User login
Opioid reform legislation passes House committee
The House Energy & Commerce Committee has passed a comprehensive package of bills designed to curb the nation’s opioid epidemic.
Eleven opioid-related bills passed the full committee by voice vote on April 27 and April 28. Key provisions of the legislation would:
• Create an interagency task force to review best practices for pain management and prescribing.
• Require annual updates of federal opioid-prescribing guidelines.
• Authorize grants to test coprescribing opioids with buprenorphine or naloxone.
• Limit the number of pills prescribed.
• Increase the number of patients that a qualified addiction treatment specialist could see annually.
• Require an FDA advisory committee to review any new opioid proposed without abuse-deterrent properties.
• Require a detailed assessment of currently available inpatient and outpatient treatment beds.
• Prohibit the sale dextromethorphan-containing products to minors.
The full Senate also has a package of opioid-related bills to consider. On March 17, the Senate Committee on Health, Education, Labor and Pensions moved similar legislation to the Senate floor, including bills that would increase addiction patient panels, require coprescribing, and mandate insurance coverage of addiction treatment as required by current mental health parity laws.
Earlier this year, in a near unanimous vote, the Senate passed the Comprehensive Addiction and Recovery Act, which calls for the creation of a federal pain management best practices interagency task force. No funding was attached to the legislation, however, and companion legislation remains in committee in the House.
Although the opioid bills had bipartisan support in the Energy & Commerce Committee, rancor may yet surface. During mark-up, three amendments were defeated mostly along party lines. The amendments would have increased the number of patients each qualified provider can treat with buprenorphine to a variety of levels – one amendment called for a maximum of 250 patients while others called for as many as 300 or 500. Supporters of the amendments said higher numbers would ensure treatment for many more patients while opponents expressed concern about sacrificing quality of care for quantity.
Another defeated amendment called for a $1 billion appropriation for increased opioid treatment, echoing President Obama’s call earlier this year. Opponents painted the proposal as “fiscally irresponsible.”
At press time, the House had not scheduled consideration on the opioid bills.
On Twitter @whitneymcknight
The House Energy & Commerce Committee has passed a comprehensive package of bills designed to curb the nation’s opioid epidemic.
Eleven opioid-related bills passed the full committee by voice vote on April 27 and April 28. Key provisions of the legislation would:
• Create an interagency task force to review best practices for pain management and prescribing.
• Require annual updates of federal opioid-prescribing guidelines.
• Authorize grants to test coprescribing opioids with buprenorphine or naloxone.
• Limit the number of pills prescribed.
• Increase the number of patients that a qualified addiction treatment specialist could see annually.
• Require an FDA advisory committee to review any new opioid proposed without abuse-deterrent properties.
• Require a detailed assessment of currently available inpatient and outpatient treatment beds.
• Prohibit the sale dextromethorphan-containing products to minors.
The full Senate also has a package of opioid-related bills to consider. On March 17, the Senate Committee on Health, Education, Labor and Pensions moved similar legislation to the Senate floor, including bills that would increase addiction patient panels, require coprescribing, and mandate insurance coverage of addiction treatment as required by current mental health parity laws.
Earlier this year, in a near unanimous vote, the Senate passed the Comprehensive Addiction and Recovery Act, which calls for the creation of a federal pain management best practices interagency task force. No funding was attached to the legislation, however, and companion legislation remains in committee in the House.
Although the opioid bills had bipartisan support in the Energy & Commerce Committee, rancor may yet surface. During mark-up, three amendments were defeated mostly along party lines. The amendments would have increased the number of patients each qualified provider can treat with buprenorphine to a variety of levels – one amendment called for a maximum of 250 patients while others called for as many as 300 or 500. Supporters of the amendments said higher numbers would ensure treatment for many more patients while opponents expressed concern about sacrificing quality of care for quantity.
Another defeated amendment called for a $1 billion appropriation for increased opioid treatment, echoing President Obama’s call earlier this year. Opponents painted the proposal as “fiscally irresponsible.”
At press time, the House had not scheduled consideration on the opioid bills.
On Twitter @whitneymcknight
The House Energy & Commerce Committee has passed a comprehensive package of bills designed to curb the nation’s opioid epidemic.
Eleven opioid-related bills passed the full committee by voice vote on April 27 and April 28. Key provisions of the legislation would:
• Create an interagency task force to review best practices for pain management and prescribing.
• Require annual updates of federal opioid-prescribing guidelines.
• Authorize grants to test coprescribing opioids with buprenorphine or naloxone.
• Limit the number of pills prescribed.
• Increase the number of patients that a qualified addiction treatment specialist could see annually.
• Require an FDA advisory committee to review any new opioid proposed without abuse-deterrent properties.
• Require a detailed assessment of currently available inpatient and outpatient treatment beds.
• Prohibit the sale dextromethorphan-containing products to minors.
The full Senate also has a package of opioid-related bills to consider. On March 17, the Senate Committee on Health, Education, Labor and Pensions moved similar legislation to the Senate floor, including bills that would increase addiction patient panels, require coprescribing, and mandate insurance coverage of addiction treatment as required by current mental health parity laws.
Earlier this year, in a near unanimous vote, the Senate passed the Comprehensive Addiction and Recovery Act, which calls for the creation of a federal pain management best practices interagency task force. No funding was attached to the legislation, however, and companion legislation remains in committee in the House.
Although the opioid bills had bipartisan support in the Energy & Commerce Committee, rancor may yet surface. During mark-up, three amendments were defeated mostly along party lines. The amendments would have increased the number of patients each qualified provider can treat with buprenorphine to a variety of levels – one amendment called for a maximum of 250 patients while others called for as many as 300 or 500. Supporters of the amendments said higher numbers would ensure treatment for many more patients while opponents expressed concern about sacrificing quality of care for quantity.
Another defeated amendment called for a $1 billion appropriation for increased opioid treatment, echoing President Obama’s call earlier this year. Opponents painted the proposal as “fiscally irresponsible.”
At press time, the House had not scheduled consideration on the opioid bills.
On Twitter @whitneymcknight
FROM A HOUSE ENERGY & COMMERCE COMMITTEE HEARING
More training in suicide risk assessment needed, experts say
The rise in U.S. suicide rates to the highest levels in almost 30 years is tied to many factors. One fact is clear – some experts say – the lack of training in suicide risk assessment among mental health and substance abuse clinicians is an issue that must be addressed.
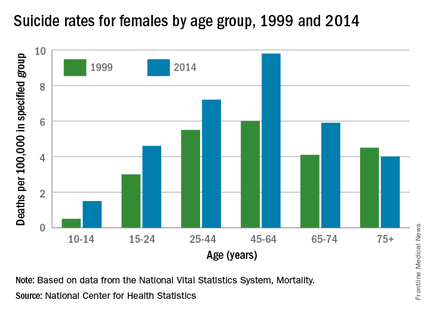
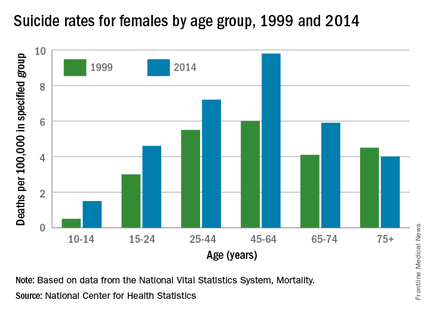
“There are mental health professionals who have little to no training in suicide risk assessment,” Dr. Michael F. Myers, professor of clinical psychiatry at State University of New York, Brooklyn, said in an interview.
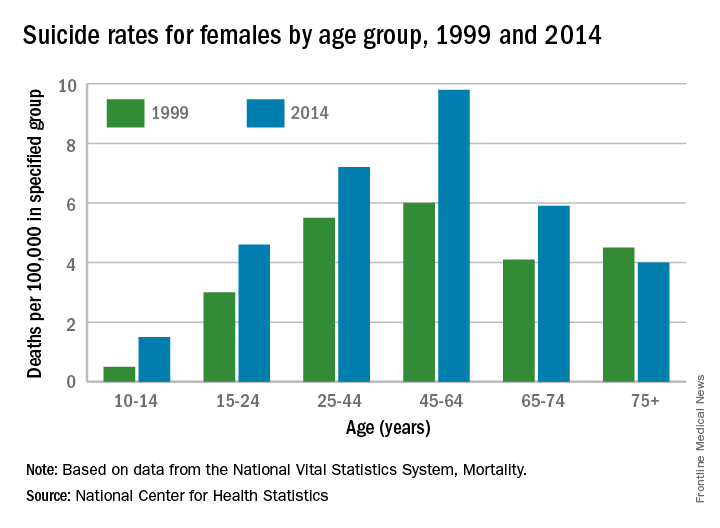
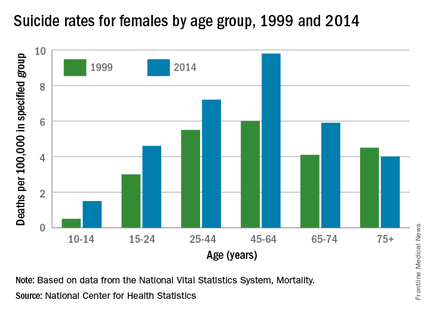
According to a report released April 22 by the Centers for Disease Control and Prevention, suicide is the 10th-leading cause of death in the United States. It increased by 24% from 1999 to 2014 overall, and the groups most dramatically affected were girls aged 10-14 years, and men aged 45-64. Women aged 45-64 and men aged 75 years and older had the highest suicide rates. About 40,000 Americans a year take their own lives, which is double the number of homicides in the country annually.
