets
- DASH
- Mediterranean
- Flexitarian and Ornish tied for third. The Ornish Diet focuses on plant-based and whole foods and limiting animal products. It recommends daily exercise and stress reduction.
Best diets for diabetes
- DASH
- Mediterranean
- Flexitarian
Best diets for bone and joint health
DASH and Mediterranean are in a first-place tie, followed by the flexitarian diet.
Best family-friendly diets
This category has a three-way tie: the flexitarian, Mediterranean, and TLC diets.
Best plant-based diets
Mediterranean was first, then flexitarian and the MIND diet. The MIND diet combines the DASH and Mediterranean diets and focuses on “brain-healthy” foods.
Easiest diets to follow
Flexitarian and TLC tied for first, followed by a tie between DASH and Mediterranean.
Best diet programs (formerly called commercial plans)
- WW
- There was a tie for second place between Jenny Craig and Noom, the latter of which focuses on low-calorie foods, with personalized calorie ranges and coaching to help meet goals.
Methodology
A variety of factors were considered, such as whether a diet includes all food groups, how easy it is to follow, whether it can be customized to meet cultural and personal preferences, and if it has a realistic timeline for weight loss.
Response from diet plans
Representatives from two plans that received mixed reviews in the rankings responded.
Jenny Craig was ranked second for best diet program but much lower for family friendly, landing at 22nd place of 24.
“Our program is designed to address the needs of the individual through personalized experiences,” Jenny Craig CEO Mandy Dowson said. “We have many families that participate in our program together but are still evaluated separately to determine appropriate individual goals.”
Its high ranking for best diet program reflects feedback from satisfied members, she said. Among advances will be the new Jenny Fresh program, a line of entrées prepared fresh and delivered to customers’ doors.
Atkins got second place for best fast weight loss but ranked near the bottom for best overall, best weight loss, diabetes, healthy eating, and heart health. In response, Colette Heimowitz, vice president of nutrition and education for Simply Good Foods, which makes Atkins’s food products, said that low-carb eating approaches are a viable option for anyone today.
“There are more than 130 independent, peer-reviewed published studies that show the efficacy and safety of low-carb eating,” she said. “The studies have been conducted for several decades and counting.”
Expert perspective
Samantha Cassetty, a registered dietitian, nutritionist, and wellness expert in New York and author of Sugar Shock, reviewed the report for this news organization. She was not involved in the rankings.
“I think what this shows you is, the best diet overall is also the best for various conditions,” she said. For instance, the Mediterranean, the No. 1 overall, also got high ranking for diabetes, heart health, and bone and joint health.
For consumers trying to lose weight: “If you see fast weight loss, that should be a red flag. A healthy diet for weight loss is one you can sustain,” she said.
She’s not a fan of the programs with prepackaged foods. “It takes the guesswork out, but the portion sizes tend to be unsatisfying. They don’t teach you how to deal with some of the challenges [such as realizing an ‘ideal’ portion size].”
How to use the report
Ms. Schueller’s advice: “Recognize that no diet fits everyone.” When considering which plan to choose, she suggests thinking long-term.
“Whatever we choose has to work in the long run,” she said.
Consumers should consider expenses, meal prep time, and whether the diet fits their lifestyle.
Ideally, she said, the best diet “teaches you smart food preparation and how to make healthy choices, allows the flexibility to be social and eat with groups, whether family or friends.”
Before choosing a diet to follow, consult a medical professional for input on the decision, U.S. News cautioned.
A version of this article first appeared on Medscape.com.
After all, weight loss usually lands one of the top spots on New Year’s resolution surveys.
And just in time, there’s guidance to pick the best plan, as U.S. News & World Report’s annual rankings of the best diet plans were released on Jan. 3.
Once again, the Mediterranean diet, which emphasizes fruits, vegetables, olive oil, and fish, got the top spot, as best diet overall. It’s the sixth consecutive year for that win. But many other diets got top marks as well.
In 2023, U.S. News, with the help of more than 30 nutritionists, doctors, and epidemiologists, ranked 24 diets in several categories to help people find a plan that meets their goals, whether it’s finding the best weight loss diet, easiest one to follow, or plans for other goals, such as managing diabetes or heart disease. Two new categories were added: Best Diets for Bone & Joint Health and Best Family-Friendly Diets.
In previous years, the publication ranked 40 diets. Even if a diet is no longer ranked, its profile with detailed information remains on the site.
“Each year we ask ourselves what we can do better or differently next time,” said Gretel Schueller, managing editor of health for U.S. News. When the publication got feedback from their experts this year, they had requests to consider sustainability of diets and whether they meet a busy family’s needs, in addition to considering many other factors.
This year’s report ranks plans in 11 categories.
The winners and the categories:
Best diets overall
After the Mediterranean diet, two others tied for second place:
- DASH (Dietary Approaches to Stop Hypertension) diet, which fights high blood pressure and emphasizes fruits, vegetables, whole grains, lean protein, and low-fat dairy.
- Flexitarian diet, which focuses on fruits, vegetables, and other healthy foods but also allows occasional meat.
Best weight-loss diets
WW, formerly known as Weight Watchers, got first place. The plan emphasizes not only weight loss but healthier eating and regular activity. The Points program, which assigns specific points to foods, with a daily Points budget, is more personalized than in the past.
- DASH got second place.
- Mayo Clinic Diet and TLC diet tied for third place. The Mayo Clinic Diet focuses on fruits, vegetables, and whole grains. It helps people improve their eating habits. The TLC diet (Therapeutic Lifestyle Changes) focuses on vegetables, fruit, lean protein, and reducing cholesterol levels.
Best fast weight-loss diets
The keto diet got first place. It’s a high-fat, low-carb diet that aims to achieve weight loss through fat burning. Four others tied for second place:
- Atkins, a diet created by the cardiologist Robert Atkins, which begins with very few carbs and then recommends progressively eating more until the weight loss goal is achieved
- Nutrisystem, a commercial program that includes prepackaged meals and focuses on high-protein, lower-glycemic foods to stabilize blood sugar levels
- Optavia, a plan focused on low-carb, low-calorie foods and including fortified meal replacements
- SlimFast Diet, a plan of shakes, smoothies, and meal bars to replace two of three meals a day
Best diets for healthy eating
- Mediterranean
- DASH
- Flexitarian
Best heart-healthy diets
- DASH
- Mediterranean
- Flexitarian and Ornish tied for third. The Ornish Diet focuses on plant-based and whole foods and limiting animal products. It recommends daily exercise and stress reduction.
Best diets for diabetes
- DASH
- Mediterranean
- Flexitarian
Best diets for bone and joint health
DASH and Mediterranean are in a first-place tie, followed by the flexitarian diet.
Best family-friendly diets
This category has a three-way tie: the flexitarian, Mediterranean, and TLC diets.
Best plant-based diets
Mediterranean was first, then flexitarian and the MIND diet. The MIND diet combines the DASH and Mediterranean diets and focuses on “brain-healthy” foods.
Easiest diets to follow
Flexitarian and TLC tied for first, followed by a tie between DASH and Mediterranean.
Best diet programs (formerly called commercial plans)
- WW
- There was a tie for second place between Jenny Craig and Noom, the latter of which focuses on low-calorie foods, with personalized calorie ranges and coaching to help meet goals.
Methodology
A variety of factors were considered, such as whether a diet includes all food groups, how easy it is to follow, whether it can be customized to meet cultural and personal preferences, and if it has a realistic timeline for weight loss.
Response from diet plans
Representatives from two plans that received mixed reviews in the rankings responded.
Jenny Craig was ranked second for best diet program but much lower for family friendly, landing at 22nd place of 24.
“Our program is designed to address the needs of the individual through personalized experiences,” Jenny Craig CEO Mandy Dowson said. “We have many families that participate in our program together but are still evaluated separately to determine appropriate individual goals.”
Its high ranking for best diet program reflects feedback from satisfied members, she said. Among advances will be the new Jenny Fresh program, a line of entrées prepared fresh and delivered to customers’ doors.
Atkins got second place for best fast weight loss but ranked near the bottom for best overall, best weight loss, diabetes, healthy eating, and heart health. In response, Colette Heimowitz, vice president of nutrition and education for Simply Good Foods, which makes Atkins’s food products, said that low-carb eating approaches are a viable option for anyone today.
“There are more than 130 independent, peer-reviewed published studies that show the efficacy and safety of low-carb eating,” she said. “The studies have been conducted for several decades and counting.”
Expert perspective
Samantha Cassetty, a registered dietitian, nutritionist, and wellness expert in New York and author of Sugar Shock, reviewed the report for this news organization. She was not involved in the rankings.
“I think what this shows you is, the best diet overall is also the best for various conditions,” she said. For instance, the Mediterranean, the No. 1 overall, also got high ranking for diabetes, heart health, and bone and joint health.
For consumers trying to lose weight: “If you see fast weight loss, that should be a red flag. A healthy diet for weight loss is one you can sustain,” she said.
She’s not a fan of the programs with prepackaged foods. “It takes the guesswork out, but the portion sizes tend to be unsatisfying. They don’t teach you how to deal with some of the challenges [such as realizing an ‘ideal’ portion size].”
How to use the report
Ms. Schueller’s advice: “Recognize that no diet fits everyone.” When considering which plan to choose, she suggests thinking long-term.
“Whatever we choose has to work in the long run,” she said.
Consumers should consider expenses, meal prep time, and whether the diet fits their lifestyle.
Ideally, she said, the best diet “teaches you smart food preparation and how to make healthy choices, allows the flexibility to be social and eat with groups, whether family or friends.”
Before choosing a diet to follow, consult a medical professional for input on the decision, U.S. News cautioned.
A version of this article first appeared on Medscape.com.
After all, weight loss usually lands one of the top spots on New Year’s resolution surveys.
And just in time, there’s guidance to pick the best plan, as U.S. News & World Report’s annual rankings of the best diet plans were released on Jan. 3.
Once again, the Mediterranean diet, which emphasizes fruits, vegetables, olive oil, and fish, got the top spot, as best diet overall. It’s the sixth consecutive year for that win. But many other diets got top marks as well.
In 2023, U.S. News, with the help of more than 30 nutritionists, doctors, and epidemiologists, ranked 24 diets in several categories to help people find a plan that meets their goals, whether it’s finding the best weight loss diet, easiest one to follow, or plans for other goals, such as managing diabetes or heart disease. Two new categories were added: Best Diets for Bone & Joint Health and Best Family-Friendly Diets.
In previous years, the publication ranked 40 diets. Even if a diet is no longer ranked, its profile with detailed information remains on the site.
“Each year we ask ourselves what we can do better or differently next time,” said Gretel Schueller, managing editor of health for U.S. News. When the publication got feedback from their experts this year, they had requests to consider sustainability of diets and whether they meet a busy family’s needs, in addition to considering many other factors.
This year’s report ranks plans in 11 categories.
The winners and the categories:
Best diets overall
After the Mediterranean diet, two others tied for second place:
- DASH (Dietary Approaches to Stop Hypertension) diet, which fights high blood pressure and emphasizes fruits, vegetables, whole grains, lean protein, and low-fat dairy.
- Flexitarian diet, which focuses on fruits, vegetables, and other healthy foods but also allows occasional meat.
