User login
The rise in U.S. suicide rates to the highest levels in almost 30 years is tied to many factors. One fact is clear – some experts say – the lack of training in suicide risk assessment among mental health and substance abuse clinicians is an issue that must be addressed.
“There are mental health professionals who have little to no training in suicide risk assessment,” Dr. Michael F. Myers, professor of clinical psychiatry at State University of New York, Brooklyn, said in an interview.
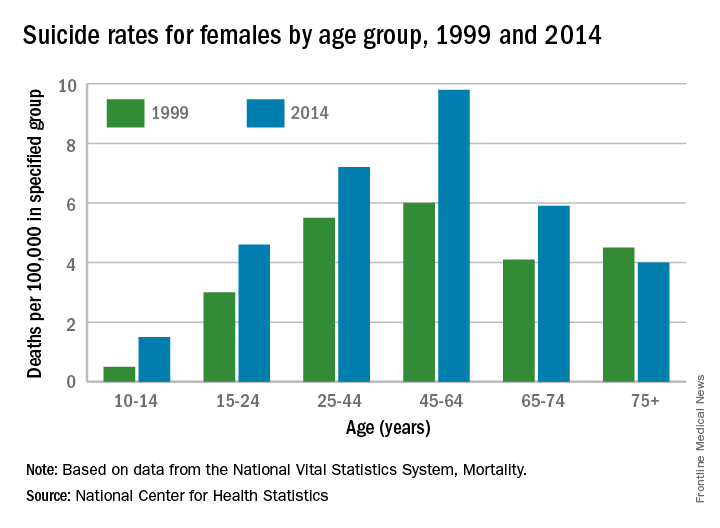
According to a report released April 22 by the Centers for Disease Control and Prevention, suicide is the 10th-leading cause of death in the United States. It increased by 24% from 1999 to 2014 overall, and the groups most dramatically affected were girls aged 10-14 years, and men aged 45-64. Women aged 45-64 and men aged 75 years and older had the highest suicide rates. About 40,000 Americans a year take their own lives, which is double the number of homicides in the country annually.
After 2006 – against the backdrop of a tough economy and a burgeoning opioid crisis – the suicide rate accelerated. Meanwhile, overall mortality from causes such as cardiovascular disease and cancer is on the decline, according to the CDC report.
Standards vary
In 2012, the American Association of Suicidology reported in its suicide prevention recommendations that less than a quarter of social workers had received any formal suicide prevention training which, when offered, usually lasted 4 hours or fewer. Only 6% of marriage and family therapists had received any such training. Psychiatry residency programs were found to offer training 91% of the time.
But in 2014, the U.S. Preventive Services Task Force (USPSTF) recommendation statement on the efficacy of suicide risk screening concluded that the evidence was insufficient to warrant allocating resources to it (Ann Int Med. 2014;160[10]:719-26). The USPSTF, however, does recommend that primary care professionals screen for depression in adults and adolescents, and earlier this year, updated its recommendations to screen pregnant women in particular (JAMA. 2016;315[4]380-7).
Also, this year, the Centers for Medicare & Medicaid Services required its providers to screen patients for depression using the Patient Health Questionnaire-9 (PHQ-9).
Dr. Myers thinks this is a good starting point, but said that adding more suicide-specific questions to the depression screening process could save more lives.
Despite the USPSTF’s recommendation, investigators for a systematic review published in 2005 concluded that “Physician education in depression recognition and treatment and restricting access to lethal methods reduce suicide rates” (JAMA. 2005;294[16];2064-74). There is some federal support for implementation of suicide prevention in the primary and mental health care settings. In 2012, the U.S. Surgeon General’s office and the National Action Alliance for Suicide Prevention jointly released the National Strategy for Suicide Prevention, which cited as its No. 1 priority, the integration of suicide prevention into health care reform through initiatives such as the Zero Suicide campaign. Sponsored by the Suicide Prevention Resource Council, and funded in part by the Substance Abuse and Mental Health Services Administration (SAMHSA), the program aims to close the gaps in care that distract or otherwise hinder caring for and following through with patients who are at risk for suicide.