After 2006 – against the backdrop of a tough economy and a burgeoning opioid crisis – the suicide rate accelerated. Meanwhile, overall mortality from causes such as cardiovascular disease and cancer is on the decline, according to the CDC report.
Standards vary
In 2012, the American Association of Suicidology reported in its suicide prevention recommendations that less than a quarter of social workers had received any formal suicide prevention training which, when offered, usually lasted 4 hours or fewer. Only 6% of marriage and family therapists had received any such training. Psychiatry residency programs were found to offer training 91% of the time.
But in 2014, the U.S. Preventive Services Task Force (USPSTF) recommendation statement on the efficacy of suicide risk screening concluded that the evidence was insufficient to warrant allocating resources to it (Ann Int Med. 2014;160[10]:719-26). The USPSTF, however, does recommend that primary care professionals screen for depression in adults and adolescents, and earlier this year, updated its recommendations to screen pregnant women in particular (JAMA. 2016;315[4]380-7).
Also, this year, the Centers for Medicare & Medicaid Services required its providers to screen patients for depression using the Patient Health Questionnaire-9 (PHQ-9).
Dr. Myers thinks this is a good starting point, but said that adding more suicide-specific questions to the depression screening process could save more lives.
Despite the USPSTF’s recommendation, investigators for a systematic review published in 2005 concluded that “Physician education in depression recognition and treatment and restricting access to lethal methods reduce suicide rates” (JAMA. 2005;294[16];2064-74). There is some federal support for implementation of suicide prevention in the primary and mental health care settings. In 2012, the U.S. Surgeon General’s office and the National Action Alliance for Suicide Prevention jointly released the National Strategy for Suicide Prevention, which cited as its No. 1 priority, the integration of suicide prevention into health care reform through initiatives such as the Zero Suicide campaign. Sponsored by the Suicide Prevention Resource Council, and funded in part by the Substance Abuse and Mental Health Services Administration (SAMHSA), the program aims to close the gaps in care that distract or otherwise hinder caring for and following through with patients who are at risk for suicide.
An unevenly trained mental health workforce was targeted earlier this month by members of the National Academies of Sciences who, in a report, criticized the current state of siloed mental health care, saying it results in stigmatization and undertreatment of mental illness. The authors urged Congress to empower the U.S. Department of Health and Human Services to oversee better implementation and coordination of evidence-based services to prevent and treat mental disorders that lead to outcomes such as suicide. The report cites successful federal initiatives in England, Australia, and Canada that have notably improved mental health care in those countries. Those improvements took decades, the report notes.
Earlier prevention efforts
In 1999, then–Surgeon General David Satcher issued his Call to Action to Prevent Suicide, which lays out a comprehensive and integrated approach. In 2012, former Surgeon General Regina M. Benjamin published a National Strategy for Suicide Prevention. But without federal policy behind those efforts, the recommendations have not been implemented.
“This is not dissimilar to what happened in the HIV/AIDS epidemic, where finally, the medical community had to be mandated to get trained to treat the illness,” said Paul Quinnett, Ph.D., a clinical psychologist at the University of Washington, Spokane, and founder and CEO of the QPR Institute, a suicide prevention nonprofit.
Dr. Quinnett admits that what he sees as a lack of political will among many of his colleagues to address the suicide crisis angers him. “We can’t afford to look the other way and pretend this isn’t happening. These numbers are just crushing.”
Currently, however, Washington and Kentucky are the only states with suicide-specific requirements for licensure. Recent efforts to mandate training in California failed when Gov. Jerry Brown (D) vetoed the measure after heavy lobbying efforts by various mental health professional organizations, including the California chapter of the National Association of Social Workers, which argued that it should be entrusted to train its members on a volunteer, as-needed basis.
Even when clinicians have received proper training and met all standards of practice, some patients still may be lost, said Dr. Myers, who also is immediate past vice chair for education and residency training director at SUNY Downstate Medical Center. “You can’t save everyone,” he said. “Some patients are just hell-bent on killing themselves and will very cleverly pull the wool over our eyes.”
He also pointed to the gaps in care that training alone cannot prevent, specifically citing the instances in which people complete a suicide because of a lack of follow-up – the kind of intensive discharge planning that might include several daily phone calls and plans for whom to talk to when thoughts of suicide arise. Those kinds of protocols are not widely used, Dr. Myers said, partly because of the cost.
But Dr. Myers also points to a failing that, while not documented, he said is well-known among his mental health peers: calculated avoidance of at-risk patients.
“There are those, therapists especially, who are cherry picking their patients. They try to make sure they don’t have to look after suicidal people. They do their best to avoid them, and will even screen referrals to avoid them,” said Dr. Myers, who has written extensively about suicide. “It’s equivalent to an oncologist saying to a referring physician: ‘Sure, I will see your patient with breast cancer, but she doesn’t have metastasis, does she?’ It’s unconscionable.”
It would help if there were guidelines for care similar to oncology or cardiology, he said, to help clinicians better balance science with instinct.
Dr. Quinnett thinks the crisis is likely to worsen before it gets better. At least one study has shown strong associations between rates of joblessness in the United States and suicide rates (Soc Sci Med. 2014 Sep;116:22-31). “I’m particularly worried about those people whose lives have been economically hollowed out by the Great Recession,” said Dr. Quinnett, also of the department of psychiatry and behavioral sciences at the University of Washington. “There are men who are aging out [of the workforce] without retirement plans or any other fallback [and who], face losing their dignity and self-esteem, and will need handouts. It’s going to be very ugly.”
Dr. Myers has written several books, including “Touched by Suicide: Hope and Healing After Loss” (New York: Gotham/Penguin, 2006). Dr. Quinnett’s suicide prevention nonprofit, the QPR Institute, is listed on SAMHSA’s National Registry of Evidence-based Programs and Practices.
Coming soon: A national suicide registry?
At the National Institutes of Health, a movement is afoot to create a national suicide registry.
“Registries can help us in all kinds of conditions. That’s how we got ahead in cancer,” Jane Pearson, Ph.D., the National Institute of Mental Health’s program chief for Suicide Treatment and Preventive Interventions Research, said in an interview.
It’s early days yet, but Dr. Pearson and her colleagues are looking into how to leverage data already collected, how to determine the quality of those data, and whom to task with its oversight and interpretation. Then there is the need to know what questions matter most, either to create new registries or to cull patterns from currently available data.
Dr. Pearson said a dedicated suicide data collection effort in a large health care system or a single state would, theoretically, allow patterns to emerge that would help create infrastructures to support specific populations at risk for suicide and guidelines for referral to support.
“Mental health issues have always been a challenge for primary care. As long as they have a partner they can refer to, it’s a much easier [task],” she said. “We wouldn’t ask them to be cardiovascular specialists. When a patient has a stroke, they figure it out and move people along. The registry ideas encompasses that. It’s about creating a whole system for how we are going to do better.”
On Twitter @whitneymcknight
When analyzing these numbers, it is important to keep them in perspective, Dr. Carl C. Bell, who has served on the National Strategy for Suicide Prevention Task Force, said in an interview. The problem is that suicide rates doubling, for example, means the rates went from 11/100,000 up to 22/100,000, or if they tripled they went from 11/100,000 up to 33/100,000.
The reality is there is not statistical difference between those three numbers. The differences could be attributable to just chance and numbers bouncing around, so to apply a meaning to the “increase” is spurious. These suicide and homicide numbers bounce up and down, but they might not mean anything, as the event is such a rare occurrence.
Ultimately, we must examine ways to strengthen protective factors around people who are most vulnerable, such as those with signs and symptoms of depression and substance abuse.
Dr. Bell is staff psychiatrist at Jackson Park Hospital Family Medicine Clinic and former president/CEO of Community Mental Health Council both in Chicago.
When analyzing these numbers, it is important to keep them in perspective, Dr. Carl C. Bell, who has served on the National Strategy for Suicide Prevention Task Force, said in an interview. The problem is that suicide rates doubling, for example, means the rates went from 11/100,000 up to 22/100,000, or if they tripled they went from 11/100,000 up to 33/100,000.
The reality is there is not statistical difference between those three numbers. The differences could be attributable to just chance and numbers bouncing around, so to apply a meaning to the “increase” is spurious. These suicide and homicide numbers bounce up and down, but they might not mean anything, as the event is such a rare occurrence.
Ultimately, we must examine ways to strengthen protective factors around people who are most vulnerable, such as those with signs and symptoms of depression and substance abuse.
Dr. Bell is staff psychiatrist at Jackson Park Hospital Family Medicine Clinic and former president/CEO of Community Mental Health Council both in Chicago.
When analyzing these numbers, it is important to keep them in perspective, Dr. Carl C. Bell, who has served on the National Strategy for Suicide Prevention Task Force, said in an interview. The problem is that suicide rates doubling, for example, means the rates went from 11/100,000 up to 22/100,000, or if they tripled they went from 11/100,000 up to 33/100,000.
The reality is there is not statistical difference between those three numbers. The differences could be attributable to just chance and numbers bouncing around, so to apply a meaning to the “increase” is spurious. These suicide and homicide numbers bounce up and down, but they might not mean anything, as the event is such a rare occurrence.