Best weight-loss diets
WW, formerly known as Weight Watchers, got first place. The plan emphasizes not only weight loss but healthier eating and regular activity. The Points program, which assigns specific points to foods, with a daily Points budget, is more personalized than in the past.
- DASH got second place.
- Mayo Clinic Diet and TLC diet tied for third place. The Mayo Clinic Diet focuses on fruits, vegetables, and whole grains. It helps people improve their eating habits. The TLC diet (Therapeutic Lifestyle Changes) focuses on vegetables, fruit, lean protein, and reducing cholesterol levels.
Best fast weight-loss diets
The keto diet got first place. It’s a high-fat, low-carb diet that aims to achieve weight loss through fat burning. Four others tied for second place:
- Atkins, a diet created by the cardiologist Robert Atkins, which begins with very few carbs and then recommends progressively eating more until the weight loss goal is achieved
- Nutrisystem, a commercial program that includes prepackaged meals and focuses on high-protein, lower-glycemic foods to stabilize blood sugar levels
- Optavia, a plan focused on low-carb, low-calorie foods and including fortified meal replacements
- SlimFast Diet, a plan of shakes, smoothies, and meal bars to replace two of three meals a day
Best diets for healthy eating
- Mediterranean
- DASH
- Flexitarian
Best heart-healthy diets
- DASH
- Mediterranean
- Flexitarian and Ornish tied for third. The Ornish Diet focuses on plant-based and whole foods and limiting animal products. It recommends daily exercise and stress reduction.
Best diets for diabetes
- DASH
- Mediterranean
- Flexitarian
Best diets for bone and joint health
DASH and Mediterranean are in a first-place tie, followed by the flexitarian diet.
Best family-friendly diets
This category has a three-way tie: the flexitarian, Mediterranean, and TLC diets.
Best plant-based diets
Mediterranean was first, then flexitarian and the MIND diet. The MIND diet combines the DASH and Mediterranean diets and focuses on “brain-healthy” foods.
Easiest diets to follow
Flexitarian and TLC tied for first, followed by a tie between DASH and Mediterranean.
Best diet programs (formerly called commercial plans)
- WW
- There was a tie for second place between Jenny Craig and Noom, the latter of which focuses on low-calorie foods, with personalized calorie ranges and coaching to help meet goals.
Methodology
A variety of factors were considered, such as whether a diet includes all food groups, how easy it is to follow, whether it can be customized to meet cultural and personal preferences, and if it has a realistic timeline for weight loss.
Response from diet plans
Representatives from two plans that received mixed reviews in the rankings responded.
Jenny Craig was ranked second for best diet program but much lower for family friendly, landing at 22nd place of 24.
“Our program is designed to address the needs of the individual through personalized experiences,” Jenny Craig CEO Mandy Dowson said. “We have many families that participate in our program together but are still evaluated separately to determine appropriate individual goals.”
Its high ranking for best diet program reflects feedback from satisfied members, she said. Among advances will be the new Jenny Fresh program, a line of entrées prepared fresh and delivered to customers’ doors.
Atkins got second place for best fast weight loss but ranked near the bottom for best overall, best weight loss, diabetes, healthy eating, and heart health. In response, Colette Heimowitz, vice president of nutrition and education for Simply Good Foods, which makes Atkins’s food products, said that low-carb eating approaches are a viable option for anyone today.
“There are more than 130 independent, peer-reviewed published studies that show the efficacy and safety of low-carb eating,” she said. “The studies have been conducted for several decades and counting.”
Expert perspective
Samantha Cassetty, a registered dietitian, nutritionist, and wellness expert in New York and author of Sugar Shock, reviewed the report for this news organization. She was not involved in the rankings.
“I think what this shows you is, the best diet overall is also the best for various conditions,” she said. For instance, the Mediterranean, the No. 1 overall, also got high ranking for diabetes, heart health, and bone and joint health.
For consumers trying to lose weight: “If you see fast weight loss, that should be a red flag. A healthy diet for weight loss is one you can sustain,” she said.
She’s not a fan of the programs with prepackaged foods. “It takes the guesswork out, but the portion sizes tend to be unsatisfying. They don’t teach you how to deal with some of the challenges [such as realizing an ‘ideal’ portion size].”
How to use the report
Ms. Schueller’s advice: “Recognize that no diet fits everyone.” When considering which plan to choose, she suggests thinking long-term.
“Whatever we choose has to work in the long run,” she said.
Consumers should consider expenses, meal prep time, and whether the diet fits their lifestyle.
Ideally, she said, the best diet “teaches you smart food preparation and how to make healthy choices, allows the flexibility to be social and eat with groups, whether family or friends.”
Before choosing a diet to follow, consult a medical professional for input on the decision, U.S. News cautioned.
A version of this article first appeared on Medscape.com.
Children and COVID: New cases fell as the old year ended
The end of 2022 saw a drop in new COVID-19 cases in children, even as rates of emergency department visits continued upward trends that began in late October.
New cases for the week of Dec. 23-29 fell for the first time since late November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP/CHA analysis of publicly available state data differs somewhat from figures reported by the Centers for Disease Control and Prevention, which has new cases for the latest available week, Dec.18-24, at just over 27,000 after 3 straight weeks of declines from a count of almost 63,000 for the week ending Nov. 26. The CDC, however, updates previously reported data on a regular basis, so that 27,000 is likely to increase in the coming weeks.
The CDC line on the graph also shows a peak for the week of Oct. 30 to Nov. 5 when new cases reached almost 50,000, compared with almost 30,000 reported for the week of Oct. 28 to Nov. 3 by the AAP and CHA in their report of state-level data. The AAP and CHA put the total number of child COVID cases since the start of the pandemic at 15.2 million as of Dec. 29, while the CDC reports 16.2 million cases as of Dec. 28.
There have been 1,975 deaths from COVID-19 in children aged 0-17 years, according to the CDC, which amounts to just over 0.2% of all COVID deaths for which age group data were available.
CDC data on emergency department visits involving diagnosed COVID-19 have been rising since late October. In children aged 0-11 years, for example, COVID was involved in 1.0% of ED visits (7-day average) as late as Nov. 4, but by Dec. 27 that rate was 2.6%. Children aged 12-15 years went from 0.6% on Oct. 28 to 1.5% on Dec. 27, while 16- to 17-year-olds had ED visit rates of 0.6% on Oct. 19 and 1.7% on Dec. 27, the CDC said on its COVID Data Tracker.
New hospital admissions with diagnosed COVID, which had been following the same upward trend as ED visits since late October, halted that rise in children aged 0-17 years and have gone no higher than 0.29 per 100,000 population since Dec. 9, the CDC data show.
The end of 2022 saw a drop in new COVID-19 cases in children, even as rates of emergency department visits continued upward trends that began in late October.
New cases for the week of Dec. 23-29 fell for the first time since late November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP/CHA analysis of publicly available state data differs somewhat from figures reported by the Centers for Disease Control and Prevention, which has new cases for the latest available week, Dec.18-24, at just over 27,000 after 3 straight weeks of declines from a count of almost 63,000 for the week ending Nov. 26. The CDC, however, updates previously reported data on a regular basis, so that 27,000 is likely to increase in the coming weeks.
The CDC line on the graph also shows a peak for the week of Oct. 30 to Nov. 5 when new cases reached almost 50,000, compared with almost 30,000 reported for the week of Oct. 28 to Nov. 3 by the AAP and CHA in their report of state-level data. The AAP and CHA put the total number of child COVID cases since the start of the pandemic at 15.2 million as of Dec. 29, while the CDC reports 16.2 million cases as of Dec. 28.
There have been 1,975 deaths from COVID-19 in children aged 0-17 years, according to the CDC, which amounts to just over 0.2% of all COVID deaths for which age group data were available.
CDC data on emergency department visits involving diagnosed COVID-19 have been rising since late October. In children aged 0-11 years, for example, COVID was involved in 1.0% of ED visits (7-day average) as late as Nov. 4, but by Dec. 27 that rate was 2.6%. Children aged 12-15 years went from 0.6% on Oct. 28 to 1.5% on Dec. 27, while 16- to 17-year-olds had ED visit rates of 0.6% on Oct. 19 and 1.7% on Dec. 27, the CDC said on its COVID Data Tracker.
New hospital admissions with diagnosed COVID, which had been following the same upward trend as ED visits since late October, halted that rise in children aged 0-17 years and have gone no higher than 0.29 per 100,000 population since Dec. 9, the CDC data show.
The end of 2022 saw a drop in new COVID-19 cases in children, even as rates of emergency department visits continued upward trends that began in late October.
New cases for the week of Dec. 23-29 fell for the first time since late November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP/CHA analysis of publicly available state data differs somewhat from figures reported by the Centers for Disease Control and Prevention, which has new cases for the latest available week, Dec.18-24, at just over 27,000 after 3 straight weeks of declines from a count of almost 63,000 for the week ending Nov. 26. The CDC, however, updates previously reported data on a regular basis, so that 27,000 is likely to increase in the coming weeks.
The CDC line on the graph also shows a peak for the week of Oct. 30 to Nov. 5 when new cases reached almost 50,000, compared with almost 30,000 reported for the week of Oct. 28 to Nov. 3 by the AAP and CHA in their report of state-level data. The AAP and CHA put the total number of child COVID cases since the start of the pandemic at 15.2 million as of Dec. 29, while the CDC reports 16.2 million cases as of Dec. 28.
There have been 1,975 deaths from COVID-19 in children aged 0-17 years, according to the CDC, which amounts to just over 0.2% of all COVID deaths for which age group data were available.
CDC data on emergency department visits involving diagnosed COVID-19 have been rising since late October. In children aged 0-11 years, for example, COVID was involved in 1.0% of ED visits (7-day average) as late as Nov. 4, but by Dec. 27 that rate was 2.6%. Children aged 12-15 years went from 0.6% on Oct. 28 to 1.5% on Dec. 27, while 16- to 17-year-olds had ED visit rates of 0.6% on Oct. 19 and 1.7% on Dec. 27, the CDC said on its COVID Data Tracker.
New hospital admissions with diagnosed COVID, which had been following the same upward trend as ED visits since late October, halted that rise in children aged 0-17 years and have gone no higher than 0.29 per 100,000 population since Dec. 9, the CDC data show.
Cervical cancer rise in White women: A ‘canary in the coal mine’
Cervical cancer appears to be rising more rapidly in White women than in Black women in the United States, according to two independent studies. Researchers puzzling over this counterintuitive finding say that, if true, the findings may be a “canary in the coal mine,” signaling problems with U.S. health care that go way beyond women’s health.
Cervical cancer incidence in the United States has plateaued since 2010 and now stands at 7.5 per 100,000 people. Well-known disparities exist: Compared with White women, Black women are more likely to have distant-stage disease at diagnosis and more commonly die of their cancer.
However, two unconnected studies published in the past 5 months suggest that White women are catching up fast.
Cervical cancer rates in White women aged 30-34 are rising 2.8% a year, but holding steady for Black women, according to a recent study led by Ashish A. Deshmukh, PhD, of the Medical University of South Carolina, Charleston. His team analyzed the 2001-2019 National Program of Cancer Registries (NPCR) and Surveillance, Epidemiology, and End Results (SEER) dataset, which covers 98% of the U.S. population and 227,062 cervical cancer cases.