An unevenly trained mental health workforce was targeted earlier this month by members of the National Academies of Sciences who, in a report, criticized the current state of siloed mental health care, saying it results in stigmatization and undertreatment of mental illness. The authors urged Congress to empower the U.S. Department of Health and Human Services to oversee better implementation and coordination of evidence-based services to prevent and treat mental disorders that lead to outcomes such as suicide. The report cites successful federal initiatives in England, Australia, and Canada that have notably improved mental health care in those countries. Those improvements took decades, the report notes.
Earlier prevention efforts
In 1999, then–Surgeon General David Satcher issued his Call to Action to Prevent Suicide, which lays out a comprehensive and integrated approach. In 2012, former Surgeon General Regina M. Benjamin published a National Strategy for Suicide Prevention. But without federal policy behind those efforts, the recommendations have not been implemented.
“This is not dissimilar to what happened in the HIV/AIDS epidemic, where finally, the medical community had to be mandated to get trained to treat the illness,” said Paul Quinnett, Ph.D., a clinical psychologist at the University of Washington, Spokane, and founder and CEO of the QPR Institute, a suicide prevention nonprofit.
Dr. Quinnett admits that what he sees as a lack of political will among many of his colleagues to address the suicide crisis angers him. “We can’t afford to look the other way and pretend this isn’t happening. These numbers are just crushing.”
Currently, however, Washington and Kentucky are the only states with suicide-specific requirements for licensure. Recent efforts to mandate training in California failed when Gov. Jerry Brown (D) vetoed the measure after heavy lobbying efforts by various mental health professional organizations, including the California chapter of the National Association of Social Workers, which argued that it should be entrusted to train its members on a volunteer, as-needed basis.
Even when clinicians have received proper training and met all standards of practice, some patients still may be lost, said Dr. Myers, who also is immediate past vice chair for education and residency training director at SUNY Downstate Medical Center. “You can’t save everyone,” he said. “Some patients are just hell-bent on killing themselves and will very cleverly pull the wool over our eyes.”
He also pointed to the gaps in care that training alone cannot prevent, specifically citing the instances in which people complete a suicide because of a lack of follow-up – the kind of intensive discharge planning that might include several daily phone calls and plans for whom to talk to when thoughts of suicide arise. Those kinds of protocols are not widely used, Dr. Myers said, partly because of the cost.
But Dr. Myers also points to a failing that, while not documented, he said is well-known among his mental health peers: calculated avoidance of at-risk patients.
“There are those, therapists especially, who are cherry picking their patients. They try to make sure they don’t have to look after suicidal people. They do their best to avoid them, and will even screen referrals to avoid them,” said Dr. Myers, who has written extensively about suicide. “It’s equivalent to an oncologist saying to a referring physician: ‘Sure, I will see your patient with breast cancer, but she doesn’t have metastasis, does she?’ It’s unconscionable.”
It would help if there were guidelines for care similar to oncology or cardiology, he said, to help clinicians better balance science with instinct.
Dr. Quinnett thinks the crisis is likely to worsen before it gets better. At least one study has shown strong associations between rates of joblessness in the United States and suicide rates (Soc Sci Med. 2014 Sep;116:22-31). “I’m particularly worried about those people whose lives have been economically hollowed out by the Great Recession,” said Dr. Quinnett, also of the department of psychiatry and behavioral sciences at the University of Washington. “There are men who are aging out [of the workforce] without retirement plans or any other fallback [and who], face losing their dignity and self-esteem, and will need handouts. It’s going to be very ugly.”
Dr. Myers has written several books, including “Touched by Suicide: Hope and Healing After Loss” (New York: Gotham/Penguin, 2006). Dr. Quinnett’s suicide prevention nonprofit, the QPR Institute, is listed on SAMHSA’s National Registry of Evidence-based Programs and Practices.