Ultimately, we must examine ways to strengthen protective factors around people who are most vulnerable, such as those with signs and symptoms of depression and substance abuse.
Dr. Bell is staff psychiatrist at Jackson Park Hospital Family Medicine Clinic and former president/CEO of Community Mental Health Council both in Chicago.
The rise in U.S. suicide rates to the highest levels in almost 30 years is tied to many factors. One fact is clear – some experts say – the lack of training in suicide risk assessment among mental health and substance abuse clinicians is an issue that must be addressed.
“There are mental health professionals who have little to no training in suicide risk assessment,” Dr. Michael F. Myers, professor of clinical psychiatry at State University of New York, Brooklyn, said in an interview.
According to a report released April 22 by the Centers for Disease Control and Prevention, suicide is the 10th-leading cause of death in the United States. It increased by 24% from 1999 to 2014 overall, and the groups most dramatically affected were girls aged 10-14 years, and men aged 45-64. Women aged 45-64 and men aged 75 years and older had the highest suicide rates. About 40,000 Americans a year take their own lives, which is double the number of homicides in the country annually.
After 2006 – against the backdrop of a tough economy and a burgeoning opioid crisis – the suicide rate accelerated. Meanwhile, overall mortality from causes such as cardiovascular disease and cancer is on the decline, according to the CDC report.
Standards vary
In 2012, the American Association of Suicidology reported in its suicide prevention recommendations that less than a quarter of social workers had received any formal suicide prevention training which, when offered, usually lasted 4 hours or fewer. Only 6% of marriage and family therapists had received any such training. Psychiatry residency programs were found to offer training 91% of the time.
But in 2014, the U.S. Preventive Services Task Force (USPSTF) recommendation statement on the efficacy of suicide risk screening concluded that the evidence was insufficient to warrant allocating resources to it (Ann Int Med. 2014;160[10]:719-26). The USPSTF, however, does recommend that primary care professionals screen for depression in adults and adolescents, and earlier this year, updated its recommendations to screen pregnant women in particular (JAMA. 2016;315[4]380-7).
Also, this year, the Centers for Medicare & Medicaid Services required its providers to screen patients for depression using the Patient Health Questionnaire-9 (PHQ-9).
Dr. Myers thinks this is a good starting point, but said that adding more suicide-specific questions to the depression screening process could save more lives.
Despite the USPSTF’s recommendation, investigators for a systematic review published in 2005 concluded that “Physician education in depression recognition and treatment and restricting access to lethal methods reduce suicide rates” (JAMA. 2005;294[16];2064-74). There is some federal support for implementation of suicide prevention in the primary and mental health care settings. In 2012, the U.S. Surgeon General’s office and the National Action Alliance for Suicide Prevention jointly released the National Strategy for Suicide Prevention, which cited as its No. 1 priority, the integration of suicide prevention into health care reform through initiatives such as the Zero Suicide campaign. Sponsored by the Suicide Prevention Resource Council, and funded in part by the Substance Abuse and Mental Health Services Administration (SAMHSA), the program aims to close the gaps in care that distract or otherwise hinder caring for and following through with patients who are at risk for suicide.
An unevenly trained mental health workforce was targeted earlier this month by members of the National Academies of Sciences who, in a report, criticized the current state of siloed mental health care, saying it results in stigmatization and undertreatment of mental illness. The authors urged Congress to empower the U.S. Department of Health and Human Services to oversee better implementation and coordination of evidence-based services to prevent and treat mental disorders that lead to outcomes such as suicide. The report cites successful federal initiatives in England, Australia, and Canada that have notably improved mental health care in those countries. Those improvements took decades, the report notes.
Earlier prevention efforts
In 1999, then–Surgeon General David Satcher issued his Call to Action to Prevent Suicide, which lays out a comprehensive and integrated approach. In 2012, former Surgeon General Regina M. Benjamin published a National Strategy for Suicide Prevention. But without federal policy behind those efforts, the recommendations have not been implemented.
“This is not dissimilar to what happened in the HIV/AIDS epidemic, where finally, the medical community had to be mandated to get trained to treat the illness,” said Paul Quinnett, Ph.D., a clinical psychologist at the University of Washington, Spokane, and founder and CEO of the QPR Institute, a suicide prevention nonprofit.
Dr. Quinnett admits that what he sees as a lack of political will among many of his colleagues to address the suicide crisis angers him. “We can’t afford to look the other way and pretend this isn’t happening. These numbers are just crushing.”
Currently, however, Washington and Kentucky are the only states with suicide-specific requirements for licensure. Recent efforts to mandate training in California failed when Gov. Jerry Brown (D) vetoed the measure after heavy lobbying efforts by various mental health professional organizations, including the California chapter of the National Association of Social Workers, which argued that it should be entrusted to train its members on a volunteer, as-needed basis.
Even when clinicians have received proper training and met all standards of practice, some patients still may be lost, said Dr. Myers, who also is immediate past vice chair for education and residency training director at SUNY Downstate Medical Center. “You can’t save everyone,” he said. “Some patients are just hell-bent on killing themselves and will very cleverly pull the wool over our eyes.”
He also pointed to the gaps in care that training alone cannot prevent, specifically citing the instances in which people complete a suicide because of a lack of follow-up – the kind of intensive discharge planning that might include several daily phone calls and plans for whom to talk to when thoughts of suicide arise. Those kinds of protocols are not widely used, Dr. Myers said, partly because of the cost.
But Dr. Myers also points to a failing that, while not documented, he said is well-known among his mental health peers: calculated avoidance of at-risk patients.
“There are those, therapists especially, who are cherry picking their patients. They try to make sure they don’t have to look after suicidal people. They do their best to avoid them, and will even screen referrals to avoid them,” said Dr. Myers, who has written extensively about suicide. “It’s equivalent to an oncologist saying to a referring physician: ‘Sure, I will see your patient with breast cancer, but she doesn’t have metastasis, does she?’ It’s unconscionable.”
It would help if there were guidelines for care similar to oncology or cardiology, he said, to help clinicians better balance science with instinct.
Dr. Quinnett thinks the crisis is likely to worsen before it gets better. At least one study has shown strong associations between rates of joblessness in the United States and suicide rates (Soc Sci Med. 2014 Sep;116:22-31). “I’m particularly worried about those people whose lives have been economically hollowed out by the Great Recession,” said Dr. Quinnett, also of the department of psychiatry and behavioral sciences at the University of Washington. “There are men who are aging out [of the workforce] without retirement plans or any other fallback [and who], face losing their dignity and self-esteem, and will need handouts. It’s going to be very ugly.”
Dr. Myers has written several books, including “Touched by Suicide: Hope and Healing After Loss” (New York: Gotham/Penguin, 2006). Dr. Quinnett’s suicide prevention nonprofit, the QPR Institute, is listed on SAMHSA’s National Registry of Evidence-based Programs and Practices.
Coming soon: A national suicide registry?
At the National Institutes of Health, a movement is afoot to create a national suicide registry.
“Registries can help us in all kinds of conditions. That’s how we got ahead in cancer,” Jane Pearson, Ph.D., the National Institute of Mental Health’s program chief for Suicide Treatment and Preventive Interventions Research, said in an interview.
It’s early days yet, but Dr. Pearson and her colleagues are looking into how to leverage data already collected, how to determine the quality of those data, and whom to task with its oversight and interpretation. Then there is the need to know what questions matter most, either to create new registries or to cull patterns from currently available data.
Dr. Pearson said a dedicated suicide data collection effort in a large health care system or a single state would, theoretically, allow patterns to emerge that would help create infrastructures to support specific populations at risk for suicide and guidelines for referral to support.
“Mental health issues have always been a challenge for primary care. As long as they have a partner they can refer to, it’s a much easier [task],” she said. “We wouldn’t ask them to be cardiovascular specialists. When a patient has a stroke, they figure it out and move people along. The registry ideas encompasses that. It’s about creating a whole system for how we are going to do better.”
On Twitter @whitneymcknight
The rise in U.S. suicide rates to the highest levels in almost 30 years is tied to many factors. One fact is clear – some experts say – the lack of training in suicide risk assessment among mental health and substance abuse clinicians is an issue that must be addressed.
“There are mental health professionals who have little to no training in suicide risk assessment,” Dr. Michael F. Myers, professor of clinical psychiatry at State University of New York, Brooklyn, said in an interview.
According to a report released April 22 by the Centers for Disease Control and Prevention, suicide is the 10th-leading cause of death in the United States. It increased by 24% from 1999 to 2014 overall, and the groups most dramatically affected were girls aged 10-14 years, and men aged 45-64. Women aged 45-64 and men aged 75 years and older had the highest suicide rates. About 40,000 Americans a year take their own lives, which is double the number of homicides in the country annually.
After 2006 – against the backdrop of a tough economy and a burgeoning opioid crisis – the suicide rate accelerated. Meanwhile, overall mortality from causes such as cardiovascular disease and cancer is on the decline, according to the CDC report.
Standards vary
In 2012, the American Association of Suicidology reported in its suicide prevention recommendations that less than a quarter of social workers had received any formal suicide prevention training which, when offered, usually lasted 4 hours or fewer. Only 6% of marriage and family therapists had received any such training. Psychiatry residency programs were found to offer training 91% of the time.