These findings were echoed by an analysis of the same database for 2001-2018 by the University of California, Los Angeles (UCLA), suggesting that distant-stage cervical cancer (defined as disease that has spread to the bladder and/or rectum at diagnosis) is climbing 1.69% a year in White people versus 0.67% in Black individuals.
The UCLA researchers, headed by Alex Francoeur, MD, a resident in the department of obstetrics and gynecology, found that disparities were most stark in adenocarcinoma, with an annual increase of 3.40% a year among White women and 1.71% in Black women.
Such findings have equity researchers scratching their heads. In cancer, it’s rare to see evidence that Black patients are doing better than their White counterparts.
One theoretical explanation is that the data are flawed, Ahmedin Jemal, DVM, PhD, senior vice president of surveillance and health equity science at the American Cancer Society, told this news organization. For example, the UCLA analysis may have been fogged by changes in staging definitions over time, Dr. Jemal said, although this would not explain the racial disparities per se.
Dr. Deshmukh stands by his data and said that, for him, the message is clear: “If rising incidence is not for localized-stage disease, but for advanced stages, that means it’s attributable to lack of screening,” he told this news organization.
However, this ‘simple’ explanation generates even more questions, Dr. Deshmukh said: “Screening is not a one-time procedure [but] a spectrum of timely cervical precancer treatment if [required]. We don’t know when exactly non-Hispanic White women are falling behind on that spectrum.”
The UCLA study supports Dr. Deshmukh’s conclusions. Using data from the Behavioral Risk Factor Surveillance System to calculate trends in “nonguideline screening,” the researchers found that White women were almost twice as likely to report that they were not following screening guidelines compared with Black women over the period of 2001-2016 (26.6% vs. 13.8%; P < .001).
“It’s not an artifact, it’s real,” said Timothy Rebbeck, PhD, the Vincent L. Gregory Jr. Professor of Cancer Prevention at Harvard TH Chan School of Public Health, Boston, who was not an author of either study and was approached for comment.
“The data are correct but there are so many things going on that might explain these patterns,” he told this news organization.
“This is a great example of complex changes in our social system, political system, health care system that are having really clear, measurable effects,” Dr. Rebbeck said. “Cervical cancer is almost a canary in the coal mine for some of this because it’s so preventable.”
(The saying “canary in a coal mine” is a warning of danger or trouble ahead. It comes from the time when coal miners would carry a caged canary down into the tunnels to warn them of noxious gases, which would kill the bird but give men time to escape.)
For example, Dr. Rebbeck said, recent turmoil in U.S. health care has left many people distrustful of the system. Although he acknowledged this was “high speculation,” he suggested that some women may have become less willing to participate in any mass health care intervention because of their political beliefs.
The UCLA study found that distant cervical cancer was rising fastest in middle-aged White women in the U.S. South, at a rate of 4.5% per year (P < .001).
Dr. Rebbeck also suggested that Medicaid expansion – the broadening of health insurance coverage in some states since the Affordable Care Act in 2014 – could be implicated. Of the 11 states that have not yet expanded Medicaid, eight are in the South.
“White populations who are in states that didn’t expand Medicaid are not getting a lot of the standard treatment and care that you would expect ...” Dr. Rebbeck said. “You could very well imagine that Medicaid nonexpanding states would have all kinds of patterns that would lead to more aggressive disease.”
In fact, there is already evidence that Medicaid expansion has affected racial disparities, disproportionately benefiting Black and Hispanic families, as for example, from an analysis of 65 studies by the Kaiser Family Foundation in 2020.
Commenting on these data, Dr. Rebbeck said, “Does that mean that the patterns of advanced cervical cancer had a smaller effect on Black women in this period because there was a greater shift in access to care? This is again a speculation, but it does fit with the ‘canary in a coal mine’ concept that advanced cervical cancer may be more rapidly influenced by health care access than other health conditions.”
The authors of the UCLA study suggested another explanation for their results: Differing enthusiasm for human papillomavirus (HPV) vaccination among White and Black families. The team also analyzed data on HPV vaccination, which offers protection against cervical cancer. The researchers found that vaccination rates were lowest, at 66.1%, among White teenagers aged 13-17 years, compared with Hispanics at 75.3%, Black teenagers at 74.6%, and Asians at 68.1%.
However, this theory was dismissed by both Dr. Jemal and Dr. Rebbeck due to timing. HPV vaccines have been around for approximately 15 years, so women who benefited (or didn’t benefit) from vaccination would be only in their late 20s today, they pointed out.
“Ninety-five percent of the cervical cancer cases we see now are in women who have not been vaccinated,” said Dr. Jemal, “So that’s out of the equation.”
Dr. Rebbeck agreed: “HPV may or may not be a thing here because it’s [got] such a latency.”
HPV vaccination may be out of the picture, but what about the epidemiology of HPV itself? Could the virus directly or indirectly be boosting advanced cervical cancer in White women?
Dr. Deshmukh thinks that it might be doing so.
He published an analysis of 2000-2018 SEER data showing that U.S. counties with the highest incidences of HPV-associated cancers also had the highest levels of smoking.
Other recent data suggest that middle-aged White women in the United States are more likely to reach for a smoke than are Black women.
Dr. Deshmukh acknowledges that the link is speculative but reasonable: “We don’t know exactly what the impact of smoking would be in terms of ... the ability to clear HPV infection. It may inhibit apoptosis, promoting tumor growth. There’s no causal association. It’s a cofactor risk.”
Dr. Rebbeck is also suspicious that smoking patterns might be a factor, pointing out that “smoking is certainly associated with both health behaviors and advanced cervical cancer.”
Both Dr. Rebbeck and Dr. Deshmukh concluded that, at this point, we can only speculate on what’s driving the puzzling acceleration of cervical cancer in White women in the United States.
However, whether it’s political aversion to screening, smoking-boosted HPV infection, Medicaid expansion or lack of it, or something else, they all agree that this canary in the coal mine clearly needs urgent medical attention.
Dr. Rebbeck and Dr. Jemal have declared no conflicts of interest. Dr. Deshmukh has declared consultant or advisory roles for Merck and Value Analytics Labs. None of the authors of the UCLA study have declared competing interests.
A version of this article first appeared on Medscape.com.
Cervical cancer appears to be rising more rapidly in White women than in Black women in the United States, according to two independent studies. Researchers puzzling over this counterintuitive finding say that, if true, the findings may be a “canary in the coal mine,” signaling problems with U.S. health care that go way beyond women’s health.
Cervical cancer incidence in the United States has plateaued since 2010 and now stands at 7.5 per 100,000 people. Well-known disparities exist: Compared with White women, Black women are more likely to have distant-stage disease at diagnosis and more commonly die of their cancer.
However, two unconnected studies published in the past 5 months suggest that White women are catching up fast.
Cervical cancer rates in White women aged 30-34 are rising 2.8% a year, but holding steady for Black women, according to a recent study led by Ashish A. Deshmukh, PhD, of the Medical University of South Carolina, Charleston. His team analyzed the 2001-2019 National Program of Cancer Registries (NPCR) and Surveillance, Epidemiology, and End Results (SEER) dataset, which covers 98% of the U.S. population and 227,062 cervical cancer cases.
These findings were echoed by an analysis of the same database for 2001-2018 by the University of California, Los Angeles (UCLA), suggesting that distant-stage cervical cancer (defined as disease that has spread to the bladder and/or rectum at diagnosis) is climbing 1.69% a year in White people versus 0.67% in Black individuals.
The UCLA researchers, headed by Alex Francoeur, MD, a resident in the department of obstetrics and gynecology, found that disparities were most stark in adenocarcinoma, with an annual increase of 3.40% a year among White women and 1.71% in Black women.
Such findings have equity researchers scratching their heads. In cancer, it’s rare to see evidence that Black patients are doing better than their White counterparts.
One theoretical explanation is that the data are flawed, Ahmedin Jemal, DVM, PhD, senior vice president of surveillance and health equity science at the American Cancer Society, told this news organization. For example, the UCLA analysis may have been fogged by changes in staging definitions over time, Dr. Jemal said, although this would not explain the racial disparities per se.
Dr. Deshmukh stands by his data and said that, for him, the message is clear: “If rising incidence is not for localized-stage disease, but for advanced stages, that means it’s attributable to lack of screening,” he told this news organization.
However, this ‘simple’ explanation generates even more questions, Dr. Deshmukh said: “Screening is not a one-time procedure [but] a spectrum of timely cervical precancer treatment if [required]. We don’t know when exactly non-Hispanic White women are falling behind on that spectrum.”
The UCLA study supports Dr. Deshmukh’s conclusions. Using data from the Behavioral Risk Factor Surveillance System to calculate trends in “nonguideline screening,” the researchers found that White women were almost twice as likely to report that they were not following screening guidelines compared with Black women over the period of 2001-2016 (26.6% vs. 13.8%; P < .001).
“It’s not an artifact, it’s real,” said Timothy Rebbeck, PhD, the Vincent L. Gregory Jr. Professor of Cancer Prevention at Harvard TH Chan School of Public Health, Boston, who was not an author of either study and was approached for comment.
“The data are correct but there are so many things going on that might explain these patterns,” he told this news organization.
“This is a great example of complex changes in our social system, political system, health care system that are having really clear, measurable effects,” Dr. Rebbeck said. “Cervical cancer is almost a canary in the coal mine for some of this because it’s so preventable.”
(The saying “canary in a coal mine” is a warning of danger or trouble ahead. It comes from the time when coal miners would carry a caged canary down into the tunnels to warn them of noxious gases, which would kill the bird but give men time to escape.)
For example, Dr. Rebbeck said, recent turmoil in U.S. health care has left many people distrustful of the system. Although he acknowledged this was “high speculation,” he suggested that some women may have become less willing to participate in any mass health care intervention because of their political beliefs.
The UCLA study found that distant cervical cancer was rising fastest in middle-aged White women in the U.S. South, at a rate of 4.5% per year (P < .001).
Dr. Rebbeck also suggested that Medicaid expansion – the broadening of health insurance coverage in some states since the Affordable Care Act in 2014 – could be implicated. Of the 11 states that have not yet expanded Medicaid, eight are in the South.
“White populations who are in states that didn’t expand Medicaid are not getting a lot of the standard treatment and care that you would expect ...” Dr. Rebbeck said. “You could very well imagine that Medicaid nonexpanding states would have all kinds of patterns that would lead to more aggressive disease.”
In fact, there is already evidence that Medicaid expansion has affected racial disparities, disproportionately benefiting Black and Hispanic families, as for example, from an analysis of 65 studies by the Kaiser Family Foundation in 2020.
Commenting on these data, Dr. Rebbeck said, “Does that mean that the patterns of advanced cervical cancer had a smaller effect on Black women in this period because there was a greater shift in access to care? This is again a speculation, but it does fit with the ‘canary in a coal mine’ concept that advanced cervical cancer may be more rapidly influenced by health care access than other health conditions.”