Coming soon: A national suicide registry?
At the National Institutes of Health, a movement is afoot to create a national suicide registry.
“Registries can help us in all kinds of conditions. That’s how we got ahead in cancer,” Jane Pearson, Ph.D., the National Institute of Mental Health’s program chief for Suicide Treatment and Preventive Interventions Research, said in an interview.
It’s early days yet, but Dr. Pearson and her colleagues are looking into how to leverage data already collected, how to determine the quality of those data, and whom to task with its oversight and interpretation. Then there is the need to know what questions matter most, either to create new registries or to cull patterns from currently available data.
Dr. Pearson said a dedicated suicide data collection effort in a large health care system or a single state would, theoretically, allow patterns to emerge that would help create infrastructures to support specific populations at risk for suicide and guidelines for referral to support.
“Mental health issues have always been a challenge for primary care. As long as they have a partner they can refer to, it’s a much easier [task],” she said. “We wouldn’t ask them to be cardiovascular specialists. When a patient has a stroke, they figure it out and move people along. The registry ideas encompasses that. It’s about creating a whole system for how we are going to do better.”
On Twitter @whitneymcknight
When analyzing these numbers, it is important to keep them in perspective, Dr. Carl C. Bell, who has served on the National Strategy for Suicide Prevention Task Force, said in an interview. The problem is that suicide rates doubling, for example, means the rates went from 11/100,000 up to 22/100,000, or if they tripled they went from 11/100,000 up to 33/100,000.
The reality is there is not statistical difference between those three numbers. The differences could be attributable to just chance and numbers bouncing around, so to apply a meaning to the “increase” is spurious. These suicide and homicide numbers bounce up and down, but they might not mean anything, as the event is such a rare occurrence.
Ultimately, we must examine ways to strengthen protective factors around people who are most vulnerable, such as those with signs and symptoms of depression and substance abuse.
Dr. Bell is staff psychiatrist at Jackson Park Hospital Family Medicine Clinic and former president/CEO of Community Mental Health Council both in Chicago.
When analyzing these numbers, it is important to keep them in perspective, Dr. Carl C. Bell, who has served on the National Strategy for Suicide Prevention Task Force, said in an interview. The problem is that suicide rates doubling, for example, means the rates went from 11/100,000 up to 22/100,000, or if they tripled they went from 11/100,000 up to 33/100,000.
The reality is there is not statistical difference between those three numbers. The differences could be attributable to just chance and numbers bouncing around, so to apply a meaning to the “increase” is spurious. These suicide and homicide numbers bounce up and down, but they might not mean anything, as the event is such a rare occurrence.
Ultimately, we must examine ways to strengthen protective factors around people who are most vulnerable, such as those with signs and symptoms of depression and substance abuse.
Dr. Bell is staff psychiatrist at Jackson Park Hospital Family Medicine Clinic and former president/CEO of Community Mental Health Council both in Chicago.
When analyzing these numbers, it is important to keep them in perspective, Dr. Carl C. Bell, who has served on the National Strategy for Suicide Prevention Task Force, said in an interview. The problem is that suicide rates doubling, for example, means the rates went from 11/100,000 up to 22/100,000, or if they tripled they went from 11/100,000 up to 33/100,000.
The reality is there is not statistical difference between those three numbers. The differences could be attributable to just chance and numbers bouncing around, so to apply a meaning to the “increase” is spurious. These suicide and homicide numbers bounce up and down, but they might not mean anything, as the event is such a rare occurrence.
Ultimately, we must examine ways to strengthen protective factors around people who are most vulnerable, such as those with signs and symptoms of depression and substance abuse.
Dr. Bell is staff psychiatrist at Jackson Park Hospital Family Medicine Clinic and former president/CEO of Community Mental Health Council both in Chicago.