But in 2014, the U.S. Preventive Services Task Force (USPSTF) recommendation statement on the efficacy of suicide risk screening concluded that the evidence was insufficient to warrant allocating resources to it (Ann Int Med. 2014;160[10]:719-26). The USPSTF, however, does recommend that primary care professionals screen for depression in adults and adolescents, and earlier this year, updated its recommendations to screen pregnant women in particular (JAMA. 2016;315[4]380-7).
Also, this year, the Centers for Medicare & Medicaid Services required its providers to screen patients for depression using the Patient Health Questionnaire-9 (PHQ-9).
Dr. Myers thinks this is a good starting point, but said that adding more suicide-specific questions to the depression screening process could save more lives.
Despite the USPSTF’s recommendation, investigators for a systematic review published in 2005 concluded that “Physician education in depression recognition and treatment and restricting access to lethal methods reduce suicide rates” (JAMA. 2005;294[16];2064-74). There is some federal support for implementation of suicide prevention in the primary and mental health care settings. In 2012, the U.S. Surgeon General’s office and the National Action Alliance for Suicide Prevention jointly released the National Strategy for Suicide Prevention, which cited as its No. 1 priority, the integration of suicide prevention into health care reform through initiatives such as the Zero Suicide campaign. Sponsored by the Suicide Prevention Resource Council, and funded in part by the Substance Abuse and Mental Health Services Administration (SAMHSA), the program aims to close the gaps in care that distract or otherwise hinder caring for and following through with patients who are at risk for suicide.
An unevenly trained mental health workforce was targeted earlier this month by members of the National Academies of Sciences who, in a report, criticized the current state of siloed mental health care, saying it results in stigmatization and undertreatment of mental illness. The authors urged Congress to empower the U.S. Department of Health and Human Services to oversee better implementation and coordination of evidence-based services to prevent and treat mental disorders that lead to outcomes such as suicide. The report cites successful federal initiatives in England, Australia, and Canada that have notably improved mental health care in those countries. Those improvements took decades, the report notes.
Earlier prevention efforts
In 1999, then–Surgeon General David Satcher issued his Call to Action to Prevent Suicide, which lays out a comprehensive and integrated approach. In 2012, former Surgeon General Regina M. Benjamin published a National Strategy for Suicide Prevention. But without federal policy behind those efforts, the recommendations have not been implemented.
“This is not dissimilar to what happened in the HIV/AIDS epidemic, where finally, the medical community had to be mandated to get trained to treat the illness,” said Paul Quinnett, Ph.D., a clinical psychologist at the University of Washington, Spokane, and founder and CEO of the QPR Institute, a suicide prevention nonprofit.
Dr. Quinnett admits that what he sees as a lack of political will among many of his colleagues to address the suicide crisis angers him. “We can’t afford to look the other way and pretend this isn’t happening. These numbers are just crushing.”
Currently, however, Washington and Kentucky are the only states with suicide-specific requirements for licensure. Recent efforts to mandate training in California failed when Gov. Jerry Brown (D) vetoed the measure after heavy lobbying efforts by various mental health professional organizations, including the California chapter of the National Association of Social Workers, which argued that it should be entrusted to train its members on a volunteer, as-needed basis.
Even when clinicians have received proper training and met all standards of practice, some patients still may be lost, said Dr. Myers, who also is immediate past vice chair for education and residency training director at SUNY Downstate Medical Center. “You can’t save everyone,” he said. “Some patients are just hell-bent on killing themselves and will very cleverly pull the wool over our eyes.”
He also pointed to the gaps in care that training alone cannot prevent, specifically citing the instances in which people complete a suicide because of a lack of follow-up – the kind of intensive discharge planning that might include several daily phone calls and plans for whom to talk to when thoughts of suicide arise. Those kinds of protocols are not widely used, Dr. Myers said, partly because of the cost.
But Dr. Myers also points to a failing that, while not documented, he said is well-known among his mental health peers: calculated avoidance of at-risk patients.
“There are those, therapists especially, who are cherry picking their patients. They try to make sure they don’t have to look after suicidal people. They do their best to avoid them, and will even screen referrals to avoid them,” said Dr. Myers, who has written extensively about suicide. “It’s equivalent to an oncologist saying to a referring physician: ‘Sure, I will see your patient with breast cancer, but she doesn’t have metastasis, does she?’ It’s unconscionable.”
It would help if there were guidelines for care similar to oncology or cardiology, he said, to help clinicians better balance science with instinct.
Dr. Quinnett thinks the crisis is likely to worsen before it gets better. At least one study has shown strong associations between rates of joblessness in the United States and suicide rates (Soc Sci Med. 2014 Sep;116:22-31). “I’m particularly worried about those people whose lives have been economically hollowed out by the Great Recession,” said Dr. Quinnett, also of the department of psychiatry and behavioral sciences at the University of Washington. “There are men who are aging out [of the workforce] without retirement plans or any other fallback [and who], face losing their dignity and self-esteem, and will need handouts. It’s going to be very ugly.”
Dr. Myers has written several books, including “Touched by Suicide: Hope and Healing After Loss” (New York: Gotham/Penguin, 2006). Dr. Quinnett’s suicide prevention nonprofit, the QPR Institute, is listed on SAMHSA’s National Registry of Evidence-based Programs and Practices.
Coming soon: A national suicide registry?
At the National Institutes of Health, a movement is afoot to create a national suicide registry.
“Registries can help us in all kinds of conditions. That’s how we got ahead in cancer,” Jane Pearson, Ph.D., the National Institute of Mental Health’s program chief for Suicide Treatment and Preventive Interventions Research, said in an interview.
It’s early days yet, but Dr. Pearson and her colleagues are looking into how to leverage data already collected, how to determine the quality of those data, and whom to task with its oversight and interpretation. Then there is the need to know what questions matter most, either to create new registries or to cull patterns from currently available data.
Dr. Pearson said a dedicated suicide data collection effort in a large health care system or a single state would, theoretically, allow patterns to emerge that would help create infrastructures to support specific populations at risk for suicide and guidelines for referral to support.
“Mental health issues have always been a challenge for primary care. As long as they have a partner they can refer to, it’s a much easier [task],” she said. “We wouldn’t ask them to be cardiovascular specialists. When a patient has a stroke, they figure it out and move people along. The registry ideas encompasses that. It’s about creating a whole system for how we are going to do better.”
On Twitter @whitneymcknight
How to Personalize Pain Management in Era of Opioids
WASHINGTON – As the prescription opioid crisis rages, how physicians evaluate, define, and treat chronic pain is evolving.
“In the science books, there’s a definition of pain,” explained Dr. Patrice Harris, psychiatrist and chair of the American Medical Association’s Task Force to Reduce Prescription Opioid Abuse. But how individuals actually perceive pain in different situations is very complex. No matter what kind of measuring tool physicians apply, she noted, “pain is going to be personal.”
In a candid interview, Dr. Harris discussed the limitation of pain scales, the value of conversations between physicians and their patients, and the importance of cultural competency to alleviate suffering and avoid unintentional harm.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – As the prescription opioid crisis rages, how physicians evaluate, define, and treat chronic pain is evolving.
“In the science books, there’s a definition of pain,” explained Dr. Patrice Harris, psychiatrist and chair of the American Medical Association’s Task Force to Reduce Prescription Opioid Abuse. But how individuals actually perceive pain in different situations is very complex. No matter what kind of measuring tool physicians apply, she noted, “pain is going to be personal.”
In a candid interview, Dr. Harris discussed the limitation of pain scales, the value of conversations between physicians and their patients, and the importance of cultural competency to alleviate suffering and avoid unintentional harm.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – As the prescription opioid crisis rages, how physicians evaluate, define, and treat chronic pain is evolving.
“In the science books, there’s a definition of pain,” explained Dr. Patrice Harris, psychiatrist and chair of the American Medical Association’s Task Force to Reduce Prescription Opioid Abuse. But how individuals actually perceive pain in different situations is very complex. No matter what kind of measuring tool physicians apply, she noted, “pain is going to be personal.”
In a candid interview, Dr. Harris discussed the limitation of pain scales, the value of conversations between physicians and their patients, and the importance of cultural competency to alleviate suffering and avoid unintentional harm.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO: How to personalize pain management in era of opioids
WASHINGTON – As the prescription opioid crisis rages, how physicians evaluate, define, and treat chronic pain is evolving.
“In the science books, there’s a definition of pain,” explained Dr. Patrice Harris, psychiatrist and chair of the American Medical Association’s Task Force to Reduce Prescription Opioid Abuse. But how individuals actually perceive pain in different situations is very complex. No matter what kind of measuring tool physicians apply, she noted, “pain is going to be personal.”
In a candid interview, Dr. Harris discussed the limitation of pain scales, the value of conversations between physicians and their patients, and the importance of cultural competency to alleviate suffering and avoid unintentional harm.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
WASHINGTON – As the prescription opioid crisis rages, how physicians evaluate, define, and treat chronic pain is evolving.
“In the science books, there’s a definition of pain,” explained Dr. Patrice Harris, psychiatrist and chair of the American Medical Association’s Task Force to Reduce Prescription Opioid Abuse. But how individuals actually perceive pain in different situations is very complex. No matter what kind of measuring tool physicians apply, she noted, “pain is going to be personal.”
In a candid interview, Dr. Harris discussed the limitation of pain scales, the value of conversations between physicians and their patients, and the importance of cultural competency to alleviate suffering and avoid unintentional harm.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
WASHINGTON – As the prescription opioid crisis rages, how physicians evaluate, define, and treat chronic pain is evolving.