The authors of the UCLA study suggested another explanation for their results: Differing enthusiasm for human papillomavirus (HPV) vaccination among White and Black families. The team also analyzed data on HPV vaccination, which offers protection against cervical cancer. The researchers found that vaccination rates were lowest, at 66.1%, among White teenagers aged 13-17 years, compared with Hispanics at 75.3%, Black teenagers at 74.6%, and Asians at 68.1%.
However, this theory was dismissed by both Dr. Jemal and Dr. Rebbeck due to timing. HPV vaccines have been around for approximately 15 years, so women who benefited (or didn’t benefit) from vaccination would be only in their late 20s today, they pointed out.
“Ninety-five percent of the cervical cancer cases we see now are in women who have not been vaccinated,” said Dr. Jemal, “So that’s out of the equation.”
Dr. Rebbeck agreed: “HPV may or may not be a thing here because it’s [got] such a latency.”
HPV vaccination may be out of the picture, but what about the epidemiology of HPV itself? Could the virus directly or indirectly be boosting advanced cervical cancer in White women?
Dr. Deshmukh thinks that it might be doing so.
He published an analysis of 2000-2018 SEER data showing that U.S. counties with the highest incidences of HPV-associated cancers also had the highest levels of smoking.
Other recent data suggest that middle-aged White women in the United States are more likely to reach for a smoke than are Black women.
Dr. Deshmukh acknowledges that the link is speculative but reasonable: “We don’t know exactly what the impact of smoking would be in terms of ... the ability to clear HPV infection. It may inhibit apoptosis, promoting tumor growth. There’s no causal association. It’s a cofactor risk.”
Dr. Rebbeck is also suspicious that smoking patterns might be a factor, pointing out that “smoking is certainly associated with both health behaviors and advanced cervical cancer.”
Both Dr. Rebbeck and Dr. Deshmukh concluded that, at this point, we can only speculate on what’s driving the puzzling acceleration of cervical cancer in White women in the United States.
However, whether it’s political aversion to screening, smoking-boosted HPV infection, Medicaid expansion or lack of it, or something else, they all agree that this canary in the coal mine clearly needs urgent medical attention.
Dr. Rebbeck and Dr. Jemal have declared no conflicts of interest. Dr. Deshmukh has declared consultant or advisory roles for Merck and Value Analytics Labs. None of the authors of the UCLA study have declared competing interests.
A version of this article first appeared on Medscape.com.
Cervical cancer appears to be rising more rapidly in White women than in Black women in the United States, according to two independent studies. Researchers puzzling over this counterintuitive finding say that, if true, the findings may be a “canary in the coal mine,” signaling problems with U.S. health care that go way beyond women’s health.
Cervical cancer incidence in the United States has plateaued since 2010 and now stands at 7.5 per 100,000 people. Well-known disparities exist: Compared with White women, Black women are more likely to have distant-stage disease at diagnosis and more commonly die of their cancer.
However, two unconnected studies published in the past 5 months suggest that White women are catching up fast.
Cervical cancer rates in White women aged 30-34 are rising 2.8% a year, but holding steady for Black women, according to a recent study led by Ashish A. Deshmukh, PhD, of the Medical University of South Carolina, Charleston. His team analyzed the 2001-2019 National Program of Cancer Registries (NPCR) and Surveillance, Epidemiology, and End Results (SEER) dataset, which covers 98% of the U.S. population and 227,062 cervical cancer cases.
These findings were echoed by an analysis of the same database for 2001-2018 by the University of California, Los Angeles (UCLA), suggesting that distant-stage cervical cancer (defined as disease that has spread to the bladder and/or rectum at diagnosis) is climbing 1.69% a year in White people versus 0.67% in Black individuals.
The UCLA researchers, headed by Alex Francoeur, MD, a resident in the department of obstetrics and gynecology, found that disparities were most stark in adenocarcinoma, with an annual increase of 3.40% a year among White women and 1.71% in Black women.
Such findings have equity researchers scratching their heads. In cancer, it’s rare to see evidence that Black patients are doing better than their White counterparts.
One theoretical explanation is that the data are flawed, Ahmedin Jemal, DVM, PhD, senior vice president of surveillance and health equity science at the American Cancer Society, told this news organization. For example, the UCLA analysis may have been fogged by changes in staging definitions over time, Dr. Jemal said, although this would not explain the racial disparities per se.
Dr. Deshmukh stands by his data and said that, for him, the message is clear: “If rising incidence is not for localized-stage disease, but for advanced stages, that means it’s attributable to lack of screening,” he told this news organization.
However, this ‘simple’ explanation generates even more questions, Dr. Deshmukh said: “Screening is not a one-time procedure [but] a spectrum of timely cervical precancer treatment if [required]. We don’t know when exactly non-Hispanic White women are falling behind on that spectrum.”
The UCLA study supports Dr. Deshmukh’s conclusions. Using data from the Behavioral Risk Factor Surveillance System to calculate trends in “nonguideline screening,” the researchers found that White women were almost twice as likely to report that they were not following screening guidelines compared with Black women over the period of 2001-2016 (26.6% vs. 13.8%; P < .001).
“It’s not an artifact, it’s real,” said Timothy Rebbeck, PhD, the Vincent L. Gregory Jr. Professor of Cancer Prevention at Harvard TH Chan School of Public Health, Boston, who was not an author of either study and was approached for comment.
“The data are correct but there are so many things going on that might explain these patterns,” he told this news organization.
“This is a great example of complex changes in our social system, political system, health care system that are having really clear, measurable effects,” Dr. Rebbeck said. “Cervical cancer is almost a canary in the coal mine for some of this because it’s so preventable.”
(The saying “canary in a coal mine” is a warning of danger or trouble ahead. It comes from the time when coal miners would carry a caged canary down into the tunnels to warn them of noxious gases, which would kill the bird but give men time to escape.)
For example, Dr. Rebbeck said, recent turmoil in U.S. health care has left many people distrustful of the system. Although he acknowledged this was “high speculation,” he suggested that some women may have become less willing to participate in any mass health care intervention because of their political beliefs.
The UCLA study found that distant cervical cancer was rising fastest in middle-aged White women in the U.S. South, at a rate of 4.5% per year (P < .001).
Dr. Rebbeck also suggested that Medicaid expansion – the broadening of health insurance coverage in some states since the Affordable Care Act in 2014 – could be implicated. Of the 11 states that have not yet expanded Medicaid, eight are in the South.
“White populations who are in states that didn’t expand Medicaid are not getting a lot of the standard treatment and care that you would expect ...” Dr. Rebbeck said. “You could very well imagine that Medicaid nonexpanding states would have all kinds of patterns that would lead to more aggressive disease.”
In fact, there is already evidence that Medicaid expansion has affected racial disparities, disproportionately benefiting Black and Hispanic families, as for example, from an analysis of 65 studies by the Kaiser Family Foundation in 2020.
Commenting on these data, Dr. Rebbeck said, “Does that mean that the patterns of advanced cervical cancer had a smaller effect on Black women in this period because there was a greater shift in access to care? This is again a speculation, but it does fit with the ‘canary in a coal mine’ concept that advanced cervical cancer may be more rapidly influenced by health care access than other health conditions.”
The authors of the UCLA study suggested another explanation for their results: Differing enthusiasm for human papillomavirus (HPV) vaccination among White and Black families. The team also analyzed data on HPV vaccination, which offers protection against cervical cancer. The researchers found that vaccination rates were lowest, at 66.1%, among White teenagers aged 13-17 years, compared with Hispanics at 75.3%, Black teenagers at 74.6%, and Asians at 68.1%.
However, this theory was dismissed by both Dr. Jemal and Dr. Rebbeck due to timing. HPV vaccines have been around for approximately 15 years, so women who benefited (or didn’t benefit) from vaccination would be only in their late 20s today, they pointed out.
“Ninety-five percent of the cervical cancer cases we see now are in women who have not been vaccinated,” said Dr. Jemal, “So that’s out of the equation.”
Dr. Rebbeck agreed: “HPV may or may not be a thing here because it’s [got] such a latency.”
HPV vaccination may be out of the picture, but what about the epidemiology of HPV itself? Could the virus directly or indirectly be boosting advanced cervical cancer in White women?
Dr. Deshmukh thinks that it might be doing so.
He published an analysis of 2000-2018 SEER data showing that U.S. counties with the highest incidences of HPV-associated cancers also had the highest levels of smoking.
Other recent data suggest that middle-aged White women in the United States are more likely to reach for a smoke than are Black women.
Dr. Deshmukh acknowledges that the link is speculative but reasonable: “We don’t know exactly what the impact of smoking would be in terms of ... the ability to clear HPV infection. It may inhibit apoptosis, promoting tumor growth. There’s no causal association. It’s a cofactor risk.”
Dr. Rebbeck is also suspicious that smoking patterns might be a factor, pointing out that “smoking is certainly associated with both health behaviors and advanced cervical cancer.”
Both Dr. Rebbeck and Dr. Deshmukh concluded that, at this point, we can only speculate on what’s driving the puzzling acceleration of cervical cancer in White women in the United States.
However, whether it’s political aversion to screening, smoking-boosted HPV infection, Medicaid expansion or lack of it, or something else, they all agree that this canary in the coal mine clearly needs urgent medical attention.
Dr. Rebbeck and Dr. Jemal have declared no conflicts of interest. Dr. Deshmukh has declared consultant or advisory roles for Merck and Value Analytics Labs. None of the authors of the UCLA study have declared competing interests.
A version of this article first appeared on Medscape.com.
SARS-CoV-2 seroprevalence grew rapidly in pandemic’s early waves
By August 2022, two-and-a-half years into the COVID-19 pandemic, most children as well as most adults under age 60 years had evidence of SARS-CoV-2 vaccination and/or infection, a Canadian seroprevalence study of almost 14,000 people over the first seven waves of the pandemic reports.
However, fewer than 50% people older than age 60, the age group most vulnerable to severe outcomes, showed evidence of immunity from infection or vaccination. The authors noted that older adults – who have the lowest infection rates but highest risk of severe outcomes – continue to warrant prioritized vaccination, writing online in the Canadian Medical Association Journal.
Previous evidence suggests that a combination of both infection and vaccination exposure may induce more robust and durable hybrid immunity than either exposure alone, according to lead author Danuta M. Skowronski, MD, MHSc, an epidemiologist at the British Columbia Centre for Disease Control in Vancouver.
“Our main objective was to chronicle the changing proportion of the population considered immunologically naive and therefore susceptible to SARS-CoV-2,” Dr. Skowronski said in an interview. “It’s relevant for risk assessment to know what proportion have acquired some priming for more efficient immune memory response to the virus because that reduces the likelihood of severe outcomes.” Standardized seroprevalence studies are essential to inform COVID-19 response, particularly in resource-limited regions.
The study
Conducted in British Columbia’s Greater Vancouver and Fraser Valley, the analysis found that in the first year of the pandemic, when extraordinary measures were in place to curtail transmission, virtually everyone remained immunologically naive. Thereafter, however, age-based vaccine rollouts dramatically changed the immuno-epidemiological landscape so that by September 2021, more than 80% of the study population had antibody evidence of immunological priming, while more than 85% remained uninfected.
By August 2022, after the Omicron-variant waves, overall vaccine- and infection-induced seroprevalence exceeded 95%, with 60% having been actually infected, including at least three-quarters of children. Fewer than 50% of older adults, however, showed immunological evidence of exposure.