The rise in U.S. suicide rates to the highest levels in almost 30 years is tied to many factors. One fact is clear – some experts say – the lack of training in suicide risk assessment among mental health and substance abuse clinicians is an issue that must be addressed.
“There are mental health professionals who have little to no training in suicide risk assessment,” Dr. Michael F. Myers, professor of clinical psychiatry at State University of New York, Brooklyn, said in an interview.
According to a report released April 22 by the Centers for Disease Control and Prevention, suicide is the 10th-leading cause of death in the United States. It increased by 24% from 1999 to 2014 overall, and the groups most dramatically affected were girls aged 10-14 years, and men aged 45-64. Women aged 45-64 and men aged 75 years and older had the highest suicide rates. About 40,000 Americans a year take their own lives, which is double the number of homicides in the country annually.
After 2006 – against the backdrop of a tough economy and a burgeoning opioid crisis – the suicide rate accelerated. Meanwhile, overall mortality from causes such as cardiovascular disease and cancer is on the decline, according to the CDC report.
Standards vary
In 2012, the American Association of Suicidology reported in its suicide prevention recommendations that less than a quarter of social workers had received any formal suicide prevention training which, when offered, usually lasted 4 hours or fewer. Only 6% of marriage and family therapists had received any such training. Psychiatry residency programs were found to offer training 91% of the time.
But in 2014, the U.S. Preventive Services Task Force (USPSTF) recommendation statement on the efficacy of suicide risk screening concluded that the evidence was insufficient to warrant allocating resources to it (Ann Int Med. 2014;160[10]:719-26). The USPSTF, however, does recommend that primary care professionals screen for depression in adults and adolescents, and earlier this year, updated its recommendations to screen pregnant women in particular (JAMA. 2016;315[4]380-7).
Also, this year, the Centers for Medicare & Medicaid Services required its providers to screen patients for depression using the Patient Health Questionnaire-9 (PHQ-9).
Dr. Myers thinks this is a good starting point, but said that adding more suicide-specific questions to the depression screening process could save more lives.
Despite the USPSTF’s recommendation, investigators for a systematic review published in 2005 concluded that “Physician education in depression recognition and treatment and restricting access to lethal methods reduce suicide rates” (JAMA. 2005;294[16];2064-74). There is some federal support for implementation of suicide prevention in the primary and mental health care settings. In 2012, the U.S. Surgeon General’s office and the National Action Alliance for Suicide Prevention jointly released the National Strategy for Suicide Prevention, which cited as its No. 1 priority, the integration of suicide prevention into health care reform through initiatives such as the Zero Suicide campaign. Sponsored by the Suicide Prevention Resource Council, and funded in part by the Substance Abuse and Mental Health Services Administration (SAMHSA), the program aims to close the gaps in care that distract or otherwise hinder caring for and following through with patients who are at risk for suicide.
An unevenly trained mental health workforce was targeted earlier this month by members of the National Academies of Sciences who, in a report, criticized the current state of siloed mental health care, saying it results in stigmatization and undertreatment of mental illness. The authors urged Congress to empower the U.S. Department of Health and Human Services to oversee better implementation and coordination of evidence-based services to prevent and treat mental disorders that lead to outcomes such as suicide. The report cites successful federal initiatives in England, Australia, and Canada that have notably improved mental health care in those countries. Those improvements took decades, the report notes.
Earlier prevention efforts
In 1999, then–Surgeon General David Satcher issued his Call to Action to Prevent Suicide, which lays out a comprehensive and integrated approach. In 2012, former Surgeon General Regina M. Benjamin published a National Strategy for Suicide Prevention. But without federal policy behind those efforts, the recommendations have not been implemented.
“This is not dissimilar to what happened in the HIV/AIDS epidemic, where finally, the medical community had to be mandated to get trained to treat the illness,” said Paul Quinnett, Ph.D., a clinical psychologist at the University of Washington, Spokane, and founder and CEO of the QPR Institute, a suicide prevention nonprofit.