“In the science books, there’s a definition of pain,” explained Dr. Patrice Harris, psychiatrist and chair of the American Medical Association’s Task Force to Reduce Prescription Opioid Abuse. But how individuals actually perceive pain in different situations is very complex. No matter what kind of measuring tool physicians apply, she noted, “pain is going to be personal.”
In a candid interview, Dr. Harris discussed the limitation of pain scales, the value of conversations between physicians and their patients, and the importance of cultural competency to alleviate suffering and avoid unintentional harm.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
Heavy marijuana use by male adolescents tied to higher mortality risk
Heavy marijuana use by men aged 18 or 19 years is associated with a greater risk of mortality by age 60, a longitudinal study of more than 45,000 subjects shows.
The findings, published online April 22, might surprise some, wrote Dr. Edison Manrique-Garcia, a researcher at the Karolinska Institutet, Stockholm, and his colleagues, because a previous study of the same cohort found no such associations. “However, in this longer-term follow-up, the cohort members had reached an age where the detrimental somatic effects of cannabis use were more likely to be apparent,” they wrote (Am J Psychiatry. 2016 Apr 22. doi: 10.1176/appi.ajp.2016.14050637).
Using the Swedish National Cause of Death Register, Dr. Manrique-Garcia and his colleagues analyzed data from a cohort of 50,373 male 18- and 19-year-olds who entered compulsory military service in 1969 and 1970. Because marijuana use information on 4,998 of the subjects was missing, the final analysis included 45,375 subjects.
Dr. Manrique-Garcia and his coauthors found that, from the time of conscription to 2011, there had been 3,918 deaths out of the 45,375 men. Those who had reported ever using marijuana were shown to have died earlier than those who had never used the drug. After adjusting for confounders, the investigators also found a significantly higher risk of death, with a hazard ratio of 1.4, in those who had used marijuana 50 or more times, compared with a hazard ratio of 0.9 in those who had used it 1-50 times.
All marijuana users in the study also were found to have sustained higher rates of mortal injuries, whether accidental or purposefully inflicted, when compared with those who had never used the drug, although the investigators reported that they did not find a correlation between increased suicide risk and marijuana use.
Dr. Manrique-Garcia and his colleagues also reported that, although they found a three- to fourfold greater mortality risk among men with a diagnosis of psychosis, “the risk did not differ between marijuana users and nonusers.” In addition, the investigators did not find a significant interaction between marijuana use and psychotic disorder diagnoses with regard to an increased mortality risk.
The investigators said that their results, while valuable, are limited by the lack of data on lifetime use of marijuana. The results also are limited by the absence of information about tobacco smoking and risky alcohol use among the men after conscription.
“Study limitations notwithstanding, we found that subjects with a baseline history of heavy use of cannabis have an increased risk of death over the course of follow-up,” they wrote.
The study was funded by grants from the Swedish Council for Working Life and Social Research and the Stockholm County Council. The authors reported no financial conflicts.
On Twitter @whitneymcknight
Heavy marijuana use by men aged 18 or 19 years is associated with a greater risk of mortality by age 60, a longitudinal study of more than 45,000 subjects shows.
The findings, published online April 22, might surprise some, wrote Dr. Edison Manrique-Garcia, a researcher at the Karolinska Institutet, Stockholm, and his colleagues, because a previous study of the same cohort found no such associations. “However, in this longer-term follow-up, the cohort members had reached an age where the detrimental somatic effects of cannabis use were more likely to be apparent,” they wrote (Am J Psychiatry. 2016 Apr 22. doi: 10.1176/appi.ajp.2016.14050637).
Using the Swedish National Cause of Death Register, Dr. Manrique-Garcia and his colleagues analyzed data from a cohort of 50,373 male 18- and 19-year-olds who entered compulsory military service in 1969 and 1970. Because marijuana use information on 4,998 of the subjects was missing, the final analysis included 45,375 subjects.
Dr. Manrique-Garcia and his coauthors found that, from the time of conscription to 2011, there had been 3,918 deaths out of the 45,375 men. Those who had reported ever using marijuana were shown to have died earlier than those who had never used the drug. After adjusting for confounders, the investigators also found a significantly higher risk of death, with a hazard ratio of 1.4, in those who had used marijuana 50 or more times, compared with a hazard ratio of 0.9 in those who had used it 1-50 times.
All marijuana users in the study also were found to have sustained higher rates of mortal injuries, whether accidental or purposefully inflicted, when compared with those who had never used the drug, although the investigators reported that they did not find a correlation between increased suicide risk and marijuana use.
Dr. Manrique-Garcia and his colleagues also reported that, although they found a three- to fourfold greater mortality risk among men with a diagnosis of psychosis, “the risk did not differ between marijuana users and nonusers.” In addition, the investigators did not find a significant interaction between marijuana use and psychotic disorder diagnoses with regard to an increased mortality risk.
The investigators said that their results, while valuable, are limited by the lack of data on lifetime use of marijuana. The results also are limited by the absence of information about tobacco smoking and risky alcohol use among the men after conscription.
“Study limitations notwithstanding, we found that subjects with a baseline history of heavy use of cannabis have an increased risk of death over the course of follow-up,” they wrote.
The study was funded by grants from the Swedish Council for Working Life and Social Research and the Stockholm County Council. The authors reported no financial conflicts.
On Twitter @whitneymcknight
Heavy marijuana use by men aged 18 or 19 years is associated with a greater risk of mortality by age 60, a longitudinal study of more than 45,000 subjects shows.
The findings, published online April 22, might surprise some, wrote Dr. Edison Manrique-Garcia, a researcher at the Karolinska Institutet, Stockholm, and his colleagues, because a previous study of the same cohort found no such associations. “However, in this longer-term follow-up, the cohort members had reached an age where the detrimental somatic effects of cannabis use were more likely to be apparent,” they wrote (Am J Psychiatry. 2016 Apr 22. doi: 10.1176/appi.ajp.2016.14050637).
Using the Swedish National Cause of Death Register, Dr. Manrique-Garcia and his colleagues analyzed data from a cohort of 50,373 male 18- and 19-year-olds who entered compulsory military service in 1969 and 1970. Because marijuana use information on 4,998 of the subjects was missing, the final analysis included 45,375 subjects.
Dr. Manrique-Garcia and his coauthors found that, from the time of conscription to 2011, there had been 3,918 deaths out of the 45,375 men. Those who had reported ever using marijuana were shown to have died earlier than those who had never used the drug. After adjusting for confounders, the investigators also found a significantly higher risk of death, with a hazard ratio of 1.4, in those who had used marijuana 50 or more times, compared with a hazard ratio of 0.9 in those who had used it 1-50 times.
All marijuana users in the study also were found to have sustained higher rates of mortal injuries, whether accidental or purposefully inflicted, when compared with those who had never used the drug, although the investigators reported that they did not find a correlation between increased suicide risk and marijuana use.
Dr. Manrique-Garcia and his colleagues also reported that, although they found a three- to fourfold greater mortality risk among men with a diagnosis of psychosis, “the risk did not differ between marijuana users and nonusers.” In addition, the investigators did not find a significant interaction between marijuana use and psychotic disorder diagnoses with regard to an increased mortality risk.
The investigators said that their results, while valuable, are limited by the lack of data on lifetime use of marijuana. The results also are limited by the absence of information about tobacco smoking and risky alcohol use among the men after conscription.
“Study limitations notwithstanding, we found that subjects with a baseline history of heavy use of cannabis have an increased risk of death over the course of follow-up,” they wrote.
The study was funded by grants from the Swedish Council for Working Life and Social Research and the Stockholm County Council. The authors reported no financial conflicts.
On Twitter @whitneymcknight
FROM THE AMERICAN JOURNAL OF PSYCHIATRY
Key clinical point: Men who use marijuana more than 50 times in adolescence are at a greater risk of dying by age 60 yesrs than those who do not have a history of marijuana use.
Major finding: Compared with the male subjects who never used marijuana, all categories of users had an increased hazard ratio for mortality. “The association persisted only for heavy users,” the investigators reported (hazard ratio, 1.4; 95% confidence interval,1.1-1.8).
Data source: Longitudinal study of 45,375 Swedish males aged 18 and 19 years.
Disclosures: The study was funded by grants from the Swedish Council for Working Life and Social Research and the Stockholm County Council. Dr. Manrique-Garcia and his coauthors reported no financial disclosures.
HHS urged to lead efforts to destigmatize mental, behavioral disorders
In order for the United States to succeed in reducing the stigma associated with mental illness and substance use disorders, the Department of Health & Human Services should lead the way, according to a National Academies of Sciences report.
The report said U.S. campaigns tied to HIV/AIDS and antistigma campaigns in countries such as England, Canada, and Australia show that “a coordinated and sustained effort over 2 or more decades” is needed.
“Changing stigma in a lasting way will require coordinated efforts, which are based on the best possible evidence, supported at the national level with multiyear funding, and planned and implemented by an effective coalition of representative stakeholders,” Dr. David H. Wegman, chair of the committee that issued the report, said in a statement. Dr. Wegman is professor emeritus in the department of work environment at the University of Massachusetts in Lowell.