The study results were based on anonymized residual sera from children and adults in an outpatient laboratory network. At least three immunoassays per serosurvey were used to detect antibodies to SARS-CoV-2 spike (from vaccine) and to nucleocapsid antibodies (from infection).
The researchers assessed any seroprevalence – vaccine-, infection-induced, or both – as defined by positivity on any two assays. Infection-induced seroprevalence was also defined by dual-assay positivity but required both antinucleocapsid and antispike detection. Their estimates of infection-induced seroprevalence indicated considerable under-ascertainment of infections by standard surveillance case reports.
Results
During the first year of the pandemic, fewer than 1% manifested seroprevalence during the first three snapshots and fewer than 5% by January 2021. With vaccine rollout, however, seroprevalence increased dramatically during the first half of 2021 to 56% by May/June 2021 and to 83% by September/October 2021.
In addition, infection-induced seroprevalence was low at less than 15% in September/October 2021 until the arrival of the Omicron waves, after which it rose to 42% by March 2022 and 61% by July/August 2022. Combined seroprevalence for vaccination or infection was more than 95% by the summer, with most children but less than half of adults older than 60 years showing evidence of having been infected.
“We found the highest infection rates among children, closely followed by young adults, which may reflect their greater interconnectedness, including between siblings and parents in the household, as well as with peers in schools and the community,” the authors wrote, adding that the low cumulative infection rates among older adults may reflect their higher vaccination rates and greater social isolation.
U.S. data show similar age-related infection rates, but data among children from other Canadian provinces are limited, the authors said.
Commenting on the survey but not involved in it, infectious diseases expert Marc Germain, MD, PhD, a vice president at Héma-Québec in Quebec City, believes the pattern observed in British Columbia is fairly representative of what happened across Canada and the United States, including the sweeping effect of the Omicron variant and the differential impact according to age.
“But regional differences might very well exist – for example, due to differential vaccine uptake – and are also probably related in part to the different testing platforms being used,” Dr. Germain told this news organization.
Caroline Quach-Tanh, MD, PhD, a pediatrician and epidemiologist/infectologist at the University of Montreal, pointed out that Quebec seroprevalence surveys using residual blood samples from children and adults visiting emergency departments for any reason showed higher rates of prior infection than did the BC surveys. “But Dr. Skowronski’s findings are likely applicable to settings where some nonpharmacological interventions were put in place, but without strict confinement – and thus are likely applicable to most settings in the U.S. and Canada.”
Dr. Quach-Tanh added that there is always a risk of bias with the use of residual blood samples, “but the fact that the study method was stable should have captured a similar population from time to time. It would be unlikely to result in a major overestimation in the proportion of individuals positive for SARS-CoV-2 antibodies.”
A recent global meta-analysis found that while global seroprevalence has risen considerably, albeit variably by region, more than a third of the world’s population is still seronegative to the SARS-CoV-2 virus.
Dr. Skowronski reported institutional grants from the Canadian Institutes of Health Research and the British Columbia Centre for Disease Control Foundation for Public Health for other SARSCoV-2 work. Coauthor Romina C. Reyes, MD, chairs the BC Diagnostic Accreditation Program committee. Coauthor Mel Krajden, MD, reported institutional grants from Roche, Hologic, and Siemens. Dr. Germain and Dr. Quach-Tanh disclosed no competing interests relevant to their comments.
By August 2022, two-and-a-half years into the COVID-19 pandemic, most children as well as most adults under age 60 years had evidence of SARS-CoV-2 vaccination and/or infection, a Canadian seroprevalence study of almost 14,000 people over the first seven waves of the pandemic reports.
However, fewer than 50% people older than age 60, the age group most vulnerable to severe outcomes, showed evidence of immunity from infection or vaccination. The authors noted that older adults – who have the lowest infection rates but highest risk of severe outcomes – continue to warrant prioritized vaccination, writing online in the Canadian Medical Association Journal.
Previous evidence suggests that a combination of both infection and vaccination exposure may induce more robust and durable hybrid immunity than either exposure alone, according to lead author Danuta M. Skowronski, MD, MHSc, an epidemiologist at the British Columbia Centre for Disease Control in Vancouver.
“Our main objective was to chronicle the changing proportion of the population considered immunologically naive and therefore susceptible to SARS-CoV-2,” Dr. Skowronski said in an interview. “It’s relevant for risk assessment to know what proportion have acquired some priming for more efficient immune memory response to the virus because that reduces the likelihood of severe outcomes.” Standardized seroprevalence studies are essential to inform COVID-19 response, particularly in resource-limited regions.
The study
Conducted in British Columbia’s Greater Vancouver and Fraser Valley, the analysis found that in the first year of the pandemic, when extraordinary measures were in place to curtail transmission, virtually everyone remained immunologically naive. Thereafter, however, age-based vaccine rollouts dramatically changed the immuno-epidemiological landscape so that by September 2021, more than 80% of the study population had antibody evidence of immunological priming, while more than 85% remained uninfected.
By August 2022, after the Omicron-variant waves, overall vaccine- and infection-induced seroprevalence exceeded 95%, with 60% having been actually infected, including at least three-quarters of children. Fewer than 50% of older adults, however, showed immunological evidence of exposure.
The study results were based on anonymized residual sera from children and adults in an outpatient laboratory network. At least three immunoassays per serosurvey were used to detect antibodies to SARS-CoV-2 spike (from vaccine) and to nucleocapsid antibodies (from infection).
The researchers assessed any seroprevalence – vaccine-, infection-induced, or both – as defined by positivity on any two assays. Infection-induced seroprevalence was also defined by dual-assay positivity but required both antinucleocapsid and antispike detection. Their estimates of infection-induced seroprevalence indicated considerable under-ascertainment of infections by standard surveillance case reports.
Results
During the first year of the pandemic, fewer than 1% manifested seroprevalence during the first three snapshots and fewer than 5% by January 2021. With vaccine rollout, however, seroprevalence increased dramatically during the first half of 2021 to 56% by May/June 2021 and to 83% by September/October 2021.
In addition, infection-induced seroprevalence was low at less than 15% in September/October 2021 until the arrival of the Omicron waves, after which it rose to 42% by March 2022 and 61% by July/August 2022. Combined seroprevalence for vaccination or infection was more than 95% by the summer, with most children but less than half of adults older than 60 years showing evidence of having been infected.
“We found the highest infection rates among children, closely followed by young adults, which may reflect their greater interconnectedness, including between siblings and parents in the household, as well as with peers in schools and the community,” the authors wrote, adding that the low cumulative infection rates among older adults may reflect their higher vaccination rates and greater social isolation.
U.S. data show similar age-related infection rates, but data among children from other Canadian provinces are limited, the authors said.
Commenting on the survey but not involved in it, infectious diseases expert Marc Germain, MD, PhD, a vice president at Héma-Québec in Quebec City, believes the pattern observed in British Columbia is fairly representative of what happened across Canada and the United States, including the sweeping effect of the Omicron variant and the differential impact according to age.
“But regional differences might very well exist – for example, due to differential vaccine uptake – and are also probably related in part to the different testing platforms being used,” Dr. Germain told this news organization.
Caroline Quach-Tanh, MD, PhD, a pediatrician and epidemiologist/infectologist at the University of Montreal, pointed out that Quebec seroprevalence surveys using residual blood samples from children and adults visiting emergency departments for any reason showed higher rates of prior infection than did the BC surveys. “But Dr. Skowronski’s findings are likely applicable to settings where some nonpharmacological interventions were put in place, but without strict confinement – and thus are likely applicable to most settings in the U.S. and Canada.”
Dr. Quach-Tanh added that there is always a risk of bias with the use of residual blood samples, “but the fact that the study method was stable should have captured a similar population from time to time. It would be unlikely to result in a major overestimation in the proportion of individuals positive for SARS-CoV-2 antibodies.”
A recent global meta-analysis found that while global seroprevalence has risen considerably, albeit variably by region, more than a third of the world’s population is still seronegative to the SARS-CoV-2 virus.
Dr. Skowronski reported institutional grants from the Canadian Institutes of Health Research and the British Columbia Centre for Disease Control Foundation for Public Health for other SARSCoV-2 work. Coauthor Romina C. Reyes, MD, chairs the BC Diagnostic Accreditation Program committee. Coauthor Mel Krajden, MD, reported institutional grants from Roche, Hologic, and Siemens. Dr. Germain and Dr. Quach-Tanh disclosed no competing interests relevant to their comments.
By August 2022, two-and-a-half years into the COVID-19 pandemic, most children as well as most adults under age 60 years had evidence of SARS-CoV-2 vaccination and/or infection, a Canadian seroprevalence study of almost 14,000 people over the first seven waves of the pandemic reports.
However, fewer than 50% people older than age 60, the age group most vulnerable to severe outcomes, showed evidence of immunity from infection or vaccination. The authors noted that older adults – who have the lowest infection rates but highest risk of severe outcomes – continue to warrant prioritized vaccination, writing online in the Canadian Medical Association Journal.
Previous evidence suggests that a combination of both infection and vaccination exposure may induce more robust and durable hybrid immunity than either exposure alone, according to lead author Danuta M. Skowronski, MD, MHSc, an epidemiologist at the British Columbia Centre for Disease Control in Vancouver.
“Our main objective was to chronicle the changing proportion of the population considered immunologically naive and therefore susceptible to SARS-CoV-2,” Dr. Skowronski said in an interview. “It’s relevant for risk assessment to know what proportion have acquired some priming for more efficient immune memory response to the virus because that reduces the likelihood of severe outcomes.” Standardized seroprevalence studies are essential to inform COVID-19 response, particularly in resource-limited regions.
The study
Conducted in British Columbia’s Greater Vancouver and Fraser Valley, the analysis found that in the first year of the pandemic, when extraordinary measures were in place to curtail transmission, virtually everyone remained immunologically naive. Thereafter, however, age-based vaccine rollouts dramatically changed the immuno-epidemiological landscape so that by September 2021, more than 80% of the study population had antibody evidence of immunological priming, while more than 85% remained uninfected.
By August 2022, after the Omicron-variant waves, overall vaccine- and infection-induced seroprevalence exceeded 95%, with 60% having been actually infected, including at least three-quarters of children. Fewer than 50% of older adults, however, showed immunological evidence of exposure.
The study results were based on anonymized residual sera from children and adults in an outpatient laboratory network. At least three immunoassays per serosurvey were used to detect antibodies to SARS-CoV-2 spike (from vaccine) and to nucleocapsid antibodies (from infection).
The researchers assessed any seroprevalence – vaccine-, infection-induced, or both – as defined by positivity on any two assays. Infection-induced seroprevalence was also defined by dual-assay positivity but required both antinucleocapsid and antispike detection. Their estimates of infection-induced seroprevalence indicated considerable under-ascertainment of infections by standard surveillance case reports.
Results
During the first year of the pandemic, fewer than 1% manifested seroprevalence during the first three snapshots and fewer than 5% by January 2021. With vaccine rollout, however, seroprevalence increased dramatically during the first half of 2021 to 56% by May/June 2021 and to 83% by September/October 2021.