Dr. Quinnett admits that what he sees as a lack of political will among many of his colleagues to address the suicide crisis angers him. “We can’t afford to look the other way and pretend this isn’t happening. These numbers are just crushing.”
Currently, however, Washington and Kentucky are the only states with suicide-specific requirements for licensure. Recent efforts to mandate training in California failed when Gov. Jerry Brown (D) vetoed the measure after heavy lobbying efforts by various mental health professional organizations, including the California chapter of the National Association of Social Workers, which argued that it should be entrusted to train its members on a volunteer, as-needed basis.
Even when clinicians have received proper training and met all standards of practice, some patients still may be lost, said Dr. Myers, who also is immediate past vice chair for education and residency training director at SUNY Downstate Medical Center. “You can’t save everyone,” he said. “Some patients are just hell-bent on killing themselves and will very cleverly pull the wool over our eyes.”
He also pointed to the gaps in care that training alone cannot prevent, specifically citing the instances in which people complete a suicide because of a lack of follow-up – the kind of intensive discharge planning that might include several daily phone calls and plans for whom to talk to when thoughts of suicide arise. Those kinds of protocols are not widely used, Dr. Myers said, partly because of the cost.
But Dr. Myers also points to a failing that, while not documented, he said is well-known among his mental health peers: calculated avoidance of at-risk patients.
“There are those, therapists especially, who are cherry picking their patients. They try to make sure they don’t have to look after suicidal people. They do their best to avoid them, and will even screen referrals to avoid them,” said Dr. Myers, who has written extensively about suicide. “It’s equivalent to an oncologist saying to a referring physician: ‘Sure, I will see your patient with breast cancer, but she doesn’t have metastasis, does she?’ It’s unconscionable.”
It would help if there were guidelines for care similar to oncology or cardiology, he said, to help clinicians better balance science with instinct.
Dr. Quinnett thinks the crisis is likely to worsen before it gets better. At least one study has shown strong associations between rates of joblessness in the United States and suicide rates (Soc Sci Med. 2014 Sep;116:22-31). “I’m particularly worried about those people whose lives have been economically hollowed out by the Great Recession,” said Dr. Quinnett, also of the department of psychiatry and behavioral sciences at the University of Washington. “There are men who are aging out [of the workforce] without retirement plans or any other fallback [and who], face losing their dignity and self-esteem, and will need handouts. It’s going to be very ugly.”
Dr. Myers has written several books, including “Touched by Suicide: Hope and Healing After Loss” (New York: Gotham/Penguin, 2006). Dr. Quinnett’s suicide prevention nonprofit, the QPR Institute, is listed on SAMHSA’s National Registry of Evidence-based Programs and Practices.
Coming soon: A national suicide registry?
At the National Institutes of Health, a movement is afoot to create a national suicide registry.
“Registries can help us in all kinds of conditions. That’s how we got ahead in cancer,” Jane Pearson, Ph.D., the National Institute of Mental Health’s program chief for Suicide Treatment and Preventive Interventions Research, said in an interview.
It’s early days yet, but Dr. Pearson and her colleagues are looking into how to leverage data already collected, how to determine the quality of those data, and whom to task with its oversight and interpretation. Then there is the need to know what questions matter most, either to create new registries or to cull patterns from currently available data.
Dr. Pearson said a dedicated suicide data collection effort in a large health care system or a single state would, theoretically, allow patterns to emerge that would help create infrastructures to support specific populations at risk for suicide and guidelines for referral to support.
“Mental health issues have always been a challenge for primary care. As long as they have a partner they can refer to, it’s a much easier [task],” she said. “We wouldn’t ask them to be cardiovascular specialists. When a patient has a stroke, they figure it out and move people along. The registry ideas encompasses that. It’s about creating a whole system for how we are going to do better.”