The report’s authors said a federal policy that culls from current, evidence-based methods already in use by many organizations – including eight federal agencies – can help change misconceptions about mental and behavioral illness (National Academies of Sciences, Engineering, and Medicine, “Ending Discrimination Against People with Mental and Substance Use Disorders: The Evidence for Stigma Change,” Washington: The National Academies Press, 2016 [doi: 10.17226/23442]).
In addition, the report said, efforts toward integrating behavioral health and primary (and other physical) care in the country’s health care system “offer possibilities for breaking down the walls that separate physical health from mental health in treatment and in the education of health care professionals.”
“This is an important document that will rival former Surgeon General David Satcher’s report on mental health,” Patrick W. Corrigan, Psy.D., part of the panel that the National Academies convened to produce the report, said in an interview.
Up to a quarter of the U.S. population will experience mental health problems, including addiction, at some point in their lives, according to the Centers for Disease Control and Prevention. Meanwhile, a survey conducted by the National Institute on Drug Abuse showed that 17 million Americans reported alcohol dependence or misuse. However, while more than half of those who responded to a nationwide survey said that people with mental illness deserved compassion, only a quarter of those in the throes of mental disease felt they were treated compassionately.
The country’s fragmented approach to treatment, prevention, and allocation of necessary resources for mental illness stems, in part, from an overall lack of agreement on how actually to define mental illness, Dr. Wegman and his coauthors suggested. An approach by the HHS-led Substance Abuse and Mental Health Services Administration (SAMHSA) could help frame the dialogue around the many aspects of mental illness diagnosis, by including the discrete categorizations of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the authors said. They also said the emerging science that indicates the role of trauma, neurobiology, cultural influences, and the dimensionality emphasized in the National Institute of Mental Health’s Research Domain Criteria (RDoC) could help toward that end.
SAMHSA’s role as envisioned by the National Academies also would include coordinating national efforts for peer training, determining the need for specific research around the relationship between attitudes and behaviors toward those with mental illness, and developing targeted messaging aimed at dispelling myths about mental illness.
Dr. Corrigan said it is important for antistigma programs to be led by people who are harmed by stigma, for example, people with mental illness and or substance use disorders. These antistigma efforts also need to “combine insights of broad-scale public health/communication campaigns with grassroots strategies that promote contact. Research is essential to move this agenda forward,” said Dr. Corrigan, Distinguished Professor of Psychology at the Illinois Institute of Technology, Chicago.
The report was written by the National Academies’ Committee on the Science of Changing Behavioral Health Social Norms; board on behavioral, cognitive, and sensory sciences; and division of behavioral and social sciences and education.
On Twitter @whitneymcknight
In order for the United States to succeed in reducing the stigma associated with mental illness and substance use disorders, the Department of Health & Human Services should lead the way, according to a National Academies of Sciences report.
The report said U.S. campaigns tied to HIV/AIDS and antistigma campaigns in countries such as England, Canada, and Australia show that “a coordinated and sustained effort over 2 or more decades” is needed.
“Changing stigma in a lasting way will require coordinated efforts, which are based on the best possible evidence, supported at the national level with multiyear funding, and planned and implemented by an effective coalition of representative stakeholders,” Dr. David H. Wegman, chair of the committee that issued the report, said in a statement. Dr. Wegman is professor emeritus in the department of work environment at the University of Massachusetts in Lowell.
The report’s authors said a federal policy that culls from current, evidence-based methods already in use by many organizations – including eight federal agencies – can help change misconceptions about mental and behavioral illness (National Academies of Sciences, Engineering, and Medicine, “Ending Discrimination Against People with Mental and Substance Use Disorders: The Evidence for Stigma Change,” Washington: The National Academies Press, 2016 [doi: 10.17226/23442]).
In addition, the report said, efforts toward integrating behavioral health and primary (and other physical) care in the country’s health care system “offer possibilities for breaking down the walls that separate physical health from mental health in treatment and in the education of health care professionals.”
“This is an important document that will rival former Surgeon General David Satcher’s report on mental health,” Patrick W. Corrigan, Psy.D., part of the panel that the National Academies convened to produce the report, said in an interview.
Up to a quarter of the U.S. population will experience mental health problems, including addiction, at some point in their lives, according to the Centers for Disease Control and Prevention. Meanwhile, a survey conducted by the National Institute on Drug Abuse showed that 17 million Americans reported alcohol dependence or misuse. However, while more than half of those who responded to a nationwide survey said that people with mental illness deserved compassion, only a quarter of those in the throes of mental disease felt they were treated compassionately.
The country’s fragmented approach to treatment, prevention, and allocation of necessary resources for mental illness stems, in part, from an overall lack of agreement on how actually to define mental illness, Dr. Wegman and his coauthors suggested. An approach by the HHS-led Substance Abuse and Mental Health Services Administration (SAMHSA) could help frame the dialogue around the many aspects of mental illness diagnosis, by including the discrete categorizations of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the authors said. They also said the emerging science that indicates the role of trauma, neurobiology, cultural influences, and the dimensionality emphasized in the National Institute of Mental Health’s Research Domain Criteria (RDoC) could help toward that end.
SAMHSA’s role as envisioned by the National Academies also would include coordinating national efforts for peer training, determining the need for specific research around the relationship between attitudes and behaviors toward those with mental illness, and developing targeted messaging aimed at dispelling myths about mental illness.
Dr. Corrigan said it is important for antistigma programs to be led by people who are harmed by stigma, for example, people with mental illness and or substance use disorders. These antistigma efforts also need to “combine insights of broad-scale public health/communication campaigns with grassroots strategies that promote contact. Research is essential to move this agenda forward,” said Dr. Corrigan, Distinguished Professor of Psychology at the Illinois Institute of Technology, Chicago.
The report was written by the National Academies’ Committee on the Science of Changing Behavioral Health Social Norms; board on behavioral, cognitive, and sensory sciences; and division of behavioral and social sciences and education.
On Twitter @whitneymcknight
In order for the United States to succeed in reducing the stigma associated with mental illness and substance use disorders, the Department of Health & Human Services should lead the way, according to a National Academies of Sciences report.
The report said U.S. campaigns tied to HIV/AIDS and antistigma campaigns in countries such as England, Canada, and Australia show that “a coordinated and sustained effort over 2 or more decades” is needed.
“Changing stigma in a lasting way will require coordinated efforts, which are based on the best possible evidence, supported at the national level with multiyear funding, and planned and implemented by an effective coalition of representative stakeholders,” Dr. David H. Wegman, chair of the committee that issued the report, said in a statement. Dr. Wegman is professor emeritus in the department of work environment at the University of Massachusetts in Lowell.
The report’s authors said a federal policy that culls from current, evidence-based methods already in use by many organizations – including eight federal agencies – can help change misconceptions about mental and behavioral illness (National Academies of Sciences, Engineering, and Medicine, “Ending Discrimination Against People with Mental and Substance Use Disorders: The Evidence for Stigma Change,” Washington: The National Academies Press, 2016 [doi: 10.17226/23442]).
In addition, the report said, efforts toward integrating behavioral health and primary (and other physical) care in the country’s health care system “offer possibilities for breaking down the walls that separate physical health from mental health in treatment and in the education of health care professionals.”
“This is an important document that will rival former Surgeon General David Satcher’s report on mental health,” Patrick W. Corrigan, Psy.D., part of the panel that the National Academies convened to produce the report, said in an interview.
Up to a quarter of the U.S. population will experience mental health problems, including addiction, at some point in their lives, according to the Centers for Disease Control and Prevention. Meanwhile, a survey conducted by the National Institute on Drug Abuse showed that 17 million Americans reported alcohol dependence or misuse. However, while more than half of those who responded to a nationwide survey said that people with mental illness deserved compassion, only a quarter of those in the throes of mental disease felt they were treated compassionately.
The country’s fragmented approach to treatment, prevention, and allocation of necessary resources for mental illness stems, in part, from an overall lack of agreement on how actually to define mental illness, Dr. Wegman and his coauthors suggested. An approach by the HHS-led Substance Abuse and Mental Health Services Administration (SAMHSA) could help frame the dialogue around the many aspects of mental illness diagnosis, by including the discrete categorizations of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the authors said. They also said the emerging science that indicates the role of trauma, neurobiology, cultural influences, and the dimensionality emphasized in the National Institute of Mental Health’s Research Domain Criteria (RDoC) could help toward that end.
SAMHSA’s role as envisioned by the National Academies also would include coordinating national efforts for peer training, determining the need for specific research around the relationship between attitudes and behaviors toward those with mental illness, and developing targeted messaging aimed at dispelling myths about mental illness.
Dr. Corrigan said it is important for antistigma programs to be led by people who are harmed by stigma, for example, people with mental illness and or substance use disorders. These antistigma efforts also need to “combine insights of broad-scale public health/communication campaigns with grassroots strategies that promote contact. Research is essential to move this agenda forward,” said Dr. Corrigan, Distinguished Professor of Psychology at the Illinois Institute of Technology, Chicago.
The report was written by the National Academies’ Committee on the Science of Changing Behavioral Health Social Norms; board on behavioral, cognitive, and sensory sciences; and division of behavioral and social sciences and education.
On Twitter @whitneymcknight
UnitedHealth Group leaving most ACA marketplaces
UnitedHealth Group will not sell policies next year in most of the health insurance marketplaces created by the Affordable Care Act, CEO Stephen Helmsley announced during an April 19 earnings call.
“Next year, we will remain in only a handful of states, and we will not carry financial exposure from exchanges into 2017,” Mr. Helmsley said, citing the company’s inability to offset the “shorter-term, higher-risk” population covered by the ACA exchange plans with large enough risk pools.