In addition, infection-induced seroprevalence was low at less than 15% in September/October 2021 until the arrival of the Omicron waves, after which it rose to 42% by March 2022 and 61% by July/August 2022. Combined seroprevalence for vaccination or infection was more than 95% by the summer, with most children but less than half of adults older than 60 years showing evidence of having been infected.
“We found the highest infection rates among children, closely followed by young adults, which may reflect their greater interconnectedness, including between siblings and parents in the household, as well as with peers in schools and the community,” the authors wrote, adding that the low cumulative infection rates among older adults may reflect their higher vaccination rates and greater social isolation.
U.S. data show similar age-related infection rates, but data among children from other Canadian provinces are limited, the authors said.
Commenting on the survey but not involved in it, infectious diseases expert Marc Germain, MD, PhD, a vice president at Héma-Québec in Quebec City, believes the pattern observed in British Columbia is fairly representative of what happened across Canada and the United States, including the sweeping effect of the Omicron variant and the differential impact according to age.
“But regional differences might very well exist – for example, due to differential vaccine uptake – and are also probably related in part to the different testing platforms being used,” Dr. Germain told this news organization.
Caroline Quach-Tanh, MD, PhD, a pediatrician and epidemiologist/infectologist at the University of Montreal, pointed out that Quebec seroprevalence surveys using residual blood samples from children and adults visiting emergency departments for any reason showed higher rates of prior infection than did the BC surveys. “But Dr. Skowronski’s findings are likely applicable to settings where some nonpharmacological interventions were put in place, but without strict confinement – and thus are likely applicable to most settings in the U.S. and Canada.”
Dr. Quach-Tanh added that there is always a risk of bias with the use of residual blood samples, “but the fact that the study method was stable should have captured a similar population from time to time. It would be unlikely to result in a major overestimation in the proportion of individuals positive for SARS-CoV-2 antibodies.”
A recent global meta-analysis found that while global seroprevalence has risen considerably, albeit variably by region, more than a third of the world’s population is still seronegative to the SARS-CoV-2 virus.
Dr. Skowronski reported institutional grants from the Canadian Institutes of Health Research and the British Columbia Centre for Disease Control Foundation for Public Health for other SARSCoV-2 work. Coauthor Romina C. Reyes, MD, chairs the BC Diagnostic Accreditation Program committee. Coauthor Mel Krajden, MD, reported institutional grants from Roche, Hologic, and Siemens. Dr. Germain and Dr. Quach-Tanh disclosed no competing interests relevant to their comments.
FROM THE CANADIAN MEDICAL ASSOCIATION JOURNAL
Diabetes surge expected in young people
according to a new study published in Diabetes Care.
It is expected that as many as 526,000 people younger than 20 years in the United States will have diabetes by 2060, researchers from the Centers for Disease Control and Prevention report. Their projections found that the number of young people with diabetes will increase 12%, from 213,000 in 2017 to 239,000 in 2060.
The estimates include a 673% rise in the number of youth with type 2 diabetes and a 65% increase in cases of type 1 diabetes over the next 4 decades.
Most of the new cases are projected to occur among non-Hispanic Blacks, exacerbating the already significant racial disparities in type 2 diabetes in particular, the study found.
“This study’s startling projections of type 2 diabetes increases show why it is crucial to advance health equity and reduce the widespread disparities that already take a toll on people’s health,” Christopher Holliday, PhD, MPH, FACHE, director of CDC’s Division of Diabetes Translation, said in a press release about the new estimates.
Even if trends remain the same in coming decades, researchers said diagnoses of type 2 diabetes will rise almost 70% and that diagnoses of type 1 diabetes will increase by 3%.
The researchers attribute the increase in diabetes cases among youth to a variety of factors, including the growing prevalence of childhood obesity and the presence of diabetes in women of childbearing age, which is linked to obesity in their offspring.
Debra Houry, MD, MPH, acting principal director of the CDC, said the focus should be on prevention.
“This new research should serve as a wake-up call for all of us. It’s vital that we focus our efforts to ensure all Americans, especially our young people, are the healthiest they can be,” she said in a press release.
The findings come from the SEARCH for Diabetes in Youth study, funded by the CDC and the National Institutes of Health. Dr. Houry and Dr. Holliday report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new study published in Diabetes Care.
It is expected that as many as 526,000 people younger than 20 years in the United States will have diabetes by 2060, researchers from the Centers for Disease Control and Prevention report. Their projections found that the number of young people with diabetes will increase 12%, from 213,000 in 2017 to 239,000 in 2060.
The estimates include a 673% rise in the number of youth with type 2 diabetes and a 65% increase in cases of type 1 diabetes over the next 4 decades.
Most of the new cases are projected to occur among non-Hispanic Blacks, exacerbating the already significant racial disparities in type 2 diabetes in particular, the study found.
“This study’s startling projections of type 2 diabetes increases show why it is crucial to advance health equity and reduce the widespread disparities that already take a toll on people’s health,” Christopher Holliday, PhD, MPH, FACHE, director of CDC’s Division of Diabetes Translation, said in a press release about the new estimates.
Even if trends remain the same in coming decades, researchers said diagnoses of type 2 diabetes will rise almost 70% and that diagnoses of type 1 diabetes will increase by 3%.
The researchers attribute the increase in diabetes cases among youth to a variety of factors, including the growing prevalence of childhood obesity and the presence of diabetes in women of childbearing age, which is linked to obesity in their offspring.
Debra Houry, MD, MPH, acting principal director of the CDC, said the focus should be on prevention.
“This new research should serve as a wake-up call for all of us. It’s vital that we focus our efforts to ensure all Americans, especially our young people, are the healthiest they can be,” she said in a press release.
The findings come from the SEARCH for Diabetes in Youth study, funded by the CDC and the National Institutes of Health. Dr. Houry and Dr. Holliday report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new study published in Diabetes Care.
It is expected that as many as 526,000 people younger than 20 years in the United States will have diabetes by 2060, researchers from the Centers for Disease Control and Prevention report. Their projections found that the number of young people with diabetes will increase 12%, from 213,000 in 2017 to 239,000 in 2060.
The estimates include a 673% rise in the number of youth with type 2 diabetes and a 65% increase in cases of type 1 diabetes over the next 4 decades.
Most of the new cases are projected to occur among non-Hispanic Blacks, exacerbating the already significant racial disparities in type 2 diabetes in particular, the study found.
“This study’s startling projections of type 2 diabetes increases show why it is crucial to advance health equity and reduce the widespread disparities that already take a toll on people’s health,” Christopher Holliday, PhD, MPH, FACHE, director of CDC’s Division of Diabetes Translation, said in a press release about the new estimates.
Even if trends remain the same in coming decades, researchers said diagnoses of type 2 diabetes will rise almost 70% and that diagnoses of type 1 diabetes will increase by 3%.
The researchers attribute the increase in diabetes cases among youth to a variety of factors, including the growing prevalence of childhood obesity and the presence of diabetes in women of childbearing age, which is linked to obesity in their offspring.
Debra Houry, MD, MPH, acting principal director of the CDC, said the focus should be on prevention.
“This new research should serve as a wake-up call for all of us. It’s vital that we focus our efforts to ensure all Americans, especially our young people, are the healthiest they can be,” she said in a press release.
The findings come from the SEARCH for Diabetes in Youth study, funded by the CDC and the National Institutes of Health. Dr. Houry and Dr. Holliday report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM DIABETES CARE
Heart benefits begin at well under 10,000 daily steps
– and the benefits accrue at well below the widely promoted threshold of 10,000 steps per day, new research shows.
Among adults aged 60 and older, those who took roughly 6,000 to 9,000 steps per day had a 40% to 50% lower risk of CVD, compared with peers logging just 2,000 steps per day.
“We hope this study will contribute evidence to future public health and clinical guidance on how many steps we need for health,” Amanda Paluch, PhD, with University of Massachusetts Amherst, told this news organization.
Getting in more steps per day can lower an individual’s risk for heart disease – but it’s not an “all or nothing” situation, Dr. Paluch said.
“The heart health benefits begin at lower than 10,000 steps per day. So, for the many adults that may find 10,000 steps a bit out of reach, it is important to promote that even small increases in steps can be beneficial for health,” Dr. Paluch said.
The study was published online in Circulation.
Attainable step goals
As part of the Steps for Health Collaborative, Dr. Paluch and colleagues examined the dose-response relationship between steps per day and CVD in a meta-analysis of eight prospective studies involving 20,152 adults (mean age 63, 52% women).
Steps were measured in each study using one of five different commercially available step-measuring devices. Adults aged 60 years and older took a median of 4,323 steps per day (interquartile range, 2,760-6,924), while younger adults walked a bit more (median 6,911 daily steps; IQR, 4,783-9,794).
During follow-up lasting an average of 6.2 years, a total of 1,523 CVD events were reported.
In the final adjusted model, for older adults, compared with those in quartile 1 who got the fewest steps per day (median 1,811), the risk of CVD was 20% lower in those in quartile 2, who got a median of 3,823 steps per day (hazard ratio, 0.80; 95% confidence interval, 0.69-0.93).
CVD risk was 38% lower in older adults in quartile 3 who got a median of 5,520 steps per day (HR, 0.62; 95% CI, 0.52-0.74) and 49% lower in those in quartile 4 who walked the most (a median of 9,259 steps per day; HR, 0.51; 95% CI, 0.41-0.63).
Restricting the analysis to individuals without known CVD at baseline showed similar results.
Among six studies that excluded adults with a history of CVD at baseline, compared with the lowest quartile, the HR for incident CVD events was 0.74 (95% CI, 0.60-0.91) in the second quartile, 0.60 (95% CI, 0.47-0.77) in the third quartile, and 0.55 (95% CI, 0.40-0.76) in the fourth quartile.
Despite the inverse association of steps with CVD in older adults, there was no association in younger adults. The researchers caution, however, that CVD is a disease of aging, and the follow-up period in these studies may not have been long enough to capture CVD incidence in younger adults.
Stepping rate (pace or cadence) was not associated with CVD risk beyond that of total steps per day. However, only four of the eight studies reported data on stepping rate, so this finding should be viewed as preliminary, Dr. Paluch and colleagues say.
Start small and go from there
Dr. Paluch said the take-home message from this study and numerous others is simple.
“Move more and sit less! Being physically active, by getting in your steps, is an important part of keeping your heart healthy,” she said in an interview.
For adults who are currently inactive, Dr. Paluch suggests finding small ways to get in a few more steps per day. “It does not need to be drastic changes. Consider a brief 5- to 10-minute walking break at lunch, taking the stairs, or playing a game of hide and seek with the grandchildren,” Dr. Paluch advised.
“For adults starting at 3,000 steps a day, set a goal of 4,000, and then 5,000. Each improvement can lead to better heart health,” Dr. Paluch said. “And for those who are already active, keep it up, as there are benefits with higher volumes of steps per day as well.”
Support for this research was provided by the Intergovernmental Personnel Act Agreement through the Centers for Disease Control and Prevention. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
– and the benefits accrue at well below the widely promoted threshold of 10,000 steps per day, new research shows.
Among adults aged 60 and older, those who took roughly 6,000 to 9,000 steps per day had a 40% to 50% lower risk of CVD, compared with peers logging just 2,000 steps per day.