On Twitter @whitneymcknight
The rise in U.S. suicide rates to the highest levels in almost 30 years is tied to many factors. One fact is clear – some experts say – the lack of training in suicide risk assessment among mental health and substance abuse clinicians is an issue that must be addressed.
“There are mental health professionals who have little to no training in suicide risk assessment,” Dr. Michael F. Myers, professor of clinical psychiatry at State University of New York, Brooklyn, said in an interview.
According to a report released April 22 by the Centers for Disease Control and Prevention, suicide is the 10th-leading cause of death in the United States. It increased by 24% from 1999 to 2014 overall, and the groups most dramatically affected were girls aged 10-14 years, and men aged 45-64. Women aged 45-64 and men aged 75 years and older had the highest suicide rates. About 40,000 Americans a year take their own lives, which is double the number of homicides in the country annually.
After 2006 – against the backdrop of a tough economy and a burgeoning opioid crisis – the suicide rate accelerated. Meanwhile, overall mortality from causes such as cardiovascular disease and cancer is on the decline, according to the CDC report.
Standards vary
In 2012, the American Association of Suicidology reported in its suicide prevention recommendations that less than a quarter of social workers had received any formal suicide prevention training which, when offered, usually lasted 4 hours or fewer. Only 6% of marriage and family therapists had received any such training. Psychiatry residency programs were found to offer training 91% of the time.
But in 2014, the U.S. Preventive Services Task Force (USPSTF) recommendation statement on the efficacy of suicide risk screening concluded that the evidence was insufficient to warrant allocating resources to it (Ann Int Med. 2014;160[10]:719-26). The USPSTF, however, does recommend that primary care professionals screen for depression in adults and adolescents, and earlier this year, updated its recommendations to screen pregnant women in particular (JAMA. 2016;315[4]380-7).
Also, this year, the Centers for Medicare & Medicaid Services required its providers to screen patients for depression using the Patient Health Questionnaire-9 (PHQ-9).
Dr. Myers thinks this is a good starting point, but said that adding more suicide-specific questions to the depression screening process could save more lives.
Despite the USPSTF’s recommendation, investigators for a systematic review published in 2005 concluded that “Physician education in depression recognition and treatment and restricting access to lethal methods reduce suicide rates” (JAMA. 2005;294[16];2064-74). There is some federal support for implementation of suicide prevention in the primary and mental health care settings. In 2012, the U.S. Surgeon General’s office and the National Action Alliance for Suicide Prevention jointly released the National Strategy for Suicide Prevention, which cited as its No. 1 priority, the integration of suicide prevention into health care reform through initiatives such as the Zero Suicide campaign. Sponsored by the Suicide Prevention Resource Council, and funded in part by the Substance Abuse and Mental Health Services Administration (SAMHSA), the program aims to close the gaps in care that distract or otherwise hinder caring for and following through with patients who are at risk for suicide.
An unevenly trained mental health workforce was targeted earlier this month by members of the National Academies of Sciences who, in a report, criticized the current state of siloed mental health care, saying it results in stigmatization and undertreatment of mental illness. The authors urged Congress to empower the U.S. Department of Health and Human Services to oversee better implementation and coordination of evidence-based services to prevent and treat mental disorders that lead to outcomes such as suicide. The report cites successful federal initiatives in England, Australia, and Canada that have notably improved mental health care in those countries. Those improvements took decades, the report notes.
Earlier prevention efforts
In 1999, then–Surgeon General David Satcher issued his Call to Action to Prevent Suicide, which lays out a comprehensive and integrated approach. In 2012, former Surgeon General Regina M. Benjamin published a National Strategy for Suicide Prevention. But without federal policy behind those efforts, the recommendations have not been implemented.
“This is not dissimilar to what happened in the HIV/AIDS epidemic, where finally, the medical community had to be mandated to get trained to treat the illness,” said Paul Quinnett, Ph.D., a clinical psychologist at the University of Washington, Spokane, and founder and CEO of the QPR Institute, a suicide prevention nonprofit.