Mr. Helmsley did not say in which state marketplaces UnitedHealth Group (UHG) will continue to offer coverage.
Areas that could be hardest hit by the UHG withdrawal include Alabama, Arizona, Arkansas, Nebraska, North Carolina, and Tennessee, according to an analysis from the Kaiser Family Foundation.
For now, the decision by UHG is not likely to impact the average benchmark premium by more than a 1% increase, according to the analysis. That’s because the insurer was less likely than its competitors to offer lower-cost silver plans; when silver plans were offered, they were offered at or very near to the competitors’ prices. However, in states where the withdrawal of UHG means that two or fewer insurers are participating in the marketplace, benchmark premiums could rise substantially, according to the study.
The long-term effect of the UHG exit from most marketplaces is not clear, according to Kaiser’s analysts. “In areas with limited insurer participation, the remaining plans after a United exit may have more market power relative to providers, but in the absence of insurer competition, those savings may not be passed along to consumers,” they wrote.
ACA measures such as rate reviews and medical loss ratio provisions could mitigate adverse effects on consumers in these markets, giving regulators the power to force insurers to issue rebates if premiums outstrip the cost of care.
The insurer’s decision is simply evidence that typical market forces are in play, according to Jonathan Gold, a spokesperson for the Centers for Medicare & Medicaid Services.
“As with any new market, we expect changes and adjustments in the early years with issuers both entering and exiting states,” Mr. Gold said in an interview. The UHG decision was not unexpected, as company officials said they were contemplating the move last November.
“We have full confidence, based on data, that the marketplaces will continue to thrive for years ahead,” he said, noting that in 2016, 39 insurers exited the marketplace, while 40 entered.
On Twitter @whitneymcknight
UnitedHealth Group will not sell policies next year in most of the health insurance marketplaces created by the Affordable Care Act, CEO Stephen Helmsley announced during an April 19 earnings call.
“Next year, we will remain in only a handful of states, and we will not carry financial exposure from exchanges into 2017,” Mr. Helmsley said, citing the company’s inability to offset the “shorter-term, higher-risk” population covered by the ACA exchange plans with large enough risk pools.
Mr. Helmsley did not say in which state marketplaces UnitedHealth Group (UHG) will continue to offer coverage.
Areas that could be hardest hit by the UHG withdrawal include Alabama, Arizona, Arkansas, Nebraska, North Carolina, and Tennessee, according to an analysis from the Kaiser Family Foundation.
For now, the decision by UHG is not likely to impact the average benchmark premium by more than a 1% increase, according to the analysis. That’s because the insurer was less likely than its competitors to offer lower-cost silver plans; when silver plans were offered, they were offered at or very near to the competitors’ prices. However, in states where the withdrawal of UHG means that two or fewer insurers are participating in the marketplace, benchmark premiums could rise substantially, according to the study.
The long-term effect of the UHG exit from most marketplaces is not clear, according to Kaiser’s analysts. “In areas with limited insurer participation, the remaining plans after a United exit may have more market power relative to providers, but in the absence of insurer competition, those savings may not be passed along to consumers,” they wrote.
ACA measures such as rate reviews and medical loss ratio provisions could mitigate adverse effects on consumers in these markets, giving regulators the power to force insurers to issue rebates if premiums outstrip the cost of care.
The insurer’s decision is simply evidence that typical market forces are in play, according to Jonathan Gold, a spokesperson for the Centers for Medicare & Medicaid Services.
“As with any new market, we expect changes and adjustments in the early years with issuers both entering and exiting states,” Mr. Gold said in an interview. The UHG decision was not unexpected, as company officials said they were contemplating the move last November.
“We have full confidence, based on data, that the marketplaces will continue to thrive for years ahead,” he said, noting that in 2016, 39 insurers exited the marketplace, while 40 entered.
On Twitter @whitneymcknight
UnitedHealth Group will not sell policies next year in most of the health insurance marketplaces created by the Affordable Care Act, CEO Stephen Helmsley announced during an April 19 earnings call.
“Next year, we will remain in only a handful of states, and we will not carry financial exposure from exchanges into 2017,” Mr. Helmsley said, citing the company’s inability to offset the “shorter-term, higher-risk” population covered by the ACA exchange plans with large enough risk pools.
Mr. Helmsley did not say in which state marketplaces UnitedHealth Group (UHG) will continue to offer coverage.
Areas that could be hardest hit by the UHG withdrawal include Alabama, Arizona, Arkansas, Nebraska, North Carolina, and Tennessee, according to an analysis from the Kaiser Family Foundation.
For now, the decision by UHG is not likely to impact the average benchmark premium by more than a 1% increase, according to the analysis. That’s because the insurer was less likely than its competitors to offer lower-cost silver plans; when silver plans were offered, they were offered at or very near to the competitors’ prices. However, in states where the withdrawal of UHG means that two or fewer insurers are participating in the marketplace, benchmark premiums could rise substantially, according to the study.
The long-term effect of the UHG exit from most marketplaces is not clear, according to Kaiser’s analysts. “In areas with limited insurer participation, the remaining plans after a United exit may have more market power relative to providers, but in the absence of insurer competition, those savings may not be passed along to consumers,” they wrote.
ACA measures such as rate reviews and medical loss ratio provisions could mitigate adverse effects on consumers in these markets, giving regulators the power to force insurers to issue rebates if premiums outstrip the cost of care.
The insurer’s decision is simply evidence that typical market forces are in play, according to Jonathan Gold, a spokesperson for the Centers for Medicare & Medicaid Services.
“As with any new market, we expect changes and adjustments in the early years with issuers both entering and exiting states,” Mr. Gold said in an interview. The UHG decision was not unexpected, as company officials said they were contemplating the move last November.
“We have full confidence, based on data, that the marketplaces will continue to thrive for years ahead,” he said, noting that in 2016, 39 insurers exited the marketplace, while 40 entered.
On Twitter @whitneymcknight
Don’t forget liver disease often has mental health component
PHILADELPHIA – To help ensure the best outcomes in patients with a range of liver pathologies, be alert for signs of neurologic and psychiatric abnormalities caused by hepatic encephalopathy, according to an expert.
“The patient doesn’t have to have cirrhosis or liver disease, but can just have portosystemic shunting with absolutely no liver disease, and still have hepatic encephalopathy,” Dr. Jasmohan S. Bajaj said at the meeting held by Global Academy for Medical Education and Rutgers, the State University of New Jersey.
Hepatic encephalopathy is believed to be due to dysbiosis caused by an altered bile acid profile, leading to an impaired intestinal barrier, which allows high levels of ammonia to circulate through the bloodstream, contributing to systemic inflammation and brain dysfunction, according to Dr. Bajaj, an associate professor of medicine at Virginia Commonwealth University and McGuire VA Medical Center, Richmond, Va.
“Ultimately, all the manifestations that we see are because of neuronal dysfunction, which is why the patient is depressed, anxious, sleepy, and has tremors,” Dr. Bajaj said.
Guidelines issued by the American Association for the Study of Liver Diseases stratify hepatic encephalopathy into four grades, the first being the difficult-to-detect subclinical form that is present in up at as many as 60% of patients with hepatic pathologies.
Because covert hepatic encephalopathy will likely progress to a more overt form, adversely impacting a patient’s quality of life and other outcomes, Dr. Bajaj emphasized the importance of testing for it.
One means of detection is to evaluate a patient’s response time using a modified version of the psychiatric Stroop test that measures cognitive dysfunction. Another is to consider collaborative care with a psychologist who can test for and diagnose cognitive impairment. Patients who select at least four items in the Sickness Impact Profile are “80% likely” to have covert hepatic encephalopathy, according to Dr. Bajaj.
Overt manifestations of hepatic encephalopathy include obvious signs of altered mental status, usually reported by the caregiver. Clinicians should consider as part of their differential diagnosis for overt hepatic encephalopathy whether the patient is diabetic, intoxicated, suffering an electrolyte disorder, or is experiencing intracranial bleeding or stroke, and should consider precipitating factors such as an infection, gastrointestinal bleeding, or an overdose of diuretics.
Avoid treatment decisions based on blood ammonia status superseding a patient’s mental status because “there are many people who are completely alert who have high ammonia levels,” Dr. Bajaj said. “When the patient presents at the emergency [department] with confusion but has a completely normal ammonia level, that is the only time ammonia levels are useful.”
Treating hepatic encephalopathy is possible by reducing the nitrogenous load in the gut with lactulose, rifaximin, probiotics, or laxatives, according to Dr. Bajaj, who noted that most overt hepatic encephalopathy patients will require inpatient evaluation, and that in cases with recurrent precipitating factors, patients should be considered for liver transplant suitability.
Dr. Bajaj said he receives grant support from Grifols, Norgine, and Salix.
Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
PHILADELPHIA – To help ensure the best outcomes in patients with a range of liver pathologies, be alert for signs of neurologic and psychiatric abnormalities caused by hepatic encephalopathy, according to an expert.
“The patient doesn’t have to have cirrhosis or liver disease, but can just have portosystemic shunting with absolutely no liver disease, and still have hepatic encephalopathy,” Dr. Jasmohan S. Bajaj said at the meeting held by Global Academy for Medical Education and Rutgers, the State University of New Jersey.