“We hope this study will contribute evidence to future public health and clinical guidance on how many steps we need for health,” Amanda Paluch, PhD, with University of Massachusetts Amherst, told this news organization.
Getting in more steps per day can lower an individual’s risk for heart disease – but it’s not an “all or nothing” situation, Dr. Paluch said.
“The heart health benefits begin at lower than 10,000 steps per day. So, for the many adults that may find 10,000 steps a bit out of reach, it is important to promote that even small increases in steps can be beneficial for health,” Dr. Paluch said.
The study was published online in Circulation.
Attainable step goals
As part of the Steps for Health Collaborative, Dr. Paluch and colleagues examined the dose-response relationship between steps per day and CVD in a meta-analysis of eight prospective studies involving 20,152 adults (mean age 63, 52% women).
Steps were measured in each study using one of five different commercially available step-measuring devices. Adults aged 60 years and older took a median of 4,323 steps per day (interquartile range, 2,760-6,924), while younger adults walked a bit more (median 6,911 daily steps; IQR, 4,783-9,794).
During follow-up lasting an average of 6.2 years, a total of 1,523 CVD events were reported.
In the final adjusted model, for older adults, compared with those in quartile 1 who got the fewest steps per day (median 1,811), the risk of CVD was 20% lower in those in quartile 2, who got a median of 3,823 steps per day (hazard ratio, 0.80; 95% confidence interval, 0.69-0.93).
CVD risk was 38% lower in older adults in quartile 3 who got a median of 5,520 steps per day (HR, 0.62; 95% CI, 0.52-0.74) and 49% lower in those in quartile 4 who walked the most (a median of 9,259 steps per day; HR, 0.51; 95% CI, 0.41-0.63).
Restricting the analysis to individuals without known CVD at baseline showed similar results.
Among six studies that excluded adults with a history of CVD at baseline, compared with the lowest quartile, the HR for incident CVD events was 0.74 (95% CI, 0.60-0.91) in the second quartile, 0.60 (95% CI, 0.47-0.77) in the third quartile, and 0.55 (95% CI, 0.40-0.76) in the fourth quartile.
Despite the inverse association of steps with CVD in older adults, there was no association in younger adults. The researchers caution, however, that CVD is a disease of aging, and the follow-up period in these studies may not have been long enough to capture CVD incidence in younger adults.
Stepping rate (pace or cadence) was not associated with CVD risk beyond that of total steps per day. However, only four of the eight studies reported data on stepping rate, so this finding should be viewed as preliminary, Dr. Paluch and colleagues say.
Start small and go from there
Dr. Paluch said the take-home message from this study and numerous others is simple.
“Move more and sit less! Being physically active, by getting in your steps, is an important part of keeping your heart healthy,” she said in an interview.
For adults who are currently inactive, Dr. Paluch suggests finding small ways to get in a few more steps per day. “It does not need to be drastic changes. Consider a brief 5- to 10-minute walking break at lunch, taking the stairs, or playing a game of hide and seek with the grandchildren,” Dr. Paluch advised.
“For adults starting at 3,000 steps a day, set a goal of 4,000, and then 5,000. Each improvement can lead to better heart health,” Dr. Paluch said. “And for those who are already active, keep it up, as there are benefits with higher volumes of steps per day as well.”
Support for this research was provided by the Intergovernmental Personnel Act Agreement through the Centers for Disease Control and Prevention. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
– and the benefits accrue at well below the widely promoted threshold of 10,000 steps per day, new research shows.
Among adults aged 60 and older, those who took roughly 6,000 to 9,000 steps per day had a 40% to 50% lower risk of CVD, compared with peers logging just 2,000 steps per day.
“We hope this study will contribute evidence to future public health and clinical guidance on how many steps we need for health,” Amanda Paluch, PhD, with University of Massachusetts Amherst, told this news organization.
Getting in more steps per day can lower an individual’s risk for heart disease – but it’s not an “all or nothing” situation, Dr. Paluch said.
“The heart health benefits begin at lower than 10,000 steps per day. So, for the many adults that may find 10,000 steps a bit out of reach, it is important to promote that even small increases in steps can be beneficial for health,” Dr. Paluch said.
The study was published online in Circulation.
Attainable step goals
As part of the Steps for Health Collaborative, Dr. Paluch and colleagues examined the dose-response relationship between steps per day and CVD in a meta-analysis of eight prospective studies involving 20,152 adults (mean age 63, 52% women).
Steps were measured in each study using one of five different commercially available step-measuring devices. Adults aged 60 years and older took a median of 4,323 steps per day (interquartile range, 2,760-6,924), while younger adults walked a bit more (median 6,911 daily steps; IQR, 4,783-9,794).
During follow-up lasting an average of 6.2 years, a total of 1,523 CVD events were reported.
In the final adjusted model, for older adults, compared with those in quartile 1 who got the fewest steps per day (median 1,811), the risk of CVD was 20% lower in those in quartile 2, who got a median of 3,823 steps per day (hazard ratio, 0.80; 95% confidence interval, 0.69-0.93).
CVD risk was 38% lower in older adults in quartile 3 who got a median of 5,520 steps per day (HR, 0.62; 95% CI, 0.52-0.74) and 49% lower in those in quartile 4 who walked the most (a median of 9,259 steps per day; HR, 0.51; 95% CI, 0.41-0.63).
Restricting the analysis to individuals without known CVD at baseline showed similar results.
Among six studies that excluded adults with a history of CVD at baseline, compared with the lowest quartile, the HR for incident CVD events was 0.74 (95% CI, 0.60-0.91) in the second quartile, 0.60 (95% CI, 0.47-0.77) in the third quartile, and 0.55 (95% CI, 0.40-0.76) in the fourth quartile.
Despite the inverse association of steps with CVD in older adults, there was no association in younger adults. The researchers caution, however, that CVD is a disease of aging, and the follow-up period in these studies may not have been long enough to capture CVD incidence in younger adults.
Stepping rate (pace or cadence) was not associated with CVD risk beyond that of total steps per day. However, only four of the eight studies reported data on stepping rate, so this finding should be viewed as preliminary, Dr. Paluch and colleagues say.
Start small and go from there
Dr. Paluch said the take-home message from this study and numerous others is simple.
“Move more and sit less! Being physically active, by getting in your steps, is an important part of keeping your heart healthy,” she said in an interview.
For adults who are currently inactive, Dr. Paluch suggests finding small ways to get in a few more steps per day. “It does not need to be drastic changes. Consider a brief 5- to 10-minute walking break at lunch, taking the stairs, or playing a game of hide and seek with the grandchildren,” Dr. Paluch advised.
“For adults starting at 3,000 steps a day, set a goal of 4,000, and then 5,000. Each improvement can lead to better heart health,” Dr. Paluch said. “And for those who are already active, keep it up, as there are benefits with higher volumes of steps per day as well.”
Support for this research was provided by the Intergovernmental Personnel Act Agreement through the Centers for Disease Control and Prevention. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CIRCULATION
Women with cycle disorders across their life span may be at increased risk of cardiovascular disease
This finding is demonstrated in a new analysis of the Nurses’ Health Study II.
“To date, several studies have reported increased risks of cardiovascular risk factors or cardiovascular disease in connection with cycle disorders,” Yi-Xin Wang, MD, PhD, a research fellow in nutrition, and associates from the Harvard School of Public Health, Boston, wrote in an article published in JAMA Network Open.
Ute Seeland, MD, speaker of the Gender Medicine in Cardiology Working Group of the German Cardiology Society, said in an interview“We know that women who have indicated in their medical history that they have irregular menstrual cycles, invariably in connection with polycystic ovary syndrome (PCOS), more commonly develop diabetes and other metabolic disorders, as well as cardiovascular diseases.”
Cycle disorders’ role
However, the role that irregular or especially long cycles play at different points of a woman’s reproductive life span was unclear. Therefore, the research group investigated the associations in the Nurses’ Health Study II between cycle irregularity and cycle length in women of different age groups who later experienced cardiovascular events.
At the end of this study in 1989, the participants also provided information regarding the length and irregularity of their menstrual cycle from ages 14 to 17 years and again from ages 18 to 22 years. The information was updated in 1993 when the participants were aged 29-46 years. The data from 2019 to 2022 were analyzed.
“This kind of long-term cohort study is extremely rare and therefore something special,” said Dr. Seeland, who conducts research at the Institute for Social Medicine, Epidemiology, and Health Economics at the Charité – University Hospital Berlin.
The investigators used the following cycle classifications: very regular (no more than 3 or 4 days before or after the expected date), regular (within 5-7 days), usually irregular, always irregular, or no periods.
The cycle lengths were divided into the following categories: less than 21 days, 21-25 days, 26-31 days, 32-39 days, 40-50 days, more than 50 days, and too irregular to estimate the length.
The onset of cardiovascular diseases was determined using information from the participants and was confirmed by reviewing the medical files. Relevant to the study were lethal and nonlethal coronary heart diseases (such as myocardial infarction or coronary artery revascularization), as well as strokes.
Significant in adulthood
The data from 80,630 study participants were included in the analysis. At study inclusion, the average age of the participants was 37.7 years, and the average body mass index (BMI) was 25.1. “Since it was predominantly White nurses who took part in the study, the data are not transferable to other, more diverse populations,” said Dr. Seeland.
Over 24 years, 1,816 women (2.4%) had a cardiovascular event. “We observed an increased rate of cardiovascular events in women with an irregular cycle and longer cycle, both in early an in mid-adulthood,” wrote Dr. Wang and associates. “Similar trends were also observed for cycle disorders when younger, but this association was weaker than in adulthood.”
Compared with women with very regular cycles, women with irregular cycles or without periods who were aged 14-17 years, 18-22 years, or 29-49 years exhibited a 15%, 36%, and 40% higher risk of a cardiovascular event, respectively.
Similarly, women aged 18-22 years or 29-46 years with long cycles of 40 days or more had a 44% or 30% higher risk of cardiovascular disease, respectively, compared with women with cycle lengths of 26-31 days.
“The coronary heart diseases were decisive for the increase, and less so, the strokes,” wrote the researchers.
Classic risk factors?
Dr. Seeland praised the fact that the study authors tried to determine the role that classic cardiovascular risk factors played. “Compared with women with a regular cycle, women with an irregular cycle had a higher BMI, more frequently increased cholesterol levels, and an elevated blood pressure,” she said. Women with a long cycle displayed a similar pattern.
It can be assumed from this that over a woman’s life span, BMI affects the risk of cardiovascular disease. Therefore, Dr. Wang and coauthors adjusted the results on the basis of BMI, which varies over time.
Regarding other classic risk factors that may have played a role, “hypercholesterolemia, chronic high blood pressure, and type 2 diabetes were only responsible in 5.4%-13.5% of the associations,” wrote the researchers.
“Our results suggest that certain characteristics of the menstrual cycle across a woman’s reproductive lifespan may constitute additional risk markers for cardiovascular disease,” according to the authors.
The highest rates of cardiovascular disease were among women with permanently irregular or long cycles in early to mid adulthood, as well as women who had regular cycles when younger but had irregular cycles in mid adulthood. “This indicates that the change from one cycle phenotype to another could be a surrogate marker for metabolic changes, which in turn contribute to the formation of cardiovascular diseases,” wrote the authors.