Dr. Quinnett admits that what he sees as a lack of political will among many of his colleagues to address the suicide crisis angers him. “We can’t afford to look the other way and pretend this isn’t happening. These numbers are just crushing.”
Currently, however, Washington and Kentucky are the only states with suicide-specific requirements for licensure. Recent efforts to mandate training in California failed when Gov. Jerry Brown (D) vetoed the measure after heavy lobbying efforts by various mental health professional organizations, including the California chapter of the National Association of Social Workers, which argued that it should be entrusted to train its members on a volunteer, as-needed basis.
Even when clinicians have received proper training and met all standards of practice, some patients still may be lost, said Dr. Myers, who also is immediate past vice chair for education and residency training director at SUNY Downstate Medical Center. “You can’t save everyone,” he said. “Some patients are just hell-bent on killing themselves and will very cleverly pull the wool over our eyes.”
He also pointed to the gaps in care that training alone cannot prevent, specifically citing the instances in which people complete a suicide because of a lack of follow-up – the kind of intensive discharge planning that might include several daily phone calls and plans for whom to talk to when thoughts of suicide arise. Those kinds of protocols are not widely used, Dr. Myers said, partly because of the cost.
But Dr. Myers also points to a failing that, while not documented, he said is well-known among his mental health peers: calculated avoidance of at-risk patients.
“There are those, therapists especially, who are cherry picking their patients. They try to make sure they don’t have to look after suicidal people. They do their best to avoid them, and will even screen referrals to avoid them,” said Dr. Myers, who has written extensively about suicide. “It’s equivalent to an oncologist saying to a referring physician: ‘Sure, I will see your patient with breast cancer, but she doesn’t have metastasis, does she?’ It’s unconscionable.”
It would help if there were guidelines for care similar to oncology or cardiology, he said, to help clinicians better balance science with instinct.
Dr. Quinnett thinks the crisis is likely to worsen before it gets better. At least one study has shown strong associations between rates of joblessness in the United States and suicide rates (Soc Sci Med. 2014 Sep;116:22-31). “I’m particularly worried about those people whose lives have been economically hollowed out by the Great Recession,” said Dr. Quinnett, also of the department of psychiatry and behavioral sciences at the University of Washington. “There are men who are aging out [of the workforce] without retirement plans or any other fallback [and who], face losing their dignity and self-esteem, and will need handouts. It’s going to be very ugly.”
Dr. Myers has written several books, including “Touched by Suicide: Hope and Healing After Loss” (New York: Gotham/Penguin, 2006). Dr. Quinnett’s suicide prevention nonprofit, the QPR Institute, is listed on SAMHSA’s National Registry of Evidence-based Programs and Practices.
Coming soon: A national suicide registry?
At the National Institutes of Health, a movement is afoot to create a national suicide registry.
“Registries can help us in all kinds of conditions. That’s how we got ahead in cancer,” Jane Pearson, Ph.D., the National Institute of Mental Health’s program chief for Suicide Treatment and Preventive Interventions Research, said in an interview.
It’s early days yet, but Dr. Pearson and her colleagues are looking into how to leverage data already collected, how to determine the quality of those data, and whom to task with its oversight and interpretation. Then there is the need to know what questions matter most, either to create new registries or to cull patterns from currently available data.
Dr. Pearson said a dedicated suicide data collection effort in a large health care system or a single state would, theoretically, allow patterns to emerge that would help create infrastructures to support specific populations at risk for suicide and guidelines for referral to support.
“Mental health issues have always been a challenge for primary care. As long as they have a partner they can refer to, it’s a much easier [task],” she said. “We wouldn’t ask them to be cardiovascular specialists. When a patient has a stroke, they figure it out and move people along. The registry ideas encompasses that. It’s about creating a whole system for how we are going to do better.”
On Twitter @whitneymcknight