Hepatic encephalopathy is believed to be due to dysbiosis caused by an altered bile acid profile, leading to an impaired intestinal barrier, which allows high levels of ammonia to circulate through the bloodstream, contributing to systemic inflammation and brain dysfunction, according to Dr. Bajaj, an associate professor of medicine at Virginia Commonwealth University and McGuire VA Medical Center, Richmond, Va.
“Ultimately, all the manifestations that we see are because of neuronal dysfunction, which is why the patient is depressed, anxious, sleepy, and has tremors,” Dr. Bajaj said.
Guidelines issued by the American Association for the Study of Liver Diseases stratify hepatic encephalopathy into four grades, the first being the difficult-to-detect subclinical form that is present in up at as many as 60% of patients with hepatic pathologies.
Because covert hepatic encephalopathy will likely progress to a more overt form, adversely impacting a patient’s quality of life and other outcomes, Dr. Bajaj emphasized the importance of testing for it.
One means of detection is to evaluate a patient’s response time using a modified version of the psychiatric Stroop test that measures cognitive dysfunction. Another is to consider collaborative care with a psychologist who can test for and diagnose cognitive impairment. Patients who select at least four items in the Sickness Impact Profile are “80% likely” to have covert hepatic encephalopathy, according to Dr. Bajaj.
Overt manifestations of hepatic encephalopathy include obvious signs of altered mental status, usually reported by the caregiver. Clinicians should consider as part of their differential diagnosis for overt hepatic encephalopathy whether the patient is diabetic, intoxicated, suffering an electrolyte disorder, or is experiencing intracranial bleeding or stroke, and should consider precipitating factors such as an infection, gastrointestinal bleeding, or an overdose of diuretics.
Avoid treatment decisions based on blood ammonia status superseding a patient’s mental status because “there are many people who are completely alert who have high ammonia levels,” Dr. Bajaj said. “When the patient presents at the emergency [department] with confusion but has a completely normal ammonia level, that is the only time ammonia levels are useful.”
Treating hepatic encephalopathy is possible by reducing the nitrogenous load in the gut with lactulose, rifaximin, probiotics, or laxatives, according to Dr. Bajaj, who noted that most overt hepatic encephalopathy patients will require inpatient evaluation, and that in cases with recurrent precipitating factors, patients should be considered for liver transplant suitability.
Dr. Bajaj said he receives grant support from Grifols, Norgine, and Salix.
Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
PHILADELPHIA – To help ensure the best outcomes in patients with a range of liver pathologies, be alert for signs of neurologic and psychiatric abnormalities caused by hepatic encephalopathy, according to an expert.
“The patient doesn’t have to have cirrhosis or liver disease, but can just have portosystemic shunting with absolutely no liver disease, and still have hepatic encephalopathy,” Dr. Jasmohan S. Bajaj said at the meeting held by Global Academy for Medical Education and Rutgers, the State University of New Jersey.
Hepatic encephalopathy is believed to be due to dysbiosis caused by an altered bile acid profile, leading to an impaired intestinal barrier, which allows high levels of ammonia to circulate through the bloodstream, contributing to systemic inflammation and brain dysfunction, according to Dr. Bajaj, an associate professor of medicine at Virginia Commonwealth University and McGuire VA Medical Center, Richmond, Va.
“Ultimately, all the manifestations that we see are because of neuronal dysfunction, which is why the patient is depressed, anxious, sleepy, and has tremors,” Dr. Bajaj said.
Guidelines issued by the American Association for the Study of Liver Diseases stratify hepatic encephalopathy into four grades, the first being the difficult-to-detect subclinical form that is present in up at as many as 60% of patients with hepatic pathologies.
Because covert hepatic encephalopathy will likely progress to a more overt form, adversely impacting a patient’s quality of life and other outcomes, Dr. Bajaj emphasized the importance of testing for it.
One means of detection is to evaluate a patient’s response time using a modified version of the psychiatric Stroop test that measures cognitive dysfunction. Another is to consider collaborative care with a psychologist who can test for and diagnose cognitive impairment. Patients who select at least four items in the Sickness Impact Profile are “80% likely” to have covert hepatic encephalopathy, according to Dr. Bajaj.
Overt manifestations of hepatic encephalopathy include obvious signs of altered mental status, usually reported by the caregiver. Clinicians should consider as part of their differential diagnosis for overt hepatic encephalopathy whether the patient is diabetic, intoxicated, suffering an electrolyte disorder, or is experiencing intracranial bleeding or stroke, and should consider precipitating factors such as an infection, gastrointestinal bleeding, or an overdose of diuretics.
Avoid treatment decisions based on blood ammonia status superseding a patient’s mental status because “there are many people who are completely alert who have high ammonia levels,” Dr. Bajaj said. “When the patient presents at the emergency [department] with confusion but has a completely normal ammonia level, that is the only time ammonia levels are useful.”
Treating hepatic encephalopathy is possible by reducing the nitrogenous load in the gut with lactulose, rifaximin, probiotics, or laxatives, according to Dr. Bajaj, who noted that most overt hepatic encephalopathy patients will require inpatient evaluation, and that in cases with recurrent precipitating factors, patients should be considered for liver transplant suitability.
Dr. Bajaj said he receives grant support from Grifols, Norgine, and Salix.
Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
AT DIGESTIVE DISEASES: NEW ADVANCES
VIDEO: Stenting to improve quality of life in esophageal cancer
PHILADELPHIA – An esophageal stent can improve quality of life for patients with advanced esophageal cancer, according to Dr. Sushil Ahlawat, director of endoscopy at Rutgers University, New Brunswick, N.J.
“An esophageal stent can be an important modality for palliating patients’ dysphagia, [which] can happen because the tumor is obstructing the esophagus,” says Dr. Ahlawat in this video. He also discusses how this minimally invasive procedure can support those undergoing chemoradiation therapy or surgery for esophageal cancer.
The video was recorded at this year’s meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy for Medical Education and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
PHILADELPHIA – An esophageal stent can improve quality of life for patients with advanced esophageal cancer, according to Dr. Sushil Ahlawat, director of endoscopy at Rutgers University, New Brunswick, N.J.
“An esophageal stent can be an important modality for palliating patients’ dysphagia, [which] can happen because the tumor is obstructing the esophagus,” says Dr. Ahlawat in this video. He also discusses how this minimally invasive procedure can support those undergoing chemoradiation therapy or surgery for esophageal cancer.
The video was recorded at this year’s meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy for Medical Education and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
PHILADELPHIA – An esophageal stent can improve quality of life for patients with advanced esophageal cancer, according to Dr. Sushil Ahlawat, director of endoscopy at Rutgers University, New Brunswick, N.J.
“An esophageal stent can be an important modality for palliating patients’ dysphagia, [which] can happen because the tumor is obstructing the esophagus,” says Dr. Ahlawat in this video. He also discusses how this minimally invasive procedure can support those undergoing chemoradiation therapy or surgery for esophageal cancer.
The video was recorded at this year’s meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy for Medical Education and this news organization are owned by the same company.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM DIGESTIVE DISEASES: NEW ADVANCES
VIDEO: How to recognize and treat nonalcoholic fatty liver disease
PHILADELPHIA – Nonalcoholic fatty liver disease is on the rise worldwide, but many clinicians are unaware of how to recognize this potentially fatal condition, in part because it can be difficult to separate from common comorbidities such as obesity and diabetes.
In an interview at the Digestive Diseases: New Advances 2016 meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey, Dr. Zobair M. Younossi, chairman of the department of medicine at Inova Fairfax (Va.) Hospital, discussed what clinicians should know in order to screen for and treat this disease.
Dr. Younossi said he is a consultant to Conatus Pharmaceuticals, Enterome Bioscience, and Gilead, and on the advisory boards of Janssen, Salix Pharmaceuticals, and Vertex Pharmaceuticals.
Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
PHILADELPHIA – Nonalcoholic fatty liver disease is on the rise worldwide, but many clinicians are unaware of how to recognize this potentially fatal condition, in part because it can be difficult to separate from common comorbidities such as obesity and diabetes.
In an interview at the Digestive Diseases: New Advances 2016 meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey, Dr. Zobair M. Younossi, chairman of the department of medicine at Inova Fairfax (Va.) Hospital, discussed what clinicians should know in order to screen for and treat this disease.
Dr. Younossi said he is a consultant to Conatus Pharmaceuticals, Enterome Bioscience, and Gilead, and on the advisory boards of Janssen, Salix Pharmaceuticals, and Vertex Pharmaceuticals.
Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
PHILADELPHIA – Nonalcoholic fatty liver disease is on the rise worldwide, but many clinicians are unaware of how to recognize this potentially fatal condition, in part because it can be difficult to separate from common comorbidities such as obesity and diabetes.
In an interview at the Digestive Diseases: New Advances 2016 meeting, held by Global Academy for Medical Education and Rutgers, the State University of New Jersey, Dr. Zobair M. Younossi, chairman of the department of medicine at Inova Fairfax (Va.) Hospital, discussed what clinicians should know in order to screen for and treat this disease.
Dr. Younossi said he is a consultant to Conatus Pharmaceuticals, Enterome Bioscience, and Gilead, and on the advisory boards of Janssen, Salix Pharmaceuticals, and Vertex Pharmaceuticals.
Global Academy and this news organization are owned by the same company.
On Twitter @whitneymcknight
AT DIGESTIVE DISEASES: NEW ADVANCES 2016