The study was observational and so conclusions cannot be drawn regarding causal relationships. But Dr. Wang and associates indicate that the most common cause of an irregular menstrual cycle may be PCOS. “Roughly 90% of women with cycle disorders or oligomenorrhea have signs of PCOS. And it was shown that women with PCOS have an increased risk of cardiovascular disease.”
They concluded that “the associations observed between irregular and long cycles in early to mid-adulthood and cardiovascular diseases are likely attributable to underlying PCOS.”
For Dr. Seeland, however, this conclusion is “too monocausal. At no point in time did there seem to be any direct information regarding the frequency of PCOS during the data collection by the respondents.”
For now, we can only speculate about the mechanisms. “The association between a very irregular and long cycle and the increased risk of cardiovascular diseases has now only been described. More research should be done on the causes,” said Dr. Seeland.
This article was translated from the Medscape German edition. A version of this article first appeared on Medscape.com.
This finding is demonstrated in a new analysis of the Nurses’ Health Study II.
“To date, several studies have reported increased risks of cardiovascular risk factors or cardiovascular disease in connection with cycle disorders,” Yi-Xin Wang, MD, PhD, a research fellow in nutrition, and associates from the Harvard School of Public Health, Boston, wrote in an article published in JAMA Network Open.
Ute Seeland, MD, speaker of the Gender Medicine in Cardiology Working Group of the German Cardiology Society, said in an interview“We know that women who have indicated in their medical history that they have irregular menstrual cycles, invariably in connection with polycystic ovary syndrome (PCOS), more commonly develop diabetes and other metabolic disorders, as well as cardiovascular diseases.”
Cycle disorders’ role
However, the role that irregular or especially long cycles play at different points of a woman’s reproductive life span was unclear. Therefore, the research group investigated the associations in the Nurses’ Health Study II between cycle irregularity and cycle length in women of different age groups who later experienced cardiovascular events.
At the end of this study in 1989, the participants also provided information regarding the length and irregularity of their menstrual cycle from ages 14 to 17 years and again from ages 18 to 22 years. The information was updated in 1993 when the participants were aged 29-46 years. The data from 2019 to 2022 were analyzed.
“This kind of long-term cohort study is extremely rare and therefore something special,” said Dr. Seeland, who conducts research at the Institute for Social Medicine, Epidemiology, and Health Economics at the Charité – University Hospital Berlin.
The investigators used the following cycle classifications: very regular (no more than 3 or 4 days before or after the expected date), regular (within 5-7 days), usually irregular, always irregular, or no periods.
The cycle lengths were divided into the following categories: less than 21 days, 21-25 days, 26-31 days, 32-39 days, 40-50 days, more than 50 days, and too irregular to estimate the length.
The onset of cardiovascular diseases was determined using information from the participants and was confirmed by reviewing the medical files. Relevant to the study were lethal and nonlethal coronary heart diseases (such as myocardial infarction or coronary artery revascularization), as well as strokes.
Significant in adulthood
The data from 80,630 study participants were included in the analysis. At study inclusion, the average age of the participants was 37.7 years, and the average body mass index (BMI) was 25.1. “Since it was predominantly White nurses who took part in the study, the data are not transferable to other, more diverse populations,” said Dr. Seeland.
Over 24 years, 1,816 women (2.4%) had a cardiovascular event. “We observed an increased rate of cardiovascular events in women with an irregular cycle and longer cycle, both in early an in mid-adulthood,” wrote Dr. Wang and associates. “Similar trends were also observed for cycle disorders when younger, but this association was weaker than in adulthood.”
Compared with women with very regular cycles, women with irregular cycles or without periods who were aged 14-17 years, 18-22 years, or 29-49 years exhibited a 15%, 36%, and 40% higher risk of a cardiovascular event, respectively.
Similarly, women aged 18-22 years or 29-46 years with long cycles of 40 days or more had a 44% or 30% higher risk of cardiovascular disease, respectively, compared with women with cycle lengths of 26-31 days.
“The coronary heart diseases were decisive for the increase, and less so, the strokes,” wrote the researchers.
Classic risk factors?
Dr. Seeland praised the fact that the study authors tried to determine the role that classic cardiovascular risk factors played. “Compared with women with a regular cycle, women with an irregular cycle had a higher BMI, more frequently increased cholesterol levels, and an elevated blood pressure,” she said. Women with a long cycle displayed a similar pattern.
It can be assumed from this that over a woman’s life span, BMI affects the risk of cardiovascular disease. Therefore, Dr. Wang and coauthors adjusted the results on the basis of BMI, which varies over time.
Regarding other classic risk factors that may have played a role, “hypercholesterolemia, chronic high blood pressure, and type 2 diabetes were only responsible in 5.4%-13.5% of the associations,” wrote the researchers.
“Our results suggest that certain characteristics of the menstrual cycle across a woman’s reproductive lifespan may constitute additional risk markers for cardiovascular disease,” according to the authors.
The highest rates of cardiovascular disease were among women with permanently irregular or long cycles in early to mid adulthood, as well as women who had regular cycles when younger but had irregular cycles in mid adulthood. “This indicates that the change from one cycle phenotype to another could be a surrogate marker for metabolic changes, which in turn contribute to the formation of cardiovascular diseases,” wrote the authors.
The study was observational and so conclusions cannot be drawn regarding causal relationships. But Dr. Wang and associates indicate that the most common cause of an irregular menstrual cycle may be PCOS. “Roughly 90% of women with cycle disorders or oligomenorrhea have signs of PCOS. And it was shown that women with PCOS have an increased risk of cardiovascular disease.”
They concluded that “the associations observed between irregular and long cycles in early to mid-adulthood and cardiovascular diseases are likely attributable to underlying PCOS.”
For Dr. Seeland, however, this conclusion is “too monocausal. At no point in time did there seem to be any direct information regarding the frequency of PCOS during the data collection by the respondents.”
For now, we can only speculate about the mechanisms. “The association between a very irregular and long cycle and the increased risk of cardiovascular diseases has now only been described. More research should be done on the causes,” said Dr. Seeland.
This article was translated from the Medscape German edition. A version of this article first appeared on Medscape.com.
This finding is demonstrated in a new analysis of the Nurses’ Health Study II.
“To date, several studies have reported increased risks of cardiovascular risk factors or cardiovascular disease in connection with cycle disorders,” Yi-Xin Wang, MD, PhD, a research fellow in nutrition, and associates from the Harvard School of Public Health, Boston, wrote in an article published in JAMA Network Open.
Ute Seeland, MD, speaker of the Gender Medicine in Cardiology Working Group of the German Cardiology Society, said in an interview“We know that women who have indicated in their medical history that they have irregular menstrual cycles, invariably in connection with polycystic ovary syndrome (PCOS), more commonly develop diabetes and other metabolic disorders, as well as cardiovascular diseases.”
Cycle disorders’ role
However, the role that irregular or especially long cycles play at different points of a woman’s reproductive life span was unclear. Therefore, the research group investigated the associations in the Nurses’ Health Study II between cycle irregularity and cycle length in women of different age groups who later experienced cardiovascular events.
At the end of this study in 1989, the participants also provided information regarding the length and irregularity of their menstrual cycle from ages 14 to 17 years and again from ages 18 to 22 years. The information was updated in 1993 when the participants were aged 29-46 years. The data from 2019 to 2022 were analyzed.
“This kind of long-term cohort study is extremely rare and therefore something special,” said Dr. Seeland, who conducts research at the Institute for Social Medicine, Epidemiology, and Health Economics at the Charité – University Hospital Berlin.
The investigators used the following cycle classifications: very regular (no more than 3 or 4 days before or after the expected date), regular (within 5-7 days), usually irregular, always irregular, or no periods.
The cycle lengths were divided into the following categories: less than 21 days, 21-25 days, 26-31 days, 32-39 days, 40-50 days, more than 50 days, and too irregular to estimate the length.
The onset of cardiovascular diseases was determined using information from the participants and was confirmed by reviewing the medical files. Relevant to the study were lethal and nonlethal coronary heart diseases (such as myocardial infarction or coronary artery revascularization), as well as strokes.
Significant in adulthood
The data from 80,630 study participants were included in the analysis. At study inclusion, the average age of the participants was 37.7 years, and the average body mass index (BMI) was 25.1. “Since it was predominantly White nurses who took part in the study, the data are not transferable to other, more diverse populations,” said Dr. Seeland.
Over 24 years, 1,816 women (2.4%) had a cardiovascular event. “We observed an increased rate of cardiovascular events in women with an irregular cycle and longer cycle, both in early an in mid-adulthood,” wrote Dr. Wang and associates. “Similar trends were also observed for cycle disorders when younger, but this association was weaker than in adulthood.”
Compared with women with very regular cycles, women with irregular cycles or without periods who were aged 14-17 years, 18-22 years, or 29-49 years exhibited a 15%, 36%, and 40% higher risk of a cardiovascular event, respectively.
Similarly, women aged 18-22 years or 29-46 years with long cycles of 40 days or more had a 44% or 30% higher risk of cardiovascular disease, respectively, compared with women with cycle lengths of 26-31 days.
“The coronary heart diseases were decisive for the increase, and less so, the strokes,” wrote the researchers.
Classic risk factors?
Dr. Seeland praised the fact that the study authors tried to determine the role that classic cardiovascular risk factors played. “Compared with women with a regular cycle, women with an irregular cycle had a higher BMI, more frequently increased cholesterol levels, and an elevated blood pressure,” she said. Women with a long cycle displayed a similar pattern.
It can be assumed from this that over a woman’s life span, BMI affects the risk of cardiovascular disease. Therefore, Dr. Wang and coauthors adjusted the results on the basis of BMI, which varies over time.
Regarding other classic risk factors that may have played a role, “hypercholesterolemia, chronic high blood pressure, and type 2 diabetes were only responsible in 5.4%-13.5% of the associations,” wrote the researchers.
“Our results suggest that certain characteristics of the menstrual cycle across a woman’s reproductive lifespan may constitute additional risk markers for cardiovascular disease,” according to the authors.
The highest rates of cardiovascular disease were among women with permanently irregular or long cycles in early to mid adulthood, as well as women who had regular cycles when younger but had irregular cycles in mid adulthood. “This indicates that the change from one cycle phenotype to another could be a surrogate marker for metabolic changes, which in turn contribute to the formation of cardiovascular diseases,” wrote the authors.
The study was observational and so conclusions cannot be drawn regarding causal relationships. But Dr. Wang and associates indicate that the most common cause of an irregular menstrual cycle may be PCOS. “Roughly 90% of women with cycle disorders or oligomenorrhea have signs of PCOS. And it was shown that women with PCOS have an increased risk of cardiovascular disease.”
They concluded that “the associations observed between irregular and long cycles in early to mid-adulthood and cardiovascular diseases are likely attributable to underlying PCOS.”
For Dr. Seeland, however, this conclusion is “too monocausal. At no point in time did there seem to be any direct information regarding the frequency of PCOS during the data collection by the respondents.”
For now, we can only speculate about the mechanisms. “The association between a very irregular and long cycle and the increased risk of cardiovascular diseases has now only been described. More research should be done on the causes,” said Dr. Seeland.
This article was translated from the Medscape German edition. A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN